User login
RUC panel aims for transparency
The RUC, seen by many as vaguely mysterious – but very influential – advisors to Medicare on the value of physician services, is trying to be more open about its process.
Formally known as the Relative Value Scale Update Committee, the RUC will begin posting votes totals for each CPT code it considers and publishing its meeting minutes, starting in November. It also plans to publicize its meeting more widely.
According to the American Medical Association, which operates the committee jointly with the medical specialty societies, the RUC is already transparent in its operations with more than 300 individuals attending each of its meetings. That said, the panel often has been criticized as being secretive.
Dr. Barbara Levy, the RUC chairwoman, said that, over her entire time on the panel, she has never denied a request for an individual to attend a meeting. However, she added, those wishing to attend a RUC meeting must register. The group does not employ a completely open meeting process, as a way to protect its expert members from lobbying by groups or companies with a stake in how the codes are valued.
The RUC also has a confidentiality policy that bars its members and meeting attendees from publicizing the specifics of the panel’s discussions. This policy is to protect the "deliberative process," Dr. Levy said.
Dr. Yul D. Ejnes, an internist who serves as an alternate for the RUC primary care rotating seat, said that the panel has to strike a tough balance.
"The challenge for the RUC is to try to respond to all the concerns regarding transparency and accountability, while at the same time allowing the RUC to remain an effective body," he said.
As a new member to the RUC, Dr. Ejnes said he was struck by the fact that, before he got to know the individuals on the panel, he couldn’t tell which specialty they represented based on their comments.
RUC members are not there to "protect their own" specialty, Dr. Ejnes said.
Not everyone, though, is impressed by the panel’s efforts. Dr. Paul M. Fischer, a family physician in Augusta, Ga., who is part of an effort to replace the RUC, said the changes are simply "window dressing" that will not do anything to change the fundamental structure of the panel or its bias toward procedural specialties. Dr. Fischer previously filed an unsuccessful lawsuit against the RUC, claiming that it violates the Federal Advisory Committee Act.
The RUC also voted to make other changes, including updating its methodology on physician surveys.
The panel is increasing the minimum number of respondents required for each survey of commonly performed CPT codes. For instance, for physician services that are performed more than 1 million times each year among Medicare patients, at least 75 physicians must complete the survey. At least 50 physicians must be surveyed if the services are performed more than 100,000 times each year.
The panel also will begin using a centralized online survey process operated by the AMA, rather than relying on individual medical specialty societies to collect and report on survey results.
Part of the reason for the change is to make the survey process uniform across specialties, but it’s also an attempt to address the appearance of the "fox guarding the hen house" that comes from having specialty societies control the collection of data so important to determining how their members get paid, Dr. Levy said.
Although they haven’t had any problems with the old procedure, they wanted to avoid any appearance of conflict, she said.
"We’re consistently looking at our own processes and trying to improve them," Dr. Levy said.
What’s the RUC?
The Relative Value Scale Update Committee, better known as the RUC, is one of the most powerful panels in medicine that many physicians know nothing about.
The expert panel is run by the American Medical Association in conjunction with medical specialty societies and offers advice to the Centers for Medicare and Medicaid Services (CMS) on how to set the relative values for services performed by physicians, based on CPT code.
As a result, decisions made by the RUC have a major impact on how much physicians get paid both by Medicare and by private insurers, which often follow Medicare’s lead.
The CMS doesn’t accept all of the annual RUC recommendations, but the panel’s success rate is very high. The agency has adopted 95% of the RUC’s work relative value recommendations, according to the AMA.
The RUC is comprised of 31 members, 28 of whom vote. The bulk of the seats (25) are appointed by major national medical specialty societies.
Four of those 25 seats rotate every 2 years. This year, the rotating seats are filled by representatives from infectious disease, oncology/hematology, pediatric surgery, and primary care.
The remaining six seats are reserved for the RUC chair, a representative of the Health Care Professionals Advisory Committee Review Board, a representative from the Practice Expense Review Committee, a representative from the CPT Editorial Panel, an AMA representative, and a representative of the American Osteopathic Association.
The AMA Board of Trustees selects the RUC chair; RUC members are nominated by their specialty societies and approved by the AMA.
The RUC has been criticized as lacking adequate representation from primary care. The AMA tried to address some of that criticism in 2012 by adding a permanent seat for geriatrics and a rotating seat for a primary care representative.
Members of the RUC are appointed as technical experts, not as representatives of an individual medical society. Recommendations must be approved by two-thirds of the RUC to be sent on to CMS.
On Twitter @MaryEllenNY
The RUC, seen by many as vaguely mysterious – but very influential – advisors to Medicare on the value of physician services, is trying to be more open about its process.
Formally known as the Relative Value Scale Update Committee, the RUC will begin posting votes totals for each CPT code it considers and publishing its meeting minutes, starting in November. It also plans to publicize its meeting more widely.
According to the American Medical Association, which operates the committee jointly with the medical specialty societies, the RUC is already transparent in its operations with more than 300 individuals attending each of its meetings. That said, the panel often has been criticized as being secretive.
Dr. Barbara Levy, the RUC chairwoman, said that, over her entire time on the panel, she has never denied a request for an individual to attend a meeting. However, she added, those wishing to attend a RUC meeting must register. The group does not employ a completely open meeting process, as a way to protect its expert members from lobbying by groups or companies with a stake in how the codes are valued.
The RUC also has a confidentiality policy that bars its members and meeting attendees from publicizing the specifics of the panel’s discussions. This policy is to protect the "deliberative process," Dr. Levy said.
Dr. Yul D. Ejnes, an internist who serves as an alternate for the RUC primary care rotating seat, said that the panel has to strike a tough balance.
"The challenge for the RUC is to try to respond to all the concerns regarding transparency and accountability, while at the same time allowing the RUC to remain an effective body," he said.
As a new member to the RUC, Dr. Ejnes said he was struck by the fact that, before he got to know the individuals on the panel, he couldn’t tell which specialty they represented based on their comments.
RUC members are not there to "protect their own" specialty, Dr. Ejnes said.
Not everyone, though, is impressed by the panel’s efforts. Dr. Paul M. Fischer, a family physician in Augusta, Ga., who is part of an effort to replace the RUC, said the changes are simply "window dressing" that will not do anything to change the fundamental structure of the panel or its bias toward procedural specialties. Dr. Fischer previously filed an unsuccessful lawsuit against the RUC, claiming that it violates the Federal Advisory Committee Act.
The RUC also voted to make other changes, including updating its methodology on physician surveys.
The panel is increasing the minimum number of respondents required for each survey of commonly performed CPT codes. For instance, for physician services that are performed more than 1 million times each year among Medicare patients, at least 75 physicians must complete the survey. At least 50 physicians must be surveyed if the services are performed more than 100,000 times each year.
The panel also will begin using a centralized online survey process operated by the AMA, rather than relying on individual medical specialty societies to collect and report on survey results.
Part of the reason for the change is to make the survey process uniform across specialties, but it’s also an attempt to address the appearance of the "fox guarding the hen house" that comes from having specialty societies control the collection of data so important to determining how their members get paid, Dr. Levy said.
Although they haven’t had any problems with the old procedure, they wanted to avoid any appearance of conflict, she said.
"We’re consistently looking at our own processes and trying to improve them," Dr. Levy said.
What’s the RUC?
The Relative Value Scale Update Committee, better known as the RUC, is one of the most powerful panels in medicine that many physicians know nothing about.
The expert panel is run by the American Medical Association in conjunction with medical specialty societies and offers advice to the Centers for Medicare and Medicaid Services (CMS) on how to set the relative values for services performed by physicians, based on CPT code.
As a result, decisions made by the RUC have a major impact on how much physicians get paid both by Medicare and by private insurers, which often follow Medicare’s lead.
The CMS doesn’t accept all of the annual RUC recommendations, but the panel’s success rate is very high. The agency has adopted 95% of the RUC’s work relative value recommendations, according to the AMA.
The RUC is comprised of 31 members, 28 of whom vote. The bulk of the seats (25) are appointed by major national medical specialty societies.
Four of those 25 seats rotate every 2 years. This year, the rotating seats are filled by representatives from infectious disease, oncology/hematology, pediatric surgery, and primary care.
The remaining six seats are reserved for the RUC chair, a representative of the Health Care Professionals Advisory Committee Review Board, a representative from the Practice Expense Review Committee, a representative from the CPT Editorial Panel, an AMA representative, and a representative of the American Osteopathic Association.
The AMA Board of Trustees selects the RUC chair; RUC members are nominated by their specialty societies and approved by the AMA.
The RUC has been criticized as lacking adequate representation from primary care. The AMA tried to address some of that criticism in 2012 by adding a permanent seat for geriatrics and a rotating seat for a primary care representative.
Members of the RUC are appointed as technical experts, not as representatives of an individual medical society. Recommendations must be approved by two-thirds of the RUC to be sent on to CMS.
On Twitter @MaryEllenNY
The RUC, seen by many as vaguely mysterious – but very influential – advisors to Medicare on the value of physician services, is trying to be more open about its process.
Formally known as the Relative Value Scale Update Committee, the RUC will begin posting votes totals for each CPT code it considers and publishing its meeting minutes, starting in November. It also plans to publicize its meeting more widely.
According to the American Medical Association, which operates the committee jointly with the medical specialty societies, the RUC is already transparent in its operations with more than 300 individuals attending each of its meetings. That said, the panel often has been criticized as being secretive.
Dr. Barbara Levy, the RUC chairwoman, said that, over her entire time on the panel, she has never denied a request for an individual to attend a meeting. However, she added, those wishing to attend a RUC meeting must register. The group does not employ a completely open meeting process, as a way to protect its expert members from lobbying by groups or companies with a stake in how the codes are valued.
The RUC also has a confidentiality policy that bars its members and meeting attendees from publicizing the specifics of the panel’s discussions. This policy is to protect the "deliberative process," Dr. Levy said.
Dr. Yul D. Ejnes, an internist who serves as an alternate for the RUC primary care rotating seat, said that the panel has to strike a tough balance.
"The challenge for the RUC is to try to respond to all the concerns regarding transparency and accountability, while at the same time allowing the RUC to remain an effective body," he said.
As a new member to the RUC, Dr. Ejnes said he was struck by the fact that, before he got to know the individuals on the panel, he couldn’t tell which specialty they represented based on their comments.
RUC members are not there to "protect their own" specialty, Dr. Ejnes said.
Not everyone, though, is impressed by the panel’s efforts. Dr. Paul M. Fischer, a family physician in Augusta, Ga., who is part of an effort to replace the RUC, said the changes are simply "window dressing" that will not do anything to change the fundamental structure of the panel or its bias toward procedural specialties. Dr. Fischer previously filed an unsuccessful lawsuit against the RUC, claiming that it violates the Federal Advisory Committee Act.
The RUC also voted to make other changes, including updating its methodology on physician surveys.
The panel is increasing the minimum number of respondents required for each survey of commonly performed CPT codes. For instance, for physician services that are performed more than 1 million times each year among Medicare patients, at least 75 physicians must complete the survey. At least 50 physicians must be surveyed if the services are performed more than 100,000 times each year.
The panel also will begin using a centralized online survey process operated by the AMA, rather than relying on individual medical specialty societies to collect and report on survey results.
Part of the reason for the change is to make the survey process uniform across specialties, but it’s also an attempt to address the appearance of the "fox guarding the hen house" that comes from having specialty societies control the collection of data so important to determining how their members get paid, Dr. Levy said.
Although they haven’t had any problems with the old procedure, they wanted to avoid any appearance of conflict, she said.
"We’re consistently looking at our own processes and trying to improve them," Dr. Levy said.
What’s the RUC?
The Relative Value Scale Update Committee, better known as the RUC, is one of the most powerful panels in medicine that many physicians know nothing about.
The expert panel is run by the American Medical Association in conjunction with medical specialty societies and offers advice to the Centers for Medicare and Medicaid Services (CMS) on how to set the relative values for services performed by physicians, based on CPT code.
As a result, decisions made by the RUC have a major impact on how much physicians get paid both by Medicare and by private insurers, which often follow Medicare’s lead.
The CMS doesn’t accept all of the annual RUC recommendations, but the panel’s success rate is very high. The agency has adopted 95% of the RUC’s work relative value recommendations, according to the AMA.
The RUC is comprised of 31 members, 28 of whom vote. The bulk of the seats (25) are appointed by major national medical specialty societies.
Four of those 25 seats rotate every 2 years. This year, the rotating seats are filled by representatives from infectious disease, oncology/hematology, pediatric surgery, and primary care.
The remaining six seats are reserved for the RUC chair, a representative of the Health Care Professionals Advisory Committee Review Board, a representative from the Practice Expense Review Committee, a representative from the CPT Editorial Panel, an AMA representative, and a representative of the American Osteopathic Association.
The AMA Board of Trustees selects the RUC chair; RUC members are nominated by their specialty societies and approved by the AMA.
The RUC has been criticized as lacking adequate representation from primary care. The AMA tried to address some of that criticism in 2012 by adding a permanent seat for geriatrics and a rotating seat for a primary care representative.
Members of the RUC are appointed as technical experts, not as representatives of an individual medical society. Recommendations must be approved by two-thirds of the RUC to be sent on to CMS.
On Twitter @MaryEllenNY
Lawmakers unveil bipartisan SGR repeal plan
A new bipartisan, bicameral plan to repeal the Medicare Sustainable Growth Rate formula has surfaced on Capitol Hill.
On Oct. 30, the Senate Finance Committee and the House Ways and Means Committee jointly released a legislative framework that would scrap Medicare’s Sustainable Growth Rate (SGR) formula and freeze physician payments for the next decade.
Starting in 2017, physicians would see their payments tied to cost and quality of care using a single quality incentive program. Under the proposal, Medicare would create the Value-Based Performance Payment Program to adjust physician payments based on quality, resource use, clinical practice improvement activities, and the use of electronic health records.
Since the program is budget neutral, some physicians would see increases while others would see cuts.
At the end of 2016, Medicare would end a group of existing incentive programs including the Physician Quality Reporting System; the Value-Based Modifier Program; and the Electronic Health Record (EHR) Incentive Program, which requires the meaningful use of certified EHR technology.
Physicians who treat few Medicare patients or who receive a significant portion of their payments from advanced alternative payment models, such as accountable care organizations, would be excluded from the new Value-Based Performance Payment Program. Physicians in ACOs and other models that involved taking on financial risk and reporting on quality measures would instead be eligible for bonus payments under the proposal.
After 2023, physicians who participate in these advanced alternative payment models would see an annual 2% payment increase, and other physicians would earn updates of 1% each year, according to the proposal circulated by the two committees.
"This discussion draft is an important step in a long-term solution to this failed policy," Rep. Dave Camp, chairman of the House Ways and Means Committee, said in a statement. "Creating a policy that rewards providers for delivering high-quality, efficient health care is the ultimate goal, and this draft brings us one step closer to that reality."
The release of the proposal follows a summer of feverish activity in the House on the issue of the SGR. After months of hearings, the Energy and Commerce Committee unanimously approved a bill on July 31 (H.R. 2810) that would repeal the SGR and provide 0.5% payment increases for physicians through 2018.
Momentum slowed after Labor Day with the continuing debate over the Affordable Care Act and the federal government shutdown that began on Oct. 1. This latest plan incorporates ideas from both the Democratic-led Senate and the GOP-controlled House.
While physician groups were still reviewing the proposal at press time, they hailed the renewed focus on the SGR as a move in the right direction.
"Congress is demonstrating that they understand that ending the failed SGR this year is fiscally responsible, and that the current Medicare payment system is a barrier to adoption of health care delivery and payment reforms that will improve health care for America’s seniors and rein in overall costs," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
Physicians can comment on the proposal until Nov. 12. Send comments to the Senate Finance Committee at [email protected] and to the House Ways and Means Committee at [email protected].
A new bipartisan, bicameral plan to repeal the Medicare Sustainable Growth Rate formula has surfaced on Capitol Hill.
On Oct. 30, the Senate Finance Committee and the House Ways and Means Committee jointly released a legislative framework that would scrap Medicare’s Sustainable Growth Rate (SGR) formula and freeze physician payments for the next decade.
Starting in 2017, physicians would see their payments tied to cost and quality of care using a single quality incentive program. Under the proposal, Medicare would create the Value-Based Performance Payment Program to adjust physician payments based on quality, resource use, clinical practice improvement activities, and the use of electronic health records.
Since the program is budget neutral, some physicians would see increases while others would see cuts.
At the end of 2016, Medicare would end a group of existing incentive programs including the Physician Quality Reporting System; the Value-Based Modifier Program; and the Electronic Health Record (EHR) Incentive Program, which requires the meaningful use of certified EHR technology.
Physicians who treat few Medicare patients or who receive a significant portion of their payments from advanced alternative payment models, such as accountable care organizations, would be excluded from the new Value-Based Performance Payment Program. Physicians in ACOs and other models that involved taking on financial risk and reporting on quality measures would instead be eligible for bonus payments under the proposal.
After 2023, physicians who participate in these advanced alternative payment models would see an annual 2% payment increase, and other physicians would earn updates of 1% each year, according to the proposal circulated by the two committees.
"This discussion draft is an important step in a long-term solution to this failed policy," Rep. Dave Camp, chairman of the House Ways and Means Committee, said in a statement. "Creating a policy that rewards providers for delivering high-quality, efficient health care is the ultimate goal, and this draft brings us one step closer to that reality."
The release of the proposal follows a summer of feverish activity in the House on the issue of the SGR. After months of hearings, the Energy and Commerce Committee unanimously approved a bill on July 31 (H.R. 2810) that would repeal the SGR and provide 0.5% payment increases for physicians through 2018.
Momentum slowed after Labor Day with the continuing debate over the Affordable Care Act and the federal government shutdown that began on Oct. 1. This latest plan incorporates ideas from both the Democratic-led Senate and the GOP-controlled House.
While physician groups were still reviewing the proposal at press time, they hailed the renewed focus on the SGR as a move in the right direction.
"Congress is demonstrating that they understand that ending the failed SGR this year is fiscally responsible, and that the current Medicare payment system is a barrier to adoption of health care delivery and payment reforms that will improve health care for America’s seniors and rein in overall costs," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
Physicians can comment on the proposal until Nov. 12. Send comments to the Senate Finance Committee at [email protected] and to the House Ways and Means Committee at [email protected].
A new bipartisan, bicameral plan to repeal the Medicare Sustainable Growth Rate formula has surfaced on Capitol Hill.
On Oct. 30, the Senate Finance Committee and the House Ways and Means Committee jointly released a legislative framework that would scrap Medicare’s Sustainable Growth Rate (SGR) formula and freeze physician payments for the next decade.
Starting in 2017, physicians would see their payments tied to cost and quality of care using a single quality incentive program. Under the proposal, Medicare would create the Value-Based Performance Payment Program to adjust physician payments based on quality, resource use, clinical practice improvement activities, and the use of electronic health records.
Since the program is budget neutral, some physicians would see increases while others would see cuts.
At the end of 2016, Medicare would end a group of existing incentive programs including the Physician Quality Reporting System; the Value-Based Modifier Program; and the Electronic Health Record (EHR) Incentive Program, which requires the meaningful use of certified EHR technology.
Physicians who treat few Medicare patients or who receive a significant portion of their payments from advanced alternative payment models, such as accountable care organizations, would be excluded from the new Value-Based Performance Payment Program. Physicians in ACOs and other models that involved taking on financial risk and reporting on quality measures would instead be eligible for bonus payments under the proposal.
After 2023, physicians who participate in these advanced alternative payment models would see an annual 2% payment increase, and other physicians would earn updates of 1% each year, according to the proposal circulated by the two committees.
"This discussion draft is an important step in a long-term solution to this failed policy," Rep. Dave Camp, chairman of the House Ways and Means Committee, said in a statement. "Creating a policy that rewards providers for delivering high-quality, efficient health care is the ultimate goal, and this draft brings us one step closer to that reality."
The release of the proposal follows a summer of feverish activity in the House on the issue of the SGR. After months of hearings, the Energy and Commerce Committee unanimously approved a bill on July 31 (H.R. 2810) that would repeal the SGR and provide 0.5% payment increases for physicians through 2018.
Momentum slowed after Labor Day with the continuing debate over the Affordable Care Act and the federal government shutdown that began on Oct. 1. This latest plan incorporates ideas from both the Democratic-led Senate and the GOP-controlled House.
While physician groups were still reviewing the proposal at press time, they hailed the renewed focus on the SGR as a move in the right direction.
"Congress is demonstrating that they understand that ending the failed SGR this year is fiscally responsible, and that the current Medicare payment system is a barrier to adoption of health care delivery and payment reforms that will improve health care for America’s seniors and rein in overall costs," Dr. Ardis Dee Hoven, president of the American Medical Association, said in a statement.
Physicians can comment on the proposal until Nov. 12. Send comments to the Senate Finance Committee at [email protected] and to the House Ways and Means Committee at [email protected].
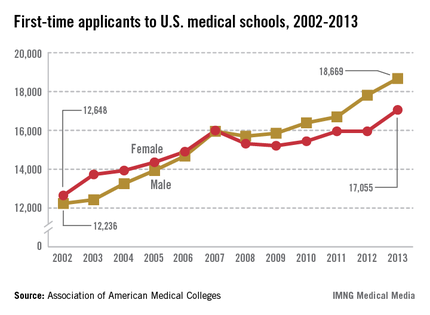
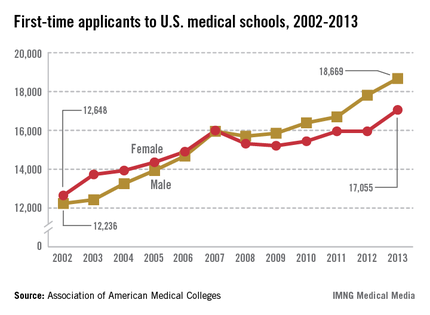
Med school applications spike
The number of students applying to medical school hit an all-time high this year, according to figures from the Association of American Medical Colleges.
More than 48,000 students applied to enter U.S. medical schools in 2013, a jump of 6% from the previous year. Most of the aspiring doctors – more than 35,000 – are first-time applicants.
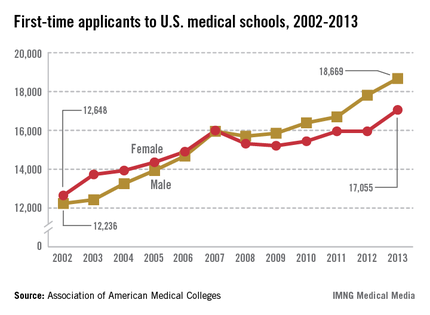
"We haven’t seen a level like this since 1996," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges (AAMC).
First-time medical school enrollment also set records this year. More than 20,000 students enrolled in their first year of medical school, a nearly 3% rise over the 2012 figures.
Dr. Kirch said college students are "voting with their feet" because they view medicine as an attractive career choice.
Medical schools have been able to accommodate this renewed interested in medicine because existing programs have expanded and some new medical schools have opened. This year, 14 medical schools increased their class sizes by more than 10% and four new medical schools opened their doors, according to the AAMC.
The enrollment and application numbers are good news as the nation faces a shortage of physicians, Dr. Kirch said. But the surge in students entering medical school won’t mean anything if they don’t have residency programs to go to after graduation, he said.
The problem is that residency training programs aren’t growing because Congress capped federal funding for residency training back in 1997. The funding restrictions severely limit the number of new slots that academic medical centers can afford to support, he said.
Dr. Kirch called on lawmakers to pass federal legislation that would lift the funding caps.
"If they don’t do it, we could face a serious shortage of physicians across the board," he said.
On Twitter @MaryEllenNY
The number of students applying to medical school hit an all-time high this year, according to figures from the Association of American Medical Colleges.
More than 48,000 students applied to enter U.S. medical schools in 2013, a jump of 6% from the previous year. Most of the aspiring doctors – more than 35,000 – are first-time applicants.
"We haven’t seen a level like this since 1996," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges (AAMC).
First-time medical school enrollment also set records this year. More than 20,000 students enrolled in their first year of medical school, a nearly 3% rise over the 2012 figures.
Dr. Kirch said college students are "voting with their feet" because they view medicine as an attractive career choice.
Medical schools have been able to accommodate this renewed interested in medicine because existing programs have expanded and some new medical schools have opened. This year, 14 medical schools increased their class sizes by more than 10% and four new medical schools opened their doors, according to the AAMC.
The enrollment and application numbers are good news as the nation faces a shortage of physicians, Dr. Kirch said. But the surge in students entering medical school won’t mean anything if they don’t have residency programs to go to after graduation, he said.
The problem is that residency training programs aren’t growing because Congress capped federal funding for residency training back in 1997. The funding restrictions severely limit the number of new slots that academic medical centers can afford to support, he said.
Dr. Kirch called on lawmakers to pass federal legislation that would lift the funding caps.
"If they don’t do it, we could face a serious shortage of physicians across the board," he said.
On Twitter @MaryEllenNY
The number of students applying to medical school hit an all-time high this year, according to figures from the Association of American Medical Colleges.
More than 48,000 students applied to enter U.S. medical schools in 2013, a jump of 6% from the previous year. Most of the aspiring doctors – more than 35,000 – are first-time applicants.
"We haven’t seen a level like this since 1996," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges (AAMC).
First-time medical school enrollment also set records this year. More than 20,000 students enrolled in their first year of medical school, a nearly 3% rise over the 2012 figures.
Dr. Kirch said college students are "voting with their feet" because they view medicine as an attractive career choice.
Medical schools have been able to accommodate this renewed interested in medicine because existing programs have expanded and some new medical schools have opened. This year, 14 medical schools increased their class sizes by more than 10% and four new medical schools opened their doors, according to the AAMC.
The enrollment and application numbers are good news as the nation faces a shortage of physicians, Dr. Kirch said. But the surge in students entering medical school won’t mean anything if they don’t have residency programs to go to after graduation, he said.
The problem is that residency training programs aren’t growing because Congress capped federal funding for residency training back in 1997. The funding restrictions severely limit the number of new slots that academic medical centers can afford to support, he said.
Dr. Kirch called on lawmakers to pass federal legislation that would lift the funding caps.
"If they don’t do it, we could face a serious shortage of physicians across the board," he said.
On Twitter @MaryEllenNY
Family doc’s coalition brings care to city’s neediest
In one of the poorest cities in the United States, Dr. Jeffrey Brenner is spearheading an innovative approach to primary care, using health data to identify hospital frequent flyers and deploying teams of nurses and health coaches to get patients’ health – and health care costs – under control.
His work in Camden, N.J., has been slowly drawing attention from health policy experts around the country. And it got a big boost in September when the MacArthur Foundation named him one of its 2013 fellows.
Dr. Brenner, a family physician, joins 23 others – including artists, scientists, and economists – who have been honored for their contributions to "American creativity." Each of the fellows will receive a "no strings attached" stipend of $625,000 to be paid out over 5 years.
The MacArthur Foundation singled out Dr. Brenner's work in founding the Camden Coalition of Healthcare Providers and called his approach to health care delivery "an important contribution to the national conversation on health care reform."
Data are key
It started in 2002 when a small group of Camden-area primary care providers started meeting for breakfast to share their frustration with the barriers they faced in practicing medicine in a fragmented, inefficient system. Fast forward a year and the group had grown to include nurses, physician assistants, podiatrists, and more. They soon formed a nonprofit organization – the Camden Coalition of Healthcare Providers – to tackle some of the systems issues they all encountered.
It took a few more years, but Dr. Brenner, who had signed on as executive director, eventually succeeded in getting to what the coalition members saw as the key to breaking down the silos of care: health data.
Today, the coalition operates a health information exchange that includes patient-level claims data from all three of Camden’s hospitals. They have real-time access to admission and diagnosis information for every Camden resident. Using that data, they target patients who need extra social and medical support.
Here’s how it works: the coalition receives a data feed on hospital admissions each day. Staff members identify the patients most in need of support and deploy a team of nurses, social workers, and health coaches to meet with the patient at the bedside. If the patient enrolls with the coalition, the next step is a home visit at discharge for medication review, but also to ensure that the patient’s home and social service needs are met. A team member accompanies the patient on follow-up visits to the primary care doctor and on specialist visits.
"We stick to them for about 90 days," Dr. Brenner, 44, said in an interview. "Then we graduate them."
The idea is to heap resources on the patients whose complex medical needs and lack of social support land them repeatedly in the emergency department, when what they really need is high-quality primary care. The Camden data demonstrate the realities of American health care: a small group of patients use most of the health care resources and cost the system money. In Camden, about 90% of the cost of hospital and ED care is spent on 20% of the patients, according to coalition data.
For patients who want to break the cycle of uncontrolled chronic disease and frequent ED visits, the coalition’s approach can make a big difference, Dr. Brenner said.
"If a patient is tired of being sick and tired you can go from 20 [hospital] visits to none," he said. The tricky part is how to help patients who aren’t primed for change and don’t trust the system. How to reach these patients is a problem they continue to work on in Camden and in other cities around the country. The coalition is working with organizations in Allentown, Pa.; Aurora, Colo.; Kansas City, Mo.; San Diego; and six other communities to adapt the Camden model.
Industrializing health care
One of the biggest problems the coalition has run into, and that others are finding around the country, is that once they identify patients who want to make changes in their health care, there aren’t enough well-run primary care practices to take on their care, Dr. Brenner said.
Even certified patient-centered medical homes don’t always do enough when it comes to incorporating clinical care teams, relying on health data, and reaching out to complex, recently hospitalized patients, Dr. Brenner said.
"The medical home is a good idea, but we’re not quite getting it right yet," he said.
There are lots of reasons why primary care isn’t there yet, Dr. Brenner said. Most offices haven’t built the right kind of clinical care teams, they lack the data systems, and physicians don’t have training in this area. Primary care physicians could take lessons from their colleagues in addiction and behavioral health on how to coordinate care for these patients, he said.
"We talk about the bio-psycho-social model, but I don’t know that we have all the components and the team and the training to fully pull it off yet," Dr. Brenner said.
The coalition has been working with local primary care physicians to try to get there, embedding nurses in their offices and helping them to create protocols for the adjustment and management of medications for blood pressure, cholesterol, and diabetes.
The idea is to create standardized protocols for common clinical scenarios and then delegate as much of the work as possible to nurses and other providers, freeing up physicians to take on the complex cases. Dr. Brenner said that in an ideal primary care practice, RNs would handle the well-child visits, the sore throats, and the simple medication adjustments.
"We need to industrialize primary care so that it becomes highly reliable, it becomes protocolized, standardized, and delegated so that we can stand out on a limb and customize and individualize for the sickest and most challenging patients," Dr. Brenner said.
And he wants to see nurses and project managers given the chance to run clinical care teams.
The Camden coalition uses licensed practical nurses, RNs, and community health workers. The coalition also relies heavily on Americorps volunteers, typically 22-year-told college graduates who are taking a year off before going to graduate school to be nurses, doctors, or public health workers. Many of the tasks that physicians stay late to do – or those that often fall through the cracks – can be delegated to these other providers, he said.
"It’s time we got out of the way and let our nurse colleagues get into the game," Dr. Brenner said. "I think their training is much better suited, frankly, for running teams, for working collaboratively, and for really improving quality and reducing costs."
Working harder doesn’t work
Instead of handing off less complex patients to clinical team members, most primary care physicians try to do it all, Dr. Brenner said. They stay in the room longer, make extra phone calls, and stay late at the office for a family conference. But this is "ad hoc work" that physicians do when they can find the time or the energy. It’s not something that they can do for every patient, he said.
"We’ve got to turn all that special sauce, all that ad hoc work into standardized, protocolized, structured work that always happens for everyone," Dr. Brenner said. "The only way we’re going to do that is to delegate and delegate and delegate."
Dr. Brenner said that he knows firsthand what’s like to try to do it all – that was his approach in his own practice. He had a completely paperless office and open-access scheduling, but he tried to make everything work by simply working harder. Ultimately, declining reimbursement from payers made it impossible to keep the doors open.
"I was trying as hard as I could but honestly I wasn’t doing all the things that I said. I wasn’t delegating, I wasn’t building a high-reliability team," he said. "I was trying to just work harder personally."
As the Affordable Care Act pushes new models for care coordination, including accountable care organizations, Dr. Brenner said he sees primary care physicians playing a major role. But they will need to delegate and to get more training to be successful, he said.
"I’ve been very fortunate. I’ve been at the right place at the right time," he said. "I think there are lots of other family docs who have the same skill sets and could do the same kind of work."
On Twitter @MaryEllenNY
In one of the poorest cities in the United States, Dr. Jeffrey Brenner is spearheading an innovative approach to primary care, using health data to identify hospital frequent flyers and deploying teams of nurses and health coaches to get patients’ health – and health care costs – under control.
His work in Camden, N.J., has been slowly drawing attention from health policy experts around the country. And it got a big boost in September when the MacArthur Foundation named him one of its 2013 fellows.
Dr. Brenner, a family physician, joins 23 others – including artists, scientists, and economists – who have been honored for their contributions to "American creativity." Each of the fellows will receive a "no strings attached" stipend of $625,000 to be paid out over 5 years.
The MacArthur Foundation singled out Dr. Brenner's work in founding the Camden Coalition of Healthcare Providers and called his approach to health care delivery "an important contribution to the national conversation on health care reform."
Data are key
It started in 2002 when a small group of Camden-area primary care providers started meeting for breakfast to share their frustration with the barriers they faced in practicing medicine in a fragmented, inefficient system. Fast forward a year and the group had grown to include nurses, physician assistants, podiatrists, and more. They soon formed a nonprofit organization – the Camden Coalition of Healthcare Providers – to tackle some of the systems issues they all encountered.
It took a few more years, but Dr. Brenner, who had signed on as executive director, eventually succeeded in getting to what the coalition members saw as the key to breaking down the silos of care: health data.
Today, the coalition operates a health information exchange that includes patient-level claims data from all three of Camden’s hospitals. They have real-time access to admission and diagnosis information for every Camden resident. Using that data, they target patients who need extra social and medical support.
Here’s how it works: the coalition receives a data feed on hospital admissions each day. Staff members identify the patients most in need of support and deploy a team of nurses, social workers, and health coaches to meet with the patient at the bedside. If the patient enrolls with the coalition, the next step is a home visit at discharge for medication review, but also to ensure that the patient’s home and social service needs are met. A team member accompanies the patient on follow-up visits to the primary care doctor and on specialist visits.
"We stick to them for about 90 days," Dr. Brenner, 44, said in an interview. "Then we graduate them."
The idea is to heap resources on the patients whose complex medical needs and lack of social support land them repeatedly in the emergency department, when what they really need is high-quality primary care. The Camden data demonstrate the realities of American health care: a small group of patients use most of the health care resources and cost the system money. In Camden, about 90% of the cost of hospital and ED care is spent on 20% of the patients, according to coalition data.
For patients who want to break the cycle of uncontrolled chronic disease and frequent ED visits, the coalition’s approach can make a big difference, Dr. Brenner said.
"If a patient is tired of being sick and tired you can go from 20 [hospital] visits to none," he said. The tricky part is how to help patients who aren’t primed for change and don’t trust the system. How to reach these patients is a problem they continue to work on in Camden and in other cities around the country. The coalition is working with organizations in Allentown, Pa.; Aurora, Colo.; Kansas City, Mo.; San Diego; and six other communities to adapt the Camden model.
Industrializing health care
One of the biggest problems the coalition has run into, and that others are finding around the country, is that once they identify patients who want to make changes in their health care, there aren’t enough well-run primary care practices to take on their care, Dr. Brenner said.
Even certified patient-centered medical homes don’t always do enough when it comes to incorporating clinical care teams, relying on health data, and reaching out to complex, recently hospitalized patients, Dr. Brenner said.
"The medical home is a good idea, but we’re not quite getting it right yet," he said.
There are lots of reasons why primary care isn’t there yet, Dr. Brenner said. Most offices haven’t built the right kind of clinical care teams, they lack the data systems, and physicians don’t have training in this area. Primary care physicians could take lessons from their colleagues in addiction and behavioral health on how to coordinate care for these patients, he said.
"We talk about the bio-psycho-social model, but I don’t know that we have all the components and the team and the training to fully pull it off yet," Dr. Brenner said.
The coalition has been working with local primary care physicians to try to get there, embedding nurses in their offices and helping them to create protocols for the adjustment and management of medications for blood pressure, cholesterol, and diabetes.
The idea is to create standardized protocols for common clinical scenarios and then delegate as much of the work as possible to nurses and other providers, freeing up physicians to take on the complex cases. Dr. Brenner said that in an ideal primary care practice, RNs would handle the well-child visits, the sore throats, and the simple medication adjustments.
"We need to industrialize primary care so that it becomes highly reliable, it becomes protocolized, standardized, and delegated so that we can stand out on a limb and customize and individualize for the sickest and most challenging patients," Dr. Brenner said.
And he wants to see nurses and project managers given the chance to run clinical care teams.
The Camden coalition uses licensed practical nurses, RNs, and community health workers. The coalition also relies heavily on Americorps volunteers, typically 22-year-told college graduates who are taking a year off before going to graduate school to be nurses, doctors, or public health workers. Many of the tasks that physicians stay late to do – or those that often fall through the cracks – can be delegated to these other providers, he said.
"It’s time we got out of the way and let our nurse colleagues get into the game," Dr. Brenner said. "I think their training is much better suited, frankly, for running teams, for working collaboratively, and for really improving quality and reducing costs."
Working harder doesn’t work
Instead of handing off less complex patients to clinical team members, most primary care physicians try to do it all, Dr. Brenner said. They stay in the room longer, make extra phone calls, and stay late at the office for a family conference. But this is "ad hoc work" that physicians do when they can find the time or the energy. It’s not something that they can do for every patient, he said.
"We’ve got to turn all that special sauce, all that ad hoc work into standardized, protocolized, structured work that always happens for everyone," Dr. Brenner said. "The only way we’re going to do that is to delegate and delegate and delegate."
Dr. Brenner said that he knows firsthand what’s like to try to do it all – that was his approach in his own practice. He had a completely paperless office and open-access scheduling, but he tried to make everything work by simply working harder. Ultimately, declining reimbursement from payers made it impossible to keep the doors open.
"I was trying as hard as I could but honestly I wasn’t doing all the things that I said. I wasn’t delegating, I wasn’t building a high-reliability team," he said. "I was trying to just work harder personally."
As the Affordable Care Act pushes new models for care coordination, including accountable care organizations, Dr. Brenner said he sees primary care physicians playing a major role. But they will need to delegate and to get more training to be successful, he said.
"I’ve been very fortunate. I’ve been at the right place at the right time," he said. "I think there are lots of other family docs who have the same skill sets and could do the same kind of work."
On Twitter @MaryEllenNY
In one of the poorest cities in the United States, Dr. Jeffrey Brenner is spearheading an innovative approach to primary care, using health data to identify hospital frequent flyers and deploying teams of nurses and health coaches to get patients’ health – and health care costs – under control.
His work in Camden, N.J., has been slowly drawing attention from health policy experts around the country. And it got a big boost in September when the MacArthur Foundation named him one of its 2013 fellows.
Dr. Brenner, a family physician, joins 23 others – including artists, scientists, and economists – who have been honored for their contributions to "American creativity." Each of the fellows will receive a "no strings attached" stipend of $625,000 to be paid out over 5 years.
The MacArthur Foundation singled out Dr. Brenner's work in founding the Camden Coalition of Healthcare Providers and called his approach to health care delivery "an important contribution to the national conversation on health care reform."
Data are key
It started in 2002 when a small group of Camden-area primary care providers started meeting for breakfast to share their frustration with the barriers they faced in practicing medicine in a fragmented, inefficient system. Fast forward a year and the group had grown to include nurses, physician assistants, podiatrists, and more. They soon formed a nonprofit organization – the Camden Coalition of Healthcare Providers – to tackle some of the systems issues they all encountered.
It took a few more years, but Dr. Brenner, who had signed on as executive director, eventually succeeded in getting to what the coalition members saw as the key to breaking down the silos of care: health data.
Today, the coalition operates a health information exchange that includes patient-level claims data from all three of Camden’s hospitals. They have real-time access to admission and diagnosis information for every Camden resident. Using that data, they target patients who need extra social and medical support.
Here’s how it works: the coalition receives a data feed on hospital admissions each day. Staff members identify the patients most in need of support and deploy a team of nurses, social workers, and health coaches to meet with the patient at the bedside. If the patient enrolls with the coalition, the next step is a home visit at discharge for medication review, but also to ensure that the patient’s home and social service needs are met. A team member accompanies the patient on follow-up visits to the primary care doctor and on specialist visits.
"We stick to them for about 90 days," Dr. Brenner, 44, said in an interview. "Then we graduate them."
The idea is to heap resources on the patients whose complex medical needs and lack of social support land them repeatedly in the emergency department, when what they really need is high-quality primary care. The Camden data demonstrate the realities of American health care: a small group of patients use most of the health care resources and cost the system money. In Camden, about 90% of the cost of hospital and ED care is spent on 20% of the patients, according to coalition data.
For patients who want to break the cycle of uncontrolled chronic disease and frequent ED visits, the coalition’s approach can make a big difference, Dr. Brenner said.
"If a patient is tired of being sick and tired you can go from 20 [hospital] visits to none," he said. The tricky part is how to help patients who aren’t primed for change and don’t trust the system. How to reach these patients is a problem they continue to work on in Camden and in other cities around the country. The coalition is working with organizations in Allentown, Pa.; Aurora, Colo.; Kansas City, Mo.; San Diego; and six other communities to adapt the Camden model.
Industrializing health care
One of the biggest problems the coalition has run into, and that others are finding around the country, is that once they identify patients who want to make changes in their health care, there aren’t enough well-run primary care practices to take on their care, Dr. Brenner said.
Even certified patient-centered medical homes don’t always do enough when it comes to incorporating clinical care teams, relying on health data, and reaching out to complex, recently hospitalized patients, Dr. Brenner said.
"The medical home is a good idea, but we’re not quite getting it right yet," he said.
There are lots of reasons why primary care isn’t there yet, Dr. Brenner said. Most offices haven’t built the right kind of clinical care teams, they lack the data systems, and physicians don’t have training in this area. Primary care physicians could take lessons from their colleagues in addiction and behavioral health on how to coordinate care for these patients, he said.
"We talk about the bio-psycho-social model, but I don’t know that we have all the components and the team and the training to fully pull it off yet," Dr. Brenner said.
The coalition has been working with local primary care physicians to try to get there, embedding nurses in their offices and helping them to create protocols for the adjustment and management of medications for blood pressure, cholesterol, and diabetes.
The idea is to create standardized protocols for common clinical scenarios and then delegate as much of the work as possible to nurses and other providers, freeing up physicians to take on the complex cases. Dr. Brenner said that in an ideal primary care practice, RNs would handle the well-child visits, the sore throats, and the simple medication adjustments.
"We need to industrialize primary care so that it becomes highly reliable, it becomes protocolized, standardized, and delegated so that we can stand out on a limb and customize and individualize for the sickest and most challenging patients," Dr. Brenner said.
And he wants to see nurses and project managers given the chance to run clinical care teams.
The Camden coalition uses licensed practical nurses, RNs, and community health workers. The coalition also relies heavily on Americorps volunteers, typically 22-year-told college graduates who are taking a year off before going to graduate school to be nurses, doctors, or public health workers. Many of the tasks that physicians stay late to do – or those that often fall through the cracks – can be delegated to these other providers, he said.
"It’s time we got out of the way and let our nurse colleagues get into the game," Dr. Brenner said. "I think their training is much better suited, frankly, for running teams, for working collaboratively, and for really improving quality and reducing costs."
Working harder doesn’t work
Instead of handing off less complex patients to clinical team members, most primary care physicians try to do it all, Dr. Brenner said. They stay in the room longer, make extra phone calls, and stay late at the office for a family conference. But this is "ad hoc work" that physicians do when they can find the time or the energy. It’s not something that they can do for every patient, he said.
"We’ve got to turn all that special sauce, all that ad hoc work into standardized, protocolized, structured work that always happens for everyone," Dr. Brenner said. "The only way we’re going to do that is to delegate and delegate and delegate."
Dr. Brenner said that he knows firsthand what’s like to try to do it all – that was his approach in his own practice. He had a completely paperless office and open-access scheduling, but he tried to make everything work by simply working harder. Ultimately, declining reimbursement from payers made it impossible to keep the doors open.
"I was trying as hard as I could but honestly I wasn’t doing all the things that I said. I wasn’t delegating, I wasn’t building a high-reliability team," he said. "I was trying to just work harder personally."
As the Affordable Care Act pushes new models for care coordination, including accountable care organizations, Dr. Brenner said he sees primary care physicians playing a major role. But they will need to delegate and to get more training to be successful, he said.
"I’ve been very fortunate. I’ve been at the right place at the right time," he said. "I think there are lots of other family docs who have the same skill sets and could do the same kind of work."
On Twitter @MaryEllenNY
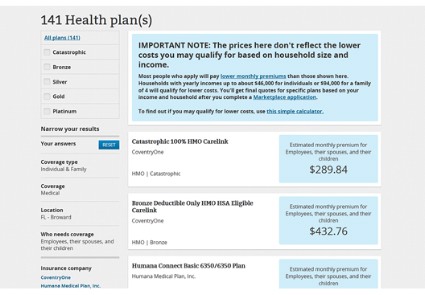
HHS: Healthcare.gov fixes underway
Three weeks after the launch of the health insurance exchanges, federal officials said they are working around-the-clock to improve the functionality of the healthcare.gov website.
The Health and Human Services (HHS) department has been working to increase the site’s bandwidth to accommodate heavier-than-expected web traffic, improve the site’s architecture to make it easier for consumers to create online accounts, and ramp up testing of the system as each of the changes is made, Centers for Medicare and Medicaid Services (CMS) spokeswoman Julie Bataille said during a press conference Oct. 24.
And the federal data hub, which provides information used in determining eligibility for tax credits, is performing well with responses in seconds, she said.
"It is getting better every day," Ms. Bataille said. "We are making incremental improvements."
Consumers will notice a smoother and more consistent experience on healthcare.gov over time, Ms. Bataille said. And she added that consumers would be able to enroll in health insurance by Dec. 15 in order have coverage in place on Jan. 1.
The healthcare.gov site, which is the portal for accessing the 34 federally run health exchanges, has been plagued by glitches since its launch on Oct. 1, with consumers complaining that the site would freeze, go blank, or send error messages when they tried to create an account.
Some of those problems have been resolved, and more consumers are now able to create online accounts to apply for insurance, Ms. Bataille said.
In the first 3 weeks, consumers have completed about 700,000 applications for insurance across the state- and federally run health insurance exchanges, she said. That means that they have completed the application phase and received information on whether they are eligible for federal premium subsidies. However, Ms. Bataille said CMS would not release information on the number of people who have actually enrolled in health plans until November.
Federal officials are urging consumers who have trouble with the website to call 1-800-318-2596 instead. That hotline has received about 1.6 million calls since Oct. 1.
Three weeks after the launch of the health insurance exchanges, federal officials said they are working around-the-clock to improve the functionality of the healthcare.gov website.
The Health and Human Services (HHS) department has been working to increase the site’s bandwidth to accommodate heavier-than-expected web traffic, improve the site’s architecture to make it easier for consumers to create online accounts, and ramp up testing of the system as each of the changes is made, Centers for Medicare and Medicaid Services (CMS) spokeswoman Julie Bataille said during a press conference Oct. 24.
And the federal data hub, which provides information used in determining eligibility for tax credits, is performing well with responses in seconds, she said.
"It is getting better every day," Ms. Bataille said. "We are making incremental improvements."
Consumers will notice a smoother and more consistent experience on healthcare.gov over time, Ms. Bataille said. And she added that consumers would be able to enroll in health insurance by Dec. 15 in order have coverage in place on Jan. 1.
The healthcare.gov site, which is the portal for accessing the 34 federally run health exchanges, has been plagued by glitches since its launch on Oct. 1, with consumers complaining that the site would freeze, go blank, or send error messages when they tried to create an account.
Some of those problems have been resolved, and more consumers are now able to create online accounts to apply for insurance, Ms. Bataille said.
In the first 3 weeks, consumers have completed about 700,000 applications for insurance across the state- and federally run health insurance exchanges, she said. That means that they have completed the application phase and received information on whether they are eligible for federal premium subsidies. However, Ms. Bataille said CMS would not release information on the number of people who have actually enrolled in health plans until November.
Federal officials are urging consumers who have trouble with the website to call 1-800-318-2596 instead. That hotline has received about 1.6 million calls since Oct. 1.
Three weeks after the launch of the health insurance exchanges, federal officials said they are working around-the-clock to improve the functionality of the healthcare.gov website.
The Health and Human Services (HHS) department has been working to increase the site’s bandwidth to accommodate heavier-than-expected web traffic, improve the site’s architecture to make it easier for consumers to create online accounts, and ramp up testing of the system as each of the changes is made, Centers for Medicare and Medicaid Services (CMS) spokeswoman Julie Bataille said during a press conference Oct. 24.
And the federal data hub, which provides information used in determining eligibility for tax credits, is performing well with responses in seconds, she said.
"It is getting better every day," Ms. Bataille said. "We are making incremental improvements."
Consumers will notice a smoother and more consistent experience on healthcare.gov over time, Ms. Bataille said. And she added that consumers would be able to enroll in health insurance by Dec. 15 in order have coverage in place on Jan. 1.
The healthcare.gov site, which is the portal for accessing the 34 federally run health exchanges, has been plagued by glitches since its launch on Oct. 1, with consumers complaining that the site would freeze, go blank, or send error messages when they tried to create an account.
Some of those problems have been resolved, and more consumers are now able to create online accounts to apply for insurance, Ms. Bataille said.
In the first 3 weeks, consumers have completed about 700,000 applications for insurance across the state- and federally run health insurance exchanges, she said. That means that they have completed the application phase and received information on whether they are eligible for federal premium subsidies. However, Ms. Bataille said CMS would not release information on the number of people who have actually enrolled in health plans until November.
Federal officials are urging consumers who have trouble with the website to call 1-800-318-2596 instead. That hotline has received about 1.6 million calls since Oct. 1.
NCQA: Docs still overusing antibiotics
Physicians continue to overuse antibiotics in adults and children, according to a health care quality report card released Oct. 23 by the National Committee for Quality Assurance.
The report, which looked at health plan quality data from 2012, shows that among adults under age 65 who were diagnosed with acute bronchitis, more than three-quarters were given a prescription for antibiotics.
Performance on this quality metric has been stagnant over the past 3 years and has actually worsened since 2006, according to the report.
"We’re not making progress here," NCQA President Margaret E. O’Kane said during a press conference. "We’ve got to up our game."
On the pediatric side, physicians appear to be doing a much better job of reining in inappropriate antibiotic use. Among children with upper respiratory infections, only about 15% are receiving prescriptions for antibiotics. But the figures show virtually no improvement over the past several years.
The NCQA findings come just after the Centers for Disease Control and Prevention warned in September that the overuse of antibiotics is creating antibiotic-resistant bacteria that are sickening at least 2 million people each year.
The rest of the NCQA report card found mixed results on quality measures, with improvements in tackling obesity in adults and children, increases in children’s vaccinations for influenza, but stagnant performance in other childhood vaccinations.
The report showed that:
• The percentage of adults aged 18-74 years who had an outpatient visit where their body mass index (BMI) was documented increased significantly, jumping from 55% to 66% in commercial health maintenance organizations (HMOs).
• For the first time, more than half of children and adolescents in commercial HMO plans were counseled about nutrition and physical activity.
• The percentage of children being immunized against influenza and rotavirus rose for the second year in a row in all types of health plans.
• The percentage of children (age 2) in commercial HMOs who had received the Combination 2 vaccine was up from the previous year at 80% in 2012, but down from a high of 81% in 2008.
• About 75% of adults with low back pain did not have imaging performed to confirm their diagnosis, but performance has been relatively unchanged over the past five years.
• Less than half of current adult smokers were offered strategies for quitting.
The NCQA report is based on the 2012 Healthcare Effectiveness Data and Information Set (HEDIS) measure performance for more than 1,000 health plans. The data set includes information on commercial and public plans covering about 136 million Americans.
Physicians continue to overuse antibiotics in adults and children, according to a health care quality report card released Oct. 23 by the National Committee for Quality Assurance.
The report, which looked at health plan quality data from 2012, shows that among adults under age 65 who were diagnosed with acute bronchitis, more than three-quarters were given a prescription for antibiotics.
Performance on this quality metric has been stagnant over the past 3 years and has actually worsened since 2006, according to the report.
"We’re not making progress here," NCQA President Margaret E. O’Kane said during a press conference. "We’ve got to up our game."
On the pediatric side, physicians appear to be doing a much better job of reining in inappropriate antibiotic use. Among children with upper respiratory infections, only about 15% are receiving prescriptions for antibiotics. But the figures show virtually no improvement over the past several years.
The NCQA findings come just after the Centers for Disease Control and Prevention warned in September that the overuse of antibiotics is creating antibiotic-resistant bacteria that are sickening at least 2 million people each year.
The rest of the NCQA report card found mixed results on quality measures, with improvements in tackling obesity in adults and children, increases in children’s vaccinations for influenza, but stagnant performance in other childhood vaccinations.
The report showed that:
• The percentage of adults aged 18-74 years who had an outpatient visit where their body mass index (BMI) was documented increased significantly, jumping from 55% to 66% in commercial health maintenance organizations (HMOs).
• For the first time, more than half of children and adolescents in commercial HMO plans were counseled about nutrition and physical activity.
• The percentage of children being immunized against influenza and rotavirus rose for the second year in a row in all types of health plans.
• The percentage of children (age 2) in commercial HMOs who had received the Combination 2 vaccine was up from the previous year at 80% in 2012, but down from a high of 81% in 2008.
• About 75% of adults with low back pain did not have imaging performed to confirm their diagnosis, but performance has been relatively unchanged over the past five years.
• Less than half of current adult smokers were offered strategies for quitting.
The NCQA report is based on the 2012 Healthcare Effectiveness Data and Information Set (HEDIS) measure performance for more than 1,000 health plans. The data set includes information on commercial and public plans covering about 136 million Americans.
Physicians continue to overuse antibiotics in adults and children, according to a health care quality report card released Oct. 23 by the National Committee for Quality Assurance.
The report, which looked at health plan quality data from 2012, shows that among adults under age 65 who were diagnosed with acute bronchitis, more than three-quarters were given a prescription for antibiotics.
Performance on this quality metric has been stagnant over the past 3 years and has actually worsened since 2006, according to the report.
"We’re not making progress here," NCQA President Margaret E. O’Kane said during a press conference. "We’ve got to up our game."
On the pediatric side, physicians appear to be doing a much better job of reining in inappropriate antibiotic use. Among children with upper respiratory infections, only about 15% are receiving prescriptions for antibiotics. But the figures show virtually no improvement over the past several years.
The NCQA findings come just after the Centers for Disease Control and Prevention warned in September that the overuse of antibiotics is creating antibiotic-resistant bacteria that are sickening at least 2 million people each year.
The rest of the NCQA report card found mixed results on quality measures, with improvements in tackling obesity in adults and children, increases in children’s vaccinations for influenza, but stagnant performance in other childhood vaccinations.
The report showed that:
• The percentage of adults aged 18-74 years who had an outpatient visit where their body mass index (BMI) was documented increased significantly, jumping from 55% to 66% in commercial health maintenance organizations (HMOs).
• For the first time, more than half of children and adolescents in commercial HMO plans were counseled about nutrition and physical activity.
• The percentage of children being immunized against influenza and rotavirus rose for the second year in a row in all types of health plans.
• The percentage of children (age 2) in commercial HMOs who had received the Combination 2 vaccine was up from the previous year at 80% in 2012, but down from a high of 81% in 2008.
• About 75% of adults with low back pain did not have imaging performed to confirm their diagnosis, but performance has been relatively unchanged over the past five years.
• Less than half of current adult smokers were offered strategies for quitting.
The NCQA report is based on the 2012 Healthcare Effectiveness Data and Information Set (HEDIS) measure performance for more than 1,000 health plans. The data set includes information on commercial and public plans covering about 136 million Americans.
Congress approves deal to open government, leaves health reform intact
Congress has approved a deal to fully reopen the federal government and keep the nation from defaulting on its debt. The agreement does not delay or defund the Affordable Care Act.
On Oct. 16 – 16 days into the government shutdown and about a day before the United States was set to breach its debt ceiling – the Senate voted 81-18 to approve a bipartisan compromise brokered by Senate Majority Leader Harry Reid (D-Nev.) and Minority Leader Mitch McConnell (R-Ky.). Later that night, the House approved the bill 285-144. The president signed the legislation in the early hours of Oct. 17.
The law funds the federal government at its current levels until Jan. 15, 2014, keeping the sequestration cuts in effect. It also allows the government to continue to borrow money to meet its financial obligations until Feb. 7, 2014. In the meantime, lawmakers have agreed to convene a budget conference to work out a long-range budget plan by mid-December.
Although the bill does not fundamentally change the Affordable Care Act (ACA), it does require the Department of Health and Human Services to beef up its income verification for individuals seeking subsidies to purchase insurance on the exchanges.
Last July, the agency announced that it would not verify the income of every applicant who applied for federal subsidies through the exchanges. Instead, federal officials planned to audit a sample of applications to ensure that individuals were getting the appropriate federal insurance subsidies. GOP lawmakers objected to this approach, saying that relying too heavily on the honor system in determining federal subsidies would leave the government open to fraud.
Under the new law, HHS must submit a report to Congress on its verification procedures by Jan. 1, 2014, and the HHS Inspector General must submit a progress report by July 2014 on the effectiveness of the new procedures.
Although the new law doesn’t do anything to hamper the implementation of the ACA, opponents have not given up. Sen. McConnell, who negotiated the deal with Democrats, said that Republicans will keep trying to repeal the ACA.
"This law is ravaging our economy, killing jobs, driving up premiums, and driving people off the health care plans they have and like in droves," he said on the Senate floor. "Its disastrous rollout is a sign of even worse things to come. And the Democrat refusal to delay it reflects a stubborn ideological obsession that will do untold damage to our country."
On Twitter @MaryEllenNY
Congress has approved a deal to fully reopen the federal government and keep the nation from defaulting on its debt. The agreement does not delay or defund the Affordable Care Act.
On Oct. 16 – 16 days into the government shutdown and about a day before the United States was set to breach its debt ceiling – the Senate voted 81-18 to approve a bipartisan compromise brokered by Senate Majority Leader Harry Reid (D-Nev.) and Minority Leader Mitch McConnell (R-Ky.). Later that night, the House approved the bill 285-144. The president signed the legislation in the early hours of Oct. 17.
The law funds the federal government at its current levels until Jan. 15, 2014, keeping the sequestration cuts in effect. It also allows the government to continue to borrow money to meet its financial obligations until Feb. 7, 2014. In the meantime, lawmakers have agreed to convene a budget conference to work out a long-range budget plan by mid-December.
Although the bill does not fundamentally change the Affordable Care Act (ACA), it does require the Department of Health and Human Services to beef up its income verification for individuals seeking subsidies to purchase insurance on the exchanges.
Last July, the agency announced that it would not verify the income of every applicant who applied for federal subsidies through the exchanges. Instead, federal officials planned to audit a sample of applications to ensure that individuals were getting the appropriate federal insurance subsidies. GOP lawmakers objected to this approach, saying that relying too heavily on the honor system in determining federal subsidies would leave the government open to fraud.
Under the new law, HHS must submit a report to Congress on its verification procedures by Jan. 1, 2014, and the HHS Inspector General must submit a progress report by July 2014 on the effectiveness of the new procedures.
Although the new law doesn’t do anything to hamper the implementation of the ACA, opponents have not given up. Sen. McConnell, who negotiated the deal with Democrats, said that Republicans will keep trying to repeal the ACA.
"This law is ravaging our economy, killing jobs, driving up premiums, and driving people off the health care plans they have and like in droves," he said on the Senate floor. "Its disastrous rollout is a sign of even worse things to come. And the Democrat refusal to delay it reflects a stubborn ideological obsession that will do untold damage to our country."
On Twitter @MaryEllenNY
Congress has approved a deal to fully reopen the federal government and keep the nation from defaulting on its debt. The agreement does not delay or defund the Affordable Care Act.
On Oct. 16 – 16 days into the government shutdown and about a day before the United States was set to breach its debt ceiling – the Senate voted 81-18 to approve a bipartisan compromise brokered by Senate Majority Leader Harry Reid (D-Nev.) and Minority Leader Mitch McConnell (R-Ky.). Later that night, the House approved the bill 285-144. The president signed the legislation in the early hours of Oct. 17.
The law funds the federal government at its current levels until Jan. 15, 2014, keeping the sequestration cuts in effect. It also allows the government to continue to borrow money to meet its financial obligations until Feb. 7, 2014. In the meantime, lawmakers have agreed to convene a budget conference to work out a long-range budget plan by mid-December.
Although the bill does not fundamentally change the Affordable Care Act (ACA), it does require the Department of Health and Human Services to beef up its income verification for individuals seeking subsidies to purchase insurance on the exchanges.
Last July, the agency announced that it would not verify the income of every applicant who applied for federal subsidies through the exchanges. Instead, federal officials planned to audit a sample of applications to ensure that individuals were getting the appropriate federal insurance subsidies. GOP lawmakers objected to this approach, saying that relying too heavily on the honor system in determining federal subsidies would leave the government open to fraud.
Under the new law, HHS must submit a report to Congress on its verification procedures by Jan. 1, 2014, and the HHS Inspector General must submit a progress report by July 2014 on the effectiveness of the new procedures.
Although the new law doesn’t do anything to hamper the implementation of the ACA, opponents have not given up. Sen. McConnell, who negotiated the deal with Democrats, said that Republicans will keep trying to repeal the ACA.
"This law is ravaging our economy, killing jobs, driving up premiums, and driving people off the health care plans they have and like in droves," he said on the Senate floor. "Its disastrous rollout is a sign of even worse things to come. And the Democrat refusal to delay it reflects a stubborn ideological obsession that will do untold damage to our country."
On Twitter @MaryEllenNY
ACA exchanges limp along after 2 weeks
The online health insurance marketplaces that are the centerpiece of the Affordable Care Act are off to a rocky start.
In the first 2 weeks of operation, consumers complained about problems using the federally run website – healthcare.gov. They reported trouble getting on the website as well as creating the accounts needed to enroll in health plans.
Health and Human Services (HHS) department officials have acknowledged what they call "glitches" in the system, but said they are working on improving the website as quickly as possible, often through overnight maintenance sessions.
"We have greatly reduced, and even eliminated, wait times at the registration stage, and more people are actively shopping and comparing plans," HHS spokeswoman Joanne Peters said.
The agency is also offering other options for signing up for insurance. Consumers can use the HHS call center (1-800-318-2596) to apply for and enroll over the phone. They can also use the website’s Find Local Help feature to find someone who will work with them in person.
HHS officials cite heavy demand as the major reason for the website’s poor performance. In the first 10 days of operation, the site had 14.6 million unique visitors, according to the agency.
But some technology experts said the problem may go deeper. Now GOP lawmakers in the House and the Senate are launching investigations into how the website was designed and tested, and what problems the administration detected in the months leading up to the Oct. 1 launch.
Rep. Michael Burgess (R-Tex.), who serves on the House Energy and Commerce Committee, said HHS officials need to come to Congress and explain what is happening with the federally run exchanges.
"Members of the administration need to come to the Energy and Commerce Committee and start telling us the truth about this information architecture," Rep. Burgess said. "Taxpayers have spent money – a lot of money – to build these sites. If they’ve been sold a pig in a poke, they need to know."
But while the federally run exchanges have been under fire, the state-run health exchanges have, for the most part, been running more smoothly.
Access Health Connecticut, for example, reported that it had more than 126,000 visitors to its website and has processed almost 2,000 applications. In California, about a million people visited the state’s exchange site in the first 5 days. California consumers submitted 40,000 applications. About 16,000 of those were completed, according to the state.
Officials in Kentucky reported that its exchange site, called Kynect, had 4 million page views in the first 10 days and about 9,000 enrollees. And in Washington state, nearly 10,000 residents had enrolled in either health plans or Medicaid coverage through the state’s exchange.
Currently, there are no data on how many Americans have purchased health insurance through the federally run exchanges. While HHS has released information on traffic to the healthcare.gov site, it will not release enrollment data until November. After that, the administration plans to provide monthly reports.
Individuals have until Dec. 15 to apply for coverage that begins on Jan. 1, 2014. But consumers can continue to enroll in plans through the end of March 2014.
Alicia Ault contributed to this report.
The online health insurance marketplaces that are the centerpiece of the Affordable Care Act are off to a rocky start.
In the first 2 weeks of operation, consumers complained about problems using the federally run website – healthcare.gov. They reported trouble getting on the website as well as creating the accounts needed to enroll in health plans.
Health and Human Services (HHS) department officials have acknowledged what they call "glitches" in the system, but said they are working on improving the website as quickly as possible, often through overnight maintenance sessions.
"We have greatly reduced, and even eliminated, wait times at the registration stage, and more people are actively shopping and comparing plans," HHS spokeswoman Joanne Peters said.
The agency is also offering other options for signing up for insurance. Consumers can use the HHS call center (1-800-318-2596) to apply for and enroll over the phone. They can also use the website’s Find Local Help feature to find someone who will work with them in person.
HHS officials cite heavy demand as the major reason for the website’s poor performance. In the first 10 days of operation, the site had 14.6 million unique visitors, according to the agency.
But some technology experts said the problem may go deeper. Now GOP lawmakers in the House and the Senate are launching investigations into how the website was designed and tested, and what problems the administration detected in the months leading up to the Oct. 1 launch.
Rep. Michael Burgess (R-Tex.), who serves on the House Energy and Commerce Committee, said HHS officials need to come to Congress and explain what is happening with the federally run exchanges.
"Members of the administration need to come to the Energy and Commerce Committee and start telling us the truth about this information architecture," Rep. Burgess said. "Taxpayers have spent money – a lot of money – to build these sites. If they’ve been sold a pig in a poke, they need to know."
But while the federally run exchanges have been under fire, the state-run health exchanges have, for the most part, been running more smoothly.
Access Health Connecticut, for example, reported that it had more than 126,000 visitors to its website and has processed almost 2,000 applications. In California, about a million people visited the state’s exchange site in the first 5 days. California consumers submitted 40,000 applications. About 16,000 of those were completed, according to the state.
Officials in Kentucky reported that its exchange site, called Kynect, had 4 million page views in the first 10 days and about 9,000 enrollees. And in Washington state, nearly 10,000 residents had enrolled in either health plans or Medicaid coverage through the state’s exchange.
Currently, there are no data on how many Americans have purchased health insurance through the federally run exchanges. While HHS has released information on traffic to the healthcare.gov site, it will not release enrollment data until November. After that, the administration plans to provide monthly reports.
Individuals have until Dec. 15 to apply for coverage that begins on Jan. 1, 2014. But consumers can continue to enroll in plans through the end of March 2014.
Alicia Ault contributed to this report.
The online health insurance marketplaces that are the centerpiece of the Affordable Care Act are off to a rocky start.
In the first 2 weeks of operation, consumers complained about problems using the federally run website – healthcare.gov. They reported trouble getting on the website as well as creating the accounts needed to enroll in health plans.
Health and Human Services (HHS) department officials have acknowledged what they call "glitches" in the system, but said they are working on improving the website as quickly as possible, often through overnight maintenance sessions.
"We have greatly reduced, and even eliminated, wait times at the registration stage, and more people are actively shopping and comparing plans," HHS spokeswoman Joanne Peters said.
The agency is also offering other options for signing up for insurance. Consumers can use the HHS call center (1-800-318-2596) to apply for and enroll over the phone. They can also use the website’s Find Local Help feature to find someone who will work with them in person.
HHS officials cite heavy demand as the major reason for the website’s poor performance. In the first 10 days of operation, the site had 14.6 million unique visitors, according to the agency.
But some technology experts said the problem may go deeper. Now GOP lawmakers in the House and the Senate are launching investigations into how the website was designed and tested, and what problems the administration detected in the months leading up to the Oct. 1 launch.
Rep. Michael Burgess (R-Tex.), who serves on the House Energy and Commerce Committee, said HHS officials need to come to Congress and explain what is happening with the federally run exchanges.
"Members of the administration need to come to the Energy and Commerce Committee and start telling us the truth about this information architecture," Rep. Burgess said. "Taxpayers have spent money – a lot of money – to build these sites. If they’ve been sold a pig in a poke, they need to know."
But while the federally run exchanges have been under fire, the state-run health exchanges have, for the most part, been running more smoothly.
Access Health Connecticut, for example, reported that it had more than 126,000 visitors to its website and has processed almost 2,000 applications. In California, about a million people visited the state’s exchange site in the first 5 days. California consumers submitted 40,000 applications. About 16,000 of those were completed, according to the state.
Officials in Kentucky reported that its exchange site, called Kynect, had 4 million page views in the first 10 days and about 9,000 enrollees. And in Washington state, nearly 10,000 residents had enrolled in either health plans or Medicaid coverage through the state’s exchange.
Currently, there are no data on how many Americans have purchased health insurance through the federally run exchanges. While HHS has released information on traffic to the healthcare.gov site, it will not release enrollment data until November. After that, the administration plans to provide monthly reports.
Individuals have until Dec. 15 to apply for coverage that begins on Jan. 1, 2014. But consumers can continue to enroll in plans through the end of March 2014.
Alicia Ault contributed to this report.
Obamacare exchanges open for enrollment during shutdown
Despite the federal government shutdown, the Affordable Care Act’s insurance marketplaces opened for enrollment on Oct. 1.
The online health marketplaces were up and running for just a few hours when complaints starting circulating about glitches. Consumers got error messages and had trouble logging in. And when they did get in, the websites for the various state and federal exchanges ran slowly.
A large part of the problem was the high volume of traffic to the websites, federal officials said.
As of late afternoon on Oct. 1, about 2.8 million visits were logged to healthcare.gov, the clearinghouse that serves the federally run marketplaces and links consumers to the state-run online marketplaces. That’s about seven times more users than Medicare.gov has ever had at any one time, Marilyn Tavenner, the administrator of the Centers for Medicare and Medicaid Services, said during a news conference.
Additionally, the Health and Human Services department received more than 80,000 calls to its help line and more than 60,000 requests for online chats to help enroll in health plans.
HHS would not release figures on how many Americans had enrolled in health plans through the federal and state marketplaces. Ms. Tavenner said that data would be released later, but that consumers were successfully enrolling.
States also reported heavy web traffic. Officials in New York reported that their state exchanges website had 2 million visits in the first 2 hours of operation. Due to the high volume, they posted a notice to consumers to come back later if they had trouble logging in.
"This gives you a sense of how important this is to millions of Americans," President Obama said during a news conference in the Rose Garden.
The president admitted that there have been "glitches" with the enrollment process, but vowed that they would be fixed.
Ms. Tavenner said federal officials had been working throughout the day to correct problems, including adding capacity to healthcare.gov. They also made adjustments to resolve problems that consumers had creating accounts. Some states, including Maryland and Hawaii, had some technical problems that kept consumers from enrolling in health plans on Oct. 1, HHS officials said.
Individuals will have until March 31, 2014, to enroll in a health plan through the marketplaces. However, they must enroll by Dec. 15 to have their coverage begin on Jan. 1, 2014.
Despite the federal government shutdown, the Affordable Care Act’s insurance marketplaces opened for enrollment on Oct. 1.
The online health marketplaces were up and running for just a few hours when complaints starting circulating about glitches. Consumers got error messages and had trouble logging in. And when they did get in, the websites for the various state and federal exchanges ran slowly.
A large part of the problem was the high volume of traffic to the websites, federal officials said.
As of late afternoon on Oct. 1, about 2.8 million visits were logged to healthcare.gov, the clearinghouse that serves the federally run marketplaces and links consumers to the state-run online marketplaces. That’s about seven times more users than Medicare.gov has ever had at any one time, Marilyn Tavenner, the administrator of the Centers for Medicare and Medicaid Services, said during a news conference.
Additionally, the Health and Human Services department received more than 80,000 calls to its help line and more than 60,000 requests for online chats to help enroll in health plans.
HHS would not release figures on how many Americans had enrolled in health plans through the federal and state marketplaces. Ms. Tavenner said that data would be released later, but that consumers were successfully enrolling.
States also reported heavy web traffic. Officials in New York reported that their state exchanges website had 2 million visits in the first 2 hours of operation. Due to the high volume, they posted a notice to consumers to come back later if they had trouble logging in.
"This gives you a sense of how important this is to millions of Americans," President Obama said during a news conference in the Rose Garden.
The president admitted that there have been "glitches" with the enrollment process, but vowed that they would be fixed.
Ms. Tavenner said federal officials had been working throughout the day to correct problems, including adding capacity to healthcare.gov. They also made adjustments to resolve problems that consumers had creating accounts. Some states, including Maryland and Hawaii, had some technical problems that kept consumers from enrolling in health plans on Oct. 1, HHS officials said.
Individuals will have until March 31, 2014, to enroll in a health plan through the marketplaces. However, they must enroll by Dec. 15 to have their coverage begin on Jan. 1, 2014.
Despite the federal government shutdown, the Affordable Care Act’s insurance marketplaces opened for enrollment on Oct. 1.
The online health marketplaces were up and running for just a few hours when complaints starting circulating about glitches. Consumers got error messages and had trouble logging in. And when they did get in, the websites for the various state and federal exchanges ran slowly.
A large part of the problem was the high volume of traffic to the websites, federal officials said.
As of late afternoon on Oct. 1, about 2.8 million visits were logged to healthcare.gov, the clearinghouse that serves the federally run marketplaces and links consumers to the state-run online marketplaces. That’s about seven times more users than Medicare.gov has ever had at any one time, Marilyn Tavenner, the administrator of the Centers for Medicare and Medicaid Services, said during a news conference.
Additionally, the Health and Human Services department received more than 80,000 calls to its help line and more than 60,000 requests for online chats to help enroll in health plans.
HHS would not release figures on how many Americans had enrolled in health plans through the federal and state marketplaces. Ms. Tavenner said that data would be released later, but that consumers were successfully enrolling.
States also reported heavy web traffic. Officials in New York reported that their state exchanges website had 2 million visits in the first 2 hours of operation. Due to the high volume, they posted a notice to consumers to come back later if they had trouble logging in.
"This gives you a sense of how important this is to millions of Americans," President Obama said during a news conference in the Rose Garden.
The president admitted that there have been "glitches" with the enrollment process, but vowed that they would be fixed.
Ms. Tavenner said federal officials had been working throughout the day to correct problems, including adding capacity to healthcare.gov. They also made adjustments to resolve problems that consumers had creating accounts. Some states, including Maryland and Hawaii, had some technical problems that kept consumers from enrolling in health plans on Oct. 1, HHS officials said.
Individuals will have until March 31, 2014, to enroll in a health plan through the marketplaces. However, they must enroll by Dec. 15 to have their coverage begin on Jan. 1, 2014.
Federal shutdown begins; health programs impacted
With lawmakers unable to make a deal on how to fund the government, federal agencies began a partial shutdown on Oct. 1.
The government closure should not hit doctors in the pocketbook. Medicare is expected to continue "largely without disruption" in the short term, according to the Health and Human Services department contingency plan for operating during a shutdown. Payments for Medicaid and the Children’s Health Insurance Program should also be unaffected, since federal monies for that program were previously set aside.
But the shutdown will impact many of the day-to-day functions at federal health agencies, from grant making to disease surveillance.
Doctors and other health care providers at the National Institutes of Health continue to care for current patients but are now unable to admit new patients unless it is deemed medically necessary by the NIH director. The agency is providing only minimal support for ongoing research protocols and has halted approval of new grant applications.
Some staffers at the Centers for Disease Control and Prevention are on duty to respond to disease outbreaks and other emergencies; however, seasonal influenza monitoring is on hold, as is technical support to states for infectious disease surveillance.
The Vaccines for Children program, mandated by law, continues despite the shutdown.
Graduate medical training at children’s hospitals is on hold since the Health Resources and Services Administration cannot make payments to the Children’s Hospitals Graduate Medical Education Payment Program during the shutdown.
Health care advocacy groups began sounding off Oct. 1 on the shutdown’s impact on public health.
"We encourage policymakers to consider the dramatic impact that funding cuts to medical research and doctor training will have on the health of the country and the millions of patients who depend on the lifesaving research conducted at, and critical health care services provided by, the nation’s medical schools and teaching hospitals," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges.
In the meantime, despite the government shutdown, enrollment in the Affordable Care Act’s health exchanges began as scheduled.
With lawmakers unable to make a deal on how to fund the government, federal agencies began a partial shutdown on Oct. 1.
The government closure should not hit doctors in the pocketbook. Medicare is expected to continue "largely without disruption" in the short term, according to the Health and Human Services department contingency plan for operating during a shutdown. Payments for Medicaid and the Children’s Health Insurance Program should also be unaffected, since federal monies for that program were previously set aside.
But the shutdown will impact many of the day-to-day functions at federal health agencies, from grant making to disease surveillance.
Doctors and other health care providers at the National Institutes of Health continue to care for current patients but are now unable to admit new patients unless it is deemed medically necessary by the NIH director. The agency is providing only minimal support for ongoing research protocols and has halted approval of new grant applications.
Some staffers at the Centers for Disease Control and Prevention are on duty to respond to disease outbreaks and other emergencies; however, seasonal influenza monitoring is on hold, as is technical support to states for infectious disease surveillance.
The Vaccines for Children program, mandated by law, continues despite the shutdown.
Graduate medical training at children’s hospitals is on hold since the Health Resources and Services Administration cannot make payments to the Children’s Hospitals Graduate Medical Education Payment Program during the shutdown.
Health care advocacy groups began sounding off Oct. 1 on the shutdown’s impact on public health.
"We encourage policymakers to consider the dramatic impact that funding cuts to medical research and doctor training will have on the health of the country and the millions of patients who depend on the lifesaving research conducted at, and critical health care services provided by, the nation’s medical schools and teaching hospitals," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges.
In the meantime, despite the government shutdown, enrollment in the Affordable Care Act’s health exchanges began as scheduled.
With lawmakers unable to make a deal on how to fund the government, federal agencies began a partial shutdown on Oct. 1.
The government closure should not hit doctors in the pocketbook. Medicare is expected to continue "largely without disruption" in the short term, according to the Health and Human Services department contingency plan for operating during a shutdown. Payments for Medicaid and the Children’s Health Insurance Program should also be unaffected, since federal monies for that program were previously set aside.
But the shutdown will impact many of the day-to-day functions at federal health agencies, from grant making to disease surveillance.
Doctors and other health care providers at the National Institutes of Health continue to care for current patients but are now unable to admit new patients unless it is deemed medically necessary by the NIH director. The agency is providing only minimal support for ongoing research protocols and has halted approval of new grant applications.
Some staffers at the Centers for Disease Control and Prevention are on duty to respond to disease outbreaks and other emergencies; however, seasonal influenza monitoring is on hold, as is technical support to states for infectious disease surveillance.
The Vaccines for Children program, mandated by law, continues despite the shutdown.
Graduate medical training at children’s hospitals is on hold since the Health Resources and Services Administration cannot make payments to the Children’s Hospitals Graduate Medical Education Payment Program during the shutdown.
Health care advocacy groups began sounding off Oct. 1 on the shutdown’s impact on public health.
"We encourage policymakers to consider the dramatic impact that funding cuts to medical research and doctor training will have on the health of the country and the millions of patients who depend on the lifesaving research conducted at, and critical health care services provided by, the nation’s medical schools and teaching hospitals," said Dr. Darrell G. Kirch, president and CEO of the Association of American Medical Colleges.
In the meantime, despite the government shutdown, enrollment in the Affordable Care Act’s health exchanges began as scheduled.