User login
The VA Research Enterprise: A Platform for National Partnerships Toward Evidence Building and Scientific Innovation
The US Department of Veterans Affairs (VA) plays a substantial role in the nation’s public health through the Veterans Health Administration (VHA). Its statutory missions of teaching, clinical care, and research enable it to serve a foundational role in the US biomedical enterprise.1 Throughout its extensive network of VA medical centers (VAMCs) and partnering academic affiliates, thousands of clinicians and researchers have been trained to improve the lives of veterans and benefit the lives of all Americans. In supporting the largest US integrated health care system, the VA also has numerous capabilities and resources that distinctively position it to produce scientific and clinical results specifically within the context of providing care. The VA has formed partnerships with other federal agencies, industry, and nonprofit entities. Its ability to be a nexus of health care and practice, scientific discovery, and innovative ways to integrate shared interests in these areas have led to many transformative endeavors that save lives and improve the quality of care for veterans and the public.
The COVID-19 pandemic triggered another mission: service in times of national emergency. Known as the Fourth Mission, the VA rapidly shifted to highlight how its health care and research enterprises could apply strengths in a unique, coordinated manner. While the Fourth Mission is typically considered in the context of clinical care, the VA’s movement toward greater integration facilitated the role of research as a key component in efforts under a learning health care model.2
VA Office of Research and Development
Within the VHA, the Office of Research and Development (ORD) develops research policy and oversees interdisciplinary efforts focused on generating evidence to improve veteran health.3 These activities span at least 100 of 171 VAMCs and include thousands of investigators and staff across all major health research disciplines. Many of these investigators are also clinicians who provide patient care and are experts in the prevention, diagnosis, and treatment of diseases and disorders affecting veterans.
The ORD has invested in a range of scientific, operational, regulatory, and technological assets and infrastructure as part of its enterprise. These strengths come from a nearly 100-year history originating as part of a set of hospital-based medical studies. This established the model for a culture of cooperative research within the VA and with external groups who benefit from the VA’s foundational role in multisite clinical trials.2,4,5 Today, the VA prioritizes bench-to-bedside research covering a broad spectrum of investigations, which are integrated with clinical operations and systems that deliver care.3 The VA supports an extensive range of work that covers core areas in preclinical and clinical studies to health services research, rehabilitation and implementation science, establishing expertise in genomic and data sciences, and more recent activities in artificial intelligence.
In 2017, the ORD began a focused strategy to transform into a national enterprise that capitalized on its place within the VA and its particular ability to translate and implement scientific findings into real impact for veteran health and care through 5 initiatives: (1) enhancing veteran access to high-quality clinical trials; (2) increasing the substantial real-world impact of VA Research; (3) putting VA data to work for veteran health; (4) promoting diversity, equity, and inclusion within our sphere of influence; and (5) building community through research. These activities are interrelated and, where possible, the ORD works with other VA clinical and operational offices to accomplish multiple goals and coordinate within the health care system. As such, the VA continually seeks to increase efficiencies and improve abilities that provide veterans with best-in-class health care. While still in its early stages, this strategy and its initiatives established a path for the ORD response to the pandemic.
Within 2 weeks of the World Health Organization and the US declaring a COVID-19 pandemic, the ORD began to address the developing needs and challenges of the yet unknown emerging public health threat. This included outreach to and contact from federal, academic, and industry partners. At the same time, the ORD maintained its focus and energy to support its ongoing veteran-centric research portfolio and VHA health care system needs across its broad scope of activities.
This article discusses how the pandemic accelerated the VA’s research enterprise strategy and enacted a response, highlighting the advantages and strengths of this direction. We demonstrate how this evolving strategy enabled the VA to quickly leverage partnerships during a health emergency. While the ORD and VA Research have been used interchangeably, we will attempt to distinguish between the office that serves as headquarters for the national enterprise—the ORD—and the components of that enterprise composed of scientific personnel, equipment, operational units, and partners—VA Research. Finally, we present lessons from this experience toward a broader, post–COVID-19, enterprise-wide approach that the VA has for providing evidence-based care. These experiences may enrich our understanding of postpandemic future research opportunities with the VA as a leader and partner who leverages its commitment to veterans to improve the nation’s health.
ORGANIZING THE VA COVID-19 RESEARCH RESPONSE
VA Research seeks to internally standardize and integrate collaborations with clinical and operational partners throughout the agency. When possible, it seeks to streamline partnership efforts involving external groups less familiar with how the VA operates or its policies, as well as its capabilities. This need was more obvious during the pandemic, and the ORD assembled its COVID-19 response quickly.6
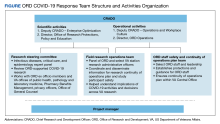
In early January 2020, VA offices, including the ORD, were carefully observing COVID-19. On March 4, 2020, a week before the World Health Organization declared COVID-19 a pandemic, the ORD and its National Research Advisory Council arranged a briefing from VA public health leaders to deal with reported cases of COVID-19 and VA plans. Immediately afterward, the ORD Chief Research and Development Officer gathered a team of experts in clinical research, infectious disease, and public health to strategize a broader research enterprise approach to the pandemic. This group quickly framed 3 key targets: (1) identify critical research questions to prioritize; (2) provide operational guidance to the research community; and (3) uphold VA research staff safety. This discussion led to the creation of a larger ORD COVID-19 Research Response Team that managed activities within this scope. This team included other ORD leaders and staff with operational, scientific, and regulatory expertise charged with enterprise-level planning and execution for all research activities addressing or affected by the pandemic (Figure).
Effective and timely communication was chief among key ORD responsibilities. On March 19, 2020, the Response Team informed the VA Research community about ORD plans for organizing the VA COVID-19 research response.7 It also mobilized VA research programs and investigators to support an enterprise approach that would be coordinated centrally. We achieved communication goals by developing a dedicated website, which provided a means to distribute up-to-date notices and guidance, answer frequently asked questions, and alert investigators about research opportunities. The site enabled the field to report on its efforts, which enhanced leadership and community awareness. A working group of ORD and field personnel managed communications. Given the volume of existing non–COVID-19 research, we established a research continuity of operations plan to provide guidelines for study participant and research staff safety. The ORD issued an unprecedented full-stop administrative hold on in-person research activities after the global announcement of the pandemic. This policy provided formal protections for research programs to safeguard staff and research participants and to determine appropriate alternatives to conduct research activities within necessary social distancing, safety, and other clinical care parameters. It also aligned with guidance and requirements that local VAMCs issued for their operations and care priorities.
The Response Team also established a scientific steering committee of VA infectious disease, critical care, informatics, and epidemiology experts to prioritize research questions, identify research opportunities, and evaluate proposals using a modified expeditious scientific review process. This group also minimized duplicate scientific efforts that might be expected from a large pool of investigators simultaneously pursuing similar research questions. Committee recommendations set up a portfolio that included basic science efforts in diagnostics, clinical trials, population studies, and research infrastructure.
Leveraging Existing Infrastructure
Besides quickly organizing a central touchpoint for the VA COVID-19 research response, the ORD capitalized on its extensive nationwide infrastructure. One key component was the Cooperative Studies Program (CSP); the longstanding VA clinical research enterprise that supports the planning and conduct of large multicenter clinical trials and epidemiological studies. The CSP includes experts at 5 data and statistical coordinating centers, a clinical research pharmacy coordinating center, and 4 epidemiological resource centers.8 CSP studies provide definitive evidence for clinical practice and care of veterans and the nation. CSP’s CONFIRM trial (CSP 577) is the largest VA interventional study with > 50,000 veterans.9 CONFIRM followed the Trial of Varicella Zoster Vaccine for the Prevention of Herpes Zoster and Its Complications (CSP 403), which involved > 38,000 participants to evaluate a vaccine to reduce the burden of illness-associated herpes zoster (shingles). In the study, the vaccine markedly reduced the shingles burden of illness among older adults.10 These studies highlight the CSP cohort development ability as evidenced by the Million Veteran Program.11
VA Research, particularly through the CSP, contributed to multiple federal actions for COVID-19. The CSP had already established partnerships with federal and industry groups in multisite clinical trials and observational studies. During COVID-19, the ORD established a COVID-19 clinical trial master protocol framework: the VA CoronavirUs Research & Efficacy Studies network.9 The CSP also supported studies by the Coronavirus Prevention Network, the National Institute of Allergy and Infectious Disease (NIAID), and the US Food and Drug Administration (FDA). As such, the VA could translate requirements in working with an industry sponsor on the rapid execution of studies within a federal health care system. Much of the success arose when there was either earlier engagement in planning and/or existing familiarity among parties with operational and regulatory requirements.
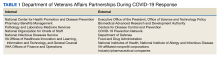
Before the pandemic, the ORD had also been working on various external partnerships to increase opportunities for veterans in clinical trial participation, particularly for cancer, which Caroff and colleagues discuss further.12 A newly emerging Partnered Research Program (PRP) offered a strategy for participation in the major COVID-19 vaccine efficacy clinical trials. VA Research, through PRP and CSP, rapidly engaged others and managed critical communication (Table 1). In quickly pivoting to COVID-19 clinical studies, the VA also used the Networks of Dedicated Enrollment Sites (NODES), its site-based, CSP-supported infrastructure of existing investigators and coordinators with clinical, operational, and regulatory proficiency for large trials.13,14 Together, the CSP and PRP solidified the VA’s scientific, operational, and regulatory support basis for working with industry partners and federal agencies to conduct therapeutic and vaccine trials.
Speed, Knowledge, and Safety
The scope of VA Research partnerships covers several goals but can be broadly categorized in the following ways: research aimed at evaluating the efficacy of new treatments; development of infrastructure to facilitate more rapid and innovative approaches to research; and building connections within the health care system to take an enterprise approach to research.
Activities are not limited to COVID-19. The VA partners with federal entities on research primarily through interagency agreements whose authorities are derived from the Economy Act (31 USC § 1535). For industry and nonfederal groups, the VA enters into Cooperative Research and Development Agreements that are rooted in the Federal Technology Transfer Act (15 USC § 3710). Although the VA has experience in each of these processes, COVID-19 prompted many groups, existing partners and new ones, to engage with the VA. Consequently, the ORD needed to quickly understand the complexities of how to handle such engagements on a larger scale. The VA Research enterprise strategy also focused on facilitating these processes.
As part of VA integration goals, ORD leaders engaged VA clinical leaders, especially in Public Health, Preventive Medicine, Pharmacy Benefits Management, and Pathology and Laboratory services. The ORD also worked closely with operational leaders, including those responsible for the Veterans Integrated Service Networks and VAMC chiefs of staff and network chief medical officers. The ORD’s familiarity with coordinating complex activities for research further helped to organize nonresearch responses for clinical needs and resources to support the VA COVID-19 response. The Office of the Under Secretary for Health recognized VA Research’s critical role as part of the VA health care system. In turn, it served as a major champion to drive success among the active research efforts, especially the partnered efforts, responding to COVID-19. Continuously communicating support and offering resources for the agency’s overall COVID-19 response reinforced the positive impact of VA Research that extended beyond its traditional roles. That is, the research component of VHA was highlighted as an integral part of the COVID-19 response along with its clinical operations. This integrated approach was perhaps best demonstrated in a VHA-wide push to start and conduct the national vaccine efficacy trials.
Other COVID-19 research supported by the ORD included participation in the Mayo Clinic–led convalescent plasma expanded access treatment protocol, which had emerged as a potential therapeutic option.15 The ORD provided centralized regulatory support to nearly 100 VAMCs, helping to reduce inconsistencies in protocol approval processes for what was hoped to be a promising treatment for COVID-19.16 This rapid approach to address a real-time treatment option demonstrated the VA Research capability for swift mobilization in an emergency.
The ORD also coordinated with other federal agencies. For example, it collaborated with the US Department of Defense to begin a parallel observational study on COVID-19 infections and potential severe outcomes. The study enrolled > 3000 veterans who are being followed for up to 2 years to better understand the natural history and course of COVID-19.17 Other interagency efforts focused on vaccine and therapeutic trials, including Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) with the National Institutes of Health. In these activities, VA Research helped increase recruitment, particularly of a more diverse patient population, in helping to assess promising treatments.10
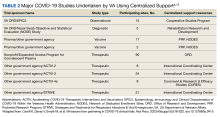
Motivated by its expanding portfolio of COVID-19 intervention studies, the VA also created a COVID-19 research registry for all VA investigators. This registry included almost 59,000 veterans who indicated a willingness to volunteer for clinical studies. This registry exemplified a long-standing tradition of veterans willing to serve their nation again in a time of need. Iaquinto and colleagues showcased how VHA programs (eg, Office of Healthcare Innovation and Learning) collaborated by expediting a study on 3D-printed swabs to address supply chain shortages. The study, which involved the FDA, showed that the printed swabs were as effective as commercially available ones.18 It provided evidence supporting the production and dissemination of a greater number of testing swabs to the public while also reducing the cost and time requirements (Table 2).
Altogether, these collaborative efforts advanced a transformative approach within the VA that was already happening but was accelerated by the pandemic. Such activities enabled greater understanding throughout the VA for how research is not merely complementary but an integrated part of how veterans receive health care. By giving opportunities to veterans to participate in studies, especially clinical studies, the VA created a path in which such expectations, understanding, and operations were more fluid.
Future Directions
The VA continues to work for veterans by emphasizing its strategic goals and strengths in clinical, data science, and other pioneering activities at an enterprise level to provide the highest quality evidence for care. These capabilities perpetuate a scientific and learning environment that also builds toward the future by giving junior investigators and others opportunities to work within a national health care setting. In turn, this provides a more focused perspective on endeavors that align with the VA mission through ORD-supported career development, merit review (independent investigator submissions), and CSP.19 Preclinical, health services, genomic, and implementation research were given insights into more effective operational and methodological partnerships to help inform the health care system. The pandemic also served to strengthen our ability to mobilize and prepare even faster for emergencies and other potential disease outbreaks, including newer pandemic concerns (eg, mpox, Ebola) from research and public health perspectives.
Conclusions
Throughout its 100-year history, VA Research has been a critical, enduring institution within the national medical landscape. The ability to collaborate with partners has helped us to design and create even better processes, optimize and maximize our infrastructure, and learn more about common research interests that can be even more responsive to national health care needs. As an enterprise, VA Research also aims to continually learn and expand on these valuable lessons gained from internal, interagency, and industry collaborations to effectively meet and exceed our mission to serve our veterans.
Acknowledgments
The authors acknowledge Daphne Swancutt for her contribution as copywriter for this manuscript.
1. US Department of Veterans Affairs. Functional organization manual: description of organization, structure, missions, functions, tasks, and authorities. Version 6. 2020. Accessed September 11, 2023. https://www.va.gov/VA-Functional-Organization-Manual-2020-4.pdf
2. Kilbourne AM, Schmidt J, Edmunds M, Vega R, Bowersox N, Atkins D. How the VA is training the next-generation workforce for learning health systems. Learn Health Syst. 2022;6(4):e10333. Published 2022 Aug 16. doi:10.1002/lrh2.10333
3. O’Leary TJ, Dominitz JA, Chang KM. Veterans Affairs office of research and development: research programs and emerging opportunities in digestive diseases research. Gastroenterology. 2015;149(7):1652-1661. doi:10.1053/j.gastro.2015.10.021
4. Tucker WB. The evolution of the cooperative studies in the chemotherapy of tuberculosis of the Veterans Administration and armed forces of the U.S.A. An account of the evolving education of the physician in clinical pharmacology. Bibl Tuberc. 1960;15:1-68.
5. Hays MT; Veterans Health Administration. A historical look at the establishment of the Department of Veterans Affairs research & development program. https://www.research.va.gov/pubs/docs/ORD-85yrHistory.pdf
6. US Department of Veterans Affairs, Veterans Health Administration. Coronavirus Disease 2019 (COVID-19) response report – annex a. May 10, 2021. Accessed September 11, 2023. https://www.va.gov/health/docs/VHA-COVID-19-Response-2021.pdf
7. US Department of Veterans Affairs, Veterans Health Administration. ORD Research Response to COVID-19. US Department of Veterans Affairs. Updated March 24, 2020. Accessed September 11, 2023. www.research.va.gov/programs/orppe/education/webinars/orppe-031920.cfm
8. Burnaska DR, Huang GD, O’Leary TJ. Clinical trials proposed for the VA cooperative studies program: success rates and factors impacting approval. Contemp Clin Trials Commun. 2021;23:100811. Published 2021 Jul 9. doi:10.1016/j.conctc.2021.100811
9. US Department of Veterans Affairs. VA CoronavirUs Research & Efficacy Studies (VA CURES). Updated January 6, 2022. Accessed September 11, 2023. https://www.research.va.gov/services/csrd/va_cures/default.cfm
10. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352(22):2271-2284. doi:10.1056/NEJMoa051016
11. Whitbourne SB, Moser J, Cho K, et al. Leveraging the Million Veteran Program infrastructure and data for a rapid research response to COVID-19. Fed Pract. 2023;40(suppl 5):S23-S28. doi:10.12788/fp.0416
12. Caroff K, Davey V, Smyth M, et al. VA lessons from partnering in COVID-19 clinical trials. Fed Pract. 2023;40(suppl 5): S18-S22. doi:10.12788/fp.0415
13. Condon DL, Beck D, Kenworthy-Heinige T, et al. A cross-cutting approach to enhancing clinical trial site success: the Department of Veterans Affairs’ network of dedicated enrollment sites (NODES) model. Contemp Clin Trials Commun. 2017;6:78-84. Published 2017 Mar 29. doi:10.1016/j.conctc.2017.03.006
14. McClure J, Asghar A, Krajec A, et al. Clinical trial facilitators: a novel approach to support the execution of clinical research at the study site level. Contemp Clin Trials Commun. 2023;33:101106. doi:10.1016/j.conctc.2023.101106
15. Joyner M. Expanded access to convalescent plasma for the treatment of patients with COVID-19. ClinicalTrials.gov identifier: NCT04338360. April 8, 2020. Updated September 2, 2020. Accessed September 11, 2023. https://clinicaltrials.gov/ct2/show/NCT04338360
16. Joyner MJ, Wright RS, Fairweather D, et al. Early safety indicators of COVID-19 convalescent plasma in 5000 patients. J Clin Invest. 2020;130(9):4791-4797. doi:10.1172/JCI140200
17. Lee JS, Smith NL. Epidemiology, immunology and clinical characteristics of COVID-19 (EPIC3). ClinicalTrials.gov identifier: NCT05764083. March 10, 2023. Updated August 1, 2023. Accessed September 11, 2023. https://clinicaltrials.gov/ct2/show/NCT05764083
18. Iaquinto J, Ripley B, Dorn PA. How VA innovative partnerships and health care system can respond to national needs: NOSE trial example. Fed Pract. 2023;40(suppl 5):S52-S56. doi:10.12788/fp.0418
19. US Department of Veterans Affairs. Health Services Research & Development research career development program. Updated March 4, 2021. Accessed September 11, 2023. https://hsrd.research.va.gov/cdp/
The US Department of Veterans Affairs (VA) plays a substantial role in the nation’s public health through the Veterans Health Administration (VHA). Its statutory missions of teaching, clinical care, and research enable it to serve a foundational role in the US biomedical enterprise.1 Throughout its extensive network of VA medical centers (VAMCs) and partnering academic affiliates, thousands of clinicians and researchers have been trained to improve the lives of veterans and benefit the lives of all Americans. In supporting the largest US integrated health care system, the VA also has numerous capabilities and resources that distinctively position it to produce scientific and clinical results specifically within the context of providing care. The VA has formed partnerships with other federal agencies, industry, and nonprofit entities. Its ability to be a nexus of health care and practice, scientific discovery, and innovative ways to integrate shared interests in these areas have led to many transformative endeavors that save lives and improve the quality of care for veterans and the public.
The COVID-19 pandemic triggered another mission: service in times of national emergency. Known as the Fourth Mission, the VA rapidly shifted to highlight how its health care and research enterprises could apply strengths in a unique, coordinated manner. While the Fourth Mission is typically considered in the context of clinical care, the VA’s movement toward greater integration facilitated the role of research as a key component in efforts under a learning health care model.2
VA Office of Research and Development
Within the VHA, the Office of Research and Development (ORD) develops research policy and oversees interdisciplinary efforts focused on generating evidence to improve veteran health.3 These activities span at least 100 of 171 VAMCs and include thousands of investigators and staff across all major health research disciplines. Many of these investigators are also clinicians who provide patient care and are experts in the prevention, diagnosis, and treatment of diseases and disorders affecting veterans.
The ORD has invested in a range of scientific, operational, regulatory, and technological assets and infrastructure as part of its enterprise. These strengths come from a nearly 100-year history originating as part of a set of hospital-based medical studies. This established the model for a culture of cooperative research within the VA and with external groups who benefit from the VA’s foundational role in multisite clinical trials.2,4,5 Today, the VA prioritizes bench-to-bedside research covering a broad spectrum of investigations, which are integrated with clinical operations and systems that deliver care.3 The VA supports an extensive range of work that covers core areas in preclinical and clinical studies to health services research, rehabilitation and implementation science, establishing expertise in genomic and data sciences, and more recent activities in artificial intelligence.
In 2017, the ORD began a focused strategy to transform into a national enterprise that capitalized on its place within the VA and its particular ability to translate and implement scientific findings into real impact for veteran health and care through 5 initiatives: (1) enhancing veteran access to high-quality clinical trials; (2) increasing the substantial real-world impact of VA Research; (3) putting VA data to work for veteran health; (4) promoting diversity, equity, and inclusion within our sphere of influence; and (5) building community through research. These activities are interrelated and, where possible, the ORD works with other VA clinical and operational offices to accomplish multiple goals and coordinate within the health care system. As such, the VA continually seeks to increase efficiencies and improve abilities that provide veterans with best-in-class health care. While still in its early stages, this strategy and its initiatives established a path for the ORD response to the pandemic.
Within 2 weeks of the World Health Organization and the US declaring a COVID-19 pandemic, the ORD began to address the developing needs and challenges of the yet unknown emerging public health threat. This included outreach to and contact from federal, academic, and industry partners. At the same time, the ORD maintained its focus and energy to support its ongoing veteran-centric research portfolio and VHA health care system needs across its broad scope of activities.
This article discusses how the pandemic accelerated the VA’s research enterprise strategy and enacted a response, highlighting the advantages and strengths of this direction. We demonstrate how this evolving strategy enabled the VA to quickly leverage partnerships during a health emergency. While the ORD and VA Research have been used interchangeably, we will attempt to distinguish between the office that serves as headquarters for the national enterprise—the ORD—and the components of that enterprise composed of scientific personnel, equipment, operational units, and partners—VA Research. Finally, we present lessons from this experience toward a broader, post–COVID-19, enterprise-wide approach that the VA has for providing evidence-based care. These experiences may enrich our understanding of postpandemic future research opportunities with the VA as a leader and partner who leverages its commitment to veterans to improve the nation’s health.
ORGANIZING THE VA COVID-19 RESEARCH RESPONSE
VA Research seeks to internally standardize and integrate collaborations with clinical and operational partners throughout the agency. When possible, it seeks to streamline partnership efforts involving external groups less familiar with how the VA operates or its policies, as well as its capabilities. This need was more obvious during the pandemic, and the ORD assembled its COVID-19 response quickly.6
In early January 2020, VA offices, including the ORD, were carefully observing COVID-19. On March 4, 2020, a week before the World Health Organization declared COVID-19 a pandemic, the ORD and its National Research Advisory Council arranged a briefing from VA public health leaders to deal with reported cases of COVID-19 and VA plans. Immediately afterward, the ORD Chief Research and Development Officer gathered a team of experts in clinical research, infectious disease, and public health to strategize a broader research enterprise approach to the pandemic. This group quickly framed 3 key targets: (1) identify critical research questions to prioritize; (2) provide operational guidance to the research community; and (3) uphold VA research staff safety. This discussion led to the creation of a larger ORD COVID-19 Research Response Team that managed activities within this scope. This team included other ORD leaders and staff with operational, scientific, and regulatory expertise charged with enterprise-level planning and execution for all research activities addressing or affected by the pandemic (Figure).
Effective and timely communication was chief among key ORD responsibilities. On March 19, 2020, the Response Team informed the VA Research community about ORD plans for organizing the VA COVID-19 research response.7 It also mobilized VA research programs and investigators to support an enterprise approach that would be coordinated centrally. We achieved communication goals by developing a dedicated website, which provided a means to distribute up-to-date notices and guidance, answer frequently asked questions, and alert investigators about research opportunities. The site enabled the field to report on its efforts, which enhanced leadership and community awareness. A working group of ORD and field personnel managed communications. Given the volume of existing non–COVID-19 research, we established a research continuity of operations plan to provide guidelines for study participant and research staff safety. The ORD issued an unprecedented full-stop administrative hold on in-person research activities after the global announcement of the pandemic. This policy provided formal protections for research programs to safeguard staff and research participants and to determine appropriate alternatives to conduct research activities within necessary social distancing, safety, and other clinical care parameters. It also aligned with guidance and requirements that local VAMCs issued for their operations and care priorities.
The Response Team also established a scientific steering committee of VA infectious disease, critical care, informatics, and epidemiology experts to prioritize research questions, identify research opportunities, and evaluate proposals using a modified expeditious scientific review process. This group also minimized duplicate scientific efforts that might be expected from a large pool of investigators simultaneously pursuing similar research questions. Committee recommendations set up a portfolio that included basic science efforts in diagnostics, clinical trials, population studies, and research infrastructure.
Leveraging Existing Infrastructure
Besides quickly organizing a central touchpoint for the VA COVID-19 research response, the ORD capitalized on its extensive nationwide infrastructure. One key component was the Cooperative Studies Program (CSP); the longstanding VA clinical research enterprise that supports the planning and conduct of large multicenter clinical trials and epidemiological studies. The CSP includes experts at 5 data and statistical coordinating centers, a clinical research pharmacy coordinating center, and 4 epidemiological resource centers.8 CSP studies provide definitive evidence for clinical practice and care of veterans and the nation. CSP’s CONFIRM trial (CSP 577) is the largest VA interventional study with > 50,000 veterans.9 CONFIRM followed the Trial of Varicella Zoster Vaccine for the Prevention of Herpes Zoster and Its Complications (CSP 403), which involved > 38,000 participants to evaluate a vaccine to reduce the burden of illness-associated herpes zoster (shingles). In the study, the vaccine markedly reduced the shingles burden of illness among older adults.10 These studies highlight the CSP cohort development ability as evidenced by the Million Veteran Program.11
VA Research, particularly through the CSP, contributed to multiple federal actions for COVID-19. The CSP had already established partnerships with federal and industry groups in multisite clinical trials and observational studies. During COVID-19, the ORD established a COVID-19 clinical trial master protocol framework: the VA CoronavirUs Research & Efficacy Studies network.9 The CSP also supported studies by the Coronavirus Prevention Network, the National Institute of Allergy and Infectious Disease (NIAID), and the US Food and Drug Administration (FDA). As such, the VA could translate requirements in working with an industry sponsor on the rapid execution of studies within a federal health care system. Much of the success arose when there was either earlier engagement in planning and/or existing familiarity among parties with operational and regulatory requirements.
Before the pandemic, the ORD had also been working on various external partnerships to increase opportunities for veterans in clinical trial participation, particularly for cancer, which Caroff and colleagues discuss further.12 A newly emerging Partnered Research Program (PRP) offered a strategy for participation in the major COVID-19 vaccine efficacy clinical trials. VA Research, through PRP and CSP, rapidly engaged others and managed critical communication (Table 1). In quickly pivoting to COVID-19 clinical studies, the VA also used the Networks of Dedicated Enrollment Sites (NODES), its site-based, CSP-supported infrastructure of existing investigators and coordinators with clinical, operational, and regulatory proficiency for large trials.13,14 Together, the CSP and PRP solidified the VA’s scientific, operational, and regulatory support basis for working with industry partners and federal agencies to conduct therapeutic and vaccine trials.
Speed, Knowledge, and Safety
The scope of VA Research partnerships covers several goals but can be broadly categorized in the following ways: research aimed at evaluating the efficacy of new treatments; development of infrastructure to facilitate more rapid and innovative approaches to research; and building connections within the health care system to take an enterprise approach to research.
Activities are not limited to COVID-19. The VA partners with federal entities on research primarily through interagency agreements whose authorities are derived from the Economy Act (31 USC § 1535). For industry and nonfederal groups, the VA enters into Cooperative Research and Development Agreements that are rooted in the Federal Technology Transfer Act (15 USC § 3710). Although the VA has experience in each of these processes, COVID-19 prompted many groups, existing partners and new ones, to engage with the VA. Consequently, the ORD needed to quickly understand the complexities of how to handle such engagements on a larger scale. The VA Research enterprise strategy also focused on facilitating these processes.
As part of VA integration goals, ORD leaders engaged VA clinical leaders, especially in Public Health, Preventive Medicine, Pharmacy Benefits Management, and Pathology and Laboratory services. The ORD also worked closely with operational leaders, including those responsible for the Veterans Integrated Service Networks and VAMC chiefs of staff and network chief medical officers. The ORD’s familiarity with coordinating complex activities for research further helped to organize nonresearch responses for clinical needs and resources to support the VA COVID-19 response. The Office of the Under Secretary for Health recognized VA Research’s critical role as part of the VA health care system. In turn, it served as a major champion to drive success among the active research efforts, especially the partnered efforts, responding to COVID-19. Continuously communicating support and offering resources for the agency’s overall COVID-19 response reinforced the positive impact of VA Research that extended beyond its traditional roles. That is, the research component of VHA was highlighted as an integral part of the COVID-19 response along with its clinical operations. This integrated approach was perhaps best demonstrated in a VHA-wide push to start and conduct the national vaccine efficacy trials.
Other COVID-19 research supported by the ORD included participation in the Mayo Clinic–led convalescent plasma expanded access treatment protocol, which had emerged as a potential therapeutic option.15 The ORD provided centralized regulatory support to nearly 100 VAMCs, helping to reduce inconsistencies in protocol approval processes for what was hoped to be a promising treatment for COVID-19.16 This rapid approach to address a real-time treatment option demonstrated the VA Research capability for swift mobilization in an emergency.
The ORD also coordinated with other federal agencies. For example, it collaborated with the US Department of Defense to begin a parallel observational study on COVID-19 infections and potential severe outcomes. The study enrolled > 3000 veterans who are being followed for up to 2 years to better understand the natural history and course of COVID-19.17 Other interagency efforts focused on vaccine and therapeutic trials, including Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) with the National Institutes of Health. In these activities, VA Research helped increase recruitment, particularly of a more diverse patient population, in helping to assess promising treatments.10
Motivated by its expanding portfolio of COVID-19 intervention studies, the VA also created a COVID-19 research registry for all VA investigators. This registry included almost 59,000 veterans who indicated a willingness to volunteer for clinical studies. This registry exemplified a long-standing tradition of veterans willing to serve their nation again in a time of need. Iaquinto and colleagues showcased how VHA programs (eg, Office of Healthcare Innovation and Learning) collaborated by expediting a study on 3D-printed swabs to address supply chain shortages. The study, which involved the FDA, showed that the printed swabs were as effective as commercially available ones.18 It provided evidence supporting the production and dissemination of a greater number of testing swabs to the public while also reducing the cost and time requirements (Table 2).
Altogether, these collaborative efforts advanced a transformative approach within the VA that was already happening but was accelerated by the pandemic. Such activities enabled greater understanding throughout the VA for how research is not merely complementary but an integrated part of how veterans receive health care. By giving opportunities to veterans to participate in studies, especially clinical studies, the VA created a path in which such expectations, understanding, and operations were more fluid.
Future Directions
The VA continues to work for veterans by emphasizing its strategic goals and strengths in clinical, data science, and other pioneering activities at an enterprise level to provide the highest quality evidence for care. These capabilities perpetuate a scientific and learning environment that also builds toward the future by giving junior investigators and others opportunities to work within a national health care setting. In turn, this provides a more focused perspective on endeavors that align with the VA mission through ORD-supported career development, merit review (independent investigator submissions), and CSP.19 Preclinical, health services, genomic, and implementation research were given insights into more effective operational and methodological partnerships to help inform the health care system. The pandemic also served to strengthen our ability to mobilize and prepare even faster for emergencies and other potential disease outbreaks, including newer pandemic concerns (eg, mpox, Ebola) from research and public health perspectives.
Conclusions
Throughout its 100-year history, VA Research has been a critical, enduring institution within the national medical landscape. The ability to collaborate with partners has helped us to design and create even better processes, optimize and maximize our infrastructure, and learn more about common research interests that can be even more responsive to national health care needs. As an enterprise, VA Research also aims to continually learn and expand on these valuable lessons gained from internal, interagency, and industry collaborations to effectively meet and exceed our mission to serve our veterans.
Acknowledgments
The authors acknowledge Daphne Swancutt for her contribution as copywriter for this manuscript.
The US Department of Veterans Affairs (VA) plays a substantial role in the nation’s public health through the Veterans Health Administration (VHA). Its statutory missions of teaching, clinical care, and research enable it to serve a foundational role in the US biomedical enterprise.1 Throughout its extensive network of VA medical centers (VAMCs) and partnering academic affiliates, thousands of clinicians and researchers have been trained to improve the lives of veterans and benefit the lives of all Americans. In supporting the largest US integrated health care system, the VA also has numerous capabilities and resources that distinctively position it to produce scientific and clinical results specifically within the context of providing care. The VA has formed partnerships with other federal agencies, industry, and nonprofit entities. Its ability to be a nexus of health care and practice, scientific discovery, and innovative ways to integrate shared interests in these areas have led to many transformative endeavors that save lives and improve the quality of care for veterans and the public.
The COVID-19 pandemic triggered another mission: service in times of national emergency. Known as the Fourth Mission, the VA rapidly shifted to highlight how its health care and research enterprises could apply strengths in a unique, coordinated manner. While the Fourth Mission is typically considered in the context of clinical care, the VA’s movement toward greater integration facilitated the role of research as a key component in efforts under a learning health care model.2
VA Office of Research and Development
Within the VHA, the Office of Research and Development (ORD) develops research policy and oversees interdisciplinary efforts focused on generating evidence to improve veteran health.3 These activities span at least 100 of 171 VAMCs and include thousands of investigators and staff across all major health research disciplines. Many of these investigators are also clinicians who provide patient care and are experts in the prevention, diagnosis, and treatment of diseases and disorders affecting veterans.
The ORD has invested in a range of scientific, operational, regulatory, and technological assets and infrastructure as part of its enterprise. These strengths come from a nearly 100-year history originating as part of a set of hospital-based medical studies. This established the model for a culture of cooperative research within the VA and with external groups who benefit from the VA’s foundational role in multisite clinical trials.2,4,5 Today, the VA prioritizes bench-to-bedside research covering a broad spectrum of investigations, which are integrated with clinical operations and systems that deliver care.3 The VA supports an extensive range of work that covers core areas in preclinical and clinical studies to health services research, rehabilitation and implementation science, establishing expertise in genomic and data sciences, and more recent activities in artificial intelligence.
In 2017, the ORD began a focused strategy to transform into a national enterprise that capitalized on its place within the VA and its particular ability to translate and implement scientific findings into real impact for veteran health and care through 5 initiatives: (1) enhancing veteran access to high-quality clinical trials; (2) increasing the substantial real-world impact of VA Research; (3) putting VA data to work for veteran health; (4) promoting diversity, equity, and inclusion within our sphere of influence; and (5) building community through research. These activities are interrelated and, where possible, the ORD works with other VA clinical and operational offices to accomplish multiple goals and coordinate within the health care system. As such, the VA continually seeks to increase efficiencies and improve abilities that provide veterans with best-in-class health care. While still in its early stages, this strategy and its initiatives established a path for the ORD response to the pandemic.
Within 2 weeks of the World Health Organization and the US declaring a COVID-19 pandemic, the ORD began to address the developing needs and challenges of the yet unknown emerging public health threat. This included outreach to and contact from federal, academic, and industry partners. At the same time, the ORD maintained its focus and energy to support its ongoing veteran-centric research portfolio and VHA health care system needs across its broad scope of activities.
This article discusses how the pandemic accelerated the VA’s research enterprise strategy and enacted a response, highlighting the advantages and strengths of this direction. We demonstrate how this evolving strategy enabled the VA to quickly leverage partnerships during a health emergency. While the ORD and VA Research have been used interchangeably, we will attempt to distinguish between the office that serves as headquarters for the national enterprise—the ORD—and the components of that enterprise composed of scientific personnel, equipment, operational units, and partners—VA Research. Finally, we present lessons from this experience toward a broader, post–COVID-19, enterprise-wide approach that the VA has for providing evidence-based care. These experiences may enrich our understanding of postpandemic future research opportunities with the VA as a leader and partner who leverages its commitment to veterans to improve the nation’s health.
ORGANIZING THE VA COVID-19 RESEARCH RESPONSE
VA Research seeks to internally standardize and integrate collaborations with clinical and operational partners throughout the agency. When possible, it seeks to streamline partnership efforts involving external groups less familiar with how the VA operates or its policies, as well as its capabilities. This need was more obvious during the pandemic, and the ORD assembled its COVID-19 response quickly.6
In early January 2020, VA offices, including the ORD, were carefully observing COVID-19. On March 4, 2020, a week before the World Health Organization declared COVID-19 a pandemic, the ORD and its National Research Advisory Council arranged a briefing from VA public health leaders to deal with reported cases of COVID-19 and VA plans. Immediately afterward, the ORD Chief Research and Development Officer gathered a team of experts in clinical research, infectious disease, and public health to strategize a broader research enterprise approach to the pandemic. This group quickly framed 3 key targets: (1) identify critical research questions to prioritize; (2) provide operational guidance to the research community; and (3) uphold VA research staff safety. This discussion led to the creation of a larger ORD COVID-19 Research Response Team that managed activities within this scope. This team included other ORD leaders and staff with operational, scientific, and regulatory expertise charged with enterprise-level planning and execution for all research activities addressing or affected by the pandemic (Figure).
Effective and timely communication was chief among key ORD responsibilities. On March 19, 2020, the Response Team informed the VA Research community about ORD plans for organizing the VA COVID-19 research response.7 It also mobilized VA research programs and investigators to support an enterprise approach that would be coordinated centrally. We achieved communication goals by developing a dedicated website, which provided a means to distribute up-to-date notices and guidance, answer frequently asked questions, and alert investigators about research opportunities. The site enabled the field to report on its efforts, which enhanced leadership and community awareness. A working group of ORD and field personnel managed communications. Given the volume of existing non–COVID-19 research, we established a research continuity of operations plan to provide guidelines for study participant and research staff safety. The ORD issued an unprecedented full-stop administrative hold on in-person research activities after the global announcement of the pandemic. This policy provided formal protections for research programs to safeguard staff and research participants and to determine appropriate alternatives to conduct research activities within necessary social distancing, safety, and other clinical care parameters. It also aligned with guidance and requirements that local VAMCs issued for their operations and care priorities.
The Response Team also established a scientific steering committee of VA infectious disease, critical care, informatics, and epidemiology experts to prioritize research questions, identify research opportunities, and evaluate proposals using a modified expeditious scientific review process. This group also minimized duplicate scientific efforts that might be expected from a large pool of investigators simultaneously pursuing similar research questions. Committee recommendations set up a portfolio that included basic science efforts in diagnostics, clinical trials, population studies, and research infrastructure.
Leveraging Existing Infrastructure
Besides quickly organizing a central touchpoint for the VA COVID-19 research response, the ORD capitalized on its extensive nationwide infrastructure. One key component was the Cooperative Studies Program (CSP); the longstanding VA clinical research enterprise that supports the planning and conduct of large multicenter clinical trials and epidemiological studies. The CSP includes experts at 5 data and statistical coordinating centers, a clinical research pharmacy coordinating center, and 4 epidemiological resource centers.8 CSP studies provide definitive evidence for clinical practice and care of veterans and the nation. CSP’s CONFIRM trial (CSP 577) is the largest VA interventional study with > 50,000 veterans.9 CONFIRM followed the Trial of Varicella Zoster Vaccine for the Prevention of Herpes Zoster and Its Complications (CSP 403), which involved > 38,000 participants to evaluate a vaccine to reduce the burden of illness-associated herpes zoster (shingles). In the study, the vaccine markedly reduced the shingles burden of illness among older adults.10 These studies highlight the CSP cohort development ability as evidenced by the Million Veteran Program.11
VA Research, particularly through the CSP, contributed to multiple federal actions for COVID-19. The CSP had already established partnerships with federal and industry groups in multisite clinical trials and observational studies. During COVID-19, the ORD established a COVID-19 clinical trial master protocol framework: the VA CoronavirUs Research & Efficacy Studies network.9 The CSP also supported studies by the Coronavirus Prevention Network, the National Institute of Allergy and Infectious Disease (NIAID), and the US Food and Drug Administration (FDA). As such, the VA could translate requirements in working with an industry sponsor on the rapid execution of studies within a federal health care system. Much of the success arose when there was either earlier engagement in planning and/or existing familiarity among parties with operational and regulatory requirements.
Before the pandemic, the ORD had also been working on various external partnerships to increase opportunities for veterans in clinical trial participation, particularly for cancer, which Caroff and colleagues discuss further.12 A newly emerging Partnered Research Program (PRP) offered a strategy for participation in the major COVID-19 vaccine efficacy clinical trials. VA Research, through PRP and CSP, rapidly engaged others and managed critical communication (Table 1). In quickly pivoting to COVID-19 clinical studies, the VA also used the Networks of Dedicated Enrollment Sites (NODES), its site-based, CSP-supported infrastructure of existing investigators and coordinators with clinical, operational, and regulatory proficiency for large trials.13,14 Together, the CSP and PRP solidified the VA’s scientific, operational, and regulatory support basis for working with industry partners and federal agencies to conduct therapeutic and vaccine trials.
Speed, Knowledge, and Safety
The scope of VA Research partnerships covers several goals but can be broadly categorized in the following ways: research aimed at evaluating the efficacy of new treatments; development of infrastructure to facilitate more rapid and innovative approaches to research; and building connections within the health care system to take an enterprise approach to research.
Activities are not limited to COVID-19. The VA partners with federal entities on research primarily through interagency agreements whose authorities are derived from the Economy Act (31 USC § 1535). For industry and nonfederal groups, the VA enters into Cooperative Research and Development Agreements that are rooted in the Federal Technology Transfer Act (15 USC § 3710). Although the VA has experience in each of these processes, COVID-19 prompted many groups, existing partners and new ones, to engage with the VA. Consequently, the ORD needed to quickly understand the complexities of how to handle such engagements on a larger scale. The VA Research enterprise strategy also focused on facilitating these processes.
As part of VA integration goals, ORD leaders engaged VA clinical leaders, especially in Public Health, Preventive Medicine, Pharmacy Benefits Management, and Pathology and Laboratory services. The ORD also worked closely with operational leaders, including those responsible for the Veterans Integrated Service Networks and VAMC chiefs of staff and network chief medical officers. The ORD’s familiarity with coordinating complex activities for research further helped to organize nonresearch responses for clinical needs and resources to support the VA COVID-19 response. The Office of the Under Secretary for Health recognized VA Research’s critical role as part of the VA health care system. In turn, it served as a major champion to drive success among the active research efforts, especially the partnered efforts, responding to COVID-19. Continuously communicating support and offering resources for the agency’s overall COVID-19 response reinforced the positive impact of VA Research that extended beyond its traditional roles. That is, the research component of VHA was highlighted as an integral part of the COVID-19 response along with its clinical operations. This integrated approach was perhaps best demonstrated in a VHA-wide push to start and conduct the national vaccine efficacy trials.
Other COVID-19 research supported by the ORD included participation in the Mayo Clinic–led convalescent plasma expanded access treatment protocol, which had emerged as a potential therapeutic option.15 The ORD provided centralized regulatory support to nearly 100 VAMCs, helping to reduce inconsistencies in protocol approval processes for what was hoped to be a promising treatment for COVID-19.16 This rapid approach to address a real-time treatment option demonstrated the VA Research capability for swift mobilization in an emergency.
The ORD also coordinated with other federal agencies. For example, it collaborated with the US Department of Defense to begin a parallel observational study on COVID-19 infections and potential severe outcomes. The study enrolled > 3000 veterans who are being followed for up to 2 years to better understand the natural history and course of COVID-19.17 Other interagency efforts focused on vaccine and therapeutic trials, including Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) with the National Institutes of Health. In these activities, VA Research helped increase recruitment, particularly of a more diverse patient population, in helping to assess promising treatments.10
Motivated by its expanding portfolio of COVID-19 intervention studies, the VA also created a COVID-19 research registry for all VA investigators. This registry included almost 59,000 veterans who indicated a willingness to volunteer for clinical studies. This registry exemplified a long-standing tradition of veterans willing to serve their nation again in a time of need. Iaquinto and colleagues showcased how VHA programs (eg, Office of Healthcare Innovation and Learning) collaborated by expediting a study on 3D-printed swabs to address supply chain shortages. The study, which involved the FDA, showed that the printed swabs were as effective as commercially available ones.18 It provided evidence supporting the production and dissemination of a greater number of testing swabs to the public while also reducing the cost and time requirements (Table 2).
Altogether, these collaborative efforts advanced a transformative approach within the VA that was already happening but was accelerated by the pandemic. Such activities enabled greater understanding throughout the VA for how research is not merely complementary but an integrated part of how veterans receive health care. By giving opportunities to veterans to participate in studies, especially clinical studies, the VA created a path in which such expectations, understanding, and operations were more fluid.
Future Directions
The VA continues to work for veterans by emphasizing its strategic goals and strengths in clinical, data science, and other pioneering activities at an enterprise level to provide the highest quality evidence for care. These capabilities perpetuate a scientific and learning environment that also builds toward the future by giving junior investigators and others opportunities to work within a national health care setting. In turn, this provides a more focused perspective on endeavors that align with the VA mission through ORD-supported career development, merit review (independent investigator submissions), and CSP.19 Preclinical, health services, genomic, and implementation research were given insights into more effective operational and methodological partnerships to help inform the health care system. The pandemic also served to strengthen our ability to mobilize and prepare even faster for emergencies and other potential disease outbreaks, including newer pandemic concerns (eg, mpox, Ebola) from research and public health perspectives.
Conclusions
Throughout its 100-year history, VA Research has been a critical, enduring institution within the national medical landscape. The ability to collaborate with partners has helped us to design and create even better processes, optimize and maximize our infrastructure, and learn more about common research interests that can be even more responsive to national health care needs. As an enterprise, VA Research also aims to continually learn and expand on these valuable lessons gained from internal, interagency, and industry collaborations to effectively meet and exceed our mission to serve our veterans.
Acknowledgments
The authors acknowledge Daphne Swancutt for her contribution as copywriter for this manuscript.
1. US Department of Veterans Affairs. Functional organization manual: description of organization, structure, missions, functions, tasks, and authorities. Version 6. 2020. Accessed September 11, 2023. https://www.va.gov/VA-Functional-Organization-Manual-2020-4.pdf
2. Kilbourne AM, Schmidt J, Edmunds M, Vega R, Bowersox N, Atkins D. How the VA is training the next-generation workforce for learning health systems. Learn Health Syst. 2022;6(4):e10333. Published 2022 Aug 16. doi:10.1002/lrh2.10333
3. O’Leary TJ, Dominitz JA, Chang KM. Veterans Affairs office of research and development: research programs and emerging opportunities in digestive diseases research. Gastroenterology. 2015;149(7):1652-1661. doi:10.1053/j.gastro.2015.10.021
4. Tucker WB. The evolution of the cooperative studies in the chemotherapy of tuberculosis of the Veterans Administration and armed forces of the U.S.A. An account of the evolving education of the physician in clinical pharmacology. Bibl Tuberc. 1960;15:1-68.
5. Hays MT; Veterans Health Administration. A historical look at the establishment of the Department of Veterans Affairs research & development program. https://www.research.va.gov/pubs/docs/ORD-85yrHistory.pdf
6. US Department of Veterans Affairs, Veterans Health Administration. Coronavirus Disease 2019 (COVID-19) response report – annex a. May 10, 2021. Accessed September 11, 2023. https://www.va.gov/health/docs/VHA-COVID-19-Response-2021.pdf
7. US Department of Veterans Affairs, Veterans Health Administration. ORD Research Response to COVID-19. US Department of Veterans Affairs. Updated March 24, 2020. Accessed September 11, 2023. www.research.va.gov/programs/orppe/education/webinars/orppe-031920.cfm
8. Burnaska DR, Huang GD, O’Leary TJ. Clinical trials proposed for the VA cooperative studies program: success rates and factors impacting approval. Contemp Clin Trials Commun. 2021;23:100811. Published 2021 Jul 9. doi:10.1016/j.conctc.2021.100811
9. US Department of Veterans Affairs. VA CoronavirUs Research & Efficacy Studies (VA CURES). Updated January 6, 2022. Accessed September 11, 2023. https://www.research.va.gov/services/csrd/va_cures/default.cfm
10. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352(22):2271-2284. doi:10.1056/NEJMoa051016
11. Whitbourne SB, Moser J, Cho K, et al. Leveraging the Million Veteran Program infrastructure and data for a rapid research response to COVID-19. Fed Pract. 2023;40(suppl 5):S23-S28. doi:10.12788/fp.0416
12. Caroff K, Davey V, Smyth M, et al. VA lessons from partnering in COVID-19 clinical trials. Fed Pract. 2023;40(suppl 5): S18-S22. doi:10.12788/fp.0415
13. Condon DL, Beck D, Kenworthy-Heinige T, et al. A cross-cutting approach to enhancing clinical trial site success: the Department of Veterans Affairs’ network of dedicated enrollment sites (NODES) model. Contemp Clin Trials Commun. 2017;6:78-84. Published 2017 Mar 29. doi:10.1016/j.conctc.2017.03.006
14. McClure J, Asghar A, Krajec A, et al. Clinical trial facilitators: a novel approach to support the execution of clinical research at the study site level. Contemp Clin Trials Commun. 2023;33:101106. doi:10.1016/j.conctc.2023.101106
15. Joyner M. Expanded access to convalescent plasma for the treatment of patients with COVID-19. ClinicalTrials.gov identifier: NCT04338360. April 8, 2020. Updated September 2, 2020. Accessed September 11, 2023. https://clinicaltrials.gov/ct2/show/NCT04338360
16. Joyner MJ, Wright RS, Fairweather D, et al. Early safety indicators of COVID-19 convalescent plasma in 5000 patients. J Clin Invest. 2020;130(9):4791-4797. doi:10.1172/JCI140200
17. Lee JS, Smith NL. Epidemiology, immunology and clinical characteristics of COVID-19 (EPIC3). ClinicalTrials.gov identifier: NCT05764083. March 10, 2023. Updated August 1, 2023. Accessed September 11, 2023. https://clinicaltrials.gov/ct2/show/NCT05764083
18. Iaquinto J, Ripley B, Dorn PA. How VA innovative partnerships and health care system can respond to national needs: NOSE trial example. Fed Pract. 2023;40(suppl 5):S52-S56. doi:10.12788/fp.0418
19. US Department of Veterans Affairs. Health Services Research & Development research career development program. Updated March 4, 2021. Accessed September 11, 2023. https://hsrd.research.va.gov/cdp/
1. US Department of Veterans Affairs. Functional organization manual: description of organization, structure, missions, functions, tasks, and authorities. Version 6. 2020. Accessed September 11, 2023. https://www.va.gov/VA-Functional-Organization-Manual-2020-4.pdf
2. Kilbourne AM, Schmidt J, Edmunds M, Vega R, Bowersox N, Atkins D. How the VA is training the next-generation workforce for learning health systems. Learn Health Syst. 2022;6(4):e10333. Published 2022 Aug 16. doi:10.1002/lrh2.10333
3. O’Leary TJ, Dominitz JA, Chang KM. Veterans Affairs office of research and development: research programs and emerging opportunities in digestive diseases research. Gastroenterology. 2015;149(7):1652-1661. doi:10.1053/j.gastro.2015.10.021
4. Tucker WB. The evolution of the cooperative studies in the chemotherapy of tuberculosis of the Veterans Administration and armed forces of the U.S.A. An account of the evolving education of the physician in clinical pharmacology. Bibl Tuberc. 1960;15:1-68.
5. Hays MT; Veterans Health Administration. A historical look at the establishment of the Department of Veterans Affairs research & development program. https://www.research.va.gov/pubs/docs/ORD-85yrHistory.pdf
6. US Department of Veterans Affairs, Veterans Health Administration. Coronavirus Disease 2019 (COVID-19) response report – annex a. May 10, 2021. Accessed September 11, 2023. https://www.va.gov/health/docs/VHA-COVID-19-Response-2021.pdf
7. US Department of Veterans Affairs, Veterans Health Administration. ORD Research Response to COVID-19. US Department of Veterans Affairs. Updated March 24, 2020. Accessed September 11, 2023. www.research.va.gov/programs/orppe/education/webinars/orppe-031920.cfm
8. Burnaska DR, Huang GD, O’Leary TJ. Clinical trials proposed for the VA cooperative studies program: success rates and factors impacting approval. Contemp Clin Trials Commun. 2021;23:100811. Published 2021 Jul 9. doi:10.1016/j.conctc.2021.100811
9. US Department of Veterans Affairs. VA CoronavirUs Research & Efficacy Studies (VA CURES). Updated January 6, 2022. Accessed September 11, 2023. https://www.research.va.gov/services/csrd/va_cures/default.cfm
10. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352(22):2271-2284. doi:10.1056/NEJMoa051016
11. Whitbourne SB, Moser J, Cho K, et al. Leveraging the Million Veteran Program infrastructure and data for a rapid research response to COVID-19. Fed Pract. 2023;40(suppl 5):S23-S28. doi:10.12788/fp.0416
12. Caroff K, Davey V, Smyth M, et al. VA lessons from partnering in COVID-19 clinical trials. Fed Pract. 2023;40(suppl 5): S18-S22. doi:10.12788/fp.0415
13. Condon DL, Beck D, Kenworthy-Heinige T, et al. A cross-cutting approach to enhancing clinical trial site success: the Department of Veterans Affairs’ network of dedicated enrollment sites (NODES) model. Contemp Clin Trials Commun. 2017;6:78-84. Published 2017 Mar 29. doi:10.1016/j.conctc.2017.03.006
14. McClure J, Asghar A, Krajec A, et al. Clinical trial facilitators: a novel approach to support the execution of clinical research at the study site level. Contemp Clin Trials Commun. 2023;33:101106. doi:10.1016/j.conctc.2023.101106
15. Joyner M. Expanded access to convalescent plasma for the treatment of patients with COVID-19. ClinicalTrials.gov identifier: NCT04338360. April 8, 2020. Updated September 2, 2020. Accessed September 11, 2023. https://clinicaltrials.gov/ct2/show/NCT04338360
16. Joyner MJ, Wright RS, Fairweather D, et al. Early safety indicators of COVID-19 convalescent plasma in 5000 patients. J Clin Invest. 2020;130(9):4791-4797. doi:10.1172/JCI140200
17. Lee JS, Smith NL. Epidemiology, immunology and clinical characteristics of COVID-19 (EPIC3). ClinicalTrials.gov identifier: NCT05764083. March 10, 2023. Updated August 1, 2023. Accessed September 11, 2023. https://clinicaltrials.gov/ct2/show/NCT05764083
18. Iaquinto J, Ripley B, Dorn PA. How VA innovative partnerships and health care system can respond to national needs: NOSE trial example. Fed Pract. 2023;40(suppl 5):S52-S56. doi:10.12788/fp.0418
19. US Department of Veterans Affairs. Health Services Research & Development research career development program. Updated March 4, 2021. Accessed September 11, 2023. https://hsrd.research.va.gov/cdp/
Introduction
Bad times have a scientific value. These are occasions a good learner would not miss.
Ralph Waldo Emerson
Like the flip of a light switch, the world in March 2020 went into lockdown. Suddenly the novel coronavirus disease (COVID-19) was ever-present and everywhere. At a time when very little was certain, scientific inquiry—along with its related skills and disciplines—offered a much-needed pathway for navigating the virus’s myriad unknowns.
From the pandemic’s onset, the Veterans Health Administration (VHA) of the US Department of Veterans Affairs (VA) made singular contributions to the advancement and acceleration of national and international research activity. This special issue of Federal Practitioner demonstrates how the VHA, through its Office of Research and Development (ORD), took advantage of its newly deployed enterprise strategy to meet the unprecedented demands of this public health emergency.
Launched in 2017, the ORD enterprise strategy enabled the VHA not only to capitalize on existing collaborations—both internal and external—but also move swiftly in forging new ones. Additionally, the strategy was key to leveraging unique VHA assets as the nation’s largest integrated health care system, including: (1) nationwide clinical trials infrastructure, including its longstanding Cooperative Studies Program; (2) a tightly integrated system of clinical care and research that serves as a ready platform for big data science, the world’s largest genomic database, and emergent capabilities; and (3) an established innovation ecosystem that worked with VA research to address rapidly changing circumstances.
In The VA Research Enterprise (p. S12), Garcia and colleagues demonstrate how the VHA pandemic response “arose from an enterprise strategy that was already in motion and aimed at identifying needs for supporting the clinical care mission, more rapidly leveraging resources, and coordinating research across the national VA health care system.” Thus, the VHA took a “model for a culture of cooperative research within the VA and with external groups” and translated it beyond the scope of clinical trials, which had been its foundation.
Led by Chief Research and Development Officer Rachel Ramoni, DMD, ScD, this strategy forged 121 VA medical centers conducting research into an integrated enterprise that could respond to needs for scientific evidence in a coordinated fashion, thereby translating research into practice for real impact on veterans. This approach built on relationships with not only scientific communities but also clinical and operational partners working within the VA to address the immediate pandemic-related needs.
In tandem with its physical infrastructure, the VA’s longstanding network of collaborators, physical infrastructure, and ability to develop new partnerships became drivers of success. Because of previous, ongoing, multisite clinical trials and observational studies, the VA had already partnered with numerous federal government agencies and industry groups and was able to quickly set up a VA COVID-19 clinical trial master protocol framework called the CURES (VA Coronavirus Research and Efficacy studies) network. The ORD enterprise strategy is noted by several other authors, including Caroff and colleagues, who show how the VA efforts to broaden partnerships prepandemic were critical to its participation in 7 large-scale COVID-19 therapeutic and vaccine trials (p. S18).
Similarly, in discussing the VA Million Veteran Program (MVP), Whitbourne and colleagues (p. S23) demonstrate how the VA research strategy and infrastructure were key to leveraging “unique MVP and VA electronic health record data to drive rapid scientific discovery and inform clinical operations.”
Launched in 2011, the MVP is one of the world’s largest genomic cohorts, with more than 985,000 veterans enrolled. MVP developers had the prescience to foresee how a robust genomic database could inform public health emergencies. Whitbourne and colleagues show the many ways the MVP facilitated the VHA COVID-19 response. By extending the MVP centralized recruitment and enrollment infrastructure, an ORD COVID-19 volunteer registry successfully registered 50,000 veterans interested in volunteering for clinical trials.
This tight integration between research and clinical care is one of the VHA’s greatest assets as a health care system. More than 60% of VA researchers are also clinicians who provide direct patient care. This enables VA physician-researchers to learn directly from veteran patients and quickly translate new findings into improved care. It also supported numerous capabilities that played a key role during the pandemic.
For example, in the article VA Big Data Science (p. S39), Young-Xu and colleagues note that the VA use of health care data proved medical research could be performed “quickly and judiciously.” Foundational to this research was a data sharing framework, electronic health record, and VA Corporate Data Warehouse that were accessible to all VA researchers. Researchers had access to clinical data and patient health records that allowed them to perform targeted, time-sensitive research. By building a cohort of 1,363,180 veterans who received ≥ 1 vaccine dose by March 7, 2021, VA researchers added significantly to our understanding of the real-world COVID-19 vaccine clinical performance.
In addition to leveraging existing capabilities, VHA clinicians and researchers created new ones in response. Krishnan and colleagues discuss the launch of 2 clinical and research consortiums focused on COVID-19 genomic surveillance (p. S44). SeqFORCE positioned the VHA to rapidly detect emergent variants and better inform the care of patients with COVID-19. SeqCURE focused on the broader study and trends of variants through sequencing.
The tightly integrated nature of VA care also supported the creation of a large-scale biorepository of specimens with accompanying clinical data to advance research and improve diagnostic and therapeutic research. Epstein and colleagues share the developmental history of the VA SHIELD biorepository, its structure, and its current and future contributions to research science (p. S48).
Finally, the same forward-learning culture which gave rise to the ORD enterprise strategy also resulted in an innovation ecosystem that was well established prior to March 2020. Now a firmly established portfolio within the VHA Office of Healthcare Innovation and Learning (OHIL), the VHA Innovation Ecosystem engages frontline clinicians in reimagining veteran health care. Iaquinto and colleagues discuss how the ecosystem’s preexisting partnerships were critical to addressing shortages in personal protective equipment and other vital resources (p. S52). The OHIL provided the quality system and manufacturing oversight and delivery of swabs for testing, while the ORD furnished research infrastructure and human subjects oversight. Together, these offices not only addressed the shortage by producing swabs but also validated the swabs’ safety and efficacy in the clinical setting.
The articles in this special issue chronicle how the VA quickly mobilized its considerable enterprise-wide resources—especially during the pandemic’s acute phases—to contribute to timely veteran, national, and global evidence about what interventions were effective, what factors were associated with better care and outcomes, and how to flip the switch back to a nonemergency response. As Emerson might have observed, the scientific value of these recent “bad times” did not go unnoticed by VHA learners. In addition to catalyzing opportunities that accelerated the VHA enterprise strategy, the pandemic strengthened existing partnerships, led to new ones, and yielded lessons learned. With variants of the virus continuing to circulate, the VHA continues to harness the lessons learned from the emergency response perspective of the pandemic in order to effectively meet and exceed our mission to serve veterans.
The 35 authors whose work is featured in this issue—and their 3665 colleagues across the VHA research enterprise—offer testament not only to the power of scientific inquiry but of dedication to the mission by the individuals whose lives and families were also impacted by the pandemic.
VA Research continues working to unravel the ongoing impact of COVID-19. As the nation observes an increase in cases again, the VA is ready and well positioned to help lead and address needs for this and other public health crises.
Acknowledgments
This special issue is dedicated to Mitchell (Mitch) Mirkin and his enduring legacy at VA Research, helping to make the contributions of VA Research known as broadly as possible. A superb writer and “editor’s editor,” Mitch had an outstanding ability to translate complex scientific findings into layman’s terms. From the start of the pandemic to his unexpected passing in 2022, Mitch was Acting Director of VA Research Communications. He was a key member of the VA Office of Research and Development COVID-19 research response team. His contributions included his work leading to the generation of this Issue.
Bad times have a scientific value. These are occasions a good learner would not miss.
Ralph Waldo Emerson
Like the flip of a light switch, the world in March 2020 went into lockdown. Suddenly the novel coronavirus disease (COVID-19) was ever-present and everywhere. At a time when very little was certain, scientific inquiry—along with its related skills and disciplines—offered a much-needed pathway for navigating the virus’s myriad unknowns.
From the pandemic’s onset, the Veterans Health Administration (VHA) of the US Department of Veterans Affairs (VA) made singular contributions to the advancement and acceleration of national and international research activity. This special issue of Federal Practitioner demonstrates how the VHA, through its Office of Research and Development (ORD), took advantage of its newly deployed enterprise strategy to meet the unprecedented demands of this public health emergency.
Launched in 2017, the ORD enterprise strategy enabled the VHA not only to capitalize on existing collaborations—both internal and external—but also move swiftly in forging new ones. Additionally, the strategy was key to leveraging unique VHA assets as the nation’s largest integrated health care system, including: (1) nationwide clinical trials infrastructure, including its longstanding Cooperative Studies Program; (2) a tightly integrated system of clinical care and research that serves as a ready platform for big data science, the world’s largest genomic database, and emergent capabilities; and (3) an established innovation ecosystem that worked with VA research to address rapidly changing circumstances.
In The VA Research Enterprise (p. S12), Garcia and colleagues demonstrate how the VHA pandemic response “arose from an enterprise strategy that was already in motion and aimed at identifying needs for supporting the clinical care mission, more rapidly leveraging resources, and coordinating research across the national VA health care system.” Thus, the VHA took a “model for a culture of cooperative research within the VA and with external groups” and translated it beyond the scope of clinical trials, which had been its foundation.
Led by Chief Research and Development Officer Rachel Ramoni, DMD, ScD, this strategy forged 121 VA medical centers conducting research into an integrated enterprise that could respond to needs for scientific evidence in a coordinated fashion, thereby translating research into practice for real impact on veterans. This approach built on relationships with not only scientific communities but also clinical and operational partners working within the VA to address the immediate pandemic-related needs.
In tandem with its physical infrastructure, the VA’s longstanding network of collaborators, physical infrastructure, and ability to develop new partnerships became drivers of success. Because of previous, ongoing, multisite clinical trials and observational studies, the VA had already partnered with numerous federal government agencies and industry groups and was able to quickly set up a VA COVID-19 clinical trial master protocol framework called the CURES (VA Coronavirus Research and Efficacy studies) network. The ORD enterprise strategy is noted by several other authors, including Caroff and colleagues, who show how the VA efforts to broaden partnerships prepandemic were critical to its participation in 7 large-scale COVID-19 therapeutic and vaccine trials (p. S18).
Similarly, in discussing the VA Million Veteran Program (MVP), Whitbourne and colleagues (p. S23) demonstrate how the VA research strategy and infrastructure were key to leveraging “unique MVP and VA electronic health record data to drive rapid scientific discovery and inform clinical operations.”
Launched in 2011, the MVP is one of the world’s largest genomic cohorts, with more than 985,000 veterans enrolled. MVP developers had the prescience to foresee how a robust genomic database could inform public health emergencies. Whitbourne and colleagues show the many ways the MVP facilitated the VHA COVID-19 response. By extending the MVP centralized recruitment and enrollment infrastructure, an ORD COVID-19 volunteer registry successfully registered 50,000 veterans interested in volunteering for clinical trials.
This tight integration between research and clinical care is one of the VHA’s greatest assets as a health care system. More than 60% of VA researchers are also clinicians who provide direct patient care. This enables VA physician-researchers to learn directly from veteran patients and quickly translate new findings into improved care. It also supported numerous capabilities that played a key role during the pandemic.
For example, in the article VA Big Data Science (p. S39), Young-Xu and colleagues note that the VA use of health care data proved medical research could be performed “quickly and judiciously.” Foundational to this research was a data sharing framework, electronic health record, and VA Corporate Data Warehouse that were accessible to all VA researchers. Researchers had access to clinical data and patient health records that allowed them to perform targeted, time-sensitive research. By building a cohort of 1,363,180 veterans who received ≥ 1 vaccine dose by March 7, 2021, VA researchers added significantly to our understanding of the real-world COVID-19 vaccine clinical performance.
In addition to leveraging existing capabilities, VHA clinicians and researchers created new ones in response. Krishnan and colleagues discuss the launch of 2 clinical and research consortiums focused on COVID-19 genomic surveillance (p. S44). SeqFORCE positioned the VHA to rapidly detect emergent variants and better inform the care of patients with COVID-19. SeqCURE focused on the broader study and trends of variants through sequencing.
The tightly integrated nature of VA care also supported the creation of a large-scale biorepository of specimens with accompanying clinical data to advance research and improve diagnostic and therapeutic research. Epstein and colleagues share the developmental history of the VA SHIELD biorepository, its structure, and its current and future contributions to research science (p. S48).
Finally, the same forward-learning culture which gave rise to the ORD enterprise strategy also resulted in an innovation ecosystem that was well established prior to March 2020. Now a firmly established portfolio within the VHA Office of Healthcare Innovation and Learning (OHIL), the VHA Innovation Ecosystem engages frontline clinicians in reimagining veteran health care. Iaquinto and colleagues discuss how the ecosystem’s preexisting partnerships were critical to addressing shortages in personal protective equipment and other vital resources (p. S52). The OHIL provided the quality system and manufacturing oversight and delivery of swabs for testing, while the ORD furnished research infrastructure and human subjects oversight. Together, these offices not only addressed the shortage by producing swabs but also validated the swabs’ safety and efficacy in the clinical setting.
The articles in this special issue chronicle how the VA quickly mobilized its considerable enterprise-wide resources—especially during the pandemic’s acute phases—to contribute to timely veteran, national, and global evidence about what interventions were effective, what factors were associated with better care and outcomes, and how to flip the switch back to a nonemergency response. As Emerson might have observed, the scientific value of these recent “bad times” did not go unnoticed by VHA learners. In addition to catalyzing opportunities that accelerated the VHA enterprise strategy, the pandemic strengthened existing partnerships, led to new ones, and yielded lessons learned. With variants of the virus continuing to circulate, the VHA continues to harness the lessons learned from the emergency response perspective of the pandemic in order to effectively meet and exceed our mission to serve veterans.
The 35 authors whose work is featured in this issue—and their 3665 colleagues across the VHA research enterprise—offer testament not only to the power of scientific inquiry but of dedication to the mission by the individuals whose lives and families were also impacted by the pandemic.
VA Research continues working to unravel the ongoing impact of COVID-19. As the nation observes an increase in cases again, the VA is ready and well positioned to help lead and address needs for this and other public health crises.
Acknowledgments
This special issue is dedicated to Mitchell (Mitch) Mirkin and his enduring legacy at VA Research, helping to make the contributions of VA Research known as broadly as possible. A superb writer and “editor’s editor,” Mitch had an outstanding ability to translate complex scientific findings into layman’s terms. From the start of the pandemic to his unexpected passing in 2022, Mitch was Acting Director of VA Research Communications. He was a key member of the VA Office of Research and Development COVID-19 research response team. His contributions included his work leading to the generation of this Issue.
Bad times have a scientific value. These are occasions a good learner would not miss.
Ralph Waldo Emerson
Like the flip of a light switch, the world in March 2020 went into lockdown. Suddenly the novel coronavirus disease (COVID-19) was ever-present and everywhere. At a time when very little was certain, scientific inquiry—along with its related skills and disciplines—offered a much-needed pathway for navigating the virus’s myriad unknowns.
From the pandemic’s onset, the Veterans Health Administration (VHA) of the US Department of Veterans Affairs (VA) made singular contributions to the advancement and acceleration of national and international research activity. This special issue of Federal Practitioner demonstrates how the VHA, through its Office of Research and Development (ORD), took advantage of its newly deployed enterprise strategy to meet the unprecedented demands of this public health emergency.
Launched in 2017, the ORD enterprise strategy enabled the VHA not only to capitalize on existing collaborations—both internal and external—but also move swiftly in forging new ones. Additionally, the strategy was key to leveraging unique VHA assets as the nation’s largest integrated health care system, including: (1) nationwide clinical trials infrastructure, including its longstanding Cooperative Studies Program; (2) a tightly integrated system of clinical care and research that serves as a ready platform for big data science, the world’s largest genomic database, and emergent capabilities; and (3) an established innovation ecosystem that worked with VA research to address rapidly changing circumstances.
In The VA Research Enterprise (p. S12), Garcia and colleagues demonstrate how the VHA pandemic response “arose from an enterprise strategy that was already in motion and aimed at identifying needs for supporting the clinical care mission, more rapidly leveraging resources, and coordinating research across the national VA health care system.” Thus, the VHA took a “model for a culture of cooperative research within the VA and with external groups” and translated it beyond the scope of clinical trials, which had been its foundation.
Led by Chief Research and Development Officer Rachel Ramoni, DMD, ScD, this strategy forged 121 VA medical centers conducting research into an integrated enterprise that could respond to needs for scientific evidence in a coordinated fashion, thereby translating research into practice for real impact on veterans. This approach built on relationships with not only scientific communities but also clinical and operational partners working within the VA to address the immediate pandemic-related needs.
In tandem with its physical infrastructure, the VA’s longstanding network of collaborators, physical infrastructure, and ability to develop new partnerships became drivers of success. Because of previous, ongoing, multisite clinical trials and observational studies, the VA had already partnered with numerous federal government agencies and industry groups and was able to quickly set up a VA COVID-19 clinical trial master protocol framework called the CURES (VA Coronavirus Research and Efficacy studies) network. The ORD enterprise strategy is noted by several other authors, including Caroff and colleagues, who show how the VA efforts to broaden partnerships prepandemic were critical to its participation in 7 large-scale COVID-19 therapeutic and vaccine trials (p. S18).
Similarly, in discussing the VA Million Veteran Program (MVP), Whitbourne and colleagues (p. S23) demonstrate how the VA research strategy and infrastructure were key to leveraging “unique MVP and VA electronic health record data to drive rapid scientific discovery and inform clinical operations.”
Launched in 2011, the MVP is one of the world’s largest genomic cohorts, with more than 985,000 veterans enrolled. MVP developers had the prescience to foresee how a robust genomic database could inform public health emergencies. Whitbourne and colleagues show the many ways the MVP facilitated the VHA COVID-19 response. By extending the MVP centralized recruitment and enrollment infrastructure, an ORD COVID-19 volunteer registry successfully registered 50,000 veterans interested in volunteering for clinical trials.
This tight integration between research and clinical care is one of the VHA’s greatest assets as a health care system. More than 60% of VA researchers are also clinicians who provide direct patient care. This enables VA physician-researchers to learn directly from veteran patients and quickly translate new findings into improved care. It also supported numerous capabilities that played a key role during the pandemic.
For example, in the article VA Big Data Science (p. S39), Young-Xu and colleagues note that the VA use of health care data proved medical research could be performed “quickly and judiciously.” Foundational to this research was a data sharing framework, electronic health record, and VA Corporate Data Warehouse that were accessible to all VA researchers. Researchers had access to clinical data and patient health records that allowed them to perform targeted, time-sensitive research. By building a cohort of 1,363,180 veterans who received ≥ 1 vaccine dose by March 7, 2021, VA researchers added significantly to our understanding of the real-world COVID-19 vaccine clinical performance.
In addition to leveraging existing capabilities, VHA clinicians and researchers created new ones in response. Krishnan and colleagues discuss the launch of 2 clinical and research consortiums focused on COVID-19 genomic surveillance (p. S44). SeqFORCE positioned the VHA to rapidly detect emergent variants and better inform the care of patients with COVID-19. SeqCURE focused on the broader study and trends of variants through sequencing.
The tightly integrated nature of VA care also supported the creation of a large-scale biorepository of specimens with accompanying clinical data to advance research and improve diagnostic and therapeutic research. Epstein and colleagues share the developmental history of the VA SHIELD biorepository, its structure, and its current and future contributions to research science (p. S48).
Finally, the same forward-learning culture which gave rise to the ORD enterprise strategy also resulted in an innovation ecosystem that was well established prior to March 2020. Now a firmly established portfolio within the VHA Office of Healthcare Innovation and Learning (OHIL), the VHA Innovation Ecosystem engages frontline clinicians in reimagining veteran health care. Iaquinto and colleagues discuss how the ecosystem’s preexisting partnerships were critical to addressing shortages in personal protective equipment and other vital resources (p. S52). The OHIL provided the quality system and manufacturing oversight and delivery of swabs for testing, while the ORD furnished research infrastructure and human subjects oversight. Together, these offices not only addressed the shortage by producing swabs but also validated the swabs’ safety and efficacy in the clinical setting.
The articles in this special issue chronicle how the VA quickly mobilized its considerable enterprise-wide resources—especially during the pandemic’s acute phases—to contribute to timely veteran, national, and global evidence about what interventions were effective, what factors were associated with better care and outcomes, and how to flip the switch back to a nonemergency response. As Emerson might have observed, the scientific value of these recent “bad times” did not go unnoticed by VHA learners. In addition to catalyzing opportunities that accelerated the VHA enterprise strategy, the pandemic strengthened existing partnerships, led to new ones, and yielded lessons learned. With variants of the virus continuing to circulate, the VHA continues to harness the lessons learned from the emergency response perspective of the pandemic in order to effectively meet and exceed our mission to serve veterans.
The 35 authors whose work is featured in this issue—and their 3665 colleagues across the VHA research enterprise—offer testament not only to the power of scientific inquiry but of dedication to the mission by the individuals whose lives and families were also impacted by the pandemic.
VA Research continues working to unravel the ongoing impact of COVID-19. As the nation observes an increase in cases again, the VA is ready and well positioned to help lead and address needs for this and other public health crises.
Acknowledgments
This special issue is dedicated to Mitchell (Mitch) Mirkin and his enduring legacy at VA Research, helping to make the contributions of VA Research known as broadly as possible. A superb writer and “editor’s editor,” Mitch had an outstanding ability to translate complex scientific findings into layman’s terms. From the start of the pandemic to his unexpected passing in 2022, Mitch was Acting Director of VA Research Communications. He was a key member of the VA Office of Research and Development COVID-19 research response team. His contributions included his work leading to the generation of this Issue.
Introduction: Precision Oncology Changes the Game for VA Health Care (FULL)
For US Army veteran Tam Huynh, the US Department of Veterans Affairs (VA) precision oncology program has been the proverbial game changer. Diagnosed in 2016 with stage IV lung cancer and physically depleted by chemotherapy, Huynh learned that treatment based on the precise molecular makeup of his tumors held the potential for improving quality of life. Through the VA National Precision Oncology Program (NPOP), Huynh was matched to a medication shown to help patients whose tumors had the same genetic mutation as Huynh’s tumors. Today, Huynh is not only free of chemotherapy’s debilitating adverse effects, but able to enjoy time with his family and return to work.
Huynh is one of 400,000 veterans treated for cancer annually at the VA. The life-changing treatment he received is due to the legacy of research, integrated care, and collaboration that is the hallmark of the VA health care system. The NPOP is a natural outgrowth of this legacy, and, as Executive-in-Charge Richard Stone, MD, notes in his Foreword, part of the Veterans Health Administration’s (VHA) evolution as a learning health care system. The articles in this special issue represent a snapshot of the work underway under VHA NPOP as well as the dedication of VHA staff nationwide to provide patient-centric care to every veteran.
Leading off this special issue, NPOP director Michael J. Kelley, MD, provides context for understanding the paradigm shift represented by precision oncology.2 He also discusses how, within 5 years, the program came together from its start as a regional effort to its use today by almost every VA oncology practice. Kelley also explains the complexity behind interpreting next-generation sequencing (NGS) gene panel test results and how VA medical centers can call upon NPOP for assistance with this interpretation. Further, he states the “obligation” for new medical technology to be accessible and notes how NPOP was “intentional” during implementation to ensure rural veterans would be offered testing.2
Following Kelley’s discussion is a series of articles focused on precision oncology for prostate cancer, which affects 15,000 veterans yearly. The first, an overview of the Prostate Cancer Foundation (PCF), provides a short history of the organization and how it came to partner with the VA.3 Written by several PCF staff, including President and CEO Jonathan Simons, MD, the paper notes how the commitment of early leaders like S. Ward Casscells, MD, and Larry Stupski led to PCF’s “no veteran left behind” philosophy; ie, ensuring veteran access to clinical trials and world class care regardless of location. As the first disease-specific national network for oncology trials serving veterans, PCF aims to provide a model for all of US health care in the delivery of precision oncology care.
A critical part of PCF is the Precision Oncology Program for Cancer of the Prostate (POPCaP), which focuses on genetics and genomic testing. Bruce Montgomery, MD, and Matthew Retting, MD—VHA’s leading experts in prostate cancer—shine the spotlight on VA’s research track record, specifically the genomics of metastatic prostate cancer.4 They also note the program’s focus on African American veteran patients who are disproportionately affected by the disease but well represented in the VA. In discussing future directions, the authors explain the importance of expanding genetic testing for those diagnosed with prostate cancer.
Prostate cancer Analysis for Therapy Choice (PATCH) is a clinical trials network that works hand-in-hand with POPCaP to use genetic data collected by POPCaP sites to find patients for trials. In their discussion, authors Julie N. Graff, MD, and Grant D. Huang, MD, who leads VA Research’s Cooperative Studies Program, focus on 3 key areas: (1) the challenges of precision oncology when working with relatively rare mutations; (2) 2 new drug trials at VA that will help clinicians know whether certain targeted therapies work for prostate cancer; and (3) how VA is emerging as a national partner in drug discovery and the approval of precision drugs.5
Turning to lung cancer–the second leading cause of cancer death among veterans–Drew Moghanaki, MD, MPH, and Michael Hagan, MD, discuss 3 multisite initiatives launched in 2016 and 2017.6 The first trial, VA Partnership to Increase Access to Lung Cancer Screening (VA-PALS), is a multisite project sponsored by the VA’s Office of Rural Health and Bristol-Myers Squibb Foundation. The trial’s goal is to reduce lung cancer mortality through a robust early detection program. The second trial, VA Lung Cancer Surgery OR Radiation therapy (VALOR) compares whether radiation or surgery is the best for early-stage lung cancer. Notably, VALOR may be one of the most difficult randomized trial ever attempted in lung cancer research (4 previous phase 3 trials outside the VA closed prematurely). By addressing the previous challenges associated with running such a trial, the VALOR study team already has enrolled more than all of the previous phase 3 efforts combined. The third trial is VA Radiation Oncology Quality Surveillance Program (VA-ROQS), which was created in 2016 to benchmark the treatment of veterans with lung cancer. VA-ROQS aims to create a national network of Lung Cancer Centers of Excellence that work with VISNs to ensure that treatment decisions for veterans with lung cancer are based on all available molecular information.
The final group of authors, led by Maren T. Scheuner, MD, discuss how the advent of germline testing as a standard-of-care practice for certain tumor types presents opportunities and challenges for precision oncology.7 One of the primary challenges they note is the shortage of genetics professionals, both within the VA system and health care generally. To help address this issue, they recommend leveraging VA’s longstanding partnership with its academic affiliates.
Precision oncology clearly demonstrates how applying knowledge regarding one of the smallest of living matter can make a tremendous difference in the matter of living. Tam Huynh’s story is proof positive. Speaking at last year’s AMSUS (Society for Federal Health Professionals) annual meeting about his experience, Huynh said that all veterans should have access to the same life-changing treatment he received. This is exactly where the VA NPOP is heading.
1. How the VA is using AI to target cancer, https://www.theatlantic.com/sponsored/ibm-2018/watson-va-cancer/1925. Accessed August 6, 2020.
2. Kelley MJ. VA National Precision Oncology Program. Fed Pract. 2020;37 (suppl 4):S22-S27. doi:10.12788/fp.0037
3. Levine RD, Ekanayake RN, Martin AC, et al. Prostate Cancer Foundation-Department of Veterans Affairs partnership: a model of public-private collaboration to advance treatment and care of invasive cancers. Fed Pract. 2020;37(suppl 4):S32-S37. doi: 10.12788/fp.0035
4. Montgomery B, Rettig M, Kasten J, Muralidhar S, Myrie K, Ramoni R. The Precision Oncology Program for Cancer of the Prostate (POPCaP) network: a Veterans Affairs/Prostate Cancer Foundation collaboration. Fed Pract. 2020;37(suppl 4):S48-S53. doi:10.12788/fp.0021
5. Graff JN, Huang GD. Leveraging Veterans Health Administration clinical and research resources to accelerate discovery and testing in precision oncology. Fed Pract. 2020;37(suppl 4):S62-S67. doi:10.12788/fp.0028
6. Moghanaki D, Hagan M. Strategic initiatives for veterans with lung cancer. Fed Pract. 2020;37(suppl 4):S76-S80. doi:10.12788/fp.0019
7. Scheuner MT, Myrie K, Peredo J, et al. Integrating germline genetics into precision oncology practice in the Veterans Health Administration: challenges and opportunities. Fed Pract. 2020;37(suppl 4):S82-S88. doi:10.12788/fp.0033
For US Army veteran Tam Huynh, the US Department of Veterans Affairs (VA) precision oncology program has been the proverbial game changer. Diagnosed in 2016 with stage IV lung cancer and physically depleted by chemotherapy, Huynh learned that treatment based on the precise molecular makeup of his tumors held the potential for improving quality of life. Through the VA National Precision Oncology Program (NPOP), Huynh was matched to a medication shown to help patients whose tumors had the same genetic mutation as Huynh’s tumors. Today, Huynh is not only free of chemotherapy’s debilitating adverse effects, but able to enjoy time with his family and return to work.
Huynh is one of 400,000 veterans treated for cancer annually at the VA. The life-changing treatment he received is due to the legacy of research, integrated care, and collaboration that is the hallmark of the VA health care system. The NPOP is a natural outgrowth of this legacy, and, as Executive-in-Charge Richard Stone, MD, notes in his Foreword, part of the Veterans Health Administration’s (VHA) evolution as a learning health care system. The articles in this special issue represent a snapshot of the work underway under VHA NPOP as well as the dedication of VHA staff nationwide to provide patient-centric care to every veteran.
Leading off this special issue, NPOP director Michael J. Kelley, MD, provides context for understanding the paradigm shift represented by precision oncology.2 He also discusses how, within 5 years, the program came together from its start as a regional effort to its use today by almost every VA oncology practice. Kelley also explains the complexity behind interpreting next-generation sequencing (NGS) gene panel test results and how VA medical centers can call upon NPOP for assistance with this interpretation. Further, he states the “obligation” for new medical technology to be accessible and notes how NPOP was “intentional” during implementation to ensure rural veterans would be offered testing.2
Following Kelley’s discussion is a series of articles focused on precision oncology for prostate cancer, which affects 15,000 veterans yearly. The first, an overview of the Prostate Cancer Foundation (PCF), provides a short history of the organization and how it came to partner with the VA.3 Written by several PCF staff, including President and CEO Jonathan Simons, MD, the paper notes how the commitment of early leaders like S. Ward Casscells, MD, and Larry Stupski led to PCF’s “no veteran left behind” philosophy; ie, ensuring veteran access to clinical trials and world class care regardless of location. As the first disease-specific national network for oncology trials serving veterans, PCF aims to provide a model for all of US health care in the delivery of precision oncology care.
A critical part of PCF is the Precision Oncology Program for Cancer of the Prostate (POPCaP), which focuses on genetics and genomic testing. Bruce Montgomery, MD, and Matthew Retting, MD—VHA’s leading experts in prostate cancer—shine the spotlight on VA’s research track record, specifically the genomics of metastatic prostate cancer.4 They also note the program’s focus on African American veteran patients who are disproportionately affected by the disease but well represented in the VA. In discussing future directions, the authors explain the importance of expanding genetic testing for those diagnosed with prostate cancer.
Prostate cancer Analysis for Therapy Choice (PATCH) is a clinical trials network that works hand-in-hand with POPCaP to use genetic data collected by POPCaP sites to find patients for trials. In their discussion, authors Julie N. Graff, MD, and Grant D. Huang, MD, who leads VA Research’s Cooperative Studies Program, focus on 3 key areas: (1) the challenges of precision oncology when working with relatively rare mutations; (2) 2 new drug trials at VA that will help clinicians know whether certain targeted therapies work for prostate cancer; and (3) how VA is emerging as a national partner in drug discovery and the approval of precision drugs.5
Turning to lung cancer–the second leading cause of cancer death among veterans–Drew Moghanaki, MD, MPH, and Michael Hagan, MD, discuss 3 multisite initiatives launched in 2016 and 2017.6 The first trial, VA Partnership to Increase Access to Lung Cancer Screening (VA-PALS), is a multisite project sponsored by the VA’s Office of Rural Health and Bristol-Myers Squibb Foundation. The trial’s goal is to reduce lung cancer mortality through a robust early detection program. The second trial, VA Lung Cancer Surgery OR Radiation therapy (VALOR) compares whether radiation or surgery is the best for early-stage lung cancer. Notably, VALOR may be one of the most difficult randomized trial ever attempted in lung cancer research (4 previous phase 3 trials outside the VA closed prematurely). By addressing the previous challenges associated with running such a trial, the VALOR study team already has enrolled more than all of the previous phase 3 efforts combined. The third trial is VA Radiation Oncology Quality Surveillance Program (VA-ROQS), which was created in 2016 to benchmark the treatment of veterans with lung cancer. VA-ROQS aims to create a national network of Lung Cancer Centers of Excellence that work with VISNs to ensure that treatment decisions for veterans with lung cancer are based on all available molecular information.
The final group of authors, led by Maren T. Scheuner, MD, discuss how the advent of germline testing as a standard-of-care practice for certain tumor types presents opportunities and challenges for precision oncology.7 One of the primary challenges they note is the shortage of genetics professionals, both within the VA system and health care generally. To help address this issue, they recommend leveraging VA’s longstanding partnership with its academic affiliates.
Precision oncology clearly demonstrates how applying knowledge regarding one of the smallest of living matter can make a tremendous difference in the matter of living. Tam Huynh’s story is proof positive. Speaking at last year’s AMSUS (Society for Federal Health Professionals) annual meeting about his experience, Huynh said that all veterans should have access to the same life-changing treatment he received. This is exactly where the VA NPOP is heading.
For US Army veteran Tam Huynh, the US Department of Veterans Affairs (VA) precision oncology program has been the proverbial game changer. Diagnosed in 2016 with stage IV lung cancer and physically depleted by chemotherapy, Huynh learned that treatment based on the precise molecular makeup of his tumors held the potential for improving quality of life. Through the VA National Precision Oncology Program (NPOP), Huynh was matched to a medication shown to help patients whose tumors had the same genetic mutation as Huynh’s tumors. Today, Huynh is not only free of chemotherapy’s debilitating adverse effects, but able to enjoy time with his family and return to work.
Huynh is one of 400,000 veterans treated for cancer annually at the VA. The life-changing treatment he received is due to the legacy of research, integrated care, and collaboration that is the hallmark of the VA health care system. The NPOP is a natural outgrowth of this legacy, and, as Executive-in-Charge Richard Stone, MD, notes in his Foreword, part of the Veterans Health Administration’s (VHA) evolution as a learning health care system. The articles in this special issue represent a snapshot of the work underway under VHA NPOP as well as the dedication of VHA staff nationwide to provide patient-centric care to every veteran.
Leading off this special issue, NPOP director Michael J. Kelley, MD, provides context for understanding the paradigm shift represented by precision oncology.2 He also discusses how, within 5 years, the program came together from its start as a regional effort to its use today by almost every VA oncology practice. Kelley also explains the complexity behind interpreting next-generation sequencing (NGS) gene panel test results and how VA medical centers can call upon NPOP for assistance with this interpretation. Further, he states the “obligation” for new medical technology to be accessible and notes how NPOP was “intentional” during implementation to ensure rural veterans would be offered testing.2
Following Kelley’s discussion is a series of articles focused on precision oncology for prostate cancer, which affects 15,000 veterans yearly. The first, an overview of the Prostate Cancer Foundation (PCF), provides a short history of the organization and how it came to partner with the VA.3 Written by several PCF staff, including President and CEO Jonathan Simons, MD, the paper notes how the commitment of early leaders like S. Ward Casscells, MD, and Larry Stupski led to PCF’s “no veteran left behind” philosophy; ie, ensuring veteran access to clinical trials and world class care regardless of location. As the first disease-specific national network for oncology trials serving veterans, PCF aims to provide a model for all of US health care in the delivery of precision oncology care.
A critical part of PCF is the Precision Oncology Program for Cancer of the Prostate (POPCaP), which focuses on genetics and genomic testing. Bruce Montgomery, MD, and Matthew Retting, MD—VHA’s leading experts in prostate cancer—shine the spotlight on VA’s research track record, specifically the genomics of metastatic prostate cancer.4 They also note the program’s focus on African American veteran patients who are disproportionately affected by the disease but well represented in the VA. In discussing future directions, the authors explain the importance of expanding genetic testing for those diagnosed with prostate cancer.
Prostate cancer Analysis for Therapy Choice (PATCH) is a clinical trials network that works hand-in-hand with POPCaP to use genetic data collected by POPCaP sites to find patients for trials. In their discussion, authors Julie N. Graff, MD, and Grant D. Huang, MD, who leads VA Research’s Cooperative Studies Program, focus on 3 key areas: (1) the challenges of precision oncology when working with relatively rare mutations; (2) 2 new drug trials at VA that will help clinicians know whether certain targeted therapies work for prostate cancer; and (3) how VA is emerging as a national partner in drug discovery and the approval of precision drugs.5
Turning to lung cancer–the second leading cause of cancer death among veterans–Drew Moghanaki, MD, MPH, and Michael Hagan, MD, discuss 3 multisite initiatives launched in 2016 and 2017.6 The first trial, VA Partnership to Increase Access to Lung Cancer Screening (VA-PALS), is a multisite project sponsored by the VA’s Office of Rural Health and Bristol-Myers Squibb Foundation. The trial’s goal is to reduce lung cancer mortality through a robust early detection program. The second trial, VA Lung Cancer Surgery OR Radiation therapy (VALOR) compares whether radiation or surgery is the best for early-stage lung cancer. Notably, VALOR may be one of the most difficult randomized trial ever attempted in lung cancer research (4 previous phase 3 trials outside the VA closed prematurely). By addressing the previous challenges associated with running such a trial, the VALOR study team already has enrolled more than all of the previous phase 3 efforts combined. The third trial is VA Radiation Oncology Quality Surveillance Program (VA-ROQS), which was created in 2016 to benchmark the treatment of veterans with lung cancer. VA-ROQS aims to create a national network of Lung Cancer Centers of Excellence that work with VISNs to ensure that treatment decisions for veterans with lung cancer are based on all available molecular information.
The final group of authors, led by Maren T. Scheuner, MD, discuss how the advent of germline testing as a standard-of-care practice for certain tumor types presents opportunities and challenges for precision oncology.7 One of the primary challenges they note is the shortage of genetics professionals, both within the VA system and health care generally. To help address this issue, they recommend leveraging VA’s longstanding partnership with its academic affiliates.
Precision oncology clearly demonstrates how applying knowledge regarding one of the smallest of living matter can make a tremendous difference in the matter of living. Tam Huynh’s story is proof positive. Speaking at last year’s AMSUS (Society for Federal Health Professionals) annual meeting about his experience, Huynh said that all veterans should have access to the same life-changing treatment he received. This is exactly where the VA NPOP is heading.
1. How the VA is using AI to target cancer, https://www.theatlantic.com/sponsored/ibm-2018/watson-va-cancer/1925. Accessed August 6, 2020.
2. Kelley MJ. VA National Precision Oncology Program. Fed Pract. 2020;37 (suppl 4):S22-S27. doi:10.12788/fp.0037
3. Levine RD, Ekanayake RN, Martin AC, et al. Prostate Cancer Foundation-Department of Veterans Affairs partnership: a model of public-private collaboration to advance treatment and care of invasive cancers. Fed Pract. 2020;37(suppl 4):S32-S37. doi: 10.12788/fp.0035
4. Montgomery B, Rettig M, Kasten J, Muralidhar S, Myrie K, Ramoni R. The Precision Oncology Program for Cancer of the Prostate (POPCaP) network: a Veterans Affairs/Prostate Cancer Foundation collaboration. Fed Pract. 2020;37(suppl 4):S48-S53. doi:10.12788/fp.0021
5. Graff JN, Huang GD. Leveraging Veterans Health Administration clinical and research resources to accelerate discovery and testing in precision oncology. Fed Pract. 2020;37(suppl 4):S62-S67. doi:10.12788/fp.0028
6. Moghanaki D, Hagan M. Strategic initiatives for veterans with lung cancer. Fed Pract. 2020;37(suppl 4):S76-S80. doi:10.12788/fp.0019
7. Scheuner MT, Myrie K, Peredo J, et al. Integrating germline genetics into precision oncology practice in the Veterans Health Administration: challenges and opportunities. Fed Pract. 2020;37(suppl 4):S82-S88. doi:10.12788/fp.0033
1. How the VA is using AI to target cancer, https://www.theatlantic.com/sponsored/ibm-2018/watson-va-cancer/1925. Accessed August 6, 2020.
2. Kelley MJ. VA National Precision Oncology Program. Fed Pract. 2020;37 (suppl 4):S22-S27. doi:10.12788/fp.0037
3. Levine RD, Ekanayake RN, Martin AC, et al. Prostate Cancer Foundation-Department of Veterans Affairs partnership: a model of public-private collaboration to advance treatment and care of invasive cancers. Fed Pract. 2020;37(suppl 4):S32-S37. doi: 10.12788/fp.0035
4. Montgomery B, Rettig M, Kasten J, Muralidhar S, Myrie K, Ramoni R. The Precision Oncology Program for Cancer of the Prostate (POPCaP) network: a Veterans Affairs/Prostate Cancer Foundation collaboration. Fed Pract. 2020;37(suppl 4):S48-S53. doi:10.12788/fp.0021
5. Graff JN, Huang GD. Leveraging Veterans Health Administration clinical and research resources to accelerate discovery and testing in precision oncology. Fed Pract. 2020;37(suppl 4):S62-S67. doi:10.12788/fp.0028
6. Moghanaki D, Hagan M. Strategic initiatives for veterans with lung cancer. Fed Pract. 2020;37(suppl 4):S76-S80. doi:10.12788/fp.0019
7. Scheuner MT, Myrie K, Peredo J, et al. Integrating germline genetics into precision oncology practice in the Veterans Health Administration: challenges and opportunities. Fed Pract. 2020;37(suppl 4):S82-S88. doi:10.12788/fp.0033
Hospitalists & Handoffs
In the nearly 10 years since the word “hospitalist” entered our consciousness, it has been inspiring to witness the dramatic growth in the specialty and, accompanying it, the growth in the membership of SHM.1 Over this same period, the healthcare system has made progress toward ensuring that it provides the safest, highest quality healthcare possible.
In my mind, the two phenomena are related. SHM itself and—more generally—the hospitalist field have played a vital role in promoting the use of evidence-based care, improved teamwork, and health information technology. Each of these efforts has made a significant difference in the care patients receive in hospitals. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. Both organizations are working to create positive change that will improve the health and healthcare of all patients.
As their numbers continue to grow, hospitalists are becoming integral members of the inpatient care team at many hospitals.
According to a recent survey conducted by SHM, a hospitalist averaged more than 2,300 inpatient encounters in 2005—a 7% increase over 2004.2 Today, hospital medicine groups practice not only in large metropolitan areas, but also in rural regions where one in three groups began operation during 2005.
In addition to their inpatient care responsibilities, the 15,000 hospitalists who practice today in the United States and Canada serve in key physician leadership roles that directly influence quality improvement and patient safety. Most hospitalists—86%—participate in quality improvement. More than half are involved in implementing information technology (54%) and teaching house staff (51%), and more than one-third—35%—are responsible for their organization’s rapid response team. The SHM survey found that nearly all hospital medicine groups provide round-the-clock patient care at their hospitals.
In this article I will emphasize two key areas relevant to improving patient safety for hospitalized patients: patient handoffs and communication.
Responsibility for Patient Handoffs
Hospitalists’ clinical and leadership roles are significant responsibilities for patient safety, including the critical period known as patient handoff or sign-out.
Patient handoffs refer to the interaction, communication, and planning required to achieve a seamless transition from one clinician to the next.3 When executed in a timely and thorough manner, patient handoffs can reduce the likelihood of medical errors and misinformation, prevent lost or missing clinical information, and maintain a high level of medical care.
Given today’s short hospital stays and the complex medical nature of the care necessary for many patients, timely and effective handoffs demand that hospitalists develop skills that extend beyond superior clinical care. They include:
- Communicating in an effective and efficient manner during patient sign-out;
- Demonstrating the use of “read-back” skills when communicating tasks;
- Developing oral and written patient summaries, including characteristics of the patient, provider, and time of the sign-out;
- Evaluating all medications for indication, dosing, and planned duration at the time of sign-out; and
- Anticipating what may go wrong with a patient after a transition in care occurs and clearly communicating this concern to the receiving clinician.
A Fumbled Handoff: A Case Study
A breakdown in communications—notably an error of omission in the patient handoff—contributed to a poor outcome for an elderly patient who was admitted to the hospital for an elective sigmoid resection.
The case, which was published in the AHRQ’s “Morbidity and Mortality Rounds on the Web” (developed by hospital medicine expert Robert Wachter, MD, and his team under contract to our agency), illustrates some of the challenges that face all clinicians in effectively transferring patient information and care responsibilities.4 It also underscores the need for close involvement by hospitalists in improving quality, teaching and supervising house staff, and implementing information systems.
According to the case study, a 73-year-old female patient with a history of hypertension, non-insulin dependent diabetes, and chronic renal insufficiency became tachycardic two days after surgery, despite receiving a low-dose beta-blocker. The same day, she informed her nurse that she had developed pain in her left leg.
Assuming the pain was related to the pre-operative epidural, the nurse contacted the anesthesia service, which responded by decreasing the epidural rate; the primary surgical team was not called. Late on the third day after surgery, the cross-covering intern was contacted about the patient’s left leg pain. No information about the intern’s findings was relayed to the primary team the following day.
On the fourth day, the patient complained to the nurse about mild chest discomfort, resulting in attention within 20 minutes by house staff and from the attending physician several hours later. The patient’s exam was unremarkable and a work-up was initiated.
Within an hour of the attending’s visit, the patient’s blood pressure dropped to 70/40, followed by a pulseless electrical activity arrest. The patient could not be resuscitated. A post-mortem examination revealed a pulmonary embolism.
Handoffs in an Era of Work-Hour Restrictions
Missing information about pain in the patient’s leg and a breakdown in communication between physicians contributed to the patient’s poor outcome. In this case, the breakdown may also have been influenced by the intern’s involvement on the third day. Like all medical residents this intern is subject to duty-hour restrictions.
Work-hour limits for all residents training in U.S. hospitals took effect in July 2003. Under these standards, created by the Accreditation Council for Graduate Medical Education (ACGME), residents are limited to a maximum of 30 consecutive work hours—known as the 30-hour rule, which includes time used for sign-out, teaching, and continuity of care. They are also prohibited from working more than 80 hours per week.
Despite the clear safety benefit of preventing fatigue-related mistakes, work-hour mandates have increased the number of patient handoffs and the potential for communication breakdowns.5 A survey of interns conducted at the hospital where this case study occurred identified a higher volume of sign-outs and the resulting potential for harm to patients as main concerns with the work-hour restrictions.6
Concerns about the quality and continuity of care that hospital patients receive are evident even among those medical residents whose work hours were restricted before the ACGME requirements took effect. (In New York state residents’ work hours have been restricted since 1998.)
A 2006 study of surgical residents at New York’s Beth Israel Hospital found that most believed that the quality of care patients received was either unchanged (63%) or worse (26%) since the work-hour restrictions took effect.7 Possible reasons for this perception include unresolved issues with continuity of care, miscommunication, and cross-coverage availability. The study concluded that interventions that target intern sign-out coverage constraints will be important for future efforts to improve the quality of care for hospital patients.
Written sign-outs appear to overcome some of the human errors that inevitably result from verbal patient summaries, such as disruptions and forgetfulness. Recent findings have, however, identified significant shortcomings in the quality and timeliness of written reports.
Critical information, such as code status and allergies, was missing in 80% of written sign-outs in one recent study.8 And in a 2006 study of the quality of discharge summaries, only 19% of hospital physicians with an outpatient practice reported being satisfied with the timeliness of discharge summaries. Only a third reported being satisfied with their quality of information. Most troubling, 41% believed that at least one of their patients hospitalized in the previous six months had experienced a preventable adverse event related to poor transfer of information at discharge.9
Use Redundancy and Simulation to Improve Safety
Given the clear challenges of providing quality and continuity of care in the inpatient setting, hospitalists are well positioned to identify strategies for safe and effective patient handoffs and advocate for a systems approach to their implementation.
Safety strategies that have been employed by industries outside of healthcare can provide a useful starting point. So-called “highly reliable” organizations use a variety of approaches to reduce the incidence of errors that occur during transitions in work staff. A recent review of transition methods used by NASA’s Johnson Space Center (Houston), Canadian nuclear power plants, and an ambulance dispatch center—organizations where lapses in transitions also have serious consequences—found that these entities used up to 21 handoff strategies.10 Techniques included verbal, face-to-face, and interactive questioning coordinated with written summaries just before a shift change.
Increasing redundancy is another technique used by highly reliable organizations to reduce the likelihood of missed, incomplete, or misinterpreted information. To create redundancy in clinical care, a physician would include more information at the outset of a procedure or medication order than is now typically provided. This additional information is then repeated and validated by other members of the care team throughout the process, reducing the likelihood of misinterpretation of an instruction or action based on incomplete information.
For example, if a physician always includes both the drug name and the condition for which it is prescribed, a medication order for “Celebrex, seizures,” instead of “Cerebyx, seizures,” would immediately indicate a mistake had occurred in ordering a pain medication instead of an anti-convulsant.11 Research has shown that increasing the amount of information about a medication order reduces the range of potentially valid clinical decisions.
Whether a hospital relies on verbal communication, written communication, computer-based communication, or a combination of all three, redundancy can be built into its sign-out processes. As PDAs become more widely used, structured sign-outs should incorporate redundancy into patient-specific checklists to include information on clinical status, recent and pending tests and study results, and similar, pertinent information.
Simulation-based training that incorporates redundancy and promotes read-back of patient information holds promise for error reduction, especially during patient handoffs.
AHRQ has recently funded research on simulation training projects that seek to:
- Reduce communication errors during patient handoffs in the emergency department by implementing a patient-specific checklist based on an electronic medical record and by testing the effect of companion simulation-based training; and
- Evaluate and improve safe communication and coordination between anesthesia providers and nurses during care transitions and during hand-offs between the operating room and the post-anesthesia care unit.12
The 24/7 role of hospital physicians brings unique experiences and insights to the challenges of patient safety that can test the feasibility of systems to reduce errors associated with care transitions. As their numbers and leadership roles expand, hospitalists are poised to make significant contributions to improving patient safety and outcomes.
We at AHRQ look forward to assisting hospitalists in making these contributions and to achieving these goals together. We also look forward to continuing our relationship with SHM and the hospitalist community as a whole. TH
Dr. Clancy is the director of the Agency for Healthcare Research and Quality.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Impact of the nation’s hospitalists continues to grow new society of hospital medicine survey says [press release]. Society of Hospital Medicine. May 4, 2006.
- Society of Hospital Medicine. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1;S1. Available at: http://onlinelibrary.wiley.com/doi/10.1002/jhm.72/pdf. Last accessed January 17, 2007.
- Vidyarthi A [commentary]. Agency for Healthcare Research and Quality Web M&M: Morbidity and Mortality Rounds on the Web. Fumbled handoff. March 2004. Available at: www.webmm.ahrq.gov/case.aspx?caseID=55. Last accessed January 17, 2007.
- Wachter RM, Shojania KG. Internal Bleeding: The Truth Behind America’s Terrifying Epidemic of Medical Mistakes. New York: Rugged Land LLG; 2004.
- Vidyarthi A. Morbidity and Mortality Rounds on the Web, “Fumbled Handoff,” unpublished data, 2004.
- Biller CK, Antonacci AC, Pelletier S, et al. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006 Oct;135(2):275-281. Epub 2006 Aug 24.
- Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11(12):753-755.
- O’Leary KJ, Leibovitz DM, Feinglass J, et al. Outpatient physicians’ satisfaction with discharge summaries and perceived need for an electronic discharge summary. J Hosp Med. 2006;1:317-320. Published online Oct. 11, 2006.
- Reason JT. Managing the Risks of Organizational Accidents. Aldershot, England: Ashgate Publishing Company; 1997:135.
- Bar-Yam Y. System care: multiscale analysis of medical errors–eliminating errors and improving organizational capabilities. New England Complex Systems Institute: Technical Report; Sept 2004. Available at: http://necsi.org/projects/yaneer/NECSITechnicalReport2004-09.pdf. Last accessed January 17, 2007.
- Agency for Healthcare Research and Quality. Improving patient safety through simulation research. 2006 Simulation Projects. Available at: www.ahrq.gov/qual/simulproj.htm. Last accessed January 17, 2007.
In the nearly 10 years since the word “hospitalist” entered our consciousness, it has been inspiring to witness the dramatic growth in the specialty and, accompanying it, the growth in the membership of SHM.1 Over this same period, the healthcare system has made progress toward ensuring that it provides the safest, highest quality healthcare possible.
In my mind, the two phenomena are related. SHM itself and—more generally—the hospitalist field have played a vital role in promoting the use of evidence-based care, improved teamwork, and health information technology. Each of these efforts has made a significant difference in the care patients receive in hospitals. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. Both organizations are working to create positive change that will improve the health and healthcare of all patients.
As their numbers continue to grow, hospitalists are becoming integral members of the inpatient care team at many hospitals.
According to a recent survey conducted by SHM, a hospitalist averaged more than 2,300 inpatient encounters in 2005—a 7% increase over 2004.2 Today, hospital medicine groups practice not only in large metropolitan areas, but also in rural regions where one in three groups began operation during 2005.
In addition to their inpatient care responsibilities, the 15,000 hospitalists who practice today in the United States and Canada serve in key physician leadership roles that directly influence quality improvement and patient safety. Most hospitalists—86%—participate in quality improvement. More than half are involved in implementing information technology (54%) and teaching house staff (51%), and more than one-third—35%—are responsible for their organization’s rapid response team. The SHM survey found that nearly all hospital medicine groups provide round-the-clock patient care at their hospitals.
In this article I will emphasize two key areas relevant to improving patient safety for hospitalized patients: patient handoffs and communication.
Responsibility for Patient Handoffs
Hospitalists’ clinical and leadership roles are significant responsibilities for patient safety, including the critical period known as patient handoff or sign-out.
Patient handoffs refer to the interaction, communication, and planning required to achieve a seamless transition from one clinician to the next.3 When executed in a timely and thorough manner, patient handoffs can reduce the likelihood of medical errors and misinformation, prevent lost or missing clinical information, and maintain a high level of medical care.
Given today’s short hospital stays and the complex medical nature of the care necessary for many patients, timely and effective handoffs demand that hospitalists develop skills that extend beyond superior clinical care. They include:
- Communicating in an effective and efficient manner during patient sign-out;
- Demonstrating the use of “read-back” skills when communicating tasks;
- Developing oral and written patient summaries, including characteristics of the patient, provider, and time of the sign-out;
- Evaluating all medications for indication, dosing, and planned duration at the time of sign-out; and
- Anticipating what may go wrong with a patient after a transition in care occurs and clearly communicating this concern to the receiving clinician.
A Fumbled Handoff: A Case Study
A breakdown in communications—notably an error of omission in the patient handoff—contributed to a poor outcome for an elderly patient who was admitted to the hospital for an elective sigmoid resection.
The case, which was published in the AHRQ’s “Morbidity and Mortality Rounds on the Web” (developed by hospital medicine expert Robert Wachter, MD, and his team under contract to our agency), illustrates some of the challenges that face all clinicians in effectively transferring patient information and care responsibilities.4 It also underscores the need for close involvement by hospitalists in improving quality, teaching and supervising house staff, and implementing information systems.
According to the case study, a 73-year-old female patient with a history of hypertension, non-insulin dependent diabetes, and chronic renal insufficiency became tachycardic two days after surgery, despite receiving a low-dose beta-blocker. The same day, she informed her nurse that she had developed pain in her left leg.
Assuming the pain was related to the pre-operative epidural, the nurse contacted the anesthesia service, which responded by decreasing the epidural rate; the primary surgical team was not called. Late on the third day after surgery, the cross-covering intern was contacted about the patient’s left leg pain. No information about the intern’s findings was relayed to the primary team the following day.
On the fourth day, the patient complained to the nurse about mild chest discomfort, resulting in attention within 20 minutes by house staff and from the attending physician several hours later. The patient’s exam was unremarkable and a work-up was initiated.
Within an hour of the attending’s visit, the patient’s blood pressure dropped to 70/40, followed by a pulseless electrical activity arrest. The patient could not be resuscitated. A post-mortem examination revealed a pulmonary embolism.
Handoffs in an Era of Work-Hour Restrictions
Missing information about pain in the patient’s leg and a breakdown in communication between physicians contributed to the patient’s poor outcome. In this case, the breakdown may also have been influenced by the intern’s involvement on the third day. Like all medical residents this intern is subject to duty-hour restrictions.
Work-hour limits for all residents training in U.S. hospitals took effect in July 2003. Under these standards, created by the Accreditation Council for Graduate Medical Education (ACGME), residents are limited to a maximum of 30 consecutive work hours—known as the 30-hour rule, which includes time used for sign-out, teaching, and continuity of care. They are also prohibited from working more than 80 hours per week.
Despite the clear safety benefit of preventing fatigue-related mistakes, work-hour mandates have increased the number of patient handoffs and the potential for communication breakdowns.5 A survey of interns conducted at the hospital where this case study occurred identified a higher volume of sign-outs and the resulting potential for harm to patients as main concerns with the work-hour restrictions.6
Concerns about the quality and continuity of care that hospital patients receive are evident even among those medical residents whose work hours were restricted before the ACGME requirements took effect. (In New York state residents’ work hours have been restricted since 1998.)
A 2006 study of surgical residents at New York’s Beth Israel Hospital found that most believed that the quality of care patients received was either unchanged (63%) or worse (26%) since the work-hour restrictions took effect.7 Possible reasons for this perception include unresolved issues with continuity of care, miscommunication, and cross-coverage availability. The study concluded that interventions that target intern sign-out coverage constraints will be important for future efforts to improve the quality of care for hospital patients.
Written sign-outs appear to overcome some of the human errors that inevitably result from verbal patient summaries, such as disruptions and forgetfulness. Recent findings have, however, identified significant shortcomings in the quality and timeliness of written reports.
Critical information, such as code status and allergies, was missing in 80% of written sign-outs in one recent study.8 And in a 2006 study of the quality of discharge summaries, only 19% of hospital physicians with an outpatient practice reported being satisfied with the timeliness of discharge summaries. Only a third reported being satisfied with their quality of information. Most troubling, 41% believed that at least one of their patients hospitalized in the previous six months had experienced a preventable adverse event related to poor transfer of information at discharge.9
Use Redundancy and Simulation to Improve Safety
Given the clear challenges of providing quality and continuity of care in the inpatient setting, hospitalists are well positioned to identify strategies for safe and effective patient handoffs and advocate for a systems approach to their implementation.
Safety strategies that have been employed by industries outside of healthcare can provide a useful starting point. So-called “highly reliable” organizations use a variety of approaches to reduce the incidence of errors that occur during transitions in work staff. A recent review of transition methods used by NASA’s Johnson Space Center (Houston), Canadian nuclear power plants, and an ambulance dispatch center—organizations where lapses in transitions also have serious consequences—found that these entities used up to 21 handoff strategies.10 Techniques included verbal, face-to-face, and interactive questioning coordinated with written summaries just before a shift change.
Increasing redundancy is another technique used by highly reliable organizations to reduce the likelihood of missed, incomplete, or misinterpreted information. To create redundancy in clinical care, a physician would include more information at the outset of a procedure or medication order than is now typically provided. This additional information is then repeated and validated by other members of the care team throughout the process, reducing the likelihood of misinterpretation of an instruction or action based on incomplete information.
For example, if a physician always includes both the drug name and the condition for which it is prescribed, a medication order for “Celebrex, seizures,” instead of “Cerebyx, seizures,” would immediately indicate a mistake had occurred in ordering a pain medication instead of an anti-convulsant.11 Research has shown that increasing the amount of information about a medication order reduces the range of potentially valid clinical decisions.
Whether a hospital relies on verbal communication, written communication, computer-based communication, or a combination of all three, redundancy can be built into its sign-out processes. As PDAs become more widely used, structured sign-outs should incorporate redundancy into patient-specific checklists to include information on clinical status, recent and pending tests and study results, and similar, pertinent information.
Simulation-based training that incorporates redundancy and promotes read-back of patient information holds promise for error reduction, especially during patient handoffs.
AHRQ has recently funded research on simulation training projects that seek to:
- Reduce communication errors during patient handoffs in the emergency department by implementing a patient-specific checklist based on an electronic medical record and by testing the effect of companion simulation-based training; and
- Evaluate and improve safe communication and coordination between anesthesia providers and nurses during care transitions and during hand-offs between the operating room and the post-anesthesia care unit.12
The 24/7 role of hospital physicians brings unique experiences and insights to the challenges of patient safety that can test the feasibility of systems to reduce errors associated with care transitions. As their numbers and leadership roles expand, hospitalists are poised to make significant contributions to improving patient safety and outcomes.
We at AHRQ look forward to assisting hospitalists in making these contributions and to achieving these goals together. We also look forward to continuing our relationship with SHM and the hospitalist community as a whole. TH
Dr. Clancy is the director of the Agency for Healthcare Research and Quality.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Impact of the nation’s hospitalists continues to grow new society of hospital medicine survey says [press release]. Society of Hospital Medicine. May 4, 2006.
- Society of Hospital Medicine. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1;S1. Available at: http://onlinelibrary.wiley.com/doi/10.1002/jhm.72/pdf. Last accessed January 17, 2007.
- Vidyarthi A [commentary]. Agency for Healthcare Research and Quality Web M&M: Morbidity and Mortality Rounds on the Web. Fumbled handoff. March 2004. Available at: www.webmm.ahrq.gov/case.aspx?caseID=55. Last accessed January 17, 2007.
- Wachter RM, Shojania KG. Internal Bleeding: The Truth Behind America’s Terrifying Epidemic of Medical Mistakes. New York: Rugged Land LLG; 2004.
- Vidyarthi A. Morbidity and Mortality Rounds on the Web, “Fumbled Handoff,” unpublished data, 2004.
- Biller CK, Antonacci AC, Pelletier S, et al. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006 Oct;135(2):275-281. Epub 2006 Aug 24.
- Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11(12):753-755.
- O’Leary KJ, Leibovitz DM, Feinglass J, et al. Outpatient physicians’ satisfaction with discharge summaries and perceived need for an electronic discharge summary. J Hosp Med. 2006;1:317-320. Published online Oct. 11, 2006.
- Reason JT. Managing the Risks of Organizational Accidents. Aldershot, England: Ashgate Publishing Company; 1997:135.
- Bar-Yam Y. System care: multiscale analysis of medical errors–eliminating errors and improving organizational capabilities. New England Complex Systems Institute: Technical Report; Sept 2004. Available at: http://necsi.org/projects/yaneer/NECSITechnicalReport2004-09.pdf. Last accessed January 17, 2007.
- Agency for Healthcare Research and Quality. Improving patient safety through simulation research. 2006 Simulation Projects. Available at: www.ahrq.gov/qual/simulproj.htm. Last accessed January 17, 2007.
In the nearly 10 years since the word “hospitalist” entered our consciousness, it has been inspiring to witness the dramatic growth in the specialty and, accompanying it, the growth in the membership of SHM.1 Over this same period, the healthcare system has made progress toward ensuring that it provides the safest, highest quality healthcare possible.
In my mind, the two phenomena are related. SHM itself and—more generally—the hospitalist field have played a vital role in promoting the use of evidence-based care, improved teamwork, and health information technology. Each of these efforts has made a significant difference in the care patients receive in hospitals. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of healthcare for all Americans. Both organizations are working to create positive change that will improve the health and healthcare of all patients.
As their numbers continue to grow, hospitalists are becoming integral members of the inpatient care team at many hospitals.
According to a recent survey conducted by SHM, a hospitalist averaged more than 2,300 inpatient encounters in 2005—a 7% increase over 2004.2 Today, hospital medicine groups practice not only in large metropolitan areas, but also in rural regions where one in three groups began operation during 2005.
In addition to their inpatient care responsibilities, the 15,000 hospitalists who practice today in the United States and Canada serve in key physician leadership roles that directly influence quality improvement and patient safety. Most hospitalists—86%—participate in quality improvement. More than half are involved in implementing information technology (54%) and teaching house staff (51%), and more than one-third—35%—are responsible for their organization’s rapid response team. The SHM survey found that nearly all hospital medicine groups provide round-the-clock patient care at their hospitals.
In this article I will emphasize two key areas relevant to improving patient safety for hospitalized patients: patient handoffs and communication.
Responsibility for Patient Handoffs
Hospitalists’ clinical and leadership roles are significant responsibilities for patient safety, including the critical period known as patient handoff or sign-out.
Patient handoffs refer to the interaction, communication, and planning required to achieve a seamless transition from one clinician to the next.3 When executed in a timely and thorough manner, patient handoffs can reduce the likelihood of medical errors and misinformation, prevent lost or missing clinical information, and maintain a high level of medical care.
Given today’s short hospital stays and the complex medical nature of the care necessary for many patients, timely and effective handoffs demand that hospitalists develop skills that extend beyond superior clinical care. They include:
- Communicating in an effective and efficient manner during patient sign-out;
- Demonstrating the use of “read-back” skills when communicating tasks;
- Developing oral and written patient summaries, including characteristics of the patient, provider, and time of the sign-out;
- Evaluating all medications for indication, dosing, and planned duration at the time of sign-out; and
- Anticipating what may go wrong with a patient after a transition in care occurs and clearly communicating this concern to the receiving clinician.
A Fumbled Handoff: A Case Study
A breakdown in communications—notably an error of omission in the patient handoff—contributed to a poor outcome for an elderly patient who was admitted to the hospital for an elective sigmoid resection.
The case, which was published in the AHRQ’s “Morbidity and Mortality Rounds on the Web” (developed by hospital medicine expert Robert Wachter, MD, and his team under contract to our agency), illustrates some of the challenges that face all clinicians in effectively transferring patient information and care responsibilities.4 It also underscores the need for close involvement by hospitalists in improving quality, teaching and supervising house staff, and implementing information systems.
According to the case study, a 73-year-old female patient with a history of hypertension, non-insulin dependent diabetes, and chronic renal insufficiency became tachycardic two days after surgery, despite receiving a low-dose beta-blocker. The same day, she informed her nurse that she had developed pain in her left leg.
Assuming the pain was related to the pre-operative epidural, the nurse contacted the anesthesia service, which responded by decreasing the epidural rate; the primary surgical team was not called. Late on the third day after surgery, the cross-covering intern was contacted about the patient’s left leg pain. No information about the intern’s findings was relayed to the primary team the following day.
On the fourth day, the patient complained to the nurse about mild chest discomfort, resulting in attention within 20 minutes by house staff and from the attending physician several hours later. The patient’s exam was unremarkable and a work-up was initiated.
Within an hour of the attending’s visit, the patient’s blood pressure dropped to 70/40, followed by a pulseless electrical activity arrest. The patient could not be resuscitated. A post-mortem examination revealed a pulmonary embolism.
Handoffs in an Era of Work-Hour Restrictions
Missing information about pain in the patient’s leg and a breakdown in communication between physicians contributed to the patient’s poor outcome. In this case, the breakdown may also have been influenced by the intern’s involvement on the third day. Like all medical residents this intern is subject to duty-hour restrictions.
Work-hour limits for all residents training in U.S. hospitals took effect in July 2003. Under these standards, created by the Accreditation Council for Graduate Medical Education (ACGME), residents are limited to a maximum of 30 consecutive work hours—known as the 30-hour rule, which includes time used for sign-out, teaching, and continuity of care. They are also prohibited from working more than 80 hours per week.
Despite the clear safety benefit of preventing fatigue-related mistakes, work-hour mandates have increased the number of patient handoffs and the potential for communication breakdowns.5 A survey of interns conducted at the hospital where this case study occurred identified a higher volume of sign-outs and the resulting potential for harm to patients as main concerns with the work-hour restrictions.6
Concerns about the quality and continuity of care that hospital patients receive are evident even among those medical residents whose work hours were restricted before the ACGME requirements took effect. (In New York state residents’ work hours have been restricted since 1998.)
A 2006 study of surgical residents at New York’s Beth Israel Hospital found that most believed that the quality of care patients received was either unchanged (63%) or worse (26%) since the work-hour restrictions took effect.7 Possible reasons for this perception include unresolved issues with continuity of care, miscommunication, and cross-coverage availability. The study concluded that interventions that target intern sign-out coverage constraints will be important for future efforts to improve the quality of care for hospital patients.
Written sign-outs appear to overcome some of the human errors that inevitably result from verbal patient summaries, such as disruptions and forgetfulness. Recent findings have, however, identified significant shortcomings in the quality and timeliness of written reports.
Critical information, such as code status and allergies, was missing in 80% of written sign-outs in one recent study.8 And in a 2006 study of the quality of discharge summaries, only 19% of hospital physicians with an outpatient practice reported being satisfied with the timeliness of discharge summaries. Only a third reported being satisfied with their quality of information. Most troubling, 41% believed that at least one of their patients hospitalized in the previous six months had experienced a preventable adverse event related to poor transfer of information at discharge.9
Use Redundancy and Simulation to Improve Safety
Given the clear challenges of providing quality and continuity of care in the inpatient setting, hospitalists are well positioned to identify strategies for safe and effective patient handoffs and advocate for a systems approach to their implementation.
Safety strategies that have been employed by industries outside of healthcare can provide a useful starting point. So-called “highly reliable” organizations use a variety of approaches to reduce the incidence of errors that occur during transitions in work staff. A recent review of transition methods used by NASA’s Johnson Space Center (Houston), Canadian nuclear power plants, and an ambulance dispatch center—organizations where lapses in transitions also have serious consequences—found that these entities used up to 21 handoff strategies.10 Techniques included verbal, face-to-face, and interactive questioning coordinated with written summaries just before a shift change.
Increasing redundancy is another technique used by highly reliable organizations to reduce the likelihood of missed, incomplete, or misinterpreted information. To create redundancy in clinical care, a physician would include more information at the outset of a procedure or medication order than is now typically provided. This additional information is then repeated and validated by other members of the care team throughout the process, reducing the likelihood of misinterpretation of an instruction or action based on incomplete information.
For example, if a physician always includes both the drug name and the condition for which it is prescribed, a medication order for “Celebrex, seizures,” instead of “Cerebyx, seizures,” would immediately indicate a mistake had occurred in ordering a pain medication instead of an anti-convulsant.11 Research has shown that increasing the amount of information about a medication order reduces the range of potentially valid clinical decisions.
Whether a hospital relies on verbal communication, written communication, computer-based communication, or a combination of all three, redundancy can be built into its sign-out processes. As PDAs become more widely used, structured sign-outs should incorporate redundancy into patient-specific checklists to include information on clinical status, recent and pending tests and study results, and similar, pertinent information.
Simulation-based training that incorporates redundancy and promotes read-back of patient information holds promise for error reduction, especially during patient handoffs.
AHRQ has recently funded research on simulation training projects that seek to:
- Reduce communication errors during patient handoffs in the emergency department by implementing a patient-specific checklist based on an electronic medical record and by testing the effect of companion simulation-based training; and
- Evaluate and improve safe communication and coordination between anesthesia providers and nurses during care transitions and during hand-offs between the operating room and the post-anesthesia care unit.12
The 24/7 role of hospital physicians brings unique experiences and insights to the challenges of patient safety that can test the feasibility of systems to reduce errors associated with care transitions. As their numbers and leadership roles expand, hospitalists are poised to make significant contributions to improving patient safety and outcomes.
We at AHRQ look forward to assisting hospitalists in making these contributions and to achieving these goals together. We also look forward to continuing our relationship with SHM and the hospitalist community as a whole. TH
Dr. Clancy is the director of the Agency for Healthcare Research and Quality.
References
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996 Aug 15;335(7):514-517.
- Impact of the nation’s hospitalists continues to grow new society of hospital medicine survey says [press release]. Society of Hospital Medicine. May 4, 2006.
- Society of Hospital Medicine. The core competencies in hospital medicine: a framework for curriculum development by the society of hospital medicine. J Hosp Med. 2006;1;S1. Available at: http://onlinelibrary.wiley.com/doi/10.1002/jhm.72/pdf. Last accessed January 17, 2007.
- Vidyarthi A [commentary]. Agency for Healthcare Research and Quality Web M&M: Morbidity and Mortality Rounds on the Web. Fumbled handoff. March 2004. Available at: www.webmm.ahrq.gov/case.aspx?caseID=55. Last accessed January 17, 2007.
- Wachter RM, Shojania KG. Internal Bleeding: The Truth Behind America’s Terrifying Epidemic of Medical Mistakes. New York: Rugged Land LLG; 2004.
- Vidyarthi A. Morbidity and Mortality Rounds on the Web, “Fumbled Handoff,” unpublished data, 2004.
- Biller CK, Antonacci AC, Pelletier S, et al. The 80-hour work guidelines and resident survey perceptions of quality. J Surg Res. 2006 Oct;135(2):275-281. Epub 2006 Aug 24.
- Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11(12):753-755.
- O’Leary KJ, Leibovitz DM, Feinglass J, et al. Outpatient physicians’ satisfaction with discharge summaries and perceived need for an electronic discharge summary. J Hosp Med. 2006;1:317-320. Published online Oct. 11, 2006.
- Reason JT. Managing the Risks of Organizational Accidents. Aldershot, England: Ashgate Publishing Company; 1997:135.
- Bar-Yam Y. System care: multiscale analysis of medical errors–eliminating errors and improving organizational capabilities. New England Complex Systems Institute: Technical Report; Sept 2004. Available at: http://necsi.org/projects/yaneer/NECSITechnicalReport2004-09.pdf. Last accessed January 17, 2007.
- Agency for Healthcare Research and Quality. Improving patient safety through simulation research. 2006 Simulation Projects. Available at: www.ahrq.gov/qual/simulproj.htm. Last accessed January 17, 2007.
AHRQ Overview
In the nearly 10 years since Bob Wachter and Lee Goldman coined the word hospitalist,1 it has been inspiring to see the dramatic growth of this specialty and with it, the growth in membership of the Society of Hospital Medicine.
Over the same period, the health care system has made progress toward ensuring that it provides the safest, highest‐quality health care possible.
In my mind, the two phenomena are related. The Society of Hospital Medicine, along with the hospitalist field more generally, has played a critical role in promoting the use of evidence‐based care, improved teamwork, and health information technology, which can make a significant difference in the care patients receive in the hospital. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of health care for all Americans. So, both of our organizations are working to create positive change that will improve the health and health care of all patients.
As a research agency, we support studies, systematic reviews, and evaluations that help to build the foundation of evidence for health care. However, our work goes beyond simply conducting, supporting, and disseminating health services research. At its heart, our mission is helping the health care system translate research into improved practice and policy. We do not see research as an end in itself but rather a vehicle to improve health care and health. We achieve our goals by working with our public‐ and private‐sector partners to translate the research we support and conduct into knowledge and information that can be used immediately to improve health care for all Americans.
Health Information Technology
This commentary features AHRQ's quality‐related initiatives, including promoting the use of health information technology to improve quality and safety, providing the tools to assess health care quality, and expanding training to promote quality improvement in local communities. Many of these tools are ideal for hospitalists to use in their mission to ensure high‐quality care and an efficient and thorough handoff at discharge.
AHRQ is at the leading edge of President Bush's vision of a health care system that harnesses the power of health information technology (IT) to improve quality. AHRQ has invested more than $166 million in more than 100 projects to promote the use of health IT, with a special focus on rural hospitals and communities. These projects will enable providers to improve patient safety and reduce medication errors by eliminating handwritten prescriptions, help to ensure that important information follows patients as they move among health care settings, and reduce duplicative and unnecessary testing.
As part of this investment, AHRQ has awarded multiyear contracts totaling nearly $30 million to Colorado, Delaware, Indiana, Rhode Island, Tennessee, and Utah to help in the development of statewide networks that are secure, ensure privacy, and make information more accessible. Participants in the networks include major purchasers of health care, public and private payers, hospitals, ambulatory care facilities, home health care providers, and long‐term care providers.
In addition, AHRQ created the AHRQ National Resource Center for Health Information Technology (
Effective Health Care Program
However, as we all know, health IT is not a magic bullet or the sole answer to the quality and safety problems facing the American health care system. It is a means to an end. Although health IT has the great potential to deliver evidence to clinicians, patients, and other health care decision makers when they need it, one challenge is to ensure the evidence base is readily available.
To that end, AHRQ's new Effective Health Care Program, authorized under Section 1013 of the Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003, is conducting research with a focus on outcomes, comparative clinical effectiveness, and appropriateness of pharmaceuticals, devices, and health care services. At press time, AHRQ had released two effectiveness reports, Comparative Effectiveness of Management Strategies for Gastroesophageal Reflux Disease2 and Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities.3
The AHRQ Effective Health Care Program takes three approaches to research on the comparative effectiveness of different treatments and clinical practices:
-
Review and synthesize knowledge. AHRQ's Evidence‐Based Practice Centers systematically review published and unpublished scientific evidence to develop evidence reports.
-
Promote and generate knowledge. A new AHRQ‐supported research network called DEcIDE (Developing Evidence to Inform Decisions about Effectiveness) conducts accelerated practical studies of new scientific evidence and analytic tools.
-
Compile the findings and translate knowledge. The John M. Eisenberg Clinical Decisions and Communications Science Center compiles the research results into a variety of useful formats for stakeholders.
Interested readers should go to the Effective Health Care Web site,
Patient Safety and Quality
Since 2001, AHRQ has been the leading funder of patient safety research, and I am proud that our $165 million patient safety research program is bearing fruit.
For example, Bob Wachterin his spare timeand his team at the University of California, San Francisco, under contract to AHRQ, developed AHRQ's Patient Safety Network, which can be found at
Readers of JHM also will be interested in AHRQ's Hospital Survey on Patient Safety Culture, which we released in partnership with Premier, Inc., the Department of Defense (DoD), and the American Hospital Association. The survey can be used to evaluate employees' attitudes about patient safety in their facilities or within specific units. It addresses a critical aspect of patient safety improvement: measuring organizational conditions that can lead to adverse events and patient harm. The survey, which is being used in the DoD's medical facilities, is available at
In another quality initiative, AHRQ also has developed a series of software tools that can help hospitals gauge the quality of care they provide. AHRQ's Prevention Quality Indicators allow hospitals to detect potentially avoidable hospital admissions for illnesses that can be effectively treated with high‐quality, community‐based primary care.
Another tool is the Inpatient Quality Indicators, 29 measures that can be used to help hospitals identify potential problem areas and to provide a proxy measure of hospital quality of care. The Patient Safety Indicators can help hospitals enhance their performance by quickly detecting potential medical errors in patients who have undergone medical or surgical care. Staff can then investigate to determine whether the problems detected by the indicators were caused by potentially preventable medical errors or have some other explanation.
Building on its long track record of developing surveys to gauge consumers' experiences in the health care system, AHRQ has developed H‐CAHPS, a survey tool that hospitals, employers, states, and others can use to assess the perceptions of hospital patients about the quality of the care they receive. This information is designed to help patients, their employers, and other purchasers make informed decisions and give hospitals feedback they can use to improve care. The Centers for Medicare & Medicaid Services, in partnership with the nation's major hospital trade groups, is using H‐CAHPS as part of their collaborative Hospital Quality Alliance to develop comparative information about hospitals.
In the future, AHRQ plans to create other surveys, including Ambulatory CAHPS, In‐Center Hemodialysis CAHPS, and Nursing Home CAHPS.
AHRQ also is now working in partnership with the Department of Veterans Affairs to train the third class of state and hospital teams participating in the Patient Safety Improvement Corps. The program was created because states asked us for help in areas such as conducting effective investigations of reports of medical errors and developing interventions and changes in standard clinical practice. When trained, the teams return to their local communities armed with the knowledge to improve patient safety.
National Health Care Quality and Disparities Reports
Finally, in January 2006, AHRQ released the third annual National Healthcare Quality Report (NHQR) and the National Healthcare Disparities Report. These reports provide data on the quality of health care and disparities in the use of health care services associated with patient characteristics, including race, ethnicity, income, education, and area of residence.45 In March 2006, AHRQ released a Web‐based tool called State Snapshots for states to use in measuring health care quality. The State Snapshots provides quick and easy access to the many measures and tables of the 2005 NHQR and also provides trend data that can help in the understanding of the quality of health care in individual states, including strengths, weaknesses, and opportunities for improvement. The reports and the State Snapshots are available on AHRQ's QualityTools Web site at
I hope this article has provided a glimpse into the quality improvement initiatives and activities supported by AHRQ. For ongoing information on these activities, I urge readers to go to AHRQ's Web site and sign up for our electronic newsletter (
AHRQ's aim is to make doing the right thing the easy thing to do for the health care system. We look forward to working with readers of the Journal of Hospital Medicine to achieve that goal.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,, et al.Comparative Effectiveness of Management Strategies for Gastroesophageal Reflux Disease. Evidence Report/Technology Assessment No. 1. (prepared by Tufts‐New England Medical Center Evidence‐Based Practice Center under Contract No. 290‐02‐0022.);Rockville, MD:Agency for Healthcare Research and Quality,2005.
- ,,,,,.Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities. Comparative Effectiveness Review No. 2 (prepared by ECRI Evidence‐Based Practice Center under Contract No. 290‐02‐0019);Rockville, MD:Agency for Healthcare Research and Quality,2006.
- National Healthcare Quality Report,2005.Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/qual/nhqr05/nhqr05.htm.
- National Healthcare Disparities Report,2005.Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/qual/nhdr05/nhdr05.htm.
In the nearly 10 years since Bob Wachter and Lee Goldman coined the word hospitalist,1 it has been inspiring to see the dramatic growth of this specialty and with it, the growth in membership of the Society of Hospital Medicine.
Over the same period, the health care system has made progress toward ensuring that it provides the safest, highest‐quality health care possible.
In my mind, the two phenomena are related. The Society of Hospital Medicine, along with the hospitalist field more generally, has played a critical role in promoting the use of evidence‐based care, improved teamwork, and health information technology, which can make a significant difference in the care patients receive in the hospital. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of health care for all Americans. So, both of our organizations are working to create positive change that will improve the health and health care of all patients.
As a research agency, we support studies, systematic reviews, and evaluations that help to build the foundation of evidence for health care. However, our work goes beyond simply conducting, supporting, and disseminating health services research. At its heart, our mission is helping the health care system translate research into improved practice and policy. We do not see research as an end in itself but rather a vehicle to improve health care and health. We achieve our goals by working with our public‐ and private‐sector partners to translate the research we support and conduct into knowledge and information that can be used immediately to improve health care for all Americans.
Health Information Technology
This commentary features AHRQ's quality‐related initiatives, including promoting the use of health information technology to improve quality and safety, providing the tools to assess health care quality, and expanding training to promote quality improvement in local communities. Many of these tools are ideal for hospitalists to use in their mission to ensure high‐quality care and an efficient and thorough handoff at discharge.
AHRQ is at the leading edge of President Bush's vision of a health care system that harnesses the power of health information technology (IT) to improve quality. AHRQ has invested more than $166 million in more than 100 projects to promote the use of health IT, with a special focus on rural hospitals and communities. These projects will enable providers to improve patient safety and reduce medication errors by eliminating handwritten prescriptions, help to ensure that important information follows patients as they move among health care settings, and reduce duplicative and unnecessary testing.
As part of this investment, AHRQ has awarded multiyear contracts totaling nearly $30 million to Colorado, Delaware, Indiana, Rhode Island, Tennessee, and Utah to help in the development of statewide networks that are secure, ensure privacy, and make information more accessible. Participants in the networks include major purchasers of health care, public and private payers, hospitals, ambulatory care facilities, home health care providers, and long‐term care providers.
In addition, AHRQ created the AHRQ National Resource Center for Health Information Technology (
Effective Health Care Program
However, as we all know, health IT is not a magic bullet or the sole answer to the quality and safety problems facing the American health care system. It is a means to an end. Although health IT has the great potential to deliver evidence to clinicians, patients, and other health care decision makers when they need it, one challenge is to ensure the evidence base is readily available.
To that end, AHRQ's new Effective Health Care Program, authorized under Section 1013 of the Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003, is conducting research with a focus on outcomes, comparative clinical effectiveness, and appropriateness of pharmaceuticals, devices, and health care services. At press time, AHRQ had released two effectiveness reports, Comparative Effectiveness of Management Strategies for Gastroesophageal Reflux Disease2 and Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities.3
The AHRQ Effective Health Care Program takes three approaches to research on the comparative effectiveness of different treatments and clinical practices:
-
Review and synthesize knowledge. AHRQ's Evidence‐Based Practice Centers systematically review published and unpublished scientific evidence to develop evidence reports.
-
Promote and generate knowledge. A new AHRQ‐supported research network called DEcIDE (Developing Evidence to Inform Decisions about Effectiveness) conducts accelerated practical studies of new scientific evidence and analytic tools.
-
Compile the findings and translate knowledge. The John M. Eisenberg Clinical Decisions and Communications Science Center compiles the research results into a variety of useful formats for stakeholders.
Interested readers should go to the Effective Health Care Web site,
Patient Safety and Quality
Since 2001, AHRQ has been the leading funder of patient safety research, and I am proud that our $165 million patient safety research program is bearing fruit.
For example, Bob Wachterin his spare timeand his team at the University of California, San Francisco, under contract to AHRQ, developed AHRQ's Patient Safety Network, which can be found at
Readers of JHM also will be interested in AHRQ's Hospital Survey on Patient Safety Culture, which we released in partnership with Premier, Inc., the Department of Defense (DoD), and the American Hospital Association. The survey can be used to evaluate employees' attitudes about patient safety in their facilities or within specific units. It addresses a critical aspect of patient safety improvement: measuring organizational conditions that can lead to adverse events and patient harm. The survey, which is being used in the DoD's medical facilities, is available at
In another quality initiative, AHRQ also has developed a series of software tools that can help hospitals gauge the quality of care they provide. AHRQ's Prevention Quality Indicators allow hospitals to detect potentially avoidable hospital admissions for illnesses that can be effectively treated with high‐quality, community‐based primary care.
Another tool is the Inpatient Quality Indicators, 29 measures that can be used to help hospitals identify potential problem areas and to provide a proxy measure of hospital quality of care. The Patient Safety Indicators can help hospitals enhance their performance by quickly detecting potential medical errors in patients who have undergone medical or surgical care. Staff can then investigate to determine whether the problems detected by the indicators were caused by potentially preventable medical errors or have some other explanation.
Building on its long track record of developing surveys to gauge consumers' experiences in the health care system, AHRQ has developed H‐CAHPS, a survey tool that hospitals, employers, states, and others can use to assess the perceptions of hospital patients about the quality of the care they receive. This information is designed to help patients, their employers, and other purchasers make informed decisions and give hospitals feedback they can use to improve care. The Centers for Medicare & Medicaid Services, in partnership with the nation's major hospital trade groups, is using H‐CAHPS as part of their collaborative Hospital Quality Alliance to develop comparative information about hospitals.
In the future, AHRQ plans to create other surveys, including Ambulatory CAHPS, In‐Center Hemodialysis CAHPS, and Nursing Home CAHPS.
AHRQ also is now working in partnership with the Department of Veterans Affairs to train the third class of state and hospital teams participating in the Patient Safety Improvement Corps. The program was created because states asked us for help in areas such as conducting effective investigations of reports of medical errors and developing interventions and changes in standard clinical practice. When trained, the teams return to their local communities armed with the knowledge to improve patient safety.
National Health Care Quality and Disparities Reports
Finally, in January 2006, AHRQ released the third annual National Healthcare Quality Report (NHQR) and the National Healthcare Disparities Report. These reports provide data on the quality of health care and disparities in the use of health care services associated with patient characteristics, including race, ethnicity, income, education, and area of residence.45 In March 2006, AHRQ released a Web‐based tool called State Snapshots for states to use in measuring health care quality. The State Snapshots provides quick and easy access to the many measures and tables of the 2005 NHQR and also provides trend data that can help in the understanding of the quality of health care in individual states, including strengths, weaknesses, and opportunities for improvement. The reports and the State Snapshots are available on AHRQ's QualityTools Web site at
I hope this article has provided a glimpse into the quality improvement initiatives and activities supported by AHRQ. For ongoing information on these activities, I urge readers to go to AHRQ's Web site and sign up for our electronic newsletter (
AHRQ's aim is to make doing the right thing the easy thing to do for the health care system. We look forward to working with readers of the Journal of Hospital Medicine to achieve that goal.
In the nearly 10 years since Bob Wachter and Lee Goldman coined the word hospitalist,1 it has been inspiring to see the dramatic growth of this specialty and with it, the growth in membership of the Society of Hospital Medicine.
Over the same period, the health care system has made progress toward ensuring that it provides the safest, highest‐quality health care possible.
In my mind, the two phenomena are related. The Society of Hospital Medicine, along with the hospitalist field more generally, has played a critical role in promoting the use of evidence‐based care, improved teamwork, and health information technology, which can make a significant difference in the care patients receive in the hospital. Similarly, the mission of the Agency for Healthcare Research and Quality (AHRQ) is to improve the quality, safety, efficiency, and effectiveness of health care for all Americans. So, both of our organizations are working to create positive change that will improve the health and health care of all patients.
As a research agency, we support studies, systematic reviews, and evaluations that help to build the foundation of evidence for health care. However, our work goes beyond simply conducting, supporting, and disseminating health services research. At its heart, our mission is helping the health care system translate research into improved practice and policy. We do not see research as an end in itself but rather a vehicle to improve health care and health. We achieve our goals by working with our public‐ and private‐sector partners to translate the research we support and conduct into knowledge and information that can be used immediately to improve health care for all Americans.
Health Information Technology
This commentary features AHRQ's quality‐related initiatives, including promoting the use of health information technology to improve quality and safety, providing the tools to assess health care quality, and expanding training to promote quality improvement in local communities. Many of these tools are ideal for hospitalists to use in their mission to ensure high‐quality care and an efficient and thorough handoff at discharge.
AHRQ is at the leading edge of President Bush's vision of a health care system that harnesses the power of health information technology (IT) to improve quality. AHRQ has invested more than $166 million in more than 100 projects to promote the use of health IT, with a special focus on rural hospitals and communities. These projects will enable providers to improve patient safety and reduce medication errors by eliminating handwritten prescriptions, help to ensure that important information follows patients as they move among health care settings, and reduce duplicative and unnecessary testing.
As part of this investment, AHRQ has awarded multiyear contracts totaling nearly $30 million to Colorado, Delaware, Indiana, Rhode Island, Tennessee, and Utah to help in the development of statewide networks that are secure, ensure privacy, and make information more accessible. Participants in the networks include major purchasers of health care, public and private payers, hospitals, ambulatory care facilities, home health care providers, and long‐term care providers.
In addition, AHRQ created the AHRQ National Resource Center for Health Information Technology (
Effective Health Care Program
However, as we all know, health IT is not a magic bullet or the sole answer to the quality and safety problems facing the American health care system. It is a means to an end. Although health IT has the great potential to deliver evidence to clinicians, patients, and other health care decision makers when they need it, one challenge is to ensure the evidence base is readily available.
To that end, AHRQ's new Effective Health Care Program, authorized under Section 1013 of the Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003, is conducting research with a focus on outcomes, comparative clinical effectiveness, and appropriateness of pharmaceuticals, devices, and health care services. At press time, AHRQ had released two effectiveness reports, Comparative Effectiveness of Management Strategies for Gastroesophageal Reflux Disease2 and Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities.3
The AHRQ Effective Health Care Program takes three approaches to research on the comparative effectiveness of different treatments and clinical practices:
-
Review and synthesize knowledge. AHRQ's Evidence‐Based Practice Centers systematically review published and unpublished scientific evidence to develop evidence reports.
-
Promote and generate knowledge. A new AHRQ‐supported research network called DEcIDE (Developing Evidence to Inform Decisions about Effectiveness) conducts accelerated practical studies of new scientific evidence and analytic tools.
-
Compile the findings and translate knowledge. The John M. Eisenberg Clinical Decisions and Communications Science Center compiles the research results into a variety of useful formats for stakeholders.
Interested readers should go to the Effective Health Care Web site,
Patient Safety and Quality
Since 2001, AHRQ has been the leading funder of patient safety research, and I am proud that our $165 million patient safety research program is bearing fruit.
For example, Bob Wachterin his spare timeand his team at the University of California, San Francisco, under contract to AHRQ, developed AHRQ's Patient Safety Network, which can be found at
Readers of JHM also will be interested in AHRQ's Hospital Survey on Patient Safety Culture, which we released in partnership with Premier, Inc., the Department of Defense (DoD), and the American Hospital Association. The survey can be used to evaluate employees' attitudes about patient safety in their facilities or within specific units. It addresses a critical aspect of patient safety improvement: measuring organizational conditions that can lead to adverse events and patient harm. The survey, which is being used in the DoD's medical facilities, is available at
In another quality initiative, AHRQ also has developed a series of software tools that can help hospitals gauge the quality of care they provide. AHRQ's Prevention Quality Indicators allow hospitals to detect potentially avoidable hospital admissions for illnesses that can be effectively treated with high‐quality, community‐based primary care.
Another tool is the Inpatient Quality Indicators, 29 measures that can be used to help hospitals identify potential problem areas and to provide a proxy measure of hospital quality of care. The Patient Safety Indicators can help hospitals enhance their performance by quickly detecting potential medical errors in patients who have undergone medical or surgical care. Staff can then investigate to determine whether the problems detected by the indicators were caused by potentially preventable medical errors or have some other explanation.
Building on its long track record of developing surveys to gauge consumers' experiences in the health care system, AHRQ has developed H‐CAHPS, a survey tool that hospitals, employers, states, and others can use to assess the perceptions of hospital patients about the quality of the care they receive. This information is designed to help patients, their employers, and other purchasers make informed decisions and give hospitals feedback they can use to improve care. The Centers for Medicare & Medicaid Services, in partnership with the nation's major hospital trade groups, is using H‐CAHPS as part of their collaborative Hospital Quality Alliance to develop comparative information about hospitals.
In the future, AHRQ plans to create other surveys, including Ambulatory CAHPS, In‐Center Hemodialysis CAHPS, and Nursing Home CAHPS.
AHRQ also is now working in partnership with the Department of Veterans Affairs to train the third class of state and hospital teams participating in the Patient Safety Improvement Corps. The program was created because states asked us for help in areas such as conducting effective investigations of reports of medical errors and developing interventions and changes in standard clinical practice. When trained, the teams return to their local communities armed with the knowledge to improve patient safety.
National Health Care Quality and Disparities Reports
Finally, in January 2006, AHRQ released the third annual National Healthcare Quality Report (NHQR) and the National Healthcare Disparities Report. These reports provide data on the quality of health care and disparities in the use of health care services associated with patient characteristics, including race, ethnicity, income, education, and area of residence.45 In March 2006, AHRQ released a Web‐based tool called State Snapshots for states to use in measuring health care quality. The State Snapshots provides quick and easy access to the many measures and tables of the 2005 NHQR and also provides trend data that can help in the understanding of the quality of health care in individual states, including strengths, weaknesses, and opportunities for improvement. The reports and the State Snapshots are available on AHRQ's QualityTools Web site at
I hope this article has provided a glimpse into the quality improvement initiatives and activities supported by AHRQ. For ongoing information on these activities, I urge readers to go to AHRQ's Web site and sign up for our electronic newsletter (
AHRQ's aim is to make doing the right thing the easy thing to do for the health care system. We look forward to working with readers of the Journal of Hospital Medicine to achieve that goal.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,, et al.Comparative Effectiveness of Management Strategies for Gastroesophageal Reflux Disease. Evidence Report/Technology Assessment No. 1. (prepared by Tufts‐New England Medical Center Evidence‐Based Practice Center under Contract No. 290‐02‐0022.);Rockville, MD:Agency for Healthcare Research and Quality,2005.
- ,,,,,.Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities. Comparative Effectiveness Review No. 2 (prepared by ECRI Evidence‐Based Practice Center under Contract No. 290‐02‐0019);Rockville, MD:Agency for Healthcare Research and Quality,2006.
- National Healthcare Quality Report,2005.Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/qual/nhqr05/nhqr05.htm.
- National Healthcare Disparities Report,2005.Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/qual/nhdr05/nhdr05.htm.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- ,,,, et al.Comparative Effectiveness of Management Strategies for Gastroesophageal Reflux Disease. Evidence Report/Technology Assessment No. 1. (prepared by Tufts‐New England Medical Center Evidence‐Based Practice Center under Contract No. 290‐02‐0022.);Rockville, MD:Agency for Healthcare Research and Quality,2005.
- ,,,,,.Effectiveness of Noninvasive Diagnostic Tests for Breast Abnormalities. Comparative Effectiveness Review No. 2 (prepared by ECRI Evidence‐Based Practice Center under Contract No. 290‐02‐0019);Rockville, MD:Agency for Healthcare Research and Quality,2006.
- National Healthcare Quality Report,2005.Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/qual/nhqr05/nhqr05.htm.
- National Healthcare Disparities Report,2005.Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/qual/nhdr05/nhdr05.htm.