User login
In type 2 diabetes, chronotype may affect depressive symptoms
ORLANDO – For patients with type 2 diabetes, larks may have an edge on owls when it comes to mood, according to a new study. Significantly more depressive symptoms were seen in owls – individuals whose sleep time preference, or chronotype, was later-to-bed and later-to-rise – in a cohort of 476 patients with type 2 diabetes.
In work that accounted for regional differences in chronotype by drawing from two different geographic regions, a later chronotype was associated with a higher score on the Center for Epidemiologic Studies Depression scale (CES-D), after controlling for potentially confounding factors (P = .045 for each cohort).
The study’s senior author, Sirimon Reutrakul, MD, of the faculty of medicine at Mahidol University, Bangkok, Thailand, said that previous work had also shown that when depression in patients with diabetes is untreated, self-care and blood glucose control can suffer, and more complications of diabetes are seen.
Dr. Reutrakul’s facility teamed with Rush University School of Medicine in Chicago, administering questionnaires designed to assess where patients fell along the morningness-eveningness scale. For the Chicago cohort (n = 194, 70% female), the Morningness-Eveningness Questionnaire (MEQ) was administered, while the Thailand cohort (n = 282, 57% female) completed the Composite Score of Morningness (CSM). Both groups completed the CES-D to assess depressive symptoms and the Pittsburgh Sleep Quality Index (PSQI); hemoglobin A1c values for both groups were ascertained by medical record review.
The mean age for the two cohorts was similar (Chicago, 58.3 plus or minus 13.0 years; Thailand, 55.7 plus or minus 11.6 years). The Chicago patients who scored higher on the CES-D, indicating that they had more depressive symptoms, were more likely to have a later chronotype on unadjusted analysis (P = .001). They were also likely to be younger (P = .005) and to have poorer sleep quality (P less than .001). Patients with more depressive symptoms were significantly more likely to be female, non-white, to use insulin, and to have poor glycemic control.
For the patients in Thailand, more depressive symptoms were also associated with a later chronotype on unadjusted analysis (P less than .001); younger age (P = .019), and poor sleep quality (P less than .001) were also associated with more depressive symptoms. Correction for a number of potentially confounding variables yielded modest statistical significance (P = .045) of the depressive symptoms-later chronotype relationship in both cohorts.
The Chicago patients were at approximately latitude 42N, while the patients in Thailand were at about latitude 13N, much closer to the equator. Populations that live closer to the equator, where days and nights are of approximately equal length year-round, tend to have more larks than owls, wrote Dr. Reutrakul and her colleagues.
In these two cohorts, which differed both by ethnic composition and geographic distance from the equator, “later chronotype was found to be independently associated with depressive symptoms” for patients with type 2 diabetes, wrote Dr. Reutrakul and her coauthors in the abstract accompanying the presentation. “In addition, sleep disturbances, more prevalent in evening types, have been associated with depression,” which is common in type 2 diabetes, the investigators wrote.
Dr. Reutrakul acknowledged that the work found an “only modest,” though consistent, association between eveningness and depressive symptoms. “We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” she said in a press statement preceding her presentation. “Learning more about the relationship between depression and circadian functioning might help us figure out strategies to improve physical and mental health for patients with diabetes…We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” Dr. Reutrakul said.
Dr. Reutrakul reported financial relationships with Medtronic Minimed, Novo Nordisk, Merck, and Sanofi.
[email protected]
On Twitter @karioakes
ORLANDO – For patients with type 2 diabetes, larks may have an edge on owls when it comes to mood, according to a new study. Significantly more depressive symptoms were seen in owls – individuals whose sleep time preference, or chronotype, was later-to-bed and later-to-rise – in a cohort of 476 patients with type 2 diabetes.
In work that accounted for regional differences in chronotype by drawing from two different geographic regions, a later chronotype was associated with a higher score on the Center for Epidemiologic Studies Depression scale (CES-D), after controlling for potentially confounding factors (P = .045 for each cohort).
The study’s senior author, Sirimon Reutrakul, MD, of the faculty of medicine at Mahidol University, Bangkok, Thailand, said that previous work had also shown that when depression in patients with diabetes is untreated, self-care and blood glucose control can suffer, and more complications of diabetes are seen.
Dr. Reutrakul’s facility teamed with Rush University School of Medicine in Chicago, administering questionnaires designed to assess where patients fell along the morningness-eveningness scale. For the Chicago cohort (n = 194, 70% female), the Morningness-Eveningness Questionnaire (MEQ) was administered, while the Thailand cohort (n = 282, 57% female) completed the Composite Score of Morningness (CSM). Both groups completed the CES-D to assess depressive symptoms and the Pittsburgh Sleep Quality Index (PSQI); hemoglobin A1c values for both groups were ascertained by medical record review.
The mean age for the two cohorts was similar (Chicago, 58.3 plus or minus 13.0 years; Thailand, 55.7 plus or minus 11.6 years). The Chicago patients who scored higher on the CES-D, indicating that they had more depressive symptoms, were more likely to have a later chronotype on unadjusted analysis (P = .001). They were also likely to be younger (P = .005) and to have poorer sleep quality (P less than .001). Patients with more depressive symptoms were significantly more likely to be female, non-white, to use insulin, and to have poor glycemic control.
For the patients in Thailand, more depressive symptoms were also associated with a later chronotype on unadjusted analysis (P less than .001); younger age (P = .019), and poor sleep quality (P less than .001) were also associated with more depressive symptoms. Correction for a number of potentially confounding variables yielded modest statistical significance (P = .045) of the depressive symptoms-later chronotype relationship in both cohorts.
The Chicago patients were at approximately latitude 42N, while the patients in Thailand were at about latitude 13N, much closer to the equator. Populations that live closer to the equator, where days and nights are of approximately equal length year-round, tend to have more larks than owls, wrote Dr. Reutrakul and her colleagues.
In these two cohorts, which differed both by ethnic composition and geographic distance from the equator, “later chronotype was found to be independently associated with depressive symptoms” for patients with type 2 diabetes, wrote Dr. Reutrakul and her coauthors in the abstract accompanying the presentation. “In addition, sleep disturbances, more prevalent in evening types, have been associated with depression,” which is common in type 2 diabetes, the investigators wrote.
Dr. Reutrakul acknowledged that the work found an “only modest,” though consistent, association between eveningness and depressive symptoms. “We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” she said in a press statement preceding her presentation. “Learning more about the relationship between depression and circadian functioning might help us figure out strategies to improve physical and mental health for patients with diabetes…We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” Dr. Reutrakul said.
Dr. Reutrakul reported financial relationships with Medtronic Minimed, Novo Nordisk, Merck, and Sanofi.
[email protected]
On Twitter @karioakes
ORLANDO – For patients with type 2 diabetes, larks may have an edge on owls when it comes to mood, according to a new study. Significantly more depressive symptoms were seen in owls – individuals whose sleep time preference, or chronotype, was later-to-bed and later-to-rise – in a cohort of 476 patients with type 2 diabetes.
In work that accounted for regional differences in chronotype by drawing from two different geographic regions, a later chronotype was associated with a higher score on the Center for Epidemiologic Studies Depression scale (CES-D), after controlling for potentially confounding factors (P = .045 for each cohort).
The study’s senior author, Sirimon Reutrakul, MD, of the faculty of medicine at Mahidol University, Bangkok, Thailand, said that previous work had also shown that when depression in patients with diabetes is untreated, self-care and blood glucose control can suffer, and more complications of diabetes are seen.
Dr. Reutrakul’s facility teamed with Rush University School of Medicine in Chicago, administering questionnaires designed to assess where patients fell along the morningness-eveningness scale. For the Chicago cohort (n = 194, 70% female), the Morningness-Eveningness Questionnaire (MEQ) was administered, while the Thailand cohort (n = 282, 57% female) completed the Composite Score of Morningness (CSM). Both groups completed the CES-D to assess depressive symptoms and the Pittsburgh Sleep Quality Index (PSQI); hemoglobin A1c values for both groups were ascertained by medical record review.
The mean age for the two cohorts was similar (Chicago, 58.3 plus or minus 13.0 years; Thailand, 55.7 plus or minus 11.6 years). The Chicago patients who scored higher on the CES-D, indicating that they had more depressive symptoms, were more likely to have a later chronotype on unadjusted analysis (P = .001). They were also likely to be younger (P = .005) and to have poorer sleep quality (P less than .001). Patients with more depressive symptoms were significantly more likely to be female, non-white, to use insulin, and to have poor glycemic control.
For the patients in Thailand, more depressive symptoms were also associated with a later chronotype on unadjusted analysis (P less than .001); younger age (P = .019), and poor sleep quality (P less than .001) were also associated with more depressive symptoms. Correction for a number of potentially confounding variables yielded modest statistical significance (P = .045) of the depressive symptoms-later chronotype relationship in both cohorts.
The Chicago patients were at approximately latitude 42N, while the patients in Thailand were at about latitude 13N, much closer to the equator. Populations that live closer to the equator, where days and nights are of approximately equal length year-round, tend to have more larks than owls, wrote Dr. Reutrakul and her colleagues.
In these two cohorts, which differed both by ethnic composition and geographic distance from the equator, “later chronotype was found to be independently associated with depressive symptoms” for patients with type 2 diabetes, wrote Dr. Reutrakul and her coauthors in the abstract accompanying the presentation. “In addition, sleep disturbances, more prevalent in evening types, have been associated with depression,” which is common in type 2 diabetes, the investigators wrote.
Dr. Reutrakul acknowledged that the work found an “only modest,” though consistent, association between eveningness and depressive symptoms. “We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” she said in a press statement preceding her presentation. “Learning more about the relationship between depression and circadian functioning might help us figure out strategies to improve physical and mental health for patients with diabetes…We need further research to explore a combination of interventions that help with circadian timing, such as light therapy and melatonin,” Dr. Reutrakul said.
Dr. Reutrakul reported financial relationships with Medtronic Minimed, Novo Nordisk, Merck, and Sanofi.
[email protected]
On Twitter @karioakes
AT ENDO 2017
Key clinical point:
Major finding: Later chronotype was associated with more depressive symptoms in 2 cohorts with type 2 diabetes (P = .045)
Data source: Cross-sectional study of 476 patients with type 2 diabetes in Chicago and Thailand..
Disclosures: Dr. Reutrakul reported financial relationships with Medtronic Minimed, Merck, Novo Nordisk, and Sanofi.
VIDEO: When early-stage vulvar cancer recurs, the prognosis is poor
NATIONAL HARBOR, MD – Cancer of the vulva is becoming more common, and as incidence is rising, so are death rates from the relatively rare malignancy. A new examination of women with early-stage vulvar cancer showed that recurrence was common, and carried a poor prognosis.
Cancer in “nearly 25% of women with stage IB squamous cell carcinoma of the vulva will recur within 3 years of initial diagnosis,” said the study’s lead author, Rebecca Stone, MD, at the annual meeting of the Society of Gynecologic Oncology. Although most (85%) of the cancers that recur do so locally, salvage rates for patients with recurrences are poor, she said in a video interview.
Dr. Stone of Johns Hopkins University, Baltimore, said that the study looked at the subset of 59 patients with recurrence of their stage IB vulvar cancer, drawing from a total of 244 stage IB patients for whom complete data were available.
Current National Comprehensive Cancer Network (NCCN) guidelines for the treatment of early-stage vulvar squamous cell carcinoma (meaning T1 or 4 cm or smaller T2 lesions) call for adjuvant radiotherapy for patients with positive margins or unresectable lesions. For patients with negative margins after the primary procedure or re-excision, the guidelines say that radiotherapy decisions should be guided by risk factors including margin width, tumor size, the presence of lymphovascular invasion, and the pattern and depth of invasion.
However, Dr. Stone said, “There’s a knowledge gap in our current management of early-stage disease.” Some unknowns include what the threshold should be for tumor recurrence in terms of depth of invasion and size of tumor, whether perineural invasion is a risk factor, and whether adverse clinical factors are important. Also, she said, it’s not known how risk factors combine to increase recurrence risk.
Tumor size, invasion depth over 6 mm, and patient age were all risk factors identified by the study; perineural and lymphovascular invasion were also potential risk factors for recurrence.
The retrospective study, said Dr. Stone, is the largest multi-institutional cohort study examining stage IB vulvar cancer that has been completed, and it accomplished a detailed examination of which patients have recurrences, factors associated with recurrence, and postrecurrence salvage rates.
Dr. Stone reported no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD – Cancer of the vulva is becoming more common, and as incidence is rising, so are death rates from the relatively rare malignancy. A new examination of women with early-stage vulvar cancer showed that recurrence was common, and carried a poor prognosis.
Cancer in “nearly 25% of women with stage IB squamous cell carcinoma of the vulva will recur within 3 years of initial diagnosis,” said the study’s lead author, Rebecca Stone, MD, at the annual meeting of the Society of Gynecologic Oncology. Although most (85%) of the cancers that recur do so locally, salvage rates for patients with recurrences are poor, she said in a video interview.
Dr. Stone of Johns Hopkins University, Baltimore, said that the study looked at the subset of 59 patients with recurrence of their stage IB vulvar cancer, drawing from a total of 244 stage IB patients for whom complete data were available.
Current National Comprehensive Cancer Network (NCCN) guidelines for the treatment of early-stage vulvar squamous cell carcinoma (meaning T1 or 4 cm or smaller T2 lesions) call for adjuvant radiotherapy for patients with positive margins or unresectable lesions. For patients with negative margins after the primary procedure or re-excision, the guidelines say that radiotherapy decisions should be guided by risk factors including margin width, tumor size, the presence of lymphovascular invasion, and the pattern and depth of invasion.
However, Dr. Stone said, “There’s a knowledge gap in our current management of early-stage disease.” Some unknowns include what the threshold should be for tumor recurrence in terms of depth of invasion and size of tumor, whether perineural invasion is a risk factor, and whether adverse clinical factors are important. Also, she said, it’s not known how risk factors combine to increase recurrence risk.
Tumor size, invasion depth over 6 mm, and patient age were all risk factors identified by the study; perineural and lymphovascular invasion were also potential risk factors for recurrence.
The retrospective study, said Dr. Stone, is the largest multi-institutional cohort study examining stage IB vulvar cancer that has been completed, and it accomplished a detailed examination of which patients have recurrences, factors associated with recurrence, and postrecurrence salvage rates.
Dr. Stone reported no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD – Cancer of the vulva is becoming more common, and as incidence is rising, so are death rates from the relatively rare malignancy. A new examination of women with early-stage vulvar cancer showed that recurrence was common, and carried a poor prognosis.
Cancer in “nearly 25% of women with stage IB squamous cell carcinoma of the vulva will recur within 3 years of initial diagnosis,” said the study’s lead author, Rebecca Stone, MD, at the annual meeting of the Society of Gynecologic Oncology. Although most (85%) of the cancers that recur do so locally, salvage rates for patients with recurrences are poor, she said in a video interview.
Dr. Stone of Johns Hopkins University, Baltimore, said that the study looked at the subset of 59 patients with recurrence of their stage IB vulvar cancer, drawing from a total of 244 stage IB patients for whom complete data were available.
Current National Comprehensive Cancer Network (NCCN) guidelines for the treatment of early-stage vulvar squamous cell carcinoma (meaning T1 or 4 cm or smaller T2 lesions) call for adjuvant radiotherapy for patients with positive margins or unresectable lesions. For patients with negative margins after the primary procedure or re-excision, the guidelines say that radiotherapy decisions should be guided by risk factors including margin width, tumor size, the presence of lymphovascular invasion, and the pattern and depth of invasion.
However, Dr. Stone said, “There’s a knowledge gap in our current management of early-stage disease.” Some unknowns include what the threshold should be for tumor recurrence in terms of depth of invasion and size of tumor, whether perineural invasion is a risk factor, and whether adverse clinical factors are important. Also, she said, it’s not known how risk factors combine to increase recurrence risk.
Tumor size, invasion depth over 6 mm, and patient age were all risk factors identified by the study; perineural and lymphovascular invasion were also potential risk factors for recurrence.
The retrospective study, said Dr. Stone, is the largest multi-institutional cohort study examining stage IB vulvar cancer that has been completed, and it accomplished a detailed examination of which patients have recurrences, factors associated with recurrence, and postrecurrence salvage rates.
Dr. Stone reported no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN’S CANCER
VIDEO: How to start an oncology sexual health clinic
NATIONAL HARBOR, MD – Start small, but anticipate growth. Engage your administration from the start. Be smart about resources, and consider using advanced practice providers to keep costs down. Above all, keep lines of communication open with physicians and other members of the care team.
In a video interview, Joanne Rash, PA-C, a certified physician assistant at the University of Wisconsin–Madison offers these and other tips. She explains her collaborative work with David Kushner, MD, director of the gynecologic oncology program and professor at the University of Wisconsin School of Medicine and Public Health, and a colleague to develop the Women’s Integrative Sexual Health (WISH) program.
WISH is modeled on the University of Chicago’s Program in Integrative Sex and Medicine for Women and Girls with Cancer (PRISM) and participates in the PRISM registry, which studies ways to prevent and treat sexual problems for women and girls with cancer.
“I think what makes the WISH program unique is that we carve time out,” said Ms. Rash. “Of course, we address some of these issues in my gynecologic oncology practice, but, when we do it in WISH, the format is different,” and there’s just more time for discussion.
Communication is key to the model’s success in safe integration of sexual health into cancer care, she said. “We certainly don’t want to do something that compromises cancer care, and so, it’s important that we have those conversations with that woman’s team. And now we get to be a part of that team, which is a real privilege.”
Ms. Rash reported no conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD – Start small, but anticipate growth. Engage your administration from the start. Be smart about resources, and consider using advanced practice providers to keep costs down. Above all, keep lines of communication open with physicians and other members of the care team.
In a video interview, Joanne Rash, PA-C, a certified physician assistant at the University of Wisconsin–Madison offers these and other tips. She explains her collaborative work with David Kushner, MD, director of the gynecologic oncology program and professor at the University of Wisconsin School of Medicine and Public Health, and a colleague to develop the Women’s Integrative Sexual Health (WISH) program.
WISH is modeled on the University of Chicago’s Program in Integrative Sex and Medicine for Women and Girls with Cancer (PRISM) and participates in the PRISM registry, which studies ways to prevent and treat sexual problems for women and girls with cancer.
“I think what makes the WISH program unique is that we carve time out,” said Ms. Rash. “Of course, we address some of these issues in my gynecologic oncology practice, but, when we do it in WISH, the format is different,” and there’s just more time for discussion.
Communication is key to the model’s success in safe integration of sexual health into cancer care, she said. “We certainly don’t want to do something that compromises cancer care, and so, it’s important that we have those conversations with that woman’s team. And now we get to be a part of that team, which is a real privilege.”
Ms. Rash reported no conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD – Start small, but anticipate growth. Engage your administration from the start. Be smart about resources, and consider using advanced practice providers to keep costs down. Above all, keep lines of communication open with physicians and other members of the care team.
In a video interview, Joanne Rash, PA-C, a certified physician assistant at the University of Wisconsin–Madison offers these and other tips. She explains her collaborative work with David Kushner, MD, director of the gynecologic oncology program and professor at the University of Wisconsin School of Medicine and Public Health, and a colleague to develop the Women’s Integrative Sexual Health (WISH) program.
WISH is modeled on the University of Chicago’s Program in Integrative Sex and Medicine for Women and Girls with Cancer (PRISM) and participates in the PRISM registry, which studies ways to prevent and treat sexual problems for women and girls with cancer.
“I think what makes the WISH program unique is that we carve time out,” said Ms. Rash. “Of course, we address some of these issues in my gynecologic oncology practice, but, when we do it in WISH, the format is different,” and there’s just more time for discussion.
Communication is key to the model’s success in safe integration of sexual health into cancer care, she said. “We certainly don’t want to do something that compromises cancer care, and so, it’s important that we have those conversations with that woman’s team. And now we get to be a part of that team, which is a real privilege.”
Ms. Rash reported no conflicts of interest.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Novel protein biomarker could accelerate ALS research
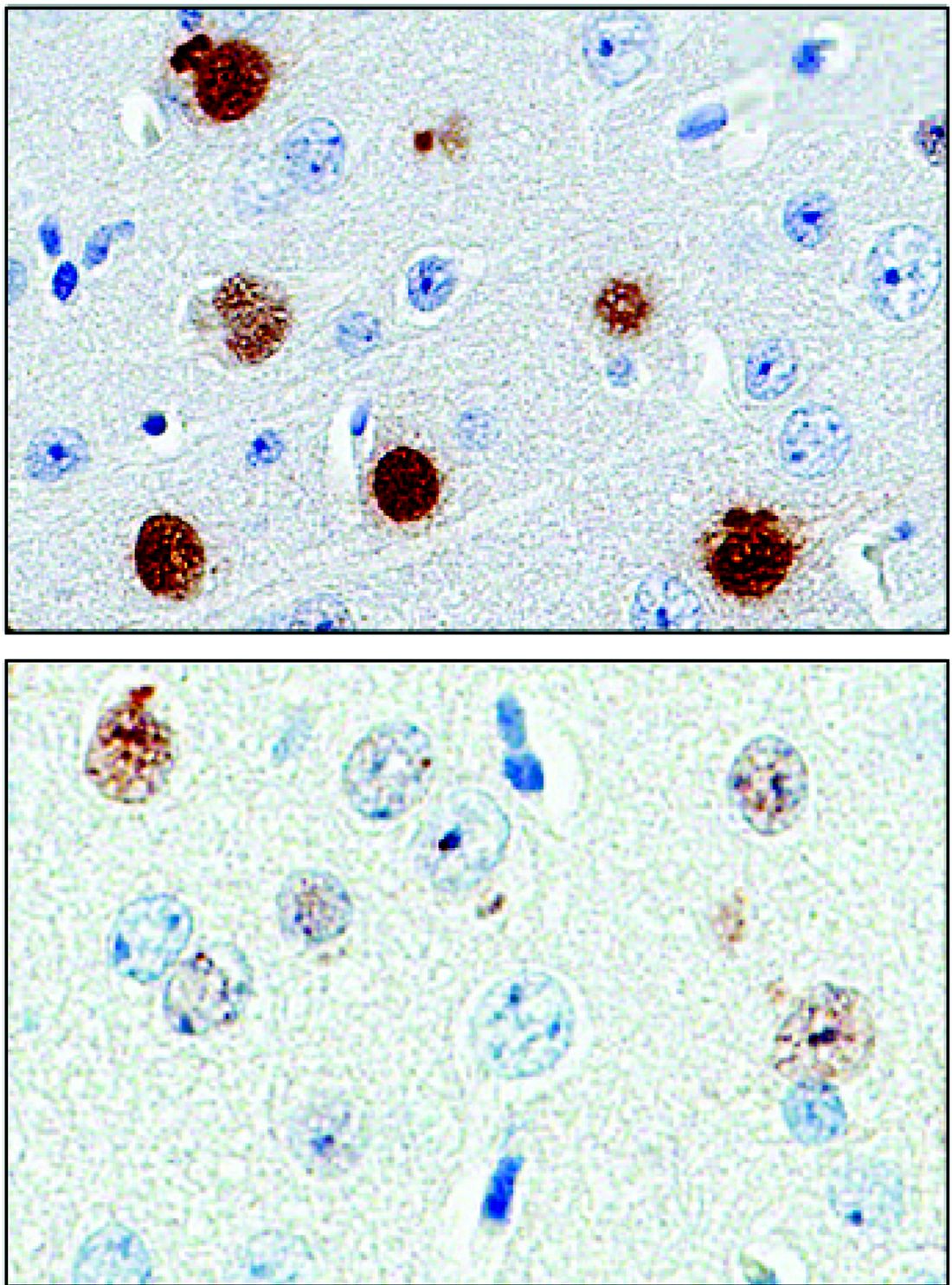
A protein found in the cerebrospinal fluid and peripheral blood cells of patients with a common type of amyotrophic lateral sclerosis may serve as a “pharmacodynamic marker,” providing a mechanism to assess RNA-based therapies that are now in clinical trials.
The protein, poly(GP), is expressed in patients who have a mutation in the gene chromosome 9 open reading frame 72 (C9ORF72), which causes one type of amyotrophic lateral sclerosis (ALS). This means that detecting poly(GP) also, eventually, may help to identify “presymptomatic individuals who are expected to benefit from early therapeutic interventions,” wrote the authors of a newly published paper (Sci Transl Med. 2017;9[383]:eaai7866).
Tania Gendron, PhD, of the department of neuroscience at the Mayo Clinic, Jacksonville, Fla., and her colleagues noted that poly(GP) was found in the cerebrospinal fluid (CSF) of both symptomatic and asymptomatic patients who carried the C9ORF72 mutation. The mutation can cause ALS, and is also associated with frontotemporal dementia (FTD) in a pattern with incomplete overlap with ALS.
However, “A limitation in moving such treatments from bench to bedside is a lack of pharmacodynamics markers for use in clinical trials,” Dr. Gendron and her collaborators wrote. The discovery that poly(GP) tracks well with C9ORF72 means that it has the potential to serve as the kind of biomarker that’s been missing in drug development for this family of neurodegenerative diseases, they said.
“To prepare for upcoming clinical trials for c9ALS, the present study used patient CSF and several preclinical models to investigate the hypothesis that poly(GP) proteins could serve as an urgently needed pharmacodynamics marker for developing and testing therapies for treating c9ALS,” Dr. Gendron and her colleagues wrote.
They looked at CSF samples from 83 patients with c9ALS and 27 patients who were asymptomatic C9ORF72 repeat expansion carriers, as well as 24 carriers who had a neurologic disease besides ALS or FTD (total n = 134). They also examined CSF samples from 120 study participants who lacked the mutation, 48 of whom were healthy controls; the remainder had ALS (n = 57) or another neurological disease.
The investigators, who were blinded to individuals’ disease status in each study arm, found that CSF poly(GP) levels were significantly higher in patients who had the C9ORF72 mutation (P less than .0001 in unadjusted and adjusted analyses). Poly(GP) was present in both asymptomatic and symptomatic carriers of the mutation, and not significantly different between these groups when data were adjusted for multiple comparisons, age, and gender.
When Dr. Gendron and her colleagues looked at poly(GP) levels over time for patients whose longitudinal data were available, they found that levels for an individual study participant were “relatively constant,” without any significant change over the median 12.9 months that these levels were tracked (P = .84).
However, “poly(GP) is not a prognostic marker,” wrote Dr. Gendron and her colleagues. They found no consistent association between levels of the protein and disease severity of progression, age at onset, or the development of FTD. Women were more likely to have lower levels, but the significance of that finding is not known, they said. There was a trend, which lost significance after statistical adjustment, for patients with cognitive impairment to have higher poly(GP) levels (adjusted P = .12).
Treatments under investigation for ALS and FTD include the use of an antisense oligonucleotide (ASO) to bind to the repeated RNA sequences and negate their ill effects. The investigators wrote that in vitro investigations using patient-derived cell models showed that poly(GP) levels dropped when cells were exposed to an ASO for 10 days. “The data indicate that poly(GP) production mirrors expression of repeat-containing C9ORF72 transcripts in lymphoblastoid cell lines,” they wrote.
The authors reported multiple governmental and private foundation sources of support for the research. Dr. Gendron and several of her coauthors are investigators in clinical trials for an ASO to target C9ORF72. Several authors reported paid and unpaid relationships and stock positions with pharmaceutical companies, including ones developing treatments for ALS and FTD.
[email protected]
On Twitter @karioakes
A protein found in the cerebrospinal fluid and peripheral blood cells of patients with a common type of amyotrophic lateral sclerosis may serve as a “pharmacodynamic marker,” providing a mechanism to assess RNA-based therapies that are now in clinical trials.
The protein, poly(GP), is expressed in patients who have a mutation in the gene chromosome 9 open reading frame 72 (C9ORF72), which causes one type of amyotrophic lateral sclerosis (ALS). This means that detecting poly(GP) also, eventually, may help to identify “presymptomatic individuals who are expected to benefit from early therapeutic interventions,” wrote the authors of a newly published paper (Sci Transl Med. 2017;9[383]:eaai7866).
Tania Gendron, PhD, of the department of neuroscience at the Mayo Clinic, Jacksonville, Fla., and her colleagues noted that poly(GP) was found in the cerebrospinal fluid (CSF) of both symptomatic and asymptomatic patients who carried the C9ORF72 mutation. The mutation can cause ALS, and is also associated with frontotemporal dementia (FTD) in a pattern with incomplete overlap with ALS.
However, “A limitation in moving such treatments from bench to bedside is a lack of pharmacodynamics markers for use in clinical trials,” Dr. Gendron and her collaborators wrote. The discovery that poly(GP) tracks well with C9ORF72 means that it has the potential to serve as the kind of biomarker that’s been missing in drug development for this family of neurodegenerative diseases, they said.
“To prepare for upcoming clinical trials for c9ALS, the present study used patient CSF and several preclinical models to investigate the hypothesis that poly(GP) proteins could serve as an urgently needed pharmacodynamics marker for developing and testing therapies for treating c9ALS,” Dr. Gendron and her colleagues wrote.
They looked at CSF samples from 83 patients with c9ALS and 27 patients who were asymptomatic C9ORF72 repeat expansion carriers, as well as 24 carriers who had a neurologic disease besides ALS or FTD (total n = 134). They also examined CSF samples from 120 study participants who lacked the mutation, 48 of whom were healthy controls; the remainder had ALS (n = 57) or another neurological disease.
The investigators, who were blinded to individuals’ disease status in each study arm, found that CSF poly(GP) levels were significantly higher in patients who had the C9ORF72 mutation (P less than .0001 in unadjusted and adjusted analyses). Poly(GP) was present in both asymptomatic and symptomatic carriers of the mutation, and not significantly different between these groups when data were adjusted for multiple comparisons, age, and gender.
When Dr. Gendron and her colleagues looked at poly(GP) levels over time for patients whose longitudinal data were available, they found that levels for an individual study participant were “relatively constant,” without any significant change over the median 12.9 months that these levels were tracked (P = .84).
However, “poly(GP) is not a prognostic marker,” wrote Dr. Gendron and her colleagues. They found no consistent association between levels of the protein and disease severity of progression, age at onset, or the development of FTD. Women were more likely to have lower levels, but the significance of that finding is not known, they said. There was a trend, which lost significance after statistical adjustment, for patients with cognitive impairment to have higher poly(GP) levels (adjusted P = .12).
Treatments under investigation for ALS and FTD include the use of an antisense oligonucleotide (ASO) to bind to the repeated RNA sequences and negate their ill effects. The investigators wrote that in vitro investigations using patient-derived cell models showed that poly(GP) levels dropped when cells were exposed to an ASO for 10 days. “The data indicate that poly(GP) production mirrors expression of repeat-containing C9ORF72 transcripts in lymphoblastoid cell lines,” they wrote.
The authors reported multiple governmental and private foundation sources of support for the research. Dr. Gendron and several of her coauthors are investigators in clinical trials for an ASO to target C9ORF72. Several authors reported paid and unpaid relationships and stock positions with pharmaceutical companies, including ones developing treatments for ALS and FTD.
[email protected]
On Twitter @karioakes
A protein found in the cerebrospinal fluid and peripheral blood cells of patients with a common type of amyotrophic lateral sclerosis may serve as a “pharmacodynamic marker,” providing a mechanism to assess RNA-based therapies that are now in clinical trials.
The protein, poly(GP), is expressed in patients who have a mutation in the gene chromosome 9 open reading frame 72 (C9ORF72), which causes one type of amyotrophic lateral sclerosis (ALS). This means that detecting poly(GP) also, eventually, may help to identify “presymptomatic individuals who are expected to benefit from early therapeutic interventions,” wrote the authors of a newly published paper (Sci Transl Med. 2017;9[383]:eaai7866).
Tania Gendron, PhD, of the department of neuroscience at the Mayo Clinic, Jacksonville, Fla., and her colleagues noted that poly(GP) was found in the cerebrospinal fluid (CSF) of both symptomatic and asymptomatic patients who carried the C9ORF72 mutation. The mutation can cause ALS, and is also associated with frontotemporal dementia (FTD) in a pattern with incomplete overlap with ALS.
However, “A limitation in moving such treatments from bench to bedside is a lack of pharmacodynamics markers for use in clinical trials,” Dr. Gendron and her collaborators wrote. The discovery that poly(GP) tracks well with C9ORF72 means that it has the potential to serve as the kind of biomarker that’s been missing in drug development for this family of neurodegenerative diseases, they said.
“To prepare for upcoming clinical trials for c9ALS, the present study used patient CSF and several preclinical models to investigate the hypothesis that poly(GP) proteins could serve as an urgently needed pharmacodynamics marker for developing and testing therapies for treating c9ALS,” Dr. Gendron and her colleagues wrote.
They looked at CSF samples from 83 patients with c9ALS and 27 patients who were asymptomatic C9ORF72 repeat expansion carriers, as well as 24 carriers who had a neurologic disease besides ALS or FTD (total n = 134). They also examined CSF samples from 120 study participants who lacked the mutation, 48 of whom were healthy controls; the remainder had ALS (n = 57) or another neurological disease.
The investigators, who were blinded to individuals’ disease status in each study arm, found that CSF poly(GP) levels were significantly higher in patients who had the C9ORF72 mutation (P less than .0001 in unadjusted and adjusted analyses). Poly(GP) was present in both asymptomatic and symptomatic carriers of the mutation, and not significantly different between these groups when data were adjusted for multiple comparisons, age, and gender.
When Dr. Gendron and her colleagues looked at poly(GP) levels over time for patients whose longitudinal data were available, they found that levels for an individual study participant were “relatively constant,” without any significant change over the median 12.9 months that these levels were tracked (P = .84).
However, “poly(GP) is not a prognostic marker,” wrote Dr. Gendron and her colleagues. They found no consistent association between levels of the protein and disease severity of progression, age at onset, or the development of FTD. Women were more likely to have lower levels, but the significance of that finding is not known, they said. There was a trend, which lost significance after statistical adjustment, for patients with cognitive impairment to have higher poly(GP) levels (adjusted P = .12).
Treatments under investigation for ALS and FTD include the use of an antisense oligonucleotide (ASO) to bind to the repeated RNA sequences and negate their ill effects. The investigators wrote that in vitro investigations using patient-derived cell models showed that poly(GP) levels dropped when cells were exposed to an ASO for 10 days. “The data indicate that poly(GP) production mirrors expression of repeat-containing C9ORF72 transcripts in lymphoblastoid cell lines,” they wrote.
The authors reported multiple governmental and private foundation sources of support for the research. Dr. Gendron and several of her coauthors are investigators in clinical trials for an ASO to target C9ORF72. Several authors reported paid and unpaid relationships and stock positions with pharmaceutical companies, including ones developing treatments for ALS and FTD.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: Patients with a mutation predisposing them to ALS had significantly higher levels of the protein poly(GP) (P less than .0001 in unadjusted and adjusted analyses).
Data source: Prospective blinded study of CSF samples from 83 patients with c9ALS, 27 patients who were asymptomatic C9ORF72 repeat expansion carriers, 24 carriers who had a neurologic disease besides ALS or FTD, and 120 study participants who lacked the C9ORF72 mutation.
Disclosures: The authors reported multiple governmental and private foundation sources of support for their research. Dr. Gendron and several of her coauthors are investigators in clinical trials for an ASO to target C9ORF72. Several authors reported paid and unpaid relationships and stock positions with pharmaceutical companies, including ones developing treatments for ALS and FTD.
VIDEO: Sex, intimacy part of history in gynecologic oncology care
NATIONAL HARBOR, MD. – Cancer care can feel like a sequence of crises, large and small; a comprehensive cancer care approach can keep the patient at the center of this flurry of events. But understanding a patient’s sexual history and assessing how a gynecologic malignancy has affected that patient’s sexual health can, too often, get lost in the shuffle, said Don Dizon, MD, of Massachusetts General Hospital, Boston.
“I think there are multiple reasons for that, but it has to be the job of the clinician – not necessarily the oncologist-physician – but somebody has to be able to say, ‘What is your sexual history? Can I ask about your sexual history?’ ” he said in a video interview at the annual meeting of the Society of Gynecologic Oncology.
Dr. Dizon, director of the Oncology Sexual Health Clinic at Massachusetts General Hospital*, emphasized the importance of providing sensitive sexual health care while staying true to one’s own framework of care. “I teach clinicians not to run away from their schema,” he said. “Having said that, the job of a clinician is to normalize the history, and to normalize that sex, intimacy, relationships are a part of someone’s history.”
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
[email protected]
On Twitter @karioakes
*A previous version of this article misstated Dr. Dizon's affiliation.
NATIONAL HARBOR, MD. – Cancer care can feel like a sequence of crises, large and small; a comprehensive cancer care approach can keep the patient at the center of this flurry of events. But understanding a patient’s sexual history and assessing how a gynecologic malignancy has affected that patient’s sexual health can, too often, get lost in the shuffle, said Don Dizon, MD, of Massachusetts General Hospital, Boston.
“I think there are multiple reasons for that, but it has to be the job of the clinician – not necessarily the oncologist-physician – but somebody has to be able to say, ‘What is your sexual history? Can I ask about your sexual history?’ ” he said in a video interview at the annual meeting of the Society of Gynecologic Oncology.
Dr. Dizon, director of the Oncology Sexual Health Clinic at Massachusetts General Hospital*, emphasized the importance of providing sensitive sexual health care while staying true to one’s own framework of care. “I teach clinicians not to run away from their schema,” he said. “Having said that, the job of a clinician is to normalize the history, and to normalize that sex, intimacy, relationships are a part of someone’s history.”
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
[email protected]
On Twitter @karioakes
*A previous version of this article misstated Dr. Dizon's affiliation.
NATIONAL HARBOR, MD. – Cancer care can feel like a sequence of crises, large and small; a comprehensive cancer care approach can keep the patient at the center of this flurry of events. But understanding a patient’s sexual history and assessing how a gynecologic malignancy has affected that patient’s sexual health can, too often, get lost in the shuffle, said Don Dizon, MD, of Massachusetts General Hospital, Boston.
“I think there are multiple reasons for that, but it has to be the job of the clinician – not necessarily the oncologist-physician – but somebody has to be able to say, ‘What is your sexual history? Can I ask about your sexual history?’ ” he said in a video interview at the annual meeting of the Society of Gynecologic Oncology.
Dr. Dizon, director of the Oncology Sexual Health Clinic at Massachusetts General Hospital*, emphasized the importance of providing sensitive sexual health care while staying true to one’s own framework of care. “I teach clinicians not to run away from their schema,” he said. “Having said that, the job of a clinician is to normalize the history, and to normalize that sex, intimacy, relationships are a part of someone’s history.”
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
[email protected]
On Twitter @karioakes
*A previous version of this article misstated Dr. Dizon's affiliation.
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Video: Try ‘PLISSIT’ to address postcancer sexual health
NATIONAL HARBOR, MD. – Comprehensive care of patients with gynecologic malignancies should include a sensitive and thorough assessment of sexual health.
In a video interview at the annual meeting of the Society of Gynecologic Oncology, Don Dizon, MD, of Massachusetts General Hospital, Boston, gives a series of practical tips to help physicians take a thorough sexual health history and provide information and guidance for patients and their partners.
Dr. Dizon, professor of gynecologic oncology and director of the oncology sexual health clinic at Brigham and Women’s Hospital, also in Boston, said that he likes to begin with the PLISSIT model, where patients are given permission (P) to talk about sexual problems. Then, the clinician gives the patient limited (LI) scientific or clinical information about the situation, followed by specific suggestions (SS) that might help. Finally, patients may be referred to mental health providers or sex counselors for intensive therapy (IT) if needed.
“It’s also important not to confuse terminology,” said Dr. Dizon. “Intimacy is experienced very differently between men and women. Women experience intimacy through arousal, desire, and, when desire is satisfied, that’s intimacy. Intercourse is not a part of that equation.” For men, he said, intimacy is more often experienced through intercourse. “So the disconnect is greater after cancer is diagnosed,” making it especially important to acknowledge problems sensitively, and to helps patients and partners find a way forward.
“The word I like to use is ‘play,’ ” said Dr. Dizon. When a renegotiation of an intimate relationship is framed in terms of play, the pressure is off, and “men can wrap their hands around that idea,” he said.
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Comprehensive care of patients with gynecologic malignancies should include a sensitive and thorough assessment of sexual health.
In a video interview at the annual meeting of the Society of Gynecologic Oncology, Don Dizon, MD, of Massachusetts General Hospital, Boston, gives a series of practical tips to help physicians take a thorough sexual health history and provide information and guidance for patients and their partners.
Dr. Dizon, professor of gynecologic oncology and director of the oncology sexual health clinic at Brigham and Women’s Hospital, also in Boston, said that he likes to begin with the PLISSIT model, where patients are given permission (P) to talk about sexual problems. Then, the clinician gives the patient limited (LI) scientific or clinical information about the situation, followed by specific suggestions (SS) that might help. Finally, patients may be referred to mental health providers or sex counselors for intensive therapy (IT) if needed.
“It’s also important not to confuse terminology,” said Dr. Dizon. “Intimacy is experienced very differently between men and women. Women experience intimacy through arousal, desire, and, when desire is satisfied, that’s intimacy. Intercourse is not a part of that equation.” For men, he said, intimacy is more often experienced through intercourse. “So the disconnect is greater after cancer is diagnosed,” making it especially important to acknowledge problems sensitively, and to helps patients and partners find a way forward.
“The word I like to use is ‘play,’ ” said Dr. Dizon. When a renegotiation of an intimate relationship is framed in terms of play, the pressure is off, and “men can wrap their hands around that idea,” he said.
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Comprehensive care of patients with gynecologic malignancies should include a sensitive and thorough assessment of sexual health.
In a video interview at the annual meeting of the Society of Gynecologic Oncology, Don Dizon, MD, of Massachusetts General Hospital, Boston, gives a series of practical tips to help physicians take a thorough sexual health history and provide information and guidance for patients and their partners.
Dr. Dizon, professor of gynecologic oncology and director of the oncology sexual health clinic at Brigham and Women’s Hospital, also in Boston, said that he likes to begin with the PLISSIT model, where patients are given permission (P) to talk about sexual problems. Then, the clinician gives the patient limited (LI) scientific or clinical information about the situation, followed by specific suggestions (SS) that might help. Finally, patients may be referred to mental health providers or sex counselors for intensive therapy (IT) if needed.
“It’s also important not to confuse terminology,” said Dr. Dizon. “Intimacy is experienced very differently between men and women. Women experience intimacy through arousal, desire, and, when desire is satisfied, that’s intimacy. Intercourse is not a part of that equation.” For men, he said, intimacy is more often experienced through intercourse. “So the disconnect is greater after cancer is diagnosed,” making it especially important to acknowledge problems sensitively, and to helps patients and partners find a way forward.
“The word I like to use is ‘play,’ ” said Dr. Dizon. When a renegotiation of an intimate relationship is framed in terms of play, the pressure is off, and “men can wrap their hands around that idea,” he said.
Dr. Dizon sits on the board of the Patty Brisben Foundation and the Young Survival Coalition.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN’S CANCER
VIDEO: Pain and impaired QOL persist after open endometrial cancer surgery
NATIONAL HARBOR, MD. – Patient-reported outcomes from a prospective cohort study of minimally invasive versus open surgery for women with endometrial cancer showed that the disability from open surgery persisted for longer than had previously been recognized. Further, for a subset of patients, impairment in sexual functioning was significant, and persistent, regardless of the type of surgery.
At 3 weeks after surgery, patients who had open surgery had greater pain as measured by the Brief Pain Inventory (minimally important difference greater than 1, P = .0004). By 3 months post surgery, responses on the Functional Assessment of Cancer Therapy–General were still significantly lower for the open-surgery group, compared with the minimally invasive group (P = .0011).
Although patients’ pain and overall state of health were better at 3 weeks post surgery, regardless of whether women had open, laparoscopic, or robotic surgery, the reduced overall quality of life experienced by patients who had open surgery persisted.
“What was a bit different from other studies … is that we found that this is maintained even at 3 months, and it was clinically and statistically different,” Sarah Ferguson, MD, said in a video interview at the annual meeting of the Society of Gynecologic Oncology. “So that was really, I think, an interesting finding, that this doesn’t just impact the very short term. Three months is a fairly long time after a primary surgery, and [it’s] important for women to know this.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Patients in the eight-center study had histologically confirmed clinical stage I or II endometrial cancer. The open-surgery arm of the study involved 106 patients, and 414 had minimally invasive surgery (168 laparascopic, 246 robotic).
The robotic and laparoscopic arms showed no statistically significant differences for any patient-reported outcome, even after adjusting for potentially confounding variables, said Dr. Ferguson of Princess Margaret Cancer Centre at the University of Toronto. Accordingly, investigators compared both minimally invasive arms grouped together against open surgery.
Overall, about 80% of patients completed the quality-of-life questionnaires. The response rate for the sexual-functioning questionnaires, however, was much lower, ranging from about a quarter to a half of the participants.
When Dr. Ferguson and her colleagues examined the characteristics of the patients who did complete the sexual-functioning questionnaires, they found that these women were more likely to be younger, partnered, premenopausal and sexually active at the time of diagnosis. Both of the surgical groups “met the clinical cutoff for sexual dysfunction” on the Female Sexual Function Index questionnaire, she said.
For the sexual function questionnaires, differences between the open and minimally invasive groups were not significant at any time point throughout the 26 weeks that patients were studied. “Though it’s a small population, I think these results are important,” said Dr. Ferguson. “These variables may be helpful for us to target patients in our practice, or in future studies, who require intervention.”
Though the study was not randomized, Dr. Ferguson said that the baseline characteristics were similar between groups, and the investigators’ intention-to-treat analysis used a statistical model that adjusted for many potential confounding variables.
Dr. Ferguson reported having no conflicts of interest.
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Patient-reported outcomes from a prospective cohort study of minimally invasive versus open surgery for women with endometrial cancer showed that the disability from open surgery persisted for longer than had previously been recognized. Further, for a subset of patients, impairment in sexual functioning was significant, and persistent, regardless of the type of surgery.
At 3 weeks after surgery, patients who had open surgery had greater pain as measured by the Brief Pain Inventory (minimally important difference greater than 1, P = .0004). By 3 months post surgery, responses on the Functional Assessment of Cancer Therapy–General were still significantly lower for the open-surgery group, compared with the minimally invasive group (P = .0011).
Although patients’ pain and overall state of health were better at 3 weeks post surgery, regardless of whether women had open, laparoscopic, or robotic surgery, the reduced overall quality of life experienced by patients who had open surgery persisted.
“What was a bit different from other studies … is that we found that this is maintained even at 3 months, and it was clinically and statistically different,” Sarah Ferguson, MD, said in a video interview at the annual meeting of the Society of Gynecologic Oncology. “So that was really, I think, an interesting finding, that this doesn’t just impact the very short term. Three months is a fairly long time after a primary surgery, and [it’s] important for women to know this.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Patients in the eight-center study had histologically confirmed clinical stage I or II endometrial cancer. The open-surgery arm of the study involved 106 patients, and 414 had minimally invasive surgery (168 laparascopic, 246 robotic).
The robotic and laparoscopic arms showed no statistically significant differences for any patient-reported outcome, even after adjusting for potentially confounding variables, said Dr. Ferguson of Princess Margaret Cancer Centre at the University of Toronto. Accordingly, investigators compared both minimally invasive arms grouped together against open surgery.
Overall, about 80% of patients completed the quality-of-life questionnaires. The response rate for the sexual-functioning questionnaires, however, was much lower, ranging from about a quarter to a half of the participants.
When Dr. Ferguson and her colleagues examined the characteristics of the patients who did complete the sexual-functioning questionnaires, they found that these women were more likely to be younger, partnered, premenopausal and sexually active at the time of diagnosis. Both of the surgical groups “met the clinical cutoff for sexual dysfunction” on the Female Sexual Function Index questionnaire, she said.
For the sexual function questionnaires, differences between the open and minimally invasive groups were not significant at any time point throughout the 26 weeks that patients were studied. “Though it’s a small population, I think these results are important,” said Dr. Ferguson. “These variables may be helpful for us to target patients in our practice, or in future studies, who require intervention.”
Though the study was not randomized, Dr. Ferguson said that the baseline characteristics were similar between groups, and the investigators’ intention-to-treat analysis used a statistical model that adjusted for many potential confounding variables.
Dr. Ferguson reported having no conflicts of interest.
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Patient-reported outcomes from a prospective cohort study of minimally invasive versus open surgery for women with endometrial cancer showed that the disability from open surgery persisted for longer than had previously been recognized. Further, for a subset of patients, impairment in sexual functioning was significant, and persistent, regardless of the type of surgery.
At 3 weeks after surgery, patients who had open surgery had greater pain as measured by the Brief Pain Inventory (minimally important difference greater than 1, P = .0004). By 3 months post surgery, responses on the Functional Assessment of Cancer Therapy–General were still significantly lower for the open-surgery group, compared with the minimally invasive group (P = .0011).
Although patients’ pain and overall state of health were better at 3 weeks post surgery, regardless of whether women had open, laparoscopic, or robotic surgery, the reduced overall quality of life experienced by patients who had open surgery persisted.
“What was a bit different from other studies … is that we found that this is maintained even at 3 months, and it was clinically and statistically different,” Sarah Ferguson, MD, said in a video interview at the annual meeting of the Society of Gynecologic Oncology. “So that was really, I think, an interesting finding, that this doesn’t just impact the very short term. Three months is a fairly long time after a primary surgery, and [it’s] important for women to know this.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Patients in the eight-center study had histologically confirmed clinical stage I or II endometrial cancer. The open-surgery arm of the study involved 106 patients, and 414 had minimally invasive surgery (168 laparascopic, 246 robotic).
The robotic and laparoscopic arms showed no statistically significant differences for any patient-reported outcome, even after adjusting for potentially confounding variables, said Dr. Ferguson of Princess Margaret Cancer Centre at the University of Toronto. Accordingly, investigators compared both minimally invasive arms grouped together against open surgery.
Overall, about 80% of patients completed the quality-of-life questionnaires. The response rate for the sexual-functioning questionnaires, however, was much lower, ranging from about a quarter to a half of the participants.
When Dr. Ferguson and her colleagues examined the characteristics of the patients who did complete the sexual-functioning questionnaires, they found that these women were more likely to be younger, partnered, premenopausal and sexually active at the time of diagnosis. Both of the surgical groups “met the clinical cutoff for sexual dysfunction” on the Female Sexual Function Index questionnaire, she said.
For the sexual function questionnaires, differences between the open and minimally invasive groups were not significant at any time point throughout the 26 weeks that patients were studied. “Though it’s a small population, I think these results are important,” said Dr. Ferguson. “These variables may be helpful for us to target patients in our practice, or in future studies, who require intervention.”
Though the study was not randomized, Dr. Ferguson said that the baseline characteristics were similar between groups, and the investigators’ intention-to-treat analysis used a statistical model that adjusted for many potential confounding variables.
Dr. Ferguson reported having no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN'S CANCER
Parental reasons for HPV nonvaccination are shifting
NATIONAL HARBOR, MD. – Parents are now less concerned about whether their daughters are sexually active when weighing whether to vaccinate against human papillomavirus (HPV), compared with just a few years ago.
This shift in parental attitudes can inform physician guidance and shift the HPV vaccination discussion, Anna Beavis, MD, a clinical fellow in gynecologic oncology at Johns Hopkins Medicine, Baltimore, said at the annual meeting of the Society of Gynecologic Oncology.
About 90% of cervical cancer is preventable with the HPV vaccine, but “U.S. vaccination rates are still suboptimal,” putting the United States far behind many other developed countries, Dr. Beavis said.
It’s been shown that the physician recommendation is one of the strongest predictors of whether an adolescent will be immunized against HPV, yet many providers remain reluctant to raise the issue, she said. Discomfort about discussing adolescent sexuality with the teen and with parents has been cited by physicians as a primary barrier.
To evaluate why parents of adolescent girls would opt out of HPV vaccination and to identify whether the reasons had changed over time, Dr. Beavis and her colleagues formulated a study that compared parent responses to a nationwide survey about HPV vaccination given in 2014 to those in 2010.
The study drew from the National Immunization Survey–Teen, a random digit-dialing survey administered by the Centers for Disease Control and Prevention. Only data pertaining to girls aged 13-17 years was included in the analysis, and for the sake of accuracy, only provider-verified responses were used.
Of the 49,345 responses that could be provider verified during the period from 2010 to 2014, 54% had received at least one HPV vaccination. Of the remaining responses, 55% of the parents said they had no intention of vaccinating their daughters.
During this period, vaccination rates have climbed slowly, from a little less than half in 2010 to about 60% in 2014 (test of trend, P less than .001), according to Dr. Beavis.
However, the reasons parents gave for declining vaccination has shifted over time, she said. The primary reason given in 2010 was concern about safety or side effects, followed by the sense that the vaccine was not necessary. These remained the top two reasons in 2014, though they had swapped places.
In 2010, the third most common reason parents gave for declining the HPV vaccination was that their daughters were not sexually active. By 2014, this reason had slid to the bottom of the top five reasons, and now was given by fewer than 10% of parents (test of trend, P less than .01).
This is important information for physicians, Dr. Beavis said in a video interview. If a physician has been reluctant to start the HPV discussion for fear of stepping into awkward territory with parents of teen girls, they should know that it’s significantly less likely that issues of sexuality will be on the parental radar when talking about HPV vaccination.
Looking deeper into the data, the investigators found that white race, younger patient age, and living above the poverty level were risk factors for nonvaccination. This means, Dr. Beavis said, that physicians should consider “developing a targeted HPV message” for families at higher risk of nonvaccination.
“This vaccine message should focus on cancer prevention, necessity, and the safety of the HPV vaccine,” Dr. Beavis said.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Parents are now less concerned about whether their daughters are sexually active when weighing whether to vaccinate against human papillomavirus (HPV), compared with just a few years ago.
This shift in parental attitudes can inform physician guidance and shift the HPV vaccination discussion, Anna Beavis, MD, a clinical fellow in gynecologic oncology at Johns Hopkins Medicine, Baltimore, said at the annual meeting of the Society of Gynecologic Oncology.
About 90% of cervical cancer is preventable with the HPV vaccine, but “U.S. vaccination rates are still suboptimal,” putting the United States far behind many other developed countries, Dr. Beavis said.
It’s been shown that the physician recommendation is one of the strongest predictors of whether an adolescent will be immunized against HPV, yet many providers remain reluctant to raise the issue, she said. Discomfort about discussing adolescent sexuality with the teen and with parents has been cited by physicians as a primary barrier.
To evaluate why parents of adolescent girls would opt out of HPV vaccination and to identify whether the reasons had changed over time, Dr. Beavis and her colleagues formulated a study that compared parent responses to a nationwide survey about HPV vaccination given in 2014 to those in 2010.
The study drew from the National Immunization Survey–Teen, a random digit-dialing survey administered by the Centers for Disease Control and Prevention. Only data pertaining to girls aged 13-17 years was included in the analysis, and for the sake of accuracy, only provider-verified responses were used.
Of the 49,345 responses that could be provider verified during the period from 2010 to 2014, 54% had received at least one HPV vaccination. Of the remaining responses, 55% of the parents said they had no intention of vaccinating their daughters.
During this period, vaccination rates have climbed slowly, from a little less than half in 2010 to about 60% in 2014 (test of trend, P less than .001), according to Dr. Beavis.
However, the reasons parents gave for declining vaccination has shifted over time, she said. The primary reason given in 2010 was concern about safety or side effects, followed by the sense that the vaccine was not necessary. These remained the top two reasons in 2014, though they had swapped places.
In 2010, the third most common reason parents gave for declining the HPV vaccination was that their daughters were not sexually active. By 2014, this reason had slid to the bottom of the top five reasons, and now was given by fewer than 10% of parents (test of trend, P less than .01).
This is important information for physicians, Dr. Beavis said in a video interview. If a physician has been reluctant to start the HPV discussion for fear of stepping into awkward territory with parents of teen girls, they should know that it’s significantly less likely that issues of sexuality will be on the parental radar when talking about HPV vaccination.
Looking deeper into the data, the investigators found that white race, younger patient age, and living above the poverty level were risk factors for nonvaccination. This means, Dr. Beavis said, that physicians should consider “developing a targeted HPV message” for families at higher risk of nonvaccination.
“This vaccine message should focus on cancer prevention, necessity, and the safety of the HPV vaccine,” Dr. Beavis said.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Parents are now less concerned about whether their daughters are sexually active when weighing whether to vaccinate against human papillomavirus (HPV), compared with just a few years ago.
This shift in parental attitudes can inform physician guidance and shift the HPV vaccination discussion, Anna Beavis, MD, a clinical fellow in gynecologic oncology at Johns Hopkins Medicine, Baltimore, said at the annual meeting of the Society of Gynecologic Oncology.
About 90% of cervical cancer is preventable with the HPV vaccine, but “U.S. vaccination rates are still suboptimal,” putting the United States far behind many other developed countries, Dr. Beavis said.
It’s been shown that the physician recommendation is one of the strongest predictors of whether an adolescent will be immunized against HPV, yet many providers remain reluctant to raise the issue, she said. Discomfort about discussing adolescent sexuality with the teen and with parents has been cited by physicians as a primary barrier.
To evaluate why parents of adolescent girls would opt out of HPV vaccination and to identify whether the reasons had changed over time, Dr. Beavis and her colleagues formulated a study that compared parent responses to a nationwide survey about HPV vaccination given in 2014 to those in 2010.
The study drew from the National Immunization Survey–Teen, a random digit-dialing survey administered by the Centers for Disease Control and Prevention. Only data pertaining to girls aged 13-17 years was included in the analysis, and for the sake of accuracy, only provider-verified responses were used.
Of the 49,345 responses that could be provider verified during the period from 2010 to 2014, 54% had received at least one HPV vaccination. Of the remaining responses, 55% of the parents said they had no intention of vaccinating their daughters.
During this period, vaccination rates have climbed slowly, from a little less than half in 2010 to about 60% in 2014 (test of trend, P less than .001), according to Dr. Beavis.
However, the reasons parents gave for declining vaccination has shifted over time, she said. The primary reason given in 2010 was concern about safety or side effects, followed by the sense that the vaccine was not necessary. These remained the top two reasons in 2014, though they had swapped places.
In 2010, the third most common reason parents gave for declining the HPV vaccination was that their daughters were not sexually active. By 2014, this reason had slid to the bottom of the top five reasons, and now was given by fewer than 10% of parents (test of trend, P less than .01).
This is important information for physicians, Dr. Beavis said in a video interview. If a physician has been reluctant to start the HPV discussion for fear of stepping into awkward territory with parents of teen girls, they should know that it’s significantly less likely that issues of sexuality will be on the parental radar when talking about HPV vaccination.
Looking deeper into the data, the investigators found that white race, younger patient age, and living above the poverty level were risk factors for nonvaccination. This means, Dr. Beavis said, that physicians should consider “developing a targeted HPV message” for families at higher risk of nonvaccination.
“This vaccine message should focus on cancer prevention, necessity, and the safety of the HPV vaccine,” Dr. Beavis said.
She reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Maintenance taxane therapy of no benefit in advanced ovarian cancer
NATIONAL HARBOR, MD. – Using either a polymerized formulation of paclitaxel or paclitaxel alone as maintenance therapy conferred no survival benefit for women with advanced ovarian, fallopian tube, or peritoneal cancer.
In a phase III randomized trial, patients survived a median 54.8 months with surveillance alone, 51.3 months with maintenance paclitaxel, and 60.0 months with maintenance paclitaxel poliglumex; these differences were not statistically significant.
In a presentation at the annual meeting of the Society of Gynecologic Oncology, Larry Copeland, MD, a professor of gynecologic oncology at Ohio State University, Columbus, said that treatment with surgery and chemotherapy yields a clinical complete response in many patients with these cancers. However, he said, recurrent progressive disease is still very common; the rationale behind maintenance chemotherapy is that it may “reduce the risk of recurrence and extend survival.”
There had been promising earlier data supporting this approach from a previous phase III comparison trial that evaluated the difference in clinical complete response between 3 or 12 cycles of paclitaxel, said Dr. Copeland. The results of a predefined interim analysis prompted the data monitoring committee to close that study (J Clin Oncol. 2003;21[13]:2460-5) since the 12-cycle, 7-month arm of the study had better progression-free survival. However, the 12-cycle protocol did not confer a benefit in overall survival, the investigators later reported (Gynecol Oncol 2009;114[2]:195-8).
The current stage III randomized trial enrolled women with stage III or IV ovarian, fallopian tube, or peritoneal cancer who had had five to eight cycles of chemotherapy and achieved clinical complete response. If patients had neuropathy, it could not exceed grade 1, and their cancer performance status scores could not exceed 2, Dr. Copeland said.
Patients were randomized 1:1:1 to a surveillance arm, to receive paclitaxel as a 3-hour infusion, or to receive paclitaxel poliglumex as a 10- to 20-minute infusion. Both study drugs were dosed at 35 mg/m2 every 28 days for 12 cycles.
The study ran from March 2005 to January 2014, enrolling 1,157 patients who were followed for a median of 71 months. Over 80% of patients in each study arm had ovarian cancer, and a similar number had stage III cancer and serous histology. Over 90% of patients in each arm had grade 2 or higher histology.
The study was designed as a superiority design, and patients were not to receive other cancer treatments until they had disease progression. Primary clinical endpoints for the study included overall survival, quality of life as measured by the Ovarian Specific Questionnaire Quality of Life–Cancer, and patient-reported neurotoxicity as reported on the Functional Assessment of Cancer Therapy/Gynecologic Oncology Group/Neurotoxicity questionnaire.
The third scheduled interim analysis, in May 2016, examined the primary endpoint of overall survival, triggered when at least 200 deaths occurred in the surveillance group. The overall final analysis had been scheduled for the point at which at least 301 deaths happened in the surveillance group. In the abstract accompanying the presentation, Dr. Copeland wrote that the data at the point of this interim analysis indicated that “the relative death hazards passed the futility boundaries for both taxane regimens.”
“The log-rank statistic for each taxane regimen was below the interval specific in the study design, making it unlikely either of the taxane regimens has superior overall survival compared to surveillance,” said Dr. Copeland.
The hazard ratio for overall survival of the paclitaxel group compared to surveillance was 1.104, with a 97.5% confidence interval (CI) of 0.884-1.38. For the paclitaxel poliglumex group, the hazard ratio compared to surveillance alone was 0.979 (97.5% CI, 0.781-1.23).
Dr. Copeland and his colleagues also looked at progression-free survival, not a primary endpoint of the study. For the paclitaxel patients compared to surveillance, the HR for progression-free survival was 0.783 (95% CI, 0.666-0.921). For paclitaxel poliglumex, the HR was 0.847 (95% CI, 0.666-0.921).
Not unexpectedly, more patients who received taxane treatment than those in the surveillance arm experienced adverse events, said Dr. Copeland. The most common adverse events were hypersensitivity or allergic reactions, fatigue, alopecia, nausea, constipation, and sensory neuropathies. Grade 2 alopecia was experienced by about a quarter of the paclitaxel poliglumex cohort, and by a little less than half of the paclitaxel cohort. Neurologic adverse events were very common, reported by three quarters of the paclitaxel poliglumex cohort, four in five of the paclitaxel group, and by a little over half of the surveillance cohort.
Overall quality of life scores did not differ significantly among the treatment arms.
In an exploratory analysis, Dr. Copeland and his colleagues determined that patients with no residual disease (R0 patients) after initial cytoreductive surgery fared better, with a median 70 months of survival compared to a median 43.6 months for individuals with gross residual disease. When those patients were sorted out by treatment arm, there was no significant difference in OS for R0 patients who received any intervention or surveillance.
“Overall survival was not improved with taxane maintenance, though progression-free survival is slightly delayed,” Dr. Copeland concluded.
In discussion after the presentation, he said that he is not sure that further investigations will be pursued for paclitaxel poliglumex in the treatment of ovarian cancers.
Paclitaxel poliglumex (CT-2103; Opaxio) is paclitaxel conjugated to a polyglutamate polymer, a formulation that may enhance tumor penetration and retention, and that allows shorter infusion at a peripheral site. Previous work had shown that CT-2103’s structure enhanced pharmacokinetics and potentially decreased toxicity (Expert Opin Investig Drugs. 2004 Nov;13[11]:1501-8).
Dr. Copeland reported receiving consulting or honoraria fees from Clovis, Advaxis, Janssen, and Tesaro, and is a stockholder or shareholder in Merck, Eli Lilly, and Cardinal Health. The study was sponsored by the Cancer Therapy Evaluation Program of the National Cancer Institute and by Cell Therapeutics, which plans to market paclitaxel poliglumex.
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Using either a polymerized formulation of paclitaxel or paclitaxel alone as maintenance therapy conferred no survival benefit for women with advanced ovarian, fallopian tube, or peritoneal cancer.
In a phase III randomized trial, patients survived a median 54.8 months with surveillance alone, 51.3 months with maintenance paclitaxel, and 60.0 months with maintenance paclitaxel poliglumex; these differences were not statistically significant.
In a presentation at the annual meeting of the Society of Gynecologic Oncology, Larry Copeland, MD, a professor of gynecologic oncology at Ohio State University, Columbus, said that treatment with surgery and chemotherapy yields a clinical complete response in many patients with these cancers. However, he said, recurrent progressive disease is still very common; the rationale behind maintenance chemotherapy is that it may “reduce the risk of recurrence and extend survival.”
There had been promising earlier data supporting this approach from a previous phase III comparison trial that evaluated the difference in clinical complete response between 3 or 12 cycles of paclitaxel, said Dr. Copeland. The results of a predefined interim analysis prompted the data monitoring committee to close that study (J Clin Oncol. 2003;21[13]:2460-5) since the 12-cycle, 7-month arm of the study had better progression-free survival. However, the 12-cycle protocol did not confer a benefit in overall survival, the investigators later reported (Gynecol Oncol 2009;114[2]:195-8).
The current stage III randomized trial enrolled women with stage III or IV ovarian, fallopian tube, or peritoneal cancer who had had five to eight cycles of chemotherapy and achieved clinical complete response. If patients had neuropathy, it could not exceed grade 1, and their cancer performance status scores could not exceed 2, Dr. Copeland said.
Patients were randomized 1:1:1 to a surveillance arm, to receive paclitaxel as a 3-hour infusion, or to receive paclitaxel poliglumex as a 10- to 20-minute infusion. Both study drugs were dosed at 35 mg/m2 every 28 days for 12 cycles.
The study ran from March 2005 to January 2014, enrolling 1,157 patients who were followed for a median of 71 months. Over 80% of patients in each study arm had ovarian cancer, and a similar number had stage III cancer and serous histology. Over 90% of patients in each arm had grade 2 or higher histology.
The study was designed as a superiority design, and patients were not to receive other cancer treatments until they had disease progression. Primary clinical endpoints for the study included overall survival, quality of life as measured by the Ovarian Specific Questionnaire Quality of Life–Cancer, and patient-reported neurotoxicity as reported on the Functional Assessment of Cancer Therapy/Gynecologic Oncology Group/Neurotoxicity questionnaire.
The third scheduled interim analysis, in May 2016, examined the primary endpoint of overall survival, triggered when at least 200 deaths occurred in the surveillance group. The overall final analysis had been scheduled for the point at which at least 301 deaths happened in the surveillance group. In the abstract accompanying the presentation, Dr. Copeland wrote that the data at the point of this interim analysis indicated that “the relative death hazards passed the futility boundaries for both taxane regimens.”
“The log-rank statistic for each taxane regimen was below the interval specific in the study design, making it unlikely either of the taxane regimens has superior overall survival compared to surveillance,” said Dr. Copeland.
The hazard ratio for overall survival of the paclitaxel group compared to surveillance was 1.104, with a 97.5% confidence interval (CI) of 0.884-1.38. For the paclitaxel poliglumex group, the hazard ratio compared to surveillance alone was 0.979 (97.5% CI, 0.781-1.23).
Dr. Copeland and his colleagues also looked at progression-free survival, not a primary endpoint of the study. For the paclitaxel patients compared to surveillance, the HR for progression-free survival was 0.783 (95% CI, 0.666-0.921). For paclitaxel poliglumex, the HR was 0.847 (95% CI, 0.666-0.921).
Not unexpectedly, more patients who received taxane treatment than those in the surveillance arm experienced adverse events, said Dr. Copeland. The most common adverse events were hypersensitivity or allergic reactions, fatigue, alopecia, nausea, constipation, and sensory neuropathies. Grade 2 alopecia was experienced by about a quarter of the paclitaxel poliglumex cohort, and by a little less than half of the paclitaxel cohort. Neurologic adverse events were very common, reported by three quarters of the paclitaxel poliglumex cohort, four in five of the paclitaxel group, and by a little over half of the surveillance cohort.
Overall quality of life scores did not differ significantly among the treatment arms.
In an exploratory analysis, Dr. Copeland and his colleagues determined that patients with no residual disease (R0 patients) after initial cytoreductive surgery fared better, with a median 70 months of survival compared to a median 43.6 months for individuals with gross residual disease. When those patients were sorted out by treatment arm, there was no significant difference in OS for R0 patients who received any intervention or surveillance.
“Overall survival was not improved with taxane maintenance, though progression-free survival is slightly delayed,” Dr. Copeland concluded.
In discussion after the presentation, he said that he is not sure that further investigations will be pursued for paclitaxel poliglumex in the treatment of ovarian cancers.
Paclitaxel poliglumex (CT-2103; Opaxio) is paclitaxel conjugated to a polyglutamate polymer, a formulation that may enhance tumor penetration and retention, and that allows shorter infusion at a peripheral site. Previous work had shown that CT-2103’s structure enhanced pharmacokinetics and potentially decreased toxicity (Expert Opin Investig Drugs. 2004 Nov;13[11]:1501-8).
Dr. Copeland reported receiving consulting or honoraria fees from Clovis, Advaxis, Janssen, and Tesaro, and is a stockholder or shareholder in Merck, Eli Lilly, and Cardinal Health. The study was sponsored by the Cancer Therapy Evaluation Program of the National Cancer Institute and by Cell Therapeutics, which plans to market paclitaxel poliglumex.
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Using either a polymerized formulation of paclitaxel or paclitaxel alone as maintenance therapy conferred no survival benefit for women with advanced ovarian, fallopian tube, or peritoneal cancer.
In a phase III randomized trial, patients survived a median 54.8 months with surveillance alone, 51.3 months with maintenance paclitaxel, and 60.0 months with maintenance paclitaxel poliglumex; these differences were not statistically significant.
In a presentation at the annual meeting of the Society of Gynecologic Oncology, Larry Copeland, MD, a professor of gynecologic oncology at Ohio State University, Columbus, said that treatment with surgery and chemotherapy yields a clinical complete response in many patients with these cancers. However, he said, recurrent progressive disease is still very common; the rationale behind maintenance chemotherapy is that it may “reduce the risk of recurrence and extend survival.”
There had been promising earlier data supporting this approach from a previous phase III comparison trial that evaluated the difference in clinical complete response between 3 or 12 cycles of paclitaxel, said Dr. Copeland. The results of a predefined interim analysis prompted the data monitoring committee to close that study (J Clin Oncol. 2003;21[13]:2460-5) since the 12-cycle, 7-month arm of the study had better progression-free survival. However, the 12-cycle protocol did not confer a benefit in overall survival, the investigators later reported (Gynecol Oncol 2009;114[2]:195-8).
The current stage III randomized trial enrolled women with stage III or IV ovarian, fallopian tube, or peritoneal cancer who had had five to eight cycles of chemotherapy and achieved clinical complete response. If patients had neuropathy, it could not exceed grade 1, and their cancer performance status scores could not exceed 2, Dr. Copeland said.
Patients were randomized 1:1:1 to a surveillance arm, to receive paclitaxel as a 3-hour infusion, or to receive paclitaxel poliglumex as a 10- to 20-minute infusion. Both study drugs were dosed at 35 mg/m2 every 28 days for 12 cycles.
The study ran from March 2005 to January 2014, enrolling 1,157 patients who were followed for a median of 71 months. Over 80% of patients in each study arm had ovarian cancer, and a similar number had stage III cancer and serous histology. Over 90% of patients in each arm had grade 2 or higher histology.
The study was designed as a superiority design, and patients were not to receive other cancer treatments until they had disease progression. Primary clinical endpoints for the study included overall survival, quality of life as measured by the Ovarian Specific Questionnaire Quality of Life–Cancer, and patient-reported neurotoxicity as reported on the Functional Assessment of Cancer Therapy/Gynecologic Oncology Group/Neurotoxicity questionnaire.
The third scheduled interim analysis, in May 2016, examined the primary endpoint of overall survival, triggered when at least 200 deaths occurred in the surveillance group. The overall final analysis had been scheduled for the point at which at least 301 deaths happened in the surveillance group. In the abstract accompanying the presentation, Dr. Copeland wrote that the data at the point of this interim analysis indicated that “the relative death hazards passed the futility boundaries for both taxane regimens.”
“The log-rank statistic for each taxane regimen was below the interval specific in the study design, making it unlikely either of the taxane regimens has superior overall survival compared to surveillance,” said Dr. Copeland.
The hazard ratio for overall survival of the paclitaxel group compared to surveillance was 1.104, with a 97.5% confidence interval (CI) of 0.884-1.38. For the paclitaxel poliglumex group, the hazard ratio compared to surveillance alone was 0.979 (97.5% CI, 0.781-1.23).
Dr. Copeland and his colleagues also looked at progression-free survival, not a primary endpoint of the study. For the paclitaxel patients compared to surveillance, the HR for progression-free survival was 0.783 (95% CI, 0.666-0.921). For paclitaxel poliglumex, the HR was 0.847 (95% CI, 0.666-0.921).
Not unexpectedly, more patients who received taxane treatment than those in the surveillance arm experienced adverse events, said Dr. Copeland. The most common adverse events were hypersensitivity or allergic reactions, fatigue, alopecia, nausea, constipation, and sensory neuropathies. Grade 2 alopecia was experienced by about a quarter of the paclitaxel poliglumex cohort, and by a little less than half of the paclitaxel cohort. Neurologic adverse events were very common, reported by three quarters of the paclitaxel poliglumex cohort, four in five of the paclitaxel group, and by a little over half of the surveillance cohort.
Overall quality of life scores did not differ significantly among the treatment arms.
In an exploratory analysis, Dr. Copeland and his colleagues determined that patients with no residual disease (R0 patients) after initial cytoreductive surgery fared better, with a median 70 months of survival compared to a median 43.6 months for individuals with gross residual disease. When those patients were sorted out by treatment arm, there was no significant difference in OS for R0 patients who received any intervention or surveillance.
“Overall survival was not improved with taxane maintenance, though progression-free survival is slightly delayed,” Dr. Copeland concluded.
In discussion after the presentation, he said that he is not sure that further investigations will be pursued for paclitaxel poliglumex in the treatment of ovarian cancers.
Paclitaxel poliglumex (CT-2103; Opaxio) is paclitaxel conjugated to a polyglutamate polymer, a formulation that may enhance tumor penetration and retention, and that allows shorter infusion at a peripheral site. Previous work had shown that CT-2103’s structure enhanced pharmacokinetics and potentially decreased toxicity (Expert Opin Investig Drugs. 2004 Nov;13[11]:1501-8).
Dr. Copeland reported receiving consulting or honoraria fees from Clovis, Advaxis, Janssen, and Tesaro, and is a stockholder or shareholder in Merck, Eli Lilly, and Cardinal Health. The study was sponsored by the Cancer Therapy Evaluation Program of the National Cancer Institute and by Cell Therapeutics, which plans to market paclitaxel poliglumex.
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN’S CANCER
Key clinical point:
Major finding: There was no statistically significant overall survival benefit of maintenance taxane therapy for advanced ovarian, fallopian tube, or peritoneal cancer, compared with surveillance.
Data source: Phase III randomized trial of 1,157 patients with advanced ovarian, fallopian tube, or peritoneal cancer.
Disclosures: Dr. Copeland reported receiving consulting or honoraria fees from Clovis, Advaxis, Janssen, and Tesaro, and is a stockholder or shareholder in Merck, Eli Lilly, and Cardinal Health. The study was sponsored by the Cancer Therapy Evaluation Program of the National Cancer Institute and by Cell Therapeutics, which plans to market paclitaxel poliglumex.
Auto-HCT patients run high risks for myeloid neoplasms
ORLANDO – For post–autologous hematopoietic cell transplant (auto-HCT) patients, the 10-year risk of developing a myeloid neoplasm was as high as 6%, based on a recent review of two large cancer databases.
Older age at transplant, receiving total body irradiation, and receiving multiple lines of chemotherapy before transplant all upped the risk of later cancers, according to a study presented by Shahrukh Hashmi, MD, and his collaborators at the combined annual meetings of the Center for International Blood & Marrow Transplant Research (CIBMTR) and the American Society for Blood and Marrow Transplantation.
“The guidelines for autologous stem cell transplantation for surveillance for AML [acute myeloid leukemia] and MDS [myelodysplastic syndrome] need to be clearly formulated. We are doing 30,000 autologous transplants a year globally and these patients are at risk for the most feared cancer, which is leukemia and MDS, for which outcomes are very poor,” said Dr. Hashmi of the Mayo Clinic in Rochester, Minn.
The researchers examined data from auto-HCT patients with diagnoses of non-Hodgkin lymphoma (NHL), Hodgkin lymphoma, and multiple myeloma to determine the relative risks of developing AML and MDS. The study also explored which patient characteristics and aspects of the conditioning regimen might affect risk for later myeloid neoplasms.
In the dataset of 9,108 patients that Dr. Hashmi and his colleagues obtained from CIBMTR, 3,540 patients had NHL.
“As age progresses, the risk of acquiring myeloid neoplasms increases significantly,” he said, noting that the relative risk (RR) rose to 4.52 for patients aged 55 years and older at the time of transplant (95% confidence interval [CI], 2.63-7.77; P less than .0001).
Patients with NHL who received more than two lines of chemotherapy had approximately double the rate of myeloid cancers (RR, 1.93; 95% CI, 1.34-2.78; P = .0004).
The type of conditioning regimen made a difference for NHL patients as well. With total-body irradiation set as the reference at RR = 1, carmustine-etoposide-cytarabine-melphalan (BEAM) or similar therapies were relatively protective, with an RR of 0.59 (95% CI, 0.40-0.87; P = .0083). Also protective were cyclophosphamide-carmustine-etoposide (CBV) and similar therapies (RR, 0.57; 95% CI, 0.33-0.99; P = .0463).
Age at transplant was a factor among the 4,653 patients with multiple myeloma, with an RR of 2.47 for those transplanted at age 55 years or older (95% CI, 1.55-3.93; P = .0001). Multiple lines of chemotherapy also increased risk, with patients who received more than two lines having an RR of 1.77 for neoplasm (95% CI, 0.04-2.06; P = .0302). Women had less than half the risk of recurrence as men (RR, 0.44; 95% CI, 0.28-0.69; P = .0003).
Among the 915 study patients with Hodgkin lymphoma, patients aged 45 years and older at the time of transplant carried an RR of 5.59 for new myeloid neoplasms (95% CI, 2.98-11.70; P less than .0001).
Total-body irradiation was received by 14% of patients with non-Hodgkin lymphoma and by 5% of patients with multiple myeloma and Hodgkin lymphoma. Total-body irradiation was associated with a fourfold increase in neoplasm risk (RR, 4.02; 95% CI, 1.40-11.55; P = .0096).
Dr. Hashmi and his colleagues then examined the incidence rates for myelodysplastic syndrome and acute myelogenous leukemia in the Surveillance, Epidemiology, and End Results (SEER) database , finding that, even at baseline, the rates of myeloid neoplasms were higher for patients with NHL, Hodgkin lymphoma, or MM patients than for the general population of cancer survivors. “Post NHL, Hodgkin lymphoma, and myeloma, the risks are significantly higher to begin with. … We saw a high risk of AML and MDS compared to the SEER controls – risks as high as 100 times greater for auto-transplant patients,” said Dr. Hashmi. “A risk of one hundred times more for MDS was astounding, surprising, unexpected,” he said. The risk of AML, he said, was elevated about 10-50 times in the CIBMTR data.
The cumulative incidence of MDS or AML for NHL was 6% at 10 years post transplant, 4% for Hodgkin lymphoma, and 3% for multiple myeloma.
A limitation of the study, said Dr. Hashmi, was that the investigators did not assess for post-transplant maintenance chemotherapy.
“We have to prospectively assess our transplant patients in a fashion to detect changes early. Or maybe they were present at the time of transplant and we never did sophisticated methods [like] next-generation sequencing” to detect them, he said.
Dr. Hashmi reported no conflicts of interest.
[email protected]
On Twitter @karioakes
ORLANDO – For post–autologous hematopoietic cell transplant (auto-HCT) patients, the 10-year risk of developing a myeloid neoplasm was as high as 6%, based on a recent review of two large cancer databases.
Older age at transplant, receiving total body irradiation, and receiving multiple lines of chemotherapy before transplant all upped the risk of later cancers, according to a study presented by Shahrukh Hashmi, MD, and his collaborators at the combined annual meetings of the Center for International Blood & Marrow Transplant Research (CIBMTR) and the American Society for Blood and Marrow Transplantation.
“The guidelines for autologous stem cell transplantation for surveillance for AML [acute myeloid leukemia] and MDS [myelodysplastic syndrome] need to be clearly formulated. We are doing 30,000 autologous transplants a year globally and these patients are at risk for the most feared cancer, which is leukemia and MDS, for which outcomes are very poor,” said Dr. Hashmi of the Mayo Clinic in Rochester, Minn.
The researchers examined data from auto-HCT patients with diagnoses of non-Hodgkin lymphoma (NHL), Hodgkin lymphoma, and multiple myeloma to determine the relative risks of developing AML and MDS. The study also explored which patient characteristics and aspects of the conditioning regimen might affect risk for later myeloid neoplasms.
In the dataset of 9,108 patients that Dr. Hashmi and his colleagues obtained from CIBMTR, 3,540 patients had NHL.
“As age progresses, the risk of acquiring myeloid neoplasms increases significantly,” he said, noting that the relative risk (RR) rose to 4.52 for patients aged 55 years and older at the time of transplant (95% confidence interval [CI], 2.63-7.77; P less than .0001).
Patients with NHL who received more than two lines of chemotherapy had approximately double the rate of myeloid cancers (RR, 1.93; 95% CI, 1.34-2.78; P = .0004).
The type of conditioning regimen made a difference for NHL patients as well. With total-body irradiation set as the reference at RR = 1, carmustine-etoposide-cytarabine-melphalan (BEAM) or similar therapies were relatively protective, with an RR of 0.59 (95% CI, 0.40-0.87; P = .0083). Also protective were cyclophosphamide-carmustine-etoposide (CBV) and similar therapies (RR, 0.57; 95% CI, 0.33-0.99; P = .0463).
Age at transplant was a factor among the 4,653 patients with multiple myeloma, with an RR of 2.47 for those transplanted at age 55 years or older (95% CI, 1.55-3.93; P = .0001). Multiple lines of chemotherapy also increased risk, with patients who received more than two lines having an RR of 1.77 for neoplasm (95% CI, 0.04-2.06; P = .0302). Women had less than half the risk of recurrence as men (RR, 0.44; 95% CI, 0.28-0.69; P = .0003).
Among the 915 study patients with Hodgkin lymphoma, patients aged 45 years and older at the time of transplant carried an RR of 5.59 for new myeloid neoplasms (95% CI, 2.98-11.70; P less than .0001).
Total-body irradiation was received by 14% of patients with non-Hodgkin lymphoma and by 5% of patients with multiple myeloma and Hodgkin lymphoma. Total-body irradiation was associated with a fourfold increase in neoplasm risk (RR, 4.02; 95% CI, 1.40-11.55; P = .0096).
Dr. Hashmi and his colleagues then examined the incidence rates for myelodysplastic syndrome and acute myelogenous leukemia in the Surveillance, Epidemiology, and End Results (SEER) database , finding that, even at baseline, the rates of myeloid neoplasms were higher for patients with NHL, Hodgkin lymphoma, or MM patients than for the general population of cancer survivors. “Post NHL, Hodgkin lymphoma, and myeloma, the risks are significantly higher to begin with. … We saw a high risk of AML and MDS compared to the SEER controls – risks as high as 100 times greater for auto-transplant patients,” said Dr. Hashmi. “A risk of one hundred times more for MDS was astounding, surprising, unexpected,” he said. The risk of AML, he said, was elevated about 10-50 times in the CIBMTR data.
The cumulative incidence of MDS or AML for NHL was 6% at 10 years post transplant, 4% for Hodgkin lymphoma, and 3% for multiple myeloma.
A limitation of the study, said Dr. Hashmi, was that the investigators did not assess for post-transplant maintenance chemotherapy.
“We have to prospectively assess our transplant patients in a fashion to detect changes early. Or maybe they were present at the time of transplant and we never did sophisticated methods [like] next-generation sequencing” to detect them, he said.
Dr. Hashmi reported no conflicts of interest.
[email protected]
On Twitter @karioakes
ORLANDO – For post–autologous hematopoietic cell transplant (auto-HCT) patients, the 10-year risk of developing a myeloid neoplasm was as high as 6%, based on a recent review of two large cancer databases.
Older age at transplant, receiving total body irradiation, and receiving multiple lines of chemotherapy before transplant all upped the risk of later cancers, according to a study presented by Shahrukh Hashmi, MD, and his collaborators at the combined annual meetings of the Center for International Blood & Marrow Transplant Research (CIBMTR) and the American Society for Blood and Marrow Transplantation.
“The guidelines for autologous stem cell transplantation for surveillance for AML [acute myeloid leukemia] and MDS [myelodysplastic syndrome] need to be clearly formulated. We are doing 30,000 autologous transplants a year globally and these patients are at risk for the most feared cancer, which is leukemia and MDS, for which outcomes are very poor,” said Dr. Hashmi of the Mayo Clinic in Rochester, Minn.
The researchers examined data from auto-HCT patients with diagnoses of non-Hodgkin lymphoma (NHL), Hodgkin lymphoma, and multiple myeloma to determine the relative risks of developing AML and MDS. The study also explored which patient characteristics and aspects of the conditioning regimen might affect risk for later myeloid neoplasms.
In the dataset of 9,108 patients that Dr. Hashmi and his colleagues obtained from CIBMTR, 3,540 patients had NHL.
“As age progresses, the risk of acquiring myeloid neoplasms increases significantly,” he said, noting that the relative risk (RR) rose to 4.52 for patients aged 55 years and older at the time of transplant (95% confidence interval [CI], 2.63-7.77; P less than .0001).
Patients with NHL who received more than two lines of chemotherapy had approximately double the rate of myeloid cancers (RR, 1.93; 95% CI, 1.34-2.78; P = .0004).
The type of conditioning regimen made a difference for NHL patients as well. With total-body irradiation set as the reference at RR = 1, carmustine-etoposide-cytarabine-melphalan (BEAM) or similar therapies were relatively protective, with an RR of 0.59 (95% CI, 0.40-0.87; P = .0083). Also protective were cyclophosphamide-carmustine-etoposide (CBV) and similar therapies (RR, 0.57; 95% CI, 0.33-0.99; P = .0463).
Age at transplant was a factor among the 4,653 patients with multiple myeloma, with an RR of 2.47 for those transplanted at age 55 years or older (95% CI, 1.55-3.93; P = .0001). Multiple lines of chemotherapy also increased risk, with patients who received more than two lines having an RR of 1.77 for neoplasm (95% CI, 0.04-2.06; P = .0302). Women had less than half the risk of recurrence as men (RR, 0.44; 95% CI, 0.28-0.69; P = .0003).
Among the 915 study patients with Hodgkin lymphoma, patients aged 45 years and older at the time of transplant carried an RR of 5.59 for new myeloid neoplasms (95% CI, 2.98-11.70; P less than .0001).
Total-body irradiation was received by 14% of patients with non-Hodgkin lymphoma and by 5% of patients with multiple myeloma and Hodgkin lymphoma. Total-body irradiation was associated with a fourfold increase in neoplasm risk (RR, 4.02; 95% CI, 1.40-11.55; P = .0096).
Dr. Hashmi and his colleagues then examined the incidence rates for myelodysplastic syndrome and acute myelogenous leukemia in the Surveillance, Epidemiology, and End Results (SEER) database , finding that, even at baseline, the rates of myeloid neoplasms were higher for patients with NHL, Hodgkin lymphoma, or MM patients than for the general population of cancer survivors. “Post NHL, Hodgkin lymphoma, and myeloma, the risks are significantly higher to begin with. … We saw a high risk of AML and MDS compared to the SEER controls – risks as high as 100 times greater for auto-transplant patients,” said Dr. Hashmi. “A risk of one hundred times more for MDS was astounding, surprising, unexpected,” he said. The risk of AML, he said, was elevated about 10-50 times in the CIBMTR data.
The cumulative incidence of MDS or AML for NHL was 6% at 10 years post transplant, 4% for Hodgkin lymphoma, and 3% for multiple myeloma.
A limitation of the study, said Dr. Hashmi, was that the investigators did not assess for post-transplant maintenance chemotherapy.
“We have to prospectively assess our transplant patients in a fashion to detect changes early. Or maybe they were present at the time of transplant and we never did sophisticated methods [like] next-generation sequencing” to detect them, he said.
Dr. Hashmi reported no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE BMT TANDEM MEETINGS
Key clinical point:
Major finding: The 10-year cumulative risk for auto-HCT patients with Hodgkin or non-Hodgkin lymphoma or multiple myeloma was as high at 6%.
Data source: Review of 9,108 patients from an international transplant database.
Disclosures: Dr. Hashmi reported no conflicts of interest.