User login
Pediatric Hospital Medicine Core Competencies
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding tubes | Communication |
| Bone and joint infections | Respiratory failure | Newborn care and delivery room management | Fluids and electrolyte management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology‐dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence‐based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health information systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary tract infections | Pediatric advanced life support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and certifying societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric hospital medicine fellowship directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- .Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine, PA 19130;2009.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?.Am J Med.2004;117:446–450.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
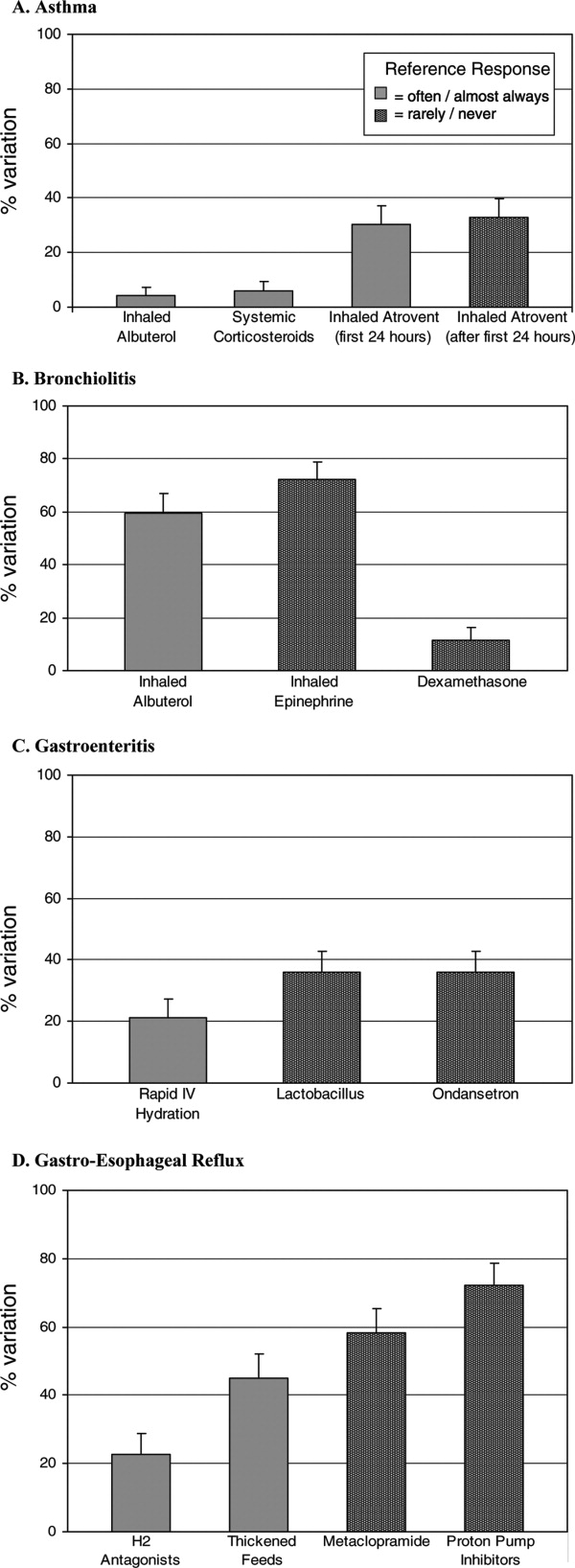
- , , , , .Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- , , .Pediatric hospitalists: Training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- , .Standardize to excellence: improving the quality and safety of care with clinical pathways.Pediatr Clin North Am.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- , , , , , , et al.Pediatric hospitalists: report of a leadership conference.Pediatrics.2006;117(4):1122–1130.
- , , , , e.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and answers regarding ABIM recognition of focused practice in hospital medicine through maintenance of certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive pediatric hospital medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance measurement initiatives. http://www. jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards frequently asked questions: comprehensive accreditation manual for critical access hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccess Hospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- , , , , .Infectious disease hospitalizations among infants in the United States.Pediatrics.2008;121(2):244–252.
- , , , .Procedures in U.S. hospitals, 1997.HCUP fact book no. 2. In:agency for healthcare research and quality,Rockville, MD;2001.
- Anderson L, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR, et al., editors.A taxonomy for learning, teaching, and assessing. In: A Revision of Bloom's Taxonomy of Educational Objectives.Upper Saddle River, NJ: Addison Wesley Longman, Inc. Pearson Education USA;2001.
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding tubes | Communication |
| Bone and joint infections | Respiratory failure | Newborn care and delivery room management | Fluids and electrolyte management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology‐dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence‐based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health information systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary tract infections | Pediatric advanced life support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and certifying societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric hospital medicine fellowship directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding tubes | Communication |
| Bone and joint infections | Respiratory failure | Newborn care and delivery room management | Fluids and electrolyte management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology‐dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence‐based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health information systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary tract infections | Pediatric advanced life support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and certifying societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric hospital medicine fellowship directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- .Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine, PA 19130;2009.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?.Am J Med.2004;117:446–450.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- , , .Pediatric hospitalists: Training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- , .Standardize to excellence: improving the quality and safety of care with clinical pathways.Pediatr Clin North Am.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- , , , , , , et al.Pediatric hospitalists: report of a leadership conference.Pediatrics.2006;117(4):1122–1130.
- , , , , e.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and answers regarding ABIM recognition of focused practice in hospital medicine through maintenance of certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive pediatric hospital medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance measurement initiatives. http://www. jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards frequently asked questions: comprehensive accreditation manual for critical access hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccess Hospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- , , , , .Infectious disease hospitalizations among infants in the United States.Pediatrics.2008;121(2):244–252.
- , , , .Procedures in U.S. hospitals, 1997.HCUP fact book no. 2. In:agency for healthcare research and quality,Rockville, MD;2001.
- Anderson L, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR, et al., editors.A taxonomy for learning, teaching, and assessing. In: A Revision of Bloom's Taxonomy of Educational Objectives.Upper Saddle River, NJ: Addison Wesley Longman, Inc. Pearson Education USA;2001.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- .Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine, PA 19130;2009.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?.Am J Med.2004;117:446–450.
- , .The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- , , , , .Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.J Hosp Med.2008;3(4):292–298.
- , , .Pediatric hospitalists: Training, current practice, and career goals.J Hosp Med.2009;4(3):179–186.
- , .Standardize to excellence: improving the quality and safety of care with clinical pathways.Pediatr Clin North Am.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- , , , , , , et al.Pediatric hospitalists: report of a leadership conference.Pediatrics.2006;117(4):1122–1130.
- , , , , e.The core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and answers regarding ABIM recognition of focused practice in hospital medicine through maintenance of certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive pediatric hospital medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance measurement initiatives. http://www. jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards frequently asked questions: comprehensive accreditation manual for critical access hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccess Hospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- , , , , .Infectious disease hospitalizations among infants in the United States.Pediatrics.2008;121(2):244–252.
- , , , .Procedures in U.S. hospitals, 1997.HCUP fact book no. 2. In:agency for healthcare research and quality,Rockville, MD;2001.
- Anderson L, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR, et al., editors.A taxonomy for learning, teaching, and assessing. In: A Revision of Bloom's Taxonomy of Educational Objectives.Upper Saddle River, NJ: Addison Wesley Longman, Inc. Pearson Education USA;2001.
Copyright © 2010 Society of Hospital Medicine
Pediatric Hospital Medicine Core Competencies
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal Jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding Tubes | Communication |
| Bone and joint infections | Respiratory Failure | Newborn care and delivery room management | Fluids and Electrolyte Management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health Information Systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary Tract infections | Pediatric Advanced Life Support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and Certifying Societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric Hospital Medicine Fellowship Directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- Todd von Deak MBA CAE Vice President Membership and Marketing.Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine National Office 1500 Spring Garden, Suite 501, Philadelphia, PA 19130;2009.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,,.Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.Journal of Hospital Medicine.2008;3(4):292–298.
- ,,.Pediatric hospitalists: Training, current practice, and career goals.Journal of Hospital Medicine.2009;4(3):179–186.
- ,.Standardize to Excellence: Improving the Quality and Safety of Care with Clinical Pathways.Pediatric Clinics of North America.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- ,,,,,, et al.Pediatric Hospitalists: Report of a Leadership Conference.Pediatrics.2006;117(4):1122–1130.
- ,,,, e.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and Answers regarding ABIM Recognition of Focused Practice in Hospital Medicine through Maintenance of Certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive Pediatric Hospital Medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance Measurement Initiatives. http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards Frequently Asked Questions: Comprehensive Accreditation Manual for Critical Access Hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccessHospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- ,,,,.Infectious Disease Hospitalizations Among Infants in the United States.Pediatrics.2008;121(2):244–252.
- ,,,.Procedures in U.S. Hospitals, 1997.HCUP Fact Book No. 2. In:Agency for Healthcare Research and Quality,Rockville, MD;2001.
- Anderson L,Krathwohl DR,Airasian PW,Cruikshank KA,Mayer RE,Pintrich PR, et al., editors.A Taxonomy for Learning, Teaching, and Assessing — A Revision of Bloom's Taxonomy of Educational Objectives.Addison Wesley Longman, Inc.Pearson Education USA, One Lake Street Upper Saddle River, NJ; (2001).
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal Jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding Tubes | Communication |
| Bone and joint infections | Respiratory Failure | Newborn care and delivery room management | Fluids and Electrolyte Management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health Information Systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary Tract infections | Pediatric Advanced Life Support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and Certifying Societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric Hospital Medicine Fellowship Directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
Introduction
The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the comprehensive general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to Hospital Medicine.1 It is estimated that there are up to 2500 pediatric hospitalists in the United States, with continued growth due to the converging needs for a dedicated focus on patient safety, quality improvement, hospital throughput, and inpatient teaching.2‐9 (Pediatric Hospital Medicine (PHM), as defined today, has been practiced in the United States for at least 30 years10 and continues to evolve as an area of specialization, with the refinement of a distinct knowledgebase and skill set focused on the provision of high quality general pediatric care in the inpatient setting. PHM is the latest site‐specific specialty to emerge from the field of general pediatrics it's development analogous to the evolution of critical care or emergency medicine during previous decades.11 Adult hospital medicine has defined itself within the field of general internal medicine12 and has recently received approval to provide a recognized focus of practice exam in 2010 for those re‐certifying with the American Board of Internal Medicine,13 PHM is creating an identity as a subspecialty practice with distinct focus on inpatient care for children within the larger context of general pediatric care.8, 14
The Pediatric Hospital Medicine Core Competencies were created to help define the roles and expectations for pediatric hospitalists, regardless of practice setting. The intent is to provide a unified approach toward identifying the specific body of knowledge and measurable skills needed to assure delivery of the highest quality of care for all hospitalized pediatric patients. Most children requiring hospitalization in the United States are hospitalized in community settings where subspecialty support is more limited and many pediatric services may be unavailable. Children with complex, chronic medical problems, however, are more likely to be hospitalized at a tertiary care or academic institutions. In order to unify pediatric hospitalists who work in different practice environments, the PHM Core Competencies were constructed to represent the knowledge, skills, attitudes, and systems improvements that all pediatric hospitalists can be expected to acquire and maintain.
Furthermore, the content of the PHM Core Competencies reflect the fact that children are a vulnerable population. Their care requires attention to many elements which distinguishes it from that given to the majority of the adult population: dependency, differences in developmental physiology and behavior, occurrence of congenital genetic disorders and age‐based clinical conditions, impact of chronic disease states on whole child development, and weight‐based medication dosing often with limited guidance from pediatric studies, to name a few. Awareness of these needs must be heightened when a child enters the hospital where diagnoses, procedures, and treatments often include use of high‐risk modalities and require coordination of care across multiple providers.
Pediatric hospitalists commonly work to improve the systems of care in which they operate and therefore both clinical and non‐clinical topics are included. The 54 chapters address the fundamental and most common components of inpatient care but are not an extensive review of all aspects of inpatient medicine encountered by those caring for hospitalized children. Finally, the PHM Core Competencies are not intended for use in assessing proficiency immediately post‐residency, but do provide a framework for the education and evaluation of both physicians‐in‐training and practicing hospitalists. Meeting these competencies is anticipated to take from one to three years of active practice in pediatric hospital medicine, and may be reached through a combination of practice experience, course work, self‐directed work, and/or formalized training.
Methods
Timeline
In 2002, SHM convened an educational summit from which there was a resolution to create core competencies. Following the summit, the SHM Pediatric Core Curriculum Task Force (CCTF) was created, which included 12 pediatric hospitalists practicing in academic and community facilities, as well as teaching and non‐teaching settings, and occupying leadership positions within institutions of varied size and geographic location. Shortly thereafter, in November 2003, approximately 130 pediatric hospitalists attended the first PHM meeting in San Antonio, Texas.11 At this meeting, with support from leaders in pediatric emergency medicine, first discussions regarding PHM scope of practice were held.
Formal development of the competencies began in 2005 in parallel to but distinct from SHM's adult work, which culminated in The Core Competencies in Hospital Medicine: A Framework for Curriculum Development published in 2006. The CCTF divided into three groups, focused on clinical, procedural, and systems‐based topics. Face‐to‐face meetings were held at the SHM annual meetings, with most work being completed by phone and electronically in the interim periods. In 2007, due to the overlapping interests of the three core pediatric societies, the work was transferred to leaders within the APA. In 2008 the work was transferred back to the leadership within SHM. Since that time, external reviewers were solicited, new chapters created, sections re‐aligned, internal and external reviewer comments incorporated, and final edits for taxonomy, content, and formatting were completed (Table 1).
| Date | Event |
|---|---|
| Feb 2002 | SHM Educational Summit held and CCTF created |
| Oct 2003 | 1st PHM meeting held in San Antonio |
| 2003‐2007 | Chapter focus determined; contributors engaged |
| 2007‐2008 | APA PHM Special Interest Group (SIG) review; creation of separate PHM Fellowship Competencies (not in this document) |
| Aug 2008‐Oct 2008 | SHM Pediatric Committee and CCTF members resume work; editorial review |
| Oct 2008‐Mar 2009 | Internal review: PHM Fellowship Director, AAP, APA, and SHM section/committee leader, and key national PHM leader reviews solicited and returned |
| Mar 2009 | PHM Fellowship Director comments addressed; editorial review |
| Mar‐Apr 2009 | External reviewers solicited from national agencies and societies relevant to PHM |
| Apr‐July 2009 | External reviewer comments returned |
| July‐Oct 2009 | Contributor review of all comments; editorial review, sections revised |
| Oct 2009 | Final review: Chapters to SHM subcommittees and Board |
Areas of Focused Practice
The PHM Core Competencies were conceptualized similarly to the SHM adult core competencies. Initial sections were divided into clinical conditions, procedures, and systems. However as content developed and reviewer comments were addressed, the four final sections were modified to those noted in Table 2. For the Common Clinical Diagnoses and Conditions, the goal was to select conditions most commonly encountered by pediatric hospitalists. Non‐surgical diagnosis‐related group (DRG) conditions were selected from the following sources: The Joint Commission's (TJC) Oryx Performance Measures Report15‐16 (asthma, abdominal pain, acute gastroenteritis, simple pneumonia); Child Health Corporation of America's Pediatric Health Information System Dataset (CHCA PHIS, Shawnee Mission, KS), and relevant publications on common pediatric hospitalizations.17 These data were compared to billing data from randomly‐selected practicing hospitalists representing free‐standing children's and community hospitals, teaching and non‐teaching settings, and urban and rural locations. The 22 clinical conditions chosen by the CCTF were those most relevant to the practice of pediatric hospital medicine.
| Common Clinical Diagnoses and Conditions | Specialized Clinical Services | Core Skills | Healthcare Systems: Supporting and Advancing Child Health | |
|---|---|---|---|---|
| Acute abdominal pain and the acute abdomen | Neonatal fever | Child abuse and neglect | Bladder catheterization/suprapubic bladder tap | Advocacy |
| Apparent life‐threatening event | Neonatal Jaundice | Hospice and palliative care | Electrocardiogram interpretation | Business practices |
| Asthma | Pneumonia | Leading a healthcare team | Feeding Tubes | Communication |
| Bone and joint infections | Respiratory Failure | Newborn care and delivery room management | Fluids and Electrolyte Management | Continuous quality improvement |
| Bronchiolitis | Seizures | Technology dependent children | Intravenous access and phlebotomy | Cost‐effective care |
| Central nervous system infections | Shock | Transport of the critically ill child | Lumbar puncture | Education |
| Diabetes mellitus | Sickle cell disease | Non‐invasive monitoring | Ethics | |
| Failure to thrive | Skin and soft tissue infection | Nutrition | Evidence based medicine | |
| Fever of unknown origin | Toxic ingestion | Oxygen delivery and airway management | Health Information Systems | |
| Gastroenteritis | Upper airway infections | Pain management | Legal issues/risk management | |
| Kawasaki disease | Urinary Tract infections | Pediatric Advanced Life Support | Patient safety |
The Specialized Clinical Servicessection addresses important components of care that are not DRG‐based and reflect the unique needs of hospitalized children, as assessed by the CCTF, editors, and contributors. Core Skillswere chosen based on the HCUP Factbook 2 Procedures,18 billing data from randomly‐selected practicing hospitalists representing the same settings listed above, and critical input from reviewers. Depending on the individual setting, pediatric hospitalists may require skills in areas not found in these 11 chapters, such as chest tube placement or ventilator management. The list is therefore not exhaustive, but rather representative of skills most pediatric hospitalists should maintain.
The Healthcare Systems: Supporting and Advancing Child Healthchapters are likely the most dissimilar to any core content taught in traditional residency programs. While residency graduates are versed in some components listed in these chapters, comprehensive education in most of these competencies is currently lacking. Improvement of healthcare systems is an essential element of pediatric hospital medicine, and unifies all pediatric hospitalists regardless of practice environment or patient population. Therefore, this section includes chapters that not only focus on systems of care, but also on advancing child health through advocacy, research, education, evidence‐based medicine, and ethical practice. These chapters were drawn from a combination of several sources: expectations of external agencies (TJC, Center for Medicaid and Medicare) related to the specific nonclinical work in which pediatric hospitalists are integrally involved; expectations for advocacy as best defined by the AAP and the National Association of Children's Hospitals and Related Institutions (NACHRI); the six core competency domains mandated by the Accrediting Council on Graduate Medical Education (ACGME), the American Board of Pediatrics (ABP), and hospital medical staff offices as part of Focused Professional Practice Evaluation (FPPE) and Ongoing Professional Practice Evaluation (OPPE)16; and assessment of responsibilities and leadership roles fulfilled by pediatric hospitalists in all venues. In keeping with the intent of the competencies to be timeless, the competency elements call out the need to attend to the changing goals of these groups as well as those of the Institute of Healthcare Improvement (IHI), the Alliance for Pediatric Quality (which consists of ABP, AAP, TJC, CHCA, NACHRI), and local hospital systems leaders.
Contributors and Review
The CCTF selected section (associate) editors from SHM based on established expertise in each area, with input from the SHM Pediatric and Education Committees and the SHM Board. As a collaborative effort, authors for various chapters were solicited in consultation with experts from the AAP, APA, and SHM, and included non‐hospitalists with reputations as experts in various fields. Numerous SHM Pediatric Committee and CCTF conference calls were held to review hospital and academic appointments, presentations given, and affiliations relevant to the practice of pediatric hospital medicine. This vetting process resulted in a robust author list representing diverse geographic and practice settings. Contributors were provided with structure (Knowledge, Skills, Attitudes, and Systems subsections) and content (timeless, competency based) guidelines.
The review process was rigorous, and included both internal and external reviewers. The APA review in 2007 included the PHM Special Interest Group as well as the PHM Fellowship Directors (Table 1). After return to SHM and further editing, the internal review commenced which focused on content and scope. The editors addressed the resulting suggestions and worked to standardize formatting and use of Bloom's taxonomy.19 A list of common terms and phrases were created to add consistency between chapters. External reviewers were first mailed a letter requesting interest, which was followed up by emails, letters, and phone calls to encourage feedback. External review included 29 solicited agencies and societies (Table 3), with overall response rate of 66% (41% for Groups I and II). Individual contributors then reviewed comments specific to their chapters, with associate editor overview of their respective sections. The editors reviewed each chapter individually multiple times throughout the 2007‐2009 years, contacting individual contributors and reviewers by email and phone. Editors concluded a final comprehensive review of all chapters in late 2009.
| I. Academic and Certifying Societies |
| Academic Pediatric Association |
| Accreditation Council for Graduate Medical Education, Pediatric Residency Review Committee |
| American Academy of Family Physicians |
| American Academy of Pediatrics Board |
| American Academy of Pediatrics National Committee on Hospital Care |
| American Association of Critical Care Nursing |
| American Board of Family Medicine |
| American Board of Pediatrics |
| American College of Emergency Physicians |
| American Pediatric Society |
| Association of American Medical Colleges |
| Association of Medical School Pediatric Department Chairs (AMSPDC) |
| Association of Pediatric Program Directors |
| Council on Teaching Hospitals |
| Society of Pediatric Research |
| II. Stakeholder agencies |
| Agency for Healthcare Research and Quality |
| American Association of Critical Care Nursing |
| American College of Emergency Physicians |
| American Hospital Association (AHA) |
| American Nurses Association |
| American Society of Health‐System Pharmacists |
| Child Health Corporation of America (CHCA) |
| Institute for Healthcare Improvement |
| National Association for Children's Hospitals and Related Institutions (NACHRI) |
| National Association of Pediatric Nurse Practitioners (NAPNAP) |
| National Initiative for Children's Healthcare Quality (NICHQ) |
| National Quality Forum |
| Quality Resources International |
| Robert Wood Johnson Foundation |
| The Joint Commission for Accreditation of Hospitals and Organizations (TJC) |
| III. Pediatric Hospital Medicine Fellowship Directors |
| Boston Children's |
| Children's Hospital Los Angeles |
| Children's National D.C. |
| Emory |
| Hospital for Sick Kids Toronto |
| Rady Children's San Diego University of California San Diego |
| Riley Children's Hospital Indiana |
| University of South Florida, All Children's Hospital |
| Texas Children's Hospital, Baylor College of Medicine |
| IV. SHM, APA, AAP Leadership and committee chairs |
| American Academy of Pediatrics Section on Hospital Medicine |
| Academic Pediatric Association PHM Special Interest Group |
| SHM Board |
| SHM Education Committee |
| SHM Family Practice Committee |
| SHM Hospital Quality and Patient Safety Committee |
| SHM IT Task Force |
| SHM Journal Editorial Board |
| SHM Palliative Care Task Force |
| SHM Practice Analysis Committee |
| SHM Public Policy Committee |
| SHM Research Committee |
Chapter Content
Each of the 54 chapters within the four sections of these competencies is presented in the educational theory of learning domains: Knowledge, Skills, Attitudes, with a final Systems domain added to reflect the emphasis of hospitalist practice on improving healthcare systems. Each chapter is designed to stand alone, which may assist with development of curriculum at individual practice locations. Certain key phrases are apparent throughout, such as lead, coordinate, or participate in and work with hospital and community leaders to which were designed to note the varied roles in different practice settings. Some chapters specifically comment on the application of competency bullets given the unique and differing roles and expectations of pediatric hospitalists, such as research and education. Chapters state specific proficiencies expected wherever possible, with phrases and wording selected to help guide learning activities to achieve the competency.
Application and Future Directions
Although pediatric hospitalists care for children in many settings, these core competencies address the common expectations for any venue. Pediatric hospital medicine requires skills in acute care clinical medicine that attend to the changing needs of hospitalized children. The core of pediatric hospital medicine is dedicated to the care of children in the geographic hospital environment between emergency medicine and tertiary pediatric and neonatal intensive care units. Pediatric hospitalists provide care in related clinical service programs that are linked to hospital systems. In performing these activities, pediatric hospitalists consistently partner with ambulatory providers and subspecialists to render coordinated care across the continuum for a given child. Pediatric hospital medicine is an interdisciplinary practice, with focus on processes of care and clinical quality outcomes based in evidence. Engagement in local, state, and national initiatives to improve child health outcomes is a cornerstone of pediatric hospitalists' practice. These competencies provide the framework for creation of curricula that can reflect local issues and react to changing evidence.
As providers of systems‐based care, pediatric hospitalists are called upon more and more to render care and provide leadership in clinical arenas that are integral to healthcare organizations, such as home health care, sub‐acute care facilities, and hospice and palliative care programs. The practice of pediatric hospital medicine has evolved to its current state through efforts of many represented in the competencies as contributors, associate editors, editors, and reviewers. Pediatric hospitalists are committed to leading change in healthcare for hospitalized children, and are positioned well to address the interests and needs of community and urban, teaching and non‐teaching facilities, and the children and families they serve. These competencies reflect the areas of focused practice which, similar to pediatric emergency medicine, will no doubt be refined but not fundamentally changed in future years. The intent, we hope, is clear: to provide excellence in clinical care, accountability for practice, and lead improvements in healthcare for hospitalized children.
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- Todd von Deak MBA CAE Vice President Membership and Marketing.Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine National Office 1500 Spring Garden, Suite 501, Philadelphia, PA 19130;2009.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,,.Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.Journal of Hospital Medicine.2008;3(4):292–298.
- ,,.Pediatric hospitalists: Training, current practice, and career goals.Journal of Hospital Medicine.2009;4(3):179–186.
- ,.Standardize to Excellence: Improving the Quality and Safety of Care with Clinical Pathways.Pediatric Clinics of North America.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- ,,,,,, et al.Pediatric Hospitalists: Report of a Leadership Conference.Pediatrics.2006;117(4):1122–1130.
- ,,,, e.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and Answers regarding ABIM Recognition of Focused Practice in Hospital Medicine through Maintenance of Certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive Pediatric Hospital Medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance Measurement Initiatives. http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards Frequently Asked Questions: Comprehensive Accreditation Manual for Critical Access Hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccessHospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- ,,,,.Infectious Disease Hospitalizations Among Infants in the United States.Pediatrics.2008;121(2):244–252.
- ,,,.Procedures in U.S. Hospitals, 1997.HCUP Fact Book No. 2. In:Agency for Healthcare Research and Quality,Rockville, MD;2001.
- Anderson L,Krathwohl DR,Airasian PW,Cruikshank KA,Mayer RE,Pintrich PR, et al., editors.A Taxonomy for Learning, Teaching, and Assessing — A Revision of Bloom's Taxonomy of Educational Objectives.Addison Wesley Longman, Inc.Pearson Education USA, One Lake Street Upper Saddle River, NJ; (2001).
- Society of Hospital Medicine (SHM). Definition of a Hospitalist. http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information 2009.
- Todd von Deak MBA CAE Vice President Membership and Marketing.Pediatric Hospitalists Membership Numbers. In.Philadelphia:Society of Hospital Medicine National Office 1500 Spring Garden, Suite 501, Philadelphia, PA 19130;2009.
- ,.The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- .The future of hospital medicine: evolution or revolution?Am J Med.2004;117:446–450.
- ,.The hospitalist movement 5 years later.JAMA.2002;287:487–494.
- ,,,,.Variation in pediatric hospitalists' use of proven and unproven therapies: A study from the Pediatric Research in Inpatient Settings (PRIS) network.Journal of Hospital Medicine.2008;3(4):292–298.
- ,,.Pediatric hospitalists: Training, current practice, and career goals.Journal of Hospital Medicine.2009;4(3):179–186.
- ,.Standardize to Excellence: Improving the Quality and Safety of Care with Clinical Pathways.Pediatric Clinics of North America.2009;56(4):893–904.
- .Evolution of a new specialty ‐ a twenty year pediatric hospitalist experience [Abstract]. In:National Association of Inpatient Physicians (now Society of Hospital Medicine).New Orleans, Louisiana;1999.
- ,,,,,, et al.Pediatric Hospitalists: Report of a Leadership Conference.Pediatrics.2006;117(4):1122–1130.
- ,,,, e.The Core Competencies in Hospital Medicine: A Framework for Curriculum Development.J Hosp Med.2006;1(Suppl 1).
- American Board of Internal Medicine. Questions and Answers regarding ABIM Recognition of Focused Practice in Hospital Medicine through Maintenance of Certification. http://www.abim.org/news/news/focused‐practice‐hospital‐medicine‐qa.aspx. Published 2010. Accessed January 6,2010.
- .Comprehensive Pediatric Hospital Medicine.N Engl J Med.2008;358(21):2301–2302.
- The Joint Commission. Performance Measurement Initiatives. http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/. Published 2010. Accessed December 5,2010.
- The Joint Commission. Standards Frequently Asked Questions: Comprehensive Accreditation Manual for Critical Access Hospitals (CAMCAH). http://www.jointcommission.org/AccreditationPrograms/CriticalAccessHospitals/Standards/09_FAQs/default.htm. Accessed December 5,2008; December 14, 2009.
- ,,,,.Infectious Disease Hospitalizations Among Infants in the United States.Pediatrics.2008;121(2):244–252.
- ,,,.Procedures in U.S. Hospitals, 1997.HCUP Fact Book No. 2. In:Agency for Healthcare Research and Quality,Rockville, MD;2001.
- Anderson L,Krathwohl DR,Airasian PW,Cruikshank KA,Mayer RE,Pintrich PR, et al., editors.A Taxonomy for Learning, Teaching, and Assessing — A Revision of Bloom's Taxonomy of Educational Objectives.Addison Wesley Longman, Inc.Pearson Education USA, One Lake Street Upper Saddle River, NJ; (2001).
Pediatric Hospitalist Variation in Care
Reduction of undesirable variation in care has been a major focus of systematic efforts to improve the quality of the healthcare system.13 The emergence of hospitalists, physicians specializing in the care of hospitalized patients, was spurred by a desire to streamline care and reduce variability in hospital management of common diseases.4, 5 Over the past decade, hospitalist systems have become a leading vehicle for care delivery.4, 6, 7 It remains unclear, however, whether implementation of hospitalist systems has lessened undesirable variation in the inpatient management of common diseases.
While systematic reviews have found costs and hospital length of stay to be 10‐15% lower in both pediatric and internal medicine hospitalist systems, few studies have adequately assessed the processes or quality of care in hospitalist systems.8, 9 Two internal medicine studies have found decreased mortality in hospitalist systems, but the mechanism by which hospitalists apparently achieved these gains is unclear.10, 11 Even less is known about care processes or quality in pediatric hospitalist systems. Death is a rare occurrence in pediatric ward settings, and the seven studies conducted to date comparing pediatric hospitalist and traditional systems have been universally underpowered to detect differences in mortality.9, 1218 There is a need to better understand care processes as a first step in understanding and improving quality of care in hospitalist systems.19
The Pediatric Research in Inpatient Settings (PRIS) Network was formed to improve the quality of care for hospitalized children through collaborative clinical research. In this study, we sought to study variation in the care of common pediatric conditions among a cohort of pediatric hospitalists. We have previously reported that less variability exists in hospitalists' reported management of inpatient conditions than in the reported management of these same conditions by community‐based pediatricians,20 but we were concerned that substantial undesirable variation (ie, variation in practice due to uncertainty or unsubstantiated local practice traditions, rather than justified variation in care based on different risks of harms or benefits in different patients) may still exist among hospitalists. We therefore conducted a study: 1) to investigate variation in hospitalists' reported use of common inpatient therapies, and 2) to test the hypothesis that greater variation exists in hospitalists' reported use of inpatient therapies of unproven benefit than in those therapies proven to be beneficial.
METHODS
Survey Design and Administration
In 2003, we designed the PRIS Survey to collect data on hospitalists' backgrounds, practices, and training needs, as well as their management of common pediatric conditions. For the current study, we chose a priori to evaluate hospitalists' use of 14 therapies in the management of 4 common conditions: asthma, bronchiolitis, gastroenteritis, and gastro‐esophageal reflux disease (GERD) (Table 1). These four conditions were chosen for study because they were among the top discharge diagnoses (primary and secondary) from the inpatient services at 2 of the authors' institutions (Children's Hospital Boston and Children's Hospital San Diego) during the year before administration of the survey, and because a discrete set of therapeutic agents are commonly used in their management. Respondents were asked to report the frequency with which they used each of the 14 therapies of interest on 5‐point Likert scales (from 1=never to 5=almost always). The survey initially developed was piloted with a small group of hospitalists and pediatricians, and a final version incorporating revisions was subsequently administered to all pediatric hospitalists in the US and Canada identified through any of 3 sources: 1) the Pediatric Research in Inpatient Settings (PRIS) list of participants; 2) the Society for Hospital Medicine (SHM) pediatric hospital medicine e‐mail listserv; and 3) the list of all attendees of the first national pediatric hospitalist conference sponsored by the Ambulatory Pediatrics Association (APA), SHM, and American Academy of Pediatrics (AAP); this meeting was held in San Antonio, Texas, USA in November 2003. Individuals identified through more than 1 of these groups were counted only once. Potential participants were assured that individual responses would be kept confidential, and were e‐mailed an access code to participate in the online survey, using a secure web‐based interface; a paper‐based version was also made available to those who preferred to respond in this manner. Regular reminder notices were sent to all non‐responders. Further details regarding PRIS Survey recruitment and study methods have been published previously.20
| Condition | Therapy | BMJ clinical evidence Treatment effect categorization* | Study classification |
|---|---|---|---|
| |||
| Asthma | Inhaled albuterol | Beneficial | Proven |
| Systemic corticosteroids | Beneficial | Proven | |
| Inhaled ipratropium in the first 24 hours of hospitalization | Beneficial | Proven | |
| Inhaled ipratropium after the first 24 hours of hospitalization | Unknown effectiveness | Unproven | |
| Bronchiolitis | Inhaled albuterol | Unknown effectiveness | Unproven |
| Inhaled epinephrine | Unknown effectiveness | Unproven | |
| Systemic corticosteroids | Unknown effectiveness | Unproven | |
| Gastroenteritis | Intravenous hydration | Beneficial | Proven |
| Lactobacillus | Not assessed | Unproven | |
| Ondansetron | Not assessed | Unproven | |
| Gastro‐Esophageal Reflux Disease (GERD) | H2 histamine‐receptor antagonists | Unknown effectiveness | Unproven |
| Thickened feeds | Unknown effectiveness Likely to be beneficial | Unproven Proven | |
| Metoclopramide | Unknown effectiveness | Unproven | |
| Proton‐pump inhibitors | Unknown effectiveness | Unproven | |
DefinitionsReference Responses and Percent Variation
To measure variation in reported management, we first sought to determine a reference response for each therapy of interest. Since the evidence base for most of the therapies we studied is weak, it was not possible to determine a gold standard response for each therapy. Instead, we sought to measure the degree of divergence from a reference response for each therapy in the following manner. First, to simplify analyses, we collapsed our five‐category Likert scale into three categories (never/rarely, sometimes, and often/almost always). We then defined the reference response for each therapy to be never/rarely or often/almost always, whichever of the 2 was more frequently selected by respondents; sometimes was not used as a reference category, as reporting use of a particular therapy sometimes indicated substantial variability even within an individual's own practice.
Classification of therapies as proven or unproven.
To classify each of the 14 studied therapies as being of proven or unproven, we used the British Medical Journal's publication Clinical Evidence.19 We chose to use Clinical Evidence as an evidence‐based reference because it provides rigorously developed, systematic analyses of therapeutic management options for multiple common pediatric conditions, and organizes recommendations in a straightforward manner. Four of the 14 therapies had been determined on systematic review to be proven beneficial at the time of study design: systemic corticosteroids, inhaled albuterol, and ipratropium (in the first 24 h) in the care of children with asthma; and IV hydration in the care of children with acute gastroenteritis. The remaining 10 therapies were either considered to be of unknown effectiveness or had not been formally evaluated by Clinical Evidence, and were hence considered unproven for this study (Table 1). Of note, the use of thickened feeds in the treatment of children with GERD had been determined to be of unknown effectiveness at the time of study design, but was reclassified as likely to be beneficial during the course of the study.
Analyses
Descriptive statistics were used to report respondents' demographic characteristics and work environments, as well as variation in their reported use of each of the 14 therapies. Variation in hospitalists' use of proven versus unproven therapies was compared using the Wilcoxon rank sum test, as it was distributed non‐normally. For our primary analysis, the use of thickened feeds in GERD was considered unproven, but a sensitivity analysis was conducted reclassifying it as proven in light of the evolving literature on its use and its consequent reclassification in Clinical Evidence.(SAS Version 9.1, Cary, NC) was used for statistical analyses.
RESULTS
213 of the 320 individuals identified through the 3 lists of pediatric hospitalists (67%) responded to the survey. Of these, 198 (93%) identified themselves as hospitalists and were therefore included. As previously reported,20 53% of respondents were male, 55% worked in academic training environments, and 47% had completed advanced training (fellowship) beyond their core pediatric training (residency training); respondents reported completing residency training 11 9 (mean, standard deviation) years prior to the survey, and spending 176 72 days per year in the care of hospitalized patients.
Variation in reported management: asthma
(Figure 1, Panel A). Relatively little variation existed in reported use of the 4 asthma therapies studied. Only 4.4% (95% CI, 1.4‐7.4%) of respondents did not provide the reference response of using inhaled albuterol often or almost always in the care of inpatients with asthma, and only 6.0% (2.5‐9.5%) of respondents did not report using systemic corticosteroids often or almost always. Variation in reported use of ipratropium was somewhat higher.
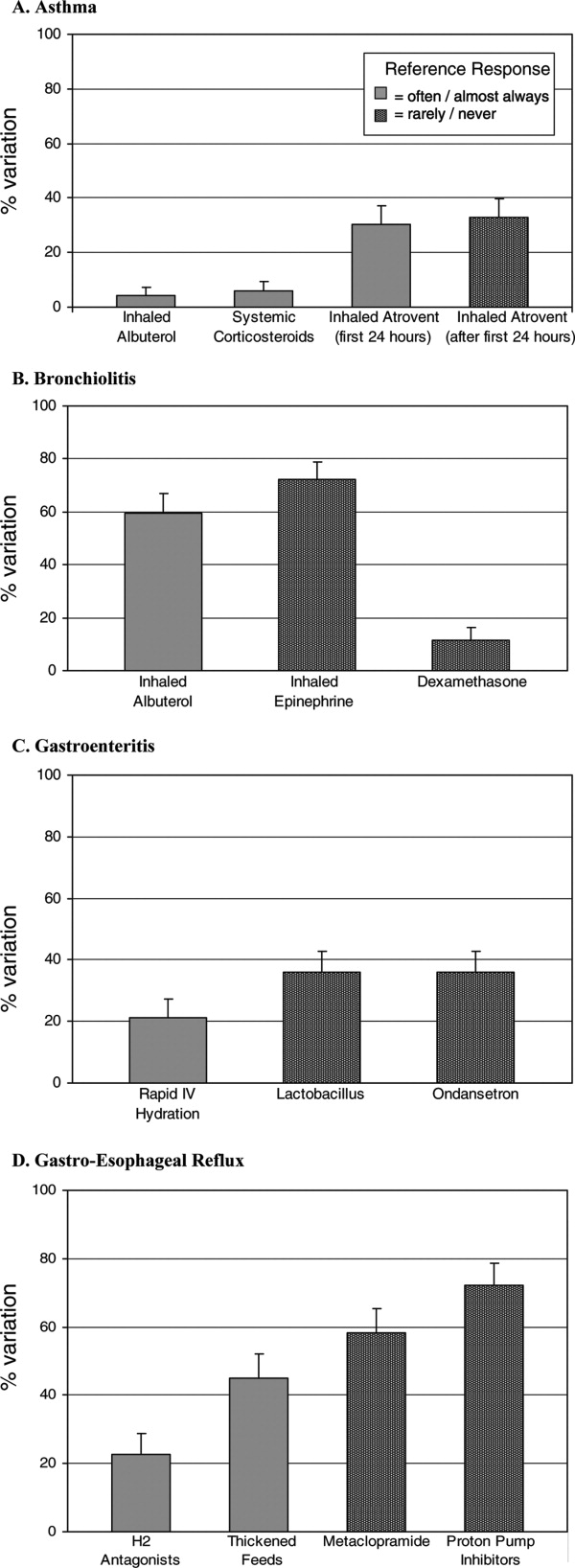
Bronchiolitis
(Figure 1B). By contrast, variation in reported use of inhaled therapies for bronchiolitis was high, with many respondents reporting that they often or always used inhaled albuterol or epinephrine, while many others reported rarely or never using them. There was 59.6% (52.4‐66.8%) variation from the reference response of often/almost always using inhaled albuterol, and 72.2% (65.6‐78.8%) variation from the reference response of never/rarely using inhaled epinephrine. Only 11.6% (6.9‐16.3%) of respondents, however, varied from the reference response of using dexamethasone more than rarely in the care of children with bronchiolitis.
Gastroenteritis
(Figure 1C). Moderate variability existed in the reported use of the 3 studied therapies for children hospitalized with gastroenteritis. 21.1% (15.1‐27.1%) of respondents did not provide the reference response of often/almost always using IV hydration; 35.9% (28.9‐42.9%) did not provide the reference response of never or rarely using lactobacillus; likewise, 35.9% (28.9‐42.9%) did not provide the reference response of never or rarely using ondansetron.
Gastro‐Esophageal Reflux Disease
(Figure 1, Panel D). There was moderate to high variability in the reported management of GERD. 22.8% (16.7‐28.9%) of respondents did not provide the reference response of often/almost always using H2 antagonists, and 44.9% (37.6‐52.2%) did not report often/almost always using thickened feeds in the care of these children. 58.3% (51.1‐65.5%) and 72.1% (65.5‐78.7%) of respondents did not provide the reference response of never/rarely using metoclopramide and proton pump inhibitors, respectively.
Proven vs. Unproven Therapies
(Figure 2). Variation in reported use of therapies of unproven benefit was significantly higher than variation in reported use of the 4 proven therapies (albuterol, corticosteroids, and ipratropium in the first 24 h for asthma; IV re‐hydration for gastroenteritis). The mean variation in reported use of unproven therapies was 44.6 20.5%, compared with 15.5 12.5% variation in reported use of therapies of proven benefit (p = 0.02).
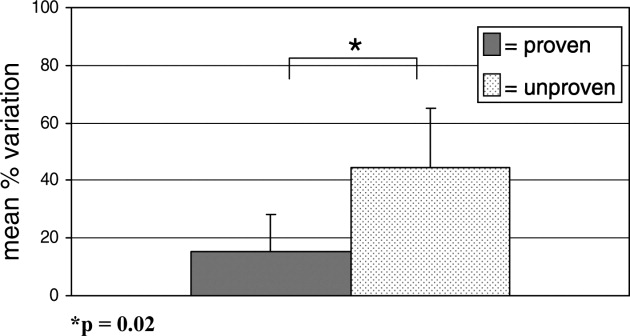
As a sensitivity analysis, the use of thickened feeds as a therapy for GERD was re‐categorized as proven and the above analysis repeated, for the reasons outlined in the methods section. This did not alter the identified relationship between variability and the evidence base fundamentally; hospitalists' reported variation in use of therapies of unproven benefit in this sensitivity analysis was 44.6 21.7%, compared with 21.4 17.0% variation in reported use of proven therapies (p = 0.05).
DISCUSSION
Substantial variation exists in the inpatient management of common pediatric diseases. Although we have previously found less reported variability in pediatric hospitalists' practices than in those of community‐based pediatricians,20 the current study demonstrates a high degree of reported variation even among a cohort of inpatient specialists. Importantly, however, reported variation was found to be significantly less for those inpatient therapies supported by a robust evidence base.
Bronchiolitis, gastroenteritis, asthma, and GERD are extremely common causes of pediatric hospitalization throughout the developed world.2125 Our finding of high reported variability in the routine care of all of these conditions except asthma is concerning, as it suggests that experts do not agree on how to manage children hospitalized with even the most common childhood diseases. While we hypothesized that there would be some variation in the use of therapies whose benefit has not been well established, the high degree of variation observed is of concern because it indicates that an insufficient evidentiary base exists to support much of our day‐to‐day practice. Some variation in practice in response to differing clinical presentations is both expected and desirable, but it is remarkable that variance in practice was significantly less for the most evidence‐based therapies than for those grounded less firmly in science, suggesting that the variation identified here is not justifiable variation based on appropriate responses to atypical clinical presentations, but uncertainty in the absence of clear data. Such undesired variability may decrease system reliability (introducing avoidable opportunity for error),26 and lead to under‐use of needed therapies as well as overuse of unnecessary therapies.1
Our work extends prior research that has identified wide variation in patterns of hospital admission, use of hospital resources, and processes of inpatient care,2732 by documenting reported variation in the use of common inpatient therapies. Rates of hospital admission may vary by as much as 7‐fold across regions.33 Our study demonstrates that wide variation exists not only in admission rates, but in reported inpatient care processes for some of the most common diseases seen in pediatric hospitals. Our study also supports the hypothesis that variation in care may be driven by gaps in knowledge.32 Among hospitalists, we found the strength of the evidence base to be a major determinant of reported variability.
Our study has several limitations. First, the data presented here are derived from provider self‐reports, which may not fully reflect actual practice. In the case of the few proven therapies studied, reporting bias could lead to an over‐reporting of adherence to evidence‐based standards of care. Like our study, however, prior studies have found that hospital‐based providers fairly consistently comply with evidence‐based practice recommendations for acute asthma care,34, 35 supporting our finding that variation in acute asthma care (which represented 3 of our 4 proven therapies) is low in this setting.
Another limitation is that classifications of therapies as proven or unproven change as the evidence base evolves. Of particular relevance to this study, the use of thickened feeds as a therapy for GERD, originally classified as being of unknown effectiveness, was reclassified by Clinical Evidence during the course of the study as likely to be beneficial. The relationship we identified between proven therapies and degree of variability in care did not change when we conducted a sensitivity analysis re‐categorizing this therapy as proven, but precisely quantifying variation is complicated by continuous changes in the state of the evidence.
Pediatric hospitalist systems have been found consistently to improve the efficiency of care,9 yet this study suggests that considerable variation in hospitalists' management of key conditions remains. The Pediatric Research in Inpatient Settings (PRIS) Network was formed in 2002 to improve the care of hospitalized children and the quality of inpatient practice by developing an evidence base for inpatient pediatric care. Ongoing multi‐center research efforts through PRIS and other research networks are beginning to critically evaluate therapies used in the management of common pediatric conditions. Rigorous studies of the processes and outcomes of pediatric hospital care will inform inpatient pediatric practice, and ultimately improve the care of hospitalized children. The current study strongly affirms the urgent need to establish such an evidence base. Without data to inform optimal care, efforts to reduce undesirable variation in care and improve care quality cannot be fully realized.
Acknowledgements
The authors would like to extend their thanks to the hospitalists and members of the Pediatric Research in Inpatient Settings Network who participated in this research, as well as the Children's National Medical Center and Children's Hospital Boston Inpatient Pediatrics Services, who provided funding to support this study. Special thanks to the Ambulatory Pediatrics Association (APA), for its core support of the PRIS Network. Dr. Landrigan is the recipient of a career development award from the Agency for Healthcare Research and Quality (AHRQ K08 HS13333). Dr. Conway is the recipient of a Robert Wood Johnson Clinical Scholars Grant. All researchers were independent from the funding agencies; the academic medical centers named above, APA, and AHRQ had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
- Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, D.C.:National Academic Press,2001.
- ..Reducing variation in surgical care.BMJ2005;330:1401–1402.
- ,,,.Variation in use of video assisted thoracic surgery in the United Kingdom.BMJ2004;329:1011–1012.
- ,..The emerging role of “hospitalists” in the American health care system.N. Engl J Med1996;335:514–517.
- ,..Hospitalism in the USA.Lancet1999;353:1902.
- Society of Hospital Medicine. Growth of Hospital Medicine Nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed April 11,2007.
- .The changing face of hospital practice.Med Econ2002;79:72–79.
- ,..The hospitalist movement 5 years later.JAMA2002;287:487–494.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics2006;117:1736–1744.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med2002;137:859–865.
- ,,,,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med2002;137:866–874.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics2000;105:478–484.
- ,,,,,,, and .Impact of an HMO hospitalist system in academic pediatrics.Pediatrics2002;110:720–728.
- ,, and .Evaluation of a pediatric hospitalist service by APR‐DRG's: impact on length of stay and hospital charges.Pediatr Research2001;49(suppl),691.
- ,,.Pediatric hospitalists: quality care for the underserved?Am J Med Qual2001;16:174–180.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr (Phila)2001;40:653–660.
- ,,, and .Hospitalist care of medically complex children.Pediatr Research2004;55(suppl),1789.
- ,,.Hospital‐based and community pediatricians: comparing outcomes for asthma and bronchiolitis.J Clin Outcomes Manage1997;4:21–24.
- Godlee F,Tovey D,Bedford M, et al., eds.Clinical Evidence: The International Source of the Best Available Evidence for Effective Health Care.London, United Kingdom:BMJ Publishing Group;2004.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics2006;118:441–447.
- ,,,,.Contribution of RSV to bronchiolitis and pneumonia‐associated hospitalizations in English children, April 1995‐March 1998.Epidemiol Infect2002;129:99–106.
- ,,.Direct medical costs of bronchiolitis hospitalizations in the United States.Pediatrics2006;118:2418–2423.
- ,,,,,.Multicenter Prospective Study of the Burden of Rotavirus Acute Gastroenteritis in Europe, 2004‐2005: The REVEAL Study.J Infect Dis2007;195Suppl 1:S4–S16.
- .The state of childhood asthma, United States, 1980‐2005.Adv.Data.2006;1–24.
- ,.Gastroesophageal reflux in children: pathogenesis, prevalence, diagnosis, and role of proton pump inhibitors in treatment.Paediatr Drugs2002;4:673–685.
- ,,,.Reliability science and patient safety.Pediatr Clin North Am2006;53:1121–1133.
- Wennberg JE and McAndrew Cooper M, eds.The Dartmouth Atlas of Health Care in the United States.Hanover, NH, USA:Health Forum, Inc.,1999.
- ,,,,,.Variations in rates of hospitalization of children in three urban communities.N Engl J Med1989;320:1183–1187.
- ,,,,,.Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States.BMJ2004;328:607.
- ,,,,,, et al.Variations in practice and outcomes in the Canadian NICU network: 1996‐1997.Pediatrics2000;106:1070–1079.
- ,,,.Evaluation of febrile children with petechial rashes: is there consensus among pediatricians?Pediatr Infect Dis J1998;17:1135–1140.
- ,,,,,, et al.Practice variation among pediatric emergency departments in the treatment of bronchiolitis.Acad Emerg Med2004;11:353–360.
- ,,,.Paediatric inpatient utilisation in a district general hospital.Arch Dis Child1994;70:488–492.
- ,,,.Emergency department asthma: compliance with an evidence‐based management algorithm.Ann Acad Med Singapore2002;31:419–424.
- ,,.Is the practice of paediatric inpatient medicine evidence‐based?J Paediatr Child Health2002;38:347–351.
Reduction of undesirable variation in care has been a major focus of systematic efforts to improve the quality of the healthcare system.13 The emergence of hospitalists, physicians specializing in the care of hospitalized patients, was spurred by a desire to streamline care and reduce variability in hospital management of common diseases.4, 5 Over the past decade, hospitalist systems have become a leading vehicle for care delivery.4, 6, 7 It remains unclear, however, whether implementation of hospitalist systems has lessened undesirable variation in the inpatient management of common diseases.
While systematic reviews have found costs and hospital length of stay to be 10‐15% lower in both pediatric and internal medicine hospitalist systems, few studies have adequately assessed the processes or quality of care in hospitalist systems.8, 9 Two internal medicine studies have found decreased mortality in hospitalist systems, but the mechanism by which hospitalists apparently achieved these gains is unclear.10, 11 Even less is known about care processes or quality in pediatric hospitalist systems. Death is a rare occurrence in pediatric ward settings, and the seven studies conducted to date comparing pediatric hospitalist and traditional systems have been universally underpowered to detect differences in mortality.9, 1218 There is a need to better understand care processes as a first step in understanding and improving quality of care in hospitalist systems.19
The Pediatric Research in Inpatient Settings (PRIS) Network was formed to improve the quality of care for hospitalized children through collaborative clinical research. In this study, we sought to study variation in the care of common pediatric conditions among a cohort of pediatric hospitalists. We have previously reported that less variability exists in hospitalists' reported management of inpatient conditions than in the reported management of these same conditions by community‐based pediatricians,20 but we were concerned that substantial undesirable variation (ie, variation in practice due to uncertainty or unsubstantiated local practice traditions, rather than justified variation in care based on different risks of harms or benefits in different patients) may still exist among hospitalists. We therefore conducted a study: 1) to investigate variation in hospitalists' reported use of common inpatient therapies, and 2) to test the hypothesis that greater variation exists in hospitalists' reported use of inpatient therapies of unproven benefit than in those therapies proven to be beneficial.
METHODS
Survey Design and Administration
In 2003, we designed the PRIS Survey to collect data on hospitalists' backgrounds, practices, and training needs, as well as their management of common pediatric conditions. For the current study, we chose a priori to evaluate hospitalists' use of 14 therapies in the management of 4 common conditions: asthma, bronchiolitis, gastroenteritis, and gastro‐esophageal reflux disease (GERD) (Table 1). These four conditions were chosen for study because they were among the top discharge diagnoses (primary and secondary) from the inpatient services at 2 of the authors' institutions (Children's Hospital Boston and Children's Hospital San Diego) during the year before administration of the survey, and because a discrete set of therapeutic agents are commonly used in their management. Respondents were asked to report the frequency with which they used each of the 14 therapies of interest on 5‐point Likert scales (from 1=never to 5=almost always). The survey initially developed was piloted with a small group of hospitalists and pediatricians, and a final version incorporating revisions was subsequently administered to all pediatric hospitalists in the US and Canada identified through any of 3 sources: 1) the Pediatric Research in Inpatient Settings (PRIS) list of participants; 2) the Society for Hospital Medicine (SHM) pediatric hospital medicine e‐mail listserv; and 3) the list of all attendees of the first national pediatric hospitalist conference sponsored by the Ambulatory Pediatrics Association (APA), SHM, and American Academy of Pediatrics (AAP); this meeting was held in San Antonio, Texas, USA in November 2003. Individuals identified through more than 1 of these groups were counted only once. Potential participants were assured that individual responses would be kept confidential, and were e‐mailed an access code to participate in the online survey, using a secure web‐based interface; a paper‐based version was also made available to those who preferred to respond in this manner. Regular reminder notices were sent to all non‐responders. Further details regarding PRIS Survey recruitment and study methods have been published previously.20
| Condition | Therapy | BMJ clinical evidence Treatment effect categorization* | Study classification |
|---|---|---|---|
| |||
| Asthma | Inhaled albuterol | Beneficial | Proven |
| Systemic corticosteroids | Beneficial | Proven | |
| Inhaled ipratropium in the first 24 hours of hospitalization | Beneficial | Proven | |
| Inhaled ipratropium after the first 24 hours of hospitalization | Unknown effectiveness | Unproven | |
| Bronchiolitis | Inhaled albuterol | Unknown effectiveness | Unproven |
| Inhaled epinephrine | Unknown effectiveness | Unproven | |
| Systemic corticosteroids | Unknown effectiveness | Unproven | |
| Gastroenteritis | Intravenous hydration | Beneficial | Proven |
| Lactobacillus | Not assessed | Unproven | |
| Ondansetron | Not assessed | Unproven | |
| Gastro‐Esophageal Reflux Disease (GERD) | H2 histamine‐receptor antagonists | Unknown effectiveness | Unproven |
| Thickened feeds | Unknown effectiveness Likely to be beneficial | Unproven Proven | |
| Metoclopramide | Unknown effectiveness | Unproven | |
| Proton‐pump inhibitors | Unknown effectiveness | Unproven | |
DefinitionsReference Responses and Percent Variation
To measure variation in reported management, we first sought to determine a reference response for each therapy of interest. Since the evidence base for most of the therapies we studied is weak, it was not possible to determine a gold standard response for each therapy. Instead, we sought to measure the degree of divergence from a reference response for each therapy in the following manner. First, to simplify analyses, we collapsed our five‐category Likert scale into three categories (never/rarely, sometimes, and often/almost always). We then defined the reference response for each therapy to be never/rarely or often/almost always, whichever of the 2 was more frequently selected by respondents; sometimes was not used as a reference category, as reporting use of a particular therapy sometimes indicated substantial variability even within an individual's own practice.
Classification of therapies as proven or unproven.
To classify each of the 14 studied therapies as being of proven or unproven, we used the British Medical Journal's publication Clinical Evidence.19 We chose to use Clinical Evidence as an evidence‐based reference because it provides rigorously developed, systematic analyses of therapeutic management options for multiple common pediatric conditions, and organizes recommendations in a straightforward manner. Four of the 14 therapies had been determined on systematic review to be proven beneficial at the time of study design: systemic corticosteroids, inhaled albuterol, and ipratropium (in the first 24 h) in the care of children with asthma; and IV hydration in the care of children with acute gastroenteritis. The remaining 10 therapies were either considered to be of unknown effectiveness or had not been formally evaluated by Clinical Evidence, and were hence considered unproven for this study (Table 1). Of note, the use of thickened feeds in the treatment of children with GERD had been determined to be of unknown effectiveness at the time of study design, but was reclassified as likely to be beneficial during the course of the study.
Analyses
Descriptive statistics were used to report respondents' demographic characteristics and work environments, as well as variation in their reported use of each of the 14 therapies. Variation in hospitalists' use of proven versus unproven therapies was compared using the Wilcoxon rank sum test, as it was distributed non‐normally. For our primary analysis, the use of thickened feeds in GERD was considered unproven, but a sensitivity analysis was conducted reclassifying it as proven in light of the evolving literature on its use and its consequent reclassification in Clinical Evidence.(SAS Version 9.1, Cary, NC) was used for statistical analyses.
RESULTS
213 of the 320 individuals identified through the 3 lists of pediatric hospitalists (67%) responded to the survey. Of these, 198 (93%) identified themselves as hospitalists and were therefore included. As previously reported,20 53% of respondents were male, 55% worked in academic training environments, and 47% had completed advanced training (fellowship) beyond their core pediatric training (residency training); respondents reported completing residency training 11 9 (mean, standard deviation) years prior to the survey, and spending 176 72 days per year in the care of hospitalized patients.
Variation in reported management: asthma
(Figure 1, Panel A). Relatively little variation existed in reported use of the 4 asthma therapies studied. Only 4.4% (95% CI, 1.4‐7.4%) of respondents did not provide the reference response of using inhaled albuterol often or almost always in the care of inpatients with asthma, and only 6.0% (2.5‐9.5%) of respondents did not report using systemic corticosteroids often or almost always. Variation in reported use of ipratropium was somewhat higher.
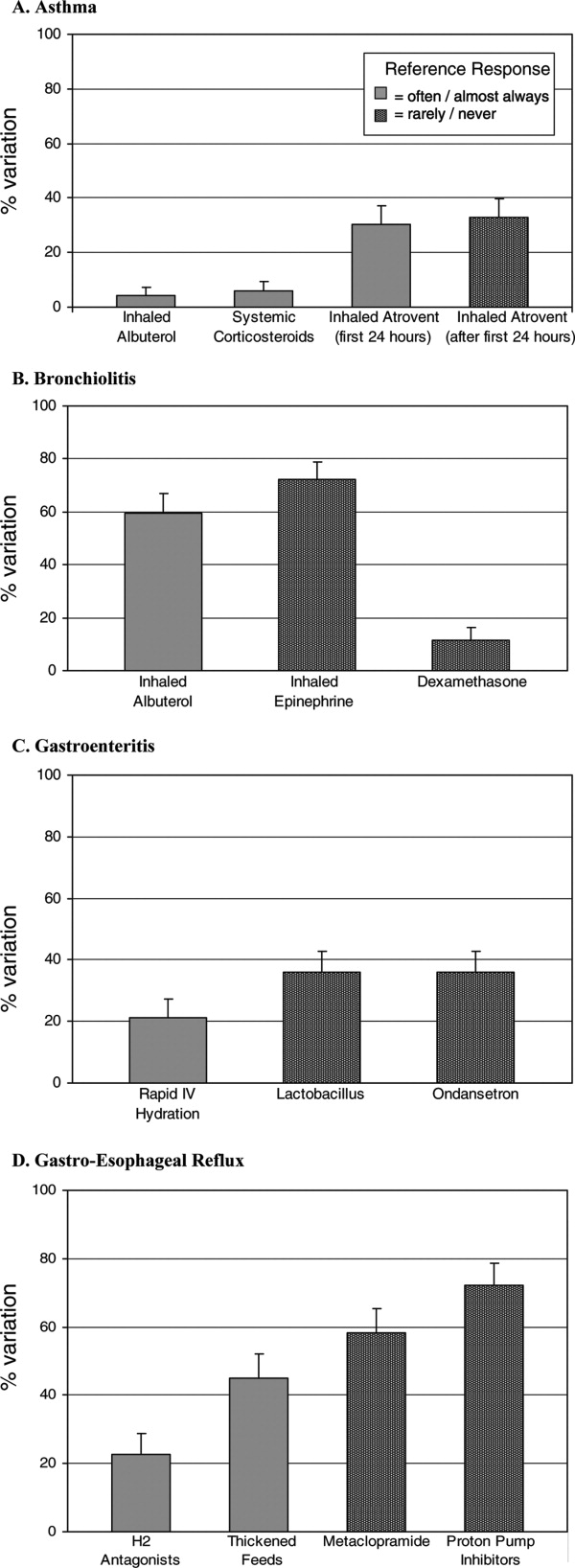
Bronchiolitis
(Figure 1B). By contrast, variation in reported use of inhaled therapies for bronchiolitis was high, with many respondents reporting that they often or always used inhaled albuterol or epinephrine, while many others reported rarely or never using them. There was 59.6% (52.4‐66.8%) variation from the reference response of often/almost always using inhaled albuterol, and 72.2% (65.6‐78.8%) variation from the reference response of never/rarely using inhaled epinephrine. Only 11.6% (6.9‐16.3%) of respondents, however, varied from the reference response of using dexamethasone more than rarely in the care of children with bronchiolitis.
Gastroenteritis
(Figure 1C). Moderate variability existed in the reported use of the 3 studied therapies for children hospitalized with gastroenteritis. 21.1% (15.1‐27.1%) of respondents did not provide the reference response of often/almost always using IV hydration; 35.9% (28.9‐42.9%) did not provide the reference response of never or rarely using lactobacillus; likewise, 35.9% (28.9‐42.9%) did not provide the reference response of never or rarely using ondansetron.
Gastro‐Esophageal Reflux Disease
(Figure 1, Panel D). There was moderate to high variability in the reported management of GERD. 22.8% (16.7‐28.9%) of respondents did not provide the reference response of often/almost always using H2 antagonists, and 44.9% (37.6‐52.2%) did not report often/almost always using thickened feeds in the care of these children. 58.3% (51.1‐65.5%) and 72.1% (65.5‐78.7%) of respondents did not provide the reference response of never/rarely using metoclopramide and proton pump inhibitors, respectively.
Proven vs. Unproven Therapies
(Figure 2). Variation in reported use of therapies of unproven benefit was significantly higher than variation in reported use of the 4 proven therapies (albuterol, corticosteroids, and ipratropium in the first 24 h for asthma; IV re‐hydration for gastroenteritis). The mean variation in reported use of unproven therapies was 44.6 20.5%, compared with 15.5 12.5% variation in reported use of therapies of proven benefit (p = 0.02).
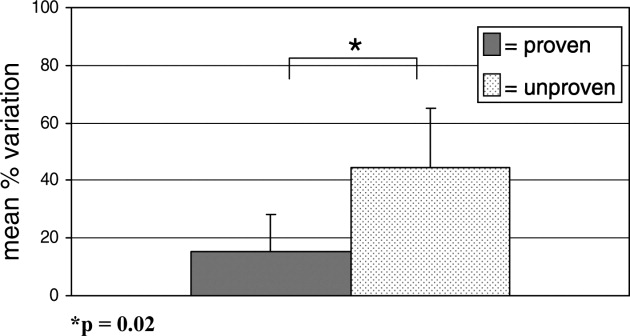
As a sensitivity analysis, the use of thickened feeds as a therapy for GERD was re‐categorized as proven and the above analysis repeated, for the reasons outlined in the methods section. This did not alter the identified relationship between variability and the evidence base fundamentally; hospitalists' reported variation in use of therapies of unproven benefit in this sensitivity analysis was 44.6 21.7%, compared with 21.4 17.0% variation in reported use of proven therapies (p = 0.05).
DISCUSSION
Substantial variation exists in the inpatient management of common pediatric diseases. Although we have previously found less reported variability in pediatric hospitalists' practices than in those of community‐based pediatricians,20 the current study demonstrates a high degree of reported variation even among a cohort of inpatient specialists. Importantly, however, reported variation was found to be significantly less for those inpatient therapies supported by a robust evidence base.
Bronchiolitis, gastroenteritis, asthma, and GERD are extremely common causes of pediatric hospitalization throughout the developed world.2125 Our finding of high reported variability in the routine care of all of these conditions except asthma is concerning, as it suggests that experts do not agree on how to manage children hospitalized with even the most common childhood diseases. While we hypothesized that there would be some variation in the use of therapies whose benefit has not been well established, the high degree of variation observed is of concern because it indicates that an insufficient evidentiary base exists to support much of our day‐to‐day practice. Some variation in practice in response to differing clinical presentations is both expected and desirable, but it is remarkable that variance in practice was significantly less for the most evidence‐based therapies than for those grounded less firmly in science, suggesting that the variation identified here is not justifiable variation based on appropriate responses to atypical clinical presentations, but uncertainty in the absence of clear data. Such undesired variability may decrease system reliability (introducing avoidable opportunity for error),26 and lead to under‐use of needed therapies as well as overuse of unnecessary therapies.1
Our work extends prior research that has identified wide variation in patterns of hospital admission, use of hospital resources, and processes of inpatient care,2732 by documenting reported variation in the use of common inpatient therapies. Rates of hospital admission may vary by as much as 7‐fold across regions.33 Our study demonstrates that wide variation exists not only in admission rates, but in reported inpatient care processes for some of the most common diseases seen in pediatric hospitals. Our study also supports the hypothesis that variation in care may be driven by gaps in knowledge.32 Among hospitalists, we found the strength of the evidence base to be a major determinant of reported variability.
Our study has several limitations. First, the data presented here are derived from provider self‐reports, which may not fully reflect actual practice. In the case of the few proven therapies studied, reporting bias could lead to an over‐reporting of adherence to evidence‐based standards of care. Like our study, however, prior studies have found that hospital‐based providers fairly consistently comply with evidence‐based practice recommendations for acute asthma care,34, 35 supporting our finding that variation in acute asthma care (which represented 3 of our 4 proven therapies) is low in this setting.
Another limitation is that classifications of therapies as proven or unproven change as the evidence base evolves. Of particular relevance to this study, the use of thickened feeds as a therapy for GERD, originally classified as being of unknown effectiveness, was reclassified by Clinical Evidence during the course of the study as likely to be beneficial. The relationship we identified between proven therapies and degree of variability in care did not change when we conducted a sensitivity analysis re‐categorizing this therapy as proven, but precisely quantifying variation is complicated by continuous changes in the state of the evidence.
Pediatric hospitalist systems have been found consistently to improve the efficiency of care,9 yet this study suggests that considerable variation in hospitalists' management of key conditions remains. The Pediatric Research in Inpatient Settings (PRIS) Network was formed in 2002 to improve the care of hospitalized children and the quality of inpatient practice by developing an evidence base for inpatient pediatric care. Ongoing multi‐center research efforts through PRIS and other research networks are beginning to critically evaluate therapies used in the management of common pediatric conditions. Rigorous studies of the processes and outcomes of pediatric hospital care will inform inpatient pediatric practice, and ultimately improve the care of hospitalized children. The current study strongly affirms the urgent need to establish such an evidence base. Without data to inform optimal care, efforts to reduce undesirable variation in care and improve care quality cannot be fully realized.
Acknowledgements
The authors would like to extend their thanks to the hospitalists and members of the Pediatric Research in Inpatient Settings Network who participated in this research, as well as the Children's National Medical Center and Children's Hospital Boston Inpatient Pediatrics Services, who provided funding to support this study. Special thanks to the Ambulatory Pediatrics Association (APA), for its core support of the PRIS Network. Dr. Landrigan is the recipient of a career development award from the Agency for Healthcare Research and Quality (AHRQ K08 HS13333). Dr. Conway is the recipient of a Robert Wood Johnson Clinical Scholars Grant. All researchers were independent from the funding agencies; the academic medical centers named above, APA, and AHRQ had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Reduction of undesirable variation in care has been a major focus of systematic efforts to improve the quality of the healthcare system.13 The emergence of hospitalists, physicians specializing in the care of hospitalized patients, was spurred by a desire to streamline care and reduce variability in hospital management of common diseases.4, 5 Over the past decade, hospitalist systems have become a leading vehicle for care delivery.4, 6, 7 It remains unclear, however, whether implementation of hospitalist systems has lessened undesirable variation in the inpatient management of common diseases.
While systematic reviews have found costs and hospital length of stay to be 10‐15% lower in both pediatric and internal medicine hospitalist systems, few studies have adequately assessed the processes or quality of care in hospitalist systems.8, 9 Two internal medicine studies have found decreased mortality in hospitalist systems, but the mechanism by which hospitalists apparently achieved these gains is unclear.10, 11 Even less is known about care processes or quality in pediatric hospitalist systems. Death is a rare occurrence in pediatric ward settings, and the seven studies conducted to date comparing pediatric hospitalist and traditional systems have been universally underpowered to detect differences in mortality.9, 1218 There is a need to better understand care processes as a first step in understanding and improving quality of care in hospitalist systems.19
The Pediatric Research in Inpatient Settings (PRIS) Network was formed to improve the quality of care for hospitalized children through collaborative clinical research. In this study, we sought to study variation in the care of common pediatric conditions among a cohort of pediatric hospitalists. We have previously reported that less variability exists in hospitalists' reported management of inpatient conditions than in the reported management of these same conditions by community‐based pediatricians,20 but we were concerned that substantial undesirable variation (ie, variation in practice due to uncertainty or unsubstantiated local practice traditions, rather than justified variation in care based on different risks of harms or benefits in different patients) may still exist among hospitalists. We therefore conducted a study: 1) to investigate variation in hospitalists' reported use of common inpatient therapies, and 2) to test the hypothesis that greater variation exists in hospitalists' reported use of inpatient therapies of unproven benefit than in those therapies proven to be beneficial.
METHODS
Survey Design and Administration
In 2003, we designed the PRIS Survey to collect data on hospitalists' backgrounds, practices, and training needs, as well as their management of common pediatric conditions. For the current study, we chose a priori to evaluate hospitalists' use of 14 therapies in the management of 4 common conditions: asthma, bronchiolitis, gastroenteritis, and gastro‐esophageal reflux disease (GERD) (Table 1). These four conditions were chosen for study because they were among the top discharge diagnoses (primary and secondary) from the inpatient services at 2 of the authors' institutions (Children's Hospital Boston and Children's Hospital San Diego) during the year before administration of the survey, and because a discrete set of therapeutic agents are commonly used in their management. Respondents were asked to report the frequency with which they used each of the 14 therapies of interest on 5‐point Likert scales (from 1=never to 5=almost always). The survey initially developed was piloted with a small group of hospitalists and pediatricians, and a final version incorporating revisions was subsequently administered to all pediatric hospitalists in the US and Canada identified through any of 3 sources: 1) the Pediatric Research in Inpatient Settings (PRIS) list of participants; 2) the Society for Hospital Medicine (SHM) pediatric hospital medicine e‐mail listserv; and 3) the list of all attendees of the first national pediatric hospitalist conference sponsored by the Ambulatory Pediatrics Association (APA), SHM, and American Academy of Pediatrics (AAP); this meeting was held in San Antonio, Texas, USA in November 2003. Individuals identified through more than 1 of these groups were counted only once. Potential participants were assured that individual responses would be kept confidential, and were e‐mailed an access code to participate in the online survey, using a secure web‐based interface; a paper‐based version was also made available to those who preferred to respond in this manner. Regular reminder notices were sent to all non‐responders. Further details regarding PRIS Survey recruitment and study methods have been published previously.20
| Condition | Therapy | BMJ clinical evidence Treatment effect categorization* | Study classification |
|---|---|---|---|
| |||
| Asthma | Inhaled albuterol | Beneficial | Proven |
| Systemic corticosteroids | Beneficial | Proven | |
| Inhaled ipratropium in the first 24 hours of hospitalization | Beneficial | Proven | |
| Inhaled ipratropium after the first 24 hours of hospitalization | Unknown effectiveness | Unproven | |
| Bronchiolitis | Inhaled albuterol | Unknown effectiveness | Unproven |
| Inhaled epinephrine | Unknown effectiveness | Unproven | |
| Systemic corticosteroids | Unknown effectiveness | Unproven | |
| Gastroenteritis | Intravenous hydration | Beneficial | Proven |
| Lactobacillus | Not assessed | Unproven | |
| Ondansetron | Not assessed | Unproven | |
| Gastro‐Esophageal Reflux Disease (GERD) | H2 histamine‐receptor antagonists | Unknown effectiveness | Unproven |
| Thickened feeds | Unknown effectiveness Likely to be beneficial | Unproven Proven | |
| Metoclopramide | Unknown effectiveness | Unproven | |
| Proton‐pump inhibitors | Unknown effectiveness | Unproven | |
DefinitionsReference Responses and Percent Variation
To measure variation in reported management, we first sought to determine a reference response for each therapy of interest. Since the evidence base for most of the therapies we studied is weak, it was not possible to determine a gold standard response for each therapy. Instead, we sought to measure the degree of divergence from a reference response for each therapy in the following manner. First, to simplify analyses, we collapsed our five‐category Likert scale into three categories (never/rarely, sometimes, and often/almost always). We then defined the reference response for each therapy to be never/rarely or often/almost always, whichever of the 2 was more frequently selected by respondents; sometimes was not used as a reference category, as reporting use of a particular therapy sometimes indicated substantial variability even within an individual's own practice.
Classification of therapies as proven or unproven.
To classify each of the 14 studied therapies as being of proven or unproven, we used the British Medical Journal's publication Clinical Evidence.19 We chose to use Clinical Evidence as an evidence‐based reference because it provides rigorously developed, systematic analyses of therapeutic management options for multiple common pediatric conditions, and organizes recommendations in a straightforward manner. Four of the 14 therapies had been determined on systematic review to be proven beneficial at the time of study design: systemic corticosteroids, inhaled albuterol, and ipratropium (in the first 24 h) in the care of children with asthma; and IV hydration in the care of children with acute gastroenteritis. The remaining 10 therapies were either considered to be of unknown effectiveness or had not been formally evaluated by Clinical Evidence, and were hence considered unproven for this study (Table 1). Of note, the use of thickened feeds in the treatment of children with GERD had been determined to be of unknown effectiveness at the time of study design, but was reclassified as likely to be beneficial during the course of the study.
Analyses
Descriptive statistics were used to report respondents' demographic characteristics and work environments, as well as variation in their reported use of each of the 14 therapies. Variation in hospitalists' use of proven versus unproven therapies was compared using the Wilcoxon rank sum test, as it was distributed non‐normally. For our primary analysis, the use of thickened feeds in GERD was considered unproven, but a sensitivity analysis was conducted reclassifying it as proven in light of the evolving literature on its use and its consequent reclassification in Clinical Evidence.(SAS Version 9.1, Cary, NC) was used for statistical analyses.
RESULTS
213 of the 320 individuals identified through the 3 lists of pediatric hospitalists (67%) responded to the survey. Of these, 198 (93%) identified themselves as hospitalists and were therefore included. As previously reported,20 53% of respondents were male, 55% worked in academic training environments, and 47% had completed advanced training (fellowship) beyond their core pediatric training (residency training); respondents reported completing residency training 11 9 (mean, standard deviation) years prior to the survey, and spending 176 72 days per year in the care of hospitalized patients.
Variation in reported management: asthma
(Figure 1, Panel A). Relatively little variation existed in reported use of the 4 asthma therapies studied. Only 4.4% (95% CI, 1.4‐7.4%) of respondents did not provide the reference response of using inhaled albuterol often or almost always in the care of inpatients with asthma, and only 6.0% (2.5‐9.5%) of respondents did not report using systemic corticosteroids often or almost always. Variation in reported use of ipratropium was somewhat higher.
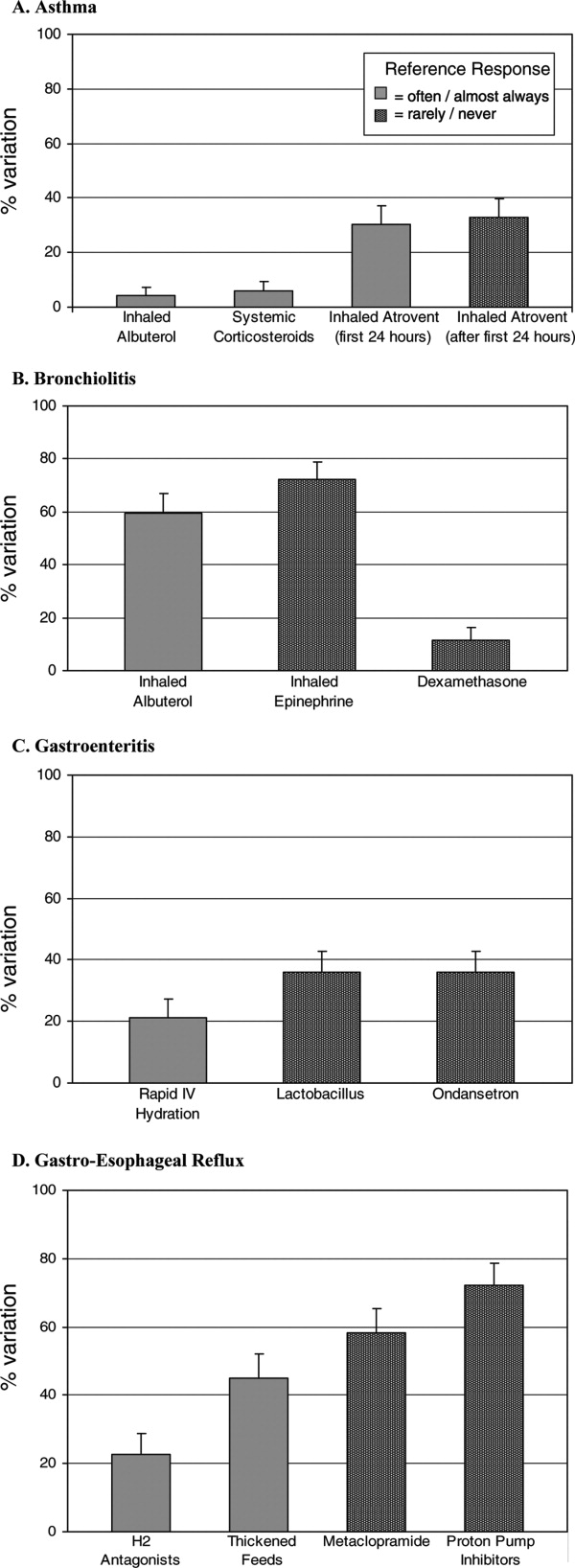
Bronchiolitis
(Figure 1B). By contrast, variation in reported use of inhaled therapies for bronchiolitis was high, with many respondents reporting that they often or always used inhaled albuterol or epinephrine, while many others reported rarely or never using them. There was 59.6% (52.4‐66.8%) variation from the reference response of often/almost always using inhaled albuterol, and 72.2% (65.6‐78.8%) variation from the reference response of never/rarely using inhaled epinephrine. Only 11.6% (6.9‐16.3%) of respondents, however, varied from the reference response of using dexamethasone more than rarely in the care of children with bronchiolitis.
Gastroenteritis
(Figure 1C). Moderate variability existed in the reported use of the 3 studied therapies for children hospitalized with gastroenteritis. 21.1% (15.1‐27.1%) of respondents did not provide the reference response of often/almost always using IV hydration; 35.9% (28.9‐42.9%) did not provide the reference response of never or rarely using lactobacillus; likewise, 35.9% (28.9‐42.9%) did not provide the reference response of never or rarely using ondansetron.
Gastro‐Esophageal Reflux Disease
(Figure 1, Panel D). There was moderate to high variability in the reported management of GERD. 22.8% (16.7‐28.9%) of respondents did not provide the reference response of often/almost always using H2 antagonists, and 44.9% (37.6‐52.2%) did not report often/almost always using thickened feeds in the care of these children. 58.3% (51.1‐65.5%) and 72.1% (65.5‐78.7%) of respondents did not provide the reference response of never/rarely using metoclopramide and proton pump inhibitors, respectively.
Proven vs. Unproven Therapies
(Figure 2). Variation in reported use of therapies of unproven benefit was significantly higher than variation in reported use of the 4 proven therapies (albuterol, corticosteroids, and ipratropium in the first 24 h for asthma; IV re‐hydration for gastroenteritis). The mean variation in reported use of unproven therapies was 44.6 20.5%, compared with 15.5 12.5% variation in reported use of therapies of proven benefit (p = 0.02).
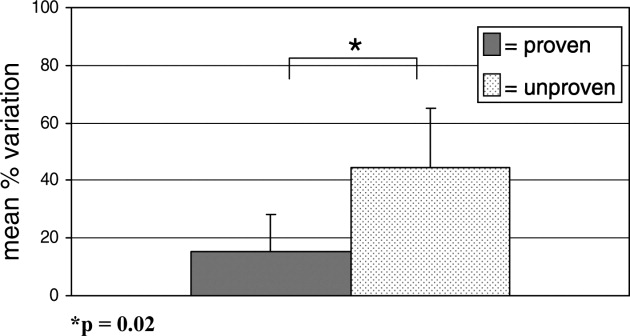
As a sensitivity analysis, the use of thickened feeds as a therapy for GERD was re‐categorized as proven and the above analysis repeated, for the reasons outlined in the methods section. This did not alter the identified relationship between variability and the evidence base fundamentally; hospitalists' reported variation in use of therapies of unproven benefit in this sensitivity analysis was 44.6 21.7%, compared with 21.4 17.0% variation in reported use of proven therapies (p = 0.05).
DISCUSSION
Substantial variation exists in the inpatient management of common pediatric diseases. Although we have previously found less reported variability in pediatric hospitalists' practices than in those of community‐based pediatricians,20 the current study demonstrates a high degree of reported variation even among a cohort of inpatient specialists. Importantly, however, reported variation was found to be significantly less for those inpatient therapies supported by a robust evidence base.
Bronchiolitis, gastroenteritis, asthma, and GERD are extremely common causes of pediatric hospitalization throughout the developed world.2125 Our finding of high reported variability in the routine care of all of these conditions except asthma is concerning, as it suggests that experts do not agree on how to manage children hospitalized with even the most common childhood diseases. While we hypothesized that there would be some variation in the use of therapies whose benefit has not been well established, the high degree of variation observed is of concern because it indicates that an insufficient evidentiary base exists to support much of our day‐to‐day practice. Some variation in practice in response to differing clinical presentations is both expected and desirable, but it is remarkable that variance in practice was significantly less for the most evidence‐based therapies than for those grounded less firmly in science, suggesting that the variation identified here is not justifiable variation based on appropriate responses to atypical clinical presentations, but uncertainty in the absence of clear data. Such undesired variability may decrease system reliability (introducing avoidable opportunity for error),26 and lead to under‐use of needed therapies as well as overuse of unnecessary therapies.1
Our work extends prior research that has identified wide variation in patterns of hospital admission, use of hospital resources, and processes of inpatient care,2732 by documenting reported variation in the use of common inpatient therapies. Rates of hospital admission may vary by as much as 7‐fold across regions.33 Our study demonstrates that wide variation exists not only in admission rates, but in reported inpatient care processes for some of the most common diseases seen in pediatric hospitals. Our study also supports the hypothesis that variation in care may be driven by gaps in knowledge.32 Among hospitalists, we found the strength of the evidence base to be a major determinant of reported variability.
Our study has several limitations. First, the data presented here are derived from provider self‐reports, which may not fully reflect actual practice. In the case of the few proven therapies studied, reporting bias could lead to an over‐reporting of adherence to evidence‐based standards of care. Like our study, however, prior studies have found that hospital‐based providers fairly consistently comply with evidence‐based practice recommendations for acute asthma care,34, 35 supporting our finding that variation in acute asthma care (which represented 3 of our 4 proven therapies) is low in this setting.
Another limitation is that classifications of therapies as proven or unproven change as the evidence base evolves. Of particular relevance to this study, the use of thickened feeds as a therapy for GERD, originally classified as being of unknown effectiveness, was reclassified by Clinical Evidence during the course of the study as likely to be beneficial. The relationship we identified between proven therapies and degree of variability in care did not change when we conducted a sensitivity analysis re‐categorizing this therapy as proven, but precisely quantifying variation is complicated by continuous changes in the state of the evidence.
Pediatric hospitalist systems have been found consistently to improve the efficiency of care,9 yet this study suggests that considerable variation in hospitalists' management of key conditions remains. The Pediatric Research in Inpatient Settings (PRIS) Network was formed in 2002 to improve the care of hospitalized children and the quality of inpatient practice by developing an evidence base for inpatient pediatric care. Ongoing multi‐center research efforts through PRIS and other research networks are beginning to critically evaluate therapies used in the management of common pediatric conditions. Rigorous studies of the processes and outcomes of pediatric hospital care will inform inpatient pediatric practice, and ultimately improve the care of hospitalized children. The current study strongly affirms the urgent need to establish such an evidence base. Without data to inform optimal care, efforts to reduce undesirable variation in care and improve care quality cannot be fully realized.
Acknowledgements
The authors would like to extend their thanks to the hospitalists and members of the Pediatric Research in Inpatient Settings Network who participated in this research, as well as the Children's National Medical Center and Children's Hospital Boston Inpatient Pediatrics Services, who provided funding to support this study. Special thanks to the Ambulatory Pediatrics Association (APA), for its core support of the PRIS Network. Dr. Landrigan is the recipient of a career development award from the Agency for Healthcare Research and Quality (AHRQ K08 HS13333). Dr. Conway is the recipient of a Robert Wood Johnson Clinical Scholars Grant. All researchers were independent from the funding agencies; the academic medical centers named above, APA, and AHRQ had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
- Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, D.C.:National Academic Press,2001.
- ..Reducing variation in surgical care.BMJ2005;330:1401–1402.
- ,,,.Variation in use of video assisted thoracic surgery in the United Kingdom.BMJ2004;329:1011–1012.
- ,..The emerging role of “hospitalists” in the American health care system.N. Engl J Med1996;335:514–517.
- ,..Hospitalism in the USA.Lancet1999;353:1902.
- Society of Hospital Medicine. Growth of Hospital Medicine Nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed April 11,2007.
- .The changing face of hospital practice.Med Econ2002;79:72–79.
- ,..The hospitalist movement 5 years later.JAMA2002;287:487–494.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics2006;117:1736–1744.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med2002;137:859–865.
- ,,,,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med2002;137:866–874.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics2000;105:478–484.
- ,,,,,,, and .Impact of an HMO hospitalist system in academic pediatrics.Pediatrics2002;110:720–728.
- ,, and .Evaluation of a pediatric hospitalist service by APR‐DRG's: impact on length of stay and hospital charges.Pediatr Research2001;49(suppl),691.
- ,,.Pediatric hospitalists: quality care for the underserved?Am J Med Qual2001;16:174–180.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr (Phila)2001;40:653–660.
- ,,, and .Hospitalist care of medically complex children.Pediatr Research2004;55(suppl),1789.
- ,,.Hospital‐based and community pediatricians: comparing outcomes for asthma and bronchiolitis.J Clin Outcomes Manage1997;4:21–24.
- Godlee F,Tovey D,Bedford M, et al., eds.Clinical Evidence: The International Source of the Best Available Evidence for Effective Health Care.London, United Kingdom:BMJ Publishing Group;2004.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics2006;118:441–447.
- ,,,,.Contribution of RSV to bronchiolitis and pneumonia‐associated hospitalizations in English children, April 1995‐March 1998.Epidemiol Infect2002;129:99–106.
- ,,.Direct medical costs of bronchiolitis hospitalizations in the United States.Pediatrics2006;118:2418–2423.
- ,,,,,.Multicenter Prospective Study of the Burden of Rotavirus Acute Gastroenteritis in Europe, 2004‐2005: The REVEAL Study.J Infect Dis2007;195Suppl 1:S4–S16.
- .The state of childhood asthma, United States, 1980‐2005.Adv.Data.2006;1–24.
- ,.Gastroesophageal reflux in children: pathogenesis, prevalence, diagnosis, and role of proton pump inhibitors in treatment.Paediatr Drugs2002;4:673–685.
- ,,,.Reliability science and patient safety.Pediatr Clin North Am2006;53:1121–1133.
- Wennberg JE and McAndrew Cooper M, eds.The Dartmouth Atlas of Health Care in the United States.Hanover, NH, USA:Health Forum, Inc.,1999.
- ,,,,,.Variations in rates of hospitalization of children in three urban communities.N Engl J Med1989;320:1183–1187.
- ,,,,,.Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States.BMJ2004;328:607.
- ,,,,,, et al.Variations in practice and outcomes in the Canadian NICU network: 1996‐1997.Pediatrics2000;106:1070–1079.
- ,,,.Evaluation of febrile children with petechial rashes: is there consensus among pediatricians?Pediatr Infect Dis J1998;17:1135–1140.
- ,,,,,, et al.Practice variation among pediatric emergency departments in the treatment of bronchiolitis.Acad Emerg Med2004;11:353–360.
- ,,,.Paediatric inpatient utilisation in a district general hospital.Arch Dis Child1994;70:488–492.
- ,,,.Emergency department asthma: compliance with an evidence‐based management algorithm.Ann Acad Med Singapore2002;31:419–424.
- ,,.Is the practice of paediatric inpatient medicine evidence‐based?J Paediatr Child Health2002;38:347–351.
- Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, D.C.:National Academic Press,2001.
- ..Reducing variation in surgical care.BMJ2005;330:1401–1402.
- ,,,.Variation in use of video assisted thoracic surgery in the United Kingdom.BMJ2004;329:1011–1012.
- ,..The emerging role of “hospitalists” in the American health care system.N. Engl J Med1996;335:514–517.
- ,..Hospitalism in the USA.Lancet1999;353:1902.
- Society of Hospital Medicine. Growth of Hospital Medicine Nationwide. Available at: http://www.hospitalmedicine.org/Content/NavigationMenu/Media/GrowthofHospitalMedicineNationwide/Growth_of_Hospital_M.htm. Accessed April 11,2007.
- .The changing face of hospital practice.Med Econ2002;79:72–79.
- ,..The hospitalist movement 5 years later.JAMA2002;287:487–494.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics2006;117:1736–1744.
- ,,,,,.Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med2002;137:859–865.
- ,,,,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med2002;137:866–874.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics2000;105:478–484.
- ,,,,,,, and .Impact of an HMO hospitalist system in academic pediatrics.Pediatrics2002;110:720–728.
- ,, and .Evaluation of a pediatric hospitalist service by APR‐DRG's: impact on length of stay and hospital charges.Pediatr Research2001;49(suppl),691.
- ,,.Pediatric hospitalists: quality care for the underserved?Am J Med Qual2001;16:174–180.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr (Phila)2001;40:653–660.
- ,,, and .Hospitalist care of medically complex children.Pediatr Research2004;55(suppl),1789.
- ,,.Hospital‐based and community pediatricians: comparing outcomes for asthma and bronchiolitis.J Clin Outcomes Manage1997;4:21–24.
- Godlee F,Tovey D,Bedford M, et al., eds.Clinical Evidence: The International Source of the Best Available Evidence for Effective Health Care.London, United Kingdom:BMJ Publishing Group;2004.
- ,,,,,.Variations in management of common inpatient pediatric illnesses: hospitalists and community pediatricians.Pediatrics2006;118:441–447.
- ,,,,.Contribution of RSV to bronchiolitis and pneumonia‐associated hospitalizations in English children, April 1995‐March 1998.Epidemiol Infect2002;129:99–106.
- ,,.Direct medical costs of bronchiolitis hospitalizations in the United States.Pediatrics2006;118:2418–2423.
- ,,,,,.Multicenter Prospective Study of the Burden of Rotavirus Acute Gastroenteritis in Europe, 2004‐2005: The REVEAL Study.J Infect Dis2007;195Suppl 1:S4–S16.
- .The state of childhood asthma, United States, 1980‐2005.Adv.Data.2006;1–24.
- ,.Gastroesophageal reflux in children: pathogenesis, prevalence, diagnosis, and role of proton pump inhibitors in treatment.Paediatr Drugs2002;4:673–685.
- ,,,.Reliability science and patient safety.Pediatr Clin North Am2006;53:1121–1133.
- Wennberg JE and McAndrew Cooper M, eds.The Dartmouth Atlas of Health Care in the United States.Hanover, NH, USA:Health Forum, Inc.,1999.
- ,,,,,.Variations in rates of hospitalization of children in three urban communities.N Engl J Med1989;320:1183–1187.
- ,,,,,.Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States.BMJ2004;328:607.
- ,,,,,, et al.Variations in practice and outcomes in the Canadian NICU network: 1996‐1997.Pediatrics2000;106:1070–1079.
- ,,,.Evaluation of febrile children with petechial rashes: is there consensus among pediatricians?Pediatr Infect Dis J1998;17:1135–1140.
- ,,,,,, et al.Practice variation among pediatric emergency departments in the treatment of bronchiolitis.Acad Emerg Med2004;11:353–360.
- ,,,.Paediatric inpatient utilisation in a district general hospital.Arch Dis Child1994;70:488–492.
- ,,,.Emergency department asthma: compliance with an evidence‐based management algorithm.Ann Acad Med Singapore2002;31:419–424.
- ,,.Is the practice of paediatric inpatient medicine evidence‐based?J Paediatr Child Health2002;38:347–351.
Copyright © 2008 Society of Hospital Medicine
PEDIATRIC SPECIAL SECTION: Children’s National Medical Center’sHospitalist Division
Although pediatric resident graduates are well prepared to care for many ill children who require hospitalization, there are clinical, academic, and administrative skills that aren’t a standard part of residency, but are necessary for long-term academic success. The Children’s National Medical Center (CNMC) Hospitalist Fellowship program is structured over three years, through a combination of formal course work, seminars, clinical work, and mentored independent study.
Fellows work under the supervision of faculty in our 20-member Hospitalist Division, with inpatient pediatric services at five hospitals in Washington D.C., and suburban Maryland. A faculty appointment as a clinical instructor of the George Washington University (GWU) School of Medicine and Health Sciences qualifies the fellow to complete a Masters in Public Health, taking 15-18 credits per year. In addition to specific clinical, research, and didactic learning objectives, participation in committees and quality improvement and epidemiologic projects will facilitate study of hospital administration, budget, epidemiology and infection control.
The fellow must be a successful graduate of an American Council of Graduate Medical Education approved pediatric residency.
Clinical Training
Fellows spend approximately three months during the three year fellowship in the pediatric intensive care unit, two weeks in anesthesia, and two months in the emergency department to gain increased confidence, knowledge, and skill in airway management, placement of central lines, evaluation and management of the severely ill/injured child (respiratory failure and shock), conscious sedation, and pain management.
In addition, fellows spend 12 weeks per year on the CNMC hospitalist service. They co-attend with a CNMC hospitalist and lead a team of residents and students to practice an evidence-based approach to the acute evaluation and management of common inpatient problems such as bronchiolitis; asthma; gastroenteritis and dehydration; pneumonia; UTI; ALTE; common head, neck, skin and musculoskeletal infections; metabolic disorders; HIV infection; rheumatologic disease; and child abuse. Fellows also devote eight weeks per year to studying the process of providing coordinated care for the medically complex/technology dependent patients at CNMC and at rehab/subacute care hospital units that focus on improving care for children with multiorgan system disease. They also learn about complications associated with use of technology. Fellows’ elective clinical time may focus on delivery room management skills and well-baby teaching and management issues at one of our community hospital sites with 8,000 deliveries annually.
Research Training
CNMC fellows learn to plan, implement, analyze, and present results of a research study to answer a question relevant to hospitalists. By the end of the fellowship the fellows have an article accepted for publication in a peer-reviewed journal and present findings at a national meeting. To gain knowledge and skill needed to conduct an independent research project the fellows complete coursework in the School of Public Health at GWU and work under faculty mentors at CNMC.
Didactic Training
Four faculty members of our Hospitalist Division have completed the CNMC Master Teacher Certificate program with the GWU School of Education. In seminars taught by master teachers, fellows learn to lead, teach, and develop educational programs effectively. Faculty observe the fellow’s teaching skills in a variety of settings and provide feedback. Fellows have the opportunity to participate and develop computerized and standardized patient simulations to assess residents’ and students’ ability to care for pediatric inpatients.
PEDIATRIC SPECIAL SECTION
In the Literature
Formula Supplementation Prophylaxis for Jaundice in Breastfed Newborns
Gourley GR, Li Z, Kreamer BL, et al. A controlled, randomized, double-blind trial of prophylaxis against jaundice among breastfed newborns. Pediatrics. 2005;116(2):385-391.
Question: In breastfed newborns does oral beta-glucuronidase inhibitors during the first week after birth increase fecal bilirubin excretion and reduce jaundice without affecting breastfeeding deleteriously?
Design: Randomized (randomization table), double-blinded (supplements were prepared by a third party and labeled by a code) controlled trial.
Setting: Clinic.
Patients: 69 newborns, Caucasian, >37 week of gestation who were exclusively breastfed.
Intervention: Patients were randomly assigned to four groups: breastfeeding only (control), L-aspartic acid supplementation (L-aspartic), enzymatically hydrolyzed casein (EHC), and whey/casein-supplement without beta-glucuronidase inhibitor (W/C).
Main outcome measure: Daily transcutaneous and fecal bilirubin levels were obtained. Long-term follow-up assessments included age at first formula feeding, breastfeeding cessation age, and mother’s subjective impression of study.
Main results: Infants in all supplementation groups had significantly lower transcutaneous bilirubin levels in the first week of life than the nonsupplemented infants. The EHC and W/C groups both excreted more bilirubin diglucuronide and bilirubin monoglucuronide than the control group, and the L-aspartic acid had increased bilirubin monoglucuronide excretion compared with the control group. No negative effects from the supplementations were noted.
Conclusions: There is a significant reduction in transcutaneous bilirubin levels, with no negative effects on breastfeeding through the administration of specific supplements that are currently found in infant formulas.
Conflict of interest: None declared.
Commentary: The study describes a possible method of reducing hyperbilirubinemia associated with breastfeeding that employs small-volume supplementations of ingredients found in common infant formulas. The study did not reveal any negative effects on breastfeeding. Though the study was described as blinded the authors do not comment on how the exclusively breastfed infant group was blinded from the researchers and family.
The other control group (W/C) not fed a supplement without a beta-glucuronidase inhibitor yielded the unexpected significant reduction in transcutaneous bilirubin level compared with the control. This may mean that there is at least one other mechanism for the reduction of bilirubin in formula-fed infants than initially proposed by the authors.
In their conclusion, the authors pose a hypothesis explaining this result. They also correctly point out that due to this small study population, larger studies are needed to confirm these results.
This study used transcutaneous bilirubin measurements raising the question of reliability of this method compared to serum bilirubin measurements. A search of Medline using the terms “bilirubin and transcutaneous” produced a technical report.1 One section of this article reviewed available studies on the accuracy of transcutaneous bilirubin measurements concluding that the transcutaneous measurement has a linear correlation to serum bilirubin and its use for hyperbilirubinemia screening is reliable.
Reference
Ip S, Chung M, Kulig J, et al. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. Pediatrics. 2004;Jul;114(1):e130-153.
Comparing Controllers: Montelukast and Fluticasone in Mild Persistent Asthma
Garcia Garcia ML, Wahn U, Gilles L, et al. Montelukast, compared with fluticasone, for control of asthma among 6- to 14-year-old patients with mild asthma: the MOSAIC study. Pediatrics. 2005;116(2):360-369.
Question: In children with mild asthma is the use of an antileukotriene medication as effective as an anti-inflammatory agent in maintaining number of days without the need of a rescue medication or utilization of asthma-related health resources?
Design: Multicenter, double-blind, double-dummy, randomized, parallel-group study. A four-week, single-blind, placebo run-in period was done prior to the initiation of the double-blind portion of the study. This run-in period included three clinic visits. During this time all participants discontinued any asthma controller medications and received image-matching, single-blind, montelukast and fluticasone. A short acting beta-agonist medication (open label) was also provided. Medication usage teaching was done during this time period. There was no placebo control group.
Setting: 104 study sites in 24 countries.
Patients: Patients (six-14 years of age) with mild persistent asthma as defined by the Global Initiative for Asthma (GINA) guidelines and otherwise in good health. Patients were required to have a FEV1 of ≥80% while the beta-receptor agonist was withheld for more than six hours in the first two visits and ≥70% on the third visit of the run-in period.
Intervention: Patients were randomized to receive either montelukast (5 mg oral before bedtime or 10 mg for patients ≥15) or fluticasone (100 mcg through MDI twice a day) and the appropriate placeboes.
Main outcome measures: Percentage of asthma rescue-free days (RFD).
RFD was defined as a day without:
- The use of a rescue medication: defined as any day during which a beta-receptor agonist, a systemic corticosteroid, or other rescue medications were used; and
- The use of an asthma health resource: defined as an unscheduled visit to a physician, an urgent/emergency care center or a hospital.
Main results: The number of RFDs were statistically similar between both groups. Mean percentage of RFD was 84% in the montelukast group and 86.7% in the fluticasone group.
Conflict of interest: Two of the study authors were employees of Merck and Company, which markets montelukast.
Commentary: This is an extensive study with multiple outcome measures. The study mimics actual clinical experience by using clinically relevant end points as primary outcomes. The study does not have a placebo control group. Overall the study showed that there is no significant difference between montelukast and fluticasone with regard to the primary outcome of RFDs, but there were some differences favoring fluticasone in secondary outcome measures, including number of days of beta-receptor agonist use and improvement of the average score of the control domain of the Pediatric Asthma Therapy Assessment Questionnaire.
K. Kingae Causes Osteomyelitis/Septic Arthritis
Kiang KM, Ogunmodede F, Juni BA, et al. Outbreak of osteomyelitis/septic arthritis caused by Kingella kingae among child care center attendees. Pediatrics. 2005;116;e206-213.
Review by Julia Simmons, MD
Kingella kingae (K. kingae), a gram-negative organism known to colonize the oropharynx, may cause invasive diseases, such as septic arthritis and osteomyelitis in children who were previously healthy. In this article, the authors describe the first reported outbreak of K. kingae causing osteomyelitis/septic arthritis.
In October 2003 the Minnesota Department of Health was notified of an outbreak of K. kingae at a daycare facility. There were two culture positive cases and one culture negative but clinically presumed to be secondary to K. kingae. The children were all in the same classroom (toddler classroom 1) and were between the ages of 17 and 21 months. The previously healthy children presented with fever and limp.
In this cohort study, the authors investigated risk factors for invasive disease and for colonization with K. kingae. They also determined the prevalence of asymptomatic colonization at the daycare involving the confirmed cases and at a second daycare facility, which served as the control. Culture samples were analyzed at the Minnesota Department of Health Public Health Laboratory. The laboratory performed confirmation, pulsed-field gel electrophoresis, DNA sequencing, and antimicrobial testing specifically with rifampin, penicillin, and azithromycin.
At the study facility 115/122 (94%) children and 28/29 (97%) adult staff members were cultured. Fifteen (13 %) of the children were colonized. The prevalence of colonization was 45% (9 children) in the toddler 1 classroom, which is the classroom of the confirmed cases. The three case patients had negative oropharyngeal cultures; however, all three had been pretreated with antibiotic therapy. The pulsed-field gel electrophoresis was indistinguishable in the confirmed cases and the colonized students. The authors did not discover any risk factors for invasive disease. This information was gathered from a list of questions regarding past medical history, which the parents discussed on the telephone with the investigators. Rifampin, penicillin, and azithromycin all had low MICs
At the control care center, 45/118 (38%) of people were cultured from the oropharynx. Seven (16%) were colonized. The pulsed-field gel electrophoresis was the same for the control care facility, but varied from the electrophoresis pattern at the study facility.
In conclusion, the authors summarized the findings of K. kingae osteomyelitis/septic arthritis in a daycare facility. There were no identifiable risk factors for invasive disease or for asymptomatic carrier state. It is important to remember that up to 50% of culture negative cases of septic arthritis in patients less than two years of age may be attributed to K. kingae. Thus, the clinician must maintain a high index of suspicion and relay this information to the laboratory so that appropriate measures are taken to ensure the optimal growth environment for the bacteria.
Although the study size was small, the investigators provide initial documentation regarding outbreaks of invasive K. kingae infections. Further studies will be useful to clarify the exact mode of transmission and appropriate duration of antimicrobial therapy.
Systematic Review of Therapy for Pediatric Migraine
Damen L, Bruijn JKJ, Verhagen AP, et al. Symptomatic treatment of migraine in children: a systematic review of medication trials. Pediatrics. 2005;116(2):295-302.
Migraines affect 3%-5% of prepubescent children. The symptoms frequently include unilateral throbbing headache associated with nausea and vomiting. If poorly controlled, the headaches can cause students to miss school and have a decreased quality of life. Symptomatic pharmacologic interventions involve analgesics, triptans, and antiemetics. Nonpharmacologic interventions include dietary changes, biofeedback, and exercise. Treatment is tailored to the patient; however, there are limited studies providing evidence describing the most efficacious pharmacologic treatment for managing symptomatic migraines.
The authors conducted a retrospective literature review to evaluate the evidence from randomized controlled trials (RCT) and clinical controlled trials (CCT) regarding the treatment of symptomatic migraine in children younger than 18. The primary outcome measure was headache clinical improvement defined as a headache decline by >50%. Secondary measures included headache intensity, frequency, duration, and headache index. The authors searched Medline, Embase, PsychInfo, Web of Science, and Cinahl from the start of the databases to June 2004. They used appropriate search terms including “headache,” “migraine,” “child” and variations thereof. Further, they searched reference lists of the articles and the included studies. Two authors independently reviewed the titles and abstracts to determine acceptability in the study. They also used the Delphi list to assess the methodologic quality of the included trials.
Of 3,492 relevant studies, 10 met the inclusion criteria specified by the authors. There were a total of 1,575 patients with a mean age of 11.7 +/- 2.2 years included in the study. A mean of 19.8% of subjects did not complete participation in their respective studies. Overall, the percentage of male and female participants was equal. Six studies were considered to be of high quality by the authors. They found moderate evidence that ibuprofen and acetaminophen were more effective in decreasing headache symptoms one and two hours after ingestion in comparison with a placebo. Further, the nasal spray sumatriptan was more efficacious in diminishing headache than placebo; however, it was associated with more side effects. Intravenous prochlorperazine was more effective than intravenous ketorolac in diminishing symptoms one hour after intake.
While accomplishing a sound systematic review of the available controlled trials, the authors conclude that there are insufficient trials of adequate quality to fully elucidate the most efficacious symptomatic pharmacologic therapy for pediatric patients suffering from migraine headaches. A large randomized prospective trial comparing analgesics, triptans, and antiemetics against placebo is needed. TH
Although pediatric resident graduates are well prepared to care for many ill children who require hospitalization, there are clinical, academic, and administrative skills that aren’t a standard part of residency, but are necessary for long-term academic success. The Children’s National Medical Center (CNMC) Hospitalist Fellowship program is structured over three years, through a combination of formal course work, seminars, clinical work, and mentored independent study.
Fellows work under the supervision of faculty in our 20-member Hospitalist Division, with inpatient pediatric services at five hospitals in Washington D.C., and suburban Maryland. A faculty appointment as a clinical instructor of the George Washington University (GWU) School of Medicine and Health Sciences qualifies the fellow to complete a Masters in Public Health, taking 15-18 credits per year. In addition to specific clinical, research, and didactic learning objectives, participation in committees and quality improvement and epidemiologic projects will facilitate study of hospital administration, budget, epidemiology and infection control.
The fellow must be a successful graduate of an American Council of Graduate Medical Education approved pediatric residency.
Clinical Training
Fellows spend approximately three months during the three year fellowship in the pediatric intensive care unit, two weeks in anesthesia, and two months in the emergency department to gain increased confidence, knowledge, and skill in airway management, placement of central lines, evaluation and management of the severely ill/injured child (respiratory failure and shock), conscious sedation, and pain management.
In addition, fellows spend 12 weeks per year on the CNMC hospitalist service. They co-attend with a CNMC hospitalist and lead a team of residents and students to practice an evidence-based approach to the acute evaluation and management of common inpatient problems such as bronchiolitis; asthma; gastroenteritis and dehydration; pneumonia; UTI; ALTE; common head, neck, skin and musculoskeletal infections; metabolic disorders; HIV infection; rheumatologic disease; and child abuse. Fellows also devote eight weeks per year to studying the process of providing coordinated care for the medically complex/technology dependent patients at CNMC and at rehab/subacute care hospital units that focus on improving care for children with multiorgan system disease. They also learn about complications associated with use of technology. Fellows’ elective clinical time may focus on delivery room management skills and well-baby teaching and management issues at one of our community hospital sites with 8,000 deliveries annually.
Research Training
CNMC fellows learn to plan, implement, analyze, and present results of a research study to answer a question relevant to hospitalists. By the end of the fellowship the fellows have an article accepted for publication in a peer-reviewed journal and present findings at a national meeting. To gain knowledge and skill needed to conduct an independent research project the fellows complete coursework in the School of Public Health at GWU and work under faculty mentors at CNMC.
Didactic Training
Four faculty members of our Hospitalist Division have completed the CNMC Master Teacher Certificate program with the GWU School of Education. In seminars taught by master teachers, fellows learn to lead, teach, and develop educational programs effectively. Faculty observe the fellow’s teaching skills in a variety of settings and provide feedback. Fellows have the opportunity to participate and develop computerized and standardized patient simulations to assess residents’ and students’ ability to care for pediatric inpatients.
PEDIATRIC SPECIAL SECTION
In the Literature
Formula Supplementation Prophylaxis for Jaundice in Breastfed Newborns
Gourley GR, Li Z, Kreamer BL, et al. A controlled, randomized, double-blind trial of prophylaxis against jaundice among breastfed newborns. Pediatrics. 2005;116(2):385-391.
Question: In breastfed newborns does oral beta-glucuronidase inhibitors during the first week after birth increase fecal bilirubin excretion and reduce jaundice without affecting breastfeeding deleteriously?
Design: Randomized (randomization table), double-blinded (supplements were prepared by a third party and labeled by a code) controlled trial.
Setting: Clinic.
Patients: 69 newborns, Caucasian, >37 week of gestation who were exclusively breastfed.
Intervention: Patients were randomly assigned to four groups: breastfeeding only (control), L-aspartic acid supplementation (L-aspartic), enzymatically hydrolyzed casein (EHC), and whey/casein-supplement without beta-glucuronidase inhibitor (W/C).
Main outcome measure: Daily transcutaneous and fecal bilirubin levels were obtained. Long-term follow-up assessments included age at first formula feeding, breastfeeding cessation age, and mother’s subjective impression of study.
Main results: Infants in all supplementation groups had significantly lower transcutaneous bilirubin levels in the first week of life than the nonsupplemented infants. The EHC and W/C groups both excreted more bilirubin diglucuronide and bilirubin monoglucuronide than the control group, and the L-aspartic acid had increased bilirubin monoglucuronide excretion compared with the control group. No negative effects from the supplementations were noted.
Conclusions: There is a significant reduction in transcutaneous bilirubin levels, with no negative effects on breastfeeding through the administration of specific supplements that are currently found in infant formulas.
Conflict of interest: None declared.
Commentary: The study describes a possible method of reducing hyperbilirubinemia associated with breastfeeding that employs small-volume supplementations of ingredients found in common infant formulas. The study did not reveal any negative effects on breastfeeding. Though the study was described as blinded the authors do not comment on how the exclusively breastfed infant group was blinded from the researchers and family.
The other control group (W/C) not fed a supplement without a beta-glucuronidase inhibitor yielded the unexpected significant reduction in transcutaneous bilirubin level compared with the control. This may mean that there is at least one other mechanism for the reduction of bilirubin in formula-fed infants than initially proposed by the authors.
In their conclusion, the authors pose a hypothesis explaining this result. They also correctly point out that due to this small study population, larger studies are needed to confirm these results.
This study used transcutaneous bilirubin measurements raising the question of reliability of this method compared to serum bilirubin measurements. A search of Medline using the terms “bilirubin and transcutaneous” produced a technical report.1 One section of this article reviewed available studies on the accuracy of transcutaneous bilirubin measurements concluding that the transcutaneous measurement has a linear correlation to serum bilirubin and its use for hyperbilirubinemia screening is reliable.
Reference
Ip S, Chung M, Kulig J, et al. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. Pediatrics. 2004;Jul;114(1):e130-153.
Comparing Controllers: Montelukast and Fluticasone in Mild Persistent Asthma
Garcia Garcia ML, Wahn U, Gilles L, et al. Montelukast, compared with fluticasone, for control of asthma among 6- to 14-year-old patients with mild asthma: the MOSAIC study. Pediatrics. 2005;116(2):360-369.
Question: In children with mild asthma is the use of an antileukotriene medication as effective as an anti-inflammatory agent in maintaining number of days without the need of a rescue medication or utilization of asthma-related health resources?
Design: Multicenter, double-blind, double-dummy, randomized, parallel-group study. A four-week, single-blind, placebo run-in period was done prior to the initiation of the double-blind portion of the study. This run-in period included three clinic visits. During this time all participants discontinued any asthma controller medications and received image-matching, single-blind, montelukast and fluticasone. A short acting beta-agonist medication (open label) was also provided. Medication usage teaching was done during this time period. There was no placebo control group.
Setting: 104 study sites in 24 countries.
Patients: Patients (six-14 years of age) with mild persistent asthma as defined by the Global Initiative for Asthma (GINA) guidelines and otherwise in good health. Patients were required to have a FEV1 of ≥80% while the beta-receptor agonist was withheld for more than six hours in the first two visits and ≥70% on the third visit of the run-in period.
Intervention: Patients were randomized to receive either montelukast (5 mg oral before bedtime or 10 mg for patients ≥15) or fluticasone (100 mcg through MDI twice a day) and the appropriate placeboes.
Main outcome measures: Percentage of asthma rescue-free days (RFD).
RFD was defined as a day without:
- The use of a rescue medication: defined as any day during which a beta-receptor agonist, a systemic corticosteroid, or other rescue medications were used; and
- The use of an asthma health resource: defined as an unscheduled visit to a physician, an urgent/emergency care center or a hospital.
Main results: The number of RFDs were statistically similar between both groups. Mean percentage of RFD was 84% in the montelukast group and 86.7% in the fluticasone group.
Conflict of interest: Two of the study authors were employees of Merck and Company, which markets montelukast.
Commentary: This is an extensive study with multiple outcome measures. The study mimics actual clinical experience by using clinically relevant end points as primary outcomes. The study does not have a placebo control group. Overall the study showed that there is no significant difference between montelukast and fluticasone with regard to the primary outcome of RFDs, but there were some differences favoring fluticasone in secondary outcome measures, including number of days of beta-receptor agonist use and improvement of the average score of the control domain of the Pediatric Asthma Therapy Assessment Questionnaire.
K. Kingae Causes Osteomyelitis/Septic Arthritis
Kiang KM, Ogunmodede F, Juni BA, et al. Outbreak of osteomyelitis/septic arthritis caused by Kingella kingae among child care center attendees. Pediatrics. 2005;116;e206-213.
Review by Julia Simmons, MD
Kingella kingae (K. kingae), a gram-negative organism known to colonize the oropharynx, may cause invasive diseases, such as septic arthritis and osteomyelitis in children who were previously healthy. In this article, the authors describe the first reported outbreak of K. kingae causing osteomyelitis/septic arthritis.
In October 2003 the Minnesota Department of Health was notified of an outbreak of K. kingae at a daycare facility. There were two culture positive cases and one culture negative but clinically presumed to be secondary to K. kingae. The children were all in the same classroom (toddler classroom 1) and were between the ages of 17 and 21 months. The previously healthy children presented with fever and limp.
In this cohort study, the authors investigated risk factors for invasive disease and for colonization with K. kingae. They also determined the prevalence of asymptomatic colonization at the daycare involving the confirmed cases and at a second daycare facility, which served as the control. Culture samples were analyzed at the Minnesota Department of Health Public Health Laboratory. The laboratory performed confirmation, pulsed-field gel electrophoresis, DNA sequencing, and antimicrobial testing specifically with rifampin, penicillin, and azithromycin.
At the study facility 115/122 (94%) children and 28/29 (97%) adult staff members were cultured. Fifteen (13 %) of the children were colonized. The prevalence of colonization was 45% (9 children) in the toddler 1 classroom, which is the classroom of the confirmed cases. The three case patients had negative oropharyngeal cultures; however, all three had been pretreated with antibiotic therapy. The pulsed-field gel electrophoresis was indistinguishable in the confirmed cases and the colonized students. The authors did not discover any risk factors for invasive disease. This information was gathered from a list of questions regarding past medical history, which the parents discussed on the telephone with the investigators. Rifampin, penicillin, and azithromycin all had low MICs
At the control care center, 45/118 (38%) of people were cultured from the oropharynx. Seven (16%) were colonized. The pulsed-field gel electrophoresis was the same for the control care facility, but varied from the electrophoresis pattern at the study facility.
In conclusion, the authors summarized the findings of K. kingae osteomyelitis/septic arthritis in a daycare facility. There were no identifiable risk factors for invasive disease or for asymptomatic carrier state. It is important to remember that up to 50% of culture negative cases of septic arthritis in patients less than two years of age may be attributed to K. kingae. Thus, the clinician must maintain a high index of suspicion and relay this information to the laboratory so that appropriate measures are taken to ensure the optimal growth environment for the bacteria.
Although the study size was small, the investigators provide initial documentation regarding outbreaks of invasive K. kingae infections. Further studies will be useful to clarify the exact mode of transmission and appropriate duration of antimicrobial therapy.
Systematic Review of Therapy for Pediatric Migraine
Damen L, Bruijn JKJ, Verhagen AP, et al. Symptomatic treatment of migraine in children: a systematic review of medication trials. Pediatrics. 2005;116(2):295-302.
Migraines affect 3%-5% of prepubescent children. The symptoms frequently include unilateral throbbing headache associated with nausea and vomiting. If poorly controlled, the headaches can cause students to miss school and have a decreased quality of life. Symptomatic pharmacologic interventions involve analgesics, triptans, and antiemetics. Nonpharmacologic interventions include dietary changes, biofeedback, and exercise. Treatment is tailored to the patient; however, there are limited studies providing evidence describing the most efficacious pharmacologic treatment for managing symptomatic migraines.
The authors conducted a retrospective literature review to evaluate the evidence from randomized controlled trials (RCT) and clinical controlled trials (CCT) regarding the treatment of symptomatic migraine in children younger than 18. The primary outcome measure was headache clinical improvement defined as a headache decline by >50%. Secondary measures included headache intensity, frequency, duration, and headache index. The authors searched Medline, Embase, PsychInfo, Web of Science, and Cinahl from the start of the databases to June 2004. They used appropriate search terms including “headache,” “migraine,” “child” and variations thereof. Further, they searched reference lists of the articles and the included studies. Two authors independently reviewed the titles and abstracts to determine acceptability in the study. They also used the Delphi list to assess the methodologic quality of the included trials.
Of 3,492 relevant studies, 10 met the inclusion criteria specified by the authors. There were a total of 1,575 patients with a mean age of 11.7 +/- 2.2 years included in the study. A mean of 19.8% of subjects did not complete participation in their respective studies. Overall, the percentage of male and female participants was equal. Six studies were considered to be of high quality by the authors. They found moderate evidence that ibuprofen and acetaminophen were more effective in decreasing headache symptoms one and two hours after ingestion in comparison with a placebo. Further, the nasal spray sumatriptan was more efficacious in diminishing headache than placebo; however, it was associated with more side effects. Intravenous prochlorperazine was more effective than intravenous ketorolac in diminishing symptoms one hour after intake.
While accomplishing a sound systematic review of the available controlled trials, the authors conclude that there are insufficient trials of adequate quality to fully elucidate the most efficacious symptomatic pharmacologic therapy for pediatric patients suffering from migraine headaches. A large randomized prospective trial comparing analgesics, triptans, and antiemetics against placebo is needed. TH
Although pediatric resident graduates are well prepared to care for many ill children who require hospitalization, there are clinical, academic, and administrative skills that aren’t a standard part of residency, but are necessary for long-term academic success. The Children’s National Medical Center (CNMC) Hospitalist Fellowship program is structured over three years, through a combination of formal course work, seminars, clinical work, and mentored independent study.
Fellows work under the supervision of faculty in our 20-member Hospitalist Division, with inpatient pediatric services at five hospitals in Washington D.C., and suburban Maryland. A faculty appointment as a clinical instructor of the George Washington University (GWU) School of Medicine and Health Sciences qualifies the fellow to complete a Masters in Public Health, taking 15-18 credits per year. In addition to specific clinical, research, and didactic learning objectives, participation in committees and quality improvement and epidemiologic projects will facilitate study of hospital administration, budget, epidemiology and infection control.
The fellow must be a successful graduate of an American Council of Graduate Medical Education approved pediatric residency.
Clinical Training
Fellows spend approximately three months during the three year fellowship in the pediatric intensive care unit, two weeks in anesthesia, and two months in the emergency department to gain increased confidence, knowledge, and skill in airway management, placement of central lines, evaluation and management of the severely ill/injured child (respiratory failure and shock), conscious sedation, and pain management.
In addition, fellows spend 12 weeks per year on the CNMC hospitalist service. They co-attend with a CNMC hospitalist and lead a team of residents and students to practice an evidence-based approach to the acute evaluation and management of common inpatient problems such as bronchiolitis; asthma; gastroenteritis and dehydration; pneumonia; UTI; ALTE; common head, neck, skin and musculoskeletal infections; metabolic disorders; HIV infection; rheumatologic disease; and child abuse. Fellows also devote eight weeks per year to studying the process of providing coordinated care for the medically complex/technology dependent patients at CNMC and at rehab/subacute care hospital units that focus on improving care for children with multiorgan system disease. They also learn about complications associated with use of technology. Fellows’ elective clinical time may focus on delivery room management skills and well-baby teaching and management issues at one of our community hospital sites with 8,000 deliveries annually.
Research Training
CNMC fellows learn to plan, implement, analyze, and present results of a research study to answer a question relevant to hospitalists. By the end of the fellowship the fellows have an article accepted for publication in a peer-reviewed journal and present findings at a national meeting. To gain knowledge and skill needed to conduct an independent research project the fellows complete coursework in the School of Public Health at GWU and work under faculty mentors at CNMC.
Didactic Training
Four faculty members of our Hospitalist Division have completed the CNMC Master Teacher Certificate program with the GWU School of Education. In seminars taught by master teachers, fellows learn to lead, teach, and develop educational programs effectively. Faculty observe the fellow’s teaching skills in a variety of settings and provide feedback. Fellows have the opportunity to participate and develop computerized and standardized patient simulations to assess residents’ and students’ ability to care for pediatric inpatients.
PEDIATRIC SPECIAL SECTION
In the Literature
Formula Supplementation Prophylaxis for Jaundice in Breastfed Newborns
Gourley GR, Li Z, Kreamer BL, et al. A controlled, randomized, double-blind trial of prophylaxis against jaundice among breastfed newborns. Pediatrics. 2005;116(2):385-391.
Question: In breastfed newborns does oral beta-glucuronidase inhibitors during the first week after birth increase fecal bilirubin excretion and reduce jaundice without affecting breastfeeding deleteriously?
Design: Randomized (randomization table), double-blinded (supplements were prepared by a third party and labeled by a code) controlled trial.
Setting: Clinic.
Patients: 69 newborns, Caucasian, >37 week of gestation who were exclusively breastfed.
Intervention: Patients were randomly assigned to four groups: breastfeeding only (control), L-aspartic acid supplementation (L-aspartic), enzymatically hydrolyzed casein (EHC), and whey/casein-supplement without beta-glucuronidase inhibitor (W/C).
Main outcome measure: Daily transcutaneous and fecal bilirubin levels were obtained. Long-term follow-up assessments included age at first formula feeding, breastfeeding cessation age, and mother’s subjective impression of study.
Main results: Infants in all supplementation groups had significantly lower transcutaneous bilirubin levels in the first week of life than the nonsupplemented infants. The EHC and W/C groups both excreted more bilirubin diglucuronide and bilirubin monoglucuronide than the control group, and the L-aspartic acid had increased bilirubin monoglucuronide excretion compared with the control group. No negative effects from the supplementations were noted.
Conclusions: There is a significant reduction in transcutaneous bilirubin levels, with no negative effects on breastfeeding through the administration of specific supplements that are currently found in infant formulas.
Conflict of interest: None declared.
Commentary: The study describes a possible method of reducing hyperbilirubinemia associated with breastfeeding that employs small-volume supplementations of ingredients found in common infant formulas. The study did not reveal any negative effects on breastfeeding. Though the study was described as blinded the authors do not comment on how the exclusively breastfed infant group was blinded from the researchers and family.
The other control group (W/C) not fed a supplement without a beta-glucuronidase inhibitor yielded the unexpected significant reduction in transcutaneous bilirubin level compared with the control. This may mean that there is at least one other mechanism for the reduction of bilirubin in formula-fed infants than initially proposed by the authors.
In their conclusion, the authors pose a hypothesis explaining this result. They also correctly point out that due to this small study population, larger studies are needed to confirm these results.
This study used transcutaneous bilirubin measurements raising the question of reliability of this method compared to serum bilirubin measurements. A search of Medline using the terms “bilirubin and transcutaneous” produced a technical report.1 One section of this article reviewed available studies on the accuracy of transcutaneous bilirubin measurements concluding that the transcutaneous measurement has a linear correlation to serum bilirubin and its use for hyperbilirubinemia screening is reliable.
Reference
Ip S, Chung M, Kulig J, et al. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. Pediatrics. 2004;Jul;114(1):e130-153.
Comparing Controllers: Montelukast and Fluticasone in Mild Persistent Asthma
Garcia Garcia ML, Wahn U, Gilles L, et al. Montelukast, compared with fluticasone, for control of asthma among 6- to 14-year-old patients with mild asthma: the MOSAIC study. Pediatrics. 2005;116(2):360-369.
Question: In children with mild asthma is the use of an antileukotriene medication as effective as an anti-inflammatory agent in maintaining number of days without the need of a rescue medication or utilization of asthma-related health resources?
Design: Multicenter, double-blind, double-dummy, randomized, parallel-group study. A four-week, single-blind, placebo run-in period was done prior to the initiation of the double-blind portion of the study. This run-in period included three clinic visits. During this time all participants discontinued any asthma controller medications and received image-matching, single-blind, montelukast and fluticasone. A short acting beta-agonist medication (open label) was also provided. Medication usage teaching was done during this time period. There was no placebo control group.
Setting: 104 study sites in 24 countries.
Patients: Patients (six-14 years of age) with mild persistent asthma as defined by the Global Initiative for Asthma (GINA) guidelines and otherwise in good health. Patients were required to have a FEV1 of ≥80% while the beta-receptor agonist was withheld for more than six hours in the first two visits and ≥70% on the third visit of the run-in period.
Intervention: Patients were randomized to receive either montelukast (5 mg oral before bedtime or 10 mg for patients ≥15) or fluticasone (100 mcg through MDI twice a day) and the appropriate placeboes.
Main outcome measures: Percentage of asthma rescue-free days (RFD).
RFD was defined as a day without:
- The use of a rescue medication: defined as any day during which a beta-receptor agonist, a systemic corticosteroid, or other rescue medications were used; and
- The use of an asthma health resource: defined as an unscheduled visit to a physician, an urgent/emergency care center or a hospital.
Main results: The number of RFDs were statistically similar between both groups. Mean percentage of RFD was 84% in the montelukast group and 86.7% in the fluticasone group.
Conflict of interest: Two of the study authors were employees of Merck and Company, which markets montelukast.
Commentary: This is an extensive study with multiple outcome measures. The study mimics actual clinical experience by using clinically relevant end points as primary outcomes. The study does not have a placebo control group. Overall the study showed that there is no significant difference between montelukast and fluticasone with regard to the primary outcome of RFDs, but there were some differences favoring fluticasone in secondary outcome measures, including number of days of beta-receptor agonist use and improvement of the average score of the control domain of the Pediatric Asthma Therapy Assessment Questionnaire.
K. Kingae Causes Osteomyelitis/Septic Arthritis
Kiang KM, Ogunmodede F, Juni BA, et al. Outbreak of osteomyelitis/septic arthritis caused by Kingella kingae among child care center attendees. Pediatrics. 2005;116;e206-213.
Review by Julia Simmons, MD
Kingella kingae (K. kingae), a gram-negative organism known to colonize the oropharynx, may cause invasive diseases, such as septic arthritis and osteomyelitis in children who were previously healthy. In this article, the authors describe the first reported outbreak of K. kingae causing osteomyelitis/septic arthritis.
In October 2003 the Minnesota Department of Health was notified of an outbreak of K. kingae at a daycare facility. There were two culture positive cases and one culture negative but clinically presumed to be secondary to K. kingae. The children were all in the same classroom (toddler classroom 1) and were between the ages of 17 and 21 months. The previously healthy children presented with fever and limp.
In this cohort study, the authors investigated risk factors for invasive disease and for colonization with K. kingae. They also determined the prevalence of asymptomatic colonization at the daycare involving the confirmed cases and at a second daycare facility, which served as the control. Culture samples were analyzed at the Minnesota Department of Health Public Health Laboratory. The laboratory performed confirmation, pulsed-field gel electrophoresis, DNA sequencing, and antimicrobial testing specifically with rifampin, penicillin, and azithromycin.
At the study facility 115/122 (94%) children and 28/29 (97%) adult staff members were cultured. Fifteen (13 %) of the children were colonized. The prevalence of colonization was 45% (9 children) in the toddler 1 classroom, which is the classroom of the confirmed cases. The three case patients had negative oropharyngeal cultures; however, all three had been pretreated with antibiotic therapy. The pulsed-field gel electrophoresis was indistinguishable in the confirmed cases and the colonized students. The authors did not discover any risk factors for invasive disease. This information was gathered from a list of questions regarding past medical history, which the parents discussed on the telephone with the investigators. Rifampin, penicillin, and azithromycin all had low MICs
At the control care center, 45/118 (38%) of people were cultured from the oropharynx. Seven (16%) were colonized. The pulsed-field gel electrophoresis was the same for the control care facility, but varied from the electrophoresis pattern at the study facility.
In conclusion, the authors summarized the findings of K. kingae osteomyelitis/septic arthritis in a daycare facility. There were no identifiable risk factors for invasive disease or for asymptomatic carrier state. It is important to remember that up to 50% of culture negative cases of septic arthritis in patients less than two years of age may be attributed to K. kingae. Thus, the clinician must maintain a high index of suspicion and relay this information to the laboratory so that appropriate measures are taken to ensure the optimal growth environment for the bacteria.
Although the study size was small, the investigators provide initial documentation regarding outbreaks of invasive K. kingae infections. Further studies will be useful to clarify the exact mode of transmission and appropriate duration of antimicrobial therapy.
Systematic Review of Therapy for Pediatric Migraine
Damen L, Bruijn JKJ, Verhagen AP, et al. Symptomatic treatment of migraine in children: a systematic review of medication trials. Pediatrics. 2005;116(2):295-302.
Migraines affect 3%-5% of prepubescent children. The symptoms frequently include unilateral throbbing headache associated with nausea and vomiting. If poorly controlled, the headaches can cause students to miss school and have a decreased quality of life. Symptomatic pharmacologic interventions involve analgesics, triptans, and antiemetics. Nonpharmacologic interventions include dietary changes, biofeedback, and exercise. Treatment is tailored to the patient; however, there are limited studies providing evidence describing the most efficacious pharmacologic treatment for managing symptomatic migraines.
The authors conducted a retrospective literature review to evaluate the evidence from randomized controlled trials (RCT) and clinical controlled trials (CCT) regarding the treatment of symptomatic migraine in children younger than 18. The primary outcome measure was headache clinical improvement defined as a headache decline by >50%. Secondary measures included headache intensity, frequency, duration, and headache index. The authors searched Medline, Embase, PsychInfo, Web of Science, and Cinahl from the start of the databases to June 2004. They used appropriate search terms including “headache,” “migraine,” “child” and variations thereof. Further, they searched reference lists of the articles and the included studies. Two authors independently reviewed the titles and abstracts to determine acceptability in the study. They also used the Delphi list to assess the methodologic quality of the included trials.
Of 3,492 relevant studies, 10 met the inclusion criteria specified by the authors. There were a total of 1,575 patients with a mean age of 11.7 +/- 2.2 years included in the study. A mean of 19.8% of subjects did not complete participation in their respective studies. Overall, the percentage of male and female participants was equal. Six studies were considered to be of high quality by the authors. They found moderate evidence that ibuprofen and acetaminophen were more effective in decreasing headache symptoms one and two hours after ingestion in comparison with a placebo. Further, the nasal spray sumatriptan was more efficacious in diminishing headache than placebo; however, it was associated with more side effects. Intravenous prochlorperazine was more effective than intravenous ketorolac in diminishing symptoms one hour after intake.
While accomplishing a sound systematic review of the available controlled trials, the authors conclude that there are insufficient trials of adequate quality to fully elucidate the most efficacious symptomatic pharmacologic therapy for pediatric patients suffering from migraine headaches. A large randomized prospective trial comparing analgesics, triptans, and antiemetics against placebo is needed. TH