User login
House budget includes SGR patch; permanent fix sails through committees
WASHINGTON – Congress has moved the ball forward on permanently replacing the Medicare Sustainable Growth Rate formula, but with time short for a fix by year’s end the House has voted to approve a temporary 3-month reprieve from the 20% cut due to take effect Jan. 1.
In a 332-94 vote, with eight abstentions, the House on Dec. 12 approved the Bipartisan Budget Act of 2013, a wide-ranging budget agreement that includes the 3-month patch. The bill also would increase physician pay by 0.5% through March.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. The fix would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
It also would extend the 2% sequestration cuts for Medicare providers by 2 years, from 2021 to 2023.
The Senate has yet to consider the budget package including the SGR patch; it is expected to do so before its holiday recess. President Obama has said that he supports the deal.
The agreement, brokered by House Budget Committee Chairman Paul Ryan (R-Wisc.) and Senate Budget Committee Chairman Patty Murray (D-Wash.), adds about $63 billion in discretionary federal spending over 2 years and makes targeted cuts and fee hikes to bring about overall deficit reduction of about $23 billion.
Although physician groups aren’t thrilled about the continuation of the Medicare cuts under sequestration, most favor the temporary SGR reprieve and the restoration of some funding to federal health programs.
Dr. Ardis Dee Hoven, president of the American Medical Association, said that the continuation of the sequester cuts in Medicare is "frustrating" and poses the risk of destabilizing physician practices. "The concept of the sequester is probably not the best way to rein in spending," she said.
Dr. Clifford A. Hudis, president of the American Society of Clinical Oncology, praised the agreement for providing funds that could restore cuts in medical research and cancer care at the National Institutes of Health. He expressed disappointment, however, that the bill does not reverse cuts to Medicare, including reductions in the payments for physician-administered drugs under Medicare Part B.
"Oncologists are doing everything possible to continue providing care for Medicare patients, but this reduction has forced many in private practice to send patients to hospitals for chemotherapy because they cannot afford to administer these drugs in their office," Dr. Hudis said in a statement.
Physician organizations viewed the patch as necessary while Congress continues to work on a permanent SGR fix. Both the House and Senate took steps toward that goal on Dec. 12.
The House Ways and Means Committee voted 39-0 to approve its replacement proposal, which essentially adds on to the bill approved by the House Energy and Commerce Committee in July.
"This may not be the final step, it’s a very important step forward," said Rep. Kevin Brady (R-Tex.), chairman of the Ways and Means Health Subcommittee.
The House did not address how to pay for the permanent replacement. House Ways and Means Chairman Dave Camp (R-Mich.) noted that the Congressional Budget Office has estimated that it will cost $116 billion over 10 years to repeal the SGR, which is "more than half the cost 2 years ago." Even though that is the lowest estimate ever, "I am of no illusion that finding pay-fors will be an easy task," he said.
The Senate Finance Committee also did not include a way to pay for repeal in its proposal.
The bill had widespread bipartisan support in the committee, but some Senators raised concerns about the lack of a funding mechanism. Sen. Pat Roberts (R-Kan.) said that he wouldn’t support the bill until he could see how it would be funded.
Sen. Orrin Hatch (R- Utah), the committee’s top-ranking Republican, said that the offsets would be worked out once the bill had cleared the initial policymaking phase.
"This bill will be offset, period, or it’s not going to go through both houses," he said. "This bill will be paid for."
The panel agreed to add a provision aimed at expanding access to community mental health services. The amendment, offered by Sen. Debbie Stabenow (D-Mich.) and Sen. Roy Blunt (R-Mo.), would create pilot programs in 10 states to ensure that community behavioral health clinics offer a full range of mental health services, including 24-hour crisis care, substance abuse treatment, and expanded support for families.
Physician groups praised the continued congressional action.
The AMA "strongly commends members of the House Ways and Means Committee and the Senate Finance Committee for the tremendous progress they have made toward repealing Medicare’s failed Sustainable Growth Rate (SGR) formula and creating a stronger Medicare program," Dr. Hoven said in a statement. "The AMA will continue to work collaboratively with Congress so that a bipartisan agreement can be signed into law early next year to repeal the failed SGR payment formula."
The American College of Physicians said that it, too, would work to ensure that a bill moves through Congress and gets to the White House for approval soon.
"The bills reported today ... will help ensure that Medicare patients continue to have access to their physicians," said Dr. Charles Cutler, chairman of the ACP Board of Regents. "Their efforts will work to stabilize payments, provide multiple pathways for physicians to qualify for positive updates and to participate in alternative payment models, create positive incentives for patient-centered medical homes, provide assistance to small practices, and needed funding for development of quality measures."
The American College of Cardiology said in a statement that the proposals accomplished two of its highest priorities: eliminating the SGR and including provisions that will emphasize quality of care, including "provisions that emphasize the importance of clinical data registries, quality measure development, and appropriate use criteria to promote evidence-based care."
"We caution that our final support rests upon the caveat that paying for this legislation must not cause harm to patients and the physicians who care for them," Dr. John Gordon Harold, ACC president, said in the statement.
Legislators from the Finance Committee and the Ways and Means Committee celebrated their votes in a joint statement. In the statement, Sen. Hatch also issued a word of caution.
"Now that this legislation moves out of Committee and onto the floor, we need to continue to work together to ensure that this smart policy becomes law and ensure that it doesn’t add one dime to our nation’s debt."
WASHINGTON – Congress has moved the ball forward on permanently replacing the Medicare Sustainable Growth Rate formula, but with time short for a fix by year’s end the House has voted to approve a temporary 3-month reprieve from the 20% cut due to take effect Jan. 1.
In a 332-94 vote, with eight abstentions, the House on Dec. 12 approved the Bipartisan Budget Act of 2013, a wide-ranging budget agreement that includes the 3-month patch. The bill also would increase physician pay by 0.5% through March.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. The fix would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
It also would extend the 2% sequestration cuts for Medicare providers by 2 years, from 2021 to 2023.
The Senate has yet to consider the budget package including the SGR patch; it is expected to do so before its holiday recess. President Obama has said that he supports the deal.
The agreement, brokered by House Budget Committee Chairman Paul Ryan (R-Wisc.) and Senate Budget Committee Chairman Patty Murray (D-Wash.), adds about $63 billion in discretionary federal spending over 2 years and makes targeted cuts and fee hikes to bring about overall deficit reduction of about $23 billion.
Although physician groups aren’t thrilled about the continuation of the Medicare cuts under sequestration, most favor the temporary SGR reprieve and the restoration of some funding to federal health programs.
Dr. Ardis Dee Hoven, president of the American Medical Association, said that the continuation of the sequester cuts in Medicare is "frustrating" and poses the risk of destabilizing physician practices. "The concept of the sequester is probably not the best way to rein in spending," she said.
Dr. Clifford A. Hudis, president of the American Society of Clinical Oncology, praised the agreement for providing funds that could restore cuts in medical research and cancer care at the National Institutes of Health. He expressed disappointment, however, that the bill does not reverse cuts to Medicare, including reductions in the payments for physician-administered drugs under Medicare Part B.
"Oncologists are doing everything possible to continue providing care for Medicare patients, but this reduction has forced many in private practice to send patients to hospitals for chemotherapy because they cannot afford to administer these drugs in their office," Dr. Hudis said in a statement.
Physician organizations viewed the patch as necessary while Congress continues to work on a permanent SGR fix. Both the House and Senate took steps toward that goal on Dec. 12.
The House Ways and Means Committee voted 39-0 to approve its replacement proposal, which essentially adds on to the bill approved by the House Energy and Commerce Committee in July.
"This may not be the final step, it’s a very important step forward," said Rep. Kevin Brady (R-Tex.), chairman of the Ways and Means Health Subcommittee.
The House did not address how to pay for the permanent replacement. House Ways and Means Chairman Dave Camp (R-Mich.) noted that the Congressional Budget Office has estimated that it will cost $116 billion over 10 years to repeal the SGR, which is "more than half the cost 2 years ago." Even though that is the lowest estimate ever, "I am of no illusion that finding pay-fors will be an easy task," he said.
The Senate Finance Committee also did not include a way to pay for repeal in its proposal.
The bill had widespread bipartisan support in the committee, but some Senators raised concerns about the lack of a funding mechanism. Sen. Pat Roberts (R-Kan.) said that he wouldn’t support the bill until he could see how it would be funded.
Sen. Orrin Hatch (R- Utah), the committee’s top-ranking Republican, said that the offsets would be worked out once the bill had cleared the initial policymaking phase.
"This bill will be offset, period, or it’s not going to go through both houses," he said. "This bill will be paid for."
The panel agreed to add a provision aimed at expanding access to community mental health services. The amendment, offered by Sen. Debbie Stabenow (D-Mich.) and Sen. Roy Blunt (R-Mo.), would create pilot programs in 10 states to ensure that community behavioral health clinics offer a full range of mental health services, including 24-hour crisis care, substance abuse treatment, and expanded support for families.
Physician groups praised the continued congressional action.
The AMA "strongly commends members of the House Ways and Means Committee and the Senate Finance Committee for the tremendous progress they have made toward repealing Medicare’s failed Sustainable Growth Rate (SGR) formula and creating a stronger Medicare program," Dr. Hoven said in a statement. "The AMA will continue to work collaboratively with Congress so that a bipartisan agreement can be signed into law early next year to repeal the failed SGR payment formula."
The American College of Physicians said that it, too, would work to ensure that a bill moves through Congress and gets to the White House for approval soon.
"The bills reported today ... will help ensure that Medicare patients continue to have access to their physicians," said Dr. Charles Cutler, chairman of the ACP Board of Regents. "Their efforts will work to stabilize payments, provide multiple pathways for physicians to qualify for positive updates and to participate in alternative payment models, create positive incentives for patient-centered medical homes, provide assistance to small practices, and needed funding for development of quality measures."
The American College of Cardiology said in a statement that the proposals accomplished two of its highest priorities: eliminating the SGR and including provisions that will emphasize quality of care, including "provisions that emphasize the importance of clinical data registries, quality measure development, and appropriate use criteria to promote evidence-based care."
"We caution that our final support rests upon the caveat that paying for this legislation must not cause harm to patients and the physicians who care for them," Dr. John Gordon Harold, ACC president, said in the statement.
Legislators from the Finance Committee and the Ways and Means Committee celebrated their votes in a joint statement. In the statement, Sen. Hatch also issued a word of caution.
"Now that this legislation moves out of Committee and onto the floor, we need to continue to work together to ensure that this smart policy becomes law and ensure that it doesn’t add one dime to our nation’s debt."
WASHINGTON – Congress has moved the ball forward on permanently replacing the Medicare Sustainable Growth Rate formula, but with time short for a fix by year’s end the House has voted to approve a temporary 3-month reprieve from the 20% cut due to take effect Jan. 1.
In a 332-94 vote, with eight abstentions, the House on Dec. 12 approved the Bipartisan Budget Act of 2013, a wide-ranging budget agreement that includes the 3-month patch. The bill also would increase physician pay by 0.5% through March.
The Congressional Budget Office estimated that the temporary fix would cost $3.3 billion in 2014 and a total of $7.3 billion through 2023. The fix would be paid for by cutting Medicaid payments for hospital-based charity care and to long-term care hospitals.
It also would extend the 2% sequestration cuts for Medicare providers by 2 years, from 2021 to 2023.
The Senate has yet to consider the budget package including the SGR patch; it is expected to do so before its holiday recess. President Obama has said that he supports the deal.
The agreement, brokered by House Budget Committee Chairman Paul Ryan (R-Wisc.) and Senate Budget Committee Chairman Patty Murray (D-Wash.), adds about $63 billion in discretionary federal spending over 2 years and makes targeted cuts and fee hikes to bring about overall deficit reduction of about $23 billion.
Although physician groups aren’t thrilled about the continuation of the Medicare cuts under sequestration, most favor the temporary SGR reprieve and the restoration of some funding to federal health programs.
Dr. Ardis Dee Hoven, president of the American Medical Association, said that the continuation of the sequester cuts in Medicare is "frustrating" and poses the risk of destabilizing physician practices. "The concept of the sequester is probably not the best way to rein in spending," she said.
Dr. Clifford A. Hudis, president of the American Society of Clinical Oncology, praised the agreement for providing funds that could restore cuts in medical research and cancer care at the National Institutes of Health. He expressed disappointment, however, that the bill does not reverse cuts to Medicare, including reductions in the payments for physician-administered drugs under Medicare Part B.
"Oncologists are doing everything possible to continue providing care for Medicare patients, but this reduction has forced many in private practice to send patients to hospitals for chemotherapy because they cannot afford to administer these drugs in their office," Dr. Hudis said in a statement.
Physician organizations viewed the patch as necessary while Congress continues to work on a permanent SGR fix. Both the House and Senate took steps toward that goal on Dec. 12.
The House Ways and Means Committee voted 39-0 to approve its replacement proposal, which essentially adds on to the bill approved by the House Energy and Commerce Committee in July.
"This may not be the final step, it’s a very important step forward," said Rep. Kevin Brady (R-Tex.), chairman of the Ways and Means Health Subcommittee.
The House did not address how to pay for the permanent replacement. House Ways and Means Chairman Dave Camp (R-Mich.) noted that the Congressional Budget Office has estimated that it will cost $116 billion over 10 years to repeal the SGR, which is "more than half the cost 2 years ago." Even though that is the lowest estimate ever, "I am of no illusion that finding pay-fors will be an easy task," he said.
The Senate Finance Committee also did not include a way to pay for repeal in its proposal.
The bill had widespread bipartisan support in the committee, but some Senators raised concerns about the lack of a funding mechanism. Sen. Pat Roberts (R-Kan.) said that he wouldn’t support the bill until he could see how it would be funded.
Sen. Orrin Hatch (R- Utah), the committee’s top-ranking Republican, said that the offsets would be worked out once the bill had cleared the initial policymaking phase.
"This bill will be offset, period, or it’s not going to go through both houses," he said. "This bill will be paid for."
The panel agreed to add a provision aimed at expanding access to community mental health services. The amendment, offered by Sen. Debbie Stabenow (D-Mich.) and Sen. Roy Blunt (R-Mo.), would create pilot programs in 10 states to ensure that community behavioral health clinics offer a full range of mental health services, including 24-hour crisis care, substance abuse treatment, and expanded support for families.
Physician groups praised the continued congressional action.
The AMA "strongly commends members of the House Ways and Means Committee and the Senate Finance Committee for the tremendous progress they have made toward repealing Medicare’s failed Sustainable Growth Rate (SGR) formula and creating a stronger Medicare program," Dr. Hoven said in a statement. "The AMA will continue to work collaboratively with Congress so that a bipartisan agreement can be signed into law early next year to repeal the failed SGR payment formula."
The American College of Physicians said that it, too, would work to ensure that a bill moves through Congress and gets to the White House for approval soon.
"The bills reported today ... will help ensure that Medicare patients continue to have access to their physicians," said Dr. Charles Cutler, chairman of the ACP Board of Regents. "Their efforts will work to stabilize payments, provide multiple pathways for physicians to qualify for positive updates and to participate in alternative payment models, create positive incentives for patient-centered medical homes, provide assistance to small practices, and needed funding for development of quality measures."
The American College of Cardiology said in a statement that the proposals accomplished two of its highest priorities: eliminating the SGR and including provisions that will emphasize quality of care, including "provisions that emphasize the importance of clinical data registries, quality measure development, and appropriate use criteria to promote evidence-based care."
"We caution that our final support rests upon the caveat that paying for this legislation must not cause harm to patients and the physicians who care for them," Dr. John Gordon Harold, ACC president, said in the statement.
Legislators from the Finance Committee and the Ways and Means Committee celebrated their votes in a joint statement. In the statement, Sen. Hatch also issued a word of caution.
"Now that this legislation moves out of Committee and onto the floor, we need to continue to work together to ensure that this smart policy becomes law and ensure that it doesn’t add one dime to our nation’s debt."
NIH launches national stroke trials network
The National Institutes of Health is launching a network of regional stroke centers with the aim of quickly advancing research from early testing to late-stage clinical trials.
The new national network, which will be funded and managed by the National Institute of Neurological Disorders and Stroke (NINDS), includes 25 regional stroke centers and nearby satellite facilities. Each of the centers will receive $250,000 annually for 3 years to cover research costs and training. NINDS will award additional funding as the centers complete milestones set by the agency.
"The new system is intended to streamline stroke research, by centralizing approval and review, lessening time and costs of clinical trials, and assembling a comprehensive data sharing system," Dr. Petra Kaufman, associate director for clinical research at NINDS, said in a statement.
The effort will be coordinated by the University of Cincinnati, which will oversee the institutional review board and all master trial agreements.
The goal is to initiate up to five phase I and II clinical trials and up to four phase III trials over the next 5 years, according to NINDS.
The National Institutes of Health is launching a network of regional stroke centers with the aim of quickly advancing research from early testing to late-stage clinical trials.
The new national network, which will be funded and managed by the National Institute of Neurological Disorders and Stroke (NINDS), includes 25 regional stroke centers and nearby satellite facilities. Each of the centers will receive $250,000 annually for 3 years to cover research costs and training. NINDS will award additional funding as the centers complete milestones set by the agency.
"The new system is intended to streamline stroke research, by centralizing approval and review, lessening time and costs of clinical trials, and assembling a comprehensive data sharing system," Dr. Petra Kaufman, associate director for clinical research at NINDS, said in a statement.
The effort will be coordinated by the University of Cincinnati, which will oversee the institutional review board and all master trial agreements.
The goal is to initiate up to five phase I and II clinical trials and up to four phase III trials over the next 5 years, according to NINDS.
The National Institutes of Health is launching a network of regional stroke centers with the aim of quickly advancing research from early testing to late-stage clinical trials.
The new national network, which will be funded and managed by the National Institute of Neurological Disorders and Stroke (NINDS), includes 25 regional stroke centers and nearby satellite facilities. Each of the centers will receive $250,000 annually for 3 years to cover research costs and training. NINDS will award additional funding as the centers complete milestones set by the agency.
"The new system is intended to streamline stroke research, by centralizing approval and review, lessening time and costs of clinical trials, and assembling a comprehensive data sharing system," Dr. Petra Kaufman, associate director for clinical research at NINDS, said in a statement.
The effort will be coordinated by the University of Cincinnati, which will oversee the institutional review board and all master trial agreements.
The goal is to initiate up to five phase I and II clinical trials and up to four phase III trials over the next 5 years, according to NINDS.
Dartmouth Atlas: Wide variation in children’s health care
Just as with adults, the quality of health care that children receive often depends more on their zip code than their health status.
A new report from the Dartmouth Atlas Project found dramatic variation in outpatient physician services, hospitalizations, common surgical procedures, imaging, and prescriptions for infants and children living in Maine, New Hampshire, and Vermont.
The Dartmouth Atlas Project has issued a series of reports over the past 20 years showing wide geographic variation in the care of elderly adults, but this is the first time that the group has focused on infants and children under age 18 who have either commercial insurance or coverage through their state Medicaid programs.
The researchers focused specifically on Maine, New Hampshire, and Vermont because they are the only states that mandate the collection of insurance claims data from both commercial plans and Medicaid. The study looks at services provided from 2007 through 2010.
The researchers found that there is as much variation in pediatric health care as they found previously in care of the elderly, according to Dr. David C. Goodman, the lead author of the study and a professor of pediatrics at the Geisel School of Medicine at Dartmouth in Hanover, N.H.
"Health care has a general problem, which is reflected in essentially any population that we study," Dr. Goodman said.
The problem is that well-meaning physicians often don’t have the information they need to understand what kind of care they are providing and how it differs from what’s being done by their peers, he said.
While some of the variation detected in the study is explained by socioeconomic differences, most of it reflects distinctive practice styles across the different health care systems in the region, Dr. Goodman explained during a Dec. 11 press conference to release the Dartmouth Atlas findings.
In some cases, the findings show underuse of recommended treatments and services, such as lead screening for the Medicaid population and follow-up visits for children who are taking medications for attention-deficit/hyperactivity disorder (ADHD).
Across the three northern New England states analyzed, nearly 44% of children who were prescribed ADHD medication had a recommended follow-up appointment within 30 days in 2009-2010. But individual regions varied greatly. In Newport, Vt., nearly 70% of children had an initial follow-up, compared with only 35% in Lewiston, Maine.
Common surgical procedures also tended to vary widely based on the individual practice styles of physicians and surgeons, Dr. Goodman said, resulting in both under- and overuse.
For instance, tympanostomy tube insertion procedures for ear infections were performed more than four times as often in Middlebury, Vt., than in Bangor, Maine. In Middlebury, physicians performed 15.2 procedures per 1,000 children, compared with 3.4 procedures per 1,000 children in Bangor.
The report also revealed wide variations in access to care. And the result is that in areas where there were a high number of visits to physician offices, trips to the emergency department (ED) were much less common.
The average annual office visit rate, including visits to primary care and subspecialty offices and clinics, was 2.8 visits per child across the three New England states. But the visit rates varied more than threefold across the different regions.
The annual ED visit rate was 359 per 1,000 children during 2007-2010. Similarly, ED visits varied nearly threefold across the various regions. The common causes for ED visits included upper respiratory infections, minor injuries such as contusions and sprains, otitis media, and open wounds.
Dr. Goodman said he hopes that physicians will see the new data and become curious about the type of care they are providing. Physicians and hospitals can be "powerful change agents" when they start asking themselves what is driving their care practices, he said.
The Dartmouth Atlas Project, which is located at the Dartmouth Institute for Health Policy and Clinical Practice, is principally funded by the Robert Wood Johnson Foundation, with support from a consortium of funders. The new pediatric report was supported by a grant from the Charles H. Hood Foundation.
Just as with adults, the quality of health care that children receive often depends more on their zip code than their health status.
A new report from the Dartmouth Atlas Project found dramatic variation in outpatient physician services, hospitalizations, common surgical procedures, imaging, and prescriptions for infants and children living in Maine, New Hampshire, and Vermont.
The Dartmouth Atlas Project has issued a series of reports over the past 20 years showing wide geographic variation in the care of elderly adults, but this is the first time that the group has focused on infants and children under age 18 who have either commercial insurance or coverage through their state Medicaid programs.
The researchers focused specifically on Maine, New Hampshire, and Vermont because they are the only states that mandate the collection of insurance claims data from both commercial plans and Medicaid. The study looks at services provided from 2007 through 2010.
The researchers found that there is as much variation in pediatric health care as they found previously in care of the elderly, according to Dr. David C. Goodman, the lead author of the study and a professor of pediatrics at the Geisel School of Medicine at Dartmouth in Hanover, N.H.
"Health care has a general problem, which is reflected in essentially any population that we study," Dr. Goodman said.
The problem is that well-meaning physicians often don’t have the information they need to understand what kind of care they are providing and how it differs from what’s being done by their peers, he said.
While some of the variation detected in the study is explained by socioeconomic differences, most of it reflects distinctive practice styles across the different health care systems in the region, Dr. Goodman explained during a Dec. 11 press conference to release the Dartmouth Atlas findings.
In some cases, the findings show underuse of recommended treatments and services, such as lead screening for the Medicaid population and follow-up visits for children who are taking medications for attention-deficit/hyperactivity disorder (ADHD).
Across the three northern New England states analyzed, nearly 44% of children who were prescribed ADHD medication had a recommended follow-up appointment within 30 days in 2009-2010. But individual regions varied greatly. In Newport, Vt., nearly 70% of children had an initial follow-up, compared with only 35% in Lewiston, Maine.
Common surgical procedures also tended to vary widely based on the individual practice styles of physicians and surgeons, Dr. Goodman said, resulting in both under- and overuse.
For instance, tympanostomy tube insertion procedures for ear infections were performed more than four times as often in Middlebury, Vt., than in Bangor, Maine. In Middlebury, physicians performed 15.2 procedures per 1,000 children, compared with 3.4 procedures per 1,000 children in Bangor.
The report also revealed wide variations in access to care. And the result is that in areas where there were a high number of visits to physician offices, trips to the emergency department (ED) were much less common.
The average annual office visit rate, including visits to primary care and subspecialty offices and clinics, was 2.8 visits per child across the three New England states. But the visit rates varied more than threefold across the different regions.
The annual ED visit rate was 359 per 1,000 children during 2007-2010. Similarly, ED visits varied nearly threefold across the various regions. The common causes for ED visits included upper respiratory infections, minor injuries such as contusions and sprains, otitis media, and open wounds.
Dr. Goodman said he hopes that physicians will see the new data and become curious about the type of care they are providing. Physicians and hospitals can be "powerful change agents" when they start asking themselves what is driving their care practices, he said.
The Dartmouth Atlas Project, which is located at the Dartmouth Institute for Health Policy and Clinical Practice, is principally funded by the Robert Wood Johnson Foundation, with support from a consortium of funders. The new pediatric report was supported by a grant from the Charles H. Hood Foundation.
Just as with adults, the quality of health care that children receive often depends more on their zip code than their health status.
A new report from the Dartmouth Atlas Project found dramatic variation in outpatient physician services, hospitalizations, common surgical procedures, imaging, and prescriptions for infants and children living in Maine, New Hampshire, and Vermont.
The Dartmouth Atlas Project has issued a series of reports over the past 20 years showing wide geographic variation in the care of elderly adults, but this is the first time that the group has focused on infants and children under age 18 who have either commercial insurance or coverage through their state Medicaid programs.
The researchers focused specifically on Maine, New Hampshire, and Vermont because they are the only states that mandate the collection of insurance claims data from both commercial plans and Medicaid. The study looks at services provided from 2007 through 2010.
The researchers found that there is as much variation in pediatric health care as they found previously in care of the elderly, according to Dr. David C. Goodman, the lead author of the study and a professor of pediatrics at the Geisel School of Medicine at Dartmouth in Hanover, N.H.
"Health care has a general problem, which is reflected in essentially any population that we study," Dr. Goodman said.
The problem is that well-meaning physicians often don’t have the information they need to understand what kind of care they are providing and how it differs from what’s being done by their peers, he said.
While some of the variation detected in the study is explained by socioeconomic differences, most of it reflects distinctive practice styles across the different health care systems in the region, Dr. Goodman explained during a Dec. 11 press conference to release the Dartmouth Atlas findings.
In some cases, the findings show underuse of recommended treatments and services, such as lead screening for the Medicaid population and follow-up visits for children who are taking medications for attention-deficit/hyperactivity disorder (ADHD).
Across the three northern New England states analyzed, nearly 44% of children who were prescribed ADHD medication had a recommended follow-up appointment within 30 days in 2009-2010. But individual regions varied greatly. In Newport, Vt., nearly 70% of children had an initial follow-up, compared with only 35% in Lewiston, Maine.
Common surgical procedures also tended to vary widely based on the individual practice styles of physicians and surgeons, Dr. Goodman said, resulting in both under- and overuse.
For instance, tympanostomy tube insertion procedures for ear infections were performed more than four times as often in Middlebury, Vt., than in Bangor, Maine. In Middlebury, physicians performed 15.2 procedures per 1,000 children, compared with 3.4 procedures per 1,000 children in Bangor.
The report also revealed wide variations in access to care. And the result is that in areas where there were a high number of visits to physician offices, trips to the emergency department (ED) were much less common.
The average annual office visit rate, including visits to primary care and subspecialty offices and clinics, was 2.8 visits per child across the three New England states. But the visit rates varied more than threefold across the different regions.
The annual ED visit rate was 359 per 1,000 children during 2007-2010. Similarly, ED visits varied nearly threefold across the various regions. The common causes for ED visits included upper respiratory infections, minor injuries such as contusions and sprains, otitis media, and open wounds.
Dr. Goodman said he hopes that physicians will see the new data and become curious about the type of care they are providing. Physicians and hospitals can be "powerful change agents" when they start asking themselves what is driving their care practices, he said.
The Dartmouth Atlas Project, which is located at the Dartmouth Institute for Health Policy and Clinical Practice, is principally funded by the Robert Wood Johnson Foundation, with support from a consortium of funders. The new pediatric report was supported by a grant from the Charles H. Hood Foundation.
CMS extends Stage 2 ‘meaningful use’ reporting through 2016
Medicare officials have extended Stage 2 of the "meaningful use" Electronic Health Record Incentive Program through the end of 2016.
The change, announced on Dec. 6, means that the earliest that physicians will progress to Stage 3 of the meaningful use requirements will be in January 2017. Officials at the Centers for Medicare and Medicaid Services are still developing the Stage 3 requirements and expect to issue a proposed rule sometime in the fall of 2014.
The extension primarily affects physicians who began attesting to meaningful EHR use in 2011 and 2012. Those physicians were scheduled to advance to Stage 3 in 2016, after 2 years of working on Stage 2. The change means that they will have an additional year at Stage 2.
"The goal of this change is twofold: First, to allow CMS and [the Office of the National Coordinator for Health Information Technology] to focus efforts on the successful implementation of the enhanced patient engagement, interoperability, and health information exchange requirements in Stage 2; and second, to utilize data from Stage 2 participation to inform policy decisions for Stage 3," Robert Tagalicod, director of the office of e-Health Standards and Services at the CMS, and Dr. Jacob Reider, acting National Coordinator for Health Information Technology, wrote in a blog post announcing the change.
Over the last several months, a growing number of physician organizations and some lawmakers have called on the government to give physicians more time to meet Stage 2 requirements, saying that pushing forward with the aggressive timetable would leave many rural physicians behind.
"This new proposed timeline tracks ongoing conversations we at CMS and [the Office of the National Coordinator] have had with providers, consumers, health care associations, EHR developers, and other stakeholders in the health care industry," Mr. Tagalicod and Dr. Reider wrote. "This timeline allows for enhanced program analysis of Stage 2 data to inform the improvements in care delivery outcomes in Stage 3."
But Thomas A. Leary, vice president for government relations at HIMSS, said that while the extension of Stage 2 meaningful use is a positive step, his organization still wants to see Medicare officials give physicians a few more months to report on their first year of Stage 2 implementation. The extra time would help physicians, hospitals, and vendors who are having difficulty upgrading to the 2014 EHR certification requirements, according to HIMSS.
On Twitter @MaryEllenNY
Medicare officials have extended Stage 2 of the "meaningful use" Electronic Health Record Incentive Program through the end of 2016.
The change, announced on Dec. 6, means that the earliest that physicians will progress to Stage 3 of the meaningful use requirements will be in January 2017. Officials at the Centers for Medicare and Medicaid Services are still developing the Stage 3 requirements and expect to issue a proposed rule sometime in the fall of 2014.
The extension primarily affects physicians who began attesting to meaningful EHR use in 2011 and 2012. Those physicians were scheduled to advance to Stage 3 in 2016, after 2 years of working on Stage 2. The change means that they will have an additional year at Stage 2.
"The goal of this change is twofold: First, to allow CMS and [the Office of the National Coordinator for Health Information Technology] to focus efforts on the successful implementation of the enhanced patient engagement, interoperability, and health information exchange requirements in Stage 2; and second, to utilize data from Stage 2 participation to inform policy decisions for Stage 3," Robert Tagalicod, director of the office of e-Health Standards and Services at the CMS, and Dr. Jacob Reider, acting National Coordinator for Health Information Technology, wrote in a blog post announcing the change.
Over the last several months, a growing number of physician organizations and some lawmakers have called on the government to give physicians more time to meet Stage 2 requirements, saying that pushing forward with the aggressive timetable would leave many rural physicians behind.
"This new proposed timeline tracks ongoing conversations we at CMS and [the Office of the National Coordinator] have had with providers, consumers, health care associations, EHR developers, and other stakeholders in the health care industry," Mr. Tagalicod and Dr. Reider wrote. "This timeline allows for enhanced program analysis of Stage 2 data to inform the improvements in care delivery outcomes in Stage 3."
But Thomas A. Leary, vice president for government relations at HIMSS, said that while the extension of Stage 2 meaningful use is a positive step, his organization still wants to see Medicare officials give physicians a few more months to report on their first year of Stage 2 implementation. The extra time would help physicians, hospitals, and vendors who are having difficulty upgrading to the 2014 EHR certification requirements, according to HIMSS.
On Twitter @MaryEllenNY
Medicare officials have extended Stage 2 of the "meaningful use" Electronic Health Record Incentive Program through the end of 2016.
The change, announced on Dec. 6, means that the earliest that physicians will progress to Stage 3 of the meaningful use requirements will be in January 2017. Officials at the Centers for Medicare and Medicaid Services are still developing the Stage 3 requirements and expect to issue a proposed rule sometime in the fall of 2014.
The extension primarily affects physicians who began attesting to meaningful EHR use in 2011 and 2012. Those physicians were scheduled to advance to Stage 3 in 2016, after 2 years of working on Stage 2. The change means that they will have an additional year at Stage 2.
"The goal of this change is twofold: First, to allow CMS and [the Office of the National Coordinator for Health Information Technology] to focus efforts on the successful implementation of the enhanced patient engagement, interoperability, and health information exchange requirements in Stage 2; and second, to utilize data from Stage 2 participation to inform policy decisions for Stage 3," Robert Tagalicod, director of the office of e-Health Standards and Services at the CMS, and Dr. Jacob Reider, acting National Coordinator for Health Information Technology, wrote in a blog post announcing the change.
Over the last several months, a growing number of physician organizations and some lawmakers have called on the government to give physicians more time to meet Stage 2 requirements, saying that pushing forward with the aggressive timetable would leave many rural physicians behind.
"This new proposed timeline tracks ongoing conversations we at CMS and [the Office of the National Coordinator] have had with providers, consumers, health care associations, EHR developers, and other stakeholders in the health care industry," Mr. Tagalicod and Dr. Reider wrote. "This timeline allows for enhanced program analysis of Stage 2 data to inform the improvements in care delivery outcomes in Stage 3."
But Thomas A. Leary, vice president for government relations at HIMSS, said that while the extension of Stage 2 meaningful use is a positive step, his organization still wants to see Medicare officials give physicians a few more months to report on their first year of Stage 2 implementation. The extra time would help physicians, hospitals, and vendors who are having difficulty upgrading to the 2014 EHR certification requirements, according to HIMSS.
On Twitter @MaryEllenNY
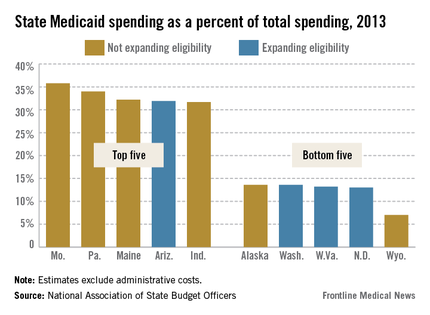
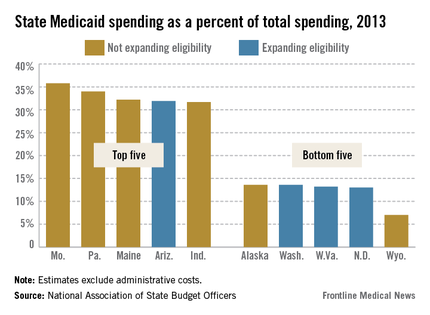
States take different paths in Medicaid expansion
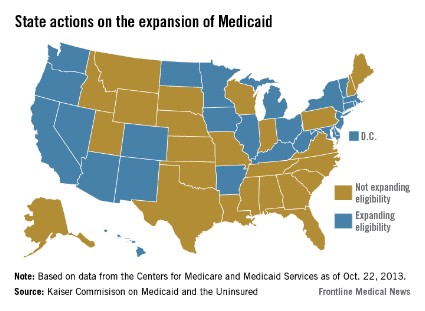
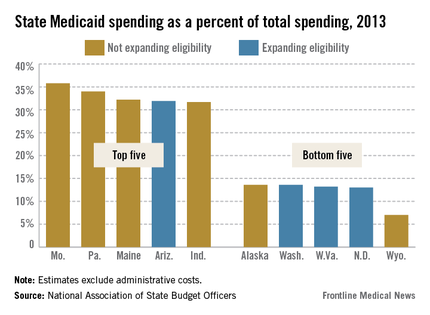
When the Supreme Court upheld the constitutionality of the Affordable Care Act in 2012, it also ruled that states could choose whether to substantially expand their Medicaid programs. That decision has created a split across the country, with about half of the states choosing to take federal dollars to expand their programs and the others opting out.
There’s no deadline on Medicaid expansion, so those states that have opted out so far can always choose to expand at a later date.

Here’s a look at two bellwether states: California, which has accepted federal money to expand its Medi-Cal program, and Texas, which has opted out of the expansion.
California Gov. Jerry Brown (D), a strong supporter of the ACA, announced that his state would expand Medicaid to include low-income individuals up to 138% of the federal poverty level starting on Jan. 1, 2014. All of the new enrollees – likely 1 million Californians – will be added to the state’s growing Medicaid managed care program.
Conversely, Texas Gov. Rick Perry (R) deemed Medicaid expansion "a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare."
California: Pay cuts complicate expansion
Physicians in California are bracing for a significant Medicaid pay cut at the same time as about a million residents are set to join the program.
The pending cuts are just one part of a complex health care picture in California, where experts are far from certain about what the expansion of Medi-Cal will mean for physicians and patients.
"I think we’re going to have a real problem in California with all the new Medi-Cal patients," said Dr. Mark Dressner, who works at a federally qualified health center in Long Beach and is the president of the California Academy of Family Physicians. "Who is going to see them when there’s going to be so many other people in the system?"
The Kaiser Family Foundation estimates that between 990,000 and 1.4 million individuals, mostly single adults, will enter Medi-Cal by 2019 because of the ACA-permitted expansion. Currently, about 8.5 million residents are enrolled. Newly eligible individuals will be enrolled in the program’s managed care health plans.
These new patients could have a hard time finding a doctor. Medi-Cal is one of the lowest payers in the nation, paying between $18 and $24 for an office visit, according to the California Medical Association.
That’s about to be compounded by a pay cut approved by the state and the Centers for Medicare and Medicaid Services in 2011. Physicians tried unsuccessfully to fight the cut in court. Now the state is implementing it retroactively, which means that Medi-Cal payments could be cut 15%-20% over the next few years.
"It really undermines efforts to successfully implement the Affordable Care Act in California," said Lisa Folberg, vice president of medical and regulatory policy at the California Medical Association.
There are broad exceptions to the cut. It does not apply to most primary care services in either managed care plans or fee-for-service Medi-Cal, or to specialty services provided through managed care plans, Ms. Folberg said. And some managed care companies have announced that they will use their discretion in setting payment rates to shield their contracted physicians from the cuts.
"Unfortunately, that doesn’t help the cancer patient on Medi-Cal in Bakersfield who has fee-for-service Medi-Cal and can’t find an oncologist," Ms. Folberg said.
Dr. Darin Latimore, president of the California chapter of the American College of Physicians, said large health systems likely will be able to work around the cuts, using group visits and physician extenders. But small physician practices in rural areas aren’t equipped to make those changes, he said.
"They are not in a position to move work on to others in order to be more efficient and see more Medi-Cal patients," said Dr. Latimore, associate dean of medicine at the University of California Davis.
The result will be that physicians who work outside of the state’s safety net system will be less likely to participate in the Medi-Cal program or will strictly limit the number of patients they see. That will translate to longer waits to get an appointment and shorter visits for Medi-Cal patients.
Another concern: Patients entering Medi-Cal managed care plans might not have access to a broad network of physicians. While California has network adequacy laws, state oversight is inadequate, according to Ms. Folberg. For the most part, the plans are on an honor system.
There are some bright spots for the Medi-Cal expansion. The ACA includes an increase in Medicaid payments to physicians for 146 primary care services provided in 2013 and 2014. The provision temporarily raises payments up to Medicare rates, which for California physicians means a 136% hike on average, according to an analysis from the Kaiser Family Foundation.
But those payments were delayed, with the first checks going out to physicians in November 2013. That delay could cost the state in physician participation.
"I think the longer it takes to implement that, the less likely it is that it will affect any decisions about whether to participate more fully in the program than you would have otherwise," said Christopher Perrone, deputy director of the health reform and public programs initiative at the California HealthCare Foundation.
And the temporary nature of the pay increase adds to the problem, Mr. Perrone said. "I don’t see California sustaining that increase on its own and I haven’t heard anyone suggest that the federal government would sustain it after the 2 years."
Mr. Perrone said it’s more likely that physicians who are already committed to participating in Medi-Cal will use the money to invest in electronic health records and other telemedicine features, and hire medical assistants.
But with so many small and solo physicians shying away from Medi-Cal because of low payments, community clinics and health centers will have to pick up the slack.
"All these issues together really point to the importance of the community health centers and the role we are going to be playing in ensuring access," said Carmela Castellano-Garcia, president and CEO of the California Primary Care Association.
Federally qualified health centers are in a better position financially because they are paid an enhanced Medicaid rate and won’t be subject to the coming Medi-Cal cuts, Ms. Castellano-Garcia said. And the ACA has directed an influx of cash to these centers as well – more than $500 million in California alone to establish new sites, expand services, and support major capital improvement projects, according to the Health and Human Services department.
Texas: No expansion means doctors will keep feeling pressure
Texas has the highest number of uninsured residents in the United States – a quarter of its 26 million residents lacking coverage – but Gov. Rick Perry (R) refused to expand Medicaid, which could cover as many as 500,000 to 1 million Texans.
The governor’s decision will stay in place at least until 2015, when the state legislature reconvenes.
Some physicians in Texas are not upset by the decision – they consider Medicaid to be low-paying program and full of bureaucratic hassles.
Others – including many of the primary care organizations – disagree.
The Texas Medical Association, the Texas Academy of Family Physicians, and the Texas chapter of the American Congress of Obstetricians and Gynecologists all support the expansion of Medicaid allowed by the ACA.
In April, Gov. Perry reiterated his position. "Medicaid expansion is a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare," he said in a statement. Instead of expansion, he favors flexibility for the state to manage its Medicaid program.
State Rep. John Zerwas (R-Simonton), an anesthesiologist, introduced H.B. 3791 that would give that flexibility, but it did not get consideration by the full House before the legislature adjourned in May.
The TMA supported Dr. Zerwas’ proposal, but also is in favor of expanding Medicaid, said Dr. Stephen L. Brotherton, TMA president. More people would have some type of insurance, but they might not necessarily have good access to care, he said.
That’s because Texas has a shortage of primary care physicians. The number of primary care physicians per capita is lower than the national average – at about 70/100,000 in 2011, compared with 80/100,000 nationally, according to the Texas Department of State Health Services, in the publication "Supply Trends Among Licensed Health Professions, Texas, 1980-2011. In rural areas, it’s even lower – about 50/100,000.
Then there’s the question of just how many physicians will take Medicaid. A 2012 TMA survey found that only 31% of doctors in the state were accepting new Medicaid patients.
Medicaid payment rates are so low that Dr. Brotherton, who practices in Ft. Worth, said that he treats Medicaid patients as charity care. "It’s much less expensive for me to do it for nothing as donated time," he said.
Dr. Moss Hampton, chairman of District XI of ACOG, added, "Medicaid doesn’t cover the cost of taking care of the patient."
For Medicaid expansion to eventually be successful, "there would have to be a better payment rate and less of a hassle factor," said Dr. Hampton, chairman of the obstetrics and gynecology department at Texas Tech Health Sciences Center at the Permian Basin in Odessa.
"It’s hard to get doctors to accept Medicaid because of the rates they pay," agreed Dr. Clare Hawkins, TAFP president, who added that Texas physicians also feel that it’s hard to comply with differing rules among various Medicaid managed care programs.
Even so, expansion will mean getting more patients into preventive care, and a reduction in emergency department visits and more expensive hospital care – costs that are being borne by all Texans, including physicians, said Dr. Hawkins, who is program director of the San Jacinto Methodist Hospital Family Medicine Residency Program in Baytown, Texas.
Although uninsured Texas residents are already receiving care – in emergency departments and at clinics – Medicaid expansion could bring a big uptick in office visits, especially to ob.gyn. practices, Dr. Hampton said. The need for those services is growing with a state law that went into effect on Oct. 29 that makes it prohibitive for most Planned Parenthood clinics and other community clinics that provide abortion services to stay open.
"What that’s done is cut out a very large group of providers, and now we’re trying to find providers to help take care of those folks," who normally use those clinics, she said.
In the absence of Medicaid expansion, Texas physicians are hoping to start receiving higher Medicaid payments that were due to start in Jan. 2013. An estimated 25,000 Texas doctors are eligible for Medicaid pay that will be on par with Medicare. But Texas has not begun to distribute that money and will not likely do so until March, according to the TMA.
When the Supreme Court upheld the constitutionality of the Affordable Care Act in 2012, it also ruled that states could choose whether to substantially expand their Medicaid programs. That decision has created a split across the country, with about half of the states choosing to take federal dollars to expand their programs and the others opting out.
There’s no deadline on Medicaid expansion, so those states that have opted out so far can always choose to expand at a later date.

Here’s a look at two bellwether states: California, which has accepted federal money to expand its Medi-Cal program, and Texas, which has opted out of the expansion.
California Gov. Jerry Brown (D), a strong supporter of the ACA, announced that his state would expand Medicaid to include low-income individuals up to 138% of the federal poverty level starting on Jan. 1, 2014. All of the new enrollees – likely 1 million Californians – will be added to the state’s growing Medicaid managed care program.
Conversely, Texas Gov. Rick Perry (R) deemed Medicaid expansion "a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare."
California: Pay cuts complicate expansion
Physicians in California are bracing for a significant Medicaid pay cut at the same time as about a million residents are set to join the program.
The pending cuts are just one part of a complex health care picture in California, where experts are far from certain about what the expansion of Medi-Cal will mean for physicians and patients.
"I think we’re going to have a real problem in California with all the new Medi-Cal patients," said Dr. Mark Dressner, who works at a federally qualified health center in Long Beach and is the president of the California Academy of Family Physicians. "Who is going to see them when there’s going to be so many other people in the system?"
The Kaiser Family Foundation estimates that between 990,000 and 1.4 million individuals, mostly single adults, will enter Medi-Cal by 2019 because of the ACA-permitted expansion. Currently, about 8.5 million residents are enrolled. Newly eligible individuals will be enrolled in the program’s managed care health plans.
These new patients could have a hard time finding a doctor. Medi-Cal is one of the lowest payers in the nation, paying between $18 and $24 for an office visit, according to the California Medical Association.
That’s about to be compounded by a pay cut approved by the state and the Centers for Medicare and Medicaid Services in 2011. Physicians tried unsuccessfully to fight the cut in court. Now the state is implementing it retroactively, which means that Medi-Cal payments could be cut 15%-20% over the next few years.
"It really undermines efforts to successfully implement the Affordable Care Act in California," said Lisa Folberg, vice president of medical and regulatory policy at the California Medical Association.
There are broad exceptions to the cut. It does not apply to most primary care services in either managed care plans or fee-for-service Medi-Cal, or to specialty services provided through managed care plans, Ms. Folberg said. And some managed care companies have announced that they will use their discretion in setting payment rates to shield their contracted physicians from the cuts.
"Unfortunately, that doesn’t help the cancer patient on Medi-Cal in Bakersfield who has fee-for-service Medi-Cal and can’t find an oncologist," Ms. Folberg said.
Dr. Darin Latimore, president of the California chapter of the American College of Physicians, said large health systems likely will be able to work around the cuts, using group visits and physician extenders. But small physician practices in rural areas aren’t equipped to make those changes, he said.
"They are not in a position to move work on to others in order to be more efficient and see more Medi-Cal patients," said Dr. Latimore, associate dean of medicine at the University of California Davis.
The result will be that physicians who work outside of the state’s safety net system will be less likely to participate in the Medi-Cal program or will strictly limit the number of patients they see. That will translate to longer waits to get an appointment and shorter visits for Medi-Cal patients.
Another concern: Patients entering Medi-Cal managed care plans might not have access to a broad network of physicians. While California has network adequacy laws, state oversight is inadequate, according to Ms. Folberg. For the most part, the plans are on an honor system.
There are some bright spots for the Medi-Cal expansion. The ACA includes an increase in Medicaid payments to physicians for 146 primary care services provided in 2013 and 2014. The provision temporarily raises payments up to Medicare rates, which for California physicians means a 136% hike on average, according to an analysis from the Kaiser Family Foundation.
But those payments were delayed, with the first checks going out to physicians in November 2013. That delay could cost the state in physician participation.
"I think the longer it takes to implement that, the less likely it is that it will affect any decisions about whether to participate more fully in the program than you would have otherwise," said Christopher Perrone, deputy director of the health reform and public programs initiative at the California HealthCare Foundation.
And the temporary nature of the pay increase adds to the problem, Mr. Perrone said. "I don’t see California sustaining that increase on its own and I haven’t heard anyone suggest that the federal government would sustain it after the 2 years."
Mr. Perrone said it’s more likely that physicians who are already committed to participating in Medi-Cal will use the money to invest in electronic health records and other telemedicine features, and hire medical assistants.
But with so many small and solo physicians shying away from Medi-Cal because of low payments, community clinics and health centers will have to pick up the slack.
"All these issues together really point to the importance of the community health centers and the role we are going to be playing in ensuring access," said Carmela Castellano-Garcia, president and CEO of the California Primary Care Association.
Federally qualified health centers are in a better position financially because they are paid an enhanced Medicaid rate and won’t be subject to the coming Medi-Cal cuts, Ms. Castellano-Garcia said. And the ACA has directed an influx of cash to these centers as well – more than $500 million in California alone to establish new sites, expand services, and support major capital improvement projects, according to the Health and Human Services department.
Texas: No expansion means doctors will keep feeling pressure
Texas has the highest number of uninsured residents in the United States – a quarter of its 26 million residents lacking coverage – but Gov. Rick Perry (R) refused to expand Medicaid, which could cover as many as 500,000 to 1 million Texans.
The governor’s decision will stay in place at least until 2015, when the state legislature reconvenes.
Some physicians in Texas are not upset by the decision – they consider Medicaid to be low-paying program and full of bureaucratic hassles.
Others – including many of the primary care organizations – disagree.
The Texas Medical Association, the Texas Academy of Family Physicians, and the Texas chapter of the American Congress of Obstetricians and Gynecologists all support the expansion of Medicaid allowed by the ACA.
In April, Gov. Perry reiterated his position. "Medicaid expansion is a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare," he said in a statement. Instead of expansion, he favors flexibility for the state to manage its Medicaid program.
State Rep. John Zerwas (R-Simonton), an anesthesiologist, introduced H.B. 3791 that would give that flexibility, but it did not get consideration by the full House before the legislature adjourned in May.
The TMA supported Dr. Zerwas’ proposal, but also is in favor of expanding Medicaid, said Dr. Stephen L. Brotherton, TMA president. More people would have some type of insurance, but they might not necessarily have good access to care, he said.
That’s because Texas has a shortage of primary care physicians. The number of primary care physicians per capita is lower than the national average – at about 70/100,000 in 2011, compared with 80/100,000 nationally, according to the Texas Department of State Health Services, in the publication "Supply Trends Among Licensed Health Professions, Texas, 1980-2011. In rural areas, it’s even lower – about 50/100,000.
Then there’s the question of just how many physicians will take Medicaid. A 2012 TMA survey found that only 31% of doctors in the state were accepting new Medicaid patients.
Medicaid payment rates are so low that Dr. Brotherton, who practices in Ft. Worth, said that he treats Medicaid patients as charity care. "It’s much less expensive for me to do it for nothing as donated time," he said.
Dr. Moss Hampton, chairman of District XI of ACOG, added, "Medicaid doesn’t cover the cost of taking care of the patient."
For Medicaid expansion to eventually be successful, "there would have to be a better payment rate and less of a hassle factor," said Dr. Hampton, chairman of the obstetrics and gynecology department at Texas Tech Health Sciences Center at the Permian Basin in Odessa.
"It’s hard to get doctors to accept Medicaid because of the rates they pay," agreed Dr. Clare Hawkins, TAFP president, who added that Texas physicians also feel that it’s hard to comply with differing rules among various Medicaid managed care programs.
Even so, expansion will mean getting more patients into preventive care, and a reduction in emergency department visits and more expensive hospital care – costs that are being borne by all Texans, including physicians, said Dr. Hawkins, who is program director of the San Jacinto Methodist Hospital Family Medicine Residency Program in Baytown, Texas.
Although uninsured Texas residents are already receiving care – in emergency departments and at clinics – Medicaid expansion could bring a big uptick in office visits, especially to ob.gyn. practices, Dr. Hampton said. The need for those services is growing with a state law that went into effect on Oct. 29 that makes it prohibitive for most Planned Parenthood clinics and other community clinics that provide abortion services to stay open.
"What that’s done is cut out a very large group of providers, and now we’re trying to find providers to help take care of those folks," who normally use those clinics, she said.
In the absence of Medicaid expansion, Texas physicians are hoping to start receiving higher Medicaid payments that were due to start in Jan. 2013. An estimated 25,000 Texas doctors are eligible for Medicaid pay that will be on par with Medicare. But Texas has not begun to distribute that money and will not likely do so until March, according to the TMA.
When the Supreme Court upheld the constitutionality of the Affordable Care Act in 2012, it also ruled that states could choose whether to substantially expand their Medicaid programs. That decision has created a split across the country, with about half of the states choosing to take federal dollars to expand their programs and the others opting out.
There’s no deadline on Medicaid expansion, so those states that have opted out so far can always choose to expand at a later date.

Here’s a look at two bellwether states: California, which has accepted federal money to expand its Medi-Cal program, and Texas, which has opted out of the expansion.
California Gov. Jerry Brown (D), a strong supporter of the ACA, announced that his state would expand Medicaid to include low-income individuals up to 138% of the federal poverty level starting on Jan. 1, 2014. All of the new enrollees – likely 1 million Californians – will be added to the state’s growing Medicaid managed care program.
Conversely, Texas Gov. Rick Perry (R) deemed Medicaid expansion "a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare."
California: Pay cuts complicate expansion
Physicians in California are bracing for a significant Medicaid pay cut at the same time as about a million residents are set to join the program.
The pending cuts are just one part of a complex health care picture in California, where experts are far from certain about what the expansion of Medi-Cal will mean for physicians and patients.
"I think we’re going to have a real problem in California with all the new Medi-Cal patients," said Dr. Mark Dressner, who works at a federally qualified health center in Long Beach and is the president of the California Academy of Family Physicians. "Who is going to see them when there’s going to be so many other people in the system?"
The Kaiser Family Foundation estimates that between 990,000 and 1.4 million individuals, mostly single adults, will enter Medi-Cal by 2019 because of the ACA-permitted expansion. Currently, about 8.5 million residents are enrolled. Newly eligible individuals will be enrolled in the program’s managed care health plans.
These new patients could have a hard time finding a doctor. Medi-Cal is one of the lowest payers in the nation, paying between $18 and $24 for an office visit, according to the California Medical Association.
That’s about to be compounded by a pay cut approved by the state and the Centers for Medicare and Medicaid Services in 2011. Physicians tried unsuccessfully to fight the cut in court. Now the state is implementing it retroactively, which means that Medi-Cal payments could be cut 15%-20% over the next few years.
"It really undermines efforts to successfully implement the Affordable Care Act in California," said Lisa Folberg, vice president of medical and regulatory policy at the California Medical Association.
There are broad exceptions to the cut. It does not apply to most primary care services in either managed care plans or fee-for-service Medi-Cal, or to specialty services provided through managed care plans, Ms. Folberg said. And some managed care companies have announced that they will use their discretion in setting payment rates to shield their contracted physicians from the cuts.
"Unfortunately, that doesn’t help the cancer patient on Medi-Cal in Bakersfield who has fee-for-service Medi-Cal and can’t find an oncologist," Ms. Folberg said.
Dr. Darin Latimore, president of the California chapter of the American College of Physicians, said large health systems likely will be able to work around the cuts, using group visits and physician extenders. But small physician practices in rural areas aren’t equipped to make those changes, he said.
"They are not in a position to move work on to others in order to be more efficient and see more Medi-Cal patients," said Dr. Latimore, associate dean of medicine at the University of California Davis.
The result will be that physicians who work outside of the state’s safety net system will be less likely to participate in the Medi-Cal program or will strictly limit the number of patients they see. That will translate to longer waits to get an appointment and shorter visits for Medi-Cal patients.
Another concern: Patients entering Medi-Cal managed care plans might not have access to a broad network of physicians. While California has network adequacy laws, state oversight is inadequate, according to Ms. Folberg. For the most part, the plans are on an honor system.
There are some bright spots for the Medi-Cal expansion. The ACA includes an increase in Medicaid payments to physicians for 146 primary care services provided in 2013 and 2014. The provision temporarily raises payments up to Medicare rates, which for California physicians means a 136% hike on average, according to an analysis from the Kaiser Family Foundation.
But those payments were delayed, with the first checks going out to physicians in November 2013. That delay could cost the state in physician participation.
"I think the longer it takes to implement that, the less likely it is that it will affect any decisions about whether to participate more fully in the program than you would have otherwise," said Christopher Perrone, deputy director of the health reform and public programs initiative at the California HealthCare Foundation.
And the temporary nature of the pay increase adds to the problem, Mr. Perrone said. "I don’t see California sustaining that increase on its own and I haven’t heard anyone suggest that the federal government would sustain it after the 2 years."
Mr. Perrone said it’s more likely that physicians who are already committed to participating in Medi-Cal will use the money to invest in electronic health records and other telemedicine features, and hire medical assistants.
But with so many small and solo physicians shying away from Medi-Cal because of low payments, community clinics and health centers will have to pick up the slack.
"All these issues together really point to the importance of the community health centers and the role we are going to be playing in ensuring access," said Carmela Castellano-Garcia, president and CEO of the California Primary Care Association.
Federally qualified health centers are in a better position financially because they are paid an enhanced Medicaid rate and won’t be subject to the coming Medi-Cal cuts, Ms. Castellano-Garcia said. And the ACA has directed an influx of cash to these centers as well – more than $500 million in California alone to establish new sites, expand services, and support major capital improvement projects, according to the Health and Human Services department.
Texas: No expansion means doctors will keep feeling pressure
Texas has the highest number of uninsured residents in the United States – a quarter of its 26 million residents lacking coverage – but Gov. Rick Perry (R) refused to expand Medicaid, which could cover as many as 500,000 to 1 million Texans.
The governor’s decision will stay in place at least until 2015, when the state legislature reconvenes.
Some physicians in Texas are not upset by the decision – they consider Medicaid to be low-paying program and full of bureaucratic hassles.
Others – including many of the primary care organizations – disagree.
The Texas Medical Association, the Texas Academy of Family Physicians, and the Texas chapter of the American Congress of Obstetricians and Gynecologists all support the expansion of Medicaid allowed by the ACA.
In April, Gov. Perry reiterated his position. "Medicaid expansion is a misguided, and ultimately doomed, attempt to mask the shortcomings of Obamacare," he said in a statement. Instead of expansion, he favors flexibility for the state to manage its Medicaid program.
State Rep. John Zerwas (R-Simonton), an anesthesiologist, introduced H.B. 3791 that would give that flexibility, but it did not get consideration by the full House before the legislature adjourned in May.
The TMA supported Dr. Zerwas’ proposal, but also is in favor of expanding Medicaid, said Dr. Stephen L. Brotherton, TMA president. More people would have some type of insurance, but they might not necessarily have good access to care, he said.
That’s because Texas has a shortage of primary care physicians. The number of primary care physicians per capita is lower than the national average – at about 70/100,000 in 2011, compared with 80/100,000 nationally, according to the Texas Department of State Health Services, in the publication "Supply Trends Among Licensed Health Professions, Texas, 1980-2011. In rural areas, it’s even lower – about 50/100,000.
Then there’s the question of just how many physicians will take Medicaid. A 2012 TMA survey found that only 31% of doctors in the state were accepting new Medicaid patients.
Medicaid payment rates are so low that Dr. Brotherton, who practices in Ft. Worth, said that he treats Medicaid patients as charity care. "It’s much less expensive for me to do it for nothing as donated time," he said.
Dr. Moss Hampton, chairman of District XI of ACOG, added, "Medicaid doesn’t cover the cost of taking care of the patient."
For Medicaid expansion to eventually be successful, "there would have to be a better payment rate and less of a hassle factor," said Dr. Hampton, chairman of the obstetrics and gynecology department at Texas Tech Health Sciences Center at the Permian Basin in Odessa.
"It’s hard to get doctors to accept Medicaid because of the rates they pay," agreed Dr. Clare Hawkins, TAFP president, who added that Texas physicians also feel that it’s hard to comply with differing rules among various Medicaid managed care programs.
Even so, expansion will mean getting more patients into preventive care, and a reduction in emergency department visits and more expensive hospital care – costs that are being borne by all Texans, including physicians, said Dr. Hawkins, who is program director of the San Jacinto Methodist Hospital Family Medicine Residency Program in Baytown, Texas.
Although uninsured Texas residents are already receiving care – in emergency departments and at clinics – Medicaid expansion could bring a big uptick in office visits, especially to ob.gyn. practices, Dr. Hampton said. The need for those services is growing with a state law that went into effect on Oct. 29 that makes it prohibitive for most Planned Parenthood clinics and other community clinics that provide abortion services to stay open.
"What that’s done is cut out a very large group of providers, and now we’re trying to find providers to help take care of those folks," who normally use those clinics, she said.
In the absence of Medicaid expansion, Texas physicians are hoping to start receiving higher Medicaid payments that were due to start in Jan. 2013. An estimated 25,000 Texas doctors are eligible for Medicaid pay that will be on par with Medicare. But Texas has not begun to distribute that money and will not likely do so until March, according to the TMA.
Bipartisan SGR repeal plan unveiled
The Senate Finance Committee and the House Ways and Means Committee jointly released a legislative framework that would scrap Medicare’s Sustainable Growth Rate (SGR) formula and freeze physician payments for the next decade.
Starting in 2017, physicians would see their payments tied to cost and quality of care using a single quality incentive program. Under the proposal, Medicare would create the Value-Based Performance Payment Program to adjust physician payments based on quality, resource use, clinical practice improvement activities, and the use of electronic health records.
Since the program is budget neutral, some physicians would see increases while others would see cuts.
At the end of 2016, Medicare would end a group of existing incentive programs including the Physician Quality Reporting System; the Value-Based Modifier Program; and the Electronic Health Record (EHR) Incentive Program, which requires the meaningful use of certified EHR technology.
Physicians who treat few Medicare patients or who receive a significant portion of their payments from advanced alternative payment models, such as accountable care organizations, would be excluded from the new Value-Based Performance Payment Program. Physicians in ACOs and other models that involved taking on financial risk and reporting on quality measures would instead be eligible for bonus payments under the proposal.
After 2023, physicians who participate in these advanced alternative payment models would see an annual 2% payment increase, and other physicians would earn updates of 1% each year, according to the proposal circulated by the two committees.
"This discussion draft is an important step in a long-term solution to this failed policy," Rep. Dave Camp, chairman of the House Ways and Means Committee, said in a statement. "Creating a policy that rewards providers for delivering high-quality, efficient health care is the ultimate goal, and this draft brings us one step closer to that reality."
The release of the proposal follows a summer of feverish activity in the House on the issue of the SGR. After months of hearings, the Energy and Commerce Committee unanimously approved a bill on July 31 (H.R. 2810) that would repeal the SGR and provide 0.5% payment increases for physicians through 2018.
This latest plan incorporates ideas from both the Democratic-led Senate and the GOP-controlled House.
"Congress is demonstrating that they understand that ending the failed SGR this year is fiscally responsible, and that the current Medicare payment system is a barrier to adoption of health care delivery and payment reforms that will improve health care for America’s seniors and rein in overall costs," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
The Senate Finance Committee and the House Ways and Means Committee jointly released a legislative framework that would scrap Medicare’s Sustainable Growth Rate (SGR) formula and freeze physician payments for the next decade.
Starting in 2017, physicians would see their payments tied to cost and quality of care using a single quality incentive program. Under the proposal, Medicare would create the Value-Based Performance Payment Program to adjust physician payments based on quality, resource use, clinical practice improvement activities, and the use of electronic health records.
Since the program is budget neutral, some physicians would see increases while others would see cuts.
At the end of 2016, Medicare would end a group of existing incentive programs including the Physician Quality Reporting System; the Value-Based Modifier Program; and the Electronic Health Record (EHR) Incentive Program, which requires the meaningful use of certified EHR technology.
Physicians who treat few Medicare patients or who receive a significant portion of their payments from advanced alternative payment models, such as accountable care organizations, would be excluded from the new Value-Based Performance Payment Program. Physicians in ACOs and other models that involved taking on financial risk and reporting on quality measures would instead be eligible for bonus payments under the proposal.
After 2023, physicians who participate in these advanced alternative payment models would see an annual 2% payment increase, and other physicians would earn updates of 1% each year, according to the proposal circulated by the two committees.
"This discussion draft is an important step in a long-term solution to this failed policy," Rep. Dave Camp, chairman of the House Ways and Means Committee, said in a statement. "Creating a policy that rewards providers for delivering high-quality, efficient health care is the ultimate goal, and this draft brings us one step closer to that reality."
The release of the proposal follows a summer of feverish activity in the House on the issue of the SGR. After months of hearings, the Energy and Commerce Committee unanimously approved a bill on July 31 (H.R. 2810) that would repeal the SGR and provide 0.5% payment increases for physicians through 2018.
This latest plan incorporates ideas from both the Democratic-led Senate and the GOP-controlled House.
"Congress is demonstrating that they understand that ending the failed SGR this year is fiscally responsible, and that the current Medicare payment system is a barrier to adoption of health care delivery and payment reforms that will improve health care for America’s seniors and rein in overall costs," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
The Senate Finance Committee and the House Ways and Means Committee jointly released a legislative framework that would scrap Medicare’s Sustainable Growth Rate (SGR) formula and freeze physician payments for the next decade.
Starting in 2017, physicians would see their payments tied to cost and quality of care using a single quality incentive program. Under the proposal, Medicare would create the Value-Based Performance Payment Program to adjust physician payments based on quality, resource use, clinical practice improvement activities, and the use of electronic health records.
Since the program is budget neutral, some physicians would see increases while others would see cuts.
At the end of 2016, Medicare would end a group of existing incentive programs including the Physician Quality Reporting System; the Value-Based Modifier Program; and the Electronic Health Record (EHR) Incentive Program, which requires the meaningful use of certified EHR technology.
Physicians who treat few Medicare patients or who receive a significant portion of their payments from advanced alternative payment models, such as accountable care organizations, would be excluded from the new Value-Based Performance Payment Program. Physicians in ACOs and other models that involved taking on financial risk and reporting on quality measures would instead be eligible for bonus payments under the proposal.
After 2023, physicians who participate in these advanced alternative payment models would see an annual 2% payment increase, and other physicians would earn updates of 1% each year, according to the proposal circulated by the two committees.
"This discussion draft is an important step in a long-term solution to this failed policy," Rep. Dave Camp, chairman of the House Ways and Means Committee, said in a statement. "Creating a policy that rewards providers for delivering high-quality, efficient health care is the ultimate goal, and this draft brings us one step closer to that reality."
The release of the proposal follows a summer of feverish activity in the House on the issue of the SGR. After months of hearings, the Energy and Commerce Committee unanimously approved a bill on July 31 (H.R. 2810) that would repeal the SGR and provide 0.5% payment increases for physicians through 2018.
This latest plan incorporates ideas from both the Democratic-led Senate and the GOP-controlled House.
"Congress is demonstrating that they understand that ending the failed SGR this year is fiscally responsible, and that the current Medicare payment system is a barrier to adoption of health care delivery and payment reforms that will improve health care for America’s seniors and rein in overall costs," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
Medicaid enrollment up 15% in October due to ACA
Medicaid applications were up more than 15% in October in states that are expanding their Medicaid programs under the Affordable Care Act.
The preliminary data, released by the Health and Human Services department Dec. 3, shows that while Americans have been slow to enroll in private health plans through the online exchanges, many low-income individuals are getting access to insurance coverage through the Medicaid program.
As of October, 23 states and the District of Columbia had expanded their Medicaid programs to include individuals with incomes up to 133% of the federal poverty level. That coverage will begin on Jan. 1, 2014. Two more states – Ohio and Michigan – recently announced plans to expand their programs but have not yet begun enrollment.
During October, the number of applications to Medicaid programs and the Children’s Health Insurance Program (CHIP) were up 15.5% overall in states expanding their eligibility, compared with the average monthly number of applications received from July through September. The figures include both individuals who are newly eligible under the ACA and those who were eligible previously. Comparatively, states that opted not to expand their Medicaid programs saw an increase in applications of 4.1%.
Across all states, more than 2.4 million applications were submitted to state Medicaid and CHIP agencies during October. More than 1.4 million individuals were deemed eligible for the programs.
The figures released by the HHS provide a partial picture of Medicaid enrollment under the ACA. Individuals also are applying to the program through the online insurance exchanges. From Oct. 1 to Nov. 2, 396,261 were determined to be eligible for Medicaid or CHIP after applying for insurance through either a state-based exchange or healthcare.gov, according to the HHS.
On Twitter @MaryEllenNY
Medicaid applications were up more than 15% in October in states that are expanding their Medicaid programs under the Affordable Care Act.
The preliminary data, released by the Health and Human Services department Dec. 3, shows that while Americans have been slow to enroll in private health plans through the online exchanges, many low-income individuals are getting access to insurance coverage through the Medicaid program.
As of October, 23 states and the District of Columbia had expanded their Medicaid programs to include individuals with incomes up to 133% of the federal poverty level. That coverage will begin on Jan. 1, 2014. Two more states – Ohio and Michigan – recently announced plans to expand their programs but have not yet begun enrollment.
During October, the number of applications to Medicaid programs and the Children’s Health Insurance Program (CHIP) were up 15.5% overall in states expanding their eligibility, compared with the average monthly number of applications received from July through September. The figures include both individuals who are newly eligible under the ACA and those who were eligible previously. Comparatively, states that opted not to expand their Medicaid programs saw an increase in applications of 4.1%.
Across all states, more than 2.4 million applications were submitted to state Medicaid and CHIP agencies during October. More than 1.4 million individuals were deemed eligible for the programs.
The figures released by the HHS provide a partial picture of Medicaid enrollment under the ACA. Individuals also are applying to the program through the online insurance exchanges. From Oct. 1 to Nov. 2, 396,261 were determined to be eligible for Medicaid or CHIP after applying for insurance through either a state-based exchange or healthcare.gov, according to the HHS.
On Twitter @MaryEllenNY
Medicaid applications were up more than 15% in October in states that are expanding their Medicaid programs under the Affordable Care Act.
The preliminary data, released by the Health and Human Services department Dec. 3, shows that while Americans have been slow to enroll in private health plans through the online exchanges, many low-income individuals are getting access to insurance coverage through the Medicaid program.
As of October, 23 states and the District of Columbia had expanded their Medicaid programs to include individuals with incomes up to 133% of the federal poverty level. That coverage will begin on Jan. 1, 2014. Two more states – Ohio and Michigan – recently announced plans to expand their programs but have not yet begun enrollment.
During October, the number of applications to Medicaid programs and the Children’s Health Insurance Program (CHIP) were up 15.5% overall in states expanding their eligibility, compared with the average monthly number of applications received from July through September. The figures include both individuals who are newly eligible under the ACA and those who were eligible previously. Comparatively, states that opted not to expand their Medicaid programs saw an increase in applications of 4.1%.
Across all states, more than 2.4 million applications were submitted to state Medicaid and CHIP agencies during October. More than 1.4 million individuals were deemed eligible for the programs.
The figures released by the HHS provide a partial picture of Medicaid enrollment under the ACA. Individuals also are applying to the program through the online insurance exchanges. From Oct. 1 to Nov. 2, 396,261 were determined to be eligible for Medicaid or CHIP after applying for insurance through either a state-based exchange or healthcare.gov, according to the HHS.
On Twitter @MaryEllenNY
Medicare finalizes plan for non-face-to-face payments
Starting in 2015, primary care physicians will get paid for some of the chronic care management work they do outside of office visits.
As part of the 2014 Medicare physician fee schedule final rule, officials at the Centers for Medicare and Medicaid Services (CMS) finalized plans to begin paying physicians separately for services such as development and revision of a care plan, communication with other treating providers, review of lab results, and adjustment of medications.
The agency established a new G-code that physicians can use to bill for non-face-to-face care management services for Medicare patients with two or more significant chronic conditions. The code, which will apply to 20 minutes or more of chronic care management services during a 30-day period, takes effect on Jan. 1, 2015.
Physicians who wish to use the new code will have to meet a series of requirements laid out by the CMS, including providing 24-7 access, coordination with home- and community-based service providers, and patient access to the practice through secure messaging or patient portals.
The new codes are part of a recent move by Medicare officials to emphasize primary care and to pay for services that happen outside of the traditional office visit. In 2012, the CMS established codes for transitional care management services for patients moving from a hospital or skilled nursing facility to home. Those codes, which took effect this year, included payment for some non-face-to-face activities.
The news was greeted as a step in the right direction by the American Academy of Family Physicians.
"Elderly and disabled patients have complex, multiple, and chronic health conditions that require the whole-person medical attention available only through primary care physicians," Dr. Reid Blackwelder, AAFP president, said in a statement. "Placing appropriate value on the primary care services these patients require and establishing codes for chronic care management are important steps in meeting their needs."
The final fee schedule rule also provides a new estimate for how deep the Sustainable Growth Rate (SGR) formula cut will be in 2014. The across-the-board cut, which will take effect on Jan. 1 unless Congress takes action to avert it, will be 20.1%, down from an earlier estimate of 24.4%.
The somewhat smaller cut was not seen as good news by physician groups, which are increasingly fed up with the SGR formula.
The American Medical Association urged Congress to act quickly, not on a temporary patch, but on a permanent repeal of the SGR formula.
"The clock is ticking," Dr. Ardis Dee Hoven, AMA president, said in a statement. "At stake are innovations that would make Medicare more cost effective for current and future generations of seniors. These innovations are not possible if physicians are worried about drastic cuts to Medicare rates that have remained almost flat since 2001, while the cost of caring for patients has gone up by 25 percent."
The 2014 fee schedule also continues to phase in the Physician Value-Based Payment Modifier program. The program links Medicare payments to performance on cost and quality of care. The first payment adjustments will come in January 2015 for practices of 100 or more providers. In January 2016, the program will extend to groups with 10 or more eligible professionals. The CMS estimates that nearly 60% of physicians will be paid under the value-based payment modifier program in 2016. The remainder of physicians will be included in the program starting in January 2017.
But the CMS urged physicians to plan ahead. While payments won’t be affected until those dates, the performance measurement will occur earlier. For instance, for small group practices that will enter the program in 2017, the performance year is 2015. Physicians in small practices should use 2014 as a "practice year" and report to the Physician Quality Reporting System (PQRS) program so that they will be ready in 2015, according to the CMS.
The fee schedule will be published in the Federal Register on Dec. 10. The deadline for public comments on the rule is Jan. 27, 2014.
Starting in 2015, primary care physicians will get paid for some of the chronic care management work they do outside of office visits.
As part of the 2014 Medicare physician fee schedule final rule, officials at the Centers for Medicare and Medicaid Services (CMS) finalized plans to begin paying physicians separately for services such as development and revision of a care plan, communication with other treating providers, review of lab results, and adjustment of medications.
The agency established a new G-code that physicians can use to bill for non-face-to-face care management services for Medicare patients with two or more significant chronic conditions. The code, which will apply to 20 minutes or more of chronic care management services during a 30-day period, takes effect on Jan. 1, 2015.
Physicians who wish to use the new code will have to meet a series of requirements laid out by the CMS, including providing 24-7 access, coordination with home- and community-based service providers, and patient access to the practice through secure messaging or patient portals.
The new codes are part of a recent move by Medicare officials to emphasize primary care and to pay for services that happen outside of the traditional office visit. In 2012, the CMS established codes for transitional care management services for patients moving from a hospital or skilled nursing facility to home. Those codes, which took effect this year, included payment for some non-face-to-face activities.
The news was greeted as a step in the right direction by the American Academy of Family Physicians.
"Elderly and disabled patients have complex, multiple, and chronic health conditions that require the whole-person medical attention available only through primary care physicians," Dr. Reid Blackwelder, AAFP president, said in a statement. "Placing appropriate value on the primary care services these patients require and establishing codes for chronic care management are important steps in meeting their needs."
The final fee schedule rule also provides a new estimate for how deep the Sustainable Growth Rate (SGR) formula cut will be in 2014. The across-the-board cut, which will take effect on Jan. 1 unless Congress takes action to avert it, will be 20.1%, down from an earlier estimate of 24.4%.
The somewhat smaller cut was not seen as good news by physician groups, which are increasingly fed up with the SGR formula.
The American Medical Association urged Congress to act quickly, not on a temporary patch, but on a permanent repeal of the SGR formula.
"The clock is ticking," Dr. Ardis Dee Hoven, AMA president, said in a statement. "At stake are innovations that would make Medicare more cost effective for current and future generations of seniors. These innovations are not possible if physicians are worried about drastic cuts to Medicare rates that have remained almost flat since 2001, while the cost of caring for patients has gone up by 25 percent."
The 2014 fee schedule also continues to phase in the Physician Value-Based Payment Modifier program. The program links Medicare payments to performance on cost and quality of care. The first payment adjustments will come in January 2015 for practices of 100 or more providers. In January 2016, the program will extend to groups with 10 or more eligible professionals. The CMS estimates that nearly 60% of physicians will be paid under the value-based payment modifier program in 2016. The remainder of physicians will be included in the program starting in January 2017.
But the CMS urged physicians to plan ahead. While payments won’t be affected until those dates, the performance measurement will occur earlier. For instance, for small group practices that will enter the program in 2017, the performance year is 2015. Physicians in small practices should use 2014 as a "practice year" and report to the Physician Quality Reporting System (PQRS) program so that they will be ready in 2015, according to the CMS.
The fee schedule will be published in the Federal Register on Dec. 10. The deadline for public comments on the rule is Jan. 27, 2014.
Starting in 2015, primary care physicians will get paid for some of the chronic care management work they do outside of office visits.
As part of the 2014 Medicare physician fee schedule final rule, officials at the Centers for Medicare and Medicaid Services (CMS) finalized plans to begin paying physicians separately for services such as development and revision of a care plan, communication with other treating providers, review of lab results, and adjustment of medications.
The agency established a new G-code that physicians can use to bill for non-face-to-face care management services for Medicare patients with two or more significant chronic conditions. The code, which will apply to 20 minutes or more of chronic care management services during a 30-day period, takes effect on Jan. 1, 2015.
Physicians who wish to use the new code will have to meet a series of requirements laid out by the CMS, including providing 24-7 access, coordination with home- and community-based service providers, and patient access to the practice through secure messaging or patient portals.
The new codes are part of a recent move by Medicare officials to emphasize primary care and to pay for services that happen outside of the traditional office visit. In 2012, the CMS established codes for transitional care management services for patients moving from a hospital or skilled nursing facility to home. Those codes, which took effect this year, included payment for some non-face-to-face activities.
The news was greeted as a step in the right direction by the American Academy of Family Physicians.
"Elderly and disabled patients have complex, multiple, and chronic health conditions that require the whole-person medical attention available only through primary care physicians," Dr. Reid Blackwelder, AAFP president, said in a statement. "Placing appropriate value on the primary care services these patients require and establishing codes for chronic care management are important steps in meeting their needs."
The final fee schedule rule also provides a new estimate for how deep the Sustainable Growth Rate (SGR) formula cut will be in 2014. The across-the-board cut, which will take effect on Jan. 1 unless Congress takes action to avert it, will be 20.1%, down from an earlier estimate of 24.4%.
The somewhat smaller cut was not seen as good news by physician groups, which are increasingly fed up with the SGR formula.
The American Medical Association urged Congress to act quickly, not on a temporary patch, but on a permanent repeal of the SGR formula.
"The clock is ticking," Dr. Ardis Dee Hoven, AMA president, said in a statement. "At stake are innovations that would make Medicare more cost effective for current and future generations of seniors. These innovations are not possible if physicians are worried about drastic cuts to Medicare rates that have remained almost flat since 2001, while the cost of caring for patients has gone up by 25 percent."
The 2014 fee schedule also continues to phase in the Physician Value-Based Payment Modifier program. The program links Medicare payments to performance on cost and quality of care. The first payment adjustments will come in January 2015 for practices of 100 or more providers. In January 2016, the program will extend to groups with 10 or more eligible professionals. The CMS estimates that nearly 60% of physicians will be paid under the value-based payment modifier program in 2016. The remainder of physicians will be included in the program starting in January 2017.
But the CMS urged physicians to plan ahead. While payments won’t be affected until those dates, the performance measurement will occur earlier. For instance, for small group practices that will enter the program in 2017, the performance year is 2015. Physicians in small practices should use 2014 as a "practice year" and report to the Physician Quality Reporting System (PQRS) program so that they will be ready in 2015, according to the CMS.
The fee schedule will be published in the Federal Register on Dec. 10. The deadline for public comments on the rule is Jan. 27, 2014.
Feds make significant progress on HealthCare.gov
The federal insurance website, HealthCare.gov, is now faster and more reliable, but more work still needs to be done, according to an assessment by the Centers for Medicare and Medicaid Services.
About 80% of users are now able to complete the online application and enrollment process, meeting the goal set by the agency to get the website running smoothly for the majority of users by the end of November, Julie Bataille, director of the office of communications at CMS, said at a Dec. 1 press briefing.
CMS officials reported that they have improved the website’s response times, decreased the per-page error rate, and improved system stability and capacity. The improved performance is a "night and day" difference from how the site operated during October, according to Jeff Zients, a consultant brought in to improve the website.
Response time to user requests has been reduced from about 8 seconds in late October to 1 second on Nov. 30, Ms. Bataille reported. Similar reductions have been made to the error rate (percentage of per page system time outs and failures). In early October, the error rate was more than 6%; on Nov. 30, it was less than 1%.
Site stability also has improved, Ms. Bataille said, meaning that HealthCare.gov is "up" more than 90% of the time now – excluding scheduled maintenance – in comparison to 42.9% of the time in early November.
Federal officials said they are hopeful that the site will be able to handle a surge in users in December as the enrollment deadline approaches for consumers who want insurance coverage on Jan. 1. They have increased capacity on the site to about 50,000 simultaneous users and more than 800,000 users per day.
Mr. Zients said that, even with the improvements, the website may not have enough capacity to handle some peak user loads. As a result, CMS has put in place a queuing system that will serve users in order. The system will e-mail those users who could not get through and invite them back to the site when it’s not as busy.
Mr. Zients said that he expects consumers will continue to encounter glitches. However, the issues should be resolved much quicker now that they will have a rapid response team monitoring and responding to problems 24 hours a day.
On Twitter @MaryEllenNY
The federal insurance website, HealthCare.gov, is now faster and more reliable, but more work still needs to be done, according to an assessment by the Centers for Medicare and Medicaid Services.
About 80% of users are now able to complete the online application and enrollment process, meeting the goal set by the agency to get the website running smoothly for the majority of users by the end of November, Julie Bataille, director of the office of communications at CMS, said at a Dec. 1 press briefing.
CMS officials reported that they have improved the website’s response times, decreased the per-page error rate, and improved system stability and capacity. The improved performance is a "night and day" difference from how the site operated during October, according to Jeff Zients, a consultant brought in to improve the website.
Response time to user requests has been reduced from about 8 seconds in late October to 1 second on Nov. 30, Ms. Bataille reported. Similar reductions have been made to the error rate (percentage of per page system time outs and failures). In early October, the error rate was more than 6%; on Nov. 30, it was less than 1%.
Site stability also has improved, Ms. Bataille said, meaning that HealthCare.gov is "up" more than 90% of the time now – excluding scheduled maintenance – in comparison to 42.9% of the time in early November.
Federal officials said they are hopeful that the site will be able to handle a surge in users in December as the enrollment deadline approaches for consumers who want insurance coverage on Jan. 1. They have increased capacity on the site to about 50,000 simultaneous users and more than 800,000 users per day.
Mr. Zients said that, even with the improvements, the website may not have enough capacity to handle some peak user loads. As a result, CMS has put in place a queuing system that will serve users in order. The system will e-mail those users who could not get through and invite them back to the site when it’s not as busy.
Mr. Zients said that he expects consumers will continue to encounter glitches. However, the issues should be resolved much quicker now that they will have a rapid response team monitoring and responding to problems 24 hours a day.
On Twitter @MaryEllenNY
The federal insurance website, HealthCare.gov, is now faster and more reliable, but more work still needs to be done, according to an assessment by the Centers for Medicare and Medicaid Services.
About 80% of users are now able to complete the online application and enrollment process, meeting the goal set by the agency to get the website running smoothly for the majority of users by the end of November, Julie Bataille, director of the office of communications at CMS, said at a Dec. 1 press briefing.
CMS officials reported that they have improved the website’s response times, decreased the per-page error rate, and improved system stability and capacity. The improved performance is a "night and day" difference from how the site operated during October, according to Jeff Zients, a consultant brought in to improve the website.
Response time to user requests has been reduced from about 8 seconds in late October to 1 second on Nov. 30, Ms. Bataille reported. Similar reductions have been made to the error rate (percentage of per page system time outs and failures). In early October, the error rate was more than 6%; on Nov. 30, it was less than 1%.
Site stability also has improved, Ms. Bataille said, meaning that HealthCare.gov is "up" more than 90% of the time now – excluding scheduled maintenance – in comparison to 42.9% of the time in early November.
Federal officials said they are hopeful that the site will be able to handle a surge in users in December as the enrollment deadline approaches for consumers who want insurance coverage on Jan. 1. They have increased capacity on the site to about 50,000 simultaneous users and more than 800,000 users per day.
Mr. Zients said that, even with the improvements, the website may not have enough capacity to handle some peak user loads. As a result, CMS has put in place a queuing system that will serve users in order. The system will e-mail those users who could not get through and invite them back to the site when it’s not as busy.
Mr. Zients said that he expects consumers will continue to encounter glitches. However, the issues should be resolved much quicker now that they will have a rapid response team monitoring and responding to problems 24 hours a day.
On Twitter @MaryEllenNY
Feds delay online enrollment in small business exchange for 1 year
Small employers seeking health insurance through the Affordable Care Act’s small business marketplace will have to wait another year to enroll online.
Officials at the Centers for Medicare and Medicaid Services (CMS) announced on Nov. 27 that online enrollment would be delayed until November 2014, though enrollment will continue through paper applications. Employers will also be able to sign up for insurance through insurance brokers or agents, and directly through health plans.
The administration delayed the Small Business Health Options Program (SHOP) Marketplace to prioritize fixes to healthcare.gov, the tech-plagued federal marketplace used by individuals purchasing insurance, according to Julie Bataille, director of CMS’ Office of Communications.
The SHOP Marketplace allows small businesses with 50 or fewer full-time-equivalent employees to choose health plan options. For 2014, employers will only be able to select one plan.
Businesses with 50 or fewer employees are not required to offer insurance under the Affordable Care Act, though their employees must have coverage in place by March 31, 2014, in order to avoid a penalty under the health law.
In the meantime, federal health officials said they are still "on track" to meet their self-imposed deadline of Nov. 30 for getting healthcare.gov working well for the vast majority of users. By the end of November, healthcare.gov will be able to handle about 50,000 users at one time and more than 800,000 over the course of a day. But officials also stressed that Nov. 30 does not represent a relaunch of the website.
"It is not a magical date," Ms. Bataille said.
Small employers seeking health insurance through the Affordable Care Act’s small business marketplace will have to wait another year to enroll online.
Officials at the Centers for Medicare and Medicaid Services (CMS) announced on Nov. 27 that online enrollment would be delayed until November 2014, though enrollment will continue through paper applications. Employers will also be able to sign up for insurance through insurance brokers or agents, and directly through health plans.
The administration delayed the Small Business Health Options Program (SHOP) Marketplace to prioritize fixes to healthcare.gov, the tech-plagued federal marketplace used by individuals purchasing insurance, according to Julie Bataille, director of CMS’ Office of Communications.
The SHOP Marketplace allows small businesses with 50 or fewer full-time-equivalent employees to choose health plan options. For 2014, employers will only be able to select one plan.
Businesses with 50 or fewer employees are not required to offer insurance under the Affordable Care Act, though their employees must have coverage in place by March 31, 2014, in order to avoid a penalty under the health law.
In the meantime, federal health officials said they are still "on track" to meet their self-imposed deadline of Nov. 30 for getting healthcare.gov working well for the vast majority of users. By the end of November, healthcare.gov will be able to handle about 50,000 users at one time and more than 800,000 over the course of a day. But officials also stressed that Nov. 30 does not represent a relaunch of the website.
"It is not a magical date," Ms. Bataille said.
Small employers seeking health insurance through the Affordable Care Act’s small business marketplace will have to wait another year to enroll online.
Officials at the Centers for Medicare and Medicaid Services (CMS) announced on Nov. 27 that online enrollment would be delayed until November 2014, though enrollment will continue through paper applications. Employers will also be able to sign up for insurance through insurance brokers or agents, and directly through health plans.
The administration delayed the Small Business Health Options Program (SHOP) Marketplace to prioritize fixes to healthcare.gov, the tech-plagued federal marketplace used by individuals purchasing insurance, according to Julie Bataille, director of CMS’ Office of Communications.
The SHOP Marketplace allows small businesses with 50 or fewer full-time-equivalent employees to choose health plan options. For 2014, employers will only be able to select one plan.
Businesses with 50 or fewer employees are not required to offer insurance under the Affordable Care Act, though their employees must have coverage in place by March 31, 2014, in order to avoid a penalty under the health law.
In the meantime, federal health officials said they are still "on track" to meet their self-imposed deadline of Nov. 30 for getting healthcare.gov working well for the vast majority of users. By the end of November, healthcare.gov will be able to handle about 50,000 users at one time and more than 800,000 over the course of a day. But officials also stressed that Nov. 30 does not represent a relaunch of the website.
"It is not a magical date," Ms. Bataille said.