User login
Current Perspectives on Transport Medicine in Pediatric Hospital Medicine Fellowships
Transport medicine (TM) involves the provision of care to patients who require transfer to a healthcare facility that can deliver definitive treatment.1 Pediatric interfacility transport occurs in approximately 10% of nonneonatal, nonpregnancy pediatric hospitalizations in the United States.2 Studies document a decline in resident participation in pediatric transports and variability in curricular content.3,4
The Pediatric Hospital Medicine (PHM) Core Competencies include “Transport of the Critically Ill Child.”7 Additionally, the Curriculum Committee of the PHM Fellowship Directors Council proposed a curricular framework that includes a required clinical experience in “Care and Stabilization of the Critically Ill Child,”8 which can occur in a variety of practice settings, including TM. TM is also listed as a potential elective rotation.
In 2014, 60% of PHM fellowships included a required or optional TM rotation.9 A recent study of pediatric emergency, critical care, and neonatal medicine fellowships revealed a paucity of formal or published TM curricula in these programs.10 Furthermore, no standard or published TM curricula have been established for PHM fellowships. The primary objective of our study is to determine attitudes regarding TM training among PHM fellows, recent PHM fellowship graduates, and PHM fellowship program directors (PDs). The secondary objective is to identify how the perspectives of these fellowship stakeholders could influence the design of a TM curriculum.
METHODS
This cross-sectional study focused on 3 stakeholder groups related to PHM fellowships. The subjects included in the study were physicians enrolled in a PHM fellowship (fellow) during the 2015-2016 academic year, graduates of fellowship (graduate) between 2010 and 2015, and fellowship program directors (PD). Unique web-based, anonymous surveys for each group were developed, reviewed by content and methodology experts, and piloted with local pediatric hospitalists. Surveys consisted of unfolding multiple-choice questions and ranking items along Likert scales and the Dreyfus model.
Questions were designed to elicit demographic data, perspectives, and experience related to TM education in PHM fellowships across all respondent groups. Depending on the context, identical or similar questions were asked among the groups. For example, all groups were asked to prioritize learning objectives for a TM rotation. Graduates and PDs reported the most effective teaching methods for use during a TM rotation. Fellows rated their own interest in a TM elective, and PDs were asked to rate the level of interest among their fellows.
Participant contact information was obtained from a website (phmfellows.org) and databases of fellows and graduates, which are maintained by the PHM Fellowship Directors Council (personal communication, Jayne Truckenbrod, DO; February 2, 2017). Between February and April 2016, the participants were individually emailed a link to their respective surveys, and 3 reminder e-mails were sent to nonresponders. The survey was administered through SurveyMonkey (www.surveymonkey.com).
SPSS (IBM SPSS Statistics, IBM Corporation, Armonk, New York) was used for statistical analysis. Descriptive data were presented using mean and standard deviation. Comparisons among fellows, graduates, and PDs were conducted using one-way analyses of variance or Mann-Whitney U test. Frequency of application and self-evaluation of core competency skills before and after the rotation were evaluated using paired sample t-tests. The study protocol was deemed exempt from review by our local Institutional Review Board.
RESULTS
Forty of 70 (57%) fellows, 32 of 87 graduates (37%), and 14 of 32 PDs (44%) responded to the survey. The majority of the participants described their respective programs as 2 years in duration (59% for fellows, 56% for graduates, and 85% for PDs). Most programs (85%) were based at children’s hospitals. Most graduates (84%) practiced in a children’s hospital, and 12% of them practiced in a community site or a combination of sites.
Both fellows and graduates reported limited involvement in several aspects of TM prior to fellowship. Fellows’ interest in completing a TM rotation during fellowship is greater than the interest as perceived by PDs (3.03+1.00 vs. 2.38+1.19, P = .061). Prior TM exposure in residency or perceived proficiency in TM was not associated with lack of interest. Twenty-five percent of graduates completed a TM rotation during PHM fellowship. Many graduates agreed (41%) or strongly agreed (16%) with the statement “I recommend participating in a TM rotation during PHM fellowship.” Graduates who had completed a TM rotation were more likely to agree with this statement (P = .001).
There were similarities between reservations about participating in a TM rotation among fellows and barriers identified by graduates and PDs (Table). However, no graduates cited lack of relevance to a career in PHM as a barrier to participation in a TM rotation. Fellows, graduates, and PDs reported concordant responses regarding the prioritization of learning objectives for a TM rotation (Table). Both graduates and PDs ranked active learning strategies, such as direct patient care and simulation, as the most effective methods for teaching TM.
Discordance was noted between how frequently fellows participated in aspects of TM during fellowship and graduates’ current practice of PHM (Figure). With regard to select TM-related PHM core competencies, such as respiratory failure, shock, and leading a healthcare team, most (63%–90%, depending on the competency) fellows perceived themselves as “competent” prior to the start of the fellowship. Nevertheless, more than 70% of fellows remained very or extremely interested in gaining additional experience in each competency during fellowship.
DISCUSSION
Survey respondents demonstrate variable levels of interest and engagement in TM training; in particular, fellows and graduates often reported greater interest and value in a TM rotation than PDs. Similar to fellows in related fields,10 PHM fellows and graduates selected clinical topics as the most essential elements of TM training. In accordance with the literature, our findings suggest that direct patient care, one-on-one instruction, and simulation would be appropriate and popular methods for delivering this type of educational content.10,11
Curriculum design for a TM rotation should reinforce clinical PHM competencies related to TM while focusing on topics that are specific to the transport environment, such as methods of interfacility transport, handoffs, transitions of care, and team leadership.2,7,12 Trainee comfort level with different forms of transport (eg, fear of flying, motion sickness) and local and state policies regarding interfacility transfer should also be considered. In addition, fellows could engage in clinical research and quality improvement projects related to TM given the overall paucity of literature in the field.13
Several reasons can explain why fellows and graduates place a greater value on a TM rotation than PDs. Fellows and graduates may perceive inherent value in gaining particular knowledge and skills, such as greater understanding of the logistics and personnel involved in transferring patients and experience working with a healthcare team in a unique and dynamic setting.3,10,14
PDs may not be aware of the extent of participation in elements of transport among graduates. A recent workforce survey of pediatric interfacility transport systems indicated that although medical directors are from the fields of emergency, critical care, and neonatal medicine, 20% of medical control physicians are pediatric hospitalists.4 Given that the majority of PHM fellowships are based at children’s hospitals and transport teams are often associated with intensive care or emergency medicine units, PDs may have limited exposure to transport systems that incorporate hospitalists.
Pediatric hospitalists at all practice sites must have clinical and systems skills related to TM. However, the scope of practice for those working at community sites may be more likely to include distinct elements of TM.6 Currently, most fellowship graduates work at free-standing children’s or university-affiliated hospitals and have pursued careers in academic medicine.15 As the field evolves, the number of fellowship-trained pediatric hospitalists working at community sites may increase, making the acquisition of skills relevant to TM during fellowship training more crucial.
This study has several limitations. We attempted to identify all recent PHM fellowship graduates, but sampling bias may exist. Response bias may have been introduced by the self-reporting of skill and proficiency as well as by the small sample size and response rate for some stakeholder groups. The latter may be exacerbated by the fact that we do not have data on the degree or distribution of program representation among the fellow and graduate groups, given the lack of identifying information collected. Finally, we did not collect specific information about existing TM curricula in PHM fellowships.
We report a variable level of interest and engagement in TM among fellowship stakeholders, even though “Transport of the Critically Ill Child” is a PHM Core Competency. Fellows are interested in TM but unsure of its relevance to a PHM career. Graduates support the acquisition of transport skills during fellowship training.
ACKNOWLEDGMENTS
The authors would like to thank Tony Woodward, MD for reviewing the survey tools; Sheree Schrager, PhD and Margaret Trost, MD for their valuable insights into the results; and Grant Christman, MD for reviewing the manuscript.
Disclosures
The authors declare no potential conflicts of interest.
Funding
No funding was secured for this study.
1. Insoft RM, Schwartz HP, Romito J. Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients., 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2016.
2. Rosenthal JL, Romano PS, Kokroko J, Gu W, Okumura MJ. Profiling interfacility transfers for hospitalized pediatric patients. Hosp Pediatr. 2017;7(6):335-343. PubMed
3. Kline-Krammes S, Wheeler DS, Schwartz HP, Forbes M, Bigham MT. Missed opportunities during pediatric residency training. Report of a 10-year follow-up survey in critical care transport medicine. Pediatr Emerg Care. 2012;28(1):1-5. PubMed
4. Tanem J, Triscari D, Chan M, Meyer MT. Workforce survey of pediatric interfacility transport systems in the United States. Pediatr Emer Care. 2016;32(6):364-370. PubMed
5. Freed GL, Dunham KM. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179-186. PubMed
6. Roberts KB. Pediatric hospitalists in community hospitals: hospital-based generalists with expanded roles. Hosp Pediatr. 2015;5(5):290-292. PubMed
7. Stucky ER, Maniscalco J, Ottolini MC, et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i-xv, 1-114. PubMed
8. Jerardi KE, Fisher E, Rassbach C, et al. Development of a Curricular Framework for Pediatric Hospital Medicine Fellowships. Pediatrics. 2017;140(1):1-8. PubMed
9. Shah NH, Rhim HJH, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: A survey of program directors. J Hosp Med. 2016;11(5):324-328. PubMed
10. Mickells GE, Goodman DM, Rozenfeld RA. Education of pediatric subspecialty fellows in transport medicine: a national survey. BMC Pediatrics. 2017;17(1):13. PubMed
11. Cross B, Wilson D. High-fidelity simulation for transport team training and competency evaluation. Newborn Inf Nurs Rev. 2009;9(4):200-206.
12. Weingart C, Herstich T, Baker P, et al. Making good better: implementing a standardized handoff in pediatric transport. Air Med J. 2013;32(1):40-46. PubMed
13. Kandil SB, Sanford HA, Northrup V, Bigham MT, Giuliano Jr. JS. Transport disposition using transport risk assessment in pediatrics (TRAP) score. Prehosp Emerg Care. 2012;16(3):366-373. PubMed
14. Giardino AP, Tran XG, King J, Giardino ER, Woodward GA, Durbin DR. A longitudinal view of resident education in pediatric emergency interhospital transport. Pediatr Emerg Care. 2010;26(9):653-658. PubMed
15. Oshimurua JM, Bauer BD, Shah N, Nguyen N, Maniscalco J. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-637 PubMed
Transport medicine (TM) involves the provision of care to patients who require transfer to a healthcare facility that can deliver definitive treatment.1 Pediatric interfacility transport occurs in approximately 10% of nonneonatal, nonpregnancy pediatric hospitalizations in the United States.2 Studies document a decline in resident participation in pediatric transports and variability in curricular content.3,4
The Pediatric Hospital Medicine (PHM) Core Competencies include “Transport of the Critically Ill Child.”7 Additionally, the Curriculum Committee of the PHM Fellowship Directors Council proposed a curricular framework that includes a required clinical experience in “Care and Stabilization of the Critically Ill Child,”8 which can occur in a variety of practice settings, including TM. TM is also listed as a potential elective rotation.
In 2014, 60% of PHM fellowships included a required or optional TM rotation.9 A recent study of pediatric emergency, critical care, and neonatal medicine fellowships revealed a paucity of formal or published TM curricula in these programs.10 Furthermore, no standard or published TM curricula have been established for PHM fellowships. The primary objective of our study is to determine attitudes regarding TM training among PHM fellows, recent PHM fellowship graduates, and PHM fellowship program directors (PDs). The secondary objective is to identify how the perspectives of these fellowship stakeholders could influence the design of a TM curriculum.
METHODS
This cross-sectional study focused on 3 stakeholder groups related to PHM fellowships. The subjects included in the study were physicians enrolled in a PHM fellowship (fellow) during the 2015-2016 academic year, graduates of fellowship (graduate) between 2010 and 2015, and fellowship program directors (PD). Unique web-based, anonymous surveys for each group were developed, reviewed by content and methodology experts, and piloted with local pediatric hospitalists. Surveys consisted of unfolding multiple-choice questions and ranking items along Likert scales and the Dreyfus model.
Questions were designed to elicit demographic data, perspectives, and experience related to TM education in PHM fellowships across all respondent groups. Depending on the context, identical or similar questions were asked among the groups. For example, all groups were asked to prioritize learning objectives for a TM rotation. Graduates and PDs reported the most effective teaching methods for use during a TM rotation. Fellows rated their own interest in a TM elective, and PDs were asked to rate the level of interest among their fellows.
Participant contact information was obtained from a website (phmfellows.org) and databases of fellows and graduates, which are maintained by the PHM Fellowship Directors Council (personal communication, Jayne Truckenbrod, DO; February 2, 2017). Between February and April 2016, the participants were individually emailed a link to their respective surveys, and 3 reminder e-mails were sent to nonresponders. The survey was administered through SurveyMonkey (www.surveymonkey.com).
SPSS (IBM SPSS Statistics, IBM Corporation, Armonk, New York) was used for statistical analysis. Descriptive data were presented using mean and standard deviation. Comparisons among fellows, graduates, and PDs were conducted using one-way analyses of variance or Mann-Whitney U test. Frequency of application and self-evaluation of core competency skills before and after the rotation were evaluated using paired sample t-tests. The study protocol was deemed exempt from review by our local Institutional Review Board.
RESULTS
Forty of 70 (57%) fellows, 32 of 87 graduates (37%), and 14 of 32 PDs (44%) responded to the survey. The majority of the participants described their respective programs as 2 years in duration (59% for fellows, 56% for graduates, and 85% for PDs). Most programs (85%) were based at children’s hospitals. Most graduates (84%) practiced in a children’s hospital, and 12% of them practiced in a community site or a combination of sites.
Both fellows and graduates reported limited involvement in several aspects of TM prior to fellowship. Fellows’ interest in completing a TM rotation during fellowship is greater than the interest as perceived by PDs (3.03+1.00 vs. 2.38+1.19, P = .061). Prior TM exposure in residency or perceived proficiency in TM was not associated with lack of interest. Twenty-five percent of graduates completed a TM rotation during PHM fellowship. Many graduates agreed (41%) or strongly agreed (16%) with the statement “I recommend participating in a TM rotation during PHM fellowship.” Graduates who had completed a TM rotation were more likely to agree with this statement (P = .001).
There were similarities between reservations about participating in a TM rotation among fellows and barriers identified by graduates and PDs (Table). However, no graduates cited lack of relevance to a career in PHM as a barrier to participation in a TM rotation. Fellows, graduates, and PDs reported concordant responses regarding the prioritization of learning objectives for a TM rotation (Table). Both graduates and PDs ranked active learning strategies, such as direct patient care and simulation, as the most effective methods for teaching TM.
Discordance was noted between how frequently fellows participated in aspects of TM during fellowship and graduates’ current practice of PHM (Figure). With regard to select TM-related PHM core competencies, such as respiratory failure, shock, and leading a healthcare team, most (63%–90%, depending on the competency) fellows perceived themselves as “competent” prior to the start of the fellowship. Nevertheless, more than 70% of fellows remained very or extremely interested in gaining additional experience in each competency during fellowship.
DISCUSSION
Survey respondents demonstrate variable levels of interest and engagement in TM training; in particular, fellows and graduates often reported greater interest and value in a TM rotation than PDs. Similar to fellows in related fields,10 PHM fellows and graduates selected clinical topics as the most essential elements of TM training. In accordance with the literature, our findings suggest that direct patient care, one-on-one instruction, and simulation would be appropriate and popular methods for delivering this type of educational content.10,11
Curriculum design for a TM rotation should reinforce clinical PHM competencies related to TM while focusing on topics that are specific to the transport environment, such as methods of interfacility transport, handoffs, transitions of care, and team leadership.2,7,12 Trainee comfort level with different forms of transport (eg, fear of flying, motion sickness) and local and state policies regarding interfacility transfer should also be considered. In addition, fellows could engage in clinical research and quality improvement projects related to TM given the overall paucity of literature in the field.13
Several reasons can explain why fellows and graduates place a greater value on a TM rotation than PDs. Fellows and graduates may perceive inherent value in gaining particular knowledge and skills, such as greater understanding of the logistics and personnel involved in transferring patients and experience working with a healthcare team in a unique and dynamic setting.3,10,14
PDs may not be aware of the extent of participation in elements of transport among graduates. A recent workforce survey of pediatric interfacility transport systems indicated that although medical directors are from the fields of emergency, critical care, and neonatal medicine, 20% of medical control physicians are pediatric hospitalists.4 Given that the majority of PHM fellowships are based at children’s hospitals and transport teams are often associated with intensive care or emergency medicine units, PDs may have limited exposure to transport systems that incorporate hospitalists.
Pediatric hospitalists at all practice sites must have clinical and systems skills related to TM. However, the scope of practice for those working at community sites may be more likely to include distinct elements of TM.6 Currently, most fellowship graduates work at free-standing children’s or university-affiliated hospitals and have pursued careers in academic medicine.15 As the field evolves, the number of fellowship-trained pediatric hospitalists working at community sites may increase, making the acquisition of skills relevant to TM during fellowship training more crucial.
This study has several limitations. We attempted to identify all recent PHM fellowship graduates, but sampling bias may exist. Response bias may have been introduced by the self-reporting of skill and proficiency as well as by the small sample size and response rate for some stakeholder groups. The latter may be exacerbated by the fact that we do not have data on the degree or distribution of program representation among the fellow and graduate groups, given the lack of identifying information collected. Finally, we did not collect specific information about existing TM curricula in PHM fellowships.
We report a variable level of interest and engagement in TM among fellowship stakeholders, even though “Transport of the Critically Ill Child” is a PHM Core Competency. Fellows are interested in TM but unsure of its relevance to a PHM career. Graduates support the acquisition of transport skills during fellowship training.
ACKNOWLEDGMENTS
The authors would like to thank Tony Woodward, MD for reviewing the survey tools; Sheree Schrager, PhD and Margaret Trost, MD for their valuable insights into the results; and Grant Christman, MD for reviewing the manuscript.
Disclosures
The authors declare no potential conflicts of interest.
Funding
No funding was secured for this study.
Transport medicine (TM) involves the provision of care to patients who require transfer to a healthcare facility that can deliver definitive treatment.1 Pediatric interfacility transport occurs in approximately 10% of nonneonatal, nonpregnancy pediatric hospitalizations in the United States.2 Studies document a decline in resident participation in pediatric transports and variability in curricular content.3,4
The Pediatric Hospital Medicine (PHM) Core Competencies include “Transport of the Critically Ill Child.”7 Additionally, the Curriculum Committee of the PHM Fellowship Directors Council proposed a curricular framework that includes a required clinical experience in “Care and Stabilization of the Critically Ill Child,”8 which can occur in a variety of practice settings, including TM. TM is also listed as a potential elective rotation.
In 2014, 60% of PHM fellowships included a required or optional TM rotation.9 A recent study of pediatric emergency, critical care, and neonatal medicine fellowships revealed a paucity of formal or published TM curricula in these programs.10 Furthermore, no standard or published TM curricula have been established for PHM fellowships. The primary objective of our study is to determine attitudes regarding TM training among PHM fellows, recent PHM fellowship graduates, and PHM fellowship program directors (PDs). The secondary objective is to identify how the perspectives of these fellowship stakeholders could influence the design of a TM curriculum.
METHODS
This cross-sectional study focused on 3 stakeholder groups related to PHM fellowships. The subjects included in the study were physicians enrolled in a PHM fellowship (fellow) during the 2015-2016 academic year, graduates of fellowship (graduate) between 2010 and 2015, and fellowship program directors (PD). Unique web-based, anonymous surveys for each group were developed, reviewed by content and methodology experts, and piloted with local pediatric hospitalists. Surveys consisted of unfolding multiple-choice questions and ranking items along Likert scales and the Dreyfus model.
Questions were designed to elicit demographic data, perspectives, and experience related to TM education in PHM fellowships across all respondent groups. Depending on the context, identical or similar questions were asked among the groups. For example, all groups were asked to prioritize learning objectives for a TM rotation. Graduates and PDs reported the most effective teaching methods for use during a TM rotation. Fellows rated their own interest in a TM elective, and PDs were asked to rate the level of interest among their fellows.
Participant contact information was obtained from a website (phmfellows.org) and databases of fellows and graduates, which are maintained by the PHM Fellowship Directors Council (personal communication, Jayne Truckenbrod, DO; February 2, 2017). Between February and April 2016, the participants were individually emailed a link to their respective surveys, and 3 reminder e-mails were sent to nonresponders. The survey was administered through SurveyMonkey (www.surveymonkey.com).
SPSS (IBM SPSS Statistics, IBM Corporation, Armonk, New York) was used for statistical analysis. Descriptive data were presented using mean and standard deviation. Comparisons among fellows, graduates, and PDs were conducted using one-way analyses of variance or Mann-Whitney U test. Frequency of application and self-evaluation of core competency skills before and after the rotation were evaluated using paired sample t-tests. The study protocol was deemed exempt from review by our local Institutional Review Board.
RESULTS
Forty of 70 (57%) fellows, 32 of 87 graduates (37%), and 14 of 32 PDs (44%) responded to the survey. The majority of the participants described their respective programs as 2 years in duration (59% for fellows, 56% for graduates, and 85% for PDs). Most programs (85%) were based at children’s hospitals. Most graduates (84%) practiced in a children’s hospital, and 12% of them practiced in a community site or a combination of sites.
Both fellows and graduates reported limited involvement in several aspects of TM prior to fellowship. Fellows’ interest in completing a TM rotation during fellowship is greater than the interest as perceived by PDs (3.03+1.00 vs. 2.38+1.19, P = .061). Prior TM exposure in residency or perceived proficiency in TM was not associated with lack of interest. Twenty-five percent of graduates completed a TM rotation during PHM fellowship. Many graduates agreed (41%) or strongly agreed (16%) with the statement “I recommend participating in a TM rotation during PHM fellowship.” Graduates who had completed a TM rotation were more likely to agree with this statement (P = .001).
There were similarities between reservations about participating in a TM rotation among fellows and barriers identified by graduates and PDs (Table). However, no graduates cited lack of relevance to a career in PHM as a barrier to participation in a TM rotation. Fellows, graduates, and PDs reported concordant responses regarding the prioritization of learning objectives for a TM rotation (Table). Both graduates and PDs ranked active learning strategies, such as direct patient care and simulation, as the most effective methods for teaching TM.
Discordance was noted between how frequently fellows participated in aspects of TM during fellowship and graduates’ current practice of PHM (Figure). With regard to select TM-related PHM core competencies, such as respiratory failure, shock, and leading a healthcare team, most (63%–90%, depending on the competency) fellows perceived themselves as “competent” prior to the start of the fellowship. Nevertheless, more than 70% of fellows remained very or extremely interested in gaining additional experience in each competency during fellowship.
DISCUSSION
Survey respondents demonstrate variable levels of interest and engagement in TM training; in particular, fellows and graduates often reported greater interest and value in a TM rotation than PDs. Similar to fellows in related fields,10 PHM fellows and graduates selected clinical topics as the most essential elements of TM training. In accordance with the literature, our findings suggest that direct patient care, one-on-one instruction, and simulation would be appropriate and popular methods for delivering this type of educational content.10,11
Curriculum design for a TM rotation should reinforce clinical PHM competencies related to TM while focusing on topics that are specific to the transport environment, such as methods of interfacility transport, handoffs, transitions of care, and team leadership.2,7,12 Trainee comfort level with different forms of transport (eg, fear of flying, motion sickness) and local and state policies regarding interfacility transfer should also be considered. In addition, fellows could engage in clinical research and quality improvement projects related to TM given the overall paucity of literature in the field.13
Several reasons can explain why fellows and graduates place a greater value on a TM rotation than PDs. Fellows and graduates may perceive inherent value in gaining particular knowledge and skills, such as greater understanding of the logistics and personnel involved in transferring patients and experience working with a healthcare team in a unique and dynamic setting.3,10,14
PDs may not be aware of the extent of participation in elements of transport among graduates. A recent workforce survey of pediatric interfacility transport systems indicated that although medical directors are from the fields of emergency, critical care, and neonatal medicine, 20% of medical control physicians are pediatric hospitalists.4 Given that the majority of PHM fellowships are based at children’s hospitals and transport teams are often associated with intensive care or emergency medicine units, PDs may have limited exposure to transport systems that incorporate hospitalists.
Pediatric hospitalists at all practice sites must have clinical and systems skills related to TM. However, the scope of practice for those working at community sites may be more likely to include distinct elements of TM.6 Currently, most fellowship graduates work at free-standing children’s or university-affiliated hospitals and have pursued careers in academic medicine.15 As the field evolves, the number of fellowship-trained pediatric hospitalists working at community sites may increase, making the acquisition of skills relevant to TM during fellowship training more crucial.
This study has several limitations. We attempted to identify all recent PHM fellowship graduates, but sampling bias may exist. Response bias may have been introduced by the self-reporting of skill and proficiency as well as by the small sample size and response rate for some stakeholder groups. The latter may be exacerbated by the fact that we do not have data on the degree or distribution of program representation among the fellow and graduate groups, given the lack of identifying information collected. Finally, we did not collect specific information about existing TM curricula in PHM fellowships.
We report a variable level of interest and engagement in TM among fellowship stakeholders, even though “Transport of the Critically Ill Child” is a PHM Core Competency. Fellows are interested in TM but unsure of its relevance to a PHM career. Graduates support the acquisition of transport skills during fellowship training.
ACKNOWLEDGMENTS
The authors would like to thank Tony Woodward, MD for reviewing the survey tools; Sheree Schrager, PhD and Margaret Trost, MD for their valuable insights into the results; and Grant Christman, MD for reviewing the manuscript.
Disclosures
The authors declare no potential conflicts of interest.
Funding
No funding was secured for this study.
1. Insoft RM, Schwartz HP, Romito J. Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients., 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2016.
2. Rosenthal JL, Romano PS, Kokroko J, Gu W, Okumura MJ. Profiling interfacility transfers for hospitalized pediatric patients. Hosp Pediatr. 2017;7(6):335-343. PubMed
3. Kline-Krammes S, Wheeler DS, Schwartz HP, Forbes M, Bigham MT. Missed opportunities during pediatric residency training. Report of a 10-year follow-up survey in critical care transport medicine. Pediatr Emerg Care. 2012;28(1):1-5. PubMed
4. Tanem J, Triscari D, Chan M, Meyer MT. Workforce survey of pediatric interfacility transport systems in the United States. Pediatr Emer Care. 2016;32(6):364-370. PubMed
5. Freed GL, Dunham KM. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179-186. PubMed
6. Roberts KB. Pediatric hospitalists in community hospitals: hospital-based generalists with expanded roles. Hosp Pediatr. 2015;5(5):290-292. PubMed
7. Stucky ER, Maniscalco J, Ottolini MC, et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i-xv, 1-114. PubMed
8. Jerardi KE, Fisher E, Rassbach C, et al. Development of a Curricular Framework for Pediatric Hospital Medicine Fellowships. Pediatrics. 2017;140(1):1-8. PubMed
9. Shah NH, Rhim HJH, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: A survey of program directors. J Hosp Med. 2016;11(5):324-328. PubMed
10. Mickells GE, Goodman DM, Rozenfeld RA. Education of pediatric subspecialty fellows in transport medicine: a national survey. BMC Pediatrics. 2017;17(1):13. PubMed
11. Cross B, Wilson D. High-fidelity simulation for transport team training and competency evaluation. Newborn Inf Nurs Rev. 2009;9(4):200-206.
12. Weingart C, Herstich T, Baker P, et al. Making good better: implementing a standardized handoff in pediatric transport. Air Med J. 2013;32(1):40-46. PubMed
13. Kandil SB, Sanford HA, Northrup V, Bigham MT, Giuliano Jr. JS. Transport disposition using transport risk assessment in pediatrics (TRAP) score. Prehosp Emerg Care. 2012;16(3):366-373. PubMed
14. Giardino AP, Tran XG, King J, Giardino ER, Woodward GA, Durbin DR. A longitudinal view of resident education in pediatric emergency interhospital transport. Pediatr Emerg Care. 2010;26(9):653-658. PubMed
15. Oshimurua JM, Bauer BD, Shah N, Nguyen N, Maniscalco J. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-637 PubMed
1. Insoft RM, Schwartz HP, Romito J. Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients., 4th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2016.
2. Rosenthal JL, Romano PS, Kokroko J, Gu W, Okumura MJ. Profiling interfacility transfers for hospitalized pediatric patients. Hosp Pediatr. 2017;7(6):335-343. PubMed
3. Kline-Krammes S, Wheeler DS, Schwartz HP, Forbes M, Bigham MT. Missed opportunities during pediatric residency training. Report of a 10-year follow-up survey in critical care transport medicine. Pediatr Emerg Care. 2012;28(1):1-5. PubMed
4. Tanem J, Triscari D, Chan M, Meyer MT. Workforce survey of pediatric interfacility transport systems in the United States. Pediatr Emer Care. 2016;32(6):364-370. PubMed
5. Freed GL, Dunham KM. Pediatric hospitalists: training, current practice, and career goals. J Hosp Med. 2009;4(3):179-186. PubMed
6. Roberts KB. Pediatric hospitalists in community hospitals: hospital-based generalists with expanded roles. Hosp Pediatr. 2015;5(5):290-292. PubMed
7. Stucky ER, Maniscalco J, Ottolini MC, et al. The Pediatric Hospital Medicine Core Competencies Supplement: a Framework for Curriculum Development by the Society of Hospital Medicine with acknowledgement to pediatric hospitalists from the American Academy of Pediatrics and the Academic Pediatric Association. J Hosp Med. 2010;5(suppl 2):i-xv, 1-114. PubMed
8. Jerardi KE, Fisher E, Rassbach C, et al. Development of a Curricular Framework for Pediatric Hospital Medicine Fellowships. Pediatrics. 2017;140(1):1-8. PubMed
9. Shah NH, Rhim HJH, Maniscalco J, Wilson K, Rassbach C. The current state of pediatric hospital medicine fellowships: A survey of program directors. J Hosp Med. 2016;11(5):324-328. PubMed
10. Mickells GE, Goodman DM, Rozenfeld RA. Education of pediatric subspecialty fellows in transport medicine: a national survey. BMC Pediatrics. 2017;17(1):13. PubMed
11. Cross B, Wilson D. High-fidelity simulation for transport team training and competency evaluation. Newborn Inf Nurs Rev. 2009;9(4):200-206.
12. Weingart C, Herstich T, Baker P, et al. Making good better: implementing a standardized handoff in pediatric transport. Air Med J. 2013;32(1):40-46. PubMed
13. Kandil SB, Sanford HA, Northrup V, Bigham MT, Giuliano Jr. JS. Transport disposition using transport risk assessment in pediatrics (TRAP) score. Prehosp Emerg Care. 2012;16(3):366-373. PubMed
14. Giardino AP, Tran XG, King J, Giardino ER, Woodward GA, Durbin DR. A longitudinal view of resident education in pediatric emergency interhospital transport. Pediatr Emerg Care. 2010;26(9):653-658. PubMed
15. Oshimurua JM, Bauer BD, Shah N, Nguyen N, Maniscalco J. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-637 PubMed
© 2018 Society of Hospital Medicine
The Current State of PHM Fellowships
Pediatric hospital medicine (PHM) fellowship programs came into existence approximately 20 years ago in Canada,[1] and since that time the number of programs in North America has grown dramatically. The first 3 PHM fellowship programs in the United States were initiated in 2003, and by 2008 there were 7 active programs. Just 5 years later in 2013, there were 20 fellowship programs in existence. Now, in 2015, there are over 30 programs, with several more in development. The goal of postresidency training in PHM is to improve the care of hospitalized children by training future hospitalists to provide high‐quality, evidence‐based clinical care and to generate new knowledge and scholarship in areas such as clinical research, patient safety and quality improvement, medical education, practice management, and patient outcomes.[2] Many pediatric hospitalists want to be able to perform research or quality improvement, but feel that they lack the time, skills, resources, and mentorship to do so.[3] To date, fellowship‐trained hospitalists have a demonstrated track record of contributing to the body of literature that is shaping the care of hospitalized children.[4, 5]
At present, PHM is not a recognized subspecialty of the American Board of Pediatrics (ABP) and therefore does not fall under the purview of the Accreditation Council of Graduate Medical Education (ACGME), leading to concern from some about the variability in depth and breadth of training across programs.[1] The development and publication of the PHM Core Competencies in 2010 helped define the scope of practice of pediatric hospitalists and provide guidelines for training programs, specifically with respect to clinical and nonclinical areas for assessment of competency.[6] Furthermore, studies of early career hospitalists have identified areas for future fellowship curriculum development, such as core procedural skills, quality improvement, and practice management.[7]
In an effort to address training variability across programs, PHM fellowship directors (FDs) have come together as an organized group, first meeting in 2008, with the primary goal of defining training standards and sharing curricular resources. Annual meetings of the FDs, sponsored by the American Academy of Pediatrics Section on Hospital Medicine (AAP‐SOHM), began in 2012. A key objective of this annual meeting has been to develop a standardized fellowship curriculum for use across programs as well as to determine gaps in training that need to be addressed. During this process, we have received input from key stakeholders including community hospitalists, internal medicine‐pediatrics hospitalists, and the PHM Certification Steering Committee, which organized the application for subspecialty certification to the ABP. To inform this process of curriculum standardization, we fielded a survey of PHM fellowship directors. The purpose of this article is to summarize the current curricula, operations, and logistics of PHM fellowship programs.
METHODS
This was a cross‐sectional study of 31 PHM fellowship programs across the United States and Canada in April 2014. Inclusion criteria included all pediatric fellowships that were self‐identified to the AAP‐SOHM as providing a hospital medicine fellowship option. This included both PHM fellowships as well as academic general pediatric fellowships with a hospitalist track. A web‐based survey (SurveyMonkey, Inc.) was distributed by e‐mail to the FDs at the 31 training programs (see Supporting Information in the online version of this article). To enhance content validity of survey responses, survey questions were designed using an iterative consensus process among the authors, who included junior and senior FDs and represented the 2014 annual FD meeting planning committee. Items were created to gather feedback on the following key areas of PHM fellowships: program demographics, types of required and elective clinical rotations, graduate coursework offerings, amount of time spent in clinical activities, fellow billing practices, and description of fellows' research activities. The survey consisted of 30 multiple‐choice and short‐answer questions. Follow‐up e‐mail reminders were sent to all FDs 2 weeks and 4 weeks after the initial request was sent. Survey completion was voluntary, and no incentives were offered. The study was determined to be exempt by the Stanford University Institutional Review Board. Data were summarized using frequency distributions. No subgroup comparisons were made.
RESULTS
Program directors from 27/31 (87%) PHM fellowship programs responded to the survey; 25 were active programs, and 2 were under development. Responding programs represented all 4 major regions of the country and Canada, with varying program initiation dates, ranging from 1997 to 2013.
Program Demographics
The duration of most programs (17/27) was 2 years (63%), with 6 (22%) 1‐year programs and 4 (15%) 3‐year programs making up the remainder. Four programs described variable lengths, which could be tailored based on the fellow's individual interest. Two of the programs are 2 years in length, but offer a 1‐year option for fellows who wish to focus on enhancing clinical skills without an academic focus. The other 2 programs are 2 years in length, but will offer an extension to a third year for those pursuing a graduate degree.
Fellow Clinical Activities
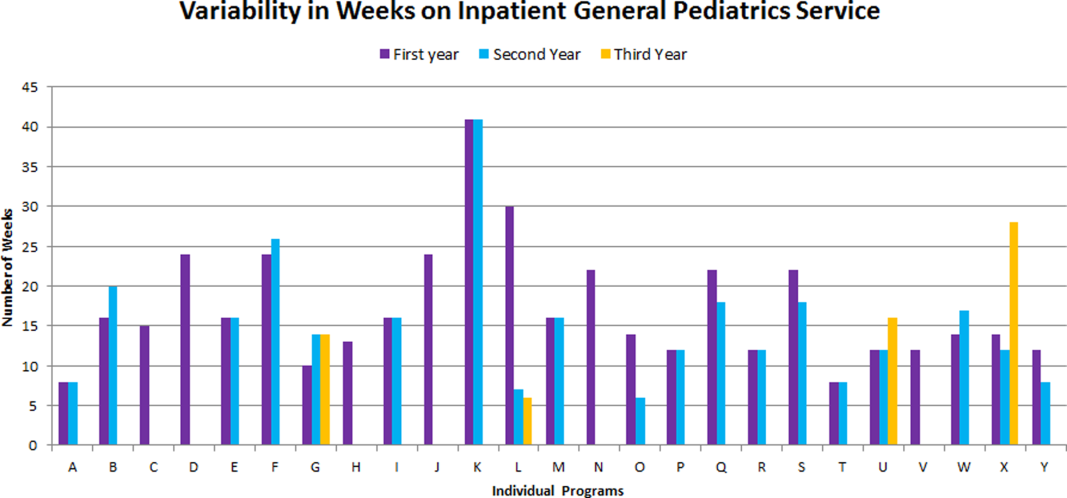
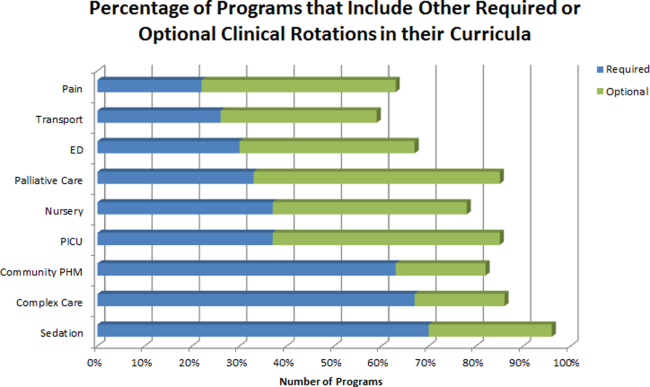
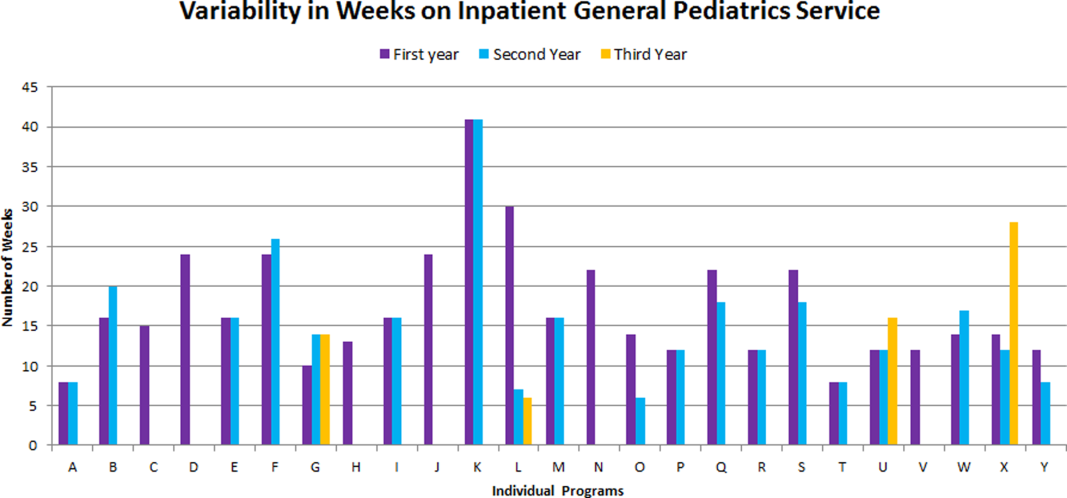
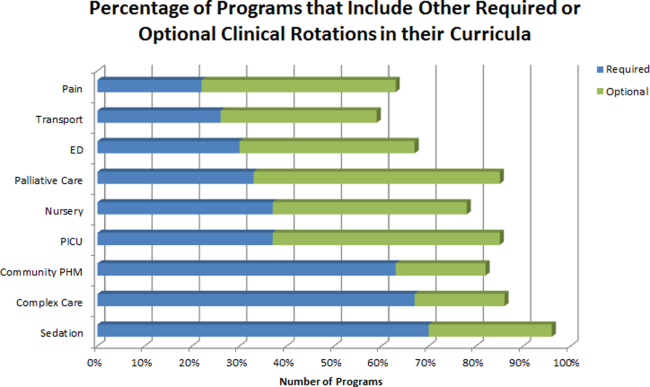
The average amount of total clinical time (weeks on service) across responding programs was 50% (range, 20%65%). When looking specifically at time on the inpatient general pediatric service, number of weeks varied by year of training and by institution, with 12 to 41 weeks in the first year of fellowship, 6 to 41 weeks in the second year of fellowship, and 6 to 28 weeks in the third year of fellowship (Figure 1). Though the range is large, on average, fellows spend 17 weeks on inpatient general pediatrics service during each year of training. Of note, the median number of weeks on inpatient general pediatrics service by year of training was 15 weeks, 16 weeks, and 16.5 weeks, respectively. In addition to inpatient general pediatrics service time, most programs require other clinical rotations, with sedation, complex care, and inpatient pediatrics at community sites being the most frequent (Figure 2). Of the 6 responding 1‐year programs, 5 (83%) allow fellows to bill/generate clinical revenue at some point during their training. Of the 15 responding 2‐year programs, 11 (73%) allow fellows to bill/generate clinical revenue at some point during their training. Of the 4 responding 3‐year programs, 2 (50%) allow their fellows to bill/generate clinical revenue at some point during their training.
Fellow Scholarly Activities
With respect to time dedicated to research, the majority of programs offer coursework such as courses for credit, noncredit courses, or certificate courses. In addition, 11 programs offer fellows a masters' degree in areas including public health, clinical science, epidemiology, education, academic sciences, healthcare quality, clinical and translational research, or health services administration. The majority of these degrees are paid for by departmental funds, with tuition reimbursement, university support, training grants, and personal funds making up the remainder. Twenty‐one (81%) programs provide a scholarship oversight committee for their fellows. Current fellows' (n = 63) primary areas of research are varied and include clinical research (36%), quality‐improvement research (22%), medical education research (20%), health services research (16%), and other areas (6%).
DISCUSSION
This is the most comprehensive description of pediatric hospital medicine fellowship curricula to date. Understanding the scope of these programs is an important first step in developing a standardized curriculum that can be used by all. The results of this survey indicate that although there is variability among PHM fellowship curricular content, several common themes exist.
The number of clinical weeks on the inpatient general pediatrics service varied from program to program, though the majority of programs require fellows to spend 15 to 16 weeks each year of training. The variability may be due in part to the way in which respondents defined the term week on clinical service. For example, if the fellow is primarily on a shift schedule, then he/she may only work 2 to 3 shifts in 1 week, which may have been viewed similarly to daily presence on a more traditional inpatient teaching service with 5 to 7 consecutive days of service. The current study did not explore the details of inpatient general pediatric clinical activities or exposure to opportunities to hone procedural skills, areas that are worth investigating as we move forward to better understand the needs of trainees.
Most residency training programs in general pediatrics require a significant amount of inpatient clinical time, specifically a minimum of 10 units or months, though only half of this time is required to be in inpatient general pediatrics.[8] Although nonfellowship trained early career hospitalists may feel adequately prepared to manage the clinical care of some hospitalized children, perceived competency is significantly lower than their fellowship‐trained colleagues with regard to care of the child with medical complexity and technology‐dependence, and with regard to provision of sedation for procedures.[7] The majority of FDs surveyed in our study indicated that additional clinical experience with sedation, complex care, and inpatient pediatrics at community sites were required of their fellows. Of note, many of these rotations are not commonly required in pediatric residency training programs; however, the PHM core competencies suggest that hospitalists should demonstrate proficiency in these areas to provide optimal care for hospitalized children. Our results suggest that current PHM fellowship curricula help address these clinical gaps. The requirement of these particular specialized experiences may reflect the clinical scope of practice that is expected from potential employers or may be related to staffing needs. It is well documented that the inpatient demographic of large pediatric tertiary care referral centers has changed over the past decade, with an increasing prevalence of children with medical complexity.[9, 10] In both tertiary referral centers and community hospitals, the expansion of the role of the hospitalist in providing specialized clinical services, such as sedation or surgical comanagement, has been significantly driven by financial factors, though a more recent focus on improvement of efficiency and quality of care within the hospital system has relied heavily on hospitalist input.[11, 12, 13] Important next steps in curriculum standardization include ensuring that training programs allow for adequate clinical exposure and proper assessment of competency in these areas, and determining the full complement of clinical training experiences that will produce hospitalists with a well‐defined scope of practice that adequately addresses the needs of hospitalized children.
Most fellowship‐trained hospitalists work primarily in university‐affiliated institutions with expectations for scholarly productivity.[5, 7] Fellowship‐trained hospitalists have made large contributions to the growing body of PHM literature, specifically in the realms of medical education, healthcare quality, clinical pediatrics, and healthcare outcomes.[4] Many PHM fellowship‐trained hospitalists have educational or administrative leadership roles.[2] Our results indicate that current PHM fellows continue to be active in a variety of research activities. In addition, FDs reported that the vast majority of programs included scholarship oversight committees, which ensure a mentored and structured research experience. Finally, most programs require or offer additional coursework, and many programs with university affiliations allow for attainment of graduate degrees. Inclusion of robust research training and infrastructure in all programs is a paramount goal of PHM fellowship training. This will allow graduates to be successful researchers, generating new knowledge and supporting the provision of high‐quality, evidence‐based, and value‐driven care for hospitalized children.
A unique feature of several PHM fellowship programs is that fellows are allowed to bill for clinical encounters. Many programs rely on clinical revenue to support fellow salaries.[14] For some programs, a portion of this clinical revenue comes from fellows billing for clinical encounters.[15] Programs that allow fellows to bill/generate clinical revenue have fellows working in attending roles without direct supervision, whereas nonbilling fellows have direct supervision by an attending.[15] In the current ABP training model, subspecialty fellows cannot independently bill for clinical encounters within their own subspecialty, though they can moonlight as long as they meet the duty hour requirements set forth by the ACGME.[16] FDs will need to consider the impact of this requirement on fellow autonomy and on financial revenue for funding fellow salaries if the field achieves ABP subspecialty status.
Regardless of whether or not PHM becomes a designated subspecialty of the ABP, FDs will continue to work together to develop a standard core curriculum that incorporates elements of clinical and nonclinical training to ensure that graduates not only provide high‐quality care for hospitalized children, but also generate new knowledge that advances the field in care delivery and quality of care in any setting. The results of this study will not only help to inform curriculum standardization, but also assessment and evaluation methods. Currently, PHM FDs meet annually and are nearing consensus on a standard 2‐year curriculum based on the PHM Core Competencies that incorporates core clinical, systems, and scholarly domains. We continue to solicit the input of stakeholders, including new FDs, community hospitalist leaders, internal medicine‐pediatrics hospitalist leaders, the Joint Council of Pediatric Hospital Medicine, and leaders of national organizations, such as the American Academy of Pediatrics, Academic Pediatrics Association, and Society of Hospital Medicine. Additional work around standardizing the fellowship application and recruitment process has resulted in our recent acceptance into the Fall Subspecialty Match through the National Residency Match Program, as well as development and implementation of a common fellowship application form. The FD group has recently formalized, voting into place an executive steering committee, which is responsible for the development and execution of long‐term goals that include finalizing a standardized curriculum, refining program and fellow assessment methods through critical evaluation of fellow metrics and outcomes, and standardization of evaluation methods.
Adopting a standard 2‐year curriculum may affect some programs, specifically those that are currently 1 year in duration. These programs would need to extend the length of their fellowship to allow for the breadth of experiences expected with a standardized 2‐year curriculum. This could result in significant financial challenges, effectively increasing the cost to administer the program. In addition, at present, programs have the flexibility to highlight individual areas of strength to attract candidates, allowing fellows to gain an in‐depth experience in domains such as clinical research, quality improvement, medical education, or health services research. With a standardized curriculum, some programs may have to assemble specific clinical and nonclinical experiences to meet the agreed‐upon expectations for PHM fellowship training. If these resources are not available, programs may need to seek relationships with other institutions to complete their offerings, a possibility that is being actively explored by this group. FDs continue to work with each other to share resources, identify training opportunities, and partner with each other to ensure that the requirements of a standard curriculum can be met.
This study has several limitations. First, it was a voluntary survey of program directors, and though we captured over 80% of programs at the time of the survey, there are currently more programs that have come into existence and more still that are in the development stage, leading to potential sampling error. Second, variable effort or accuracy by participants may have led to some degree of response error, such as content error or nonreporting error. Third, the survey questions focused on high‐level information, making it difficult to make nuanced comparisons between curricular elements or determine best curricular practice. In addition, this survey did not explore medical education and quality improvement activities of fellows, 2 major areas in which hospitalists play a major role in the inpatient setting.[1, 17, 18, 19, 20]
CONCLUSION
PHM fellowship programs have grown and continue to grow at a rapid rate. Variability in training is evident, both in clinical experiences and research experiences, though several common elements were identified in this study. The majority of programs are 2 years, and clinical experience comprises approximately 50% of training time, often including key rotations such as sedation, complex care, and rotations at community hospitals. Future directions include standardizing clinical training and expectations for scholarship, formulating appropriate methods for assessment of competency that can be used across programs, and seeking sustainable sources of funding.
Disclosure
Nothing to report.
- , . Characteristics of pediatric hospital medicine fellowships and training programs. J Hosp Med. 2009;4(3):157–163.
- , . Pediatric hospitalists in medical education: current roles and future directions. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):120–126.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , , , . Pediatric hospital medicine fellowships: outcomes and future directions. Paper presented at: Pediatric Hospital Medicine 2014; July 26, 2014; Orlando, FL.
- , , . Pediatric hospitalist research productivity: predictors of success at presenting abstracts and publishing peer‐reviewed manuscripts among pediatric hospitalists. Hosp Pediatr. 2012;2(3):149–160.
- , , . Pediatric hospital medicine core competencies: development and methodology. J Hosp Med. 2010;5:339–343.
- , , , . Perceived core competency achievements of fellowship and non‐fellowship early career pediatric hospitalists. J Hosp Med. 2015;10(6):373–389.
- Accreditation Council of Graduate Medical Education. ACGME program requirements for graduate medical education in pediatrics. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013‐PR‐FAQ‐PIF/320_pediatrics_07012013.pdf. Published September 30, 2012. Accessed July 7, 2015.
- , , , , , . Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646.
- , , , et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136:591–596.
- , , , , , . Pediatric hospitalist comanagement of spinal fusion surgery patients. J Hosp Med. 2007;2(1):23–30.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , . Sources of funding and support for pediatric hospital medicine fellowship programs. Poster presented at: Pediatric Hospital Medicine 2014; July 27, 2014; Orlando, FL.
- Council of Pediatric Hospital Medicine Fellowship Directors. Pediatric Hospital Medicine Fellowship Directors Annual Meeting: funding and return on investment. July 24, 2014.
- Accreditation Council of Graduate Medical Education. Frequently asked questions: ACGME common duty hour requirements. Available at: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh‐faqs2011.pdf. Updated June 18, 2014. Accessed July 7, 2015.
- , . Pediatric hospitalists: training, current practice and career goals. J Hosp Med. 2009;4(3):179–186.
- , . The hospitalist movement and its implications for the care of hospitalized children. Pediatrics. 1999;103:473–477.
- . Pediatric hospitalists and medical education. Pediatr Ann. 2014;43(7):e151–e156
- , , , et al. Quality improvement research in pediatric hospital medicine and the role of the Pediatric Research in Inpatient Settings (PRIS) network. Acad Pediatr. 2013;13(6):S54–S60.
Pediatric hospital medicine (PHM) fellowship programs came into existence approximately 20 years ago in Canada,[1] and since that time the number of programs in North America has grown dramatically. The first 3 PHM fellowship programs in the United States were initiated in 2003, and by 2008 there were 7 active programs. Just 5 years later in 2013, there were 20 fellowship programs in existence. Now, in 2015, there are over 30 programs, with several more in development. The goal of postresidency training in PHM is to improve the care of hospitalized children by training future hospitalists to provide high‐quality, evidence‐based clinical care and to generate new knowledge and scholarship in areas such as clinical research, patient safety and quality improvement, medical education, practice management, and patient outcomes.[2] Many pediatric hospitalists want to be able to perform research or quality improvement, but feel that they lack the time, skills, resources, and mentorship to do so.[3] To date, fellowship‐trained hospitalists have a demonstrated track record of contributing to the body of literature that is shaping the care of hospitalized children.[4, 5]
At present, PHM is not a recognized subspecialty of the American Board of Pediatrics (ABP) and therefore does not fall under the purview of the Accreditation Council of Graduate Medical Education (ACGME), leading to concern from some about the variability in depth and breadth of training across programs.[1] The development and publication of the PHM Core Competencies in 2010 helped define the scope of practice of pediatric hospitalists and provide guidelines for training programs, specifically with respect to clinical and nonclinical areas for assessment of competency.[6] Furthermore, studies of early career hospitalists have identified areas for future fellowship curriculum development, such as core procedural skills, quality improvement, and practice management.[7]
In an effort to address training variability across programs, PHM fellowship directors (FDs) have come together as an organized group, first meeting in 2008, with the primary goal of defining training standards and sharing curricular resources. Annual meetings of the FDs, sponsored by the American Academy of Pediatrics Section on Hospital Medicine (AAP‐SOHM), began in 2012. A key objective of this annual meeting has been to develop a standardized fellowship curriculum for use across programs as well as to determine gaps in training that need to be addressed. During this process, we have received input from key stakeholders including community hospitalists, internal medicine‐pediatrics hospitalists, and the PHM Certification Steering Committee, which organized the application for subspecialty certification to the ABP. To inform this process of curriculum standardization, we fielded a survey of PHM fellowship directors. The purpose of this article is to summarize the current curricula, operations, and logistics of PHM fellowship programs.
METHODS
This was a cross‐sectional study of 31 PHM fellowship programs across the United States and Canada in April 2014. Inclusion criteria included all pediatric fellowships that were self‐identified to the AAP‐SOHM as providing a hospital medicine fellowship option. This included both PHM fellowships as well as academic general pediatric fellowships with a hospitalist track. A web‐based survey (SurveyMonkey, Inc.) was distributed by e‐mail to the FDs at the 31 training programs (see Supporting Information in the online version of this article). To enhance content validity of survey responses, survey questions were designed using an iterative consensus process among the authors, who included junior and senior FDs and represented the 2014 annual FD meeting planning committee. Items were created to gather feedback on the following key areas of PHM fellowships: program demographics, types of required and elective clinical rotations, graduate coursework offerings, amount of time spent in clinical activities, fellow billing practices, and description of fellows' research activities. The survey consisted of 30 multiple‐choice and short‐answer questions. Follow‐up e‐mail reminders were sent to all FDs 2 weeks and 4 weeks after the initial request was sent. Survey completion was voluntary, and no incentives were offered. The study was determined to be exempt by the Stanford University Institutional Review Board. Data were summarized using frequency distributions. No subgroup comparisons were made.
RESULTS
Program directors from 27/31 (87%) PHM fellowship programs responded to the survey; 25 were active programs, and 2 were under development. Responding programs represented all 4 major regions of the country and Canada, with varying program initiation dates, ranging from 1997 to 2013.
Program Demographics
The duration of most programs (17/27) was 2 years (63%), with 6 (22%) 1‐year programs and 4 (15%) 3‐year programs making up the remainder. Four programs described variable lengths, which could be tailored based on the fellow's individual interest. Two of the programs are 2 years in length, but offer a 1‐year option for fellows who wish to focus on enhancing clinical skills without an academic focus. The other 2 programs are 2 years in length, but will offer an extension to a third year for those pursuing a graduate degree.
Fellow Clinical Activities
The average amount of total clinical time (weeks on service) across responding programs was 50% (range, 20%65%). When looking specifically at time on the inpatient general pediatric service, number of weeks varied by year of training and by institution, with 12 to 41 weeks in the first year of fellowship, 6 to 41 weeks in the second year of fellowship, and 6 to 28 weeks in the third year of fellowship (Figure 1). Though the range is large, on average, fellows spend 17 weeks on inpatient general pediatrics service during each year of training. Of note, the median number of weeks on inpatient general pediatrics service by year of training was 15 weeks, 16 weeks, and 16.5 weeks, respectively. In addition to inpatient general pediatrics service time, most programs require other clinical rotations, with sedation, complex care, and inpatient pediatrics at community sites being the most frequent (Figure 2). Of the 6 responding 1‐year programs, 5 (83%) allow fellows to bill/generate clinical revenue at some point during their training. Of the 15 responding 2‐year programs, 11 (73%) allow fellows to bill/generate clinical revenue at some point during their training. Of the 4 responding 3‐year programs, 2 (50%) allow their fellows to bill/generate clinical revenue at some point during their training.
Fellow Scholarly Activities
With respect to time dedicated to research, the majority of programs offer coursework such as courses for credit, noncredit courses, or certificate courses. In addition, 11 programs offer fellows a masters' degree in areas including public health, clinical science, epidemiology, education, academic sciences, healthcare quality, clinical and translational research, or health services administration. The majority of these degrees are paid for by departmental funds, with tuition reimbursement, university support, training grants, and personal funds making up the remainder. Twenty‐one (81%) programs provide a scholarship oversight committee for their fellows. Current fellows' (n = 63) primary areas of research are varied and include clinical research (36%), quality‐improvement research (22%), medical education research (20%), health services research (16%), and other areas (6%).
DISCUSSION
This is the most comprehensive description of pediatric hospital medicine fellowship curricula to date. Understanding the scope of these programs is an important first step in developing a standardized curriculum that can be used by all. The results of this survey indicate that although there is variability among PHM fellowship curricular content, several common themes exist.
The number of clinical weeks on the inpatient general pediatrics service varied from program to program, though the majority of programs require fellows to spend 15 to 16 weeks each year of training. The variability may be due in part to the way in which respondents defined the term week on clinical service. For example, if the fellow is primarily on a shift schedule, then he/she may only work 2 to 3 shifts in 1 week, which may have been viewed similarly to daily presence on a more traditional inpatient teaching service with 5 to 7 consecutive days of service. The current study did not explore the details of inpatient general pediatric clinical activities or exposure to opportunities to hone procedural skills, areas that are worth investigating as we move forward to better understand the needs of trainees.
Most residency training programs in general pediatrics require a significant amount of inpatient clinical time, specifically a minimum of 10 units or months, though only half of this time is required to be in inpatient general pediatrics.[8] Although nonfellowship trained early career hospitalists may feel adequately prepared to manage the clinical care of some hospitalized children, perceived competency is significantly lower than their fellowship‐trained colleagues with regard to care of the child with medical complexity and technology‐dependence, and with regard to provision of sedation for procedures.[7] The majority of FDs surveyed in our study indicated that additional clinical experience with sedation, complex care, and inpatient pediatrics at community sites were required of their fellows. Of note, many of these rotations are not commonly required in pediatric residency training programs; however, the PHM core competencies suggest that hospitalists should demonstrate proficiency in these areas to provide optimal care for hospitalized children. Our results suggest that current PHM fellowship curricula help address these clinical gaps. The requirement of these particular specialized experiences may reflect the clinical scope of practice that is expected from potential employers or may be related to staffing needs. It is well documented that the inpatient demographic of large pediatric tertiary care referral centers has changed over the past decade, with an increasing prevalence of children with medical complexity.[9, 10] In both tertiary referral centers and community hospitals, the expansion of the role of the hospitalist in providing specialized clinical services, such as sedation or surgical comanagement, has been significantly driven by financial factors, though a more recent focus on improvement of efficiency and quality of care within the hospital system has relied heavily on hospitalist input.[11, 12, 13] Important next steps in curriculum standardization include ensuring that training programs allow for adequate clinical exposure and proper assessment of competency in these areas, and determining the full complement of clinical training experiences that will produce hospitalists with a well‐defined scope of practice that adequately addresses the needs of hospitalized children.
Most fellowship‐trained hospitalists work primarily in university‐affiliated institutions with expectations for scholarly productivity.[5, 7] Fellowship‐trained hospitalists have made large contributions to the growing body of PHM literature, specifically in the realms of medical education, healthcare quality, clinical pediatrics, and healthcare outcomes.[4] Many PHM fellowship‐trained hospitalists have educational or administrative leadership roles.[2] Our results indicate that current PHM fellows continue to be active in a variety of research activities. In addition, FDs reported that the vast majority of programs included scholarship oversight committees, which ensure a mentored and structured research experience. Finally, most programs require or offer additional coursework, and many programs with university affiliations allow for attainment of graduate degrees. Inclusion of robust research training and infrastructure in all programs is a paramount goal of PHM fellowship training. This will allow graduates to be successful researchers, generating new knowledge and supporting the provision of high‐quality, evidence‐based, and value‐driven care for hospitalized children.
A unique feature of several PHM fellowship programs is that fellows are allowed to bill for clinical encounters. Many programs rely on clinical revenue to support fellow salaries.[14] For some programs, a portion of this clinical revenue comes from fellows billing for clinical encounters.[15] Programs that allow fellows to bill/generate clinical revenue have fellows working in attending roles without direct supervision, whereas nonbilling fellows have direct supervision by an attending.[15] In the current ABP training model, subspecialty fellows cannot independently bill for clinical encounters within their own subspecialty, though they can moonlight as long as they meet the duty hour requirements set forth by the ACGME.[16] FDs will need to consider the impact of this requirement on fellow autonomy and on financial revenue for funding fellow salaries if the field achieves ABP subspecialty status.
Regardless of whether or not PHM becomes a designated subspecialty of the ABP, FDs will continue to work together to develop a standard core curriculum that incorporates elements of clinical and nonclinical training to ensure that graduates not only provide high‐quality care for hospitalized children, but also generate new knowledge that advances the field in care delivery and quality of care in any setting. The results of this study will not only help to inform curriculum standardization, but also assessment and evaluation methods. Currently, PHM FDs meet annually and are nearing consensus on a standard 2‐year curriculum based on the PHM Core Competencies that incorporates core clinical, systems, and scholarly domains. We continue to solicit the input of stakeholders, including new FDs, community hospitalist leaders, internal medicine‐pediatrics hospitalist leaders, the Joint Council of Pediatric Hospital Medicine, and leaders of national organizations, such as the American Academy of Pediatrics, Academic Pediatrics Association, and Society of Hospital Medicine. Additional work around standardizing the fellowship application and recruitment process has resulted in our recent acceptance into the Fall Subspecialty Match through the National Residency Match Program, as well as development and implementation of a common fellowship application form. The FD group has recently formalized, voting into place an executive steering committee, which is responsible for the development and execution of long‐term goals that include finalizing a standardized curriculum, refining program and fellow assessment methods through critical evaluation of fellow metrics and outcomes, and standardization of evaluation methods.
Adopting a standard 2‐year curriculum may affect some programs, specifically those that are currently 1 year in duration. These programs would need to extend the length of their fellowship to allow for the breadth of experiences expected with a standardized 2‐year curriculum. This could result in significant financial challenges, effectively increasing the cost to administer the program. In addition, at present, programs have the flexibility to highlight individual areas of strength to attract candidates, allowing fellows to gain an in‐depth experience in domains such as clinical research, quality improvement, medical education, or health services research. With a standardized curriculum, some programs may have to assemble specific clinical and nonclinical experiences to meet the agreed‐upon expectations for PHM fellowship training. If these resources are not available, programs may need to seek relationships with other institutions to complete their offerings, a possibility that is being actively explored by this group. FDs continue to work with each other to share resources, identify training opportunities, and partner with each other to ensure that the requirements of a standard curriculum can be met.
This study has several limitations. First, it was a voluntary survey of program directors, and though we captured over 80% of programs at the time of the survey, there are currently more programs that have come into existence and more still that are in the development stage, leading to potential sampling error. Second, variable effort or accuracy by participants may have led to some degree of response error, such as content error or nonreporting error. Third, the survey questions focused on high‐level information, making it difficult to make nuanced comparisons between curricular elements or determine best curricular practice. In addition, this survey did not explore medical education and quality improvement activities of fellows, 2 major areas in which hospitalists play a major role in the inpatient setting.[1, 17, 18, 19, 20]
CONCLUSION
PHM fellowship programs have grown and continue to grow at a rapid rate. Variability in training is evident, both in clinical experiences and research experiences, though several common elements were identified in this study. The majority of programs are 2 years, and clinical experience comprises approximately 50% of training time, often including key rotations such as sedation, complex care, and rotations at community hospitals. Future directions include standardizing clinical training and expectations for scholarship, formulating appropriate methods for assessment of competency that can be used across programs, and seeking sustainable sources of funding.
Disclosure
Nothing to report.
Pediatric hospital medicine (PHM) fellowship programs came into existence approximately 20 years ago in Canada,[1] and since that time the number of programs in North America has grown dramatically. The first 3 PHM fellowship programs in the United States were initiated in 2003, and by 2008 there were 7 active programs. Just 5 years later in 2013, there were 20 fellowship programs in existence. Now, in 2015, there are over 30 programs, with several more in development. The goal of postresidency training in PHM is to improve the care of hospitalized children by training future hospitalists to provide high‐quality, evidence‐based clinical care and to generate new knowledge and scholarship in areas such as clinical research, patient safety and quality improvement, medical education, practice management, and patient outcomes.[2] Many pediatric hospitalists want to be able to perform research or quality improvement, but feel that they lack the time, skills, resources, and mentorship to do so.[3] To date, fellowship‐trained hospitalists have a demonstrated track record of contributing to the body of literature that is shaping the care of hospitalized children.[4, 5]
At present, PHM is not a recognized subspecialty of the American Board of Pediatrics (ABP) and therefore does not fall under the purview of the Accreditation Council of Graduate Medical Education (ACGME), leading to concern from some about the variability in depth and breadth of training across programs.[1] The development and publication of the PHM Core Competencies in 2010 helped define the scope of practice of pediatric hospitalists and provide guidelines for training programs, specifically with respect to clinical and nonclinical areas for assessment of competency.[6] Furthermore, studies of early career hospitalists have identified areas for future fellowship curriculum development, such as core procedural skills, quality improvement, and practice management.[7]
In an effort to address training variability across programs, PHM fellowship directors (FDs) have come together as an organized group, first meeting in 2008, with the primary goal of defining training standards and sharing curricular resources. Annual meetings of the FDs, sponsored by the American Academy of Pediatrics Section on Hospital Medicine (AAP‐SOHM), began in 2012. A key objective of this annual meeting has been to develop a standardized fellowship curriculum for use across programs as well as to determine gaps in training that need to be addressed. During this process, we have received input from key stakeholders including community hospitalists, internal medicine‐pediatrics hospitalists, and the PHM Certification Steering Committee, which organized the application for subspecialty certification to the ABP. To inform this process of curriculum standardization, we fielded a survey of PHM fellowship directors. The purpose of this article is to summarize the current curricula, operations, and logistics of PHM fellowship programs.
METHODS
This was a cross‐sectional study of 31 PHM fellowship programs across the United States and Canada in April 2014. Inclusion criteria included all pediatric fellowships that were self‐identified to the AAP‐SOHM as providing a hospital medicine fellowship option. This included both PHM fellowships as well as academic general pediatric fellowships with a hospitalist track. A web‐based survey (SurveyMonkey, Inc.) was distributed by e‐mail to the FDs at the 31 training programs (see Supporting Information in the online version of this article). To enhance content validity of survey responses, survey questions were designed using an iterative consensus process among the authors, who included junior and senior FDs and represented the 2014 annual FD meeting planning committee. Items were created to gather feedback on the following key areas of PHM fellowships: program demographics, types of required and elective clinical rotations, graduate coursework offerings, amount of time spent in clinical activities, fellow billing practices, and description of fellows' research activities. The survey consisted of 30 multiple‐choice and short‐answer questions. Follow‐up e‐mail reminders were sent to all FDs 2 weeks and 4 weeks after the initial request was sent. Survey completion was voluntary, and no incentives were offered. The study was determined to be exempt by the Stanford University Institutional Review Board. Data were summarized using frequency distributions. No subgroup comparisons were made.
RESULTS
Program directors from 27/31 (87%) PHM fellowship programs responded to the survey; 25 were active programs, and 2 were under development. Responding programs represented all 4 major regions of the country and Canada, with varying program initiation dates, ranging from 1997 to 2013.
Program Demographics
The duration of most programs (17/27) was 2 years (63%), with 6 (22%) 1‐year programs and 4 (15%) 3‐year programs making up the remainder. Four programs described variable lengths, which could be tailored based on the fellow's individual interest. Two of the programs are 2 years in length, but offer a 1‐year option for fellows who wish to focus on enhancing clinical skills without an academic focus. The other 2 programs are 2 years in length, but will offer an extension to a third year for those pursuing a graduate degree.
Fellow Clinical Activities
The average amount of total clinical time (weeks on service) across responding programs was 50% (range, 20%65%). When looking specifically at time on the inpatient general pediatric service, number of weeks varied by year of training and by institution, with 12 to 41 weeks in the first year of fellowship, 6 to 41 weeks in the second year of fellowship, and 6 to 28 weeks in the third year of fellowship (Figure 1). Though the range is large, on average, fellows spend 17 weeks on inpatient general pediatrics service during each year of training. Of note, the median number of weeks on inpatient general pediatrics service by year of training was 15 weeks, 16 weeks, and 16.5 weeks, respectively. In addition to inpatient general pediatrics service time, most programs require other clinical rotations, with sedation, complex care, and inpatient pediatrics at community sites being the most frequent (Figure 2). Of the 6 responding 1‐year programs, 5 (83%) allow fellows to bill/generate clinical revenue at some point during their training. Of the 15 responding 2‐year programs, 11 (73%) allow fellows to bill/generate clinical revenue at some point during their training. Of the 4 responding 3‐year programs, 2 (50%) allow their fellows to bill/generate clinical revenue at some point during their training.
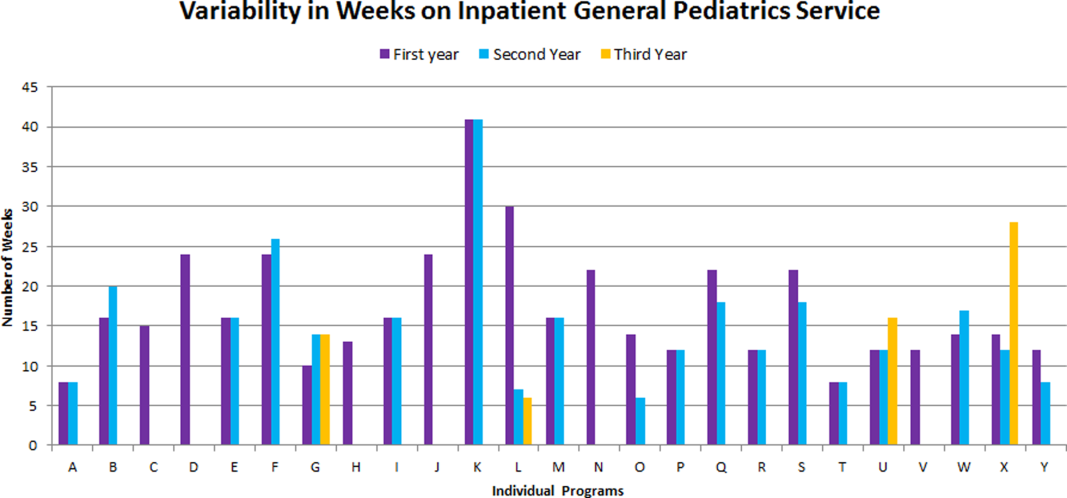
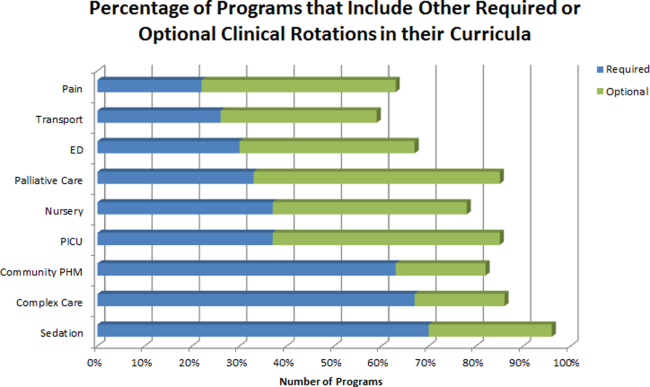
Fellow Scholarly Activities
With respect to time dedicated to research, the majority of programs offer coursework such as courses for credit, noncredit courses, or certificate courses. In addition, 11 programs offer fellows a masters' degree in areas including public health, clinical science, epidemiology, education, academic sciences, healthcare quality, clinical and translational research, or health services administration. The majority of these degrees are paid for by departmental funds, with tuition reimbursement, university support, training grants, and personal funds making up the remainder. Twenty‐one (81%) programs provide a scholarship oversight committee for their fellows. Current fellows' (n = 63) primary areas of research are varied and include clinical research (36%), quality‐improvement research (22%), medical education research (20%), health services research (16%), and other areas (6%).
DISCUSSION
This is the most comprehensive description of pediatric hospital medicine fellowship curricula to date. Understanding the scope of these programs is an important first step in developing a standardized curriculum that can be used by all. The results of this survey indicate that although there is variability among PHM fellowship curricular content, several common themes exist.
The number of clinical weeks on the inpatient general pediatrics service varied from program to program, though the majority of programs require fellows to spend 15 to 16 weeks each year of training. The variability may be due in part to the way in which respondents defined the term week on clinical service. For example, if the fellow is primarily on a shift schedule, then he/she may only work 2 to 3 shifts in 1 week, which may have been viewed similarly to daily presence on a more traditional inpatient teaching service with 5 to 7 consecutive days of service. The current study did not explore the details of inpatient general pediatric clinical activities or exposure to opportunities to hone procedural skills, areas that are worth investigating as we move forward to better understand the needs of trainees.
Most residency training programs in general pediatrics require a significant amount of inpatient clinical time, specifically a minimum of 10 units or months, though only half of this time is required to be in inpatient general pediatrics.[8] Although nonfellowship trained early career hospitalists may feel adequately prepared to manage the clinical care of some hospitalized children, perceived competency is significantly lower than their fellowship‐trained colleagues with regard to care of the child with medical complexity and technology‐dependence, and with regard to provision of sedation for procedures.[7] The majority of FDs surveyed in our study indicated that additional clinical experience with sedation, complex care, and inpatient pediatrics at community sites were required of their fellows. Of note, many of these rotations are not commonly required in pediatric residency training programs; however, the PHM core competencies suggest that hospitalists should demonstrate proficiency in these areas to provide optimal care for hospitalized children. Our results suggest that current PHM fellowship curricula help address these clinical gaps. The requirement of these particular specialized experiences may reflect the clinical scope of practice that is expected from potential employers or may be related to staffing needs. It is well documented that the inpatient demographic of large pediatric tertiary care referral centers has changed over the past decade, with an increasing prevalence of children with medical complexity.[9, 10] In both tertiary referral centers and community hospitals, the expansion of the role of the hospitalist in providing specialized clinical services, such as sedation or surgical comanagement, has been significantly driven by financial factors, though a more recent focus on improvement of efficiency and quality of care within the hospital system has relied heavily on hospitalist input.[11, 12, 13] Important next steps in curriculum standardization include ensuring that training programs allow for adequate clinical exposure and proper assessment of competency in these areas, and determining the full complement of clinical training experiences that will produce hospitalists with a well‐defined scope of practice that adequately addresses the needs of hospitalized children.
Most fellowship‐trained hospitalists work primarily in university‐affiliated institutions with expectations for scholarly productivity.[5, 7] Fellowship‐trained hospitalists have made large contributions to the growing body of PHM literature, specifically in the realms of medical education, healthcare quality, clinical pediatrics, and healthcare outcomes.[4] Many PHM fellowship‐trained hospitalists have educational or administrative leadership roles.[2] Our results indicate that current PHM fellows continue to be active in a variety of research activities. In addition, FDs reported that the vast majority of programs included scholarship oversight committees, which ensure a mentored and structured research experience. Finally, most programs require or offer additional coursework, and many programs with university affiliations allow for attainment of graduate degrees. Inclusion of robust research training and infrastructure in all programs is a paramount goal of PHM fellowship training. This will allow graduates to be successful researchers, generating new knowledge and supporting the provision of high‐quality, evidence‐based, and value‐driven care for hospitalized children.
A unique feature of several PHM fellowship programs is that fellows are allowed to bill for clinical encounters. Many programs rely on clinical revenue to support fellow salaries.[14] For some programs, a portion of this clinical revenue comes from fellows billing for clinical encounters.[15] Programs that allow fellows to bill/generate clinical revenue have fellows working in attending roles without direct supervision, whereas nonbilling fellows have direct supervision by an attending.[15] In the current ABP training model, subspecialty fellows cannot independently bill for clinical encounters within their own subspecialty, though they can moonlight as long as they meet the duty hour requirements set forth by the ACGME.[16] FDs will need to consider the impact of this requirement on fellow autonomy and on financial revenue for funding fellow salaries if the field achieves ABP subspecialty status.
Regardless of whether or not PHM becomes a designated subspecialty of the ABP, FDs will continue to work together to develop a standard core curriculum that incorporates elements of clinical and nonclinical training to ensure that graduates not only provide high‐quality care for hospitalized children, but also generate new knowledge that advances the field in care delivery and quality of care in any setting. The results of this study will not only help to inform curriculum standardization, but also assessment and evaluation methods. Currently, PHM FDs meet annually and are nearing consensus on a standard 2‐year curriculum based on the PHM Core Competencies that incorporates core clinical, systems, and scholarly domains. We continue to solicit the input of stakeholders, including new FDs, community hospitalist leaders, internal medicine‐pediatrics hospitalist leaders, the Joint Council of Pediatric Hospital Medicine, and leaders of national organizations, such as the American Academy of Pediatrics, Academic Pediatrics Association, and Society of Hospital Medicine. Additional work around standardizing the fellowship application and recruitment process has resulted in our recent acceptance into the Fall Subspecialty Match through the National Residency Match Program, as well as development and implementation of a common fellowship application form. The FD group has recently formalized, voting into place an executive steering committee, which is responsible for the development and execution of long‐term goals that include finalizing a standardized curriculum, refining program and fellow assessment methods through critical evaluation of fellow metrics and outcomes, and standardization of evaluation methods.
Adopting a standard 2‐year curriculum may affect some programs, specifically those that are currently 1 year in duration. These programs would need to extend the length of their fellowship to allow for the breadth of experiences expected with a standardized 2‐year curriculum. This could result in significant financial challenges, effectively increasing the cost to administer the program. In addition, at present, programs have the flexibility to highlight individual areas of strength to attract candidates, allowing fellows to gain an in‐depth experience in domains such as clinical research, quality improvement, medical education, or health services research. With a standardized curriculum, some programs may have to assemble specific clinical and nonclinical experiences to meet the agreed‐upon expectations for PHM fellowship training. If these resources are not available, programs may need to seek relationships with other institutions to complete their offerings, a possibility that is being actively explored by this group. FDs continue to work with each other to share resources, identify training opportunities, and partner with each other to ensure that the requirements of a standard curriculum can be met.
This study has several limitations. First, it was a voluntary survey of program directors, and though we captured over 80% of programs at the time of the survey, there are currently more programs that have come into existence and more still that are in the development stage, leading to potential sampling error. Second, variable effort or accuracy by participants may have led to some degree of response error, such as content error or nonreporting error. Third, the survey questions focused on high‐level information, making it difficult to make nuanced comparisons between curricular elements or determine best curricular practice. In addition, this survey did not explore medical education and quality improvement activities of fellows, 2 major areas in which hospitalists play a major role in the inpatient setting.[1, 17, 18, 19, 20]
CONCLUSION
PHM fellowship programs have grown and continue to grow at a rapid rate. Variability in training is evident, both in clinical experiences and research experiences, though several common elements were identified in this study. The majority of programs are 2 years, and clinical experience comprises approximately 50% of training time, often including key rotations such as sedation, complex care, and rotations at community hospitals. Future directions include standardizing clinical training and expectations for scholarship, formulating appropriate methods for assessment of competency that can be used across programs, and seeking sustainable sources of funding.
Disclosure
Nothing to report.
- , . Characteristics of pediatric hospital medicine fellowships and training programs. J Hosp Med. 2009;4(3):157–163.
- , . Pediatric hospitalists in medical education: current roles and future directions. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):120–126.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , , , . Pediatric hospital medicine fellowships: outcomes and future directions. Paper presented at: Pediatric Hospital Medicine 2014; July 26, 2014; Orlando, FL.
- , , . Pediatric hospitalist research productivity: predictors of success at presenting abstracts and publishing peer‐reviewed manuscripts among pediatric hospitalists. Hosp Pediatr. 2012;2(3):149–160.
- , , . Pediatric hospital medicine core competencies: development and methodology. J Hosp Med. 2010;5:339–343.
- , , , . Perceived core competency achievements of fellowship and non‐fellowship early career pediatric hospitalists. J Hosp Med. 2015;10(6):373–389.
- Accreditation Council of Graduate Medical Education. ACGME program requirements for graduate medical education in pediatrics. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013‐PR‐FAQ‐PIF/320_pediatrics_07012013.pdf. Published September 30, 2012. Accessed July 7, 2015.
- , , , , , . Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646.
- , , , et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136:591–596.
- , , , , , . Pediatric hospitalist comanagement of spinal fusion surgery patients. J Hosp Med. 2007;2(1):23–30.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , . Sources of funding and support for pediatric hospital medicine fellowship programs. Poster presented at: Pediatric Hospital Medicine 2014; July 27, 2014; Orlando, FL.
- Council of Pediatric Hospital Medicine Fellowship Directors. Pediatric Hospital Medicine Fellowship Directors Annual Meeting: funding and return on investment. July 24, 2014.
- Accreditation Council of Graduate Medical Education. Frequently asked questions: ACGME common duty hour requirements. Available at: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh‐faqs2011.pdf. Updated June 18, 2014. Accessed July 7, 2015.
- , . Pediatric hospitalists: training, current practice and career goals. J Hosp Med. 2009;4(3):179–186.
- , . The hospitalist movement and its implications for the care of hospitalized children. Pediatrics. 1999;103:473–477.
- . Pediatric hospitalists and medical education. Pediatr Ann. 2014;43(7):e151–e156
- , , , et al. Quality improvement research in pediatric hospital medicine and the role of the Pediatric Research in Inpatient Settings (PRIS) network. Acad Pediatr. 2013;13(6):S54–S60.
- , . Characteristics of pediatric hospital medicine fellowships and training programs. J Hosp Med. 2009;4(3):157–163.
- , . Pediatric hospitalists in medical education: current roles and future directions. Curr Probl Pediatr Adolesc Health Care. 2012;42(5):120–126.
- , , . Research needs of pediatric hospitalists. Hosp Pediatr. 2011;1(1):38–44.
- , , , . Pediatric hospital medicine fellowships: outcomes and future directions. Paper presented at: Pediatric Hospital Medicine 2014; July 26, 2014; Orlando, FL.
- , , . Pediatric hospitalist research productivity: predictors of success at presenting abstracts and publishing peer‐reviewed manuscripts among pediatric hospitalists. Hosp Pediatr. 2012;2(3):149–160.
- , , . Pediatric hospital medicine core competencies: development and methodology. J Hosp Med. 2010;5:339–343.
- , , , . Perceived core competency achievements of fellowship and non‐fellowship early career pediatric hospitalists. J Hosp Med. 2015;10(6):373–389.
- Accreditation Council of Graduate Medical Education. ACGME program requirements for graduate medical education in pediatrics. Available at: https://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013‐PR‐FAQ‐PIF/320_pediatrics_07012013.pdf. Published September 30, 2012. Accessed July 7, 2015.
- , , , , , . Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126(4):638–646.
- , , , et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655.
- , . The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136:591–596.
- , , , , , . Pediatric hospitalist comanagement of spinal fusion surgery patients. J Hosp Med. 2007;2(1):23–30.
- , , , , . Development of a pediatric hospitalist sedation service: training and implementation. J Hosp Med. 2012;7(4):335–339.
- , . Sources of funding and support for pediatric hospital medicine fellowship programs. Poster presented at: Pediatric Hospital Medicine 2014; July 27, 2014; Orlando, FL.
- Council of Pediatric Hospital Medicine Fellowship Directors. Pediatric Hospital Medicine Fellowship Directors Annual Meeting: funding and return on investment. July 24, 2014.
- Accreditation Council of Graduate Medical Education. Frequently asked questions: ACGME common duty hour requirements. Available at: https://www.acgme.org/acgmeweb/Portals/0/PDFs/dh‐faqs2011.pdf. Updated June 18, 2014. Accessed July 7, 2015.
- , . Pediatric hospitalists: training, current practice and career goals. J Hosp Med. 2009;4(3):179–186.
- , . The hospitalist movement and its implications for the care of hospitalized children. Pediatrics. 1999;103:473–477.
- . Pediatric hospitalists and medical education. Pediatr Ann. 2014;43(7):e151–e156
- , , , et al. Quality improvement research in pediatric hospital medicine and the role of the Pediatric Research in Inpatient Settings (PRIS) network. Acad Pediatr. 2013;13(6):S54–S60.
© 2016 Society of Hospital Medicine
Pediatric Hospital Medicine Core Competencies
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding tubes | Communication |
| Bone and joint infections | Respiratory failure | Newborn care and delivery room management | Fluids and electrolyte management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology‐dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence‐based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health information systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary tract infections | Pediatric advanced life support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and certifying societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric hospital medicine fellowship directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- .Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine, PA 19130;2009.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?.Am J Med.2004;117:446–450.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- , , .Pediatric hospitalists: Training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- , .Standardize to excellence: improving the quality and safety of care with clinical pathways.Pediatr Clin North Am.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- , , , , , , et al.Pediatric hospitalists: report of a leadership conference.Pediatrics.2006;117(4):1122–1130.
- , , , , e.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and answers regarding ABIM recognition of focused practice in hospital medicine through maintenance of certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive pediatric hospital medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance measurement initiatives. http://www. jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards frequently asked questions: comprehensive accreditation manual for critical access hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccess Hospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- , , , , .Infectious disease hospitalizations among infants in the United States.Pediatrics.2008;121(2):244–252.
- , , , .Procedures in U.S. hospitals, 1997.HCUP fact book no. 2. In:agency for healthcare research and quality,Rockville, MD;2001.
- Anderson L, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR, et al., editors.A taxonomy for learning, teaching, and assessing. In: A Revision of Bloom's Taxonomy of Educational Objectives.Upper Saddle River, NJ: Addison Wesley Longman, Inc. Pearson Education USA;2001.
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding tubes | Communication |
| Bone and joint infections | Respiratory failure | Newborn care and delivery room management | Fluids and electrolyte management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology‐dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence‐based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health information systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary tract infections | Pediatric advanced life support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and certifying societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric hospital medicine fellowship directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding tubes | Communication |
| Bone and joint infections | Respiratory failure | Newborn care and delivery room management | Fluids and electrolyte management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology‐dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence‐based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health information systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary tract infections | Pediatric advanced life support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and certifying societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric hospital medicine fellowship directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- .Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine, PA 19130;2009.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?.Am J Med.2004;117:446–450.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- , , .Pediatric hospitalists: Training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- , .Standardize to excellence: improving the quality and safety of care with clinical pathways.Pediatr Clin North Am.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- , , , , , , et al.Pediatric hospitalists: report of a leadership conference.Pediatrics.2006;117(4):1122–1130.
- , , , , e.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and answers regarding ABIM recognition of focused practice in hospital medicine through maintenance of certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive pediatric hospital medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance measurement initiatives. http://www. jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards frequently asked questions: comprehensive accreditation manual for critical access hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccess Hospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- , , , , .Infectious disease hospitalizations among infants in the United States.Pediatrics.2008;121(2):244–252.
- , , , .Procedures in U.S. hospitals, 1997.HCUP fact book no. 2. In:agency for healthcare research and quality,Rockville, MD;2001.
- Anderson L, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR, et al., editors.A taxonomy for learning, teaching, and assessing. In: A Revision of Bloom's Taxonomy of Educational Objectives.Upper Saddle River, NJ: Addison Wesley Longman, Inc. Pearson Education USA;2001.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- .Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine, PA 19130;2009.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?.Am J Med.2004;117:446–450.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- , , .Pediatric hospitalists: Training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- , .Standardize to excellence: improving the quality and safety of care with clinical pathways.Pediatr Clin North Am.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- , , , , , , et al.Pediatric hospitalists: report of a leadership conference.Pediatrics.2006;117(4):1122–1130.
- , , , , e.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and answers regarding ABIM recognition of focused practice in hospital medicine through maintenance of certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive pediatric hospital medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance measurement initiatives. http://www. jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards frequently asked questions: comprehensive accreditation manual for critical access hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccess Hospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- , , , , .Infectious disease hospitalizations among infants in the United States.Pediatrics.2008;121(2):244–252.
- , , , .Procedures in U.S. hospitals, 1997.HCUP fact book no. 2. In:agency for healthcare research and quality,Rockville, MD;2001.
- Anderson L, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR, et al., editors.A taxonomy for learning, teaching, and assessing. In: A Revision of Bloom's Taxonomy of Educational Objectives.Upper Saddle River, NJ: Addison Wesley Longman, Inc. Pearson Education USA;2001.
Copyright © 2010 Society of Hospital Medicine
Pediatric Hospital Medicine Core Competencies
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal Jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding Tubes | Communication |
| Bone and joint infections | Respiratory Failure | Newborn care and delivery room management | Fluids and Electrolyte Management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health Information Systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary Tract infections | Pediatric Advanced Life Support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and Certifying Societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric Hospital Medicine Fellowship Directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- Todd von Deak MBA CAE Vice President Membership and Marketing.Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine National Office 1500 Spring Garden, Suite 501, Philadelphia, PA 19130;2009.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,,.Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.Journal of Hospital Medicine.2008;3(4):292–298.
- ,,.Pediatric hospitalists: Training, current practice, and career goals.Journal of Hospital Medicine.2009;4(3):179–186.
- ,.Standardize to Excellence: Improving the Quality and Safety of Care with Clinical Pathways.Pediatric Clinics of North America.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- ,,,,,, et al.Pediatric Hospitalists: Report of a Leadership Conference.Pediatrics.2006;117(4):1122–1130.
- ,,,, e.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and Answers regarding ABIM Recognition of Focused Practice in Hospital Medicine through Maintenance of Certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive Pediatric Hospital Medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance Measurement Initiatives. http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards Frequently Asked Questions: Comprehensive Accreditation Manual for Critical Access Hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccessHospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- ,,,,.Infectious Disease Hospitalizations Among Infants in the United States.Pediatrics.2008;121(2):244–252.
- ,,,.Procedures in U.S. Hospitals, 1997.HCUP Fact Book No. 2. In:Agency for Healthcare Research and Quality,Rockville, MD;2001.
- Anderson L,Krathwohl DR,Airasian PW,Cruikshank KA,Mayer RE,Pintrich PR, et al., editors.A Taxonomy for Learning, Teaching, and Assessing — A Revision of Bloom's Taxonomy of Educational Objectives.Addison Wesley Longman, Inc.Pearson Education USA, One Lake Street Upper Saddle River, NJ; (2001).
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal Jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding Tubes | Communication |
| Bone and joint infections | Respiratory Failure | Newborn care and delivery room management | Fluids and Electrolyte Management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health Information Systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary Tract infections | Pediatric Advanced Life Support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and Certifying Societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric Hospital Medicine Fellowship Directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal Jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding Tubes | Communication |
| Bone and joint infections | Respiratory Failure | Newborn care and delivery room management | Fluids and Electrolyte Management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health Information Systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary Tract infections | Pediatric Advanced Life Support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and Certifying Societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric Hospital Medicine Fellowship Directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- Todd von Deak MBA CAE Vice President Membership and Marketing.Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine National Office 1500 Spring Garden, Suite 501, Philadelphia, PA 19130;2009.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,,.Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.Journal of Hospital Medicine.2008;3(4):292–298.
- ,,.Pediatric hospitalists: Training, current practice, and career goals.Journal of Hospital Medicine.2009;4(3):179–186.
- ,.Standardize to Excellence: Improving the Quality and Safety of Care with Clinical Pathways.Pediatric Clinics of North America.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- ,,,,,, et al.Pediatric Hospitalists: Report of a Leadership Conference.Pediatrics.2006;117(4):1122–1130.
- ,,,, e.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and Answers regarding ABIM Recognition of Focused Practice in Hospital Medicine through Maintenance of Certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive Pediatric Hospital Medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance Measurement Initiatives. http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards Frequently Asked Questions: Comprehensive Accreditation Manual for Critical Access Hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccessHospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- ,,,,.Infectious Disease Hospitalizations Among Infants in the United States.Pediatrics.2008;121(2):244–252.
- ,,,.Procedures in U.S. Hospitals, 1997.HCUP Fact Book No. 2. In:Agency for Healthcare Research and Quality,Rockville, MD;2001.
- Anderson L,Krathwohl DR,Airasian PW,Cruikshank KA,Mayer RE,Pintrich PR, et al., editors.A Taxonomy for Learning, Teaching, and Assessing — A Revision of Bloom's Taxonomy of Educational Objectives.Addison Wesley Longman, Inc.Pearson Education USA, One Lake Street Upper Saddle River, NJ; (2001).
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- Todd von Deak MBA CAE Vice President Membership and Marketing.Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine National Office 1500 Spring Garden, Suite 501, Philadelphia, PA 19130;2009.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,,.Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.Journal of Hospital Medicine.2008;3(4):292–298.
- ,,.Pediatric hospitalists: Training, current practice, and career goals.Journal of Hospital Medicine.2009;4(3):179–186.
- ,.Standardize to Excellence: Improving the Quality and Safety of Care with Clinical Pathways.Pediatric Clinics of North America.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- ,,,,,, et al.Pediatric Hospitalists: Report of a Leadership Conference.Pediatrics.2006;117(4):1122–1130.
- ,,,, e.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and Answers regarding ABIM Recognition of Focused Practice in Hospital Medicine through Maintenance of Certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive Pediatric Hospital Medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance Measurement Initiatives. http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards Frequently Asked Questions: Comprehensive Accreditation Manual for Critical Access Hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccessHospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- ,,,,.Infectious Disease Hospitalizations Among Infants in the United States.Pediatrics.2008;121(2):244–252.
- ,,,.Procedures in U.S. Hospitals, 1997.HCUP Fact Book No. 2. In:Agency for Healthcare Research and Quality,Rockville, MD;2001.
- Anderson L,Krathwohl DR,Airasian PW,Cruikshank KA,Mayer RE,Pintrich PR, et al., editors.A Taxonomy for Learning, Teaching, and Assessing — A Revision of Bloom's Taxonomy of Educational Objectives.Addison Wesley Longman, Inc.Pearson Education USA, One Lake Street Upper Saddle River, NJ; (2001).