User login
AVAHO Encourages Members to Make Voices Heard
Advocacy for veterans with cancer has always been a central part of the Association for VA Hematology/Oncology (AVAHO) mission, but that advocacy has now taken on a new focus: the fate of US Department of Veterans Affairs (VA) employees. The advocacy portal provides templated letters, a search function to find local Senators and Members of Congress, a search function to find regional media outlets, updates on voting and elections, and information on key legislation relevant to VA health care.
To ensure its members’ concerns are heard, AVAHO is encouraging members, in their own time and as private citizens, to contact their local representatives to inform them about the real impact of recent policy changes on VA employees and the veterans they care for. Members can select any of 4 letters focused on reductions in force, cancellation of VA contracts, the return to office mandate, and the National Institutes of Health’s proposed cap on indirect cost for research grants: “AVAHO recognizes the power of the individual voice. Our members have an important role in shaping the health care services provided to veterans across our nation.”
"The contracts that have been canceled and continue to be canceled included critical services related to cancer care," AVAHO notes on its Advocacy page. "We know these impacted contracts have hindered the VA’s ability to implement research protocols, process and report pharmacogenomic results, manage Electronic Health Record Modernization workgroups responsible for safety improvements, and execute new oncology services through the Close to Me initiative, just to name a few."
Advocacy for veterans with cancer has always been a central part of the Association for VA Hematology/Oncology (AVAHO) mission, but that advocacy has now taken on a new focus: the fate of US Department of Veterans Affairs (VA) employees. The advocacy portal provides templated letters, a search function to find local Senators and Members of Congress, a search function to find regional media outlets, updates on voting and elections, and information on key legislation relevant to VA health care.
To ensure its members’ concerns are heard, AVAHO is encouraging members, in their own time and as private citizens, to contact their local representatives to inform them about the real impact of recent policy changes on VA employees and the veterans they care for. Members can select any of 4 letters focused on reductions in force, cancellation of VA contracts, the return to office mandate, and the National Institutes of Health’s proposed cap on indirect cost for research grants: “AVAHO recognizes the power of the individual voice. Our members have an important role in shaping the health care services provided to veterans across our nation.”
"The contracts that have been canceled and continue to be canceled included critical services related to cancer care," AVAHO notes on its Advocacy page. "We know these impacted contracts have hindered the VA’s ability to implement research protocols, process and report pharmacogenomic results, manage Electronic Health Record Modernization workgroups responsible for safety improvements, and execute new oncology services through the Close to Me initiative, just to name a few."
Advocacy for veterans with cancer has always been a central part of the Association for VA Hematology/Oncology (AVAHO) mission, but that advocacy has now taken on a new focus: the fate of US Department of Veterans Affairs (VA) employees. The advocacy portal provides templated letters, a search function to find local Senators and Members of Congress, a search function to find regional media outlets, updates on voting and elections, and information on key legislation relevant to VA health care.
To ensure its members’ concerns are heard, AVAHO is encouraging members, in their own time and as private citizens, to contact their local representatives to inform them about the real impact of recent policy changes on VA employees and the veterans they care for. Members can select any of 4 letters focused on reductions in force, cancellation of VA contracts, the return to office mandate, and the National Institutes of Health’s proposed cap on indirect cost for research grants: “AVAHO recognizes the power of the individual voice. Our members have an important role in shaping the health care services provided to veterans across our nation.”
"The contracts that have been canceled and continue to be canceled included critical services related to cancer care," AVAHO notes on its Advocacy page. "We know these impacted contracts have hindered the VA’s ability to implement research protocols, process and report pharmacogenomic results, manage Electronic Health Record Modernization workgroups responsible for safety improvements, and execute new oncology services through the Close to Me initiative, just to name a few."
Veterans and Nonveterans Show Similar Mammogram Rates
TOPLINE: A national survey of 8996 females reveals comparable mammography screening rates between those who identify as veterans (57.9%) and nonveterans (55.2%).
METHODOLOGY:
Researchers analyzed data from the 2019 National Health Interview Survey, a cross-sectional national survey tracking health information.
Female respondents aged 40 to 74 years without history of breast cancer were included in the analysis.
Analysis evaluated the association between screening and veteran status through logistic regression, adjusting for potential confounders.
Survey procedures accounted for complex sampling design to obtain valid estimates for the civilian, noninstitutionalized US population.
TAKEAWAY:
Analysis included 8996 female survey respondents, including 169 veterans (1.9%) and 320 (3.2%) reported having military health coverage.
Mammography screening rates within the last year were comparable between veterans (57.9%) and nonveterans (55.2%).
Veteran status showed no significant association with differences in mammography screening percentages (P = .96).
Among insured participants, military health insurance demonstrated no significant association with mammography screening percentages (P = .13).
The authors suggest that radiology practices should design proactive outreach strategies to address the needs of the growing number of female veterans who may face increased breast cancer risk due to military environmental exposures.
IN PRACTICE: “Although the results from our study demonstrate comparable mammography screening percentages, veterans may face additional risk factors for breast cancer due to occupational,” the authors argue.
SOURCE: This summary is based on a preprint published online in the Journal of the American College of Radiology: Milton A, Miles R, Gettle LM, Van Geertruyden P, Narayan AK. Utilization of Mammography Screening in Female Veterans: Cross-Sectional Survey Results from the National Health Interview Survey. J Am Coll Radiol. Published online April 24, 2025. doi:10.1016/j.jacr.2025.04.017
LIMITATIONS: The study relied on self-reported adherence data, which could overestimate screening percentages. Data collection occurred prior to updated United States Preventive Services Task Force guidelines recommending routine mammography screening for women starting at age 40 years every 2 years. The relatively small number of female veteran respondents limited the precision of population estimates. Additionally, the data were collected before the COVID-19 pandemic, which has been associated with reduced mammographic screening, particularly in medically underserved populations.
DISCLOSURES: Anand Narayan disclosed receiving financial support from Susan G. Komen Breast Cancer Foundation and National Academy of Medicine. The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The remaining authors reported no potential conflicts of interest. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE: A national survey of 8996 females reveals comparable mammography screening rates between those who identify as veterans (57.9%) and nonveterans (55.2%).
METHODOLOGY:
Researchers analyzed data from the 2019 National Health Interview Survey, a cross-sectional national survey tracking health information.
Female respondents aged 40 to 74 years without history of breast cancer were included in the analysis.
Analysis evaluated the association between screening and veteran status through logistic regression, adjusting for potential confounders.
Survey procedures accounted for complex sampling design to obtain valid estimates for the civilian, noninstitutionalized US population.
TAKEAWAY:
Analysis included 8996 female survey respondents, including 169 veterans (1.9%) and 320 (3.2%) reported having military health coverage.
Mammography screening rates within the last year were comparable between veterans (57.9%) and nonveterans (55.2%).
Veteran status showed no significant association with differences in mammography screening percentages (P = .96).
Among insured participants, military health insurance demonstrated no significant association with mammography screening percentages (P = .13).
The authors suggest that radiology practices should design proactive outreach strategies to address the needs of the growing number of female veterans who may face increased breast cancer risk due to military environmental exposures.
IN PRACTICE: “Although the results from our study demonstrate comparable mammography screening percentages, veterans may face additional risk factors for breast cancer due to occupational,” the authors argue.
SOURCE: This summary is based on a preprint published online in the Journal of the American College of Radiology: Milton A, Miles R, Gettle LM, Van Geertruyden P, Narayan AK. Utilization of Mammography Screening in Female Veterans: Cross-Sectional Survey Results from the National Health Interview Survey. J Am Coll Radiol. Published online April 24, 2025. doi:10.1016/j.jacr.2025.04.017
LIMITATIONS: The study relied on self-reported adherence data, which could overestimate screening percentages. Data collection occurred prior to updated United States Preventive Services Task Force guidelines recommending routine mammography screening for women starting at age 40 years every 2 years. The relatively small number of female veteran respondents limited the precision of population estimates. Additionally, the data were collected before the COVID-19 pandemic, which has been associated with reduced mammographic screening, particularly in medically underserved populations.
DISCLOSURES: Anand Narayan disclosed receiving financial support from Susan G. Komen Breast Cancer Foundation and National Academy of Medicine. The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The remaining authors reported no potential conflicts of interest. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
TOPLINE: A national survey of 8996 females reveals comparable mammography screening rates between those who identify as veterans (57.9%) and nonveterans (55.2%).
METHODOLOGY:
Researchers analyzed data from the 2019 National Health Interview Survey, a cross-sectional national survey tracking health information.
Female respondents aged 40 to 74 years without history of breast cancer were included in the analysis.
Analysis evaluated the association between screening and veteran status through logistic regression, adjusting for potential confounders.
Survey procedures accounted for complex sampling design to obtain valid estimates for the civilian, noninstitutionalized US population.
TAKEAWAY:
Analysis included 8996 female survey respondents, including 169 veterans (1.9%) and 320 (3.2%) reported having military health coverage.
Mammography screening rates within the last year were comparable between veterans (57.9%) and nonveterans (55.2%).
Veteran status showed no significant association with differences in mammography screening percentages (P = .96).
Among insured participants, military health insurance demonstrated no significant association with mammography screening percentages (P = .13).
The authors suggest that radiology practices should design proactive outreach strategies to address the needs of the growing number of female veterans who may face increased breast cancer risk due to military environmental exposures.
IN PRACTICE: “Although the results from our study demonstrate comparable mammography screening percentages, veterans may face additional risk factors for breast cancer due to occupational,” the authors argue.
SOURCE: This summary is based on a preprint published online in the Journal of the American College of Radiology: Milton A, Miles R, Gettle LM, Van Geertruyden P, Narayan AK. Utilization of Mammography Screening in Female Veterans: Cross-Sectional Survey Results from the National Health Interview Survey. J Am Coll Radiol. Published online April 24, 2025. doi:10.1016/j.jacr.2025.04.017
LIMITATIONS: The study relied on self-reported adherence data, which could overestimate screening percentages. Data collection occurred prior to updated United States Preventive Services Task Force guidelines recommending routine mammography screening for women starting at age 40 years every 2 years. The relatively small number of female veteran respondents limited the precision of population estimates. Additionally, the data were collected before the COVID-19 pandemic, which has been associated with reduced mammographic screening, particularly in medically underserved populations.
DISCLOSURES: Anand Narayan disclosed receiving financial support from Susan G. Komen Breast Cancer Foundation and National Academy of Medicine. The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The remaining authors reported no potential conflicts of interest. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
PSA Screening in VA Patients After Age 70 Years
TOPLINE: Most men receiving care through the Veterans Health Administration (VHA) continue prostate-specific antigen (PSA) screening after aged 70 years despite low absolute risk for prostate cancer-specific mortality (PCSM), even among Black men in the healthiest quintile.
METHODOLOGY:
Researchers conducted a cohort study of 921,609 men aged 70 years receiving VHA care between 2008 and 2020, who had normal screening PSA values (< 4 ng/mL) between ages 65-69 years.
- Analysis included electronic health record data from VHA Corporate Data Warehouse, linked Medicare claims data, and VHA community care data.
- Investigators examined the value of PSA levels, race and ethnicity, and competing mortality in risk stratification for PCSM and mPCa using regression modeling.
TAKEAWAY:
The 10-year cumulative incidence of PCSM was 0.26% overall, with 95% of men having a 10-year risk < 0.73%, and higher baseline PSA levels associated with increased risk (0.79% for 3.00-3.99 ng/mL vs 0.10% for 0.20-0.99 ng/mL).
- Race and ethnicity showed modest association with PCSM risk: Black patients had a 0.79% risk of mPCa vs 0.38% for White patients. The risk of PCSM was 0.36% for Black patients vs 0.25% for White patients.
- Most patients (87%) continued PSA screening after age 70 years, with little variation by competing mortality risk or race and ethnicity.
- Low PSA (0.20-0.99 ng/mL) identified very low-risk populations with < 1% 10-year risk for prostate biopsy, clinically significant prostate cancer diagnosis, and treatment.
IN PRACTICE: "Our data suggest that a simple assessment of personal risk based on PSA values before age 70 years captures a large proportion of relevant prognostic information with respect to mPCa and PCSM risk ... Low PSA (0.20-0.99 ng/mL) was associated with very low PCSM and mPCa risk, even among the healthiest Black men," wrote the authors of the study.
SOURCE: The study was led by Alex K. Bryant,MD, MAS and the Veterans Affairs Center for Clinical Management Research in Ann Arbor. It was published online on February 14 in JAMA Network Open.
LIMITATIONS: According to the authors, any potential PCSM or mPCa reduction from continued PSA screening > age 70 years remains unproven due to lack of randomized trial data. The study relied on death certificates to define PCSM, which may have introduced misclassification error. Family history of prostate cancer was not included due to unreliable electronic medical record data availability. Additionally, veterans have higher comorbidity burdens than the general population and unique military-related environmental exposures, potentially limiting result generalizability.
DISCLOSURES: The study was supported by grants U01CA253915, PSOCA097186, R35CA274442, and R50CA221836 from the National Cancer Institute. Matthew J. Schipper, MD, reported receiving consulting fees from Innovative Analytics. Phoebe A. Tsao, MD, disclosed receiving grants from the Prostate Cancer Foundation outside the submitted work. Kristian D. Stensland, MD, reported receiving a grant from the National Institutes of Health during the conduct of the study.
TOPLINE: Most men receiving care through the Veterans Health Administration (VHA) continue prostate-specific antigen (PSA) screening after aged 70 years despite low absolute risk for prostate cancer-specific mortality (PCSM), even among Black men in the healthiest quintile.
METHODOLOGY:
Researchers conducted a cohort study of 921,609 men aged 70 years receiving VHA care between 2008 and 2020, who had normal screening PSA values (< 4 ng/mL) between ages 65-69 years.
- Analysis included electronic health record data from VHA Corporate Data Warehouse, linked Medicare claims data, and VHA community care data.
- Investigators examined the value of PSA levels, race and ethnicity, and competing mortality in risk stratification for PCSM and mPCa using regression modeling.
TAKEAWAY:
The 10-year cumulative incidence of PCSM was 0.26% overall, with 95% of men having a 10-year risk < 0.73%, and higher baseline PSA levels associated with increased risk (0.79% for 3.00-3.99 ng/mL vs 0.10% for 0.20-0.99 ng/mL).
- Race and ethnicity showed modest association with PCSM risk: Black patients had a 0.79% risk of mPCa vs 0.38% for White patients. The risk of PCSM was 0.36% for Black patients vs 0.25% for White patients.
- Most patients (87%) continued PSA screening after age 70 years, with little variation by competing mortality risk or race and ethnicity.
- Low PSA (0.20-0.99 ng/mL) identified very low-risk populations with < 1% 10-year risk for prostate biopsy, clinically significant prostate cancer diagnosis, and treatment.
IN PRACTICE: "Our data suggest that a simple assessment of personal risk based on PSA values before age 70 years captures a large proportion of relevant prognostic information with respect to mPCa and PCSM risk ... Low PSA (0.20-0.99 ng/mL) was associated with very low PCSM and mPCa risk, even among the healthiest Black men," wrote the authors of the study.
SOURCE: The study was led by Alex K. Bryant,MD, MAS and the Veterans Affairs Center for Clinical Management Research in Ann Arbor. It was published online on February 14 in JAMA Network Open.
LIMITATIONS: According to the authors, any potential PCSM or mPCa reduction from continued PSA screening > age 70 years remains unproven due to lack of randomized trial data. The study relied on death certificates to define PCSM, which may have introduced misclassification error. Family history of prostate cancer was not included due to unreliable electronic medical record data availability. Additionally, veterans have higher comorbidity burdens than the general population and unique military-related environmental exposures, potentially limiting result generalizability.
DISCLOSURES: The study was supported by grants U01CA253915, PSOCA097186, R35CA274442, and R50CA221836 from the National Cancer Institute. Matthew J. Schipper, MD, reported receiving consulting fees from Innovative Analytics. Phoebe A. Tsao, MD, disclosed receiving grants from the Prostate Cancer Foundation outside the submitted work. Kristian D. Stensland, MD, reported receiving a grant from the National Institutes of Health during the conduct of the study.
TOPLINE: Most men receiving care through the Veterans Health Administration (VHA) continue prostate-specific antigen (PSA) screening after aged 70 years despite low absolute risk for prostate cancer-specific mortality (PCSM), even among Black men in the healthiest quintile.
METHODOLOGY:
Researchers conducted a cohort study of 921,609 men aged 70 years receiving VHA care between 2008 and 2020, who had normal screening PSA values (< 4 ng/mL) between ages 65-69 years.
- Analysis included electronic health record data from VHA Corporate Data Warehouse, linked Medicare claims data, and VHA community care data.
- Investigators examined the value of PSA levels, race and ethnicity, and competing mortality in risk stratification for PCSM and mPCa using regression modeling.
TAKEAWAY:
The 10-year cumulative incidence of PCSM was 0.26% overall, with 95% of men having a 10-year risk < 0.73%, and higher baseline PSA levels associated with increased risk (0.79% for 3.00-3.99 ng/mL vs 0.10% for 0.20-0.99 ng/mL).
- Race and ethnicity showed modest association with PCSM risk: Black patients had a 0.79% risk of mPCa vs 0.38% for White patients. The risk of PCSM was 0.36% for Black patients vs 0.25% for White patients.
- Most patients (87%) continued PSA screening after age 70 years, with little variation by competing mortality risk or race and ethnicity.
- Low PSA (0.20-0.99 ng/mL) identified very low-risk populations with < 1% 10-year risk for prostate biopsy, clinically significant prostate cancer diagnosis, and treatment.
IN PRACTICE: "Our data suggest that a simple assessment of personal risk based on PSA values before age 70 years captures a large proportion of relevant prognostic information with respect to mPCa and PCSM risk ... Low PSA (0.20-0.99 ng/mL) was associated with very low PCSM and mPCa risk, even among the healthiest Black men," wrote the authors of the study.
SOURCE: The study was led by Alex K. Bryant,MD, MAS and the Veterans Affairs Center for Clinical Management Research in Ann Arbor. It was published online on February 14 in JAMA Network Open.
LIMITATIONS: According to the authors, any potential PCSM or mPCa reduction from continued PSA screening > age 70 years remains unproven due to lack of randomized trial data. The study relied on death certificates to define PCSM, which may have introduced misclassification error. Family history of prostate cancer was not included due to unreliable electronic medical record data availability. Additionally, veterans have higher comorbidity burdens than the general population and unique military-related environmental exposures, potentially limiting result generalizability.
DISCLOSURES: The study was supported by grants U01CA253915, PSOCA097186, R35CA274442, and R50CA221836 from the National Cancer Institute. Matthew J. Schipper, MD, reported receiving consulting fees from Innovative Analytics. Phoebe A. Tsao, MD, disclosed receiving grants from the Prostate Cancer Foundation outside the submitted work. Kristian D. Stensland, MD, reported receiving a grant from the National Institutes of Health during the conduct of the study.
No Racial Disparities in CVD Outcomes For VA Patients with Prostate Cancer Receiving ADT
TOPLINE: Veterans treated in the Veterans Health Administration (VHA) who had preexisting cardiometabolic disease and received androgen deprivation therapy (ADT) with radiation therapy developed major adverse cardiovascular events (MACE) at 4 times the rate compared to those without cardiometabolic disease. Black and White veterans showed similar cardiovascular outcomes regardless of treatment type.
METHODOLOGY:
Researchers conducted a retrospective cohort study examining 39,580 veterans in the VHA system diagnosed with prostate cancer between 2000 and 2015, following them for a median of 9.6 years to assess time to MACE diagnosis.
- Analysis utilized a 1:1 propensity score matching process to compare outcomes between treatment types (ADT with radiation therapy vs radiation therapy alone) and racial groups (Black vs White men).
- Participants had a mean age of 65.9 years at diagnosis; 68% identified as White and 32% as Black, and 83% had stage 2 disease classified with 43.1% intermediate risk. Most lived in nonrural zip codes
- Primary outcome measure was time to MACE, defined as a composite of cardiovascular death, myocardial infarction, or ischemic stroke, with patients censored at non-cardiovascular death or study end.
TAKEAWAY:
Compared to those without CMD, the hazard ratio (HR) for MACE for men with preexisting CMD who received ADT was 4.2. Those receiving radiation alone had an HR of 2.5.
- Patients diagnosed between 2010 and 2015 showed significantly lower MACE rates compared to those diagnosed in 2000 to 2005: HR, 0.23; 95% CI, 0.08-0.71 for White patients; and HR, 0.23; 95% CI, 0.07-0.77 for Black patients.
- Multiple comorbidities were associated with doubled MACE risk (HR, 2.22; 95% CI, 1.08-4.59) compared to those without comorbidities.
- No significant differences in MACE rates were observed between Black and White veterans, regardless of treatment type.
IN PRACTICE: “Within the VHA, men treated with ADT + radiation therapy for prostate cancer do not appear to be at greater risk for MACE than those receiving radiation therapy alone. Black men have similar risk of MACE as White men, whether receiving radiation therapy alone or in combination with ADT," the authors wrote.
SOURCE: The study was led by Alexander R. Lucas, Virginia Commonwealth University School of Public Health in Richmond. It was published online on February 6 in Cardio-Oncology.
LIMITATIONS: According to the authors, the retrospective nature of the data may have limited their ability to detect MACE events occurring outside the VHA. Additionally, the study was limited to men who initiated ADT prior to radiation therapy, excluding those who had surgery or radiation before ADT. The researchers also note that the analysis did not compare outcomes between different types of ADT treatments, such as GnRH agonists vs antagonists, which may have different cardiovascular risk profiles.
DISCLOSURES: Alexander R. Lucas’s work was partly funded by grants 1KO1HL161419 and NRG FP00019789. Ashit K. Paul disclosed receiving honorarium for serving on scientific consultancy panels of SANOFI-Genzyme, Bayer, and Tempus & Cardinal Health. Additional disclosures are noted but not specified in the article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication
TOPLINE: Veterans treated in the Veterans Health Administration (VHA) who had preexisting cardiometabolic disease and received androgen deprivation therapy (ADT) with radiation therapy developed major adverse cardiovascular events (MACE) at 4 times the rate compared to those without cardiometabolic disease. Black and White veterans showed similar cardiovascular outcomes regardless of treatment type.
METHODOLOGY:
Researchers conducted a retrospective cohort study examining 39,580 veterans in the VHA system diagnosed with prostate cancer between 2000 and 2015, following them for a median of 9.6 years to assess time to MACE diagnosis.
- Analysis utilized a 1:1 propensity score matching process to compare outcomes between treatment types (ADT with radiation therapy vs radiation therapy alone) and racial groups (Black vs White men).
- Participants had a mean age of 65.9 years at diagnosis; 68% identified as White and 32% as Black, and 83% had stage 2 disease classified with 43.1% intermediate risk. Most lived in nonrural zip codes
- Primary outcome measure was time to MACE, defined as a composite of cardiovascular death, myocardial infarction, or ischemic stroke, with patients censored at non-cardiovascular death or study end.
TAKEAWAY:
Compared to those without CMD, the hazard ratio (HR) for MACE for men with preexisting CMD who received ADT was 4.2. Those receiving radiation alone had an HR of 2.5.
- Patients diagnosed between 2010 and 2015 showed significantly lower MACE rates compared to those diagnosed in 2000 to 2005: HR, 0.23; 95% CI, 0.08-0.71 for White patients; and HR, 0.23; 95% CI, 0.07-0.77 for Black patients.
- Multiple comorbidities were associated with doubled MACE risk (HR, 2.22; 95% CI, 1.08-4.59) compared to those without comorbidities.
- No significant differences in MACE rates were observed between Black and White veterans, regardless of treatment type.
IN PRACTICE: “Within the VHA, men treated with ADT + radiation therapy for prostate cancer do not appear to be at greater risk for MACE than those receiving radiation therapy alone. Black men have similar risk of MACE as White men, whether receiving radiation therapy alone or in combination with ADT," the authors wrote.
SOURCE: The study was led by Alexander R. Lucas, Virginia Commonwealth University School of Public Health in Richmond. It was published online on February 6 in Cardio-Oncology.
LIMITATIONS: According to the authors, the retrospective nature of the data may have limited their ability to detect MACE events occurring outside the VHA. Additionally, the study was limited to men who initiated ADT prior to radiation therapy, excluding those who had surgery or radiation before ADT. The researchers also note that the analysis did not compare outcomes between different types of ADT treatments, such as GnRH agonists vs antagonists, which may have different cardiovascular risk profiles.
DISCLOSURES: Alexander R. Lucas’s work was partly funded by grants 1KO1HL161419 and NRG FP00019789. Ashit K. Paul disclosed receiving honorarium for serving on scientific consultancy panels of SANOFI-Genzyme, Bayer, and Tempus & Cardinal Health. Additional disclosures are noted but not specified in the article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication
TOPLINE: Veterans treated in the Veterans Health Administration (VHA) who had preexisting cardiometabolic disease and received androgen deprivation therapy (ADT) with radiation therapy developed major adverse cardiovascular events (MACE) at 4 times the rate compared to those without cardiometabolic disease. Black and White veterans showed similar cardiovascular outcomes regardless of treatment type.
METHODOLOGY:
Researchers conducted a retrospective cohort study examining 39,580 veterans in the VHA system diagnosed with prostate cancer between 2000 and 2015, following them for a median of 9.6 years to assess time to MACE diagnosis.
- Analysis utilized a 1:1 propensity score matching process to compare outcomes between treatment types (ADT with radiation therapy vs radiation therapy alone) and racial groups (Black vs White men).
- Participants had a mean age of 65.9 years at diagnosis; 68% identified as White and 32% as Black, and 83% had stage 2 disease classified with 43.1% intermediate risk. Most lived in nonrural zip codes
- Primary outcome measure was time to MACE, defined as a composite of cardiovascular death, myocardial infarction, or ischemic stroke, with patients censored at non-cardiovascular death or study end.
TAKEAWAY:
Compared to those without CMD, the hazard ratio (HR) for MACE for men with preexisting CMD who received ADT was 4.2. Those receiving radiation alone had an HR of 2.5.
- Patients diagnosed between 2010 and 2015 showed significantly lower MACE rates compared to those diagnosed in 2000 to 2005: HR, 0.23; 95% CI, 0.08-0.71 for White patients; and HR, 0.23; 95% CI, 0.07-0.77 for Black patients.
- Multiple comorbidities were associated with doubled MACE risk (HR, 2.22; 95% CI, 1.08-4.59) compared to those without comorbidities.
- No significant differences in MACE rates were observed between Black and White veterans, regardless of treatment type.
IN PRACTICE: “Within the VHA, men treated with ADT + radiation therapy for prostate cancer do not appear to be at greater risk for MACE than those receiving radiation therapy alone. Black men have similar risk of MACE as White men, whether receiving radiation therapy alone or in combination with ADT," the authors wrote.
SOURCE: The study was led by Alexander R. Lucas, Virginia Commonwealth University School of Public Health in Richmond. It was published online on February 6 in Cardio-Oncology.
LIMITATIONS: According to the authors, the retrospective nature of the data may have limited their ability to detect MACE events occurring outside the VHA. Additionally, the study was limited to men who initiated ADT prior to radiation therapy, excluding those who had surgery or radiation before ADT. The researchers also note that the analysis did not compare outcomes between different types of ADT treatments, such as GnRH agonists vs antagonists, which may have different cardiovascular risk profiles.
DISCLOSURES: Alexander R. Lucas’s work was partly funded by grants 1KO1HL161419 and NRG FP00019789. Ashit K. Paul disclosed receiving honorarium for serving on scientific consultancy panels of SANOFI-Genzyme, Bayer, and Tempus & Cardinal Health. Additional disclosures are noted but not specified in the article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication
AVAHO Implores VA Secretary Collins to Use Caution Amid Rapid Changes
The Association of VA Hematology/Oncology outlined its concerns over “unintended consequences” to recent changes at the US Department of Veterans Affairs (VA) in a March 3, 2025, letter to Secretary Doug A. Collins. “Indiscriminate cuts to contracts and personnel could have unforeseen consequences in many research areas within the VA, so we implore scrutiny,” the letter warns.
“We have already seen specific examples this past week of swift contract cuts impairing the VA’s ability to implement research protocols, process and report pharmacogenomic results, management of Electronic Health Record Modernization (EHRM) council workgroups, and execute new oncology services through the Close to Me initiative,” AVAHO Executive Director Julie Lawson said.
As Lawson noted, the return-to-office order for the staff of the Clinical Resource Hubs (CRHs) and the National Tele-Oncology programs could significantly impair their ability to function. Both departments have been fully remote since their start and are key elements of VA care for rural veterans. In fiscal year 2024, > 500,000 veterans received > 1.4 million CRH encounters. Nearly 20,000 veterans have utilized the National Tele-Oncology program in > 80,000 cancer-care encounters.
“We have significant concern that a blanket return to office of these fully remote programs, without an adequate plan for office space, teleworking equipment, and clinical and administrative support could have significant disruption and impairment in their delivery of care, negatively impacting veteran outcomes,” Lawson said.
AVAHO also strongly urged Collins to continue VA investment in clinical trials specifically and research in general: "To implement and execute research, there must be an adequte system in place to support these research programs."
The Association of VA Hematology/Oncology outlined its concerns over “unintended consequences” to recent changes at the US Department of Veterans Affairs (VA) in a March 3, 2025, letter to Secretary Doug A. Collins. “Indiscriminate cuts to contracts and personnel could have unforeseen consequences in many research areas within the VA, so we implore scrutiny,” the letter warns.
“We have already seen specific examples this past week of swift contract cuts impairing the VA’s ability to implement research protocols, process and report pharmacogenomic results, management of Electronic Health Record Modernization (EHRM) council workgroups, and execute new oncology services through the Close to Me initiative,” AVAHO Executive Director Julie Lawson said.
As Lawson noted, the return-to-office order for the staff of the Clinical Resource Hubs (CRHs) and the National Tele-Oncology programs could significantly impair their ability to function. Both departments have been fully remote since their start and are key elements of VA care for rural veterans. In fiscal year 2024, > 500,000 veterans received > 1.4 million CRH encounters. Nearly 20,000 veterans have utilized the National Tele-Oncology program in > 80,000 cancer-care encounters.
“We have significant concern that a blanket return to office of these fully remote programs, without an adequate plan for office space, teleworking equipment, and clinical and administrative support could have significant disruption and impairment in their delivery of care, negatively impacting veteran outcomes,” Lawson said.
AVAHO also strongly urged Collins to continue VA investment in clinical trials specifically and research in general: "To implement and execute research, there must be an adequte system in place to support these research programs."
The Association of VA Hematology/Oncology outlined its concerns over “unintended consequences” to recent changes at the US Department of Veterans Affairs (VA) in a March 3, 2025, letter to Secretary Doug A. Collins. “Indiscriminate cuts to contracts and personnel could have unforeseen consequences in many research areas within the VA, so we implore scrutiny,” the letter warns.
“We have already seen specific examples this past week of swift contract cuts impairing the VA’s ability to implement research protocols, process and report pharmacogenomic results, management of Electronic Health Record Modernization (EHRM) council workgroups, and execute new oncology services through the Close to Me initiative,” AVAHO Executive Director Julie Lawson said.
As Lawson noted, the return-to-office order for the staff of the Clinical Resource Hubs (CRHs) and the National Tele-Oncology programs could significantly impair their ability to function. Both departments have been fully remote since their start and are key elements of VA care for rural veterans. In fiscal year 2024, > 500,000 veterans received > 1.4 million CRH encounters. Nearly 20,000 veterans have utilized the National Tele-Oncology program in > 80,000 cancer-care encounters.
“We have significant concern that a blanket return to office of these fully remote programs, without an adequate plan for office space, teleworking equipment, and clinical and administrative support could have significant disruption and impairment in their delivery of care, negatively impacting veteran outcomes,” Lawson said.
AVAHO also strongly urged Collins to continue VA investment in clinical trials specifically and research in general: "To implement and execute research, there must be an adequte system in place to support these research programs."
Collins Confirmed as VA Secretary
Collins Confirmed as VA Secretary
The U.S. Senate confirmed former Georgia congressman Doug Collins as the Secretary for the US Department of Veterans Affairs (VA) on Feb. 4 in a comfortable 77 to 23 vote. Collins received votes from every Republican Senator and 23 Democratic Senators.
“The MISSION Act, the VA Accountability and Whistleblower Protection Act and the PACT Act are 3 of the most important veterans laws in recent history,” Collins said during his confirmation hearing. “They received widespread bipartisan support because their focus is exactly where VA’s focus should be: on veteran convenience and accountability for the department.”
Collins pledged to keep the VA strong but also to expand community care, noting: “I believe you can have both, you can have a strong VA as it currently exists, and you can have the community care aspect.”
Sen. Richard Blumenthal (D-CT), who voted to confirm Collins, urged the secretary to exempt all VA employees from the Trump Administration’s recent hiring freeze; ensure that financial assistance programs for veterans are exempt from funding pauses; work with President Trump to reappoint VA Inspector General Mike Missal, who was removed from office by the President in January; and to ensure all VA employees receive due process amid recent directives from the Office of Personnel Management.
The VA also announced a number of new political appointees, including Chris Syrek, who set to serve as chief of staff; Cheryl Mason is slated to serve as senior advisory to Secretary Collins; and Lynda Davis is set to serve as the chief officer with VA's Veterans Experience Office. No nominations have been made for the Undersecretary of Health to date.
The U.S. Senate confirmed former Georgia congressman Doug Collins as the Secretary for the US Department of Veterans Affairs (VA) on Feb. 4 in a comfortable 77 to 23 vote. Collins received votes from every Republican Senator and 23 Democratic Senators.
“The MISSION Act, the VA Accountability and Whistleblower Protection Act and the PACT Act are 3 of the most important veterans laws in recent history,” Collins said during his confirmation hearing. “They received widespread bipartisan support because their focus is exactly where VA’s focus should be: on veteran convenience and accountability for the department.”
Collins pledged to keep the VA strong but also to expand community care, noting: “I believe you can have both, you can have a strong VA as it currently exists, and you can have the community care aspect.”
Sen. Richard Blumenthal (D-CT), who voted to confirm Collins, urged the secretary to exempt all VA employees from the Trump Administration’s recent hiring freeze; ensure that financial assistance programs for veterans are exempt from funding pauses; work with President Trump to reappoint VA Inspector General Mike Missal, who was removed from office by the President in January; and to ensure all VA employees receive due process amid recent directives from the Office of Personnel Management.
The VA also announced a number of new political appointees, including Chris Syrek, who set to serve as chief of staff; Cheryl Mason is slated to serve as senior advisory to Secretary Collins; and Lynda Davis is set to serve as the chief officer with VA's Veterans Experience Office. No nominations have been made for the Undersecretary of Health to date.
The U.S. Senate confirmed former Georgia congressman Doug Collins as the Secretary for the US Department of Veterans Affairs (VA) on Feb. 4 in a comfortable 77 to 23 vote. Collins received votes from every Republican Senator and 23 Democratic Senators.
“The MISSION Act, the VA Accountability and Whistleblower Protection Act and the PACT Act are 3 of the most important veterans laws in recent history,” Collins said during his confirmation hearing. “They received widespread bipartisan support because their focus is exactly where VA’s focus should be: on veteran convenience and accountability for the department.”
Collins pledged to keep the VA strong but also to expand community care, noting: “I believe you can have both, you can have a strong VA as it currently exists, and you can have the community care aspect.”
Sen. Richard Blumenthal (D-CT), who voted to confirm Collins, urged the secretary to exempt all VA employees from the Trump Administration’s recent hiring freeze; ensure that financial assistance programs for veterans are exempt from funding pauses; work with President Trump to reappoint VA Inspector General Mike Missal, who was removed from office by the President in January; and to ensure all VA employees receive due process amid recent directives from the Office of Personnel Management.
The VA also announced a number of new political appointees, including Chris Syrek, who set to serve as chief of staff; Cheryl Mason is slated to serve as senior advisory to Secretary Collins; and Lynda Davis is set to serve as the chief officer with VA's Veterans Experience Office. No nominations have been made for the Undersecretary of Health to date.
Collins Confirmed as VA Secretary
Collins Confirmed as VA Secretary
Leaders Outline DHA “Market” Transition
One theme emerged from multiple military healthy system (MHS) leaders at the recent AMSUS annual conference: Significant change is coming to the MHS, and military health care providers can either embrace and shape that change or somebody else will. “If we don’t shape our future, others will step in and do it for us,” Tom McCaffrey, Assistant Secretary of Defense for Health Affairs; Defense Health Agency (DHA), and the Uniformed Service University for the Health Sciences (USU) told the audience.
The “historic” changes are underway, as the DHA has already begun to take over control of many military treatment facilities (MTFs) that were formerly operated by the separate services. In the next step of the transition, nearly 250 individual MTFs will be combined—along with TRICARE providers—in 21 geographically based “markets” in order to streamline management and avoid redundancies.
The exact details of the changes in store have not been released. McCaffrey noted that US Department of Defense (DoD) leadership will submit the “framework” for their assessment of the MHS to Congress “very soon, and at that point we will begin the hard work of detailed implementation of the results of that assessment and recommendations from the department.” Changes are expected to continue through fiscal year 2021, and some sources have estimated that as many as 18,000 jobs could be eliminated in the process.
Although Congress drove these changes in the National Defense Authorization Act of 2017, MHS leaders insist they are determining how to make the transformation without hurting medical readiness. “We the senior leadership of the MHS must continue to work together to shape our system to meet the challenges of the new environment,” McCaffrey insisted.
It seems as though all elements of the MHS are on the table. One report has suggested that the USU budget could be cut by a third. “Given the USU’s track record of excellence, we were alarmed to learn that the department is considering cuts as high as 30% to the university’s budget for research, development, testing, and evaluation, and 34% to university operations and maintenance... includ[ing] the cancellation of a $445 million military construction project and closure of the USU medical school,” US senators Chris Van Hollen (D-MD), Ben Cardin (D-MD.), Jack Reed (D-RI), and Congressman Jamie Raskin (D-MD) wrote in a November 21, 2019, letter to US Department of Defense Secretary Mark Esper. “These cuts, even if only partially implemented or scaled back, will adversely impact the enterprise across recruitment, retention, access to research funding, and severely impact medical readiness at a time when demand is increasing.”
The medical readiness of military health care providers remains one of the thorniest challenges revolving around the DHA transition. “As an infantryman, from my perspective if you can't maintain effectiveness on the trauma side than it is not worth getting more efficient,” argued LTG (Ret) Jeffrey S. Buchannon, who formerly served as senior commander of Fort Sam Houston, which includes Brooke Army Medical Center, the military’s only level 1 trauma center and 1 of only 2 trauma centers in San Antonio. “We need the home game in order to prepare for the away game,”
In its review, DoD is looking at how the MTFs support inpatient and/or outpatient services to maintain medical force readiness. “We need to identify those areas where we can expand capacity at MTFs that offer potential for sustaining the skills and knowledge of our members,” said McCaffrey. “But we also must examine those areas where facilities do not offer now and likely will not be able to offer in the future a platform for maximizing capabilities to support medical readiness. In those situations, we must be open to right sizing MTF services and capabilities so as to ensure that we are using finite resources most efficiently while not compromising our ability to meet the mission.”
“Our military healthy system is the envy of the world. Any great power competitor would trade its health care and battlefield medicine capabilities for the system you have built,” McCaffrey said. “But just as America’s combat supremacy is not guaranteed nor is the supremacy of the MHS.” The US faces new global security challenges, McCaffrey argued, and “we must adapt and evolve if we are to successfully meet these challenges.”
One theme emerged from multiple military healthy system (MHS) leaders at the recent AMSUS annual conference: Significant change is coming to the MHS, and military health care providers can either embrace and shape that change or somebody else will. “If we don’t shape our future, others will step in and do it for us,” Tom McCaffrey, Assistant Secretary of Defense for Health Affairs; Defense Health Agency (DHA), and the Uniformed Service University for the Health Sciences (USU) told the audience.
The “historic” changes are underway, as the DHA has already begun to take over control of many military treatment facilities (MTFs) that were formerly operated by the separate services. In the next step of the transition, nearly 250 individual MTFs will be combined—along with TRICARE providers—in 21 geographically based “markets” in order to streamline management and avoid redundancies.
The exact details of the changes in store have not been released. McCaffrey noted that US Department of Defense (DoD) leadership will submit the “framework” for their assessment of the MHS to Congress “very soon, and at that point we will begin the hard work of detailed implementation of the results of that assessment and recommendations from the department.” Changes are expected to continue through fiscal year 2021, and some sources have estimated that as many as 18,000 jobs could be eliminated in the process.
Although Congress drove these changes in the National Defense Authorization Act of 2017, MHS leaders insist they are determining how to make the transformation without hurting medical readiness. “We the senior leadership of the MHS must continue to work together to shape our system to meet the challenges of the new environment,” McCaffrey insisted.
It seems as though all elements of the MHS are on the table. One report has suggested that the USU budget could be cut by a third. “Given the USU’s track record of excellence, we were alarmed to learn that the department is considering cuts as high as 30% to the university’s budget for research, development, testing, and evaluation, and 34% to university operations and maintenance... includ[ing] the cancellation of a $445 million military construction project and closure of the USU medical school,” US senators Chris Van Hollen (D-MD), Ben Cardin (D-MD.), Jack Reed (D-RI), and Congressman Jamie Raskin (D-MD) wrote in a November 21, 2019, letter to US Department of Defense Secretary Mark Esper. “These cuts, even if only partially implemented or scaled back, will adversely impact the enterprise across recruitment, retention, access to research funding, and severely impact medical readiness at a time when demand is increasing.”
The medical readiness of military health care providers remains one of the thorniest challenges revolving around the DHA transition. “As an infantryman, from my perspective if you can't maintain effectiveness on the trauma side than it is not worth getting more efficient,” argued LTG (Ret) Jeffrey S. Buchannon, who formerly served as senior commander of Fort Sam Houston, which includes Brooke Army Medical Center, the military’s only level 1 trauma center and 1 of only 2 trauma centers in San Antonio. “We need the home game in order to prepare for the away game,”
In its review, DoD is looking at how the MTFs support inpatient and/or outpatient services to maintain medical force readiness. “We need to identify those areas where we can expand capacity at MTFs that offer potential for sustaining the skills and knowledge of our members,” said McCaffrey. “But we also must examine those areas where facilities do not offer now and likely will not be able to offer in the future a platform for maximizing capabilities to support medical readiness. In those situations, we must be open to right sizing MTF services and capabilities so as to ensure that we are using finite resources most efficiently while not compromising our ability to meet the mission.”
“Our military healthy system is the envy of the world. Any great power competitor would trade its health care and battlefield medicine capabilities for the system you have built,” McCaffrey said. “But just as America’s combat supremacy is not guaranteed nor is the supremacy of the MHS.” The US faces new global security challenges, McCaffrey argued, and “we must adapt and evolve if we are to successfully meet these challenges.”
One theme emerged from multiple military healthy system (MHS) leaders at the recent AMSUS annual conference: Significant change is coming to the MHS, and military health care providers can either embrace and shape that change or somebody else will. “If we don’t shape our future, others will step in and do it for us,” Tom McCaffrey, Assistant Secretary of Defense for Health Affairs; Defense Health Agency (DHA), and the Uniformed Service University for the Health Sciences (USU) told the audience.
The “historic” changes are underway, as the DHA has already begun to take over control of many military treatment facilities (MTFs) that were formerly operated by the separate services. In the next step of the transition, nearly 250 individual MTFs will be combined—along with TRICARE providers—in 21 geographically based “markets” in order to streamline management and avoid redundancies.
The exact details of the changes in store have not been released. McCaffrey noted that US Department of Defense (DoD) leadership will submit the “framework” for their assessment of the MHS to Congress “very soon, and at that point we will begin the hard work of detailed implementation of the results of that assessment and recommendations from the department.” Changes are expected to continue through fiscal year 2021, and some sources have estimated that as many as 18,000 jobs could be eliminated in the process.
Although Congress drove these changes in the National Defense Authorization Act of 2017, MHS leaders insist they are determining how to make the transformation without hurting medical readiness. “We the senior leadership of the MHS must continue to work together to shape our system to meet the challenges of the new environment,” McCaffrey insisted.
It seems as though all elements of the MHS are on the table. One report has suggested that the USU budget could be cut by a third. “Given the USU’s track record of excellence, we were alarmed to learn that the department is considering cuts as high as 30% to the university’s budget for research, development, testing, and evaluation, and 34% to university operations and maintenance... includ[ing] the cancellation of a $445 million military construction project and closure of the USU medical school,” US senators Chris Van Hollen (D-MD), Ben Cardin (D-MD.), Jack Reed (D-RI), and Congressman Jamie Raskin (D-MD) wrote in a November 21, 2019, letter to US Department of Defense Secretary Mark Esper. “These cuts, even if only partially implemented or scaled back, will adversely impact the enterprise across recruitment, retention, access to research funding, and severely impact medical readiness at a time when demand is increasing.”
The medical readiness of military health care providers remains one of the thorniest challenges revolving around the DHA transition. “As an infantryman, from my perspective if you can't maintain effectiveness on the trauma side than it is not worth getting more efficient,” argued LTG (Ret) Jeffrey S. Buchannon, who formerly served as senior commander of Fort Sam Houston, which includes Brooke Army Medical Center, the military’s only level 1 trauma center and 1 of only 2 trauma centers in San Antonio. “We need the home game in order to prepare for the away game,”
In its review, DoD is looking at how the MTFs support inpatient and/or outpatient services to maintain medical force readiness. “We need to identify those areas where we can expand capacity at MTFs that offer potential for sustaining the skills and knowledge of our members,” said McCaffrey. “But we also must examine those areas where facilities do not offer now and likely will not be able to offer in the future a platform for maximizing capabilities to support medical readiness. In those situations, we must be open to right sizing MTF services and capabilities so as to ensure that we are using finite resources most efficiently while not compromising our ability to meet the mission.”
“Our military healthy system is the envy of the world. Any great power competitor would trade its health care and battlefield medicine capabilities for the system you have built,” McCaffrey said. “But just as America’s combat supremacy is not guaranteed nor is the supremacy of the MHS.” The US faces new global security challenges, McCaffrey argued, and “we must adapt and evolve if we are to successfully meet these challenges.”
Peer-Review Transparency
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff ([email protected]) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
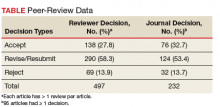
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at [email protected].
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff ([email protected]) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at [email protected].
Federal health care providers live under a microscope, so it seems only fair that we at Fed Pract honor that reality and open ourselves up to scrutiny as well.1 We hope that by shedding light on our peer-review process and manuscript acceptance rate, we will not only highlight our accomplishments, but identify areas for improvement.
Free access to Fed Pract content has always been our priority. While many journals charge authors or readers, Fed Pract has been and will remain free for readers and authors.2 Advertising enables the journal to support this free model of publishing, but we take care to ensure that advertisements do not influence content in any way. Our advertising policy can be found at www.mdedge.com/fedprac/page/advertising.
In January 2019, Fed Pract placed > 400 peer-reviewed articles published since January 2015 in the PubMed Central (PMC) database (ncbi.nlm.nih.gov/pmc). The full text of these and all future Fed Pract peer-reviewed articles will be available at PMC (no registration required), and the citations also will be included in PubMed. We hope that this process will make it even easier for anyone to access our authors’ works.
In 2018 about 36,000 federal health care providers (HCPs) received hard copies of this journal. The print journal is free, but circulation is limited to HCPs who work at the US Department of Veterans Affairs (VA), US Department of Defense (DoD), and the US Public Health Service (PHS). The mdedge.com/fedprac website, which includes every article published since 2003, had 1.4 million page views in 2018. After reading 3 online articles, readers in the US are asked to complete a simple registration form to help us better customize the reader experience. In some cases, international readers may be asked to pay for access to articles online; however, any VA, DoD, or PHS officer stationed overseas can contact the editorial staff ([email protected]) to ensure that they can access the articles for free.
In 2018 the journal received 164 manuscripts and published 94 articles written by 357 different federal HCPs. The 164 manuscript submissions represented a 45% growth over previous years. Not surprisingly, the increased rate of submissions began shortly after the May 2018 announcement that journal articles would be included in PMC. Most of those articles (83%) were submitted unsolicited.
Fed Pract has always prided itself on being an early promoter of interdisciplinary health care professional publications. Nearly half of its listed authors were physicians (48%), while pharmacists made up the next largest cohort (18%). There were smaller numbers of PhDs, nurses, social workers, and physical therapists. The majority were written by HCPs affiliated with the VA (95% of articles and 93% of authors), and no articles in 2018 were written by PHS officers. Physicians comprise about two-thirds of the audience, while pharmacists make up 17% and nurses 9%. PHS and DoD HCPs make up 19% of the Fed Pract audience, suggesting that the journal needs to do more work to encourage these HCPs to contribute articles to the journal.3
Articles published in 2018 covered a broad range of topics from “Anesthesia Care Practice Models in the VHA” and “Army Behavioral Health System” to “Vitreous Hemorrhage in the Setting of a Vascular Loop” and “A Workforce Assessment of VA Home-Based Primary Care Pharmacists.” Categorizing the articles is a challenge. Few health care topics fit neatly into a single topic or specialty. This is especially true in federal health care where much of the care is delivered by multidisciplinary patient-centered medical homes or patient aligned care teams. Nevertheless, a few broad outlines can be discerned. Articles were roughly split between primary care and hospital-based and/or specialty care topics; one-quarter of the articles were case studies or case series articles, and about 20% were editorials or opinion columns. Nineteen articles dealt explicitly with chronic conditions, and 10 articles focused on mental health care.
Peer reviewers are an essential part of the process. Reviewers are blinded to the identityof the authors, ensuring fairness and reducing potential conflicts of interest. We are extremely grateful to each and every reviewer for the time and energy they contribute to the journal. Peer reviewers do not get nearly enough recognition for their important work. In 2018 Fed Pract invited 1,205 reviewers for 164 manuscript submissions and 94 manuscript revisions. More than 200 different reviewers submitted 487 reviews with a median (SD) of 2 reviews (1.8) and a range of 1 to 10. The top 20 reviewers completed 134 reviews with a median (SD) of 6 reviews (1.2). The results stand in contrast to some journals that must offer many invitations per review and depend on a small number of reviewers.1,4-6
The reviewers recommended to reject 14% and to revise 26% of the articles, which is a much lower rejection rate than many other journals (Table).4
These data suggest that Fed Pract and its peer-review process is on a sound foundation but needs to make improvements. Moving into 2019, the journal expects that an increasing number of submissions will require a higher rejection rate. Moreover, we will need to do a better job reaching out to underrepresented portions of our audience. To decrease the time to publication for accepted manuscripts, in 2019 we will publish more articles online ahead of the print publication as we strive to improve the experience for authors, reviewers, readers, and the entire Fed Pract audience.
None of this work can be done without our small and dedicated staff. I would like to thank Managing Editor Joyce Brody who sent out each and every one of those reviewer invitations, Deputy Editor Robert Fee, who manages the special issues, Web Editor Teraya Smith, who runs our entire digital operation, and of course, Editor in Chief Cynthia Geppert, who oversees it all. Finally, it is important that you let us know how we are doing and whether we are meeting your needs. Visit mdedge.com/fedprac to take the readership survey or reach out to me at [email protected].
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
1. Geppert CMA. Caring under a microscope. Fed Pract. 2018;35(7):6-7.
2. Smith R. Peer review: a flawed process at the heart of science and journals. J R Soc Med. 2006;99(4):178-182.
3. BPA Worldwide. Federal Practitioner brand report for the 6 month period ending June 2018. https://www.frontlinemedcom.com/wp-content/uploads/FEDPRAC_BPA.pdf. Updated June 2018. Accessed March 5, 2019.
4. Fontanarosa PB, Bauchner H, Golub RM. Thank you to JAMA authors, peer reviewers, and readers. JAMA. 2017;317(8):812-813.
5. Publons, Clarivate Analytics. 2018 global state of peer review. https://publons.com/static/Publons-Global-State-Of-Peer-Review-2018.pdf. Published September 2018. Accessed March 5, 2019.
6. Malcom D. It’s time we fix the peer review system. Am J Pharm Educ. 2018;82(5):7144.
Breaking News: Trump Upends Federal Pay for 2019
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
In a letter to Congressional leaders, President Trump has announced a pay freeze for all civilian federal employees in 2019. The decision will not impact active duty service members who are still are expected to receive a 2.6% pay raise next year.
The decision aims to circumvent a 2.1% across the board increase and additional locality pay increases that would average 25.7%. "We must maintain efforts to put our Nation on a fiscally sustainable course, and Federal agency budgets cannot sustain such increases. Accordingly, I have determined that it is appropriate to exercise my authority to set alternative across-the-board and locality pay adjustments for 2019."
In the letter, the President disputed the notion that locality pay was important for keeping and attracting quality applicants for positions. Currently, the Veterans Health Administration has more than 40,000 job openings.
"I have determined that for 2019, both across‑the‑board pay increases and locality pay increases will be set at zero. These alternative pay plan decisions will not materially affect our ability to attract and retain a well‑qualified Federal workforce.
President Trump had already included the pay freeze in his budget proposal. While Congress can override the President's decision, congressional action is not expected.
Singing Praises, Naming Names
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.