User login
Getting the most out of a psychiatric consultation
You’ve been struggling with what to do for a patient who has a significant mental health problem and really would love to have some help. You’re willing to fill out the requisite referral forms and wait your turn for what seems like an excruciating amount of time. But how do you ensure that you, your patient, and the family get the most out of the consultative experience so that everyone’s questions are answered and ongoing care, if needed, can continue?
To be fair, most of the burden of doing a good psychiatric or mental health consultation rests on the consultant, not the person making the request. It is their job to do a thorough evaluation and to identify any additional pieces of information that may be missing before a strong conclusion can be made. That said, however, this is the real world where everyone is busy and few have the time to track down every loose end that may exist regarding a patient’s history.
To that end, here are some recommendations for how to increase the chance that the outcome of your consultation with a child psychiatrist or other mental health professional will be maximally helpful for everyone involved. These tips are based on having been on the receiving end of psychiatric consultations for almost 2 decades and having worked closely with primary care clinicians in a number of different capacities.
The first question to ask yourself, and this may be the most important one of all, is whether or not you really need an actual psychiatrist at all at this stage versus another type of mental health professional. Physicians often are most comfortable dealing with other physicians. If a pediatrician has a question about a patient’s heart, it’s logical to consult a cardiologist. Thus if there’s a question about mental health, the knee-jerk reaction is to consult a psychiatrist. While understandable, looking first to a psychiatrist to help with a patient’s mental health struggles often is not the best move. Psychiatrists make up only one small part of all mental health professionals that also include psychologists, counselors, and clinical social workers, among others. The availability of child and adolescent psychiatrists can been exceedingly sparse while other types of mental health professionals generally are much more available. Moreover, these other types of mental health professionals also can do a great job at assessment and treatment. It is true that most can’t prescribe medication, but best practice recommendations for most of the common mental health diagnoses in youth (anxiety, depression, obsessive compulsive disorder, etc.) explicitly outline that nonpharmacologic treatments should be used first. It breaks my heart every time I do a consult for a family who has waited 6 months only to have me recommend a good therapist they could have seen right off in a week.
Get to know the mental health resources of your community beyond the small number of psychiatrists who might be there. And if you aren’t sure whether or not a referral might best go first to a mental health professional who is not a psychiatrist, just ask. That quick phone call or email might save the family a needless delay in treatment and a lot of aggravation for you.
If you are confident that it is a child & adolescent psychiatrist you want your patient to see, here are some things that will help you get the most out of that consultation and help you avoid the disappointment (for both you and the family) of an evaluation that completely misses the mark.
Select the best site (if you have an option)
Broadly speaking, psychiatrists often can be found in three main areas: academic clinics, private practice, and community mental health centers. While of course there is huge variation of clinicians at each of the sites, some generalizations regarding typical advantages and disadvantages of each setting are probably fair.
Academic settings often have psychiatrists who are local or even national experts on particular topics and can be good places to get evaluations for patients with complicated histories. At the same time, however, these settings typically rely on trainees to do much of the actual work. Many of the residents and fellows are excellent, but they turn over quickly because of graduation and finishing rotations, which can force patients to get to know a lot of different people. Academic centers also can be quite a distance from a family’s home, which often makes follow-up care a challenge (especially when we go back to more in-person visits).
Private practice psychiatrists can provide a more local option and can give families access to experienced clinicians, but many of these practices (especially the ones that take insurance) have practice models that involve seeing a lot of patients for short amounts of time and with less coordination with other types of services.
Finally, psychiatrists working at community mental health centers often work in teams that can help families get access to a lot of useful ancillary services (case management, home supports, etc.) but are part of a public mental health system that sadly is all too often overstretched and underfunded.
If you have choices for where to go for psychiatric services, keeping these things in mind can help you find the best fit for families.
Provide a medication history
While I’m not a big fan of the “what medicine do I try next?” consultation, don’t rely on families to provide this information accurately. Medications are confusing, and I can’t tell you how many times I’ve heard: “I tried the little blue pill and then the big white capsule.” Nobody feels good if the end result of a long consultative process includes a recommendation for a medication that the patient has already tried and failed. Some EMRs now have this information in a way that can be more easily packaged and shared.
State what you are looking for
If you really want the psychiatrist to take over the care of the patient, are just looking for some guidance for what to do next, or are seeking a second opinion for a patient that already works with a psychiatrist, stating so specifically can help tailor the consultation to best address the situation.
Send along past evaluations
Many patients have accumulated detailed psychological or educational evaluations over time that can include some really important information like cognitive profiles, other diagnostic impressions, and past treatment recommendations that may or may not have been implemented. Having these available to the consulting psychiatrist (of course parents need to give permission to send these along) can help the consultant avoid asking redundant questions or recommend things that already have been tried.
Rule outs of medical causes
There are a lot of psychiatric symptoms that can be caused by nonpsychiatric causes. Sometimes, there can be an assumption on the part of the psychiatrist that the pediatrician already has evaluated for these possibilities while the pediatrician assumes that the psychiatrist will work those up if needed. This is how the care of some patients fall through the cracks, and how those unflattering stories of how patients were forced to live with undiagnosed ailments (seizures, encephalopathy, Lyme disease, etc.) for years are generated. Being clear what work-up and tests already have been done to look for other causes can help everyone involved decide what should be done next and who should do it.
Yes, it is true that most of the recommendations specified here involve more work that the quick “behavioral problems: eval and treat” note that may be tempting to write when consulting with a mental health professional, but they will help avoid a lot of headaches for you down the road and, most importantly, get patients and families the timely and comprehensive care they deserve.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Dr. Rettew said he had no relevant financial disclosures. Email Dr. Rettew at [email protected].
You’ve been struggling with what to do for a patient who has a significant mental health problem and really would love to have some help. You’re willing to fill out the requisite referral forms and wait your turn for what seems like an excruciating amount of time. But how do you ensure that you, your patient, and the family get the most out of the consultative experience so that everyone’s questions are answered and ongoing care, if needed, can continue?
To be fair, most of the burden of doing a good psychiatric or mental health consultation rests on the consultant, not the person making the request. It is their job to do a thorough evaluation and to identify any additional pieces of information that may be missing before a strong conclusion can be made. That said, however, this is the real world where everyone is busy and few have the time to track down every loose end that may exist regarding a patient’s history.
To that end, here are some recommendations for how to increase the chance that the outcome of your consultation with a child psychiatrist or other mental health professional will be maximally helpful for everyone involved. These tips are based on having been on the receiving end of psychiatric consultations for almost 2 decades and having worked closely with primary care clinicians in a number of different capacities.
The first question to ask yourself, and this may be the most important one of all, is whether or not you really need an actual psychiatrist at all at this stage versus another type of mental health professional. Physicians often are most comfortable dealing with other physicians. If a pediatrician has a question about a patient’s heart, it’s logical to consult a cardiologist. Thus if there’s a question about mental health, the knee-jerk reaction is to consult a psychiatrist. While understandable, looking first to a psychiatrist to help with a patient’s mental health struggles often is not the best move. Psychiatrists make up only one small part of all mental health professionals that also include psychologists, counselors, and clinical social workers, among others. The availability of child and adolescent psychiatrists can been exceedingly sparse while other types of mental health professionals generally are much more available. Moreover, these other types of mental health professionals also can do a great job at assessment and treatment. It is true that most can’t prescribe medication, but best practice recommendations for most of the common mental health diagnoses in youth (anxiety, depression, obsessive compulsive disorder, etc.) explicitly outline that nonpharmacologic treatments should be used first. It breaks my heart every time I do a consult for a family who has waited 6 months only to have me recommend a good therapist they could have seen right off in a week.
Get to know the mental health resources of your community beyond the small number of psychiatrists who might be there. And if you aren’t sure whether or not a referral might best go first to a mental health professional who is not a psychiatrist, just ask. That quick phone call or email might save the family a needless delay in treatment and a lot of aggravation for you.
If you are confident that it is a child & adolescent psychiatrist you want your patient to see, here are some things that will help you get the most out of that consultation and help you avoid the disappointment (for both you and the family) of an evaluation that completely misses the mark.
Select the best site (if you have an option)
Broadly speaking, psychiatrists often can be found in three main areas: academic clinics, private practice, and community mental health centers. While of course there is huge variation of clinicians at each of the sites, some generalizations regarding typical advantages and disadvantages of each setting are probably fair.
Academic settings often have psychiatrists who are local or even national experts on particular topics and can be good places to get evaluations for patients with complicated histories. At the same time, however, these settings typically rely on trainees to do much of the actual work. Many of the residents and fellows are excellent, but they turn over quickly because of graduation and finishing rotations, which can force patients to get to know a lot of different people. Academic centers also can be quite a distance from a family’s home, which often makes follow-up care a challenge (especially when we go back to more in-person visits).
Private practice psychiatrists can provide a more local option and can give families access to experienced clinicians, but many of these practices (especially the ones that take insurance) have practice models that involve seeing a lot of patients for short amounts of time and with less coordination with other types of services.
Finally, psychiatrists working at community mental health centers often work in teams that can help families get access to a lot of useful ancillary services (case management, home supports, etc.) but are part of a public mental health system that sadly is all too often overstretched and underfunded.
If you have choices for where to go for psychiatric services, keeping these things in mind can help you find the best fit for families.
Provide a medication history
While I’m not a big fan of the “what medicine do I try next?” consultation, don’t rely on families to provide this information accurately. Medications are confusing, and I can’t tell you how many times I’ve heard: “I tried the little blue pill and then the big white capsule.” Nobody feels good if the end result of a long consultative process includes a recommendation for a medication that the patient has already tried and failed. Some EMRs now have this information in a way that can be more easily packaged and shared.
State what you are looking for
If you really want the psychiatrist to take over the care of the patient, are just looking for some guidance for what to do next, or are seeking a second opinion for a patient that already works with a psychiatrist, stating so specifically can help tailor the consultation to best address the situation.
Send along past evaluations
Many patients have accumulated detailed psychological or educational evaluations over time that can include some really important information like cognitive profiles, other diagnostic impressions, and past treatment recommendations that may or may not have been implemented. Having these available to the consulting psychiatrist (of course parents need to give permission to send these along) can help the consultant avoid asking redundant questions or recommend things that already have been tried.
Rule outs of medical causes
There are a lot of psychiatric symptoms that can be caused by nonpsychiatric causes. Sometimes, there can be an assumption on the part of the psychiatrist that the pediatrician already has evaluated for these possibilities while the pediatrician assumes that the psychiatrist will work those up if needed. This is how the care of some patients fall through the cracks, and how those unflattering stories of how patients were forced to live with undiagnosed ailments (seizures, encephalopathy, Lyme disease, etc.) for years are generated. Being clear what work-up and tests already have been done to look for other causes can help everyone involved decide what should be done next and who should do it.
Yes, it is true that most of the recommendations specified here involve more work that the quick “behavioral problems: eval and treat” note that may be tempting to write when consulting with a mental health professional, but they will help avoid a lot of headaches for you down the road and, most importantly, get patients and families the timely and comprehensive care they deserve.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Dr. Rettew said he had no relevant financial disclosures. Email Dr. Rettew at [email protected].
You’ve been struggling with what to do for a patient who has a significant mental health problem and really would love to have some help. You’re willing to fill out the requisite referral forms and wait your turn for what seems like an excruciating amount of time. But how do you ensure that you, your patient, and the family get the most out of the consultative experience so that everyone’s questions are answered and ongoing care, if needed, can continue?
To be fair, most of the burden of doing a good psychiatric or mental health consultation rests on the consultant, not the person making the request. It is their job to do a thorough evaluation and to identify any additional pieces of information that may be missing before a strong conclusion can be made. That said, however, this is the real world where everyone is busy and few have the time to track down every loose end that may exist regarding a patient’s history.
To that end, here are some recommendations for how to increase the chance that the outcome of your consultation with a child psychiatrist or other mental health professional will be maximally helpful for everyone involved. These tips are based on having been on the receiving end of psychiatric consultations for almost 2 decades and having worked closely with primary care clinicians in a number of different capacities.
The first question to ask yourself, and this may be the most important one of all, is whether or not you really need an actual psychiatrist at all at this stage versus another type of mental health professional. Physicians often are most comfortable dealing with other physicians. If a pediatrician has a question about a patient’s heart, it’s logical to consult a cardiologist. Thus if there’s a question about mental health, the knee-jerk reaction is to consult a psychiatrist. While understandable, looking first to a psychiatrist to help with a patient’s mental health struggles often is not the best move. Psychiatrists make up only one small part of all mental health professionals that also include psychologists, counselors, and clinical social workers, among others. The availability of child and adolescent psychiatrists can been exceedingly sparse while other types of mental health professionals generally are much more available. Moreover, these other types of mental health professionals also can do a great job at assessment and treatment. It is true that most can’t prescribe medication, but best practice recommendations for most of the common mental health diagnoses in youth (anxiety, depression, obsessive compulsive disorder, etc.) explicitly outline that nonpharmacologic treatments should be used first. It breaks my heart every time I do a consult for a family who has waited 6 months only to have me recommend a good therapist they could have seen right off in a week.
Get to know the mental health resources of your community beyond the small number of psychiatrists who might be there. And if you aren’t sure whether or not a referral might best go first to a mental health professional who is not a psychiatrist, just ask. That quick phone call or email might save the family a needless delay in treatment and a lot of aggravation for you.
If you are confident that it is a child & adolescent psychiatrist you want your patient to see, here are some things that will help you get the most out of that consultation and help you avoid the disappointment (for both you and the family) of an evaluation that completely misses the mark.
Select the best site (if you have an option)
Broadly speaking, psychiatrists often can be found in three main areas: academic clinics, private practice, and community mental health centers. While of course there is huge variation of clinicians at each of the sites, some generalizations regarding typical advantages and disadvantages of each setting are probably fair.
Academic settings often have psychiatrists who are local or even national experts on particular topics and can be good places to get evaluations for patients with complicated histories. At the same time, however, these settings typically rely on trainees to do much of the actual work. Many of the residents and fellows are excellent, but they turn over quickly because of graduation and finishing rotations, which can force patients to get to know a lot of different people. Academic centers also can be quite a distance from a family’s home, which often makes follow-up care a challenge (especially when we go back to more in-person visits).
Private practice psychiatrists can provide a more local option and can give families access to experienced clinicians, but many of these practices (especially the ones that take insurance) have practice models that involve seeing a lot of patients for short amounts of time and with less coordination with other types of services.
Finally, psychiatrists working at community mental health centers often work in teams that can help families get access to a lot of useful ancillary services (case management, home supports, etc.) but are part of a public mental health system that sadly is all too often overstretched and underfunded.
If you have choices for where to go for psychiatric services, keeping these things in mind can help you find the best fit for families.
Provide a medication history
While I’m not a big fan of the “what medicine do I try next?” consultation, don’t rely on families to provide this information accurately. Medications are confusing, and I can’t tell you how many times I’ve heard: “I tried the little blue pill and then the big white capsule.” Nobody feels good if the end result of a long consultative process includes a recommendation for a medication that the patient has already tried and failed. Some EMRs now have this information in a way that can be more easily packaged and shared.
State what you are looking for
If you really want the psychiatrist to take over the care of the patient, are just looking for some guidance for what to do next, or are seeking a second opinion for a patient that already works with a psychiatrist, stating so specifically can help tailor the consultation to best address the situation.
Send along past evaluations
Many patients have accumulated detailed psychological or educational evaluations over time that can include some really important information like cognitive profiles, other diagnostic impressions, and past treatment recommendations that may or may not have been implemented. Having these available to the consulting psychiatrist (of course parents need to give permission to send these along) can help the consultant avoid asking redundant questions or recommend things that already have been tried.
Rule outs of medical causes
There are a lot of psychiatric symptoms that can be caused by nonpsychiatric causes. Sometimes, there can be an assumption on the part of the psychiatrist that the pediatrician already has evaluated for these possibilities while the pediatrician assumes that the psychiatrist will work those up if needed. This is how the care of some patients fall through the cracks, and how those unflattering stories of how patients were forced to live with undiagnosed ailments (seizures, encephalopathy, Lyme disease, etc.) for years are generated. Being clear what work-up and tests already have been done to look for other causes can help everyone involved decide what should be done next and who should do it.
Yes, it is true that most of the recommendations specified here involve more work that the quick “behavioral problems: eval and treat” note that may be tempting to write when consulting with a mental health professional, but they will help avoid a lot of headaches for you down the road and, most importantly, get patients and families the timely and comprehensive care they deserve.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Dr. Rettew said he had no relevant financial disclosures. Email Dr. Rettew at [email protected].
Pediatricians take on more mental health care
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
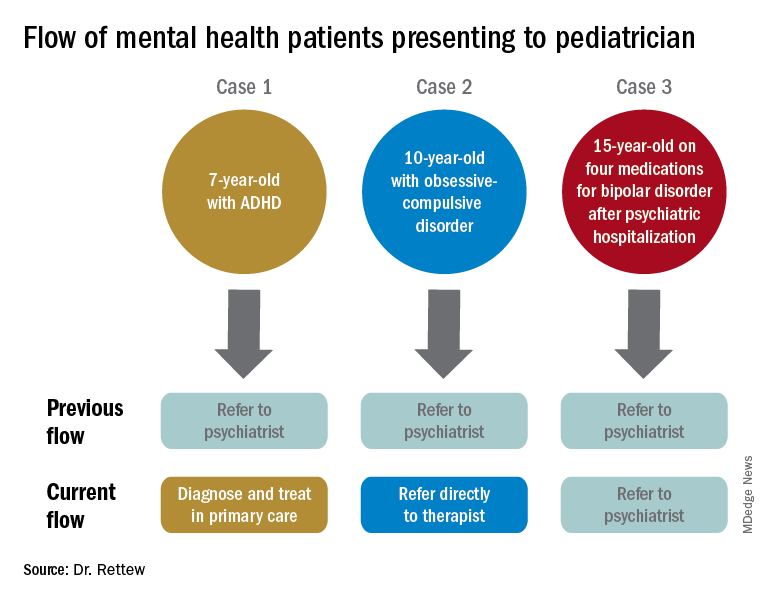
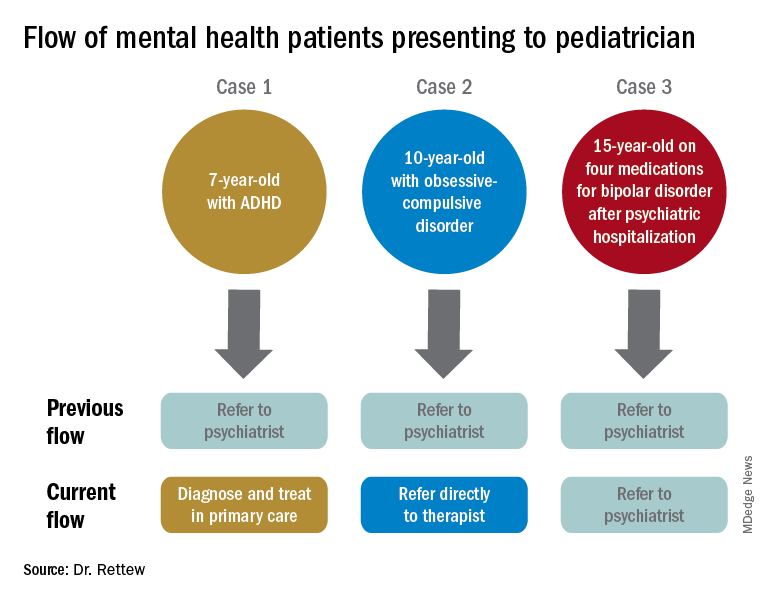
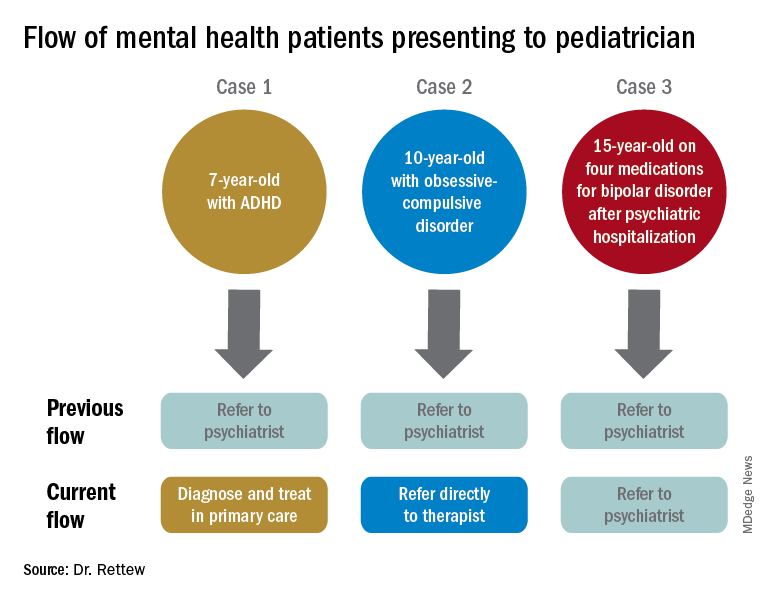
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected]. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected]. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Assessment and treatment of many of the more common behavioral disorders in childhood, such as ADHD and anxiety, should be considered within a pediatrician’s scope of practice, a stance made very clear by a recent policy statement published by the American Academy of Pediatrics entitled “Mental health competencies for pediatric practice.”1 These competencies include medication treatment. As stated in the article, “certain disorders (ADHD, common anxiety disorders, depression), if associated with no more than moderate impairment, are amenable to primary care medication management because there are indicated medications with a well-established safety profile.”
This shift to shared ownership when it comes to mental health care is likely coming from multiple sources, not the least of them being necessity and an acknowledgment that there simply aren’t enough psychiatrists to take over the mental health care of every youth with a diagnosable psychiatric disorder. While the number of child and adolescent psychiatrists remains relatively flat, the youth suicide rate is rising, as are the numbers presenting to emergency departments in crisis – all for reasons still to be fully understood. And these trends all are occurring as the medical community overall is appreciating more and more that good mental health is a cornerstone of all health.
The response from the pediatric community, whether it be because of personal conviction or simply a lack of options, largely has been to step up to the plate and take on these new responsibilities and challenges while trying to get up to speed with the latest information about mental health best practices. From my own experience doing evaluations and consultations from area primary care clinicians for over 15 years, the shift is noticeable. The typical patient now coming in has already seen a mental health counselor and tried at least one medication, while evaluations for diagnosis and treatment recommendations for things like uncomplicated and treatment-naive ADHD symptoms, for example, are becoming much more infrequent – although still far from extinct.
Nevertheless, there remain concerns about the extent of these new charges. Joe Nasca, MD, an experienced pediatrician who has been practicing in rural Vermont for decades, is worried that there is simply too much already for pediatricians to know and do to be able to add extensive mental health care. “There is so much to know in general peds [pediatrics] that I would guess a year or more of additional residency and experience would adequately prepare me to take this on,” he said in an interview. In comparing psychiatric care to other specialties, Dr. Nasca went on to say that, “I would not presume to treat chronic renal failure without the help of a nephrologist or a dilated aortic arch without a cardiologist.”
In a similar vein, however, it also is true that a significant percentage of children presenting to pediatricians for orthopedic problems, infections, asthma, and rashes are managed without referrals to specialists. The right balance, of course, will vary from clinician to clinician based on that pediatrician’s level of interest, experience, and available resources in the community. The AAP position papers don’t mandate or even encourage the notion that all pediatricians need to be at the same place when it comes to competency in assessment and treatment of mental health problems, although it is probably fair to say that there is a push for the pediatric community as a whole to raise the collective bar at least a notch or two.
In response, the mental health community has moved to support the primary care community in their expanded role. These efforts have taken many forms, most notably the model of integrated care, in which mental health clinicians of various types see patients in primary care offices rather than making patients come to them. There also are new consultation programs that provide easy access to a child psychiatrist or other mental health professional for case-related questions delivered by phone, email, or for single in-person consultations. Additional training and educational offerings also are now available for pediatricians either in training and for those already in practice. These initiatives are bolstered by research showing that, not only can good mental health care be delivered in pediatric settings, but there are cost savings that can be realized, particularly for nonpsychiatric medical care.2 Despite these promising leads, however, there will remain some for whom anything less than the increased availability of a psychiatrist to “take over” a patient’s mental health care will be seen as a falling short of the clinical need.
To illustrate how things have and continue to change, consider the following three common clinical scenarios that generally present to a pediatrician:
- New presentation of ADHD symptoms.
- Anxiety or obsessive-compulsive problems.
- Return of a patient who has been psychiatrically hospitalized and now is taking multiple medications.
In the past, all three cases often would have resulted in a referral to a psychiatrist. Today, however, it is quite likely that only one of these cases would be referred because ADHD could be well diagnosed and managed within the primary care setting, and problems like anxiety and obsessive-compulsive disorder are sent first not to a psychiatrist but to a non-MD psychotherapist.
Moving forward, today’s pediatricians are expected to do more for the mental health care of patients themselves instead of referring to a psychiatrist. Most already do, despite having had little in the way of formal training. As the evidence grows that the promotion of mental well-being can be a key to future overall health, as well as to the cost of future health care, there are many reasons to be optimistic that support for pediatricians and collaborative care models for clinicians trying to fulfill these new responsibilities will get only stronger.
References
1. Pediatrics. 2019 Nov;144(5). pii: e20192757.
2. Pediatrics. 2019 Jul;144(1). pii: e20183243.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected]. Looking for more mental health training? Attend the 14th annual Child Psychiatry in Primary Care conference in Burlington on May 8, 2020 (http://www.med.uvm.edu/cme/conferences).
Consider caffeine effects on children and adolescents
Less clinical attention has been paid to caffeine lately as the medical community works to overcome the negative effects of substances such as opiates and cannabis. Quietly, however, caffeine continues to be widely consumed among children and adolescents, and its use often flies under the radar for pediatricians who have so many other topics to address. To help clinicians decide whether more focus on caffeine use is needed, a review was published in the Journal of the American Academy of Child & Adolescent Psychiatry (2019;58[1]:36-45). A synopsis of this paper which summarizes 90 individual studies on caffeine use in children and adolescents is provided here.
Caffeine usage in children and adolescents
Caffeine continues to be one of the most commonly used substances in youth, with about 75% of older children and adolescents consuming it regularly, often at an average dose of about 25 mg/day for children aged 6-11 years and 50 mg/day for adolescents. Because most people have trouble quickly converting commonly used products into milligrams of caffeine, the following guide can be useful:
- Soda (12 oz). About 40 mg caffeine.
- Coffee (8 oz). About 100 mg caffeine.
- Tea (8 oz). About 48 mg caffeine.
- Energy drinks (12 oz). About 150 mg caffeine plus, with 5-Hour Energy being around 215 mg caffeine, according to a Consumer Reports study.
It is important to pay attention to the serving size, as the actual volume consumed of products like coffee or soft drinks often are much higher.
With regards to caffeine trends over time, a surprising observation is that total caffeine consumption among youth over the past decade or so looks relatively flat and may even be decreasing. This trend has occurred despite the aggressive marketing to youth of many energy drinks that contain high amounts of caffeine. In many ways, the pattern of caffeine use fits with what we know about substance use in general in adolescents, with rates dropping for many commonly used substances – with the exception of cannabis.
Effects of caffeine
As many know, caffeine is a stimulant and is known to increase arousal, alertness, and amount of motor behavior. While many youth drink caffeine in an effort to improve cognitive performance, the evidence that it does so directly is modest. There are some studies that show improvements on some cognitive tests when children take moderate doses of caffeine, but these effects tend to be most pronounced for kids who are more naive to caffeine at baseline. Of course, caffeine also can temporarily reduce feelings of fatigue and sleepiness.
Anecdotally, many youth and parents will report that caffeine is a way to “self-medicate” various symptoms of ADHD. While many will report some benefit, there is a surprising lack of rigorous data about the effects of caffeine for youth who meet criteria for ADHD, according to this review.
There also are some well-known negative effects of caffeine use. One of the most important ones is that caffeine can interfere with sleep onset, thereby inducing a cycle that reinforces more caffeine use in the day in an effort to compensate for poor sleep at night. A less obvious negative effect that has been documented is that caffeine added to sweetened beverages can increase consumption of similar sugary foods, even if they don’t have caffeine.
A number of adverse effects have been observed when youth consume caffeine at excessive doses, which tend to be around a threshold of 400 mg/day for teens and about 100 mg/day for younger children. These can include both behavioral and nonbehavioral changes such as agitation or irritability, anxiety, heart arrhythmias, and hypertension. Concern over high caffeine intake also was raised in relation to a number of cases of sudden death, although these events fortunately are rare. The review mentions that one factor that could increase the risk of a serious medical event related to caffeine use is the presence of an underlying cardiac problem which may go undetected until a negative outcome occurs. In thinking about these risks associated with “excessive” caffeine consumption, it can be important to go back to the guides and see just how easily an adolescent can get to a level of 400 mg or more. A couple large cups of coffee per day or two to three specific “energy-boosting” products can be all that it takes.
There also are a few large longitudinal studies that have shown a significant association between increased caffeine consumption and future problems with anger, aggression, risky sexual behavior, and substance use. Energy drinks, which can deliver a lot of caffeine quickly, were singled out as particularly problematic in some of these studies, although these naturalistic studies are unable to determine causation, and it also is possible that teens who are already prone towards behavioral problems tend to consume more caffeine. However, the review also mentions animal studies that have demonstrated that caffeine may prime the brain to use other substances like amphetamines or cocaine. Finally, another concern raised about energy drinks in particular is that they also often contain other substances which may have similar physiological effects but are relatively untested when it comes to safety.
Conclusions
This review, like the current position of the Food and Drug Administration, considers caffeine as generally safe at low doses because there does not appear to be much evidence that low or moderate use in youth leads to significant problems. The conclusion changes, however, with higher levels of consumption, as more frequent and more serious risks are encountered. The article recommends that both parents and doctors be more vigilant in monitoring the amount of caffeine that a child consumes as well as the timing of that use during the day. Some quick calculations can be done to give adolescents and their parents an estimate of their caffeine use in milligrams. And while caffeine may not rise to the level of public health concern as substances like opiates or alcohol, there is evidence that it can cause some real problems in children and teens, especially in higher amounts, and thus shouldn’t be given a total pass by parents and doctors alike.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at [email protected]. Follow him on Twitter @PediPsych. Looking for more mental health training? Attend the 13th annual Child Psychiatry in Primary Care conference in Burlington, Vt., May 3, 2019 (http://www.med.uvm.edu/cme/conferences).
Less clinical attention has been paid to caffeine lately as the medical community works to overcome the negative effects of substances such as opiates and cannabis. Quietly, however, caffeine continues to be widely consumed among children and adolescents, and its use often flies under the radar for pediatricians who have so many other topics to address. To help clinicians decide whether more focus on caffeine use is needed, a review was published in the Journal of the American Academy of Child & Adolescent Psychiatry (2019;58[1]:36-45). A synopsis of this paper which summarizes 90 individual studies on caffeine use in children and adolescents is provided here.
Caffeine usage in children and adolescents
Caffeine continues to be one of the most commonly used substances in youth, with about 75% of older children and adolescents consuming it regularly, often at an average dose of about 25 mg/day for children aged 6-11 years and 50 mg/day for adolescents. Because most people have trouble quickly converting commonly used products into milligrams of caffeine, the following guide can be useful:
- Soda (12 oz). About 40 mg caffeine.
- Coffee (8 oz). About 100 mg caffeine.
- Tea (8 oz). About 48 mg caffeine.
- Energy drinks (12 oz). About 150 mg caffeine plus, with 5-Hour Energy being around 215 mg caffeine, according to a Consumer Reports study.
It is important to pay attention to the serving size, as the actual volume consumed of products like coffee or soft drinks often are much higher.
With regards to caffeine trends over time, a surprising observation is that total caffeine consumption among youth over the past decade or so looks relatively flat and may even be decreasing. This trend has occurred despite the aggressive marketing to youth of many energy drinks that contain high amounts of caffeine. In many ways, the pattern of caffeine use fits with what we know about substance use in general in adolescents, with rates dropping for many commonly used substances – with the exception of cannabis.
Effects of caffeine
As many know, caffeine is a stimulant and is known to increase arousal, alertness, and amount of motor behavior. While many youth drink caffeine in an effort to improve cognitive performance, the evidence that it does so directly is modest. There are some studies that show improvements on some cognitive tests when children take moderate doses of caffeine, but these effects tend to be most pronounced for kids who are more naive to caffeine at baseline. Of course, caffeine also can temporarily reduce feelings of fatigue and sleepiness.
Anecdotally, many youth and parents will report that caffeine is a way to “self-medicate” various symptoms of ADHD. While many will report some benefit, there is a surprising lack of rigorous data about the effects of caffeine for youth who meet criteria for ADHD, according to this review.
There also are some well-known negative effects of caffeine use. One of the most important ones is that caffeine can interfere with sleep onset, thereby inducing a cycle that reinforces more caffeine use in the day in an effort to compensate for poor sleep at night. A less obvious negative effect that has been documented is that caffeine added to sweetened beverages can increase consumption of similar sugary foods, even if they don’t have caffeine.
A number of adverse effects have been observed when youth consume caffeine at excessive doses, which tend to be around a threshold of 400 mg/day for teens and about 100 mg/day for younger children. These can include both behavioral and nonbehavioral changes such as agitation or irritability, anxiety, heart arrhythmias, and hypertension. Concern over high caffeine intake also was raised in relation to a number of cases of sudden death, although these events fortunately are rare. The review mentions that one factor that could increase the risk of a serious medical event related to caffeine use is the presence of an underlying cardiac problem which may go undetected until a negative outcome occurs. In thinking about these risks associated with “excessive” caffeine consumption, it can be important to go back to the guides and see just how easily an adolescent can get to a level of 400 mg or more. A couple large cups of coffee per day or two to three specific “energy-boosting” products can be all that it takes.
There also are a few large longitudinal studies that have shown a significant association between increased caffeine consumption and future problems with anger, aggression, risky sexual behavior, and substance use. Energy drinks, which can deliver a lot of caffeine quickly, were singled out as particularly problematic in some of these studies, although these naturalistic studies are unable to determine causation, and it also is possible that teens who are already prone towards behavioral problems tend to consume more caffeine. However, the review also mentions animal studies that have demonstrated that caffeine may prime the brain to use other substances like amphetamines or cocaine. Finally, another concern raised about energy drinks in particular is that they also often contain other substances which may have similar physiological effects but are relatively untested when it comes to safety.
Conclusions
This review, like the current position of the Food and Drug Administration, considers caffeine as generally safe at low doses because there does not appear to be much evidence that low or moderate use in youth leads to significant problems. The conclusion changes, however, with higher levels of consumption, as more frequent and more serious risks are encountered. The article recommends that both parents and doctors be more vigilant in monitoring the amount of caffeine that a child consumes as well as the timing of that use during the day. Some quick calculations can be done to give adolescents and their parents an estimate of their caffeine use in milligrams. And while caffeine may not rise to the level of public health concern as substances like opiates or alcohol, there is evidence that it can cause some real problems in children and teens, especially in higher amounts, and thus shouldn’t be given a total pass by parents and doctors alike.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at [email protected]. Follow him on Twitter @PediPsych. Looking for more mental health training? Attend the 13th annual Child Psychiatry in Primary Care conference in Burlington, Vt., May 3, 2019 (http://www.med.uvm.edu/cme/conferences).
Less clinical attention has been paid to caffeine lately as the medical community works to overcome the negative effects of substances such as opiates and cannabis. Quietly, however, caffeine continues to be widely consumed among children and adolescents, and its use often flies under the radar for pediatricians who have so many other topics to address. To help clinicians decide whether more focus on caffeine use is needed, a review was published in the Journal of the American Academy of Child & Adolescent Psychiatry (2019;58[1]:36-45). A synopsis of this paper which summarizes 90 individual studies on caffeine use in children and adolescents is provided here.
Caffeine usage in children and adolescents
Caffeine continues to be one of the most commonly used substances in youth, with about 75% of older children and adolescents consuming it regularly, often at an average dose of about 25 mg/day for children aged 6-11 years and 50 mg/day for adolescents. Because most people have trouble quickly converting commonly used products into milligrams of caffeine, the following guide can be useful:
- Soda (12 oz). About 40 mg caffeine.
- Coffee (8 oz). About 100 mg caffeine.
- Tea (8 oz). About 48 mg caffeine.
- Energy drinks (12 oz). About 150 mg caffeine plus, with 5-Hour Energy being around 215 mg caffeine, according to a Consumer Reports study.
It is important to pay attention to the serving size, as the actual volume consumed of products like coffee or soft drinks often are much higher.
With regards to caffeine trends over time, a surprising observation is that total caffeine consumption among youth over the past decade or so looks relatively flat and may even be decreasing. This trend has occurred despite the aggressive marketing to youth of many energy drinks that contain high amounts of caffeine. In many ways, the pattern of caffeine use fits with what we know about substance use in general in adolescents, with rates dropping for many commonly used substances – with the exception of cannabis.
Effects of caffeine
As many know, caffeine is a stimulant and is known to increase arousal, alertness, and amount of motor behavior. While many youth drink caffeine in an effort to improve cognitive performance, the evidence that it does so directly is modest. There are some studies that show improvements on some cognitive tests when children take moderate doses of caffeine, but these effects tend to be most pronounced for kids who are more naive to caffeine at baseline. Of course, caffeine also can temporarily reduce feelings of fatigue and sleepiness.
Anecdotally, many youth and parents will report that caffeine is a way to “self-medicate” various symptoms of ADHD. While many will report some benefit, there is a surprising lack of rigorous data about the effects of caffeine for youth who meet criteria for ADHD, according to this review.
There also are some well-known negative effects of caffeine use. One of the most important ones is that caffeine can interfere with sleep onset, thereby inducing a cycle that reinforces more caffeine use in the day in an effort to compensate for poor sleep at night. A less obvious negative effect that has been documented is that caffeine added to sweetened beverages can increase consumption of similar sugary foods, even if they don’t have caffeine.
A number of adverse effects have been observed when youth consume caffeine at excessive doses, which tend to be around a threshold of 400 mg/day for teens and about 100 mg/day for younger children. These can include both behavioral and nonbehavioral changes such as agitation or irritability, anxiety, heart arrhythmias, and hypertension. Concern over high caffeine intake also was raised in relation to a number of cases of sudden death, although these events fortunately are rare. The review mentions that one factor that could increase the risk of a serious medical event related to caffeine use is the presence of an underlying cardiac problem which may go undetected until a negative outcome occurs. In thinking about these risks associated with “excessive” caffeine consumption, it can be important to go back to the guides and see just how easily an adolescent can get to a level of 400 mg or more. A couple large cups of coffee per day or two to three specific “energy-boosting” products can be all that it takes.
There also are a few large longitudinal studies that have shown a significant association between increased caffeine consumption and future problems with anger, aggression, risky sexual behavior, and substance use. Energy drinks, which can deliver a lot of caffeine quickly, were singled out as particularly problematic in some of these studies, although these naturalistic studies are unable to determine causation, and it also is possible that teens who are already prone towards behavioral problems tend to consume more caffeine. However, the review also mentions animal studies that have demonstrated that caffeine may prime the brain to use other substances like amphetamines or cocaine. Finally, another concern raised about energy drinks in particular is that they also often contain other substances which may have similar physiological effects but are relatively untested when it comes to safety.
Conclusions
This review, like the current position of the Food and Drug Administration, considers caffeine as generally safe at low doses because there does not appear to be much evidence that low or moderate use in youth leads to significant problems. The conclusion changes, however, with higher levels of consumption, as more frequent and more serious risks are encountered. The article recommends that both parents and doctors be more vigilant in monitoring the amount of caffeine that a child consumes as well as the timing of that use during the day. Some quick calculations can be done to give adolescents and their parents an estimate of their caffeine use in milligrams. And while caffeine may not rise to the level of public health concern as substances like opiates or alcohol, there is evidence that it can cause some real problems in children and teens, especially in higher amounts, and thus shouldn’t be given a total pass by parents and doctors alike.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at [email protected]. Follow him on Twitter @PediPsych. Looking for more mental health training? Attend the 13th annual Child Psychiatry in Primary Care conference in Burlington, Vt., May 3, 2019 (http://www.med.uvm.edu/cme/conferences).
Anxiety disorders: Psychopharmacologic treatment update
Anxiety disorders, including separation anxiety disorder, social anxiety disorder, and generalized anxiety disorder, are some of the most common psychiatric conditions of childhood and adolescence, affecting up to 20% of youth.1 Patients commonly present with a mix of symptoms that often span multiple anxiety disorder diagnoses. While this pattern can present somewhat of a diagnostic conundrum, it can be reassuring to know that such constellations of symptoms are the rule rather than the exception. Further, given that both the pharmacologic and nonpharmacologic treatment strategies don’t change much among the various anxiety disorders, the lack of a definitive single diagnosis should not delay intervention. Be alert to the possibility that anxiety and anxiety disorders can be the engine that drives what on the surface appears to be more disruptive and oppositional behavior.
Although medications can be a useful part of treatment, they are not recommended as a stand-alone intervention. Nonpharmacologic treatments generally should be tried before medications are considered. Among the different types of psychotherapy, cognitive-behavioral therapy (CBT) has the most empirical support from research trials, although other modalities such as mindfulness-based treatments show some promise. As anxiety disorders often run in families, it also can be very useful to explore the possibility that one or more parents also struggle with an anxiety disorder, which, if untreated, might complicate the child’s course.
With regard to medications, it is being increasingly appreciated that, despite SSRIs being most popularly known as antidepressants, these medications actually may be as efficacious or even more efficacious in the management of anxiety disorders. This class remains the cornerstone of medication treatment, and a brief review of current options follows.
SSRIs and SNRIs
A 2015 meta-analysis that examined nine randomized controlled trials of SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs) for pediatric anxiety disorders concluded that these agents provided a benefit of modest effect size. No significant increase in treatment-emergent suicidality was found, and the medications were generally well tolerated.2 This analysis also found some evidence that greater efficacy was related to a medication with more specific serotonergic properties, suggesting improved response with “true” SSRIs versus SNRIs such as venlafaxine and duloxetine. One major study using sertraline found that, at least in the short term, combined use of sertraline with CBT resulted in better efficacy than either treatment alone.3 Dosing of SSRIs should start low: A general rule is to begin at half of the smallest dosage made, depending on the age and size of the patient. One question that often comes up after a successful trial is how long to continue the medications. A recent meta-analysis in adults concluded that there was evidence that stopping medication prior to 1 year resulted in an increased risk of relapse with little to guide clinicians after that 1-year mark.4
Benzodiazepines
Even though benzodiazepines have been around for a long time, data supporting their efficacy and safety in pediatric populations remain extremely limited, and what has been reported has not been particularly positive. Thus, most experts do not suggest using benzodiazepines for anxiety disorders, with the exception of helping children through single or rare events, such as medical procedures or enabling an adolescent who has been fearful of attending school to get to the building on the first day back after a long absence.
Guanfacine
In a recent exploratory trial of guanfacine for children with mixed anxiety disorders,5 the medication was well tolerated overall but did not result in statistically significant improvement relative to placebo on primary anxiety rating scales. However, a higher number of children were rated as improved on a clinician-rated scale. This medication is usually started at 0.5 mg/day and increased as tolerated, while checking vital signs, to a maximum of 4 mg/day.
Atomoxetine
A randomized control trial of pediatric patients with both ADHD and an anxiety disorder showed reductions in both symptom domains with atomoxetine dosed at an average of 1.3 mg/kg per day.6 There is little evidence to suggest its use in primary anxiety disorders without comorbid ADHD.
Buspirone
This 5-hydroxytryptamine 1a agonist has Food and Drug Administration approval for generalized anxiety disorder in adults and is generally well tolerated. Unfortunately, two randomized controlled studies in children and adolescents did not find statistically significant improvement relative to placebo, although some methodological problems may have played a role.7
Antipsychotics
Although sometimes used to augment an SSRI in adult anxiety disorders, there are little data to support the use of antipsychotics in pediatric populations, especially given the antecedent risks of the drugs.
Summary
Pharmacotherapy for anxiety disorders often includes the advice that, if medications are indicated in conjunction with psychotherapy, to start with an SSRI; and if that is not effective to try a different one.7 An SNRI such as venlafaxine or duloxetine may then be a third-line alternative, although for youth with comorbid ADHD, consideration of either atomoxetine or guanfacine is also reasonable. Beyond that point, there unfortunately are little systematic data to guide pharmacologic decision making, and increased potential risks of other classes of medications suggest the need for caution and consultation.
Looking for more mental health training? Attend the 12th annual Child Psychiatry in Primary Care conference in Burlington, on May 4, 2018,organized by the University of Vermont with Dr. Rettew as course director. Go to http://www.med.uvm.edu/cme/conferences.
References
1. Merikangas KR et al. J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.
2. Strawn JR et al. Depress Anxiety. 2015 Mar;32(3):149-57.
3. Walkup J et al. N Engl J Med. 2008 Dec 25;359(26):2753-66.
4. Batelaan N et al. BMJ. 2017 Sep 13;358:j3927.
5. Strawn JR et al. J Child Adolesc Psychopharm. 2017 Feb;27(1): 29-37..
6. Geller D et al. J Am Acad Child Adolesc Psychiatry. 2007 Sep;46(9):1119-27.
7. Strawn JR et al. J Child Adolesc Psychopharm. 2017 Feb;28(1): 2-9.
Anxiety disorders, including separation anxiety disorder, social anxiety disorder, and generalized anxiety disorder, are some of the most common psychiatric conditions of childhood and adolescence, affecting up to 20% of youth.1 Patients commonly present with a mix of symptoms that often span multiple anxiety disorder diagnoses. While this pattern can present somewhat of a diagnostic conundrum, it can be reassuring to know that such constellations of symptoms are the rule rather than the exception. Further, given that both the pharmacologic and nonpharmacologic treatment strategies don’t change much among the various anxiety disorders, the lack of a definitive single diagnosis should not delay intervention. Be alert to the possibility that anxiety and anxiety disorders can be the engine that drives what on the surface appears to be more disruptive and oppositional behavior.
Although medications can be a useful part of treatment, they are not recommended as a stand-alone intervention. Nonpharmacologic treatments generally should be tried before medications are considered. Among the different types of psychotherapy, cognitive-behavioral therapy (CBT) has the most empirical support from research trials, although other modalities such as mindfulness-based treatments show some promise. As anxiety disorders often run in families, it also can be very useful to explore the possibility that one or more parents also struggle with an anxiety disorder, which, if untreated, might complicate the child’s course.
With regard to medications, it is being increasingly appreciated that, despite SSRIs being most popularly known as antidepressants, these medications actually may be as efficacious or even more efficacious in the management of anxiety disorders. This class remains the cornerstone of medication treatment, and a brief review of current options follows.
SSRIs and SNRIs
A 2015 meta-analysis that examined nine randomized controlled trials of SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs) for pediatric anxiety disorders concluded that these agents provided a benefit of modest effect size. No significant increase in treatment-emergent suicidality was found, and the medications were generally well tolerated.2 This analysis also found some evidence that greater efficacy was related to a medication with more specific serotonergic properties, suggesting improved response with “true” SSRIs versus SNRIs such as venlafaxine and duloxetine. One major study using sertraline found that, at least in the short term, combined use of sertraline with CBT resulted in better efficacy than either treatment alone.3 Dosing of SSRIs should start low: A general rule is to begin at half of the smallest dosage made, depending on the age and size of the patient. One question that often comes up after a successful trial is how long to continue the medications. A recent meta-analysis in adults concluded that there was evidence that stopping medication prior to 1 year resulted in an increased risk of relapse with little to guide clinicians after that 1-year mark.4
Benzodiazepines
Even though benzodiazepines have been around for a long time, data supporting their efficacy and safety in pediatric populations remain extremely limited, and what has been reported has not been particularly positive. Thus, most experts do not suggest using benzodiazepines for anxiety disorders, with the exception of helping children through single or rare events, such as medical procedures or enabling an adolescent who has been fearful of attending school to get to the building on the first day back after a long absence.
Guanfacine
In a recent exploratory trial of guanfacine for children with mixed anxiety disorders,5 the medication was well tolerated overall but did not result in statistically significant improvement relative to placebo on primary anxiety rating scales. However, a higher number of children were rated as improved on a clinician-rated scale. This medication is usually started at 0.5 mg/day and increased as tolerated, while checking vital signs, to a maximum of 4 mg/day.
Atomoxetine
A randomized control trial of pediatric patients with both ADHD and an anxiety disorder showed reductions in both symptom domains with atomoxetine dosed at an average of 1.3 mg/kg per day.6 There is little evidence to suggest its use in primary anxiety disorders without comorbid ADHD.
Buspirone
This 5-hydroxytryptamine 1a agonist has Food and Drug Administration approval for generalized anxiety disorder in adults and is generally well tolerated. Unfortunately, two randomized controlled studies in children and adolescents did not find statistically significant improvement relative to placebo, although some methodological problems may have played a role.7
Antipsychotics
Although sometimes used to augment an SSRI in adult anxiety disorders, there are little data to support the use of antipsychotics in pediatric populations, especially given the antecedent risks of the drugs.
Summary
Pharmacotherapy for anxiety disorders often includes the advice that, if medications are indicated in conjunction with psychotherapy, to start with an SSRI; and if that is not effective to try a different one.7 An SNRI such as venlafaxine or duloxetine may then be a third-line alternative, although for youth with comorbid ADHD, consideration of either atomoxetine or guanfacine is also reasonable. Beyond that point, there unfortunately are little systematic data to guide pharmacologic decision making, and increased potential risks of other classes of medications suggest the need for caution and consultation.
Looking for more mental health training? Attend the 12th annual Child Psychiatry in Primary Care conference in Burlington, on May 4, 2018,organized by the University of Vermont with Dr. Rettew as course director. Go to http://www.med.uvm.edu/cme/conferences.
References
1. Merikangas KR et al. J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.
2. Strawn JR et al. Depress Anxiety. 2015 Mar;32(3):149-57.
3. Walkup J et al. N Engl J Med. 2008 Dec 25;359(26):2753-66.
4. Batelaan N et al. BMJ. 2017 Sep 13;358:j3927.
5. Strawn JR et al. J Child Adolesc Psychopharm. 2017 Feb;27(1): 29-37..
6. Geller D et al. J Am Acad Child Adolesc Psychiatry. 2007 Sep;46(9):1119-27.
7. Strawn JR et al. J Child Adolesc Psychopharm. 2017 Feb;28(1): 2-9.
Anxiety disorders, including separation anxiety disorder, social anxiety disorder, and generalized anxiety disorder, are some of the most common psychiatric conditions of childhood and adolescence, affecting up to 20% of youth.1 Patients commonly present with a mix of symptoms that often span multiple anxiety disorder diagnoses. While this pattern can present somewhat of a diagnostic conundrum, it can be reassuring to know that such constellations of symptoms are the rule rather than the exception. Further, given that both the pharmacologic and nonpharmacologic treatment strategies don’t change much among the various anxiety disorders, the lack of a definitive single diagnosis should not delay intervention. Be alert to the possibility that anxiety and anxiety disorders can be the engine that drives what on the surface appears to be more disruptive and oppositional behavior.
Although medications can be a useful part of treatment, they are not recommended as a stand-alone intervention. Nonpharmacologic treatments generally should be tried before medications are considered. Among the different types of psychotherapy, cognitive-behavioral therapy (CBT) has the most empirical support from research trials, although other modalities such as mindfulness-based treatments show some promise. As anxiety disorders often run in families, it also can be very useful to explore the possibility that one or more parents also struggle with an anxiety disorder, which, if untreated, might complicate the child’s course.
With regard to medications, it is being increasingly appreciated that, despite SSRIs being most popularly known as antidepressants, these medications actually may be as efficacious or even more efficacious in the management of anxiety disorders. This class remains the cornerstone of medication treatment, and a brief review of current options follows.
SSRIs and SNRIs
A 2015 meta-analysis that examined nine randomized controlled trials of SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs) for pediatric anxiety disorders concluded that these agents provided a benefit of modest effect size. No significant increase in treatment-emergent suicidality was found, and the medications were generally well tolerated.2 This analysis also found some evidence that greater efficacy was related to a medication with more specific serotonergic properties, suggesting improved response with “true” SSRIs versus SNRIs such as venlafaxine and duloxetine. One major study using sertraline found that, at least in the short term, combined use of sertraline with CBT resulted in better efficacy than either treatment alone.3 Dosing of SSRIs should start low: A general rule is to begin at half of the smallest dosage made, depending on the age and size of the patient. One question that often comes up after a successful trial is how long to continue the medications. A recent meta-analysis in adults concluded that there was evidence that stopping medication prior to 1 year resulted in an increased risk of relapse with little to guide clinicians after that 1-year mark.4
Benzodiazepines
Even though benzodiazepines have been around for a long time, data supporting their efficacy and safety in pediatric populations remain extremely limited, and what has been reported has not been particularly positive. Thus, most experts do not suggest using benzodiazepines for anxiety disorders, with the exception of helping children through single or rare events, such as medical procedures or enabling an adolescent who has been fearful of attending school to get to the building on the first day back after a long absence.
Guanfacine
In a recent exploratory trial of guanfacine for children with mixed anxiety disorders,5 the medication was well tolerated overall but did not result in statistically significant improvement relative to placebo on primary anxiety rating scales. However, a higher number of children were rated as improved on a clinician-rated scale. This medication is usually started at 0.5 mg/day and increased as tolerated, while checking vital signs, to a maximum of 4 mg/day.
Atomoxetine
A randomized control trial of pediatric patients with both ADHD and an anxiety disorder showed reductions in both symptom domains with atomoxetine dosed at an average of 1.3 mg/kg per day.6 There is little evidence to suggest its use in primary anxiety disorders without comorbid ADHD.
Buspirone
This 5-hydroxytryptamine 1a agonist has Food and Drug Administration approval for generalized anxiety disorder in adults and is generally well tolerated. Unfortunately, two randomized controlled studies in children and adolescents did not find statistically significant improvement relative to placebo, although some methodological problems may have played a role.7
Antipsychotics
Although sometimes used to augment an SSRI in adult anxiety disorders, there are little data to support the use of antipsychotics in pediatric populations, especially given the antecedent risks of the drugs.
Summary
Pharmacotherapy for anxiety disorders often includes the advice that, if medications are indicated in conjunction with psychotherapy, to start with an SSRI; and if that is not effective to try a different one.7 An SNRI such as venlafaxine or duloxetine may then be a third-line alternative, although for youth with comorbid ADHD, consideration of either atomoxetine or guanfacine is also reasonable. Beyond that point, there unfortunately are little systematic data to guide pharmacologic decision making, and increased potential risks of other classes of medications suggest the need for caution and consultation.
Looking for more mental health training? Attend the 12th annual Child Psychiatry in Primary Care conference in Burlington, on May 4, 2018,organized by the University of Vermont with Dr. Rettew as course director. Go to http://www.med.uvm.edu/cme/conferences.
References
1. Merikangas KR et al. J Am Acad Child Adolesc Psychiatry. 2010 Oct;49(10):980-9.
2. Strawn JR et al. Depress Anxiety. 2015 Mar;32(3):149-57.
3. Walkup J et al. N Engl J Med. 2008 Dec 25;359(26):2753-66.
4. Batelaan N et al. BMJ. 2017 Sep 13;358:j3927.
5. Strawn JR et al. J Child Adolesc Psychopharm. 2017 Feb;27(1): 29-37..
6. Geller D et al. J Am Acad Child Adolesc Psychiatry. 2007 Sep;46(9):1119-27.
7. Strawn JR et al. J Child Adolesc Psychopharm. 2017 Feb;28(1): 2-9.
Nature versus nurture: 50 years of a popular debate
This basic question has been debated at settings ranging from scientific conferences to dinner tables for many decades. The media also has covered it in forms ranging from documentaries to the popular comedy movie “Trading Places” (1983). Yet, despite so much attention and so much research devoted to resolving this timeless debate, the arguments continue to this day.
A lack of a clear answer, however, by no means implies that we have not made major advances in our understanding. This short review takes a look at the progression of this seemingly eternal question by categorizing the development of the nature versus nurture question into three main stages. While such a partitioning is somewhat oversimplified with regard to what the various positions on this issue have been at different times, it does illustrate the way that the debate has gradually evolved.
Part 1: Nature versus nurture
The origins of the nature versus nurture debate date back far beyond the past 50 years. The ancient Greek philosopher Galen postulated that personality traits were driven by the relative concentrations of four bodily fluids or “humours.” In 1874, Sir Francis Galton published “English Men of Science: Their Nature and Nurture,” in which he advanced his ideas about the dominance of hereditary factors in intelligence and character at the beginning of the eugenics movement.1 These ideas were in stark opposition to the perspective of earlier scholars, such as the philosopher John Locke, who popularized the theory that children are born a “blank slate” and from there develop their traits and intellectual abilities through their environment and experiences.
The other primary school of thought in the mid-1960s was psychoanalysis, which was based on the ideas of Sigmund Freud, MD. Psychoanalysis maintains that the way that unconscious sexual and aggressive drives were channeled through various defense mechanisms was of primary importance to the understanding of both psychopathology and typical human behavior.
While these two perspectives were often very much in opposition to each other, they shared in common the view that the environment and a person’s individual experiences, i.e. nurture, were the prevailing forces in development. In the background, more biologically oriented research and clinical work was slowly beginning to work its way into the field, especially at certain institutions, such as Washington University in St. Louis. Several medications of various types were then available, including chlorpromazine, imipramine, and diazepam.
Overall, however, it is probably fair to say that, 50 years ago, it was the nurture perspective that held the most sway since psychodynamic treatment and behaviorist research dominated, while the emerging fields of genetics and neuroscience were only beginning to take hold.
Part 2: Nature and nurture
From the 1970s to the end of the 20th century, a noticeable shift occurred as knowledge of the brain and genetics – supported by remarkable advances in research techniques – began to swing the pendulum back toward an increased appreciation of nature as a critical influence on a person’s thoughts, feelings, and behavior.
Researchers Stella Chess, MD, and Alexander Thomas, MD, for example, conducted the New York Longitudinal Study, in which they closely observed a group of young children over many years. Their studies compelled them to argue for the significance of more innate temperament traits as critical aspects of a youth’s overall adjustment.2 The Human Genome Project was launched in 1990, and the entire decade was designated as the “Decade of the Brain.” During this time, neuroscience research exploded as techniques, such as MRI and PET, allowed scientists to view the living brain like never before.
The type of research investigation that perhaps was most directly relevant to the nature-nurture debate and that became quite popular during this time was the twin study. By comparing the relative similarities among monozygotic and dizygotic twins raised in the same household, it became possible to calculate directly the degree to which a variable of interest (intelligence, height, aggressive behavior) could be attributed to genetic versus environmental factors. When it came to behavioral variables, a repeated finding that emerged was that both genetic and environmental influences are important, often at close to a 50/50 split in terms of magnitude.3,4 These studies were complemented by molecular genetic studies, which were beginning to be able to identify specific genes that conveyed usually small amounts of risk for a wide range of psychiatric disorders.
Yet, while twin studies and many other lines of research made it increasingly difficult to argue for the overwhelming supremacy of either nature or nurture, the two domains generally were treated as being independent of each other. Specific traits or symptoms in an individual often were thought of as being the result of either psychological (nurture) or biological (nature) causes. Terms such as “endogenous depression,” for example, were used to distinguish those who had symptoms that were thought generally to be out of reach for “psychological” treatments, such as psychotherapy. Looking back, it might be fair to say that one of the principle flaws in this perspective was the commonly held belief that, if something was brain based or biological, then it therefore implied a kind of automatic “wiring” of the brain that was generally driven by genes and beyond the influence of environmental factors.
Part 3: Nature is nurture (and vice versa)
As the science progressed, it became increasingly clear that the nature and nurture domains were hopelessly intertwined with one another. From early PET-scan studies showing that both medications and psychotherapy not only changed the brain but also did so in ways similar to behavioral-genetic studies showing how genetically influenced behaviors actually cause certain environmental events to be more likely to occur, research continued to demonstrate the bidirectional influences of genetic and environmental factors on development.5,6 This appreciation rose to even greater heights with advances in the field of epigenetics, which was able to document some of the specific mechanisms through which environmental factors cause genes involved in regulating the plasticity of the brain to turn on and off.7
In thinking through some of this complexity, however, it is important to remember the hopeful message that is contained in this rich understanding. All of these complicated, interacting genetic and environmental factors give us many avenues for positive intervention. Now we understand that not only might a medication help strengthen some of the brain connections needed to reduce and cope with that child’s anxiety, but so could mindfulness, exercise, and addressing his parents’ symptoms. When the families ask me whether their child’s struggles are behavioral or psychological, the answer I tend to give them is “yes.”
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington.
Email him at [email protected]. Follow him on Twitter @pedipsych.
References
1. “English Men of Science: Their Nature and Nurture” (London: MacMillan & Co., 1874)
2. “Temperament: Theory and Practice” (New York: Brunner/Mazel, 1996)
3. “Nature and Nurture during Infancy and Early Childhood” (New York: Cambridge University Press, 1988)
4. Nat Genet. 2015;47(7):702-9.
5. Arch Gen Psychiatry. 1992;49(9):681-9.
6. Dev Psychopathol. 1997 Spring;9(2):335-64.
7. JAMA Psychiatry. 2017;74(6):551-2.
This basic question has been debated at settings ranging from scientific conferences to dinner tables for many decades. The media also has covered it in forms ranging from documentaries to the popular comedy movie “Trading Places” (1983). Yet, despite so much attention and so much research devoted to resolving this timeless debate, the arguments continue to this day.
A lack of a clear answer, however, by no means implies that we have not made major advances in our understanding. This short review takes a look at the progression of this seemingly eternal question by categorizing the development of the nature versus nurture question into three main stages. While such a partitioning is somewhat oversimplified with regard to what the various positions on this issue have been at different times, it does illustrate the way that the debate has gradually evolved.
Part 1: Nature versus nurture
The origins of the nature versus nurture debate date back far beyond the past 50 years. The ancient Greek philosopher Galen postulated that personality traits were driven by the relative concentrations of four bodily fluids or “humours.” In 1874, Sir Francis Galton published “English Men of Science: Their Nature and Nurture,” in which he advanced his ideas about the dominance of hereditary factors in intelligence and character at the beginning of the eugenics movement.1 These ideas were in stark opposition to the perspective of earlier scholars, such as the philosopher John Locke, who popularized the theory that children are born a “blank slate” and from there develop their traits and intellectual abilities through their environment and experiences.
The other primary school of thought in the mid-1960s was psychoanalysis, which was based on the ideas of Sigmund Freud, MD. Psychoanalysis maintains that the way that unconscious sexual and aggressive drives were channeled through various defense mechanisms was of primary importance to the understanding of both psychopathology and typical human behavior.
While these two perspectives were often very much in opposition to each other, they shared in common the view that the environment and a person’s individual experiences, i.e. nurture, were the prevailing forces in development. In the background, more biologically oriented research and clinical work was slowly beginning to work its way into the field, especially at certain institutions, such as Washington University in St. Louis. Several medications of various types were then available, including chlorpromazine, imipramine, and diazepam.
Overall, however, it is probably fair to say that, 50 years ago, it was the nurture perspective that held the most sway since psychodynamic treatment and behaviorist research dominated, while the emerging fields of genetics and neuroscience were only beginning to take hold.
Part 2: Nature and nurture
From the 1970s to the end of the 20th century, a noticeable shift occurred as knowledge of the brain and genetics – supported by remarkable advances in research techniques – began to swing the pendulum back toward an increased appreciation of nature as a critical influence on a person’s thoughts, feelings, and behavior.
Researchers Stella Chess, MD, and Alexander Thomas, MD, for example, conducted the New York Longitudinal Study, in which they closely observed a group of young children over many years. Their studies compelled them to argue for the significance of more innate temperament traits as critical aspects of a youth’s overall adjustment.2 The Human Genome Project was launched in 1990, and the entire decade was designated as the “Decade of the Brain.” During this time, neuroscience research exploded as techniques, such as MRI and PET, allowed scientists to view the living brain like never before.
The type of research investigation that perhaps was most directly relevant to the nature-nurture debate and that became quite popular during this time was the twin study. By comparing the relative similarities among monozygotic and dizygotic twins raised in the same household, it became possible to calculate directly the degree to which a variable of interest (intelligence, height, aggressive behavior) could be attributed to genetic versus environmental factors. When it came to behavioral variables, a repeated finding that emerged was that both genetic and environmental influences are important, often at close to a 50/50 split in terms of magnitude.3,4 These studies were complemented by molecular genetic studies, which were beginning to be able to identify specific genes that conveyed usually small amounts of risk for a wide range of psychiatric disorders.
Yet, while twin studies and many other lines of research made it increasingly difficult to argue for the overwhelming supremacy of either nature or nurture, the two domains generally were treated as being independent of each other. Specific traits or symptoms in an individual often were thought of as being the result of either psychological (nurture) or biological (nature) causes. Terms such as “endogenous depression,” for example, were used to distinguish those who had symptoms that were thought generally to be out of reach for “psychological” treatments, such as psychotherapy. Looking back, it might be fair to say that one of the principle flaws in this perspective was the commonly held belief that, if something was brain based or biological, then it therefore implied a kind of automatic “wiring” of the brain that was generally driven by genes and beyond the influence of environmental factors.
Part 3: Nature is nurture (and vice versa)
As the science progressed, it became increasingly clear that the nature and nurture domains were hopelessly intertwined with one another. From early PET-scan studies showing that both medications and psychotherapy not only changed the brain but also did so in ways similar to behavioral-genetic studies showing how genetically influenced behaviors actually cause certain environmental events to be more likely to occur, research continued to demonstrate the bidirectional influences of genetic and environmental factors on development.5,6 This appreciation rose to even greater heights with advances in the field of epigenetics, which was able to document some of the specific mechanisms through which environmental factors cause genes involved in regulating the plasticity of the brain to turn on and off.7
In thinking through some of this complexity, however, it is important to remember the hopeful message that is contained in this rich understanding. All of these complicated, interacting genetic and environmental factors give us many avenues for positive intervention. Now we understand that not only might a medication help strengthen some of the brain connections needed to reduce and cope with that child’s anxiety, but so could mindfulness, exercise, and addressing his parents’ symptoms. When the families ask me whether their child’s struggles are behavioral or psychological, the answer I tend to give them is “yes.”
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington.
Email him at [email protected]. Follow him on Twitter @pedipsych.
References
1. “English Men of Science: Their Nature and Nurture” (London: MacMillan & Co., 1874)
2. “Temperament: Theory and Practice” (New York: Brunner/Mazel, 1996)
3. “Nature and Nurture during Infancy and Early Childhood” (New York: Cambridge University Press, 1988)
4. Nat Genet. 2015;47(7):702-9.
5. Arch Gen Psychiatry. 1992;49(9):681-9.
6. Dev Psychopathol. 1997 Spring;9(2):335-64.
7. JAMA Psychiatry. 2017;74(6):551-2.
This basic question has been debated at settings ranging from scientific conferences to dinner tables for many decades. The media also has covered it in forms ranging from documentaries to the popular comedy movie “Trading Places” (1983). Yet, despite so much attention and so much research devoted to resolving this timeless debate, the arguments continue to this day.
A lack of a clear answer, however, by no means implies that we have not made major advances in our understanding. This short review takes a look at the progression of this seemingly eternal question by categorizing the development of the nature versus nurture question into three main stages. While such a partitioning is somewhat oversimplified with regard to what the various positions on this issue have been at different times, it does illustrate the way that the debate has gradually evolved.
Part 1: Nature versus nurture
The origins of the nature versus nurture debate date back far beyond the past 50 years. The ancient Greek philosopher Galen postulated that personality traits were driven by the relative concentrations of four bodily fluids or “humours.” In 1874, Sir Francis Galton published “English Men of Science: Their Nature and Nurture,” in which he advanced his ideas about the dominance of hereditary factors in intelligence and character at the beginning of the eugenics movement.1 These ideas were in stark opposition to the perspective of earlier scholars, such as the philosopher John Locke, who popularized the theory that children are born a “blank slate” and from there develop their traits and intellectual abilities through their environment and experiences.
The other primary school of thought in the mid-1960s was psychoanalysis, which was based on the ideas of Sigmund Freud, MD. Psychoanalysis maintains that the way that unconscious sexual and aggressive drives were channeled through various defense mechanisms was of primary importance to the understanding of both psychopathology and typical human behavior.
While these two perspectives were often very much in opposition to each other, they shared in common the view that the environment and a person’s individual experiences, i.e. nurture, were the prevailing forces in development. In the background, more biologically oriented research and clinical work was slowly beginning to work its way into the field, especially at certain institutions, such as Washington University in St. Louis. Several medications of various types were then available, including chlorpromazine, imipramine, and diazepam.
Overall, however, it is probably fair to say that, 50 years ago, it was the nurture perspective that held the most sway since psychodynamic treatment and behaviorist research dominated, while the emerging fields of genetics and neuroscience were only beginning to take hold.
Part 2: Nature and nurture
From the 1970s to the end of the 20th century, a noticeable shift occurred as knowledge of the brain and genetics – supported by remarkable advances in research techniques – began to swing the pendulum back toward an increased appreciation of nature as a critical influence on a person’s thoughts, feelings, and behavior.
Researchers Stella Chess, MD, and Alexander Thomas, MD, for example, conducted the New York Longitudinal Study, in which they closely observed a group of young children over many years. Their studies compelled them to argue for the significance of more innate temperament traits as critical aspects of a youth’s overall adjustment.2 The Human Genome Project was launched in 1990, and the entire decade was designated as the “Decade of the Brain.” During this time, neuroscience research exploded as techniques, such as MRI and PET, allowed scientists to view the living brain like never before.
The type of research investigation that perhaps was most directly relevant to the nature-nurture debate and that became quite popular during this time was the twin study. By comparing the relative similarities among monozygotic and dizygotic twins raised in the same household, it became possible to calculate directly the degree to which a variable of interest (intelligence, height, aggressive behavior) could be attributed to genetic versus environmental factors. When it came to behavioral variables, a repeated finding that emerged was that both genetic and environmental influences are important, often at close to a 50/50 split in terms of magnitude.3,4 These studies were complemented by molecular genetic studies, which were beginning to be able to identify specific genes that conveyed usually small amounts of risk for a wide range of psychiatric disorders.
Yet, while twin studies and many other lines of research made it increasingly difficult to argue for the overwhelming supremacy of either nature or nurture, the two domains generally were treated as being independent of each other. Specific traits or symptoms in an individual often were thought of as being the result of either psychological (nurture) or biological (nature) causes. Terms such as “endogenous depression,” for example, were used to distinguish those who had symptoms that were thought generally to be out of reach for “psychological” treatments, such as psychotherapy. Looking back, it might be fair to say that one of the principle flaws in this perspective was the commonly held belief that, if something was brain based or biological, then it therefore implied a kind of automatic “wiring” of the brain that was generally driven by genes and beyond the influence of environmental factors.
Part 3: Nature is nurture (and vice versa)
As the science progressed, it became increasingly clear that the nature and nurture domains were hopelessly intertwined with one another. From early PET-scan studies showing that both medications and psychotherapy not only changed the brain but also did so in ways similar to behavioral-genetic studies showing how genetically influenced behaviors actually cause certain environmental events to be more likely to occur, research continued to demonstrate the bidirectional influences of genetic and environmental factors on development.5,6 This appreciation rose to even greater heights with advances in the field of epigenetics, which was able to document some of the specific mechanisms through which environmental factors cause genes involved in regulating the plasticity of the brain to turn on and off.7
In thinking through some of this complexity, however, it is important to remember the hopeful message that is contained in this rich understanding. All of these complicated, interacting genetic and environmental factors give us many avenues for positive intervention. Now we understand that not only might a medication help strengthen some of the brain connections needed to reduce and cope with that child’s anxiety, but so could mindfulness, exercise, and addressing his parents’ symptoms. When the families ask me whether their child’s struggles are behavioral or psychological, the answer I tend to give them is “yes.”
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington.
Email him at [email protected]. Follow him on Twitter @pedipsych.
References
1. “English Men of Science: Their Nature and Nurture” (London: MacMillan & Co., 1874)
2. “Temperament: Theory and Practice” (New York: Brunner/Mazel, 1996)
3. “Nature and Nurture during Infancy and Early Childhood” (New York: Cambridge University Press, 1988)
4. Nat Genet. 2015;47(7):702-9.
5. Arch Gen Psychiatry. 1992;49(9):681-9.
6. Dev Psychopathol. 1997 Spring;9(2):335-64.
7. JAMA Psychiatry. 2017;74(6):551-2.
Discussing the ADHD ‘controversy’ with patients and parents
There are many topics within the child psychiatry community that are controversial. How many kids really deserve a diagnosis of bipolar disorder? Which type of therapy works best? Is cannabis a gateway drug? The existence of attention-deficit/hyperactivity disorder as a legitimate psychiatric entity, however, is not one of them.
Despite this fact, there remains considerable controversy in the public about how “real” ADHD actually is. Social media, blogs, and even entire books have been written that disparage the diagnosis and even suggest that ADHD was fabricated by the pharmaceutical industry to sell medications. Although these publications and posts generally ignore the scientific literature or at least twist it beyond recognition, there are several aspects of ADHD that legitimately cause more confusion and less confidence about the diagnosis, relative to other common pediatric problems. This column attempts to describe and contextualize these elements so that pediatricians can be more fully informed when they are called to respond to some of the allegations against ADHD that often are brought up by families.
Case summary
Hunter is a 6-year-old boy who presents with his mother and father for “behavioral concerns.” He always has been an energetic child, but the school has been having increasing difficulties with his behavior. Hunter struggles to stay in his seat and take part in quiet activities. His teacher needs to give multiple reminders per day about not interrupting others or speaking out in class. Without redirection, Hunter typically loses focus in class and does not complete his work. Because of these difficulties, the question of ADHD arose during a recent parent-teacher conference. While Hunter’s mother acknowledges these behaviors and notes similar ones at home, the father is resisting any further evaluation, claiming that Hunter “is just being a boy.” The father notes that he acted similarly as a child and “turned out okay.” When the mother tried to research ADHD online, she encountered several sites that claimed that the diagnosis of ADHD was “made up” by drug companies wanting “to turn kids into zombies.” At the appointment, the parents state that they want their son to succeed and be happy, but are concerned about some of the things they have read on the Internet.
Discussion
This example represents a common dilemma for parents who encounter so many mixed messages when doing background research on ADHD. Although the legitimacy of ADHD has been supported in literally hundreds of research studies that have examined areas such as genetics, neuropsychological testing, and brain imaging1,2, some of the lingering doubts about ADHD validity are rooted in characteristics of the diagnosis that do differ from some nonpsychiatric diagnoses. At the same time, however, further inspection reveals that these qualities exist for many other entities that have received far less public criticism. Three of these main qualities include the following:
1. ADHD is a dimensional rather than binary entity. Despite the fact that the current nomenclature continues to frame ADHD as an all-or-nothing diagnosis, there is now overwhelming scientific evidence that it is much more accurately conceptualized as a dimension3. As such, there is no clear-cut boundary between what should be judged as “typical” levels of attention and activity and ADHD. As written in a previous column4, in some ways the label of ADHD is a lot like the label of someone being tall, with some individuals clearly falling into the category of “tall” or “not tall,” while many others could be considered in-between. However, many of the most common nonpsychiatric conditions such as hypertension and hypercholesterolemia also exist this way without high levels of public controversy.
2. ADHD lacks a specific known neurobiologic marker that can be measured by a lab or neuroimaging test. As mentioned, there is a vast literature supporting the idea that the brains of people with ADHD are different from those without ADHD, but these differences tend to describe quantitative differences in regional brain volume, cortical thickness, activity levels, or connectivity rather than a discrete “thing” that a radiologist can point to on a scan. Given the dimensional nature of ADHD and the broad brain processes required for complex functions such as attention and motor activity, the lack of a specific and universal “lesion” underlying ADHD is to be expected, yet it still remains easy ammunition for those who criticize the diagnosis. Again, very similar cases can be made for other entities such as autism or low intelligence, which few argue are not real but also have no reliable biomarker to support them.
3. Medications often are used to treat ADHD. The diagnosis of ADHD would probably be far less controversial if one of its primary treatments did not involve psychiatric medications. While it is probably fair to say that the many nonpharmacologic approaches to ADHD are quite underutilized, it seems a stretch to use potential overreliance on medication as a legitimate reason to question the validity of a diagnosis. Opiate abuse also is a problem in this country, but that doesn’t mean a person’s pain doesn’t exist. As a practical tip, it can be reassuring for families to hear explicitly from their physician that “zombification” is not considered an acceptable medical outcome and that the prescribing clinician will promptly deal with any side effects that might occur with treatment5.
Understanding these aspects about ADHD and how they are misinterpreted in the media can help families make more informed and comfortable decisions about their child’s care in collaboration with their pediatrician. It also is important for pediatricians to be proactive in distributing reliable and science-backed material to the public in this new age of information overload.
Case follow-up
The pediatrician hears the family’s concerns and discusses the evidence supporting the scientific legitimacy of ADHD, as well as some of the qualities of the diagnosis that have led to its controversy. The parents are reassured but would like to proceed carefully and cautiously with further work-up and treatment. The pediatrician sends the family home with some quantitative rating scales to be completed by Hunter’s parents and teacher. She also makes a plan to begin monitoring several health promotion areas that could be impacting Hunter’s behavior including sleep quality, physical activity, screen time, and nutrition.
References
1. Psychiatr Clin North Am. 2010 Mar;33(1):159-80.
2. Dev Neuropsychol. 2013;38(4):211-25.3. Can Fam Physician. 2016 Dec;62(12):979-82.
4. ADHD boundaries with normal behavior. Pediatric News; published online Aug. 27, 2014.
5. Zombification is not an acceptable medical outcome. Psychology Today, ABCs of Child Psychiatry blog; published online Oct. 18, 2013.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych.
There are many topics within the child psychiatry community that are controversial. How many kids really deserve a diagnosis of bipolar disorder? Which type of therapy works best? Is cannabis a gateway drug? The existence of attention-deficit/hyperactivity disorder as a legitimate psychiatric entity, however, is not one of them.
Despite this fact, there remains considerable controversy in the public about how “real” ADHD actually is. Social media, blogs, and even entire books have been written that disparage the diagnosis and even suggest that ADHD was fabricated by the pharmaceutical industry to sell medications. Although these publications and posts generally ignore the scientific literature or at least twist it beyond recognition, there are several aspects of ADHD that legitimately cause more confusion and less confidence about the diagnosis, relative to other common pediatric problems. This column attempts to describe and contextualize these elements so that pediatricians can be more fully informed when they are called to respond to some of the allegations against ADHD that often are brought up by families.
Case summary
Hunter is a 6-year-old boy who presents with his mother and father for “behavioral concerns.” He always has been an energetic child, but the school has been having increasing difficulties with his behavior. Hunter struggles to stay in his seat and take part in quiet activities. His teacher needs to give multiple reminders per day about not interrupting others or speaking out in class. Without redirection, Hunter typically loses focus in class and does not complete his work. Because of these difficulties, the question of ADHD arose during a recent parent-teacher conference. While Hunter’s mother acknowledges these behaviors and notes similar ones at home, the father is resisting any further evaluation, claiming that Hunter “is just being a boy.” The father notes that he acted similarly as a child and “turned out okay.” When the mother tried to research ADHD online, she encountered several sites that claimed that the diagnosis of ADHD was “made up” by drug companies wanting “to turn kids into zombies.” At the appointment, the parents state that they want their son to succeed and be happy, but are concerned about some of the things they have read on the Internet.
Discussion
This example represents a common dilemma for parents who encounter so many mixed messages when doing background research on ADHD. Although the legitimacy of ADHD has been supported in literally hundreds of research studies that have examined areas such as genetics, neuropsychological testing, and brain imaging1,2, some of the lingering doubts about ADHD validity are rooted in characteristics of the diagnosis that do differ from some nonpsychiatric diagnoses. At the same time, however, further inspection reveals that these qualities exist for many other entities that have received far less public criticism. Three of these main qualities include the following:
1. ADHD is a dimensional rather than binary entity. Despite the fact that the current nomenclature continues to frame ADHD as an all-or-nothing diagnosis, there is now overwhelming scientific evidence that it is much more accurately conceptualized as a dimension3. As such, there is no clear-cut boundary between what should be judged as “typical” levels of attention and activity and ADHD. As written in a previous column4, in some ways the label of ADHD is a lot like the label of someone being tall, with some individuals clearly falling into the category of “tall” or “not tall,” while many others could be considered in-between. However, many of the most common nonpsychiatric conditions such as hypertension and hypercholesterolemia also exist this way without high levels of public controversy.
2. ADHD lacks a specific known neurobiologic marker that can be measured by a lab or neuroimaging test. As mentioned, there is a vast literature supporting the idea that the brains of people with ADHD are different from those without ADHD, but these differences tend to describe quantitative differences in regional brain volume, cortical thickness, activity levels, or connectivity rather than a discrete “thing” that a radiologist can point to on a scan. Given the dimensional nature of ADHD and the broad brain processes required for complex functions such as attention and motor activity, the lack of a specific and universal “lesion” underlying ADHD is to be expected, yet it still remains easy ammunition for those who criticize the diagnosis. Again, very similar cases can be made for other entities such as autism or low intelligence, which few argue are not real but also have no reliable biomarker to support them.
3. Medications often are used to treat ADHD. The diagnosis of ADHD would probably be far less controversial if one of its primary treatments did not involve psychiatric medications. While it is probably fair to say that the many nonpharmacologic approaches to ADHD are quite underutilized, it seems a stretch to use potential overreliance on medication as a legitimate reason to question the validity of a diagnosis. Opiate abuse also is a problem in this country, but that doesn’t mean a person’s pain doesn’t exist. As a practical tip, it can be reassuring for families to hear explicitly from their physician that “zombification” is not considered an acceptable medical outcome and that the prescribing clinician will promptly deal with any side effects that might occur with treatment5.
Understanding these aspects about ADHD and how they are misinterpreted in the media can help families make more informed and comfortable decisions about their child’s care in collaboration with their pediatrician. It also is important for pediatricians to be proactive in distributing reliable and science-backed material to the public in this new age of information overload.
Case follow-up
The pediatrician hears the family’s concerns and discusses the evidence supporting the scientific legitimacy of ADHD, as well as some of the qualities of the diagnosis that have led to its controversy. The parents are reassured but would like to proceed carefully and cautiously with further work-up and treatment. The pediatrician sends the family home with some quantitative rating scales to be completed by Hunter’s parents and teacher. She also makes a plan to begin monitoring several health promotion areas that could be impacting Hunter’s behavior including sleep quality, physical activity, screen time, and nutrition.
References
1. Psychiatr Clin North Am. 2010 Mar;33(1):159-80.
2. Dev Neuropsychol. 2013;38(4):211-25.3. Can Fam Physician. 2016 Dec;62(12):979-82.
4. ADHD boundaries with normal behavior. Pediatric News; published online Aug. 27, 2014.
5. Zombification is not an acceptable medical outcome. Psychology Today, ABCs of Child Psychiatry blog; published online Oct. 18, 2013.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych.
There are many topics within the child psychiatry community that are controversial. How many kids really deserve a diagnosis of bipolar disorder? Which type of therapy works best? Is cannabis a gateway drug? The existence of attention-deficit/hyperactivity disorder as a legitimate psychiatric entity, however, is not one of them.
Despite this fact, there remains considerable controversy in the public about how “real” ADHD actually is. Social media, blogs, and even entire books have been written that disparage the diagnosis and even suggest that ADHD was fabricated by the pharmaceutical industry to sell medications. Although these publications and posts generally ignore the scientific literature or at least twist it beyond recognition, there are several aspects of ADHD that legitimately cause more confusion and less confidence about the diagnosis, relative to other common pediatric problems. This column attempts to describe and contextualize these elements so that pediatricians can be more fully informed when they are called to respond to some of the allegations against ADHD that often are brought up by families.
Case summary
Hunter is a 6-year-old boy who presents with his mother and father for “behavioral concerns.” He always has been an energetic child, but the school has been having increasing difficulties with his behavior. Hunter struggles to stay in his seat and take part in quiet activities. His teacher needs to give multiple reminders per day about not interrupting others or speaking out in class. Without redirection, Hunter typically loses focus in class and does not complete his work. Because of these difficulties, the question of ADHD arose during a recent parent-teacher conference. While Hunter’s mother acknowledges these behaviors and notes similar ones at home, the father is resisting any further evaluation, claiming that Hunter “is just being a boy.” The father notes that he acted similarly as a child and “turned out okay.” When the mother tried to research ADHD online, she encountered several sites that claimed that the diagnosis of ADHD was “made up” by drug companies wanting “to turn kids into zombies.” At the appointment, the parents state that they want their son to succeed and be happy, but are concerned about some of the things they have read on the Internet.
Discussion
This example represents a common dilemma for parents who encounter so many mixed messages when doing background research on ADHD. Although the legitimacy of ADHD has been supported in literally hundreds of research studies that have examined areas such as genetics, neuropsychological testing, and brain imaging1,2, some of the lingering doubts about ADHD validity are rooted in characteristics of the diagnosis that do differ from some nonpsychiatric diagnoses. At the same time, however, further inspection reveals that these qualities exist for many other entities that have received far less public criticism. Three of these main qualities include the following:
1. ADHD is a dimensional rather than binary entity. Despite the fact that the current nomenclature continues to frame ADHD as an all-or-nothing diagnosis, there is now overwhelming scientific evidence that it is much more accurately conceptualized as a dimension3. As such, there is no clear-cut boundary between what should be judged as “typical” levels of attention and activity and ADHD. As written in a previous column4, in some ways the label of ADHD is a lot like the label of someone being tall, with some individuals clearly falling into the category of “tall” or “not tall,” while many others could be considered in-between. However, many of the most common nonpsychiatric conditions such as hypertension and hypercholesterolemia also exist this way without high levels of public controversy.
2. ADHD lacks a specific known neurobiologic marker that can be measured by a lab or neuroimaging test. As mentioned, there is a vast literature supporting the idea that the brains of people with ADHD are different from those without ADHD, but these differences tend to describe quantitative differences in regional brain volume, cortical thickness, activity levels, or connectivity rather than a discrete “thing” that a radiologist can point to on a scan. Given the dimensional nature of ADHD and the broad brain processes required for complex functions such as attention and motor activity, the lack of a specific and universal “lesion” underlying ADHD is to be expected, yet it still remains easy ammunition for those who criticize the diagnosis. Again, very similar cases can be made for other entities such as autism or low intelligence, which few argue are not real but also have no reliable biomarker to support them.
3. Medications often are used to treat ADHD. The diagnosis of ADHD would probably be far less controversial if one of its primary treatments did not involve psychiatric medications. While it is probably fair to say that the many nonpharmacologic approaches to ADHD are quite underutilized, it seems a stretch to use potential overreliance on medication as a legitimate reason to question the validity of a diagnosis. Opiate abuse also is a problem in this country, but that doesn’t mean a person’s pain doesn’t exist. As a practical tip, it can be reassuring for families to hear explicitly from their physician that “zombification” is not considered an acceptable medical outcome and that the prescribing clinician will promptly deal with any side effects that might occur with treatment5.
Understanding these aspects about ADHD and how they are misinterpreted in the media can help families make more informed and comfortable decisions about their child’s care in collaboration with their pediatrician. It also is important for pediatricians to be proactive in distributing reliable and science-backed material to the public in this new age of information overload.
Case follow-up
The pediatrician hears the family’s concerns and discusses the evidence supporting the scientific legitimacy of ADHD, as well as some of the qualities of the diagnosis that have led to its controversy. The parents are reassured but would like to proceed carefully and cautiously with further work-up and treatment. The pediatrician sends the family home with some quantitative rating scales to be completed by Hunter’s parents and teacher. She also makes a plan to begin monitoring several health promotion areas that could be impacting Hunter’s behavior including sleep quality, physical activity, screen time, and nutrition.
References
1. Psychiatr Clin North Am. 2010 Mar;33(1):159-80.
2. Dev Neuropsychol. 2013;38(4):211-25.3. Can Fam Physician. 2016 Dec;62(12):979-82.
4. ADHD boundaries with normal behavior. Pediatric News; published online Aug. 27, 2014.
5. Zombification is not an acceptable medical outcome. Psychology Today, ABCs of Child Psychiatry blog; published online Oct. 18, 2013.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych.
ADHD versus anxiety? An approach for pediatricians
This month’s column comes directly by request from a pediatric colleague. She asked about a common diagnostic dilemma for pediatricians that involves what at least on the surface appears like disruptive or oppositional behavior at the home, school, or both, but is complicated by the possibility that the primary engine of this behavior is anxiety. This is an important challenge to try and get right because the treatment plan will take different paths, depending on the final call that is made.
Case summary
Devin is a 6-year-old boy who comes in with his parents for concerns about his behavior. His parents note that he has always been “high strung” but not disruptive or aggressive. When he was younger, Devin was quite sensitive to sounds, textures, and tactile sensations, but this has improved on its own. Thunderstorms continue to bother him quite a bit, though, and he often will ask his parents repeated questions when it is cloudy about the possibility of a thunderstorm. With some extra teacher and parent support, Devin made the transition to kindergarten fairly well. Now, however, he is struggling in a larger 1st grade class. His teacher states that he often seems distracted, fidgety, and easily frustrated, causing him to “shut down” and refuse to do his work. This past week, during a more challenging assignment, he crawled under his desk and would not come out. The teacher is now recommending an evaluation for attention-deficit/hyperactivity disorder (ADHD).
Discussion
1. Are there other times in the child’s life when clearly he is very anxious? The presence of developmentally elevated levels of anxiety in areas outside the particular situations in question can provide a clue that anxiety is contributing to what otherwise might be seen as more oppositional behavior. In this case, the high levels of anxiety about thunderstorms show that anxiety is present in the child and could be playing a role in his disruptive behavior at school.
2. When he’s not focusing on the task at hand, what is he thinking about? Nonanxious children with or without ADHD can frequently daydream and go “off task,” but the content of those thoughts frequently involves anticipation for more preferred activities, reminisces of positive events from the past, or attention to other stimuli in the environment (for example, the bird in a tree outside). More anxious children, by contrast, may have more worried and ruminating thoughts about poor performance, possible bad events that might happen in the future, or “what if?” kinds of concerns.
3. Is there a family history of anxiety? While one should not over-rely on family history, the presence of one or more family members with clinically significant anxiety does raise the possibility of anxiety in the identified patient. Research indicates that the heritability of anxiety is about 50%,1,2 but that a significant amount of the transmission of anxiety from parent to child comes from environmental mechanisms.3
4. Is there a consistent trigger to his outbursts? For anxious children, meltdowns are frequently provoked by situations in which a child feels uncomfortable, overstimulated, or overwhelmed, and the outburst is a reflection of those intense feelings that are difficult to manage. An outburst like that above, which occurs when a child is pushed to finish difficult work, might be a good example of one that is triggered by anxiety.
5. What does the rating scale show? A broad-based rating scale that assesses multiple domains of symptoms can be a big help for diagnostic dilemmas such as this one. Our clinic uses the Child Behavior Checklist4 which has subscales for both anxiety and attention problems. Evidence of a spike in either of those domains, or both, really can help guide our thinking.
Of course, it is very possible that the answer to the ADHD versus anxiety question is that both are present. This is a common conclusion when it comes to mental health assessment, and it is different from the traditional “this or that” thinking present in more classic differential diagnosis decision making. Research indicates that the ADHD and anxiety disorders frequently co-occur.5 When that happens, concurrent evidence-based psychotherapy for anxiety in conjunction with multimodal treatment for ADHD has been recommended as a first step.6
Case follow-up
Based on all the information, the pediatrician judges that Devin’s disruptive behavior is in large part being driven by his level of anxiety. She makes a referral to a child psychologist to begin evidence-based psychotherapy and recommends that the school consider some modifications and accommodations that may help his behavior at school. At a follow-up appointment, Devin’s difficulties have improved, and there is little evidence of ADHD now that the anxiety has been fully addressed.
References
1. Genes Brain Behav. 2005;4(8):466-81.
2. J Am Acad Child Adolesc Psychiatry. 2010;49(3):248-55.
3. Am J Psychiatry. 2015;172(7):630-7.
4. Manual for the ASEBA School-Age Forms & Profiles (Burlington, Vt.: University of Vermont, Research Center for Children, Youth, and Families, 2001).
5. J Anxiety Disord. 1997;11(4):377-94.
6. J Abnorm Child Psychol. 2000;28(6):527-41.
Dr. Rettew is a child and adolescent psychiatrist and assistant professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected].
This month’s column comes directly by request from a pediatric colleague. She asked about a common diagnostic dilemma for pediatricians that involves what at least on the surface appears like disruptive or oppositional behavior at the home, school, or both, but is complicated by the possibility that the primary engine of this behavior is anxiety. This is an important challenge to try and get right because the treatment plan will take different paths, depending on the final call that is made.
Case summary
Devin is a 6-year-old boy who comes in with his parents for concerns about his behavior. His parents note that he has always been “high strung” but not disruptive or aggressive. When he was younger, Devin was quite sensitive to sounds, textures, and tactile sensations, but this has improved on its own. Thunderstorms continue to bother him quite a bit, though, and he often will ask his parents repeated questions when it is cloudy about the possibility of a thunderstorm. With some extra teacher and parent support, Devin made the transition to kindergarten fairly well. Now, however, he is struggling in a larger 1st grade class. His teacher states that he often seems distracted, fidgety, and easily frustrated, causing him to “shut down” and refuse to do his work. This past week, during a more challenging assignment, he crawled under his desk and would not come out. The teacher is now recommending an evaluation for attention-deficit/hyperactivity disorder (ADHD).
Discussion
1. Are there other times in the child’s life when clearly he is very anxious? The presence of developmentally elevated levels of anxiety in areas outside the particular situations in question can provide a clue that anxiety is contributing to what otherwise might be seen as more oppositional behavior. In this case, the high levels of anxiety about thunderstorms show that anxiety is present in the child and could be playing a role in his disruptive behavior at school.
2. When he’s not focusing on the task at hand, what is he thinking about? Nonanxious children with or without ADHD can frequently daydream and go “off task,” but the content of those thoughts frequently involves anticipation for more preferred activities, reminisces of positive events from the past, or attention to other stimuli in the environment (for example, the bird in a tree outside). More anxious children, by contrast, may have more worried and ruminating thoughts about poor performance, possible bad events that might happen in the future, or “what if?” kinds of concerns.
3. Is there a family history of anxiety? While one should not over-rely on family history, the presence of one or more family members with clinically significant anxiety does raise the possibility of anxiety in the identified patient. Research indicates that the heritability of anxiety is about 50%,1,2 but that a significant amount of the transmission of anxiety from parent to child comes from environmental mechanisms.3
4. Is there a consistent trigger to his outbursts? For anxious children, meltdowns are frequently provoked by situations in which a child feels uncomfortable, overstimulated, or overwhelmed, and the outburst is a reflection of those intense feelings that are difficult to manage. An outburst like that above, which occurs when a child is pushed to finish difficult work, might be a good example of one that is triggered by anxiety.
5. What does the rating scale show? A broad-based rating scale that assesses multiple domains of symptoms can be a big help for diagnostic dilemmas such as this one. Our clinic uses the Child Behavior Checklist4 which has subscales for both anxiety and attention problems. Evidence of a spike in either of those domains, or both, really can help guide our thinking.
Of course, it is very possible that the answer to the ADHD versus anxiety question is that both are present. This is a common conclusion when it comes to mental health assessment, and it is different from the traditional “this or that” thinking present in more classic differential diagnosis decision making. Research indicates that the ADHD and anxiety disorders frequently co-occur.5 When that happens, concurrent evidence-based psychotherapy for anxiety in conjunction with multimodal treatment for ADHD has been recommended as a first step.6
Case follow-up
Based on all the information, the pediatrician judges that Devin’s disruptive behavior is in large part being driven by his level of anxiety. She makes a referral to a child psychologist to begin evidence-based psychotherapy and recommends that the school consider some modifications and accommodations that may help his behavior at school. At a follow-up appointment, Devin’s difficulties have improved, and there is little evidence of ADHD now that the anxiety has been fully addressed.
References
1. Genes Brain Behav. 2005;4(8):466-81.
2. J Am Acad Child Adolesc Psychiatry. 2010;49(3):248-55.
3. Am J Psychiatry. 2015;172(7):630-7.
4. Manual for the ASEBA School-Age Forms & Profiles (Burlington, Vt.: University of Vermont, Research Center for Children, Youth, and Families, 2001).
5. J Anxiety Disord. 1997;11(4):377-94.
6. J Abnorm Child Psychol. 2000;28(6):527-41.
Dr. Rettew is a child and adolescent psychiatrist and assistant professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected].
This month’s column comes directly by request from a pediatric colleague. She asked about a common diagnostic dilemma for pediatricians that involves what at least on the surface appears like disruptive or oppositional behavior at the home, school, or both, but is complicated by the possibility that the primary engine of this behavior is anxiety. This is an important challenge to try and get right because the treatment plan will take different paths, depending on the final call that is made.
Case summary
Devin is a 6-year-old boy who comes in with his parents for concerns about his behavior. His parents note that he has always been “high strung” but not disruptive or aggressive. When he was younger, Devin was quite sensitive to sounds, textures, and tactile sensations, but this has improved on its own. Thunderstorms continue to bother him quite a bit, though, and he often will ask his parents repeated questions when it is cloudy about the possibility of a thunderstorm. With some extra teacher and parent support, Devin made the transition to kindergarten fairly well. Now, however, he is struggling in a larger 1st grade class. His teacher states that he often seems distracted, fidgety, and easily frustrated, causing him to “shut down” and refuse to do his work. This past week, during a more challenging assignment, he crawled under his desk and would not come out. The teacher is now recommending an evaluation for attention-deficit/hyperactivity disorder (ADHD).
Discussion
1. Are there other times in the child’s life when clearly he is very anxious? The presence of developmentally elevated levels of anxiety in areas outside the particular situations in question can provide a clue that anxiety is contributing to what otherwise might be seen as more oppositional behavior. In this case, the high levels of anxiety about thunderstorms show that anxiety is present in the child and could be playing a role in his disruptive behavior at school.
2. When he’s not focusing on the task at hand, what is he thinking about? Nonanxious children with or without ADHD can frequently daydream and go “off task,” but the content of those thoughts frequently involves anticipation for more preferred activities, reminisces of positive events from the past, or attention to other stimuli in the environment (for example, the bird in a tree outside). More anxious children, by contrast, may have more worried and ruminating thoughts about poor performance, possible bad events that might happen in the future, or “what if?” kinds of concerns.
3. Is there a family history of anxiety? While one should not over-rely on family history, the presence of one or more family members with clinically significant anxiety does raise the possibility of anxiety in the identified patient. Research indicates that the heritability of anxiety is about 50%,1,2 but that a significant amount of the transmission of anxiety from parent to child comes from environmental mechanisms.3
4. Is there a consistent trigger to his outbursts? For anxious children, meltdowns are frequently provoked by situations in which a child feels uncomfortable, overstimulated, or overwhelmed, and the outburst is a reflection of those intense feelings that are difficult to manage. An outburst like that above, which occurs when a child is pushed to finish difficult work, might be a good example of one that is triggered by anxiety.
5. What does the rating scale show? A broad-based rating scale that assesses multiple domains of symptoms can be a big help for diagnostic dilemmas such as this one. Our clinic uses the Child Behavior Checklist4 which has subscales for both anxiety and attention problems. Evidence of a spike in either of those domains, or both, really can help guide our thinking.
Of course, it is very possible that the answer to the ADHD versus anxiety question is that both are present. This is a common conclusion when it comes to mental health assessment, and it is different from the traditional “this or that” thinking present in more classic differential diagnosis decision making. Research indicates that the ADHD and anxiety disorders frequently co-occur.5 When that happens, concurrent evidence-based psychotherapy for anxiety in conjunction with multimodal treatment for ADHD has been recommended as a first step.6
Case follow-up
Based on all the information, the pediatrician judges that Devin’s disruptive behavior is in large part being driven by his level of anxiety. She makes a referral to a child psychologist to begin evidence-based psychotherapy and recommends that the school consider some modifications and accommodations that may help his behavior at school. At a follow-up appointment, Devin’s difficulties have improved, and there is little evidence of ADHD now that the anxiety has been fully addressed.
References
1. Genes Brain Behav. 2005;4(8):466-81.
2. J Am Acad Child Adolesc Psychiatry. 2010;49(3):248-55.
3. Am J Psychiatry. 2015;172(7):630-7.
4. Manual for the ASEBA School-Age Forms & Profiles (Burlington, Vt.: University of Vermont, Research Center for Children, Youth, and Families, 2001).
5. J Anxiety Disord. 1997;11(4):377-94.
6. J Abnorm Child Psychol. 2000;28(6):527-41.
Dr. Rettew is a child and adolescent psychiatrist and assistant professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. Email him at [email protected].
Parenting: Tips on discussing a tough but important topic
It seems like the field of psychiatry has been all over the map when it comes to viewing the importance of parenting with regard to child behavioral problems and disorders. For decades, we heard that parents, particularly mothers, were to blame for everything from childhood autism to excessive temper tantrums.1 Then, parenting somehow got somewhat pushed aside as the genetic and biological underpinnings of behavior became increasingly appreciated. For a while, parenting was nearly relegated to epiphenomenon status – that is, an almost irrelevant reaction to genetically driven child behavior.
More recently, it appears that some semblance of balance has been restored with parenting behavior being appreciated as critically important in the development of a child, but in the context of many other mutually interacting factors.2 There also is a far greater understanding that child behavior and parent behavior is very much a two-way street.
These more nuanced and neuroscience-backed perspectives, however, don’t make bringing up the subject of parenting any easier. In part because of how seriously most mothers, fathers, and other caretakers take their job as a parent, it can be easy to put parents on the defensive, especially when one of their children is struggling behaviorally. At the same time, taking the easy way out by giving boilerplate advice, or even avoiding the topic of parenting completely, is a huge missed opportunity to engage families who often are desperately seeking some guidance.
Case summary
Emily is a healthy 6-year-old girl who comes in with her single mother and her two younger siblings for an annual exam. Her mother proudly reports that she is doing great at school, but seems reluctant to say much about her home life. The mother seems somewhat frazzled, and the interview is difficult because the three siblings are arguing with each other. After Emily and her sister fight over reading the same book, the mother suddenly and quite loudly says, “Can you just let me talk for 1 second!”
Discussion
Pediatricians often have strong suspicions that parents are struggling with a child’s behavior but can have trouble knowing how exactly to bring up the subject of parenting. Some specific suggestions for having productive discussions on parenting include the following:
• Think about the statements embedded in your questions. A screening question about parenting such as, “Can you tell me about the areas of parenting that you are most proud of and the areas where you feel you need the most help?” helps a parent understand that you assume that no parent is perfect and that everyone has areas of strength and weakness.
• Compliment when you can. Related to the above, find those areas of positive parenting, even if it involves effort more than results, and communicate that you have noticed them. This can make talking about the weaknesses a little easier to hear for the parent.
• Frame the issue in terms of surpluses rather than deficits. Instead of coming from the perspective that a parent is deficient in their basic parenting skills, reframe the challenge as someone needing “superparent” skills to manage multiple or more challenging children. The often-heard statements that “kids don’t come with instruction books” or “you need to earn a license to drive a car but not raise a child” are almost cliché these days, but still convey to parents that you understand how difficult parenting can be. In some cases, it may be appropriate to disclose some parenting challenges you have experienced firsthand.
• Get details. Before launching into specific recommendations, ask yourself if you are able to really see the issue a parent is describing. Rather than reviewing a laundry list of sleep hygiene recommendations, for example, it can be very worthwhile to ask, “How exactly does bedtime work at your home?” Getting all the details can not only build empathy, but allow you to really see specific areas for improvement. If you can’t paint a picture of how a scene might really look at this patient’s home, there likely is more to learn.
Of course, one of the key challenges here is time. Really giving these parenting concerns the time they deserve usually means going beyond the precious few minutes pediatricians have for a well visit. In these instances, it may be worth scheduling a future appointment that is exclusively devoted to this issue. Alternatively, a referral can be made to a therapist, counselor, or parent “coach” to give a family greater opportunity to work 1:1 with a professional. When you do this, be clear that you are looking for a therapist to work with the whole family, ideally using many of the evidence-based techniques that have been shown to be effective. A list of manual-based treatments as well as some books that parents could read on their own to address oppositional-defiant behavior is available, including a guide for families from the American Academy from Child and Adolescent Psychiatry.3
Case follow-up
The pediatrician finds another book to satisfy the younger sibling and says to the mother, “I’m glad to see that at least they are fighting over a book. That’s great that you have taught them to like reading.” They commiserate about how difficult it is to raise three young children as a single parent, and the mother then begins to open up about Emily’s defiant and disrespectful behavior at home that the mother blames on herself. The pediatrician offers a referral to see a local family therapist, which the mother gratefully accepts.
References
1. Am J Orthopsychiatry. 1985 Jul;55(3):345-53.
2. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78.
3. American Academy of Child and Adolescent Psychiatry. (2009). Oppositional Defiant Disorder: A Guide for Families.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at [email protected].
It seems like the field of psychiatry has been all over the map when it comes to viewing the importance of parenting with regard to child behavioral problems and disorders. For decades, we heard that parents, particularly mothers, were to blame for everything from childhood autism to excessive temper tantrums.1 Then, parenting somehow got somewhat pushed aside as the genetic and biological underpinnings of behavior became increasingly appreciated. For a while, parenting was nearly relegated to epiphenomenon status – that is, an almost irrelevant reaction to genetically driven child behavior.
More recently, it appears that some semblance of balance has been restored with parenting behavior being appreciated as critically important in the development of a child, but in the context of many other mutually interacting factors.2 There also is a far greater understanding that child behavior and parent behavior is very much a two-way street.
These more nuanced and neuroscience-backed perspectives, however, don’t make bringing up the subject of parenting any easier. In part because of how seriously most mothers, fathers, and other caretakers take their job as a parent, it can be easy to put parents on the defensive, especially when one of their children is struggling behaviorally. At the same time, taking the easy way out by giving boilerplate advice, or even avoiding the topic of parenting completely, is a huge missed opportunity to engage families who often are desperately seeking some guidance.
Case summary
Emily is a healthy 6-year-old girl who comes in with her single mother and her two younger siblings for an annual exam. Her mother proudly reports that she is doing great at school, but seems reluctant to say much about her home life. The mother seems somewhat frazzled, and the interview is difficult because the three siblings are arguing with each other. After Emily and her sister fight over reading the same book, the mother suddenly and quite loudly says, “Can you just let me talk for 1 second!”
Discussion
Pediatricians often have strong suspicions that parents are struggling with a child’s behavior but can have trouble knowing how exactly to bring up the subject of parenting. Some specific suggestions for having productive discussions on parenting include the following:
• Think about the statements embedded in your questions. A screening question about parenting such as, “Can you tell me about the areas of parenting that you are most proud of and the areas where you feel you need the most help?” helps a parent understand that you assume that no parent is perfect and that everyone has areas of strength and weakness.
• Compliment when you can. Related to the above, find those areas of positive parenting, even if it involves effort more than results, and communicate that you have noticed them. This can make talking about the weaknesses a little easier to hear for the parent.
• Frame the issue in terms of surpluses rather than deficits. Instead of coming from the perspective that a parent is deficient in their basic parenting skills, reframe the challenge as someone needing “superparent” skills to manage multiple or more challenging children. The often-heard statements that “kids don’t come with instruction books” or “you need to earn a license to drive a car but not raise a child” are almost cliché these days, but still convey to parents that you understand how difficult parenting can be. In some cases, it may be appropriate to disclose some parenting challenges you have experienced firsthand.
• Get details. Before launching into specific recommendations, ask yourself if you are able to really see the issue a parent is describing. Rather than reviewing a laundry list of sleep hygiene recommendations, for example, it can be very worthwhile to ask, “How exactly does bedtime work at your home?” Getting all the details can not only build empathy, but allow you to really see specific areas for improvement. If you can’t paint a picture of how a scene might really look at this patient’s home, there likely is more to learn.
Of course, one of the key challenges here is time. Really giving these parenting concerns the time they deserve usually means going beyond the precious few minutes pediatricians have for a well visit. In these instances, it may be worth scheduling a future appointment that is exclusively devoted to this issue. Alternatively, a referral can be made to a therapist, counselor, or parent “coach” to give a family greater opportunity to work 1:1 with a professional. When you do this, be clear that you are looking for a therapist to work with the whole family, ideally using many of the evidence-based techniques that have been shown to be effective. A list of manual-based treatments as well as some books that parents could read on their own to address oppositional-defiant behavior is available, including a guide for families from the American Academy from Child and Adolescent Psychiatry.3
Case follow-up
The pediatrician finds another book to satisfy the younger sibling and says to the mother, “I’m glad to see that at least they are fighting over a book. That’s great that you have taught them to like reading.” They commiserate about how difficult it is to raise three young children as a single parent, and the mother then begins to open up about Emily’s defiant and disrespectful behavior at home that the mother blames on herself. The pediatrician offers a referral to see a local family therapist, which the mother gratefully accepts.
References
1. Am J Orthopsychiatry. 1985 Jul;55(3):345-53.
2. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78.
3. American Academy of Child and Adolescent Psychiatry. (2009). Oppositional Defiant Disorder: A Guide for Families.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at [email protected].
It seems like the field of psychiatry has been all over the map when it comes to viewing the importance of parenting with regard to child behavioral problems and disorders. For decades, we heard that parents, particularly mothers, were to blame for everything from childhood autism to excessive temper tantrums.1 Then, parenting somehow got somewhat pushed aside as the genetic and biological underpinnings of behavior became increasingly appreciated. For a while, parenting was nearly relegated to epiphenomenon status – that is, an almost irrelevant reaction to genetically driven child behavior.
More recently, it appears that some semblance of balance has been restored with parenting behavior being appreciated as critically important in the development of a child, but in the context of many other mutually interacting factors.2 There also is a far greater understanding that child behavior and parent behavior is very much a two-way street.
These more nuanced and neuroscience-backed perspectives, however, don’t make bringing up the subject of parenting any easier. In part because of how seriously most mothers, fathers, and other caretakers take their job as a parent, it can be easy to put parents on the defensive, especially when one of their children is struggling behaviorally. At the same time, taking the easy way out by giving boilerplate advice, or even avoiding the topic of parenting completely, is a huge missed opportunity to engage families who often are desperately seeking some guidance.
Case summary
Emily is a healthy 6-year-old girl who comes in with her single mother and her two younger siblings for an annual exam. Her mother proudly reports that she is doing great at school, but seems reluctant to say much about her home life. The mother seems somewhat frazzled, and the interview is difficult because the three siblings are arguing with each other. After Emily and her sister fight over reading the same book, the mother suddenly and quite loudly says, “Can you just let me talk for 1 second!”
Discussion
Pediatricians often have strong suspicions that parents are struggling with a child’s behavior but can have trouble knowing how exactly to bring up the subject of parenting. Some specific suggestions for having productive discussions on parenting include the following:
• Think about the statements embedded in your questions. A screening question about parenting such as, “Can you tell me about the areas of parenting that you are most proud of and the areas where you feel you need the most help?” helps a parent understand that you assume that no parent is perfect and that everyone has areas of strength and weakness.
• Compliment when you can. Related to the above, find those areas of positive parenting, even if it involves effort more than results, and communicate that you have noticed them. This can make talking about the weaknesses a little easier to hear for the parent.
• Frame the issue in terms of surpluses rather than deficits. Instead of coming from the perspective that a parent is deficient in their basic parenting skills, reframe the challenge as someone needing “superparent” skills to manage multiple or more challenging children. The often-heard statements that “kids don’t come with instruction books” or “you need to earn a license to drive a car but not raise a child” are almost cliché these days, but still convey to parents that you understand how difficult parenting can be. In some cases, it may be appropriate to disclose some parenting challenges you have experienced firsthand.
• Get details. Before launching into specific recommendations, ask yourself if you are able to really see the issue a parent is describing. Rather than reviewing a laundry list of sleep hygiene recommendations, for example, it can be very worthwhile to ask, “How exactly does bedtime work at your home?” Getting all the details can not only build empathy, but allow you to really see specific areas for improvement. If you can’t paint a picture of how a scene might really look at this patient’s home, there likely is more to learn.
Of course, one of the key challenges here is time. Really giving these parenting concerns the time they deserve usually means going beyond the precious few minutes pediatricians have for a well visit. In these instances, it may be worth scheduling a future appointment that is exclusively devoted to this issue. Alternatively, a referral can be made to a therapist, counselor, or parent “coach” to give a family greater opportunity to work 1:1 with a professional. When you do this, be clear that you are looking for a therapist to work with the whole family, ideally using many of the evidence-based techniques that have been shown to be effective. A list of manual-based treatments as well as some books that parents could read on their own to address oppositional-defiant behavior is available, including a guide for families from the American Academy from Child and Adolescent Psychiatry.3
Case follow-up
The pediatrician finds another book to satisfy the younger sibling and says to the mother, “I’m glad to see that at least they are fighting over a book. That’s great that you have taught them to like reading.” They commiserate about how difficult it is to raise three young children as a single parent, and the mother then begins to open up about Emily’s defiant and disrespectful behavior at home that the mother blames on herself. The pediatrician offers a referral to see a local family therapist, which the mother gratefully accepts.
References
1. Am J Orthopsychiatry. 1985 Jul;55(3):345-53.
2. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78.
3. American Academy of Child and Adolescent Psychiatry. (2009). Oppositional Defiant Disorder: A Guide for Families.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Email him at [email protected].
Mental health of transgender youth
There has been quite a bit of discussion and controversy lately about transgender individuals. The debate has extended to the diagnosis itself and whether it should be maintained as an official entity. The previous edition of the Diagnostic and Statistical Manual included the diagnosis of gender identity disorder, which was modified to the current diagnosis of gender dysphoria that describes individuals who show a persistent desire to be the “other” gender and/or an insistence that their gender is different from their birth sex.
One question at the heart of this discussion is the degree to which psychiatric symptoms and disorders are inherent in the gender dysphoria itself or whether most, if not all, of the noted links to things like anxiety, depression, and suicidal behavior stem from the hostility and abuse that many of these youth endure.
As has been reported in the Pediatric News column LGBT Youth Consult, research is now focusing on the mental health of transgender youth, although the data are not entirely consistent. One recent study of 298 transgender women between the ages of 16 and 29 years, of whom nearly three-quarters had received crossgender hormones, showed quite high rates of psychiatric disorders including depression (35%), anxiety (8%), and substance abuse (11%).1 Moderate to high levels of suicidality in the past month were found in 20% of the sample. Although one cannot conclude from this study that psychopathology is intrinsic to transgender individuals, it does suggest that difficulties can certainly persist among those who have socially transitioned to their affirmed gender.
In contrast, another study from the TransYouth Project showed much more hopeful results.2 In this younger sample of 73 prepubescent children, 70% of whom were natal males and all of whom had been supported in the social transition to their affirmed gender at a relatively young age, levels of depressed symptoms were no different from those in 73 controls, and scores on an anxiety scale were only slightly elevated, but did not reach clinical or even subclinical levels as a group. The authors of this study concluded that psychiatric symptoms are not “synonymous” with being transgender. They suggest that supporting youth in their transition at earlier ages could possibly prevent the occurrence of mental health problems in the future.
There is wide acknowledgment that gender-nonconforming youth are at much heightened risk from what can be vicious and cruel maltreatment from peers and the wider community. Similarly, there is good consensus that “conversion therapy” approaches that actively try to discourage youth from their affirmed gender are misguided and unethical. What remains in question among well-meaning parents and clinicians alike, however, is at what age should social transition be supported and how encompassing should it be with regard to pronoun use, bathroom and dressing room access, clothing, and so on. Studies have shown that gender atypical behavior can be quite common in young children, with the vast majority eventually developing gender identities that are in line with their natal sex. Parents may worry that promoting a premature gender transition might expose their child to bullying and harassment that could otherwise be avoided. On the other hand, parents may worry that not supporting gender transition will be experienced as rejecting and critical, which could lead to increased feelings of depression and isolation. Although both views represent valid concerns, it is probably fair to say that among clinicians and researchers who work with transgender youth, there seems to be some movement toward more active acceptance and encouragement of a child’s gender expression at the time, with the understanding that for many, there can be continued movement in one’s gender “journey” across development.
Interestingly, these studies are being published in parallel with some neuroimaging research investigating sex differences with regard to the brain. A recent study from the Proceedings of the National Academy of Sciences found that, among many different regions that are known to show some sex differences with regard to size or connectivity to other regions, the typical human brain shows a “mosaic” pattern in which some regions look more typically male while others look more typically female.3
References
1. JAMA Pediatr. 2016 May 1;170(5):481-6.
2. Pediatrics. 2016;137(3):1-8.
3. PNAS. 2015;112(50):15468-73
Dr. Rettew is an associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @pedipsych.
There has been quite a bit of discussion and controversy lately about transgender individuals. The debate has extended to the diagnosis itself and whether it should be maintained as an official entity. The previous edition of the Diagnostic and Statistical Manual included the diagnosis of gender identity disorder, which was modified to the current diagnosis of gender dysphoria that describes individuals who show a persistent desire to be the “other” gender and/or an insistence that their gender is different from their birth sex.
One question at the heart of this discussion is the degree to which psychiatric symptoms and disorders are inherent in the gender dysphoria itself or whether most, if not all, of the noted links to things like anxiety, depression, and suicidal behavior stem from the hostility and abuse that many of these youth endure.
As has been reported in the Pediatric News column LGBT Youth Consult, research is now focusing on the mental health of transgender youth, although the data are not entirely consistent. One recent study of 298 transgender women between the ages of 16 and 29 years, of whom nearly three-quarters had received crossgender hormones, showed quite high rates of psychiatric disorders including depression (35%), anxiety (8%), and substance abuse (11%).1 Moderate to high levels of suicidality in the past month were found in 20% of the sample. Although one cannot conclude from this study that psychopathology is intrinsic to transgender individuals, it does suggest that difficulties can certainly persist among those who have socially transitioned to their affirmed gender.
In contrast, another study from the TransYouth Project showed much more hopeful results.2 In this younger sample of 73 prepubescent children, 70% of whom were natal males and all of whom had been supported in the social transition to their affirmed gender at a relatively young age, levels of depressed symptoms were no different from those in 73 controls, and scores on an anxiety scale were only slightly elevated, but did not reach clinical or even subclinical levels as a group. The authors of this study concluded that psychiatric symptoms are not “synonymous” with being transgender. They suggest that supporting youth in their transition at earlier ages could possibly prevent the occurrence of mental health problems in the future.
There is wide acknowledgment that gender-nonconforming youth are at much heightened risk from what can be vicious and cruel maltreatment from peers and the wider community. Similarly, there is good consensus that “conversion therapy” approaches that actively try to discourage youth from their affirmed gender are misguided and unethical. What remains in question among well-meaning parents and clinicians alike, however, is at what age should social transition be supported and how encompassing should it be with regard to pronoun use, bathroom and dressing room access, clothing, and so on. Studies have shown that gender atypical behavior can be quite common in young children, with the vast majority eventually developing gender identities that are in line with their natal sex. Parents may worry that promoting a premature gender transition might expose their child to bullying and harassment that could otherwise be avoided. On the other hand, parents may worry that not supporting gender transition will be experienced as rejecting and critical, which could lead to increased feelings of depression and isolation. Although both views represent valid concerns, it is probably fair to say that among clinicians and researchers who work with transgender youth, there seems to be some movement toward more active acceptance and encouragement of a child’s gender expression at the time, with the understanding that for many, there can be continued movement in one’s gender “journey” across development.
Interestingly, these studies are being published in parallel with some neuroimaging research investigating sex differences with regard to the brain. A recent study from the Proceedings of the National Academy of Sciences found that, among many different regions that are known to show some sex differences with regard to size or connectivity to other regions, the typical human brain shows a “mosaic” pattern in which some regions look more typically male while others look more typically female.3
References
1. JAMA Pediatr. 2016 May 1;170(5):481-6.
2. Pediatrics. 2016;137(3):1-8.
3. PNAS. 2015;112(50):15468-73
Dr. Rettew is an associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @pedipsych.
There has been quite a bit of discussion and controversy lately about transgender individuals. The debate has extended to the diagnosis itself and whether it should be maintained as an official entity. The previous edition of the Diagnostic and Statistical Manual included the diagnosis of gender identity disorder, which was modified to the current diagnosis of gender dysphoria that describes individuals who show a persistent desire to be the “other” gender and/or an insistence that their gender is different from their birth sex.
One question at the heart of this discussion is the degree to which psychiatric symptoms and disorders are inherent in the gender dysphoria itself or whether most, if not all, of the noted links to things like anxiety, depression, and suicidal behavior stem from the hostility and abuse that many of these youth endure.
As has been reported in the Pediatric News column LGBT Youth Consult, research is now focusing on the mental health of transgender youth, although the data are not entirely consistent. One recent study of 298 transgender women between the ages of 16 and 29 years, of whom nearly three-quarters had received crossgender hormones, showed quite high rates of psychiatric disorders including depression (35%), anxiety (8%), and substance abuse (11%).1 Moderate to high levels of suicidality in the past month were found in 20% of the sample. Although one cannot conclude from this study that psychopathology is intrinsic to transgender individuals, it does suggest that difficulties can certainly persist among those who have socially transitioned to their affirmed gender.
In contrast, another study from the TransYouth Project showed much more hopeful results.2 In this younger sample of 73 prepubescent children, 70% of whom were natal males and all of whom had been supported in the social transition to their affirmed gender at a relatively young age, levels of depressed symptoms were no different from those in 73 controls, and scores on an anxiety scale were only slightly elevated, but did not reach clinical or even subclinical levels as a group. The authors of this study concluded that psychiatric symptoms are not “synonymous” with being transgender. They suggest that supporting youth in their transition at earlier ages could possibly prevent the occurrence of mental health problems in the future.
There is wide acknowledgment that gender-nonconforming youth are at much heightened risk from what can be vicious and cruel maltreatment from peers and the wider community. Similarly, there is good consensus that “conversion therapy” approaches that actively try to discourage youth from their affirmed gender are misguided and unethical. What remains in question among well-meaning parents and clinicians alike, however, is at what age should social transition be supported and how encompassing should it be with regard to pronoun use, bathroom and dressing room access, clothing, and so on. Studies have shown that gender atypical behavior can be quite common in young children, with the vast majority eventually developing gender identities that are in line with their natal sex. Parents may worry that promoting a premature gender transition might expose their child to bullying and harassment that could otherwise be avoided. On the other hand, parents may worry that not supporting gender transition will be experienced as rejecting and critical, which could lead to increased feelings of depression and isolation. Although both views represent valid concerns, it is probably fair to say that among clinicians and researchers who work with transgender youth, there seems to be some movement toward more active acceptance and encouragement of a child’s gender expression at the time, with the understanding that for many, there can be continued movement in one’s gender “journey” across development.
Interestingly, these studies are being published in parallel with some neuroimaging research investigating sex differences with regard to the brain. A recent study from the Proceedings of the National Academy of Sciences found that, among many different regions that are known to show some sex differences with regard to size or connectivity to other regions, the typical human brain shows a “mosaic” pattern in which some regions look more typically male while others look more typically female.3
References
1. JAMA Pediatr. 2016 May 1;170(5):481-6.
2. Pediatrics. 2016;137(3):1-8.
3. PNAS. 2015;112(50):15468-73
Dr. Rettew is an associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @pedipsych.
Behavior problems in youth: Are things worse today than in the past?
Every generation of adults seems to worry that the next generation of youth is in trouble. The perception of kids today is no different, with theories abounding as to why the mental health of the newest generation is slipping, compared with previous standards. From mobile phones to helicopter parents, it might seem like a foregone conclusion that our current crop of young people is destined to be insecure, inattentive, and unable to cope with challenges and stress. Many news headlines on the latest mass shooting or standardized test results often seem to confirm these widespread concerns.
Pediatricians often hear parents lamenting the “good old days” when such things as corporal punishment were more easily accepted to help keep kids in line. But taking a step back, it may be worth a more objective look to examine the assumption that child behavioral problems are worse than ever. Measuring overall mental health is not an easy task, but looking at several important metrics indicate that things may not be nearly as bad as many people think.
Substance use
From the latest data from the Monitoring the Future Study, one of the nation’s most reliable sources on teen substance use, the use of both alcohol and tobacco among youth is at the lowest level since the study began in 1975. Use of drugs like heroin and ecstasy also are declining. The only major exception to this trend seems to be cannabis use, which has generally shown stable rates during this climate of marijuana decriminalization and, for some states, legalization.
Teen pregnancy rates
One area where there continues to be sustained progress is in teen pregnancy. According to the government’s Centers for Disease Control and Prevention, the overall pregnancy rate among adolescent females has been cut in half from 1991 to 2011, across many different ethnic groups. The rate fell from 61.8/1,000 teenagers aged 15-19 years to 31.3/1,000 teenagers.
Delinquency
Far fewer adolescents are being held against their will in juvenile detention centers. The number of youth who are incarcerated have dropped from a high of 381/100,000 in 1995 to 225/100,000 in 2010, according to a report by the Annie E. Casey Foundation.
Bullying
Bullying has been increasingly recognized as the public health problem that it is. The use of online technology also has created many new settings in which bullying can take place. Nevertheless, there is reason to be optimistic. From the National Center for Education Statistics and the National Crime Victimization Survey, the number of students who report being bullied at school has dropped from 32% in 2007 to an all-time low of 22% in 2013. Another recent study reached similar conclusions for bullying and many other forms of child victimization between 2003 and 2011 (JAMA Pediatr. 2014 Jun;168[6]:540-6).
Suicide
According to the CDC, the rate of completed suicide in youth peaked in the early1990s and then dropped and stabilized before starting to creep up again over the past 5 or so years. The trends are somewhat different, based on gender and the specific age group that is examined. The majority of completed youth suicides occur in males, with current rates still well below those historical highs.
Psychiatric disorders
This one is particularly tricky. While the rates of many specific psychiatric disorders such as ADHD and bipolar disorder have been rising in youth, as well as the use of psychiatric medications, it is much less clear whether this represents a true rise in these disorders versus other factors such as improved detection and a lower diagnostic threshold. One study by Achenbach et al. that measured quantitative levels of child behavior problems from the same rating scale over a 23-year time span found some increases in overall levels from the 1970s to the early 1990s, but then levels began to fall by the end of the millennium (J Abnorm Child Psychol. 2003 Feb;31[1]:1-11).
Of course, these hopeful trends in many significant areas do not mean that these problems have been overcome. While much work remains to be done on many fronts, it is still worth keeping in mind that the overall condition of youth mental health may not be as dire as we might be led to believe and that there is evidence that our efforts, perhaps, are leading to some progress.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. He said he has no relevant financial disclosures. Follow him on Twitter @pedipsych. E-mail him at [email protected].
Every generation of adults seems to worry that the next generation of youth is in trouble. The perception of kids today is no different, with theories abounding as to why the mental health of the newest generation is slipping, compared with previous standards. From mobile phones to helicopter parents, it might seem like a foregone conclusion that our current crop of young people is destined to be insecure, inattentive, and unable to cope with challenges and stress. Many news headlines on the latest mass shooting or standardized test results often seem to confirm these widespread concerns.
Pediatricians often hear parents lamenting the “good old days” when such things as corporal punishment were more easily accepted to help keep kids in line. But taking a step back, it may be worth a more objective look to examine the assumption that child behavioral problems are worse than ever. Measuring overall mental health is not an easy task, but looking at several important metrics indicate that things may not be nearly as bad as many people think.
Substance use
From the latest data from the Monitoring the Future Study, one of the nation’s most reliable sources on teen substance use, the use of both alcohol and tobacco among youth is at the lowest level since the study began in 1975. Use of drugs like heroin and ecstasy also are declining. The only major exception to this trend seems to be cannabis use, which has generally shown stable rates during this climate of marijuana decriminalization and, for some states, legalization.
Teen pregnancy rates
One area where there continues to be sustained progress is in teen pregnancy. According to the government’s Centers for Disease Control and Prevention, the overall pregnancy rate among adolescent females has been cut in half from 1991 to 2011, across many different ethnic groups. The rate fell from 61.8/1,000 teenagers aged 15-19 years to 31.3/1,000 teenagers.
Delinquency
Far fewer adolescents are being held against their will in juvenile detention centers. The number of youth who are incarcerated have dropped from a high of 381/100,000 in 1995 to 225/100,000 in 2010, according to a report by the Annie E. Casey Foundation.
Bullying
Bullying has been increasingly recognized as the public health problem that it is. The use of online technology also has created many new settings in which bullying can take place. Nevertheless, there is reason to be optimistic. From the National Center for Education Statistics and the National Crime Victimization Survey, the number of students who report being bullied at school has dropped from 32% in 2007 to an all-time low of 22% in 2013. Another recent study reached similar conclusions for bullying and many other forms of child victimization between 2003 and 2011 (JAMA Pediatr. 2014 Jun;168[6]:540-6).
Suicide
According to the CDC, the rate of completed suicide in youth peaked in the early1990s and then dropped and stabilized before starting to creep up again over the past 5 or so years. The trends are somewhat different, based on gender and the specific age group that is examined. The majority of completed youth suicides occur in males, with current rates still well below those historical highs.
Psychiatric disorders
This one is particularly tricky. While the rates of many specific psychiatric disorders such as ADHD and bipolar disorder have been rising in youth, as well as the use of psychiatric medications, it is much less clear whether this represents a true rise in these disorders versus other factors such as improved detection and a lower diagnostic threshold. One study by Achenbach et al. that measured quantitative levels of child behavior problems from the same rating scale over a 23-year time span found some increases in overall levels from the 1970s to the early 1990s, but then levels began to fall by the end of the millennium (J Abnorm Child Psychol. 2003 Feb;31[1]:1-11).
Of course, these hopeful trends in many significant areas do not mean that these problems have been overcome. While much work remains to be done on many fronts, it is still worth keeping in mind that the overall condition of youth mental health may not be as dire as we might be led to believe and that there is evidence that our efforts, perhaps, are leading to some progress.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. He said he has no relevant financial disclosures. Follow him on Twitter @pedipsych. E-mail him at [email protected].
Every generation of adults seems to worry that the next generation of youth is in trouble. The perception of kids today is no different, with theories abounding as to why the mental health of the newest generation is slipping, compared with previous standards. From mobile phones to helicopter parents, it might seem like a foregone conclusion that our current crop of young people is destined to be insecure, inattentive, and unable to cope with challenges and stress. Many news headlines on the latest mass shooting or standardized test results often seem to confirm these widespread concerns.
Pediatricians often hear parents lamenting the “good old days” when such things as corporal punishment were more easily accepted to help keep kids in line. But taking a step back, it may be worth a more objective look to examine the assumption that child behavioral problems are worse than ever. Measuring overall mental health is not an easy task, but looking at several important metrics indicate that things may not be nearly as bad as many people think.
Substance use
From the latest data from the Monitoring the Future Study, one of the nation’s most reliable sources on teen substance use, the use of both alcohol and tobacco among youth is at the lowest level since the study began in 1975. Use of drugs like heroin and ecstasy also are declining. The only major exception to this trend seems to be cannabis use, which has generally shown stable rates during this climate of marijuana decriminalization and, for some states, legalization.
Teen pregnancy rates
One area where there continues to be sustained progress is in teen pregnancy. According to the government’s Centers for Disease Control and Prevention, the overall pregnancy rate among adolescent females has been cut in half from 1991 to 2011, across many different ethnic groups. The rate fell from 61.8/1,000 teenagers aged 15-19 years to 31.3/1,000 teenagers.
Delinquency
Far fewer adolescents are being held against their will in juvenile detention centers. The number of youth who are incarcerated have dropped from a high of 381/100,000 in 1995 to 225/100,000 in 2010, according to a report by the Annie E. Casey Foundation.
Bullying
Bullying has been increasingly recognized as the public health problem that it is. The use of online technology also has created many new settings in which bullying can take place. Nevertheless, there is reason to be optimistic. From the National Center for Education Statistics and the National Crime Victimization Survey, the number of students who report being bullied at school has dropped from 32% in 2007 to an all-time low of 22% in 2013. Another recent study reached similar conclusions for bullying and many other forms of child victimization between 2003 and 2011 (JAMA Pediatr. 2014 Jun;168[6]:540-6).
Suicide
According to the CDC, the rate of completed suicide in youth peaked in the early1990s and then dropped and stabilized before starting to creep up again over the past 5 or so years. The trends are somewhat different, based on gender and the specific age group that is examined. The majority of completed youth suicides occur in males, with current rates still well below those historical highs.
Psychiatric disorders
This one is particularly tricky. While the rates of many specific psychiatric disorders such as ADHD and bipolar disorder have been rising in youth, as well as the use of psychiatric medications, it is much less clear whether this represents a true rise in these disorders versus other factors such as improved detection and a lower diagnostic threshold. One study by Achenbach et al. that measured quantitative levels of child behavior problems from the same rating scale over a 23-year time span found some increases in overall levels from the 1970s to the early 1990s, but then levels began to fall by the end of the millennium (J Abnorm Child Psychol. 2003 Feb;31[1]:1-11).
Of course, these hopeful trends in many significant areas do not mean that these problems have been overcome. While much work remains to be done on many fronts, it is still worth keeping in mind that the overall condition of youth mental health may not be as dire as we might be led to believe and that there is evidence that our efforts, perhaps, are leading to some progress.
Dr. Rettew is associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. He said he has no relevant financial disclosures. Follow him on Twitter @pedipsych. E-mail him at [email protected].