User login
Adjuvant chemotherapy alone may suffice for some high-risk early cervical cancers
National Harbor, MD. – Patients, even those with surgically-confirmed risk factors, fared well when they received adjuvant chemotherapy without radiotherapy for early-stage cervical cancer.
In a retrospective review of 101 patients, Kwang-Beom Lee, MD, and his associates found that patients with known surgical risk factors had a posttreatment disease-free survival rate of 94.6%, a 5-year overall survival rate of 90.6%. and a disease-specific 5-year survival rate of 96.2%. These figures compare with survival rates of 79.4%, 90.6%, and 90.6%, respectively, for early-stage cervical cancer patients with lymph node metastasis.
Dr. Lee, professor of obstetrics and gynecology at Gachon University School of Medicine, Incheon, South Korea, said that about 3,600 cases of cervical cancer are diagnosed each year in Korea, and a little more than half (58%) are early-stage cancers. Most Korean patients with International Federation of Gynecology and Obstetrics (FIGO) stage IA2-IIA cancer will receive a radical hysterectomy with lymphadenectomy, he said at the annual meeting of the Society of Gynecologic Oncology.
Dr. Lee and his colleagues sought to ascertain morbidity when patients with early cervical cancer received either adjuvant radiotherapy or concurrent chemoradiotherapy (CCRT), and to explore the potential role that chemotherapy alone might play in these patients.
Accordingly, one of the primary outcomes of the study was to determine outcomes of adjuvant chemotherapy alone for patients with FIGO stage IB-IIA cervical cancer who had surgically-confirmed risk factors, and who received radical surgery.
The surgically-confirmed factors included lymphovascular space invasion, depth of penetration, and tumor size.
Currently, Dr. Lee said, evidence indicates that CCRT for patients with high risk factors improves both progression-free survival and overall survival. For patients with intermediate risk factors, radiotherapy is associated with increased progression-free survival.
The researchers examined 101 patients in this category who were treated between March of 2006 and December of 2014 at two Korean academic medical centers, excluding patients who had positive tumor margins, who received neoadjuvant chemotherapy, or who had microscopic parametrium involvement.
The mean age of the patients was 47.1 years (range, 23-73 years). Their mean body mass index was 23.1, and two thirds of patients were premenopausal. Most patients (73.3%, n = 74) had stage IB1 cancer, while 23 (22.8%) had stage IB2 cancer, and 4 (3.9%) had stage IIA cancer. Most patients (74.3%, n = 75) had squamous cell cancer.
The radical procedure performed was a type C radical hysterectomy; patients underwent pelvic lymph node dissection, with or without para-aortic node dissection. Pelvic nodes included all of the common iliac nodes, the external and internal iliac chains, and the obturator nodes. Para-aortic node dissection included dissection up to the level of the inferior mesenteric artery.
A total of 50 patients received pelvic lymph node and para-aortic lymph node dissection, with a mean 54.5 tumors retrieved per patient. A mean of 4.58 pelvic nodes were assessed as metastatic. A mean of 11.2 para-aortic nodes were retrieved, and of these, a mean 5.3 were metastatic.
All together, 76 patients had a combination of three surgically-confirmed risk factors without positive lymph nodes; the remaining 25 patients had positive lymph nodes (4 with pelvic and para-aortic involvement, the remaining with pelvic involvement alone), and were included irrespective of whether they met other risk factor criteria.
Dr. Lee said that the protocol for chemotherapy paralelled Protocol 92 from the Gynecologic Oncology Group; patients received chemotherapy if the combination of tumor diameter, depth of stromal invasion, and lymphovascular space invasion met Protocol 92 criteria for treatment, or if more than one lymph node metastasis was found.
The chemotherapy regime for intermediate-risk patients called for six cycles of either platinum alone (n = 47), or platinum with paclitaxel (n = 54). High-risk patients received six cycles of paclitaxel and platinum.
Patients were followed for a median of 65 months, and a total of 14 patients had a recurrence.
Dr. Lee reported no conflicts of interest.
[email protected]
On Twitter @karioakes
National Harbor, MD. – Patients, even those with surgically-confirmed risk factors, fared well when they received adjuvant chemotherapy without radiotherapy for early-stage cervical cancer.
In a retrospective review of 101 patients, Kwang-Beom Lee, MD, and his associates found that patients with known surgical risk factors had a posttreatment disease-free survival rate of 94.6%, a 5-year overall survival rate of 90.6%. and a disease-specific 5-year survival rate of 96.2%. These figures compare with survival rates of 79.4%, 90.6%, and 90.6%, respectively, for early-stage cervical cancer patients with lymph node metastasis.
Dr. Lee, professor of obstetrics and gynecology at Gachon University School of Medicine, Incheon, South Korea, said that about 3,600 cases of cervical cancer are diagnosed each year in Korea, and a little more than half (58%) are early-stage cancers. Most Korean patients with International Federation of Gynecology and Obstetrics (FIGO) stage IA2-IIA cancer will receive a radical hysterectomy with lymphadenectomy, he said at the annual meeting of the Society of Gynecologic Oncology.
Dr. Lee and his colleagues sought to ascertain morbidity when patients with early cervical cancer received either adjuvant radiotherapy or concurrent chemoradiotherapy (CCRT), and to explore the potential role that chemotherapy alone might play in these patients.
Accordingly, one of the primary outcomes of the study was to determine outcomes of adjuvant chemotherapy alone for patients with FIGO stage IB-IIA cervical cancer who had surgically-confirmed risk factors, and who received radical surgery.
The surgically-confirmed factors included lymphovascular space invasion, depth of penetration, and tumor size.
Currently, Dr. Lee said, evidence indicates that CCRT for patients with high risk factors improves both progression-free survival and overall survival. For patients with intermediate risk factors, radiotherapy is associated with increased progression-free survival.
The researchers examined 101 patients in this category who were treated between March of 2006 and December of 2014 at two Korean academic medical centers, excluding patients who had positive tumor margins, who received neoadjuvant chemotherapy, or who had microscopic parametrium involvement.
The mean age of the patients was 47.1 years (range, 23-73 years). Their mean body mass index was 23.1, and two thirds of patients were premenopausal. Most patients (73.3%, n = 74) had stage IB1 cancer, while 23 (22.8%) had stage IB2 cancer, and 4 (3.9%) had stage IIA cancer. Most patients (74.3%, n = 75) had squamous cell cancer.
The radical procedure performed was a type C radical hysterectomy; patients underwent pelvic lymph node dissection, with or without para-aortic node dissection. Pelvic nodes included all of the common iliac nodes, the external and internal iliac chains, and the obturator nodes. Para-aortic node dissection included dissection up to the level of the inferior mesenteric artery.
A total of 50 patients received pelvic lymph node and para-aortic lymph node dissection, with a mean 54.5 tumors retrieved per patient. A mean of 4.58 pelvic nodes were assessed as metastatic. A mean of 11.2 para-aortic nodes were retrieved, and of these, a mean 5.3 were metastatic.
All together, 76 patients had a combination of three surgically-confirmed risk factors without positive lymph nodes; the remaining 25 patients had positive lymph nodes (4 with pelvic and para-aortic involvement, the remaining with pelvic involvement alone), and were included irrespective of whether they met other risk factor criteria.
Dr. Lee said that the protocol for chemotherapy paralelled Protocol 92 from the Gynecologic Oncology Group; patients received chemotherapy if the combination of tumor diameter, depth of stromal invasion, and lymphovascular space invasion met Protocol 92 criteria for treatment, or if more than one lymph node metastasis was found.
The chemotherapy regime for intermediate-risk patients called for six cycles of either platinum alone (n = 47), or platinum with paclitaxel (n = 54). High-risk patients received six cycles of paclitaxel and platinum.
Patients were followed for a median of 65 months, and a total of 14 patients had a recurrence.
Dr. Lee reported no conflicts of interest.
[email protected]
On Twitter @karioakes
National Harbor, MD. – Patients, even those with surgically-confirmed risk factors, fared well when they received adjuvant chemotherapy without radiotherapy for early-stage cervical cancer.
In a retrospective review of 101 patients, Kwang-Beom Lee, MD, and his associates found that patients with known surgical risk factors had a posttreatment disease-free survival rate of 94.6%, a 5-year overall survival rate of 90.6%. and a disease-specific 5-year survival rate of 96.2%. These figures compare with survival rates of 79.4%, 90.6%, and 90.6%, respectively, for early-stage cervical cancer patients with lymph node metastasis.
Dr. Lee, professor of obstetrics and gynecology at Gachon University School of Medicine, Incheon, South Korea, said that about 3,600 cases of cervical cancer are diagnosed each year in Korea, and a little more than half (58%) are early-stage cancers. Most Korean patients with International Federation of Gynecology and Obstetrics (FIGO) stage IA2-IIA cancer will receive a radical hysterectomy with lymphadenectomy, he said at the annual meeting of the Society of Gynecologic Oncology.
Dr. Lee and his colleagues sought to ascertain morbidity when patients with early cervical cancer received either adjuvant radiotherapy or concurrent chemoradiotherapy (CCRT), and to explore the potential role that chemotherapy alone might play in these patients.
Accordingly, one of the primary outcomes of the study was to determine outcomes of adjuvant chemotherapy alone for patients with FIGO stage IB-IIA cervical cancer who had surgically-confirmed risk factors, and who received radical surgery.
The surgically-confirmed factors included lymphovascular space invasion, depth of penetration, and tumor size.
Currently, Dr. Lee said, evidence indicates that CCRT for patients with high risk factors improves both progression-free survival and overall survival. For patients with intermediate risk factors, radiotherapy is associated with increased progression-free survival.
The researchers examined 101 patients in this category who were treated between March of 2006 and December of 2014 at two Korean academic medical centers, excluding patients who had positive tumor margins, who received neoadjuvant chemotherapy, or who had microscopic parametrium involvement.
The mean age of the patients was 47.1 years (range, 23-73 years). Their mean body mass index was 23.1, and two thirds of patients were premenopausal. Most patients (73.3%, n = 74) had stage IB1 cancer, while 23 (22.8%) had stage IB2 cancer, and 4 (3.9%) had stage IIA cancer. Most patients (74.3%, n = 75) had squamous cell cancer.
The radical procedure performed was a type C radical hysterectomy; patients underwent pelvic lymph node dissection, with or without para-aortic node dissection. Pelvic nodes included all of the common iliac nodes, the external and internal iliac chains, and the obturator nodes. Para-aortic node dissection included dissection up to the level of the inferior mesenteric artery.
A total of 50 patients received pelvic lymph node and para-aortic lymph node dissection, with a mean 54.5 tumors retrieved per patient. A mean of 4.58 pelvic nodes were assessed as metastatic. A mean of 11.2 para-aortic nodes were retrieved, and of these, a mean 5.3 were metastatic.
All together, 76 patients had a combination of three surgically-confirmed risk factors without positive lymph nodes; the remaining 25 patients had positive lymph nodes (4 with pelvic and para-aortic involvement, the remaining with pelvic involvement alone), and were included irrespective of whether they met other risk factor criteria.
Dr. Lee said that the protocol for chemotherapy paralelled Protocol 92 from the Gynecologic Oncology Group; patients received chemotherapy if the combination of tumor diameter, depth of stromal invasion, and lymphovascular space invasion met Protocol 92 criteria for treatment, or if more than one lymph node metastasis was found.
The chemotherapy regime for intermediate-risk patients called for six cycles of either platinum alone (n = 47), or platinum with paclitaxel (n = 54). High-risk patients received six cycles of paclitaxel and platinum.
Patients were followed for a median of 65 months, and a total of 14 patients had a recurrence.
Dr. Lee reported no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE ANNUAL MEETING ON WOMEN’S CANCERS
Key clinical point:
Major finding: Patients with known surgical risk factors had a posttreatment disease-free survival rate of 94.6%.
Data source: Retrospective, two-center review of patients with early cervical cancer and multiple risk factors or pelvic node involvement.
Disclosures: Dr. Lee reported no conflicts of interest.
No advantage seen in pelvic node dissection for early cervical cancer
NATIONAL HARBOR, MD. – Patients with early cervical cancer with negative sentinel lymph node biopsy who did not receive pelvic lymphadenectomy experienced less postsurgical morbidity than patients who underwent lymphadenectomy, with no drop in overall or recurrence-free survival, investigators report.
In SENTICOL2, a 30-center prospective randomized study that compared sentinel lymph node (SLN) biopsy alone with SLN biopsy plus pelvic lymph node dissection for patients with early cervical cancer, recurrence-free survival at 3 years was 92% for patients receiving SLN only, compared with 95% in patients who had pelvic node dissection.
Overall survival at 3 years was 98% for the SLN-only patients, compared with 99% for those who had pelvic node dissection. None of these differences were statistically significant, and there were no significant differences between the study arms’ non-censored progression-free and overall survival rates at 6 years, Patrice Mathevet, MD, reported at the annual meeting of the Society of Gynecologic Oncology.
The study’s primary objective, said Dr. Mathevet, professor of obstetrics and gynecology at the University of Lausanne, Switzerland, was to compare the surgical morbidity experienced in each study arm, including quality of life and lymphedema–related signs and symptoms. A secondary objective was to assess and compare both overall survival and the 3-year recurrence-free rate for each study arm.
Patients were included if they had cervical cancer at International Federation of Gynecology and Obstetrics stage IA, IB1, or IIA1, with no sign of regional or distant metastases. Pregnant patients were excluded.
SLN scintigraphy was performed using the combined technetium and patent blue dye method. Patients with no identified or unilateral SLNs were excluded from the study and underwent pelvic lymph node dissection, as were patients in whom SLN scintigraphy was not performed.
Once SLNs were identified for the remaining patients, any patients with SLN metastases found on frozen section were excluded as well, while patients with grossly non-suspicious nodes and those with negative nodes on frozen section were randomized to receive just SLN biopsy with or without hysterectomy, or to receive pelvic lymph node dissection with or without hysterectomy.
SLNs in both study arms were examined by 200 micrometer serial sectioning with immunohistochemistry. For the pelvic node dissection arm, the nodes were submitted for pathology examination according to the study institution’s standard of care.
Over a 40-month period from March 2009 to July 2012, 267 patients with early cervical cancer were recruited. In the end, 206 patients were included in the study and 61 patients with positive or absent SLN results became ineligible according to the protocol criteria.
Of the eligible patients, 105 were randomized to the SLN biopsy–only arm, while 101 were allocated to the SLN biopsy plus pelvic lymph node dissection arm. Taking both study arms together, the median number of SLNs taken was three per patient, with a median one node per side.
When Dr. Mathevet and his colleagues looked at pathology from the pelvic lymph node dissection arm, they found that there were no false negatives, meaning that all patients with negative SLNs also had negative pelvic nodes.
Patient quality of life as assessed by the Short Form Health Survey (SF-36) was significantly lower for patients who received pelvic lymph node dissection. Lower extremity lymphedema signs and symptoms were also more common in patients who had pelvic lymph node dissection, indicated by the larger mean mid-thigh circumference and more common patient-reported leg heaviness and leg fatigue in the pelvic node dissection group.
The lymphedema findings were encapsulated in a global lymphatic morbidity score of 33 for the SLN-only group, compared with 52 for the pelvic node dissection group (P = .0046).
“Sentinel lymph node biopsy may improve the management of early cervical cancer, as sentinel lymph node biopsy alone induced less surgical morbidity than full pelvic lymph node dissection,” said Dr. Mathevet.
Patients were followed for a mean of 51 months post-procedure, with a total of 16 patients lost to follow-up. Patients in the SLN-only arm had a total of 11 recurrences, of which 5 were metastatic, 4 were local, and 2 were pelvic nodal. One of the pelvic nodal recurrences led to the patient’s death.
In the patients receiving pelvic node dissection, there were four metastatic and two local recurrences, but the difference in recurrence rates between the two groups was not statistically significant.
“This study leads to the morbidity-sparing approach in cervical cancer treatment while omitting the full pelvic lymph node dissection if the sentinel lymph nodes are negative,” said Dr. Mathevet.
Dr. Mathevet reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Patients with early cervical cancer with negative sentinel lymph node biopsy who did not receive pelvic lymphadenectomy experienced less postsurgical morbidity than patients who underwent lymphadenectomy, with no drop in overall or recurrence-free survival, investigators report.
In SENTICOL2, a 30-center prospective randomized study that compared sentinel lymph node (SLN) biopsy alone with SLN biopsy plus pelvic lymph node dissection for patients with early cervical cancer, recurrence-free survival at 3 years was 92% for patients receiving SLN only, compared with 95% in patients who had pelvic node dissection.
Overall survival at 3 years was 98% for the SLN-only patients, compared with 99% for those who had pelvic node dissection. None of these differences were statistically significant, and there were no significant differences between the study arms’ non-censored progression-free and overall survival rates at 6 years, Patrice Mathevet, MD, reported at the annual meeting of the Society of Gynecologic Oncology.
The study’s primary objective, said Dr. Mathevet, professor of obstetrics and gynecology at the University of Lausanne, Switzerland, was to compare the surgical morbidity experienced in each study arm, including quality of life and lymphedema–related signs and symptoms. A secondary objective was to assess and compare both overall survival and the 3-year recurrence-free rate for each study arm.
Patients were included if they had cervical cancer at International Federation of Gynecology and Obstetrics stage IA, IB1, or IIA1, with no sign of regional or distant metastases. Pregnant patients were excluded.
SLN scintigraphy was performed using the combined technetium and patent blue dye method. Patients with no identified or unilateral SLNs were excluded from the study and underwent pelvic lymph node dissection, as were patients in whom SLN scintigraphy was not performed.
Once SLNs were identified for the remaining patients, any patients with SLN metastases found on frozen section were excluded as well, while patients with grossly non-suspicious nodes and those with negative nodes on frozen section were randomized to receive just SLN biopsy with or without hysterectomy, or to receive pelvic lymph node dissection with or without hysterectomy.
SLNs in both study arms were examined by 200 micrometer serial sectioning with immunohistochemistry. For the pelvic node dissection arm, the nodes were submitted for pathology examination according to the study institution’s standard of care.
Over a 40-month period from March 2009 to July 2012, 267 patients with early cervical cancer were recruited. In the end, 206 patients were included in the study and 61 patients with positive or absent SLN results became ineligible according to the protocol criteria.
Of the eligible patients, 105 were randomized to the SLN biopsy–only arm, while 101 were allocated to the SLN biopsy plus pelvic lymph node dissection arm. Taking both study arms together, the median number of SLNs taken was three per patient, with a median one node per side.
When Dr. Mathevet and his colleagues looked at pathology from the pelvic lymph node dissection arm, they found that there were no false negatives, meaning that all patients with negative SLNs also had negative pelvic nodes.
Patient quality of life as assessed by the Short Form Health Survey (SF-36) was significantly lower for patients who received pelvic lymph node dissection. Lower extremity lymphedema signs and symptoms were also more common in patients who had pelvic lymph node dissection, indicated by the larger mean mid-thigh circumference and more common patient-reported leg heaviness and leg fatigue in the pelvic node dissection group.
The lymphedema findings were encapsulated in a global lymphatic morbidity score of 33 for the SLN-only group, compared with 52 for the pelvic node dissection group (P = .0046).
“Sentinel lymph node biopsy may improve the management of early cervical cancer, as sentinel lymph node biopsy alone induced less surgical morbidity than full pelvic lymph node dissection,” said Dr. Mathevet.
Patients were followed for a mean of 51 months post-procedure, with a total of 16 patients lost to follow-up. Patients in the SLN-only arm had a total of 11 recurrences, of which 5 were metastatic, 4 were local, and 2 were pelvic nodal. One of the pelvic nodal recurrences led to the patient’s death.
In the patients receiving pelvic node dissection, there were four metastatic and two local recurrences, but the difference in recurrence rates between the two groups was not statistically significant.
“This study leads to the morbidity-sparing approach in cervical cancer treatment while omitting the full pelvic lymph node dissection if the sentinel lymph nodes are negative,” said Dr. Mathevet.
Dr. Mathevet reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
NATIONAL HARBOR, MD. – Patients with early cervical cancer with negative sentinel lymph node biopsy who did not receive pelvic lymphadenectomy experienced less postsurgical morbidity than patients who underwent lymphadenectomy, with no drop in overall or recurrence-free survival, investigators report.
In SENTICOL2, a 30-center prospective randomized study that compared sentinel lymph node (SLN) biopsy alone with SLN biopsy plus pelvic lymph node dissection for patients with early cervical cancer, recurrence-free survival at 3 years was 92% for patients receiving SLN only, compared with 95% in patients who had pelvic node dissection.
Overall survival at 3 years was 98% for the SLN-only patients, compared with 99% for those who had pelvic node dissection. None of these differences were statistically significant, and there were no significant differences between the study arms’ non-censored progression-free and overall survival rates at 6 years, Patrice Mathevet, MD, reported at the annual meeting of the Society of Gynecologic Oncology.
The study’s primary objective, said Dr. Mathevet, professor of obstetrics and gynecology at the University of Lausanne, Switzerland, was to compare the surgical morbidity experienced in each study arm, including quality of life and lymphedema–related signs and symptoms. A secondary objective was to assess and compare both overall survival and the 3-year recurrence-free rate for each study arm.
Patients were included if they had cervical cancer at International Federation of Gynecology and Obstetrics stage IA, IB1, or IIA1, with no sign of regional or distant metastases. Pregnant patients were excluded.
SLN scintigraphy was performed using the combined technetium and patent blue dye method. Patients with no identified or unilateral SLNs were excluded from the study and underwent pelvic lymph node dissection, as were patients in whom SLN scintigraphy was not performed.
Once SLNs were identified for the remaining patients, any patients with SLN metastases found on frozen section were excluded as well, while patients with grossly non-suspicious nodes and those with negative nodes on frozen section were randomized to receive just SLN biopsy with or without hysterectomy, or to receive pelvic lymph node dissection with or without hysterectomy.
SLNs in both study arms were examined by 200 micrometer serial sectioning with immunohistochemistry. For the pelvic node dissection arm, the nodes were submitted for pathology examination according to the study institution’s standard of care.
Over a 40-month period from March 2009 to July 2012, 267 patients with early cervical cancer were recruited. In the end, 206 patients were included in the study and 61 patients with positive or absent SLN results became ineligible according to the protocol criteria.
Of the eligible patients, 105 were randomized to the SLN biopsy–only arm, while 101 were allocated to the SLN biopsy plus pelvic lymph node dissection arm. Taking both study arms together, the median number of SLNs taken was three per patient, with a median one node per side.
When Dr. Mathevet and his colleagues looked at pathology from the pelvic lymph node dissection arm, they found that there were no false negatives, meaning that all patients with negative SLNs also had negative pelvic nodes.
Patient quality of life as assessed by the Short Form Health Survey (SF-36) was significantly lower for patients who received pelvic lymph node dissection. Lower extremity lymphedema signs and symptoms were also more common in patients who had pelvic lymph node dissection, indicated by the larger mean mid-thigh circumference and more common patient-reported leg heaviness and leg fatigue in the pelvic node dissection group.
The lymphedema findings were encapsulated in a global lymphatic morbidity score of 33 for the SLN-only group, compared with 52 for the pelvic node dissection group (P = .0046).
“Sentinel lymph node biopsy may improve the management of early cervical cancer, as sentinel lymph node biopsy alone induced less surgical morbidity than full pelvic lymph node dissection,” said Dr. Mathevet.
Patients were followed for a mean of 51 months post-procedure, with a total of 16 patients lost to follow-up. Patients in the SLN-only arm had a total of 11 recurrences, of which 5 were metastatic, 4 were local, and 2 were pelvic nodal. One of the pelvic nodal recurrences led to the patient’s death.
In the patients receiving pelvic node dissection, there were four metastatic and two local recurrences, but the difference in recurrence rates between the two groups was not statistically significant.
“This study leads to the morbidity-sparing approach in cervical cancer treatment while omitting the full pelvic lymph node dissection if the sentinel lymph nodes are negative,” said Dr. Mathevet.
Dr. Mathevet reported no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: Pelvic node dissection gave no significant survival or recurrence benefit over sentinel lymph node biopsy alone.
Data source: Randomized, prospective, multicenter trial of 206 patients with early-stage cervical cancer.
Disclosures: Dr. Mathevet reported no conflicts of interest.
APA task force urges caution in off-label use of ketamine for mood disorders
A new consensus statement on the use of ketamine as an off-label treatment for mood disorders provides psychiatrists some guidance for patient selection and evaluation, as well as dosing and duration of therapy. The statement was issued against the backdrop of newer studies showing ketamine’s rapid, though not durable, efficacy in treating depression and anxiety disorders.
From start to end, however, the statement urges caution and marks out areas for further study, citing a paucity of data on longer-term efficacy and safety and a literature largely made up of smaller studies.
Dr. Sanacora, professor of psychiatry at Yale University, New Haven, Conn., and his coauthors made clear that “this report is not intended to serve as a standard, guideline, clinical policy, or absolute requirement.” Rather, the document identifies the current state of the field and identifies factors to consider in determining the appropriateness of ketamine therapy.
When a clinician is considering giving ketamine to a patient, a preprocedural evaluation is recommended, both to assess whether ketamine is likely to benefit the patient and to evaluate potential risks. Recommended components include a comprehensive psychiatric diagnostic assessment, paying particular attention to substance use and psychosis history, if any; assessment of baseline symptom severity; history of prior antidepressant treatment; review of systems to assess risk factors; physical examination and laboratory screening that follows accepted guidelines for the anticipated level of sedation, with the recommended addition of a baseline urine toxicology screen; and records review and family corroboration with a particular eye to past substance use.
Finally, the informed consent process should ensure that the patient is aware not only of potential treatment risks, but also of the relatively limited data on the off-label use of ketamine for mood disorders. Thorough written documentation is recommended.
Regarding the appropriate amount of experience and training a clinician should have before administering ketamine, Dr. Sanacora and his coauthors noted that the subanesthetic doses of ketamine that are used to treat mood disorders have been found generally very safe in the limited studies that have been done. Typical peak plasma concentrations will not induce general anesthesia. However, systolic and diastolic blood pressure and heart rate elevations are not uncommon. The statement cites a study that found “blood pressure levels exceeding 180/100 mm Hg or heart rates exceeding 110 beats per minute in approximately 30% of the patients treated.”
Accordingly, the statement recommends that clinicians administering ketamine have Advanced Cardiac Life Support certification and be able to administer Drug Enforcement Administration Schedule III medications. Individual organizations, according to the statement, should follow accepted standards of practice for granting privileges to administer ketamine. A statement developed by the American Society of Anesthesiologists on granting privileges for conscious sedation to nonanesthesia professionals may be used for guidance.
The most-studied dose of ketamine in the treatment of mood disorders is 0.5 mg/kg, administered intravenously over 40 minutes. Though other routes, and lower doses, have been studied, Dr. Sanacora and his colleagues wrote that they consider that “insufficient benefit was provided in those studies to allow any meaningful analysis of any specific dose or route of treatment compared with the standard dose.”
The statement includes a strong recommendation to develop a site-specific–standard operating procedure for the administration of ketamine that incorporates the preprocedural evaluation. In addition, the procedure should assess baseline vital signs, include criteria for acceptable vital signs, and incorporate a “time-out” procedure before initiating ketamine treatment.
Also, standard operating procedures should include continued assessment of respiratory, cardiovascular, and mental status throughout the infusion. Stopping criteria should be clearly defined, as should a plan aimed at managing any cardiovascular or behavioral problems. Discharge procedures should include documentation of vital signs and mental status, ensuring that an adult caregiver can take the patient home, and a thorough review of discharge instructions.
The statement’s section on follow-up and assessments noted: “The existing data surrounding the benefits of repeated infusions of ketamine remain limited.” However, some studies have shown that twice-weekly infusions were as efficacious as infusions given three times a week. In terms of longer-term treatment, the data are sparse, wrote Dr. Sanacora and his coauthors. Some clinics, they said, are giving ketamine two or three times weekly for 2 or 3 weeks, then tapering or adjusting the regimen based on clinical response, but high-quality studies are lacking.” The scarcity of this information is one of the major drawbacks to be considered before initiating ketamine therapy for patients with mood disorders and should be discussed with the patient before beginning treatment,” they wrote.
The known risks of cognitive impairment and cystitis with more chronic high-frequency ketamine use, taken together with the significant potential for abuse, mean that ketamine should be discontinued if more than once-weekly dosing is required after 2 months of treatment. “The goal remains to eventually taper and discontinue treatment until more long-term safety data can be collected,” wrote Dr. Sanacora and his coauthors.
The statement, while acknowledging the hope and excitement that currently surround the use of ketamine for mood disorders, calls for further research that would include a patient registry and coordinated data collection to facilitate answering the many important questions remaining about ketamine’s efficacy and safety.
The report was neither endorsed nor promulgated as policy of the APA. Dr. Sanacora reported multiple relationships with pharmaceutical companies, as did all of his coauthors.
[email protected]
On Twitter @karioakes
A clear need exists for better treatments for the up to one-third of patients with major depression who do not respond to currently available therapies. Ketamine, which can produce rapid antidepressant effects, holds promise for this population and is increasingly being used off-label.
However, clinical guidance is lacking, and the small studies done to date leave many knowledge gaps. Though ketamine is known to be an N-methyl-D-aspartate (NMDA) glutamate receptor antagonist, rodent studies show that its action, or perhaps that of its metabolites, on another glutamate pathway may primarily underlie its antidepressant effects. Also, researchers are trialling adjunctive agents such as clonidine to help mute the undesirable psychomimetic and cardiorespiratory effects of ketamine. As the science rapidly develops, more targeted rapid treatments may become available, an evolution that could fundamentally change many aspects of the practice of psychiatry.
Uncertainty created by the current limitations in knowledge permeates the consensus statement and appropriately so. The authors provide clinical guidance based on what data are available but call for caution and transparency when treating mood disorder patients with ketamine. Gaps in data can be ameliorated by the formation of a patient registry for coordinated data collection and safety monitoring.
Charles F. Zorumski, MD, and Charles R. Conway, MD, are professors of psychiatry at Washington University in St. Louis, where Dr. Zorumski also holds an appointment in the department of neuroscience. Dr. Zorumski reported serving on the scientific advisory board of Sage Therapeutics, which also has funded research conducted by both authors. Dr. Conway reported serving as an unpaid consultant to LivaNova. These remarks were drawn from invited commentary accompanying the consensus statement.
A clear need exists for better treatments for the up to one-third of patients with major depression who do not respond to currently available therapies. Ketamine, which can produce rapid antidepressant effects, holds promise for this population and is increasingly being used off-label.
However, clinical guidance is lacking, and the small studies done to date leave many knowledge gaps. Though ketamine is known to be an N-methyl-D-aspartate (NMDA) glutamate receptor antagonist, rodent studies show that its action, or perhaps that of its metabolites, on another glutamate pathway may primarily underlie its antidepressant effects. Also, researchers are trialling adjunctive agents such as clonidine to help mute the undesirable psychomimetic and cardiorespiratory effects of ketamine. As the science rapidly develops, more targeted rapid treatments may become available, an evolution that could fundamentally change many aspects of the practice of psychiatry.
Uncertainty created by the current limitations in knowledge permeates the consensus statement and appropriately so. The authors provide clinical guidance based on what data are available but call for caution and transparency when treating mood disorder patients with ketamine. Gaps in data can be ameliorated by the formation of a patient registry for coordinated data collection and safety monitoring.
Charles F. Zorumski, MD, and Charles R. Conway, MD, are professors of psychiatry at Washington University in St. Louis, where Dr. Zorumski also holds an appointment in the department of neuroscience. Dr. Zorumski reported serving on the scientific advisory board of Sage Therapeutics, which also has funded research conducted by both authors. Dr. Conway reported serving as an unpaid consultant to LivaNova. These remarks were drawn from invited commentary accompanying the consensus statement.
A clear need exists for better treatments for the up to one-third of patients with major depression who do not respond to currently available therapies. Ketamine, which can produce rapid antidepressant effects, holds promise for this population and is increasingly being used off-label.
However, clinical guidance is lacking, and the small studies done to date leave many knowledge gaps. Though ketamine is known to be an N-methyl-D-aspartate (NMDA) glutamate receptor antagonist, rodent studies show that its action, or perhaps that of its metabolites, on another glutamate pathway may primarily underlie its antidepressant effects. Also, researchers are trialling adjunctive agents such as clonidine to help mute the undesirable psychomimetic and cardiorespiratory effects of ketamine. As the science rapidly develops, more targeted rapid treatments may become available, an evolution that could fundamentally change many aspects of the practice of psychiatry.
Uncertainty created by the current limitations in knowledge permeates the consensus statement and appropriately so. The authors provide clinical guidance based on what data are available but call for caution and transparency when treating mood disorder patients with ketamine. Gaps in data can be ameliorated by the formation of a patient registry for coordinated data collection and safety monitoring.
Charles F. Zorumski, MD, and Charles R. Conway, MD, are professors of psychiatry at Washington University in St. Louis, where Dr. Zorumski also holds an appointment in the department of neuroscience. Dr. Zorumski reported serving on the scientific advisory board of Sage Therapeutics, which also has funded research conducted by both authors. Dr. Conway reported serving as an unpaid consultant to LivaNova. These remarks were drawn from invited commentary accompanying the consensus statement.
A new consensus statement on the use of ketamine as an off-label treatment for mood disorders provides psychiatrists some guidance for patient selection and evaluation, as well as dosing and duration of therapy. The statement was issued against the backdrop of newer studies showing ketamine’s rapid, though not durable, efficacy in treating depression and anxiety disorders.
From start to end, however, the statement urges caution and marks out areas for further study, citing a paucity of data on longer-term efficacy and safety and a literature largely made up of smaller studies.
Dr. Sanacora, professor of psychiatry at Yale University, New Haven, Conn., and his coauthors made clear that “this report is not intended to serve as a standard, guideline, clinical policy, or absolute requirement.” Rather, the document identifies the current state of the field and identifies factors to consider in determining the appropriateness of ketamine therapy.
When a clinician is considering giving ketamine to a patient, a preprocedural evaluation is recommended, both to assess whether ketamine is likely to benefit the patient and to evaluate potential risks. Recommended components include a comprehensive psychiatric diagnostic assessment, paying particular attention to substance use and psychosis history, if any; assessment of baseline symptom severity; history of prior antidepressant treatment; review of systems to assess risk factors; physical examination and laboratory screening that follows accepted guidelines for the anticipated level of sedation, with the recommended addition of a baseline urine toxicology screen; and records review and family corroboration with a particular eye to past substance use.
Finally, the informed consent process should ensure that the patient is aware not only of potential treatment risks, but also of the relatively limited data on the off-label use of ketamine for mood disorders. Thorough written documentation is recommended.
Regarding the appropriate amount of experience and training a clinician should have before administering ketamine, Dr. Sanacora and his coauthors noted that the subanesthetic doses of ketamine that are used to treat mood disorders have been found generally very safe in the limited studies that have been done. Typical peak plasma concentrations will not induce general anesthesia. However, systolic and diastolic blood pressure and heart rate elevations are not uncommon. The statement cites a study that found “blood pressure levels exceeding 180/100 mm Hg or heart rates exceeding 110 beats per minute in approximately 30% of the patients treated.”
Accordingly, the statement recommends that clinicians administering ketamine have Advanced Cardiac Life Support certification and be able to administer Drug Enforcement Administration Schedule III medications. Individual organizations, according to the statement, should follow accepted standards of practice for granting privileges to administer ketamine. A statement developed by the American Society of Anesthesiologists on granting privileges for conscious sedation to nonanesthesia professionals may be used for guidance.
The most-studied dose of ketamine in the treatment of mood disorders is 0.5 mg/kg, administered intravenously over 40 minutes. Though other routes, and lower doses, have been studied, Dr. Sanacora and his colleagues wrote that they consider that “insufficient benefit was provided in those studies to allow any meaningful analysis of any specific dose or route of treatment compared with the standard dose.”
The statement includes a strong recommendation to develop a site-specific–standard operating procedure for the administration of ketamine that incorporates the preprocedural evaluation. In addition, the procedure should assess baseline vital signs, include criteria for acceptable vital signs, and incorporate a “time-out” procedure before initiating ketamine treatment.
Also, standard operating procedures should include continued assessment of respiratory, cardiovascular, and mental status throughout the infusion. Stopping criteria should be clearly defined, as should a plan aimed at managing any cardiovascular or behavioral problems. Discharge procedures should include documentation of vital signs and mental status, ensuring that an adult caregiver can take the patient home, and a thorough review of discharge instructions.
The statement’s section on follow-up and assessments noted: “The existing data surrounding the benefits of repeated infusions of ketamine remain limited.” However, some studies have shown that twice-weekly infusions were as efficacious as infusions given three times a week. In terms of longer-term treatment, the data are sparse, wrote Dr. Sanacora and his coauthors. Some clinics, they said, are giving ketamine two or three times weekly for 2 or 3 weeks, then tapering or adjusting the regimen based on clinical response, but high-quality studies are lacking.” The scarcity of this information is one of the major drawbacks to be considered before initiating ketamine therapy for patients with mood disorders and should be discussed with the patient before beginning treatment,” they wrote.
The known risks of cognitive impairment and cystitis with more chronic high-frequency ketamine use, taken together with the significant potential for abuse, mean that ketamine should be discontinued if more than once-weekly dosing is required after 2 months of treatment. “The goal remains to eventually taper and discontinue treatment until more long-term safety data can be collected,” wrote Dr. Sanacora and his coauthors.
The statement, while acknowledging the hope and excitement that currently surround the use of ketamine for mood disorders, calls for further research that would include a patient registry and coordinated data collection to facilitate answering the many important questions remaining about ketamine’s efficacy and safety.
The report was neither endorsed nor promulgated as policy of the APA. Dr. Sanacora reported multiple relationships with pharmaceutical companies, as did all of his coauthors.
[email protected]
On Twitter @karioakes
A new consensus statement on the use of ketamine as an off-label treatment for mood disorders provides psychiatrists some guidance for patient selection and evaluation, as well as dosing and duration of therapy. The statement was issued against the backdrop of newer studies showing ketamine’s rapid, though not durable, efficacy in treating depression and anxiety disorders.
From start to end, however, the statement urges caution and marks out areas for further study, citing a paucity of data on longer-term efficacy and safety and a literature largely made up of smaller studies.
Dr. Sanacora, professor of psychiatry at Yale University, New Haven, Conn., and his coauthors made clear that “this report is not intended to serve as a standard, guideline, clinical policy, or absolute requirement.” Rather, the document identifies the current state of the field and identifies factors to consider in determining the appropriateness of ketamine therapy.
When a clinician is considering giving ketamine to a patient, a preprocedural evaluation is recommended, both to assess whether ketamine is likely to benefit the patient and to evaluate potential risks. Recommended components include a comprehensive psychiatric diagnostic assessment, paying particular attention to substance use and psychosis history, if any; assessment of baseline symptom severity; history of prior antidepressant treatment; review of systems to assess risk factors; physical examination and laboratory screening that follows accepted guidelines for the anticipated level of sedation, with the recommended addition of a baseline urine toxicology screen; and records review and family corroboration with a particular eye to past substance use.
Finally, the informed consent process should ensure that the patient is aware not only of potential treatment risks, but also of the relatively limited data on the off-label use of ketamine for mood disorders. Thorough written documentation is recommended.
Regarding the appropriate amount of experience and training a clinician should have before administering ketamine, Dr. Sanacora and his coauthors noted that the subanesthetic doses of ketamine that are used to treat mood disorders have been found generally very safe in the limited studies that have been done. Typical peak plasma concentrations will not induce general anesthesia. However, systolic and diastolic blood pressure and heart rate elevations are not uncommon. The statement cites a study that found “blood pressure levels exceeding 180/100 mm Hg or heart rates exceeding 110 beats per minute in approximately 30% of the patients treated.”
Accordingly, the statement recommends that clinicians administering ketamine have Advanced Cardiac Life Support certification and be able to administer Drug Enforcement Administration Schedule III medications. Individual organizations, according to the statement, should follow accepted standards of practice for granting privileges to administer ketamine. A statement developed by the American Society of Anesthesiologists on granting privileges for conscious sedation to nonanesthesia professionals may be used for guidance.
The most-studied dose of ketamine in the treatment of mood disorders is 0.5 mg/kg, administered intravenously over 40 minutes. Though other routes, and lower doses, have been studied, Dr. Sanacora and his colleagues wrote that they consider that “insufficient benefit was provided in those studies to allow any meaningful analysis of any specific dose or route of treatment compared with the standard dose.”
The statement includes a strong recommendation to develop a site-specific–standard operating procedure for the administration of ketamine that incorporates the preprocedural evaluation. In addition, the procedure should assess baseline vital signs, include criteria for acceptable vital signs, and incorporate a “time-out” procedure before initiating ketamine treatment.
Also, standard operating procedures should include continued assessment of respiratory, cardiovascular, and mental status throughout the infusion. Stopping criteria should be clearly defined, as should a plan aimed at managing any cardiovascular or behavioral problems. Discharge procedures should include documentation of vital signs and mental status, ensuring that an adult caregiver can take the patient home, and a thorough review of discharge instructions.
The statement’s section on follow-up and assessments noted: “The existing data surrounding the benefits of repeated infusions of ketamine remain limited.” However, some studies have shown that twice-weekly infusions were as efficacious as infusions given three times a week. In terms of longer-term treatment, the data are sparse, wrote Dr. Sanacora and his coauthors. Some clinics, they said, are giving ketamine two or three times weekly for 2 or 3 weeks, then tapering or adjusting the regimen based on clinical response, but high-quality studies are lacking.” The scarcity of this information is one of the major drawbacks to be considered before initiating ketamine therapy for patients with mood disorders and should be discussed with the patient before beginning treatment,” they wrote.
The known risks of cognitive impairment and cystitis with more chronic high-frequency ketamine use, taken together with the significant potential for abuse, mean that ketamine should be discontinued if more than once-weekly dosing is required after 2 months of treatment. “The goal remains to eventually taper and discontinue treatment until more long-term safety data can be collected,” wrote Dr. Sanacora and his coauthors.
The statement, while acknowledging the hope and excitement that currently surround the use of ketamine for mood disorders, calls for further research that would include a patient registry and coordinated data collection to facilitate answering the many important questions remaining about ketamine’s efficacy and safety.
The report was neither endorsed nor promulgated as policy of the APA. Dr. Sanacora reported multiple relationships with pharmaceutical companies, as did all of his coauthors.
[email protected]
On Twitter @karioakes
FROM JAMA PSYCHIATRY
Cervicovaginal microbiota correlates with preterm birth rate
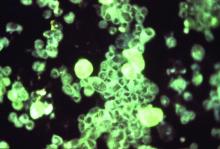
LAS VEGAS – Certain cervicovaginal microbiota predispose women to spontaneous preterm birth, according to a new study, while other microbiota were found to be protective against preterm delivery.
The findings stand in contrast to previous clinical trials that “targeted uterine activity and/or uterine infection,” said Michal Elovitz, MD, the first author of a study presented at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
To answer the question, Dr. Elovitz and her colleagues conducted a large prospective cohort and validation study, testing the hypothesis that cervicovaginal microbial communities in women “destined to have a preterm birth” would differ from those of control patients.
The Motherhood and the Microbiome study enrolled 1,500 women aged 13-50 years with singleton pregnancies to constitute the prospective cohort. Cervicovaginal swabs were obtained at three time points: at gestational weeks 16-20, 20-24, and 24-28. Dr. Elovitz, professor of ob.gyn. at the University of Pennsylvania, Philadelphia, was the study adjudicator for determining preterm births.
Within the prospective cohort, Dr. Elovitz and her collaborators identified 83 cases of spontaneous preterm birth (SPTB), and frequency matched them by race to 336 patients who had term deliveries in a 4:1 ratio. The cervicovaginal microbiota of these patients was characterized by performing 165 rRNA gene analyses. Once the bacterial composition and structure had been identified, the investigators then calculated the effect of cervicovaginal bacterial composition on the risk of SPTB by using the log ratio between the mean relative abundance of a given phylotype for the SPTB, compared with the term birth samples.
A second prospective cohort of 616 women was formed for validation; cervicovaginal specimens in this cohort were collected between 22 and 32 weeks of gestation.
Taking both cohorts together, a total of 127 phylotypes were found in all samples. A total of 13 bacterial species were positively associated with an increased risk of spontaneous preterm birth in the primary cohort; 37 species were significantly associated with a decreased risk of spontaneous preterm birth.
“Bifidobacterium species were noted to be significantly protective against SPTB at all gestational time points,” wrote Dr. Elovitz and her collaborators in the abstract accompanying the presentation. On the other hand, they wrote, “BVAB2, BVAB3, and Mobiluncus were associated with a dramatic increase[d] risk of SPTB (all q-values less than 0.0001).”
Abundant Mobiluncus mulieris, in particular, was associated with significantly increased risk of SPTB at all time points during the study. The odds ratio for SPTB with a positive mobiluncus swab at visit one was 9.21.
Since the study examined both relative and absolute abundance of individual bacterial species, the investigators were able to determine that when Bifidobacterium breve was present, the incidence of BVAB3-associated preterm birth dropped from more than 30% to less than 10% (P = .006).
The notion that specific cervicovaginal bacterial species can be associated with increased rate of SPTB represents a different finding than most previous work in this field, said Dr. Elovitz, adding that much of the research on the vaginal microbiome during the reproductive years has focused on groupings of predominant bacteria, termed community state types (CSTs). “Classification of communities into CST, as performed in the nonpregnant woman, is not revealing for PTB,” Dr. Elovitz said.
Future research into cervicovaginal microbial communities and spontaneous preterm birth are likely to produce new methods to risk-stratify women and potential new therapeutics to reduce the rate of spontaneous preterm birth, she added.
The presentation won the conference’s March of Dimes award for best abstract in prematurity.
Dr. Elovitz reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
LAS VEGAS – Certain cervicovaginal microbiota predispose women to spontaneous preterm birth, according to a new study, while other microbiota were found to be protective against preterm delivery.
The findings stand in contrast to previous clinical trials that “targeted uterine activity and/or uterine infection,” said Michal Elovitz, MD, the first author of a study presented at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
To answer the question, Dr. Elovitz and her colleagues conducted a large prospective cohort and validation study, testing the hypothesis that cervicovaginal microbial communities in women “destined to have a preterm birth” would differ from those of control patients.
The Motherhood and the Microbiome study enrolled 1,500 women aged 13-50 years with singleton pregnancies to constitute the prospective cohort. Cervicovaginal swabs were obtained at three time points: at gestational weeks 16-20, 20-24, and 24-28. Dr. Elovitz, professor of ob.gyn. at the University of Pennsylvania, Philadelphia, was the study adjudicator for determining preterm births.
Within the prospective cohort, Dr. Elovitz and her collaborators identified 83 cases of spontaneous preterm birth (SPTB), and frequency matched them by race to 336 patients who had term deliveries in a 4:1 ratio. The cervicovaginal microbiota of these patients was characterized by performing 165 rRNA gene analyses. Once the bacterial composition and structure had been identified, the investigators then calculated the effect of cervicovaginal bacterial composition on the risk of SPTB by using the log ratio between the mean relative abundance of a given phylotype for the SPTB, compared with the term birth samples.
A second prospective cohort of 616 women was formed for validation; cervicovaginal specimens in this cohort were collected between 22 and 32 weeks of gestation.
Taking both cohorts together, a total of 127 phylotypes were found in all samples. A total of 13 bacterial species were positively associated with an increased risk of spontaneous preterm birth in the primary cohort; 37 species were significantly associated with a decreased risk of spontaneous preterm birth.
“Bifidobacterium species were noted to be significantly protective against SPTB at all gestational time points,” wrote Dr. Elovitz and her collaborators in the abstract accompanying the presentation. On the other hand, they wrote, “BVAB2, BVAB3, and Mobiluncus were associated with a dramatic increase[d] risk of SPTB (all q-values less than 0.0001).”
Abundant Mobiluncus mulieris, in particular, was associated with significantly increased risk of SPTB at all time points during the study. The odds ratio for SPTB with a positive mobiluncus swab at visit one was 9.21.
Since the study examined both relative and absolute abundance of individual bacterial species, the investigators were able to determine that when Bifidobacterium breve was present, the incidence of BVAB3-associated preterm birth dropped from more than 30% to less than 10% (P = .006).
The notion that specific cervicovaginal bacterial species can be associated with increased rate of SPTB represents a different finding than most previous work in this field, said Dr. Elovitz, adding that much of the research on the vaginal microbiome during the reproductive years has focused on groupings of predominant bacteria, termed community state types (CSTs). “Classification of communities into CST, as performed in the nonpregnant woman, is not revealing for PTB,” Dr. Elovitz said.
Future research into cervicovaginal microbial communities and spontaneous preterm birth are likely to produce new methods to risk-stratify women and potential new therapeutics to reduce the rate of spontaneous preterm birth, she added.
The presentation won the conference’s March of Dimes award for best abstract in prematurity.
Dr. Elovitz reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
LAS VEGAS – Certain cervicovaginal microbiota predispose women to spontaneous preterm birth, according to a new study, while other microbiota were found to be protective against preterm delivery.
The findings stand in contrast to previous clinical trials that “targeted uterine activity and/or uterine infection,” said Michal Elovitz, MD, the first author of a study presented at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
To answer the question, Dr. Elovitz and her colleagues conducted a large prospective cohort and validation study, testing the hypothesis that cervicovaginal microbial communities in women “destined to have a preterm birth” would differ from those of control patients.
The Motherhood and the Microbiome study enrolled 1,500 women aged 13-50 years with singleton pregnancies to constitute the prospective cohort. Cervicovaginal swabs were obtained at three time points: at gestational weeks 16-20, 20-24, and 24-28. Dr. Elovitz, professor of ob.gyn. at the University of Pennsylvania, Philadelphia, was the study adjudicator for determining preterm births.
Within the prospective cohort, Dr. Elovitz and her collaborators identified 83 cases of spontaneous preterm birth (SPTB), and frequency matched them by race to 336 patients who had term deliveries in a 4:1 ratio. The cervicovaginal microbiota of these patients was characterized by performing 165 rRNA gene analyses. Once the bacterial composition and structure had been identified, the investigators then calculated the effect of cervicovaginal bacterial composition on the risk of SPTB by using the log ratio between the mean relative abundance of a given phylotype for the SPTB, compared with the term birth samples.
A second prospective cohort of 616 women was formed for validation; cervicovaginal specimens in this cohort were collected between 22 and 32 weeks of gestation.
Taking both cohorts together, a total of 127 phylotypes were found in all samples. A total of 13 bacterial species were positively associated with an increased risk of spontaneous preterm birth in the primary cohort; 37 species were significantly associated with a decreased risk of spontaneous preterm birth.
“Bifidobacterium species were noted to be significantly protective against SPTB at all gestational time points,” wrote Dr. Elovitz and her collaborators in the abstract accompanying the presentation. On the other hand, they wrote, “BVAB2, BVAB3, and Mobiluncus were associated with a dramatic increase[d] risk of SPTB (all q-values less than 0.0001).”
Abundant Mobiluncus mulieris, in particular, was associated with significantly increased risk of SPTB at all time points during the study. The odds ratio for SPTB with a positive mobiluncus swab at visit one was 9.21.
Since the study examined both relative and absolute abundance of individual bacterial species, the investigators were able to determine that when Bifidobacterium breve was present, the incidence of BVAB3-associated preterm birth dropped from more than 30% to less than 10% (P = .006).
The notion that specific cervicovaginal bacterial species can be associated with increased rate of SPTB represents a different finding than most previous work in this field, said Dr. Elovitz, adding that much of the research on the vaginal microbiome during the reproductive years has focused on groupings of predominant bacteria, termed community state types (CSTs). “Classification of communities into CST, as performed in the nonpregnant woman, is not revealing for PTB,” Dr. Elovitz said.
Future research into cervicovaginal microbial communities and spontaneous preterm birth are likely to produce new methods to risk-stratify women and potential new therapeutics to reduce the rate of spontaneous preterm birth, she added.
The presentation won the conference’s March of Dimes award for best abstract in prematurity.
Dr. Elovitz reported having no relevant financial disclosures.
[email protected]
On Twitter @karioakes
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: Mobiluncus mulieris in the cervicovaginal space was associated with an odds ratio of 9.21 for spontaneous preterm birth.
Data source: Nested case-control study of 83 cases of spontaneous preterm birth matched with 336 term deliveries, drawn from 1,500 patients participating in the National Institute of Nursing Research–sponsored Motherhood and Microbiome study.
Disclosures: Dr. Elovitz reported having no relevant financial disclosures.
Adding rituximab to reduced intensity conditioning boosts PFS
ORLANDO – Rituximab conferred a significant progression-free survival benefit in reduced intensity conditioning regimens for patients with B-cell non-Hodgkin lymphoma who underwent allogeneic hematopoietic cell transplantation, based on data from the Center for International Blood & Marrow Transplant Research.
Further, higher cumulative rituximab doses appeared to confer a benefit in overall survival.
Rituximab is frequently a component of reduced intensity conditioning (RIC) regimens in allogeneic hematopoietic cell transplantation (HCT), but there has been a “paucity of comparative data” for rituximab-containing (R-RIC) versus non–R-RIC conditioning regimens for allogeneic transplant patients, Narendranath Epperla, MD, of the Medical College of Wisconsin, Milwaukee, said during the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
Using data from the Center for International Blood & Marrow Transplant Research, Dr. Epperla and his colleagues identified 1,022 patients who received rituximab and 379 patients who did not with diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and marginal zone lymphoma. The patients received their first RIC or non-myeloablative allogeneic HCT between 2008 and 2014. The donors were matched, and either related or 8x8 allele-matched unrelated; the graft source could be bone marrow or peripheral blood. Graft versus host disease (GVHD) suppression was calcineurin inhibitor based.
Patients who had received myeloablative conditioning, or who had received radioimmunotherapy or alemtuzumab were excluded, as were those who received alternative donor allografts.
Dr. Epperla and his colleagues factored in patient and disease characteristics, as well as differences in transplant regimen, in determining the adjusted cumulative incidence of relapse or progression, as well as the incidence of nonrelapse mortality.
In the multivariable analysis, overall survival did not differ between the R-RIC and the non–R-RIC cohorts (relative risk [RR] of all-cause mortality, R-RIC = 0.83, 95% CI 0.67-1.03, P = .09).
Based on the cumulative dose of rituximab that patients had received, though, “we noted that patients who got higher doses of rituximab had lower risk of nonrelapse mortality,” Dr. Epperla said. “Higher cumulative doses of rituximab seem to confer overall survival benefit.” This was true even though the higher rituximab doses had no significant effect on the risk of therapy failure, nonrelapse mortality, or the risk of progression/relapse.
When the cumulative rituximab dose was 2,000 to 3,375 mg/m2, the hazard ratio for all-cause mortality fell to 0.43 compared to a cumulative rituximab dose of less than 1,000 mg/m2 (95% confidence interval [CI] 0.21-0.90, P = .02).
Among the R-RIC group, there was a nonsignificant trend toward reduced risk of progression or relapse (relative risk of progression/relapse, R-RIC = 0.79, 95% CI 0.63-1.01, P = .055). However, the R-RIC group fared significantly better in terms of progression-free survival (RR of PFS, R-RIC = 0.76, 95% CI 0.62-0.92, P = .006).
After transplant, patients in the R-RIC group were no more likely than those in the non–R-RIC group to experience chronic GVHD (RR of GVHD, R-RIC = 1.15, 95% CI 0.96-1.39, P = .13). There was no difference in the adjusted curves of nonrelapse mortality between the groups (RR of nonrelapse mortality, R-RIC = 0.90, 95% CI 0.67-1.22, P = .51).
Also, there were no fatal cytopenias in the R-RIC arm, although the literature warrants some concern for increased risk of infection with rituximab, Dr. Epperla said.
At baseline, there were no significant differences in demographic characteristics between the nonrituximab and rituximab arms of the study population. More than 90% of patients were white, and 65% were male; the median age was 57 years (range, 18-74).
Patients had been diagnosed about 3 years before receiving HCT; about 60% of patients had a baseline Karnofsky performance score greater than 90, and the HCT comorbidity index was 2. About 86% of patients were chemosensitive, and patients in both study arms had received a median of three prior lines of therapy.
There were some differences in conditioning regimens between the two groups. “There were a significantly higher number of patients in the nonrituximab group who received fludarabine/busulfan, while there were a significantly high number in the rituximab group who received a fludarabine/cyclophosphamide-based conditioning regimen,” Dr. Epperla said. Follicular lymphomas were more common in the R-RIC arm, while diffuse large B-cell lymphomas were seen more in the non–R-RIC arm.
Given the survival benefit and similar rates of chronic GVHD seen in the retrospective analysis, a prospective, randomized head-to-head trial of R-RIC versus non–R-RIC is warranted, Dr. Epperla concluded.
During the postpresentation discussion, Dr. Epperla acknowledged the variability of the lymphomas in the study, but that there was no significant statistical effect of specific histologies on the findings in a subgroup analysis. Dr. Epperla added that the chemosensitivity status at transplant was checked to account for patient exposure to rituximab before RIC, and that there was no effect of prior rituximab exposure on the outcomes examined.
Dr. Epperla reported no conflicts of interest.
[email protected]
On Twitter @karioakes
ORLANDO – Rituximab conferred a significant progression-free survival benefit in reduced intensity conditioning regimens for patients with B-cell non-Hodgkin lymphoma who underwent allogeneic hematopoietic cell transplantation, based on data from the Center for International Blood & Marrow Transplant Research.
Further, higher cumulative rituximab doses appeared to confer a benefit in overall survival.
Rituximab is frequently a component of reduced intensity conditioning (RIC) regimens in allogeneic hematopoietic cell transplantation (HCT), but there has been a “paucity of comparative data” for rituximab-containing (R-RIC) versus non–R-RIC conditioning regimens for allogeneic transplant patients, Narendranath Epperla, MD, of the Medical College of Wisconsin, Milwaukee, said during the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
Using data from the Center for International Blood & Marrow Transplant Research, Dr. Epperla and his colleagues identified 1,022 patients who received rituximab and 379 patients who did not with diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and marginal zone lymphoma. The patients received their first RIC or non-myeloablative allogeneic HCT between 2008 and 2014. The donors were matched, and either related or 8x8 allele-matched unrelated; the graft source could be bone marrow or peripheral blood. Graft versus host disease (GVHD) suppression was calcineurin inhibitor based.
Patients who had received myeloablative conditioning, or who had received radioimmunotherapy or alemtuzumab were excluded, as were those who received alternative donor allografts.
Dr. Epperla and his colleagues factored in patient and disease characteristics, as well as differences in transplant regimen, in determining the adjusted cumulative incidence of relapse or progression, as well as the incidence of nonrelapse mortality.
In the multivariable analysis, overall survival did not differ between the R-RIC and the non–R-RIC cohorts (relative risk [RR] of all-cause mortality, R-RIC = 0.83, 95% CI 0.67-1.03, P = .09).
Based on the cumulative dose of rituximab that patients had received, though, “we noted that patients who got higher doses of rituximab had lower risk of nonrelapse mortality,” Dr. Epperla said. “Higher cumulative doses of rituximab seem to confer overall survival benefit.” This was true even though the higher rituximab doses had no significant effect on the risk of therapy failure, nonrelapse mortality, or the risk of progression/relapse.
When the cumulative rituximab dose was 2,000 to 3,375 mg/m2, the hazard ratio for all-cause mortality fell to 0.43 compared to a cumulative rituximab dose of less than 1,000 mg/m2 (95% confidence interval [CI] 0.21-0.90, P = .02).
Among the R-RIC group, there was a nonsignificant trend toward reduced risk of progression or relapse (relative risk of progression/relapse, R-RIC = 0.79, 95% CI 0.63-1.01, P = .055). However, the R-RIC group fared significantly better in terms of progression-free survival (RR of PFS, R-RIC = 0.76, 95% CI 0.62-0.92, P = .006).
After transplant, patients in the R-RIC group were no more likely than those in the non–R-RIC group to experience chronic GVHD (RR of GVHD, R-RIC = 1.15, 95% CI 0.96-1.39, P = .13). There was no difference in the adjusted curves of nonrelapse mortality between the groups (RR of nonrelapse mortality, R-RIC = 0.90, 95% CI 0.67-1.22, P = .51).
Also, there were no fatal cytopenias in the R-RIC arm, although the literature warrants some concern for increased risk of infection with rituximab, Dr. Epperla said.
At baseline, there were no significant differences in demographic characteristics between the nonrituximab and rituximab arms of the study population. More than 90% of patients were white, and 65% were male; the median age was 57 years (range, 18-74).
Patients had been diagnosed about 3 years before receiving HCT; about 60% of patients had a baseline Karnofsky performance score greater than 90, and the HCT comorbidity index was 2. About 86% of patients were chemosensitive, and patients in both study arms had received a median of three prior lines of therapy.
There were some differences in conditioning regimens between the two groups. “There were a significantly higher number of patients in the nonrituximab group who received fludarabine/busulfan, while there were a significantly high number in the rituximab group who received a fludarabine/cyclophosphamide-based conditioning regimen,” Dr. Epperla said. Follicular lymphomas were more common in the R-RIC arm, while diffuse large B-cell lymphomas were seen more in the non–R-RIC arm.
Given the survival benefit and similar rates of chronic GVHD seen in the retrospective analysis, a prospective, randomized head-to-head trial of R-RIC versus non–R-RIC is warranted, Dr. Epperla concluded.
During the postpresentation discussion, Dr. Epperla acknowledged the variability of the lymphomas in the study, but that there was no significant statistical effect of specific histologies on the findings in a subgroup analysis. Dr. Epperla added that the chemosensitivity status at transplant was checked to account for patient exposure to rituximab before RIC, and that there was no effect of prior rituximab exposure on the outcomes examined.
Dr. Epperla reported no conflicts of interest.
[email protected]
On Twitter @karioakes
ORLANDO – Rituximab conferred a significant progression-free survival benefit in reduced intensity conditioning regimens for patients with B-cell non-Hodgkin lymphoma who underwent allogeneic hematopoietic cell transplantation, based on data from the Center for International Blood & Marrow Transplant Research.
Further, higher cumulative rituximab doses appeared to confer a benefit in overall survival.
Rituximab is frequently a component of reduced intensity conditioning (RIC) regimens in allogeneic hematopoietic cell transplantation (HCT), but there has been a “paucity of comparative data” for rituximab-containing (R-RIC) versus non–R-RIC conditioning regimens for allogeneic transplant patients, Narendranath Epperla, MD, of the Medical College of Wisconsin, Milwaukee, said during the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
Using data from the Center for International Blood & Marrow Transplant Research, Dr. Epperla and his colleagues identified 1,022 patients who received rituximab and 379 patients who did not with diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and marginal zone lymphoma. The patients received their first RIC or non-myeloablative allogeneic HCT between 2008 and 2014. The donors were matched, and either related or 8x8 allele-matched unrelated; the graft source could be bone marrow or peripheral blood. Graft versus host disease (GVHD) suppression was calcineurin inhibitor based.
Patients who had received myeloablative conditioning, or who had received radioimmunotherapy or alemtuzumab were excluded, as were those who received alternative donor allografts.
Dr. Epperla and his colleagues factored in patient and disease characteristics, as well as differences in transplant regimen, in determining the adjusted cumulative incidence of relapse or progression, as well as the incidence of nonrelapse mortality.
In the multivariable analysis, overall survival did not differ between the R-RIC and the non–R-RIC cohorts (relative risk [RR] of all-cause mortality, R-RIC = 0.83, 95% CI 0.67-1.03, P = .09).
Based on the cumulative dose of rituximab that patients had received, though, “we noted that patients who got higher doses of rituximab had lower risk of nonrelapse mortality,” Dr. Epperla said. “Higher cumulative doses of rituximab seem to confer overall survival benefit.” This was true even though the higher rituximab doses had no significant effect on the risk of therapy failure, nonrelapse mortality, or the risk of progression/relapse.
When the cumulative rituximab dose was 2,000 to 3,375 mg/m2, the hazard ratio for all-cause mortality fell to 0.43 compared to a cumulative rituximab dose of less than 1,000 mg/m2 (95% confidence interval [CI] 0.21-0.90, P = .02).
Among the R-RIC group, there was a nonsignificant trend toward reduced risk of progression or relapse (relative risk of progression/relapse, R-RIC = 0.79, 95% CI 0.63-1.01, P = .055). However, the R-RIC group fared significantly better in terms of progression-free survival (RR of PFS, R-RIC = 0.76, 95% CI 0.62-0.92, P = .006).
After transplant, patients in the R-RIC group were no more likely than those in the non–R-RIC group to experience chronic GVHD (RR of GVHD, R-RIC = 1.15, 95% CI 0.96-1.39, P = .13). There was no difference in the adjusted curves of nonrelapse mortality between the groups (RR of nonrelapse mortality, R-RIC = 0.90, 95% CI 0.67-1.22, P = .51).
Also, there were no fatal cytopenias in the R-RIC arm, although the literature warrants some concern for increased risk of infection with rituximab, Dr. Epperla said.
At baseline, there were no significant differences in demographic characteristics between the nonrituximab and rituximab arms of the study population. More than 90% of patients were white, and 65% were male; the median age was 57 years (range, 18-74).
Patients had been diagnosed about 3 years before receiving HCT; about 60% of patients had a baseline Karnofsky performance score greater than 90, and the HCT comorbidity index was 2. About 86% of patients were chemosensitive, and patients in both study arms had received a median of three prior lines of therapy.
There were some differences in conditioning regimens between the two groups. “There were a significantly higher number of patients in the nonrituximab group who received fludarabine/busulfan, while there were a significantly high number in the rituximab group who received a fludarabine/cyclophosphamide-based conditioning regimen,” Dr. Epperla said. Follicular lymphomas were more common in the R-RIC arm, while diffuse large B-cell lymphomas were seen more in the non–R-RIC arm.
Given the survival benefit and similar rates of chronic GVHD seen in the retrospective analysis, a prospective, randomized head-to-head trial of R-RIC versus non–R-RIC is warranted, Dr. Epperla concluded.
During the postpresentation discussion, Dr. Epperla acknowledged the variability of the lymphomas in the study, but that there was no significant statistical effect of specific histologies on the findings in a subgroup analysis. Dr. Epperla added that the chemosensitivity status at transplant was checked to account for patient exposure to rituximab before RIC, and that there was no effect of prior rituximab exposure on the outcomes examined.
Dr. Epperla reported no conflicts of interest.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: Patients with rituximab-containing RIC regimens had better progression-free survival (PFS; relative risk of PFS, non–R-RIC=1, R-RIC=076, 95% CI 0.62-092, P = .006).
Data source: Retrospective review of 1,022 allogeneic HCT B-cell non-Hodgkin lymphoma patients who received rituximab and 379 who did not.
Disclosures: The data were obtained from the Center for International Blood & Marrow Transplant Research. Dr. Epperla reported no disclosures.
Antihypertensive protocol cuts eclampsia rates
LAS VEGAS – A multisite trial that implemented a protocol for use of intravenous hydralazine or labetalol together with magnesium sulfate for critically high blood pressures in pregnancy saw maternal eclampsia rates fall by 46% and severe maternal morbidity fall by 17%, as the protocol compliance rate rose to almost 90% of deliveries by study’s end.
Hypertensive disorders of pregnancy (HDP) are seen in up to 10% of all births and are collectively a major cause of severe maternal morbidity, according to Laurence E. Shields, MD, a perinatologist at Marian Regional Medical Center, Santa Maria, Calif. Eclampsia, seen as a complication of HDP, can have a set of disastrous maternal neurologic, cognitive, and cardiac sequelae, he added.
Recently, both state and national guidelines have called for more attention to and aggressive treatment of critically elevated blood pressure in pregnant women, Dr. Shields said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
As part of a global pregnancy complications assessment and treatment algorithm termed the Maternal Early Warning Tool (MEWT), Dignity Health, which owns Dr. Shields’ home institution, put in place a protocol to manage hypertension in pregnancy.
For pregnant women with sustained blood pressures greater than 160 mm Hg systolic and/or 110 mm Hg diastolic, the protocol calls for intravenous hydralazine or labetalol together with magnesium sulfate. The protocol also calls for “appropriate labs” to be ordered, and permits oral medication if the patient does not have intravenous access.
These steps were taken regardless of the type of hypertension the patient had, Dr. Shields said. Patients with HDP who were treated with antihypertensives were also scheduled for postpartum follow-up within 7 days of delivery.
Originally, the MEWT trial had included a total of 29 perinatal centers, 6 of which instituted the blood pressure management protocol (“trial hospitals”). Dr. Shields said that for the present study, “we wanted to determine if we could replicate the reduction in the rate of eclampsia that we noted in the 6 MEWT trial sites after initiating similar hypertension treatment recommendations in the 23 non-MEWT sites.” He and his colleagues also wanted to determine whether using the hypertension protocol would reduce severe maternal morbidity.
Compliance with the three metrics of antihypertensive administration and magnesium sulfate administration for critical blood pressure elevations and early follow-up was assessed with an “all or none” judgment.
The study was broken into three broad phases. First, recommendations were distributed to all hospitals without monitoring compliance. Eight months later, the researchers conducted a retrospective assessment of institutional compliance with the protocol. They also monitored eclampsia rates and the incidence of severe maternal mortality, using Centers for Disease Control and Prevention (CDC) criteria. Finally, after 6 months of retrospective monitoring, a prospective assessment of compliance, rates of eclampsia, and incidence of severe maternal mortality was conducted, and the results were compared with the preintervention figures.
For data analysis, protocol compliance was assessed as a primary outcome measure, but also broken down so investigators could track rates of appropriate blood pressure medication administration and appropriate treatment with magnesium sulfate. Eclampsia and severe maternal morbidity rates were the other two outcome measures.
Delivery volume at the hospitals ranged from 150 to 5,000 per year. Hispanic patients made up 42% of the study population; white and Asian patients each made up 23%; 7% were African American, and the remainder identified as “other.”
Over the study period, compliance with all three metrics rose from a baseline of 50.5%, to a midpoint rate of 73.4%, to a final rate of 88.5%. The number of deliveries was approximately the same in all time periods.
There was an overall 10.5% increase in magnesium sulfate use, with the proportion of patients being appropriately treated with magnesium sulfate rising from 85.4% at baseline to 96.2% by the end of the trial (P less than .01).
Significantly more patients were appropriately treated with blood pressure medications by the trial’s end as well; just 56.9% of patients received appropriate hypertensive medication at baseline, but that grew to 90.1% by study’s end (P less than .01). This represented a 33.2% increase in the appropriate use of antihypertensives, Dr. Shields said.
Labetalol use increased from 44% of patients treated at baseline to 64% by the end of the study (P less than .01). Hydralazine use decreased from 39% to 26% (P less than .01), and fewer oral agents were used by the end of the study (17% compared with 10%; P less than .02).
This shift was accompanied by a decrease in eclampsia rates, with overall rates per 1,000 births decreasing from 1.15 to 0.62 by the end of the study (–46%; P = .02). Severe maternal morbidity also fell from 2.4 per 100 births to 2.0 per 1,000 patients (–16.8%; P less than .01).
About 40% of the reduction in eclampsia rates could be attributed to the improved magnesium sulfate administration rates, Dr. Shields said. “This finding would suggest that the combination of blood pressure treatment and magnesium sulfate produced a synergistic effect on the reduction of eclampsia.”
“Compliance with state and national recommendations for treatment of critically elevated blood pressures is poor without monitoring,” Dr. Shields said. But with education and monitoring, physician and nurse behavior can be modified in a relatively short time period, he said.
Dr. Shields did not report financial disclosure information.
[email protected]
On Twitter @karioakes
LAS VEGAS – A multisite trial that implemented a protocol for use of intravenous hydralazine or labetalol together with magnesium sulfate for critically high blood pressures in pregnancy saw maternal eclampsia rates fall by 46% and severe maternal morbidity fall by 17%, as the protocol compliance rate rose to almost 90% of deliveries by study’s end.
Hypertensive disorders of pregnancy (HDP) are seen in up to 10% of all births and are collectively a major cause of severe maternal morbidity, according to Laurence E. Shields, MD, a perinatologist at Marian Regional Medical Center, Santa Maria, Calif. Eclampsia, seen as a complication of HDP, can have a set of disastrous maternal neurologic, cognitive, and cardiac sequelae, he added.
Recently, both state and national guidelines have called for more attention to and aggressive treatment of critically elevated blood pressure in pregnant women, Dr. Shields said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
As part of a global pregnancy complications assessment and treatment algorithm termed the Maternal Early Warning Tool (MEWT), Dignity Health, which owns Dr. Shields’ home institution, put in place a protocol to manage hypertension in pregnancy.
For pregnant women with sustained blood pressures greater than 160 mm Hg systolic and/or 110 mm Hg diastolic, the protocol calls for intravenous hydralazine or labetalol together with magnesium sulfate. The protocol also calls for “appropriate labs” to be ordered, and permits oral medication if the patient does not have intravenous access.
These steps were taken regardless of the type of hypertension the patient had, Dr. Shields said. Patients with HDP who were treated with antihypertensives were also scheduled for postpartum follow-up within 7 days of delivery.
Originally, the MEWT trial had included a total of 29 perinatal centers, 6 of which instituted the blood pressure management protocol (“trial hospitals”). Dr. Shields said that for the present study, “we wanted to determine if we could replicate the reduction in the rate of eclampsia that we noted in the 6 MEWT trial sites after initiating similar hypertension treatment recommendations in the 23 non-MEWT sites.” He and his colleagues also wanted to determine whether using the hypertension protocol would reduce severe maternal morbidity.
Compliance with the three metrics of antihypertensive administration and magnesium sulfate administration for critical blood pressure elevations and early follow-up was assessed with an “all or none” judgment.
The study was broken into three broad phases. First, recommendations were distributed to all hospitals without monitoring compliance. Eight months later, the researchers conducted a retrospective assessment of institutional compliance with the protocol. They also monitored eclampsia rates and the incidence of severe maternal mortality, using Centers for Disease Control and Prevention (CDC) criteria. Finally, after 6 months of retrospective monitoring, a prospective assessment of compliance, rates of eclampsia, and incidence of severe maternal mortality was conducted, and the results were compared with the preintervention figures.
For data analysis, protocol compliance was assessed as a primary outcome measure, but also broken down so investigators could track rates of appropriate blood pressure medication administration and appropriate treatment with magnesium sulfate. Eclampsia and severe maternal morbidity rates were the other two outcome measures.
Delivery volume at the hospitals ranged from 150 to 5,000 per year. Hispanic patients made up 42% of the study population; white and Asian patients each made up 23%; 7% were African American, and the remainder identified as “other.”
Over the study period, compliance with all three metrics rose from a baseline of 50.5%, to a midpoint rate of 73.4%, to a final rate of 88.5%. The number of deliveries was approximately the same in all time periods.
There was an overall 10.5% increase in magnesium sulfate use, with the proportion of patients being appropriately treated with magnesium sulfate rising from 85.4% at baseline to 96.2% by the end of the trial (P less than .01).
Significantly more patients were appropriately treated with blood pressure medications by the trial’s end as well; just 56.9% of patients received appropriate hypertensive medication at baseline, but that grew to 90.1% by study’s end (P less than .01). This represented a 33.2% increase in the appropriate use of antihypertensives, Dr. Shields said.
Labetalol use increased from 44% of patients treated at baseline to 64% by the end of the study (P less than .01). Hydralazine use decreased from 39% to 26% (P less than .01), and fewer oral agents were used by the end of the study (17% compared with 10%; P less than .02).
This shift was accompanied by a decrease in eclampsia rates, with overall rates per 1,000 births decreasing from 1.15 to 0.62 by the end of the study (–46%; P = .02). Severe maternal morbidity also fell from 2.4 per 100 births to 2.0 per 1,000 patients (–16.8%; P less than .01).
About 40% of the reduction in eclampsia rates could be attributed to the improved magnesium sulfate administration rates, Dr. Shields said. “This finding would suggest that the combination of blood pressure treatment and magnesium sulfate produced a synergistic effect on the reduction of eclampsia.”
“Compliance with state and national recommendations for treatment of critically elevated blood pressures is poor without monitoring,” Dr. Shields said. But with education and monitoring, physician and nurse behavior can be modified in a relatively short time period, he said.
Dr. Shields did not report financial disclosure information.
[email protected]
On Twitter @karioakes
LAS VEGAS – A multisite trial that implemented a protocol for use of intravenous hydralazine or labetalol together with magnesium sulfate for critically high blood pressures in pregnancy saw maternal eclampsia rates fall by 46% and severe maternal morbidity fall by 17%, as the protocol compliance rate rose to almost 90% of deliveries by study’s end.
Hypertensive disorders of pregnancy (HDP) are seen in up to 10% of all births and are collectively a major cause of severe maternal morbidity, according to Laurence E. Shields, MD, a perinatologist at Marian Regional Medical Center, Santa Maria, Calif. Eclampsia, seen as a complication of HDP, can have a set of disastrous maternal neurologic, cognitive, and cardiac sequelae, he added.
Recently, both state and national guidelines have called for more attention to and aggressive treatment of critically elevated blood pressure in pregnant women, Dr. Shields said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
As part of a global pregnancy complications assessment and treatment algorithm termed the Maternal Early Warning Tool (MEWT), Dignity Health, which owns Dr. Shields’ home institution, put in place a protocol to manage hypertension in pregnancy.
For pregnant women with sustained blood pressures greater than 160 mm Hg systolic and/or 110 mm Hg diastolic, the protocol calls for intravenous hydralazine or labetalol together with magnesium sulfate. The protocol also calls for “appropriate labs” to be ordered, and permits oral medication if the patient does not have intravenous access.
These steps were taken regardless of the type of hypertension the patient had, Dr. Shields said. Patients with HDP who were treated with antihypertensives were also scheduled for postpartum follow-up within 7 days of delivery.
Originally, the MEWT trial had included a total of 29 perinatal centers, 6 of which instituted the blood pressure management protocol (“trial hospitals”). Dr. Shields said that for the present study, “we wanted to determine if we could replicate the reduction in the rate of eclampsia that we noted in the 6 MEWT trial sites after initiating similar hypertension treatment recommendations in the 23 non-MEWT sites.” He and his colleagues also wanted to determine whether using the hypertension protocol would reduce severe maternal morbidity.
Compliance with the three metrics of antihypertensive administration and magnesium sulfate administration for critical blood pressure elevations and early follow-up was assessed with an “all or none” judgment.
The study was broken into three broad phases. First, recommendations were distributed to all hospitals without monitoring compliance. Eight months later, the researchers conducted a retrospective assessment of institutional compliance with the protocol. They also monitored eclampsia rates and the incidence of severe maternal mortality, using Centers for Disease Control and Prevention (CDC) criteria. Finally, after 6 months of retrospective monitoring, a prospective assessment of compliance, rates of eclampsia, and incidence of severe maternal mortality was conducted, and the results were compared with the preintervention figures.
For data analysis, protocol compliance was assessed as a primary outcome measure, but also broken down so investigators could track rates of appropriate blood pressure medication administration and appropriate treatment with magnesium sulfate. Eclampsia and severe maternal morbidity rates were the other two outcome measures.
Delivery volume at the hospitals ranged from 150 to 5,000 per year. Hispanic patients made up 42% of the study population; white and Asian patients each made up 23%; 7% were African American, and the remainder identified as “other.”
Over the study period, compliance with all three metrics rose from a baseline of 50.5%, to a midpoint rate of 73.4%, to a final rate of 88.5%. The number of deliveries was approximately the same in all time periods.
There was an overall 10.5% increase in magnesium sulfate use, with the proportion of patients being appropriately treated with magnesium sulfate rising from 85.4% at baseline to 96.2% by the end of the trial (P less than .01).
Significantly more patients were appropriately treated with blood pressure medications by the trial’s end as well; just 56.9% of patients received appropriate hypertensive medication at baseline, but that grew to 90.1% by study’s end (P less than .01). This represented a 33.2% increase in the appropriate use of antihypertensives, Dr. Shields said.
Labetalol use increased from 44% of patients treated at baseline to 64% by the end of the study (P less than .01). Hydralazine use decreased from 39% to 26% (P less than .01), and fewer oral agents were used by the end of the study (17% compared with 10%; P less than .02).
This shift was accompanied by a decrease in eclampsia rates, with overall rates per 1,000 births decreasing from 1.15 to 0.62 by the end of the study (–46%; P = .02). Severe maternal morbidity also fell from 2.4 per 100 births to 2.0 per 1,000 patients (–16.8%; P less than .01).
About 40% of the reduction in eclampsia rates could be attributed to the improved magnesium sulfate administration rates, Dr. Shields said. “This finding would suggest that the combination of blood pressure treatment and magnesium sulfate produced a synergistic effect on the reduction of eclampsia.”
“Compliance with state and national recommendations for treatment of critically elevated blood pressures is poor without monitoring,” Dr. Shields said. But with education and monitoring, physician and nurse behavior can be modified in a relatively short time period, he said.
Dr. Shields did not report financial disclosure information.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: Maternal eclampsia rates fell by 46% after the protocol was instituted (P = .02).
Data source: Prospective study of 29 perinatal centers in a single health care system.
Disclosures: Dr. Shields did not report financial disclosure information.
Older AML patients benefit from frailty assessment and interventions
ORLANDO – Performing a comprehensive geriatric assessment of patients with acute myeloid leukemia (AML) does more than provide fine-tuned risk stratification; spotting areas of vulnerability and frailty can also identify targets for prehabilitation, support, and remediation as older patients face transplant.
A program at the University of Chicago termed the Transplant Optimization Program, or TOP, uses the geriatric assessment as the foundation of an interdisciplinary, customized intervention for older adults facing hematopoietic cell transplant (HCT). The team includes the transplant physician and a geriatric oncologist; however, social work, dietetics, psychology, and physical therapy professionals also are brought on board.
“High comorbidities and functional limitations influence overall survival,” Dr. Artz said. “Non-relapse mortality remains a major barrier; of course, the attendant morbidity before it is perhaps a bigger concern, and our patients’ concern.”
Dr. Artz said that he and his colleagues at the University of Chicago, where he is a professor of medicine, had adapted the geriatric assessment developed by the Cancer and Aging Group, and now administer it to all prospective transplant patients aged 50 years and older. Dr. Artz said that, at his center, they have found that 25% of patients aged 50 and older were frail according to the Fried Frailty Index. “That’s what we expect for people in the community who are aged 80 and older, so we’re painting a picture of accelerated aging for patients before they undergo allograft,” he said.
Results of the assessment are then reviewed by a multidisciplinary team, and an individualized prehabilitation and support program is developed based on those results. “Using chronologic and physiologic age in transplant can help us better risk stratify, and think about strategies to mitigate some of those risks,” Dr. Artz said.
The staging tool currently used at the University of Chicago examines seven domains and uses objective tools to deliver information in each domain. Comorbidities are assessed by the Hematopoietic Cell Transplant–Specific Comorbidity Index (HCT-CI) and the Older Americans Resources and Services (OARS) scale. “We are trying to use standardized tools such as the geriatric assessment, because our ‘eyeball test’ is quite poor,” he said.
Physical function is assessed by measuring four-meter walk speed and grip strength; by asking about falls and capacity for instrumental activities of daily living; and by administering the Karnofsky Performance Scale–MD. Patients are given the Mental Health Inventory–17 to assess psychological health.
Neurocognitive testing and the Blessed Orientation-Memory-Concentration test are used to assess cognitive function. The Medical Outcomes Study Social Activity and Social Limitations scales give an idea about social support.
Biomarkers that are tracked include C-reactive protein and ferritin, among others, Dr. Artz said. Nutritional status is assessed by measuring serum albumin as well as any weight loss.
Once the full geriatric assessment data about a patient are gathered, a plan is formulated for impairments in any given domain. For example, if significant comorbid conditions exist, the TOP team seeks subspecialty consultation for management advice in the context of transplant. “This is a consultation – not a clearance!” Dr. Artz said.
Physical and functional impairments are addressed with prehabilitation if time permits, and the home assessment is aligned with patient expectations. Sometimes, the inactivity associated with peritransplant period can worsen conditions such as osteoarthritis, so a patient who’s been functional may find themselves very stiff when going home. Caregivers can encourage early activity to help minimize this effect, Dr. Artz said.
For patients at nutritional risk, it’s vital to have a good nutrition plan for transplant and to make sure medications or social factors aren’t standing in the way of adequate nutrition, Dr. Artz said. “Don’t forget to ask about dentures,” he said, since mucositis can make dentures unbearable in the immediate posttransplant period.
It’s important to be careful when unpacking findings of cognitive impairment, Dr. Artz said, since untreated depression and anxiety can manifest as forgetfulness and perseveration. Eliminating unnecessary medication, having a good delirium protocol in place, and keeping a family member in the room with the patient can help minimize a cognitive downturn during transplant.
As patients age, it can be more common for them to have limited social support. The TOP team calls a family meeting to assess resources and appoint a “team captain” among the patient’s social circle. “We work to enlarge that circle,” by pulling in as many family members and friends as possible, Dr. Artz said. In a discussion after the talk, he said that he feels that having a family member in the hospital with the older transplant patient is important for many reasons. Not only is the patient less likely to fall, he or she may also eat better and feel better. In addition, he said he has a sense that when the caregiver has seen the patient at his or her nadir, taking that patient home isn’t as scary, since it’s easier to see that the trajectory is headed upward by the time of discharge.
Dr. Artz said that other facilities are now beginning to send patients for TOP evaluations; “the aging evaluation informs physiologic age, candidacy for transplant, and may permit optimizing outcomes,” he said. “We’re trying to ... optimize patients both before and after transplant. It’s one thing to say you’re vulnerable, but how do you take that vulnerable patient and improve their outcomes? That’s the question.” Though the proportion of older individuals receiving allogeneic transplants is growing rapidly, research is not keeping up, Dr. Artz said, calling for more prospective studies in older adults.
Dr. Artz reported that he has received research funding from Miltenyi Biotech.
[email protected]
On Twitter @karioakes
ORLANDO – Performing a comprehensive geriatric assessment of patients with acute myeloid leukemia (AML) does more than provide fine-tuned risk stratification; spotting areas of vulnerability and frailty can also identify targets for prehabilitation, support, and remediation as older patients face transplant.
A program at the University of Chicago termed the Transplant Optimization Program, or TOP, uses the geriatric assessment as the foundation of an interdisciplinary, customized intervention for older adults facing hematopoietic cell transplant (HCT). The team includes the transplant physician and a geriatric oncologist; however, social work, dietetics, psychology, and physical therapy professionals also are brought on board.
“High comorbidities and functional limitations influence overall survival,” Dr. Artz said. “Non-relapse mortality remains a major barrier; of course, the attendant morbidity before it is perhaps a bigger concern, and our patients’ concern.”
Dr. Artz said that he and his colleagues at the University of Chicago, where he is a professor of medicine, had adapted the geriatric assessment developed by the Cancer and Aging Group, and now administer it to all prospective transplant patients aged 50 years and older. Dr. Artz said that, at his center, they have found that 25% of patients aged 50 and older were frail according to the Fried Frailty Index. “That’s what we expect for people in the community who are aged 80 and older, so we’re painting a picture of accelerated aging for patients before they undergo allograft,” he said.
Results of the assessment are then reviewed by a multidisciplinary team, and an individualized prehabilitation and support program is developed based on those results. “Using chronologic and physiologic age in transplant can help us better risk stratify, and think about strategies to mitigate some of those risks,” Dr. Artz said.
The staging tool currently used at the University of Chicago examines seven domains and uses objective tools to deliver information in each domain. Comorbidities are assessed by the Hematopoietic Cell Transplant–Specific Comorbidity Index (HCT-CI) and the Older Americans Resources and Services (OARS) scale. “We are trying to use standardized tools such as the geriatric assessment, because our ‘eyeball test’ is quite poor,” he said.
Physical function is assessed by measuring four-meter walk speed and grip strength; by asking about falls and capacity for instrumental activities of daily living; and by administering the Karnofsky Performance Scale–MD. Patients are given the Mental Health Inventory–17 to assess psychological health.
Neurocognitive testing and the Blessed Orientation-Memory-Concentration test are used to assess cognitive function. The Medical Outcomes Study Social Activity and Social Limitations scales give an idea about social support.
Biomarkers that are tracked include C-reactive protein and ferritin, among others, Dr. Artz said. Nutritional status is assessed by measuring serum albumin as well as any weight loss.
Once the full geriatric assessment data about a patient are gathered, a plan is formulated for impairments in any given domain. For example, if significant comorbid conditions exist, the TOP team seeks subspecialty consultation for management advice in the context of transplant. “This is a consultation – not a clearance!” Dr. Artz said.
Physical and functional impairments are addressed with prehabilitation if time permits, and the home assessment is aligned with patient expectations. Sometimes, the inactivity associated with peritransplant period can worsen conditions such as osteoarthritis, so a patient who’s been functional may find themselves very stiff when going home. Caregivers can encourage early activity to help minimize this effect, Dr. Artz said.
For patients at nutritional risk, it’s vital to have a good nutrition plan for transplant and to make sure medications or social factors aren’t standing in the way of adequate nutrition, Dr. Artz said. “Don’t forget to ask about dentures,” he said, since mucositis can make dentures unbearable in the immediate posttransplant period.
It’s important to be careful when unpacking findings of cognitive impairment, Dr. Artz said, since untreated depression and anxiety can manifest as forgetfulness and perseveration. Eliminating unnecessary medication, having a good delirium protocol in place, and keeping a family member in the room with the patient can help minimize a cognitive downturn during transplant.
As patients age, it can be more common for them to have limited social support. The TOP team calls a family meeting to assess resources and appoint a “team captain” among the patient’s social circle. “We work to enlarge that circle,” by pulling in as many family members and friends as possible, Dr. Artz said. In a discussion after the talk, he said that he feels that having a family member in the hospital with the older transplant patient is important for many reasons. Not only is the patient less likely to fall, he or she may also eat better and feel better. In addition, he said he has a sense that when the caregiver has seen the patient at his or her nadir, taking that patient home isn’t as scary, since it’s easier to see that the trajectory is headed upward by the time of discharge.
Dr. Artz said that other facilities are now beginning to send patients for TOP evaluations; “the aging evaluation informs physiologic age, candidacy for transplant, and may permit optimizing outcomes,” he said. “We’re trying to ... optimize patients both before and after transplant. It’s one thing to say you’re vulnerable, but how do you take that vulnerable patient and improve their outcomes? That’s the question.” Though the proportion of older individuals receiving allogeneic transplants is growing rapidly, research is not keeping up, Dr. Artz said, calling for more prospective studies in older adults.
Dr. Artz reported that he has received research funding from Miltenyi Biotech.
[email protected]
On Twitter @karioakes
ORLANDO – Performing a comprehensive geriatric assessment of patients with acute myeloid leukemia (AML) does more than provide fine-tuned risk stratification; spotting areas of vulnerability and frailty can also identify targets for prehabilitation, support, and remediation as older patients face transplant.
A program at the University of Chicago termed the Transplant Optimization Program, or TOP, uses the geriatric assessment as the foundation of an interdisciplinary, customized intervention for older adults facing hematopoietic cell transplant (HCT). The team includes the transplant physician and a geriatric oncologist; however, social work, dietetics, psychology, and physical therapy professionals also are brought on board.
“High comorbidities and functional limitations influence overall survival,” Dr. Artz said. “Non-relapse mortality remains a major barrier; of course, the attendant morbidity before it is perhaps a bigger concern, and our patients’ concern.”
Dr. Artz said that he and his colleagues at the University of Chicago, where he is a professor of medicine, had adapted the geriatric assessment developed by the Cancer and Aging Group, and now administer it to all prospective transplant patients aged 50 years and older. Dr. Artz said that, at his center, they have found that 25% of patients aged 50 and older were frail according to the Fried Frailty Index. “That’s what we expect for people in the community who are aged 80 and older, so we’re painting a picture of accelerated aging for patients before they undergo allograft,” he said.
Results of the assessment are then reviewed by a multidisciplinary team, and an individualized prehabilitation and support program is developed based on those results. “Using chronologic and physiologic age in transplant can help us better risk stratify, and think about strategies to mitigate some of those risks,” Dr. Artz said.
The staging tool currently used at the University of Chicago examines seven domains and uses objective tools to deliver information in each domain. Comorbidities are assessed by the Hematopoietic Cell Transplant–Specific Comorbidity Index (HCT-CI) and the Older Americans Resources and Services (OARS) scale. “We are trying to use standardized tools such as the geriatric assessment, because our ‘eyeball test’ is quite poor,” he said.
Physical function is assessed by measuring four-meter walk speed and grip strength; by asking about falls and capacity for instrumental activities of daily living; and by administering the Karnofsky Performance Scale–MD. Patients are given the Mental Health Inventory–17 to assess psychological health.
Neurocognitive testing and the Blessed Orientation-Memory-Concentration test are used to assess cognitive function. The Medical Outcomes Study Social Activity and Social Limitations scales give an idea about social support.
Biomarkers that are tracked include C-reactive protein and ferritin, among others, Dr. Artz said. Nutritional status is assessed by measuring serum albumin as well as any weight loss.
Once the full geriatric assessment data about a patient are gathered, a plan is formulated for impairments in any given domain. For example, if significant comorbid conditions exist, the TOP team seeks subspecialty consultation for management advice in the context of transplant. “This is a consultation – not a clearance!” Dr. Artz said.
Physical and functional impairments are addressed with prehabilitation if time permits, and the home assessment is aligned with patient expectations. Sometimes, the inactivity associated with peritransplant period can worsen conditions such as osteoarthritis, so a patient who’s been functional may find themselves very stiff when going home. Caregivers can encourage early activity to help minimize this effect, Dr. Artz said.
For patients at nutritional risk, it’s vital to have a good nutrition plan for transplant and to make sure medications or social factors aren’t standing in the way of adequate nutrition, Dr. Artz said. “Don’t forget to ask about dentures,” he said, since mucositis can make dentures unbearable in the immediate posttransplant period.
It’s important to be careful when unpacking findings of cognitive impairment, Dr. Artz said, since untreated depression and anxiety can manifest as forgetfulness and perseveration. Eliminating unnecessary medication, having a good delirium protocol in place, and keeping a family member in the room with the patient can help minimize a cognitive downturn during transplant.
As patients age, it can be more common for them to have limited social support. The TOP team calls a family meeting to assess resources and appoint a “team captain” among the patient’s social circle. “We work to enlarge that circle,” by pulling in as many family members and friends as possible, Dr. Artz said. In a discussion after the talk, he said that he feels that having a family member in the hospital with the older transplant patient is important for many reasons. Not only is the patient less likely to fall, he or she may also eat better and feel better. In addition, he said he has a sense that when the caregiver has seen the patient at his or her nadir, taking that patient home isn’t as scary, since it’s easier to see that the trajectory is headed upward by the time of discharge.
Dr. Artz said that other facilities are now beginning to send patients for TOP evaluations; “the aging evaluation informs physiologic age, candidacy for transplant, and may permit optimizing outcomes,” he said. “We’re trying to ... optimize patients both before and after transplant. It’s one thing to say you’re vulnerable, but how do you take that vulnerable patient and improve their outcomes? That’s the question.” Though the proportion of older individuals receiving allogeneic transplants is growing rapidly, research is not keeping up, Dr. Artz said, calling for more prospective studies in older adults.
Dr. Artz reported that he has received research funding from Miltenyi Biotech.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM THE 2017 BMT TANDEM MEETINGS
Fewer post-transplant CMV infections with novel antiviral prophylaxis
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
[email protected]
On Twitter @karioakes
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
[email protected]
On Twitter @karioakes
ORLANDO – A first-in-class antiviral drug was safe and effective when used to prevent clinically significant cytomegalovirus infections in adults undergoing hematopoietic cell transplantation.
At 24 weeks post-transplant, 38% (122/325) of those receiving the novel antiviral letermovir were considered treatment failures, compared with 61% (103/170) of those receiving placebo (P less than .0001). All-cause mortality was 10% (n=32/325) for patients receiving letermovir and 16%, (n=27/170) for the placebo group (log rank two-sided P = 0.0317).
The study findings show that “we [can] prevent patients from getting CMV infections from the beginning of the transplant and that [result can] confer a mortality benefit,” lead author Francisco Marty, MD, said in an interview.
Dr. Marty said that letermovir has received fast-track status both from the Food and Drug Administration and from the European Medicines Agency.
HCT recipients who are CMV-positive but who do not have clinically significant disease are not preemptively treated in current practice. “Previously, there wasn’t a primary prevention strategy in bone marrow transplantation. When myelosuppressive drugs were tried such as ganciclovir, any benefit was offset by increased myelosuppression, with resulting increases in bacterial and fungal infections,” said Dr. Marty, professor of medicine at Harvard Medical School, Boston.
Letermovir was generally well-tolerated in the clinical trial; myelotoxicity and nephrotoxicity levels were comparable in patients receiving letermovir and placebo. Letermovir targets the terminase complex, which is a viral replication process specific to CMV and not otherwise present in humans. That fact may explain, in part, letermovir’s limited toxicity, Dr. Marty said. The primary outcome measure of the phase III randomized, double-blind, placebo-controlled trial was the stratum-adjusted proportion of patients who had clinically significant CMV at post-transplant week 24, examining only the patients in the trials who had no detectable CMV DNA at the time of randomization. If patients did not complete the study, or had missing data at week 24, they were considered to have failed the trial.
Overall, 31% of patients were considered at high risk for CMV disease. Half of the patients received myeloablative conditioning, and about a third (35%) received antithymocyte globulin. Donor sources, whose characteristics were balanced between study arms, included 14% mismatched unrelated donors, 13% haploidentical donors, and 4% cord blood.
The multinational study’s 24-week results were presented at the combined annual meetings of the Center for International Blood & Marrow Transplant Research and the American Society of Blood and Marrow Transplantation.
“This was an international study, conducted at multiple sites in multiple countries. We used two-to-one randomization, and stratified participants by their risk of CMV disease and by study sites. We wanted to make sure the groups were balanced by disease risk and by study sites, to account for regional variations in bone marrow transplant procedures and CMV treatment patterns,” said Dr. Marty.
For the study, clinically significant CMV infection was defined as either CMV disease, such as pneumonia, colitis, or hepatitis, or CMV viremia that would trigger preemptive treatment.
Letermovir, which can be administered orally or intravenously, was dosed at 480 mg per day. Because of the risk for a drug-drug interaction, patients on cyclosporine received 240 mg of letermovir per day. Having intravenous dosing as an option helped patients who were not tolerating oral intake to stay on the study drug during the post-transplant period, he said.
The study drug was begun a median of 9 days post-transplant. Some patients received letermovir or placebo as early as the day of transplant; all patients began the study drug by 28 days post-transplant. The study drug was continued through week 14, or until at least 100 days post-transplant. Overall, 37% of patients had engrafted at the time they began the study drug.
Patients had weekly serum CMV assays performed until week 14, with biweekly sampling done through week 24. If patients developed clinically significant CMV, or if their serum samples yielded CMV DNA warranting preemptive treatment, they discontinued the study drug and began treatment for CMV.
The safety analysis, which was carried through week 48, tracked adverse events from the first dose of study drug until 14 days after discontinuation. Adverse events that were more common with letermovir than placebo included vomiting (19% versus 14%), edema (15% versus 9%), atrial arrhythmias (10% versus 5%), and having alanine aspartate levels more than five times the upper limit of normal (4% versus 2%). Graft versus host disease occurred in 39% of patients in each group; diarrhea and nausea occurred in approximately one fourth of patients in each group.
In response to a question after the presentation, Dr. Marty said, “The higher the risk of CMV disease, the higher the benefit in terms of survival.” Answering another question, about who should receive letermovir. Dr. Marty replied, “Like acyclovir, we should give it during times of risk. And CMV risk is different for different populations. It’s a matter of managing risks and benefits.”
Though letermovir was safe and well-tolerated in this trial, it’s different from acyclovir in that “it’s not a one dollar a day drug,” Dr. Marty acknowledged.
Merck, which plans to market letermovir, was the sponsor of the study and plans to submit applications for approval in both the United States and in the European Union in 2017. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
This article was updated 2/27/17.
[email protected]
On Twitter @karioakes
AT THE 2017 BMT TANDEM MEETINGS
Key clinical point:
Major finding: Cytomegalovirus (CMV) infection or viremia occurred in 38% of patients receiving post-HCT letermovir, compared with 61% of controls.
Data source: Randomized, double-blind, placebo-controlled study of 495 patients seropositive for CMV with no detectable CMV DNA at the time of HCT.
Disclosures: Merck, which plans to market letermovir, was the sponsor of the study. Dr. Marty reported receiving research grants from Merck as well as Astellas, Chimerix, and Shire. Additionally, he has received honoraria from Alexion, Chimerix, LFB, Merck, Roche Molecular Diagnostics, and Shire.
Pregnancy medical home reduces hospital visits, overall costs
LAS VEGAS – Women and their newborns who received care through a pregnancy medical home model used the emergency department less and had fewer inpatient stays, resulting in significant cost savings to a state health insurance plan.
In the single-center, retrospective cohort study, women who had at least one medical home visit had 897 emergency department visits per 1,000 member months, compared with 1,969/1,000 member months for patients who had no medical home visits (P less than .01). Newborns in the medical home group had fewer inpatient days per 1,000 member months as well, compared with non–medical home infants (698 vs. 1,799 days/member month, P less than .01). Inpatient stays for pregnant women receiving medical home care were also reduced (4,279 vs. 2,939 inpatient days, P less than .01).
The pregnancy medical home project was conducted jointly by the Texas Children’s Health Plan and Baylor College of Medicine. The care delivery model, offered from the Baylor Center for Children and Women, gave pregnant women enhanced access, used evidence-based protocols for treatment, and emphasized both quality care and the patient experience, said Dr. Suhag, professor of ob.gyn. at Baylor College of Medicine, Houston.
The pregnancy medical home includes extended hours, walk-in appointments, 24-hour nurse availability for triage, and a laborist model for hospital coverage.
From a payment perspective, the medical home is a fully capitated, full-risk model. “Our center is paid on a monthly basis to provide care to members of our panel,” Dr. Suhag said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The primary outcomes measured by the study were the number of inpatient days and the rate of emergency department usage among pregnancy medical home participants, compared with nonparticipating pregnant women and newborns seen at the Center for Children and Women. Annualized cost savings for the pregnancy medical home model was a secondary outcome measure.
Over a 1-year period, the study examined claims data for pregnant women and newborns who were enrolled in the Texas Children’s Health Plan and were assigned to the pregnancy medical home panel. In total, 27,912 member months (including care for both women and newborns) were examined; of these, about 37% (10,402) were for women and newborns who had at least one medical home visit, and 63% (17,510) of the member months accrued to patients who had no medical home visits. Women and their infants were excluded from the cohort if they received care billed to another health plan.
Participation in the medical home group resulted in lower costs, with annualized estimated emergency department cost savings of $330,161 and $30,739 for pregnant women and newborns, respectively. The reduced number of inpatient days in the medical home group resulted in a total savings of $494,313 for pregnant women and $1,606,392 for newborns in this cohort.
The integrated care model, which used a care coordinator and provided care from multiple specialties at a single site, was likely the key to success, Dr. Suhag said. “With this access, 40% of our pregnant moms were able to access prenatal care in the first trimester, which likely improved outcomes and contributed to the cost savings,” she said.
The control group in the study was made up of individuals who had been randomized to the medical home, but who had chosen care from another provider instead. Because the researchers were relying on health claims data, they were not able to perform a detailed comparison between the two groups, leaving open the possibility that patient characteristics may have accounted for part of the differences in outcomes. Women “could self-select to receive care at the Center for Children and Women,” Dr. Suhag said in an interview. “It is possible that they are different than the women who did not choose care in our clinic.”
A strength of the study, Dr. Suhag said, is that it evaluated outcomes from the medical home model by comparing it to several other medical practices caring for a similar demographic in the same geographic area.
The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Dr. Suhag reported having no outside sources of funding beyond the study’s two sponsoring organizations and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Women and their newborns who received care through a pregnancy medical home model used the emergency department less and had fewer inpatient stays, resulting in significant cost savings to a state health insurance plan.
In the single-center, retrospective cohort study, women who had at least one medical home visit had 897 emergency department visits per 1,000 member months, compared with 1,969/1,000 member months for patients who had no medical home visits (P less than .01). Newborns in the medical home group had fewer inpatient days per 1,000 member months as well, compared with non–medical home infants (698 vs. 1,799 days/member month, P less than .01). Inpatient stays for pregnant women receiving medical home care were also reduced (4,279 vs. 2,939 inpatient days, P less than .01).
The pregnancy medical home project was conducted jointly by the Texas Children’s Health Plan and Baylor College of Medicine. The care delivery model, offered from the Baylor Center for Children and Women, gave pregnant women enhanced access, used evidence-based protocols for treatment, and emphasized both quality care and the patient experience, said Dr. Suhag, professor of ob.gyn. at Baylor College of Medicine, Houston.
The pregnancy medical home includes extended hours, walk-in appointments, 24-hour nurse availability for triage, and a laborist model for hospital coverage.
From a payment perspective, the medical home is a fully capitated, full-risk model. “Our center is paid on a monthly basis to provide care to members of our panel,” Dr. Suhag said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The primary outcomes measured by the study were the number of inpatient days and the rate of emergency department usage among pregnancy medical home participants, compared with nonparticipating pregnant women and newborns seen at the Center for Children and Women. Annualized cost savings for the pregnancy medical home model was a secondary outcome measure.
Over a 1-year period, the study examined claims data for pregnant women and newborns who were enrolled in the Texas Children’s Health Plan and were assigned to the pregnancy medical home panel. In total, 27,912 member months (including care for both women and newborns) were examined; of these, about 37% (10,402) were for women and newborns who had at least one medical home visit, and 63% (17,510) of the member months accrued to patients who had no medical home visits. Women and their infants were excluded from the cohort if they received care billed to another health plan.
Participation in the medical home group resulted in lower costs, with annualized estimated emergency department cost savings of $330,161 and $30,739 for pregnant women and newborns, respectively. The reduced number of inpatient days in the medical home group resulted in a total savings of $494,313 for pregnant women and $1,606,392 for newborns in this cohort.
The integrated care model, which used a care coordinator and provided care from multiple specialties at a single site, was likely the key to success, Dr. Suhag said. “With this access, 40% of our pregnant moms were able to access prenatal care in the first trimester, which likely improved outcomes and contributed to the cost savings,” she said.
The control group in the study was made up of individuals who had been randomized to the medical home, but who had chosen care from another provider instead. Because the researchers were relying on health claims data, they were not able to perform a detailed comparison between the two groups, leaving open the possibility that patient characteristics may have accounted for part of the differences in outcomes. Women “could self-select to receive care at the Center for Children and Women,” Dr. Suhag said in an interview. “It is possible that they are different than the women who did not choose care in our clinic.”
A strength of the study, Dr. Suhag said, is that it evaluated outcomes from the medical home model by comparing it to several other medical practices caring for a similar demographic in the same geographic area.
The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Dr. Suhag reported having no outside sources of funding beyond the study’s two sponsoring organizations and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Women and their newborns who received care through a pregnancy medical home model used the emergency department less and had fewer inpatient stays, resulting in significant cost savings to a state health insurance plan.
In the single-center, retrospective cohort study, women who had at least one medical home visit had 897 emergency department visits per 1,000 member months, compared with 1,969/1,000 member months for patients who had no medical home visits (P less than .01). Newborns in the medical home group had fewer inpatient days per 1,000 member months as well, compared with non–medical home infants (698 vs. 1,799 days/member month, P less than .01). Inpatient stays for pregnant women receiving medical home care were also reduced (4,279 vs. 2,939 inpatient days, P less than .01).
The pregnancy medical home project was conducted jointly by the Texas Children’s Health Plan and Baylor College of Medicine. The care delivery model, offered from the Baylor Center for Children and Women, gave pregnant women enhanced access, used evidence-based protocols for treatment, and emphasized both quality care and the patient experience, said Dr. Suhag, professor of ob.gyn. at Baylor College of Medicine, Houston.
The pregnancy medical home includes extended hours, walk-in appointments, 24-hour nurse availability for triage, and a laborist model for hospital coverage.
From a payment perspective, the medical home is a fully capitated, full-risk model. “Our center is paid on a monthly basis to provide care to members of our panel,” Dr. Suhag said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The primary outcomes measured by the study were the number of inpatient days and the rate of emergency department usage among pregnancy medical home participants, compared with nonparticipating pregnant women and newborns seen at the Center for Children and Women. Annualized cost savings for the pregnancy medical home model was a secondary outcome measure.
Over a 1-year period, the study examined claims data for pregnant women and newborns who were enrolled in the Texas Children’s Health Plan and were assigned to the pregnancy medical home panel. In total, 27,912 member months (including care for both women and newborns) were examined; of these, about 37% (10,402) were for women and newborns who had at least one medical home visit, and 63% (17,510) of the member months accrued to patients who had no medical home visits. Women and their infants were excluded from the cohort if they received care billed to another health plan.
Participation in the medical home group resulted in lower costs, with annualized estimated emergency department cost savings of $330,161 and $30,739 for pregnant women and newborns, respectively. The reduced number of inpatient days in the medical home group resulted in a total savings of $494,313 for pregnant women and $1,606,392 for newborns in this cohort.
The integrated care model, which used a care coordinator and provided care from multiple specialties at a single site, was likely the key to success, Dr. Suhag said. “With this access, 40% of our pregnant moms were able to access prenatal care in the first trimester, which likely improved outcomes and contributed to the cost savings,” she said.
The control group in the study was made up of individuals who had been randomized to the medical home, but who had chosen care from another provider instead. Because the researchers were relying on health claims data, they were not able to perform a detailed comparison between the two groups, leaving open the possibility that patient characteristics may have accounted for part of the differences in outcomes. Women “could self-select to receive care at the Center for Children and Women,” Dr. Suhag said in an interview. “It is possible that they are different than the women who did not choose care in our clinic.”
A strength of the study, Dr. Suhag said, is that it evaluated outcomes from the medical home model by comparing it to several other medical practices caring for a similar demographic in the same geographic area.
The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Dr. Suhag reported having no outside sources of funding beyond the study’s two sponsoring organizations and no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: Medical home patients had 897 emergency department visits, compared with 1,969 per 1,000 member months for non–medical home patients (P less than .01).
Data source: A retrospective cohort study of 27,912 patient member months comparing pregnancy medical home patients with non–medical home patients.
Disclosures: The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Weekend births linked to higher maternal-fetal mortality
LAS VEGAS – Weekend deliveries were associated with a significantly increased risk of maternal-fetal morbidity and death, according to a review of all U.S. deliveries over the past decade.
“Maternal morbidity and mortality were increased on weekends, compared to weekdays, and stillbirth and neonatal morbidity were also increased in infants delivered on weekends. Both of these findings occur against a background of lower intrinsic risk among weekend deliveries,” Amirhossein Moaddab, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Study objectives included measuring both maternal and fetal mortality ratios by the day and month of death or delivery; the study also tracked maternal and neonatal morbidities according to the day of the week the delivery occurred.
Using publicly available data sets (the National Vital Statistics System and the Centers for Disease Control and Prevention WONDER online database), Dr. Moaddab and his colleagues examined all live births and all maternal and fetal deaths in all 50 states and the District of Columbia for the period from 2004 to 2014.
In total, there were 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths during this period.
On weekdays, the maternal mortality rate was 15.3/100,000 live births; the rate rose to 22.8 maternal deaths per 100,000 live births on the weekends (P less than .001). Fetal mortality followed a similar pattern: The weekday fetal mortality rate was 5.85/1,000 live births, compared with 7.21/1,000 live births on the weekends (P less than .001).
A wide range of maternal and fetal morbidities were also more common when deliveries happened on the weekend. For mothers, the adjusted relative risk (aRR) ranged from 1.41 for maternal transfusion to 1.166 for perineal lacerations with Saturday or Sunday deliveries. Unplanned hysterectomy, however, was less likely on the weekend (aRR, 0.810).
Neonatal morbidities with a higher adjusted relative risk included gestational age less than 28 weeks (aRR, 1.481), a 5-minute Apgar score less than 7 (aRR, 1.251), and being placed on a ventilator or admitted to the neonatal intensive care unit (aRRs, 1.219 and 1.199, respectively). The odds of having a chromosomal abnormality were lower for infants delivered on weekends (aRR, 0.864), a result consistent with the increased likelihood of planned delivery for fetuses whose chromosomal status was known, said Dr. Moaddab, a postdoctoral fellow in obstetrics and gynecology at the Baylor College of Medicine, Houston .
Examining maternal characteristics, Dr. Moaddab and his colleagues did find some significant differences between those delivering on weekdays and weekends. However, because the weekend group was healthier overall than the weekday group, these differences were not likely to account for the worse weekend outcomes.
“We were able to control for pregnancy complications, and found that most women with pregnancy complications known to lead to death actually deliver on weekdays, suggesting that the total problem with weekend deliveries is even greater,” said Dr. Clark, professor of ob.gyn. at Baylor College of Medicine.
For example, women delivering on weekends were less likely to be smokers, have diabetes or gestational diabetes, or have chronic or gestational hypertension; they were also less likely to have had a previous cesarean delivery (all P equal to or less than .0001). They were, however, more likely to be nulliparous and to have eclampsia (P equal to or less than .0001).
Dr. Moaddab said that his group’s examination of monthly variations in maternal and fetal morbidity and mortality showed no sign of the “July phenomenon,” the worsening in outcomes seen in some specialties when new interns take to the wards and clinics.
The “weekend effect,” said Dr. Moaddab, has been documented elsewhere as well. In the United Kingdom, a recent observational study of obstetric outcomes found “increases in the rates of death and other complications for both women and babies born at weekends,” he said (BMJ. 2015;351:h5774).
Though Dr. Moaddab’s descriptive study couldn’t get at underlying causes, he said that there are many possible culprits. These can include the divided physician attention and reduced provider availability that can come with weekend staffing, as well as the possibility that the experience level of both physician and nurse staff drops on weekends. Long work hours that come with call may also contribute, he said.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Weekend deliveries were associated with a significantly increased risk of maternal-fetal morbidity and death, according to a review of all U.S. deliveries over the past decade.
“Maternal morbidity and mortality were increased on weekends, compared to weekdays, and stillbirth and neonatal morbidity were also increased in infants delivered on weekends. Both of these findings occur against a background of lower intrinsic risk among weekend deliveries,” Amirhossein Moaddab, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Study objectives included measuring both maternal and fetal mortality ratios by the day and month of death or delivery; the study also tracked maternal and neonatal morbidities according to the day of the week the delivery occurred.
Using publicly available data sets (the National Vital Statistics System and the Centers for Disease Control and Prevention WONDER online database), Dr. Moaddab and his colleagues examined all live births and all maternal and fetal deaths in all 50 states and the District of Columbia for the period from 2004 to 2014.
In total, there were 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths during this period.
On weekdays, the maternal mortality rate was 15.3/100,000 live births; the rate rose to 22.8 maternal deaths per 100,000 live births on the weekends (P less than .001). Fetal mortality followed a similar pattern: The weekday fetal mortality rate was 5.85/1,000 live births, compared with 7.21/1,000 live births on the weekends (P less than .001).
A wide range of maternal and fetal morbidities were also more common when deliveries happened on the weekend. For mothers, the adjusted relative risk (aRR) ranged from 1.41 for maternal transfusion to 1.166 for perineal lacerations with Saturday or Sunday deliveries. Unplanned hysterectomy, however, was less likely on the weekend (aRR, 0.810).
Neonatal morbidities with a higher adjusted relative risk included gestational age less than 28 weeks (aRR, 1.481), a 5-minute Apgar score less than 7 (aRR, 1.251), and being placed on a ventilator or admitted to the neonatal intensive care unit (aRRs, 1.219 and 1.199, respectively). The odds of having a chromosomal abnormality were lower for infants delivered on weekends (aRR, 0.864), a result consistent with the increased likelihood of planned delivery for fetuses whose chromosomal status was known, said Dr. Moaddab, a postdoctoral fellow in obstetrics and gynecology at the Baylor College of Medicine, Houston .
Examining maternal characteristics, Dr. Moaddab and his colleagues did find some significant differences between those delivering on weekdays and weekends. However, because the weekend group was healthier overall than the weekday group, these differences were not likely to account for the worse weekend outcomes.
“We were able to control for pregnancy complications, and found that most women with pregnancy complications known to lead to death actually deliver on weekdays, suggesting that the total problem with weekend deliveries is even greater,” said Dr. Clark, professor of ob.gyn. at Baylor College of Medicine.
For example, women delivering on weekends were less likely to be smokers, have diabetes or gestational diabetes, or have chronic or gestational hypertension; they were also less likely to have had a previous cesarean delivery (all P equal to or less than .0001). They were, however, more likely to be nulliparous and to have eclampsia (P equal to or less than .0001).
Dr. Moaddab said that his group’s examination of monthly variations in maternal and fetal morbidity and mortality showed no sign of the “July phenomenon,” the worsening in outcomes seen in some specialties when new interns take to the wards and clinics.
The “weekend effect,” said Dr. Moaddab, has been documented elsewhere as well. In the United Kingdom, a recent observational study of obstetric outcomes found “increases in the rates of death and other complications for both women and babies born at weekends,” he said (BMJ. 2015;351:h5774).
Though Dr. Moaddab’s descriptive study couldn’t get at underlying causes, he said that there are many possible culprits. These can include the divided physician attention and reduced provider availability that can come with weekend staffing, as well as the possibility that the experience level of both physician and nurse staff drops on weekends. Long work hours that come with call may also contribute, he said.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Weekend deliveries were associated with a significantly increased risk of maternal-fetal morbidity and death, according to a review of all U.S. deliveries over the past decade.
“Maternal morbidity and mortality were increased on weekends, compared to weekdays, and stillbirth and neonatal morbidity were also increased in infants delivered on weekends. Both of these findings occur against a background of lower intrinsic risk among weekend deliveries,” Amirhossein Moaddab, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Study objectives included measuring both maternal and fetal mortality ratios by the day and month of death or delivery; the study also tracked maternal and neonatal morbidities according to the day of the week the delivery occurred.
Using publicly available data sets (the National Vital Statistics System and the Centers for Disease Control and Prevention WONDER online database), Dr. Moaddab and his colleagues examined all live births and all maternal and fetal deaths in all 50 states and the District of Columbia for the period from 2004 to 2014.
In total, there were 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths during this period.
On weekdays, the maternal mortality rate was 15.3/100,000 live births; the rate rose to 22.8 maternal deaths per 100,000 live births on the weekends (P less than .001). Fetal mortality followed a similar pattern: The weekday fetal mortality rate was 5.85/1,000 live births, compared with 7.21/1,000 live births on the weekends (P less than .001).
A wide range of maternal and fetal morbidities were also more common when deliveries happened on the weekend. For mothers, the adjusted relative risk (aRR) ranged from 1.41 for maternal transfusion to 1.166 for perineal lacerations with Saturday or Sunday deliveries. Unplanned hysterectomy, however, was less likely on the weekend (aRR, 0.810).
Neonatal morbidities with a higher adjusted relative risk included gestational age less than 28 weeks (aRR, 1.481), a 5-minute Apgar score less than 7 (aRR, 1.251), and being placed on a ventilator or admitted to the neonatal intensive care unit (aRRs, 1.219 and 1.199, respectively). The odds of having a chromosomal abnormality were lower for infants delivered on weekends (aRR, 0.864), a result consistent with the increased likelihood of planned delivery for fetuses whose chromosomal status was known, said Dr. Moaddab, a postdoctoral fellow in obstetrics and gynecology at the Baylor College of Medicine, Houston .
Examining maternal characteristics, Dr. Moaddab and his colleagues did find some significant differences between those delivering on weekdays and weekends. However, because the weekend group was healthier overall than the weekday group, these differences were not likely to account for the worse weekend outcomes.
“We were able to control for pregnancy complications, and found that most women with pregnancy complications known to lead to death actually deliver on weekdays, suggesting that the total problem with weekend deliveries is even greater,” said Dr. Clark, professor of ob.gyn. at Baylor College of Medicine.
For example, women delivering on weekends were less likely to be smokers, have diabetes or gestational diabetes, or have chronic or gestational hypertension; they were also less likely to have had a previous cesarean delivery (all P equal to or less than .0001). They were, however, more likely to be nulliparous and to have eclampsia (P equal to or less than .0001).
Dr. Moaddab said that his group’s examination of monthly variations in maternal and fetal morbidity and mortality showed no sign of the “July phenomenon,” the worsening in outcomes seen in some specialties when new interns take to the wards and clinics.
The “weekend effect,” said Dr. Moaddab, has been documented elsewhere as well. In the United Kingdom, a recent observational study of obstetric outcomes found “increases in the rates of death and other complications for both women and babies born at weekends,” he said (BMJ. 2015;351:h5774).
Though Dr. Moaddab’s descriptive study couldn’t get at underlying causes, he said that there are many possible culprits. These can include the divided physician attention and reduced provider availability that can come with weekend staffing, as well as the possibility that the experience level of both physician and nurse staff drops on weekends. Long work hours that come with call may also contribute, he said.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: On weekends, the maternal death rate was 22.8/100,000 live births, compared with a weekday rate of 15.3/100,000 (P less than .001).
Data source: A retrospective study of U.S. publicly available maternal-fetal data, including 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths from 2004 to 2014.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.