User login
New and Emerging Treatments for Major Depressive Disorder
Outside of treating major depressive disorder (MDD) through the monoamine system with selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, exploration of other treatment pathways has opened the possibility of faster onset of action and fewer side effects.
In this ReCAP, Dr Joseph Goldberg, from Mount Sinai Hospital in New York, NY, outlines how a better understanding of the glutamate system has led to the emergence of ketamine and esketamine as important treatment options, as well as the combination therapy of dextromethorphan with bupropion.
Dr Goldberg also discusses new results from serotonin system modulation through the 5HT1A receptor with gepirone, or the 5HT2A receptor with psilocybin. He also reports on a new compound esmethadone, known as REL-1017. Finally, he discusses the first approval of a digital therapeutic app designed to augment pharmacotherapy, and the dopamine partial agonist cariprazine as an adjunctive therapy.
--
Joseph F. Goldberg, MD, Clinical Professor, Department of Psychiatry, Icahn School of Medicine at Mount Sinai; Teaching Attending, Department of Psychiatry, Mount Sinai Hospital, New York, NY
Joseph F. Goldberg, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AbbVie; Genomind; Luye Pharma; Neuroma; Neurelis; Otsuka; Sunovion
Serve(d) as a speaker or a member of a speakers bureau for: AbbVie; Alkermes; Axsome; Intracellular Therapies
Receive(d) royalties from: American Psychiatric Publishing; Cambridge University Press
Outside of treating major depressive disorder (MDD) through the monoamine system with selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, exploration of other treatment pathways has opened the possibility of faster onset of action and fewer side effects.
In this ReCAP, Dr Joseph Goldberg, from Mount Sinai Hospital in New York, NY, outlines how a better understanding of the glutamate system has led to the emergence of ketamine and esketamine as important treatment options, as well as the combination therapy of dextromethorphan with bupropion.
Dr Goldberg also discusses new results from serotonin system modulation through the 5HT1A receptor with gepirone, or the 5HT2A receptor with psilocybin. He also reports on a new compound esmethadone, known as REL-1017. Finally, he discusses the first approval of a digital therapeutic app designed to augment pharmacotherapy, and the dopamine partial agonist cariprazine as an adjunctive therapy.
--
Joseph F. Goldberg, MD, Clinical Professor, Department of Psychiatry, Icahn School of Medicine at Mount Sinai; Teaching Attending, Department of Psychiatry, Mount Sinai Hospital, New York, NY
Joseph F. Goldberg, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AbbVie; Genomind; Luye Pharma; Neuroma; Neurelis; Otsuka; Sunovion
Serve(d) as a speaker or a member of a speakers bureau for: AbbVie; Alkermes; Axsome; Intracellular Therapies
Receive(d) royalties from: American Psychiatric Publishing; Cambridge University Press
Outside of treating major depressive disorder (MDD) through the monoamine system with selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors, exploration of other treatment pathways has opened the possibility of faster onset of action and fewer side effects.
In this ReCAP, Dr Joseph Goldberg, from Mount Sinai Hospital in New York, NY, outlines how a better understanding of the glutamate system has led to the emergence of ketamine and esketamine as important treatment options, as well as the combination therapy of dextromethorphan with bupropion.
Dr Goldberg also discusses new results from serotonin system modulation through the 5HT1A receptor with gepirone, or the 5HT2A receptor with psilocybin. He also reports on a new compound esmethadone, known as REL-1017. Finally, he discusses the first approval of a digital therapeutic app designed to augment pharmacotherapy, and the dopamine partial agonist cariprazine as an adjunctive therapy.
--
Joseph F. Goldberg, MD, Clinical Professor, Department of Psychiatry, Icahn School of Medicine at Mount Sinai; Teaching Attending, Department of Psychiatry, Mount Sinai Hospital, New York, NY
Joseph F. Goldberg, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AbbVie; Genomind; Luye Pharma; Neuroma; Neurelis; Otsuka; Sunovion
Serve(d) as a speaker or a member of a speakers bureau for: AbbVie; Alkermes; Axsome; Intracellular Therapies
Receive(d) royalties from: American Psychiatric Publishing; Cambridge University Press

GLP-1 agonists for weight loss: What you need to know
Obesity and overweight, with or without metabolic dysregulation, pose vexing problems for many patients with mood, anxiety, or psychotic disorders. More than one-half of individuals with severe mental illnesses are obese or overweight,1 resulting from multiple factors that may include psychiatric symptoms (eg, anergia and hyperphagia), poor dietary choices, sedentary lifestyle, underlying inflammatory processes, medical comorbidities, and iatrogenic consequences of certain medications. Unfortunately, numerous psychotropic medications can increase weight and appetite due to a variety of mechanisms, including antihistaminergic effects, direct appetite-stimulating effects, and proclivities to cause insulin resistance. While individual agents can vary, a recent review identified an overall 2-fold increased risk for rapid, significant weight gain during treatment with antipsychotics as a class.2 In addition to lifestyle modifications (diet and exercise), many pharmacologic strategies have been proposed to counter iatrogenic weight gain, including appetite suppressants (eg, pro-dopaminergic agents such as phentermine, stimulants, and amantadine), pro-anorectant anticonvulsants (eg, topiramate or zonisamide), opioid receptor antagonists (eg, olanzapine/samidorphan or naltrexone) and oral hypoglycemics such as metformin. However, the magnitude of impact for most of these agents to reverse iatrogenic weight gain tends to be modest, particularly once significant weight gain (ie, ≥7% of initial body weight) has already occurred.
Pharmacologic strategies to modulate or enhance the effects of insulin hold particular importance for combatting psychotropic-associated weight gain. Insulin transports glucose from the intravascular space to end organs for fuel consumption; to varying degrees, second-generation antipsychotics (SGAs) and some other psychotropic medications can cause insulin resistance. This in turn leads to excessive storage of underutilized glucose in the liver (glycogenesis), the potential for developing fatty liver (ie, nonalcoholic steatohepatitis), and conversion of excess carbohydrates to fatty acids and triglycerides, with subsequent storage in adipose tissue. Medications that can enhance the activity of insulin (so-called incretin mimetics) can help to overcome insulin resistance caused by SGAs (and potentially by other psychotropic medications) and essentially lead to weight loss through enhanced “fuel efficiency.”
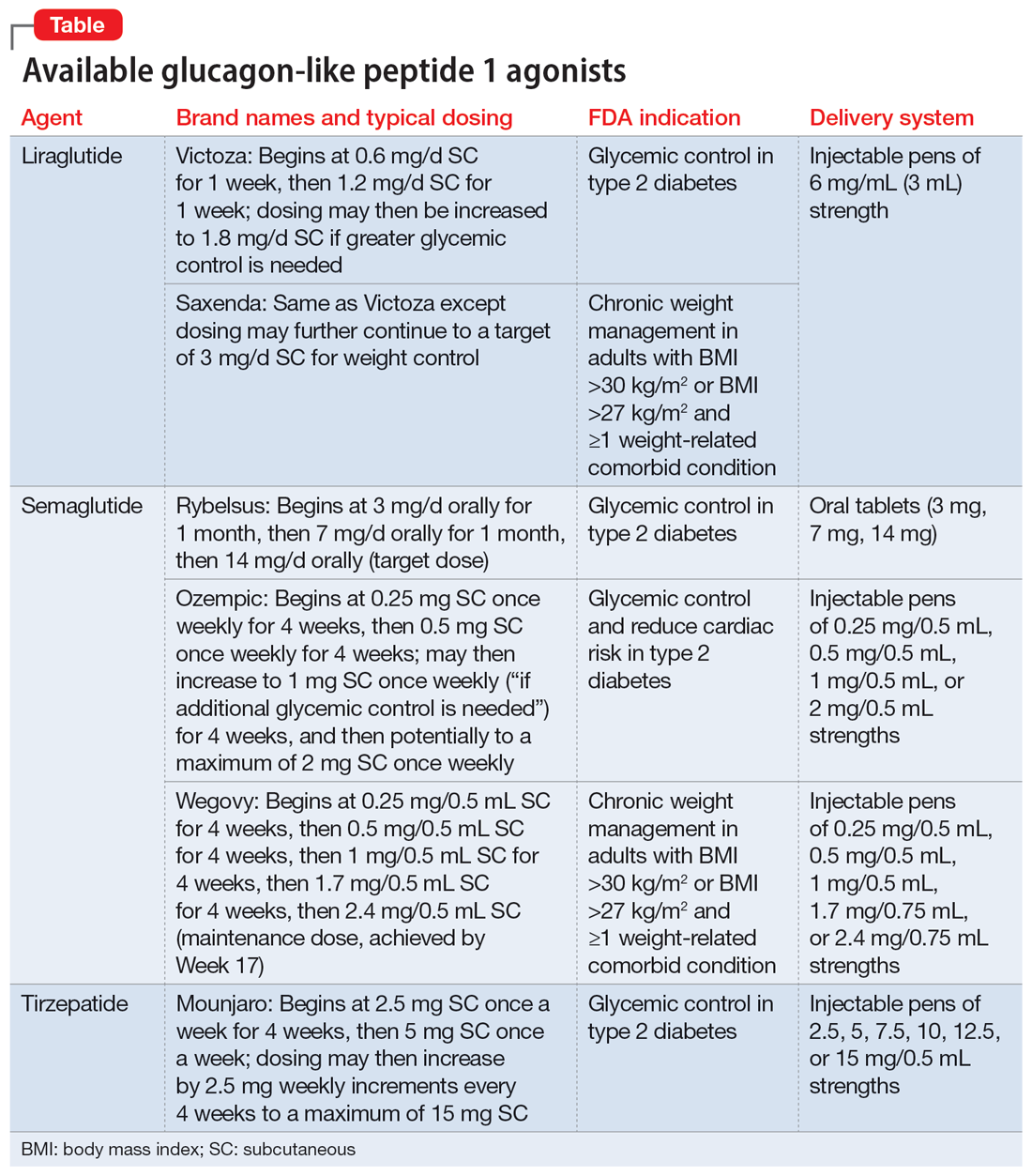
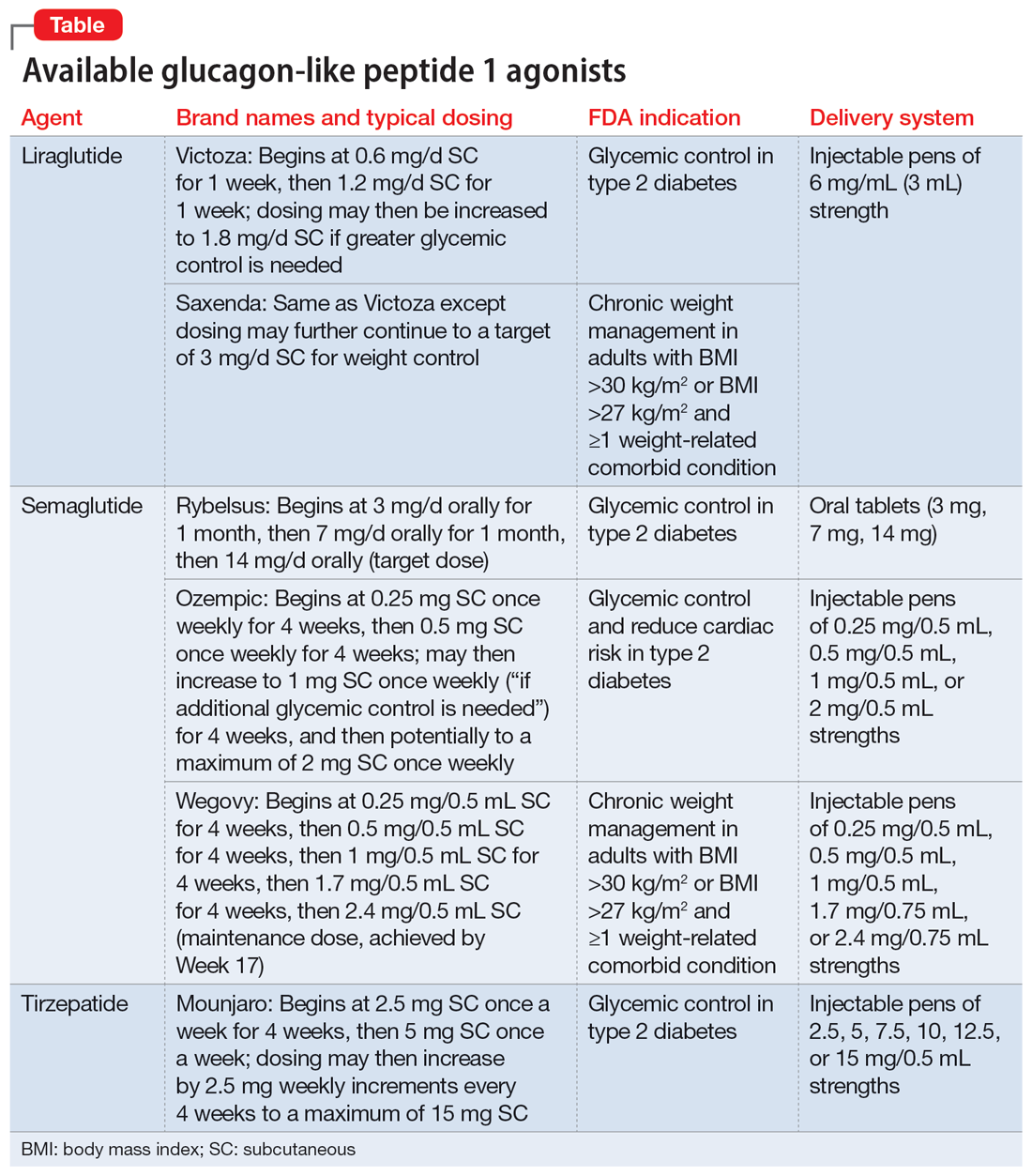
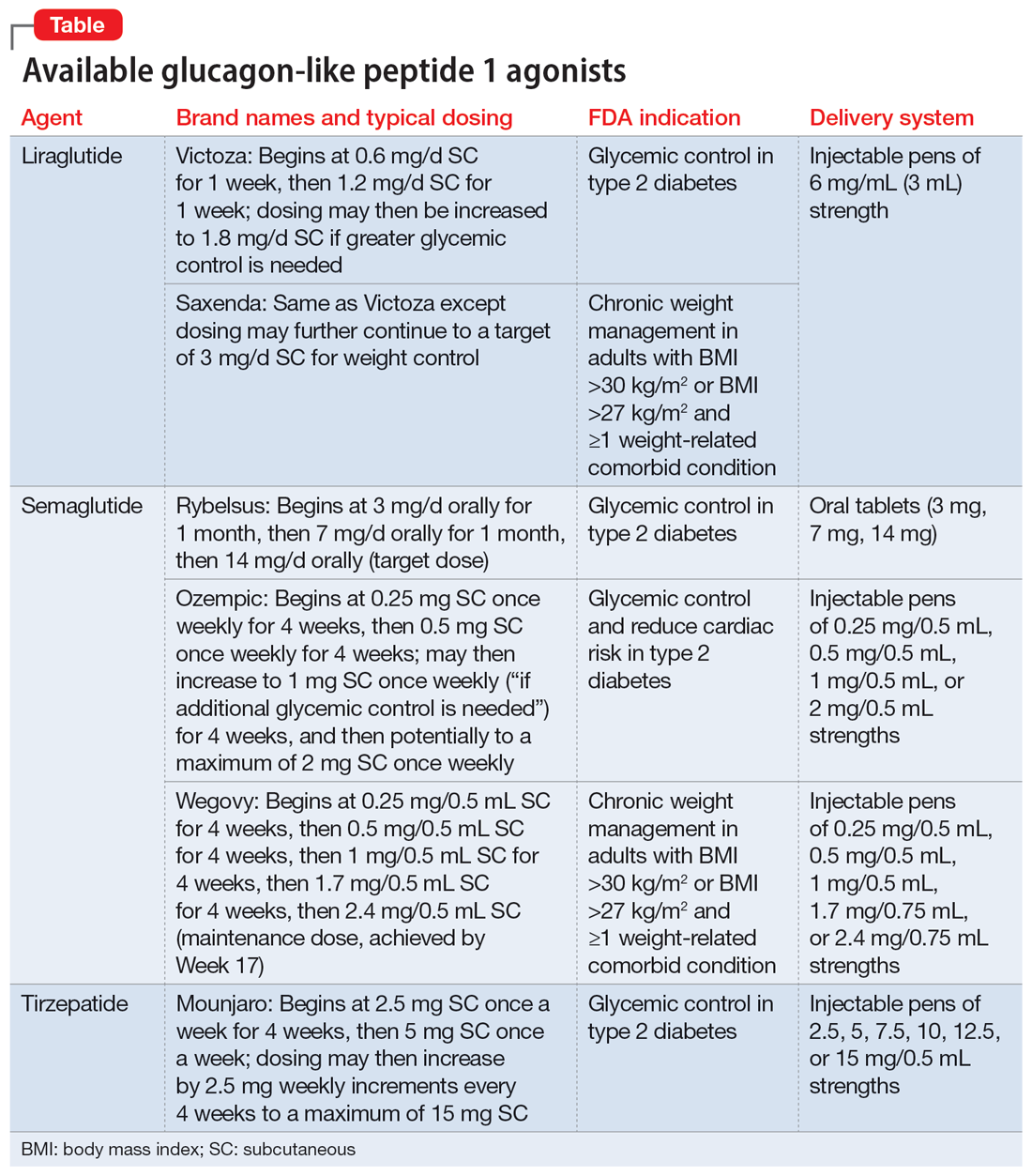
Metformin, typically dosed up to 1,000 mg twice daily with meals, has increasingly become recognized as a first-line strategy to attenuate weight gain and glycemic dysregulation from SGAs via its ability to reduce insulin resistance. Yet meta-analyses have shown that although results are significantly better than placebo, overall long-term weight loss from metformin alone tends to be rather modest (<4 kg) and associated with a reduction in body mass index (BMI) of only approximately 1 point.3 Psychiatrists (and other clinicians who prescribe psychotropic medications that can cause weight gain or metabolic dysregulation) therefore need to become familiar with alternative or adjunctive weight loss options. The use of a relatively new class of incretin mimetics called glucagon-like peptide 1 (GLP-1) agonists (Table) has been associated with profound and often dramatic weight loss and improvement of glycemic parameters in patients with obesity and glycemic dysregulation.
What are GLP-1 agonists?
GLP-1 is a hormone secreted by L cells in the intestinal mucosa in response to food. GLP-1 agonists reduce blood sugar by increasing insulin secretion, decreasing glucagon release (thus downregulating further increases in blood sugar), and reducing insulin resistance. GLP-1 agonists also reduce appetite by directly stimulating the satiety center and slowing gastric emptying and GI motility. In addition to GLP-1 agonism, some medications in this family (notably tirzepatide) also agonize a second hormone, glucose-dependent insulinotropic polypeptide, which can further induce insulin secretion as well as decrease stomach acid secretion, potentially delivering an even more substantial reduction in appetite and weight.
Routes of administration and FDA indications
Due to limited bioavailability, most GLP-1 agonists require subcutaneous (SC) injections (the sole exception is the Rybelsus brand of semaglutide, which comes in a daily pill form). Most are FDA-approved not specifically for weight loss but for patients with type 2 diabetes (defined as a hemoglobin A1C ≥6.5% or a fasting blood glucose level ≥126 mg/dL). Weight loss represents a secondary outcome for GLP-1 agonists FDA-approved for glycemic control in patients with type 2 diabetes. The 2 current exceptions to this classification are the Wegovy brand of semaglutide (ie, dosing of 2.4 mg) and the Saxenda brand of liraglutide, both of which carry FDA indications for chronic weight management alone (when paired with dietary and lifestyle modification) in individuals who are obese (BMI >30 kg/m2) regardless of the presence or absence of diabetes, or for persons who are overweight (BMI >27 kg/m2) and have ≥1 weight-related comorbid condition (eg, hypertension, type 2 diabetes, or dyslipidemia). Although patients at risk for diabetes (ie, prediabetes, defined as a hemoglobin A1C 5.7% to 6.4% or a fasting blood glucose level 100 to 125 mg/dL) were included in FDA registration trials of Saxenda or Wegovy, prediabetes is not an FDA indication for any GLP-1 agonist.
Data in weight loss
Most of the existing empirical data on weight loss with GLP-1 agonists come from studies of individuals who are overweight or obese, with or without type 2 diabetes, rather than from studies using these agents to counteract iatrogenic weight gain. In a retrospective cohort study of patients with type 2 diabetes, coadministration with serotonergic antidepressants (eg, citalopram/escitalopram) was associated with attenuation of the weight loss effects of GLP-1 agonists.4
Liraglutide currently is the sole GLP-1 agonist studied for treating SGA-associated weight gain. A 16-week randomized trial compared once-daily SC injected liraglutide vs placebo in patients with schizophrenia who incurred weight gain and prediabetes after taking olanzapine or clozapine.5 Significantly more patients taking liraglutide than placebo developed normal glucose tolerance (64% vs 16%), and body weight decreased by a mean of 5.3 kg.
Continue to: In studies of semaglutide...
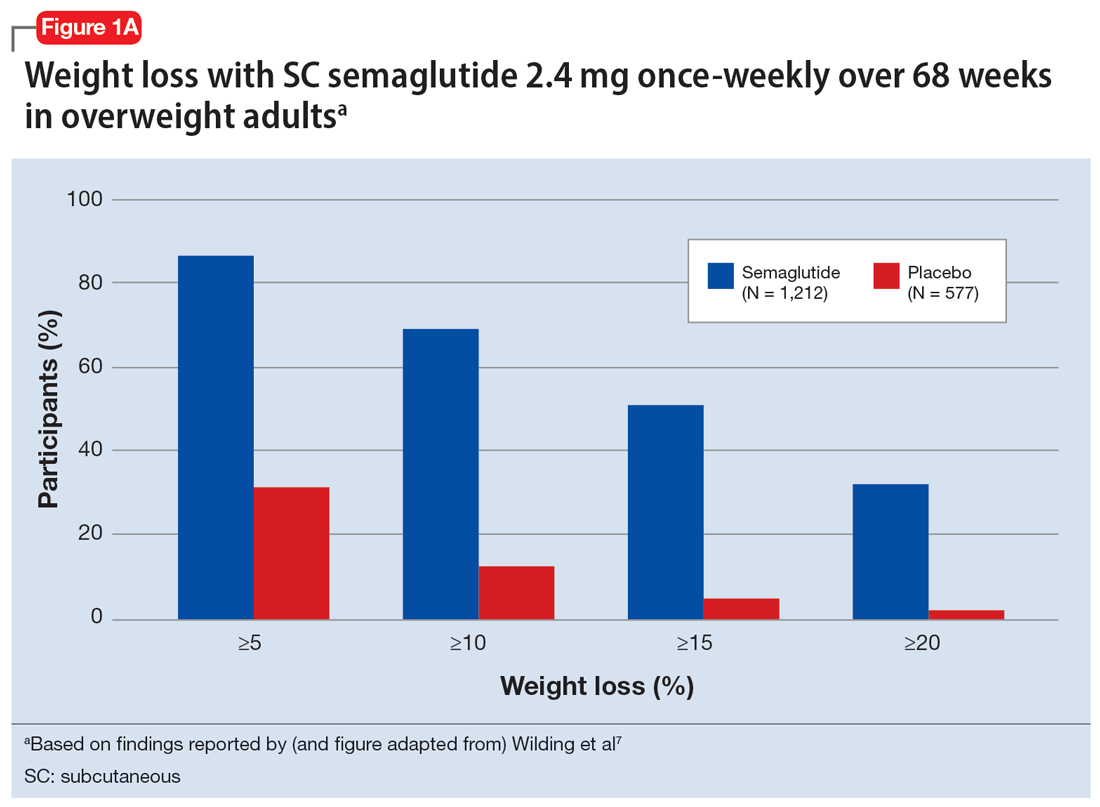
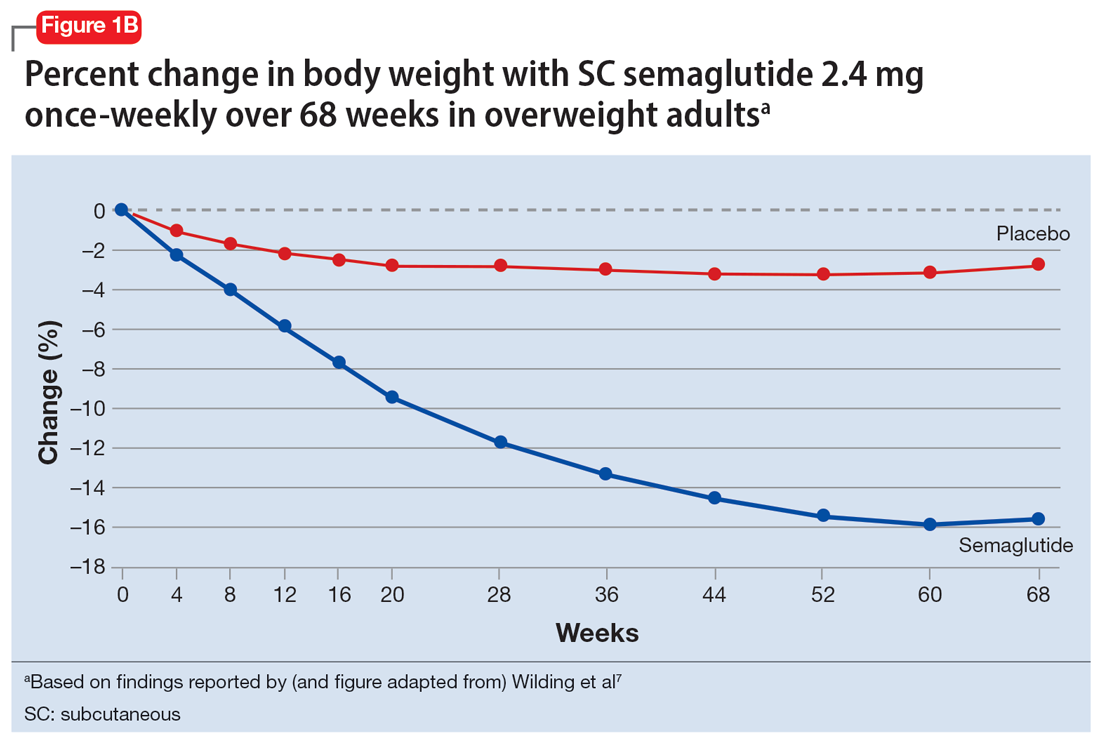
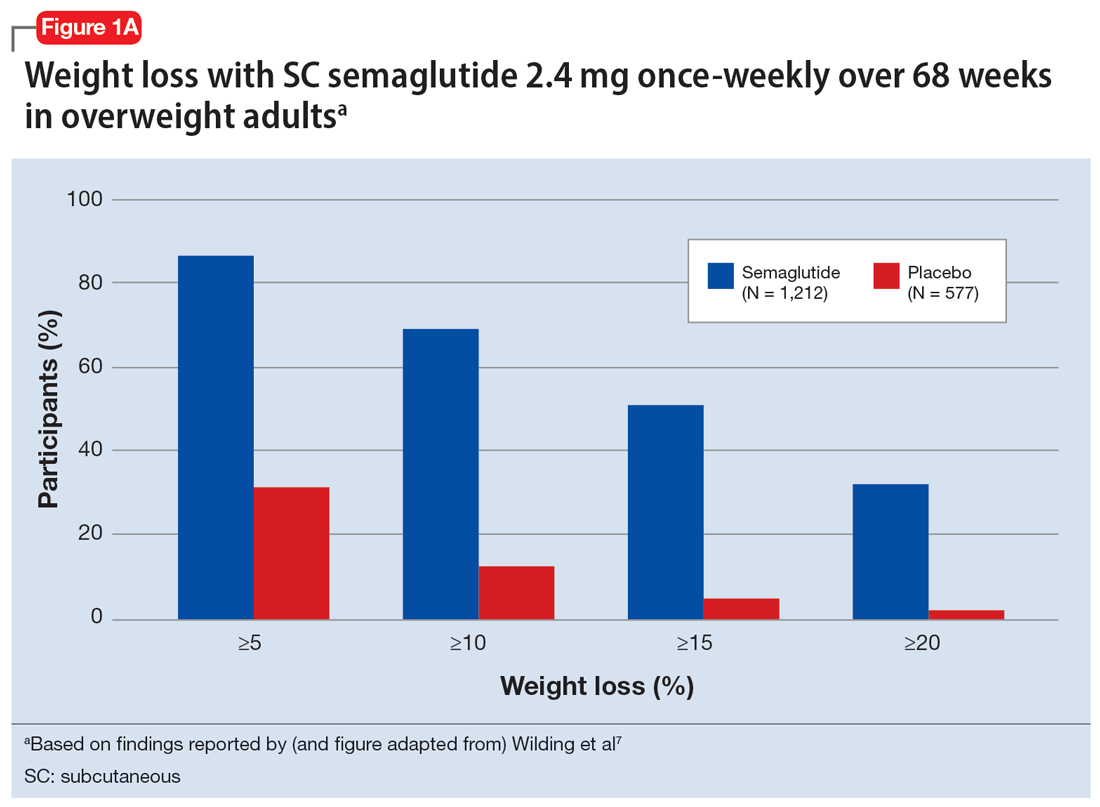
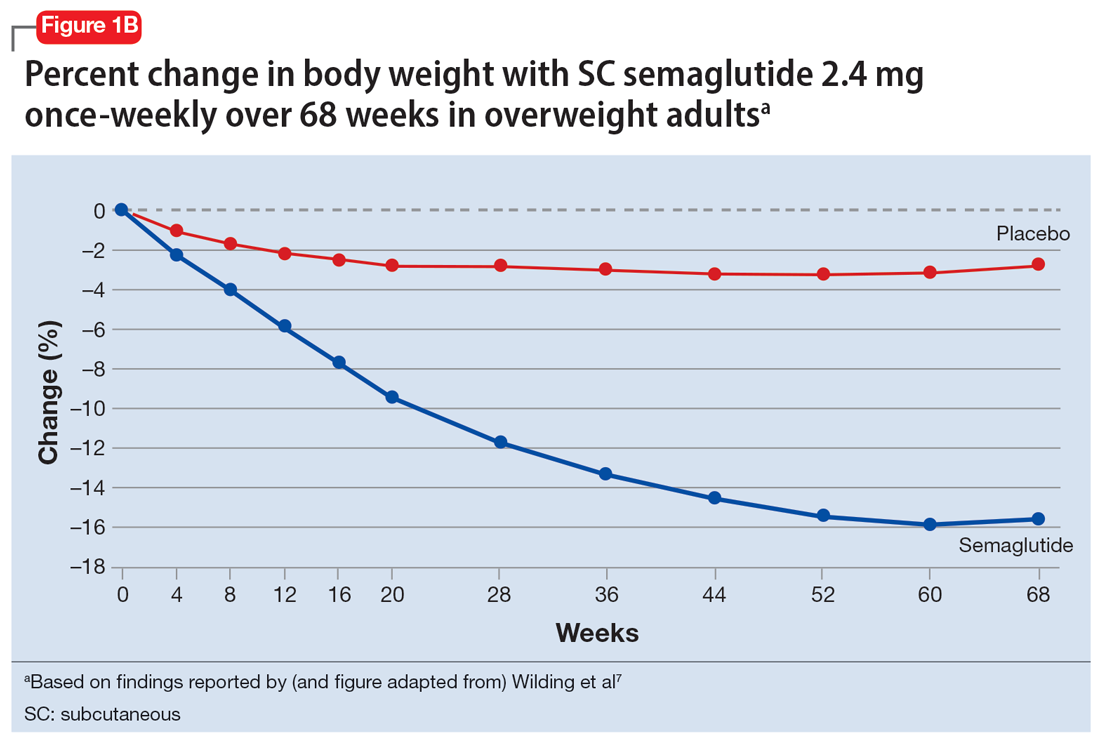
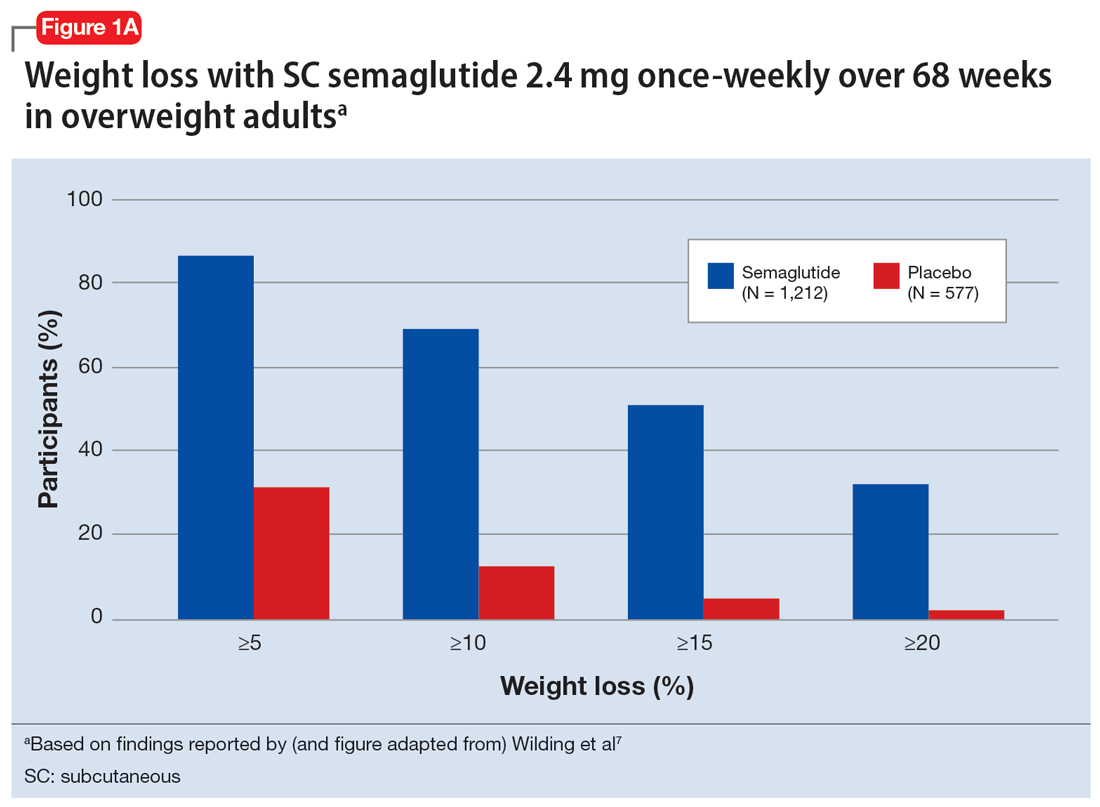
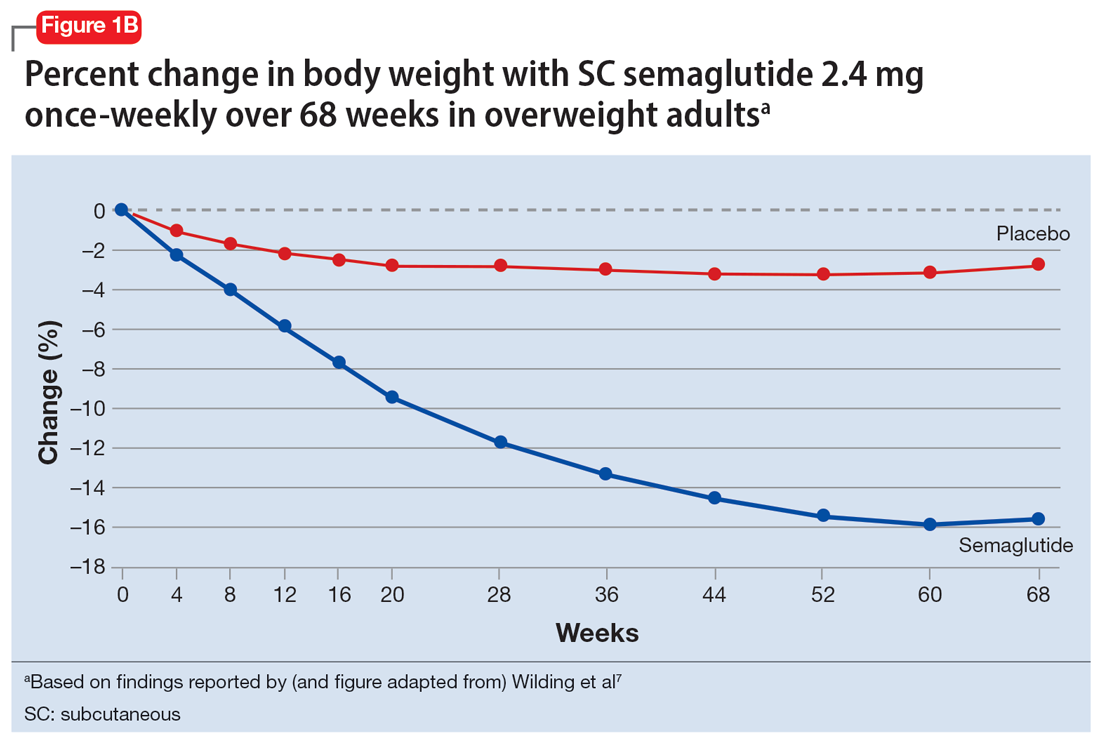
In studies of semaglutide for overweight/obese patients with type 2 diabetes or prediabetes, clinical trials of oral semaglutide (Rybelsus) found a mean weight loss over 26 weeks of -1.0 kg with dosing at 7 mg/d and -2.6 kg with dosing at 14 mg/d.6 A 68-week placebo-controlled trial of semaglutide (dosed at 2.4 mg SC weekly) for overweight/obese adults who did not have diabetes yielded a -15.3 kg weight loss (vs -2.6 kg with placebo); one-half of those who received semaglutide lost 15% of their initial body weight (Figure 1A and Figure 1B).7 Similar findings with semaglutide 2.4 mg SC weekly (Wegovy) were observed in overweight/obese adolescents, with 73% of participants losing ≥5% of their baseline weight.8 A comparative randomized trial in patients with type 2 diabetes also found modestly but significantly greater weight loss with oral semaglutide than with SC liraglutide.9
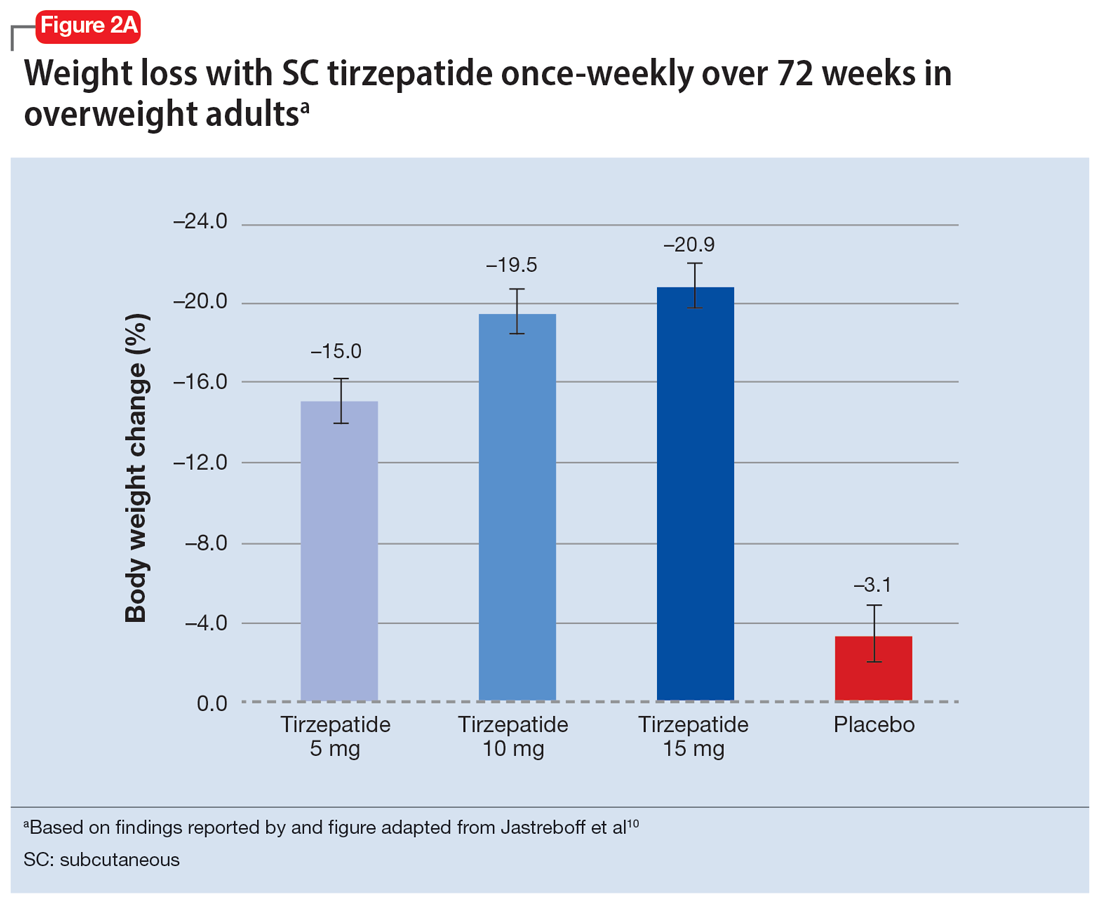
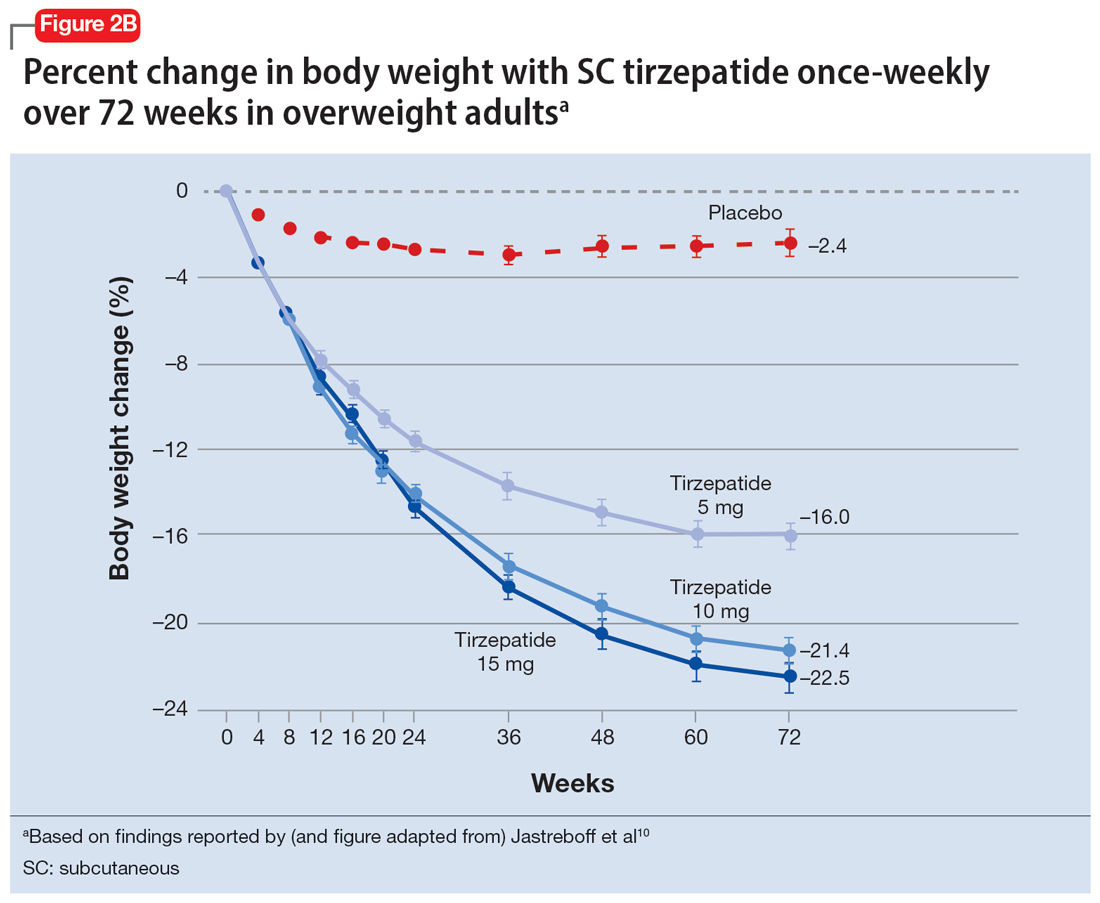
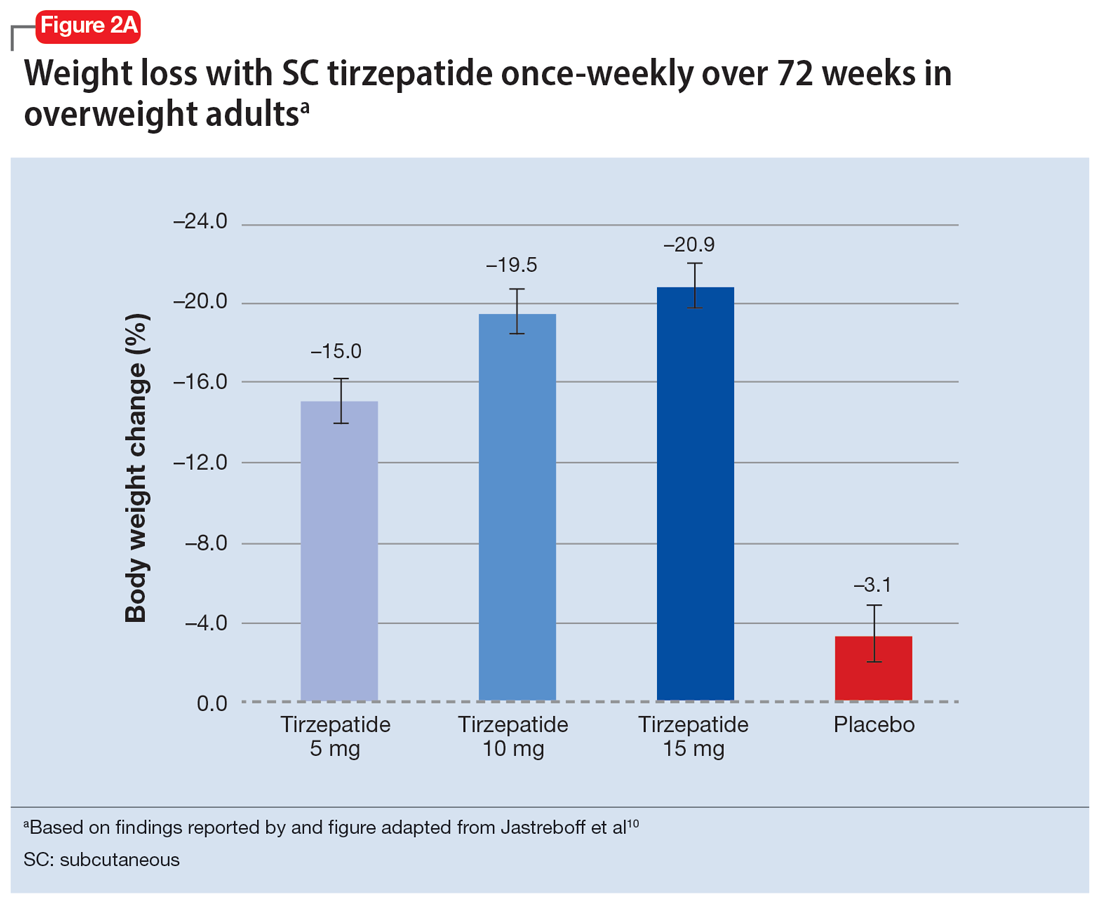
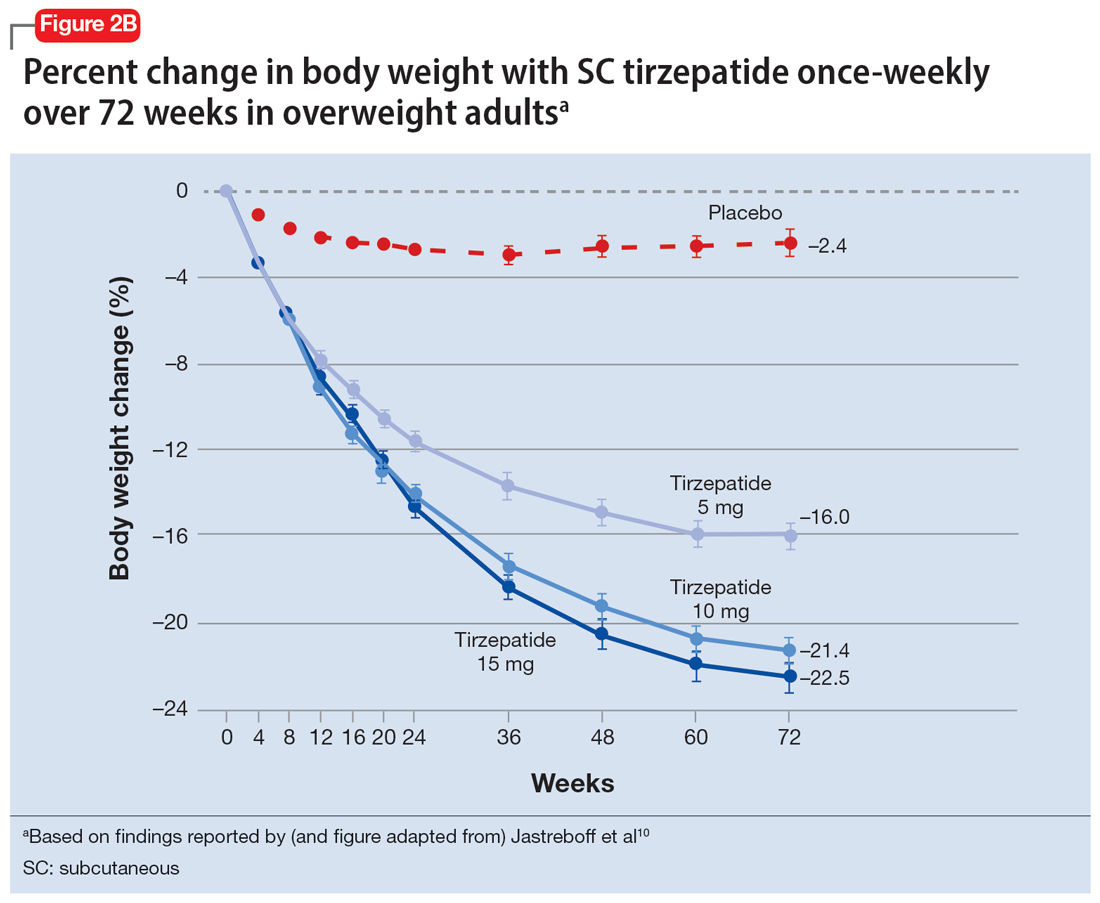
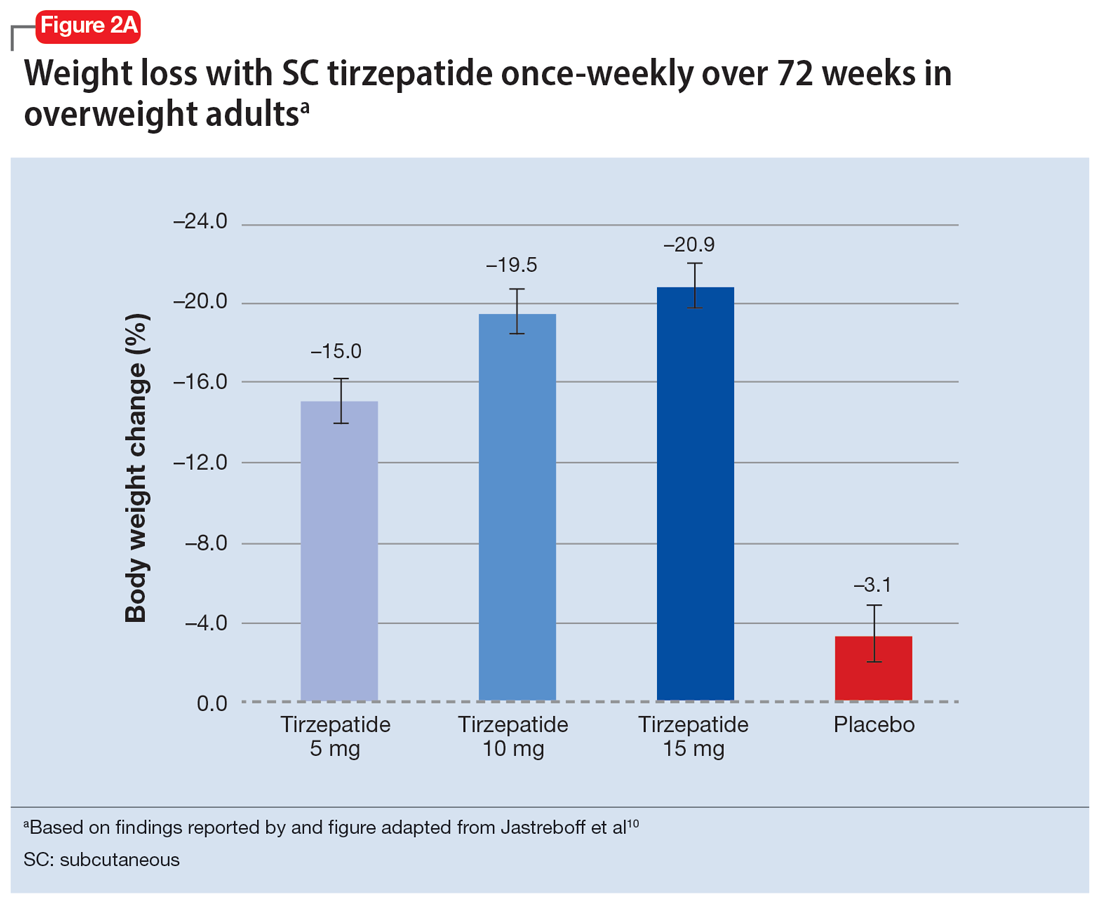
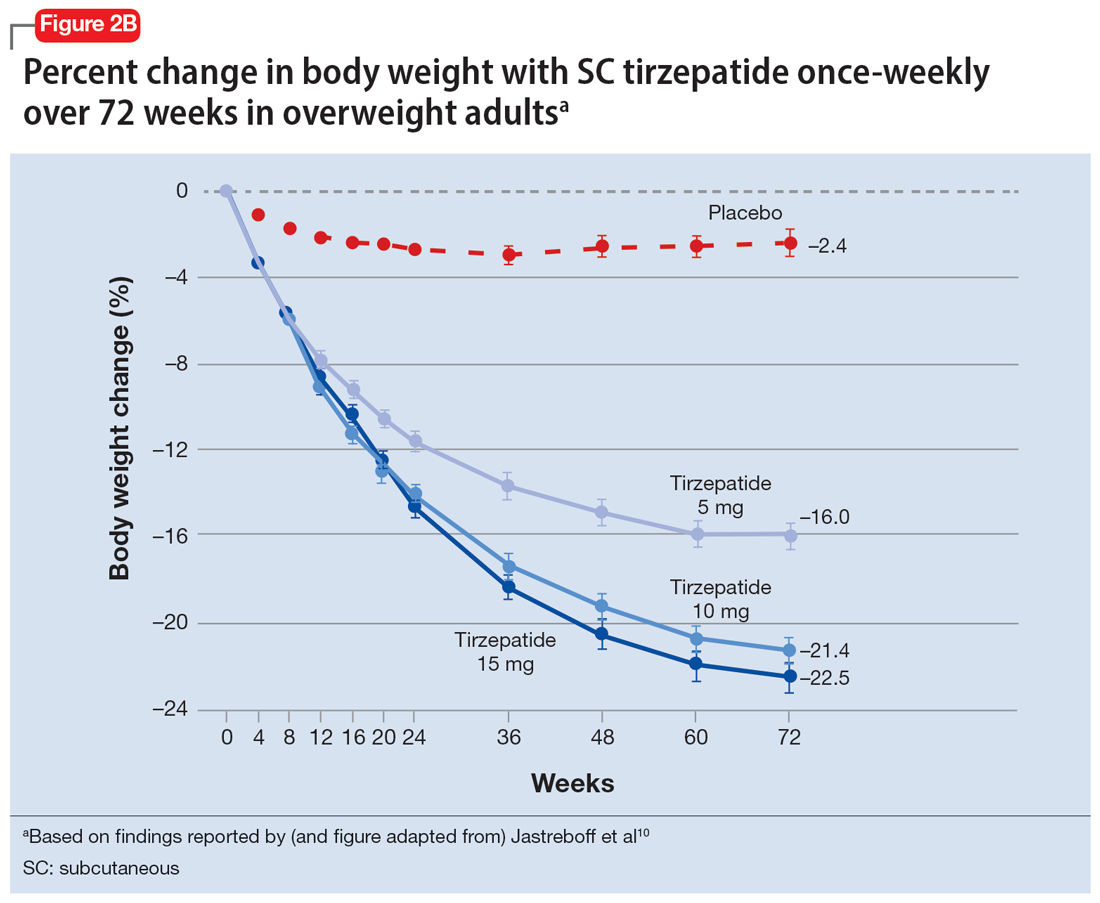
In a 72-week study of tirzepatide specifically for weight loss in nondiabetic patients who were overweight or obese, findings were especially dramatic (Figure 2A and Figure 2B).10 An overall 15% decrease in body weight was observed with 5 mg/week dosing alongside a 19.5% decrease in body weight with 10 mg/week dosing and a 20.9% weight reduction with 15 mg/week dosing.10 As noted in Figure 2B, the observed pattern of weight loss occurred along an exponential decay curve. Notably, a comparative study of tirzepatide vs once-weekly semaglutide (1 mg) in patients with type 2 diabetes11 found significantly greater dose-dependent weight loss with tirzepatide than semaglutide (-1.9 kg at 5 mg, -3.6 kg at 10 mg, and -5.5 kg at 15 mg)—although the somewhat low dosing of semaglutide may have limited its optimal possible weight loss benefit.
Tolerability
Adverse effects with GLP-1 agonists are mainly gastrointestinal (eg, nausea, vomiting, abdominal pain, diarrhea, or constipation)5-11 and generally transient. SC administration is performed in fatty tissue of the abdomen, thigh, or upper arm; site rotation is recommended to minimize injection site pain. All GLP-1 agonists carry manufacturers’ warning and precaution statements identifying the rare potential for acute pancreatitis, acute gall bladder disease, acute kidney injury, and hypoglycemia. Animal studies also have suggested an increased, dose-dependent risk for thyroid C-cell tumors with GLP-1 agonists; this has not been observed in human trials, although postmarketing pharmacovigilance reports have identified cases of medullary thyroid carcinoma in patients who took liraglutide. A manufacturer’s boxed warning indicates that a personal or family history of medullary carcinoma of the thyroid poses a contraindication for taking semaglutide, liraglutide, or tirzepatide.
Initial evidence prompts additional questions
GLP-1 agonists represent an emerging class of novel agents that can modulate glycemic dysregulation and overweight/obesity, often with dramatic results whose magnitude rivals the efficacy of bariatric surgery. Once-weekly formulations of semaglutide (Wegovy) and daily liraglutide (Saxenda) are FDA-approved for weight loss in patients who are overweight or obese while other existing formulations are approved solely for patients with type 2 diabetes, although it is likely that broader indications for weight loss (regardless of glycemic status) are forthcoming. Targeted use of GLP-1 agonists to counteract SGA-associated weight gain is supported by a handful of preliminary reports, with additional studies likely to come. Unanswered questions include:
- When should GLP-1 agonists be considered within a treatment algorithm for iatrogenic weight gain relative to other antidote strategies such as metformin or appetite-suppressing anticonvulsants?
- How effective might GLP-1 agonists be for iatrogenic weight gain from non-SGA psychotropic medications, such as serotonergic antidepressants?
- When and how can GLP-1 agonists be safely coprescribed with other nonincretin mimetic weight loss medications?
- When should psychiatrists prescribe GLP-1 agonists, or do so collaboratively with primary care physicians or endocrinologists, particularly in patients with metabolic syndrome?
Followers of the rapidly emerging literature in this area will likely find themselves best positioned to address these and other questions about optimal management of psychotropic-induced weight gain for the patients they treat.
Bottom Line
The use of glucagon-like peptide 1 (GLP-1) agonists, a relatively new class of incretin mimetics, has been associated with profound and often dramatic weight loss and improvement of glycemic parameters in patients with obesity and glycemic dysregulation. Preliminary reports support the potential targeted use of GLP-1 agonists to counteract weight gain associated with second-generation antipsychotics.
Related Resources
- Singh F, Allen A, Ianni A. Managing metabolic syndrome in patients with schizophrenia. Current Psychiatry. 2020;19(12):20-24,26. doi:10.12788/cp.0064
- Ard J, Fitch A, Fruh S, et al. Weight loss and maintenance related to the mechanism of action of glucagon-like peptide 1 receptor agonists. Adv Ther. 2021;38(6):2821- 2839. doi:10.1007/s12325-021-01710-0
Drug Brand Names
Amantadine • Gocovri
Citalopram • Celexa
Clozapine • Clozaril
Escitalopram • Lexapro
Liraglutide • Victoza, Saxenda
Metformin • Glucophage
Naltrexone • ReVia
Olanzapine • Zyprexa
Olanzapine/samidorphan • Lybalvi
Phentermine • Ionamin
Semaglutide • Rybelsus, Ozempic, Wegovy
Tirzepatide • Mounjaro
Topiramate • Topamax
Zonisamide • Zonegran
1. Afzal M, Siddiqi N, Ahmad B, et al. Prevalence of overweight and obesity in people with severe mental illness: systematic review and meta-analysis. Front Endocrinol (Lausanne). 2021;25;12:769309.
2. Barton BB, Segger F, Fischer K, et al. Update on weight-gain caused by antipsychotics: a systematic review and meta-analysis. Expert Opin Drug Safety. 2020;19(3):295-314.
3. de Silva AV, Suraweera C, Ratnatunga SS, et al. Metformin in prevention and treatment of antipsychotic induced weight gain: a systematic review and meta-analysis. BMC Psychiatry. 2016;16(1):341.
4. Durell N, Franks R, Coon S, et al. Effects of antidepressants on glucagon-like peptide-1 receptor agonist-related weight loss. J Pharm Technol. 2022;38(5):283-288.
5. Larsen JR, Vedtofte L, Jakobsen MSL, et al. Effect of liraglutide treatment on prediabetes and overweight or obesity in clozapine- or olanzapine-treated patients with schizophrenia spectrum disorder: a randomized clinical trial. JAMA Psychiatry. 2017;74(7):719-728.
6. Aroda VR, Rosenstock J, Terauchi Y, et al. PIONEER 1: randomized clinical trial of the efficacy and safety of oral semaglutide monotherapy in comparison with placebo in patients with type 2 diabetes. Diabetes Care. 2019;42(9):1724-1732.
7. Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989-1002.
8. Weghuber D, Barrett T, Barrientos-Pérez M, et al. Once-weekly semaglutide in adolescents with obesity. N Engl J Med. Published online November 2, 2022. doi:10.1056/NEJMoa2208601.
9. Pratley R, Amod A, Hoff ST, et al. Oral semaglutide versus subcutaneous liraglutide and placebo in type 2 diabetes (PIONEER 4): a randomized, double-blind, phase 3a trial. Lancet. 2019;394(10192):39-50.
10. Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387(3):205-216.
11. Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503-515.
Obesity and overweight, with or without metabolic dysregulation, pose vexing problems for many patients with mood, anxiety, or psychotic disorders. More than one-half of individuals with severe mental illnesses are obese or overweight,1 resulting from multiple factors that may include psychiatric symptoms (eg, anergia and hyperphagia), poor dietary choices, sedentary lifestyle, underlying inflammatory processes, medical comorbidities, and iatrogenic consequences of certain medications. Unfortunately, numerous psychotropic medications can increase weight and appetite due to a variety of mechanisms, including antihistaminergic effects, direct appetite-stimulating effects, and proclivities to cause insulin resistance. While individual agents can vary, a recent review identified an overall 2-fold increased risk for rapid, significant weight gain during treatment with antipsychotics as a class.2 In addition to lifestyle modifications (diet and exercise), many pharmacologic strategies have been proposed to counter iatrogenic weight gain, including appetite suppressants (eg, pro-dopaminergic agents such as phentermine, stimulants, and amantadine), pro-anorectant anticonvulsants (eg, topiramate or zonisamide), opioid receptor antagonists (eg, olanzapine/samidorphan or naltrexone) and oral hypoglycemics such as metformin. However, the magnitude of impact for most of these agents to reverse iatrogenic weight gain tends to be modest, particularly once significant weight gain (ie, ≥7% of initial body weight) has already occurred.
Pharmacologic strategies to modulate or enhance the effects of insulin hold particular importance for combatting psychotropic-associated weight gain. Insulin transports glucose from the intravascular space to end organs for fuel consumption; to varying degrees, second-generation antipsychotics (SGAs) and some other psychotropic medications can cause insulin resistance. This in turn leads to excessive storage of underutilized glucose in the liver (glycogenesis), the potential for developing fatty liver (ie, nonalcoholic steatohepatitis), and conversion of excess carbohydrates to fatty acids and triglycerides, with subsequent storage in adipose tissue. Medications that can enhance the activity of insulin (so-called incretin mimetics) can help to overcome insulin resistance caused by SGAs (and potentially by other psychotropic medications) and essentially lead to weight loss through enhanced “fuel efficiency.”
Metformin, typically dosed up to 1,000 mg twice daily with meals, has increasingly become recognized as a first-line strategy to attenuate weight gain and glycemic dysregulation from SGAs via its ability to reduce insulin resistance. Yet meta-analyses have shown that although results are significantly better than placebo, overall long-term weight loss from metformin alone tends to be rather modest (<4 kg) and associated with a reduction in body mass index (BMI) of only approximately 1 point.3 Psychiatrists (and other clinicians who prescribe psychotropic medications that can cause weight gain or metabolic dysregulation) therefore need to become familiar with alternative or adjunctive weight loss options. The use of a relatively new class of incretin mimetics called glucagon-like peptide 1 (GLP-1) agonists (Table) has been associated with profound and often dramatic weight loss and improvement of glycemic parameters in patients with obesity and glycemic dysregulation.
What are GLP-1 agonists?
GLP-1 is a hormone secreted by L cells in the intestinal mucosa in response to food. GLP-1 agonists reduce blood sugar by increasing insulin secretion, decreasing glucagon release (thus downregulating further increases in blood sugar), and reducing insulin resistance. GLP-1 agonists also reduce appetite by directly stimulating the satiety center and slowing gastric emptying and GI motility. In addition to GLP-1 agonism, some medications in this family (notably tirzepatide) also agonize a second hormone, glucose-dependent insulinotropic polypeptide, which can further induce insulin secretion as well as decrease stomach acid secretion, potentially delivering an even more substantial reduction in appetite and weight.
Routes of administration and FDA indications
Due to limited bioavailability, most GLP-1 agonists require subcutaneous (SC) injections (the sole exception is the Rybelsus brand of semaglutide, which comes in a daily pill form). Most are FDA-approved not specifically for weight loss but for patients with type 2 diabetes (defined as a hemoglobin A1C ≥6.5% or a fasting blood glucose level ≥126 mg/dL). Weight loss represents a secondary outcome for GLP-1 agonists FDA-approved for glycemic control in patients with type 2 diabetes. The 2 current exceptions to this classification are the Wegovy brand of semaglutide (ie, dosing of 2.4 mg) and the Saxenda brand of liraglutide, both of which carry FDA indications for chronic weight management alone (when paired with dietary and lifestyle modification) in individuals who are obese (BMI >30 kg/m2) regardless of the presence or absence of diabetes, or for persons who are overweight (BMI >27 kg/m2) and have ≥1 weight-related comorbid condition (eg, hypertension, type 2 diabetes, or dyslipidemia). Although patients at risk for diabetes (ie, prediabetes, defined as a hemoglobin A1C 5.7% to 6.4% or a fasting blood glucose level 100 to 125 mg/dL) were included in FDA registration trials of Saxenda or Wegovy, prediabetes is not an FDA indication for any GLP-1 agonist.
Data in weight loss
Most of the existing empirical data on weight loss with GLP-1 agonists come from studies of individuals who are overweight or obese, with or without type 2 diabetes, rather than from studies using these agents to counteract iatrogenic weight gain. In a retrospective cohort study of patients with type 2 diabetes, coadministration with serotonergic antidepressants (eg, citalopram/escitalopram) was associated with attenuation of the weight loss effects of GLP-1 agonists.4
Liraglutide currently is the sole GLP-1 agonist studied for treating SGA-associated weight gain. A 16-week randomized trial compared once-daily SC injected liraglutide vs placebo in patients with schizophrenia who incurred weight gain and prediabetes after taking olanzapine or clozapine.5 Significantly more patients taking liraglutide than placebo developed normal glucose tolerance (64% vs 16%), and body weight decreased by a mean of 5.3 kg.
Continue to: In studies of semaglutide...
In studies of semaglutide for overweight/obese patients with type 2 diabetes or prediabetes, clinical trials of oral semaglutide (Rybelsus) found a mean weight loss over 26 weeks of -1.0 kg with dosing at 7 mg/d and -2.6 kg with dosing at 14 mg/d.6 A 68-week placebo-controlled trial of semaglutide (dosed at 2.4 mg SC weekly) for overweight/obese adults who did not have diabetes yielded a -15.3 kg weight loss (vs -2.6 kg with placebo); one-half of those who received semaglutide lost 15% of their initial body weight (Figure 1A and Figure 1B).7 Similar findings with semaglutide 2.4 mg SC weekly (Wegovy) were observed in overweight/obese adolescents, with 73% of participants losing ≥5% of their baseline weight.8 A comparative randomized trial in patients with type 2 diabetes also found modestly but significantly greater weight loss with oral semaglutide than with SC liraglutide.9
In a 72-week study of tirzepatide specifically for weight loss in nondiabetic patients who were overweight or obese, findings were especially dramatic (Figure 2A and Figure 2B).10 An overall 15% decrease in body weight was observed with 5 mg/week dosing alongside a 19.5% decrease in body weight with 10 mg/week dosing and a 20.9% weight reduction with 15 mg/week dosing.10 As noted in Figure 2B, the observed pattern of weight loss occurred along an exponential decay curve. Notably, a comparative study of tirzepatide vs once-weekly semaglutide (1 mg) in patients with type 2 diabetes11 found significantly greater dose-dependent weight loss with tirzepatide than semaglutide (-1.9 kg at 5 mg, -3.6 kg at 10 mg, and -5.5 kg at 15 mg)—although the somewhat low dosing of semaglutide may have limited its optimal possible weight loss benefit.
Tolerability
Adverse effects with GLP-1 agonists are mainly gastrointestinal (eg, nausea, vomiting, abdominal pain, diarrhea, or constipation)5-11 and generally transient. SC administration is performed in fatty tissue of the abdomen, thigh, or upper arm; site rotation is recommended to minimize injection site pain. All GLP-1 agonists carry manufacturers’ warning and precaution statements identifying the rare potential for acute pancreatitis, acute gall bladder disease, acute kidney injury, and hypoglycemia. Animal studies also have suggested an increased, dose-dependent risk for thyroid C-cell tumors with GLP-1 agonists; this has not been observed in human trials, although postmarketing pharmacovigilance reports have identified cases of medullary thyroid carcinoma in patients who took liraglutide. A manufacturer’s boxed warning indicates that a personal or family history of medullary carcinoma of the thyroid poses a contraindication for taking semaglutide, liraglutide, or tirzepatide.
Initial evidence prompts additional questions
GLP-1 agonists represent an emerging class of novel agents that can modulate glycemic dysregulation and overweight/obesity, often with dramatic results whose magnitude rivals the efficacy of bariatric surgery. Once-weekly formulations of semaglutide (Wegovy) and daily liraglutide (Saxenda) are FDA-approved for weight loss in patients who are overweight or obese while other existing formulations are approved solely for patients with type 2 diabetes, although it is likely that broader indications for weight loss (regardless of glycemic status) are forthcoming. Targeted use of GLP-1 agonists to counteract SGA-associated weight gain is supported by a handful of preliminary reports, with additional studies likely to come. Unanswered questions include:
- When should GLP-1 agonists be considered within a treatment algorithm for iatrogenic weight gain relative to other antidote strategies such as metformin or appetite-suppressing anticonvulsants?
- How effective might GLP-1 agonists be for iatrogenic weight gain from non-SGA psychotropic medications, such as serotonergic antidepressants?
- When and how can GLP-1 agonists be safely coprescribed with other nonincretin mimetic weight loss medications?
- When should psychiatrists prescribe GLP-1 agonists, or do so collaboratively with primary care physicians or endocrinologists, particularly in patients with metabolic syndrome?
Followers of the rapidly emerging literature in this area will likely find themselves best positioned to address these and other questions about optimal management of psychotropic-induced weight gain for the patients they treat.
Bottom Line
The use of glucagon-like peptide 1 (GLP-1) agonists, a relatively new class of incretin mimetics, has been associated with profound and often dramatic weight loss and improvement of glycemic parameters in patients with obesity and glycemic dysregulation. Preliminary reports support the potential targeted use of GLP-1 agonists to counteract weight gain associated with second-generation antipsychotics.
Related Resources
- Singh F, Allen A, Ianni A. Managing metabolic syndrome in patients with schizophrenia. Current Psychiatry. 2020;19(12):20-24,26. doi:10.12788/cp.0064
- Ard J, Fitch A, Fruh S, et al. Weight loss and maintenance related to the mechanism of action of glucagon-like peptide 1 receptor agonists. Adv Ther. 2021;38(6):2821- 2839. doi:10.1007/s12325-021-01710-0
Drug Brand Names
Amantadine • Gocovri
Citalopram • Celexa
Clozapine • Clozaril
Escitalopram • Lexapro
Liraglutide • Victoza, Saxenda
Metformin • Glucophage
Naltrexone • ReVia
Olanzapine • Zyprexa
Olanzapine/samidorphan • Lybalvi
Phentermine • Ionamin
Semaglutide • Rybelsus, Ozempic, Wegovy
Tirzepatide • Mounjaro
Topiramate • Topamax
Zonisamide • Zonegran
Obesity and overweight, with or without metabolic dysregulation, pose vexing problems for many patients with mood, anxiety, or psychotic disorders. More than one-half of individuals with severe mental illnesses are obese or overweight,1 resulting from multiple factors that may include psychiatric symptoms (eg, anergia and hyperphagia), poor dietary choices, sedentary lifestyle, underlying inflammatory processes, medical comorbidities, and iatrogenic consequences of certain medications. Unfortunately, numerous psychotropic medications can increase weight and appetite due to a variety of mechanisms, including antihistaminergic effects, direct appetite-stimulating effects, and proclivities to cause insulin resistance. While individual agents can vary, a recent review identified an overall 2-fold increased risk for rapid, significant weight gain during treatment with antipsychotics as a class.2 In addition to lifestyle modifications (diet and exercise), many pharmacologic strategies have been proposed to counter iatrogenic weight gain, including appetite suppressants (eg, pro-dopaminergic agents such as phentermine, stimulants, and amantadine), pro-anorectant anticonvulsants (eg, topiramate or zonisamide), opioid receptor antagonists (eg, olanzapine/samidorphan or naltrexone) and oral hypoglycemics such as metformin. However, the magnitude of impact for most of these agents to reverse iatrogenic weight gain tends to be modest, particularly once significant weight gain (ie, ≥7% of initial body weight) has already occurred.
Pharmacologic strategies to modulate or enhance the effects of insulin hold particular importance for combatting psychotropic-associated weight gain. Insulin transports glucose from the intravascular space to end organs for fuel consumption; to varying degrees, second-generation antipsychotics (SGAs) and some other psychotropic medications can cause insulin resistance. This in turn leads to excessive storage of underutilized glucose in the liver (glycogenesis), the potential for developing fatty liver (ie, nonalcoholic steatohepatitis), and conversion of excess carbohydrates to fatty acids and triglycerides, with subsequent storage in adipose tissue. Medications that can enhance the activity of insulin (so-called incretin mimetics) can help to overcome insulin resistance caused by SGAs (and potentially by other psychotropic medications) and essentially lead to weight loss through enhanced “fuel efficiency.”
Metformin, typically dosed up to 1,000 mg twice daily with meals, has increasingly become recognized as a first-line strategy to attenuate weight gain and glycemic dysregulation from SGAs via its ability to reduce insulin resistance. Yet meta-analyses have shown that although results are significantly better than placebo, overall long-term weight loss from metformin alone tends to be rather modest (<4 kg) and associated with a reduction in body mass index (BMI) of only approximately 1 point.3 Psychiatrists (and other clinicians who prescribe psychotropic medications that can cause weight gain or metabolic dysregulation) therefore need to become familiar with alternative or adjunctive weight loss options. The use of a relatively new class of incretin mimetics called glucagon-like peptide 1 (GLP-1) agonists (Table) has been associated with profound and often dramatic weight loss and improvement of glycemic parameters in patients with obesity and glycemic dysregulation.
What are GLP-1 agonists?
GLP-1 is a hormone secreted by L cells in the intestinal mucosa in response to food. GLP-1 agonists reduce blood sugar by increasing insulin secretion, decreasing glucagon release (thus downregulating further increases in blood sugar), and reducing insulin resistance. GLP-1 agonists also reduce appetite by directly stimulating the satiety center and slowing gastric emptying and GI motility. In addition to GLP-1 agonism, some medications in this family (notably tirzepatide) also agonize a second hormone, glucose-dependent insulinotropic polypeptide, which can further induce insulin secretion as well as decrease stomach acid secretion, potentially delivering an even more substantial reduction in appetite and weight.
Routes of administration and FDA indications
Due to limited bioavailability, most GLP-1 agonists require subcutaneous (SC) injections (the sole exception is the Rybelsus brand of semaglutide, which comes in a daily pill form). Most are FDA-approved not specifically for weight loss but for patients with type 2 diabetes (defined as a hemoglobin A1C ≥6.5% or a fasting blood glucose level ≥126 mg/dL). Weight loss represents a secondary outcome for GLP-1 agonists FDA-approved for glycemic control in patients with type 2 diabetes. The 2 current exceptions to this classification are the Wegovy brand of semaglutide (ie, dosing of 2.4 mg) and the Saxenda brand of liraglutide, both of which carry FDA indications for chronic weight management alone (when paired with dietary and lifestyle modification) in individuals who are obese (BMI >30 kg/m2) regardless of the presence or absence of diabetes, or for persons who are overweight (BMI >27 kg/m2) and have ≥1 weight-related comorbid condition (eg, hypertension, type 2 diabetes, or dyslipidemia). Although patients at risk for diabetes (ie, prediabetes, defined as a hemoglobin A1C 5.7% to 6.4% or a fasting blood glucose level 100 to 125 mg/dL) were included in FDA registration trials of Saxenda or Wegovy, prediabetes is not an FDA indication for any GLP-1 agonist.
Data in weight loss
Most of the existing empirical data on weight loss with GLP-1 agonists come from studies of individuals who are overweight or obese, with or without type 2 diabetes, rather than from studies using these agents to counteract iatrogenic weight gain. In a retrospective cohort study of patients with type 2 diabetes, coadministration with serotonergic antidepressants (eg, citalopram/escitalopram) was associated with attenuation of the weight loss effects of GLP-1 agonists.4
Liraglutide currently is the sole GLP-1 agonist studied for treating SGA-associated weight gain. A 16-week randomized trial compared once-daily SC injected liraglutide vs placebo in patients with schizophrenia who incurred weight gain and prediabetes after taking olanzapine or clozapine.5 Significantly more patients taking liraglutide than placebo developed normal glucose tolerance (64% vs 16%), and body weight decreased by a mean of 5.3 kg.
Continue to: In studies of semaglutide...
In studies of semaglutide for overweight/obese patients with type 2 diabetes or prediabetes, clinical trials of oral semaglutide (Rybelsus) found a mean weight loss over 26 weeks of -1.0 kg with dosing at 7 mg/d and -2.6 kg with dosing at 14 mg/d.6 A 68-week placebo-controlled trial of semaglutide (dosed at 2.4 mg SC weekly) for overweight/obese adults who did not have diabetes yielded a -15.3 kg weight loss (vs -2.6 kg with placebo); one-half of those who received semaglutide lost 15% of their initial body weight (Figure 1A and Figure 1B).7 Similar findings with semaglutide 2.4 mg SC weekly (Wegovy) were observed in overweight/obese adolescents, with 73% of participants losing ≥5% of their baseline weight.8 A comparative randomized trial in patients with type 2 diabetes also found modestly but significantly greater weight loss with oral semaglutide than with SC liraglutide.9
In a 72-week study of tirzepatide specifically for weight loss in nondiabetic patients who were overweight or obese, findings were especially dramatic (Figure 2A and Figure 2B).10 An overall 15% decrease in body weight was observed with 5 mg/week dosing alongside a 19.5% decrease in body weight with 10 mg/week dosing and a 20.9% weight reduction with 15 mg/week dosing.10 As noted in Figure 2B, the observed pattern of weight loss occurred along an exponential decay curve. Notably, a comparative study of tirzepatide vs once-weekly semaglutide (1 mg) in patients with type 2 diabetes11 found significantly greater dose-dependent weight loss with tirzepatide than semaglutide (-1.9 kg at 5 mg, -3.6 kg at 10 mg, and -5.5 kg at 15 mg)—although the somewhat low dosing of semaglutide may have limited its optimal possible weight loss benefit.
Tolerability
Adverse effects with GLP-1 agonists are mainly gastrointestinal (eg, nausea, vomiting, abdominal pain, diarrhea, or constipation)5-11 and generally transient. SC administration is performed in fatty tissue of the abdomen, thigh, or upper arm; site rotation is recommended to minimize injection site pain. All GLP-1 agonists carry manufacturers’ warning and precaution statements identifying the rare potential for acute pancreatitis, acute gall bladder disease, acute kidney injury, and hypoglycemia. Animal studies also have suggested an increased, dose-dependent risk for thyroid C-cell tumors with GLP-1 agonists; this has not been observed in human trials, although postmarketing pharmacovigilance reports have identified cases of medullary thyroid carcinoma in patients who took liraglutide. A manufacturer’s boxed warning indicates that a personal or family history of medullary carcinoma of the thyroid poses a contraindication for taking semaglutide, liraglutide, or tirzepatide.
Initial evidence prompts additional questions
GLP-1 agonists represent an emerging class of novel agents that can modulate glycemic dysregulation and overweight/obesity, often with dramatic results whose magnitude rivals the efficacy of bariatric surgery. Once-weekly formulations of semaglutide (Wegovy) and daily liraglutide (Saxenda) are FDA-approved for weight loss in patients who are overweight or obese while other existing formulations are approved solely for patients with type 2 diabetes, although it is likely that broader indications for weight loss (regardless of glycemic status) are forthcoming. Targeted use of GLP-1 agonists to counteract SGA-associated weight gain is supported by a handful of preliminary reports, with additional studies likely to come. Unanswered questions include:
- When should GLP-1 agonists be considered within a treatment algorithm for iatrogenic weight gain relative to other antidote strategies such as metformin or appetite-suppressing anticonvulsants?
- How effective might GLP-1 agonists be for iatrogenic weight gain from non-SGA psychotropic medications, such as serotonergic antidepressants?
- When and how can GLP-1 agonists be safely coprescribed with other nonincretin mimetic weight loss medications?
- When should psychiatrists prescribe GLP-1 agonists, or do so collaboratively with primary care physicians or endocrinologists, particularly in patients with metabolic syndrome?
Followers of the rapidly emerging literature in this area will likely find themselves best positioned to address these and other questions about optimal management of psychotropic-induced weight gain for the patients they treat.
Bottom Line
The use of glucagon-like peptide 1 (GLP-1) agonists, a relatively new class of incretin mimetics, has been associated with profound and often dramatic weight loss and improvement of glycemic parameters in patients with obesity and glycemic dysregulation. Preliminary reports support the potential targeted use of GLP-1 agonists to counteract weight gain associated with second-generation antipsychotics.
Related Resources
- Singh F, Allen A, Ianni A. Managing metabolic syndrome in patients with schizophrenia. Current Psychiatry. 2020;19(12):20-24,26. doi:10.12788/cp.0064
- Ard J, Fitch A, Fruh S, et al. Weight loss and maintenance related to the mechanism of action of glucagon-like peptide 1 receptor agonists. Adv Ther. 2021;38(6):2821- 2839. doi:10.1007/s12325-021-01710-0
Drug Brand Names
Amantadine • Gocovri
Citalopram • Celexa
Clozapine • Clozaril
Escitalopram • Lexapro
Liraglutide • Victoza, Saxenda
Metformin • Glucophage
Naltrexone • ReVia
Olanzapine • Zyprexa
Olanzapine/samidorphan • Lybalvi
Phentermine • Ionamin
Semaglutide • Rybelsus, Ozempic, Wegovy
Tirzepatide • Mounjaro
Topiramate • Topamax
Zonisamide • Zonegran
1. Afzal M, Siddiqi N, Ahmad B, et al. Prevalence of overweight and obesity in people with severe mental illness: systematic review and meta-analysis. Front Endocrinol (Lausanne). 2021;25;12:769309.
2. Barton BB, Segger F, Fischer K, et al. Update on weight-gain caused by antipsychotics: a systematic review and meta-analysis. Expert Opin Drug Safety. 2020;19(3):295-314.
3. de Silva AV, Suraweera C, Ratnatunga SS, et al. Metformin in prevention and treatment of antipsychotic induced weight gain: a systematic review and meta-analysis. BMC Psychiatry. 2016;16(1):341.
4. Durell N, Franks R, Coon S, et al. Effects of antidepressants on glucagon-like peptide-1 receptor agonist-related weight loss. J Pharm Technol. 2022;38(5):283-288.
5. Larsen JR, Vedtofte L, Jakobsen MSL, et al. Effect of liraglutide treatment on prediabetes and overweight or obesity in clozapine- or olanzapine-treated patients with schizophrenia spectrum disorder: a randomized clinical trial. JAMA Psychiatry. 2017;74(7):719-728.
6. Aroda VR, Rosenstock J, Terauchi Y, et al. PIONEER 1: randomized clinical trial of the efficacy and safety of oral semaglutide monotherapy in comparison with placebo in patients with type 2 diabetes. Diabetes Care. 2019;42(9):1724-1732.
7. Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989-1002.
8. Weghuber D, Barrett T, Barrientos-Pérez M, et al. Once-weekly semaglutide in adolescents with obesity. N Engl J Med. Published online November 2, 2022. doi:10.1056/NEJMoa2208601.
9. Pratley R, Amod A, Hoff ST, et al. Oral semaglutide versus subcutaneous liraglutide and placebo in type 2 diabetes (PIONEER 4): a randomized, double-blind, phase 3a trial. Lancet. 2019;394(10192):39-50.
10. Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387(3):205-216.
11. Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503-515.
1. Afzal M, Siddiqi N, Ahmad B, et al. Prevalence of overweight and obesity in people with severe mental illness: systematic review and meta-analysis. Front Endocrinol (Lausanne). 2021;25;12:769309.
2. Barton BB, Segger F, Fischer K, et al. Update on weight-gain caused by antipsychotics: a systematic review and meta-analysis. Expert Opin Drug Safety. 2020;19(3):295-314.
3. de Silva AV, Suraweera C, Ratnatunga SS, et al. Metformin in prevention and treatment of antipsychotic induced weight gain: a systematic review and meta-analysis. BMC Psychiatry. 2016;16(1):341.
4. Durell N, Franks R, Coon S, et al. Effects of antidepressants on glucagon-like peptide-1 receptor agonist-related weight loss. J Pharm Technol. 2022;38(5):283-288.
5. Larsen JR, Vedtofte L, Jakobsen MSL, et al. Effect of liraglutide treatment on prediabetes and overweight or obesity in clozapine- or olanzapine-treated patients with schizophrenia spectrum disorder: a randomized clinical trial. JAMA Psychiatry. 2017;74(7):719-728.
6. Aroda VR, Rosenstock J, Terauchi Y, et al. PIONEER 1: randomized clinical trial of the efficacy and safety of oral semaglutide monotherapy in comparison with placebo in patients with type 2 diabetes. Diabetes Care. 2019;42(9):1724-1732.
7. Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989-1002.
8. Weghuber D, Barrett T, Barrientos-Pérez M, et al. Once-weekly semaglutide in adolescents with obesity. N Engl J Med. Published online November 2, 2022. doi:10.1056/NEJMoa2208601.
9. Pratley R, Amod A, Hoff ST, et al. Oral semaglutide versus subcutaneous liraglutide and placebo in type 2 diabetes (PIONEER 4): a randomized, double-blind, phase 3a trial. Lancet. 2019;394(10192):39-50.
10. Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387(3):205-216.
11. Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503-515.
What to Do When Your Depressed Patient Develops Mania
This article has been adapted from an article originally published in Current Psychiatry (http://currentpsychiatry.com):Current Psychiatry. 2015;14(10):29-32,35-40,e6.
When a known depressed patient newly develops signs of mania or hypomania, a cascade of diagnostic and therapeutic questions ensues: Does the event “automatically” signify the presence of bipolar disorder (BD), or could manic symptoms be secondary to another underlying medical problem, a prescribed antidepressant or non-psychotropic medication, or illicit substances?
Even more questions confront the clinician: If mania symptoms are nothing more than an adverse drug reaction, will they go away by stopping the presumed offending agent? Or do symptoms always indicate the unmasking of a bipolar diathesis? Should anti-manic medication be prescribed immediately? If so, which one(s) and for how long? How extensive a medical or neurologic workup is indicated?
And how do you differentiate ambiguous hypomania symptoms (irritability, insomnia, agitation) from other phenomena, such as akathisia, anxiety, and overstimulation?
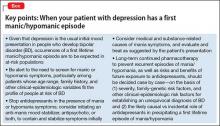
In this article, we present an overview of how to approach and answer these key questions, so that you can identify, comprehend, and manage manic symptoms that arise in the course of your patient’s treatment for depression (Box).
Does Disease Exist on a Unipolar-Bipolar Continuum.
There has been a resurgence of interest in Kraepelin’s original notion of mania and depression as falling along a continuum, rather than being distinct categories of pathology. True bipolar mania has its own identifiable epidemiology, familiality, and treatment, but symptomatic shades of gray often pose a formidable diagnostic and therapeutic challenge.
For example, the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) relaxed its definition of “mixed” episodes of BD to include subsyndromal mania features in unipolar depression. When a patient with unipolar depression develops a full, unequivocal manic episode, there usually isn’t much ambiguity or confusion about initial management: assure a safe environment, stop any antidepressants, rule out drug- or medically induced causes, and begin an acute anti-manic medication.
Next steps can, sometimes, be murkier:
- Formulate a definitive, overarching diagnosis
- Provide psycho-education
- Forecast return to work or school
- Discuss prognosis and likelihood of relapse
- Address necessary lifestyle modifications (eg, sleep hygiene, elimination of alcohol and illicit drug use)
- Determine whether indefinite maintenance pharmacotherapy is indicated—and, if so, with which medication(s).
A Diagnostic Formulation Isn’t Always Black and White
Ms. J, age 56, a medically healthy woman, has a 10-year history of depression and anxiety that has been treated effectively for most of that time with venlafaxine,
225 mg/d. The mother of 4 grown children, Ms. J has worked steadily for > 20 years as a flight attendant for an international airline.
Today, Ms. J is brought by ambulance from work to the emergency department in a paranoid and agitated state. The admission follows her having e-blasted airline corporate executives with a voluminous manifesto that she worked on around the clock the preceding week, in which she explained her bold ideas to revolutionize the airline industry, under her leadership.
Ms. J’s family history is unremarkable for psychiatric illness.
How Does One Approach A Case Such As Ms. J's?
Stark examples of classical mania, as depicted in this case vignette, are easy to recognize but not necessarily straightforward, nosologically. Consider the following not-so-straightforward elements of Ms. J’s case:
- A first-lifetime episode of mania or hypomania is rare after age 50
- Ms. J took a serotonin-norepinephrine reuptake inhibitor (SNRI) for many years without evidence of mood destabilization
- Years of repetitive chronobiological stress (including probable frequent time zone changes with likely sleep disruption) apparently did not trigger mood destabilization
- None of Ms. J’s 4 pregnancies led to postpartum mood episodes
- At least on the surface, there are no obvious features that point to likely causes of a secondary mania (eg, drug-induced, toxic, metabolic, or medical)
- Ms. J has no known family history of BD or any other mood disorder.
Approaching a case such as Ms. J’s must involve a systematic strategy that can best be broken into 2 segments: (1) a period of acute initial assessment and treatment and (2) later efforts focused on broader diagnostic evaluation and longer-term relapse prevention.
Initial Assessment and Treatment
Immediate assessment and management hinges on initial triage and forming a working diagnostic impression. Although full-blown mania usually is obvious (sometimes even without a formal interview), be alert to patients who might minimize or altogether disavow mania symptoms—often because of denial of illness, misidentification of symptoms, or impaired insight about changes in thinking, mood, or behavior.
Because florid mania, by definition, impairs psychosocial functioning, the context of an initial presentation often holds diagnostic relevance. Manic patients who display disruptive behaviors often are brought to treatment by a third party, whereas a less severely ill patient might be more inclined to seek treatment for herself (himself) when psychosis is absent and insight is less compromised or when the patient feels she (he) might be depressed.
It is not uncommon for a manic patient to report “depression” as the chief complaint or to omit elements related to psychomotor acceleration (such as racing thoughts or psychomotor agitation) in the description of symptoms. An accurate diagnosis often requires clinical probing and clarification of symptoms (eg, differentiating simple insomnia with consequent next-day fatigue from loss of the need for sleep with intact or even enhanced next-day energy) or discriminating racing thoughts from anxious ruminations that might be more intrusive than rapid.
Presentations of frank mania also can come to light as a consequence of symptoms, rather than as symptoms per se (eg, conflict in relationships, problems at work, financial reversals).
Particularly in patients who do not have a history of mania, avoid the temptation to begin or modify existing pharmacotherapy until you have performed a basic initial evaluation. Immediate considerations for initial assessment and management include the following:
Provide containment. Ensure a safe setting, level of care, and frequency of monitoring. Evaluate suicide risk (particularly when mixed features are present), and risk of withdrawal from any psychoactive substances.
Engage significant others. Close family members can provide essential history, particularly when a patient’s insight about her illness and need for treatment are impaired. Family members and significant others also often play important roles in helping to restrict access to finances, fostering medication adherence, preventing access to weapons in the home, and sharing information with providers about substance use or high-risk behavior.
Systematically assess for DSM-5 symptoms of mania and depression. DSM-5 modified criteria for mania/hypomania to necessitate increased energy, in addition to change in mood, to make a syndromal diagnosis. Useful during a clinical interview is the popular mnemonic DIGFAST to aid recognition of core mania symptoms:
- Distractibility
- Indiscretion/impulsivity
- Grandiosity
- Flight of ideas
- Activity increase
- Sleep deficit
- Talkativeness.
These symptoms should represent a departure from normal baseline characteristics; it often is helpful to ask a significant other or collateral historian how the
present symptoms differ from the patient’s usual state.
Assess for unstable medical conditions or toxicity states. When evaluating an acute change in mental status, toxicology screening is relatively standard and the absence of illicit substances should seldom, if ever, be taken for granted—especially because occult substance use can lead to identification of false-positive BD “cases.”1
Stop any antidepressant. During a manic episode, continuing antidepressant medication serves no purpose other than to contribute to or exacerbate mania symptoms. Nonetheless, observational studies demonstrate that approximately 15% of syndromally manic patients continue to receive an antidepressant, often when a clinician perceives more severe depression during mania, multiple prior depressive episodes,current anxiety, or rapid cycling.2
Importantly, antidepressants have been shown to harm, rather than alleviate, presentations that involve a mixed state, and have no demonstrated value in preventing post-manic depression.3 Mere elimination of an antidepressant might ease symptoms during a manic or mixed episode.4
In some cases, it might be advisable to taper, not abruptly stop, a short halflife serotonergic antidepressant, even in the setting of mania, to minimize the potential for aggravating autonomic dysregulation that can result from antidepressant discontinuation effects.
Begin anti-manic pharmacotherapy. Initiation of an anti-manic mood stabilizer, such as lithium and divalproex, has been standard in the treatment of acute mania.
In the 1990s, protocols for oral loading of divalproex (20 to 30 mg/kg/d) gained popularity for achieving more rapid symptom improvement than might occur with lithium. In the current era, atypical antipsychotics have all but replaced mood stabilizers as an initial intervention to contain mania symptoms quickly (and with less risk than firstgeneration antipsychotics for acute adverse motor effects from so-called rapid neuroleptization).
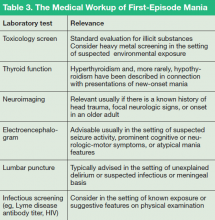
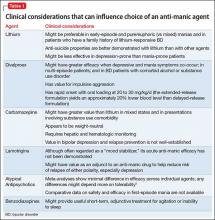
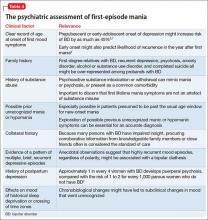
Because atypical antipsychotics often rapidly subdue mania, psychosis, and agitation, regardless of the underlying process, many practitioners might feel more comfortable initiating them than a mood stabilizer when the diagnosis is ambiguous or provisional, although their longer-term efficacy and safety, relative to traditional mood stabilizers, remains contested. Considerations for choosing from among feasible anti-manic pharmacotherapies are summarized in Table 1.
Normalize the sleep-wake cycle. Chronobiological and circadian variables, such as irregular sleep patterns, are thought to contribute to the pathophysiology of affective switch in BD. Behavioral and pharmacotherapeutic efforts to impose a normal sleep-wake schedule are considered fundamental to stabilizing acute mania.
Facilitate next steps after acute stabilization. For inpatients, this might involve step-down to a partial hospitalization or intensive outpatient program, alongside taking steps to ensure continued treatment adherence and minimize relapse.
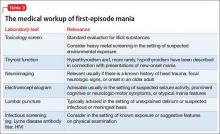
What Medical and Neurologic Workup is Appropriate?
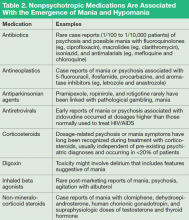
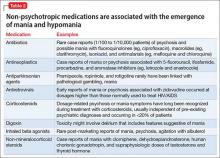
Not every first lifetime presentation of mania requires extensive medical and neurologic workup, particularly among patients who have a history of depression and those whose presentation neatly fits the demographic and clinical profile of newly emergent BD. Basic assessment should determine whether any new medication has been started that could plausibly contribute to abnormal mental status (Table 2).
Nevertheless, evaluation of almost all first presentations of mania should include:
- Urine toxicology screen
- Complete blood count
- Comprehensive metabolic panel
- Thyroid-stimulating hormone assay
- Serum vitamin B12 level assay
- Serum folic acid level assay
- Rapid plasma reagin test.
Clinical features that usually lead a clinician to pursue a more detailed medical and neurologic evaluation of first-episode mania include:
- Onset age > 40
- Absence of a family history of mood disorder
- Symptoms arising during a major medical illness
- Multiple medications
- Suspicion of a degenerative or hereditary neurologic disorder
- Altered state of consciousness
- Signs of cortical or diffuse subcortical dysfunction (eg, cognitive deficits, motor deficits, tremor)
- Abnormal vital signs.
Depending on the presentation, additional testing might include:
- Tests of HIV antibody, immune autoantibodies, and Lyme disease antibody
- Heavy metal screening (when suggested by environmental exposure)
- Lumbar puncture (eg, in a setting of manic delirium or suspected central nervous system infection or paraneoplastic syndrome)
- Neuroimaging (note: MRI provides better visualization than CT of white matter pathology and small vessel cerebrovascular disease) electroencephalography.
Making An Overarching Diagnosis: Is Mania Always Bipolar Disorder?
Mania is considered a manifestation of BD when symptoms cannot be attributed to another psychiatric condition, another underlying medical or neurologic condition, or a toxic-metabolic state (Tables 3 and 4). Classification of mania that occurs soon after antidepressant exposure in patients without a known history of BD continues to be the subject of debate, varying in its conceptualization across editions of DSM.
The National Institute of Mental Health (NIMH) Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, observed a fairly low (approximately 10%) incidence of switch from depression to mania when an antidepressant is added to a mood stabilizer; the study authors concluded that much of what is presumed to be antidepressant-induced mania might simply be the natural course of illness.10
Notably, several reports suggest that antidepressants might pose a greater risk of mood destabilization in people with BD I than with either BD II or other suspected variants on the bipolar spectrum.
DSM-5 advises that a diagnosis of substance-induced mood disorder appropriately describes symptoms that spontaneously dissipate once an antidepressant has been discontinued, whereas a diagnosis of BD can be made when manic or hypomanic symptoms persist at a syndromal level after an antidepressant has been stopped and its physiological effects are no longer present. With respect to time course, the International Society of Bipolar Disorders proposes that, beyond 12 to 16 weeks after an antidepressant has been started or the dosage has been increased, it is unlikely that new-onset mania/hypomania can reasonably be attributed to “triggering” by an antidepressant (although antidepressants should be stopped when symptoms of mania emerge).11 Several clinical features have been linked in the literature with an increased susceptibility to BD after an initial depressive episode, including:
- Early (pre-adolescent) age at onset of first mood disorder episode6
- Family history of BD, highly recurrent depression, or psychosis12,13
- Psychosis when depressed.7,14
A number of other characteristics of depressive illness—including seasonal depression, atypical depressive features, suicidality, irritability, anxiety or substance use comorbidity, postpartum mood episodes, and brief recurrent depressive episodes—have been described in the literature as potential correlates of a bipolar diathesis; none have proved to be robust or pathognomonic of a BD diagnosis, as opposed to a unipolar diagnosis.
Data from the NIMH Collaborative Depression Study suggest that recurrent mania/hypomania after an antidepressant-associated polarity switch is greater when a family history of BD is present; other clinical variables might hold less predictive value.15 In addition, although some practitioners consider a history of nonresponse to trials of multiple antidepressants suggestive of an underlying bipolar process, polarity is only one of many variables that must be considered in the differential diagnosis of antidepressantresistant depression. Likewise, molecular genetic studies do not support a link between antidepressant nonresponse and the likelihood of a diagnosis of BD.16
Indefinite Pharmacotherapy for Bipolar Disorder
An important but nagging issue when diagnosing BD after a first manic (or hypomanic) episode is the implied need for indefinite pharmacotherapy to sustain remission and prevent relapse and recurrence.
The likelihood of subsequent depression or mania/hypomania remains high after an index manic/hypomanic episode, particularly for 6 to 8 months after recovery.8,17 Natural history data suggest that, during the year that follows a first lifetime mania, approximately 40% of patients experience a second manic episode.8 A second lifetime mania might be especially likely in patients whose index episode involved mood-congruent psychosis, low premorbid work functioning, and an initial manic episode, as opposed to a mixed episode or early age at onset.8,17
In the absence of randomized, placebo-controlled studies of maintenance pharmacotherapy after a first lifetime manic episode, clinical judgment often drives decisions about the duration of continuing pharmacotherapy after initial symptoms resolve. The Texas Medication Algorithm Project for BD advises that:
General practice at this time is lifetime medication following 2 manic episodes, or 1 episode if it was a severe episode and/or significant family history of bipolar or major depressive disorder is present. For a first episode of bipolar mania with no family history of bipolar or major depressive disorders, medication tapering and discontinuation may be considered after the continuation period is completed (usually 6 months in remission), depending on the severity of the first episode, surrounding factors, and prodromal history.18
Similarly, in the most recent (2004) Expert Consensus Guideline Series for the Treatment of Bipolar Disorder, 84% of practitioner−respondents favored indefinite mood stabilizer therapy after a second lifetime manic episode.19 No recommendation was made about the duration of maintenance pharmacotherapy after a first lifetime manic/hypomanic episode.
Avoid or Reintroduce an Antidepressant if Depression Recurs After a First Mania?
Controversies surrounding antidepressant use in BD are extensive; detailed discussion is beyond the scope of this review (Goldberg and Ghaemi provided a broader discussion of risks and benefits of antidepressants in BD).20 Although the main clinical concern regarding antidepressant use was, at one time, the potential to induce mania or accelerate the frequency of recurrent episodes, more recent, empirical studies suggest that the greater risk of using antidepressants for BD is lack of efficacy.10,21
If a careful longitudinal history and clinical evaluation reveal that an initial manic episode heralds the onset of BD, decisions about whether to avoid an antidepressant (as opposed to using other, more evidence-based interventions for bipolar depression) depend on a number of variables, including establishing whether the index episode was manic or hypomanic; ruling out current subthreshold mixed features; and clarifying how recently mania developed. Decisions about future antidepressant use (or avoidance) might be less clear if an index manic/hypomanic episode was brief and self-limited once the antidepressant was stopped.
Although some experts eschew antidepressant monotherapy after such occurrences, there is no body of literature to inform decisions about the safety or efficacy of undertaking a future antidepressant trial in such patients. That said, reasonable judgment probably includes several considerations:
- Re-exposure to the same antidepressant that was associated with an induction of mania is likely riskier than choosing a different antidepressant; in general, purely serotonergic antidepressants or bupropion are considered to pose less risk of mood destabilization than is seen with an SNRI or tricyclic antidepressant.
- After a manic episode, a subsequent antidepressant trial generally shouldn’t be attempted without concurrent anti-manic medication.
- Introducing any antidepressant is probably ill-advised in the recent (~2 months) aftermath of acute manic/hypomanic symptoms.22
- Patients and their significant other should be apprised of the risk of emerging symptoms of mania or hypomania, or mixed features, and should be familiar with key target symptoms to watch for. Prospective mood charting can be helpful.
- Patients should be monitored closely both for an exacerbation of depression and recurrence of mania/hypomania symptoms.
- Any antidepressant should be discontinued promptly at the first sign of psychomotor acceleration or the emergence of mixed features, as defined by DSM-5
Psychoeducation and Forecasting
Functional recovery from a manic episode can lag behind symptomatic recovery. Subsyndromal symptoms often persist after a full episode subsides.
Mania often is followed by a depressive episode, and questions inevitably arise about how to prevent and treat these episodes. Because the median duration of a manic episode is approximately 13 weeks, it is crucial for patients and their immediate family to recognize that recovery might be gradual, and that it will likely take time before she (he) can resume full-time responsibilities at work or school or in the home.23
Today, a patient who is hospitalized for severe acute mania (as Ms. J was, in the case vignette) seldom remains an inpatient long enough to achieve remission of symptoms; sometimes, she (he) might continue to manifest significant symptoms, even though decisions about the “medical necessity” of ongoing inpatient care tend to be governed mainly by issues of safety and imminent danger. (See this article at CurrentPsychiatry.com for a Table of considerations when making the transition from the acute phase to the continuation phase of treatment.20,24,25)
To minimize risk of relapse, psycho-education should include discussion of:
- Psychiatrically deleterious effects of alcohol and illicit drug use
- Suicide risk, including what to do in an emergency
- Protecting a regular sleep schedule and avoiding sleep deprivation
- The potential for poor medication adherence and management of side effects
- The role of adjunctive psychotherapy and effective stress management
- Familiarity with symptoms that serve as warning signs, and how to monitor their onset.
Click here to read the digital edition.
1. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder in patients with mood instability. J Clin Psychiatry. 2008;69(11): 1751-1757.
2. Rosa AR, Cruz B, Franco C, et al. Why do clinicians maintain antidepressants in some patients with acute mania? Hints from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM), a large naturalistic study. J Clin Psychiatry. 2010;71(8):1000-1006.
3. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355.
4. Bowers MB Jr, McKay BG, Mazure CM. Discontinuation of antidepressants in newly admitted psychotic patients. J Neuropsychiatr Clin Neurosci. 2003;15(2):227-230.
5. Perlis RH, Welge JA, Vornik LA, et al. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4): 509-516.
6. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective followup of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158(1): 125-127.
7. Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158(8):1265-1270.
8. Yatham LN, Kauer-Sant’Anna M, Bond DJ, et al. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Project for Early Mania project. Can J Psychiatry. 2009;54(2):105-112.
9. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar
disorder: a review. J Clin Psychiatry. 2003;64(11):1284-1292.
10. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711-1722.
11. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11(15):453-473.
12. Schulze TG, Hedeker D, Zandi P, et al. What is familial about familial bipolar disorder? Resemblance among relatives across a broad spectrum of phenotypic characteristics. Arch Gen Psychiatry. 2006;63(12):1368-1376.
13. Song J, Bergen SE, Kuja-Halkola R, et al. Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord. 2015;7(2):184-193.
14. Goes FS, Sadler B, Toolan J, et al. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007;9(8):901-906.
15. Fiedorowicz JG, Endicott J, Solomon DA, et al. Course of illness following prospectively observed mania or hypomania in individuals presenting with unipolar depression. Bipolar Disord. 2007;14(6):664-671.
16. Tansey KE, Guipponi M, Domenici E, et al. Genetic susceptibility for bipolar disorder and response to antidepressants in major depressive disorder. Am J Med Genetics B Neuropsychiatr Genet. 2014;165B(1):77-83.
17. Tohen M, Zarate CA Jr, Hennen J, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160(12):2099-2107.
18. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas Consensus Conference Panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry. 2002; 63(4):288-299.
19. Keck PE Jr, Perlis RH, Otto MW, et al. The Expert Consensus Guideline Series: treatment of bipolar disorder 2004. Postgrad Med Special Report. 2004:1-120.
20. Goldberg JF, Ghaemi SN. Benefits and limitations of antidepressants and traditional mood stabilizers for treatment of bipolar depression. Bipolar Disord. 2005; 7(suppl 5):3-12.
21. Sidor MM, MacQueen GM. Antidepressants for the acute treatment of bipolar
depression: a systematic review and meta-analysis. J Clin Psychiatry. 2011;72(2): 156-167.
22. MacQueen GM, Trevor Young L, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105(6):414-418.
23. Solomon DA, Leon AC, Coryell WH, et al. Longitudinal course of bipolar I disorder: duration of mood episodes. Arch Gen Psychiatry. 2010;67(4):339-347.
24. Tohen M, Chengappa KN, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry. 2004;184:337-345.
25. Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry. 2009;166(4): 476-488.
Note: Page numbers differ between the print issue and digital edition.
This article has been adapted from an article originally published in Current Psychiatry (http://currentpsychiatry.com):Current Psychiatry. 2015;14(10):29-32,35-40,e6.
When a known depressed patient newly develops signs of mania or hypomania, a cascade of diagnostic and therapeutic questions ensues: Does the event “automatically” signify the presence of bipolar disorder (BD), or could manic symptoms be secondary to another underlying medical problem, a prescribed antidepressant or non-psychotropic medication, or illicit substances?
Even more questions confront the clinician: If mania symptoms are nothing more than an adverse drug reaction, will they go away by stopping the presumed offending agent? Or do symptoms always indicate the unmasking of a bipolar diathesis? Should anti-manic medication be prescribed immediately? If so, which one(s) and for how long? How extensive a medical or neurologic workup is indicated?
And how do you differentiate ambiguous hypomania symptoms (irritability, insomnia, agitation) from other phenomena, such as akathisia, anxiety, and overstimulation?
In this article, we present an overview of how to approach and answer these key questions, so that you can identify, comprehend, and manage manic symptoms that arise in the course of your patient’s treatment for depression (Box).
Does Disease Exist on a Unipolar-Bipolar Continuum.
There has been a resurgence of interest in Kraepelin’s original notion of mania and depression as falling along a continuum, rather than being distinct categories of pathology. True bipolar mania has its own identifiable epidemiology, familiality, and treatment, but symptomatic shades of gray often pose a formidable diagnostic and therapeutic challenge.
For example, the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) relaxed its definition of “mixed” episodes of BD to include subsyndromal mania features in unipolar depression. When a patient with unipolar depression develops a full, unequivocal manic episode, there usually isn’t much ambiguity or confusion about initial management: assure a safe environment, stop any antidepressants, rule out drug- or medically induced causes, and begin an acute anti-manic medication.
Next steps can, sometimes, be murkier:
- Formulate a definitive, overarching diagnosis
- Provide psycho-education
- Forecast return to work or school
- Discuss prognosis and likelihood of relapse
- Address necessary lifestyle modifications (eg, sleep hygiene, elimination of alcohol and illicit drug use)
- Determine whether indefinite maintenance pharmacotherapy is indicated—and, if so, with which medication(s).
A Diagnostic Formulation Isn’t Always Black and White
Ms. J, age 56, a medically healthy woman, has a 10-year history of depression and anxiety that has been treated effectively for most of that time with venlafaxine,
225 mg/d. The mother of 4 grown children, Ms. J has worked steadily for > 20 years as a flight attendant for an international airline.
Today, Ms. J is brought by ambulance from work to the emergency department in a paranoid and agitated state. The admission follows her having e-blasted airline corporate executives with a voluminous manifesto that she worked on around the clock the preceding week, in which she explained her bold ideas to revolutionize the airline industry, under her leadership.
Ms. J’s family history is unremarkable for psychiatric illness.
How Does One Approach A Case Such As Ms. J's?
Stark examples of classical mania, as depicted in this case vignette, are easy to recognize but not necessarily straightforward, nosologically. Consider the following not-so-straightforward elements of Ms. J’s case:
- A first-lifetime episode of mania or hypomania is rare after age 50
- Ms. J took a serotonin-norepinephrine reuptake inhibitor (SNRI) for many years without evidence of mood destabilization
- Years of repetitive chronobiological stress (including probable frequent time zone changes with likely sleep disruption) apparently did not trigger mood destabilization
- None of Ms. J’s 4 pregnancies led to postpartum mood episodes
- At least on the surface, there are no obvious features that point to likely causes of a secondary mania (eg, drug-induced, toxic, metabolic, or medical)
- Ms. J has no known family history of BD or any other mood disorder.
Approaching a case such as Ms. J’s must involve a systematic strategy that can best be broken into 2 segments: (1) a period of acute initial assessment and treatment and (2) later efforts focused on broader diagnostic evaluation and longer-term relapse prevention.
Initial Assessment and Treatment
Immediate assessment and management hinges on initial triage and forming a working diagnostic impression. Although full-blown mania usually is obvious (sometimes even without a formal interview), be alert to patients who might minimize or altogether disavow mania symptoms—often because of denial of illness, misidentification of symptoms, or impaired insight about changes in thinking, mood, or behavior.
Because florid mania, by definition, impairs psychosocial functioning, the context of an initial presentation often holds diagnostic relevance. Manic patients who display disruptive behaviors often are brought to treatment by a third party, whereas a less severely ill patient might be more inclined to seek treatment for herself (himself) when psychosis is absent and insight is less compromised or when the patient feels she (he) might be depressed.
It is not uncommon for a manic patient to report “depression” as the chief complaint or to omit elements related to psychomotor acceleration (such as racing thoughts or psychomotor agitation) in the description of symptoms. An accurate diagnosis often requires clinical probing and clarification of symptoms (eg, differentiating simple insomnia with consequent next-day fatigue from loss of the need for sleep with intact or even enhanced next-day energy) or discriminating racing thoughts from anxious ruminations that might be more intrusive than rapid.
Presentations of frank mania also can come to light as a consequence of symptoms, rather than as symptoms per se (eg, conflict in relationships, problems at work, financial reversals).
Particularly in patients who do not have a history of mania, avoid the temptation to begin or modify existing pharmacotherapy until you have performed a basic initial evaluation. Immediate considerations for initial assessment and management include the following:
Provide containment. Ensure a safe setting, level of care, and frequency of monitoring. Evaluate suicide risk (particularly when mixed features are present), and risk of withdrawal from any psychoactive substances.
Engage significant others. Close family members can provide essential history, particularly when a patient’s insight about her illness and need for treatment are impaired. Family members and significant others also often play important roles in helping to restrict access to finances, fostering medication adherence, preventing access to weapons in the home, and sharing information with providers about substance use or high-risk behavior.
Systematically assess for DSM-5 symptoms of mania and depression. DSM-5 modified criteria for mania/hypomania to necessitate increased energy, in addition to change in mood, to make a syndromal diagnosis. Useful during a clinical interview is the popular mnemonic DIGFAST to aid recognition of core mania symptoms:
- Distractibility
- Indiscretion/impulsivity
- Grandiosity
- Flight of ideas
- Activity increase
- Sleep deficit
- Talkativeness.
These symptoms should represent a departure from normal baseline characteristics; it often is helpful to ask a significant other or collateral historian how the
present symptoms differ from the patient’s usual state.
Assess for unstable medical conditions or toxicity states. When evaluating an acute change in mental status, toxicology screening is relatively standard and the absence of illicit substances should seldom, if ever, be taken for granted—especially because occult substance use can lead to identification of false-positive BD “cases.”1
Stop any antidepressant. During a manic episode, continuing antidepressant medication serves no purpose other than to contribute to or exacerbate mania symptoms. Nonetheless, observational studies demonstrate that approximately 15% of syndromally manic patients continue to receive an antidepressant, often when a clinician perceives more severe depression during mania, multiple prior depressive episodes,current anxiety, or rapid cycling.2
Importantly, antidepressants have been shown to harm, rather than alleviate, presentations that involve a mixed state, and have no demonstrated value in preventing post-manic depression.3 Mere elimination of an antidepressant might ease symptoms during a manic or mixed episode.4
In some cases, it might be advisable to taper, not abruptly stop, a short halflife serotonergic antidepressant, even in the setting of mania, to minimize the potential for aggravating autonomic dysregulation that can result from antidepressant discontinuation effects.
Begin anti-manic pharmacotherapy. Initiation of an anti-manic mood stabilizer, such as lithium and divalproex, has been standard in the treatment of acute mania.
In the 1990s, protocols for oral loading of divalproex (20 to 30 mg/kg/d) gained popularity for achieving more rapid symptom improvement than might occur with lithium. In the current era, atypical antipsychotics have all but replaced mood stabilizers as an initial intervention to contain mania symptoms quickly (and with less risk than firstgeneration antipsychotics for acute adverse motor effects from so-called rapid neuroleptization).
Because atypical antipsychotics often rapidly subdue mania, psychosis, and agitation, regardless of the underlying process, many practitioners might feel more comfortable initiating them than a mood stabilizer when the diagnosis is ambiguous or provisional, although their longer-term efficacy and safety, relative to traditional mood stabilizers, remains contested. Considerations for choosing from among feasible anti-manic pharmacotherapies are summarized in Table 1.
Normalize the sleep-wake cycle. Chronobiological and circadian variables, such as irregular sleep patterns, are thought to contribute to the pathophysiology of affective switch in BD. Behavioral and pharmacotherapeutic efforts to impose a normal sleep-wake schedule are considered fundamental to stabilizing acute mania.
Facilitate next steps after acute stabilization. For inpatients, this might involve step-down to a partial hospitalization or intensive outpatient program, alongside taking steps to ensure continued treatment adherence and minimize relapse.
What Medical and Neurologic Workup is Appropriate?
Not every first lifetime presentation of mania requires extensive medical and neurologic workup, particularly among patients who have a history of depression and those whose presentation neatly fits the demographic and clinical profile of newly emergent BD. Basic assessment should determine whether any new medication has been started that could plausibly contribute to abnormal mental status (Table 2).
Nevertheless, evaluation of almost all first presentations of mania should include:
- Urine toxicology screen
- Complete blood count
- Comprehensive metabolic panel
- Thyroid-stimulating hormone assay
- Serum vitamin B12 level assay
- Serum folic acid level assay
- Rapid plasma reagin test.
Clinical features that usually lead a clinician to pursue a more detailed medical and neurologic evaluation of first-episode mania include:
- Onset age > 40
- Absence of a family history of mood disorder
- Symptoms arising during a major medical illness
- Multiple medications
- Suspicion of a degenerative or hereditary neurologic disorder
- Altered state of consciousness
- Signs of cortical or diffuse subcortical dysfunction (eg, cognitive deficits, motor deficits, tremor)
- Abnormal vital signs.
Depending on the presentation, additional testing might include:
- Tests of HIV antibody, immune autoantibodies, and Lyme disease antibody
- Heavy metal screening (when suggested by environmental exposure)
- Lumbar puncture (eg, in a setting of manic delirium or suspected central nervous system infection or paraneoplastic syndrome)
- Neuroimaging (note: MRI provides better visualization than CT of white matter pathology and small vessel cerebrovascular disease) electroencephalography.
Making An Overarching Diagnosis: Is Mania Always Bipolar Disorder?
Mania is considered a manifestation of BD when symptoms cannot be attributed to another psychiatric condition, another underlying medical or neurologic condition, or a toxic-metabolic state (Tables 3 and 4). Classification of mania that occurs soon after antidepressant exposure in patients without a known history of BD continues to be the subject of debate, varying in its conceptualization across editions of DSM.
The National Institute of Mental Health (NIMH) Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, observed a fairly low (approximately 10%) incidence of switch from depression to mania when an antidepressant is added to a mood stabilizer; the study authors concluded that much of what is presumed to be antidepressant-induced mania might simply be the natural course of illness.10
Notably, several reports suggest that antidepressants might pose a greater risk of mood destabilization in people with BD I than with either BD II or other suspected variants on the bipolar spectrum.
DSM-5 advises that a diagnosis of substance-induced mood disorder appropriately describes symptoms that spontaneously dissipate once an antidepressant has been discontinued, whereas a diagnosis of BD can be made when manic or hypomanic symptoms persist at a syndromal level after an antidepressant has been stopped and its physiological effects are no longer present. With respect to time course, the International Society of Bipolar Disorders proposes that, beyond 12 to 16 weeks after an antidepressant has been started or the dosage has been increased, it is unlikely that new-onset mania/hypomania can reasonably be attributed to “triggering” by an antidepressant (although antidepressants should be stopped when symptoms of mania emerge).11 Several clinical features have been linked in the literature with an increased susceptibility to BD after an initial depressive episode, including:
- Early (pre-adolescent) age at onset of first mood disorder episode6
- Family history of BD, highly recurrent depression, or psychosis12,13
- Psychosis when depressed.7,14
A number of other characteristics of depressive illness—including seasonal depression, atypical depressive features, suicidality, irritability, anxiety or substance use comorbidity, postpartum mood episodes, and brief recurrent depressive episodes—have been described in the literature as potential correlates of a bipolar diathesis; none have proved to be robust or pathognomonic of a BD diagnosis, as opposed to a unipolar diagnosis.
Data from the NIMH Collaborative Depression Study suggest that recurrent mania/hypomania after an antidepressant-associated polarity switch is greater when a family history of BD is present; other clinical variables might hold less predictive value.15 In addition, although some practitioners consider a history of nonresponse to trials of multiple antidepressants suggestive of an underlying bipolar process, polarity is only one of many variables that must be considered in the differential diagnosis of antidepressantresistant depression. Likewise, molecular genetic studies do not support a link between antidepressant nonresponse and the likelihood of a diagnosis of BD.16
Indefinite Pharmacotherapy for Bipolar Disorder
An important but nagging issue when diagnosing BD after a first manic (or hypomanic) episode is the implied need for indefinite pharmacotherapy to sustain remission and prevent relapse and recurrence.
The likelihood of subsequent depression or mania/hypomania remains high after an index manic/hypomanic episode, particularly for 6 to 8 months after recovery.8,17 Natural history data suggest that, during the year that follows a first lifetime mania, approximately 40% of patients experience a second manic episode.8 A second lifetime mania might be especially likely in patients whose index episode involved mood-congruent psychosis, low premorbid work functioning, and an initial manic episode, as opposed to a mixed episode or early age at onset.8,17
In the absence of randomized, placebo-controlled studies of maintenance pharmacotherapy after a first lifetime manic episode, clinical judgment often drives decisions about the duration of continuing pharmacotherapy after initial symptoms resolve. The Texas Medication Algorithm Project for BD advises that:
General practice at this time is lifetime medication following 2 manic episodes, or 1 episode if it was a severe episode and/or significant family history of bipolar or major depressive disorder is present. For a first episode of bipolar mania with no family history of bipolar or major depressive disorders, medication tapering and discontinuation may be considered after the continuation period is completed (usually 6 months in remission), depending on the severity of the first episode, surrounding factors, and prodromal history.18
Similarly, in the most recent (2004) Expert Consensus Guideline Series for the Treatment of Bipolar Disorder, 84% of practitioner−respondents favored indefinite mood stabilizer therapy after a second lifetime manic episode.19 No recommendation was made about the duration of maintenance pharmacotherapy after a first lifetime manic/hypomanic episode.
Avoid or Reintroduce an Antidepressant if Depression Recurs After a First Mania?
Controversies surrounding antidepressant use in BD are extensive; detailed discussion is beyond the scope of this review (Goldberg and Ghaemi provided a broader discussion of risks and benefits of antidepressants in BD).20 Although the main clinical concern regarding antidepressant use was, at one time, the potential to induce mania or accelerate the frequency of recurrent episodes, more recent, empirical studies suggest that the greater risk of using antidepressants for BD is lack of efficacy.10,21
If a careful longitudinal history and clinical evaluation reveal that an initial manic episode heralds the onset of BD, decisions about whether to avoid an antidepressant (as opposed to using other, more evidence-based interventions for bipolar depression) depend on a number of variables, including establishing whether the index episode was manic or hypomanic; ruling out current subthreshold mixed features; and clarifying how recently mania developed. Decisions about future antidepressant use (or avoidance) might be less clear if an index manic/hypomanic episode was brief and self-limited once the antidepressant was stopped.
Although some experts eschew antidepressant monotherapy after such occurrences, there is no body of literature to inform decisions about the safety or efficacy of undertaking a future antidepressant trial in such patients. That said, reasonable judgment probably includes several considerations:
- Re-exposure to the same antidepressant that was associated with an induction of mania is likely riskier than choosing a different antidepressant; in general, purely serotonergic antidepressants or bupropion are considered to pose less risk of mood destabilization than is seen with an SNRI or tricyclic antidepressant.
- After a manic episode, a subsequent antidepressant trial generally shouldn’t be attempted without concurrent anti-manic medication.
- Introducing any antidepressant is probably ill-advised in the recent (~2 months) aftermath of acute manic/hypomanic symptoms.22
- Patients and their significant other should be apprised of the risk of emerging symptoms of mania or hypomania, or mixed features, and should be familiar with key target symptoms to watch for. Prospective mood charting can be helpful.
- Patients should be monitored closely both for an exacerbation of depression and recurrence of mania/hypomania symptoms.
- Any antidepressant should be discontinued promptly at the first sign of psychomotor acceleration or the emergence of mixed features, as defined by DSM-5
Psychoeducation and Forecasting
Functional recovery from a manic episode can lag behind symptomatic recovery. Subsyndromal symptoms often persist after a full episode subsides.
Mania often is followed by a depressive episode, and questions inevitably arise about how to prevent and treat these episodes. Because the median duration of a manic episode is approximately 13 weeks, it is crucial for patients and their immediate family to recognize that recovery might be gradual, and that it will likely take time before she (he) can resume full-time responsibilities at work or school or in the home.23
Today, a patient who is hospitalized for severe acute mania (as Ms. J was, in the case vignette) seldom remains an inpatient long enough to achieve remission of symptoms; sometimes, she (he) might continue to manifest significant symptoms, even though decisions about the “medical necessity” of ongoing inpatient care tend to be governed mainly by issues of safety and imminent danger. (See this article at CurrentPsychiatry.com for a Table of considerations when making the transition from the acute phase to the continuation phase of treatment.20,24,25)
To minimize risk of relapse, psycho-education should include discussion of:
- Psychiatrically deleterious effects of alcohol and illicit drug use
- Suicide risk, including what to do in an emergency
- Protecting a regular sleep schedule and avoiding sleep deprivation
- The potential for poor medication adherence and management of side effects
- The role of adjunctive psychotherapy and effective stress management
- Familiarity with symptoms that serve as warning signs, and how to monitor their onset.
Click here to read the digital edition.
This article has been adapted from an article originally published in Current Psychiatry (http://currentpsychiatry.com):Current Psychiatry. 2015;14(10):29-32,35-40,e6.
When a known depressed patient newly develops signs of mania or hypomania, a cascade of diagnostic and therapeutic questions ensues: Does the event “automatically” signify the presence of bipolar disorder (BD), or could manic symptoms be secondary to another underlying medical problem, a prescribed antidepressant or non-psychotropic medication, or illicit substances?
Even more questions confront the clinician: If mania symptoms are nothing more than an adverse drug reaction, will they go away by stopping the presumed offending agent? Or do symptoms always indicate the unmasking of a bipolar diathesis? Should anti-manic medication be prescribed immediately? If so, which one(s) and for how long? How extensive a medical or neurologic workup is indicated?
And how do you differentiate ambiguous hypomania symptoms (irritability, insomnia, agitation) from other phenomena, such as akathisia, anxiety, and overstimulation?
In this article, we present an overview of how to approach and answer these key questions, so that you can identify, comprehend, and manage manic symptoms that arise in the course of your patient’s treatment for depression (Box).
Does Disease Exist on a Unipolar-Bipolar Continuum.
There has been a resurgence of interest in Kraepelin’s original notion of mania and depression as falling along a continuum, rather than being distinct categories of pathology. True bipolar mania has its own identifiable epidemiology, familiality, and treatment, but symptomatic shades of gray often pose a formidable diagnostic and therapeutic challenge.
For example, the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) relaxed its definition of “mixed” episodes of BD to include subsyndromal mania features in unipolar depression. When a patient with unipolar depression develops a full, unequivocal manic episode, there usually isn’t much ambiguity or confusion about initial management: assure a safe environment, stop any antidepressants, rule out drug- or medically induced causes, and begin an acute anti-manic medication.
Next steps can, sometimes, be murkier:
- Formulate a definitive, overarching diagnosis
- Provide psycho-education
- Forecast return to work or school
- Discuss prognosis and likelihood of relapse
- Address necessary lifestyle modifications (eg, sleep hygiene, elimination of alcohol and illicit drug use)
- Determine whether indefinite maintenance pharmacotherapy is indicated—and, if so, with which medication(s).
A Diagnostic Formulation Isn’t Always Black and White
Ms. J, age 56, a medically healthy woman, has a 10-year history of depression and anxiety that has been treated effectively for most of that time with venlafaxine,
225 mg/d. The mother of 4 grown children, Ms. J has worked steadily for > 20 years as a flight attendant for an international airline.
Today, Ms. J is brought by ambulance from work to the emergency department in a paranoid and agitated state. The admission follows her having e-blasted airline corporate executives with a voluminous manifesto that she worked on around the clock the preceding week, in which she explained her bold ideas to revolutionize the airline industry, under her leadership.
Ms. J’s family history is unremarkable for psychiatric illness.
How Does One Approach A Case Such As Ms. J's?
Stark examples of classical mania, as depicted in this case vignette, are easy to recognize but not necessarily straightforward, nosologically. Consider the following not-so-straightforward elements of Ms. J’s case:
- A first-lifetime episode of mania or hypomania is rare after age 50
- Ms. J took a serotonin-norepinephrine reuptake inhibitor (SNRI) for many years without evidence of mood destabilization
- Years of repetitive chronobiological stress (including probable frequent time zone changes with likely sleep disruption) apparently did not trigger mood destabilization
- None of Ms. J’s 4 pregnancies led to postpartum mood episodes
- At least on the surface, there are no obvious features that point to likely causes of a secondary mania (eg, drug-induced, toxic, metabolic, or medical)
- Ms. J has no known family history of BD or any other mood disorder.
Approaching a case such as Ms. J’s must involve a systematic strategy that can best be broken into 2 segments: (1) a period of acute initial assessment and treatment and (2) later efforts focused on broader diagnostic evaluation and longer-term relapse prevention.
Initial Assessment and Treatment
Immediate assessment and management hinges on initial triage and forming a working diagnostic impression. Although full-blown mania usually is obvious (sometimes even without a formal interview), be alert to patients who might minimize or altogether disavow mania symptoms—often because of denial of illness, misidentification of symptoms, or impaired insight about changes in thinking, mood, or behavior.
Because florid mania, by definition, impairs psychosocial functioning, the context of an initial presentation often holds diagnostic relevance. Manic patients who display disruptive behaviors often are brought to treatment by a third party, whereas a less severely ill patient might be more inclined to seek treatment for herself (himself) when psychosis is absent and insight is less compromised or when the patient feels she (he) might be depressed.
It is not uncommon for a manic patient to report “depression” as the chief complaint or to omit elements related to psychomotor acceleration (such as racing thoughts or psychomotor agitation) in the description of symptoms. An accurate diagnosis often requires clinical probing and clarification of symptoms (eg, differentiating simple insomnia with consequent next-day fatigue from loss of the need for sleep with intact or even enhanced next-day energy) or discriminating racing thoughts from anxious ruminations that might be more intrusive than rapid.
Presentations of frank mania also can come to light as a consequence of symptoms, rather than as symptoms per se (eg, conflict in relationships, problems at work, financial reversals).
Particularly in patients who do not have a history of mania, avoid the temptation to begin or modify existing pharmacotherapy until you have performed a basic initial evaluation. Immediate considerations for initial assessment and management include the following:
Provide containment. Ensure a safe setting, level of care, and frequency of monitoring. Evaluate suicide risk (particularly when mixed features are present), and risk of withdrawal from any psychoactive substances.
Engage significant others. Close family members can provide essential history, particularly when a patient’s insight about her illness and need for treatment are impaired. Family members and significant others also often play important roles in helping to restrict access to finances, fostering medication adherence, preventing access to weapons in the home, and sharing information with providers about substance use or high-risk behavior.
Systematically assess for DSM-5 symptoms of mania and depression. DSM-5 modified criteria for mania/hypomania to necessitate increased energy, in addition to change in mood, to make a syndromal diagnosis. Useful during a clinical interview is the popular mnemonic DIGFAST to aid recognition of core mania symptoms:
- Distractibility
- Indiscretion/impulsivity
- Grandiosity
- Flight of ideas
- Activity increase
- Sleep deficit
- Talkativeness.
These symptoms should represent a departure from normal baseline characteristics; it often is helpful to ask a significant other or collateral historian how the
present symptoms differ from the patient’s usual state.
Assess for unstable medical conditions or toxicity states. When evaluating an acute change in mental status, toxicology screening is relatively standard and the absence of illicit substances should seldom, if ever, be taken for granted—especially because occult substance use can lead to identification of false-positive BD “cases.”1
Stop any antidepressant. During a manic episode, continuing antidepressant medication serves no purpose other than to contribute to or exacerbate mania symptoms. Nonetheless, observational studies demonstrate that approximately 15% of syndromally manic patients continue to receive an antidepressant, often when a clinician perceives more severe depression during mania, multiple prior depressive episodes,current anxiety, or rapid cycling.2
Importantly, antidepressants have been shown to harm, rather than alleviate, presentations that involve a mixed state, and have no demonstrated value in preventing post-manic depression.3 Mere elimination of an antidepressant might ease symptoms during a manic or mixed episode.4
In some cases, it might be advisable to taper, not abruptly stop, a short halflife serotonergic antidepressant, even in the setting of mania, to minimize the potential for aggravating autonomic dysregulation that can result from antidepressant discontinuation effects.
Begin anti-manic pharmacotherapy. Initiation of an anti-manic mood stabilizer, such as lithium and divalproex, has been standard in the treatment of acute mania.
In the 1990s, protocols for oral loading of divalproex (20 to 30 mg/kg/d) gained popularity for achieving more rapid symptom improvement than might occur with lithium. In the current era, atypical antipsychotics have all but replaced mood stabilizers as an initial intervention to contain mania symptoms quickly (and with less risk than firstgeneration antipsychotics for acute adverse motor effects from so-called rapid neuroleptization).
Because atypical antipsychotics often rapidly subdue mania, psychosis, and agitation, regardless of the underlying process, many practitioners might feel more comfortable initiating them than a mood stabilizer when the diagnosis is ambiguous or provisional, although their longer-term efficacy and safety, relative to traditional mood stabilizers, remains contested. Considerations for choosing from among feasible anti-manic pharmacotherapies are summarized in Table 1.
Normalize the sleep-wake cycle. Chronobiological and circadian variables, such as irregular sleep patterns, are thought to contribute to the pathophysiology of affective switch in BD. Behavioral and pharmacotherapeutic efforts to impose a normal sleep-wake schedule are considered fundamental to stabilizing acute mania.
Facilitate next steps after acute stabilization. For inpatients, this might involve step-down to a partial hospitalization or intensive outpatient program, alongside taking steps to ensure continued treatment adherence and minimize relapse.
What Medical and Neurologic Workup is Appropriate?
Not every first lifetime presentation of mania requires extensive medical and neurologic workup, particularly among patients who have a history of depression and those whose presentation neatly fits the demographic and clinical profile of newly emergent BD. Basic assessment should determine whether any new medication has been started that could plausibly contribute to abnormal mental status (Table 2).
Nevertheless, evaluation of almost all first presentations of mania should include:
- Urine toxicology screen
- Complete blood count
- Comprehensive metabolic panel
- Thyroid-stimulating hormone assay
- Serum vitamin B12 level assay
- Serum folic acid level assay
- Rapid plasma reagin test.
Clinical features that usually lead a clinician to pursue a more detailed medical and neurologic evaluation of first-episode mania include:
- Onset age > 40
- Absence of a family history of mood disorder
- Symptoms arising during a major medical illness
- Multiple medications
- Suspicion of a degenerative or hereditary neurologic disorder
- Altered state of consciousness
- Signs of cortical or diffuse subcortical dysfunction (eg, cognitive deficits, motor deficits, tremor)
- Abnormal vital signs.
Depending on the presentation, additional testing might include:
- Tests of HIV antibody, immune autoantibodies, and Lyme disease antibody
- Heavy metal screening (when suggested by environmental exposure)
- Lumbar puncture (eg, in a setting of manic delirium or suspected central nervous system infection or paraneoplastic syndrome)
- Neuroimaging (note: MRI provides better visualization than CT of white matter pathology and small vessel cerebrovascular disease) electroencephalography.
Making An Overarching Diagnosis: Is Mania Always Bipolar Disorder?
Mania is considered a manifestation of BD when symptoms cannot be attributed to another psychiatric condition, another underlying medical or neurologic condition, or a toxic-metabolic state (Tables 3 and 4). Classification of mania that occurs soon after antidepressant exposure in patients without a known history of BD continues to be the subject of debate, varying in its conceptualization across editions of DSM.
The National Institute of Mental Health (NIMH) Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, observed a fairly low (approximately 10%) incidence of switch from depression to mania when an antidepressant is added to a mood stabilizer; the study authors concluded that much of what is presumed to be antidepressant-induced mania might simply be the natural course of illness.10
Notably, several reports suggest that antidepressants might pose a greater risk of mood destabilization in people with BD I than with either BD II or other suspected variants on the bipolar spectrum.
DSM-5 advises that a diagnosis of substance-induced mood disorder appropriately describes symptoms that spontaneously dissipate once an antidepressant has been discontinued, whereas a diagnosis of BD can be made when manic or hypomanic symptoms persist at a syndromal level after an antidepressant has been stopped and its physiological effects are no longer present. With respect to time course, the International Society of Bipolar Disorders proposes that, beyond 12 to 16 weeks after an antidepressant has been started or the dosage has been increased, it is unlikely that new-onset mania/hypomania can reasonably be attributed to “triggering” by an antidepressant (although antidepressants should be stopped when symptoms of mania emerge).11 Several clinical features have been linked in the literature with an increased susceptibility to BD after an initial depressive episode, including:
- Early (pre-adolescent) age at onset of first mood disorder episode6
- Family history of BD, highly recurrent depression, or psychosis12,13
- Psychosis when depressed.7,14
A number of other characteristics of depressive illness—including seasonal depression, atypical depressive features, suicidality, irritability, anxiety or substance use comorbidity, postpartum mood episodes, and brief recurrent depressive episodes—have been described in the literature as potential correlates of a bipolar diathesis; none have proved to be robust or pathognomonic of a BD diagnosis, as opposed to a unipolar diagnosis.
Data from the NIMH Collaborative Depression Study suggest that recurrent mania/hypomania after an antidepressant-associated polarity switch is greater when a family history of BD is present; other clinical variables might hold less predictive value.15 In addition, although some practitioners consider a history of nonresponse to trials of multiple antidepressants suggestive of an underlying bipolar process, polarity is only one of many variables that must be considered in the differential diagnosis of antidepressantresistant depression. Likewise, molecular genetic studies do not support a link between antidepressant nonresponse and the likelihood of a diagnosis of BD.16
Indefinite Pharmacotherapy for Bipolar Disorder
An important but nagging issue when diagnosing BD after a first manic (or hypomanic) episode is the implied need for indefinite pharmacotherapy to sustain remission and prevent relapse and recurrence.
The likelihood of subsequent depression or mania/hypomania remains high after an index manic/hypomanic episode, particularly for 6 to 8 months after recovery.8,17 Natural history data suggest that, during the year that follows a first lifetime mania, approximately 40% of patients experience a second manic episode.8 A second lifetime mania might be especially likely in patients whose index episode involved mood-congruent psychosis, low premorbid work functioning, and an initial manic episode, as opposed to a mixed episode or early age at onset.8,17
In the absence of randomized, placebo-controlled studies of maintenance pharmacotherapy after a first lifetime manic episode, clinical judgment often drives decisions about the duration of continuing pharmacotherapy after initial symptoms resolve. The Texas Medication Algorithm Project for BD advises that:
General practice at this time is lifetime medication following 2 manic episodes, or 1 episode if it was a severe episode and/or significant family history of bipolar or major depressive disorder is present. For a first episode of bipolar mania with no family history of bipolar or major depressive disorders, medication tapering and discontinuation may be considered after the continuation period is completed (usually 6 months in remission), depending on the severity of the first episode, surrounding factors, and prodromal history.18
Similarly, in the most recent (2004) Expert Consensus Guideline Series for the Treatment of Bipolar Disorder, 84% of practitioner−respondents favored indefinite mood stabilizer therapy after a second lifetime manic episode.19 No recommendation was made about the duration of maintenance pharmacotherapy after a first lifetime manic/hypomanic episode.
Avoid or Reintroduce an Antidepressant if Depression Recurs After a First Mania?
Controversies surrounding antidepressant use in BD are extensive; detailed discussion is beyond the scope of this review (Goldberg and Ghaemi provided a broader discussion of risks and benefits of antidepressants in BD).20 Although the main clinical concern regarding antidepressant use was, at one time, the potential to induce mania or accelerate the frequency of recurrent episodes, more recent, empirical studies suggest that the greater risk of using antidepressants for BD is lack of efficacy.10,21
If a careful longitudinal history and clinical evaluation reveal that an initial manic episode heralds the onset of BD, decisions about whether to avoid an antidepressant (as opposed to using other, more evidence-based interventions for bipolar depression) depend on a number of variables, including establishing whether the index episode was manic or hypomanic; ruling out current subthreshold mixed features; and clarifying how recently mania developed. Decisions about future antidepressant use (or avoidance) might be less clear if an index manic/hypomanic episode was brief and self-limited once the antidepressant was stopped.
Although some experts eschew antidepressant monotherapy after such occurrences, there is no body of literature to inform decisions about the safety or efficacy of undertaking a future antidepressant trial in such patients. That said, reasonable judgment probably includes several considerations:
- Re-exposure to the same antidepressant that was associated with an induction of mania is likely riskier than choosing a different antidepressant; in general, purely serotonergic antidepressants or bupropion are considered to pose less risk of mood destabilization than is seen with an SNRI or tricyclic antidepressant.
- After a manic episode, a subsequent antidepressant trial generally shouldn’t be attempted without concurrent anti-manic medication.
- Introducing any antidepressant is probably ill-advised in the recent (~2 months) aftermath of acute manic/hypomanic symptoms.22
- Patients and their significant other should be apprised of the risk of emerging symptoms of mania or hypomania, or mixed features, and should be familiar with key target symptoms to watch for. Prospective mood charting can be helpful.
- Patients should be monitored closely both for an exacerbation of depression and recurrence of mania/hypomania symptoms.
- Any antidepressant should be discontinued promptly at the first sign of psychomotor acceleration or the emergence of mixed features, as defined by DSM-5
Psychoeducation and Forecasting
Functional recovery from a manic episode can lag behind symptomatic recovery. Subsyndromal symptoms often persist after a full episode subsides.
Mania often is followed by a depressive episode, and questions inevitably arise about how to prevent and treat these episodes. Because the median duration of a manic episode is approximately 13 weeks, it is crucial for patients and their immediate family to recognize that recovery might be gradual, and that it will likely take time before she (he) can resume full-time responsibilities at work or school or in the home.23
Today, a patient who is hospitalized for severe acute mania (as Ms. J was, in the case vignette) seldom remains an inpatient long enough to achieve remission of symptoms; sometimes, she (he) might continue to manifest significant symptoms, even though decisions about the “medical necessity” of ongoing inpatient care tend to be governed mainly by issues of safety and imminent danger. (See this article at CurrentPsychiatry.com for a Table of considerations when making the transition from the acute phase to the continuation phase of treatment.20,24,25)
To minimize risk of relapse, psycho-education should include discussion of:
- Psychiatrically deleterious effects of alcohol and illicit drug use
- Suicide risk, including what to do in an emergency
- Protecting a regular sleep schedule and avoiding sleep deprivation
- The potential for poor medication adherence and management of side effects
- The role of adjunctive psychotherapy and effective stress management
- Familiarity with symptoms that serve as warning signs, and how to monitor their onset.
Click here to read the digital edition.
1. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder in patients with mood instability. J Clin Psychiatry. 2008;69(11): 1751-1757.
2. Rosa AR, Cruz B, Franco C, et al. Why do clinicians maintain antidepressants in some patients with acute mania? Hints from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM), a large naturalistic study. J Clin Psychiatry. 2010;71(8):1000-1006.
3. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355.
4. Bowers MB Jr, McKay BG, Mazure CM. Discontinuation of antidepressants in newly admitted psychotic patients. J Neuropsychiatr Clin Neurosci. 2003;15(2):227-230.
5. Perlis RH, Welge JA, Vornik LA, et al. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4): 509-516.
6. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective followup of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158(1): 125-127.
7. Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158(8):1265-1270.
8. Yatham LN, Kauer-Sant’Anna M, Bond DJ, et al. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Project for Early Mania project. Can J Psychiatry. 2009;54(2):105-112.
9. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar
disorder: a review. J Clin Psychiatry. 2003;64(11):1284-1292.
10. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711-1722.
11. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11(15):453-473.
12. Schulze TG, Hedeker D, Zandi P, et al. What is familial about familial bipolar disorder? Resemblance among relatives across a broad spectrum of phenotypic characteristics. Arch Gen Psychiatry. 2006;63(12):1368-1376.
13. Song J, Bergen SE, Kuja-Halkola R, et al. Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord. 2015;7(2):184-193.
14. Goes FS, Sadler B, Toolan J, et al. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007;9(8):901-906.
15. Fiedorowicz JG, Endicott J, Solomon DA, et al. Course of illness following prospectively observed mania or hypomania in individuals presenting with unipolar depression. Bipolar Disord. 2007;14(6):664-671.
16. Tansey KE, Guipponi M, Domenici E, et al. Genetic susceptibility for bipolar disorder and response to antidepressants in major depressive disorder. Am J Med Genetics B Neuropsychiatr Genet. 2014;165B(1):77-83.
17. Tohen M, Zarate CA Jr, Hennen J, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160(12):2099-2107.
18. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas Consensus Conference Panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry. 2002; 63(4):288-299.
19. Keck PE Jr, Perlis RH, Otto MW, et al. The Expert Consensus Guideline Series: treatment of bipolar disorder 2004. Postgrad Med Special Report. 2004:1-120.
20. Goldberg JF, Ghaemi SN. Benefits and limitations of antidepressants and traditional mood stabilizers for treatment of bipolar depression. Bipolar Disord. 2005; 7(suppl 5):3-12.
21. Sidor MM, MacQueen GM. Antidepressants for the acute treatment of bipolar
depression: a systematic review and meta-analysis. J Clin Psychiatry. 2011;72(2): 156-167.
22. MacQueen GM, Trevor Young L, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105(6):414-418.
23. Solomon DA, Leon AC, Coryell WH, et al. Longitudinal course of bipolar I disorder: duration of mood episodes. Arch Gen Psychiatry. 2010;67(4):339-347.
24. Tohen M, Chengappa KN, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry. 2004;184:337-345.
25. Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry. 2009;166(4): 476-488.
Note: Page numbers differ between the print issue and digital edition.
1. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder in patients with mood instability. J Clin Psychiatry. 2008;69(11): 1751-1757.
2. Rosa AR, Cruz B, Franco C, et al. Why do clinicians maintain antidepressants in some patients with acute mania? Hints from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM), a large naturalistic study. J Clin Psychiatry. 2010;71(8):1000-1006.
3. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355.
4. Bowers MB Jr, McKay BG, Mazure CM. Discontinuation of antidepressants in newly admitted psychotic patients. J Neuropsychiatr Clin Neurosci. 2003;15(2):227-230.
5. Perlis RH, Welge JA, Vornik LA, et al. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4): 509-516.
6. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective followup of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158(1): 125-127.
7. Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158(8):1265-1270.
8. Yatham LN, Kauer-Sant’Anna M, Bond DJ, et al. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Project for Early Mania project. Can J Psychiatry. 2009;54(2):105-112.
9. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar
disorder: a review. J Clin Psychiatry. 2003;64(11):1284-1292.
10. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711-1722.
11. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11(15):453-473.
12. Schulze TG, Hedeker D, Zandi P, et al. What is familial about familial bipolar disorder? Resemblance among relatives across a broad spectrum of phenotypic characteristics. Arch Gen Psychiatry. 2006;63(12):1368-1376.
13. Song J, Bergen SE, Kuja-Halkola R, et al. Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord. 2015;7(2):184-193.
14. Goes FS, Sadler B, Toolan J, et al. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007;9(8):901-906.
15. Fiedorowicz JG, Endicott J, Solomon DA, et al. Course of illness following prospectively observed mania or hypomania in individuals presenting with unipolar depression. Bipolar Disord. 2007;14(6):664-671.
16. Tansey KE, Guipponi M, Domenici E, et al. Genetic susceptibility for bipolar disorder and response to antidepressants in major depressive disorder. Am J Med Genetics B Neuropsychiatr Genet. 2014;165B(1):77-83.
17. Tohen M, Zarate CA Jr, Hennen J, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160(12):2099-2107.
18. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas Consensus Conference Panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry. 2002; 63(4):288-299.
19. Keck PE Jr, Perlis RH, Otto MW, et al. The Expert Consensus Guideline Series: treatment of bipolar disorder 2004. Postgrad Med Special Report. 2004:1-120.
20. Goldberg JF, Ghaemi SN. Benefits and limitations of antidepressants and traditional mood stabilizers for treatment of bipolar depression. Bipolar Disord. 2005; 7(suppl 5):3-12.
21. Sidor MM, MacQueen GM. Antidepressants for the acute treatment of bipolar
depression: a systematic review and meta-analysis. J Clin Psychiatry. 2011;72(2): 156-167.
22. MacQueen GM, Trevor Young L, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105(6):414-418.
23. Solomon DA, Leon AC, Coryell WH, et al. Longitudinal course of bipolar I disorder: duration of mood episodes. Arch Gen Psychiatry. 2010;67(4):339-347.
24. Tohen M, Chengappa KN, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry. 2004;184:337-345.
25. Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry. 2009;166(4): 476-488.
Note: Page numbers differ between the print issue and digital edition.
What to do when your depressed patient develops mania
When a known depressed patient newly develops signs of mania or hypomania, a cascade of diagnostic and therapeutic questions ensues: Does the event “automatically” signify the presence of bipolar disorder (BD), or could manic symptoms be secondary to another underlying medical problem, a prescribed antidepressant or non-psychotropic medication, or illicit substances?
Even more questions confront the clinician: If mania symptoms are nothing more than an adverse drug reaction, will they go away by stopping the presumed offending agent? Or do symptoms always indicate the unmasking of a bipolar diathesis? Should anti-manic medication be prescribed immediately? If so, which one(s) and for how long? How extensive a medical or neurologic workup is indicated?
And, how do you differentiate ambiguous hypomania symptoms (irritability, insomnia, agitation) from other phenomena, such as akathisia, anxiety, and overstimulation?
In this article, we present an overview of how to approach and answer these key questions, so that you can identify, comprehend, and manage manic symptoms that arise in the course of your patient’s treatment for depression (Box).
Does disease exist on a unipolar−bipolar continuum?
There has been a resurgence of interest in Kraepelin’s original notion of mania and depression as falling along a continuum, rather than being distinct categories of pathology. True bipolar mania has its own identifiable epidemiology, familiality, and treatment, but symptomatic shades of gray often pose a formidable diagnostic and therapeutic challenge.
For example, DSM-5 relaxed its definition of “mixed” episodes of BD to include subsyndromal mania features in unipolar depression. When a patient with unipolar depression develops a full, unequivocal manic episode, there usually isn’t much ambiguity or confusion about initial management: assure a safe environment, stop any antidepressants, rule out drug- or medically induced causes, and begin an acute anti-manic medication.
Next steps can, sometimes, be murkier:
• formulate a definitive, overarching diagnosis
• provide psycho-education
• forecast return to work or school
• discuss prognosis and likelihood of relapse
• address necessary lifestyle modifications (eg, sleep hygiene, elimination of alcohol and illicit drug use)
• determine whether indefinite maintenance pharmacotherapy is indicated— and, if so, with which medication(s).
CASE A diagnostic formulation isn’t always black and white
Ms. J, age 56, a medically healthy woman, has a 10-year history of depression and anxiety that has been treated effectively for most of that time with venlafaxine, 225 mg/d. The mother of 4 grown children, Ms. J has worked steadily for >20 years as a flight attendant for an international airline.
Today, Ms. J is brought by ambulance from work to the emergency department in a paranoid and agitated state. The admission follows her having e-blasted airline corporate executives with a voluminous manifesto that she worked on around the clock the preceding week, in which she explained her bold ideas to revolutionize the airline industry, under her leadership.
Ms. J’s family history is unremarkable for psychiatric illness.
How does one approach a case such as Ms. J’s?
Stark examples of classical mania, as depicted in this case vignette, are easy to recognize but not necessarily straightforward, nosologically. Consider the following not-so-straightforward elements of Ms. J’s case:
• a first-lifetime episode of mania or hypomania is rare after age 50
• Ms. J took a serotonin-norepinephrine reuptake inhibitor (SNRI) for many years without evidence of mood destabilization
• years of repetitive chronobiological stress (including probable frequent time zone changes with likely sleep disruption) apparently did not trigger mood destabilization
• none of Ms. J’s 4 pregnancies led to postpartum mood episodes
• at least on the surface, there are no obvious features that point to likely causes of a secondary mania (eg, drug-induced, toxic, metabolic, or medical)
• Ms. J has no known family history of BD or any other mood disorder.
Approaching a case such as Ms. J’s must involve a systematic strategy that can best be broken into 2 segments: (1) a period of acute initial assessment and treatment and (2) later efforts focused on broader diagnostic evaluation and longer-term relapse prevention.
Initial assessment and treatment
Immediate assessment and management hinges on initial triage and forming a working diagnostic impression. Although full-blown mania usually is obvious (sometimes even without a formal interview), be alert to patients who might minimize or altogether disavow mania symptoms—often because of denial of illness, misidentification of symptoms, or impaired insight about changes in thinking, mood, or behavior.
Because florid mania, by definition, impairs psychosocial functioning, the context of an initial presentation often holds diagnostic relevance. Manic patients who display disruptive behaviors often are brought to treatment by a third party, whereas a less severely ill patient might be more inclined to seek treatment for herself (himself) when psychosis is absent and insight is less compromised or when the patient feels she (he) might be depressed.
It is not uncommon for a manic patient to report “depression” as the chief complaint or to omit elements related to psychomotor acceleration (such as racing thoughts or psychomotor agitation) in the description of symptoms. An accurate diagnosis often requires clinical probing and clarification of symptoms (eg, differentiating simple insomnia with consequent next-day fatigue from loss of the need for sleep with intact or even enhanced next-day energy) or discriminating racing thoughts from anxious ruminations that might be more intrusive than rapid.
Presentations of frank mania also can come to light as a consequence of symptoms, rather than as symptoms per se (eg, conflict in relationships, problems at work, financial reversals).
Particularly in patients who do not have a history of mania, avoid the temptation to begin or modify existing pharmacotherapy until you have performed a basic initial evaluation. Immediate considerations for initial assessment and management include the following:
Provide containment. Ensure a safe setting, level of care, and frequency of monitoring. Evaluate suicide risk (particularly when mixed features are present), and risk of withdrawal from any psychoactive substances.
Engage significant others. Close family members can provide essential history, particularly when a patient’s insight about her illness and need for treatment are impaired. Family members and significant others also often play important roles in helping to restrict access to finances, fostering medication adherence, preventing access to weapons in the home, and sharing information with providers about substance use or high-risk behavior.
Systematically assess for DSM-5 symptoms of mania and depression. DSM-5 modified criteria for mania/hypomania to necessitate increased energy, in addition to change in mood, to make a syndromal diagnosis. Useful during a clinical interview is the popular mnemonic DIGFAST to aid recognition of core mania symptomsa:
• Distractibility
• Indiscretion/impulsivity
• Grandiosity
• Flight of ideas
• Activity increase
• Sleep deficit
• Talkativeness.
aAlso see: “Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis,” in the October 2008 issue Current Psychiatry and in the archive at CurrentPsychiatry.com.
These symptoms should represent a departure from normal baseline characteristics; it often is helpful to ask a significant other or collateral historian how the present symptoms differ from the patient’s usual state.
Assess for unstable medical conditions or toxicity states. When evaluating an acute change in mental status, toxicology screening is relatively standard and the absence of illicit substances should seldom, if ever, be taken for granted—especially because occult substance use can lead to identification of false-positive BD “cases.”1
Stop any antidepressant. During a manic episode, continuing antidepressant medication serves no purpose other than to contribute to or exacerbate mania symptoms. Nonetheless, observational studies demonstrate that approximately 15% of syndromally manic patients continue to receive an antidepressant, often when a clinician perceives more severe depression during mania, multiple prior depressive episodes, current anxiety, or rapid cycling.2
Importantly, antidepressants have been shown to harm, rather than alleviate, presentations that involve a mixed state,3 and have no demonstrated value in preventing post-manic depression. Mere elimination of an antidepressant might ease symptoms during a manic or mixed episode.4
In some cases, it might be advisable to taper, not abruptly stop, a short half-life serotonergic antidepressant, even in the setting of mania, to minimize the potential for aggravating autonomic dysregulation that can result from antidepressant discontinuation effects.
Begin anti-manic pharmacotherapy. Initiation of an anti-manic mood stabilizer, such as lithium and divalproex, has been standard in the treatment of acute mania.
In the 1990s, protocols for oral loading of divalproex (20 to 30 mg/kg/d) gained popularity for achieving more rapid symptom improvement than might occur with lithium. In the current era, atypical antipsychotics have all but replaced mood stabilizers as an initial intervention to contain mania symptoms quickly (and with less risk than first-generation antipsychotics for acute adverse motor effects from so-called rapid neuroleptization).
Because atypical antipsychotics often rapidly subdue mania, psychosis, and agitation, regardless of the underlying process, many practitioners might feel more comfortable initiating them than a mood stabilizer when the diagnosis is ambiguous or provisional, although their longer-term efficacy and safety, relative to traditional mood stabilizers, remains contested. Considerations for choosing from among feasible anti-manic pharmacotherapies are summarized in Table 1.5
Normalize the sleep-wake cycle. Chronobiological and circadian variables, such as irregular sleep patterns, are thought to contribute to the pathophysiology of affective switch in BD. Behavioral and pharmacotherapeutic efforts to impose a normal sleep−wake schedule are considered fundamental to stabilizing acute mania.
Facilitate next steps after acute stabilization. For inpatients, this might involve step-down to a partial hospitalization or intensive outpatient program, alongside taking steps to ensure continued treatment adherence and minimize relapse.
What medical and neurologic workup is appropriate?
Not every first lifetime presentation of mania requires extensive medical and neurologic workup, particularly among patients who have a history of depression and those whose presentation neatly fits the demographic and clinical profile of newly emergent BD. Basic assessment should determine whether any new medication has been started that could plausibly contribute to abnormal mental status (Table 2).
Nevertheless, evaluation of almost all first presentations of mania should include:
• urine toxicology screen
• complete blood count
• comprehensive metabolic panel
• thyroid-stimulating hormone assay
• serum vitamin B12 level assay
• serum folic acid level assay
• rapid plasma reagin test.
Clinical features that usually lead a clinician to pursue a more detailed medical and neurologic evaluation of first-episode mania include:
• onset age >40
• absence of a family history of mood disorder
• symptoms arising during a major medical illness
• multiple medications
• suspicion of a degenerative or hereditary neurologic disorder
• altered state of consciousness
• signs of cortical or diffuse subcortical dysfunction (eg, cognitive deficits, motor deficits, tremor)
• abnormal vital signs.
Depending on the presentation, additional testing might include:
• tests of HIV antibody, immune autoantibodies, and Lyme disease antibody
• heavy metal screening (when suggested by environmental exposure)
• lumbar puncture (eg, in a setting of manic delirium or suspected central nervous system infection or paraneoplastic syndrome)
• neuroimaging (note: MRI provides better visualization than CT of white matter pathology and small vessel cerebrovascular disease) electroencephalography.
Making an overarching diagnosis: Is mania always bipolar disorder?
Mania is considered a manifestation of BD when symptoms cannot be attributed to another psychiatric condition, another underlying medical or neurologic condition, or a toxic-metabolic state (Table 3 and Table 46-9). Classification of mania that occurs soon after antidepressant exposure in patients without a known history of BD continues to be the subject of debate, varying in its conceptualization across editions of DSM.
The National Institute of Mental Health (NIMH) Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, observed a fairly low (approximately 10%) incidence of switch from depression to mania when an antidepressant is added to a mood stabilizer; the study authors concluded that much of what is presumed to be antidepressant-induced mania might simply be the natural course of illness.10
Notably, several reports suggest that antidepressants might pose a greater risk of mood destabilization in people with BD I than with either BD II or other suspected variants on the bipolar spectrum.
DSM-5 advises that a diagnosis of substance-induced mood disorder appropriately describes symptoms that spontaneously dissipate once an antidepressant has been discontinued, whereas a diagnosis of BD can be made when manic or hypomanic symptoms persist at a syndromal level after an antidepressant has been stopped and its physiological effects are no longer present. With respect to time course, the International Society of Bipolar Disorders proposes that, beyond 12 to 16 weeks after an antidepressant has been started or the dosage has been increased, it is unlikely that new-onset mania/hypomania can reasonably be attributed to “triggering” by an antidepressant11 (although antidepressants should be stopped when symptoms of mania emerge).
Several clinical features have been linked in the literature with an increased susceptibility to BD after an initial depressive episode, including:
• early (pre-adolescent) age at onset of first mood disorder episode6
• family history of BD, highly recurrent depression, or psychosis12,13
• psychosis when depressed.7,14
A number of other characteristics of depressive illness—including seasonal depression, atypical depressive features, suicidality, irritability, anxiety or substance use comorbidity, postpartum mood episodes, and brief recurrent depressive episodes—have been described in the literature as potential correlates of a bipolar diathesis; none have proved to be robust or pathognomonic of a BD diagnosis, as opposed to a unipolar diagnosis.
Data from the NIMH Collaborative Depression Study suggest that recurrent mania/hypomania after an antidepressant-associated polarity switch is greater when a family history of BD is present; other clinical variables might hold less predictive value.15
In addition, although some practitioners consider a history of nonresponse to trials of multiple antidepressants suggestive of an underlying bipolar process, polarity is only one of many variables that must be considered in the differential diagnosis of antidepressant-resistant depression.b Likewise, molecular genetic studies do not support a link between antidepressant nonresponse and the likelihood of a diagnosis of BD.16
bSee “A practical approach to subtyping depression among your patients” in the April 2014 issue of Current Psychiatry or in the archive at CurrentPsychiatry.com.
Indefinite pharmacotherapy for bipolar disorder?
An important but nagging issue when diagnosing BD after a first manic (or hypomanic) episode is the implied need for indefinite pharmacotherapy to sustain remission and prevent relapse and recurrence.
The likelihood of subsequent depression or mania/hypomania remains high after an index manic/hypomanic episode, particularly for 6 to 8 months after recovery.8,17 Natural history data suggest that, during the year that follows a first lifetime mania, approximately 40% of patients experience a second manic episode.8 A second lifetime mania might be especially likely in patients whose index episode involved mood-congruent psychosis, low premorbid work functioning, and an initial manic episode, as opposed to a mixed episode17 or early age at onset.8
In the absence of randomized, placebo-controlled studies of maintenance pharmacotherapy after a first lifetime manic episode, clinical judgment often drives decisions about the duration of continuing pharmacotherapy after initial symptoms resolve. The Texas Medication Algorithm Project for BD advises that:
Similarly, in the most recent (2004) Expert Consensus Guideline Series for the Treatment of Bipolar Disorder,19 84% of practitioner−respondents favored indefinite mood stabilizer therapy after a second lifetime manic episode. No recommendation was made about the duration of maintenance pharmacotherapy after a first lifetime manic/hypomanic episode.
Avoid or reintroduce an antidepressant if depression recurs after a first mania?
Controversies surrounding antidepressant use in BD are extensive; detailed discussion is beyond the scope of this review (Goldberg and Ghaemi provided a broader discussion of risks and benefits of antidepressants in BD20). Although the main clinical concern regarding antidepressant use was, at one time, the potential to induce mania or accelerate the frequency of recurrent episodes, more recent, empirical studies suggest that the greater risk of using antidepressants for BD is lack of efficacy.10,21
If a careful longitudinal history and clinical evaluation reveal that an initial manic episode heralds the onset of BD, decisions about whether to avoid an antidepressant (as opposed to using other, more evidence-based interventions for bipolar depression) depend on a number of variables, including establishing whether the index episode was manic or hypomanic; ruling out current subthreshold mixed features; and clarifying how recently mania developed. Decisions about future antidepressant use (or avoidance) might be less clear if an index manic/hypomanic episode was brief and self-limited once the antidepressant was stopped.
Although some experts eschew antidepressant monotherapy after such occurrences, there is no body of literature to inform decisions about the safety or efficacy of undertaking a future antidepressant trial in such patients. That said, reasonable judgment probably includes several considerations:
• Re-exposure to the same antidepressant that was associated with an induction of mania is likely riskier than choosing a different antidepressant; in general, purely serotonergic antidepressants or bupropion are considered to pose less risk of mood destabilization than is seen with an SNRI or tricyclic antidepressant.
• After a manic episode, a subsequent antidepressant trial generally shouldn’t be attempted without concurrent anti-manic medication.
• Introducing any antidepressant is probably ill-advised in the recent (~2 months) aftermath of acute manic/ hypomanic symptoms.22
• Patients and their significant other should be apprised of the risk of emerging symptoms of mania or hypomania, or mixed features, and should be familiar with key target symptoms to watch for. Prospective mood charting can be helpful.
• Patients should be monitored closely both for an exacerbation of depression and recurrence of mania/hypomania symptoms.
• Any antidepressant should be discontinued promptly at the first sign of psychomotor acceleration or the emergence of mixed features, as defined by DSM-5.
Psychoeducation and forecasting
Functional recovery from a manic episode can lag behind symptomatic recovery. Subsyndromal symptoms often persist after a full episode subsides.
Mania often is followed by a depressive episode, and questions inevitably arise about how to prevent and treat these episodes. Because the median duration of a manic episode is approximately 13 weeks,23 it is crucial for patients and their immediate family to recognize that recovery might be gradual, and that it will likely take time before she (he) can resume full-time responsibilities at work or school or in the home.
Today, a patient who is hospitalized for severe acute mania (as Ms. J was, in the case vignette) seldom remains an inpatient long enough to achieve remission of symptoms; sometimes, she (he) might continue to manifest significant symptoms, even though decisions about the “medical necessity” of ongoing inpatient care tend to be governed mainly by issues of safety and imminent danger. (This web exclusive Table20,24,25 provides considerations when making the transition from the acute phase to the continuation phase of treatment.)
To minimize risk of relapse, psycho-education should include discussion of:
• psychiatrically deleterious effects of alcohol and illicit drug use
• suicide risk, including what to do in an emergency
• protecting a regular sleep schedule and avoiding sleep deprivation
• the potential for poor medication adherence and management of side effects
• the need for periodic laboratory monitoring, as needed
• the role of adjunctive psychotherapy and effective stress management
• familiarity with symptoms that serve as warning signs, and how to monitor their onset.
Bottom Line
When a patient being treated for depression develops signs of mania or hypomania, stop any antidepressant and consider initiating a mood stabilizer, antipsychotic, or both, to contain and stabilize symptoms. Entertain medical and substance-related causes of mania symptoms, and evaluate and treat as suggested by the patient’s presentation. Long-term drug therapy to prevent recurrence of mania/hypomania, as well as risks and benefits of future exposure to antidepressants, should be decided case by case.
Related Resources
• Proudfoot J, Whitton A, Parker G, et al. Triggers of mania and depression in young adults with bipolar disorder. J Affect Disord. 2012;143(1-3):196-202.
• Stange JP, Sylvia LG, Magalhães PV, et al. Extreme attributions predict transition from depression to mania or hypomania in bipolar disorder. J Psychiatr Res. 2013;47(10):1329-1336.
Drug Brand Names
Albuterol • Proventil, Ventolin
Anastrozole • Arimidex
Aripiprazole • Abilify
Bupropion • Wellbutrin
Carbamazepine • Tegretol
Chloroquine • Aralen
Ciprofloxacin • Cipro
Clarithromycin • Biaxin
Clomiphene • Clomid
Digoxin • Digox, Lanoxin
Divalproex • Depakote
5-Fluorouracil • Carac, Efudex
Human chorionic gonadotropin • Novarel, Pregnyl
Ifosfamide • Ifex
Isoniazid • Nydrazid
Lamotrigine • Lamictal
Letrozole • Femara
Lithium • Eskalith, Lithobid
Lurasidone • Latuda
Mefloquine • Lariam
Olanzapine • Zyprexa
Olanzapine/fluoxetine combination • Symbyax
ramipexole • Mirapex
Procarbazine • Matulane
Quetiapine • Seroquel
Ropinirole • Requip
Rotigotine • Neupro
Venlafaxine • Effexor
Zidovudine • Retrovir
Disclosures
Dr. Goldberg is a consultant to Merck & Co. and Sunovion. He is a member of the speakers’ bureau of AstraZeneca, Janssen, Merck & Co., Takeda and Lundbeck, and Sunovion.
Dr. Ernst reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder in patients with mood instability. J Clin Psychiatry. 2008;69(11):1751-1757.
2. Rosa AR, Cruz B, Franco C, et al. Why do clinicians maintain antidepressants in some patients with acute mania? Hints from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM), a large naturalistic study. J Clin Psychiatry. 2010;71(8):1000-1006.
3. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355.
4. Bowers MB Jr, McKay BG, Mazure CM. Discontinuation of antidepressants in newly admitted psychotic patients. J Neuropsychiatr Clin Neurosci. 2003;15(2):227-230.
5. Perlis RH, Welge JA, Vornik LA, et al. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4):509-516.
6. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158(1):125-127.
7. Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158(8):1265-1270.
8. Yatham LN, Kauer-Sant’Anna M, Bond DJ, et al. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Project for Early Mania project. Can J Psychiatry. 2009;54(2):105-112.
9. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry 2003;64(11):1284-1292.
10. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711-1722.
11. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11(15):453-473.
12. Schulze TG, Hedeker D, Zandi P, et al. What is familial about familial bipolar disorder? Resemblance among relatives across a broad spectrum of phenotypic characteristics. Arch Gen Psychiatry. 2006;63(12):1368-1376.
13. Song J, Bergen SE, Kuja-Halkola R, et al. Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord. 2015;7(2):184-193.
14. Goes FS, Sadler B, Toolan J, et al. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007;9(8):901-906.
15. Fiedorowicz JG, Endicott J, Solomon DA, et al. Course of illness following prospectively observed mania or hypomania in individuals presenting with unipolar depression. Bipolar Disord. 2007;14(6):664-671.
16. Tansey KE, Guipponi M, Domenici E, et al. Genetic susceptibility for bipolar disorder and response to antidepressants in major depressive disorder. Am J Med Genetics B Neuropsychiatr Genet. 2014;165B(1):77-83.
17. Tohen M, Zarate CA Jr, Hennen J, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160(12):2099-2107.
18. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas Consensus Conference Panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry. 2002;63(4):288-299.
19. Keck PE Jr, Perlis RH, Otto MW, et al. The Expert Consensus Guideline Series: treatment of bipolar disorder 2004. Postgrad Med Special Report. 2004:1-120.
20. Goldberg JF, Ghaemi SN. Benefits and limitations of antidepressants and traditional mood stabilizers for treatment of bipolar depression. Bipolar Disord. 2005;7(suppl 5):3-12.
21. Sidor MM, MacQueen GM. Antidepressants for the acute treatment of bipolar depression: a systematic review and meta-analysis. J Clin Psychiatry. 2011;72(2):156-167.
22. MacQueen GM, Trevor Young L, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105(6):414-418.
23. Solomon DA, Leon AC, Coryell WH, et al. Longitudinal course of bipolar I disorder: duration of mood episodes. Arch Gen Psychiatry. 2010;67(4):339-347.
24. Tohen M, Chengappa KN, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry. 2004;184:337-345.
25. Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry. 2009;166(4):476-488.
When a known depressed patient newly develops signs of mania or hypomania, a cascade of diagnostic and therapeutic questions ensues: Does the event “automatically” signify the presence of bipolar disorder (BD), or could manic symptoms be secondary to another underlying medical problem, a prescribed antidepressant or non-psychotropic medication, or illicit substances?
Even more questions confront the clinician: If mania symptoms are nothing more than an adverse drug reaction, will they go away by stopping the presumed offending agent? Or do symptoms always indicate the unmasking of a bipolar diathesis? Should anti-manic medication be prescribed immediately? If so, which one(s) and for how long? How extensive a medical or neurologic workup is indicated?
And, how do you differentiate ambiguous hypomania symptoms (irritability, insomnia, agitation) from other phenomena, such as akathisia, anxiety, and overstimulation?
In this article, we present an overview of how to approach and answer these key questions, so that you can identify, comprehend, and manage manic symptoms that arise in the course of your patient’s treatment for depression (Box).
Does disease exist on a unipolar−bipolar continuum?
There has been a resurgence of interest in Kraepelin’s original notion of mania and depression as falling along a continuum, rather than being distinct categories of pathology. True bipolar mania has its own identifiable epidemiology, familiality, and treatment, but symptomatic shades of gray often pose a formidable diagnostic and therapeutic challenge.
For example, DSM-5 relaxed its definition of “mixed” episodes of BD to include subsyndromal mania features in unipolar depression. When a patient with unipolar depression develops a full, unequivocal manic episode, there usually isn’t much ambiguity or confusion about initial management: assure a safe environment, stop any antidepressants, rule out drug- or medically induced causes, and begin an acute anti-manic medication.
Next steps can, sometimes, be murkier:
• formulate a definitive, overarching diagnosis
• provide psycho-education
• forecast return to work or school
• discuss prognosis and likelihood of relapse
• address necessary lifestyle modifications (eg, sleep hygiene, elimination of alcohol and illicit drug use)
• determine whether indefinite maintenance pharmacotherapy is indicated— and, if so, with which medication(s).
CASE A diagnostic formulation isn’t always black and white
Ms. J, age 56, a medically healthy woman, has a 10-year history of depression and anxiety that has been treated effectively for most of that time with venlafaxine, 225 mg/d. The mother of 4 grown children, Ms. J has worked steadily for >20 years as a flight attendant for an international airline.
Today, Ms. J is brought by ambulance from work to the emergency department in a paranoid and agitated state. The admission follows her having e-blasted airline corporate executives with a voluminous manifesto that she worked on around the clock the preceding week, in which she explained her bold ideas to revolutionize the airline industry, under her leadership.
Ms. J’s family history is unremarkable for psychiatric illness.
How does one approach a case such as Ms. J’s?
Stark examples of classical mania, as depicted in this case vignette, are easy to recognize but not necessarily straightforward, nosologically. Consider the following not-so-straightforward elements of Ms. J’s case:
• a first-lifetime episode of mania or hypomania is rare after age 50
• Ms. J took a serotonin-norepinephrine reuptake inhibitor (SNRI) for many years without evidence of mood destabilization
• years of repetitive chronobiological stress (including probable frequent time zone changes with likely sleep disruption) apparently did not trigger mood destabilization
• none of Ms. J’s 4 pregnancies led to postpartum mood episodes
• at least on the surface, there are no obvious features that point to likely causes of a secondary mania (eg, drug-induced, toxic, metabolic, or medical)
• Ms. J has no known family history of BD or any other mood disorder.
Approaching a case such as Ms. J’s must involve a systematic strategy that can best be broken into 2 segments: (1) a period of acute initial assessment and treatment and (2) later efforts focused on broader diagnostic evaluation and longer-term relapse prevention.
Initial assessment and treatment
Immediate assessment and management hinges on initial triage and forming a working diagnostic impression. Although full-blown mania usually is obvious (sometimes even without a formal interview), be alert to patients who might minimize or altogether disavow mania symptoms—often because of denial of illness, misidentification of symptoms, or impaired insight about changes in thinking, mood, or behavior.
Because florid mania, by definition, impairs psychosocial functioning, the context of an initial presentation often holds diagnostic relevance. Manic patients who display disruptive behaviors often are brought to treatment by a third party, whereas a less severely ill patient might be more inclined to seek treatment for herself (himself) when psychosis is absent and insight is less compromised or when the patient feels she (he) might be depressed.
It is not uncommon for a manic patient to report “depression” as the chief complaint or to omit elements related to psychomotor acceleration (such as racing thoughts or psychomotor agitation) in the description of symptoms. An accurate diagnosis often requires clinical probing and clarification of symptoms (eg, differentiating simple insomnia with consequent next-day fatigue from loss of the need for sleep with intact or even enhanced next-day energy) or discriminating racing thoughts from anxious ruminations that might be more intrusive than rapid.
Presentations of frank mania also can come to light as a consequence of symptoms, rather than as symptoms per se (eg, conflict in relationships, problems at work, financial reversals).
Particularly in patients who do not have a history of mania, avoid the temptation to begin or modify existing pharmacotherapy until you have performed a basic initial evaluation. Immediate considerations for initial assessment and management include the following:
Provide containment. Ensure a safe setting, level of care, and frequency of monitoring. Evaluate suicide risk (particularly when mixed features are present), and risk of withdrawal from any psychoactive substances.
Engage significant others. Close family members can provide essential history, particularly when a patient’s insight about her illness and need for treatment are impaired. Family members and significant others also often play important roles in helping to restrict access to finances, fostering medication adherence, preventing access to weapons in the home, and sharing information with providers about substance use or high-risk behavior.
Systematically assess for DSM-5 symptoms of mania and depression. DSM-5 modified criteria for mania/hypomania to necessitate increased energy, in addition to change in mood, to make a syndromal diagnosis. Useful during a clinical interview is the popular mnemonic DIGFAST to aid recognition of core mania symptomsa:
• Distractibility
• Indiscretion/impulsivity
• Grandiosity
• Flight of ideas
• Activity increase
• Sleep deficit
• Talkativeness.
aAlso see: “Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis,” in the October 2008 issue Current Psychiatry and in the archive at CurrentPsychiatry.com.
These symptoms should represent a departure from normal baseline characteristics; it often is helpful to ask a significant other or collateral historian how the present symptoms differ from the patient’s usual state.
Assess for unstable medical conditions or toxicity states. When evaluating an acute change in mental status, toxicology screening is relatively standard and the absence of illicit substances should seldom, if ever, be taken for granted—especially because occult substance use can lead to identification of false-positive BD “cases.”1
Stop any antidepressant. During a manic episode, continuing antidepressant medication serves no purpose other than to contribute to or exacerbate mania symptoms. Nonetheless, observational studies demonstrate that approximately 15% of syndromally manic patients continue to receive an antidepressant, often when a clinician perceives more severe depression during mania, multiple prior depressive episodes, current anxiety, or rapid cycling.2
Importantly, antidepressants have been shown to harm, rather than alleviate, presentations that involve a mixed state,3 and have no demonstrated value in preventing post-manic depression. Mere elimination of an antidepressant might ease symptoms during a manic or mixed episode.4
In some cases, it might be advisable to taper, not abruptly stop, a short half-life serotonergic antidepressant, even in the setting of mania, to minimize the potential for aggravating autonomic dysregulation that can result from antidepressant discontinuation effects.
Begin anti-manic pharmacotherapy. Initiation of an anti-manic mood stabilizer, such as lithium and divalproex, has been standard in the treatment of acute mania.
In the 1990s, protocols for oral loading of divalproex (20 to 30 mg/kg/d) gained popularity for achieving more rapid symptom improvement than might occur with lithium. In the current era, atypical antipsychotics have all but replaced mood stabilizers as an initial intervention to contain mania symptoms quickly (and with less risk than first-generation antipsychotics for acute adverse motor effects from so-called rapid neuroleptization).
Because atypical antipsychotics often rapidly subdue mania, psychosis, and agitation, regardless of the underlying process, many practitioners might feel more comfortable initiating them than a mood stabilizer when the diagnosis is ambiguous or provisional, although their longer-term efficacy and safety, relative to traditional mood stabilizers, remains contested. Considerations for choosing from among feasible anti-manic pharmacotherapies are summarized in Table 1.5
Normalize the sleep-wake cycle. Chronobiological and circadian variables, such as irregular sleep patterns, are thought to contribute to the pathophysiology of affective switch in BD. Behavioral and pharmacotherapeutic efforts to impose a normal sleep−wake schedule are considered fundamental to stabilizing acute mania.
Facilitate next steps after acute stabilization. For inpatients, this might involve step-down to a partial hospitalization or intensive outpatient program, alongside taking steps to ensure continued treatment adherence and minimize relapse.
What medical and neurologic workup is appropriate?
Not every first lifetime presentation of mania requires extensive medical and neurologic workup, particularly among patients who have a history of depression and those whose presentation neatly fits the demographic and clinical profile of newly emergent BD. Basic assessment should determine whether any new medication has been started that could plausibly contribute to abnormal mental status (Table 2).
Nevertheless, evaluation of almost all first presentations of mania should include:
• urine toxicology screen
• complete blood count
• comprehensive metabolic panel
• thyroid-stimulating hormone assay
• serum vitamin B12 level assay
• serum folic acid level assay
• rapid plasma reagin test.
Clinical features that usually lead a clinician to pursue a more detailed medical and neurologic evaluation of first-episode mania include:
• onset age >40
• absence of a family history of mood disorder
• symptoms arising during a major medical illness
• multiple medications
• suspicion of a degenerative or hereditary neurologic disorder
• altered state of consciousness
• signs of cortical or diffuse subcortical dysfunction (eg, cognitive deficits, motor deficits, tremor)
• abnormal vital signs.
Depending on the presentation, additional testing might include:
• tests of HIV antibody, immune autoantibodies, and Lyme disease antibody
• heavy metal screening (when suggested by environmental exposure)
• lumbar puncture (eg, in a setting of manic delirium or suspected central nervous system infection or paraneoplastic syndrome)
• neuroimaging (note: MRI provides better visualization than CT of white matter pathology and small vessel cerebrovascular disease) electroencephalography.
Making an overarching diagnosis: Is mania always bipolar disorder?
Mania is considered a manifestation of BD when symptoms cannot be attributed to another psychiatric condition, another underlying medical or neurologic condition, or a toxic-metabolic state (Table 3 and Table 46-9). Classification of mania that occurs soon after antidepressant exposure in patients without a known history of BD continues to be the subject of debate, varying in its conceptualization across editions of DSM.
The National Institute of Mental Health (NIMH) Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, observed a fairly low (approximately 10%) incidence of switch from depression to mania when an antidepressant is added to a mood stabilizer; the study authors concluded that much of what is presumed to be antidepressant-induced mania might simply be the natural course of illness.10
Notably, several reports suggest that antidepressants might pose a greater risk of mood destabilization in people with BD I than with either BD II or other suspected variants on the bipolar spectrum.
DSM-5 advises that a diagnosis of substance-induced mood disorder appropriately describes symptoms that spontaneously dissipate once an antidepressant has been discontinued, whereas a diagnosis of BD can be made when manic or hypomanic symptoms persist at a syndromal level after an antidepressant has been stopped and its physiological effects are no longer present. With respect to time course, the International Society of Bipolar Disorders proposes that, beyond 12 to 16 weeks after an antidepressant has been started or the dosage has been increased, it is unlikely that new-onset mania/hypomania can reasonably be attributed to “triggering” by an antidepressant11 (although antidepressants should be stopped when symptoms of mania emerge).
Several clinical features have been linked in the literature with an increased susceptibility to BD after an initial depressive episode, including:
• early (pre-adolescent) age at onset of first mood disorder episode6
• family history of BD, highly recurrent depression, or psychosis12,13
• psychosis when depressed.7,14
A number of other characteristics of depressive illness—including seasonal depression, atypical depressive features, suicidality, irritability, anxiety or substance use comorbidity, postpartum mood episodes, and brief recurrent depressive episodes—have been described in the literature as potential correlates of a bipolar diathesis; none have proved to be robust or pathognomonic of a BD diagnosis, as opposed to a unipolar diagnosis.
Data from the NIMH Collaborative Depression Study suggest that recurrent mania/hypomania after an antidepressant-associated polarity switch is greater when a family history of BD is present; other clinical variables might hold less predictive value.15
In addition, although some practitioners consider a history of nonresponse to trials of multiple antidepressants suggestive of an underlying bipolar process, polarity is only one of many variables that must be considered in the differential diagnosis of antidepressant-resistant depression.b Likewise, molecular genetic studies do not support a link between antidepressant nonresponse and the likelihood of a diagnosis of BD.16
bSee “A practical approach to subtyping depression among your patients” in the April 2014 issue of Current Psychiatry or in the archive at CurrentPsychiatry.com.
Indefinite pharmacotherapy for bipolar disorder?
An important but nagging issue when diagnosing BD after a first manic (or hypomanic) episode is the implied need for indefinite pharmacotherapy to sustain remission and prevent relapse and recurrence.
The likelihood of subsequent depression or mania/hypomania remains high after an index manic/hypomanic episode, particularly for 6 to 8 months after recovery.8,17 Natural history data suggest that, during the year that follows a first lifetime mania, approximately 40% of patients experience a second manic episode.8 A second lifetime mania might be especially likely in patients whose index episode involved mood-congruent psychosis, low premorbid work functioning, and an initial manic episode, as opposed to a mixed episode17 or early age at onset.8
In the absence of randomized, placebo-controlled studies of maintenance pharmacotherapy after a first lifetime manic episode, clinical judgment often drives decisions about the duration of continuing pharmacotherapy after initial symptoms resolve. The Texas Medication Algorithm Project for BD advises that:
Similarly, in the most recent (2004) Expert Consensus Guideline Series for the Treatment of Bipolar Disorder,19 84% of practitioner−respondents favored indefinite mood stabilizer therapy after a second lifetime manic episode. No recommendation was made about the duration of maintenance pharmacotherapy after a first lifetime manic/hypomanic episode.
Avoid or reintroduce an antidepressant if depression recurs after a first mania?
Controversies surrounding antidepressant use in BD are extensive; detailed discussion is beyond the scope of this review (Goldberg and Ghaemi provided a broader discussion of risks and benefits of antidepressants in BD20). Although the main clinical concern regarding antidepressant use was, at one time, the potential to induce mania or accelerate the frequency of recurrent episodes, more recent, empirical studies suggest that the greater risk of using antidepressants for BD is lack of efficacy.10,21
If a careful longitudinal history and clinical evaluation reveal that an initial manic episode heralds the onset of BD, decisions about whether to avoid an antidepressant (as opposed to using other, more evidence-based interventions for bipolar depression) depend on a number of variables, including establishing whether the index episode was manic or hypomanic; ruling out current subthreshold mixed features; and clarifying how recently mania developed. Decisions about future antidepressant use (or avoidance) might be less clear if an index manic/hypomanic episode was brief and self-limited once the antidepressant was stopped.
Although some experts eschew antidepressant monotherapy after such occurrences, there is no body of literature to inform decisions about the safety or efficacy of undertaking a future antidepressant trial in such patients. That said, reasonable judgment probably includes several considerations:
• Re-exposure to the same antidepressant that was associated with an induction of mania is likely riskier than choosing a different antidepressant; in general, purely serotonergic antidepressants or bupropion are considered to pose less risk of mood destabilization than is seen with an SNRI or tricyclic antidepressant.
• After a manic episode, a subsequent antidepressant trial generally shouldn’t be attempted without concurrent anti-manic medication.
• Introducing any antidepressant is probably ill-advised in the recent (~2 months) aftermath of acute manic/ hypomanic symptoms.22
• Patients and their significant other should be apprised of the risk of emerging symptoms of mania or hypomania, or mixed features, and should be familiar with key target symptoms to watch for. Prospective mood charting can be helpful.
• Patients should be monitored closely both for an exacerbation of depression and recurrence of mania/hypomania symptoms.
• Any antidepressant should be discontinued promptly at the first sign of psychomotor acceleration or the emergence of mixed features, as defined by DSM-5.
Psychoeducation and forecasting
Functional recovery from a manic episode can lag behind symptomatic recovery. Subsyndromal symptoms often persist after a full episode subsides.
Mania often is followed by a depressive episode, and questions inevitably arise about how to prevent and treat these episodes. Because the median duration of a manic episode is approximately 13 weeks,23 it is crucial for patients and their immediate family to recognize that recovery might be gradual, and that it will likely take time before she (he) can resume full-time responsibilities at work or school or in the home.
Today, a patient who is hospitalized for severe acute mania (as Ms. J was, in the case vignette) seldom remains an inpatient long enough to achieve remission of symptoms; sometimes, she (he) might continue to manifest significant symptoms, even though decisions about the “medical necessity” of ongoing inpatient care tend to be governed mainly by issues of safety and imminent danger. (This web exclusive Table20,24,25 provides considerations when making the transition from the acute phase to the continuation phase of treatment.)
To minimize risk of relapse, psycho-education should include discussion of:
• psychiatrically deleterious effects of alcohol and illicit drug use
• suicide risk, including what to do in an emergency
• protecting a regular sleep schedule and avoiding sleep deprivation
• the potential for poor medication adherence and management of side effects
• the need for periodic laboratory monitoring, as needed
• the role of adjunctive psychotherapy and effective stress management
• familiarity with symptoms that serve as warning signs, and how to monitor their onset.
Bottom Line
When a patient being treated for depression develops signs of mania or hypomania, stop any antidepressant and consider initiating a mood stabilizer, antipsychotic, or both, to contain and stabilize symptoms. Entertain medical and substance-related causes of mania symptoms, and evaluate and treat as suggested by the patient’s presentation. Long-term drug therapy to prevent recurrence of mania/hypomania, as well as risks and benefits of future exposure to antidepressants, should be decided case by case.
Related Resources
• Proudfoot J, Whitton A, Parker G, et al. Triggers of mania and depression in young adults with bipolar disorder. J Affect Disord. 2012;143(1-3):196-202.
• Stange JP, Sylvia LG, Magalhães PV, et al. Extreme attributions predict transition from depression to mania or hypomania in bipolar disorder. J Psychiatr Res. 2013;47(10):1329-1336.
Drug Brand Names
Albuterol • Proventil, Ventolin
Anastrozole • Arimidex
Aripiprazole • Abilify
Bupropion • Wellbutrin
Carbamazepine • Tegretol
Chloroquine • Aralen
Ciprofloxacin • Cipro
Clarithromycin • Biaxin
Clomiphene • Clomid
Digoxin • Digox, Lanoxin
Divalproex • Depakote
5-Fluorouracil • Carac, Efudex
Human chorionic gonadotropin • Novarel, Pregnyl
Ifosfamide • Ifex
Isoniazid • Nydrazid
Lamotrigine • Lamictal
Letrozole • Femara
Lithium • Eskalith, Lithobid
Lurasidone • Latuda
Mefloquine • Lariam
Olanzapine • Zyprexa
Olanzapine/fluoxetine combination • Symbyax
ramipexole • Mirapex
Procarbazine • Matulane
Quetiapine • Seroquel
Ropinirole • Requip
Rotigotine • Neupro
Venlafaxine • Effexor
Zidovudine • Retrovir
Disclosures
Dr. Goldberg is a consultant to Merck & Co. and Sunovion. He is a member of the speakers’ bureau of AstraZeneca, Janssen, Merck & Co., Takeda and Lundbeck, and Sunovion.
Dr. Ernst reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
When a known depressed patient newly develops signs of mania or hypomania, a cascade of diagnostic and therapeutic questions ensues: Does the event “automatically” signify the presence of bipolar disorder (BD), or could manic symptoms be secondary to another underlying medical problem, a prescribed antidepressant or non-psychotropic medication, or illicit substances?
Even more questions confront the clinician: If mania symptoms are nothing more than an adverse drug reaction, will they go away by stopping the presumed offending agent? Or do symptoms always indicate the unmasking of a bipolar diathesis? Should anti-manic medication be prescribed immediately? If so, which one(s) and for how long? How extensive a medical or neurologic workup is indicated?
And, how do you differentiate ambiguous hypomania symptoms (irritability, insomnia, agitation) from other phenomena, such as akathisia, anxiety, and overstimulation?
In this article, we present an overview of how to approach and answer these key questions, so that you can identify, comprehend, and manage manic symptoms that arise in the course of your patient’s treatment for depression (Box).
Does disease exist on a unipolar−bipolar continuum?
There has been a resurgence of interest in Kraepelin’s original notion of mania and depression as falling along a continuum, rather than being distinct categories of pathology. True bipolar mania has its own identifiable epidemiology, familiality, and treatment, but symptomatic shades of gray often pose a formidable diagnostic and therapeutic challenge.
For example, DSM-5 relaxed its definition of “mixed” episodes of BD to include subsyndromal mania features in unipolar depression. When a patient with unipolar depression develops a full, unequivocal manic episode, there usually isn’t much ambiguity or confusion about initial management: assure a safe environment, stop any antidepressants, rule out drug- or medically induced causes, and begin an acute anti-manic medication.
Next steps can, sometimes, be murkier:
• formulate a definitive, overarching diagnosis
• provide psycho-education
• forecast return to work or school
• discuss prognosis and likelihood of relapse
• address necessary lifestyle modifications (eg, sleep hygiene, elimination of alcohol and illicit drug use)
• determine whether indefinite maintenance pharmacotherapy is indicated— and, if so, with which medication(s).
CASE A diagnostic formulation isn’t always black and white
Ms. J, age 56, a medically healthy woman, has a 10-year history of depression and anxiety that has been treated effectively for most of that time with venlafaxine, 225 mg/d. The mother of 4 grown children, Ms. J has worked steadily for >20 years as a flight attendant for an international airline.
Today, Ms. J is brought by ambulance from work to the emergency department in a paranoid and agitated state. The admission follows her having e-blasted airline corporate executives with a voluminous manifesto that she worked on around the clock the preceding week, in which she explained her bold ideas to revolutionize the airline industry, under her leadership.
Ms. J’s family history is unremarkable for psychiatric illness.
How does one approach a case such as Ms. J’s?
Stark examples of classical mania, as depicted in this case vignette, are easy to recognize but not necessarily straightforward, nosologically. Consider the following not-so-straightforward elements of Ms. J’s case:
• a first-lifetime episode of mania or hypomania is rare after age 50
• Ms. J took a serotonin-norepinephrine reuptake inhibitor (SNRI) for many years without evidence of mood destabilization
• years of repetitive chronobiological stress (including probable frequent time zone changes with likely sleep disruption) apparently did not trigger mood destabilization
• none of Ms. J’s 4 pregnancies led to postpartum mood episodes
• at least on the surface, there are no obvious features that point to likely causes of a secondary mania (eg, drug-induced, toxic, metabolic, or medical)
• Ms. J has no known family history of BD or any other mood disorder.
Approaching a case such as Ms. J’s must involve a systematic strategy that can best be broken into 2 segments: (1) a period of acute initial assessment and treatment and (2) later efforts focused on broader diagnostic evaluation and longer-term relapse prevention.
Initial assessment and treatment
Immediate assessment and management hinges on initial triage and forming a working diagnostic impression. Although full-blown mania usually is obvious (sometimes even without a formal interview), be alert to patients who might minimize or altogether disavow mania symptoms—often because of denial of illness, misidentification of symptoms, or impaired insight about changes in thinking, mood, or behavior.
Because florid mania, by definition, impairs psychosocial functioning, the context of an initial presentation often holds diagnostic relevance. Manic patients who display disruptive behaviors often are brought to treatment by a third party, whereas a less severely ill patient might be more inclined to seek treatment for herself (himself) when psychosis is absent and insight is less compromised or when the patient feels she (he) might be depressed.
It is not uncommon for a manic patient to report “depression” as the chief complaint or to omit elements related to psychomotor acceleration (such as racing thoughts or psychomotor agitation) in the description of symptoms. An accurate diagnosis often requires clinical probing and clarification of symptoms (eg, differentiating simple insomnia with consequent next-day fatigue from loss of the need for sleep with intact or even enhanced next-day energy) or discriminating racing thoughts from anxious ruminations that might be more intrusive than rapid.
Presentations of frank mania also can come to light as a consequence of symptoms, rather than as symptoms per se (eg, conflict in relationships, problems at work, financial reversals).
Particularly in patients who do not have a history of mania, avoid the temptation to begin or modify existing pharmacotherapy until you have performed a basic initial evaluation. Immediate considerations for initial assessment and management include the following:
Provide containment. Ensure a safe setting, level of care, and frequency of monitoring. Evaluate suicide risk (particularly when mixed features are present), and risk of withdrawal from any psychoactive substances.
Engage significant others. Close family members can provide essential history, particularly when a patient’s insight about her illness and need for treatment are impaired. Family members and significant others also often play important roles in helping to restrict access to finances, fostering medication adherence, preventing access to weapons in the home, and sharing information with providers about substance use or high-risk behavior.
Systematically assess for DSM-5 symptoms of mania and depression. DSM-5 modified criteria for mania/hypomania to necessitate increased energy, in addition to change in mood, to make a syndromal diagnosis. Useful during a clinical interview is the popular mnemonic DIGFAST to aid recognition of core mania symptomsa:
• Distractibility
• Indiscretion/impulsivity
• Grandiosity
• Flight of ideas
• Activity increase
• Sleep deficit
• Talkativeness.
aAlso see: “Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis,” in the October 2008 issue Current Psychiatry and in the archive at CurrentPsychiatry.com.
These symptoms should represent a departure from normal baseline characteristics; it often is helpful to ask a significant other or collateral historian how the present symptoms differ from the patient’s usual state.
Assess for unstable medical conditions or toxicity states. When evaluating an acute change in mental status, toxicology screening is relatively standard and the absence of illicit substances should seldom, if ever, be taken for granted—especially because occult substance use can lead to identification of false-positive BD “cases.”1
Stop any antidepressant. During a manic episode, continuing antidepressant medication serves no purpose other than to contribute to or exacerbate mania symptoms. Nonetheless, observational studies demonstrate that approximately 15% of syndromally manic patients continue to receive an antidepressant, often when a clinician perceives more severe depression during mania, multiple prior depressive episodes, current anxiety, or rapid cycling.2
Importantly, antidepressants have been shown to harm, rather than alleviate, presentations that involve a mixed state,3 and have no demonstrated value in preventing post-manic depression. Mere elimination of an antidepressant might ease symptoms during a manic or mixed episode.4
In some cases, it might be advisable to taper, not abruptly stop, a short half-life serotonergic antidepressant, even in the setting of mania, to minimize the potential for aggravating autonomic dysregulation that can result from antidepressant discontinuation effects.
Begin anti-manic pharmacotherapy. Initiation of an anti-manic mood stabilizer, such as lithium and divalproex, has been standard in the treatment of acute mania.
In the 1990s, protocols for oral loading of divalproex (20 to 30 mg/kg/d) gained popularity for achieving more rapid symptom improvement than might occur with lithium. In the current era, atypical antipsychotics have all but replaced mood stabilizers as an initial intervention to contain mania symptoms quickly (and with less risk than first-generation antipsychotics for acute adverse motor effects from so-called rapid neuroleptization).
Because atypical antipsychotics often rapidly subdue mania, psychosis, and agitation, regardless of the underlying process, many practitioners might feel more comfortable initiating them than a mood stabilizer when the diagnosis is ambiguous or provisional, although their longer-term efficacy and safety, relative to traditional mood stabilizers, remains contested. Considerations for choosing from among feasible anti-manic pharmacotherapies are summarized in Table 1.5
Normalize the sleep-wake cycle. Chronobiological and circadian variables, such as irregular sleep patterns, are thought to contribute to the pathophysiology of affective switch in BD. Behavioral and pharmacotherapeutic efforts to impose a normal sleep−wake schedule are considered fundamental to stabilizing acute mania.
Facilitate next steps after acute stabilization. For inpatients, this might involve step-down to a partial hospitalization or intensive outpatient program, alongside taking steps to ensure continued treatment adherence and minimize relapse.
What medical and neurologic workup is appropriate?
Not every first lifetime presentation of mania requires extensive medical and neurologic workup, particularly among patients who have a history of depression and those whose presentation neatly fits the demographic and clinical profile of newly emergent BD. Basic assessment should determine whether any new medication has been started that could plausibly contribute to abnormal mental status (Table 2).
Nevertheless, evaluation of almost all first presentations of mania should include:
• urine toxicology screen
• complete blood count
• comprehensive metabolic panel
• thyroid-stimulating hormone assay
• serum vitamin B12 level assay
• serum folic acid level assay
• rapid plasma reagin test.
Clinical features that usually lead a clinician to pursue a more detailed medical and neurologic evaluation of first-episode mania include:
• onset age >40
• absence of a family history of mood disorder
• symptoms arising during a major medical illness
• multiple medications
• suspicion of a degenerative or hereditary neurologic disorder
• altered state of consciousness
• signs of cortical or diffuse subcortical dysfunction (eg, cognitive deficits, motor deficits, tremor)
• abnormal vital signs.
Depending on the presentation, additional testing might include:
• tests of HIV antibody, immune autoantibodies, and Lyme disease antibody
• heavy metal screening (when suggested by environmental exposure)
• lumbar puncture (eg, in a setting of manic delirium or suspected central nervous system infection or paraneoplastic syndrome)
• neuroimaging (note: MRI provides better visualization than CT of white matter pathology and small vessel cerebrovascular disease) electroencephalography.
Making an overarching diagnosis: Is mania always bipolar disorder?
Mania is considered a manifestation of BD when symptoms cannot be attributed to another psychiatric condition, another underlying medical or neurologic condition, or a toxic-metabolic state (Table 3 and Table 46-9). Classification of mania that occurs soon after antidepressant exposure in patients without a known history of BD continues to be the subject of debate, varying in its conceptualization across editions of DSM.
The National Institute of Mental Health (NIMH) Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, observed a fairly low (approximately 10%) incidence of switch from depression to mania when an antidepressant is added to a mood stabilizer; the study authors concluded that much of what is presumed to be antidepressant-induced mania might simply be the natural course of illness.10
Notably, several reports suggest that antidepressants might pose a greater risk of mood destabilization in people with BD I than with either BD II or other suspected variants on the bipolar spectrum.
DSM-5 advises that a diagnosis of substance-induced mood disorder appropriately describes symptoms that spontaneously dissipate once an antidepressant has been discontinued, whereas a diagnosis of BD can be made when manic or hypomanic symptoms persist at a syndromal level after an antidepressant has been stopped and its physiological effects are no longer present. With respect to time course, the International Society of Bipolar Disorders proposes that, beyond 12 to 16 weeks after an antidepressant has been started or the dosage has been increased, it is unlikely that new-onset mania/hypomania can reasonably be attributed to “triggering” by an antidepressant11 (although antidepressants should be stopped when symptoms of mania emerge).
Several clinical features have been linked in the literature with an increased susceptibility to BD after an initial depressive episode, including:
• early (pre-adolescent) age at onset of first mood disorder episode6
• family history of BD, highly recurrent depression, or psychosis12,13
• psychosis when depressed.7,14
A number of other characteristics of depressive illness—including seasonal depression, atypical depressive features, suicidality, irritability, anxiety or substance use comorbidity, postpartum mood episodes, and brief recurrent depressive episodes—have been described in the literature as potential correlates of a bipolar diathesis; none have proved to be robust or pathognomonic of a BD diagnosis, as opposed to a unipolar diagnosis.
Data from the NIMH Collaborative Depression Study suggest that recurrent mania/hypomania after an antidepressant-associated polarity switch is greater when a family history of BD is present; other clinical variables might hold less predictive value.15
In addition, although some practitioners consider a history of nonresponse to trials of multiple antidepressants suggestive of an underlying bipolar process, polarity is only one of many variables that must be considered in the differential diagnosis of antidepressant-resistant depression.b Likewise, molecular genetic studies do not support a link between antidepressant nonresponse and the likelihood of a diagnosis of BD.16
bSee “A practical approach to subtyping depression among your patients” in the April 2014 issue of Current Psychiatry or in the archive at CurrentPsychiatry.com.
Indefinite pharmacotherapy for bipolar disorder?
An important but nagging issue when diagnosing BD after a first manic (or hypomanic) episode is the implied need for indefinite pharmacotherapy to sustain remission and prevent relapse and recurrence.
The likelihood of subsequent depression or mania/hypomania remains high after an index manic/hypomanic episode, particularly for 6 to 8 months after recovery.8,17 Natural history data suggest that, during the year that follows a first lifetime mania, approximately 40% of patients experience a second manic episode.8 A second lifetime mania might be especially likely in patients whose index episode involved mood-congruent psychosis, low premorbid work functioning, and an initial manic episode, as opposed to a mixed episode17 or early age at onset.8
In the absence of randomized, placebo-controlled studies of maintenance pharmacotherapy after a first lifetime manic episode, clinical judgment often drives decisions about the duration of continuing pharmacotherapy after initial symptoms resolve. The Texas Medication Algorithm Project for BD advises that:
Similarly, in the most recent (2004) Expert Consensus Guideline Series for the Treatment of Bipolar Disorder,19 84% of practitioner−respondents favored indefinite mood stabilizer therapy after a second lifetime manic episode. No recommendation was made about the duration of maintenance pharmacotherapy after a first lifetime manic/hypomanic episode.
Avoid or reintroduce an antidepressant if depression recurs after a first mania?
Controversies surrounding antidepressant use in BD are extensive; detailed discussion is beyond the scope of this review (Goldberg and Ghaemi provided a broader discussion of risks and benefits of antidepressants in BD20). Although the main clinical concern regarding antidepressant use was, at one time, the potential to induce mania or accelerate the frequency of recurrent episodes, more recent, empirical studies suggest that the greater risk of using antidepressants for BD is lack of efficacy.10,21
If a careful longitudinal history and clinical evaluation reveal that an initial manic episode heralds the onset of BD, decisions about whether to avoid an antidepressant (as opposed to using other, more evidence-based interventions for bipolar depression) depend on a number of variables, including establishing whether the index episode was manic or hypomanic; ruling out current subthreshold mixed features; and clarifying how recently mania developed. Decisions about future antidepressant use (or avoidance) might be less clear if an index manic/hypomanic episode was brief and self-limited once the antidepressant was stopped.
Although some experts eschew antidepressant monotherapy after such occurrences, there is no body of literature to inform decisions about the safety or efficacy of undertaking a future antidepressant trial in such patients. That said, reasonable judgment probably includes several considerations:
• Re-exposure to the same antidepressant that was associated with an induction of mania is likely riskier than choosing a different antidepressant; in general, purely serotonergic antidepressants or bupropion are considered to pose less risk of mood destabilization than is seen with an SNRI or tricyclic antidepressant.
• After a manic episode, a subsequent antidepressant trial generally shouldn’t be attempted without concurrent anti-manic medication.
• Introducing any antidepressant is probably ill-advised in the recent (~2 months) aftermath of acute manic/ hypomanic symptoms.22
• Patients and their significant other should be apprised of the risk of emerging symptoms of mania or hypomania, or mixed features, and should be familiar with key target symptoms to watch for. Prospective mood charting can be helpful.
• Patients should be monitored closely both for an exacerbation of depression and recurrence of mania/hypomania symptoms.
• Any antidepressant should be discontinued promptly at the first sign of psychomotor acceleration or the emergence of mixed features, as defined by DSM-5.
Psychoeducation and forecasting
Functional recovery from a manic episode can lag behind symptomatic recovery. Subsyndromal symptoms often persist after a full episode subsides.
Mania often is followed by a depressive episode, and questions inevitably arise about how to prevent and treat these episodes. Because the median duration of a manic episode is approximately 13 weeks,23 it is crucial for patients and their immediate family to recognize that recovery might be gradual, and that it will likely take time before she (he) can resume full-time responsibilities at work or school or in the home.
Today, a patient who is hospitalized for severe acute mania (as Ms. J was, in the case vignette) seldom remains an inpatient long enough to achieve remission of symptoms; sometimes, she (he) might continue to manifest significant symptoms, even though decisions about the “medical necessity” of ongoing inpatient care tend to be governed mainly by issues of safety and imminent danger. (This web exclusive Table20,24,25 provides considerations when making the transition from the acute phase to the continuation phase of treatment.)
To minimize risk of relapse, psycho-education should include discussion of:
• psychiatrically deleterious effects of alcohol and illicit drug use
• suicide risk, including what to do in an emergency
• protecting a regular sleep schedule and avoiding sleep deprivation
• the potential for poor medication adherence and management of side effects
• the need for periodic laboratory monitoring, as needed
• the role of adjunctive psychotherapy and effective stress management
• familiarity with symptoms that serve as warning signs, and how to monitor their onset.
Bottom Line
When a patient being treated for depression develops signs of mania or hypomania, stop any antidepressant and consider initiating a mood stabilizer, antipsychotic, or both, to contain and stabilize symptoms. Entertain medical and substance-related causes of mania symptoms, and evaluate and treat as suggested by the patient’s presentation. Long-term drug therapy to prevent recurrence of mania/hypomania, as well as risks and benefits of future exposure to antidepressants, should be decided case by case.
Related Resources
• Proudfoot J, Whitton A, Parker G, et al. Triggers of mania and depression in young adults with bipolar disorder. J Affect Disord. 2012;143(1-3):196-202.
• Stange JP, Sylvia LG, Magalhães PV, et al. Extreme attributions predict transition from depression to mania or hypomania in bipolar disorder. J Psychiatr Res. 2013;47(10):1329-1336.
Drug Brand Names
Albuterol • Proventil, Ventolin
Anastrozole • Arimidex
Aripiprazole • Abilify
Bupropion • Wellbutrin
Carbamazepine • Tegretol
Chloroquine • Aralen
Ciprofloxacin • Cipro
Clarithromycin • Biaxin
Clomiphene • Clomid
Digoxin • Digox, Lanoxin
Divalproex • Depakote
5-Fluorouracil • Carac, Efudex
Human chorionic gonadotropin • Novarel, Pregnyl
Ifosfamide • Ifex
Isoniazid • Nydrazid
Lamotrigine • Lamictal
Letrozole • Femara
Lithium • Eskalith, Lithobid
Lurasidone • Latuda
Mefloquine • Lariam
Olanzapine • Zyprexa
Olanzapine/fluoxetine combination • Symbyax
ramipexole • Mirapex
Procarbazine • Matulane
Quetiapine • Seroquel
Ropinirole • Requip
Rotigotine • Neupro
Venlafaxine • Effexor
Zidovudine • Retrovir
Disclosures
Dr. Goldberg is a consultant to Merck & Co. and Sunovion. He is a member of the speakers’ bureau of AstraZeneca, Janssen, Merck & Co., Takeda and Lundbeck, and Sunovion.
Dr. Ernst reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder in patients with mood instability. J Clin Psychiatry. 2008;69(11):1751-1757.
2. Rosa AR, Cruz B, Franco C, et al. Why do clinicians maintain antidepressants in some patients with acute mania? Hints from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM), a large naturalistic study. J Clin Psychiatry. 2010;71(8):1000-1006.
3. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355.
4. Bowers MB Jr, McKay BG, Mazure CM. Discontinuation of antidepressants in newly admitted psychotic patients. J Neuropsychiatr Clin Neurosci. 2003;15(2):227-230.
5. Perlis RH, Welge JA, Vornik LA, et al. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4):509-516.
6. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158(1):125-127.
7. Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158(8):1265-1270.
8. Yatham LN, Kauer-Sant’Anna M, Bond DJ, et al. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Project for Early Mania project. Can J Psychiatry. 2009;54(2):105-112.
9. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry 2003;64(11):1284-1292.
10. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711-1722.
11. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11(15):453-473.
12. Schulze TG, Hedeker D, Zandi P, et al. What is familial about familial bipolar disorder? Resemblance among relatives across a broad spectrum of phenotypic characteristics. Arch Gen Psychiatry. 2006;63(12):1368-1376.
13. Song J, Bergen SE, Kuja-Halkola R, et al. Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord. 2015;7(2):184-193.
14. Goes FS, Sadler B, Toolan J, et al. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007;9(8):901-906.
15. Fiedorowicz JG, Endicott J, Solomon DA, et al. Course of illness following prospectively observed mania or hypomania in individuals presenting with unipolar depression. Bipolar Disord. 2007;14(6):664-671.
16. Tansey KE, Guipponi M, Domenici E, et al. Genetic susceptibility for bipolar disorder and response to antidepressants in major depressive disorder. Am J Med Genetics B Neuropsychiatr Genet. 2014;165B(1):77-83.
17. Tohen M, Zarate CA Jr, Hennen J, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160(12):2099-2107.
18. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas Consensus Conference Panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry. 2002;63(4):288-299.
19. Keck PE Jr, Perlis RH, Otto MW, et al. The Expert Consensus Guideline Series: treatment of bipolar disorder 2004. Postgrad Med Special Report. 2004:1-120.
20. Goldberg JF, Ghaemi SN. Benefits and limitations of antidepressants and traditional mood stabilizers for treatment of bipolar depression. Bipolar Disord. 2005;7(suppl 5):3-12.
21. Sidor MM, MacQueen GM. Antidepressants for the acute treatment of bipolar depression: a systematic review and meta-analysis. J Clin Psychiatry. 2011;72(2):156-167.
22. MacQueen GM, Trevor Young L, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105(6):414-418.
23. Solomon DA, Leon AC, Coryell WH, et al. Longitudinal course of bipolar I disorder: duration of mood episodes. Arch Gen Psychiatry. 2010;67(4):339-347.
24. Tohen M, Chengappa KN, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry. 2004;184:337-345.
25. Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry. 2009;166(4):476-488.
1. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder in patients with mood instability. J Clin Psychiatry. 2008;69(11):1751-1757.
2. Rosa AR, Cruz B, Franco C, et al. Why do clinicians maintain antidepressants in some patients with acute mania? Hints from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM), a large naturalistic study. J Clin Psychiatry. 2010;71(8):1000-1006.
3. Goldberg JF, Perlis RH, Ghaemi SN, et al. Adjunctive antidepressant use and symptomatic recovery among bipolar depressed patients with concomitant manic symptoms: findings from the STEP-BD. Am J Psychiatry. 2007;164(9):1348-1355.
4. Bowers MB Jr, McKay BG, Mazure CM. Discontinuation of antidepressants in newly admitted psychotic patients. J Neuropsychiatr Clin Neurosci. 2003;15(2):227-230.
5. Perlis RH, Welge JA, Vornik LA, et al. Atypical antipsychotics in the treatment of mania: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2006;67(4):509-516.
6. Geller B, Zimmerman B, Williams M, et al. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158(1):125-127.
7. Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158(8):1265-1270.
8. Yatham LN, Kauer-Sant’Anna M, Bond DJ, et al. Course and outcome after the first manic episode in patients with bipolar disorder: prospective 12-month data from the Systematic Treatment Optimization Project for Early Mania project. Can J Psychiatry. 2009;54(2):105-112.
9. Chaudron LH, Pies RW. The relationship between postpartum psychosis and bipolar disorder: a review. J Clin Psychiatry 2003;64(11):1284-1292.
10. Sachs GS, Nierenberg AA, Calabrese JR, et al. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356(17):1711-1722.
11. Tohen M, Frank E, Bowden CL, et al. The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord. 2009;11(15):453-473.
12. Schulze TG, Hedeker D, Zandi P, et al. What is familial about familial bipolar disorder? Resemblance among relatives across a broad spectrum of phenotypic characteristics. Arch Gen Psychiatry. 2006;63(12):1368-1376.
13. Song J, Bergen SE, Kuja-Halkola R, et al. Bipolar disorder and its relation to major psychiatric disorders: a family-based study in the Swedish population. Bipolar Disord. 2015;7(2):184-193.
14. Goes FS, Sadler B, Toolan J, et al. Psychotic features in bipolar and unipolar depression. Bipolar Disord. 2007;9(8):901-906.
15. Fiedorowicz JG, Endicott J, Solomon DA, et al. Course of illness following prospectively observed mania or hypomania in individuals presenting with unipolar depression. Bipolar Disord. 2007;14(6):664-671.
16. Tansey KE, Guipponi M, Domenici E, et al. Genetic susceptibility for bipolar disorder and response to antidepressants in major depressive disorder. Am J Med Genetics B Neuropsychiatr Genet. 2014;165B(1):77-83.
17. Tohen M, Zarate CA Jr, Hennen J, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160(12):2099-2107.
18. Suppes T, Dennehy EB, Swann AC, et al. Report of the Texas Consensus Conference Panel on medication treatment of bipolar disorder 2000. J Clin Psychiatry. 2002;63(4):288-299.
19. Keck PE Jr, Perlis RH, Otto MW, et al. The Expert Consensus Guideline Series: treatment of bipolar disorder 2004. Postgrad Med Special Report. 2004:1-120.
20. Goldberg JF, Ghaemi SN. Benefits and limitations of antidepressants and traditional mood stabilizers for treatment of bipolar depression. Bipolar Disord. 2005;7(suppl 5):3-12.
21. Sidor MM, MacQueen GM. Antidepressants for the acute treatment of bipolar depression: a systematic review and meta-analysis. J Clin Psychiatry. 2011;72(2):156-167.
22. MacQueen GM, Trevor Young L, Marriott M, et al. Previous mood state predicts response and switch rates in patients with bipolar depression. Acta Psychiatr Scand. 2002;105(6):414-418.
23. Solomon DA, Leon AC, Coryell WH, et al. Longitudinal course of bipolar I disorder: duration of mood episodes. Arch Gen Psychiatry. 2010;67(4):339-347.
24. Tohen M, Chengappa KN, Suppes T, et al. Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry. 2004;184:337-345.
25. Suppes T, Vieta E, Liu S, et al. Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry. 2009;166(4):476-488.
Novel treatments for depression
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Second of 2 parts: A practical approach to subtyping depression among your patients
Depression—sad, empty, or irritable mood accompanied by somatic or cognitive changes—is not a homogeneous condition. Recognizing subtypes of depressive illness can guide treatment and relieve your patient’s suffering. In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular subgroups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonresponse or partial response, often hinges on clinical subtyping.
The second part of this article examines “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder. Treatments for these subtypes for which there is evidence, or a clinical rationale, are given in the Table.
‘Situational depression’
In recent decades, the phenomenon of nonsyndromal depression after a life stress has undergone many name changes but little conceptional revision: “situational,” “reactive,” and “neurotic” labels for depression that were used before DSM-III became “adjustment disorders” in DSM-IV-TR and then “stress response syndromes” in DSM-5. These names all connote presentations of depressed mood after an environmental stressor, without either the full constellation of symptoms that define major depression or the chronicity of dysthymic disorder.
Paucity of guidance. There has been little research to identify vulnerability variables for adjustment disorders in the aftermath of particular stressors. Similarly, extensive data are lacking on 1) the likely progression of such disorders to a syndromal form of depression or 2) protective factors against developing clinically significant depression after a life stress. The extent to which adjustment disorders lie on a continuum with major mood disorders is not well-established, although subthreshold levels of depression can predispose to major depression or suicidal behaviors.1
Models of behavioral sensitization posit that stressful life events more often precede first or early episodes of depression than subsequent recurrences.2 At the same time, non-melancholic depressions that are preceded by “situational stresses” tend to recur in similar fashion.3
Medical therapy of value? Psychotherapy without medication—apart from occasional sedative−hypnotic drugs as needed for insomnia, anxiety, or distress—is considered the standard of care for treating an adjustment disorder. No drug has demonstrated superiority to placebo for alleviating symptoms of an adjustment disorder, but some clinicians nonetheless sometimes feel compelled to “up-code” the diagnosis of an adjustment disorder to the status of a major affective disorder, even when syndromal criteria for major depressive disorder (MDD) or dysthymia are absent.
Treatment-resistant depression
Disease staging models for depression and other psychiatric disordersa make note that, elsewhere in medicine, distinct clinical entities often are identified based on their responsivity to treatment (eg, classifying infections as antibiotic-sensitive or -resistant). Within the study and management of mood disorders, “treatment resistance” sometimes is a catch-all description of situations in which past treatment 1) yielded no improvement or partial improvement or 2) was marked by intolerance. Poor outcomes due to past medication intolerance or an aborted trial often are commingled with cases of true lack of improvement after an adequate treatment trial.
aSee “Staging psychiatric disorders: A clinico-biologic model,” Current Psychiatry, May 2013, at CurrentPsychiatry.com.
It is useful, therefore, to define terminology precisely when describing “treatment-resistant depression” and “treatment-refractory depression.” True past nonresponse to appropriate treatment often carries prognostic importance and bears on future treatment decisions.
Few interventions are FDA approved for treatment-resistant depression (Table).
Neuromodulation techniques are attracting interest in this area, although repetitive transcranial magnetic stimulation appears inferior to electroconvulsive therapy (ECT) for this indication.4
Melancholic depression
Melancholia involves the cardinal symptoms of anhedonia and lack of mood reactivity, alongside such features as distinct quality of mood, diurnal variation, excessive guilt, and severe weight loss. It most closely approximates pre-DSM-III “endogenous depression” and can involve 1) greater genetic loading5 and 2) structural and functional abnormalities in frontostriatal pathways.6,7
Melancholic features do not necessarily recur across successive episodes8 but carry an increased risk of psychosis9 and high-lethality suicidal behavior.10 Melancholia implies necessity for pharmacotherapy or ECT rather than psychosocial treatment alone; some researchers have suggested that tricyclic antidepressants (TCAs) might yield better results than selective serotonin reuptake inhibitors (SSRIs).11
Agitated depression
The Research Diagnostic Criteria (a forerunner in the 1970s to DSM-III) described agitated depression, but the disorder was not included in any DSM editions—although it is a “clinical modification” for MDD in the 10th revision of the International Statistical Classification of Diseases and Related Health Problems.
Agitated depression refers to a major depressive episode involving motor or psychic agitation, intense inner tension, and racing or “crowded” thoughts. Some experts believe that it represents a variant of psychotic depression or a bipolar mixed state, but the construct does not specify that criteria for a full manic or hypomanic episode exist.
Recovery from agitated depression tends to be slower than in non-agitated depression. Treatment usually entails an antidepressant plus an antipsychotic, although some believe that antidepressants can exacerbate, not alleviate, symptoms and, instead, favor antipsychotics, mood stabilizers, or ECT.12
Anxious depression
Anxiety symptoms or syndromes occur in at least one-half of outpatients who have major depression, and might account for a substantial percentage of nonresponse to first-line antidepressant therapies.13 The construct of a mixed anxiety−depressive disorder is, in fact, well-represented in the literature, particularly in primary care medicine, but its poor inter-rater reliability in DSM-5 field trials led to its exclusion there as a formal diagnosis.14
Serotonergic antidepressants remain the mainstay of treatment for depression with anxiety, although (contrary to popular perception) bupropion exerts an anxiolytic effect that is comparable to the effect of SSRIs.15 Notably, high somatic anxiety during depression might predict a poor outcome from ECT.16
Atypical depression
Often closely linked with early onset and chronicity, the construct of atypical depression has been defined in the literature by the symptom constellation of:
• mood reactiveness to environmental circumstances (unlike melancholia)
• heightened interpersonal sensitivity
• hypersomnia
• hyperphagia
• profound fatigue or a sense of physical heaviness.
Some authorities regard atypical features as being especially common in bipolar depression, or in depression among people who have borderline personality disorder.
Particular interest in this construct grew from studies that suggested that atypical depression is more responsive to a monoamine oxidase inhibitor (MAOI) than to a TCA, but also that SSRIs are not clearly superior to MAOIs.17 Response to ECT might also be better in atypical than in typical depression.18
Depression with a substance use disorder
Although not a distinct diagnostic entity, depression with a coexisting substance use disorder poses special challenges with regard to the source of symptom emergence (that is, when does depression lead to drug or alcohol use to “self medicate,” and when does drug use cause depression?) and treatment. Debate continues about whether 1) medicines that treat depression are effective and worthwhile in the setting of active substance use or 2) aggressive treatment of substance misuse is a prerequisite for subsequent pharmacotherapy for depression that is “uncontaminated” by the psychotoxic effects of concurrent substances of abuse.
Meta-analysis of controlled trials of antidepressants for patients who have MDD or a dysthymic disorder plus a comorbid alcohol use disorder found that antidepressants were, overall, superior to placebo unless a patient is actively drinking.19 Of the various classes of antidepressants, TCAs and nefazodone were found to be superior to placebo but, surprisingly, SSRIs were not. Another meta-analysis of adjunctive antidepressant outcomes for opiate-dependent, depressed patients who are receiving methadone maintenance therapy found no difference between antidepressants and placebo in their effect on depression symptom outcomes.20
Premenstrual dysphoric disorder
A new category in DSM-5, premenstrual dysphoric disorder (PMDD) represents a variant of premenstrual syndrome that arises during the luteal phase and ends with menstruation. Symptoms include several of those identified with MDD (without duration criteria), as well as mood swings, panic attacks, and physical complaints.
SSRIs—but not bupropion21 or TCAs22— and, sometimes, low-estrogen oral contraceptives are mainstays of treatment; so is cognitive-behavioral therapy, as well as lifestyle modifications (eg, exercise and changes to diet). Phototherapy has not shown robust efficacy for PMDD.23
Secondary depression
In DSM-5, depressive episodes that arise secondary to a general medical condition (eg, hypothyroidism and other endocrinopathies, cerebrovascular accidents, malignancies) or iatrogenically from medications (eg, corticosteroids, some anticonvulsants, interinterferon) are viewed as distinct from MDD in regard to risk of recurrence, genetic underpinnings, and possible neurodegenerative pathophysiology.b Unlike MDD, patient-specific risk factors are poorly defined for anticipating that a secondary depression is more or less likely to develop in the context of an exogenous substance or medical illness.
bFor further discussion, see “Is a medical illness causing your patient’s depression? Current Psychiatry, August 2009, at CurrentPsychiatry.com.
Treating secondary depression involves addressing the underlying condition and might include antidepressant medication.
Seasonal affective disorder
DSM-5 identifies “with seasonal pattern” as a specifier for recurrent major depression. Phototherapy remains a standard treatment, although a Cochrane Review identified comparable outcomes with fluoxetine, but inconclusive data for other, newer antidepressants.24 Small open trials have suggested that MAOIs and TCAs can be efficacious.
Note: Phototherapy lacks demonstrated efficacy in non-seasonal forms of depression.25
What does the future hold for classifying depressive disorders?
Recent initiatives have attempted to classify depression less by traditional clinical signs and more by focusing on possible underlying neurobiological substrates.c In the future, subtyping of mood disorders might focus on such constructs as:
• positive and negative valence systems and attentional domains
• treatment-responsivity relative to genotypic variants (for example, the serotonin transporter gene locus [SLC6A4] or prediction of L-methylfolate-responsive depression based on the genotype of the methylenetetrahydrofolate reductase [MTHFR] polymorphism)
• disrupted neural plasticity in brain circuits believed to regulate emotion.
cAn example is the Research Domain Criteria [RDoC],www. nimh.nih.gov/research-priorities/rdoc/index.shtml.
Until robust biomarkers for depression are identified and validated, however, such advances in nosology remain experimental and speculative.
BOTTOM LINE
Depressive disorders comprise a range of conditions that can be viewed along many dimensions, including “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder, among other classifications. Clinical characteristics vary across subtypes—as do corresponding preferred treatments, which should be tailored to the needs of your patients.
Editor’s note: The first part of Dr. Goldberg’s review of depression subtypes—focusing on major and minor depression, chronicity, polarity, severity, and psychosis—appeared in the April 2014 issue.
Related Resources
• Kosinski EC, Rothschild AJ. Monoamine oxidase inhibitors: Forgotten treatment for depression. Current Psychiatry. 2012;11(12):20-26.
• Rodgers S, Grosse Holtforth M, Müller M, et al. Symptom-based subtypes of depression and their psychosocial correlates: a person-centered approach focusing on the influence of sex. J Affect Disord. 2014;156:92-103.
Drug Brand Names
Aripiprazole • Abilify Mirtazapine • Remeron
Bupropion • Wellbutrin Nefazodone • Serzone
Fluoxetine • Prozac Olanzapine/fluoxetine • Symbyax
Ketamine • Ketalar Pramipexole • Mirapex
L-Methylfolate • Deplin Quetiapine • Seroquel
Lamotrigine • Lamictal Riluzole • Rilutek
Lithium • Eskalith, Lithobid Vortioxetine • Brintellix
Methadone • Dolophine
Disclosure
Dr. Goldberg has been a consultant to Avanir Pharmaceuticals and Merck; has served on the speakers’ bureau for AstraZeneca, Merck, Novartis, Sunovion Pharmaceuticals, Takeda-Lundbeck; and has received royalties from American Psychiatric Publishing and honoraria from Medscape and WebMD.
1. Fergusson DM, Horwood LJ, Ridder EM, et al. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62(1):66-72.
2. Mitchell PB, Parker GB, Gladstone GL, et al. Severity of stressful life events in first and subsequent episodes of depression: the relevance of depressive subtypes. J Affect Disord. 2003;73(3):245-252.
3. Coryell W, Winokur G, Maser JD, et al. Recurrently situational (reactive) depression: a study of course, phenomenology and familial psychopathology. J Affect Disord. 1994;31(3):203-210.
4. Slotema CW, Blom JD, Hoek HW, et al. Should we expand the toolbox of psychiatric treatment methods to include Repetitive Transcranial Magnetic Stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders. J Clin Psychiatry. 2010;71(7):873-884.
5. Kendler KS. The diagnostic validity of melancholic major depression in a population-based sample of female twins. Arch Gen Psychiatry. 1997;54(4):299-304.
6. Bracht T, Horn H, Strik W, et al. White matter microstructure alterations of the medial forebrain bundle in melancholic depression. J Affect Disord. 2014;155:186-193.
7. Pizzagalli DA, Oakes TR, Fox AS, et al. Functional but not structural subgenual prefrontal cortex abnormalities in melancholia. Mol Psychiatry. 2004;9(4):325, 393-405.
8. Melartin T, Leskelä U, Rytsälä H, et al. Co-morbidity and stability of melancholic features in DSM-IV major depressive disorder. Psychol Med. 2004;34(8):1443-1452.
9. Caldieraro MA, Baeza FL, Pinheiro DO, et al. Prevalence of psychotic symptoms in those with melancholic and nonmelancholic depression. J Nerv Ment Dis. 2013;201(10):855-859.
10. Grunebaum MF, Galfalvy HC, Oquendo MA, et al. Melancholia and the probability and lethality of suicide attempts. Br J Psychiatry. 2004;184:534-535.
11. Roose SP, Glassman AH, Attia E, et al. Comparative efficacy of selective serotonin reuptake inhibitors and tricyclics in the treatment of melancholia. Am J Psychiatry. 1994;151(12):1735-1739.
12. Koukopoulos A, Sani G, Koukopoulos AE, et al. Melancholia agitata and mixed depression. Acta Psychiatr Scand Suppl. 2007;(433):50-57.
13. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008; 165(3):342-351.
14. Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170(1):59-70.
15. Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology. 2001;25(1):131-138.
16. Rasmussen KG, Snyder KA, Knapp RG, et al. Relationship between somatization and remission with ECT. Psychiatry Res. 2004;129(3):293-295.
17. Henkel V, Mergl R, Allgaier AK, et al. Treatment of depression with atypical features: a meta-analytic approach. Psychiatry Res. 2006;141(1):89-101.
18. Husain MM, McClintock SM, Rush AJ, et al. The efficacy of acute electroconvulsive therapy in atypical depression. J Clin Psychiatry. 2008;69(3):406-411.
19. Iovieno N, Tedeschini E, Bentley KH, et al. Antidepressants for major depressive disorder and dysthymic disorder in patients with comorbid alcohol use disorders: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72(8):1144-1151.
20. Pedrelli P, Iovieno N, Vitali M, et al. Treatment of major depressive disorder and dysthymic disorder with antidepressants in patients with comorbid opiate use disorders enrolled in methadone maintenance therapy: a meta-analysis. J Clin Psychopharmacol. 2011;31(5):582-586.
21. Pearlstein TB, Stone AB, Lund SA, et al. Comparison of fluoxetine, bupropion, and placebo in the treatment of premenstrual dysphoric disorder. J Clin Psychopharmacol. 1997;17(4):261-266.
22. Freeman EW, Rickels K, Sondheimer SJ, et al. Differential response to antidepressants in women with premenstrual syndrome/premenstrual dysphoric disorder: a randomized controlled trial. Arch Gen Psychiatry. 1999;56(10):932-939.
23. Krasnik C, Montori VM, Guyatt GH, et al. The effect of bright light therapy on depression associated with premenstrual dysphoric disorder. Am J Obstet Gynecol. 2005;193(3, pt 1):658-661.
24. Thaler K, Delivuk M, Chapman A, et al. Second-generation antidepressants for seasonal affective disorder. Cochrane Database Syst Rev. 2011;7(12):CD008591.
25. Thalén BE, Kjellman BF, Mørkid L, et al. Light treatment in seasonal and nonseasonal depression. Acta Psychiatr Scand. 1995;91(5):352-360.
Depression—sad, empty, or irritable mood accompanied by somatic or cognitive changes—is not a homogeneous condition. Recognizing subtypes of depressive illness can guide treatment and relieve your patient’s suffering. In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular subgroups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonresponse or partial response, often hinges on clinical subtyping.
The second part of this article examines “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder. Treatments for these subtypes for which there is evidence, or a clinical rationale, are given in the Table.
‘Situational depression’
In recent decades, the phenomenon of nonsyndromal depression after a life stress has undergone many name changes but little conceptional revision: “situational,” “reactive,” and “neurotic” labels for depression that were used before DSM-III became “adjustment disorders” in DSM-IV-TR and then “stress response syndromes” in DSM-5. These names all connote presentations of depressed mood after an environmental stressor, without either the full constellation of symptoms that define major depression or the chronicity of dysthymic disorder.
Paucity of guidance. There has been little research to identify vulnerability variables for adjustment disorders in the aftermath of particular stressors. Similarly, extensive data are lacking on 1) the likely progression of such disorders to a syndromal form of depression or 2) protective factors against developing clinically significant depression after a life stress. The extent to which adjustment disorders lie on a continuum with major mood disorders is not well-established, although subthreshold levels of depression can predispose to major depression or suicidal behaviors.1
Models of behavioral sensitization posit that stressful life events more often precede first or early episodes of depression than subsequent recurrences.2 At the same time, non-melancholic depressions that are preceded by “situational stresses” tend to recur in similar fashion.3
Medical therapy of value? Psychotherapy without medication—apart from occasional sedative−hypnotic drugs as needed for insomnia, anxiety, or distress—is considered the standard of care for treating an adjustment disorder. No drug has demonstrated superiority to placebo for alleviating symptoms of an adjustment disorder, but some clinicians nonetheless sometimes feel compelled to “up-code” the diagnosis of an adjustment disorder to the status of a major affective disorder, even when syndromal criteria for major depressive disorder (MDD) or dysthymia are absent.
Treatment-resistant depression
Disease staging models for depression and other psychiatric disordersa make note that, elsewhere in medicine, distinct clinical entities often are identified based on their responsivity to treatment (eg, classifying infections as antibiotic-sensitive or -resistant). Within the study and management of mood disorders, “treatment resistance” sometimes is a catch-all description of situations in which past treatment 1) yielded no improvement or partial improvement or 2) was marked by intolerance. Poor outcomes due to past medication intolerance or an aborted trial often are commingled with cases of true lack of improvement after an adequate treatment trial.
aSee “Staging psychiatric disorders: A clinico-biologic model,” Current Psychiatry, May 2013, at CurrentPsychiatry.com.
It is useful, therefore, to define terminology precisely when describing “treatment-resistant depression” and “treatment-refractory depression.” True past nonresponse to appropriate treatment often carries prognostic importance and bears on future treatment decisions.
Few interventions are FDA approved for treatment-resistant depression (Table).
Neuromodulation techniques are attracting interest in this area, although repetitive transcranial magnetic stimulation appears inferior to electroconvulsive therapy (ECT) for this indication.4
Melancholic depression
Melancholia involves the cardinal symptoms of anhedonia and lack of mood reactivity, alongside such features as distinct quality of mood, diurnal variation, excessive guilt, and severe weight loss. It most closely approximates pre-DSM-III “endogenous depression” and can involve 1) greater genetic loading5 and 2) structural and functional abnormalities in frontostriatal pathways.6,7
Melancholic features do not necessarily recur across successive episodes8 but carry an increased risk of psychosis9 and high-lethality suicidal behavior.10 Melancholia implies necessity for pharmacotherapy or ECT rather than psychosocial treatment alone; some researchers have suggested that tricyclic antidepressants (TCAs) might yield better results than selective serotonin reuptake inhibitors (SSRIs).11
Agitated depression
The Research Diagnostic Criteria (a forerunner in the 1970s to DSM-III) described agitated depression, but the disorder was not included in any DSM editions—although it is a “clinical modification” for MDD in the 10th revision of the International Statistical Classification of Diseases and Related Health Problems.
Agitated depression refers to a major depressive episode involving motor or psychic agitation, intense inner tension, and racing or “crowded” thoughts. Some experts believe that it represents a variant of psychotic depression or a bipolar mixed state, but the construct does not specify that criteria for a full manic or hypomanic episode exist.
Recovery from agitated depression tends to be slower than in non-agitated depression. Treatment usually entails an antidepressant plus an antipsychotic, although some believe that antidepressants can exacerbate, not alleviate, symptoms and, instead, favor antipsychotics, mood stabilizers, or ECT.12
Anxious depression
Anxiety symptoms or syndromes occur in at least one-half of outpatients who have major depression, and might account for a substantial percentage of nonresponse to first-line antidepressant therapies.13 The construct of a mixed anxiety−depressive disorder is, in fact, well-represented in the literature, particularly in primary care medicine, but its poor inter-rater reliability in DSM-5 field trials led to its exclusion there as a formal diagnosis.14
Serotonergic antidepressants remain the mainstay of treatment for depression with anxiety, although (contrary to popular perception) bupropion exerts an anxiolytic effect that is comparable to the effect of SSRIs.15 Notably, high somatic anxiety during depression might predict a poor outcome from ECT.16
Atypical depression
Often closely linked with early onset and chronicity, the construct of atypical depression has been defined in the literature by the symptom constellation of:
• mood reactiveness to environmental circumstances (unlike melancholia)
• heightened interpersonal sensitivity
• hypersomnia
• hyperphagia
• profound fatigue or a sense of physical heaviness.
Some authorities regard atypical features as being especially common in bipolar depression, or in depression among people who have borderline personality disorder.
Particular interest in this construct grew from studies that suggested that atypical depression is more responsive to a monoamine oxidase inhibitor (MAOI) than to a TCA, but also that SSRIs are not clearly superior to MAOIs.17 Response to ECT might also be better in atypical than in typical depression.18
Depression with a substance use disorder
Although not a distinct diagnostic entity, depression with a coexisting substance use disorder poses special challenges with regard to the source of symptom emergence (that is, when does depression lead to drug or alcohol use to “self medicate,” and when does drug use cause depression?) and treatment. Debate continues about whether 1) medicines that treat depression are effective and worthwhile in the setting of active substance use or 2) aggressive treatment of substance misuse is a prerequisite for subsequent pharmacotherapy for depression that is “uncontaminated” by the psychotoxic effects of concurrent substances of abuse.
Meta-analysis of controlled trials of antidepressants for patients who have MDD or a dysthymic disorder plus a comorbid alcohol use disorder found that antidepressants were, overall, superior to placebo unless a patient is actively drinking.19 Of the various classes of antidepressants, TCAs and nefazodone were found to be superior to placebo but, surprisingly, SSRIs were not. Another meta-analysis of adjunctive antidepressant outcomes for opiate-dependent, depressed patients who are receiving methadone maintenance therapy found no difference between antidepressants and placebo in their effect on depression symptom outcomes.20
Premenstrual dysphoric disorder
A new category in DSM-5, premenstrual dysphoric disorder (PMDD) represents a variant of premenstrual syndrome that arises during the luteal phase and ends with menstruation. Symptoms include several of those identified with MDD (without duration criteria), as well as mood swings, panic attacks, and physical complaints.
SSRIs—but not bupropion21 or TCAs22— and, sometimes, low-estrogen oral contraceptives are mainstays of treatment; so is cognitive-behavioral therapy, as well as lifestyle modifications (eg, exercise and changes to diet). Phototherapy has not shown robust efficacy for PMDD.23
Secondary depression
In DSM-5, depressive episodes that arise secondary to a general medical condition (eg, hypothyroidism and other endocrinopathies, cerebrovascular accidents, malignancies) or iatrogenically from medications (eg, corticosteroids, some anticonvulsants, interinterferon) are viewed as distinct from MDD in regard to risk of recurrence, genetic underpinnings, and possible neurodegenerative pathophysiology.b Unlike MDD, patient-specific risk factors are poorly defined for anticipating that a secondary depression is more or less likely to develop in the context of an exogenous substance or medical illness.
bFor further discussion, see “Is a medical illness causing your patient’s depression? Current Psychiatry, August 2009, at CurrentPsychiatry.com.
Treating secondary depression involves addressing the underlying condition and might include antidepressant medication.
Seasonal affective disorder
DSM-5 identifies “with seasonal pattern” as a specifier for recurrent major depression. Phototherapy remains a standard treatment, although a Cochrane Review identified comparable outcomes with fluoxetine, but inconclusive data for other, newer antidepressants.24 Small open trials have suggested that MAOIs and TCAs can be efficacious.
Note: Phototherapy lacks demonstrated efficacy in non-seasonal forms of depression.25
What does the future hold for classifying depressive disorders?
Recent initiatives have attempted to classify depression less by traditional clinical signs and more by focusing on possible underlying neurobiological substrates.c In the future, subtyping of mood disorders might focus on such constructs as:
• positive and negative valence systems and attentional domains
• treatment-responsivity relative to genotypic variants (for example, the serotonin transporter gene locus [SLC6A4] or prediction of L-methylfolate-responsive depression based on the genotype of the methylenetetrahydrofolate reductase [MTHFR] polymorphism)
• disrupted neural plasticity in brain circuits believed to regulate emotion.
cAn example is the Research Domain Criteria [RDoC],www. nimh.nih.gov/research-priorities/rdoc/index.shtml.
Until robust biomarkers for depression are identified and validated, however, such advances in nosology remain experimental and speculative.
BOTTOM LINE
Depressive disorders comprise a range of conditions that can be viewed along many dimensions, including “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder, among other classifications. Clinical characteristics vary across subtypes—as do corresponding preferred treatments, which should be tailored to the needs of your patients.
Editor’s note: The first part of Dr. Goldberg’s review of depression subtypes—focusing on major and minor depression, chronicity, polarity, severity, and psychosis—appeared in the April 2014 issue.
Related Resources
• Kosinski EC, Rothschild AJ. Monoamine oxidase inhibitors: Forgotten treatment for depression. Current Psychiatry. 2012;11(12):20-26.
• Rodgers S, Grosse Holtforth M, Müller M, et al. Symptom-based subtypes of depression and their psychosocial correlates: a person-centered approach focusing on the influence of sex. J Affect Disord. 2014;156:92-103.
Drug Brand Names
Aripiprazole • Abilify Mirtazapine • Remeron
Bupropion • Wellbutrin Nefazodone • Serzone
Fluoxetine • Prozac Olanzapine/fluoxetine • Symbyax
Ketamine • Ketalar Pramipexole • Mirapex
L-Methylfolate • Deplin Quetiapine • Seroquel
Lamotrigine • Lamictal Riluzole • Rilutek
Lithium • Eskalith, Lithobid Vortioxetine • Brintellix
Methadone • Dolophine
Disclosure
Dr. Goldberg has been a consultant to Avanir Pharmaceuticals and Merck; has served on the speakers’ bureau for AstraZeneca, Merck, Novartis, Sunovion Pharmaceuticals, Takeda-Lundbeck; and has received royalties from American Psychiatric Publishing and honoraria from Medscape and WebMD.
Depression—sad, empty, or irritable mood accompanied by somatic or cognitive changes—is not a homogeneous condition. Recognizing subtypes of depressive illness can guide treatment and relieve your patient’s suffering. In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular subgroups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonresponse or partial response, often hinges on clinical subtyping.
The second part of this article examines “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder. Treatments for these subtypes for which there is evidence, or a clinical rationale, are given in the Table.
‘Situational depression’
In recent decades, the phenomenon of nonsyndromal depression after a life stress has undergone many name changes but little conceptional revision: “situational,” “reactive,” and “neurotic” labels for depression that were used before DSM-III became “adjustment disorders” in DSM-IV-TR and then “stress response syndromes” in DSM-5. These names all connote presentations of depressed mood after an environmental stressor, without either the full constellation of symptoms that define major depression or the chronicity of dysthymic disorder.
Paucity of guidance. There has been little research to identify vulnerability variables for adjustment disorders in the aftermath of particular stressors. Similarly, extensive data are lacking on 1) the likely progression of such disorders to a syndromal form of depression or 2) protective factors against developing clinically significant depression after a life stress. The extent to which adjustment disorders lie on a continuum with major mood disorders is not well-established, although subthreshold levels of depression can predispose to major depression or suicidal behaviors.1
Models of behavioral sensitization posit that stressful life events more often precede first or early episodes of depression than subsequent recurrences.2 At the same time, non-melancholic depressions that are preceded by “situational stresses” tend to recur in similar fashion.3
Medical therapy of value? Psychotherapy without medication—apart from occasional sedative−hypnotic drugs as needed for insomnia, anxiety, or distress—is considered the standard of care for treating an adjustment disorder. No drug has demonstrated superiority to placebo for alleviating symptoms of an adjustment disorder, but some clinicians nonetheless sometimes feel compelled to “up-code” the diagnosis of an adjustment disorder to the status of a major affective disorder, even when syndromal criteria for major depressive disorder (MDD) or dysthymia are absent.
Treatment-resistant depression
Disease staging models for depression and other psychiatric disordersa make note that, elsewhere in medicine, distinct clinical entities often are identified based on their responsivity to treatment (eg, classifying infections as antibiotic-sensitive or -resistant). Within the study and management of mood disorders, “treatment resistance” sometimes is a catch-all description of situations in which past treatment 1) yielded no improvement or partial improvement or 2) was marked by intolerance. Poor outcomes due to past medication intolerance or an aborted trial often are commingled with cases of true lack of improvement after an adequate treatment trial.
aSee “Staging psychiatric disorders: A clinico-biologic model,” Current Psychiatry, May 2013, at CurrentPsychiatry.com.
It is useful, therefore, to define terminology precisely when describing “treatment-resistant depression” and “treatment-refractory depression.” True past nonresponse to appropriate treatment often carries prognostic importance and bears on future treatment decisions.
Few interventions are FDA approved for treatment-resistant depression (Table).
Neuromodulation techniques are attracting interest in this area, although repetitive transcranial magnetic stimulation appears inferior to electroconvulsive therapy (ECT) for this indication.4
Melancholic depression
Melancholia involves the cardinal symptoms of anhedonia and lack of mood reactivity, alongside such features as distinct quality of mood, diurnal variation, excessive guilt, and severe weight loss. It most closely approximates pre-DSM-III “endogenous depression” and can involve 1) greater genetic loading5 and 2) structural and functional abnormalities in frontostriatal pathways.6,7
Melancholic features do not necessarily recur across successive episodes8 but carry an increased risk of psychosis9 and high-lethality suicidal behavior.10 Melancholia implies necessity for pharmacotherapy or ECT rather than psychosocial treatment alone; some researchers have suggested that tricyclic antidepressants (TCAs) might yield better results than selective serotonin reuptake inhibitors (SSRIs).11
Agitated depression
The Research Diagnostic Criteria (a forerunner in the 1970s to DSM-III) described agitated depression, but the disorder was not included in any DSM editions—although it is a “clinical modification” for MDD in the 10th revision of the International Statistical Classification of Diseases and Related Health Problems.
Agitated depression refers to a major depressive episode involving motor or psychic agitation, intense inner tension, and racing or “crowded” thoughts. Some experts believe that it represents a variant of psychotic depression or a bipolar mixed state, but the construct does not specify that criteria for a full manic or hypomanic episode exist.
Recovery from agitated depression tends to be slower than in non-agitated depression. Treatment usually entails an antidepressant plus an antipsychotic, although some believe that antidepressants can exacerbate, not alleviate, symptoms and, instead, favor antipsychotics, mood stabilizers, or ECT.12
Anxious depression
Anxiety symptoms or syndromes occur in at least one-half of outpatients who have major depression, and might account for a substantial percentage of nonresponse to first-line antidepressant therapies.13 The construct of a mixed anxiety−depressive disorder is, in fact, well-represented in the literature, particularly in primary care medicine, but its poor inter-rater reliability in DSM-5 field trials led to its exclusion there as a formal diagnosis.14
Serotonergic antidepressants remain the mainstay of treatment for depression with anxiety, although (contrary to popular perception) bupropion exerts an anxiolytic effect that is comparable to the effect of SSRIs.15 Notably, high somatic anxiety during depression might predict a poor outcome from ECT.16
Atypical depression
Often closely linked with early onset and chronicity, the construct of atypical depression has been defined in the literature by the symptom constellation of:
• mood reactiveness to environmental circumstances (unlike melancholia)
• heightened interpersonal sensitivity
• hypersomnia
• hyperphagia
• profound fatigue or a sense of physical heaviness.
Some authorities regard atypical features as being especially common in bipolar depression, or in depression among people who have borderline personality disorder.
Particular interest in this construct grew from studies that suggested that atypical depression is more responsive to a monoamine oxidase inhibitor (MAOI) than to a TCA, but also that SSRIs are not clearly superior to MAOIs.17 Response to ECT might also be better in atypical than in typical depression.18
Depression with a substance use disorder
Although not a distinct diagnostic entity, depression with a coexisting substance use disorder poses special challenges with regard to the source of symptom emergence (that is, when does depression lead to drug or alcohol use to “self medicate,” and when does drug use cause depression?) and treatment. Debate continues about whether 1) medicines that treat depression are effective and worthwhile in the setting of active substance use or 2) aggressive treatment of substance misuse is a prerequisite for subsequent pharmacotherapy for depression that is “uncontaminated” by the psychotoxic effects of concurrent substances of abuse.
Meta-analysis of controlled trials of antidepressants for patients who have MDD or a dysthymic disorder plus a comorbid alcohol use disorder found that antidepressants were, overall, superior to placebo unless a patient is actively drinking.19 Of the various classes of antidepressants, TCAs and nefazodone were found to be superior to placebo but, surprisingly, SSRIs were not. Another meta-analysis of adjunctive antidepressant outcomes for opiate-dependent, depressed patients who are receiving methadone maintenance therapy found no difference between antidepressants and placebo in their effect on depression symptom outcomes.20
Premenstrual dysphoric disorder
A new category in DSM-5, premenstrual dysphoric disorder (PMDD) represents a variant of premenstrual syndrome that arises during the luteal phase and ends with menstruation. Symptoms include several of those identified with MDD (without duration criteria), as well as mood swings, panic attacks, and physical complaints.
SSRIs—but not bupropion21 or TCAs22— and, sometimes, low-estrogen oral contraceptives are mainstays of treatment; so is cognitive-behavioral therapy, as well as lifestyle modifications (eg, exercise and changes to diet). Phototherapy has not shown robust efficacy for PMDD.23
Secondary depression
In DSM-5, depressive episodes that arise secondary to a general medical condition (eg, hypothyroidism and other endocrinopathies, cerebrovascular accidents, malignancies) or iatrogenically from medications (eg, corticosteroids, some anticonvulsants, interinterferon) are viewed as distinct from MDD in regard to risk of recurrence, genetic underpinnings, and possible neurodegenerative pathophysiology.b Unlike MDD, patient-specific risk factors are poorly defined for anticipating that a secondary depression is more or less likely to develop in the context of an exogenous substance or medical illness.
bFor further discussion, see “Is a medical illness causing your patient’s depression? Current Psychiatry, August 2009, at CurrentPsychiatry.com.
Treating secondary depression involves addressing the underlying condition and might include antidepressant medication.
Seasonal affective disorder
DSM-5 identifies “with seasonal pattern” as a specifier for recurrent major depression. Phototherapy remains a standard treatment, although a Cochrane Review identified comparable outcomes with fluoxetine, but inconclusive data for other, newer antidepressants.24 Small open trials have suggested that MAOIs and TCAs can be efficacious.
Note: Phototherapy lacks demonstrated efficacy in non-seasonal forms of depression.25
What does the future hold for classifying depressive disorders?
Recent initiatives have attempted to classify depression less by traditional clinical signs and more by focusing on possible underlying neurobiological substrates.c In the future, subtyping of mood disorders might focus on such constructs as:
• positive and negative valence systems and attentional domains
• treatment-responsivity relative to genotypic variants (for example, the serotonin transporter gene locus [SLC6A4] or prediction of L-methylfolate-responsive depression based on the genotype of the methylenetetrahydrofolate reductase [MTHFR] polymorphism)
• disrupted neural plasticity in brain circuits believed to regulate emotion.
cAn example is the Research Domain Criteria [RDoC],www. nimh.nih.gov/research-priorities/rdoc/index.shtml.
Until robust biomarkers for depression are identified and validated, however, such advances in nosology remain experimental and speculative.
BOTTOM LINE
Depressive disorders comprise a range of conditions that can be viewed along many dimensions, including “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder, among other classifications. Clinical characteristics vary across subtypes—as do corresponding preferred treatments, which should be tailored to the needs of your patients.
Editor’s note: The first part of Dr. Goldberg’s review of depression subtypes—focusing on major and minor depression, chronicity, polarity, severity, and psychosis—appeared in the April 2014 issue.
Related Resources
• Kosinski EC, Rothschild AJ. Monoamine oxidase inhibitors: Forgotten treatment for depression. Current Psychiatry. 2012;11(12):20-26.
• Rodgers S, Grosse Holtforth M, Müller M, et al. Symptom-based subtypes of depression and their psychosocial correlates: a person-centered approach focusing on the influence of sex. J Affect Disord. 2014;156:92-103.
Drug Brand Names
Aripiprazole • Abilify Mirtazapine • Remeron
Bupropion • Wellbutrin Nefazodone • Serzone
Fluoxetine • Prozac Olanzapine/fluoxetine • Symbyax
Ketamine • Ketalar Pramipexole • Mirapex
L-Methylfolate • Deplin Quetiapine • Seroquel
Lamotrigine • Lamictal Riluzole • Rilutek
Lithium • Eskalith, Lithobid Vortioxetine • Brintellix
Methadone • Dolophine
Disclosure
Dr. Goldberg has been a consultant to Avanir Pharmaceuticals and Merck; has served on the speakers’ bureau for AstraZeneca, Merck, Novartis, Sunovion Pharmaceuticals, Takeda-Lundbeck; and has received royalties from American Psychiatric Publishing and honoraria from Medscape and WebMD.
1. Fergusson DM, Horwood LJ, Ridder EM, et al. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62(1):66-72.
2. Mitchell PB, Parker GB, Gladstone GL, et al. Severity of stressful life events in first and subsequent episodes of depression: the relevance of depressive subtypes. J Affect Disord. 2003;73(3):245-252.
3. Coryell W, Winokur G, Maser JD, et al. Recurrently situational (reactive) depression: a study of course, phenomenology and familial psychopathology. J Affect Disord. 1994;31(3):203-210.
4. Slotema CW, Blom JD, Hoek HW, et al. Should we expand the toolbox of psychiatric treatment methods to include Repetitive Transcranial Magnetic Stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders. J Clin Psychiatry. 2010;71(7):873-884.
5. Kendler KS. The diagnostic validity of melancholic major depression in a population-based sample of female twins. Arch Gen Psychiatry. 1997;54(4):299-304.
6. Bracht T, Horn H, Strik W, et al. White matter microstructure alterations of the medial forebrain bundle in melancholic depression. J Affect Disord. 2014;155:186-193.
7. Pizzagalli DA, Oakes TR, Fox AS, et al. Functional but not structural subgenual prefrontal cortex abnormalities in melancholia. Mol Psychiatry. 2004;9(4):325, 393-405.
8. Melartin T, Leskelä U, Rytsälä H, et al. Co-morbidity and stability of melancholic features in DSM-IV major depressive disorder. Psychol Med. 2004;34(8):1443-1452.
9. Caldieraro MA, Baeza FL, Pinheiro DO, et al. Prevalence of psychotic symptoms in those with melancholic and nonmelancholic depression. J Nerv Ment Dis. 2013;201(10):855-859.
10. Grunebaum MF, Galfalvy HC, Oquendo MA, et al. Melancholia and the probability and lethality of suicide attempts. Br J Psychiatry. 2004;184:534-535.
11. Roose SP, Glassman AH, Attia E, et al. Comparative efficacy of selective serotonin reuptake inhibitors and tricyclics in the treatment of melancholia. Am J Psychiatry. 1994;151(12):1735-1739.
12. Koukopoulos A, Sani G, Koukopoulos AE, et al. Melancholia agitata and mixed depression. Acta Psychiatr Scand Suppl. 2007;(433):50-57.
13. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008; 165(3):342-351.
14. Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170(1):59-70.
15. Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology. 2001;25(1):131-138.
16. Rasmussen KG, Snyder KA, Knapp RG, et al. Relationship between somatization and remission with ECT. Psychiatry Res. 2004;129(3):293-295.
17. Henkel V, Mergl R, Allgaier AK, et al. Treatment of depression with atypical features: a meta-analytic approach. Psychiatry Res. 2006;141(1):89-101.
18. Husain MM, McClintock SM, Rush AJ, et al. The efficacy of acute electroconvulsive therapy in atypical depression. J Clin Psychiatry. 2008;69(3):406-411.
19. Iovieno N, Tedeschini E, Bentley KH, et al. Antidepressants for major depressive disorder and dysthymic disorder in patients with comorbid alcohol use disorders: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72(8):1144-1151.
20. Pedrelli P, Iovieno N, Vitali M, et al. Treatment of major depressive disorder and dysthymic disorder with antidepressants in patients with comorbid opiate use disorders enrolled in methadone maintenance therapy: a meta-analysis. J Clin Psychopharmacol. 2011;31(5):582-586.
21. Pearlstein TB, Stone AB, Lund SA, et al. Comparison of fluoxetine, bupropion, and placebo in the treatment of premenstrual dysphoric disorder. J Clin Psychopharmacol. 1997;17(4):261-266.
22. Freeman EW, Rickels K, Sondheimer SJ, et al. Differential response to antidepressants in women with premenstrual syndrome/premenstrual dysphoric disorder: a randomized controlled trial. Arch Gen Psychiatry. 1999;56(10):932-939.
23. Krasnik C, Montori VM, Guyatt GH, et al. The effect of bright light therapy on depression associated with premenstrual dysphoric disorder. Am J Obstet Gynecol. 2005;193(3, pt 1):658-661.
24. Thaler K, Delivuk M, Chapman A, et al. Second-generation antidepressants for seasonal affective disorder. Cochrane Database Syst Rev. 2011;7(12):CD008591.
25. Thalén BE, Kjellman BF, Mørkid L, et al. Light treatment in seasonal and nonseasonal depression. Acta Psychiatr Scand. 1995;91(5):352-360.
1. Fergusson DM, Horwood LJ, Ridder EM, et al. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62(1):66-72.
2. Mitchell PB, Parker GB, Gladstone GL, et al. Severity of stressful life events in first and subsequent episodes of depression: the relevance of depressive subtypes. J Affect Disord. 2003;73(3):245-252.
3. Coryell W, Winokur G, Maser JD, et al. Recurrently situational (reactive) depression: a study of course, phenomenology and familial psychopathology. J Affect Disord. 1994;31(3):203-210.
4. Slotema CW, Blom JD, Hoek HW, et al. Should we expand the toolbox of psychiatric treatment methods to include Repetitive Transcranial Magnetic Stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders. J Clin Psychiatry. 2010;71(7):873-884.
5. Kendler KS. The diagnostic validity of melancholic major depression in a population-based sample of female twins. Arch Gen Psychiatry. 1997;54(4):299-304.
6. Bracht T, Horn H, Strik W, et al. White matter microstructure alterations of the medial forebrain bundle in melancholic depression. J Affect Disord. 2014;155:186-193.
7. Pizzagalli DA, Oakes TR, Fox AS, et al. Functional but not structural subgenual prefrontal cortex abnormalities in melancholia. Mol Psychiatry. 2004;9(4):325, 393-405.
8. Melartin T, Leskelä U, Rytsälä H, et al. Co-morbidity and stability of melancholic features in DSM-IV major depressive disorder. Psychol Med. 2004;34(8):1443-1452.
9. Caldieraro MA, Baeza FL, Pinheiro DO, et al. Prevalence of psychotic symptoms in those with melancholic and nonmelancholic depression. J Nerv Ment Dis. 2013;201(10):855-859.
10. Grunebaum MF, Galfalvy HC, Oquendo MA, et al. Melancholia and the probability and lethality of suicide attempts. Br J Psychiatry. 2004;184:534-535.
11. Roose SP, Glassman AH, Attia E, et al. Comparative efficacy of selective serotonin reuptake inhibitors and tricyclics in the treatment of melancholia. Am J Psychiatry. 1994;151(12):1735-1739.
12. Koukopoulos A, Sani G, Koukopoulos AE, et al. Melancholia agitata and mixed depression. Acta Psychiatr Scand Suppl. 2007;(433):50-57.
13. Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008; 165(3):342-351.
14. Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170(1):59-70.
15. Rush AJ, Trivedi MH, Carmody TJ, et al. Response in relation to baseline anxiety levels in major depressive disorder treated with bupropion sustained release or sertraline. Neuropsychopharmacology. 2001;25(1):131-138.
16. Rasmussen KG, Snyder KA, Knapp RG, et al. Relationship between somatization and remission with ECT. Psychiatry Res. 2004;129(3):293-295.
17. Henkel V, Mergl R, Allgaier AK, et al. Treatment of depression with atypical features: a meta-analytic approach. Psychiatry Res. 2006;141(1):89-101.
18. Husain MM, McClintock SM, Rush AJ, et al. The efficacy of acute electroconvulsive therapy in atypical depression. J Clin Psychiatry. 2008;69(3):406-411.
19. Iovieno N, Tedeschini E, Bentley KH, et al. Antidepressants for major depressive disorder and dysthymic disorder in patients with comorbid alcohol use disorders: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72(8):1144-1151.
20. Pedrelli P, Iovieno N, Vitali M, et al. Treatment of major depressive disorder and dysthymic disorder with antidepressants in patients with comorbid opiate use disorders enrolled in methadone maintenance therapy: a meta-analysis. J Clin Psychopharmacol. 2011;31(5):582-586.
21. Pearlstein TB, Stone AB, Lund SA, et al. Comparison of fluoxetine, bupropion, and placebo in the treatment of premenstrual dysphoric disorder. J Clin Psychopharmacol. 1997;17(4):261-266.
22. Freeman EW, Rickels K, Sondheimer SJ, et al. Differential response to antidepressants in women with premenstrual syndrome/premenstrual dysphoric disorder: a randomized controlled trial. Arch Gen Psychiatry. 1999;56(10):932-939.
23. Krasnik C, Montori VM, Guyatt GH, et al. The effect of bright light therapy on depression associated with premenstrual dysphoric disorder. Am J Obstet Gynecol. 2005;193(3, pt 1):658-661.
24. Thaler K, Delivuk M, Chapman A, et al. Second-generation antidepressants for seasonal affective disorder. Cochrane Database Syst Rev. 2011;7(12):CD008591.
25. Thalén BE, Kjellman BF, Mørkid L, et al. Light treatment in seasonal and nonseasonal depression. Acta Psychiatr Scand. 1995;91(5):352-360.
Value of subtyping depression
The first of 2 parts: A practical approach to subtyping depression among your patients
Depression carries a wide differential diagnosis. Practitioners sometimes think polarity is the fundamental distinction when they conceptualize depression as a clinical entity; in fact, many nosologic frameworks have been described for defining and subtyping clinically meaningful forms of depression, and each waxed and waned in popularity.
Kraepelin, writing in the early 20th century, linked manic-depressive illness with “the greater part of the morbid states termed melancholia,”1 but many features other than polarity remain important components of depression, and those features often carry implications for how individual patients respond to treatment.
In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular subgroups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonresponse or partial response, often hinges on clinical subtyping.
The first part of this article examines major depressive disorder (MDD), minor depression, chronic depression, depression in bipolar disorder, depression that is severe or mild, and psychotic depression. Treatments for these subtypes for which there is evidence, or a clinical rationale, are given in the Table.
The subtypes of depression that I’ll discuss in the second part of the article are listed on page 47.
Major and minor depression
MDD has been the focus of most drug trials seeking FDA approval. As a syndrome, MDD is defined by a constellation of features that are related not only to mood but also to sleep, energy, cognition, motivation, and motor behavior, persisting for ≥2 weeks.
DSM-5 has imposed few changes to the basic definition of MDD:
• bereavement (the aftermath of death of a loved one), formerly an exclusion criterion, no longer precludes making a diagnosis of MDD when syndromal criteria are otherwise fulfilled
• “with anxious distress” is a new course specifier that designates prominent anxiety features (feeling worried, restless, tense, or keyed up; fearful of losing control or something terrible happening)
• “with mixed features” is a new course specifier pertinent when ≥3 mania or hypomania symptoms coexist (that is, might be a subsyndromal mania or hypomania) with a depressive syndrome; the mixed features specifier can be applied to depressed patients whether or not they have ever had a manic or hypomanic episode, but MDD—rather than bipolar disorder— remains the overarching diagnosis, unless criteria have ever been met for a full mania or hypomania.
More than 2 dozen medications are FDA-approved to treat MDD. Evidence-based psychotherapies (eg, cognitive-behavioral therapy [CBT] and interpersonal therapy), as adjuncts to pharmacotherapy, further improve outcomes, but with only modest additional effect.2
Minor depression. Depressive states that involve 2 to 4 associated symptoms lasting ≥2 weeks but <2 years are sometimes described as minor depression, captured within DSM-5 as “depression not elsewhere defined.” The terminology of so-called “minor depression” generally is shunned, in part because it might wrongly connote low severity and therefore discourage treatment—even though it confers more than a 5-fold increase in risk of MDD.3
Chronicity
DSM-IV-TR identified long-standing depression by 2 constructs:
• chronic major depression (an episode of MDD lasting ≥2 years in adults, ≥1 year in children and adolescents)
• dysthymic disorder (2 to 4 depressive symptoms for ≥2 years in adults and ≥1 year in children and adolescents), affecting 3% to 6% of adults and carrying a 2-fold increased risk of MDD, eventually.4
Depression that begins as dysthymic disorder and blossoms into syndromal MDD is described as “double depression”—although it is not recognized as a unique condition in any edition of the DSM. Subsequent incomplete recovery may revert to dysthymic disorder. DSM-5 has subsumed chronic major depression and dysthymia under the unified heading of persistent depressive disorder.
There are no FDA-approved drugs for treating dysthymia. A meta-analysis of 9 controlled trials of off-label use of antidepressants to treat dysthymia revealed an overall response rate of 52.4%, compared with 29.9% for placebo.5 Notably, although the active drug response rate in these studies is comparable to what seen in MDD, the placebo response rate was approximately 10% lower than what was seen in major depression.
Positive therapeutic findings (typically, treatment for 6 to 12 weeks) have been reported in so-called “pure” dysthymic disorder with sertraline, fluoxetine, imipramine, ritanserin, moclobemide (not approved for use in the United States), and phenelzine; the results of additional, positive placebo-controlled studies support the utility of duloxetine6 and paroxetine.7 Randomized trials have reported negative findings for desipramine,8 fluoxetine,9 and escitalopram10 escitalopram10—although the sample size in these latter studies might have been too small to detect a drug-placebo difference.
In dysthymic and minor-depressive middle-age and older adult men who have a low serum level of testosterone, hormone replacement was shown to be superior to placebo in several randomized trials.11 Studies of adjunctive atypical antipsychotics for dysthymic disorder are scarce; a Cochrane review identified controlled data only with amisulpride (not approved for use in the United States), which yielded a modest therapeutic effect.12
Polarity
In recent years, depression in bipolar disorder (BD) has been contrasted with unipolar MDD based on a difference in:
• duration (briefer in BD)
• severity (worse in BD)
• risk of suicide (higher)
• comorbidity (more extensive)
• family history (often present for BD and highly recurrent depression)
• treatment outcome (generally less favorable).
DSM-5 has at least somewhat blurred the distinctions in polarity by way of the new construct of “major depression with mixed features” (see the discussion of MDD above), identifiable even when a person has never had a full manic or hypomanic episode.
No randomized trials have been conducted to identify the best treatments for such presentations, which has invited extrapolation from the literature in regard to bipolar mixed episodes, and suggesting that 1) some mood stabilizers (eg, divalproex) might have value and 2) antidepressants might exacerbate manic symptoms.
Perhaps most noteworthy in regard to treating bipolar depression is the unresolved, but hotly debated, controversy over whether and, if so, when, an antidepressant is inappropriate (based on concerns about possible induction or exacerbation of manic symptoms). In addition, nearly all of the large, randomized controlled trials of antidepressants for bipolar depression have shown that they offer no advantage over placebo.
Some authors argue that a lack of response to antidepressants might, itself, be a “soft” indicator of “bipolarity.” However, nonresponse to antidepressants should prompt a wider assessment of features other than polarity—including psychosis, anxiety, substance abuse, a personality disorder, psychiatric adverse effects from concomitant medications, medical comor bidity, adequacy of trials of medical therapy, and potential non-adherence to such trials—to account for poor antidepressant outcomes.
Severity
Severity of depression warrants consideration when formulating impressions about the nature and treatment of all presentations of depression.
High-severity forms prompt decisions about treatment setting (inpatient or outpatient); suicide assessment; and therapeutic modalities (eg, electroconvulsive therapy is more appropriate than psychotherapy for catatonic depression).
Mild forms. A recent meta-analysis of 6 randomized trials (each of >6 weeks’ duration) of antidepressants for mild depression demonstrated that these agents exert only a modest effect compared with placebo, owing largely to higher placebo-responsivity in mild depressive episodes than in moderate and severe episodes.13 In contrast, another meta-analysis of subjects who had “mild” baseline depression severity scores found that antidepressant medication had greater efficacy than placebo in 4 of 6 randomized trials.14 Higher depression severity levels typically diminish the placebo response rate but also reduce the magnitude of drug efficacy.
Psychosis
Before DSM-III, psychotic (as opposed to neurotic) depression was perhaps the key nosologic distinction when characterizing forms of depression. The presence of psychosis and related components (eg, mood-congruence) is closely linked with the severity of depression (high) and prognosis and longitudinal outcome (poorer), and has implications for treatment (Table).
Bottom Line
Depressive disorders comprise a range of conditions that can be viewed along many dimensions, including polarity, chronicity, recurrence, psychosis, treatment resistance, comorbidity, and atypicality, among other classifications. Clinical characteristics vary across subtypes—and so do corresponding preferred treatments, which should be tailored to the needs of each of your patients.
Related Resources
• Goldberg JF, Thase ME. Monoamine oxidase inhibitors revisited: what you should know. J Clin Psychiatry. 2013;74(2):189-191.
• Goldberg JF. Antidepressants in bipolar disorder: 7 myths and realities. Current Psychiatry. 2010;9(5):41-49.
• Ketamine cousin rapidly lifts depression without side effects. National Institute of Mental Health. http://www. nimh.nih.gov/news/science-news/2013/ketamine-cousin-rapidly-lifts-depression-without-side-effects.shtml. Published May 23, 2013. Accessed March 20, 2014.
• Research Domain Criteria (RDoC). National Institute of Mental Health. http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml?u tm_ source = govdelivery&utm_medium=email&utm_campaign= govdelivery. Accessed March 20, 2014.
Drug Brand Names
Amisulpride • Amazeo, Lurasidone • Latuda
Amival, Amipride, Sulpitax Mirtazapine • Remeron
Aripiprazole • Abilify Moclobemide • Amira,
Armodafinil • Nuvigil Aurorix, Clobemix,
Bupropion • Wellbutrin Depnil, Manerix
Desipramine • Norpramin Modafinil • Provigil
Divalproex • Depakote, Olanzapine/fluoxetine
Depakene • Symbyax
Duloxetine • Cymbalta Paroxetine • Paxil
Escitalopram • Lexapro Phenelzine • Nardil
Fluoxetine • Prozac Pramipexole • Mirapex
Imipramine • Tofranil Quetiapine • Seroquel
Ketamine • Ketalar Riluzole • Rilutek
Lamotrigine • Lamictal Sertraline • Zoloft
Lithium • Eskalith, Lithobid Vortioxetine • Brintellix
Disclosure
Dr. Goldberg has been a consultant to Avanir Pharmaceuticals and Merck; has served on the speakers’ bureau for AstraZeneca, Merck, Novartis, Sunovion
Pharmaceuticals, and Takeda and Lundbeck; and has received royalties from American Psychiatric Publishing and honoraria from Medscape and WebMD.
Editor’s note: The second part of Dr. Goldberg’s review of depression subtypes—focusing on “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder—will appear in the May 2014 issue of Current Psychiatry.
1. Kraepelin E. Manic-depressive insanity and paranoia. Barclay RM, trans. Robertson GM, ed. Edinburgh, Scotland: E&S Livingstone; 1921:1.
2. Cuijpers P, Dekker J, Hollon SD, et al. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis. J Clin Psychiatry. 2009;70(9):1219-1229.
3. Fogel J, Eaton WW, Ford DE. Minor depression as a predictor of the first onset of major depressive disorder over a 15-year follow-up. Acta Psychiatr Scand. 2006; 113(1):36-43.
4. Cuijpers P, de Graaf R, van Dorsselaer S. Minor depression: risk profiles, functional disability, health care use and risk of developing major depression. J Affect Disord. 2004;79(1-3):71-79.
5. Levkovitz Y, Tedeschini E, Papakostas GI. Efficacy of antidepressants for dysthymia: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72(4):509-514.
6. Hellerstein DJ, Stewart JW, McGrath PJ, et al. A randomized controlled trial of duloxetine versus placebo in the treatment of nonmajor chronic depression. J Clin Psychiatry. 2012;73(7):984-991.
7. Ravindran AV, Cameron C, Bhatla R, et al. Paroxetine in the treatment of dysthymic disorder without co-morbidities: a double-blind, placebo-controlled, flexible-dose study. Asian J Psychiatry. 2013;6(2):157-161.
8. Stewart JW, McGrath PJ, Liebowitz MR, et al. Treatment outcome validation of DSM-III depressive subtypes. Clinical usefulness in outpatients with mild to moderate depression. Arch Gen Psychiatry. 1985;42(12):1148-1153.
9. Serrano-Blanco A, Gabarron E, Garcia-Bayo I, et al. Effectiveness and cost-effectiveness of antidepressant treatment in primary health care: a six-month randomised study comparing fluoxetine to imipramine. J Affect Disord. 2006;91(2-3):153-163.
10. Hellerstein DJ, Batchelder ST, Hyler S, et al. Escitalopram versus placebo in the treatment of dysthymic disorders. Int Clin Psychopharmacol. 2010;25(3):143-148.
11. Seidman SN, Orr G, Raviv G, et al. Effects of testosterone replacement in middle-aged men with dysthymia: a randomized, placebo-controlled clinical trial. J Clin Psychopharmacol. 2009;29(3):216-221.
12. Komossa K, Depping AM, Gaudchau A, et al. Second-generation antipsychotics for major depressive disorder and dysthymia. Cochrane Database Syst Rev. 2010; 8:(12):CD008121.
13. Fournier JC, DeRubeis RJ, Hollom SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47-53.
14. Stewart JA, Deliyannides DA, Hellerstein DJ, et al. Can people with nonsevere major depression benefit from antidepressant medication? J Clin Psychiatry. 2012;73(4):518-525.
Depression carries a wide differential diagnosis. Practitioners sometimes think polarity is the fundamental distinction when they conceptualize depression as a clinical entity; in fact, many nosologic frameworks have been described for defining and subtyping clinically meaningful forms of depression, and each waxed and waned in popularity.
Kraepelin, writing in the early 20th century, linked manic-depressive illness with “the greater part of the morbid states termed melancholia,”1 but many features other than polarity remain important components of depression, and those features often carry implications for how individual patients respond to treatment.
In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular subgroups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonresponse or partial response, often hinges on clinical subtyping.
The first part of this article examines major depressive disorder (MDD), minor depression, chronic depression, depression in bipolar disorder, depression that is severe or mild, and psychotic depression. Treatments for these subtypes for which there is evidence, or a clinical rationale, are given in the Table.
The subtypes of depression that I’ll discuss in the second part of the article are listed on page 47.
Major and minor depression
MDD has been the focus of most drug trials seeking FDA approval. As a syndrome, MDD is defined by a constellation of features that are related not only to mood but also to sleep, energy, cognition, motivation, and motor behavior, persisting for ≥2 weeks.
DSM-5 has imposed few changes to the basic definition of MDD:
• bereavement (the aftermath of death of a loved one), formerly an exclusion criterion, no longer precludes making a diagnosis of MDD when syndromal criteria are otherwise fulfilled
• “with anxious distress” is a new course specifier that designates prominent anxiety features (feeling worried, restless, tense, or keyed up; fearful of losing control or something terrible happening)
• “with mixed features” is a new course specifier pertinent when ≥3 mania or hypomania symptoms coexist (that is, might be a subsyndromal mania or hypomania) with a depressive syndrome; the mixed features specifier can be applied to depressed patients whether or not they have ever had a manic or hypomanic episode, but MDD—rather than bipolar disorder— remains the overarching diagnosis, unless criteria have ever been met for a full mania or hypomania.
More than 2 dozen medications are FDA-approved to treat MDD. Evidence-based psychotherapies (eg, cognitive-behavioral therapy [CBT] and interpersonal therapy), as adjuncts to pharmacotherapy, further improve outcomes, but with only modest additional effect.2
Minor depression. Depressive states that involve 2 to 4 associated symptoms lasting ≥2 weeks but <2 years are sometimes described as minor depression, captured within DSM-5 as “depression not elsewhere defined.” The terminology of so-called “minor depression” generally is shunned, in part because it might wrongly connote low severity and therefore discourage treatment—even though it confers more than a 5-fold increase in risk of MDD.3
Chronicity
DSM-IV-TR identified long-standing depression by 2 constructs:
• chronic major depression (an episode of MDD lasting ≥2 years in adults, ≥1 year in children and adolescents)
• dysthymic disorder (2 to 4 depressive symptoms for ≥2 years in adults and ≥1 year in children and adolescents), affecting 3% to 6% of adults and carrying a 2-fold increased risk of MDD, eventually.4
Depression that begins as dysthymic disorder and blossoms into syndromal MDD is described as “double depression”—although it is not recognized as a unique condition in any edition of the DSM. Subsequent incomplete recovery may revert to dysthymic disorder. DSM-5 has subsumed chronic major depression and dysthymia under the unified heading of persistent depressive disorder.
There are no FDA-approved drugs for treating dysthymia. A meta-analysis of 9 controlled trials of off-label use of antidepressants to treat dysthymia revealed an overall response rate of 52.4%, compared with 29.9% for placebo.5 Notably, although the active drug response rate in these studies is comparable to what seen in MDD, the placebo response rate was approximately 10% lower than what was seen in major depression.
Positive therapeutic findings (typically, treatment for 6 to 12 weeks) have been reported in so-called “pure” dysthymic disorder with sertraline, fluoxetine, imipramine, ritanserin, moclobemide (not approved for use in the United States), and phenelzine; the results of additional, positive placebo-controlled studies support the utility of duloxetine6 and paroxetine.7 Randomized trials have reported negative findings for desipramine,8 fluoxetine,9 and escitalopram10 escitalopram10—although the sample size in these latter studies might have been too small to detect a drug-placebo difference.
In dysthymic and minor-depressive middle-age and older adult men who have a low serum level of testosterone, hormone replacement was shown to be superior to placebo in several randomized trials.11 Studies of adjunctive atypical antipsychotics for dysthymic disorder are scarce; a Cochrane review identified controlled data only with amisulpride (not approved for use in the United States), which yielded a modest therapeutic effect.12
Polarity
In recent years, depression in bipolar disorder (BD) has been contrasted with unipolar MDD based on a difference in:
• duration (briefer in BD)
• severity (worse in BD)
• risk of suicide (higher)
• comorbidity (more extensive)
• family history (often present for BD and highly recurrent depression)
• treatment outcome (generally less favorable).
DSM-5 has at least somewhat blurred the distinctions in polarity by way of the new construct of “major depression with mixed features” (see the discussion of MDD above), identifiable even when a person has never had a full manic or hypomanic episode.
No randomized trials have been conducted to identify the best treatments for such presentations, which has invited extrapolation from the literature in regard to bipolar mixed episodes, and suggesting that 1) some mood stabilizers (eg, divalproex) might have value and 2) antidepressants might exacerbate manic symptoms.
Perhaps most noteworthy in regard to treating bipolar depression is the unresolved, but hotly debated, controversy over whether and, if so, when, an antidepressant is inappropriate (based on concerns about possible induction or exacerbation of manic symptoms). In addition, nearly all of the large, randomized controlled trials of antidepressants for bipolar depression have shown that they offer no advantage over placebo.
Some authors argue that a lack of response to antidepressants might, itself, be a “soft” indicator of “bipolarity.” However, nonresponse to antidepressants should prompt a wider assessment of features other than polarity—including psychosis, anxiety, substance abuse, a personality disorder, psychiatric adverse effects from concomitant medications, medical comor bidity, adequacy of trials of medical therapy, and potential non-adherence to such trials—to account for poor antidepressant outcomes.
Severity
Severity of depression warrants consideration when formulating impressions about the nature and treatment of all presentations of depression.
High-severity forms prompt decisions about treatment setting (inpatient or outpatient); suicide assessment; and therapeutic modalities (eg, electroconvulsive therapy is more appropriate than psychotherapy for catatonic depression).
Mild forms. A recent meta-analysis of 6 randomized trials (each of >6 weeks’ duration) of antidepressants for mild depression demonstrated that these agents exert only a modest effect compared with placebo, owing largely to higher placebo-responsivity in mild depressive episodes than in moderate and severe episodes.13 In contrast, another meta-analysis of subjects who had “mild” baseline depression severity scores found that antidepressant medication had greater efficacy than placebo in 4 of 6 randomized trials.14 Higher depression severity levels typically diminish the placebo response rate but also reduce the magnitude of drug efficacy.
Psychosis
Before DSM-III, psychotic (as opposed to neurotic) depression was perhaps the key nosologic distinction when characterizing forms of depression. The presence of psychosis and related components (eg, mood-congruence) is closely linked with the severity of depression (high) and prognosis and longitudinal outcome (poorer), and has implications for treatment (Table).
Bottom Line
Depressive disorders comprise a range of conditions that can be viewed along many dimensions, including polarity, chronicity, recurrence, psychosis, treatment resistance, comorbidity, and atypicality, among other classifications. Clinical characteristics vary across subtypes—and so do corresponding preferred treatments, which should be tailored to the needs of each of your patients.
Related Resources
• Goldberg JF, Thase ME. Monoamine oxidase inhibitors revisited: what you should know. J Clin Psychiatry. 2013;74(2):189-191.
• Goldberg JF. Antidepressants in bipolar disorder: 7 myths and realities. Current Psychiatry. 2010;9(5):41-49.
• Ketamine cousin rapidly lifts depression without side effects. National Institute of Mental Health. http://www. nimh.nih.gov/news/science-news/2013/ketamine-cousin-rapidly-lifts-depression-without-side-effects.shtml. Published May 23, 2013. Accessed March 20, 2014.
• Research Domain Criteria (RDoC). National Institute of Mental Health. http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml?u tm_ source = govdelivery&utm_medium=email&utm_campaign= govdelivery. Accessed March 20, 2014.
Drug Brand Names
Amisulpride • Amazeo, Lurasidone • Latuda
Amival, Amipride, Sulpitax Mirtazapine • Remeron
Aripiprazole • Abilify Moclobemide • Amira,
Armodafinil • Nuvigil Aurorix, Clobemix,
Bupropion • Wellbutrin Depnil, Manerix
Desipramine • Norpramin Modafinil • Provigil
Divalproex • Depakote, Olanzapine/fluoxetine
Depakene • Symbyax
Duloxetine • Cymbalta Paroxetine • Paxil
Escitalopram • Lexapro Phenelzine • Nardil
Fluoxetine • Prozac Pramipexole • Mirapex
Imipramine • Tofranil Quetiapine • Seroquel
Ketamine • Ketalar Riluzole • Rilutek
Lamotrigine • Lamictal Sertraline • Zoloft
Lithium • Eskalith, Lithobid Vortioxetine • Brintellix
Disclosure
Dr. Goldberg has been a consultant to Avanir Pharmaceuticals and Merck; has served on the speakers’ bureau for AstraZeneca, Merck, Novartis, Sunovion
Pharmaceuticals, and Takeda and Lundbeck; and has received royalties from American Psychiatric Publishing and honoraria from Medscape and WebMD.
Editor’s note: The second part of Dr. Goldberg’s review of depression subtypes—focusing on “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder—will appear in the May 2014 issue of Current Psychiatry.
Depression carries a wide differential diagnosis. Practitioners sometimes think polarity is the fundamental distinction when they conceptualize depression as a clinical entity; in fact, many nosologic frameworks have been described for defining and subtyping clinically meaningful forms of depression, and each waxed and waned in popularity.
Kraepelin, writing in the early 20th century, linked manic-depressive illness with “the greater part of the morbid states termed melancholia,”1 but many features other than polarity remain important components of depression, and those features often carry implications for how individual patients respond to treatment.
In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular subgroups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonresponse or partial response, often hinges on clinical subtyping.
The first part of this article examines major depressive disorder (MDD), minor depression, chronic depression, depression in bipolar disorder, depression that is severe or mild, and psychotic depression. Treatments for these subtypes for which there is evidence, or a clinical rationale, are given in the Table.
The subtypes of depression that I’ll discuss in the second part of the article are listed on page 47.
Major and minor depression
MDD has been the focus of most drug trials seeking FDA approval. As a syndrome, MDD is defined by a constellation of features that are related not only to mood but also to sleep, energy, cognition, motivation, and motor behavior, persisting for ≥2 weeks.
DSM-5 has imposed few changes to the basic definition of MDD:
• bereavement (the aftermath of death of a loved one), formerly an exclusion criterion, no longer precludes making a diagnosis of MDD when syndromal criteria are otherwise fulfilled
• “with anxious distress” is a new course specifier that designates prominent anxiety features (feeling worried, restless, tense, or keyed up; fearful of losing control or something terrible happening)
• “with mixed features” is a new course specifier pertinent when ≥3 mania or hypomania symptoms coexist (that is, might be a subsyndromal mania or hypomania) with a depressive syndrome; the mixed features specifier can be applied to depressed patients whether or not they have ever had a manic or hypomanic episode, but MDD—rather than bipolar disorder— remains the overarching diagnosis, unless criteria have ever been met for a full mania or hypomania.
More than 2 dozen medications are FDA-approved to treat MDD. Evidence-based psychotherapies (eg, cognitive-behavioral therapy [CBT] and interpersonal therapy), as adjuncts to pharmacotherapy, further improve outcomes, but with only modest additional effect.2
Minor depression. Depressive states that involve 2 to 4 associated symptoms lasting ≥2 weeks but <2 years are sometimes described as minor depression, captured within DSM-5 as “depression not elsewhere defined.” The terminology of so-called “minor depression” generally is shunned, in part because it might wrongly connote low severity and therefore discourage treatment—even though it confers more than a 5-fold increase in risk of MDD.3
Chronicity
DSM-IV-TR identified long-standing depression by 2 constructs:
• chronic major depression (an episode of MDD lasting ≥2 years in adults, ≥1 year in children and adolescents)
• dysthymic disorder (2 to 4 depressive symptoms for ≥2 years in adults and ≥1 year in children and adolescents), affecting 3% to 6% of adults and carrying a 2-fold increased risk of MDD, eventually.4
Depression that begins as dysthymic disorder and blossoms into syndromal MDD is described as “double depression”—although it is not recognized as a unique condition in any edition of the DSM. Subsequent incomplete recovery may revert to dysthymic disorder. DSM-5 has subsumed chronic major depression and dysthymia under the unified heading of persistent depressive disorder.
There are no FDA-approved drugs for treating dysthymia. A meta-analysis of 9 controlled trials of off-label use of antidepressants to treat dysthymia revealed an overall response rate of 52.4%, compared with 29.9% for placebo.5 Notably, although the active drug response rate in these studies is comparable to what seen in MDD, the placebo response rate was approximately 10% lower than what was seen in major depression.
Positive therapeutic findings (typically, treatment for 6 to 12 weeks) have been reported in so-called “pure” dysthymic disorder with sertraline, fluoxetine, imipramine, ritanserin, moclobemide (not approved for use in the United States), and phenelzine; the results of additional, positive placebo-controlled studies support the utility of duloxetine6 and paroxetine.7 Randomized trials have reported negative findings for desipramine,8 fluoxetine,9 and escitalopram10 escitalopram10—although the sample size in these latter studies might have been too small to detect a drug-placebo difference.
In dysthymic and minor-depressive middle-age and older adult men who have a low serum level of testosterone, hormone replacement was shown to be superior to placebo in several randomized trials.11 Studies of adjunctive atypical antipsychotics for dysthymic disorder are scarce; a Cochrane review identified controlled data only with amisulpride (not approved for use in the United States), which yielded a modest therapeutic effect.12
Polarity
In recent years, depression in bipolar disorder (BD) has been contrasted with unipolar MDD based on a difference in:
• duration (briefer in BD)
• severity (worse in BD)
• risk of suicide (higher)
• comorbidity (more extensive)
• family history (often present for BD and highly recurrent depression)
• treatment outcome (generally less favorable).
DSM-5 has at least somewhat blurred the distinctions in polarity by way of the new construct of “major depression with mixed features” (see the discussion of MDD above), identifiable even when a person has never had a full manic or hypomanic episode.
No randomized trials have been conducted to identify the best treatments for such presentations, which has invited extrapolation from the literature in regard to bipolar mixed episodes, and suggesting that 1) some mood stabilizers (eg, divalproex) might have value and 2) antidepressants might exacerbate manic symptoms.
Perhaps most noteworthy in regard to treating bipolar depression is the unresolved, but hotly debated, controversy over whether and, if so, when, an antidepressant is inappropriate (based on concerns about possible induction or exacerbation of manic symptoms). In addition, nearly all of the large, randomized controlled trials of antidepressants for bipolar depression have shown that they offer no advantage over placebo.
Some authors argue that a lack of response to antidepressants might, itself, be a “soft” indicator of “bipolarity.” However, nonresponse to antidepressants should prompt a wider assessment of features other than polarity—including psychosis, anxiety, substance abuse, a personality disorder, psychiatric adverse effects from concomitant medications, medical comor bidity, adequacy of trials of medical therapy, and potential non-adherence to such trials—to account for poor antidepressant outcomes.
Severity
Severity of depression warrants consideration when formulating impressions about the nature and treatment of all presentations of depression.
High-severity forms prompt decisions about treatment setting (inpatient or outpatient); suicide assessment; and therapeutic modalities (eg, electroconvulsive therapy is more appropriate than psychotherapy for catatonic depression).
Mild forms. A recent meta-analysis of 6 randomized trials (each of >6 weeks’ duration) of antidepressants for mild depression demonstrated that these agents exert only a modest effect compared with placebo, owing largely to higher placebo-responsivity in mild depressive episodes than in moderate and severe episodes.13 In contrast, another meta-analysis of subjects who had “mild” baseline depression severity scores found that antidepressant medication had greater efficacy than placebo in 4 of 6 randomized trials.14 Higher depression severity levels typically diminish the placebo response rate but also reduce the magnitude of drug efficacy.
Psychosis
Before DSM-III, psychotic (as opposed to neurotic) depression was perhaps the key nosologic distinction when characterizing forms of depression. The presence of psychosis and related components (eg, mood-congruence) is closely linked with the severity of depression (high) and prognosis and longitudinal outcome (poorer), and has implications for treatment (Table).
Bottom Line
Depressive disorders comprise a range of conditions that can be viewed along many dimensions, including polarity, chronicity, recurrence, psychosis, treatment resistance, comorbidity, and atypicality, among other classifications. Clinical characteristics vary across subtypes—and so do corresponding preferred treatments, which should be tailored to the needs of each of your patients.
Related Resources
• Goldberg JF, Thase ME. Monoamine oxidase inhibitors revisited: what you should know. J Clin Psychiatry. 2013;74(2):189-191.
• Goldberg JF. Antidepressants in bipolar disorder: 7 myths and realities. Current Psychiatry. 2010;9(5):41-49.
• Ketamine cousin rapidly lifts depression without side effects. National Institute of Mental Health. http://www. nimh.nih.gov/news/science-news/2013/ketamine-cousin-rapidly-lifts-depression-without-side-effects.shtml. Published May 23, 2013. Accessed March 20, 2014.
• Research Domain Criteria (RDoC). National Institute of Mental Health. http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml?u tm_ source = govdelivery&utm_medium=email&utm_campaign= govdelivery. Accessed March 20, 2014.
Drug Brand Names
Amisulpride • Amazeo, Lurasidone • Latuda
Amival, Amipride, Sulpitax Mirtazapine • Remeron
Aripiprazole • Abilify Moclobemide • Amira,
Armodafinil • Nuvigil Aurorix, Clobemix,
Bupropion • Wellbutrin Depnil, Manerix
Desipramine • Norpramin Modafinil • Provigil
Divalproex • Depakote, Olanzapine/fluoxetine
Depakene • Symbyax
Duloxetine • Cymbalta Paroxetine • Paxil
Escitalopram • Lexapro Phenelzine • Nardil
Fluoxetine • Prozac Pramipexole • Mirapex
Imipramine • Tofranil Quetiapine • Seroquel
Ketamine • Ketalar Riluzole • Rilutek
Lamotrigine • Lamictal Sertraline • Zoloft
Lithium • Eskalith, Lithobid Vortioxetine • Brintellix
Disclosure
Dr. Goldberg has been a consultant to Avanir Pharmaceuticals and Merck; has served on the speakers’ bureau for AstraZeneca, Merck, Novartis, Sunovion
Pharmaceuticals, and Takeda and Lundbeck; and has received royalties from American Psychiatric Publishing and honoraria from Medscape and WebMD.
Editor’s note: The second part of Dr. Goldberg’s review of depression subtypes—focusing on “situational,” treatment-resistant, melancholic, agitated, anxious, and atypical depression; depression occurring with a substance use disorder; premenstrual dysphoric disorder; and seasonal affective disorder—will appear in the May 2014 issue of Current Psychiatry.
1. Kraepelin E. Manic-depressive insanity and paranoia. Barclay RM, trans. Robertson GM, ed. Edinburgh, Scotland: E&S Livingstone; 1921:1.
2. Cuijpers P, Dekker J, Hollon SD, et al. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis. J Clin Psychiatry. 2009;70(9):1219-1229.
3. Fogel J, Eaton WW, Ford DE. Minor depression as a predictor of the first onset of major depressive disorder over a 15-year follow-up. Acta Psychiatr Scand. 2006; 113(1):36-43.
4. Cuijpers P, de Graaf R, van Dorsselaer S. Minor depression: risk profiles, functional disability, health care use and risk of developing major depression. J Affect Disord. 2004;79(1-3):71-79.
5. Levkovitz Y, Tedeschini E, Papakostas GI. Efficacy of antidepressants for dysthymia: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72(4):509-514.
6. Hellerstein DJ, Stewart JW, McGrath PJ, et al. A randomized controlled trial of duloxetine versus placebo in the treatment of nonmajor chronic depression. J Clin Psychiatry. 2012;73(7):984-991.
7. Ravindran AV, Cameron C, Bhatla R, et al. Paroxetine in the treatment of dysthymic disorder without co-morbidities: a double-blind, placebo-controlled, flexible-dose study. Asian J Psychiatry. 2013;6(2):157-161.
8. Stewart JW, McGrath PJ, Liebowitz MR, et al. Treatment outcome validation of DSM-III depressive subtypes. Clinical usefulness in outpatients with mild to moderate depression. Arch Gen Psychiatry. 1985;42(12):1148-1153.
9. Serrano-Blanco A, Gabarron E, Garcia-Bayo I, et al. Effectiveness and cost-effectiveness of antidepressant treatment in primary health care: a six-month randomised study comparing fluoxetine to imipramine. J Affect Disord. 2006;91(2-3):153-163.
10. Hellerstein DJ, Batchelder ST, Hyler S, et al. Escitalopram versus placebo in the treatment of dysthymic disorders. Int Clin Psychopharmacol. 2010;25(3):143-148.
11. Seidman SN, Orr G, Raviv G, et al. Effects of testosterone replacement in middle-aged men with dysthymia: a randomized, placebo-controlled clinical trial. J Clin Psychopharmacol. 2009;29(3):216-221.
12. Komossa K, Depping AM, Gaudchau A, et al. Second-generation antipsychotics for major depressive disorder and dysthymia. Cochrane Database Syst Rev. 2010; 8:(12):CD008121.
13. Fournier JC, DeRubeis RJ, Hollom SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47-53.
14. Stewart JA, Deliyannides DA, Hellerstein DJ, et al. Can people with nonsevere major depression benefit from antidepressant medication? J Clin Psychiatry. 2012;73(4):518-525.
1. Kraepelin E. Manic-depressive insanity and paranoia. Barclay RM, trans. Robertson GM, ed. Edinburgh, Scotland: E&S Livingstone; 1921:1.
2. Cuijpers P, Dekker J, Hollon SD, et al. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis. J Clin Psychiatry. 2009;70(9):1219-1229.
3. Fogel J, Eaton WW, Ford DE. Minor depression as a predictor of the first onset of major depressive disorder over a 15-year follow-up. Acta Psychiatr Scand. 2006; 113(1):36-43.
4. Cuijpers P, de Graaf R, van Dorsselaer S. Minor depression: risk profiles, functional disability, health care use and risk of developing major depression. J Affect Disord. 2004;79(1-3):71-79.
5. Levkovitz Y, Tedeschini E, Papakostas GI. Efficacy of antidepressants for dysthymia: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry. 2011;72(4):509-514.
6. Hellerstein DJ, Stewart JW, McGrath PJ, et al. A randomized controlled trial of duloxetine versus placebo in the treatment of nonmajor chronic depression. J Clin Psychiatry. 2012;73(7):984-991.
7. Ravindran AV, Cameron C, Bhatla R, et al. Paroxetine in the treatment of dysthymic disorder without co-morbidities: a double-blind, placebo-controlled, flexible-dose study. Asian J Psychiatry. 2013;6(2):157-161.
8. Stewart JW, McGrath PJ, Liebowitz MR, et al. Treatment outcome validation of DSM-III depressive subtypes. Clinical usefulness in outpatients with mild to moderate depression. Arch Gen Psychiatry. 1985;42(12):1148-1153.
9. Serrano-Blanco A, Gabarron E, Garcia-Bayo I, et al. Effectiveness and cost-effectiveness of antidepressant treatment in primary health care: a six-month randomised study comparing fluoxetine to imipramine. J Affect Disord. 2006;91(2-3):153-163.
10. Hellerstein DJ, Batchelder ST, Hyler S, et al. Escitalopram versus placebo in the treatment of dysthymic disorders. Int Clin Psychopharmacol. 2010;25(3):143-148.
11. Seidman SN, Orr G, Raviv G, et al. Effects of testosterone replacement in middle-aged men with dysthymia: a randomized, placebo-controlled clinical trial. J Clin Psychopharmacol. 2009;29(3):216-221.
12. Komossa K, Depping AM, Gaudchau A, et al. Second-generation antipsychotics for major depressive disorder and dysthymia. Cochrane Database Syst Rev. 2010; 8:(12):CD008121.
13. Fournier JC, DeRubeis RJ, Hollom SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303(1):47-53.
14. Stewart JA, Deliyannides DA, Hellerstein DJ, et al. Can people with nonsevere major depression benefit from antidepressant medication? J Clin Psychiatry. 2012;73(4):518-525.
Treating patients with suspected ultra-rapid cycling bipolar disorder
Ultra-rapid cycling bipolar disorder: A critical look
Ultra-rapid cycling (URC) entered the psychiatric lexicon in the 1990s as a proposed descriptor for manic/hypomanic, mixed, or depressed episodes of bipolar disorder (BD) that occur every few days or weeks. DSM-IV-TR incorporates rapid cycling (RC)—but not URC—as a course specifier that occurs in 10% to 15% of patients with BD who have ≥4 distinct affective episodes per year, each fulfilling duration criteria and separated by identifiable recovery periods (unless an episode directly changes polarity). Since then, the terms RC and URC have seemingly metamorphosed into imprecise, popular colloquialisms meant to loosely describe frequent mood changes rather than distinct episodes over extended time periods, with little regard for the associated signs that define manic or hypomanic episodes.
This article examines the meaning and validity of URC in BD, its relevance and differentiation from rapid mood shifts in patients without BD, and concepts relevant to treatment extrapolated from studies of RC BD.
Imprecise nomenclature
Post et al1 coined the terms “ultra-rapid cycling” and “ultra-ultra-rapid cycling” (also called “ultradian cycling”) to describe mood episodes that occur monthly (URC) or over the course of as little as 1 day (ultradian cycling). These constructs are controversial because they lack demonstrated content validity and discriminant validity relative to other disorders. (“Content validity” refers to whether the features thought to comprise an entity of interest accurately and meaningfully do so; “discriminant validity” tells researchers and clinicians whether the proposed description of a clinical entity uniquely differentiates it from other disorders—avoiding “false-positive” suspected cases.) Clinicians therefore must pay careful attention to non-bipolar psychiatric problems that can present with rapid mood changes but without the psychomotor and related signs that define bipolar mood episodes. In their looser, nontechnical meanings, “rapid cycling” or “ultra-rapid cycling” may be synonymous with affective lability. RC is neither a diagnosis in itself nor a criterion for diagnosing BD. Rather, it is a course specifier to describe episode frequency in patients with past unambiguous manic or hypomanic episodes.
In children and adolescents, whose presentations often are atypical and can be hard to differentiate from other forms of behavioral or temperamental dysregulation, severe non-episodic mood dysregulation without signs of mania or hypomania may indicate a phenomenon separate from BD.2 Geller and colleagues3 proposed using the term “episodes” to frame the duration of a DSM-IV-defined syndrome of mania/hypomania or depression, while reserving the term “cycling” to connote patterns of mood alternation within a given episode. It is not clear whether this concept of “cycling” differs qualitatively from mood lability that arises during a mood episode in children or adults, and notably, this perspective does not account for changes in psychomotor signs in conjunction with changes in mood.
Clinicians also sometimes blur the concept of “mixed episodes” with RC or URC. DSM-IV-TR defines mixed episodes within bipolar I disorder (BD I) based on criteria for a simultaneous manic and depressive episode, rather than on frequent oscillations between affective poles. These and other differential diagnostic considerations for suspected URC are summarized in Table 1.4
A further concern regarding nomenclature involves the distinction between cyclicity (ie, successive episodes regardless of pole direction) and changes in polarity (ie, switches from depression to mania/hypomania or vice versa). Some mood disorder patients may have rapid oscillations from euthymia to depression while never changing polarity to mania/hypomania and may be best described as having recurrent brief depression.
Table 1
Differential diagnosis in suspected URC
| Phenomenon | Considerations for assessment |
|---|---|
| Mixed episodes in bipolar I disorder, or mixed depressive episodes in bipolar II disorder | DSM-IV-TR mixed episodes entail the co-occurrence of manic and depressive symptoms during the same episode without an intervening period of recovery. ICD-10 includes “rapid alternation of manic, hypomanic or depressive symptoms…from day to day or even hour to hour” in its definition of a mixed episode |
| Distress responses to acute environmental adversities (eg, adjustment disorders with mixed disturbance of emotions and conduct) | One would expect an absence of corresponding sleep-wake cycle changes or speech-language and psychomotor disturbances |
| Intoxication/withdrawal from psychoactive substances or drug-induced mental status changes (eg, corticosteroids, amphetamine, cocaine); a history of substance abuse also may be associated with development of URC in BD patients4 | Substance-induced mood fluctuations caused by intoxication/withdrawal can mimic affective cycling |
| Disinhibition states and frontal lobe syndromes as seen in traumatic brain injury and other CNS disorders, such as multiple sclerosis | Assess for signs of perseveration and history of head trauma or neurologic damage from cumulative toxic-metabolic insults (eg, chronic alcoholism) |
| Autonomic hyperarousal, emotional volatility, and hyperreactivity to environmental stresses, suggestive of PTSD | Determine the presence of a trauma history and review whether DSM-IV-TR symptoms and associated features of PTSD exist, including re-experiencing/reliving and avoidance, as well as paranoid thinking, dissociation, and nightmares |
| Recurrent mood shifts related to premenstrual dysphoric disorder may mimic URC. Other endocrine dysfunctions also may present with URC (eg, thyroid or ovarian malignancies) | Affirm the independent presence of BD before inferring its manifestations solely from premenstrual mood changes |
| Trait affective instability associated with borderline personality disorder | Trait mood instability is more chronic and enduring than episodic, and would not be expected to occur in tandem with signs of psychomotor activation that define mania/hypomania |
| BD: bipolar disorder; ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th revision; PTSD: posttraumatic stress disorder; URC: ultra-rapid cycling | |
Duration criteria
Clinicians and researchers have debated the minimum duration criteria for identifying manic or hypomanic episodes, and the extent to which suspected hypomanic periods of short duration constitute distinct illness phases. Although DSM-IV-TR designates 4 days as a minimum time for classifying an episode of hypomania, empirical studies suggest that mood symptoms lasting as few as 2 days may comprise a valid and reliably distinct entity relevant to RC.5 More limited data (mainly case observations) identify “affective oscillations” and “mood shifts” occurring faster than once per 24 hours in BD patients without comorbid personality disorders.6 Phenomenologic studies that have focused on 24- to 48-hour switch cycles have described new-onset URC arising spontaneously or following closed head injuries.7 In children and younger adolescents, reports have identified long index manic episodes (mean durations as long as 80 weeks)8 that involve continual (ultradian) mood cycling in as many as 80% of cases.9
Is URC a valid construct?
A central controversy surrounding the validity and meaningfulness of URC as a BD subtype involves its sole focus on mood variation rather than the fuller constellation of associated signs and symptoms that define episodes of mania/hypomania or depression. Abrupt, sudden, drastic, or dramatic mood shifts from one moment to the next are nowhere to be found in the DSM-IV-TR definition of BD, and the construct of mood lability or affective instability is neither a cardinal nor defining element of BD. Although individuals with BD I or bipolar II disorder (BD II) may have periods of affective lability, rapid shifts in mood are neither necessary nor sufficient for a BD diagnosis, and may indicate other types of psychopathology when affective instability occurs in the absence of a history of discernible manic or hypomanic episodes.
Studies by our group10 and others11 have shown that overattention to mood variation without considering associated cognitive, speech-language, chronobiologic, and motor signs of mania/hypomania accounts for substantial overdiagnosis of BD in patients with non-specific mood disturbances, particularly in those with active substance abuse or borderline personality disorder (BPD). Whereas the construct of RC BD attempts to account for changes in energy and psychomotor function as part of recurrent syndromes of mania/hypomania, existing literature on URC does not. Assessing mood changes in <24 hours also precludes assessing associated phenomena that occur over longer periods, such as changes in the sleep-wake cycle.
A rigorous, systematic approach to differential diagnosis for patients with affective instability is essential.
Borderline personality disorder
A common diagnostic debate regarding URC involves how to differentiate it from the chronic mood instability and reactivity inherent to BPD. Although some authors have suggested that RC BD and affective instability in BPD may be the same entity,12 others object to unifying the 2 conditions without considering their phenomenologic and other clinical differences. For example, affective instability arising from borderline character organization is thought to reflect a patient’s impaired capacity to self-regulate his or her internal state and emotional responses to interpersonal and other environmental stresses, or difficulty managing impulses. By contrast, manic or depressive phases of BD tend not to be “triggered” by interpersonal conflicts or frustrations. Furthermore, reframing intense mood reactions to the environment as bipolar variants carries several pitfalls: doing so wrongly accords patients a passive role in their reactions to life events, inaccurately reinforces a sense of victimization in response to stress, and diverts inquiry away from a patient’s active role in life decisions and circumstances that may be unsatisfying, self-defeating, or volatile.
Two key considerations may be helpful in discriminating rapid mood changes in BD vs BPD. First, some longitudinal studies indicate that RC often is a transient, rather than enduring, phenomenon in BD,13 in contrast to the nonvarying, trait feature of affective instability in persons with BPD. It is unknown whether URC is more enduring than transient. Notably, whereas bipolar mood episodes constitute deviations from a baseline state, affective instability in BPD is a baseline characteristic, rather than a deviation from it. Second, by definition, a BPD diagnosis hinges on additional elements unrelated to mood disturbances, such as interpersonal styles or defense mechanisms that involve splitting, projection, and projective identification, feelings of numbness, boredom, or emptiness, identity diffusion, fears of abandonment, and proclivities toward self-mutilation or other self-injurious behaviors as a means to alleviate tension and stress. These characteristics do not overlap with the core elements of BD.
Affective lability in patients with BPD entails prominent oscillations between anger and anxiety, or depression and anxiety, but not depression and elation14; by contrast, affective instability in BD has been linked with greater oscillations between euthymia and depression, and euthymia and elation, but not euthymia and anger.15 Moreover, daily mood fluctuations in patients with BD appear to occur in a relatively random fashion,16 whereas in BPD mood fluctuations are reactions that appear intimately linked to distressing interpersonal experiences.
See the table below, entitled “Rapid cycling and ultra-rapid cycling BD: A comparison,” comparing the phenomenology of RC and URC and a discussion of studies that explored genetic markers or family patterns that may be related to RC or URC.
Treatment considerations
No systematic studies exist for treating URC. Because most clinical trials of BD focus on treatment or prevention of a single episode rather than changes of mood over time, it is difficult to draw inferences about the ability of any treatment to attenuate marked, day-to-day mood variations. Some antimanic drugs, such as carbamazepine, have been suggested to offer better prophylactic efficacy compared with lithium for “non-classical” BD presentations, although the efficacy of carbamazepine has not been studied in URC.
Broadly speaking, treatment for URC, similar to RC, pragmatically involves:
- identifying and eliminating sources of mood destabilization (eg, substance abuse, erratic sleep patterns)
- treating medical comorbidities such as hypothyroidism
- optimizing treatment with mood stabilizing agents
- exercising caution when using antidepressants (see below).
Interestingly, despite frequent allusion to certain medications as “mood stabilizers,” no controlled study has examined mood instability on a day-to-day basis as a primary outcome measure in BD treatment, which limits the ability to surmise that any drug could be expected to diminish mood oscillations that occur over the course of days, or within a single day. However, a post hoc analysis by our group17 compared randomized treatment with lamotrigine or placebo over 6 months in RC BD I or BD II. Using prospective life charting, we found patients who received lamotrigine were almost twice as likely as those receiving placebo to achieve euthymia from one week to the next, which suggests the possibility that lamotrigine may offer benefit for affective instability in BD I or BD II patients, in addition to preventing discrete mood episodes.
Antidepressant controversy. Concerns that antidepressants might acutely induce mania or accelerate cycling frequency over long time periods have led to a contentious, long-standing debate within psychopharmacology. As noted in the box below, several long-term naturalistic follow-up studies have reported RC as a perceived consequence of antidepressants in most RC patients, although efforts to differentiate cycle acceleration caused by antidepressants (or other iatrogenic factors) from the natural course of illness remains exceedingly difficult without prospective randomized trials. (Antidepressants might cause more affective recurrences, but having multiple episodes may also cause more antidepressant prescriptions.) Some researchers (eg, Schneck et al18) have reported more frequent episodes among patients taking antidepressants but did not consider that patients with multiple episodes may be more likely to receive antidepressants, which fail to ameliorate acute or recurrent affective episodes. Importantly, a recent multi-site randomized trial by Ghaemi et al19 found that after a favorable acute response to antidepressants plus mood stabilizers, patients with preexisting RC who were randomized to continue antidepressants for up to 1 year had a 3-fold increased likelihood of developing a new depressive episode, which affirms suggestions that antidepressants do not help—but may exacerbate—cycling in patients with RC. No studies in BD have examined whether URC is more likely to arise as a consequence of antidepressant use.
Mood stabilizers and other biologic therapies. A small body of literature specifically addresses pharmacotherapy of URC in patients with BD (Table 2).19-26 A limitation of most existing literature is its focus on case reports, small open trials, or anecdotal observations rather than large, randomized controlled trials using systematic outcome measures. Extrapolation from reports focusing on patients with DSM-IV-TR RC is limited because it is uncertain whether URC differs fundamentally from RC and studies of DSM-IV-TR RC typically examine acute response during an index episode or time until relapse during maintenance therapy, rather than impact on mood changes over time.
Psychotherapy. A limited database on the efficacy of adjunctive cognitive-behavioral therapy (CBT) in RC BD describes improvement in depressive symptoms over short-term follow-up.27 No long-term studies of CBT or other structured psychotherapies have focused on RC or URC. Intuitively, one might expect that psychoeducation targeting sleep hygiene, substance use, stress management and coping skills, medication adherence, and prodrome recognition would be of value to patients with BD who experience frequent mood episodes, especially in those who may be unaware of or unfamiliar with basic concepts related to BD. In addition, relevant concepts from dialectical behavior therapy may be beneficial for BD patients with possible URC, such as skills to enhance emotional regulation, distress tolerance, mindfulness, and interpersonal effectiveness.
Table 2
Evidence-based treatments for ultra-rapid cycling BD
| Intervention | Strength of evidence | Comment |
|---|---|---|
| Antidepressant elimination | Cycling frequency may lengthen during antidepressant-free periods among patients with RC20; long-term (up to 1 year) antidepressant use in RC patients may increase the likelihood of depressive recurrences19 | Findings based mostly on small sample sizes; no controlled trials of antidepressant cessation as an intervention specifically for URC |
| Lithium | Single case report of ECT-induced URC resolved by lithium augmentation during continued ECT22 | No large-scale or randomized trials |
| Carbamazepine | No controlled trials or case reports | Possible anti-cycling benefits relevant for URC could be inferred from post hoc studies among patients with RC |
| Divalproex | Single case report describing resolution of a 48-hour cycle after augmentation of lithium with divalproex23 | No large-scale or randomized trials |
| Lamotrigine | Single case report of 100 mg/d lamotrigine augmentation to divalproex yielded 8 months of remission in a 25-year-old man with BD II and a long-standing pattern of 3 days of hypomania followed by 5 days of depression24 | No large-scale or randomized trials |
| Topiramate | Single case report in URC describing reduction of cycling frequency over 3 years25 | Multiple large scale placebo-controlled studies in bipolar mania have been negative |
| Second-generation antipsychotics | No controlled trials or case reports | Possible anti-cycling benefits relevant for URC could be inferred from post hoc studies in RC |
| Combinations of ≥2 mood stabilizing drugs | No controlled trials or case reports | Combining multiple anti-cycling agents is intuitively logical but largely unstudied |
| Nimodipine | 1 unipolar and 11 BD patients treated in randomized, off-on-off-on fashion (begun at 90 mg/d, increased up to 720 mg/d, mean duration of 12 weeks on active drug)26 | Response in 5 of 9 completers. Findings await replication with larger sample sizes |
| Hypermetabolic thyroid hormone (levothyroxine) | Findings from a small (N = 11) study of adjunctive high-dose levothyroxine (0.15 to 0.4 mg/d, with dosages increased by 0.05 to 0.1 mg/d every 1 to 2 weeks); an unspecified subgroup had “a very rapid cycling pattern” (reviewed by Bauer et al21) | 10 of 11 RC patients had reductions in depressive symptoms, 5 of 7 had improvement from baseline manic symptoms (observation period >60 days) |
| ECT | Case reports of improvement with ECT in refractory RC that was presumed secondary to tricyclic antidepressants | Reports of induction of URC by ECT22; whether or not ECT would more likely improve or exacerbate cyclicity for a given patient may require empirical determination |
| BD: bipolar disorder; BD II: bipolar II disorder; ECT: electroconvulsive therapy; RC: rapid cycling; URC: ultra-rapid cycling | ||
Treatment monitoring. Prospective life charting allows patients to systematically record manic/hypomanic and depressive symptoms day-to-day and week-to-week, thus creating a measure that may be particularly relevant for patients whose moods change rapidly. Simple mood charts (see Related Resources) typically take into account the severity of symptoms of either polarity with ratings of mild, moderate, or severe. Such visual records permit simple calculations over the course of a given interval (eg, week-by-week or across months) of several important parameters, including:
- number of days euthymic
- number of days with depression
- number of days with abnormal mood elevation
- number of occasions in which moods of both polarities occur on the same day.
Tracking these parameters during a treatment allows clinicians to make quantitative comparisons over time as a method of determining whether or not meaningful changes are occurring in cyclicity. See the figure below for an example of a completed mood chart and its interpretation.
Additional recommendations for assessing and managing cyclicity in BD are summarized in Table 3.
Table 3
Tips for managing suspected ultra-rapid cycling BD
| Do’s | Don’ts |
|---|---|
| Ascertain a history of ≥1 lifetime manic or hypomanic episode to diagnose BD | Diagnose BD solely on the presence of rapid mood fluctuations |
| Determine the presence of changes in sleep, energy, speech-language, and related behavior as correlates of mood to differentiate syndromes from isolated variation in mood | Ignore constellations of associated signs and symptoms of mania/hypomania |
| Obtain patient history to assess for head trauma or other medical and neurologic events that could have affective or other psychiatric manifestations | Disregard possible medical etiologies for new-onset affective dysregulation |
| Ascertain the resolution of 1 episode before counting the resurgence of symptoms as constituting a new episode; a waxing and waning course may reflect illness chronicity with incomplete recovery rather than true cyclicity | Misidentify incomplete recovery from an existing episode as the occurrence of new multiple episodes, which would inflate false-positive cases of RC or URC |
| Advise patients to refrain from alcohol or illicit substances that could destabilize mood | Assume that comorbid alcohol or illicit substance abuse will remit only after mood stabilization has been achieved, rather than the reverse |
| Monitor changes in sleep-wake cycles and the effects of erratic sleep or sleep deprivation on mood | Ignore the effects of poor sleep hygiene on mood |
| Minimize antidepressant exposure in patients with RC or URC | Continue long-term antidepressant maintenance therapy in patients with manic or mixed features or ongoing oscillations between mania/hypomania and depression |
| Assure euthyroid status and consider the potential utility of hypermetabolic levothyroxine | Assume that RC or URC will resolve solely by normalizing or optimizing thyroid function |
| Use rational, pharmacodynamically nonredundant anti-cycling drugs | Ignore the cumulative burden of adverse effects of multiple drugs |
| Consider the potential role for ECT as a strategy to arrest URC during any phase of BD | Assume ECT has value only during acute depressive phases of BD |
| Use prospective mood charting to document the evolution of mood changes over time, particularly when gauging treatment efficacy | Rely solely on impressionistic recall of mood states or polarity changes as reflecting distinct phasic changes |
| BD: bipolar disorder; ECT: electroconvulsive therapy; RC: rapid cycling; URC: ultra-rapid cycling | |
Table
Rapid cycling and ultra-rapid cycling BD: A comparison
| Construct | Rapid cycling | Ultra-rapid cycling |
|---|---|---|
| Bipolar I vs II | Predominantly BD IIa | No systematic data |
| Sex | Predominantly women | No systematic data |
| Longitudinal course | May be a transient phenomenon that can occur at any timeb or an enduring phenomenon that may persist for yearsc | Ultradian patterns may be more common across the first several episodes among pediatric BD patientsd |
| Age at onset | Associated with younger age at onsete | May be more evident in prepubescent onset mood disordersd; ultradian cycling more likely when onset occurs before age 13 than in adulthoode |
| Diurnal variation in mood | Morning-to-evening mood switches usually involve depression to mania/hypomania, with the opposite typifying evening-to-morning mood switchesf | Not reported |
| Relationship to environmental stresses | Life stresses may precede initial affective episodes but may be less important as subsequent episodes arise with increasing automaticity | No systematic data |
| Relationship to menstrual cycle | Despite case reports and self-reported links between RC and menstrual mood exacerbations, prospective data do not identify associations between RC and menstrual patternsg,h | No systematic data |
| Subclinical hypothyroidism | Bauer and Whybrow identified hypothyroidism independent of lithium use in 60% of 30 rapidly cycling BD patients, with evidence of improvement in a separate study of 11 RC patients given suprametabolic levothyroxine (reviewed by Bauer et ali) | No systematic data |
| Relationship to psychosis | Nonea | No systematic data |
| Relationship to antidepressant use | Naturalistic observations suggest RC may occur later in the illness course as a result of antidepressant use.c Small open case series data suggest shorter intermorbid intervals on antidepressants with longer intervals off antidepressants.j RC patients often receive antidepressants, but causal relationships are not well-documented.k Some case-control data dispute links between antidepressant use and RCl | No specific published cases |
| Considerations for suicide risk | RC linked with more serious suicide attemptsl | Suicide attempts may be associated with cycling within an episodem or rapid shifting in moodn |
| Time course for judging treatment efficacy | Efforts to diminish acute affective instability may be measured over the course of days to weeks | By definition, treatment of RC involves relapse prevention over the course of 1 year |
| BD: bipolar disorder; RC: rapid cycling | ||
| References a. Schneck CD, Miklowitz DJ, Calabrese JR, et al. Phenomenology of rapid-cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry. 2004;161(10):1902-1908. b. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131. c. Koukopoulos A, Sani G, Koukopoulos AE, et al. Duration and stability of the rapid-cycling course: a long-term personal follow-up of 109 patients. J Affect Disord. 2003;73(1-2):75-85. d. Geller B, Tillman R, Bolhofner K, et al. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry. 2008;65(10):1125-1133. e. Post RM, Leverich GS, Kupka RW, et al. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry. 2010;71(7):864-872. f. Feldman-Naim S, Turner EH, Leibenluft E. Diurnal variation in the direction of mood switches in patients with rapid-cycling bipolar disorder. J Clin Psychiatry. 1997;58(2):79-84. g. Leibenluft E, Ashman SB, Feldman-Naim S, et al. Lack of relationship between menstrual cycle phase and mood in a sample of women with rapid cycling bipolar disorder. Biol Psychiatry. 1999;46(4):577-580. h. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145(2):179-184. i. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162. j. Wehr TA, Goodwin FK. Can antidepressants cause mania and worsen the course of affective illness? Am J Psychiatry. 1987;144(11):1403-1411. k. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165(3):370-377. l. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003;60(9):914-920. m. Fawcett J, Scheftner W, Clark D, et al. Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry. 1987;144(1):35-40. n. MacKinnon DF, Potash JB, McMahon FJ, et al. Rapid mood switching and suicidality in familial bipolar disorder. Bipolar Disord. 2005;7(5):441-448. | ||
From a biologic perspective, a handful of preliminary studies have examined genetic markers or familial patterns that might be related to rapid cycling (RC) or ultra-rapid cycling (URC). These include a reported link between URC and the low activity variant of the catechol-o-methyltransferase gene polymorphism in a small group of patients with velo-cardio-facial syndrome,a although this finding was not replicated in a larger sample.a Other preliminary reports on RC have implicated both the long (l) and short (s) allelic variants of the serotonin transporter gene (SLC6A4), the val66met variant of the brain-derived neurotrophic factor gene, and the circadian cryptochrome 2 (CRY2) gene (reviewed by Bauer et alb). These candidate loci have been examined in RC but not URC.
URC has not been examined as a familial entity, although in the National Institute of Mental Health Collaborative Depression Study, DSM-IV-TR RC did not occur with elevated frequency in bipolar pedigrees.c Rapid mood switches—abrupt rather than gradual transitions from one affective pole to another—appear to be only slightly, nonsignificantly more common in first-degree bipolar relatives of BD patients who themselves have rapid rather than gradual transitions from one affective pole to the other.d
Neuroimaging studies in BD seldom focus on subpopulations with RC or URC, and have been confined mainly to case reports that have yielded limited, non-generalizable observations, such as state-dependent variations in prefrontal activity during tasks of facial recognition (reviewed by Bauer et alb).
References
a. Papolos DF, Veit S, Faedda GL, et al. Ultra-ultra rapid cycling bipolar disorder is associated with the low activity catecholamine-O-methyltransferase allele. Mol Psychiatry. 1998;3(4):346-349.
b. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162.
c. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131.
d. MacKinnon DF, Potash JB, McMahon FJ, et al. Rapid mood switching and suicidality in familial bipolar disorder. Bipolar Disord. 2005;7(5):441-448.
Figure: Example of prospective mood charting to document changes in manic/hypomanic and depressive symptoms across time
In the above example, the prevalence and severity of mood symptoms are identified over 21 days. Note the distinctly separate phases of mood elevation followed by depression, whereas euthymia was present only 6 of 21 days (29% of the time). Symptoms of at least moderate severity were more prominently depressive (5 of 21 days, or 24% of the time) than manic/hypomanic (2 of 21 days, or approximately 10% of the time). Mood charting does not capture associate DSM-IV-TR criteria for a mood episode but instead focuses solely on longitudinal changes in mood elevation or depression
Related Resources
- American Psychiatric Association practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry. 2002;159(4 suppl):1-50.
- Massachusetts General Hospital Bipolar Clinic and Research Program. Sample mood chart (downloadable). www.manicdepressive.org/moodchart.html.
Drug Brand Names
- Carbamazepine • Equetro, Tegretol
- Divalproex • Depakote
- Lamotrigine • Lamictal
- Levothyroxine • Synthroid
- Lithium • Lithobid
- Nimodipine • Nimotop
- Topiramate • Topamax
Disclosures
Dr. Goldberg is on the speakers’ bureaus for AstraZeneca, Dey Pharmaceuticals, Eli Lilly and Company, Merck, and Sunovion and is a consultant for Axon Advisors, Dey Pharmaceuticals, Eli Lilly and Company, and Grünenthal Group.
Acknowledgment
The author wishes to thank David L. Dunner, MD, for his helpful comments regarding this article.
1. Kramlinger KG, Post RM. Ultra-rapid and ultradian cycling in bipolar affective illness. Br J Psychiatry. 1996;168(3):314-323.
2. Leibenluft E. Severe mood dysregulation irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168(2):129-142.
3. Geller B, Tillman R, Bolhofner K. Proposed definitions of bipolar I disorder episodes and daily rapid cycling phenomena in preschoolers school-aged children, adolescents, and adults. J Child Adolesc Psychopharmacol. 2007;17(2):217-222.
4. Feinman JA, Dunner DL. The effect of alcohol and substance abuse on the course of bipolar affective disorder. J Affect Disord. 1996;37(1):43-49.
5. Maj M, Pirozzi R, Formicola AM, et al. Reliability and validity of four alternative definitions of rapid-cycling bipolar disorder. Am J Psychiatry. 1999;156(9):1421-1424.
6. Jenner FA, Gjessing LR, Cox JR, et al. A manic depressive psychotic with a persistent forty-eight hour cycle. Br J Psychiatry. 1967;113(501):895-910.
7. Zwil AS, McAllister TW, Cohen I, et al. Ultra-rapid cycling bipolar affective disorder following a closed-head injury. Brain Inj. 1993;7(2):147-152.
8. Geller B, Tillman R, Craney JL, et al. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry. 2004;61(5):459-467.
9. Geller B, Sun K, Zimerman B, et al. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord. 1995;34(4):259-268.
10. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder inpatients with mood instability. J Clin Psychiatry. 2008;69(11):1751-1757.
11. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
12. MacKinnon DF, Pies R. Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006;8(1):1-14.
13. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131.
14. Koenigsberg HW, Harvey PD, Mitropoulou V, et al. Characterizing affective instability in borderline personality disorder. Am J Psychiatry. 2002;159(5):784-788.
15. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35(6):307-312.
16. Gottschalk A, Bauer MS, Whybrow PC. Evidence of chaotic mood variation in bipolar disorder. Arch Gen Psychiatry. 1995;52(11):947-959.
17. Goldberg JF, Bowden CL, Calabrese JR, et al. Six-month prospective life charting of mood symptoms with lamotrigine monotherapy versus placebo in rapid cycling bipolar disorder. Biol Psychiatry. 2008;63(1):125-130.
18. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165(3):370-377.
19. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. 2010;71(4):372-380.
20. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145(2):179-184.
21. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162.
22. Zavorotnyy M, Diemer J, Patzelt J, et al. Occurrence of ultra-rapid cycling during electroconvulsive therapy in bipolar depression. World J Biol Psychiatry. 2009;10(4 Pt 3):987-990.
23. Lepkifker E, Iancu I, Dannon P, et al. Valproic acid in ultra-rapid cycling: a case report. Clin Neuropharmacol. 1995;18(1):72-75.
24. Woo YS, Chae JH, Jun TY, et al. Lamotrigine added to valproate successfully treated a case of ultra-rapid cycling bipolar disorder. Psychiatry Clin Neurosci. 2007;61(1):130-131.
25. Karama S, Lal S. Adjunctive topiramate in ultradian cycling bipolar disorder: case report with 3-year follow-up. Eur Psychiatry. 2006;21(4):280-281.
26. Pazzaglia PJ, Post RM, Ketter TA, et al. Preliminary controlled trial of nimodipine in ultra-rapid cycling affective dysregulation. Psychiatry Res. 1993;49(3):257-272.
27. Reilly-Harrington NA, Deckersbach T, Knauz R, et al. Cognitive behavioral therapy for rapid-cycling bipolar disorder: a pilot study. J Psychiatr Pract. 2007;13(5):291-297.
Ultra-rapid cycling (URC) entered the psychiatric lexicon in the 1990s as a proposed descriptor for manic/hypomanic, mixed, or depressed episodes of bipolar disorder (BD) that occur every few days or weeks. DSM-IV-TR incorporates rapid cycling (RC)—but not URC—as a course specifier that occurs in 10% to 15% of patients with BD who have ≥4 distinct affective episodes per year, each fulfilling duration criteria and separated by identifiable recovery periods (unless an episode directly changes polarity). Since then, the terms RC and URC have seemingly metamorphosed into imprecise, popular colloquialisms meant to loosely describe frequent mood changes rather than distinct episodes over extended time periods, with little regard for the associated signs that define manic or hypomanic episodes.
This article examines the meaning and validity of URC in BD, its relevance and differentiation from rapid mood shifts in patients without BD, and concepts relevant to treatment extrapolated from studies of RC BD.
Imprecise nomenclature
Post et al1 coined the terms “ultra-rapid cycling” and “ultra-ultra-rapid cycling” (also called “ultradian cycling”) to describe mood episodes that occur monthly (URC) or over the course of as little as 1 day (ultradian cycling). These constructs are controversial because they lack demonstrated content validity and discriminant validity relative to other disorders. (“Content validity” refers to whether the features thought to comprise an entity of interest accurately and meaningfully do so; “discriminant validity” tells researchers and clinicians whether the proposed description of a clinical entity uniquely differentiates it from other disorders—avoiding “false-positive” suspected cases.) Clinicians therefore must pay careful attention to non-bipolar psychiatric problems that can present with rapid mood changes but without the psychomotor and related signs that define bipolar mood episodes. In their looser, nontechnical meanings, “rapid cycling” or “ultra-rapid cycling” may be synonymous with affective lability. RC is neither a diagnosis in itself nor a criterion for diagnosing BD. Rather, it is a course specifier to describe episode frequency in patients with past unambiguous manic or hypomanic episodes.
In children and adolescents, whose presentations often are atypical and can be hard to differentiate from other forms of behavioral or temperamental dysregulation, severe non-episodic mood dysregulation without signs of mania or hypomania may indicate a phenomenon separate from BD.2 Geller and colleagues3 proposed using the term “episodes” to frame the duration of a DSM-IV-defined syndrome of mania/hypomania or depression, while reserving the term “cycling” to connote patterns of mood alternation within a given episode. It is not clear whether this concept of “cycling” differs qualitatively from mood lability that arises during a mood episode in children or adults, and notably, this perspective does not account for changes in psychomotor signs in conjunction with changes in mood.
Clinicians also sometimes blur the concept of “mixed episodes” with RC or URC. DSM-IV-TR defines mixed episodes within bipolar I disorder (BD I) based on criteria for a simultaneous manic and depressive episode, rather than on frequent oscillations between affective poles. These and other differential diagnostic considerations for suspected URC are summarized in Table 1.4
A further concern regarding nomenclature involves the distinction between cyclicity (ie, successive episodes regardless of pole direction) and changes in polarity (ie, switches from depression to mania/hypomania or vice versa). Some mood disorder patients may have rapid oscillations from euthymia to depression while never changing polarity to mania/hypomania and may be best described as having recurrent brief depression.
Table 1
Differential diagnosis in suspected URC
| Phenomenon | Considerations for assessment |
|---|---|
| Mixed episodes in bipolar I disorder, or mixed depressive episodes in bipolar II disorder | DSM-IV-TR mixed episodes entail the co-occurrence of manic and depressive symptoms during the same episode without an intervening period of recovery. ICD-10 includes “rapid alternation of manic, hypomanic or depressive symptoms…from day to day or even hour to hour” in its definition of a mixed episode |
| Distress responses to acute environmental adversities (eg, adjustment disorders with mixed disturbance of emotions and conduct) | One would expect an absence of corresponding sleep-wake cycle changes or speech-language and psychomotor disturbances |
| Intoxication/withdrawal from psychoactive substances or drug-induced mental status changes (eg, corticosteroids, amphetamine, cocaine); a history of substance abuse also may be associated with development of URC in BD patients4 | Substance-induced mood fluctuations caused by intoxication/withdrawal can mimic affective cycling |
| Disinhibition states and frontal lobe syndromes as seen in traumatic brain injury and other CNS disorders, such as multiple sclerosis | Assess for signs of perseveration and history of head trauma or neurologic damage from cumulative toxic-metabolic insults (eg, chronic alcoholism) |
| Autonomic hyperarousal, emotional volatility, and hyperreactivity to environmental stresses, suggestive of PTSD | Determine the presence of a trauma history and review whether DSM-IV-TR symptoms and associated features of PTSD exist, including re-experiencing/reliving and avoidance, as well as paranoid thinking, dissociation, and nightmares |
| Recurrent mood shifts related to premenstrual dysphoric disorder may mimic URC. Other endocrine dysfunctions also may present with URC (eg, thyroid or ovarian malignancies) | Affirm the independent presence of BD before inferring its manifestations solely from premenstrual mood changes |
| Trait affective instability associated with borderline personality disorder | Trait mood instability is more chronic and enduring than episodic, and would not be expected to occur in tandem with signs of psychomotor activation that define mania/hypomania |
| BD: bipolar disorder; ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th revision; PTSD: posttraumatic stress disorder; URC: ultra-rapid cycling | |
Duration criteria
Clinicians and researchers have debated the minimum duration criteria for identifying manic or hypomanic episodes, and the extent to which suspected hypomanic periods of short duration constitute distinct illness phases. Although DSM-IV-TR designates 4 days as a minimum time for classifying an episode of hypomania, empirical studies suggest that mood symptoms lasting as few as 2 days may comprise a valid and reliably distinct entity relevant to RC.5 More limited data (mainly case observations) identify “affective oscillations” and “mood shifts” occurring faster than once per 24 hours in BD patients without comorbid personality disorders.6 Phenomenologic studies that have focused on 24- to 48-hour switch cycles have described new-onset URC arising spontaneously or following closed head injuries.7 In children and younger adolescents, reports have identified long index manic episodes (mean durations as long as 80 weeks)8 that involve continual (ultradian) mood cycling in as many as 80% of cases.9
Is URC a valid construct?
A central controversy surrounding the validity and meaningfulness of URC as a BD subtype involves its sole focus on mood variation rather than the fuller constellation of associated signs and symptoms that define episodes of mania/hypomania or depression. Abrupt, sudden, drastic, or dramatic mood shifts from one moment to the next are nowhere to be found in the DSM-IV-TR definition of BD, and the construct of mood lability or affective instability is neither a cardinal nor defining element of BD. Although individuals with BD I or bipolar II disorder (BD II) may have periods of affective lability, rapid shifts in mood are neither necessary nor sufficient for a BD diagnosis, and may indicate other types of psychopathology when affective instability occurs in the absence of a history of discernible manic or hypomanic episodes.
Studies by our group10 and others11 have shown that overattention to mood variation without considering associated cognitive, speech-language, chronobiologic, and motor signs of mania/hypomania accounts for substantial overdiagnosis of BD in patients with non-specific mood disturbances, particularly in those with active substance abuse or borderline personality disorder (BPD). Whereas the construct of RC BD attempts to account for changes in energy and psychomotor function as part of recurrent syndromes of mania/hypomania, existing literature on URC does not. Assessing mood changes in <24 hours also precludes assessing associated phenomena that occur over longer periods, such as changes in the sleep-wake cycle.
A rigorous, systematic approach to differential diagnosis for patients with affective instability is essential.
Borderline personality disorder
A common diagnostic debate regarding URC involves how to differentiate it from the chronic mood instability and reactivity inherent to BPD. Although some authors have suggested that RC BD and affective instability in BPD may be the same entity,12 others object to unifying the 2 conditions without considering their phenomenologic and other clinical differences. For example, affective instability arising from borderline character organization is thought to reflect a patient’s impaired capacity to self-regulate his or her internal state and emotional responses to interpersonal and other environmental stresses, or difficulty managing impulses. By contrast, manic or depressive phases of BD tend not to be “triggered” by interpersonal conflicts or frustrations. Furthermore, reframing intense mood reactions to the environment as bipolar variants carries several pitfalls: doing so wrongly accords patients a passive role in their reactions to life events, inaccurately reinforces a sense of victimization in response to stress, and diverts inquiry away from a patient’s active role in life decisions and circumstances that may be unsatisfying, self-defeating, or volatile.
Two key considerations may be helpful in discriminating rapid mood changes in BD vs BPD. First, some longitudinal studies indicate that RC often is a transient, rather than enduring, phenomenon in BD,13 in contrast to the nonvarying, trait feature of affective instability in persons with BPD. It is unknown whether URC is more enduring than transient. Notably, whereas bipolar mood episodes constitute deviations from a baseline state, affective instability in BPD is a baseline characteristic, rather than a deviation from it. Second, by definition, a BPD diagnosis hinges on additional elements unrelated to mood disturbances, such as interpersonal styles or defense mechanisms that involve splitting, projection, and projective identification, feelings of numbness, boredom, or emptiness, identity diffusion, fears of abandonment, and proclivities toward self-mutilation or other self-injurious behaviors as a means to alleviate tension and stress. These characteristics do not overlap with the core elements of BD.
Affective lability in patients with BPD entails prominent oscillations between anger and anxiety, or depression and anxiety, but not depression and elation14; by contrast, affective instability in BD has been linked with greater oscillations between euthymia and depression, and euthymia and elation, but not euthymia and anger.15 Moreover, daily mood fluctuations in patients with BD appear to occur in a relatively random fashion,16 whereas in BPD mood fluctuations are reactions that appear intimately linked to distressing interpersonal experiences.
See the table below, entitled “Rapid cycling and ultra-rapid cycling BD: A comparison,” comparing the phenomenology of RC and URC and a discussion of studies that explored genetic markers or family patterns that may be related to RC or URC.
Treatment considerations
No systematic studies exist for treating URC. Because most clinical trials of BD focus on treatment or prevention of a single episode rather than changes of mood over time, it is difficult to draw inferences about the ability of any treatment to attenuate marked, day-to-day mood variations. Some antimanic drugs, such as carbamazepine, have been suggested to offer better prophylactic efficacy compared with lithium for “non-classical” BD presentations, although the efficacy of carbamazepine has not been studied in URC.
Broadly speaking, treatment for URC, similar to RC, pragmatically involves:
- identifying and eliminating sources of mood destabilization (eg, substance abuse, erratic sleep patterns)
- treating medical comorbidities such as hypothyroidism
- optimizing treatment with mood stabilizing agents
- exercising caution when using antidepressants (see below).
Interestingly, despite frequent allusion to certain medications as “mood stabilizers,” no controlled study has examined mood instability on a day-to-day basis as a primary outcome measure in BD treatment, which limits the ability to surmise that any drug could be expected to diminish mood oscillations that occur over the course of days, or within a single day. However, a post hoc analysis by our group17 compared randomized treatment with lamotrigine or placebo over 6 months in RC BD I or BD II. Using prospective life charting, we found patients who received lamotrigine were almost twice as likely as those receiving placebo to achieve euthymia from one week to the next, which suggests the possibility that lamotrigine may offer benefit for affective instability in BD I or BD II patients, in addition to preventing discrete mood episodes.
Antidepressant controversy. Concerns that antidepressants might acutely induce mania or accelerate cycling frequency over long time periods have led to a contentious, long-standing debate within psychopharmacology. As noted in the box below, several long-term naturalistic follow-up studies have reported RC as a perceived consequence of antidepressants in most RC patients, although efforts to differentiate cycle acceleration caused by antidepressants (or other iatrogenic factors) from the natural course of illness remains exceedingly difficult without prospective randomized trials. (Antidepressants might cause more affective recurrences, but having multiple episodes may also cause more antidepressant prescriptions.) Some researchers (eg, Schneck et al18) have reported more frequent episodes among patients taking antidepressants but did not consider that patients with multiple episodes may be more likely to receive antidepressants, which fail to ameliorate acute or recurrent affective episodes. Importantly, a recent multi-site randomized trial by Ghaemi et al19 found that after a favorable acute response to antidepressants plus mood stabilizers, patients with preexisting RC who were randomized to continue antidepressants for up to 1 year had a 3-fold increased likelihood of developing a new depressive episode, which affirms suggestions that antidepressants do not help—but may exacerbate—cycling in patients with RC. No studies in BD have examined whether URC is more likely to arise as a consequence of antidepressant use.
Mood stabilizers and other biologic therapies. A small body of literature specifically addresses pharmacotherapy of URC in patients with BD (Table 2).19-26 A limitation of most existing literature is its focus on case reports, small open trials, or anecdotal observations rather than large, randomized controlled trials using systematic outcome measures. Extrapolation from reports focusing on patients with DSM-IV-TR RC is limited because it is uncertain whether URC differs fundamentally from RC and studies of DSM-IV-TR RC typically examine acute response during an index episode or time until relapse during maintenance therapy, rather than impact on mood changes over time.
Psychotherapy. A limited database on the efficacy of adjunctive cognitive-behavioral therapy (CBT) in RC BD describes improvement in depressive symptoms over short-term follow-up.27 No long-term studies of CBT or other structured psychotherapies have focused on RC or URC. Intuitively, one might expect that psychoeducation targeting sleep hygiene, substance use, stress management and coping skills, medication adherence, and prodrome recognition would be of value to patients with BD who experience frequent mood episodes, especially in those who may be unaware of or unfamiliar with basic concepts related to BD. In addition, relevant concepts from dialectical behavior therapy may be beneficial for BD patients with possible URC, such as skills to enhance emotional regulation, distress tolerance, mindfulness, and interpersonal effectiveness.
Table 2
Evidence-based treatments for ultra-rapid cycling BD
| Intervention | Strength of evidence | Comment |
|---|---|---|
| Antidepressant elimination | Cycling frequency may lengthen during antidepressant-free periods among patients with RC20; long-term (up to 1 year) antidepressant use in RC patients may increase the likelihood of depressive recurrences19 | Findings based mostly on small sample sizes; no controlled trials of antidepressant cessation as an intervention specifically for URC |
| Lithium | Single case report of ECT-induced URC resolved by lithium augmentation during continued ECT22 | No large-scale or randomized trials |
| Carbamazepine | No controlled trials or case reports | Possible anti-cycling benefits relevant for URC could be inferred from post hoc studies among patients with RC |
| Divalproex | Single case report describing resolution of a 48-hour cycle after augmentation of lithium with divalproex23 | No large-scale or randomized trials |
| Lamotrigine | Single case report of 100 mg/d lamotrigine augmentation to divalproex yielded 8 months of remission in a 25-year-old man with BD II and a long-standing pattern of 3 days of hypomania followed by 5 days of depression24 | No large-scale or randomized trials |
| Topiramate | Single case report in URC describing reduction of cycling frequency over 3 years25 | Multiple large scale placebo-controlled studies in bipolar mania have been negative |
| Second-generation antipsychotics | No controlled trials or case reports | Possible anti-cycling benefits relevant for URC could be inferred from post hoc studies in RC |
| Combinations of ≥2 mood stabilizing drugs | No controlled trials or case reports | Combining multiple anti-cycling agents is intuitively logical but largely unstudied |
| Nimodipine | 1 unipolar and 11 BD patients treated in randomized, off-on-off-on fashion (begun at 90 mg/d, increased up to 720 mg/d, mean duration of 12 weeks on active drug)26 | Response in 5 of 9 completers. Findings await replication with larger sample sizes |
| Hypermetabolic thyroid hormone (levothyroxine) | Findings from a small (N = 11) study of adjunctive high-dose levothyroxine (0.15 to 0.4 mg/d, with dosages increased by 0.05 to 0.1 mg/d every 1 to 2 weeks); an unspecified subgroup had “a very rapid cycling pattern” (reviewed by Bauer et al21) | 10 of 11 RC patients had reductions in depressive symptoms, 5 of 7 had improvement from baseline manic symptoms (observation period >60 days) |
| ECT | Case reports of improvement with ECT in refractory RC that was presumed secondary to tricyclic antidepressants | Reports of induction of URC by ECT22; whether or not ECT would more likely improve or exacerbate cyclicity for a given patient may require empirical determination |
| BD: bipolar disorder; BD II: bipolar II disorder; ECT: electroconvulsive therapy; RC: rapid cycling; URC: ultra-rapid cycling | ||
Treatment monitoring. Prospective life charting allows patients to systematically record manic/hypomanic and depressive symptoms day-to-day and week-to-week, thus creating a measure that may be particularly relevant for patients whose moods change rapidly. Simple mood charts (see Related Resources) typically take into account the severity of symptoms of either polarity with ratings of mild, moderate, or severe. Such visual records permit simple calculations over the course of a given interval (eg, week-by-week or across months) of several important parameters, including:
- number of days euthymic
- number of days with depression
- number of days with abnormal mood elevation
- number of occasions in which moods of both polarities occur on the same day.
Tracking these parameters during a treatment allows clinicians to make quantitative comparisons over time as a method of determining whether or not meaningful changes are occurring in cyclicity. See the figure below for an example of a completed mood chart and its interpretation.
Additional recommendations for assessing and managing cyclicity in BD are summarized in Table 3.
Table 3
Tips for managing suspected ultra-rapid cycling BD
| Do’s | Don’ts |
|---|---|
| Ascertain a history of ≥1 lifetime manic or hypomanic episode to diagnose BD | Diagnose BD solely on the presence of rapid mood fluctuations |
| Determine the presence of changes in sleep, energy, speech-language, and related behavior as correlates of mood to differentiate syndromes from isolated variation in mood | Ignore constellations of associated signs and symptoms of mania/hypomania |
| Obtain patient history to assess for head trauma or other medical and neurologic events that could have affective or other psychiatric manifestations | Disregard possible medical etiologies for new-onset affective dysregulation |
| Ascertain the resolution of 1 episode before counting the resurgence of symptoms as constituting a new episode; a waxing and waning course may reflect illness chronicity with incomplete recovery rather than true cyclicity | Misidentify incomplete recovery from an existing episode as the occurrence of new multiple episodes, which would inflate false-positive cases of RC or URC |
| Advise patients to refrain from alcohol or illicit substances that could destabilize mood | Assume that comorbid alcohol or illicit substance abuse will remit only after mood stabilization has been achieved, rather than the reverse |
| Monitor changes in sleep-wake cycles and the effects of erratic sleep or sleep deprivation on mood | Ignore the effects of poor sleep hygiene on mood |
| Minimize antidepressant exposure in patients with RC or URC | Continue long-term antidepressant maintenance therapy in patients with manic or mixed features or ongoing oscillations between mania/hypomania and depression |
| Assure euthyroid status and consider the potential utility of hypermetabolic levothyroxine | Assume that RC or URC will resolve solely by normalizing or optimizing thyroid function |
| Use rational, pharmacodynamically nonredundant anti-cycling drugs | Ignore the cumulative burden of adverse effects of multiple drugs |
| Consider the potential role for ECT as a strategy to arrest URC during any phase of BD | Assume ECT has value only during acute depressive phases of BD |
| Use prospective mood charting to document the evolution of mood changes over time, particularly when gauging treatment efficacy | Rely solely on impressionistic recall of mood states or polarity changes as reflecting distinct phasic changes |
| BD: bipolar disorder; ECT: electroconvulsive therapy; RC: rapid cycling; URC: ultra-rapid cycling | |
Table
Rapid cycling and ultra-rapid cycling BD: A comparison
| Construct | Rapid cycling | Ultra-rapid cycling |
|---|---|---|
| Bipolar I vs II | Predominantly BD IIa | No systematic data |
| Sex | Predominantly women | No systematic data |
| Longitudinal course | May be a transient phenomenon that can occur at any timeb or an enduring phenomenon that may persist for yearsc | Ultradian patterns may be more common across the first several episodes among pediatric BD patientsd |
| Age at onset | Associated with younger age at onsete | May be more evident in prepubescent onset mood disordersd; ultradian cycling more likely when onset occurs before age 13 than in adulthoode |
| Diurnal variation in mood | Morning-to-evening mood switches usually involve depression to mania/hypomania, with the opposite typifying evening-to-morning mood switchesf | Not reported |
| Relationship to environmental stresses | Life stresses may precede initial affective episodes but may be less important as subsequent episodes arise with increasing automaticity | No systematic data |
| Relationship to menstrual cycle | Despite case reports and self-reported links between RC and menstrual mood exacerbations, prospective data do not identify associations between RC and menstrual patternsg,h | No systematic data |
| Subclinical hypothyroidism | Bauer and Whybrow identified hypothyroidism independent of lithium use in 60% of 30 rapidly cycling BD patients, with evidence of improvement in a separate study of 11 RC patients given suprametabolic levothyroxine (reviewed by Bauer et ali) | No systematic data |
| Relationship to psychosis | Nonea | No systematic data |
| Relationship to antidepressant use | Naturalistic observations suggest RC may occur later in the illness course as a result of antidepressant use.c Small open case series data suggest shorter intermorbid intervals on antidepressants with longer intervals off antidepressants.j RC patients often receive antidepressants, but causal relationships are not well-documented.k Some case-control data dispute links between antidepressant use and RCl | No specific published cases |
| Considerations for suicide risk | RC linked with more serious suicide attemptsl | Suicide attempts may be associated with cycling within an episodem or rapid shifting in moodn |
| Time course for judging treatment efficacy | Efforts to diminish acute affective instability may be measured over the course of days to weeks | By definition, treatment of RC involves relapse prevention over the course of 1 year |
| BD: bipolar disorder; RC: rapid cycling | ||
| References a. Schneck CD, Miklowitz DJ, Calabrese JR, et al. Phenomenology of rapid-cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry. 2004;161(10):1902-1908. b. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131. c. Koukopoulos A, Sani G, Koukopoulos AE, et al. Duration and stability of the rapid-cycling course: a long-term personal follow-up of 109 patients. J Affect Disord. 2003;73(1-2):75-85. d. Geller B, Tillman R, Bolhofner K, et al. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry. 2008;65(10):1125-1133. e. Post RM, Leverich GS, Kupka RW, et al. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry. 2010;71(7):864-872. f. Feldman-Naim S, Turner EH, Leibenluft E. Diurnal variation in the direction of mood switches in patients with rapid-cycling bipolar disorder. J Clin Psychiatry. 1997;58(2):79-84. g. Leibenluft E, Ashman SB, Feldman-Naim S, et al. Lack of relationship between menstrual cycle phase and mood in a sample of women with rapid cycling bipolar disorder. Biol Psychiatry. 1999;46(4):577-580. h. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145(2):179-184. i. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162. j. Wehr TA, Goodwin FK. Can antidepressants cause mania and worsen the course of affective illness? Am J Psychiatry. 1987;144(11):1403-1411. k. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165(3):370-377. l. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003;60(9):914-920. m. Fawcett J, Scheftner W, Clark D, et al. Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry. 1987;144(1):35-40. n. MacKinnon DF, Potash JB, McMahon FJ, et al. Rapid mood switching and suicidality in familial bipolar disorder. Bipolar Disord. 2005;7(5):441-448. | ||
From a biologic perspective, a handful of preliminary studies have examined genetic markers or familial patterns that might be related to rapid cycling (RC) or ultra-rapid cycling (URC). These include a reported link between URC and the low activity variant of the catechol-o-methyltransferase gene polymorphism in a small group of patients with velo-cardio-facial syndrome,a although this finding was not replicated in a larger sample.a Other preliminary reports on RC have implicated both the long (l) and short (s) allelic variants of the serotonin transporter gene (SLC6A4), the val66met variant of the brain-derived neurotrophic factor gene, and the circadian cryptochrome 2 (CRY2) gene (reviewed by Bauer et alb). These candidate loci have been examined in RC but not URC.
URC has not been examined as a familial entity, although in the National Institute of Mental Health Collaborative Depression Study, DSM-IV-TR RC did not occur with elevated frequency in bipolar pedigrees.c Rapid mood switches—abrupt rather than gradual transitions from one affective pole to another—appear to be only slightly, nonsignificantly more common in first-degree bipolar relatives of BD patients who themselves have rapid rather than gradual transitions from one affective pole to the other.d
Neuroimaging studies in BD seldom focus on subpopulations with RC or URC, and have been confined mainly to case reports that have yielded limited, non-generalizable observations, such as state-dependent variations in prefrontal activity during tasks of facial recognition (reviewed by Bauer et alb).
References
a. Papolos DF, Veit S, Faedda GL, et al. Ultra-ultra rapid cycling bipolar disorder is associated with the low activity catecholamine-O-methyltransferase allele. Mol Psychiatry. 1998;3(4):346-349.
b. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162.
c. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131.
d. MacKinnon DF, Potash JB, McMahon FJ, et al. Rapid mood switching and suicidality in familial bipolar disorder. Bipolar Disord. 2005;7(5):441-448.
Figure: Example of prospective mood charting to document changes in manic/hypomanic and depressive symptoms across time
In the above example, the prevalence and severity of mood symptoms are identified over 21 days. Note the distinctly separate phases of mood elevation followed by depression, whereas euthymia was present only 6 of 21 days (29% of the time). Symptoms of at least moderate severity were more prominently depressive (5 of 21 days, or 24% of the time) than manic/hypomanic (2 of 21 days, or approximately 10% of the time). Mood charting does not capture associate DSM-IV-TR criteria for a mood episode but instead focuses solely on longitudinal changes in mood elevation or depression
Related Resources
- American Psychiatric Association practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry. 2002;159(4 suppl):1-50.
- Massachusetts General Hospital Bipolar Clinic and Research Program. Sample mood chart (downloadable). www.manicdepressive.org/moodchart.html.
Drug Brand Names
- Carbamazepine • Equetro, Tegretol
- Divalproex • Depakote
- Lamotrigine • Lamictal
- Levothyroxine • Synthroid
- Lithium • Lithobid
- Nimodipine • Nimotop
- Topiramate • Topamax
Disclosures
Dr. Goldberg is on the speakers’ bureaus for AstraZeneca, Dey Pharmaceuticals, Eli Lilly and Company, Merck, and Sunovion and is a consultant for Axon Advisors, Dey Pharmaceuticals, Eli Lilly and Company, and Grünenthal Group.
Acknowledgment
The author wishes to thank David L. Dunner, MD, for his helpful comments regarding this article.
Ultra-rapid cycling (URC) entered the psychiatric lexicon in the 1990s as a proposed descriptor for manic/hypomanic, mixed, or depressed episodes of bipolar disorder (BD) that occur every few days or weeks. DSM-IV-TR incorporates rapid cycling (RC)—but not URC—as a course specifier that occurs in 10% to 15% of patients with BD who have ≥4 distinct affective episodes per year, each fulfilling duration criteria and separated by identifiable recovery periods (unless an episode directly changes polarity). Since then, the terms RC and URC have seemingly metamorphosed into imprecise, popular colloquialisms meant to loosely describe frequent mood changes rather than distinct episodes over extended time periods, with little regard for the associated signs that define manic or hypomanic episodes.
This article examines the meaning and validity of URC in BD, its relevance and differentiation from rapid mood shifts in patients without BD, and concepts relevant to treatment extrapolated from studies of RC BD.
Imprecise nomenclature
Post et al1 coined the terms “ultra-rapid cycling” and “ultra-ultra-rapid cycling” (also called “ultradian cycling”) to describe mood episodes that occur monthly (URC) or over the course of as little as 1 day (ultradian cycling). These constructs are controversial because they lack demonstrated content validity and discriminant validity relative to other disorders. (“Content validity” refers to whether the features thought to comprise an entity of interest accurately and meaningfully do so; “discriminant validity” tells researchers and clinicians whether the proposed description of a clinical entity uniquely differentiates it from other disorders—avoiding “false-positive” suspected cases.) Clinicians therefore must pay careful attention to non-bipolar psychiatric problems that can present with rapid mood changes but without the psychomotor and related signs that define bipolar mood episodes. In their looser, nontechnical meanings, “rapid cycling” or “ultra-rapid cycling” may be synonymous with affective lability. RC is neither a diagnosis in itself nor a criterion for diagnosing BD. Rather, it is a course specifier to describe episode frequency in patients with past unambiguous manic or hypomanic episodes.
In children and adolescents, whose presentations often are atypical and can be hard to differentiate from other forms of behavioral or temperamental dysregulation, severe non-episodic mood dysregulation without signs of mania or hypomania may indicate a phenomenon separate from BD.2 Geller and colleagues3 proposed using the term “episodes” to frame the duration of a DSM-IV-defined syndrome of mania/hypomania or depression, while reserving the term “cycling” to connote patterns of mood alternation within a given episode. It is not clear whether this concept of “cycling” differs qualitatively from mood lability that arises during a mood episode in children or adults, and notably, this perspective does not account for changes in psychomotor signs in conjunction with changes in mood.
Clinicians also sometimes blur the concept of “mixed episodes” with RC or URC. DSM-IV-TR defines mixed episodes within bipolar I disorder (BD I) based on criteria for a simultaneous manic and depressive episode, rather than on frequent oscillations between affective poles. These and other differential diagnostic considerations for suspected URC are summarized in Table 1.4
A further concern regarding nomenclature involves the distinction between cyclicity (ie, successive episodes regardless of pole direction) and changes in polarity (ie, switches from depression to mania/hypomania or vice versa). Some mood disorder patients may have rapid oscillations from euthymia to depression while never changing polarity to mania/hypomania and may be best described as having recurrent brief depression.
Table 1
Differential diagnosis in suspected URC
| Phenomenon | Considerations for assessment |
|---|---|
| Mixed episodes in bipolar I disorder, or mixed depressive episodes in bipolar II disorder | DSM-IV-TR mixed episodes entail the co-occurrence of manic and depressive symptoms during the same episode without an intervening period of recovery. ICD-10 includes “rapid alternation of manic, hypomanic or depressive symptoms…from day to day or even hour to hour” in its definition of a mixed episode |
| Distress responses to acute environmental adversities (eg, adjustment disorders with mixed disturbance of emotions and conduct) | One would expect an absence of corresponding sleep-wake cycle changes or speech-language and psychomotor disturbances |
| Intoxication/withdrawal from psychoactive substances or drug-induced mental status changes (eg, corticosteroids, amphetamine, cocaine); a history of substance abuse also may be associated with development of URC in BD patients4 | Substance-induced mood fluctuations caused by intoxication/withdrawal can mimic affective cycling |
| Disinhibition states and frontal lobe syndromes as seen in traumatic brain injury and other CNS disorders, such as multiple sclerosis | Assess for signs of perseveration and history of head trauma or neurologic damage from cumulative toxic-metabolic insults (eg, chronic alcoholism) |
| Autonomic hyperarousal, emotional volatility, and hyperreactivity to environmental stresses, suggestive of PTSD | Determine the presence of a trauma history and review whether DSM-IV-TR symptoms and associated features of PTSD exist, including re-experiencing/reliving and avoidance, as well as paranoid thinking, dissociation, and nightmares |
| Recurrent mood shifts related to premenstrual dysphoric disorder may mimic URC. Other endocrine dysfunctions also may present with URC (eg, thyroid or ovarian malignancies) | Affirm the independent presence of BD before inferring its manifestations solely from premenstrual mood changes |
| Trait affective instability associated with borderline personality disorder | Trait mood instability is more chronic and enduring than episodic, and would not be expected to occur in tandem with signs of psychomotor activation that define mania/hypomania |
| BD: bipolar disorder; ICD-10: International Statistical Classification of Diseases and Related Health Problems, 10th revision; PTSD: posttraumatic stress disorder; URC: ultra-rapid cycling | |
Duration criteria
Clinicians and researchers have debated the minimum duration criteria for identifying manic or hypomanic episodes, and the extent to which suspected hypomanic periods of short duration constitute distinct illness phases. Although DSM-IV-TR designates 4 days as a minimum time for classifying an episode of hypomania, empirical studies suggest that mood symptoms lasting as few as 2 days may comprise a valid and reliably distinct entity relevant to RC.5 More limited data (mainly case observations) identify “affective oscillations” and “mood shifts” occurring faster than once per 24 hours in BD patients without comorbid personality disorders.6 Phenomenologic studies that have focused on 24- to 48-hour switch cycles have described new-onset URC arising spontaneously or following closed head injuries.7 In children and younger adolescents, reports have identified long index manic episodes (mean durations as long as 80 weeks)8 that involve continual (ultradian) mood cycling in as many as 80% of cases.9
Is URC a valid construct?
A central controversy surrounding the validity and meaningfulness of URC as a BD subtype involves its sole focus on mood variation rather than the fuller constellation of associated signs and symptoms that define episodes of mania/hypomania or depression. Abrupt, sudden, drastic, or dramatic mood shifts from one moment to the next are nowhere to be found in the DSM-IV-TR definition of BD, and the construct of mood lability or affective instability is neither a cardinal nor defining element of BD. Although individuals with BD I or bipolar II disorder (BD II) may have periods of affective lability, rapid shifts in mood are neither necessary nor sufficient for a BD diagnosis, and may indicate other types of psychopathology when affective instability occurs in the absence of a history of discernible manic or hypomanic episodes.
Studies by our group10 and others11 have shown that overattention to mood variation without considering associated cognitive, speech-language, chronobiologic, and motor signs of mania/hypomania accounts for substantial overdiagnosis of BD in patients with non-specific mood disturbances, particularly in those with active substance abuse or borderline personality disorder (BPD). Whereas the construct of RC BD attempts to account for changes in energy and psychomotor function as part of recurrent syndromes of mania/hypomania, existing literature on URC does not. Assessing mood changes in <24 hours also precludes assessing associated phenomena that occur over longer periods, such as changes in the sleep-wake cycle.
A rigorous, systematic approach to differential diagnosis for patients with affective instability is essential.
Borderline personality disorder
A common diagnostic debate regarding URC involves how to differentiate it from the chronic mood instability and reactivity inherent to BPD. Although some authors have suggested that RC BD and affective instability in BPD may be the same entity,12 others object to unifying the 2 conditions without considering their phenomenologic and other clinical differences. For example, affective instability arising from borderline character organization is thought to reflect a patient’s impaired capacity to self-regulate his or her internal state and emotional responses to interpersonal and other environmental stresses, or difficulty managing impulses. By contrast, manic or depressive phases of BD tend not to be “triggered” by interpersonal conflicts or frustrations. Furthermore, reframing intense mood reactions to the environment as bipolar variants carries several pitfalls: doing so wrongly accords patients a passive role in their reactions to life events, inaccurately reinforces a sense of victimization in response to stress, and diverts inquiry away from a patient’s active role in life decisions and circumstances that may be unsatisfying, self-defeating, or volatile.
Two key considerations may be helpful in discriminating rapid mood changes in BD vs BPD. First, some longitudinal studies indicate that RC often is a transient, rather than enduring, phenomenon in BD,13 in contrast to the nonvarying, trait feature of affective instability in persons with BPD. It is unknown whether URC is more enduring than transient. Notably, whereas bipolar mood episodes constitute deviations from a baseline state, affective instability in BPD is a baseline characteristic, rather than a deviation from it. Second, by definition, a BPD diagnosis hinges on additional elements unrelated to mood disturbances, such as interpersonal styles or defense mechanisms that involve splitting, projection, and projective identification, feelings of numbness, boredom, or emptiness, identity diffusion, fears of abandonment, and proclivities toward self-mutilation or other self-injurious behaviors as a means to alleviate tension and stress. These characteristics do not overlap with the core elements of BD.
Affective lability in patients with BPD entails prominent oscillations between anger and anxiety, or depression and anxiety, but not depression and elation14; by contrast, affective instability in BD has been linked with greater oscillations between euthymia and depression, and euthymia and elation, but not euthymia and anger.15 Moreover, daily mood fluctuations in patients with BD appear to occur in a relatively random fashion,16 whereas in BPD mood fluctuations are reactions that appear intimately linked to distressing interpersonal experiences.
See the table below, entitled “Rapid cycling and ultra-rapid cycling BD: A comparison,” comparing the phenomenology of RC and URC and a discussion of studies that explored genetic markers or family patterns that may be related to RC or URC.
Treatment considerations
No systematic studies exist for treating URC. Because most clinical trials of BD focus on treatment or prevention of a single episode rather than changes of mood over time, it is difficult to draw inferences about the ability of any treatment to attenuate marked, day-to-day mood variations. Some antimanic drugs, such as carbamazepine, have been suggested to offer better prophylactic efficacy compared with lithium for “non-classical” BD presentations, although the efficacy of carbamazepine has not been studied in URC.
Broadly speaking, treatment for URC, similar to RC, pragmatically involves:
- identifying and eliminating sources of mood destabilization (eg, substance abuse, erratic sleep patterns)
- treating medical comorbidities such as hypothyroidism
- optimizing treatment with mood stabilizing agents
- exercising caution when using antidepressants (see below).
Interestingly, despite frequent allusion to certain medications as “mood stabilizers,” no controlled study has examined mood instability on a day-to-day basis as a primary outcome measure in BD treatment, which limits the ability to surmise that any drug could be expected to diminish mood oscillations that occur over the course of days, or within a single day. However, a post hoc analysis by our group17 compared randomized treatment with lamotrigine or placebo over 6 months in RC BD I or BD II. Using prospective life charting, we found patients who received lamotrigine were almost twice as likely as those receiving placebo to achieve euthymia from one week to the next, which suggests the possibility that lamotrigine may offer benefit for affective instability in BD I or BD II patients, in addition to preventing discrete mood episodes.
Antidepressant controversy. Concerns that antidepressants might acutely induce mania or accelerate cycling frequency over long time periods have led to a contentious, long-standing debate within psychopharmacology. As noted in the box below, several long-term naturalistic follow-up studies have reported RC as a perceived consequence of antidepressants in most RC patients, although efforts to differentiate cycle acceleration caused by antidepressants (or other iatrogenic factors) from the natural course of illness remains exceedingly difficult without prospective randomized trials. (Antidepressants might cause more affective recurrences, but having multiple episodes may also cause more antidepressant prescriptions.) Some researchers (eg, Schneck et al18) have reported more frequent episodes among patients taking antidepressants but did not consider that patients with multiple episodes may be more likely to receive antidepressants, which fail to ameliorate acute or recurrent affective episodes. Importantly, a recent multi-site randomized trial by Ghaemi et al19 found that after a favorable acute response to antidepressants plus mood stabilizers, patients with preexisting RC who were randomized to continue antidepressants for up to 1 year had a 3-fold increased likelihood of developing a new depressive episode, which affirms suggestions that antidepressants do not help—but may exacerbate—cycling in patients with RC. No studies in BD have examined whether URC is more likely to arise as a consequence of antidepressant use.
Mood stabilizers and other biologic therapies. A small body of literature specifically addresses pharmacotherapy of URC in patients with BD (Table 2).19-26 A limitation of most existing literature is its focus on case reports, small open trials, or anecdotal observations rather than large, randomized controlled trials using systematic outcome measures. Extrapolation from reports focusing on patients with DSM-IV-TR RC is limited because it is uncertain whether URC differs fundamentally from RC and studies of DSM-IV-TR RC typically examine acute response during an index episode or time until relapse during maintenance therapy, rather than impact on mood changes over time.
Psychotherapy. A limited database on the efficacy of adjunctive cognitive-behavioral therapy (CBT) in RC BD describes improvement in depressive symptoms over short-term follow-up.27 No long-term studies of CBT or other structured psychotherapies have focused on RC or URC. Intuitively, one might expect that psychoeducation targeting sleep hygiene, substance use, stress management and coping skills, medication adherence, and prodrome recognition would be of value to patients with BD who experience frequent mood episodes, especially in those who may be unaware of or unfamiliar with basic concepts related to BD. In addition, relevant concepts from dialectical behavior therapy may be beneficial for BD patients with possible URC, such as skills to enhance emotional regulation, distress tolerance, mindfulness, and interpersonal effectiveness.
Table 2
Evidence-based treatments for ultra-rapid cycling BD
| Intervention | Strength of evidence | Comment |
|---|---|---|
| Antidepressant elimination | Cycling frequency may lengthen during antidepressant-free periods among patients with RC20; long-term (up to 1 year) antidepressant use in RC patients may increase the likelihood of depressive recurrences19 | Findings based mostly on small sample sizes; no controlled trials of antidepressant cessation as an intervention specifically for URC |
| Lithium | Single case report of ECT-induced URC resolved by lithium augmentation during continued ECT22 | No large-scale or randomized trials |
| Carbamazepine | No controlled trials or case reports | Possible anti-cycling benefits relevant for URC could be inferred from post hoc studies among patients with RC |
| Divalproex | Single case report describing resolution of a 48-hour cycle after augmentation of lithium with divalproex23 | No large-scale or randomized trials |
| Lamotrigine | Single case report of 100 mg/d lamotrigine augmentation to divalproex yielded 8 months of remission in a 25-year-old man with BD II and a long-standing pattern of 3 days of hypomania followed by 5 days of depression24 | No large-scale or randomized trials |
| Topiramate | Single case report in URC describing reduction of cycling frequency over 3 years25 | Multiple large scale placebo-controlled studies in bipolar mania have been negative |
| Second-generation antipsychotics | No controlled trials or case reports | Possible anti-cycling benefits relevant for URC could be inferred from post hoc studies in RC |
| Combinations of ≥2 mood stabilizing drugs | No controlled trials or case reports | Combining multiple anti-cycling agents is intuitively logical but largely unstudied |
| Nimodipine | 1 unipolar and 11 BD patients treated in randomized, off-on-off-on fashion (begun at 90 mg/d, increased up to 720 mg/d, mean duration of 12 weeks on active drug)26 | Response in 5 of 9 completers. Findings await replication with larger sample sizes |
| Hypermetabolic thyroid hormone (levothyroxine) | Findings from a small (N = 11) study of adjunctive high-dose levothyroxine (0.15 to 0.4 mg/d, with dosages increased by 0.05 to 0.1 mg/d every 1 to 2 weeks); an unspecified subgroup had “a very rapid cycling pattern” (reviewed by Bauer et al21) | 10 of 11 RC patients had reductions in depressive symptoms, 5 of 7 had improvement from baseline manic symptoms (observation period >60 days) |
| ECT | Case reports of improvement with ECT in refractory RC that was presumed secondary to tricyclic antidepressants | Reports of induction of URC by ECT22; whether or not ECT would more likely improve or exacerbate cyclicity for a given patient may require empirical determination |
| BD: bipolar disorder; BD II: bipolar II disorder; ECT: electroconvulsive therapy; RC: rapid cycling; URC: ultra-rapid cycling | ||
Treatment monitoring. Prospective life charting allows patients to systematically record manic/hypomanic and depressive symptoms day-to-day and week-to-week, thus creating a measure that may be particularly relevant for patients whose moods change rapidly. Simple mood charts (see Related Resources) typically take into account the severity of symptoms of either polarity with ratings of mild, moderate, or severe. Such visual records permit simple calculations over the course of a given interval (eg, week-by-week or across months) of several important parameters, including:
- number of days euthymic
- number of days with depression
- number of days with abnormal mood elevation
- number of occasions in which moods of both polarities occur on the same day.
Tracking these parameters during a treatment allows clinicians to make quantitative comparisons over time as a method of determining whether or not meaningful changes are occurring in cyclicity. See the figure below for an example of a completed mood chart and its interpretation.
Additional recommendations for assessing and managing cyclicity in BD are summarized in Table 3.
Table 3
Tips for managing suspected ultra-rapid cycling BD
| Do’s | Don’ts |
|---|---|
| Ascertain a history of ≥1 lifetime manic or hypomanic episode to diagnose BD | Diagnose BD solely on the presence of rapid mood fluctuations |
| Determine the presence of changes in sleep, energy, speech-language, and related behavior as correlates of mood to differentiate syndromes from isolated variation in mood | Ignore constellations of associated signs and symptoms of mania/hypomania |
| Obtain patient history to assess for head trauma or other medical and neurologic events that could have affective or other psychiatric manifestations | Disregard possible medical etiologies for new-onset affective dysregulation |
| Ascertain the resolution of 1 episode before counting the resurgence of symptoms as constituting a new episode; a waxing and waning course may reflect illness chronicity with incomplete recovery rather than true cyclicity | Misidentify incomplete recovery from an existing episode as the occurrence of new multiple episodes, which would inflate false-positive cases of RC or URC |
| Advise patients to refrain from alcohol or illicit substances that could destabilize mood | Assume that comorbid alcohol or illicit substance abuse will remit only after mood stabilization has been achieved, rather than the reverse |
| Monitor changes in sleep-wake cycles and the effects of erratic sleep or sleep deprivation on mood | Ignore the effects of poor sleep hygiene on mood |
| Minimize antidepressant exposure in patients with RC or URC | Continue long-term antidepressant maintenance therapy in patients with manic or mixed features or ongoing oscillations between mania/hypomania and depression |
| Assure euthyroid status and consider the potential utility of hypermetabolic levothyroxine | Assume that RC or URC will resolve solely by normalizing or optimizing thyroid function |
| Use rational, pharmacodynamically nonredundant anti-cycling drugs | Ignore the cumulative burden of adverse effects of multiple drugs |
| Consider the potential role for ECT as a strategy to arrest URC during any phase of BD | Assume ECT has value only during acute depressive phases of BD |
| Use prospective mood charting to document the evolution of mood changes over time, particularly when gauging treatment efficacy | Rely solely on impressionistic recall of mood states or polarity changes as reflecting distinct phasic changes |
| BD: bipolar disorder; ECT: electroconvulsive therapy; RC: rapid cycling; URC: ultra-rapid cycling | |
Table
Rapid cycling and ultra-rapid cycling BD: A comparison
| Construct | Rapid cycling | Ultra-rapid cycling |
|---|---|---|
| Bipolar I vs II | Predominantly BD IIa | No systematic data |
| Sex | Predominantly women | No systematic data |
| Longitudinal course | May be a transient phenomenon that can occur at any timeb or an enduring phenomenon that may persist for yearsc | Ultradian patterns may be more common across the first several episodes among pediatric BD patientsd |
| Age at onset | Associated with younger age at onsete | May be more evident in prepubescent onset mood disordersd; ultradian cycling more likely when onset occurs before age 13 than in adulthoode |
| Diurnal variation in mood | Morning-to-evening mood switches usually involve depression to mania/hypomania, with the opposite typifying evening-to-morning mood switchesf | Not reported |
| Relationship to environmental stresses | Life stresses may precede initial affective episodes but may be less important as subsequent episodes arise with increasing automaticity | No systematic data |
| Relationship to menstrual cycle | Despite case reports and self-reported links between RC and menstrual mood exacerbations, prospective data do not identify associations between RC and menstrual patternsg,h | No systematic data |
| Subclinical hypothyroidism | Bauer and Whybrow identified hypothyroidism independent of lithium use in 60% of 30 rapidly cycling BD patients, with evidence of improvement in a separate study of 11 RC patients given suprametabolic levothyroxine (reviewed by Bauer et ali) | No systematic data |
| Relationship to psychosis | Nonea | No systematic data |
| Relationship to antidepressant use | Naturalistic observations suggest RC may occur later in the illness course as a result of antidepressant use.c Small open case series data suggest shorter intermorbid intervals on antidepressants with longer intervals off antidepressants.j RC patients often receive antidepressants, but causal relationships are not well-documented.k Some case-control data dispute links between antidepressant use and RCl | No specific published cases |
| Considerations for suicide risk | RC linked with more serious suicide attemptsl | Suicide attempts may be associated with cycling within an episodem or rapid shifting in moodn |
| Time course for judging treatment efficacy | Efforts to diminish acute affective instability may be measured over the course of days to weeks | By definition, treatment of RC involves relapse prevention over the course of 1 year |
| BD: bipolar disorder; RC: rapid cycling | ||
| References a. Schneck CD, Miklowitz DJ, Calabrese JR, et al. Phenomenology of rapid-cycling bipolar disorder: data from the first 500 participants in the Systematic Treatment Enhancement Program. Am J Psychiatry. 2004;161(10):1902-1908. b. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131. c. Koukopoulos A, Sani G, Koukopoulos AE, et al. Duration and stability of the rapid-cycling course: a long-term personal follow-up of 109 patients. J Affect Disord. 2003;73(1-2):75-85. d. Geller B, Tillman R, Bolhofner K, et al. Child bipolar I disorder: prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry. 2008;65(10):1125-1133. e. Post RM, Leverich GS, Kupka RW, et al. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry. 2010;71(7):864-872. f. Feldman-Naim S, Turner EH, Leibenluft E. Diurnal variation in the direction of mood switches in patients with rapid-cycling bipolar disorder. J Clin Psychiatry. 1997;58(2):79-84. g. Leibenluft E, Ashman SB, Feldman-Naim S, et al. Lack of relationship between menstrual cycle phase and mood in a sample of women with rapid cycling bipolar disorder. Biol Psychiatry. 1999;46(4):577-580. h. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145(2):179-184. i. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162. j. Wehr TA, Goodwin FK. Can antidepressants cause mania and worsen the course of affective illness? Am J Psychiatry. 1987;144(11):1403-1411. k. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165(3):370-377. l. Coryell W, Solomon D, Turvey C, et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003;60(9):914-920. m. Fawcett J, Scheftner W, Clark D, et al. Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry. 1987;144(1):35-40. n. MacKinnon DF, Potash JB, McMahon FJ, et al. Rapid mood switching and suicidality in familial bipolar disorder. Bipolar Disord. 2005;7(5):441-448. | ||
From a biologic perspective, a handful of preliminary studies have examined genetic markers or familial patterns that might be related to rapid cycling (RC) or ultra-rapid cycling (URC). These include a reported link between URC and the low activity variant of the catechol-o-methyltransferase gene polymorphism in a small group of patients with velo-cardio-facial syndrome,a although this finding was not replicated in a larger sample.a Other preliminary reports on RC have implicated both the long (l) and short (s) allelic variants of the serotonin transporter gene (SLC6A4), the val66met variant of the brain-derived neurotrophic factor gene, and the circadian cryptochrome 2 (CRY2) gene (reviewed by Bauer et alb). These candidate loci have been examined in RC but not URC.
URC has not been examined as a familial entity, although in the National Institute of Mental Health Collaborative Depression Study, DSM-IV-TR RC did not occur with elevated frequency in bipolar pedigrees.c Rapid mood switches—abrupt rather than gradual transitions from one affective pole to another—appear to be only slightly, nonsignificantly more common in first-degree bipolar relatives of BD patients who themselves have rapid rather than gradual transitions from one affective pole to the other.d
Neuroimaging studies in BD seldom focus on subpopulations with RC or URC, and have been confined mainly to case reports that have yielded limited, non-generalizable observations, such as state-dependent variations in prefrontal activity during tasks of facial recognition (reviewed by Bauer et alb).
References
a. Papolos DF, Veit S, Faedda GL, et al. Ultra-ultra rapid cycling bipolar disorder is associated with the low activity catecholamine-O-methyltransferase allele. Mol Psychiatry. 1998;3(4):346-349.
b. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162.
c. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics, diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131.
d. MacKinnon DF, Potash JB, McMahon FJ, et al. Rapid mood switching and suicidality in familial bipolar disorder. Bipolar Disord. 2005;7(5):441-448.
Figure: Example of prospective mood charting to document changes in manic/hypomanic and depressive symptoms across time
In the above example, the prevalence and severity of mood symptoms are identified over 21 days. Note the distinctly separate phases of mood elevation followed by depression, whereas euthymia was present only 6 of 21 days (29% of the time). Symptoms of at least moderate severity were more prominently depressive (5 of 21 days, or 24% of the time) than manic/hypomanic (2 of 21 days, or approximately 10% of the time). Mood charting does not capture associate DSM-IV-TR criteria for a mood episode but instead focuses solely on longitudinal changes in mood elevation or depression
Related Resources
- American Psychiatric Association practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry. 2002;159(4 suppl):1-50.
- Massachusetts General Hospital Bipolar Clinic and Research Program. Sample mood chart (downloadable). www.manicdepressive.org/moodchart.html.
Drug Brand Names
- Carbamazepine • Equetro, Tegretol
- Divalproex • Depakote
- Lamotrigine • Lamictal
- Levothyroxine • Synthroid
- Lithium • Lithobid
- Nimodipine • Nimotop
- Topiramate • Topamax
Disclosures
Dr. Goldberg is on the speakers’ bureaus for AstraZeneca, Dey Pharmaceuticals, Eli Lilly and Company, Merck, and Sunovion and is a consultant for Axon Advisors, Dey Pharmaceuticals, Eli Lilly and Company, and Grünenthal Group.
Acknowledgment
The author wishes to thank David L. Dunner, MD, for his helpful comments regarding this article.
1. Kramlinger KG, Post RM. Ultra-rapid and ultradian cycling in bipolar affective illness. Br J Psychiatry. 1996;168(3):314-323.
2. Leibenluft E. Severe mood dysregulation irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168(2):129-142.
3. Geller B, Tillman R, Bolhofner K. Proposed definitions of bipolar I disorder episodes and daily rapid cycling phenomena in preschoolers school-aged children, adolescents, and adults. J Child Adolesc Psychopharmacol. 2007;17(2):217-222.
4. Feinman JA, Dunner DL. The effect of alcohol and substance abuse on the course of bipolar affective disorder. J Affect Disord. 1996;37(1):43-49.
5. Maj M, Pirozzi R, Formicola AM, et al. Reliability and validity of four alternative definitions of rapid-cycling bipolar disorder. Am J Psychiatry. 1999;156(9):1421-1424.
6. Jenner FA, Gjessing LR, Cox JR, et al. A manic depressive psychotic with a persistent forty-eight hour cycle. Br J Psychiatry. 1967;113(501):895-910.
7. Zwil AS, McAllister TW, Cohen I, et al. Ultra-rapid cycling bipolar affective disorder following a closed-head injury. Brain Inj. 1993;7(2):147-152.
8. Geller B, Tillman R, Craney JL, et al. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry. 2004;61(5):459-467.
9. Geller B, Sun K, Zimerman B, et al. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord. 1995;34(4):259-268.
10. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder inpatients with mood instability. J Clin Psychiatry. 2008;69(11):1751-1757.
11. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
12. MacKinnon DF, Pies R. Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006;8(1):1-14.
13. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131.
14. Koenigsberg HW, Harvey PD, Mitropoulou V, et al. Characterizing affective instability in borderline personality disorder. Am J Psychiatry. 2002;159(5):784-788.
15. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35(6):307-312.
16. Gottschalk A, Bauer MS, Whybrow PC. Evidence of chaotic mood variation in bipolar disorder. Arch Gen Psychiatry. 1995;52(11):947-959.
17. Goldberg JF, Bowden CL, Calabrese JR, et al. Six-month prospective life charting of mood symptoms with lamotrigine monotherapy versus placebo in rapid cycling bipolar disorder. Biol Psychiatry. 2008;63(1):125-130.
18. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165(3):370-377.
19. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. 2010;71(4):372-380.
20. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145(2):179-184.
21. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162.
22. Zavorotnyy M, Diemer J, Patzelt J, et al. Occurrence of ultra-rapid cycling during electroconvulsive therapy in bipolar depression. World J Biol Psychiatry. 2009;10(4 Pt 3):987-990.
23. Lepkifker E, Iancu I, Dannon P, et al. Valproic acid in ultra-rapid cycling: a case report. Clin Neuropharmacol. 1995;18(1):72-75.
24. Woo YS, Chae JH, Jun TY, et al. Lamotrigine added to valproate successfully treated a case of ultra-rapid cycling bipolar disorder. Psychiatry Clin Neurosci. 2007;61(1):130-131.
25. Karama S, Lal S. Adjunctive topiramate in ultradian cycling bipolar disorder: case report with 3-year follow-up. Eur Psychiatry. 2006;21(4):280-281.
26. Pazzaglia PJ, Post RM, Ketter TA, et al. Preliminary controlled trial of nimodipine in ultra-rapid cycling affective dysregulation. Psychiatry Res. 1993;49(3):257-272.
27. Reilly-Harrington NA, Deckersbach T, Knauz R, et al. Cognitive behavioral therapy for rapid-cycling bipolar disorder: a pilot study. J Psychiatr Pract. 2007;13(5):291-297.
1. Kramlinger KG, Post RM. Ultra-rapid and ultradian cycling in bipolar affective illness. Br J Psychiatry. 1996;168(3):314-323.
2. Leibenluft E. Severe mood dysregulation irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 2011;168(2):129-142.
3. Geller B, Tillman R, Bolhofner K. Proposed definitions of bipolar I disorder episodes and daily rapid cycling phenomena in preschoolers school-aged children, adolescents, and adults. J Child Adolesc Psychopharmacol. 2007;17(2):217-222.
4. Feinman JA, Dunner DL. The effect of alcohol and substance abuse on the course of bipolar affective disorder. J Affect Disord. 1996;37(1):43-49.
5. Maj M, Pirozzi R, Formicola AM, et al. Reliability and validity of four alternative definitions of rapid-cycling bipolar disorder. Am J Psychiatry. 1999;156(9):1421-1424.
6. Jenner FA, Gjessing LR, Cox JR, et al. A manic depressive psychotic with a persistent forty-eight hour cycle. Br J Psychiatry. 1967;113(501):895-910.
7. Zwil AS, McAllister TW, Cohen I, et al. Ultra-rapid cycling bipolar affective disorder following a closed-head injury. Brain Inj. 1993;7(2):147-152.
8. Geller B, Tillman R, Craney JL, et al. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Arch Gen Psychiatry. 2004;61(5):459-467.
9. Geller B, Sun K, Zimerman B, et al. Complex and rapid-cycling in bipolar children and adolescents: a preliminary study. J Affect Disord. 1995;34(4):259-268.
10. Goldberg JF, Garno JL, Callahan AM, et al. Overdiagnosis of bipolar disorder among substance use disorder inpatients with mood instability. J Clin Psychiatry. 2008;69(11):1751-1757.
11. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
12. MacKinnon DF, Pies R. Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders. Bipolar Disord. 2006;8(1):1-14.
13. Coryell W, Endicott J, Keller M. Rapidly cycling affective disorder. Demographics diagnosis, family history, and course. Arch Gen Psychiatry. 1992;49(2):126-131.
14. Koenigsberg HW, Harvey PD, Mitropoulou V, et al. Characterizing affective instability in borderline personality disorder. Am J Psychiatry. 2002;159(5):784-788.
15. Henry C, Mitropoulou V, New AS, et al. Affective instability and impulsivity in borderline personality and bipolar II disorders: similarities and differences. J Psychiatr Res. 2001;35(6):307-312.
16. Gottschalk A, Bauer MS, Whybrow PC. Evidence of chaotic mood variation in bipolar disorder. Arch Gen Psychiatry. 1995;52(11):947-959.
17. Goldberg JF, Bowden CL, Calabrese JR, et al. Six-month prospective life charting of mood symptoms with lamotrigine monotherapy versus placebo in rapid cycling bipolar disorder. Biol Psychiatry. 2008;63(1):125-130.
18. Schneck CD, Miklowitz DJ, Miyahara S, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008;165(3):370-377.
19. Ghaemi SN, Ostacher MM, El-Mallakh RS, et al. Antidepressant discontinuation in bipolar depression: a Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) randomized clinical trial of long-term effectiveness and safety. J Clin Psychiatry. 2010;71(4):372-380.
20. Wehr TA, Sack DA, Rosenthal NE, et al. Rapid cycling affective disorder: contributing factors and treatment responses in 51 patients. Am J Psychiatry. 1988;145(2):179-184.
21. Bauer M, Beaulieu S, Dunner DL, et al. Rapid cycling bipolar disorder—diagnostic concepts. Bipolar Disord. 2008;10(1 Pt 2):153-162.
22. Zavorotnyy M, Diemer J, Patzelt J, et al. Occurrence of ultra-rapid cycling during electroconvulsive therapy in bipolar depression. World J Biol Psychiatry. 2009;10(4 Pt 3):987-990.
23. Lepkifker E, Iancu I, Dannon P, et al. Valproic acid in ultra-rapid cycling: a case report. Clin Neuropharmacol. 1995;18(1):72-75.
24. Woo YS, Chae JH, Jun TY, et al. Lamotrigine added to valproate successfully treated a case of ultra-rapid cycling bipolar disorder. Psychiatry Clin Neurosci. 2007;61(1):130-131.
25. Karama S, Lal S. Adjunctive topiramate in ultradian cycling bipolar disorder: case report with 3-year follow-up. Eur Psychiatry. 2006;21(4):280-281.
26. Pazzaglia PJ, Post RM, Ketter TA, et al. Preliminary controlled trial of nimodipine in ultra-rapid cycling affective dysregulation. Psychiatry Res. 1993;49(3):257-272.
27. Reilly-Harrington NA, Deckersbach T, Knauz R, et al. Cognitive behavioral therapy for rapid-cycling bipolar disorder: a pilot study. J Psychiatr Pract. 2007;13(5):291-297.