User login
Poor diet causes 70% of type 2 diabetes, says new study
Poor diets account for most newly diagnosed type 2 diabetes cases worldwide, a new analysis has found.
More specifically, the modeling study showed that roughly 14 million cases of type 2 diabetes – or 70% of total type 2 diabetes diagnoses in 2018 – were linked with a poor diet, found Meghan O’Hearn, a doctoral student at the Friedman School of Nutrition Science and Policy, Tufts University, Boston, and colleagues. The study was published online in Nature Medicine.
The results also indicate that the greatest burdens of type 2 diabetes were accounted for by excess wheat intake and refined rice (24.6%), excess processed meat consumption (20.3%), and inadequate whole-grain consumption (26.1%). Factors such as drinking too much fruit juice and not eating enough nonstarchy vegetables, nuts, or seeds, had less of an impact on new cases of the disease, the researchers determined.
“These findings can help inform nutritional priorities for clinicians, policymakers, and private sector actors as they encourage healthier dietary choices that address this global epidemic,” Ms. O’Hearn said in a press release.
Prior research has suggested that poor diet contributes to about 40% of type 2 diabetes cases worldwide, the researchers note.
The team attributes their finding of a 70% contribution to the new information in their analysis, such as the first-ever inclusion of refined grains, which was one of the top contributors to diabetes burden, and updated data on dietary habits based on national individual-level dietary surveys rather than agricultural estimates.
“Our study suggests poor carbohydrate quality is a leading driver of diet-attributable type 2 diabetes globally and with important variation by nation and over time,” said senior author Dariush Mozaffarian, MD, DrPh, MPH, who is the Jean Mayer Professor of Nutrition at the Friedman School of Nutrition Science and Policy.
“These new findings reveal critical areas for national and global focus to improve nutrition and reduce devastating burdens of diabetes,” he noted.
“Left unchecked and with incidence only projected to rise, type 2 diabetes will continue to impact population health, economic productivity, [and] health care system capacity, [as well as] drive health inequities worldwide,” Ms. O’Hearn said.
It’s about reducing harmful dietary components
Ms. O’Hearn and colleagues set out to fill information gaps in knowledge about how the global burden of diet-associated type 2 diabetes is impacted by disparities and other factors known to influence risk, including dietary components.
They used information from the Global Dietary Database to study dietary intake in 184 nations from 1990 to 2018. They also studied demographics from multiple sources, estimates of type 2 diabetes incidence around the world, and data on food choices, including the effect of 11 dietary factors, from prior research.
They found that there were 8.6 million more cases of type 2 diabetes in 2018 than in 1990 because of poor diet.
Regionally, Central and Eastern Europe and Central Asia had the greatest number of type 2 diabetes cases linked to diet, particularly Poland and Russia, where diets tend to be rich in red meat, processed meat, and potatoes. Incidence was also high in Latin America and the Caribbean, especially in Colombia and Mexico, which was attributed to high consumption of sugary drinks and processed meat and low intake of whole grains.
Regions where diet had less of an impact on type 2 diabetes cases included South Asia and sub-Saharan Africa, although the largest increases in type 2 diabetes due to poor diet between 1990 and 2018 were observed in sub-Saharan Africa.
Diet-attributable type 2 diabetes was generally larger among urban versus rural residents and higher versus lower educated individuals, except in high-income countries, Central and Eastern Europe, and Central Asia, where burdens were larger in rural residents and in lower educated individuals.
Notably, women had lower proportions of diet-related type 2 diabetes, compared with men, and these proportions were inversely related to age.
Excess intake of harmful dietary factors contributed a greater percentage of the burden of type 2 diabetes globally (60.8%) than did insufficient intake of protective dietary factors (39.2%).
“Future research should address whether more complex diet–type 2 diabetes dose–response relationships exist,” the authors conclude.
Ms. O’Hearn has reported receiving research funding from the Gates Foundation, as well as the National Institutes of Health and Vail Innovative Global Research and employment with Food Systems for the Future. Dr. Mozaffarian has reported receiving funding from the National Institutes of Health, the Gates Foundation, the Rockefeller Foundation, Vail Innovative Global Research, and the Kaiser Permanente Fund at East Bay Community Foundation; personal fees from Acasti Pharma, Barilla, Danone, and Motif FoodWorks; is on the scientific advisory board for Beren Therapeutics, Brightseed, Calibrate, DiscernDx, Elysium Health, Filtricine, HumanCo, January, Perfect Day, Tiny Organics and (ended) Day Two and Season Health; has stock ownership in Calibrate and HumanCo; and receives chapter royalties from UpToDate.
A version of this article first appeared on Medscape.com.
Poor diets account for most newly diagnosed type 2 diabetes cases worldwide, a new analysis has found.
More specifically, the modeling study showed that roughly 14 million cases of type 2 diabetes – or 70% of total type 2 diabetes diagnoses in 2018 – were linked with a poor diet, found Meghan O’Hearn, a doctoral student at the Friedman School of Nutrition Science and Policy, Tufts University, Boston, and colleagues. The study was published online in Nature Medicine.
The results also indicate that the greatest burdens of type 2 diabetes were accounted for by excess wheat intake and refined rice (24.6%), excess processed meat consumption (20.3%), and inadequate whole-grain consumption (26.1%). Factors such as drinking too much fruit juice and not eating enough nonstarchy vegetables, nuts, or seeds, had less of an impact on new cases of the disease, the researchers determined.
“These findings can help inform nutritional priorities for clinicians, policymakers, and private sector actors as they encourage healthier dietary choices that address this global epidemic,” Ms. O’Hearn said in a press release.
Prior research has suggested that poor diet contributes to about 40% of type 2 diabetes cases worldwide, the researchers note.
The team attributes their finding of a 70% contribution to the new information in their analysis, such as the first-ever inclusion of refined grains, which was one of the top contributors to diabetes burden, and updated data on dietary habits based on national individual-level dietary surveys rather than agricultural estimates.
“Our study suggests poor carbohydrate quality is a leading driver of diet-attributable type 2 diabetes globally and with important variation by nation and over time,” said senior author Dariush Mozaffarian, MD, DrPh, MPH, who is the Jean Mayer Professor of Nutrition at the Friedman School of Nutrition Science and Policy.
“These new findings reveal critical areas for national and global focus to improve nutrition and reduce devastating burdens of diabetes,” he noted.
“Left unchecked and with incidence only projected to rise, type 2 diabetes will continue to impact population health, economic productivity, [and] health care system capacity, [as well as] drive health inequities worldwide,” Ms. O’Hearn said.
It’s about reducing harmful dietary components
Ms. O’Hearn and colleagues set out to fill information gaps in knowledge about how the global burden of diet-associated type 2 diabetes is impacted by disparities and other factors known to influence risk, including dietary components.
They used information from the Global Dietary Database to study dietary intake in 184 nations from 1990 to 2018. They also studied demographics from multiple sources, estimates of type 2 diabetes incidence around the world, and data on food choices, including the effect of 11 dietary factors, from prior research.
They found that there were 8.6 million more cases of type 2 diabetes in 2018 than in 1990 because of poor diet.
Regionally, Central and Eastern Europe and Central Asia had the greatest number of type 2 diabetes cases linked to diet, particularly Poland and Russia, where diets tend to be rich in red meat, processed meat, and potatoes. Incidence was also high in Latin America and the Caribbean, especially in Colombia and Mexico, which was attributed to high consumption of sugary drinks and processed meat and low intake of whole grains.
Regions where diet had less of an impact on type 2 diabetes cases included South Asia and sub-Saharan Africa, although the largest increases in type 2 diabetes due to poor diet between 1990 and 2018 were observed in sub-Saharan Africa.
Diet-attributable type 2 diabetes was generally larger among urban versus rural residents and higher versus lower educated individuals, except in high-income countries, Central and Eastern Europe, and Central Asia, where burdens were larger in rural residents and in lower educated individuals.
Notably, women had lower proportions of diet-related type 2 diabetes, compared with men, and these proportions were inversely related to age.
Excess intake of harmful dietary factors contributed a greater percentage of the burden of type 2 diabetes globally (60.8%) than did insufficient intake of protective dietary factors (39.2%).
“Future research should address whether more complex diet–type 2 diabetes dose–response relationships exist,” the authors conclude.
Ms. O’Hearn has reported receiving research funding from the Gates Foundation, as well as the National Institutes of Health and Vail Innovative Global Research and employment with Food Systems for the Future. Dr. Mozaffarian has reported receiving funding from the National Institutes of Health, the Gates Foundation, the Rockefeller Foundation, Vail Innovative Global Research, and the Kaiser Permanente Fund at East Bay Community Foundation; personal fees from Acasti Pharma, Barilla, Danone, and Motif FoodWorks; is on the scientific advisory board for Beren Therapeutics, Brightseed, Calibrate, DiscernDx, Elysium Health, Filtricine, HumanCo, January, Perfect Day, Tiny Organics and (ended) Day Two and Season Health; has stock ownership in Calibrate and HumanCo; and receives chapter royalties from UpToDate.
A version of this article first appeared on Medscape.com.
Poor diets account for most newly diagnosed type 2 diabetes cases worldwide, a new analysis has found.
More specifically, the modeling study showed that roughly 14 million cases of type 2 diabetes – or 70% of total type 2 diabetes diagnoses in 2018 – were linked with a poor diet, found Meghan O’Hearn, a doctoral student at the Friedman School of Nutrition Science and Policy, Tufts University, Boston, and colleagues. The study was published online in Nature Medicine.
The results also indicate that the greatest burdens of type 2 diabetes were accounted for by excess wheat intake and refined rice (24.6%), excess processed meat consumption (20.3%), and inadequate whole-grain consumption (26.1%). Factors such as drinking too much fruit juice and not eating enough nonstarchy vegetables, nuts, or seeds, had less of an impact on new cases of the disease, the researchers determined.
“These findings can help inform nutritional priorities for clinicians, policymakers, and private sector actors as they encourage healthier dietary choices that address this global epidemic,” Ms. O’Hearn said in a press release.
Prior research has suggested that poor diet contributes to about 40% of type 2 diabetes cases worldwide, the researchers note.
The team attributes their finding of a 70% contribution to the new information in their analysis, such as the first-ever inclusion of refined grains, which was one of the top contributors to diabetes burden, and updated data on dietary habits based on national individual-level dietary surveys rather than agricultural estimates.
“Our study suggests poor carbohydrate quality is a leading driver of diet-attributable type 2 diabetes globally and with important variation by nation and over time,” said senior author Dariush Mozaffarian, MD, DrPh, MPH, who is the Jean Mayer Professor of Nutrition at the Friedman School of Nutrition Science and Policy.
“These new findings reveal critical areas for national and global focus to improve nutrition and reduce devastating burdens of diabetes,” he noted.
“Left unchecked and with incidence only projected to rise, type 2 diabetes will continue to impact population health, economic productivity, [and] health care system capacity, [as well as] drive health inequities worldwide,” Ms. O’Hearn said.
It’s about reducing harmful dietary components
Ms. O’Hearn and colleagues set out to fill information gaps in knowledge about how the global burden of diet-associated type 2 diabetes is impacted by disparities and other factors known to influence risk, including dietary components.
They used information from the Global Dietary Database to study dietary intake in 184 nations from 1990 to 2018. They also studied demographics from multiple sources, estimates of type 2 diabetes incidence around the world, and data on food choices, including the effect of 11 dietary factors, from prior research.
They found that there were 8.6 million more cases of type 2 diabetes in 2018 than in 1990 because of poor diet.
Regionally, Central and Eastern Europe and Central Asia had the greatest number of type 2 diabetes cases linked to diet, particularly Poland and Russia, where diets tend to be rich in red meat, processed meat, and potatoes. Incidence was also high in Latin America and the Caribbean, especially in Colombia and Mexico, which was attributed to high consumption of sugary drinks and processed meat and low intake of whole grains.
Regions where diet had less of an impact on type 2 diabetes cases included South Asia and sub-Saharan Africa, although the largest increases in type 2 diabetes due to poor diet between 1990 and 2018 were observed in sub-Saharan Africa.
Diet-attributable type 2 diabetes was generally larger among urban versus rural residents and higher versus lower educated individuals, except in high-income countries, Central and Eastern Europe, and Central Asia, where burdens were larger in rural residents and in lower educated individuals.
Notably, women had lower proportions of diet-related type 2 diabetes, compared with men, and these proportions were inversely related to age.
Excess intake of harmful dietary factors contributed a greater percentage of the burden of type 2 diabetes globally (60.8%) than did insufficient intake of protective dietary factors (39.2%).
“Future research should address whether more complex diet–type 2 diabetes dose–response relationships exist,” the authors conclude.
Ms. O’Hearn has reported receiving research funding from the Gates Foundation, as well as the National Institutes of Health and Vail Innovative Global Research and employment with Food Systems for the Future. Dr. Mozaffarian has reported receiving funding from the National Institutes of Health, the Gates Foundation, the Rockefeller Foundation, Vail Innovative Global Research, and the Kaiser Permanente Fund at East Bay Community Foundation; personal fees from Acasti Pharma, Barilla, Danone, and Motif FoodWorks; is on the scientific advisory board for Beren Therapeutics, Brightseed, Calibrate, DiscernDx, Elysium Health, Filtricine, HumanCo, January, Perfect Day, Tiny Organics and (ended) Day Two and Season Health; has stock ownership in Calibrate and HumanCo; and receives chapter royalties from UpToDate.
A version of this article first appeared on Medscape.com.
FROM NATURE MEDICINE
Optimal time period for weight loss drugs: Debate continues
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
After bariatric surgery in 2014, Kristal Hartman still struggled to manage her weight long term. It took her over a year to lose 100 pounds, a loss she initially maintained, but then gradually her body mass index (BMI) started creeping up again.
“The body kind of has a set point, and you have to constantly trick it because it is going to start to gain weight again,” Ms. Hartman, who is on the national board of directors for the Obesity Action Coalition, said in an interview.
So, 2.5 years after her surgery, Ms. Hartman began weekly subcutaneous injections of the glucagonlike peptide–1 (GLP-1) agonist semaglutide, a medication that is now almost infamous because of its popularity among celebrities and social media influencers.
Branded as Ozempic for type 2 diabetes and Wegovy for obesity, both contain semaglutide but in slightly different doses. The popularity of the medication has led to shortages for those living with type 2 diabetes and/or obesity. And other medications are waiting in the wings that work on GLP-1 and other hormones that regulate appetite, such as the twincretin tirzepatide (Mounjaro), another weekly injection, approved by the Food and Drug Administration in May 2022 for type 2 diabetes and awaiting approval for obesity.
Ms. Hartman said taking semaglutide helped her not only lose weight but also “curb [her] obsessive thoughts over food.” To maintain a BMI within the healthy range, as well as taking the GLP-1 agonist, Ms. Hartman relies on other strategies, including exercise, and mental health support.
“Physicians really need to be open to these FDA-approved medications as one of many tools in the toolbox for patients with obesity. It’s just like any other chronic disease state, when they are thinking of using these, they need to think about long-term use ... in patients who have obesity, not just [among those people] who just want to lose 5-10 pounds. That’s not what these drugs are designed for. They are for people who are actually living with the chronic disease of obesity every day of their lives,” she emphasized.
On average, patients lose 25%-40% of their total body weight following bariatric surgery, said Teresa LeMasters, MD, president of the American Society for Metabolic & Bariatric Surgery. However, there typically is a “small” weight regain after surgery.
“For most patients, it is a small 5-10 pounds, but for some others, it can be significant,” said Dr. LeMasters, a bariatric surgeon at UnityPoint Clinic, Des Moines, Iowa.
“We do still see some patients– anywhere from 10% to 30% – who will have some [significant] weight regain, and so then we will look at that,” she noted. In those cases, the disease of obesity “is definitely still present.”
Medications can counter weight regain after surgery
For patients who don’t reach their weight loss goals after bariatric surgery, Dr. LeMasters said it’s appropriate to consider adding an anti-obesity medication. The newer GLP-1 agonists can lead to a loss of around 15% of body weight in some patients.
or even just to optimize their initial response to surgery if they are starting at a very, very severe point of disease,” she explained.
She noted, however, that some patients shouldn’t be prescribed GLP-1 agonists, including those with a history of thyroid cancer or pancreatitis.
Caroline M. Apovian, MD, codirector of the center for weight management and wellness and professor of medicine at Harvard Medical School, Boston, said in an interview that the physiology behind bariatric surgery and that of the newer obesity medications is somewhat aligned.
“In order to reduce ... body weight permanently you need adjustments. We learned that you need the adjustments of the hormones [that affect appetite, such as GLP-1], and that’s why bariatric surgery works because ... [it] provides the most durable and the most effective treatment for obesity ... because [with surgery] you are adjusting the secretion and timing of many of the hormones that regulate body weight,” she explained.
So, when people are taking GLP-1 agonists for obesity, with or without surgery, these medications “are meant and were approved by the FDA to be taken indefinitely. They are not [for the] short term,” Dr. Apovian noted.
Benjamin O’Donnell, MD, an associate professor at Ohio State University Wexner Medical Center, Columbus, agreed that the newer anti-obesity medications can be very effective; however, he expressed uncertainty about prescribing these medications for years and years.
“If somebody has obesity, they need medicine to help them manage appetite and maintain a lower, healthier weight. It would make sense that they would just stay on the medicine,” he noted.
But he qualified: “I have a hard time committing to saying that someone should take this medication for the rest of their life. Part of my hesitation is that the medications are expensive, so we’ve had a hard time with people staying on them, mostly because of insurance formulary changes.”
Why stop the medications? Side effects and lack of insurance coverage
Many people have to discontinue these newer medications for that exact reason.
When Ms. Hartman’s insurance coverage lapsed, she had to go without semaglutide for a while.
“At that time, I absolutely gained weight back up into an abnormal BMI range,” Ms. Hartman said. When she was able to resume the medication, she lost weight again and her BMI returned to normal range.
These medications currently cost around $1,400 per month in the United States, unless patients can access initiatives such as company coupons. Some insurers, including state-subsidized Medicare and Medicaid, don’t cover the new medications.
Dr. O’Donnell said, “More accessibility for more people would help in the big picture.”
Other patients stop taking GLP-1 agonists because they experience side effects, such as nausea.
“Gastrointestinal complaints ... are the number one reason for people to come off the medication,” said Disha Narang, MD, an endocrinologist and obesity medicine specialist at Northwestern Medicine Lake Forest (Ill.) Hospital.
“It is an elective therapy, so it is not mandatory that someone take it. So if they are not feeling well or they are sick, then that’s a major reason for coming off of it,” she said.
Dan Bessesen, MD, professor of medicine at the University of Colorado at Denver, Aurora, and chief of endocrinology, agreed.
Patients are unlikely to stay on these medications if they feel nauseous or experience vomiting, he said. Although he noted there are options to try to counter this, such as starting patients on a very low dose of the drug and up-titrating slowly. This method requires good coordination between the patient and physician.
Goutham Rao, MD, a professor of medicine at Case Western Reserve University and head of the weight-loss initiative Fitter Me at University Hospitals, both in Cleveland, said that prior to prescribing GLP-1 agonists for weight loss, he sets four basic, nonnegotiable goals for patients: “to have breakfast within 30 minutes of getting up, to drink just water, no food or drink after 7:00 p.m. except for water, and 30 minutes of continuous exercise per day, which is typically, for older clientele, walking.”
This, he said, can help establish good habits because if “patients are not engaged psychologically in weight loss ... they expect the medication to do [all] the work.”
Most regain weight after stopping obesity medications
As Ms. Hartman’s story illustrates, discontinuing the medications often leads to weight regain.
“Without the medicine, there are a variety of things that will happen. Appetite will tend to increase, and so [patients] will gradually tend to eat more over time,” Dr. Bessesen noted.
“So it may take a long time for the weight regain to happen, but in every study where an obesity medicine has been used, and then it is stopped, the weight goes back to where it was on lifestyle alone,” he added.
In the STEP 1 trial, almost 2,000 patients who were either overweight or living with obesity were randomized 2:1 to semaglutide, titrated up to 2.4 mg each week by week 16, or placebo in addition to lifestyle modification. After 68 weeks, those in the semaglutide group had a mean weight loss of 14.9%, compared with 2.4% in the placebo group.
Patients were also followed in a 1-year extension of the trial, published in Diabetes, Obesity, and Metabolism.
Within 1 year of stopping treatment, participants regained two thirds of the weight they had initially lost.
Hence, Dr. Bessesen stressed that a total rethink of how obesity is approached is needed among most physicians.
“I think in the future treating obesity with medications should be like treating hypertension and diabetes, something most primary care doctors are comfortable doing, but that’s going to take a little work and practice on the part of clinicians to really have a comfortable conversation about risks, and benefits, with patients,” he said.
“I would encourage primary care doctors to learn more about the treatment of obesity, and learn more about bias and stigma, and think about how they can deliver care that is compassionate and competent,” he concluded.
A version of this article first appeared on Medscape.com.
STEMI times to treatment usually miss established goals
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).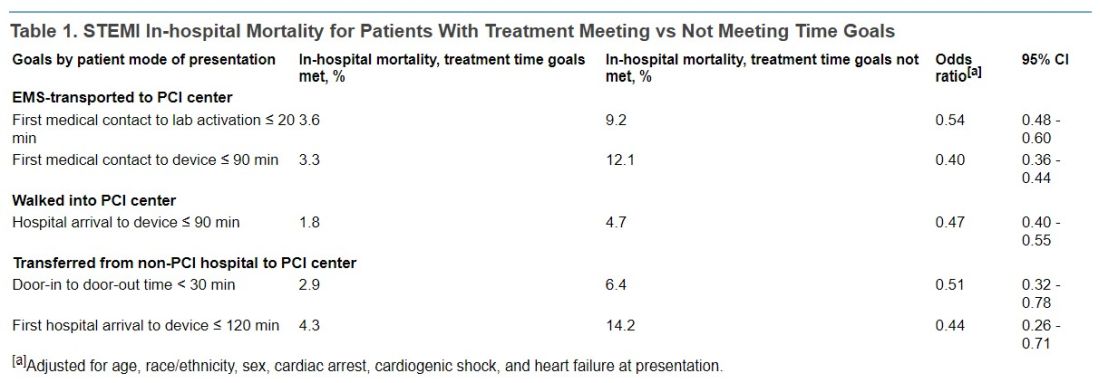
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).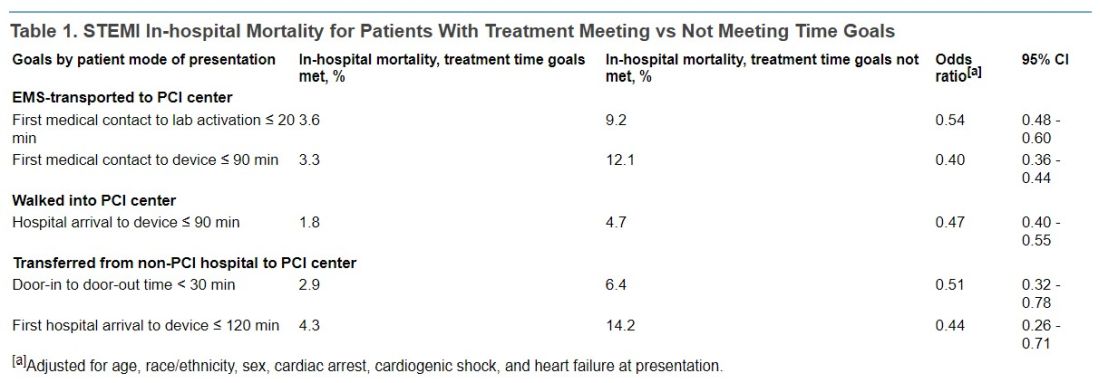
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).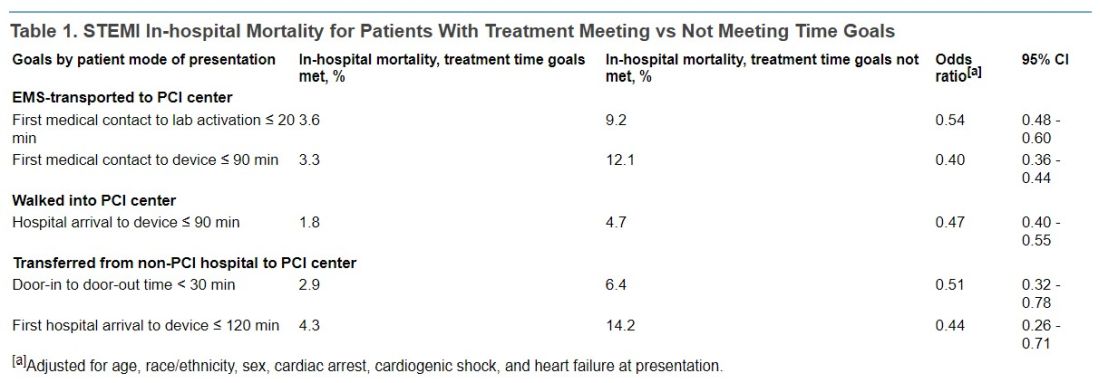
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
FROM JAMA
‘The Whale’: Is this new movie fat-phobic or fat-friendly?
“I could relate to many, many, many of the experiences and emotions that Charlie, which is Brendan Fraser’s character, was portraying,” Patricia Nece recalls after watching a preview copy of the new film “The Whale.”
Much of the movie “rang true and hit home for me as things that I, too, had experienced,” Ms. Nece, the board of directors’ chair of the Obesity Action Coalition (OAC) and a person living with obesity, shares with this news organization.
In theaters as of December 9, The Whale chronicles the experience of a 600-lb, middle-aged man named Charlie. Throughout the film, Charlie seeks to rebuild his relationship with his estranged teenage daughter. Charlie had left his daughter and family to pursue a relationship with a man, who eventually died. As he navigates the pain surrounding his partner’s death and his lack of community, Charlie turns to food for comfort.
When the movie premiered at the Venice Film Festival, Mr. Fraser received a 6-minute standing ovation. However, activists criticized the movie for casting Fraser over an actor with obesity as well as its depiction of people with obesity.
Representatives from the National Association to Advance Fat Acceptance contend that casting an actor without obesity only contributes to ongoing bias against people of size. “Medical weight stigma and other socio-political determinants of health for people of all sizes cause far more harm to fat people than body fat does. Bias endangers fat people’s health. Anti-obesity organizations, such as those consulted with for this movie, contribute to stigma rather than reducing it as they claim,” NAAFA wrote in a statement to this news organization.
And they added that though the fat suit used in the movie may be superior to previous ones, it is still not an accurate depiction: “The creators of The Whale consider its CGI-generated fat suit to be superior to tactile fat suits, but we don’t. The issue with fat suits in Hollywood is not that they aren’t realistic enough. The issue is that they are used rather than using performers who actually live in bodies like the ones being depicted. If there is a 600-pound character in a movie, there should be a 600-pound human in that role. Rather than concentrate on the hype around the fake fat body created for The Whale, we want to see Hollywood create more opportunities for fat people across the size spectrum, both in front of the camera and behind the scenes.”
Prosthetics vs. reality?
Ms. Nece says she understands the controversy surrounding the use of fat suits but believes that it was not done in poor taste.
“OAC got involved with the movie after Brendan was already chosen for the part, and we never would have gotten involved with it had the prosthetics or fat suit been used to ridicule or make fun of people with obesity, which is usually the case,” she explains.
“But we knew from the start that that was never the intent of anyone involved with The Whale. And I think that’s shown by the fact that Brendan and Darren Aronofsky, the director, reached out to people who live with obesity on a daily basis to find out and learn more about it and to educate themselves about it,” Ms. Nece continues.
In a Daily Mail article, Mr. Fraser credited his son Griffin, who is autistic and obese, with helping him understand the struggles that people with obesity face.
Rachel Goldman, PhD, a clinical psychologist in private practice in New York and a professor in the psychology department at New York University, notes that there are other considerations that played into casting. “I know there was some pushback in terms of could, a say 600-lb individual, even be able to go to be on set every day and do this kind of work, and the answer is we don’t know.”
“I’m sure Darren chose Brendan for many reasons above and beyond just his body. I think that’s very important to keep in mind that just as much as representation is very important, I think it is also about finding the right person for the right role,” adds Dr. Goldman, who served as a consultant to the film.
Fat suits, extreme weight gains all to play a role
About 42% of adults in the United States have obesity, according to the 2017-2020 National Health and Nutrition Examination Survey, but that reality is not reflected in films or television.
A study of 1018 major television characters found that 24% of men and 14% of women had either overweight or obesity – far below the national average. And when characters with obesity are portrayed, actors often wear prosthetics, like Gwyneth Paltrow in Shallow Hal or Eddie Murphy in the Nutty Professor.
But unlike Mr. Fraser, some actors gain weight quickly instead.
This practice is unhealthy, says Jaime Almandoz, MD, an associate professor at the University of Texas Southwestern Medical Center, Dallas, and a nonsurgical weight management expert. In interviews, actors have shared how they increased calorie intake by drinking two milkshakes per day, going to fast food places regularly, or, in Mark Walhberg’s case, consuming 7,000 calories per day to gain 30 pounds for his role as boxer-turned-priest in the movie Father Stu.
This method provides their bodies with excess calories they are unable to burn off. “Then the amount of sugar and fat that streams into the blood as a result creates problems both directly and indirectly as your body tries to store it. It basically ends up using overflow warehouses for fat storage, like the liver for example, so we can create a condition called fatty liver, or in the muscle and other places, and this excess sugar and fat in the bloodstream cause several factors that are both insulin resistance causing,” Dr. Almandoz explains.
Though gaining weight helps the actor understand the character’s life experience, it may also be risky.
“To have an actor deliberately put his own health at risk and gain a certain amount of weight and whatever that might entail, one – that’s not necessarily the safest thing for that actor – but two, it’s also important to highlight the authentic experience of someone who has dealt with this chronic disease as well,” says Disha Narang, MD, a quadruple-board certified endocrinologist, obesity medicine, and culinary medicine specialist at Northwestern Medicine Lake Forest Hospital, Chicago.
These extreme fluctuations in weight may create problems. “It is typically not something we recommend because there could be metabolic damages as well as health concerns when patients are trying to gain weight quickly, just as we don’t want patients to lose weight quickly,” says Kurt Hong, MD, PhD, board-certified in internal medicine and clinical nutrition at the University of Southern California, Los Angeles.
Dr. Hong notes that it may be difficult for individuals to experience sudden weight gain because the body works hard to maintain a state of homeostasis.
“Similarly, to someone trying to gain weight you overeat, initially your body will try to again, maybe enhance its metabolic efficiency to hold the body stable,” Dr. Hong adds.
Dietary choices that may contribute to insulin resistance or promote high blood sugar can contribute to inflammation and a number of other adverse health outcomes, notes Dr. Almandoz. “The things that actors need to do in order to gain this magnitude of weight and they want to do it in the most time-effective manner is often not helpful for our bodies, it can be very problematic, the same thing goes for weight loss when actors need to lose significant amounts of weight for roles,” says Dr. Almandoz.
And Dr. Hong explained that for patients trying to lose weight, they may cut calories, but the body will try to compensate by slowing down the metabolism to keep their weight the same.
‘Your own worst bully’
In “The Whale,” Charlie appears to suffer from internalized weight bias, which is common to many people living with obesity, Ms. Nece says.
“Internalized weight bias is when the person of size takes all that negativity and turns it on themselves. The easiest way to describe that is to tell you that I became my own worst bully because I started believing all the negative things people said to me about my weight,” Ms. Nece adds.
Her hope is that the film will bring attention to the harm that this bias creates, especially when it derives from other people. “There’s no telling whether it will, but what Charlie experiences in bias and stigma from others clearly happens. It’s realistic. Those of us in large bodies have experienced what he is experiencing, so some people have said the movie is fat-phobic, but I see it as I can relate to those experiences because I have them too, so they are very realistic.”
Ms. Nece notes that it is important for clinicians to understand that obesity is a multifaceted and sensitive topic. “For those medical professionals who do not already know that obesity is complex, I hope the film will begin to open their eyes to the many different facets involved in obesity and their patients with obesity, I hope it will help them empathize and show compassion to their patients with obesity,” she concludes.
A version of this article first appeared on Medscape.com.
“I could relate to many, many, many of the experiences and emotions that Charlie, which is Brendan Fraser’s character, was portraying,” Patricia Nece recalls after watching a preview copy of the new film “The Whale.”
Much of the movie “rang true and hit home for me as things that I, too, had experienced,” Ms. Nece, the board of directors’ chair of the Obesity Action Coalition (OAC) and a person living with obesity, shares with this news organization.
In theaters as of December 9, The Whale chronicles the experience of a 600-lb, middle-aged man named Charlie. Throughout the film, Charlie seeks to rebuild his relationship with his estranged teenage daughter. Charlie had left his daughter and family to pursue a relationship with a man, who eventually died. As he navigates the pain surrounding his partner’s death and his lack of community, Charlie turns to food for comfort.
When the movie premiered at the Venice Film Festival, Mr. Fraser received a 6-minute standing ovation. However, activists criticized the movie for casting Fraser over an actor with obesity as well as its depiction of people with obesity.
Representatives from the National Association to Advance Fat Acceptance contend that casting an actor without obesity only contributes to ongoing bias against people of size. “Medical weight stigma and other socio-political determinants of health for people of all sizes cause far more harm to fat people than body fat does. Bias endangers fat people’s health. Anti-obesity organizations, such as those consulted with for this movie, contribute to stigma rather than reducing it as they claim,” NAAFA wrote in a statement to this news organization.
And they added that though the fat suit used in the movie may be superior to previous ones, it is still not an accurate depiction: “The creators of The Whale consider its CGI-generated fat suit to be superior to tactile fat suits, but we don’t. The issue with fat suits in Hollywood is not that they aren’t realistic enough. The issue is that they are used rather than using performers who actually live in bodies like the ones being depicted. If there is a 600-pound character in a movie, there should be a 600-pound human in that role. Rather than concentrate on the hype around the fake fat body created for The Whale, we want to see Hollywood create more opportunities for fat people across the size spectrum, both in front of the camera and behind the scenes.”
Prosthetics vs. reality?
Ms. Nece says she understands the controversy surrounding the use of fat suits but believes that it was not done in poor taste.
“OAC got involved with the movie after Brendan was already chosen for the part, and we never would have gotten involved with it had the prosthetics or fat suit been used to ridicule or make fun of people with obesity, which is usually the case,” she explains.
“But we knew from the start that that was never the intent of anyone involved with The Whale. And I think that’s shown by the fact that Brendan and Darren Aronofsky, the director, reached out to people who live with obesity on a daily basis to find out and learn more about it and to educate themselves about it,” Ms. Nece continues.
In a Daily Mail article, Mr. Fraser credited his son Griffin, who is autistic and obese, with helping him understand the struggles that people with obesity face.
Rachel Goldman, PhD, a clinical psychologist in private practice in New York and a professor in the psychology department at New York University, notes that there are other considerations that played into casting. “I know there was some pushback in terms of could, a say 600-lb individual, even be able to go to be on set every day and do this kind of work, and the answer is we don’t know.”
“I’m sure Darren chose Brendan for many reasons above and beyond just his body. I think that’s very important to keep in mind that just as much as representation is very important, I think it is also about finding the right person for the right role,” adds Dr. Goldman, who served as a consultant to the film.
Fat suits, extreme weight gains all to play a role
About 42% of adults in the United States have obesity, according to the 2017-2020 National Health and Nutrition Examination Survey, but that reality is not reflected in films or television.
A study of 1018 major television characters found that 24% of men and 14% of women had either overweight or obesity – far below the national average. And when characters with obesity are portrayed, actors often wear prosthetics, like Gwyneth Paltrow in Shallow Hal or Eddie Murphy in the Nutty Professor.
But unlike Mr. Fraser, some actors gain weight quickly instead.
This practice is unhealthy, says Jaime Almandoz, MD, an associate professor at the University of Texas Southwestern Medical Center, Dallas, and a nonsurgical weight management expert. In interviews, actors have shared how they increased calorie intake by drinking two milkshakes per day, going to fast food places regularly, or, in Mark Walhberg’s case, consuming 7,000 calories per day to gain 30 pounds for his role as boxer-turned-priest in the movie Father Stu.
This method provides their bodies with excess calories they are unable to burn off. “Then the amount of sugar and fat that streams into the blood as a result creates problems both directly and indirectly as your body tries to store it. It basically ends up using overflow warehouses for fat storage, like the liver for example, so we can create a condition called fatty liver, or in the muscle and other places, and this excess sugar and fat in the bloodstream cause several factors that are both insulin resistance causing,” Dr. Almandoz explains.
Though gaining weight helps the actor understand the character’s life experience, it may also be risky.
“To have an actor deliberately put his own health at risk and gain a certain amount of weight and whatever that might entail, one – that’s not necessarily the safest thing for that actor – but two, it’s also important to highlight the authentic experience of someone who has dealt with this chronic disease as well,” says Disha Narang, MD, a quadruple-board certified endocrinologist, obesity medicine, and culinary medicine specialist at Northwestern Medicine Lake Forest Hospital, Chicago.
These extreme fluctuations in weight may create problems. “It is typically not something we recommend because there could be metabolic damages as well as health concerns when patients are trying to gain weight quickly, just as we don’t want patients to lose weight quickly,” says Kurt Hong, MD, PhD, board-certified in internal medicine and clinical nutrition at the University of Southern California, Los Angeles.
Dr. Hong notes that it may be difficult for individuals to experience sudden weight gain because the body works hard to maintain a state of homeostasis.
“Similarly, to someone trying to gain weight you overeat, initially your body will try to again, maybe enhance its metabolic efficiency to hold the body stable,” Dr. Hong adds.
Dietary choices that may contribute to insulin resistance or promote high blood sugar can contribute to inflammation and a number of other adverse health outcomes, notes Dr. Almandoz. “The things that actors need to do in order to gain this magnitude of weight and they want to do it in the most time-effective manner is often not helpful for our bodies, it can be very problematic, the same thing goes for weight loss when actors need to lose significant amounts of weight for roles,” says Dr. Almandoz.
And Dr. Hong explained that for patients trying to lose weight, they may cut calories, but the body will try to compensate by slowing down the metabolism to keep their weight the same.
‘Your own worst bully’
In “The Whale,” Charlie appears to suffer from internalized weight bias, which is common to many people living with obesity, Ms. Nece says.
“Internalized weight bias is when the person of size takes all that negativity and turns it on themselves. The easiest way to describe that is to tell you that I became my own worst bully because I started believing all the negative things people said to me about my weight,” Ms. Nece adds.
Her hope is that the film will bring attention to the harm that this bias creates, especially when it derives from other people. “There’s no telling whether it will, but what Charlie experiences in bias and stigma from others clearly happens. It’s realistic. Those of us in large bodies have experienced what he is experiencing, so some people have said the movie is fat-phobic, but I see it as I can relate to those experiences because I have them too, so they are very realistic.”
Ms. Nece notes that it is important for clinicians to understand that obesity is a multifaceted and sensitive topic. “For those medical professionals who do not already know that obesity is complex, I hope the film will begin to open their eyes to the many different facets involved in obesity and their patients with obesity, I hope it will help them empathize and show compassion to their patients with obesity,” she concludes.
A version of this article first appeared on Medscape.com.
“I could relate to many, many, many of the experiences and emotions that Charlie, which is Brendan Fraser’s character, was portraying,” Patricia Nece recalls after watching a preview copy of the new film “The Whale.”
Much of the movie “rang true and hit home for me as things that I, too, had experienced,” Ms. Nece, the board of directors’ chair of the Obesity Action Coalition (OAC) and a person living with obesity, shares with this news organization.
In theaters as of December 9, The Whale chronicles the experience of a 600-lb, middle-aged man named Charlie. Throughout the film, Charlie seeks to rebuild his relationship with his estranged teenage daughter. Charlie had left his daughter and family to pursue a relationship with a man, who eventually died. As he navigates the pain surrounding his partner’s death and his lack of community, Charlie turns to food for comfort.
When the movie premiered at the Venice Film Festival, Mr. Fraser received a 6-minute standing ovation. However, activists criticized the movie for casting Fraser over an actor with obesity as well as its depiction of people with obesity.
Representatives from the National Association to Advance Fat Acceptance contend that casting an actor without obesity only contributes to ongoing bias against people of size. “Medical weight stigma and other socio-political determinants of health for people of all sizes cause far more harm to fat people than body fat does. Bias endangers fat people’s health. Anti-obesity organizations, such as those consulted with for this movie, contribute to stigma rather than reducing it as they claim,” NAAFA wrote in a statement to this news organization.
And they added that though the fat suit used in the movie may be superior to previous ones, it is still not an accurate depiction: “The creators of The Whale consider its CGI-generated fat suit to be superior to tactile fat suits, but we don’t. The issue with fat suits in Hollywood is not that they aren’t realistic enough. The issue is that they are used rather than using performers who actually live in bodies like the ones being depicted. If there is a 600-pound character in a movie, there should be a 600-pound human in that role. Rather than concentrate on the hype around the fake fat body created for The Whale, we want to see Hollywood create more opportunities for fat people across the size spectrum, both in front of the camera and behind the scenes.”
Prosthetics vs. reality?
Ms. Nece says she understands the controversy surrounding the use of fat suits but believes that it was not done in poor taste.
“OAC got involved with the movie after Brendan was already chosen for the part, and we never would have gotten involved with it had the prosthetics or fat suit been used to ridicule or make fun of people with obesity, which is usually the case,” she explains.
“But we knew from the start that that was never the intent of anyone involved with The Whale. And I think that’s shown by the fact that Brendan and Darren Aronofsky, the director, reached out to people who live with obesity on a daily basis to find out and learn more about it and to educate themselves about it,” Ms. Nece continues.
In a Daily Mail article, Mr. Fraser credited his son Griffin, who is autistic and obese, with helping him understand the struggles that people with obesity face.
Rachel Goldman, PhD, a clinical psychologist in private practice in New York and a professor in the psychology department at New York University, notes that there are other considerations that played into casting. “I know there was some pushback in terms of could, a say 600-lb individual, even be able to go to be on set every day and do this kind of work, and the answer is we don’t know.”
“I’m sure Darren chose Brendan for many reasons above and beyond just his body. I think that’s very important to keep in mind that just as much as representation is very important, I think it is also about finding the right person for the right role,” adds Dr. Goldman, who served as a consultant to the film.
Fat suits, extreme weight gains all to play a role
About 42% of adults in the United States have obesity, according to the 2017-2020 National Health and Nutrition Examination Survey, but that reality is not reflected in films or television.
A study of 1018 major television characters found that 24% of men and 14% of women had either overweight or obesity – far below the national average. And when characters with obesity are portrayed, actors often wear prosthetics, like Gwyneth Paltrow in Shallow Hal or Eddie Murphy in the Nutty Professor.
But unlike Mr. Fraser, some actors gain weight quickly instead.
This practice is unhealthy, says Jaime Almandoz, MD, an associate professor at the University of Texas Southwestern Medical Center, Dallas, and a nonsurgical weight management expert. In interviews, actors have shared how they increased calorie intake by drinking two milkshakes per day, going to fast food places regularly, or, in Mark Walhberg’s case, consuming 7,000 calories per day to gain 30 pounds for his role as boxer-turned-priest in the movie Father Stu.
This method provides their bodies with excess calories they are unable to burn off. “Then the amount of sugar and fat that streams into the blood as a result creates problems both directly and indirectly as your body tries to store it. It basically ends up using overflow warehouses for fat storage, like the liver for example, so we can create a condition called fatty liver, or in the muscle and other places, and this excess sugar and fat in the bloodstream cause several factors that are both insulin resistance causing,” Dr. Almandoz explains.
Though gaining weight helps the actor understand the character’s life experience, it may also be risky.
“To have an actor deliberately put his own health at risk and gain a certain amount of weight and whatever that might entail, one – that’s not necessarily the safest thing for that actor – but two, it’s also important to highlight the authentic experience of someone who has dealt with this chronic disease as well,” says Disha Narang, MD, a quadruple-board certified endocrinologist, obesity medicine, and culinary medicine specialist at Northwestern Medicine Lake Forest Hospital, Chicago.
These extreme fluctuations in weight may create problems. “It is typically not something we recommend because there could be metabolic damages as well as health concerns when patients are trying to gain weight quickly, just as we don’t want patients to lose weight quickly,” says Kurt Hong, MD, PhD, board-certified in internal medicine and clinical nutrition at the University of Southern California, Los Angeles.
Dr. Hong notes that it may be difficult for individuals to experience sudden weight gain because the body works hard to maintain a state of homeostasis.
“Similarly, to someone trying to gain weight you overeat, initially your body will try to again, maybe enhance its metabolic efficiency to hold the body stable,” Dr. Hong adds.
Dietary choices that may contribute to insulin resistance or promote high blood sugar can contribute to inflammation and a number of other adverse health outcomes, notes Dr. Almandoz. “The things that actors need to do in order to gain this magnitude of weight and they want to do it in the most time-effective manner is often not helpful for our bodies, it can be very problematic, the same thing goes for weight loss when actors need to lose significant amounts of weight for roles,” says Dr. Almandoz.
And Dr. Hong explained that for patients trying to lose weight, they may cut calories, but the body will try to compensate by slowing down the metabolism to keep their weight the same.
‘Your own worst bully’
In “The Whale,” Charlie appears to suffer from internalized weight bias, which is common to many people living with obesity, Ms. Nece says.
“Internalized weight bias is when the person of size takes all that negativity and turns it on themselves. The easiest way to describe that is to tell you that I became my own worst bully because I started believing all the negative things people said to me about my weight,” Ms. Nece adds.
Her hope is that the film will bring attention to the harm that this bias creates, especially when it derives from other people. “There’s no telling whether it will, but what Charlie experiences in bias and stigma from others clearly happens. It’s realistic. Those of us in large bodies have experienced what he is experiencing, so some people have said the movie is fat-phobic, but I see it as I can relate to those experiences because I have them too, so they are very realistic.”
Ms. Nece notes that it is important for clinicians to understand that obesity is a multifaceted and sensitive topic. “For those medical professionals who do not already know that obesity is complex, I hope the film will begin to open their eyes to the many different facets involved in obesity and their patients with obesity, I hope it will help them empathize and show compassion to their patients with obesity,” she concludes.
A version of this article first appeared on Medscape.com.
Green Mediterranean diet lowers visceral adipose tissue
according to a new analysis of the 18-month Dietary Intervention Randomized Controlled Trial Polyphenols Unprocessed (DIRECT-PLUS) trial.
The new results indicate that the green Mediterranean diet lowered visceral fat by twice as much as the standard Mediterranean diet (14% vs. 7%), reported Iris Shai, PhD, of Ben-Gurion University of the Negev in Be’er Sheva, Israel, and colleagues.
“This study may suggest an improved dietary protocol for treating visceral adiposity,” the authors wrote in their article, published recently in BMC Medicine.
“A healthy lifestyle is a strong basis for any weight-loss program. We learned from the results of our experiment that the quality of food is no less important than the number of calories consumed and the goal today is to understand the mechanisms of various nutrients, for example, positive ones such as the polyphenols, and negative ones such as empty carbohydrates and processed red meat, on the pace of fat cell differentiation and their aggregation in the viscera,” Dr. Shai said in a press release from Ben‐Gurion University.
“A 14% reduction in visceral fat is a dramatic achievement for making simple changes to your diet and lifestyle. Weight loss is an important goal only if it is accompanied by impressive results in reducing adipose tissue,” added coauthor Hila Zelicha, RD, PhD, also of Ben‐Gurion University of the Negev.
Previous randomized controlled trials have shown that dietary changes with a higher polyphenol content tend to produce better cardiometabolic outcomes and appear to mobilize particular ectopic fat depots, the researchers noted.
The main results of the DIRECT-PLUS trial were published in 2020 in Heart. Almost 300 participants with abdominal obesity/dyslipidemia were randomized to one of three diet groups (all accompanied by physical activity): standard healthy dietary guidelines (HDG), standard Mediterranean diet, and the so-called green Mediterranean diet. The mean age of participants was 51 years, and men comprised 88% of the study cohort.
Participants in both Mediterranean diet groups ate 28 grams/day of walnuts, which accounted for about 440 mg/day of polyphenols. Participants in the green Mediterranean group also ate 100 grams/day of frozen cubes of a Wolffia globosa (duckweed strain) plant green shake, and three to four cups/day of green tea, which contributed to consumption of 800 mg/day of polyphenols, and decreased red meat consumption.
Both the green and standard Mediterranean diet groups achieved similar weight loss (–6.2 kg and –5.4 kg) compared with the HDG group (–1.5 kg; P < .001). However, the green Mediterranean diet group had a greater reduction in waist circumference (–8.6 cm) than the standard Mediterranean diet group (–6.8 cm; P = .033) and HDG group (–4.3 cm; P < .001). Stratification by gender showed these differences were significant only among men.
Explaining the rationale for the study, the researchers noted that visceral adipose tissue accumulation is a key factor that differentiates metabolic healthy and unhealthy obese individuals, is closely related to the development of multiple cardiovascular risk factors, including hypertension, dyslipidemia, and type 2 diabetes, and is an independent marker of mortality.
Now, their latest data show the green Mediterranean diet group lost approximately twice as much visceral adipose tissue compared with the standard Mediterranean diet and HDG groups (−14.1%, −6.0%, and − 4.2%; P < .05 independent of weight loss, sex, waist circumference, or age).
Lower red meat consumption, greater dietary consumption of walnuts, Wolffia globosa, and green tea, increased urine urolithin A polyphenol, and elevated total plasma polyphenols were significantly associated with greater visceral adipose tissue loss (P < .05, multivariate models).
“A green Mediterranean diet enriched with polyphenols and decreased red meat consumption might serve as an improved version of the Mediterranean diet for targeted VAT reduction. Future studies are needed to explore the exact mechanisms of specific polyphenol-rich foods on visceral adiposity,” the study authors concluded.
A version of this article first appeared on Medscape.com.
according to a new analysis of the 18-month Dietary Intervention Randomized Controlled Trial Polyphenols Unprocessed (DIRECT-PLUS) trial.
The new results indicate that the green Mediterranean diet lowered visceral fat by twice as much as the standard Mediterranean diet (14% vs. 7%), reported Iris Shai, PhD, of Ben-Gurion University of the Negev in Be’er Sheva, Israel, and colleagues.
“This study may suggest an improved dietary protocol for treating visceral adiposity,” the authors wrote in their article, published recently in BMC Medicine.
“A healthy lifestyle is a strong basis for any weight-loss program. We learned from the results of our experiment that the quality of food is no less important than the number of calories consumed and the goal today is to understand the mechanisms of various nutrients, for example, positive ones such as the polyphenols, and negative ones such as empty carbohydrates and processed red meat, on the pace of fat cell differentiation and their aggregation in the viscera,” Dr. Shai said in a press release from Ben‐Gurion University.
“A 14% reduction in visceral fat is a dramatic achievement for making simple changes to your diet and lifestyle. Weight loss is an important goal only if it is accompanied by impressive results in reducing adipose tissue,” added coauthor Hila Zelicha, RD, PhD, also of Ben‐Gurion University of the Negev.
Previous randomized controlled trials have shown that dietary changes with a higher polyphenol content tend to produce better cardiometabolic outcomes and appear to mobilize particular ectopic fat depots, the researchers noted.
The main results of the DIRECT-PLUS trial were published in 2020 in Heart. Almost 300 participants with abdominal obesity/dyslipidemia were randomized to one of three diet groups (all accompanied by physical activity): standard healthy dietary guidelines (HDG), standard Mediterranean diet, and the so-called green Mediterranean diet. The mean age of participants was 51 years, and men comprised 88% of the study cohort.
Participants in both Mediterranean diet groups ate 28 grams/day of walnuts, which accounted for about 440 mg/day of polyphenols. Participants in the green Mediterranean group also ate 100 grams/day of frozen cubes of a Wolffia globosa (duckweed strain) plant green shake, and three to four cups/day of green tea, which contributed to consumption of 800 mg/day of polyphenols, and decreased red meat consumption.
Both the green and standard Mediterranean diet groups achieved similar weight loss (–6.2 kg and –5.4 kg) compared with the HDG group (–1.5 kg; P < .001). However, the green Mediterranean diet group had a greater reduction in waist circumference (–8.6 cm) than the standard Mediterranean diet group (–6.8 cm; P = .033) and HDG group (–4.3 cm; P < .001). Stratification by gender showed these differences were significant only among men.
Explaining the rationale for the study, the researchers noted that visceral adipose tissue accumulation is a key factor that differentiates metabolic healthy and unhealthy obese individuals, is closely related to the development of multiple cardiovascular risk factors, including hypertension, dyslipidemia, and type 2 diabetes, and is an independent marker of mortality.
Now, their latest data show the green Mediterranean diet group lost approximately twice as much visceral adipose tissue compared with the standard Mediterranean diet and HDG groups (−14.1%, −6.0%, and − 4.2%; P < .05 independent of weight loss, sex, waist circumference, or age).
Lower red meat consumption, greater dietary consumption of walnuts, Wolffia globosa, and green tea, increased urine urolithin A polyphenol, and elevated total plasma polyphenols were significantly associated with greater visceral adipose tissue loss (P < .05, multivariate models).
“A green Mediterranean diet enriched with polyphenols and decreased red meat consumption might serve as an improved version of the Mediterranean diet for targeted VAT reduction. Future studies are needed to explore the exact mechanisms of specific polyphenol-rich foods on visceral adiposity,” the study authors concluded.
A version of this article first appeared on Medscape.com.
according to a new analysis of the 18-month Dietary Intervention Randomized Controlled Trial Polyphenols Unprocessed (DIRECT-PLUS) trial.
The new results indicate that the green Mediterranean diet lowered visceral fat by twice as much as the standard Mediterranean diet (14% vs. 7%), reported Iris Shai, PhD, of Ben-Gurion University of the Negev in Be’er Sheva, Israel, and colleagues.
“This study may suggest an improved dietary protocol for treating visceral adiposity,” the authors wrote in their article, published recently in BMC Medicine.
“A healthy lifestyle is a strong basis for any weight-loss program. We learned from the results of our experiment that the quality of food is no less important than the number of calories consumed and the goal today is to understand the mechanisms of various nutrients, for example, positive ones such as the polyphenols, and negative ones such as empty carbohydrates and processed red meat, on the pace of fat cell differentiation and their aggregation in the viscera,” Dr. Shai said in a press release from Ben‐Gurion University.
“A 14% reduction in visceral fat is a dramatic achievement for making simple changes to your diet and lifestyle. Weight loss is an important goal only if it is accompanied by impressive results in reducing adipose tissue,” added coauthor Hila Zelicha, RD, PhD, also of Ben‐Gurion University of the Negev.
Previous randomized controlled trials have shown that dietary changes with a higher polyphenol content tend to produce better cardiometabolic outcomes and appear to mobilize particular ectopic fat depots, the researchers noted.
The main results of the DIRECT-PLUS trial were published in 2020 in Heart. Almost 300 participants with abdominal obesity/dyslipidemia were randomized to one of three diet groups (all accompanied by physical activity): standard healthy dietary guidelines (HDG), standard Mediterranean diet, and the so-called green Mediterranean diet. The mean age of participants was 51 years, and men comprised 88% of the study cohort.
Participants in both Mediterranean diet groups ate 28 grams/day of walnuts, which accounted for about 440 mg/day of polyphenols. Participants in the green Mediterranean group also ate 100 grams/day of frozen cubes of a Wolffia globosa (duckweed strain) plant green shake, and three to four cups/day of green tea, which contributed to consumption of 800 mg/day of polyphenols, and decreased red meat consumption.
Both the green and standard Mediterranean diet groups achieved similar weight loss (–6.2 kg and –5.4 kg) compared with the HDG group (–1.5 kg; P < .001). However, the green Mediterranean diet group had a greater reduction in waist circumference (–8.6 cm) than the standard Mediterranean diet group (–6.8 cm; P = .033) and HDG group (–4.3 cm; P < .001). Stratification by gender showed these differences were significant only among men.
Explaining the rationale for the study, the researchers noted that visceral adipose tissue accumulation is a key factor that differentiates metabolic healthy and unhealthy obese individuals, is closely related to the development of multiple cardiovascular risk factors, including hypertension, dyslipidemia, and type 2 diabetes, and is an independent marker of mortality.
Now, their latest data show the green Mediterranean diet group lost approximately twice as much visceral adipose tissue compared with the standard Mediterranean diet and HDG groups (−14.1%, −6.0%, and − 4.2%; P < .05 independent of weight loss, sex, waist circumference, or age).
Lower red meat consumption, greater dietary consumption of walnuts, Wolffia globosa, and green tea, increased urine urolithin A polyphenol, and elevated total plasma polyphenols were significantly associated with greater visceral adipose tissue loss (P < .05, multivariate models).
“A green Mediterranean diet enriched with polyphenols and decreased red meat consumption might serve as an improved version of the Mediterranean diet for targeted VAT reduction. Future studies are needed to explore the exact mechanisms of specific polyphenol-rich foods on visceral adiposity,” the study authors concluded.
A version of this article first appeared on Medscape.com.
FROM BMC MEDICINE
Night lights in the city link to increased risk of diabetes
Higher levels of exposure to outdoor artificial light at night are significantly linked with markers of diabetes and impaired glucose homeostasis, in a new national, cross-sectional study from China.
The results showed a 7% significant increase in diabetes prevalence per quintile exposure to artificial light at night (prevalence ratio, 1.07), report Ruizhi Zheng, PhD, of the Shanghai (China) Jiaotong University School of Medicine, and colleagues. People living in areas with the most exposure to light at night had a 28% higher prevalence of diabetes than those living in places with the lowest exposure (PR, 1.28), the researchers found.
The study was published online in Diabetologia.
Previous animal studies have shown that exposure to light at night may interfere with circadian rhythms and affect glucose homeostasis, the study team note. Other research has demonstrated that chronic exposure to moderate indoor light during sleep elevated the prevalence of diabetes in older adults, compared with those sleeping in a dim setting, the authors add.
“Our findings contribute to the growing literature suggesting that artificial light at night is detrimental to health and demonstrate that artificial light at night may be a potential novel risk factor for diabetes,” they write.
“Considering the coexistence of the diabetes epidemic and the widespread influence of light pollution at night, the positive associations indicate an urgent need for countries and governments to develop effective prevention and intervention policies and to protect people from the adverse health effects of light pollution at night,” the study authors stress.
Gareth Nye, PhD, senior lecturer at the University of Chester, England, agreed that prior research has found an association between metabolic conditions, such as diabetes, and artificial light at night, with most theories as to the cause focusing on the body’s natural circadian cycle.
He said that internal clocks regulate a variety of bodily processes, such as metabolism and hormone synthesis. They also affect sleep patterns by interfering with synthesis of the hormone melatonin, which is essential for sound sleep, Dr. Nye told the UK Science Media Centre.
However, he stressed that much more research is needed before any link can be considered definitive.
Outdoor night light exposure linked to fasting glucose, A1c
The Chinese researchers set out to approximate the relationships between diabetes prevalence and glucose homeostasis with chronic exposure to outdoor light at night.
They assessed 98,658 participants from the China Noncommunicable Disease Surveillance Study across 162 sites. The mean age of participants was 42.7 years. Female participants comprised 49.2% of the study cohort.
Diabetes was defined based on American Diabetes Association criteria. Satellite data were used to determine exposure to outdoor light at night in 2010. The associations between light exposure at night and indicators of glucose homeostasis were investigated.
Prevalence ratios were calculated and adjusted for sex, age, smoking status, education, body mass index, physical activity, household income, family history of diabetes, rural/urban areas, drinking status, and use of lipid-lowering prescription drugs (primarily statins) or antihypertensives.
The findings showed exposure levels to outdoor light at night were positively linked with 2-hour and fasting glucose concentrations, A1c, and insulin resistance (measured using homeostatic model assessment [HOMA]), but negatively related to β-cell function (measured using HOMA).
More research needed
“We advise caution against causal interpretation of the findings and call for further studies involving direct measurement of individual exposure to light at night,” the researchers conclude.
Dr. Nye agreed.
“One issue with this study is that the areas with the highest outdoor artificial light levels are likely to be those in urban areas and bigger cities. It has been known for a long time now that living in an urbanized area increases your risk of obesity through increased access to high-fat and convenience food, less physical activity levels due to transport links, and less social activities. The authors also state this and the fact participants tended to be older,” he noted.
Large datasets are used in this investigation, however, which generally increases the reliability of the data, he observed.
But it is also “unclear as to whether the population here was selected for this study or was retrospectively analyzed, which poses reliability issues, as does the selection of the representative sample, as it is not discussed,” he noted.
Ultimately, there is no confirmed evidence of the link, and until further work is done to directly link light exposure and diabetes in humans, “the link will remain an association only,” he concluded.
A version of this article first appeared on Medscape.com.
Higher levels of exposure to outdoor artificial light at night are significantly linked with markers of diabetes and impaired glucose homeostasis, in a new national, cross-sectional study from China.
The results showed a 7% significant increase in diabetes prevalence per quintile exposure to artificial light at night (prevalence ratio, 1.07), report Ruizhi Zheng, PhD, of the Shanghai (China) Jiaotong University School of Medicine, and colleagues. People living in areas with the most exposure to light at night had a 28% higher prevalence of diabetes than those living in places with the lowest exposure (PR, 1.28), the researchers found.
The study was published online in Diabetologia.
Previous animal studies have shown that exposure to light at night may interfere with circadian rhythms and affect glucose homeostasis, the study team note. Other research has demonstrated that chronic exposure to moderate indoor light during sleep elevated the prevalence of diabetes in older adults, compared with those sleeping in a dim setting, the authors add.
“Our findings contribute to the growing literature suggesting that artificial light at night is detrimental to health and demonstrate that artificial light at night may be a potential novel risk factor for diabetes,” they write.
“Considering the coexistence of the diabetes epidemic and the widespread influence of light pollution at night, the positive associations indicate an urgent need for countries and governments to develop effective prevention and intervention policies and to protect people from the adverse health effects of light pollution at night,” the study authors stress.
Gareth Nye, PhD, senior lecturer at the University of Chester, England, agreed that prior research has found an association between metabolic conditions, such as diabetes, and artificial light at night, with most theories as to the cause focusing on the body’s natural circadian cycle.
He said that internal clocks regulate a variety of bodily processes, such as metabolism and hormone synthesis. They also affect sleep patterns by interfering with synthesis of the hormone melatonin, which is essential for sound sleep, Dr. Nye told the UK Science Media Centre.
However, he stressed that much more research is needed before any link can be considered definitive.
Outdoor night light exposure linked to fasting glucose, A1c
The Chinese researchers set out to approximate the relationships between diabetes prevalence and glucose homeostasis with chronic exposure to outdoor light at night.
They assessed 98,658 participants from the China Noncommunicable Disease Surveillance Study across 162 sites. The mean age of participants was 42.7 years. Female participants comprised 49.2% of the study cohort.
Diabetes was defined based on American Diabetes Association criteria. Satellite data were used to determine exposure to outdoor light at night in 2010. The associations between light exposure at night and indicators of glucose homeostasis were investigated.
Prevalence ratios were calculated and adjusted for sex, age, smoking status, education, body mass index, physical activity, household income, family history of diabetes, rural/urban areas, drinking status, and use of lipid-lowering prescription drugs (primarily statins) or antihypertensives.
The findings showed exposure levels to outdoor light at night were positively linked with 2-hour and fasting glucose concentrations, A1c, and insulin resistance (measured using homeostatic model assessment [HOMA]), but negatively related to β-cell function (measured using HOMA).
More research needed
“We advise caution against causal interpretation of the findings and call for further studies involving direct measurement of individual exposure to light at night,” the researchers conclude.
Dr. Nye agreed.
“One issue with this study is that the areas with the highest outdoor artificial light levels are likely to be those in urban areas and bigger cities. It has been known for a long time now that living in an urbanized area increases your risk of obesity through increased access to high-fat and convenience food, less physical activity levels due to transport links, and less social activities. The authors also state this and the fact participants tended to be older,” he noted.
Large datasets are used in this investigation, however, which generally increases the reliability of the data, he observed.
But it is also “unclear as to whether the population here was selected for this study or was retrospectively analyzed, which poses reliability issues, as does the selection of the representative sample, as it is not discussed,” he noted.
Ultimately, there is no confirmed evidence of the link, and until further work is done to directly link light exposure and diabetes in humans, “the link will remain an association only,” he concluded.
A version of this article first appeared on Medscape.com.
Higher levels of exposure to outdoor artificial light at night are significantly linked with markers of diabetes and impaired glucose homeostasis, in a new national, cross-sectional study from China.
The results showed a 7% significant increase in diabetes prevalence per quintile exposure to artificial light at night (prevalence ratio, 1.07), report Ruizhi Zheng, PhD, of the Shanghai (China) Jiaotong University School of Medicine, and colleagues. People living in areas with the most exposure to light at night had a 28% higher prevalence of diabetes than those living in places with the lowest exposure (PR, 1.28), the researchers found.
The study was published online in Diabetologia.
Previous animal studies have shown that exposure to light at night may interfere with circadian rhythms and affect glucose homeostasis, the study team note. Other research has demonstrated that chronic exposure to moderate indoor light during sleep elevated the prevalence of diabetes in older adults, compared with those sleeping in a dim setting, the authors add.
“Our findings contribute to the growing literature suggesting that artificial light at night is detrimental to health and demonstrate that artificial light at night may be a potential novel risk factor for diabetes,” they write.
“Considering the coexistence of the diabetes epidemic and the widespread influence of light pollution at night, the positive associations indicate an urgent need for countries and governments to develop effective prevention and intervention policies and to protect people from the adverse health effects of light pollution at night,” the study authors stress.
Gareth Nye, PhD, senior lecturer at the University of Chester, England, agreed that prior research has found an association between metabolic conditions, such as diabetes, and artificial light at night, with most theories as to the cause focusing on the body’s natural circadian cycle.
He said that internal clocks regulate a variety of bodily processes, such as metabolism and hormone synthesis. They also affect sleep patterns by interfering with synthesis of the hormone melatonin, which is essential for sound sleep, Dr. Nye told the UK Science Media Centre.
However, he stressed that much more research is needed before any link can be considered definitive.
Outdoor night light exposure linked to fasting glucose, A1c
The Chinese researchers set out to approximate the relationships between diabetes prevalence and glucose homeostasis with chronic exposure to outdoor light at night.
They assessed 98,658 participants from the China Noncommunicable Disease Surveillance Study across 162 sites. The mean age of participants was 42.7 years. Female participants comprised 49.2% of the study cohort.
Diabetes was defined based on American Diabetes Association criteria. Satellite data were used to determine exposure to outdoor light at night in 2010. The associations between light exposure at night and indicators of glucose homeostasis were investigated.
Prevalence ratios were calculated and adjusted for sex, age, smoking status, education, body mass index, physical activity, household income, family history of diabetes, rural/urban areas, drinking status, and use of lipid-lowering prescription drugs (primarily statins) or antihypertensives.
The findings showed exposure levels to outdoor light at night were positively linked with 2-hour and fasting glucose concentrations, A1c, and insulin resistance (measured using homeostatic model assessment [HOMA]), but negatively related to β-cell function (measured using HOMA).
More research needed
“We advise caution against causal interpretation of the findings and call for further studies involving direct measurement of individual exposure to light at night,” the researchers conclude.
Dr. Nye agreed.
“One issue with this study is that the areas with the highest outdoor artificial light levels are likely to be those in urban areas and bigger cities. It has been known for a long time now that living in an urbanized area increases your risk of obesity through increased access to high-fat and convenience food, less physical activity levels due to transport links, and less social activities. The authors also state this and the fact participants tended to be older,” he noted.
Large datasets are used in this investigation, however, which generally increases the reliability of the data, he observed.
But it is also “unclear as to whether the population here was selected for this study or was retrospectively analyzed, which poses reliability issues, as does the selection of the representative sample, as it is not discussed,” he noted.
Ultimately, there is no confirmed evidence of the link, and until further work is done to directly link light exposure and diabetes in humans, “the link will remain an association only,” he concluded.
A version of this article first appeared on Medscape.com.
It’s about location: PCOS symptoms differ depending where you live
Geographic location within the United States appears to have an impact on the specific symptoms of polycystic ovary syndrome (PCOS) that any one particular woman will develop, according to a new prospective cohort study.
Women in California were more likely to exhibit high levels of testosterone (hyperandrogenism), while women in Alabama with PCOS had more metabolic dysfunction and hirsutism.
And although the women in Alabama were younger and had a higher body mass index (BMI), even after adjusting for these factors, the clinical differences were still present between the geographic locations, the authors said.
“This study suggests there are regional differences in hormonal and metabolic parameters in women with PCOS in California and Alabama, highlighting the impact of differing genetic and environmental modulators on PCOS development,” Katherine VanHise, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote in their article, published online in the Journal of Clinical Endocrinology and Metabolism.
Genetic and environmental factors play a role
Prior research has looked at variations in symptoms of PCOS across countries and identified differences in hirsutism and its prevalence, which is greater in Middle Eastern, Mediterranean, and Indian women, noted senior author Margareta D. Pisarska, MD.
And women of some other backgrounds “are at increased risk of developing metabolic syndrome and insulin resistance, including South Asian, African, and Hispanic women, so they are at a greater risk trajectory of developing manifestations later on in life that can ultimately lead to adverse outcomes in overall health,” Dr. Pisarska, director of the division of reproductive endocrinology and infertility in obstetrics and gynecology at Cedars-Sinai, told this news organization.
“We do see regional differences in the diagnosis of PCOS [in the United States] as well as the manifestations of PCOS including high andrenoemia, hirsutism, and metabolic parameters ... and we need to better understand it because, at least in the entire population, weight was not the entire factor contributing to these differences,” she explained.
“So there are definitely environmental factors and possibly genetic factors that we need to take into consideration as we try to study these women and try to help them decrease their risk of metabolic syndrome later in life,” she noted.
Differences not attributable to race either
PCOS is a common endocrine disorder affecting women and female adolescents worldwide. Diagnosis usually requires at least two of the following to be present: ovulatory dysfunction, hyperandrogenism, and/or polycystic ovarian morphology.
Because of the prior work that had identified differences in symptoms among women with PCOS in different countries, the investigators set out to determine if women of the same race would have distinct hormonal and metabolic traits of PCOS in two geographical locations in the United States, suggesting geo-epidemiologic contributors of the disease
They evaluated 889 women at the University of Alabama at Birmingham and 721 at Cedars-Sinai Medical Center. Participants in Birmingham were a mean age of 28 years, had a mean BMI of 33.1 kg/m2, a mean waist-to-hip ratio of 0.8, and a mean hirsute rate of 84.6%. Participants in California were a mean age of 29.5 years, had an average BMI of 30.1 kg/m2, a mean waist-to-hip ratio of 0.9, and a mean hirsute rate of 72.8%.
The study team gathered data on menstrual cycle history, metabolic and hormonal parameters, and demographic data for each participant. They assessed hirsutism based on modified Ferriman-Gallwey scores of four or more. Patients were classified as having hyperandrogenemia if they had elevated androgen values greater than the 95th percentile of all values or androgen values that exceeded laboratory reference ranges.
The findings showed that Alabama women with PCOS had elevated homeostatic model assessment for insulin resistance scores (adjusted beta coefficient, 3.6; P < .001) and were more likely to be hirsute (adjusted odds ratio, 1.8; P < .001) after adjustment for BMI and age than those in California.
In contrast, women with PCOS in California were more likely to have elevated free testosterone and total testosterone values than women in Alabama (both P < .001). These findings persisted after adjusting for age and BMI.
When stratified by White race, these findings were similar. Notably, BMI and waist-to-hip ratio did not vary between regions in Black women with PCOS, although variations in metabolic dysfunction and androgen profiles persisted.
“This study supports regional differences in hormonal and metabolic parameters in women with PCOS in the United States, highlighting the impact of the environment on PCOS phenotype. Individuals of the same race in different geographical locations of the United States may have differing genetic predispositions for developing diseases such as PCOS,” the researchers said.
“Ongoing research is needed to identify modifiable environmental risk factors for PCOS that may be race and ethnic specific to bring precision medicine to the management of PCOS,” they conclude.
This work was supported in part by grants from the National Institutes of Health and an endowment of the Helping Hand of Los Angeles. Dr. VanHise reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Geographic location within the United States appears to have an impact on the specific symptoms of polycystic ovary syndrome (PCOS) that any one particular woman will develop, according to a new prospective cohort study.
Women in California were more likely to exhibit high levels of testosterone (hyperandrogenism), while women in Alabama with PCOS had more metabolic dysfunction and hirsutism.
And although the women in Alabama were younger and had a higher body mass index (BMI), even after adjusting for these factors, the clinical differences were still present between the geographic locations, the authors said.
“This study suggests there are regional differences in hormonal and metabolic parameters in women with PCOS in California and Alabama, highlighting the impact of differing genetic and environmental modulators on PCOS development,” Katherine VanHise, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote in their article, published online in the Journal of Clinical Endocrinology and Metabolism.
Genetic and environmental factors play a role
Prior research has looked at variations in symptoms of PCOS across countries and identified differences in hirsutism and its prevalence, which is greater in Middle Eastern, Mediterranean, and Indian women, noted senior author Margareta D. Pisarska, MD.
And women of some other backgrounds “are at increased risk of developing metabolic syndrome and insulin resistance, including South Asian, African, and Hispanic women, so they are at a greater risk trajectory of developing manifestations later on in life that can ultimately lead to adverse outcomes in overall health,” Dr. Pisarska, director of the division of reproductive endocrinology and infertility in obstetrics and gynecology at Cedars-Sinai, told this news organization.
“We do see regional differences in the diagnosis of PCOS [in the United States] as well as the manifestations of PCOS including high andrenoemia, hirsutism, and metabolic parameters ... and we need to better understand it because, at least in the entire population, weight was not the entire factor contributing to these differences,” she explained.
“So there are definitely environmental factors and possibly genetic factors that we need to take into consideration as we try to study these women and try to help them decrease their risk of metabolic syndrome later in life,” she noted.
Differences not attributable to race either
PCOS is a common endocrine disorder affecting women and female adolescents worldwide. Diagnosis usually requires at least two of the following to be present: ovulatory dysfunction, hyperandrogenism, and/or polycystic ovarian morphology.
Because of the prior work that had identified differences in symptoms among women with PCOS in different countries, the investigators set out to determine if women of the same race would have distinct hormonal and metabolic traits of PCOS in two geographical locations in the United States, suggesting geo-epidemiologic contributors of the disease
They evaluated 889 women at the University of Alabama at Birmingham and 721 at Cedars-Sinai Medical Center. Participants in Birmingham were a mean age of 28 years, had a mean BMI of 33.1 kg/m2, a mean waist-to-hip ratio of 0.8, and a mean hirsute rate of 84.6%. Participants in California were a mean age of 29.5 years, had an average BMI of 30.1 kg/m2, a mean waist-to-hip ratio of 0.9, and a mean hirsute rate of 72.8%.
The study team gathered data on menstrual cycle history, metabolic and hormonal parameters, and demographic data for each participant. They assessed hirsutism based on modified Ferriman-Gallwey scores of four or more. Patients were classified as having hyperandrogenemia if they had elevated androgen values greater than the 95th percentile of all values or androgen values that exceeded laboratory reference ranges.
The findings showed that Alabama women with PCOS had elevated homeostatic model assessment for insulin resistance scores (adjusted beta coefficient, 3.6; P < .001) and were more likely to be hirsute (adjusted odds ratio, 1.8; P < .001) after adjustment for BMI and age than those in California.
In contrast, women with PCOS in California were more likely to have elevated free testosterone and total testosterone values than women in Alabama (both P < .001). These findings persisted after adjusting for age and BMI.
When stratified by White race, these findings were similar. Notably, BMI and waist-to-hip ratio did not vary between regions in Black women with PCOS, although variations in metabolic dysfunction and androgen profiles persisted.
“This study supports regional differences in hormonal and metabolic parameters in women with PCOS in the United States, highlighting the impact of the environment on PCOS phenotype. Individuals of the same race in different geographical locations of the United States may have differing genetic predispositions for developing diseases such as PCOS,” the researchers said.
“Ongoing research is needed to identify modifiable environmental risk factors for PCOS that may be race and ethnic specific to bring precision medicine to the management of PCOS,” they conclude.
This work was supported in part by grants from the National Institutes of Health and an endowment of the Helping Hand of Los Angeles. Dr. VanHise reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Geographic location within the United States appears to have an impact on the specific symptoms of polycystic ovary syndrome (PCOS) that any one particular woman will develop, according to a new prospective cohort study.
Women in California were more likely to exhibit high levels of testosterone (hyperandrogenism), while women in Alabama with PCOS had more metabolic dysfunction and hirsutism.
And although the women in Alabama were younger and had a higher body mass index (BMI), even after adjusting for these factors, the clinical differences were still present between the geographic locations, the authors said.
“This study suggests there are regional differences in hormonal and metabolic parameters in women with PCOS in California and Alabama, highlighting the impact of differing genetic and environmental modulators on PCOS development,” Katherine VanHise, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote in their article, published online in the Journal of Clinical Endocrinology and Metabolism.
Genetic and environmental factors play a role
Prior research has looked at variations in symptoms of PCOS across countries and identified differences in hirsutism and its prevalence, which is greater in Middle Eastern, Mediterranean, and Indian women, noted senior author Margareta D. Pisarska, MD.
And women of some other backgrounds “are at increased risk of developing metabolic syndrome and insulin resistance, including South Asian, African, and Hispanic women, so they are at a greater risk trajectory of developing manifestations later on in life that can ultimately lead to adverse outcomes in overall health,” Dr. Pisarska, director of the division of reproductive endocrinology and infertility in obstetrics and gynecology at Cedars-Sinai, told this news organization.
“We do see regional differences in the diagnosis of PCOS [in the United States] as well as the manifestations of PCOS including high andrenoemia, hirsutism, and metabolic parameters ... and we need to better understand it because, at least in the entire population, weight was not the entire factor contributing to these differences,” she explained.
“So there are definitely environmental factors and possibly genetic factors that we need to take into consideration as we try to study these women and try to help them decrease their risk of metabolic syndrome later in life,” she noted.
Differences not attributable to race either
PCOS is a common endocrine disorder affecting women and female adolescents worldwide. Diagnosis usually requires at least two of the following to be present: ovulatory dysfunction, hyperandrogenism, and/or polycystic ovarian morphology.
Because of the prior work that had identified differences in symptoms among women with PCOS in different countries, the investigators set out to determine if women of the same race would have distinct hormonal and metabolic traits of PCOS in two geographical locations in the United States, suggesting geo-epidemiologic contributors of the disease
They evaluated 889 women at the University of Alabama at Birmingham and 721 at Cedars-Sinai Medical Center. Participants in Birmingham were a mean age of 28 years, had a mean BMI of 33.1 kg/m2, a mean waist-to-hip ratio of 0.8, and a mean hirsute rate of 84.6%. Participants in California were a mean age of 29.5 years, had an average BMI of 30.1 kg/m2, a mean waist-to-hip ratio of 0.9, and a mean hirsute rate of 72.8%.
The study team gathered data on menstrual cycle history, metabolic and hormonal parameters, and demographic data for each participant. They assessed hirsutism based on modified Ferriman-Gallwey scores of four or more. Patients were classified as having hyperandrogenemia if they had elevated androgen values greater than the 95th percentile of all values or androgen values that exceeded laboratory reference ranges.
The findings showed that Alabama women with PCOS had elevated homeostatic model assessment for insulin resistance scores (adjusted beta coefficient, 3.6; P < .001) and were more likely to be hirsute (adjusted odds ratio, 1.8; P < .001) after adjustment for BMI and age than those in California.
In contrast, women with PCOS in California were more likely to have elevated free testosterone and total testosterone values than women in Alabama (both P < .001). These findings persisted after adjusting for age and BMI.
When stratified by White race, these findings were similar. Notably, BMI and waist-to-hip ratio did not vary between regions in Black women with PCOS, although variations in metabolic dysfunction and androgen profiles persisted.
“This study supports regional differences in hormonal and metabolic parameters in women with PCOS in the United States, highlighting the impact of the environment on PCOS phenotype. Individuals of the same race in different geographical locations of the United States may have differing genetic predispositions for developing diseases such as PCOS,” the researchers said.
“Ongoing research is needed to identify modifiable environmental risk factors for PCOS that may be race and ethnic specific to bring precision medicine to the management of PCOS,” they conclude.
This work was supported in part by grants from the National Institutes of Health and an endowment of the Helping Hand of Los Angeles. Dr. VanHise reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
Who are the patients with longstanding ankylosing spondylitis without syndesmophytes?
Syndesmophytes are not present in a subgroup of patients with ankylosing spondylitis (AS) and sacroiliac (SI) joint fusion who have had the disease for 20 years or longer, according to findings from a nested case-control study.
Syndesmophytes did not occur in only 23 (7%) of 354 patients, and these patients without spinal-fusing bone growths were less likely to be female but very likely to be HLA-B27 positive, Lauren K. Ridley, MD, a rheumatologist at the University of Texas Health Science Center at Houston, and colleagues reported in The Journal of Rheumatology.
“Women appear to have a different phenotype in AS; we found that they are less likely to form syndesmophytes despite fused SI joints with at least 20 years of disease duration. We do not understand the reasons behind these differences among the possibilities of genetic, hormonal, and bio-mechanical factors,” the authors wrote.
AS is a heterogenous disease that affects different people in various ways, Dr. Ridley noted. “Prior research has shown that and hasn’t really elucidated how different people manifest their disease. Previous research has shown that women tend to have more nonradiographic spondylitis,” Dr. Ridley said in an interview.
“This is still a very heterogenous disease. We don’t fully understand it, and we don’t know why some patients present with SI joint disease [and] no syndesmophytes, or some patients have the opposite. Truly, we do need to do more studies to find out why some patients behave differently and if there are ways we can try to alter that,” Dr. Ridley continued.
The researchers evaluated 354 patients from the Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS). Of these patients, 23 did not have syndesmophytes. Patients were selected if they had fused SI joints (bilateral grade 4 sacroiliac joint disease) and had a disease course lasting 20 years or more. The researchers identified risk factors for syndesmophytes using classification and regression trees (CART) analysis and then reassessed their validity with univariable logistic regression models.
All 23 patients who had no syndesmophytes were HLA-B27 positive, and all patients older than 45 years at symptom onset had syndesmophytes.
The results also highlighted age of disease onset as an important predictor of syndesmophytes in males. Syndesmophytes were less likely to be reported in males with a disease onset at 16 years or younger.
The presence of syndesmophytes was linked with an age older than 16 years at symptom onset (OR, 2.72; 95% confidence interval, 1.15-6.45), and syndesmophytes were less likely to occur among HLA-B27 positive individuals (P = .03).
Females were less likely than males to have syndesmophytes, as verified by univariable analysis (odds ratio, 0.17; 95% confidence interval, 0.07-0.41).
“There is likely a complex interplay of factors leading to differences in radiographic damage between the sacroiliac joints and the spine in AS, and it is interesting to consider if HLA-B27 may have more effect on sacroiliac joint damage than spinal damage,” the authors noted.
Some limitations of the study include the researchers’ choice to compare a subtype with overt spinal involvement and a subtype with limited spinal involvement when other criteria could have been used to separate cases, and their use of the modified Stoke Ankylosing Spondylitis Scoring System (mSaSSS) to examine radiographic changes over time, as the mSaSSS does not take into account radiographic variation in the zygaphophyseal joints and thoracic spine (and were not part of the dataset). Another limitation was the relatively small cohort size, the researchers noted.
“This was a small study, and further studies are needed to elucidate why AS disease may behave differently in this and other subgroups,” Dr. Ridley and colleagues concluded.
Expert commentary
Researchers agree that spinal structural damage is a predictor of further damage in patients with radiographic AS, Marina Magrey, MD, the Roland W. Moskowitz Professor in Rheumatic Diseases at Case Western Reserve University, Cleveland, said in an interview. She pointed out that previous literature has shown that longer disease durations make it more likely that patients will have syndesmophytes.
Previous research has also shown that there was an association between structural damage in the SI joints and the function and mobility of the spine. This observation was independent of the disease activity and prior structural damage in the spine, Dr. Magrey noted.
“This is a very complex disease with very diverse manifestations. Traditionally, it was thought to be a disease of men, but now we believe it is equally common between men and women. The burden is equal between men and women, and they need to be treated equally. Both of them need to be treated early on to prevent this radiographic damage,” she said.
Looking ahead, there need to be more translational studies looking for answers as to why there are phenotypic differences between men and women, as well as why men have spinal fusion more often than women. Bed-to-the-bench studies are warranted to get more answers, she said.
The study was supported by an NIH Centers for Translational Science Award grant. The researchers declared having no conflicts of interest related to the study. One author is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases Intramural Research Program, and another by the Spondyloarthritis Association of America and the University of Texas Health Center for Clinical and Translational Sciences KL2 program. Another author is an adviser for AbbVie, Eli Lilly, Gilead, Janssen, MoonLake, Novartis, Pfizer, and UCB, and has grant support from Novartis, Pfizer, and UCB.
Dr. Magrey disclosed being a consultant for Novartis, UCB, Pfizer, AbbVie, Janssen, Bristol-Myers Squibb, and Eli Lilly.
Syndesmophytes are not present in a subgroup of patients with ankylosing spondylitis (AS) and sacroiliac (SI) joint fusion who have had the disease for 20 years or longer, according to findings from a nested case-control study.
Syndesmophytes did not occur in only 23 (7%) of 354 patients, and these patients without spinal-fusing bone growths were less likely to be female but very likely to be HLA-B27 positive, Lauren K. Ridley, MD, a rheumatologist at the University of Texas Health Science Center at Houston, and colleagues reported in The Journal of Rheumatology.
“Women appear to have a different phenotype in AS; we found that they are less likely to form syndesmophytes despite fused SI joints with at least 20 years of disease duration. We do not understand the reasons behind these differences among the possibilities of genetic, hormonal, and bio-mechanical factors,” the authors wrote.
AS is a heterogenous disease that affects different people in various ways, Dr. Ridley noted. “Prior research has shown that and hasn’t really elucidated how different people manifest their disease. Previous research has shown that women tend to have more nonradiographic spondylitis,” Dr. Ridley said in an interview.
“This is still a very heterogenous disease. We don’t fully understand it, and we don’t know why some patients present with SI joint disease [and] no syndesmophytes, or some patients have the opposite. Truly, we do need to do more studies to find out why some patients behave differently and if there are ways we can try to alter that,” Dr. Ridley continued.
The researchers evaluated 354 patients from the Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS). Of these patients, 23 did not have syndesmophytes. Patients were selected if they had fused SI joints (bilateral grade 4 sacroiliac joint disease) and had a disease course lasting 20 years or more. The researchers identified risk factors for syndesmophytes using classification and regression trees (CART) analysis and then reassessed their validity with univariable logistic regression models.
All 23 patients who had no syndesmophytes were HLA-B27 positive, and all patients older than 45 years at symptom onset had syndesmophytes.
The results also highlighted age of disease onset as an important predictor of syndesmophytes in males. Syndesmophytes were less likely to be reported in males with a disease onset at 16 years or younger.
The presence of syndesmophytes was linked with an age older than 16 years at symptom onset (OR, 2.72; 95% confidence interval, 1.15-6.45), and syndesmophytes were less likely to occur among HLA-B27 positive individuals (P = .03).
Females were less likely than males to have syndesmophytes, as verified by univariable analysis (odds ratio, 0.17; 95% confidence interval, 0.07-0.41).
“There is likely a complex interplay of factors leading to differences in radiographic damage between the sacroiliac joints and the spine in AS, and it is interesting to consider if HLA-B27 may have more effect on sacroiliac joint damage than spinal damage,” the authors noted.
Some limitations of the study include the researchers’ choice to compare a subtype with overt spinal involvement and a subtype with limited spinal involvement when other criteria could have been used to separate cases, and their use of the modified Stoke Ankylosing Spondylitis Scoring System (mSaSSS) to examine radiographic changes over time, as the mSaSSS does not take into account radiographic variation in the zygaphophyseal joints and thoracic spine (and were not part of the dataset). Another limitation was the relatively small cohort size, the researchers noted.
“This was a small study, and further studies are needed to elucidate why AS disease may behave differently in this and other subgroups,” Dr. Ridley and colleagues concluded.
Expert commentary
Researchers agree that spinal structural damage is a predictor of further damage in patients with radiographic AS, Marina Magrey, MD, the Roland W. Moskowitz Professor in Rheumatic Diseases at Case Western Reserve University, Cleveland, said in an interview. She pointed out that previous literature has shown that longer disease durations make it more likely that patients will have syndesmophytes.
Previous research has also shown that there was an association between structural damage in the SI joints and the function and mobility of the spine. This observation was independent of the disease activity and prior structural damage in the spine, Dr. Magrey noted.
“This is a very complex disease with very diverse manifestations. Traditionally, it was thought to be a disease of men, but now we believe it is equally common between men and women. The burden is equal between men and women, and they need to be treated equally. Both of them need to be treated early on to prevent this radiographic damage,” she said.
Looking ahead, there need to be more translational studies looking for answers as to why there are phenotypic differences between men and women, as well as why men have spinal fusion more often than women. Bed-to-the-bench studies are warranted to get more answers, she said.
The study was supported by an NIH Centers for Translational Science Award grant. The researchers declared having no conflicts of interest related to the study. One author is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases Intramural Research Program, and another by the Spondyloarthritis Association of America and the University of Texas Health Center for Clinical and Translational Sciences KL2 program. Another author is an adviser for AbbVie, Eli Lilly, Gilead, Janssen, MoonLake, Novartis, Pfizer, and UCB, and has grant support from Novartis, Pfizer, and UCB.
Dr. Magrey disclosed being a consultant for Novartis, UCB, Pfizer, AbbVie, Janssen, Bristol-Myers Squibb, and Eli Lilly.
Syndesmophytes are not present in a subgroup of patients with ankylosing spondylitis (AS) and sacroiliac (SI) joint fusion who have had the disease for 20 years or longer, according to findings from a nested case-control study.
Syndesmophytes did not occur in only 23 (7%) of 354 patients, and these patients without spinal-fusing bone growths were less likely to be female but very likely to be HLA-B27 positive, Lauren K. Ridley, MD, a rheumatologist at the University of Texas Health Science Center at Houston, and colleagues reported in The Journal of Rheumatology.
“Women appear to have a different phenotype in AS; we found that they are less likely to form syndesmophytes despite fused SI joints with at least 20 years of disease duration. We do not understand the reasons behind these differences among the possibilities of genetic, hormonal, and bio-mechanical factors,” the authors wrote.
AS is a heterogenous disease that affects different people in various ways, Dr. Ridley noted. “Prior research has shown that and hasn’t really elucidated how different people manifest their disease. Previous research has shown that women tend to have more nonradiographic spondylitis,” Dr. Ridley said in an interview.
“This is still a very heterogenous disease. We don’t fully understand it, and we don’t know why some patients present with SI joint disease [and] no syndesmophytes, or some patients have the opposite. Truly, we do need to do more studies to find out why some patients behave differently and if there are ways we can try to alter that,” Dr. Ridley continued.
The researchers evaluated 354 patients from the Prospective Study of Outcomes in Ankylosing Spondylitis (PSOAS). Of these patients, 23 did not have syndesmophytes. Patients were selected if they had fused SI joints (bilateral grade 4 sacroiliac joint disease) and had a disease course lasting 20 years or more. The researchers identified risk factors for syndesmophytes using classification and regression trees (CART) analysis and then reassessed their validity with univariable logistic regression models.
All 23 patients who had no syndesmophytes were HLA-B27 positive, and all patients older than 45 years at symptom onset had syndesmophytes.
The results also highlighted age of disease onset as an important predictor of syndesmophytes in males. Syndesmophytes were less likely to be reported in males with a disease onset at 16 years or younger.
The presence of syndesmophytes was linked with an age older than 16 years at symptom onset (OR, 2.72; 95% confidence interval, 1.15-6.45), and syndesmophytes were less likely to occur among HLA-B27 positive individuals (P = .03).
Females were less likely than males to have syndesmophytes, as verified by univariable analysis (odds ratio, 0.17; 95% confidence interval, 0.07-0.41).
“There is likely a complex interplay of factors leading to differences in radiographic damage between the sacroiliac joints and the spine in AS, and it is interesting to consider if HLA-B27 may have more effect on sacroiliac joint damage than spinal damage,” the authors noted.
Some limitations of the study include the researchers’ choice to compare a subtype with overt spinal involvement and a subtype with limited spinal involvement when other criteria could have been used to separate cases, and their use of the modified Stoke Ankylosing Spondylitis Scoring System (mSaSSS) to examine radiographic changes over time, as the mSaSSS does not take into account radiographic variation in the zygaphophyseal joints and thoracic spine (and were not part of the dataset). Another limitation was the relatively small cohort size, the researchers noted.
“This was a small study, and further studies are needed to elucidate why AS disease may behave differently in this and other subgroups,” Dr. Ridley and colleagues concluded.
Expert commentary
Researchers agree that spinal structural damage is a predictor of further damage in patients with radiographic AS, Marina Magrey, MD, the Roland W. Moskowitz Professor in Rheumatic Diseases at Case Western Reserve University, Cleveland, said in an interview. She pointed out that previous literature has shown that longer disease durations make it more likely that patients will have syndesmophytes.
Previous research has also shown that there was an association between structural damage in the SI joints and the function and mobility of the spine. This observation was independent of the disease activity and prior structural damage in the spine, Dr. Magrey noted.
“This is a very complex disease with very diverse manifestations. Traditionally, it was thought to be a disease of men, but now we believe it is equally common between men and women. The burden is equal between men and women, and they need to be treated equally. Both of them need to be treated early on to prevent this radiographic damage,” she said.
Looking ahead, there need to be more translational studies looking for answers as to why there are phenotypic differences between men and women, as well as why men have spinal fusion more often than women. Bed-to-the-bench studies are warranted to get more answers, she said.
The study was supported by an NIH Centers for Translational Science Award grant. The researchers declared having no conflicts of interest related to the study. One author is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases Intramural Research Program, and another by the Spondyloarthritis Association of America and the University of Texas Health Center for Clinical and Translational Sciences KL2 program. Another author is an adviser for AbbVie, Eli Lilly, Gilead, Janssen, MoonLake, Novartis, Pfizer, and UCB, and has grant support from Novartis, Pfizer, and UCB.
Dr. Magrey disclosed being a consultant for Novartis, UCB, Pfizer, AbbVie, Janssen, Bristol-Myers Squibb, and Eli Lilly.
FROM THE JOURNAL OF RHEUMATOLOGY
Ultra-processed food intake by moms linked with childhood obesity
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
A mother’s consumption of ultra-processed foods appears to be related to an increased risk of overweight or obesity in her children, according to new research.
Among the 19,958 mother-child pairs studied, 12.4% of children developed obesity or overweight in the full analytic study group, and the offspring of those mothers who ate the most ultra-processed foods had a 26% higher risk of obesity/overweight (12.1 servings/day), compared with those with the lowest consumption (3.4 servings/day), report Andrew T. Chan, MD, MPH, professor of medicine at Harvard Medical School, Boston, and colleagues.
This study demonstrates the possible advantages of restricting ultra-processed food consumption among women and mothers who are in their reproductive years to potentially lower the risk of childhood obesity, the investigators note.
“These data support the importance of refining dietary recommendations and the development of programs to improve nutrition for women of reproductive age to promote offspring health,” they write in their article, published in BMJ.
“As a medical and public health community, we have to understand that the period of time in which a woman is carrying a child or ... the time when she is raising her children represents a unique opportunity to potentially intervene to affect both the health of the mother and also the health of the children,” Dr. Chan said in an interview.
It is important to address these trends both on an individual clinician level and on a societal level, noted Dr. Chan.
“This is a good opportunity to counsel patients about the potential linkage between their consumption of ultra-processed food for not just themselves but also their kids, and I think that added counseling and awareness may motivate individuals to think about their diets in a more favorable way,” he added.
But ultra-processed foods are affordable and convenient, and many communities are not able to easily access fresh and healthy foods, so “it is incumbent upon [clinicians] to make it a priority and to break down those social and economic barriers, which make it difficult to have healthy and less processed food,” Dr. Chan elaborated.
Assessment of maternal junk food intake during peri-pregnancy and childhood
Modern Western diets frequently include ultra-processed foods – such as packaged baked goods and snacks, fizzy drinks, and sugary cereals – which are linked to adult weight increase. The relationship between parental consumption of highly processed meals and offspring weight is, however, unclear across generations, the researchers note.
Hence, they set out to determine whether eating ultra-processed foods during peri-pregnancy and while raising children increased the risk of being overweight or having obesity among children and teens.
The study team assessed 14,553 mothers and their 19,958 children from the Growing Up Today Study (GUTS I and II) and Nurses’ Health Study II (NHS II) in the United States. Males accounted for 45% of the children in the study, and the children’s ages ranged from 7 to 17 years.
The NHS II is a continuing investigation following the lifestyle and health choices of over 100,000 female registered nurses in the United States in 1989, while the GUTS I involved about 17,000 children of the nurses in the NHS II. Participants in GUTS I filled out an initial lifestyle and health survey and were evaluated annually between 1997 and 2001 and every 2 years thereafter.
Roughly 11,000 children from the NHS II were included in the GUTS II. The children were further evaluated in 2006, 2008, and 2011, as well as every 2 years thereafter.
Participants were followed until the children reached 18 years of age or experienced obesity and overweight onset. A subcohort consisted of 2,925 mother-child pairs with data on peri-pregnancy eating patterns.
Maternal intake of ultra-processed foods while raising children was linked with obesity or overweight in children. Moreover, compared with the lowest consumption cohort (3.4 servings/day), there was a 26% greater risk for the greatest maternal ultra-processed food intake cohort (12.1 servings/day) after adjusting for child’s sedentary time, ultra-processed food intake, physical activity, and established maternal risk factors.
Even though rates were elevated, ultra-processed food intake during pregnancy was not significantly linked to a higher risk of obesity or overweight in children (P for trend = .07).
Sex, birth weight, age, gestational age, or maternal body weight had no effect on these correlations either.
The study’s limitations include the fact that some of the children in the pairs were lost during follow-up; there may have been data misreporting, as the weight and diet measures were provided via self-reported questionnaires; and potential residual confounding given the observational study design, the researchers note.
Other limitations include that the mothers involved in the study came from similar socioeconomic backgrounds, had similar personal and familial educational statuses, and were primarily White, which limits the generalizability of these data to other ethnic groups, the authors add.
“Further studies are warranted to investigate specific biological mechanisms and socioeconomic determinants underlying the observed associations between maternal ultra-processed food intake and offspring overweight and obesity,” the researchers conclude.
A version of this article first appeared on Medscape.com.
Trial shows olokizumab’s effect in nonresponders to TNF inhibitors in RA
Treatment of rheumatoid arthritis with olokizumab combined with methotrexate led to significantly more patients with improved signs and symptoms than did methotrexate plus placebo in circumstances where previous treatment with one or more tumor necrosis factor (TNF) inhibitors yielded inadequate responses, results from a phase 3 randomized trial show.
At the week 12 primary endpoint, 40.6% of patients receiving placebo had at least 20% improvement in American College of Rheumatology response criteria (ACR 20), compared with 60.9% of patients receiving olokizumab 64 mg every 2 weeks and 59.6% of patients receiving olokizumab 64 mg every 4 weeks (P <.01 for both comparisons), senior author Roy M. Fleischmann, MD, of the University of Texas Southwestern Medical Center in Dallas and colleagues reported in Annals of the Rheumatic Diseases.
Dr. Fleischmann said that given the existing literature on the investigational interleukin (IL)-6 inhibitor olokizumab shows that it is superior to placebo and noninferior to adalimumab (Humira) in patients who have an inadequate response to methotrexate and that it was superior to methotrexate alone for patients who have failed one or more TNF inhibitors in this current trial, the most likely use of olokizumab in clinical practice if it is approved is for those with inadequate responses to TNF inhibitors.
“If olokizumab is approved in the U.S., it is a reasonable choice when considering an inhibitor of IL-6. As it does affect IL-6 directly, rather than the receptor, much less protein needs to be administered with a convenient dosing interval of either every 2 or 4 weeks subcutaneously,” Dr. Fleischmann said in an interview.
The 24-week, double-blind, multicenter study, dubbed Clinical Rheumatoid Arthritis Development for Olokizumab (CREDO 3), involved 161 patients receiving 64 mg of olokizumab subcutaneously every 4 weeks, 138 receiving 64 mg of olokizumab subcutaneously once every 2 weeks, and 69 receiving placebo. At week 16, the researchers randomized participants in the placebo group to receive either olokizumab regimen.
All patients received methotrexate, and NSAIDs and glucocorticoids (< 10 mg/day prednisone or equivalent) were allowed in stable doses. Mean age was about 53 years across all three arms, and females accounted for the majority for each arm.
Significantly more patients in both olokizumab arms achieved the main secondary endpoint of Disease Activity Score in 28 joints based on C-reactive protein less than 3.2 at week 12, compared with placebo.
Notably, patients who moved from placebo at week 16 experienced improvement that was sustained over the remaining 8 weeks.
Serious treatment-emergent adverse events with olokizumab occurred in 3.2% receiving the drug every 4 weeks and in 7% receiving it every 2 weeks but in none who received placebo.
The study’s limitations included the high placebo response rate, the short timeframe for placebo, and its fairly small sample size, which limits the generalizability of the results, the authors noted.
Expert commentary
There are currently two biologics on the market that inhibit the IL-6 receptor, tocilizumab (Actemra), and sarilumab (Kevzara), but olokizumab is unique in that “it does not block the receptor. It binds directly to the cytokine,” noted Larry Moreland, MD, a professor of medicine and orthopedics in the division of rheumatology at the University of Colorado at Denver in Aurora, who was not involved in the study.
Tocilizumab and sarilumab had a similar clinical trial portfolio when they were studied in people who failed anti-TNF therapy, so this is the standard study a company would do prior to seeking approval, Dr. Moreland said.
“The fact that there is another IL-6 blocker that is showing promise means that there are more opportunities for researchers and clinicians to use these agents not only for rheumatoid arthritis but also hopefully study them in other diseases,” he said.
The CREDO 3 trial was sponsored by R-Pharm. Some of the authors are employees of R-Pharm. Dr. Fleischmann and some of his coauthors reported financial ties to R-Pharm and other pharmaceutical companies. Dr. Moreland reported having no relevant competing interests.
Treatment of rheumatoid arthritis with olokizumab combined with methotrexate led to significantly more patients with improved signs and symptoms than did methotrexate plus placebo in circumstances where previous treatment with one or more tumor necrosis factor (TNF) inhibitors yielded inadequate responses, results from a phase 3 randomized trial show.
At the week 12 primary endpoint, 40.6% of patients receiving placebo had at least 20% improvement in American College of Rheumatology response criteria (ACR 20), compared with 60.9% of patients receiving olokizumab 64 mg every 2 weeks and 59.6% of patients receiving olokizumab 64 mg every 4 weeks (P <.01 for both comparisons), senior author Roy M. Fleischmann, MD, of the University of Texas Southwestern Medical Center in Dallas and colleagues reported in Annals of the Rheumatic Diseases.
Dr. Fleischmann said that given the existing literature on the investigational interleukin (IL)-6 inhibitor olokizumab shows that it is superior to placebo and noninferior to adalimumab (Humira) in patients who have an inadequate response to methotrexate and that it was superior to methotrexate alone for patients who have failed one or more TNF inhibitors in this current trial, the most likely use of olokizumab in clinical practice if it is approved is for those with inadequate responses to TNF inhibitors.
“If olokizumab is approved in the U.S., it is a reasonable choice when considering an inhibitor of IL-6. As it does affect IL-6 directly, rather than the receptor, much less protein needs to be administered with a convenient dosing interval of either every 2 or 4 weeks subcutaneously,” Dr. Fleischmann said in an interview.
The 24-week, double-blind, multicenter study, dubbed Clinical Rheumatoid Arthritis Development for Olokizumab (CREDO 3), involved 161 patients receiving 64 mg of olokizumab subcutaneously every 4 weeks, 138 receiving 64 mg of olokizumab subcutaneously once every 2 weeks, and 69 receiving placebo. At week 16, the researchers randomized participants in the placebo group to receive either olokizumab regimen.
All patients received methotrexate, and NSAIDs and glucocorticoids (< 10 mg/day prednisone or equivalent) were allowed in stable doses. Mean age was about 53 years across all three arms, and females accounted for the majority for each arm.
Significantly more patients in both olokizumab arms achieved the main secondary endpoint of Disease Activity Score in 28 joints based on C-reactive protein less than 3.2 at week 12, compared with placebo.
Notably, patients who moved from placebo at week 16 experienced improvement that was sustained over the remaining 8 weeks.
Serious treatment-emergent adverse events with olokizumab occurred in 3.2% receiving the drug every 4 weeks and in 7% receiving it every 2 weeks but in none who received placebo.
The study’s limitations included the high placebo response rate, the short timeframe for placebo, and its fairly small sample size, which limits the generalizability of the results, the authors noted.
Expert commentary
There are currently two biologics on the market that inhibit the IL-6 receptor, tocilizumab (Actemra), and sarilumab (Kevzara), but olokizumab is unique in that “it does not block the receptor. It binds directly to the cytokine,” noted Larry Moreland, MD, a professor of medicine and orthopedics in the division of rheumatology at the University of Colorado at Denver in Aurora, who was not involved in the study.
Tocilizumab and sarilumab had a similar clinical trial portfolio when they were studied in people who failed anti-TNF therapy, so this is the standard study a company would do prior to seeking approval, Dr. Moreland said.
“The fact that there is another IL-6 blocker that is showing promise means that there are more opportunities for researchers and clinicians to use these agents not only for rheumatoid arthritis but also hopefully study them in other diseases,” he said.
The CREDO 3 trial was sponsored by R-Pharm. Some of the authors are employees of R-Pharm. Dr. Fleischmann and some of his coauthors reported financial ties to R-Pharm and other pharmaceutical companies. Dr. Moreland reported having no relevant competing interests.
Treatment of rheumatoid arthritis with olokizumab combined with methotrexate led to significantly more patients with improved signs and symptoms than did methotrexate plus placebo in circumstances where previous treatment with one or more tumor necrosis factor (TNF) inhibitors yielded inadequate responses, results from a phase 3 randomized trial show.
At the week 12 primary endpoint, 40.6% of patients receiving placebo had at least 20% improvement in American College of Rheumatology response criteria (ACR 20), compared with 60.9% of patients receiving olokizumab 64 mg every 2 weeks and 59.6% of patients receiving olokizumab 64 mg every 4 weeks (P <.01 for both comparisons), senior author Roy M. Fleischmann, MD, of the University of Texas Southwestern Medical Center in Dallas and colleagues reported in Annals of the Rheumatic Diseases.
Dr. Fleischmann said that given the existing literature on the investigational interleukin (IL)-6 inhibitor olokizumab shows that it is superior to placebo and noninferior to adalimumab (Humira) in patients who have an inadequate response to methotrexate and that it was superior to methotrexate alone for patients who have failed one or more TNF inhibitors in this current trial, the most likely use of olokizumab in clinical practice if it is approved is for those with inadequate responses to TNF inhibitors.
“If olokizumab is approved in the U.S., it is a reasonable choice when considering an inhibitor of IL-6. As it does affect IL-6 directly, rather than the receptor, much less protein needs to be administered with a convenient dosing interval of either every 2 or 4 weeks subcutaneously,” Dr. Fleischmann said in an interview.
The 24-week, double-blind, multicenter study, dubbed Clinical Rheumatoid Arthritis Development for Olokizumab (CREDO 3), involved 161 patients receiving 64 mg of olokizumab subcutaneously every 4 weeks, 138 receiving 64 mg of olokizumab subcutaneously once every 2 weeks, and 69 receiving placebo. At week 16, the researchers randomized participants in the placebo group to receive either olokizumab regimen.
All patients received methotrexate, and NSAIDs and glucocorticoids (< 10 mg/day prednisone or equivalent) were allowed in stable doses. Mean age was about 53 years across all three arms, and females accounted for the majority for each arm.
Significantly more patients in both olokizumab arms achieved the main secondary endpoint of Disease Activity Score in 28 joints based on C-reactive protein less than 3.2 at week 12, compared with placebo.
Notably, patients who moved from placebo at week 16 experienced improvement that was sustained over the remaining 8 weeks.
Serious treatment-emergent adverse events with olokizumab occurred in 3.2% receiving the drug every 4 weeks and in 7% receiving it every 2 weeks but in none who received placebo.
The study’s limitations included the high placebo response rate, the short timeframe for placebo, and its fairly small sample size, which limits the generalizability of the results, the authors noted.
Expert commentary
There are currently two biologics on the market that inhibit the IL-6 receptor, tocilizumab (Actemra), and sarilumab (Kevzara), but olokizumab is unique in that “it does not block the receptor. It binds directly to the cytokine,” noted Larry Moreland, MD, a professor of medicine and orthopedics in the division of rheumatology at the University of Colorado at Denver in Aurora, who was not involved in the study.
Tocilizumab and sarilumab had a similar clinical trial portfolio when they were studied in people who failed anti-TNF therapy, so this is the standard study a company would do prior to seeking approval, Dr. Moreland said.
“The fact that there is another IL-6 blocker that is showing promise means that there are more opportunities for researchers and clinicians to use these agents not only for rheumatoid arthritis but also hopefully study them in other diseases,” he said.
The CREDO 3 trial was sponsored by R-Pharm. Some of the authors are employees of R-Pharm. Dr. Fleischmann and some of his coauthors reported financial ties to R-Pharm and other pharmaceutical companies. Dr. Moreland reported having no relevant competing interests.
FROM ANNALS OF THE RHEUMATIC DISEASES





