User login
Psychiatric symptoms of dementia: Treatable, but no silver bullet
Your 84-year-old patient's son is distraught. “I know Mom has dementia, but I don’t understand why she cannot relax. She is busy all night long, taking out the silverware, packing her clothes, and trying to leave the house. Sometimes she tells me that there are little children in the room. These hallucinations scare me, although they do not seem to bother her very much. She keeps me awake; I’m often late to work because I’m up much of the night. I’m afraid I’m going to lose my job; and I don’t want to put Mom into a nursing home. Please give her a medication for this behavior.”
Another of your patients, an 82-year-old man, is admitted to a nursing home after an emergency hospitalization in the geriatric psychiatry unit. His daughter left him alone with her boyfriend one morning while she went to work. Not recognizing him, your patient attacked the young man with a kitchen knife. The police initially arrested your patient and then had him admitted to the psychiatric unit. He is discharged 2 weeks later to the nursing home.
Can anything be done for these patients?
A GROWING PROBLEM
Dementia is a growing problem with the aging of the population. At the time of the 2000 census there were 4.5 million people in the United States with Alzheimer disease, the most common type of dementia,1 and the prevalence is expected to increase to 13.2 million by the year 2050.1
CONSERVATIVE MEASURES ARE THE MAINSTAY OF TREATMENT
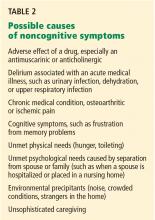
As for offending drugs, removing an antimuscarinic or anticholinergic drug may resolve hallucinations; stopping propoxyphene (Darvon) may improve sleep.
No drugs are approved for treating hallucinations, agitation, or other distressing behavior in neurodegenerative diseases such as Alzheimer dementia. Rather, the mainstay of treatment is behavioral and environmental modification.7 In an environment optimized to maximize comfort, reduce stress, and permit safe wandering, behavioral medications may be unnecessary.
Nevertheless, environments are not always optimal, and physicians may offer medications to treat behavioral symptoms to improve quality of life and to let patients keep living in the community.
Below, we discuss the drugs used to treat behavioral problems in dementia, evidence for the efficacy of these drugs, and their potential for adverse effects.
ANTIPSYCHOTIC DRUGS: SMALL BENEFIT, BIG RISK
Although antipsychotic drugs, both typical and atypical, are often used to treat dementia- related behaviors, their beneficial effects are minimal and adverse effects are common.8,9
Aggression has been considered a symptom that might respond to an atypical antipsychotic drug.10 However, the Clinical Antipsychotic Trials of Intervention Effectiveness—Alzheimer’s Disease (CATIE-AD) trial11 found no differences in efficacy between placebo and the atypical antipsychotics olanzapine (Zyprexa), quetiapine (Seroquel), and risperidone (Risperdal) in treating psychosis, aggression, and agitation in dementia. In that study, rates of drug discontinuation due to adverse effects ranged from 5% for placebo to 24% for olanzapine. Overall, 82% of the patients stopped taking their initially assigned medications during the 36-week period of the trial.11
Antipsychotic drugs may cause more adverse effects in patients with Parkinson disease or dementia with Lewy bodies, and medications with the least dopamine D2 receptor blockade are chosen to reduce the impact on the parkinsonism. Patients with movement disorders were excluded from the CATIE-AD study, and data on this topic are very limited. Quetiapine and olanzapine are often used as alternatives to clozapine (Clozaril) for treating psychosis in Parkinson disease and may have a role in dementia with Lewy bodies.12,13
Atypical antipsychotics carry significant risk of illness and even death. The US Food and Drug Administration (FDA) has published advisories about hyperglycemia, cerebrovascular events, and death.14 Returning to the older, “typical” antipsychotics is not a solution either, given their high incidence of extrapyramidal symptoms15 and potentially higher risk of death.16,17
Even if effective, try stopping the drug
Even in the few situations in dementia in which antipsychotics prove efficacious, a trial of dose-reduction and possible discontinuation is a part of the appropriate plan of care. Symptoms such as aggression and delusions may decrease as the underlying dementia progresses.2 A consensus statement on antipsychotic drug use in the elderly18 recommended stopping antipsychotic drugs as follows:
- If given for delirium—discontinue the drug after 1 week
- For agitated dementia—taper within 3 to 6 months to determine the lowest effective maintenance dose
- For psychotic major depression—discontinue after 6 months
- For mania with psychosis—discontinue after 3 months.18
Disorders for which antipsychotics are not recommended are irritability, hostility, generalized anxiety, and insomnia. In contrast with recommendations for dementia-related behaviors, the psychosis of schizophrenia is treated lifelong at the lowest effective dose of medication.
ANTIDEPRESSANTS: MANY CHOICES, LITTLE EVIDENCE
Depression is hard to assess in a patient with dementia, particularly since apathy is a common symptom in both dementia and depression and may confuse the presentation. Additionally, screening tests for depression have not been validated in the demented elderly.
Depression in dementia is associated with poorer quality of life, greater disability in activities of daily living, a faster cognitive decline, a high rate of nursing home placement, a higher death rate, and a higher frequency of depression and burden in caregivers.19 Quality of life may improve with antidepressant treatment even if the patient does not meet all the criteria for a major depressive disorder. Provisional recommendations for diagnosing depression in dementia suggest using three (instead of five) or more criteria, and include irritability or social isolation as additional criteria.20
Choosing an antidepressant
Only a few randomized controlled trials of antidepressants for depression with dementia have been completed, each with a small number of patients.
Mirtazapine (Remeron) is what we recommend to improve sleep and appetite and restore lost weight.21 It can be used in patients with Parkinson disease or parkinsonian symptoms who experience increased tremors or bradykinesia with selective serotonin reuptake inhibitors (SSRIs). On the other hand, it may not be the best option for those with diabetes mellitus, metabolic syndrome, hyperlipidemia, or obesity. It may rarely also cause a reversible agranulocytosis.
Venlafaxine (Effexor) and duloxetine (Cymbalta) are serotonin-norepinephrine reuptake inhibitors (SNRIs) and may help in concomitant pain syndromes.22 Either drug can cause anorexia at any dose and can elevate blood pressure at higher doses. Venlafaxine may also cause insomnia in some patients.
Bupropion (Wellbutrin) can be difficult to titrate to an effective dose in an older person with unsuspected renal insufficiency, and it may interact at the P450 complex.23 The risk of seizures is greater at higher bupropion serum levels. There is also a high incidence of weight loss. Frail elderly patients, those with hypertension, and those vulnerable to hallucinations will likely do better with another drug.
Nefazodone is a third- or fourth-line antidepressive choice because of the risk of hepatic failure. However, it can help reduce disabling anxiety associated with depression. The FDA requires periodic liver function testing if this drug is used.
Trazodone in low doses (≤ 100 mg) each evening may help with sleep, but it cannot be titrated to antidepressive doses in older adults because of orthostatic effects.
Nortriptyline is recommended by some geriatricians for depression or pathologic crying in patients with mixed vascular dementia. However, it often causes cardiac conduction delays with reflex sympathetic tachycardia and anticholinergic side effects.
Monoamine oxidase inhibitors interact with many foods and drugs, limiting their use in older adults.
Methylphenidate (Ritalin) at low doses is used off-label for depression in palliative care, with noted rapid improvements in mood and appetite.24 Monitoring for increases in blood pressure, heart rate, and respiratory rate is essential if this stimulant is chosen. Patients who respond may make a transition to other traditional drugs after 2 to 4 weeks.
Caveats with SSRIs
- Despite the safety profile of SSRIs in older adults, care must be taken when prescribing them to frail elderly patients, given recent data associating SSRIs with falls and fragility fractures25,26 and urinary incontinence.27
- SSRIs may decrease appetite during initial treatment.
- Sertraline (Zoloft) may have to be started at a very low dose to decrease possible adverse gastrointestinal symptoms, such as diarrhea.
- Paroxetine (Paxil) has multiple interactions at the cytochrome P450 complex and has the most anticholinergic properties of the SSRIs, rendering it more likely to cause adverse drug reactions, constipation, and delirium.
- Daily fluoxetine (Prozac) may not be appropriate in older adults because of its long half-life and the risk of insomnia and agitation.28
- Tremors can emerge with all the SSRIs; akathisia, dystonia, and parkinsonism are also possible.29
- Hyponatremia, bruising, and increased bleeding time can occur with any SSRI.
- Abrupt cessation of any SSRI except fluoxetine (due to its long half-life) or of SNRIs may cause a very unpleasant flu-like withdrawal syndrome.
- Apathy can be a reversible, dose-dependent adverse effect of SSRIs in young persons30; there are no data on the dose at which this adverse effect might emerge in demented elderly patients.
In a systematic review, Sink et al31 found citalopram (Celexa) to help reduce nondepressive agitation.
How long should depression be treated?
Antidepressant treatment is typically for 6 to 12 months. However, the optimal duration in an older adult with dementia is not known and is not addressed in either the American Psychiatric Association practice guideline on dementia32 or the position statement of the American Association for Geriatric Psychiatry.33
Patients with executive dysfunction, particularly those with perseveration and diminished inhibition, may be less likely to respond to antidepressants, and the symptoms are more likely to recur if they do respond.34 It may be appropriate to treat them for a year and then withdraw the drug and monitor for recurrence. Some patients may need indefinite treatment.
No data on treating apathy
Apathy in elderly patients with dementia is common. It is found in nearly half of elderly patients with mild dementia and in nearly all of those with severe dementia. If accompanied by depressive symptoms such as sadness, guilt, feelings of worthlessness, passive or active death wish, changes in sleep or appetite, or tearfulness, apathy and other depressive symptoms may respond to antidepressive treatment—both behavioral and pharmacologic. When present in dementia without depressive symptomatology, apathy is unlikely to respond to antidepressants. In particular, SSRIs may actually induce or worsen apathy through their effect on the angular gyrus. Apathy can be very frustrating to family members but not troublesome at all to the patient.
No medication carries an indication for apathy in dementia. Although stimulants such as methylphenidate and modafinil (Provigil) have been used, there is no evidence to date from any controlled study of efficacy and safety in this population.
Try nondrug measures concomitantly
Given the limited evidence of efficacy of antidepressive therapy in demented elderly patients, nonpharmacologic therapy should be offered concomitantly.
Evidence-based nonpharmacologic treatment for depression in dementia includes increasing enjoyable activities and socialization with people and pets, reducing the need to perform frustrating activities, redirecting perseverative behaviors and speech, and addressing caregiver needs.34 Exercise may improve physical functioning in depression with dementia.35 A comprehensive sleep program may improve associated sleep disorders.36
An intensive collaborative-care intervention37 resulted in more demented elderly patients in the intervention group receiving a cholinesterase inhibitor and an antidepressive than in the usual-care group. Outcomes included fewer behavioral symptoms, less caregiver distress, and less caregiver depression.
So far, no randomized trial has shown electroconvulsive therapy to be effective in elderly patients with depression and dementia.38
ANTICONVULSANT DRUGS MAY STABILIZE MOOD
On the basis of small studies with some contradictory outcomes,39 both older and newer anticonvulsants have been used in nonpsychotic agitation, aggression, and impulsivity in a variety of psychiatric disorders, brain injury, and dementia.40 Most of the data are on the older drugs such as valproic acid and carbamazepine (Tegretol).
Valproic acid is associated with an adverse metabolic profile (hyperglycemia, weight gain, and hyperlipidemia),41,42 dose-related orthostasis, sedation, and worsening cognitive performance. In addition, the possibility of thrombocytopenia and blood level fluctuations requires monitoring. Older adults may tolerate 250 to 500 mg/day with minimal adverse effects.
Carbamazepine reduced aggression in a blinded, placebo-controlled study in nursing home patients.43 Use of carbamazepine requires monitoring of hematologic and liver profiles, alters the metabolism of itself and other drugs, and is associated with dose-related sedation.
Lamotrigine (Lamictal) takes a long time to titrate but may help with nonpsychotic agitation and impulsivity; it is a relatively new drug, and there are limited data to support its use at this time in the elderly.
Gabapentin (Gabarone), in case reports at doses primarily from 600 to 1,200 mg/day, reduced behavioral and psychological problems of patients with dementia and with good renal clearance.44 Some patients may experience tremors or oversedation.
Phenytoin (Dilantin) is not a good choice for behavioral problems because of unwanted effects on teeth, bones, and balance.
Levetiracetam (Keppra) may cause behavioral disturbances to emerge or worsen.45
Emerging evidence suggests that all anticonvulsants may also be associated with an increased risk of depressive symptoms.
COGNITIVE ENHANCERS MAY IMPROVE BEHAVIOR
Acetylcholinesterase inhibitors may improve some behavioral symptoms of dementia. In an open-label retrospective trial, delusionality, irritability, anxiety, disinhibition, and agitation improved in some patients on these drugs.46 Patients most likely to respond were those with the most impairment from these behaviors and those with depressive or apathetic symptoms.46 A Cochrane review found a modest beneficial effect on behavior.47
Acetylcholinesterase inhibitors may reduce symptoms of apathy. Additionally, they actually improve depressive symptoms in mild to moderate dementia independent of any effect on cognition.48
Memantine (Namenda), approved for the treatment of moderate to severe dementia, may reduce the prevalence and incidence of agitation, particularly in more advanced dementia.49
The cognitive enhancers all require several weeks for titration and are not helpful for the acute management of behavioral or depressive symptoms.
OTHER DRUGS
Beta-blockers50 and estrogen51 have been studied as off-label, nonneuroleptic treatments for male aggression. Use of progesterone in men with inappropriate sexual behavior52 may have benefit; further interventions are reviewed by Srinivasan and Weinberg.53 These recommendations are based on small case series. In addition, the hormonal treatments may carry significant morbidity.
Sedative hypnotics were evaluated for sleep difficulties in demented patients in a meta-analysis by Glass et al,54 who found adverse cognitive events, psychomotor events, and daytime fatigue more common (5, 2.6, and 3.8 times, respectively) in the sedative group than in the placebo group.
For agitation in delirium, haloperidol (Haldol) is preferable to benzodiazepines, based on studies from the 1970s.55 Although benzodiazepines carry an indication for anxiety, newly prescribed benzodiazepines and those with a longer half-life are associated with hip fractures in older adults,56 possibly from sedation.
WHAT TO DO FOR YOUR PATIENTS
The 84-year-old woman
For the 84-year-old woman who is keeping her son awake all night, recommend making the environment safe for her to wander, including placing a bolt on the doors leading to the basement and outdoors and moving the knives to an area that she cannot reach, to avoid accidents. Recommend that she be given things to do that are repetitive, such as folding towels and arranging drawers. Referring her to day care may improve socialization and increase physical activity during the day, possibly improving her sleep time at night.
The 82-year-old man
Let’s assume the 82-year-old man arrested and then hospitalized is placed on risperidone 1 mg twice daily prior to discharge to the nursing home. In the nursing home, he becomes irritable with any change in his routine: the door has to be open by exactly 6 inches; his meals have to be identical and served on time; the newspaper needs to arrive by 8 AM. Since routine is paramount in the nursing home, the staff accommodates his need for a very regular schedule. Donepezil (Aricept) and memantine can be added as cognitive enhancers, and citalopram can be added for possible depression and obsessive features. The daughter should then be approached about reducing the risperidone dose and, hopefully, discontinuing it in the future.
Comment. A stable, routine environment is the most important intervention for managing this aggressive resident’s behavior, although he may have been helped to some degree by the adjunct medications. Once he is stable, the daughter may be able to bring him home for weekends and holidays, as long as she is advised never to surprise him with an unexpected visit or to bring home unexpected guests.
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol 2003; 60:1119–1122.
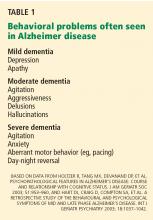
- Holtzer R, Tang MX, Devanand DP, et al. Psychopathological features in Alzheimer's disease: course and relationship with cognitive status. J Am Geriatr Soc 2003; 51:953–960.
- Hart DJ, Craig D, Compton SA, et al. A retrospective study of the behavioural and psychological symptoms of mid and late phase Alzheimer's disease. Int J Geriatr Psychiatry 2003; 18:1037–1042.
- McKeith I, Cummings J. Behavioural changes and psychological symptoms in dementia disorders. Lancet Neurol 2005; 4:735–742.
- Stern Y, Albert M, Brandt J, et al. Utility of extrapyramidal signs and psychosis as predictors of cognitive and functional decline, nursing home admission, and death in Alzheimer's disease: prospective analyses from the Predictors Study. Neurology 1994; 44:2300–2307.
- Chibnall JT, Tait RC, Harman B, Luebbert RA. Effect of acetaminophen on behavior, well-being, and psychotropic medication use in nursing home residents with moderate-to-severe dementia. J Am Geriatr Soc 2005; 53:1921–1929.
- Doody RS, Stevens JC, Beck C, et al. Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2001; 56:1154–1166.
- Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry 2006; 14:191–210.
- Jeste DV, Dolder CR, Nayak GV, Salzman C. Atypical antipsychotics in elderly patients with dementia or schizophrenia: review of recent literature. Harv Rev Psychiatry 2005; 13:340–351.
- Rabinowitz J, Katz IR, De Deyn PP, Brodaty H, Greenspan A, Davidson M. Behavioral and psychological symptoms in patients with dementia as a target for pharmacotherapy with risperidone. J Clin Psychiatry 2004; 65:1329–1334.
- Schneider LS, Tariot PN, Dagerman KS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer's disease. N Engl J Med 2006; 355:1525–1538.
- Fernandez HH, Trieschmann ME, Burke MA, Friedman JH. Quetiapine for psychosis in Parkinson's disease versus dementia with Lewy bodies. J Clin Psychiatry 2002; 63:513–515.
- Cummings JL, Street J, Masterman D, Clark WS. Efficacy of olanzapine in the treatment of psychosis in dementia with Lewy bodies. Dement Geriatr Cogn Disord 2002; 13:67–73.
- US Food and Drug Administration. FDA Public Health Advisory—Deaths with Antipsychotics in Elderly Patients with Behavioral Disturbances: FDA/Center for Drug Evaluation and Research; April 11 2005.
- Lonergan E, Luxenberg J, Colford J. Haloperidol for agitation in dementia. Cochrane Database Syst Rev 2001; (4):CD002852.
- Wang PS, Schneeweiss S, Avorn J, et al. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med 2005; 353:2335–2341.
- Gill SS, Bronskill SE, Normand SL, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med 2007; 146:775–786.
- Alexopoulos GS, Streim J, Carpenter D, Docherty JP; Expert Consensus Panel for Using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry 2004; 65(suppl 2):5–99.
- Starkstein SE, Mizrahi R. Depression in Alzheimer's disease. Expert Rev Neurother 2006; 6:887–895.
- Olin JT, Katz IR, Meyers BS, Schneider LS, Lebowitz BD. Provisional diagnostic criteria for depression of Alzheimer disease: rationale and background. Am J Geriatr Psychiatry 2002; 10:129–141.
- Aronne LJ, Segal KR. Weight gain in the treatment of mood disorders. J Clin Psychiatry 2003; 64(suppl 8):22–29.
- Barkin RL, Barkin S. The role of venlafaxine and duloxetine in the treatment of depression with decremental changes in somatic symptoms of pain, chronic pain, and the pharmacokinetics and clinical considerations of duloxetine pharmacotherapy. Am J Ther 2005; 12:431–438.
- Wilkes S. Bupropion. Drugs Today (Barc) 2006; 42:671–681.
- Homsi J, Walsh D, Nelson KA, LeGrand S, Davis M. Methylphenidate for depression in hospice practice: a case series. Am J Hosp Palliat Care 2000; 17:393–398.
- Kallin K, Lundin-Olsson L, Jensen J, Nyberg L, Gustafson Y. Predisposing and precipitating factors for falls among older people in residential care. Public Health 2002; 116:263–271.
- Richards JB, Papaioannou A, Adachi JD, et al; Canadian Multicentre Osteoporosis Study Research Group. Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med 2007; 167:188–194.
- Movig KL, Leufkens HG, Belitser SV, Lenderink AW, Egberts ACG. Selective serotonin reuptake inhibitor-induced urinary incontinence. Pharmacoepidemiol Drug Saf 2002; 11:271–279.
- Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 2003; 163:2716–2724.
- Leo RJ. Movement disorders associated with the serotonin selective reuptake inhibitors. J Clin Psychiatry 1996; 57:449–454.
- Barnhart WJ, Makela EH, Latocha MJ. SSRI-induced apathy syndrome: a clinical review. J Psychiatr Pract 2004; 10:196–199.
- Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA 2005; 293:596–608.
- American Psychiatric Association. Practice Guideline and Resources for Treatment of Patients with Alzheimer's Disease and Other Dementias, 2nd Edition. October 2007. www.psychiatryonline.com/pracGuide/pracGuideTopic_3.aspx. Accessed 2/2/2009.
- Lyketsos CG, Colenda CC, Beck C, et al; Task Force of American Association for Geriatric Psychiatry. Position Statement of the American Association for Geriatric Psychiatry regarding principles of care for patients with dementia resulting from Alzheimer disease. Am J Geriatr Psychiatry 2006; 14:561–572.
- Potter GG, Steffens DC. Contribution of depression to cognitive impairment and dementia in older adults. Neurologist 2007; 13:105– 117.
- Teri L, Gibbons LE, McCurry SM, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA 2003; 290:2015–2022.
- McCurry SM, Gibbons LE, Logsdon RG, Vitiello MV, Teri L. Nighttime insomnia treatment and education for Alzheimer's disease: a randomized, controlled trial. J Am Geriatr Soc 2005; 53:793–802.
- Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA 2006; 295:2148–2157.
- Van der Wurff FB, Stek ML, Hoogendijk WL, Beekman AT. Electroconvulsive therapy for the depressed elderly. Cochrane Database Syst Rev 2003; ( 2):CD003593.
- Tariot PN, Raman R, Jakimovich L, et al. Divalproex sodium in nursing home residents with possible or probable Alzheimer disease complicated by agitation: a randomized, controlled trial. Am J Geriatr Psychiatry 2005; 13:942–949.
- Kim E. The use of newer anticonvulsants in neuropsychiatric disorders. Curr Psychiatry Rep 2002; 4:331–337.
- Ness-Abramof R, Apovian CM. Drug-induced weight gain. Drugs Today (Barc) 2005; 41:547–555.
- Biton V. Weight change and antiepileptic drugs: health issues and criteria for appropriate selection of an antiepileptic agent. Neurologist 2006; 12:163–167.
- Tariot PN, Erb R, Podgorski CA, et al. Efficacy and tolerability of carbamazepine for agitation and aggression in dementia. Am J Psychiatry 1998; 155:54–61.
- Miller LJ. Gabapentin for treatment of behavioral and psychological symptoms of dementia. Ann Pharmacother 2001; 35:427–431.
- White JR, Walczak TS, Leppik IE, et al. Discontinuation of levetiracetam because of behavioral side effects: a case-control study. Neurology 2003; 61:1218–1221.
- Mega S, Masterman DM, O'Connor SM, Barclay TR, Cummings JL. The spectrum of behavioral responses to cholinesterase inhibitor therapy in Alzheimer disease. Arch Neurol 1999; 56:1388–1393.
- Birks J. Cholinesterase inhibitors for Alzheimer's disease. Cochrane Database of Syst Rev 2006; (1):CD005593.
- Rozzini L, Vicini Chilovi B, Bertoletti E, Trabucchi M, Padovani A. Acetyl-cholinesterase inhibitors and depressive symptoms in patients with mild to moderate Alzheimer's disease. Aging Clin Exp Res 2007; 19:220–223.
- McShane R, Areosa Sastre A, Minakaran N. Memantine for dementia. Cochrane Database Syst Rev 2006; (2):CD003154.
- Peskind ER, Tsuang DW, Bonner LT, et al. Propranolol for disruptive behaviors in nursing home residents with probable or possible Alzheimer disease: a placebo-controlled study. Alzheimer Dis Assoc Disord 2005; 19:23–28.
- Hall KA, Keks NA, O'Connor DW. Transdermal estrogen patches for aggressive behavior in male patients with dementia: a randomized, controlled trial. Int Psychogeriatr 2005; 17:165–178.
- Light SA, Holroyd S. The use of medroxyprogesterone acetate for the treatment of sexually inappropriate behaviour in patients with dementia. J Psychiatry Neurosci 2006; 31:132–134.
- Srinivasan S, Weinberg A. Pharmacologic treatment of sexual inappropriateness in long-term care residents with dementia. Ann Long-Term Care: Clin Care Aging 2006; 14:20–28.
- Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 2005; 331:1169.
- Kirven LE, Montero EF. Comparison of thioridazine and diazepam in the control of nonpsychotic symptoms associated with senility: double-blind study. J Am Geriatr Soc 1973; 21:546–551.
- Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs 2003; 17:825–837.
Your 84-year-old patient's son is distraught. “I know Mom has dementia, but I don’t understand why she cannot relax. She is busy all night long, taking out the silverware, packing her clothes, and trying to leave the house. Sometimes she tells me that there are little children in the room. These hallucinations scare me, although they do not seem to bother her very much. She keeps me awake; I’m often late to work because I’m up much of the night. I’m afraid I’m going to lose my job; and I don’t want to put Mom into a nursing home. Please give her a medication for this behavior.”
Another of your patients, an 82-year-old man, is admitted to a nursing home after an emergency hospitalization in the geriatric psychiatry unit. His daughter left him alone with her boyfriend one morning while she went to work. Not recognizing him, your patient attacked the young man with a kitchen knife. The police initially arrested your patient and then had him admitted to the psychiatric unit. He is discharged 2 weeks later to the nursing home.
Can anything be done for these patients?
A GROWING PROBLEM
Dementia is a growing problem with the aging of the population. At the time of the 2000 census there were 4.5 million people in the United States with Alzheimer disease, the most common type of dementia,1 and the prevalence is expected to increase to 13.2 million by the year 2050.1
CONSERVATIVE MEASURES ARE THE MAINSTAY OF TREATMENT
As for offending drugs, removing an antimuscarinic or anticholinergic drug may resolve hallucinations; stopping propoxyphene (Darvon) may improve sleep.
No drugs are approved for treating hallucinations, agitation, or other distressing behavior in neurodegenerative diseases such as Alzheimer dementia. Rather, the mainstay of treatment is behavioral and environmental modification.7 In an environment optimized to maximize comfort, reduce stress, and permit safe wandering, behavioral medications may be unnecessary.
Nevertheless, environments are not always optimal, and physicians may offer medications to treat behavioral symptoms to improve quality of life and to let patients keep living in the community.
Below, we discuss the drugs used to treat behavioral problems in dementia, evidence for the efficacy of these drugs, and their potential for adverse effects.
ANTIPSYCHOTIC DRUGS: SMALL BENEFIT, BIG RISK
Although antipsychotic drugs, both typical and atypical, are often used to treat dementia- related behaviors, their beneficial effects are minimal and adverse effects are common.8,9
Aggression has been considered a symptom that might respond to an atypical antipsychotic drug.10 However, the Clinical Antipsychotic Trials of Intervention Effectiveness—Alzheimer’s Disease (CATIE-AD) trial11 found no differences in efficacy between placebo and the atypical antipsychotics olanzapine (Zyprexa), quetiapine (Seroquel), and risperidone (Risperdal) in treating psychosis, aggression, and agitation in dementia. In that study, rates of drug discontinuation due to adverse effects ranged from 5% for placebo to 24% for olanzapine. Overall, 82% of the patients stopped taking their initially assigned medications during the 36-week period of the trial.11
Antipsychotic drugs may cause more adverse effects in patients with Parkinson disease or dementia with Lewy bodies, and medications with the least dopamine D2 receptor blockade are chosen to reduce the impact on the parkinsonism. Patients with movement disorders were excluded from the CATIE-AD study, and data on this topic are very limited. Quetiapine and olanzapine are often used as alternatives to clozapine (Clozaril) for treating psychosis in Parkinson disease and may have a role in dementia with Lewy bodies.12,13
Atypical antipsychotics carry significant risk of illness and even death. The US Food and Drug Administration (FDA) has published advisories about hyperglycemia, cerebrovascular events, and death.14 Returning to the older, “typical” antipsychotics is not a solution either, given their high incidence of extrapyramidal symptoms15 and potentially higher risk of death.16,17
Even if effective, try stopping the drug
Even in the few situations in dementia in which antipsychotics prove efficacious, a trial of dose-reduction and possible discontinuation is a part of the appropriate plan of care. Symptoms such as aggression and delusions may decrease as the underlying dementia progresses.2 A consensus statement on antipsychotic drug use in the elderly18 recommended stopping antipsychotic drugs as follows:
- If given for delirium—discontinue the drug after 1 week
- For agitated dementia—taper within 3 to 6 months to determine the lowest effective maintenance dose
- For psychotic major depression—discontinue after 6 months
- For mania with psychosis—discontinue after 3 months.18
Disorders for which antipsychotics are not recommended are irritability, hostility, generalized anxiety, and insomnia. In contrast with recommendations for dementia-related behaviors, the psychosis of schizophrenia is treated lifelong at the lowest effective dose of medication.
ANTIDEPRESSANTS: MANY CHOICES, LITTLE EVIDENCE
Depression is hard to assess in a patient with dementia, particularly since apathy is a common symptom in both dementia and depression and may confuse the presentation. Additionally, screening tests for depression have not been validated in the demented elderly.
Depression in dementia is associated with poorer quality of life, greater disability in activities of daily living, a faster cognitive decline, a high rate of nursing home placement, a higher death rate, and a higher frequency of depression and burden in caregivers.19 Quality of life may improve with antidepressant treatment even if the patient does not meet all the criteria for a major depressive disorder. Provisional recommendations for diagnosing depression in dementia suggest using three (instead of five) or more criteria, and include irritability or social isolation as additional criteria.20
Choosing an antidepressant
Only a few randomized controlled trials of antidepressants for depression with dementia have been completed, each with a small number of patients.
Mirtazapine (Remeron) is what we recommend to improve sleep and appetite and restore lost weight.21 It can be used in patients with Parkinson disease or parkinsonian symptoms who experience increased tremors or bradykinesia with selective serotonin reuptake inhibitors (SSRIs). On the other hand, it may not be the best option for those with diabetes mellitus, metabolic syndrome, hyperlipidemia, or obesity. It may rarely also cause a reversible agranulocytosis.
Venlafaxine (Effexor) and duloxetine (Cymbalta) are serotonin-norepinephrine reuptake inhibitors (SNRIs) and may help in concomitant pain syndromes.22 Either drug can cause anorexia at any dose and can elevate blood pressure at higher doses. Venlafaxine may also cause insomnia in some patients.
Bupropion (Wellbutrin) can be difficult to titrate to an effective dose in an older person with unsuspected renal insufficiency, and it may interact at the P450 complex.23 The risk of seizures is greater at higher bupropion serum levels. There is also a high incidence of weight loss. Frail elderly patients, those with hypertension, and those vulnerable to hallucinations will likely do better with another drug.
Nefazodone is a third- or fourth-line antidepressive choice because of the risk of hepatic failure. However, it can help reduce disabling anxiety associated with depression. The FDA requires periodic liver function testing if this drug is used.
Trazodone in low doses (≤ 100 mg) each evening may help with sleep, but it cannot be titrated to antidepressive doses in older adults because of orthostatic effects.
Nortriptyline is recommended by some geriatricians for depression or pathologic crying in patients with mixed vascular dementia. However, it often causes cardiac conduction delays with reflex sympathetic tachycardia and anticholinergic side effects.
Monoamine oxidase inhibitors interact with many foods and drugs, limiting their use in older adults.
Methylphenidate (Ritalin) at low doses is used off-label for depression in palliative care, with noted rapid improvements in mood and appetite.24 Monitoring for increases in blood pressure, heart rate, and respiratory rate is essential if this stimulant is chosen. Patients who respond may make a transition to other traditional drugs after 2 to 4 weeks.
Caveats with SSRIs
- Despite the safety profile of SSRIs in older adults, care must be taken when prescribing them to frail elderly patients, given recent data associating SSRIs with falls and fragility fractures25,26 and urinary incontinence.27
- SSRIs may decrease appetite during initial treatment.
- Sertraline (Zoloft) may have to be started at a very low dose to decrease possible adverse gastrointestinal symptoms, such as diarrhea.
- Paroxetine (Paxil) has multiple interactions at the cytochrome P450 complex and has the most anticholinergic properties of the SSRIs, rendering it more likely to cause adverse drug reactions, constipation, and delirium.
- Daily fluoxetine (Prozac) may not be appropriate in older adults because of its long half-life and the risk of insomnia and agitation.28
- Tremors can emerge with all the SSRIs; akathisia, dystonia, and parkinsonism are also possible.29
- Hyponatremia, bruising, and increased bleeding time can occur with any SSRI.
- Abrupt cessation of any SSRI except fluoxetine (due to its long half-life) or of SNRIs may cause a very unpleasant flu-like withdrawal syndrome.
- Apathy can be a reversible, dose-dependent adverse effect of SSRIs in young persons30; there are no data on the dose at which this adverse effect might emerge in demented elderly patients.
In a systematic review, Sink et al31 found citalopram (Celexa) to help reduce nondepressive agitation.
How long should depression be treated?
Antidepressant treatment is typically for 6 to 12 months. However, the optimal duration in an older adult with dementia is not known and is not addressed in either the American Psychiatric Association practice guideline on dementia32 or the position statement of the American Association for Geriatric Psychiatry.33
Patients with executive dysfunction, particularly those with perseveration and diminished inhibition, may be less likely to respond to antidepressants, and the symptoms are more likely to recur if they do respond.34 It may be appropriate to treat them for a year and then withdraw the drug and monitor for recurrence. Some patients may need indefinite treatment.
No data on treating apathy
Apathy in elderly patients with dementia is common. It is found in nearly half of elderly patients with mild dementia and in nearly all of those with severe dementia. If accompanied by depressive symptoms such as sadness, guilt, feelings of worthlessness, passive or active death wish, changes in sleep or appetite, or tearfulness, apathy and other depressive symptoms may respond to antidepressive treatment—both behavioral and pharmacologic. When present in dementia without depressive symptomatology, apathy is unlikely to respond to antidepressants. In particular, SSRIs may actually induce or worsen apathy through their effect on the angular gyrus. Apathy can be very frustrating to family members but not troublesome at all to the patient.
No medication carries an indication for apathy in dementia. Although stimulants such as methylphenidate and modafinil (Provigil) have been used, there is no evidence to date from any controlled study of efficacy and safety in this population.
Try nondrug measures concomitantly
Given the limited evidence of efficacy of antidepressive therapy in demented elderly patients, nonpharmacologic therapy should be offered concomitantly.
Evidence-based nonpharmacologic treatment for depression in dementia includes increasing enjoyable activities and socialization with people and pets, reducing the need to perform frustrating activities, redirecting perseverative behaviors and speech, and addressing caregiver needs.34 Exercise may improve physical functioning in depression with dementia.35 A comprehensive sleep program may improve associated sleep disorders.36
An intensive collaborative-care intervention37 resulted in more demented elderly patients in the intervention group receiving a cholinesterase inhibitor and an antidepressive than in the usual-care group. Outcomes included fewer behavioral symptoms, less caregiver distress, and less caregiver depression.
So far, no randomized trial has shown electroconvulsive therapy to be effective in elderly patients with depression and dementia.38
ANTICONVULSANT DRUGS MAY STABILIZE MOOD
On the basis of small studies with some contradictory outcomes,39 both older and newer anticonvulsants have been used in nonpsychotic agitation, aggression, and impulsivity in a variety of psychiatric disorders, brain injury, and dementia.40 Most of the data are on the older drugs such as valproic acid and carbamazepine (Tegretol).
Valproic acid is associated with an adverse metabolic profile (hyperglycemia, weight gain, and hyperlipidemia),41,42 dose-related orthostasis, sedation, and worsening cognitive performance. In addition, the possibility of thrombocytopenia and blood level fluctuations requires monitoring. Older adults may tolerate 250 to 500 mg/day with minimal adverse effects.
Carbamazepine reduced aggression in a blinded, placebo-controlled study in nursing home patients.43 Use of carbamazepine requires monitoring of hematologic and liver profiles, alters the metabolism of itself and other drugs, and is associated with dose-related sedation.
Lamotrigine (Lamictal) takes a long time to titrate but may help with nonpsychotic agitation and impulsivity; it is a relatively new drug, and there are limited data to support its use at this time in the elderly.
Gabapentin (Gabarone), in case reports at doses primarily from 600 to 1,200 mg/day, reduced behavioral and psychological problems of patients with dementia and with good renal clearance.44 Some patients may experience tremors or oversedation.
Phenytoin (Dilantin) is not a good choice for behavioral problems because of unwanted effects on teeth, bones, and balance.
Levetiracetam (Keppra) may cause behavioral disturbances to emerge or worsen.45
Emerging evidence suggests that all anticonvulsants may also be associated with an increased risk of depressive symptoms.
COGNITIVE ENHANCERS MAY IMPROVE BEHAVIOR
Acetylcholinesterase inhibitors may improve some behavioral symptoms of dementia. In an open-label retrospective trial, delusionality, irritability, anxiety, disinhibition, and agitation improved in some patients on these drugs.46 Patients most likely to respond were those with the most impairment from these behaviors and those with depressive or apathetic symptoms.46 A Cochrane review found a modest beneficial effect on behavior.47
Acetylcholinesterase inhibitors may reduce symptoms of apathy. Additionally, they actually improve depressive symptoms in mild to moderate dementia independent of any effect on cognition.48
Memantine (Namenda), approved for the treatment of moderate to severe dementia, may reduce the prevalence and incidence of agitation, particularly in more advanced dementia.49
The cognitive enhancers all require several weeks for titration and are not helpful for the acute management of behavioral or depressive symptoms.
OTHER DRUGS
Beta-blockers50 and estrogen51 have been studied as off-label, nonneuroleptic treatments for male aggression. Use of progesterone in men with inappropriate sexual behavior52 may have benefit; further interventions are reviewed by Srinivasan and Weinberg.53 These recommendations are based on small case series. In addition, the hormonal treatments may carry significant morbidity.
Sedative hypnotics were evaluated for sleep difficulties in demented patients in a meta-analysis by Glass et al,54 who found adverse cognitive events, psychomotor events, and daytime fatigue more common (5, 2.6, and 3.8 times, respectively) in the sedative group than in the placebo group.
For agitation in delirium, haloperidol (Haldol) is preferable to benzodiazepines, based on studies from the 1970s.55 Although benzodiazepines carry an indication for anxiety, newly prescribed benzodiazepines and those with a longer half-life are associated with hip fractures in older adults,56 possibly from sedation.
WHAT TO DO FOR YOUR PATIENTS
The 84-year-old woman
For the 84-year-old woman who is keeping her son awake all night, recommend making the environment safe for her to wander, including placing a bolt on the doors leading to the basement and outdoors and moving the knives to an area that she cannot reach, to avoid accidents. Recommend that she be given things to do that are repetitive, such as folding towels and arranging drawers. Referring her to day care may improve socialization and increase physical activity during the day, possibly improving her sleep time at night.
The 82-year-old man
Let’s assume the 82-year-old man arrested and then hospitalized is placed on risperidone 1 mg twice daily prior to discharge to the nursing home. In the nursing home, he becomes irritable with any change in his routine: the door has to be open by exactly 6 inches; his meals have to be identical and served on time; the newspaper needs to arrive by 8 AM. Since routine is paramount in the nursing home, the staff accommodates his need for a very regular schedule. Donepezil (Aricept) and memantine can be added as cognitive enhancers, and citalopram can be added for possible depression and obsessive features. The daughter should then be approached about reducing the risperidone dose and, hopefully, discontinuing it in the future.
Comment. A stable, routine environment is the most important intervention for managing this aggressive resident’s behavior, although he may have been helped to some degree by the adjunct medications. Once he is stable, the daughter may be able to bring him home for weekends and holidays, as long as she is advised never to surprise him with an unexpected visit or to bring home unexpected guests.
Your 84-year-old patient's son is distraught. “I know Mom has dementia, but I don’t understand why she cannot relax. She is busy all night long, taking out the silverware, packing her clothes, and trying to leave the house. Sometimes she tells me that there are little children in the room. These hallucinations scare me, although they do not seem to bother her very much. She keeps me awake; I’m often late to work because I’m up much of the night. I’m afraid I’m going to lose my job; and I don’t want to put Mom into a nursing home. Please give her a medication for this behavior.”
Another of your patients, an 82-year-old man, is admitted to a nursing home after an emergency hospitalization in the geriatric psychiatry unit. His daughter left him alone with her boyfriend one morning while she went to work. Not recognizing him, your patient attacked the young man with a kitchen knife. The police initially arrested your patient and then had him admitted to the psychiatric unit. He is discharged 2 weeks later to the nursing home.
Can anything be done for these patients?
A GROWING PROBLEM
Dementia is a growing problem with the aging of the population. At the time of the 2000 census there were 4.5 million people in the United States with Alzheimer disease, the most common type of dementia,1 and the prevalence is expected to increase to 13.2 million by the year 2050.1
CONSERVATIVE MEASURES ARE THE MAINSTAY OF TREATMENT
As for offending drugs, removing an antimuscarinic or anticholinergic drug may resolve hallucinations; stopping propoxyphene (Darvon) may improve sleep.
No drugs are approved for treating hallucinations, agitation, or other distressing behavior in neurodegenerative diseases such as Alzheimer dementia. Rather, the mainstay of treatment is behavioral and environmental modification.7 In an environment optimized to maximize comfort, reduce stress, and permit safe wandering, behavioral medications may be unnecessary.
Nevertheless, environments are not always optimal, and physicians may offer medications to treat behavioral symptoms to improve quality of life and to let patients keep living in the community.
Below, we discuss the drugs used to treat behavioral problems in dementia, evidence for the efficacy of these drugs, and their potential for adverse effects.
ANTIPSYCHOTIC DRUGS: SMALL BENEFIT, BIG RISK
Although antipsychotic drugs, both typical and atypical, are often used to treat dementia- related behaviors, their beneficial effects are minimal and adverse effects are common.8,9
Aggression has been considered a symptom that might respond to an atypical antipsychotic drug.10 However, the Clinical Antipsychotic Trials of Intervention Effectiveness—Alzheimer’s Disease (CATIE-AD) trial11 found no differences in efficacy between placebo and the atypical antipsychotics olanzapine (Zyprexa), quetiapine (Seroquel), and risperidone (Risperdal) in treating psychosis, aggression, and agitation in dementia. In that study, rates of drug discontinuation due to adverse effects ranged from 5% for placebo to 24% for olanzapine. Overall, 82% of the patients stopped taking their initially assigned medications during the 36-week period of the trial.11
Antipsychotic drugs may cause more adverse effects in patients with Parkinson disease or dementia with Lewy bodies, and medications with the least dopamine D2 receptor blockade are chosen to reduce the impact on the parkinsonism. Patients with movement disorders were excluded from the CATIE-AD study, and data on this topic are very limited. Quetiapine and olanzapine are often used as alternatives to clozapine (Clozaril) for treating psychosis in Parkinson disease and may have a role in dementia with Lewy bodies.12,13
Atypical antipsychotics carry significant risk of illness and even death. The US Food and Drug Administration (FDA) has published advisories about hyperglycemia, cerebrovascular events, and death.14 Returning to the older, “typical” antipsychotics is not a solution either, given their high incidence of extrapyramidal symptoms15 and potentially higher risk of death.16,17
Even if effective, try stopping the drug
Even in the few situations in dementia in which antipsychotics prove efficacious, a trial of dose-reduction and possible discontinuation is a part of the appropriate plan of care. Symptoms such as aggression and delusions may decrease as the underlying dementia progresses.2 A consensus statement on antipsychotic drug use in the elderly18 recommended stopping antipsychotic drugs as follows:
- If given for delirium—discontinue the drug after 1 week
- For agitated dementia—taper within 3 to 6 months to determine the lowest effective maintenance dose
- For psychotic major depression—discontinue after 6 months
- For mania with psychosis—discontinue after 3 months.18
Disorders for which antipsychotics are not recommended are irritability, hostility, generalized anxiety, and insomnia. In contrast with recommendations for dementia-related behaviors, the psychosis of schizophrenia is treated lifelong at the lowest effective dose of medication.
ANTIDEPRESSANTS: MANY CHOICES, LITTLE EVIDENCE
Depression is hard to assess in a patient with dementia, particularly since apathy is a common symptom in both dementia and depression and may confuse the presentation. Additionally, screening tests for depression have not been validated in the demented elderly.
Depression in dementia is associated with poorer quality of life, greater disability in activities of daily living, a faster cognitive decline, a high rate of nursing home placement, a higher death rate, and a higher frequency of depression and burden in caregivers.19 Quality of life may improve with antidepressant treatment even if the patient does not meet all the criteria for a major depressive disorder. Provisional recommendations for diagnosing depression in dementia suggest using three (instead of five) or more criteria, and include irritability or social isolation as additional criteria.20
Choosing an antidepressant
Only a few randomized controlled trials of antidepressants for depression with dementia have been completed, each with a small number of patients.
Mirtazapine (Remeron) is what we recommend to improve sleep and appetite and restore lost weight.21 It can be used in patients with Parkinson disease or parkinsonian symptoms who experience increased tremors or bradykinesia with selective serotonin reuptake inhibitors (SSRIs). On the other hand, it may not be the best option for those with diabetes mellitus, metabolic syndrome, hyperlipidemia, or obesity. It may rarely also cause a reversible agranulocytosis.
Venlafaxine (Effexor) and duloxetine (Cymbalta) are serotonin-norepinephrine reuptake inhibitors (SNRIs) and may help in concomitant pain syndromes.22 Either drug can cause anorexia at any dose and can elevate blood pressure at higher doses. Venlafaxine may also cause insomnia in some patients.
Bupropion (Wellbutrin) can be difficult to titrate to an effective dose in an older person with unsuspected renal insufficiency, and it may interact at the P450 complex.23 The risk of seizures is greater at higher bupropion serum levels. There is also a high incidence of weight loss. Frail elderly patients, those with hypertension, and those vulnerable to hallucinations will likely do better with another drug.
Nefazodone is a third- or fourth-line antidepressive choice because of the risk of hepatic failure. However, it can help reduce disabling anxiety associated with depression. The FDA requires periodic liver function testing if this drug is used.
Trazodone in low doses (≤ 100 mg) each evening may help with sleep, but it cannot be titrated to antidepressive doses in older adults because of orthostatic effects.
Nortriptyline is recommended by some geriatricians for depression or pathologic crying in patients with mixed vascular dementia. However, it often causes cardiac conduction delays with reflex sympathetic tachycardia and anticholinergic side effects.
Monoamine oxidase inhibitors interact with many foods and drugs, limiting their use in older adults.
Methylphenidate (Ritalin) at low doses is used off-label for depression in palliative care, with noted rapid improvements in mood and appetite.24 Monitoring for increases in blood pressure, heart rate, and respiratory rate is essential if this stimulant is chosen. Patients who respond may make a transition to other traditional drugs after 2 to 4 weeks.
Caveats with SSRIs
- Despite the safety profile of SSRIs in older adults, care must be taken when prescribing them to frail elderly patients, given recent data associating SSRIs with falls and fragility fractures25,26 and urinary incontinence.27
- SSRIs may decrease appetite during initial treatment.
- Sertraline (Zoloft) may have to be started at a very low dose to decrease possible adverse gastrointestinal symptoms, such as diarrhea.
- Paroxetine (Paxil) has multiple interactions at the cytochrome P450 complex and has the most anticholinergic properties of the SSRIs, rendering it more likely to cause adverse drug reactions, constipation, and delirium.
- Daily fluoxetine (Prozac) may not be appropriate in older adults because of its long half-life and the risk of insomnia and agitation.28
- Tremors can emerge with all the SSRIs; akathisia, dystonia, and parkinsonism are also possible.29
- Hyponatremia, bruising, and increased bleeding time can occur with any SSRI.
- Abrupt cessation of any SSRI except fluoxetine (due to its long half-life) or of SNRIs may cause a very unpleasant flu-like withdrawal syndrome.
- Apathy can be a reversible, dose-dependent adverse effect of SSRIs in young persons30; there are no data on the dose at which this adverse effect might emerge in demented elderly patients.
In a systematic review, Sink et al31 found citalopram (Celexa) to help reduce nondepressive agitation.
How long should depression be treated?
Antidepressant treatment is typically for 6 to 12 months. However, the optimal duration in an older adult with dementia is not known and is not addressed in either the American Psychiatric Association practice guideline on dementia32 or the position statement of the American Association for Geriatric Psychiatry.33
Patients with executive dysfunction, particularly those with perseveration and diminished inhibition, may be less likely to respond to antidepressants, and the symptoms are more likely to recur if they do respond.34 It may be appropriate to treat them for a year and then withdraw the drug and monitor for recurrence. Some patients may need indefinite treatment.
No data on treating apathy
Apathy in elderly patients with dementia is common. It is found in nearly half of elderly patients with mild dementia and in nearly all of those with severe dementia. If accompanied by depressive symptoms such as sadness, guilt, feelings of worthlessness, passive or active death wish, changes in sleep or appetite, or tearfulness, apathy and other depressive symptoms may respond to antidepressive treatment—both behavioral and pharmacologic. When present in dementia without depressive symptomatology, apathy is unlikely to respond to antidepressants. In particular, SSRIs may actually induce or worsen apathy through their effect on the angular gyrus. Apathy can be very frustrating to family members but not troublesome at all to the patient.
No medication carries an indication for apathy in dementia. Although stimulants such as methylphenidate and modafinil (Provigil) have been used, there is no evidence to date from any controlled study of efficacy and safety in this population.
Try nondrug measures concomitantly
Given the limited evidence of efficacy of antidepressive therapy in demented elderly patients, nonpharmacologic therapy should be offered concomitantly.
Evidence-based nonpharmacologic treatment for depression in dementia includes increasing enjoyable activities and socialization with people and pets, reducing the need to perform frustrating activities, redirecting perseverative behaviors and speech, and addressing caregiver needs.34 Exercise may improve physical functioning in depression with dementia.35 A comprehensive sleep program may improve associated sleep disorders.36
An intensive collaborative-care intervention37 resulted in more demented elderly patients in the intervention group receiving a cholinesterase inhibitor and an antidepressive than in the usual-care group. Outcomes included fewer behavioral symptoms, less caregiver distress, and less caregiver depression.
So far, no randomized trial has shown electroconvulsive therapy to be effective in elderly patients with depression and dementia.38
ANTICONVULSANT DRUGS MAY STABILIZE MOOD
On the basis of small studies with some contradictory outcomes,39 both older and newer anticonvulsants have been used in nonpsychotic agitation, aggression, and impulsivity in a variety of psychiatric disorders, brain injury, and dementia.40 Most of the data are on the older drugs such as valproic acid and carbamazepine (Tegretol).
Valproic acid is associated with an adverse metabolic profile (hyperglycemia, weight gain, and hyperlipidemia),41,42 dose-related orthostasis, sedation, and worsening cognitive performance. In addition, the possibility of thrombocytopenia and blood level fluctuations requires monitoring. Older adults may tolerate 250 to 500 mg/day with minimal adverse effects.
Carbamazepine reduced aggression in a blinded, placebo-controlled study in nursing home patients.43 Use of carbamazepine requires monitoring of hematologic and liver profiles, alters the metabolism of itself and other drugs, and is associated with dose-related sedation.
Lamotrigine (Lamictal) takes a long time to titrate but may help with nonpsychotic agitation and impulsivity; it is a relatively new drug, and there are limited data to support its use at this time in the elderly.
Gabapentin (Gabarone), in case reports at doses primarily from 600 to 1,200 mg/day, reduced behavioral and psychological problems of patients with dementia and with good renal clearance.44 Some patients may experience tremors or oversedation.
Phenytoin (Dilantin) is not a good choice for behavioral problems because of unwanted effects on teeth, bones, and balance.
Levetiracetam (Keppra) may cause behavioral disturbances to emerge or worsen.45
Emerging evidence suggests that all anticonvulsants may also be associated with an increased risk of depressive symptoms.
COGNITIVE ENHANCERS MAY IMPROVE BEHAVIOR
Acetylcholinesterase inhibitors may improve some behavioral symptoms of dementia. In an open-label retrospective trial, delusionality, irritability, anxiety, disinhibition, and agitation improved in some patients on these drugs.46 Patients most likely to respond were those with the most impairment from these behaviors and those with depressive or apathetic symptoms.46 A Cochrane review found a modest beneficial effect on behavior.47
Acetylcholinesterase inhibitors may reduce symptoms of apathy. Additionally, they actually improve depressive symptoms in mild to moderate dementia independent of any effect on cognition.48
Memantine (Namenda), approved for the treatment of moderate to severe dementia, may reduce the prevalence and incidence of agitation, particularly in more advanced dementia.49
The cognitive enhancers all require several weeks for titration and are not helpful for the acute management of behavioral or depressive symptoms.
OTHER DRUGS
Beta-blockers50 and estrogen51 have been studied as off-label, nonneuroleptic treatments for male aggression. Use of progesterone in men with inappropriate sexual behavior52 may have benefit; further interventions are reviewed by Srinivasan and Weinberg.53 These recommendations are based on small case series. In addition, the hormonal treatments may carry significant morbidity.
Sedative hypnotics were evaluated for sleep difficulties in demented patients in a meta-analysis by Glass et al,54 who found adverse cognitive events, psychomotor events, and daytime fatigue more common (5, 2.6, and 3.8 times, respectively) in the sedative group than in the placebo group.
For agitation in delirium, haloperidol (Haldol) is preferable to benzodiazepines, based on studies from the 1970s.55 Although benzodiazepines carry an indication for anxiety, newly prescribed benzodiazepines and those with a longer half-life are associated with hip fractures in older adults,56 possibly from sedation.
WHAT TO DO FOR YOUR PATIENTS
The 84-year-old woman
For the 84-year-old woman who is keeping her son awake all night, recommend making the environment safe for her to wander, including placing a bolt on the doors leading to the basement and outdoors and moving the knives to an area that she cannot reach, to avoid accidents. Recommend that she be given things to do that are repetitive, such as folding towels and arranging drawers. Referring her to day care may improve socialization and increase physical activity during the day, possibly improving her sleep time at night.
The 82-year-old man
Let’s assume the 82-year-old man arrested and then hospitalized is placed on risperidone 1 mg twice daily prior to discharge to the nursing home. In the nursing home, he becomes irritable with any change in his routine: the door has to be open by exactly 6 inches; his meals have to be identical and served on time; the newspaper needs to arrive by 8 AM. Since routine is paramount in the nursing home, the staff accommodates his need for a very regular schedule. Donepezil (Aricept) and memantine can be added as cognitive enhancers, and citalopram can be added for possible depression and obsessive features. The daughter should then be approached about reducing the risperidone dose and, hopefully, discontinuing it in the future.
Comment. A stable, routine environment is the most important intervention for managing this aggressive resident’s behavior, although he may have been helped to some degree by the adjunct medications. Once he is stable, the daughter may be able to bring him home for weekends and holidays, as long as she is advised never to surprise him with an unexpected visit or to bring home unexpected guests.
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol 2003; 60:1119–1122.
- Holtzer R, Tang MX, Devanand DP, et al. Psychopathological features in Alzheimer's disease: course and relationship with cognitive status. J Am Geriatr Soc 2003; 51:953–960.
- Hart DJ, Craig D, Compton SA, et al. A retrospective study of the behavioural and psychological symptoms of mid and late phase Alzheimer's disease. Int J Geriatr Psychiatry 2003; 18:1037–1042.
- McKeith I, Cummings J. Behavioural changes and psychological symptoms in dementia disorders. Lancet Neurol 2005; 4:735–742.
- Stern Y, Albert M, Brandt J, et al. Utility of extrapyramidal signs and psychosis as predictors of cognitive and functional decline, nursing home admission, and death in Alzheimer's disease: prospective analyses from the Predictors Study. Neurology 1994; 44:2300–2307.
- Chibnall JT, Tait RC, Harman B, Luebbert RA. Effect of acetaminophen on behavior, well-being, and psychotropic medication use in nursing home residents with moderate-to-severe dementia. J Am Geriatr Soc 2005; 53:1921–1929.
- Doody RS, Stevens JC, Beck C, et al. Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2001; 56:1154–1166.
- Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry 2006; 14:191–210.
- Jeste DV, Dolder CR, Nayak GV, Salzman C. Atypical antipsychotics in elderly patients with dementia or schizophrenia: review of recent literature. Harv Rev Psychiatry 2005; 13:340–351.
- Rabinowitz J, Katz IR, De Deyn PP, Brodaty H, Greenspan A, Davidson M. Behavioral and psychological symptoms in patients with dementia as a target for pharmacotherapy with risperidone. J Clin Psychiatry 2004; 65:1329–1334.
- Schneider LS, Tariot PN, Dagerman KS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer's disease. N Engl J Med 2006; 355:1525–1538.
- Fernandez HH, Trieschmann ME, Burke MA, Friedman JH. Quetiapine for psychosis in Parkinson's disease versus dementia with Lewy bodies. J Clin Psychiatry 2002; 63:513–515.
- Cummings JL, Street J, Masterman D, Clark WS. Efficacy of olanzapine in the treatment of psychosis in dementia with Lewy bodies. Dement Geriatr Cogn Disord 2002; 13:67–73.
- US Food and Drug Administration. FDA Public Health Advisory—Deaths with Antipsychotics in Elderly Patients with Behavioral Disturbances: FDA/Center for Drug Evaluation and Research; April 11 2005.
- Lonergan E, Luxenberg J, Colford J. Haloperidol for agitation in dementia. Cochrane Database Syst Rev 2001; (4):CD002852.
- Wang PS, Schneeweiss S, Avorn J, et al. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med 2005; 353:2335–2341.
- Gill SS, Bronskill SE, Normand SL, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med 2007; 146:775–786.
- Alexopoulos GS, Streim J, Carpenter D, Docherty JP; Expert Consensus Panel for Using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry 2004; 65(suppl 2):5–99.
- Starkstein SE, Mizrahi R. Depression in Alzheimer's disease. Expert Rev Neurother 2006; 6:887–895.
- Olin JT, Katz IR, Meyers BS, Schneider LS, Lebowitz BD. Provisional diagnostic criteria for depression of Alzheimer disease: rationale and background. Am J Geriatr Psychiatry 2002; 10:129–141.
- Aronne LJ, Segal KR. Weight gain in the treatment of mood disorders. J Clin Psychiatry 2003; 64(suppl 8):22–29.
- Barkin RL, Barkin S. The role of venlafaxine and duloxetine in the treatment of depression with decremental changes in somatic symptoms of pain, chronic pain, and the pharmacokinetics and clinical considerations of duloxetine pharmacotherapy. Am J Ther 2005; 12:431–438.
- Wilkes S. Bupropion. Drugs Today (Barc) 2006; 42:671–681.
- Homsi J, Walsh D, Nelson KA, LeGrand S, Davis M. Methylphenidate for depression in hospice practice: a case series. Am J Hosp Palliat Care 2000; 17:393–398.
- Kallin K, Lundin-Olsson L, Jensen J, Nyberg L, Gustafson Y. Predisposing and precipitating factors for falls among older people in residential care. Public Health 2002; 116:263–271.
- Richards JB, Papaioannou A, Adachi JD, et al; Canadian Multicentre Osteoporosis Study Research Group. Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med 2007; 167:188–194.
- Movig KL, Leufkens HG, Belitser SV, Lenderink AW, Egberts ACG. Selective serotonin reuptake inhibitor-induced urinary incontinence. Pharmacoepidemiol Drug Saf 2002; 11:271–279.
- Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 2003; 163:2716–2724.
- Leo RJ. Movement disorders associated with the serotonin selective reuptake inhibitors. J Clin Psychiatry 1996; 57:449–454.
- Barnhart WJ, Makela EH, Latocha MJ. SSRI-induced apathy syndrome: a clinical review. J Psychiatr Pract 2004; 10:196–199.
- Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA 2005; 293:596–608.
- American Psychiatric Association. Practice Guideline and Resources for Treatment of Patients with Alzheimer's Disease and Other Dementias, 2nd Edition. October 2007. www.psychiatryonline.com/pracGuide/pracGuideTopic_3.aspx. Accessed 2/2/2009.
- Lyketsos CG, Colenda CC, Beck C, et al; Task Force of American Association for Geriatric Psychiatry. Position Statement of the American Association for Geriatric Psychiatry regarding principles of care for patients with dementia resulting from Alzheimer disease. Am J Geriatr Psychiatry 2006; 14:561–572.
- Potter GG, Steffens DC. Contribution of depression to cognitive impairment and dementia in older adults. Neurologist 2007; 13:105– 117.
- Teri L, Gibbons LE, McCurry SM, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA 2003; 290:2015–2022.
- McCurry SM, Gibbons LE, Logsdon RG, Vitiello MV, Teri L. Nighttime insomnia treatment and education for Alzheimer's disease: a randomized, controlled trial. J Am Geriatr Soc 2005; 53:793–802.
- Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA 2006; 295:2148–2157.
- Van der Wurff FB, Stek ML, Hoogendijk WL, Beekman AT. Electroconvulsive therapy for the depressed elderly. Cochrane Database Syst Rev 2003; ( 2):CD003593.
- Tariot PN, Raman R, Jakimovich L, et al. Divalproex sodium in nursing home residents with possible or probable Alzheimer disease complicated by agitation: a randomized, controlled trial. Am J Geriatr Psychiatry 2005; 13:942–949.
- Kim E. The use of newer anticonvulsants in neuropsychiatric disorders. Curr Psychiatry Rep 2002; 4:331–337.
- Ness-Abramof R, Apovian CM. Drug-induced weight gain. Drugs Today (Barc) 2005; 41:547–555.
- Biton V. Weight change and antiepileptic drugs: health issues and criteria for appropriate selection of an antiepileptic agent. Neurologist 2006; 12:163–167.
- Tariot PN, Erb R, Podgorski CA, et al. Efficacy and tolerability of carbamazepine for agitation and aggression in dementia. Am J Psychiatry 1998; 155:54–61.
- Miller LJ. Gabapentin for treatment of behavioral and psychological symptoms of dementia. Ann Pharmacother 2001; 35:427–431.
- White JR, Walczak TS, Leppik IE, et al. Discontinuation of levetiracetam because of behavioral side effects: a case-control study. Neurology 2003; 61:1218–1221.
- Mega S, Masterman DM, O'Connor SM, Barclay TR, Cummings JL. The spectrum of behavioral responses to cholinesterase inhibitor therapy in Alzheimer disease. Arch Neurol 1999; 56:1388–1393.
- Birks J. Cholinesterase inhibitors for Alzheimer's disease. Cochrane Database of Syst Rev 2006; (1):CD005593.
- Rozzini L, Vicini Chilovi B, Bertoletti E, Trabucchi M, Padovani A. Acetyl-cholinesterase inhibitors and depressive symptoms in patients with mild to moderate Alzheimer's disease. Aging Clin Exp Res 2007; 19:220–223.
- McShane R, Areosa Sastre A, Minakaran N. Memantine for dementia. Cochrane Database Syst Rev 2006; (2):CD003154.
- Peskind ER, Tsuang DW, Bonner LT, et al. Propranolol for disruptive behaviors in nursing home residents with probable or possible Alzheimer disease: a placebo-controlled study. Alzheimer Dis Assoc Disord 2005; 19:23–28.
- Hall KA, Keks NA, O'Connor DW. Transdermal estrogen patches for aggressive behavior in male patients with dementia: a randomized, controlled trial. Int Psychogeriatr 2005; 17:165–178.
- Light SA, Holroyd S. The use of medroxyprogesterone acetate for the treatment of sexually inappropriate behaviour in patients with dementia. J Psychiatry Neurosci 2006; 31:132–134.
- Srinivasan S, Weinberg A. Pharmacologic treatment of sexual inappropriateness in long-term care residents with dementia. Ann Long-Term Care: Clin Care Aging 2006; 14:20–28.
- Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 2005; 331:1169.
- Kirven LE, Montero EF. Comparison of thioridazine and diazepam in the control of nonpsychotic symptoms associated with senility: double-blind study. J Am Geriatr Soc 1973; 21:546–551.
- Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs 2003; 17:825–837.
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol 2003; 60:1119–1122.
- Holtzer R, Tang MX, Devanand DP, et al. Psychopathological features in Alzheimer's disease: course and relationship with cognitive status. J Am Geriatr Soc 2003; 51:953–960.
- Hart DJ, Craig D, Compton SA, et al. A retrospective study of the behavioural and psychological symptoms of mid and late phase Alzheimer's disease. Int J Geriatr Psychiatry 2003; 18:1037–1042.
- McKeith I, Cummings J. Behavioural changes and psychological symptoms in dementia disorders. Lancet Neurol 2005; 4:735–742.
- Stern Y, Albert M, Brandt J, et al. Utility of extrapyramidal signs and psychosis as predictors of cognitive and functional decline, nursing home admission, and death in Alzheimer's disease: prospective analyses from the Predictors Study. Neurology 1994; 44:2300–2307.
- Chibnall JT, Tait RC, Harman B, Luebbert RA. Effect of acetaminophen on behavior, well-being, and psychotropic medication use in nursing home residents with moderate-to-severe dementia. J Am Geriatr Soc 2005; 53:1921–1929.
- Doody RS, Stevens JC, Beck C, et al. Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2001; 56:1154–1166.
- Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry 2006; 14:191–210.
- Jeste DV, Dolder CR, Nayak GV, Salzman C. Atypical antipsychotics in elderly patients with dementia or schizophrenia: review of recent literature. Harv Rev Psychiatry 2005; 13:340–351.
- Rabinowitz J, Katz IR, De Deyn PP, Brodaty H, Greenspan A, Davidson M. Behavioral and psychological symptoms in patients with dementia as a target for pharmacotherapy with risperidone. J Clin Psychiatry 2004; 65:1329–1334.
- Schneider LS, Tariot PN, Dagerman KS, et al. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer's disease. N Engl J Med 2006; 355:1525–1538.
- Fernandez HH, Trieschmann ME, Burke MA, Friedman JH. Quetiapine for psychosis in Parkinson's disease versus dementia with Lewy bodies. J Clin Psychiatry 2002; 63:513–515.
- Cummings JL, Street J, Masterman D, Clark WS. Efficacy of olanzapine in the treatment of psychosis in dementia with Lewy bodies. Dement Geriatr Cogn Disord 2002; 13:67–73.
- US Food and Drug Administration. FDA Public Health Advisory—Deaths with Antipsychotics in Elderly Patients with Behavioral Disturbances: FDA/Center for Drug Evaluation and Research; April 11 2005.
- Lonergan E, Luxenberg J, Colford J. Haloperidol for agitation in dementia. Cochrane Database Syst Rev 2001; (4):CD002852.
- Wang PS, Schneeweiss S, Avorn J, et al. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med 2005; 353:2335–2341.
- Gill SS, Bronskill SE, Normand SL, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med 2007; 146:775–786.
- Alexopoulos GS, Streim J, Carpenter D, Docherty JP; Expert Consensus Panel for Using Antipsychotic Drugs in Older Patients. Using antipsychotic agents in older patients. J Clin Psychiatry 2004; 65(suppl 2):5–99.
- Starkstein SE, Mizrahi R. Depression in Alzheimer's disease. Expert Rev Neurother 2006; 6:887–895.
- Olin JT, Katz IR, Meyers BS, Schneider LS, Lebowitz BD. Provisional diagnostic criteria for depression of Alzheimer disease: rationale and background. Am J Geriatr Psychiatry 2002; 10:129–141.
- Aronne LJ, Segal KR. Weight gain in the treatment of mood disorders. J Clin Psychiatry 2003; 64(suppl 8):22–29.
- Barkin RL, Barkin S. The role of venlafaxine and duloxetine in the treatment of depression with decremental changes in somatic symptoms of pain, chronic pain, and the pharmacokinetics and clinical considerations of duloxetine pharmacotherapy. Am J Ther 2005; 12:431–438.
- Wilkes S. Bupropion. Drugs Today (Barc) 2006; 42:671–681.
- Homsi J, Walsh D, Nelson KA, LeGrand S, Davis M. Methylphenidate for depression in hospice practice: a case series. Am J Hosp Palliat Care 2000; 17:393–398.
- Kallin K, Lundin-Olsson L, Jensen J, Nyberg L, Gustafson Y. Predisposing and precipitating factors for falls among older people in residential care. Public Health 2002; 116:263–271.
- Richards JB, Papaioannou A, Adachi JD, et al; Canadian Multicentre Osteoporosis Study Research Group. Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med 2007; 167:188–194.
- Movig KL, Leufkens HG, Belitser SV, Lenderink AW, Egberts ACG. Selective serotonin reuptake inhibitor-induced urinary incontinence. Pharmacoepidemiol Drug Saf 2002; 11:271–279.
- Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 2003; 163:2716–2724.
- Leo RJ. Movement disorders associated with the serotonin selective reuptake inhibitors. J Clin Psychiatry 1996; 57:449–454.
- Barnhart WJ, Makela EH, Latocha MJ. SSRI-induced apathy syndrome: a clinical review. J Psychiatr Pract 2004; 10:196–199.
- Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA 2005; 293:596–608.
- American Psychiatric Association. Practice Guideline and Resources for Treatment of Patients with Alzheimer's Disease and Other Dementias, 2nd Edition. October 2007. www.psychiatryonline.com/pracGuide/pracGuideTopic_3.aspx. Accessed 2/2/2009.
- Lyketsos CG, Colenda CC, Beck C, et al; Task Force of American Association for Geriatric Psychiatry. Position Statement of the American Association for Geriatric Psychiatry regarding principles of care for patients with dementia resulting from Alzheimer disease. Am J Geriatr Psychiatry 2006; 14:561–572.
- Potter GG, Steffens DC. Contribution of depression to cognitive impairment and dementia in older adults. Neurologist 2007; 13:105– 117.
- Teri L, Gibbons LE, McCurry SM, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial. JAMA 2003; 290:2015–2022.
- McCurry SM, Gibbons LE, Logsdon RG, Vitiello MV, Teri L. Nighttime insomnia treatment and education for Alzheimer's disease: a randomized, controlled trial. J Am Geriatr Soc 2005; 53:793–802.
- Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA 2006; 295:2148–2157.
- Van der Wurff FB, Stek ML, Hoogendijk WL, Beekman AT. Electroconvulsive therapy for the depressed elderly. Cochrane Database Syst Rev 2003; ( 2):CD003593.
- Tariot PN, Raman R, Jakimovich L, et al. Divalproex sodium in nursing home residents with possible or probable Alzheimer disease complicated by agitation: a randomized, controlled trial. Am J Geriatr Psychiatry 2005; 13:942–949.
- Kim E. The use of newer anticonvulsants in neuropsychiatric disorders. Curr Psychiatry Rep 2002; 4:331–337.
- Ness-Abramof R, Apovian CM. Drug-induced weight gain. Drugs Today (Barc) 2005; 41:547–555.
- Biton V. Weight change and antiepileptic drugs: health issues and criteria for appropriate selection of an antiepileptic agent. Neurologist 2006; 12:163–167.
- Tariot PN, Erb R, Podgorski CA, et al. Efficacy and tolerability of carbamazepine for agitation and aggression in dementia. Am J Psychiatry 1998; 155:54–61.
- Miller LJ. Gabapentin for treatment of behavioral and psychological symptoms of dementia. Ann Pharmacother 2001; 35:427–431.
- White JR, Walczak TS, Leppik IE, et al. Discontinuation of levetiracetam because of behavioral side effects: a case-control study. Neurology 2003; 61:1218–1221.
- Mega S, Masterman DM, O'Connor SM, Barclay TR, Cummings JL. The spectrum of behavioral responses to cholinesterase inhibitor therapy in Alzheimer disease. Arch Neurol 1999; 56:1388–1393.
- Birks J. Cholinesterase inhibitors for Alzheimer's disease. Cochrane Database of Syst Rev 2006; (1):CD005593.
- Rozzini L, Vicini Chilovi B, Bertoletti E, Trabucchi M, Padovani A. Acetyl-cholinesterase inhibitors and depressive symptoms in patients with mild to moderate Alzheimer's disease. Aging Clin Exp Res 2007; 19:220–223.
- McShane R, Areosa Sastre A, Minakaran N. Memantine for dementia. Cochrane Database Syst Rev 2006; (2):CD003154.
- Peskind ER, Tsuang DW, Bonner LT, et al. Propranolol for disruptive behaviors in nursing home residents with probable or possible Alzheimer disease: a placebo-controlled study. Alzheimer Dis Assoc Disord 2005; 19:23–28.
- Hall KA, Keks NA, O'Connor DW. Transdermal estrogen patches for aggressive behavior in male patients with dementia: a randomized, controlled trial. Int Psychogeriatr 2005; 17:165–178.
- Light SA, Holroyd S. The use of medroxyprogesterone acetate for the treatment of sexually inappropriate behaviour in patients with dementia. J Psychiatry Neurosci 2006; 31:132–134.
- Srinivasan S, Weinberg A. Pharmacologic treatment of sexual inappropriateness in long-term care residents with dementia. Ann Long-Term Care: Clin Care Aging 2006; 14:20–28.
- Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ 2005; 331:1169.
- Kirven LE, Montero EF. Comparison of thioridazine and diazepam in the control of nonpsychotic symptoms associated with senility: double-blind study. J Am Geriatr Soc 1973; 21:546–551.
- Cumming RG, Le Couteur DG. Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs 2003; 17:825–837.
KEY POINTS
- No drug specifically addresses wandering, hoarding, or resistance to care, behaviors that are particularly frustrating to caregivers.
- Many drugs are sedating and increase the risk of falling and injury; antipsychotic use is off-label for dementia and carries significant and possibly lethal adverse effects.
- Managing the behavioral symptoms of dementia requires attention to the environmental and psychosocial context in which they occur, as well as to comorbidities and potential adverse drug effects.
- Evidence for the efficacy of antidepressants for depression in dementia is limited.