User login
Neonatal Early-Onset Sepsis: Revised Evaluation Guidelines Save Money
BOSTON – Implementation of a revised algorithm for the identification of early-onset sepsis in newborn infants significantly improves resource allocation and decreases overall health care costs, a study has shown.
To gauge the efficiency of the updated algorithm, which is based on the 2010 Centers for Disease Control and Prevention guidelines for the prevention of perinatal group B streptococcal (GBS) disease, Dr. Sagori Mukhopadhyay of Children’s Hospital, Boston, and colleagues conducted a retrospective time-series analysis to compare the frequency of early-onset sepsis (EOS) evaluations during two 5-month time periods – one in 2009, when the 2002 iteration of the guidelines were followed, and one in 2011, when the 2010 guidelines were followed – measuring differences in resource utilization and costs.
"We performed a retrospective economic evaluation to determine the cost difference between periods, using individual patient data, a third-party payer perspective, and a cost-minimization approach," she reported at the annual meeting of the Pediatric Academic Societies.
"We determined the costs associated with the early-onset sepsis evaluation, including laboratory, medication, and physician fees, and time spent in evaluation, specifically nursing costs," Dr. Mukhopadhyay said.
During the periods of study, 6,504 infants were born at or beyond 36 weeks’ gestation, including 662 who were evaluated for EOS. The overall incidence of EOS was 0.62/1,000 infants.
Importantly, "the frequency of evaluation for inadequate intrapartum antibiotic prophylaxis decreased significantly from 33/1,000 in 2009 to 3/1,000 in 2011," she said, with the remaining evaluations during both time periods conducted primarily because of maternal intrapartum fever. The reduction in evaluations for inadequate intrapartum prophylaxis translated into a significant reduction in overall costs associated with EOS evaluation, from $27,883.06 in 2009 to $2,434.64 in 2011. The findings may help hospitals transition to the revised recommendations in terms of anticipated staffing needs and resource allocation, she said.
Although the incidence of perinatal early-onset GBS has decreased since the CDC issued the first iteration of its prevention guidelines in 1996, GBS remained the leading cause of early-onset neonatal sepsis in 2010, prompting the revision of the 2002 guidelines.
Under the revised algorithm, all newborns with signs of sepsis should undergo a full diagnostic evaluation, including a blood culture, a complete blood count with white blood cell differential and platelet count, a chest radiograph in the presence of any abnormal respiratory signs, and a lumbar puncture if the newborn is stable enough to tolerate the procedure and sepsis is suspected. Further, the algorithm provides for the administration of antibiotics active against GBS, including intravenous ampicillin, and other organisms that could cause sepsis, such as Escherichia coli, pending the results of the evaluation.
Additional components of the algorithm include:
• A limited evaluation (consisting of blood culture and CBC) and antibiotic treatment – pending culture results – in well-appearing newborns whose mothers had suspected chorioamnionitis.
• Routine clinical care for well-appearing infants whose mothers had no chorioamnionitis and no indication for GBS prophylaxis.
• A minimum 48 hours of observation but no routine diagnostic testing in well-appearing infants of any gestational age whose mother received adequate intrapartum GBS prophylaxis consisting of at least 4 hours of intravenous penicillin, ampicillin, or cefazolin prior to delivery.
• Observation in well-appearing infants at least 37 weeks’ gestational age whose mothers had an indication for GBS prophylaxis but who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was less than 18 hours.
• Limited evaluation as above and a minimum of 48 hours of observation in well-appearing infants less than 37 weeks’ gestation born to mothers with an indication for prophylaxis who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was more than 18 hours.
Dr. Mukhopadhyay reported having no relevant financial disclosures.
BOSTON – Implementation of a revised algorithm for the identification of early-onset sepsis in newborn infants significantly improves resource allocation and decreases overall health care costs, a study has shown.
To gauge the efficiency of the updated algorithm, which is based on the 2010 Centers for Disease Control and Prevention guidelines for the prevention of perinatal group B streptococcal (GBS) disease, Dr. Sagori Mukhopadhyay of Children’s Hospital, Boston, and colleagues conducted a retrospective time-series analysis to compare the frequency of early-onset sepsis (EOS) evaluations during two 5-month time periods – one in 2009, when the 2002 iteration of the guidelines were followed, and one in 2011, when the 2010 guidelines were followed – measuring differences in resource utilization and costs.
"We performed a retrospective economic evaluation to determine the cost difference between periods, using individual patient data, a third-party payer perspective, and a cost-minimization approach," she reported at the annual meeting of the Pediatric Academic Societies.
"We determined the costs associated with the early-onset sepsis evaluation, including laboratory, medication, and physician fees, and time spent in evaluation, specifically nursing costs," Dr. Mukhopadhyay said.
During the periods of study, 6,504 infants were born at or beyond 36 weeks’ gestation, including 662 who were evaluated for EOS. The overall incidence of EOS was 0.62/1,000 infants.
Importantly, "the frequency of evaluation for inadequate intrapartum antibiotic prophylaxis decreased significantly from 33/1,000 in 2009 to 3/1,000 in 2011," she said, with the remaining evaluations during both time periods conducted primarily because of maternal intrapartum fever. The reduction in evaluations for inadequate intrapartum prophylaxis translated into a significant reduction in overall costs associated with EOS evaluation, from $27,883.06 in 2009 to $2,434.64 in 2011. The findings may help hospitals transition to the revised recommendations in terms of anticipated staffing needs and resource allocation, she said.
Although the incidence of perinatal early-onset GBS has decreased since the CDC issued the first iteration of its prevention guidelines in 1996, GBS remained the leading cause of early-onset neonatal sepsis in 2010, prompting the revision of the 2002 guidelines.
Under the revised algorithm, all newborns with signs of sepsis should undergo a full diagnostic evaluation, including a blood culture, a complete blood count with white blood cell differential and platelet count, a chest radiograph in the presence of any abnormal respiratory signs, and a lumbar puncture if the newborn is stable enough to tolerate the procedure and sepsis is suspected. Further, the algorithm provides for the administration of antibiotics active against GBS, including intravenous ampicillin, and other organisms that could cause sepsis, such as Escherichia coli, pending the results of the evaluation.
Additional components of the algorithm include:
• A limited evaluation (consisting of blood culture and CBC) and antibiotic treatment – pending culture results – in well-appearing newborns whose mothers had suspected chorioamnionitis.
• Routine clinical care for well-appearing infants whose mothers had no chorioamnionitis and no indication for GBS prophylaxis.
• A minimum 48 hours of observation but no routine diagnostic testing in well-appearing infants of any gestational age whose mother received adequate intrapartum GBS prophylaxis consisting of at least 4 hours of intravenous penicillin, ampicillin, or cefazolin prior to delivery.
• Observation in well-appearing infants at least 37 weeks’ gestational age whose mothers had an indication for GBS prophylaxis but who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was less than 18 hours.
• Limited evaluation as above and a minimum of 48 hours of observation in well-appearing infants less than 37 weeks’ gestation born to mothers with an indication for prophylaxis who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was more than 18 hours.
Dr. Mukhopadhyay reported having no relevant financial disclosures.
BOSTON – Implementation of a revised algorithm for the identification of early-onset sepsis in newborn infants significantly improves resource allocation and decreases overall health care costs, a study has shown.
To gauge the efficiency of the updated algorithm, which is based on the 2010 Centers for Disease Control and Prevention guidelines for the prevention of perinatal group B streptococcal (GBS) disease, Dr. Sagori Mukhopadhyay of Children’s Hospital, Boston, and colleagues conducted a retrospective time-series analysis to compare the frequency of early-onset sepsis (EOS) evaluations during two 5-month time periods – one in 2009, when the 2002 iteration of the guidelines were followed, and one in 2011, when the 2010 guidelines were followed – measuring differences in resource utilization and costs.
"We performed a retrospective economic evaluation to determine the cost difference between periods, using individual patient data, a third-party payer perspective, and a cost-minimization approach," she reported at the annual meeting of the Pediatric Academic Societies.
"We determined the costs associated with the early-onset sepsis evaluation, including laboratory, medication, and physician fees, and time spent in evaluation, specifically nursing costs," Dr. Mukhopadhyay said.
During the periods of study, 6,504 infants were born at or beyond 36 weeks’ gestation, including 662 who were evaluated for EOS. The overall incidence of EOS was 0.62/1,000 infants.
Importantly, "the frequency of evaluation for inadequate intrapartum antibiotic prophylaxis decreased significantly from 33/1,000 in 2009 to 3/1,000 in 2011," she said, with the remaining evaluations during both time periods conducted primarily because of maternal intrapartum fever. The reduction in evaluations for inadequate intrapartum prophylaxis translated into a significant reduction in overall costs associated with EOS evaluation, from $27,883.06 in 2009 to $2,434.64 in 2011. The findings may help hospitals transition to the revised recommendations in terms of anticipated staffing needs and resource allocation, she said.
Although the incidence of perinatal early-onset GBS has decreased since the CDC issued the first iteration of its prevention guidelines in 1996, GBS remained the leading cause of early-onset neonatal sepsis in 2010, prompting the revision of the 2002 guidelines.
Under the revised algorithm, all newborns with signs of sepsis should undergo a full diagnostic evaluation, including a blood culture, a complete blood count with white blood cell differential and platelet count, a chest radiograph in the presence of any abnormal respiratory signs, and a lumbar puncture if the newborn is stable enough to tolerate the procedure and sepsis is suspected. Further, the algorithm provides for the administration of antibiotics active against GBS, including intravenous ampicillin, and other organisms that could cause sepsis, such as Escherichia coli, pending the results of the evaluation.
Additional components of the algorithm include:
• A limited evaluation (consisting of blood culture and CBC) and antibiotic treatment – pending culture results – in well-appearing newborns whose mothers had suspected chorioamnionitis.
• Routine clinical care for well-appearing infants whose mothers had no chorioamnionitis and no indication for GBS prophylaxis.
• A minimum 48 hours of observation but no routine diagnostic testing in well-appearing infants of any gestational age whose mother received adequate intrapartum GBS prophylaxis consisting of at least 4 hours of intravenous penicillin, ampicillin, or cefazolin prior to delivery.
• Observation in well-appearing infants at least 37 weeks’ gestational age whose mothers had an indication for GBS prophylaxis but who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was less than 18 hours.
• Limited evaluation as above and a minimum of 48 hours of observation in well-appearing infants less than 37 weeks’ gestation born to mothers with an indication for prophylaxis who received inadequate or no prophylaxis and in whom the duration of membrane rupture prior to delivery was more than 18 hours.
Dr. Mukhopadhyay reported having no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: The frequency of newborn evaluation for inadequate intrapartum antibiotic prophylaxis at an academic medical center decreased significantly from 33/1,000 births during a 5-month period in 2009 under 2002 CDC guidelines to 3/1,000 during a 5-month period in 2011 under revised 2010 CDC guidelines. The overall costs associated with early-onset sepsis evaluations decreased from $27,883.06 in 2009 to $2,434.64 in 2011.
Data Source: A retrospective economic analysis of two 5-month periods to measure differences in resource utilization and costs associated with the transition to the 2010 guidelines.
Disclosures: Dr. Mukhopadhyay reported having no relevant financial disclosures.
Consider Narrow Fluconazole Strategy if Candida Incidence Is Low
BOSTON – A narrow, targeted approach to fluconazole prophylaxis prevents most cases of neonatal candidiasis among extremely low-birth-weight infants in centers with a low incidence of the fungal infection, a study has shown.
Because of the high rates of mortality and neurodevelopmental impairment associated with candidiasis infection in at-risk infants, the Infectious Diseases Society of America recommends that centers with a high incidence of the infection consider routine fluconazole prophylaxis for extremely low-birth-weight neonates (less than 1,000 g at birth). The recommendation does not extend to low-incidence centers, however, because of the unknown risks for neurologic and cognitive disorders after fluconazole exposure in premature infants, said Dr. Karen M. Puopolo, a neonatologist at Brigham and Women’s Hospital in Boston.
To assess the theoretical efficacy of fluconazole prophylaxis in extremely low-birth-weight (ELBW) infants in a low-incidence center, Dr. Puopolo and her colleagues reviewed the clinical details of blood culture–proven neonatal Candida infections that occurred in a single tertiary care neonatal intensive care unit (NICU) from January 2003 to October 2010.
Using demographic data and antibiotic exposure information gleaned from medical and administrative records of nearly 1,400 ELBW infants, "we developed four different possible criteria for fluconazole prophylaxis, including fluconazole prophylaxis for all babies born with a birth weight less than 1,000 g, all babies born with a birth weight less than 1,000 g who also received 7 or more days of antibiotics, all babies born with a birth weight less than 750 g, and all babies born with a birth weight less than 750 g who also received 7 or more days of antibiotics," she explained at the annual meeting of the Pediatric Academic Societies.
For the number needed to treat (NNT) calculations, the investigators assumed that fluconazole prophylaxis would be 100% effective, and for the antibiotic exposure calculation, which was based on a review of antibiotic use in the NICU, they assumed that 50% of the infants with a birth weight less than 1,000 g and 80% with a birth weight less than 750 g would be treated with antibiotics for 7 or more days, Dr. Puopolo said.
During the period of study, 1,381 ELBW infants were exposed to fluconazole prophylaxis, including 878 weighing less than 1,000 g at birth, of which 293 had a minimum of 7 days of antibiotic therapy, and 393 weighing less than 750 g at birth, of which 179 had a minimum of 7 days of antibiotic therapy, Dr. Puopolo said. "Twenty cases of neonatal candidiasis were identified, with 18 [3%] occurring in ELBW infants surviving beyond 72 hours of life," she said. The mean birth weight of the infected infants was 702 g, and the mean gestational age and age at infection were 24.5 weeks and 21.4 weeks.
With respect to the number needed to treat analysis, the narrowest targeted approach – routine fluconazole prophylaxis in neonates weighing less than 750 g who had been exposed to a minimum of 7 days of antibiotic therapy – was the most efficient. In this subgroup, according to Dr. Puopolo, "we would need to treat 13 infants to prevent one fungal infection." The NNT in the 750-g, 1000-g with 7 or more days of antibiotic exposure, and 1,000-g groups were 15, 19, and 33, respectively.
If this approach were applied to the number of babies in each of the four prophylaxis categories, all 18 infections would have been targeted in the most liberal exposure group, while 567 of the babies would have been unnecessarily exposed to the antifungal drug. In the increasingly narrower exposure groups, 16, 15, and 14 of the infections would have been targeted. Although 2, 3, and 4 of the infections, respectively, would have been missed in these groups, far fewer babies would have been unnecessarily exposed to fluconazole, said Dr. Puopolo.
National guidelines do not recommend fluconazole prophylaxis in centers with a lower-than-average incidence of neonatal invasive Candida infections in the NICU, but "our findings suggest that individual NICUs should consider different approaches to fluconazole prophylaxis based on their incidence of candidiasis," Dr. Puopolo said. "A narrow targeted approach can prevent most cases of neonatal candidiasis with the lowest number needed to treat."
Dr. Puopolo said she had no relevant financial disclosures.
BOSTON – A narrow, targeted approach to fluconazole prophylaxis prevents most cases of neonatal candidiasis among extremely low-birth-weight infants in centers with a low incidence of the fungal infection, a study has shown.
Because of the high rates of mortality and neurodevelopmental impairment associated with candidiasis infection in at-risk infants, the Infectious Diseases Society of America recommends that centers with a high incidence of the infection consider routine fluconazole prophylaxis for extremely low-birth-weight neonates (less than 1,000 g at birth). The recommendation does not extend to low-incidence centers, however, because of the unknown risks for neurologic and cognitive disorders after fluconazole exposure in premature infants, said Dr. Karen M. Puopolo, a neonatologist at Brigham and Women’s Hospital in Boston.
To assess the theoretical efficacy of fluconazole prophylaxis in extremely low-birth-weight (ELBW) infants in a low-incidence center, Dr. Puopolo and her colleagues reviewed the clinical details of blood culture–proven neonatal Candida infections that occurred in a single tertiary care neonatal intensive care unit (NICU) from January 2003 to October 2010.
Using demographic data and antibiotic exposure information gleaned from medical and administrative records of nearly 1,400 ELBW infants, "we developed four different possible criteria for fluconazole prophylaxis, including fluconazole prophylaxis for all babies born with a birth weight less than 1,000 g, all babies born with a birth weight less than 1,000 g who also received 7 or more days of antibiotics, all babies born with a birth weight less than 750 g, and all babies born with a birth weight less than 750 g who also received 7 or more days of antibiotics," she explained at the annual meeting of the Pediatric Academic Societies.
For the number needed to treat (NNT) calculations, the investigators assumed that fluconazole prophylaxis would be 100% effective, and for the antibiotic exposure calculation, which was based on a review of antibiotic use in the NICU, they assumed that 50% of the infants with a birth weight less than 1,000 g and 80% with a birth weight less than 750 g would be treated with antibiotics for 7 or more days, Dr. Puopolo said.
During the period of study, 1,381 ELBW infants were exposed to fluconazole prophylaxis, including 878 weighing less than 1,000 g at birth, of which 293 had a minimum of 7 days of antibiotic therapy, and 393 weighing less than 750 g at birth, of which 179 had a minimum of 7 days of antibiotic therapy, Dr. Puopolo said. "Twenty cases of neonatal candidiasis were identified, with 18 [3%] occurring in ELBW infants surviving beyond 72 hours of life," she said. The mean birth weight of the infected infants was 702 g, and the mean gestational age and age at infection were 24.5 weeks and 21.4 weeks.
With respect to the number needed to treat analysis, the narrowest targeted approach – routine fluconazole prophylaxis in neonates weighing less than 750 g who had been exposed to a minimum of 7 days of antibiotic therapy – was the most efficient. In this subgroup, according to Dr. Puopolo, "we would need to treat 13 infants to prevent one fungal infection." The NNT in the 750-g, 1000-g with 7 or more days of antibiotic exposure, and 1,000-g groups were 15, 19, and 33, respectively.
If this approach were applied to the number of babies in each of the four prophylaxis categories, all 18 infections would have been targeted in the most liberal exposure group, while 567 of the babies would have been unnecessarily exposed to the antifungal drug. In the increasingly narrower exposure groups, 16, 15, and 14 of the infections would have been targeted. Although 2, 3, and 4 of the infections, respectively, would have been missed in these groups, far fewer babies would have been unnecessarily exposed to fluconazole, said Dr. Puopolo.
National guidelines do not recommend fluconazole prophylaxis in centers with a lower-than-average incidence of neonatal invasive Candida infections in the NICU, but "our findings suggest that individual NICUs should consider different approaches to fluconazole prophylaxis based on their incidence of candidiasis," Dr. Puopolo said. "A narrow targeted approach can prevent most cases of neonatal candidiasis with the lowest number needed to treat."
Dr. Puopolo said she had no relevant financial disclosures.
BOSTON – A narrow, targeted approach to fluconazole prophylaxis prevents most cases of neonatal candidiasis among extremely low-birth-weight infants in centers with a low incidence of the fungal infection, a study has shown.
Because of the high rates of mortality and neurodevelopmental impairment associated with candidiasis infection in at-risk infants, the Infectious Diseases Society of America recommends that centers with a high incidence of the infection consider routine fluconazole prophylaxis for extremely low-birth-weight neonates (less than 1,000 g at birth). The recommendation does not extend to low-incidence centers, however, because of the unknown risks for neurologic and cognitive disorders after fluconazole exposure in premature infants, said Dr. Karen M. Puopolo, a neonatologist at Brigham and Women’s Hospital in Boston.
To assess the theoretical efficacy of fluconazole prophylaxis in extremely low-birth-weight (ELBW) infants in a low-incidence center, Dr. Puopolo and her colleagues reviewed the clinical details of blood culture–proven neonatal Candida infections that occurred in a single tertiary care neonatal intensive care unit (NICU) from January 2003 to October 2010.
Using demographic data and antibiotic exposure information gleaned from medical and administrative records of nearly 1,400 ELBW infants, "we developed four different possible criteria for fluconazole prophylaxis, including fluconazole prophylaxis for all babies born with a birth weight less than 1,000 g, all babies born with a birth weight less than 1,000 g who also received 7 or more days of antibiotics, all babies born with a birth weight less than 750 g, and all babies born with a birth weight less than 750 g who also received 7 or more days of antibiotics," she explained at the annual meeting of the Pediatric Academic Societies.
For the number needed to treat (NNT) calculations, the investigators assumed that fluconazole prophylaxis would be 100% effective, and for the antibiotic exposure calculation, which was based on a review of antibiotic use in the NICU, they assumed that 50% of the infants with a birth weight less than 1,000 g and 80% with a birth weight less than 750 g would be treated with antibiotics for 7 or more days, Dr. Puopolo said.
During the period of study, 1,381 ELBW infants were exposed to fluconazole prophylaxis, including 878 weighing less than 1,000 g at birth, of which 293 had a minimum of 7 days of antibiotic therapy, and 393 weighing less than 750 g at birth, of which 179 had a minimum of 7 days of antibiotic therapy, Dr. Puopolo said. "Twenty cases of neonatal candidiasis were identified, with 18 [3%] occurring in ELBW infants surviving beyond 72 hours of life," she said. The mean birth weight of the infected infants was 702 g, and the mean gestational age and age at infection were 24.5 weeks and 21.4 weeks.
With respect to the number needed to treat analysis, the narrowest targeted approach – routine fluconazole prophylaxis in neonates weighing less than 750 g who had been exposed to a minimum of 7 days of antibiotic therapy – was the most efficient. In this subgroup, according to Dr. Puopolo, "we would need to treat 13 infants to prevent one fungal infection." The NNT in the 750-g, 1000-g with 7 or more days of antibiotic exposure, and 1,000-g groups were 15, 19, and 33, respectively.
If this approach were applied to the number of babies in each of the four prophylaxis categories, all 18 infections would have been targeted in the most liberal exposure group, while 567 of the babies would have been unnecessarily exposed to the antifungal drug. In the increasingly narrower exposure groups, 16, 15, and 14 of the infections would have been targeted. Although 2, 3, and 4 of the infections, respectively, would have been missed in these groups, far fewer babies would have been unnecessarily exposed to fluconazole, said Dr. Puopolo.
National guidelines do not recommend fluconazole prophylaxis in centers with a lower-than-average incidence of neonatal invasive Candida infections in the NICU, but "our findings suggest that individual NICUs should consider different approaches to fluconazole prophylaxis based on their incidence of candidiasis," Dr. Puopolo said. "A narrow targeted approach can prevent most cases of neonatal candidiasis with the lowest number needed to treat."
Dr. Puopolo said she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: In 179 premature neonates weighing 750 g who received at least 7 days of antibiotic therapy, fluconazole prophylaxis would have targeted 14 of 18 invasive Candida infections, based on the findings of a theoretical efficacy evaluation showing the number of prophylaxis exposures needed to prevent 1 such infection in this patient group was 13. In contrast, the number needed to treat in a broader group of all neonates weighing 1,000 g at birth was 33.
Data Source: The medical and administrative records of nearly 1,400 ELBW babies in a single tertiary care NICU were reviewed to determine the theoretical efficacy of various fluconazole prophylaxis practices.
Disclosures: Dr. Puopolo said she had no relevant financial disclosures.
FDA Warns of 'Liberation Therapy' Dangers for Multiple Sclerosis
An experimental procedure that attempts to improve venous blood flow may cause significant damage or death in patients with multiple sclerosis, according to an alert issued by the Food and Drug Administration.
"Liberation therapy," which involves balloon angioplasty or stenting of veins in the neck and chest, has been used but not proven as a treatment for chronic cerebrospinal venous insufficiency (CCSVI), a condition characterized by stenosis of the veins draining blood from the brain and upper spinal cord. Despite the lack of a definitive link between CCSVI and multiple sclerosis (MS), the former has been suggested as a cause of or contributing factor in the development of the progressive, immune-mediated neurologic disorder (Ann. Neurol. 2010;67:286-90).
Since its introduction in 2009 (J. Vasc. Surg. 2009;50:1348-58), the liberation procedure has been linked to multiple complications, including stroke, stent detachment and migration, impairment of the treated vein, cranial nerve damage, blood clots, abdominal bleeding, and death, according to a statement issued by the FDA. The complications have been reported through the agency’s Safety Information and Adverse Event Reporting Program.
In the absence of rigorous, targeted research establishing an association between the two conditions or reliable evidence from controlled clinical trials demonstrating the efficacy of liberation-type procedures in MS, "patients are encouraged to discuss the potential risks and benefits of this procedure with a neurologist or other physician who is familiar with MS and CCSVI, including the CCSVI procedures and their outcomes," Dr. William Maisel, chief scientist in the FDA’s Center for Devices and Radiological Health, emphasized in the alert.
The statement also stresses that physicians and clinical investigators considering or conducting trials of devices to treat CCSVI are obligated to comply with regulations for investigational devices.
Currently, no devices for use in liberation therapy have received FDA approval for that indication, although doctors can and have offered the procedure to their patients, Dr. Maisel said in an interview. "We don’t know exactly how many individuals have had the treatment, because there is no central patient registry."
An experimental procedure that attempts to improve venous blood flow may cause significant damage or death in patients with multiple sclerosis, according to an alert issued by the Food and Drug Administration.
"Liberation therapy," which involves balloon angioplasty or stenting of veins in the neck and chest, has been used but not proven as a treatment for chronic cerebrospinal venous insufficiency (CCSVI), a condition characterized by stenosis of the veins draining blood from the brain and upper spinal cord. Despite the lack of a definitive link between CCSVI and multiple sclerosis (MS), the former has been suggested as a cause of or contributing factor in the development of the progressive, immune-mediated neurologic disorder (Ann. Neurol. 2010;67:286-90).
Since its introduction in 2009 (J. Vasc. Surg. 2009;50:1348-58), the liberation procedure has been linked to multiple complications, including stroke, stent detachment and migration, impairment of the treated vein, cranial nerve damage, blood clots, abdominal bleeding, and death, according to a statement issued by the FDA. The complications have been reported through the agency’s Safety Information and Adverse Event Reporting Program.
In the absence of rigorous, targeted research establishing an association between the two conditions or reliable evidence from controlled clinical trials demonstrating the efficacy of liberation-type procedures in MS, "patients are encouraged to discuss the potential risks and benefits of this procedure with a neurologist or other physician who is familiar with MS and CCSVI, including the CCSVI procedures and their outcomes," Dr. William Maisel, chief scientist in the FDA’s Center for Devices and Radiological Health, emphasized in the alert.
The statement also stresses that physicians and clinical investigators considering or conducting trials of devices to treat CCSVI are obligated to comply with regulations for investigational devices.
Currently, no devices for use in liberation therapy have received FDA approval for that indication, although doctors can and have offered the procedure to their patients, Dr. Maisel said in an interview. "We don’t know exactly how many individuals have had the treatment, because there is no central patient registry."
An experimental procedure that attempts to improve venous blood flow may cause significant damage or death in patients with multiple sclerosis, according to an alert issued by the Food and Drug Administration.
"Liberation therapy," which involves balloon angioplasty or stenting of veins in the neck and chest, has been used but not proven as a treatment for chronic cerebrospinal venous insufficiency (CCSVI), a condition characterized by stenosis of the veins draining blood from the brain and upper spinal cord. Despite the lack of a definitive link between CCSVI and multiple sclerosis (MS), the former has been suggested as a cause of or contributing factor in the development of the progressive, immune-mediated neurologic disorder (Ann. Neurol. 2010;67:286-90).
Since its introduction in 2009 (J. Vasc. Surg. 2009;50:1348-58), the liberation procedure has been linked to multiple complications, including stroke, stent detachment and migration, impairment of the treated vein, cranial nerve damage, blood clots, abdominal bleeding, and death, according to a statement issued by the FDA. The complications have been reported through the agency’s Safety Information and Adverse Event Reporting Program.
In the absence of rigorous, targeted research establishing an association between the two conditions or reliable evidence from controlled clinical trials demonstrating the efficacy of liberation-type procedures in MS, "patients are encouraged to discuss the potential risks and benefits of this procedure with a neurologist or other physician who is familiar with MS and CCSVI, including the CCSVI procedures and their outcomes," Dr. William Maisel, chief scientist in the FDA’s Center for Devices and Radiological Health, emphasized in the alert.
The statement also stresses that physicians and clinical investigators considering or conducting trials of devices to treat CCSVI are obligated to comply with regulations for investigational devices.
Currently, no devices for use in liberation therapy have received FDA approval for that indication, although doctors can and have offered the procedure to their patients, Dr. Maisel said in an interview. "We don’t know exactly how many individuals have had the treatment, because there is no central patient registry."
Prenatal Screen Predicts Maternal Risk of Traumatic Death
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
BOSTON – A screening tool designed to identify medical and psychosocial risk factors associated with poor pregnancy outcomes also seems to predict maternal traumatic pregnancy–associated death, according to Dr. Nancy S. Hardt.
The Florida Healthy Start Prenatal Risk Screen has been validated for the identification of women who are at risk for preterm delivery or for delivering a low-birth-weight infant. Even low levels of risk on the screening test, which has been offered to all pregnant women in Florida at their first prenatal visit as per state legislative statute since 1991, appear to be associated with an increased likelihood of traumatic maternal death, Dr. Hardt said at the annual meeting of the Pediatric Academic Societies.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death," she said. "It doesn’t take a whole lot of practice change to address some of the factors that might be putting the moms at risk, such as dispelling the myth that pregnant women shouldn’t wear seatbelts, asking patients if they feel safe in their homes, and stressing the dangers of substance use and abuse, including prescription drug use."
Dr. Hardt and her colleagues reviewed 600,000 Healthy Start screens from 1999 to 2005, as well as linked data for the concurrent period from Florida’s Enhanced Maternal Mortality Reporting Database. Of the women who died during the period of study, 144 experienced traumatic deaths. These included accidents, homicides, suicides, and drug overdoses, she said, noting that the top four causes of maternal deaths were trauma related.
"It’s possible that services targeting the reduction of adverse infant outcomes may simultaneously lower pregnant women’s risk of traumatic death."
Specifically, the causes of death that had the greatest maternal mortality ratios were transport accidents (13.3), homicide (5.5), accidental poisoning (3.3), and suicide (2.9).
"We have to go through quite a few categories of traumatic deaths before we get to the obstetric-related deaths," such as hypertension disorders (2.7), hemorrhage (2.2), thrombotic embolism (2.2), and infection (2.0), observed Dr. Hardt, professor of pathology and ob.gyn. at the University of Florida in Gainesville.
To evaluate the predictive value of the Healthy Start screen for identifying risk of traumatic death, the investigators used the same screening threshold as that used for identifying women at risk for poor pregnancy outcomes, Dr. Hardt said. "A score of 4 or higher on the [15-item] weighted measure, which includes demographic as well as environmental and social factors, indicates a positive screen for risk of preterm or low-birth-weight delivery and triggers referral to Healthy Start services," Dr. Hardt explained. "We hypothesized that the risk factors for these infant problems would be the same as for maternal death, and as such the screening instruments would work for identifying at-risk moms."
An analysis of the data showed that as a woman’s risk score increased, the probability of traumatic death also increased. In fact, "a woman with a risk score of 4 had nearly 12 times the risk of traumatic death compared to a women with a risk score of zero, and a woman with a risk score of 9 had 52 times the risk of traumatic death compared to one who scored zero," Dr. Hardt said. "What we observed is that with each increase in score of 1, the relative risk of death increased 1.5 to 2 times."
What this means, in terms of a prediction tool, "is that for every 100,000 women with a score of 4, expect nearly 48 traumatic maternal deaths, and for every one with a score of 9, expect 215 traumatic deaths," according to Dr. Hardt.
Many of the specific risk determinants associated with poor pregnancy outcomes are likely the same as those that are predictive of maternal traumatic death, including mental health, substance use, domestic violence, education, and employment/family income status, Dr. Hardt said.
Dr. Hardt said she had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
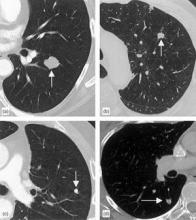
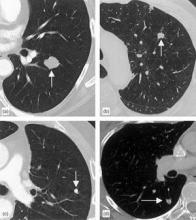
NCCN Affirms CT Scans For Heavy Smokers
The benefits of routine lung cancer screening in high-risk individuals outweigh the potential risks, according to members of a National Comprehensive Cancer Network guidelines panel that recommended low-dose helical CT screening of two high-risk groups.
Mary E. Reid, Ph.D., of the Roswell Park Cancer Institute in Buffalo, N.Y., acknowledged the burdens – in particular, the cost and requisite resource utilization – associated with following all high-risk patients who screen positive. But, she said, "the evidence [in favor of] the recommendations is really strong and supports their implementation."
Lung cancer, she noted, is the only one of the top four deadliest cancers (lung, prostate, breast, and colorectal) that is not currently subject to routine screening.
Dr. Reid and colleagues on the National Comprehensive Cancer Network (NCCN) Guidelines Panel for Lung Cancer Screening presented the update at the NCCN annual conference March 14-18 in Hollywood, Fla. It had been issued in October 2011 and followed a New England Journal of Medicine report that low-dose CT screening of heavy smokers reduced lung cancer mortality by 20%, compared with annual chest x-rays, in the National Lung Screening Trial (NLST).
The revised guidelines recommend annual low-dose helical CT screening for the following two groups of high-risk individuals:
• Those aged 55-74 years with a minimum smoking history of 30 pack-years who either are current smokers or quit within the past 15 years.
• Those aged 50 years or older with a minimum smoking history of 20 pack-years plus one additional lung cancer risk factor, excluding secondhand exposure.
Evidence from the randomized, controlled NLST suggests that early detection via screening reduced lung-cancer specific mortality in the former risk group, which characterizes the NLST patient population. Specifically, 1 in 100 high-risk individuals who were enrolled in the study screened positive on their first low-dose CT exam, and one life was saved for every 320 high-risk individuals screened over 2 years (three screens) (N. Engl. J. Med. 2011;365:395-409). The NCCN recommendation for this group is category 1, the highest level.
The recommendation for annual screening in the second high-risk group is based on less-robust evidence and a nonuniform consensus of the NCCN panel members, Dr. Reid said. As such, it is a less-emphatic category 2B recommendation.
The NCCN screening recommendations have been deemed by some experts to be premature in the absence of cost-efficacy analysis, particularly because of the high false-positive rates observed in both the CT group (96.4%) and the radiography group (94.5%), as well as the potentially harmful effects of radiation exposure associated with low-dose CT screening.
Despite the favorable outcome of their study, the NLST authors stressed the need for rigorous cost-effectiveness analyses before the crafting of public policy recommendations. "The reductions in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote. "The cost component of low-dose CT screening includes not only the screening examination itself but also the diagnostic follow-up and treatment."
In addition to recommending appropriate candidates for routine screening and the proposed frequency of the scans, the new NCCN guidelines outline lung cancer risk factors, address the risks and benefits of screening as well as screening accuracy, and offer an algorithm for the evaluation and follow-up of positive screens. Specifically, the guidelines recommend the following:
• Basing the frequency of low-dose CT in high-risk patients on the size and status (solid, nonsolid, part-solid, ground-glass, ground-glass opacity) of the nodule on baseline CT.
• Excising all nodules that increase in size or become solid or part-solid during follow-up.
• Considering PET with CT for nodules 8 mm or larger at baseline.
• Performing biopsy or excision of nodules that are suspicious for lung cancer, based on PET with CT findings.
• Reexamining within 1 month solid endobronchial nodules with low-dose CT immediately after vigorous coughing.
• Counseling smokers to quit.
The NCCN is the first professional organization to recommend routine low-dose CT screening for individuals who are considered to be at high-risk for lung cancer, according to Dr. Reid. Last summer, the International Association for the Study of Lung Cancer issued a call for physicians to discuss lung cancer screening with patients who match the high-risk smoking history of those enrolled in the NSLT.
Dr. Reid reported having no financial conflicts of interest.
The benefits of routine lung cancer screening in high-risk individuals outweigh the potential risks, according to members of a National Comprehensive Cancer Network guidelines panel that recommended low-dose helical CT screening of two high-risk groups.
Mary E. Reid, Ph.D., of the Roswell Park Cancer Institute in Buffalo, N.Y., acknowledged the burdens – in particular, the cost and requisite resource utilization – associated with following all high-risk patients who screen positive. But, she said, "the evidence [in favor of] the recommendations is really strong and supports their implementation."
Lung cancer, she noted, is the only one of the top four deadliest cancers (lung, prostate, breast, and colorectal) that is not currently subject to routine screening.
Dr. Reid and colleagues on the National Comprehensive Cancer Network (NCCN) Guidelines Panel for Lung Cancer Screening presented the update at the NCCN annual conference March 14-18 in Hollywood, Fla. It had been issued in October 2011 and followed a New England Journal of Medicine report that low-dose CT screening of heavy smokers reduced lung cancer mortality by 20%, compared with annual chest x-rays, in the National Lung Screening Trial (NLST).
The revised guidelines recommend annual low-dose helical CT screening for the following two groups of high-risk individuals:
• Those aged 55-74 years with a minimum smoking history of 30 pack-years who either are current smokers or quit within the past 15 years.
• Those aged 50 years or older with a minimum smoking history of 20 pack-years plus one additional lung cancer risk factor, excluding secondhand exposure.
Evidence from the randomized, controlled NLST suggests that early detection via screening reduced lung-cancer specific mortality in the former risk group, which characterizes the NLST patient population. Specifically, 1 in 100 high-risk individuals who were enrolled in the study screened positive on their first low-dose CT exam, and one life was saved for every 320 high-risk individuals screened over 2 years (three screens) (N. Engl. J. Med. 2011;365:395-409). The NCCN recommendation for this group is category 1, the highest level.
The recommendation for annual screening in the second high-risk group is based on less-robust evidence and a nonuniform consensus of the NCCN panel members, Dr. Reid said. As such, it is a less-emphatic category 2B recommendation.
The NCCN screening recommendations have been deemed by some experts to be premature in the absence of cost-efficacy analysis, particularly because of the high false-positive rates observed in both the CT group (96.4%) and the radiography group (94.5%), as well as the potentially harmful effects of radiation exposure associated with low-dose CT screening.
Despite the favorable outcome of their study, the NLST authors stressed the need for rigorous cost-effectiveness analyses before the crafting of public policy recommendations. "The reductions in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote. "The cost component of low-dose CT screening includes not only the screening examination itself but also the diagnostic follow-up and treatment."
In addition to recommending appropriate candidates for routine screening and the proposed frequency of the scans, the new NCCN guidelines outline lung cancer risk factors, address the risks and benefits of screening as well as screening accuracy, and offer an algorithm for the evaluation and follow-up of positive screens. Specifically, the guidelines recommend the following:
• Basing the frequency of low-dose CT in high-risk patients on the size and status (solid, nonsolid, part-solid, ground-glass, ground-glass opacity) of the nodule on baseline CT.
• Excising all nodules that increase in size or become solid or part-solid during follow-up.
• Considering PET with CT for nodules 8 mm or larger at baseline.
• Performing biopsy or excision of nodules that are suspicious for lung cancer, based on PET with CT findings.
• Reexamining within 1 month solid endobronchial nodules with low-dose CT immediately after vigorous coughing.
• Counseling smokers to quit.
The NCCN is the first professional organization to recommend routine low-dose CT screening for individuals who are considered to be at high-risk for lung cancer, according to Dr. Reid. Last summer, the International Association for the Study of Lung Cancer issued a call for physicians to discuss lung cancer screening with patients who match the high-risk smoking history of those enrolled in the NSLT.
Dr. Reid reported having no financial conflicts of interest.
The benefits of routine lung cancer screening in high-risk individuals outweigh the potential risks, according to members of a National Comprehensive Cancer Network guidelines panel that recommended low-dose helical CT screening of two high-risk groups.
Mary E. Reid, Ph.D., of the Roswell Park Cancer Institute in Buffalo, N.Y., acknowledged the burdens – in particular, the cost and requisite resource utilization – associated with following all high-risk patients who screen positive. But, she said, "the evidence [in favor of] the recommendations is really strong and supports their implementation."
Lung cancer, she noted, is the only one of the top four deadliest cancers (lung, prostate, breast, and colorectal) that is not currently subject to routine screening.
Dr. Reid and colleagues on the National Comprehensive Cancer Network (NCCN) Guidelines Panel for Lung Cancer Screening presented the update at the NCCN annual conference March 14-18 in Hollywood, Fla. It had been issued in October 2011 and followed a New England Journal of Medicine report that low-dose CT screening of heavy smokers reduced lung cancer mortality by 20%, compared with annual chest x-rays, in the National Lung Screening Trial (NLST).
The revised guidelines recommend annual low-dose helical CT screening for the following two groups of high-risk individuals:
• Those aged 55-74 years with a minimum smoking history of 30 pack-years who either are current smokers or quit within the past 15 years.
• Those aged 50 years or older with a minimum smoking history of 20 pack-years plus one additional lung cancer risk factor, excluding secondhand exposure.
Evidence from the randomized, controlled NLST suggests that early detection via screening reduced lung-cancer specific mortality in the former risk group, which characterizes the NLST patient population. Specifically, 1 in 100 high-risk individuals who were enrolled in the study screened positive on their first low-dose CT exam, and one life was saved for every 320 high-risk individuals screened over 2 years (three screens) (N. Engl. J. Med. 2011;365:395-409). The NCCN recommendation for this group is category 1, the highest level.
The recommendation for annual screening in the second high-risk group is based on less-robust evidence and a nonuniform consensus of the NCCN panel members, Dr. Reid said. As such, it is a less-emphatic category 2B recommendation.
The NCCN screening recommendations have been deemed by some experts to be premature in the absence of cost-efficacy analysis, particularly because of the high false-positive rates observed in both the CT group (96.4%) and the radiography group (94.5%), as well as the potentially harmful effects of radiation exposure associated with low-dose CT screening.
Despite the favorable outcome of their study, the NLST authors stressed the need for rigorous cost-effectiveness analyses before the crafting of public policy recommendations. "The reductions in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote. "The cost component of low-dose CT screening includes not only the screening examination itself but also the diagnostic follow-up and treatment."
In addition to recommending appropriate candidates for routine screening and the proposed frequency of the scans, the new NCCN guidelines outline lung cancer risk factors, address the risks and benefits of screening as well as screening accuracy, and offer an algorithm for the evaluation and follow-up of positive screens. Specifically, the guidelines recommend the following:
• Basing the frequency of low-dose CT in high-risk patients on the size and status (solid, nonsolid, part-solid, ground-glass, ground-glass opacity) of the nodule on baseline CT.
• Excising all nodules that increase in size or become solid or part-solid during follow-up.
• Considering PET with CT for nodules 8 mm or larger at baseline.
• Performing biopsy or excision of nodules that are suspicious for lung cancer, based on PET with CT findings.
• Reexamining within 1 month solid endobronchial nodules with low-dose CT immediately after vigorous coughing.
• Counseling smokers to quit.
The NCCN is the first professional organization to recommend routine low-dose CT screening for individuals who are considered to be at high-risk for lung cancer, according to Dr. Reid. Last summer, the International Association for the Study of Lung Cancer issued a call for physicians to discuss lung cancer screening with patients who match the high-risk smoking history of those enrolled in the NSLT.
Dr. Reid reported having no financial conflicts of interest.
NCCN Affirms CT Scans For Heavy Smokers
The benefits of routine lung cancer screening in high-risk individuals outweigh the potential risks, according to members of a National Comprehensive Cancer Network guidelines panel that recommended low-dose helical CT screening of two high-risk groups.
Mary E. Reid, Ph.D., of the Roswell Park Cancer Institute in Buffalo, N.Y., acknowledged the burdens – in particular, the cost and requisite resource utilization – associated with following all high-risk patients who screen positive. But, she said, "the evidence [in favor of] the recommendations is really strong and supports their implementation."
Lung cancer, she noted, is the only one of the top four deadliest cancers (lung, prostate, breast, and colorectal) that is not currently subject to routine screening.
Dr. Reid and colleagues on the National Comprehensive Cancer Network (NCCN) Guidelines Panel for Lung Cancer Screening presented the update at the NCCN annual conference March 14-18 in Hollywood, Fla. It had been issued in October 2011 and followed a New England Journal of Medicine report that low-dose CT screening of heavy smokers reduced lung cancer mortality by 20%, compared with annual chest x-rays, in the National Lung Screening Trial (NLST).
The revised guidelines recommend annual low-dose helical CT screening for the following two groups of high-risk individuals:
• Those aged 55-74 years with a minimum smoking history of 30 pack-years who either are current smokers or quit within the past 15 years.
• Those aged 50 years or older with a minimum smoking history of 20 pack-years plus one additional lung cancer risk factor, excluding secondhand exposure.
Evidence from the randomized, controlled NLST suggests that early detection via screening reduced lung-cancer specific mortality in the former risk group, which characterizes the NLST patient population. Specifically, 1 in 100 high-risk individuals who were enrolled in the study screened positive on their first low-dose CT exam, and one life was saved for every 320 high-risk individuals screened over 2 years (three screens) (N. Engl. J. Med. 2011;365:395-409). The NCCN recommendation for this group is category 1, the highest level.
The recommendation for annual screening in the second high-risk group is based on less-robust evidence and a nonuniform consensus of the NCCN panel members, Dr. Reid said. As such, it is a less-emphatic category 2B recommendation.
The NCCN screening recommendations have been deemed by some experts to be premature in the absence of cost-efficacy analysis, particularly because of the high false-positive rates observed in both the CT group (96.4%) and the radiography group (94.5%), as well as the potentially harmful effects of radiation exposure associated with low-dose CT screening.
Despite the favorable outcome of their study, the NLST authors stressed the need for rigorous cost-effectiveness analyses before the crafting of public policy recommendations. "The reductions in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote. "The cost component of low-dose CT screening includes not only the screening examination itself but also the diagnostic follow-up and treatment."
In addition to recommending appropriate candidates for routine screening and the proposed frequency of the scans, the new NCCN guidelines outline lung cancer risk factors, address the risks and benefits of screening as well as screening accuracy, and offer an algorithm for the evaluation and follow-up of positive screens. Specifically, the guidelines recommend the following:
• Basing the frequency of low-dose CT in high-risk patients on the size and status (solid, nonsolid, part-solid, ground-glass, ground-glass opacity) of the nodule on baseline CT.
• Excising all nodules that increase in size or become solid or part-solid during follow-up.
• Considering PET with CT for nodules 8 mm or larger at baseline.
• Performing biopsy or excision of nodules that are suspicious for lung cancer, based on PET with CT findings.
• Reexamining within 1 month solid endobronchial nodules with low-dose CT immediately after vigorous coughing.
• Counseling smokers to quit.
The NCCN is the first professional organization to recommend routine low-dose CT screening for individuals who are considered to be at high-risk for lung cancer, according to Dr. Reid. Last summer, the International Association for the Study of Lung Cancer issued a call for physicians to discuss lung cancer screening with patients who match the high-risk smoking history of those enrolled in the NSLT.
Dr. Reid reported having no financial conflicts of interest.
The benefits of routine lung cancer screening in high-risk individuals outweigh the potential risks, according to members of a National Comprehensive Cancer Network guidelines panel that recommended low-dose helical CT screening of two high-risk groups.
Mary E. Reid, Ph.D., of the Roswell Park Cancer Institute in Buffalo, N.Y., acknowledged the burdens – in particular, the cost and requisite resource utilization – associated with following all high-risk patients who screen positive. But, she said, "the evidence [in favor of] the recommendations is really strong and supports their implementation."
Lung cancer, she noted, is the only one of the top four deadliest cancers (lung, prostate, breast, and colorectal) that is not currently subject to routine screening.
Dr. Reid and colleagues on the National Comprehensive Cancer Network (NCCN) Guidelines Panel for Lung Cancer Screening presented the update at the NCCN annual conference March 14-18 in Hollywood, Fla. It had been issued in October 2011 and followed a New England Journal of Medicine report that low-dose CT screening of heavy smokers reduced lung cancer mortality by 20%, compared with annual chest x-rays, in the National Lung Screening Trial (NLST).
The revised guidelines recommend annual low-dose helical CT screening for the following two groups of high-risk individuals:
• Those aged 55-74 years with a minimum smoking history of 30 pack-years who either are current smokers or quit within the past 15 years.
• Those aged 50 years or older with a minimum smoking history of 20 pack-years plus one additional lung cancer risk factor, excluding secondhand exposure.
Evidence from the randomized, controlled NLST suggests that early detection via screening reduced lung-cancer specific mortality in the former risk group, which characterizes the NLST patient population. Specifically, 1 in 100 high-risk individuals who were enrolled in the study screened positive on their first low-dose CT exam, and one life was saved for every 320 high-risk individuals screened over 2 years (three screens) (N. Engl. J. Med. 2011;365:395-409). The NCCN recommendation for this group is category 1, the highest level.
The recommendation for annual screening in the second high-risk group is based on less-robust evidence and a nonuniform consensus of the NCCN panel members, Dr. Reid said. As such, it is a less-emphatic category 2B recommendation.
The NCCN screening recommendations have been deemed by some experts to be premature in the absence of cost-efficacy analysis, particularly because of the high false-positive rates observed in both the CT group (96.4%) and the radiography group (94.5%), as well as the potentially harmful effects of radiation exposure associated with low-dose CT screening.
Despite the favorable outcome of their study, the NLST authors stressed the need for rigorous cost-effectiveness analyses before the crafting of public policy recommendations. "The reductions in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote. "The cost component of low-dose CT screening includes not only the screening examination itself but also the diagnostic follow-up and treatment."
In addition to recommending appropriate candidates for routine screening and the proposed frequency of the scans, the new NCCN guidelines outline lung cancer risk factors, address the risks and benefits of screening as well as screening accuracy, and offer an algorithm for the evaluation and follow-up of positive screens. Specifically, the guidelines recommend the following:
• Basing the frequency of low-dose CT in high-risk patients on the size and status (solid, nonsolid, part-solid, ground-glass, ground-glass opacity) of the nodule on baseline CT.
• Excising all nodules that increase in size or become solid or part-solid during follow-up.
• Considering PET with CT for nodules 8 mm or larger at baseline.
• Performing biopsy or excision of nodules that are suspicious for lung cancer, based on PET with CT findings.
• Reexamining within 1 month solid endobronchial nodules with low-dose CT immediately after vigorous coughing.
• Counseling smokers to quit.
The NCCN is the first professional organization to recommend routine low-dose CT screening for individuals who are considered to be at high-risk for lung cancer, according to Dr. Reid. Last summer, the International Association for the Study of Lung Cancer issued a call for physicians to discuss lung cancer screening with patients who match the high-risk smoking history of those enrolled in the NSLT.
Dr. Reid reported having no financial conflicts of interest.
The benefits of routine lung cancer screening in high-risk individuals outweigh the potential risks, according to members of a National Comprehensive Cancer Network guidelines panel that recommended low-dose helical CT screening of two high-risk groups.
Mary E. Reid, Ph.D., of the Roswell Park Cancer Institute in Buffalo, N.Y., acknowledged the burdens – in particular, the cost and requisite resource utilization – associated with following all high-risk patients who screen positive. But, she said, "the evidence [in favor of] the recommendations is really strong and supports their implementation."
Lung cancer, she noted, is the only one of the top four deadliest cancers (lung, prostate, breast, and colorectal) that is not currently subject to routine screening.
Dr. Reid and colleagues on the National Comprehensive Cancer Network (NCCN) Guidelines Panel for Lung Cancer Screening presented the update at the NCCN annual conference March 14-18 in Hollywood, Fla. It had been issued in October 2011 and followed a New England Journal of Medicine report that low-dose CT screening of heavy smokers reduced lung cancer mortality by 20%, compared with annual chest x-rays, in the National Lung Screening Trial (NLST).
The revised guidelines recommend annual low-dose helical CT screening for the following two groups of high-risk individuals:
• Those aged 55-74 years with a minimum smoking history of 30 pack-years who either are current smokers or quit within the past 15 years.
• Those aged 50 years or older with a minimum smoking history of 20 pack-years plus one additional lung cancer risk factor, excluding secondhand exposure.
Evidence from the randomized, controlled NLST suggests that early detection via screening reduced lung-cancer specific mortality in the former risk group, which characterizes the NLST patient population. Specifically, 1 in 100 high-risk individuals who were enrolled in the study screened positive on their first low-dose CT exam, and one life was saved for every 320 high-risk individuals screened over 2 years (three screens) (N. Engl. J. Med. 2011;365:395-409). The NCCN recommendation for this group is category 1, the highest level.
The recommendation for annual screening in the second high-risk group is based on less-robust evidence and a nonuniform consensus of the NCCN panel members, Dr. Reid said. As such, it is a less-emphatic category 2B recommendation.
The NCCN screening recommendations have been deemed by some experts to be premature in the absence of cost-efficacy analysis, particularly because of the high false-positive rates observed in both the CT group (96.4%) and the radiography group (94.5%), as well as the potentially harmful effects of radiation exposure associated with low-dose CT screening.
Despite the favorable outcome of their study, the NLST authors stressed the need for rigorous cost-effectiveness analyses before the crafting of public policy recommendations. "The reductions in lung-cancer mortality must be weighed against the harms from positive screening results and overdiagnosis, as well as the costs," they wrote. "The cost component of low-dose CT screening includes not only the screening examination itself but also the diagnostic follow-up and treatment."
In addition to recommending appropriate candidates for routine screening and the proposed frequency of the scans, the new NCCN guidelines outline lung cancer risk factors, address the risks and benefits of screening as well as screening accuracy, and offer an algorithm for the evaluation and follow-up of positive screens. Specifically, the guidelines recommend the following:
• Basing the frequency of low-dose CT in high-risk patients on the size and status (solid, nonsolid, part-solid, ground-glass, ground-glass opacity) of the nodule on baseline CT.
• Excising all nodules that increase in size or become solid or part-solid during follow-up.
• Considering PET with CT for nodules 8 mm or larger at baseline.
• Performing biopsy or excision of nodules that are suspicious for lung cancer, based on PET with CT findings.
• Reexamining within 1 month solid endobronchial nodules with low-dose CT immediately after vigorous coughing.
• Counseling smokers to quit.
The NCCN is the first professional organization to recommend routine low-dose CT screening for individuals who are considered to be at high-risk for lung cancer, according to Dr. Reid. Last summer, the International Association for the Study of Lung Cancer issued a call for physicians to discuss lung cancer screening with patients who match the high-risk smoking history of those enrolled in the NSLT.
Dr. Reid reported having no financial conflicts of interest.
Project GREAT Educates Clinicians, Empowers Patients
What is "great" about the Georgia Recovery-Based Educational Approach to Teaching, in addition to its acronym, is the sense of hope it fosters among psychiatric patients by making them full partners in their own care rather than passive recipients of symptomatic treatment, P. Alex Mabe, Ph.D., says.
In fact, shared decision-making and empowerment are the lynchpins of the psychoeducational model, which recently earned the 2012 Award for Creativity in Psychiatric Education from the American College of Psychiatrists.
Project GREAT, conceived by Dr. Peter F. Buckley, former chair of the department of psychiatry and health behavior and current dean of the medical college at Georgia Health Sciences University in Atlanta, is a recovery-oriented treatment program designed to not only change the nature of patient involvement in their own care, but also to change the way in which providers think about treatment, said Dr. Mabe, faculty leader of the program.
Recovery-oriented treatment programs – those that focus on promoting the ability of individuals to cope with their mental illness and to recover meaningful roles and quality of life in the community – began to emerge in the late 1980s. But Project GREAT is among the first to attempt to change clinical services and educational curriculum, Dr. Mabe said. Specifically, the project comprises both an educational/curriculum development and a treatment component, he said.
With respect to provider education, the team has developed a workshop curriculum made up of role plays, live and video presentations, and interactive discussions created and presented by providers and patients working together, Dr. Mabe explained. "Psychiatrists and psychologists teach along side certified peer specialists (CPS) – individuals who have experienced the disabling symptoms of severe mental illness and have gained control over their lives."
Through the multimedia presentations, workshop participants gain an understanding of the recovery model and obtain the tools to put the concepts into practice immediately, including the pre-assessment process, intake interview, and follow-up appointment documentation that stresses self-directed treatment planning and a focus on strengths and hope rather than on psychopathology and symptoms, he said.
"Conventional psychiatry has tended to focus exclusively on diagnosis and symptom treatment, without a consideration of well-being and overall quality of life," Dr. Mabe said. "Through Project GREAT, our goal is to empower patients to gain some measure of control over their lives and to have meaningful goals."
Toward this end, the treatment component of the program is built on shared decision making. In this regard, the CPS members of the treatment team are mission-critical. Their role is tri-fold: provide direct support to patients; educate and provide feedback to residents and other providers with respect to listening to, collaborating with, empowering, and fostering a partnership with patients; and represent the project in the community through participation on advisory boards.
By sharing their own stories, the treatment team members help to dispel patients’ negative self images, an all-too-frequent byproduct of societal stigmatization of mental illness, he said.
"Through Project GREAT, our goal is to empower patients to gain some measure of control over their lives and to have meaningful goals."
"Because these specialists have themselves successfully engaged in the recovery process, they are able to instill hope in the consumers in a more powerful way than someone who has not been on that journey would be able to, including providers."
Time and resource restraints are often cited as obstacles to new program acceptance, but "there is no difference in the treatment course or duration between Project GREAT and conventional care," Dr. Mabe said. The differences lie in the underlying philosophy and the nature of its implementation.
"Financially, the main economic question will center around the peer specialists and whether they can be sustained in terms of their own income," he said. "Many states have funding through Medicaid, but the rates are fairly low at this point. Although we haven’t yet done a financial assessment of the program, which we began in earnest in 2007, it’s easy to see how recovery-based care in the long-run will reduce recidivism and actually make systems more efficient."
Curiously, although initial skepticism among providers that a recovery-based treatment approach is feasible in mental health practice is among the implementation challenges, one of the more stubborn obstacles is the pervasive stigmatizing attitudes that providers have toward their patients, Dr. Mabe said. "Unfortunately, the research is quite clear that providers still have trouble being hopeful about outcomes, particularly with people who have serious or chronic mental illness."
This is exacerbated by the paternalistic perspective that continues to be taught by the traditional model "So shifting this attitude and getting providers to see their patients as capable and helping them instill hope is not at all intuitive or easy," he said.
"What we’re finding, though, is that the more contact providers have with the consumer, and particularly the CPS, the more they are able to see and appreciate a more promising outlook: that recovery is possible and that people can reclaim their lives, so this constant exposure is very valuable."
Although the model, which is being implemented at the Medical College of Georgia and its affiliated hospital as well as at a traditional mental health public hospital in Atlanta, is still new enough to preclude comprehensive outcome studies in the scientific domain, "our program evaluation materials suggest we’re on the right track," Dr. Mabe said. "The scores for the questions on our patient satisfaction measures that are most relevant to Project GREAT, including, ‘Does my doctor understand me? Does my doctor give a good explanation of the treatment options? Am I allowed to be an active participant in the decision-making process?’ have risen from the mid-80% range prior to 2007 to the 95% and higher range since 2007."
Further, in an assessment of the Project GREAT curriculum’s effectiveness for instilling knowledge about recovery and promoting recovery-based attitudes among psychiatrists and psychologists, investigators showed that the recovery principles were effectively taught and that when patients and CPS shared their recovery stories, provider attitudes "shifted toward recovery," Dr. Mabe said (Community Ment. Health J. 2009;45:239-45).
Project GREAT continues to be a work in progress. "Right now, we are piloting a new seminar on shared decision making in psychiatry and looking at the impact on attitudes in practice," Dr. Mabe said. Looking 5-10 years out, "our hope is that by then, there will be a solid skill base in faculty and students where they are really integrating the holistic perspective into their practice by considering life purpose and meaning rather than just symptoms," he said.
"Also, we hope collaboration and shared decision-making are established, valued clinical skills."
Dr. Mabe disclosed having no financial conflicts of interest.
What is "great" about the Georgia Recovery-Based Educational Approach to Teaching, in addition to its acronym, is the sense of hope it fosters among psychiatric patients by making them full partners in their own care rather than passive recipients of symptomatic treatment, P. Alex Mabe, Ph.D., says.
In fact, shared decision-making and empowerment are the lynchpins of the psychoeducational model, which recently earned the 2012 Award for Creativity in Psychiatric Education from the American College of Psychiatrists.
Project GREAT, conceived by Dr. Peter F. Buckley, former chair of the department of psychiatry and health behavior and current dean of the medical college at Georgia Health Sciences University in Atlanta, is a recovery-oriented treatment program designed to not only change the nature of patient involvement in their own care, but also to change the way in which providers think about treatment, said Dr. Mabe, faculty leader of the program.
Recovery-oriented treatment programs – those that focus on promoting the ability of individuals to cope with their mental illness and to recover meaningful roles and quality of life in the community – began to emerge in the late 1980s. But Project GREAT is among the first to attempt to change clinical services and educational curriculum, Dr. Mabe said. Specifically, the project comprises both an educational/curriculum development and a treatment component, he said.
With respect to provider education, the team has developed a workshop curriculum made up of role plays, live and video presentations, and interactive discussions created and presented by providers and patients working together, Dr. Mabe explained. "Psychiatrists and psychologists teach along side certified peer specialists (CPS) – individuals who have experienced the disabling symptoms of severe mental illness and have gained control over their lives."
Through the multimedia presentations, workshop participants gain an understanding of the recovery model and obtain the tools to put the concepts into practice immediately, including the pre-assessment process, intake interview, and follow-up appointment documentation that stresses self-directed treatment planning and a focus on strengths and hope rather than on psychopathology and symptoms, he said.
"Conventional psychiatry has tended to focus exclusively on diagnosis and symptom treatment, without a consideration of well-being and overall quality of life," Dr. Mabe said. "Through Project GREAT, our goal is to empower patients to gain some measure of control over their lives and to have meaningful goals."
Toward this end, the treatment component of the program is built on shared decision making. In this regard, the CPS members of the treatment team are mission-critical. Their role is tri-fold: provide direct support to patients; educate and provide feedback to residents and other providers with respect to listening to, collaborating with, empowering, and fostering a partnership with patients; and represent the project in the community through participation on advisory boards.
By sharing their own stories, the treatment team members help to dispel patients’ negative self images, an all-too-frequent byproduct of societal stigmatization of mental illness, he said.
"Through Project GREAT, our goal is to empower patients to gain some measure of control over their lives and to have meaningful goals."
"Because these specialists have themselves successfully engaged in the recovery process, they are able to instill hope in the consumers in a more powerful way than someone who has not been on that journey would be able to, including providers."
Time and resource restraints are often cited as obstacles to new program acceptance, but "there is no difference in the treatment course or duration between Project GREAT and conventional care," Dr. Mabe said. The differences lie in the underlying philosophy and the nature of its implementation.
"Financially, the main economic question will center around the peer specialists and whether they can be sustained in terms of their own income," he said. "Many states have funding through Medicaid, but the rates are fairly low at this point. Although we haven’t yet done a financial assessment of the program, which we began in earnest in 2007, it’s easy to see how recovery-based care in the long-run will reduce recidivism and actually make systems more efficient."
Curiously, although initial skepticism among providers that a recovery-based treatment approach is feasible in mental health practice is among the implementation challenges, one of the more stubborn obstacles is the pervasive stigmatizing attitudes that providers have toward their patients, Dr. Mabe said. "Unfortunately, the research is quite clear that providers still have trouble being hopeful about outcomes, particularly with people who have serious or chronic mental illness."
This is exacerbated by the paternalistic perspective that continues to be taught by the traditional model "So shifting this attitude and getting providers to see their patients as capable and helping them instill hope is not at all intuitive or easy," he said.
"What we’re finding, though, is that the more contact providers have with the consumer, and particularly the CPS, the more they are able to see and appreciate a more promising outlook: that recovery is possible and that people can reclaim their lives, so this constant exposure is very valuable."
Although the model, which is being implemented at the Medical College of Georgia and its affiliated hospital as well as at a traditional mental health public hospital in Atlanta, is still new enough to preclude comprehensive outcome studies in the scientific domain, "our program evaluation materials suggest we’re on the right track," Dr. Mabe said. "The scores for the questions on our patient satisfaction measures that are most relevant to Project GREAT, including, ‘Does my doctor understand me? Does my doctor give a good explanation of the treatment options? Am I allowed to be an active participant in the decision-making process?’ have risen from the mid-80% range prior to 2007 to the 95% and higher range since 2007."
Further, in an assessment of the Project GREAT curriculum’s effectiveness for instilling knowledge about recovery and promoting recovery-based attitudes among psychiatrists and psychologists, investigators showed that the recovery principles were effectively taught and that when patients and CPS shared their recovery stories, provider attitudes "shifted toward recovery," Dr. Mabe said (Community Ment. Health J. 2009;45:239-45).
Project GREAT continues to be a work in progress. "Right now, we are piloting a new seminar on shared decision making in psychiatry and looking at the impact on attitudes in practice," Dr. Mabe said. Looking 5-10 years out, "our hope is that by then, there will be a solid skill base in faculty and students where they are really integrating the holistic perspective into their practice by considering life purpose and meaning rather than just symptoms," he said.
"Also, we hope collaboration and shared decision-making are established, valued clinical skills."
Dr. Mabe disclosed having no financial conflicts of interest.
What is "great" about the Georgia Recovery-Based Educational Approach to Teaching, in addition to its acronym, is the sense of hope it fosters among psychiatric patients by making them full partners in their own care rather than passive recipients of symptomatic treatment, P. Alex Mabe, Ph.D., says.
In fact, shared decision-making and empowerment are the lynchpins of the psychoeducational model, which recently earned the 2012 Award for Creativity in Psychiatric Education from the American College of Psychiatrists.
Project GREAT, conceived by Dr. Peter F. Buckley, former chair of the department of psychiatry and health behavior and current dean of the medical college at Georgia Health Sciences University in Atlanta, is a recovery-oriented treatment program designed to not only change the nature of patient involvement in their own care, but also to change the way in which providers think about treatment, said Dr. Mabe, faculty leader of the program.
Recovery-oriented treatment programs – those that focus on promoting the ability of individuals to cope with their mental illness and to recover meaningful roles and quality of life in the community – began to emerge in the late 1980s. But Project GREAT is among the first to attempt to change clinical services and educational curriculum, Dr. Mabe said. Specifically, the project comprises both an educational/curriculum development and a treatment component, he said.
With respect to provider education, the team has developed a workshop curriculum made up of role plays, live and video presentations, and interactive discussions created and presented by providers and patients working together, Dr. Mabe explained. "Psychiatrists and psychologists teach along side certified peer specialists (CPS) – individuals who have experienced the disabling symptoms of severe mental illness and have gained control over their lives."
Through the multimedia presentations, workshop participants gain an understanding of the recovery model and obtain the tools to put the concepts into practice immediately, including the pre-assessment process, intake interview, and follow-up appointment documentation that stresses self-directed treatment planning and a focus on strengths and hope rather than on psychopathology and symptoms, he said.
"Conventional psychiatry has tended to focus exclusively on diagnosis and symptom treatment, without a consideration of well-being and overall quality of life," Dr. Mabe said. "Through Project GREAT, our goal is to empower patients to gain some measure of control over their lives and to have meaningful goals."
Toward this end, the treatment component of the program is built on shared decision making. In this regard, the CPS members of the treatment team are mission-critical. Their role is tri-fold: provide direct support to patients; educate and provide feedback to residents and other providers with respect to listening to, collaborating with, empowering, and fostering a partnership with patients; and represent the project in the community through participation on advisory boards.
By sharing their own stories, the treatment team members help to dispel patients’ negative self images, an all-too-frequent byproduct of societal stigmatization of mental illness, he said.
"Through Project GREAT, our goal is to empower patients to gain some measure of control over their lives and to have meaningful goals."
"Because these specialists have themselves successfully engaged in the recovery process, they are able to instill hope in the consumers in a more powerful way than someone who has not been on that journey would be able to, including providers."
Time and resource restraints are often cited as obstacles to new program acceptance, but "there is no difference in the treatment course or duration between Project GREAT and conventional care," Dr. Mabe said. The differences lie in the underlying philosophy and the nature of its implementation.
"Financially, the main economic question will center around the peer specialists and whether they can be sustained in terms of their own income," he said. "Many states have funding through Medicaid, but the rates are fairly low at this point. Although we haven’t yet done a financial assessment of the program, which we began in earnest in 2007, it’s easy to see how recovery-based care in the long-run will reduce recidivism and actually make systems more efficient."
Curiously, although initial skepticism among providers that a recovery-based treatment approach is feasible in mental health practice is among the implementation challenges, one of the more stubborn obstacles is the pervasive stigmatizing attitudes that providers have toward their patients, Dr. Mabe said. "Unfortunately, the research is quite clear that providers still have trouble being hopeful about outcomes, particularly with people who have serious or chronic mental illness."
This is exacerbated by the paternalistic perspective that continues to be taught by the traditional model "So shifting this attitude and getting providers to see their patients as capable and helping them instill hope is not at all intuitive or easy," he said.
"What we’re finding, though, is that the more contact providers have with the consumer, and particularly the CPS, the more they are able to see and appreciate a more promising outlook: that recovery is possible and that people can reclaim their lives, so this constant exposure is very valuable."
Although the model, which is being implemented at the Medical College of Georgia and its affiliated hospital as well as at a traditional mental health public hospital in Atlanta, is still new enough to preclude comprehensive outcome studies in the scientific domain, "our program evaluation materials suggest we’re on the right track," Dr. Mabe said. "The scores for the questions on our patient satisfaction measures that are most relevant to Project GREAT, including, ‘Does my doctor understand me? Does my doctor give a good explanation of the treatment options? Am I allowed to be an active participant in the decision-making process?’ have risen from the mid-80% range prior to 2007 to the 95% and higher range since 2007."
Further, in an assessment of the Project GREAT curriculum’s effectiveness for instilling knowledge about recovery and promoting recovery-based attitudes among psychiatrists and psychologists, investigators showed that the recovery principles were effectively taught and that when patients and CPS shared their recovery stories, provider attitudes "shifted toward recovery," Dr. Mabe said (Community Ment. Health J. 2009;45:239-45).
Project GREAT continues to be a work in progress. "Right now, we are piloting a new seminar on shared decision making in psychiatry and looking at the impact on attitudes in practice," Dr. Mabe said. Looking 5-10 years out, "our hope is that by then, there will be a solid skill base in faculty and students where they are really integrating the holistic perspective into their practice by considering life purpose and meaning rather than just symptoms," he said.
"Also, we hope collaboration and shared decision-making are established, valued clinical skills."
Dr. Mabe disclosed having no financial conflicts of interest.
Gloves Not Enough for Infection Control in Preterm Newborns
BOSTON – Supplementing appropriate hand hygiene with nonsterile gloving can help keep late-onset infections at bay in preterm infants.
In a randomized, controlled trial reported at the annual meeting of the Pediatric Academic Societies, preterm infants in the neonatal intensive care unit of an academic hospital whose caregivers were directed to don nonsterile gloves after standard hand washing and prior to contact with the infants or with their central or peripheral lines were significantly less likely to develop bloodstream infections after 72 hours than those cared for by individuals who practiced appropriate hand hygiene only.
Specifically, the rate of gram-positive bloodstream infections among the 60 newborns randomized to gloved treatment was approximately 40% less than in the 60 newborns randomized to hand hygiene-only care, according to lead investigator David A. Kaufman of the University of Virginia in Charlottesville.
Further, "gloving after hand hygiene with all patient line contact was associated with a 60% decrease in central line associated blood stream infections and a 50% decrease in UTIs [urinary tract infections]," he said.
In previous studies, gloving plus hand hygiene has reduced the transmission of methicillin-resistant Staphylococcus aureus (MRSA) and other infections, "but we haven’t seen many randomized controlled trials in the NICU," said Dr. Kaufman. Such investigations are especially warranted in light of evidence that microorganisms often persist despite appropriate hand hygiene practices as well as the increased risk of infection and consequent morbidity and mortality among preterm infants weighing less than 1,000 g at birth.
For the current study, preterm newborns who weighed less than 1,000 g at birth or who were born at or before 28 weeks’ gestation were randomized to the gloving plus hand hygiene or hand hygiene-only group within 7 days after birth and continuing for 4 weeks or until intravenous access was no longer necessary, Dr. Kaufman said. Hand hygiene was defined as using alcohol hand rub or washing hands with antimicrobial soap. Outcome measures included the incidence of one or more episodes of blood stream infection, urinary tract infection, meningitis, and/or necrotizing enterocolitis after 72 hours.
The baseline characteristics of both groups of infants were similar, Dr. Kaufman reported, noting that gestational age and body weight of infants in the gloved group were 25.7 weeks and 790 g, respectively, compared with 25.9 weeks and 803 g in the hand hygiene-only group. While the rates for one or more episode of blood stream infection, UTI, meningitis, and necrotizing enterocolitis were similar between the groups, the odds ratio for gram-positive bloodstream infections in the gloving group was 0.42, and the odds ratio of possible central line-associated blood stream infection – defined as one or more positive culture and a central line in place – was 0.31 in the gloving group, he said.
The findings suggest that gloving is a simple, effective approach for preventing invasive infections in high-risk infants with lines in place, said Dr. Kaufmann. The resulting reduction in infection rates could improve outcomes while reducing hospital stays and overall health care costs in this population.
Dr. Kaufmann said he had no relevant financial conflicts to disclose.
BOSTON – Supplementing appropriate hand hygiene with nonsterile gloving can help keep late-onset infections at bay in preterm infants.
In a randomized, controlled trial reported at the annual meeting of the Pediatric Academic Societies, preterm infants in the neonatal intensive care unit of an academic hospital whose caregivers were directed to don nonsterile gloves after standard hand washing and prior to contact with the infants or with their central or peripheral lines were significantly less likely to develop bloodstream infections after 72 hours than those cared for by individuals who practiced appropriate hand hygiene only.
Specifically, the rate of gram-positive bloodstream infections among the 60 newborns randomized to gloved treatment was approximately 40% less than in the 60 newborns randomized to hand hygiene-only care, according to lead investigator David A. Kaufman of the University of Virginia in Charlottesville.
Further, "gloving after hand hygiene with all patient line contact was associated with a 60% decrease in central line associated blood stream infections and a 50% decrease in UTIs [urinary tract infections]," he said.
In previous studies, gloving plus hand hygiene has reduced the transmission of methicillin-resistant Staphylococcus aureus (MRSA) and other infections, "but we haven’t seen many randomized controlled trials in the NICU," said Dr. Kaufman. Such investigations are especially warranted in light of evidence that microorganisms often persist despite appropriate hand hygiene practices as well as the increased risk of infection and consequent morbidity and mortality among preterm infants weighing less than 1,000 g at birth.
For the current study, preterm newborns who weighed less than 1,000 g at birth or who were born at or before 28 weeks’ gestation were randomized to the gloving plus hand hygiene or hand hygiene-only group within 7 days after birth and continuing for 4 weeks or until intravenous access was no longer necessary, Dr. Kaufman said. Hand hygiene was defined as using alcohol hand rub or washing hands with antimicrobial soap. Outcome measures included the incidence of one or more episodes of blood stream infection, urinary tract infection, meningitis, and/or necrotizing enterocolitis after 72 hours.
The baseline characteristics of both groups of infants were similar, Dr. Kaufman reported, noting that gestational age and body weight of infants in the gloved group were 25.7 weeks and 790 g, respectively, compared with 25.9 weeks and 803 g in the hand hygiene-only group. While the rates for one or more episode of blood stream infection, UTI, meningitis, and necrotizing enterocolitis were similar between the groups, the odds ratio for gram-positive bloodstream infections in the gloving group was 0.42, and the odds ratio of possible central line-associated blood stream infection – defined as one or more positive culture and a central line in place – was 0.31 in the gloving group, he said.
The findings suggest that gloving is a simple, effective approach for preventing invasive infections in high-risk infants with lines in place, said Dr. Kaufmann. The resulting reduction in infection rates could improve outcomes while reducing hospital stays and overall health care costs in this population.
Dr. Kaufmann said he had no relevant financial conflicts to disclose.
BOSTON – Supplementing appropriate hand hygiene with nonsterile gloving can help keep late-onset infections at bay in preterm infants.
In a randomized, controlled trial reported at the annual meeting of the Pediatric Academic Societies, preterm infants in the neonatal intensive care unit of an academic hospital whose caregivers were directed to don nonsterile gloves after standard hand washing and prior to contact with the infants or with their central or peripheral lines were significantly less likely to develop bloodstream infections after 72 hours than those cared for by individuals who practiced appropriate hand hygiene only.
Specifically, the rate of gram-positive bloodstream infections among the 60 newborns randomized to gloved treatment was approximately 40% less than in the 60 newborns randomized to hand hygiene-only care, according to lead investigator David A. Kaufman of the University of Virginia in Charlottesville.
Further, "gloving after hand hygiene with all patient line contact was associated with a 60% decrease in central line associated blood stream infections and a 50% decrease in UTIs [urinary tract infections]," he said.
In previous studies, gloving plus hand hygiene has reduced the transmission of methicillin-resistant Staphylococcus aureus (MRSA) and other infections, "but we haven’t seen many randomized controlled trials in the NICU," said Dr. Kaufman. Such investigations are especially warranted in light of evidence that microorganisms often persist despite appropriate hand hygiene practices as well as the increased risk of infection and consequent morbidity and mortality among preterm infants weighing less than 1,000 g at birth.
For the current study, preterm newborns who weighed less than 1,000 g at birth or who were born at or before 28 weeks’ gestation were randomized to the gloving plus hand hygiene or hand hygiene-only group within 7 days after birth and continuing for 4 weeks or until intravenous access was no longer necessary, Dr. Kaufman said. Hand hygiene was defined as using alcohol hand rub or washing hands with antimicrobial soap. Outcome measures included the incidence of one or more episodes of blood stream infection, urinary tract infection, meningitis, and/or necrotizing enterocolitis after 72 hours.
The baseline characteristics of both groups of infants were similar, Dr. Kaufman reported, noting that gestational age and body weight of infants in the gloved group were 25.7 weeks and 790 g, respectively, compared with 25.9 weeks and 803 g in the hand hygiene-only group. While the rates for one or more episode of blood stream infection, UTI, meningitis, and necrotizing enterocolitis were similar between the groups, the odds ratio for gram-positive bloodstream infections in the gloving group was 0.42, and the odds ratio of possible central line-associated blood stream infection – defined as one or more positive culture and a central line in place – was 0.31 in the gloving group, he said.
The findings suggest that gloving is a simple, effective approach for preventing invasive infections in high-risk infants with lines in place, said Dr. Kaufmann. The resulting reduction in infection rates could improve outcomes while reducing hospital stays and overall health care costs in this population.
Dr. Kaufmann said he had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE PEDIATRIC ACADEMIC SOCIETIES
Major Finding: Gram-positive bloodstream infections were more than 40% lower in preterm infants whose NICU caregivers donned nonsterile gloves after hand hygiene relative to appropriate hand hygiene alone prior to patient and peripheral and central line contact.
Data Source: This was a randomized controlled trial of 120 preterm infants.
Disclosures: Dr. Kaufmann said he had no relevant financial conflicts to disclose.
Fast-Acting Erectile Dysfunction Drug Approved
The fast-acting erectile dysfunction medication avanafil was approved by the Food and Drug Administration April 30 on the basis of findings from multiple phase-III trials demonstrating the safety and efficacy of the phosphodiesterase type 5 inhibitor, according to a statement from the agency.
The first new entry in the erectile dysfunction (ED) marketplace in nearly 10 years, avanafil (Stendra) joins the ranks of other PDE5 inhibitors approved for the treatment of ED and is expected to be a formidable competitor in the marketplace because it is a faster-acting agent associated with fewer side effects than the currently available options, including sildenafil citrate (Viagra), vardenafil (Levitra), and tadalafil (Cialis), according to Dr. Irwin Goldstein, director of the sexual medicine program at Alvarado Hospital in San Diego.
Dr. Goldstein was the lead investigator of the pivotal phase-III Research Evaluating an Investigational Medication for Erectile Dysfunction (REVIVE) trial in which 646 men with a history of ED for at least 6 months were randomized to 50-mg, 100-mg, or 200-mg of avanafil or placebo (J. Sex. Med. 2012;9:1122-33).
"We observed significant improvements in erectile function and low rates of side effects common to [the PDE5] drug class," Dr. Goldstein said in an interview. "Importantly, the majority of patients who attempted intercourse within 15 minutes of dosing were successful at all dosage levels," he said, noting that successful attempts were reported 64%, 67%, and 71% of the time with 50-mg, 100-mg, and 200-mg doses, respectively, compared with 27% for placebo.
In addition to the REVIVE trial, the avanafil development program included the REVIVE-Diabetes trial comprising 390 men with ED and diabetes and the REVIVE-RP trial comprising 298 men with ED following radical prostatectomy, as well as a year-long safety study of 712 continuation patients from the REVIVE and REVIVE-Diabetes trials, according to a statement issued by Vivus, manufacturer of the drug.
The combined highlights of the various studies showed statistically significant improvements relative to placebo in measures of erectile function, vaginal penetration, and successful intercourse at all three dosages, according the FDA.
The most common side effects, reported in more than 2% of the patients, were headache, facial flushing, nasal congestion, and back pain; there were no drug-related serious adverse events reported, the FDA said.
In the continuation study of patients who received up to 40 additional weeks of treatment, initially at the 100-mg dose and eventually maintained, increased, or decreased based on individual patient response, the side effects did not appear to worsen over time.
Dr. Goldstein disclosed financial relationships with BioSante, Boehringer Ingelheim, Medtronic, Pfizer, VIVUS, Alagin, Shionogi, Slate, Abbott, Ascend, Auxilium, Coloplast, and Warner Chilcott.
The fast-acting erectile dysfunction medication avanafil was approved by the Food and Drug Administration April 30 on the basis of findings from multiple phase-III trials demonstrating the safety and efficacy of the phosphodiesterase type 5 inhibitor, according to a statement from the agency.
The first new entry in the erectile dysfunction (ED) marketplace in nearly 10 years, avanafil (Stendra) joins the ranks of other PDE5 inhibitors approved for the treatment of ED and is expected to be a formidable competitor in the marketplace because it is a faster-acting agent associated with fewer side effects than the currently available options, including sildenafil citrate (Viagra), vardenafil (Levitra), and tadalafil (Cialis), according to Dr. Irwin Goldstein, director of the sexual medicine program at Alvarado Hospital in San Diego.
Dr. Goldstein was the lead investigator of the pivotal phase-III Research Evaluating an Investigational Medication for Erectile Dysfunction (REVIVE) trial in which 646 men with a history of ED for at least 6 months were randomized to 50-mg, 100-mg, or 200-mg of avanafil or placebo (J. Sex. Med. 2012;9:1122-33).
"We observed significant improvements in erectile function and low rates of side effects common to [the PDE5] drug class," Dr. Goldstein said in an interview. "Importantly, the majority of patients who attempted intercourse within 15 minutes of dosing were successful at all dosage levels," he said, noting that successful attempts were reported 64%, 67%, and 71% of the time with 50-mg, 100-mg, and 200-mg doses, respectively, compared with 27% for placebo.
In addition to the REVIVE trial, the avanafil development program included the REVIVE-Diabetes trial comprising 390 men with ED and diabetes and the REVIVE-RP trial comprising 298 men with ED following radical prostatectomy, as well as a year-long safety study of 712 continuation patients from the REVIVE and REVIVE-Diabetes trials, according to a statement issued by Vivus, manufacturer of the drug.
The combined highlights of the various studies showed statistically significant improvements relative to placebo in measures of erectile function, vaginal penetration, and successful intercourse at all three dosages, according the FDA.
The most common side effects, reported in more than 2% of the patients, were headache, facial flushing, nasal congestion, and back pain; there were no drug-related serious adverse events reported, the FDA said.
In the continuation study of patients who received up to 40 additional weeks of treatment, initially at the 100-mg dose and eventually maintained, increased, or decreased based on individual patient response, the side effects did not appear to worsen over time.
Dr. Goldstein disclosed financial relationships with BioSante, Boehringer Ingelheim, Medtronic, Pfizer, VIVUS, Alagin, Shionogi, Slate, Abbott, Ascend, Auxilium, Coloplast, and Warner Chilcott.
The fast-acting erectile dysfunction medication avanafil was approved by the Food and Drug Administration April 30 on the basis of findings from multiple phase-III trials demonstrating the safety and efficacy of the phosphodiesterase type 5 inhibitor, according to a statement from the agency.
The first new entry in the erectile dysfunction (ED) marketplace in nearly 10 years, avanafil (Stendra) joins the ranks of other PDE5 inhibitors approved for the treatment of ED and is expected to be a formidable competitor in the marketplace because it is a faster-acting agent associated with fewer side effects than the currently available options, including sildenafil citrate (Viagra), vardenafil (Levitra), and tadalafil (Cialis), according to Dr. Irwin Goldstein, director of the sexual medicine program at Alvarado Hospital in San Diego.
Dr. Goldstein was the lead investigator of the pivotal phase-III Research Evaluating an Investigational Medication for Erectile Dysfunction (REVIVE) trial in which 646 men with a history of ED for at least 6 months were randomized to 50-mg, 100-mg, or 200-mg of avanafil or placebo (J. Sex. Med. 2012;9:1122-33).
"We observed significant improvements in erectile function and low rates of side effects common to [the PDE5] drug class," Dr. Goldstein said in an interview. "Importantly, the majority of patients who attempted intercourse within 15 minutes of dosing were successful at all dosage levels," he said, noting that successful attempts were reported 64%, 67%, and 71% of the time with 50-mg, 100-mg, and 200-mg doses, respectively, compared with 27% for placebo.
In addition to the REVIVE trial, the avanafil development program included the REVIVE-Diabetes trial comprising 390 men with ED and diabetes and the REVIVE-RP trial comprising 298 men with ED following radical prostatectomy, as well as a year-long safety study of 712 continuation patients from the REVIVE and REVIVE-Diabetes trials, according to a statement issued by Vivus, manufacturer of the drug.
The combined highlights of the various studies showed statistically significant improvements relative to placebo in measures of erectile function, vaginal penetration, and successful intercourse at all three dosages, according the FDA.
The most common side effects, reported in more than 2% of the patients, were headache, facial flushing, nasal congestion, and back pain; there were no drug-related serious adverse events reported, the FDA said.
In the continuation study of patients who received up to 40 additional weeks of treatment, initially at the 100-mg dose and eventually maintained, increased, or decreased based on individual patient response, the side effects did not appear to worsen over time.
Dr. Goldstein disclosed financial relationships with BioSante, Boehringer Ingelheim, Medtronic, Pfizer, VIVUS, Alagin, Shionogi, Slate, Abbott, Ascend, Auxilium, Coloplast, and Warner Chilcott.
Maintenance Immunotherapy Extends Survival in Multiple Advanced Cancers
CHICAGO – Maintenance immunotherapy with low-dose interleukin-2 and 13-cis-retinoic acid demonstrated an "unexpected" survival benefit in a phase II trial among 500 patients who had derived clinical benefit from chemotherapy for a variety of stage IV cancers, investigators from Italy reported.
The 15-year disease-free survival and overall survival rates reached 32.6% and 36.8%, respectively, in the open, nonrandomized trial, and a breakdown by tumor type showed better outcomes than seen in historic controls, Dr. Francesco Recchia reported at the annual meeting of the American Association for Cancer Research.
Comparing their data with outcomes for the most commonly treated metastatic cancers in the Surveillance, Epidemiology, and End Results (SEER) database in the United States, the investigators found their 5-year overall survival rates were 42.7% vs. 23.3% for breast cancer, 26.4% vs. 3.6% for lung cancer, 43.6% vs. 11.7% for colorectal cancer, and 23% vs. 11% for renal cancer.
"The good and unexpected results of this immunotherapy regimen were seen in all types of cancer: ovarian cancer and recurrent ovarian cancer, non–small cell lung cancer, cardiac metastases of sarcoma, colorectal cancer, gastric cancer, renal cell carcinoma, melanoma, head and neck cancer, breast cancer, and pancreatic cancer," said Dr. Recchia, director of oncology at the Civilian Hospital in Avezzano (Italy).
"The best merit of our research is the low cost of this therapy," he added.
The impetus for the phase II trial was an observation, in 1995, that a patient, who could not tolerate standard high-dose (18 x 106 IU/m2) IL-2 therapy for metastatic melanoma, experienced a long-lasting response to low-dose subcutaneous IL-2. Dr. Recchia and his colleagues conducted a series of phase I and II randomized studies of low-dose IL-2 with and without retinoic acid, ultimately determining that the combination of the two agents was most effective in increasing natural killer (NK) cell populations and decreasing vascular endothelial growth factor (VEGF) expression.
In the current study, after a median follow-up of 60 months, Dr. Recchia and his colleagues observed a statistically significant increase in the number of NK cells – mediators of lytic activity against cancer cell lines – from a baseline mean of 309/mm3 to a mean of 579/mm3. They also found a statistically significant decrease in VEGF expression, from a baseline mean of 520 pg/mm3 to a mean of 150 pg/mm3 in the study participants.
"Both of these mechanisms are associated with slowing cancer growth," he said in an interview.
All of the patients enrolled in the study were in chemotherapy-induced remission, with good performance status, from stage IV cancer, and all (median age 61 years) were treated for 1 year with self-administered subcutaneous IL-2 (1.8 x 106 IU) and oral 13-cis-retinoic acid (0.5 mg/kg) 5 days per week for two consecutive 3-week cycles, with a 1-week rest. This was followed by continued intermittently scheduled therapy for 5 years or until disease progression, with assessment of NK cells, serum VEGF, tumor response, and toxicity every 4 months, Dr. Recchia said.
The study’s primary end point was NK cell and VEGF response, he added, noting that disease-free survival, overall survival, and toxicity in various tumor types were secondary end points.
The treatment was not associated with any World Health Organization grade 3 or 4 toxicities, Dr. Recchia reported. Grade 2 cutaneous toxicity (20%), fever (13%), mild hypothyroidism (5%), and triglyceride elevation (15%) were observed, he said; one patient discontinued treatment because of grade 2 urticaria.
Prior to using the maintenance regimen in clinical practice, the findings of the current study have to be validated in a blinded, controlled, randomized trial, said Dr. Recchia, noting that a phase III study is underway in patients with advanced breast cancer.
Dr. Recchia reported having no relevant financial conflicts of interest.
CHICAGO – Maintenance immunotherapy with low-dose interleukin-2 and 13-cis-retinoic acid demonstrated an "unexpected" survival benefit in a phase II trial among 500 patients who had derived clinical benefit from chemotherapy for a variety of stage IV cancers, investigators from Italy reported.
The 15-year disease-free survival and overall survival rates reached 32.6% and 36.8%, respectively, in the open, nonrandomized trial, and a breakdown by tumor type showed better outcomes than seen in historic controls, Dr. Francesco Recchia reported at the annual meeting of the American Association for Cancer Research.
Comparing their data with outcomes for the most commonly treated metastatic cancers in the Surveillance, Epidemiology, and End Results (SEER) database in the United States, the investigators found their 5-year overall survival rates were 42.7% vs. 23.3% for breast cancer, 26.4% vs. 3.6% for lung cancer, 43.6% vs. 11.7% for colorectal cancer, and 23% vs. 11% for renal cancer.
"The good and unexpected results of this immunotherapy regimen were seen in all types of cancer: ovarian cancer and recurrent ovarian cancer, non–small cell lung cancer, cardiac metastases of sarcoma, colorectal cancer, gastric cancer, renal cell carcinoma, melanoma, head and neck cancer, breast cancer, and pancreatic cancer," said Dr. Recchia, director of oncology at the Civilian Hospital in Avezzano (Italy).
"The best merit of our research is the low cost of this therapy," he added.
The impetus for the phase II trial was an observation, in 1995, that a patient, who could not tolerate standard high-dose (18 x 106 IU/m2) IL-2 therapy for metastatic melanoma, experienced a long-lasting response to low-dose subcutaneous IL-2. Dr. Recchia and his colleagues conducted a series of phase I and II randomized studies of low-dose IL-2 with and without retinoic acid, ultimately determining that the combination of the two agents was most effective in increasing natural killer (NK) cell populations and decreasing vascular endothelial growth factor (VEGF) expression.
In the current study, after a median follow-up of 60 months, Dr. Recchia and his colleagues observed a statistically significant increase in the number of NK cells – mediators of lytic activity against cancer cell lines – from a baseline mean of 309/mm3 to a mean of 579/mm3. They also found a statistically significant decrease in VEGF expression, from a baseline mean of 520 pg/mm3 to a mean of 150 pg/mm3 in the study participants.
"Both of these mechanisms are associated with slowing cancer growth," he said in an interview.
All of the patients enrolled in the study were in chemotherapy-induced remission, with good performance status, from stage IV cancer, and all (median age 61 years) were treated for 1 year with self-administered subcutaneous IL-2 (1.8 x 106 IU) and oral 13-cis-retinoic acid (0.5 mg/kg) 5 days per week for two consecutive 3-week cycles, with a 1-week rest. This was followed by continued intermittently scheduled therapy for 5 years or until disease progression, with assessment of NK cells, serum VEGF, tumor response, and toxicity every 4 months, Dr. Recchia said.
The study’s primary end point was NK cell and VEGF response, he added, noting that disease-free survival, overall survival, and toxicity in various tumor types were secondary end points.
The treatment was not associated with any World Health Organization grade 3 or 4 toxicities, Dr. Recchia reported. Grade 2 cutaneous toxicity (20%), fever (13%), mild hypothyroidism (5%), and triglyceride elevation (15%) were observed, he said; one patient discontinued treatment because of grade 2 urticaria.
Prior to using the maintenance regimen in clinical practice, the findings of the current study have to be validated in a blinded, controlled, randomized trial, said Dr. Recchia, noting that a phase III study is underway in patients with advanced breast cancer.
Dr. Recchia reported having no relevant financial conflicts of interest.
CHICAGO – Maintenance immunotherapy with low-dose interleukin-2 and 13-cis-retinoic acid demonstrated an "unexpected" survival benefit in a phase II trial among 500 patients who had derived clinical benefit from chemotherapy for a variety of stage IV cancers, investigators from Italy reported.
The 15-year disease-free survival and overall survival rates reached 32.6% and 36.8%, respectively, in the open, nonrandomized trial, and a breakdown by tumor type showed better outcomes than seen in historic controls, Dr. Francesco Recchia reported at the annual meeting of the American Association for Cancer Research.
Comparing their data with outcomes for the most commonly treated metastatic cancers in the Surveillance, Epidemiology, and End Results (SEER) database in the United States, the investigators found their 5-year overall survival rates were 42.7% vs. 23.3% for breast cancer, 26.4% vs. 3.6% for lung cancer, 43.6% vs. 11.7% for colorectal cancer, and 23% vs. 11% for renal cancer.
"The good and unexpected results of this immunotherapy regimen were seen in all types of cancer: ovarian cancer and recurrent ovarian cancer, non–small cell lung cancer, cardiac metastases of sarcoma, colorectal cancer, gastric cancer, renal cell carcinoma, melanoma, head and neck cancer, breast cancer, and pancreatic cancer," said Dr. Recchia, director of oncology at the Civilian Hospital in Avezzano (Italy).
"The best merit of our research is the low cost of this therapy," he added.
The impetus for the phase II trial was an observation, in 1995, that a patient, who could not tolerate standard high-dose (18 x 106 IU/m2) IL-2 therapy for metastatic melanoma, experienced a long-lasting response to low-dose subcutaneous IL-2. Dr. Recchia and his colleagues conducted a series of phase I and II randomized studies of low-dose IL-2 with and without retinoic acid, ultimately determining that the combination of the two agents was most effective in increasing natural killer (NK) cell populations and decreasing vascular endothelial growth factor (VEGF) expression.
In the current study, after a median follow-up of 60 months, Dr. Recchia and his colleagues observed a statistically significant increase in the number of NK cells – mediators of lytic activity against cancer cell lines – from a baseline mean of 309/mm3 to a mean of 579/mm3. They also found a statistically significant decrease in VEGF expression, from a baseline mean of 520 pg/mm3 to a mean of 150 pg/mm3 in the study participants.
"Both of these mechanisms are associated with slowing cancer growth," he said in an interview.
All of the patients enrolled in the study were in chemotherapy-induced remission, with good performance status, from stage IV cancer, and all (median age 61 years) were treated for 1 year with self-administered subcutaneous IL-2 (1.8 x 106 IU) and oral 13-cis-retinoic acid (0.5 mg/kg) 5 days per week for two consecutive 3-week cycles, with a 1-week rest. This was followed by continued intermittently scheduled therapy for 5 years or until disease progression, with assessment of NK cells, serum VEGF, tumor response, and toxicity every 4 months, Dr. Recchia said.
The study’s primary end point was NK cell and VEGF response, he added, noting that disease-free survival, overall survival, and toxicity in various tumor types were secondary end points.
The treatment was not associated with any World Health Organization grade 3 or 4 toxicities, Dr. Recchia reported. Grade 2 cutaneous toxicity (20%), fever (13%), mild hypothyroidism (5%), and triglyceride elevation (15%) were observed, he said; one patient discontinued treatment because of grade 2 urticaria.
Prior to using the maintenance regimen in clinical practice, the findings of the current study have to be validated in a blinded, controlled, randomized trial, said Dr. Recchia, noting that a phase III study is underway in patients with advanced breast cancer.
Dr. Recchia reported having no relevant financial conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR CANCER RESEARCH