User login
When a child won’t speak
- Good-quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
- Assess children with selective mutism for severe social anxiety (C).
- Drug therapy for anxiety and depressive conditions related to selective mutism and collaboration with school personnel and parents can help a child increase her frequency and audibility of speech in public settings (C).
- Exposure-based practices can help children with selective mutism to speak in public places (C).
Lucy’s parents were having difficulty reconciling the child they knew at home with the one they sent to school. At home, the 7-year-old spoke easily with her parents and siblings. At school and in other public places such as the supermarket, mall, or park, she would not speak at all. This had been going on for several years.
While Lucy was attending school without difficulty, she seemed sullen and withdrawn to her teachers. Lucy had friends at school, but would communicate with them by writing messages on paper or drawing letters in the air. Although Lucy had passed first grade on the basis of her written work, her parents worried about her ability to succeed in second grade, where her teachers expected her to participate in class and she would need to take standardized tests that required audible verbal responses. At the urging of a school counselor, Lucy’s parents took her to their family physician. They needed help in drawing her out so that the rest of the world could get to know the Lucy that they knew and loved.
Lucy’s case is typical of selective mutism
Lucy was suffering from selective mutism, the persistent failure to speak in specific social situations where speaking is expected, such as at school and with playmates.1 Lucy’s case is typical in that children with selective mutism speak well in other situations, typically at home. Thus, the disorder is not due to a communication disorder such as stuttering and it is not due to a lack of knowledge or comfort with language.
To meet diagnostic criteria, the disorder must last at least 1 month, though it can last for several years, and must interfere with a child’s education or ability to communicate socially.1
A little known disorder makes national headlines
Selective mutism occurs in 0.2%–2.0% of children, affects boys and girls equally, and often begins at 3 to 6 years of age.2-9 The disorder gained national attention this past spring when it was revealed that the shooter in the Virginia Tech massacre—Seung-Hui Cho—had, as an adolescent, been diagnosed with selective mutism.10 Though his diagnosis made plenty of headlines, the disorder itself occupies little space in the pediatric literature.11
What we do know is that selective mutism can have a chronic course that affects a child’s ability to form friendships, complete academic tasks, develop appropriate language and social skills, and participate in standardized testing.2-9 While parents often attribute their child’s behavior to shyness, this disorder goes beyond that. While shy children function, those with selective mutism struggle socially, emotionally, and academically. Children with selective mutism say the words won’t come out and their body won’t let them speak. One father of a 7-year-old girl with selective mutism said that his daughter “describes it as the words get stuck in her toes.”12
Many researchers theorize that children with selective mutism have severe social anxiety, and assessment and treatment strategies are typically based on this notion. Reports in the literature have also suggested that selective mutism is related to a developmental disorder or delay, as seen in autistic spectrum disorders, as well as anxiety disorders and depression.13 In addition, selective mutism has been linked to oppositional defiant disorder and subtle language impairments.14,15
Begin by excluding competing explanations
If a family is referred to you for possible selective mutism, you’ll first need to exclude competing explanations for the problem, such as hearing difficulties, speech and language disorders, school-based threats, and medical problems, such as asthma, which could prevent a child from speaking comfortably in a public setting. Assuming you are able to exclude these, and other competing explanations, you’ll need to ask 8 questions of parents and school officials. The answers you get will help you to screen for selective mutism and identify key antecedents and consequences to the behavior that are important in addressing the problem.
8 questions you’ll need to ask
1. What specific settings involve failure to speak? Children with selective mutism typically have difficulties in school, on the playground, in malls, and at restaurants.
2. Has the mutism lasted at least one month? Brief refusal to speak is not uncommon in children.
3. Does the child speak well at home with people she knows well? Most children with selective mutism speak well at home with family members, which belies a communication disorder.
4. Is failure to speak significantly interfering with the child’s academic or social development? Selective mutism must involve a significant interference in daily functioning.
5. What circumstances surround each episode of mutism? In particular, is the mutism associated with the desire to increase social attention or stimulation from others, decrease anxiety, or avoid or withdraw from adult commands or requests? A full understanding of selective mutism must include a review of triggers like these.
6. Can the child be encouraged to speak audibly in any way in certain public settings? Children with selective mutism who can speak to some extent in public situations may have a better prognosis than those who do not.9
7. How do others respond to, or compensate for, the child’s mutism? Do they complete tasks for the child? Order food for her? Allow whispers or communication via writing? Excessive accommodations enable a child with selective mutism to maintain the behavior.
8. Does the child appear anxious or depressed in situations involving mutism? Mutism is often linked to poor affect and social anxiety.
Still suspect selective mutism? Make a referral
If after asking these 8 questions you still suspect selective mutism, you will need to make a referral to a child psychologist or other mental health professional who specializes in behavioral strategies to treat selective mutism. The psychologist will meet with the child and utilize more formal methods of assessment.
The psychologist may use the Anxiety Disorders Interview Schedule for DSM-IV-TR (child and parent versions), a structured interview that emphasizes anxiety-based disorders and includes a section for selective mutism based on DSM-IV-TR criteria.16 Another helpful tool is the Functional Diagnostic Profile for Selective Mutism, which helps to assess contextual factors that surround refusal to speak.17 The challenge, of course, in conducting these interviews is that many children will not answer the psychologist’s questions verbally, but may communicate via nonverbal gestures, writing, or other creative ways such as drawing letters in the air.
Parent and teacher logs provide valuable insight
Ongoing behavioral observations or daily logbooks completed by parents and teachers are also important in treating a child with selective mutism. If parents aren’t doing so already at the suggestion of the therapist, ask them to keep a logbook and encourage them to ask the child’s teachers to keep one, as well. This log should include the number and volume of words spoken, to whom the child has spoken, where the child spoke, how others reacted (ie, Did they pay extra attention to the child?), and the child’s compensatory behaviors such as whispering, pointing, crying, nodding, or frowning.18 Parents and teachers should also note the antecedents to mutism, including demands (or requests) from others, or the presence of unfamiliar people.
A focus on systematic desensitization
Much of the literature regarding the treatment of selective mutism consists of case reports and small-scale studies.19 The paucity of data is, in part, a reflection of the rarity of the problem as well as a historical lack of consensus among researchers about the nature and diagnostic criteria for selective mutism.
The studies we do have on selective mutism indicate that behavior modification can be effective for these patients. Behavioral treatment primarily involves child- and parent-based practices.20
Child-based practices include management of physical sensations of anxiety often via relaxation training and breathing retraining. Neither technique requires verbal input from a child. In addition, the therapist will have the child practice audible words in progressively more difficult settings via systematic desensitization. These settings often include the following, in order: the child’s home (with the therapist), the therapist’s office, community settings such as a mall or a restaurant, and finally, school.
In these settings, the therapist might, for example, encourage the patient to:
- speak on the telephone or answer the door at home.
- stay at the therapist’s office until at least one word is audibly spoken. (One approach that the therapist may use to increase rapport and provide opportunities to prompt speech is to play games with the child.)
- order her own food at a local restaurant.
- read a story aloud to classmates at school.
In addition to systematic desensitization, the therapist may use audio or videotapes to help the youngster. In one scenario, the therapist may ask the parents to bring in an audiotape or videotape of the child at home when she is speaking. The therapist then provides ample reinforcement for the child’s speech by praising the child for having a beautiful voice and for making the tape. Audio and videotapes may also be used to help the child speak louder or work on her articulation.
Reinforce the positive, avoid “shaming”
Parent-based practices include reinforcing the child’s speech in different settings, developing new and independent exposures to generalize speech, and consulting with school officials on an ongoing basis to address social and academic problems from poor use of speech.
The therapist is likely to remind the parent that positive reinforcement is key, while punishing or “shaming” the child is ineffective.11 Some therapists will make use of a technique called “token economy,” where the child’s progress earns her colored chips that can be redeemed for a trip to a video game center, or a special treat, such as a sleep-over with a trusted friend.11
With the therapist’s help, parents can also model appropriate social interactions for a child with selective mutism because social skills may not be sufficiently developed. For example, the parent might encourage the child to answer the door or telephone. The parent might also monitor the child’s interactions with friends and provide feedback. In addition, the therapist may encourage the parents to ignore inappropriate compensatory behaviors as treatment progresses. Instead, a child with selective mutism may be increasingly challenged to provide audible speech to make requests or otherwise communicate.21
Drug therapy may include MAOIs and SSRIs
Medical treatment for selective mutism may include monoamine oxidase inhibitors (MAOIs) such as phenelzine (30–60 mg/day) or selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (10–60 mg/day), sertraline (100 mg/day), fluvoxamine (50–100 mg/day), citalopram (20–40 mg/day), or paroxetine (5 mg/day).22 However, no large-scale studies of pharmacotherapy for selective mutism have been conducted and medication effects are quite variable. The literature in this area has consisted largely of case studies.
After 9 months of treatment, Lucy speaks up at school
Lucy’s therapist (JLV) utilized many of the behavioral procedures described in this article. Treatment included exposure-based practices at home, in a clinic, in various community settings, and at school. By the end of her 9 months of treatment, Lucy was speaking independently to her classmates and teachers, though ongoing praise by her teachers was needed to encourage her to maintain an appropriate speech volume.
The literature on selective mutism suggests Lucy’s case was not unusual; it typically takes several months for these young patients to improve. Ongoing communication issues, though, often linger.9
- What specific settings involve failure to speak?
- Has the mutism lasted at least one month?
- Does the child speak well at home with people she knows well?
- Is failure to speak significantly interfering with the child’s academic or social development?
- What circumstances surround each episode of mutism?
- Can the child be encouraged to speak audibly in any way in certain public settings?
- How do others respond to, or compensate for, the child’s mutism?
- Does the child appear anxious or depressed in situations involving mutism?
Correspondence
Christopher A. Kearney, PhD, Department of Psychology, University of Nevada, Las Vegas, 4505 maryland Parkway, Las Vegas, Nv 89154-5030; [email protected]
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text revision). Washington, DC: Author.
2. Andersson CB, Thomsen PH. Electively mute children: an analysis of 37 Danish cases. Nordic J Psychiatry 1998;52:231-238.
3. Bergman RL, Piacentini J, McCracken JT. Prevalence and description of selective mutism in a school-based study. J Am Acad Child Adolesc Psychiatry 2002;41:938-946.
4. Black B, Uhde TW. Elective mutism as a variant of social phobia. J Am Acad Child Adolesc Psychiatry 1992;1090-1094.
5. Ford MA, Sladeczeck IE, Carlson J. Selective mutism: phenomenological characteristics. School Psychol Quarterly 1998;13:192-227.
6. Kopp S, Gillberg C. Selective mutism: a population-based study: a research note. J Child Psychol Psychiatry 1997;38:257-262.
7. Krysanski V. A brief review of selective mutism literature. J Psychol 2003;137:29-40.
8. Kumpulainen K, Rasanen E, Raaska H, Somppi V. Selective mutism among second-graders in elementary school. Euro Child Adolesc Psychiatry 1998;7:24-29.
9. Remschmidt H, Poller M, Herpertz-Dahlmann B, Hennighausen K, Gutenbrenner C. A follow-up study of 45 patients with elective mutism. European Archives of Psychiatry and Clinical Neuroscience 2001;251:284-296.
10. Urbina I. Virginia Tech criticized for actions in shooting. The New York Times. August 30, 2007. Available at: www.nytimes.com/2007/08/30/us/30school.html. Accessed on October 10, 2007.
11. Schwartz RH, Shipon-Blum E. “Shy”child? Don’t overlook selective mutism. Contemp Peds 2005;22(7):30-39.
12. ABC News. Selective mutism: When your child can’t speak. Available at: abcnews.go.com/GmA/AmericanFamily/story?id=1770308&page=1. Accessed on September 26, 2007.
13. Vecchio J, Kearney CA. Selective mutism in children: comparison to youths with and without anxiety disorders. J Psychopath Beh Assess 2005;28:139-144.
14. Yeganeh R, Beidel DC, Turner SM. Selective mutism: more than social anxiety? Depress Anx 2006;23:117-123.
15. Manassis K, Fung D, Tannock R, Sloman L, Fiksenbaum L, McInnes A. Characterizing selective mutism: is it more than social anxiety? Depress Anx 2003;18:153-161.
16. Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV, child and parent versions. New York: oxford University Press;1996.
17. Schill MT, Kratochwill TR, Gardner WI. An assessment protocol for selective mutism: analogue assessment using parents as facilitators. J Sch Psychol 1996;34:1-21.
18. Jackson MF, Allen RS, Boothe AB, Nava ML, Coates A. Innovative analyses and interventions in the treatment of selective mutism. Clin Case Studies 2005;4:81-112.
19. Cohan SL, Chavira DA, Stein MB. Practitioner review: psychosocial interventions for children with selective mutism: a critical evaluation of the literature from 1990-2005. J Child Psychol Psychiatry 2006;47:1085-1097.
20. Rye MS, Ullman D. The successful treatment of long-term selective mutism: a case study. J Beh Ther Exp Psychiatry 1999;30:313-323.
21. Fisak BJ, Oliveros A, Ehrenreich JT. Assessment and behavioral treatment of selective mutism. Clin Case Studies 2006;5:382-402.
22. Kumpulainen K. Phenomenology and treatment of selective mutism. CNS Drugs 2002;16:175-180.
- Good-quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
- Assess children with selective mutism for severe social anxiety (C).
- Drug therapy for anxiety and depressive conditions related to selective mutism and collaboration with school personnel and parents can help a child increase her frequency and audibility of speech in public settings (C).
- Exposure-based practices can help children with selective mutism to speak in public places (C).
Lucy’s parents were having difficulty reconciling the child they knew at home with the one they sent to school. At home, the 7-year-old spoke easily with her parents and siblings. At school and in other public places such as the supermarket, mall, or park, she would not speak at all. This had been going on for several years.
While Lucy was attending school without difficulty, she seemed sullen and withdrawn to her teachers. Lucy had friends at school, but would communicate with them by writing messages on paper or drawing letters in the air. Although Lucy had passed first grade on the basis of her written work, her parents worried about her ability to succeed in second grade, where her teachers expected her to participate in class and she would need to take standardized tests that required audible verbal responses. At the urging of a school counselor, Lucy’s parents took her to their family physician. They needed help in drawing her out so that the rest of the world could get to know the Lucy that they knew and loved.
Lucy’s case is typical of selective mutism
Lucy was suffering from selective mutism, the persistent failure to speak in specific social situations where speaking is expected, such as at school and with playmates.1 Lucy’s case is typical in that children with selective mutism speak well in other situations, typically at home. Thus, the disorder is not due to a communication disorder such as stuttering and it is not due to a lack of knowledge or comfort with language.
To meet diagnostic criteria, the disorder must last at least 1 month, though it can last for several years, and must interfere with a child’s education or ability to communicate socially.1
A little known disorder makes national headlines
Selective mutism occurs in 0.2%–2.0% of children, affects boys and girls equally, and often begins at 3 to 6 years of age.2-9 The disorder gained national attention this past spring when it was revealed that the shooter in the Virginia Tech massacre—Seung-Hui Cho—had, as an adolescent, been diagnosed with selective mutism.10 Though his diagnosis made plenty of headlines, the disorder itself occupies little space in the pediatric literature.11
What we do know is that selective mutism can have a chronic course that affects a child’s ability to form friendships, complete academic tasks, develop appropriate language and social skills, and participate in standardized testing.2-9 While parents often attribute their child’s behavior to shyness, this disorder goes beyond that. While shy children function, those with selective mutism struggle socially, emotionally, and academically. Children with selective mutism say the words won’t come out and their body won’t let them speak. One father of a 7-year-old girl with selective mutism said that his daughter “describes it as the words get stuck in her toes.”12
Many researchers theorize that children with selective mutism have severe social anxiety, and assessment and treatment strategies are typically based on this notion. Reports in the literature have also suggested that selective mutism is related to a developmental disorder or delay, as seen in autistic spectrum disorders, as well as anxiety disorders and depression.13 In addition, selective mutism has been linked to oppositional defiant disorder and subtle language impairments.14,15
Begin by excluding competing explanations
If a family is referred to you for possible selective mutism, you’ll first need to exclude competing explanations for the problem, such as hearing difficulties, speech and language disorders, school-based threats, and medical problems, such as asthma, which could prevent a child from speaking comfortably in a public setting. Assuming you are able to exclude these, and other competing explanations, you’ll need to ask 8 questions of parents and school officials. The answers you get will help you to screen for selective mutism and identify key antecedents and consequences to the behavior that are important in addressing the problem.
8 questions you’ll need to ask
1. What specific settings involve failure to speak? Children with selective mutism typically have difficulties in school, on the playground, in malls, and at restaurants.
2. Has the mutism lasted at least one month? Brief refusal to speak is not uncommon in children.
3. Does the child speak well at home with people she knows well? Most children with selective mutism speak well at home with family members, which belies a communication disorder.
4. Is failure to speak significantly interfering with the child’s academic or social development? Selective mutism must involve a significant interference in daily functioning.
5. What circumstances surround each episode of mutism? In particular, is the mutism associated with the desire to increase social attention or stimulation from others, decrease anxiety, or avoid or withdraw from adult commands or requests? A full understanding of selective mutism must include a review of triggers like these.
6. Can the child be encouraged to speak audibly in any way in certain public settings? Children with selective mutism who can speak to some extent in public situations may have a better prognosis than those who do not.9
7. How do others respond to, or compensate for, the child’s mutism? Do they complete tasks for the child? Order food for her? Allow whispers or communication via writing? Excessive accommodations enable a child with selective mutism to maintain the behavior.
8. Does the child appear anxious or depressed in situations involving mutism? Mutism is often linked to poor affect and social anxiety.
Still suspect selective mutism? Make a referral
If after asking these 8 questions you still suspect selective mutism, you will need to make a referral to a child psychologist or other mental health professional who specializes in behavioral strategies to treat selective mutism. The psychologist will meet with the child and utilize more formal methods of assessment.
The psychologist may use the Anxiety Disorders Interview Schedule for DSM-IV-TR (child and parent versions), a structured interview that emphasizes anxiety-based disorders and includes a section for selective mutism based on DSM-IV-TR criteria.16 Another helpful tool is the Functional Diagnostic Profile for Selective Mutism, which helps to assess contextual factors that surround refusal to speak.17 The challenge, of course, in conducting these interviews is that many children will not answer the psychologist’s questions verbally, but may communicate via nonverbal gestures, writing, or other creative ways such as drawing letters in the air.
Parent and teacher logs provide valuable insight
Ongoing behavioral observations or daily logbooks completed by parents and teachers are also important in treating a child with selective mutism. If parents aren’t doing so already at the suggestion of the therapist, ask them to keep a logbook and encourage them to ask the child’s teachers to keep one, as well. This log should include the number and volume of words spoken, to whom the child has spoken, where the child spoke, how others reacted (ie, Did they pay extra attention to the child?), and the child’s compensatory behaviors such as whispering, pointing, crying, nodding, or frowning.18 Parents and teachers should also note the antecedents to mutism, including demands (or requests) from others, or the presence of unfamiliar people.
A focus on systematic desensitization
Much of the literature regarding the treatment of selective mutism consists of case reports and small-scale studies.19 The paucity of data is, in part, a reflection of the rarity of the problem as well as a historical lack of consensus among researchers about the nature and diagnostic criteria for selective mutism.
The studies we do have on selective mutism indicate that behavior modification can be effective for these patients. Behavioral treatment primarily involves child- and parent-based practices.20
Child-based practices include management of physical sensations of anxiety often via relaxation training and breathing retraining. Neither technique requires verbal input from a child. In addition, the therapist will have the child practice audible words in progressively more difficult settings via systematic desensitization. These settings often include the following, in order: the child’s home (with the therapist), the therapist’s office, community settings such as a mall or a restaurant, and finally, school.
In these settings, the therapist might, for example, encourage the patient to:
- speak on the telephone or answer the door at home.
- stay at the therapist’s office until at least one word is audibly spoken. (One approach that the therapist may use to increase rapport and provide opportunities to prompt speech is to play games with the child.)
- order her own food at a local restaurant.
- read a story aloud to classmates at school.
In addition to systematic desensitization, the therapist may use audio or videotapes to help the youngster. In one scenario, the therapist may ask the parents to bring in an audiotape or videotape of the child at home when she is speaking. The therapist then provides ample reinforcement for the child’s speech by praising the child for having a beautiful voice and for making the tape. Audio and videotapes may also be used to help the child speak louder or work on her articulation.
Reinforce the positive, avoid “shaming”
Parent-based practices include reinforcing the child’s speech in different settings, developing new and independent exposures to generalize speech, and consulting with school officials on an ongoing basis to address social and academic problems from poor use of speech.
The therapist is likely to remind the parent that positive reinforcement is key, while punishing or “shaming” the child is ineffective.11 Some therapists will make use of a technique called “token economy,” where the child’s progress earns her colored chips that can be redeemed for a trip to a video game center, or a special treat, such as a sleep-over with a trusted friend.11
With the therapist’s help, parents can also model appropriate social interactions for a child with selective mutism because social skills may not be sufficiently developed. For example, the parent might encourage the child to answer the door or telephone. The parent might also monitor the child’s interactions with friends and provide feedback. In addition, the therapist may encourage the parents to ignore inappropriate compensatory behaviors as treatment progresses. Instead, a child with selective mutism may be increasingly challenged to provide audible speech to make requests or otherwise communicate.21
Drug therapy may include MAOIs and SSRIs
Medical treatment for selective mutism may include monoamine oxidase inhibitors (MAOIs) such as phenelzine (30–60 mg/day) or selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (10–60 mg/day), sertraline (100 mg/day), fluvoxamine (50–100 mg/day), citalopram (20–40 mg/day), or paroxetine (5 mg/day).22 However, no large-scale studies of pharmacotherapy for selective mutism have been conducted and medication effects are quite variable. The literature in this area has consisted largely of case studies.
After 9 months of treatment, Lucy speaks up at school
Lucy’s therapist (JLV) utilized many of the behavioral procedures described in this article. Treatment included exposure-based practices at home, in a clinic, in various community settings, and at school. By the end of her 9 months of treatment, Lucy was speaking independently to her classmates and teachers, though ongoing praise by her teachers was needed to encourage her to maintain an appropriate speech volume.
The literature on selective mutism suggests Lucy’s case was not unusual; it typically takes several months for these young patients to improve. Ongoing communication issues, though, often linger.9
- What specific settings involve failure to speak?
- Has the mutism lasted at least one month?
- Does the child speak well at home with people she knows well?
- Is failure to speak significantly interfering with the child’s academic or social development?
- What circumstances surround each episode of mutism?
- Can the child be encouraged to speak audibly in any way in certain public settings?
- How do others respond to, or compensate for, the child’s mutism?
- Does the child appear anxious or depressed in situations involving mutism?
Correspondence
Christopher A. Kearney, PhD, Department of Psychology, University of Nevada, Las Vegas, 4505 maryland Parkway, Las Vegas, Nv 89154-5030; [email protected]
- Good-quality patient-oriented evidence
- Inconsistent or limited-quality patient-oriented evidence
- Consensus, usual practice, opinion, disease-oriented evidence, case series
- Assess children with selective mutism for severe social anxiety (C).
- Drug therapy for anxiety and depressive conditions related to selective mutism and collaboration with school personnel and parents can help a child increase her frequency and audibility of speech in public settings (C).
- Exposure-based practices can help children with selective mutism to speak in public places (C).
Lucy’s parents were having difficulty reconciling the child they knew at home with the one they sent to school. At home, the 7-year-old spoke easily with her parents and siblings. At school and in other public places such as the supermarket, mall, or park, she would not speak at all. This had been going on for several years.
While Lucy was attending school without difficulty, she seemed sullen and withdrawn to her teachers. Lucy had friends at school, but would communicate with them by writing messages on paper or drawing letters in the air. Although Lucy had passed first grade on the basis of her written work, her parents worried about her ability to succeed in second grade, where her teachers expected her to participate in class and she would need to take standardized tests that required audible verbal responses. At the urging of a school counselor, Lucy’s parents took her to their family physician. They needed help in drawing her out so that the rest of the world could get to know the Lucy that they knew and loved.
Lucy’s case is typical of selective mutism
Lucy was suffering from selective mutism, the persistent failure to speak in specific social situations where speaking is expected, such as at school and with playmates.1 Lucy’s case is typical in that children with selective mutism speak well in other situations, typically at home. Thus, the disorder is not due to a communication disorder such as stuttering and it is not due to a lack of knowledge or comfort with language.
To meet diagnostic criteria, the disorder must last at least 1 month, though it can last for several years, and must interfere with a child’s education or ability to communicate socially.1
A little known disorder makes national headlines
Selective mutism occurs in 0.2%–2.0% of children, affects boys and girls equally, and often begins at 3 to 6 years of age.2-9 The disorder gained national attention this past spring when it was revealed that the shooter in the Virginia Tech massacre—Seung-Hui Cho—had, as an adolescent, been diagnosed with selective mutism.10 Though his diagnosis made plenty of headlines, the disorder itself occupies little space in the pediatric literature.11
What we do know is that selective mutism can have a chronic course that affects a child’s ability to form friendships, complete academic tasks, develop appropriate language and social skills, and participate in standardized testing.2-9 While parents often attribute their child’s behavior to shyness, this disorder goes beyond that. While shy children function, those with selective mutism struggle socially, emotionally, and academically. Children with selective mutism say the words won’t come out and their body won’t let them speak. One father of a 7-year-old girl with selective mutism said that his daughter “describes it as the words get stuck in her toes.”12
Many researchers theorize that children with selective mutism have severe social anxiety, and assessment and treatment strategies are typically based on this notion. Reports in the literature have also suggested that selective mutism is related to a developmental disorder or delay, as seen in autistic spectrum disorders, as well as anxiety disorders and depression.13 In addition, selective mutism has been linked to oppositional defiant disorder and subtle language impairments.14,15
Begin by excluding competing explanations
If a family is referred to you for possible selective mutism, you’ll first need to exclude competing explanations for the problem, such as hearing difficulties, speech and language disorders, school-based threats, and medical problems, such as asthma, which could prevent a child from speaking comfortably in a public setting. Assuming you are able to exclude these, and other competing explanations, you’ll need to ask 8 questions of parents and school officials. The answers you get will help you to screen for selective mutism and identify key antecedents and consequences to the behavior that are important in addressing the problem.
8 questions you’ll need to ask
1. What specific settings involve failure to speak? Children with selective mutism typically have difficulties in school, on the playground, in malls, and at restaurants.
2. Has the mutism lasted at least one month? Brief refusal to speak is not uncommon in children.
3. Does the child speak well at home with people she knows well? Most children with selective mutism speak well at home with family members, which belies a communication disorder.
4. Is failure to speak significantly interfering with the child’s academic or social development? Selective mutism must involve a significant interference in daily functioning.
5. What circumstances surround each episode of mutism? In particular, is the mutism associated with the desire to increase social attention or stimulation from others, decrease anxiety, or avoid or withdraw from adult commands or requests? A full understanding of selective mutism must include a review of triggers like these.
6. Can the child be encouraged to speak audibly in any way in certain public settings? Children with selective mutism who can speak to some extent in public situations may have a better prognosis than those who do not.9
7. How do others respond to, or compensate for, the child’s mutism? Do they complete tasks for the child? Order food for her? Allow whispers or communication via writing? Excessive accommodations enable a child with selective mutism to maintain the behavior.
8. Does the child appear anxious or depressed in situations involving mutism? Mutism is often linked to poor affect and social anxiety.
Still suspect selective mutism? Make a referral
If after asking these 8 questions you still suspect selective mutism, you will need to make a referral to a child psychologist or other mental health professional who specializes in behavioral strategies to treat selective mutism. The psychologist will meet with the child and utilize more formal methods of assessment.
The psychologist may use the Anxiety Disorders Interview Schedule for DSM-IV-TR (child and parent versions), a structured interview that emphasizes anxiety-based disorders and includes a section for selective mutism based on DSM-IV-TR criteria.16 Another helpful tool is the Functional Diagnostic Profile for Selective Mutism, which helps to assess contextual factors that surround refusal to speak.17 The challenge, of course, in conducting these interviews is that many children will not answer the psychologist’s questions verbally, but may communicate via nonverbal gestures, writing, or other creative ways such as drawing letters in the air.
Parent and teacher logs provide valuable insight
Ongoing behavioral observations or daily logbooks completed by parents and teachers are also important in treating a child with selective mutism. If parents aren’t doing so already at the suggestion of the therapist, ask them to keep a logbook and encourage them to ask the child’s teachers to keep one, as well. This log should include the number and volume of words spoken, to whom the child has spoken, where the child spoke, how others reacted (ie, Did they pay extra attention to the child?), and the child’s compensatory behaviors such as whispering, pointing, crying, nodding, or frowning.18 Parents and teachers should also note the antecedents to mutism, including demands (or requests) from others, or the presence of unfamiliar people.
A focus on systematic desensitization
Much of the literature regarding the treatment of selective mutism consists of case reports and small-scale studies.19 The paucity of data is, in part, a reflection of the rarity of the problem as well as a historical lack of consensus among researchers about the nature and diagnostic criteria for selective mutism.
The studies we do have on selective mutism indicate that behavior modification can be effective for these patients. Behavioral treatment primarily involves child- and parent-based practices.20
Child-based practices include management of physical sensations of anxiety often via relaxation training and breathing retraining. Neither technique requires verbal input from a child. In addition, the therapist will have the child practice audible words in progressively more difficult settings via systematic desensitization. These settings often include the following, in order: the child’s home (with the therapist), the therapist’s office, community settings such as a mall or a restaurant, and finally, school.
In these settings, the therapist might, for example, encourage the patient to:
- speak on the telephone or answer the door at home.
- stay at the therapist’s office until at least one word is audibly spoken. (One approach that the therapist may use to increase rapport and provide opportunities to prompt speech is to play games with the child.)
- order her own food at a local restaurant.
- read a story aloud to classmates at school.
In addition to systematic desensitization, the therapist may use audio or videotapes to help the youngster. In one scenario, the therapist may ask the parents to bring in an audiotape or videotape of the child at home when she is speaking. The therapist then provides ample reinforcement for the child’s speech by praising the child for having a beautiful voice and for making the tape. Audio and videotapes may also be used to help the child speak louder or work on her articulation.
Reinforce the positive, avoid “shaming”
Parent-based practices include reinforcing the child’s speech in different settings, developing new and independent exposures to generalize speech, and consulting with school officials on an ongoing basis to address social and academic problems from poor use of speech.
The therapist is likely to remind the parent that positive reinforcement is key, while punishing or “shaming” the child is ineffective.11 Some therapists will make use of a technique called “token economy,” where the child’s progress earns her colored chips that can be redeemed for a trip to a video game center, or a special treat, such as a sleep-over with a trusted friend.11
With the therapist’s help, parents can also model appropriate social interactions for a child with selective mutism because social skills may not be sufficiently developed. For example, the parent might encourage the child to answer the door or telephone. The parent might also monitor the child’s interactions with friends and provide feedback. In addition, the therapist may encourage the parents to ignore inappropriate compensatory behaviors as treatment progresses. Instead, a child with selective mutism may be increasingly challenged to provide audible speech to make requests or otherwise communicate.21
Drug therapy may include MAOIs and SSRIs
Medical treatment for selective mutism may include monoamine oxidase inhibitors (MAOIs) such as phenelzine (30–60 mg/day) or selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (10–60 mg/day), sertraline (100 mg/day), fluvoxamine (50–100 mg/day), citalopram (20–40 mg/day), or paroxetine (5 mg/day).22 However, no large-scale studies of pharmacotherapy for selective mutism have been conducted and medication effects are quite variable. The literature in this area has consisted largely of case studies.
After 9 months of treatment, Lucy speaks up at school
Lucy’s therapist (JLV) utilized many of the behavioral procedures described in this article. Treatment included exposure-based practices at home, in a clinic, in various community settings, and at school. By the end of her 9 months of treatment, Lucy was speaking independently to her classmates and teachers, though ongoing praise by her teachers was needed to encourage her to maintain an appropriate speech volume.
The literature on selective mutism suggests Lucy’s case was not unusual; it typically takes several months for these young patients to improve. Ongoing communication issues, though, often linger.9
- What specific settings involve failure to speak?
- Has the mutism lasted at least one month?
- Does the child speak well at home with people she knows well?
- Is failure to speak significantly interfering with the child’s academic or social development?
- What circumstances surround each episode of mutism?
- Can the child be encouraged to speak audibly in any way in certain public settings?
- How do others respond to, or compensate for, the child’s mutism?
- Does the child appear anxious or depressed in situations involving mutism?
Correspondence
Christopher A. Kearney, PhD, Department of Psychology, University of Nevada, Las Vegas, 4505 maryland Parkway, Las Vegas, Nv 89154-5030; [email protected]
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text revision). Washington, DC: Author.
2. Andersson CB, Thomsen PH. Electively mute children: an analysis of 37 Danish cases. Nordic J Psychiatry 1998;52:231-238.
3. Bergman RL, Piacentini J, McCracken JT. Prevalence and description of selective mutism in a school-based study. J Am Acad Child Adolesc Psychiatry 2002;41:938-946.
4. Black B, Uhde TW. Elective mutism as a variant of social phobia. J Am Acad Child Adolesc Psychiatry 1992;1090-1094.
5. Ford MA, Sladeczeck IE, Carlson J. Selective mutism: phenomenological characteristics. School Psychol Quarterly 1998;13:192-227.
6. Kopp S, Gillberg C. Selective mutism: a population-based study: a research note. J Child Psychol Psychiatry 1997;38:257-262.
7. Krysanski V. A brief review of selective mutism literature. J Psychol 2003;137:29-40.
8. Kumpulainen K, Rasanen E, Raaska H, Somppi V. Selective mutism among second-graders in elementary school. Euro Child Adolesc Psychiatry 1998;7:24-29.
9. Remschmidt H, Poller M, Herpertz-Dahlmann B, Hennighausen K, Gutenbrenner C. A follow-up study of 45 patients with elective mutism. European Archives of Psychiatry and Clinical Neuroscience 2001;251:284-296.
10. Urbina I. Virginia Tech criticized for actions in shooting. The New York Times. August 30, 2007. Available at: www.nytimes.com/2007/08/30/us/30school.html. Accessed on October 10, 2007.
11. Schwartz RH, Shipon-Blum E. “Shy”child? Don’t overlook selective mutism. Contemp Peds 2005;22(7):30-39.
12. ABC News. Selective mutism: When your child can’t speak. Available at: abcnews.go.com/GmA/AmericanFamily/story?id=1770308&page=1. Accessed on September 26, 2007.
13. Vecchio J, Kearney CA. Selective mutism in children: comparison to youths with and without anxiety disorders. J Psychopath Beh Assess 2005;28:139-144.
14. Yeganeh R, Beidel DC, Turner SM. Selective mutism: more than social anxiety? Depress Anx 2006;23:117-123.
15. Manassis K, Fung D, Tannock R, Sloman L, Fiksenbaum L, McInnes A. Characterizing selective mutism: is it more than social anxiety? Depress Anx 2003;18:153-161.
16. Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV, child and parent versions. New York: oxford University Press;1996.
17. Schill MT, Kratochwill TR, Gardner WI. An assessment protocol for selective mutism: analogue assessment using parents as facilitators. J Sch Psychol 1996;34:1-21.
18. Jackson MF, Allen RS, Boothe AB, Nava ML, Coates A. Innovative analyses and interventions in the treatment of selective mutism. Clin Case Studies 2005;4:81-112.
19. Cohan SL, Chavira DA, Stein MB. Practitioner review: psychosocial interventions for children with selective mutism: a critical evaluation of the literature from 1990-2005. J Child Psychol Psychiatry 2006;47:1085-1097.
20. Rye MS, Ullman D. The successful treatment of long-term selective mutism: a case study. J Beh Ther Exp Psychiatry 1999;30:313-323.
21. Fisak BJ, Oliveros A, Ehrenreich JT. Assessment and behavioral treatment of selective mutism. Clin Case Studies 2006;5:382-402.
22. Kumpulainen K. Phenomenology and treatment of selective mutism. CNS Drugs 2002;16:175-180.
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed, text revision). Washington, DC: Author.
2. Andersson CB, Thomsen PH. Electively mute children: an analysis of 37 Danish cases. Nordic J Psychiatry 1998;52:231-238.
3. Bergman RL, Piacentini J, McCracken JT. Prevalence and description of selective mutism in a school-based study. J Am Acad Child Adolesc Psychiatry 2002;41:938-946.
4. Black B, Uhde TW. Elective mutism as a variant of social phobia. J Am Acad Child Adolesc Psychiatry 1992;1090-1094.
5. Ford MA, Sladeczeck IE, Carlson J. Selective mutism: phenomenological characteristics. School Psychol Quarterly 1998;13:192-227.
6. Kopp S, Gillberg C. Selective mutism: a population-based study: a research note. J Child Psychol Psychiatry 1997;38:257-262.
7. Krysanski V. A brief review of selective mutism literature. J Psychol 2003;137:29-40.
8. Kumpulainen K, Rasanen E, Raaska H, Somppi V. Selective mutism among second-graders in elementary school. Euro Child Adolesc Psychiatry 1998;7:24-29.
9. Remschmidt H, Poller M, Herpertz-Dahlmann B, Hennighausen K, Gutenbrenner C. A follow-up study of 45 patients with elective mutism. European Archives of Psychiatry and Clinical Neuroscience 2001;251:284-296.
10. Urbina I. Virginia Tech criticized for actions in shooting. The New York Times. August 30, 2007. Available at: www.nytimes.com/2007/08/30/us/30school.html. Accessed on October 10, 2007.
11. Schwartz RH, Shipon-Blum E. “Shy”child? Don’t overlook selective mutism. Contemp Peds 2005;22(7):30-39.
12. ABC News. Selective mutism: When your child can’t speak. Available at: abcnews.go.com/GmA/AmericanFamily/story?id=1770308&page=1. Accessed on September 26, 2007.
13. Vecchio J, Kearney CA. Selective mutism in children: comparison to youths with and without anxiety disorders. J Psychopath Beh Assess 2005;28:139-144.
14. Yeganeh R, Beidel DC, Turner SM. Selective mutism: more than social anxiety? Depress Anx 2006;23:117-123.
15. Manassis K, Fung D, Tannock R, Sloman L, Fiksenbaum L, McInnes A. Characterizing selective mutism: is it more than social anxiety? Depress Anx 2003;18:153-161.
16. Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV, child and parent versions. New York: oxford University Press;1996.
17. Schill MT, Kratochwill TR, Gardner WI. An assessment protocol for selective mutism: analogue assessment using parents as facilitators. J Sch Psychol 1996;34:1-21.
18. Jackson MF, Allen RS, Boothe AB, Nava ML, Coates A. Innovative analyses and interventions in the treatment of selective mutism. Clin Case Studies 2005;4:81-112.
19. Cohan SL, Chavira DA, Stein MB. Practitioner review: psychosocial interventions for children with selective mutism: a critical evaluation of the literature from 1990-2005. J Child Psychol Psychiatry 2006;47:1085-1097.
20. Rye MS, Ullman D. The successful treatment of long-term selective mutism: a case study. J Beh Ther Exp Psychiatry 1999;30:313-323.
21. Fisak BJ, Oliveros A, Ehrenreich JT. Assessment and behavioral treatment of selective mutism. Clin Case Studies 2006;5:382-402.
22. Kumpulainen K. Phenomenology and treatment of selective mutism. CNS Drugs 2002;16:175-180.
Solutions to school refusal for parents and kids
Case: 'He's okay on weekends'
Nathan, age 13, is referred by his parents for recent school refusal behavior. He has had difficulty adjusting to middle school and has been marked absent one-third of school days this academic year. These absences come in the form of tardiness, skipped classes, and full-day absences.
Nathan complains of headaches and stomachaches and says he feels upset and nervous while in school. His parents, however, complain that Nathan seems fine on weekends and holidays and seems to be embellishing symptoms to miss school. Nathan’s parents are concerned that their son may have some physical or mental condition that is preventing his school attendance and that might be remediated with medication.
Child-motivated refusal to attend school or remain in class an entire day is not uncommon, affecting 5% to 28% of youths at some time in their lives.1,2
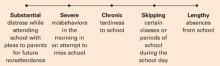
The behavior may be viewed along a spectrum of absenteeism (Figure), and a child may exhibit all forms of absenteeism at one time or another. In Nathan’s case, for example, he could be anxious during school on Monday, arrive late to school on Tuesday, skip afternoon classes on Wednesday, and fail to attend school completely on Thursday and Friday.
In this article you will learn characteristics of school refusal behavior to watch for and assess, and treatment strategies for youths ages 5 to 17. You will also find advice and techniques to offer parents.
Figure A child might exhibit each behavior on this spectrum at different times
Refusal behavior characteristics
School refusal behavior encompasses all subsets of problematic absenteeism, such as truancy, school phobia, and separation anxiety.3 Children and adolescents of all ages, boys and girls alike, can exhibit school refusal behavior. The most common age of onset is 10 to 13 years. Youths such as Nathan who are entering a school building for the first time—especially elementary and middle school—are at particular risk for school refusal behavior. Little information is available regarding ethnic differences, although school dropout rates for Hispanics are often considerably elevated compared with other ethnic groups.4,5
School refusal behavior covers a range of symptoms, diagnoses, somatic complaints, and medical conditions (Tables 1-3).6-12 Longitudinal studies indicate that school refusal behavior, if left unaddressed, can lead to serious short-term problems, such as distress, academic decline, alienation from peers, family conflict, and financial and legal consequences. Common long-term problems include school dropout, delinquent behaviors, economic deprivation, social isolation, marital problems, and difficulty maintaining employment. Approximately 52% of adolescents with school refusal behavior meet criteria for an anxiety, depressive, conduct-personality, or other psychiatric disorder later in life.13-16
Table 1
Common symptoms that could signal school refusal behavior
| Internalizing/covert symptoms | Externalizing/overt symptoms |
|---|---|
| Depression | Aggression |
| Fatigue/tiredness | Clinging to an adult |
| Fear and panic | Excessive reassurance-seeking behavior |
| General and social anxiety | Noncompliance and defiance |
| Self-consciousness | Refusal to move in the morning |
| Somatization | Running away from school or home |
| Worry | Temper tantrums and crying |
Table 2
Primary psychiatric disorders among youths with school refusal behavior
| Diagnosis | Percentage |
|---|---|
| None | 32.9% |
| Separation anxiety disorder | 22.4% |
| Generalized anxiety disorder | 10.5% |
| Oppositional defiant disorder | 8.4% |
| Major depression | 4.9% |
| Specific phobia | 4.2% |
| Social anxiety disorder | 3.5% |
| Conduct disorder | 2.8% |
| Attention deficit/hyperactivity disorder | 1.4% |
| Panic disorder | 1.4% |
| Enuresis | 0.7% |
| Posttraumatic stress disorder | 0.7% |
| Source: Reference 7 | |
Table 3
Somatic complaints and medical conditions
commonly associated with school refusal behavior
| Somatic complaints | Medical conditions |
|---|---|
| Diarrhea/irritable bowel | Allergic rhinitis |
| Fatigue | Asthma and respiratory illness |
| Headache and stomachache | Chronic pain and illness (notably cancer, Crohn’s disease, dyspepsia, hemophilia, chronic fatigue syndrome) |
| Nausea and vomiting | Diabetes |
| Palpitations and perspiration | Dysmenorrhea |
| Recurrent abdominal pain or other pain | Head louse infestation |
| Shaking or trembling | Influenza |
| Sleep problems | Orodental disease |
Finding a reason for school refusal
If a child has somatic complaints, you can expect to find that the child is:
- suffering from a true physical malady
- embellishing low-grade physical symptoms from stress or attention-seeking behavior
- reporting physical problems that have no medical basis.
A full medical examination is always recommended to rule out organic problems or to properly treat true medical conditions.
Four functions. If no medical condition is found, explore the reasons a particular child refuses school. A common model of conceptualizing school refusal behavior involves reinforcers:1,2
- to avoid school-based stimuli that provoke a sense of negative affectivity, or combined anxiety and depression; examples of key stimuli include teachers, peers, bus, cafeteria, classroom, and transitions between classes
- to escape aversive social or evaluative situations such as conversing or otherwise interacting with others or performing before others as in class presentations
- to pursue attention from significant others, such as wanting to stay home or go to work with parents
- to pursue tangible reinforcers outside of school, such as sleeping late, watching television, playing with friends, or engaging in delinquent behavior or substance use.
The first 2 functions are maintained by negative reinforcement or a desire to leave anxiety-provoking stimuli. The latter 2 functions are maintained by positive reinforcement, or a desire to pursue rewards outside of school. Youths may also refuse school for a combination of these reasons.17 In Nathan’s case, he was initially anxious about school in general (the first function). After his parents allowed him to stay home for a few days, however, he was refusing school to enjoy fun activities such as video games at home (the last function).
Violence on school campuses across the country naturally makes many parents skittish about possible copycat incidents. In fact, some parents acquiesce to their children’s pleas to remain home on school shooting anniversaries—particularly the Columbine tragedy of April 20, 1999.
Student and parental fears likely are exacerbated by new episodes of violence, such as three school shootings in 2006:
- On September 27, a 53-year-old man entered a high school in Bailey, Colorado, and shot one girl before killing himself.
- On September 29, a high school student near Madison, Wisconsin, killed his principal after being disciplined for carrying tobacco.
- On October 2, a heavily armed man barricaded himself in a one-room Amish schoolhouse in Paradise, Pennsylvania. He bound and shot 11 girls before killing himself, and five of the girls died.
Compared with highly publicized school violence, however, personal victimization is a much stronger factor in absenteeism.32 Specifically, school violence is related to school absenteeism especially for youths who have been previously victimized. The literature shows:
- Students who have been bullied are 2.1 times more likely than other students to feel unsafe at school.
- 20% of elementary school children report they would skip school to avoid being bullied.33
- High school students’ fear of attending classes because of violence is directly associated with victimization by teachers or other students.
- Missing school because of feeling unsafe is a strong risk factor for asthma and, potentially, being sent home early from school.34
Assessment scale. One method for quickly assessing the role of these functions is the School Refusal Assessment Scale-Revised.18,19 This scale poses 24 questions, the answers to which measure the relative strength of each of the 4 functions. Versions are available for children and parents, who complete their respective scales separately (see Related resources). Item means are calculated across the measures to help determine the primary reason for a child’s school refusal.
In addition to using the assessment scale, you may ask interview questions regarding the form and function of school refusal behavior (Tables 4,5). Take care to assess attendance history and patterns, comorbid conditions, instances of legitimate absenteeism, family disruption, and a child’s social and academic status. Specific questions about function can help narrow the reason for school refusal.
Assess specific school-related stimuli that provoke absenteeism such as social and evaluative situations, whether a child could attend school with a parent (evidence of attention-seeking), and what tangible rewards a child receives for absenteeism throughout the school day. Information about the form and function of school refusal behavior may also be evident during in-office observations of the family. Data from the School Refusal Assessment Scale-Revised, interviews, and observations can then be used to recommend particular treatment options.
Table 4
Questions related to forms of school refusal behavior
| What are the child’s specific forms of absenteeism, and how do these forms change daily? | What specific school-related stimuli are provoking the child’s concern about going to school? |
| Is a child’s school refusal behavior relatively acute or chronic in nature (in related fashion, how did the child’s school refusal behavior develop over time)? | Is the child’s refusal to attend school legitimate or understandable in some way (eg, school-based threat, bullying, inadequate school climate)? |
| What comorbid conditions occur with a child’s school refusal behavior (Table 3), including substance abuse? | What family disruption or conflict has occurred as a result of a child’s school refusal behavior? |
| What is the child’s degree of anxiety or misbehavior upon entering school, and what specific misbehaviors are present in the morning before school (Table 2)? | What is the child’s academic and social status? (This should include a review of academic records, formal evaluation reports, attendance records, and individualized education plans or 504 plans as applicable.) |
Table 5
Questions related to functions of school refusal behavior
| Have recent or traumatic home or school events influenced a child’s school refusal behavior? | Is the child willing to attend school if a parent accompanies him or her? |
| Are symptoms of school refusal behavior evident on weekends and holidays? | What specific tangible rewards does the child pursue outside of school that cause him or her to miss school? |
| Are there any nonschool situations where anxiety or attention-seeking behavior occurs? | Is the child willing to attend school if incentives are provided for attendance? |
| What specific social and/or evaluative situations at school are avoided? |
Treating youths who refuse school
Treatment success will be better assured if you work closely with school personnel and parents to gather and share information, coordinate a plan for returning a child to school, and address familial issues and the child’s comorbid medical problems that impact attendance.
Medications have proven useful in alleviating severe cases of anxiety and depression, and cognitive management techniques can be applied to the child, the parents, and the family together.
Anxiolytics or antidepressants. Pharmacotherapy research for school refusal behavior is in its infancy. Some investigators have found, however, that a tricyclic antidepressant (TCA) such as imipramine, 3 mg/kg/d, may be useful in some cases20,21—generally for youths ages 10 to 17 years with better attendance records and fewer symptoms of social avoidance and separation anxiety.22 Researchers speculate that TCAs, which are not always effective in children, may influence symptoms such as anhedonia or sleep problems that contribute to school refusal behavior.
With respect to substantial child anxiety and depression without school refusal behavior, researchers have focused on selective serotonin reuptake inhibitors (SSRIs). In particular, fluoxetine, 10 to 20 mg/d, fluvoxamine, 50 to 250 mg/d, sertraline, 85 to 160 mg/d, and paroxetine, 10 to 50 mg/d, have been useful for youths with symptoms of general and social anxiety and depression.23,24
Youths often do not respond to these medications as well as adults do, however, because of the fluid and amorphous nature of anxious and depressive symptomatology in children and adolescents. Careful monitoring is required when treating youth with SSRIs, which have been associated with an increased risk of suicidal behavior.
Psychological techniques. Sophisticated clinical controlled studies have addressed the treatment of diverse youths with school refusal behavior.25-28 Options for this population may be arranged according to function or the primary reinforcers maintaining absenteeism:
- child-based techniques to manage anxiety in a school setting
- parent-based techniques to manage contingencies for school attendance and nonattendance
- family-based techniques to manage incentives and disincentives for school attendance and nonattendance.
Child-based anxiety management techniques include relaxation training, breathing retraining, cognitive therapy (generally for youths ages 9 to 17), and exposure-based practices to gradually reintroduce a child to school. These techniques have been strongly supported by randomized controlled trials specific to school refusal behavior2 and are useful for treating general anxiety and depression as well.
Parent-based contingency management techniques include establishing morning and evening routines, modifying parental commands toward brevity and clarity, providing attention-based consequences for school nonattendance (such as early bedtime, limited time with a parent at night), reducing excessive child questioning or reassurance-seeking behavior, and engaging in forced school attendance under strict conditions. Parent-based techniques have received strong support in the literature in general29 but have been applied less frequently than child-based techniques to youths with school refusal behavior.
Family-based techniques include developing written contracts to increase incentives for school attendance and decrease incentives for nonattendance, escorting a child to school and classes, and teaching youths to refuse offers from peers to miss school.30 As with parent-based techniques, family-based techniques have received strong support in the literature in general, but have been applied less frequently than child-based techniques to youths with school refusal behavior.
Gradual reintroduction to school
A preferred approach to resolve school refusal behavior usually involves gradual reintegration to school and classes. This may include initial attendance at lunchtime, 1 or 2 favorite classes, or in an alternative classroom setting such as a guidance counselor’s office or school library. Gradual reintegration into regular classrooms may then proceed.
If possible, a child should remain in school during the day and not be sent home unless intense medical symptoms are present.30 A recommended list of intense symptoms includes:
- frequent vomiting
- bleeding
- temperature >100° F
- severe diarrhea
- lice
- acute flu-like symptoms
- extreme medical conditions such as intense pain.
Case continued: a full-time student.
A structured diagnostic interview and other behavioral assessment measures show that Nathan meets criteria for generalized anxiety disorder. He worries excessively about his social and academic performance at school and displays several somatic complaints related to anxiety. His treatment thus involves a two-pronged approach:
- sertraline, 50 mg/d, which has been found to significantly reduce symptoms of generalized anxiety disorder in youths ages 5 to 17.
- child-based anxiety management techniques and family therapy to increase incentives for school attendance and limit fun activities during a school day spent at home.
His therapist and family physician collaborate with school personnel to gradually reintroduce Nathan to a full-time academic schedule.
- Copies of the child and parent versions of the School Refusal Assessment Scale-Revised are available at www.jfponline.com/Pages.asp?AID=4322&UID=.
- King NJ, Bernstein GA. School refusal in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 2001;40:197-205.
- Kearney CA. School refusal behavior in youth: a functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
- Kearney CA, Albano AM. When children refuse school: a cognitive-behavioral therapy approach. Parent workbook/therapist’s guide. New York: Oxford University Press; 2000.
Drug brand names
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Paroxetine • Paxil
- Sertraline • Zoloft
Acknowledgment
Adapted and reprinted with permission from The Journal of Family Practice, August 2006, p 685-92.
1. Kearney CA, Silverman WK. The evolution and reconciliation of taxonomic strategies for school refusal behavior. Clin Psychol: Sci Prac 1996;3:339-54.
2. Kearney CA. School refusal behavior in youth: a functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
3. Hansen C, Sanders SL, Massaro S, Last CG. Predictors of severity of absenteeism in children with anxiety-based school refusal. J Clin Child Psychol 1998;27:246-54.
4. Franklin CG, Soto I. Keeping Hispanic youths in school. Children & Schools 2002;24:139-43.
5. Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: a community study. J Am Acad Child Adolesc Psychiatry 2003;42:797-807.
6. McShane G, Walter G, Rey JM. Characteristics of adolescents with school refusal. Aust New Zeal J Psychiatry 2001;35:822-6.
7. Kearney CA, Albano AM. The functional profiles of school refusal behavior: diagnostic aspects. Behav Modif 2004;28:147-61.
8. Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchardt CM, Crosby RD. Somatic symptoms in anxious-depressed school refusers. J Am Acad Child Adolesc Psychiatry 1997;36:661-8.
9. Gilliland FD, Berhane K, Islam T, et al. Environmental tobacco smoke and absenteeism related to respiratory illness in school children. Am J Epidemiology 2003;157:861-9.
10. Glaab LA, Brown R, Daneman D. School attendance in children with type I diabetes. Diabetic Med 2005;22:421-6.
11. Levy RL, Whitehead WE, Walker LS, et al. Increased somatic complaints and health-care utilization in children: effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterology 2004;99:2442-51.
12. Buitelaar JK, van Andel H, Duyx JHM, van Strien DC. Depressive and anxiety disorders in adolescence: a follow-up study of adolescents with school refusal. Acta Paedopsychiatrica 1994;56:249-53.
13. Flakierska-Praquin N, Lindstrom M, Gillberg C. School phobia with separation anxiety disorder: a comparative 20- to 29-year follow-up study of 35 school refusers. Comp Psychiatry 1997;38:17-22.
14. Hibbett A, Fogelman K. Future lives of truants: family formation and health-related behaviour. Brit J Educ Psychology 1990;60:171-9.
15. Hibbett A, Fogelman K, Manor O. Occupational outcomes of truancy. Brit J Educ Psychology 1990;60:23-36.
16. Kearney CA. Bridging the gap among professionals who address youth with school absenteeism: overview and suggestions for consensus. Prof Psychol Res Prac 2003;34:57-65.
17. King NJ, Heyne D, Tonge B, Gullone E, Ollendick TH. School refusal: categorical diagnoses, functional analysis and treatment planning. Clin Psychol Psychother 2001;8:352-60.
18. Kearney CA. Identifying the function of school refusal behavior: a revision of the School Refusal Assessment Scale. J Psychopathol Behav Assess 2002;24:235-45.
19. Kearney CA. Confirmatory factor analysis of the School Refusal Assessment Scale-Revised: child and parent versions. J Psychopathol Behav Assess 2006; in press.
20. Bernstein GA, Borchardt CM, Perwein AR, et al. Imipramine plus cognitive-behavioral therapy in the treatment of school refusal. J Am Acad Chil Adol Psychiatry 2000;39:276-83.
21. Kearney CA, Silverman WK. A critical review of pharmacotherapy for youth with anxiety disorders: things are not as they seem. J Anxiety Disord 1998;12:83-102.
22. Layne AE, Bernstein GA, Egan EA, Kushner MG. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Am Acad Chil Adol Psychiatry 2003;42:319-26.
23. Compton SN, Grant PJ, Chrisman AK, et al. Sertraline in children and adolescents with social anxiety disorder: an open trial. J Am Acad Chil Adol Psychiatry 2001;40:564-71.
24. Whittington CJ, Kendall T, Fonagy T, et al. Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. Lancet 2004;363:1341-5.
25. Kearney CA, Silverman WK. Functionally-based prescriptive and nonprescriptive treatment for children and adolescents with school refusal behavior. Behav Ther 1999;30:673-95.
26. King NJ, Tonge BJ, Heyne D, et al. Cognitive-behavioral treatment of school-refusing children: A controlled evaluation. J Am Acad Chil Adol Psychiatry 1998;37:395-403.
27. Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Am Acad Chil Adol Psychiatry 1998;37:404-11.
28. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-20.
29. Kearney CA, Roblek TL. Parent training in the treatment of school refusal behavior. In: Briesmeister JM, Schaefer CE, eds. Handbook of parent training: parents as co-therapists for children’s behavior problems, 2nd ed. New York: Wiley; 1998:225-56.
30. Kearney CA, Albano AM. When children refuse school: A cognitive-behavioral therapy approach/Therapist’s guide. San Antonio: Psychological Corporation, 2000.
31. Kearney CA, Bates M. Addressing school refusal behavior: Suggestions for frontline professionals. Children & Schools 2005;27:207-16.
32. Astor RA, Benbenishty R, Zeira A, Vinokur A. School climate, observed risky behaviors, and victimization as predictors of high school students’ fear and judgments of school violence as a problem. Health Educ Behav 2002;29:716-36.
33. Glew GM, Fan M-Y, Katon W, Rivara FP, Kernic MA. Bullying, psychosocial adjustment, and academic performance in elementary school. Arch Pediatr Adolesc Med 2005;159:1026-31.
34. Swahn MH, Bossarte RM. The associations between victimization, feeling unsafe, and asthma episodes among US high-school students. Am J Public Health 2006;96:802-4.
Case: 'He's okay on weekends'
Nathan, age 13, is referred by his parents for recent school refusal behavior. He has had difficulty adjusting to middle school and has been marked absent one-third of school days this academic year. These absences come in the form of tardiness, skipped classes, and full-day absences.
Nathan complains of headaches and stomachaches and says he feels upset and nervous while in school. His parents, however, complain that Nathan seems fine on weekends and holidays and seems to be embellishing symptoms to miss school. Nathan’s parents are concerned that their son may have some physical or mental condition that is preventing his school attendance and that might be remediated with medication.
Child-motivated refusal to attend school or remain in class an entire day is not uncommon, affecting 5% to 28% of youths at some time in their lives.1,2
The behavior may be viewed along a spectrum of absenteeism (Figure), and a child may exhibit all forms of absenteeism at one time or another. In Nathan’s case, for example, he could be anxious during school on Monday, arrive late to school on Tuesday, skip afternoon classes on Wednesday, and fail to attend school completely on Thursday and Friday.
In this article you will learn characteristics of school refusal behavior to watch for and assess, and treatment strategies for youths ages 5 to 17. You will also find advice and techniques to offer parents.
Figure A child might exhibit each behavior on this spectrum at different times
Refusal behavior characteristics
School refusal behavior encompasses all subsets of problematic absenteeism, such as truancy, school phobia, and separation anxiety.3 Children and adolescents of all ages, boys and girls alike, can exhibit school refusal behavior. The most common age of onset is 10 to 13 years. Youths such as Nathan who are entering a school building for the first time—especially elementary and middle school—are at particular risk for school refusal behavior. Little information is available regarding ethnic differences, although school dropout rates for Hispanics are often considerably elevated compared with other ethnic groups.4,5
School refusal behavior covers a range of symptoms, diagnoses, somatic complaints, and medical conditions (Tables 1-3).6-12 Longitudinal studies indicate that school refusal behavior, if left unaddressed, can lead to serious short-term problems, such as distress, academic decline, alienation from peers, family conflict, and financial and legal consequences. Common long-term problems include school dropout, delinquent behaviors, economic deprivation, social isolation, marital problems, and difficulty maintaining employment. Approximately 52% of adolescents with school refusal behavior meet criteria for an anxiety, depressive, conduct-personality, or other psychiatric disorder later in life.13-16
Table 1
Common symptoms that could signal school refusal behavior
| Internalizing/covert symptoms | Externalizing/overt symptoms |
|---|---|
| Depression | Aggression |
| Fatigue/tiredness | Clinging to an adult |
| Fear and panic | Excessive reassurance-seeking behavior |
| General and social anxiety | Noncompliance and defiance |
| Self-consciousness | Refusal to move in the morning |
| Somatization | Running away from school or home |
| Worry | Temper tantrums and crying |
Table 2
Primary psychiatric disorders among youths with school refusal behavior
| Diagnosis | Percentage |
|---|---|
| None | 32.9% |
| Separation anxiety disorder | 22.4% |
| Generalized anxiety disorder | 10.5% |
| Oppositional defiant disorder | 8.4% |
| Major depression | 4.9% |
| Specific phobia | 4.2% |
| Social anxiety disorder | 3.5% |
| Conduct disorder | 2.8% |
| Attention deficit/hyperactivity disorder | 1.4% |
| Panic disorder | 1.4% |
| Enuresis | 0.7% |
| Posttraumatic stress disorder | 0.7% |
| Source: Reference 7 | |
Table 3
Somatic complaints and medical conditions
commonly associated with school refusal behavior
| Somatic complaints | Medical conditions |
|---|---|
| Diarrhea/irritable bowel | Allergic rhinitis |
| Fatigue | Asthma and respiratory illness |
| Headache and stomachache | Chronic pain and illness (notably cancer, Crohn’s disease, dyspepsia, hemophilia, chronic fatigue syndrome) |
| Nausea and vomiting | Diabetes |
| Palpitations and perspiration | Dysmenorrhea |
| Recurrent abdominal pain or other pain | Head louse infestation |
| Shaking or trembling | Influenza |
| Sleep problems | Orodental disease |
Finding a reason for school refusal
If a child has somatic complaints, you can expect to find that the child is:
- suffering from a true physical malady
- embellishing low-grade physical symptoms from stress or attention-seeking behavior
- reporting physical problems that have no medical basis.
A full medical examination is always recommended to rule out organic problems or to properly treat true medical conditions.
Four functions. If no medical condition is found, explore the reasons a particular child refuses school. A common model of conceptualizing school refusal behavior involves reinforcers:1,2
- to avoid school-based stimuli that provoke a sense of negative affectivity, or combined anxiety and depression; examples of key stimuli include teachers, peers, bus, cafeteria, classroom, and transitions between classes
- to escape aversive social or evaluative situations such as conversing or otherwise interacting with others or performing before others as in class presentations
- to pursue attention from significant others, such as wanting to stay home or go to work with parents
- to pursue tangible reinforcers outside of school, such as sleeping late, watching television, playing with friends, or engaging in delinquent behavior or substance use.
The first 2 functions are maintained by negative reinforcement or a desire to leave anxiety-provoking stimuli. The latter 2 functions are maintained by positive reinforcement, or a desire to pursue rewards outside of school. Youths may also refuse school for a combination of these reasons.17 In Nathan’s case, he was initially anxious about school in general (the first function). After his parents allowed him to stay home for a few days, however, he was refusing school to enjoy fun activities such as video games at home (the last function).
Violence on school campuses across the country naturally makes many parents skittish about possible copycat incidents. In fact, some parents acquiesce to their children’s pleas to remain home on school shooting anniversaries—particularly the Columbine tragedy of April 20, 1999.
Student and parental fears likely are exacerbated by new episodes of violence, such as three school shootings in 2006:
- On September 27, a 53-year-old man entered a high school in Bailey, Colorado, and shot one girl before killing himself.
- On September 29, a high school student near Madison, Wisconsin, killed his principal after being disciplined for carrying tobacco.
- On October 2, a heavily armed man barricaded himself in a one-room Amish schoolhouse in Paradise, Pennsylvania. He bound and shot 11 girls before killing himself, and five of the girls died.
Compared with highly publicized school violence, however, personal victimization is a much stronger factor in absenteeism.32 Specifically, school violence is related to school absenteeism especially for youths who have been previously victimized. The literature shows:
- Students who have been bullied are 2.1 times more likely than other students to feel unsafe at school.
- 20% of elementary school children report they would skip school to avoid being bullied.33
- High school students’ fear of attending classes because of violence is directly associated with victimization by teachers or other students.
- Missing school because of feeling unsafe is a strong risk factor for asthma and, potentially, being sent home early from school.34
Assessment scale. One method for quickly assessing the role of these functions is the School Refusal Assessment Scale-Revised.18,19 This scale poses 24 questions, the answers to which measure the relative strength of each of the 4 functions. Versions are available for children and parents, who complete their respective scales separately (see Related resources). Item means are calculated across the measures to help determine the primary reason for a child’s school refusal.
In addition to using the assessment scale, you may ask interview questions regarding the form and function of school refusal behavior (Tables 4,5). Take care to assess attendance history and patterns, comorbid conditions, instances of legitimate absenteeism, family disruption, and a child’s social and academic status. Specific questions about function can help narrow the reason for school refusal.
Assess specific school-related stimuli that provoke absenteeism such as social and evaluative situations, whether a child could attend school with a parent (evidence of attention-seeking), and what tangible rewards a child receives for absenteeism throughout the school day. Information about the form and function of school refusal behavior may also be evident during in-office observations of the family. Data from the School Refusal Assessment Scale-Revised, interviews, and observations can then be used to recommend particular treatment options.
Table 4
Questions related to forms of school refusal behavior
| What are the child’s specific forms of absenteeism, and how do these forms change daily? | What specific school-related stimuli are provoking the child’s concern about going to school? |
| Is a child’s school refusal behavior relatively acute or chronic in nature (in related fashion, how did the child’s school refusal behavior develop over time)? | Is the child’s refusal to attend school legitimate or understandable in some way (eg, school-based threat, bullying, inadequate school climate)? |
| What comorbid conditions occur with a child’s school refusal behavior (Table 3), including substance abuse? | What family disruption or conflict has occurred as a result of a child’s school refusal behavior? |
| What is the child’s degree of anxiety or misbehavior upon entering school, and what specific misbehaviors are present in the morning before school (Table 2)? | What is the child’s academic and social status? (This should include a review of academic records, formal evaluation reports, attendance records, and individualized education plans or 504 plans as applicable.) |
Table 5
Questions related to functions of school refusal behavior
| Have recent or traumatic home or school events influenced a child’s school refusal behavior? | Is the child willing to attend school if a parent accompanies him or her? |
| Are symptoms of school refusal behavior evident on weekends and holidays? | What specific tangible rewards does the child pursue outside of school that cause him or her to miss school? |
| Are there any nonschool situations where anxiety or attention-seeking behavior occurs? | Is the child willing to attend school if incentives are provided for attendance? |
| What specific social and/or evaluative situations at school are avoided? |
Treating youths who refuse school
Treatment success will be better assured if you work closely with school personnel and parents to gather and share information, coordinate a plan for returning a child to school, and address familial issues and the child’s comorbid medical problems that impact attendance.
Medications have proven useful in alleviating severe cases of anxiety and depression, and cognitive management techniques can be applied to the child, the parents, and the family together.
Anxiolytics or antidepressants. Pharmacotherapy research for school refusal behavior is in its infancy. Some investigators have found, however, that a tricyclic antidepressant (TCA) such as imipramine, 3 mg/kg/d, may be useful in some cases20,21—generally for youths ages 10 to 17 years with better attendance records and fewer symptoms of social avoidance and separation anxiety.22 Researchers speculate that TCAs, which are not always effective in children, may influence symptoms such as anhedonia or sleep problems that contribute to school refusal behavior.
With respect to substantial child anxiety and depression without school refusal behavior, researchers have focused on selective serotonin reuptake inhibitors (SSRIs). In particular, fluoxetine, 10 to 20 mg/d, fluvoxamine, 50 to 250 mg/d, sertraline, 85 to 160 mg/d, and paroxetine, 10 to 50 mg/d, have been useful for youths with symptoms of general and social anxiety and depression.23,24
Youths often do not respond to these medications as well as adults do, however, because of the fluid and amorphous nature of anxious and depressive symptomatology in children and adolescents. Careful monitoring is required when treating youth with SSRIs, which have been associated with an increased risk of suicidal behavior.
Psychological techniques. Sophisticated clinical controlled studies have addressed the treatment of diverse youths with school refusal behavior.25-28 Options for this population may be arranged according to function or the primary reinforcers maintaining absenteeism:
- child-based techniques to manage anxiety in a school setting
- parent-based techniques to manage contingencies for school attendance and nonattendance
- family-based techniques to manage incentives and disincentives for school attendance and nonattendance.
Child-based anxiety management techniques include relaxation training, breathing retraining, cognitive therapy (generally for youths ages 9 to 17), and exposure-based practices to gradually reintroduce a child to school. These techniques have been strongly supported by randomized controlled trials specific to school refusal behavior2 and are useful for treating general anxiety and depression as well.
Parent-based contingency management techniques include establishing morning and evening routines, modifying parental commands toward brevity and clarity, providing attention-based consequences for school nonattendance (such as early bedtime, limited time with a parent at night), reducing excessive child questioning or reassurance-seeking behavior, and engaging in forced school attendance under strict conditions. Parent-based techniques have received strong support in the literature in general29 but have been applied less frequently than child-based techniques to youths with school refusal behavior.
Family-based techniques include developing written contracts to increase incentives for school attendance and decrease incentives for nonattendance, escorting a child to school and classes, and teaching youths to refuse offers from peers to miss school.30 As with parent-based techniques, family-based techniques have received strong support in the literature in general, but have been applied less frequently than child-based techniques to youths with school refusal behavior.
Gradual reintroduction to school
A preferred approach to resolve school refusal behavior usually involves gradual reintegration to school and classes. This may include initial attendance at lunchtime, 1 or 2 favorite classes, or in an alternative classroom setting such as a guidance counselor’s office or school library. Gradual reintegration into regular classrooms may then proceed.
If possible, a child should remain in school during the day and not be sent home unless intense medical symptoms are present.30 A recommended list of intense symptoms includes:
- frequent vomiting
- bleeding
- temperature >100° F
- severe diarrhea
- lice
- acute flu-like symptoms
- extreme medical conditions such as intense pain.
Case continued: a full-time student.
A structured diagnostic interview and other behavioral assessment measures show that Nathan meets criteria for generalized anxiety disorder. He worries excessively about his social and academic performance at school and displays several somatic complaints related to anxiety. His treatment thus involves a two-pronged approach:
- sertraline, 50 mg/d, which has been found to significantly reduce symptoms of generalized anxiety disorder in youths ages 5 to 17.
- child-based anxiety management techniques and family therapy to increase incentives for school attendance and limit fun activities during a school day spent at home.
His therapist and family physician collaborate with school personnel to gradually reintroduce Nathan to a full-time academic schedule.
- Copies of the child and parent versions of the School Refusal Assessment Scale-Revised are available at www.jfponline.com/Pages.asp?AID=4322&UID=.
- King NJ, Bernstein GA. School refusal in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 2001;40:197-205.
- Kearney CA. School refusal behavior in youth: a functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
- Kearney CA, Albano AM. When children refuse school: a cognitive-behavioral therapy approach. Parent workbook/therapist’s guide. New York: Oxford University Press; 2000.
Drug brand names
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Paroxetine • Paxil
- Sertraline • Zoloft
Acknowledgment
Adapted and reprinted with permission from The Journal of Family Practice, August 2006, p 685-92.
Case: 'He's okay on weekends'
Nathan, age 13, is referred by his parents for recent school refusal behavior. He has had difficulty adjusting to middle school and has been marked absent one-third of school days this academic year. These absences come in the form of tardiness, skipped classes, and full-day absences.
Nathan complains of headaches and stomachaches and says he feels upset and nervous while in school. His parents, however, complain that Nathan seems fine on weekends and holidays and seems to be embellishing symptoms to miss school. Nathan’s parents are concerned that their son may have some physical or mental condition that is preventing his school attendance and that might be remediated with medication.
Child-motivated refusal to attend school or remain in class an entire day is not uncommon, affecting 5% to 28% of youths at some time in their lives.1,2
The behavior may be viewed along a spectrum of absenteeism (Figure), and a child may exhibit all forms of absenteeism at one time or another. In Nathan’s case, for example, he could be anxious during school on Monday, arrive late to school on Tuesday, skip afternoon classes on Wednesday, and fail to attend school completely on Thursday and Friday.
In this article you will learn characteristics of school refusal behavior to watch for and assess, and treatment strategies for youths ages 5 to 17. You will also find advice and techniques to offer parents.
Figure A child might exhibit each behavior on this spectrum at different times
Refusal behavior characteristics
School refusal behavior encompasses all subsets of problematic absenteeism, such as truancy, school phobia, and separation anxiety.3 Children and adolescents of all ages, boys and girls alike, can exhibit school refusal behavior. The most common age of onset is 10 to 13 years. Youths such as Nathan who are entering a school building for the first time—especially elementary and middle school—are at particular risk for school refusal behavior. Little information is available regarding ethnic differences, although school dropout rates for Hispanics are often considerably elevated compared with other ethnic groups.4,5
School refusal behavior covers a range of symptoms, diagnoses, somatic complaints, and medical conditions (Tables 1-3).6-12 Longitudinal studies indicate that school refusal behavior, if left unaddressed, can lead to serious short-term problems, such as distress, academic decline, alienation from peers, family conflict, and financial and legal consequences. Common long-term problems include school dropout, delinquent behaviors, economic deprivation, social isolation, marital problems, and difficulty maintaining employment. Approximately 52% of adolescents with school refusal behavior meet criteria for an anxiety, depressive, conduct-personality, or other psychiatric disorder later in life.13-16
Table 1
Common symptoms that could signal school refusal behavior
| Internalizing/covert symptoms | Externalizing/overt symptoms |
|---|---|
| Depression | Aggression |
| Fatigue/tiredness | Clinging to an adult |
| Fear and panic | Excessive reassurance-seeking behavior |
| General and social anxiety | Noncompliance and defiance |
| Self-consciousness | Refusal to move in the morning |
| Somatization | Running away from school or home |
| Worry | Temper tantrums and crying |
Table 2
Primary psychiatric disorders among youths with school refusal behavior
| Diagnosis | Percentage |
|---|---|
| None | 32.9% |
| Separation anxiety disorder | 22.4% |
| Generalized anxiety disorder | 10.5% |
| Oppositional defiant disorder | 8.4% |
| Major depression | 4.9% |
| Specific phobia | 4.2% |
| Social anxiety disorder | 3.5% |
| Conduct disorder | 2.8% |
| Attention deficit/hyperactivity disorder | 1.4% |
| Panic disorder | 1.4% |
| Enuresis | 0.7% |
| Posttraumatic stress disorder | 0.7% |
| Source: Reference 7 | |
Table 3
Somatic complaints and medical conditions
commonly associated with school refusal behavior
| Somatic complaints | Medical conditions |
|---|---|
| Diarrhea/irritable bowel | Allergic rhinitis |
| Fatigue | Asthma and respiratory illness |
| Headache and stomachache | Chronic pain and illness (notably cancer, Crohn’s disease, dyspepsia, hemophilia, chronic fatigue syndrome) |
| Nausea and vomiting | Diabetes |
| Palpitations and perspiration | Dysmenorrhea |
| Recurrent abdominal pain or other pain | Head louse infestation |
| Shaking or trembling | Influenza |
| Sleep problems | Orodental disease |
Finding a reason for school refusal
If a child has somatic complaints, you can expect to find that the child is:
- suffering from a true physical malady
- embellishing low-grade physical symptoms from stress or attention-seeking behavior
- reporting physical problems that have no medical basis.
A full medical examination is always recommended to rule out organic problems or to properly treat true medical conditions.
Four functions. If no medical condition is found, explore the reasons a particular child refuses school. A common model of conceptualizing school refusal behavior involves reinforcers:1,2
- to avoid school-based stimuli that provoke a sense of negative affectivity, or combined anxiety and depression; examples of key stimuli include teachers, peers, bus, cafeteria, classroom, and transitions between classes
- to escape aversive social or evaluative situations such as conversing or otherwise interacting with others or performing before others as in class presentations
- to pursue attention from significant others, such as wanting to stay home or go to work with parents
- to pursue tangible reinforcers outside of school, such as sleeping late, watching television, playing with friends, or engaging in delinquent behavior or substance use.
The first 2 functions are maintained by negative reinforcement or a desire to leave anxiety-provoking stimuli. The latter 2 functions are maintained by positive reinforcement, or a desire to pursue rewards outside of school. Youths may also refuse school for a combination of these reasons.17 In Nathan’s case, he was initially anxious about school in general (the first function). After his parents allowed him to stay home for a few days, however, he was refusing school to enjoy fun activities such as video games at home (the last function).
Violence on school campuses across the country naturally makes many parents skittish about possible copycat incidents. In fact, some parents acquiesce to their children’s pleas to remain home on school shooting anniversaries—particularly the Columbine tragedy of April 20, 1999.
Student and parental fears likely are exacerbated by new episodes of violence, such as three school shootings in 2006:
- On September 27, a 53-year-old man entered a high school in Bailey, Colorado, and shot one girl before killing himself.
- On September 29, a high school student near Madison, Wisconsin, killed his principal after being disciplined for carrying tobacco.
- On October 2, a heavily armed man barricaded himself in a one-room Amish schoolhouse in Paradise, Pennsylvania. He bound and shot 11 girls before killing himself, and five of the girls died.
Compared with highly publicized school violence, however, personal victimization is a much stronger factor in absenteeism.32 Specifically, school violence is related to school absenteeism especially for youths who have been previously victimized. The literature shows:
- Students who have been bullied are 2.1 times more likely than other students to feel unsafe at school.
- 20% of elementary school children report they would skip school to avoid being bullied.33
- High school students’ fear of attending classes because of violence is directly associated with victimization by teachers or other students.
- Missing school because of feeling unsafe is a strong risk factor for asthma and, potentially, being sent home early from school.34
Assessment scale. One method for quickly assessing the role of these functions is the School Refusal Assessment Scale-Revised.18,19 This scale poses 24 questions, the answers to which measure the relative strength of each of the 4 functions. Versions are available for children and parents, who complete their respective scales separately (see Related resources). Item means are calculated across the measures to help determine the primary reason for a child’s school refusal.
In addition to using the assessment scale, you may ask interview questions regarding the form and function of school refusal behavior (Tables 4,5). Take care to assess attendance history and patterns, comorbid conditions, instances of legitimate absenteeism, family disruption, and a child’s social and academic status. Specific questions about function can help narrow the reason for school refusal.
Assess specific school-related stimuli that provoke absenteeism such as social and evaluative situations, whether a child could attend school with a parent (evidence of attention-seeking), and what tangible rewards a child receives for absenteeism throughout the school day. Information about the form and function of school refusal behavior may also be evident during in-office observations of the family. Data from the School Refusal Assessment Scale-Revised, interviews, and observations can then be used to recommend particular treatment options.
Table 4
Questions related to forms of school refusal behavior
| What are the child’s specific forms of absenteeism, and how do these forms change daily? | What specific school-related stimuli are provoking the child’s concern about going to school? |
| Is a child’s school refusal behavior relatively acute or chronic in nature (in related fashion, how did the child’s school refusal behavior develop over time)? | Is the child’s refusal to attend school legitimate or understandable in some way (eg, school-based threat, bullying, inadequate school climate)? |
| What comorbid conditions occur with a child’s school refusal behavior (Table 3), including substance abuse? | What family disruption or conflict has occurred as a result of a child’s school refusal behavior? |
| What is the child’s degree of anxiety or misbehavior upon entering school, and what specific misbehaviors are present in the morning before school (Table 2)? | What is the child’s academic and social status? (This should include a review of academic records, formal evaluation reports, attendance records, and individualized education plans or 504 plans as applicable.) |
Table 5
Questions related to functions of school refusal behavior
| Have recent or traumatic home or school events influenced a child’s school refusal behavior? | Is the child willing to attend school if a parent accompanies him or her? |
| Are symptoms of school refusal behavior evident on weekends and holidays? | What specific tangible rewards does the child pursue outside of school that cause him or her to miss school? |
| Are there any nonschool situations where anxiety or attention-seeking behavior occurs? | Is the child willing to attend school if incentives are provided for attendance? |
| What specific social and/or evaluative situations at school are avoided? |
Treating youths who refuse school
Treatment success will be better assured if you work closely with school personnel and parents to gather and share information, coordinate a plan for returning a child to school, and address familial issues and the child’s comorbid medical problems that impact attendance.
Medications have proven useful in alleviating severe cases of anxiety and depression, and cognitive management techniques can be applied to the child, the parents, and the family together.
Anxiolytics or antidepressants. Pharmacotherapy research for school refusal behavior is in its infancy. Some investigators have found, however, that a tricyclic antidepressant (TCA) such as imipramine, 3 mg/kg/d, may be useful in some cases20,21—generally for youths ages 10 to 17 years with better attendance records and fewer symptoms of social avoidance and separation anxiety.22 Researchers speculate that TCAs, which are not always effective in children, may influence symptoms such as anhedonia or sleep problems that contribute to school refusal behavior.
With respect to substantial child anxiety and depression without school refusal behavior, researchers have focused on selective serotonin reuptake inhibitors (SSRIs). In particular, fluoxetine, 10 to 20 mg/d, fluvoxamine, 50 to 250 mg/d, sertraline, 85 to 160 mg/d, and paroxetine, 10 to 50 mg/d, have been useful for youths with symptoms of general and social anxiety and depression.23,24
Youths often do not respond to these medications as well as adults do, however, because of the fluid and amorphous nature of anxious and depressive symptomatology in children and adolescents. Careful monitoring is required when treating youth with SSRIs, which have been associated with an increased risk of suicidal behavior.
Psychological techniques. Sophisticated clinical controlled studies have addressed the treatment of diverse youths with school refusal behavior.25-28 Options for this population may be arranged according to function or the primary reinforcers maintaining absenteeism:
- child-based techniques to manage anxiety in a school setting
- parent-based techniques to manage contingencies for school attendance and nonattendance
- family-based techniques to manage incentives and disincentives for school attendance and nonattendance.
Child-based anxiety management techniques include relaxation training, breathing retraining, cognitive therapy (generally for youths ages 9 to 17), and exposure-based practices to gradually reintroduce a child to school. These techniques have been strongly supported by randomized controlled trials specific to school refusal behavior2 and are useful for treating general anxiety and depression as well.
Parent-based contingency management techniques include establishing morning and evening routines, modifying parental commands toward brevity and clarity, providing attention-based consequences for school nonattendance (such as early bedtime, limited time with a parent at night), reducing excessive child questioning or reassurance-seeking behavior, and engaging in forced school attendance under strict conditions. Parent-based techniques have received strong support in the literature in general29 but have been applied less frequently than child-based techniques to youths with school refusal behavior.
Family-based techniques include developing written contracts to increase incentives for school attendance and decrease incentives for nonattendance, escorting a child to school and classes, and teaching youths to refuse offers from peers to miss school.30 As with parent-based techniques, family-based techniques have received strong support in the literature in general, but have been applied less frequently than child-based techniques to youths with school refusal behavior.
Gradual reintroduction to school
A preferred approach to resolve school refusal behavior usually involves gradual reintegration to school and classes. This may include initial attendance at lunchtime, 1 or 2 favorite classes, or in an alternative classroom setting such as a guidance counselor’s office or school library. Gradual reintegration into regular classrooms may then proceed.
If possible, a child should remain in school during the day and not be sent home unless intense medical symptoms are present.30 A recommended list of intense symptoms includes:
- frequent vomiting
- bleeding
- temperature >100° F
- severe diarrhea
- lice
- acute flu-like symptoms
- extreme medical conditions such as intense pain.
Case continued: a full-time student.
A structured diagnostic interview and other behavioral assessment measures show that Nathan meets criteria for generalized anxiety disorder. He worries excessively about his social and academic performance at school and displays several somatic complaints related to anxiety. His treatment thus involves a two-pronged approach:
- sertraline, 50 mg/d, which has been found to significantly reduce symptoms of generalized anxiety disorder in youths ages 5 to 17.
- child-based anxiety management techniques and family therapy to increase incentives for school attendance and limit fun activities during a school day spent at home.
His therapist and family physician collaborate with school personnel to gradually reintroduce Nathan to a full-time academic schedule.
- Copies of the child and parent versions of the School Refusal Assessment Scale-Revised are available at www.jfponline.com/Pages.asp?AID=4322&UID=.
- King NJ, Bernstein GA. School refusal in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 2001;40:197-205.
- Kearney CA. School refusal behavior in youth: a functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
- Kearney CA, Albano AM. When children refuse school: a cognitive-behavioral therapy approach. Parent workbook/therapist’s guide. New York: Oxford University Press; 2000.
Drug brand names
- Fluoxetine • Prozac
- Fluvoxamine • Luvox
- Imipramine • Tofranil
- Paroxetine • Paxil
- Sertraline • Zoloft
Acknowledgment
Adapted and reprinted with permission from The Journal of Family Practice, August 2006, p 685-92.
1. Kearney CA, Silverman WK. The evolution and reconciliation of taxonomic strategies for school refusal behavior. Clin Psychol: Sci Prac 1996;3:339-54.
2. Kearney CA. School refusal behavior in youth: a functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
3. Hansen C, Sanders SL, Massaro S, Last CG. Predictors of severity of absenteeism in children with anxiety-based school refusal. J Clin Child Psychol 1998;27:246-54.
4. Franklin CG, Soto I. Keeping Hispanic youths in school. Children & Schools 2002;24:139-43.
5. Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: a community study. J Am Acad Child Adolesc Psychiatry 2003;42:797-807.
6. McShane G, Walter G, Rey JM. Characteristics of adolescents with school refusal. Aust New Zeal J Psychiatry 2001;35:822-6.
7. Kearney CA, Albano AM. The functional profiles of school refusal behavior: diagnostic aspects. Behav Modif 2004;28:147-61.
8. Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchardt CM, Crosby RD. Somatic symptoms in anxious-depressed school refusers. J Am Acad Child Adolesc Psychiatry 1997;36:661-8.
9. Gilliland FD, Berhane K, Islam T, et al. Environmental tobacco smoke and absenteeism related to respiratory illness in school children. Am J Epidemiology 2003;157:861-9.
10. Glaab LA, Brown R, Daneman D. School attendance in children with type I diabetes. Diabetic Med 2005;22:421-6.
11. Levy RL, Whitehead WE, Walker LS, et al. Increased somatic complaints and health-care utilization in children: effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterology 2004;99:2442-51.
12. Buitelaar JK, van Andel H, Duyx JHM, van Strien DC. Depressive and anxiety disorders in adolescence: a follow-up study of adolescents with school refusal. Acta Paedopsychiatrica 1994;56:249-53.
13. Flakierska-Praquin N, Lindstrom M, Gillberg C. School phobia with separation anxiety disorder: a comparative 20- to 29-year follow-up study of 35 school refusers. Comp Psychiatry 1997;38:17-22.
14. Hibbett A, Fogelman K. Future lives of truants: family formation and health-related behaviour. Brit J Educ Psychology 1990;60:171-9.
15. Hibbett A, Fogelman K, Manor O. Occupational outcomes of truancy. Brit J Educ Psychology 1990;60:23-36.
16. Kearney CA. Bridging the gap among professionals who address youth with school absenteeism: overview and suggestions for consensus. Prof Psychol Res Prac 2003;34:57-65.
17. King NJ, Heyne D, Tonge B, Gullone E, Ollendick TH. School refusal: categorical diagnoses, functional analysis and treatment planning. Clin Psychol Psychother 2001;8:352-60.
18. Kearney CA. Identifying the function of school refusal behavior: a revision of the School Refusal Assessment Scale. J Psychopathol Behav Assess 2002;24:235-45.
19. Kearney CA. Confirmatory factor analysis of the School Refusal Assessment Scale-Revised: child and parent versions. J Psychopathol Behav Assess 2006; in press.
20. Bernstein GA, Borchardt CM, Perwein AR, et al. Imipramine plus cognitive-behavioral therapy in the treatment of school refusal. J Am Acad Chil Adol Psychiatry 2000;39:276-83.
21. Kearney CA, Silverman WK. A critical review of pharmacotherapy for youth with anxiety disorders: things are not as they seem. J Anxiety Disord 1998;12:83-102.
22. Layne AE, Bernstein GA, Egan EA, Kushner MG. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Am Acad Chil Adol Psychiatry 2003;42:319-26.
23. Compton SN, Grant PJ, Chrisman AK, et al. Sertraline in children and adolescents with social anxiety disorder: an open trial. J Am Acad Chil Adol Psychiatry 2001;40:564-71.
24. Whittington CJ, Kendall T, Fonagy T, et al. Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. Lancet 2004;363:1341-5.
25. Kearney CA, Silverman WK. Functionally-based prescriptive and nonprescriptive treatment for children and adolescents with school refusal behavior. Behav Ther 1999;30:673-95.
26. King NJ, Tonge BJ, Heyne D, et al. Cognitive-behavioral treatment of school-refusing children: A controlled evaluation. J Am Acad Chil Adol Psychiatry 1998;37:395-403.
27. Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Am Acad Chil Adol Psychiatry 1998;37:404-11.
28. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-20.
29. Kearney CA, Roblek TL. Parent training in the treatment of school refusal behavior. In: Briesmeister JM, Schaefer CE, eds. Handbook of parent training: parents as co-therapists for children’s behavior problems, 2nd ed. New York: Wiley; 1998:225-56.
30. Kearney CA, Albano AM. When children refuse school: A cognitive-behavioral therapy approach/Therapist’s guide. San Antonio: Psychological Corporation, 2000.
31. Kearney CA, Bates M. Addressing school refusal behavior: Suggestions for frontline professionals. Children & Schools 2005;27:207-16.
32. Astor RA, Benbenishty R, Zeira A, Vinokur A. School climate, observed risky behaviors, and victimization as predictors of high school students’ fear and judgments of school violence as a problem. Health Educ Behav 2002;29:716-36.
33. Glew GM, Fan M-Y, Katon W, Rivara FP, Kernic MA. Bullying, psychosocial adjustment, and academic performance in elementary school. Arch Pediatr Adolesc Med 2005;159:1026-31.
34. Swahn MH, Bossarte RM. The associations between victimization, feeling unsafe, and asthma episodes among US high-school students. Am J Public Health 2006;96:802-4.
1. Kearney CA, Silverman WK. The evolution and reconciliation of taxonomic strategies for school refusal behavior. Clin Psychol: Sci Prac 1996;3:339-54.
2. Kearney CA. School refusal behavior in youth: a functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
3. Hansen C, Sanders SL, Massaro S, Last CG. Predictors of severity of absenteeism in children with anxiety-based school refusal. J Clin Child Psychol 1998;27:246-54.
4. Franklin CG, Soto I. Keeping Hispanic youths in school. Children & Schools 2002;24:139-43.
5. Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: a community study. J Am Acad Child Adolesc Psychiatry 2003;42:797-807.
6. McShane G, Walter G, Rey JM. Characteristics of adolescents with school refusal. Aust New Zeal J Psychiatry 2001;35:822-6.
7. Kearney CA, Albano AM. The functional profiles of school refusal behavior: diagnostic aspects. Behav Modif 2004;28:147-61.
8. Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchardt CM, Crosby RD. Somatic symptoms in anxious-depressed school refusers. J Am Acad Child Adolesc Psychiatry 1997;36:661-8.
9. Gilliland FD, Berhane K, Islam T, et al. Environmental tobacco smoke and absenteeism related to respiratory illness in school children. Am J Epidemiology 2003;157:861-9.
10. Glaab LA, Brown R, Daneman D. School attendance in children with type I diabetes. Diabetic Med 2005;22:421-6.
11. Levy RL, Whitehead WE, Walker LS, et al. Increased somatic complaints and health-care utilization in children: effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterology 2004;99:2442-51.
12. Buitelaar JK, van Andel H, Duyx JHM, van Strien DC. Depressive and anxiety disorders in adolescence: a follow-up study of adolescents with school refusal. Acta Paedopsychiatrica 1994;56:249-53.
13. Flakierska-Praquin N, Lindstrom M, Gillberg C. School phobia with separation anxiety disorder: a comparative 20- to 29-year follow-up study of 35 school refusers. Comp Psychiatry 1997;38:17-22.
14. Hibbett A, Fogelman K. Future lives of truants: family formation and health-related behaviour. Brit J Educ Psychology 1990;60:171-9.
15. Hibbett A, Fogelman K, Manor O. Occupational outcomes of truancy. Brit J Educ Psychology 1990;60:23-36.
16. Kearney CA. Bridging the gap among professionals who address youth with school absenteeism: overview and suggestions for consensus. Prof Psychol Res Prac 2003;34:57-65.
17. King NJ, Heyne D, Tonge B, Gullone E, Ollendick TH. School refusal: categorical diagnoses, functional analysis and treatment planning. Clin Psychol Psychother 2001;8:352-60.
18. Kearney CA. Identifying the function of school refusal behavior: a revision of the School Refusal Assessment Scale. J Psychopathol Behav Assess 2002;24:235-45.
19. Kearney CA. Confirmatory factor analysis of the School Refusal Assessment Scale-Revised: child and parent versions. J Psychopathol Behav Assess 2006; in press.
20. Bernstein GA, Borchardt CM, Perwein AR, et al. Imipramine plus cognitive-behavioral therapy in the treatment of school refusal. J Am Acad Chil Adol Psychiatry 2000;39:276-83.
21. Kearney CA, Silverman WK. A critical review of pharmacotherapy for youth with anxiety disorders: things are not as they seem. J Anxiety Disord 1998;12:83-102.
22. Layne AE, Bernstein GA, Egan EA, Kushner MG. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Am Acad Chil Adol Psychiatry 2003;42:319-26.
23. Compton SN, Grant PJ, Chrisman AK, et al. Sertraline in children and adolescents with social anxiety disorder: an open trial. J Am Acad Chil Adol Psychiatry 2001;40:564-71.
24. Whittington CJ, Kendall T, Fonagy T, et al. Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data. Lancet 2004;363:1341-5.
25. Kearney CA, Silverman WK. Functionally-based prescriptive and nonprescriptive treatment for children and adolescents with school refusal behavior. Behav Ther 1999;30:673-95.
26. King NJ, Tonge BJ, Heyne D, et al. Cognitive-behavioral treatment of school-refusing children: A controlled evaluation. J Am Acad Chil Adol Psychiatry 1998;37:395-403.
27. Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Am Acad Chil Adol Psychiatry 1998;37:404-11.
28. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Fam Pract 2004;53:111-20.
29. Kearney CA, Roblek TL. Parent training in the treatment of school refusal behavior. In: Briesmeister JM, Schaefer CE, eds. Handbook of parent training: parents as co-therapists for children’s behavior problems, 2nd ed. New York: Wiley; 1998:225-56.
30. Kearney CA, Albano AM. When children refuse school: A cognitive-behavioral therapy approach/Therapist’s guide. San Antonio: Psychological Corporation, 2000.
31. Kearney CA, Bates M. Addressing school refusal behavior: Suggestions for frontline professionals. Children & Schools 2005;27:207-16.
32. Astor RA, Benbenishty R, Zeira A, Vinokur A. School climate, observed risky behaviors, and victimization as predictors of high school students’ fear and judgments of school violence as a problem. Health Educ Behav 2002;29:716-36.
33. Glew GM, Fan M-Y, Katon W, Rivara FP, Kernic MA. Bullying, psychosocial adjustment, and academic performance in elementary school. Arch Pediatr Adolesc Med 2005;159:1026-31.
34. Swahn MH, Bossarte RM. The associations between victimization, feeling unsafe, and asthma episodes among US high-school students. Am J Public Health 2006;96:802-4.
Dealing with school refusal behavior: A primer for family physicians
- You can help assess forms of a child’s school refusal behavior as well as reinforcers that maintain the problem (B).
- All youths with school refusal behavior should be assessed for severe anxiety and depression (C).
- You can treat medical conditions associated with school refusal behavior, provide pharmacotherapy for severe anxiety and depression, and work with school-based personnel and a clinical child psychologist to gradually reintroduce a child to school and address comorbid educational, psychological, and familial problems (A).
Nathan is a 13-year-old boy referred by his parents to a family physician for recent school refusal behavior. Nathan has had difficulty adjusting to middle school and has already been marked absent one-third of school days this academic year. These absences have come in the form of tardiness, skipped classes, and full-day absences. Nathan complains of headaches and stomachaches and says he feels upset and nervous while in school. His parents, however, complain that Nathan seems fine on weekends and holidays and seems to be embellishing symptoms to miss school. Nathan’s parents are concerned that their son may have some physical or mental condition that is preventing his school attendance and that might be remediated with medication.
Child-motivated refusal to attend school or to remain in classes for an entire day is not that uncommon. The problem affects 5% to 28% of youths at some time during their lives and is often referred first by parents to the attention of a family physician.1-2
The behavior may be viewed along a spectrum of absenteeism ( FIGURE), and a child may exhibit all forms of absenteeism at one time or another. In Nathan’s case, for example, he could be anxious during school on Monday, arrive late to school on Tuesday, skip afternoon classes on Wednesday, and fail to attend school completely on Thursday and Friday.
In this article you will learn characteristics of school refusal behavior to watch for and assess, and treatment strategies for youths aged 5 to 17 years. You will also find advice and techniques to offer parents.
FIGURE
A child may exhibit each behavior on this spectrum at different times
Characteristics of youths with school refusal behavior
School refusal behavior is a term than encompasses all subsets of problematic absenteeism, such as truancy, school phobia, and separation anxiety.3 Children and adolescents of all ages, and boys and girls alike, can exhibit school refusal behavior. The most common age of onset, however, is 10 to 13 years. In addition, youths who are entering a school building for the first time, especially elementary and middle school (as was the case for Nathan), are at particular risk for school refusal behavior. Little information is available regarding ethnic differences, although school dropout rates for Hispanics are often considerably elevated compared with other ethnic groups.4-5
School refusal behavior covers a range of symptoms, diagnoses, somatic complaints, and medical conditions (TABLES 1-3).6-12 Longitudinal studies indicate that, if left unaddressed, school refusal behavior can lead to serious short-term problems such as distress, academic decline, alienation from peers, family conflict, and financial and legal consequences. Common long-term problems include school dropout, delinquent behaviors, economic deprivation, social isolation, marital problems, and difficulty maintaining employment. Approximately 52% of adolescents with school refusal behavior meet criteria for an anxiety, depressive, conduct-personality, or other psychiatric disorder later in life.13-16
TABLE 1
Common symptoms that could signal school refusal behavior
| INTERNALIZING/COVERT SYMPTOM | EXTERNALIZING/OVERT SYMPTOM |
|---|---|
| Depression | Aggression |
| Fatigue/tiredness | Clinging to an adult |
| Fear and panic | Excessive reassurance-seeking behavior |
| General and social anxiety | Noncompliance and defiance |
| Self-consciousness | Refusal to move in the morning |
| Somatization | Running away from school or home |
| Worry | Temper tantrums and crying |
TABLE 2
Primary psychiatric disorders among youths with school refusal behavior
| DIAGNOSIS | PERCENTAGE |
|---|---|
| No diagnosis | 32.9 |
| Separation anxiety disorder | 22.4 |
| Generalized anxiety disorder | 10.5 |
| Oppositional defiant disorder | 8.4 |
| Major depression | 4.9 |
| Specific phobia | 4.2 |
| Social anxiety disorder | 3.5 |
| Conduct disorder | 2.8 |
| Attention deficit/hyperactivity disorder | 1.4 |
| Panic disorder | 1.4 |
| Enuresis | 0.7 |
| Posttraumatic stress disorder | 0.7 |
| Source: Adapted from Kearney and Albano (2004). | |
TABLE 3
Rule out these somatic complaints and medical conditions commonly associated with school refusal behavior
| SOMATIC COMPLAINT | MEDICAL CONDITION |
|---|---|
| Diarrhea/irritable bowel | Allergic rhinitis |
| Fatigue | Asthma and respiratory illness |
| Headache and stomachache | Chronic pain and illness (notably cancer, Crohn’s disease, dyspepsia, hemophilia, chronic fatigue syndrome) |
| Nausea and vomiting | Diabetes |
| Palpitations and perspiration | Dysmenorrhea |
| Recurrent abdominal pain or other pain | Head louse infestation |
| Shaking or trembling | Influenza |
| Sleep problems | Orodental disease |
Getting to the bottom of school refusal behavior
If a child has somatic complaints, you can expect to find that the child is (1) suffering from a true physical malady, (2) embellishing low-grade physical symptoms from stress or attention-seeking behavior, or (3) reporting physical problems that have no medical basis. A full medical examination is always recommended to rule out organic problems or to properly treat true medical conditions.
If no medical condition is found, explore the reasons a particular child refuses school. A common model of conceptualizing school refusal behavior involves reinforcers1-2:
- To avoid school-based stimuli that provoke a sense of negative affectivity, or combined anxiety and depression; examples of key stimuli include teachers, peers, bus, cafeteria, classroom, and transitions between classes
- To escape aversive social or evaluative situations such as conversing or otherwise interacting with others or performing before others as in class presentations
- To pursue attention from significant others, such as wanting to stay home or go to work with parents
- To pursue tangible reinforcers outside of school, such as sleeping late, watching television, playing with friends, or engaging in delinquent behavior or substance use.
The first 2 functions are maintained by negative reinforcement, or a desire to leave anxiety-provoking stimuli. The latter 2 functions are maintained by positive reinforcement, or a desire to pursue rewards outside of school. Youths may also refuse school for a combination of these reasons.17 In Nathan’s case, he was initially anxious about school in general (function 1) but, after his parents allowed him to stay home for a few days, was refusing school as well to enjoy fun activities (eg, video games) at home (function 4).
One method for quickly assessing the role of these 4 functions is the School Refusal Assessment Scale–Revised.18,19 This scale poses 24 questions, the answers to which measure the relative strength of each of the 4 functions. Versions are available for children and parents, who complete their respective scales separately (TABLES 4-5). Item means are calculated across the measures to help determine the primary reason for a child’s school refusal.
In addition to using the School Refusal Assessment Scale–Revised, you may ask interview questions regarding the form and function of school refusal behavior (TABLE 6). Take care to assess attendance history and patterns, comorbid conditions, instances of legitimate absenteeism, family disruption, and a child’s social and academic status. Specific questions about function can help narrow the reason for school refusal.
Assess specific school-related stimuli that provoke absenteeism (eg, social and evaluative situations), whether a child could attend school with a parent (evidence of attention-seeking), and what tangible rewards a child receives for absenteeism throughout the school day. Information about the form and function of school refusal behavior may also be evident during in-office observations of the family. Data from the School Refusal Assessment Scale-Revised, interviews, and observations can then be used to recommend particular treatment options.
TABLE 4
Child version of the School Refusal Assessment Scale–Revised
|
| NOTE: (1)=avoidance of school-related stimuli that provoke a sense of negative affectivity, (2)=escape aversive social and/or evaluative situations, (3) pursuit of attention from significant others, (4) pursuit of tangible reinforcers outside of school. |
| NOTE: Items are scored on a 0-6 scale where 0=never, 1=seldom, 2=sometimes, 3=half the time, 4=usually, 5=almost always, and 6=always. |
TABLE 5
Parent version of the School Refusal Assessment Scale–Revised
|
| NOTE: (1)=avoidance of school-related stimuli that provoke a sense of negative affectivity, (2)=escape aversive social and/or evaluative situations, (3) pursuit of attention from significant others, (4) pursuit of tangible reinforcers outside of school. |
| NOTE: Items are scored on a 0-6 scale where 0=never, 1=seldom, 2=sometimes, 3=half the time, 4=usually, 5=almost always, and 6=always. |
TABLE 6
Sample questions and targets of assessment regarding the forms of school refusal behavior
| QUESTIONS RELATED TO THE FORM OF SCHOOL REFUSAL BEHAVIOR |
| What are the child’s specific forms of absenteeism, and how do these forms change daily? |
| Is a child’s school refusal behavior relatively acute or chronic in nature (in related fashion, how did the child’s school refusal behavior develop over time)? |
| What comorbid conditions occur with a child’s school refusal behavior (see TABLE 3), including substance abuse? |
| What is the child’s degree of anxiety or misbehavior upon entering school, and what specific misbehaviors are present in the morning before school (see TABLES 2 AND 4)? |
| What specific school-related stimuli are provoking the child’s concern about going to school? |
| Is the child’s refusal to attend school legitimate or understandable in some way (eg, school-based threat, bullying, inadequate school climate)? |
| What family disruption or conflict has occurred as a result of a child’s school refusal behavior? |
| What is the child’s academic and social status (this should include a review of academic records, formal evaluation reports, attendance records, and individualized education plans or 504 plans as applicable)? |
| QUESTIONS RELATED TO THE FUNCTION OF SCHOOL REFUSAL BEHAVIOR |
| Have recent or traumatic home or school events occurred to influence a child’s school refusal behavior? |
| Are symptoms of school refusal behavior evident on weekends and holidays? |
| Are there any non-school situations where anxiety or attention-seeking behavior occurs? |
| What specific social and/or evaluative situations at school are avoided? |
| Is the child willing to attend school if a parent accompanied him or her? |
| What specific tangible rewards does the child pursue outside of school that causes him or her to miss school? |
| Is the child willing to attend school if incentives were provided for attendance? |
Treating youths with school refusal behavior
Should you choose to address more than a diagnosed physical condition contributing to school refusal behavior, various resources are available to you. Medications have proven useful in alleviating severe cases of anxiety and depression. And cognitive management techniques can be applied to the child, the parents, and the family together.
Treatment success will be better assured, too, if you work closely with school personnel and a clinical child psychologist to gather and share information, coordinate a plan for returning a child to school, and address familial and comorbid psychological problems that impact attendance.
When to consider anxiolytics or antidepressants
Pharmacotherapy research for school refusal behavior is in its infancy. However, some investigators have found that tricyclic antidepressant such as imipramine may be useful in some cases20-21—generally for children with better attendance records and fewer symptoms of social avoidance and separation anxiety.22
With respect to substantial child anxiety and depression without school refusal behavior, researchers have focused on selective serotonin reuptake inhibitors. In particular, fluoxetine, fluvoxamine, sertraline, and paroxetine have been useful for youths with symptoms of general and social anxiety and depression,23,24 However, youths often do not respond to these medications as well as adults because of the fluid and amorphous nature of anxious and depressive symptomatology in children and adolescents.
Useful psychological techniques
Sophisticated Level 1 clinical controlled studies on treatment of diverse youths with school refusal behavior have appeared in recent literature.25-28 Options for this population may be generally arranged according to function or the set of reinforcers primarily maintaining absenteeism:
- Child-based techniques to manage anxiety in a school setting
- Parent-based techniques to manage contingencies for school attendance and nonattendance
- Family-based techniques to manage incentives and disincentives for school attendance and nonattendance.
Child-based anxiety management techniques include relaxation training, breathing retraining, cognitive therapy (generally for youths aged 9–17 years), and exposure-based practices to gradually reintroduce a child to school. These techniques have been strongly supported by randomized controlled trials specific to school refusal behavior (see above) and are useful for treating general anxiety and depression in these youths as well.
Parent-based contingency management techniques include establishing morning and evening routines, modifying parental commands toward brevity and clarity, providing attention-based consequences for school nonattendance (eg, early bedtime, limited time with a parent at night), reducing excessive child questioning or reassurance-seeking behavior, and engaging in forced school attendance under strict conditions. Parent-based techniques have received strong support in the literature in general, but have been applied specifically to youths with school refusal behavior less frequently than child-based techniques.
Family-based techniques include developing written contracts to increase incentives for school attendance and decrease incentives for nonattendance, escorting a child to school and classes, and teaching youths to refuse offers from peers to miss school.29 As with parent-based techniques, family-based techniques have received strong support in the literature in general, but have been applied specifically to youths with school refusal behavior less frequently than child-based techniques.
Gradual reintroduction to school
A preferred approach to resolve school refusal behavior usually involves gradual reintegration to school and classes. This may include initial attendance at lunchtime, 1 or 2 favorite classes, or in an alternative classroom setting such as a guidance counselor’s office or school library. Gradual reintegration into a regular classroom setting may then proceed.
If possible, a child should remain in the school setting during the day and not be sent home unless intense medical symptoms are present.30 A recommended list regarding the latter includes frequent vomiting, bleeding, temperature greater than 100°F, severe diarrhea, lice, acute flu-like symptoms, or an extreme medical condition such as intense pain.
The outcome for Nathan
Using a structured diagnostic interview and other behavioral assessment measures, Nathan’s psychologist concluded that the teenager met criteria for generalized anxiety disorder. He worried excessively about his social and academic performance at school and displayed several somatic complaints related to anxiety. His treatment thus involved a two-pronged approach.
Nathan’s physician placed him on a regimen of sertraline, 50 mg/d, which has been found to significantly reduce symptoms of generalized anxiety disorder in youths aged 5 to 17 years. In addition, Nathan’s psychologist implemented child-based anxiety management techniques as well as family therapy to increase incentives for school attendance and limit fun activities during a school day spent at home. The physician and psychologist collaborated with school personnel as well to gradually reintroduce Nathan to a full-time academic schedule.
Final comments
School refusal behavior sometimes is severe and intransigent, and requires a multidisciplinary approach. Cooperation and communication among parents, physicians, mental health professionals, and school officials is often crucial for resolving any particular case of school refusal behavior. The references at the end of this article provide more detailed information and note advances in the field.
CORRESPONDENCE
Christopher A. Kearney, PhD, Department of Psychology, University of Nevada, Las Vegas, 4505 Maryland Parkway, Las Vegas, NV 89154-5030. E-mail: [email protected]
1. Kearney CA, Silverman WK. The evolution and reconciliation of taxonomic strategies for school refusal behavior. Clin Psychol: Sci Prac 1996;3:339-354.
2. Kearney CA. School refusal behavior in youth: A functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
3. Hansen C, Sanders SL, Massaro S, Last CG. Predictors of severity of absenteeism in children with anxiety-based school refusal. J Clin Child Psychol 1998;27:246-254.
4. Franklin CG, Soto I. Keeping Hispanic youths in school. Children & Schools 2002;24:139-143.
5. Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: A community study. J Am Acad Child Adolesc Psychiatry 2003;42:797-807.
6. McShane G, Walter G, Rey JM. Characteristics of adolescents with school refusal. Aust New Zeal J Psychiatry 2001;35:822-826.
7. Kearney CA, Albano AM. The functional profiles of school refusal behavior: Diagnostic aspects. Behav Modif 2004;28:147-161.
8. Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchardt CM, Crosby RD. Somatic symptoms in anxious-depressed school refusers. J Amer Acad Child Adolesc Psychiatry 1997;36:661-668.
9. Gilliland FD, Berhane K, Islam T, et al. Environmental tobacco smoke and absenteeism related to respiratory illness in schoolchildren. Am J Epidemiology 2003;157:861-869.
10. Glaab LA, Brown R, Daneman D. School attendance in children with type I diabetes. Diabetic Med 2005;22:421-426.
11. Levy RL, Whitehead WE, Walker LS, et al. Increased somatic complaints and health-care utilization in children: Effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterology 2004;99:2442-2451.
12. Buitelaar JK, van Andel H, Duyx, JHM, van Strien DC. Depressive and anxiety disorders in adolescence: A follow-up study of adolescents with school refusal. Acta Paedopsychiatrica 1994;56:249-253.
13. Flakierska-Praquin N, Lindstrom M, Gillberg C. School phobia with separation anxiety disorder: A comparative 20- to 29-year follow-up study of 35 school refusers. Comp Psychiatry 1997;38:17-22.
14. Hibbett A, Fogelman K. Future lives of truants: Family formation and health-related behaviour. Brit J Educ Psychology 1990;60:171-179.
15. Hibbett A, Fogelman K, Manor O. Occupational outcomes of truancy. Brit J Educ Psychology 1990;60:23-36.
16. Kearney CA. Bridging the gap among professionals who address youth with school absenteeism: Overview and suggestions for consensus. Prof Psychol Res Prac 2003;34:57-65.
17. King NJ, Heyne D, Tonge B, Gullone E, Ollendick TH. School refusal: Categorical diagnoses, functional analysis and treatment planning. Clin Psychol Psychother 2001;8:352-360.
18. Kearney CA. Identifying the function of school refusal behavior: A revision of the School Refusal Assessment Scale. J Psychopathol Behav Assess 2002;24:235-245.
19. Kearney CA. Confirmatory factor analysis of the School Refusal Assessment Scale-Revised: Child and parent versions. J Psychopathol Behav Assess 2006; in press.
20. Bernstein GA, Borchardt CM, Perwein AR, et al. Imipramine plus cognitive-behavioral therapy in the treatment of school refusal. J Amer Acad Chil Adol Psychiatry 2000;39:276-283.
21. Kearney CA, Silverman WK. A critical review of pharmacotherapy for youth with anxiety disorders: Things are not as they seem. J Anx Dis 1998;12:83-102.
22. Layne AE, Bernstein GA, Egan EA, Kushner MG. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Amer Acad Chil Adol Psychiatry 2003;42:319-326.
23. Compton SN, Grant PJ, Chrisman AK, Gammon PJ, Brown VL, March JS. Sertraline in children and adolescents with social anxiety disorder: An open trial. J Amer Acad Chil Adol Psychiatry 2001;40:564-571.
24. Whittington CJ, Kendall T, Fonagy T, Cottrell D, Cotgrove A, Boddington E. Selective serotonin reuptake inhibitors in childhood depression: Systematic review of published versus unpublished data. Lancet 2004;363:1341-1345.
25. Kearney CA, Silverman WK. Functionally-based prescriptive and nonprescriptive treatment for children and adolescents with school refusal behavior. Behav Ther 1999;30:673-695.
26. King NJ, Tonge BJ, Heyne D, et al. Cognitive-behavioral treatment of school-refusing children: A controlled evaluation. J Amer Acad Chil Adol Psychiatry 1998;37:395-403.
27. Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Amer Acad Chil Adol Psychiatry 1998;37:404-411.
28. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature J Fam Pract 2004;53:111-120.
29. Kearney CA, Albano AM. When children refuse school: A cognitive-behavioral therapy approach/Therapist’s guide. San Antonio, Tex: Psychological Corporation, 2000.
30. Kearney CA, Bates M. Addressing school refusal behavior: Suggestions for frontline professionals. Children & Schools 2005;27:207-216.
31. Seidel L, Walkup JT. Selective serotonin reuptake inhibitor use in the treatment of the pediatric non-obsessive-compulsive disorder anxiety diagnoses. J Child Adol Psychopharm 2006;16:171-179.
- You can help assess forms of a child’s school refusal behavior as well as reinforcers that maintain the problem (B).
- All youths with school refusal behavior should be assessed for severe anxiety and depression (C).
- You can treat medical conditions associated with school refusal behavior, provide pharmacotherapy for severe anxiety and depression, and work with school-based personnel and a clinical child psychologist to gradually reintroduce a child to school and address comorbid educational, psychological, and familial problems (A).
Nathan is a 13-year-old boy referred by his parents to a family physician for recent school refusal behavior. Nathan has had difficulty adjusting to middle school and has already been marked absent one-third of school days this academic year. These absences have come in the form of tardiness, skipped classes, and full-day absences. Nathan complains of headaches and stomachaches and says he feels upset and nervous while in school. His parents, however, complain that Nathan seems fine on weekends and holidays and seems to be embellishing symptoms to miss school. Nathan’s parents are concerned that their son may have some physical or mental condition that is preventing his school attendance and that might be remediated with medication.
Child-motivated refusal to attend school or to remain in classes for an entire day is not that uncommon. The problem affects 5% to 28% of youths at some time during their lives and is often referred first by parents to the attention of a family physician.1-2
The behavior may be viewed along a spectrum of absenteeism ( FIGURE), and a child may exhibit all forms of absenteeism at one time or another. In Nathan’s case, for example, he could be anxious during school on Monday, arrive late to school on Tuesday, skip afternoon classes on Wednesday, and fail to attend school completely on Thursday and Friday.
In this article you will learn characteristics of school refusal behavior to watch for and assess, and treatment strategies for youths aged 5 to 17 years. You will also find advice and techniques to offer parents.
FIGURE
A child may exhibit each behavior on this spectrum at different times
Characteristics of youths with school refusal behavior
School refusal behavior is a term than encompasses all subsets of problematic absenteeism, such as truancy, school phobia, and separation anxiety.3 Children and adolescents of all ages, and boys and girls alike, can exhibit school refusal behavior. The most common age of onset, however, is 10 to 13 years. In addition, youths who are entering a school building for the first time, especially elementary and middle school (as was the case for Nathan), are at particular risk for school refusal behavior. Little information is available regarding ethnic differences, although school dropout rates for Hispanics are often considerably elevated compared with other ethnic groups.4-5
School refusal behavior covers a range of symptoms, diagnoses, somatic complaints, and medical conditions (TABLES 1-3).6-12 Longitudinal studies indicate that, if left unaddressed, school refusal behavior can lead to serious short-term problems such as distress, academic decline, alienation from peers, family conflict, and financial and legal consequences. Common long-term problems include school dropout, delinquent behaviors, economic deprivation, social isolation, marital problems, and difficulty maintaining employment. Approximately 52% of adolescents with school refusal behavior meet criteria for an anxiety, depressive, conduct-personality, or other psychiatric disorder later in life.13-16
TABLE 1
Common symptoms that could signal school refusal behavior
| INTERNALIZING/COVERT SYMPTOM | EXTERNALIZING/OVERT SYMPTOM |
|---|---|
| Depression | Aggression |
| Fatigue/tiredness | Clinging to an adult |
| Fear and panic | Excessive reassurance-seeking behavior |
| General and social anxiety | Noncompliance and defiance |
| Self-consciousness | Refusal to move in the morning |
| Somatization | Running away from school or home |
| Worry | Temper tantrums and crying |
TABLE 2
Primary psychiatric disorders among youths with school refusal behavior
| DIAGNOSIS | PERCENTAGE |
|---|---|
| No diagnosis | 32.9 |
| Separation anxiety disorder | 22.4 |
| Generalized anxiety disorder | 10.5 |
| Oppositional defiant disorder | 8.4 |
| Major depression | 4.9 |
| Specific phobia | 4.2 |
| Social anxiety disorder | 3.5 |
| Conduct disorder | 2.8 |
| Attention deficit/hyperactivity disorder | 1.4 |
| Panic disorder | 1.4 |
| Enuresis | 0.7 |
| Posttraumatic stress disorder | 0.7 |
| Source: Adapted from Kearney and Albano (2004). | |
TABLE 3
Rule out these somatic complaints and medical conditions commonly associated with school refusal behavior
| SOMATIC COMPLAINT | MEDICAL CONDITION |
|---|---|
| Diarrhea/irritable bowel | Allergic rhinitis |
| Fatigue | Asthma and respiratory illness |
| Headache and stomachache | Chronic pain and illness (notably cancer, Crohn’s disease, dyspepsia, hemophilia, chronic fatigue syndrome) |
| Nausea and vomiting | Diabetes |
| Palpitations and perspiration | Dysmenorrhea |
| Recurrent abdominal pain or other pain | Head louse infestation |
| Shaking or trembling | Influenza |
| Sleep problems | Orodental disease |
Getting to the bottom of school refusal behavior
If a child has somatic complaints, you can expect to find that the child is (1) suffering from a true physical malady, (2) embellishing low-grade physical symptoms from stress or attention-seeking behavior, or (3) reporting physical problems that have no medical basis. A full medical examination is always recommended to rule out organic problems or to properly treat true medical conditions.
If no medical condition is found, explore the reasons a particular child refuses school. A common model of conceptualizing school refusal behavior involves reinforcers1-2:
- To avoid school-based stimuli that provoke a sense of negative affectivity, or combined anxiety and depression; examples of key stimuli include teachers, peers, bus, cafeteria, classroom, and transitions between classes
- To escape aversive social or evaluative situations such as conversing or otherwise interacting with others or performing before others as in class presentations
- To pursue attention from significant others, such as wanting to stay home or go to work with parents
- To pursue tangible reinforcers outside of school, such as sleeping late, watching television, playing with friends, or engaging in delinquent behavior or substance use.
The first 2 functions are maintained by negative reinforcement, or a desire to leave anxiety-provoking stimuli. The latter 2 functions are maintained by positive reinforcement, or a desire to pursue rewards outside of school. Youths may also refuse school for a combination of these reasons.17 In Nathan’s case, he was initially anxious about school in general (function 1) but, after his parents allowed him to stay home for a few days, was refusing school as well to enjoy fun activities (eg, video games) at home (function 4).
One method for quickly assessing the role of these 4 functions is the School Refusal Assessment Scale–Revised.18,19 This scale poses 24 questions, the answers to which measure the relative strength of each of the 4 functions. Versions are available for children and parents, who complete their respective scales separately (TABLES 4-5). Item means are calculated across the measures to help determine the primary reason for a child’s school refusal.
In addition to using the School Refusal Assessment Scale–Revised, you may ask interview questions regarding the form and function of school refusal behavior (TABLE 6). Take care to assess attendance history and patterns, comorbid conditions, instances of legitimate absenteeism, family disruption, and a child’s social and academic status. Specific questions about function can help narrow the reason for school refusal.
Assess specific school-related stimuli that provoke absenteeism (eg, social and evaluative situations), whether a child could attend school with a parent (evidence of attention-seeking), and what tangible rewards a child receives for absenteeism throughout the school day. Information about the form and function of school refusal behavior may also be evident during in-office observations of the family. Data from the School Refusal Assessment Scale-Revised, interviews, and observations can then be used to recommend particular treatment options.
TABLE 4
Child version of the School Refusal Assessment Scale–Revised
|
| NOTE: (1)=avoidance of school-related stimuli that provoke a sense of negative affectivity, (2)=escape aversive social and/or evaluative situations, (3) pursuit of attention from significant others, (4) pursuit of tangible reinforcers outside of school. |
| NOTE: Items are scored on a 0-6 scale where 0=never, 1=seldom, 2=sometimes, 3=half the time, 4=usually, 5=almost always, and 6=always. |
TABLE 5
Parent version of the School Refusal Assessment Scale–Revised
|
| NOTE: (1)=avoidance of school-related stimuli that provoke a sense of negative affectivity, (2)=escape aversive social and/or evaluative situations, (3) pursuit of attention from significant others, (4) pursuit of tangible reinforcers outside of school. |
| NOTE: Items are scored on a 0-6 scale where 0=never, 1=seldom, 2=sometimes, 3=half the time, 4=usually, 5=almost always, and 6=always. |
TABLE 6
Sample questions and targets of assessment regarding the forms of school refusal behavior
| QUESTIONS RELATED TO THE FORM OF SCHOOL REFUSAL BEHAVIOR |
| What are the child’s specific forms of absenteeism, and how do these forms change daily? |
| Is a child’s school refusal behavior relatively acute or chronic in nature (in related fashion, how did the child’s school refusal behavior develop over time)? |
| What comorbid conditions occur with a child’s school refusal behavior (see TABLE 3), including substance abuse? |
| What is the child’s degree of anxiety or misbehavior upon entering school, and what specific misbehaviors are present in the morning before school (see TABLES 2 AND 4)? |
| What specific school-related stimuli are provoking the child’s concern about going to school? |
| Is the child’s refusal to attend school legitimate or understandable in some way (eg, school-based threat, bullying, inadequate school climate)? |
| What family disruption or conflict has occurred as a result of a child’s school refusal behavior? |
| What is the child’s academic and social status (this should include a review of academic records, formal evaluation reports, attendance records, and individualized education plans or 504 plans as applicable)? |
| QUESTIONS RELATED TO THE FUNCTION OF SCHOOL REFUSAL BEHAVIOR |
| Have recent or traumatic home or school events occurred to influence a child’s school refusal behavior? |
| Are symptoms of school refusal behavior evident on weekends and holidays? |
| Are there any non-school situations where anxiety or attention-seeking behavior occurs? |
| What specific social and/or evaluative situations at school are avoided? |
| Is the child willing to attend school if a parent accompanied him or her? |
| What specific tangible rewards does the child pursue outside of school that causes him or her to miss school? |
| Is the child willing to attend school if incentives were provided for attendance? |
Treating youths with school refusal behavior
Should you choose to address more than a diagnosed physical condition contributing to school refusal behavior, various resources are available to you. Medications have proven useful in alleviating severe cases of anxiety and depression. And cognitive management techniques can be applied to the child, the parents, and the family together.
Treatment success will be better assured, too, if you work closely with school personnel and a clinical child psychologist to gather and share information, coordinate a plan for returning a child to school, and address familial and comorbid psychological problems that impact attendance.
When to consider anxiolytics or antidepressants
Pharmacotherapy research for school refusal behavior is in its infancy. However, some investigators have found that tricyclic antidepressant such as imipramine may be useful in some cases20-21—generally for children with better attendance records and fewer symptoms of social avoidance and separation anxiety.22
With respect to substantial child anxiety and depression without school refusal behavior, researchers have focused on selective serotonin reuptake inhibitors. In particular, fluoxetine, fluvoxamine, sertraline, and paroxetine have been useful for youths with symptoms of general and social anxiety and depression,23,24 However, youths often do not respond to these medications as well as adults because of the fluid and amorphous nature of anxious and depressive symptomatology in children and adolescents.
Useful psychological techniques
Sophisticated Level 1 clinical controlled studies on treatment of diverse youths with school refusal behavior have appeared in recent literature.25-28 Options for this population may be generally arranged according to function or the set of reinforcers primarily maintaining absenteeism:
- Child-based techniques to manage anxiety in a school setting
- Parent-based techniques to manage contingencies for school attendance and nonattendance
- Family-based techniques to manage incentives and disincentives for school attendance and nonattendance.
Child-based anxiety management techniques include relaxation training, breathing retraining, cognitive therapy (generally for youths aged 9–17 years), and exposure-based practices to gradually reintroduce a child to school. These techniques have been strongly supported by randomized controlled trials specific to school refusal behavior (see above) and are useful for treating general anxiety and depression in these youths as well.
Parent-based contingency management techniques include establishing morning and evening routines, modifying parental commands toward brevity and clarity, providing attention-based consequences for school nonattendance (eg, early bedtime, limited time with a parent at night), reducing excessive child questioning or reassurance-seeking behavior, and engaging in forced school attendance under strict conditions. Parent-based techniques have received strong support in the literature in general, but have been applied specifically to youths with school refusal behavior less frequently than child-based techniques.
Family-based techniques include developing written contracts to increase incentives for school attendance and decrease incentives for nonattendance, escorting a child to school and classes, and teaching youths to refuse offers from peers to miss school.29 As with parent-based techniques, family-based techniques have received strong support in the literature in general, but have been applied specifically to youths with school refusal behavior less frequently than child-based techniques.
Gradual reintroduction to school
A preferred approach to resolve school refusal behavior usually involves gradual reintegration to school and classes. This may include initial attendance at lunchtime, 1 or 2 favorite classes, or in an alternative classroom setting such as a guidance counselor’s office or school library. Gradual reintegration into a regular classroom setting may then proceed.
If possible, a child should remain in the school setting during the day and not be sent home unless intense medical symptoms are present.30 A recommended list regarding the latter includes frequent vomiting, bleeding, temperature greater than 100°F, severe diarrhea, lice, acute flu-like symptoms, or an extreme medical condition such as intense pain.
The outcome for Nathan
Using a structured diagnostic interview and other behavioral assessment measures, Nathan’s psychologist concluded that the teenager met criteria for generalized anxiety disorder. He worried excessively about his social and academic performance at school and displayed several somatic complaints related to anxiety. His treatment thus involved a two-pronged approach.
Nathan’s physician placed him on a regimen of sertraline, 50 mg/d, which has been found to significantly reduce symptoms of generalized anxiety disorder in youths aged 5 to 17 years. In addition, Nathan’s psychologist implemented child-based anxiety management techniques as well as family therapy to increase incentives for school attendance and limit fun activities during a school day spent at home. The physician and psychologist collaborated with school personnel as well to gradually reintroduce Nathan to a full-time academic schedule.
Final comments
School refusal behavior sometimes is severe and intransigent, and requires a multidisciplinary approach. Cooperation and communication among parents, physicians, mental health professionals, and school officials is often crucial for resolving any particular case of school refusal behavior. The references at the end of this article provide more detailed information and note advances in the field.
CORRESPONDENCE
Christopher A. Kearney, PhD, Department of Psychology, University of Nevada, Las Vegas, 4505 Maryland Parkway, Las Vegas, NV 89154-5030. E-mail: [email protected]
- You can help assess forms of a child’s school refusal behavior as well as reinforcers that maintain the problem (B).
- All youths with school refusal behavior should be assessed for severe anxiety and depression (C).
- You can treat medical conditions associated with school refusal behavior, provide pharmacotherapy for severe anxiety and depression, and work with school-based personnel and a clinical child psychologist to gradually reintroduce a child to school and address comorbid educational, psychological, and familial problems (A).
Nathan is a 13-year-old boy referred by his parents to a family physician for recent school refusal behavior. Nathan has had difficulty adjusting to middle school and has already been marked absent one-third of school days this academic year. These absences have come in the form of tardiness, skipped classes, and full-day absences. Nathan complains of headaches and stomachaches and says he feels upset and nervous while in school. His parents, however, complain that Nathan seems fine on weekends and holidays and seems to be embellishing symptoms to miss school. Nathan’s parents are concerned that their son may have some physical or mental condition that is preventing his school attendance and that might be remediated with medication.
Child-motivated refusal to attend school or to remain in classes for an entire day is not that uncommon. The problem affects 5% to 28% of youths at some time during their lives and is often referred first by parents to the attention of a family physician.1-2
The behavior may be viewed along a spectrum of absenteeism ( FIGURE), and a child may exhibit all forms of absenteeism at one time or another. In Nathan’s case, for example, he could be anxious during school on Monday, arrive late to school on Tuesday, skip afternoon classes on Wednesday, and fail to attend school completely on Thursday and Friday.
In this article you will learn characteristics of school refusal behavior to watch for and assess, and treatment strategies for youths aged 5 to 17 years. You will also find advice and techniques to offer parents.
FIGURE
A child may exhibit each behavior on this spectrum at different times
Characteristics of youths with school refusal behavior
School refusal behavior is a term than encompasses all subsets of problematic absenteeism, such as truancy, school phobia, and separation anxiety.3 Children and adolescents of all ages, and boys and girls alike, can exhibit school refusal behavior. The most common age of onset, however, is 10 to 13 years. In addition, youths who are entering a school building for the first time, especially elementary and middle school (as was the case for Nathan), are at particular risk for school refusal behavior. Little information is available regarding ethnic differences, although school dropout rates for Hispanics are often considerably elevated compared with other ethnic groups.4-5
School refusal behavior covers a range of symptoms, diagnoses, somatic complaints, and medical conditions (TABLES 1-3).6-12 Longitudinal studies indicate that, if left unaddressed, school refusal behavior can lead to serious short-term problems such as distress, academic decline, alienation from peers, family conflict, and financial and legal consequences. Common long-term problems include school dropout, delinquent behaviors, economic deprivation, social isolation, marital problems, and difficulty maintaining employment. Approximately 52% of adolescents with school refusal behavior meet criteria for an anxiety, depressive, conduct-personality, or other psychiatric disorder later in life.13-16
TABLE 1
Common symptoms that could signal school refusal behavior
| INTERNALIZING/COVERT SYMPTOM | EXTERNALIZING/OVERT SYMPTOM |
|---|---|
| Depression | Aggression |
| Fatigue/tiredness | Clinging to an adult |
| Fear and panic | Excessive reassurance-seeking behavior |
| General and social anxiety | Noncompliance and defiance |
| Self-consciousness | Refusal to move in the morning |
| Somatization | Running away from school or home |
| Worry | Temper tantrums and crying |
TABLE 2
Primary psychiatric disorders among youths with school refusal behavior
| DIAGNOSIS | PERCENTAGE |
|---|---|
| No diagnosis | 32.9 |
| Separation anxiety disorder | 22.4 |
| Generalized anxiety disorder | 10.5 |
| Oppositional defiant disorder | 8.4 |
| Major depression | 4.9 |
| Specific phobia | 4.2 |
| Social anxiety disorder | 3.5 |
| Conduct disorder | 2.8 |
| Attention deficit/hyperactivity disorder | 1.4 |
| Panic disorder | 1.4 |
| Enuresis | 0.7 |
| Posttraumatic stress disorder | 0.7 |
| Source: Adapted from Kearney and Albano (2004). | |
TABLE 3
Rule out these somatic complaints and medical conditions commonly associated with school refusal behavior
| SOMATIC COMPLAINT | MEDICAL CONDITION |
|---|---|
| Diarrhea/irritable bowel | Allergic rhinitis |
| Fatigue | Asthma and respiratory illness |
| Headache and stomachache | Chronic pain and illness (notably cancer, Crohn’s disease, dyspepsia, hemophilia, chronic fatigue syndrome) |
| Nausea and vomiting | Diabetes |
| Palpitations and perspiration | Dysmenorrhea |
| Recurrent abdominal pain or other pain | Head louse infestation |
| Shaking or trembling | Influenza |
| Sleep problems | Orodental disease |
Getting to the bottom of school refusal behavior
If a child has somatic complaints, you can expect to find that the child is (1) suffering from a true physical malady, (2) embellishing low-grade physical symptoms from stress or attention-seeking behavior, or (3) reporting physical problems that have no medical basis. A full medical examination is always recommended to rule out organic problems or to properly treat true medical conditions.
If no medical condition is found, explore the reasons a particular child refuses school. A common model of conceptualizing school refusal behavior involves reinforcers1-2:
- To avoid school-based stimuli that provoke a sense of negative affectivity, or combined anxiety and depression; examples of key stimuli include teachers, peers, bus, cafeteria, classroom, and transitions between classes
- To escape aversive social or evaluative situations such as conversing or otherwise interacting with others or performing before others as in class presentations
- To pursue attention from significant others, such as wanting to stay home or go to work with parents
- To pursue tangible reinforcers outside of school, such as sleeping late, watching television, playing with friends, or engaging in delinquent behavior or substance use.
The first 2 functions are maintained by negative reinforcement, or a desire to leave anxiety-provoking stimuli. The latter 2 functions are maintained by positive reinforcement, or a desire to pursue rewards outside of school. Youths may also refuse school for a combination of these reasons.17 In Nathan’s case, he was initially anxious about school in general (function 1) but, after his parents allowed him to stay home for a few days, was refusing school as well to enjoy fun activities (eg, video games) at home (function 4).
One method for quickly assessing the role of these 4 functions is the School Refusal Assessment Scale–Revised.18,19 This scale poses 24 questions, the answers to which measure the relative strength of each of the 4 functions. Versions are available for children and parents, who complete their respective scales separately (TABLES 4-5). Item means are calculated across the measures to help determine the primary reason for a child’s school refusal.
In addition to using the School Refusal Assessment Scale–Revised, you may ask interview questions regarding the form and function of school refusal behavior (TABLE 6). Take care to assess attendance history and patterns, comorbid conditions, instances of legitimate absenteeism, family disruption, and a child’s social and academic status. Specific questions about function can help narrow the reason for school refusal.
Assess specific school-related stimuli that provoke absenteeism (eg, social and evaluative situations), whether a child could attend school with a parent (evidence of attention-seeking), and what tangible rewards a child receives for absenteeism throughout the school day. Information about the form and function of school refusal behavior may also be evident during in-office observations of the family. Data from the School Refusal Assessment Scale-Revised, interviews, and observations can then be used to recommend particular treatment options.
TABLE 4
Child version of the School Refusal Assessment Scale–Revised
|
| NOTE: (1)=avoidance of school-related stimuli that provoke a sense of negative affectivity, (2)=escape aversive social and/or evaluative situations, (3) pursuit of attention from significant others, (4) pursuit of tangible reinforcers outside of school. |
| NOTE: Items are scored on a 0-6 scale where 0=never, 1=seldom, 2=sometimes, 3=half the time, 4=usually, 5=almost always, and 6=always. |
TABLE 5
Parent version of the School Refusal Assessment Scale–Revised
|
| NOTE: (1)=avoidance of school-related stimuli that provoke a sense of negative affectivity, (2)=escape aversive social and/or evaluative situations, (3) pursuit of attention from significant others, (4) pursuit of tangible reinforcers outside of school. |
| NOTE: Items are scored on a 0-6 scale where 0=never, 1=seldom, 2=sometimes, 3=half the time, 4=usually, 5=almost always, and 6=always. |
TABLE 6
Sample questions and targets of assessment regarding the forms of school refusal behavior
| QUESTIONS RELATED TO THE FORM OF SCHOOL REFUSAL BEHAVIOR |
| What are the child’s specific forms of absenteeism, and how do these forms change daily? |
| Is a child’s school refusal behavior relatively acute or chronic in nature (in related fashion, how did the child’s school refusal behavior develop over time)? |
| What comorbid conditions occur with a child’s school refusal behavior (see TABLE 3), including substance abuse? |
| What is the child’s degree of anxiety or misbehavior upon entering school, and what specific misbehaviors are present in the morning before school (see TABLES 2 AND 4)? |
| What specific school-related stimuli are provoking the child’s concern about going to school? |
| Is the child’s refusal to attend school legitimate or understandable in some way (eg, school-based threat, bullying, inadequate school climate)? |
| What family disruption or conflict has occurred as a result of a child’s school refusal behavior? |
| What is the child’s academic and social status (this should include a review of academic records, formal evaluation reports, attendance records, and individualized education plans or 504 plans as applicable)? |
| QUESTIONS RELATED TO THE FUNCTION OF SCHOOL REFUSAL BEHAVIOR |
| Have recent or traumatic home or school events occurred to influence a child’s school refusal behavior? |
| Are symptoms of school refusal behavior evident on weekends and holidays? |
| Are there any non-school situations where anxiety or attention-seeking behavior occurs? |
| What specific social and/or evaluative situations at school are avoided? |
| Is the child willing to attend school if a parent accompanied him or her? |
| What specific tangible rewards does the child pursue outside of school that causes him or her to miss school? |
| Is the child willing to attend school if incentives were provided for attendance? |
Treating youths with school refusal behavior
Should you choose to address more than a diagnosed physical condition contributing to school refusal behavior, various resources are available to you. Medications have proven useful in alleviating severe cases of anxiety and depression. And cognitive management techniques can be applied to the child, the parents, and the family together.
Treatment success will be better assured, too, if you work closely with school personnel and a clinical child psychologist to gather and share information, coordinate a plan for returning a child to school, and address familial and comorbid psychological problems that impact attendance.
When to consider anxiolytics or antidepressants
Pharmacotherapy research for school refusal behavior is in its infancy. However, some investigators have found that tricyclic antidepressant such as imipramine may be useful in some cases20-21—generally for children with better attendance records and fewer symptoms of social avoidance and separation anxiety.22
With respect to substantial child anxiety and depression without school refusal behavior, researchers have focused on selective serotonin reuptake inhibitors. In particular, fluoxetine, fluvoxamine, sertraline, and paroxetine have been useful for youths with symptoms of general and social anxiety and depression,23,24 However, youths often do not respond to these medications as well as adults because of the fluid and amorphous nature of anxious and depressive symptomatology in children and adolescents.
Useful psychological techniques
Sophisticated Level 1 clinical controlled studies on treatment of diverse youths with school refusal behavior have appeared in recent literature.25-28 Options for this population may be generally arranged according to function or the set of reinforcers primarily maintaining absenteeism:
- Child-based techniques to manage anxiety in a school setting
- Parent-based techniques to manage contingencies for school attendance and nonattendance
- Family-based techniques to manage incentives and disincentives for school attendance and nonattendance.
Child-based anxiety management techniques include relaxation training, breathing retraining, cognitive therapy (generally for youths aged 9–17 years), and exposure-based practices to gradually reintroduce a child to school. These techniques have been strongly supported by randomized controlled trials specific to school refusal behavior (see above) and are useful for treating general anxiety and depression in these youths as well.
Parent-based contingency management techniques include establishing morning and evening routines, modifying parental commands toward brevity and clarity, providing attention-based consequences for school nonattendance (eg, early bedtime, limited time with a parent at night), reducing excessive child questioning or reassurance-seeking behavior, and engaging in forced school attendance under strict conditions. Parent-based techniques have received strong support in the literature in general, but have been applied specifically to youths with school refusal behavior less frequently than child-based techniques.
Family-based techniques include developing written contracts to increase incentives for school attendance and decrease incentives for nonattendance, escorting a child to school and classes, and teaching youths to refuse offers from peers to miss school.29 As with parent-based techniques, family-based techniques have received strong support in the literature in general, but have been applied specifically to youths with school refusal behavior less frequently than child-based techniques.
Gradual reintroduction to school
A preferred approach to resolve school refusal behavior usually involves gradual reintegration to school and classes. This may include initial attendance at lunchtime, 1 or 2 favorite classes, or in an alternative classroom setting such as a guidance counselor’s office or school library. Gradual reintegration into a regular classroom setting may then proceed.
If possible, a child should remain in the school setting during the day and not be sent home unless intense medical symptoms are present.30 A recommended list regarding the latter includes frequent vomiting, bleeding, temperature greater than 100°F, severe diarrhea, lice, acute flu-like symptoms, or an extreme medical condition such as intense pain.
The outcome for Nathan
Using a structured diagnostic interview and other behavioral assessment measures, Nathan’s psychologist concluded that the teenager met criteria for generalized anxiety disorder. He worried excessively about his social and academic performance at school and displayed several somatic complaints related to anxiety. His treatment thus involved a two-pronged approach.
Nathan’s physician placed him on a regimen of sertraline, 50 mg/d, which has been found to significantly reduce symptoms of generalized anxiety disorder in youths aged 5 to 17 years. In addition, Nathan’s psychologist implemented child-based anxiety management techniques as well as family therapy to increase incentives for school attendance and limit fun activities during a school day spent at home. The physician and psychologist collaborated with school personnel as well to gradually reintroduce Nathan to a full-time academic schedule.
Final comments
School refusal behavior sometimes is severe and intransigent, and requires a multidisciplinary approach. Cooperation and communication among parents, physicians, mental health professionals, and school officials is often crucial for resolving any particular case of school refusal behavior. The references at the end of this article provide more detailed information and note advances in the field.
CORRESPONDENCE
Christopher A. Kearney, PhD, Department of Psychology, University of Nevada, Las Vegas, 4505 Maryland Parkway, Las Vegas, NV 89154-5030. E-mail: [email protected]
1. Kearney CA, Silverman WK. The evolution and reconciliation of taxonomic strategies for school refusal behavior. Clin Psychol: Sci Prac 1996;3:339-354.
2. Kearney CA. School refusal behavior in youth: A functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
3. Hansen C, Sanders SL, Massaro S, Last CG. Predictors of severity of absenteeism in children with anxiety-based school refusal. J Clin Child Psychol 1998;27:246-254.
4. Franklin CG, Soto I. Keeping Hispanic youths in school. Children & Schools 2002;24:139-143.
5. Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: A community study. J Am Acad Child Adolesc Psychiatry 2003;42:797-807.
6. McShane G, Walter G, Rey JM. Characteristics of adolescents with school refusal. Aust New Zeal J Psychiatry 2001;35:822-826.
7. Kearney CA, Albano AM. The functional profiles of school refusal behavior: Diagnostic aspects. Behav Modif 2004;28:147-161.
8. Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchardt CM, Crosby RD. Somatic symptoms in anxious-depressed school refusers. J Amer Acad Child Adolesc Psychiatry 1997;36:661-668.
9. Gilliland FD, Berhane K, Islam T, et al. Environmental tobacco smoke and absenteeism related to respiratory illness in schoolchildren. Am J Epidemiology 2003;157:861-869.
10. Glaab LA, Brown R, Daneman D. School attendance in children with type I diabetes. Diabetic Med 2005;22:421-426.
11. Levy RL, Whitehead WE, Walker LS, et al. Increased somatic complaints and health-care utilization in children: Effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterology 2004;99:2442-2451.
12. Buitelaar JK, van Andel H, Duyx, JHM, van Strien DC. Depressive and anxiety disorders in adolescence: A follow-up study of adolescents with school refusal. Acta Paedopsychiatrica 1994;56:249-253.
13. Flakierska-Praquin N, Lindstrom M, Gillberg C. School phobia with separation anxiety disorder: A comparative 20- to 29-year follow-up study of 35 school refusers. Comp Psychiatry 1997;38:17-22.
14. Hibbett A, Fogelman K. Future lives of truants: Family formation and health-related behaviour. Brit J Educ Psychology 1990;60:171-179.
15. Hibbett A, Fogelman K, Manor O. Occupational outcomes of truancy. Brit J Educ Psychology 1990;60:23-36.
16. Kearney CA. Bridging the gap among professionals who address youth with school absenteeism: Overview and suggestions for consensus. Prof Psychol Res Prac 2003;34:57-65.
17. King NJ, Heyne D, Tonge B, Gullone E, Ollendick TH. School refusal: Categorical diagnoses, functional analysis and treatment planning. Clin Psychol Psychother 2001;8:352-360.
18. Kearney CA. Identifying the function of school refusal behavior: A revision of the School Refusal Assessment Scale. J Psychopathol Behav Assess 2002;24:235-245.
19. Kearney CA. Confirmatory factor analysis of the School Refusal Assessment Scale-Revised: Child and parent versions. J Psychopathol Behav Assess 2006; in press.
20. Bernstein GA, Borchardt CM, Perwein AR, et al. Imipramine plus cognitive-behavioral therapy in the treatment of school refusal. J Amer Acad Chil Adol Psychiatry 2000;39:276-283.
21. Kearney CA, Silverman WK. A critical review of pharmacotherapy for youth with anxiety disorders: Things are not as they seem. J Anx Dis 1998;12:83-102.
22. Layne AE, Bernstein GA, Egan EA, Kushner MG. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Amer Acad Chil Adol Psychiatry 2003;42:319-326.
23. Compton SN, Grant PJ, Chrisman AK, Gammon PJ, Brown VL, March JS. Sertraline in children and adolescents with social anxiety disorder: An open trial. J Amer Acad Chil Adol Psychiatry 2001;40:564-571.
24. Whittington CJ, Kendall T, Fonagy T, Cottrell D, Cotgrove A, Boddington E. Selective serotonin reuptake inhibitors in childhood depression: Systematic review of published versus unpublished data. Lancet 2004;363:1341-1345.
25. Kearney CA, Silverman WK. Functionally-based prescriptive and nonprescriptive treatment for children and adolescents with school refusal behavior. Behav Ther 1999;30:673-695.
26. King NJ, Tonge BJ, Heyne D, et al. Cognitive-behavioral treatment of school-refusing children: A controlled evaluation. J Amer Acad Chil Adol Psychiatry 1998;37:395-403.
27. Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Amer Acad Chil Adol Psychiatry 1998;37:404-411.
28. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature J Fam Pract 2004;53:111-120.
29. Kearney CA, Albano AM. When children refuse school: A cognitive-behavioral therapy approach/Therapist’s guide. San Antonio, Tex: Psychological Corporation, 2000.
30. Kearney CA, Bates M. Addressing school refusal behavior: Suggestions for frontline professionals. Children & Schools 2005;27:207-216.
31. Seidel L, Walkup JT. Selective serotonin reuptake inhibitor use in the treatment of the pediatric non-obsessive-compulsive disorder anxiety diagnoses. J Child Adol Psychopharm 2006;16:171-179.
1. Kearney CA, Silverman WK. The evolution and reconciliation of taxonomic strategies for school refusal behavior. Clin Psychol: Sci Prac 1996;3:339-354.
2. Kearney CA. School refusal behavior in youth: A functional approach to assessment and treatment. Washington, DC: American Psychological Association; 2001.
3. Hansen C, Sanders SL, Massaro S, Last CG. Predictors of severity of absenteeism in children with anxiety-based school refusal. J Clin Child Psychol 1998;27:246-254.
4. Franklin CG, Soto I. Keeping Hispanic youths in school. Children & Schools 2002;24:139-143.
5. Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: A community study. J Am Acad Child Adolesc Psychiatry 2003;42:797-807.
6. McShane G, Walter G, Rey JM. Characteristics of adolescents with school refusal. Aust New Zeal J Psychiatry 2001;35:822-826.
7. Kearney CA, Albano AM. The functional profiles of school refusal behavior: Diagnostic aspects. Behav Modif 2004;28:147-161.
8. Bernstein GA, Massie ED, Thuras PD, Perwien AR, Borchardt CM, Crosby RD. Somatic symptoms in anxious-depressed school refusers. J Amer Acad Child Adolesc Psychiatry 1997;36:661-668.
9. Gilliland FD, Berhane K, Islam T, et al. Environmental tobacco smoke and absenteeism related to respiratory illness in schoolchildren. Am J Epidemiology 2003;157:861-869.
10. Glaab LA, Brown R, Daneman D. School attendance in children with type I diabetes. Diabetic Med 2005;22:421-426.
11. Levy RL, Whitehead WE, Walker LS, et al. Increased somatic complaints and health-care utilization in children: Effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterology 2004;99:2442-2451.
12. Buitelaar JK, van Andel H, Duyx, JHM, van Strien DC. Depressive and anxiety disorders in adolescence: A follow-up study of adolescents with school refusal. Acta Paedopsychiatrica 1994;56:249-253.
13. Flakierska-Praquin N, Lindstrom M, Gillberg C. School phobia with separation anxiety disorder: A comparative 20- to 29-year follow-up study of 35 school refusers. Comp Psychiatry 1997;38:17-22.
14. Hibbett A, Fogelman K. Future lives of truants: Family formation and health-related behaviour. Brit J Educ Psychology 1990;60:171-179.
15. Hibbett A, Fogelman K, Manor O. Occupational outcomes of truancy. Brit J Educ Psychology 1990;60:23-36.
16. Kearney CA. Bridging the gap among professionals who address youth with school absenteeism: Overview and suggestions for consensus. Prof Psychol Res Prac 2003;34:57-65.
17. King NJ, Heyne D, Tonge B, Gullone E, Ollendick TH. School refusal: Categorical diagnoses, functional analysis and treatment planning. Clin Psychol Psychother 2001;8:352-360.
18. Kearney CA. Identifying the function of school refusal behavior: A revision of the School Refusal Assessment Scale. J Psychopathol Behav Assess 2002;24:235-245.
19. Kearney CA. Confirmatory factor analysis of the School Refusal Assessment Scale-Revised: Child and parent versions. J Psychopathol Behav Assess 2006; in press.
20. Bernstein GA, Borchardt CM, Perwein AR, et al. Imipramine plus cognitive-behavioral therapy in the treatment of school refusal. J Amer Acad Chil Adol Psychiatry 2000;39:276-283.
21. Kearney CA, Silverman WK. A critical review of pharmacotherapy for youth with anxiety disorders: Things are not as they seem. J Anx Dis 1998;12:83-102.
22. Layne AE, Bernstein GA, Egan EA, Kushner MG. Predictors of treatment response in anxious-depressed adolescents with school refusal. J Amer Acad Chil Adol Psychiatry 2003;42:319-326.
23. Compton SN, Grant PJ, Chrisman AK, Gammon PJ, Brown VL, March JS. Sertraline in children and adolescents with social anxiety disorder: An open trial. J Amer Acad Chil Adol Psychiatry 2001;40:564-571.
24. Whittington CJ, Kendall T, Fonagy T, Cottrell D, Cotgrove A, Boddington E. Selective serotonin reuptake inhibitors in childhood depression: Systematic review of published versus unpublished data. Lancet 2004;363:1341-1345.
25. Kearney CA, Silverman WK. Functionally-based prescriptive and nonprescriptive treatment for children and adolescents with school refusal behavior. Behav Ther 1999;30:673-695.
26. King NJ, Tonge BJ, Heyne D, et al. Cognitive-behavioral treatment of school-refusing children: A controlled evaluation. J Amer Acad Chil Adol Psychiatry 1998;37:395-403.
27. Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Amer Acad Chil Adol Psychiatry 1998;37:404-411.
28. Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature J Fam Pract 2004;53:111-120.
29. Kearney CA, Albano AM. When children refuse school: A cognitive-behavioral therapy approach/Therapist’s guide. San Antonio, Tex: Psychological Corporation, 2000.
30. Kearney CA, Bates M. Addressing school refusal behavior: Suggestions for frontline professionals. Children & Schools 2005;27:207-216.
31. Seidel L, Walkup JT. Selective serotonin reuptake inhibitor use in the treatment of the pediatric non-obsessive-compulsive disorder anxiety diagnoses. J Child Adol Psychopharm 2006;16:171-179.