User login
Up to 90% of gout hospitalizations might be preventable
BOSTON – Nearly all hospitalizations of people who were discharged with a primary diagnosis of gout were likely preventable, based on the results of a retrospective analysis of 79 cases at a single institution.
Because most of these patients presented to the emergency department rather than their doctor’s office, and were in pain and had other comorbidities, admission seemed the correct medical care decision, said Dr. Thomas Olenginski of the Geisinger Health System and one of the study’s lead authors. If the ED had gotten a rheumatology consult during the patients’ observation periods, however, the diagnosis could have been confirmed and most of these admissions would likely have been avoided, with a potential savings of over $200,000 in total hospitalization-related costs, Dr. Olenginski said at the annual meeting of the American College of Rheumatology.
Further, most of these patients were not adherent to their prescribed gout medications. Better clinical care and compliance with gout therapy might prevent most gout flareups that result in hospitalization, he added.
As a result of these findings, Geisinger has reassessed its approach to gout patients, especially those who present to the ED. For identified gout patients, they have ramped up efforts to make sure patients are adhering to therapy and are at goal, as well as educating them about their disease and how it can worsen without adherence. Rheumatologists are available to the ED by pager, encouraging arthrocentesis and crystal confirmation, thereby allowing the ED to focus on treating any associated skin infections and comorbidities, Dr. Olenginski said.
Of 56 gout-related admissions to their hospital, the Geisinger researchers found that 50 (89%) met the study’s definition of a preventable admission. A preventable admission was defined as one with a primary admitting diagnosis of mono- or polyarthritis subsequently diagnosed as gout and without any concomitant illness warranting admission on presentation.
The clinical diagnoses included 76% septic arthritis, 14% inflammatory polyarthritis, and 8% cellulitis.
Of the 50 preventable admissions, 33 patients underwent arthrocentesis, 24 of which were performed in the ED where the diagnosis could have been made based on crystal-confirmed diagnosis, he said.
Among the 35 patients with a prior history of gout, there were 23 patients whose serum uric acid levels were recorded within 1 year of their hospitalization, and 18 (78%) did not reach the goal of less than 6 mg/dL. Of 15 patients on long-term gout treatment, 5 (33%) were noncompliant with their treatment plans.
The total additive length of stay for the preventable gout admissions was 171 days with a mean stay of 3.42 days. Total hospitalization-related costs of these admissions were $208,000, with an average cost per admission of $4,160.
The study was performed as a quality initiative at Geisinger Health System. Dr. Olenginski had no relevant financial disclosures.
BOSTON – Nearly all hospitalizations of people who were discharged with a primary diagnosis of gout were likely preventable, based on the results of a retrospective analysis of 79 cases at a single institution.
Because most of these patients presented to the emergency department rather than their doctor’s office, and were in pain and had other comorbidities, admission seemed the correct medical care decision, said Dr. Thomas Olenginski of the Geisinger Health System and one of the study’s lead authors. If the ED had gotten a rheumatology consult during the patients’ observation periods, however, the diagnosis could have been confirmed and most of these admissions would likely have been avoided, with a potential savings of over $200,000 in total hospitalization-related costs, Dr. Olenginski said at the annual meeting of the American College of Rheumatology.
Further, most of these patients were not adherent to their prescribed gout medications. Better clinical care and compliance with gout therapy might prevent most gout flareups that result in hospitalization, he added.
As a result of these findings, Geisinger has reassessed its approach to gout patients, especially those who present to the ED. For identified gout patients, they have ramped up efforts to make sure patients are adhering to therapy and are at goal, as well as educating them about their disease and how it can worsen without adherence. Rheumatologists are available to the ED by pager, encouraging arthrocentesis and crystal confirmation, thereby allowing the ED to focus on treating any associated skin infections and comorbidities, Dr. Olenginski said.
Of 56 gout-related admissions to their hospital, the Geisinger researchers found that 50 (89%) met the study’s definition of a preventable admission. A preventable admission was defined as one with a primary admitting diagnosis of mono- or polyarthritis subsequently diagnosed as gout and without any concomitant illness warranting admission on presentation.
The clinical diagnoses included 76% septic arthritis, 14% inflammatory polyarthritis, and 8% cellulitis.
Of the 50 preventable admissions, 33 patients underwent arthrocentesis, 24 of which were performed in the ED where the diagnosis could have been made based on crystal-confirmed diagnosis, he said.
Among the 35 patients with a prior history of gout, there were 23 patients whose serum uric acid levels were recorded within 1 year of their hospitalization, and 18 (78%) did not reach the goal of less than 6 mg/dL. Of 15 patients on long-term gout treatment, 5 (33%) were noncompliant with their treatment plans.
The total additive length of stay for the preventable gout admissions was 171 days with a mean stay of 3.42 days. Total hospitalization-related costs of these admissions were $208,000, with an average cost per admission of $4,160.
The study was performed as a quality initiative at Geisinger Health System. Dr. Olenginski had no relevant financial disclosures.
BOSTON – Nearly all hospitalizations of people who were discharged with a primary diagnosis of gout were likely preventable, based on the results of a retrospective analysis of 79 cases at a single institution.
Because most of these patients presented to the emergency department rather than their doctor’s office, and were in pain and had other comorbidities, admission seemed the correct medical care decision, said Dr. Thomas Olenginski of the Geisinger Health System and one of the study’s lead authors. If the ED had gotten a rheumatology consult during the patients’ observation periods, however, the diagnosis could have been confirmed and most of these admissions would likely have been avoided, with a potential savings of over $200,000 in total hospitalization-related costs, Dr. Olenginski said at the annual meeting of the American College of Rheumatology.
Further, most of these patients were not adherent to their prescribed gout medications. Better clinical care and compliance with gout therapy might prevent most gout flareups that result in hospitalization, he added.
As a result of these findings, Geisinger has reassessed its approach to gout patients, especially those who present to the ED. For identified gout patients, they have ramped up efforts to make sure patients are adhering to therapy and are at goal, as well as educating them about their disease and how it can worsen without adherence. Rheumatologists are available to the ED by pager, encouraging arthrocentesis and crystal confirmation, thereby allowing the ED to focus on treating any associated skin infections and comorbidities, Dr. Olenginski said.
Of 56 gout-related admissions to their hospital, the Geisinger researchers found that 50 (89%) met the study’s definition of a preventable admission. A preventable admission was defined as one with a primary admitting diagnosis of mono- or polyarthritis subsequently diagnosed as gout and without any concomitant illness warranting admission on presentation.
The clinical diagnoses included 76% septic arthritis, 14% inflammatory polyarthritis, and 8% cellulitis.
Of the 50 preventable admissions, 33 patients underwent arthrocentesis, 24 of which were performed in the ED where the diagnosis could have been made based on crystal-confirmed diagnosis, he said.
Among the 35 patients with a prior history of gout, there were 23 patients whose serum uric acid levels were recorded within 1 year of their hospitalization, and 18 (78%) did not reach the goal of less than 6 mg/dL. Of 15 patients on long-term gout treatment, 5 (33%) were noncompliant with their treatment plans.
The total additive length of stay for the preventable gout admissions was 171 days with a mean stay of 3.42 days. Total hospitalization-related costs of these admissions were $208,000, with an average cost per admission of $4,160.
The study was performed as a quality initiative at Geisinger Health System. Dr. Olenginski had no relevant financial disclosures.
AT THE ACR ANNUAL MEETING
Key clinical point: Gout patients are often admitted to the hospital via the emergency department; most of these admissions could be avoidable.
Major finding: Of 56 gout-related admissions to their hospital, the Geisinger researchers found that 50 (89%) met the study’s definition of a preventable admission.
Data source: A retrospective analysis of 79 cases of gout at a single institution.
Disclosures: The study was performed as a quality initiative at Geisinger Health System. Dr. Olenginski had no relevant financial disclosures.
VIDEO: Lower heart failure risk seen in users of tumor necrosis factor inhibitors
BOSTON – Rheumatoid arthritis patients taking tumor necrosis factor inhibitors ran a lower risk of developing congestive heart failure than did those on nonbiologic disease-modifying antirheumatic drugs, based on data from a large British registry.
Dr. Alper van Sijl of the University of Manchester (England) reported that, among comparable RA patients who have not yet developed CHF, fully adjusted propensity scores showed a reduced risk for developing CHF in those taking TNF inhibitors. He explained the possible reasons for the findings and described next steps in new studies designed to cut the risk of CHF in RA patients during an interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Rheumatoid arthritis patients taking tumor necrosis factor inhibitors ran a lower risk of developing congestive heart failure than did those on nonbiologic disease-modifying antirheumatic drugs, based on data from a large British registry.
Dr. Alper van Sijl of the University of Manchester (England) reported that, among comparable RA patients who have not yet developed CHF, fully adjusted propensity scores showed a reduced risk for developing CHF in those taking TNF inhibitors. He explained the possible reasons for the findings and described next steps in new studies designed to cut the risk of CHF in RA patients during an interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Rheumatoid arthritis patients taking tumor necrosis factor inhibitors ran a lower risk of developing congestive heart failure than did those on nonbiologic disease-modifying antirheumatic drugs, based on data from a large British registry.
Dr. Alper van Sijl of the University of Manchester (England) reported that, among comparable RA patients who have not yet developed CHF, fully adjusted propensity scores showed a reduced risk for developing CHF in those taking TNF inhibitors. He explained the possible reasons for the findings and described next steps in new studies designed to cut the risk of CHF in RA patients during an interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE ACR ANNUAL MEETING
VIDEO: Herpes Zoster Vaccination: Is it Safe for Rheumatology Patients Over Age 30 on Biologics?
BOSTON– The herpes zoster vaccine may be safe to give to patients who are taking biologic therapies and have quiescent rheumatologic disorders, based on preliminary data from two studies presented at the annual meeting of the American College of Rheumatology.
Dr. Jeffrey Curtis of the University of Alabama at Birmingham presented data about the extent of the increased risk for herpes zoster in rheumatology patients, especially those with systemic lupus erythematosus, and some intriguing results on 630 patients on biologic therapies who inadvertently got the vaccine.
Dr. Stephen Lindsey of Ochsner Health System in Baton Rouge, La., said that he continues to evolve a protocol for herpes zoster vaccination of his patients with rheumatologic disorders.
In our exclusive interview at ACR14, the two researchers discussed the implications of their separate studies on the subject and revealed the next steps of a prospective study of herpes zoster vaccination in patients with rheumatologic disorders that is just getting underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The herpes zoster vaccine may be safe to give to patients who are taking biologic therapies and have quiescent rheumatologic disorders, based on preliminary data from two studies presented at the annual meeting of the American College of Rheumatology.
Dr. Jeffrey Curtis of the University of Alabama at Birmingham presented data about the extent of the increased risk for herpes zoster in rheumatology patients, especially those with systemic lupus erythematosus, and some intriguing results on 630 patients on biologic therapies who inadvertently got the vaccine.
Dr. Stephen Lindsey of Ochsner Health System in Baton Rouge, La., said that he continues to evolve a protocol for herpes zoster vaccination of his patients with rheumatologic disorders.
In our exclusive interview at ACR14, the two researchers discussed the implications of their separate studies on the subject and revealed the next steps of a prospective study of herpes zoster vaccination in patients with rheumatologic disorders that is just getting underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The herpes zoster vaccine may be safe to give to patients who are taking biologic therapies and have quiescent rheumatologic disorders, based on preliminary data from two studies presented at the annual meeting of the American College of Rheumatology.
Dr. Jeffrey Curtis of the University of Alabama at Birmingham presented data about the extent of the increased risk for herpes zoster in rheumatology patients, especially those with systemic lupus erythematosus, and some intriguing results on 630 patients on biologic therapies who inadvertently got the vaccine.
Dr. Stephen Lindsey of Ochsner Health System in Baton Rouge, La., said that he continues to evolve a protocol for herpes zoster vaccination of his patients with rheumatologic disorders.
In our exclusive interview at ACR14, the two researchers discussed the implications of their separate studies on the subject and revealed the next steps of a prospective study of herpes zoster vaccination in patients with rheumatologic disorders that is just getting underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACR 2014
VIDEO: Herpes zoster vaccination: Is it safe for rheumatology patients over age 30 on biologics?
BOSTON– The herpes zoster vaccine may be safe to give to patients who are taking biologic therapies and have quiescent rheumatologic disorders, based on preliminary data from two studies presented at the annual meeting of the American College of Rheumatology.
Dr. Jeffrey Curtis of the University of Alabama at Birmingham presented data about the extent of the increased risk for herpes zoster in rheumatology patients, especially those with systemic lupus erythematosus, and some intriguing results on 630 patients on biologic therapies who inadvertently got the vaccine.
Dr. Stephen Lindsey of Ochsner Health System in Baton Rouge, La., said that he continues to evolve a protocol for herpes zoster vaccination of his patients with rheumatologic disorders.
In our exclusive interview at ACR14, the two researchers discussed the implications of their separate studies on the subject and revealed the next steps of a prospective study of herpes zoster vaccination in patients with rheumatologic disorders that is just getting underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The herpes zoster vaccine may be safe to give to patients who are taking biologic therapies and have quiescent rheumatologic disorders, based on preliminary data from two studies presented at the annual meeting of the American College of Rheumatology.
Dr. Jeffrey Curtis of the University of Alabama at Birmingham presented data about the extent of the increased risk for herpes zoster in rheumatology patients, especially those with systemic lupus erythematosus, and some intriguing results on 630 patients on biologic therapies who inadvertently got the vaccine.
Dr. Stephen Lindsey of Ochsner Health System in Baton Rouge, La., said that he continues to evolve a protocol for herpes zoster vaccination of his patients with rheumatologic disorders.
In our exclusive interview at ACR14, the two researchers discussed the implications of their separate studies on the subject and revealed the next steps of a prospective study of herpes zoster vaccination in patients with rheumatologic disorders that is just getting underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON– The herpes zoster vaccine may be safe to give to patients who are taking biologic therapies and have quiescent rheumatologic disorders, based on preliminary data from two studies presented at the annual meeting of the American College of Rheumatology.
Dr. Jeffrey Curtis of the University of Alabama at Birmingham presented data about the extent of the increased risk for herpes zoster in rheumatology patients, especially those with systemic lupus erythematosus, and some intriguing results on 630 patients on biologic therapies who inadvertently got the vaccine.
Dr. Stephen Lindsey of Ochsner Health System in Baton Rouge, La., said that he continues to evolve a protocol for herpes zoster vaccination of his patients with rheumatologic disorders.
In our exclusive interview at ACR14, the two researchers discussed the implications of their separate studies on the subject and revealed the next steps of a prospective study of herpes zoster vaccination in patients with rheumatologic disorders that is just getting underway.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACR 2014
RA increases mortality, particularly for respiratory causes, in women
BOSTON – A diagnosis of rheumatoid arthritis doubled the risk of death from any cause over the risk for those without RA, based on 34 years of follow-up data from women in the Nurses’ Health Study.
Incident RA was associated with a 40% increase in the risk of death, and seropositive RA was associated with a 51% increase in the risk of death, Dr. Jeffrey A. Sparks of Brigham and Women’s Hospital, Boston, reported at the annual meeting of the American College of Rheumatology.
The data also revealed a much stronger link between RA and the risk of death due to respiratory causes. That rate was sixfold higher in seropositive women with RA. While there is an appreciation of an increased risk for cardiovascular disease and cancer in RA patients, deaths due to respiratory disease are “an underappreciated cause of death” that warrant more focus in these patients, he said.
Among the 25,699 deaths that took place during the course of the study, 261 of them occurred in the 960 women who developed RA after they enrolled in the study. Among the women with RA, cancer was the cause of death in 29%, cardiovascular disease in 22%, and respiratory causes in 16%.
The study allows direct comparisons of RA patients and controls over a prolonged time with detailed data on clinical, lifestyle, and serologic factors, he said. Compared with women without RA, all-cause mortality was significantly higher in women with RA after adjustment for age and other potentially confounding factors (hazard ratio, 2.07; 95% CI, 1.83-2.35).
The variables used to adjust the analyses were age, questionnaire period, U.S. region, race/ethnicity, education, husband’s education, body mass index (<18.5, 18.5-24.9, 25-29.9, ≥30 kg/m2), cigarette smoking pack-years (never, 0-10, 10.1-20, >20), postmenopausal hormone use, physical activity, healthy eating index, cancer, cardiovascular disease, diabetes, family history of diabetes, family history of cancer, family history of myocardial infarction before age 60 years, and aspirin use. Modifiable factors were adjusted up to RA diagnosis (cigarette smoking pack-years, physical activity, and BMI).
The mortality rate was higher for women with seropositive disease than it was for those without RA (HR, 2.33; 95% CI, 2.00-2.71), as was the rate for seronegative RA (HR, 1.60; 95% CI, 1.30-1.98).
For every 5 years of RA duration, mortality risk increased 32% (95% CI, 27%-36%) compared with unaffected women. Women with RA had significantly increased risks for mortality from CVD (HR, 1.87; 95% CI, 1.44-2.43), cancer (HR, 1.35; 95% CI, 1.07-1.69), and respiratory causes (HR, 4.50; 95% CI, 3.28-6.17), compared with women without the disease.
Respiratory mortality for women with seropositive RA was sixfold higher than it was for non-RA women (HR, 6.23; 95% CI, 4.38-8.85). Among women with RA, there were 43 respiratory deaths caused by pneumonia (11), emphysema (8), chronic interstitial lung disease (5), asthma (1), and other respiratory diseases (18).
Dr. Sparks had no relevant financial disclosures. The National Institutes of Health and the Rheumatology Research Foundation funded the study.
BOSTON – A diagnosis of rheumatoid arthritis doubled the risk of death from any cause over the risk for those without RA, based on 34 years of follow-up data from women in the Nurses’ Health Study.
Incident RA was associated with a 40% increase in the risk of death, and seropositive RA was associated with a 51% increase in the risk of death, Dr. Jeffrey A. Sparks of Brigham and Women’s Hospital, Boston, reported at the annual meeting of the American College of Rheumatology.
The data also revealed a much stronger link between RA and the risk of death due to respiratory causes. That rate was sixfold higher in seropositive women with RA. While there is an appreciation of an increased risk for cardiovascular disease and cancer in RA patients, deaths due to respiratory disease are “an underappreciated cause of death” that warrant more focus in these patients, he said.
Among the 25,699 deaths that took place during the course of the study, 261 of them occurred in the 960 women who developed RA after they enrolled in the study. Among the women with RA, cancer was the cause of death in 29%, cardiovascular disease in 22%, and respiratory causes in 16%.
The study allows direct comparisons of RA patients and controls over a prolonged time with detailed data on clinical, lifestyle, and serologic factors, he said. Compared with women without RA, all-cause mortality was significantly higher in women with RA after adjustment for age and other potentially confounding factors (hazard ratio, 2.07; 95% CI, 1.83-2.35).
The variables used to adjust the analyses were age, questionnaire period, U.S. region, race/ethnicity, education, husband’s education, body mass index (<18.5, 18.5-24.9, 25-29.9, ≥30 kg/m2), cigarette smoking pack-years (never, 0-10, 10.1-20, >20), postmenopausal hormone use, physical activity, healthy eating index, cancer, cardiovascular disease, diabetes, family history of diabetes, family history of cancer, family history of myocardial infarction before age 60 years, and aspirin use. Modifiable factors were adjusted up to RA diagnosis (cigarette smoking pack-years, physical activity, and BMI).
The mortality rate was higher for women with seropositive disease than it was for those without RA (HR, 2.33; 95% CI, 2.00-2.71), as was the rate for seronegative RA (HR, 1.60; 95% CI, 1.30-1.98).
For every 5 years of RA duration, mortality risk increased 32% (95% CI, 27%-36%) compared with unaffected women. Women with RA had significantly increased risks for mortality from CVD (HR, 1.87; 95% CI, 1.44-2.43), cancer (HR, 1.35; 95% CI, 1.07-1.69), and respiratory causes (HR, 4.50; 95% CI, 3.28-6.17), compared with women without the disease.
Respiratory mortality for women with seropositive RA was sixfold higher than it was for non-RA women (HR, 6.23; 95% CI, 4.38-8.85). Among women with RA, there were 43 respiratory deaths caused by pneumonia (11), emphysema (8), chronic interstitial lung disease (5), asthma (1), and other respiratory diseases (18).
Dr. Sparks had no relevant financial disclosures. The National Institutes of Health and the Rheumatology Research Foundation funded the study.
BOSTON – A diagnosis of rheumatoid arthritis doubled the risk of death from any cause over the risk for those without RA, based on 34 years of follow-up data from women in the Nurses’ Health Study.
Incident RA was associated with a 40% increase in the risk of death, and seropositive RA was associated with a 51% increase in the risk of death, Dr. Jeffrey A. Sparks of Brigham and Women’s Hospital, Boston, reported at the annual meeting of the American College of Rheumatology.
The data also revealed a much stronger link between RA and the risk of death due to respiratory causes. That rate was sixfold higher in seropositive women with RA. While there is an appreciation of an increased risk for cardiovascular disease and cancer in RA patients, deaths due to respiratory disease are “an underappreciated cause of death” that warrant more focus in these patients, he said.
Among the 25,699 deaths that took place during the course of the study, 261 of them occurred in the 960 women who developed RA after they enrolled in the study. Among the women with RA, cancer was the cause of death in 29%, cardiovascular disease in 22%, and respiratory causes in 16%.
The study allows direct comparisons of RA patients and controls over a prolonged time with detailed data on clinical, lifestyle, and serologic factors, he said. Compared with women without RA, all-cause mortality was significantly higher in women with RA after adjustment for age and other potentially confounding factors (hazard ratio, 2.07; 95% CI, 1.83-2.35).
The variables used to adjust the analyses were age, questionnaire period, U.S. region, race/ethnicity, education, husband’s education, body mass index (<18.5, 18.5-24.9, 25-29.9, ≥30 kg/m2), cigarette smoking pack-years (never, 0-10, 10.1-20, >20), postmenopausal hormone use, physical activity, healthy eating index, cancer, cardiovascular disease, diabetes, family history of diabetes, family history of cancer, family history of myocardial infarction before age 60 years, and aspirin use. Modifiable factors were adjusted up to RA diagnosis (cigarette smoking pack-years, physical activity, and BMI).
The mortality rate was higher for women with seropositive disease than it was for those without RA (HR, 2.33; 95% CI, 2.00-2.71), as was the rate for seronegative RA (HR, 1.60; 95% CI, 1.30-1.98).
For every 5 years of RA duration, mortality risk increased 32% (95% CI, 27%-36%) compared with unaffected women. Women with RA had significantly increased risks for mortality from CVD (HR, 1.87; 95% CI, 1.44-2.43), cancer (HR, 1.35; 95% CI, 1.07-1.69), and respiratory causes (HR, 4.50; 95% CI, 3.28-6.17), compared with women without the disease.
Respiratory mortality for women with seropositive RA was sixfold higher than it was for non-RA women (HR, 6.23; 95% CI, 4.38-8.85). Among women with RA, there were 43 respiratory deaths caused by pneumonia (11), emphysema (8), chronic interstitial lung disease (5), asthma (1), and other respiratory diseases (18).
Dr. Sparks had no relevant financial disclosures. The National Institutes of Health and the Rheumatology Research Foundation funded the study.
AT THE ACR ANNUAL MEETING
Key clinical point: All-cause mortality was significantly higher in women with RA after adjustment for age and other factors.
Major finding: For every 5 years of RA duration, mortality risk increased 32% (95% CI, 27%-36%), compared with women without RA.
Data source: A study of RA and mortality among 121,700 women followed from 1976 to 2010 in the Nurses’ Health Study.
Disclosures: Dr. Sparks had no relevant disclosures. The National Institutes of Health and the Rheumatology Research Foundation funded the study.
Treat-to-target approach cuts mortality risk in RA patients
BOSTON – Aggressive treatment of rheumatoid arthritis patients aimed at achieving Disease Activity Scores of 2.4 or less was associated with mortality rates that were not significantly different from those seen in the general population, based on the results of a 10-year Dutch study.
Irrespective of the treatment regimen, keeping the DAS (Disease Activity Score) at 2.4 or below is associated with lower inflammation, according to Dr. Iris Markusse of Leiden University Medical Center. “Historically, mortality risk in RA was significantly increased when inflammation was not as effectively suppressed ... [but with intensified treatment] inflammation can be so well controlled that it no longer affects overall survival.”
In the Behandel Strategieen (BeST) study, 508 patients with recent active-onset RA were randomized to one of four treatment approaches. Patients received either sequential monotherapy with methotrexate, step-up therapy with methotrexate, methotrexate plus sulfasalazine and prednisone, or methotrexate and infliximab. For all patients, the treatment target was a DAS of 2.4 or less, and follow-up occurred at 3-month intervals.
Patients who started on methotrexate monotherapy and had a DAS exceeding 2.4 received the next step in therapy, which included adding or switching to other therapies as needed. Conversely, if low disease activity was seen for at least 6 consecutive months, combination therapy was tapered to maintenance monotherapy. After the third year of the trial, patients who had at least 6 consecutive months on maintenance monotherapy had to stop that drug as well.
Over the course of the study, 80% of participants had low disease activity, 45% were in remission, and 15% were in drug-free remission, she reported at a press conference during the annual meeting of the American College of Rheumatology.
Of the 508 patients, 72 died at a mean age of 75 years; the deaths occurred in 16 of 126 patients on methotrexate monotherapy, 15 of 121 on step-up methotrexate, 21 of 133 on methotrexate plus sulfasalazine and prednisone, and 20 of 128 on methotrexate and infliximab. Based on the general Dutch population, 62 deaths would have been expected.
While mortality risk was not significantly different among the treatment arms; mortality risk was higher for patients who were older at baseline, male, smokers, and those with poorer scores on a baseline health assessment questionnaire. The most significant risk factor was smoking at baseline (hazard ratio, 5.19; 95% confidence interval, 3.08-8.75).
Encouraging patients to quit smoking might be effective for reducing mortality, she added.
Dr. Markusse declared having no relevant financial disclosures. Funding for the study included a government grant from the Dutch College of Health Insurance Companies, with additional funding from Schering-Plough/MSD and Centocor/Janssen.
BOSTON – Aggressive treatment of rheumatoid arthritis patients aimed at achieving Disease Activity Scores of 2.4 or less was associated with mortality rates that were not significantly different from those seen in the general population, based on the results of a 10-year Dutch study.
Irrespective of the treatment regimen, keeping the DAS (Disease Activity Score) at 2.4 or below is associated with lower inflammation, according to Dr. Iris Markusse of Leiden University Medical Center. “Historically, mortality risk in RA was significantly increased when inflammation was not as effectively suppressed ... [but with intensified treatment] inflammation can be so well controlled that it no longer affects overall survival.”
In the Behandel Strategieen (BeST) study, 508 patients with recent active-onset RA were randomized to one of four treatment approaches. Patients received either sequential monotherapy with methotrexate, step-up therapy with methotrexate, methotrexate plus sulfasalazine and prednisone, or methotrexate and infliximab. For all patients, the treatment target was a DAS of 2.4 or less, and follow-up occurred at 3-month intervals.
Patients who started on methotrexate monotherapy and had a DAS exceeding 2.4 received the next step in therapy, which included adding or switching to other therapies as needed. Conversely, if low disease activity was seen for at least 6 consecutive months, combination therapy was tapered to maintenance monotherapy. After the third year of the trial, patients who had at least 6 consecutive months on maintenance monotherapy had to stop that drug as well.
Over the course of the study, 80% of participants had low disease activity, 45% were in remission, and 15% were in drug-free remission, she reported at a press conference during the annual meeting of the American College of Rheumatology.
Of the 508 patients, 72 died at a mean age of 75 years; the deaths occurred in 16 of 126 patients on methotrexate monotherapy, 15 of 121 on step-up methotrexate, 21 of 133 on methotrexate plus sulfasalazine and prednisone, and 20 of 128 on methotrexate and infliximab. Based on the general Dutch population, 62 deaths would have been expected.
While mortality risk was not significantly different among the treatment arms; mortality risk was higher for patients who were older at baseline, male, smokers, and those with poorer scores on a baseline health assessment questionnaire. The most significant risk factor was smoking at baseline (hazard ratio, 5.19; 95% confidence interval, 3.08-8.75).
Encouraging patients to quit smoking might be effective for reducing mortality, she added.
Dr. Markusse declared having no relevant financial disclosures. Funding for the study included a government grant from the Dutch College of Health Insurance Companies, with additional funding from Schering-Plough/MSD and Centocor/Janssen.
BOSTON – Aggressive treatment of rheumatoid arthritis patients aimed at achieving Disease Activity Scores of 2.4 or less was associated with mortality rates that were not significantly different from those seen in the general population, based on the results of a 10-year Dutch study.
Irrespective of the treatment regimen, keeping the DAS (Disease Activity Score) at 2.4 or below is associated with lower inflammation, according to Dr. Iris Markusse of Leiden University Medical Center. “Historically, mortality risk in RA was significantly increased when inflammation was not as effectively suppressed ... [but with intensified treatment] inflammation can be so well controlled that it no longer affects overall survival.”
In the Behandel Strategieen (BeST) study, 508 patients with recent active-onset RA were randomized to one of four treatment approaches. Patients received either sequential monotherapy with methotrexate, step-up therapy with methotrexate, methotrexate plus sulfasalazine and prednisone, or methotrexate and infliximab. For all patients, the treatment target was a DAS of 2.4 or less, and follow-up occurred at 3-month intervals.
Patients who started on methotrexate monotherapy and had a DAS exceeding 2.4 received the next step in therapy, which included adding or switching to other therapies as needed. Conversely, if low disease activity was seen for at least 6 consecutive months, combination therapy was tapered to maintenance monotherapy. After the third year of the trial, patients who had at least 6 consecutive months on maintenance monotherapy had to stop that drug as well.
Over the course of the study, 80% of participants had low disease activity, 45% were in remission, and 15% were in drug-free remission, she reported at a press conference during the annual meeting of the American College of Rheumatology.
Of the 508 patients, 72 died at a mean age of 75 years; the deaths occurred in 16 of 126 patients on methotrexate monotherapy, 15 of 121 on step-up methotrexate, 21 of 133 on methotrexate plus sulfasalazine and prednisone, and 20 of 128 on methotrexate and infliximab. Based on the general Dutch population, 62 deaths would have been expected.
While mortality risk was not significantly different among the treatment arms; mortality risk was higher for patients who were older at baseline, male, smokers, and those with poorer scores on a baseline health assessment questionnaire. The most significant risk factor was smoking at baseline (hazard ratio, 5.19; 95% confidence interval, 3.08-8.75).
Encouraging patients to quit smoking might be effective for reducing mortality, she added.
Dr. Markusse declared having no relevant financial disclosures. Funding for the study included a government grant from the Dutch College of Health Insurance Companies, with additional funding from Schering-Plough/MSD and Centocor/Janssen.
AT THE ACR ANNUAL MEETING
Key clinical point: Keeping Disease Activity Scores low, irrespective of the treatment regimen selected, is associated with reduced mortality risk.
Major finding: The most significant risk factor for mortality was smoking at baseline (HR 5.19, 95% CI 3.08-8.75).
Data source: The Behandel Strategieen (BeST) study of 508 patients with recent active-onset RA followed for 10 years.
Disclosures: Dr. Markusse declared having no relevant financial disclosures. Funding for the study included a government grant from the Dutch College of Health Insurance Companies, with additional funding from Schering-Plough/MSD and Centocor/Janssen.
Novel program improves RA care, cuts costs
BOSTON– A bundle of eight measures was effective in improving the quality of rheumatoid arthritis care while reducing costs, Dr. Eric D. Newman reported at the annual meeting of the American College of Rheumatology.
At the start of the program, 22% of roughly 2,400 RA patients had achieved all of the applicable quality measures that were integrated into the program. After 22 months in the program, 40% had met all of the measures.
Using routine disease measures, the program was successful for de-escalating use of biologics among the patients. After 1 year, the associated savings came to $720,000; a savings estimate of $1.2 million is projected for 2014.
“We recognized the importance of objectively and routinely measuring disease activity, and using that information to engage our patients and drive a new systematic strategic approach to rheumatoid arthritis care,” said Dr. Newman, director of rheumatology for the Geisinger Health System, Wilkes-Barre, Penn., and the program’s designer.
The AIM FARTHER (Attribution, Integration, Measurement, Finances and Reporting of Therapies) model was designed and implemented for about 2,400 RA patients cared for by the 17 rheumatologists within the Geisinger Health System. The eight measures included disease activity measures (RA on DMARD, active RA on DMARD, RA with CDAI [Clinical Disease Activity Index], and RA at low disease activity); drug safety measures (TB testing if on a biologic agent, yearly influenza vaccination, and pneumococcal vaccination), and a comorbidity measure (check of LDL cholesterol).
Individual patient scorecards were developed via patient responses on a touch-screen questionnaire and input from physicians, nurses, and the electronic health record. The data were used to measure RA patient care gaps to be resolved. The measures were shared and analyzed to close care gaps as well as create provider and department performance reports.
Before the start of the program, measures were high for the percentage of RA patients and the percentage of patients with active RA on a DMARD as well as the percentage of patients who had their LDLs checked. As a result, only modest further improvements were seen after 22 months of the program (from 88% at baseline to 90% for the percentage of RA patients on a DMARD, from 92% to 93% for RA patients with active disease on a DMARD, and from 93% to 95 for LDL checks).
Significant improvements in other measures were seen, however, including a rise in the use of CDAI measures from 52% to 84%, a rise in TB testing for those on a biologic from 83% to 93%, an increase in yearly influenza vaccination from 59% to 75%, and a rise in pneumococcal vaccination from 59% to 72%.
As a care model, AIM FARTHER seeks to employ provider engagement, process redesign, measurement, and information technology, Dr. Newman said. The components of the program include establishing a registry, defining roles and attribution, integrating primary and specialty care, defining a strategic approach to RA care, developing an RA quality measure bundle, task management and performance reporting, and a financial incentive model.
The success of AIM FARTHER “is not due to any one individual, but [relies on] meaningful involvement of all members of the rheumatology team, holding ourselves accountable, dedicating the time needed to perform the work, and creating an internal forum to discuss quality improvement on a regular basis. This approach moved our rheumatology team from engagement to buy-in to ownership. The result is an RA population management program that is sustainable yet evolving, as we challenge ourselves to continuously improve the quality of care for our patients with rheumatic disease,” Dr. Newman said.
The authors had no disclosures. The work was internally funded by the Geisinger Health System.
BOSTON– A bundle of eight measures was effective in improving the quality of rheumatoid arthritis care while reducing costs, Dr. Eric D. Newman reported at the annual meeting of the American College of Rheumatology.
At the start of the program, 22% of roughly 2,400 RA patients had achieved all of the applicable quality measures that were integrated into the program. After 22 months in the program, 40% had met all of the measures.
Using routine disease measures, the program was successful for de-escalating use of biologics among the patients. After 1 year, the associated savings came to $720,000; a savings estimate of $1.2 million is projected for 2014.
“We recognized the importance of objectively and routinely measuring disease activity, and using that information to engage our patients and drive a new systematic strategic approach to rheumatoid arthritis care,” said Dr. Newman, director of rheumatology for the Geisinger Health System, Wilkes-Barre, Penn., and the program’s designer.
The AIM FARTHER (Attribution, Integration, Measurement, Finances and Reporting of Therapies) model was designed and implemented for about 2,400 RA patients cared for by the 17 rheumatologists within the Geisinger Health System. The eight measures included disease activity measures (RA on DMARD, active RA on DMARD, RA with CDAI [Clinical Disease Activity Index], and RA at low disease activity); drug safety measures (TB testing if on a biologic agent, yearly influenza vaccination, and pneumococcal vaccination), and a comorbidity measure (check of LDL cholesterol).
Individual patient scorecards were developed via patient responses on a touch-screen questionnaire and input from physicians, nurses, and the electronic health record. The data were used to measure RA patient care gaps to be resolved. The measures were shared and analyzed to close care gaps as well as create provider and department performance reports.
Before the start of the program, measures were high for the percentage of RA patients and the percentage of patients with active RA on a DMARD as well as the percentage of patients who had their LDLs checked. As a result, only modest further improvements were seen after 22 months of the program (from 88% at baseline to 90% for the percentage of RA patients on a DMARD, from 92% to 93% for RA patients with active disease on a DMARD, and from 93% to 95 for LDL checks).
Significant improvements in other measures were seen, however, including a rise in the use of CDAI measures from 52% to 84%, a rise in TB testing for those on a biologic from 83% to 93%, an increase in yearly influenza vaccination from 59% to 75%, and a rise in pneumococcal vaccination from 59% to 72%.
As a care model, AIM FARTHER seeks to employ provider engagement, process redesign, measurement, and information technology, Dr. Newman said. The components of the program include establishing a registry, defining roles and attribution, integrating primary and specialty care, defining a strategic approach to RA care, developing an RA quality measure bundle, task management and performance reporting, and a financial incentive model.
The success of AIM FARTHER “is not due to any one individual, but [relies on] meaningful involvement of all members of the rheumatology team, holding ourselves accountable, dedicating the time needed to perform the work, and creating an internal forum to discuss quality improvement on a regular basis. This approach moved our rheumatology team from engagement to buy-in to ownership. The result is an RA population management program that is sustainable yet evolving, as we challenge ourselves to continuously improve the quality of care for our patients with rheumatic disease,” Dr. Newman said.
The authors had no disclosures. The work was internally funded by the Geisinger Health System.
BOSTON– A bundle of eight measures was effective in improving the quality of rheumatoid arthritis care while reducing costs, Dr. Eric D. Newman reported at the annual meeting of the American College of Rheumatology.
At the start of the program, 22% of roughly 2,400 RA patients had achieved all of the applicable quality measures that were integrated into the program. After 22 months in the program, 40% had met all of the measures.
Using routine disease measures, the program was successful for de-escalating use of biologics among the patients. After 1 year, the associated savings came to $720,000; a savings estimate of $1.2 million is projected for 2014.
“We recognized the importance of objectively and routinely measuring disease activity, and using that information to engage our patients and drive a new systematic strategic approach to rheumatoid arthritis care,” said Dr. Newman, director of rheumatology for the Geisinger Health System, Wilkes-Barre, Penn., and the program’s designer.
The AIM FARTHER (Attribution, Integration, Measurement, Finances and Reporting of Therapies) model was designed and implemented for about 2,400 RA patients cared for by the 17 rheumatologists within the Geisinger Health System. The eight measures included disease activity measures (RA on DMARD, active RA on DMARD, RA with CDAI [Clinical Disease Activity Index], and RA at low disease activity); drug safety measures (TB testing if on a biologic agent, yearly influenza vaccination, and pneumococcal vaccination), and a comorbidity measure (check of LDL cholesterol).
Individual patient scorecards were developed via patient responses on a touch-screen questionnaire and input from physicians, nurses, and the electronic health record. The data were used to measure RA patient care gaps to be resolved. The measures were shared and analyzed to close care gaps as well as create provider and department performance reports.
Before the start of the program, measures were high for the percentage of RA patients and the percentage of patients with active RA on a DMARD as well as the percentage of patients who had their LDLs checked. As a result, only modest further improvements were seen after 22 months of the program (from 88% at baseline to 90% for the percentage of RA patients on a DMARD, from 92% to 93% for RA patients with active disease on a DMARD, and from 93% to 95 for LDL checks).
Significant improvements in other measures were seen, however, including a rise in the use of CDAI measures from 52% to 84%, a rise in TB testing for those on a biologic from 83% to 93%, an increase in yearly influenza vaccination from 59% to 75%, and a rise in pneumococcal vaccination from 59% to 72%.
As a care model, AIM FARTHER seeks to employ provider engagement, process redesign, measurement, and information technology, Dr. Newman said. The components of the program include establishing a registry, defining roles and attribution, integrating primary and specialty care, defining a strategic approach to RA care, developing an RA quality measure bundle, task management and performance reporting, and a financial incentive model.
The success of AIM FARTHER “is not due to any one individual, but [relies on] meaningful involvement of all members of the rheumatology team, holding ourselves accountable, dedicating the time needed to perform the work, and creating an internal forum to discuss quality improvement on a regular basis. This approach moved our rheumatology team from engagement to buy-in to ownership. The result is an RA population management program that is sustainable yet evolving, as we challenge ourselves to continuously improve the quality of care for our patients with rheumatic disease,” Dr. Newman said.
The authors had no disclosures. The work was internally funded by the Geisinger Health System.
AT THE ACR ANNUAL MEETING
Key clinical point: Quality programs can improve care and save costs for rheumatoid arthritis patients.
Major finding: After 1 year, the savings came to $720,000; a savings estimate of $1.2 million is projected for 2014.
Data source: Nearly 2,400 RA patients receiving care in central Pennsylvania through the Geisinger Health Care system.
Disclosures: The authors declared no financial disclosures. The work was internally funded by the Geisinger Health System.
VIDEO: BeST: Does a treat-to-target approach reduce RA mortality?
BOSTON - With follow up every 3 months, the survival rates of RA patients were comparable to those of the general population in a 10-year study of patients in the Netherlands. Dr. Iris Markusse of Leiden University Medical Center credits regimens that were tailored to keep the Disease Activity Score at levels of 2.4 or lower. Further, the medications used in this strategy did not increase patient mortality. Dr. Markusse discusses the findings of BeST in an exclusive interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON - With follow up every 3 months, the survival rates of RA patients were comparable to those of the general population in a 10-year study of patients in the Netherlands. Dr. Iris Markusse of Leiden University Medical Center credits regimens that were tailored to keep the Disease Activity Score at levels of 2.4 or lower. Further, the medications used in this strategy did not increase patient mortality. Dr. Markusse discusses the findings of BeST in an exclusive interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON - With follow up every 3 months, the survival rates of RA patients were comparable to those of the general population in a 10-year study of patients in the Netherlands. Dr. Iris Markusse of Leiden University Medical Center credits regimens that were tailored to keep the Disease Activity Score at levels of 2.4 or lower. Further, the medications used in this strategy did not increase patient mortality. Dr. Markusse discusses the findings of BeST in an exclusive interview at the annual meeting of the American College of Rheumatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACR 2014
VIDEO: RA linked to increased mortality in Nurses’ Health Study
BOSTON – Rheumatoid arthritis has been linked to increased risk for death in one of the first studies to directly compare RA patients with controls over a prolonged period of time. In women who developed RA after enrollment in the Nurses’ Health Study, seropositive disease was strongly associated with worse outcomes. Also, some surprising findings emerged about RA and the risk for fatal respiratory disease in women.
In our exclusive interview, one of the study’s lead authors, Dr. Jeffrey A. Sparks of Brigham and Women’s Hospital, Boston, discusses how the findings may begin to influence the clinical management of women with RA.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Rheumatoid arthritis has been linked to increased risk for death in one of the first studies to directly compare RA patients with controls over a prolonged period of time. In women who developed RA after enrollment in the Nurses’ Health Study, seropositive disease was strongly associated with worse outcomes. Also, some surprising findings emerged about RA and the risk for fatal respiratory disease in women.
In our exclusive interview, one of the study’s lead authors, Dr. Jeffrey A. Sparks of Brigham and Women’s Hospital, Boston, discusses how the findings may begin to influence the clinical management of women with RA.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Rheumatoid arthritis has been linked to increased risk for death in one of the first studies to directly compare RA patients with controls over a prolonged period of time. In women who developed RA after enrollment in the Nurses’ Health Study, seropositive disease was strongly associated with worse outcomes. Also, some surprising findings emerged about RA and the risk for fatal respiratory disease in women.
In our exclusive interview, one of the study’s lead authors, Dr. Jeffrey A. Sparks of Brigham and Women’s Hospital, Boston, discusses how the findings may begin to influence the clinical management of women with RA.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ACR 2014
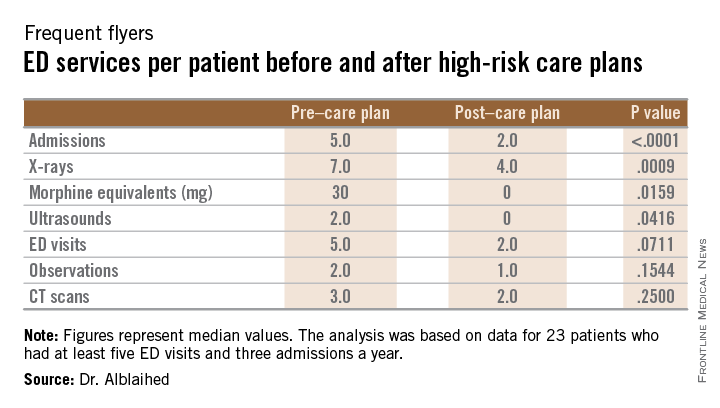
High-risk care plans reduced ED testing, admissions
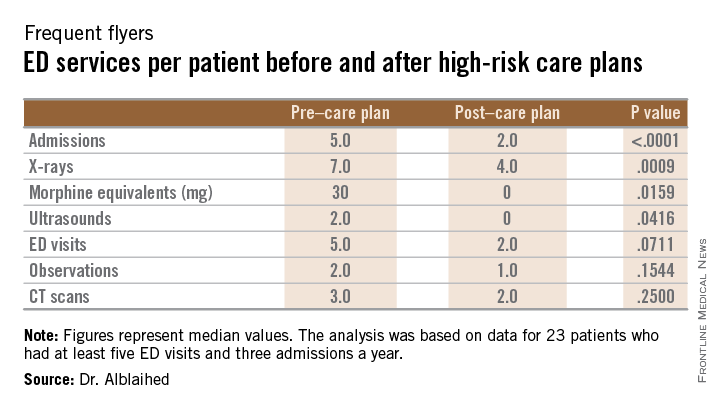
CHICAGO – Frequent flyers, patients with a history of at least five visits per year to the emergency department, might benefit from high-risk care plans, based on research from the University of Maryland health care system.
The plans are designed to improve patient safety by reducing exposure to ionizing radiation and have the additional benefit of reducing the costs of care, Dr. Leen Alblaihed, a resident physician at the university, reported at the annual meeting of the American College of Emergency Physicians.
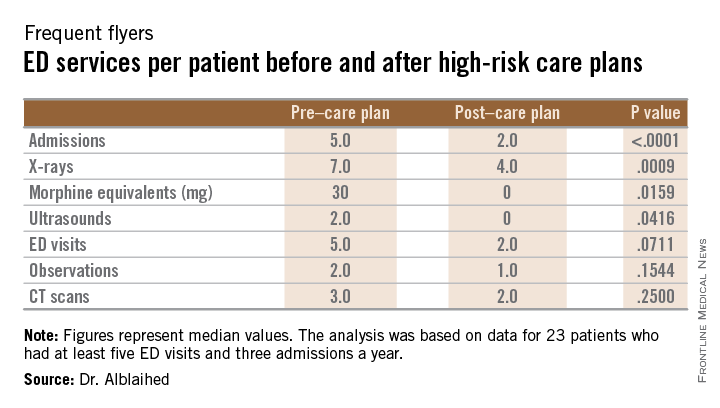
After high-risk care plans were put into the emergency physician work flow for 41 patients with a history of high emergency department utilization, unneeded tests declined. Other important outcomes were statistically significant reductions in hospitalizations and quantities of prescribed opioids.
he patients considered for the study had to have at least five ED visits and three admissions per year. Based on the electronic medical record data of the university’s two suburban medical centers, a total of 845 patients met that definition.
The high-risk care plans for the management of the 41 patients were developed by a multi-disciplinary team of case managers, emergency physicians, and hospitalists. The plans were then integrated into the physician electronic documentation and work flow.
The data analysis was based on 23 of the patients, 10 men and 13 women with a median age of 48 years, who had 6 months of data before and 6 months of data after the care plan was instituted. The primary outcome measures were a reduction in ionizing radiation. Secondary outcome measures were reductions in ED visits, hospital admissions, observation stays, and opioid prescriptions based on morphine equivalent totals.
Compared to the data before the care plan was instituted, the 23 patients had nearly half as many x-rays and CT scans and a nearly sixfold reduction in prescribing of morphine equivalents. While ED visits decreased modestly from 116 to 82, the admission rates dropped from 99 to 37 and observation stays declined from 43 to 28.
The study group had decreases in all measures after high-risk care plans. X-ray studies decreased from 202 to 106, CT scans declined from 107 to 50, and opiate prescribing decreased from 3824 mg to 675 mg in morphine equivalents.
Because the outcomes were not normally distributed, medians and interquartile ranges were analyzed using the Wilcoxon signed-rank test to compare the pre/post median values (see table).
CHICAGO – Frequent flyers, patients with a history of at least five visits per year to the emergency department, might benefit from high-risk care plans, based on research from the University of Maryland health care system.
The plans are designed to improve patient safety by reducing exposure to ionizing radiation and have the additional benefit of reducing the costs of care, Dr. Leen Alblaihed, a resident physician at the university, reported at the annual meeting of the American College of Emergency Physicians.
After high-risk care plans were put into the emergency physician work flow for 41 patients with a history of high emergency department utilization, unneeded tests declined. Other important outcomes were statistically significant reductions in hospitalizations and quantities of prescribed opioids.
he patients considered for the study had to have at least five ED visits and three admissions per year. Based on the electronic medical record data of the university’s two suburban medical centers, a total of 845 patients met that definition.
The high-risk care plans for the management of the 41 patients were developed by a multi-disciplinary team of case managers, emergency physicians, and hospitalists. The plans were then integrated into the physician electronic documentation and work flow.
The data analysis was based on 23 of the patients, 10 men and 13 women with a median age of 48 years, who had 6 months of data before and 6 months of data after the care plan was instituted. The primary outcome measures were a reduction in ionizing radiation. Secondary outcome measures were reductions in ED visits, hospital admissions, observation stays, and opioid prescriptions based on morphine equivalent totals.
Compared to the data before the care plan was instituted, the 23 patients had nearly half as many x-rays and CT scans and a nearly sixfold reduction in prescribing of morphine equivalents. While ED visits decreased modestly from 116 to 82, the admission rates dropped from 99 to 37 and observation stays declined from 43 to 28.
The study group had decreases in all measures after high-risk care plans. X-ray studies decreased from 202 to 106, CT scans declined from 107 to 50, and opiate prescribing decreased from 3824 mg to 675 mg in morphine equivalents.
Because the outcomes were not normally distributed, medians and interquartile ranges were analyzed using the Wilcoxon signed-rank test to compare the pre/post median values (see table).
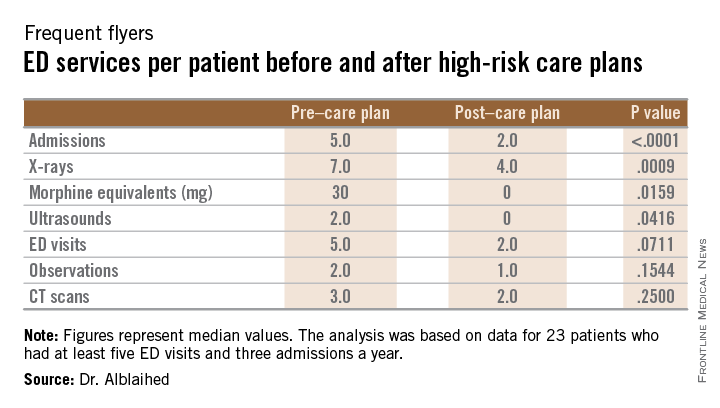
CHICAGO – Frequent flyers, patients with a history of at least five visits per year to the emergency department, might benefit from high-risk care plans, based on research from the University of Maryland health care system.
The plans are designed to improve patient safety by reducing exposure to ionizing radiation and have the additional benefit of reducing the costs of care, Dr. Leen Alblaihed, a resident physician at the university, reported at the annual meeting of the American College of Emergency Physicians.
After high-risk care plans were put into the emergency physician work flow for 41 patients with a history of high emergency department utilization, unneeded tests declined. Other important outcomes were statistically significant reductions in hospitalizations and quantities of prescribed opioids.
he patients considered for the study had to have at least five ED visits and three admissions per year. Based on the electronic medical record data of the university’s two suburban medical centers, a total of 845 patients met that definition.
The high-risk care plans for the management of the 41 patients were developed by a multi-disciplinary team of case managers, emergency physicians, and hospitalists. The plans were then integrated into the physician electronic documentation and work flow.
The data analysis was based on 23 of the patients, 10 men and 13 women with a median age of 48 years, who had 6 months of data before and 6 months of data after the care plan was instituted. The primary outcome measures were a reduction in ionizing radiation. Secondary outcome measures were reductions in ED visits, hospital admissions, observation stays, and opioid prescriptions based on morphine equivalent totals.
Compared to the data before the care plan was instituted, the 23 patients had nearly half as many x-rays and CT scans and a nearly sixfold reduction in prescribing of morphine equivalents. While ED visits decreased modestly from 116 to 82, the admission rates dropped from 99 to 37 and observation stays declined from 43 to 28.
The study group had decreases in all measures after high-risk care plans. X-ray studies decreased from 202 to 106, CT scans declined from 107 to 50, and opiate prescribing decreased from 3824 mg to 675 mg in morphine equivalents.
Because the outcomes were not normally distributed, medians and interquartile ranges were analyzed using the Wilcoxon signed-rank test to compare the pre/post median values (see table).
AT ACEP14