User login
A Common Pancreatic Condition That Few Have Heard Of
— a disorder experienced by roughly one fifth of the world’s population. Although it is more common than type 2 diabetes, pancreatitis, and pancreatic cancer combined, it has remained relatively obscure.
By contrast, fatty liver — once called nonalcoholic fatty liver disease and recently renamed metabolic dysfunction–associated steatotic liver disease (MASLD) — is well-known.
“When it comes to diseases of the liver and pancreas, the liver is the big brother that has gotten all the attention, while the pancreas is the neglected little stepbrother that’s not sufficiently profiled in most medical textbooks and gets very little attention,” Max Petrov, MD, MPH, PhD, professor of pancreatology, University of Auckland, New Zealand, said in an interview. “The phenomenon of fatty pancreas has been observed for decades, but it is underappreciated and underrecognized.”
As early as 1926, fat depositions were identified during autopsies, but the condition remained relatively unknown, Mohammad Bilal, MD, associate professor of medicine-gastroenterology, University of Colorado Anschutz Medical Campus, Aurora, said in an interview. “Fortunately, FPD has recently been receiving more focus.”
Generally, healthy individuals have small amounts of fat in their pancreas. IPFD is defined as “the diffuse presence of fat in the pancreas, measured on a continuous scale,” and FPD refers to IPFD above the upper limit of normal. While there is no clear consensus as to what the normal range is, studies suggest it’s a pancreatic fat content ranging from 1.8% to 10.4%.
FPD’s “most important implication is that it can be a precursor for more challenging and burdensome diseases of the pancreas,” Petrov said.
Fatty changes in the pancreas affect both its endocrine and exocrine systems. FPD is associated with type 2 diabetes, the most common disease of the endocrine pancreas, as well as pancreatitis and pancreatic cancer, the most common diseases of the exocrine pancreas. It’s also implicated in the development of carotid atherosclerosis, pancreatic fistula following surgery, and exocrine pancreatic insufficiency (EPI).
A ‘Pandora’s Box’
Up to half of people with fatty pancreas are lean. The condition isn’t merely caused by an overflow of fat from the liver into the pancreas in people who consume more calories than they burn, Petrov said. Neither robust postmortem nor biopsy studies have found a statistically significant association between fatty deposition in the pancreas and liver fat.
Compared with the way people accumulate liver fat, the development of FPD is more complex, Petrov said.
“Hepatic fat is a relatively simple process: Lipid droplets accumulate in the hepatocytes; but, in the pancreas, there are several ways by which fat may accumulate,” he said.
One relates to the location of the pancreas within visceral, retroperitoneal fat, Petrov said. That fat can migrate and build up between pancreatic lobules.
Fat also can accumulate inside the lobes. This process can involve a buildup of fat droplets in acinar and stellate cells on the exocrine side and in the islets of Langerhans on the endocrine side. Additionally, when functional pancreatic cells die, particularly acinar cells, adult stem cells may replace them with adipocytes. Transformation of acinar cells into fat cells — a process called acinar-to-adipocyte transdifferentiation — also may be a way fat accumulates inside the lobes, Petrov said.
The accumulation of fat is a response to a wide array of insults to the pancreas over time. For example, obesity and metabolic syndrome lead to the accumulation of adipocytes and fat infiltration, whereas alcohol abuse and viral infections may lead to the death of acinar cells, which produce digestive enzymes.
Ultimately, the negative changes produced by excess fat in the pancreas are the origin of all common noninherited pancreatic diseases, bringing them under one umbrella, Petrov maintained. He dubbed this hypothesis PANcreatic Diseases Originating from intRapancreatic fAt (PANDORA).
The type of cells involved has implications for which disease may arise. For example, fat infiltration in stellate cells may promote pancreatic cancer, whereas its accumulation in the islets of Langerhans, which produce insulin and glucagon, is associated with type 2 diabetes.
The PANDORA hypothesis has eight foundational principles:
- Fatty pancreas is a key driver of pancreatic diseases in most people.
- Inflammation within the pancreatic microenvironment results from overwhelming lipotoxicity fueled by fatty pancreas.
- Aberrant communication between acinar cells involving lipid droplets drives acute pancreatitis.
- The pancreas responds to lipotoxicity with fibrosis and calcification — the hallmarks of chronic pancreatitis.
- Fat deposition affects signaling between stellate cells and other components of the microenvironment in ways that raise the risk for pancreatic cancer.
- The development of diabetes of the exocrine pancreas and EPI is affected by the presence of fatty pancreas.
- The higher risk for pancreatic disease in older adults is influenced by fatty pancreas.
- The multipronged nature of intrapancreatic fat deposition accounts for the common development of one pancreatic disease after another.
The idea that all common pancreatic diseases are the result of pathways emanating from FPD could “explain the bidirectional relationship between diabetes and pancreatitis or pancreatic cancer,” Petrov said.
Risk Factors, Symptoms, and Diagnosis
A variety of risk factors are involved in the accumulation of fat that may lead to pancreatic diseases, including aging, cholelithiasis, dyslipidemia, drugs/toxins (eg, steroids), genetic predisposition, iron overload, diet (eg, fatty foods, ultraprocessed foods), heavy alcohol use, overweight/obesity, pancreatic duct obstruction, tobacco use, viral infection (eg, hepatitis B, COVID-19), severe malnutrition, prediabetes, and dysglycemia.
Petrov described FPD as a “silent disease” that’s often asymptomatic, with its presence emerging as an incidental finding during abdominal ultrasonography for other reasons. However, patients may sometimes experience stomach pain or nausea if they have concurrent diseases of the pancreas, he said.
There are no currently available lab tests that can definitively detect the presence of FPD. Rather, the gold standard for a noninvasive diagnosis of FPD is MRI, with CT as the second-best choice, Petrov said.
In countries where advanced imaging is not available, a low-cost alternative might be a simple abdominal ultrasound, but it is not definitive, he said. “It’s operator-dependent and can be subjective.”
Some risk factors, such as derangements of glucose and lipid metabolism, especially in the presence of heavy alcohol use and a high-fat diet, can “be detected on lab tests,” Petrov said. “This, in combination with the abdominal ultrasound, might suggest the patients will benefit from deeper investigation, including MRI.”
Because the exocrine pancreas helps with digestion of fatty food, intralobular fatty deposits or replacement of pancreatic exocrine cells with adipose cells can lead to steatorrhea, Bilal said.
“Fat within the stool or oily diarrhea is a clue to the presence of FPD,” Bilal said.
Although this symptom isn’t unique to FPD and is found in other types of pancreatic conditions, its presence suggests that further investigation for FPD is warranted, he added.
Common-Sense Treatment Approaches
At present, there are no US Food and Drug Administration–approved treatments for FPD, Petrov said.
“What might be recommended is something along the lines of treatment of MASLD — appropriate diet and physical activity,” he said. Petrov hopes that as the disease entity garners more research attention, more clinical drug trials will be initiated, and new medications are found and approved.
Petrov suggested that there could be a “theoretical rationale” for the use of glucagon-like peptide 1 receptor agonists (GLP-1 RAs) as a treatment, given their effectiveness in multiple conditions, including MASLD, but no human trials have robustly shown specific benefits of these drugs for FPD.
Petrov added that, to date, 12 classes of drugs have been investigated for reducing IPFD: biguanides, sulfonylureas, GLP-1 RAs, thiazolidinediones, dipeptidyl peptidase–4 (DPP-4) inhibitors, sodium-glucose cotransporter 2 inhibitors, statins, fibrates, pancreatic lipase inhibitors, angiotensin II receptor blockers, somatostatin receptor agonists, and antioxidants.
Of these, most have shown promise in preclinical animal models. But only thiazolidinediones, GLP-1 RAs, DPP-4 inhibitors, and somatostatin receptor agonists have been investigated in randomized controlled trials in humans. The findings have been inconsistent, with the active treatment often not achieving statistically significant improvements.
“At this stage of our knowledge, we can’t recommend a specific pharmacotherapy,” Petrov said. But we can suggest dietary changes, such as saturated fat reduction, alcohol reduction, smoking cessation, reduction in consumption of ultraprocessed food, physical exercise, and addressing obesity and other drivers of metabolic disease.
Bilal, who is also a spokesperson for AGA, suggested that pancreatic enzyme replacement therapy, often used to treat pancreatic EPI, may treat some symptoms of FPD such as diarrhea.
Bariatric surgery has shown promise for FPD, in that it can decrease the patient’s body mass and potentially reduce the fat in the pancreas as well as it can improve metabolic diseases and hyperlipidemia. One study showed that it significantly decreased IPFD, fatty acid uptake, and blood flow, and these improvements were associated with more favorable glucose homeostasis and beta-cell function.
However, bariatric surgery is only appropriate for certain patients; is associated with potentially adverse sequelae including malnutrition, anemia, and digestive tract stenosis; and is currently not indicated for FPD.
Bilal advises clinicians to “keep an eye on FPD” if it’s detected incidentally and to screen patients more carefully for MASLD, metabolic disease, and diabetes.
“Although there are no consensus guidelines and recommendations for managing FPD at present, these common-sense approaches will benefit the patient’s overall health and hopefully will have a beneficial impact on pancreatic health as well,” he said.
Petrov reported no relevant financial relationships. Bilal reported being a consultant for Boston Scientific, Steris Endoscopy, and Cook Medical.
A version of this article first appeared on Medscape.com.
— a disorder experienced by roughly one fifth of the world’s population. Although it is more common than type 2 diabetes, pancreatitis, and pancreatic cancer combined, it has remained relatively obscure.
By contrast, fatty liver — once called nonalcoholic fatty liver disease and recently renamed metabolic dysfunction–associated steatotic liver disease (MASLD) — is well-known.
“When it comes to diseases of the liver and pancreas, the liver is the big brother that has gotten all the attention, while the pancreas is the neglected little stepbrother that’s not sufficiently profiled in most medical textbooks and gets very little attention,” Max Petrov, MD, MPH, PhD, professor of pancreatology, University of Auckland, New Zealand, said in an interview. “The phenomenon of fatty pancreas has been observed for decades, but it is underappreciated and underrecognized.”
As early as 1926, fat depositions were identified during autopsies, but the condition remained relatively unknown, Mohammad Bilal, MD, associate professor of medicine-gastroenterology, University of Colorado Anschutz Medical Campus, Aurora, said in an interview. “Fortunately, FPD has recently been receiving more focus.”
Generally, healthy individuals have small amounts of fat in their pancreas. IPFD is defined as “the diffuse presence of fat in the pancreas, measured on a continuous scale,” and FPD refers to IPFD above the upper limit of normal. While there is no clear consensus as to what the normal range is, studies suggest it’s a pancreatic fat content ranging from 1.8% to 10.4%.
FPD’s “most important implication is that it can be a precursor for more challenging and burdensome diseases of the pancreas,” Petrov said.
Fatty changes in the pancreas affect both its endocrine and exocrine systems. FPD is associated with type 2 diabetes, the most common disease of the endocrine pancreas, as well as pancreatitis and pancreatic cancer, the most common diseases of the exocrine pancreas. It’s also implicated in the development of carotid atherosclerosis, pancreatic fistula following surgery, and exocrine pancreatic insufficiency (EPI).
A ‘Pandora’s Box’
Up to half of people with fatty pancreas are lean. The condition isn’t merely caused by an overflow of fat from the liver into the pancreas in people who consume more calories than they burn, Petrov said. Neither robust postmortem nor biopsy studies have found a statistically significant association between fatty deposition in the pancreas and liver fat.
Compared with the way people accumulate liver fat, the development of FPD is more complex, Petrov said.
“Hepatic fat is a relatively simple process: Lipid droplets accumulate in the hepatocytes; but, in the pancreas, there are several ways by which fat may accumulate,” he said.
One relates to the location of the pancreas within visceral, retroperitoneal fat, Petrov said. That fat can migrate and build up between pancreatic lobules.
Fat also can accumulate inside the lobes. This process can involve a buildup of fat droplets in acinar and stellate cells on the exocrine side and in the islets of Langerhans on the endocrine side. Additionally, when functional pancreatic cells die, particularly acinar cells, adult stem cells may replace them with adipocytes. Transformation of acinar cells into fat cells — a process called acinar-to-adipocyte transdifferentiation — also may be a way fat accumulates inside the lobes, Petrov said.
The accumulation of fat is a response to a wide array of insults to the pancreas over time. For example, obesity and metabolic syndrome lead to the accumulation of adipocytes and fat infiltration, whereas alcohol abuse and viral infections may lead to the death of acinar cells, which produce digestive enzymes.
Ultimately, the negative changes produced by excess fat in the pancreas are the origin of all common noninherited pancreatic diseases, bringing them under one umbrella, Petrov maintained. He dubbed this hypothesis PANcreatic Diseases Originating from intRapancreatic fAt (PANDORA).
The type of cells involved has implications for which disease may arise. For example, fat infiltration in stellate cells may promote pancreatic cancer, whereas its accumulation in the islets of Langerhans, which produce insulin and glucagon, is associated with type 2 diabetes.
The PANDORA hypothesis has eight foundational principles:
- Fatty pancreas is a key driver of pancreatic diseases in most people.
- Inflammation within the pancreatic microenvironment results from overwhelming lipotoxicity fueled by fatty pancreas.
- Aberrant communication between acinar cells involving lipid droplets drives acute pancreatitis.
- The pancreas responds to lipotoxicity with fibrosis and calcification — the hallmarks of chronic pancreatitis.
- Fat deposition affects signaling between stellate cells and other components of the microenvironment in ways that raise the risk for pancreatic cancer.
- The development of diabetes of the exocrine pancreas and EPI is affected by the presence of fatty pancreas.
- The higher risk for pancreatic disease in older adults is influenced by fatty pancreas.
- The multipronged nature of intrapancreatic fat deposition accounts for the common development of one pancreatic disease after another.
The idea that all common pancreatic diseases are the result of pathways emanating from FPD could “explain the bidirectional relationship between diabetes and pancreatitis or pancreatic cancer,” Petrov said.
Risk Factors, Symptoms, and Diagnosis
A variety of risk factors are involved in the accumulation of fat that may lead to pancreatic diseases, including aging, cholelithiasis, dyslipidemia, drugs/toxins (eg, steroids), genetic predisposition, iron overload, diet (eg, fatty foods, ultraprocessed foods), heavy alcohol use, overweight/obesity, pancreatic duct obstruction, tobacco use, viral infection (eg, hepatitis B, COVID-19), severe malnutrition, prediabetes, and dysglycemia.
Petrov described FPD as a “silent disease” that’s often asymptomatic, with its presence emerging as an incidental finding during abdominal ultrasonography for other reasons. However, patients may sometimes experience stomach pain or nausea if they have concurrent diseases of the pancreas, he said.
There are no currently available lab tests that can definitively detect the presence of FPD. Rather, the gold standard for a noninvasive diagnosis of FPD is MRI, with CT as the second-best choice, Petrov said.
In countries where advanced imaging is not available, a low-cost alternative might be a simple abdominal ultrasound, but it is not definitive, he said. “It’s operator-dependent and can be subjective.”
Some risk factors, such as derangements of glucose and lipid metabolism, especially in the presence of heavy alcohol use and a high-fat diet, can “be detected on lab tests,” Petrov said. “This, in combination with the abdominal ultrasound, might suggest the patients will benefit from deeper investigation, including MRI.”
Because the exocrine pancreas helps with digestion of fatty food, intralobular fatty deposits or replacement of pancreatic exocrine cells with adipose cells can lead to steatorrhea, Bilal said.
“Fat within the stool or oily diarrhea is a clue to the presence of FPD,” Bilal said.
Although this symptom isn’t unique to FPD and is found in other types of pancreatic conditions, its presence suggests that further investigation for FPD is warranted, he added.
Common-Sense Treatment Approaches
At present, there are no US Food and Drug Administration–approved treatments for FPD, Petrov said.
“What might be recommended is something along the lines of treatment of MASLD — appropriate diet and physical activity,” he said. Petrov hopes that as the disease entity garners more research attention, more clinical drug trials will be initiated, and new medications are found and approved.
Petrov suggested that there could be a “theoretical rationale” for the use of glucagon-like peptide 1 receptor agonists (GLP-1 RAs) as a treatment, given their effectiveness in multiple conditions, including MASLD, but no human trials have robustly shown specific benefits of these drugs for FPD.
Petrov added that, to date, 12 classes of drugs have been investigated for reducing IPFD: biguanides, sulfonylureas, GLP-1 RAs, thiazolidinediones, dipeptidyl peptidase–4 (DPP-4) inhibitors, sodium-glucose cotransporter 2 inhibitors, statins, fibrates, pancreatic lipase inhibitors, angiotensin II receptor blockers, somatostatin receptor agonists, and antioxidants.
Of these, most have shown promise in preclinical animal models. But only thiazolidinediones, GLP-1 RAs, DPP-4 inhibitors, and somatostatin receptor agonists have been investigated in randomized controlled trials in humans. The findings have been inconsistent, with the active treatment often not achieving statistically significant improvements.
“At this stage of our knowledge, we can’t recommend a specific pharmacotherapy,” Petrov said. But we can suggest dietary changes, such as saturated fat reduction, alcohol reduction, smoking cessation, reduction in consumption of ultraprocessed food, physical exercise, and addressing obesity and other drivers of metabolic disease.
Bilal, who is also a spokesperson for AGA, suggested that pancreatic enzyme replacement therapy, often used to treat pancreatic EPI, may treat some symptoms of FPD such as diarrhea.
Bariatric surgery has shown promise for FPD, in that it can decrease the patient’s body mass and potentially reduce the fat in the pancreas as well as it can improve metabolic diseases and hyperlipidemia. One study showed that it significantly decreased IPFD, fatty acid uptake, and blood flow, and these improvements were associated with more favorable glucose homeostasis and beta-cell function.
However, bariatric surgery is only appropriate for certain patients; is associated with potentially adverse sequelae including malnutrition, anemia, and digestive tract stenosis; and is currently not indicated for FPD.
Bilal advises clinicians to “keep an eye on FPD” if it’s detected incidentally and to screen patients more carefully for MASLD, metabolic disease, and diabetes.
“Although there are no consensus guidelines and recommendations for managing FPD at present, these common-sense approaches will benefit the patient’s overall health and hopefully will have a beneficial impact on pancreatic health as well,” he said.
Petrov reported no relevant financial relationships. Bilal reported being a consultant for Boston Scientific, Steris Endoscopy, and Cook Medical.
A version of this article first appeared on Medscape.com.
— a disorder experienced by roughly one fifth of the world’s population. Although it is more common than type 2 diabetes, pancreatitis, and pancreatic cancer combined, it has remained relatively obscure.
By contrast, fatty liver — once called nonalcoholic fatty liver disease and recently renamed metabolic dysfunction–associated steatotic liver disease (MASLD) — is well-known.
“When it comes to diseases of the liver and pancreas, the liver is the big brother that has gotten all the attention, while the pancreas is the neglected little stepbrother that’s not sufficiently profiled in most medical textbooks and gets very little attention,” Max Petrov, MD, MPH, PhD, professor of pancreatology, University of Auckland, New Zealand, said in an interview. “The phenomenon of fatty pancreas has been observed for decades, but it is underappreciated and underrecognized.”
As early as 1926, fat depositions were identified during autopsies, but the condition remained relatively unknown, Mohammad Bilal, MD, associate professor of medicine-gastroenterology, University of Colorado Anschutz Medical Campus, Aurora, said in an interview. “Fortunately, FPD has recently been receiving more focus.”
Generally, healthy individuals have small amounts of fat in their pancreas. IPFD is defined as “the diffuse presence of fat in the pancreas, measured on a continuous scale,” and FPD refers to IPFD above the upper limit of normal. While there is no clear consensus as to what the normal range is, studies suggest it’s a pancreatic fat content ranging from 1.8% to 10.4%.
FPD’s “most important implication is that it can be a precursor for more challenging and burdensome diseases of the pancreas,” Petrov said.
Fatty changes in the pancreas affect both its endocrine and exocrine systems. FPD is associated with type 2 diabetes, the most common disease of the endocrine pancreas, as well as pancreatitis and pancreatic cancer, the most common diseases of the exocrine pancreas. It’s also implicated in the development of carotid atherosclerosis, pancreatic fistula following surgery, and exocrine pancreatic insufficiency (EPI).
A ‘Pandora’s Box’
Up to half of people with fatty pancreas are lean. The condition isn’t merely caused by an overflow of fat from the liver into the pancreas in people who consume more calories than they burn, Petrov said. Neither robust postmortem nor biopsy studies have found a statistically significant association between fatty deposition in the pancreas and liver fat.
Compared with the way people accumulate liver fat, the development of FPD is more complex, Petrov said.
“Hepatic fat is a relatively simple process: Lipid droplets accumulate in the hepatocytes; but, in the pancreas, there are several ways by which fat may accumulate,” he said.
One relates to the location of the pancreas within visceral, retroperitoneal fat, Petrov said. That fat can migrate and build up between pancreatic lobules.
Fat also can accumulate inside the lobes. This process can involve a buildup of fat droplets in acinar and stellate cells on the exocrine side and in the islets of Langerhans on the endocrine side. Additionally, when functional pancreatic cells die, particularly acinar cells, adult stem cells may replace them with adipocytes. Transformation of acinar cells into fat cells — a process called acinar-to-adipocyte transdifferentiation — also may be a way fat accumulates inside the lobes, Petrov said.
The accumulation of fat is a response to a wide array of insults to the pancreas over time. For example, obesity and metabolic syndrome lead to the accumulation of adipocytes and fat infiltration, whereas alcohol abuse and viral infections may lead to the death of acinar cells, which produce digestive enzymes.
Ultimately, the negative changes produced by excess fat in the pancreas are the origin of all common noninherited pancreatic diseases, bringing them under one umbrella, Petrov maintained. He dubbed this hypothesis PANcreatic Diseases Originating from intRapancreatic fAt (PANDORA).
The type of cells involved has implications for which disease may arise. For example, fat infiltration in stellate cells may promote pancreatic cancer, whereas its accumulation in the islets of Langerhans, which produce insulin and glucagon, is associated with type 2 diabetes.
The PANDORA hypothesis has eight foundational principles:
- Fatty pancreas is a key driver of pancreatic diseases in most people.
- Inflammation within the pancreatic microenvironment results from overwhelming lipotoxicity fueled by fatty pancreas.
- Aberrant communication between acinar cells involving lipid droplets drives acute pancreatitis.
- The pancreas responds to lipotoxicity with fibrosis and calcification — the hallmarks of chronic pancreatitis.
- Fat deposition affects signaling between stellate cells and other components of the microenvironment in ways that raise the risk for pancreatic cancer.
- The development of diabetes of the exocrine pancreas and EPI is affected by the presence of fatty pancreas.
- The higher risk for pancreatic disease in older adults is influenced by fatty pancreas.
- The multipronged nature of intrapancreatic fat deposition accounts for the common development of one pancreatic disease after another.
The idea that all common pancreatic diseases are the result of pathways emanating from FPD could “explain the bidirectional relationship between diabetes and pancreatitis or pancreatic cancer,” Petrov said.
Risk Factors, Symptoms, and Diagnosis
A variety of risk factors are involved in the accumulation of fat that may lead to pancreatic diseases, including aging, cholelithiasis, dyslipidemia, drugs/toxins (eg, steroids), genetic predisposition, iron overload, diet (eg, fatty foods, ultraprocessed foods), heavy alcohol use, overweight/obesity, pancreatic duct obstruction, tobacco use, viral infection (eg, hepatitis B, COVID-19), severe malnutrition, prediabetes, and dysglycemia.
Petrov described FPD as a “silent disease” that’s often asymptomatic, with its presence emerging as an incidental finding during abdominal ultrasonography for other reasons. However, patients may sometimes experience stomach pain or nausea if they have concurrent diseases of the pancreas, he said.
There are no currently available lab tests that can definitively detect the presence of FPD. Rather, the gold standard for a noninvasive diagnosis of FPD is MRI, with CT as the second-best choice, Petrov said.
In countries where advanced imaging is not available, a low-cost alternative might be a simple abdominal ultrasound, but it is not definitive, he said. “It’s operator-dependent and can be subjective.”
Some risk factors, such as derangements of glucose and lipid metabolism, especially in the presence of heavy alcohol use and a high-fat diet, can “be detected on lab tests,” Petrov said. “This, in combination with the abdominal ultrasound, might suggest the patients will benefit from deeper investigation, including MRI.”
Because the exocrine pancreas helps with digestion of fatty food, intralobular fatty deposits or replacement of pancreatic exocrine cells with adipose cells can lead to steatorrhea, Bilal said.
“Fat within the stool or oily diarrhea is a clue to the presence of FPD,” Bilal said.
Although this symptom isn’t unique to FPD and is found in other types of pancreatic conditions, its presence suggests that further investigation for FPD is warranted, he added.
Common-Sense Treatment Approaches
At present, there are no US Food and Drug Administration–approved treatments for FPD, Petrov said.
“What might be recommended is something along the lines of treatment of MASLD — appropriate diet and physical activity,” he said. Petrov hopes that as the disease entity garners more research attention, more clinical drug trials will be initiated, and new medications are found and approved.
Petrov suggested that there could be a “theoretical rationale” for the use of glucagon-like peptide 1 receptor agonists (GLP-1 RAs) as a treatment, given their effectiveness in multiple conditions, including MASLD, but no human trials have robustly shown specific benefits of these drugs for FPD.
Petrov added that, to date, 12 classes of drugs have been investigated for reducing IPFD: biguanides, sulfonylureas, GLP-1 RAs, thiazolidinediones, dipeptidyl peptidase–4 (DPP-4) inhibitors, sodium-glucose cotransporter 2 inhibitors, statins, fibrates, pancreatic lipase inhibitors, angiotensin II receptor blockers, somatostatin receptor agonists, and antioxidants.
Of these, most have shown promise in preclinical animal models. But only thiazolidinediones, GLP-1 RAs, DPP-4 inhibitors, and somatostatin receptor agonists have been investigated in randomized controlled trials in humans. The findings have been inconsistent, with the active treatment often not achieving statistically significant improvements.
“At this stage of our knowledge, we can’t recommend a specific pharmacotherapy,” Petrov said. But we can suggest dietary changes, such as saturated fat reduction, alcohol reduction, smoking cessation, reduction in consumption of ultraprocessed food, physical exercise, and addressing obesity and other drivers of metabolic disease.
Bilal, who is also a spokesperson for AGA, suggested that pancreatic enzyme replacement therapy, often used to treat pancreatic EPI, may treat some symptoms of FPD such as diarrhea.
Bariatric surgery has shown promise for FPD, in that it can decrease the patient’s body mass and potentially reduce the fat in the pancreas as well as it can improve metabolic diseases and hyperlipidemia. One study showed that it significantly decreased IPFD, fatty acid uptake, and blood flow, and these improvements were associated with more favorable glucose homeostasis and beta-cell function.
However, bariatric surgery is only appropriate for certain patients; is associated with potentially adverse sequelae including malnutrition, anemia, and digestive tract stenosis; and is currently not indicated for FPD.
Bilal advises clinicians to “keep an eye on FPD” if it’s detected incidentally and to screen patients more carefully for MASLD, metabolic disease, and diabetes.
“Although there are no consensus guidelines and recommendations for managing FPD at present, these common-sense approaches will benefit the patient’s overall health and hopefully will have a beneficial impact on pancreatic health as well,” he said.
Petrov reported no relevant financial relationships. Bilal reported being a consultant for Boston Scientific, Steris Endoscopy, and Cook Medical.
A version of this article first appeared on Medscape.com.
Newborn Screening Programs: What Do Clinicians Need to Know?
Newborn screening programs are public health services aimed at ensuring that the close to 4 million infants born each year in the United States are screened for certain serious disorders at birth. These disorders, albeit rare, are detected in roughly 12,500 newborn babies every year.
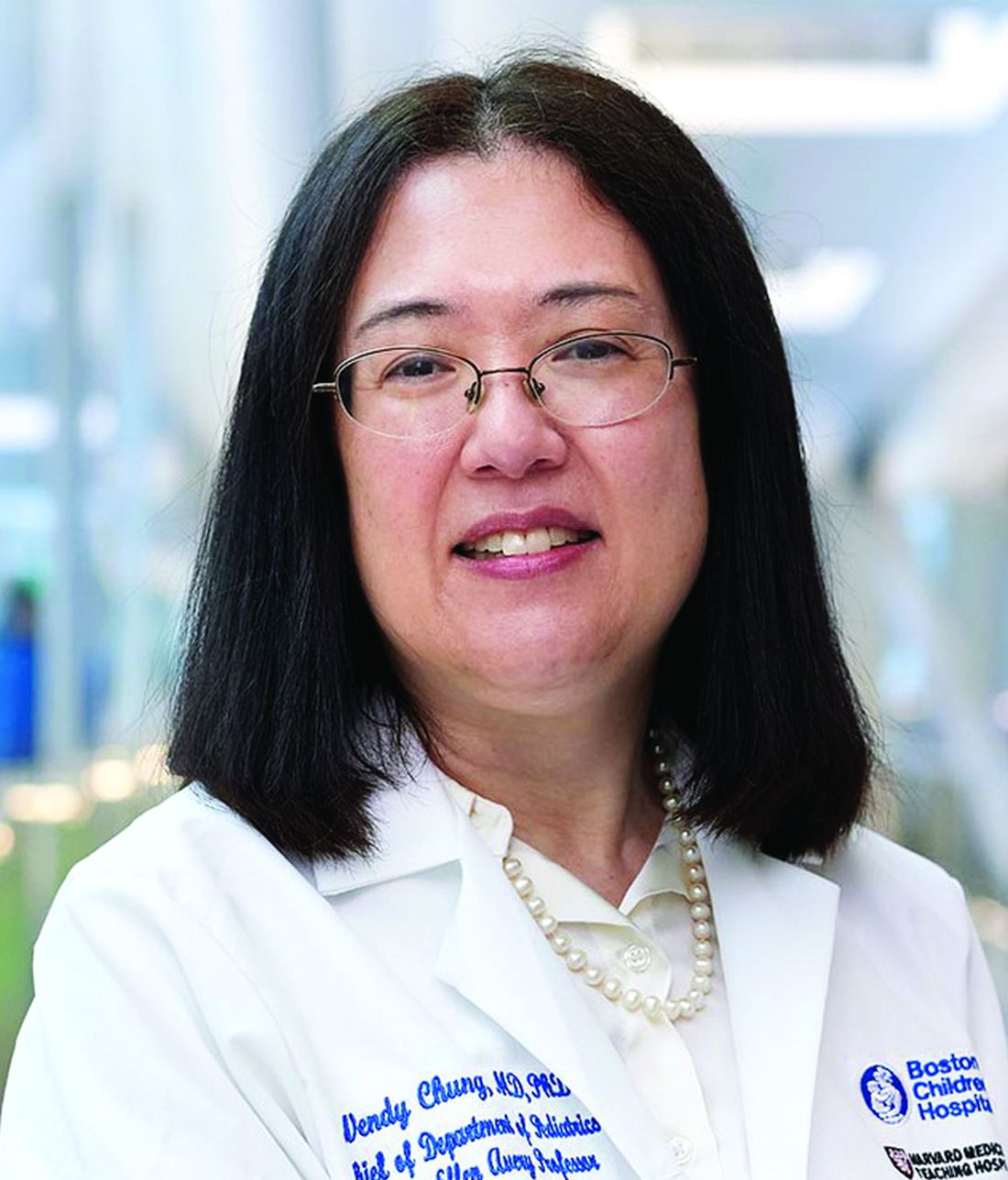
Newborn screening isn’t new, although it has expanded and transformed over the decades. The first newborn screening test was developed in the 1960s to detect phenylketonuria (PKU).1 Since then, the number of conditions screened for has increased, with programs in every US state and territory. “Newborn screening is well established now, not experimental or newfangled,” Wendy Chung, MD, PhD, professor of pediatrics, Harvard Medical School, Boston, Massachusetts, told Neurology Reviews.
In newborn screening, blood drawn from the baby’s heel is applied to specialized filter paper, which is then subjected to several analytical methods, including tandem mass spectrometry and molecular analyses to detect biomarkers for the diseases.2 More recently, genomic sequencing is being piloted as part of consented research studies.3
Newborn screening includes not only biochemical and genetic testing, but also includes noninvasive screening for hearing loss or for critical congenital heart disease using pulse oximetry. And newborn screening goes beyond analysis of a single drop of blood. Rather, “it’s an entire system, with the goal of identifying babies with genetic disorders who otherwise have no obvious symptoms,” said Dr. Chung. Left undetected and untreated, these conditions can be associated with serious adverse outcomes and even death.
Dr. Chung described newborn screening as a “one of the most successful public health programs, supporting health equity by screening almost every US baby after birth and then bringing timely treatments when relevant even before the baby develops symptoms of a disorder.” In this way, newborn screening has “saved lives and decreased disease burdens.”
There are at present 38 core conditions that the Department of Health and Human Services (HHS) regards as the most critical to screen for and 26 secondary conditions associated with these core disorders. This is called the Recommended Uniform Screening Panel (RUSP). Guidance regarding the most appropriate application of newborn screening tests, technologies and standards are provided by the Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC).
Each state “independently determines which screening tests are performed and what follow-up is provided.”4 Information about which tests are provided by which states can be found on the “Report Card” of the National Organization for Rare Diseases (NORD).
Challenges in Expanding the Current Newborn Screening
One of the major drawbacks in the current system is that “we don’t screen for enough diseases,” according to Zhanzhi Hu, PhD, of the Department of Systems Biology and the Department of Biomedical Information, Columbia University, New York City. “There are over 10,000 rare genetic diseases, but we’re currently screening for fewer than 100,” he told Neurology Reviews. Although in the United States, there are about 700-800 drugs approved for genetic diseases, “we can’t identify patients with these diseases early enough for the ideal window when treatments are most effective.”
Moreover, it’s a “lengthy process” to add new diseases to RUSP. “New conditions are added at the pace of less than one per year, on average — even for the hundreds of diseases for which there are treatments,” he said. “If we keep going at the current pace, we won’t be able to screen for those diseases for another few hundred years.”
Speeding up the pace of including new diseases in newborn screening is challenging because “we have more diseases than we have development dollars for,” Dr. Hu said. “Big pharmaceutical companies are reluctant to invest in rare diseases because the population is so small and it’s hard and expensive to develop such drugs. So if we can identify patients first, there will be more interest in developing treatments down the road.”
On the other hand, for trials to take place, these babies have to be identified in a timely manner — which requires testing. “Right now, we have a deadlock,” Dr. Hu said. “To nominate a disease, you need an approved treatment. But to get a treatment developed, you need to identify patients suitable for a clinical trial. If you have to wait for the symptoms to show up, the damage has already manifested and is irreversible. Our chance is to recognize the disease before symptom onset and then start treatment. I would call this a ‘chicken-and-egg’ problem.”
Dr. Hu is passionate about expanding newborn screening, and he has a very personal reason. Two of his children have a rare genetic disease. “My younger son, now 13 years old, was diagnosed at a much earlier age than my older son, although he had very few symptoms at the time, because his older brother was known to have the disease. As a result of this, his outcome was much better.” By contrast, Dr. Hu’s oldest son — now age 16 — wasn’t diagnosed until he became symptomatic.
His quest led him to join forces with Dr. Chung in conducting the Genomic Uniform-screening Against Rare Disease in All Newborns (Guardian) study, which screens newborns for more than 450 genetic conditions not currently screened as part of the standard newborn screening. To date, the study — which focuses on babies born in New York City — has screened about 11,000 infants.
“To accumulate enough evidence requires screening at least 100,000 babies because one requirement for nominating a disease for national inclusion in RUSP is an ‘N of 1’ study — meaning, to identify at least one positive patient using the proposed screening method in a prospective study,” Dr. Hu explained. “Most are rare diseases with an incidence rate of around one in 100,000. So getting to that magic number of 100,000 participants should enable us to hit that ‘N of 1’ for most diseases.”
The most challenging part, according to Dr. Hu, is the requirement of a prospective study, which means that you have to conduct a large-scale study enrolling tens of thousands of families and babies. If done for individual diseases (as has been the case in the past), “this is a huge cost and very inefficient.”
In reality, he added, the true incidence of these diseases is unclear. “Incidence rates are based on historical data rather than prospective studies. We’ve already seen some diseases show up more frequently than previously recorded, while others have shown up less frequently.”
For example, in the 11,000 babies screened to date, at least three girls with Rett syndrome have been identified, which is “quite a bit higher” than what has previously been identified in the literature (ie, one in 10,000-12,000 births). “This is a highly unmet need for these families because if you can initiate early treatment — at age 1, or even younger — the outcome will be better.”
He noted that there is at least one clinical trial underway for treating Rett syndrome, which has yielded “promising” data.5 “We’re hoping that by screening for diseases like Rett and identifying patients early, this will go hand-in-hand with clinical drug development. It can speed both the approval of the treatment and the addition to the newborn screening list,” Dr. Hu stated.
Screening and Drug Development Working in Tandem
Sequencing technologies have advanced and become more sophisticated as well as less costly, so interest in expanding newborn screening through newborn genome sequencing has increased. In fact, many states currently have incorporated genetic testing into newborn screening for conditions without biochemical markers. Additionally, newborn genomic sequencing is also used for further testing in infants with abnormal biochemical screening results.6
Genomic sequencing “identifies nucleotide changes that are the underlying etiology of monogenic disorders.”6 Its use could potentially enable identification of over 500 genetic disorders for which an newborn screening assay is not currently available, said Dr. Hu.
“Molecular DNA analysis has been integrated into newborn testing either as a first- or second-tier test for several conditions, including cystic fibrosis, severe combined immunodeficiency, and spinal muscular atrophy (SMA),” Dr. Hu said.
Dr. Hu pointed to SMA to illustrate the power and potential of newborn screening working hand-in-hand with the development of new treatments. SMA is a neurodegenerative disorder caused by mutations in SMN1, which encodes survival motor neuron protein (SMN).7 Deficiencies in SMN results in loss of motor neurons with muscle weakness and, often, early death.7A pilot study, on which Dr. Chung was the senior author, used both biochemical and genetic testing of close to 4000 newborns and found an SMA carrier frequency of 1.5%. One newborn was identified who had a homozygous SMN1 gene deletion and two copies of SMN2, strongly suggesting the presence of a severe type 1 SMA phenotype.8
At age 15 days, the baby was treated with nusinersen, an injection administered into the fluid surrounding the spinal cord, and the first FDA-approved genetic treatment for SMA. At the time of study publication, the baby was 12 months old, “meeting all developmental milestones and free of any respiratory issues,” the authors report.
“Screening for SMA — which was added to the RUSP in 2018 — has dramatically transformed what used to be the most common genetic cause of death in children under the age of 2,” Dr. Chung said. “Now, a once-and-done IV infusion of genetic therapy right after screening has transformed everything, taking what used to be a lethal condition and allowing children to grow up healthy.”
Advocating for Inclusion of Diseases With No Current Treatment
At present, any condition included in the RUSP is required to have a treatment, which can be dietary, surgical/procedural, or an FDA-approved drug-based agent. Unfortunately, a wide range of neurodevelopmental diseases still have no known treatments. But lack of availability of treatment shouldn’t invalidate a disease from being included in the RUSP, because even if there is no specific treatment for the condition itself, early intervention can still be initiated to prevent some of the manifestations of the condition, said Dr. Hu.
“For example, most patients with these diseases will sooner or later undergo seizures,” Dr. Hu remarked. “We know that repeated seizures can cause brain damage. If we can diagnose the disease before the seizures start to take place, we can put preventive seizure control interventions in place, even if there is no direct ‘treatment’ for the condition itself.”
Early identification can lead to early intervention, which can have other benefits, Dr. Hu noted. “If we train the brain at a young age, when the brain is most receptive, even though a disease may be progressive and will worsen, those abilities acquired earlier will last longer and remain in place longer. When these skills are acquired later, they’re forgotten sooner. This isn’t a ‘cure,’ but it will help with functional improvement.”
Moreover, parents are “interested in knowing that their child has a condition, even if no treatment is currently available for that disorder, according to our research,” Dr. Chung said. “We found that the parents we interviewed endorsed the nonmedical utility of having access to information, even in the absence of a ‘cure,’ so they could prepare for medical issues that might arise down the road and make informed choices.”9
Nina Gold, MD, director of Prenatal Medical Genetics and associate director for Research for Massachusetts General Brigham Personalized Medicine, Boston, obtained similar findings in her own research, which is currently under review for publication. “We conducted focus groups and one-on-one interviews with parents from diverse racial and socioeconomic backgrounds. At least one parent said they didn’t want to compare their child to other children if their child might have a different developmental trajectory. They stressed that the information would be helpful, even if there was no immediate clinical utility.”
Additionally, there are an “increasing number of fetal therapies for rare disorders, so information about a genetic disease in an older child can be helpful for parents who may go on to have another pregnancy,” Dr. Gold noted.
Dr. Hu detailed several other reasons for including a wider range of disorders in the RUSP. Doing so helps families avoid a “stressful and expensive diagnostic odyssey and also provides equitable access to a diagnosis.” And if these patients are identified early, “we can connect the family with clinical trials already underway or connect them to an organization such as the Accelerating Medicines Partnership (AMP) Program Bespoke Gene Therapy Consortium (AMP BGTC). Bespoke “brings together partners from the public, private, and nonprofit sectors to foster development of gene therapies intended to treat rare genetic diseases, which affect populations too small for viable commercial development.”
Next Steps Following Screening
Rebecca Sponberg, NP, of the Children’s Hospital of Orange County, UC Irvine School of Medicine, California, is part of a broader multidisciplinary team that interfaces with parents whose newborns have screened positive for a genetic disorder. The team also includes a biochemical geneticist, a pediatric neurologist, a pediatric endocrinologist, a genetic counselor, and a social worker.
Different states and locations have different procedures for receiving test results, said Dr. Chung. In some, pediatricians are the ones who receive the results, and they are tasked with the responsibility of making sure the children can start getting appropriate care. In particular, these pediatricians are associated with centers of excellence that specialize in working with families around these conditions. Other facilities have multidisciplinary teams.
Ms. Sponberg gave an example of how the process unfolded with X-linked adrenoleukodystrophy, a rare genetic disorder that affects the white matter of the nervous system and the adrenal cortex.10 “This is the most common peroxisomal disorder, affecting one in 20,000 males,” she said. “There are several different forms of the disorder, but males are most at risk for having the cerebral form, which can lead to neurological regression and hasten death. But the regression does not appear until 4 to 12 years of age.”
A baby who screens positive on the initial newborn screening has repeat testing; and if it’s confirmed, the family meets the entire team to help them understand what the disorder is, what to expect, and how it’s monitored and managed. “Children have to be followed closely with a brain MRI every 6 months to detect brain abnormalities quickly,” Ms. Sponberg explained “And we do regular bloodwork to look for adrenocortical insufficiency.”
A child who shows concerning changes on the MRI or abnormal blood test findings is immediately seen by the relevant specialist. “So far, our center has had one patient who had MRI changes consistent with the cerebral form of the disease and the patient was immediately able to receive a bone marrow transplant,” she reported. “We don’t think this child’s condition would have been picked up so quickly or treatment initiated so rapidly if we hadn’t known about it through newborn screening.”
Educating and Involving Families
Part of the role of clinicians is to provide education regarding newborn screening to families, according to Ms. Sponberg. “In my role, I have to call parents to tell them their child screened positive for a genetic condition and that we need to proceed with confirmatory testing,” she said. “We let them know if there’s a high concern that this might be a true positive for the condition, and we offer them information so they know what to expect.”
Unfortunately, Ms. Sponberg said, in the absence of education, some families are skeptical. “When I call families directly, some think it’s a scam and it can be hard to earn their trust. We need to do a better job educating families, especially our pregnant individuals, that testing will occur and if anything is abnormal, they will receive a call.”
References
1. Levy HL. Robert Guthrie and the Trials and Tribulations of Newborn Screening. Int J Neonatal Screen. 2021 Jan 19;7(1):5. doi: 10.3390/ijns7010005.
2. Chace DH et al. Clinical Chemistry and Dried Blood Spots: Increasing Laboratory Utilization by Improved Understanding of Quantitative Challenges. Bioanalysis. 2014;6(21):2791-2794. doi: 10.4155/bio.14.237.
3. Gold NB et al. Perspectives of Rare Disease Experts on Newborn Genome Sequencing. JAMA Netw Open. 2023 May 1;6(5):e2312231. doi: 10.1001/jamanetworkopen.2023.12231.
4. Weismiller DG. Expanded Newborn Screening: Information and Resources for the Family Physician. Am Fam Physician. 2017 Jun 1;95(11):703-709. https://www.aafp.org/pubs/afp/issues/2017/0601/p703.html.
5. Neul JL et al. Trofinetide for the Treatment of Rett Syndrome: A Randomized Phase 3 Study. Nat Med. 2023 Jun;29(6):1468-1475. doi: 10.1038/s41591-023-02398-1.
6. Chen T et al. Genomic Sequencing as a First-Tier Screening Test and Outcomes of Newborn Screening. JAMA Netw Open. 2023 Sep 5;6(9):e2331162. doi: 10.1001/jamanetworkopen.2023.31162.
7. Mercuri E et al. Spinal Muscular Atrophy. Nat Rev Dis Primers. 2022 Aug 4;8(1):52. doi: 10.1038/s41572-022-00380-8.
8. Kraszewski JN et al. Pilot Study of Population-Based Newborn Screening for Spinal Muscular Atrophy in New York State. Genet Med. 2018 Jun;20(6):608-613. doi: 10.1038/gim.2017.152.
9. Timmins GT et al. Diverse Parental Perspectives of the Social and Educational Needs for Expanding Newborn Screening Through Genomic Sequencing. Public Health Genomics. 2022 Sep 15:1-8. doi: 10.1159/000526382.
10. Turk BR et al. X-linked Adrenoleukodystrophy: Pathology, Pathophysiology, Diagnostic Testing, Newborn Screening and Therapies. Int J Dev Neurosci. 2020 Feb;80(1):52-72. doi: 10.1002/jdn.10003.
Newborn screening programs are public health services aimed at ensuring that the close to 4 million infants born each year in the United States are screened for certain serious disorders at birth. These disorders, albeit rare, are detected in roughly 12,500 newborn babies every year.
Newborn screening isn’t new, although it has expanded and transformed over the decades. The first newborn screening test was developed in the 1960s to detect phenylketonuria (PKU).1 Since then, the number of conditions screened for has increased, with programs in every US state and territory. “Newborn screening is well established now, not experimental or newfangled,” Wendy Chung, MD, PhD, professor of pediatrics, Harvard Medical School, Boston, Massachusetts, told Neurology Reviews.
In newborn screening, blood drawn from the baby’s heel is applied to specialized filter paper, which is then subjected to several analytical methods, including tandem mass spectrometry and molecular analyses to detect biomarkers for the diseases.2 More recently, genomic sequencing is being piloted as part of consented research studies.3
Newborn screening includes not only biochemical and genetic testing, but also includes noninvasive screening for hearing loss or for critical congenital heart disease using pulse oximetry. And newborn screening goes beyond analysis of a single drop of blood. Rather, “it’s an entire system, with the goal of identifying babies with genetic disorders who otherwise have no obvious symptoms,” said Dr. Chung. Left undetected and untreated, these conditions can be associated with serious adverse outcomes and even death.
Dr. Chung described newborn screening as a “one of the most successful public health programs, supporting health equity by screening almost every US baby after birth and then bringing timely treatments when relevant even before the baby develops symptoms of a disorder.” In this way, newborn screening has “saved lives and decreased disease burdens.”
There are at present 38 core conditions that the Department of Health and Human Services (HHS) regards as the most critical to screen for and 26 secondary conditions associated with these core disorders. This is called the Recommended Uniform Screening Panel (RUSP). Guidance regarding the most appropriate application of newborn screening tests, technologies and standards are provided by the Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC).
Each state “independently determines which screening tests are performed and what follow-up is provided.”4 Information about which tests are provided by which states can be found on the “Report Card” of the National Organization for Rare Diseases (NORD).
Challenges in Expanding the Current Newborn Screening
One of the major drawbacks in the current system is that “we don’t screen for enough diseases,” according to Zhanzhi Hu, PhD, of the Department of Systems Biology and the Department of Biomedical Information, Columbia University, New York City. “There are over 10,000 rare genetic diseases, but we’re currently screening for fewer than 100,” he told Neurology Reviews. Although in the United States, there are about 700-800 drugs approved for genetic diseases, “we can’t identify patients with these diseases early enough for the ideal window when treatments are most effective.”
Moreover, it’s a “lengthy process” to add new diseases to RUSP. “New conditions are added at the pace of less than one per year, on average — even for the hundreds of diseases for which there are treatments,” he said. “If we keep going at the current pace, we won’t be able to screen for those diseases for another few hundred years.”
Speeding up the pace of including new diseases in newborn screening is challenging because “we have more diseases than we have development dollars for,” Dr. Hu said. “Big pharmaceutical companies are reluctant to invest in rare diseases because the population is so small and it’s hard and expensive to develop such drugs. So if we can identify patients first, there will be more interest in developing treatments down the road.”
On the other hand, for trials to take place, these babies have to be identified in a timely manner — which requires testing. “Right now, we have a deadlock,” Dr. Hu said. “To nominate a disease, you need an approved treatment. But to get a treatment developed, you need to identify patients suitable for a clinical trial. If you have to wait for the symptoms to show up, the damage has already manifested and is irreversible. Our chance is to recognize the disease before symptom onset and then start treatment. I would call this a ‘chicken-and-egg’ problem.”
Dr. Hu is passionate about expanding newborn screening, and he has a very personal reason. Two of his children have a rare genetic disease. “My younger son, now 13 years old, was diagnosed at a much earlier age than my older son, although he had very few symptoms at the time, because his older brother was known to have the disease. As a result of this, his outcome was much better.” By contrast, Dr. Hu’s oldest son — now age 16 — wasn’t diagnosed until he became symptomatic.
His quest led him to join forces with Dr. Chung in conducting the Genomic Uniform-screening Against Rare Disease in All Newborns (Guardian) study, which screens newborns for more than 450 genetic conditions not currently screened as part of the standard newborn screening. To date, the study — which focuses on babies born in New York City — has screened about 11,000 infants.
“To accumulate enough evidence requires screening at least 100,000 babies because one requirement for nominating a disease for national inclusion in RUSP is an ‘N of 1’ study — meaning, to identify at least one positive patient using the proposed screening method in a prospective study,” Dr. Hu explained. “Most are rare diseases with an incidence rate of around one in 100,000. So getting to that magic number of 100,000 participants should enable us to hit that ‘N of 1’ for most diseases.”
The most challenging part, according to Dr. Hu, is the requirement of a prospective study, which means that you have to conduct a large-scale study enrolling tens of thousands of families and babies. If done for individual diseases (as has been the case in the past), “this is a huge cost and very inefficient.”
In reality, he added, the true incidence of these diseases is unclear. “Incidence rates are based on historical data rather than prospective studies. We’ve already seen some diseases show up more frequently than previously recorded, while others have shown up less frequently.”
For example, in the 11,000 babies screened to date, at least three girls with Rett syndrome have been identified, which is “quite a bit higher” than what has previously been identified in the literature (ie, one in 10,000-12,000 births). “This is a highly unmet need for these families because if you can initiate early treatment — at age 1, or even younger — the outcome will be better.”
He noted that there is at least one clinical trial underway for treating Rett syndrome, which has yielded “promising” data.5 “We’re hoping that by screening for diseases like Rett and identifying patients early, this will go hand-in-hand with clinical drug development. It can speed both the approval of the treatment and the addition to the newborn screening list,” Dr. Hu stated.
Screening and Drug Development Working in Tandem
Sequencing technologies have advanced and become more sophisticated as well as less costly, so interest in expanding newborn screening through newborn genome sequencing has increased. In fact, many states currently have incorporated genetic testing into newborn screening for conditions without biochemical markers. Additionally, newborn genomic sequencing is also used for further testing in infants with abnormal biochemical screening results.6
Genomic sequencing “identifies nucleotide changes that are the underlying etiology of monogenic disorders.”6 Its use could potentially enable identification of over 500 genetic disorders for which an newborn screening assay is not currently available, said Dr. Hu.
“Molecular DNA analysis has been integrated into newborn testing either as a first- or second-tier test for several conditions, including cystic fibrosis, severe combined immunodeficiency, and spinal muscular atrophy (SMA),” Dr. Hu said.
Dr. Hu pointed to SMA to illustrate the power and potential of newborn screening working hand-in-hand with the development of new treatments. SMA is a neurodegenerative disorder caused by mutations in SMN1, which encodes survival motor neuron protein (SMN).7 Deficiencies in SMN results in loss of motor neurons with muscle weakness and, often, early death.7A pilot study, on which Dr. Chung was the senior author, used both biochemical and genetic testing of close to 4000 newborns and found an SMA carrier frequency of 1.5%. One newborn was identified who had a homozygous SMN1 gene deletion and two copies of SMN2, strongly suggesting the presence of a severe type 1 SMA phenotype.8
At age 15 days, the baby was treated with nusinersen, an injection administered into the fluid surrounding the spinal cord, and the first FDA-approved genetic treatment for SMA. At the time of study publication, the baby was 12 months old, “meeting all developmental milestones and free of any respiratory issues,” the authors report.
“Screening for SMA — which was added to the RUSP in 2018 — has dramatically transformed what used to be the most common genetic cause of death in children under the age of 2,” Dr. Chung said. “Now, a once-and-done IV infusion of genetic therapy right after screening has transformed everything, taking what used to be a lethal condition and allowing children to grow up healthy.”
Advocating for Inclusion of Diseases With No Current Treatment
At present, any condition included in the RUSP is required to have a treatment, which can be dietary, surgical/procedural, or an FDA-approved drug-based agent. Unfortunately, a wide range of neurodevelopmental diseases still have no known treatments. But lack of availability of treatment shouldn’t invalidate a disease from being included in the RUSP, because even if there is no specific treatment for the condition itself, early intervention can still be initiated to prevent some of the manifestations of the condition, said Dr. Hu.
“For example, most patients with these diseases will sooner or later undergo seizures,” Dr. Hu remarked. “We know that repeated seizures can cause brain damage. If we can diagnose the disease before the seizures start to take place, we can put preventive seizure control interventions in place, even if there is no direct ‘treatment’ for the condition itself.”
Early identification can lead to early intervention, which can have other benefits, Dr. Hu noted. “If we train the brain at a young age, when the brain is most receptive, even though a disease may be progressive and will worsen, those abilities acquired earlier will last longer and remain in place longer. When these skills are acquired later, they’re forgotten sooner. This isn’t a ‘cure,’ but it will help with functional improvement.”
Moreover, parents are “interested in knowing that their child has a condition, even if no treatment is currently available for that disorder, according to our research,” Dr. Chung said. “We found that the parents we interviewed endorsed the nonmedical utility of having access to information, even in the absence of a ‘cure,’ so they could prepare for medical issues that might arise down the road and make informed choices.”9
Nina Gold, MD, director of Prenatal Medical Genetics and associate director for Research for Massachusetts General Brigham Personalized Medicine, Boston, obtained similar findings in her own research, which is currently under review for publication. “We conducted focus groups and one-on-one interviews with parents from diverse racial and socioeconomic backgrounds. At least one parent said they didn’t want to compare their child to other children if their child might have a different developmental trajectory. They stressed that the information would be helpful, even if there was no immediate clinical utility.”
Additionally, there are an “increasing number of fetal therapies for rare disorders, so information about a genetic disease in an older child can be helpful for parents who may go on to have another pregnancy,” Dr. Gold noted.
Dr. Hu detailed several other reasons for including a wider range of disorders in the RUSP. Doing so helps families avoid a “stressful and expensive diagnostic odyssey and also provides equitable access to a diagnosis.” And if these patients are identified early, “we can connect the family with clinical trials already underway or connect them to an organization such as the Accelerating Medicines Partnership (AMP) Program Bespoke Gene Therapy Consortium (AMP BGTC). Bespoke “brings together partners from the public, private, and nonprofit sectors to foster development of gene therapies intended to treat rare genetic diseases, which affect populations too small for viable commercial development.”
Next Steps Following Screening
Rebecca Sponberg, NP, of the Children’s Hospital of Orange County, UC Irvine School of Medicine, California, is part of a broader multidisciplinary team that interfaces with parents whose newborns have screened positive for a genetic disorder. The team also includes a biochemical geneticist, a pediatric neurologist, a pediatric endocrinologist, a genetic counselor, and a social worker.
Different states and locations have different procedures for receiving test results, said Dr. Chung. In some, pediatricians are the ones who receive the results, and they are tasked with the responsibility of making sure the children can start getting appropriate care. In particular, these pediatricians are associated with centers of excellence that specialize in working with families around these conditions. Other facilities have multidisciplinary teams.
Ms. Sponberg gave an example of how the process unfolded with X-linked adrenoleukodystrophy, a rare genetic disorder that affects the white matter of the nervous system and the adrenal cortex.10 “This is the most common peroxisomal disorder, affecting one in 20,000 males,” she said. “There are several different forms of the disorder, but males are most at risk for having the cerebral form, which can lead to neurological regression and hasten death. But the regression does not appear until 4 to 12 years of age.”
A baby who screens positive on the initial newborn screening has repeat testing; and if it’s confirmed, the family meets the entire team to help them understand what the disorder is, what to expect, and how it’s monitored and managed. “Children have to be followed closely with a brain MRI every 6 months to detect brain abnormalities quickly,” Ms. Sponberg explained “And we do regular bloodwork to look for adrenocortical insufficiency.”
A child who shows concerning changes on the MRI or abnormal blood test findings is immediately seen by the relevant specialist. “So far, our center has had one patient who had MRI changes consistent with the cerebral form of the disease and the patient was immediately able to receive a bone marrow transplant,” she reported. “We don’t think this child’s condition would have been picked up so quickly or treatment initiated so rapidly if we hadn’t known about it through newborn screening.”
Educating and Involving Families
Part of the role of clinicians is to provide education regarding newborn screening to families, according to Ms. Sponberg. “In my role, I have to call parents to tell them their child screened positive for a genetic condition and that we need to proceed with confirmatory testing,” she said. “We let them know if there’s a high concern that this might be a true positive for the condition, and we offer them information so they know what to expect.”
Unfortunately, Ms. Sponberg said, in the absence of education, some families are skeptical. “When I call families directly, some think it’s a scam and it can be hard to earn their trust. We need to do a better job educating families, especially our pregnant individuals, that testing will occur and if anything is abnormal, they will receive a call.”
References
1. Levy HL. Robert Guthrie and the Trials and Tribulations of Newborn Screening. Int J Neonatal Screen. 2021 Jan 19;7(1):5. doi: 10.3390/ijns7010005.
2. Chace DH et al. Clinical Chemistry and Dried Blood Spots: Increasing Laboratory Utilization by Improved Understanding of Quantitative Challenges. Bioanalysis. 2014;6(21):2791-2794. doi: 10.4155/bio.14.237.
3. Gold NB et al. Perspectives of Rare Disease Experts on Newborn Genome Sequencing. JAMA Netw Open. 2023 May 1;6(5):e2312231. doi: 10.1001/jamanetworkopen.2023.12231.
4. Weismiller DG. Expanded Newborn Screening: Information and Resources for the Family Physician. Am Fam Physician. 2017 Jun 1;95(11):703-709. https://www.aafp.org/pubs/afp/issues/2017/0601/p703.html.
5. Neul JL et al. Trofinetide for the Treatment of Rett Syndrome: A Randomized Phase 3 Study. Nat Med. 2023 Jun;29(6):1468-1475. doi: 10.1038/s41591-023-02398-1.
6. Chen T et al. Genomic Sequencing as a First-Tier Screening Test and Outcomes of Newborn Screening. JAMA Netw Open. 2023 Sep 5;6(9):e2331162. doi: 10.1001/jamanetworkopen.2023.31162.
7. Mercuri E et al. Spinal Muscular Atrophy. Nat Rev Dis Primers. 2022 Aug 4;8(1):52. doi: 10.1038/s41572-022-00380-8.
8. Kraszewski JN et al. Pilot Study of Population-Based Newborn Screening for Spinal Muscular Atrophy in New York State. Genet Med. 2018 Jun;20(6):608-613. doi: 10.1038/gim.2017.152.
9. Timmins GT et al. Diverse Parental Perspectives of the Social and Educational Needs for Expanding Newborn Screening Through Genomic Sequencing. Public Health Genomics. 2022 Sep 15:1-8. doi: 10.1159/000526382.
10. Turk BR et al. X-linked Adrenoleukodystrophy: Pathology, Pathophysiology, Diagnostic Testing, Newborn Screening and Therapies. Int J Dev Neurosci. 2020 Feb;80(1):52-72. doi: 10.1002/jdn.10003.
Newborn screening programs are public health services aimed at ensuring that the close to 4 million infants born each year in the United States are screened for certain serious disorders at birth. These disorders, albeit rare, are detected in roughly 12,500 newborn babies every year.
Newborn screening isn’t new, although it has expanded and transformed over the decades. The first newborn screening test was developed in the 1960s to detect phenylketonuria (PKU).1 Since then, the number of conditions screened for has increased, with programs in every US state and territory. “Newborn screening is well established now, not experimental or newfangled,” Wendy Chung, MD, PhD, professor of pediatrics, Harvard Medical School, Boston, Massachusetts, told Neurology Reviews.
In newborn screening, blood drawn from the baby’s heel is applied to specialized filter paper, which is then subjected to several analytical methods, including tandem mass spectrometry and molecular analyses to detect biomarkers for the diseases.2 More recently, genomic sequencing is being piloted as part of consented research studies.3
Newborn screening includes not only biochemical and genetic testing, but also includes noninvasive screening for hearing loss or for critical congenital heart disease using pulse oximetry. And newborn screening goes beyond analysis of a single drop of blood. Rather, “it’s an entire system, with the goal of identifying babies with genetic disorders who otherwise have no obvious symptoms,” said Dr. Chung. Left undetected and untreated, these conditions can be associated with serious adverse outcomes and even death.
Dr. Chung described newborn screening as a “one of the most successful public health programs, supporting health equity by screening almost every US baby after birth and then bringing timely treatments when relevant even before the baby develops symptoms of a disorder.” In this way, newborn screening has “saved lives and decreased disease burdens.”
There are at present 38 core conditions that the Department of Health and Human Services (HHS) regards as the most critical to screen for and 26 secondary conditions associated with these core disorders. This is called the Recommended Uniform Screening Panel (RUSP). Guidance regarding the most appropriate application of newborn screening tests, technologies and standards are provided by the Advisory Committee on Heritable Disorders in Newborns and Children (ACHDNC).
Each state “independently determines which screening tests are performed and what follow-up is provided.”4 Information about which tests are provided by which states can be found on the “Report Card” of the National Organization for Rare Diseases (NORD).
Challenges in Expanding the Current Newborn Screening
One of the major drawbacks in the current system is that “we don’t screen for enough diseases,” according to Zhanzhi Hu, PhD, of the Department of Systems Biology and the Department of Biomedical Information, Columbia University, New York City. “There are over 10,000 rare genetic diseases, but we’re currently screening for fewer than 100,” he told Neurology Reviews. Although in the United States, there are about 700-800 drugs approved for genetic diseases, “we can’t identify patients with these diseases early enough for the ideal window when treatments are most effective.”
Moreover, it’s a “lengthy process” to add new diseases to RUSP. “New conditions are added at the pace of less than one per year, on average — even for the hundreds of diseases for which there are treatments,” he said. “If we keep going at the current pace, we won’t be able to screen for those diseases for another few hundred years.”
Speeding up the pace of including new diseases in newborn screening is challenging because “we have more diseases than we have development dollars for,” Dr. Hu said. “Big pharmaceutical companies are reluctant to invest in rare diseases because the population is so small and it’s hard and expensive to develop such drugs. So if we can identify patients first, there will be more interest in developing treatments down the road.”
On the other hand, for trials to take place, these babies have to be identified in a timely manner — which requires testing. “Right now, we have a deadlock,” Dr. Hu said. “To nominate a disease, you need an approved treatment. But to get a treatment developed, you need to identify patients suitable for a clinical trial. If you have to wait for the symptoms to show up, the damage has already manifested and is irreversible. Our chance is to recognize the disease before symptom onset and then start treatment. I would call this a ‘chicken-and-egg’ problem.”
Dr. Hu is passionate about expanding newborn screening, and he has a very personal reason. Two of his children have a rare genetic disease. “My younger son, now 13 years old, was diagnosed at a much earlier age than my older son, although he had very few symptoms at the time, because his older brother was known to have the disease. As a result of this, his outcome was much better.” By contrast, Dr. Hu’s oldest son — now age 16 — wasn’t diagnosed until he became symptomatic.
His quest led him to join forces with Dr. Chung in conducting the Genomic Uniform-screening Against Rare Disease in All Newborns (Guardian) study, which screens newborns for more than 450 genetic conditions not currently screened as part of the standard newborn screening. To date, the study — which focuses on babies born in New York City — has screened about 11,000 infants.
“To accumulate enough evidence requires screening at least 100,000 babies because one requirement for nominating a disease for national inclusion in RUSP is an ‘N of 1’ study — meaning, to identify at least one positive patient using the proposed screening method in a prospective study,” Dr. Hu explained. “Most are rare diseases with an incidence rate of around one in 100,000. So getting to that magic number of 100,000 participants should enable us to hit that ‘N of 1’ for most diseases.”
The most challenging part, according to Dr. Hu, is the requirement of a prospective study, which means that you have to conduct a large-scale study enrolling tens of thousands of families and babies. If done for individual diseases (as has been the case in the past), “this is a huge cost and very inefficient.”
In reality, he added, the true incidence of these diseases is unclear. “Incidence rates are based on historical data rather than prospective studies. We’ve already seen some diseases show up more frequently than previously recorded, while others have shown up less frequently.”
For example, in the 11,000 babies screened to date, at least three girls with Rett syndrome have been identified, which is “quite a bit higher” than what has previously been identified in the literature (ie, one in 10,000-12,000 births). “This is a highly unmet need for these families because if you can initiate early treatment — at age 1, or even younger — the outcome will be better.”
He noted that there is at least one clinical trial underway for treating Rett syndrome, which has yielded “promising” data.5 “We’re hoping that by screening for diseases like Rett and identifying patients early, this will go hand-in-hand with clinical drug development. It can speed both the approval of the treatment and the addition to the newborn screening list,” Dr. Hu stated.
Screening and Drug Development Working in Tandem
Sequencing technologies have advanced and become more sophisticated as well as less costly, so interest in expanding newborn screening through newborn genome sequencing has increased. In fact, many states currently have incorporated genetic testing into newborn screening for conditions without biochemical markers. Additionally, newborn genomic sequencing is also used for further testing in infants with abnormal biochemical screening results.6
Genomic sequencing “identifies nucleotide changes that are the underlying etiology of monogenic disorders.”6 Its use could potentially enable identification of over 500 genetic disorders for which an newborn screening assay is not currently available, said Dr. Hu.
“Molecular DNA analysis has been integrated into newborn testing either as a first- or second-tier test for several conditions, including cystic fibrosis, severe combined immunodeficiency, and spinal muscular atrophy (SMA),” Dr. Hu said.
Dr. Hu pointed to SMA to illustrate the power and potential of newborn screening working hand-in-hand with the development of new treatments. SMA is a neurodegenerative disorder caused by mutations in SMN1, which encodes survival motor neuron protein (SMN).7 Deficiencies in SMN results in loss of motor neurons with muscle weakness and, often, early death.7A pilot study, on which Dr. Chung was the senior author, used both biochemical and genetic testing of close to 4000 newborns and found an SMA carrier frequency of 1.5%. One newborn was identified who had a homozygous SMN1 gene deletion and two copies of SMN2, strongly suggesting the presence of a severe type 1 SMA phenotype.8
At age 15 days, the baby was treated with nusinersen, an injection administered into the fluid surrounding the spinal cord, and the first FDA-approved genetic treatment for SMA. At the time of study publication, the baby was 12 months old, “meeting all developmental milestones and free of any respiratory issues,” the authors report.
“Screening for SMA — which was added to the RUSP in 2018 — has dramatically transformed what used to be the most common genetic cause of death in children under the age of 2,” Dr. Chung said. “Now, a once-and-done IV infusion of genetic therapy right after screening has transformed everything, taking what used to be a lethal condition and allowing children to grow up healthy.”
Advocating for Inclusion of Diseases With No Current Treatment
At present, any condition included in the RUSP is required to have a treatment, which can be dietary, surgical/procedural, or an FDA-approved drug-based agent. Unfortunately, a wide range of neurodevelopmental diseases still have no known treatments. But lack of availability of treatment shouldn’t invalidate a disease from being included in the RUSP, because even if there is no specific treatment for the condition itself, early intervention can still be initiated to prevent some of the manifestations of the condition, said Dr. Hu.
“For example, most patients with these diseases will sooner or later undergo seizures,” Dr. Hu remarked. “We know that repeated seizures can cause brain damage. If we can diagnose the disease before the seizures start to take place, we can put preventive seizure control interventions in place, even if there is no direct ‘treatment’ for the condition itself.”
Early identification can lead to early intervention, which can have other benefits, Dr. Hu noted. “If we train the brain at a young age, when the brain is most receptive, even though a disease may be progressive and will worsen, those abilities acquired earlier will last longer and remain in place longer. When these skills are acquired later, they’re forgotten sooner. This isn’t a ‘cure,’ but it will help with functional improvement.”
Moreover, parents are “interested in knowing that their child has a condition, even if no treatment is currently available for that disorder, according to our research,” Dr. Chung said. “We found that the parents we interviewed endorsed the nonmedical utility of having access to information, even in the absence of a ‘cure,’ so they could prepare for medical issues that might arise down the road and make informed choices.”9
Nina Gold, MD, director of Prenatal Medical Genetics and associate director for Research for Massachusetts General Brigham Personalized Medicine, Boston, obtained similar findings in her own research, which is currently under review for publication. “We conducted focus groups and one-on-one interviews with parents from diverse racial and socioeconomic backgrounds. At least one parent said they didn’t want to compare their child to other children if their child might have a different developmental trajectory. They stressed that the information would be helpful, even if there was no immediate clinical utility.”
Additionally, there are an “increasing number of fetal therapies for rare disorders, so information about a genetic disease in an older child can be helpful for parents who may go on to have another pregnancy,” Dr. Gold noted.
Dr. Hu detailed several other reasons for including a wider range of disorders in the RUSP. Doing so helps families avoid a “stressful and expensive diagnostic odyssey and also provides equitable access to a diagnosis.” And if these patients are identified early, “we can connect the family with clinical trials already underway or connect them to an organization such as the Accelerating Medicines Partnership (AMP) Program Bespoke Gene Therapy Consortium (AMP BGTC). Bespoke “brings together partners from the public, private, and nonprofit sectors to foster development of gene therapies intended to treat rare genetic diseases, which affect populations too small for viable commercial development.”
Next Steps Following Screening
Rebecca Sponberg, NP, of the Children’s Hospital of Orange County, UC Irvine School of Medicine, California, is part of a broader multidisciplinary team that interfaces with parents whose newborns have screened positive for a genetic disorder. The team also includes a biochemical geneticist, a pediatric neurologist, a pediatric endocrinologist, a genetic counselor, and a social worker.
Different states and locations have different procedures for receiving test results, said Dr. Chung. In some, pediatricians are the ones who receive the results, and they are tasked with the responsibility of making sure the children can start getting appropriate care. In particular, these pediatricians are associated with centers of excellence that specialize in working with families around these conditions. Other facilities have multidisciplinary teams.
Ms. Sponberg gave an example of how the process unfolded with X-linked adrenoleukodystrophy, a rare genetic disorder that affects the white matter of the nervous system and the adrenal cortex.10 “This is the most common peroxisomal disorder, affecting one in 20,000 males,” she said. “There are several different forms of the disorder, but males are most at risk for having the cerebral form, which can lead to neurological regression and hasten death. But the regression does not appear until 4 to 12 years of age.”
A baby who screens positive on the initial newborn screening has repeat testing; and if it’s confirmed, the family meets the entire team to help them understand what the disorder is, what to expect, and how it’s monitored and managed. “Children have to be followed closely with a brain MRI every 6 months to detect brain abnormalities quickly,” Ms. Sponberg explained “And we do regular bloodwork to look for adrenocortical insufficiency.”
A child who shows concerning changes on the MRI or abnormal blood test findings is immediately seen by the relevant specialist. “So far, our center has had one patient who had MRI changes consistent with the cerebral form of the disease and the patient was immediately able to receive a bone marrow transplant,” she reported. “We don’t think this child’s condition would have been picked up so quickly or treatment initiated so rapidly if we hadn’t known about it through newborn screening.”
Educating and Involving Families
Part of the role of clinicians is to provide education regarding newborn screening to families, according to Ms. Sponberg. “In my role, I have to call parents to tell them their child screened positive for a genetic condition and that we need to proceed with confirmatory testing,” she said. “We let them know if there’s a high concern that this might be a true positive for the condition, and we offer them information so they know what to expect.”
Unfortunately, Ms. Sponberg said, in the absence of education, some families are skeptical. “When I call families directly, some think it’s a scam and it can be hard to earn their trust. We need to do a better job educating families, especially our pregnant individuals, that testing will occur and if anything is abnormal, they will receive a call.”
References
1. Levy HL. Robert Guthrie and the Trials and Tribulations of Newborn Screening. Int J Neonatal Screen. 2021 Jan 19;7(1):5. doi: 10.3390/ijns7010005.
2. Chace DH et al. Clinical Chemistry and Dried Blood Spots: Increasing Laboratory Utilization by Improved Understanding of Quantitative Challenges. Bioanalysis. 2014;6(21):2791-2794. doi: 10.4155/bio.14.237.
3. Gold NB et al. Perspectives of Rare Disease Experts on Newborn Genome Sequencing. JAMA Netw Open. 2023 May 1;6(5):e2312231. doi: 10.1001/jamanetworkopen.2023.12231.
4. Weismiller DG. Expanded Newborn Screening: Information and Resources for the Family Physician. Am Fam Physician. 2017 Jun 1;95(11):703-709. https://www.aafp.org/pubs/afp/issues/2017/0601/p703.html.
5. Neul JL et al. Trofinetide for the Treatment of Rett Syndrome: A Randomized Phase 3 Study. Nat Med. 2023 Jun;29(6):1468-1475. doi: 10.1038/s41591-023-02398-1.
6. Chen T et al. Genomic Sequencing as a First-Tier Screening Test and Outcomes of Newborn Screening. JAMA Netw Open. 2023 Sep 5;6(9):e2331162. doi: 10.1001/jamanetworkopen.2023.31162.
7. Mercuri E et al. Spinal Muscular Atrophy. Nat Rev Dis Primers. 2022 Aug 4;8(1):52. doi: 10.1038/s41572-022-00380-8.
8. Kraszewski JN et al. Pilot Study of Population-Based Newborn Screening for Spinal Muscular Atrophy in New York State. Genet Med. 2018 Jun;20(6):608-613. doi: 10.1038/gim.2017.152.
9. Timmins GT et al. Diverse Parental Perspectives of the Social and Educational Needs for Expanding Newborn Screening Through Genomic Sequencing. Public Health Genomics. 2022 Sep 15:1-8. doi: 10.1159/000526382.
10. Turk BR et al. X-linked Adrenoleukodystrophy: Pathology, Pathophysiology, Diagnostic Testing, Newborn Screening and Therapies. Int J Dev Neurosci. 2020 Feb;80(1):52-72. doi: 10.1002/jdn.10003.
Teen Cannabis Use Tied to Dramatic Increased Risk for Psychosis
, new research showed.
Investigators at the University of Toronto, The Centre for Addiction and Mental Health (CAMH), and the Institute for Clinical Evaluative Sciences (ICES), in Canada, linked recent population-based survey data from more than 11,000 youngsters to health service use records, including hospitalizations, emergency department (ED) visits, and outpatient visits.
“We found a very strong association between cannabis use and risk of psychotic disorder in adolescence [although] surprisingly, we didn’t find evidence of association in young adulthood,” lead author André J. McDonald, PhD, currently a postdoctoral fellow at the Peter Boris Centre for Addictions Research and the Michael G. DeGroote Centre for Medicinal Cannabis Research, McMaster University, Hamilton, Ontario, Canada, said in a news release.
“These findings are consistent with the neurodevelopmental theory that teens are especially vulnerable to the effects of cannabis,” said Dr. McDonald, who conducted the research.
The study was published online in Psychological Medicine.
Increased Potency
“Epidemiologic research suggests that cannabis use may be a significant risk factor for psychotic disorders,” the authors wrote. However, methodological limitations of previous studies make it difficult to estimate the strength of association, with the current evidence base relying largely on cannabis use during the twentieth century, when the drug was “significantly less potent.” It’s plausible that the strength of association has increased due to increased cannabis potency.
The researchers believe youth cannabis use and psychotic disorders is “a critical public health issue,” especially as more jurisdictions liberalize cannabis use and the perception of harm declines among youth.
To estimate the association between cannabis use during youth and the risk for a psychotic disorder diagnosis, using recent population-based data, they used data from the 2009-2012 cycles of the Canadian Community Health Survey (CCHS) linked to administrative health data at ICES to study noninstitutionalized Ontario residents, aged 12-24 years, who had completed the CCHS during that period.
They excluded respondents who used health services for psychotic disorders during the 6 years prior to their CCHS interview date.
Respondents (n = 11,363; 51% men; mean age [SD], 18.3 [15.2-21.3] years) were followed for 6-9 years, with days to first hospitalization, ED visit, or outpatient visit related to a psychotic disorder as the primary outcome.
The researchers estimated age-specific hazard ratios during adolescence (12-19 years) and young adulthood (20-33 years) and conducted sensitivity analyses to explore alternative model conditions, including restricting the outcome to hospitalizations and ED visits, to increase specificity.
Compared with no cannabis use, cannabis use was significantly associated with an 11-fold increased risk for psychotic disorders during adolescence, although not during young adulthood (adjusted hazard ratio [aHR], 11.2; 95% CI, 4.6-27.3 and aHR, 1.3; 95% CI, 0.6-2.6, respectively).
Perception of Harm Declining
When the researchers restricted the outcome to hospitalizations and ED visits only, the strength of association “increased markedly” during adolescence, with a 26-fold higher association in cannabis users than in nonusers (aHR, 26.7; 95% CI, 7.7-92.8). However, there was no meaningful change during young adulthood (aHR, 1.8; 95% CI, 0.6-5.4).
“Many have hypothesized that adolescence is a more sensitive risk period than adulthood for the effect of cannabis use on psychotic disorder development, yet prior to this study, little epidemiologic evidence existed to support this view,” the authors wrote.
The data also suggest that cannabis use is “more strongly associated with more severe psychotic outcomes, as the strength of association during adolescence increased markedly when we restricted the outcome to hospitalizations and ED visits (the most severe types of health service use),” the investigators noted.
The authors noted several limitations. For instance, it’s unclear to what extent unmeasured confounders including genetic predisposition, family history of psychotic disorders, and trauma might have biased the results. In addition, they could not assess the potential confounding impact of genetic predisposition to psychotic disorders. The possibility of reverse causality also cannot be ruled out. It’s possible, they noted, that individuals with “psychotic dispositions” may self-medicate or show greater disposition to cannabis use.
Moreover, the dataset neither captured important factors regarding the cannabis itself, including delta-9-tetrahydrocannabinol potency, mode of use, product type, or cannabis dependence, nor captured institutionalized and homeless youth.
Nevertheless, they pointed to the findings as supporting a “precautionary principle” — as more jurisdictions move to liberalize cannabis use and perception of harm declines among youth, the findings suggest that evidence-based cannabis prevention strategies for adolescents are warranted.
This study was supported by CAMH, the University of Toronto, and ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care. The authors declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
, new research showed.
Investigators at the University of Toronto, The Centre for Addiction and Mental Health (CAMH), and the Institute for Clinical Evaluative Sciences (ICES), in Canada, linked recent population-based survey data from more than 11,000 youngsters to health service use records, including hospitalizations, emergency department (ED) visits, and outpatient visits.
“We found a very strong association between cannabis use and risk of psychotic disorder in adolescence [although] surprisingly, we didn’t find evidence of association in young adulthood,” lead author André J. McDonald, PhD, currently a postdoctoral fellow at the Peter Boris Centre for Addictions Research and the Michael G. DeGroote Centre for Medicinal Cannabis Research, McMaster University, Hamilton, Ontario, Canada, said in a news release.
“These findings are consistent with the neurodevelopmental theory that teens are especially vulnerable to the effects of cannabis,” said Dr. McDonald, who conducted the research.
The study was published online in Psychological Medicine.
Increased Potency
“Epidemiologic research suggests that cannabis use may be a significant risk factor for psychotic disorders,” the authors wrote. However, methodological limitations of previous studies make it difficult to estimate the strength of association, with the current evidence base relying largely on cannabis use during the twentieth century, when the drug was “significantly less potent.” It’s plausible that the strength of association has increased due to increased cannabis potency.
The researchers believe youth cannabis use and psychotic disorders is “a critical public health issue,” especially as more jurisdictions liberalize cannabis use and the perception of harm declines among youth.
To estimate the association between cannabis use during youth and the risk for a psychotic disorder diagnosis, using recent population-based data, they used data from the 2009-2012 cycles of the Canadian Community Health Survey (CCHS) linked to administrative health data at ICES to study noninstitutionalized Ontario residents, aged 12-24 years, who had completed the CCHS during that period.
They excluded respondents who used health services for psychotic disorders during the 6 years prior to their CCHS interview date.
Respondents (n = 11,363; 51% men; mean age [SD], 18.3 [15.2-21.3] years) were followed for 6-9 years, with days to first hospitalization, ED visit, or outpatient visit related to a psychotic disorder as the primary outcome.
The researchers estimated age-specific hazard ratios during adolescence (12-19 years) and young adulthood (20-33 years) and conducted sensitivity analyses to explore alternative model conditions, including restricting the outcome to hospitalizations and ED visits, to increase specificity.
Compared with no cannabis use, cannabis use was significantly associated with an 11-fold increased risk for psychotic disorders during adolescence, although not during young adulthood (adjusted hazard ratio [aHR], 11.2; 95% CI, 4.6-27.3 and aHR, 1.3; 95% CI, 0.6-2.6, respectively).
Perception of Harm Declining
When the researchers restricted the outcome to hospitalizations and ED visits only, the strength of association “increased markedly” during adolescence, with a 26-fold higher association in cannabis users than in nonusers (aHR, 26.7; 95% CI, 7.7-92.8). However, there was no meaningful change during young adulthood (aHR, 1.8; 95% CI, 0.6-5.4).
“Many have hypothesized that adolescence is a more sensitive risk period than adulthood for the effect of cannabis use on psychotic disorder development, yet prior to this study, little epidemiologic evidence existed to support this view,” the authors wrote.
The data also suggest that cannabis use is “more strongly associated with more severe psychotic outcomes, as the strength of association during adolescence increased markedly when we restricted the outcome to hospitalizations and ED visits (the most severe types of health service use),” the investigators noted.
The authors noted several limitations. For instance, it’s unclear to what extent unmeasured confounders including genetic predisposition, family history of psychotic disorders, and trauma might have biased the results. In addition, they could not assess the potential confounding impact of genetic predisposition to psychotic disorders. The possibility of reverse causality also cannot be ruled out. It’s possible, they noted, that individuals with “psychotic dispositions” may self-medicate or show greater disposition to cannabis use.
Moreover, the dataset neither captured important factors regarding the cannabis itself, including delta-9-tetrahydrocannabinol potency, mode of use, product type, or cannabis dependence, nor captured institutionalized and homeless youth.
Nevertheless, they pointed to the findings as supporting a “precautionary principle” — as more jurisdictions move to liberalize cannabis use and perception of harm declines among youth, the findings suggest that evidence-based cannabis prevention strategies for adolescents are warranted.
This study was supported by CAMH, the University of Toronto, and ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care. The authors declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
, new research showed.
Investigators at the University of Toronto, The Centre for Addiction and Mental Health (CAMH), and the Institute for Clinical Evaluative Sciences (ICES), in Canada, linked recent population-based survey data from more than 11,000 youngsters to health service use records, including hospitalizations, emergency department (ED) visits, and outpatient visits.
“We found a very strong association between cannabis use and risk of psychotic disorder in adolescence [although] surprisingly, we didn’t find evidence of association in young adulthood,” lead author André J. McDonald, PhD, currently a postdoctoral fellow at the Peter Boris Centre for Addictions Research and the Michael G. DeGroote Centre for Medicinal Cannabis Research, McMaster University, Hamilton, Ontario, Canada, said in a news release.
“These findings are consistent with the neurodevelopmental theory that teens are especially vulnerable to the effects of cannabis,” said Dr. McDonald, who conducted the research.
The study was published online in Psychological Medicine.
Increased Potency
“Epidemiologic research suggests that cannabis use may be a significant risk factor for psychotic disorders,” the authors wrote. However, methodological limitations of previous studies make it difficult to estimate the strength of association, with the current evidence base relying largely on cannabis use during the twentieth century, when the drug was “significantly less potent.” It’s plausible that the strength of association has increased due to increased cannabis potency.
The researchers believe youth cannabis use and psychotic disorders is “a critical public health issue,” especially as more jurisdictions liberalize cannabis use and the perception of harm declines among youth.
To estimate the association between cannabis use during youth and the risk for a psychotic disorder diagnosis, using recent population-based data, they used data from the 2009-2012 cycles of the Canadian Community Health Survey (CCHS) linked to administrative health data at ICES to study noninstitutionalized Ontario residents, aged 12-24 years, who had completed the CCHS during that period.
They excluded respondents who used health services for psychotic disorders during the 6 years prior to their CCHS interview date.
Respondents (n = 11,363; 51% men; mean age [SD], 18.3 [15.2-21.3] years) were followed for 6-9 years, with days to first hospitalization, ED visit, or outpatient visit related to a psychotic disorder as the primary outcome.
The researchers estimated age-specific hazard ratios during adolescence (12-19 years) and young adulthood (20-33 years) and conducted sensitivity analyses to explore alternative model conditions, including restricting the outcome to hospitalizations and ED visits, to increase specificity.
Compared with no cannabis use, cannabis use was significantly associated with an 11-fold increased risk for psychotic disorders during adolescence, although not during young adulthood (adjusted hazard ratio [aHR], 11.2; 95% CI, 4.6-27.3 and aHR, 1.3; 95% CI, 0.6-2.6, respectively).
Perception of Harm Declining
When the researchers restricted the outcome to hospitalizations and ED visits only, the strength of association “increased markedly” during adolescence, with a 26-fold higher association in cannabis users than in nonusers (aHR, 26.7; 95% CI, 7.7-92.8). However, there was no meaningful change during young adulthood (aHR, 1.8; 95% CI, 0.6-5.4).
“Many have hypothesized that adolescence is a more sensitive risk period than adulthood for the effect of cannabis use on psychotic disorder development, yet prior to this study, little epidemiologic evidence existed to support this view,” the authors wrote.
The data also suggest that cannabis use is “more strongly associated with more severe psychotic outcomes, as the strength of association during adolescence increased markedly when we restricted the outcome to hospitalizations and ED visits (the most severe types of health service use),” the investigators noted.
The authors noted several limitations. For instance, it’s unclear to what extent unmeasured confounders including genetic predisposition, family history of psychotic disorders, and trauma might have biased the results. In addition, they could not assess the potential confounding impact of genetic predisposition to psychotic disorders. The possibility of reverse causality also cannot be ruled out. It’s possible, they noted, that individuals with “psychotic dispositions” may self-medicate or show greater disposition to cannabis use.
Moreover, the dataset neither captured important factors regarding the cannabis itself, including delta-9-tetrahydrocannabinol potency, mode of use, product type, or cannabis dependence, nor captured institutionalized and homeless youth.
Nevertheless, they pointed to the findings as supporting a “precautionary principle” — as more jurisdictions move to liberalize cannabis use and perception of harm declines among youth, the findings suggest that evidence-based cannabis prevention strategies for adolescents are warranted.
This study was supported by CAMH, the University of Toronto, and ICES, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care. The authors declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
Dramatic Increase in College Student Suicide Rates
TOPLINE:
, a new study by the National Collegiate Athletic Association (NCAA) found.
METHODOLOGY:
- Investigators analyzed deaths between 2002 and 2022, using Poisson regression models to assess changes in incidence rates over time.
- Data were drawn from the NCAA death database, which includes death from any cause, and included demographic characteristics such as age and race and sporting discipline.
- They utilized linear and quadratic fits between year and suicide incidence for men and women.
- Given the low incidence of suicide deaths per year, the incidence rate was multiplied by 100,000 to calculate the incidence per 100,000 athlete-years (AYs).
TAKEAWAY:
- Of 1102 total deaths, 11.6% were due to suicide (98 men, 30 women).
- Athletes who died by suicide ranged in age from 17 to 24 years (mean, 20 years) were predominantly men (77%) and White (59%), with the highest suicide incidence rate among male cross-country athletes (1:29 per 815 AYs).
- The overall incidence of suicide was 1:71 per 145 AYs.
- Over the last 10 years, suicide was the second most common cause of death after accidents, with the proportion of deaths by suicide doubling from the first to the second decades (7.6% to 15.3%).
- Among men, the suicide incidence rate increased in a linear fashion (5-year incidence rate ratio, 1.32; 95% CI, 1.14-1.53), while among women, a quadratic association was identified (P = .002), with the incidence rate reaching its lowest point in women from 2010 to 2011 and increasing thereafter.
IN PRACTICE:
“Athletes are generally thought of as one of the healthiest populations in our society, yet the pressures of school, internal and external performance expectations, time demands, injury, athletic identity, and physical fatigue can lead to depression, mental health problems, and suicide,” the authors wrote. “Although the rate of suicide among collegiate athletes remains lower than the general population, it is important to recognize the parallel increase to ensure this population is not overlooked when assessing for risk factors and implementing prevention strategies.”
SOURCE:
Bridget M. Whelan, MPH, research scientist in the Department of Family Medicine, Sports Medicine Section, University of Washington School of Medicine, Seattle, was the lead and corresponding author on the study, which was published online in the British Journal of Sports Medicine.
LIMITATIONS:
There is no mandatory reporting system for athlete deaths in the United States, and investigators’ search identified 16 deaths with unknown causes, suggesting reported suicide incidence rates may be underestimated. Additionally, in cases of overdose that were not clearly intentional, the death was listed as “overdose,” possibly resulting in underreporting of suicide.
DISCLOSURES:
No source of study funding was listed. The authors disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, a new study by the National Collegiate Athletic Association (NCAA) found.
METHODOLOGY:
- Investigators analyzed deaths between 2002 and 2022, using Poisson regression models to assess changes in incidence rates over time.
- Data were drawn from the NCAA death database, which includes death from any cause, and included demographic characteristics such as age and race and sporting discipline.
- They utilized linear and quadratic fits between year and suicide incidence for men and women.
- Given the low incidence of suicide deaths per year, the incidence rate was multiplied by 100,000 to calculate the incidence per 100,000 athlete-years (AYs).
TAKEAWAY:
- Of 1102 total deaths, 11.6% were due to suicide (98 men, 30 women).
- Athletes who died by suicide ranged in age from 17 to 24 years (mean, 20 years) were predominantly men (77%) and White (59%), with the highest suicide incidence rate among male cross-country athletes (1:29 per 815 AYs).
- The overall incidence of suicide was 1:71 per 145 AYs.
- Over the last 10 years, suicide was the second most common cause of death after accidents, with the proportion of deaths by suicide doubling from the first to the second decades (7.6% to 15.3%).
- Among men, the suicide incidence rate increased in a linear fashion (5-year incidence rate ratio, 1.32; 95% CI, 1.14-1.53), while among women, a quadratic association was identified (P = .002), with the incidence rate reaching its lowest point in women from 2010 to 2011 and increasing thereafter.
IN PRACTICE:
“Athletes are generally thought of as one of the healthiest populations in our society, yet the pressures of school, internal and external performance expectations, time demands, injury, athletic identity, and physical fatigue can lead to depression, mental health problems, and suicide,” the authors wrote. “Although the rate of suicide among collegiate athletes remains lower than the general population, it is important to recognize the parallel increase to ensure this population is not overlooked when assessing for risk factors and implementing prevention strategies.”
SOURCE:
Bridget M. Whelan, MPH, research scientist in the Department of Family Medicine, Sports Medicine Section, University of Washington School of Medicine, Seattle, was the lead and corresponding author on the study, which was published online in the British Journal of Sports Medicine.
LIMITATIONS:
There is no mandatory reporting system for athlete deaths in the United States, and investigators’ search identified 16 deaths with unknown causes, suggesting reported suicide incidence rates may be underestimated. Additionally, in cases of overdose that were not clearly intentional, the death was listed as “overdose,” possibly resulting in underreporting of suicide.
DISCLOSURES:
No source of study funding was listed. The authors disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, a new study by the National Collegiate Athletic Association (NCAA) found.
METHODOLOGY:
- Investigators analyzed deaths between 2002 and 2022, using Poisson regression models to assess changes in incidence rates over time.
- Data were drawn from the NCAA death database, which includes death from any cause, and included demographic characteristics such as age and race and sporting discipline.
- They utilized linear and quadratic fits between year and suicide incidence for men and women.
- Given the low incidence of suicide deaths per year, the incidence rate was multiplied by 100,000 to calculate the incidence per 100,000 athlete-years (AYs).
TAKEAWAY:
- Of 1102 total deaths, 11.6% were due to suicide (98 men, 30 women).
- Athletes who died by suicide ranged in age from 17 to 24 years (mean, 20 years) were predominantly men (77%) and White (59%), with the highest suicide incidence rate among male cross-country athletes (1:29 per 815 AYs).
- The overall incidence of suicide was 1:71 per 145 AYs.
- Over the last 10 years, suicide was the second most common cause of death after accidents, with the proportion of deaths by suicide doubling from the first to the second decades (7.6% to 15.3%).
- Among men, the suicide incidence rate increased in a linear fashion (5-year incidence rate ratio, 1.32; 95% CI, 1.14-1.53), while among women, a quadratic association was identified (P = .002), with the incidence rate reaching its lowest point in women from 2010 to 2011 and increasing thereafter.
IN PRACTICE:
“Athletes are generally thought of as one of the healthiest populations in our society, yet the pressures of school, internal and external performance expectations, time demands, injury, athletic identity, and physical fatigue can lead to depression, mental health problems, and suicide,” the authors wrote. “Although the rate of suicide among collegiate athletes remains lower than the general population, it is important to recognize the parallel increase to ensure this population is not overlooked when assessing for risk factors and implementing prevention strategies.”
SOURCE:
Bridget M. Whelan, MPH, research scientist in the Department of Family Medicine, Sports Medicine Section, University of Washington School of Medicine, Seattle, was the lead and corresponding author on the study, which was published online in the British Journal of Sports Medicine.
LIMITATIONS:
There is no mandatory reporting system for athlete deaths in the United States, and investigators’ search identified 16 deaths with unknown causes, suggesting reported suicide incidence rates may be underestimated. Additionally, in cases of overdose that were not clearly intentional, the death was listed as “overdose,” possibly resulting in underreporting of suicide.
DISCLOSURES:
No source of study funding was listed. The authors disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Antidepressants and Dementia Risk: Reassuring Data
TOPLINE:
, new research suggests.
METHODOLOGY:
- Investigators studied 5511 individuals (58% women; mean age, 71 years) from the Rotterdam study, an ongoing prospective population-based cohort study.
- Participants were free from dementia at baseline, and incident dementia was monitored from baseline until 2018 with repeated cognitive assessments using the Mini-Mental Status Examination (MMSE) and the Geriatric Mental Schedule, as well as MRIs.
- Information on participants’ antidepressant use was extracted from pharmacy records from 1992 until baseline (2002-2008).
- During a mean follow-up of 10 years, 12% of participants developed dementia.
TAKEAWAY:
- Overall, 17% of participants had used antidepressants during the roughly 10-year period prior to baseline, and 4.1% were still using antidepressants at baseline.
- Medication use at baseline was more common in women than in men (21% vs 18%), and use increased with age: From 2.1% in participants aged between 45 and 50 years to 4.5% in those older than 80 years.
- After adjustment for confounders, there was no association between antidepressant use and dementia risk (hazard ratio [HR], 1.14; 95% CI, 0.92-1.41), accelerated cognitive decline, or atrophy of white and gray matter.
- However, tricyclic antidepressant use was associated with increased dementia risk (HR, 1.36; 95% CI, 1.01-1.83) compared with the use of selective serotonin reuptake inhibitors (HR, 1.12; 95% CI, 0.81-1.54).
IN PRACTICE:
“Although prescription of antidepressant medication in older individuals, in particular those with some cognitive impairment, may have acute symptomatic anticholinergic effects that warrant consideration in clinical practice, our results show that long-term antidepressant use does not have lasting effects on cognition or brain health in older adults without indication of cognitive impairment,” the authors wrote.
SOURCE:
Frank J. Wolters, MD, of the Department of Epidemiology and the Department of Radiology and Nuclear Medicine and Alzheimer Center, Erasmus University Medical Center, Rotterdam, the Netherlands, was the senior author on this study that was published online in Alzheimer’s and Dementia.
LIMITATIONS:
Limitations included the concern that although exclusion of participants with MMSE < 26 at baseline prevented reversed causation (ie, antidepressant use in response to depression during the prodromal phase of dementia), it may have introduced selection bias by disregarding the effects of antidepressant use prior to baseline and excluding participants with lower education.
DISCLOSURES:
This study was conducted as part of the Netherlands Consortium of Dementia Cohorts, which receives funding in the context of Deltaplan Dementie from ZonMW Memorabel and Alzheimer Nederland. Further funding was also obtained from the Stichting Erasmus Trustfonds. This study was further supported by a 2020 NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation. The authors reported no conflicts of interest or relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, new research suggests.
METHODOLOGY:
- Investigators studied 5511 individuals (58% women; mean age, 71 years) from the Rotterdam study, an ongoing prospective population-based cohort study.
- Participants were free from dementia at baseline, and incident dementia was monitored from baseline until 2018 with repeated cognitive assessments using the Mini-Mental Status Examination (MMSE) and the Geriatric Mental Schedule, as well as MRIs.
- Information on participants’ antidepressant use was extracted from pharmacy records from 1992 until baseline (2002-2008).
- During a mean follow-up of 10 years, 12% of participants developed dementia.
TAKEAWAY:
- Overall, 17% of participants had used antidepressants during the roughly 10-year period prior to baseline, and 4.1% were still using antidepressants at baseline.
- Medication use at baseline was more common in women than in men (21% vs 18%), and use increased with age: From 2.1% in participants aged between 45 and 50 years to 4.5% in those older than 80 years.
- After adjustment for confounders, there was no association between antidepressant use and dementia risk (hazard ratio [HR], 1.14; 95% CI, 0.92-1.41), accelerated cognitive decline, or atrophy of white and gray matter.
- However, tricyclic antidepressant use was associated with increased dementia risk (HR, 1.36; 95% CI, 1.01-1.83) compared with the use of selective serotonin reuptake inhibitors (HR, 1.12; 95% CI, 0.81-1.54).
IN PRACTICE:
“Although prescription of antidepressant medication in older individuals, in particular those with some cognitive impairment, may have acute symptomatic anticholinergic effects that warrant consideration in clinical practice, our results show that long-term antidepressant use does not have lasting effects on cognition or brain health in older adults without indication of cognitive impairment,” the authors wrote.
SOURCE:
Frank J. Wolters, MD, of the Department of Epidemiology and the Department of Radiology and Nuclear Medicine and Alzheimer Center, Erasmus University Medical Center, Rotterdam, the Netherlands, was the senior author on this study that was published online in Alzheimer’s and Dementia.
LIMITATIONS:
Limitations included the concern that although exclusion of participants with MMSE < 26 at baseline prevented reversed causation (ie, antidepressant use in response to depression during the prodromal phase of dementia), it may have introduced selection bias by disregarding the effects of antidepressant use prior to baseline and excluding participants with lower education.
DISCLOSURES:
This study was conducted as part of the Netherlands Consortium of Dementia Cohorts, which receives funding in the context of Deltaplan Dementie from ZonMW Memorabel and Alzheimer Nederland. Further funding was also obtained from the Stichting Erasmus Trustfonds. This study was further supported by a 2020 NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation. The authors reported no conflicts of interest or relevant financial relationships.
A version of this article appeared on Medscape.com.
TOPLINE:
, new research suggests.
METHODOLOGY:
- Investigators studied 5511 individuals (58% women; mean age, 71 years) from the Rotterdam study, an ongoing prospective population-based cohort study.
- Participants were free from dementia at baseline, and incident dementia was monitored from baseline until 2018 with repeated cognitive assessments using the Mini-Mental Status Examination (MMSE) and the Geriatric Mental Schedule, as well as MRIs.
- Information on participants’ antidepressant use was extracted from pharmacy records from 1992 until baseline (2002-2008).
- During a mean follow-up of 10 years, 12% of participants developed dementia.
TAKEAWAY:
- Overall, 17% of participants had used antidepressants during the roughly 10-year period prior to baseline, and 4.1% were still using antidepressants at baseline.
- Medication use at baseline was more common in women than in men (21% vs 18%), and use increased with age: From 2.1% in participants aged between 45 and 50 years to 4.5% in those older than 80 years.
- After adjustment for confounders, there was no association between antidepressant use and dementia risk (hazard ratio [HR], 1.14; 95% CI, 0.92-1.41), accelerated cognitive decline, or atrophy of white and gray matter.
- However, tricyclic antidepressant use was associated with increased dementia risk (HR, 1.36; 95% CI, 1.01-1.83) compared with the use of selective serotonin reuptake inhibitors (HR, 1.12; 95% CI, 0.81-1.54).
IN PRACTICE:
“Although prescription of antidepressant medication in older individuals, in particular those with some cognitive impairment, may have acute symptomatic anticholinergic effects that warrant consideration in clinical practice, our results show that long-term antidepressant use does not have lasting effects on cognition or brain health in older adults without indication of cognitive impairment,” the authors wrote.
SOURCE:
Frank J. Wolters, MD, of the Department of Epidemiology and the Department of Radiology and Nuclear Medicine and Alzheimer Center, Erasmus University Medical Center, Rotterdam, the Netherlands, was the senior author on this study that was published online in Alzheimer’s and Dementia.
LIMITATIONS:
Limitations included the concern that although exclusion of participants with MMSE < 26 at baseline prevented reversed causation (ie, antidepressant use in response to depression during the prodromal phase of dementia), it may have introduced selection bias by disregarding the effects of antidepressant use prior to baseline and excluding participants with lower education.
DISCLOSURES:
This study was conducted as part of the Netherlands Consortium of Dementia Cohorts, which receives funding in the context of Deltaplan Dementie from ZonMW Memorabel and Alzheimer Nederland. Further funding was also obtained from the Stichting Erasmus Trustfonds. This study was further supported by a 2020 NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation. The authors reported no conflicts of interest or relevant financial relationships.
A version of this article appeared on Medscape.com.
Mandatory DMV Reporting Tied to Dementia Underdiagnosis
, new research suggests.
Investigators found that primary care physicians (PCPs) in states with clinician reporting mandates had a 59% higher probability of underdiagnosing dementia compared with their counterparts in states that require patients to self-report or that have no reporting mandates.
“Our findings in this cross-sectional study raise concerns about potential adverse effects of mandatory clinician reporting for dementia diagnosis and underscore the need for careful consideration of the effect of such policies,” wrote the investigators, led by Soeren Mattke, MD, DSc, director of the USC Brain Health Observatory and research professor of economics at the University of Southern California, Los Angeles.
The study was published online in JAMA Network Open.
Lack of Guidance
As the US population ages, the number of older drivers is increasing, with 55.8 million drivers 65 years old or older. Approximately 7 million people in this age group have dementia — an estimate that is expected to increase to nearly 12 million by 2040.
The aging population raises a “critical policy question” about how to ensure road safety. Although the American Medical Association’s Code of Ethics outlines a physician’s obligation to identify drivers with medical impairments that impede safe driving, guidance restricting cognitively impaired drivers from driving is lacking.
In addition, evidence as to whether cognitive impairment indeed poses a threat to driving safety is mixed and has led to a lack of uniform policies with respect to reporting dementia.
Four states explicitly require clinicians to report dementia diagnoses to the DMV, which will then determine the patient’s fitness to drive, whereas 14 states require people with dementia to self-report. The remaining states have no explicit reporting requirements.
The issue of mandatory reporting is controversial, the researchers noted. On the one hand, physicians could protect patients and others by reporting potentially unsafe drivers.
On the other hand, evidence of an association with lower accident risks in patients with dementia is sparse and mandatory reporting may adversely affect physician-patient relationships. Empirical evidence for unintended consequences of reporting laws is lacking.
To examine the potential link between dementia underdiagnosis and mandatory reporting policies, the investigators analyzed the 100% data from the Medicare fee-for-service program and Medicare Advantage plans from 2017 to 2019, which included 223,036 PCPs with a panel of 25 or more Medicare patients.
The researchers examined dementia diagnosis rates in the patient panel of PCPs, rather than neurologists or gerontologists, regardless of who documented the diagnosis. Dr. Mattke said that it is possible that the diagnosis was established after referral to a specialist.
Each physician’s expected number of dementia cases was estimated using a predictive model based on patient characteristics. The researchers then compared the estimate with observed dementia diagnoses, thereby identifying clinicians who underdiagnosed dementia after sampling errors were accounted for.
‘Heavy-Handed Interference’
The researchers adjusted for several covariates potentially associated with a clinician’s probability of underdiagnosing dementia. These included sex, office location, practice specialty, racial/ethnic composition of the patient panel, and percentage of patients dually eligible for Medicare and Medicaid. The table shows PCP characteristics.
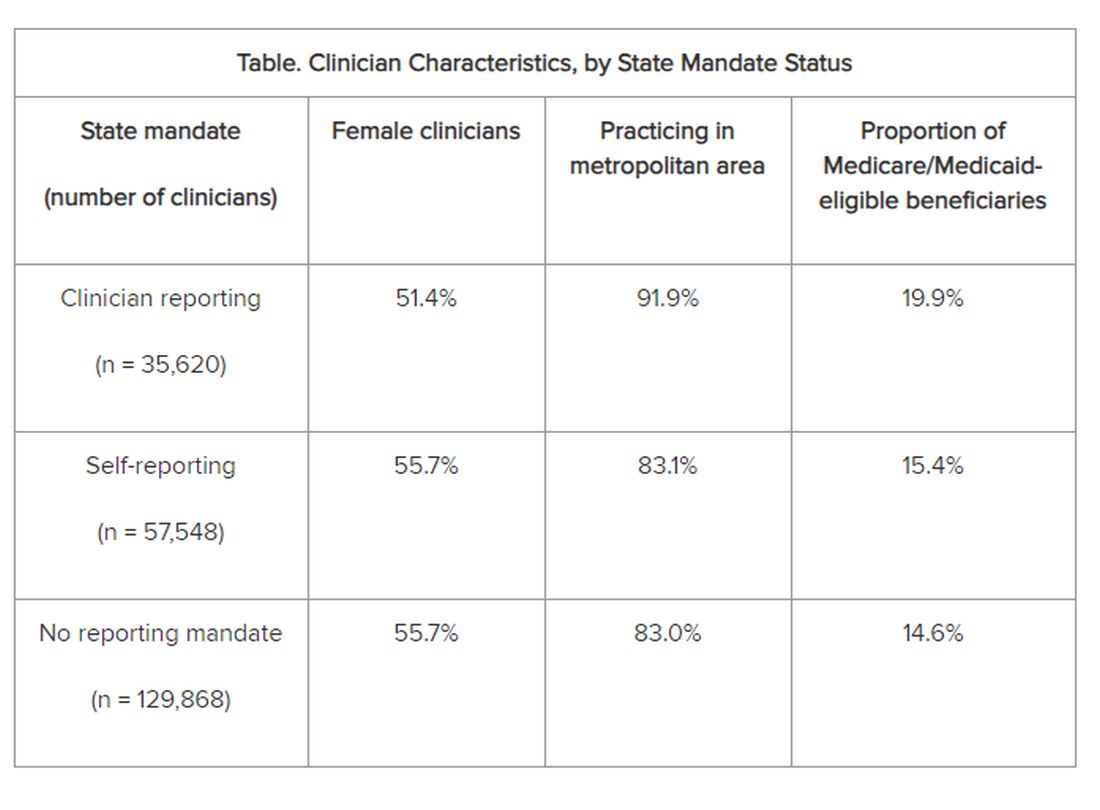
Adjusted results showed that PCPs practicing in states with clinician reporting mandates had a 12.4% (95% confidence interval [CI], 10.5%-14.2%) probability of underdiagnosing dementia versus 7.8% (95% CI, 6.9%-8.7%) in states with self-reporting and 7.7% (95% CI, 6.9%-8.4%) in states with no mandates, translating into a 4–percentage point difference (P < .001).
“Our study is the first to provide empirical evidence for the potential adverse effects of reporting policies,” the researchers noted. “Although we found that some clinicians underdiagnosed dementia regardless of state mandates, the key finding of this study reveals that primary care clinicians who practice in states with clinician reporting mandates were 59% more likely to do so…compared with those states with no reporting requirements…or driver self-reporting requirements.”
The investigators suggested that one potential explanation for underdiagnosis is patient resistance to cognitive testing. If patients were aware that the clinician was obligated by law to report their dementia diagnosis to the DMV, “they might be more inclined to conceal their symptoms or refuse further assessments, in addition to the general stigma and resistance to a formal assessment after a positive dementia screening result.”
“The findings suggest that policymakers might want to rethink those physician reporting mandates, since we also could not find conclusive evidence that they improve road safety,” Dr. Mattke said. “Maybe patients and their physicians can arrive at a sensible approach to determine driving fitness without such heavy-handed interference.”
However, he cautioned that the findings are not definitive and further study is needed before firm recommendations either for or against mandatory reporting.
In addition, the researchers noted several study limitations. One is that dementia underdiagnosis may also be associated with factors not captured in their model, including physician-patient relationships, health literacy, or language barriers.
However, Dr. Mattke noted, “ my sense is that those unobservable factors are not systematically related to state reporting policies and having omitted them would therefore not bias our results.”
Experts Weigh In
Commenting on the research, Morgan Daven, MA, the Alzheimer’s Association vice president of health systems, said that dementia is widely and significantly underdiagnosed, and not only in the states with dementia reporting mandates. Many factors may contribute to underdiagnosis, and although the study shows an association between reporting mandates and underdiagnosis, it does not demonstrate causation.
That said, Mr. Daven added, “fear and stigma related to dementia may inhibit the clinician, the patient, and their family from pursuing detection and diagnosis for dementia. As a society, we need to address dementia fear and stigma for all parties.”
He noted that useful tools include healthcare policies, workforce training, public awareness and education, and public policies to mitigate fear and stigma and their negative effects on diagnosis, care, support, and communication.
A potential study limitation is that it relied only on diagnoses by PCPs. Mr. Daven noted that the diagnosis of Alzheimer’ disease — the most common cause of dementia — is confirmation of amyloid buildup via a biomarker test, using PET or cerebrospinal fluid analysis.
“Both of these tests are extremely limited in their use and accessibility in a primary care setting. Inclusion of diagnoses by dementia specialists would provide a more complete picture,” he said.
Mr. Daven added that the Alzheimer’s Association encourages families to proactively discuss driving and other disease-related safety concerns as soon as possible. The Alzheimer’s Association Dementia and Driving webpage offers tips and strategies to discuss driving concerns with a family member.
In an accompanying editorial, Donald Redelmeier, MD, MS(HSR), and Vidhi Bhatt, BSc, both of the Department of Medicine, University of Toronto, differentiate the mandate for physicians to warn patients with dementia about traffic safety from the mandate for reporting child maltreatment, gunshot victims, or communicable diseases. They noted that mandated warnings “are not easy, can engender patient dissatisfaction, and need to be handled with tact.”
Yet, they pointed out, “breaking bad news is what practicing medicine entails.” They emphasized that, regardless of government mandates, “counseling patients for more road safety is an essential skill for clinicians in diverse states who hope to help their patients avoid becoming more traffic statistics.”
Research reported in this publication was supported by Genentech, a member of the Roche Group, and a grant from the National Institute on Aging of the National Institutes of Health. Dr. Mattke reported receiving grants from Genentech for a research contract with USC during the conduct of the study; personal fees from Eisai, Biogen, C2N, Novo Nordisk, Novartis, and Roche Genentech; and serving on the Senscio Systems board of directors, ALZpath scientific advisory board, AiCure scientific advisory board, and Boston Millennia Partners scientific advisory board outside the submitted work. The other authors’ disclosures are listed on the original paper. The editorial was supported by the Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, Kimel-Schatzky Traumatic Brain Injury Research Fund, and the Graduate Diploma Program in Health Research at the University of Toronto. The editorial authors report no other relevant financial relationships.
A version of this article appeared on Medscape.com.
, new research suggests.
Investigators found that primary care physicians (PCPs) in states with clinician reporting mandates had a 59% higher probability of underdiagnosing dementia compared with their counterparts in states that require patients to self-report or that have no reporting mandates.
“Our findings in this cross-sectional study raise concerns about potential adverse effects of mandatory clinician reporting for dementia diagnosis and underscore the need for careful consideration of the effect of such policies,” wrote the investigators, led by Soeren Mattke, MD, DSc, director of the USC Brain Health Observatory and research professor of economics at the University of Southern California, Los Angeles.
The study was published online in JAMA Network Open.
Lack of Guidance
As the US population ages, the number of older drivers is increasing, with 55.8 million drivers 65 years old or older. Approximately 7 million people in this age group have dementia — an estimate that is expected to increase to nearly 12 million by 2040.
The aging population raises a “critical policy question” about how to ensure road safety. Although the American Medical Association’s Code of Ethics outlines a physician’s obligation to identify drivers with medical impairments that impede safe driving, guidance restricting cognitively impaired drivers from driving is lacking.
In addition, evidence as to whether cognitive impairment indeed poses a threat to driving safety is mixed and has led to a lack of uniform policies with respect to reporting dementia.
Four states explicitly require clinicians to report dementia diagnoses to the DMV, which will then determine the patient’s fitness to drive, whereas 14 states require people with dementia to self-report. The remaining states have no explicit reporting requirements.
The issue of mandatory reporting is controversial, the researchers noted. On the one hand, physicians could protect patients and others by reporting potentially unsafe drivers.
On the other hand, evidence of an association with lower accident risks in patients with dementia is sparse and mandatory reporting may adversely affect physician-patient relationships. Empirical evidence for unintended consequences of reporting laws is lacking.
To examine the potential link between dementia underdiagnosis and mandatory reporting policies, the investigators analyzed the 100% data from the Medicare fee-for-service program and Medicare Advantage plans from 2017 to 2019, which included 223,036 PCPs with a panel of 25 or more Medicare patients.
The researchers examined dementia diagnosis rates in the patient panel of PCPs, rather than neurologists or gerontologists, regardless of who documented the diagnosis. Dr. Mattke said that it is possible that the diagnosis was established after referral to a specialist.
Each physician’s expected number of dementia cases was estimated using a predictive model based on patient characteristics. The researchers then compared the estimate with observed dementia diagnoses, thereby identifying clinicians who underdiagnosed dementia after sampling errors were accounted for.
‘Heavy-Handed Interference’
The researchers adjusted for several covariates potentially associated with a clinician’s probability of underdiagnosing dementia. These included sex, office location, practice specialty, racial/ethnic composition of the patient panel, and percentage of patients dually eligible for Medicare and Medicaid. The table shows PCP characteristics.
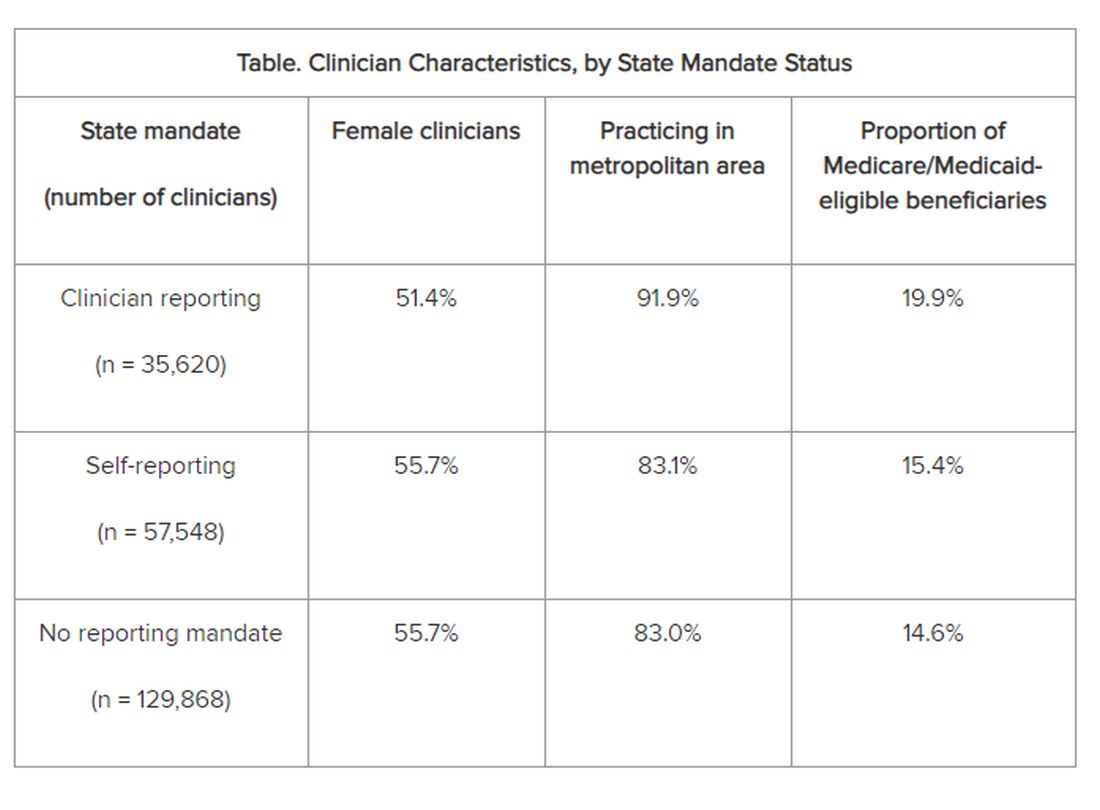
Adjusted results showed that PCPs practicing in states with clinician reporting mandates had a 12.4% (95% confidence interval [CI], 10.5%-14.2%) probability of underdiagnosing dementia versus 7.8% (95% CI, 6.9%-8.7%) in states with self-reporting and 7.7% (95% CI, 6.9%-8.4%) in states with no mandates, translating into a 4–percentage point difference (P < .001).
“Our study is the first to provide empirical evidence for the potential adverse effects of reporting policies,” the researchers noted. “Although we found that some clinicians underdiagnosed dementia regardless of state mandates, the key finding of this study reveals that primary care clinicians who practice in states with clinician reporting mandates were 59% more likely to do so…compared with those states with no reporting requirements…or driver self-reporting requirements.”
The investigators suggested that one potential explanation for underdiagnosis is patient resistance to cognitive testing. If patients were aware that the clinician was obligated by law to report their dementia diagnosis to the DMV, “they might be more inclined to conceal their symptoms or refuse further assessments, in addition to the general stigma and resistance to a formal assessment after a positive dementia screening result.”
“The findings suggest that policymakers might want to rethink those physician reporting mandates, since we also could not find conclusive evidence that they improve road safety,” Dr. Mattke said. “Maybe patients and their physicians can arrive at a sensible approach to determine driving fitness without such heavy-handed interference.”
However, he cautioned that the findings are not definitive and further study is needed before firm recommendations either for or against mandatory reporting.
In addition, the researchers noted several study limitations. One is that dementia underdiagnosis may also be associated with factors not captured in their model, including physician-patient relationships, health literacy, or language barriers.
However, Dr. Mattke noted, “ my sense is that those unobservable factors are not systematically related to state reporting policies and having omitted them would therefore not bias our results.”
Experts Weigh In
Commenting on the research, Morgan Daven, MA, the Alzheimer’s Association vice president of health systems, said that dementia is widely and significantly underdiagnosed, and not only in the states with dementia reporting mandates. Many factors may contribute to underdiagnosis, and although the study shows an association between reporting mandates and underdiagnosis, it does not demonstrate causation.
That said, Mr. Daven added, “fear and stigma related to dementia may inhibit the clinician, the patient, and their family from pursuing detection and diagnosis for dementia. As a society, we need to address dementia fear and stigma for all parties.”
He noted that useful tools include healthcare policies, workforce training, public awareness and education, and public policies to mitigate fear and stigma and their negative effects on diagnosis, care, support, and communication.
A potential study limitation is that it relied only on diagnoses by PCPs. Mr. Daven noted that the diagnosis of Alzheimer’ disease — the most common cause of dementia — is confirmation of amyloid buildup via a biomarker test, using PET or cerebrospinal fluid analysis.
“Both of these tests are extremely limited in their use and accessibility in a primary care setting. Inclusion of diagnoses by dementia specialists would provide a more complete picture,” he said.
Mr. Daven added that the Alzheimer’s Association encourages families to proactively discuss driving and other disease-related safety concerns as soon as possible. The Alzheimer’s Association Dementia and Driving webpage offers tips and strategies to discuss driving concerns with a family member.
In an accompanying editorial, Donald Redelmeier, MD, MS(HSR), and Vidhi Bhatt, BSc, both of the Department of Medicine, University of Toronto, differentiate the mandate for physicians to warn patients with dementia about traffic safety from the mandate for reporting child maltreatment, gunshot victims, or communicable diseases. They noted that mandated warnings “are not easy, can engender patient dissatisfaction, and need to be handled with tact.”
Yet, they pointed out, “breaking bad news is what practicing medicine entails.” They emphasized that, regardless of government mandates, “counseling patients for more road safety is an essential skill for clinicians in diverse states who hope to help their patients avoid becoming more traffic statistics.”
Research reported in this publication was supported by Genentech, a member of the Roche Group, and a grant from the National Institute on Aging of the National Institutes of Health. Dr. Mattke reported receiving grants from Genentech for a research contract with USC during the conduct of the study; personal fees from Eisai, Biogen, C2N, Novo Nordisk, Novartis, and Roche Genentech; and serving on the Senscio Systems board of directors, ALZpath scientific advisory board, AiCure scientific advisory board, and Boston Millennia Partners scientific advisory board outside the submitted work. The other authors’ disclosures are listed on the original paper. The editorial was supported by the Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, Kimel-Schatzky Traumatic Brain Injury Research Fund, and the Graduate Diploma Program in Health Research at the University of Toronto. The editorial authors report no other relevant financial relationships.
A version of this article appeared on Medscape.com.
, new research suggests.
Investigators found that primary care physicians (PCPs) in states with clinician reporting mandates had a 59% higher probability of underdiagnosing dementia compared with their counterparts in states that require patients to self-report or that have no reporting mandates.
“Our findings in this cross-sectional study raise concerns about potential adverse effects of mandatory clinician reporting for dementia diagnosis and underscore the need for careful consideration of the effect of such policies,” wrote the investigators, led by Soeren Mattke, MD, DSc, director of the USC Brain Health Observatory and research professor of economics at the University of Southern California, Los Angeles.
The study was published online in JAMA Network Open.
Lack of Guidance
As the US population ages, the number of older drivers is increasing, with 55.8 million drivers 65 years old or older. Approximately 7 million people in this age group have dementia — an estimate that is expected to increase to nearly 12 million by 2040.
The aging population raises a “critical policy question” about how to ensure road safety. Although the American Medical Association’s Code of Ethics outlines a physician’s obligation to identify drivers with medical impairments that impede safe driving, guidance restricting cognitively impaired drivers from driving is lacking.
In addition, evidence as to whether cognitive impairment indeed poses a threat to driving safety is mixed and has led to a lack of uniform policies with respect to reporting dementia.
Four states explicitly require clinicians to report dementia diagnoses to the DMV, which will then determine the patient’s fitness to drive, whereas 14 states require people with dementia to self-report. The remaining states have no explicit reporting requirements.
The issue of mandatory reporting is controversial, the researchers noted. On the one hand, physicians could protect patients and others by reporting potentially unsafe drivers.
On the other hand, evidence of an association with lower accident risks in patients with dementia is sparse and mandatory reporting may adversely affect physician-patient relationships. Empirical evidence for unintended consequences of reporting laws is lacking.
To examine the potential link between dementia underdiagnosis and mandatory reporting policies, the investigators analyzed the 100% data from the Medicare fee-for-service program and Medicare Advantage plans from 2017 to 2019, which included 223,036 PCPs with a panel of 25 or more Medicare patients.
The researchers examined dementia diagnosis rates in the patient panel of PCPs, rather than neurologists or gerontologists, regardless of who documented the diagnosis. Dr. Mattke said that it is possible that the diagnosis was established after referral to a specialist.
Each physician’s expected number of dementia cases was estimated using a predictive model based on patient characteristics. The researchers then compared the estimate with observed dementia diagnoses, thereby identifying clinicians who underdiagnosed dementia after sampling errors were accounted for.
‘Heavy-Handed Interference’
The researchers adjusted for several covariates potentially associated with a clinician’s probability of underdiagnosing dementia. These included sex, office location, practice specialty, racial/ethnic composition of the patient panel, and percentage of patients dually eligible for Medicare and Medicaid. The table shows PCP characteristics.
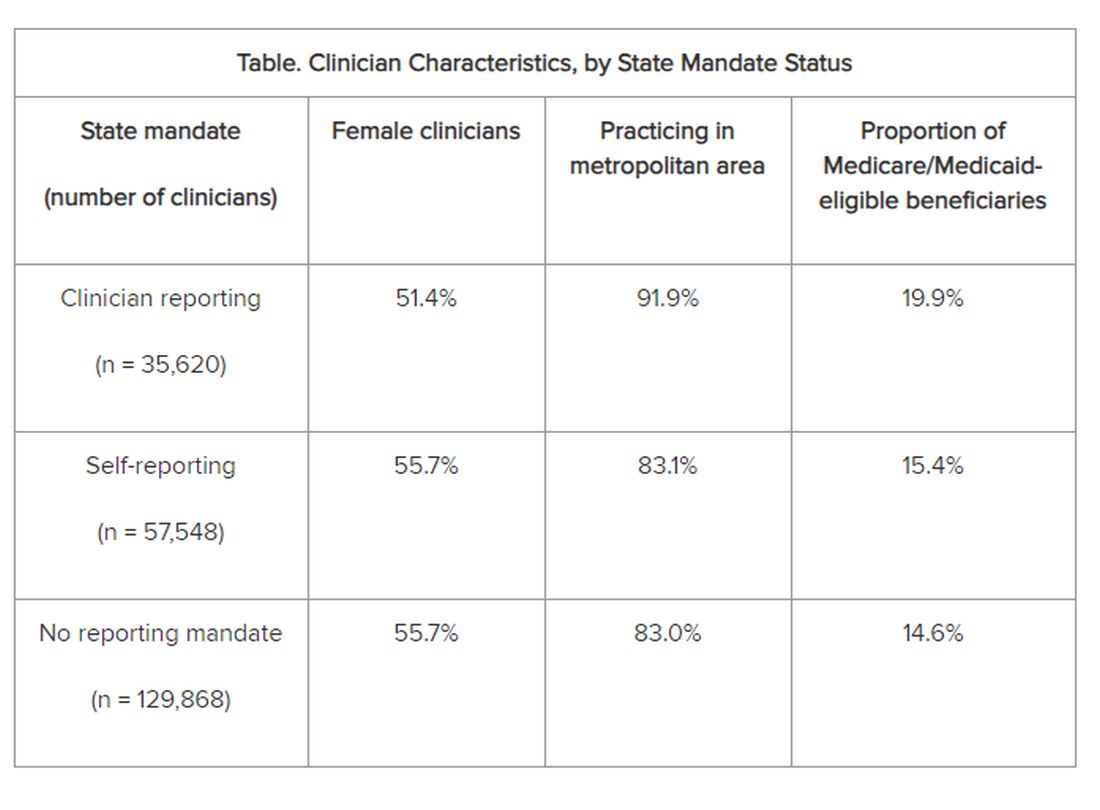
Adjusted results showed that PCPs practicing in states with clinician reporting mandates had a 12.4% (95% confidence interval [CI], 10.5%-14.2%) probability of underdiagnosing dementia versus 7.8% (95% CI, 6.9%-8.7%) in states with self-reporting and 7.7% (95% CI, 6.9%-8.4%) in states with no mandates, translating into a 4–percentage point difference (P < .001).
“Our study is the first to provide empirical evidence for the potential adverse effects of reporting policies,” the researchers noted. “Although we found that some clinicians underdiagnosed dementia regardless of state mandates, the key finding of this study reveals that primary care clinicians who practice in states with clinician reporting mandates were 59% more likely to do so…compared with those states with no reporting requirements…or driver self-reporting requirements.”
The investigators suggested that one potential explanation for underdiagnosis is patient resistance to cognitive testing. If patients were aware that the clinician was obligated by law to report their dementia diagnosis to the DMV, “they might be more inclined to conceal their symptoms or refuse further assessments, in addition to the general stigma and resistance to a formal assessment after a positive dementia screening result.”
“The findings suggest that policymakers might want to rethink those physician reporting mandates, since we also could not find conclusive evidence that they improve road safety,” Dr. Mattke said. “Maybe patients and their physicians can arrive at a sensible approach to determine driving fitness without such heavy-handed interference.”
However, he cautioned that the findings are not definitive and further study is needed before firm recommendations either for or against mandatory reporting.
In addition, the researchers noted several study limitations. One is that dementia underdiagnosis may also be associated with factors not captured in their model, including physician-patient relationships, health literacy, or language barriers.
However, Dr. Mattke noted, “ my sense is that those unobservable factors are not systematically related to state reporting policies and having omitted them would therefore not bias our results.”
Experts Weigh In
Commenting on the research, Morgan Daven, MA, the Alzheimer’s Association vice president of health systems, said that dementia is widely and significantly underdiagnosed, and not only in the states with dementia reporting mandates. Many factors may contribute to underdiagnosis, and although the study shows an association between reporting mandates and underdiagnosis, it does not demonstrate causation.
That said, Mr. Daven added, “fear and stigma related to dementia may inhibit the clinician, the patient, and their family from pursuing detection and diagnosis for dementia. As a society, we need to address dementia fear and stigma for all parties.”
He noted that useful tools include healthcare policies, workforce training, public awareness and education, and public policies to mitigate fear and stigma and their negative effects on diagnosis, care, support, and communication.
A potential study limitation is that it relied only on diagnoses by PCPs. Mr. Daven noted that the diagnosis of Alzheimer’ disease — the most common cause of dementia — is confirmation of amyloid buildup via a biomarker test, using PET or cerebrospinal fluid analysis.
“Both of these tests are extremely limited in their use and accessibility in a primary care setting. Inclusion of diagnoses by dementia specialists would provide a more complete picture,” he said.
Mr. Daven added that the Alzheimer’s Association encourages families to proactively discuss driving and other disease-related safety concerns as soon as possible. The Alzheimer’s Association Dementia and Driving webpage offers tips and strategies to discuss driving concerns with a family member.
In an accompanying editorial, Donald Redelmeier, MD, MS(HSR), and Vidhi Bhatt, BSc, both of the Department of Medicine, University of Toronto, differentiate the mandate for physicians to warn patients with dementia about traffic safety from the mandate for reporting child maltreatment, gunshot victims, or communicable diseases. They noted that mandated warnings “are not easy, can engender patient dissatisfaction, and need to be handled with tact.”
Yet, they pointed out, “breaking bad news is what practicing medicine entails.” They emphasized that, regardless of government mandates, “counseling patients for more road safety is an essential skill for clinicians in diverse states who hope to help their patients avoid becoming more traffic statistics.”
Research reported in this publication was supported by Genentech, a member of the Roche Group, and a grant from the National Institute on Aging of the National Institutes of Health. Dr. Mattke reported receiving grants from Genentech for a research contract with USC during the conduct of the study; personal fees from Eisai, Biogen, C2N, Novo Nordisk, Novartis, and Roche Genentech; and serving on the Senscio Systems board of directors, ALZpath scientific advisory board, AiCure scientific advisory board, and Boston Millennia Partners scientific advisory board outside the submitted work. The other authors’ disclosures are listed on the original paper. The editorial was supported by the Canada Research Chair in Medical Decision Sciences, the Canadian Institutes of Health Research, Kimel-Schatzky Traumatic Brain Injury Research Fund, and the Graduate Diploma Program in Health Research at the University of Toronto. The editorial authors report no other relevant financial relationships.
A version of this article appeared on Medscape.com.
From JAMA Network Open
Vaccine Safety and DMT for Highly Active Multiple Sclerosis: New Data
, new research shows.
The study, the first to examine vaccine safety and immunogenicity in highly active MS, revealed high seroprotection rates following receipt of vaccines for COVID-19 and hepatitis A and B, regardless of the duration of treatment with natalizumab.
On the basis of these findings, investigators created an algorithm that clinicians can use to map an immunization schedule in patients who might otherwise delay initiation of disease-modifying therapy until they are fully vaccinated.
“We observed seroprotection rates exceeding 90% for hepatitis A and B, and mRNA COVID-19 vaccines, and all vaccines demonstrated a favorable safety profile, with no exacerbation of disease activity detected,” said lead author René Carvajal, MD, of the Department of Neurology-Neuroimmunology, Multiple Sclerosis Centre of Catalonia (Cemcat), Hospital Universitari Vall d’Hebron, Universitat Autònoma de Barcelona, Barcelona, Spain. “This points to potential benefits for patients with highly active MS who require both immunization and high-efficacy therapies that may impact vaccine responses.”
The study was published online in JAMA Network Open.
A Controversial Issue
Today’s high-efficacy therapies for MS may increase the risk of acquiring new infections, reactivate latent pathogens, or worsen ongoing infectious conditions, and immunogenicity of vaccination can be compromised by immunosuppressive agents, particularly CD20 therapies, researchers noted.
As a result, many clinicians opt to delay initiation of such therapies until vaccination schedules are complete to avoid exposure to vaccine-preventable infections. But delaying treatment can potentially affect disease progression.
Reports of disease worsening following vaccination “have raised controversy around vaccine safety,” the authors wrote. The issue is especially relevant to those with highly active MS due to the scarcity of available data in this population.
The motivation for the study “stemmed from the complex balance clinicians face between initiating highly effective therapies promptly in patients with highly active MS and ensuring adequate protection against preventable infections through vaccination,” Dr. Carvajal said.
High Seroprotection Rate
Researchers analyzed data on 60 patients (mean age, 43 years; 44 female; mean disease duration, 17 years) participating in one of two prospectively followed cohorts: The Barcelona Clinically Isolated Syndromes Inception Cohort and the Barcelona Treatment Cohort. Data included demographic, clinical, radiologic, and biological data as well as regular clinical assessments, evaluations of the Expanded Disability Status Scale (EDSS), and MRI scans.
Patients enrolled in the current study had received at least one of these vaccines between September 2016 and February 2022: hepatitis A virus (HAV), hepatitis B virus (HBV; enhanced immunity high load or adjuvanted), or COVID-19 (BNT162b2 [Pfizer-BioNTech], mRAN-1273 [Moderna], or ChAdOx1-S [recombinant; AstraZeneca]).
The researchers conducted a retrospective, self-controlled analysis to compare the annualized relapse rate, EDSS score, and new T2 lesions counts during the 12 months before and after vaccination in patients with short- and long-term treatment duration.
They also compared John Cunningham virus serostatus between the two periods, as well as immunoglobulin G titers for each vaccine.
The global seroprotection rate was 93% (95% CI, 86%-98%). Individual vaccine rates were 92% for HAV, 93% for HBV, and 100% for COVID-19.
There was a significant reduction between the pre- and postvaccination periods in mean relapse rates (P = .004) and median number of new T2 lesions (P = .01).
There were no changes in EDSS scores before and after vaccinations and duration of natalizumab treatment had no impact on safety and immunogenicity.
‘Viable Option’
The researchers used their findings to create a proposed algorithm to inform immunization decisions in patients with highly active MS who require prompt initiation of high-efficacy disease-modifying therapy.
The algorithm is “integrated into a risk-minimization strategy tailored for patients with highly active MS, emphasizing in this case the pivotal role of natalizumab in averting treatment delays and providing adequate protection against potentially severe infections,” Dr. Carvajal said.
Participants who initiated or continued treatment with natalizumab completed their vaccination regimen without any incidents of progressive multifocal leukoencephalopathy (PML) or disease activity rebound following natalizumab discontinuation.
This suggests that using natalizumab for a brief duration might be a “viable option to contemplate,” the authors noted.
Commenting on the findings, Grace Gombolay, MD, assistant professor of pediatrics in the Division of Pediatric Neurology and director of the Pediatric Neuroimmunology and Multiple Sclerosis Clinic, Emory University, Atlanta, Georgia, said the study “demonstrates that vaccines are safe and do not trigger attacks in patients with MS on natalizumab, and that immunity — as measured by antibodies — is preserved in MS patients who receive natalizumab.”
This “contrasts with other treatments, as decreased antibody responses in COVID-19 are noted in certain treatments,” said Dr. Gombolay, who was not part of the study. “If both disease control and immunity against infection are the goals for the patient, then natalizumab is a reasonable option.”
“However, this must be balanced with other considerations,” she added, including the risk for PML and pregnancy.
This study was supported by grants from the European Committee for Treatment and Research in Multiple Sclerosis, Instituto de Salud Carlos III, and the European Union. Dr. Carvajal reported receiving grants from Vall d’Hebron Institut de Recerca and the European Committee for Treatment and Research in Multiple Sclerosis and honoraria from Roche, Novartis, BIIB-Colombia, Merck, and Sanofi outside the submitted work. Dr. Gombolay serves as media editor for Pediatric Neurology and as associate editor of the Annals of the Child Neurology Society. She is also a part-time CDC consultant for acute flaccid myelitis and received an honorarium as a speaker at the Georgia Neurological Society meeting, sponsored by Academic CME and TG Therapeutics.
A version of this article appeared on Medscape.com.
, new research shows.
The study, the first to examine vaccine safety and immunogenicity in highly active MS, revealed high seroprotection rates following receipt of vaccines for COVID-19 and hepatitis A and B, regardless of the duration of treatment with natalizumab.
On the basis of these findings, investigators created an algorithm that clinicians can use to map an immunization schedule in patients who might otherwise delay initiation of disease-modifying therapy until they are fully vaccinated.
“We observed seroprotection rates exceeding 90% for hepatitis A and B, and mRNA COVID-19 vaccines, and all vaccines demonstrated a favorable safety profile, with no exacerbation of disease activity detected,” said lead author René Carvajal, MD, of the Department of Neurology-Neuroimmunology, Multiple Sclerosis Centre of Catalonia (Cemcat), Hospital Universitari Vall d’Hebron, Universitat Autònoma de Barcelona, Barcelona, Spain. “This points to potential benefits for patients with highly active MS who require both immunization and high-efficacy therapies that may impact vaccine responses.”
The study was published online in JAMA Network Open.
A Controversial Issue
Today’s high-efficacy therapies for MS may increase the risk of acquiring new infections, reactivate latent pathogens, or worsen ongoing infectious conditions, and immunogenicity of vaccination can be compromised by immunosuppressive agents, particularly CD20 therapies, researchers noted.
As a result, many clinicians opt to delay initiation of such therapies until vaccination schedules are complete to avoid exposure to vaccine-preventable infections. But delaying treatment can potentially affect disease progression.
Reports of disease worsening following vaccination “have raised controversy around vaccine safety,” the authors wrote. The issue is especially relevant to those with highly active MS due to the scarcity of available data in this population.
The motivation for the study “stemmed from the complex balance clinicians face between initiating highly effective therapies promptly in patients with highly active MS and ensuring adequate protection against preventable infections through vaccination,” Dr. Carvajal said.
High Seroprotection Rate
Researchers analyzed data on 60 patients (mean age, 43 years; 44 female; mean disease duration, 17 years) participating in one of two prospectively followed cohorts: The Barcelona Clinically Isolated Syndromes Inception Cohort and the Barcelona Treatment Cohort. Data included demographic, clinical, radiologic, and biological data as well as regular clinical assessments, evaluations of the Expanded Disability Status Scale (EDSS), and MRI scans.
Patients enrolled in the current study had received at least one of these vaccines between September 2016 and February 2022: hepatitis A virus (HAV), hepatitis B virus (HBV; enhanced immunity high load or adjuvanted), or COVID-19 (BNT162b2 [Pfizer-BioNTech], mRAN-1273 [Moderna], or ChAdOx1-S [recombinant; AstraZeneca]).
The researchers conducted a retrospective, self-controlled analysis to compare the annualized relapse rate, EDSS score, and new T2 lesions counts during the 12 months before and after vaccination in patients with short- and long-term treatment duration.
They also compared John Cunningham virus serostatus between the two periods, as well as immunoglobulin G titers for each vaccine.
The global seroprotection rate was 93% (95% CI, 86%-98%). Individual vaccine rates were 92% for HAV, 93% for HBV, and 100% for COVID-19.
There was a significant reduction between the pre- and postvaccination periods in mean relapse rates (P = .004) and median number of new T2 lesions (P = .01).
There were no changes in EDSS scores before and after vaccinations and duration of natalizumab treatment had no impact on safety and immunogenicity.
‘Viable Option’
The researchers used their findings to create a proposed algorithm to inform immunization decisions in patients with highly active MS who require prompt initiation of high-efficacy disease-modifying therapy.
The algorithm is “integrated into a risk-minimization strategy tailored for patients with highly active MS, emphasizing in this case the pivotal role of natalizumab in averting treatment delays and providing adequate protection against potentially severe infections,” Dr. Carvajal said.
Participants who initiated or continued treatment with natalizumab completed their vaccination regimen without any incidents of progressive multifocal leukoencephalopathy (PML) or disease activity rebound following natalizumab discontinuation.
This suggests that using natalizumab for a brief duration might be a “viable option to contemplate,” the authors noted.
Commenting on the findings, Grace Gombolay, MD, assistant professor of pediatrics in the Division of Pediatric Neurology and director of the Pediatric Neuroimmunology and Multiple Sclerosis Clinic, Emory University, Atlanta, Georgia, said the study “demonstrates that vaccines are safe and do not trigger attacks in patients with MS on natalizumab, and that immunity — as measured by antibodies — is preserved in MS patients who receive natalizumab.”
This “contrasts with other treatments, as decreased antibody responses in COVID-19 are noted in certain treatments,” said Dr. Gombolay, who was not part of the study. “If both disease control and immunity against infection are the goals for the patient, then natalizumab is a reasonable option.”
“However, this must be balanced with other considerations,” she added, including the risk for PML and pregnancy.
This study was supported by grants from the European Committee for Treatment and Research in Multiple Sclerosis, Instituto de Salud Carlos III, and the European Union. Dr. Carvajal reported receiving grants from Vall d’Hebron Institut de Recerca and the European Committee for Treatment and Research in Multiple Sclerosis and honoraria from Roche, Novartis, BIIB-Colombia, Merck, and Sanofi outside the submitted work. Dr. Gombolay serves as media editor for Pediatric Neurology and as associate editor of the Annals of the Child Neurology Society. She is also a part-time CDC consultant for acute flaccid myelitis and received an honorarium as a speaker at the Georgia Neurological Society meeting, sponsored by Academic CME and TG Therapeutics.
A version of this article appeared on Medscape.com.
, new research shows.
The study, the first to examine vaccine safety and immunogenicity in highly active MS, revealed high seroprotection rates following receipt of vaccines for COVID-19 and hepatitis A and B, regardless of the duration of treatment with natalizumab.
On the basis of these findings, investigators created an algorithm that clinicians can use to map an immunization schedule in patients who might otherwise delay initiation of disease-modifying therapy until they are fully vaccinated.
“We observed seroprotection rates exceeding 90% for hepatitis A and B, and mRNA COVID-19 vaccines, and all vaccines demonstrated a favorable safety profile, with no exacerbation of disease activity detected,” said lead author René Carvajal, MD, of the Department of Neurology-Neuroimmunology, Multiple Sclerosis Centre of Catalonia (Cemcat), Hospital Universitari Vall d’Hebron, Universitat Autònoma de Barcelona, Barcelona, Spain. “This points to potential benefits for patients with highly active MS who require both immunization and high-efficacy therapies that may impact vaccine responses.”
The study was published online in JAMA Network Open.
A Controversial Issue
Today’s high-efficacy therapies for MS may increase the risk of acquiring new infections, reactivate latent pathogens, or worsen ongoing infectious conditions, and immunogenicity of vaccination can be compromised by immunosuppressive agents, particularly CD20 therapies, researchers noted.
As a result, many clinicians opt to delay initiation of such therapies until vaccination schedules are complete to avoid exposure to vaccine-preventable infections. But delaying treatment can potentially affect disease progression.
Reports of disease worsening following vaccination “have raised controversy around vaccine safety,” the authors wrote. The issue is especially relevant to those with highly active MS due to the scarcity of available data in this population.
The motivation for the study “stemmed from the complex balance clinicians face between initiating highly effective therapies promptly in patients with highly active MS and ensuring adequate protection against preventable infections through vaccination,” Dr. Carvajal said.
High Seroprotection Rate
Researchers analyzed data on 60 patients (mean age, 43 years; 44 female; mean disease duration, 17 years) participating in one of two prospectively followed cohorts: The Barcelona Clinically Isolated Syndromes Inception Cohort and the Barcelona Treatment Cohort. Data included demographic, clinical, radiologic, and biological data as well as regular clinical assessments, evaluations of the Expanded Disability Status Scale (EDSS), and MRI scans.
Patients enrolled in the current study had received at least one of these vaccines between September 2016 and February 2022: hepatitis A virus (HAV), hepatitis B virus (HBV; enhanced immunity high load or adjuvanted), or COVID-19 (BNT162b2 [Pfizer-BioNTech], mRAN-1273 [Moderna], or ChAdOx1-S [recombinant; AstraZeneca]).
The researchers conducted a retrospective, self-controlled analysis to compare the annualized relapse rate, EDSS score, and new T2 lesions counts during the 12 months before and after vaccination in patients with short- and long-term treatment duration.
They also compared John Cunningham virus serostatus between the two periods, as well as immunoglobulin G titers for each vaccine.
The global seroprotection rate was 93% (95% CI, 86%-98%). Individual vaccine rates were 92% for HAV, 93% for HBV, and 100% for COVID-19.
There was a significant reduction between the pre- and postvaccination periods in mean relapse rates (P = .004) and median number of new T2 lesions (P = .01).
There were no changes in EDSS scores before and after vaccinations and duration of natalizumab treatment had no impact on safety and immunogenicity.
‘Viable Option’
The researchers used their findings to create a proposed algorithm to inform immunization decisions in patients with highly active MS who require prompt initiation of high-efficacy disease-modifying therapy.
The algorithm is “integrated into a risk-minimization strategy tailored for patients with highly active MS, emphasizing in this case the pivotal role of natalizumab in averting treatment delays and providing adequate protection against potentially severe infections,” Dr. Carvajal said.
Participants who initiated or continued treatment with natalizumab completed their vaccination regimen without any incidents of progressive multifocal leukoencephalopathy (PML) or disease activity rebound following natalizumab discontinuation.
This suggests that using natalizumab for a brief duration might be a “viable option to contemplate,” the authors noted.
Commenting on the findings, Grace Gombolay, MD, assistant professor of pediatrics in the Division of Pediatric Neurology and director of the Pediatric Neuroimmunology and Multiple Sclerosis Clinic, Emory University, Atlanta, Georgia, said the study “demonstrates that vaccines are safe and do not trigger attacks in patients with MS on natalizumab, and that immunity — as measured by antibodies — is preserved in MS patients who receive natalizumab.”
This “contrasts with other treatments, as decreased antibody responses in COVID-19 are noted in certain treatments,” said Dr. Gombolay, who was not part of the study. “If both disease control and immunity against infection are the goals for the patient, then natalizumab is a reasonable option.”
“However, this must be balanced with other considerations,” she added, including the risk for PML and pregnancy.
This study was supported by grants from the European Committee for Treatment and Research in Multiple Sclerosis, Instituto de Salud Carlos III, and the European Union. Dr. Carvajal reported receiving grants from Vall d’Hebron Institut de Recerca and the European Committee for Treatment and Research in Multiple Sclerosis and honoraria from Roche, Novartis, BIIB-Colombia, Merck, and Sanofi outside the submitted work. Dr. Gombolay serves as media editor for Pediatric Neurology and as associate editor of the Annals of the Child Neurology Society. She is also a part-time CDC consultant for acute flaccid myelitis and received an honorarium as a speaker at the Georgia Neurological Society meeting, sponsored by Academic CME and TG Therapeutics.
A version of this article appeared on Medscape.com.
FROM JAMA OPEN NETWORK
Device Uses Sleep Data to Pinpoint Stress Risk
TOPLINE:
Decreased total sleep time (TST) and increased resting heart rate (RHR), heart rate variability (HRV), and average nightly respiratory rate (ARR) as measured by a multisensor device worn during sleep accurately correlated with self-reported stress levels in college students, a new study suggests.
METHODOLOGY:
- First-semester college students (n = 525; aged 18-24 years) enrolled in the Lived Experiences measured Using Rings Study (LEMURS) provided continuous biometric data via a wearable device (Oura Ring; Oura Health) and answered weekly surveys regarding stress levels.
- The researchers used mixed-effects regression models to identify associations between perceived stress scores and average nightly TST, RHR, HRV, and ARR.
TAKEAWAY:
- Consistent associations were found between perceived stress scores and TST, RHR, HRV, and ARR, which persisted even after controlling for gender and week of the semester.
- Risk for moderate to high stress decreased by 38% with every additional hour of TST (P < .01) and by 1.2% with each millisecond increase in HRV (P < .05).
- Moderate to high stress risk increased by 3.6% with each beat-per-minute-increase in RHR (P < .01) and by 23% with each additional breath-per-minute increase in ARR (P < .01).
- Participants who identified as female, nonbinary, or transgender reported significantly higher stress throughout the study.
IN PRACTICE:
“The present work highlights the potential utility of monitoring sleep, suggesting that these measures may identify within individual changes that are concerning for stress. As the demand for mental health services grows, determining which wearable-derived sleep estimates provide information about well-being and can predict worsening mental health in young adults is an important area of study,” study authors wrote.
SOURCE:
The study, led by Laura S.P. Bloomfield, University of Vermont, Burlington, Vermont, was published online in PLOS Digital Health.
LIMITATIONS:
The study focused on raw sleep measures; the researchers suggest that future studies evaluate additional sleep variables (eg, daytime naps), which have been associated with mental health in college students. In addition, the researchers did not have stress or sleep data before participants started college, so they could not assess the impact of starting college on participants’ sleep.
DISCLOSURES:
Bloomfield was supported by the Gund Fellowship and received a partial salary from the Mass Mutual Insurance Wellness Initiative. Other authors’ funding is reported in the original article.
A version of this article appeared on Medscape.com.
TOPLINE:
Decreased total sleep time (TST) and increased resting heart rate (RHR), heart rate variability (HRV), and average nightly respiratory rate (ARR) as measured by a multisensor device worn during sleep accurately correlated with self-reported stress levels in college students, a new study suggests.
METHODOLOGY:
- First-semester college students (n = 525; aged 18-24 years) enrolled in the Lived Experiences measured Using Rings Study (LEMURS) provided continuous biometric data via a wearable device (Oura Ring; Oura Health) and answered weekly surveys regarding stress levels.
- The researchers used mixed-effects regression models to identify associations between perceived stress scores and average nightly TST, RHR, HRV, and ARR.
TAKEAWAY:
- Consistent associations were found between perceived stress scores and TST, RHR, HRV, and ARR, which persisted even after controlling for gender and week of the semester.
- Risk for moderate to high stress decreased by 38% with every additional hour of TST (P < .01) and by 1.2% with each millisecond increase in HRV (P < .05).
- Moderate to high stress risk increased by 3.6% with each beat-per-minute-increase in RHR (P < .01) and by 23% with each additional breath-per-minute increase in ARR (P < .01).
- Participants who identified as female, nonbinary, or transgender reported significantly higher stress throughout the study.
IN PRACTICE:
“The present work highlights the potential utility of monitoring sleep, suggesting that these measures may identify within individual changes that are concerning for stress. As the demand for mental health services grows, determining which wearable-derived sleep estimates provide information about well-being and can predict worsening mental health in young adults is an important area of study,” study authors wrote.
SOURCE:
The study, led by Laura S.P. Bloomfield, University of Vermont, Burlington, Vermont, was published online in PLOS Digital Health.
LIMITATIONS:
The study focused on raw sleep measures; the researchers suggest that future studies evaluate additional sleep variables (eg, daytime naps), which have been associated with mental health in college students. In addition, the researchers did not have stress or sleep data before participants started college, so they could not assess the impact of starting college on participants’ sleep.
DISCLOSURES:
Bloomfield was supported by the Gund Fellowship and received a partial salary from the Mass Mutual Insurance Wellness Initiative. Other authors’ funding is reported in the original article.
A version of this article appeared on Medscape.com.
TOPLINE:
Decreased total sleep time (TST) and increased resting heart rate (RHR), heart rate variability (HRV), and average nightly respiratory rate (ARR) as measured by a multisensor device worn during sleep accurately correlated with self-reported stress levels in college students, a new study suggests.
METHODOLOGY:
- First-semester college students (n = 525; aged 18-24 years) enrolled in the Lived Experiences measured Using Rings Study (LEMURS) provided continuous biometric data via a wearable device (Oura Ring; Oura Health) and answered weekly surveys regarding stress levels.
- The researchers used mixed-effects regression models to identify associations between perceived stress scores and average nightly TST, RHR, HRV, and ARR.
TAKEAWAY:
- Consistent associations were found between perceived stress scores and TST, RHR, HRV, and ARR, which persisted even after controlling for gender and week of the semester.
- Risk for moderate to high stress decreased by 38% with every additional hour of TST (P < .01) and by 1.2% with each millisecond increase in HRV (P < .05).
- Moderate to high stress risk increased by 3.6% with each beat-per-minute-increase in RHR (P < .01) and by 23% with each additional breath-per-minute increase in ARR (P < .01).
- Participants who identified as female, nonbinary, or transgender reported significantly higher stress throughout the study.
IN PRACTICE:
“The present work highlights the potential utility of monitoring sleep, suggesting that these measures may identify within individual changes that are concerning for stress. As the demand for mental health services grows, determining which wearable-derived sleep estimates provide information about well-being and can predict worsening mental health in young adults is an important area of study,” study authors wrote.
SOURCE:
The study, led by Laura S.P. Bloomfield, University of Vermont, Burlington, Vermont, was published online in PLOS Digital Health.
LIMITATIONS:
The study focused on raw sleep measures; the researchers suggest that future studies evaluate additional sleep variables (eg, daytime naps), which have been associated with mental health in college students. In addition, the researchers did not have stress or sleep data before participants started college, so they could not assess the impact of starting college on participants’ sleep.
DISCLOSURES:
Bloomfield was supported by the Gund Fellowship and received a partial salary from the Mass Mutual Insurance Wellness Initiative. Other authors’ funding is reported in the original article.
A version of this article appeared on Medscape.com.
Disadvantaged Neighborhoods Tied to Higher Dementia Risk, Brain Aging
Living in a disadvantaged neighborhood is associated with accelerated brain aging and a higher risk for early dementia, regardless of income level or education, new research suggested.
“If you want to prevent dementia and you’re not asking someone about their neighborhood, you’re missing information that’s important to know,” lead author Aaron Reuben, PhD, postdoctoral scholar in neuropsychology and environmental health at Duke University, Durham, North Carolina, said in a news release.
The study was published online in Alzheimer’s & Dementia.
Higher Risk in Men
Few interventions exist to halt or delay the progression of Alzheimer’s disease and related dementias (ADRD), which has increasingly led to a focus on primary prevention.
Although previous research pointed to a link between socioeconomically disadvantaged neighborhoods and a greater risk for cognitive deficits, mild cognitive impairment, dementia, and poor brain health, the timeline for the emergence of that risk is unknown.
To fill in the gaps, investigators studied data on all 1.4 million New Zealand residents, dividing neighborhoods into quintiles based on level of disadvantage (assessed by the New Zealand Index of Deprivation) to see whether dementia diagnoses followed neighborhood socioeconomic gradients.
After adjusting for covariates, they found that overall, those living in disadvantaged areas were slightly more likely to develop dementia across the 20-year study period (adjusted hazard ratio [HR], 1.09; 95% CI, 1.08-1.10).
The more disadvantaged the neighborhood, the higher the dementia risk, with a 43% higher risk for ADRD among those in the highest quintile than among those in the lowest quintile (HR, 1.43; 95% CI, 1.36-1.49).
The effect was larger in men than in women and in younger vs older individuals, with the youngest age group showing 21% greater risk in women and 26% greater risk in men vs the oldest age group.
Dementia Prevention Starts Early
Researchers then turned to the Dunedin Study, a cohort of 938 New Zealanders (50% female) followed from birth to age 45 to track their psychological, social, and physiological health with brain scans, memory tests, and cognitive self-assessments.
The analysis suggested that by age 45, those living in more disadvantaged neighborhoods across adulthood had accumulated a significantly greater number of midlife risk factors for later ADRD.
They also had worse structural brain integrity, with each standard deviation increase in neighborhood disadvantage resulting in a thinner cortex, greater white matter hyperintensities volume, and older brain age.
Those living in poorer areas had lower cognitive test scores, reported more issues with everyday cognitive function, and showed a greater reduction in IQ from childhood to midlife. Analysis of brain scans also revealed mean brain ages 2.98 years older than those living in the least disadvantaged areas (P = .001).
Limitations included the study’s observational design, which could not establish causation, and the fact that the researchers did not have access to individual-level socioeconomic information for the entire population. Additionally, brain-integrity measures in the Dunedin Study were largely cross-sectional.
“If you want to truly prevent dementia, you’ve got to start early because 20 years before anyone will get a diagnosis, we’re seeing dementia’s emergence,” Dr. Reuben said. “And it could be even earlier.”
Funding for the study was provided by the National Institutes for Health; UK Medical Research Council; Health Research Council of New Zealand; Brain Research New Zealand; New Zealand Ministry of Business, Innovation, & Employment; and the Duke University and the University of North Carolina Alzheimer’s Disease Research Center. The authors declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
Living in a disadvantaged neighborhood is associated with accelerated brain aging and a higher risk for early dementia, regardless of income level or education, new research suggested.
“If you want to prevent dementia and you’re not asking someone about their neighborhood, you’re missing information that’s important to know,” lead author Aaron Reuben, PhD, postdoctoral scholar in neuropsychology and environmental health at Duke University, Durham, North Carolina, said in a news release.
The study was published online in Alzheimer’s & Dementia.
Higher Risk in Men
Few interventions exist to halt or delay the progression of Alzheimer’s disease and related dementias (ADRD), which has increasingly led to a focus on primary prevention.
Although previous research pointed to a link between socioeconomically disadvantaged neighborhoods and a greater risk for cognitive deficits, mild cognitive impairment, dementia, and poor brain health, the timeline for the emergence of that risk is unknown.
To fill in the gaps, investigators studied data on all 1.4 million New Zealand residents, dividing neighborhoods into quintiles based on level of disadvantage (assessed by the New Zealand Index of Deprivation) to see whether dementia diagnoses followed neighborhood socioeconomic gradients.
After adjusting for covariates, they found that overall, those living in disadvantaged areas were slightly more likely to develop dementia across the 20-year study period (adjusted hazard ratio [HR], 1.09; 95% CI, 1.08-1.10).
The more disadvantaged the neighborhood, the higher the dementia risk, with a 43% higher risk for ADRD among those in the highest quintile than among those in the lowest quintile (HR, 1.43; 95% CI, 1.36-1.49).
The effect was larger in men than in women and in younger vs older individuals, with the youngest age group showing 21% greater risk in women and 26% greater risk in men vs the oldest age group.
Dementia Prevention Starts Early
Researchers then turned to the Dunedin Study, a cohort of 938 New Zealanders (50% female) followed from birth to age 45 to track their psychological, social, and physiological health with brain scans, memory tests, and cognitive self-assessments.
The analysis suggested that by age 45, those living in more disadvantaged neighborhoods across adulthood had accumulated a significantly greater number of midlife risk factors for later ADRD.
They also had worse structural brain integrity, with each standard deviation increase in neighborhood disadvantage resulting in a thinner cortex, greater white matter hyperintensities volume, and older brain age.
Those living in poorer areas had lower cognitive test scores, reported more issues with everyday cognitive function, and showed a greater reduction in IQ from childhood to midlife. Analysis of brain scans also revealed mean brain ages 2.98 years older than those living in the least disadvantaged areas (P = .001).
Limitations included the study’s observational design, which could not establish causation, and the fact that the researchers did not have access to individual-level socioeconomic information for the entire population. Additionally, brain-integrity measures in the Dunedin Study were largely cross-sectional.
“If you want to truly prevent dementia, you’ve got to start early because 20 years before anyone will get a diagnosis, we’re seeing dementia’s emergence,” Dr. Reuben said. “And it could be even earlier.”
Funding for the study was provided by the National Institutes for Health; UK Medical Research Council; Health Research Council of New Zealand; Brain Research New Zealand; New Zealand Ministry of Business, Innovation, & Employment; and the Duke University and the University of North Carolina Alzheimer’s Disease Research Center. The authors declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
Living in a disadvantaged neighborhood is associated with accelerated brain aging and a higher risk for early dementia, regardless of income level or education, new research suggested.
“If you want to prevent dementia and you’re not asking someone about their neighborhood, you’re missing information that’s important to know,” lead author Aaron Reuben, PhD, postdoctoral scholar in neuropsychology and environmental health at Duke University, Durham, North Carolina, said in a news release.
The study was published online in Alzheimer’s & Dementia.
Higher Risk in Men
Few interventions exist to halt or delay the progression of Alzheimer’s disease and related dementias (ADRD), which has increasingly led to a focus on primary prevention.
Although previous research pointed to a link between socioeconomically disadvantaged neighborhoods and a greater risk for cognitive deficits, mild cognitive impairment, dementia, and poor brain health, the timeline for the emergence of that risk is unknown.
To fill in the gaps, investigators studied data on all 1.4 million New Zealand residents, dividing neighborhoods into quintiles based on level of disadvantage (assessed by the New Zealand Index of Deprivation) to see whether dementia diagnoses followed neighborhood socioeconomic gradients.
After adjusting for covariates, they found that overall, those living in disadvantaged areas were slightly more likely to develop dementia across the 20-year study period (adjusted hazard ratio [HR], 1.09; 95% CI, 1.08-1.10).
The more disadvantaged the neighborhood, the higher the dementia risk, with a 43% higher risk for ADRD among those in the highest quintile than among those in the lowest quintile (HR, 1.43; 95% CI, 1.36-1.49).
The effect was larger in men than in women and in younger vs older individuals, with the youngest age group showing 21% greater risk in women and 26% greater risk in men vs the oldest age group.
Dementia Prevention Starts Early
Researchers then turned to the Dunedin Study, a cohort of 938 New Zealanders (50% female) followed from birth to age 45 to track their psychological, social, and physiological health with brain scans, memory tests, and cognitive self-assessments.
The analysis suggested that by age 45, those living in more disadvantaged neighborhoods across adulthood had accumulated a significantly greater number of midlife risk factors for later ADRD.
They also had worse structural brain integrity, with each standard deviation increase in neighborhood disadvantage resulting in a thinner cortex, greater white matter hyperintensities volume, and older brain age.
Those living in poorer areas had lower cognitive test scores, reported more issues with everyday cognitive function, and showed a greater reduction in IQ from childhood to midlife. Analysis of brain scans also revealed mean brain ages 2.98 years older than those living in the least disadvantaged areas (P = .001).
Limitations included the study’s observational design, which could not establish causation, and the fact that the researchers did not have access to individual-level socioeconomic information for the entire population. Additionally, brain-integrity measures in the Dunedin Study were largely cross-sectional.
“If you want to truly prevent dementia, you’ve got to start early because 20 years before anyone will get a diagnosis, we’re seeing dementia’s emergence,” Dr. Reuben said. “And it could be even earlier.”
Funding for the study was provided by the National Institutes for Health; UK Medical Research Council; Health Research Council of New Zealand; Brain Research New Zealand; New Zealand Ministry of Business, Innovation, & Employment; and the Duke University and the University of North Carolina Alzheimer’s Disease Research Center. The authors declared no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM ALZHEIMER’S AND DEMENTIA
Stimulants for ADHD Not Linked to Prescription Drug Misuse
TOPLINE:
The use of stimulant therapy by adolescents with attention-deficit/hyperactivity disorder (ADHD) was not associated with later prescription drug misuse (PDM), a new study showed. However, misuse of prescription stimulants during adolescence was associated with significantly higher odds of later PDM.
METHODOLOGY:
- Data came from 11,066 participants in the ongoing Monitoring the Future panel study (baseline cohort years 2005-2017), a multicohort US national longitudinal study of adolescents followed into adulthood, in which procedures and measures are kept consistent across time.
- Participants (ages 17 and 18 years, 51.7% female, 11.2% Black, 15.7% Hispanic, and 59.6% White) completed self-administered questionnaires, with biennial follow-up during young adulthood (ages 19-24 years).
- The questionnaires asked about the number of occasions (if any) in which respondents used a prescription drug (benzodiazepine, opioid, or stimulant) on their own, without a physician’s order.
- Baseline covariates included sex, race, ethnicity, grade point average during high school, parental education, past 2-week binge drinking, past-month cigarette use, and past-year marijuana use, as well as demographic factors.
TAKEAWAY:
- Overall, 9.9% of participants reported lifetime stimulant therapy for ADHD, and 18.6% reported lifetime prescription stimulant misuse at baseline.
- Adolescents who received stimulant therapy for ADHD were less likely to report past-year prescription stimulant misuse as young adults compared with their same-age peers who did not receive stimulant therapy (adjusted odds ratio, 0.71; 95% CI, 0.52-0.99).
- The researchers found no significant differences between adolescents with or without lifetime stimulants in later incidence or prevalence of past-year PDM during young adulthood.
- The most robust predictor of prescription stimulant misuse during young adulthood was prescription stimulant misuse during adolescence; similarly, the most robust predictors of prescription opioid and prescription benzodiazepine misuse during young adulthood were prescription opioid and prescription benzodiazepine misuse (respectively) during adolescence.
IN PRACTICE:
“These findings amplify accumulating evidence suggesting that careful monitoring and screening during adolescence could identify individuals who are at relatively greater risk for PDM and need more comprehensive substance use assessment,” the authors wrote.
SOURCE:
Sean Esteban McCabe, PhD, professor and director, Center for the Study of Drugs, Alcohol, Smoking and Health, University of Michigan School of Nursing, Ann Arbor, was the lead and corresponding author of the study. It was published online on February 7 in Psychiatric Sciences.
LIMITATIONS:
Some subpopulations with higher rates of substance use, including youths who left school before completion and institutionalized populations, were excluded from the study, which may have led to an underestimation of PDM. Moreover, some potential confounders (eg, comorbid psychiatric conditions) were not assessed.
DISCLOSURES:
This study was supported by a research award from the US Food and Drug Administration and research awards from the National Institute on Drug Abuse of the NIH. Dr. McCabe reported no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
The use of stimulant therapy by adolescents with attention-deficit/hyperactivity disorder (ADHD) was not associated with later prescription drug misuse (PDM), a new study showed. However, misuse of prescription stimulants during adolescence was associated with significantly higher odds of later PDM.
METHODOLOGY:
- Data came from 11,066 participants in the ongoing Monitoring the Future panel study (baseline cohort years 2005-2017), a multicohort US national longitudinal study of adolescents followed into adulthood, in which procedures and measures are kept consistent across time.
- Participants (ages 17 and 18 years, 51.7% female, 11.2% Black, 15.7% Hispanic, and 59.6% White) completed self-administered questionnaires, with biennial follow-up during young adulthood (ages 19-24 years).
- The questionnaires asked about the number of occasions (if any) in which respondents used a prescription drug (benzodiazepine, opioid, or stimulant) on their own, without a physician’s order.
- Baseline covariates included sex, race, ethnicity, grade point average during high school, parental education, past 2-week binge drinking, past-month cigarette use, and past-year marijuana use, as well as demographic factors.
TAKEAWAY:
- Overall, 9.9% of participants reported lifetime stimulant therapy for ADHD, and 18.6% reported lifetime prescription stimulant misuse at baseline.
- Adolescents who received stimulant therapy for ADHD were less likely to report past-year prescription stimulant misuse as young adults compared with their same-age peers who did not receive stimulant therapy (adjusted odds ratio, 0.71; 95% CI, 0.52-0.99).
- The researchers found no significant differences between adolescents with or without lifetime stimulants in later incidence or prevalence of past-year PDM during young adulthood.
- The most robust predictor of prescription stimulant misuse during young adulthood was prescription stimulant misuse during adolescence; similarly, the most robust predictors of prescription opioid and prescription benzodiazepine misuse during young adulthood were prescription opioid and prescription benzodiazepine misuse (respectively) during adolescence.
IN PRACTICE:
“These findings amplify accumulating evidence suggesting that careful monitoring and screening during adolescence could identify individuals who are at relatively greater risk for PDM and need more comprehensive substance use assessment,” the authors wrote.
SOURCE:
Sean Esteban McCabe, PhD, professor and director, Center for the Study of Drugs, Alcohol, Smoking and Health, University of Michigan School of Nursing, Ann Arbor, was the lead and corresponding author of the study. It was published online on February 7 in Psychiatric Sciences.
LIMITATIONS:
Some subpopulations with higher rates of substance use, including youths who left school before completion and institutionalized populations, were excluded from the study, which may have led to an underestimation of PDM. Moreover, some potential confounders (eg, comorbid psychiatric conditions) were not assessed.
DISCLOSURES:
This study was supported by a research award from the US Food and Drug Administration and research awards from the National Institute on Drug Abuse of the NIH. Dr. McCabe reported no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.
TOPLINE:
The use of stimulant therapy by adolescents with attention-deficit/hyperactivity disorder (ADHD) was not associated with later prescription drug misuse (PDM), a new study showed. However, misuse of prescription stimulants during adolescence was associated with significantly higher odds of later PDM.
METHODOLOGY:
- Data came from 11,066 participants in the ongoing Monitoring the Future panel study (baseline cohort years 2005-2017), a multicohort US national longitudinal study of adolescents followed into adulthood, in which procedures and measures are kept consistent across time.
- Participants (ages 17 and 18 years, 51.7% female, 11.2% Black, 15.7% Hispanic, and 59.6% White) completed self-administered questionnaires, with biennial follow-up during young adulthood (ages 19-24 years).
- The questionnaires asked about the number of occasions (if any) in which respondents used a prescription drug (benzodiazepine, opioid, or stimulant) on their own, without a physician’s order.
- Baseline covariates included sex, race, ethnicity, grade point average during high school, parental education, past 2-week binge drinking, past-month cigarette use, and past-year marijuana use, as well as demographic factors.
TAKEAWAY:
- Overall, 9.9% of participants reported lifetime stimulant therapy for ADHD, and 18.6% reported lifetime prescription stimulant misuse at baseline.
- Adolescents who received stimulant therapy for ADHD were less likely to report past-year prescription stimulant misuse as young adults compared with their same-age peers who did not receive stimulant therapy (adjusted odds ratio, 0.71; 95% CI, 0.52-0.99).
- The researchers found no significant differences between adolescents with or without lifetime stimulants in later incidence or prevalence of past-year PDM during young adulthood.
- The most robust predictor of prescription stimulant misuse during young adulthood was prescription stimulant misuse during adolescence; similarly, the most robust predictors of prescription opioid and prescription benzodiazepine misuse during young adulthood were prescription opioid and prescription benzodiazepine misuse (respectively) during adolescence.
IN PRACTICE:
“These findings amplify accumulating evidence suggesting that careful monitoring and screening during adolescence could identify individuals who are at relatively greater risk for PDM and need more comprehensive substance use assessment,” the authors wrote.
SOURCE:
Sean Esteban McCabe, PhD, professor and director, Center for the Study of Drugs, Alcohol, Smoking and Health, University of Michigan School of Nursing, Ann Arbor, was the lead and corresponding author of the study. It was published online on February 7 in Psychiatric Sciences.
LIMITATIONS:
Some subpopulations with higher rates of substance use, including youths who left school before completion and institutionalized populations, were excluded from the study, which may have led to an underestimation of PDM. Moreover, some potential confounders (eg, comorbid psychiatric conditions) were not assessed.
DISCLOSURES:
This study was supported by a research award from the US Food and Drug Administration and research awards from the National Institute on Drug Abuse of the NIH. Dr. McCabe reported no relevant financial relationships. The other authors’ disclosures are listed in the original paper.
A version of this article appeared on Medscape.com.