User login
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Time-based billing allows hospitalists to avoid
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
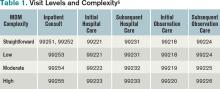
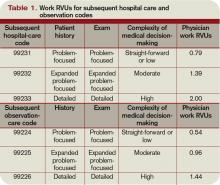
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
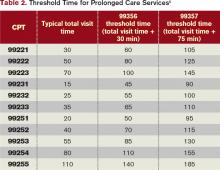
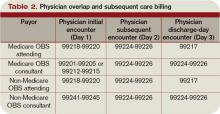
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Medical Decision-Making Factors Include Quantity of Information, Complexity
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
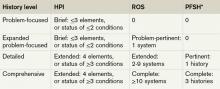
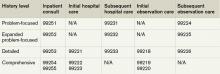
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Physicians should formulate a complete and accurate description of a patient’s condition with an equivalent plan of care for each encounter. While acuity and severity can be inferred by healthcare professionals without excessive detail or repetitive documentation of previously entered information, adequate documentation for every service date assists in conveying patient complexity during medical record review.
Regardless of how complex a patient’s condition might be, physicians tend to undervalue their services. This is due, in part, to the routine nature of patient care for seasoned physicians; it is also due in part to a general lack of understanding with respect to the documentation guidelines.
Consider the following scenario: A 68-year-old male with diabetes and a history of chronic obstructive bronchitis was hospitalized after a five-day history of progressive cough with increasing purulent sputum, shortness of breath, and fever. He was treated for an exacerbation of chronic bronchitis within the past six weeks. Upon admission, the patient had an increased temperature (102°F), increased heart rate (96 beats per minute), and increased respiratory rate (28 shallow breaths per minute). His breath sounds included in the right lower lobe rhonchi, and his pulse oximetry was 89% on room air. Chest X-ray confirmed right lower lobe infiltrates along with chronic changes.
Although some physicians would consider this “low complexity” due to the frequency in which they encounter this type of case, others will more appropriately identify this as moderately complex.
MDM Categories
Medical decision-making (MDM) remains consistent in both the 1995 and 1997 guidelines.1,2 Complexity is categorized as straightforward, low, moderate, or high, based on the content of physician documentation. Each visit level is associated with a particular level of complexity. Only the care plan for a given date of service is considered when assigning MDM complexity. For each encounter, the physician receives credit for the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality (see Table 1).
Number of diagnoses or treatment options. Physicians should document problems addressed and managed daily despite any changes to the treatment plan. Credit is provided for each problem with an associated plan, even if the plan states “continue treatment.” Credit also depends upon the quantity of problems addressed, as well as the problem type. An established problem in which the care plan has been established by the physician or group practice member during the current hospitalization is less complex than a new problem for which a diagnosis, prognosis, or plan has not been determined. Severity of the problem affects the weight of complexity. A worsening problem is more complex than an improving problem. Physician documentation should:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined;
- Indicate the management/treatment option(s) for each problem; and
- When documentation indicates a continuation of current management options (e.g. “continue meds”), be sure that the management options to be continued are noted somewhere in the progress note for that encounter (e.g. medication list).
The plan of care outlines problems that the physician personally manages and those that impact management options, even if another physician directly oversees the problem. For example, the hospitalist might primarily manage diabetes, while the pulmonologist manages pneumonia. Since the pneumonia may impact the hospitalist’s plan for diabetic management, the hospitalist can receive credit for the pneumonia diagnosis if there is a non-overlapping, hospitalist-related care plan or comment about the pneumonia.
Amount and/or complexity of data ordered/reviewed. “Data” is classified as pathology/laboratory testing, radiology, and medicine-based diagnostics. Pertinent orders or results could be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note. To receive credit:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Document test review by including a brief entry in the progress note (e.g. “elevated glucose levels” or “CXR shows RLL infiltrates”);
- Summarize key points when reviewing old records or obtaining history from someone other than the patient, as necessary;
- Indicate when images, tracings, or specimens are “personally reviewed”; and
- Summarize any discussions of unexpected or contradictory test results with the physician performing the procedure or diagnostic study.
Risks of complication and/or morbidity or mortality. Risk involves the patient’s presenting problem, diagnostic procedures ordered, and management options selected. It is measured as minimal, low, moderate, or high when compared with corresponding items assigned to each risk level (see Table 2). The highest individual item detected on the table determines the overall patient risk for that encounter.
Chronic conditions and invasive procedures pose more risk than acute, uncomplicated illnesses or non-invasive procedures. Stable or improving problems are not as menacing as progressing problems; minor exacerbations are less hazardous than severe exacerbations; and medication risk varies with the type and potential for adverse effects. A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change. Physicians should:
- Status all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), when applicable;
- Document all diagnostic or therapeutic procedures considered;
- Identify surgical risk factors involving comorbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding medication (e.g. “Continue Coumadin, monitor PT/INR”).
Determining complexity of medical decision-making. The final complexity of MDM depends upon the second-highest MDM category. The physician does not have to meet the requirements for all three MDM categories. For example, if a physician satisfies the requirements for a “multiple” number of diagnoses/treatment options, “limited” data, and “high” risk, the physician achieves moderate complexity decision-making (see Table 3). Remember that decision-making is just one of three components in evaluation and management services, along with history and exam.
Beware of payor variation, as it could have a significant impact on visit-level selection.3 Become acquainted with rules applicable to the geographical area. Review insurer websites for guidelines, policies, and “frequently asked questions” that can help improve documentation skills and support billing practices.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Nov. 14, 2011.
- Centers for Medicare and Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Nov. 14, 2011.
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
Exam Guidelines
The extent of the exam should correspond to the nature of the presenting problem, the standard of care, and the physicians’ clinical judgment. Remember, medical necessity issues can arise if the physician performs and submits a claim for a comprehensive service involving a self-limiting problem. The easiest way to demonstrate the medical necessity for evaluation and management (E/M) services is through medical decision-making. It prevents a third party from making accusations that a Level 5 service was reported solely based upon a comprehensive history and examination that was not warranted by the patient’s presenting problem (e.g. the common cold).1
1995 Exam Guidelines
The 1995 guidelines differentiate 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory, gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).2 Physicians are permitted to perform and comment without mandate, as appropriate, but with a few minor directives:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems.
- Elaborate abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Documentation Guidelines
The 1997 guidelines are formatted as organ systems with corresponding, bulleted items referred to as “elements.”3 Additionally, a few elements have a numeric requirement to be achieved before satisfying the documentation of that particular element. For example, credit for the “vital signs element” (located within the constitutional system) is only awarded after documentation of three individual measurements (e.g. blood pressure, heart rate, and respiratory rate). Failure to document the specified criterion (e.g. two measurements: “blood pressure and heart rate only,” or a single nonspecific comment: “vital signs stable”) leads to failure to assign credit.
Take note that these specified criterion do not resonate within the 1995 guidelines. Numerical requirements also are indicated for the lymphatic system. The physician must examine and document findings associated with two or more lymphatic areas (e.g. “no lymphadenopathy noted in the neck or axillae”).
In the absence of numeric criterion, some elements contain multiple components, which require documentation of at least one component. For example, one listed psychiatric element designates the assessment of the patient’s “mood and affect.” The physician receives credit for a comment regarding the patient’s mood (e.g. “appears depressed”) without identification of a flat (or normal).
The 1997 Documentation Guide-lines comprise the following systems and elements:
Constitutional
- Measurement of any three of the following seven vital signs:
- Sitting or standing blood pressure;
- Supine blood pressure;
- Pulse rate and regularity;
- Respiration;
- Temperature;
- Height; or
- Weight (can be measured and recorded by ancillary staff).
- General appearance of patient (e.g. development, nutrition, body habitus, deformities, attention to grooming)
Eyes
- Inspection of conjunctivae and lids;
- Examination of pupils and irises (e.g. reaction to light and accommodation, size, symmetry); and
- Ophthalmoscopic examination of optic discs (e.g. size, C/D ratio, appearance) and posterior segments (e.g. vessel changes, exudates, hemorrhages).
Ears, Nose, Mouth, and Throat
- External inspection of ears and nose (e.g. overall appearance, scars, lesions, masses);
- Otoscopic examination of external auditory canals and tympanic membranes;
- Assessment of hearing (e.g. whispered voice, finger rub, tuning fork);
- Inspection of nasal mucosa, septum, and turbinates;
- Inspection of lips, teeth, and gums; and
- Examination of oropharynx: oral mucosa, salivary glands, hard and soft palates, tongue, tonsils, and posterior pharynx.
Neck
- Examination of neck (e.g. masses, overall appearance, symmetry, tracheal position, crepitus); and
- Examination of thyroid (e.g. enlargement, tenderness, mass).
Respiratory
- Assessment of respiratory effort (e.g. intercostal retractions, use of accessory muscles, diaphragmatic movement);
- Percussion of chest (e.g. dullness, flatness, hyperresonance);
- Palpation of chest (e.g. tactile fremitus); and
- Auscultation of lungs (e.g. breath sounds, adventitious sounds, rubs).
Cardiovascular
- Palpation of heart (e.g. location, size, thrills);
- Auscultation of heart with notation of abnormal sounds and murmurs; and
- Examination of:
- Carotid arteries (e.g. pulse amplitude, bruits);
- Abdominal aorta (e.g. size, bruits);
- Femoral arteries (e.g. pulse amplitude, bruits);
- Pedal pulses (e.g. pulse amplitude); and
- Extremities for edema and/or varicosities.
Chest
- Inspection of breasts (e.g. symmetry, nipple discharge); and
- Palpation of breasts and axillae (e.g. masses or lumps, tenderness).
Gastrointestinal
- Examination of abdomen with notation of presence of masses or tenderness;
- Examination of liver and spleen;
- Examination for presence or absence of hernia;
- Examination (when indicated) of anus, perineum, and rectum, including sphincter tone, presence of hemorrhoids, and rectal masses; and
- Obtain stool sample for occult blood test when indicated.
Genitourinary (Male)
- Examination of the scrotal contents (e.g. hydrocele, spermatocele, tenderness of cord, testicular mass);
- Examination of the penis; and
- Digital rectal examination of prostate gland (e.g. size, symmetry, nodularity, tenderness).
Genitourinary (Female)
- Pelvic examination (with or without specimen collection for smears and cultures), including:
- Examination of external genitalia (e.g. general appearance, hair distribution, lesions) and vagina (e.g. general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, rectocele);
- Examination of urethra (e.g. masses, tenderness, scarring);
- Examination of bladder (e.g. fullness, masses, tenderness);
- Cervix (e.g. general appearance, lesions, discharge);
- Uterus (e.g. size, contour, position, mobility, tenderness, consistency, descent or support); and
- Adnexa/parametria (e.g. masses, tenderness, organomegaly, nodularity).
- Lymphatic Palpation of lymph nodes in two or more areas: Neck, axillae, groin, other.
Musculoskeletal
- Examination of gait and station;
- Inspection and/or palpation of digits and nails (e.g. clubbing, cyanosis, inflammatory conditions, petechiae, ischemia, infections, nodes);
- Examination of joints, bones and muscles of one or more of the following six areas:
- head and neck;
- spine, ribs and pelvis;
- right upper extremity;
- left upper extremity;
- right lower extremity; and
- left lower extremity.
The examination of a given area includes:
- Inspection and/or palpation with notation of presence of any misalignment, asymmetry, crepitation, defects, tenderness, masses, effusions;
- Assessment of range of motion with notation of any pain, crepitation or contracture;
- Assessment of stability with notation of any dislocation (luxation), subluxation or laxity; and
- Assessment of muscle strength and tone (e.g. flaccid, cog wheel, spastic) with notation of any atrophy or abnormal movements.
Skin
- Inspection of skin and subcutaneous tissue (e.g. rashes, lesions, ulcers); and
- Palpation of skin and subcutaneous tissue (e.g. induration, subcutaneous nodules, tightening).
Neurologic
- Test cranial nerves with notation of any deficits;
- Examination of deep tendon reflexes with notation of pathological reflexes (e.g. Babinski); and
- Examination of sensation (e.g. by touch, pin, vibration, proprioception).
Psychiatric
- Description of patient’s judgment and insight;
- Brief assessment of mental status, including:
- Orientation to time, place, and person;
- Recent and remote memory; and
- Mood and affect (e.g. depression, anxiety, agitation).
Considerations
The 1997 Documentation Guidelines often are criticized for their “specific” nature. Although this assists the auditor, it hinders the physician. The consequence is difficulty and frustration with remembering the explicit comments and number of elements associated with each level of exam. As a solution, consider documentation templates—paper or electronic—that incorporate cues and prompts for normal exam findings with adequate space for elaboration of abnormal findings.
Remember that both sets of guidelines apply to visit level selection, and physicians may utilize either set when documenting their services. Auditors will review documentation with each of the guidelines, and assign the final audited result as the highest visit level supported during the comparison. Physicians should use the set that is best for their patients, practice, and peace of mind.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, Ill.: American College of Chest Physicians; 2009:87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Sept. 12, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Sept. 12, 2011.
- Highmark Medicare Services. Frequently Asked Questions: Evaluation And Management Services (Part B). Available at: http://www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html#10. Accessed Sept. 14, 2011.
- Centers for Medicare & Medicaid Services. Transmittal 2282: Clarification of Evaluation and Management Payment Policy. Available at: http://www.cms.gov/transmittals/downloads/R2282CP.pdf. Accessed Sept. 15, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
The extent of the exam should correspond to the nature of the presenting problem, the standard of care, and the physicians’ clinical judgment. Remember, medical necessity issues can arise if the physician performs and submits a claim for a comprehensive service involving a self-limiting problem. The easiest way to demonstrate the medical necessity for evaluation and management (E/M) services is through medical decision-making. It prevents a third party from making accusations that a Level 5 service was reported solely based upon a comprehensive history and examination that was not warranted by the patient’s presenting problem (e.g. the common cold).1
1995 Exam Guidelines
The 1995 guidelines differentiate 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory, gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).2 Physicians are permitted to perform and comment without mandate, as appropriate, but with a few minor directives:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems.
- Elaborate abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Documentation Guidelines
The 1997 guidelines are formatted as organ systems with corresponding, bulleted items referred to as “elements.”3 Additionally, a few elements have a numeric requirement to be achieved before satisfying the documentation of that particular element. For example, credit for the “vital signs element” (located within the constitutional system) is only awarded after documentation of three individual measurements (e.g. blood pressure, heart rate, and respiratory rate). Failure to document the specified criterion (e.g. two measurements: “blood pressure and heart rate only,” or a single nonspecific comment: “vital signs stable”) leads to failure to assign credit.
Take note that these specified criterion do not resonate within the 1995 guidelines. Numerical requirements also are indicated for the lymphatic system. The physician must examine and document findings associated with two or more lymphatic areas (e.g. “no lymphadenopathy noted in the neck or axillae”).
In the absence of numeric criterion, some elements contain multiple components, which require documentation of at least one component. For example, one listed psychiatric element designates the assessment of the patient’s “mood and affect.” The physician receives credit for a comment regarding the patient’s mood (e.g. “appears depressed”) without identification of a flat (or normal).
The 1997 Documentation Guide-lines comprise the following systems and elements:
Constitutional
- Measurement of any three of the following seven vital signs:
- Sitting or standing blood pressure;
- Supine blood pressure;
- Pulse rate and regularity;
- Respiration;
- Temperature;
- Height; or
- Weight (can be measured and recorded by ancillary staff).
- General appearance of patient (e.g. development, nutrition, body habitus, deformities, attention to grooming)
Eyes
- Inspection of conjunctivae and lids;
- Examination of pupils and irises (e.g. reaction to light and accommodation, size, symmetry); and
- Ophthalmoscopic examination of optic discs (e.g. size, C/D ratio, appearance) and posterior segments (e.g. vessel changes, exudates, hemorrhages).
Ears, Nose, Mouth, and Throat
- External inspection of ears and nose (e.g. overall appearance, scars, lesions, masses);
- Otoscopic examination of external auditory canals and tympanic membranes;
- Assessment of hearing (e.g. whispered voice, finger rub, tuning fork);
- Inspection of nasal mucosa, septum, and turbinates;
- Inspection of lips, teeth, and gums; and
- Examination of oropharynx: oral mucosa, salivary glands, hard and soft palates, tongue, tonsils, and posterior pharynx.
Neck
- Examination of neck (e.g. masses, overall appearance, symmetry, tracheal position, crepitus); and
- Examination of thyroid (e.g. enlargement, tenderness, mass).
Respiratory
- Assessment of respiratory effort (e.g. intercostal retractions, use of accessory muscles, diaphragmatic movement);
- Percussion of chest (e.g. dullness, flatness, hyperresonance);
- Palpation of chest (e.g. tactile fremitus); and
- Auscultation of lungs (e.g. breath sounds, adventitious sounds, rubs).
Cardiovascular
- Palpation of heart (e.g. location, size, thrills);
- Auscultation of heart with notation of abnormal sounds and murmurs; and
- Examination of:
- Carotid arteries (e.g. pulse amplitude, bruits);
- Abdominal aorta (e.g. size, bruits);
- Femoral arteries (e.g. pulse amplitude, bruits);
- Pedal pulses (e.g. pulse amplitude); and
- Extremities for edema and/or varicosities.
Chest
- Inspection of breasts (e.g. symmetry, nipple discharge); and
- Palpation of breasts and axillae (e.g. masses or lumps, tenderness).
Gastrointestinal
- Examination of abdomen with notation of presence of masses or tenderness;
- Examination of liver and spleen;
- Examination for presence or absence of hernia;
- Examination (when indicated) of anus, perineum, and rectum, including sphincter tone, presence of hemorrhoids, and rectal masses; and
- Obtain stool sample for occult blood test when indicated.
Genitourinary (Male)
- Examination of the scrotal contents (e.g. hydrocele, spermatocele, tenderness of cord, testicular mass);
- Examination of the penis; and
- Digital rectal examination of prostate gland (e.g. size, symmetry, nodularity, tenderness).
Genitourinary (Female)
- Pelvic examination (with or without specimen collection for smears and cultures), including:
- Examination of external genitalia (e.g. general appearance, hair distribution, lesions) and vagina (e.g. general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, rectocele);
- Examination of urethra (e.g. masses, tenderness, scarring);
- Examination of bladder (e.g. fullness, masses, tenderness);
- Cervix (e.g. general appearance, lesions, discharge);
- Uterus (e.g. size, contour, position, mobility, tenderness, consistency, descent or support); and
- Adnexa/parametria (e.g. masses, tenderness, organomegaly, nodularity).
- Lymphatic Palpation of lymph nodes in two or more areas: Neck, axillae, groin, other.
Musculoskeletal
- Examination of gait and station;
- Inspection and/or palpation of digits and nails (e.g. clubbing, cyanosis, inflammatory conditions, petechiae, ischemia, infections, nodes);
- Examination of joints, bones and muscles of one or more of the following six areas:
- head and neck;
- spine, ribs and pelvis;
- right upper extremity;
- left upper extremity;
- right lower extremity; and
- left lower extremity.
The examination of a given area includes:
- Inspection and/or palpation with notation of presence of any misalignment, asymmetry, crepitation, defects, tenderness, masses, effusions;
- Assessment of range of motion with notation of any pain, crepitation or contracture;
- Assessment of stability with notation of any dislocation (luxation), subluxation or laxity; and
- Assessment of muscle strength and tone (e.g. flaccid, cog wheel, spastic) with notation of any atrophy or abnormal movements.
Skin
- Inspection of skin and subcutaneous tissue (e.g. rashes, lesions, ulcers); and
- Palpation of skin and subcutaneous tissue (e.g. induration, subcutaneous nodules, tightening).
Neurologic
- Test cranial nerves with notation of any deficits;
- Examination of deep tendon reflexes with notation of pathological reflexes (e.g. Babinski); and
- Examination of sensation (e.g. by touch, pin, vibration, proprioception).
Psychiatric
- Description of patient’s judgment and insight;
- Brief assessment of mental status, including:
- Orientation to time, place, and person;
- Recent and remote memory; and
- Mood and affect (e.g. depression, anxiety, agitation).
Considerations
The 1997 Documentation Guidelines often are criticized for their “specific” nature. Although this assists the auditor, it hinders the physician. The consequence is difficulty and frustration with remembering the explicit comments and number of elements associated with each level of exam. As a solution, consider documentation templates—paper or electronic—that incorporate cues and prompts for normal exam findings with adequate space for elaboration of abnormal findings.
Remember that both sets of guidelines apply to visit level selection, and physicians may utilize either set when documenting their services. Auditors will review documentation with each of the guidelines, and assign the final audited result as the highest visit level supported during the comparison. Physicians should use the set that is best for their patients, practice, and peace of mind.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, Ill.: American College of Chest Physicians; 2009:87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Sept. 12, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Sept. 12, 2011.
- Highmark Medicare Services. Frequently Asked Questions: Evaluation And Management Services (Part B). Available at: http://www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html#10. Accessed Sept. 14, 2011.
- Centers for Medicare & Medicaid Services. Transmittal 2282: Clarification of Evaluation and Management Payment Policy. Available at: http://www.cms.gov/transmittals/downloads/R2282CP.pdf. Accessed Sept. 15, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
The extent of the exam should correspond to the nature of the presenting problem, the standard of care, and the physicians’ clinical judgment. Remember, medical necessity issues can arise if the physician performs and submits a claim for a comprehensive service involving a self-limiting problem. The easiest way to demonstrate the medical necessity for evaluation and management (E/M) services is through medical decision-making. It prevents a third party from making accusations that a Level 5 service was reported solely based upon a comprehensive history and examination that was not warranted by the patient’s presenting problem (e.g. the common cold).1
1995 Exam Guidelines
The 1995 guidelines differentiate 10 body areas (head and face; neck; chest, breast, and axillae; abdomen; genitalia, groin, and buttocks; back and spine; right upper extremity; left upper extremity; right lower extremity; and left lower extremity) from 12 organ systems (constitutional; eyes; ears, nose, mouth, and throat; cardiovascular; respiratory, gastrointestinal; genitourinary; musculoskeletal; integumentary; neurological; psychiatric; hematologic, lymphatic, and immunologic).2 Physicians are permitted to perform and comment without mandate, as appropriate, but with a few minor directives:
- Document relevant negative findings. Commenting that a system or area is “negative” or “normal” is acceptable when referring to unaffected areas or asymptomatic organ systems.
- Elaborate abnormal findings. Commenting that a system or area is “abnormal” is not sufficient unless additional comments describing the abnormality are documented.
1997 Documentation Guidelines
The 1997 guidelines are formatted as organ systems with corresponding, bulleted items referred to as “elements.”3 Additionally, a few elements have a numeric requirement to be achieved before satisfying the documentation of that particular element. For example, credit for the “vital signs element” (located within the constitutional system) is only awarded after documentation of three individual measurements (e.g. blood pressure, heart rate, and respiratory rate). Failure to document the specified criterion (e.g. two measurements: “blood pressure and heart rate only,” or a single nonspecific comment: “vital signs stable”) leads to failure to assign credit.
Take note that these specified criterion do not resonate within the 1995 guidelines. Numerical requirements also are indicated for the lymphatic system. The physician must examine and document findings associated with two or more lymphatic areas (e.g. “no lymphadenopathy noted in the neck or axillae”).
In the absence of numeric criterion, some elements contain multiple components, which require documentation of at least one component. For example, one listed psychiatric element designates the assessment of the patient’s “mood and affect.” The physician receives credit for a comment regarding the patient’s mood (e.g. “appears depressed”) without identification of a flat (or normal).
The 1997 Documentation Guide-lines comprise the following systems and elements:
Constitutional
- Measurement of any three of the following seven vital signs:
- Sitting or standing blood pressure;
- Supine blood pressure;
- Pulse rate and regularity;
- Respiration;
- Temperature;
- Height; or
- Weight (can be measured and recorded by ancillary staff).
- General appearance of patient (e.g. development, nutrition, body habitus, deformities, attention to grooming)
Eyes
- Inspection of conjunctivae and lids;
- Examination of pupils and irises (e.g. reaction to light and accommodation, size, symmetry); and
- Ophthalmoscopic examination of optic discs (e.g. size, C/D ratio, appearance) and posterior segments (e.g. vessel changes, exudates, hemorrhages).
Ears, Nose, Mouth, and Throat
- External inspection of ears and nose (e.g. overall appearance, scars, lesions, masses);
- Otoscopic examination of external auditory canals and tympanic membranes;
- Assessment of hearing (e.g. whispered voice, finger rub, tuning fork);
- Inspection of nasal mucosa, septum, and turbinates;
- Inspection of lips, teeth, and gums; and
- Examination of oropharynx: oral mucosa, salivary glands, hard and soft palates, tongue, tonsils, and posterior pharynx.
Neck
- Examination of neck (e.g. masses, overall appearance, symmetry, tracheal position, crepitus); and
- Examination of thyroid (e.g. enlargement, tenderness, mass).
Respiratory
- Assessment of respiratory effort (e.g. intercostal retractions, use of accessory muscles, diaphragmatic movement);
- Percussion of chest (e.g. dullness, flatness, hyperresonance);
- Palpation of chest (e.g. tactile fremitus); and
- Auscultation of lungs (e.g. breath sounds, adventitious sounds, rubs).
Cardiovascular
- Palpation of heart (e.g. location, size, thrills);
- Auscultation of heart with notation of abnormal sounds and murmurs; and
- Examination of:
- Carotid arteries (e.g. pulse amplitude, bruits);
- Abdominal aorta (e.g. size, bruits);
- Femoral arteries (e.g. pulse amplitude, bruits);
- Pedal pulses (e.g. pulse amplitude); and
- Extremities for edema and/or varicosities.
Chest
- Inspection of breasts (e.g. symmetry, nipple discharge); and
- Palpation of breasts and axillae (e.g. masses or lumps, tenderness).
Gastrointestinal
- Examination of abdomen with notation of presence of masses or tenderness;
- Examination of liver and spleen;
- Examination for presence or absence of hernia;
- Examination (when indicated) of anus, perineum, and rectum, including sphincter tone, presence of hemorrhoids, and rectal masses; and
- Obtain stool sample for occult blood test when indicated.
Genitourinary (Male)
- Examination of the scrotal contents (e.g. hydrocele, spermatocele, tenderness of cord, testicular mass);
- Examination of the penis; and
- Digital rectal examination of prostate gland (e.g. size, symmetry, nodularity, tenderness).
Genitourinary (Female)
- Pelvic examination (with or without specimen collection for smears and cultures), including:
- Examination of external genitalia (e.g. general appearance, hair distribution, lesions) and vagina (e.g. general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, rectocele);
- Examination of urethra (e.g. masses, tenderness, scarring);
- Examination of bladder (e.g. fullness, masses, tenderness);
- Cervix (e.g. general appearance, lesions, discharge);
- Uterus (e.g. size, contour, position, mobility, tenderness, consistency, descent or support); and
- Adnexa/parametria (e.g. masses, tenderness, organomegaly, nodularity).
- Lymphatic Palpation of lymph nodes in two or more areas: Neck, axillae, groin, other.
Musculoskeletal
- Examination of gait and station;
- Inspection and/or palpation of digits and nails (e.g. clubbing, cyanosis, inflammatory conditions, petechiae, ischemia, infections, nodes);
- Examination of joints, bones and muscles of one or more of the following six areas:
- head and neck;
- spine, ribs and pelvis;
- right upper extremity;
- left upper extremity;
- right lower extremity; and
- left lower extremity.
The examination of a given area includes:
- Inspection and/or palpation with notation of presence of any misalignment, asymmetry, crepitation, defects, tenderness, masses, effusions;
- Assessment of range of motion with notation of any pain, crepitation or contracture;
- Assessment of stability with notation of any dislocation (luxation), subluxation or laxity; and
- Assessment of muscle strength and tone (e.g. flaccid, cog wheel, spastic) with notation of any atrophy or abnormal movements.
Skin
- Inspection of skin and subcutaneous tissue (e.g. rashes, lesions, ulcers); and
- Palpation of skin and subcutaneous tissue (e.g. induration, subcutaneous nodules, tightening).
Neurologic
- Test cranial nerves with notation of any deficits;
- Examination of deep tendon reflexes with notation of pathological reflexes (e.g. Babinski); and
- Examination of sensation (e.g. by touch, pin, vibration, proprioception).
Psychiatric
- Description of patient’s judgment and insight;
- Brief assessment of mental status, including:
- Orientation to time, place, and person;
- Recent and remote memory; and
- Mood and affect (e.g. depression, anxiety, agitation).
Considerations
The 1997 Documentation Guidelines often are criticized for their “specific” nature. Although this assists the auditor, it hinders the physician. The consequence is difficulty and frustration with remembering the explicit comments and number of elements associated with each level of exam. As a solution, consider documentation templates—paper or electronic—that incorporate cues and prompts for normal exam findings with adequate space for elaboration of abnormal findings.
Remember that both sets of guidelines apply to visit level selection, and physicians may utilize either set when documenting their services. Auditors will review documentation with each of the guidelines, and assign the final audited result as the highest visit level supported during the comparison. Physicians should use the set that is best for their patients, practice, and peace of mind.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, Ill.: American College of Chest Physicians; 2009:87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.gov/MLNProducts/Downloads/1995dg.pdf. Accessed Sept. 12, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. Available at: http://www.cms.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed Sept. 12, 2011.
- Highmark Medicare Services. Frequently Asked Questions: Evaluation And Management Services (Part B). Available at: http://www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html#10. Accessed Sept. 14, 2011.
- Centers for Medicare & Medicaid Services. Transmittal 2282: Clarification of Evaluation and Management Payment Policy. Available at: http://www.cms.gov/transmittals/downloads/R2282CP.pdf. Accessed Sept. 15, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011:1-20.
A Brief History
Each visit category and level of service has corresponding documentation requirements.1 Selecting an evaluation and management (E/M) level is based upon 1) the content of the three “key” components: history, exam, and decision-making, or 2) time, but only when counseling or coordination of care dominates more than 50% of the physician’s total visit time. Failure to document any essential element in a given visit level (e.g. family history required but missing for 99222 and 99223) could result in downcoding or service denial. Be aware of what an auditor expects when reviewing the key component of “history.”
Documentation Options
Auditors recognize two sets of documentation guidelines: “1995” and “1997” guidelines.2,3,4 Each set of guidelines has received valid criticism. The 1995 guidelines undoubtedly are vague and subjective in some areas, whereas the 1997 guidelines are known for arduous specificity.
However, to benefit all physicians and specialties, both sets of guidelines apply to visit-level selection. In other words, physicians can utilize either set when documenting their services, and auditors must review provider records against both styles. The final audited outcome reflects the highest visit level supported upon comparison.
Elements of History2,3,4
Chief complaint. The chief complaint (CC) is the reason for the visit, as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
History of present illness (HPI). The HPI is a description of the patient’s present illness as it developed. It characteristically is referenced as location, quality, severity, timing, context, modifying factors, and associated signs/symptoms, as related to the chief complaint. The 1997 guidelines allow physicians to receive HPI credit for providing the status of the patient’s chronic or inactive conditions, such as “extrinsic asthma without acute exacerbation in past six months.” An auditor will not assign HPI credit to a chronic or inactive condition that does not have a corresponding status (e.g. “asthma”). This will be considered “past medical history.”
The HPI is classified as brief (a comment on <3 HPI elements, or the status of <2 conditions) or extended (a comment on >4 HPI elements, or the status of >3 conditions). Consider these examples of an extended HPI:
- “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90.” (Status of three chronic conditions.)
Physicians receive credit for confirming and personally documenting the HPI, or linking to documentation recorded by residents (residents, fellows, interns) or nonphysician providers (NPPs) when performing services according to the Teaching Physician Rules or Split-Shared Billing Rules, respectively. An auditor will not assign physician credit for HPI elements documented by ancillary staff (registered nurses, medical assistants) or students.
Review of systems (ROS). The ROS is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient: constitutional; eyes, ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/ lymphatic; and allergic/immunologic. Auditors classify the ROS as brief (a comment on one system), extended (a comment on two to nine systems), or complete (a comment on >10 systems). Physicians can document a complete ROS by noting individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal); and occasional runny nose (ears, nose, mouth, throat),” or by eliciting a complete system review but documenting only the positive and pertinent negative findings related to the chief complaint, along with an additional comment that “all other systems are negative.”
Although the latter method is formally included in Medicare’s documentation guidelines and accepted by some Medicare contractors (e.g. Highmark, WPS), be aware that it is not universally accepted.5,6
Documentation involving the ROS can be provided by anyone, including the patient. The physician should reference ROS information that is completed by individuals other than residents or NPPs during services provided under the Teaching Physician Rules or Split-Shared Billing Rules. Physician duplication of ROS information is unnecessary unless an update or revision is required.
Past, family, and social history (PFSH). The PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH could be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). The physician merely needs a single comment associated with each history for the PFSH to be regarded as complete. Refrain from using “noncontributory” to describe any of the histories, as previous misuse of this term has resulted in its prohibition. An example of a complete PFSH documentation includes: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
Similar to the ROS, PFSH documentation can be provided by anyone, including the patient, and the physician should reference the documented PFSH in his own progress note. Redocumentation of the PFSH is not necessary unless a revision is required.
PFSH documentation is only required for initial care services (i.e. initial hospital care, initial observation care, consultations). It is not warranted in subsequent care services unless additional, pertinent information is obtained during the hospital stay that impacts care.
Considerations
When a physician cannot elicit historical information from the patient directly, and no other source is available, they should document “unable to obtain” the history. A comment regarding the circumstances surrounding this problem (e.g. patient confused, no caregiver present) should be provided, along with the available information from the limited resources (e.g. emergency medical technicians, previous hospitalizations at the same facility). Some contractors will not penalize the physician for the inability to ascertain complete historical information, as long as a proven attempt to obtain the information is evident.
Never document any item for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed July 7, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed July 7, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
- History of E/M (Q&As). WPS Health Insurance website. Available at: http://www.wpsmedicare.com/j5macpartb/resources/provider_types/2009_0526_emqahistory.shtml. Accessed July 11, 2011.
- Frequently Asked Questions: Evaluation and Management Services (Part B). Highmark Medicare Services website. Available at: www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed on July 11, 2011.
Each visit category and level of service has corresponding documentation requirements.1 Selecting an evaluation and management (E/M) level is based upon 1) the content of the three “key” components: history, exam, and decision-making, or 2) time, but only when counseling or coordination of care dominates more than 50% of the physician’s total visit time. Failure to document any essential element in a given visit level (e.g. family history required but missing for 99222 and 99223) could result in downcoding or service denial. Be aware of what an auditor expects when reviewing the key component of “history.”
Documentation Options
Auditors recognize two sets of documentation guidelines: “1995” and “1997” guidelines.2,3,4 Each set of guidelines has received valid criticism. The 1995 guidelines undoubtedly are vague and subjective in some areas, whereas the 1997 guidelines are known for arduous specificity.
However, to benefit all physicians and specialties, both sets of guidelines apply to visit-level selection. In other words, physicians can utilize either set when documenting their services, and auditors must review provider records against both styles. The final audited outcome reflects the highest visit level supported upon comparison.
Elements of History2,3,4
Chief complaint. The chief complaint (CC) is the reason for the visit, as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
History of present illness (HPI). The HPI is a description of the patient’s present illness as it developed. It characteristically is referenced as location, quality, severity, timing, context, modifying factors, and associated signs/symptoms, as related to the chief complaint. The 1997 guidelines allow physicians to receive HPI credit for providing the status of the patient’s chronic or inactive conditions, such as “extrinsic asthma without acute exacerbation in past six months.” An auditor will not assign HPI credit to a chronic or inactive condition that does not have a corresponding status (e.g. “asthma”). This will be considered “past medical history.”
The HPI is classified as brief (a comment on <3 HPI elements, or the status of <2 conditions) or extended (a comment on >4 HPI elements, or the status of >3 conditions). Consider these examples of an extended HPI:
- “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90.” (Status of three chronic conditions.)
Physicians receive credit for confirming and personally documenting the HPI, or linking to documentation recorded by residents (residents, fellows, interns) or nonphysician providers (NPPs) when performing services according to the Teaching Physician Rules or Split-Shared Billing Rules, respectively. An auditor will not assign physician credit for HPI elements documented by ancillary staff (registered nurses, medical assistants) or students.
Review of systems (ROS). The ROS is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient: constitutional; eyes, ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/ lymphatic; and allergic/immunologic. Auditors classify the ROS as brief (a comment on one system), extended (a comment on two to nine systems), or complete (a comment on >10 systems). Physicians can document a complete ROS by noting individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal); and occasional runny nose (ears, nose, mouth, throat),” or by eliciting a complete system review but documenting only the positive and pertinent negative findings related to the chief complaint, along with an additional comment that “all other systems are negative.”
Although the latter method is formally included in Medicare’s documentation guidelines and accepted by some Medicare contractors (e.g. Highmark, WPS), be aware that it is not universally accepted.5,6
Documentation involving the ROS can be provided by anyone, including the patient. The physician should reference ROS information that is completed by individuals other than residents or NPPs during services provided under the Teaching Physician Rules or Split-Shared Billing Rules. Physician duplication of ROS information is unnecessary unless an update or revision is required.
Past, family, and social history (PFSH). The PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH could be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). The physician merely needs a single comment associated with each history for the PFSH to be regarded as complete. Refrain from using “noncontributory” to describe any of the histories, as previous misuse of this term has resulted in its prohibition. An example of a complete PFSH documentation includes: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
Similar to the ROS, PFSH documentation can be provided by anyone, including the patient, and the physician should reference the documented PFSH in his own progress note. Redocumentation of the PFSH is not necessary unless a revision is required.
PFSH documentation is only required for initial care services (i.e. initial hospital care, initial observation care, consultations). It is not warranted in subsequent care services unless additional, pertinent information is obtained during the hospital stay that impacts care.
Considerations
When a physician cannot elicit historical information from the patient directly, and no other source is available, they should document “unable to obtain” the history. A comment regarding the circumstances surrounding this problem (e.g. patient confused, no caregiver present) should be provided, along with the available information from the limited resources (e.g. emergency medical technicians, previous hospitalizations at the same facility). Some contractors will not penalize the physician for the inability to ascertain complete historical information, as long as a proven attempt to obtain the information is evident.
Never document any item for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed July 7, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed July 7, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
- History of E/M (Q&As). WPS Health Insurance website. Available at: http://www.wpsmedicare.com/j5macpartb/resources/provider_types/2009_0526_emqahistory.shtml. Accessed July 11, 2011.
- Frequently Asked Questions: Evaluation and Management Services (Part B). Highmark Medicare Services website. Available at: www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed on July 11, 2011.
Each visit category and level of service has corresponding documentation requirements.1 Selecting an evaluation and management (E/M) level is based upon 1) the content of the three “key” components: history, exam, and decision-making, or 2) time, but only when counseling or coordination of care dominates more than 50% of the physician’s total visit time. Failure to document any essential element in a given visit level (e.g. family history required but missing for 99222 and 99223) could result in downcoding or service denial. Be aware of what an auditor expects when reviewing the key component of “history.”
Documentation Options
Auditors recognize two sets of documentation guidelines: “1995” and “1997” guidelines.2,3,4 Each set of guidelines has received valid criticism. The 1995 guidelines undoubtedly are vague and subjective in some areas, whereas the 1997 guidelines are known for arduous specificity.
However, to benefit all physicians and specialties, both sets of guidelines apply to visit-level selection. In other words, physicians can utilize either set when documenting their services, and auditors must review provider records against both styles. The final audited outcome reflects the highest visit level supported upon comparison.
Elements of History2,3,4
Chief complaint. The chief complaint (CC) is the reason for the visit, as stated in the patient’s own words. Every encounter, regardless of visit type, must include a CC. The physician must personally document and/or validate the CC with reference to a specific condition or symptom (e.g. patient complains of abdominal pain).
History of present illness (HPI). The HPI is a description of the patient’s present illness as it developed. It characteristically is referenced as location, quality, severity, timing, context, modifying factors, and associated signs/symptoms, as related to the chief complaint. The 1997 guidelines allow physicians to receive HPI credit for providing the status of the patient’s chronic or inactive conditions, such as “extrinsic asthma without acute exacerbation in past six months.” An auditor will not assign HPI credit to a chronic or inactive condition that does not have a corresponding status (e.g. “asthma”). This will be considered “past medical history.”
The HPI is classified as brief (a comment on <3 HPI elements, or the status of <2 conditions) or extended (a comment on >4 HPI elements, or the status of >3 conditions). Consider these examples of an extended HPI:
- “The patient has intermittent (duration), sharp (quality) pain in the right upper quadrant (location) without associated nausea, vomiting, or diarrhea (associated signs/symptoms).”
- “Diabetes controlled by oral medication; hyperlipidemia stable on simvastatin with increased dietary efforts; hypertension stable with pressures ranging from 130-140/80-90.” (Status of three chronic conditions.)
Physicians receive credit for confirming and personally documenting the HPI, or linking to documentation recorded by residents (residents, fellows, interns) or nonphysician providers (NPPs) when performing services according to the Teaching Physician Rules or Split-Shared Billing Rules, respectively. An auditor will not assign physician credit for HPI elements documented by ancillary staff (registered nurses, medical assistants) or students.
Review of systems (ROS). The ROS is a series of questions used to elicit information about additional signs, symptoms, or problems currently or previously experienced by the patient: constitutional; eyes, ears, nose, mouth, throat; cardiovascular; respiratory; gastrointestinal; genitourinary; musculoskeletal; integumentary (including skin and/or breast); neurological; psychiatric; endocrine; hematologic/ lymphatic; and allergic/immunologic. Auditors classify the ROS as brief (a comment on one system), extended (a comment on two to nine systems), or complete (a comment on >10 systems). Physicians can document a complete ROS by noting individual systems: “no fever/chills (constitutional) or blurred vision (eyes); no chest pain (cardiovascular) or shortness of breath (respiratory); intermittent nausea (gastrointestinal); and occasional runny nose (ears, nose, mouth, throat),” or by eliciting a complete system review but documenting only the positive and pertinent negative findings related to the chief complaint, along with an additional comment that “all other systems are negative.”
Although the latter method is formally included in Medicare’s documentation guidelines and accepted by some Medicare contractors (e.g. Highmark, WPS), be aware that it is not universally accepted.5,6
Documentation involving the ROS can be provided by anyone, including the patient. The physician should reference ROS information that is completed by individuals other than residents or NPPs during services provided under the Teaching Physician Rules or Split-Shared Billing Rules. Physician duplication of ROS information is unnecessary unless an update or revision is required.
Past, family, and social history (PFSH). The PFSH involves data obtained about the patient’s previous illness or medical conditions/therapies, family occurrences with illness, and relevant patient activities. The PFSH could be classified as pertinent (a comment on one history) or complete (a comment in each of the three histories). The physician merely needs a single comment associated with each history for the PFSH to be regarded as complete. Refrain from using “noncontributory” to describe any of the histories, as previous misuse of this term has resulted in its prohibition. An example of a complete PFSH documentation includes: “Patient currently on Prilosec 20 mg daily; family history of Barrett’s esophagus; no tobacco or alcohol use.”
Similar to the ROS, PFSH documentation can be provided by anyone, including the patient, and the physician should reference the documented PFSH in his own progress note. Redocumentation of the PFSH is not necessary unless a revision is required.
PFSH documentation is only required for initial care services (i.e. initial hospital care, initial observation care, consultations). It is not warranted in subsequent care services unless additional, pertinent information is obtained during the hospital stay that impacts care.
Considerations
When a physician cannot elicit historical information from the patient directly, and no other source is available, they should document “unable to obtain” the history. A comment regarding the circumstances surrounding this problem (e.g. patient confused, no caregiver present) should be provided, along with the available information from the limited resources (e.g. emergency medical technicians, previous hospitalizations at the same facility). Some contractors will not penalize the physician for the inability to ascertain complete historical information, as long as a proven attempt to obtain the information is evident.
Never document any item for the purpose of “getting paid.” Only document information that is clinically relevant, lends to the quality of care provided, or demonstrates the delivery of healthcare services. This prevents accusations of fraud and abuse, promotes billing compliance, and supports medical necessity for the services provided.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Pohlig, C. Documentation and Coding Evaluation and Management Services. In: Coding for Chest Medicine 2010. Northbrook, IL: American College of Chest Physicians, 2009; 87-118.
- Centers for Medicare & Medicaid Services. 1995 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf. Accessed July 7, 2011.
- Centers for Medicare & Medicaid Services. 1997 Documentation Guidelines for Evaluation & Management Services. CMS website. Available at: http://www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.pdf. Accessed July 7, 2011.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
- History of E/M (Q&As). WPS Health Insurance website. Available at: http://www.wpsmedicare.com/j5macpartb/resources/provider_types/2009_0526_emqahistory.shtml. Accessed July 11, 2011.
- Frequently Asked Questions: Evaluation and Management Services (Part B). Highmark Medicare Services website. Available at: www.highmarkmedicareservices.com/faq/partb/pet/lpet-evaluation_management_services.html. Accessed on July 11, 2011.
Academic Institutions
Hospitalists work in many types of facilities, including academic centers that utilize residents (including interns) in healthcare delivery. Medical and surgical services furnished by a resident within the scope of the training program are covered as provider services and paid by Medicare through direct Graduate Medical Education (GME) and Indirect Medical Education (IME) payments; the services of the resident may not be billed or paid for using the Medicare Physician Fee Schedule.
Similarly, the teaching physician is not paid for the resident’s work. The teaching physician is paid for their participation in patient care. In other words, payment is provided to the teaching physician for services that are:
- Furnished by a physician who is not a resident; or
- Furnished by a resident with a teaching physician physically present during the critical or key portion(s) of the service.
Teaching physicians participate in evaluation and management (E/M) services with residents in several ways. Consider the following teaching physician scenarios:
Scenario 1: “Stand-Alone” Service
The resident sees a patient in the morning. The teaching physician independently sees the patient later that same day, performing all required elements to support their own bill (e.g. 99233: subsequent hospital care, per day, which requires at least two of these three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making). When documenting, the teaching physician can write their own note with or without any of the residents’ information. The attending note “stands alone” in support of the reported visit level. Alternatively, the teaching physician might “link to” the resident note, instead of personally redocumenting the entire service.
Appropriate documentation includes teaching physician notation of the provided critical or key portion(s) of the service and the involvement in patient management. The visit level is based upon the combined documentation, both teaching physician and resident.
Using Medicare-approved linkage statements will ensure compliance with teaching physician rules. Examples:
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of the above linkage statements is acceptable, and “more is always better.” The last example best identifies the teaching physician’s involvement in patient management and best supports other regulatory goals and quality initiatives of the current healthcare environment.
Scenario 2: “Supervised” Service
The resident and the teaching physician see the patient at the same time. The teaching physician supervises the resident’s performance of the required service elements or personally performs elements separate from those completed by the resident. Despite personal supervision, the attending still must document their presence during the encounter, performance of the critical or key portion(s) of the service, and involvement in patient management. The visit level is based upon the combined documentation.
Medicare-accepted teaching physician statements associated with this scenario include:
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
These generalized statements will be accepted for billing under teaching physician rules. However, documenting patient-specific elements of the assessment and plan unequivocally demonstrates teaching- physician involvement in patient care and the quality of care provided.
Scenario 3: The “Shared” Service
The resident performs a portion or all of the required service elements without teaching-physician presence and documents this service. The teaching physician then independently performs only the critical or key portion(s) of the service and, as appropriate, discusses the case with the resident. As in the other scenarios, the attending documents the presence and performance of the critical or key portion(s) of the service, as well as involvement in patient management. The teaching physician selects the visit level based upon the combined documentation of the teaching physician and resident.
Such Medicare-approved statements for use by teaching physicians under this scenario include:
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Regardless of the timing between the attending and the resident encounter represented in each scenario, the teaching physician cannot “link to” a resident note that has not been written. More specifically, if the resident’s note has not been documented at the time the teaching physician writes their note, the teaching physician can’t link to the resident’s note or consider it for billing purposes.
Time-Based Exception
Time-based E/M services (e.g. critical-care services, discharge-day management, prolonged care, etc.) do not follow the same guideline as the standard E/M services, which are selected upon the level of history, exam, and decision-making. Only the billing provider’s time counts toward the reported visit level. This means that the teaching physician must be present for the entire period of time for which the claim is made. Documentation should identify the teaching physician’s total visit time (spent on the unit/floor for inpatient services), including face-to-face time with the patient. Time spent by the resident without the presence of the teaching physician does not count toward the teaching physician’s reported time. Additionally, time spent “teaching” the resident cannot be attributed to the teaching physician’s visit time.
Student Notes
Per Medicare guidelines, students (medical, nurse practitioner, etc.) can document services in the medical record. However, the teaching physician can only refer to medical student documentation associated with the review of systems and/or past/family/social history. The teaching physician cannot refer to a student’s documentation of physical exam findings or medical decision-making.
If the medical student documents E/M services, the teaching physician must verify and redocument the history of present illness, as well as perform and redocument the physical exam and medical decision-making activities of the service. The teaching physician then selects the visit level and documents service. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Guidelines for Teaching Physicians, Interns, Residents. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed May 6, 2011.
- Medicare Claims Processing Manual: Chapter 12, Section 100. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2011.
- Medicare Benefit Policy Manual: Chapter 15, Section 30.2. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed May 6, 2011.
- Manaker, S. Teaching Physician Regulations. In: Coding for Chest Medicine 2008. Northbrook, IL: American College of Chest Physicians, 2008; 279-285.
- Pohlig, C. Evaluation & Management Services: An Overview. In: Coding for Chest Medicine 2011. Northbrook, IL: American College of Chest Physicians, 2010; 323-330.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists work in many types of facilities, including academic centers that utilize residents (including interns) in healthcare delivery. Medical and surgical services furnished by a resident within the scope of the training program are covered as provider services and paid by Medicare through direct Graduate Medical Education (GME) and Indirect Medical Education (IME) payments; the services of the resident may not be billed or paid for using the Medicare Physician Fee Schedule.
Similarly, the teaching physician is not paid for the resident’s work. The teaching physician is paid for their participation in patient care. In other words, payment is provided to the teaching physician for services that are:
- Furnished by a physician who is not a resident; or
- Furnished by a resident with a teaching physician physically present during the critical or key portion(s) of the service.
Teaching physicians participate in evaluation and management (E/M) services with residents in several ways. Consider the following teaching physician scenarios:
Scenario 1: “Stand-Alone” Service
The resident sees a patient in the morning. The teaching physician independently sees the patient later that same day, performing all required elements to support their own bill (e.g. 99233: subsequent hospital care, per day, which requires at least two of these three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making). When documenting, the teaching physician can write their own note with or without any of the residents’ information. The attending note “stands alone” in support of the reported visit level. Alternatively, the teaching physician might “link to” the resident note, instead of personally redocumenting the entire service.
Appropriate documentation includes teaching physician notation of the provided critical or key portion(s) of the service and the involvement in patient management. The visit level is based upon the combined documentation, both teaching physician and resident.
Using Medicare-approved linkage statements will ensure compliance with teaching physician rules. Examples:
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of the above linkage statements is acceptable, and “more is always better.” The last example best identifies the teaching physician’s involvement in patient management and best supports other regulatory goals and quality initiatives of the current healthcare environment.
Scenario 2: “Supervised” Service
The resident and the teaching physician see the patient at the same time. The teaching physician supervises the resident’s performance of the required service elements or personally performs elements separate from those completed by the resident. Despite personal supervision, the attending still must document their presence during the encounter, performance of the critical or key portion(s) of the service, and involvement in patient management. The visit level is based upon the combined documentation.
Medicare-accepted teaching physician statements associated with this scenario include:
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
These generalized statements will be accepted for billing under teaching physician rules. However, documenting patient-specific elements of the assessment and plan unequivocally demonstrates teaching- physician involvement in patient care and the quality of care provided.
Scenario 3: The “Shared” Service
The resident performs a portion or all of the required service elements without teaching-physician presence and documents this service. The teaching physician then independently performs only the critical or key portion(s) of the service and, as appropriate, discusses the case with the resident. As in the other scenarios, the attending documents the presence and performance of the critical or key portion(s) of the service, as well as involvement in patient management. The teaching physician selects the visit level based upon the combined documentation of the teaching physician and resident.
Such Medicare-approved statements for use by teaching physicians under this scenario include:
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Regardless of the timing between the attending and the resident encounter represented in each scenario, the teaching physician cannot “link to” a resident note that has not been written. More specifically, if the resident’s note has not been documented at the time the teaching physician writes their note, the teaching physician can’t link to the resident’s note or consider it for billing purposes.
Time-Based Exception
Time-based E/M services (e.g. critical-care services, discharge-day management, prolonged care, etc.) do not follow the same guideline as the standard E/M services, which are selected upon the level of history, exam, and decision-making. Only the billing provider’s time counts toward the reported visit level. This means that the teaching physician must be present for the entire period of time for which the claim is made. Documentation should identify the teaching physician’s total visit time (spent on the unit/floor for inpatient services), including face-to-face time with the patient. Time spent by the resident without the presence of the teaching physician does not count toward the teaching physician’s reported time. Additionally, time spent “teaching” the resident cannot be attributed to the teaching physician’s visit time.
Student Notes
Per Medicare guidelines, students (medical, nurse practitioner, etc.) can document services in the medical record. However, the teaching physician can only refer to medical student documentation associated with the review of systems and/or past/family/social history. The teaching physician cannot refer to a student’s documentation of physical exam findings or medical decision-making.
If the medical student documents E/M services, the teaching physician must verify and redocument the history of present illness, as well as perform and redocument the physical exam and medical decision-making activities of the service. The teaching physician then selects the visit level and documents service. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Guidelines for Teaching Physicians, Interns, Residents. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed May 6, 2011.
- Medicare Claims Processing Manual: Chapter 12, Section 100. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2011.
- Medicare Benefit Policy Manual: Chapter 15, Section 30.2. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed May 6, 2011.
- Manaker, S. Teaching Physician Regulations. In: Coding for Chest Medicine 2008. Northbrook, IL: American College of Chest Physicians, 2008; 279-285.
- Pohlig, C. Evaluation & Management Services: An Overview. In: Coding for Chest Medicine 2011. Northbrook, IL: American College of Chest Physicians, 2010; 323-330.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists work in many types of facilities, including academic centers that utilize residents (including interns) in healthcare delivery. Medical and surgical services furnished by a resident within the scope of the training program are covered as provider services and paid by Medicare through direct Graduate Medical Education (GME) and Indirect Medical Education (IME) payments; the services of the resident may not be billed or paid for using the Medicare Physician Fee Schedule.
Similarly, the teaching physician is not paid for the resident’s work. The teaching physician is paid for their participation in patient care. In other words, payment is provided to the teaching physician for services that are:
- Furnished by a physician who is not a resident; or
- Furnished by a resident with a teaching physician physically present during the critical or key portion(s) of the service.
Teaching physicians participate in evaluation and management (E/M) services with residents in several ways. Consider the following teaching physician scenarios:
Scenario 1: “Stand-Alone” Service
The resident sees a patient in the morning. The teaching physician independently sees the patient later that same day, performing all required elements to support their own bill (e.g. 99233: subsequent hospital care, per day, which requires at least two of these three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making). When documenting, the teaching physician can write their own note with or without any of the residents’ information. The attending note “stands alone” in support of the reported visit level. Alternatively, the teaching physician might “link to” the resident note, instead of personally redocumenting the entire service.
Appropriate documentation includes teaching physician notation of the provided critical or key portion(s) of the service and the involvement in patient management. The visit level is based upon the combined documentation, both teaching physician and resident.
Using Medicare-approved linkage statements will ensure compliance with teaching physician rules. Examples:
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of the above linkage statements is acceptable, and “more is always better.” The last example best identifies the teaching physician’s involvement in patient management and best supports other regulatory goals and quality initiatives of the current healthcare environment.
Scenario 2: “Supervised” Service
The resident and the teaching physician see the patient at the same time. The teaching physician supervises the resident’s performance of the required service elements or personally performs elements separate from those completed by the resident. Despite personal supervision, the attending still must document their presence during the encounter, performance of the critical or key portion(s) of the service, and involvement in patient management. The visit level is based upon the combined documentation.
Medicare-accepted teaching physician statements associated with this scenario include:
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
These generalized statements will be accepted for billing under teaching physician rules. However, documenting patient-specific elements of the assessment and plan unequivocally demonstrates teaching- physician involvement in patient care and the quality of care provided.
Scenario 3: The “Shared” Service
The resident performs a portion or all of the required service elements without teaching-physician presence and documents this service. The teaching physician then independently performs only the critical or key portion(s) of the service and, as appropriate, discusses the case with the resident. As in the other scenarios, the attending documents the presence and performance of the critical or key portion(s) of the service, as well as involvement in patient management. The teaching physician selects the visit level based upon the combined documentation of the teaching physician and resident.
Such Medicare-approved statements for use by teaching physicians under this scenario include:
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Regardless of the timing between the attending and the resident encounter represented in each scenario, the teaching physician cannot “link to” a resident note that has not been written. More specifically, if the resident’s note has not been documented at the time the teaching physician writes their note, the teaching physician can’t link to the resident’s note or consider it for billing purposes.
Time-Based Exception
Time-based E/M services (e.g. critical-care services, discharge-day management, prolonged care, etc.) do not follow the same guideline as the standard E/M services, which are selected upon the level of history, exam, and decision-making. Only the billing provider’s time counts toward the reported visit level. This means that the teaching physician must be present for the entire period of time for which the claim is made. Documentation should identify the teaching physician’s total visit time (spent on the unit/floor for inpatient services), including face-to-face time with the patient. Time spent by the resident without the presence of the teaching physician does not count toward the teaching physician’s reported time. Additionally, time spent “teaching” the resident cannot be attributed to the teaching physician’s visit time.
Student Notes
Per Medicare guidelines, students (medical, nurse practitioner, etc.) can document services in the medical record. However, the teaching physician can only refer to medical student documentation associated with the review of systems and/or past/family/social history. The teaching physician cannot refer to a student’s documentation of physical exam findings or medical decision-making.
If the medical student documents E/M services, the teaching physician must verify and redocument the history of present illness, as well as perform and redocument the physical exam and medical decision-making activities of the service. The teaching physician then selects the visit level and documents service. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Guidelines for Teaching Physicians, Interns, Residents. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed May 6, 2011.
- Medicare Claims Processing Manual: Chapter 12, Section 100. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2011.
- Medicare Benefit Policy Manual: Chapter 15, Section 30.2. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed May 6, 2011.
- Manaker, S. Teaching Physician Regulations. In: Coding for Chest Medicine 2008. Northbrook, IL: American College of Chest Physicians, 2008; 279-285.
- Pohlig, C. Evaluation & Management Services: An Overview. In: Coding for Chest Medicine 2011. Northbrook, IL: American College of Chest Physicians, 2010; 323-330.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2011.
Due Diligence: Denials
Before submitting a claim, hospitalists should ensure that the service is rendered, that it is completely and accurately documented in the medical record, that the correct information is entered on the claim form, and that it is a covered benefit and eligible for payment.
Although the latter two elements typically are delegated to the billing team, hospitalists should encourage or request feedback regarding payment and denials. The ensuing open dialogue between physicians and billers might prove helpful in understanding and resolving future billing issues. Less-experienced billers first respond to claim denials by submitting documentation (i.e. “appeal with paper”) despite the inappropriateness of this action. If the denial is upheld, this attempt is viewed as unsuccessful and, without further consideration, “written off.” However, careful examination of the payor’s initial claim determination could elicit a more suitable response.
Service Provider
Provider enrollment issues can sidetrack claim submissions. Physicians must register their NPI (national provider identifier) with the correct practice location and group assignment, particularly when previously practicing physicians join a new group practice. Failure to do so is an infrequent, yet valid, cause for denial.
Alternatively, enrollment issues play a greater role when services involve nurse practitioners (NPs) and physician assistants (PAs) who are enrolled with Medicare but might be prohibited from enrolling with other payors. For example, an NP independently provides subsequent hospital care (e.g. 99232) to a Medicare beneficiary. The claim is submitted in the NP’s name and reimbursed at the correct amount by Medicare as the primary insurer. The remaining balance is submitted to the secondary insurer, who does not enroll NPPs. The claim is rejected. If the physician group has a contractual agreement to recognize NPP services by reporting them under the collaborating physician’s name, the claim can be resubmitted in the physician’s name. In absence of such an agreement, the claim should be written off.
Location
The place of service (POS) must match the reported service/procedure code. For example, a hospitalist is asked to see a patient in the ED. The patient requires further testing but does not meet the criterion for an inpatient stay. The hospitalist admits the patient to observation, treats him, and discharges him to home.
Hospitalists need to avoid the common mistake of mismatching the service code with the location/POS. Observation services performed by the “physician of record” should be reported with the corresponding codes: initial observation care (99218-99220), subsequent observation care (99224-99226), or observation discharge (99217), as appropriate.1 The correct POS should be reported as outpatient hospital (POS 22), not inpatient hospital (POS 21). Trying to report outpatient codes with an inpatient POS will result in claim denial.
A similar denial occurs when trying to report inpatient codes (99231-99233) in an outpatient location (e.g. 23-ED). These denials require claim resubmission with the correct POS and/or service/procedure code. A complete list of POS codes and corresponding definitions can be obtained from Chapter 26, Section 10.5 of the Medicare Claims Processing Manual, available at www.cms.hhs.gov/manuals/downloads/clm104c26.pdf.
Diagnosis
Denials involving diagnoses produce issues of “medical necessity.”1 Examine these denials carefully. Consider the service/procedure code when trying to formulate a response to the denial. The diagnosis code represents the reason for the service or procedure and might be a sign, symptom, or condition with which the patient presents. Medicare reimburses for procedures and services that are deemed “reasonable and necessary.”
In an effort to unify standards, Medicare has developed national coverage determinations (NCDs) to identify coverage requirements for frequent or problematic procedures or services. These coverage requirements can identify specific conditions (i.e. ICD-9-CM codes) for which the services or procedures are considered medically necessary. In the absence of a national coverage policy, an item or service could be covered at the discretion of Medicare contractors based on a local coverage determination (LCD), which varies by contractor.
Medical necessity denials often involve a mismatched or missing diagnosis. For example, a payor might deny a claim for cardiopulmonary resuscitation (92950) that is associated with a diagnosis code of congestive heart failure (428.0), despite this being the underlying condition that prompted the decline in the patient’s condition. The payor might only accept “cardiac arrest” (427.5) as the “medically necessary” diagnosis for cardiopulmonary resuscitation, as this is the direct reason necessitating the procedure. After reviewing the documentation to ensure that the documentation supports the diagnosis, the claim can be resubmitted with a confirmed and corrected diagnosis code.
Initial-Request Response
While diagnoses can lead to medical necessity issues, not all medical necessity denials are due to incorrect diagnoses. Some “medical necessity” denials result from a failure to respond to a payor request. More specifically, if the “medical necessity” denial involves a covered evaluation and management visit, the denial is more likely the result of a failure to respond to a prepayment request for documentation.
Medicare typically issues prepayment requests for documentation for the following inpatient CPT codes: 99223, 99233, 99232, 99239, and 99292.1 If the documentation is not provided to the Medicare review department within a designated time frame (e.g. 30-45 days), the claim is automatically denied. The reason for denial is cited as being “not deemed a medical necessity.” These claims do not require electronic resubmission, and instead require submission of documentation to the Medicare appeals department. Once the supporting documentation is reviewed, reimbursement is issued.
Supportive Documentation
There are times when payor requests for additional information or documentation is handled in a timely fashion. However, the paper submission might have been incomplete, as the encounter note itself might not contain the cumulative information representing the reported service.
For example, other pieces of pertinent information may be obtained from the data or order section of the chart. If the individual responsible for gathering the requested documentation does not review it before submission, important or referenced entries may be missed, and the complexity of the billed service might be sacrificed. The provider should submit any entry with the same date as the requested documentation in support: labs, diagnostic testing, physician orders, patient instructions, nursing notes, resident notes, notes by other physicians in the same group, discharge summaries, etc.
Legibility of the encounter note is crucial when the documentation is sent for review. Most reviewers will seek another reviewer’s assistance in translating, but they are not obligated to do this. If the note is deemed incomprehensible, the service is denied, resulting in a nonpayment or a refund. Electronic medical records (EMRs) are assisting physicians and other providers with legibility issues and improving review findings. If a physician is still writing notes by hand, a transcription might be sent along with the documentation to prevent unnecessary denials. Only consider this for requests involving providers with problematic handwriting. A legible signature is required. If a denial ensues in absence of a signature, the provider can submit an appeal with an acceptable attestation.
Modifier Considerations
Some services are denied for being “incidental/integral” to another reimbursed service (i.e. bundled). Payors implement electronic payment edits that disallow separate payment for “related” services. The industry standard, known as the National Correct Coding Initiative (NCCI), identifies code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When a claim is denied for this reason, billers tend to automatically and erroneously resubmit the claim with a modifier appended to the disallowed or “bundled” procedure code. Documentation should be reviewed to determine if the denied service is separately reportable from the paid service. The biller might append the appropriate modifier and resubmit the claim only when well supported by documentation.
For example, the hospitalist evaluated a patient with congestive heart failure and pleural effusions. The hospitalist determined that the patient requires placement of a central venous catheter (36556). Because the patient’s underlying condition was evaluated, and resulted in the decision to place a catheter, both the visit (99233) and the procedure (36556) can be reported. If submitted without modifiers, some payors will deny payment for the visit for being integral to the catheter placement. In this case, the claim should be resubmitted with modifier 25 appended to the visit. Payors might still require documentation review to ensure legitimacy of this modifier before the claim is paid. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Reference
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: AMA Press; 2011.
Before submitting a claim, hospitalists should ensure that the service is rendered, that it is completely and accurately documented in the medical record, that the correct information is entered on the claim form, and that it is a covered benefit and eligible for payment.
Although the latter two elements typically are delegated to the billing team, hospitalists should encourage or request feedback regarding payment and denials. The ensuing open dialogue between physicians and billers might prove helpful in understanding and resolving future billing issues. Less-experienced billers first respond to claim denials by submitting documentation (i.e. “appeal with paper”) despite the inappropriateness of this action. If the denial is upheld, this attempt is viewed as unsuccessful and, without further consideration, “written off.” However, careful examination of the payor’s initial claim determination could elicit a more suitable response.
Service Provider
Provider enrollment issues can sidetrack claim submissions. Physicians must register their NPI (national provider identifier) with the correct practice location and group assignment, particularly when previously practicing physicians join a new group practice. Failure to do so is an infrequent, yet valid, cause for denial.
Alternatively, enrollment issues play a greater role when services involve nurse practitioners (NPs) and physician assistants (PAs) who are enrolled with Medicare but might be prohibited from enrolling with other payors. For example, an NP independently provides subsequent hospital care (e.g. 99232) to a Medicare beneficiary. The claim is submitted in the NP’s name and reimbursed at the correct amount by Medicare as the primary insurer. The remaining balance is submitted to the secondary insurer, who does not enroll NPPs. The claim is rejected. If the physician group has a contractual agreement to recognize NPP services by reporting them under the collaborating physician’s name, the claim can be resubmitted in the physician’s name. In absence of such an agreement, the claim should be written off.
Location
The place of service (POS) must match the reported service/procedure code. For example, a hospitalist is asked to see a patient in the ED. The patient requires further testing but does not meet the criterion for an inpatient stay. The hospitalist admits the patient to observation, treats him, and discharges him to home.
Hospitalists need to avoid the common mistake of mismatching the service code with the location/POS. Observation services performed by the “physician of record” should be reported with the corresponding codes: initial observation care (99218-99220), subsequent observation care (99224-99226), or observation discharge (99217), as appropriate.1 The correct POS should be reported as outpatient hospital (POS 22), not inpatient hospital (POS 21). Trying to report outpatient codes with an inpatient POS will result in claim denial.
A similar denial occurs when trying to report inpatient codes (99231-99233) in an outpatient location (e.g. 23-ED). These denials require claim resubmission with the correct POS and/or service/procedure code. A complete list of POS codes and corresponding definitions can be obtained from Chapter 26, Section 10.5 of the Medicare Claims Processing Manual, available at www.cms.hhs.gov/manuals/downloads/clm104c26.pdf.
Diagnosis
Denials involving diagnoses produce issues of “medical necessity.”1 Examine these denials carefully. Consider the service/procedure code when trying to formulate a response to the denial. The diagnosis code represents the reason for the service or procedure and might be a sign, symptom, or condition with which the patient presents. Medicare reimburses for procedures and services that are deemed “reasonable and necessary.”
In an effort to unify standards, Medicare has developed national coverage determinations (NCDs) to identify coverage requirements for frequent or problematic procedures or services. These coverage requirements can identify specific conditions (i.e. ICD-9-CM codes) for which the services or procedures are considered medically necessary. In the absence of a national coverage policy, an item or service could be covered at the discretion of Medicare contractors based on a local coverage determination (LCD), which varies by contractor.
Medical necessity denials often involve a mismatched or missing diagnosis. For example, a payor might deny a claim for cardiopulmonary resuscitation (92950) that is associated with a diagnosis code of congestive heart failure (428.0), despite this being the underlying condition that prompted the decline in the patient’s condition. The payor might only accept “cardiac arrest” (427.5) as the “medically necessary” diagnosis for cardiopulmonary resuscitation, as this is the direct reason necessitating the procedure. After reviewing the documentation to ensure that the documentation supports the diagnosis, the claim can be resubmitted with a confirmed and corrected diagnosis code.
Initial-Request Response
While diagnoses can lead to medical necessity issues, not all medical necessity denials are due to incorrect diagnoses. Some “medical necessity” denials result from a failure to respond to a payor request. More specifically, if the “medical necessity” denial involves a covered evaluation and management visit, the denial is more likely the result of a failure to respond to a prepayment request for documentation.
Medicare typically issues prepayment requests for documentation for the following inpatient CPT codes: 99223, 99233, 99232, 99239, and 99292.1 If the documentation is not provided to the Medicare review department within a designated time frame (e.g. 30-45 days), the claim is automatically denied. The reason for denial is cited as being “not deemed a medical necessity.” These claims do not require electronic resubmission, and instead require submission of documentation to the Medicare appeals department. Once the supporting documentation is reviewed, reimbursement is issued.
Supportive Documentation
There are times when payor requests for additional information or documentation is handled in a timely fashion. However, the paper submission might have been incomplete, as the encounter note itself might not contain the cumulative information representing the reported service.
For example, other pieces of pertinent information may be obtained from the data or order section of the chart. If the individual responsible for gathering the requested documentation does not review it before submission, important or referenced entries may be missed, and the complexity of the billed service might be sacrificed. The provider should submit any entry with the same date as the requested documentation in support: labs, diagnostic testing, physician orders, patient instructions, nursing notes, resident notes, notes by other physicians in the same group, discharge summaries, etc.
Legibility of the encounter note is crucial when the documentation is sent for review. Most reviewers will seek another reviewer’s assistance in translating, but they are not obligated to do this. If the note is deemed incomprehensible, the service is denied, resulting in a nonpayment or a refund. Electronic medical records (EMRs) are assisting physicians and other providers with legibility issues and improving review findings. If a physician is still writing notes by hand, a transcription might be sent along with the documentation to prevent unnecessary denials. Only consider this for requests involving providers with problematic handwriting. A legible signature is required. If a denial ensues in absence of a signature, the provider can submit an appeal with an acceptable attestation.
Modifier Considerations
Some services are denied for being “incidental/integral” to another reimbursed service (i.e. bundled). Payors implement electronic payment edits that disallow separate payment for “related” services. The industry standard, known as the National Correct Coding Initiative (NCCI), identifies code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When a claim is denied for this reason, billers tend to automatically and erroneously resubmit the claim with a modifier appended to the disallowed or “bundled” procedure code. Documentation should be reviewed to determine if the denied service is separately reportable from the paid service. The biller might append the appropriate modifier and resubmit the claim only when well supported by documentation.
For example, the hospitalist evaluated a patient with congestive heart failure and pleural effusions. The hospitalist determined that the patient requires placement of a central venous catheter (36556). Because the patient’s underlying condition was evaluated, and resulted in the decision to place a catheter, both the visit (99233) and the procedure (36556) can be reported. If submitted without modifiers, some payors will deny payment for the visit for being integral to the catheter placement. In this case, the claim should be resubmitted with modifier 25 appended to the visit. Payors might still require documentation review to ensure legitimacy of this modifier before the claim is paid. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Reference
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: AMA Press; 2011.
Before submitting a claim, hospitalists should ensure that the service is rendered, that it is completely and accurately documented in the medical record, that the correct information is entered on the claim form, and that it is a covered benefit and eligible for payment.
Although the latter two elements typically are delegated to the billing team, hospitalists should encourage or request feedback regarding payment and denials. The ensuing open dialogue between physicians and billers might prove helpful in understanding and resolving future billing issues. Less-experienced billers first respond to claim denials by submitting documentation (i.e. “appeal with paper”) despite the inappropriateness of this action. If the denial is upheld, this attempt is viewed as unsuccessful and, without further consideration, “written off.” However, careful examination of the payor’s initial claim determination could elicit a more suitable response.
Service Provider
Provider enrollment issues can sidetrack claim submissions. Physicians must register their NPI (national provider identifier) with the correct practice location and group assignment, particularly when previously practicing physicians join a new group practice. Failure to do so is an infrequent, yet valid, cause for denial.
Alternatively, enrollment issues play a greater role when services involve nurse practitioners (NPs) and physician assistants (PAs) who are enrolled with Medicare but might be prohibited from enrolling with other payors. For example, an NP independently provides subsequent hospital care (e.g. 99232) to a Medicare beneficiary. The claim is submitted in the NP’s name and reimbursed at the correct amount by Medicare as the primary insurer. The remaining balance is submitted to the secondary insurer, who does not enroll NPPs. The claim is rejected. If the physician group has a contractual agreement to recognize NPP services by reporting them under the collaborating physician’s name, the claim can be resubmitted in the physician’s name. In absence of such an agreement, the claim should be written off.
Location
The place of service (POS) must match the reported service/procedure code. For example, a hospitalist is asked to see a patient in the ED. The patient requires further testing but does not meet the criterion for an inpatient stay. The hospitalist admits the patient to observation, treats him, and discharges him to home.
Hospitalists need to avoid the common mistake of mismatching the service code with the location/POS. Observation services performed by the “physician of record” should be reported with the corresponding codes: initial observation care (99218-99220), subsequent observation care (99224-99226), or observation discharge (99217), as appropriate.1 The correct POS should be reported as outpatient hospital (POS 22), not inpatient hospital (POS 21). Trying to report outpatient codes with an inpatient POS will result in claim denial.
A similar denial occurs when trying to report inpatient codes (99231-99233) in an outpatient location (e.g. 23-ED). These denials require claim resubmission with the correct POS and/or service/procedure code. A complete list of POS codes and corresponding definitions can be obtained from Chapter 26, Section 10.5 of the Medicare Claims Processing Manual, available at www.cms.hhs.gov/manuals/downloads/clm104c26.pdf.
Diagnosis
Denials involving diagnoses produce issues of “medical necessity.”1 Examine these denials carefully. Consider the service/procedure code when trying to formulate a response to the denial. The diagnosis code represents the reason for the service or procedure and might be a sign, symptom, or condition with which the patient presents. Medicare reimburses for procedures and services that are deemed “reasonable and necessary.”
In an effort to unify standards, Medicare has developed national coverage determinations (NCDs) to identify coverage requirements for frequent or problematic procedures or services. These coverage requirements can identify specific conditions (i.e. ICD-9-CM codes) for which the services or procedures are considered medically necessary. In the absence of a national coverage policy, an item or service could be covered at the discretion of Medicare contractors based on a local coverage determination (LCD), which varies by contractor.
Medical necessity denials often involve a mismatched or missing diagnosis. For example, a payor might deny a claim for cardiopulmonary resuscitation (92950) that is associated with a diagnosis code of congestive heart failure (428.0), despite this being the underlying condition that prompted the decline in the patient’s condition. The payor might only accept “cardiac arrest” (427.5) as the “medically necessary” diagnosis for cardiopulmonary resuscitation, as this is the direct reason necessitating the procedure. After reviewing the documentation to ensure that the documentation supports the diagnosis, the claim can be resubmitted with a confirmed and corrected diagnosis code.
Initial-Request Response
While diagnoses can lead to medical necessity issues, not all medical necessity denials are due to incorrect diagnoses. Some “medical necessity” denials result from a failure to respond to a payor request. More specifically, if the “medical necessity” denial involves a covered evaluation and management visit, the denial is more likely the result of a failure to respond to a prepayment request for documentation.
Medicare typically issues prepayment requests for documentation for the following inpatient CPT codes: 99223, 99233, 99232, 99239, and 99292.1 If the documentation is not provided to the Medicare review department within a designated time frame (e.g. 30-45 days), the claim is automatically denied. The reason for denial is cited as being “not deemed a medical necessity.” These claims do not require electronic resubmission, and instead require submission of documentation to the Medicare appeals department. Once the supporting documentation is reviewed, reimbursement is issued.
Supportive Documentation
There are times when payor requests for additional information or documentation is handled in a timely fashion. However, the paper submission might have been incomplete, as the encounter note itself might not contain the cumulative information representing the reported service.
For example, other pieces of pertinent information may be obtained from the data or order section of the chart. If the individual responsible for gathering the requested documentation does not review it before submission, important or referenced entries may be missed, and the complexity of the billed service might be sacrificed. The provider should submit any entry with the same date as the requested documentation in support: labs, diagnostic testing, physician orders, patient instructions, nursing notes, resident notes, notes by other physicians in the same group, discharge summaries, etc.
Legibility of the encounter note is crucial when the documentation is sent for review. Most reviewers will seek another reviewer’s assistance in translating, but they are not obligated to do this. If the note is deemed incomprehensible, the service is denied, resulting in a nonpayment or a refund. Electronic medical records (EMRs) are assisting physicians and other providers with legibility issues and improving review findings. If a physician is still writing notes by hand, a transcription might be sent along with the documentation to prevent unnecessary denials. Only consider this for requests involving providers with problematic handwriting. A legible signature is required. If a denial ensues in absence of a signature, the provider can submit an appeal with an acceptable attestation.
Modifier Considerations
Some services are denied for being “incidental/integral” to another reimbursed service (i.e. bundled). Payors implement electronic payment edits that disallow separate payment for “related” services. The industry standard, known as the National Correct Coding Initiative (NCCI), identifies code pairs that should not be reported together on the same date by either a single physician or physicians of the same specialty within a provider group.
When a claim is denied for this reason, billers tend to automatically and erroneously resubmit the claim with a modifier appended to the disallowed or “bundled” procedure code. Documentation should be reviewed to determine if the denied service is separately reportable from the paid service. The biller might append the appropriate modifier and resubmit the claim only when well supported by documentation.
For example, the hospitalist evaluated a patient with congestive heart failure and pleural effusions. The hospitalist determined that the patient requires placement of a central venous catheter (36556). Because the patient’s underlying condition was evaluated, and resulted in the decision to place a catheter, both the visit (99233) and the procedure (36556) can be reported. If submitted without modifiers, some payors will deny payment for the visit for being integral to the catheter placement. In this case, the claim should be resubmitted with modifier 25 appended to the visit. Payors might still require documentation review to ensure legitimacy of this modifier before the claim is paid. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Reference
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology Professional Edition. Chicago: AMA Press; 2011.
CPT 2011 Update
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
In the past, observation services typically did not exceed 24 hours or two calendar days. However, changes in healthcare policy coupled with the impetus to reduce wasteful spending have spurred an atmosphere of scrutiny over hospital admissions. Sometimes there are discrepancies between a hospital’s utilization review committee and a payor’s utilization review committee in determining the appropriateness of healthcare services and supplies, in accordance with each party’s definition of medical necessity. This situation has caused an increase in both the number and cost of observation stays.
In response, subsequent observation-care codes (99224-99226) were developed and published in the 2011 edition of Current Procedural Terminology (CPT).1
Codes and Their Uses
CPT outlines three subsequent observation care codes:
- 99224: Subsequent observation care, per day, for the evaluation and management (E/M) of a patient, which requires at least two of these three key components: problem-focused interval history; problem-focused examination; and medical decision-making that is straightforward or of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is stable, recovering, or improving. Physicians typically spend 15 minutes at the bedside and on the patient’s hospital floor or unit.
- 99225: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: expanded problem focused interval history; expanded problem focused examination; and medical decision-making of moderate complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is responding inadequately to therapy or has developed a minor complication. Physicians typically spend 25 minutes at the bedside and on the patient’s hospital floor or unit.
- 99226: Subsequent observation care, per day, for the E/M of a patient, which requires at least two of these three key components: detailed interval history; detailed examination; and medical decision-making of high complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the patient is unstable or has developed a significant complication or a significant new problem. Physicians typically spend 35 minutes at the bedside and on the patient’s hospital floor or unit.
Subsequent observation-care codes replicate the key components and time requirements established for subsequent hospital care services (99231-99233). However, the relative value units (RVUs) of physician work associated with subsequent observation care are not weighted equally (see Table 1, below). Subsequent observation care is a less-intense service, and therefore is valued at a lesser rate.
The attending of record writes the orders to admit the patient to observation (OBS); indicates the reason for the stay; outlines the plan of care; and manages the patient during the stay. Specialists typically are called onto an OBS case for their opinion/advice (i.e. consultants) but do not function as the attending of record.
According to CPT 2011, subsequent OBS care codes can be reported by both the attending physician of record and specialists who provide medically necessary, nonoverlapping care to patients on any day other than the admission or discharge day (see Table 2, above). At press time, CMS and private payors had not provided written clarification on the use of subsequent observation-care codes. Therefore, it is imperative to monitor payments, denials, and policy clarifications providing further billing instruction.
On the Horizon
Prior reporting guidelines required the reporting of subsequent observation-care days with established outpatient codes (99212-99215). Some member plans insisted on referrals for all outpatient visits regardless nature of the service. Without the mandated referral for established patient visits performed in the observation setting, physician services were denied for coverage.
The creation of subsequent observation codes might play a role in decreasing these denials. Be sure to review the private payors’ fee schedules for inclusion of 99224-99226 codes. If missing, contact the payor or include it as an agenda item during your contract negotiations.
For more information on observation care services, check out “Observation Care” in the July 2010 issue of The Hospitalist. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is faculty for SHM’s inpatient coding course.
References
- Abraham M, Ahlman J, Boudreau A, Connelly J, Evans D. Current Procedural Terminology: Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.8. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 16, 2011.
Shared/Split Service
In response to internal and external pressures to minimize length of stay, adhere to limitations on the maximum number of admitted patients, focus on evidence-based care, and improve outcomes of care, hospitalists have incorporated nonphysician providers (NPPs), such as acute-care nurse practitioners (ACNPs), into their group practices.1 HM groups employing these practitioners must be aware of state and federal regulations, as well as billing and documentation standards surrounding NPP services.
Consider the following common hospitalist scenario: A nurse practitioner evaluates a 67-year-old patient admitted for chronic obstructive bronchitis and progressing shortness of breath. The nurse practitioner documents the service and provides the attending physician with an update on the patient’s status. Later in the day, the physician makes rounds and concurs with the patient’s current plan of care.
The above scenario represents a shared/split service in which two providers from the same group perform a service for the same patient on the same calendar day. The Centers for Medicare & Medicaid Services (CMS) allows these visits to be combined and reported under a single provider’s name if the shared/split billing criteria are met and appropriately documented.
Eligible Providers
The shared/split billing option only applies to services rendered by the attending physician and specified NPPs: nurse practitioners, physician assistants, clinical nurse specialists, and certified nurse-midwives. Both the attending physician and the NPP must be part of the same group practice, either through direct employment or a leased arrangement that contractually links the two individuals. The “leased” relationship often occurs when the facility directly employs the NPP but arranges for the NPP to provide services exclusively for the physician group. It is imperative that the bills for the NPP services are captured and reported by one entity—the hospitalist group.
Several other NPPs (e.g. clinical psychologists or certified registered nurse anesthetists) are recognized by CMS but are ineligible for shared/split billing and must report their services under a different Medicare billing option. Additionally, shared/split services do not apply to physicians in training (interns, residents, fellows) or students.
Qualifying Services
Medicare reimburses services that are considered reasonable and necessary and not otherwise excluded from coverage. From a clinical perspective, NPPs might provide any service permitted by the state scope of practice and performed under the appropriate level of supervision or collaboration as depicted in licensure requirements. These typically comprise visits or procedures rendered by ancillary staff or considered a “physician” service.
Alternatively, shared/split billing regulations limit the types of services that can be reported under this methodology, recognizing only evaluation and management (E/M) services provided in explicit facility-based settings: EDs, outpatient hospital clinics, or inpatient hospitals. Critical-care services and procedures are excluded.
Physician Involvement
The NPP and the physician must have a face-to-face encounter with the same patient on the same calendar day, and there are no constraints on which provider should perform the initial encounter of the day.2
The extent of each provider’s involvement is left to provider discretion and/or local Medicare contractor requirements. Some contractors refer to the physician performing a “substantive” service but do not elaborate with specific service parameters, leaving the physician to determine the critical or key portion of his/her service. A corresponding, detailed notation alleviates any misconceptions of physician involvement.
Documentation by the attending physician should include an attestation that unequivocally demonstrates their personal encounter with the patient—for example, “Patient seen and examined by me.” Additionally, both the NPP and the physician should document the name of the individual with whom the service is shared/split—for example, “Agree with note by ____.” This allows for better charge capture; alerts coders, auditors, and payor representatives to consider both notes in support of the billed service; and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Each provider must document their portion of the rendered service, date and legibly sign their corresponding note, and select the visit level supported by the cumulative encounter—for example, “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR.”
Only one claim can be submitted for a shared/split service. The services might either be reported with the physician’s NPI or the NPP’s NPI. Reimbursement is dependent upon this designation. The physician NPI generates 100% of the Medicare allowable rate; the NPP NPI limits reimbursement to 85% of the allowable physician rate.
Non-Medicare Claims
The shared/split billing policy only applies to Medicare beneficiaries. Due to excessive costs of NPP credentialing and enrollment, most non-Medicare insurers do not issue NPP provider numbers.
Effective June 1, 2010, Aetna began to enroll and reimburse NPP services, but it has not yet outlined a policy that parallels Medicare’s shared/split billing policy. However, lack of payor policy does not preclude payment for shared NPP services; it necessitates additional—and initial—efforts to obtain recognition and corresponding reimbursement.
After determining which insurers have applicable shared/split billing policies, develop a reasonable guideline to offer those payors who do not recognize the billing option. Alert the payor, in writing, that policy implementation will take place in a predetermined timeframe unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option:
- Types of NPP involved in patient care;
- Category of services provided (e.g. E/M, procedures);
- Service location(s) (ED, inpatient, or outpatient hospital);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
This can be performed for any of the NPP billing options and is not limited to shared/split billing. Be sure to obtain payor response before initiating the shared/split billing process.
Summary
NPPs are involved in numerous services within the hospital, and often share/split services with hospitalists. Successful reporting requires understanding of and adherence to federal, state, and billing guidelines.
It is important to identify NPP employment relationships, the NPP’s role in the provision of services, the state supervisory or collaborative rules, and local payor interpretations to prevent misrepresentations, misunderstandings, or erroneous reporting. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Howie JN, Erickson M. Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J Crit Care. 2002; 11(5):448-458.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2010.
- Pohlig, C. Nonphysician providers in your practice. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2010.
- Medicare Benefit Policy Manual: Chapter 15, Section 190-200. CMS website. Available at: www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Nov. 14, 2010.
In response to internal and external pressures to minimize length of stay, adhere to limitations on the maximum number of admitted patients, focus on evidence-based care, and improve outcomes of care, hospitalists have incorporated nonphysician providers (NPPs), such as acute-care nurse practitioners (ACNPs), into their group practices.1 HM groups employing these practitioners must be aware of state and federal regulations, as well as billing and documentation standards surrounding NPP services.
Consider the following common hospitalist scenario: A nurse practitioner evaluates a 67-year-old patient admitted for chronic obstructive bronchitis and progressing shortness of breath. The nurse practitioner documents the service and provides the attending physician with an update on the patient’s status. Later in the day, the physician makes rounds and concurs with the patient’s current plan of care.
The above scenario represents a shared/split service in which two providers from the same group perform a service for the same patient on the same calendar day. The Centers for Medicare & Medicaid Services (CMS) allows these visits to be combined and reported under a single provider’s name if the shared/split billing criteria are met and appropriately documented.
Eligible Providers
The shared/split billing option only applies to services rendered by the attending physician and specified NPPs: nurse practitioners, physician assistants, clinical nurse specialists, and certified nurse-midwives. Both the attending physician and the NPP must be part of the same group practice, either through direct employment or a leased arrangement that contractually links the two individuals. The “leased” relationship often occurs when the facility directly employs the NPP but arranges for the NPP to provide services exclusively for the physician group. It is imperative that the bills for the NPP services are captured and reported by one entity—the hospitalist group.
Several other NPPs (e.g. clinical psychologists or certified registered nurse anesthetists) are recognized by CMS but are ineligible for shared/split billing and must report their services under a different Medicare billing option. Additionally, shared/split services do not apply to physicians in training (interns, residents, fellows) or students.
Qualifying Services
Medicare reimburses services that are considered reasonable and necessary and not otherwise excluded from coverage. From a clinical perspective, NPPs might provide any service permitted by the state scope of practice and performed under the appropriate level of supervision or collaboration as depicted in licensure requirements. These typically comprise visits or procedures rendered by ancillary staff or considered a “physician” service.
Alternatively, shared/split billing regulations limit the types of services that can be reported under this methodology, recognizing only evaluation and management (E/M) services provided in explicit facility-based settings: EDs, outpatient hospital clinics, or inpatient hospitals. Critical-care services and procedures are excluded.
Physician Involvement
The NPP and the physician must have a face-to-face encounter with the same patient on the same calendar day, and there are no constraints on which provider should perform the initial encounter of the day.2
The extent of each provider’s involvement is left to provider discretion and/or local Medicare contractor requirements. Some contractors refer to the physician performing a “substantive” service but do not elaborate with specific service parameters, leaving the physician to determine the critical or key portion of his/her service. A corresponding, detailed notation alleviates any misconceptions of physician involvement.
Documentation by the attending physician should include an attestation that unequivocally demonstrates their personal encounter with the patient—for example, “Patient seen and examined by me.” Additionally, both the NPP and the physician should document the name of the individual with whom the service is shared/split—for example, “Agree with note by ____.” This allows for better charge capture; alerts coders, auditors, and payor representatives to consider both notes in support of the billed service; and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Each provider must document their portion of the rendered service, date and legibly sign their corresponding note, and select the visit level supported by the cumulative encounter—for example, “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR.”
Only one claim can be submitted for a shared/split service. The services might either be reported with the physician’s NPI or the NPP’s NPI. Reimbursement is dependent upon this designation. The physician NPI generates 100% of the Medicare allowable rate; the NPP NPI limits reimbursement to 85% of the allowable physician rate.
Non-Medicare Claims
The shared/split billing policy only applies to Medicare beneficiaries. Due to excessive costs of NPP credentialing and enrollment, most non-Medicare insurers do not issue NPP provider numbers.
Effective June 1, 2010, Aetna began to enroll and reimburse NPP services, but it has not yet outlined a policy that parallels Medicare’s shared/split billing policy. However, lack of payor policy does not preclude payment for shared NPP services; it necessitates additional—and initial—efforts to obtain recognition and corresponding reimbursement.
After determining which insurers have applicable shared/split billing policies, develop a reasonable guideline to offer those payors who do not recognize the billing option. Alert the payor, in writing, that policy implementation will take place in a predetermined timeframe unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option:
- Types of NPP involved in patient care;
- Category of services provided (e.g. E/M, procedures);
- Service location(s) (ED, inpatient, or outpatient hospital);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
This can be performed for any of the NPP billing options and is not limited to shared/split billing. Be sure to obtain payor response before initiating the shared/split billing process.
Summary
NPPs are involved in numerous services within the hospital, and often share/split services with hospitalists. Successful reporting requires understanding of and adherence to federal, state, and billing guidelines.
It is important to identify NPP employment relationships, the NPP’s role in the provision of services, the state supervisory or collaborative rules, and local payor interpretations to prevent misrepresentations, misunderstandings, or erroneous reporting. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Howie JN, Erickson M. Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J Crit Care. 2002; 11(5):448-458.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2010.
- Pohlig, C. Nonphysician providers in your practice. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2010.
- Medicare Benefit Policy Manual: Chapter 15, Section 190-200. CMS website. Available at: www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Nov. 14, 2010.
In response to internal and external pressures to minimize length of stay, adhere to limitations on the maximum number of admitted patients, focus on evidence-based care, and improve outcomes of care, hospitalists have incorporated nonphysician providers (NPPs), such as acute-care nurse practitioners (ACNPs), into their group practices.1 HM groups employing these practitioners must be aware of state and federal regulations, as well as billing and documentation standards surrounding NPP services.
Consider the following common hospitalist scenario: A nurse practitioner evaluates a 67-year-old patient admitted for chronic obstructive bronchitis and progressing shortness of breath. The nurse practitioner documents the service and provides the attending physician with an update on the patient’s status. Later in the day, the physician makes rounds and concurs with the patient’s current plan of care.
The above scenario represents a shared/split service in which two providers from the same group perform a service for the same patient on the same calendar day. The Centers for Medicare & Medicaid Services (CMS) allows these visits to be combined and reported under a single provider’s name if the shared/split billing criteria are met and appropriately documented.
Eligible Providers
The shared/split billing option only applies to services rendered by the attending physician and specified NPPs: nurse practitioners, physician assistants, clinical nurse specialists, and certified nurse-midwives. Both the attending physician and the NPP must be part of the same group practice, either through direct employment or a leased arrangement that contractually links the two individuals. The “leased” relationship often occurs when the facility directly employs the NPP but arranges for the NPP to provide services exclusively for the physician group. It is imperative that the bills for the NPP services are captured and reported by one entity—the hospitalist group.
Several other NPPs (e.g. clinical psychologists or certified registered nurse anesthetists) are recognized by CMS but are ineligible for shared/split billing and must report their services under a different Medicare billing option. Additionally, shared/split services do not apply to physicians in training (interns, residents, fellows) or students.
Qualifying Services
Medicare reimburses services that are considered reasonable and necessary and not otherwise excluded from coverage. From a clinical perspective, NPPs might provide any service permitted by the state scope of practice and performed under the appropriate level of supervision or collaboration as depicted in licensure requirements. These typically comprise visits or procedures rendered by ancillary staff or considered a “physician” service.
Alternatively, shared/split billing regulations limit the types of services that can be reported under this methodology, recognizing only evaluation and management (E/M) services provided in explicit facility-based settings: EDs, outpatient hospital clinics, or inpatient hospitals. Critical-care services and procedures are excluded.
Physician Involvement
The NPP and the physician must have a face-to-face encounter with the same patient on the same calendar day, and there are no constraints on which provider should perform the initial encounter of the day.2
The extent of each provider’s involvement is left to provider discretion and/or local Medicare contractor requirements. Some contractors refer to the physician performing a “substantive” service but do not elaborate with specific service parameters, leaving the physician to determine the critical or key portion of his/her service. A corresponding, detailed notation alleviates any misconceptions of physician involvement.
Documentation by the attending physician should include an attestation that unequivocally demonstrates their personal encounter with the patient—for example, “Patient seen and examined by me.” Additionally, both the NPP and the physician should document the name of the individual with whom the service is shared/split—for example, “Agree with note by ____.” This allows for better charge capture; alerts coders, auditors, and payor representatives to consider both notes in support of the billed service; and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Each provider must document their portion of the rendered service, date and legibly sign their corresponding note, and select the visit level supported by the cumulative encounter—for example, “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR.”
Only one claim can be submitted for a shared/split service. The services might either be reported with the physician’s NPI or the NPP’s NPI. Reimbursement is dependent upon this designation. The physician NPI generates 100% of the Medicare allowable rate; the NPP NPI limits reimbursement to 85% of the allowable physician rate.
Non-Medicare Claims
The shared/split billing policy only applies to Medicare beneficiaries. Due to excessive costs of NPP credentialing and enrollment, most non-Medicare insurers do not issue NPP provider numbers.
Effective June 1, 2010, Aetna began to enroll and reimburse NPP services, but it has not yet outlined a policy that parallels Medicare’s shared/split billing policy. However, lack of payor policy does not preclude payment for shared NPP services; it necessitates additional—and initial—efforts to obtain recognition and corresponding reimbursement.
After determining which insurers have applicable shared/split billing policies, develop a reasonable guideline to offer those payors who do not recognize the billing option. Alert the payor, in writing, that policy implementation will take place in a predetermined timeframe unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option:
- Types of NPP involved in patient care;
- Category of services provided (e.g. E/M, procedures);
- Service location(s) (ED, inpatient, or outpatient hospital);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
This can be performed for any of the NPP billing options and is not limited to shared/split billing. Be sure to obtain payor response before initiating the shared/split billing process.
Summary
NPPs are involved in numerous services within the hospital, and often share/split services with hospitalists. Successful reporting requires understanding of and adherence to federal, state, and billing guidelines.
It is important to identify NPP employment relationships, the NPP’s role in the provision of services, the state supervisory or collaborative rules, and local payor interpretations to prevent misrepresentations, misunderstandings, or erroneous reporting. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Howie JN, Erickson M. Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J Crit Care. 2002; 11(5):448-458.
- Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare and Medicaid Services website. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Nov. 14, 2010.
- Pohlig, C. Nonphysician providers in your practice. In: Coding for Chest Medicine 2009. Northbrook, Ill.: American College of Chest Physicians; 2010.
- Medicare Benefit Policy Manual: Chapter 15, Section 190-200. CMS website. Available at: www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Nov. 14, 2010.
Concurrent Care
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Back to Basics
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.
Let’s examine a documentation case for hospitalists providing daily care: A 65-year-old male patient is admitted with a left hip fracture. The patient also has hypertension and Type 2 diabetes, which might complicate his care. The orthopedic surgeon manages the patient’s perioperative course for the fracture while the hospitalist provides daily post-op care for hypertension and diabetes.
A common scenario is the hospitalist will provide concurrent care, along with a varying number of specialists, depending on the complexity of the patient’s presenting problems and existing comorbidities. Payors define concurrent care as more than one physician providing care to the same patient on the same date, or during the same hospitalization. Payors often consider two key principles before reimbursing concurrent care:
- Does the patient’s condition warrant more than one physician? and
- Are the services provided by each physician reasonable and necessary?1
When more than one medical condition exists and each physician actively treats the condition related to their expertise, each physician can demonstrate medical necessity. As in the above example, the orthopedic surgeon cares for the patient’s fracture while the hospitalist oversees diabetes and hypertension management. Claim submission follows the same logic. Report each subsequent hospital care code (99231-99233) with the corresponding diagnosis each physician primarily manages (i.e., orthopedic surgeon: 9923x with 820.8; hospitalist: 9923x with 250.00, 401.1).
When each physician assigns a different primary diagnosis code to the visit code, each is more likely to receive payment. Because each of these physicians are in different specialties and different provider groups, most payors do not require modifier 25 (separately identifiable E/M service on the same day as a procedure or other service) appended to the visit code. However, some managed-care payors require each physician to append modifier 25 to the concurrent E/M visit code (i.e., 99232-25) despite claim submission under different tax identification numbers.
Unfortunately, the physicians might not realize this until a claim rejection has been issued. Furthermore, payors might want to see the proof before rendering payment. In other words, they pay the first claim received and deny any subsequent claim in order to confirm medical necessity of the concurrent visit. Appeal denied such claims rejections with supporting documentation that distinguishes each physician visit, if possible. This assists the payors in understanding each physician’s contribution to care.
Reasons for Denial
Concurrent care services are more easily distinguished when separate diagnoses are reported with each service. Conversely, payors are likely to deny services that are hard to differentiate. Furthermore, payors frequently deny concurrent care services for the following reasons:
- Services exceed normal frequency or duration for a given condition without documented circumstances requiring additional care; or
- Services by one physician duplicate or overlap those of another provider without recognizable distinction.2
For example, a hospitalist might be involved in the post-op care of patients with fractures and no other identifiable chronic or acute conditions or complications. In these cases, the hospitalist’s continued involvement might constitute a facility policy (e.g., quality of care, risk reduction, etc.) rather than active clinical management. Claim submission could erroneously occur with each physician reporting 9923x for 820.8. Payors deny medically unnecessary services, or request refunds for inappropriate payments.
Hospitalists might attempt to negotiate other terms with the facility to account for the unpaid time and effort directed toward these types of cases.
Group Practice
Physicians in the same group practice with the same specialty designation must report, and are paid, as a single physician. Multiple visits to the same patient can occur on the same day by members of the same group (e.g., hospitalist A evaluates the patient in the morning, and hospitalist B reviews test results and the resulting course of treatment in the afternoon). However, only one subsequent hospital care service can be reported for the day.
The hospitalists should select the visit level representative of the combined services and submit one appropriately determined code (e.g., 99233), thereby capturing the medically necessary efforts of each physician. To complicate matters, the hospitalists must determine which name to report on the claim: the physician who provided the first encounter, or the physician who provided the most extensive or best-documented encounter.
Tracking productivity for these cases proves challenging. Some practices develop an internal accounting system and credit each physician for their medically necessary efforts (a labor-intensive task for administrators and physicians). TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Medicare Benefit Policy Manual: Concurrent Care. Chapter 15, Section 30.E. CMS website. Available at: www.cms.gov/manuals/Downloads/bp102c15.pdf. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Physicians in Group Practice. Chapter 12, Section 30.6.5. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Pohlig, C. Daily care conundrums. The Hospitalist website. Available at: www.the-hospitalist.org/details/article/188735/Daily_Care_Conundrums_.html. Accessed July 9, 2010.
- Medicare Claims Processing Manual: Hospital Visits Same Day But by Different Physicians. Chapter 12, Section 30.6.9.C. CMS website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed July 9, 2010.
- Abraham M, Beebe M, Dalton J, Evans D, Glenn R. Current Procedural Terminology Professional Edition. Chicago: American Medical Association Press; 2010:15.