User login
COVID-19 drives innovation in addiction treatment
With the onset of the COVID-19 pandemic, there has been a rapid uptick in virtual recovery programs and telemedicine counseling sessions for patients with substance use disorders (SUDs). New research shows that these programs are acceptable and effective alternatives to in-person sessions.
Study results from three research teams at the University of South Carolina School of Medicine Greenville (USCSM-G) show that SUD counselors in the state were satisfied with their experience with telehealth and virtual recovery meetings.
In one of the studies, five counselors who utilized a virtual meeting platform after the COVID-19 pandemic made in-person visits unsafe were surveyed. The respondents said they much preferred in-person meetings. However, they could also see that virtual meetings were filling an important need for their patients.
Two other studies echoed the results from the first. Clinicians who were leery of the new technology at first became more enthusiastic after they gained experience using it.
“We have lived in a society where there has been one right way, which has always been in-person meetings for recovery, such as Alcoholics Anonymous. It is a very structured process,” lead author Haley Fulton, a fourth-year medical student at USCSM-G, said in an interview.
“The onset of COVID really upended a lot of things, but ... now there may not be just one right way for recovery. There are alternatives to offer,” Ms. Fulton said.
The findings were presented at the annual meeting of the American Academy of Addiction Psychiatry, which was held online this year because of the pandemic.
Huge need
“Virtual meetings may not be ideal, but some version of recovery is better than none. If we can make these meetings accessible to more people, this could promote recovery from substance use disorder,” Ms. Fulton said.
There is a huge need for counseling, and past research has shown that failure to attend meetings can precipitate relapse in many individuals.
In Ms. Fulton’s study, counselors were asked to describe how they perceived the efficacy of virtual recovery meetings, compared with that of in-person meetings.
The investigators analyzed how often certain words, phrases, or issues came up during seven in-person recovery meetings held before the COVID-19 pandemic as well as observational data from seven virtual recovery-support meetings held during the pandemic.
On the pro side, the respondents cited convenience, comfort at home, and increased accessibility to counseling for patients.
In addition, because there was no need to travel, virtual meetings were cost effective. Such meetings could expand the recovery world, inasmuch as individuals could attend recovery meetings in other parts of the country.
Perceived disadvantages included challenges involving technology, because learning new apps such as Zoom could be a problem for some patients. Distractions at home and lack of privacy were also cited, but for many, the most important drawback to virtual meetings was the lessening of emotional connection with others.
Impact on SUD treatment
In a second study, another team from USCSM-G reported similar findings when it explored the impact of telehealth on counselors as well as on patients who were undergoing SUD treatment during the pandemic.
Led by fourth-year medical students Elizabeth Whiteside and Kyleigh Connolly, the researchers assessed data from a focus group of six behavioral health counselors representing rural and city agencies throughout South Carolina.
Themes that emerged included concerns about mental health – counselors and patients were experiencing increased stress, depression, and anxiety.
“People had to now home school, there were job layoffs, increased responsibilities at home. Also, Narcan [naloxone] distribution was decreased, and this contributed to rising overdose rates,” Ms. Whiteside said in an interview.
The focus group concluded that the advantages of telehealth included greater ability to accept new patients, an increase in scheduling flexibility, and cost-effectiveness because it obviated the need for child care or transportation.
Disadvantages included problems involving privacy, because for many patients who were undergoing SUD recovery, it was impossible to be alone in a room or a designated area of their own.
“Before COVID happened, [health care] barriers included transport to the actual center and finding care for children,” Ms. Connolly said in an interview.
“That’s where telehealth really bridged the gap for these people, and it actually became a lot easier for them to get in contact with their counselors, get into group meetings, and access other services,” she said.
Many of the study participants were not very optimistic about telehealth at first, Ms. Connolly noted. “They felt a little odd going on telehealth at first, but by the end, everybody said that they loved having it.”
“One of the things that came out often was that patients felt they could be more open and honest because they weren’t looking their counselor right in the face. They didn’t feel so horrible sharing,” Ms. Whiteside added.
Some counselors reported that some clients shared more details with them and that there was an ease of connecting. If a patient was a few minutes late to an appointment, telehealth would put in a call to find out where that patient was.
The counselors also had the ability to determine which of their patients would be good candidates for telehealth counseling and which patients would not do well with telehealth and would instead need in-patient care.
“This is something that really helped the experience go better for the counselors. They were able to determine which patient fit the mold for telehealth working for them. Obviously, patients who have more acute periods of mental health problems would do better with in-person care,” Ms. Whiteside said.
Here to stay?
In the third study from USCSM-G, investigators evaluated data from a focus group of four providers of medications for opioid use disorder (MOUD) who practiced in urban and rural areas throughout the state.
The respondents reflected on their experiences in using telemedicine for prescribing MOUD.
As in the previous studies, the providers had positive experiences with telemedicine. It increased patient access, participation, and satisfaction with treatment, and the benefits of telemedicine outweighed its potential limitations.
Still, technology was cited as a barrier to care, especially in rural areas.
“We found that there was a lack of good internet in certain rural parts of South Carolina, and that lack of the proper electronic devices ... could also make it difficult to access telemedicine,” lead author Kellie Shell said in an interview.
As noted in the other studies, the providers expressed a desire that telemedicine incorporate safeguards that would enable clinicians to identify a particular patient’s location in order that authorities could be dispatched if an emergency were to arise.
The clinicians also said that monitoring for diversion and performing pill counts were more difficult to do via telemedicine.
“We definitely have to improve infrastructure, especially in rural areas, so that all people have access to telemedicine,” Ms. Shell said.
“Overall, the providers were won over with telemedicine, and some predicted telehealth and virtual visits were here to stay, even after COVID,” she added.
The three posters provide useful insight into the potential advantages and disadvantages of telehealth in SUD settings, experts said.
Telehealth data ‘very limited’
Commenting on the research, Lewei (Allison) Lin, MD, University of Michigan, Ann Arbor, noted that “there is such limited information” about the use of telehealth for patients with SUD.
“These insights are helpful for us to start understanding the things that need to be considered, including clinician attitudes and perceptions,” said Dr. Lin, who was not involved with the studies.
“It will be key to have data as use of telemedicine increases during COVID-19 to help us see exactly how it should be used and to better understand the actual impacts and whether or not it is increasing accessibility, and for which patients,” she added.
David Kan, MD, chief medical officer at Bright Heart Health, San Ramon, Calif., has had experience with telehealth for SUD and has found that conducting pill counts with his patients has not been a problem.
“The Shell poster covers telemedicine well,” Dr. Kan said in an interview.
However, “I disagree with their point that diversion prevention is harder via telemedicine. In my experience, it is easier, as you can do pill or wrapper counts almost on demand. You can also do daily observed dosing with pill counts if diversion is suspected,” he said.
Dr. Kan also suggested ways to cope with problems involving privacy. “Privacy concerns are always an issue but can be mitigated with headphones and a scan of the room with the telehealth technology if a privacy concern arises.”
He acknowledged that in-person meetings, especially through well-established programs, such as Alcoholics Anonymous (AA), will always be important. But he pointed out that people are finding ways to meet safely and have in-person connections.
“The AA has been providing virtual recovery meetings long before COVID. The common complaint is the loss of fellowship associated with recovery groups. I don’t know of a way to get around this short of vaccines,” Dr. Kan said. However, “people have adapted impressively with masked outdoor meetings and other forms of safe gathering.”
The investigators, Dr. Lin, and Dr. Kan reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
With the onset of the COVID-19 pandemic, there has been a rapid uptick in virtual recovery programs and telemedicine counseling sessions for patients with substance use disorders (SUDs). New research shows that these programs are acceptable and effective alternatives to in-person sessions.
Study results from three research teams at the University of South Carolina School of Medicine Greenville (USCSM-G) show that SUD counselors in the state were satisfied with their experience with telehealth and virtual recovery meetings.
In one of the studies, five counselors who utilized a virtual meeting platform after the COVID-19 pandemic made in-person visits unsafe were surveyed. The respondents said they much preferred in-person meetings. However, they could also see that virtual meetings were filling an important need for their patients.
Two other studies echoed the results from the first. Clinicians who were leery of the new technology at first became more enthusiastic after they gained experience using it.
“We have lived in a society where there has been one right way, which has always been in-person meetings for recovery, such as Alcoholics Anonymous. It is a very structured process,” lead author Haley Fulton, a fourth-year medical student at USCSM-G, said in an interview.
“The onset of COVID really upended a lot of things, but ... now there may not be just one right way for recovery. There are alternatives to offer,” Ms. Fulton said.
The findings were presented at the annual meeting of the American Academy of Addiction Psychiatry, which was held online this year because of the pandemic.
Huge need
“Virtual meetings may not be ideal, but some version of recovery is better than none. If we can make these meetings accessible to more people, this could promote recovery from substance use disorder,” Ms. Fulton said.
There is a huge need for counseling, and past research has shown that failure to attend meetings can precipitate relapse in many individuals.
In Ms. Fulton’s study, counselors were asked to describe how they perceived the efficacy of virtual recovery meetings, compared with that of in-person meetings.
The investigators analyzed how often certain words, phrases, or issues came up during seven in-person recovery meetings held before the COVID-19 pandemic as well as observational data from seven virtual recovery-support meetings held during the pandemic.
On the pro side, the respondents cited convenience, comfort at home, and increased accessibility to counseling for patients.
In addition, because there was no need to travel, virtual meetings were cost effective. Such meetings could expand the recovery world, inasmuch as individuals could attend recovery meetings in other parts of the country.
Perceived disadvantages included challenges involving technology, because learning new apps such as Zoom could be a problem for some patients. Distractions at home and lack of privacy were also cited, but for many, the most important drawback to virtual meetings was the lessening of emotional connection with others.
Impact on SUD treatment
In a second study, another team from USCSM-G reported similar findings when it explored the impact of telehealth on counselors as well as on patients who were undergoing SUD treatment during the pandemic.
Led by fourth-year medical students Elizabeth Whiteside and Kyleigh Connolly, the researchers assessed data from a focus group of six behavioral health counselors representing rural and city agencies throughout South Carolina.
Themes that emerged included concerns about mental health – counselors and patients were experiencing increased stress, depression, and anxiety.
“People had to now home school, there were job layoffs, increased responsibilities at home. Also, Narcan [naloxone] distribution was decreased, and this contributed to rising overdose rates,” Ms. Whiteside said in an interview.
The focus group concluded that the advantages of telehealth included greater ability to accept new patients, an increase in scheduling flexibility, and cost-effectiveness because it obviated the need for child care or transportation.
Disadvantages included problems involving privacy, because for many patients who were undergoing SUD recovery, it was impossible to be alone in a room or a designated area of their own.
“Before COVID happened, [health care] barriers included transport to the actual center and finding care for children,” Ms. Connolly said in an interview.
“That’s where telehealth really bridged the gap for these people, and it actually became a lot easier for them to get in contact with their counselors, get into group meetings, and access other services,” she said.
Many of the study participants were not very optimistic about telehealth at first, Ms. Connolly noted. “They felt a little odd going on telehealth at first, but by the end, everybody said that they loved having it.”
“One of the things that came out often was that patients felt they could be more open and honest because they weren’t looking their counselor right in the face. They didn’t feel so horrible sharing,” Ms. Whiteside added.
Some counselors reported that some clients shared more details with them and that there was an ease of connecting. If a patient was a few minutes late to an appointment, telehealth would put in a call to find out where that patient was.
The counselors also had the ability to determine which of their patients would be good candidates for telehealth counseling and which patients would not do well with telehealth and would instead need in-patient care.
“This is something that really helped the experience go better for the counselors. They were able to determine which patient fit the mold for telehealth working for them. Obviously, patients who have more acute periods of mental health problems would do better with in-person care,” Ms. Whiteside said.
Here to stay?
In the third study from USCSM-G, investigators evaluated data from a focus group of four providers of medications for opioid use disorder (MOUD) who practiced in urban and rural areas throughout the state.
The respondents reflected on their experiences in using telemedicine for prescribing MOUD.
As in the previous studies, the providers had positive experiences with telemedicine. It increased patient access, participation, and satisfaction with treatment, and the benefits of telemedicine outweighed its potential limitations.
Still, technology was cited as a barrier to care, especially in rural areas.
“We found that there was a lack of good internet in certain rural parts of South Carolina, and that lack of the proper electronic devices ... could also make it difficult to access telemedicine,” lead author Kellie Shell said in an interview.
As noted in the other studies, the providers expressed a desire that telemedicine incorporate safeguards that would enable clinicians to identify a particular patient’s location in order that authorities could be dispatched if an emergency were to arise.
The clinicians also said that monitoring for diversion and performing pill counts were more difficult to do via telemedicine.
“We definitely have to improve infrastructure, especially in rural areas, so that all people have access to telemedicine,” Ms. Shell said.
“Overall, the providers were won over with telemedicine, and some predicted telehealth and virtual visits were here to stay, even after COVID,” she added.
The three posters provide useful insight into the potential advantages and disadvantages of telehealth in SUD settings, experts said.
Telehealth data ‘very limited’
Commenting on the research, Lewei (Allison) Lin, MD, University of Michigan, Ann Arbor, noted that “there is such limited information” about the use of telehealth for patients with SUD.
“These insights are helpful for us to start understanding the things that need to be considered, including clinician attitudes and perceptions,” said Dr. Lin, who was not involved with the studies.
“It will be key to have data as use of telemedicine increases during COVID-19 to help us see exactly how it should be used and to better understand the actual impacts and whether or not it is increasing accessibility, and for which patients,” she added.
David Kan, MD, chief medical officer at Bright Heart Health, San Ramon, Calif., has had experience with telehealth for SUD and has found that conducting pill counts with his patients has not been a problem.
“The Shell poster covers telemedicine well,” Dr. Kan said in an interview.
However, “I disagree with their point that diversion prevention is harder via telemedicine. In my experience, it is easier, as you can do pill or wrapper counts almost on demand. You can also do daily observed dosing with pill counts if diversion is suspected,” he said.
Dr. Kan also suggested ways to cope with problems involving privacy. “Privacy concerns are always an issue but can be mitigated with headphones and a scan of the room with the telehealth technology if a privacy concern arises.”
He acknowledged that in-person meetings, especially through well-established programs, such as Alcoholics Anonymous (AA), will always be important. But he pointed out that people are finding ways to meet safely and have in-person connections.
“The AA has been providing virtual recovery meetings long before COVID. The common complaint is the loss of fellowship associated with recovery groups. I don’t know of a way to get around this short of vaccines,” Dr. Kan said. However, “people have adapted impressively with masked outdoor meetings and other forms of safe gathering.”
The investigators, Dr. Lin, and Dr. Kan reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
With the onset of the COVID-19 pandemic, there has been a rapid uptick in virtual recovery programs and telemedicine counseling sessions for patients with substance use disorders (SUDs). New research shows that these programs are acceptable and effective alternatives to in-person sessions.
Study results from three research teams at the University of South Carolina School of Medicine Greenville (USCSM-G) show that SUD counselors in the state were satisfied with their experience with telehealth and virtual recovery meetings.
In one of the studies, five counselors who utilized a virtual meeting platform after the COVID-19 pandemic made in-person visits unsafe were surveyed. The respondents said they much preferred in-person meetings. However, they could also see that virtual meetings were filling an important need for their patients.
Two other studies echoed the results from the first. Clinicians who were leery of the new technology at first became more enthusiastic after they gained experience using it.
“We have lived in a society where there has been one right way, which has always been in-person meetings for recovery, such as Alcoholics Anonymous. It is a very structured process,” lead author Haley Fulton, a fourth-year medical student at USCSM-G, said in an interview.
“The onset of COVID really upended a lot of things, but ... now there may not be just one right way for recovery. There are alternatives to offer,” Ms. Fulton said.
The findings were presented at the annual meeting of the American Academy of Addiction Psychiatry, which was held online this year because of the pandemic.
Huge need
“Virtual meetings may not be ideal, but some version of recovery is better than none. If we can make these meetings accessible to more people, this could promote recovery from substance use disorder,” Ms. Fulton said.
There is a huge need for counseling, and past research has shown that failure to attend meetings can precipitate relapse in many individuals.
In Ms. Fulton’s study, counselors were asked to describe how they perceived the efficacy of virtual recovery meetings, compared with that of in-person meetings.
The investigators analyzed how often certain words, phrases, or issues came up during seven in-person recovery meetings held before the COVID-19 pandemic as well as observational data from seven virtual recovery-support meetings held during the pandemic.
On the pro side, the respondents cited convenience, comfort at home, and increased accessibility to counseling for patients.
In addition, because there was no need to travel, virtual meetings were cost effective. Such meetings could expand the recovery world, inasmuch as individuals could attend recovery meetings in other parts of the country.
Perceived disadvantages included challenges involving technology, because learning new apps such as Zoom could be a problem for some patients. Distractions at home and lack of privacy were also cited, but for many, the most important drawback to virtual meetings was the lessening of emotional connection with others.
Impact on SUD treatment
In a second study, another team from USCSM-G reported similar findings when it explored the impact of telehealth on counselors as well as on patients who were undergoing SUD treatment during the pandemic.
Led by fourth-year medical students Elizabeth Whiteside and Kyleigh Connolly, the researchers assessed data from a focus group of six behavioral health counselors representing rural and city agencies throughout South Carolina.
Themes that emerged included concerns about mental health – counselors and patients were experiencing increased stress, depression, and anxiety.
“People had to now home school, there were job layoffs, increased responsibilities at home. Also, Narcan [naloxone] distribution was decreased, and this contributed to rising overdose rates,” Ms. Whiteside said in an interview.
The focus group concluded that the advantages of telehealth included greater ability to accept new patients, an increase in scheduling flexibility, and cost-effectiveness because it obviated the need for child care or transportation.
Disadvantages included problems involving privacy, because for many patients who were undergoing SUD recovery, it was impossible to be alone in a room or a designated area of their own.
“Before COVID happened, [health care] barriers included transport to the actual center and finding care for children,” Ms. Connolly said in an interview.
“That’s where telehealth really bridged the gap for these people, and it actually became a lot easier for them to get in contact with their counselors, get into group meetings, and access other services,” she said.
Many of the study participants were not very optimistic about telehealth at first, Ms. Connolly noted. “They felt a little odd going on telehealth at first, but by the end, everybody said that they loved having it.”
“One of the things that came out often was that patients felt they could be more open and honest because they weren’t looking their counselor right in the face. They didn’t feel so horrible sharing,” Ms. Whiteside added.
Some counselors reported that some clients shared more details with them and that there was an ease of connecting. If a patient was a few minutes late to an appointment, telehealth would put in a call to find out where that patient was.
The counselors also had the ability to determine which of their patients would be good candidates for telehealth counseling and which patients would not do well with telehealth and would instead need in-patient care.
“This is something that really helped the experience go better for the counselors. They were able to determine which patient fit the mold for telehealth working for them. Obviously, patients who have more acute periods of mental health problems would do better with in-person care,” Ms. Whiteside said.
Here to stay?
In the third study from USCSM-G, investigators evaluated data from a focus group of four providers of medications for opioid use disorder (MOUD) who practiced in urban and rural areas throughout the state.
The respondents reflected on their experiences in using telemedicine for prescribing MOUD.
As in the previous studies, the providers had positive experiences with telemedicine. It increased patient access, participation, and satisfaction with treatment, and the benefits of telemedicine outweighed its potential limitations.
Still, technology was cited as a barrier to care, especially in rural areas.
“We found that there was a lack of good internet in certain rural parts of South Carolina, and that lack of the proper electronic devices ... could also make it difficult to access telemedicine,” lead author Kellie Shell said in an interview.
As noted in the other studies, the providers expressed a desire that telemedicine incorporate safeguards that would enable clinicians to identify a particular patient’s location in order that authorities could be dispatched if an emergency were to arise.
The clinicians also said that monitoring for diversion and performing pill counts were more difficult to do via telemedicine.
“We definitely have to improve infrastructure, especially in rural areas, so that all people have access to telemedicine,” Ms. Shell said.
“Overall, the providers were won over with telemedicine, and some predicted telehealth and virtual visits were here to stay, even after COVID,” she added.
The three posters provide useful insight into the potential advantages and disadvantages of telehealth in SUD settings, experts said.
Telehealth data ‘very limited’
Commenting on the research, Lewei (Allison) Lin, MD, University of Michigan, Ann Arbor, noted that “there is such limited information” about the use of telehealth for patients with SUD.
“These insights are helpful for us to start understanding the things that need to be considered, including clinician attitudes and perceptions,” said Dr. Lin, who was not involved with the studies.
“It will be key to have data as use of telemedicine increases during COVID-19 to help us see exactly how it should be used and to better understand the actual impacts and whether or not it is increasing accessibility, and for which patients,” she added.
David Kan, MD, chief medical officer at Bright Heart Health, San Ramon, Calif., has had experience with telehealth for SUD and has found that conducting pill counts with his patients has not been a problem.
“The Shell poster covers telemedicine well,” Dr. Kan said in an interview.
However, “I disagree with their point that diversion prevention is harder via telemedicine. In my experience, it is easier, as you can do pill or wrapper counts almost on demand. You can also do daily observed dosing with pill counts if diversion is suspected,” he said.
Dr. Kan also suggested ways to cope with problems involving privacy. “Privacy concerns are always an issue but can be mitigated with headphones and a scan of the room with the telehealth technology if a privacy concern arises.”
He acknowledged that in-person meetings, especially through well-established programs, such as Alcoholics Anonymous (AA), will always be important. But he pointed out that people are finding ways to meet safely and have in-person connections.
“The AA has been providing virtual recovery meetings long before COVID. The common complaint is the loss of fellowship associated with recovery groups. I don’t know of a way to get around this short of vaccines,” Dr. Kan said. However, “people have adapted impressively with masked outdoor meetings and other forms of safe gathering.”
The investigators, Dr. Lin, and Dr. Kan reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
New reports guide return to play in athletes with COVID-19
Increasingly, clinicians are being called upon to advise athletes who have recovered from COVID-19 on when it is safe for them to return to play.
Now, they have two reports that offer more insights into the cardiotoxic effects of COVID-19 on the athletic heart.
In the first report, researchers report a high prevalence of pericardial involvement in college-student athletes who have recovered from COVID-19 and give their practical advice on how to let these athletes return to play safely.
In the second report, an expert panel of sports cardiologists provides a comprehensive guide to the appropriate imaging of athletes who may have cardiovascular complications from COVID-19.
Both are published in JACC: Cardiovascular Imaging.
“We were asked by the editors of JACC to submit this paper, and the impetus for it was the fact that there are so many athletes returning after being infected with COVID-19, we need to try and give guidance to cardiologists as to how best to evaluate these athletes,” Dermot Phelan, MD, PhD, Sanger Heart and Vascular Institute, Atrium Health, Charlotte, N.C., and lead author of the consensus statement, said in an interview.
The consensus statement acknowledges that information about the cardiovascular complications of COVID-19 continues to evolve. Meanwhile, pathologies such as myocarditis, pericarditis, and right ventricular dysfunction, in the absence of significant clinical symptoms, in athletes who have been affected by COVID-19 remain of considerable concern.
It also emphasizes the unique challenges the average cardiologist faces in distinguishing between what is normal for an athlete’s heart and what is true pathology after COVID-19 infection; details how different imaging modalities can help in screening, evaluating, and monitoring athletes with suspected cardiovascular complications of COVID-19 infection; and discusses the strengths and limitations of these modalities.
Finally, the consensus statement provides some well-needed guidance on return-to-play decision-making, for both the athlete and the clinician.
Athletic remodeling or covid-19 damage?
Athletes can develop certain cardiovascular characteristics because of their athletic activity, and sometimes, this can cloud the diagnostic picture.
“Is this change due to the effects of COVID-19, or is it just because this is an athlete’s heart? This was an international expert consensus, made up of sports cardiologists from all over the world who have a lot of experience in dealing with athletes,” Dr. Phelan said. “We were trying to relay the important information to the cardiologist who is not used to dealing with athletes on a day-to-day basis, as to what they might expect to find in that athlete, and what is not an expected finding and should be tested further.”
Phelan, a sports cardiologist, is familiar with what is normal for an athlete’s heart and what is pathology.
“We know that athletes, particularly long-term endurance athletes, develop changes in the heart that can affect not only the electrics but the structure of the heart, and sometimes, that overlaps with abnormalities with pathology. This can be a challenge for the nonsports cardiologist to differentiate,” he said.
Phelan and his group have written two other consensus documents on the management of cardiovascular problems that develop in some athletes who have been infected with COVID-19.
The first was published in May in JAMA Cardiology, and the second, which revised some of the original recommendations made in the first document, was published online Oct. 26 in JAMA Cardiology.
The first set of recommendations called for imaging studies to be done in all athletes, but the second set states that athletes who recover and are asymptomatic do not need extensive (and expensive) imaging tests.
“These two papers work hand in hand,” Dr. Phelan said. “In May, we had very little experience with COVID, and there was a lot of concern about hospitalized patients having a very high incidence of heart disease. We published those recommendations, but we recognized at the time that we had very little data and that we would reconsider once we had more experience with data.
“This current set of recommendations that we have put forth here are for those athletes who do need to get further testing, so it’s a step beyond,” Dr. Phelan added. “So the second iteration states that young athletes who had mild or no symptoms didn’t need to go through all of that cardiac testing, but others do need it.”
To do widespread cardiovascular imaging for many individuals would be very costly. Realistically, there are not that many centers in the United States that have all the sophisticated equipment required to do such testing, Dr. Phelan noted.
“One of our major points is difficulty obtaining the test, but also the cost; these are very expensive tests. There are limitations. They are useful when used in the correct context,” he said.
To play or not to play, that is the question
Partho P. Sengupta, MD, DM, had to answer that question for more than 50 young athletes who were returning to college at West Virginia University, anxious to be back with their teams and on the playing field. They had been infected with COVID-19 and needed to know when they could return to play.
Dr. Sengupta, who is also an author for the Phelan et al consensus statement on imaging, said there was a lot of pressure – from all the various stakeholders, and from anxious parents, worried college athletes, their teammates, and the university – to determine if the youngsters could return to play.
The fear was that COVID-19 infection left the young athlete’s heart vulnerable to myocarditis and, thus, sudden death on the playing field after strenuous activity.
“At the time we were doing this imaging, there was a lot of concern in the media, and papers were coming out reporting a lot of cardiac involvement or myocarditis associated with COVID-19. Nobody really knew what to do,” he explained.
“There were all kinds of questions, concerns. The parents were putting pressure on us, the athletes wanted to know, the teams, the university. So we put together a team and completed all of the examinations, including testing of blood markers, within a 2-week period. These young athletes, they’re scared, they’re worried and anxious, they don’t know what’s going to happen with their scholarship, so there was some urgency to this work,” Dr. Sengupta said.
“We had to screen all comers within a very short period. We had 54 consecutive patients, gave them full screening, full battery of tests, blood tests, all in a 2-week period,” he said.
Speed was of the essence, and Dr. Sengupta and his team rolled up their sleeves and got to work “We had to know who was safe to clear to return to play and who might need extra follow-up.”
Screening echocardiograms
They performed screening echocardiograms on 54 consecutive college athletes who had tested positive for COVID-19 on reverse transcription polymerase chain reaction nasal swab testing or who showed that they had IgG antibodies against COVID-19. The screening echocardiograms were done after the athletes had quarantined for at least 14 days and were no longer infectious.
Most (85%) were male, and the mean age was 19 years. A total of 16 (30%) athletes were asymptomatic, 36 (66%) reported mild COVID-19 related symptoms, and two (4%) reported moderate symptoms.
Of the 54 athletes who were initially screened with echocardiography, 48 (11 asymptomatic, 37 symptomatic), went on to have cardiac magnetic resonance imaging.
Results showed that more than half the athletes (27; 56.3%), showed some cardiac abnormality. The most common was pericardial late enhancement with associated pericardial effusion, affecting 19 (39.5%) athletes.
Of these, six (12.5%) had reduced global longitudinal strain (GLS) or an increased native T1.
One patient showed myocardial enhancement.
Additionally, seven athletes (14.6%) had reduced left ventricular ejection fraction or reduced GLS with or without increased native T1. Native T2 levels were normal in all subjects and no specific imaging features of myocardial inflammation were identified.
Participants were brought back to receive the results of their tests and to get an individualized plan about their safe return to play 3 to 5 weeks after they had ceased to be infectious with COVID-19.
“We saw pericardial inflammation that was resolving. We did not see any blood biomarkers to suggest that there was active inflammation going on,” he said. “We also did not see any muscle inflammation, but we did see pockets of fluid in over a third of our athletes.”
Fortunately, most were deemed able to get back to playing safely, despite having evidence of pericardial inflammation.
This was on strict condition that they be monitored very closely for any adverse events that might occur as they began to exercise again.
“Once they go back to the field to start exercising and practicing, it is under great supervision. We instructed all of our sports physicians and other team managers that these people need to be observed very carefully. So as long as they were asymptomatic, even though the signs of pericardial inflammation were there, if there were no signs of inflammation in the blood, we let them go back to play, closely monitored,” Dr. Sengupta said.
A small number remained very symptomatic at the end of the 5 weeks and were referred to cardiac rehabilitation, Dr. Sengupta said. “They were tired, fatigued, short of breath, even 5 weeks after they got over COVID, so we sent them for cardiac rehab to help them get conditioned again.”
The researchers plan to reevaluate and reimage all of the athletes in another 3 months to monitor their cardiac health.
Dr. Sengupta acknowledged the limitations of this single-center, nonrandomized, controlled report, but insists reports such as this add a bit more to what we are learning about COVID-19 every day.
“These kids were coming to us and asking questions. You have to use the best science you have available to you at that point in time. Some people ask why we did not have a control group, but how do you design a control population in the midst of a pandemic? The science may or may not be perfect, I agree, but the information we obtained is important,” he said.
“Right now, I don’t think we have enough science, and we are still learning. It is very difficult to predict who will develop the heart muscle disease or the pericardial disease,” Dr. Sengupta said. “We had to do our work quickly to give answers to the young athletes, their parents, their teammates, their university, as soon as possible, and we were doing this under pandemic conditions.”
The work was supported by the National Science Foundation National Institute of General Medical Sciences of the National Institutes of Health. Dr. Phelan reported no relevant financial relationships. Dr. Sengupta reported that he is a consultant for HeartSciences, Kencor Health, and Ultromics.
This article first appeared on Medscape.com.
Increasingly, clinicians are being called upon to advise athletes who have recovered from COVID-19 on when it is safe for them to return to play.
Now, they have two reports that offer more insights into the cardiotoxic effects of COVID-19 on the athletic heart.
In the first report, researchers report a high prevalence of pericardial involvement in college-student athletes who have recovered from COVID-19 and give their practical advice on how to let these athletes return to play safely.
In the second report, an expert panel of sports cardiologists provides a comprehensive guide to the appropriate imaging of athletes who may have cardiovascular complications from COVID-19.
Both are published in JACC: Cardiovascular Imaging.
“We were asked by the editors of JACC to submit this paper, and the impetus for it was the fact that there are so many athletes returning after being infected with COVID-19, we need to try and give guidance to cardiologists as to how best to evaluate these athletes,” Dermot Phelan, MD, PhD, Sanger Heart and Vascular Institute, Atrium Health, Charlotte, N.C., and lead author of the consensus statement, said in an interview.
The consensus statement acknowledges that information about the cardiovascular complications of COVID-19 continues to evolve. Meanwhile, pathologies such as myocarditis, pericarditis, and right ventricular dysfunction, in the absence of significant clinical symptoms, in athletes who have been affected by COVID-19 remain of considerable concern.
It also emphasizes the unique challenges the average cardiologist faces in distinguishing between what is normal for an athlete’s heart and what is true pathology after COVID-19 infection; details how different imaging modalities can help in screening, evaluating, and monitoring athletes with suspected cardiovascular complications of COVID-19 infection; and discusses the strengths and limitations of these modalities.
Finally, the consensus statement provides some well-needed guidance on return-to-play decision-making, for both the athlete and the clinician.
Athletic remodeling or covid-19 damage?
Athletes can develop certain cardiovascular characteristics because of their athletic activity, and sometimes, this can cloud the diagnostic picture.
“Is this change due to the effects of COVID-19, or is it just because this is an athlete’s heart? This was an international expert consensus, made up of sports cardiologists from all over the world who have a lot of experience in dealing with athletes,” Dr. Phelan said. “We were trying to relay the important information to the cardiologist who is not used to dealing with athletes on a day-to-day basis, as to what they might expect to find in that athlete, and what is not an expected finding and should be tested further.”
Phelan, a sports cardiologist, is familiar with what is normal for an athlete’s heart and what is pathology.
“We know that athletes, particularly long-term endurance athletes, develop changes in the heart that can affect not only the electrics but the structure of the heart, and sometimes, that overlaps with abnormalities with pathology. This can be a challenge for the nonsports cardiologist to differentiate,” he said.
Phelan and his group have written two other consensus documents on the management of cardiovascular problems that develop in some athletes who have been infected with COVID-19.
The first was published in May in JAMA Cardiology, and the second, which revised some of the original recommendations made in the first document, was published online Oct. 26 in JAMA Cardiology.
The first set of recommendations called for imaging studies to be done in all athletes, but the second set states that athletes who recover and are asymptomatic do not need extensive (and expensive) imaging tests.
“These two papers work hand in hand,” Dr. Phelan said. “In May, we had very little experience with COVID, and there was a lot of concern about hospitalized patients having a very high incidence of heart disease. We published those recommendations, but we recognized at the time that we had very little data and that we would reconsider once we had more experience with data.
“This current set of recommendations that we have put forth here are for those athletes who do need to get further testing, so it’s a step beyond,” Dr. Phelan added. “So the second iteration states that young athletes who had mild or no symptoms didn’t need to go through all of that cardiac testing, but others do need it.”
To do widespread cardiovascular imaging for many individuals would be very costly. Realistically, there are not that many centers in the United States that have all the sophisticated equipment required to do such testing, Dr. Phelan noted.
“One of our major points is difficulty obtaining the test, but also the cost; these are very expensive tests. There are limitations. They are useful when used in the correct context,” he said.
To play or not to play, that is the question
Partho P. Sengupta, MD, DM, had to answer that question for more than 50 young athletes who were returning to college at West Virginia University, anxious to be back with their teams and on the playing field. They had been infected with COVID-19 and needed to know when they could return to play.
Dr. Sengupta, who is also an author for the Phelan et al consensus statement on imaging, said there was a lot of pressure – from all the various stakeholders, and from anxious parents, worried college athletes, their teammates, and the university – to determine if the youngsters could return to play.
The fear was that COVID-19 infection left the young athlete’s heart vulnerable to myocarditis and, thus, sudden death on the playing field after strenuous activity.
“At the time we were doing this imaging, there was a lot of concern in the media, and papers were coming out reporting a lot of cardiac involvement or myocarditis associated with COVID-19. Nobody really knew what to do,” he explained.
“There were all kinds of questions, concerns. The parents were putting pressure on us, the athletes wanted to know, the teams, the university. So we put together a team and completed all of the examinations, including testing of blood markers, within a 2-week period. These young athletes, they’re scared, they’re worried and anxious, they don’t know what’s going to happen with their scholarship, so there was some urgency to this work,” Dr. Sengupta said.
“We had to screen all comers within a very short period. We had 54 consecutive patients, gave them full screening, full battery of tests, blood tests, all in a 2-week period,” he said.
Speed was of the essence, and Dr. Sengupta and his team rolled up their sleeves and got to work “We had to know who was safe to clear to return to play and who might need extra follow-up.”
Screening echocardiograms
They performed screening echocardiograms on 54 consecutive college athletes who had tested positive for COVID-19 on reverse transcription polymerase chain reaction nasal swab testing or who showed that they had IgG antibodies against COVID-19. The screening echocardiograms were done after the athletes had quarantined for at least 14 days and were no longer infectious.
Most (85%) were male, and the mean age was 19 years. A total of 16 (30%) athletes were asymptomatic, 36 (66%) reported mild COVID-19 related symptoms, and two (4%) reported moderate symptoms.
Of the 54 athletes who were initially screened with echocardiography, 48 (11 asymptomatic, 37 symptomatic), went on to have cardiac magnetic resonance imaging.
Results showed that more than half the athletes (27; 56.3%), showed some cardiac abnormality. The most common was pericardial late enhancement with associated pericardial effusion, affecting 19 (39.5%) athletes.
Of these, six (12.5%) had reduced global longitudinal strain (GLS) or an increased native T1.
One patient showed myocardial enhancement.
Additionally, seven athletes (14.6%) had reduced left ventricular ejection fraction or reduced GLS with or without increased native T1. Native T2 levels were normal in all subjects and no specific imaging features of myocardial inflammation were identified.
Participants were brought back to receive the results of their tests and to get an individualized plan about their safe return to play 3 to 5 weeks after they had ceased to be infectious with COVID-19.
“We saw pericardial inflammation that was resolving. We did not see any blood biomarkers to suggest that there was active inflammation going on,” he said. “We also did not see any muscle inflammation, but we did see pockets of fluid in over a third of our athletes.”
Fortunately, most were deemed able to get back to playing safely, despite having evidence of pericardial inflammation.
This was on strict condition that they be monitored very closely for any adverse events that might occur as they began to exercise again.
“Once they go back to the field to start exercising and practicing, it is under great supervision. We instructed all of our sports physicians and other team managers that these people need to be observed very carefully. So as long as they were asymptomatic, even though the signs of pericardial inflammation were there, if there were no signs of inflammation in the blood, we let them go back to play, closely monitored,” Dr. Sengupta said.
A small number remained very symptomatic at the end of the 5 weeks and were referred to cardiac rehabilitation, Dr. Sengupta said. “They were tired, fatigued, short of breath, even 5 weeks after they got over COVID, so we sent them for cardiac rehab to help them get conditioned again.”
The researchers plan to reevaluate and reimage all of the athletes in another 3 months to monitor their cardiac health.
Dr. Sengupta acknowledged the limitations of this single-center, nonrandomized, controlled report, but insists reports such as this add a bit more to what we are learning about COVID-19 every day.
“These kids were coming to us and asking questions. You have to use the best science you have available to you at that point in time. Some people ask why we did not have a control group, but how do you design a control population in the midst of a pandemic? The science may or may not be perfect, I agree, but the information we obtained is important,” he said.
“Right now, I don’t think we have enough science, and we are still learning. It is very difficult to predict who will develop the heart muscle disease or the pericardial disease,” Dr. Sengupta said. “We had to do our work quickly to give answers to the young athletes, their parents, their teammates, their university, as soon as possible, and we were doing this under pandemic conditions.”
The work was supported by the National Science Foundation National Institute of General Medical Sciences of the National Institutes of Health. Dr. Phelan reported no relevant financial relationships. Dr. Sengupta reported that he is a consultant for HeartSciences, Kencor Health, and Ultromics.
This article first appeared on Medscape.com.
Increasingly, clinicians are being called upon to advise athletes who have recovered from COVID-19 on when it is safe for them to return to play.
Now, they have two reports that offer more insights into the cardiotoxic effects of COVID-19 on the athletic heart.
In the first report, researchers report a high prevalence of pericardial involvement in college-student athletes who have recovered from COVID-19 and give their practical advice on how to let these athletes return to play safely.
In the second report, an expert panel of sports cardiologists provides a comprehensive guide to the appropriate imaging of athletes who may have cardiovascular complications from COVID-19.
Both are published in JACC: Cardiovascular Imaging.
“We were asked by the editors of JACC to submit this paper, and the impetus for it was the fact that there are so many athletes returning after being infected with COVID-19, we need to try and give guidance to cardiologists as to how best to evaluate these athletes,” Dermot Phelan, MD, PhD, Sanger Heart and Vascular Institute, Atrium Health, Charlotte, N.C., and lead author of the consensus statement, said in an interview.
The consensus statement acknowledges that information about the cardiovascular complications of COVID-19 continues to evolve. Meanwhile, pathologies such as myocarditis, pericarditis, and right ventricular dysfunction, in the absence of significant clinical symptoms, in athletes who have been affected by COVID-19 remain of considerable concern.
It also emphasizes the unique challenges the average cardiologist faces in distinguishing between what is normal for an athlete’s heart and what is true pathology after COVID-19 infection; details how different imaging modalities can help in screening, evaluating, and monitoring athletes with suspected cardiovascular complications of COVID-19 infection; and discusses the strengths and limitations of these modalities.
Finally, the consensus statement provides some well-needed guidance on return-to-play decision-making, for both the athlete and the clinician.
Athletic remodeling or covid-19 damage?
Athletes can develop certain cardiovascular characteristics because of their athletic activity, and sometimes, this can cloud the diagnostic picture.
“Is this change due to the effects of COVID-19, or is it just because this is an athlete’s heart? This was an international expert consensus, made up of sports cardiologists from all over the world who have a lot of experience in dealing with athletes,” Dr. Phelan said. “We were trying to relay the important information to the cardiologist who is not used to dealing with athletes on a day-to-day basis, as to what they might expect to find in that athlete, and what is not an expected finding and should be tested further.”
Phelan, a sports cardiologist, is familiar with what is normal for an athlete’s heart and what is pathology.
“We know that athletes, particularly long-term endurance athletes, develop changes in the heart that can affect not only the electrics but the structure of the heart, and sometimes, that overlaps with abnormalities with pathology. This can be a challenge for the nonsports cardiologist to differentiate,” he said.
Phelan and his group have written two other consensus documents on the management of cardiovascular problems that develop in some athletes who have been infected with COVID-19.
The first was published in May in JAMA Cardiology, and the second, which revised some of the original recommendations made in the first document, was published online Oct. 26 in JAMA Cardiology.
The first set of recommendations called for imaging studies to be done in all athletes, but the second set states that athletes who recover and are asymptomatic do not need extensive (and expensive) imaging tests.
“These two papers work hand in hand,” Dr. Phelan said. “In May, we had very little experience with COVID, and there was a lot of concern about hospitalized patients having a very high incidence of heart disease. We published those recommendations, but we recognized at the time that we had very little data and that we would reconsider once we had more experience with data.
“This current set of recommendations that we have put forth here are for those athletes who do need to get further testing, so it’s a step beyond,” Dr. Phelan added. “So the second iteration states that young athletes who had mild or no symptoms didn’t need to go through all of that cardiac testing, but others do need it.”
To do widespread cardiovascular imaging for many individuals would be very costly. Realistically, there are not that many centers in the United States that have all the sophisticated equipment required to do such testing, Dr. Phelan noted.
“One of our major points is difficulty obtaining the test, but also the cost; these are very expensive tests. There are limitations. They are useful when used in the correct context,” he said.
To play or not to play, that is the question
Partho P. Sengupta, MD, DM, had to answer that question for more than 50 young athletes who were returning to college at West Virginia University, anxious to be back with their teams and on the playing field. They had been infected with COVID-19 and needed to know when they could return to play.
Dr. Sengupta, who is also an author for the Phelan et al consensus statement on imaging, said there was a lot of pressure – from all the various stakeholders, and from anxious parents, worried college athletes, their teammates, and the university – to determine if the youngsters could return to play.
The fear was that COVID-19 infection left the young athlete’s heart vulnerable to myocarditis and, thus, sudden death on the playing field after strenuous activity.
“At the time we were doing this imaging, there was a lot of concern in the media, and papers were coming out reporting a lot of cardiac involvement or myocarditis associated with COVID-19. Nobody really knew what to do,” he explained.
“There were all kinds of questions, concerns. The parents were putting pressure on us, the athletes wanted to know, the teams, the university. So we put together a team and completed all of the examinations, including testing of blood markers, within a 2-week period. These young athletes, they’re scared, they’re worried and anxious, they don’t know what’s going to happen with their scholarship, so there was some urgency to this work,” Dr. Sengupta said.
“We had to screen all comers within a very short period. We had 54 consecutive patients, gave them full screening, full battery of tests, blood tests, all in a 2-week period,” he said.
Speed was of the essence, and Dr. Sengupta and his team rolled up their sleeves and got to work “We had to know who was safe to clear to return to play and who might need extra follow-up.”
Screening echocardiograms
They performed screening echocardiograms on 54 consecutive college athletes who had tested positive for COVID-19 on reverse transcription polymerase chain reaction nasal swab testing or who showed that they had IgG antibodies against COVID-19. The screening echocardiograms were done after the athletes had quarantined for at least 14 days and were no longer infectious.
Most (85%) were male, and the mean age was 19 years. A total of 16 (30%) athletes were asymptomatic, 36 (66%) reported mild COVID-19 related symptoms, and two (4%) reported moderate symptoms.
Of the 54 athletes who were initially screened with echocardiography, 48 (11 asymptomatic, 37 symptomatic), went on to have cardiac magnetic resonance imaging.
Results showed that more than half the athletes (27; 56.3%), showed some cardiac abnormality. The most common was pericardial late enhancement with associated pericardial effusion, affecting 19 (39.5%) athletes.
Of these, six (12.5%) had reduced global longitudinal strain (GLS) or an increased native T1.
One patient showed myocardial enhancement.
Additionally, seven athletes (14.6%) had reduced left ventricular ejection fraction or reduced GLS with or without increased native T1. Native T2 levels were normal in all subjects and no specific imaging features of myocardial inflammation were identified.
Participants were brought back to receive the results of their tests and to get an individualized plan about their safe return to play 3 to 5 weeks after they had ceased to be infectious with COVID-19.
“We saw pericardial inflammation that was resolving. We did not see any blood biomarkers to suggest that there was active inflammation going on,” he said. “We also did not see any muscle inflammation, but we did see pockets of fluid in over a third of our athletes.”
Fortunately, most were deemed able to get back to playing safely, despite having evidence of pericardial inflammation.
This was on strict condition that they be monitored very closely for any adverse events that might occur as they began to exercise again.
“Once they go back to the field to start exercising and practicing, it is under great supervision. We instructed all of our sports physicians and other team managers that these people need to be observed very carefully. So as long as they were asymptomatic, even though the signs of pericardial inflammation were there, if there were no signs of inflammation in the blood, we let them go back to play, closely monitored,” Dr. Sengupta said.
A small number remained very symptomatic at the end of the 5 weeks and were referred to cardiac rehabilitation, Dr. Sengupta said. “They were tired, fatigued, short of breath, even 5 weeks after they got over COVID, so we sent them for cardiac rehab to help them get conditioned again.”
The researchers plan to reevaluate and reimage all of the athletes in another 3 months to monitor their cardiac health.
Dr. Sengupta acknowledged the limitations of this single-center, nonrandomized, controlled report, but insists reports such as this add a bit more to what we are learning about COVID-19 every day.
“These kids were coming to us and asking questions. You have to use the best science you have available to you at that point in time. Some people ask why we did not have a control group, but how do you design a control population in the midst of a pandemic? The science may or may not be perfect, I agree, but the information we obtained is important,” he said.
“Right now, I don’t think we have enough science, and we are still learning. It is very difficult to predict who will develop the heart muscle disease or the pericardial disease,” Dr. Sengupta said. “We had to do our work quickly to give answers to the young athletes, their parents, their teammates, their university, as soon as possible, and we were doing this under pandemic conditions.”
The work was supported by the National Science Foundation National Institute of General Medical Sciences of the National Institutes of Health. Dr. Phelan reported no relevant financial relationships. Dr. Sengupta reported that he is a consultant for HeartSciences, Kencor Health, and Ultromics.
This article first appeared on Medscape.com.
New return-to-play recommendations for athletes with COVID-19
The latest recommendations from sports cardiologists on getting athletes with COVID-19 back on the playing field safely emphasize a more judicious approach to screening for cardiac injury.
The new recommendations, made by the American College of Cardiology’s Sports and Exercise Cardiology Section, are for adult athletes in competitive sports and also for two important groups: younger athletes taking part in competitive high school sports and older athletes aged 35 and older, the Masters athletes, who continue to be active throughout their lives. The document was published online in JAMA Cardiology.
Because of the evolving nature of knowledge about COVID-19, updates on recommendations for safe return to play for athletes of all ages will continue to be made, senior author Aaron L. Baggish, MD, director of the cardiovascular performance program at Massachusetts General Hospital, Boston, said.
“The recommendations we released in May were entirely based on our experience taking care of hospitalized patients with COVID-19; we had no athletes in this population. We used a lot of conservative guesswork around how this would apply to otherwise healthy athletes,” Dr. Baggish said in an interview.
“But as sports started to open up, and we started to see large numbers of first professional and then college athletes come back into training, we realized that we needed to stop and ask whether the recommendations we put forward back in May were still appropriate,” Dr. Baggish said.
“Once we started to actually get into the trenches with these athletes, literally hundreds of them, and applying the testing strategies that we had initially recommended in everybody, we realized that we probably had some room for improvement, and that’s why we reconvened, to make these revisions,” he said.
Essentially, the recommendations now urge less cardiac testing. “Cardiac injury is not as common as we may have originally thought,” said Dr. Baggish.
“In the early days of COVID, people who were hospitalized had evidence of heart injury, and so we wondered if that prevalence would also be applicable to otherwise young, healthy people who got COVID. If that had been the case, we would have been in big trouble with respect to getting people back into sports. So this is why we started with a conservative screening approach and a lot of testing in order to not miss a huge burden of disease,” he said.
“But what we’ve learned over the past few months is that young people who get either asymptomatic or mild infection appear to have very, very low risk of having associated heart injury, so the need for testing in that population, when people who have infections recover fully, is almost certainly not going to be high yield,” Dr. Baggish said.
First iteration of the recommendations
Published in May in the early weeks of the pandemic, the first recommendations for safe return to play said that all athletes should stop training for at least 2 weeks after their symptoms resolve, then undergo “careful, clinical cardiovascular evaluation in combination with cardiac biomarkers and imaging.”
Additional testing with cardiac MRI, exercise testing, or ambulatory rhythm monitoring was to be done “based on the clinical course and initial testing.”
But experts caution that monitoring on such a scale in everyone is unnecessary and could even be counterproductive.
“Sending young athletes for extensive testing is not warranted and could send them to unnecessary testing, cardiac imaging, and so on,” Dr. Baggish said.
Only those athletes who continue to have symptoms or whose symptoms return when they get back to their athletic activities should go on for more screening.
“There, in essence, is the single main change from May, and that is a move away from screening with testing everyone, [and instead] confining that to the people who had moderate or greater severity disease,” he said.
Both iterations of the recommendations end with the same message.
“We are at the beginning of our knowledge about the cardiotoxic effects of COVID-19 but we are gathering evidence every day,” said Dr. Baggish. “Just as they did earlier, we acknowledge that our approaches are subject to change when we learn more about how COVID affects the heart, and specifically the hearts of athletes. This will be an ongoing process.”
Something to lean on
The recommendations are welcome, said James E. Udelson, MD, chief of the division of cardiology at Tufts Medical Center, Boston, coauthor of an accompanying editorial.
“It was a bit of the wild west out there, because each university, each college, all with good intentions, had been all struggling to figure out what to do, and how much to do. Probably the most important message from this new paper is the fact that now there is something out there that all coaches, athletes, families, schools, trainers can get some guidance from,” Dr. Udelson said in an interview.
Refining the cardiac screening criteria was a necessary step, Dr. Udelson said.
“How much cardiac imaging do you do? That is a matter of controversy,” said Dr. Udelson, who coauthored the commentary with Tufts cardiologist Ethan Rowin, MD, and Michael A. Curtis, MEd, a certified strength and conditioning specialist at the University of Virginia, Charlottesville. “The problem is that if you use a very sensitive imaging test on a lot of people, sometimes you find things that you really didn’t need to know about. They’re really not important. And now, the athlete is told he or she cannot play for 3 months because they might have myocarditis.
“Should we be too sensitive, meaning do we want to pick up anything no matter whether it’s important or not?” he added. “There will be a lot of false positives, and we are going to disqualify a lot of people. Or do you tune it a different way?”
Dr. Udelson said he would like to see commercial sports donate money to support research into the potential cardiotoxicity of COVID-19.
“If the organizations that benefit from these athletes, like the National Collegiate Athletic Association and professional sports leagues, can fund some of this research, that would be a huge help,” Dr. Udelson said.
“These are the top sports cardiologists in the country, and they have to start somewhere, and these are all based on what we know right now, as well as their own extensive experience. We all know that we are just at the beginning of our knowledge of this. But we have to have something to guide this huge community out there that is really thirsty for help.”
Dr. Baggish reports receiving research funding for the study of athletes in competitive sports from the National Heart, Lung, and Blood Institute; the National Football League Players Association; and the American Heart Association and receiving compensation for his role as team cardiologist from the US Olympic Committee/US Olympic Training Centers, US Soccer, US Rowing, the New England Patriots, the Boston Bruins, the New England Revolution, and Harvard University. Dr. Udelson has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The latest recommendations from sports cardiologists on getting athletes with COVID-19 back on the playing field safely emphasize a more judicious approach to screening for cardiac injury.
The new recommendations, made by the American College of Cardiology’s Sports and Exercise Cardiology Section, are for adult athletes in competitive sports and also for two important groups: younger athletes taking part in competitive high school sports and older athletes aged 35 and older, the Masters athletes, who continue to be active throughout their lives. The document was published online in JAMA Cardiology.
Because of the evolving nature of knowledge about COVID-19, updates on recommendations for safe return to play for athletes of all ages will continue to be made, senior author Aaron L. Baggish, MD, director of the cardiovascular performance program at Massachusetts General Hospital, Boston, said.
“The recommendations we released in May were entirely based on our experience taking care of hospitalized patients with COVID-19; we had no athletes in this population. We used a lot of conservative guesswork around how this would apply to otherwise healthy athletes,” Dr. Baggish said in an interview.
“But as sports started to open up, and we started to see large numbers of first professional and then college athletes come back into training, we realized that we needed to stop and ask whether the recommendations we put forward back in May were still appropriate,” Dr. Baggish said.
“Once we started to actually get into the trenches with these athletes, literally hundreds of them, and applying the testing strategies that we had initially recommended in everybody, we realized that we probably had some room for improvement, and that’s why we reconvened, to make these revisions,” he said.
Essentially, the recommendations now urge less cardiac testing. “Cardiac injury is not as common as we may have originally thought,” said Dr. Baggish.
“In the early days of COVID, people who were hospitalized had evidence of heart injury, and so we wondered if that prevalence would also be applicable to otherwise young, healthy people who got COVID. If that had been the case, we would have been in big trouble with respect to getting people back into sports. So this is why we started with a conservative screening approach and a lot of testing in order to not miss a huge burden of disease,” he said.
“But what we’ve learned over the past few months is that young people who get either asymptomatic or mild infection appear to have very, very low risk of having associated heart injury, so the need for testing in that population, when people who have infections recover fully, is almost certainly not going to be high yield,” Dr. Baggish said.
First iteration of the recommendations
Published in May in the early weeks of the pandemic, the first recommendations for safe return to play said that all athletes should stop training for at least 2 weeks after their symptoms resolve, then undergo “careful, clinical cardiovascular evaluation in combination with cardiac biomarkers and imaging.”
Additional testing with cardiac MRI, exercise testing, or ambulatory rhythm monitoring was to be done “based on the clinical course and initial testing.”
But experts caution that monitoring on such a scale in everyone is unnecessary and could even be counterproductive.
“Sending young athletes for extensive testing is not warranted and could send them to unnecessary testing, cardiac imaging, and so on,” Dr. Baggish said.
Only those athletes who continue to have symptoms or whose symptoms return when they get back to their athletic activities should go on for more screening.
“There, in essence, is the single main change from May, and that is a move away from screening with testing everyone, [and instead] confining that to the people who had moderate or greater severity disease,” he said.
Both iterations of the recommendations end with the same message.
“We are at the beginning of our knowledge about the cardiotoxic effects of COVID-19 but we are gathering evidence every day,” said Dr. Baggish. “Just as they did earlier, we acknowledge that our approaches are subject to change when we learn more about how COVID affects the heart, and specifically the hearts of athletes. This will be an ongoing process.”
Something to lean on
The recommendations are welcome, said James E. Udelson, MD, chief of the division of cardiology at Tufts Medical Center, Boston, coauthor of an accompanying editorial.
“It was a bit of the wild west out there, because each university, each college, all with good intentions, had been all struggling to figure out what to do, and how much to do. Probably the most important message from this new paper is the fact that now there is something out there that all coaches, athletes, families, schools, trainers can get some guidance from,” Dr. Udelson said in an interview.
Refining the cardiac screening criteria was a necessary step, Dr. Udelson said.
“How much cardiac imaging do you do? That is a matter of controversy,” said Dr. Udelson, who coauthored the commentary with Tufts cardiologist Ethan Rowin, MD, and Michael A. Curtis, MEd, a certified strength and conditioning specialist at the University of Virginia, Charlottesville. “The problem is that if you use a very sensitive imaging test on a lot of people, sometimes you find things that you really didn’t need to know about. They’re really not important. And now, the athlete is told he or she cannot play for 3 months because they might have myocarditis.
“Should we be too sensitive, meaning do we want to pick up anything no matter whether it’s important or not?” he added. “There will be a lot of false positives, and we are going to disqualify a lot of people. Or do you tune it a different way?”
Dr. Udelson said he would like to see commercial sports donate money to support research into the potential cardiotoxicity of COVID-19.
“If the organizations that benefit from these athletes, like the National Collegiate Athletic Association and professional sports leagues, can fund some of this research, that would be a huge help,” Dr. Udelson said.
“These are the top sports cardiologists in the country, and they have to start somewhere, and these are all based on what we know right now, as well as their own extensive experience. We all know that we are just at the beginning of our knowledge of this. But we have to have something to guide this huge community out there that is really thirsty for help.”
Dr. Baggish reports receiving research funding for the study of athletes in competitive sports from the National Heart, Lung, and Blood Institute; the National Football League Players Association; and the American Heart Association and receiving compensation for his role as team cardiologist from the US Olympic Committee/US Olympic Training Centers, US Soccer, US Rowing, the New England Patriots, the Boston Bruins, the New England Revolution, and Harvard University. Dr. Udelson has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The latest recommendations from sports cardiologists on getting athletes with COVID-19 back on the playing field safely emphasize a more judicious approach to screening for cardiac injury.
The new recommendations, made by the American College of Cardiology’s Sports and Exercise Cardiology Section, are for adult athletes in competitive sports and also for two important groups: younger athletes taking part in competitive high school sports and older athletes aged 35 and older, the Masters athletes, who continue to be active throughout their lives. The document was published online in JAMA Cardiology.
Because of the evolving nature of knowledge about COVID-19, updates on recommendations for safe return to play for athletes of all ages will continue to be made, senior author Aaron L. Baggish, MD, director of the cardiovascular performance program at Massachusetts General Hospital, Boston, said.
“The recommendations we released in May were entirely based on our experience taking care of hospitalized patients with COVID-19; we had no athletes in this population. We used a lot of conservative guesswork around how this would apply to otherwise healthy athletes,” Dr. Baggish said in an interview.
“But as sports started to open up, and we started to see large numbers of first professional and then college athletes come back into training, we realized that we needed to stop and ask whether the recommendations we put forward back in May were still appropriate,” Dr. Baggish said.
“Once we started to actually get into the trenches with these athletes, literally hundreds of them, and applying the testing strategies that we had initially recommended in everybody, we realized that we probably had some room for improvement, and that’s why we reconvened, to make these revisions,” he said.
Essentially, the recommendations now urge less cardiac testing. “Cardiac injury is not as common as we may have originally thought,” said Dr. Baggish.
“In the early days of COVID, people who were hospitalized had evidence of heart injury, and so we wondered if that prevalence would also be applicable to otherwise young, healthy people who got COVID. If that had been the case, we would have been in big trouble with respect to getting people back into sports. So this is why we started with a conservative screening approach and a lot of testing in order to not miss a huge burden of disease,” he said.
“But what we’ve learned over the past few months is that young people who get either asymptomatic or mild infection appear to have very, very low risk of having associated heart injury, so the need for testing in that population, when people who have infections recover fully, is almost certainly not going to be high yield,” Dr. Baggish said.
First iteration of the recommendations
Published in May in the early weeks of the pandemic, the first recommendations for safe return to play said that all athletes should stop training for at least 2 weeks after their symptoms resolve, then undergo “careful, clinical cardiovascular evaluation in combination with cardiac biomarkers and imaging.”
Additional testing with cardiac MRI, exercise testing, or ambulatory rhythm monitoring was to be done “based on the clinical course and initial testing.”
But experts caution that monitoring on such a scale in everyone is unnecessary and could even be counterproductive.
“Sending young athletes for extensive testing is not warranted and could send them to unnecessary testing, cardiac imaging, and so on,” Dr. Baggish said.
Only those athletes who continue to have symptoms or whose symptoms return when they get back to their athletic activities should go on for more screening.
“There, in essence, is the single main change from May, and that is a move away from screening with testing everyone, [and instead] confining that to the people who had moderate or greater severity disease,” he said.
Both iterations of the recommendations end with the same message.
“We are at the beginning of our knowledge about the cardiotoxic effects of COVID-19 but we are gathering evidence every day,” said Dr. Baggish. “Just as they did earlier, we acknowledge that our approaches are subject to change when we learn more about how COVID affects the heart, and specifically the hearts of athletes. This will be an ongoing process.”
Something to lean on
The recommendations are welcome, said James E. Udelson, MD, chief of the division of cardiology at Tufts Medical Center, Boston, coauthor of an accompanying editorial.
“It was a bit of the wild west out there, because each university, each college, all with good intentions, had been all struggling to figure out what to do, and how much to do. Probably the most important message from this new paper is the fact that now there is something out there that all coaches, athletes, families, schools, trainers can get some guidance from,” Dr. Udelson said in an interview.
Refining the cardiac screening criteria was a necessary step, Dr. Udelson said.
“How much cardiac imaging do you do? That is a matter of controversy,” said Dr. Udelson, who coauthored the commentary with Tufts cardiologist Ethan Rowin, MD, and Michael A. Curtis, MEd, a certified strength and conditioning specialist at the University of Virginia, Charlottesville. “The problem is that if you use a very sensitive imaging test on a lot of people, sometimes you find things that you really didn’t need to know about. They’re really not important. And now, the athlete is told he or she cannot play for 3 months because they might have myocarditis.
“Should we be too sensitive, meaning do we want to pick up anything no matter whether it’s important or not?” he added. “There will be a lot of false positives, and we are going to disqualify a lot of people. Or do you tune it a different way?”
Dr. Udelson said he would like to see commercial sports donate money to support research into the potential cardiotoxicity of COVID-19.
“If the organizations that benefit from these athletes, like the National Collegiate Athletic Association and professional sports leagues, can fund some of this research, that would be a huge help,” Dr. Udelson said.
“These are the top sports cardiologists in the country, and they have to start somewhere, and these are all based on what we know right now, as well as their own extensive experience. We all know that we are just at the beginning of our knowledge of this. But we have to have something to guide this huge community out there that is really thirsty for help.”
Dr. Baggish reports receiving research funding for the study of athletes in competitive sports from the National Heart, Lung, and Blood Institute; the National Football League Players Association; and the American Heart Association and receiving compensation for his role as team cardiologist from the US Olympic Committee/US Olympic Training Centers, US Soccer, US Rowing, the New England Patriots, the Boston Bruins, the New England Revolution, and Harvard University. Dr. Udelson has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Being HIV positive increases risk of death from COVID-19
compared with people without HIV.
A comparison of outcomes of people with HIV to people without HIV who were hospitalized in the United Kingdom with COVID-19 from Jan. 17 to June 4 showed that HIV-positive status was associated with a 63% increased risk of day 28 mortality.
This was especially true for HIV+ patients younger than 70 years of age, said Anna Maria Geretti, MD, PhD, professor of virology and infectious diseases, University of Liverpool, England.
The results are from an analysis of data from the ISARIC World Health Organization (WHO) Clinical Characterisation Protocol (UK) study, and were presented at the HIV Glasgow annual meeting, held virtually this year because of the pandemic.
“We investigated whether HIV status could be important in COVID-19 outcomes because there was anxiety on the part of our patients, and we wanted to gather some evidence-based information in order to help guide them,” Dr. Geretti said in an interview.
“ISARIC is an international protocol and the UK is one of the nations participating. We applied for access to its very large database, which connects data from all patients who are hospitalized with either known or suspected COVID-19. We wanted to see specifically how the presentation and outcomes of patients with HIV compared with the rest of the population without HIV. It afforded us an ideal opportunity to start to answer this question, and this is our first analysis in what will be an ongoing process. Importantly, we showed that there is a need to really look more carefully at the population with HIV,” she said.
Out of a total of 47,539 patients in the database, 115 (0.24%) had confirmed HIV-positive status, and 103 of those 115, or 89.6%, had a record of being on antiretroviral therapy.
On admission, the patients with HIV were younger, with a median age of 55 compared with 74 for patients without HIV (P < .001). They also had a higher prevalence of obesity, moderate to severe liver disease, higher lymphocyte counts and C-reactive protein, as well as more systemic symptoms.
There were no differences in respiratory rate, need for oxygen, or prevalence of chest infiltrates.
The cumulative incidence of mortality at day 28 was 25.2% in HIV-positive patients compared with 32.1% in HIV-negative patients (P = .12).
But when the researchers looked more closely, they noticed that the mortality rate was actually higher in younger HIV+ patients compared with HIV-negative patients.
Stratified by age, 28-day mortality was significantly higher in HIV+ patients aged <50 years (P =.004); and those aged 50 to 59 years (P = .05).
“So below the age of 70, the risk of mortality was double in people with HIV. The people with HIV who died often had diabetes with complications and also more frequent obesity, but this was not the only explanation,” Dr. Geretti said. “There is something to do with the HIV status per se.”
Next steps will be to expand the data set and repeat the analysis with an additional 100 patients “at least” she said.
The researchers also hope to zero in on what about being HIV+ is increasing the mortality risk from COVID-19.
“Right now we need greater numbers and we hope that the research community will be stimulated to take a closer look at this information, and merge other data so that we can strengthen confidence in the data and tease out what factors are causing this increased risk for mortality,” Dr. Geretti said.
She also emphasized that all patients admitted to hospital with COVID-19 should be asked about their HIV status.
“It is important that the HIV status be recorded if we want to increase our ability to understand how HIV impacts survival,” she stressed. “In our experience we found that most of the hospital records were not doing that. Since HIV+ patients seem to be at increased risk, HIV status should be factored into the clinical management. Ask patients if they are HIV+, and if it is not known, then do a test. That would be good practice.”
Dr. Geretti reported no relevant financial relationships. The work was supported by grants from the National Institute of Health Research, the Medical Research Council, the Wellcome Trust, the Department for International Development, and the Bill and Melinda Gates Foundation.
A version of this article originally appeared on Medscape.com.
compared with people without HIV.
A comparison of outcomes of people with HIV to people without HIV who were hospitalized in the United Kingdom with COVID-19 from Jan. 17 to June 4 showed that HIV-positive status was associated with a 63% increased risk of day 28 mortality.
This was especially true for HIV+ patients younger than 70 years of age, said Anna Maria Geretti, MD, PhD, professor of virology and infectious diseases, University of Liverpool, England.
The results are from an analysis of data from the ISARIC World Health Organization (WHO) Clinical Characterisation Protocol (UK) study, and were presented at the HIV Glasgow annual meeting, held virtually this year because of the pandemic.
“We investigated whether HIV status could be important in COVID-19 outcomes because there was anxiety on the part of our patients, and we wanted to gather some evidence-based information in order to help guide them,” Dr. Geretti said in an interview.
“ISARIC is an international protocol and the UK is one of the nations participating. We applied for access to its very large database, which connects data from all patients who are hospitalized with either known or suspected COVID-19. We wanted to see specifically how the presentation and outcomes of patients with HIV compared with the rest of the population without HIV. It afforded us an ideal opportunity to start to answer this question, and this is our first analysis in what will be an ongoing process. Importantly, we showed that there is a need to really look more carefully at the population with HIV,” she said.
Out of a total of 47,539 patients in the database, 115 (0.24%) had confirmed HIV-positive status, and 103 of those 115, or 89.6%, had a record of being on antiretroviral therapy.
On admission, the patients with HIV were younger, with a median age of 55 compared with 74 for patients without HIV (P < .001). They also had a higher prevalence of obesity, moderate to severe liver disease, higher lymphocyte counts and C-reactive protein, as well as more systemic symptoms.
There were no differences in respiratory rate, need for oxygen, or prevalence of chest infiltrates.
The cumulative incidence of mortality at day 28 was 25.2% in HIV-positive patients compared with 32.1% in HIV-negative patients (P = .12).
But when the researchers looked more closely, they noticed that the mortality rate was actually higher in younger HIV+ patients compared with HIV-negative patients.
Stratified by age, 28-day mortality was significantly higher in HIV+ patients aged <50 years (P =.004); and those aged 50 to 59 years (P = .05).
“So below the age of 70, the risk of mortality was double in people with HIV. The people with HIV who died often had diabetes with complications and also more frequent obesity, but this was not the only explanation,” Dr. Geretti said. “There is something to do with the HIV status per se.”
Next steps will be to expand the data set and repeat the analysis with an additional 100 patients “at least” she said.
The researchers also hope to zero in on what about being HIV+ is increasing the mortality risk from COVID-19.
“Right now we need greater numbers and we hope that the research community will be stimulated to take a closer look at this information, and merge other data so that we can strengthen confidence in the data and tease out what factors are causing this increased risk for mortality,” Dr. Geretti said.
She also emphasized that all patients admitted to hospital with COVID-19 should be asked about their HIV status.
“It is important that the HIV status be recorded if we want to increase our ability to understand how HIV impacts survival,” she stressed. “In our experience we found that most of the hospital records were not doing that. Since HIV+ patients seem to be at increased risk, HIV status should be factored into the clinical management. Ask patients if they are HIV+, and if it is not known, then do a test. That would be good practice.”
Dr. Geretti reported no relevant financial relationships. The work was supported by grants from the National Institute of Health Research, the Medical Research Council, the Wellcome Trust, the Department for International Development, and the Bill and Melinda Gates Foundation.
A version of this article originally appeared on Medscape.com.
compared with people without HIV.
A comparison of outcomes of people with HIV to people without HIV who were hospitalized in the United Kingdom with COVID-19 from Jan. 17 to June 4 showed that HIV-positive status was associated with a 63% increased risk of day 28 mortality.
This was especially true for HIV+ patients younger than 70 years of age, said Anna Maria Geretti, MD, PhD, professor of virology and infectious diseases, University of Liverpool, England.
The results are from an analysis of data from the ISARIC World Health Organization (WHO) Clinical Characterisation Protocol (UK) study, and were presented at the HIV Glasgow annual meeting, held virtually this year because of the pandemic.
“We investigated whether HIV status could be important in COVID-19 outcomes because there was anxiety on the part of our patients, and we wanted to gather some evidence-based information in order to help guide them,” Dr. Geretti said in an interview.
“ISARIC is an international protocol and the UK is one of the nations participating. We applied for access to its very large database, which connects data from all patients who are hospitalized with either known or suspected COVID-19. We wanted to see specifically how the presentation and outcomes of patients with HIV compared with the rest of the population without HIV. It afforded us an ideal opportunity to start to answer this question, and this is our first analysis in what will be an ongoing process. Importantly, we showed that there is a need to really look more carefully at the population with HIV,” she said.
Out of a total of 47,539 patients in the database, 115 (0.24%) had confirmed HIV-positive status, and 103 of those 115, or 89.6%, had a record of being on antiretroviral therapy.
On admission, the patients with HIV were younger, with a median age of 55 compared with 74 for patients without HIV (P < .001). They also had a higher prevalence of obesity, moderate to severe liver disease, higher lymphocyte counts and C-reactive protein, as well as more systemic symptoms.
There were no differences in respiratory rate, need for oxygen, or prevalence of chest infiltrates.
The cumulative incidence of mortality at day 28 was 25.2% in HIV-positive patients compared with 32.1% in HIV-negative patients (P = .12).
But when the researchers looked more closely, they noticed that the mortality rate was actually higher in younger HIV+ patients compared with HIV-negative patients.
Stratified by age, 28-day mortality was significantly higher in HIV+ patients aged <50 years (P =.004); and those aged 50 to 59 years (P = .05).
“So below the age of 70, the risk of mortality was double in people with HIV. The people with HIV who died often had diabetes with complications and also more frequent obesity, but this was not the only explanation,” Dr. Geretti said. “There is something to do with the HIV status per se.”
Next steps will be to expand the data set and repeat the analysis with an additional 100 patients “at least” she said.
The researchers also hope to zero in on what about being HIV+ is increasing the mortality risk from COVID-19.
“Right now we need greater numbers and we hope that the research community will be stimulated to take a closer look at this information, and merge other data so that we can strengthen confidence in the data and tease out what factors are causing this increased risk for mortality,” Dr. Geretti said.
She also emphasized that all patients admitted to hospital with COVID-19 should be asked about their HIV status.
“It is important that the HIV status be recorded if we want to increase our ability to understand how HIV impacts survival,” she stressed. “In our experience we found that most of the hospital records were not doing that. Since HIV+ patients seem to be at increased risk, HIV status should be factored into the clinical management. Ask patients if they are HIV+, and if it is not known, then do a test. That would be good practice.”
Dr. Geretti reported no relevant financial relationships. The work was supported by grants from the National Institute of Health Research, the Medical Research Council, the Wellcome Trust, the Department for International Development, and the Bill and Melinda Gates Foundation.
A version of this article originally appeared on Medscape.com.
Novel therapy an effective alternative to ECT for suicidality in TRD?
Magnetic seizure therapy (MST) appears to be a viable alternative to electroconvulsive therapy (ECT) in reducing suicide risk in patients with treatment-resistant depression (TRD), early research suggests.
In a single-center, open-label study, MST produced complete remission from suicidality in almost half of the patients who received the treatment.
“The results are promising,” lead author Cory R. Weissman, MD, Centre for Addiction and Mental Health, University of Toronto, told Medscape Medical News.
“The field needs new ways of approaching suicidality because it’s becoming a bigger issue and a major concern, especially now with COVID. These are early but promising results that need to be followed up,” Weissman said.
The study was published online August 18 in JAMA Network Open.
Fewer side effects, less stigma
However, ECT is underutilized – fewer than 1% of patients with TRD receive the treatment – because of stigma and/or a perceived risk of cognitive adverse effects, he said.
“MST is a focal magnetic pulse that leads to discharge or depolarization within the frontal lobe of the brain with the goal of inducing a seizure. It works quite similarly to ECT, which we know is quite a good anti-suicidal treatment, especially in depression,” Weissman explained
However, MST has fewer side effects, particularly on cognition, and less stigma compared to ECT. It also has a different mechanism of action, with a “more focal treatment target in the brain than ECT to induce seizures,” Weissman said.
The Toronto group has been studying MST in various mood disorders for several years. As previously reported by Medscape Medical News, MST is effective in reducing suicidal thoughts in treatment-resistant bipolar disorder.
The current study is a post hoc secondary analysis of data from the group’s original trial of MST as a treatment for treatment resistant depression in patients initially referred for ECT. The trial ran from February 2012 through June 2019 and with a post-treatment 6-month follow-up.
The secondary analysis was performed from January 2019 to November 2019.
The secondary analysis included 67 patients who underwent MST 2 to 3 times per week until they achieved remission from a depressive episode or until they reached a maximum of 24 sessions. All had baseline suicidality, as defined by a score greater than 0 on the Beck Scale for Suicidal Ideation (Beck SSI).
MST was administered using the MagPro MST device with Twin Coil-XS (MagVenture) applied over the frontal cortex at 100% machine output with low (25 Hz), moderate (50 or 60 Hz), or high (100 Hz) frequency.
“It’s very similar to ECT. The actual seizure lasts about a minute or two, and patients recover in about 10 to 15 minutes and they go home afterwards,” Weissman said.
The main outcome was remission from suicidality as measured by an end-point score of 0 on the Beck SSI. Of the 67 patients, 32 (47.8%) achieved remission from suicidality.
Low and moderate frequencies appeared to be more effective for suicidality; 16 of 29 patients (55.2%) receiving low frequency MST achieved remission, as did 12 of 22 patients (54.5%) receiving moderate frequency MST. Four of 16 patients (25%) who received high frequency MST achieved remission from suicidality.
A “valuable contribution”
Commenting on the findings for Medscape Medical News, Manish K. Jha, MD, Icahn School of Medicine at Mount Sinai in New York City, said there is an urgent need to develop safe and effective treatment for patients with treatment-resistant depression (TRD).
“The Sequenced Treatment Alternative to Relieve Depression (STAR*D) trial showed that after inadequate improvement with two antidepressants, the likelihood of improvement with a third or fourth antidepressant trial was very low. Therefore, we need effective treatment for TRD,” noted Jha, who was not involved in the research.
The current study represents a “valuable contribution, as it shows improvement in suicidal ideation with magnetic seizure therapy,” he added.
The study’s findings suggest that MST may offer a “viable new treatment” for patients with TRD. He added that the upcoming results of an ongoing clinical trial testing MST against ECT are of “great interest to the field.”
Although the findings are compelling, Jha also noted the study had several limitations, include a relatively “modest” sample size and no sham or active comparator.
In addition, he said, the level of suicidality in this study was limited because of eligibility restrictions, such as exclusion of individuals who had attempted suicide in the prior 6 months.
“While authors use a broad term of ‘suicidality,’ their study is focused on suicidal ideation. Future studies that target suicide behavior are urgently needed. This may mean that we need to study individuals with recent suicide attempts in settings such as emergency rooms and inpatient units,” said Jha.
The study had no specific funding. Weissman has disclosed no relevant financial relationships. Several other study authors reported relationships with industry. The full list can be found with the original article. Jha has received contract research grants from Acadia Pharmaceuticals and Janssen Research & Development, and honoraria for CME presentations from North American Center for Continuing Medical Education and Global Medical Education.
This article first appeared on Medscape.com.
Magnetic seizure therapy (MST) appears to be a viable alternative to electroconvulsive therapy (ECT) in reducing suicide risk in patients with treatment-resistant depression (TRD), early research suggests.
In a single-center, open-label study, MST produced complete remission from suicidality in almost half of the patients who received the treatment.
“The results are promising,” lead author Cory R. Weissman, MD, Centre for Addiction and Mental Health, University of Toronto, told Medscape Medical News.
“The field needs new ways of approaching suicidality because it’s becoming a bigger issue and a major concern, especially now with COVID. These are early but promising results that need to be followed up,” Weissman said.
The study was published online August 18 in JAMA Network Open.
Fewer side effects, less stigma
However, ECT is underutilized – fewer than 1% of patients with TRD receive the treatment – because of stigma and/or a perceived risk of cognitive adverse effects, he said.
“MST is a focal magnetic pulse that leads to discharge or depolarization within the frontal lobe of the brain with the goal of inducing a seizure. It works quite similarly to ECT, which we know is quite a good anti-suicidal treatment, especially in depression,” Weissman explained
However, MST has fewer side effects, particularly on cognition, and less stigma compared to ECT. It also has a different mechanism of action, with a “more focal treatment target in the brain than ECT to induce seizures,” Weissman said.
The Toronto group has been studying MST in various mood disorders for several years. As previously reported by Medscape Medical News, MST is effective in reducing suicidal thoughts in treatment-resistant bipolar disorder.
The current study is a post hoc secondary analysis of data from the group’s original trial of MST as a treatment for treatment resistant depression in patients initially referred for ECT. The trial ran from February 2012 through June 2019 and with a post-treatment 6-month follow-up.
The secondary analysis was performed from January 2019 to November 2019.
The secondary analysis included 67 patients who underwent MST 2 to 3 times per week until they achieved remission from a depressive episode or until they reached a maximum of 24 sessions. All had baseline suicidality, as defined by a score greater than 0 on the Beck Scale for Suicidal Ideation (Beck SSI).
MST was administered using the MagPro MST device with Twin Coil-XS (MagVenture) applied over the frontal cortex at 100% machine output with low (25 Hz), moderate (50 or 60 Hz), or high (100 Hz) frequency.
“It’s very similar to ECT. The actual seizure lasts about a minute or two, and patients recover in about 10 to 15 minutes and they go home afterwards,” Weissman said.
The main outcome was remission from suicidality as measured by an end-point score of 0 on the Beck SSI. Of the 67 patients, 32 (47.8%) achieved remission from suicidality.
Low and moderate frequencies appeared to be more effective for suicidality; 16 of 29 patients (55.2%) receiving low frequency MST achieved remission, as did 12 of 22 patients (54.5%) receiving moderate frequency MST. Four of 16 patients (25%) who received high frequency MST achieved remission from suicidality.
A “valuable contribution”
Commenting on the findings for Medscape Medical News, Manish K. Jha, MD, Icahn School of Medicine at Mount Sinai in New York City, said there is an urgent need to develop safe and effective treatment for patients with treatment-resistant depression (TRD).
“The Sequenced Treatment Alternative to Relieve Depression (STAR*D) trial showed that after inadequate improvement with two antidepressants, the likelihood of improvement with a third or fourth antidepressant trial was very low. Therefore, we need effective treatment for TRD,” noted Jha, who was not involved in the research.
The current study represents a “valuable contribution, as it shows improvement in suicidal ideation with magnetic seizure therapy,” he added.
The study’s findings suggest that MST may offer a “viable new treatment” for patients with TRD. He added that the upcoming results of an ongoing clinical trial testing MST against ECT are of “great interest to the field.”
Although the findings are compelling, Jha also noted the study had several limitations, include a relatively “modest” sample size and no sham or active comparator.
In addition, he said, the level of suicidality in this study was limited because of eligibility restrictions, such as exclusion of individuals who had attempted suicide in the prior 6 months.
“While authors use a broad term of ‘suicidality,’ their study is focused on suicidal ideation. Future studies that target suicide behavior are urgently needed. This may mean that we need to study individuals with recent suicide attempts in settings such as emergency rooms and inpatient units,” said Jha.
The study had no specific funding. Weissman has disclosed no relevant financial relationships. Several other study authors reported relationships with industry. The full list can be found with the original article. Jha has received contract research grants from Acadia Pharmaceuticals and Janssen Research & Development, and honoraria for CME presentations from North American Center for Continuing Medical Education and Global Medical Education.
This article first appeared on Medscape.com.
Magnetic seizure therapy (MST) appears to be a viable alternative to electroconvulsive therapy (ECT) in reducing suicide risk in patients with treatment-resistant depression (TRD), early research suggests.
In a single-center, open-label study, MST produced complete remission from suicidality in almost half of the patients who received the treatment.
“The results are promising,” lead author Cory R. Weissman, MD, Centre for Addiction and Mental Health, University of Toronto, told Medscape Medical News.
“The field needs new ways of approaching suicidality because it’s becoming a bigger issue and a major concern, especially now with COVID. These are early but promising results that need to be followed up,” Weissman said.
The study was published online August 18 in JAMA Network Open.
Fewer side effects, less stigma
However, ECT is underutilized – fewer than 1% of patients with TRD receive the treatment – because of stigma and/or a perceived risk of cognitive adverse effects, he said.
“MST is a focal magnetic pulse that leads to discharge or depolarization within the frontal lobe of the brain with the goal of inducing a seizure. It works quite similarly to ECT, which we know is quite a good anti-suicidal treatment, especially in depression,” Weissman explained
However, MST has fewer side effects, particularly on cognition, and less stigma compared to ECT. It also has a different mechanism of action, with a “more focal treatment target in the brain than ECT to induce seizures,” Weissman said.
The Toronto group has been studying MST in various mood disorders for several years. As previously reported by Medscape Medical News, MST is effective in reducing suicidal thoughts in treatment-resistant bipolar disorder.
The current study is a post hoc secondary analysis of data from the group’s original trial of MST as a treatment for treatment resistant depression in patients initially referred for ECT. The trial ran from February 2012 through June 2019 and with a post-treatment 6-month follow-up.
The secondary analysis was performed from January 2019 to November 2019.
The secondary analysis included 67 patients who underwent MST 2 to 3 times per week until they achieved remission from a depressive episode or until they reached a maximum of 24 sessions. All had baseline suicidality, as defined by a score greater than 0 on the Beck Scale for Suicidal Ideation (Beck SSI).
MST was administered using the MagPro MST device with Twin Coil-XS (MagVenture) applied over the frontal cortex at 100% machine output with low (25 Hz), moderate (50 or 60 Hz), or high (100 Hz) frequency.
“It’s very similar to ECT. The actual seizure lasts about a minute or two, and patients recover in about 10 to 15 minutes and they go home afterwards,” Weissman said.
The main outcome was remission from suicidality as measured by an end-point score of 0 on the Beck SSI. Of the 67 patients, 32 (47.8%) achieved remission from suicidality.
Low and moderate frequencies appeared to be more effective for suicidality; 16 of 29 patients (55.2%) receiving low frequency MST achieved remission, as did 12 of 22 patients (54.5%) receiving moderate frequency MST. Four of 16 patients (25%) who received high frequency MST achieved remission from suicidality.
A “valuable contribution”
Commenting on the findings for Medscape Medical News, Manish K. Jha, MD, Icahn School of Medicine at Mount Sinai in New York City, said there is an urgent need to develop safe and effective treatment for patients with treatment-resistant depression (TRD).
“The Sequenced Treatment Alternative to Relieve Depression (STAR*D) trial showed that after inadequate improvement with two antidepressants, the likelihood of improvement with a third or fourth antidepressant trial was very low. Therefore, we need effective treatment for TRD,” noted Jha, who was not involved in the research.
The current study represents a “valuable contribution, as it shows improvement in suicidal ideation with magnetic seizure therapy,” he added.
The study’s findings suggest that MST may offer a “viable new treatment” for patients with TRD. He added that the upcoming results of an ongoing clinical trial testing MST against ECT are of “great interest to the field.”
Although the findings are compelling, Jha also noted the study had several limitations, include a relatively “modest” sample size and no sham or active comparator.
In addition, he said, the level of suicidality in this study was limited because of eligibility restrictions, such as exclusion of individuals who had attempted suicide in the prior 6 months.
“While authors use a broad term of ‘suicidality,’ their study is focused on suicidal ideation. Future studies that target suicide behavior are urgently needed. This may mean that we need to study individuals with recent suicide attempts in settings such as emergency rooms and inpatient units,” said Jha.
The study had no specific funding. Weissman has disclosed no relevant financial relationships. Several other study authors reported relationships with industry. The full list can be found with the original article. Jha has received contract research grants from Acadia Pharmaceuticals and Janssen Research & Development, and honoraria for CME presentations from North American Center for Continuing Medical Education and Global Medical Education.
This article first appeared on Medscape.com.
Cardiorespiratory fitness may alter AFib ablation outcomes
Higher baseline cardiorespiratory fitness (CRF) is associated with better outcomes after atrial fibrillation (AFib) ablation, according to new research.
In a single-center, retrospective cohort study, patients with the highest level of baseline CRF had significantly lower rates of arrhythmia recurrence and death than did patients with lower levels of CRF.
“It is stunning how just a simple measure, in this case walking on a treadmill, can predict whether atrial fibrillation ablation will be a successful endeavor or if it will fail,” senior author Wael A. Jaber, MD, professor of medicine, Cleveland Clinic, said in an interview.
“We found that ablation was not successful in most patients who had poor functional class and, conversely, that it was successful in most patients who were in tip-top shape when they walked on the treadmill. Our results can help clinicians inform patients about what they can expect after the procedure, depending on the baseline fitness level,” Dr. Jaber said.
The study was published online Aug. 2 in Heart Rhythm.
Several studies have shown a reduction in AFib incidence among individuals who report a physically active lifestyle, but the extent to which baseline CRF influences arrhythmia rates after AFib ablation is unknown, the authors note.
For the study, Dr. Jaber and colleagues analyzed results in 591 consecutive patients (mean age, 66.5 years; 75% male) with symptomatic paroxysmal or persistent AFib who underwent de novo AFib ablation at their institution. Only patients who had undergone an exercise stress test in the 12 months before AFib ablation (average, 4.5 months) were included.
Age- and sex-specific predicted metabolic equivalents (METs) were calculated using the St. James model for women and the Veterans Affairs referral model for men. The number of METs achieved was then divided by the predicted METs, and the patients were categorized into low (<85% predicted; n = 152), adequate (85%-100% predicted; n = 115), and high (>100% predicted; n = 324) CRF groups. Functional capacity was characterized as poor in 56 patients (9.5%), fair in 94 (16.0%), average in 225 (38.1%), good in 169 (28.6%), and high in 47 (8.0%).
During a mean follow-up of 32 months, arrhythmia recurrence was observed in 79% of patients in the low-CRF group, 54% of patients in the adequate-CRF group, and 27.5% of patients in the high-CRF group (P < .0001). Rates of repeat arrhythmia-related hospitalization, repeat rhythm-control procedures, and the need for ongoing antiarrhythmic therapy (ATT) were significantly lower in the high-CRF group. Specifically, ATT was stopped in 56% of patients in the high-CRF group, compared with 24% in the adequate-CRF group and 11% in the low-CRF group (P < .0001). Rehospitalization for arrhythmia was required in 18.5%, 38.0%, and 60.5% of cases, respectively, and repeat direct-current cardioversion or ablation was performed in 26.0%, 49.0%, and 65.0%, respectively (P < .0001 for both).
Death occurred in 11% of the low-CRF group, compared with 4% in the adequate-CRF group and 2.5% in the high-CRF group. Most (70%) of the deaths were caused by cardiovascular events, including heart failure, cardiac arrest, and coronary artery disease. The most common cause of noncardiac death was respiratory failure (13%), followed by sepsis (10%), malignancy (3%), and complications of Parkinson’s disease (3%).
“Although there was a statistically significant association between higher CRF and lower mortality in this cohort, the findings are to be viewed through the prism of a small sample size and relatively low death rate,” the authors wrote.
Don’t “overpromise” results
“The important message for clinicians is that when, you are discussing what to expect after atrial fibrillation ablation with your patients, do not overpromise the results. You can inform them that the success of the procedure depends more on how they perform on the baseline exercise test, and less on the ablation itself,” Dr. Jaber said.
Clinicians might want to consider advising their patients to become more active and increase their fitness level before undergoing the procedure, but whether doing so will improve outcomes is still unknown.
“This is what we don’t know. It makes sense. Hopefully, our results will encourage people to be more active before they arrive here for the procedure,” he said. “Our study is retrospective and is hypothesis generating, but we are planning a prospective study where patients will be referred to cardiac rehab prior to having ablation to try to improve their functional class to see if this will improve outcomes.”
Survival of the fittest
In an accompanying editorial commentary, Eric Black-Maier, MD, and Jonathan P. Piccini Sr, MD, from Duke University Medical Center, Durham, N.C., wrote that the findings have “important implications for clinical practice and raise important additional questions.”
They note that catheter ablation as a first-line rhythm-control strategy, per current recommendations, “seems reasonable” in individuals with high baseline cardiorespiratory fitness, but that the benefit is less clear for patients with poor baseline CRF and uncontrolled risk factors.
“Significant limitations in functional status may be at least partially attributable to uncontrolled [AFib], and patients with limited exercise capacity may stand to gain most from successful catheter ablation,” the editorialists wrote.
“Furthermore, because shorter time from [AFib] diagnosis to catheter ablation has been associated with improved outcomes, the decision to postpone ablation in favor of lifestyle modification is not without potential adverse consequences,” they added.
Dr. Black-Maier and Dr. Piccini agree with the need for additional prospective randomized clinical trials to confirm that exercise training to improve cardiorespiratory fitness before AFib ablation is practical and effective for reducing arrhythmia recurrence.
“Over the past 50-plus years, our understanding of cardiorespiratory fitness, exercise capacity, and arrhythmia occurrence in patients with [AFib] continues to evolve,” the editorialists concluded. Data from the study “clearly demonstrate that arrhythmia-free survival is indeed survival of the fittest. Time will tell if exercise training and improvements in cardiorespiratory fitness can change outcomes after ablation.”
The study was sponsored by the Cleveland Clinic. Dr. Jaber and Dr. Black-Maier report no relevant financial relationships. Dr. Piccini receives grants for clinical research from Abbott, the American Heart Association, the Association for the Advancement of Medical Instrumentation, Bayer, Boston Scientific, and Philips and serves as a consultant to Abbott, Allergan, ARCA Biopharma, Biotronik, Boston Scientific, LivaNova, Medtronic, Milestone, MyoKardia, Sanofi, Philips, and UpToDate.
A version of this story originally appeared on Medscape.com.
Higher baseline cardiorespiratory fitness (CRF) is associated with better outcomes after atrial fibrillation (AFib) ablation, according to new research.
In a single-center, retrospective cohort study, patients with the highest level of baseline CRF had significantly lower rates of arrhythmia recurrence and death than did patients with lower levels of CRF.
“It is stunning how just a simple measure, in this case walking on a treadmill, can predict whether atrial fibrillation ablation will be a successful endeavor or if it will fail,” senior author Wael A. Jaber, MD, professor of medicine, Cleveland Clinic, said in an interview.
“We found that ablation was not successful in most patients who had poor functional class and, conversely, that it was successful in most patients who were in tip-top shape when they walked on the treadmill. Our results can help clinicians inform patients about what they can expect after the procedure, depending on the baseline fitness level,” Dr. Jaber said.
The study was published online Aug. 2 in Heart Rhythm.
Several studies have shown a reduction in AFib incidence among individuals who report a physically active lifestyle, but the extent to which baseline CRF influences arrhythmia rates after AFib ablation is unknown, the authors note.
For the study, Dr. Jaber and colleagues analyzed results in 591 consecutive patients (mean age, 66.5 years; 75% male) with symptomatic paroxysmal or persistent AFib who underwent de novo AFib ablation at their institution. Only patients who had undergone an exercise stress test in the 12 months before AFib ablation (average, 4.5 months) were included.
Age- and sex-specific predicted metabolic equivalents (METs) were calculated using the St. James model for women and the Veterans Affairs referral model for men. The number of METs achieved was then divided by the predicted METs, and the patients were categorized into low (<85% predicted; n = 152), adequate (85%-100% predicted; n = 115), and high (>100% predicted; n = 324) CRF groups. Functional capacity was characterized as poor in 56 patients (9.5%), fair in 94 (16.0%), average in 225 (38.1%), good in 169 (28.6%), and high in 47 (8.0%).
During a mean follow-up of 32 months, arrhythmia recurrence was observed in 79% of patients in the low-CRF group, 54% of patients in the adequate-CRF group, and 27.5% of patients in the high-CRF group (P < .0001). Rates of repeat arrhythmia-related hospitalization, repeat rhythm-control procedures, and the need for ongoing antiarrhythmic therapy (ATT) were significantly lower in the high-CRF group. Specifically, ATT was stopped in 56% of patients in the high-CRF group, compared with 24% in the adequate-CRF group and 11% in the low-CRF group (P < .0001). Rehospitalization for arrhythmia was required in 18.5%, 38.0%, and 60.5% of cases, respectively, and repeat direct-current cardioversion or ablation was performed in 26.0%, 49.0%, and 65.0%, respectively (P < .0001 for both).
Death occurred in 11% of the low-CRF group, compared with 4% in the adequate-CRF group and 2.5% in the high-CRF group. Most (70%) of the deaths were caused by cardiovascular events, including heart failure, cardiac arrest, and coronary artery disease. The most common cause of noncardiac death was respiratory failure (13%), followed by sepsis (10%), malignancy (3%), and complications of Parkinson’s disease (3%).
“Although there was a statistically significant association between higher CRF and lower mortality in this cohort, the findings are to be viewed through the prism of a small sample size and relatively low death rate,” the authors wrote.
Don’t “overpromise” results
“The important message for clinicians is that when, you are discussing what to expect after atrial fibrillation ablation with your patients, do not overpromise the results. You can inform them that the success of the procedure depends more on how they perform on the baseline exercise test, and less on the ablation itself,” Dr. Jaber said.
Clinicians might want to consider advising their patients to become more active and increase their fitness level before undergoing the procedure, but whether doing so will improve outcomes is still unknown.
“This is what we don’t know. It makes sense. Hopefully, our results will encourage people to be more active before they arrive here for the procedure,” he said. “Our study is retrospective and is hypothesis generating, but we are planning a prospective study where patients will be referred to cardiac rehab prior to having ablation to try to improve their functional class to see if this will improve outcomes.”
Survival of the fittest
In an accompanying editorial commentary, Eric Black-Maier, MD, and Jonathan P. Piccini Sr, MD, from Duke University Medical Center, Durham, N.C., wrote that the findings have “important implications for clinical practice and raise important additional questions.”
They note that catheter ablation as a first-line rhythm-control strategy, per current recommendations, “seems reasonable” in individuals with high baseline cardiorespiratory fitness, but that the benefit is less clear for patients with poor baseline CRF and uncontrolled risk factors.
“Significant limitations in functional status may be at least partially attributable to uncontrolled [AFib], and patients with limited exercise capacity may stand to gain most from successful catheter ablation,” the editorialists wrote.
“Furthermore, because shorter time from [AFib] diagnosis to catheter ablation has been associated with improved outcomes, the decision to postpone ablation in favor of lifestyle modification is not without potential adverse consequences,” they added.
Dr. Black-Maier and Dr. Piccini agree with the need for additional prospective randomized clinical trials to confirm that exercise training to improve cardiorespiratory fitness before AFib ablation is practical and effective for reducing arrhythmia recurrence.
“Over the past 50-plus years, our understanding of cardiorespiratory fitness, exercise capacity, and arrhythmia occurrence in patients with [AFib] continues to evolve,” the editorialists concluded. Data from the study “clearly demonstrate that arrhythmia-free survival is indeed survival of the fittest. Time will tell if exercise training and improvements in cardiorespiratory fitness can change outcomes after ablation.”
The study was sponsored by the Cleveland Clinic. Dr. Jaber and Dr. Black-Maier report no relevant financial relationships. Dr. Piccini receives grants for clinical research from Abbott, the American Heart Association, the Association for the Advancement of Medical Instrumentation, Bayer, Boston Scientific, and Philips and serves as a consultant to Abbott, Allergan, ARCA Biopharma, Biotronik, Boston Scientific, LivaNova, Medtronic, Milestone, MyoKardia, Sanofi, Philips, and UpToDate.
A version of this story originally appeared on Medscape.com.
Higher baseline cardiorespiratory fitness (CRF) is associated with better outcomes after atrial fibrillation (AFib) ablation, according to new research.
In a single-center, retrospective cohort study, patients with the highest level of baseline CRF had significantly lower rates of arrhythmia recurrence and death than did patients with lower levels of CRF.
“It is stunning how just a simple measure, in this case walking on a treadmill, can predict whether atrial fibrillation ablation will be a successful endeavor or if it will fail,” senior author Wael A. Jaber, MD, professor of medicine, Cleveland Clinic, said in an interview.
“We found that ablation was not successful in most patients who had poor functional class and, conversely, that it was successful in most patients who were in tip-top shape when they walked on the treadmill. Our results can help clinicians inform patients about what they can expect after the procedure, depending on the baseline fitness level,” Dr. Jaber said.
The study was published online Aug. 2 in Heart Rhythm.
Several studies have shown a reduction in AFib incidence among individuals who report a physically active lifestyle, but the extent to which baseline CRF influences arrhythmia rates after AFib ablation is unknown, the authors note.
For the study, Dr. Jaber and colleagues analyzed results in 591 consecutive patients (mean age, 66.5 years; 75% male) with symptomatic paroxysmal or persistent AFib who underwent de novo AFib ablation at their institution. Only patients who had undergone an exercise stress test in the 12 months before AFib ablation (average, 4.5 months) were included.
Age- and sex-specific predicted metabolic equivalents (METs) were calculated using the St. James model for women and the Veterans Affairs referral model for men. The number of METs achieved was then divided by the predicted METs, and the patients were categorized into low (<85% predicted; n = 152), adequate (85%-100% predicted; n = 115), and high (>100% predicted; n = 324) CRF groups. Functional capacity was characterized as poor in 56 patients (9.5%), fair in 94 (16.0%), average in 225 (38.1%), good in 169 (28.6%), and high in 47 (8.0%).
During a mean follow-up of 32 months, arrhythmia recurrence was observed in 79% of patients in the low-CRF group, 54% of patients in the adequate-CRF group, and 27.5% of patients in the high-CRF group (P < .0001). Rates of repeat arrhythmia-related hospitalization, repeat rhythm-control procedures, and the need for ongoing antiarrhythmic therapy (ATT) were significantly lower in the high-CRF group. Specifically, ATT was stopped in 56% of patients in the high-CRF group, compared with 24% in the adequate-CRF group and 11% in the low-CRF group (P < .0001). Rehospitalization for arrhythmia was required in 18.5%, 38.0%, and 60.5% of cases, respectively, and repeat direct-current cardioversion or ablation was performed in 26.0%, 49.0%, and 65.0%, respectively (P < .0001 for both).
Death occurred in 11% of the low-CRF group, compared with 4% in the adequate-CRF group and 2.5% in the high-CRF group. Most (70%) of the deaths were caused by cardiovascular events, including heart failure, cardiac arrest, and coronary artery disease. The most common cause of noncardiac death was respiratory failure (13%), followed by sepsis (10%), malignancy (3%), and complications of Parkinson’s disease (3%).
“Although there was a statistically significant association between higher CRF and lower mortality in this cohort, the findings are to be viewed through the prism of a small sample size and relatively low death rate,” the authors wrote.
Don’t “overpromise” results
“The important message for clinicians is that when, you are discussing what to expect after atrial fibrillation ablation with your patients, do not overpromise the results. You can inform them that the success of the procedure depends more on how they perform on the baseline exercise test, and less on the ablation itself,” Dr. Jaber said.
Clinicians might want to consider advising their patients to become more active and increase their fitness level before undergoing the procedure, but whether doing so will improve outcomes is still unknown.
“This is what we don’t know. It makes sense. Hopefully, our results will encourage people to be more active before they arrive here for the procedure,” he said. “Our study is retrospective and is hypothesis generating, but we are planning a prospective study where patients will be referred to cardiac rehab prior to having ablation to try to improve their functional class to see if this will improve outcomes.”
Survival of the fittest
In an accompanying editorial commentary, Eric Black-Maier, MD, and Jonathan P. Piccini Sr, MD, from Duke University Medical Center, Durham, N.C., wrote that the findings have “important implications for clinical practice and raise important additional questions.”
They note that catheter ablation as a first-line rhythm-control strategy, per current recommendations, “seems reasonable” in individuals with high baseline cardiorespiratory fitness, but that the benefit is less clear for patients with poor baseline CRF and uncontrolled risk factors.
“Significant limitations in functional status may be at least partially attributable to uncontrolled [AFib], and patients with limited exercise capacity may stand to gain most from successful catheter ablation,” the editorialists wrote.
“Furthermore, because shorter time from [AFib] diagnosis to catheter ablation has been associated with improved outcomes, the decision to postpone ablation in favor of lifestyle modification is not without potential adverse consequences,” they added.
Dr. Black-Maier and Dr. Piccini agree with the need for additional prospective randomized clinical trials to confirm that exercise training to improve cardiorespiratory fitness before AFib ablation is practical and effective for reducing arrhythmia recurrence.
“Over the past 50-plus years, our understanding of cardiorespiratory fitness, exercise capacity, and arrhythmia occurrence in patients with [AFib] continues to evolve,” the editorialists concluded. Data from the study “clearly demonstrate that arrhythmia-free survival is indeed survival of the fittest. Time will tell if exercise training and improvements in cardiorespiratory fitness can change outcomes after ablation.”
The study was sponsored by the Cleveland Clinic. Dr. Jaber and Dr. Black-Maier report no relevant financial relationships. Dr. Piccini receives grants for clinical research from Abbott, the American Heart Association, the Association for the Advancement of Medical Instrumentation, Bayer, Boston Scientific, and Philips and serves as a consultant to Abbott, Allergan, ARCA Biopharma, Biotronik, Boston Scientific, LivaNova, Medtronic, Milestone, MyoKardia, Sanofi, Philips, and UpToDate.
A version of this story originally appeared on Medscape.com.
New long-term data for antipsychotic in pediatric bipolar depression
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.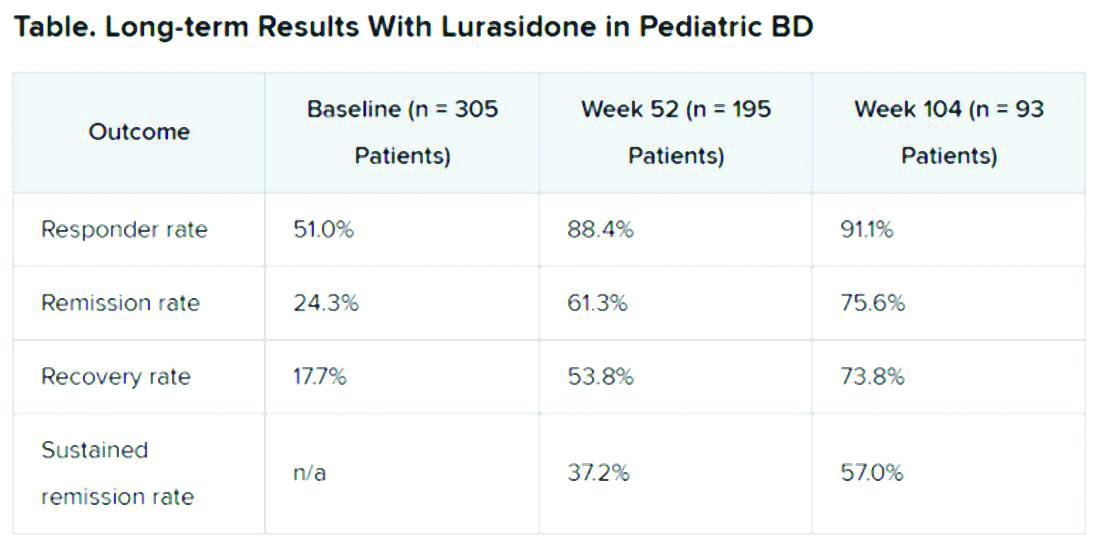
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.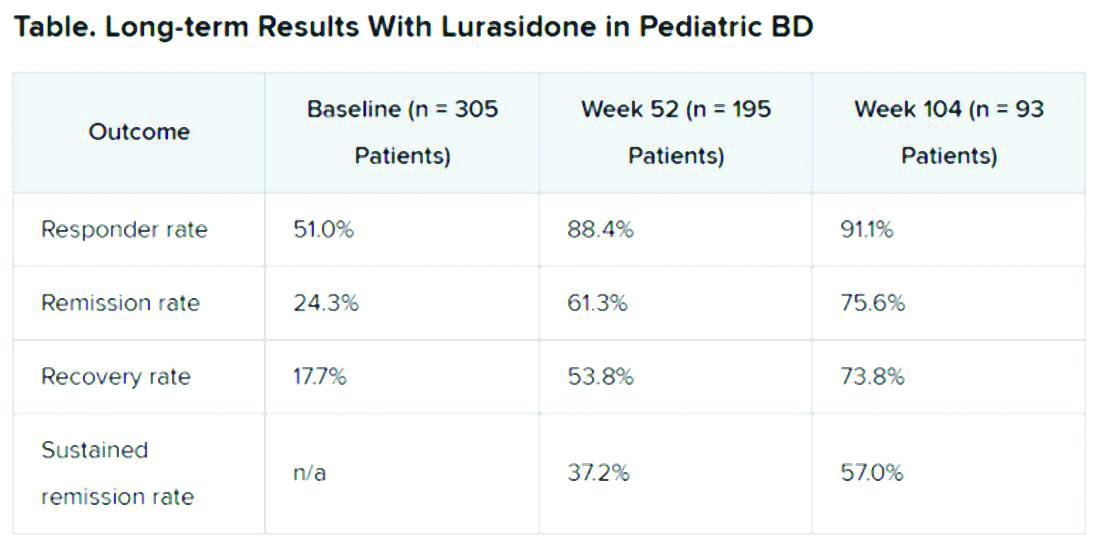
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
The antipsychotic lurasidone (Latuda, Sunovion Pharmaceuticals) has long-term efficacy in the treatment of bipolar depression (BD) in children and adolescents, new research suggests.
In an open-label extension study involving patients aged 10-17 years, up to 2 years of treatment with lurasidone was associated with continued improvement in depressive symptoms. There were progressively higher rates of remission, recovery, and sustained remission.
Coinvestigator Manpreet K. Singh, MD, director of the Stanford Pediatric Mood Disorders Program, Stanford (Calif.) University, noted that early onset of BD is common. Although in pediatric populations, prevalence has been fairly stable at around 1.8%, these patients have “a very limited number of treatment options available for the depressed phases of BD,” which is often predominant and can be difficult to identify.
“A lot of youths who are experiencing depressive symptoms in the context of having had a manic episode will often have a relapsing and remitting course, even after the acute phase of treatment, so because kids can be on medications for long periods of time, a better understanding of what works ... is very important,” Dr. Singh said in an interview.
The findings were presented at the virtual American Society of Clinical Psychopharmacology (ASCP) 2020 annual meeting.
Long-term Efficacy
The Food and Drug Administration approved lurasidone as monotherapy for BD in children and adolescents in 2018. The aim of the current study was to evaluate the drug’s long-term efficacy in achieving response or remission in this population.
A total of 305 children who completed an initial 6-week double-blind study of lurasidone versus placebo entered the 2-year, open-label extension study. In the extension, they either continued taking lurasidone or were switched from placebo to lurasidone 20-80 mg/day. Of this group, 195 children completed 52 weeks of treatment, and 93 completed 104 weeks of treatment.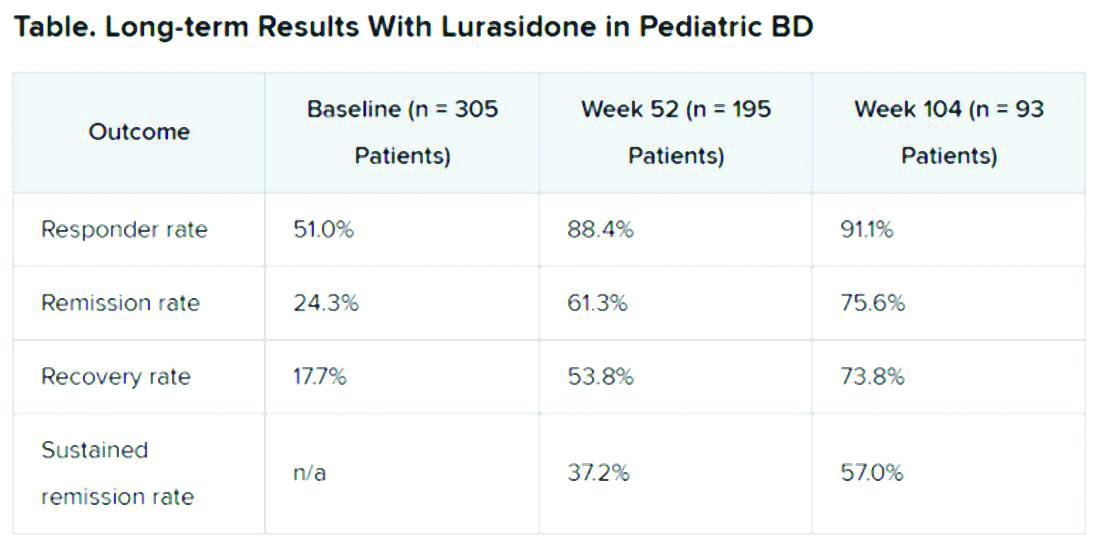
Efficacy was measured with the Children’s Depression Rating Scale, Revised (CDRS-R) and the Clinical Global Impression, Bipolar Depression Severity scale (CGI-BP-S). Functioning was evaluated with the clinician-rated Children’s Global Assessment Scale (CGAS); on that scale, a score of 70 or higher indicates no clinically meaningful functional impairment.
Remission criteria were met if a patient achieved a CDRS-R total score of 28 or less, a Young Mania Rating Scale (YMRS) total score of 8 or less, and a CGI-BP-S depression score of 3 or less.
Recovery criteria were met if a patient achieved remission and had a CGAS score of at least 70.
Sustained remission, a more stringent outcome, required that the patient meet remission criteria for at least 24 consecutive weeks.
In addition, there was a strong inverse correlation (r = –0.71) between depression severity, as measured by CDRS-R total score, and functioning, as measured by the CGAS.
“That’s the cool thing: As the depression symptoms and severity came down, the overall functioning in these kids improved,” Dr. Singh noted.
“This improvement in functioning ends up being much more clinically relevant and useful to clinicians than just showing an improvement in a set of symptoms because what brings a kid – or even an adult, for that matter – to see a clinician to get treatment is because something about their symptoms is causing significant functional impairment,” she said.
“So this is the take-home message: You can see that lurasidone ... demonstrates not just recovery from depressive symptoms but that this reduction in depressive symptoms corresponds to an improvement in functioning for these youths,” she added.
Potential Limitations
Commenting on the study, Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charite Universitatsmedizin, Berlin, Germany, noted that BD is difficult to treat, especially for patients who are going through “a developmentally vulnerable phase of their lives.”
“Lurasidone is the only monotherapy approved for bipolar depression in youth and is fairly well tolerated,” said Dr. Correll, who was not part of the research. He added that the long-term effectiveness data on response and remission “add relevant information” to the field.
However, he noted that it is not clear whether the high and increasing rates of response and remission were based on the reporting of observed cases or on last-observation-carried-forward analyses. “Given the naturally high dropout rate in such a long-term study and the potential for a survival bias, this is a relevant methodological question that affects the interpretation of the data,” he said.
“Nevertheless, the very favorable results for cumulative response, remission, and sustained remission add to the evidence that lurasidone is an effective treatment for youth with bipolar depression. Since efficacy cannot be interpreted in isolation, data describing the tolerability, including long-term cardiometabolic effects, will be important complementary data to consider,” Dr. Correll said.
The study was funded by Sunovion Pharmaceuticals. Dr. Singh is on the advisory board for Sunovion, is a consultant for Google X and Limbix, and receives royalties from American Psychiatric Association Publishing. She has also received research support from Stanford’s Maternal Child Health Research Institute and Department of Psychiatry, the National Institute of Mental Health, the National Institute on Aging, Johnson and Johnson, Allergan, PCORI, and the Brain and Behavior Research Foundation. Dr. Correll has been a consultant or adviser to and has received honoraria from Sunovion, as well as Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
FROM ASCP 2020
Irritability strongly linked to suicidal behavior in major depression
Irritability in adults with major depressive disorder (MDD) and stimulant use disorder (SUD) is strongly linked to suicidality and should be assessed by clinicians.
Three clinical trials of adults with MDD and one trial of adults with SUD showed that the link between irritability and suicidality was stronger than the association between depression severity and suicidal behaviors.
“Irritability is an important construct that is not often studied in adults with major depressive disorder,” Manish K. Jha, MD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“If you look at current diagnostic convention, irritability is not considered a symptom of major depressive episodes in adults, but below age 18, it is considered one of the two main symptoms,” Dr. Jha said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2020 annual Meeting.
Clinically useful
Irritability is assessed using age-related norms of behavior, Dr. Jha said.
“The best way to conceptualize it is that it is the propensity to get angry easily or more frequently as compared to peers in response to frustration. I have a 2½-year old, and if he throws a tantrum, that is perfectly age appropriate. But if I do the same thing, it would be extreme irritability. The pediatric literature uses the word ‘grouchiness,’ but it is a little bit difficult to define, in part because it hasn’t been studied extensively,” he said.
To better understand the potential association between irritability and suicidality, the investigators reviewed results of three trials involving adults with MDD. These trials were CO-MED (Combining Medications to Enhance Depression Outcomes), which included 665 patients; EMBARC (Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care), which included 296 patients; and SAMS (Suicide Assessment Methodology Study), which included 266 patients.
They also examined the STRIDE (Stimulant Reduction Intervention Using Dosed Exercise) study, which was conducted in 302 adults with SUD.
All studies assessed irritability using the Concise Associated Symptom Tracking scale, a 5-point Likert scale. The trials also assessed suicidality with the Concise Health Risk Tracking Suicidal Thoughts.
The investigators found that irritability and suicidality were positively correlated. The association between irritability and suicidality was 2-11 times stronger than the link to overall depression.
Higher irritability at baseline predicted higher levels of suicidality at week 9 in CO-MED (P = .011), EMBARC (P < .0001), and STRIDE (P = .007), but not in SAMS (P = .21).
Greater reduction in irritability from baseline to week 4 predicted lower levels of suicidality at week 8 in CO-MED (P = .007), EMBARC (P < .0001), and STRIDE (P < .0001), but not in SAMS (P = .065).
Similarly, lower baseline levels and greater reductions in irritability were associated with lower levels of suicidality at week 28 of CO-MED, week 16 of EMBARC, and week 36 of STRIDE.
, and he believes that measuring irritability in MDD “has clinical utility.”
A common and disabling symptom
Commenting on the study, Sanjay J. Mathew, MD, professor of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, said the findings provide further support that irritability is a relatively common and disabling symptom associated with major depression.
“The presence of significant irritability was associated with higher levels of suicidal ideation and is therefore highly relevant for clinicians to assess,” said Dr. Mathew, who was not part of the study.
“Early improvements in irritability are associated with better longer-term outcomes with antidepressant treatments, and this highlights the need for careful clinical evaluation early on in the course of antidepressant therapy, ideally within the first 2 weeks,” he said.
Dr. Jha reports financial relationships with Acadia Pharmaceuticals and Janssen Research & Development. Dr. Mathew reports financial relationships with Allergan, Vistagen, Janssen, Clexio, and Biohaven.
A version of this article originally appeared on Medscape.com.
Irritability in adults with major depressive disorder (MDD) and stimulant use disorder (SUD) is strongly linked to suicidality and should be assessed by clinicians.
Three clinical trials of adults with MDD and one trial of adults with SUD showed that the link between irritability and suicidality was stronger than the association between depression severity and suicidal behaviors.
“Irritability is an important construct that is not often studied in adults with major depressive disorder,” Manish K. Jha, MD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“If you look at current diagnostic convention, irritability is not considered a symptom of major depressive episodes in adults, but below age 18, it is considered one of the two main symptoms,” Dr. Jha said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2020 annual Meeting.
Clinically useful
Irritability is assessed using age-related norms of behavior, Dr. Jha said.
“The best way to conceptualize it is that it is the propensity to get angry easily or more frequently as compared to peers in response to frustration. I have a 2½-year old, and if he throws a tantrum, that is perfectly age appropriate. But if I do the same thing, it would be extreme irritability. The pediatric literature uses the word ‘grouchiness,’ but it is a little bit difficult to define, in part because it hasn’t been studied extensively,” he said.
To better understand the potential association between irritability and suicidality, the investigators reviewed results of three trials involving adults with MDD. These trials were CO-MED (Combining Medications to Enhance Depression Outcomes), which included 665 patients; EMBARC (Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care), which included 296 patients; and SAMS (Suicide Assessment Methodology Study), which included 266 patients.
They also examined the STRIDE (Stimulant Reduction Intervention Using Dosed Exercise) study, which was conducted in 302 adults with SUD.
All studies assessed irritability using the Concise Associated Symptom Tracking scale, a 5-point Likert scale. The trials also assessed suicidality with the Concise Health Risk Tracking Suicidal Thoughts.
The investigators found that irritability and suicidality were positively correlated. The association between irritability and suicidality was 2-11 times stronger than the link to overall depression.
Higher irritability at baseline predicted higher levels of suicidality at week 9 in CO-MED (P = .011), EMBARC (P < .0001), and STRIDE (P = .007), but not in SAMS (P = .21).
Greater reduction in irritability from baseline to week 4 predicted lower levels of suicidality at week 8 in CO-MED (P = .007), EMBARC (P < .0001), and STRIDE (P < .0001), but not in SAMS (P = .065).
Similarly, lower baseline levels and greater reductions in irritability were associated with lower levels of suicidality at week 28 of CO-MED, week 16 of EMBARC, and week 36 of STRIDE.
, and he believes that measuring irritability in MDD “has clinical utility.”
A common and disabling symptom
Commenting on the study, Sanjay J. Mathew, MD, professor of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, said the findings provide further support that irritability is a relatively common and disabling symptom associated with major depression.
“The presence of significant irritability was associated with higher levels of suicidal ideation and is therefore highly relevant for clinicians to assess,” said Dr. Mathew, who was not part of the study.
“Early improvements in irritability are associated with better longer-term outcomes with antidepressant treatments, and this highlights the need for careful clinical evaluation early on in the course of antidepressant therapy, ideally within the first 2 weeks,” he said.
Dr. Jha reports financial relationships with Acadia Pharmaceuticals and Janssen Research & Development. Dr. Mathew reports financial relationships with Allergan, Vistagen, Janssen, Clexio, and Biohaven.
A version of this article originally appeared on Medscape.com.
Irritability in adults with major depressive disorder (MDD) and stimulant use disorder (SUD) is strongly linked to suicidality and should be assessed by clinicians.
Three clinical trials of adults with MDD and one trial of adults with SUD showed that the link between irritability and suicidality was stronger than the association between depression severity and suicidal behaviors.
“Irritability is an important construct that is not often studied in adults with major depressive disorder,” Manish K. Jha, MD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“If you look at current diagnostic convention, irritability is not considered a symptom of major depressive episodes in adults, but below age 18, it is considered one of the two main symptoms,” Dr. Jha said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2020 annual Meeting.
Clinically useful
Irritability is assessed using age-related norms of behavior, Dr. Jha said.
“The best way to conceptualize it is that it is the propensity to get angry easily or more frequently as compared to peers in response to frustration. I have a 2½-year old, and if he throws a tantrum, that is perfectly age appropriate. But if I do the same thing, it would be extreme irritability. The pediatric literature uses the word ‘grouchiness,’ but it is a little bit difficult to define, in part because it hasn’t been studied extensively,” he said.
To better understand the potential association between irritability and suicidality, the investigators reviewed results of three trials involving adults with MDD. These trials were CO-MED (Combining Medications to Enhance Depression Outcomes), which included 665 patients; EMBARC (Establishing Moderators and Biosignatures of Antidepressant Response in Clinical Care), which included 296 patients; and SAMS (Suicide Assessment Methodology Study), which included 266 patients.
They also examined the STRIDE (Stimulant Reduction Intervention Using Dosed Exercise) study, which was conducted in 302 adults with SUD.
All studies assessed irritability using the Concise Associated Symptom Tracking scale, a 5-point Likert scale. The trials also assessed suicidality with the Concise Health Risk Tracking Suicidal Thoughts.
The investigators found that irritability and suicidality were positively correlated. The association between irritability and suicidality was 2-11 times stronger than the link to overall depression.
Higher irritability at baseline predicted higher levels of suicidality at week 9 in CO-MED (P = .011), EMBARC (P < .0001), and STRIDE (P = .007), but not in SAMS (P = .21).
Greater reduction in irritability from baseline to week 4 predicted lower levels of suicidality at week 8 in CO-MED (P = .007), EMBARC (P < .0001), and STRIDE (P < .0001), but not in SAMS (P = .065).
Similarly, lower baseline levels and greater reductions in irritability were associated with lower levels of suicidality at week 28 of CO-MED, week 16 of EMBARC, and week 36 of STRIDE.
, and he believes that measuring irritability in MDD “has clinical utility.”
A common and disabling symptom
Commenting on the study, Sanjay J. Mathew, MD, professor of psychiatry and behavioral sciences at Baylor College of Medicine, Houston, said the findings provide further support that irritability is a relatively common and disabling symptom associated with major depression.
“The presence of significant irritability was associated with higher levels of suicidal ideation and is therefore highly relevant for clinicians to assess,” said Dr. Mathew, who was not part of the study.
“Early improvements in irritability are associated with better longer-term outcomes with antidepressant treatments, and this highlights the need for careful clinical evaluation early on in the course of antidepressant therapy, ideally within the first 2 weeks,” he said.
Dr. Jha reports financial relationships with Acadia Pharmaceuticals and Janssen Research & Development. Dr. Mathew reports financial relationships with Allergan, Vistagen, Janssen, Clexio, and Biohaven.
A version of this article originally appeared on Medscape.com.
First-in-class antipsychotic linked to lower cardiometabolic risk
A recently approved first-in-class antipsychotic appears to have fewer adverse cardiometabolic effects than standard care with risperidone, new research suggests.
In post hoc analyses of two short-term randomized controlled trials plus an open-label long-term study, patients with schizophrenia on lumateperone (Caplyta, Intra-Cellular Therapies) had reduced rates of metabolic syndrome, compared with their counterparts taking placebo or the antipsychotic risperidone.
In the short-term studies, rates of metabolic syndrome were similar between groups at baseline, but by the end of 4 and 6 weeks of treatment, 25% of patients taking lumateperone no longer met criteria for metabolic syndrome. A similar finding occurred in 36% of patients in the 1-year open label study.
“One of the major advantages that we found during the drug’s development was that it has a very favorable profile with regard to changes in weight, and other [parameters] associated with cardiovascular disease risk, such as elevated glucose and lipids,” study investigator Andrew Satlin, MD, chief medical officer at Intra-Cellular Therapies, New York, told this news organization.
“So we went back to our data and looked to see whether the changes that we saw had an impact on either the development or the resolution of metabolic syndrome in the patients who came into our studies,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Reduced cholesterol
Lumateperone was approved in December by the Food and Drug Administration. The drug acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
The short-term studies included 511 patients randomly assigned to receive lumateperone 42 mg (n = 256 patients) or risperidone 4 mg (n = 255 patients).
At baseline, rates of metabolic syndrome were 16% in the lumateperone group and 19% in the risperidone group. At the end of treatment, metabolic syndrome was less common in the lumateperone group (13%) vs. those receiving risperidone (25%).
In addition, 46% of lumateperone patients with metabolic syndrome at baseline no longer had it at the end of the study period. This compared with 25% of patients on risperidone.
The differences in metabolic syndrome conversion rates appeared to be driven by greater reductions in total cholesterol with lumateperone, compared with risperidone (–2.8 mg/dL with lumateperone vs. 4.8 mg/dL with risperidone) and triglycerides (–0.7 mg/dL with lumateperone vs. 20.4 mg/dL with risperidone).
Greater increases in blood glucose were also seen with risperidone (7.7 mg/dL) than with lumateperone (0.9 mg/dL).
The long-term study included 602 patients with stable schizophrenia. All received lumateperone 42 mg, and 197 patients (33%) had metabolic syndrome at baseline.
At the end of the 1-year study, 72 of these patients (36%) no longer met criteria for metabolic syndrome.
“Safest antipsychotic so far”
“Lumateperone seems to be the safest antipsychotic we have seen so far,” Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charité Universitatsmedizin, Berlin, who was also involved in clinical trials of lumateperone, told this news organization.
“It seems to be very safe when it comes to cardiometabolic parameters, and it shows similar reduction in symptoms as risperidone. It is certainly an agent one should consider, particularly when a patient cannot tolerate other medications or may not be in full adherence,” said Dr. Correll, who has a joint appointment as professor of psychiatry and molecular medicine at the Zucker School of Medicine at Hofstra University in Hempstead, New York.
The drug’s safety and efficacy profile would make it a good candidate in patients initiating antipsychotic treatment, but reimbursement issues may be a barrier, at least for now, he added.
He said that the drug may prevent the onset of metabolic side effects and added that once payers are willing to reimburse the drug it should become the “first-line standard of care.”
It is well known that atypical antipsychotics are associated with adverse and rapid metabolic changes. Dr. Correll noted that particularly early-phase and first-episode patients can be “very sensitive” to the side effects of these drugs and often experience rapid weight gain and other adverse metabolic changes. Lumateperone, he added, may help avoid some of this cardiometabolic risk.
Time will tell
Jessica M. Gannon, MD, a psychiatrist at the University of Pittsburgh said in commenting on the findings that the drug’s favorable metabolic profile has previously been reported.
She also noted that there has been some interest in lumateperone because of possible “downstream effects on NMDA-type glutamate receptor activity, a larger binding ratio at dopamine-2:5HT1A receptors than other atypical antipsychotics, and presynaptic D2 partial agonism and a postsynaptic D2 antagonism.”
“This latter feature may explain the reported low extrapyramidal symptom incidence in the clinical trials,” she said .
“While I think future studies and clinical use can help determine how clinically efficacious this medication will be for our patients when compared to others on the market, its favorable metabolic and EPS profile do make it of interest,” added Gannon, who was not involved in researching the drug.
The study was funded by Intra-Cellular Therapies. Dr. Satlin is chief medical officer of Intracellular Therapies. Dr. Correll has been a consultant or advisor to and has received honoraria from Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Sunovion, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
A recently approved first-in-class antipsychotic appears to have fewer adverse cardiometabolic effects than standard care with risperidone, new research suggests.
In post hoc analyses of two short-term randomized controlled trials plus an open-label long-term study, patients with schizophrenia on lumateperone (Caplyta, Intra-Cellular Therapies) had reduced rates of metabolic syndrome, compared with their counterparts taking placebo or the antipsychotic risperidone.
In the short-term studies, rates of metabolic syndrome were similar between groups at baseline, but by the end of 4 and 6 weeks of treatment, 25% of patients taking lumateperone no longer met criteria for metabolic syndrome. A similar finding occurred in 36% of patients in the 1-year open label study.
“One of the major advantages that we found during the drug’s development was that it has a very favorable profile with regard to changes in weight, and other [parameters] associated with cardiovascular disease risk, such as elevated glucose and lipids,” study investigator Andrew Satlin, MD, chief medical officer at Intra-Cellular Therapies, New York, told this news organization.
“So we went back to our data and looked to see whether the changes that we saw had an impact on either the development or the resolution of metabolic syndrome in the patients who came into our studies,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Reduced cholesterol
Lumateperone was approved in December by the Food and Drug Administration. The drug acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
The short-term studies included 511 patients randomly assigned to receive lumateperone 42 mg (n = 256 patients) or risperidone 4 mg (n = 255 patients).
At baseline, rates of metabolic syndrome were 16% in the lumateperone group and 19% in the risperidone group. At the end of treatment, metabolic syndrome was less common in the lumateperone group (13%) vs. those receiving risperidone (25%).
In addition, 46% of lumateperone patients with metabolic syndrome at baseline no longer had it at the end of the study period. This compared with 25% of patients on risperidone.
The differences in metabolic syndrome conversion rates appeared to be driven by greater reductions in total cholesterol with lumateperone, compared with risperidone (–2.8 mg/dL with lumateperone vs. 4.8 mg/dL with risperidone) and triglycerides (–0.7 mg/dL with lumateperone vs. 20.4 mg/dL with risperidone).
Greater increases in blood glucose were also seen with risperidone (7.7 mg/dL) than with lumateperone (0.9 mg/dL).
The long-term study included 602 patients with stable schizophrenia. All received lumateperone 42 mg, and 197 patients (33%) had metabolic syndrome at baseline.
At the end of the 1-year study, 72 of these patients (36%) no longer met criteria for metabolic syndrome.
“Safest antipsychotic so far”
“Lumateperone seems to be the safest antipsychotic we have seen so far,” Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charité Universitatsmedizin, Berlin, who was also involved in clinical trials of lumateperone, told this news organization.
“It seems to be very safe when it comes to cardiometabolic parameters, and it shows similar reduction in symptoms as risperidone. It is certainly an agent one should consider, particularly when a patient cannot tolerate other medications or may not be in full adherence,” said Dr. Correll, who has a joint appointment as professor of psychiatry and molecular medicine at the Zucker School of Medicine at Hofstra University in Hempstead, New York.
The drug’s safety and efficacy profile would make it a good candidate in patients initiating antipsychotic treatment, but reimbursement issues may be a barrier, at least for now, he added.
He said that the drug may prevent the onset of metabolic side effects and added that once payers are willing to reimburse the drug it should become the “first-line standard of care.”
It is well known that atypical antipsychotics are associated with adverse and rapid metabolic changes. Dr. Correll noted that particularly early-phase and first-episode patients can be “very sensitive” to the side effects of these drugs and often experience rapid weight gain and other adverse metabolic changes. Lumateperone, he added, may help avoid some of this cardiometabolic risk.
Time will tell
Jessica M. Gannon, MD, a psychiatrist at the University of Pittsburgh said in commenting on the findings that the drug’s favorable metabolic profile has previously been reported.
She also noted that there has been some interest in lumateperone because of possible “downstream effects on NMDA-type glutamate receptor activity, a larger binding ratio at dopamine-2:5HT1A receptors than other atypical antipsychotics, and presynaptic D2 partial agonism and a postsynaptic D2 antagonism.”
“This latter feature may explain the reported low extrapyramidal symptom incidence in the clinical trials,” she said .
“While I think future studies and clinical use can help determine how clinically efficacious this medication will be for our patients when compared to others on the market, its favorable metabolic and EPS profile do make it of interest,” added Gannon, who was not involved in researching the drug.
The study was funded by Intra-Cellular Therapies. Dr. Satlin is chief medical officer of Intracellular Therapies. Dr. Correll has been a consultant or advisor to and has received honoraria from Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Sunovion, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
A recently approved first-in-class antipsychotic appears to have fewer adverse cardiometabolic effects than standard care with risperidone, new research suggests.
In post hoc analyses of two short-term randomized controlled trials plus an open-label long-term study, patients with schizophrenia on lumateperone (Caplyta, Intra-Cellular Therapies) had reduced rates of metabolic syndrome, compared with their counterparts taking placebo or the antipsychotic risperidone.
In the short-term studies, rates of metabolic syndrome were similar between groups at baseline, but by the end of 4 and 6 weeks of treatment, 25% of patients taking lumateperone no longer met criteria for metabolic syndrome. A similar finding occurred in 36% of patients in the 1-year open label study.
“One of the major advantages that we found during the drug’s development was that it has a very favorable profile with regard to changes in weight, and other [parameters] associated with cardiovascular disease risk, such as elevated glucose and lipids,” study investigator Andrew Satlin, MD, chief medical officer at Intra-Cellular Therapies, New York, told this news organization.
“So we went back to our data and looked to see whether the changes that we saw had an impact on either the development or the resolution of metabolic syndrome in the patients who came into our studies,” he said.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Reduced cholesterol
Lumateperone was approved in December by the Food and Drug Administration. The drug acts synergistically through the serotonergic, dopaminergic, and glutamatergic systems.
The short-term studies included 511 patients randomly assigned to receive lumateperone 42 mg (n = 256 patients) or risperidone 4 mg (n = 255 patients).
At baseline, rates of metabolic syndrome were 16% in the lumateperone group and 19% in the risperidone group. At the end of treatment, metabolic syndrome was less common in the lumateperone group (13%) vs. those receiving risperidone (25%).
In addition, 46% of lumateperone patients with metabolic syndrome at baseline no longer had it at the end of the study period. This compared with 25% of patients on risperidone.
The differences in metabolic syndrome conversion rates appeared to be driven by greater reductions in total cholesterol with lumateperone, compared with risperidone (–2.8 mg/dL with lumateperone vs. 4.8 mg/dL with risperidone) and triglycerides (–0.7 mg/dL with lumateperone vs. 20.4 mg/dL with risperidone).
Greater increases in blood glucose were also seen with risperidone (7.7 mg/dL) than with lumateperone (0.9 mg/dL).
The long-term study included 602 patients with stable schizophrenia. All received lumateperone 42 mg, and 197 patients (33%) had metabolic syndrome at baseline.
At the end of the 1-year study, 72 of these patients (36%) no longer met criteria for metabolic syndrome.
“Safest antipsychotic so far”
“Lumateperone seems to be the safest antipsychotic we have seen so far,” Christoph U. Correll, MD, professor of child and adolescent psychiatry, Charité Universitatsmedizin, Berlin, who was also involved in clinical trials of lumateperone, told this news organization.
“It seems to be very safe when it comes to cardiometabolic parameters, and it shows similar reduction in symptoms as risperidone. It is certainly an agent one should consider, particularly when a patient cannot tolerate other medications or may not be in full adherence,” said Dr. Correll, who has a joint appointment as professor of psychiatry and molecular medicine at the Zucker School of Medicine at Hofstra University in Hempstead, New York.
The drug’s safety and efficacy profile would make it a good candidate in patients initiating antipsychotic treatment, but reimbursement issues may be a barrier, at least for now, he added.
He said that the drug may prevent the onset of metabolic side effects and added that once payers are willing to reimburse the drug it should become the “first-line standard of care.”
It is well known that atypical antipsychotics are associated with adverse and rapid metabolic changes. Dr. Correll noted that particularly early-phase and first-episode patients can be “very sensitive” to the side effects of these drugs and often experience rapid weight gain and other adverse metabolic changes. Lumateperone, he added, may help avoid some of this cardiometabolic risk.
Time will tell
Jessica M. Gannon, MD, a psychiatrist at the University of Pittsburgh said in commenting on the findings that the drug’s favorable metabolic profile has previously been reported.
She also noted that there has been some interest in lumateperone because of possible “downstream effects on NMDA-type glutamate receptor activity, a larger binding ratio at dopamine-2:5HT1A receptors than other atypical antipsychotics, and presynaptic D2 partial agonism and a postsynaptic D2 antagonism.”
“This latter feature may explain the reported low extrapyramidal symptom incidence in the clinical trials,” she said .
“While I think future studies and clinical use can help determine how clinically efficacious this medication will be for our patients when compared to others on the market, its favorable metabolic and EPS profile do make it of interest,” added Gannon, who was not involved in researching the drug.
The study was funded by Intra-Cellular Therapies. Dr. Satlin is chief medical officer of Intracellular Therapies. Dr. Correll has been a consultant or advisor to and has received honoraria from Acadia, Alkermes, Allergan, Angelini, Axsome, Gedeon Richter, Gerson Lehrman Group, Intra-Cellular Therapies, Janssen/J&J, LB Pharma, Lundbeck, MedAvante-ProPhase, Medscape, Neurocrine, Noven, Otsuka, Pfizer, Recordati, Rovi, Sumitomo Dainippon, Sunovion, Supernus, Takeda, and Teva.
A version of this article originally appeared on Medscape.com.
Dietary intervention cuts mood swings, other bipolar symptoms
A nutritional intervention with a focus on fatty acids appears to reduce mood swings in patients with bipolar disorder (BD) when used as an adjunct to pharmacotherapy, early research suggests.
In a single-center study, patients with BD who received a diet consisting of high omega-3 plus low omega-6 fatty acids (H3-L6), in addition to usual care, showed significant reductions in mood variability, irritability, and pain, compared with their counterparts who received a diet with usual levels of omega-3 and omega-6 fatty acids commonly consumed in regular U.S. diets.
“Our findings need replication and validation in other studies,” study coinvestigator Erika Saunders, MD, professor and chair of the department of psychiatry and behavioral health at Penn State Health, Hershey, said in an interview.
“While we got really exciting findings, it’s far from confirmatory or the last word on the subject. The fatty acids do two broad things. They incorporate into the membranes of neurons in the brain and they also create signaling molecules throughout the brain and the body that interact with the immune system and the inflammatory system. And we suspect that it is through those mechanisms that this composition of fatty acids is having an effect on mood stability, but lots more work needs to be done to figure that out,” Dr. Saunders added.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Fewer mood swings
Many patients with bipolar disorder do not achieve complete mood stability with medication, making the need for additional treatments imperative, she added.
“We were interested in looking at treatments that improved mood stability in bipolar disorder that are well tolerated by patients and that can be added to pharmacological treatments. We studied this particular nutritional intervention because biologically it does some of the same things that effective medications for bipolar disorder do and it has been investigated as an effective treatment for conditions like migraine headaches, which has a lot of overlap and comorbidity with bipolar disorder.”
The researchers randomized 41 patients with BD to receive the nutritional intervention of high omega-3 plus low omega-6 (H3-L6) and 41 patients with BD to receive a control diet of usual US levels of omega-3 and omega-6 fatty acids.
The patients were aged 20-75 years (mean age, 43.5 +/– 13.9 years) and 83% were women. They had similar mean levels of mood symptoms and pain.
All patients received group-specific study foods and oils, as well as intensive dietary counseling from a dietitian, access to a website with recipes, and guidance for eating in restaurants. All participants were blinded to the composition of the food that they were eating.
Both the interventional diet and the control diet were tailored for the purposes of the study, noted coinvestigator Sarah Shahriar, a research assistant at Penn State.
“The interventional group had more fatty fish such as salmon and tuna, while the control group had more white fish and fish with less fatty acid content. The interventional group also received a different type of cooking oil, which was a blend of olive and macadamia-nut oil, which was specially formulated by a research nutritional service at the University of North Carolina,” Ms. Shahriar said in an interview.
“They also decreased their red meat consumption and received specially formulated snack foods, which were specifically prepared by [the university’s] research nutritional service. It is important to point out that these diets were for a very specific purpose. We are not saying in any way shape or form that this particular nutritional intervention is good in general,” she added.
After 12 weeks, significant reductions were seen in mood variability, energy, irritability, and pain in the H3-L6 group (P < .001). The only symptom that was significantly lowered in the control group was impulsive thoughts (P = .004).
“The best message for doctors to tell their patients at this point is one of general nutritional health and the importance of nutrition in overall body and brain health, and that [this] can be a very important component of mood,” Dr. Saunders said.
Diet matters
“Highly unsaturated fatty acids are important components of neuronal cell membranes and in cell signaling,” Jessica M. Gannon, MD, University of Pittsburgh, who was not part of the study, said in an interview.
“Omega-6 fatty acids are precursors to proinflammatory compounds. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid are thought to be competitive inhibitors of omega-6 and thought to have anti-inflammatory effects. Supplementation with omega-3 has been explored in cardiovascular disease, diabetes, and in rheumatologic disorders as well as in a host of psychiatric disorders, including bipolar disorders, where a possible treatment effect has been suggested,” Dr. Gannon said.
Dietary interventions targeting not only increasing omega-3 but also decreasing consumption of omega-6 rich foods could be both effective and attractive to patients invested in a healthy lifestyle for promotion of mental health, especially when they are not optimally controlled by prescribed medications, she added.
“This study suggests that such an intervention could prove beneficial, although significant patient support may be necessary to assure adherence to the diet. I would agree that future studies would be worth pursuing,” Dr. Gannon said.
The investigators and Dr. Gannon have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A nutritional intervention with a focus on fatty acids appears to reduce mood swings in patients with bipolar disorder (BD) when used as an adjunct to pharmacotherapy, early research suggests.
In a single-center study, patients with BD who received a diet consisting of high omega-3 plus low omega-6 fatty acids (H3-L6), in addition to usual care, showed significant reductions in mood variability, irritability, and pain, compared with their counterparts who received a diet with usual levels of omega-3 and omega-6 fatty acids commonly consumed in regular U.S. diets.
“Our findings need replication and validation in other studies,” study coinvestigator Erika Saunders, MD, professor and chair of the department of psychiatry and behavioral health at Penn State Health, Hershey, said in an interview.
“While we got really exciting findings, it’s far from confirmatory or the last word on the subject. The fatty acids do two broad things. They incorporate into the membranes of neurons in the brain and they also create signaling molecules throughout the brain and the body that interact with the immune system and the inflammatory system. And we suspect that it is through those mechanisms that this composition of fatty acids is having an effect on mood stability, but lots more work needs to be done to figure that out,” Dr. Saunders added.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Fewer mood swings
Many patients with bipolar disorder do not achieve complete mood stability with medication, making the need for additional treatments imperative, she added.
“We were interested in looking at treatments that improved mood stability in bipolar disorder that are well tolerated by patients and that can be added to pharmacological treatments. We studied this particular nutritional intervention because biologically it does some of the same things that effective medications for bipolar disorder do and it has been investigated as an effective treatment for conditions like migraine headaches, which has a lot of overlap and comorbidity with bipolar disorder.”
The researchers randomized 41 patients with BD to receive the nutritional intervention of high omega-3 plus low omega-6 (H3-L6) and 41 patients with BD to receive a control diet of usual US levels of omega-3 and omega-6 fatty acids.
The patients were aged 20-75 years (mean age, 43.5 +/– 13.9 years) and 83% were women. They had similar mean levels of mood symptoms and pain.
All patients received group-specific study foods and oils, as well as intensive dietary counseling from a dietitian, access to a website with recipes, and guidance for eating in restaurants. All participants were blinded to the composition of the food that they were eating.
Both the interventional diet and the control diet were tailored for the purposes of the study, noted coinvestigator Sarah Shahriar, a research assistant at Penn State.
“The interventional group had more fatty fish such as salmon and tuna, while the control group had more white fish and fish with less fatty acid content. The interventional group also received a different type of cooking oil, which was a blend of olive and macadamia-nut oil, which was specially formulated by a research nutritional service at the University of North Carolina,” Ms. Shahriar said in an interview.
“They also decreased their red meat consumption and received specially formulated snack foods, which were specifically prepared by [the university’s] research nutritional service. It is important to point out that these diets were for a very specific purpose. We are not saying in any way shape or form that this particular nutritional intervention is good in general,” she added.
After 12 weeks, significant reductions were seen in mood variability, energy, irritability, and pain in the H3-L6 group (P < .001). The only symptom that was significantly lowered in the control group was impulsive thoughts (P = .004).
“The best message for doctors to tell their patients at this point is one of general nutritional health and the importance of nutrition in overall body and brain health, and that [this] can be a very important component of mood,” Dr. Saunders said.
Diet matters
“Highly unsaturated fatty acids are important components of neuronal cell membranes and in cell signaling,” Jessica M. Gannon, MD, University of Pittsburgh, who was not part of the study, said in an interview.
“Omega-6 fatty acids are precursors to proinflammatory compounds. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid are thought to be competitive inhibitors of omega-6 and thought to have anti-inflammatory effects. Supplementation with omega-3 has been explored in cardiovascular disease, diabetes, and in rheumatologic disorders as well as in a host of psychiatric disorders, including bipolar disorders, where a possible treatment effect has been suggested,” Dr. Gannon said.
Dietary interventions targeting not only increasing omega-3 but also decreasing consumption of omega-6 rich foods could be both effective and attractive to patients invested in a healthy lifestyle for promotion of mental health, especially when they are not optimally controlled by prescribed medications, she added.
“This study suggests that such an intervention could prove beneficial, although significant patient support may be necessary to assure adherence to the diet. I would agree that future studies would be worth pursuing,” Dr. Gannon said.
The investigators and Dr. Gannon have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A nutritional intervention with a focus on fatty acids appears to reduce mood swings in patients with bipolar disorder (BD) when used as an adjunct to pharmacotherapy, early research suggests.
In a single-center study, patients with BD who received a diet consisting of high omega-3 plus low omega-6 fatty acids (H3-L6), in addition to usual care, showed significant reductions in mood variability, irritability, and pain, compared with their counterparts who received a diet with usual levels of omega-3 and omega-6 fatty acids commonly consumed in regular U.S. diets.
“Our findings need replication and validation in other studies,” study coinvestigator Erika Saunders, MD, professor and chair of the department of psychiatry and behavioral health at Penn State Health, Hershey, said in an interview.
“While we got really exciting findings, it’s far from confirmatory or the last word on the subject. The fatty acids do two broad things. They incorporate into the membranes of neurons in the brain and they also create signaling molecules throughout the brain and the body that interact with the immune system and the inflammatory system. And we suspect that it is through those mechanisms that this composition of fatty acids is having an effect on mood stability, but lots more work needs to be done to figure that out,” Dr. Saunders added.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Fewer mood swings
Many patients with bipolar disorder do not achieve complete mood stability with medication, making the need for additional treatments imperative, she added.
“We were interested in looking at treatments that improved mood stability in bipolar disorder that are well tolerated by patients and that can be added to pharmacological treatments. We studied this particular nutritional intervention because biologically it does some of the same things that effective medications for bipolar disorder do and it has been investigated as an effective treatment for conditions like migraine headaches, which has a lot of overlap and comorbidity with bipolar disorder.”
The researchers randomized 41 patients with BD to receive the nutritional intervention of high omega-3 plus low omega-6 (H3-L6) and 41 patients with BD to receive a control diet of usual US levels of omega-3 and omega-6 fatty acids.
The patients were aged 20-75 years (mean age, 43.5 +/– 13.9 years) and 83% were women. They had similar mean levels of mood symptoms and pain.
All patients received group-specific study foods and oils, as well as intensive dietary counseling from a dietitian, access to a website with recipes, and guidance for eating in restaurants. All participants were blinded to the composition of the food that they were eating.
Both the interventional diet and the control diet were tailored for the purposes of the study, noted coinvestigator Sarah Shahriar, a research assistant at Penn State.
“The interventional group had more fatty fish such as salmon and tuna, while the control group had more white fish and fish with less fatty acid content. The interventional group also received a different type of cooking oil, which was a blend of olive and macadamia-nut oil, which was specially formulated by a research nutritional service at the University of North Carolina,” Ms. Shahriar said in an interview.
“They also decreased their red meat consumption and received specially formulated snack foods, which were specifically prepared by [the university’s] research nutritional service. It is important to point out that these diets were for a very specific purpose. We are not saying in any way shape or form that this particular nutritional intervention is good in general,” she added.
After 12 weeks, significant reductions were seen in mood variability, energy, irritability, and pain in the H3-L6 group (P < .001). The only symptom that was significantly lowered in the control group was impulsive thoughts (P = .004).
“The best message for doctors to tell their patients at this point is one of general nutritional health and the importance of nutrition in overall body and brain health, and that [this] can be a very important component of mood,” Dr. Saunders said.
Diet matters
“Highly unsaturated fatty acids are important components of neuronal cell membranes and in cell signaling,” Jessica M. Gannon, MD, University of Pittsburgh, who was not part of the study, said in an interview.
“Omega-6 fatty acids are precursors to proinflammatory compounds. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid are thought to be competitive inhibitors of omega-6 and thought to have anti-inflammatory effects. Supplementation with omega-3 has been explored in cardiovascular disease, diabetes, and in rheumatologic disorders as well as in a host of psychiatric disorders, including bipolar disorders, where a possible treatment effect has been suggested,” Dr. Gannon said.
Dietary interventions targeting not only increasing omega-3 but also decreasing consumption of omega-6 rich foods could be both effective and attractive to patients invested in a healthy lifestyle for promotion of mental health, especially when they are not optimally controlled by prescribed medications, she added.
“This study suggests that such an intervention could prove beneficial, although significant patient support may be necessary to assure adherence to the diet. I would agree that future studies would be worth pursuing,” Dr. Gannon said.
The investigators and Dr. Gannon have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.





