User login
Jennifer Smith is the editor of Oncology Practice, part of MDedge Hematology/Oncology. She was previously the editor of Hematology Times, an editor at Principal Investigators Association, and a reporter at The Oneida Daily Dispatch. She has a BS in journalism.
Combo produces disappointing PFS, promising OS in metastatic colorectal cancer
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
NATIONAL HARBOR, MD. – An immunochemotherapy regimen produced mixed results in a phase 2 trial of patients with previously untreated metastatic colorectal cancer.
The regimen – avelumab and cetuximab plus oxaliplatin, leucovorin, and 5-fluorouracil (mFOLFOX6) – failed to meet the primary endpoint for progression-free survival (PFS) but was associated with “promising” yet “preliminary” overall survival, according to Joseph Tintelnot, MD, of University Medical Center Hamburg-Eppendorf (Germany).
Dr. Tintelnot presented these results from the AVETUX trial (NCT03174405) at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled 43 patients with previously untreated, metastatic colorectal cancer, and 39 of them had wild-type RAS and BRAF mutations. Among those 39 patients, the median age was 62 years (range, 29-82 years), 13 patients were female, and 36 patients had left-sided tumors.
A total of 30 patients had liver metastasis, 12 had lung metastasis, and 18 had lymph node metastasis. Most patients (n = 36) had microsatellite stable tumors, 2 were microsatellite instability high, and 1 was microsatellite instability low.
Patients received IV cetuximab at 250 mg/m2 over 60-90 minutes (day 1 and 8), with a first dose of 400 mg/m2; mFOLFOX6 according to local standard – IV oxaliplatin at 85 mg/m2 IV (day 1), IV leucovorin at 400 mg/m2 IV (day 1), and IV bolus 5-fluorouracil at 400 mg/m2 (day 1) and IV at 2,400 mg/m2 (days 1-3); and IV avelumab at 10 mg/kg over 60-90 minutes (day 1 from cycle 2 onward).
The median number of treatment cycles was 8 (range, 1-34) for oxaliplatin, 13 (range, 1-35) for 5-fluorouracil, 12 (range, 1-35) for cetuximab, and 16 (range, 0-34) for avelumab. The median duration of cetuximab/avelumab treatment was 5.4 months (range, 0.7-18.4 months).
The study’s primary endpoint was 12-month PFS, and the researchers expected the PFS to rise from 40% to 57%. Unfortunately, the 12-month PFS was 40%, so the primary endpoint was not met.
However, the treatment produced a “very high” overall response rate at 81% (30/37), according to Dr. Tintelnot. A total of 4 patients achieved a complete response, 26 had a partial response, 4 had stable disease, and 3 progressed.
Dr. Tintelnot also noted a “promising” but “preliminary” overall survival rate – 84% at a median follow-up of 16.2 months. He said these results suggest PFS may not be the ideal endpoint for this combination.
Dr. Tintelnot said the combination was safe, with no unexpected toxicities. The most common grade 3-4 adverse events were infection of catheter, device, urinary tract, etc. (32%); abdominal pain, diarrhea, etc. (24%); skin reaction (21%); anemia, blood disorders, and hemolytic-uremic syndrome (18%); administration, infusion-related, and allergic reactions (16%); cognitive disturbance, meningism, syncope, and psychiatric disorders (16%); and peripheral sensory polyneuropathy and paresthesia (16%).
Dr. Tintelnot and colleagues also conducted translational research evaluating programmed death-ligand 1 (PD-L1) expression and serial circulating tumor DNA in patients on this trial.
The team found no clear correlation between PFS and T-cell diversification, tumor-infiltrating lymphocytes, or tumor proportion score. Dr. Tintelnot said this suggests classical predictive factors for PD-1/PD-L1 inhibitor treatment have a limited role with this combination.
The researchers did find that circulating tumor mutations might help predict early relapse with the regimen. The team identified 26 patients with mutations detectable in their blood. There was an immediate decline of circulating tumor mutations after treatment initiation, and reemergence of mutation clones was associated with progression.
Lastly, the researchers found that avelumab, cetuximab, and mFOLFOX6 suppressed the development of epidermal growth factor receptor–resistant subclones. There were no epidermal growth factor receptor mutations detected during follow-up.
This research was sponsored by AIO-Studien-gGmbH. Dr. Tintelnot disclosed no conflicts of interest.
SOURCE: Tintelnot J et al. SITC 2019, Abstract O16.
REPORTING FROM SITC 2019
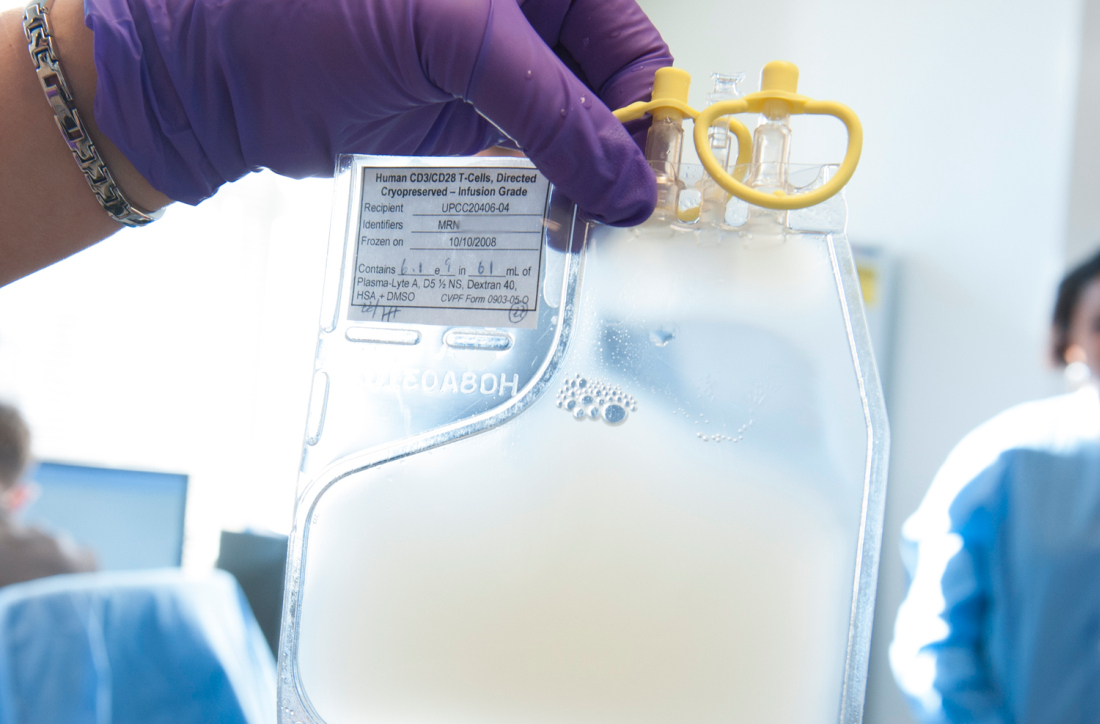
Armored CAR T cells elicit responses in NHL patients
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
NATIONAL HARBOR, MD – An armored chimeric antigen receptor (CAR) T-cell therapy has demonstrated efficacy in vitro and in patients with relapsed or refractory non-Hodgkin lymphoma (NHL), according to findings presented at the annual meeting of the Society for Immunotherapy of Cancer.
ICTCAR014, a dominant negative PD-1 armored CAR T-cell therapy, proved more cytotoxic than traditional CAR T-cell therapy in vitro and produced responses in 12 of 13 NHL patients who received it.
Xiaobin Victor Lu, PhD, of Innovative Cellular Therapeutics, Shanghai, China, presented results with ICTCAR014 at the meeting.
Dr. Lu explained that ICTCAR014 consists of CD19-targeted CAR T cells genetically engineered to overexpress a PD-1 dominant negative protein with an altered intracellular signaling domain. The dominant negative protein can act as a “decoy receptor” to bind and block the PD-L1/2 inhibitory signal, thereby enhancing the efficacy of CAR T cells.
Innovative Cellular Therapeutics is developing ICTCAR014 because there is “some room to improve” with commercially available CAR T-cell products, Dr. Lu said. Specifically, tisagenlecleucel produced a 52% response rate in the JULIET trial (N Engl J Med. 2019;380:45-56), and axicabtagene ciloleucel produced an 82% response rate in the ZUMA-1 trial (N Engl J Med. 2017;377:2531-44).
There is also evidence to suggest that PD-1 blockade can modulate and “refuel” CAR T cells in relapsed/refractory NHL patients who fail or relapse after traditional anti-CD19 CAR T-cell therapy (Blood. 2017 Feb 23;129[8]:1039-41). This finding has prompted researchers to conduct trials of PD-1 inhibitors in combination with CAR T-cell therapies. But this combination approach may be expensive and cause more side effects than the armored CAR T-cell approach, Dr. Lu said.
In preclinical studies, Dr. Lu and colleagues found that ICTCAR014 was more effective than traditional anti-CD19 CAR T cells in killing Nalm6-PDL1 cells. In addition, the PD-1 dominant negative protein protected CAR T cells from exhaustion.
Dr. Lu also presented results in 13 NHL patients who have received ICTCAR014 in a phase 1 trial in China. Eleven patients had diffuse large B-cell lymphoma (DLBCL), and two had follicular lymphoma.
The objective response rate was 92.3% (12/13), which included five partial responses (38.5%) and seven complete responses (53.8%). Both follicular lymphoma patients and five DLBCL patients achieved a complete response. Five DLBCL patients achieved a partial response, and the remaining DLBCL patient did not respond.
Dr. Lu did not present safety data. However, he reported that there was no increased incidence of cytokine release syndrome or neurotoxicity in these patients, compared with patients receiving traditional CAR T-cell therapy.
Dr. Lu is employed by Innovative Cellular Therapeutics, which funded the research and is developing ICTCAR014.
SOURCE: Lu V et al. SITC 2019, Abstract O25.
REPORTING FROM SITC 2019
Combo shows promise for checkpoint inhibitor-refractory urothelial carcinoma
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
NATIONAL HARBOR, MD. – Sitravatinib may “restore or enhance” the activity of anti-PD-1 therapy in patients with checkpoint inhibitor–refractory urothelial carcinoma, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
Clinical activity was observed with combination sitravatinib and nivolumab in patients with urothelial carcinoma who had disease progression on or after an immune checkpoint inhibitor and were previously treated with platinum-based chemotherapy.
“Up until a few years ago, the only therapies we had [for urothelial carcinoma] were cytotoxic, platinum-based chemotherapies,” said Pavlos Msaouel, MD, PhD, of the University of Texas MD Anderson Cancer Center, Houston.
“Thankfully, since 2016, immune checkpoint therapy has become part of our toolbox. But even with single-agent, approved immune checkpoint therapies, anti-PD-1/anti-PD-L1, the response rates are still low, around 20%, and durable responses are only seen in a subset of patients. So we have to do better, if possible, potentially by combining immune checkpoint therapies with other immunotherapies such as sitravatinib.”
Dr. Msaouel explained that sitravatinib inhibits a spectrum of related receptor tyrosine kinases, including TAM family receptors (TYRO3, Axl, and Mer), split family receptors (VEGFR2/PDGFR and c-KIT), and c-Met. Researchers are investigating sitravatinib in combination with nivolumab in a phase 2 trial of patients with urothelial carcinoma (NCT03606174). Dr. Msaouel presented results from one cohort on this trial – 33 patients who had previously received platinum-based chemotherapy and a PD-1/PD-L1 inhibitor.
At baseline, the patients’ median age was 68 years (range, 47-83 years), and 70% were male. Patients had metastatic (n = 30) or locally advanced (n = 3) disease. They had received a median of two (range, one to four) prior systemic therapies.
For this study, patients received oral sitravatinib at 120 mg daily and intravenous nivolumab at 240 mg every 2 weeks or 480 mg every 4 weeks on continuous 28-day cycles. Tumor assessments were performed every 8 weeks.
Results
Of the 22 patients evaluable for efficacy, 1 patient achieved a complete response, 5 had a partial response, 15 had stable disease, and 1 progressed. Eight patients had tumor regression greater than 30%.
Treatment duration exceeded 26 weeks in six patients. Nine patients, including four responders, were still on study at the data cutoff in mid-October.
“This ongoing trial continues to show promising clinical activity, including tumor regression and prolonged duration on treatment,” Dr. Msaouel said.
He added that combination sitravatinib and nivolumab has “an acceptable side effect profile, with manageable adverse events.”
Common treatment-related adverse events, in all 33 patients, were fatigue (58%), diarrhea (48%), decreased appetite (33%), dysphonia (33%), nausea (33%), and alanine aminotransferase increase (21%).
Grade 3 treatment-related adverse events included fatigue (12%), hypertension (12%), diarrhea (9%), lipase increase (9%), decreased appetite (3%), and palmar-plantar erythrodysesthesia syndrome (3%). There were no grade 4 or 5 treatment-related events.
Mirati Therapeutics sponsored the trial. Dr. Msaouel disclosed relationships with Mirati, Bristol-Myers Squibb, Exelixis, Pfizer, and Takeda.
SOURCE: Msaouel P et al. SITC 2019. Abstract O23.
REPORTING FROM SITC 2019
TLR9 agonist may overcome resistance to anti–PD-1 therapy in melanoma
NATIONAL HARBOR, MD. – A TLR9 agonist called CMP-001 can reverse resistance to anti–programmed death-1 (PD-1) therapy in patients with melanoma, a phase 1 trial suggests.
Combination CMP-001 and pembrolizumab produced durable responses in patients who had progressed on prior anti–PD-1 therapy, and the combination was considered well tolerated.
CMP-001 is a CpG-A TLR9 agonist packaged in a viruslike particle, John Kirkwood, MD, of University of Pittsburgh Medical Center, explained in a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer. CMP-001 activates tumor-associated plasmacytoid dendritic cells and induces systemic tumor-specific CD8+ T-cell responses.
Dr. Kirkwood and associates are investigating CMP-001, given alone or in combination with pembrolizumab, in a phase 1 trial (NCT02680184) of patients with metastatic or unresectable melanoma who are refractory to anti–PD-1 therapy.
Data were presented on 144 patients who received CMP-001 in combination with pembrolizumab. About 40% of patients (39.6%) had elevated lactate dehydrogenase at baseline, and 32.6% had BRAF mutations.
All patients had received prior anti–PD-1 therapy alone (75%) and/or in combination (50%). For most patients (93.1%), their last response to anti–PD-1 therapy was progression.
For this study, the patients received intratumoral CMP-001 injections at a range of doses (1 mg, 3 mg, 5 mg, 7.5 mg, and 10 mg). CMP-001 was given weekly for either 2 weeks or 7 weeks, then every 3 weeks until discontinuation. There were two different formulations of CMP-001 given – 0.01% polysorbate 20 (PS20; n = 83) and 0.00167% PS20 (n = 61).
Safety
“CMP-001 in combination with pembrolizumab is very well tolerated, with no apparent increase in autoimmune toxicities associated with anti–PD-1,” Dr. Kirkwood said.
The most common treatment-related adverse events were flulike symptoms, including chills (72%), pyrexia (56%), fatigue (51%), nausea (45%), vomiting (29%), and headache (28%). Another common event was injection-site pain (28%).
The most common grade 3 adverse events were hypotension (n = 9) and hypertension (n = 7). Grade 4 events included hypotension, aspartate aminotransferase increase, and alanine aminotransferase increase (n = 1 for all). There were no grade 5 events.
Six patients discontinued treatment because of adverse events.
Response
The overall response rate was 25% (21/83) among patients who received the 0.01% PS20 formulation of CMP-001 and 11.5% (7/61) among patients who received the 0.00167% PS20 formulation.
Responses were similar in injected and noninjected target lesions. The median duration of response has not been reached at a median follow-up of 16.9 months.
“Intratumoral CMP-001 reverses resistance to anti–PD-1 in patients who have progressed on prior anti–PD-1 therapy,” Dr. Kirkwood said, adding that these data support further clinical development of CMP-001.
The research is sponsored by Checkmate Pharmaceuticals. Dr. Kirkwood disclosed relationships with Amgen, BMS, Immunocore, Iovance, Novartis, Elsevier, Castle, Merck, and Checkmate.
SOURCE: Kirkwood J et al. SITC 2019, Abstract O85.
NATIONAL HARBOR, MD. – A TLR9 agonist called CMP-001 can reverse resistance to anti–programmed death-1 (PD-1) therapy in patients with melanoma, a phase 1 trial suggests.
Combination CMP-001 and pembrolizumab produced durable responses in patients who had progressed on prior anti–PD-1 therapy, and the combination was considered well tolerated.
CMP-001 is a CpG-A TLR9 agonist packaged in a viruslike particle, John Kirkwood, MD, of University of Pittsburgh Medical Center, explained in a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer. CMP-001 activates tumor-associated plasmacytoid dendritic cells and induces systemic tumor-specific CD8+ T-cell responses.
Dr. Kirkwood and associates are investigating CMP-001, given alone or in combination with pembrolizumab, in a phase 1 trial (NCT02680184) of patients with metastatic or unresectable melanoma who are refractory to anti–PD-1 therapy.
Data were presented on 144 patients who received CMP-001 in combination with pembrolizumab. About 40% of patients (39.6%) had elevated lactate dehydrogenase at baseline, and 32.6% had BRAF mutations.
All patients had received prior anti–PD-1 therapy alone (75%) and/or in combination (50%). For most patients (93.1%), their last response to anti–PD-1 therapy was progression.
For this study, the patients received intratumoral CMP-001 injections at a range of doses (1 mg, 3 mg, 5 mg, 7.5 mg, and 10 mg). CMP-001 was given weekly for either 2 weeks or 7 weeks, then every 3 weeks until discontinuation. There were two different formulations of CMP-001 given – 0.01% polysorbate 20 (PS20; n = 83) and 0.00167% PS20 (n = 61).
Safety
“CMP-001 in combination with pembrolizumab is very well tolerated, with no apparent increase in autoimmune toxicities associated with anti–PD-1,” Dr. Kirkwood said.
The most common treatment-related adverse events were flulike symptoms, including chills (72%), pyrexia (56%), fatigue (51%), nausea (45%), vomiting (29%), and headache (28%). Another common event was injection-site pain (28%).
The most common grade 3 adverse events were hypotension (n = 9) and hypertension (n = 7). Grade 4 events included hypotension, aspartate aminotransferase increase, and alanine aminotransferase increase (n = 1 for all). There were no grade 5 events.
Six patients discontinued treatment because of adverse events.
Response
The overall response rate was 25% (21/83) among patients who received the 0.01% PS20 formulation of CMP-001 and 11.5% (7/61) among patients who received the 0.00167% PS20 formulation.
Responses were similar in injected and noninjected target lesions. The median duration of response has not been reached at a median follow-up of 16.9 months.
“Intratumoral CMP-001 reverses resistance to anti–PD-1 in patients who have progressed on prior anti–PD-1 therapy,” Dr. Kirkwood said, adding that these data support further clinical development of CMP-001.
The research is sponsored by Checkmate Pharmaceuticals. Dr. Kirkwood disclosed relationships with Amgen, BMS, Immunocore, Iovance, Novartis, Elsevier, Castle, Merck, and Checkmate.
SOURCE: Kirkwood J et al. SITC 2019, Abstract O85.
NATIONAL HARBOR, MD. – A TLR9 agonist called CMP-001 can reverse resistance to anti–programmed death-1 (PD-1) therapy in patients with melanoma, a phase 1 trial suggests.
Combination CMP-001 and pembrolizumab produced durable responses in patients who had progressed on prior anti–PD-1 therapy, and the combination was considered well tolerated.
CMP-001 is a CpG-A TLR9 agonist packaged in a viruslike particle, John Kirkwood, MD, of University of Pittsburgh Medical Center, explained in a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer. CMP-001 activates tumor-associated plasmacytoid dendritic cells and induces systemic tumor-specific CD8+ T-cell responses.
Dr. Kirkwood and associates are investigating CMP-001, given alone or in combination with pembrolizumab, in a phase 1 trial (NCT02680184) of patients with metastatic or unresectable melanoma who are refractory to anti–PD-1 therapy.
Data were presented on 144 patients who received CMP-001 in combination with pembrolizumab. About 40% of patients (39.6%) had elevated lactate dehydrogenase at baseline, and 32.6% had BRAF mutations.
All patients had received prior anti–PD-1 therapy alone (75%) and/or in combination (50%). For most patients (93.1%), their last response to anti–PD-1 therapy was progression.
For this study, the patients received intratumoral CMP-001 injections at a range of doses (1 mg, 3 mg, 5 mg, 7.5 mg, and 10 mg). CMP-001 was given weekly for either 2 weeks or 7 weeks, then every 3 weeks until discontinuation. There were two different formulations of CMP-001 given – 0.01% polysorbate 20 (PS20; n = 83) and 0.00167% PS20 (n = 61).
Safety
“CMP-001 in combination with pembrolizumab is very well tolerated, with no apparent increase in autoimmune toxicities associated with anti–PD-1,” Dr. Kirkwood said.
The most common treatment-related adverse events were flulike symptoms, including chills (72%), pyrexia (56%), fatigue (51%), nausea (45%), vomiting (29%), and headache (28%). Another common event was injection-site pain (28%).
The most common grade 3 adverse events were hypotension (n = 9) and hypertension (n = 7). Grade 4 events included hypotension, aspartate aminotransferase increase, and alanine aminotransferase increase (n = 1 for all). There were no grade 5 events.
Six patients discontinued treatment because of adverse events.
Response
The overall response rate was 25% (21/83) among patients who received the 0.01% PS20 formulation of CMP-001 and 11.5% (7/61) among patients who received the 0.00167% PS20 formulation.
Responses were similar in injected and noninjected target lesions. The median duration of response has not been reached at a median follow-up of 16.9 months.
“Intratumoral CMP-001 reverses resistance to anti–PD-1 in patients who have progressed on prior anti–PD-1 therapy,” Dr. Kirkwood said, adding that these data support further clinical development of CMP-001.
The research is sponsored by Checkmate Pharmaceuticals. Dr. Kirkwood disclosed relationships with Amgen, BMS, Immunocore, Iovance, Novartis, Elsevier, Castle, Merck, and Checkmate.
SOURCE: Kirkwood J et al. SITC 2019, Abstract O85.
REPORTING FROM SITC 2019
Smokers with PE have higher rate of hospital readmission
NEW ORLEANS – , according to a retrospective study.
The rate of readmission was significantly higher among patients with tobacco dependence, and tobacco dependence was independently associated with an increased risk of readmission.
“This is the first study to quantify the increased rate of hospital readmission due to smoking,” said study investigator Kam Sing Ho, MD, of Mount Sinai St. Luke’s and Mount Sinai West, New York.
Dr. Ho and colleagues described this study and its results in a poster presented at the annual meeting of the American College of Chest Physicians.
The researchers analyzed data on 168,891 hospital admissions of adults with PE, 34.2% of whom had tobacco dependence. Patients with and without tobacco dependence were propensity matched for baseline characteristics (n = 24,262 in each group).
The 30-day readmission rate was significantly higher in patients with tobacco dependence than in those without it – 11.0% and 8.9%, respectively (P less than .001). The most common reason for readmission in both groups was PE.
Dr. Ho said the higher readmission rate among patients with tobacco dependence might be explained by the fact that smokers have a higher level of fibrinogen, which may affect blood viscosity and contribute to thrombus formation (Proc Am Thorac Soc. 2005;2[1]:71-7).
The investigators also found that tobacco dependence was an independent predictor of readmission (hazard ratio, 1.43; P less than .001). And the mortality rate was significantly higher after readmission than after index admission – 6.27% and 3.15%, respectively (P less than .001).
The increased risk of readmission and death among smokers highlights the importance of smoking cessation services. Dr. Ho cited previous research suggesting these services are underused in the hospital setting (BMJ Qual Improv Rep. 2014;3[1]:u204964.w2110).
“Given that smoking is a common phenomenon among patients admitted with pulmonary embolism, we suggest that more rigorous smoking cessation services are implemented prior to discharge for all active smokers,” Dr. Ho said. “[P]atients have the right to be informed on the benefits of smoking cessation and the autonomy to choose. Future research will focus on implementing inpatient smoking cessation at our hospital and its effect on local readmission rate, health resources utilization, and mortality.”
Dr. Ho has no relevant relationships to disclose.
SOURCE: Ho KS et al. CHEST 2019 October. doi: 10.1016/j.chest.2019.08.1551.
NEW ORLEANS – , according to a retrospective study.
The rate of readmission was significantly higher among patients with tobacco dependence, and tobacco dependence was independently associated with an increased risk of readmission.
“This is the first study to quantify the increased rate of hospital readmission due to smoking,” said study investigator Kam Sing Ho, MD, of Mount Sinai St. Luke’s and Mount Sinai West, New York.
Dr. Ho and colleagues described this study and its results in a poster presented at the annual meeting of the American College of Chest Physicians.
The researchers analyzed data on 168,891 hospital admissions of adults with PE, 34.2% of whom had tobacco dependence. Patients with and without tobacco dependence were propensity matched for baseline characteristics (n = 24,262 in each group).
The 30-day readmission rate was significantly higher in patients with tobacco dependence than in those without it – 11.0% and 8.9%, respectively (P less than .001). The most common reason for readmission in both groups was PE.
Dr. Ho said the higher readmission rate among patients with tobacco dependence might be explained by the fact that smokers have a higher level of fibrinogen, which may affect blood viscosity and contribute to thrombus formation (Proc Am Thorac Soc. 2005;2[1]:71-7).
The investigators also found that tobacco dependence was an independent predictor of readmission (hazard ratio, 1.43; P less than .001). And the mortality rate was significantly higher after readmission than after index admission – 6.27% and 3.15%, respectively (P less than .001).
The increased risk of readmission and death among smokers highlights the importance of smoking cessation services. Dr. Ho cited previous research suggesting these services are underused in the hospital setting (BMJ Qual Improv Rep. 2014;3[1]:u204964.w2110).
“Given that smoking is a common phenomenon among patients admitted with pulmonary embolism, we suggest that more rigorous smoking cessation services are implemented prior to discharge for all active smokers,” Dr. Ho said. “[P]atients have the right to be informed on the benefits of smoking cessation and the autonomy to choose. Future research will focus on implementing inpatient smoking cessation at our hospital and its effect on local readmission rate, health resources utilization, and mortality.”
Dr. Ho has no relevant relationships to disclose.
SOURCE: Ho KS et al. CHEST 2019 October. doi: 10.1016/j.chest.2019.08.1551.
NEW ORLEANS – , according to a retrospective study.
The rate of readmission was significantly higher among patients with tobacco dependence, and tobacco dependence was independently associated with an increased risk of readmission.
“This is the first study to quantify the increased rate of hospital readmission due to smoking,” said study investigator Kam Sing Ho, MD, of Mount Sinai St. Luke’s and Mount Sinai West, New York.
Dr. Ho and colleagues described this study and its results in a poster presented at the annual meeting of the American College of Chest Physicians.
The researchers analyzed data on 168,891 hospital admissions of adults with PE, 34.2% of whom had tobacco dependence. Patients with and without tobacco dependence were propensity matched for baseline characteristics (n = 24,262 in each group).
The 30-day readmission rate was significantly higher in patients with tobacco dependence than in those without it – 11.0% and 8.9%, respectively (P less than .001). The most common reason for readmission in both groups was PE.
Dr. Ho said the higher readmission rate among patients with tobacco dependence might be explained by the fact that smokers have a higher level of fibrinogen, which may affect blood viscosity and contribute to thrombus formation (Proc Am Thorac Soc. 2005;2[1]:71-7).
The investigators also found that tobacco dependence was an independent predictor of readmission (hazard ratio, 1.43; P less than .001). And the mortality rate was significantly higher after readmission than after index admission – 6.27% and 3.15%, respectively (P less than .001).
The increased risk of readmission and death among smokers highlights the importance of smoking cessation services. Dr. Ho cited previous research suggesting these services are underused in the hospital setting (BMJ Qual Improv Rep. 2014;3[1]:u204964.w2110).
“Given that smoking is a common phenomenon among patients admitted with pulmonary embolism, we suggest that more rigorous smoking cessation services are implemented prior to discharge for all active smokers,” Dr. Ho said. “[P]atients have the right to be informed on the benefits of smoking cessation and the autonomy to choose. Future research will focus on implementing inpatient smoking cessation at our hospital and its effect on local readmission rate, health resources utilization, and mortality.”
Dr. Ho has no relevant relationships to disclose.
SOURCE: Ho KS et al. CHEST 2019 October. doi: 10.1016/j.chest.2019.08.1551.
REPORTING FROM CHEST 2019
Molecule exhibits activity in heavily pretreated, HER2-positive solid tumors
NATIONAL HARBOR, MD – PRS-343, a 4-1BB/HER2 bispecific molecule, has demonstrated safety and antitumor activity in patients with heavily pretreated, HER2-positive solid tumors, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
In a phase 1 trial of 18 evaluable patients, PRS-343 produced partial responses in 2 patients and enabled 8 patients to maintain stable disease. PRS-343 was considered well tolerated at all doses and schedules tested.
“PRS-343 is a bispecific construct targeting HER2 as well as 4-1BB,” said Geoffrey Y. Ku, MD, of Memorial Sloan Kettering Cancer Center in New York. “The HER2 component of the molecule localizes it into the tumor microenvironment of any HER2-positive cells. If the density of the HER2 protein is high enough, that facilitates cross-linkage of 4-1BB.
“4-1BB is an immune agonist that’s present in activated T cells, and cross-linkage helps to improve T-cell exhaustion and is also critical for T-cell expansion. The idea is that, by localizing 4-1BB activation to the tumor microenvironment, we can avoid some of the systemic toxicities associated with naked 4-1BB antibodies,” Dr. Ku added.
The ongoing, phase 1 trial of PRS-343 (NCT03330561) has enrolled 53 patients with a range of HER2-positive malignancies. To be eligible, patients must have progressed on standard therapy or have a tumor for which no standard therapy is available.
The most common diagnosis among enrolled patients is gastroesophageal cancer (n = 19), followed by breast cancer (n = 14), gynecologic cancers (n = 6), colorectal cancer (n = 5), and other malignancies.
The patients’ median age at baseline was 61 years (range, 29-92 years), and a majority were female (62%). Most patients (79%) had received three or more prior lines of therapy, including anti-HER2 treatments. Breast cancer patients had received a median of four anti-HER2 treatments, and gastric cancer patients had received a median of two.
The patients have been treated with PRS-343 at 11 dose levels, ranging from 0.0005 mg/kg to 8 mg/kg, given every 3 weeks. The highest dose, 8 mg/kg, was also given every 2 weeks.
Treatment-related adverse events (TRAEs) included infusion-related reactions (9%), fatigue (9%), chills (6%), flushing (6%), nausea (6%), diarrhea (6%), vomiting (5%), and noncardiac chest pain (4%).
“This was an extremely well-tolerated drug,” Dr. Ku said. “Out of 111 TRAEs, only a tiny proportion were grade 3, and toxicities mostly clustered around infusion-related reactions, constitutional symptoms, as well as gastrointestinal symptoms.”
Grade 3 TRAEs included infusion-related reactions (2%), fatigue (1%), flushing (3%), and noncardiac chest pain (1%). There were no grade 4-5 TRAEs.
At the data cutoff (Oct. 23, 2019), 18 patients were evaluable for a response at active dose levels (2.5 mg/kg, 5 mg/kg, and 8 mg/kg).
Two patients achieved a partial response, and eight had stable disease. “This translates to a response rate of 11% and a disease control rate of 55%,” Dr. Ku noted.
Both responders received PRS-343 at 8 mg/kg every 2 weeks. One of these patients had stage 4 gastric adenocarcinoma, and one had stage 4 gynecologic carcinoma.
Of the eight patients with stable disease, three received PRS-343 at 8 mg/kg every 2 weeks, two received 8 mg/kg every 3 weeks, one received the 5 mg/kg dose, and two received the 2.5 mg/kg dose.
Dr. Ku noted that the average time on treatment significantly increased in patients who received PRS-343 at 8 mg/kg every 2 weeks. Additionally, both responders and patients with stable disease had a “clear increase” in CD8+ T cells.
“[PRS-343] has demonstrated antitumor activity in heavily pretreated patients across multiple tumor types, and the treatment history, specifically the receipt of prior anti-HER2 therapy, indicates this is a 4-1BB-driven mechanism of action,” Dr. Ku said. “Based on these results, future studies are planned for continued development in defined HER2-positive indications.”
The current study is sponsored by Pieris Pharmaceuticals. Dr. Ku disclosed relationships with Arog Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, Merck, Zymeworks, and Pieris Pharmaceuticals.
SOURCE: Ku GY et al. SITC 2019, Abstract O82.
NATIONAL HARBOR, MD – PRS-343, a 4-1BB/HER2 bispecific molecule, has demonstrated safety and antitumor activity in patients with heavily pretreated, HER2-positive solid tumors, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
In a phase 1 trial of 18 evaluable patients, PRS-343 produced partial responses in 2 patients and enabled 8 patients to maintain stable disease. PRS-343 was considered well tolerated at all doses and schedules tested.
“PRS-343 is a bispecific construct targeting HER2 as well as 4-1BB,” said Geoffrey Y. Ku, MD, of Memorial Sloan Kettering Cancer Center in New York. “The HER2 component of the molecule localizes it into the tumor microenvironment of any HER2-positive cells. If the density of the HER2 protein is high enough, that facilitates cross-linkage of 4-1BB.
“4-1BB is an immune agonist that’s present in activated T cells, and cross-linkage helps to improve T-cell exhaustion and is also critical for T-cell expansion. The idea is that, by localizing 4-1BB activation to the tumor microenvironment, we can avoid some of the systemic toxicities associated with naked 4-1BB antibodies,” Dr. Ku added.
The ongoing, phase 1 trial of PRS-343 (NCT03330561) has enrolled 53 patients with a range of HER2-positive malignancies. To be eligible, patients must have progressed on standard therapy or have a tumor for which no standard therapy is available.
The most common diagnosis among enrolled patients is gastroesophageal cancer (n = 19), followed by breast cancer (n = 14), gynecologic cancers (n = 6), colorectal cancer (n = 5), and other malignancies.
The patients’ median age at baseline was 61 years (range, 29-92 years), and a majority were female (62%). Most patients (79%) had received three or more prior lines of therapy, including anti-HER2 treatments. Breast cancer patients had received a median of four anti-HER2 treatments, and gastric cancer patients had received a median of two.
The patients have been treated with PRS-343 at 11 dose levels, ranging from 0.0005 mg/kg to 8 mg/kg, given every 3 weeks. The highest dose, 8 mg/kg, was also given every 2 weeks.
Treatment-related adverse events (TRAEs) included infusion-related reactions (9%), fatigue (9%), chills (6%), flushing (6%), nausea (6%), diarrhea (6%), vomiting (5%), and noncardiac chest pain (4%).
“This was an extremely well-tolerated drug,” Dr. Ku said. “Out of 111 TRAEs, only a tiny proportion were grade 3, and toxicities mostly clustered around infusion-related reactions, constitutional symptoms, as well as gastrointestinal symptoms.”
Grade 3 TRAEs included infusion-related reactions (2%), fatigue (1%), flushing (3%), and noncardiac chest pain (1%). There were no grade 4-5 TRAEs.
At the data cutoff (Oct. 23, 2019), 18 patients were evaluable for a response at active dose levels (2.5 mg/kg, 5 mg/kg, and 8 mg/kg).
Two patients achieved a partial response, and eight had stable disease. “This translates to a response rate of 11% and a disease control rate of 55%,” Dr. Ku noted.
Both responders received PRS-343 at 8 mg/kg every 2 weeks. One of these patients had stage 4 gastric adenocarcinoma, and one had stage 4 gynecologic carcinoma.
Of the eight patients with stable disease, three received PRS-343 at 8 mg/kg every 2 weeks, two received 8 mg/kg every 3 weeks, one received the 5 mg/kg dose, and two received the 2.5 mg/kg dose.
Dr. Ku noted that the average time on treatment significantly increased in patients who received PRS-343 at 8 mg/kg every 2 weeks. Additionally, both responders and patients with stable disease had a “clear increase” in CD8+ T cells.
“[PRS-343] has demonstrated antitumor activity in heavily pretreated patients across multiple tumor types, and the treatment history, specifically the receipt of prior anti-HER2 therapy, indicates this is a 4-1BB-driven mechanism of action,” Dr. Ku said. “Based on these results, future studies are planned for continued development in defined HER2-positive indications.”
The current study is sponsored by Pieris Pharmaceuticals. Dr. Ku disclosed relationships with Arog Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, Merck, Zymeworks, and Pieris Pharmaceuticals.
SOURCE: Ku GY et al. SITC 2019, Abstract O82.
NATIONAL HARBOR, MD – PRS-343, a 4-1BB/HER2 bispecific molecule, has demonstrated safety and antitumor activity in patients with heavily pretreated, HER2-positive solid tumors, an investigator reported at the annual meeting of the Society for Immunotherapy of Cancer.
In a phase 1 trial of 18 evaluable patients, PRS-343 produced partial responses in 2 patients and enabled 8 patients to maintain stable disease. PRS-343 was considered well tolerated at all doses and schedules tested.
“PRS-343 is a bispecific construct targeting HER2 as well as 4-1BB,” said Geoffrey Y. Ku, MD, of Memorial Sloan Kettering Cancer Center in New York. “The HER2 component of the molecule localizes it into the tumor microenvironment of any HER2-positive cells. If the density of the HER2 protein is high enough, that facilitates cross-linkage of 4-1BB.
“4-1BB is an immune agonist that’s present in activated T cells, and cross-linkage helps to improve T-cell exhaustion and is also critical for T-cell expansion. The idea is that, by localizing 4-1BB activation to the tumor microenvironment, we can avoid some of the systemic toxicities associated with naked 4-1BB antibodies,” Dr. Ku added.
The ongoing, phase 1 trial of PRS-343 (NCT03330561) has enrolled 53 patients with a range of HER2-positive malignancies. To be eligible, patients must have progressed on standard therapy or have a tumor for which no standard therapy is available.
The most common diagnosis among enrolled patients is gastroesophageal cancer (n = 19), followed by breast cancer (n = 14), gynecologic cancers (n = 6), colorectal cancer (n = 5), and other malignancies.
The patients’ median age at baseline was 61 years (range, 29-92 years), and a majority were female (62%). Most patients (79%) had received three or more prior lines of therapy, including anti-HER2 treatments. Breast cancer patients had received a median of four anti-HER2 treatments, and gastric cancer patients had received a median of two.
The patients have been treated with PRS-343 at 11 dose levels, ranging from 0.0005 mg/kg to 8 mg/kg, given every 3 weeks. The highest dose, 8 mg/kg, was also given every 2 weeks.
Treatment-related adverse events (TRAEs) included infusion-related reactions (9%), fatigue (9%), chills (6%), flushing (6%), nausea (6%), diarrhea (6%), vomiting (5%), and noncardiac chest pain (4%).
“This was an extremely well-tolerated drug,” Dr. Ku said. “Out of 111 TRAEs, only a tiny proportion were grade 3, and toxicities mostly clustered around infusion-related reactions, constitutional symptoms, as well as gastrointestinal symptoms.”
Grade 3 TRAEs included infusion-related reactions (2%), fatigue (1%), flushing (3%), and noncardiac chest pain (1%). There were no grade 4-5 TRAEs.
At the data cutoff (Oct. 23, 2019), 18 patients were evaluable for a response at active dose levels (2.5 mg/kg, 5 mg/kg, and 8 mg/kg).
Two patients achieved a partial response, and eight had stable disease. “This translates to a response rate of 11% and a disease control rate of 55%,” Dr. Ku noted.
Both responders received PRS-343 at 8 mg/kg every 2 weeks. One of these patients had stage 4 gastric adenocarcinoma, and one had stage 4 gynecologic carcinoma.
Of the eight patients with stable disease, three received PRS-343 at 8 mg/kg every 2 weeks, two received 8 mg/kg every 3 weeks, one received the 5 mg/kg dose, and two received the 2.5 mg/kg dose.
Dr. Ku noted that the average time on treatment significantly increased in patients who received PRS-343 at 8 mg/kg every 2 weeks. Additionally, both responders and patients with stable disease had a “clear increase” in CD8+ T cells.
“[PRS-343] has demonstrated antitumor activity in heavily pretreated patients across multiple tumor types, and the treatment history, specifically the receipt of prior anti-HER2 therapy, indicates this is a 4-1BB-driven mechanism of action,” Dr. Ku said. “Based on these results, future studies are planned for continued development in defined HER2-positive indications.”
The current study is sponsored by Pieris Pharmaceuticals. Dr. Ku disclosed relationships with Arog Pharmaceuticals, AstraZeneca, Bristol-Myers Squibb, Daiichi Sankyo, Eli Lilly, Merck, Zymeworks, and Pieris Pharmaceuticals.
SOURCE: Ku GY et al. SITC 2019, Abstract O82.
REPORTING FROM SITC 2019
Atezolizumab bests chemo in NSCLC patients with high PD-L1 expression
NATIONAL HARBOR, MD – interim results of a phase 3 trial suggest.
When compared with platinum-based chemotherapy, atezolizumab significantly improved OS in patients who had PD-L1 expression of 50% or greater on tumor cells (TC) or 10% or greater on tumor-infiltrating immune cells (IC).
Patients with lower levels of PD-L1 expression had a numerical, but not statistically significant, benefit in OS with atezolizumab.
Giuseppe Giaccone, MD, PhD, of Georgetown University, Washington, presented these results, from the IMpower110 trial, as a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled treatment-naive, PD-L1–selected patients with stage IV NSCLC. Patients with EGFR-positive or ALK-positive NSCLC were excluded.
The overall population consisted of 554 patients with PD-L1 expression of at least 1% on TC or IC (TC1/2/3 or IC1/2/3). There were 328 patients with PD-L1 expression of at least 5% on TC or IC (TC2/3 or IC2/3) and 205 patients with PD-L1 expression of at least 50% on TC or 10% on IC (TC3 or IC3).
All patients were randomized to receive atezolizumab or platinum-based chemotherapy. Atezolizumab was given at 1,200 mg every 3 weeks until disease progression or loss of clinical benefit. In the chemotherapy arm, patients with nonsquamous NSCLC received cisplatin or carboplatin plus pemetrexed, and patients with squamous NSCLC received cisplatin or carboplatin plus gemcitabine. Chemotherapy was given for 4-6 cycles, after which patients received pemetrexed (nonsquamous) or best supportive care (squamous) until progression.
Baseline characteristics were similar between the treatment arms and across the PD-L1 subgroups.
Overall survival
OS was evaluated hierarchically, starting with the TC3 or IC3 population. This group had a significant improvement in OS with atezolizumab. At a median follow-up of 15.7 months, the median OS was 13.1 months with chemotherapy and 20.2 months with atezolizumab (hazard ratio, 0.59; P = .0106).
The TC2/3 or IC2/3 population had a numerical, but not significant, improvement in OS with atezolizumab. At a median follow-up of 15.2 months, the median OS was 14.9 months with chemotherapy and 18.2 months with atezolizumab (HR, 0.72; P = .0416).
“The prespecified alpha boundary was not crossed in this analysis,” Dr. Giaccone said. “Therefore, it cannot be considered statistically significant, although, numerically, there is clearly an advantage with atezolizumab versus chemotherapy.”
There was no significant improvement in OS in the overall population (TC1/2/3 or IC1/2/3). At a median follow-up of 13.4 months, the median OS was 14.1 months in the chemotherapy arm and 17.5 months in the atezolizumab arm (HR, 0.83; P = .1481).
Dr. Giaccone noted that 29.6% of patients in the atezolizumab arm and 49.5% of those in the chemotherapy arm received at least one subsequent cancer therapy. The proportion of patients that received second-line cancer therapies was similar across the PD-L1 subgroups.
Progression-free survival
Progression-free survival (PFS) was significantly better with atezolizumab, regardless of PD-L1 expression.
In the TC3/IC3 population, the median PFS was 5.0 months with chemotherapy and 8.1 months with atezolizumab (HR, 0.63; P = .0070). In the TC2/3 or IC2/3 group, the median PFS was 5.5 months with chemotherapy and 7.2 months with atezolizumab (HR, 0.67; P = .0030). In the overall population, the median PFS was 5.5 months with chemotherapy and 5.7 months with atezolizumab (HR, 0.77; P = .0104).
Safety
“The safety profile of atezolizumab was consistent with prior observations,” Dr. Giaccone said.
The incidence of treatment-related adverse events (AEs) was 90.2% in the atezolizumab arm and 94.7% in the chemotherapy arm. Rates of grade 3/4 related AEs were 12.9% and 44.1%, respectively. There was one grade 5 AE in the chemotherapy arm and none in the atezolizumab arm.
AEs that were more frequent with atezolizumab included increased aspartate aminotransferase, pruritus, and hypothyroidism.
This trial is sponsored by Hoffmann-La Roche, and Dr. Giaccone disclosed grants and nonfinancial support from the company.
SOURCE: Giaccone G et al. SITC 2019, Abstract O81.
NATIONAL HARBOR, MD – interim results of a phase 3 trial suggest.
When compared with platinum-based chemotherapy, atezolizumab significantly improved OS in patients who had PD-L1 expression of 50% or greater on tumor cells (TC) or 10% or greater on tumor-infiltrating immune cells (IC).
Patients with lower levels of PD-L1 expression had a numerical, but not statistically significant, benefit in OS with atezolizumab.
Giuseppe Giaccone, MD, PhD, of Georgetown University, Washington, presented these results, from the IMpower110 trial, as a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled treatment-naive, PD-L1–selected patients with stage IV NSCLC. Patients with EGFR-positive or ALK-positive NSCLC were excluded.
The overall population consisted of 554 patients with PD-L1 expression of at least 1% on TC or IC (TC1/2/3 or IC1/2/3). There were 328 patients with PD-L1 expression of at least 5% on TC or IC (TC2/3 or IC2/3) and 205 patients with PD-L1 expression of at least 50% on TC or 10% on IC (TC3 or IC3).
All patients were randomized to receive atezolizumab or platinum-based chemotherapy. Atezolizumab was given at 1,200 mg every 3 weeks until disease progression or loss of clinical benefit. In the chemotherapy arm, patients with nonsquamous NSCLC received cisplatin or carboplatin plus pemetrexed, and patients with squamous NSCLC received cisplatin or carboplatin plus gemcitabine. Chemotherapy was given for 4-6 cycles, after which patients received pemetrexed (nonsquamous) or best supportive care (squamous) until progression.
Baseline characteristics were similar between the treatment arms and across the PD-L1 subgroups.
Overall survival
OS was evaluated hierarchically, starting with the TC3 or IC3 population. This group had a significant improvement in OS with atezolizumab. At a median follow-up of 15.7 months, the median OS was 13.1 months with chemotherapy and 20.2 months with atezolizumab (hazard ratio, 0.59; P = .0106).
The TC2/3 or IC2/3 population had a numerical, but not significant, improvement in OS with atezolizumab. At a median follow-up of 15.2 months, the median OS was 14.9 months with chemotherapy and 18.2 months with atezolizumab (HR, 0.72; P = .0416).
“The prespecified alpha boundary was not crossed in this analysis,” Dr. Giaccone said. “Therefore, it cannot be considered statistically significant, although, numerically, there is clearly an advantage with atezolizumab versus chemotherapy.”
There was no significant improvement in OS in the overall population (TC1/2/3 or IC1/2/3). At a median follow-up of 13.4 months, the median OS was 14.1 months in the chemotherapy arm and 17.5 months in the atezolizumab arm (HR, 0.83; P = .1481).
Dr. Giaccone noted that 29.6% of patients in the atezolizumab arm and 49.5% of those in the chemotherapy arm received at least one subsequent cancer therapy. The proportion of patients that received second-line cancer therapies was similar across the PD-L1 subgroups.
Progression-free survival
Progression-free survival (PFS) was significantly better with atezolizumab, regardless of PD-L1 expression.
In the TC3/IC3 population, the median PFS was 5.0 months with chemotherapy and 8.1 months with atezolizumab (HR, 0.63; P = .0070). In the TC2/3 or IC2/3 group, the median PFS was 5.5 months with chemotherapy and 7.2 months with atezolizumab (HR, 0.67; P = .0030). In the overall population, the median PFS was 5.5 months with chemotherapy and 5.7 months with atezolizumab (HR, 0.77; P = .0104).
Safety
“The safety profile of atezolizumab was consistent with prior observations,” Dr. Giaccone said.
The incidence of treatment-related adverse events (AEs) was 90.2% in the atezolizumab arm and 94.7% in the chemotherapy arm. Rates of grade 3/4 related AEs were 12.9% and 44.1%, respectively. There was one grade 5 AE in the chemotherapy arm and none in the atezolizumab arm.
AEs that were more frequent with atezolizumab included increased aspartate aminotransferase, pruritus, and hypothyroidism.
This trial is sponsored by Hoffmann-La Roche, and Dr. Giaccone disclosed grants and nonfinancial support from the company.
SOURCE: Giaccone G et al. SITC 2019, Abstract O81.
NATIONAL HARBOR, MD – interim results of a phase 3 trial suggest.
When compared with platinum-based chemotherapy, atezolizumab significantly improved OS in patients who had PD-L1 expression of 50% or greater on tumor cells (TC) or 10% or greater on tumor-infiltrating immune cells (IC).
Patients with lower levels of PD-L1 expression had a numerical, but not statistically significant, benefit in OS with atezolizumab.
Giuseppe Giaccone, MD, PhD, of Georgetown University, Washington, presented these results, from the IMpower110 trial, as a late-breaking abstract at the annual meeting of the Society for Immunotherapy of Cancer.
The trial enrolled treatment-naive, PD-L1–selected patients with stage IV NSCLC. Patients with EGFR-positive or ALK-positive NSCLC were excluded.
The overall population consisted of 554 patients with PD-L1 expression of at least 1% on TC or IC (TC1/2/3 or IC1/2/3). There were 328 patients with PD-L1 expression of at least 5% on TC or IC (TC2/3 or IC2/3) and 205 patients with PD-L1 expression of at least 50% on TC or 10% on IC (TC3 or IC3).
All patients were randomized to receive atezolizumab or platinum-based chemotherapy. Atezolizumab was given at 1,200 mg every 3 weeks until disease progression or loss of clinical benefit. In the chemotherapy arm, patients with nonsquamous NSCLC received cisplatin or carboplatin plus pemetrexed, and patients with squamous NSCLC received cisplatin or carboplatin plus gemcitabine. Chemotherapy was given for 4-6 cycles, after which patients received pemetrexed (nonsquamous) or best supportive care (squamous) until progression.
Baseline characteristics were similar between the treatment arms and across the PD-L1 subgroups.
Overall survival
OS was evaluated hierarchically, starting with the TC3 or IC3 population. This group had a significant improvement in OS with atezolizumab. At a median follow-up of 15.7 months, the median OS was 13.1 months with chemotherapy and 20.2 months with atezolizumab (hazard ratio, 0.59; P = .0106).
The TC2/3 or IC2/3 population had a numerical, but not significant, improvement in OS with atezolizumab. At a median follow-up of 15.2 months, the median OS was 14.9 months with chemotherapy and 18.2 months with atezolizumab (HR, 0.72; P = .0416).
“The prespecified alpha boundary was not crossed in this analysis,” Dr. Giaccone said. “Therefore, it cannot be considered statistically significant, although, numerically, there is clearly an advantage with atezolizumab versus chemotherapy.”
There was no significant improvement in OS in the overall population (TC1/2/3 or IC1/2/3). At a median follow-up of 13.4 months, the median OS was 14.1 months in the chemotherapy arm and 17.5 months in the atezolizumab arm (HR, 0.83; P = .1481).
Dr. Giaccone noted that 29.6% of patients in the atezolizumab arm and 49.5% of those in the chemotherapy arm received at least one subsequent cancer therapy. The proportion of patients that received second-line cancer therapies was similar across the PD-L1 subgroups.
Progression-free survival
Progression-free survival (PFS) was significantly better with atezolizumab, regardless of PD-L1 expression.
In the TC3/IC3 population, the median PFS was 5.0 months with chemotherapy and 8.1 months with atezolizumab (HR, 0.63; P = .0070). In the TC2/3 or IC2/3 group, the median PFS was 5.5 months with chemotherapy and 7.2 months with atezolizumab (HR, 0.67; P = .0030). In the overall population, the median PFS was 5.5 months with chemotherapy and 5.7 months with atezolizumab (HR, 0.77; P = .0104).
Safety
“The safety profile of atezolizumab was consistent with prior observations,” Dr. Giaccone said.
The incidence of treatment-related adverse events (AEs) was 90.2% in the atezolizumab arm and 94.7% in the chemotherapy arm. Rates of grade 3/4 related AEs were 12.9% and 44.1%, respectively. There was one grade 5 AE in the chemotherapy arm and none in the atezolizumab arm.
AEs that were more frequent with atezolizumab included increased aspartate aminotransferase, pruritus, and hypothyroidism.
This trial is sponsored by Hoffmann-La Roche, and Dr. Giaccone disclosed grants and nonfinancial support from the company.
SOURCE: Giaccone G et al. SITC 2019, Abstract O81.
REPORTING FROM SITC 2019
Dupilumab effective in early- and late-onset asthma
NEW ORLEANS – A new analysis suggests
Dupilumab may be more effective in reducing severe asthma exacerbations in patients with late-onset asthma, but the drug’s effect on lung function appeared the same regardless of asthma onset. Nicola Hanania, MD, of Baylor College of Medicine in Houston presented these results at the annual meeting of the American College of Chest Physicians.
Dr. Hanania and colleagues conducted a subanalysis of the LIBERTY ASTHMA QUEST study (NCT02414854). Previous data from this study showed that patients with uncontrolled, moderate to severe asthma who received dupilumab had fewer exacerbations and better lung function than did patients who received placebo (N Engl J Med. 2018;378:2486-96).
In their subanalysis, Dr. Hanania and his colleagues evaluated the efficacy of dupilumab, given at 200 mg or 300 mg every 2 weeks, in patients with early-onset asthma (at 40 years of age or younger) and late-onset asthma (at 41 years or older). The analysis included 919 patients with early-onset asthma who received dupilumab and 450 early-onset patients who received placebo. There were 345 patients with late-onset asthma who received dupilumab and 188 late-onset patients who received placebo.
Exacerbations
Dupilumab significantly reduced the adjusted annualized severe exacerbation rates during the 52-week treatment period. Significant reductions occurred in both early- and late-onset patients, though reductions were greater in the late-onset group.
In early-onset patients, dupilumab reduced severe exacerbations by 38% when given at 200 mg and by 37% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients, dupilumab reduced exacerbations by 64% and 69%, respectively (P less than .001 vs. placebo).
Dr. Hanania said it isn’t clear why late-onset patients appear to derive more benefit with regard to exacerbations. It may be because these patients have more comorbidities or because they aren’t using their inhalers correctly. The researchers are investigating these possibilities.
Dr. Hanania went on to note that reductions in exacerbation rates were greatest in patients with elevated blood eosinophils (150 cells/mcL or greater) or fractional exhaled nitric oxide (FeNO; 25 ppb or greater).
In patients with early-onset asthma and elevated eosinophils, dupilumab reduced severe exacerbations by 50% when given at 200 mg and by 55% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients with elevated eosinophils, dupilumab reduced exacerbations by 65% and 73%, respectively (P less than .001 vs. placebo).
In patients with early-onset asthma and elevated FeNO, dupilumab reduced severe exacerbations by 56% when given at 200 mg and by 52% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients with elevated FeNO, dupilumab reduced exacerbations by 79% and 71%, respectively (P less than .001 vs. placebo).
Lung function
Dupilumab also improved prebronchodilator forced expiratory volume in 1 second (pre-BD FEV1), compared with placebo, with similar results in early- and late-onset patients.
In early-onset patients, the P values were less than .001 for both doses of dupilumab at weeks 12 and 52. In late-onset patients, the P values were less than .001 for the 300-mg dose at week 12 and the 200-mg dose at week 52, less than .01 for the 200-mg dose at week 12, and less than .05 for the 300-mg dose at week 52.
The effects of dupilumab on pre-BD FEV1 were greatest in patients with elevated eosinophils or FeNO. At week 12, the P value was less than .001 for both doses of dupilumab in early-onset patients with elevated eosinophils or FeNO. The P value was less than .01 for both doses in late-onset patients with elevated eosinophils. And the P value was less than .001 for both doses in late-onset patients with elevated FeNO.
This research was sponsored by Sanofi and Regeneron. Dr. Hanania disclosed relationships with Genentech, Novartis, AstraZeneca, Boehringer Ingelheim, GSK, Regeneron, and Sanofi.
SOURCE: Hanania N et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.870.
NEW ORLEANS – A new analysis suggests
Dupilumab may be more effective in reducing severe asthma exacerbations in patients with late-onset asthma, but the drug’s effect on lung function appeared the same regardless of asthma onset. Nicola Hanania, MD, of Baylor College of Medicine in Houston presented these results at the annual meeting of the American College of Chest Physicians.
Dr. Hanania and colleagues conducted a subanalysis of the LIBERTY ASTHMA QUEST study (NCT02414854). Previous data from this study showed that patients with uncontrolled, moderate to severe asthma who received dupilumab had fewer exacerbations and better lung function than did patients who received placebo (N Engl J Med. 2018;378:2486-96).
In their subanalysis, Dr. Hanania and his colleagues evaluated the efficacy of dupilumab, given at 200 mg or 300 mg every 2 weeks, in patients with early-onset asthma (at 40 years of age or younger) and late-onset asthma (at 41 years or older). The analysis included 919 patients with early-onset asthma who received dupilumab and 450 early-onset patients who received placebo. There were 345 patients with late-onset asthma who received dupilumab and 188 late-onset patients who received placebo.
Exacerbations
Dupilumab significantly reduced the adjusted annualized severe exacerbation rates during the 52-week treatment period. Significant reductions occurred in both early- and late-onset patients, though reductions were greater in the late-onset group.
In early-onset patients, dupilumab reduced severe exacerbations by 38% when given at 200 mg and by 37% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients, dupilumab reduced exacerbations by 64% and 69%, respectively (P less than .001 vs. placebo).
Dr. Hanania said it isn’t clear why late-onset patients appear to derive more benefit with regard to exacerbations. It may be because these patients have more comorbidities or because they aren’t using their inhalers correctly. The researchers are investigating these possibilities.
Dr. Hanania went on to note that reductions in exacerbation rates were greatest in patients with elevated blood eosinophils (150 cells/mcL or greater) or fractional exhaled nitric oxide (FeNO; 25 ppb or greater).
In patients with early-onset asthma and elevated eosinophils, dupilumab reduced severe exacerbations by 50% when given at 200 mg and by 55% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients with elevated eosinophils, dupilumab reduced exacerbations by 65% and 73%, respectively (P less than .001 vs. placebo).
In patients with early-onset asthma and elevated FeNO, dupilumab reduced severe exacerbations by 56% when given at 200 mg and by 52% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients with elevated FeNO, dupilumab reduced exacerbations by 79% and 71%, respectively (P less than .001 vs. placebo).
Lung function
Dupilumab also improved prebronchodilator forced expiratory volume in 1 second (pre-BD FEV1), compared with placebo, with similar results in early- and late-onset patients.
In early-onset patients, the P values were less than .001 for both doses of dupilumab at weeks 12 and 52. In late-onset patients, the P values were less than .001 for the 300-mg dose at week 12 and the 200-mg dose at week 52, less than .01 for the 200-mg dose at week 12, and less than .05 for the 300-mg dose at week 52.
The effects of dupilumab on pre-BD FEV1 were greatest in patients with elevated eosinophils or FeNO. At week 12, the P value was less than .001 for both doses of dupilumab in early-onset patients with elevated eosinophils or FeNO. The P value was less than .01 for both doses in late-onset patients with elevated eosinophils. And the P value was less than .001 for both doses in late-onset patients with elevated FeNO.
This research was sponsored by Sanofi and Regeneron. Dr. Hanania disclosed relationships with Genentech, Novartis, AstraZeneca, Boehringer Ingelheim, GSK, Regeneron, and Sanofi.
SOURCE: Hanania N et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.870.
NEW ORLEANS – A new analysis suggests
Dupilumab may be more effective in reducing severe asthma exacerbations in patients with late-onset asthma, but the drug’s effect on lung function appeared the same regardless of asthma onset. Nicola Hanania, MD, of Baylor College of Medicine in Houston presented these results at the annual meeting of the American College of Chest Physicians.
Dr. Hanania and colleagues conducted a subanalysis of the LIBERTY ASTHMA QUEST study (NCT02414854). Previous data from this study showed that patients with uncontrolled, moderate to severe asthma who received dupilumab had fewer exacerbations and better lung function than did patients who received placebo (N Engl J Med. 2018;378:2486-96).
In their subanalysis, Dr. Hanania and his colleagues evaluated the efficacy of dupilumab, given at 200 mg or 300 mg every 2 weeks, in patients with early-onset asthma (at 40 years of age or younger) and late-onset asthma (at 41 years or older). The analysis included 919 patients with early-onset asthma who received dupilumab and 450 early-onset patients who received placebo. There were 345 patients with late-onset asthma who received dupilumab and 188 late-onset patients who received placebo.
Exacerbations
Dupilumab significantly reduced the adjusted annualized severe exacerbation rates during the 52-week treatment period. Significant reductions occurred in both early- and late-onset patients, though reductions were greater in the late-onset group.
In early-onset patients, dupilumab reduced severe exacerbations by 38% when given at 200 mg and by 37% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients, dupilumab reduced exacerbations by 64% and 69%, respectively (P less than .001 vs. placebo).
Dr. Hanania said it isn’t clear why late-onset patients appear to derive more benefit with regard to exacerbations. It may be because these patients have more comorbidities or because they aren’t using their inhalers correctly. The researchers are investigating these possibilities.
Dr. Hanania went on to note that reductions in exacerbation rates were greatest in patients with elevated blood eosinophils (150 cells/mcL or greater) or fractional exhaled nitric oxide (FeNO; 25 ppb or greater).
In patients with early-onset asthma and elevated eosinophils, dupilumab reduced severe exacerbations by 50% when given at 200 mg and by 55% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients with elevated eosinophils, dupilumab reduced exacerbations by 65% and 73%, respectively (P less than .001 vs. placebo).
In patients with early-onset asthma and elevated FeNO, dupilumab reduced severe exacerbations by 56% when given at 200 mg and by 52% when given at 300 mg (P less than .001 vs. placebo). In late-onset patients with elevated FeNO, dupilumab reduced exacerbations by 79% and 71%, respectively (P less than .001 vs. placebo).
Lung function
Dupilumab also improved prebronchodilator forced expiratory volume in 1 second (pre-BD FEV1), compared with placebo, with similar results in early- and late-onset patients.
In early-onset patients, the P values were less than .001 for both doses of dupilumab at weeks 12 and 52. In late-onset patients, the P values were less than .001 for the 300-mg dose at week 12 and the 200-mg dose at week 52, less than .01 for the 200-mg dose at week 12, and less than .05 for the 300-mg dose at week 52.
The effects of dupilumab on pre-BD FEV1 were greatest in patients with elevated eosinophils or FeNO. At week 12, the P value was less than .001 for both doses of dupilumab in early-onset patients with elevated eosinophils or FeNO. The P value was less than .01 for both doses in late-onset patients with elevated eosinophils. And the P value was less than .001 for both doses in late-onset patients with elevated FeNO.
This research was sponsored by Sanofi and Regeneron. Dr. Hanania disclosed relationships with Genentech, Novartis, AstraZeneca, Boehringer Ingelheim, GSK, Regeneron, and Sanofi.
SOURCE: Hanania N et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.870.
REPORTING FROM CHEST 2019
Robotic bronchoscopy beat standard techniques for targeting lung nodules
NEW ORLEANS –
A prospective study in a cadaver model showed that robotic bronchoscopy targeted nodules more effectively than electromagnetic navigation or an ultrathin bronchoscope with radial endobronchial ultrasound (UTB-rEBUS).
“This is really the first study to randomize, blind, and compare procedural outcomes between existing technologies in advanced bronchoscopy,” said Lonny Yarmus, DO, of Johns Hopkins Medicine in Baltimore.
Dr. Yarmus described this study, PRECISION-1, at the annual meeting of the American Society of Chest Physicians. The study was designed to compare the following:
- UTB-rEBUS (3.0 mm outer diameter and 1.7 mm working channel).
- Electromagnetic navigation bronchoscopy (Superdimension version 7.1).
- Robotic bronchoscopy (3.5 mm outer diameter and 2.0-mm working channel).
With all methods, a 21-gauge needle was used. For each nodule, UTB-rEBUS was done first to eliminate potential localization bias. The subsequent order of electromagnetic navigation and robotic bronchoscopy was determined based on block randomization.
Eight bronchoscopists performed a total of 60 procedures using each of the methods to target 20 nodules implanted in cadavers. The nodules were distributed across all lobes, 80% were in the outer third of the lung, and 50% had a positive bronchus sign on computed tomography (CT). The mean nodule size was 16.5 plus or minus 1.5 mm.
The study’s primary endpoint was the ability to localize and puncture target nodules within a maximum of three attempts per method. This includes center, peripheral, and distal punctures of nodules. Cone-beam CT was used to confirm that needles punctured the target lesions. The bronchoscopists were blinded to cone-beam CT results, and a blinded, independent investigator assessed whether nodule punctures were successful. The primary endpoint was met in 25% of UTB-rEBUS procedures, 45% of electromagnetic navigation procedures, and 80% of robotic bronchoscopy procedures.
The study’s secondary endpoint was localization success, which was defined as navigation to within needle biopsy distance of the nodule. This includes center, peripheral, and distal punctures of nodules, as well as adjacent punctures (touching the nodule but not within it). The secondary endpoint was met in 35% of UTB-rEBUS procedures, 65% of electromagnetic navigation procedures, and 90% of robotic bronchoscopy procedures.
The researchers also assessed successful navigation, which was defined as the provider localizing with software or radial ultrasound and passing the needle to make a biopsy attempt. Navigation was successful in 65% of UTB-rEBUS procedures, 85% of electromagnetic navigation procedures, and 100% of robotic bronchoscopy procedures.
“Utilization of robotic bronchoscopy with shape-sensing technology can significantly increase the ability to localize and puncture lesions when compared with standard existing technologies,” Dr. Yarmus said in closing.
He did note that this research was done in a cadaveric model, so “prospective, randomized, and comparative in vivo studies are needed.”
This study was funded by the Association of Interventional Pulmonary Program Directors. Dr. Yarmus disclosed government and societal funding and relationships with Boston Scientific, Veran, Medtronic, Intuitive, Auris, Erbe, Olympus, BD, Rocket, Ambu, Inspire Medical, and AstraZeneca.
SOURCE: Yarmus L et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.311.
NEW ORLEANS –
A prospective study in a cadaver model showed that robotic bronchoscopy targeted nodules more effectively than electromagnetic navigation or an ultrathin bronchoscope with radial endobronchial ultrasound (UTB-rEBUS).
“This is really the first study to randomize, blind, and compare procedural outcomes between existing technologies in advanced bronchoscopy,” said Lonny Yarmus, DO, of Johns Hopkins Medicine in Baltimore.
Dr. Yarmus described this study, PRECISION-1, at the annual meeting of the American Society of Chest Physicians. The study was designed to compare the following:
- UTB-rEBUS (3.0 mm outer diameter and 1.7 mm working channel).
- Electromagnetic navigation bronchoscopy (Superdimension version 7.1).
- Robotic bronchoscopy (3.5 mm outer diameter and 2.0-mm working channel).
With all methods, a 21-gauge needle was used. For each nodule, UTB-rEBUS was done first to eliminate potential localization bias. The subsequent order of electromagnetic navigation and robotic bronchoscopy was determined based on block randomization.
Eight bronchoscopists performed a total of 60 procedures using each of the methods to target 20 nodules implanted in cadavers. The nodules were distributed across all lobes, 80% were in the outer third of the lung, and 50% had a positive bronchus sign on computed tomography (CT). The mean nodule size was 16.5 plus or minus 1.5 mm.
The study’s primary endpoint was the ability to localize and puncture target nodules within a maximum of three attempts per method. This includes center, peripheral, and distal punctures of nodules. Cone-beam CT was used to confirm that needles punctured the target lesions. The bronchoscopists were blinded to cone-beam CT results, and a blinded, independent investigator assessed whether nodule punctures were successful. The primary endpoint was met in 25% of UTB-rEBUS procedures, 45% of electromagnetic navigation procedures, and 80% of robotic bronchoscopy procedures.
The study’s secondary endpoint was localization success, which was defined as navigation to within needle biopsy distance of the nodule. This includes center, peripheral, and distal punctures of nodules, as well as adjacent punctures (touching the nodule but not within it). The secondary endpoint was met in 35% of UTB-rEBUS procedures, 65% of electromagnetic navigation procedures, and 90% of robotic bronchoscopy procedures.
The researchers also assessed successful navigation, which was defined as the provider localizing with software or radial ultrasound and passing the needle to make a biopsy attempt. Navigation was successful in 65% of UTB-rEBUS procedures, 85% of electromagnetic navigation procedures, and 100% of robotic bronchoscopy procedures.
“Utilization of robotic bronchoscopy with shape-sensing technology can significantly increase the ability to localize and puncture lesions when compared with standard existing technologies,” Dr. Yarmus said in closing.
He did note that this research was done in a cadaveric model, so “prospective, randomized, and comparative in vivo studies are needed.”
This study was funded by the Association of Interventional Pulmonary Program Directors. Dr. Yarmus disclosed government and societal funding and relationships with Boston Scientific, Veran, Medtronic, Intuitive, Auris, Erbe, Olympus, BD, Rocket, Ambu, Inspire Medical, and AstraZeneca.
SOURCE: Yarmus L et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.311.
NEW ORLEANS –
A prospective study in a cadaver model showed that robotic bronchoscopy targeted nodules more effectively than electromagnetic navigation or an ultrathin bronchoscope with radial endobronchial ultrasound (UTB-rEBUS).
“This is really the first study to randomize, blind, and compare procedural outcomes between existing technologies in advanced bronchoscopy,” said Lonny Yarmus, DO, of Johns Hopkins Medicine in Baltimore.
Dr. Yarmus described this study, PRECISION-1, at the annual meeting of the American Society of Chest Physicians. The study was designed to compare the following:
- UTB-rEBUS (3.0 mm outer diameter and 1.7 mm working channel).
- Electromagnetic navigation bronchoscopy (Superdimension version 7.1).
- Robotic bronchoscopy (3.5 mm outer diameter and 2.0-mm working channel).
With all methods, a 21-gauge needle was used. For each nodule, UTB-rEBUS was done first to eliminate potential localization bias. The subsequent order of electromagnetic navigation and robotic bronchoscopy was determined based on block randomization.
Eight bronchoscopists performed a total of 60 procedures using each of the methods to target 20 nodules implanted in cadavers. The nodules were distributed across all lobes, 80% were in the outer third of the lung, and 50% had a positive bronchus sign on computed tomography (CT). The mean nodule size was 16.5 plus or minus 1.5 mm.
The study’s primary endpoint was the ability to localize and puncture target nodules within a maximum of three attempts per method. This includes center, peripheral, and distal punctures of nodules. Cone-beam CT was used to confirm that needles punctured the target lesions. The bronchoscopists were blinded to cone-beam CT results, and a blinded, independent investigator assessed whether nodule punctures were successful. The primary endpoint was met in 25% of UTB-rEBUS procedures, 45% of electromagnetic navigation procedures, and 80% of robotic bronchoscopy procedures.
The study’s secondary endpoint was localization success, which was defined as navigation to within needle biopsy distance of the nodule. This includes center, peripheral, and distal punctures of nodules, as well as adjacent punctures (touching the nodule but not within it). The secondary endpoint was met in 35% of UTB-rEBUS procedures, 65% of electromagnetic navigation procedures, and 90% of robotic bronchoscopy procedures.
The researchers also assessed successful navigation, which was defined as the provider localizing with software or radial ultrasound and passing the needle to make a biopsy attempt. Navigation was successful in 65% of UTB-rEBUS procedures, 85% of electromagnetic navigation procedures, and 100% of robotic bronchoscopy procedures.
“Utilization of robotic bronchoscopy with shape-sensing technology can significantly increase the ability to localize and puncture lesions when compared with standard existing technologies,” Dr. Yarmus said in closing.
He did note that this research was done in a cadaveric model, so “prospective, randomized, and comparative in vivo studies are needed.”
This study was funded by the Association of Interventional Pulmonary Program Directors. Dr. Yarmus disclosed government and societal funding and relationships with Boston Scientific, Veran, Medtronic, Intuitive, Auris, Erbe, Olympus, BD, Rocket, Ambu, Inspire Medical, and AstraZeneca.
SOURCE: Yarmus L et al. CHEST 2019. Abstract, doi: 10.1016/j.chest.2019.08.311.
REPORTING FROM CHEST 2019
Fluoroscopic system can improve targeting of lung lesions
NEW ORLEANS – A novel according to an industry-sponsored, prospective study.
The system, which incorporates fluoroscopic navigation, increased the percentage of cases in which the target overlapped with the lesion, from 60% to 83%. The percentage of cases without any target overlap decreased from 32% to 5%.
“Tomosynthesis-based fluoroscopic navigation … improves the three-dimensional convergence between the virtual target and the actual target,” said Krish Bhadra, MD, of CHI Memorial Medical Group in Chattanooga, Tenn.
Dr. Bhadra presented results with this system at the annual meeting of the American College of Chest Physicians.
He and his colleagues conducted a study of Medtronic’s superDimension navigation system (version 7.2), which provides real-time imaging with three-dimensional fluoroscopy. The system has a “local registration” feature, which uses fluoroscopy and an algorithm to update the virtual target location during the procedure. This allows the user to reposition the catheter based on the location of the lesion.
The researchers tested the system in 50 patients from two centers (NCT03585959). Patients’ lesions had to be larger than 10 mm, not visible endobronchially, and not reachable by convex endobronchial ultrasound. Lesions within 10 mm of the diaphragm were excluded.
The median lesion size was 17.0 mm, 61.2% were smaller than 20 mm, 65.3% were in the upper lobe, and 53.1% had a bronchus sign present. The median distance from lesion to pleura was 5.9 mm.
Dr. Bhadra said the system performed as designed in all cases, and the protocol-defined technical success rate was 95.9% (47/49). Local registration was attempted in 49 patients and was successful in 47 patients (95.9%). In the unsuccessful cases, local registration was not completed based on the system design because the correction distance was greater than 3.0 cm.
The study’s primary endpoint was three-dimensional overlap of the virtual target and the actual lesion, as confirmed by cone-beam computed tomography. Success was defined as greater than 0% overlap after location correction. Target overlap was achieved in 59.6% (28/47) of cases before local registration and 83.0% (39/47) of cases after.
There were six cases in which local registration was successful, but these subjects weren’t evaluable because of failed procedure recording. When those subjects were excluded, target overlap was achieved in 95.1% (39/41) of cases after local registration.
The median percent overlap between the virtual target and the actual lesion was 11.4% before local registration and 32.8% after. The percentage of cases without any target overlap decreased from 31.7% (13/41) before local registration to 4.9% (2/41) after.
Focusing on the two cases without target overlap, Dr. Bhadra noted that he was able to get a biopsy that proved a malignancy in one of those patients. In the other patient, Dr. Bhadra was able to identify features of organizing pneumonia.
“Even though we did not have overlap, we must have been close enough that we were able to get malignant tissue in one [patient] and features of organizing pneumonia in a patient who’s got no history of organizing pneumonia,” Dr. Bhadra said.
He and his colleagues did not evaluate diagnostic yield in this study, but they did assess complications up to 7 days after the procedure.
The team reported one case of pneumothorax, but the patient didn’t require a chest tube. Additionally, there were two cases of bronchopulmonary hemorrhage, but the patients didn’t require any interventions.
This study was sponsored by Medtronic. Dr. Bhadra disclosed relationships with Medtronic, Boston Scientific, BodyVision, Auris Surgical Robotics, Intuitive Surgical, Veracyte, Biodesix, Merit Medical Endotek, and Johnson & Johnson.
SOURCE: Bhadra K et al. CHEST 2019. doi: 10.1016/j.chest.2019.08.314.
NEW ORLEANS – A novel according to an industry-sponsored, prospective study.
The system, which incorporates fluoroscopic navigation, increased the percentage of cases in which the target overlapped with the lesion, from 60% to 83%. The percentage of cases without any target overlap decreased from 32% to 5%.
“Tomosynthesis-based fluoroscopic navigation … improves the three-dimensional convergence between the virtual target and the actual target,” said Krish Bhadra, MD, of CHI Memorial Medical Group in Chattanooga, Tenn.
Dr. Bhadra presented results with this system at the annual meeting of the American College of Chest Physicians.
He and his colleagues conducted a study of Medtronic’s superDimension navigation system (version 7.2), which provides real-time imaging with three-dimensional fluoroscopy. The system has a “local registration” feature, which uses fluoroscopy and an algorithm to update the virtual target location during the procedure. This allows the user to reposition the catheter based on the location of the lesion.
The researchers tested the system in 50 patients from two centers (NCT03585959). Patients’ lesions had to be larger than 10 mm, not visible endobronchially, and not reachable by convex endobronchial ultrasound. Lesions within 10 mm of the diaphragm were excluded.
The median lesion size was 17.0 mm, 61.2% were smaller than 20 mm, 65.3% were in the upper lobe, and 53.1% had a bronchus sign present. The median distance from lesion to pleura was 5.9 mm.
Dr. Bhadra said the system performed as designed in all cases, and the protocol-defined technical success rate was 95.9% (47/49). Local registration was attempted in 49 patients and was successful in 47 patients (95.9%). In the unsuccessful cases, local registration was not completed based on the system design because the correction distance was greater than 3.0 cm.
The study’s primary endpoint was three-dimensional overlap of the virtual target and the actual lesion, as confirmed by cone-beam computed tomography. Success was defined as greater than 0% overlap after location correction. Target overlap was achieved in 59.6% (28/47) of cases before local registration and 83.0% (39/47) of cases after.
There were six cases in which local registration was successful, but these subjects weren’t evaluable because of failed procedure recording. When those subjects were excluded, target overlap was achieved in 95.1% (39/41) of cases after local registration.
The median percent overlap between the virtual target and the actual lesion was 11.4% before local registration and 32.8% after. The percentage of cases without any target overlap decreased from 31.7% (13/41) before local registration to 4.9% (2/41) after.
Focusing on the two cases without target overlap, Dr. Bhadra noted that he was able to get a biopsy that proved a malignancy in one of those patients. In the other patient, Dr. Bhadra was able to identify features of organizing pneumonia.
“Even though we did not have overlap, we must have been close enough that we were able to get malignant tissue in one [patient] and features of organizing pneumonia in a patient who’s got no history of organizing pneumonia,” Dr. Bhadra said.
He and his colleagues did not evaluate diagnostic yield in this study, but they did assess complications up to 7 days after the procedure.
The team reported one case of pneumothorax, but the patient didn’t require a chest tube. Additionally, there were two cases of bronchopulmonary hemorrhage, but the patients didn’t require any interventions.
This study was sponsored by Medtronic. Dr. Bhadra disclosed relationships with Medtronic, Boston Scientific, BodyVision, Auris Surgical Robotics, Intuitive Surgical, Veracyte, Biodesix, Merit Medical Endotek, and Johnson & Johnson.
SOURCE: Bhadra K et al. CHEST 2019. doi: 10.1016/j.chest.2019.08.314.
NEW ORLEANS – A novel according to an industry-sponsored, prospective study.
The system, which incorporates fluoroscopic navigation, increased the percentage of cases in which the target overlapped with the lesion, from 60% to 83%. The percentage of cases without any target overlap decreased from 32% to 5%.
“Tomosynthesis-based fluoroscopic navigation … improves the three-dimensional convergence between the virtual target and the actual target,” said Krish Bhadra, MD, of CHI Memorial Medical Group in Chattanooga, Tenn.
Dr. Bhadra presented results with this system at the annual meeting of the American College of Chest Physicians.
He and his colleagues conducted a study of Medtronic’s superDimension navigation system (version 7.2), which provides real-time imaging with three-dimensional fluoroscopy. The system has a “local registration” feature, which uses fluoroscopy and an algorithm to update the virtual target location during the procedure. This allows the user to reposition the catheter based on the location of the lesion.
The researchers tested the system in 50 patients from two centers (NCT03585959). Patients’ lesions had to be larger than 10 mm, not visible endobronchially, and not reachable by convex endobronchial ultrasound. Lesions within 10 mm of the diaphragm were excluded.
The median lesion size was 17.0 mm, 61.2% were smaller than 20 mm, 65.3% were in the upper lobe, and 53.1% had a bronchus sign present. The median distance from lesion to pleura was 5.9 mm.
Dr. Bhadra said the system performed as designed in all cases, and the protocol-defined technical success rate was 95.9% (47/49). Local registration was attempted in 49 patients and was successful in 47 patients (95.9%). In the unsuccessful cases, local registration was not completed based on the system design because the correction distance was greater than 3.0 cm.
The study’s primary endpoint was three-dimensional overlap of the virtual target and the actual lesion, as confirmed by cone-beam computed tomography. Success was defined as greater than 0% overlap after location correction. Target overlap was achieved in 59.6% (28/47) of cases before local registration and 83.0% (39/47) of cases after.
There were six cases in which local registration was successful, but these subjects weren’t evaluable because of failed procedure recording. When those subjects were excluded, target overlap was achieved in 95.1% (39/41) of cases after local registration.
The median percent overlap between the virtual target and the actual lesion was 11.4% before local registration and 32.8% after. The percentage of cases without any target overlap decreased from 31.7% (13/41) before local registration to 4.9% (2/41) after.
Focusing on the two cases without target overlap, Dr. Bhadra noted that he was able to get a biopsy that proved a malignancy in one of those patients. In the other patient, Dr. Bhadra was able to identify features of organizing pneumonia.
“Even though we did not have overlap, we must have been close enough that we were able to get malignant tissue in one [patient] and features of organizing pneumonia in a patient who’s got no history of organizing pneumonia,” Dr. Bhadra said.
He and his colleagues did not evaluate diagnostic yield in this study, but they did assess complications up to 7 days after the procedure.
The team reported one case of pneumothorax, but the patient didn’t require a chest tube. Additionally, there were two cases of bronchopulmonary hemorrhage, but the patients didn’t require any interventions.
This study was sponsored by Medtronic. Dr. Bhadra disclosed relationships with Medtronic, Boston Scientific, BodyVision, Auris Surgical Robotics, Intuitive Surgical, Veracyte, Biodesix, Merit Medical Endotek, and Johnson & Johnson.
SOURCE: Bhadra K et al. CHEST 2019. doi: 10.1016/j.chest.2019.08.314.
REPORTING FROM CHEST 2019