User login
Dr. Whitcomb is chief medical officer of Remedy Partners. He is co-founder and past president of SHM. E-mail him at [email protected].
Win Whitcomb: Hospitalists Must Grin and Bear the Hospital-Acquired Conditions Program
The Inpatient Prospective Payment System FY2013 Final Rule charts a different future: By fiscal-year 2015 (October 2014), it will morph into a set of measures that are vetted by the National Quality Forum. Hopefully, this will be an improvement.
In recent years, hospitalists have been deluged with rules about documentation, being asked to use medical vocabulary in ways that were foreign to many of us during our training years. Much of the focus on documentation has been propelled by hospitals’ quest to optimize (“maximize” is a forbidden term) reimbursement, which is purely a function of what is written by “licensed providers” (doctors, physician assistants, and nurse practitioners) in the medical chart.
But another powerful driver of documentation practices of late is the hospital-acquired conditions (HAC) program developed by the Centers for Medicare & Medicaid Services (CMS) and enacted in 2009.
Origins of the HAC List
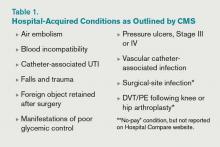
CMS disliked the fact that they were paying for conditions acquired in the hospital that were “reasonably preventable” if evidence-based—or at least “best”—practice was applied. After all, who likes to pay for a punctured gas tank when you brought the minivan in for an oil change? CMS worked with stakeholder groups, including SHM, to create a list of conditions known as hospital-acquired conditions (see Table 1, right).
(As an aside, SHM was supportive of CMS. In fact, we provided direct input into the final rule, recognizing some of the drawbacks of the CMS approach but understanding the larger objective of reengineering a flawed incentive system.)
The idea was that if a hospital submitted a bill to CMS that contained one of these conditions, the hospital would not be paid the amount by which that condition increased total reimbursement for that hospitalization. Note that if you’ve been told your hospital isn’t getting paid at all for patients with one of these conditions, that is not quite correct. Instead, your hospital may not get paid the added amount that is derived from having one of the diagnoses on the list submitted in your hospital’s bill to CMS for a given patient. At the end of the day, this might be a few hundred dollars each time one of these is documented—or $0, if your hospital biller can add another diagnosis in its place to capture the higher payment.
How big a hit to a hospital’s bottom line is this? Meddings and colleagues recently reported that a measly 0.003% of all hospitalizations in Michigan in 2009 saw payments lowered as a result of hospital-acquired catheter-associated UTI, one of the list’s HACs (Ann Int Med. 2012;157:305-312). When all the HACs are added together, one can extrapolate that they haven’t exactly had a big impact on hospital payments.
If the specter of nonpayment for one of these is not enough of a motivator (and it shouldn’t be, given the paltry financial stakes), the rate of HACs are now reported for all hospitals on the Hospital Compare website (www.hospitalcompare.hhs.gov). If a small poke to the pocketbook doesn’t work, maybe public humiliation will.
The Problem with HACs
Although CMS’ intent in creating the HAC program—to eliminate payment for “reasonably preventable” hospital-acquired conditions, thereby improving patient safety—was good, in practice, the program has turned out to be as much about documentation as it is about providing good care. For example, if I forget to write that a Stage III pressure ulcer was present on admission, it gets coded as hospital-acquired and my hospital gets dinged.
It’s important to note that HACs as quality measures were never endorsed by the National Quality Forum (NQF), and without such an endorsement, a quality measure suffers from Rodney Dangerfield syndrome: It don’t get no respect.
Finally, it is disquieting that Meddings et al showed that hospital-acquired catheter-associated UTI rates derived from chart documentation for HACs were but a small fraction of rates determined from rigorous epidemiologic studies, demonstrating that using claims data for determining rates for that specific HAC is flawed. We can only wonder how divergent reported vs. actual rates for the other HACs are.
The Future of the HAC Program
The Affordable Care Act specifies that the lowest-performing quartile of U.S. hospitals for HAC rates will see a 1% Medicare reimbursement reduction beginning in fiscal-year 2015. That’s right: Hospitals facing possible readmissions penalties and losses under value-based purchasing also will face a HAC penalty.
Thankfully, the recently released Inpatient Prospective Payment System FY2013 Final Rule, CMS’ annual update of how hospitals are paid, specifies that the HAC measures are to be removed from public reporting on the Hospital Compare website effective Oct. 1, 2014. They will be replaced by a new set of measures that will (hopefully) be more methodologically sound, because they will require the scrutiny required for endorsement by the NQF. Exactly how these measures will look is not certain, as the rule-making has not yet occurred.
We do know that the three infection measures—catheter-associated UTI, surgical-site infection, and vascular catheter infection—will be generated from clinical data and, therefore, more methodologically sound under the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network. The derivation of the other measures will have to wait until the rule is written next year.
So, until further notice, pay attention to the queries of your hospital’s documentation experts when they approach you about a potential HAC!
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The Inpatient Prospective Payment System FY2013 Final Rule charts a different future: By fiscal-year 2015 (October 2014), it will morph into a set of measures that are vetted by the National Quality Forum. Hopefully, this will be an improvement.
In recent years, hospitalists have been deluged with rules about documentation, being asked to use medical vocabulary in ways that were foreign to many of us during our training years. Much of the focus on documentation has been propelled by hospitals’ quest to optimize (“maximize” is a forbidden term) reimbursement, which is purely a function of what is written by “licensed providers” (doctors, physician assistants, and nurse practitioners) in the medical chart.
But another powerful driver of documentation practices of late is the hospital-acquired conditions (HAC) program developed by the Centers for Medicare & Medicaid Services (CMS) and enacted in 2009.
Origins of the HAC List
CMS disliked the fact that they were paying for conditions acquired in the hospital that were “reasonably preventable” if evidence-based—or at least “best”—practice was applied. After all, who likes to pay for a punctured gas tank when you brought the minivan in for an oil change? CMS worked with stakeholder groups, including SHM, to create a list of conditions known as hospital-acquired conditions (see Table 1, right).
(As an aside, SHM was supportive of CMS. In fact, we provided direct input into the final rule, recognizing some of the drawbacks of the CMS approach but understanding the larger objective of reengineering a flawed incentive system.)
The idea was that if a hospital submitted a bill to CMS that contained one of these conditions, the hospital would not be paid the amount by which that condition increased total reimbursement for that hospitalization. Note that if you’ve been told your hospital isn’t getting paid at all for patients with one of these conditions, that is not quite correct. Instead, your hospital may not get paid the added amount that is derived from having one of the diagnoses on the list submitted in your hospital’s bill to CMS for a given patient. At the end of the day, this might be a few hundred dollars each time one of these is documented—or $0, if your hospital biller can add another diagnosis in its place to capture the higher payment.
How big a hit to a hospital’s bottom line is this? Meddings and colleagues recently reported that a measly 0.003% of all hospitalizations in Michigan in 2009 saw payments lowered as a result of hospital-acquired catheter-associated UTI, one of the list’s HACs (Ann Int Med. 2012;157:305-312). When all the HACs are added together, one can extrapolate that they haven’t exactly had a big impact on hospital payments.
If the specter of nonpayment for one of these is not enough of a motivator (and it shouldn’t be, given the paltry financial stakes), the rate of HACs are now reported for all hospitals on the Hospital Compare website (www.hospitalcompare.hhs.gov). If a small poke to the pocketbook doesn’t work, maybe public humiliation will.
The Problem with HACs
Although CMS’ intent in creating the HAC program—to eliminate payment for “reasonably preventable” hospital-acquired conditions, thereby improving patient safety—was good, in practice, the program has turned out to be as much about documentation as it is about providing good care. For example, if I forget to write that a Stage III pressure ulcer was present on admission, it gets coded as hospital-acquired and my hospital gets dinged.
It’s important to note that HACs as quality measures were never endorsed by the National Quality Forum (NQF), and without such an endorsement, a quality measure suffers from Rodney Dangerfield syndrome: It don’t get no respect.
Finally, it is disquieting that Meddings et al showed that hospital-acquired catheter-associated UTI rates derived from chart documentation for HACs were but a small fraction of rates determined from rigorous epidemiologic studies, demonstrating that using claims data for determining rates for that specific HAC is flawed. We can only wonder how divergent reported vs. actual rates for the other HACs are.
The Future of the HAC Program
The Affordable Care Act specifies that the lowest-performing quartile of U.S. hospitals for HAC rates will see a 1% Medicare reimbursement reduction beginning in fiscal-year 2015. That’s right: Hospitals facing possible readmissions penalties and losses under value-based purchasing also will face a HAC penalty.
Thankfully, the recently released Inpatient Prospective Payment System FY2013 Final Rule, CMS’ annual update of how hospitals are paid, specifies that the HAC measures are to be removed from public reporting on the Hospital Compare website effective Oct. 1, 2014. They will be replaced by a new set of measures that will (hopefully) be more methodologically sound, because they will require the scrutiny required for endorsement by the NQF. Exactly how these measures will look is not certain, as the rule-making has not yet occurred.
We do know that the three infection measures—catheter-associated UTI, surgical-site infection, and vascular catheter infection—will be generated from clinical data and, therefore, more methodologically sound under the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network. The derivation of the other measures will have to wait until the rule is written next year.
So, until further notice, pay attention to the queries of your hospital’s documentation experts when they approach you about a potential HAC!
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The Inpatient Prospective Payment System FY2013 Final Rule charts a different future: By fiscal-year 2015 (October 2014), it will morph into a set of measures that are vetted by the National Quality Forum. Hopefully, this will be an improvement.
In recent years, hospitalists have been deluged with rules about documentation, being asked to use medical vocabulary in ways that were foreign to many of us during our training years. Much of the focus on documentation has been propelled by hospitals’ quest to optimize (“maximize” is a forbidden term) reimbursement, which is purely a function of what is written by “licensed providers” (doctors, physician assistants, and nurse practitioners) in the medical chart.
But another powerful driver of documentation practices of late is the hospital-acquired conditions (HAC) program developed by the Centers for Medicare & Medicaid Services (CMS) and enacted in 2009.
Origins of the HAC List
CMS disliked the fact that they were paying for conditions acquired in the hospital that were “reasonably preventable” if evidence-based—or at least “best”—practice was applied. After all, who likes to pay for a punctured gas tank when you brought the minivan in for an oil change? CMS worked with stakeholder groups, including SHM, to create a list of conditions known as hospital-acquired conditions (see Table 1, right).
(As an aside, SHM was supportive of CMS. In fact, we provided direct input into the final rule, recognizing some of the drawbacks of the CMS approach but understanding the larger objective of reengineering a flawed incentive system.)
The idea was that if a hospital submitted a bill to CMS that contained one of these conditions, the hospital would not be paid the amount by which that condition increased total reimbursement for that hospitalization. Note that if you’ve been told your hospital isn’t getting paid at all for patients with one of these conditions, that is not quite correct. Instead, your hospital may not get paid the added amount that is derived from having one of the diagnoses on the list submitted in your hospital’s bill to CMS for a given patient. At the end of the day, this might be a few hundred dollars each time one of these is documented—or $0, if your hospital biller can add another diagnosis in its place to capture the higher payment.
How big a hit to a hospital’s bottom line is this? Meddings and colleagues recently reported that a measly 0.003% of all hospitalizations in Michigan in 2009 saw payments lowered as a result of hospital-acquired catheter-associated UTI, one of the list’s HACs (Ann Int Med. 2012;157:305-312). When all the HACs are added together, one can extrapolate that they haven’t exactly had a big impact on hospital payments.
If the specter of nonpayment for one of these is not enough of a motivator (and it shouldn’t be, given the paltry financial stakes), the rate of HACs are now reported for all hospitals on the Hospital Compare website (www.hospitalcompare.hhs.gov). If a small poke to the pocketbook doesn’t work, maybe public humiliation will.
The Problem with HACs
Although CMS’ intent in creating the HAC program—to eliminate payment for “reasonably preventable” hospital-acquired conditions, thereby improving patient safety—was good, in practice, the program has turned out to be as much about documentation as it is about providing good care. For example, if I forget to write that a Stage III pressure ulcer was present on admission, it gets coded as hospital-acquired and my hospital gets dinged.
It’s important to note that HACs as quality measures were never endorsed by the National Quality Forum (NQF), and without such an endorsement, a quality measure suffers from Rodney Dangerfield syndrome: It don’t get no respect.
Finally, it is disquieting that Meddings et al showed that hospital-acquired catheter-associated UTI rates derived from chart documentation for HACs were but a small fraction of rates determined from rigorous epidemiologic studies, demonstrating that using claims data for determining rates for that specific HAC is flawed. We can only wonder how divergent reported vs. actual rates for the other HACs are.
The Future of the HAC Program
The Affordable Care Act specifies that the lowest-performing quartile of U.S. hospitals for HAC rates will see a 1% Medicare reimbursement reduction beginning in fiscal-year 2015. That’s right: Hospitals facing possible readmissions penalties and losses under value-based purchasing also will face a HAC penalty.
Thankfully, the recently released Inpatient Prospective Payment System FY2013 Final Rule, CMS’ annual update of how hospitals are paid, specifies that the HAC measures are to be removed from public reporting on the Hospital Compare website effective Oct. 1, 2014. They will be replaced by a new set of measures that will (hopefully) be more methodologically sound, because they will require the scrutiny required for endorsement by the NQF. Exactly how these measures will look is not certain, as the rule-making has not yet occurred.
We do know that the three infection measures—catheter-associated UTI, surgical-site infection, and vascular catheter infection—will be generated from clinical data and, therefore, more methodologically sound under the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network. The derivation of the other measures will have to wait until the rule is written next year.
So, until further notice, pay attention to the queries of your hospital’s documentation experts when they approach you about a potential HAC!
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Win Whitcomb: Hospital Readmissions Penalties Start Now
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
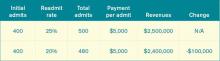
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
The uproar and confusion over readmissions penalties has consumed umpteen hours of senior leaders’ time (especially that of CFOs), not to mention that of front-line nurses, case managers, quality-improvement (QI) coordinators, hospitalists, and others involved in discharge planning and ensuring a safe transition for patients out of the hospital. For many, the math is fuzzy, and for most, the return on investment is even fuzzier. After all, avoided readmissions are lost revenue to those who are running a business known as an acute-care hospital.
Let me start with the conclusion: Eliminating avoidable readmissions is the right thing to do, period. But the financial downside to doing so is probably greater than any upside realized through avoidance of the penalties that began affecting hospital payments on Oct. 1—at least in the fee-for-service world we live in. At some point in the future, when most patients are under a global payment, the math might be clearer, but today, penalties probably won’t offset lost revenue from reduced readmissions added to the cost of paying lots of people to work in meetings (and at the bedside) to devise better care transitions. (Caveat: If your hospital is bursting at the seams with full occupancy, reducing readmissions and replacing them with higher-reimbursing patients, such as those undergoing elective major surgery, likely will be a net financial gain for your hospital.)
Part of the Affordable Care Act (ACA), the Hospital Readmissions Reduction Program (HRRP) will reduce total Medicare DRG reimbursement for hospitals beginning in fiscal-year 2013 based on actual 30-day readmission rates for myocardial infarction (MI), heart failure (HF), and pneumonia that are in excess of risk-adjusted expected rates. The reduction is capped at 1% in 2013, 2% in 2014, and 3% in 2015 and beyond. Hospital readmission rates are based on calculated baseline rates using Medicare data from July 1, 2008, to June 30, 2011.
Cost of a Readmissions-Reduction Program
How much does it cost for a hospital to implement a care-transitions program—such as SHM’s Project BOOST—to reduce readmissions? Last year, I interviewed a dozen hospitals that successfully implemented SHM’s formal mentored implementation program. The result? In the first year of the program, hospitals spent about $170,000 on training and staff time devoted to the project.
Lost Revenue
Let’s look at a sample penalty calculation, then examine a scenario sizing up how revenue is lost when a hospital is successful in reducing readmissions. The ACA defines the payments for excess readmissions as:
The number of patients with the applicable condition (HF, MI, or pneumonia) multiplied by the base DRG payment made for those patients multiplied by the percentage of readmissions beyond the expected.
As an example, let’s take a hospital that treats 500 pneumonia patients (# with the applicable condition), has a base DRG payment for pneumonia of $5,000, and a readmission rate that is 4% higher than expected (in this example, the actual rate is 25% and the expected rate is 24%; 1/25=4%). The penalty is 500 X $5,000 X .04, or $100,000. We’ll assume that the readmission rate for myocardial infarction and heart failure are less than expected, so the total penalty is $100,000.
Let’s say the hospital works hard to decrease pneumonia readmissions from 25% to 20% and avoids the penalty. As outlined in Table 1, the hospital will lose $100,000 in revenue (admittedly, reducing readmissions to 20% from 25% represents a big jump, but this is for illustration purposes—we haven’t added in lost revenue from reduced readmissions for other conditions). What’s the final cost of avoiding the $100,000 readmission penalty? Lost revenue of $100,000 plus the cost of implementing the readmission reduction program of $170,000=$270,000.
Why Are We Doing This?
I see the value in care transitions and readmissions-reduction programs, such as Project BOOST, first and foremost as a way to improve patient safety; as such, if implemented effectively, they are likely worth the investment. Second, their value lies in the preparation all hospitals and health systems should be undergoing to remain market-competitive and solvent under global payment systems. Because the penalties in the HRRP might come with lost revenues and the costs of program implementation, be clear about your team’s motivation for reducing readmissions. Your CFO will see to it if I don’t.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Win Whitcomb: Inflexible, Big-Box EHRs Endanger the QI Movement
In “The Lean Startup,” author Eric Ries notes that in its early stages, his gaming company would routinely issue new versions of their software application several times each day. Continuous deployment—the process Ries’ company used—leveraged such Lean principles as reduced batch size and continuous learning based on end-user feedback to achieve rapid improvements in their product.
Ries says companies that learn the quickest about what the customer wants, and can incorporate that information into products more efficiently, stand the greatest chance of succeeding. A software engineer by trade, Ries uses many examples of companies that have succeeded with this approach, none of which are from healthcare.
In stark relief, the chief technology hospitalists interface with daily is the electronic health record (EHR), widely recognized as a system that fails to consider the end-user experience, that is unable to interoperate with other software, and is incapable of using data for quality improvement (QI). The PDSA (“plan, do, study, act”) cycle is the foundation of QI activities and relies on rapidly incorporating observations made by those performing the work to create novel workflows and processes based on learning. EHRs, by digitizing health information, theoretically provide the ideal tool for supporting QI.
The reality is that EHRs have been a colossal disappointment with regard to QI efforts. The space in and around EHR effectively represents “dead zones” for innovation and improvement. Mandl and Kohane note:
EHR companies have followed a business model whereby they control all data, rather than liberating the data for use in innovative applications in clinical care.
Conducting a Google-style search of an EHR database usually requires involvement of a clinician’s information services department and often the specialized knowledge and cooperation of the vendor’s technical teams.
Greg Maynard, MD, MSc, SFHM, senior vice president of SHM’s Center for Hospital Innovation and Improvement, recently provided testimony to the Office of the National Coordinator for Health Information Technology about the challenges current EHRs present to QI efforts and what features EHRs need to incorporate to better serve the needs of patients and clinicians. Dr. Maynard answered a few questions for The Hospitalist:
Q: What is it about current EHRs that make continuous improvement so difficult?
A: EHRs were built for fiscal and administrative purposes, not for quality improvement and safety. The administrative/fiscal roots of today’s IT systems lead to poor availability of clinical, quality, and safety data. In many medical centers and practices, the great majority of information available is months-old administrative data, which does not lend itself to rapid cycle improvement.
Q: Why is the PDSA cycle endangered in most systems?
A: EHRs often do not facilitate rapid-cycle, PDSA-style improvements on a small pilot scale. Most improvement teams get one shot to get the clinical decision support and data-capture tools correct after months of waiting in queue and development time. Any request for revisions and refinements is treated as a failure of the improvement team, and it is often difficult or impossible to pilot new tools in a limited setting.
Q: What features would you like to see in EHRs that would facilitate QI?
A: We need a user-friendly interface for clinicians and for data analysts/reporters. Other industries have common data formats to allow for sharing of information across disparate systems. We need the same capability for clinical information in healthcare. Also, a change in architecture of EHRs and other health IT tools that allows for not just interoperability but substitutable options is required. In the more “app”-like environment, innovation and flexibility would be the rule. An underlying architecture could have different plug-and-play modules for different functions. Some companies are overcoming the current barriers to provide wonderful, easy-to-generate and useful reports, but most are stymied by proprietary systems.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
In “The Lean Startup,” author Eric Ries notes that in its early stages, his gaming company would routinely issue new versions of their software application several times each day. Continuous deployment—the process Ries’ company used—leveraged such Lean principles as reduced batch size and continuous learning based on end-user feedback to achieve rapid improvements in their product.
Ries says companies that learn the quickest about what the customer wants, and can incorporate that information into products more efficiently, stand the greatest chance of succeeding. A software engineer by trade, Ries uses many examples of companies that have succeeded with this approach, none of which are from healthcare.
In stark relief, the chief technology hospitalists interface with daily is the electronic health record (EHR), widely recognized as a system that fails to consider the end-user experience, that is unable to interoperate with other software, and is incapable of using data for quality improvement (QI). The PDSA (“plan, do, study, act”) cycle is the foundation of QI activities and relies on rapidly incorporating observations made by those performing the work to create novel workflows and processes based on learning. EHRs, by digitizing health information, theoretically provide the ideal tool for supporting QI.
The reality is that EHRs have been a colossal disappointment with regard to QI efforts. The space in and around EHR effectively represents “dead zones” for innovation and improvement. Mandl and Kohane note:
EHR companies have followed a business model whereby they control all data, rather than liberating the data for use in innovative applications in clinical care.
Conducting a Google-style search of an EHR database usually requires involvement of a clinician’s information services department and often the specialized knowledge and cooperation of the vendor’s technical teams.
Greg Maynard, MD, MSc, SFHM, senior vice president of SHM’s Center for Hospital Innovation and Improvement, recently provided testimony to the Office of the National Coordinator for Health Information Technology about the challenges current EHRs present to QI efforts and what features EHRs need to incorporate to better serve the needs of patients and clinicians. Dr. Maynard answered a few questions for The Hospitalist:
Q: What is it about current EHRs that make continuous improvement so difficult?
A: EHRs were built for fiscal and administrative purposes, not for quality improvement and safety. The administrative/fiscal roots of today’s IT systems lead to poor availability of clinical, quality, and safety data. In many medical centers and practices, the great majority of information available is months-old administrative data, which does not lend itself to rapid cycle improvement.
Q: Why is the PDSA cycle endangered in most systems?
A: EHRs often do not facilitate rapid-cycle, PDSA-style improvements on a small pilot scale. Most improvement teams get one shot to get the clinical decision support and data-capture tools correct after months of waiting in queue and development time. Any request for revisions and refinements is treated as a failure of the improvement team, and it is often difficult or impossible to pilot new tools in a limited setting.
Q: What features would you like to see in EHRs that would facilitate QI?
A: We need a user-friendly interface for clinicians and for data analysts/reporters. Other industries have common data formats to allow for sharing of information across disparate systems. We need the same capability for clinical information in healthcare. Also, a change in architecture of EHRs and other health IT tools that allows for not just interoperability but substitutable options is required. In the more “app”-like environment, innovation and flexibility would be the rule. An underlying architecture could have different plug-and-play modules for different functions. Some companies are overcoming the current barriers to provide wonderful, easy-to-generate and useful reports, but most are stymied by proprietary systems.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
In “The Lean Startup,” author Eric Ries notes that in its early stages, his gaming company would routinely issue new versions of their software application several times each day. Continuous deployment—the process Ries’ company used—leveraged such Lean principles as reduced batch size and continuous learning based on end-user feedback to achieve rapid improvements in their product.
Ries says companies that learn the quickest about what the customer wants, and can incorporate that information into products more efficiently, stand the greatest chance of succeeding. A software engineer by trade, Ries uses many examples of companies that have succeeded with this approach, none of which are from healthcare.
In stark relief, the chief technology hospitalists interface with daily is the electronic health record (EHR), widely recognized as a system that fails to consider the end-user experience, that is unable to interoperate with other software, and is incapable of using data for quality improvement (QI). The PDSA (“plan, do, study, act”) cycle is the foundation of QI activities and relies on rapidly incorporating observations made by those performing the work to create novel workflows and processes based on learning. EHRs, by digitizing health information, theoretically provide the ideal tool for supporting QI.
The reality is that EHRs have been a colossal disappointment with regard to QI efforts. The space in and around EHR effectively represents “dead zones” for innovation and improvement. Mandl and Kohane note:
EHR companies have followed a business model whereby they control all data, rather than liberating the data for use in innovative applications in clinical care.
Conducting a Google-style search of an EHR database usually requires involvement of a clinician’s information services department and often the specialized knowledge and cooperation of the vendor’s technical teams.
Greg Maynard, MD, MSc, SFHM, senior vice president of SHM’s Center for Hospital Innovation and Improvement, recently provided testimony to the Office of the National Coordinator for Health Information Technology about the challenges current EHRs present to QI efforts and what features EHRs need to incorporate to better serve the needs of patients and clinicians. Dr. Maynard answered a few questions for The Hospitalist:
Q: What is it about current EHRs that make continuous improvement so difficult?
A: EHRs were built for fiscal and administrative purposes, not for quality improvement and safety. The administrative/fiscal roots of today’s IT systems lead to poor availability of clinical, quality, and safety data. In many medical centers and practices, the great majority of information available is months-old administrative data, which does not lend itself to rapid cycle improvement.
Q: Why is the PDSA cycle endangered in most systems?
A: EHRs often do not facilitate rapid-cycle, PDSA-style improvements on a small pilot scale. Most improvement teams get one shot to get the clinical decision support and data-capture tools correct after months of waiting in queue and development time. Any request for revisions and refinements is treated as a failure of the improvement team, and it is often difficult or impossible to pilot new tools in a limited setting.
Q: What features would you like to see in EHRs that would facilitate QI?
A: We need a user-friendly interface for clinicians and for data analysts/reporters. Other industries have common data formats to allow for sharing of information across disparate systems. We need the same capability for clinical information in healthcare. Also, a change in architecture of EHRs and other health IT tools that allows for not just interoperability but substitutable options is required. In the more “app”-like environment, innovation and flexibility would be the rule. An underlying architecture could have different plug-and-play modules for different functions. Some companies are overcoming the current barriers to provide wonderful, easy-to-generate and useful reports, but most are stymied by proprietary systems.
Reference
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Win Whitcomb: Spotlight on Medical Necessity
EDITOR’S NOTE: An incorrect version of Win Whitcomb’s “On the Horizon” column was published in the July issue of The Hospitalist. We deeply regret the error. The correct version of Dr. Whitcomb’s column appears this month, with proper attribution given to hospitalist Brad Flansbaum, DO, SFHM, who contributed to the column.
Assigning the appropriate status to patients (“inpatient” or “observation”) has emerged as a front-and-center issue for hospitalists. Also known as “medical necessity,” many HM groups have been called upon to help solve the “status” problem for their institutions. With nearly 1 in 5 hospitalized patients on observation status in U.S. hospitals, appropriately assigning status is now a dominant, system-level challenge for hospitalists.
This month, we asked two experts to shed light on the nature of this beast, with a focus on the impact on the patient. Brad Flansbaum, DO, SFHM, hospitalist at Lenox Hill Hospital in New York City, and Patrick Conway, MD, FAAP, MSC, SFHM, chief medical officer at the Centers for Medicare & Medicaid Services (CMS), were kind enough to participate in the interview. We start with Dr. Flansbaum.
Dr. Whitcomb: It appears that patients are caught in the middle of the observation status challenge, at least as it relates to footing the bill. Explain the patient perspective of being unwittingly placed on observation status.
Dr. Flansbaum: Recall your last credit card statement. On it is the hotel charge from your last out-of-town CME excursion. Below the total charge, which you were expecting, is a separate line item for a $75 “recreational fee.” You call the hotel, and they inform you that, because you used the hotel gym and pool—accessed with your room key, they levied the fee. No signs, alerts, or postings denoted the policy, so you expected inclusive use of the facilities as a price of your visit. Capture the emotion of the moment, when you see that bill, feel your heart race, and think to yourself, “Get me the manager!”
WW: Why has assigning appropriate status captured the attention of hospitals?
BF: Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing patients under observation, rather than inpatient, status to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change, and much in the same way of our hotel charge, our patients experience sticker shock when they receive their bill. It is leading to confusion among providers and consternation within the Medicare recipient community.
WW: Why is there so much confusion around appropriate patient status?
BF: The dilemma stems from Medicare payment, and the key distinction between inpatient coverage (Part A) and outpatient coverage, including pharmaceuticals (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation, sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit, beneficiary charges are different. This could result in discrete—and sometimes jolting—enrollee copayments and deductibles for drugs and services.
WW: I’ve heard observation status is having a big, adverse impact on patients who go to skilled nursing facilities. Why?
BF: If a patient requires a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because the patient never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and consequently, tempers are rising. The rules for Medicare Advantage enrollees (Part C—commercial payers receive a fixed sum from CMS, and oversee parts A, B, and D for an individual beneficiary), which comprise 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional, fee-for-service in their policies and, consequently, no exemplar of success in this realm exits.
WW: Why is the number of patients on observation status growing?
BF: Hospitals have significantly increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists often are navigating without a compass. Again, fear of fraud and penalty places hospitals and, indirectly, hospitalists—who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which may change in real time during the stay, and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices, as well as the beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after the stay. Hospitalists, of course, want direction on coding, along with an understanding of the impact their decisions will have on patients and subspecialty colleagues.
Let’s now bring in Dr. Conway, a pediatric hospitalist. I thank Dr. Flansbaum, who formulated the following questions.
BF/WW: Is it tenable to keep the current system in place? Would it help to require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet to-be-determined manner?
Dr. Conway: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for beneficiary coverage post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask,” to educate beneficiaries on this issue. (Download a PDF of the pamphlet at www.medicare.gov/Publications/Pubs/pdf/11435.pdf.)
BF/WW: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
PC: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary-care, emergency medicine, and/or HM clinician.
BF/WW: Before the U.S. healthcare system matures to a more full-out, integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
PC: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
With growing attention to observation status coming from patients and provider groups (the AMA is requesting that CMS revise its coverage rules), we will no doubt be hearing more about this going forward.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
EDITOR’S NOTE: An incorrect version of Win Whitcomb’s “On the Horizon” column was published in the July issue of The Hospitalist. We deeply regret the error. The correct version of Dr. Whitcomb’s column appears this month, with proper attribution given to hospitalist Brad Flansbaum, DO, SFHM, who contributed to the column.
Assigning the appropriate status to patients (“inpatient” or “observation”) has emerged as a front-and-center issue for hospitalists. Also known as “medical necessity,” many HM groups have been called upon to help solve the “status” problem for their institutions. With nearly 1 in 5 hospitalized patients on observation status in U.S. hospitals, appropriately assigning status is now a dominant, system-level challenge for hospitalists.
This month, we asked two experts to shed light on the nature of this beast, with a focus on the impact on the patient. Brad Flansbaum, DO, SFHM, hospitalist at Lenox Hill Hospital in New York City, and Patrick Conway, MD, FAAP, MSC, SFHM, chief medical officer at the Centers for Medicare & Medicaid Services (CMS), were kind enough to participate in the interview. We start with Dr. Flansbaum.
Dr. Whitcomb: It appears that patients are caught in the middle of the observation status challenge, at least as it relates to footing the bill. Explain the patient perspective of being unwittingly placed on observation status.
Dr. Flansbaum: Recall your last credit card statement. On it is the hotel charge from your last out-of-town CME excursion. Below the total charge, which you were expecting, is a separate line item for a $75 “recreational fee.” You call the hotel, and they inform you that, because you used the hotel gym and pool—accessed with your room key, they levied the fee. No signs, alerts, or postings denoted the policy, so you expected inclusive use of the facilities as a price of your visit. Capture the emotion of the moment, when you see that bill, feel your heart race, and think to yourself, “Get me the manager!”
WW: Why has assigning appropriate status captured the attention of hospitals?
BF: Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing patients under observation, rather than inpatient, status to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change, and much in the same way of our hotel charge, our patients experience sticker shock when they receive their bill. It is leading to confusion among providers and consternation within the Medicare recipient community.
WW: Why is there so much confusion around appropriate patient status?
BF: The dilemma stems from Medicare payment, and the key distinction between inpatient coverage (Part A) and outpatient coverage, including pharmaceuticals (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation, sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit, beneficiary charges are different. This could result in discrete—and sometimes jolting—enrollee copayments and deductibles for drugs and services.
WW: I’ve heard observation status is having a big, adverse impact on patients who go to skilled nursing facilities. Why?
BF: If a patient requires a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because the patient never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and consequently, tempers are rising. The rules for Medicare Advantage enrollees (Part C—commercial payers receive a fixed sum from CMS, and oversee parts A, B, and D for an individual beneficiary), which comprise 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional, fee-for-service in their policies and, consequently, no exemplar of success in this realm exits.
WW: Why is the number of patients on observation status growing?
BF: Hospitals have significantly increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists often are navigating without a compass. Again, fear of fraud and penalty places hospitals and, indirectly, hospitalists—who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which may change in real time during the stay, and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices, as well as the beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after the stay. Hospitalists, of course, want direction on coding, along with an understanding of the impact their decisions will have on patients and subspecialty colleagues.
Let’s now bring in Dr. Conway, a pediatric hospitalist. I thank Dr. Flansbaum, who formulated the following questions.
BF/WW: Is it tenable to keep the current system in place? Would it help to require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet to-be-determined manner?
Dr. Conway: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for beneficiary coverage post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask,” to educate beneficiaries on this issue. (Download a PDF of the pamphlet at www.medicare.gov/Publications/Pubs/pdf/11435.pdf.)
BF/WW: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
PC: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary-care, emergency medicine, and/or HM clinician.
BF/WW: Before the U.S. healthcare system matures to a more full-out, integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
PC: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
With growing attention to observation status coming from patients and provider groups (the AMA is requesting that CMS revise its coverage rules), we will no doubt be hearing more about this going forward.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
EDITOR’S NOTE: An incorrect version of Win Whitcomb’s “On the Horizon” column was published in the July issue of The Hospitalist. We deeply regret the error. The correct version of Dr. Whitcomb’s column appears this month, with proper attribution given to hospitalist Brad Flansbaum, DO, SFHM, who contributed to the column.
Assigning the appropriate status to patients (“inpatient” or “observation”) has emerged as a front-and-center issue for hospitalists. Also known as “medical necessity,” many HM groups have been called upon to help solve the “status” problem for their institutions. With nearly 1 in 5 hospitalized patients on observation status in U.S. hospitals, appropriately assigning status is now a dominant, system-level challenge for hospitalists.
This month, we asked two experts to shed light on the nature of this beast, with a focus on the impact on the patient. Brad Flansbaum, DO, SFHM, hospitalist at Lenox Hill Hospital in New York City, and Patrick Conway, MD, FAAP, MSC, SFHM, chief medical officer at the Centers for Medicare & Medicaid Services (CMS), were kind enough to participate in the interview. We start with Dr. Flansbaum.
Dr. Whitcomb: It appears that patients are caught in the middle of the observation status challenge, at least as it relates to footing the bill. Explain the patient perspective of being unwittingly placed on observation status.
Dr. Flansbaum: Recall your last credit card statement. On it is the hotel charge from your last out-of-town CME excursion. Below the total charge, which you were expecting, is a separate line item for a $75 “recreational fee.” You call the hotel, and they inform you that, because you used the hotel gym and pool—accessed with your room key, they levied the fee. No signs, alerts, or postings denoted the policy, so you expected inclusive use of the facilities as a price of your visit. Capture the emotion of the moment, when you see that bill, feel your heart race, and think to yourself, “Get me the manager!”
WW: Why has assigning appropriate status captured the attention of hospitals?
BF: Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing patients under observation, rather than inpatient, status to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change, and much in the same way of our hotel charge, our patients experience sticker shock when they receive their bill. It is leading to confusion among providers and consternation within the Medicare recipient community.
WW: Why is there so much confusion around appropriate patient status?
BF: The dilemma stems from Medicare payment, and the key distinction between inpatient coverage (Part A) and outpatient coverage, including pharmaceuticals (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation, sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit, beneficiary charges are different. This could result in discrete—and sometimes jolting—enrollee copayments and deductibles for drugs and services.
WW: I’ve heard observation status is having a big, adverse impact on patients who go to skilled nursing facilities. Why?
BF: If a patient requires a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because the patient never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and consequently, tempers are rising. The rules for Medicare Advantage enrollees (Part C—commercial payers receive a fixed sum from CMS, and oversee parts A, B, and D for an individual beneficiary), which comprise 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional, fee-for-service in their policies and, consequently, no exemplar of success in this realm exits.
WW: Why is the number of patients on observation status growing?
BF: Hospitals have significantly increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists often are navigating without a compass. Again, fear of fraud and penalty places hospitals and, indirectly, hospitalists—who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which may change in real time during the stay, and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices, as well as the beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after the stay. Hospitalists, of course, want direction on coding, along with an understanding of the impact their decisions will have on patients and subspecialty colleagues.
Let’s now bring in Dr. Conway, a pediatric hospitalist. I thank Dr. Flansbaum, who formulated the following questions.
BF/WW: Is it tenable to keep the current system in place? Would it help to require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet to-be-determined manner?
Dr. Conway: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for beneficiary coverage post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask,” to educate beneficiaries on this issue. (Download a PDF of the pamphlet at www.medicare.gov/Publications/Pubs/pdf/11435.pdf.)
BF/WW: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
PC: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary-care, emergency medicine, and/or HM clinician.
BF/WW: Before the U.S. healthcare system matures to a more full-out, integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
PC: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
With growing attention to observation status coming from patients and provider groups (the AMA is requesting that CMS revise its coverage rules), we will no doubt be hearing more about this going forward.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Win Whitcomb: Staying ... and Paying
Take a minute to recall your last credit-card statement. On it, say, is the hotel charge from your last out-of-town CME excursion. Below the total charge you were expecting is a separate line-item charge of $75 for a “recreational fee.” Puzzled, you call the hotel. They inform you that because you used the gym and pool—accessed with your room key—they levied the fee. No signs, alerts, or postings to denote such a policy, you innocently expected inclusive use of the facilities in the price of your visit.
Capture the emotion of that moment. It is likely your heart will race and you will think to yourself, “Get me the manager!”
Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing Medicare patients under observation, rather than inpatient, status. This is to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change and, much in the same way as with our hotel charge, they also experience sticker shock when they get their bills. It is leading to confusion among providers, and consternation within the Medicare recipient community.
Why is this occurring? The dilemma stems from Medicare payments and the key distinction between inpatient coverage (Part A) and outpatient coverage (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation—sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit can mean that beneficiary charges are different. This could result in discrete and sometimes jolting copayments and deductibles for drugs and services.
Worse, if beneficiaries require a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because they never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and, consequently, tempers are rising.
The rules for Medicare Advantage enrollees, who make up 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional fee-for-service in their policies, and, consequently, no exemplar of success in this realm exits.
Hospitals have increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists are often left to navigate without a compass. Again, fear of fraud and penalties places hospitals—and, indirectly, hospitalists, who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which might change in real time during the stay and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices as well as beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after a stay.
Hospitalists, of course, want direction on coding and an understanding of the impact their decisions will have on patients and subspecialty colleagues. To that end, Patrick Conway, MD, SFHM, chief medical officer for the Centers for Medicare & Medicaid (CMS), offers some enlightenment on this matter:
Q: Is it tenable to keep the current system in place? However, as a fix, require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet-to-be determined manner?
A: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for coverage for beneficiaries post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask!” to educate beneficiaries on this issue. The pamphlet can found at http://www.medicare.gov/Publications/Pubs/pdf/11435.pdf.
Q: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
A: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary care, emergency medicine, and/or hospital medicine clinician.
Q: Before the U.S. healthcare system matures to a more integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
A: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
I expect we will hear more from Medicare in the near-term on this matter. Stay tuned.
For more about the patient’s perspective on this issue, please see Brad’s blog: www.hospitalmedicine.org/pmblog.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Take a minute to recall your last credit-card statement. On it, say, is the hotel charge from your last out-of-town CME excursion. Below the total charge you were expecting is a separate line-item charge of $75 for a “recreational fee.” Puzzled, you call the hotel. They inform you that because you used the gym and pool—accessed with your room key—they levied the fee. No signs, alerts, or postings to denote such a policy, you innocently expected inclusive use of the facilities in the price of your visit.
Capture the emotion of that moment. It is likely your heart will race and you will think to yourself, “Get me the manager!”
Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing Medicare patients under observation, rather than inpatient, status. This is to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change and, much in the same way as with our hotel charge, they also experience sticker shock when they get their bills. It is leading to confusion among providers, and consternation within the Medicare recipient community.
Why is this occurring? The dilemma stems from Medicare payments and the key distinction between inpatient coverage (Part A) and outpatient coverage (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation—sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit can mean that beneficiary charges are different. This could result in discrete and sometimes jolting copayments and deductibles for drugs and services.
Worse, if beneficiaries require a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because they never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and, consequently, tempers are rising.
The rules for Medicare Advantage enrollees, who make up 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional fee-for-service in their policies, and, consequently, no exemplar of success in this realm exits.
Hospitals have increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists are often left to navigate without a compass. Again, fear of fraud and penalties places hospitals—and, indirectly, hospitalists, who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which might change in real time during the stay and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices as well as beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after a stay.
Hospitalists, of course, want direction on coding and an understanding of the impact their decisions will have on patients and subspecialty colleagues. To that end, Patrick Conway, MD, SFHM, chief medical officer for the Centers for Medicare & Medicaid (CMS), offers some enlightenment on this matter:
Q: Is it tenable to keep the current system in place? However, as a fix, require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet-to-be determined manner?
A: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for coverage for beneficiaries post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask!” to educate beneficiaries on this issue. The pamphlet can found at http://www.medicare.gov/Publications/Pubs/pdf/11435.pdf.
Q: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
A: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary care, emergency medicine, and/or hospital medicine clinician.
Q: Before the U.S. healthcare system matures to a more integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
A: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
I expect we will hear more from Medicare in the near-term on this matter. Stay tuned.
For more about the patient’s perspective on this issue, please see Brad’s blog: www.hospitalmedicine.org/pmblog.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Take a minute to recall your last credit-card statement. On it, say, is the hotel charge from your last out-of-town CME excursion. Below the total charge you were expecting is a separate line-item charge of $75 for a “recreational fee.” Puzzled, you call the hotel. They inform you that because you used the gym and pool—accessed with your room key—they levied the fee. No signs, alerts, or postings to denote such a policy, you innocently expected inclusive use of the facilities in the price of your visit.
Capture the emotion of that moment. It is likely your heart will race and you will think to yourself, “Get me the manager!”
Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing Medicare patients under observation, rather than inpatient, status. This is to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change and, much in the same way as with our hotel charge, they also experience sticker shock when they get their bills. It is leading to confusion among providers, and consternation within the Medicare recipient community.
Why is this occurring? The dilemma stems from Medicare payments and the key distinction between inpatient coverage (Part A) and outpatient coverage (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation—sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit can mean that beneficiary charges are different. This could result in discrete and sometimes jolting copayments and deductibles for drugs and services.
Worse, if beneficiaries require a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because they never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and, consequently, tempers are rising.
The rules for Medicare Advantage enrollees, who make up 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional fee-for-service in their policies, and, consequently, no exemplar of success in this realm exits.
Hospitals have increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists are often left to navigate without a compass. Again, fear of fraud and penalties places hospitals—and, indirectly, hospitalists, who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which might change in real time during the stay and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices as well as beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after a stay.
Hospitalists, of course, want direction on coding and an understanding of the impact their decisions will have on patients and subspecialty colleagues. To that end, Patrick Conway, MD, SFHM, chief medical officer for the Centers for Medicare & Medicaid (CMS), offers some enlightenment on this matter:
Q: Is it tenable to keep the current system in place? However, as a fix, require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet-to-be determined manner?
A: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for coverage for beneficiaries post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask!” to educate beneficiaries on this issue. The pamphlet can found at http://www.medicare.gov/Publications/Pubs/pdf/11435.pdf.
Q: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
A: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary care, emergency medicine, and/or hospital medicine clinician.
Q: Before the U.S. healthcare system matures to a more integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
A: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
I expect we will hear more from Medicare in the near-term on this matter. Stay tuned.
For more about the patient’s perspective on this issue, please see Brad’s blog: www.hospitalmedicine.org/pmblog.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Win Whitcomb: A New Quality Paradigm
Hospital medicine has never been bashful about stating its goal to be a financial steward of the most expensive place in our healthcare system—the hospital. At the first gathering of hospitalists in April 1997, the newly formed board of directors debated whether we should promote efficiency as a primary goal of the organization and, by extension, our field. We drafted as the first line of our mission: To promote the high-quality and cost-effective care of the hospitalized patient.
Now, as the cost of healthcare approaches 18% of our nation’s gross domestic product, the jobless rate remains high, and the economic recovery underwhelms us, the emphasis of many thought leaders has shifted to cost as the single biggest barrier to ideal healthcare in the U.S.:
- The ABIM Foundation’s Choosing Wisely campaign encourages doctors and patients to “talk about medical tests and procedures that might be unnecessary, and in some instances can cause harm.” Its Physician Charter contains “wise use of finite resources” as a key element.
- In April, the American College of Physicians (ACP) announced “5 Things Internists and Patients Should Question in Internal Medicine”.
- At the Institute for Healthcare Improvement’s national meeting in December, the organization’s spiritual leader, Don Berwick, MD, had just returned from 16 months as CMS administrator and pronounced in his keynote address: “I would go so far as to say that, for the next three to five years at least, the credibility and leverage of the quality movement will rise or fall on its success in reducing the cost of healthcare … while improving patient experience. ‘Value’ improvement won’t be enough. It will take cost reduction to capture the flag. Otherwise, cutting wins.”
Cost Is the New Quality
I agree with Don: Sure, the other dimensions of quality healthcare—that it be safe, timely, equitable, effective, and person-centered—are critical. But now, efficiency is king. Looking ahead, it will require singular focus.
The problem is, who can get excited about reducing costs? (Don’t all raise your hands at once.) Well-meaning clinicians, when asked by healthcare administrators to order fewer tests or use cheaper drugs, shrug their shoulders and assume it is a ploy for the hospital or health plan to bolster profits off their backs. Or we simply feel that we have better places to focus our efforts. After all, ours is a noble profession, not a bottom-line-focused guild.
Waste Is the New Cost
The thing we can get excited about is reducing waste. We see waste every day and have the genuine wish to eliminate it. As an example, the Lean practice—borrowed from manufacturing—is a widely used tool in healthcare. Its primary focus is the recognition and elimination of waste. Lean recognizes as many types of waste as Eskimos have words for snow.
Dr. Berwick went on to outline six areas of waste in healthcare, at least three of which fall squarely on the shoulders of hospitalists:1
- Failures of care delivery, or lack of uniform adoption of best-care processes. Examples: use of a central-line insertion bundle; early, goal-directed therapy in severe sepsis.
- Failures of care coordination. Poor handoffs and follow-up cause readmissions and other harm. Example: failure to provide a reconciled medication list to patient and next provider of care after discharge.
- Overtreatment, or exposing patients to care interventions that offer no benefit and could cause harm. Examples: VTE prophylaxis in low-risk patients; endotracheal intubation in a patient who does not desire it; admitting a patient to the hospital because it is easier than arranging outpatient follow-up from the ED (see Table 1).
The other three (administrative complexity, pricing failures, and fraud and abuse) are for another day.
Go Forth and Slash
What can we do immediately to reduce waste? At a high level, HM should take on the waste challenge the same way it confronted quality and patient safety. We have had an implicit waste agenda, at least in terms of efficient hospital throughput. Now we need to make that agenda explicit, and be clear that our focus on length of stay, costs, and avoidance of overtreatment is what is needed for our patients and our system. We need a framework for moving forward, and we need leaders from our ranks to build it out.
In the meantime, let’s go to work tomorrow and implement change in the three areas Dr. Berwick mentions. He believes in us. So do I.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Reference
Hospital medicine has never been bashful about stating its goal to be a financial steward of the most expensive place in our healthcare system—the hospital. At the first gathering of hospitalists in April 1997, the newly formed board of directors debated whether we should promote efficiency as a primary goal of the organization and, by extension, our field. We drafted as the first line of our mission: To promote the high-quality and cost-effective care of the hospitalized patient.
Now, as the cost of healthcare approaches 18% of our nation’s gross domestic product, the jobless rate remains high, and the economic recovery underwhelms us, the emphasis of many thought leaders has shifted to cost as the single biggest barrier to ideal healthcare in the U.S.:
- The ABIM Foundation’s Choosing Wisely campaign encourages doctors and patients to “talk about medical tests and procedures that might be unnecessary, and in some instances can cause harm.” Its Physician Charter contains “wise use of finite resources” as a key element.
- In April, the American College of Physicians (ACP) announced “5 Things Internists and Patients Should Question in Internal Medicine”.
- At the Institute for Healthcare Improvement’s national meeting in December, the organization’s spiritual leader, Don Berwick, MD, had just returned from 16 months as CMS administrator and pronounced in his keynote address: “I would go so far as to say that, for the next three to five years at least, the credibility and leverage of the quality movement will rise or fall on its success in reducing the cost of healthcare … while improving patient experience. ‘Value’ improvement won’t be enough. It will take cost reduction to capture the flag. Otherwise, cutting wins.”
Cost Is the New Quality
I agree with Don: Sure, the other dimensions of quality healthcare—that it be safe, timely, equitable, effective, and person-centered—are critical. But now, efficiency is king. Looking ahead, it will require singular focus.
The problem is, who can get excited about reducing costs? (Don’t all raise your hands at once.) Well-meaning clinicians, when asked by healthcare administrators to order fewer tests or use cheaper drugs, shrug their shoulders and assume it is a ploy for the hospital or health plan to bolster profits off their backs. Or we simply feel that we have better places to focus our efforts. After all, ours is a noble profession, not a bottom-line-focused guild.
Waste Is the New Cost
The thing we can get excited about is reducing waste. We see waste every day and have the genuine wish to eliminate it. As an example, the Lean practice—borrowed from manufacturing—is a widely used tool in healthcare. Its primary focus is the recognition and elimination of waste. Lean recognizes as many types of waste as Eskimos have words for snow.
Dr. Berwick went on to outline six areas of waste in healthcare, at least three of which fall squarely on the shoulders of hospitalists:1
- Failures of care delivery, or lack of uniform adoption of best-care processes. Examples: use of a central-line insertion bundle; early, goal-directed therapy in severe sepsis.
- Failures of care coordination. Poor handoffs and follow-up cause readmissions and other harm. Example: failure to provide a reconciled medication list to patient and next provider of care after discharge.
- Overtreatment, or exposing patients to care interventions that offer no benefit and could cause harm. Examples: VTE prophylaxis in low-risk patients; endotracheal intubation in a patient who does not desire it; admitting a patient to the hospital because it is easier than arranging outpatient follow-up from the ED (see Table 1).
The other three (administrative complexity, pricing failures, and fraud and abuse) are for another day.
Go Forth and Slash
What can we do immediately to reduce waste? At a high level, HM should take on the waste challenge the same way it confronted quality and patient safety. We have had an implicit waste agenda, at least in terms of efficient hospital throughput. Now we need to make that agenda explicit, and be clear that our focus on length of stay, costs, and avoidance of overtreatment is what is needed for our patients and our system. We need a framework for moving forward, and we need leaders from our ranks to build it out.
In the meantime, let’s go to work tomorrow and implement change in the three areas Dr. Berwick mentions. He believes in us. So do I.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Reference
Hospital medicine has never been bashful about stating its goal to be a financial steward of the most expensive place in our healthcare system—the hospital. At the first gathering of hospitalists in April 1997, the newly formed board of directors debated whether we should promote efficiency as a primary goal of the organization and, by extension, our field. We drafted as the first line of our mission: To promote the high-quality and cost-effective care of the hospitalized patient.
Now, as the cost of healthcare approaches 18% of our nation’s gross domestic product, the jobless rate remains high, and the economic recovery underwhelms us, the emphasis of many thought leaders has shifted to cost as the single biggest barrier to ideal healthcare in the U.S.:
- The ABIM Foundation’s Choosing Wisely campaign encourages doctors and patients to “talk about medical tests and procedures that might be unnecessary, and in some instances can cause harm.” Its Physician Charter contains “wise use of finite resources” as a key element.
- In April, the American College of Physicians (ACP) announced “5 Things Internists and Patients Should Question in Internal Medicine”.
- At the Institute for Healthcare Improvement’s national meeting in December, the organization’s spiritual leader, Don Berwick, MD, had just returned from 16 months as CMS administrator and pronounced in his keynote address: “I would go so far as to say that, for the next three to five years at least, the credibility and leverage of the quality movement will rise or fall on its success in reducing the cost of healthcare … while improving patient experience. ‘Value’ improvement won’t be enough. It will take cost reduction to capture the flag. Otherwise, cutting wins.”
Cost Is the New Quality
I agree with Don: Sure, the other dimensions of quality healthcare—that it be safe, timely, equitable, effective, and person-centered—are critical. But now, efficiency is king. Looking ahead, it will require singular focus.
The problem is, who can get excited about reducing costs? (Don’t all raise your hands at once.) Well-meaning clinicians, when asked by healthcare administrators to order fewer tests or use cheaper drugs, shrug their shoulders and assume it is a ploy for the hospital or health plan to bolster profits off their backs. Or we simply feel that we have better places to focus our efforts. After all, ours is a noble profession, not a bottom-line-focused guild.
Waste Is the New Cost
The thing we can get excited about is reducing waste. We see waste every day and have the genuine wish to eliminate it. As an example, the Lean practice—borrowed from manufacturing—is a widely used tool in healthcare. Its primary focus is the recognition and elimination of waste. Lean recognizes as many types of waste as Eskimos have words for snow.
Dr. Berwick went on to outline six areas of waste in healthcare, at least three of which fall squarely on the shoulders of hospitalists:1
- Failures of care delivery, or lack of uniform adoption of best-care processes. Examples: use of a central-line insertion bundle; early, goal-directed therapy in severe sepsis.
- Failures of care coordination. Poor handoffs and follow-up cause readmissions and other harm. Example: failure to provide a reconciled medication list to patient and next provider of care after discharge.
- Overtreatment, or exposing patients to care interventions that offer no benefit and could cause harm. Examples: VTE prophylaxis in low-risk patients; endotracheal intubation in a patient who does not desire it; admitting a patient to the hospital because it is easier than arranging outpatient follow-up from the ED (see Table 1).
The other three (administrative complexity, pricing failures, and fraud and abuse) are for another day.
Go Forth and Slash
What can we do immediately to reduce waste? At a high level, HM should take on the waste challenge the same way it confronted quality and patient safety. We have had an implicit waste agenda, at least in terms of efficient hospital throughput. Now we need to make that agenda explicit, and be clear that our focus on length of stay, costs, and avoidance of overtreatment is what is needed for our patients and our system. We need a framework for moving forward, and we need leaders from our ranks to build it out.
In the meantime, let’s go to work tomorrow and implement change in the three areas Dr. Berwick mentions. He believes in us. So do I.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Reference
Win Whitcomb: Hospitalists, PCPs, and Population Health
Jan. 1 marked the official start of the Accountable Care Organization (ACO) era, with 32 Pioneer ACOs across the country beginning a three-year program embracing the “three-part aim” of improving the health of the population, enhancing patient experience, and making costs sustainable. Later this year, many more ACOs will come on line around the country under the Medicare Shared Savings Program. Perhaps the biggest challenge to ACOs will be the management of the complex medically ill, or those individuals with two or more concurrent chronic conditions that require ongoing medical attention and/or limit activities of daily living.
In 2011, SHM embarked on a groundbreaking project to improve care coordination between hospitalists and primary-care physicians (PCPs). The Complex Medically Ill Project is being carried out at three health systems and has already had a positive impact. As part of the project, SHM is working with a mobile and online physician community, QuantiaMD, to both learn and teach during the one-year project. Parenthetically, in a short time, the collaboration has yielded glimpses of the potential of mobile technology to improve healthcare, or at least learn about physician attitudes and preferences.
In November 2011, SHM queried hospitalists and PCPs about communication and care coordination between the two specialties regarding treatment of the complex medically ill patient. Remarkably, 4,000 PCPs and hospitalists responded to the survey. In less than a month, we collected more information on this crucial topic than at any other time in the past.
SHM has prepared a white paper that will provide a full picture of what we learned. Here is a preview of the survey findings:
- Improvement efforts in hospitalist-PCP communication should focus on 1) the hospital discharge and 2) the “black hole” —the time between hospital discharge and first follow-up with a PCP;
- Hospitalists and PCPs feel that the telephone currently is the best communication tool, but both groups agree that technology solutions will improve care coordination more than human resources (e.g. a transitions coach) or process improvement (e.g. checklists or discharge bundles);
- PCPs should be more involved in the inpatient care of the complex medically ill; and
- There is a high degree of alignment between PCPs and hospitalists regarding the importance of robust communication for complex medically ill patients.
As ACOs and other approaches to payment innovation expand to effectively manage the health of a population, HM must evolve its focus away from just managing the individual patient during an acute hospitalization and toward a true collaboration with PCPs and the medical home. What will this look like? In pockets across the country, there are hospitalist systems that have enabled 1990s-style managed care to survive and thrive under Medicare Advantage programs (physician groups and hospitals that have aligned incentives under capitated or global payments). They provide some of the best insight into how HM can embrace population health management. The key elements of these hospitalist programs include:
- Aligned incentives with PCPs (and in some cases specialists) and the hospital under a global payment for a population of patients;
- Active participation in disease-management programs for patients, especially the complex medically ill, across the care continuum, including the home and post-acute-care venues;
- Use of “front-end” technology to coordinate care with the PCP and other members of the care team; and
- Use of “back-end” technology to 1) track key measures of healthcare quality and population health, 2) measure and manage utilization of resources, and 3) accurately capture severity of population illness.
SHM’s Complex Medically Ill Project will be one of a number of “test tubes” for care coordination in HM as it transitions from fee-for-service to global payment and population health management. The coming months will see the start of the ACO voyage for a few hundred health systems and their hospitalist programs.
Additionally, Medicare Advantage programs continue to grow, fueling efforts at better coordination and disease management, with hospitalists squarely in the mix. Surely, each of these will represent an experiment in the design of systems for population health management.
While it is anyone’s guess as to whether these policy initiatives will have a major impact on cost containment while maintaining quality and access, it is hard to imagine the brave new world without a retooled hospitalist model that plays an integral role in population health.
Win Whitcomb, MD, MHM is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Jan. 1 marked the official start of the Accountable Care Organization (ACO) era, with 32 Pioneer ACOs across the country beginning a three-year program embracing the “three-part aim” of improving the health of the population, enhancing patient experience, and making costs sustainable. Later this year, many more ACOs will come on line around the country under the Medicare Shared Savings Program. Perhaps the biggest challenge to ACOs will be the management of the complex medically ill, or those individuals with two or more concurrent chronic conditions that require ongoing medical attention and/or limit activities of daily living.
In 2011, SHM embarked on a groundbreaking project to improve care coordination between hospitalists and primary-care physicians (PCPs). The Complex Medically Ill Project is being carried out at three health systems and has already had a positive impact. As part of the project, SHM is working with a mobile and online physician community, QuantiaMD, to both learn and teach during the one-year project. Parenthetically, in a short time, the collaboration has yielded glimpses of the potential of mobile technology to improve healthcare, or at least learn about physician attitudes and preferences.
In November 2011, SHM queried hospitalists and PCPs about communication and care coordination between the two specialties regarding treatment of the complex medically ill patient. Remarkably, 4,000 PCPs and hospitalists responded to the survey. In less than a month, we collected more information on this crucial topic than at any other time in the past.
SHM has prepared a white paper that will provide a full picture of what we learned. Here is a preview of the survey findings:
- Improvement efforts in hospitalist-PCP communication should focus on 1) the hospital discharge and 2) the “black hole” —the time between hospital discharge and first follow-up with a PCP;
- Hospitalists and PCPs feel that the telephone currently is the best communication tool, but both groups agree that technology solutions will improve care coordination more than human resources (e.g. a transitions coach) or process improvement (e.g. checklists or discharge bundles);
- PCPs should be more involved in the inpatient care of the complex medically ill; and
- There is a high degree of alignment between PCPs and hospitalists regarding the importance of robust communication for complex medically ill patients.
As ACOs and other approaches to payment innovation expand to effectively manage the health of a population, HM must evolve its focus away from just managing the individual patient during an acute hospitalization and toward a true collaboration with PCPs and the medical home. What will this look like? In pockets across the country, there are hospitalist systems that have enabled 1990s-style managed care to survive and thrive under Medicare Advantage programs (physician groups and hospitals that have aligned incentives under capitated or global payments). They provide some of the best insight into how HM can embrace population health management. The key elements of these hospitalist programs include:
- Aligned incentives with PCPs (and in some cases specialists) and the hospital under a global payment for a population of patients;
- Active participation in disease-management programs for patients, especially the complex medically ill, across the care continuum, including the home and post-acute-care venues;
- Use of “front-end” technology to coordinate care with the PCP and other members of the care team; and
- Use of “back-end” technology to 1) track key measures of healthcare quality and population health, 2) measure and manage utilization of resources, and 3) accurately capture severity of population illness.
SHM’s Complex Medically Ill Project will be one of a number of “test tubes” for care coordination in HM as it transitions from fee-for-service to global payment and population health management. The coming months will see the start of the ACO voyage for a few hundred health systems and their hospitalist programs.
Additionally, Medicare Advantage programs continue to grow, fueling efforts at better coordination and disease management, with hospitalists squarely in the mix. Surely, each of these will represent an experiment in the design of systems for population health management.
While it is anyone’s guess as to whether these policy initiatives will have a major impact on cost containment while maintaining quality and access, it is hard to imagine the brave new world without a retooled hospitalist model that plays an integral role in population health.
Win Whitcomb, MD, MHM is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Jan. 1 marked the official start of the Accountable Care Organization (ACO) era, with 32 Pioneer ACOs across the country beginning a three-year program embracing the “three-part aim” of improving the health of the population, enhancing patient experience, and making costs sustainable. Later this year, many more ACOs will come on line around the country under the Medicare Shared Savings Program. Perhaps the biggest challenge to ACOs will be the management of the complex medically ill, or those individuals with two or more concurrent chronic conditions that require ongoing medical attention and/or limit activities of daily living.
In 2011, SHM embarked on a groundbreaking project to improve care coordination between hospitalists and primary-care physicians (PCPs). The Complex Medically Ill Project is being carried out at three health systems and has already had a positive impact. As part of the project, SHM is working with a mobile and online physician community, QuantiaMD, to both learn and teach during the one-year project. Parenthetically, in a short time, the collaboration has yielded glimpses of the potential of mobile technology to improve healthcare, or at least learn about physician attitudes and preferences.
In November 2011, SHM queried hospitalists and PCPs about communication and care coordination between the two specialties regarding treatment of the complex medically ill patient. Remarkably, 4,000 PCPs and hospitalists responded to the survey. In less than a month, we collected more information on this crucial topic than at any other time in the past.
SHM has prepared a white paper that will provide a full picture of what we learned. Here is a preview of the survey findings:
- Improvement efforts in hospitalist-PCP communication should focus on 1) the hospital discharge and 2) the “black hole” —the time between hospital discharge and first follow-up with a PCP;
- Hospitalists and PCPs feel that the telephone currently is the best communication tool, but both groups agree that technology solutions will improve care coordination more than human resources (e.g. a transitions coach) or process improvement (e.g. checklists or discharge bundles);
- PCPs should be more involved in the inpatient care of the complex medically ill; and
- There is a high degree of alignment between PCPs and hospitalists regarding the importance of robust communication for complex medically ill patients.
As ACOs and other approaches to payment innovation expand to effectively manage the health of a population, HM must evolve its focus away from just managing the individual patient during an acute hospitalization and toward a true collaboration with PCPs and the medical home. What will this look like? In pockets across the country, there are hospitalist systems that have enabled 1990s-style managed care to survive and thrive under Medicare Advantage programs (physician groups and hospitals that have aligned incentives under capitated or global payments). They provide some of the best insight into how HM can embrace population health management. The key elements of these hospitalist programs include:
- Aligned incentives with PCPs (and in some cases specialists) and the hospital under a global payment for a population of patients;
- Active participation in disease-management programs for patients, especially the complex medically ill, across the care continuum, including the home and post-acute-care venues;
- Use of “front-end” technology to coordinate care with the PCP and other members of the care team; and
- Use of “back-end” technology to 1) track key measures of healthcare quality and population health, 2) measure and manage utilization of resources, and 3) accurately capture severity of population illness.
SHM’s Complex Medically Ill Project will be one of a number of “test tubes” for care coordination in HM as it transitions from fee-for-service to global payment and population health management. The coming months will see the start of the ACO voyage for a few hundred health systems and their hospitalist programs.
Additionally, Medicare Advantage programs continue to grow, fueling efforts at better coordination and disease management, with hospitalists squarely in the mix. Surely, each of these will represent an experiment in the design of systems for population health management.
While it is anyone’s guess as to whether these policy initiatives will have a major impact on cost containment while maintaining quality and access, it is hard to imagine the brave new world without a retooled hospitalist model that plays an integral role in population health.
Win Whitcomb, MD, MHM is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
WIN WHITCOMB: CMS Core Measures Program a Win-Win for Hospitalists
EDITOR’S NOTE: This month, we introduce a new column, “On the Horizon: Quality, Systems, Safety.” Herein, author Win Whitcomb, MD, MHM, one of SHM’s founders and medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., will deliver his views on all things quality and monitor the major issues affecting hospitalists today. As a companion to Dr. Whitcomb’s perspectives, you’ll find “The View from the Center.” “The View” will on occasion provide readers with news and details of how SHM’s Center for Hospital Innovation and Improvement (“the center”) is addressing implementation of healthcare reform, planning programs to improve quality and safety of care, and influencing decisions that will affect hospital medicine for years to come.
Burke Kealey, MD, SFHM, SHM board member and medical director with HealthPartners in Minneapolis, once remarked, “The core measures program is one of the greatest gifts hospital medicine has been given.” Scoring high on the Centers for Medicare & Medicaid Services (CMS) core measures has been a no-brainer for many hospitalist programs over the years; this success has allowed hospitalists to distinguish themselves from traditional PCPs in the hospital.
Looking back, many of us saw the huge opportunity created by the core measures a decade ago. What could be so hard about writing for a flu shot or ordering an echocardiogram? We joined teams, and put systems in place to ensure high performance and, ahem, figured out how to jump through documentation hoops. (Who disputes that quality improvement is two parts better care, one part managing the medical record?)
The result? A bonanza for hospitalists (as overachievers) in the process measures known as the CMS core measures. Admittedly, some of us have struggled more than others in achieving high performance on some of the measures. For example, we couldn’t for the life of us figure out how to excel in “discharge instructions” for heart failure patients at my hospital because we stunk at medication reconciliation. And, being the team sport that QI is, some of these struggles have been beyond hospitalists’ influence.
Well, times are changing, and a good number of core measures (the CMS Inpatient Quality Reporting, or IQR, Program) recently have been retired or suspended. Table 1 outlines the retired or suspended CMS measures; The Joint Commission is retiring many, but not all, of the same measures. To clarify, CMS uses Hospital IQR measures for reporting on the public website hospitalcompare.hhs.gov and, beginning in 2013, a subset will make up part of the value-based purchasing program (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1, or visit www.hospitalmedicine.org/vbp). For the commission, the measures are used as part of the survey process for hospital accreditation.
Timeline
The changes described in Table 1 denote measures that will be retired or suspended from the FY14 Hospital IQR measure set, and were reflected in hospital discharges effective Jan. 1, 2012. In other words, the changes are reflected in CMS’ collection of data from hospitals as of this year.
A few words of explanation of the table terms: “AMI,” of course, stands for acute myocardial infarction, “HF” is heart failure, and “PN” is pneumonia.
“Retire” means just that. Let’s hope so, and not what Michael Jordan meant when calling it quits the first time to try out baseball.
“Suspended” means CMS is retaining the measure in the IQR program but is not collecting data until such time that evidence shows hospital performance has unacceptably declined. Win’s word: Hard to know exactly what that means. It scares me enough that my hospital will continue data collection for internal purposes and not take our eye off the ball regarding performance.
“IMM” is short for global immunization and means that influenza and pneumococcal vaccine administration will be tracked on all hospital patients, not just those with pneumonia, who meet the age and high-risk criteria. Win’s word: You read that correctly. All inpatients require these vaccinations if they meet the criteria.
“Accountability measures” became part of The Joint Commission’s accreditation process Jan. 1. According to the commission’s website, they refer to a subset of core measures resulting in “the greatest positive impact on patient outcomes when hospitals demonstrate improvement on them.” Each accountability measure must meet these four criteria:
RESEARCH: There is strong evidence that compliance with this process of care improves outcomes.
PROXIMITY: The process being measured is “close” to the outcome (i.e. relatively few steps between the process and outcome).
ACCURACY: The measure accurately reflects that the process actually has been provided. Win’s word: In = “aspirin on arrival” and “ACE/ARB for LVSD.” Out = “smoking cessation counseling.” For smoking cessation, who knows if this was actually provided or the box was simply checked?
ADVERSE EFFECTS: The measure minimizes adverse effects. Win’s word: The “initial antibiotic timing” measure probably reduced diagnostic accuracy of pneumonia. See ya.
The other core measures will remain in their current form for now. Going forward, the IQR program provides hospitalists new opportunities to shine. These went into effect Jan. 1:
- Admit decision time to ED departure for admitted patients;
- Median time from ED arrival to ED departure for admitted patients; and
- Catheter-associated UTI rates.
As with all the measures, working in teams will be essential to success in these new measures. So go out there and hit a few more home runs (or at least a base hit or two). The season is well underway.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder of SHM and an expert in quality improvement and hospitalist practice management. Write to him at [email protected].
EDITOR’S NOTE: This month, we introduce a new column, “On the Horizon: Quality, Systems, Safety.” Herein, author Win Whitcomb, MD, MHM, one of SHM’s founders and medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., will deliver his views on all things quality and monitor the major issues affecting hospitalists today. As a companion to Dr. Whitcomb’s perspectives, you’ll find “The View from the Center.” “The View” will on occasion provide readers with news and details of how SHM’s Center for Hospital Innovation and Improvement (“the center”) is addressing implementation of healthcare reform, planning programs to improve quality and safety of care, and influencing decisions that will affect hospital medicine for years to come.
Burke Kealey, MD, SFHM, SHM board member and medical director with HealthPartners in Minneapolis, once remarked, “The core measures program is one of the greatest gifts hospital medicine has been given.” Scoring high on the Centers for Medicare & Medicaid Services (CMS) core measures has been a no-brainer for many hospitalist programs over the years; this success has allowed hospitalists to distinguish themselves from traditional PCPs in the hospital.
Looking back, many of us saw the huge opportunity created by the core measures a decade ago. What could be so hard about writing for a flu shot or ordering an echocardiogram? We joined teams, and put systems in place to ensure high performance and, ahem, figured out how to jump through documentation hoops. (Who disputes that quality improvement is two parts better care, one part managing the medical record?)
The result? A bonanza for hospitalists (as overachievers) in the process measures known as the CMS core measures. Admittedly, some of us have struggled more than others in achieving high performance on some of the measures. For example, we couldn’t for the life of us figure out how to excel in “discharge instructions” for heart failure patients at my hospital because we stunk at medication reconciliation. And, being the team sport that QI is, some of these struggles have been beyond hospitalists’ influence.
Well, times are changing, and a good number of core measures (the CMS Inpatient Quality Reporting, or IQR, Program) recently have been retired or suspended. Table 1 outlines the retired or suspended CMS measures; The Joint Commission is retiring many, but not all, of the same measures. To clarify, CMS uses Hospital IQR measures for reporting on the public website hospitalcompare.hhs.gov and, beginning in 2013, a subset will make up part of the value-based purchasing program (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1, or visit www.hospitalmedicine.org/vbp). For the commission, the measures are used as part of the survey process for hospital accreditation.
Timeline
The changes described in Table 1 denote measures that will be retired or suspended from the FY14 Hospital IQR measure set, and were reflected in hospital discharges effective Jan. 1, 2012. In other words, the changes are reflected in CMS’ collection of data from hospitals as of this year.
A few words of explanation of the table terms: “AMI,” of course, stands for acute myocardial infarction, “HF” is heart failure, and “PN” is pneumonia.
“Retire” means just that. Let’s hope so, and not what Michael Jordan meant when calling it quits the first time to try out baseball.
“Suspended” means CMS is retaining the measure in the IQR program but is not collecting data until such time that evidence shows hospital performance has unacceptably declined. Win’s word: Hard to know exactly what that means. It scares me enough that my hospital will continue data collection for internal purposes and not take our eye off the ball regarding performance.
“IMM” is short for global immunization and means that influenza and pneumococcal vaccine administration will be tracked on all hospital patients, not just those with pneumonia, who meet the age and high-risk criteria. Win’s word: You read that correctly. All inpatients require these vaccinations if they meet the criteria.
“Accountability measures” became part of The Joint Commission’s accreditation process Jan. 1. According to the commission’s website, they refer to a subset of core measures resulting in “the greatest positive impact on patient outcomes when hospitals demonstrate improvement on them.” Each accountability measure must meet these four criteria:
RESEARCH: There is strong evidence that compliance with this process of care improves outcomes.
PROXIMITY: The process being measured is “close” to the outcome (i.e. relatively few steps between the process and outcome).
ACCURACY: The measure accurately reflects that the process actually has been provided. Win’s word: In = “aspirin on arrival” and “ACE/ARB for LVSD.” Out = “smoking cessation counseling.” For smoking cessation, who knows if this was actually provided or the box was simply checked?
ADVERSE EFFECTS: The measure minimizes adverse effects. Win’s word: The “initial antibiotic timing” measure probably reduced diagnostic accuracy of pneumonia. See ya.
The other core measures will remain in their current form for now. Going forward, the IQR program provides hospitalists new opportunities to shine. These went into effect Jan. 1:
- Admit decision time to ED departure for admitted patients;
- Median time from ED arrival to ED departure for admitted patients; and
- Catheter-associated UTI rates.
As with all the measures, working in teams will be essential to success in these new measures. So go out there and hit a few more home runs (or at least a base hit or two). The season is well underway.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder of SHM and an expert in quality improvement and hospitalist practice management. Write to him at [email protected].
EDITOR’S NOTE: This month, we introduce a new column, “On the Horizon: Quality, Systems, Safety.” Herein, author Win Whitcomb, MD, MHM, one of SHM’s founders and medical director of healthcare quality at Baystate Medical Center in Springfield, Mass., will deliver his views on all things quality and monitor the major issues affecting hospitalists today. As a companion to Dr. Whitcomb’s perspectives, you’ll find “The View from the Center.” “The View” will on occasion provide readers with news and details of how SHM’s Center for Hospital Innovation and Improvement (“the center”) is addressing implementation of healthcare reform, planning programs to improve quality and safety of care, and influencing decisions that will affect hospital medicine for years to come.
Burke Kealey, MD, SFHM, SHM board member and medical director with HealthPartners in Minneapolis, once remarked, “The core measures program is one of the greatest gifts hospital medicine has been given.” Scoring high on the Centers for Medicare & Medicaid Services (CMS) core measures has been a no-brainer for many hospitalist programs over the years; this success has allowed hospitalists to distinguish themselves from traditional PCPs in the hospital.
Looking back, many of us saw the huge opportunity created by the core measures a decade ago. What could be so hard about writing for a flu shot or ordering an echocardiogram? We joined teams, and put systems in place to ensure high performance and, ahem, figured out how to jump through documentation hoops. (Who disputes that quality improvement is two parts better care, one part managing the medical record?)
The result? A bonanza for hospitalists (as overachievers) in the process measures known as the CMS core measures. Admittedly, some of us have struggled more than others in achieving high performance on some of the measures. For example, we couldn’t for the life of us figure out how to excel in “discharge instructions” for heart failure patients at my hospital because we stunk at medication reconciliation. And, being the team sport that QI is, some of these struggles have been beyond hospitalists’ influence.
Well, times are changing, and a good number of core measures (the CMS Inpatient Quality Reporting, or IQR, Program) recently have been retired or suspended. Table 1 outlines the retired or suspended CMS measures; The Joint Commission is retiring many, but not all, of the same measures. To clarify, CMS uses Hospital IQR measures for reporting on the public website hospitalcompare.hhs.gov and, beginning in 2013, a subset will make up part of the value-based purchasing program (see “Value-Based Purchasing Raises the Stakes,” May 2011, p. 1, or visit www.hospitalmedicine.org/vbp). For the commission, the measures are used as part of the survey process for hospital accreditation.
Timeline
The changes described in Table 1 denote measures that will be retired or suspended from the FY14 Hospital IQR measure set, and were reflected in hospital discharges effective Jan. 1, 2012. In other words, the changes are reflected in CMS’ collection of data from hospitals as of this year.
A few words of explanation of the table terms: “AMI,” of course, stands for acute myocardial infarction, “HF” is heart failure, and “PN” is pneumonia.
“Retire” means just that. Let’s hope so, and not what Michael Jordan meant when calling it quits the first time to try out baseball.
“Suspended” means CMS is retaining the measure in the IQR program but is not collecting data until such time that evidence shows hospital performance has unacceptably declined. Win’s word: Hard to know exactly what that means. It scares me enough that my hospital will continue data collection for internal purposes and not take our eye off the ball regarding performance.
“IMM” is short for global immunization and means that influenza and pneumococcal vaccine administration will be tracked on all hospital patients, not just those with pneumonia, who meet the age and high-risk criteria. Win’s word: You read that correctly. All inpatients require these vaccinations if they meet the criteria.
“Accountability measures” became part of The Joint Commission’s accreditation process Jan. 1. According to the commission’s website, they refer to a subset of core measures resulting in “the greatest positive impact on patient outcomes when hospitals demonstrate improvement on them.” Each accountability measure must meet these four criteria:
RESEARCH: There is strong evidence that compliance with this process of care improves outcomes.
PROXIMITY: The process being measured is “close” to the outcome (i.e. relatively few steps between the process and outcome).
ACCURACY: The measure accurately reflects that the process actually has been provided. Win’s word: In = “aspirin on arrival” and “ACE/ARB for LVSD.” Out = “smoking cessation counseling.” For smoking cessation, who knows if this was actually provided or the box was simply checked?
ADVERSE EFFECTS: The measure minimizes adverse effects. Win’s word: The “initial antibiotic timing” measure probably reduced diagnostic accuracy of pneumonia. See ya.
The other core measures will remain in their current form for now. Going forward, the IQR program provides hospitalists new opportunities to shine. These went into effect Jan. 1:
- Admit decision time to ED departure for admitted patients;
- Median time from ED arrival to ED departure for admitted patients; and
- Catheter-associated UTI rates.
As with all the measures, working in teams will be essential to success in these new measures. So go out there and hit a few more home runs (or at least a base hit or two). The season is well underway.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder of SHM and an expert in quality improvement and hospitalist practice management. Write to him at [email protected].
Career Satisfaction Toolkit
Early survey data on hospitalists, which suggest high levels of job engagement and low turnover rates, may not be as relevant as programs mature in a competitive marketplace to meet important needs such as rising census and Accreditation Council for Graduate Medical Education (ACGME) requirements. There is also a paucity of data on how different models of compensation affect hospitalists’ career satisfaction.
In 2005 the role of the hospitalist has evolved from simply improving throughput (average length of stay) to one of leadership, quality improvement, and teaching that extends beyond direct patient care. Compensation for hospitalists should not, therefore, be based solely on billing revenue. Improving the efficiency of the hospitalists work environment, which may include IT support, adequate office space, and administrative support, may not only enhance productivity but also job satisfaction. More research is needed to examine these questions.
Progress Report
One of the Career Satisfaction Task Force’s major initiatives has been developing a toolkit for the SHM membership with the purpose of providing members with an action plan for attaining a long and satisfying career in hospital medicine. The following steps are being taken in the creation of the toolkit:
- Needs assessment—questionnaire at the SHM 2005 Annual Meeting;
- Monthly conference calls;
- Timeline:
- Toolkit draft completion—Sept. 2005;
- Review SHM Membership Committee—Oct. 2005;
- Further revision;
- Submission to SHM Board for review—Nov. 2005;
- Further revision; and
- Dissemination at SHM Annual Meeting—May 2006.
- Content—four workplace domains:
- Control/Autonomy;
- Workload/Schedule;
- Community/Environment; and
- Reward/Recognition.
- Elements comprising each domain:
- Definition: specific description of workplace domain;
- Background: review of literature, expert opinion, experience-based observation, executive summary of background content;
- Guidelines: practical actionable recommendations and educational initiatives;
- Pitfalls: specific examples;
- Examples: application to different settings (community, academic, pediatric); and
- References.
Research and Timeline
In parallel to the development of the work domains for the toolkit, the Career Satisfaction Task Force is developing a questionnaire to survey hospitalist physicians on career satisfaction and “worklife.” The last survey of this type was performed in 1999. This questionnaire will allow us to assess changes in hospitalist quality of working life over time to further explore how hospitalists are faring during this critical time of rapid growth of our specialty.
The task force is developing a list of important aspects of worklife, satisfaction, and stress for hospitalists. This list will be supplemented by semi-structured interviews of SHM members and leaders in hospital medicine to include a representative viewpoint of hospitalist worklife: adult and pediatric medicine, academic and community, gender and age, directors of programs, and different employer types.
The interviews were expected to be completed in the fall of 2005. Qualitative data analysis will allow us to ascertain important themes for job performance and satisfaction to be highlighted in the survey. The questionnaire development will also consider inclusion of aspects from the prior surveys to follow results over time and when possible will use validated questions from the quality of working life literature.
We anticipate completion of the questionnaire in spring 2006 followed by surveying of a random sample of hospitalists from the SHM membership through a Web-based survey. Sampling of groups of hospitalists based on job characteristics will occur because there is significant interest and need for information about hospitalist worklife in certain work settings. The questionnaire dissemination time will overlap with the annual meeting to maximize survey response. The task force will work with SHM annual meeting committee to discuss having a dedicated computer for filling out the Web-based survey on-site.
Any SHM member who would like to participate in the questionnaire on-site, even if they were not selected for the random sample, will be encouraged to do so. Data analysis will occur in mid-late 2006. The task force will use information from the analyses to update the SHM Worklife Toolkit. We will also provide numerous forums for dissemination of the data. In particular, we plan to showcase this data at the 2007 SHM Annual Meeting followed by journal publication and Web site posting. It is our hope that this data will provide key information on the current quality of working life of hospitalist physicians to support worklife recommendations that promote sustainable, enjoyable careers in hospital medicine.
Early survey data on hospitalists, which suggest high levels of job engagement and low turnover rates, may not be as relevant as programs mature in a competitive marketplace to meet important needs such as rising census and Accreditation Council for Graduate Medical Education (ACGME) requirements. There is also a paucity of data on how different models of compensation affect hospitalists’ career satisfaction.
In 2005 the role of the hospitalist has evolved from simply improving throughput (average length of stay) to one of leadership, quality improvement, and teaching that extends beyond direct patient care. Compensation for hospitalists should not, therefore, be based solely on billing revenue. Improving the efficiency of the hospitalists work environment, which may include IT support, adequate office space, and administrative support, may not only enhance productivity but also job satisfaction. More research is needed to examine these questions.
Progress Report
One of the Career Satisfaction Task Force’s major initiatives has been developing a toolkit for the SHM membership with the purpose of providing members with an action plan for attaining a long and satisfying career in hospital medicine. The following steps are being taken in the creation of the toolkit:
- Needs assessment—questionnaire at the SHM 2005 Annual Meeting;
- Monthly conference calls;
- Timeline:
- Toolkit draft completion—Sept. 2005;
- Review SHM Membership Committee—Oct. 2005;
- Further revision;
- Submission to SHM Board for review—Nov. 2005;
- Further revision; and
- Dissemination at SHM Annual Meeting—May 2006.
- Content—four workplace domains:
- Control/Autonomy;
- Workload/Schedule;
- Community/Environment; and
- Reward/Recognition.
- Elements comprising each domain:
- Definition: specific description of workplace domain;
- Background: review of literature, expert opinion, experience-based observation, executive summary of background content;
- Guidelines: practical actionable recommendations and educational initiatives;
- Pitfalls: specific examples;
- Examples: application to different settings (community, academic, pediatric); and
- References.
Research and Timeline
In parallel to the development of the work domains for the toolkit, the Career Satisfaction Task Force is developing a questionnaire to survey hospitalist physicians on career satisfaction and “worklife.” The last survey of this type was performed in 1999. This questionnaire will allow us to assess changes in hospitalist quality of working life over time to further explore how hospitalists are faring during this critical time of rapid growth of our specialty.
The task force is developing a list of important aspects of worklife, satisfaction, and stress for hospitalists. This list will be supplemented by semi-structured interviews of SHM members and leaders in hospital medicine to include a representative viewpoint of hospitalist worklife: adult and pediatric medicine, academic and community, gender and age, directors of programs, and different employer types.
The interviews were expected to be completed in the fall of 2005. Qualitative data analysis will allow us to ascertain important themes for job performance and satisfaction to be highlighted in the survey. The questionnaire development will also consider inclusion of aspects from the prior surveys to follow results over time and when possible will use validated questions from the quality of working life literature.
We anticipate completion of the questionnaire in spring 2006 followed by surveying of a random sample of hospitalists from the SHM membership through a Web-based survey. Sampling of groups of hospitalists based on job characteristics will occur because there is significant interest and need for information about hospitalist worklife in certain work settings. The questionnaire dissemination time will overlap with the annual meeting to maximize survey response. The task force will work with SHM annual meeting committee to discuss having a dedicated computer for filling out the Web-based survey on-site.
Any SHM member who would like to participate in the questionnaire on-site, even if they were not selected for the random sample, will be encouraged to do so. Data analysis will occur in mid-late 2006. The task force will use information from the analyses to update the SHM Worklife Toolkit. We will also provide numerous forums for dissemination of the data. In particular, we plan to showcase this data at the 2007 SHM Annual Meeting followed by journal publication and Web site posting. It is our hope that this data will provide key information on the current quality of working life of hospitalist physicians to support worklife recommendations that promote sustainable, enjoyable careers in hospital medicine.
Early survey data on hospitalists, which suggest high levels of job engagement and low turnover rates, may not be as relevant as programs mature in a competitive marketplace to meet important needs such as rising census and Accreditation Council for Graduate Medical Education (ACGME) requirements. There is also a paucity of data on how different models of compensation affect hospitalists’ career satisfaction.
In 2005 the role of the hospitalist has evolved from simply improving throughput (average length of stay) to one of leadership, quality improvement, and teaching that extends beyond direct patient care. Compensation for hospitalists should not, therefore, be based solely on billing revenue. Improving the efficiency of the hospitalists work environment, which may include IT support, adequate office space, and administrative support, may not only enhance productivity but also job satisfaction. More research is needed to examine these questions.
Progress Report
One of the Career Satisfaction Task Force’s major initiatives has been developing a toolkit for the SHM membership with the purpose of providing members with an action plan for attaining a long and satisfying career in hospital medicine. The following steps are being taken in the creation of the toolkit:
- Needs assessment—questionnaire at the SHM 2005 Annual Meeting;
- Monthly conference calls;
- Timeline:
- Toolkit draft completion—Sept. 2005;
- Review SHM Membership Committee—Oct. 2005;
- Further revision;
- Submission to SHM Board for review—Nov. 2005;
- Further revision; and
- Dissemination at SHM Annual Meeting—May 2006.
- Content—four workplace domains:
- Control/Autonomy;
- Workload/Schedule;
- Community/Environment; and
- Reward/Recognition.
- Elements comprising each domain:
- Definition: specific description of workplace domain;
- Background: review of literature, expert opinion, experience-based observation, executive summary of background content;
- Guidelines: practical actionable recommendations and educational initiatives;
- Pitfalls: specific examples;
- Examples: application to different settings (community, academic, pediatric); and
- References.
Research and Timeline
In parallel to the development of the work domains for the toolkit, the Career Satisfaction Task Force is developing a questionnaire to survey hospitalist physicians on career satisfaction and “worklife.” The last survey of this type was performed in 1999. This questionnaire will allow us to assess changes in hospitalist quality of working life over time to further explore how hospitalists are faring during this critical time of rapid growth of our specialty.
The task force is developing a list of important aspects of worklife, satisfaction, and stress for hospitalists. This list will be supplemented by semi-structured interviews of SHM members and leaders in hospital medicine to include a representative viewpoint of hospitalist worklife: adult and pediatric medicine, academic and community, gender and age, directors of programs, and different employer types.
The interviews were expected to be completed in the fall of 2005. Qualitative data analysis will allow us to ascertain important themes for job performance and satisfaction to be highlighted in the survey. The questionnaire development will also consider inclusion of aspects from the prior surveys to follow results over time and when possible will use validated questions from the quality of working life literature.
We anticipate completion of the questionnaire in spring 2006 followed by surveying of a random sample of hospitalists from the SHM membership through a Web-based survey. Sampling of groups of hospitalists based on job characteristics will occur because there is significant interest and need for information about hospitalist worklife in certain work settings. The questionnaire dissemination time will overlap with the annual meeting to maximize survey response. The task force will work with SHM annual meeting committee to discuss having a dedicated computer for filling out the Web-based survey on-site.
Any SHM member who would like to participate in the questionnaire on-site, even if they were not selected for the random sample, will be encouraged to do so. Data analysis will occur in mid-late 2006. The task force will use information from the analyses to update the SHM Worklife Toolkit. We will also provide numerous forums for dissemination of the data. In particular, we plan to showcase this data at the 2007 SHM Annual Meeting followed by journal publication and Web site posting. It is our hope that this data will provide key information on the current quality of working life of hospitalist physicians to support worklife recommendations that promote sustainable, enjoyable careers in hospital medicine.
Physician Pay-for-Performance Comes to the Hospital
In January 2004, the Mercy Inpatient Medicine Service embarked on a quality-based incentive program, or “pay-for-performance.” This was spurred on by Blue Cross of Massachusetts, which contracted with all hospitals in the state to receive a substantial financial bonus for agreed-upon quality indicators.
Prior to the start date, representatives from Mercy Medical Center negotiated with Blue Cross, arriving at the following quality indicators and targets for all hospital patients for the period of January to December 2004:
- For pneumonia patients, 45% rate of pneumococcal vaccine screening and administration;
- For heart failure patients, 85% rate of documentation of ejection fraction; and
- For heart failure patients with ejection fraction <40%, prescription of an ACE-inhibitor (or documentation of a contraindication) upon discharge.
The Mercy Inpatient Medicine Service, which consisted of 10 full-time hospitalists in 2004, cared for approximately 75% of all medical inpatients at the hospital. We created a quality-based incentive program for this hospital medicine group that mirrored the incentives mentioned above for the entire hospital. We postulated that superior performance by the hospitalists would “raise the bar” for the remainder of the patients, some of whom were cared for by a separate hospital medicine group and some by traditional PCPs.
Mechanics of the Pay for Performance Program
The quality-based bonus was structured so that it would be paid out at 6-month intervals in equal parts to all full-time hospitalists. The magnitude of the bonus was set in excess of 7.5% of the hospitalists’ base salary, an amount that we felt would be large enough to influence behavior change.
From the outset of the bonus period (2004), as medical director of the group, I convened a weekly meeting with hospitalists and representatives from the Quality Improvement department, nursing, and case management. The meeting was being held amid the backdrop of a renewed institutional emphasis on all the JCAHO Core Measures and other quality/patient safety initiatives. The purpose of the meeting was to review hospital performance on all JCAHO Core Measures.
A nurse from the Quality Improvement department reviewed all charts of pneumonia and heart failure patients. For cases where pneumovax was not screened/administered, ejection fraction not assessed, and ACE-I not given, a hospitalist would review the chart and provide feedback to the physician-of-record regarding the nature of the problem. Further, I provided regular feedback to the hospital medicine group regarding their performance on the 3 indicators.
Results
The results in Figures 1–3 are for the hospitalist group, with results for the hospital as a whole slightly lower, but still in excess of the targets agreed upon with Blue Cross.
Summary
Mercy’s experience in 2004 is among the first hospitalist pay-for-performance programs reported. This quality-based incentive resulted in marked improvement in 3 quality indicators, resulting in the hospital’s attainment of the bonus paid by Blue Cross. The hospitalists were satisfied with the incentive program, because they felt appropriately rewarded for high-quality care. It is interesting to note that less-aggressive measures had been undertaken in the past to improve these indicators, but with little success. In 2004, with financial rewards at stake, more robust processes—such as a weekly meeting, ongoing chart review, and direct feedback to physicians—were put in place to ensure quality improvement.
Win Whitcomb, MD, cofounded the Society of Hospital Medicine with John Nelson, MD, in 1996. He is director of Performance Improvement at Mercy Medical Center, Springfield, MA, and can be reached at [email protected].
In January 2004, the Mercy Inpatient Medicine Service embarked on a quality-based incentive program, or “pay-for-performance.” This was spurred on by Blue Cross of Massachusetts, which contracted with all hospitals in the state to receive a substantial financial bonus for agreed-upon quality indicators.
Prior to the start date, representatives from Mercy Medical Center negotiated with Blue Cross, arriving at the following quality indicators and targets for all hospital patients for the period of January to December 2004:
- For pneumonia patients, 45% rate of pneumococcal vaccine screening and administration;
- For heart failure patients, 85% rate of documentation of ejection fraction; and
- For heart failure patients with ejection fraction <40%, prescription of an ACE-inhibitor (or documentation of a contraindication) upon discharge.
The Mercy Inpatient Medicine Service, which consisted of 10 full-time hospitalists in 2004, cared for approximately 75% of all medical inpatients at the hospital. We created a quality-based incentive program for this hospital medicine group that mirrored the incentives mentioned above for the entire hospital. We postulated that superior performance by the hospitalists would “raise the bar” for the remainder of the patients, some of whom were cared for by a separate hospital medicine group and some by traditional PCPs.
Mechanics of the Pay for Performance Program
The quality-based bonus was structured so that it would be paid out at 6-month intervals in equal parts to all full-time hospitalists. The magnitude of the bonus was set in excess of 7.5% of the hospitalists’ base salary, an amount that we felt would be large enough to influence behavior change.
From the outset of the bonus period (2004), as medical director of the group, I convened a weekly meeting with hospitalists and representatives from the Quality Improvement department, nursing, and case management. The meeting was being held amid the backdrop of a renewed institutional emphasis on all the JCAHO Core Measures and other quality/patient safety initiatives. The purpose of the meeting was to review hospital performance on all JCAHO Core Measures.
A nurse from the Quality Improvement department reviewed all charts of pneumonia and heart failure patients. For cases where pneumovax was not screened/administered, ejection fraction not assessed, and ACE-I not given, a hospitalist would review the chart and provide feedback to the physician-of-record regarding the nature of the problem. Further, I provided regular feedback to the hospital medicine group regarding their performance on the 3 indicators.
Results
The results in Figures 1–3 are for the hospitalist group, with results for the hospital as a whole slightly lower, but still in excess of the targets agreed upon with Blue Cross.
Summary
Mercy’s experience in 2004 is among the first hospitalist pay-for-performance programs reported. This quality-based incentive resulted in marked improvement in 3 quality indicators, resulting in the hospital’s attainment of the bonus paid by Blue Cross. The hospitalists were satisfied with the incentive program, because they felt appropriately rewarded for high-quality care. It is interesting to note that less-aggressive measures had been undertaken in the past to improve these indicators, but with little success. In 2004, with financial rewards at stake, more robust processes—such as a weekly meeting, ongoing chart review, and direct feedback to physicians—were put in place to ensure quality improvement.
Win Whitcomb, MD, cofounded the Society of Hospital Medicine with John Nelson, MD, in 1996. He is director of Performance Improvement at Mercy Medical Center, Springfield, MA, and can be reached at [email protected].
In January 2004, the Mercy Inpatient Medicine Service embarked on a quality-based incentive program, or “pay-for-performance.” This was spurred on by Blue Cross of Massachusetts, which contracted with all hospitals in the state to receive a substantial financial bonus for agreed-upon quality indicators.
Prior to the start date, representatives from Mercy Medical Center negotiated with Blue Cross, arriving at the following quality indicators and targets for all hospital patients for the period of January to December 2004:
- For pneumonia patients, 45% rate of pneumococcal vaccine screening and administration;
- For heart failure patients, 85% rate of documentation of ejection fraction; and
- For heart failure patients with ejection fraction <40%, prescription of an ACE-inhibitor (or documentation of a contraindication) upon discharge.
The Mercy Inpatient Medicine Service, which consisted of 10 full-time hospitalists in 2004, cared for approximately 75% of all medical inpatients at the hospital. We created a quality-based incentive program for this hospital medicine group that mirrored the incentives mentioned above for the entire hospital. We postulated that superior performance by the hospitalists would “raise the bar” for the remainder of the patients, some of whom were cared for by a separate hospital medicine group and some by traditional PCPs.
Mechanics of the Pay for Performance Program
The quality-based bonus was structured so that it would be paid out at 6-month intervals in equal parts to all full-time hospitalists. The magnitude of the bonus was set in excess of 7.5% of the hospitalists’ base salary, an amount that we felt would be large enough to influence behavior change.
From the outset of the bonus period (2004), as medical director of the group, I convened a weekly meeting with hospitalists and representatives from the Quality Improvement department, nursing, and case management. The meeting was being held amid the backdrop of a renewed institutional emphasis on all the JCAHO Core Measures and other quality/patient safety initiatives. The purpose of the meeting was to review hospital performance on all JCAHO Core Measures.
A nurse from the Quality Improvement department reviewed all charts of pneumonia and heart failure patients. For cases where pneumovax was not screened/administered, ejection fraction not assessed, and ACE-I not given, a hospitalist would review the chart and provide feedback to the physician-of-record regarding the nature of the problem. Further, I provided regular feedback to the hospital medicine group regarding their performance on the 3 indicators.
Results
The results in Figures 1–3 are for the hospitalist group, with results for the hospital as a whole slightly lower, but still in excess of the targets agreed upon with Blue Cross.
Summary
Mercy’s experience in 2004 is among the first hospitalist pay-for-performance programs reported. This quality-based incentive resulted in marked improvement in 3 quality indicators, resulting in the hospital’s attainment of the bonus paid by Blue Cross. The hospitalists were satisfied with the incentive program, because they felt appropriately rewarded for high-quality care. It is interesting to note that less-aggressive measures had been undertaken in the past to improve these indicators, but with little success. In 2004, with financial rewards at stake, more robust processes—such as a weekly meeting, ongoing chart review, and direct feedback to physicians—were put in place to ensure quality improvement.
Win Whitcomb, MD, cofounded the Society of Hospital Medicine with John Nelson, MD, in 1996. He is director of Performance Improvement at Mercy Medical Center, Springfield, MA, and can be reached at [email protected].