User login
Building a Toolkit for the Treatment of Acute Migraine
Selecting a treatment plan to deal with acute migraine attacks can be like putting together a toolkit of possible therapies, individualized for each patient, one expert said.
The toolkit should comprise reliable treatments that patients know are going to work and that act quickly, allowing them to get back to functioning normally in their daily lives, said Jessica Ailani, MD, during a talk at the 17th European Headache Congress held recently in Barcelona, Spain.
“Everyone with migraine needs acute treatment,” Dr. Ailani, who is a clinical professor of neurology at MedStar Georgetown University Hospital and director of the Georgetown Headache Center, Washington, DC, noted. “Sometimes we can reduce acute treatment with preventative agents, but some disability will remain, so we have to focus on good acute treatment, and this becomes more complex if a person has a lot of comorbidities, which is common in older patients.”
In selecting suitable treatments for migraine, consideration has to be given to the patient profile, any other conditions they have, speed of onset of the migraine attack, length of the attack, associated symptoms, and side effects of the medications, she said.
A Complex Case
As an example, Dr. Ailani described the process she used to treat one of her patients who had frequent severe migraines and other issues causing difficult decisions when selecting medications — a woman in her late 60s with several other comorbidities.
“This is the kind of case I see on a daily basis and which keeps me up at night,” she said. “Many times in clinical practice, we see complex cases like this, and through the course of a year, we may try every treatment option we have in a patient like this.”
On the first presentation, the patient had a chronic migraine with severe headaches every day. She had a history of previous cervical discectomy with fusion surgery; uncontrolled hypertension, for which she was taking an angiotensin blocker; high cholesterol, for which she was taking a statin; and diabetes with an A1c of 8. She did not smoke or drink alcohol, exercised moderately, and her body mass index was in a good range.
“Before a patient ever sees a doctor for their migraine, they will have already tried a lot of different things. Most people are already using NSAIDs and acetaminophen, the most commonly used treatments for acute migraine,” Dr. Ailani explains.
Her patient was taking a triptan and the barbiturate, butalbital. Dr. Ailani notes that the triptan is very effective, but in the United States, they are not available over the counter, and the patient is only allowed nine doses per month on her insurance, so she was supplementing with butalbital.
Over the course of a year, Dr. Ailani got her off the butalbital and started her on onabotulinum toxin A for migraine prevention, which reduced her headache days to about 15 per month (8 severe). She then added the anti-calcitonin gene-related peptide (CGRP) monoclonal antibody, galcanezumab, as another preventative, which further reduced the headache days down to 8-10 days per month (all migraine).
The attacks are rapid onset and can last multiple days. They come with photophobia and phonophobia and cause her to be bedridden, she noted.
“I was still worried about this frequency of headache and the fact she was using a triptan for acute treatment when she had uncontrolled hypertension and other cardiovascular risk factors, Dr. Ailani commented.
She explained that triptans are generally not used in individuals aged over 65 years because of a lack of data in this age group. They are also contraindicated in patients with cardiovascular (CV) disease, and caution is advised in patients with CV risk factors. Noting that migraine is an independent risk factor for stroke in healthy individuals, and this patient already had three other major risk factors for stroke, Dr. Ailani said she did not think a triptan was the best option.
When triptans do not work, Dr. Ailani said she thinks about dihydroergotamine, which she describes as “a great drug for long-lasting migraine” as it tends to have a sustained response. But it also has vasoconstrictive effects and can increase blood pressure, so it was not suitable for this patient.
CV risk is also an issue with nonsteroidal anti-inflammatory drugs (NSAIDs), one of the staple treatments for acute migraine.
“NSAIDs are available over the counter, inexpensive, quite effective, and have minimal immediate side effects,” Dr. Ailani said. But long-term adverse events include CV events, particularly in those who already have CV risk factors, and it is now thought that NSAIDs actually carry more CV risk than triptans.
She noted that out of all the NSAIDs, celecoxib carries the lowest CV risk, and in the United States, it is available as a liquid formulation. There is also a study of ketorolac nasal spray showing it to be as effective as sumatriptan nasal spray for acute migraine.
As her patient was still going to the emergency room (ER) quite frequently at this point, Dr. Ailani prescribed ketorolac nasal spray as an emergency rescue medication, which did help to reduce ER visits but did not solve the acute treatment problem.
The next option she tried was the CGRP antagonists or “gepants” because of their good tolerability.
Because her patient had long attacks, Dr. Ailani said her first choice gepant was rimegepant as it has a long half-life.
She noted that in patients who have frequent migraine attacks (> 6 migraine days per month), using rimegepant as needed has been shown to lead to migraine frequency declining over time. “This shows that if we treat acute attacks properly, we can minimize the risk of chronic migraine.”
She pointed out that if a patient has prodrome that is easy to identify or has short attacks, ubrogepant may be a good option, having shown effectiveness in preventing or reducing the onset of the headache in the recently reported PRODROME trial when given the day before migraine starts.
Then there is also zavegepant, which is available as a nasal spray, so it is a good option for patients with nausea and vomiting. Dr. Ailani suggested that zavegepant as a third-generation gepant may be worth trying in patients who have tried the other gepants, as it is a different type of molecule.
For this patient, neither rimegepant nor ubrogepant worked. “We tried treating in the prodrome, when the pain was starting, adding to other treatments, but she is not a ‘gepant’ responder. We have yet to try zavegepant,” she said.
The next consideration was lasmiditan. “This patient is a triptan responder and lasmiditan is a 5HT1 agonist, so it makes sense to try this. Also, it doesn’t have a vasoconstrictor effect as it doesn’t work on the blood vessels, so it is safe for patients with high blood pressure,” Dr. Ailani noted.
She pointed out, however, that lasmiditan has become a rescue medication in her practice because of side effect issues such as dizziness and sleepiness.
But Dr. Ailani said she has learned how to use the medication to minimize the side effects, by increasing the dose slowly and advising patients to take it later in the day.
“We start with 50 mg for a few doses then increase to 100 mg. This seems to build tolerability.”
Her patient has found good relief from lasmiditan 100 mg, but she can’t take it during the day as it makes her sleepy.
As a last resort, Dr. Ailani went back to metoclopramide, which she described as “a tried and tested old-time drug.”
While this does not make the patient sleepy, it has other adverse effects limiting the frequency of its use, she noted. “I ask her to try to limit it to twice a week, and this has been pretty effective. She can function when she uses it.”
Dr. Ailani also points out that neuromodulation should be in everyone’s tool kit. “So, we added an external combined occipital and trigeminal (eCOT device) neurostimulation device.”
The patient’s tool kit now looks like this:
- Neuromodulation device and meditation at first sign of an attack.
- Add metoclopramide 10 mg and acetaminophen 1000 mg.
- If the attack lasts into the second day, add lasmiditan 100 mg in the evening of the second day (limit 8 days a month).
- If the patient has a sudden onset severe migraine with nausea and vomiting that might make her go to the ER, add in ketorolac nasal spray (not > 5 days per month).
Dr. Ailani noted that other patients will need different toolkits, and in most cases, it is recommended to think about “situational prevention” for times when migraine attacks are predictable, which may include air travel, high-stress times (holidays, etc.), occasions when alcohol will be consumed, and at times of certain weather triggers.
Dr. Ailani disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Selecting a treatment plan to deal with acute migraine attacks can be like putting together a toolkit of possible therapies, individualized for each patient, one expert said.
The toolkit should comprise reliable treatments that patients know are going to work and that act quickly, allowing them to get back to functioning normally in their daily lives, said Jessica Ailani, MD, during a talk at the 17th European Headache Congress held recently in Barcelona, Spain.
“Everyone with migraine needs acute treatment,” Dr. Ailani, who is a clinical professor of neurology at MedStar Georgetown University Hospital and director of the Georgetown Headache Center, Washington, DC, noted. “Sometimes we can reduce acute treatment with preventative agents, but some disability will remain, so we have to focus on good acute treatment, and this becomes more complex if a person has a lot of comorbidities, which is common in older patients.”
In selecting suitable treatments for migraine, consideration has to be given to the patient profile, any other conditions they have, speed of onset of the migraine attack, length of the attack, associated symptoms, and side effects of the medications, she said.
A Complex Case
As an example, Dr. Ailani described the process she used to treat one of her patients who had frequent severe migraines and other issues causing difficult decisions when selecting medications — a woman in her late 60s with several other comorbidities.
“This is the kind of case I see on a daily basis and which keeps me up at night,” she said. “Many times in clinical practice, we see complex cases like this, and through the course of a year, we may try every treatment option we have in a patient like this.”
On the first presentation, the patient had a chronic migraine with severe headaches every day. She had a history of previous cervical discectomy with fusion surgery; uncontrolled hypertension, for which she was taking an angiotensin blocker; high cholesterol, for which she was taking a statin; and diabetes with an A1c of 8. She did not smoke or drink alcohol, exercised moderately, and her body mass index was in a good range.
“Before a patient ever sees a doctor for their migraine, they will have already tried a lot of different things. Most people are already using NSAIDs and acetaminophen, the most commonly used treatments for acute migraine,” Dr. Ailani explains.
Her patient was taking a triptan and the barbiturate, butalbital. Dr. Ailani notes that the triptan is very effective, but in the United States, they are not available over the counter, and the patient is only allowed nine doses per month on her insurance, so she was supplementing with butalbital.
Over the course of a year, Dr. Ailani got her off the butalbital and started her on onabotulinum toxin A for migraine prevention, which reduced her headache days to about 15 per month (8 severe). She then added the anti-calcitonin gene-related peptide (CGRP) monoclonal antibody, galcanezumab, as another preventative, which further reduced the headache days down to 8-10 days per month (all migraine).
The attacks are rapid onset and can last multiple days. They come with photophobia and phonophobia and cause her to be bedridden, she noted.
“I was still worried about this frequency of headache and the fact she was using a triptan for acute treatment when she had uncontrolled hypertension and other cardiovascular risk factors, Dr. Ailani commented.
She explained that triptans are generally not used in individuals aged over 65 years because of a lack of data in this age group. They are also contraindicated in patients with cardiovascular (CV) disease, and caution is advised in patients with CV risk factors. Noting that migraine is an independent risk factor for stroke in healthy individuals, and this patient already had three other major risk factors for stroke, Dr. Ailani said she did not think a triptan was the best option.
When triptans do not work, Dr. Ailani said she thinks about dihydroergotamine, which she describes as “a great drug for long-lasting migraine” as it tends to have a sustained response. But it also has vasoconstrictive effects and can increase blood pressure, so it was not suitable for this patient.
CV risk is also an issue with nonsteroidal anti-inflammatory drugs (NSAIDs), one of the staple treatments for acute migraine.
“NSAIDs are available over the counter, inexpensive, quite effective, and have minimal immediate side effects,” Dr. Ailani said. But long-term adverse events include CV events, particularly in those who already have CV risk factors, and it is now thought that NSAIDs actually carry more CV risk than triptans.
She noted that out of all the NSAIDs, celecoxib carries the lowest CV risk, and in the United States, it is available as a liquid formulation. There is also a study of ketorolac nasal spray showing it to be as effective as sumatriptan nasal spray for acute migraine.
As her patient was still going to the emergency room (ER) quite frequently at this point, Dr. Ailani prescribed ketorolac nasal spray as an emergency rescue medication, which did help to reduce ER visits but did not solve the acute treatment problem.
The next option she tried was the CGRP antagonists or “gepants” because of their good tolerability.
Because her patient had long attacks, Dr. Ailani said her first choice gepant was rimegepant as it has a long half-life.
She noted that in patients who have frequent migraine attacks (> 6 migraine days per month), using rimegepant as needed has been shown to lead to migraine frequency declining over time. “This shows that if we treat acute attacks properly, we can minimize the risk of chronic migraine.”
She pointed out that if a patient has prodrome that is easy to identify or has short attacks, ubrogepant may be a good option, having shown effectiveness in preventing or reducing the onset of the headache in the recently reported PRODROME trial when given the day before migraine starts.
Then there is also zavegepant, which is available as a nasal spray, so it is a good option for patients with nausea and vomiting. Dr. Ailani suggested that zavegepant as a third-generation gepant may be worth trying in patients who have tried the other gepants, as it is a different type of molecule.
For this patient, neither rimegepant nor ubrogepant worked. “We tried treating in the prodrome, when the pain was starting, adding to other treatments, but she is not a ‘gepant’ responder. We have yet to try zavegepant,” she said.
The next consideration was lasmiditan. “This patient is a triptan responder and lasmiditan is a 5HT1 agonist, so it makes sense to try this. Also, it doesn’t have a vasoconstrictor effect as it doesn’t work on the blood vessels, so it is safe for patients with high blood pressure,” Dr. Ailani noted.
She pointed out, however, that lasmiditan has become a rescue medication in her practice because of side effect issues such as dizziness and sleepiness.
But Dr. Ailani said she has learned how to use the medication to minimize the side effects, by increasing the dose slowly and advising patients to take it later in the day.
“We start with 50 mg for a few doses then increase to 100 mg. This seems to build tolerability.”
Her patient has found good relief from lasmiditan 100 mg, but she can’t take it during the day as it makes her sleepy.
As a last resort, Dr. Ailani went back to metoclopramide, which she described as “a tried and tested old-time drug.”
While this does not make the patient sleepy, it has other adverse effects limiting the frequency of its use, she noted. “I ask her to try to limit it to twice a week, and this has been pretty effective. She can function when she uses it.”
Dr. Ailani also points out that neuromodulation should be in everyone’s tool kit. “So, we added an external combined occipital and trigeminal (eCOT device) neurostimulation device.”
The patient’s tool kit now looks like this:
- Neuromodulation device and meditation at first sign of an attack.
- Add metoclopramide 10 mg and acetaminophen 1000 mg.
- If the attack lasts into the second day, add lasmiditan 100 mg in the evening of the second day (limit 8 days a month).
- If the patient has a sudden onset severe migraine with nausea and vomiting that might make her go to the ER, add in ketorolac nasal spray (not > 5 days per month).
Dr. Ailani noted that other patients will need different toolkits, and in most cases, it is recommended to think about “situational prevention” for times when migraine attacks are predictable, which may include air travel, high-stress times (holidays, etc.), occasions when alcohol will be consumed, and at times of certain weather triggers.
Dr. Ailani disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Selecting a treatment plan to deal with acute migraine attacks can be like putting together a toolkit of possible therapies, individualized for each patient, one expert said.
The toolkit should comprise reliable treatments that patients know are going to work and that act quickly, allowing them to get back to functioning normally in their daily lives, said Jessica Ailani, MD, during a talk at the 17th European Headache Congress held recently in Barcelona, Spain.
“Everyone with migraine needs acute treatment,” Dr. Ailani, who is a clinical professor of neurology at MedStar Georgetown University Hospital and director of the Georgetown Headache Center, Washington, DC, noted. “Sometimes we can reduce acute treatment with preventative agents, but some disability will remain, so we have to focus on good acute treatment, and this becomes more complex if a person has a lot of comorbidities, which is common in older patients.”
In selecting suitable treatments for migraine, consideration has to be given to the patient profile, any other conditions they have, speed of onset of the migraine attack, length of the attack, associated symptoms, and side effects of the medications, she said.
A Complex Case
As an example, Dr. Ailani described the process she used to treat one of her patients who had frequent severe migraines and other issues causing difficult decisions when selecting medications — a woman in her late 60s with several other comorbidities.
“This is the kind of case I see on a daily basis and which keeps me up at night,” she said. “Many times in clinical practice, we see complex cases like this, and through the course of a year, we may try every treatment option we have in a patient like this.”
On the first presentation, the patient had a chronic migraine with severe headaches every day. She had a history of previous cervical discectomy with fusion surgery; uncontrolled hypertension, for which she was taking an angiotensin blocker; high cholesterol, for which she was taking a statin; and diabetes with an A1c of 8. She did not smoke or drink alcohol, exercised moderately, and her body mass index was in a good range.
“Before a patient ever sees a doctor for their migraine, they will have already tried a lot of different things. Most people are already using NSAIDs and acetaminophen, the most commonly used treatments for acute migraine,” Dr. Ailani explains.
Her patient was taking a triptan and the barbiturate, butalbital. Dr. Ailani notes that the triptan is very effective, but in the United States, they are not available over the counter, and the patient is only allowed nine doses per month on her insurance, so she was supplementing with butalbital.
Over the course of a year, Dr. Ailani got her off the butalbital and started her on onabotulinum toxin A for migraine prevention, which reduced her headache days to about 15 per month (8 severe). She then added the anti-calcitonin gene-related peptide (CGRP) monoclonal antibody, galcanezumab, as another preventative, which further reduced the headache days down to 8-10 days per month (all migraine).
The attacks are rapid onset and can last multiple days. They come with photophobia and phonophobia and cause her to be bedridden, she noted.
“I was still worried about this frequency of headache and the fact she was using a triptan for acute treatment when she had uncontrolled hypertension and other cardiovascular risk factors, Dr. Ailani commented.
She explained that triptans are generally not used in individuals aged over 65 years because of a lack of data in this age group. They are also contraindicated in patients with cardiovascular (CV) disease, and caution is advised in patients with CV risk factors. Noting that migraine is an independent risk factor for stroke in healthy individuals, and this patient already had three other major risk factors for stroke, Dr. Ailani said she did not think a triptan was the best option.
When triptans do not work, Dr. Ailani said she thinks about dihydroergotamine, which she describes as “a great drug for long-lasting migraine” as it tends to have a sustained response. But it also has vasoconstrictive effects and can increase blood pressure, so it was not suitable for this patient.
CV risk is also an issue with nonsteroidal anti-inflammatory drugs (NSAIDs), one of the staple treatments for acute migraine.
“NSAIDs are available over the counter, inexpensive, quite effective, and have minimal immediate side effects,” Dr. Ailani said. But long-term adverse events include CV events, particularly in those who already have CV risk factors, and it is now thought that NSAIDs actually carry more CV risk than triptans.
She noted that out of all the NSAIDs, celecoxib carries the lowest CV risk, and in the United States, it is available as a liquid formulation. There is also a study of ketorolac nasal spray showing it to be as effective as sumatriptan nasal spray for acute migraine.
As her patient was still going to the emergency room (ER) quite frequently at this point, Dr. Ailani prescribed ketorolac nasal spray as an emergency rescue medication, which did help to reduce ER visits but did not solve the acute treatment problem.
The next option she tried was the CGRP antagonists or “gepants” because of their good tolerability.
Because her patient had long attacks, Dr. Ailani said her first choice gepant was rimegepant as it has a long half-life.
She noted that in patients who have frequent migraine attacks (> 6 migraine days per month), using rimegepant as needed has been shown to lead to migraine frequency declining over time. “This shows that if we treat acute attacks properly, we can minimize the risk of chronic migraine.”
She pointed out that if a patient has prodrome that is easy to identify or has short attacks, ubrogepant may be a good option, having shown effectiveness in preventing or reducing the onset of the headache in the recently reported PRODROME trial when given the day before migraine starts.
Then there is also zavegepant, which is available as a nasal spray, so it is a good option for patients with nausea and vomiting. Dr. Ailani suggested that zavegepant as a third-generation gepant may be worth trying in patients who have tried the other gepants, as it is a different type of molecule.
For this patient, neither rimegepant nor ubrogepant worked. “We tried treating in the prodrome, when the pain was starting, adding to other treatments, but she is not a ‘gepant’ responder. We have yet to try zavegepant,” she said.
The next consideration was lasmiditan. “This patient is a triptan responder and lasmiditan is a 5HT1 agonist, so it makes sense to try this. Also, it doesn’t have a vasoconstrictor effect as it doesn’t work on the blood vessels, so it is safe for patients with high blood pressure,” Dr. Ailani noted.
She pointed out, however, that lasmiditan has become a rescue medication in her practice because of side effect issues such as dizziness and sleepiness.
But Dr. Ailani said she has learned how to use the medication to minimize the side effects, by increasing the dose slowly and advising patients to take it later in the day.
“We start with 50 mg for a few doses then increase to 100 mg. This seems to build tolerability.”
Her patient has found good relief from lasmiditan 100 mg, but she can’t take it during the day as it makes her sleepy.
As a last resort, Dr. Ailani went back to metoclopramide, which she described as “a tried and tested old-time drug.”
While this does not make the patient sleepy, it has other adverse effects limiting the frequency of its use, she noted. “I ask her to try to limit it to twice a week, and this has been pretty effective. She can function when she uses it.”
Dr. Ailani also points out that neuromodulation should be in everyone’s tool kit. “So, we added an external combined occipital and trigeminal (eCOT device) neurostimulation device.”
The patient’s tool kit now looks like this:
- Neuromodulation device and meditation at first sign of an attack.
- Add metoclopramide 10 mg and acetaminophen 1000 mg.
- If the attack lasts into the second day, add lasmiditan 100 mg in the evening of the second day (limit 8 days a month).
- If the patient has a sudden onset severe migraine with nausea and vomiting that might make her go to the ER, add in ketorolac nasal spray (not > 5 days per month).
Dr. Ailani noted that other patients will need different toolkits, and in most cases, it is recommended to think about “situational prevention” for times when migraine attacks are predictable, which may include air travel, high-stress times (holidays, etc.), occasions when alcohol will be consumed, and at times of certain weather triggers.
Dr. Ailani disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM THE EUROPEAN HEADACHE CONGRESS
CGRP in migraine prodrome can stop headache, reduce severity
BARCELONA, SPAIN — In the randomized, placebo-controlled crossover PRODROME trial, treatment with ubrogepant (Ubrelvy) 100 mg, one of the new CGRP receptor antagonists, during the prodrome prevented the development of moderate/severe headache at both 24 hours and 48 hours post-dose. The medication also reduced headache of any intensity within 24 hours and functional disability compared with placebo.
“This represents a totally different way of treating a migraine attack – to treat it before the headache starts. This is a paradigm shift in the way we approach the acute treatment of migraine,” study investigator Peter Goadsby, MBBS, MD, PhD, professor of neurology at Kings College London, UK, said in an interview.
The findings were presented at 17th European Headache Congress (EHC) and were also recently published online in The Lancet.
A New Way to Manage Migraine?
The prodrome is usually the earliest phase of a migraine attack and is believed to be experienced by the vast majority of patients with migraine. It consists of various symptoms, including sensitivity to light, fatigue, mood changes, cognitive dysfunction, craving certain foods, and neck pain, which can occur several hours or days before onset.
Dr. Goadsby notes that, at present, there isn’t very much a patient can do about the prodrome.
“We advise patients if they feel an attack is coming not to do anything that might make it worse and make sure they have their acute treatment available for when the headache phase starts. So, we just advise people to prepare for the attack rather than doing anything specific to stop it. But with new data from this study, we now have something that can be done. Patients have an option,” he said.
Dr. Goadsby explained that currently patients are not encouraged to use acute migraine medications such as triptans in the prodrome phase.
“There is actually no evidence that taking a triptan during the prodromal phase works. The advice is to take a triptan as soon as the headache starts, but not before the headache starts.”
He noted that there is also the problem of medication overuse that is seen with triptans, and most other medications used to treat acute migraine, which leads to medication overuse headache, “so we don’t like to encourage patients to increase the frequency of taking triptans for this reason.”
But ubrogepant and other members of the “gepant” class do not seem to have the propensity for medication overuse problems. “Rather, the more a patient takes the less likely they are to get a headache as these drugs also have a preventative effect,” Dr. Goadsby said.
Major Reduction in Severity
The PRODROME trial was conducted at 75 sites in the United States in 518 patients who had at least a 1-year history of migraine with or without aura and a history of two to eight migraine attacks per month with moderate to severe headache in each of the 3 months before study entry.
Participants underwent a rigorous screening period during which they were required to show that they could identify prodromal symptoms that were reliably followed by migraine headache within 1-6 hours.
They were randomly assigned to receive either placebo to treat the first qualifying prodrome event and ubrogepant 100 mg to treat the second qualifying prodrome event or vice versa, with instructions to take the study drug at the onset of the prodrome event.
Efficacy assessments during the double-blind treatment period were recorded by the participant in an electronic diary. On identifying a qualifying prodrome, the patient recorded prodromal symptoms, and was then required to report the absence or presence of a headache at regular intervals up to 48 hours after the study drug dose. If a headache was reported, participants rated the intensity as mild, moderate, or severe and reported whether rescue medication was taken to treat it.
The primary endpoint was absence of moderate or severe intensity headache within 24 hours after study-drug dose. This occurred after 46% of 418 qualifying prodrome events that had been treated with ubrogepant and after 29% of 423 qualifying prodrome events that had been treated with placebo (odds ratio, 2.09; 95% CI, 1.63 - 2.69; P < .0001).
“The incidence of moderate to severe headache was almost halved when ubrogepant was taken in the prodrome,” Dr. Goadsby reported.
Ubrogepant also showed similar impressive results for the secondary endpoints in the absence of moderate to severe headache within 48 hours post-dose and the absence of any headache of any intensity at 24 hours.
Little to No Disability
The researchers also evaluated functional ability, and more participants reported “no disability or able to function normally” during the 24 hours after treatment with ubrogepant than after placebo (OR, 1.66; P < .0001).
Other findings showed that the prodromal symptoms themselves, such as light sensitivity and cognitive dysfunction, were also reduced with ubrogepant.
Dr. Goadsby said he was pleased but not surprised by the results, as the “gepant” class of drugs are used in both the acute treatment of migraine and as preventive agents, although different agents have been approved for different indications in this regard.
“The ‘gepants’ are a class of medication that can be used in almost any way in migraine — to treat an acute migraine headache, to prevent migraine if taken chronically, and now we see that they can also stop a migraine from developing if taken during the initial prodromal phase. That’s unique for a migraine medication,” he said.
While the current study was conducted with ubrogepant, Dr. Goadsby suspects that any of the “gepants” would probably have a similar effect.
He noted that the prodromal phase of migraine has only just started to be explored, with functional imaging studies showing that structural brain changes occur during this phase.
Dr. Goadsby said the current study opens up a whole new area of interest, emphasizing the clinical value of identifying the prodrome in individuals with migraine, better characterizing the symptomology of the prodrome and understanding more about how to treat it.
“It’s the ultimate way of treating migraine early, and by taking this type of medication in the prodromal phase, patients may be able to stop having pain. That’s quite an implication,” he concluded.
The PRODROME study was funded by AbbVie. Dr. Goadsby reports personal fees from AbbVie.
A version of this article appeared on Medscape.com.
BARCELONA, SPAIN — In the randomized, placebo-controlled crossover PRODROME trial, treatment with ubrogepant (Ubrelvy) 100 mg, one of the new CGRP receptor antagonists, during the prodrome prevented the development of moderate/severe headache at both 24 hours and 48 hours post-dose. The medication also reduced headache of any intensity within 24 hours and functional disability compared with placebo.
“This represents a totally different way of treating a migraine attack – to treat it before the headache starts. This is a paradigm shift in the way we approach the acute treatment of migraine,” study investigator Peter Goadsby, MBBS, MD, PhD, professor of neurology at Kings College London, UK, said in an interview.
The findings were presented at 17th European Headache Congress (EHC) and were also recently published online in The Lancet.
A New Way to Manage Migraine?
The prodrome is usually the earliest phase of a migraine attack and is believed to be experienced by the vast majority of patients with migraine. It consists of various symptoms, including sensitivity to light, fatigue, mood changes, cognitive dysfunction, craving certain foods, and neck pain, which can occur several hours or days before onset.
Dr. Goadsby notes that, at present, there isn’t very much a patient can do about the prodrome.
“We advise patients if they feel an attack is coming not to do anything that might make it worse and make sure they have their acute treatment available for when the headache phase starts. So, we just advise people to prepare for the attack rather than doing anything specific to stop it. But with new data from this study, we now have something that can be done. Patients have an option,” he said.
Dr. Goadsby explained that currently patients are not encouraged to use acute migraine medications such as triptans in the prodrome phase.
“There is actually no evidence that taking a triptan during the prodromal phase works. The advice is to take a triptan as soon as the headache starts, but not before the headache starts.”
He noted that there is also the problem of medication overuse that is seen with triptans, and most other medications used to treat acute migraine, which leads to medication overuse headache, “so we don’t like to encourage patients to increase the frequency of taking triptans for this reason.”
But ubrogepant and other members of the “gepant” class do not seem to have the propensity for medication overuse problems. “Rather, the more a patient takes the less likely they are to get a headache as these drugs also have a preventative effect,” Dr. Goadsby said.
Major Reduction in Severity
The PRODROME trial was conducted at 75 sites in the United States in 518 patients who had at least a 1-year history of migraine with or without aura and a history of two to eight migraine attacks per month with moderate to severe headache in each of the 3 months before study entry.
Participants underwent a rigorous screening period during which they were required to show that they could identify prodromal symptoms that were reliably followed by migraine headache within 1-6 hours.
They were randomly assigned to receive either placebo to treat the first qualifying prodrome event and ubrogepant 100 mg to treat the second qualifying prodrome event or vice versa, with instructions to take the study drug at the onset of the prodrome event.
Efficacy assessments during the double-blind treatment period were recorded by the participant in an electronic diary. On identifying a qualifying prodrome, the patient recorded prodromal symptoms, and was then required to report the absence or presence of a headache at regular intervals up to 48 hours after the study drug dose. If a headache was reported, participants rated the intensity as mild, moderate, or severe and reported whether rescue medication was taken to treat it.
The primary endpoint was absence of moderate or severe intensity headache within 24 hours after study-drug dose. This occurred after 46% of 418 qualifying prodrome events that had been treated with ubrogepant and after 29% of 423 qualifying prodrome events that had been treated with placebo (odds ratio, 2.09; 95% CI, 1.63 - 2.69; P < .0001).
“The incidence of moderate to severe headache was almost halved when ubrogepant was taken in the prodrome,” Dr. Goadsby reported.
Ubrogepant also showed similar impressive results for the secondary endpoints in the absence of moderate to severe headache within 48 hours post-dose and the absence of any headache of any intensity at 24 hours.
Little to No Disability
The researchers also evaluated functional ability, and more participants reported “no disability or able to function normally” during the 24 hours after treatment with ubrogepant than after placebo (OR, 1.66; P < .0001).
Other findings showed that the prodromal symptoms themselves, such as light sensitivity and cognitive dysfunction, were also reduced with ubrogepant.
Dr. Goadsby said he was pleased but not surprised by the results, as the “gepant” class of drugs are used in both the acute treatment of migraine and as preventive agents, although different agents have been approved for different indications in this regard.
“The ‘gepants’ are a class of medication that can be used in almost any way in migraine — to treat an acute migraine headache, to prevent migraine if taken chronically, and now we see that they can also stop a migraine from developing if taken during the initial prodromal phase. That’s unique for a migraine medication,” he said.
While the current study was conducted with ubrogepant, Dr. Goadsby suspects that any of the “gepants” would probably have a similar effect.
He noted that the prodromal phase of migraine has only just started to be explored, with functional imaging studies showing that structural brain changes occur during this phase.
Dr. Goadsby said the current study opens up a whole new area of interest, emphasizing the clinical value of identifying the prodrome in individuals with migraine, better characterizing the symptomology of the prodrome and understanding more about how to treat it.
“It’s the ultimate way of treating migraine early, and by taking this type of medication in the prodromal phase, patients may be able to stop having pain. That’s quite an implication,” he concluded.
The PRODROME study was funded by AbbVie. Dr. Goadsby reports personal fees from AbbVie.
A version of this article appeared on Medscape.com.
BARCELONA, SPAIN — In the randomized, placebo-controlled crossover PRODROME trial, treatment with ubrogepant (Ubrelvy) 100 mg, one of the new CGRP receptor antagonists, during the prodrome prevented the development of moderate/severe headache at both 24 hours and 48 hours post-dose. The medication also reduced headache of any intensity within 24 hours and functional disability compared with placebo.
“This represents a totally different way of treating a migraine attack – to treat it before the headache starts. This is a paradigm shift in the way we approach the acute treatment of migraine,” study investigator Peter Goadsby, MBBS, MD, PhD, professor of neurology at Kings College London, UK, said in an interview.
The findings were presented at 17th European Headache Congress (EHC) and were also recently published online in The Lancet.
A New Way to Manage Migraine?
The prodrome is usually the earliest phase of a migraine attack and is believed to be experienced by the vast majority of patients with migraine. It consists of various symptoms, including sensitivity to light, fatigue, mood changes, cognitive dysfunction, craving certain foods, and neck pain, which can occur several hours or days before onset.
Dr. Goadsby notes that, at present, there isn’t very much a patient can do about the prodrome.
“We advise patients if they feel an attack is coming not to do anything that might make it worse and make sure they have their acute treatment available for when the headache phase starts. So, we just advise people to prepare for the attack rather than doing anything specific to stop it. But with new data from this study, we now have something that can be done. Patients have an option,” he said.
Dr. Goadsby explained that currently patients are not encouraged to use acute migraine medications such as triptans in the prodrome phase.
“There is actually no evidence that taking a triptan during the prodromal phase works. The advice is to take a triptan as soon as the headache starts, but not before the headache starts.”
He noted that there is also the problem of medication overuse that is seen with triptans, and most other medications used to treat acute migraine, which leads to medication overuse headache, “so we don’t like to encourage patients to increase the frequency of taking triptans for this reason.”
But ubrogepant and other members of the “gepant” class do not seem to have the propensity for medication overuse problems. “Rather, the more a patient takes the less likely they are to get a headache as these drugs also have a preventative effect,” Dr. Goadsby said.
Major Reduction in Severity
The PRODROME trial was conducted at 75 sites in the United States in 518 patients who had at least a 1-year history of migraine with or without aura and a history of two to eight migraine attacks per month with moderate to severe headache in each of the 3 months before study entry.
Participants underwent a rigorous screening period during which they were required to show that they could identify prodromal symptoms that were reliably followed by migraine headache within 1-6 hours.
They were randomly assigned to receive either placebo to treat the first qualifying prodrome event and ubrogepant 100 mg to treat the second qualifying prodrome event or vice versa, with instructions to take the study drug at the onset of the prodrome event.
Efficacy assessments during the double-blind treatment period were recorded by the participant in an electronic diary. On identifying a qualifying prodrome, the patient recorded prodromal symptoms, and was then required to report the absence or presence of a headache at regular intervals up to 48 hours after the study drug dose. If a headache was reported, participants rated the intensity as mild, moderate, or severe and reported whether rescue medication was taken to treat it.
The primary endpoint was absence of moderate or severe intensity headache within 24 hours after study-drug dose. This occurred after 46% of 418 qualifying prodrome events that had been treated with ubrogepant and after 29% of 423 qualifying prodrome events that had been treated with placebo (odds ratio, 2.09; 95% CI, 1.63 - 2.69; P < .0001).
“The incidence of moderate to severe headache was almost halved when ubrogepant was taken in the prodrome,” Dr. Goadsby reported.
Ubrogepant also showed similar impressive results for the secondary endpoints in the absence of moderate to severe headache within 48 hours post-dose and the absence of any headache of any intensity at 24 hours.
Little to No Disability
The researchers also evaluated functional ability, and more participants reported “no disability or able to function normally” during the 24 hours after treatment with ubrogepant than after placebo (OR, 1.66; P < .0001).
Other findings showed that the prodromal symptoms themselves, such as light sensitivity and cognitive dysfunction, were also reduced with ubrogepant.
Dr. Goadsby said he was pleased but not surprised by the results, as the “gepant” class of drugs are used in both the acute treatment of migraine and as preventive agents, although different agents have been approved for different indications in this regard.
“The ‘gepants’ are a class of medication that can be used in almost any way in migraine — to treat an acute migraine headache, to prevent migraine if taken chronically, and now we see that they can also stop a migraine from developing if taken during the initial prodromal phase. That’s unique for a migraine medication,” he said.
While the current study was conducted with ubrogepant, Dr. Goadsby suspects that any of the “gepants” would probably have a similar effect.
He noted that the prodromal phase of migraine has only just started to be explored, with functional imaging studies showing that structural brain changes occur during this phase.
Dr. Goadsby said the current study opens up a whole new area of interest, emphasizing the clinical value of identifying the prodrome in individuals with migraine, better characterizing the symptomology of the prodrome and understanding more about how to treat it.
“It’s the ultimate way of treating migraine early, and by taking this type of medication in the prodromal phase, patients may be able to stop having pain. That’s quite an implication,” he concluded.
The PRODROME study was funded by AbbVie. Dr. Goadsby reports personal fees from AbbVie.
A version of this article appeared on Medscape.com.
FROM EHC 2023
New cardiology certification board: What’s the plan?
The proposal by the major cardiovascular societies in the US to form a new board of cardiovascular medicine to manage initial and ongoing certification of cardiologists represents something of a revolution in the field of continuing medical education and assessment of competency.
Five US cardiovascular societies — the American College of Cardiology (ACC), the American Heart Association (AHA), the Heart Failure Society of America (HFSA), the Heart Rhythm Society (HRS), and the Society for Cardiovascular Angiography & Interventions (SCAI) — have now joined forces to propose a new professional certification board for cardiovascular medicine, to be known as the American Board of Cardiovascular Medicine (ABCVM).
The ABCVM would be independent of the American Board of Internal Medicine (ABIM), the current organization providing maintenance of certification for cardiologists as well as many other internal medicine subspecialties. The ABIM’s maintenance of certification process has been widely criticized for many years and has been described as “needlessly burdensome and expensive.”
, according to Jeffrey Kuvin, MD, a trustee of the ACC, who has been heading up the working group to develop this plan.
Dr. Kuvin, who is chair of the cardiology at Northwell Health, Manhasset, New York, a large academic healthcare system, explained that maintenance of certification has been a topic of discussion across the cardiovascular community for many years, and the ACC has a working group focused on the next steps for evaluation of competency, which he chairs.
“The topic of evaluation of competence has been on the mind of the ACC for many years and hence a work group was developed to focus on this,” Dr. Kuvin noted. “A lot of evolution of the concepts and next steps have been drawn out of this working group. And now other cardiovascular societies have joined to show unification across the house of cardiology and that this is indeed the way that the cardiovascular profession should move.”
“Time to Separate from Internal Medicine”
The general concept behind the new cardiology board is to separate cardiology from the ABIM.
“This is rooted from the concept that cardiology has evolved so much over the last few decades into such a large multidimensional specialty that it really does demarcate itself from internal medicine, and as such, it deserves a separate board governed by cardiologists with collaboration across the entirely of cardiology,” Dr. Kuvin said.
Cardiology has had significant growth and expansion of technology, tools, medications, and the approach to patients in many specialities and subspecialties, he added. “We have defined training programs in many different areas within cardiology; we have our own guidelines, our own competency statements, and in many cases, cardiology exists as its own department outside of medicine in many institutions. It’s just time to separate cardiology from the umbrella of internal medicine.”
The new cardiology board would be separate from, and not report to, the ABIM; rather, it would report directly to the American Board of Medical Specialties (ABMS), the only recognized medical certification body in the US.
What Are the Proposed Changes
Under the present system, managed by the ABIM, clinicians must undergo two stages of certification to be a cardiologist. First, they have to pass the initial certification exam in general cardiology, and then exams in one of four subspecialties if they plan to enter one of these, including interventional cardiology, electrophysiology, advanced heart failure or adult congenital heart disease.
Next, clinicians enter the maintenance of certification phase, which can take three different forms: 1) taking another recertification exam every 10 years; 2) the collaborative maintenance pathway — a collaboration between ACC and ABIM, which includes evaluation, learning and a certified exam each year; or 3) longitudinal knowledge and assessment — in which the program interacts with the clinician on an ongoing basis, sending secured questions regularly.
All three of these pathways for maintenance of certification involve high stakes questions and a set bar for passing or failing.
Under the proposed new cardiology board, an initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured, with the new approach taking the form of continuous learning and assessment of competency.
“This is an iterative process, but we envision with a new American Board of Cardiovascular Medicine, we will pick up where the ABIM left off,” Dr. Kuvin notes. “That includes an initial certifying examination for the five areas that already exist under the ABIM system but with the opportunities to expand that to further specialties as well.”
He points out that there are several areas in cardiology that are currently not represented by these five areas that warrant some discussion, including multimodality imaging, vascular heart disease, and cardio-oncology.
“At present, everybody has to pass the general cardiology exam and then some may wish to further train and get certified in one of the other four other specific areas. But one topic that has been discussed over many years is how do we maintain competency in the areas in which clinicians practice over their lifetime as a cardiologist,” Dr. Kuvin commented.
He said the proposed cardiology board would like to adhere to some basic principles that are fundamental to the practice of medicine.
“We want to make sure that we are practicing medicine so that our patients derive the most benefit from seeing a cardiologist,” he said. “We also want to make sure, however, that this is a supportive process, supporting cardiologists to learn what they know and more importantly what they don’t know; to identify knowledge gaps in specific area; to help the cardiologist fill those knowledge gaps; to acknowledge those gaps have been filled; and then move on to another area of interest. This will be the focus of this new and improved model of continuous competency.”
The proposed new board also says it wants to make sure this is appropriate to the area in which the clinician is practicing.
“To take a closed book certified exam every 10 years on the world of cardiology as happens at the current time – or the assessments conducted in the other two pathways – is often meaningless to the cardiologist,” Dr. Kuvin says. “All three current pathways involve high stakes questions that are often irrelevant to one’s clinical practice.”
Lifelong Learning
“The crux of the changes we are proposing will be away from the focus of passing a test towards a model of helping the individual with their competency, with continuous learning and evaluation of competency to help the clinician fill in their knowledge gaps,” he explains.
He described the new approach as “lifelong learning,” adding that, instead of it being “a punitive pass/fail environment with no feedback, which causes a lot of discontent among clinicians,” it will be a supportive process, where a clinician will be helped in filling their knowledge gaps.
“I think this would be a welcome change not just for cardiology but across medical specialties,” Dr. Kuvin said.
He also pointed out the ABMS itself is considering a continuous competency approach, and the proposed new cardiology board aims to work with the ABMS to make sure that their goals of continuous competency assessment are matched.
“The world has changed. The ability to access information has changed. It is no longer imperative for a clinician to have every piece of knowledge in their brain, but rather to know how to get knowledge and to incorporate that knowledge into clinical practice,” Dr. Kuvin noted. “Competency should not involve knowledge alone as in a closed book exam. It is more about understanding the world that we live in, how to synthesize information, where we need to improve knowledge and how to do that.”
Dr. Kuvin acknowledged that asking clinicians questions is a very helpful tool to identify their knowledge base and their knowledge gaps. “But we believe the clinician needs to be given resources — that could be a conference, an article, a simulation — to fill that knowledge gap. Then we could ask clinicians some different questions and if they get those right then we have provided a service.”
Tactile skills for cardiologists needing to perform procedures – such as interventionalists or electrophysiologists may be incorporated by simulation in a technology-based scenario.
On how often these assessments would take place, Dr. Kuvin said that hadn’t been decided for sure.
“We certainly do not think an assessment every 10 years is appropriate. We envision, instead of an episodic model, it will be rather a lifelong journey of education and competency. This will involve frequent contact and making sure knowledge gaps are being filled. There are criteria being set out by the ABMS that there should be a certain number of touch points with individuals on an annual as well as a 5-year basis to make sure cardiologists are staying within specific guardrails. The exact nature of these is yet to be determined,” he said.
Dr. Kuvin added that it was not known yet what sort of hours would be required but added that “this will not be a significant time burden.”
What is the Timeframe?
The application to the ABMS for a separate cardiology board is still ongoing and has not yet received formal acceptance. Representatives from the five US cardiovascular societies are in the initial stages of formulating a transition board.
“The submission to the ABMS will take time for them to review. This could take up to a year or so,” Dr. Kuvin estimates.
This is the first time the ABMS has entertained the concept of a new board in many years, he noted. “It will be a paradigm shift for the whole country. I think that cardiology is really at the forefront and in a position where we can actually do this. If cardiovascular medicine is granted a new board, I think this will help change the approach of how physicians are assessed in terms of continuous competency not just in cardiology but across all specialties of medicine.”
He added: “We are confident that we can work within the construct of the ABMS guidelines that have been revised to be much more holistic in the approach of continuous competence across the board. This includes thinking beyond rote medical knowledge and thinking about the clinician as a whole and their abilities to communicate, act professionally, work within a complex medical system, utilize medical resources effectively. These all have to be part of continuous competence.”
How Much Will This Cost?
Noting that the ABIM has received criticism over the costs of the certification process, Dr. Kuvin said they intend to make this “as lean a machine as possible with the focus on reducing the financial [burden] as well as the time burden for cardiologists. It is very important that this is not cumbersome, that it is woven into clinical practice, and that it is not costly.”
But he pointed out that building a new board will have significant costs.
“We have to think about developing initial board certification examinations as well as changing the paradigm on continuous certification,” he said. “This will take some up-front costs, and our society partners have decided that they are willing to provide some start-up funds for this. We anticipate the initial certification will remain somewhat similar in price, but the cost of ongoing continuous competency assessment will be significantly reduced compared to today’s models.”
Dr. Kuvin said the collaboration of the five participating US cardiovascular societies was unprecedented. But he noted that while the transition board is beginning with representatives of these individual societies, it will ultimately be independent from these societies and have its own board of directors.
He suggested that other societies representing other parts of cardiology are also interested. “Cardiology has recognized how important this is,” he said. “Everybody is excited about this.”
A version of this article appeared on Medscape.com.
The proposal by the major cardiovascular societies in the US to form a new board of cardiovascular medicine to manage initial and ongoing certification of cardiologists represents something of a revolution in the field of continuing medical education and assessment of competency.
Five US cardiovascular societies — the American College of Cardiology (ACC), the American Heart Association (AHA), the Heart Failure Society of America (HFSA), the Heart Rhythm Society (HRS), and the Society for Cardiovascular Angiography & Interventions (SCAI) — have now joined forces to propose a new professional certification board for cardiovascular medicine, to be known as the American Board of Cardiovascular Medicine (ABCVM).
The ABCVM would be independent of the American Board of Internal Medicine (ABIM), the current organization providing maintenance of certification for cardiologists as well as many other internal medicine subspecialties. The ABIM’s maintenance of certification process has been widely criticized for many years and has been described as “needlessly burdensome and expensive.”
, according to Jeffrey Kuvin, MD, a trustee of the ACC, who has been heading up the working group to develop this plan.
Dr. Kuvin, who is chair of the cardiology at Northwell Health, Manhasset, New York, a large academic healthcare system, explained that maintenance of certification has been a topic of discussion across the cardiovascular community for many years, and the ACC has a working group focused on the next steps for evaluation of competency, which he chairs.
“The topic of evaluation of competence has been on the mind of the ACC for many years and hence a work group was developed to focus on this,” Dr. Kuvin noted. “A lot of evolution of the concepts and next steps have been drawn out of this working group. And now other cardiovascular societies have joined to show unification across the house of cardiology and that this is indeed the way that the cardiovascular profession should move.”
“Time to Separate from Internal Medicine”
The general concept behind the new cardiology board is to separate cardiology from the ABIM.
“This is rooted from the concept that cardiology has evolved so much over the last few decades into such a large multidimensional specialty that it really does demarcate itself from internal medicine, and as such, it deserves a separate board governed by cardiologists with collaboration across the entirely of cardiology,” Dr. Kuvin said.
Cardiology has had significant growth and expansion of technology, tools, medications, and the approach to patients in many specialities and subspecialties, he added. “We have defined training programs in many different areas within cardiology; we have our own guidelines, our own competency statements, and in many cases, cardiology exists as its own department outside of medicine in many institutions. It’s just time to separate cardiology from the umbrella of internal medicine.”
The new cardiology board would be separate from, and not report to, the ABIM; rather, it would report directly to the American Board of Medical Specialties (ABMS), the only recognized medical certification body in the US.
What Are the Proposed Changes
Under the present system, managed by the ABIM, clinicians must undergo two stages of certification to be a cardiologist. First, they have to pass the initial certification exam in general cardiology, and then exams in one of four subspecialties if they plan to enter one of these, including interventional cardiology, electrophysiology, advanced heart failure or adult congenital heart disease.
Next, clinicians enter the maintenance of certification phase, which can take three different forms: 1) taking another recertification exam every 10 years; 2) the collaborative maintenance pathway — a collaboration between ACC and ABIM, which includes evaluation, learning and a certified exam each year; or 3) longitudinal knowledge and assessment — in which the program interacts with the clinician on an ongoing basis, sending secured questions regularly.
All three of these pathways for maintenance of certification involve high stakes questions and a set bar for passing or failing.
Under the proposed new cardiology board, an initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured, with the new approach taking the form of continuous learning and assessment of competency.
“This is an iterative process, but we envision with a new American Board of Cardiovascular Medicine, we will pick up where the ABIM left off,” Dr. Kuvin notes. “That includes an initial certifying examination for the five areas that already exist under the ABIM system but with the opportunities to expand that to further specialties as well.”
He points out that there are several areas in cardiology that are currently not represented by these five areas that warrant some discussion, including multimodality imaging, vascular heart disease, and cardio-oncology.
“At present, everybody has to pass the general cardiology exam and then some may wish to further train and get certified in one of the other four other specific areas. But one topic that has been discussed over many years is how do we maintain competency in the areas in which clinicians practice over their lifetime as a cardiologist,” Dr. Kuvin commented.
He said the proposed cardiology board would like to adhere to some basic principles that are fundamental to the practice of medicine.
“We want to make sure that we are practicing medicine so that our patients derive the most benefit from seeing a cardiologist,” he said. “We also want to make sure, however, that this is a supportive process, supporting cardiologists to learn what they know and more importantly what they don’t know; to identify knowledge gaps in specific area; to help the cardiologist fill those knowledge gaps; to acknowledge those gaps have been filled; and then move on to another area of interest. This will be the focus of this new and improved model of continuous competency.”
The proposed new board also says it wants to make sure this is appropriate to the area in which the clinician is practicing.
“To take a closed book certified exam every 10 years on the world of cardiology as happens at the current time – or the assessments conducted in the other two pathways – is often meaningless to the cardiologist,” Dr. Kuvin says. “All three current pathways involve high stakes questions that are often irrelevant to one’s clinical practice.”
Lifelong Learning
“The crux of the changes we are proposing will be away from the focus of passing a test towards a model of helping the individual with their competency, with continuous learning and evaluation of competency to help the clinician fill in their knowledge gaps,” he explains.
He described the new approach as “lifelong learning,” adding that, instead of it being “a punitive pass/fail environment with no feedback, which causes a lot of discontent among clinicians,” it will be a supportive process, where a clinician will be helped in filling their knowledge gaps.
“I think this would be a welcome change not just for cardiology but across medical specialties,” Dr. Kuvin said.
He also pointed out the ABMS itself is considering a continuous competency approach, and the proposed new cardiology board aims to work with the ABMS to make sure that their goals of continuous competency assessment are matched.
“The world has changed. The ability to access information has changed. It is no longer imperative for a clinician to have every piece of knowledge in their brain, but rather to know how to get knowledge and to incorporate that knowledge into clinical practice,” Dr. Kuvin noted. “Competency should not involve knowledge alone as in a closed book exam. It is more about understanding the world that we live in, how to synthesize information, where we need to improve knowledge and how to do that.”
Dr. Kuvin acknowledged that asking clinicians questions is a very helpful tool to identify their knowledge base and their knowledge gaps. “But we believe the clinician needs to be given resources — that could be a conference, an article, a simulation — to fill that knowledge gap. Then we could ask clinicians some different questions and if they get those right then we have provided a service.”
Tactile skills for cardiologists needing to perform procedures – such as interventionalists or electrophysiologists may be incorporated by simulation in a technology-based scenario.
On how often these assessments would take place, Dr. Kuvin said that hadn’t been decided for sure.
“We certainly do not think an assessment every 10 years is appropriate. We envision, instead of an episodic model, it will be rather a lifelong journey of education and competency. This will involve frequent contact and making sure knowledge gaps are being filled. There are criteria being set out by the ABMS that there should be a certain number of touch points with individuals on an annual as well as a 5-year basis to make sure cardiologists are staying within specific guardrails. The exact nature of these is yet to be determined,” he said.
Dr. Kuvin added that it was not known yet what sort of hours would be required but added that “this will not be a significant time burden.”
What is the Timeframe?
The application to the ABMS for a separate cardiology board is still ongoing and has not yet received formal acceptance. Representatives from the five US cardiovascular societies are in the initial stages of formulating a transition board.
“The submission to the ABMS will take time for them to review. This could take up to a year or so,” Dr. Kuvin estimates.
This is the first time the ABMS has entertained the concept of a new board in many years, he noted. “It will be a paradigm shift for the whole country. I think that cardiology is really at the forefront and in a position where we can actually do this. If cardiovascular medicine is granted a new board, I think this will help change the approach of how physicians are assessed in terms of continuous competency not just in cardiology but across all specialties of medicine.”
He added: “We are confident that we can work within the construct of the ABMS guidelines that have been revised to be much more holistic in the approach of continuous competence across the board. This includes thinking beyond rote medical knowledge and thinking about the clinician as a whole and their abilities to communicate, act professionally, work within a complex medical system, utilize medical resources effectively. These all have to be part of continuous competence.”
How Much Will This Cost?
Noting that the ABIM has received criticism over the costs of the certification process, Dr. Kuvin said they intend to make this “as lean a machine as possible with the focus on reducing the financial [burden] as well as the time burden for cardiologists. It is very important that this is not cumbersome, that it is woven into clinical practice, and that it is not costly.”
But he pointed out that building a new board will have significant costs.
“We have to think about developing initial board certification examinations as well as changing the paradigm on continuous certification,” he said. “This will take some up-front costs, and our society partners have decided that they are willing to provide some start-up funds for this. We anticipate the initial certification will remain somewhat similar in price, but the cost of ongoing continuous competency assessment will be significantly reduced compared to today’s models.”
Dr. Kuvin said the collaboration of the five participating US cardiovascular societies was unprecedented. But he noted that while the transition board is beginning with representatives of these individual societies, it will ultimately be independent from these societies and have its own board of directors.
He suggested that other societies representing other parts of cardiology are also interested. “Cardiology has recognized how important this is,” he said. “Everybody is excited about this.”
A version of this article appeared on Medscape.com.
The proposal by the major cardiovascular societies in the US to form a new board of cardiovascular medicine to manage initial and ongoing certification of cardiologists represents something of a revolution in the field of continuing medical education and assessment of competency.
Five US cardiovascular societies — the American College of Cardiology (ACC), the American Heart Association (AHA), the Heart Failure Society of America (HFSA), the Heart Rhythm Society (HRS), and the Society for Cardiovascular Angiography & Interventions (SCAI) — have now joined forces to propose a new professional certification board for cardiovascular medicine, to be known as the American Board of Cardiovascular Medicine (ABCVM).
The ABCVM would be independent of the American Board of Internal Medicine (ABIM), the current organization providing maintenance of certification for cardiologists as well as many other internal medicine subspecialties. The ABIM’s maintenance of certification process has been widely criticized for many years and has been described as “needlessly burdensome and expensive.”
, according to Jeffrey Kuvin, MD, a trustee of the ACC, who has been heading up the working group to develop this plan.
Dr. Kuvin, who is chair of the cardiology at Northwell Health, Manhasset, New York, a large academic healthcare system, explained that maintenance of certification has been a topic of discussion across the cardiovascular community for many years, and the ACC has a working group focused on the next steps for evaluation of competency, which he chairs.
“The topic of evaluation of competence has been on the mind of the ACC for many years and hence a work group was developed to focus on this,” Dr. Kuvin noted. “A lot of evolution of the concepts and next steps have been drawn out of this working group. And now other cardiovascular societies have joined to show unification across the house of cardiology and that this is indeed the way that the cardiovascular profession should move.”
“Time to Separate from Internal Medicine”
The general concept behind the new cardiology board is to separate cardiology from the ABIM.
“This is rooted from the concept that cardiology has evolved so much over the last few decades into such a large multidimensional specialty that it really does demarcate itself from internal medicine, and as such, it deserves a separate board governed by cardiologists with collaboration across the entirely of cardiology,” Dr. Kuvin said.
Cardiology has had significant growth and expansion of technology, tools, medications, and the approach to patients in many specialities and subspecialties, he added. “We have defined training programs in many different areas within cardiology; we have our own guidelines, our own competency statements, and in many cases, cardiology exists as its own department outside of medicine in many institutions. It’s just time to separate cardiology from the umbrella of internal medicine.”
The new cardiology board would be separate from, and not report to, the ABIM; rather, it would report directly to the American Board of Medical Specialties (ABMS), the only recognized medical certification body in the US.
What Are the Proposed Changes
Under the present system, managed by the ABIM, clinicians must undergo two stages of certification to be a cardiologist. First, they have to pass the initial certification exam in general cardiology, and then exams in one of four subspecialties if they plan to enter one of these, including interventional cardiology, electrophysiology, advanced heart failure or adult congenital heart disease.
Next, clinicians enter the maintenance of certification phase, which can take three different forms: 1) taking another recertification exam every 10 years; 2) the collaborative maintenance pathway — a collaboration between ACC and ABIM, which includes evaluation, learning and a certified exam each year; or 3) longitudinal knowledge and assessment — in which the program interacts with the clinician on an ongoing basis, sending secured questions regularly.
All three of these pathways for maintenance of certification involve high stakes questions and a set bar for passing or failing.
Under the proposed new cardiology board, an initial certification exam would still be required after fellowship training, but the maintenance of certification process would be completely restructured, with the new approach taking the form of continuous learning and assessment of competency.
“This is an iterative process, but we envision with a new American Board of Cardiovascular Medicine, we will pick up where the ABIM left off,” Dr. Kuvin notes. “That includes an initial certifying examination for the five areas that already exist under the ABIM system but with the opportunities to expand that to further specialties as well.”
He points out that there are several areas in cardiology that are currently not represented by these five areas that warrant some discussion, including multimodality imaging, vascular heart disease, and cardio-oncology.
“At present, everybody has to pass the general cardiology exam and then some may wish to further train and get certified in one of the other four other specific areas. But one topic that has been discussed over many years is how do we maintain competency in the areas in which clinicians practice over their lifetime as a cardiologist,” Dr. Kuvin commented.
He said the proposed cardiology board would like to adhere to some basic principles that are fundamental to the practice of medicine.
“We want to make sure that we are practicing medicine so that our patients derive the most benefit from seeing a cardiologist,” he said. “We also want to make sure, however, that this is a supportive process, supporting cardiologists to learn what they know and more importantly what they don’t know; to identify knowledge gaps in specific area; to help the cardiologist fill those knowledge gaps; to acknowledge those gaps have been filled; and then move on to another area of interest. This will be the focus of this new and improved model of continuous competency.”
The proposed new board also says it wants to make sure this is appropriate to the area in which the clinician is practicing.
“To take a closed book certified exam every 10 years on the world of cardiology as happens at the current time – or the assessments conducted in the other two pathways – is often meaningless to the cardiologist,” Dr. Kuvin says. “All three current pathways involve high stakes questions that are often irrelevant to one’s clinical practice.”
Lifelong Learning
“The crux of the changes we are proposing will be away from the focus of passing a test towards a model of helping the individual with their competency, with continuous learning and evaluation of competency to help the clinician fill in their knowledge gaps,” he explains.
He described the new approach as “lifelong learning,” adding that, instead of it being “a punitive pass/fail environment with no feedback, which causes a lot of discontent among clinicians,” it will be a supportive process, where a clinician will be helped in filling their knowledge gaps.
“I think this would be a welcome change not just for cardiology but across medical specialties,” Dr. Kuvin said.
He also pointed out the ABMS itself is considering a continuous competency approach, and the proposed new cardiology board aims to work with the ABMS to make sure that their goals of continuous competency assessment are matched.
“The world has changed. The ability to access information has changed. It is no longer imperative for a clinician to have every piece of knowledge in their brain, but rather to know how to get knowledge and to incorporate that knowledge into clinical practice,” Dr. Kuvin noted. “Competency should not involve knowledge alone as in a closed book exam. It is more about understanding the world that we live in, how to synthesize information, where we need to improve knowledge and how to do that.”
Dr. Kuvin acknowledged that asking clinicians questions is a very helpful tool to identify their knowledge base and their knowledge gaps. “But we believe the clinician needs to be given resources — that could be a conference, an article, a simulation — to fill that knowledge gap. Then we could ask clinicians some different questions and if they get those right then we have provided a service.”
Tactile skills for cardiologists needing to perform procedures – such as interventionalists or electrophysiologists may be incorporated by simulation in a technology-based scenario.
On how often these assessments would take place, Dr. Kuvin said that hadn’t been decided for sure.
“We certainly do not think an assessment every 10 years is appropriate. We envision, instead of an episodic model, it will be rather a lifelong journey of education and competency. This will involve frequent contact and making sure knowledge gaps are being filled. There are criteria being set out by the ABMS that there should be a certain number of touch points with individuals on an annual as well as a 5-year basis to make sure cardiologists are staying within specific guardrails. The exact nature of these is yet to be determined,” he said.
Dr. Kuvin added that it was not known yet what sort of hours would be required but added that “this will not be a significant time burden.”
What is the Timeframe?
The application to the ABMS for a separate cardiology board is still ongoing and has not yet received formal acceptance. Representatives from the five US cardiovascular societies are in the initial stages of formulating a transition board.
“The submission to the ABMS will take time for them to review. This could take up to a year or so,” Dr. Kuvin estimates.
This is the first time the ABMS has entertained the concept of a new board in many years, he noted. “It will be a paradigm shift for the whole country. I think that cardiology is really at the forefront and in a position where we can actually do this. If cardiovascular medicine is granted a new board, I think this will help change the approach of how physicians are assessed in terms of continuous competency not just in cardiology but across all specialties of medicine.”
He added: “We are confident that we can work within the construct of the ABMS guidelines that have been revised to be much more holistic in the approach of continuous competence across the board. This includes thinking beyond rote medical knowledge and thinking about the clinician as a whole and their abilities to communicate, act professionally, work within a complex medical system, utilize medical resources effectively. These all have to be part of continuous competence.”
How Much Will This Cost?
Noting that the ABIM has received criticism over the costs of the certification process, Dr. Kuvin said they intend to make this “as lean a machine as possible with the focus on reducing the financial [burden] as well as the time burden for cardiologists. It is very important that this is not cumbersome, that it is woven into clinical practice, and that it is not costly.”
But he pointed out that building a new board will have significant costs.
“We have to think about developing initial board certification examinations as well as changing the paradigm on continuous certification,” he said. “This will take some up-front costs, and our society partners have decided that they are willing to provide some start-up funds for this. We anticipate the initial certification will remain somewhat similar in price, but the cost of ongoing continuous competency assessment will be significantly reduced compared to today’s models.”
Dr. Kuvin said the collaboration of the five participating US cardiovascular societies was unprecedented. But he noted that while the transition board is beginning with representatives of these individual societies, it will ultimately be independent from these societies and have its own board of directors.
He suggested that other societies representing other parts of cardiology are also interested. “Cardiology has recognized how important this is,” he said. “Everybody is excited about this.”
A version of this article appeared on Medscape.com.
More evidence of better outcomes with 120–mm Hg BP target
Intensive lowering of blood pressure to a systolic target less than 120 mm Hg reduced cardiovascular events among individuals at high risk for cardiovascular disease, compared with standard treatment using a target less than 140 mm Hg in the ESPRIT trial.
a 39% lower cardiovascular mortality, and 21% lower all-cause mortality than the standard treatment targeting a systolic pressure below 140 mm Hg,” reported lead investigator, Jing Li, MD, PhD, director of the department of preventive medicine at the National Center for Cardiovascular Diseases in Beijing.
The trial included patients with diabetes and those with a history of stroke, two important groups that were excluded in the previous SPRINT trial of intensive BP lowering. Results suggested that the benefit of intensive BP lowering extends to these groups.
The results translate into the prevention of 14 major vascular events and 8 deaths for every 1,000 individuals are treated for 3 years to a target systolic pressure less than 120 mm Hg rather than less than 140 mm Hg, at the cost of an additional three patients experiencing the serious adverse event of syncope, Dr. Li said.
“Our study generates new evidence about benefit and safety of treatment targeting systolic blood pressure below 120 mm Hg among a diverse Asian population, which is generally consistent with those from other ethnicities. Implementing this intensive treatment strategy for high-risk adults has the potential to save more lives and reduce the public health burden of heart disease worldwide,” she concluded.
Dr. Li presented the ESPRIT trial at the annual scientific sessions of the American Heart Association.
The ESPRIT trial included 11,255 Chinese adults (average age, 64 years; 41% women) who had a baseline systolic BP measurement of 130-180 mm Hg (average was 147/83 mm Hg) and either established cardiovascular disease or at least two major risk factors for cardiovascular disease. Of those enrolled, 39% had diabetes, and 27% had a history of stroke.
They were randomly assigned to receive intensive BP treatment, with a systolic BP target less than 120 mm Hg, or standard treatment, with a target measurement less than 140 mm Hg, over a 3-year period. After 1 year, systolic pressure was lowered to 135.6 mm Hg in the standard care group and to 120.3 mm Hg in the intensive treatment group, with values remaining at around the same level for the remainder of the follow-up.
The primary outcome was a composite of myocardial infarction, coronary or noncoronary revascularization, hospitalization/ED visit for heart failure, stroke, or cardiovascular death.
After 3.4 years of follow-up, 624 primary outcome events had occurred in the standard arm (3.6%) versus 547 events in intensive arm (3.2%), a reduction of 12% (hazard ratio, 0.88; 95% confidence interval, 0.78-0.99). This gives a number needed to treat to prevent one event of 74.
Cardiovascular death occurred in 0.5% of the standard group versus 0.3% of the intensive group (HR 0.61; 95% CI, 0.44-0.84); and all-cause death occurred in 1.1% of the standard group versus 0.9% of the intensive group (HR, 0.79; 95% CI, 0.64-0.97).
The individual endpoints of MI, stroke, and heart failure showed positive trends to a reduction with intensive BP lowering, but these did not reach statistical significance.
In terms of serious adverse events, syncope was increased in the intensive group (0.4% vs 0.1%), but there were no significant differences in hypotension, electrolyte abnormality, falls resulting in an injury, acute kidney injury, or renal failure.
Should 120 mm Hg be new target?
Commenting on the study, Paul Whelton, MD, chair in global public health at Tulane University, New Orleans, said that the results were consistent with several other trials.
“When we look at meta-analysis of trials of different levels of blood pressure reduction, all the studies show the same thing – the lower the blood pressure, the better the outcome, with those starting at higher levels gaining the greatest the benefit of blood pressure reductions,” he noted.
“There are four trials that have looked at systolic targets of less than 120 mm Hg versus less than 140 mm Hg (SPRINT, ACCORD BP, RESPECT, and now ESPRIT), and when analyzed properly, they all show a similar benefit for cardiovascular outcomes with the lower 120 target,” said Dr. Whelton, who led the SPRINT trial.
“ESPRIT is a nicely done trial. It is reassuring because it is consistent with the other trials, in that it seems that the benefits are much greater than the risk of adverse effects,” he added.
Dr. Whelton pointed out that there are three more trials to come looking at this question, two in Brazil (one in individuals with diabetes and one in stroke survivors) and another trial in China in people with diabetes. “So, we will get more information from these.”
He said that guidelines committees will have to consider a lower systolic BP of 120 mm Hg as the optimal treatment target. In the United States, at present, the target is 130 mm Hg.
The current U.S. guidelines were based on the SPRINT trial, which showed a reduction in cardiovascular events in patients treated to a systolic target of 120 mm Hg versus 140 mm Hg.
Dr. Whelton, who was chair of the 2017 American College of Cardiology/American Heart Association hypertension guidelines committee, explained that, at the time the guidelines were written, there was only one trial, SPRINT, to base the evidence on.
“The committee could all comfortably agree on the 130 mm Hg target, but it was felt that there wasn’t enough evidence at the time to make a recommendation for 120 mm Hg,” he said. “But now we have four trials.”
He said that the trials included patients with high risk for cardiovascular disease, but they all brought some differences to the table, with ACCORD BP conducted in patients with diabetes; SPRINT having enrichment with African American patients, older adults, and patients with kidney disease; RESPECT was in stroke survivors; and ESPRIT had a mix of Chinese patients.
“I think we’ve got a nice mix of different participants and they’re all showing the same signal – that 120 mm Hg is better,” Dr. Whelton said.
But he stressed that although there is now good evidence in favor of lower BP targets, these findings were not being implemented in clinical practice.
“We are doing very badly in terms of implementation. There is a big gap between science and what’s happening in the real world.”
Dr. Whelton pointed out that only 30% of patients in high-income countries are controlled to the 140/90 target and that in low- and middle-income countries, only 8.8% get to that level, never mind lower targets. “The next job is to work on implementing these findings.”
He noted that several studies have shown better results in this regard using a team approach, with nonphysicians playing a major role in following up with patients.
A version of this article appeared on Medscape.com.
Intensive lowering of blood pressure to a systolic target less than 120 mm Hg reduced cardiovascular events among individuals at high risk for cardiovascular disease, compared with standard treatment using a target less than 140 mm Hg in the ESPRIT trial.
a 39% lower cardiovascular mortality, and 21% lower all-cause mortality than the standard treatment targeting a systolic pressure below 140 mm Hg,” reported lead investigator, Jing Li, MD, PhD, director of the department of preventive medicine at the National Center for Cardiovascular Diseases in Beijing.
The trial included patients with diabetes and those with a history of stroke, two important groups that were excluded in the previous SPRINT trial of intensive BP lowering. Results suggested that the benefit of intensive BP lowering extends to these groups.
The results translate into the prevention of 14 major vascular events and 8 deaths for every 1,000 individuals are treated for 3 years to a target systolic pressure less than 120 mm Hg rather than less than 140 mm Hg, at the cost of an additional three patients experiencing the serious adverse event of syncope, Dr. Li said.
“Our study generates new evidence about benefit and safety of treatment targeting systolic blood pressure below 120 mm Hg among a diverse Asian population, which is generally consistent with those from other ethnicities. Implementing this intensive treatment strategy for high-risk adults has the potential to save more lives and reduce the public health burden of heart disease worldwide,” she concluded.
Dr. Li presented the ESPRIT trial at the annual scientific sessions of the American Heart Association.
The ESPRIT trial included 11,255 Chinese adults (average age, 64 years; 41% women) who had a baseline systolic BP measurement of 130-180 mm Hg (average was 147/83 mm Hg) and either established cardiovascular disease or at least two major risk factors for cardiovascular disease. Of those enrolled, 39% had diabetes, and 27% had a history of stroke.
They were randomly assigned to receive intensive BP treatment, with a systolic BP target less than 120 mm Hg, or standard treatment, with a target measurement less than 140 mm Hg, over a 3-year period. After 1 year, systolic pressure was lowered to 135.6 mm Hg in the standard care group and to 120.3 mm Hg in the intensive treatment group, with values remaining at around the same level for the remainder of the follow-up.
The primary outcome was a composite of myocardial infarction, coronary or noncoronary revascularization, hospitalization/ED visit for heart failure, stroke, or cardiovascular death.
After 3.4 years of follow-up, 624 primary outcome events had occurred in the standard arm (3.6%) versus 547 events in intensive arm (3.2%), a reduction of 12% (hazard ratio, 0.88; 95% confidence interval, 0.78-0.99). This gives a number needed to treat to prevent one event of 74.
Cardiovascular death occurred in 0.5% of the standard group versus 0.3% of the intensive group (HR 0.61; 95% CI, 0.44-0.84); and all-cause death occurred in 1.1% of the standard group versus 0.9% of the intensive group (HR, 0.79; 95% CI, 0.64-0.97).
The individual endpoints of MI, stroke, and heart failure showed positive trends to a reduction with intensive BP lowering, but these did not reach statistical significance.
In terms of serious adverse events, syncope was increased in the intensive group (0.4% vs 0.1%), but there were no significant differences in hypotension, electrolyte abnormality, falls resulting in an injury, acute kidney injury, or renal failure.
Should 120 mm Hg be new target?
Commenting on the study, Paul Whelton, MD, chair in global public health at Tulane University, New Orleans, said that the results were consistent with several other trials.
“When we look at meta-analysis of trials of different levels of blood pressure reduction, all the studies show the same thing – the lower the blood pressure, the better the outcome, with those starting at higher levels gaining the greatest the benefit of blood pressure reductions,” he noted.
“There are four trials that have looked at systolic targets of less than 120 mm Hg versus less than 140 mm Hg (SPRINT, ACCORD BP, RESPECT, and now ESPRIT), and when analyzed properly, they all show a similar benefit for cardiovascular outcomes with the lower 120 target,” said Dr. Whelton, who led the SPRINT trial.
“ESPRIT is a nicely done trial. It is reassuring because it is consistent with the other trials, in that it seems that the benefits are much greater than the risk of adverse effects,” he added.
Dr. Whelton pointed out that there are three more trials to come looking at this question, two in Brazil (one in individuals with diabetes and one in stroke survivors) and another trial in China in people with diabetes. “So, we will get more information from these.”
He said that guidelines committees will have to consider a lower systolic BP of 120 mm Hg as the optimal treatment target. In the United States, at present, the target is 130 mm Hg.
The current U.S. guidelines were based on the SPRINT trial, which showed a reduction in cardiovascular events in patients treated to a systolic target of 120 mm Hg versus 140 mm Hg.
Dr. Whelton, who was chair of the 2017 American College of Cardiology/American Heart Association hypertension guidelines committee, explained that, at the time the guidelines were written, there was only one trial, SPRINT, to base the evidence on.
“The committee could all comfortably agree on the 130 mm Hg target, but it was felt that there wasn’t enough evidence at the time to make a recommendation for 120 mm Hg,” he said. “But now we have four trials.”
He said that the trials included patients with high risk for cardiovascular disease, but they all brought some differences to the table, with ACCORD BP conducted in patients with diabetes; SPRINT having enrichment with African American patients, older adults, and patients with kidney disease; RESPECT was in stroke survivors; and ESPRIT had a mix of Chinese patients.
“I think we’ve got a nice mix of different participants and they’re all showing the same signal – that 120 mm Hg is better,” Dr. Whelton said.
But he stressed that although there is now good evidence in favor of lower BP targets, these findings were not being implemented in clinical practice.
“We are doing very badly in terms of implementation. There is a big gap between science and what’s happening in the real world.”
Dr. Whelton pointed out that only 30% of patients in high-income countries are controlled to the 140/90 target and that in low- and middle-income countries, only 8.8% get to that level, never mind lower targets. “The next job is to work on implementing these findings.”
He noted that several studies have shown better results in this regard using a team approach, with nonphysicians playing a major role in following up with patients.
A version of this article appeared on Medscape.com.
Intensive lowering of blood pressure to a systolic target less than 120 mm Hg reduced cardiovascular events among individuals at high risk for cardiovascular disease, compared with standard treatment using a target less than 140 mm Hg in the ESPRIT trial.
a 39% lower cardiovascular mortality, and 21% lower all-cause mortality than the standard treatment targeting a systolic pressure below 140 mm Hg,” reported lead investigator, Jing Li, MD, PhD, director of the department of preventive medicine at the National Center for Cardiovascular Diseases in Beijing.
The trial included patients with diabetes and those with a history of stroke, two important groups that were excluded in the previous SPRINT trial of intensive BP lowering. Results suggested that the benefit of intensive BP lowering extends to these groups.
The results translate into the prevention of 14 major vascular events and 8 deaths for every 1,000 individuals are treated for 3 years to a target systolic pressure less than 120 mm Hg rather than less than 140 mm Hg, at the cost of an additional three patients experiencing the serious adverse event of syncope, Dr. Li said.
“Our study generates new evidence about benefit and safety of treatment targeting systolic blood pressure below 120 mm Hg among a diverse Asian population, which is generally consistent with those from other ethnicities. Implementing this intensive treatment strategy for high-risk adults has the potential to save more lives and reduce the public health burden of heart disease worldwide,” she concluded.
Dr. Li presented the ESPRIT trial at the annual scientific sessions of the American Heart Association.
The ESPRIT trial included 11,255 Chinese adults (average age, 64 years; 41% women) who had a baseline systolic BP measurement of 130-180 mm Hg (average was 147/83 mm Hg) and either established cardiovascular disease or at least two major risk factors for cardiovascular disease. Of those enrolled, 39% had diabetes, and 27% had a history of stroke.
They were randomly assigned to receive intensive BP treatment, with a systolic BP target less than 120 mm Hg, or standard treatment, with a target measurement less than 140 mm Hg, over a 3-year period. After 1 year, systolic pressure was lowered to 135.6 mm Hg in the standard care group and to 120.3 mm Hg in the intensive treatment group, with values remaining at around the same level for the remainder of the follow-up.
The primary outcome was a composite of myocardial infarction, coronary or noncoronary revascularization, hospitalization/ED visit for heart failure, stroke, or cardiovascular death.
After 3.4 years of follow-up, 624 primary outcome events had occurred in the standard arm (3.6%) versus 547 events in intensive arm (3.2%), a reduction of 12% (hazard ratio, 0.88; 95% confidence interval, 0.78-0.99). This gives a number needed to treat to prevent one event of 74.
Cardiovascular death occurred in 0.5% of the standard group versus 0.3% of the intensive group (HR 0.61; 95% CI, 0.44-0.84); and all-cause death occurred in 1.1% of the standard group versus 0.9% of the intensive group (HR, 0.79; 95% CI, 0.64-0.97).
The individual endpoints of MI, stroke, and heart failure showed positive trends to a reduction with intensive BP lowering, but these did not reach statistical significance.
In terms of serious adverse events, syncope was increased in the intensive group (0.4% vs 0.1%), but there were no significant differences in hypotension, electrolyte abnormality, falls resulting in an injury, acute kidney injury, or renal failure.
Should 120 mm Hg be new target?
Commenting on the study, Paul Whelton, MD, chair in global public health at Tulane University, New Orleans, said that the results were consistent with several other trials.
“When we look at meta-analysis of trials of different levels of blood pressure reduction, all the studies show the same thing – the lower the blood pressure, the better the outcome, with those starting at higher levels gaining the greatest the benefit of blood pressure reductions,” he noted.
“There are four trials that have looked at systolic targets of less than 120 mm Hg versus less than 140 mm Hg (SPRINT, ACCORD BP, RESPECT, and now ESPRIT), and when analyzed properly, they all show a similar benefit for cardiovascular outcomes with the lower 120 target,” said Dr. Whelton, who led the SPRINT trial.
“ESPRIT is a nicely done trial. It is reassuring because it is consistent with the other trials, in that it seems that the benefits are much greater than the risk of adverse effects,” he added.
Dr. Whelton pointed out that there are three more trials to come looking at this question, two in Brazil (one in individuals with diabetes and one in stroke survivors) and another trial in China in people with diabetes. “So, we will get more information from these.”
He said that guidelines committees will have to consider a lower systolic BP of 120 mm Hg as the optimal treatment target. In the United States, at present, the target is 130 mm Hg.
The current U.S. guidelines were based on the SPRINT trial, which showed a reduction in cardiovascular events in patients treated to a systolic target of 120 mm Hg versus 140 mm Hg.
Dr. Whelton, who was chair of the 2017 American College of Cardiology/American Heart Association hypertension guidelines committee, explained that, at the time the guidelines were written, there was only one trial, SPRINT, to base the evidence on.
“The committee could all comfortably agree on the 130 mm Hg target, but it was felt that there wasn’t enough evidence at the time to make a recommendation for 120 mm Hg,” he said. “But now we have four trials.”
He said that the trials included patients with high risk for cardiovascular disease, but they all brought some differences to the table, with ACCORD BP conducted in patients with diabetes; SPRINT having enrichment with African American patients, older adults, and patients with kidney disease; RESPECT was in stroke survivors; and ESPRIT had a mix of Chinese patients.
“I think we’ve got a nice mix of different participants and they’re all showing the same signal – that 120 mm Hg is better,” Dr. Whelton said.
But he stressed that although there is now good evidence in favor of lower BP targets, these findings were not being implemented in clinical practice.
“We are doing very badly in terms of implementation. There is a big gap between science and what’s happening in the real world.”
Dr. Whelton pointed out that only 30% of patients in high-income countries are controlled to the 140/90 target and that in low- and middle-income countries, only 8.8% get to that level, never mind lower targets. “The next job is to work on implementing these findings.”
He noted that several studies have shown better results in this regard using a team approach, with nonphysicians playing a major role in following up with patients.
A version of this article appeared on Medscape.com.
FROM AHA 2023
Single injection reduces blood pressure for 6 months: KARDIA-1
with what appeared to be an encouraging side-effect profile, in the phase 2 dose-ranging KARDIA-1 study.
“Our study demonstrates that either quarterly or biannual doses of zilebesiran can effectively and safely lower blood pressure in patients with uncontrolled hypertension,” said senior study investigator George Bakris, MD.
“Based on these results, zilebesiran has the potential to improve medication adherence, which will, in turn, reduce cardiovascular risk in people with hypertension,” added Dr. Bakris, who is professor of medicine and director of the Comprehensive Hypertension Center at the University of Chicago Medicine.
The KARDIA-1 study was presented at the American Heart Association scientific sessions.
Dr. Bakris noted that uncontrolled hypertension is a leading cause of morbidity and mortality, and despite availability of effective antihypertensives, many adults with hypertension are untreated, and up to 80% have uncontrolled disease, both globally and in the United States.
Zilebesiran is a subcutaneous RNA interference therapeutic that binds with high affinity to the hepatic asialoglycoprotein receptor, bringing about a reduction in the synthesis of angiotensinogen, the sole precursor of all angiotensin peptides. It is hoped that its hepatocyte-targeted delivery may allow extrahepatic angiotensinogen expression to be preserved, which could limit off-target effects in the kidney and other tissues.
The KARDIA-1 trial investigated the safety and efficacy of different doses of zilebesiran in patients with mild to moderate hypertension (systolic BP of 135-160 mm Hg), who are untreated or on stable therapy with up to two antihypertensive medications.
The study included 394 such patients (average baseline systolic BP was 142 mm Hg) who were randomly assigned to receive one of four different zilebesiran doses (150 mg, 300 mg, or 600 mg once every 6 months or 300 mg once every 2 months) or a placebo. The final analysis included 377 patients (56% men, 25% Black).
Results showed sustained reductions in serum angiotensinogen (between 88% and 98%) over the 6-month follow-up period.
Ambulatory systolic BP measured over 24 hours was significantly decreased with all zilebesiran regimens, with a mean reduction from baseline to month 6 of around 10 mm Hg in the three top doses studied and by around 14 mm Hg compared with placebo.
Patients receiving zilebesiran were more likely to achieve 24-hour average systolic BP measurements of 130 mm Hg or less at 6 months.
In addition, participants in all four zilebesiran groups consistently experienced significantly greater reductions in both daytime and nighttime systolic BP.
There were four nonserious adverse reactions leading to discontinuation in the zilebesiran groups: two instances of orthostatic hypotension, one of BP elevation, and one of injection site reaction.
Most hyperkalemia adverse events, which occurred in 6% of patients, were mild, did not require intervention, and generally resolved with repeat measurement; none were associated with acute kidney injury or led to study drug discontinuation. The incidence of hypotension events was low, and no clinically relevant changes in renal or hepatic function were observed, Dr. Bakris reported.
There was one death caused by cardiopulmonary arrest in a patient receiving zilebesiran 300 mg every 3 months, but this was not classified as drug related.
Zilebesiran is being further evaluated as an add-on therapy for treatment of hypertension in the ongoing KARDIA-2 phase 2 study.
Moderator of an AHA press conference at which the study was discussed, Sandra Taler, MD, professor of medicine at the Mayo Clinic, Rochester, Minn., said that “to have an injectable medicine that gives long-term blood pressure lowering is extremely exciting.”
Dr. Taler raised the point that some patients may not return for subsequent doses, but added that with subcutaneous dosing, administration at home may be a possibility.
Also commenting at the press conference, Keith Ferdinand, MD, professor of clinical medicine at Tulane University, New Orleans, said that this study “suggests we can now target the first step in the renin-angiotensin system – angiotensinogen – which then appears to lead to robust and continued blood pressure lowering for up to 6 months, which should improve adherence.”
Noting that only 50% of patients continue to take antihypertensive drugs after 1 year, Dr. Ferdinand added: “If we can increase adherence, we will increase efficacy and perhaps protect against some of the target organ damage.”
Designated discussant of the KARDIA-1 study at the AHA late-breaking clinical trial session, Anna Dominiczak, MD, University of Glasgow, noted that hypertension affects one in three adults worldwide, but only around 20% of people have it under control.
“An increase in the number of patients effectively treated for hypertension to levels observed in high-performing countries could prevent 76 million deaths, 120 million strokes, 79 million heart attacks, and 17 million cases of heart failure between now and 2050,” she said.
Dr. Bakris has received consulting fees from Alnylam Pharmaceuticals.
A version of this article first appeared on Medscape.com.
with what appeared to be an encouraging side-effect profile, in the phase 2 dose-ranging KARDIA-1 study.
“Our study demonstrates that either quarterly or biannual doses of zilebesiran can effectively and safely lower blood pressure in patients with uncontrolled hypertension,” said senior study investigator George Bakris, MD.
“Based on these results, zilebesiran has the potential to improve medication adherence, which will, in turn, reduce cardiovascular risk in people with hypertension,” added Dr. Bakris, who is professor of medicine and director of the Comprehensive Hypertension Center at the University of Chicago Medicine.
The KARDIA-1 study was presented at the American Heart Association scientific sessions.
Dr. Bakris noted that uncontrolled hypertension is a leading cause of morbidity and mortality, and despite availability of effective antihypertensives, many adults with hypertension are untreated, and up to 80% have uncontrolled disease, both globally and in the United States.
Zilebesiran is a subcutaneous RNA interference therapeutic that binds with high affinity to the hepatic asialoglycoprotein receptor, bringing about a reduction in the synthesis of angiotensinogen, the sole precursor of all angiotensin peptides. It is hoped that its hepatocyte-targeted delivery may allow extrahepatic angiotensinogen expression to be preserved, which could limit off-target effects in the kidney and other tissues.
The KARDIA-1 trial investigated the safety and efficacy of different doses of zilebesiran in patients with mild to moderate hypertension (systolic BP of 135-160 mm Hg), who are untreated or on stable therapy with up to two antihypertensive medications.
The study included 394 such patients (average baseline systolic BP was 142 mm Hg) who were randomly assigned to receive one of four different zilebesiran doses (150 mg, 300 mg, or 600 mg once every 6 months or 300 mg once every 2 months) or a placebo. The final analysis included 377 patients (56% men, 25% Black).
Results showed sustained reductions in serum angiotensinogen (between 88% and 98%) over the 6-month follow-up period.
Ambulatory systolic BP measured over 24 hours was significantly decreased with all zilebesiran regimens, with a mean reduction from baseline to month 6 of around 10 mm Hg in the three top doses studied and by around 14 mm Hg compared with placebo.
Patients receiving zilebesiran were more likely to achieve 24-hour average systolic BP measurements of 130 mm Hg or less at 6 months.
In addition, participants in all four zilebesiran groups consistently experienced significantly greater reductions in both daytime and nighttime systolic BP.
There were four nonserious adverse reactions leading to discontinuation in the zilebesiran groups: two instances of orthostatic hypotension, one of BP elevation, and one of injection site reaction.
Most hyperkalemia adverse events, which occurred in 6% of patients, were mild, did not require intervention, and generally resolved with repeat measurement; none were associated with acute kidney injury or led to study drug discontinuation. The incidence of hypotension events was low, and no clinically relevant changes in renal or hepatic function were observed, Dr. Bakris reported.
There was one death caused by cardiopulmonary arrest in a patient receiving zilebesiran 300 mg every 3 months, but this was not classified as drug related.
Zilebesiran is being further evaluated as an add-on therapy for treatment of hypertension in the ongoing KARDIA-2 phase 2 study.
Moderator of an AHA press conference at which the study was discussed, Sandra Taler, MD, professor of medicine at the Mayo Clinic, Rochester, Minn., said that “to have an injectable medicine that gives long-term blood pressure lowering is extremely exciting.”
Dr. Taler raised the point that some patients may not return for subsequent doses, but added that with subcutaneous dosing, administration at home may be a possibility.
Also commenting at the press conference, Keith Ferdinand, MD, professor of clinical medicine at Tulane University, New Orleans, said that this study “suggests we can now target the first step in the renin-angiotensin system – angiotensinogen – which then appears to lead to robust and continued blood pressure lowering for up to 6 months, which should improve adherence.”
Noting that only 50% of patients continue to take antihypertensive drugs after 1 year, Dr. Ferdinand added: “If we can increase adherence, we will increase efficacy and perhaps protect against some of the target organ damage.”
Designated discussant of the KARDIA-1 study at the AHA late-breaking clinical trial session, Anna Dominiczak, MD, University of Glasgow, noted that hypertension affects one in three adults worldwide, but only around 20% of people have it under control.
“An increase in the number of patients effectively treated for hypertension to levels observed in high-performing countries could prevent 76 million deaths, 120 million strokes, 79 million heart attacks, and 17 million cases of heart failure between now and 2050,” she said.
Dr. Bakris has received consulting fees from Alnylam Pharmaceuticals.
A version of this article first appeared on Medscape.com.
with what appeared to be an encouraging side-effect profile, in the phase 2 dose-ranging KARDIA-1 study.
“Our study demonstrates that either quarterly or biannual doses of zilebesiran can effectively and safely lower blood pressure in patients with uncontrolled hypertension,” said senior study investigator George Bakris, MD.
“Based on these results, zilebesiran has the potential to improve medication adherence, which will, in turn, reduce cardiovascular risk in people with hypertension,” added Dr. Bakris, who is professor of medicine and director of the Comprehensive Hypertension Center at the University of Chicago Medicine.
The KARDIA-1 study was presented at the American Heart Association scientific sessions.
Dr. Bakris noted that uncontrolled hypertension is a leading cause of morbidity and mortality, and despite availability of effective antihypertensives, many adults with hypertension are untreated, and up to 80% have uncontrolled disease, both globally and in the United States.
Zilebesiran is a subcutaneous RNA interference therapeutic that binds with high affinity to the hepatic asialoglycoprotein receptor, bringing about a reduction in the synthesis of angiotensinogen, the sole precursor of all angiotensin peptides. It is hoped that its hepatocyte-targeted delivery may allow extrahepatic angiotensinogen expression to be preserved, which could limit off-target effects in the kidney and other tissues.
The KARDIA-1 trial investigated the safety and efficacy of different doses of zilebesiran in patients with mild to moderate hypertension (systolic BP of 135-160 mm Hg), who are untreated or on stable therapy with up to two antihypertensive medications.
The study included 394 such patients (average baseline systolic BP was 142 mm Hg) who were randomly assigned to receive one of four different zilebesiran doses (150 mg, 300 mg, or 600 mg once every 6 months or 300 mg once every 2 months) or a placebo. The final analysis included 377 patients (56% men, 25% Black).
Results showed sustained reductions in serum angiotensinogen (between 88% and 98%) over the 6-month follow-up period.
Ambulatory systolic BP measured over 24 hours was significantly decreased with all zilebesiran regimens, with a mean reduction from baseline to month 6 of around 10 mm Hg in the three top doses studied and by around 14 mm Hg compared with placebo.
Patients receiving zilebesiran were more likely to achieve 24-hour average systolic BP measurements of 130 mm Hg or less at 6 months.
In addition, participants in all four zilebesiran groups consistently experienced significantly greater reductions in both daytime and nighttime systolic BP.
There were four nonserious adverse reactions leading to discontinuation in the zilebesiran groups: two instances of orthostatic hypotension, one of BP elevation, and one of injection site reaction.
Most hyperkalemia adverse events, which occurred in 6% of patients, were mild, did not require intervention, and generally resolved with repeat measurement; none were associated with acute kidney injury or led to study drug discontinuation. The incidence of hypotension events was low, and no clinically relevant changes in renal or hepatic function were observed, Dr. Bakris reported.
There was one death caused by cardiopulmonary arrest in a patient receiving zilebesiran 300 mg every 3 months, but this was not classified as drug related.
Zilebesiran is being further evaluated as an add-on therapy for treatment of hypertension in the ongoing KARDIA-2 phase 2 study.
Moderator of an AHA press conference at which the study was discussed, Sandra Taler, MD, professor of medicine at the Mayo Clinic, Rochester, Minn., said that “to have an injectable medicine that gives long-term blood pressure lowering is extremely exciting.”
Dr. Taler raised the point that some patients may not return for subsequent doses, but added that with subcutaneous dosing, administration at home may be a possibility.
Also commenting at the press conference, Keith Ferdinand, MD, professor of clinical medicine at Tulane University, New Orleans, said that this study “suggests we can now target the first step in the renin-angiotensin system – angiotensinogen – which then appears to lead to robust and continued blood pressure lowering for up to 6 months, which should improve adherence.”
Noting that only 50% of patients continue to take antihypertensive drugs after 1 year, Dr. Ferdinand added: “If we can increase adherence, we will increase efficacy and perhaps protect against some of the target organ damage.”
Designated discussant of the KARDIA-1 study at the AHA late-breaking clinical trial session, Anna Dominiczak, MD, University of Glasgow, noted that hypertension affects one in three adults worldwide, but only around 20% of people have it under control.
“An increase in the number of patients effectively treated for hypertension to levels observed in high-performing countries could prevent 76 million deaths, 120 million strokes, 79 million heart attacks, and 17 million cases of heart failure between now and 2050,” she said.
Dr. Bakris has received consulting fees from Alnylam Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM AHA 2023
Low-salt diet cut BP by 6 mm Hg in 1 week: CARDIA-SSBP
The CARDIA-SSBP trial involved 213 individuals aged 50-75 years, including those with and those without hypertension, and showed that the decline in blood pressure brought about by a low-salt diet was independent of hypertension status and antihypertensive medication use. It was also generally consistent across subgroups and did not result in excess adverse events.
“The blood pressure reduction we see here is meaningful, and comparable to that produced by one antihypertensive medication,” lead investigator Deepak Gupta, MD, Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
Dr. Gupta presented the CARDIA-SSBP study on Nov. 11 at the American Heart Association scientific sessions, held in Philadelphia. The study was published online in JAMA. The exact menus used in the study are available in a supplement to the JAMA paper.
“In order to live a healthy lifestyle, understanding what we eat has important health effects. Raised blood pressure contributes to one out of every eight deaths worldwide,” Dr. Gupta noted. “If people want to lower their blood pressure, attention to dietary sodium is one part of that. If individuals can stick with a low sodium diet, they may be able to stop taking one of their antihypertensive medications, and those who are normotensive will be less likely to develop hypertension.”
Commentators said the study had significant implications for public health, but they pointed out that maintaining a low-sodium diet over the long term is challenging, given the high salt content of generally available foods.
Dr. Gupta noted that the study did use commercially available products in the low-sodium diets and the menus are available for people to follow, making it more accessible than some diets used in previous studies.
“What may also be attractive to people is that you don’t have to wait for months to see an effect. If you start to consume a low-sodium diet, you can see results on blood pressure rapidly, within a week,” he said.
The diet in this study brought about a large reduction in dietary sodium, but Dr. Gupta says any reduction in dietary sodium is likely to be beneficial.
“If you go to the level that we got to, you could expect to see a reduction of around 6 mm Hg. But it’s like walking – you don’t necessarily need to get to 10,000 steps every day. Any amount of walking or physical activity is of benefit. The same is probably true for salt: Any reduction that you can make is probably of benefit.”
For the study, participants had their blood pressure measured by 24-hour ambulatory monitoring while on their usual diets. They were then randomly assigned to either a high-sodium diet or a low-sodium diet for 1 week. Participants then crossed over to the opposite diet for 1 week, with blood pressure measured over a 24-hour period on the last day of each diet.
As assessed by 24-hour urine excretion, the usual diet of participants was found to already be high in sodium (median, 4.45 g/d). This increased to a median of 5.00 g/d when on the high-sodium diet in the study and decreased to 1.27 g/d while on the low-sodium diet.
Results found participants had a median systolic blood pressure of 125 mm Hg on their usual diets. This was raised to 126 mm Hg on the high-sodium diet and lowered to 119 mm Hg on the low-sodium diet.
The researchers also reported that 75% of individuals showed a blood pressure reduction on the low-sodium diet and are thus defined as “salt-sensitive.” This is a higher percentage than found in previous studies.
“Of those that didn’t show a blood pressure reduction with a low-sodium diet in this study, it appears that they may not have been so adherent to the diet as those who did show a blood pressure reduction,” Dr. Gupta said.
He noted that hypertension is the most common chronic disease condition worldwide, with about 1.3 billion people affected, and although it has been known for some time that dietary sodium affects blood pressure, there have been some gaps in previous studies.
For example, many studies have excluded individuals who were already taking antihypertensive medications and people with diabetes, and they have generally not included many older individuals. The current study found that all of these groups showed significant blood pressure reductions by reducing dietary sodium.
Large effect in people with diabetes
Subgroup analysis largely showed consistent results across the population, regardless of age, sex, race, and body mass index and whether participants were taking antihypertensive medication or not, but there were a couple of exceptions. Individuals with higher blood pressure at baseline seemed to have a greater effect of lowering dietary sodium, although those who were normotensive at baseline still showed significant blood pressure reduction, Dr. Gupta reported.
The researchers found a particularly large reduction in blood pressure from lowering sodium intake in people with diabetes, who made up about 21% of the overall cohort. Their average reduction in systolic blood pressure between the high and low sodium diet was close to 17 mm Hg rather than the 7-8 mm Hg in the whole cohort.
Dr. Gupta said that the results are applicable to most of the population.
“The people who will be most motivated to follow a low-sodium diet are those with hypertension. But even in normotensive individuals, there is likely to be benefit.”
To help people follow a low-sodium diet, Dr. Gupta says education campaigns are needed “to show people that they can do it and make it work.” But there are bigger structural issues that need to be addressed at policy and governmental levels.
“Most of our food available in grocery stores and restaurants is high in salt. We now have a preponderance of evidence showing us that we need to change what’s available in the food supply,” he said. “There is a push going on for this now, and the U.S. has introduced some guidelines for the food industry on sodium content of foods. These are voluntary at this point, but it’s a start.”
Difficult to maintain long term
Commenting on the study, Paul Whelton, MD, chair in global public health at Tulane University, New Orleans, noted that sodium reduction is known to reduce blood pressure, with greater sodium reductions giving greater blood pressure decreases, and that some people are more sensitive to the effects of sodium than others.
He described CARDIA-SSBP as a “well-done study.”
“They managed to get a very low sodium intake and a large difference between the two groups, which translated into a big reduction in systolic blood pressure,” Dr. Whelton said. “However, the problem with these sorts of trials where the diets are provided to the participants is that although they show proof of concept, it is difficult to generalize because we can’t normally provide patients with their meals. In this type of ‘feeding’ study, we find it difficult to maintain people on their behavioral intervention over the long term.”
Dr. Whelton said that he was more excited about this trial knowing that the food given was commercially available. “That makes it more practical, but you still have to be quite motivated to follow a diet like this. Buying low-sodium products in the supermarket does require quite a lot of work to read the labels, and sometimes the low-sodium foods are specialty products and are more expensive.”
He pointed out that older people in higher socioeconomic classes are more likely to attempt this and do better from behavioral interventions in general. “Unfortunately, people who don’t do well from behavioral interventions like this are those from lower socioeconomic groups, who are ones at most at risk for cardiovascular disease.”
Dr. Whelton noted that the food industry has been reluctant to lower sodium content because high-salt foods sell better. “Unfortunately, foods high in saturated fat and salt taste good to most people. We are generally attuned to a high salt intake. But when people have been following a low-salt diet for a while, they generally don’t like high-salt foods anymore. They become attuned to lower-sodium diet,” he added.
New U.S. sodium reduction guidelines
Discussant of the CARDIA-SSBP study at the AHA meeting, Cheryl Anderson, MD, University of California, San Diego, said that the findings were important and consistent with prior studies.
“These studies have global implications because salt is ubiquitous in the food supply in much of the world,” she noted, adding that, “Americans consume almost 50% more sodium than recommended, and there has been a persistent lack of adherence to healthy diet recommendations for reductions in salt, sugar, and fats.”
Dr. Anderson pointed out that in 2021, the Food and Drug Administration issued guidance for voluntary sodium reduction, which uses a gradual approach, with targets to reach a population goal of 3,000 mg/d of sodium by 2023 and 2,300 mg/d by 2031.
“These targets apply to 150 categories of food that are sales-weighted to focus on dominant sellers in each category. They apply to food manufacturers, restaurants and food service operations,” she concluded. “These targets serve as a basis for continued dialogue. The research community eagerly awaits the review of population-based data to help refine this approach and goals.”
This study was supported by grants from the National Heart, Lung, and Blood Institute, the National Institutes of Health, the American Heart Association, and the National Center for Advancing Translational Sciences. The authors report no disclosures.
A version of this article appeared on Medscape.com.
The CARDIA-SSBP trial involved 213 individuals aged 50-75 years, including those with and those without hypertension, and showed that the decline in blood pressure brought about by a low-salt diet was independent of hypertension status and antihypertensive medication use. It was also generally consistent across subgroups and did not result in excess adverse events.
“The blood pressure reduction we see here is meaningful, and comparable to that produced by one antihypertensive medication,” lead investigator Deepak Gupta, MD, Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
Dr. Gupta presented the CARDIA-SSBP study on Nov. 11 at the American Heart Association scientific sessions, held in Philadelphia. The study was published online in JAMA. The exact menus used in the study are available in a supplement to the JAMA paper.
“In order to live a healthy lifestyle, understanding what we eat has important health effects. Raised blood pressure contributes to one out of every eight deaths worldwide,” Dr. Gupta noted. “If people want to lower their blood pressure, attention to dietary sodium is one part of that. If individuals can stick with a low sodium diet, they may be able to stop taking one of their antihypertensive medications, and those who are normotensive will be less likely to develop hypertension.”
Commentators said the study had significant implications for public health, but they pointed out that maintaining a low-sodium diet over the long term is challenging, given the high salt content of generally available foods.
Dr. Gupta noted that the study did use commercially available products in the low-sodium diets and the menus are available for people to follow, making it more accessible than some diets used in previous studies.
“What may also be attractive to people is that you don’t have to wait for months to see an effect. If you start to consume a low-sodium diet, you can see results on blood pressure rapidly, within a week,” he said.
The diet in this study brought about a large reduction in dietary sodium, but Dr. Gupta says any reduction in dietary sodium is likely to be beneficial.
“If you go to the level that we got to, you could expect to see a reduction of around 6 mm Hg. But it’s like walking – you don’t necessarily need to get to 10,000 steps every day. Any amount of walking or physical activity is of benefit. The same is probably true for salt: Any reduction that you can make is probably of benefit.”
For the study, participants had their blood pressure measured by 24-hour ambulatory monitoring while on their usual diets. They were then randomly assigned to either a high-sodium diet or a low-sodium diet for 1 week. Participants then crossed over to the opposite diet for 1 week, with blood pressure measured over a 24-hour period on the last day of each diet.
As assessed by 24-hour urine excretion, the usual diet of participants was found to already be high in sodium (median, 4.45 g/d). This increased to a median of 5.00 g/d when on the high-sodium diet in the study and decreased to 1.27 g/d while on the low-sodium diet.
Results found participants had a median systolic blood pressure of 125 mm Hg on their usual diets. This was raised to 126 mm Hg on the high-sodium diet and lowered to 119 mm Hg on the low-sodium diet.
The researchers also reported that 75% of individuals showed a blood pressure reduction on the low-sodium diet and are thus defined as “salt-sensitive.” This is a higher percentage than found in previous studies.
“Of those that didn’t show a blood pressure reduction with a low-sodium diet in this study, it appears that they may not have been so adherent to the diet as those who did show a blood pressure reduction,” Dr. Gupta said.
He noted that hypertension is the most common chronic disease condition worldwide, with about 1.3 billion people affected, and although it has been known for some time that dietary sodium affects blood pressure, there have been some gaps in previous studies.
For example, many studies have excluded individuals who were already taking antihypertensive medications and people with diabetes, and they have generally not included many older individuals. The current study found that all of these groups showed significant blood pressure reductions by reducing dietary sodium.
Large effect in people with diabetes
Subgroup analysis largely showed consistent results across the population, regardless of age, sex, race, and body mass index and whether participants were taking antihypertensive medication or not, but there were a couple of exceptions. Individuals with higher blood pressure at baseline seemed to have a greater effect of lowering dietary sodium, although those who were normotensive at baseline still showed significant blood pressure reduction, Dr. Gupta reported.
The researchers found a particularly large reduction in blood pressure from lowering sodium intake in people with diabetes, who made up about 21% of the overall cohort. Their average reduction in systolic blood pressure between the high and low sodium diet was close to 17 mm Hg rather than the 7-8 mm Hg in the whole cohort.
Dr. Gupta said that the results are applicable to most of the population.
“The people who will be most motivated to follow a low-sodium diet are those with hypertension. But even in normotensive individuals, there is likely to be benefit.”
To help people follow a low-sodium diet, Dr. Gupta says education campaigns are needed “to show people that they can do it and make it work.” But there are bigger structural issues that need to be addressed at policy and governmental levels.
“Most of our food available in grocery stores and restaurants is high in salt. We now have a preponderance of evidence showing us that we need to change what’s available in the food supply,” he said. “There is a push going on for this now, and the U.S. has introduced some guidelines for the food industry on sodium content of foods. These are voluntary at this point, but it’s a start.”
Difficult to maintain long term
Commenting on the study, Paul Whelton, MD, chair in global public health at Tulane University, New Orleans, noted that sodium reduction is known to reduce blood pressure, with greater sodium reductions giving greater blood pressure decreases, and that some people are more sensitive to the effects of sodium than others.
He described CARDIA-SSBP as a “well-done study.”
“They managed to get a very low sodium intake and a large difference between the two groups, which translated into a big reduction in systolic blood pressure,” Dr. Whelton said. “However, the problem with these sorts of trials where the diets are provided to the participants is that although they show proof of concept, it is difficult to generalize because we can’t normally provide patients with their meals. In this type of ‘feeding’ study, we find it difficult to maintain people on their behavioral intervention over the long term.”
Dr. Whelton said that he was more excited about this trial knowing that the food given was commercially available. “That makes it more practical, but you still have to be quite motivated to follow a diet like this. Buying low-sodium products in the supermarket does require quite a lot of work to read the labels, and sometimes the low-sodium foods are specialty products and are more expensive.”
He pointed out that older people in higher socioeconomic classes are more likely to attempt this and do better from behavioral interventions in general. “Unfortunately, people who don’t do well from behavioral interventions like this are those from lower socioeconomic groups, who are ones at most at risk for cardiovascular disease.”
Dr. Whelton noted that the food industry has been reluctant to lower sodium content because high-salt foods sell better. “Unfortunately, foods high in saturated fat and salt taste good to most people. We are generally attuned to a high salt intake. But when people have been following a low-salt diet for a while, they generally don’t like high-salt foods anymore. They become attuned to lower-sodium diet,” he added.
New U.S. sodium reduction guidelines
Discussant of the CARDIA-SSBP study at the AHA meeting, Cheryl Anderson, MD, University of California, San Diego, said that the findings were important and consistent with prior studies.
“These studies have global implications because salt is ubiquitous in the food supply in much of the world,” she noted, adding that, “Americans consume almost 50% more sodium than recommended, and there has been a persistent lack of adherence to healthy diet recommendations for reductions in salt, sugar, and fats.”
Dr. Anderson pointed out that in 2021, the Food and Drug Administration issued guidance for voluntary sodium reduction, which uses a gradual approach, with targets to reach a population goal of 3,000 mg/d of sodium by 2023 and 2,300 mg/d by 2031.
“These targets apply to 150 categories of food that are sales-weighted to focus on dominant sellers in each category. They apply to food manufacturers, restaurants and food service operations,” she concluded. “These targets serve as a basis for continued dialogue. The research community eagerly awaits the review of population-based data to help refine this approach and goals.”
This study was supported by grants from the National Heart, Lung, and Blood Institute, the National Institutes of Health, the American Heart Association, and the National Center for Advancing Translational Sciences. The authors report no disclosures.
A version of this article appeared on Medscape.com.
The CARDIA-SSBP trial involved 213 individuals aged 50-75 years, including those with and those without hypertension, and showed that the decline in blood pressure brought about by a low-salt diet was independent of hypertension status and antihypertensive medication use. It was also generally consistent across subgroups and did not result in excess adverse events.
“The blood pressure reduction we see here is meaningful, and comparable to that produced by one antihypertensive medication,” lead investigator Deepak Gupta, MD, Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
Dr. Gupta presented the CARDIA-SSBP study on Nov. 11 at the American Heart Association scientific sessions, held in Philadelphia. The study was published online in JAMA. The exact menus used in the study are available in a supplement to the JAMA paper.
“In order to live a healthy lifestyle, understanding what we eat has important health effects. Raised blood pressure contributes to one out of every eight deaths worldwide,” Dr. Gupta noted. “If people want to lower their blood pressure, attention to dietary sodium is one part of that. If individuals can stick with a low sodium diet, they may be able to stop taking one of their antihypertensive medications, and those who are normotensive will be less likely to develop hypertension.”
Commentators said the study had significant implications for public health, but they pointed out that maintaining a low-sodium diet over the long term is challenging, given the high salt content of generally available foods.
Dr. Gupta noted that the study did use commercially available products in the low-sodium diets and the menus are available for people to follow, making it more accessible than some diets used in previous studies.
“What may also be attractive to people is that you don’t have to wait for months to see an effect. If you start to consume a low-sodium diet, you can see results on blood pressure rapidly, within a week,” he said.
The diet in this study brought about a large reduction in dietary sodium, but Dr. Gupta says any reduction in dietary sodium is likely to be beneficial.
“If you go to the level that we got to, you could expect to see a reduction of around 6 mm Hg. But it’s like walking – you don’t necessarily need to get to 10,000 steps every day. Any amount of walking or physical activity is of benefit. The same is probably true for salt: Any reduction that you can make is probably of benefit.”
For the study, participants had their blood pressure measured by 24-hour ambulatory monitoring while on their usual diets. They were then randomly assigned to either a high-sodium diet or a low-sodium diet for 1 week. Participants then crossed over to the opposite diet for 1 week, with blood pressure measured over a 24-hour period on the last day of each diet.
As assessed by 24-hour urine excretion, the usual diet of participants was found to already be high in sodium (median, 4.45 g/d). This increased to a median of 5.00 g/d when on the high-sodium diet in the study and decreased to 1.27 g/d while on the low-sodium diet.
Results found participants had a median systolic blood pressure of 125 mm Hg on their usual diets. This was raised to 126 mm Hg on the high-sodium diet and lowered to 119 mm Hg on the low-sodium diet.
The researchers also reported that 75% of individuals showed a blood pressure reduction on the low-sodium diet and are thus defined as “salt-sensitive.” This is a higher percentage than found in previous studies.
“Of those that didn’t show a blood pressure reduction with a low-sodium diet in this study, it appears that they may not have been so adherent to the diet as those who did show a blood pressure reduction,” Dr. Gupta said.
He noted that hypertension is the most common chronic disease condition worldwide, with about 1.3 billion people affected, and although it has been known for some time that dietary sodium affects blood pressure, there have been some gaps in previous studies.
For example, many studies have excluded individuals who were already taking antihypertensive medications and people with diabetes, and they have generally not included many older individuals. The current study found that all of these groups showed significant blood pressure reductions by reducing dietary sodium.
Large effect in people with diabetes
Subgroup analysis largely showed consistent results across the population, regardless of age, sex, race, and body mass index and whether participants were taking antihypertensive medication or not, but there were a couple of exceptions. Individuals with higher blood pressure at baseline seemed to have a greater effect of lowering dietary sodium, although those who were normotensive at baseline still showed significant blood pressure reduction, Dr. Gupta reported.
The researchers found a particularly large reduction in blood pressure from lowering sodium intake in people with diabetes, who made up about 21% of the overall cohort. Their average reduction in systolic blood pressure between the high and low sodium diet was close to 17 mm Hg rather than the 7-8 mm Hg in the whole cohort.
Dr. Gupta said that the results are applicable to most of the population.
“The people who will be most motivated to follow a low-sodium diet are those with hypertension. But even in normotensive individuals, there is likely to be benefit.”
To help people follow a low-sodium diet, Dr. Gupta says education campaigns are needed “to show people that they can do it and make it work.” But there are bigger structural issues that need to be addressed at policy and governmental levels.
“Most of our food available in grocery stores and restaurants is high in salt. We now have a preponderance of evidence showing us that we need to change what’s available in the food supply,” he said. “There is a push going on for this now, and the U.S. has introduced some guidelines for the food industry on sodium content of foods. These are voluntary at this point, but it’s a start.”
Difficult to maintain long term
Commenting on the study, Paul Whelton, MD, chair in global public health at Tulane University, New Orleans, noted that sodium reduction is known to reduce blood pressure, with greater sodium reductions giving greater blood pressure decreases, and that some people are more sensitive to the effects of sodium than others.
He described CARDIA-SSBP as a “well-done study.”
“They managed to get a very low sodium intake and a large difference between the two groups, which translated into a big reduction in systolic blood pressure,” Dr. Whelton said. “However, the problem with these sorts of trials where the diets are provided to the participants is that although they show proof of concept, it is difficult to generalize because we can’t normally provide patients with their meals. In this type of ‘feeding’ study, we find it difficult to maintain people on their behavioral intervention over the long term.”
Dr. Whelton said that he was more excited about this trial knowing that the food given was commercially available. “That makes it more practical, but you still have to be quite motivated to follow a diet like this. Buying low-sodium products in the supermarket does require quite a lot of work to read the labels, and sometimes the low-sodium foods are specialty products and are more expensive.”
He pointed out that older people in higher socioeconomic classes are more likely to attempt this and do better from behavioral interventions in general. “Unfortunately, people who don’t do well from behavioral interventions like this are those from lower socioeconomic groups, who are ones at most at risk for cardiovascular disease.”
Dr. Whelton noted that the food industry has been reluctant to lower sodium content because high-salt foods sell better. “Unfortunately, foods high in saturated fat and salt taste good to most people. We are generally attuned to a high salt intake. But when people have been following a low-salt diet for a while, they generally don’t like high-salt foods anymore. They become attuned to lower-sodium diet,” he added.
New U.S. sodium reduction guidelines
Discussant of the CARDIA-SSBP study at the AHA meeting, Cheryl Anderson, MD, University of California, San Diego, said that the findings were important and consistent with prior studies.
“These studies have global implications because salt is ubiquitous in the food supply in much of the world,” she noted, adding that, “Americans consume almost 50% more sodium than recommended, and there has been a persistent lack of adherence to healthy diet recommendations for reductions in salt, sugar, and fats.”
Dr. Anderson pointed out that in 2021, the Food and Drug Administration issued guidance for voluntary sodium reduction, which uses a gradual approach, with targets to reach a population goal of 3,000 mg/d of sodium by 2023 and 2,300 mg/d by 2031.
“These targets apply to 150 categories of food that are sales-weighted to focus on dominant sellers in each category. They apply to food manufacturers, restaurants and food service operations,” she concluded. “These targets serve as a basis for continued dialogue. The research community eagerly awaits the review of population-based data to help refine this approach and goals.”
This study was supported by grants from the National Heart, Lung, and Blood Institute, the National Institutes of Health, the American Heart Association, and the National Center for Advancing Translational Sciences. The authors report no disclosures.
A version of this article appeared on Medscape.com.
FROM AHA 2023
Apixaban cuts stroke but ups bleeding in subclinical AFib: ARTESIA
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
in the ARTESIA study.
The results appear to contrast somewhat with the recently reported NOAH-AFNET 6 trial, which failed to show a reduction in stroke with the anticoagulant edoxaban versus placebo in a similar patient group, but that trial was stopped early and so was underpowered.
However, the lead investigators of both trials say the studies actually show consistent results – both found a lower rate of stroke than expected in this population, but the confidence intervals for stroke reduction with anticoagulation overlap, suggesting there is likely some effect, albeit less than that in clinical AFib.
The big question is whether the reduction in stroke with anticoagulation outweighs the increase in major bleeding.
A new meta-analysis of the two trials showed that “oral anticoagulation with edoxaban or apixaban reduces the risk of ischemic stroke by approximately one-third and increases major bleeding by roughly double.”
In absolute numbers, there were three fewer ischemic strokes per 1,000 patient-years with anticoagulation in the two trials combined, at the cost of seven more major bleeds.
The lead investigators of the two trials have somewhat different opinions on how these findings may translate into clinical practice.
Jeff Healey, MD, Population Health Research Institute, McMaster University, Hamilton, Ont., lead investigator of the ARTESIA trial, believes that the risks and benefits need to be assessed in individual patients, but there should be some patient groups that will benefit from anticoagulation treatment.
“In patients with pacemakers or implantable loop recorders with continuous monitoring, subclinical AF[ib] is detected in about one third of patients, so this is extremely common,” he said in an interview. “The question is whether this is just a normal feature of getting older or is this like AF[ib] that we see in the clinic which increases stroke risk, and I think we can conclude from ARTESIA that this subclinical AF[ib] is associated with an increased risk of stroke, although that is lower than the risk with clinical AF[ib], and that it can be reduced by anticoagulation.”
Until recently it hasn’t been possible to quantify the risk associated with subclinical AFib, he noted. “But now we have a rich dataset to use to see if we can tease out some specifics on this. Future analyses of this dataset will help define patients where the benefits outweigh the risks of bleeding. For now, I think we can look at the data in a qualitative way and consider the totality of risk factors in each patient – their bleeding risk, stroke risk, how much AF[ib] they have, and make a decision as to whether to give anticoagulation or not.”
But Paulus Kirchhof, MD, University Heart and Vascular Center Hamburg (Germany), lead investigator of the NOAH-AFNET 6 trial said: “Both trials showed the stroke rate is low in these patients – about 1% per year – and that anticoagulation can reduce it a bit further at the expense of increasing major bleeding. I don’t believe the AF[ib] episodes picked up on these devices constitute a sufficient stroke risk to warrant anticoagulation, given the bleeding risk.”
Dr. Kirchhof suggests an alternate approach of performing further traditional AFib monitoring on these patients.
“I think going forward in my practice, when we come across this device-detected AF[ib], we will do further investigations with an established method for detecting AF[ib] involving surface ECG monitoring – maybe a 3-day or 7-day Holter. If that shows AF[ib], then we will be on firm ground to start anticoagulation. If that doesn’t show AF[ib], we will probably not use anticoagulation.”
The ARTESIA trial and the meta-analysis of the two trials were both presented at the annual scientific sessions of the American Heart Association. Both studies were also simultaneously published online – ARTESIA in the New England Journal of Medicine and the meta-analysis in Circulation.
ARTESIA
For the ARTESIA study, 4012 patients with device-detected AFib and other clinical risk factors for stroke were randomly assigned to treatment with apixaban (5 mg twice daily) or aspirin (81 mg daily).
After a mean follow-up of 3.5 years, the primary endpoint – stroke or systemic embolism – occurred in 55 patients in the apixaban group (0.78% per patient-year), compared with 86 patients in the aspirin group (1.24% per patient-year), giving a hazard ratio of 0.63 (95% confidence interval, 0.45-0.88; P = .007).
“The risk of stroke or systemic embolism was lower by 37% with apixaban than with aspirin, and the risk of disabling or fatal stroke was lower by 49%,” Dr. Healey reported.
In the “on-treatment” population, the rate of major bleeding was 1.71% per patient-year in the apixaban group and 0.94% per patient-year in the aspirin group (HR, 1.80; 95% CI, 1.26-2.57; P = .001).
Fatal bleeding occurred in five patients in the apixaban group and eight patients in the aspirin group. Symptomatic intracranial hemorrhage occurred in 12 patients with apixaban and 15 patients with aspirin.
One of the main findings of the trial is the lower-than-expected risk of ischemic stroke in this population – about 1% per year in the aspirin group, which was reduced to 0.64% per year in the apixaban group.
The authors noted that “simply counting strokes as compared with bleeding events might suggest a neutral overall effect. With apixaban as compared with aspirin, 31 fewer cases of stroke or systemic embolism were seen in the intention-to-treat analysis, as compared with 39 more major bleeding events in the on-treatment analysis.”
However, they pointed out that strokes involve permanent loss of brain tissue, whereas major bleeding is usually reversible, with most patients having complete recovery, which was the case in this study.
“Thus, on the basis of the considerably greater severity of the stroke events prevented than the bleeding events caused, we believe that these findings favor consideration of the use of oral anticoagulation for patients with risk factors for stroke in whom subclinical atrial fibrillation develops,” they concluded.
First well-powered trial addressing this question
Discussing the ARTESIA trial at an AHA press conference, Christine Albert, MD, Cedars-Sinai Medical Center, Los Angeles, said: “I want to emphasize how important this trial is.”
She explained that current guidelines do not recommend any treatment for patients with device-detected AFib that is not shown on ECG, even though it is known this confers some excess risk of stroke.
“ARTESIA is the first well-powered, long-term trial looking at this question,” she said. “It found a clear reduction in the risk of stroke/systemic embolism with apixaban vs aspirin, but there was also a significant amount of bleeding – about an 80% increase. The question is whether the benefit on stroke is worth it given the bleeding risk.”
Dr. Albert highlighted the low absolute risk of stroke in this study population of around 1.2%, pointing out that even with the 37% relative reduction with anticoagulation, stroke is only reduced in absolute terms by 0.4%.
“We are going to have to take this back to committees and guidelines and look at the balance between the benefit on stroke and the increase in bleeding,” she concluded.
Noting that observational studies have shown that the duration of AFib impacts the risk of stroke, Dr. Albert suggested that patients with longer-duration AFib may benefit from anticoagulation to a greater extent; and given that the bleeding seen in ARTESIA was mainly GI bleeding, it might be possible to screen out patients at high risk of GI bleeding.
She also pointed out that a lot of patients discontinued anticoagulation treatment in both ARTESIA and NOAH-AFNET 6, showing that this is not an easy strategy for elderly patients.
In an editorial accompanying publication of the ARTESIA trial, Emma Svennberg, MD, Karolinska Institute, Stockholm, also concluded that, “going forward, we must balance the increased bleeding risks with the risk for disabling strokes,” and that “future substudies and meta-analyses may provide further insights regarding treatment benefits in specific subgroups.”
NOAH-AFNET 6: New subgroup analysis
The previously reported NOAH-AFNET 6 study randomly assigned 2,538 patients with subclinical AFib and additional risk factors for stroke to anticoagulation with edoxaban or placebo. The trial was stopped early, so it was underpowered – but it found no difference between groups in the incidence of the composite endpoint of stroke, systemic embolism, or death from cardiovascular causes or in the incidence of stroke, although there was higher risk of major bleeding.
Again, there was a low rate of stroke in this trial with just 49 strokes in total in the whole study. The NOAH-AFNET-6 investigators concluded that these patients should not receive anticoagulation because the risk of bleeding outweighed any potential benefits.
A new subanalysis of the 259 patients who had durations of subclinical AFib of 24 hours or longer in the NOAH-AFNET 6 trial was presented at the AHA meeting, and simultaneously published online in the European Heart Journal.
This showed that the rate of stroke also appeared low in patients with these long durations of subclinical AFib, and that there was no interaction between the duration of subclinical AFib and the efficacy and safety of oral anticoagulation.
But with such a low number of events in the study as a whole and in the long duration subclinical AFib subgroup (in which there were just two strokes in each treatment group), this analysis was unlikely to show a difference, Dr. Kirchhof commented.
The subgroup analysis did, however, show that patients experiencing subclinical AFib durations of 24 hours or more were more likely to develop clinical AFib over time than those with shorter durations, suggesting the need for regular ECGs in these patients.
Dr. Kirchhof said better methods are needed to detect patients with subclinical AFib at high risk of stroke. “I don’t think our clinical stroke risk factor scores such as CHA2DS2-VASc are sufficient to detect high-risk patients. Patients in both NOAH-AFNET 6 and ARTESIA had a median CHA2DS2-VASc score of 4, but they had a stroke rate of just 1% per year,” he noted.
The meta-analysis of the two trials showed that the results from both are consistent, with an overall reduction in ischemic stroke with oral anticoagulation (relative risk, 0.68). Oral anticoagulation also reduced a composite of cardiovascular death, all-cause stroke, peripheral arterial embolism, myocardial infarction, or pulmonary embolism (RR, 0.85).
There was no significant difference in cardiovascular death (RR, 0.95) or all-cause mortality (RR, 1.08), but anticoagulation significantly increased major bleeding (RR, 1.62).
Aspirin use complicates results
Dr. Healey said further analyses of the ARTESIA data will try to tease out the effect of concomitant aspirin use in the trial.
He explained that patients in this trial were allowed to take a single antiplatelet agent on top of study therapy.
“It is difficult to work out the exact use of antiplatelet therapy as it changed throughout the study,” he said. “About two-thirds were taking antiplatelet agents at the time of enrollment into the trial, but this decreased throughout the study. Many clinicians stopped open-label antiplatelet therapy during the trial when new evidence came out to suggest that there was no added benefit of adding aspirin on top of anticoagulants.
“We need to look carefully as to what impact that may have had,” Dr. Healey added. “We know from other studies that adding an antiplatelet on top of an anticoagulant doesn’t do much to thromboembolic events, but it approximately doubles the risk of major bleeding.”
In contrast, the NOAH-AFNET trial did not allow aspirin use in the anticoagulation group and aspirin was taken by around half the patients in the placebo group who had an indication for its use.
The authors of the meta-analysis pointed out that the omission of aspirin in nearly half of the control patients in NOAH-AFNET 6 and the early termination of the trial may have led to a slightly higher estimate for excess major bleeding with anticoagulation.
The ARTESIA study was supported by the Canadian Institutes for Health Research, the Bristol Myers Squibb-Pfizer Alliance, the Heart and Stroke Foundation of Canada, the Canadian Stroke Prevention Intervention Network, Hamilton Health Sciences, the Advancing Clinical Trials Network and the Population Health Research Institute. Dr. Healey reported research grants and speaking fees from BMS/Pfizer Alliance, Servier, Novartis, Boston Scientific, Medtronic; and acts as a consultant to Bayer, Servier and Boston Scientific. The NOAH-AFNET 6 trial was an investigator-initiated trial funded by the German Center for Cardiovascular Research and Daiichi Sankyo Europe. Dr. Kirchhof reported research support from several drug and device companies active in AFib. He is also listed as an inventor on two patents held by the University of Hamburg on AFib therapy and AFib markers.
A version of this article first appeared on Medscape.com.
FROM AHA 2023
Impressive bleeding profile with factor XI inhibitor in AFib: AZALEA
; the risk of stroke was moderate to high.
The trial was stopped earlier this year because of an “overwhelming” reduction in bleeding with abelacimab in comparison to rivaroxaban. Abelacimab is a monoclonal antibody given by subcutaneous injection once a month.
“Details of the bleeding results have now shown that the 150-mg dose of abelacimab, which is the dose being carried forward to phase 3 trials, was associated with a 67% reduction in major or clinically relevant nonmajor bleeding, the primary endpoint of the study.”
In addition, major bleeding was reduced by 74%, and major gastrointestinal bleeding was reduced by 93%.
“We are seeing really profound reductions in bleeding with this agent vs. a NOAC [novel oral anticoagulant],” lead AZALEA investigator Christian Ruff, MD, professor of medicine at Brigham and Women’s Hospital, Boston, said in an interview.
“Major bleeding – effectively the type of bleeding that results in hospitalization – is reduced by more than two-thirds, and major GI bleeding – which is the most common type of bleeding experienced by AF patients on anticoagulants – is almost eliminated. This gives us real hope that we have finally found an anticoagulant that is remarkably safe and will allow us to use anticoagulation in our most vulnerable patients,” he said.
Dr. Ruff presented the full results from the AZALEA trial at the American Heart Association scientific sessions.
He noted that AFib is one of the most common medical conditions in the world and that it confers an increased risk of stroke. Anticoagulants reduce this risk very effectively, and while the NOACS, such as apixaban and rivaroxaban, are safer than warfarin, significant bleeding still occurs, and “shockingly,” he said, between 30% and 60% of patients are not prescribed an anticoagulant or discontinue treatment because of bleeding concerns.
“Clearly, we need safer anticoagulants to protect these patients. Factor XI inhibitors, of which abelacimab is one, have emerged as the most promising agents, as they are thought to provide precision anticoagulation,” Dr. Ruff said.
He explained that factor XI appears to be involved in the formation of thrombus, which blocks arteries and causes strokes and myocardial infarction (thrombosis), but not in the healing process of blood vessels after injury (hemostasis). So, it is believed that inhibiting factor XI should reduce thrombotic events without causing excess bleeding.
AZALEA, which is the largest and longest trial of a factor XI inhibitor to date, enrolled 1,287 adults with AF who were at moderate to high risk of stroke.
They were randomly assigned to receive one of three treatments: oral rivaroxaban 20 mg daily; abelacimab 90 mg; or abelacimab 150 mg. Abelacimab was given monthly by injection.
Both doses of abelacimab inhibited factor XI almost completely; 97% inhibition was achieved with the 90-mg dose, and 99% inhibition was achieved with the 150-mg dose.
Results showed that after a median follow-up of 1.8 years, there was a clear reduction in all bleeding endpoints with both doses of abelacimab, compared with rivaroxaban.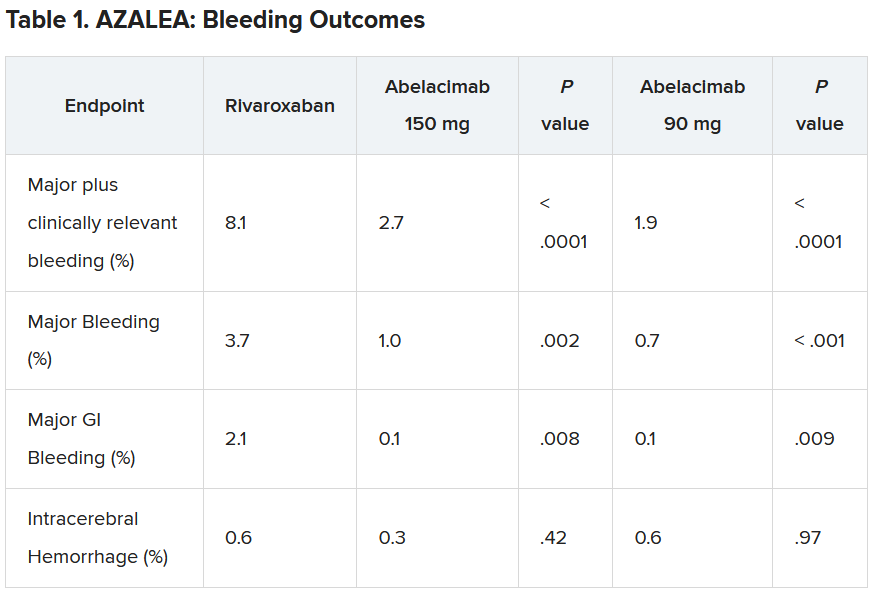
Dr. Ruff explained that the trial was powered to detect differences in bleeding, not stroke, but the investigators approached this in an exploratory way.
“As expected, the numbers were low, with just 25 strokes (23 ischemic strokes) across all three groups in the trial. So, because of this very low rate, we are really not able to compare how abelacimab compares with rivaroxaban in reducing stroke,” he commented.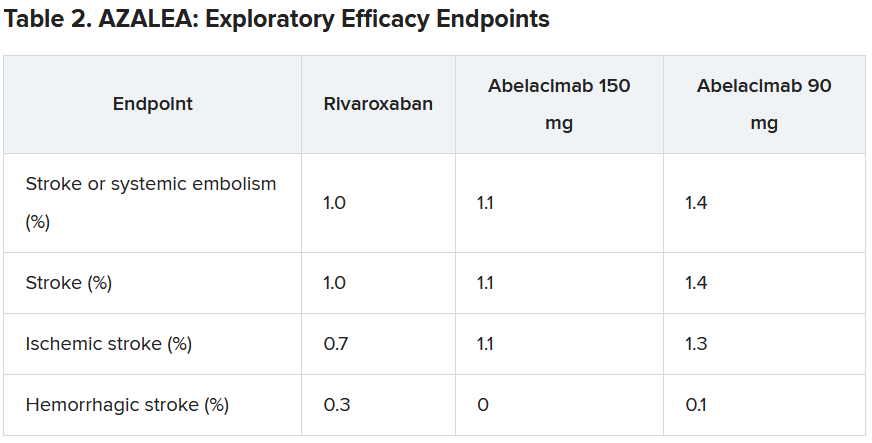
He did, however, suggest that the low stroke rate in the study was encouraging.
“If we look at the same population without anticoagulation, the stroke rate would be about 7% per year. And we see here in this trial that in all three arms, the stroke rate was just above 1% per year. I think this shows that all the patients in the trial were getting highly effective anticoagulation,” he said.
“But what this trial doesn’t answer – because the numbers are so low – is exactly how effective factor XI inhibition with abelacimab is, compared to NOACs in reducing stroke rates. That requires dedicated phase 3 trials.”
Dr. Ruff pointed out that there are some reassuring data from phase 2 trials in venous thromboembolism (VTE), in which the 150-mg dose of abelacimab was associated with an 80% reduction in VTE, compared with enoxaparin. “Historically in the development of anticoagulants, efficacy in VTE has translated into efficacy in stroke prevention, so that is very encouraging,” he commented.
“So, I think our results along with the VTE results are encouraging, but the precision regarding the relative efficacy compared to NOACs is still an open question that needs to be clarified in phase 3 trials,” he concluded.
Several phase 3 trials are now underway with abelacimab and two other small-molecule orally available factor XI inhibitors, milvexian (BMS/Janssen) and asundexian (Bayer).
The designated discussant of the AZALEA study at the AHA meeting, Manesh Patel. MD, Duke University, Durham, N.C., described the results as “an important step forward.”
“This trial, with the prior data in this field, show that factor XI inhibition as a target is biologically possible (studies showing > 95% inhibition), significantly less bleeding than NOACS. We await the phase 3 studies, but having significantly less bleeding and similar or less stroke would be a substantial step forward for the field,” he said.
John Alexander, MD, also from Duke University, said: “There were clinically important reductions in bleeding with both doses of abelacimab, compared with rivaroxaban. This is consistent to what we’ve seen with comparisons between other factor XI inhibitors and other factor Xa inhibitors.”
On the exploratory efficacy results, Dr. Alexander agreed with Dr. Ruff that it was not possible to get any idea of how abelacimab compared with rivaroxaban in reducing stroke. “The hazard ratio and confidence intervals comparing abelacimab and rivaroxaban include substantial lower rates, no difference, and substantially higher rates,” he noted.
“We need to wait for the results of phase 3 trials, with abelacimab and other factor XI inhibitors, to understand how well factor XI inhibition prevents stroke and systemic embolism in patients with atrial fibrillation,” Dr. Alexander added. “These trials are ongoing.”
Dr. Ruff concluded: “Assuming the data from ongoing phase 3 trials confirm the benefit of factor XI inhibitors for stroke prevention in people with AF, it will really be transformative for the field of cardiology.
“Our first mission in treating people with AF is to prevent stroke, and our ability to do this with a remarkably safe anticoagulant such as abelacimab would be an incredible advance,” he concluded.
Dr. Ruff receives research funding from Anthos for abelacimab trials, is on an AF executive committee for BMS/Janssen (milvexian), and has been on an advisory board for Bayer (asundexian). Dr. Patel has received grants from and acts as an advisor to Bayer and Janssen. Dr. Alexander receives research funding from Bayer.
A version of this article first appeared on Medscape.com.
; the risk of stroke was moderate to high.
The trial was stopped earlier this year because of an “overwhelming” reduction in bleeding with abelacimab in comparison to rivaroxaban. Abelacimab is a monoclonal antibody given by subcutaneous injection once a month.
“Details of the bleeding results have now shown that the 150-mg dose of abelacimab, which is the dose being carried forward to phase 3 trials, was associated with a 67% reduction in major or clinically relevant nonmajor bleeding, the primary endpoint of the study.”
In addition, major bleeding was reduced by 74%, and major gastrointestinal bleeding was reduced by 93%.
“We are seeing really profound reductions in bleeding with this agent vs. a NOAC [novel oral anticoagulant],” lead AZALEA investigator Christian Ruff, MD, professor of medicine at Brigham and Women’s Hospital, Boston, said in an interview.
“Major bleeding – effectively the type of bleeding that results in hospitalization – is reduced by more than two-thirds, and major GI bleeding – which is the most common type of bleeding experienced by AF patients on anticoagulants – is almost eliminated. This gives us real hope that we have finally found an anticoagulant that is remarkably safe and will allow us to use anticoagulation in our most vulnerable patients,” he said.
Dr. Ruff presented the full results from the AZALEA trial at the American Heart Association scientific sessions.
He noted that AFib is one of the most common medical conditions in the world and that it confers an increased risk of stroke. Anticoagulants reduce this risk very effectively, and while the NOACS, such as apixaban and rivaroxaban, are safer than warfarin, significant bleeding still occurs, and “shockingly,” he said, between 30% and 60% of patients are not prescribed an anticoagulant or discontinue treatment because of bleeding concerns.
“Clearly, we need safer anticoagulants to protect these patients. Factor XI inhibitors, of which abelacimab is one, have emerged as the most promising agents, as they are thought to provide precision anticoagulation,” Dr. Ruff said.
He explained that factor XI appears to be involved in the formation of thrombus, which blocks arteries and causes strokes and myocardial infarction (thrombosis), but not in the healing process of blood vessels after injury (hemostasis). So, it is believed that inhibiting factor XI should reduce thrombotic events without causing excess bleeding.
AZALEA, which is the largest and longest trial of a factor XI inhibitor to date, enrolled 1,287 adults with AF who were at moderate to high risk of stroke.
They were randomly assigned to receive one of three treatments: oral rivaroxaban 20 mg daily; abelacimab 90 mg; or abelacimab 150 mg. Abelacimab was given monthly by injection.
Both doses of abelacimab inhibited factor XI almost completely; 97% inhibition was achieved with the 90-mg dose, and 99% inhibition was achieved with the 150-mg dose.
Results showed that after a median follow-up of 1.8 years, there was a clear reduction in all bleeding endpoints with both doses of abelacimab, compared with rivaroxaban.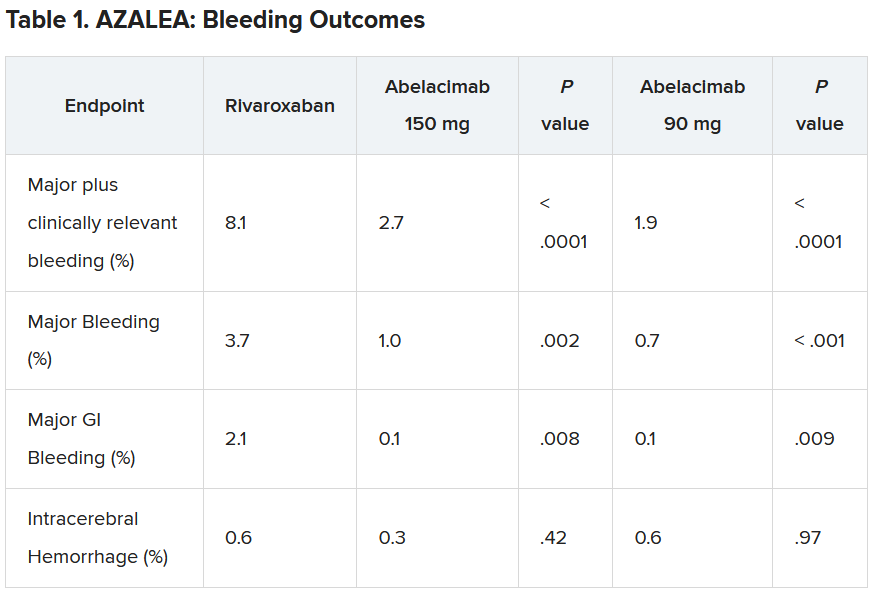
Dr. Ruff explained that the trial was powered to detect differences in bleeding, not stroke, but the investigators approached this in an exploratory way.
“As expected, the numbers were low, with just 25 strokes (23 ischemic strokes) across all three groups in the trial. So, because of this very low rate, we are really not able to compare how abelacimab compares with rivaroxaban in reducing stroke,” he commented.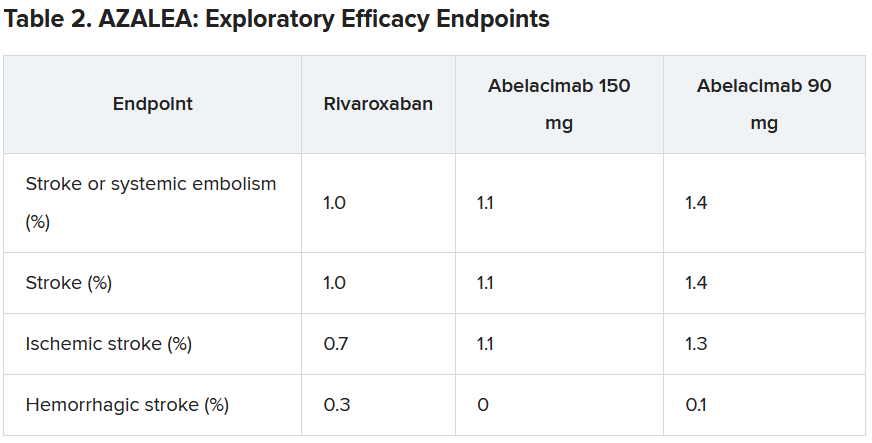
He did, however, suggest that the low stroke rate in the study was encouraging.
“If we look at the same population without anticoagulation, the stroke rate would be about 7% per year. And we see here in this trial that in all three arms, the stroke rate was just above 1% per year. I think this shows that all the patients in the trial were getting highly effective anticoagulation,” he said.
“But what this trial doesn’t answer – because the numbers are so low – is exactly how effective factor XI inhibition with abelacimab is, compared to NOACs in reducing stroke rates. That requires dedicated phase 3 trials.”
Dr. Ruff pointed out that there are some reassuring data from phase 2 trials in venous thromboembolism (VTE), in which the 150-mg dose of abelacimab was associated with an 80% reduction in VTE, compared with enoxaparin. “Historically in the development of anticoagulants, efficacy in VTE has translated into efficacy in stroke prevention, so that is very encouraging,” he commented.
“So, I think our results along with the VTE results are encouraging, but the precision regarding the relative efficacy compared to NOACs is still an open question that needs to be clarified in phase 3 trials,” he concluded.
Several phase 3 trials are now underway with abelacimab and two other small-molecule orally available factor XI inhibitors, milvexian (BMS/Janssen) and asundexian (Bayer).
The designated discussant of the AZALEA study at the AHA meeting, Manesh Patel. MD, Duke University, Durham, N.C., described the results as “an important step forward.”
“This trial, with the prior data in this field, show that factor XI inhibition as a target is biologically possible (studies showing > 95% inhibition), significantly less bleeding than NOACS. We await the phase 3 studies, but having significantly less bleeding and similar or less stroke would be a substantial step forward for the field,” he said.
John Alexander, MD, also from Duke University, said: “There were clinically important reductions in bleeding with both doses of abelacimab, compared with rivaroxaban. This is consistent to what we’ve seen with comparisons between other factor XI inhibitors and other factor Xa inhibitors.”
On the exploratory efficacy results, Dr. Alexander agreed with Dr. Ruff that it was not possible to get any idea of how abelacimab compared with rivaroxaban in reducing stroke. “The hazard ratio and confidence intervals comparing abelacimab and rivaroxaban include substantial lower rates, no difference, and substantially higher rates,” he noted.
“We need to wait for the results of phase 3 trials, with abelacimab and other factor XI inhibitors, to understand how well factor XI inhibition prevents stroke and systemic embolism in patients with atrial fibrillation,” Dr. Alexander added. “These trials are ongoing.”
Dr. Ruff concluded: “Assuming the data from ongoing phase 3 trials confirm the benefit of factor XI inhibitors for stroke prevention in people with AF, it will really be transformative for the field of cardiology.
“Our first mission in treating people with AF is to prevent stroke, and our ability to do this with a remarkably safe anticoagulant such as abelacimab would be an incredible advance,” he concluded.
Dr. Ruff receives research funding from Anthos for abelacimab trials, is on an AF executive committee for BMS/Janssen (milvexian), and has been on an advisory board for Bayer (asundexian). Dr. Patel has received grants from and acts as an advisor to Bayer and Janssen. Dr. Alexander receives research funding from Bayer.
A version of this article first appeared on Medscape.com.
; the risk of stroke was moderate to high.
The trial was stopped earlier this year because of an “overwhelming” reduction in bleeding with abelacimab in comparison to rivaroxaban. Abelacimab is a monoclonal antibody given by subcutaneous injection once a month.
“Details of the bleeding results have now shown that the 150-mg dose of abelacimab, which is the dose being carried forward to phase 3 trials, was associated with a 67% reduction in major or clinically relevant nonmajor bleeding, the primary endpoint of the study.”
In addition, major bleeding was reduced by 74%, and major gastrointestinal bleeding was reduced by 93%.
“We are seeing really profound reductions in bleeding with this agent vs. a NOAC [novel oral anticoagulant],” lead AZALEA investigator Christian Ruff, MD, professor of medicine at Brigham and Women’s Hospital, Boston, said in an interview.
“Major bleeding – effectively the type of bleeding that results in hospitalization – is reduced by more than two-thirds, and major GI bleeding – which is the most common type of bleeding experienced by AF patients on anticoagulants – is almost eliminated. This gives us real hope that we have finally found an anticoagulant that is remarkably safe and will allow us to use anticoagulation in our most vulnerable patients,” he said.
Dr. Ruff presented the full results from the AZALEA trial at the American Heart Association scientific sessions.
He noted that AFib is one of the most common medical conditions in the world and that it confers an increased risk of stroke. Anticoagulants reduce this risk very effectively, and while the NOACS, such as apixaban and rivaroxaban, are safer than warfarin, significant bleeding still occurs, and “shockingly,” he said, between 30% and 60% of patients are not prescribed an anticoagulant or discontinue treatment because of bleeding concerns.
“Clearly, we need safer anticoagulants to protect these patients. Factor XI inhibitors, of which abelacimab is one, have emerged as the most promising agents, as they are thought to provide precision anticoagulation,” Dr. Ruff said.
He explained that factor XI appears to be involved in the formation of thrombus, which blocks arteries and causes strokes and myocardial infarction (thrombosis), but not in the healing process of blood vessels after injury (hemostasis). So, it is believed that inhibiting factor XI should reduce thrombotic events without causing excess bleeding.
AZALEA, which is the largest and longest trial of a factor XI inhibitor to date, enrolled 1,287 adults with AF who were at moderate to high risk of stroke.
They were randomly assigned to receive one of three treatments: oral rivaroxaban 20 mg daily; abelacimab 90 mg; or abelacimab 150 mg. Abelacimab was given monthly by injection.
Both doses of abelacimab inhibited factor XI almost completely; 97% inhibition was achieved with the 90-mg dose, and 99% inhibition was achieved with the 150-mg dose.
Results showed that after a median follow-up of 1.8 years, there was a clear reduction in all bleeding endpoints with both doses of abelacimab, compared with rivaroxaban.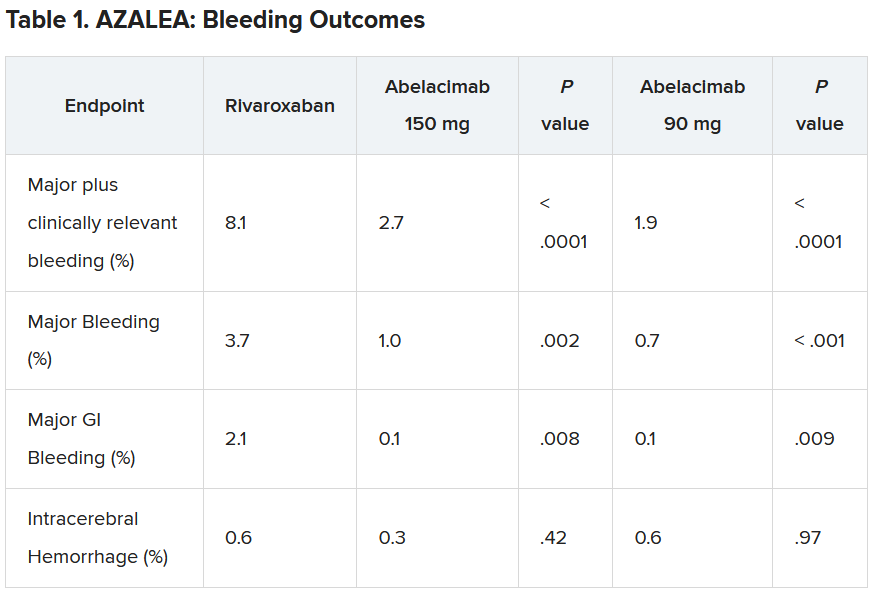
Dr. Ruff explained that the trial was powered to detect differences in bleeding, not stroke, but the investigators approached this in an exploratory way.
“As expected, the numbers were low, with just 25 strokes (23 ischemic strokes) across all three groups in the trial. So, because of this very low rate, we are really not able to compare how abelacimab compares with rivaroxaban in reducing stroke,” he commented.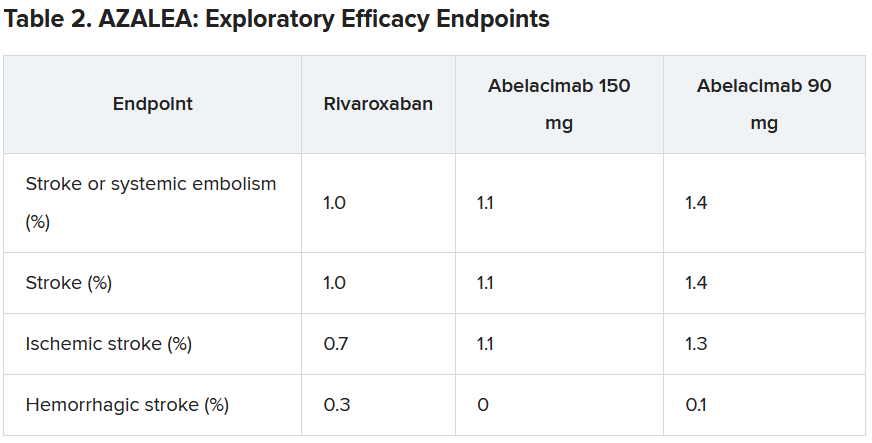
He did, however, suggest that the low stroke rate in the study was encouraging.
“If we look at the same population without anticoagulation, the stroke rate would be about 7% per year. And we see here in this trial that in all three arms, the stroke rate was just above 1% per year. I think this shows that all the patients in the trial were getting highly effective anticoagulation,” he said.
“But what this trial doesn’t answer – because the numbers are so low – is exactly how effective factor XI inhibition with abelacimab is, compared to NOACs in reducing stroke rates. That requires dedicated phase 3 trials.”
Dr. Ruff pointed out that there are some reassuring data from phase 2 trials in venous thromboembolism (VTE), in which the 150-mg dose of abelacimab was associated with an 80% reduction in VTE, compared with enoxaparin. “Historically in the development of anticoagulants, efficacy in VTE has translated into efficacy in stroke prevention, so that is very encouraging,” he commented.
“So, I think our results along with the VTE results are encouraging, but the precision regarding the relative efficacy compared to NOACs is still an open question that needs to be clarified in phase 3 trials,” he concluded.
Several phase 3 trials are now underway with abelacimab and two other small-molecule orally available factor XI inhibitors, milvexian (BMS/Janssen) and asundexian (Bayer).
The designated discussant of the AZALEA study at the AHA meeting, Manesh Patel. MD, Duke University, Durham, N.C., described the results as “an important step forward.”
“This trial, with the prior data in this field, show that factor XI inhibition as a target is biologically possible (studies showing > 95% inhibition), significantly less bleeding than NOACS. We await the phase 3 studies, but having significantly less bleeding and similar or less stroke would be a substantial step forward for the field,” he said.
John Alexander, MD, also from Duke University, said: “There were clinically important reductions in bleeding with both doses of abelacimab, compared with rivaroxaban. This is consistent to what we’ve seen with comparisons between other factor XI inhibitors and other factor Xa inhibitors.”
On the exploratory efficacy results, Dr. Alexander agreed with Dr. Ruff that it was not possible to get any idea of how abelacimab compared with rivaroxaban in reducing stroke. “The hazard ratio and confidence intervals comparing abelacimab and rivaroxaban include substantial lower rates, no difference, and substantially higher rates,” he noted.
“We need to wait for the results of phase 3 trials, with abelacimab and other factor XI inhibitors, to understand how well factor XI inhibition prevents stroke and systemic embolism in patients with atrial fibrillation,” Dr. Alexander added. “These trials are ongoing.”
Dr. Ruff concluded: “Assuming the data from ongoing phase 3 trials confirm the benefit of factor XI inhibitors for stroke prevention in people with AF, it will really be transformative for the field of cardiology.
“Our first mission in treating people with AF is to prevent stroke, and our ability to do this with a remarkably safe anticoagulant such as abelacimab would be an incredible advance,” he concluded.
Dr. Ruff receives research funding from Anthos for abelacimab trials, is on an AF executive committee for BMS/Janssen (milvexian), and has been on an advisory board for Bayer (asundexian). Dr. Patel has received grants from and acts as an advisor to Bayer and Janssen. Dr. Alexander receives research funding from Bayer.
A version of this article first appeared on Medscape.com.
FROM AHA 2023
Semaglutide ‘a new pathway’ to CVD risk reduction: SELECT
over the approximately 3-year follow-up in patients with overweight or obesity and cardiovascular disease but not diabetes.
“This is a very exciting set of results. I think it is going to have a big impact on a large number of people,” lead investigator A. Michael Lincoff, MD, vice chair for research in the department of cardiovascular medicine at the Cleveland Clinic, said in an interview.
“And from a scientific standpoint, these data show that we now have a new pathway or a new modifiable risk factor for cardiovascular disease that we can use in our patients who have overweight or obesity,” he added.
The trial involved 17,604 patients with a history of cardiovascular disease and a body mass index of 27 kg/m2 or above (mean BMI was 33), who were randomly assigned to the glucagonlike peptide–1 (GLP-1) agonist semaglutide, given by subcutaneous injection once weekly at a gradually escalating dose up to 2.4 mg daily by week 16, or placebo. The mean baseline glycated hemoglobin level was 5.8% and 66.4% of patients met the criteria for prediabetes.
Patients lost a mean of 9.4% of body weight over the first 2 years with semaglutide versus 0.88% with placebo.
The primary cardiovascular endpoint – a composite of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke – was reduced significantly, with a hazard ratio of 0.80 (95% confidence interval, 0.72-0.90; P < .001).
Death from cardiovascular causes, the first confirmatory secondary endpoint, showed a 15% reduction (HR, 0.85; P = .07) but this missed meeting criteria for statistical significance, and because of the hierarchical design of the trial, this meant that superiority testing was not performed for the remaining confirmatory secondary endpoints.
However, results showed reductions of around 20% for the heart failure composite endpoint and for all-cause mortality, with confidence intervals that did not cross 1.0, and directionally consistent effects were observed for all supportive secondary endpoints.
The HR for the heart failure composite endpoint was 0.82 (95% CI, 0.71-0.96), and the HR for death from any cause was 0.81 (95% CI, 0.71-0.93). Nonfatal MI was reduced by 28% (HR 0.72; 95% CI, 0.61-0.85).
The effects of semaglutide on the primary endpoint appeared to be similar across all prespecified subgroups.
Adverse events leading to discontinuation of treatment occurred in 16.6% in the semaglutide group, mostly gastrointestinal effects, and in 8.2% in the placebo group.
The trial results were presented by Dr. Lincoff at the annual scientific sessions of the American Heart Association . They were also simultaneously published online in the New England Journal of Medicine.
Dr. Lincoff explained that there is a growing pandemic of overweight and obesity worldwide with clear evidence for years that these conditions increase the risk of cardiovascular events – and yet there has been no evidence, until now, that any pharmacologic or lifestyle therapy can reduce the increased risk conferred by overweight/obesity.
“Patients in the trial were already taking standard of care therapies for other risk factors, such as hypertension and cholesterol, so this drug is giving additional benefit,” he said.
Dr. Lincoff believes these data will lead to a large increase in use of semaglutide, which is already available for the treatment of obesity and diabetes but can be difficult to get reimbursed.
“There is a lot of difficulty getting payors to pay for this drug for weight management. But with this new data from the SELECT trial there should be more willingness – at least in the population with a history of cardiovascular disease,” he commented. In diabetes, where it is already established that there is a cardiovascular risk reduction, it is easier to get these drugs reimbursed, he noted.
On the outcome data, Dr. Lincoff said he could not explain why cardiovascular death was not significantly reduced while all-cause mortality appeared to be cut more definitively.
“The cardiovascular death curves separated, then merged, then separated again. We don’t really know what is going on there. It may be that some deaths were misclassified. This trial was conducted through the COVID era and there may have been less information available on some patients because of that.”
But he added: “The all-cause mortality is more reassuring, as it doesn’t depend on classifying cause of death. Because of the design of the trial, we can’t formally claim a reduction in all-cause mortality, but the results do suggest there is an effect on this endpoint. And all the different types of cardiovascular events were similarly reduced in a consistent way, with similar effects seen across all subgroups. That is very reassuring.”
‘A new era’ for patients with obesity
Outside experts in the field were also impressed with the data.
Designated discussant of the trial at the AHA meeting, Ania Jastreboff, MD, associate professor medicine (endocrinology) at Yale University, New Haven, Conn., said the SELECT trial was “a turning point in the treatment of obesity and a call to action.
“Now is the time to treat obesity to improve health outcomes in people with cardiovascular disease,” she said.
Dr. Jastreboff noted that high BMI was estimated to have accounted for 4 million deaths worldwide in 2015, two-thirds of which were caused by cardiovascular disease. And she presented data showing that U.S. individuals meeting the SELECT criteria increased from 4.3 million in 2011-12 to 6.6 million in 2017-18.
She highlighted one major limitation of the SELECT trial: it enrolled a low number of women (38%) and ethnic minorities, with only 12% of the trial population being Black.
Deepak L. Bhatt, MD, director of Mount Sinai Fuster Heart Hospital, New York, described the SELECT results as “altogether a compelling package of data.”
“These results are even better than I had expected,” Dr. Bhatt said in an interview. “There is a significant reduction in MI as I had anticipated, but additionally, there is a reduction in all-cause death. One can debate the statistics, though on a common-sense level, I think it is a real finding,” he noted.
“Given that MI, heart failure, nephropathy, and revascularization are all reduced, and even stroke is numerically lower, it makes sense that all-cause mortality would be reduced,” he said. “To me, apart from the GI side effects, this counts as a home run.”
Steve Nissen, MD, chief academic officer at the Cleveland Clinic’s Heart, Vascular and Thoracic Institute, was similarly upbeat.
“These data prove what many of us have long suspected – that losing weight can reduce cardiovascular morbidity and mortality. This is great news for patients living with obesity. The obesity epidemic is out of control,” he added. “We need to have therapies that improve cardiovascular outcomes caused by obesity and this shows that semaglutide can do that. I think this is the beginning of a whole new era for patients with obesity.”
Michelle O’Donoghue, MD, associate professor of medicine at Harvard Medical School, Boston, called the results of SELECT “both intriguing and compelling. Certainly, these findings lend further support to the use of semaglutide in a much broader secondary prevention population of individuals with obesity.”
Christie Ballantyne, MD, director of the center for cardiometabolic disease prevention at Baylor College of Medicine, Houston, described the SELECT study as “a landmark trial which will change the practice of medicine in regard to how we treat obesity.”
He compared it with the landmark 4S trial in 1994, the first study in the area of cholesterol lowering therapy to show a clear benefit in reducing cardiovascular events and total mortality, and “began a drastic change in the way that physicians approached treatment of cholesterol.”
On the more robust reduction in all-cause death, compared with cardiovascular death,
Dr. Ballantyne pointed out: “Adjudication of dead or alive is something that everyone gets right. In contrast, the cause of death is sometime difficult to ascertain. Most importantly, the benefit on total mortality also provides assurance that this therapy does not have some adverse effect on increasing noncardiovascular deaths.”
Gastrointestinal adverse effects
On the side effects seen with semaglutide, Dr. Lincoff reported that 10% of patients in the semaglutide group discontinued treatment because of GI side effects versus 2% in the placebo arm. He said this was “an expected issue.”
“GI effects, such as nausea, vomiting and diarrhea, are known side effects of this whole class of drugs. The dose is slowly escalated to manage these adverse effects but there will be a proportion of patients who can’t tolerate it, although the vast majority are able to continue.”
He noted that, while dose reduction was allowed, of the patients who were still on the drug at 2 years, 77% were on the full dose, and 23% were on a reduced dose.
Dr. Lincoff pointed out that there were no serious adverse events with semaglutide. “This is the largest database by far now on the drug with a long-term follow up and we didn’t see the emergence of any new safety signals, which is very reassuring.”
Dr. Nissen said the 16% rate of patients stopping the drug because of tolerability “is not a trivial number.”
He noted that the semaglutide dose used in this study was larger than that used in diabetes.
“They did this to try to achieve more weight loss but then you get more issues with tolerability. It’s a trade-off. If patients are experiencing adverse effects, the dose can be reduced, but then you will lose some effect. All the GLP-1 agonists have GI side effects – it’s part of the way that they work.”
Just weight loss or other actions too?
Speculating on the mechanism behind the reduction in cardiovascular events with semaglutide, Dr. Lincoff does not think it is just weight reduction.
“The event curves start to diverge very soon after the start of the trial and yet the maximum weight loss doesn’t occur until about 65 weeks. I think something else is going on.”
In the paper, the researchers noted that GLP-1 agonists have been shown in animal studies to reduce inflammation, improve endothelial and left ventricular function, promote plaque stability, and decrease platelet aggregation. In this trial, semaglutide was associated with changes in multiple biomarkers of cardiovascular risk, including blood pressure, waist circumference, glycemic control, nephropathy, and levels of lipids and C-reactive protein.
Dr. Lincoff also pointed out that similar benefits were seen in patients with different levels of overweight, and in those who were prediabetic and those who weren’t, so benefit was not dependent on baseline BMI or glycated hemoglobin levels.
Dr. O’Donoghue agreed that other effects, as well as weight loss, could be involved. “The reduction in events with semaglutide appeared very early after initiation and far preceded the drug’s maximal effects on weight reduction. This might suggest that the drug offers other cardioprotective effects through pathways independent of weight loss. Certainly, semaglutide and the other GLP-1 agonists appear to attenuate inflammation, and the patterns of redistribution of adipose tissue may also be of interest.”
She also pointed out that the reduction in cardiovascular events appeared even earlier in this population of obese nondiabetic patients with cardiovascular disease than in prior studies of patients with diabetes. “It may suggest that there is particular benefit for this type of therapy in patients with an inflammatory milieu. I look forward to seeing further analyses to help tease apart the correlation between changes in inflammation, observed weight loss and cardiovascular benefit.”
Effect on clinical practice
With the majority of patients with cardiovascular disease being overweight, these results are obviously going to increase demand for semaglutide, but cost and availability are going to be an issue.
Dr. Bhatt noted that semaglutide is already very popular. “Weight loss drugs are somewhat different from other medications. I can spend 30 minutes trying to convince a patient to take a statin, but here people realize it’s going to cause weight loss and they come in asking for it even if they don’t strictly need it. I think it’s good to have cardiovascular outcome data because now at least for this population of patients, we have evidence to prescribe it.”
He agreed with Dr. Lincoff that these new data should encourage insurance companies to cover the drug, because in reducing cardiovascular events it should also improve downstream health care costs.
“It is providing clear cardiovascular and kidney benefit, so it is in the best interest to the health care system to fund this drug,” he said. “I hope insurers look at it rationally in this way, but they may also be frightened of the explosion of patients wanting this drug and now doctors wanting to prescribe it and how that would affect their shorter-term costs.”
Dr. Lincoff said it would not be easy to prioritize certain groups. “We couldn’t identify any subgroup who showed particularly more benefit than any others. But in the evolution of any therapy, there is a time period where it is in short supply and prohibitively expensive, then over time when there is some competition and pricing deals occur as more people are advocating for it, they become more available.”
‘A welcome treatment option’
In an editorial accompanying publication of the trial, Amit Khera, MD, University of Texas Southwestern Medical Center, Dallas, and Tiffany Powell-Wiley, MD, MPH, National Institutes of Health, Bethesda, noted that baseline risk factors such as LDL cholesterol (78 mg/dL) and systolic blood pressure (131 mm Hg) were not ideal in the semaglutide group in this trial, and they suggest that the benefits of semaglutide may be attenuated when these measures are better controlled.
But given that more than 20 million people in the United States have coronary artery disease, with the majority having overweight or obesity and only approximately 30% having concomitant diabetes, they said that, even in the context of well-controlled risk factors and very low LDL cholesterol levels, the residual risk of atherosclerotic cardiovascular disease in these persons is unacceptably high. “Thus, the SELECT trial provides a welcome treatment option that can be extended to millions of additional patients.”
However, the editorialists cautioned that semaglutide at current pricing comes with a significant cost to both patients and society, which makes this treatment inaccessible for many.
They added that intensive lifestyle interventions and bariatric surgery remain effective but underutilized options for obesity, and that the prevention of obesity before it develops should be the primary goal.
The SELECT trial was supported by Novo Nordisk, and several coauthors are employees of the company. Dr. Lincoff is a consultant for Novo Nordisk. Dr. Bhatt and Dr. Nissen are involved in a cardiovascular outcomes trial with a new investigational weight loss drug from Lilly. Dr. Bhatt and Dr. Ballantyne are also investigators in a Novo Nordisk trial of a new anti-inflammatory drug.
over the approximately 3-year follow-up in patients with overweight or obesity and cardiovascular disease but not diabetes.
“This is a very exciting set of results. I think it is going to have a big impact on a large number of people,” lead investigator A. Michael Lincoff, MD, vice chair for research in the department of cardiovascular medicine at the Cleveland Clinic, said in an interview.
“And from a scientific standpoint, these data show that we now have a new pathway or a new modifiable risk factor for cardiovascular disease that we can use in our patients who have overweight or obesity,” he added.
The trial involved 17,604 patients with a history of cardiovascular disease and a body mass index of 27 kg/m2 or above (mean BMI was 33), who were randomly assigned to the glucagonlike peptide–1 (GLP-1) agonist semaglutide, given by subcutaneous injection once weekly at a gradually escalating dose up to 2.4 mg daily by week 16, or placebo. The mean baseline glycated hemoglobin level was 5.8% and 66.4% of patients met the criteria for prediabetes.
Patients lost a mean of 9.4% of body weight over the first 2 years with semaglutide versus 0.88% with placebo.
The primary cardiovascular endpoint – a composite of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke – was reduced significantly, with a hazard ratio of 0.80 (95% confidence interval, 0.72-0.90; P < .001).
Death from cardiovascular causes, the first confirmatory secondary endpoint, showed a 15% reduction (HR, 0.85; P = .07) but this missed meeting criteria for statistical significance, and because of the hierarchical design of the trial, this meant that superiority testing was not performed for the remaining confirmatory secondary endpoints.
However, results showed reductions of around 20% for the heart failure composite endpoint and for all-cause mortality, with confidence intervals that did not cross 1.0, and directionally consistent effects were observed for all supportive secondary endpoints.
The HR for the heart failure composite endpoint was 0.82 (95% CI, 0.71-0.96), and the HR for death from any cause was 0.81 (95% CI, 0.71-0.93). Nonfatal MI was reduced by 28% (HR 0.72; 95% CI, 0.61-0.85).
The effects of semaglutide on the primary endpoint appeared to be similar across all prespecified subgroups.
Adverse events leading to discontinuation of treatment occurred in 16.6% in the semaglutide group, mostly gastrointestinal effects, and in 8.2% in the placebo group.
The trial results were presented by Dr. Lincoff at the annual scientific sessions of the American Heart Association . They were also simultaneously published online in the New England Journal of Medicine.
Dr. Lincoff explained that there is a growing pandemic of overweight and obesity worldwide with clear evidence for years that these conditions increase the risk of cardiovascular events – and yet there has been no evidence, until now, that any pharmacologic or lifestyle therapy can reduce the increased risk conferred by overweight/obesity.
“Patients in the trial were already taking standard of care therapies for other risk factors, such as hypertension and cholesterol, so this drug is giving additional benefit,” he said.
Dr. Lincoff believes these data will lead to a large increase in use of semaglutide, which is already available for the treatment of obesity and diabetes but can be difficult to get reimbursed.
“There is a lot of difficulty getting payors to pay for this drug for weight management. But with this new data from the SELECT trial there should be more willingness – at least in the population with a history of cardiovascular disease,” he commented. In diabetes, where it is already established that there is a cardiovascular risk reduction, it is easier to get these drugs reimbursed, he noted.
On the outcome data, Dr. Lincoff said he could not explain why cardiovascular death was not significantly reduced while all-cause mortality appeared to be cut more definitively.
“The cardiovascular death curves separated, then merged, then separated again. We don’t really know what is going on there. It may be that some deaths were misclassified. This trial was conducted through the COVID era and there may have been less information available on some patients because of that.”
But he added: “The all-cause mortality is more reassuring, as it doesn’t depend on classifying cause of death. Because of the design of the trial, we can’t formally claim a reduction in all-cause mortality, but the results do suggest there is an effect on this endpoint. And all the different types of cardiovascular events were similarly reduced in a consistent way, with similar effects seen across all subgroups. That is very reassuring.”
‘A new era’ for patients with obesity
Outside experts in the field were also impressed with the data.
Designated discussant of the trial at the AHA meeting, Ania Jastreboff, MD, associate professor medicine (endocrinology) at Yale University, New Haven, Conn., said the SELECT trial was “a turning point in the treatment of obesity and a call to action.
“Now is the time to treat obesity to improve health outcomes in people with cardiovascular disease,” she said.
Dr. Jastreboff noted that high BMI was estimated to have accounted for 4 million deaths worldwide in 2015, two-thirds of which were caused by cardiovascular disease. And she presented data showing that U.S. individuals meeting the SELECT criteria increased from 4.3 million in 2011-12 to 6.6 million in 2017-18.
She highlighted one major limitation of the SELECT trial: it enrolled a low number of women (38%) and ethnic minorities, with only 12% of the trial population being Black.
Deepak L. Bhatt, MD, director of Mount Sinai Fuster Heart Hospital, New York, described the SELECT results as “altogether a compelling package of data.”
“These results are even better than I had expected,” Dr. Bhatt said in an interview. “There is a significant reduction in MI as I had anticipated, but additionally, there is a reduction in all-cause death. One can debate the statistics, though on a common-sense level, I think it is a real finding,” he noted.
“Given that MI, heart failure, nephropathy, and revascularization are all reduced, and even stroke is numerically lower, it makes sense that all-cause mortality would be reduced,” he said. “To me, apart from the GI side effects, this counts as a home run.”
Steve Nissen, MD, chief academic officer at the Cleveland Clinic’s Heart, Vascular and Thoracic Institute, was similarly upbeat.
“These data prove what many of us have long suspected – that losing weight can reduce cardiovascular morbidity and mortality. This is great news for patients living with obesity. The obesity epidemic is out of control,” he added. “We need to have therapies that improve cardiovascular outcomes caused by obesity and this shows that semaglutide can do that. I think this is the beginning of a whole new era for patients with obesity.”
Michelle O’Donoghue, MD, associate professor of medicine at Harvard Medical School, Boston, called the results of SELECT “both intriguing and compelling. Certainly, these findings lend further support to the use of semaglutide in a much broader secondary prevention population of individuals with obesity.”
Christie Ballantyne, MD, director of the center for cardiometabolic disease prevention at Baylor College of Medicine, Houston, described the SELECT study as “a landmark trial which will change the practice of medicine in regard to how we treat obesity.”
He compared it with the landmark 4S trial in 1994, the first study in the area of cholesterol lowering therapy to show a clear benefit in reducing cardiovascular events and total mortality, and “began a drastic change in the way that physicians approached treatment of cholesterol.”
On the more robust reduction in all-cause death, compared with cardiovascular death,
Dr. Ballantyne pointed out: “Adjudication of dead or alive is something that everyone gets right. In contrast, the cause of death is sometime difficult to ascertain. Most importantly, the benefit on total mortality also provides assurance that this therapy does not have some adverse effect on increasing noncardiovascular deaths.”
Gastrointestinal adverse effects
On the side effects seen with semaglutide, Dr. Lincoff reported that 10% of patients in the semaglutide group discontinued treatment because of GI side effects versus 2% in the placebo arm. He said this was “an expected issue.”
“GI effects, such as nausea, vomiting and diarrhea, are known side effects of this whole class of drugs. The dose is slowly escalated to manage these adverse effects but there will be a proportion of patients who can’t tolerate it, although the vast majority are able to continue.”
He noted that, while dose reduction was allowed, of the patients who were still on the drug at 2 years, 77% were on the full dose, and 23% were on a reduced dose.
Dr. Lincoff pointed out that there were no serious adverse events with semaglutide. “This is the largest database by far now on the drug with a long-term follow up and we didn’t see the emergence of any new safety signals, which is very reassuring.”
Dr. Nissen said the 16% rate of patients stopping the drug because of tolerability “is not a trivial number.”
He noted that the semaglutide dose used in this study was larger than that used in diabetes.
“They did this to try to achieve more weight loss but then you get more issues with tolerability. It’s a trade-off. If patients are experiencing adverse effects, the dose can be reduced, but then you will lose some effect. All the GLP-1 agonists have GI side effects – it’s part of the way that they work.”
Just weight loss or other actions too?
Speculating on the mechanism behind the reduction in cardiovascular events with semaglutide, Dr. Lincoff does not think it is just weight reduction.
“The event curves start to diverge very soon after the start of the trial and yet the maximum weight loss doesn’t occur until about 65 weeks. I think something else is going on.”
In the paper, the researchers noted that GLP-1 agonists have been shown in animal studies to reduce inflammation, improve endothelial and left ventricular function, promote plaque stability, and decrease platelet aggregation. In this trial, semaglutide was associated with changes in multiple biomarkers of cardiovascular risk, including blood pressure, waist circumference, glycemic control, nephropathy, and levels of lipids and C-reactive protein.
Dr. Lincoff also pointed out that similar benefits were seen in patients with different levels of overweight, and in those who were prediabetic and those who weren’t, so benefit was not dependent on baseline BMI or glycated hemoglobin levels.
Dr. O’Donoghue agreed that other effects, as well as weight loss, could be involved. “The reduction in events with semaglutide appeared very early after initiation and far preceded the drug’s maximal effects on weight reduction. This might suggest that the drug offers other cardioprotective effects through pathways independent of weight loss. Certainly, semaglutide and the other GLP-1 agonists appear to attenuate inflammation, and the patterns of redistribution of adipose tissue may also be of interest.”
She also pointed out that the reduction in cardiovascular events appeared even earlier in this population of obese nondiabetic patients with cardiovascular disease than in prior studies of patients with diabetes. “It may suggest that there is particular benefit for this type of therapy in patients with an inflammatory milieu. I look forward to seeing further analyses to help tease apart the correlation between changes in inflammation, observed weight loss and cardiovascular benefit.”
Effect on clinical practice
With the majority of patients with cardiovascular disease being overweight, these results are obviously going to increase demand for semaglutide, but cost and availability are going to be an issue.
Dr. Bhatt noted that semaglutide is already very popular. “Weight loss drugs are somewhat different from other medications. I can spend 30 minutes trying to convince a patient to take a statin, but here people realize it’s going to cause weight loss and they come in asking for it even if they don’t strictly need it. I think it’s good to have cardiovascular outcome data because now at least for this population of patients, we have evidence to prescribe it.”
He agreed with Dr. Lincoff that these new data should encourage insurance companies to cover the drug, because in reducing cardiovascular events it should also improve downstream health care costs.
“It is providing clear cardiovascular and kidney benefit, so it is in the best interest to the health care system to fund this drug,” he said. “I hope insurers look at it rationally in this way, but they may also be frightened of the explosion of patients wanting this drug and now doctors wanting to prescribe it and how that would affect their shorter-term costs.”
Dr. Lincoff said it would not be easy to prioritize certain groups. “We couldn’t identify any subgroup who showed particularly more benefit than any others. But in the evolution of any therapy, there is a time period where it is in short supply and prohibitively expensive, then over time when there is some competition and pricing deals occur as more people are advocating for it, they become more available.”
‘A welcome treatment option’
In an editorial accompanying publication of the trial, Amit Khera, MD, University of Texas Southwestern Medical Center, Dallas, and Tiffany Powell-Wiley, MD, MPH, National Institutes of Health, Bethesda, noted that baseline risk factors such as LDL cholesterol (78 mg/dL) and systolic blood pressure (131 mm Hg) were not ideal in the semaglutide group in this trial, and they suggest that the benefits of semaglutide may be attenuated when these measures are better controlled.
But given that more than 20 million people in the United States have coronary artery disease, with the majority having overweight or obesity and only approximately 30% having concomitant diabetes, they said that, even in the context of well-controlled risk factors and very low LDL cholesterol levels, the residual risk of atherosclerotic cardiovascular disease in these persons is unacceptably high. “Thus, the SELECT trial provides a welcome treatment option that can be extended to millions of additional patients.”
However, the editorialists cautioned that semaglutide at current pricing comes with a significant cost to both patients and society, which makes this treatment inaccessible for many.
They added that intensive lifestyle interventions and bariatric surgery remain effective but underutilized options for obesity, and that the prevention of obesity before it develops should be the primary goal.
The SELECT trial was supported by Novo Nordisk, and several coauthors are employees of the company. Dr. Lincoff is a consultant for Novo Nordisk. Dr. Bhatt and Dr. Nissen are involved in a cardiovascular outcomes trial with a new investigational weight loss drug from Lilly. Dr. Bhatt and Dr. Ballantyne are also investigators in a Novo Nordisk trial of a new anti-inflammatory drug.
over the approximately 3-year follow-up in patients with overweight or obesity and cardiovascular disease but not diabetes.
“This is a very exciting set of results. I think it is going to have a big impact on a large number of people,” lead investigator A. Michael Lincoff, MD, vice chair for research in the department of cardiovascular medicine at the Cleveland Clinic, said in an interview.
“And from a scientific standpoint, these data show that we now have a new pathway or a new modifiable risk factor for cardiovascular disease that we can use in our patients who have overweight or obesity,” he added.
The trial involved 17,604 patients with a history of cardiovascular disease and a body mass index of 27 kg/m2 or above (mean BMI was 33), who were randomly assigned to the glucagonlike peptide–1 (GLP-1) agonist semaglutide, given by subcutaneous injection once weekly at a gradually escalating dose up to 2.4 mg daily by week 16, or placebo. The mean baseline glycated hemoglobin level was 5.8% and 66.4% of patients met the criteria for prediabetes.
Patients lost a mean of 9.4% of body weight over the first 2 years with semaglutide versus 0.88% with placebo.
The primary cardiovascular endpoint – a composite of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke – was reduced significantly, with a hazard ratio of 0.80 (95% confidence interval, 0.72-0.90; P < .001).
Death from cardiovascular causes, the first confirmatory secondary endpoint, showed a 15% reduction (HR, 0.85; P = .07) but this missed meeting criteria for statistical significance, and because of the hierarchical design of the trial, this meant that superiority testing was not performed for the remaining confirmatory secondary endpoints.
However, results showed reductions of around 20% for the heart failure composite endpoint and for all-cause mortality, with confidence intervals that did not cross 1.0, and directionally consistent effects were observed for all supportive secondary endpoints.
The HR for the heart failure composite endpoint was 0.82 (95% CI, 0.71-0.96), and the HR for death from any cause was 0.81 (95% CI, 0.71-0.93). Nonfatal MI was reduced by 28% (HR 0.72; 95% CI, 0.61-0.85).
The effects of semaglutide on the primary endpoint appeared to be similar across all prespecified subgroups.
Adverse events leading to discontinuation of treatment occurred in 16.6% in the semaglutide group, mostly gastrointestinal effects, and in 8.2% in the placebo group.
The trial results were presented by Dr. Lincoff at the annual scientific sessions of the American Heart Association . They were also simultaneously published online in the New England Journal of Medicine.
Dr. Lincoff explained that there is a growing pandemic of overweight and obesity worldwide with clear evidence for years that these conditions increase the risk of cardiovascular events – and yet there has been no evidence, until now, that any pharmacologic or lifestyle therapy can reduce the increased risk conferred by overweight/obesity.
“Patients in the trial were already taking standard of care therapies for other risk factors, such as hypertension and cholesterol, so this drug is giving additional benefit,” he said.
Dr. Lincoff believes these data will lead to a large increase in use of semaglutide, which is already available for the treatment of obesity and diabetes but can be difficult to get reimbursed.
“There is a lot of difficulty getting payors to pay for this drug for weight management. But with this new data from the SELECT trial there should be more willingness – at least in the population with a history of cardiovascular disease,” he commented. In diabetes, where it is already established that there is a cardiovascular risk reduction, it is easier to get these drugs reimbursed, he noted.
On the outcome data, Dr. Lincoff said he could not explain why cardiovascular death was not significantly reduced while all-cause mortality appeared to be cut more definitively.
“The cardiovascular death curves separated, then merged, then separated again. We don’t really know what is going on there. It may be that some deaths were misclassified. This trial was conducted through the COVID era and there may have been less information available on some patients because of that.”
But he added: “The all-cause mortality is more reassuring, as it doesn’t depend on classifying cause of death. Because of the design of the trial, we can’t formally claim a reduction in all-cause mortality, but the results do suggest there is an effect on this endpoint. And all the different types of cardiovascular events were similarly reduced in a consistent way, with similar effects seen across all subgroups. That is very reassuring.”
‘A new era’ for patients with obesity
Outside experts in the field were also impressed with the data.
Designated discussant of the trial at the AHA meeting, Ania Jastreboff, MD, associate professor medicine (endocrinology) at Yale University, New Haven, Conn., said the SELECT trial was “a turning point in the treatment of obesity and a call to action.
“Now is the time to treat obesity to improve health outcomes in people with cardiovascular disease,” she said.
Dr. Jastreboff noted that high BMI was estimated to have accounted for 4 million deaths worldwide in 2015, two-thirds of which were caused by cardiovascular disease. And she presented data showing that U.S. individuals meeting the SELECT criteria increased from 4.3 million in 2011-12 to 6.6 million in 2017-18.
She highlighted one major limitation of the SELECT trial: it enrolled a low number of women (38%) and ethnic minorities, with only 12% of the trial population being Black.
Deepak L. Bhatt, MD, director of Mount Sinai Fuster Heart Hospital, New York, described the SELECT results as “altogether a compelling package of data.”
“These results are even better than I had expected,” Dr. Bhatt said in an interview. “There is a significant reduction in MI as I had anticipated, but additionally, there is a reduction in all-cause death. One can debate the statistics, though on a common-sense level, I think it is a real finding,” he noted.
“Given that MI, heart failure, nephropathy, and revascularization are all reduced, and even stroke is numerically lower, it makes sense that all-cause mortality would be reduced,” he said. “To me, apart from the GI side effects, this counts as a home run.”
Steve Nissen, MD, chief academic officer at the Cleveland Clinic’s Heart, Vascular and Thoracic Institute, was similarly upbeat.
“These data prove what many of us have long suspected – that losing weight can reduce cardiovascular morbidity and mortality. This is great news for patients living with obesity. The obesity epidemic is out of control,” he added. “We need to have therapies that improve cardiovascular outcomes caused by obesity and this shows that semaglutide can do that. I think this is the beginning of a whole new era for patients with obesity.”
Michelle O’Donoghue, MD, associate professor of medicine at Harvard Medical School, Boston, called the results of SELECT “both intriguing and compelling. Certainly, these findings lend further support to the use of semaglutide in a much broader secondary prevention population of individuals with obesity.”
Christie Ballantyne, MD, director of the center for cardiometabolic disease prevention at Baylor College of Medicine, Houston, described the SELECT study as “a landmark trial which will change the practice of medicine in regard to how we treat obesity.”
He compared it with the landmark 4S trial in 1994, the first study in the area of cholesterol lowering therapy to show a clear benefit in reducing cardiovascular events and total mortality, and “began a drastic change in the way that physicians approached treatment of cholesterol.”
On the more robust reduction in all-cause death, compared with cardiovascular death,
Dr. Ballantyne pointed out: “Adjudication of dead or alive is something that everyone gets right. In contrast, the cause of death is sometime difficult to ascertain. Most importantly, the benefit on total mortality also provides assurance that this therapy does not have some adverse effect on increasing noncardiovascular deaths.”
Gastrointestinal adverse effects
On the side effects seen with semaglutide, Dr. Lincoff reported that 10% of patients in the semaglutide group discontinued treatment because of GI side effects versus 2% in the placebo arm. He said this was “an expected issue.”
“GI effects, such as nausea, vomiting and diarrhea, are known side effects of this whole class of drugs. The dose is slowly escalated to manage these adverse effects but there will be a proportion of patients who can’t tolerate it, although the vast majority are able to continue.”
He noted that, while dose reduction was allowed, of the patients who were still on the drug at 2 years, 77% were on the full dose, and 23% were on a reduced dose.
Dr. Lincoff pointed out that there were no serious adverse events with semaglutide. “This is the largest database by far now on the drug with a long-term follow up and we didn’t see the emergence of any new safety signals, which is very reassuring.”
Dr. Nissen said the 16% rate of patients stopping the drug because of tolerability “is not a trivial number.”
He noted that the semaglutide dose used in this study was larger than that used in diabetes.
“They did this to try to achieve more weight loss but then you get more issues with tolerability. It’s a trade-off. If patients are experiencing adverse effects, the dose can be reduced, but then you will lose some effect. All the GLP-1 agonists have GI side effects – it’s part of the way that they work.”
Just weight loss or other actions too?
Speculating on the mechanism behind the reduction in cardiovascular events with semaglutide, Dr. Lincoff does not think it is just weight reduction.
“The event curves start to diverge very soon after the start of the trial and yet the maximum weight loss doesn’t occur until about 65 weeks. I think something else is going on.”
In the paper, the researchers noted that GLP-1 agonists have been shown in animal studies to reduce inflammation, improve endothelial and left ventricular function, promote plaque stability, and decrease platelet aggregation. In this trial, semaglutide was associated with changes in multiple biomarkers of cardiovascular risk, including blood pressure, waist circumference, glycemic control, nephropathy, and levels of lipids and C-reactive protein.
Dr. Lincoff also pointed out that similar benefits were seen in patients with different levels of overweight, and in those who were prediabetic and those who weren’t, so benefit was not dependent on baseline BMI or glycated hemoglobin levels.
Dr. O’Donoghue agreed that other effects, as well as weight loss, could be involved. “The reduction in events with semaglutide appeared very early after initiation and far preceded the drug’s maximal effects on weight reduction. This might suggest that the drug offers other cardioprotective effects through pathways independent of weight loss. Certainly, semaglutide and the other GLP-1 agonists appear to attenuate inflammation, and the patterns of redistribution of adipose tissue may also be of interest.”
She also pointed out that the reduction in cardiovascular events appeared even earlier in this population of obese nondiabetic patients with cardiovascular disease than in prior studies of patients with diabetes. “It may suggest that there is particular benefit for this type of therapy in patients with an inflammatory milieu. I look forward to seeing further analyses to help tease apart the correlation between changes in inflammation, observed weight loss and cardiovascular benefit.”
Effect on clinical practice
With the majority of patients with cardiovascular disease being overweight, these results are obviously going to increase demand for semaglutide, but cost and availability are going to be an issue.
Dr. Bhatt noted that semaglutide is already very popular. “Weight loss drugs are somewhat different from other medications. I can spend 30 minutes trying to convince a patient to take a statin, but here people realize it’s going to cause weight loss and they come in asking for it even if they don’t strictly need it. I think it’s good to have cardiovascular outcome data because now at least for this population of patients, we have evidence to prescribe it.”
He agreed with Dr. Lincoff that these new data should encourage insurance companies to cover the drug, because in reducing cardiovascular events it should also improve downstream health care costs.
“It is providing clear cardiovascular and kidney benefit, so it is in the best interest to the health care system to fund this drug,” he said. “I hope insurers look at it rationally in this way, but they may also be frightened of the explosion of patients wanting this drug and now doctors wanting to prescribe it and how that would affect their shorter-term costs.”
Dr. Lincoff said it would not be easy to prioritize certain groups. “We couldn’t identify any subgroup who showed particularly more benefit than any others. But in the evolution of any therapy, there is a time period where it is in short supply and prohibitively expensive, then over time when there is some competition and pricing deals occur as more people are advocating for it, they become more available.”
‘A welcome treatment option’
In an editorial accompanying publication of the trial, Amit Khera, MD, University of Texas Southwestern Medical Center, Dallas, and Tiffany Powell-Wiley, MD, MPH, National Institutes of Health, Bethesda, noted that baseline risk factors such as LDL cholesterol (78 mg/dL) and systolic blood pressure (131 mm Hg) were not ideal in the semaglutide group in this trial, and they suggest that the benefits of semaglutide may be attenuated when these measures are better controlled.
But given that more than 20 million people in the United States have coronary artery disease, with the majority having overweight or obesity and only approximately 30% having concomitant diabetes, they said that, even in the context of well-controlled risk factors and very low LDL cholesterol levels, the residual risk of atherosclerotic cardiovascular disease in these persons is unacceptably high. “Thus, the SELECT trial provides a welcome treatment option that can be extended to millions of additional patients.”
However, the editorialists cautioned that semaglutide at current pricing comes with a significant cost to both patients and society, which makes this treatment inaccessible for many.
They added that intensive lifestyle interventions and bariatric surgery remain effective but underutilized options for obesity, and that the prevention of obesity before it develops should be the primary goal.
The SELECT trial was supported by Novo Nordisk, and several coauthors are employees of the company. Dr. Lincoff is a consultant for Novo Nordisk. Dr. Bhatt and Dr. Nissen are involved in a cardiovascular outcomes trial with a new investigational weight loss drug from Lilly. Dr. Bhatt and Dr. Ballantyne are also investigators in a Novo Nordisk trial of a new anti-inflammatory drug.
FROM AHA 2023
Women have worse outcomes in cardiogenic shock
“These data identify the need for us to continue working to identify barriers in terms of diagnosis, management, and technological innovations for women in cardiogenic shock to resolve these issues and improve outcomes,” the senior author of the study, Navin Kapur, MD, Tufts Medical Center, Boston, said in an interview.
The study is said to be the one of the largest contemporary analyses of real-world registry data on the characteristics and outcomes of women in comparison with men with cardiogenic shock.
It showed sex-specific differences in outcomes that were primarily driven by differences in heart failure–related cardiogenic shock. Women with heart failure–related cardiogenic shock had more severe cardiogenic shock, worse survival at discharge, and more vascular complications than men. Outcomes in cardiogenic shock related to MI were similar for men and women.
The study, which will be presented at the upcoming annual meeting of the American Heart Association, was published online in JACC: Heart Failure.
Dr. Kapur founded the Cardiogenic Shock Working Group in 2017 to collect quality data on the condition.
“We realized our patients were dying, and we didn’t have enough data on how best to manage them. So, we started this registry, and now have detailed data on close to 9,000 patients with cardiogenic shock from 45 hospitals in the U.S., Mexico, Australia, and Japan,” he explained.
“The primary goal is to try to investigate the questions related to cardiogenic shock that can inform management, and one of the key questions that came up was differences in how men and women present with cardiogenic shock and what their outcomes may be. This is what we are reporting in this paper,” he added.
Cardiogenic shock is defined as having a low cardiac output most commonly because of MI or an episode of acute heart failure, Dr. Kapur said. Patients with cardiogenic shock are identified by their low blood pressure or hypoperfusion evidenced by clinical exam or biomarkers, such as elevated lactate levels.
“In this analysis, we’re looking at patients presenting with cardiogenic shock, so were not looking at the incidence of the condition in men versus women,” Dr. Kapur noted. “However, we believe that cardiogenic shock is probably more underrepresented in women, who may present with an MI or acute heart failure and may or may not be identified as having low cardiac output states until quite late. The likelihood is that the incidence is similar in men and women, but women are more often undiagnosed.”
For the current study, the authors analyzed data on 5,083 patients with cardiogenic shock in the registry, of whom 1,522 (30%) were women. Compared with men, women had slightly higher body mass index (BMI) and smaller body surface area.
Results showed that women with heart failure–related cardiogenic shock had worse survival at discharge than men (69.9% vs. 74.4%) and a higher rate of refractory shock (SCAI stage E; 26% vs. 21%). Women were also less likely to undergo pulmonary artery catheterization (52.9% vs. 54.6%), heart transplantation (6.5% vs. 10.3%), or left ventricular assist device implantation (7.8% vs. 10%).
Regardless of cardiogenic shock etiology, women had more vascular complications (8.8% vs. 5.7%), bleeding (7.1% vs. 5.2%), and limb ischemia (6.8% vs. 4.5%).
“This analysis is quite revealing. We identified some important distinctions between men and women,” Dr. Kapur commented.
For many patients who present with MI-related cardiogenic shock, many of the baseline characteristics in men and women were quite similar, he said. “But in heart failure–related cardiogenic shock, we saw more differences, with typical comorbidities associated with cardiogenic shock [e.g., diabetes, chronic kidney disease, hypertension] being less common in women than in men. This suggests there may be phenotypic differences as to why women present with heart failure shock versus men.”
Dr. Kapur pointed out that differences in BMI or body surface area between men and women may play into some of the management decision-making.
“Women having a smaller stature may lead to a selection bias where we don’t want to use large-bore pumps or devices because we’re worried about causing complications. We found in the analysis that vascular complications such as bleeding or ischemia of the lower extremity where these devices typically go were more frequent in women,” he noted.
“We also found that women were less likely to receive invasive therapies in general, including pulmonary artery catheters, temporary mechanical support, and heart replacements, such as LVAD or transplants,” he added.
Further results showed that, after propensity score matching, some of the gender differences disappeared, but women continued to have a higher rate of vascular complications (10.4% women vs. 7.4% men).
But Dr. Kapur warned that the propensity-matched analysis had some caveats.
“Essentially what we are doing with propensity matching is creating two populations that are as similar as possible, and this reduced the number of patients in the analysis down to 25% of the original population,” he said. “One of the things we had to match was body surface area, and in doing this, we are taking out one of the most important differences between men and women, and as a result, a lot of the differences in outcomes go away.
“In this respect, propensity matching can be a bit of a double-edge sword,” he added. “I think the non–propensity-matched results are more interesting, as they are more of a reflection of the real world.”
Dr. Kapur concluded that these findings are compelling enough to suggest that there are important differences between women and men with cardiogenic shock in terms of outcomes as well as complication rates.
“Our decision-making around women seems to be different to that around men. I think this paper should start to trigger more awareness of that.”
Dr. Kapur also emphasized the importance of paying attention to vascular complications in women.
“The higher rates of bleeding and limb ischemia issues in women may explain the rationale for being less aggressive with invasive therapies in women,” he said. “But we need to come up with better solutions or technologies so they can be used more effectively in women. This could include adapting technology for smaller vascular sizes, which should lead to better outcome and fewer complications in women.”
He added that further granular data on this issue are needed. “We have very limited datasets in cardiogenic shock. There are few randomized controlled trials, and women are not well represented in such trials. We need to make sure we enroll women in randomized trials.”
Dr. Kapur said more women physicians who treat cardiogenic shock are also required, which would include cardiologists, critical care specialists, cardiac surgeons, and anesthesia personnel.
He pointed out that the two first authors of the current study are women – Van-Khue Ton, MD, Massachusetts General Hospital, Boston, and Manreet Kanwar, MD, Allegheny Health Network, Pittsburgh.
“We worked hard to involve women as principal investigators. They led the effort. These are investigations led by women, on women, to advance the care of women,” he commented.
Gender-related inequality
In an editorial accompanying publication of the study, Sara Kalantari, MD, and Jonathan Grinstein, MD, University of Chicago, and Robert O. Roswell, MD, Hofstra University, Hempstead, N.Y., said these results “provide valuable information about gender-related inequality in care and outcomes in the management of cardiogenic shock, although the exact mechanisms driving these observed differences still need to be elucidated.
“Broadly speaking, barriers in the care of women with heart failure and cardiogenic shock include a reduced awareness among both patients and providers, a deficiency of sex-specific objective criteria for guiding therapy, and unfavorable temporary mechanical circulatory support devices with higher rates of hemocompatibility-related complications in women,” they added.
“In the era of the multidisciplinary shock team and shock pathways with protocolized management algorithms, it is imperative that we still allow for personalization of care to match the physiologic needs of the patient in order for us to continue to close the gender gap in the care of patients presenting with cardiogenic shock,” the editorialists concluded.
A version of this article appeared on Medscape.com.
“These data identify the need for us to continue working to identify barriers in terms of diagnosis, management, and technological innovations for women in cardiogenic shock to resolve these issues and improve outcomes,” the senior author of the study, Navin Kapur, MD, Tufts Medical Center, Boston, said in an interview.
The study is said to be the one of the largest contemporary analyses of real-world registry data on the characteristics and outcomes of women in comparison with men with cardiogenic shock.
It showed sex-specific differences in outcomes that were primarily driven by differences in heart failure–related cardiogenic shock. Women with heart failure–related cardiogenic shock had more severe cardiogenic shock, worse survival at discharge, and more vascular complications than men. Outcomes in cardiogenic shock related to MI were similar for men and women.
The study, which will be presented at the upcoming annual meeting of the American Heart Association, was published online in JACC: Heart Failure.
Dr. Kapur founded the Cardiogenic Shock Working Group in 2017 to collect quality data on the condition.
“We realized our patients were dying, and we didn’t have enough data on how best to manage them. So, we started this registry, and now have detailed data on close to 9,000 patients with cardiogenic shock from 45 hospitals in the U.S., Mexico, Australia, and Japan,” he explained.
“The primary goal is to try to investigate the questions related to cardiogenic shock that can inform management, and one of the key questions that came up was differences in how men and women present with cardiogenic shock and what their outcomes may be. This is what we are reporting in this paper,” he added.
Cardiogenic shock is defined as having a low cardiac output most commonly because of MI or an episode of acute heart failure, Dr. Kapur said. Patients with cardiogenic shock are identified by their low blood pressure or hypoperfusion evidenced by clinical exam or biomarkers, such as elevated lactate levels.
“In this analysis, we’re looking at patients presenting with cardiogenic shock, so were not looking at the incidence of the condition in men versus women,” Dr. Kapur noted. “However, we believe that cardiogenic shock is probably more underrepresented in women, who may present with an MI or acute heart failure and may or may not be identified as having low cardiac output states until quite late. The likelihood is that the incidence is similar in men and women, but women are more often undiagnosed.”
For the current study, the authors analyzed data on 5,083 patients with cardiogenic shock in the registry, of whom 1,522 (30%) were women. Compared with men, women had slightly higher body mass index (BMI) and smaller body surface area.
Results showed that women with heart failure–related cardiogenic shock had worse survival at discharge than men (69.9% vs. 74.4%) and a higher rate of refractory shock (SCAI stage E; 26% vs. 21%). Women were also less likely to undergo pulmonary artery catheterization (52.9% vs. 54.6%), heart transplantation (6.5% vs. 10.3%), or left ventricular assist device implantation (7.8% vs. 10%).
Regardless of cardiogenic shock etiology, women had more vascular complications (8.8% vs. 5.7%), bleeding (7.1% vs. 5.2%), and limb ischemia (6.8% vs. 4.5%).
“This analysis is quite revealing. We identified some important distinctions between men and women,” Dr. Kapur commented.
For many patients who present with MI-related cardiogenic shock, many of the baseline characteristics in men and women were quite similar, he said. “But in heart failure–related cardiogenic shock, we saw more differences, with typical comorbidities associated with cardiogenic shock [e.g., diabetes, chronic kidney disease, hypertension] being less common in women than in men. This suggests there may be phenotypic differences as to why women present with heart failure shock versus men.”
Dr. Kapur pointed out that differences in BMI or body surface area between men and women may play into some of the management decision-making.
“Women having a smaller stature may lead to a selection bias where we don’t want to use large-bore pumps or devices because we’re worried about causing complications. We found in the analysis that vascular complications such as bleeding or ischemia of the lower extremity where these devices typically go were more frequent in women,” he noted.
“We also found that women were less likely to receive invasive therapies in general, including pulmonary artery catheters, temporary mechanical support, and heart replacements, such as LVAD or transplants,” he added.
Further results showed that, after propensity score matching, some of the gender differences disappeared, but women continued to have a higher rate of vascular complications (10.4% women vs. 7.4% men).
But Dr. Kapur warned that the propensity-matched analysis had some caveats.
“Essentially what we are doing with propensity matching is creating two populations that are as similar as possible, and this reduced the number of patients in the analysis down to 25% of the original population,” he said. “One of the things we had to match was body surface area, and in doing this, we are taking out one of the most important differences between men and women, and as a result, a lot of the differences in outcomes go away.
“In this respect, propensity matching can be a bit of a double-edge sword,” he added. “I think the non–propensity-matched results are more interesting, as they are more of a reflection of the real world.”
Dr. Kapur concluded that these findings are compelling enough to suggest that there are important differences between women and men with cardiogenic shock in terms of outcomes as well as complication rates.
“Our decision-making around women seems to be different to that around men. I think this paper should start to trigger more awareness of that.”
Dr. Kapur also emphasized the importance of paying attention to vascular complications in women.
“The higher rates of bleeding and limb ischemia issues in women may explain the rationale for being less aggressive with invasive therapies in women,” he said. “But we need to come up with better solutions or technologies so they can be used more effectively in women. This could include adapting technology for smaller vascular sizes, which should lead to better outcome and fewer complications in women.”
He added that further granular data on this issue are needed. “We have very limited datasets in cardiogenic shock. There are few randomized controlled trials, and women are not well represented in such trials. We need to make sure we enroll women in randomized trials.”
Dr. Kapur said more women physicians who treat cardiogenic shock are also required, which would include cardiologists, critical care specialists, cardiac surgeons, and anesthesia personnel.
He pointed out that the two first authors of the current study are women – Van-Khue Ton, MD, Massachusetts General Hospital, Boston, and Manreet Kanwar, MD, Allegheny Health Network, Pittsburgh.
“We worked hard to involve women as principal investigators. They led the effort. These are investigations led by women, on women, to advance the care of women,” he commented.
Gender-related inequality
In an editorial accompanying publication of the study, Sara Kalantari, MD, and Jonathan Grinstein, MD, University of Chicago, and Robert O. Roswell, MD, Hofstra University, Hempstead, N.Y., said these results “provide valuable information about gender-related inequality in care and outcomes in the management of cardiogenic shock, although the exact mechanisms driving these observed differences still need to be elucidated.
“Broadly speaking, barriers in the care of women with heart failure and cardiogenic shock include a reduced awareness among both patients and providers, a deficiency of sex-specific objective criteria for guiding therapy, and unfavorable temporary mechanical circulatory support devices with higher rates of hemocompatibility-related complications in women,” they added.
“In the era of the multidisciplinary shock team and shock pathways with protocolized management algorithms, it is imperative that we still allow for personalization of care to match the physiologic needs of the patient in order for us to continue to close the gender gap in the care of patients presenting with cardiogenic shock,” the editorialists concluded.
A version of this article appeared on Medscape.com.
“These data identify the need for us to continue working to identify barriers in terms of diagnosis, management, and technological innovations for women in cardiogenic shock to resolve these issues and improve outcomes,” the senior author of the study, Navin Kapur, MD, Tufts Medical Center, Boston, said in an interview.
The study is said to be the one of the largest contemporary analyses of real-world registry data on the characteristics and outcomes of women in comparison with men with cardiogenic shock.
It showed sex-specific differences in outcomes that were primarily driven by differences in heart failure–related cardiogenic shock. Women with heart failure–related cardiogenic shock had more severe cardiogenic shock, worse survival at discharge, and more vascular complications than men. Outcomes in cardiogenic shock related to MI were similar for men and women.
The study, which will be presented at the upcoming annual meeting of the American Heart Association, was published online in JACC: Heart Failure.
Dr. Kapur founded the Cardiogenic Shock Working Group in 2017 to collect quality data on the condition.
“We realized our patients were dying, and we didn’t have enough data on how best to manage them. So, we started this registry, and now have detailed data on close to 9,000 patients with cardiogenic shock from 45 hospitals in the U.S., Mexico, Australia, and Japan,” he explained.
“The primary goal is to try to investigate the questions related to cardiogenic shock that can inform management, and one of the key questions that came up was differences in how men and women present with cardiogenic shock and what their outcomes may be. This is what we are reporting in this paper,” he added.
Cardiogenic shock is defined as having a low cardiac output most commonly because of MI or an episode of acute heart failure, Dr. Kapur said. Patients with cardiogenic shock are identified by their low blood pressure or hypoperfusion evidenced by clinical exam or biomarkers, such as elevated lactate levels.
“In this analysis, we’re looking at patients presenting with cardiogenic shock, so were not looking at the incidence of the condition in men versus women,” Dr. Kapur noted. “However, we believe that cardiogenic shock is probably more underrepresented in women, who may present with an MI or acute heart failure and may or may not be identified as having low cardiac output states until quite late. The likelihood is that the incidence is similar in men and women, but women are more often undiagnosed.”
For the current study, the authors analyzed data on 5,083 patients with cardiogenic shock in the registry, of whom 1,522 (30%) were women. Compared with men, women had slightly higher body mass index (BMI) and smaller body surface area.
Results showed that women with heart failure–related cardiogenic shock had worse survival at discharge than men (69.9% vs. 74.4%) and a higher rate of refractory shock (SCAI stage E; 26% vs. 21%). Women were also less likely to undergo pulmonary artery catheterization (52.9% vs. 54.6%), heart transplantation (6.5% vs. 10.3%), or left ventricular assist device implantation (7.8% vs. 10%).
Regardless of cardiogenic shock etiology, women had more vascular complications (8.8% vs. 5.7%), bleeding (7.1% vs. 5.2%), and limb ischemia (6.8% vs. 4.5%).
“This analysis is quite revealing. We identified some important distinctions between men and women,” Dr. Kapur commented.
For many patients who present with MI-related cardiogenic shock, many of the baseline characteristics in men and women were quite similar, he said. “But in heart failure–related cardiogenic shock, we saw more differences, with typical comorbidities associated with cardiogenic shock [e.g., diabetes, chronic kidney disease, hypertension] being less common in women than in men. This suggests there may be phenotypic differences as to why women present with heart failure shock versus men.”
Dr. Kapur pointed out that differences in BMI or body surface area between men and women may play into some of the management decision-making.
“Women having a smaller stature may lead to a selection bias where we don’t want to use large-bore pumps or devices because we’re worried about causing complications. We found in the analysis that vascular complications such as bleeding or ischemia of the lower extremity where these devices typically go were more frequent in women,” he noted.
“We also found that women were less likely to receive invasive therapies in general, including pulmonary artery catheters, temporary mechanical support, and heart replacements, such as LVAD or transplants,” he added.
Further results showed that, after propensity score matching, some of the gender differences disappeared, but women continued to have a higher rate of vascular complications (10.4% women vs. 7.4% men).
But Dr. Kapur warned that the propensity-matched analysis had some caveats.
“Essentially what we are doing with propensity matching is creating two populations that are as similar as possible, and this reduced the number of patients in the analysis down to 25% of the original population,” he said. “One of the things we had to match was body surface area, and in doing this, we are taking out one of the most important differences between men and women, and as a result, a lot of the differences in outcomes go away.
“In this respect, propensity matching can be a bit of a double-edge sword,” he added. “I think the non–propensity-matched results are more interesting, as they are more of a reflection of the real world.”
Dr. Kapur concluded that these findings are compelling enough to suggest that there are important differences between women and men with cardiogenic shock in terms of outcomes as well as complication rates.
“Our decision-making around women seems to be different to that around men. I think this paper should start to trigger more awareness of that.”
Dr. Kapur also emphasized the importance of paying attention to vascular complications in women.
“The higher rates of bleeding and limb ischemia issues in women may explain the rationale for being less aggressive with invasive therapies in women,” he said. “But we need to come up with better solutions or technologies so they can be used more effectively in women. This could include adapting technology for smaller vascular sizes, which should lead to better outcome and fewer complications in women.”
He added that further granular data on this issue are needed. “We have very limited datasets in cardiogenic shock. There are few randomized controlled trials, and women are not well represented in such trials. We need to make sure we enroll women in randomized trials.”
Dr. Kapur said more women physicians who treat cardiogenic shock are also required, which would include cardiologists, critical care specialists, cardiac surgeons, and anesthesia personnel.
He pointed out that the two first authors of the current study are women – Van-Khue Ton, MD, Massachusetts General Hospital, Boston, and Manreet Kanwar, MD, Allegheny Health Network, Pittsburgh.
“We worked hard to involve women as principal investigators. They led the effort. These are investigations led by women, on women, to advance the care of women,” he commented.
Gender-related inequality
In an editorial accompanying publication of the study, Sara Kalantari, MD, and Jonathan Grinstein, MD, University of Chicago, and Robert O. Roswell, MD, Hofstra University, Hempstead, N.Y., said these results “provide valuable information about gender-related inequality in care and outcomes in the management of cardiogenic shock, although the exact mechanisms driving these observed differences still need to be elucidated.
“Broadly speaking, barriers in the care of women with heart failure and cardiogenic shock include a reduced awareness among both patients and providers, a deficiency of sex-specific objective criteria for guiding therapy, and unfavorable temporary mechanical circulatory support devices with higher rates of hemocompatibility-related complications in women,” they added.
“In the era of the multidisciplinary shock team and shock pathways with protocolized management algorithms, it is imperative that we still allow for personalization of care to match the physiologic needs of the patient in order for us to continue to close the gender gap in the care of patients presenting with cardiogenic shock,” the editorialists concluded.
A version of this article appeared on Medscape.com.
FROM AHA 2023


