User login
Methemoglobinemia in an HIV patient
A 45-year-old man with known human immunodeficiency virus infection presented with a 5-day history of dyspnea. When his dyspnea had become symptomatic, he had restarted his home dapsone prophylaxis, but his dyspnea had progressively worsened, and his urine became dark.
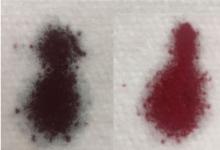
Based on these test results, the patient’s dapsone was stopped and replaced with atovaquone. Intravenous infusion of methylene blue was started, with subsequent improvement of the hypoxia and cyanosis (Figure 1). His urine became green, but it returned to a normal color in a matter of hours. He was ultimately diagnosed with P jirovecii pneumonia and completed a course of atovaquone with total resolution of his symptoms.
THE MECHANISMS BEHIND METHEMOGLOBINEMIA
Heme iron is normally in the ferrous state (Fe2+), which allows for hemoglobin to carry oxygen and release it to tissues.1 Exposure to an oxidative stress can lead to methemoglobinemia from an increase in abnormal hemoglobin that contains iron in a ferric state (Fe3+).1,2
Methemoglobin reduces oxygen-carrying capacity in two ways: it is unable to carry oxygen, and its presence shifts the oxygen dissociation curve to the left, causing any remaining normal hemoglobin to be unable to release oxygen to the tissues.1,2
Causes of acquired methemoglobinemia include topical anesthetics (eg, benzocaine, lidocaine) and antibiotics (eg, dapsone).2,3 Signs and symptoms include cyanosis, headache, fatigue, dyspnea, lethargy, respiratory distress, and dark-colored urine.1,2
MANAGEMENT
Treatment consists of intravenous methylene blue, which reduces the hemoglobin from a ferric state to a ferrous state.1–4 Methylene blue is a water-soluble dye excreted primarily in the urine, and common side effects include dizziness, nausea, and green urine.5–7 The blue pigments from methylene blue combine with urobilin (a yellow pigment in the urine), producing a green color.7 This is not pathological and requires no treatment, as the urine returns to normal color after the body fully excretes the dye.5–7
If intravenous methylene blue fails to produce a response, other treatments to consider include hemodialysis, blood transfusion, exchange transfusion, and hyperbaric oxygen therapy.2
- Umbreit J. Methemoglobin—it’s not just blue: a concise review. Am J Hematol 2007; 82:134–144.
- Ash-Bernal R, Wise R, Wright SM. Acquired methemoglobinemia: a retrospective series of 138 cases at 2 teaching hospitals. Medicine (Baltimore) 2004; 83:265–273.
- Coleman MD, Coleman NA. Drug-induced methaemoglobinaemia. Treatment issues. Drug Saf 1996; 14:394–405.
- Sikka P, Bindra VK, Kapoor S, Jain V, Saxena KK. Blue cures blue but be cautious. J Pharm Bioallied Sci 2011; 3:543–545.
- Stratta P, Barbe MC. Images in clinical medicine. Green urine. N Engl J Med 2008; 358:e12.
- Miri-Aliabad G. Green urine secondary to methylene blue. Indian J Pediatr 2014; 81:1255–1256.
- Prakash S, Saini S, Mullick P, Pawar M. Green urine: a cause for concern? J Anaesthesiol Clin Pharmacol 2017; 33:128–130.
A 45-year-old man with known human immunodeficiency virus infection presented with a 5-day history of dyspnea. When his dyspnea had become symptomatic, he had restarted his home dapsone prophylaxis, but his dyspnea had progressively worsened, and his urine became dark.
Based on these test results, the patient’s dapsone was stopped and replaced with atovaquone. Intravenous infusion of methylene blue was started, with subsequent improvement of the hypoxia and cyanosis (Figure 1). His urine became green, but it returned to a normal color in a matter of hours. He was ultimately diagnosed with P jirovecii pneumonia and completed a course of atovaquone with total resolution of his symptoms.
THE MECHANISMS BEHIND METHEMOGLOBINEMIA
Heme iron is normally in the ferrous state (Fe2+), which allows for hemoglobin to carry oxygen and release it to tissues.1 Exposure to an oxidative stress can lead to methemoglobinemia from an increase in abnormal hemoglobin that contains iron in a ferric state (Fe3+).1,2
Methemoglobin reduces oxygen-carrying capacity in two ways: it is unable to carry oxygen, and its presence shifts the oxygen dissociation curve to the left, causing any remaining normal hemoglobin to be unable to release oxygen to the tissues.1,2
Causes of acquired methemoglobinemia include topical anesthetics (eg, benzocaine, lidocaine) and antibiotics (eg, dapsone).2,3 Signs and symptoms include cyanosis, headache, fatigue, dyspnea, lethargy, respiratory distress, and dark-colored urine.1,2
MANAGEMENT
Treatment consists of intravenous methylene blue, which reduces the hemoglobin from a ferric state to a ferrous state.1–4 Methylene blue is a water-soluble dye excreted primarily in the urine, and common side effects include dizziness, nausea, and green urine.5–7 The blue pigments from methylene blue combine with urobilin (a yellow pigment in the urine), producing a green color.7 This is not pathological and requires no treatment, as the urine returns to normal color after the body fully excretes the dye.5–7
If intravenous methylene blue fails to produce a response, other treatments to consider include hemodialysis, blood transfusion, exchange transfusion, and hyperbaric oxygen therapy.2
A 45-year-old man with known human immunodeficiency virus infection presented with a 5-day history of dyspnea. When his dyspnea had become symptomatic, he had restarted his home dapsone prophylaxis, but his dyspnea had progressively worsened, and his urine became dark.
Based on these test results, the patient’s dapsone was stopped and replaced with atovaquone. Intravenous infusion of methylene blue was started, with subsequent improvement of the hypoxia and cyanosis (Figure 1). His urine became green, but it returned to a normal color in a matter of hours. He was ultimately diagnosed with P jirovecii pneumonia and completed a course of atovaquone with total resolution of his symptoms.
THE MECHANISMS BEHIND METHEMOGLOBINEMIA
Heme iron is normally in the ferrous state (Fe2+), which allows for hemoglobin to carry oxygen and release it to tissues.1 Exposure to an oxidative stress can lead to methemoglobinemia from an increase in abnormal hemoglobin that contains iron in a ferric state (Fe3+).1,2
Methemoglobin reduces oxygen-carrying capacity in two ways: it is unable to carry oxygen, and its presence shifts the oxygen dissociation curve to the left, causing any remaining normal hemoglobin to be unable to release oxygen to the tissues.1,2
Causes of acquired methemoglobinemia include topical anesthetics (eg, benzocaine, lidocaine) and antibiotics (eg, dapsone).2,3 Signs and symptoms include cyanosis, headache, fatigue, dyspnea, lethargy, respiratory distress, and dark-colored urine.1,2
MANAGEMENT
Treatment consists of intravenous methylene blue, which reduces the hemoglobin from a ferric state to a ferrous state.1–4 Methylene blue is a water-soluble dye excreted primarily in the urine, and common side effects include dizziness, nausea, and green urine.5–7 The blue pigments from methylene blue combine with urobilin (a yellow pigment in the urine), producing a green color.7 This is not pathological and requires no treatment, as the urine returns to normal color after the body fully excretes the dye.5–7
If intravenous methylene blue fails to produce a response, other treatments to consider include hemodialysis, blood transfusion, exchange transfusion, and hyperbaric oxygen therapy.2
- Umbreit J. Methemoglobin—it’s not just blue: a concise review. Am J Hematol 2007; 82:134–144.
- Ash-Bernal R, Wise R, Wright SM. Acquired methemoglobinemia: a retrospective series of 138 cases at 2 teaching hospitals. Medicine (Baltimore) 2004; 83:265–273.
- Coleman MD, Coleman NA. Drug-induced methaemoglobinaemia. Treatment issues. Drug Saf 1996; 14:394–405.
- Sikka P, Bindra VK, Kapoor S, Jain V, Saxena KK. Blue cures blue but be cautious. J Pharm Bioallied Sci 2011; 3:543–545.
- Stratta P, Barbe MC. Images in clinical medicine. Green urine. N Engl J Med 2008; 358:e12.
- Miri-Aliabad G. Green urine secondary to methylene blue. Indian J Pediatr 2014; 81:1255–1256.
- Prakash S, Saini S, Mullick P, Pawar M. Green urine: a cause for concern? J Anaesthesiol Clin Pharmacol 2017; 33:128–130.
- Umbreit J. Methemoglobin—it’s not just blue: a concise review. Am J Hematol 2007; 82:134–144.
- Ash-Bernal R, Wise R, Wright SM. Acquired methemoglobinemia: a retrospective series of 138 cases at 2 teaching hospitals. Medicine (Baltimore) 2004; 83:265–273.
- Coleman MD, Coleman NA. Drug-induced methaemoglobinaemia. Treatment issues. Drug Saf 1996; 14:394–405.
- Sikka P, Bindra VK, Kapoor S, Jain V, Saxena KK. Blue cures blue but be cautious. J Pharm Bioallied Sci 2011; 3:543–545.
- Stratta P, Barbe MC. Images in clinical medicine. Green urine. N Engl J Med 2008; 358:e12.
- Miri-Aliabad G. Green urine secondary to methylene blue. Indian J Pediatr 2014; 81:1255–1256.
- Prakash S, Saini S, Mullick P, Pawar M. Green urine: a cause for concern? J Anaesthesiol Clin Pharmacol 2017; 33:128–130.