User login
What Is Your Diagnosis? Granulocytic Sarcoma
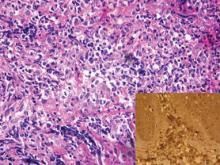
A 24-year-old man presented with a 5-cm asymptomatic, indurated, well-defined nodule with a violaceous center surrounded by a greenish halo on the lower back of 3 months’ duration, along with lymphadenopathy. There was no history of trauma, weight loss, bleeding, or systemic illness. A biopsy revealed sheets of pleomorphic cells with lobulated nuclei and detectable granular cytoplasm. Immunohistochemistry showed strong myeloperoxidase activity in neoplastic cells that were CD13- and CD56-.
The Diagnosis: Granulocytic Sarcoma
Granulocytic sarcoma (GS), sometimes known as leukemia cutis, myeloid sarcoma, or an extramedullary myeloid tumor, is a rare localized collection of immature cells of granulocytic series or the cells of each maturation step in extramedullary sites. Originally described in 1811, the condition was noted after identifying an extramedullary collection of immature granulocytes involving the orbit. Then in 1853 the term chloroma was coined because of the greenish appearance of the tumor when exposed to light due to myeloperoxidase activity in the tumor cells. Finally, in 1967 the term granulocytic sarcoma was introduced because the greenish appearance was not observed in all cases, providing a more correct term.1
Granulocytic sarcoma often manifests in patients with acute myeloid leukemia, chronic myelogenous leukemia, chronic idiopathic myelofibrosis, eosinophilia, refractory anemia, or polycythemia vera, and as an isolated form in patients without apparent hematologic disorder.2
Cutaneous manifestations of leukemia can be specific (eg, GS) or nonspecific (eg, panniculitis, generalized pruritus).2,3 The tumor often appears as a solitary mass (Figure 1); however, in rare instances it can be multifocal. It usually presents as a rapidly growing nodular mass with solid consistence, and it is seen in patients of any age but most often those aged 45 to 55 years as well as in patients younger than 15 years.4
Granulocytic sarcoma is most commonly associated with acute myeloid leukemia. However, it is interesting that the chloroma appears before the onset of leukemia. Occasionally GS is associated with acute myeloid leukemia as a presenting symptom or as a manifestation of recurrence of the disease that was usually related to poor prognosis.5 In patients with GS that is associated with myeloproliferative neoplasms, the occurrence of GS frequently is associated with acute transformation of the disease and therefore a poor prognosis.6
The most common sites of involvement are bone, soft tissue, lymph nodes, and skin. The prognosis does not vary according to location.
Cutaneous B-cell lymphoma should be considered in the differential diagnosis, as it may be clinically observed as single or multiple violaceous nodules involving the head, neck, and/or trunk. Histologically, there generally is a bottom-heavy infiltrate of lymphocytes sparing the epidermis (Figure 2). Immunohistochemistry, flow cytometry, or cytochemical stains often are needed to exclude lymphoma. Pseudochloroma is a rare disease characterized by a collection of normal hematopoietic tissue in locations other than GS. It can be distinguished from GS by its constituent of mature cells.7
Granulocytic sarcoma implies a therapeutic challenge for the clinician. It should always be considered as part of a systemic disease rather than an isolated skin disorder. In patients with evidence of leukemia and GS, systemic chemotherapy is the first line of treatment. Other effective treatment regimens include radiotherapy (electron beam radiation), either alone or in combination with systemic chemotherapy (eg, hydroxyurea, methotrexate).8 If GS persists after chemotherapy, local treatment (eg, radiotherapy, surgery) should be considered with variable results.2
1. Meis JM, Butler JJ, Osborne BM, et al. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986;58:2697-2709.
2. Sun NCJ, Ellis R. Granulocytic sarcoma of the skin. Arch Dermatol. 1980;116:800-802.
3. Campidelli C, Agostinelli C, Stitson R, et al. Myeloid sarcoma. Extramedullary manifestation of myeloid disorders. Am J Clin Pathol. 2009;132:426-437.
4. Pulsoni A, Falcucci P, Anghel G, et al. Isolated granulocytic sarcoma of the skin in an elderly patient: good response to treatment with local radiotherapy and low dose methotrexate. J Eur Acad Dermatol Venereol. 2000;14:216-218.
5. Neiman RS, Barcos M, Berard C, et al. Granulocytic sarcoma: a clinicopathologic study of 61 biopsied cases. Cancer. 1981;48:1426-1437.
6. Byrd JC, Edenfield WJ, Dow NS, et al. Extramedullary myeloid cell tumors in myelodysplastic syndromes: not a true indication of impending acute myeloid leukemia. Leukemia. 1996;21:153-159.
7. Beswick SJ, Jones EL, Mahendra P, et al. Chloroma (aleukaemic leukaemia cutis) initially diagnosed as a cutaneous lymphoma. Clin Exp Dermatol. 2002;27:272-274.
8. Chen WY, Wang CW, Chang CH, et al. Clinicopathologic features and responses to radiotherapy of myeloid sarcoma. Radiat Oncol. 2013;8:245.
A 24-year-old man presented with a 5-cm asymptomatic, indurated, well-defined nodule with a violaceous center surrounded by a greenish halo on the lower back of 3 months’ duration, along with lymphadenopathy. There was no history of trauma, weight loss, bleeding, or systemic illness. A biopsy revealed sheets of pleomorphic cells with lobulated nuclei and detectable granular cytoplasm. Immunohistochemistry showed strong myeloperoxidase activity in neoplastic cells that were CD13- and CD56-.
The Diagnosis: Granulocytic Sarcoma
Granulocytic sarcoma (GS), sometimes known as leukemia cutis, myeloid sarcoma, or an extramedullary myeloid tumor, is a rare localized collection of immature cells of granulocytic series or the cells of each maturation step in extramedullary sites. Originally described in 1811, the condition was noted after identifying an extramedullary collection of immature granulocytes involving the orbit. Then in 1853 the term chloroma was coined because of the greenish appearance of the tumor when exposed to light due to myeloperoxidase activity in the tumor cells. Finally, in 1967 the term granulocytic sarcoma was introduced because the greenish appearance was not observed in all cases, providing a more correct term.1
Granulocytic sarcoma often manifests in patients with acute myeloid leukemia, chronic myelogenous leukemia, chronic idiopathic myelofibrosis, eosinophilia, refractory anemia, or polycythemia vera, and as an isolated form in patients without apparent hematologic disorder.2
Cutaneous manifestations of leukemia can be specific (eg, GS) or nonspecific (eg, panniculitis, generalized pruritus).2,3 The tumor often appears as a solitary mass (Figure 1); however, in rare instances it can be multifocal. It usually presents as a rapidly growing nodular mass with solid consistence, and it is seen in patients of any age but most often those aged 45 to 55 years as well as in patients younger than 15 years.4
Granulocytic sarcoma is most commonly associated with acute myeloid leukemia. However, it is interesting that the chloroma appears before the onset of leukemia. Occasionally GS is associated with acute myeloid leukemia as a presenting symptom or as a manifestation of recurrence of the disease that was usually related to poor prognosis.5 In patients with GS that is associated with myeloproliferative neoplasms, the occurrence of GS frequently is associated with acute transformation of the disease and therefore a poor prognosis.6
The most common sites of involvement are bone, soft tissue, lymph nodes, and skin. The prognosis does not vary according to location.
Cutaneous B-cell lymphoma should be considered in the differential diagnosis, as it may be clinically observed as single or multiple violaceous nodules involving the head, neck, and/or trunk. Histologically, there generally is a bottom-heavy infiltrate of lymphocytes sparing the epidermis (Figure 2). Immunohistochemistry, flow cytometry, or cytochemical stains often are needed to exclude lymphoma. Pseudochloroma is a rare disease characterized by a collection of normal hematopoietic tissue in locations other than GS. It can be distinguished from GS by its constituent of mature cells.7
Granulocytic sarcoma implies a therapeutic challenge for the clinician. It should always be considered as part of a systemic disease rather than an isolated skin disorder. In patients with evidence of leukemia and GS, systemic chemotherapy is the first line of treatment. Other effective treatment regimens include radiotherapy (electron beam radiation), either alone or in combination with systemic chemotherapy (eg, hydroxyurea, methotrexate).8 If GS persists after chemotherapy, local treatment (eg, radiotherapy, surgery) should be considered with variable results.2
A 24-year-old man presented with a 5-cm asymptomatic, indurated, well-defined nodule with a violaceous center surrounded by a greenish halo on the lower back of 3 months’ duration, along with lymphadenopathy. There was no history of trauma, weight loss, bleeding, or systemic illness. A biopsy revealed sheets of pleomorphic cells with lobulated nuclei and detectable granular cytoplasm. Immunohistochemistry showed strong myeloperoxidase activity in neoplastic cells that were CD13- and CD56-.
The Diagnosis: Granulocytic Sarcoma
Granulocytic sarcoma (GS), sometimes known as leukemia cutis, myeloid sarcoma, or an extramedullary myeloid tumor, is a rare localized collection of immature cells of granulocytic series or the cells of each maturation step in extramedullary sites. Originally described in 1811, the condition was noted after identifying an extramedullary collection of immature granulocytes involving the orbit. Then in 1853 the term chloroma was coined because of the greenish appearance of the tumor when exposed to light due to myeloperoxidase activity in the tumor cells. Finally, in 1967 the term granulocytic sarcoma was introduced because the greenish appearance was not observed in all cases, providing a more correct term.1
Granulocytic sarcoma often manifests in patients with acute myeloid leukemia, chronic myelogenous leukemia, chronic idiopathic myelofibrosis, eosinophilia, refractory anemia, or polycythemia vera, and as an isolated form in patients without apparent hematologic disorder.2
Cutaneous manifestations of leukemia can be specific (eg, GS) or nonspecific (eg, panniculitis, generalized pruritus).2,3 The tumor often appears as a solitary mass (Figure 1); however, in rare instances it can be multifocal. It usually presents as a rapidly growing nodular mass with solid consistence, and it is seen in patients of any age but most often those aged 45 to 55 years as well as in patients younger than 15 years.4
Granulocytic sarcoma is most commonly associated with acute myeloid leukemia. However, it is interesting that the chloroma appears before the onset of leukemia. Occasionally GS is associated with acute myeloid leukemia as a presenting symptom or as a manifestation of recurrence of the disease that was usually related to poor prognosis.5 In patients with GS that is associated with myeloproliferative neoplasms, the occurrence of GS frequently is associated with acute transformation of the disease and therefore a poor prognosis.6
The most common sites of involvement are bone, soft tissue, lymph nodes, and skin. The prognosis does not vary according to location.
Cutaneous B-cell lymphoma should be considered in the differential diagnosis, as it may be clinically observed as single or multiple violaceous nodules involving the head, neck, and/or trunk. Histologically, there generally is a bottom-heavy infiltrate of lymphocytes sparing the epidermis (Figure 2). Immunohistochemistry, flow cytometry, or cytochemical stains often are needed to exclude lymphoma. Pseudochloroma is a rare disease characterized by a collection of normal hematopoietic tissue in locations other than GS. It can be distinguished from GS by its constituent of mature cells.7
Granulocytic sarcoma implies a therapeutic challenge for the clinician. It should always be considered as part of a systemic disease rather than an isolated skin disorder. In patients with evidence of leukemia and GS, systemic chemotherapy is the first line of treatment. Other effective treatment regimens include radiotherapy (electron beam radiation), either alone or in combination with systemic chemotherapy (eg, hydroxyurea, methotrexate).8 If GS persists after chemotherapy, local treatment (eg, radiotherapy, surgery) should be considered with variable results.2
1. Meis JM, Butler JJ, Osborne BM, et al. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986;58:2697-2709.
2. Sun NCJ, Ellis R. Granulocytic sarcoma of the skin. Arch Dermatol. 1980;116:800-802.
3. Campidelli C, Agostinelli C, Stitson R, et al. Myeloid sarcoma. Extramedullary manifestation of myeloid disorders. Am J Clin Pathol. 2009;132:426-437.
4. Pulsoni A, Falcucci P, Anghel G, et al. Isolated granulocytic sarcoma of the skin in an elderly patient: good response to treatment with local radiotherapy and low dose methotrexate. J Eur Acad Dermatol Venereol. 2000;14:216-218.
5. Neiman RS, Barcos M, Berard C, et al. Granulocytic sarcoma: a clinicopathologic study of 61 biopsied cases. Cancer. 1981;48:1426-1437.
6. Byrd JC, Edenfield WJ, Dow NS, et al. Extramedullary myeloid cell tumors in myelodysplastic syndromes: not a true indication of impending acute myeloid leukemia. Leukemia. 1996;21:153-159.
7. Beswick SJ, Jones EL, Mahendra P, et al. Chloroma (aleukaemic leukaemia cutis) initially diagnosed as a cutaneous lymphoma. Clin Exp Dermatol. 2002;27:272-274.
8. Chen WY, Wang CW, Chang CH, et al. Clinicopathologic features and responses to radiotherapy of myeloid sarcoma. Radiat Oncol. 2013;8:245.
1. Meis JM, Butler JJ, Osborne BM, et al. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986;58:2697-2709.
2. Sun NCJ, Ellis R. Granulocytic sarcoma of the skin. Arch Dermatol. 1980;116:800-802.
3. Campidelli C, Agostinelli C, Stitson R, et al. Myeloid sarcoma. Extramedullary manifestation of myeloid disorders. Am J Clin Pathol. 2009;132:426-437.
4. Pulsoni A, Falcucci P, Anghel G, et al. Isolated granulocytic sarcoma of the skin in an elderly patient: good response to treatment with local radiotherapy and low dose methotrexate. J Eur Acad Dermatol Venereol. 2000;14:216-218.
5. Neiman RS, Barcos M, Berard C, et al. Granulocytic sarcoma: a clinicopathologic study of 61 biopsied cases. Cancer. 1981;48:1426-1437.
6. Byrd JC, Edenfield WJ, Dow NS, et al. Extramedullary myeloid cell tumors in myelodysplastic syndromes: not a true indication of impending acute myeloid leukemia. Leukemia. 1996;21:153-159.
7. Beswick SJ, Jones EL, Mahendra P, et al. Chloroma (aleukaemic leukaemia cutis) initially diagnosed as a cutaneous lymphoma. Clin Exp Dermatol. 2002;27:272-274.
8. Chen WY, Wang CW, Chang CH, et al. Clinicopathologic features and responses to radiotherapy of myeloid sarcoma. Radiat Oncol. 2013;8:245.