User login
Elective Hand Surgery and Antithrombotic Use in Veterans
Patients planning plastic surgery traditionally were instructed to stop anticoagulants and antiplatelet medications during the perioperative period to avoid bleeding, which could result in flap loss, pain, skin necrosis, and blood transfusions. In the veteran patient population, anticoagulants are prescribed for the prevention of limb- and life-threatening embolic and thrombotic events.1-3 As of June 2021, > 332,000 veterans were prescribed direct oral anticoagulants.1
In 2015, the Malcom Randall Veterans Affairs Medical Center (MRVAMC) in Gainesville, Florida, Plastic Surgery Service began instructing patients planning elective hand surgery to continue their prescription anticoagulants and antiplatelets during the perioperative period. This decision was prompted by a patient who needed carpal tunnel release surgery and was prescribed coumadin for repeated thrombosis of his dialysis grafts. Hand surgery literature at the time suggested allowing patients to continue their anticoagulants and antiplatelets through the perioperative period to avoid life- and limb-threatening events and wide fluctuations in blood anticoagulant levels.4-6 The MRVAMC Plastic Surgery Service chose to accept the risk of perioperative bleeding after shared decision making with the patients rather than risk a cardiac stent obstruction, pulmonary embolism, or embolic stroke in the at-risk patients.
The objective of this study was to determine the postoperative bleeding complication rate over a 7.5-year period in the veteran patients who did not interrupt their prescription blood thinners. This would assist the MRVAMC Plastic Surgery Service with providing data-driven informed consent and determine whether this protocol should continue.
Methods
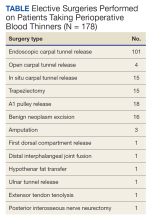
The North Florida/South Georgia Veterans Health System Research Committee and the University of Florida Institutional Review Board approved a retrospective chart review of elective hand cases performed by the MRVAMC Plastic Surgery Service from January 1, 2015, through June 30, 2022. Elective hand cases were identified based on the operation description and included nerve decompressions, tendon releases, trapeziectomy, small-joint fusion, neurectomy, elective amputations, and benign neoplasm removals (Table). Hand surgery included cubital tunnel releases (decompression of the ulnar nerve at the level of the elbow) because hand surgery fellowships, hand surgery training, and hand surgery practices traditionally include a high volume of cubital tunnel releases. We wanted this study to have real-world applications.
Patients’ histories and physicals were reviewed for prescription antithrombotics and for instructions not to interrupt these medications. Postoperative notes were reviewed for 30 days for evidence of postoperative bleeding complications.
The following prescription anticoagulants were included in the study: dabigatran, rivaroxaban, warfarin, edoxaban, and apixaban. In addition, the following prescription antiplatelets were included in the study:
Results
One hundred seventy-eight patients were identified for maintaining prescription blood thinners during their elective hand surgery. There was 1 major complication (0.6%) and 4 minor bleeding complications (2.2%). The major complication occurred when a patient had to return to surgery from the recovery room for emergent control of bleeding. The surgery was for an in situ cubital tunnel release. The patient, aged 48 years, was taking clopidogrel and aspirin and had a personal and family history of cardiovascular disease. The bleeding was controlled with bipolar cautery and Floseal, a topical haemostatic matrix made of bovine gelatin and human thrombin. The minor bleeding complications were treated in the clinic with compression, wound care, or expedited follow-up for reassurance. These included an in situ cubital tunnel release for a patient taking warfarin and aspirin, a digital inclusion cyst for a patient taking apixaban, an endoscopic carpal tunnel for a patient taking aspirin and clopidogrel, and an open carpal tunnel and ulnar tunnel release for a patient taking aspirin and clopidogrel. There were no thrombotic events during the study.
Discussion
Higher utilization of anticoagulation has been evidenced by a 30% increase in Medicare claims and a 277% increase in Medicaid anticoagulation claims between 2014 and 2019, driven by more prescriptions for direct oral anticoagulants such as apixaban and rivaroxaban.7 The MRVAMC Plastic Surgery Service began a protocol for managing perioperative anticoagulation in 2015 to avoid the risk of perioperative thrombotic events in veteran patients. Patients who choose elective hand surgery were instructed to continue their prescription blood thinners. Exceptions to this protocol were patients scheduled for a partial fasciectomy (for Dupuytren contracture) or cubital tunnel release with anterior ulnar nerve transposition. A hematoma would increase the risk for skin necrosis in the patients receiving a fasciectomy, resulting from the thin skin flaps and meticulous dissection to identify and protect the digital nerves. Worsening nerve dysfunction could result from hematoma compression and scarring in the ulnar nerve cases. If the risk of holding the blood thinner was felt to be unreasonably high, based on recommendations from the patients’ cardiologist or primary care doctor, we offered an in situ cubital tunnel release for the ulnar nerve patients.
Concerns regarding interrupting chronic anticoagulation involve the increased risk of thromboembolism and the theoretical risk of a rebound hypercoagulable effect.8 Patients prescribed warfarin have been found to unintentionally discontinue this medication after outpatient surgery at more than 1.5 times the rate of the general population.9
A systematic review of 9 published studies looking specifically at elective hand and wrist surgeries demonstrated no significant increase in perioperative bleeding risk with the continuation of anticoagulation and antiplatelet medications.10 Sardenberg and colleagues reviewed 7 studies in which 410 hand and wrist surgeries were performed in patients prescribed warfarin or aspirin and clopidogrel. These patients had a 0.7% serious complication rate, requiring surgical treatment only in patients having complex wrist surgeries (wrist arthrodesis with tenosynovectomy, resection of the distal ulna with tenosynovectomy and tendon transfer, and proximal row carpectomy).11 Bogunovic and colleagues compared 50 hand and wrist patients who were on uninterrupted warfarin with those who were not. They required patients to have an
These and our study are consistent with other disciplines, such as facial plastic surgery, dermatology, and ophthalmology, which do not support routine suspension of anticoagulants.13-16 A review of 30 cutaneous surgery studies involving > 14,000 patients recommended meticulous hemostasis over cessation of blood thinners.15 The University of Massachusetts Dermatology Clinic found a 40 times higher rate of bleeding complications in patients on clopidogrel and warfarin but still recommended continuation of these medications to avoid thrombotic events.16
Limitations
This study is a retrospective chart review and limited by what is already documented in the electronic health record. We can verify that the patients were given instructions to continue their medications up to the day of surgery but cannot be certain whether the instructions were followed. No control group was told to hold their anticoagulants for the same surgery. Once we decided on a protocol, we applied it to all patients. The study approval was for the specific time frame when the protocol was in place.
Our study was designed for elective hand cases because those surgeries can be anticipated, predicted, and patients can be given instructions during the preoperative appointments. We did incidentally find several nonelective hand cases (traumas, infections, and cancers) during the review of patients taking prescription blood thinners that had to be expedited to the operating room. Based on morbidity data during that time period, there were no additional postoperative hand surgery bleeding complications that had to return to the operating room. Future studies are indicated, but we believe our protocol can be applied to urgent and emergent hand surgeries as well as elective cases.
Conclusions
Our study supports continuing prescription anticoagulant and antiplatelet medications during the perioperative period for elective hand surgery. We found this is a safe practice in our veteran population with an acceptably low local bleeding complication rate.
Acknowledgments
This manuscript is the result of work supported with the resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
1. Allen AL, Lucas J, Parra D, et al. Shifting the paradigm: a population health approach to the management of direct oral anticoagulants. J Am Heart Assoc. 2021;10(24):e022758. doi:10.1161/JAHA.121.022758
2. Buck J, Kaboli P, Gage BF, Cram P, Vaughan Sarrazin MS. Trends in antithrombotic therapy for atrial fibrillation: data from the Veterans Health Administration health system. Am Heart J. 2016;179:186-191. doi:10.1016/j.ahj.2016.03.029
3. Kinlay S, Young MM, Sherrod R, Gagnon DR. Long-term outcomes and duration of dual antiplatelet therapy after coronary intervention with second-generation drug-eluting stents: the Veterans Affairs Extended DAPT Study. J Am Heart Assoc. 2023;12(2):e027055.
4. Bogunovic L, Gelberman RH, Goldfarb CA, Boyer MI, Calfee RP. The impact of antiplatelet medication on hand and wrist surgery. J Hand Surg Am. 2013;38(6):1063-1070. doi:10.1016/j.jhsa.2013.03.034
5. Wallace DL, Latimer MD, Belcher HJ. Stopping warfarin therapy is unnecessary for hand surgery. J Hand Surg Br. 2004;29(3):203-205. doi:10.1016/j.jhsb.2003.12.008
6. Edmunds I, Avakian Z. Hand surgery on anticoagulated patients: a prospective study of 121 operations. Hand Surg. 2010;15(2):109-113. doi:10.1142/S021881041000468
7. Duvalyan A, Pandey A, Vaduganathan M, et al. Trends in anticoagulation prescription spending among Medicare Part D and Medicaid beneficiaries between 2014 and 2019. J Am Heart Assoc. 2021;10(24):e022644. doi:10.1161/JAHA.121.022644
8. Thakur NA, Czerwein JK, Butera JN, Palumbo MA. Perioperative management of chronic anticoagulation in orthopaedic surgery. J Am Acad Orthop Surg. 2010;18(12):729-738. doi:10.5435/00124635-201012000-00003
9. Bell C, Bajca J, Bierman A, Li P, Mamdani M, Urbach D. Potentially unintended discontinuation of long-term medication use after elective surgical procedures. Arch Int Med. 2003;166(22):2525-2531.
10. Stone MJ, Wilks DJ, Wade RG. Hand and wrist surgery on anticoagulants and antiplatelets: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2020;73(8):1413-1423.
11. Sardenberg T, Deienno FS, Miranda RF, et al. Hand and wrist surgery without suspending warfarin or oral antiplatelet - systematic review. Rev Bras Ortop. 2017;52(4):390-395. doi:10.1016/j.rboe.2017.07.001
12. Bogunovic L, Gelberman RH, Goldfarb CA, Boyer MI, Calfee RP. The impact of uninterrupted warfarin on hand and wrist surgery. J Hand Surg Am. 2015;40(11):2133-2140. doi:10.1016/j.jhsa.2015.07.037
13. Kraft CT, Bellile E, Baker SR, Kim JC, Moyer JS. Anticoagulant complications in facial plastic and reconstructive surgery. JAMA Facial Plast Surg. 2015;17(2):103-107. doi:10.1001/jamafacial.2014.1147
14. He X, Chen AF, Nirwan RS, Sridhar J, Kuriyan AE. Perioperative management of anticoagulants in ocular surgeries. Int Ophthalmol Clin. 2020;60(3):3-15. doi:10.1097/IIO.0000000000000316
15. Isted A, Cooper L, Colville RJ. Bleeding on the cutting edge: a systematic review of anticoagulant and antiplatelet continuation in minor cutaneous surgery. J Plast Reconstr Aesthet Surg. 2018;71(4):455-467. doi:10.1016/j.bjps.2017.11.024
16. Bordeaux JS, Martires KJ, Goldberg D, Pattee SF, Fu P, Maloney ME. Prospective evaluation of dermatologic surgery complications including patients on multiple antiplatelet and anticoagulant medications. J Am Acad Dermatol. 2011;65(3):576-583. doi:10.1016/j.jaad.2011.02.012
Patients planning plastic surgery traditionally were instructed to stop anticoagulants and antiplatelet medications during the perioperative period to avoid bleeding, which could result in flap loss, pain, skin necrosis, and blood transfusions. In the veteran patient population, anticoagulants are prescribed for the prevention of limb- and life-threatening embolic and thrombotic events.1-3 As of June 2021, > 332,000 veterans were prescribed direct oral anticoagulants.1
In 2015, the Malcom Randall Veterans Affairs Medical Center (MRVAMC) in Gainesville, Florida, Plastic Surgery Service began instructing patients planning elective hand surgery to continue their prescription anticoagulants and antiplatelets during the perioperative period. This decision was prompted by a patient who needed carpal tunnel release surgery and was prescribed coumadin for repeated thrombosis of his dialysis grafts. Hand surgery literature at the time suggested allowing patients to continue their anticoagulants and antiplatelets through the perioperative period to avoid life- and limb-threatening events and wide fluctuations in blood anticoagulant levels.4-6 The MRVAMC Plastic Surgery Service chose to accept the risk of perioperative bleeding after shared decision making with the patients rather than risk a cardiac stent obstruction, pulmonary embolism, or embolic stroke in the at-risk patients.
The objective of this study was to determine the postoperative bleeding complication rate over a 7.5-year period in the veteran patients who did not interrupt their prescription blood thinners. This would assist the MRVAMC Plastic Surgery Service with providing data-driven informed consent and determine whether this protocol should continue.
Methods
The North Florida/South Georgia Veterans Health System Research Committee and the University of Florida Institutional Review Board approved a retrospective chart review of elective hand cases performed by the MRVAMC Plastic Surgery Service from January 1, 2015, through June 30, 2022. Elective hand cases were identified based on the operation description and included nerve decompressions, tendon releases, trapeziectomy, small-joint fusion, neurectomy, elective amputations, and benign neoplasm removals (Table). Hand surgery included cubital tunnel releases (decompression of the ulnar nerve at the level of the elbow) because hand surgery fellowships, hand surgery training, and hand surgery practices traditionally include a high volume of cubital tunnel releases. We wanted this study to have real-world applications.
Patients’ histories and physicals were reviewed for prescription antithrombotics and for instructions not to interrupt these medications. Postoperative notes were reviewed for 30 days for evidence of postoperative bleeding complications.
The following prescription anticoagulants were included in the study: dabigatran, rivaroxaban, warfarin, edoxaban, and apixaban. In addition, the following prescription antiplatelets were included in the study:
Results
One hundred seventy-eight patients were identified for maintaining prescription blood thinners during their elective hand surgery. There was 1 major complication (0.6%) and 4 minor bleeding complications (2.2%). The major complication occurred when a patient had to return to surgery from the recovery room for emergent control of bleeding. The surgery was for an in situ cubital tunnel release. The patient, aged 48 years, was taking clopidogrel and aspirin and had a personal and family history of cardiovascular disease. The bleeding was controlled with bipolar cautery and Floseal, a topical haemostatic matrix made of bovine gelatin and human thrombin. The minor bleeding complications were treated in the clinic with compression, wound care, or expedited follow-up for reassurance. These included an in situ cubital tunnel release for a patient taking warfarin and aspirin, a digital inclusion cyst for a patient taking apixaban, an endoscopic carpal tunnel for a patient taking aspirin and clopidogrel, and an open carpal tunnel and ulnar tunnel release for a patient taking aspirin and clopidogrel. There were no thrombotic events during the study.
Discussion
Higher utilization of anticoagulation has been evidenced by a 30% increase in Medicare claims and a 277% increase in Medicaid anticoagulation claims between 2014 and 2019, driven by more prescriptions for direct oral anticoagulants such as apixaban and rivaroxaban.7 The MRVAMC Plastic Surgery Service began a protocol for managing perioperative anticoagulation in 2015 to avoid the risk of perioperative thrombotic events in veteran patients. Patients who choose elective hand surgery were instructed to continue their prescription blood thinners. Exceptions to this protocol were patients scheduled for a partial fasciectomy (for Dupuytren contracture) or cubital tunnel release with anterior ulnar nerve transposition. A hematoma would increase the risk for skin necrosis in the patients receiving a fasciectomy, resulting from the thin skin flaps and meticulous dissection to identify and protect the digital nerves. Worsening nerve dysfunction could result from hematoma compression and scarring in the ulnar nerve cases. If the risk of holding the blood thinner was felt to be unreasonably high, based on recommendations from the patients’ cardiologist or primary care doctor, we offered an in situ cubital tunnel release for the ulnar nerve patients.
Concerns regarding interrupting chronic anticoagulation involve the increased risk of thromboembolism and the theoretical risk of a rebound hypercoagulable effect.8 Patients prescribed warfarin have been found to unintentionally discontinue this medication after outpatient surgery at more than 1.5 times the rate of the general population.9
A systematic review of 9 published studies looking specifically at elective hand and wrist surgeries demonstrated no significant increase in perioperative bleeding risk with the continuation of anticoagulation and antiplatelet medications.10 Sardenberg and colleagues reviewed 7 studies in which 410 hand and wrist surgeries were performed in patients prescribed warfarin or aspirin and clopidogrel. These patients had a 0.7% serious complication rate, requiring surgical treatment only in patients having complex wrist surgeries (wrist arthrodesis with tenosynovectomy, resection of the distal ulna with tenosynovectomy and tendon transfer, and proximal row carpectomy).11 Bogunovic and colleagues compared 50 hand and wrist patients who were on uninterrupted warfarin with those who were not. They required patients to have an
These and our study are consistent with other disciplines, such as facial plastic surgery, dermatology, and ophthalmology, which do not support routine suspension of anticoagulants.13-16 A review of 30 cutaneous surgery studies involving > 14,000 patients recommended meticulous hemostasis over cessation of blood thinners.15 The University of Massachusetts Dermatology Clinic found a 40 times higher rate of bleeding complications in patients on clopidogrel and warfarin but still recommended continuation of these medications to avoid thrombotic events.16
Limitations
This study is a retrospective chart review and limited by what is already documented in the electronic health record. We can verify that the patients were given instructions to continue their medications up to the day of surgery but cannot be certain whether the instructions were followed. No control group was told to hold their anticoagulants for the same surgery. Once we decided on a protocol, we applied it to all patients. The study approval was for the specific time frame when the protocol was in place.
Our study was designed for elective hand cases because those surgeries can be anticipated, predicted, and patients can be given instructions during the preoperative appointments. We did incidentally find several nonelective hand cases (traumas, infections, and cancers) during the review of patients taking prescription blood thinners that had to be expedited to the operating room. Based on morbidity data during that time period, there were no additional postoperative hand surgery bleeding complications that had to return to the operating room. Future studies are indicated, but we believe our protocol can be applied to urgent and emergent hand surgeries as well as elective cases.
Conclusions
Our study supports continuing prescription anticoagulant and antiplatelet medications during the perioperative period for elective hand surgery. We found this is a safe practice in our veteran population with an acceptably low local bleeding complication rate.
Acknowledgments
This manuscript is the result of work supported with the resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
Patients planning plastic surgery traditionally were instructed to stop anticoagulants and antiplatelet medications during the perioperative period to avoid bleeding, which could result in flap loss, pain, skin necrosis, and blood transfusions. In the veteran patient population, anticoagulants are prescribed for the prevention of limb- and life-threatening embolic and thrombotic events.1-3 As of June 2021, > 332,000 veterans were prescribed direct oral anticoagulants.1
In 2015, the Malcom Randall Veterans Affairs Medical Center (MRVAMC) in Gainesville, Florida, Plastic Surgery Service began instructing patients planning elective hand surgery to continue their prescription anticoagulants and antiplatelets during the perioperative period. This decision was prompted by a patient who needed carpal tunnel release surgery and was prescribed coumadin for repeated thrombosis of his dialysis grafts. Hand surgery literature at the time suggested allowing patients to continue their anticoagulants and antiplatelets through the perioperative period to avoid life- and limb-threatening events and wide fluctuations in blood anticoagulant levels.4-6 The MRVAMC Plastic Surgery Service chose to accept the risk of perioperative bleeding after shared decision making with the patients rather than risk a cardiac stent obstruction, pulmonary embolism, or embolic stroke in the at-risk patients.
The objective of this study was to determine the postoperative bleeding complication rate over a 7.5-year period in the veteran patients who did not interrupt their prescription blood thinners. This would assist the MRVAMC Plastic Surgery Service with providing data-driven informed consent and determine whether this protocol should continue.
Methods
The North Florida/South Georgia Veterans Health System Research Committee and the University of Florida Institutional Review Board approved a retrospective chart review of elective hand cases performed by the MRVAMC Plastic Surgery Service from January 1, 2015, through June 30, 2022. Elective hand cases were identified based on the operation description and included nerve decompressions, tendon releases, trapeziectomy, small-joint fusion, neurectomy, elective amputations, and benign neoplasm removals (Table). Hand surgery included cubital tunnel releases (decompression of the ulnar nerve at the level of the elbow) because hand surgery fellowships, hand surgery training, and hand surgery practices traditionally include a high volume of cubital tunnel releases. We wanted this study to have real-world applications.
Patients’ histories and physicals were reviewed for prescription antithrombotics and for instructions not to interrupt these medications. Postoperative notes were reviewed for 30 days for evidence of postoperative bleeding complications.
The following prescription anticoagulants were included in the study: dabigatran, rivaroxaban, warfarin, edoxaban, and apixaban. In addition, the following prescription antiplatelets were included in the study:
Results
One hundred seventy-eight patients were identified for maintaining prescription blood thinners during their elective hand surgery. There was 1 major complication (0.6%) and 4 minor bleeding complications (2.2%). The major complication occurred when a patient had to return to surgery from the recovery room for emergent control of bleeding. The surgery was for an in situ cubital tunnel release. The patient, aged 48 years, was taking clopidogrel and aspirin and had a personal and family history of cardiovascular disease. The bleeding was controlled with bipolar cautery and Floseal, a topical haemostatic matrix made of bovine gelatin and human thrombin. The minor bleeding complications were treated in the clinic with compression, wound care, or expedited follow-up for reassurance. These included an in situ cubital tunnel release for a patient taking warfarin and aspirin, a digital inclusion cyst for a patient taking apixaban, an endoscopic carpal tunnel for a patient taking aspirin and clopidogrel, and an open carpal tunnel and ulnar tunnel release for a patient taking aspirin and clopidogrel. There were no thrombotic events during the study.
Discussion
Higher utilization of anticoagulation has been evidenced by a 30% increase in Medicare claims and a 277% increase in Medicaid anticoagulation claims between 2014 and 2019, driven by more prescriptions for direct oral anticoagulants such as apixaban and rivaroxaban.7 The MRVAMC Plastic Surgery Service began a protocol for managing perioperative anticoagulation in 2015 to avoid the risk of perioperative thrombotic events in veteran patients. Patients who choose elective hand surgery were instructed to continue their prescription blood thinners. Exceptions to this protocol were patients scheduled for a partial fasciectomy (for Dupuytren contracture) or cubital tunnel release with anterior ulnar nerve transposition. A hematoma would increase the risk for skin necrosis in the patients receiving a fasciectomy, resulting from the thin skin flaps and meticulous dissection to identify and protect the digital nerves. Worsening nerve dysfunction could result from hematoma compression and scarring in the ulnar nerve cases. If the risk of holding the blood thinner was felt to be unreasonably high, based on recommendations from the patients’ cardiologist or primary care doctor, we offered an in situ cubital tunnel release for the ulnar nerve patients.
Concerns regarding interrupting chronic anticoagulation involve the increased risk of thromboembolism and the theoretical risk of a rebound hypercoagulable effect.8 Patients prescribed warfarin have been found to unintentionally discontinue this medication after outpatient surgery at more than 1.5 times the rate of the general population.9
A systematic review of 9 published studies looking specifically at elective hand and wrist surgeries demonstrated no significant increase in perioperative bleeding risk with the continuation of anticoagulation and antiplatelet medications.10 Sardenberg and colleagues reviewed 7 studies in which 410 hand and wrist surgeries were performed in patients prescribed warfarin or aspirin and clopidogrel. These patients had a 0.7% serious complication rate, requiring surgical treatment only in patients having complex wrist surgeries (wrist arthrodesis with tenosynovectomy, resection of the distal ulna with tenosynovectomy and tendon transfer, and proximal row carpectomy).11 Bogunovic and colleagues compared 50 hand and wrist patients who were on uninterrupted warfarin with those who were not. They required patients to have an
These and our study are consistent with other disciplines, such as facial plastic surgery, dermatology, and ophthalmology, which do not support routine suspension of anticoagulants.13-16 A review of 30 cutaneous surgery studies involving > 14,000 patients recommended meticulous hemostasis over cessation of blood thinners.15 The University of Massachusetts Dermatology Clinic found a 40 times higher rate of bleeding complications in patients on clopidogrel and warfarin but still recommended continuation of these medications to avoid thrombotic events.16
Limitations
This study is a retrospective chart review and limited by what is already documented in the electronic health record. We can verify that the patients were given instructions to continue their medications up to the day of surgery but cannot be certain whether the instructions were followed. No control group was told to hold their anticoagulants for the same surgery. Once we decided on a protocol, we applied it to all patients. The study approval was for the specific time frame when the protocol was in place.
Our study was designed for elective hand cases because those surgeries can be anticipated, predicted, and patients can be given instructions during the preoperative appointments. We did incidentally find several nonelective hand cases (traumas, infections, and cancers) during the review of patients taking prescription blood thinners that had to be expedited to the operating room. Based on morbidity data during that time period, there were no additional postoperative hand surgery bleeding complications that had to return to the operating room. Future studies are indicated, but we believe our protocol can be applied to urgent and emergent hand surgeries as well as elective cases.
Conclusions
Our study supports continuing prescription anticoagulant and antiplatelet medications during the perioperative period for elective hand surgery. We found this is a safe practice in our veteran population with an acceptably low local bleeding complication rate.
Acknowledgments
This manuscript is the result of work supported with the resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
1. Allen AL, Lucas J, Parra D, et al. Shifting the paradigm: a population health approach to the management of direct oral anticoagulants. J Am Heart Assoc. 2021;10(24):e022758. doi:10.1161/JAHA.121.022758
2. Buck J, Kaboli P, Gage BF, Cram P, Vaughan Sarrazin MS. Trends in antithrombotic therapy for atrial fibrillation: data from the Veterans Health Administration health system. Am Heart J. 2016;179:186-191. doi:10.1016/j.ahj.2016.03.029
3. Kinlay S, Young MM, Sherrod R, Gagnon DR. Long-term outcomes and duration of dual antiplatelet therapy after coronary intervention with second-generation drug-eluting stents: the Veterans Affairs Extended DAPT Study. J Am Heart Assoc. 2023;12(2):e027055.
4. Bogunovic L, Gelberman RH, Goldfarb CA, Boyer MI, Calfee RP. The impact of antiplatelet medication on hand and wrist surgery. J Hand Surg Am. 2013;38(6):1063-1070. doi:10.1016/j.jhsa.2013.03.034
5. Wallace DL, Latimer MD, Belcher HJ. Stopping warfarin therapy is unnecessary for hand surgery. J Hand Surg Br. 2004;29(3):203-205. doi:10.1016/j.jhsb.2003.12.008
6. Edmunds I, Avakian Z. Hand surgery on anticoagulated patients: a prospective study of 121 operations. Hand Surg. 2010;15(2):109-113. doi:10.1142/S021881041000468
7. Duvalyan A, Pandey A, Vaduganathan M, et al. Trends in anticoagulation prescription spending among Medicare Part D and Medicaid beneficiaries between 2014 and 2019. J Am Heart Assoc. 2021;10(24):e022644. doi:10.1161/JAHA.121.022644
8. Thakur NA, Czerwein JK, Butera JN, Palumbo MA. Perioperative management of chronic anticoagulation in orthopaedic surgery. J Am Acad Orthop Surg. 2010;18(12):729-738. doi:10.5435/00124635-201012000-00003
9. Bell C, Bajca J, Bierman A, Li P, Mamdani M, Urbach D. Potentially unintended discontinuation of long-term medication use after elective surgical procedures. Arch Int Med. 2003;166(22):2525-2531.
10. Stone MJ, Wilks DJ, Wade RG. Hand and wrist surgery on anticoagulants and antiplatelets: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2020;73(8):1413-1423.
11. Sardenberg T, Deienno FS, Miranda RF, et al. Hand and wrist surgery without suspending warfarin or oral antiplatelet - systematic review. Rev Bras Ortop. 2017;52(4):390-395. doi:10.1016/j.rboe.2017.07.001
12. Bogunovic L, Gelberman RH, Goldfarb CA, Boyer MI, Calfee RP. The impact of uninterrupted warfarin on hand and wrist surgery. J Hand Surg Am. 2015;40(11):2133-2140. doi:10.1016/j.jhsa.2015.07.037
13. Kraft CT, Bellile E, Baker SR, Kim JC, Moyer JS. Anticoagulant complications in facial plastic and reconstructive surgery. JAMA Facial Plast Surg. 2015;17(2):103-107. doi:10.1001/jamafacial.2014.1147
14. He X, Chen AF, Nirwan RS, Sridhar J, Kuriyan AE. Perioperative management of anticoagulants in ocular surgeries. Int Ophthalmol Clin. 2020;60(3):3-15. doi:10.1097/IIO.0000000000000316
15. Isted A, Cooper L, Colville RJ. Bleeding on the cutting edge: a systematic review of anticoagulant and antiplatelet continuation in minor cutaneous surgery. J Plast Reconstr Aesthet Surg. 2018;71(4):455-467. doi:10.1016/j.bjps.2017.11.024
16. Bordeaux JS, Martires KJ, Goldberg D, Pattee SF, Fu P, Maloney ME. Prospective evaluation of dermatologic surgery complications including patients on multiple antiplatelet and anticoagulant medications. J Am Acad Dermatol. 2011;65(3):576-583. doi:10.1016/j.jaad.2011.02.012
1. Allen AL, Lucas J, Parra D, et al. Shifting the paradigm: a population health approach to the management of direct oral anticoagulants. J Am Heart Assoc. 2021;10(24):e022758. doi:10.1161/JAHA.121.022758
2. Buck J, Kaboli P, Gage BF, Cram P, Vaughan Sarrazin MS. Trends in antithrombotic therapy for atrial fibrillation: data from the Veterans Health Administration health system. Am Heart J. 2016;179:186-191. doi:10.1016/j.ahj.2016.03.029
3. Kinlay S, Young MM, Sherrod R, Gagnon DR. Long-term outcomes and duration of dual antiplatelet therapy after coronary intervention with second-generation drug-eluting stents: the Veterans Affairs Extended DAPT Study. J Am Heart Assoc. 2023;12(2):e027055.
4. Bogunovic L, Gelberman RH, Goldfarb CA, Boyer MI, Calfee RP. The impact of antiplatelet medication on hand and wrist surgery. J Hand Surg Am. 2013;38(6):1063-1070. doi:10.1016/j.jhsa.2013.03.034
5. Wallace DL, Latimer MD, Belcher HJ. Stopping warfarin therapy is unnecessary for hand surgery. J Hand Surg Br. 2004;29(3):203-205. doi:10.1016/j.jhsb.2003.12.008
6. Edmunds I, Avakian Z. Hand surgery on anticoagulated patients: a prospective study of 121 operations. Hand Surg. 2010;15(2):109-113. doi:10.1142/S021881041000468
7. Duvalyan A, Pandey A, Vaduganathan M, et al. Trends in anticoagulation prescription spending among Medicare Part D and Medicaid beneficiaries between 2014 and 2019. J Am Heart Assoc. 2021;10(24):e022644. doi:10.1161/JAHA.121.022644
8. Thakur NA, Czerwein JK, Butera JN, Palumbo MA. Perioperative management of chronic anticoagulation in orthopaedic surgery. J Am Acad Orthop Surg. 2010;18(12):729-738. doi:10.5435/00124635-201012000-00003
9. Bell C, Bajca J, Bierman A, Li P, Mamdani M, Urbach D. Potentially unintended discontinuation of long-term medication use after elective surgical procedures. Arch Int Med. 2003;166(22):2525-2531.
10. Stone MJ, Wilks DJ, Wade RG. Hand and wrist surgery on anticoagulants and antiplatelets: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2020;73(8):1413-1423.
11. Sardenberg T, Deienno FS, Miranda RF, et al. Hand and wrist surgery without suspending warfarin or oral antiplatelet - systematic review. Rev Bras Ortop. 2017;52(4):390-395. doi:10.1016/j.rboe.2017.07.001
12. Bogunovic L, Gelberman RH, Goldfarb CA, Boyer MI, Calfee RP. The impact of uninterrupted warfarin on hand and wrist surgery. J Hand Surg Am. 2015;40(11):2133-2140. doi:10.1016/j.jhsa.2015.07.037
13. Kraft CT, Bellile E, Baker SR, Kim JC, Moyer JS. Anticoagulant complications in facial plastic and reconstructive surgery. JAMA Facial Plast Surg. 2015;17(2):103-107. doi:10.1001/jamafacial.2014.1147
14. He X, Chen AF, Nirwan RS, Sridhar J, Kuriyan AE. Perioperative management of anticoagulants in ocular surgeries. Int Ophthalmol Clin. 2020;60(3):3-15. doi:10.1097/IIO.0000000000000316
15. Isted A, Cooper L, Colville RJ. Bleeding on the cutting edge: a systematic review of anticoagulant and antiplatelet continuation in minor cutaneous surgery. J Plast Reconstr Aesthet Surg. 2018;71(4):455-467. doi:10.1016/j.bjps.2017.11.024
16. Bordeaux JS, Martires KJ, Goldberg D, Pattee SF, Fu P, Maloney ME. Prospective evaluation of dermatologic surgery complications including patients on multiple antiplatelet and anticoagulant medications. J Am Acad Dermatol. 2011;65(3):576-583. doi:10.1016/j.jaad.2011.02.012
Twenty Years of Breast Reduction Surgery at a Veterans Affairs Medical Center
Women make up an estimated 10% of the veteran population.1 The US Department of Veterans Affairs (VA) projected that there would be an increase of 18,000 female veterans per year for 10 years based on 2015 data. The number of women veterans enrolled in the VA health care increased from 397,024 to 729,989 (83.9%) between 2005 and 2015.2 This rise in the number of enrolled women veterans also increased the demand for female-specific health care services, such as breast reduction surgery, a reconstructive procedure provided at the Malcom Randall VA Medical Center (MRVAMC) federal teaching hospital in Gainesville, Florida.
Patients who experience symptomatic macromastia will report a history of neck and shoulder pain, shoulder grooving from bra straps, inframammary intertrigo, difficulty finding clothes that fit, and discomfort participating in sports. For the treatment of symptomatic macromastia, patients report a high satisfaction rate after breast reduction surgery.3-5 Unfortunately, the complications from the surgery can significantly disrupt a woman’s life due to previously unplanned hospital admissions, clinic appointments, wound care, time off work, and poor aesthetic outcome. Faculty awareness of a large number of complications for patients after breast reduction surgery prompted the MRVAMC Plastic Surgery Service to establish a stricter surgical screening protocol using body mass index (BMI) values and negative nicotine status to help patients be healthier and reduce the potential risk before offering surgery. A medical literature search did not find an existing study on veteran-specific breast reduction surgery.
Methods
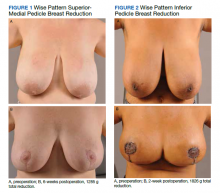
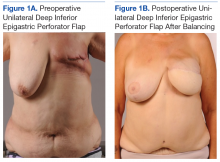
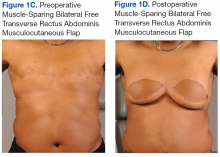
The University of Florida and North Florida/South Georgia Veterans Health System Institutional Review Board approved a retrospective chart review of all breast reduction surgeries performed at MRVAMC over a 20-year period (July 1, 2000-June 30, 2020). Electronic health records were queried for all primary bilateral breast reduction surgeries performed for symptomatic macromastia using Current Procedural Terminology code 19318. Potentially modifiable or predictable risk factors for wound complications were recorded: nicotine status, BMI, diabetes mellitus (DM) status, skin incision pattern, and pedicle location. Skin incision patterns were either vertical (periareolar plus a vertical scar from the areola to the inframammary fold) or traditional Wise pattern (also known as anchor pattern: periareolar scar, vertical scar to inframammary fold, plus a horizontal scar along the inframammary fold) as seen in Figures 1 and 2. The pedicle is the source of blood supply to the nipple, which was documented as either from the inferior aspect or the superior or superior/medial aspect.
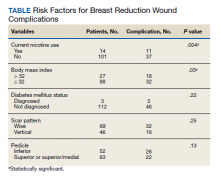
For this study, the blood supply from the superior and superior/medial was logged in the same category. Records were reviewed 3 months after surgery for documentation of local wound complications, such as hematoma, infection, wound breakdown, skin necrosis, and nipple necrosis. Major complications were defined as requiring an unplanned hospital admission or urgent return to the operating room. A χ2 test using a P value of < .05 was used to determine statistical significance between the incidence of wound complications and the individually identifiable variables.
Results
One hundred fifteen bilateral breast reduction surgeries were performed at MRVAMC over a 20-year period. Patient median age was 43 years. Median combined specimen weight was 1272 g. Forty-eight (41.7%) wound complications were documented, including 8 (7%) major complications. Most complications were identified in the first 7 years of the study before the new protocol and consult template became active. The new template resulted in the local complication rate dropping from 62% (July 2000-June 2007) to 26% (July 2007-June 2020). BMI > 32 (P = .03) and active nicotine use (P = .004) were found to be statistically significant independent risk factors for wound complications. Median BMI for all patients was 30. DM status (P = .22), skin incision pattern (P = .25), and pedicle location (P = .13) were not found to be predictors of wound complications (Table). There was no significant change in the incidence of major complications before and after the new protocols were enforced.
Discussion
Breast reduction surgery is an elective reconstructive option to treat symptomatic macromastia. There are several accepted ways to do the reduction surgical procedure where the blood supply (pedicle) to the nipple can vary and the visible scars can be in a horizontal, vertical, or Wise pattern. Technique is usually based on surgeon training, comfort, and preference. There are several known complications specific to this operation that include asymmetry, changes in nipple sensation, unattractive scars, diminished ability to breastfeed, and wound complications.5-7 Wound complications include seroma, hematoma, dehiscence, infection, wound breakdown, skin necrosis, and nipple necrosis.
This study focused on wound complications with the objective of identifying and modifying risk factors. Two known risk factors documented in the literature, nicotine use and obesity, already had been addressed by our service, and results were known anecdotally but had not been previously verified. This study also looked at other potential risk factors, including the pedicle location, skin incision, and DM status.
Residents or fellows participated in all the surgeries. An outcome analysis from The American College of Surgeons National Surgical Quality Improvement Program database from 2005 to 2011 found that resident participation was associated with morbidity, including wound complications.8 This study was performed at a federal hospital with a complexity level 1a rating, which is designated based on the highest level of patient volume, risk, teaching, research, intensive care unit beds, and specialty services.9 The hospital is closely affiliated with a level 1 trauma center and teaching hospital; therefore, resident and fellow participation is not a modifiable risk factor.
This study did not find an increased risk of wound complications in patients with DM, which has been found to be an independent risk factor in a prior study.10 DM status was indicated in only 3 histories, and they all had perioperative hemoglobin A1c levels < 8%. There is documentation of patients receiving perioperative antibiotics in 99 out of 116 of the surgical records; however, we did not include this in the analysis because the operative reports from the first year of the study were incomplete.
Smoking is a known risk factor for local wound complications in breast reduction surgery.10-15 The VA has a smoking cessation program through its mental health service that provides counseling and medication treatment options, including nicotine replacement, bupropion, and varenicline. We require patients to be at least 4 weeks nicotine free before surgery, which has been previously recommended in the literature.16
Existing studies that compare the traditional Wise pattern/inferior pedicle with vertical pattern/superior medial pedicle did not find an increased risk of wound complications.17-19 Our study separated the different incisions from the pedicle because the surgical technique among the different surgeons in the study varied, where sometimes the traditional Wise pattern was combined with the less traditional superior-medial pedicle. We did not find a statistical difference when comparing the incisions and pedicle location, which suggests that the incision type and source of blood supply to the nipple are not the determining factors for wound complications in the early postoperative period.
Obesity is a known risk factor for local wound complications.12,13,15,20-22 Studies have shown that patients who are obese benefit from breast reduction surgery; authors have argued against restricting surgery to these higher risk patients.4,23-25 Patients usually report decades of macromastia symptoms at consultation; so, we believe delaying the surgical procedure to get patients to a safer risk profile is in their best interest. We chose a cutoff BMI of 32 as a realistic value rather than 30, which is considered the definition of obesity. Patients at MRVAMC have access to MOVE!, a weight loss management program through primary care. We believe in being reasonable; so if a patient makes a significant improvement in her health but falls short of the required cutoff, we will still consider offering the surgical procedure after a full explanation of the surgical risks.
Wound complications, especially those that require admission or frequent appointments can seriously disrupt a patient’s life, creating unnecessary hardships and expense in time lost from work, travel, and child care. MRVAMC has a catchment area the size of North Carolina; so many of our patients travel hours for their appointments. The added scars and deformity from wound dehiscence and debridement can lead to asymmetry, widened scars, and future revision operations. Multiple clinic appointments for wound care not only impact that individual patient, but also has the effect of limiting access for all patients in a health care environment with high patient volume and limited providers, operating room time, and clinic appointments. As a result, minimizing predictable wound complications benefits the entire system.
Limitations and Strengths
This retrospective review comprised multiple different surgeons, including faculty and trainees, who were involved in the consultation, surgery, and postoperative care of the patients over a 20-year period; therefore, consistency in documentation is lacking. In addition, we were limited to only the information available on the charts. For example, wound size and laterality were not consistently documented. The MRVAMC complication rate was consistent with the current literature (range, 14-52%).12,18,20,24
The major strength of the study is that the veterans tend to stay within the VA, which makes complications easier to identify and follow. Patients who do not present initially to their surgeon due to travel limitations will typically contact their primary care provider or present to their local VA urgent care or emergency department provider, who will route the patient back to the surgical specialty service through the electronic health record.
Conclusions
Breast reduction surgery has a high wound complication rate, which can be predicted and improved on so that patients can receive their indicated surgical procedure with minimal inconvenience and downtime. This review confirms that preoperative weight loss and nicotine cessation were the appropriate focus of the MRVAMC plastic surgery service’s efforts to achieve a safer surgical experience. We will continue to enforce our protocol and encourage patients who are interested in breast reduction surgery and fall outside the requirements to work with their primary care provider on smoking cessation and weight loss through better nutrition and physical activity.
Acknowledgment
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
1. US Department of Veterans Affairs. Statistics at a glance. Published February 2020. Accessed June 18, 2021. https://www.va.gov/vetdata/docs/Quickfacts/Homepage_slideshow_4_6_20.PDF
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed June 18, 2020. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Crittenden TA, Watson DI, Ratcliffe J, Griffin PA, Dean NR. Outcomes of breast reduction surgery using the breast-q: a prospective study and comparison with normative data. Plast Reconstr Surg. 2019;144(5):1034-1044. doi:10.1097/PRS.0000000000006114
4. Thoma A, Sprague S, Veltri K, Duku E, Furlong W. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg. 2007;120(1):13-26. doi:10.1097/01.prs.0000263370.94191.90
5. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and quality of life following reduction mammaplasty in adolescents and young women.Plast Reconstr Surg. 2019;144(3):572-581. doi:10.1097/PRS.0000000000005907
6. Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136(4):531e-544e. doi:10.1097/PRS.0000000000001622
7. Kraut RY, Brown E, Korownyk C, et al. The impact of breast reduction surgery on breastfeeding: systematic review of observational studies. PLoS One. 2017;12(10):e0186591. doi:10.1371/journal.pone.0186591
8. Fischer JP, Wes AM, Kovach SJ. The impact of surgical resident participation in breast reduction surgery--outcome analysis from the 2005-2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):315-321. doi:10.3109/2000656X.2014.882345
9. Site Facility Name and Complexity Summary of VHA Facility. Accessed June 18, 2021. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=2793591&FileName=VA118-16-R-1059-A00002002.docx
10. Lewin R, Göransson M, Elander A, Thorarinsson A, Lundberg J, Lidén M. Risk factors for complications after breast reduction surgery. J Plast Surg Hand Surg. 2014;48(1):10-14. doi:10.3109/2000656X.2013.791625
11. Cunningham BL, Gear AJ, Kerrigan CL, Collins ED. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115(6):1597-1604. doi:10.1097/01.prs.0000160695.33457.db
12. Karamanos E, Wei B, Siddiqui A, Rubinfeld I. Tobacco use and body mass index as predictors of outcomes in patients undergoing breast reduction mammoplasty. Ann Plast Surg. 2015;75(4):383-387. doi:10.1097/SAP.0000000000000192
13. Manahan MA, Buretta KJ, Chang D, Mithani SK, Mallalieu J, Shermak MA. An outcomes analysis of 2142 breast reduction procedures. Ann Plast Surg. 2015;74(3):289-292. doi:10.1097/SAP.0b013e31829d2261
14. Hillam JS, Borsting EA, Chim JH, Thaller SR. Smoking as a risk factor for breast reduction: an analysis of 13,503 cases. J Plast Reconstr Aesthet Surg. 2017;70(6):734-740. doi:10.1016/j.bjps.2016.12.012
15. Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: a meta-analysis. PLoS One. 2016;11(12):e0167746. doi:10.1371/journal.pone.0167746
16. Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069-1079.doi:10.1097/SLA.0b013e31824f632d
17. Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle Wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg. 2013;132(5):1068-1076. doi:10.1097/PRS.0b013e3182a48b2d
18. Hunter-Smith DJ, Smoll NR, Marne B, Maung H, Findlay MW. Comparing breast-reduction techniques: time-to-event analysis and recommendations. Aesthetic Plast Surg. 2012;36(3):600-606. doi:10.1007/s00266-011-9860-3
19. Ogunleye AA, Leroux O, Morrison N, Preminger AB. Complications after reduction mammaplasty: a comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg. 2017;79(1):13-16. doi:10.1097/SAP.0000000000001059
20. Bauermeister AJ, Gill K, Zuriarrain A, Earle SA, Newman MI. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72(3):410-418. doi:10.1016/j.bjps.2018.12.004
21. Nelson JA, Fischer JP, Chung CU, et al. Obesity and early complications following reduction mammaplasty: an analysis of 4545 patients from the 2005-2011 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):334-339. doi:10.3109/2000656X.2014.886582
22. Kreithen J, Caffee H, Rosenberg J, et al. A comparison of the LeJour and Wise pattern methods of breast reduction. Ann Plast Surg. 2005;54(3):236-241. doi:10.3109/2000656X.2014.886582
23. Güemes A, Pérez E, Sousa R, et al. Quality of life and alleviation of symptoms after breast reduction for macromastia in obese patients: is surgery worth it? Aesthetic Plast Surg. 2016;40(1):62-70. doi:10.1007/s00266-015-0601-x
24. Setälä L, Papp A, Joukainen S, et al. Obesity and complications in breast reduction surgery: are restrictions justified? J Plast Reconstr Aesthet Surg. 2009;62(2):195-199. doi:10.1016/j.bjps.2007.10.043
25. Shah R, Al-Ajam Y, Stott D, Kang N. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthet Surg. 2011;64(4):508-514. doi:10.1016/j.bjps.2007.10.043
Women make up an estimated 10% of the veteran population.1 The US Department of Veterans Affairs (VA) projected that there would be an increase of 18,000 female veterans per year for 10 years based on 2015 data. The number of women veterans enrolled in the VA health care increased from 397,024 to 729,989 (83.9%) between 2005 and 2015.2 This rise in the number of enrolled women veterans also increased the demand for female-specific health care services, such as breast reduction surgery, a reconstructive procedure provided at the Malcom Randall VA Medical Center (MRVAMC) federal teaching hospital in Gainesville, Florida.
Patients who experience symptomatic macromastia will report a history of neck and shoulder pain, shoulder grooving from bra straps, inframammary intertrigo, difficulty finding clothes that fit, and discomfort participating in sports. For the treatment of symptomatic macromastia, patients report a high satisfaction rate after breast reduction surgery.3-5 Unfortunately, the complications from the surgery can significantly disrupt a woman’s life due to previously unplanned hospital admissions, clinic appointments, wound care, time off work, and poor aesthetic outcome. Faculty awareness of a large number of complications for patients after breast reduction surgery prompted the MRVAMC Plastic Surgery Service to establish a stricter surgical screening protocol using body mass index (BMI) values and negative nicotine status to help patients be healthier and reduce the potential risk before offering surgery. A medical literature search did not find an existing study on veteran-specific breast reduction surgery.
Methods
The University of Florida and North Florida/South Georgia Veterans Health System Institutional Review Board approved a retrospective chart review of all breast reduction surgeries performed at MRVAMC over a 20-year period (July 1, 2000-June 30, 2020). Electronic health records were queried for all primary bilateral breast reduction surgeries performed for symptomatic macromastia using Current Procedural Terminology code 19318. Potentially modifiable or predictable risk factors for wound complications were recorded: nicotine status, BMI, diabetes mellitus (DM) status, skin incision pattern, and pedicle location. Skin incision patterns were either vertical (periareolar plus a vertical scar from the areola to the inframammary fold) or traditional Wise pattern (also known as anchor pattern: periareolar scar, vertical scar to inframammary fold, plus a horizontal scar along the inframammary fold) as seen in Figures 1 and 2. The pedicle is the source of blood supply to the nipple, which was documented as either from the inferior aspect or the superior or superior/medial aspect.
For this study, the blood supply from the superior and superior/medial was logged in the same category. Records were reviewed 3 months after surgery for documentation of local wound complications, such as hematoma, infection, wound breakdown, skin necrosis, and nipple necrosis. Major complications were defined as requiring an unplanned hospital admission or urgent return to the operating room. A χ2 test using a P value of < .05 was used to determine statistical significance between the incidence of wound complications and the individually identifiable variables.
Results
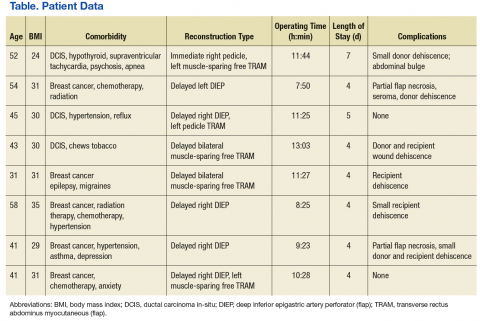
One hundred fifteen bilateral breast reduction surgeries were performed at MRVAMC over a 20-year period. Patient median age was 43 years. Median combined specimen weight was 1272 g. Forty-eight (41.7%) wound complications were documented, including 8 (7%) major complications. Most complications were identified in the first 7 years of the study before the new protocol and consult template became active. The new template resulted in the local complication rate dropping from 62% (July 2000-June 2007) to 26% (July 2007-June 2020). BMI > 32 (P = .03) and active nicotine use (P = .004) were found to be statistically significant independent risk factors for wound complications. Median BMI for all patients was 30. DM status (P = .22), skin incision pattern (P = .25), and pedicle location (P = .13) were not found to be predictors of wound complications (Table). There was no significant change in the incidence of major complications before and after the new protocols were enforced.
Discussion
Breast reduction surgery is an elective reconstructive option to treat symptomatic macromastia. There are several accepted ways to do the reduction surgical procedure where the blood supply (pedicle) to the nipple can vary and the visible scars can be in a horizontal, vertical, or Wise pattern. Technique is usually based on surgeon training, comfort, and preference. There are several known complications specific to this operation that include asymmetry, changes in nipple sensation, unattractive scars, diminished ability to breastfeed, and wound complications.5-7 Wound complications include seroma, hematoma, dehiscence, infection, wound breakdown, skin necrosis, and nipple necrosis.
This study focused on wound complications with the objective of identifying and modifying risk factors. Two known risk factors documented in the literature, nicotine use and obesity, already had been addressed by our service, and results were known anecdotally but had not been previously verified. This study also looked at other potential risk factors, including the pedicle location, skin incision, and DM status.
Residents or fellows participated in all the surgeries. An outcome analysis from The American College of Surgeons National Surgical Quality Improvement Program database from 2005 to 2011 found that resident participation was associated with morbidity, including wound complications.8 This study was performed at a federal hospital with a complexity level 1a rating, which is designated based on the highest level of patient volume, risk, teaching, research, intensive care unit beds, and specialty services.9 The hospital is closely affiliated with a level 1 trauma center and teaching hospital; therefore, resident and fellow participation is not a modifiable risk factor.
This study did not find an increased risk of wound complications in patients with DM, which has been found to be an independent risk factor in a prior study.10 DM status was indicated in only 3 histories, and they all had perioperative hemoglobin A1c levels < 8%. There is documentation of patients receiving perioperative antibiotics in 99 out of 116 of the surgical records; however, we did not include this in the analysis because the operative reports from the first year of the study were incomplete.
Smoking is a known risk factor for local wound complications in breast reduction surgery.10-15 The VA has a smoking cessation program through its mental health service that provides counseling and medication treatment options, including nicotine replacement, bupropion, and varenicline. We require patients to be at least 4 weeks nicotine free before surgery, which has been previously recommended in the literature.16
Existing studies that compare the traditional Wise pattern/inferior pedicle with vertical pattern/superior medial pedicle did not find an increased risk of wound complications.17-19 Our study separated the different incisions from the pedicle because the surgical technique among the different surgeons in the study varied, where sometimes the traditional Wise pattern was combined with the less traditional superior-medial pedicle. We did not find a statistical difference when comparing the incisions and pedicle location, which suggests that the incision type and source of blood supply to the nipple are not the determining factors for wound complications in the early postoperative period.
Obesity is a known risk factor for local wound complications.12,13,15,20-22 Studies have shown that patients who are obese benefit from breast reduction surgery; authors have argued against restricting surgery to these higher risk patients.4,23-25 Patients usually report decades of macromastia symptoms at consultation; so, we believe delaying the surgical procedure to get patients to a safer risk profile is in their best interest. We chose a cutoff BMI of 32 as a realistic value rather than 30, which is considered the definition of obesity. Patients at MRVAMC have access to MOVE!, a weight loss management program through primary care. We believe in being reasonable; so if a patient makes a significant improvement in her health but falls short of the required cutoff, we will still consider offering the surgical procedure after a full explanation of the surgical risks.
Wound complications, especially those that require admission or frequent appointments can seriously disrupt a patient’s life, creating unnecessary hardships and expense in time lost from work, travel, and child care. MRVAMC has a catchment area the size of North Carolina; so many of our patients travel hours for their appointments. The added scars and deformity from wound dehiscence and debridement can lead to asymmetry, widened scars, and future revision operations. Multiple clinic appointments for wound care not only impact that individual patient, but also has the effect of limiting access for all patients in a health care environment with high patient volume and limited providers, operating room time, and clinic appointments. As a result, minimizing predictable wound complications benefits the entire system.
Limitations and Strengths
This retrospective review comprised multiple different surgeons, including faculty and trainees, who were involved in the consultation, surgery, and postoperative care of the patients over a 20-year period; therefore, consistency in documentation is lacking. In addition, we were limited to only the information available on the charts. For example, wound size and laterality were not consistently documented. The MRVAMC complication rate was consistent with the current literature (range, 14-52%).12,18,20,24
The major strength of the study is that the veterans tend to stay within the VA, which makes complications easier to identify and follow. Patients who do not present initially to their surgeon due to travel limitations will typically contact their primary care provider or present to their local VA urgent care or emergency department provider, who will route the patient back to the surgical specialty service through the electronic health record.
Conclusions
Breast reduction surgery has a high wound complication rate, which can be predicted and improved on so that patients can receive their indicated surgical procedure with minimal inconvenience and downtime. This review confirms that preoperative weight loss and nicotine cessation were the appropriate focus of the MRVAMC plastic surgery service’s efforts to achieve a safer surgical experience. We will continue to enforce our protocol and encourage patients who are interested in breast reduction surgery and fall outside the requirements to work with their primary care provider on smoking cessation and weight loss through better nutrition and physical activity.
Acknowledgment
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
Women make up an estimated 10% of the veteran population.1 The US Department of Veterans Affairs (VA) projected that there would be an increase of 18,000 female veterans per year for 10 years based on 2015 data. The number of women veterans enrolled in the VA health care increased from 397,024 to 729,989 (83.9%) between 2005 and 2015.2 This rise in the number of enrolled women veterans also increased the demand for female-specific health care services, such as breast reduction surgery, a reconstructive procedure provided at the Malcom Randall VA Medical Center (MRVAMC) federal teaching hospital in Gainesville, Florida.
Patients who experience symptomatic macromastia will report a history of neck and shoulder pain, shoulder grooving from bra straps, inframammary intertrigo, difficulty finding clothes that fit, and discomfort participating in sports. For the treatment of symptomatic macromastia, patients report a high satisfaction rate after breast reduction surgery.3-5 Unfortunately, the complications from the surgery can significantly disrupt a woman’s life due to previously unplanned hospital admissions, clinic appointments, wound care, time off work, and poor aesthetic outcome. Faculty awareness of a large number of complications for patients after breast reduction surgery prompted the MRVAMC Plastic Surgery Service to establish a stricter surgical screening protocol using body mass index (BMI) values and negative nicotine status to help patients be healthier and reduce the potential risk before offering surgery. A medical literature search did not find an existing study on veteran-specific breast reduction surgery.
Methods
The University of Florida and North Florida/South Georgia Veterans Health System Institutional Review Board approved a retrospective chart review of all breast reduction surgeries performed at MRVAMC over a 20-year period (July 1, 2000-June 30, 2020). Electronic health records were queried for all primary bilateral breast reduction surgeries performed for symptomatic macromastia using Current Procedural Terminology code 19318. Potentially modifiable or predictable risk factors for wound complications were recorded: nicotine status, BMI, diabetes mellitus (DM) status, skin incision pattern, and pedicle location. Skin incision patterns were either vertical (periareolar plus a vertical scar from the areola to the inframammary fold) or traditional Wise pattern (also known as anchor pattern: periareolar scar, vertical scar to inframammary fold, plus a horizontal scar along the inframammary fold) as seen in Figures 1 and 2. The pedicle is the source of blood supply to the nipple, which was documented as either from the inferior aspect or the superior or superior/medial aspect.
For this study, the blood supply from the superior and superior/medial was logged in the same category. Records were reviewed 3 months after surgery for documentation of local wound complications, such as hematoma, infection, wound breakdown, skin necrosis, and nipple necrosis. Major complications were defined as requiring an unplanned hospital admission or urgent return to the operating room. A χ2 test using a P value of < .05 was used to determine statistical significance between the incidence of wound complications and the individually identifiable variables.
Results
One hundred fifteen bilateral breast reduction surgeries were performed at MRVAMC over a 20-year period. Patient median age was 43 years. Median combined specimen weight was 1272 g. Forty-eight (41.7%) wound complications were documented, including 8 (7%) major complications. Most complications were identified in the first 7 years of the study before the new protocol and consult template became active. The new template resulted in the local complication rate dropping from 62% (July 2000-June 2007) to 26% (July 2007-June 2020). BMI > 32 (P = .03) and active nicotine use (P = .004) were found to be statistically significant independent risk factors for wound complications. Median BMI for all patients was 30. DM status (P = .22), skin incision pattern (P = .25), and pedicle location (P = .13) were not found to be predictors of wound complications (Table). There was no significant change in the incidence of major complications before and after the new protocols were enforced.
Discussion
Breast reduction surgery is an elective reconstructive option to treat symptomatic macromastia. There are several accepted ways to do the reduction surgical procedure where the blood supply (pedicle) to the nipple can vary and the visible scars can be in a horizontal, vertical, or Wise pattern. Technique is usually based on surgeon training, comfort, and preference. There are several known complications specific to this operation that include asymmetry, changes in nipple sensation, unattractive scars, diminished ability to breastfeed, and wound complications.5-7 Wound complications include seroma, hematoma, dehiscence, infection, wound breakdown, skin necrosis, and nipple necrosis.
This study focused on wound complications with the objective of identifying and modifying risk factors. Two known risk factors documented in the literature, nicotine use and obesity, already had been addressed by our service, and results were known anecdotally but had not been previously verified. This study also looked at other potential risk factors, including the pedicle location, skin incision, and DM status.
Residents or fellows participated in all the surgeries. An outcome analysis from The American College of Surgeons National Surgical Quality Improvement Program database from 2005 to 2011 found that resident participation was associated with morbidity, including wound complications.8 This study was performed at a federal hospital with a complexity level 1a rating, which is designated based on the highest level of patient volume, risk, teaching, research, intensive care unit beds, and specialty services.9 The hospital is closely affiliated with a level 1 trauma center and teaching hospital; therefore, resident and fellow participation is not a modifiable risk factor.
This study did not find an increased risk of wound complications in patients with DM, which has been found to be an independent risk factor in a prior study.10 DM status was indicated in only 3 histories, and they all had perioperative hemoglobin A1c levels < 8%. There is documentation of patients receiving perioperative antibiotics in 99 out of 116 of the surgical records; however, we did not include this in the analysis because the operative reports from the first year of the study were incomplete.
Smoking is a known risk factor for local wound complications in breast reduction surgery.10-15 The VA has a smoking cessation program through its mental health service that provides counseling and medication treatment options, including nicotine replacement, bupropion, and varenicline. We require patients to be at least 4 weeks nicotine free before surgery, which has been previously recommended in the literature.16
Existing studies that compare the traditional Wise pattern/inferior pedicle with vertical pattern/superior medial pedicle did not find an increased risk of wound complications.17-19 Our study separated the different incisions from the pedicle because the surgical technique among the different surgeons in the study varied, where sometimes the traditional Wise pattern was combined with the less traditional superior-medial pedicle. We did not find a statistical difference when comparing the incisions and pedicle location, which suggests that the incision type and source of blood supply to the nipple are not the determining factors for wound complications in the early postoperative period.
Obesity is a known risk factor for local wound complications.12,13,15,20-22 Studies have shown that patients who are obese benefit from breast reduction surgery; authors have argued against restricting surgery to these higher risk patients.4,23-25 Patients usually report decades of macromastia symptoms at consultation; so, we believe delaying the surgical procedure to get patients to a safer risk profile is in their best interest. We chose a cutoff BMI of 32 as a realistic value rather than 30, which is considered the definition of obesity. Patients at MRVAMC have access to MOVE!, a weight loss management program through primary care. We believe in being reasonable; so if a patient makes a significant improvement in her health but falls short of the required cutoff, we will still consider offering the surgical procedure after a full explanation of the surgical risks.
Wound complications, especially those that require admission or frequent appointments can seriously disrupt a patient’s life, creating unnecessary hardships and expense in time lost from work, travel, and child care. MRVAMC has a catchment area the size of North Carolina; so many of our patients travel hours for their appointments. The added scars and deformity from wound dehiscence and debridement can lead to asymmetry, widened scars, and future revision operations. Multiple clinic appointments for wound care not only impact that individual patient, but also has the effect of limiting access for all patients in a health care environment with high patient volume and limited providers, operating room time, and clinic appointments. As a result, minimizing predictable wound complications benefits the entire system.
Limitations and Strengths
This retrospective review comprised multiple different surgeons, including faculty and trainees, who were involved in the consultation, surgery, and postoperative care of the patients over a 20-year period; therefore, consistency in documentation is lacking. In addition, we were limited to only the information available on the charts. For example, wound size and laterality were not consistently documented. The MRVAMC complication rate was consistent with the current literature (range, 14-52%).12,18,20,24
The major strength of the study is that the veterans tend to stay within the VA, which makes complications easier to identify and follow. Patients who do not present initially to their surgeon due to travel limitations will typically contact their primary care provider or present to their local VA urgent care or emergency department provider, who will route the patient back to the surgical specialty service through the electronic health record.
Conclusions
Breast reduction surgery has a high wound complication rate, which can be predicted and improved on so that patients can receive their indicated surgical procedure with minimal inconvenience and downtime. This review confirms that preoperative weight loss and nicotine cessation were the appropriate focus of the MRVAMC plastic surgery service’s efforts to achieve a safer surgical experience. We will continue to enforce our protocol and encourage patients who are interested in breast reduction surgery and fall outside the requirements to work with their primary care provider on smoking cessation and weight loss through better nutrition and physical activity.
Acknowledgment
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
1. US Department of Veterans Affairs. Statistics at a glance. Published February 2020. Accessed June 18, 2021. https://www.va.gov/vetdata/docs/Quickfacts/Homepage_slideshow_4_6_20.PDF
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed June 18, 2020. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Crittenden TA, Watson DI, Ratcliffe J, Griffin PA, Dean NR. Outcomes of breast reduction surgery using the breast-q: a prospective study and comparison with normative data. Plast Reconstr Surg. 2019;144(5):1034-1044. doi:10.1097/PRS.0000000000006114
4. Thoma A, Sprague S, Veltri K, Duku E, Furlong W. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg. 2007;120(1):13-26. doi:10.1097/01.prs.0000263370.94191.90
5. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and quality of life following reduction mammaplasty in adolescents and young women.Plast Reconstr Surg. 2019;144(3):572-581. doi:10.1097/PRS.0000000000005907
6. Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136(4):531e-544e. doi:10.1097/PRS.0000000000001622
7. Kraut RY, Brown E, Korownyk C, et al. The impact of breast reduction surgery on breastfeeding: systematic review of observational studies. PLoS One. 2017;12(10):e0186591. doi:10.1371/journal.pone.0186591
8. Fischer JP, Wes AM, Kovach SJ. The impact of surgical resident participation in breast reduction surgery--outcome analysis from the 2005-2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):315-321. doi:10.3109/2000656X.2014.882345
9. Site Facility Name and Complexity Summary of VHA Facility. Accessed June 18, 2021. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=2793591&FileName=VA118-16-R-1059-A00002002.docx
10. Lewin R, Göransson M, Elander A, Thorarinsson A, Lundberg J, Lidén M. Risk factors for complications after breast reduction surgery. J Plast Surg Hand Surg. 2014;48(1):10-14. doi:10.3109/2000656X.2013.791625
11. Cunningham BL, Gear AJ, Kerrigan CL, Collins ED. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115(6):1597-1604. doi:10.1097/01.prs.0000160695.33457.db
12. Karamanos E, Wei B, Siddiqui A, Rubinfeld I. Tobacco use and body mass index as predictors of outcomes in patients undergoing breast reduction mammoplasty. Ann Plast Surg. 2015;75(4):383-387. doi:10.1097/SAP.0000000000000192
13. Manahan MA, Buretta KJ, Chang D, Mithani SK, Mallalieu J, Shermak MA. An outcomes analysis of 2142 breast reduction procedures. Ann Plast Surg. 2015;74(3):289-292. doi:10.1097/SAP.0b013e31829d2261
14. Hillam JS, Borsting EA, Chim JH, Thaller SR. Smoking as a risk factor for breast reduction: an analysis of 13,503 cases. J Plast Reconstr Aesthet Surg. 2017;70(6):734-740. doi:10.1016/j.bjps.2016.12.012
15. Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: a meta-analysis. PLoS One. 2016;11(12):e0167746. doi:10.1371/journal.pone.0167746
16. Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069-1079.doi:10.1097/SLA.0b013e31824f632d
17. Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle Wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg. 2013;132(5):1068-1076. doi:10.1097/PRS.0b013e3182a48b2d
18. Hunter-Smith DJ, Smoll NR, Marne B, Maung H, Findlay MW. Comparing breast-reduction techniques: time-to-event analysis and recommendations. Aesthetic Plast Surg. 2012;36(3):600-606. doi:10.1007/s00266-011-9860-3
19. Ogunleye AA, Leroux O, Morrison N, Preminger AB. Complications after reduction mammaplasty: a comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg. 2017;79(1):13-16. doi:10.1097/SAP.0000000000001059
20. Bauermeister AJ, Gill K, Zuriarrain A, Earle SA, Newman MI. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72(3):410-418. doi:10.1016/j.bjps.2018.12.004
21. Nelson JA, Fischer JP, Chung CU, et al. Obesity and early complications following reduction mammaplasty: an analysis of 4545 patients from the 2005-2011 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):334-339. doi:10.3109/2000656X.2014.886582
22. Kreithen J, Caffee H, Rosenberg J, et al. A comparison of the LeJour and Wise pattern methods of breast reduction. Ann Plast Surg. 2005;54(3):236-241. doi:10.3109/2000656X.2014.886582
23. Güemes A, Pérez E, Sousa R, et al. Quality of life and alleviation of symptoms after breast reduction for macromastia in obese patients: is surgery worth it? Aesthetic Plast Surg. 2016;40(1):62-70. doi:10.1007/s00266-015-0601-x
24. Setälä L, Papp A, Joukainen S, et al. Obesity and complications in breast reduction surgery: are restrictions justified? J Plast Reconstr Aesthet Surg. 2009;62(2):195-199. doi:10.1016/j.bjps.2007.10.043
25. Shah R, Al-Ajam Y, Stott D, Kang N. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthet Surg. 2011;64(4):508-514. doi:10.1016/j.bjps.2007.10.043
1. US Department of Veterans Affairs. Statistics at a glance. Published February 2020. Accessed June 18, 2021. https://www.va.gov/vetdata/docs/Quickfacts/Homepage_slideshow_4_6_20.PDF
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed June 18, 2020. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Crittenden TA, Watson DI, Ratcliffe J, Griffin PA, Dean NR. Outcomes of breast reduction surgery using the breast-q: a prospective study and comparison with normative data. Plast Reconstr Surg. 2019;144(5):1034-1044. doi:10.1097/PRS.0000000000006114
4. Thoma A, Sprague S, Veltri K, Duku E, Furlong W. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg. 2007;120(1):13-26. doi:10.1097/01.prs.0000263370.94191.90
5. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and quality of life following reduction mammaplasty in adolescents and young women.Plast Reconstr Surg. 2019;144(3):572-581. doi:10.1097/PRS.0000000000005907
6. Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136(4):531e-544e. doi:10.1097/PRS.0000000000001622
7. Kraut RY, Brown E, Korownyk C, et al. The impact of breast reduction surgery on breastfeeding: systematic review of observational studies. PLoS One. 2017;12(10):e0186591. doi:10.1371/journal.pone.0186591
8. Fischer JP, Wes AM, Kovach SJ. The impact of surgical resident participation in breast reduction surgery--outcome analysis from the 2005-2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):315-321. doi:10.3109/2000656X.2014.882345
9. Site Facility Name and Complexity Summary of VHA Facility. Accessed June 18, 2021. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=2793591&FileName=VA118-16-R-1059-A00002002.docx
10. Lewin R, Göransson M, Elander A, Thorarinsson A, Lundberg J, Lidén M. Risk factors for complications after breast reduction surgery. J Plast Surg Hand Surg. 2014;48(1):10-14. doi:10.3109/2000656X.2013.791625
11. Cunningham BL, Gear AJ, Kerrigan CL, Collins ED. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115(6):1597-1604. doi:10.1097/01.prs.0000160695.33457.db
12. Karamanos E, Wei B, Siddiqui A, Rubinfeld I. Tobacco use and body mass index as predictors of outcomes in patients undergoing breast reduction mammoplasty. Ann Plast Surg. 2015;75(4):383-387. doi:10.1097/SAP.0000000000000192
13. Manahan MA, Buretta KJ, Chang D, Mithani SK, Mallalieu J, Shermak MA. An outcomes analysis of 2142 breast reduction procedures. Ann Plast Surg. 2015;74(3):289-292. doi:10.1097/SAP.0b013e31829d2261
14. Hillam JS, Borsting EA, Chim JH, Thaller SR. Smoking as a risk factor for breast reduction: an analysis of 13,503 cases. J Plast Reconstr Aesthet Surg. 2017;70(6):734-740. doi:10.1016/j.bjps.2016.12.012
15. Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: a meta-analysis. PLoS One. 2016;11(12):e0167746. doi:10.1371/journal.pone.0167746
16. Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069-1079.doi:10.1097/SLA.0b013e31824f632d
17. Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle Wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg. 2013;132(5):1068-1076. doi:10.1097/PRS.0b013e3182a48b2d
18. Hunter-Smith DJ, Smoll NR, Marne B, Maung H, Findlay MW. Comparing breast-reduction techniques: time-to-event analysis and recommendations. Aesthetic Plast Surg. 2012;36(3):600-606. doi:10.1007/s00266-011-9860-3
19. Ogunleye AA, Leroux O, Morrison N, Preminger AB. Complications after reduction mammaplasty: a comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg. 2017;79(1):13-16. doi:10.1097/SAP.0000000000001059
20. Bauermeister AJ, Gill K, Zuriarrain A, Earle SA, Newman MI. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72(3):410-418. doi:10.1016/j.bjps.2018.12.004
21. Nelson JA, Fischer JP, Chung CU, et al. Obesity and early complications following reduction mammaplasty: an analysis of 4545 patients from the 2005-2011 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):334-339. doi:10.3109/2000656X.2014.886582
22. Kreithen J, Caffee H, Rosenberg J, et al. A comparison of the LeJour and Wise pattern methods of breast reduction. Ann Plast Surg. 2005;54(3):236-241. doi:10.3109/2000656X.2014.886582
23. Güemes A, Pérez E, Sousa R, et al. Quality of life and alleviation of symptoms after breast reduction for macromastia in obese patients: is surgery worth it? Aesthetic Plast Surg. 2016;40(1):62-70. doi:10.1007/s00266-015-0601-x
24. Setälä L, Papp A, Joukainen S, et al. Obesity and complications in breast reduction surgery: are restrictions justified? J Plast Reconstr Aesthet Surg. 2009;62(2):195-199. doi:10.1016/j.bjps.2007.10.043
25. Shah R, Al-Ajam Y, Stott D, Kang N. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthet Surg. 2011;64(4):508-514. doi:10.1016/j.bjps.2007.10.043
Necrotizing Infection of the Upper Extremity: A Veterans Affairs Medical Center Experience (2008-2017)
Necrotizing infection of the extremity is a rare but potentially lethal diagnosis with a mortality rate in the range of 17% to 35%.1-4 The plastic surgery service at the Malcom Randall Veterans Affairs Medical Center (MRVAMC) treats all hand emergencies, including upper extremity infection, in the North Florida/South Georgia Veterans Heath System. There has been a well-coordinated emergency hand care system in place for several years that includes specialty templates on the electronic health record, pre-existing urgent clinic appointments, and single service surgical specialty care.5 This facilitates a fluid line of communication between primary care, emergency department (ED) providers, and surgical specialties. The objective of the study was to evaluate our identification, treatment, and outcome of these serious infections.
Methods
The MRVAMC Institutional Review Board approved a retrospective review of necrotizing infection of the upper extremity treated at the facility by the plastic surgery service. Surgical cases over a 9-year period (June 5, 2008-June 5, 2017) were identified by CPT (current procedural technology) codes for amputation and/or debridement of the upper extremity. The charts were reviewed for evidence of necrotizing infection by clinical description or pathology report. The patients’ age, sex, etiology, comorbidities from their problem list, vitals, and laboratory results were recorded upon arrival at the hospital. Time from presentation to surgery, treatment, and outcomes were recorded.
Results
Ten patients were treated for necrotizing infection of the upper extremity over a 9-year period; all were men with an average age of 64 years. Etiologies included nail biting, “bug bites,” crush injuries, burns, suspected IV drug use, and unknown. Nine of 10 patients had diabetes mellitus (DM). Most did not show evidence of hemodynamic instability on hospital arrival (Table). One patient was hypotensive with a mean arterial blood pressure < 65 mm Hg, 2 had heart rates > 100 beats/min, 1 patient had a temperature > 38° C, and 7 had elevated white blood cell (WBC) counts ranging from 11 to 24 k/cmm. Two undiagnosed patients with DM (patients 1 and 8) expressed no complaints of pain and presented with blood glucose > 450 mg/dL with hemoglobin A1c levels > 12%.
Infectious disease and critical care services were involved in the treatment of several cases when requested. A computed tomography (CT) scan was used in 2 of the patients (patients 1 and 4) to assist in the diagnosis (Figure 1).
Seven patients out of 10 were treated with surgery within 24 hours on hospital arrival. The severity of the pathology was not initially recognized in 2 of the patients earlier in the review. A third patient resisted surgical treatment until the second hospital day. Four patients had from 1 to 3 digital amputations, 2 patients had wrist disarticulations, and 1 had a distal forearm amputation.
Antibiotics were managed by critical care, hospitalist, or infectious disease services and adjusted once final cultures were returned (Table).
Discussion
Necrotizing infection of the upper extremity is a rare pathology with a substantial risk of amputation and mortality that requires a high index of suspicion and expeditious referral to a hand surgeon. It is well accepted that the key to survival is prompt surgical debridement of all necrotic tissue, ideally within 24 hours of hospital arrival.2-4,6 Death is usually secondary to sepsis.3 The classic presentation of pain out of proportion to exam, hypotension, erythema, skin necrosis, elevated WBC count, and fever may not be present and can delay diagnosis.1-4,6
DM is the most common comorbidity, and reviews have found the disease occurs more often in males, both which are consistent with our study.1-3 Diabetic infections have been found to be more likely to present as necrotizing infection than are nondiabetic infections and be at a higher risk for amputation.7 The patients with the wrist disarticulations and forearm amputation had DM. A minor trauma can be a portal for infection, which can be monomicrobial or polymicrobial.1,4 Once the diagnosis is suspected, prompt resuscitation, surgical debridement, IV antibiotics, and early intensive care are lifesaving. Hyperbaric oxygen is not available at MRVAMC and was not pursued as a transfer request due to its controversial benefit.6
There were no perioperative 30-day mortalities over a 9-year period in patients identified as having necrotizing infection of the upper extremity. This is attributed to an aggressive and well-coordinated, multisystem approach involving emergency, surgical, anesthesia, intensive care, and infectious disease services.
The hand trauma triage system in place at MRVAMC was started in 2008 and presented at the 38th Annual VA Surgeons Meeting in New Haven, Connecticut. The process starts at the level of the ED, urgent care or primary care provider and facilitates rapid access to subspecialty care by reducing unnecessary phone calls and appointment wait times.
All hand emergencies are covered by the plastic surgery service rather than the traditional split coverage between orthopedics and plastic surgery. This provides consistency and continuity for the patients and staff. The electronic health record consult template gives specific instructions to contact the on-call plastic surgeon. The resident/fellow gets called if patient is in-house, and faculty is called if the patient is outside the main hospital. The requesting provider gets instructions on treatment and follow-up. Clinic profiles have appointments reserved for urgent consults during the first hour so that patients can be sent to pre-anesthesia clinic or hand therapy, depending on the diagnosis. This triage system increased our hand trauma volume by a multiple of 6 between 2008 and 2012 but cut the appointment wait time > 1 week by half, as a percentage of consults, and did not significantly increase after-hour use of the operating room. The number of faculty and trainees stayed the same.
We did find that speed to diagnosis for necrotizing infection is an area that can be improved on with a higher clinical suspicion. There is a learning curve to the diagnosis and treatment, which can be prolonged when the index cases do not present themselves often and the patients do not appear in distress. This argues for consistency in hand-specific trauma coverage. The patients were most often initially seen by the resident and examined by a faculty member within hours. There were 4 different plastic surgery faculty involved in these cases, and they all included resident participation before, during, and after surgery. Debridement consists of wide local excision to bleeding tissue. Author review of the operative notes found the numbers of trips to the operating room for debridement can be reduced as the surgeon becomes more confident in the diagnosis and management, resulting in less “whittling” and a more definitive debridement, resulting in a faster recovery.
The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) is a tool that helps to distinguish necrotizing infection from other forms of soft tissue infection by using a point system for laboratory values that include C-reactive protein (CRP), white blood count, hemoglobin, sodium, creatinine, and glucose values.8 We do not routinely request CRP results, but 1 of the 2 patients (patient 9) who had the full complement of laboratory tests would have met high-risk criteria. The diagnostic accuracy of this tool has been questioned9; however, the authors welcome any method that can rapidly and noninvasively assist in getting the patient proper attention.
The patients were not seen for long-term follow-up, but some did return to the main hospital or clinic for other pathology and were pleased to show off their grip strength after a 3-ray amputation (patient 1) and aesthetics after upper arm and forearm debridement and skin graft reconstruction (patient 4, Figure 4).
A single-ray amputation can be expected to result in a loss of grip and pinch strength, about 43.3% and 33.6%, respectively; however, given the alternative of further loss of life or limb, this was considered a reasonable trade-off.10 One wrist disarticulation and the forearm amputation were seen by amputee clinic for prosthetic fitting many months after the amputations once the wounds were healed and edema had subsided.
Conclusion
A well-coordinated multidisciplinary effort was the key to successful identification and treatment of this serious life- and limb-threatening infection at our institution. We did identify room for improvement in making an earlier diagnosis and performing a more aggressive first debridement.
Acknowledgments
This project is the result of work supported with resources and use of facilities at the Malcom Randall VA Medical Center in Gainesville, Florida.
1. Angoules AG, Kontakis G, Drakoulakis E, Vrentzos G, Granick MS, Giannoudis PV. Necrotizing fasciitis of upper and lower limb: a systemic review. Injury. 2007;38(suppl 5):S19-S26.
2. Chauhan A, Wigton MD, Palmer BA. Necrotizing fasciitis. J Hand Surg Am. 2014;39(8):1598-1601.
3. Cheng NC, SU YM, Kuo YS, Tai HC, Tang YB. Factors affecting the mortality of necrotizing fasciitis involving the upper extremities. Surg Today. 2008;38(12):1108-1113.
4. Sunderland IR, Friedrich JB. Predictors of mortality and limb loss in necrotizing soft tissue infections of the upper extremity. J Hand Surg Am. 2009;34(10):1900-1901.
5. Coady-Fariborzian L, McGreane A. Comparison of hand emergency triage before and after specialty templates (2007 vs 2012). Hand (N Y). 2015;10(2):215-220.
6. Stevens D, Bryant A. Necrotizing soft-tissue infections. N Engl J Med. 2017;377(23):2253-2265.
7. Sharma K, Pan D, Friedman J, Yu JL, Mull A, Moore AM. Quantifying the effect of diabetes on surgical hand and forearm infections. J Hand Surg Am. 2018;43(2):105-114.
8. Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32(7):1535-1541.
9. Fernando SM, Tran A, Cheng W, et al. Necrotizing soft tissue infection: diagnostic accuracy of physical examination, imaging, and LRINEC score: a systematic review and meta-analysis. Ann Surg. 2019;269(1):58-65. 10. Bhat AK, Acharya AM, Narayanakurup JK, Kumar B, Nagpal PS, Kamath A. Functional and cosmetic outcome of single-digit ray amputation in hand. Musculoskelet Surg. 2017;101(3):275-281.
Necrotizing infection of the extremity is a rare but potentially lethal diagnosis with a mortality rate in the range of 17% to 35%.1-4 The plastic surgery service at the Malcom Randall Veterans Affairs Medical Center (MRVAMC) treats all hand emergencies, including upper extremity infection, in the North Florida/South Georgia Veterans Heath System. There has been a well-coordinated emergency hand care system in place for several years that includes specialty templates on the electronic health record, pre-existing urgent clinic appointments, and single service surgical specialty care.5 This facilitates a fluid line of communication between primary care, emergency department (ED) providers, and surgical specialties. The objective of the study was to evaluate our identification, treatment, and outcome of these serious infections.
Methods
The MRVAMC Institutional Review Board approved a retrospective review of necrotizing infection of the upper extremity treated at the facility by the plastic surgery service. Surgical cases over a 9-year period (June 5, 2008-June 5, 2017) were identified by CPT (current procedural technology) codes for amputation and/or debridement of the upper extremity. The charts were reviewed for evidence of necrotizing infection by clinical description or pathology report. The patients’ age, sex, etiology, comorbidities from their problem list, vitals, and laboratory results were recorded upon arrival at the hospital. Time from presentation to surgery, treatment, and outcomes were recorded.
Results
Ten patients were treated for necrotizing infection of the upper extremity over a 9-year period; all were men with an average age of 64 years. Etiologies included nail biting, “bug bites,” crush injuries, burns, suspected IV drug use, and unknown. Nine of 10 patients had diabetes mellitus (DM). Most did not show evidence of hemodynamic instability on hospital arrival (Table). One patient was hypotensive with a mean arterial blood pressure < 65 mm Hg, 2 had heart rates > 100 beats/min, 1 patient had a temperature > 38° C, and 7 had elevated white blood cell (WBC) counts ranging from 11 to 24 k/cmm. Two undiagnosed patients with DM (patients 1 and 8) expressed no complaints of pain and presented with blood glucose > 450 mg/dL with hemoglobin A1c levels > 12%.
Infectious disease and critical care services were involved in the treatment of several cases when requested. A computed tomography (CT) scan was used in 2 of the patients (patients 1 and 4) to assist in the diagnosis (Figure 1).
Seven patients out of 10 were treated with surgery within 24 hours on hospital arrival. The severity of the pathology was not initially recognized in 2 of the patients earlier in the review. A third patient resisted surgical treatment until the second hospital day. Four patients had from 1 to 3 digital amputations, 2 patients had wrist disarticulations, and 1 had a distal forearm amputation.
Antibiotics were managed by critical care, hospitalist, or infectious disease services and adjusted once final cultures were returned (Table).
Discussion
Necrotizing infection of the upper extremity is a rare pathology with a substantial risk of amputation and mortality that requires a high index of suspicion and expeditious referral to a hand surgeon. It is well accepted that the key to survival is prompt surgical debridement of all necrotic tissue, ideally within 24 hours of hospital arrival.2-4,6 Death is usually secondary to sepsis.3 The classic presentation of pain out of proportion to exam, hypotension, erythema, skin necrosis, elevated WBC count, and fever may not be present and can delay diagnosis.1-4,6
DM is the most common comorbidity, and reviews have found the disease occurs more often in males, both which are consistent with our study.1-3 Diabetic infections have been found to be more likely to present as necrotizing infection than are nondiabetic infections and be at a higher risk for amputation.7 The patients with the wrist disarticulations and forearm amputation had DM. A minor trauma can be a portal for infection, which can be monomicrobial or polymicrobial.1,4 Once the diagnosis is suspected, prompt resuscitation, surgical debridement, IV antibiotics, and early intensive care are lifesaving. Hyperbaric oxygen is not available at MRVAMC and was not pursued as a transfer request due to its controversial benefit.6
There were no perioperative 30-day mortalities over a 9-year period in patients identified as having necrotizing infection of the upper extremity. This is attributed to an aggressive and well-coordinated, multisystem approach involving emergency, surgical, anesthesia, intensive care, and infectious disease services.
The hand trauma triage system in place at MRVAMC was started in 2008 and presented at the 38th Annual VA Surgeons Meeting in New Haven, Connecticut. The process starts at the level of the ED, urgent care or primary care provider and facilitates rapid access to subspecialty care by reducing unnecessary phone calls and appointment wait times.
All hand emergencies are covered by the plastic surgery service rather than the traditional split coverage between orthopedics and plastic surgery. This provides consistency and continuity for the patients and staff. The electronic health record consult template gives specific instructions to contact the on-call plastic surgeon. The resident/fellow gets called if patient is in-house, and faculty is called if the patient is outside the main hospital. The requesting provider gets instructions on treatment and follow-up. Clinic profiles have appointments reserved for urgent consults during the first hour so that patients can be sent to pre-anesthesia clinic or hand therapy, depending on the diagnosis. This triage system increased our hand trauma volume by a multiple of 6 between 2008 and 2012 but cut the appointment wait time > 1 week by half, as a percentage of consults, and did not significantly increase after-hour use of the operating room. The number of faculty and trainees stayed the same.
We did find that speed to diagnosis for necrotizing infection is an area that can be improved on with a higher clinical suspicion. There is a learning curve to the diagnosis and treatment, which can be prolonged when the index cases do not present themselves often and the patients do not appear in distress. This argues for consistency in hand-specific trauma coverage. The patients were most often initially seen by the resident and examined by a faculty member within hours. There were 4 different plastic surgery faculty involved in these cases, and they all included resident participation before, during, and after surgery. Debridement consists of wide local excision to bleeding tissue. Author review of the operative notes found the numbers of trips to the operating room for debridement can be reduced as the surgeon becomes more confident in the diagnosis and management, resulting in less “whittling” and a more definitive debridement, resulting in a faster recovery.
The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) is a tool that helps to distinguish necrotizing infection from other forms of soft tissue infection by using a point system for laboratory values that include C-reactive protein (CRP), white blood count, hemoglobin, sodium, creatinine, and glucose values.8 We do not routinely request CRP results, but 1 of the 2 patients (patient 9) who had the full complement of laboratory tests would have met high-risk criteria. The diagnostic accuracy of this tool has been questioned9; however, the authors welcome any method that can rapidly and noninvasively assist in getting the patient proper attention.
The patients were not seen for long-term follow-up, but some did return to the main hospital or clinic for other pathology and were pleased to show off their grip strength after a 3-ray amputation (patient 1) and aesthetics after upper arm and forearm debridement and skin graft reconstruction (patient 4, Figure 4).
A single-ray amputation can be expected to result in a loss of grip and pinch strength, about 43.3% and 33.6%, respectively; however, given the alternative of further loss of life or limb, this was considered a reasonable trade-off.10 One wrist disarticulation and the forearm amputation were seen by amputee clinic for prosthetic fitting many months after the amputations once the wounds were healed and edema had subsided.
Conclusion
A well-coordinated multidisciplinary effort was the key to successful identification and treatment of this serious life- and limb-threatening infection at our institution. We did identify room for improvement in making an earlier diagnosis and performing a more aggressive first debridement.
Acknowledgments
This project is the result of work supported with resources and use of facilities at the Malcom Randall VA Medical Center in Gainesville, Florida.
Necrotizing infection of the extremity is a rare but potentially lethal diagnosis with a mortality rate in the range of 17% to 35%.1-4 The plastic surgery service at the Malcom Randall Veterans Affairs Medical Center (MRVAMC) treats all hand emergencies, including upper extremity infection, in the North Florida/South Georgia Veterans Heath System. There has been a well-coordinated emergency hand care system in place for several years that includes specialty templates on the electronic health record, pre-existing urgent clinic appointments, and single service surgical specialty care.5 This facilitates a fluid line of communication between primary care, emergency department (ED) providers, and surgical specialties. The objective of the study was to evaluate our identification, treatment, and outcome of these serious infections.
Methods
The MRVAMC Institutional Review Board approved a retrospective review of necrotizing infection of the upper extremity treated at the facility by the plastic surgery service. Surgical cases over a 9-year period (June 5, 2008-June 5, 2017) were identified by CPT (current procedural technology) codes for amputation and/or debridement of the upper extremity. The charts were reviewed for evidence of necrotizing infection by clinical description or pathology report. The patients’ age, sex, etiology, comorbidities from their problem list, vitals, and laboratory results were recorded upon arrival at the hospital. Time from presentation to surgery, treatment, and outcomes were recorded.
Results
Ten patients were treated for necrotizing infection of the upper extremity over a 9-year period; all were men with an average age of 64 years. Etiologies included nail biting, “bug bites,” crush injuries, burns, suspected IV drug use, and unknown. Nine of 10 patients had diabetes mellitus (DM). Most did not show evidence of hemodynamic instability on hospital arrival (Table). One patient was hypotensive with a mean arterial blood pressure < 65 mm Hg, 2 had heart rates > 100 beats/min, 1 patient had a temperature > 38° C, and 7 had elevated white blood cell (WBC) counts ranging from 11 to 24 k/cmm. Two undiagnosed patients with DM (patients 1 and 8) expressed no complaints of pain and presented with blood glucose > 450 mg/dL with hemoglobin A1c levels > 12%.
Infectious disease and critical care services were involved in the treatment of several cases when requested. A computed tomography (CT) scan was used in 2 of the patients (patients 1 and 4) to assist in the diagnosis (Figure 1).
Seven patients out of 10 were treated with surgery within 24 hours on hospital arrival. The severity of the pathology was not initially recognized in 2 of the patients earlier in the review. A third patient resisted surgical treatment until the second hospital day. Four patients had from 1 to 3 digital amputations, 2 patients had wrist disarticulations, and 1 had a distal forearm amputation.
Antibiotics were managed by critical care, hospitalist, or infectious disease services and adjusted once final cultures were returned (Table).
Discussion
Necrotizing infection of the upper extremity is a rare pathology with a substantial risk of amputation and mortality that requires a high index of suspicion and expeditious referral to a hand surgeon. It is well accepted that the key to survival is prompt surgical debridement of all necrotic tissue, ideally within 24 hours of hospital arrival.2-4,6 Death is usually secondary to sepsis.3 The classic presentation of pain out of proportion to exam, hypotension, erythema, skin necrosis, elevated WBC count, and fever may not be present and can delay diagnosis.1-4,6
DM is the most common comorbidity, and reviews have found the disease occurs more often in males, both which are consistent with our study.1-3 Diabetic infections have been found to be more likely to present as necrotizing infection than are nondiabetic infections and be at a higher risk for amputation.7 The patients with the wrist disarticulations and forearm amputation had DM. A minor trauma can be a portal for infection, which can be monomicrobial or polymicrobial.1,4 Once the diagnosis is suspected, prompt resuscitation, surgical debridement, IV antibiotics, and early intensive care are lifesaving. Hyperbaric oxygen is not available at MRVAMC and was not pursued as a transfer request due to its controversial benefit.6
There were no perioperative 30-day mortalities over a 9-year period in patients identified as having necrotizing infection of the upper extremity. This is attributed to an aggressive and well-coordinated, multisystem approach involving emergency, surgical, anesthesia, intensive care, and infectious disease services.
The hand trauma triage system in place at MRVAMC was started in 2008 and presented at the 38th Annual VA Surgeons Meeting in New Haven, Connecticut. The process starts at the level of the ED, urgent care or primary care provider and facilitates rapid access to subspecialty care by reducing unnecessary phone calls and appointment wait times.
All hand emergencies are covered by the plastic surgery service rather than the traditional split coverage between orthopedics and plastic surgery. This provides consistency and continuity for the patients and staff. The electronic health record consult template gives specific instructions to contact the on-call plastic surgeon. The resident/fellow gets called if patient is in-house, and faculty is called if the patient is outside the main hospital. The requesting provider gets instructions on treatment and follow-up. Clinic profiles have appointments reserved for urgent consults during the first hour so that patients can be sent to pre-anesthesia clinic or hand therapy, depending on the diagnosis. This triage system increased our hand trauma volume by a multiple of 6 between 2008 and 2012 but cut the appointment wait time > 1 week by half, as a percentage of consults, and did not significantly increase after-hour use of the operating room. The number of faculty and trainees stayed the same.
We did find that speed to diagnosis for necrotizing infection is an area that can be improved on with a higher clinical suspicion. There is a learning curve to the diagnosis and treatment, which can be prolonged when the index cases do not present themselves often and the patients do not appear in distress. This argues for consistency in hand-specific trauma coverage. The patients were most often initially seen by the resident and examined by a faculty member within hours. There were 4 different plastic surgery faculty involved in these cases, and they all included resident participation before, during, and after surgery. Debridement consists of wide local excision to bleeding tissue. Author review of the operative notes found the numbers of trips to the operating room for debridement can be reduced as the surgeon becomes more confident in the diagnosis and management, resulting in less “whittling” and a more definitive debridement, resulting in a faster recovery.
The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) is a tool that helps to distinguish necrotizing infection from other forms of soft tissue infection by using a point system for laboratory values that include C-reactive protein (CRP), white blood count, hemoglobin, sodium, creatinine, and glucose values.8 We do not routinely request CRP results, but 1 of the 2 patients (patient 9) who had the full complement of laboratory tests would have met high-risk criteria. The diagnostic accuracy of this tool has been questioned9; however, the authors welcome any method that can rapidly and noninvasively assist in getting the patient proper attention.
The patients were not seen for long-term follow-up, but some did return to the main hospital or clinic for other pathology and were pleased to show off their grip strength after a 3-ray amputation (patient 1) and aesthetics after upper arm and forearm debridement and skin graft reconstruction (patient 4, Figure 4).
A single-ray amputation can be expected to result in a loss of grip and pinch strength, about 43.3% and 33.6%, respectively; however, given the alternative of further loss of life or limb, this was considered a reasonable trade-off.10 One wrist disarticulation and the forearm amputation were seen by amputee clinic for prosthetic fitting many months after the amputations once the wounds were healed and edema had subsided.
Conclusion
A well-coordinated multidisciplinary effort was the key to successful identification and treatment of this serious life- and limb-threatening infection at our institution. We did identify room for improvement in making an earlier diagnosis and performing a more aggressive first debridement.
Acknowledgments
This project is the result of work supported with resources and use of facilities at the Malcom Randall VA Medical Center in Gainesville, Florida.
1. Angoules AG, Kontakis G, Drakoulakis E, Vrentzos G, Granick MS, Giannoudis PV. Necrotizing fasciitis of upper and lower limb: a systemic review. Injury. 2007;38(suppl 5):S19-S26.
2. Chauhan A, Wigton MD, Palmer BA. Necrotizing fasciitis. J Hand Surg Am. 2014;39(8):1598-1601.
3. Cheng NC, SU YM, Kuo YS, Tai HC, Tang YB. Factors affecting the mortality of necrotizing fasciitis involving the upper extremities. Surg Today. 2008;38(12):1108-1113.
4. Sunderland IR, Friedrich JB. Predictors of mortality and limb loss in necrotizing soft tissue infections of the upper extremity. J Hand Surg Am. 2009;34(10):1900-1901.
5. Coady-Fariborzian L, McGreane A. Comparison of hand emergency triage before and after specialty templates (2007 vs 2012). Hand (N Y). 2015;10(2):215-220.
6. Stevens D, Bryant A. Necrotizing soft-tissue infections. N Engl J Med. 2017;377(23):2253-2265.
7. Sharma K, Pan D, Friedman J, Yu JL, Mull A, Moore AM. Quantifying the effect of diabetes on surgical hand and forearm infections. J Hand Surg Am. 2018;43(2):105-114.
8. Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32(7):1535-1541.
9. Fernando SM, Tran A, Cheng W, et al. Necrotizing soft tissue infection: diagnostic accuracy of physical examination, imaging, and LRINEC score: a systematic review and meta-analysis. Ann Surg. 2019;269(1):58-65. 10. Bhat AK, Acharya AM, Narayanakurup JK, Kumar B, Nagpal PS, Kamath A. Functional and cosmetic outcome of single-digit ray amputation in hand. Musculoskelet Surg. 2017;101(3):275-281.
1. Angoules AG, Kontakis G, Drakoulakis E, Vrentzos G, Granick MS, Giannoudis PV. Necrotizing fasciitis of upper and lower limb: a systemic review. Injury. 2007;38(suppl 5):S19-S26.
2. Chauhan A, Wigton MD, Palmer BA. Necrotizing fasciitis. J Hand Surg Am. 2014;39(8):1598-1601.
3. Cheng NC, SU YM, Kuo YS, Tai HC, Tang YB. Factors affecting the mortality of necrotizing fasciitis involving the upper extremities. Surg Today. 2008;38(12):1108-1113.
4. Sunderland IR, Friedrich JB. Predictors of mortality and limb loss in necrotizing soft tissue infections of the upper extremity. J Hand Surg Am. 2009;34(10):1900-1901.
5. Coady-Fariborzian L, McGreane A. Comparison of hand emergency triage before and after specialty templates (2007 vs 2012). Hand (N Y). 2015;10(2):215-220.
6. Stevens D, Bryant A. Necrotizing soft-tissue infections. N Engl J Med. 2017;377(23):2253-2265.
7. Sharma K, Pan D, Friedman J, Yu JL, Mull A, Moore AM. Quantifying the effect of diabetes on surgical hand and forearm infections. J Hand Surg Am. 2018;43(2):105-114.
8. Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32(7):1535-1541.
9. Fernando SM, Tran A, Cheng W, et al. Necrotizing soft tissue infection: diagnostic accuracy of physical examination, imaging, and LRINEC score: a systematic review and meta-analysis. Ann Surg. 2019;269(1):58-65. 10. Bhat AK, Acharya AM, Narayanakurup JK, Kumar B, Nagpal PS, Kamath A. Functional and cosmetic outcome of single-digit ray amputation in hand. Musculoskelet Surg. 2017;101(3):275-281.
Assessment of Free Flap Breast Reconstructions
Free flap autologous breast reconstruction is an excellent surgical option for breast reconstruction in select patients. A free flap involves moving skin, fat, and/or muscle from a distant part of the body, based on a named blood supply (pedicle), and attaching it to another blood supply adjacent to the acquired defect. This procedure is particularly useful in areas where local tissue supply is lacking in volume or is damaged due to trauma or radiation. These reconstructions are performed largely in high-volume centers outside the VA because of the required specialized level of surgical training, manpower, and nursing support.1 The Malcom Randall VAMC in Gainesville, Florida, started offering autologous free flap breast reconstruction as an option to select patients in October 2012.
The Malcom Randall VAMC operating room (OR) does not operate 24/7, and the system has limited available OR time and surgical staff compared with the volume of patients requesting care.2 Operative planning for free flap autologous breast reconstruction must occur months ahead of surgery to balance the system limitations with the ability to offer the highest level of care. Planning includes strict patient selection, preoperative imaging, practice runs with OR staff, use of venous couplers, and frequent intensive care unit (ICU) staff in-services. Planning also includes the need to keep surgeries within the allocated OR time to avoid shift changes during critical periods. Frequent and early communication occurs between the surgical scheduler, OR nurses, and the anesthesia and critical care teams.
Studies have found that the best chance of flap salvage in the event of a thrombotic event is a rapid return to the OR.3 It is essential to minimize the risk of emergent returns to the OR because it is not staffed throughout the night. Patient risk factors for perioperative vascular complications include hypercoagulable disorders, peripheral vascular disease, use of the superficial epigastric system, and smoking.4-7
A PubMed search for free flap reconstruction solely within the VA over the past 20 years found 1 article discussing the use of free flaps in head and neck reconstruction which demonstrated an impressive success rate of 93%.8
The object of this study was to assess free flap breast reconstruction results at the Malcolm Randall VAMC to determine whether it is a realistic treatment to offer in the federal system.
Methods
The Malcolm Randall Institutional Review Board approved a retrospective chart review of all autologous free flap breast reconstructions using CPT code 19364, performed from October 2012 to June 2016. Medical records of patients who had a free flap breast reconstruction were queried during that period. Patient age; comorbidities listed on the electronic medical record “problem list;” body mass index (BMI); type of reconstruction (delayed vs immediate); length of surgery; length of stay; and complications over a 30-day period were recorded (Table). The authors looked for documentation of preoperative imaging and unplanned returns to the OR within the 30-day period.
Of 3 full-time VA plastic surgeons on staff during the study period, 2 surgeons had advanced fellowship training in either microsurgery or hand and microsurgery. Plastic surgery fellows and general surgery interns participated in the surgeries and postoperative care. The service had 1 dedicated advanced practice registered nurse involved in the surgical scheduling and perioperative care.
Results
A total of 11 abdominally based free flap breast reconstructions—6 muscle-sparing transverse rectus abdominus musculocutaneous (TRAM) and 5 deep inferior epigastric perforator (DIEP) flaps—were performed in 8 patients during the study period (Figures 1A, 1B, 1C, and 1D). Patient ages ranged from 31 to 58 years with a mean of 45.6 years. Six patients had preoperative computer tomography angiography (CTA) to define the location of the abdominal wall perforators. One muscle-sparing free flap was performed immediately after mastectomy; the other free flaps were performed as delayed reconstructions. Body mass index ranged from 24 to 35, with a mean of 30. All patients reported no tobacco use during the consultation; however, 1 patient later admitted to chewing tobacco. No urinary cotinine confirmation was requested. Two patients had 1 free flap reconstruction and 1 pedicle TRAM. This bilateral combination has been recently described in the literature and was chosen as a reasonable option to balance limited resources with abdominal wall morbidity.9 Operating room time ranged from 7 hours 50 minutes to 13 hours 3 minutes. All patients went to the ICU for hourly flap monitoring.
Length of stay ranged from 4 to 7 days, with a mean of 4.5 days. The longest stay was for a patient who had immediate reconstruction using a pedicle TRAM and muscle-sparing free TRAM. She was not a DIEP candidate because poor perforator quality had been noted during preoperative imaging.
Six patients had documentation of postoperative wound complications. One patient returned to the OR on the elective schedule 3 weeks postoperatively for a partial flap debridement. Her tissue transfer was > 1,000 g, and she required a matching reduction on the other side. There were no complete flap losses or postoperative thrombotic events; no cases went back to the OR emergently.
Discussion
With the number of women veterans steadily increasing, the number of patients in need of breast cancer surgery, including reconstruction, will rise in the VA.10 Fortunately, breast reconstruction is an elective procedure. Immediate breast reconstruction is a popular option because patients can combine surgeries and potentially avoid 2 recovery periods, and a better aesthetic outcome is possible because the skin does not have time to contract. Although immediate reconstruction has been increasing in popularity, it is associated with a higher complication rate.11 Further, reconstruction can be jeopardized if the oncologic plan is changed in the early postoperative period.
Positive margins found after an autologous reconstruction result in a more complicated postoperative course and a higher rate of wound complications.12 Unexpected radiation therapy after autologous reconstruction can severely distort a tissue flap because of fat necrosis, fibrosis, and contraction.13,14 From a practical perspective in the federal system, it is very difficult to coordinate 2 surgeons’ schedules when the system is already struggling to keep up with demand. Splitting the ablative and reconstructive surgery allows the urgent problem (cancer) to be addressed first, ensuring clear margins and allowing the patient to recover and consider all reconstructive options without feeling time pressure.
A large tertiary care center will have staff and equipment redundancy, but this study had to consider limitations in resources. The preoperative lead time allows the ICU to arrange a bed for hourly flap checks and for in-servicing new nursing staff on free flap monitoring. This was well received, and patients gave positive feedback on the staff. The OR schedulers can schedule nurses and techs who are familiar with the microscope and microsurgery instruments. The micro sets were opened, and the microscope powered on for practice runs a week before the procedures to insure no broken or missing instruments.
High-procedure volume would logically improve efficiency. Although the VA is not likely to become a tertiary center for breast reconstruction, the findings of other high-volume microsurgeons can be applied to improve speed and limit complications. Efforts to limit the OR time included use of preoperative imaging and intraoperative venous couplers. Venous couplers can result in shorter OR time, fewer returns to the OR, and excellent patency rates.15,16 One microsurgeon performed his surgery using only loupe-assisted vision (x 3.5), without use of the microscope. Pannucci and colleagues have recommended this as a way to improve access and OR efficiency.17 Use of the CTA has been found to decrease the rate of partial flap necrosis and improve speed of surgery.18-20
Careful patient selection allowed a hospital stay that averaged 4.5 days and minimized risks for return to the OR. Only patients who were nonsmokers were offered the surgery. Average BMI was 30 to prevent the known operative risks in breast surgery patients who are morbidly obese.21-23 No patients had a history of thromboembolic disease. Most patients were discharged home from the ICU. They eventually returned for elective revisions, second stages, and balancing procedures.
Conclusion
Free flap breast reconstruction can be offered as a treatment option with appropriate patient selection and planning. The most efficient way to provide this procedure within the federal system and to minimize the risk of flap loss and complications is by offering delayed reconstruction, obtaining preoperative CTA imaging, utilizing venous couplers, and frequently communicating with all involved practitioners from the OR to the ICU. This small study provides a good starting point to illustrate that tertiary-care reconstructive surgery can be offered to veterans within the federal system.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System, Gainesville, Florida.
1. Tuggle CT, Patel A, Broer N, Persing JA, Sosa JA, Au AF. Increased hospital volume is associated with improved outcomes following abdominal-based breast reconstruction. J Plast Surg Hand Surg. 2014;48(6):382-388.
2. Shulkin DJ. Beyond the VA crisis — becoming a high-performance network. N Engl J Med. 2016;374(11):1003-1005.
3. Novakovic D, Patel RS, Goldstein DP, Gullane PJ. Salvage of failed free flaps used in head and neck reconstruction. Head Neck Oncol. 2009;1:33.
4. Davison SP, Kessler CM, Al-Attar A. Microvascular free flap failure caused by unrecognized hypercoagulability. Plast Reconstr Surg. 2009;124(2):490-495.
5. Masoomi H, Clark EG, Paydar KZ, et al. Predictive risk factors of free flap thrombosis in breast reconstructive surgery. Microsurgery. 2014;34(8):589-594.
6. O’Neill AC, Haykal S, Bagher S, Zhong T, Hofer S. Predictors and consequences of intraoperative microvascular problems in autologous breast reconstruction. J Plast Reconstr Aesthet Surg. 2016;69(10):1349-1355.
7. Sanati-Mehrizy P, Massengburg BB, Rozehnal JM, Ignargiola MJ, Hernandez Rosa J, Taub PJ. Risk factors leading to free flap failure: analysis from the national surgical quality improvement program database. J Craniofac Surg. 2016;27(8):1956-1964.
8. Myers LL, Sumer BD, Defatta RJ, Minhajuddin A. Free tissue transfer reconstruction of the head and neck at a Veterans Affairs hospital. Head Neck. 2008;30(8):1007-1011.
9. Roslan EJ, Kelly EG, Zain MA, Basiron NH, Imran FH. Immediate simultaneous bilateral breast reconstruction with deep inferior epigastric (DIEP) flap and pedicled transverse rectus abdominis musculocutaneous (TRAM) pedicle flap. Med J Malaysia. 2017;72(1):85-87.
10. Leong M, Chike-Obi CJ, Basu CB, Lee EL, Albo D, Netscher DT. Effective breast reconstruction in female veterans. Am J Surg. 2009;198(5):658-663.
11. Kwok AC, Goodwin IA, Ying J, Agarwal JP. National trends and complication rates after bilateral mastectomy and immediate breast reconstruction from 2005 to 2012. Am J Surg. 2015;210(3):512-516.
12. Ochoa O, Theoharis C, Pisano S, et al. Positive margin re-excision following immediate autologous breast reconstruction: morbidity, cosmetic outcome, and oncologic significance. Aesthet Surg J. 2017; [Epub ahead of print.]
13. Garvey PB, Clemens MW, Hoy AE, et al. Muscle-sparing TRAM flap does not protect breast reconstruction from post-mastectomy radiation damage compared to DIEP flap. Plast Reconstr Surg. 2014;133(2):223-233.
14. Kronowitz SJ. Current status of autologous tissue-based breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg. 2012;130(2):282-292.
15. Fitzgerald O’Connor E, Rozen WM, Chowdhry M, et al. The microvascular anastomotic coupler for venous anastomoses in free flap breast reconstruction improves outcomes. Gland Surg. 2016;5(2):88-92.
16. Jandali S, Wu LC, Vega SJ, Kovach SJ, Serletti JM. 1000 consecutive venous anastomoses using the microvascular anastomotic coupler in breast reconstruction. Plast Reconstr Surg. 2010;125(3):792-798.
17. Pannucci CJ, Basta MN, Kovach SJ, Kanchwala SK, Wu LC, Serletti JM. Loupes-only microsurgery is a safe alternative to the operating microscope: an analysis of 1,649 consecutive free flap breast reconstruction. J Reconstr Microsurg. 2015;31(9):636-642.
18. Teunis T, Heerma van Voss MR, Kon M, van Maurik JF. CT-angiography prior to DIEP flap reconstruction: a systemic review and meta-analysis. Microsurgery. 2013;33(6):496-502.
19. Fitzgerald O’Connor E, Rozen WM, Chowdhry M, Band B, Ramakrishnan VV, Griffiths M. Preoperative computed tomography angiography for planning DIEP flap breast reconstruction reduces operative time and overall complications. Gland Surgery. 2016;5(2):93-98.
20. Malhotra A, Chhaya N, Nsiah-Sarbeng P, Mosahebi A. CT-guided deep inferior epigastric perforator (DIEP) flap localization—better for the patient, the surgeon, and the hospital. Clin Radiol. 2013;68(2):131-138.
21. Ilonzo N, Tsang A, Tsantes S, Estabrook A, Thu Ma AM. Breast reconstruction after mastectomy: a ten-year analysis of trends and immediate postoperative outcomes. Breast. 2017;32:7-12.
22. McAllister P, Teo L, Chin K, Makubate B, Alexander Munnoch D. Bilateral breast reconstruction with abdominal free flaps: a single centre, single surgeon retrospective review of 55 consecutive patients. Plast Surg Int. 2016;2016:6085624.
23. Myung Y, Heo CY. Relationship between obesity and surgical complications after reduction mammoplasty: a systemic literature review and meta-analysis. Aesthet Surg J. 2017;37(3):308-315.
Free flap autologous breast reconstruction is an excellent surgical option for breast reconstruction in select patients. A free flap involves moving skin, fat, and/or muscle from a distant part of the body, based on a named blood supply (pedicle), and attaching it to another blood supply adjacent to the acquired defect. This procedure is particularly useful in areas where local tissue supply is lacking in volume or is damaged due to trauma or radiation. These reconstructions are performed largely in high-volume centers outside the VA because of the required specialized level of surgical training, manpower, and nursing support.1 The Malcom Randall VAMC in Gainesville, Florida, started offering autologous free flap breast reconstruction as an option to select patients in October 2012.
The Malcom Randall VAMC operating room (OR) does not operate 24/7, and the system has limited available OR time and surgical staff compared with the volume of patients requesting care.2 Operative planning for free flap autologous breast reconstruction must occur months ahead of surgery to balance the system limitations with the ability to offer the highest level of care. Planning includes strict patient selection, preoperative imaging, practice runs with OR staff, use of venous couplers, and frequent intensive care unit (ICU) staff in-services. Planning also includes the need to keep surgeries within the allocated OR time to avoid shift changes during critical periods. Frequent and early communication occurs between the surgical scheduler, OR nurses, and the anesthesia and critical care teams.
Studies have found that the best chance of flap salvage in the event of a thrombotic event is a rapid return to the OR.3 It is essential to minimize the risk of emergent returns to the OR because it is not staffed throughout the night. Patient risk factors for perioperative vascular complications include hypercoagulable disorders, peripheral vascular disease, use of the superficial epigastric system, and smoking.4-7
A PubMed search for free flap reconstruction solely within the VA over the past 20 years found 1 article discussing the use of free flaps in head and neck reconstruction which demonstrated an impressive success rate of 93%.8
The object of this study was to assess free flap breast reconstruction results at the Malcolm Randall VAMC to determine whether it is a realistic treatment to offer in the federal system.
Methods
The Malcolm Randall Institutional Review Board approved a retrospective chart review of all autologous free flap breast reconstructions using CPT code 19364, performed from October 2012 to June 2016. Medical records of patients who had a free flap breast reconstruction were queried during that period. Patient age; comorbidities listed on the electronic medical record “problem list;” body mass index (BMI); type of reconstruction (delayed vs immediate); length of surgery; length of stay; and complications over a 30-day period were recorded (Table). The authors looked for documentation of preoperative imaging and unplanned returns to the OR within the 30-day period.
Of 3 full-time VA plastic surgeons on staff during the study period, 2 surgeons had advanced fellowship training in either microsurgery or hand and microsurgery. Plastic surgery fellows and general surgery interns participated in the surgeries and postoperative care. The service had 1 dedicated advanced practice registered nurse involved in the surgical scheduling and perioperative care.
Results
A total of 11 abdominally based free flap breast reconstructions—6 muscle-sparing transverse rectus abdominus musculocutaneous (TRAM) and 5 deep inferior epigastric perforator (DIEP) flaps—were performed in 8 patients during the study period (Figures 1A, 1B, 1C, and 1D). Patient ages ranged from 31 to 58 years with a mean of 45.6 years. Six patients had preoperative computer tomography angiography (CTA) to define the location of the abdominal wall perforators. One muscle-sparing free flap was performed immediately after mastectomy; the other free flaps were performed as delayed reconstructions. Body mass index ranged from 24 to 35, with a mean of 30. All patients reported no tobacco use during the consultation; however, 1 patient later admitted to chewing tobacco. No urinary cotinine confirmation was requested. Two patients had 1 free flap reconstruction and 1 pedicle TRAM. This bilateral combination has been recently described in the literature and was chosen as a reasonable option to balance limited resources with abdominal wall morbidity.9 Operating room time ranged from 7 hours 50 minutes to 13 hours 3 minutes. All patients went to the ICU for hourly flap monitoring.
Length of stay ranged from 4 to 7 days, with a mean of 4.5 days. The longest stay was for a patient who had immediate reconstruction using a pedicle TRAM and muscle-sparing free TRAM. She was not a DIEP candidate because poor perforator quality had been noted during preoperative imaging.
Six patients had documentation of postoperative wound complications. One patient returned to the OR on the elective schedule 3 weeks postoperatively for a partial flap debridement. Her tissue transfer was > 1,000 g, and she required a matching reduction on the other side. There were no complete flap losses or postoperative thrombotic events; no cases went back to the OR emergently.
Discussion
With the number of women veterans steadily increasing, the number of patients in need of breast cancer surgery, including reconstruction, will rise in the VA.10 Fortunately, breast reconstruction is an elective procedure. Immediate breast reconstruction is a popular option because patients can combine surgeries and potentially avoid 2 recovery periods, and a better aesthetic outcome is possible because the skin does not have time to contract. Although immediate reconstruction has been increasing in popularity, it is associated with a higher complication rate.11 Further, reconstruction can be jeopardized if the oncologic plan is changed in the early postoperative period.
Positive margins found after an autologous reconstruction result in a more complicated postoperative course and a higher rate of wound complications.12 Unexpected radiation therapy after autologous reconstruction can severely distort a tissue flap because of fat necrosis, fibrosis, and contraction.13,14 From a practical perspective in the federal system, it is very difficult to coordinate 2 surgeons’ schedules when the system is already struggling to keep up with demand. Splitting the ablative and reconstructive surgery allows the urgent problem (cancer) to be addressed first, ensuring clear margins and allowing the patient to recover and consider all reconstructive options without feeling time pressure.
A large tertiary care center will have staff and equipment redundancy, but this study had to consider limitations in resources. The preoperative lead time allows the ICU to arrange a bed for hourly flap checks and for in-servicing new nursing staff on free flap monitoring. This was well received, and patients gave positive feedback on the staff. The OR schedulers can schedule nurses and techs who are familiar with the microscope and microsurgery instruments. The micro sets were opened, and the microscope powered on for practice runs a week before the procedures to insure no broken or missing instruments.
High-procedure volume would logically improve efficiency. Although the VA is not likely to become a tertiary center for breast reconstruction, the findings of other high-volume microsurgeons can be applied to improve speed and limit complications. Efforts to limit the OR time included use of preoperative imaging and intraoperative venous couplers. Venous couplers can result in shorter OR time, fewer returns to the OR, and excellent patency rates.15,16 One microsurgeon performed his surgery using only loupe-assisted vision (x 3.5), without use of the microscope. Pannucci and colleagues have recommended this as a way to improve access and OR efficiency.17 Use of the CTA has been found to decrease the rate of partial flap necrosis and improve speed of surgery.18-20
Careful patient selection allowed a hospital stay that averaged 4.5 days and minimized risks for return to the OR. Only patients who were nonsmokers were offered the surgery. Average BMI was 30 to prevent the known operative risks in breast surgery patients who are morbidly obese.21-23 No patients had a history of thromboembolic disease. Most patients were discharged home from the ICU. They eventually returned for elective revisions, second stages, and balancing procedures.
Conclusion
Free flap breast reconstruction can be offered as a treatment option with appropriate patient selection and planning. The most efficient way to provide this procedure within the federal system and to minimize the risk of flap loss and complications is by offering delayed reconstruction, obtaining preoperative CTA imaging, utilizing venous couplers, and frequently communicating with all involved practitioners from the OR to the ICU. This small study provides a good starting point to illustrate that tertiary-care reconstructive surgery can be offered to veterans within the federal system.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System, Gainesville, Florida.
Free flap autologous breast reconstruction is an excellent surgical option for breast reconstruction in select patients. A free flap involves moving skin, fat, and/or muscle from a distant part of the body, based on a named blood supply (pedicle), and attaching it to another blood supply adjacent to the acquired defect. This procedure is particularly useful in areas where local tissue supply is lacking in volume or is damaged due to trauma or radiation. These reconstructions are performed largely in high-volume centers outside the VA because of the required specialized level of surgical training, manpower, and nursing support.1 The Malcom Randall VAMC in Gainesville, Florida, started offering autologous free flap breast reconstruction as an option to select patients in October 2012.
The Malcom Randall VAMC operating room (OR) does not operate 24/7, and the system has limited available OR time and surgical staff compared with the volume of patients requesting care.2 Operative planning for free flap autologous breast reconstruction must occur months ahead of surgery to balance the system limitations with the ability to offer the highest level of care. Planning includes strict patient selection, preoperative imaging, practice runs with OR staff, use of venous couplers, and frequent intensive care unit (ICU) staff in-services. Planning also includes the need to keep surgeries within the allocated OR time to avoid shift changes during critical periods. Frequent and early communication occurs between the surgical scheduler, OR nurses, and the anesthesia and critical care teams.
Studies have found that the best chance of flap salvage in the event of a thrombotic event is a rapid return to the OR.3 It is essential to minimize the risk of emergent returns to the OR because it is not staffed throughout the night. Patient risk factors for perioperative vascular complications include hypercoagulable disorders, peripheral vascular disease, use of the superficial epigastric system, and smoking.4-7
A PubMed search for free flap reconstruction solely within the VA over the past 20 years found 1 article discussing the use of free flaps in head and neck reconstruction which demonstrated an impressive success rate of 93%.8
The object of this study was to assess free flap breast reconstruction results at the Malcolm Randall VAMC to determine whether it is a realistic treatment to offer in the federal system.
Methods
The Malcolm Randall Institutional Review Board approved a retrospective chart review of all autologous free flap breast reconstructions using CPT code 19364, performed from October 2012 to June 2016. Medical records of patients who had a free flap breast reconstruction were queried during that period. Patient age; comorbidities listed on the electronic medical record “problem list;” body mass index (BMI); type of reconstruction (delayed vs immediate); length of surgery; length of stay; and complications over a 30-day period were recorded (Table). The authors looked for documentation of preoperative imaging and unplanned returns to the OR within the 30-day period.
Of 3 full-time VA plastic surgeons on staff during the study period, 2 surgeons had advanced fellowship training in either microsurgery or hand and microsurgery. Plastic surgery fellows and general surgery interns participated in the surgeries and postoperative care. The service had 1 dedicated advanced practice registered nurse involved in the surgical scheduling and perioperative care.
Results
A total of 11 abdominally based free flap breast reconstructions—6 muscle-sparing transverse rectus abdominus musculocutaneous (TRAM) and 5 deep inferior epigastric perforator (DIEP) flaps—were performed in 8 patients during the study period (Figures 1A, 1B, 1C, and 1D). Patient ages ranged from 31 to 58 years with a mean of 45.6 years. Six patients had preoperative computer tomography angiography (CTA) to define the location of the abdominal wall perforators. One muscle-sparing free flap was performed immediately after mastectomy; the other free flaps were performed as delayed reconstructions. Body mass index ranged from 24 to 35, with a mean of 30. All patients reported no tobacco use during the consultation; however, 1 patient later admitted to chewing tobacco. No urinary cotinine confirmation was requested. Two patients had 1 free flap reconstruction and 1 pedicle TRAM. This bilateral combination has been recently described in the literature and was chosen as a reasonable option to balance limited resources with abdominal wall morbidity.9 Operating room time ranged from 7 hours 50 minutes to 13 hours 3 minutes. All patients went to the ICU for hourly flap monitoring.
Length of stay ranged from 4 to 7 days, with a mean of 4.5 days. The longest stay was for a patient who had immediate reconstruction using a pedicle TRAM and muscle-sparing free TRAM. She was not a DIEP candidate because poor perforator quality had been noted during preoperative imaging.
Six patients had documentation of postoperative wound complications. One patient returned to the OR on the elective schedule 3 weeks postoperatively for a partial flap debridement. Her tissue transfer was > 1,000 g, and she required a matching reduction on the other side. There were no complete flap losses or postoperative thrombotic events; no cases went back to the OR emergently.
Discussion
With the number of women veterans steadily increasing, the number of patients in need of breast cancer surgery, including reconstruction, will rise in the VA.10 Fortunately, breast reconstruction is an elective procedure. Immediate breast reconstruction is a popular option because patients can combine surgeries and potentially avoid 2 recovery periods, and a better aesthetic outcome is possible because the skin does not have time to contract. Although immediate reconstruction has been increasing in popularity, it is associated with a higher complication rate.11 Further, reconstruction can be jeopardized if the oncologic plan is changed in the early postoperative period.
Positive margins found after an autologous reconstruction result in a more complicated postoperative course and a higher rate of wound complications.12 Unexpected radiation therapy after autologous reconstruction can severely distort a tissue flap because of fat necrosis, fibrosis, and contraction.13,14 From a practical perspective in the federal system, it is very difficult to coordinate 2 surgeons’ schedules when the system is already struggling to keep up with demand. Splitting the ablative and reconstructive surgery allows the urgent problem (cancer) to be addressed first, ensuring clear margins and allowing the patient to recover and consider all reconstructive options without feeling time pressure.
A large tertiary care center will have staff and equipment redundancy, but this study had to consider limitations in resources. The preoperative lead time allows the ICU to arrange a bed for hourly flap checks and for in-servicing new nursing staff on free flap monitoring. This was well received, and patients gave positive feedback on the staff. The OR schedulers can schedule nurses and techs who are familiar with the microscope and microsurgery instruments. The micro sets were opened, and the microscope powered on for practice runs a week before the procedures to insure no broken or missing instruments.
High-procedure volume would logically improve efficiency. Although the VA is not likely to become a tertiary center for breast reconstruction, the findings of other high-volume microsurgeons can be applied to improve speed and limit complications. Efforts to limit the OR time included use of preoperative imaging and intraoperative venous couplers. Venous couplers can result in shorter OR time, fewer returns to the OR, and excellent patency rates.15,16 One microsurgeon performed his surgery using only loupe-assisted vision (x 3.5), without use of the microscope. Pannucci and colleagues have recommended this as a way to improve access and OR efficiency.17 Use of the CTA has been found to decrease the rate of partial flap necrosis and improve speed of surgery.18-20
Careful patient selection allowed a hospital stay that averaged 4.5 days and minimized risks for return to the OR. Only patients who were nonsmokers were offered the surgery. Average BMI was 30 to prevent the known operative risks in breast surgery patients who are morbidly obese.21-23 No patients had a history of thromboembolic disease. Most patients were discharged home from the ICU. They eventually returned for elective revisions, second stages, and balancing procedures.
Conclusion
Free flap breast reconstruction can be offered as a treatment option with appropriate patient selection and planning. The most efficient way to provide this procedure within the federal system and to minimize the risk of flap loss and complications is by offering delayed reconstruction, obtaining preoperative CTA imaging, utilizing venous couplers, and frequently communicating with all involved practitioners from the OR to the ICU. This small study provides a good starting point to illustrate that tertiary-care reconstructive surgery can be offered to veterans within the federal system.
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System, Gainesville, Florida.
1. Tuggle CT, Patel A, Broer N, Persing JA, Sosa JA, Au AF. Increased hospital volume is associated with improved outcomes following abdominal-based breast reconstruction. J Plast Surg Hand Surg. 2014;48(6):382-388.
2. Shulkin DJ. Beyond the VA crisis — becoming a high-performance network. N Engl J Med. 2016;374(11):1003-1005.
3. Novakovic D, Patel RS, Goldstein DP, Gullane PJ. Salvage of failed free flaps used in head and neck reconstruction. Head Neck Oncol. 2009;1:33.
4. Davison SP, Kessler CM, Al-Attar A. Microvascular free flap failure caused by unrecognized hypercoagulability. Plast Reconstr Surg. 2009;124(2):490-495.
5. Masoomi H, Clark EG, Paydar KZ, et al. Predictive risk factors of free flap thrombosis in breast reconstructive surgery. Microsurgery. 2014;34(8):589-594.
6. O’Neill AC, Haykal S, Bagher S, Zhong T, Hofer S. Predictors and consequences of intraoperative microvascular problems in autologous breast reconstruction. J Plast Reconstr Aesthet Surg. 2016;69(10):1349-1355.
7. Sanati-Mehrizy P, Massengburg BB, Rozehnal JM, Ignargiola MJ, Hernandez Rosa J, Taub PJ. Risk factors leading to free flap failure: analysis from the national surgical quality improvement program database. J Craniofac Surg. 2016;27(8):1956-1964.
8. Myers LL, Sumer BD, Defatta RJ, Minhajuddin A. Free tissue transfer reconstruction of the head and neck at a Veterans Affairs hospital. Head Neck. 2008;30(8):1007-1011.
9. Roslan EJ, Kelly EG, Zain MA, Basiron NH, Imran FH. Immediate simultaneous bilateral breast reconstruction with deep inferior epigastric (DIEP) flap and pedicled transverse rectus abdominis musculocutaneous (TRAM) pedicle flap. Med J Malaysia. 2017;72(1):85-87.
10. Leong M, Chike-Obi CJ, Basu CB, Lee EL, Albo D, Netscher DT. Effective breast reconstruction in female veterans. Am J Surg. 2009;198(5):658-663.
11. Kwok AC, Goodwin IA, Ying J, Agarwal JP. National trends and complication rates after bilateral mastectomy and immediate breast reconstruction from 2005 to 2012. Am J Surg. 2015;210(3):512-516.
12. Ochoa O, Theoharis C, Pisano S, et al. Positive margin re-excision following immediate autologous breast reconstruction: morbidity, cosmetic outcome, and oncologic significance. Aesthet Surg J. 2017; [Epub ahead of print.]
13. Garvey PB, Clemens MW, Hoy AE, et al. Muscle-sparing TRAM flap does not protect breast reconstruction from post-mastectomy radiation damage compared to DIEP flap. Plast Reconstr Surg. 2014;133(2):223-233.
14. Kronowitz SJ. Current status of autologous tissue-based breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg. 2012;130(2):282-292.
15. Fitzgerald O’Connor E, Rozen WM, Chowdhry M, et al. The microvascular anastomotic coupler for venous anastomoses in free flap breast reconstruction improves outcomes. Gland Surg. 2016;5(2):88-92.
16. Jandali S, Wu LC, Vega SJ, Kovach SJ, Serletti JM. 1000 consecutive venous anastomoses using the microvascular anastomotic coupler in breast reconstruction. Plast Reconstr Surg. 2010;125(3):792-798.
17. Pannucci CJ, Basta MN, Kovach SJ, Kanchwala SK, Wu LC, Serletti JM. Loupes-only microsurgery is a safe alternative to the operating microscope: an analysis of 1,649 consecutive free flap breast reconstruction. J Reconstr Microsurg. 2015;31(9):636-642.
18. Teunis T, Heerma van Voss MR, Kon M, van Maurik JF. CT-angiography prior to DIEP flap reconstruction: a systemic review and meta-analysis. Microsurgery. 2013;33(6):496-502.
19. Fitzgerald O’Connor E, Rozen WM, Chowdhry M, Band B, Ramakrishnan VV, Griffiths M. Preoperative computed tomography angiography for planning DIEP flap breast reconstruction reduces operative time and overall complications. Gland Surgery. 2016;5(2):93-98.
20. Malhotra A, Chhaya N, Nsiah-Sarbeng P, Mosahebi A. CT-guided deep inferior epigastric perforator (DIEP) flap localization—better for the patient, the surgeon, and the hospital. Clin Radiol. 2013;68(2):131-138.
21. Ilonzo N, Tsang A, Tsantes S, Estabrook A, Thu Ma AM. Breast reconstruction after mastectomy: a ten-year analysis of trends and immediate postoperative outcomes. Breast. 2017;32:7-12.
22. McAllister P, Teo L, Chin K, Makubate B, Alexander Munnoch D. Bilateral breast reconstruction with abdominal free flaps: a single centre, single surgeon retrospective review of 55 consecutive patients. Plast Surg Int. 2016;2016:6085624.
23. Myung Y, Heo CY. Relationship between obesity and surgical complications after reduction mammoplasty: a systemic literature review and meta-analysis. Aesthet Surg J. 2017;37(3):308-315.
1. Tuggle CT, Patel A, Broer N, Persing JA, Sosa JA, Au AF. Increased hospital volume is associated with improved outcomes following abdominal-based breast reconstruction. J Plast Surg Hand Surg. 2014;48(6):382-388.
2. Shulkin DJ. Beyond the VA crisis — becoming a high-performance network. N Engl J Med. 2016;374(11):1003-1005.
3. Novakovic D, Patel RS, Goldstein DP, Gullane PJ. Salvage of failed free flaps used in head and neck reconstruction. Head Neck Oncol. 2009;1:33.
4. Davison SP, Kessler CM, Al-Attar A. Microvascular free flap failure caused by unrecognized hypercoagulability. Plast Reconstr Surg. 2009;124(2):490-495.
5. Masoomi H, Clark EG, Paydar KZ, et al. Predictive risk factors of free flap thrombosis in breast reconstructive surgery. Microsurgery. 2014;34(8):589-594.
6. O’Neill AC, Haykal S, Bagher S, Zhong T, Hofer S. Predictors and consequences of intraoperative microvascular problems in autologous breast reconstruction. J Plast Reconstr Aesthet Surg. 2016;69(10):1349-1355.
7. Sanati-Mehrizy P, Massengburg BB, Rozehnal JM, Ignargiola MJ, Hernandez Rosa J, Taub PJ. Risk factors leading to free flap failure: analysis from the national surgical quality improvement program database. J Craniofac Surg. 2016;27(8):1956-1964.
8. Myers LL, Sumer BD, Defatta RJ, Minhajuddin A. Free tissue transfer reconstruction of the head and neck at a Veterans Affairs hospital. Head Neck. 2008;30(8):1007-1011.
9. Roslan EJ, Kelly EG, Zain MA, Basiron NH, Imran FH. Immediate simultaneous bilateral breast reconstruction with deep inferior epigastric (DIEP) flap and pedicled transverse rectus abdominis musculocutaneous (TRAM) pedicle flap. Med J Malaysia. 2017;72(1):85-87.
10. Leong M, Chike-Obi CJ, Basu CB, Lee EL, Albo D, Netscher DT. Effective breast reconstruction in female veterans. Am J Surg. 2009;198(5):658-663.
11. Kwok AC, Goodwin IA, Ying J, Agarwal JP. National trends and complication rates after bilateral mastectomy and immediate breast reconstruction from 2005 to 2012. Am J Surg. 2015;210(3):512-516.
12. Ochoa O, Theoharis C, Pisano S, et al. Positive margin re-excision following immediate autologous breast reconstruction: morbidity, cosmetic outcome, and oncologic significance. Aesthet Surg J. 2017; [Epub ahead of print.]
13. Garvey PB, Clemens MW, Hoy AE, et al. Muscle-sparing TRAM flap does not protect breast reconstruction from post-mastectomy radiation damage compared to DIEP flap. Plast Reconstr Surg. 2014;133(2):223-233.
14. Kronowitz SJ. Current status of autologous tissue-based breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg. 2012;130(2):282-292.
15. Fitzgerald O’Connor E, Rozen WM, Chowdhry M, et al. The microvascular anastomotic coupler for venous anastomoses in free flap breast reconstruction improves outcomes. Gland Surg. 2016;5(2):88-92.
16. Jandali S, Wu LC, Vega SJ, Kovach SJ, Serletti JM. 1000 consecutive venous anastomoses using the microvascular anastomotic coupler in breast reconstruction. Plast Reconstr Surg. 2010;125(3):792-798.
17. Pannucci CJ, Basta MN, Kovach SJ, Kanchwala SK, Wu LC, Serletti JM. Loupes-only microsurgery is a safe alternative to the operating microscope: an analysis of 1,649 consecutive free flap breast reconstruction. J Reconstr Microsurg. 2015;31(9):636-642.
18. Teunis T, Heerma van Voss MR, Kon M, van Maurik JF. CT-angiography prior to DIEP flap reconstruction: a systemic review and meta-analysis. Microsurgery. 2013;33(6):496-502.
19. Fitzgerald O’Connor E, Rozen WM, Chowdhry M, Band B, Ramakrishnan VV, Griffiths M. Preoperative computed tomography angiography for planning DIEP flap breast reconstruction reduces operative time and overall complications. Gland Surgery. 2016;5(2):93-98.
20. Malhotra A, Chhaya N, Nsiah-Sarbeng P, Mosahebi A. CT-guided deep inferior epigastric perforator (DIEP) flap localization—better for the patient, the surgeon, and the hospital. Clin Radiol. 2013;68(2):131-138.
21. Ilonzo N, Tsang A, Tsantes S, Estabrook A, Thu Ma AM. Breast reconstruction after mastectomy: a ten-year analysis of trends and immediate postoperative outcomes. Breast. 2017;32:7-12.
22. McAllister P, Teo L, Chin K, Makubate B, Alexander Munnoch D. Bilateral breast reconstruction with abdominal free flaps: a single centre, single surgeon retrospective review of 55 consecutive patients. Plast Surg Int. 2016;2016:6085624.
23. Myung Y, Heo CY. Relationship between obesity and surgical complications after reduction mammoplasty: a systemic literature review and meta-analysis. Aesthet Surg J. 2017;37(3):308-315.