User login
Patient Preferences for Physician Attire: A Multicenter Study in Japan
The patient-physician relationship is critical for ensuring the delivery of high-quality healthcare. Successful patient-physician relationships arise from shared trust, knowledge, mutual respect, and effective verbal and nonverbal communication. The ways in which patients experience healthcare and their satisfaction with physicians affect a myriad of important health outcomes, such as adherence to treatment and outcomes for conditions such as hypertension and diabetes mellitus.1-5 One method for potentially enhancing patient satisfaction is through understanding how patients wish their physicians to dress6-8 and tailoring attire to match these expectations. In addition to our systematic review,9 a recent large-scale, multicenter study in the United States revealed that most patients perceive physician attire as important, but that preferences for specific types of attire are contextual.9,10 For example, elderly patients preferred physicians in formal attire and white coat, while scrubs with white coat or scrubs alone were preferred for emergency department (ED) physicians and surgeons, respectively. Moreover, regional variation regarding attire preference was also observed in the US, with preferences for more formal attire in the South and less formal in the Midwest.
Geographic variation, regarding patient preferences for physician dress, is perhaps even more relevant internationally. In particular, Japan is considered to have a highly contextualized culture that relies on nonverbal and implicit communication. However, medical professionals have no specific dress code and, thus, don many different kinds of attire. In part, this may be because it is not clear whether or how physician attire impacts patient satisfaction and perceived healthcare quality in Japan.11-13 Although previous studies in Japan have suggested that physician attire has a considerable influence on patient satisfaction, these studies either involved a single department in one hospital or a small number of respondents.14-17 Therefore, we performed a multicenter, cross-sectional study to understand patients’ preferences for physician attire in different clinical settings and in different geographic regions in Japan.
METHODS
Study Population
We conducted a cross-sectional, questionnaire-based study from 2015 to 2017, in four geographically diverse hospitals in Japan. Two of these hospitals, Tokyo Joto Hospital and Juntendo University Hospital, are located in eastern Japan whereas the others, Kurashiki Central Hospital and Akashi Medical Center, are in western Japan.
Questionnaires were printed and randomly distributed by research staff to outpatients in waiting rooms and inpatients in medical wards who were 20 years of age or older. We placed no restriction on ward site or time of questionnaire distribution. Research staff, including physicians, nurses, and medical clerks, were instructed to avoid guiding or influencing participants’ responses. Informed consent was obtained by the staff; only those who provided informed consent participated in the study. Respondents could request assistance with form completion from persons accompanying them if they had difficulties, such as physical, visual, or hearing impairments. All responses were collected anonymously. The study was approved by the ethics committees of all four hospitals.
Questionnaire
We used a modified version of the survey instrument from a prior study.10 The first section of the survey showed photographs of either a male or female physician with 7 unique forms of attire, including casual, casual with white coat, scrubs, scrubs with white coat, formal, formal with white coat, and business suit (Figure 1). Given the Japanese context of this study, the language was translated to Japanese and photographs of physicians of Japanese descent were used. Photographs were taken with attention paid to achieving constant facial expressions on the physicians as well as in other visual cues (eg, lighting, background, pose). The physician’s gender and attire in the first photograph seen by each respondent were randomized to prevent bias in ordering, priming, and anchoring; all other sections of the survey were identical.
Respondents were first asked to rate the standalone, randomized physician photograph using a 1-10 scale across five domains (ie, how knowledgeable, trustworthy, caring, and approachable the physician appeared and how comfortable the physician’s appearance made the respondent feel), with a score of 10 representing the highest rating. Respondents were subsequently given 7 photographs of the same physician wearing various forms of attire. Questions were asked regarding preference of attire in varied clinical settings (ie, primary care, ED, hospital, surgery, overall preference). To identify the influence of and respondent preferences for physician dress and white coats, a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was employed. The scale was trichotomized into “disagree” (1, 2), “neither agree nor disagree” (3), and “agree” (4, 5) for analysis. Demographic data, including age, gender, education level, nationality (Japanese or non-Japanese), and number of physicians seen in the past year were collected.
Outcomes and Sample Size Calculation
The primary outcome of attire preference was calculated as the mean composite score of the five individual rating domains (ie, knowledgeable, trustworthy, caring, approachable, and comfortable), with the highest score representing the most preferred form of attire. We also assessed variation in preferences for physician attire by respondent characteristics, such as age and gender.
Sample size estimation was based on previous survey methodology.10 The Likert scale range for identifying influence of and respondent preferences for physician dress and white coats was 1-5 (“strongly disagree” to “strongly agree”). The scale range for measuring preferences for the randomized attire photograph was 1-10. An assumption of normality was made regarding responses on the 1-10 scale. An estimated standard deviation of 2.2 was assumed, based on prior findings.10 Based on these assumptions and the inclusion of at least 816 respondents (assuming a two-sided alpha error of 0.05), we expected to have 90% capacity to detect differences for effect sizes of 0.50 on the 1-10 scale.
Statistical Analyses
Paper-based survey data were entered independently and in duplicate by the study team. Respondents were not required to answer all questions; therefore, the denominator for each question varied. Data were reported as mean and standard deviation (SD) or percentages, where appropriate. Differences in the mean composite rating scores were assessed using one-way ANOVA with the Tukey method for pairwise comparisons. Differences in proportions for categorical data were compared using the Z-test. Chi-squared tests were used for bivariate comparisons between respondent age, gender, and level of education and corresponding respondent preferences. All analyses were performed using Stata 14 MP/SE (Stata Corp., College Station, Texas, USA).
RESULTS
Characteristics of Participants
Between December 1, 2015 and October 30, 2017, a total of 2,020 surveys were completed by patients across four academic hospitals in Japan. Of those, 1,960 patients (97.0%) completed the survey in its entirety. Approximately half of the respondents were 65 years of age or older (49%), of female gender (52%), and reported receiving care in the outpatient setting (53%). Regarding use of healthcare, 91% had seen more than one physician in the year preceding the time of survey completion (Table 1).
Ratings of Physician Attire
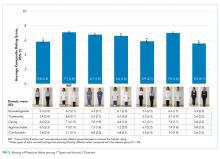
Compared with all forms of attire depicted in the survey’s first standalone photograph, respondents rated “casual attire with white coat” the highest (Figure 2). The mean composite score for “casual attire with white coat” was 7.1 (standard deviation [SD] = 1.8), and this attire was set as the referent group. Cronbach’s alpha, for the five items included in the composite score, was 0.95. However, “formal attire with white coat” was rated almost as highly as “casual attire with white coat” with an overall mean composite score of 7.0 (SD = 1.6).
Variation in Preference for Physician Attire by Clinical Setting
Preferences for physician attire varied by clinical care setting. Most respondents preferred “casual attire with white coat” or “formal attire with white coat” in both primary care and hospital settings, with a slight preference for “casual attire with white coat.” In contrast, respondents preferred “scrubs without white coat” in the ED and surgical settings. When asked about their overall preference, respondents reported they felt their physician should wear “formal attire with white coat” (35%) or “casual attire with white coat” (30%; Table 2). When comparing the group of photographs of physicians with white coats to the group without white coats (Figure 1), respondents preferred physicians wearing white coats overall and specifically when providing care in primary care and hospital settings. However, they preferred physicians without white coats when providing care in the ED (P < .001). With respect to surgeons, there was no statistically significant difference between preference for white coats and no white coats. These results were similar for photographs of both male and female physicians.
When asked whether physician dress was important to them and if physician attire influenced their satisfaction with the care received, 61% of participants agreed that physician dress was important, and 47% agreed that physician attire influenced satisfaction (Appendix Table 1). With respect to appropriateness of physicians dressing casually over the weekend in clinical settings, 52% responded that casual wear was inappropriate, while 31% had a neutral opinion.
Participants were asked whether physicians should wear a white coat in different clinical settings. Nearly two-thirds indicated a preference for white coats in the office and hospital (65% and 64%, respectively). Responses regarding whether emergency physicians should wear white coats were nearly equally divided (Agree, 37%; Disagree, 32%; Neither Agree nor Disagree, 31%). However, “scrubs without white coat” was most preferred (56%) when patients were given photographs of various attire and asked, “Which physician would you prefer to see when visiting the ER?” Responses to the question “Physicians should always wear a white coat when seeing patients in any setting” varied equally (Agree, 32%; Disagree, 34%; Neither Agree nor Disagree, 34%).
Variation in Preference for Physician Attire by Respondent Demographics
When comparing respondents by age, those 65 years or older preferred “formal attire with white coat” more so than respondents younger than 65 years (Appendix Table 2). This finding was identified in both primary care (36% vs 31%, P < .001) and hospital settings (37% vs 30%, P < .001). Additionally, physician attire had a greater impact on older respondents’ satisfaction and experience (Appendix Table 3). For example, 67% of respondents 65 years and older agreed that physician attire was important, and 54% agreed that attire influenced satisfaction. Conversely, for respondents younger than 65 years, the proportion agreeing with these statements was lower (56% and 41%, both P < .001). When comparing older and younger respondents, those 65 years and older more often preferred physicians wearing white coats in any setting (39% vs 26%, P < .001) and specifically in their office (68% vs 61%, P = .002), the ED (40% vs 34%, P < .001), and the hospital (69% vs 60%, P < .001).
When comparing male and female respondents, male respondents more often stated that physician dress was important to them (men, 64%; women, 58%; P = .002). When comparing responses to the question “Overall, which clothes do you feel a doctor should wear?”, between the eastern and western Japanese hospitals, preferences for physician attire varied.
Variation in Expectations Between Male and Female Physicians
When comparing the ratings of male and female physicians, female physicians were rated higher in how caring (P = .005) and approachable (P < .001) they appeared. However, there were no significant differences in the ratings of the three remaining domains (ie, knowledgeable, trustworthy, and comfortable) or the composite score.
DISCUSSION
Since we employed the same methodology as previous studies conducted in the US10 and Switzerland,18 a notable strength of our approach is that comparisons among these countries can be drawn. For example, physician attire appears to hold greater importance in Japan than in the US and Switzerland. Among Japanese participants, 61% agreed that physician dress is important (US, 53%; Switzerland, 36%), and 47% agreed that physician dress influenced how satisfied they were with their care (US, 36%; Switzerland, 23%).10 This result supports the notion that nonverbal and implicit communications (such as physician dress) may carry more importance among Japanese people.11-13
Regarding preference ratings for type of dress among respondents in Japan, “casual attire with white coat” received the highest mean composite score rating, with “formal attire with white coat” rated second overall. In contrast, US respondents rated “formal attire with white coat” highest and “scrubs with white coat” second.10 Our result runs counter to our expectation in that we expected Japanese respondents to prefer formal attire, since Japan is one of the most formal cultures in the world. One potential explanation for this difference is that the casual style chosen for this study was close to the smart casual style (slightly casual). Most hospitals and clinics in Japan do not allow physicians to wear jeans or polo shirts, which were chosen as the casual attire in the previous US study.
When examining various care settings and physician types, both Japanese and US respondents were more likely to prefer physicians wearing a white coat in the office or hospital.10 However, Japanese participants preferred both “casual attire with white coat” and “formal attire with white coat” equally in primary care or hospital settings. A smaller proportion of US respondents preferred “casual attire with white coat” in primary care (11%) and hospital settings (9%), but more preferred “formal attire with white coat” for primary care (44%) and hospital physicians (39%). In the ED setting, 32% of participants in Japan and 18% in the US disagreed with the idea that physicians should wear a white coat. Among Japanese participants, “scrubs without white coat” was rated highest for emergency physicians (56%) and surgeons (47%), while US preferences were 40% and 42%, respectively.10 One potential explanation is that scrubs-based attire became popular among Japanese ED and surgical contexts as a result of cultural influence and spread from western countries.19, 20
With respect to perceptions regarding physician attire on weekends, 52% of participants considered it inappropriate for a physician to dress casually over the weekend, compared with only 30% in Switzerland and 21% in the US.11,12 Given Japan’s level of formality and the fact that most Japanese physicians continue to work over the weekend,21-23 Japanese patients tend to expect their physicians to dress in more formal attire during these times.
Previous studies in Japan have demonstrated that older patients gave low ratings to scrubs and high ratings to white coat with any attire,15,17 and this was also the case in our study. Perhaps elderly patients reflect conservative values in their preferences of physician dress. Their perceptions may be less influenced by scenes portraying physicians in popular media when compared with the perceptions of younger patients. Though a 2015 systematic review and studies in other countries revealed white coats were preferred regardless of exact dress,9,24-26 they also showed variation in preferences for physician attire. For example, patients in Saudi Arabia preferred white coat and traditional ethnic dress,25 whereas mothers of pediatric patients in Saudi Arabia preferred scrubs for their pediatricians.27 Therefore, it is recommended for internationally mobile physicians to choose their dress depending on a variety of factors including country, context, and patient age group.
Our study has limitations. First, because some physicians presented the surveys to the patients, participants may have responded differently. Second, participants may have identified photographs of the male physician model as their personal healthcare provider (one author, K.K.). To avoid this possible bias, we randomly distributed 14 different versions of physician photographs in the questionnaire. Third, although physician photographs were strictly controlled, the “formal attire and white coat” and “casual attire and white coat” photographs appeared similar, especially given that the white coats were buttoned. Also, the female physician depicted in the photographs did not have the scrub shirt tucked in, while the male physician did. These nuances may have affected participant ratings between groups. Fourth,
In conclusion, patient preferences for physician attire were examined using a multicenter survey with a large sample size and robust survey methodology, thus overcoming weaknesses of previous studies into Japanese attire. Japanese patients perceive that physician attire is important and influences satisfaction with their care, more so than patients in other countries, like the US and Switzerland. Geography, settings of care, and patient age play a role in preferences. As a result, hospitals and health systems may use these findings to inform dress code policy based on patient population and context, recognizing that the appearance of their providers affects the patient-physician relationship. Future research should focus on better understanding the various cultural and societal customs that lead to patient expectations of physician attire.
Acknowledgments
The authors thank Drs. Fumi Takemoto, Masayuki Ueno, Kazuya Sakai, Saori Kinami, and Toshio Naito for their assistance with data collection at their respective sites. Additionally, the authors thank Dr. Yoko Kanamitsu for serving as a model for photographs.
1. Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201-203. https://doi.org/ 10.1056/NEJMp1211775.
2. Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
3. Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39-48. https://doi.org/10.2147/PPA.S24752.
4. Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921-31. https://doi.org/10.1056/NEJMsa080411.
5. O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144-54. https://doi.org/10.1046/j.1525-1497.2002.10431.x.
6. Chung H, Lee H, Chang DS, Kim HS, Park HJ, Chae Y. Doctor’s attire influences perceived empathy in the patient-doctor relationship. Patient Educ Couns. 2012;89(3):387-391. https://doi.org/10.1016/j.pec.2012.02.017.
7. Bianchi MT. Desiderata or dogma: what the evidence reveals about physician attire. J Gen Intern Med. 2008;23(5):641-643. https://doi.org/10.1007/s11606-008-0546-8.
8. Brandt LJ. On the value of an old dress code in the new millennium. Arch Intern Med. 2003;163(11):1277-1281. https://doi.org/10.1001/archinte.163.11.1277.
9. Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature--targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578. https://doi.org/10.1136/bmjopen-2014-006578.
10. Petrilli CM, Saint S, Jennings JJ, et al. Understanding patient preference for physician attire: a cross-sectional observational study of 10 academic medical centres in the USA. BMJ Open. 2018;8(5):e021239. https://doi.org/10.1136/bmjopen-2017-021239.
11. Rowbury R. The need for more proactive communications. Low trust and changing values mean Japan can no longer fall back on its homogeneity. The Japan Times. 2017, Oct 15;Sect. Opinion. https://www.japantimes.co.jp/opinion/2017/10/15/commentary/japan-commentary/need-proactive-communications/#.Xej7lC3MzUI. Accessed December 5, 2019.
12. Shoji Nishimura ANaST. Communication Style and Cultural Features in High/Low Context Communication Cultures: A Case Study of Finland, Japan and India. Nov 22nd, 2009.
13. Smith RMRSW. The influence of high/low-context culture and power distance on choice of communication media: Students’ media choice to communicate with Professors in Japan and America. Int J Intercultural Relations. 2007;31(4):479-501.
14. Yamada Y, Takahashi O, Ohde S, Deshpande GA, Fukui T. Patients’ preferences for doctors’ attire in Japan. Intern Med. 2010;49(15):1521-1526. https://doi.org/10.2169/internalmedicine.49.3572.
15. Ikusaka M, Kamegai M, Sunaga T, et al. Patients’ attitude toward consultations by a physician without a white coat in Japan. Intern Med. 1999;38(7):533-536. https://doi.org/10.2169/internalmedicine.38.533.
16. Lefor AK, Ohnuma T, Nunomiya S, Yokota S, Makino J, Sanui M. Physician attire in the intensive care unit in Japan influences visitors’ perception of care. J Crit Care. 2018;43:288-293.
17. Kurihara H, Maeno T. Importance of physicians’ attire: factors influencing the impression it makes on patients, a cross-sectional study. Asia Pac Fam Med. 2014;13(1):2. https://doi.org/10.1186/1447-056X-13-2.
18. Zollinger M, Houchens N, Chopra V, et al. Understanding patient preference for physician attire in ambulatory clinics: a cross-sectional observational study. BMJ Open. 2019;9(5):e026009. https://doi.org/10.1136/bmjopen-2018-026009.
19. Chung JE. Medical Dramas and Viewer Perception of Health: Testing Cultivation Effects. Hum Commun Res. 2014;40(3):333-349.
20. Michael Pfau LJM, Kirsten Garrow. The influence of television viewing on public perceptions of physicians. J Broadcast Electron Media. 1995;39(4):441-458.
21. Suzuki S. Exhausting physicians employed in hospitals in Japan assessed by a health questionnaire [in Japanese]. Sangyo Eiseigaku Zasshi. 2017;59(4):107-118. https://doi.org/10.1539/sangyoeisei.
22. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. 2018;18(1):50. https://doi.org/10.1186/s12909-018-1171-9.
23. Saijo Y, Chiba S, Yoshioka E, et al. Effects of work burden, job strain and support on depressive symptoms and burnout among Japanese physicians. Int J Occup Med Environ Health. 2014;27(6):980-992. https://doi.org/10.2478/s13382-014-0324-2.
24. Tiang KW, Razack AH, Ng KL. The ‘auxiliary’ white coat effect in hospitals: perceptions of patients and doctors. Singapore Med J. 2017;58(10):574-575. https://doi.org/10.11622/smedj.2017023.
25. Al Amry KM, Al Farrah M, Ur Rahman S, Abdulmajeed I. Patient perceptions and preferences of physicians’ attire in Saudi primary healthcare setting. J Community Hosp Intern Med Perspect. 2018;8(6):326-330. https://doi.org/10.1080/20009666.2018.1551026.
26. Healy WL. Letter to the editor: editor’s spotlight/take 5: physicians’ attire influences patients’ perceptions in the urban outpatient orthopaedic surgery setting. Clin Orthop Relat Res. 2016;474(11):2545-2546. https://doi.org/10.1007/s11999-016-5049-z.
27. Aldrees T, Alsuhaibani R, Alqaryan S, et al. Physicians’ attire. Parents preferences in a tertiary hospital. Saudi Med J. 2017;38(4):435-439. https://doi.org/10.15537/smj.2017.4.15853.
The patient-physician relationship is critical for ensuring the delivery of high-quality healthcare. Successful patient-physician relationships arise from shared trust, knowledge, mutual respect, and effective verbal and nonverbal communication. The ways in which patients experience healthcare and their satisfaction with physicians affect a myriad of important health outcomes, such as adherence to treatment and outcomes for conditions such as hypertension and diabetes mellitus.1-5 One method for potentially enhancing patient satisfaction is through understanding how patients wish their physicians to dress6-8 and tailoring attire to match these expectations. In addition to our systematic review,9 a recent large-scale, multicenter study in the United States revealed that most patients perceive physician attire as important, but that preferences for specific types of attire are contextual.9,10 For example, elderly patients preferred physicians in formal attire and white coat, while scrubs with white coat or scrubs alone were preferred for emergency department (ED) physicians and surgeons, respectively. Moreover, regional variation regarding attire preference was also observed in the US, with preferences for more formal attire in the South and less formal in the Midwest.
Geographic variation, regarding patient preferences for physician dress, is perhaps even more relevant internationally. In particular, Japan is considered to have a highly contextualized culture that relies on nonverbal and implicit communication. However, medical professionals have no specific dress code and, thus, don many different kinds of attire. In part, this may be because it is not clear whether or how physician attire impacts patient satisfaction and perceived healthcare quality in Japan.11-13 Although previous studies in Japan have suggested that physician attire has a considerable influence on patient satisfaction, these studies either involved a single department in one hospital or a small number of respondents.14-17 Therefore, we performed a multicenter, cross-sectional study to understand patients’ preferences for physician attire in different clinical settings and in different geographic regions in Japan.
METHODS
Study Population
We conducted a cross-sectional, questionnaire-based study from 2015 to 2017, in four geographically diverse hospitals in Japan. Two of these hospitals, Tokyo Joto Hospital and Juntendo University Hospital, are located in eastern Japan whereas the others, Kurashiki Central Hospital and Akashi Medical Center, are in western Japan.
Questionnaires were printed and randomly distributed by research staff to outpatients in waiting rooms and inpatients in medical wards who were 20 years of age or older. We placed no restriction on ward site or time of questionnaire distribution. Research staff, including physicians, nurses, and medical clerks, were instructed to avoid guiding or influencing participants’ responses. Informed consent was obtained by the staff; only those who provided informed consent participated in the study. Respondents could request assistance with form completion from persons accompanying them if they had difficulties, such as physical, visual, or hearing impairments. All responses were collected anonymously. The study was approved by the ethics committees of all four hospitals.
Questionnaire
We used a modified version of the survey instrument from a prior study.10 The first section of the survey showed photographs of either a male or female physician with 7 unique forms of attire, including casual, casual with white coat, scrubs, scrubs with white coat, formal, formal with white coat, and business suit (Figure 1). Given the Japanese context of this study, the language was translated to Japanese and photographs of physicians of Japanese descent were used. Photographs were taken with attention paid to achieving constant facial expressions on the physicians as well as in other visual cues (eg, lighting, background, pose). The physician’s gender and attire in the first photograph seen by each respondent were randomized to prevent bias in ordering, priming, and anchoring; all other sections of the survey were identical.
Respondents were first asked to rate the standalone, randomized physician photograph using a 1-10 scale across five domains (ie, how knowledgeable, trustworthy, caring, and approachable the physician appeared and how comfortable the physician’s appearance made the respondent feel), with a score of 10 representing the highest rating. Respondents were subsequently given 7 photographs of the same physician wearing various forms of attire. Questions were asked regarding preference of attire in varied clinical settings (ie, primary care, ED, hospital, surgery, overall preference). To identify the influence of and respondent preferences for physician dress and white coats, a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was employed. The scale was trichotomized into “disagree” (1, 2), “neither agree nor disagree” (3), and “agree” (4, 5) for analysis. Demographic data, including age, gender, education level, nationality (Japanese or non-Japanese), and number of physicians seen in the past year were collected.
Outcomes and Sample Size Calculation
The primary outcome of attire preference was calculated as the mean composite score of the five individual rating domains (ie, knowledgeable, trustworthy, caring, approachable, and comfortable), with the highest score representing the most preferred form of attire. We also assessed variation in preferences for physician attire by respondent characteristics, such as age and gender.
Sample size estimation was based on previous survey methodology.10 The Likert scale range for identifying influence of and respondent preferences for physician dress and white coats was 1-5 (“strongly disagree” to “strongly agree”). The scale range for measuring preferences for the randomized attire photograph was 1-10. An assumption of normality was made regarding responses on the 1-10 scale. An estimated standard deviation of 2.2 was assumed, based on prior findings.10 Based on these assumptions and the inclusion of at least 816 respondents (assuming a two-sided alpha error of 0.05), we expected to have 90% capacity to detect differences for effect sizes of 0.50 on the 1-10 scale.
Statistical Analyses
Paper-based survey data were entered independently and in duplicate by the study team. Respondents were not required to answer all questions; therefore, the denominator for each question varied. Data were reported as mean and standard deviation (SD) or percentages, where appropriate. Differences in the mean composite rating scores were assessed using one-way ANOVA with the Tukey method for pairwise comparisons. Differences in proportions for categorical data were compared using the Z-test. Chi-squared tests were used for bivariate comparisons between respondent age, gender, and level of education and corresponding respondent preferences. All analyses were performed using Stata 14 MP/SE (Stata Corp., College Station, Texas, USA).
RESULTS
Characteristics of Participants
Between December 1, 2015 and October 30, 2017, a total of 2,020 surveys were completed by patients across four academic hospitals in Japan. Of those, 1,960 patients (97.0%) completed the survey in its entirety. Approximately half of the respondents were 65 years of age or older (49%), of female gender (52%), and reported receiving care in the outpatient setting (53%). Regarding use of healthcare, 91% had seen more than one physician in the year preceding the time of survey completion (Table 1).
Ratings of Physician Attire
Compared with all forms of attire depicted in the survey’s first standalone photograph, respondents rated “casual attire with white coat” the highest (Figure 2). The mean composite score for “casual attire with white coat” was 7.1 (standard deviation [SD] = 1.8), and this attire was set as the referent group. Cronbach’s alpha, for the five items included in the composite score, was 0.95. However, “formal attire with white coat” was rated almost as highly as “casual attire with white coat” with an overall mean composite score of 7.0 (SD = 1.6).
Variation in Preference for Physician Attire by Clinical Setting
Preferences for physician attire varied by clinical care setting. Most respondents preferred “casual attire with white coat” or “formal attire with white coat” in both primary care and hospital settings, with a slight preference for “casual attire with white coat.” In contrast, respondents preferred “scrubs without white coat” in the ED and surgical settings. When asked about their overall preference, respondents reported they felt their physician should wear “formal attire with white coat” (35%) or “casual attire with white coat” (30%; Table 2). When comparing the group of photographs of physicians with white coats to the group without white coats (Figure 1), respondents preferred physicians wearing white coats overall and specifically when providing care in primary care and hospital settings. However, they preferred physicians without white coats when providing care in the ED (P < .001). With respect to surgeons, there was no statistically significant difference between preference for white coats and no white coats. These results were similar for photographs of both male and female physicians.
When asked whether physician dress was important to them and if physician attire influenced their satisfaction with the care received, 61% of participants agreed that physician dress was important, and 47% agreed that physician attire influenced satisfaction (Appendix Table 1). With respect to appropriateness of physicians dressing casually over the weekend in clinical settings, 52% responded that casual wear was inappropriate, while 31% had a neutral opinion.
Participants were asked whether physicians should wear a white coat in different clinical settings. Nearly two-thirds indicated a preference for white coats in the office and hospital (65% and 64%, respectively). Responses regarding whether emergency physicians should wear white coats were nearly equally divided (Agree, 37%; Disagree, 32%; Neither Agree nor Disagree, 31%). However, “scrubs without white coat” was most preferred (56%) when patients were given photographs of various attire and asked, “Which physician would you prefer to see when visiting the ER?” Responses to the question “Physicians should always wear a white coat when seeing patients in any setting” varied equally (Agree, 32%; Disagree, 34%; Neither Agree nor Disagree, 34%).
Variation in Preference for Physician Attire by Respondent Demographics
When comparing respondents by age, those 65 years or older preferred “formal attire with white coat” more so than respondents younger than 65 years (Appendix Table 2). This finding was identified in both primary care (36% vs 31%, P < .001) and hospital settings (37% vs 30%, P < .001). Additionally, physician attire had a greater impact on older respondents’ satisfaction and experience (Appendix Table 3). For example, 67% of respondents 65 years and older agreed that physician attire was important, and 54% agreed that attire influenced satisfaction. Conversely, for respondents younger than 65 years, the proportion agreeing with these statements was lower (56% and 41%, both P < .001). When comparing older and younger respondents, those 65 years and older more often preferred physicians wearing white coats in any setting (39% vs 26%, P < .001) and specifically in their office (68% vs 61%, P = .002), the ED (40% vs 34%, P < .001), and the hospital (69% vs 60%, P < .001).
When comparing male and female respondents, male respondents more often stated that physician dress was important to them (men, 64%; women, 58%; P = .002). When comparing responses to the question “Overall, which clothes do you feel a doctor should wear?”, between the eastern and western Japanese hospitals, preferences for physician attire varied.
Variation in Expectations Between Male and Female Physicians
When comparing the ratings of male and female physicians, female physicians were rated higher in how caring (P = .005) and approachable (P < .001) they appeared. However, there were no significant differences in the ratings of the three remaining domains (ie, knowledgeable, trustworthy, and comfortable) or the composite score.
DISCUSSION
Since we employed the same methodology as previous studies conducted in the US10 and Switzerland,18 a notable strength of our approach is that comparisons among these countries can be drawn. For example, physician attire appears to hold greater importance in Japan than in the US and Switzerland. Among Japanese participants, 61% agreed that physician dress is important (US, 53%; Switzerland, 36%), and 47% agreed that physician dress influenced how satisfied they were with their care (US, 36%; Switzerland, 23%).10 This result supports the notion that nonverbal and implicit communications (such as physician dress) may carry more importance among Japanese people.11-13
Regarding preference ratings for type of dress among respondents in Japan, “casual attire with white coat” received the highest mean composite score rating, with “formal attire with white coat” rated second overall. In contrast, US respondents rated “formal attire with white coat” highest and “scrubs with white coat” second.10 Our result runs counter to our expectation in that we expected Japanese respondents to prefer formal attire, since Japan is one of the most formal cultures in the world. One potential explanation for this difference is that the casual style chosen for this study was close to the smart casual style (slightly casual). Most hospitals and clinics in Japan do not allow physicians to wear jeans or polo shirts, which were chosen as the casual attire in the previous US study.
When examining various care settings and physician types, both Japanese and US respondents were more likely to prefer physicians wearing a white coat in the office or hospital.10 However, Japanese participants preferred both “casual attire with white coat” and “formal attire with white coat” equally in primary care or hospital settings. A smaller proportion of US respondents preferred “casual attire with white coat” in primary care (11%) and hospital settings (9%), but more preferred “formal attire with white coat” for primary care (44%) and hospital physicians (39%). In the ED setting, 32% of participants in Japan and 18% in the US disagreed with the idea that physicians should wear a white coat. Among Japanese participants, “scrubs without white coat” was rated highest for emergency physicians (56%) and surgeons (47%), while US preferences were 40% and 42%, respectively.10 One potential explanation is that scrubs-based attire became popular among Japanese ED and surgical contexts as a result of cultural influence and spread from western countries.19, 20
With respect to perceptions regarding physician attire on weekends, 52% of participants considered it inappropriate for a physician to dress casually over the weekend, compared with only 30% in Switzerland and 21% in the US.11,12 Given Japan’s level of formality and the fact that most Japanese physicians continue to work over the weekend,21-23 Japanese patients tend to expect their physicians to dress in more formal attire during these times.
Previous studies in Japan have demonstrated that older patients gave low ratings to scrubs and high ratings to white coat with any attire,15,17 and this was also the case in our study. Perhaps elderly patients reflect conservative values in their preferences of physician dress. Their perceptions may be less influenced by scenes portraying physicians in popular media when compared with the perceptions of younger patients. Though a 2015 systematic review and studies in other countries revealed white coats were preferred regardless of exact dress,9,24-26 they also showed variation in preferences for physician attire. For example, patients in Saudi Arabia preferred white coat and traditional ethnic dress,25 whereas mothers of pediatric patients in Saudi Arabia preferred scrubs for their pediatricians.27 Therefore, it is recommended for internationally mobile physicians to choose their dress depending on a variety of factors including country, context, and patient age group.
Our study has limitations. First, because some physicians presented the surveys to the patients, participants may have responded differently. Second, participants may have identified photographs of the male physician model as their personal healthcare provider (one author, K.K.). To avoid this possible bias, we randomly distributed 14 different versions of physician photographs in the questionnaire. Third, although physician photographs were strictly controlled, the “formal attire and white coat” and “casual attire and white coat” photographs appeared similar, especially given that the white coats were buttoned. Also, the female physician depicted in the photographs did not have the scrub shirt tucked in, while the male physician did. These nuances may have affected participant ratings between groups. Fourth,
In conclusion, patient preferences for physician attire were examined using a multicenter survey with a large sample size and robust survey methodology, thus overcoming weaknesses of previous studies into Japanese attire. Japanese patients perceive that physician attire is important and influences satisfaction with their care, more so than patients in other countries, like the US and Switzerland. Geography, settings of care, and patient age play a role in preferences. As a result, hospitals and health systems may use these findings to inform dress code policy based on patient population and context, recognizing that the appearance of their providers affects the patient-physician relationship. Future research should focus on better understanding the various cultural and societal customs that lead to patient expectations of physician attire.
Acknowledgments
The authors thank Drs. Fumi Takemoto, Masayuki Ueno, Kazuya Sakai, Saori Kinami, and Toshio Naito for their assistance with data collection at their respective sites. Additionally, the authors thank Dr. Yoko Kanamitsu for serving as a model for photographs.
The patient-physician relationship is critical for ensuring the delivery of high-quality healthcare. Successful patient-physician relationships arise from shared trust, knowledge, mutual respect, and effective verbal and nonverbal communication. The ways in which patients experience healthcare and their satisfaction with physicians affect a myriad of important health outcomes, such as adherence to treatment and outcomes for conditions such as hypertension and diabetes mellitus.1-5 One method for potentially enhancing patient satisfaction is through understanding how patients wish their physicians to dress6-8 and tailoring attire to match these expectations. In addition to our systematic review,9 a recent large-scale, multicenter study in the United States revealed that most patients perceive physician attire as important, but that preferences for specific types of attire are contextual.9,10 For example, elderly patients preferred physicians in formal attire and white coat, while scrubs with white coat or scrubs alone were preferred for emergency department (ED) physicians and surgeons, respectively. Moreover, regional variation regarding attire preference was also observed in the US, with preferences for more formal attire in the South and less formal in the Midwest.
Geographic variation, regarding patient preferences for physician dress, is perhaps even more relevant internationally. In particular, Japan is considered to have a highly contextualized culture that relies on nonverbal and implicit communication. However, medical professionals have no specific dress code and, thus, don many different kinds of attire. In part, this may be because it is not clear whether or how physician attire impacts patient satisfaction and perceived healthcare quality in Japan.11-13 Although previous studies in Japan have suggested that physician attire has a considerable influence on patient satisfaction, these studies either involved a single department in one hospital or a small number of respondents.14-17 Therefore, we performed a multicenter, cross-sectional study to understand patients’ preferences for physician attire in different clinical settings and in different geographic regions in Japan.
METHODS
Study Population
We conducted a cross-sectional, questionnaire-based study from 2015 to 2017, in four geographically diverse hospitals in Japan. Two of these hospitals, Tokyo Joto Hospital and Juntendo University Hospital, are located in eastern Japan whereas the others, Kurashiki Central Hospital and Akashi Medical Center, are in western Japan.
Questionnaires were printed and randomly distributed by research staff to outpatients in waiting rooms and inpatients in medical wards who were 20 years of age or older. We placed no restriction on ward site or time of questionnaire distribution. Research staff, including physicians, nurses, and medical clerks, were instructed to avoid guiding or influencing participants’ responses. Informed consent was obtained by the staff; only those who provided informed consent participated in the study. Respondents could request assistance with form completion from persons accompanying them if they had difficulties, such as physical, visual, or hearing impairments. All responses were collected anonymously. The study was approved by the ethics committees of all four hospitals.
Questionnaire
We used a modified version of the survey instrument from a prior study.10 The first section of the survey showed photographs of either a male or female physician with 7 unique forms of attire, including casual, casual with white coat, scrubs, scrubs with white coat, formal, formal with white coat, and business suit (Figure 1). Given the Japanese context of this study, the language was translated to Japanese and photographs of physicians of Japanese descent were used. Photographs were taken with attention paid to achieving constant facial expressions on the physicians as well as in other visual cues (eg, lighting, background, pose). The physician’s gender and attire in the first photograph seen by each respondent were randomized to prevent bias in ordering, priming, and anchoring; all other sections of the survey were identical.
Respondents were first asked to rate the standalone, randomized physician photograph using a 1-10 scale across five domains (ie, how knowledgeable, trustworthy, caring, and approachable the physician appeared and how comfortable the physician’s appearance made the respondent feel), with a score of 10 representing the highest rating. Respondents were subsequently given 7 photographs of the same physician wearing various forms of attire. Questions were asked regarding preference of attire in varied clinical settings (ie, primary care, ED, hospital, surgery, overall preference). To identify the influence of and respondent preferences for physician dress and white coats, a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was employed. The scale was trichotomized into “disagree” (1, 2), “neither agree nor disagree” (3), and “agree” (4, 5) for analysis. Demographic data, including age, gender, education level, nationality (Japanese or non-Japanese), and number of physicians seen in the past year were collected.
Outcomes and Sample Size Calculation
The primary outcome of attire preference was calculated as the mean composite score of the five individual rating domains (ie, knowledgeable, trustworthy, caring, approachable, and comfortable), with the highest score representing the most preferred form of attire. We also assessed variation in preferences for physician attire by respondent characteristics, such as age and gender.
Sample size estimation was based on previous survey methodology.10 The Likert scale range for identifying influence of and respondent preferences for physician dress and white coats was 1-5 (“strongly disagree” to “strongly agree”). The scale range for measuring preferences for the randomized attire photograph was 1-10. An assumption of normality was made regarding responses on the 1-10 scale. An estimated standard deviation of 2.2 was assumed, based on prior findings.10 Based on these assumptions and the inclusion of at least 816 respondents (assuming a two-sided alpha error of 0.05), we expected to have 90% capacity to detect differences for effect sizes of 0.50 on the 1-10 scale.
Statistical Analyses
Paper-based survey data were entered independently and in duplicate by the study team. Respondents were not required to answer all questions; therefore, the denominator for each question varied. Data were reported as mean and standard deviation (SD) or percentages, where appropriate. Differences in the mean composite rating scores were assessed using one-way ANOVA with the Tukey method for pairwise comparisons. Differences in proportions for categorical data were compared using the Z-test. Chi-squared tests were used for bivariate comparisons between respondent age, gender, and level of education and corresponding respondent preferences. All analyses were performed using Stata 14 MP/SE (Stata Corp., College Station, Texas, USA).
RESULTS
Characteristics of Participants
Between December 1, 2015 and October 30, 2017, a total of 2,020 surveys were completed by patients across four academic hospitals in Japan. Of those, 1,960 patients (97.0%) completed the survey in its entirety. Approximately half of the respondents were 65 years of age or older (49%), of female gender (52%), and reported receiving care in the outpatient setting (53%). Regarding use of healthcare, 91% had seen more than one physician in the year preceding the time of survey completion (Table 1).
Ratings of Physician Attire
Compared with all forms of attire depicted in the survey’s first standalone photograph, respondents rated “casual attire with white coat” the highest (Figure 2). The mean composite score for “casual attire with white coat” was 7.1 (standard deviation [SD] = 1.8), and this attire was set as the referent group. Cronbach’s alpha, for the five items included in the composite score, was 0.95. However, “formal attire with white coat” was rated almost as highly as “casual attire with white coat” with an overall mean composite score of 7.0 (SD = 1.6).
Variation in Preference for Physician Attire by Clinical Setting
Preferences for physician attire varied by clinical care setting. Most respondents preferred “casual attire with white coat” or “formal attire with white coat” in both primary care and hospital settings, with a slight preference for “casual attire with white coat.” In contrast, respondents preferred “scrubs without white coat” in the ED and surgical settings. When asked about their overall preference, respondents reported they felt their physician should wear “formal attire with white coat” (35%) or “casual attire with white coat” (30%; Table 2). When comparing the group of photographs of physicians with white coats to the group without white coats (Figure 1), respondents preferred physicians wearing white coats overall and specifically when providing care in primary care and hospital settings. However, they preferred physicians without white coats when providing care in the ED (P < .001). With respect to surgeons, there was no statistically significant difference between preference for white coats and no white coats. These results were similar for photographs of both male and female physicians.
When asked whether physician dress was important to them and if physician attire influenced their satisfaction with the care received, 61% of participants agreed that physician dress was important, and 47% agreed that physician attire influenced satisfaction (Appendix Table 1). With respect to appropriateness of physicians dressing casually over the weekend in clinical settings, 52% responded that casual wear was inappropriate, while 31% had a neutral opinion.
Participants were asked whether physicians should wear a white coat in different clinical settings. Nearly two-thirds indicated a preference for white coats in the office and hospital (65% and 64%, respectively). Responses regarding whether emergency physicians should wear white coats were nearly equally divided (Agree, 37%; Disagree, 32%; Neither Agree nor Disagree, 31%). However, “scrubs without white coat” was most preferred (56%) when patients were given photographs of various attire and asked, “Which physician would you prefer to see when visiting the ER?” Responses to the question “Physicians should always wear a white coat when seeing patients in any setting” varied equally (Agree, 32%; Disagree, 34%; Neither Agree nor Disagree, 34%).
Variation in Preference for Physician Attire by Respondent Demographics
When comparing respondents by age, those 65 years or older preferred “formal attire with white coat” more so than respondents younger than 65 years (Appendix Table 2). This finding was identified in both primary care (36% vs 31%, P < .001) and hospital settings (37% vs 30%, P < .001). Additionally, physician attire had a greater impact on older respondents’ satisfaction and experience (Appendix Table 3). For example, 67% of respondents 65 years and older agreed that physician attire was important, and 54% agreed that attire influenced satisfaction. Conversely, for respondents younger than 65 years, the proportion agreeing with these statements was lower (56% and 41%, both P < .001). When comparing older and younger respondents, those 65 years and older more often preferred physicians wearing white coats in any setting (39% vs 26%, P < .001) and specifically in their office (68% vs 61%, P = .002), the ED (40% vs 34%, P < .001), and the hospital (69% vs 60%, P < .001).
When comparing male and female respondents, male respondents more often stated that physician dress was important to them (men, 64%; women, 58%; P = .002). When comparing responses to the question “Overall, which clothes do you feel a doctor should wear?”, between the eastern and western Japanese hospitals, preferences for physician attire varied.
Variation in Expectations Between Male and Female Physicians
When comparing the ratings of male and female physicians, female physicians were rated higher in how caring (P = .005) and approachable (P < .001) they appeared. However, there were no significant differences in the ratings of the three remaining domains (ie, knowledgeable, trustworthy, and comfortable) or the composite score.
DISCUSSION
Since we employed the same methodology as previous studies conducted in the US10 and Switzerland,18 a notable strength of our approach is that comparisons among these countries can be drawn. For example, physician attire appears to hold greater importance in Japan than in the US and Switzerland. Among Japanese participants, 61% agreed that physician dress is important (US, 53%; Switzerland, 36%), and 47% agreed that physician dress influenced how satisfied they were with their care (US, 36%; Switzerland, 23%).10 This result supports the notion that nonverbal and implicit communications (such as physician dress) may carry more importance among Japanese people.11-13
Regarding preference ratings for type of dress among respondents in Japan, “casual attire with white coat” received the highest mean composite score rating, with “formal attire with white coat” rated second overall. In contrast, US respondents rated “formal attire with white coat” highest and “scrubs with white coat” second.10 Our result runs counter to our expectation in that we expected Japanese respondents to prefer formal attire, since Japan is one of the most formal cultures in the world. One potential explanation for this difference is that the casual style chosen for this study was close to the smart casual style (slightly casual). Most hospitals and clinics in Japan do not allow physicians to wear jeans or polo shirts, which were chosen as the casual attire in the previous US study.
When examining various care settings and physician types, both Japanese and US respondents were more likely to prefer physicians wearing a white coat in the office or hospital.10 However, Japanese participants preferred both “casual attire with white coat” and “formal attire with white coat” equally in primary care or hospital settings. A smaller proportion of US respondents preferred “casual attire with white coat” in primary care (11%) and hospital settings (9%), but more preferred “formal attire with white coat” for primary care (44%) and hospital physicians (39%). In the ED setting, 32% of participants in Japan and 18% in the US disagreed with the idea that physicians should wear a white coat. Among Japanese participants, “scrubs without white coat” was rated highest for emergency physicians (56%) and surgeons (47%), while US preferences were 40% and 42%, respectively.10 One potential explanation is that scrubs-based attire became popular among Japanese ED and surgical contexts as a result of cultural influence and spread from western countries.19, 20
With respect to perceptions regarding physician attire on weekends, 52% of participants considered it inappropriate for a physician to dress casually over the weekend, compared with only 30% in Switzerland and 21% in the US.11,12 Given Japan’s level of formality and the fact that most Japanese physicians continue to work over the weekend,21-23 Japanese patients tend to expect their physicians to dress in more formal attire during these times.
Previous studies in Japan have demonstrated that older patients gave low ratings to scrubs and high ratings to white coat with any attire,15,17 and this was also the case in our study. Perhaps elderly patients reflect conservative values in their preferences of physician dress. Their perceptions may be less influenced by scenes portraying physicians in popular media when compared with the perceptions of younger patients. Though a 2015 systematic review and studies in other countries revealed white coats were preferred regardless of exact dress,9,24-26 they also showed variation in preferences for physician attire. For example, patients in Saudi Arabia preferred white coat and traditional ethnic dress,25 whereas mothers of pediatric patients in Saudi Arabia preferred scrubs for their pediatricians.27 Therefore, it is recommended for internationally mobile physicians to choose their dress depending on a variety of factors including country, context, and patient age group.
Our study has limitations. First, because some physicians presented the surveys to the patients, participants may have responded differently. Second, participants may have identified photographs of the male physician model as their personal healthcare provider (one author, K.K.). To avoid this possible bias, we randomly distributed 14 different versions of physician photographs in the questionnaire. Third, although physician photographs were strictly controlled, the “formal attire and white coat” and “casual attire and white coat” photographs appeared similar, especially given that the white coats were buttoned. Also, the female physician depicted in the photographs did not have the scrub shirt tucked in, while the male physician did. These nuances may have affected participant ratings between groups. Fourth,
In conclusion, patient preferences for physician attire were examined using a multicenter survey with a large sample size and robust survey methodology, thus overcoming weaknesses of previous studies into Japanese attire. Japanese patients perceive that physician attire is important and influences satisfaction with their care, more so than patients in other countries, like the US and Switzerland. Geography, settings of care, and patient age play a role in preferences. As a result, hospitals and health systems may use these findings to inform dress code policy based on patient population and context, recognizing that the appearance of their providers affects the patient-physician relationship. Future research should focus on better understanding the various cultural and societal customs that lead to patient expectations of physician attire.
Acknowledgments
The authors thank Drs. Fumi Takemoto, Masayuki Ueno, Kazuya Sakai, Saori Kinami, and Toshio Naito for their assistance with data collection at their respective sites. Additionally, the authors thank Dr. Yoko Kanamitsu for serving as a model for photographs.
1. Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201-203. https://doi.org/ 10.1056/NEJMp1211775.
2. Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
3. Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39-48. https://doi.org/10.2147/PPA.S24752.
4. Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921-31. https://doi.org/10.1056/NEJMsa080411.
5. O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144-54. https://doi.org/10.1046/j.1525-1497.2002.10431.x.
6. Chung H, Lee H, Chang DS, Kim HS, Park HJ, Chae Y. Doctor’s attire influences perceived empathy in the patient-doctor relationship. Patient Educ Couns. 2012;89(3):387-391. https://doi.org/10.1016/j.pec.2012.02.017.
7. Bianchi MT. Desiderata or dogma: what the evidence reveals about physician attire. J Gen Intern Med. 2008;23(5):641-643. https://doi.org/10.1007/s11606-008-0546-8.
8. Brandt LJ. On the value of an old dress code in the new millennium. Arch Intern Med. 2003;163(11):1277-1281. https://doi.org/10.1001/archinte.163.11.1277.
9. Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature--targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578. https://doi.org/10.1136/bmjopen-2014-006578.
10. Petrilli CM, Saint S, Jennings JJ, et al. Understanding patient preference for physician attire: a cross-sectional observational study of 10 academic medical centres in the USA. BMJ Open. 2018;8(5):e021239. https://doi.org/10.1136/bmjopen-2017-021239.
11. Rowbury R. The need for more proactive communications. Low trust and changing values mean Japan can no longer fall back on its homogeneity. The Japan Times. 2017, Oct 15;Sect. Opinion. https://www.japantimes.co.jp/opinion/2017/10/15/commentary/japan-commentary/need-proactive-communications/#.Xej7lC3MzUI. Accessed December 5, 2019.
12. Shoji Nishimura ANaST. Communication Style and Cultural Features in High/Low Context Communication Cultures: A Case Study of Finland, Japan and India. Nov 22nd, 2009.
13. Smith RMRSW. The influence of high/low-context culture and power distance on choice of communication media: Students’ media choice to communicate with Professors in Japan and America. Int J Intercultural Relations. 2007;31(4):479-501.
14. Yamada Y, Takahashi O, Ohde S, Deshpande GA, Fukui T. Patients’ preferences for doctors’ attire in Japan. Intern Med. 2010;49(15):1521-1526. https://doi.org/10.2169/internalmedicine.49.3572.
15. Ikusaka M, Kamegai M, Sunaga T, et al. Patients’ attitude toward consultations by a physician without a white coat in Japan. Intern Med. 1999;38(7):533-536. https://doi.org/10.2169/internalmedicine.38.533.
16. Lefor AK, Ohnuma T, Nunomiya S, Yokota S, Makino J, Sanui M. Physician attire in the intensive care unit in Japan influences visitors’ perception of care. J Crit Care. 2018;43:288-293.
17. Kurihara H, Maeno T. Importance of physicians’ attire: factors influencing the impression it makes on patients, a cross-sectional study. Asia Pac Fam Med. 2014;13(1):2. https://doi.org/10.1186/1447-056X-13-2.
18. Zollinger M, Houchens N, Chopra V, et al. Understanding patient preference for physician attire in ambulatory clinics: a cross-sectional observational study. BMJ Open. 2019;9(5):e026009. https://doi.org/10.1136/bmjopen-2018-026009.
19. Chung JE. Medical Dramas and Viewer Perception of Health: Testing Cultivation Effects. Hum Commun Res. 2014;40(3):333-349.
20. Michael Pfau LJM, Kirsten Garrow. The influence of television viewing on public perceptions of physicians. J Broadcast Electron Media. 1995;39(4):441-458.
21. Suzuki S. Exhausting physicians employed in hospitals in Japan assessed by a health questionnaire [in Japanese]. Sangyo Eiseigaku Zasshi. 2017;59(4):107-118. https://doi.org/10.1539/sangyoeisei.
22. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. 2018;18(1):50. https://doi.org/10.1186/s12909-018-1171-9.
23. Saijo Y, Chiba S, Yoshioka E, et al. Effects of work burden, job strain and support on depressive symptoms and burnout among Japanese physicians. Int J Occup Med Environ Health. 2014;27(6):980-992. https://doi.org/10.2478/s13382-014-0324-2.
24. Tiang KW, Razack AH, Ng KL. The ‘auxiliary’ white coat effect in hospitals: perceptions of patients and doctors. Singapore Med J. 2017;58(10):574-575. https://doi.org/10.11622/smedj.2017023.
25. Al Amry KM, Al Farrah M, Ur Rahman S, Abdulmajeed I. Patient perceptions and preferences of physicians’ attire in Saudi primary healthcare setting. J Community Hosp Intern Med Perspect. 2018;8(6):326-330. https://doi.org/10.1080/20009666.2018.1551026.
26. Healy WL. Letter to the editor: editor’s spotlight/take 5: physicians’ attire influences patients’ perceptions in the urban outpatient orthopaedic surgery setting. Clin Orthop Relat Res. 2016;474(11):2545-2546. https://doi.org/10.1007/s11999-016-5049-z.
27. Aldrees T, Alsuhaibani R, Alqaryan S, et al. Physicians’ attire. Parents preferences in a tertiary hospital. Saudi Med J. 2017;38(4):435-439. https://doi.org/10.15537/smj.2017.4.15853.
1. Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201-203. https://doi.org/ 10.1056/NEJMp1211775.
2. Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
3. Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39-48. https://doi.org/10.2147/PPA.S24752.
4. Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921-31. https://doi.org/10.1056/NEJMsa080411.
5. O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med. 2002;17(2):144-54. https://doi.org/10.1046/j.1525-1497.2002.10431.x.
6. Chung H, Lee H, Chang DS, Kim HS, Park HJ, Chae Y. Doctor’s attire influences perceived empathy in the patient-doctor relationship. Patient Educ Couns. 2012;89(3):387-391. https://doi.org/10.1016/j.pec.2012.02.017.
7. Bianchi MT. Desiderata or dogma: what the evidence reveals about physician attire. J Gen Intern Med. 2008;23(5):641-643. https://doi.org/10.1007/s11606-008-0546-8.
8. Brandt LJ. On the value of an old dress code in the new millennium. Arch Intern Med. 2003;163(11):1277-1281. https://doi.org/10.1001/archinte.163.11.1277.
9. Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature--targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578. https://doi.org/10.1136/bmjopen-2014-006578.
10. Petrilli CM, Saint S, Jennings JJ, et al. Understanding patient preference for physician attire: a cross-sectional observational study of 10 academic medical centres in the USA. BMJ Open. 2018;8(5):e021239. https://doi.org/10.1136/bmjopen-2017-021239.
11. Rowbury R. The need for more proactive communications. Low trust and changing values mean Japan can no longer fall back on its homogeneity. The Japan Times. 2017, Oct 15;Sect. Opinion. https://www.japantimes.co.jp/opinion/2017/10/15/commentary/japan-commentary/need-proactive-communications/#.Xej7lC3MzUI. Accessed December 5, 2019.
12. Shoji Nishimura ANaST. Communication Style and Cultural Features in High/Low Context Communication Cultures: A Case Study of Finland, Japan and India. Nov 22nd, 2009.
13. Smith RMRSW. The influence of high/low-context culture and power distance on choice of communication media: Students’ media choice to communicate with Professors in Japan and America. Int J Intercultural Relations. 2007;31(4):479-501.
14. Yamada Y, Takahashi O, Ohde S, Deshpande GA, Fukui T. Patients’ preferences for doctors’ attire in Japan. Intern Med. 2010;49(15):1521-1526. https://doi.org/10.2169/internalmedicine.49.3572.
15. Ikusaka M, Kamegai M, Sunaga T, et al. Patients’ attitude toward consultations by a physician without a white coat in Japan. Intern Med. 1999;38(7):533-536. https://doi.org/10.2169/internalmedicine.38.533.
16. Lefor AK, Ohnuma T, Nunomiya S, Yokota S, Makino J, Sanui M. Physician attire in the intensive care unit in Japan influences visitors’ perception of care. J Crit Care. 2018;43:288-293.
17. Kurihara H, Maeno T. Importance of physicians’ attire: factors influencing the impression it makes on patients, a cross-sectional study. Asia Pac Fam Med. 2014;13(1):2. https://doi.org/10.1186/1447-056X-13-2.
18. Zollinger M, Houchens N, Chopra V, et al. Understanding patient preference for physician attire in ambulatory clinics: a cross-sectional observational study. BMJ Open. 2019;9(5):e026009. https://doi.org/10.1136/bmjopen-2018-026009.
19. Chung JE. Medical Dramas and Viewer Perception of Health: Testing Cultivation Effects. Hum Commun Res. 2014;40(3):333-349.
20. Michael Pfau LJM, Kirsten Garrow. The influence of television viewing on public perceptions of physicians. J Broadcast Electron Media. 1995;39(4):441-458.
21. Suzuki S. Exhausting physicians employed in hospitals in Japan assessed by a health questionnaire [in Japanese]. Sangyo Eiseigaku Zasshi. 2017;59(4):107-118. https://doi.org/10.1539/sangyoeisei.
22. Ogawa R, Seo E, Maeno T, Ito M, Sanuki M. The relationship between long working hours and depression among first-year residents in Japan. BMC Med Educ. 2018;18(1):50. https://doi.org/10.1186/s12909-018-1171-9.
23. Saijo Y, Chiba S, Yoshioka E, et al. Effects of work burden, job strain and support on depressive symptoms and burnout among Japanese physicians. Int J Occup Med Environ Health. 2014;27(6):980-992. https://doi.org/10.2478/s13382-014-0324-2.
24. Tiang KW, Razack AH, Ng KL. The ‘auxiliary’ white coat effect in hospitals: perceptions of patients and doctors. Singapore Med J. 2017;58(10):574-575. https://doi.org/10.11622/smedj.2017023.
25. Al Amry KM, Al Farrah M, Ur Rahman S, Abdulmajeed I. Patient perceptions and preferences of physicians’ attire in Saudi primary healthcare setting. J Community Hosp Intern Med Perspect. 2018;8(6):326-330. https://doi.org/10.1080/20009666.2018.1551026.
26. Healy WL. Letter to the editor: editor’s spotlight/take 5: physicians’ attire influences patients’ perceptions in the urban outpatient orthopaedic surgery setting. Clin Orthop Relat Res. 2016;474(11):2545-2546. https://doi.org/10.1007/s11999-016-5049-z.
27. Aldrees T, Alsuhaibani R, Alqaryan S, et al. Physicians’ attire. Parents preferences in a tertiary hospital. Saudi Med J. 2017;38(4):435-439. https://doi.org/10.15537/smj.2017.4.15853.
© 2020 Society of Hospital Medicine
Cognitive Errors in Medical Injury
Promotion of safer healthcare by patient organizations has led to an expansion of studies aimed at understanding medical errors to minimize injury through systemic improvement. These efforts have focused on identifying patient‐related factors, reducing technology failures, and improving communication.1 In contrast, factors related to cognitive errors by healthcare providers have received relatively little attention, although such errors may be an important source of preventable harm.1, 2
Limited information is available on the types and prevalence of cognitive factors in cases of medical injury, although cognitive factors may be a major risk for medical injury. If these factors were confirmed to be important factors for medical injury, better educational strategies may be needed to reduce cognitive errors among physicians and to enhance quality improvement and patient safety. Better understanding of these cognitive factors may also help to implement educational programs aimed at the improvement of cognitive performance in medical schools or teaching hospital.35
Closed‐claim files for cases of medical injury contain valuable information for investigation of the factors involved in medical errors.3 In Japan, court claims were tried and closed orders were issued by judges without a jury system until 2009. Under this system, representatives for defense and plaintiffs can present medical experts. Courts can also appoint experts independent of either party. Court opinions in Japan are considered as neutral judgments for conflicts between plaintiffs and defendants. Usually there are 3 judges who are required to be involved with each judgment in Japanese courts.
Closed‐claim files in cases of medical injury contain information about the types and prevalence of cognitive factors suggested to be causally related to the injuries by verdicts in district courts. Thus, by analyzing these files, an unbiased description of the characteristics and epidemiology of cognitive factors can be obtained for cases of medical injury, with minimization of potentially biased claims indicated by both parties; ie, plaintiffs vs. hospitals. Therefore, in this study, by using information from closed claims files at district courts in Tokyo and Osaka, Japan, we aimed to determine the important cognitive factors associated with cases of medical injury from such factors as judgment, vigilance, memory, technical competence, or knowledge. Since we anticipated that cognitive factors would dominate among the causative factors, we also explored the association of these factors with cases in which a judgment of paid compensation was made.
Methods
Study Sample
The authors acknowledge that the methodologies are based on those from the Malpractice Insurers' Medical Errors Prevention Study.6 A claim was defined as a written demand for compensation for cases of medical injury, based on a similar approach in previous studies.7, 8 Reviews were performed for closed‐claim files for cases of medical injury involving physicians from 2001 to 2005. These files were published by the Division of the Tokyo‐Osaka Medical Malpractice Lawsuits, organized by district courts in Tokyo and Osaka. The files included all closed‐claim cases of medical injury involving physicians from 2001 to 2005 at district courts in Tokyo and Osaka. The locations of delivery of care were inpatients in this study. All patients in Japan were insured during the study period.
Data Collection
Reviews were conducted by 3 board‐certified Japanese physician‐investigators specializing in internal medicine (1 chief investigator and 2 coinvestigators). The chief investigator trained the coinvestigators in 1‐day sessions with regard to the content of claims files, data collection, and the confidentiality procedure. Reviews were first performed by 1 coinvestigator and then confirmed by the chief investigator.
Data were collected for patient demographics and characteristics of adverse events, including types, locations, clinical areas, and specialties involved in the claims. Classification of specialties was based on that of Singh et al.3 Types of adverse events included minor injury for cases with complete recovery within a year, significant injury for those with complete recovery requiring more than a year, major injury for those with incomplete recovery (any physical sequelae) after more than a year, and death. Clinical areas consisted of surgery, obstetrics, missed diagnosis, delayed diagnosis, medication, and fall. Data for litigation outcomes and the amounts of paid compensation in Japanese Yen (JY) were also collected for claims that received verdicts supporting the plaintiffs.
All factors identified in the verdicts as causally related to the medical injury were recorded for data analysis. Classification of these factors was based on that of Singh et al.3 Cognitive factors were drawn from a list of categories of physicians' tasks provided by the Occupational Information Network. This network is a database of occupational requirements and worker attributes and it describes occupations in terms of the skills and knowledge required, how the work is performed, and typical work settings. The list of cognitive factor categories of physicians' tasks included judgment, vigilance, memory, technical competence, or knowledge. Accordingly, the cognitive factor category list was considered to capture the work of clinicians across the entire range of specialties.3
An example concerning failure of judgment would be that a rapid respiratory rate in initial vital signs was missed or ignored in a patient who complained of upper abdominal pain, was sent home with a diagnosis of gastritis, and eventually died at home; and an autopsy diagnosis of myocardial infarction with congestive heart failure was later confirmed. A vigilance error example would be that, in an electronic ordering system, typing an incorrect medication that has the similar commercial name of a correct medication. An example of failure of memory as a cognitive error would be that a physician forgot a result of laboratory data (positive sputum cytology of lung cancer), and so the physician did not explain it to the patient and did not perform an appropriate subsequent treatment referral. A technical incompetence example would be an operative or procedural injury due to technical problems of physicians. An example of a knowledge error would be that a contraindicated drug combination was prescribed such as the use of both selective serotonin reuptake inhibitor and monoamine oxidase inhibitor.
For systemic factors, a teamwork problem (poor teamwork) was used to describe disruptive team behavior, based on the concept of teamwork described by the Agency for Healthcare Research and Quality and the British Medical Association.9, 10 Cases with teamwork problems were defined as those in which the original reviewer had judged that 1 or more of the following contributory factors played a role in the error: communication breakdowns, supervision problems, handoff problems, failures to establish clear lines of responsibility, and conflict among clinical staff. Technology failure indicated an error of commission or omission by devices, tools, or machines.
The Japanese courts analyze medical records but they do not open the records to the public and so we could not analyze the medical records of the cases in our study. Thus, we did not judge whether the adverse outcome could have been attributed to medical errors, while we analyzed the claims files and followed the conclusions reached by the end of the claims.
Statistical Analysis
Data are given as proportions for categorical variables and means or medians for continuous variables. Cognitive factors associated with cases receiving adjudication of a compensation payment by district courts (litigation outcomes) were analyzed using a logistic regression model including 5 types of cognitive errors. Analyses were conducted with the Stata SE 10.0 statistical software package (College Station, TX). All P values are 2‐sided and P < 0.05 was considered to be statistically significant. The study was approved by the ethics review board at the institution of the chief investigator.
Results
In a total of 274 closed cases of medical injury, the mean age of the patients was 49 years old and 45% were women (Table 1). The reviews performed by the coinvestigators were all confirmed by the chief investigator without discordance of the reviews between the coinvestigators and the chief investigator. The claims involved death of patients in 45% of cases; injuries that caused significant or major disability in 10% and 24%, respectively (a total of 34%); and minor adverse outcomes of medical care in 21% (57 cases). Closing verdicts supporting the plaintiffs (patients or family) by the district courts were given in 103 claims (38%), with compensation at a median of 8,000,000 JY (100 JY = $1 US in 2005). The compensation ranged from 20,000 JY to 222,710,251 JY. The highest compensation was ordered to be paid to a 36‐year‐old woman with an obstetrics‐related major injury and the court indicated the injury was causally related to the following 3 cognitive factors: error in judgment, failure of vigilance, and lack of technical competence.
| Characteristic | n (%) |
|---|---|
| |
| Demographic of patients | |
| Women | 121 (45) |
| Men | 153 (55) |
| Age, mean SD, year | 49 22 |
| Adverse outcome | |
| Minor | 57 (21) |
| Significant | 28 (10) |
| Major | 67 (24) |
| Death | 122 (45) |
| Operative | 36 |
| Delayed diagnosis | 35 |
| Medication | 26 |
| Missed diagnosis | 16 |
| Obstetrics | 8 |
| Clinical area | |
| Operative | 120 (44) |
| Delayed diagnosis | 54 (20) |
| Medication | 50 (18) |
| Missed diagnosis | 28 (10) |
| Obstetrics | 19 (7) |
| Fall | 3 (1) |
Operative injury was the most frequent reason for claims, followed by delayed diagnosis, medication error, and missed diagnosis. General surgery, orthopedics, internal medicine, and obstetrics/gynecology were the most frequently involved specialties, comprising 30% of all cases (Table 2). The verdicts suggested cognitive factors were the most prevalent factors associated with cases of medical injury: 73% of the injuries were judged to be the result of an error in judgment (Table 3), followed by failure of vigilance (65%), lack of technical competence (34%), and lack of knowledge (31%). Verdicts indicated systemic factors in only a few cases, including poor teamwork in 4% and technology failure in 2%. Patient‐related factors were suggested in 32% of the claims.
| Specialty | Cases, n (%) |
|---|---|
| General surgery | 27 (10) |
| Orthopedic surgery | 27 (10) |
| Internal medicine | 27 (10) |
| Obstetrics‐gynecology | 26 (9) |
| Neurosurgery | 19 (7) |
| Ear, nose, and throat | 18 (7) |
| Plastic surgery | 15 (5) |
| Psychiatry | 14 (5) |
| Cardiology | 13 (5) |
| Dental care | 13 (5) |
| Ophthalmology | 12 (4) |
| Hematology or oncology | 10 (4) |
| Adult primary care | 9 (3) |
| Pediatrics | 8 (3) |
| Urology | 8 (3) |
| Cardiothoracic surgery | 8 (3) |
| Neurology | 5 (2) |
| Anesthesiology | 4 (1) |
| Physical medicine or rehabilitation | 3 (1) |
| Emergency medicine | 2 (1) |
| Infectious disease | 2 (1) |
| Dermatology | 2 (1) |
| Radiology | 1 (<1) |
| Vascular surgery | 1 (<1) |
| Contributory Factor | n (%) |
|---|---|
| |
| Cognitive factors | |
| Error in judgment | 199 (73) |
| Failure of vigilance | 177 (65) |
| Lack of technical competence | 94 (34) |
| Lack of knowledge | 86 (31) |
| Failure of memory | 5 (2) |
| System factors | |
| Poor teamwork | 11 (4) |
| Technology failure | 5 (2) |
| Patient‐related factors | 87 (32) |
In a multivariable‐adjusted logistic regression analysis of cognitive factors with a potential association with the claims with paid compensation (Table 4), only error in judgment showed a significant association (odds ratio, 1.9; 95% confidence interval [CI], 1.01‐3.40). The other four cognitive factors in the model were not associated with these claims. The odds ratio for failure of memory was high (2.8), but this factor was identified by the courts in only 5 cases and was not significantly associated with claims with paid compensation.
| Cognitive Factor | Cases With No Compensation (n = 171), n (%) | Cases With Paid Compensation (n = 103), n (%) | Odds Ratio (95% CI)* |
|---|---|---|---|
| |||
| Error in judgment | 117 (68) | 82 (80) | 1.9 (1.03.4) |
| Failure of vigilance | 111 (65) | 66 (64) | 1.0 (0.61.7) |
| Failure of memory | 2 (1) | 3 (3) | 2.8 (0.518) |
| Lack of technical competence | 58 (34) | 36 (35) | 1.1 (0.61.8) |
| Lack of knowledge | 52 (30) | 34 (33) | 1.0 (0.61.7) |
Discussion
In this study of closed claims files, we identified 2 important cognitive factors involved in cases of medical injury. Error in judgment was the most common factor, comprising about 70% of all claims, and was significantly associated with cases with paid compensation for medical injury. The second cognitive factor was failure of vigilance, which was found in 65% of the claims. Other cognitive factors, such as lack of technical competence and knowledge or failure of memory, as well as systemic factors (poor teamwork and technology failure) were less frequently found to be causally related to cases with medical injury in the verdicts examined in the study.
Reasons for the low frequency of systemic factors involved in cases of medical injury in our study are unclear. This may be the cultural characteristics such as greater emphasis to working in teams and following rules of an organization in Japan. Another possibility is that plaintiffs might have tended to generate lawsuits in cases with suspected higher frequency of individual physicians' factors in Japan. Moreover, among cognitive factors, lack of technical competence and knowledge or failure of memory was also less frequently related to cases with medical injury in our study compared to those of the previous studies.3, 11
The study design of analyzing closed claims files of cases of medical injury is noteworthy for its methodology of error assessment and provides valuable information on errors related to medical injury.3, 7 Moreover, the system of court verdicts in Japan based on decisions by a professional judge allows elimination of potential bias from stakeholders (plaintiffs vs. hospitals) involved in cases of medical injury. Thus, probable causes related to adverse events can be determined from a neutral position. Previous studies of medical error have focused on medical record reviews, surveys, and interviews;12, 13 our study corroborates and extends the findings in these studies that cognitive errors are the most frequent source of medical injury.
Error in judgment is commonly made in the course of decision making in multiple clinical areas. This type of error is referred to recently as cognitive dispositions to respond,14 which is different from bias or heuristics, since not all heuristics are biased and not all errors in judgments come from bias. There is a well‐established value of heuristics in medical diagnosis. Moreover, the properties of this type of error are likely to be distinct from those associated with performance of procedures (lack of technical competence), such as operative injury, which are directly visible and can be prevented through rapid dissemination of information on safety procedures among a medical team. However, the consequences of error in judgment are important for patients, family, and healthcare providers, and these errors are also largely preventable by implementation of educational programs.15
Possible solutions for improving clinical judgment skills may be derived from recent education theory. The theory provides a means for minimizing errors in judgment through the process of meta‐cognition, in which cognitive forcing strategies can be developed through thinking that involves active control over the process of one's own thinking.14, 15 For example, reflective practice has been suggested to be an important instrument for improving clinical judgment and may particularly improve diagnoses in situations of uncertainty and uniqueness, thereby reducing diagnostic errors.16 The capability of critical reflection in real‐time practice (reflection‐in‐action) and on our own practice (reflection‐on‐action) appears to be a key requirement for developing and maintaining medical expertise.17, 18 For instance, case‐based discussion with clinician educators can be an opportunity for enhancing critical thinking skills of medical trainees.
Based on a context‐based approach that focuses on the nature of the clinical problem, potential systemic solutions have recently been proposed for reducing errors in judgment.1 These solutions utilize advanced technology, including symptom‐oriented diagnostic decision support, internet search engines for information on possible diagnoses, and automated reminders in electronic health records.1, 19 Previous studies have shown that long work hours and sleep deprivation can decrease cognitive function, leading to failure of vigilance and increased medical errors,20 and several systemic solutions provide models for avoidance of failure of vigilance. For instance, eliminating extended work shifts and reducing the number of work hours per week was shown to reduce serious medical errors through increased sleep and decreased failure of vigilance during night work in an intensive care unit.21, 22 Taking a brief nap during work hours has also been associated with decreased medical errors in a recent study conducted in Japan.23 Despite the well‐known importance of factors of physicians' workloads, our study did not analyze these factors and thus further studies are needed to confirm their importance in Japanese medical practice.
There were also 32% of patient‐related factors suggested as contributory factors to medical injury in verdicts of the closed claims. This finding may be also important in planning educational intervention strategies to reduce medical errors. Although our data did not include the relative frequency of components related to these factors, major components of patient‐related factors may include age, severity of illnesses, comorbidity, functional status, or mental status. Educational intervention programs may help healthcare providers to evaluate patients with these risk factors and to implement preventive strategies to avoid incidents among these patients.
General surgery, orthopedic surgery, internal medicine, and obstetrics‐gynecology were the most frequently involved specialties in our study. The reasons why these specialties were highly involved in the claims are unclear and our study could not analyze these issues. However, these specialties may be related to patients with greater clinical severity and thus they may have subsequently higher risk for receiving claims. Further, physicians in these specialties may be at higher risk for having various errors because of the complexity of care for patients.
Our study has several limitations. First, the closed claims are more likely to represent cases with severe injury.3 Therefore, it is unclear if we can generalize our findings beyond cases with severe injury.3 Second, certain contributory factors may not have been suggested by the verdicts, even though they played a role. Among these potential factors, poor teamwork and communication issues are unlikely to be identified as causative in verdicts, unless the allegation of the plaintiffs documented these issues. Moreover, the Japanese courts did not open the medical records to the public and so we could not analyze the medical records of the cases. Third, we only evaluated closed verdicts given by professional judges of district courts, who are unlikely to be medical experts. However, the closed verdicts underwent an extensive process involving testimony from medical professionals and academic societies. Fourth, we, as investigators, had few members with surgical backgrounds in this study so we might have underestimated issues related to technical competence among the claims. Finally, although a small percentage of closed‐ claim cases involving team performance were identified in our study, the plaintiffs might have indicated this point to the court claims, since it might have been difficult to describe this issue as a reason for requesting compensations from defendants. Thus, despite a low proportion of team performance involvement in the verdicts, we still believe that poor team performance is a factor related to most medical injuries.
In summary, causal factors obtained from closed claims files suggest the importance of cognitive factors in cases of medical injury. Among the cognitive factors, error in judgment and failure of vigilance were the most frequent. These findings may help leaders of medical schools and hospitals to allocate more resources for research into strategies to improve cognitive performance and thereby ensure patient safety. Further research is needed to better understand the cognitive mechanisms involved in medical errors and to translate this into educational strategies.
- ,.Diagnostic errors‐the next frontier for patient safety.JAMA.2009;301(10):1060–1062.
- ,,.Diagnostic error in internal medicine.Arch Intern Med.2005;165(13):1493–1499.
- ,,,.Medical errors involving trainees: a study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167(19):2030–2036.
- ,,.Understanding diagnostic errors in medicine: a lesson from aviation.Qual Saf Health Care.2006;15(3):159–164.
- .The importance of cognitive errors in diagnosis and strategies to minimize them.Acad Med.2003;78(8):775–780.
- ,,, et al.Claims, errors, and compensation payments in medical malpractice litigation.N Engl J Med.2006;354(19):2024–2033.
- ,,,,,.Negligent care and malpractice claiming behavior in Utah and Colorado.Med Care.2000;38(3):250–260.
- ,,, et al.Incidence and types of adverse events and negligent care in Utah and Colorado.Med Care.2000;38(3):261–271.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality;2005 [updated April 2005]; Available at: http://www.ahrq.gov/qual/medteam. Accessed June 2010.
- ,.Team working in Primary Health Care. Realising Shared Aims in Patient Care.London, UK:Royal Pharmaceutical Society and British Medical Association.2005.
- ,,,,.The nature and causes of unintended events reported at ten emergency departments.BMC Emerg Med.2009;9:16.
- ,,.To Err Is Human: Building a Safer Health System.Washington, USA:National Academy Press;2000.
- ,,,.Analysis of errors reported by surgeons at three teaching hospitals.Surgery.2003;133(6):614–621.
- .Achieving quality in clinical decision making: cognitive strategies and detection of bias.Acad Emerg Med.2002;9(11):1184–1204.
- .Cognitive forcing strategies in clinical decision making.Ann Emerg Med.2003;41(1):110–120.
- ,,.Effects of reflective practice on the accuracy of medical diagnoses.Med Educ.2008;42(5):468–475.
- .The Reflective Practitioner: How Professionals Think in Action.New York, NY:Basic Books;1983.
- ,,.Diagnostic errors and reflective practice in medicine.J Eval Clin Pract.2007;13(1):138–145.
- ,,,.Caught in the web: e‐diagnosis.J Hosp Med.2009;4(4):262–266.
- ,,, et al.Extended work duration and the risk of self‐reported percutaneous injuries in interns.JAMA.2006;296(9):1055–1062.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351(18):1838–1848.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351(18):1829–1837.
- ,,, et al.Influence of Residents' Workload, Mental State and Job Satisfaction on Procedural Error: a prospective daily questionnaire‐based study.General Medicine.2008;9(2):57–64.
Promotion of safer healthcare by patient organizations has led to an expansion of studies aimed at understanding medical errors to minimize injury through systemic improvement. These efforts have focused on identifying patient‐related factors, reducing technology failures, and improving communication.1 In contrast, factors related to cognitive errors by healthcare providers have received relatively little attention, although such errors may be an important source of preventable harm.1, 2
Limited information is available on the types and prevalence of cognitive factors in cases of medical injury, although cognitive factors may be a major risk for medical injury. If these factors were confirmed to be important factors for medical injury, better educational strategies may be needed to reduce cognitive errors among physicians and to enhance quality improvement and patient safety. Better understanding of these cognitive factors may also help to implement educational programs aimed at the improvement of cognitive performance in medical schools or teaching hospital.35
Closed‐claim files for cases of medical injury contain valuable information for investigation of the factors involved in medical errors.3 In Japan, court claims were tried and closed orders were issued by judges without a jury system until 2009. Under this system, representatives for defense and plaintiffs can present medical experts. Courts can also appoint experts independent of either party. Court opinions in Japan are considered as neutral judgments for conflicts between plaintiffs and defendants. Usually there are 3 judges who are required to be involved with each judgment in Japanese courts.
Closed‐claim files in cases of medical injury contain information about the types and prevalence of cognitive factors suggested to be causally related to the injuries by verdicts in district courts. Thus, by analyzing these files, an unbiased description of the characteristics and epidemiology of cognitive factors can be obtained for cases of medical injury, with minimization of potentially biased claims indicated by both parties; ie, plaintiffs vs. hospitals. Therefore, in this study, by using information from closed claims files at district courts in Tokyo and Osaka, Japan, we aimed to determine the important cognitive factors associated with cases of medical injury from such factors as judgment, vigilance, memory, technical competence, or knowledge. Since we anticipated that cognitive factors would dominate among the causative factors, we also explored the association of these factors with cases in which a judgment of paid compensation was made.
Methods
Study Sample
The authors acknowledge that the methodologies are based on those from the Malpractice Insurers' Medical Errors Prevention Study.6 A claim was defined as a written demand for compensation for cases of medical injury, based on a similar approach in previous studies.7, 8 Reviews were performed for closed‐claim files for cases of medical injury involving physicians from 2001 to 2005. These files were published by the Division of the Tokyo‐Osaka Medical Malpractice Lawsuits, organized by district courts in Tokyo and Osaka. The files included all closed‐claim cases of medical injury involving physicians from 2001 to 2005 at district courts in Tokyo and Osaka. The locations of delivery of care were inpatients in this study. All patients in Japan were insured during the study period.
Data Collection
Reviews were conducted by 3 board‐certified Japanese physician‐investigators specializing in internal medicine (1 chief investigator and 2 coinvestigators). The chief investigator trained the coinvestigators in 1‐day sessions with regard to the content of claims files, data collection, and the confidentiality procedure. Reviews were first performed by 1 coinvestigator and then confirmed by the chief investigator.
Data were collected for patient demographics and characteristics of adverse events, including types, locations, clinical areas, and specialties involved in the claims. Classification of specialties was based on that of Singh et al.3 Types of adverse events included minor injury for cases with complete recovery within a year, significant injury for those with complete recovery requiring more than a year, major injury for those with incomplete recovery (any physical sequelae) after more than a year, and death. Clinical areas consisted of surgery, obstetrics, missed diagnosis, delayed diagnosis, medication, and fall. Data for litigation outcomes and the amounts of paid compensation in Japanese Yen (JY) were also collected for claims that received verdicts supporting the plaintiffs.
All factors identified in the verdicts as causally related to the medical injury were recorded for data analysis. Classification of these factors was based on that of Singh et al.3 Cognitive factors were drawn from a list of categories of physicians' tasks provided by the Occupational Information Network. This network is a database of occupational requirements and worker attributes and it describes occupations in terms of the skills and knowledge required, how the work is performed, and typical work settings. The list of cognitive factor categories of physicians' tasks included judgment, vigilance, memory, technical competence, or knowledge. Accordingly, the cognitive factor category list was considered to capture the work of clinicians across the entire range of specialties.3
An example concerning failure of judgment would be that a rapid respiratory rate in initial vital signs was missed or ignored in a patient who complained of upper abdominal pain, was sent home with a diagnosis of gastritis, and eventually died at home; and an autopsy diagnosis of myocardial infarction with congestive heart failure was later confirmed. A vigilance error example would be that, in an electronic ordering system, typing an incorrect medication that has the similar commercial name of a correct medication. An example of failure of memory as a cognitive error would be that a physician forgot a result of laboratory data (positive sputum cytology of lung cancer), and so the physician did not explain it to the patient and did not perform an appropriate subsequent treatment referral. A technical incompetence example would be an operative or procedural injury due to technical problems of physicians. An example of a knowledge error would be that a contraindicated drug combination was prescribed such as the use of both selective serotonin reuptake inhibitor and monoamine oxidase inhibitor.
For systemic factors, a teamwork problem (poor teamwork) was used to describe disruptive team behavior, based on the concept of teamwork described by the Agency for Healthcare Research and Quality and the British Medical Association.9, 10 Cases with teamwork problems were defined as those in which the original reviewer had judged that 1 or more of the following contributory factors played a role in the error: communication breakdowns, supervision problems, handoff problems, failures to establish clear lines of responsibility, and conflict among clinical staff. Technology failure indicated an error of commission or omission by devices, tools, or machines.
The Japanese courts analyze medical records but they do not open the records to the public and so we could not analyze the medical records of the cases in our study. Thus, we did not judge whether the adverse outcome could have been attributed to medical errors, while we analyzed the claims files and followed the conclusions reached by the end of the claims.
Statistical Analysis
Data are given as proportions for categorical variables and means or medians for continuous variables. Cognitive factors associated with cases receiving adjudication of a compensation payment by district courts (litigation outcomes) were analyzed using a logistic regression model including 5 types of cognitive errors. Analyses were conducted with the Stata SE 10.0 statistical software package (College Station, TX). All P values are 2‐sided and P < 0.05 was considered to be statistically significant. The study was approved by the ethics review board at the institution of the chief investigator.
Results
In a total of 274 closed cases of medical injury, the mean age of the patients was 49 years old and 45% were women (Table 1). The reviews performed by the coinvestigators were all confirmed by the chief investigator without discordance of the reviews between the coinvestigators and the chief investigator. The claims involved death of patients in 45% of cases; injuries that caused significant or major disability in 10% and 24%, respectively (a total of 34%); and minor adverse outcomes of medical care in 21% (57 cases). Closing verdicts supporting the plaintiffs (patients or family) by the district courts were given in 103 claims (38%), with compensation at a median of 8,000,000 JY (100 JY = $1 US in 2005). The compensation ranged from 20,000 JY to 222,710,251 JY. The highest compensation was ordered to be paid to a 36‐year‐old woman with an obstetrics‐related major injury and the court indicated the injury was causally related to the following 3 cognitive factors: error in judgment, failure of vigilance, and lack of technical competence.
| Characteristic | n (%) |
|---|---|
| |
| Demographic of patients | |
| Women | 121 (45) |
| Men | 153 (55) |
| Age, mean SD, year | 49 22 |
| Adverse outcome | |
| Minor | 57 (21) |
| Significant | 28 (10) |
| Major | 67 (24) |
| Death | 122 (45) |
| Operative | 36 |
| Delayed diagnosis | 35 |
| Medication | 26 |
| Missed diagnosis | 16 |
| Obstetrics | 8 |
| Clinical area | |
| Operative | 120 (44) |
| Delayed diagnosis | 54 (20) |
| Medication | 50 (18) |
| Missed diagnosis | 28 (10) |
| Obstetrics | 19 (7) |
| Fall | 3 (1) |
Operative injury was the most frequent reason for claims, followed by delayed diagnosis, medication error, and missed diagnosis. General surgery, orthopedics, internal medicine, and obstetrics/gynecology were the most frequently involved specialties, comprising 30% of all cases (Table 2). The verdicts suggested cognitive factors were the most prevalent factors associated with cases of medical injury: 73% of the injuries were judged to be the result of an error in judgment (Table 3), followed by failure of vigilance (65%), lack of technical competence (34%), and lack of knowledge (31%). Verdicts indicated systemic factors in only a few cases, including poor teamwork in 4% and technology failure in 2%. Patient‐related factors were suggested in 32% of the claims.
| Specialty | Cases, n (%) |
|---|---|
| General surgery | 27 (10) |
| Orthopedic surgery | 27 (10) |
| Internal medicine | 27 (10) |
| Obstetrics‐gynecology | 26 (9) |
| Neurosurgery | 19 (7) |
| Ear, nose, and throat | 18 (7) |
| Plastic surgery | 15 (5) |
| Psychiatry | 14 (5) |
| Cardiology | 13 (5) |
| Dental care | 13 (5) |
| Ophthalmology | 12 (4) |
| Hematology or oncology | 10 (4) |
| Adult primary care | 9 (3) |
| Pediatrics | 8 (3) |
| Urology | 8 (3) |
| Cardiothoracic surgery | 8 (3) |
| Neurology | 5 (2) |
| Anesthesiology | 4 (1) |
| Physical medicine or rehabilitation | 3 (1) |
| Emergency medicine | 2 (1) |
| Infectious disease | 2 (1) |
| Dermatology | 2 (1) |
| Radiology | 1 (<1) |
| Vascular surgery | 1 (<1) |
| Contributory Factor | n (%) |
|---|---|
| |
| Cognitive factors | |
| Error in judgment | 199 (73) |
| Failure of vigilance | 177 (65) |
| Lack of technical competence | 94 (34) |
| Lack of knowledge | 86 (31) |
| Failure of memory | 5 (2) |
| System factors | |
| Poor teamwork | 11 (4) |
| Technology failure | 5 (2) |
| Patient‐related factors | 87 (32) |
In a multivariable‐adjusted logistic regression analysis of cognitive factors with a potential association with the claims with paid compensation (Table 4), only error in judgment showed a significant association (odds ratio, 1.9; 95% confidence interval [CI], 1.01‐3.40). The other four cognitive factors in the model were not associated with these claims. The odds ratio for failure of memory was high (2.8), but this factor was identified by the courts in only 5 cases and was not significantly associated with claims with paid compensation.
| Cognitive Factor | Cases With No Compensation (n = 171), n (%) | Cases With Paid Compensation (n = 103), n (%) | Odds Ratio (95% CI)* |
|---|---|---|---|
| |||
| Error in judgment | 117 (68) | 82 (80) | 1.9 (1.03.4) |
| Failure of vigilance | 111 (65) | 66 (64) | 1.0 (0.61.7) |
| Failure of memory | 2 (1) | 3 (3) | 2.8 (0.518) |
| Lack of technical competence | 58 (34) | 36 (35) | 1.1 (0.61.8) |
| Lack of knowledge | 52 (30) | 34 (33) | 1.0 (0.61.7) |
Discussion
In this study of closed claims files, we identified 2 important cognitive factors involved in cases of medical injury. Error in judgment was the most common factor, comprising about 70% of all claims, and was significantly associated with cases with paid compensation for medical injury. The second cognitive factor was failure of vigilance, which was found in 65% of the claims. Other cognitive factors, such as lack of technical competence and knowledge or failure of memory, as well as systemic factors (poor teamwork and technology failure) were less frequently found to be causally related to cases with medical injury in the verdicts examined in the study.
Reasons for the low frequency of systemic factors involved in cases of medical injury in our study are unclear. This may be the cultural characteristics such as greater emphasis to working in teams and following rules of an organization in Japan. Another possibility is that plaintiffs might have tended to generate lawsuits in cases with suspected higher frequency of individual physicians' factors in Japan. Moreover, among cognitive factors, lack of technical competence and knowledge or failure of memory was also less frequently related to cases with medical injury in our study compared to those of the previous studies.3, 11
The study design of analyzing closed claims files of cases of medical injury is noteworthy for its methodology of error assessment and provides valuable information on errors related to medical injury.3, 7 Moreover, the system of court verdicts in Japan based on decisions by a professional judge allows elimination of potential bias from stakeholders (plaintiffs vs. hospitals) involved in cases of medical injury. Thus, probable causes related to adverse events can be determined from a neutral position. Previous studies of medical error have focused on medical record reviews, surveys, and interviews;12, 13 our study corroborates and extends the findings in these studies that cognitive errors are the most frequent source of medical injury.
Error in judgment is commonly made in the course of decision making in multiple clinical areas. This type of error is referred to recently as cognitive dispositions to respond,14 which is different from bias or heuristics, since not all heuristics are biased and not all errors in judgments come from bias. There is a well‐established value of heuristics in medical diagnosis. Moreover, the properties of this type of error are likely to be distinct from those associated with performance of procedures (lack of technical competence), such as operative injury, which are directly visible and can be prevented through rapid dissemination of information on safety procedures among a medical team. However, the consequences of error in judgment are important for patients, family, and healthcare providers, and these errors are also largely preventable by implementation of educational programs.15
Possible solutions for improving clinical judgment skills may be derived from recent education theory. The theory provides a means for minimizing errors in judgment through the process of meta‐cognition, in which cognitive forcing strategies can be developed through thinking that involves active control over the process of one's own thinking.14, 15 For example, reflective practice has been suggested to be an important instrument for improving clinical judgment and may particularly improve diagnoses in situations of uncertainty and uniqueness, thereby reducing diagnostic errors.16 The capability of critical reflection in real‐time practice (reflection‐in‐action) and on our own practice (reflection‐on‐action) appears to be a key requirement for developing and maintaining medical expertise.17, 18 For instance, case‐based discussion with clinician educators can be an opportunity for enhancing critical thinking skills of medical trainees.
Based on a context‐based approach that focuses on the nature of the clinical problem, potential systemic solutions have recently been proposed for reducing errors in judgment.1 These solutions utilize advanced technology, including symptom‐oriented diagnostic decision support, internet search engines for information on possible diagnoses, and automated reminders in electronic health records.1, 19 Previous studies have shown that long work hours and sleep deprivation can decrease cognitive function, leading to failure of vigilance and increased medical errors,20 and several systemic solutions provide models for avoidance of failure of vigilance. For instance, eliminating extended work shifts and reducing the number of work hours per week was shown to reduce serious medical errors through increased sleep and decreased failure of vigilance during night work in an intensive care unit.21, 22 Taking a brief nap during work hours has also been associated with decreased medical errors in a recent study conducted in Japan.23 Despite the well‐known importance of factors of physicians' workloads, our study did not analyze these factors and thus further studies are needed to confirm their importance in Japanese medical practice.
There were also 32% of patient‐related factors suggested as contributory factors to medical injury in verdicts of the closed claims. This finding may be also important in planning educational intervention strategies to reduce medical errors. Although our data did not include the relative frequency of components related to these factors, major components of patient‐related factors may include age, severity of illnesses, comorbidity, functional status, or mental status. Educational intervention programs may help healthcare providers to evaluate patients with these risk factors and to implement preventive strategies to avoid incidents among these patients.
General surgery, orthopedic surgery, internal medicine, and obstetrics‐gynecology were the most frequently involved specialties in our study. The reasons why these specialties were highly involved in the claims are unclear and our study could not analyze these issues. However, these specialties may be related to patients with greater clinical severity and thus they may have subsequently higher risk for receiving claims. Further, physicians in these specialties may be at higher risk for having various errors because of the complexity of care for patients.
Our study has several limitations. First, the closed claims are more likely to represent cases with severe injury.3 Therefore, it is unclear if we can generalize our findings beyond cases with severe injury.3 Second, certain contributory factors may not have been suggested by the verdicts, even though they played a role. Among these potential factors, poor teamwork and communication issues are unlikely to be identified as causative in verdicts, unless the allegation of the plaintiffs documented these issues. Moreover, the Japanese courts did not open the medical records to the public and so we could not analyze the medical records of the cases. Third, we only evaluated closed verdicts given by professional judges of district courts, who are unlikely to be medical experts. However, the closed verdicts underwent an extensive process involving testimony from medical professionals and academic societies. Fourth, we, as investigators, had few members with surgical backgrounds in this study so we might have underestimated issues related to technical competence among the claims. Finally, although a small percentage of closed‐ claim cases involving team performance were identified in our study, the plaintiffs might have indicated this point to the court claims, since it might have been difficult to describe this issue as a reason for requesting compensations from defendants. Thus, despite a low proportion of team performance involvement in the verdicts, we still believe that poor team performance is a factor related to most medical injuries.
In summary, causal factors obtained from closed claims files suggest the importance of cognitive factors in cases of medical injury. Among the cognitive factors, error in judgment and failure of vigilance were the most frequent. These findings may help leaders of medical schools and hospitals to allocate more resources for research into strategies to improve cognitive performance and thereby ensure patient safety. Further research is needed to better understand the cognitive mechanisms involved in medical errors and to translate this into educational strategies.
Promotion of safer healthcare by patient organizations has led to an expansion of studies aimed at understanding medical errors to minimize injury through systemic improvement. These efforts have focused on identifying patient‐related factors, reducing technology failures, and improving communication.1 In contrast, factors related to cognitive errors by healthcare providers have received relatively little attention, although such errors may be an important source of preventable harm.1, 2
Limited information is available on the types and prevalence of cognitive factors in cases of medical injury, although cognitive factors may be a major risk for medical injury. If these factors were confirmed to be important factors for medical injury, better educational strategies may be needed to reduce cognitive errors among physicians and to enhance quality improvement and patient safety. Better understanding of these cognitive factors may also help to implement educational programs aimed at the improvement of cognitive performance in medical schools or teaching hospital.35
Closed‐claim files for cases of medical injury contain valuable information for investigation of the factors involved in medical errors.3 In Japan, court claims were tried and closed orders were issued by judges without a jury system until 2009. Under this system, representatives for defense and plaintiffs can present medical experts. Courts can also appoint experts independent of either party. Court opinions in Japan are considered as neutral judgments for conflicts between plaintiffs and defendants. Usually there are 3 judges who are required to be involved with each judgment in Japanese courts.
Closed‐claim files in cases of medical injury contain information about the types and prevalence of cognitive factors suggested to be causally related to the injuries by verdicts in district courts. Thus, by analyzing these files, an unbiased description of the characteristics and epidemiology of cognitive factors can be obtained for cases of medical injury, with minimization of potentially biased claims indicated by both parties; ie, plaintiffs vs. hospitals. Therefore, in this study, by using information from closed claims files at district courts in Tokyo and Osaka, Japan, we aimed to determine the important cognitive factors associated with cases of medical injury from such factors as judgment, vigilance, memory, technical competence, or knowledge. Since we anticipated that cognitive factors would dominate among the causative factors, we also explored the association of these factors with cases in which a judgment of paid compensation was made.
Methods
Study Sample
The authors acknowledge that the methodologies are based on those from the Malpractice Insurers' Medical Errors Prevention Study.6 A claim was defined as a written demand for compensation for cases of medical injury, based on a similar approach in previous studies.7, 8 Reviews were performed for closed‐claim files for cases of medical injury involving physicians from 2001 to 2005. These files were published by the Division of the Tokyo‐Osaka Medical Malpractice Lawsuits, organized by district courts in Tokyo and Osaka. The files included all closed‐claim cases of medical injury involving physicians from 2001 to 2005 at district courts in Tokyo and Osaka. The locations of delivery of care were inpatients in this study. All patients in Japan were insured during the study period.
Data Collection
Reviews were conducted by 3 board‐certified Japanese physician‐investigators specializing in internal medicine (1 chief investigator and 2 coinvestigators). The chief investigator trained the coinvestigators in 1‐day sessions with regard to the content of claims files, data collection, and the confidentiality procedure. Reviews were first performed by 1 coinvestigator and then confirmed by the chief investigator.
Data were collected for patient demographics and characteristics of adverse events, including types, locations, clinical areas, and specialties involved in the claims. Classification of specialties was based on that of Singh et al.3 Types of adverse events included minor injury for cases with complete recovery within a year, significant injury for those with complete recovery requiring more than a year, major injury for those with incomplete recovery (any physical sequelae) after more than a year, and death. Clinical areas consisted of surgery, obstetrics, missed diagnosis, delayed diagnosis, medication, and fall. Data for litigation outcomes and the amounts of paid compensation in Japanese Yen (JY) were also collected for claims that received verdicts supporting the plaintiffs.
All factors identified in the verdicts as causally related to the medical injury were recorded for data analysis. Classification of these factors was based on that of Singh et al.3 Cognitive factors were drawn from a list of categories of physicians' tasks provided by the Occupational Information Network. This network is a database of occupational requirements and worker attributes and it describes occupations in terms of the skills and knowledge required, how the work is performed, and typical work settings. The list of cognitive factor categories of physicians' tasks included judgment, vigilance, memory, technical competence, or knowledge. Accordingly, the cognitive factor category list was considered to capture the work of clinicians across the entire range of specialties.3
An example concerning failure of judgment would be that a rapid respiratory rate in initial vital signs was missed or ignored in a patient who complained of upper abdominal pain, was sent home with a diagnosis of gastritis, and eventually died at home; and an autopsy diagnosis of myocardial infarction with congestive heart failure was later confirmed. A vigilance error example would be that, in an electronic ordering system, typing an incorrect medication that has the similar commercial name of a correct medication. An example of failure of memory as a cognitive error would be that a physician forgot a result of laboratory data (positive sputum cytology of lung cancer), and so the physician did not explain it to the patient and did not perform an appropriate subsequent treatment referral. A technical incompetence example would be an operative or procedural injury due to technical problems of physicians. An example of a knowledge error would be that a contraindicated drug combination was prescribed such as the use of both selective serotonin reuptake inhibitor and monoamine oxidase inhibitor.
For systemic factors, a teamwork problem (poor teamwork) was used to describe disruptive team behavior, based on the concept of teamwork described by the Agency for Healthcare Research and Quality and the British Medical Association.9, 10 Cases with teamwork problems were defined as those in which the original reviewer had judged that 1 or more of the following contributory factors played a role in the error: communication breakdowns, supervision problems, handoff problems, failures to establish clear lines of responsibility, and conflict among clinical staff. Technology failure indicated an error of commission or omission by devices, tools, or machines.
The Japanese courts analyze medical records but they do not open the records to the public and so we could not analyze the medical records of the cases in our study. Thus, we did not judge whether the adverse outcome could have been attributed to medical errors, while we analyzed the claims files and followed the conclusions reached by the end of the claims.
Statistical Analysis
Data are given as proportions for categorical variables and means or medians for continuous variables. Cognitive factors associated with cases receiving adjudication of a compensation payment by district courts (litigation outcomes) were analyzed using a logistic regression model including 5 types of cognitive errors. Analyses were conducted with the Stata SE 10.0 statistical software package (College Station, TX). All P values are 2‐sided and P < 0.05 was considered to be statistically significant. The study was approved by the ethics review board at the institution of the chief investigator.
Results
In a total of 274 closed cases of medical injury, the mean age of the patients was 49 years old and 45% were women (Table 1). The reviews performed by the coinvestigators were all confirmed by the chief investigator without discordance of the reviews between the coinvestigators and the chief investigator. The claims involved death of patients in 45% of cases; injuries that caused significant or major disability in 10% and 24%, respectively (a total of 34%); and minor adverse outcomes of medical care in 21% (57 cases). Closing verdicts supporting the plaintiffs (patients or family) by the district courts were given in 103 claims (38%), with compensation at a median of 8,000,000 JY (100 JY = $1 US in 2005). The compensation ranged from 20,000 JY to 222,710,251 JY. The highest compensation was ordered to be paid to a 36‐year‐old woman with an obstetrics‐related major injury and the court indicated the injury was causally related to the following 3 cognitive factors: error in judgment, failure of vigilance, and lack of technical competence.
| Characteristic | n (%) |
|---|---|
| |
| Demographic of patients | |
| Women | 121 (45) |
| Men | 153 (55) |
| Age, mean SD, year | 49 22 |
| Adverse outcome | |
| Minor | 57 (21) |
| Significant | 28 (10) |
| Major | 67 (24) |
| Death | 122 (45) |
| Operative | 36 |
| Delayed diagnosis | 35 |
| Medication | 26 |
| Missed diagnosis | 16 |
| Obstetrics | 8 |
| Clinical area | |
| Operative | 120 (44) |
| Delayed diagnosis | 54 (20) |
| Medication | 50 (18) |
| Missed diagnosis | 28 (10) |
| Obstetrics | 19 (7) |
| Fall | 3 (1) |
Operative injury was the most frequent reason for claims, followed by delayed diagnosis, medication error, and missed diagnosis. General surgery, orthopedics, internal medicine, and obstetrics/gynecology were the most frequently involved specialties, comprising 30% of all cases (Table 2). The verdicts suggested cognitive factors were the most prevalent factors associated with cases of medical injury: 73% of the injuries were judged to be the result of an error in judgment (Table 3), followed by failure of vigilance (65%), lack of technical competence (34%), and lack of knowledge (31%). Verdicts indicated systemic factors in only a few cases, including poor teamwork in 4% and technology failure in 2%. Patient‐related factors were suggested in 32% of the claims.
| Specialty | Cases, n (%) |
|---|---|
| General surgery | 27 (10) |
| Orthopedic surgery | 27 (10) |
| Internal medicine | 27 (10) |
| Obstetrics‐gynecology | 26 (9) |
| Neurosurgery | 19 (7) |
| Ear, nose, and throat | 18 (7) |
| Plastic surgery | 15 (5) |
| Psychiatry | 14 (5) |
| Cardiology | 13 (5) |
| Dental care | 13 (5) |
| Ophthalmology | 12 (4) |
| Hematology or oncology | 10 (4) |
| Adult primary care | 9 (3) |
| Pediatrics | 8 (3) |
| Urology | 8 (3) |
| Cardiothoracic surgery | 8 (3) |
| Neurology | 5 (2) |
| Anesthesiology | 4 (1) |
| Physical medicine or rehabilitation | 3 (1) |
| Emergency medicine | 2 (1) |
| Infectious disease | 2 (1) |
| Dermatology | 2 (1) |
| Radiology | 1 (<1) |
| Vascular surgery | 1 (<1) |
| Contributory Factor | n (%) |
|---|---|
| |
| Cognitive factors | |
| Error in judgment | 199 (73) |
| Failure of vigilance | 177 (65) |
| Lack of technical competence | 94 (34) |
| Lack of knowledge | 86 (31) |
| Failure of memory | 5 (2) |
| System factors | |
| Poor teamwork | 11 (4) |
| Technology failure | 5 (2) |
| Patient‐related factors | 87 (32) |
In a multivariable‐adjusted logistic regression analysis of cognitive factors with a potential association with the claims with paid compensation (Table 4), only error in judgment showed a significant association (odds ratio, 1.9; 95% confidence interval [CI], 1.01‐3.40). The other four cognitive factors in the model were not associated with these claims. The odds ratio for failure of memory was high (2.8), but this factor was identified by the courts in only 5 cases and was not significantly associated with claims with paid compensation.
| Cognitive Factor | Cases With No Compensation (n = 171), n (%) | Cases With Paid Compensation (n = 103), n (%) | Odds Ratio (95% CI)* |
|---|---|---|---|
| |||
| Error in judgment | 117 (68) | 82 (80) | 1.9 (1.03.4) |
| Failure of vigilance | 111 (65) | 66 (64) | 1.0 (0.61.7) |
| Failure of memory | 2 (1) | 3 (3) | 2.8 (0.518) |
| Lack of technical competence | 58 (34) | 36 (35) | 1.1 (0.61.8) |
| Lack of knowledge | 52 (30) | 34 (33) | 1.0 (0.61.7) |
Discussion
In this study of closed claims files, we identified 2 important cognitive factors involved in cases of medical injury. Error in judgment was the most common factor, comprising about 70% of all claims, and was significantly associated with cases with paid compensation for medical injury. The second cognitive factor was failure of vigilance, which was found in 65% of the claims. Other cognitive factors, such as lack of technical competence and knowledge or failure of memory, as well as systemic factors (poor teamwork and technology failure) were less frequently found to be causally related to cases with medical injury in the verdicts examined in the study.
Reasons for the low frequency of systemic factors involved in cases of medical injury in our study are unclear. This may be the cultural characteristics such as greater emphasis to working in teams and following rules of an organization in Japan. Another possibility is that plaintiffs might have tended to generate lawsuits in cases with suspected higher frequency of individual physicians' factors in Japan. Moreover, among cognitive factors, lack of technical competence and knowledge or failure of memory was also less frequently related to cases with medical injury in our study compared to those of the previous studies.3, 11
The study design of analyzing closed claims files of cases of medical injury is noteworthy for its methodology of error assessment and provides valuable information on errors related to medical injury.3, 7 Moreover, the system of court verdicts in Japan based on decisions by a professional judge allows elimination of potential bias from stakeholders (plaintiffs vs. hospitals) involved in cases of medical injury. Thus, probable causes related to adverse events can be determined from a neutral position. Previous studies of medical error have focused on medical record reviews, surveys, and interviews;12, 13 our study corroborates and extends the findings in these studies that cognitive errors are the most frequent source of medical injury.
Error in judgment is commonly made in the course of decision making in multiple clinical areas. This type of error is referred to recently as cognitive dispositions to respond,14 which is different from bias or heuristics, since not all heuristics are biased and not all errors in judgments come from bias. There is a well‐established value of heuristics in medical diagnosis. Moreover, the properties of this type of error are likely to be distinct from those associated with performance of procedures (lack of technical competence), such as operative injury, which are directly visible and can be prevented through rapid dissemination of information on safety procedures among a medical team. However, the consequences of error in judgment are important for patients, family, and healthcare providers, and these errors are also largely preventable by implementation of educational programs.15
Possible solutions for improving clinical judgment skills may be derived from recent education theory. The theory provides a means for minimizing errors in judgment through the process of meta‐cognition, in which cognitive forcing strategies can be developed through thinking that involves active control over the process of one's own thinking.14, 15 For example, reflective practice has been suggested to be an important instrument for improving clinical judgment and may particularly improve diagnoses in situations of uncertainty and uniqueness, thereby reducing diagnostic errors.16 The capability of critical reflection in real‐time practice (reflection‐in‐action) and on our own practice (reflection‐on‐action) appears to be a key requirement for developing and maintaining medical expertise.17, 18 For instance, case‐based discussion with clinician educators can be an opportunity for enhancing critical thinking skills of medical trainees.
Based on a context‐based approach that focuses on the nature of the clinical problem, potential systemic solutions have recently been proposed for reducing errors in judgment.1 These solutions utilize advanced technology, including symptom‐oriented diagnostic decision support, internet search engines for information on possible diagnoses, and automated reminders in electronic health records.1, 19 Previous studies have shown that long work hours and sleep deprivation can decrease cognitive function, leading to failure of vigilance and increased medical errors,20 and several systemic solutions provide models for avoidance of failure of vigilance. For instance, eliminating extended work shifts and reducing the number of work hours per week was shown to reduce serious medical errors through increased sleep and decreased failure of vigilance during night work in an intensive care unit.21, 22 Taking a brief nap during work hours has also been associated with decreased medical errors in a recent study conducted in Japan.23 Despite the well‐known importance of factors of physicians' workloads, our study did not analyze these factors and thus further studies are needed to confirm their importance in Japanese medical practice.
There were also 32% of patient‐related factors suggested as contributory factors to medical injury in verdicts of the closed claims. This finding may be also important in planning educational intervention strategies to reduce medical errors. Although our data did not include the relative frequency of components related to these factors, major components of patient‐related factors may include age, severity of illnesses, comorbidity, functional status, or mental status. Educational intervention programs may help healthcare providers to evaluate patients with these risk factors and to implement preventive strategies to avoid incidents among these patients.
General surgery, orthopedic surgery, internal medicine, and obstetrics‐gynecology were the most frequently involved specialties in our study. The reasons why these specialties were highly involved in the claims are unclear and our study could not analyze these issues. However, these specialties may be related to patients with greater clinical severity and thus they may have subsequently higher risk for receiving claims. Further, physicians in these specialties may be at higher risk for having various errors because of the complexity of care for patients.
Our study has several limitations. First, the closed claims are more likely to represent cases with severe injury.3 Therefore, it is unclear if we can generalize our findings beyond cases with severe injury.3 Second, certain contributory factors may not have been suggested by the verdicts, even though they played a role. Among these potential factors, poor teamwork and communication issues are unlikely to be identified as causative in verdicts, unless the allegation of the plaintiffs documented these issues. Moreover, the Japanese courts did not open the medical records to the public and so we could not analyze the medical records of the cases. Third, we only evaluated closed verdicts given by professional judges of district courts, who are unlikely to be medical experts. However, the closed verdicts underwent an extensive process involving testimony from medical professionals and academic societies. Fourth, we, as investigators, had few members with surgical backgrounds in this study so we might have underestimated issues related to technical competence among the claims. Finally, although a small percentage of closed‐ claim cases involving team performance were identified in our study, the plaintiffs might have indicated this point to the court claims, since it might have been difficult to describe this issue as a reason for requesting compensations from defendants. Thus, despite a low proportion of team performance involvement in the verdicts, we still believe that poor team performance is a factor related to most medical injuries.
In summary, causal factors obtained from closed claims files suggest the importance of cognitive factors in cases of medical injury. Among the cognitive factors, error in judgment and failure of vigilance were the most frequent. These findings may help leaders of medical schools and hospitals to allocate more resources for research into strategies to improve cognitive performance and thereby ensure patient safety. Further research is needed to better understand the cognitive mechanisms involved in medical errors and to translate this into educational strategies.
- ,.Diagnostic errors‐the next frontier for patient safety.JAMA.2009;301(10):1060–1062.
- ,,.Diagnostic error in internal medicine.Arch Intern Med.2005;165(13):1493–1499.
- ,,,.Medical errors involving trainees: a study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167(19):2030–2036.
- ,,.Understanding diagnostic errors in medicine: a lesson from aviation.Qual Saf Health Care.2006;15(3):159–164.
- .The importance of cognitive errors in diagnosis and strategies to minimize them.Acad Med.2003;78(8):775–780.
- ,,, et al.Claims, errors, and compensation payments in medical malpractice litigation.N Engl J Med.2006;354(19):2024–2033.
- ,,,,,.Negligent care and malpractice claiming behavior in Utah and Colorado.Med Care.2000;38(3):250–260.
- ,,, et al.Incidence and types of adverse events and negligent care in Utah and Colorado.Med Care.2000;38(3):261–271.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality;2005 [updated April 2005]; Available at: http://www.ahrq.gov/qual/medteam. Accessed June 2010.
- ,.Team working in Primary Health Care. Realising Shared Aims in Patient Care.London, UK:Royal Pharmaceutical Society and British Medical Association.2005.
- ,,,,.The nature and causes of unintended events reported at ten emergency departments.BMC Emerg Med.2009;9:16.
- ,,.To Err Is Human: Building a Safer Health System.Washington, USA:National Academy Press;2000.
- ,,,.Analysis of errors reported by surgeons at three teaching hospitals.Surgery.2003;133(6):614–621.
- .Achieving quality in clinical decision making: cognitive strategies and detection of bias.Acad Emerg Med.2002;9(11):1184–1204.
- .Cognitive forcing strategies in clinical decision making.Ann Emerg Med.2003;41(1):110–120.
- ,,.Effects of reflective practice on the accuracy of medical diagnoses.Med Educ.2008;42(5):468–475.
- .The Reflective Practitioner: How Professionals Think in Action.New York, NY:Basic Books;1983.
- ,,.Diagnostic errors and reflective practice in medicine.J Eval Clin Pract.2007;13(1):138–145.
- ,,,.Caught in the web: e‐diagnosis.J Hosp Med.2009;4(4):262–266.
- ,,, et al.Extended work duration and the risk of self‐reported percutaneous injuries in interns.JAMA.2006;296(9):1055–1062.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351(18):1838–1848.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351(18):1829–1837.
- ,,, et al.Influence of Residents' Workload, Mental State and Job Satisfaction on Procedural Error: a prospective daily questionnaire‐based study.General Medicine.2008;9(2):57–64.
- ,.Diagnostic errors‐the next frontier for patient safety.JAMA.2009;301(10):1060–1062.
- ,,.Diagnostic error in internal medicine.Arch Intern Med.2005;165(13):1493–1499.
- ,,,.Medical errors involving trainees: a study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167(19):2030–2036.
- ,,.Understanding diagnostic errors in medicine: a lesson from aviation.Qual Saf Health Care.2006;15(3):159–164.
- .The importance of cognitive errors in diagnosis and strategies to minimize them.Acad Med.2003;78(8):775–780.
- ,,, et al.Claims, errors, and compensation payments in medical malpractice litigation.N Engl J Med.2006;354(19):2024–2033.
- ,,,,,.Negligent care and malpractice claiming behavior in Utah and Colorado.Med Care.2000;38(3):250–260.
- ,,, et al.Incidence and types of adverse events and negligent care in Utah and Colorado.Med Care.2000;38(3):261–271.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality;2005 [updated April 2005]; Available at: http://www.ahrq.gov/qual/medteam. Accessed June 2010.
- ,.Team working in Primary Health Care. Realising Shared Aims in Patient Care.London, UK:Royal Pharmaceutical Society and British Medical Association.2005.
- ,,,,.The nature and causes of unintended events reported at ten emergency departments.BMC Emerg Med.2009;9:16.
- ,,.To Err Is Human: Building a Safer Health System.Washington, USA:National Academy Press;2000.
- ,,,.Analysis of errors reported by surgeons at three teaching hospitals.Surgery.2003;133(6):614–621.
- .Achieving quality in clinical decision making: cognitive strategies and detection of bias.Acad Emerg Med.2002;9(11):1184–1204.
- .Cognitive forcing strategies in clinical decision making.Ann Emerg Med.2003;41(1):110–120.
- ,,.Effects of reflective practice on the accuracy of medical diagnoses.Med Educ.2008;42(5):468–475.
- .The Reflective Practitioner: How Professionals Think in Action.New York, NY:Basic Books;1983.
- ,,.Diagnostic errors and reflective practice in medicine.J Eval Clin Pract.2007;13(1):138–145.
- ,,,.Caught in the web: e‐diagnosis.J Hosp Med.2009;4(4):262–266.
- ,,, et al.Extended work duration and the risk of self‐reported percutaneous injuries in interns.JAMA.2006;296(9):1055–1062.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351(18):1838–1848.
- ,,, et al.Effect of reducing interns' weekly work hours on sleep and attentional failures.N Engl J Med.2004;351(18):1829–1837.
- ,,, et al.Influence of Residents' Workload, Mental State and Job Satisfaction on Procedural Error: a prospective daily questionnaire‐based study.General Medicine.2008;9(2):57–64.
Copyright © 2010 Society of Hospital Medicine
Caught in the Web: e‐Diagnosis
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
A 52‐year‐old woman presented with a 3‐month history of progressive bilateral leg edema and dyspnea while climbing a flight of stairs or while walking up a steep slope. She also complained of a tingling sensation in both hands and fingers, which started about 2 months prior to the onset of edema. She did not describe sensory problems in the lower extremities and did not have any other neurological complaints. She denied fever, cough, chest pain, palpitations, orthopnea, paroxysmal nocturnal dyspnea, and dark stools. She had no history of hypertension, diabetes, dyslipidemia, or asthma and had never been hospitalized. She did not smoke or consume alcohol and used no medications, including over‐the‐counter drugs or dietary supplements. The patient was born in Japan and had not traveled outside the country since her birth. She was a homemaker and had worked occasionally as a manual laborer in sugar cane agriculture. A review of systems revealed no history of polydipsia, polyuria, or cold or heat intolerance but did identify new hair growth, especially on the extremities.
This middle‐aged woman shows progressive changes in her general health status that are characterized by edema and dyspnea on effort. The differential diagnosis of edema includes a broad spectrum of illnesses, such as cardiac, lung, renal, endocrine, and hepatic diseases. Because of the life‐threatening potential, my first concern is cardiac disease, although the patient is not experiencing typical symptoms of ischemic heart disease or congestive failure. Bilateral and distal distribution of neuropathic symptoms is likely due to diseases of peripheral nerves rather than those of the central nervous system. Her complaint of a bilateral tingling sensation in the hands may suggest carpal tunnel syndrome as a result of her long‐term agricultural work. Other possible causes include radiculopathy of the cervical spine or polyneuropathy. Clues in the physical examination may help narrow the differential diagnosis to a cardiac, hepatic, or endocrine disorder.
The patient appeared ill. Her weight had increased from 48 to 61 kg since she was last weighed 6 months previously. Her blood pressure was 140/78 mm Hg, her heart rate was 72 beats/minute with a regular rhythm, her respiratory rate was 18/minute, and her temperature was 37.5C. The jugular venous pressure was elevated at 10 cm above the sternal angle. A grade III/VI systolic ejection murmur was evident at the second interspace along the left sternal border. The second heart sound was fixed and split. There were decreased breath sounds and complete dullness to percussion over both lower lung fields. Shifting dullness was noted on abdominal examination. There was pitting edema from the feet to the thighs, with slow pit‐recovery time in both legs, and she exhibited generalized hirsutism on the face, body, and extremities. There was no lymphadenopathy. On neurological examination, her mental status was normal. The cranial nerves were normal, as was coordination. There was mild generalized distal‐dominant motor weakness with generalized hyporeflexia. Sensory testing demonstrated glove‐and‐stocking type loss of sensation to pinpricks as well as dysesthesia in all extremities. Phalen and Tinel tests were negative.
The elevated venous pressure and pitting edema with slow recovery suggest high venous pressure edema rather than hypoproteinemic edema. Complete bilateral dullness of the chest and shifting dullness of the abdomen indicate the presence of bilateral pleural effusion and ascites. Edema from high venous pressure is usually caused by right, left, or biventricular cardiac failure. A fixed splitting of the second heart sound suggests an atrial septal defect, which is a rare cause of progressive right heart failure in adults. I recommend checking the patient's thyroid function to investigate the possibility of hypothyroidism, which is a common illness among middle‐aged women and could contribute to her edema as well as hirsutism. The neurological findings suggest a generalized polyneuropathy. The unusual combination of high venous pressure edema and polyneuropathy may indicate a rare multisystem disorder such as amyloidosis. Alternatively, the patient might have developed multiple diseases during the same time period. For instance, diabetic polyneuropathy is the most common cause of polyneuropathy among the middle‐aged. Finally, the differential diagnosis of hirsutism includes ovarian, adrenal, or pituitary sources of hyperandrogenism in addition to hypothyroidism. I would first evaluate for diabetes, thyroid disease, and cardiac disease and would like to see the results of laboratory tests for thyrotropin and plasma glucose as well as chest radiography and electrocardiography.
The white‐cell count was 5400/mm3 with a normal differential. Hemoglobin was 10.7 g/dL with normal red‐cell indices, and the platelet count was 276,000/mm3. The erythrocyte sedimentation rate was 29 mm/hour. Other laboratory tests revealed the following values: total protein, 6.2 g/dL; albumin, 3.3 g/dL; blood urea nitrogen, 12 mg/dL; creatinine, 0.7 mg/dL; aspartate aminotransferase, 6 U/L; alanine aminotransferase, 2 U/L; lactate dehydrogenase, 96 U/L; alkaline phosphatase, 115 U/L; creatine phosphokinase, 60 U/L; total bilirubin, 0.9 mg/dL; glucose, 96 mg/dL; hemoglobin A1c, 4.6%; total cholesterol, 111 mg/dL; and thyrotropin, 6.32 mIU/mL (normal range, 0.50‐5.00 mIU/mL). Serum free thyroxine, triiodothyronine, and urine testosterone were normal. Serum dehydroepiandrosterone sulfate was mildly elevated for her age (864 ng/mL: normal range, 180‐750 ng/mL). Serological studies for human immunodeficiency virus, human T‐lymphotrophic virus type 1, and syphilis were negative. Urinalysis was weakly positive for protein but negative for casts and occult blood. The stool was negative for occult blood.
A chest radiograph showed bilateral pleural effusions. Computed tomography demonstrated bilateral pleural effusions, ascites, mild hepatomegaly, and small, multiple, mediastinal lymph nodes. Her electrocardiogram was normal. A transesophageal echocardiogram with agitated saline contrast demonstrated normal ventricular systolic and diastolic function and no atrial septal defect. The inferior vena cava did not collapse with inspiration, and there was no evidence of infiltrative cardiomyopathy.
These laboratory results rule out diabetes as the cause of the polyneuropathy. The subclinical hypothyroidism would not explain profound edema and hirsutism. A serum albumin level of 3.3 g/dL confirms high venous pressure edema rather than hypoproteinemic edema. Normochromic, normocytic anemia and a mildly elevated sedimentation rate point to a chronic illness or inflammatory state. The mediastinal lymphadenopathy may reflect congestion as a result of the high venous pressure or reflect a systemic disease involving lymph nodes. Normal ventricular function with high venous pressure is suggestive of heart failure from diastolic dysfunction, although the patient does not have risk factors for diastolic dysfunction, such as hypertension, and has no other echocardiographic features of diastolic impairment. The combination of hyperandrogenism and neuropathy points to a systemic process, such as a paraneoplastic syndrome. I would next investigate the source of the excess androgens.
Because serum dehydroepiandrosterone sulfate was mildly elevated, I‐131 aldosterol scintigraphy was performed, and it was negative. Electromyography showed a pattern of generalized sensorimotor polyneuropathy.
At this point, it appears that cardiac, endocrine, hepatic, and renal diseases have been largely ruled out as a cause of her symptoms. Reframing and unifying the important clinical problems for this patient may be useful in resolving this diagnostic puzzle. They include (1) systemic high venous pressure edema; (2) generalized sensorimotor polyneuropathy; (3) hirsutism; (4) normocytic, normochromic anemia; (5) an elevated erythrocyte sedimentation rate; (6) mediastinal lymphadenopathy; and (7) subclinical hypothyroidism. At this point, I cannot unify these pieces of information into a single diagnosis. I would search the medical literature, focusing on these terms.
A general internist consultant performed MEDLINE and Google Scholar searches using the key words edema, polyneuropathy, and hirsutism. This search suggested the diagnosis of Crow‐Fukase syndrome, also known as POEMS (polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes) syndrome. Subsequent evaluations were performed. First, serum protein electrophoresis revealed the presence of monoclonal proteins, although hypergammaglobulinemia was not present. Second, a bone marrow examination demonstrated increased abnormal plasma cell proliferation (7%), although a radiographic skeletal survey found no lesions suggestive of plasmacytoma. Third, cerebrospinal fluid analysis showed normal cell counts but increased protein concentration (202 mg/dL). Fourth, a blood sample referred to an outside laboratory demonstrated elevated levels of vascular endothelial growth factor (3902 pg/mL: normal range, 150‐500 pg/mL). On the basis of these findings, the diagnosis of POEMS syndrome was made. After oral prednisolone (40 mg/day) was initiated, the systemic edema improved gradually, and she did well during the 2‐year follow‐up period.
Commentary
POEMS syndrome, also known as Crow‐Fukase syndrome, is a rare multisystem disorder first described by Crow in 1956.1, 2 It is characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes, as indicated by the acronym. The diagnosis of POEMS syndrome is difficult as this syndrome is rare and requires high clinical suspicion. According to a nationwide cross‐sectional survey in Japan, the prevalence of POEMS syndrome is very low (about 3 patients per 1,000,000 persons),3 and its prevalence in Western countries is considered even lower than that in Japan. The average age at onset is around 45 to 50 years old, and men are twice as likely to have this syndrome as women.46 Table 1 shows the diagnostic criteria of POEMS syndrome, based on research by Dispenzieri and others at the Mayo Clinic, and Table 2 presents the relative frequency of these clinical features.6, 7 The initial symptomatology generally includes polyneuropathy, skin changes, and generalized edema, which are nonspecific symptoms, as are other well‐recognized associated conditions such as clubbing, weight loss, thrombocytosis, polycythemia, and hyperhidrosis. Thus, it is important to consider this syndrome when one is facing an undiagnosed illness involving multiple organ systems and to distinguish it from other conditions such as multiple myeloma, amyloidosis, and monoclonal gammopathy of undetermined significance. Vascular endothelial growth factor is thought to be involved in the edema of POEMS syndrome, as massive release from aggregated platelets increases vascular permeability and venous pressure.710
| |
| Major criteria | Polyneuropathy |
| Monoclonal plasma cell‐proliferative disorder | |
| Minor criteria | Sclerotic bone lesions |
| Castleman disease | |
| Organomegaly (splenomegaly, hepatomegaly, or lymphadenopathy) | |
| Edema (peripheral edema, pleural effusion, or ascites) | |
| Endocrinopathy (adrenal, thyroid, pituitary, gonadal, parathyroid, or pancreatic) | |
| Skin changes (hyperpigmentation, hirsutism, plethora, hemangiomata, and white nails) | |
| Papilledema | |
| Characteristic | % |
|---|---|
| |
| Peripheral neuropathy | 100 |
| Monoclonal plasma cell dyscrasia | 100 |
| Sclerotic bone lesions | 97 |
| Endocrinopathy | 71 |
| Skin changes | 68 |
| Organomegaly | 46 |
| Extravascular volume overload | 39 |
| Papilledema | 29 |
| Castleman disease | 11 |
Data regarding treatment and survival are largely observational. Overall mean survival from diagnosis in the 2003 Dispenzieri cohort was 13.7 years, with death often due to infection or cardiorespiratory failure.6 When a solitary plasmacytoma or osteosclerotic myeloma is present, radiation to the lesion can often lead to clinical remission. Other treatment options include alkylating agents and/or high‐dose chemotherapy with peripheral stem‐cell transplantation, corticosteroids, and supportive care.7
Clinicians frequently use the internet to aid in the clinical decision process. In a survey of the Royal New Zealand College of General Practitioners,11 half reported that they used the Internet to search for clinical information. Two well‐known resources are MEDLINE, which contains over 11 million references dating back to the 1960s, and internet search engines such as Google (and a more recent product, Google Scholar, which attempts to sort search results by including factors such as the author, the publication in which the article appears, and how often the article has been cited).
MEDLINE searches a well‐defined set of journals and uses the Medical Subject Headings (MeSH) vocabulary, which consists of sets of descriptive terms organized in a hierarchical structure to allow searching with various levels of specificity. For instance, entering the term heart attack will map to the MeSH term myocardial infarction and will also include more specific terms such as myocardial stunning and cardiogenic shock.
Google, in comparison, explores resources beyond journals without any clear boundary to its scope, and its advanced search functions can be occasionally unreliable. For instance, search results are occasionally marred by outdated citation information and may include materials that are not truly scholarly. However, search engines can search through the actual text of manuscripts and access the gray literature, which includes open‐source material that is usually original but not widely distributed or often easily available, such as technical reports and dissertations. A direct study comparing the results of searches in PubMed (one of the MEDLINE search engines) and Google Scholar is difficult, but the critical characteristics of each can be compared and contrasted (Table 3).
| Google Scholar | PubMed |
|---|---|
| 1. Database selection is clumped under subject areas, and it cannot be searched with unique identifiers: Con | 1. It allows one to choose a database at the outset and can search with a unique identifier (PubMed identifier): Pro |
| 2. Results cannot be filtered (ie, it does not allow multiple article selection): Con | 2. The single citation matcher allows retrieval of articles with pieces of information: Pro |
| 3. A search for related articles or similar pages is not available: Con | 3. It allows article selection by checkbox to reduce the number of articles relevant to the search query and to append the filter to search box: Pro |
| 4. It allows one to search by without words to exclude unwanted and confusing retrieved data: Pro | 4. It provides unique identifier (PubMed identifier) for each retrieved article for easy communicability: Pro |
| 5. It allows one to search a single journal/publication of interest: Pro | 5. Search are limited to journals only; it does not include the grey area of literature: Con |
| 6. Initial search results are those articles that are most cited by journals that themselves are the most cited: Pro | 6. It lists search results in chronological order and not by relevance: Con |
Internet searches may also suggest diagnoses from a compilation of clinical features, such as in this case. To be successful, such a search must complement the cognitive process; a search engine cannot completely replace clinical judgment. Clinicians must be able to identify salient clinical features and generate high‐yield search terms and then exercise skill in sifting through the citations to arrive at the appropriate diagnosis. A recent study found that Google searches revealed the correct diagnosis in 58% of the case records of the New England Journal of Medicine,12 although each search query resulted in many results, which then had to be manually reviewed for appropriateness within the case's context.
Like a traditional diagnostic test, a search can be described by sensitivity, specificity, and the number of articles needed to read.13 For example, in a study comparing the performance of search strategies to identify clinical practice guidelines in Google Scholar and SUMSearch (another freely accessible search engine), using the term guideline yielded the highest sensitivity, and using the term practice guideline generated the highest specificity and the lowest number of articles needed to read (Table 4).14
| Search Strategy | Sensitivity (%) | Specificity (%) | NNR |
|---|---|---|---|
| |||
| SUMSearch | |||
| Guideline* | 81.51 (74.5388.49) | 74.29 (72.6475.94) | 8.18 (6.9010.05) |
| Recommendation* | 60.50 (51.7269.28) | 76.28 (74.6777.89) | 9.93 (8.1412.72) |
| Practice guideline* | 40.34 (31.5249.16) | 89.45 (88.2990.61) | 6.96 (5.529.43) |
| Google Scholar | |||
| Guideline/s | 31.93 (23.5640.30) | 78.05 (76.5079.60) | 16.67 (12.7624.04) |
| Recommendation/s | 8.40 (3.4213.38) | 92.11 (91.0993.13) | 22.42 (13.9756.82) |
| Practice guideline/s | 11.76 (5.9817.54) | 95.72 (94.9696.48) | 9.29 (6.2118.38) |
Although there are several other popular hosts of web‐based search engines, a more robust decision‐support program may help physicians more efficiently consider relevant diagnoses. One program, named Isabel, has been developed through the indexing of a database of more than 11,000 diseases according to word patterns in journal articles associated with each disease, and it is updated as new and relevant articles emerge. One recent study demonstrated that the correct diagnosis was made in 48 of 50 cases (96%) with specific, key findings as search terms but in only 37 of the same 50 cases (74%) if the entire case history was simply pasted in, again emphasizing the importance of specific search terms.15
POEMS syndrome is a rare entity occasionally seen in middle‐aged individuals and marked by a multitude of nonspecific findings, particularly polyneuropathy and plasma cell dyscrasia. In this case, the diagnostic test was an internet search based on the most prominent clinical symptoms. Such a strategy can provide a powerful addition to traditional literature and MEDLINE resources. However, the efficiency of this process is heavily dependent on the quality of the search strategy and, therefore, the cognitive faculties of the treating physician to avoid the predictable shortcoming of low specificity. Garbage in, garbage out still applies whether the computer in question is the human mind or the desktop PC.
Teaching Points
-
POEMS syndrome, also known as Crow‐Fukase syndrome, is a rare multisystem disorder characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes.
-
Internet‐based searches, including Google and MEDLINE, are being used more frequently because they are widely available, quick, and freely accessed.
-
Internet searches appear most useful as adjuncts to PubMed and clinical reasoning in identifying case reports when a well‐constructed collection of symptoms and signs is used for searches.
- .Peripheral neuritis in myelomatosis.Br Med J.1956;2(4996):802–804.
- ,,,,,.Plasma cell dyscrasia with polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes: the POEMS syndrome. Report on two cases and a review of the literature.Medicine (Baltimore).1980;59(4):311–322.
- .Nationwide Epidemiologic Survey of Crow‐Fukase Syndrome in 2004.Tokyo, Japan:Japanese Ministry of Health and Welfare Government Report, 2004.
- ,,, et al.The Crow‐Fukase syndrome: a study of 102 cases in Japan.Neurology.1984;34(6):712–720.
- ,,.POEMS syndrome: a study of 25 cases and a review of the literature. French Study Group on POEMS Syndrome.Am J Med.1994;97(6):543–553.
- ,,, et al.POEMS syndrome: definitions and long‐term outcome.Blood.2003;101(7):2496–2506.
- .POEMS syndrome.Hematology.2005;1(1):360–367.
- ,,,,.Greatly raised vascular endothelial growth factor (VEGF) in POEMS syndrome.Lancet.1996;347(9002):702.
- ,.Assessment of hypoproteinaemic oedema: a simple physical sign.Br Med J.1978;1(6117):890–891.
- ,,, et al.Ratio of serum vascular endothelial growth factor to platelet count correlates with disease activity in a patient with POEMS syndrome.Eur J Intern Med.2002;13(1):70–74.
- .In search of evidence: family practitioners' use of the Internet for clinical information.J Med Libr Assoc.2002;90(4):370–379.
- ,.Googling for a diagnosis—use of Google as a diagnostic aid: internet based study.BMJ.2006;333(7579):1143–5114.
- ,,.The number needed to read—a new measure of journal value.Health Info Libr J.2005;22(2):81–82.
- ,,,.Developing search strategies for clinical practice guidelines in SUMSearch and Google Scholar and assessing their retrieval performance.BMC Med Res Methodol.2007;7:28.
- ,.Performance of a web‐based clinical diagnosis support system for internists.J Gen Intern Med.2008;23(suppl 1):37–40.
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
A 52‐year‐old woman presented with a 3‐month history of progressive bilateral leg edema and dyspnea while climbing a flight of stairs or while walking up a steep slope. She also complained of a tingling sensation in both hands and fingers, which started about 2 months prior to the onset of edema. She did not describe sensory problems in the lower extremities and did not have any other neurological complaints. She denied fever, cough, chest pain, palpitations, orthopnea, paroxysmal nocturnal dyspnea, and dark stools. She had no history of hypertension, diabetes, dyslipidemia, or asthma and had never been hospitalized. She did not smoke or consume alcohol and used no medications, including over‐the‐counter drugs or dietary supplements. The patient was born in Japan and had not traveled outside the country since her birth. She was a homemaker and had worked occasionally as a manual laborer in sugar cane agriculture. A review of systems revealed no history of polydipsia, polyuria, or cold or heat intolerance but did identify new hair growth, especially on the extremities.
This middle‐aged woman shows progressive changes in her general health status that are characterized by edema and dyspnea on effort. The differential diagnosis of edema includes a broad spectrum of illnesses, such as cardiac, lung, renal, endocrine, and hepatic diseases. Because of the life‐threatening potential, my first concern is cardiac disease, although the patient is not experiencing typical symptoms of ischemic heart disease or congestive failure. Bilateral and distal distribution of neuropathic symptoms is likely due to diseases of peripheral nerves rather than those of the central nervous system. Her complaint of a bilateral tingling sensation in the hands may suggest carpal tunnel syndrome as a result of her long‐term agricultural work. Other possible causes include radiculopathy of the cervical spine or polyneuropathy. Clues in the physical examination may help narrow the differential diagnosis to a cardiac, hepatic, or endocrine disorder.
The patient appeared ill. Her weight had increased from 48 to 61 kg since she was last weighed 6 months previously. Her blood pressure was 140/78 mm Hg, her heart rate was 72 beats/minute with a regular rhythm, her respiratory rate was 18/minute, and her temperature was 37.5C. The jugular venous pressure was elevated at 10 cm above the sternal angle. A grade III/VI systolic ejection murmur was evident at the second interspace along the left sternal border. The second heart sound was fixed and split. There were decreased breath sounds and complete dullness to percussion over both lower lung fields. Shifting dullness was noted on abdominal examination. There was pitting edema from the feet to the thighs, with slow pit‐recovery time in both legs, and she exhibited generalized hirsutism on the face, body, and extremities. There was no lymphadenopathy. On neurological examination, her mental status was normal. The cranial nerves were normal, as was coordination. There was mild generalized distal‐dominant motor weakness with generalized hyporeflexia. Sensory testing demonstrated glove‐and‐stocking type loss of sensation to pinpricks as well as dysesthesia in all extremities. Phalen and Tinel tests were negative.
The elevated venous pressure and pitting edema with slow recovery suggest high venous pressure edema rather than hypoproteinemic edema. Complete bilateral dullness of the chest and shifting dullness of the abdomen indicate the presence of bilateral pleural effusion and ascites. Edema from high venous pressure is usually caused by right, left, or biventricular cardiac failure. A fixed splitting of the second heart sound suggests an atrial septal defect, which is a rare cause of progressive right heart failure in adults. I recommend checking the patient's thyroid function to investigate the possibility of hypothyroidism, which is a common illness among middle‐aged women and could contribute to her edema as well as hirsutism. The neurological findings suggest a generalized polyneuropathy. The unusual combination of high venous pressure edema and polyneuropathy may indicate a rare multisystem disorder such as amyloidosis. Alternatively, the patient might have developed multiple diseases during the same time period. For instance, diabetic polyneuropathy is the most common cause of polyneuropathy among the middle‐aged. Finally, the differential diagnosis of hirsutism includes ovarian, adrenal, or pituitary sources of hyperandrogenism in addition to hypothyroidism. I would first evaluate for diabetes, thyroid disease, and cardiac disease and would like to see the results of laboratory tests for thyrotropin and plasma glucose as well as chest radiography and electrocardiography.
The white‐cell count was 5400/mm3 with a normal differential. Hemoglobin was 10.7 g/dL with normal red‐cell indices, and the platelet count was 276,000/mm3. The erythrocyte sedimentation rate was 29 mm/hour. Other laboratory tests revealed the following values: total protein, 6.2 g/dL; albumin, 3.3 g/dL; blood urea nitrogen, 12 mg/dL; creatinine, 0.7 mg/dL; aspartate aminotransferase, 6 U/L; alanine aminotransferase, 2 U/L; lactate dehydrogenase, 96 U/L; alkaline phosphatase, 115 U/L; creatine phosphokinase, 60 U/L; total bilirubin, 0.9 mg/dL; glucose, 96 mg/dL; hemoglobin A1c, 4.6%; total cholesterol, 111 mg/dL; and thyrotropin, 6.32 mIU/mL (normal range, 0.50‐5.00 mIU/mL). Serum free thyroxine, triiodothyronine, and urine testosterone were normal. Serum dehydroepiandrosterone sulfate was mildly elevated for her age (864 ng/mL: normal range, 180‐750 ng/mL). Serological studies for human immunodeficiency virus, human T‐lymphotrophic virus type 1, and syphilis were negative. Urinalysis was weakly positive for protein but negative for casts and occult blood. The stool was negative for occult blood.
A chest radiograph showed bilateral pleural effusions. Computed tomography demonstrated bilateral pleural effusions, ascites, mild hepatomegaly, and small, multiple, mediastinal lymph nodes. Her electrocardiogram was normal. A transesophageal echocardiogram with agitated saline contrast demonstrated normal ventricular systolic and diastolic function and no atrial septal defect. The inferior vena cava did not collapse with inspiration, and there was no evidence of infiltrative cardiomyopathy.
These laboratory results rule out diabetes as the cause of the polyneuropathy. The subclinical hypothyroidism would not explain profound edema and hirsutism. A serum albumin level of 3.3 g/dL confirms high venous pressure edema rather than hypoproteinemic edema. Normochromic, normocytic anemia and a mildly elevated sedimentation rate point to a chronic illness or inflammatory state. The mediastinal lymphadenopathy may reflect congestion as a result of the high venous pressure or reflect a systemic disease involving lymph nodes. Normal ventricular function with high venous pressure is suggestive of heart failure from diastolic dysfunction, although the patient does not have risk factors for diastolic dysfunction, such as hypertension, and has no other echocardiographic features of diastolic impairment. The combination of hyperandrogenism and neuropathy points to a systemic process, such as a paraneoplastic syndrome. I would next investigate the source of the excess androgens.
Because serum dehydroepiandrosterone sulfate was mildly elevated, I‐131 aldosterol scintigraphy was performed, and it was negative. Electromyography showed a pattern of generalized sensorimotor polyneuropathy.
At this point, it appears that cardiac, endocrine, hepatic, and renal diseases have been largely ruled out as a cause of her symptoms. Reframing and unifying the important clinical problems for this patient may be useful in resolving this diagnostic puzzle. They include (1) systemic high venous pressure edema; (2) generalized sensorimotor polyneuropathy; (3) hirsutism; (4) normocytic, normochromic anemia; (5) an elevated erythrocyte sedimentation rate; (6) mediastinal lymphadenopathy; and (7) subclinical hypothyroidism. At this point, I cannot unify these pieces of information into a single diagnosis. I would search the medical literature, focusing on these terms.
A general internist consultant performed MEDLINE and Google Scholar searches using the key words edema, polyneuropathy, and hirsutism. This search suggested the diagnosis of Crow‐Fukase syndrome, also known as POEMS (polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes) syndrome. Subsequent evaluations were performed. First, serum protein electrophoresis revealed the presence of monoclonal proteins, although hypergammaglobulinemia was not present. Second, a bone marrow examination demonstrated increased abnormal plasma cell proliferation (7%), although a radiographic skeletal survey found no lesions suggestive of plasmacytoma. Third, cerebrospinal fluid analysis showed normal cell counts but increased protein concentration (202 mg/dL). Fourth, a blood sample referred to an outside laboratory demonstrated elevated levels of vascular endothelial growth factor (3902 pg/mL: normal range, 150‐500 pg/mL). On the basis of these findings, the diagnosis of POEMS syndrome was made. After oral prednisolone (40 mg/day) was initiated, the systemic edema improved gradually, and she did well during the 2‐year follow‐up period.
Commentary
POEMS syndrome, also known as Crow‐Fukase syndrome, is a rare multisystem disorder first described by Crow in 1956.1, 2 It is characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes, as indicated by the acronym. The diagnosis of POEMS syndrome is difficult as this syndrome is rare and requires high clinical suspicion. According to a nationwide cross‐sectional survey in Japan, the prevalence of POEMS syndrome is very low (about 3 patients per 1,000,000 persons),3 and its prevalence in Western countries is considered even lower than that in Japan. The average age at onset is around 45 to 50 years old, and men are twice as likely to have this syndrome as women.46 Table 1 shows the diagnostic criteria of POEMS syndrome, based on research by Dispenzieri and others at the Mayo Clinic, and Table 2 presents the relative frequency of these clinical features.6, 7 The initial symptomatology generally includes polyneuropathy, skin changes, and generalized edema, which are nonspecific symptoms, as are other well‐recognized associated conditions such as clubbing, weight loss, thrombocytosis, polycythemia, and hyperhidrosis. Thus, it is important to consider this syndrome when one is facing an undiagnosed illness involving multiple organ systems and to distinguish it from other conditions such as multiple myeloma, amyloidosis, and monoclonal gammopathy of undetermined significance. Vascular endothelial growth factor is thought to be involved in the edema of POEMS syndrome, as massive release from aggregated platelets increases vascular permeability and venous pressure.710
| |
| Major criteria | Polyneuropathy |
| Monoclonal plasma cell‐proliferative disorder | |
| Minor criteria | Sclerotic bone lesions |
| Castleman disease | |
| Organomegaly (splenomegaly, hepatomegaly, or lymphadenopathy) | |
| Edema (peripheral edema, pleural effusion, or ascites) | |
| Endocrinopathy (adrenal, thyroid, pituitary, gonadal, parathyroid, or pancreatic) | |
| Skin changes (hyperpigmentation, hirsutism, plethora, hemangiomata, and white nails) | |
| Papilledema | |
| Characteristic | % |
|---|---|
| |
| Peripheral neuropathy | 100 |
| Monoclonal plasma cell dyscrasia | 100 |
| Sclerotic bone lesions | 97 |
| Endocrinopathy | 71 |
| Skin changes | 68 |
| Organomegaly | 46 |
| Extravascular volume overload | 39 |
| Papilledema | 29 |
| Castleman disease | 11 |
Data regarding treatment and survival are largely observational. Overall mean survival from diagnosis in the 2003 Dispenzieri cohort was 13.7 years, with death often due to infection or cardiorespiratory failure.6 When a solitary plasmacytoma or osteosclerotic myeloma is present, radiation to the lesion can often lead to clinical remission. Other treatment options include alkylating agents and/or high‐dose chemotherapy with peripheral stem‐cell transplantation, corticosteroids, and supportive care.7
Clinicians frequently use the internet to aid in the clinical decision process. In a survey of the Royal New Zealand College of General Practitioners,11 half reported that they used the Internet to search for clinical information. Two well‐known resources are MEDLINE, which contains over 11 million references dating back to the 1960s, and internet search engines such as Google (and a more recent product, Google Scholar, which attempts to sort search results by including factors such as the author, the publication in which the article appears, and how often the article has been cited).
MEDLINE searches a well‐defined set of journals and uses the Medical Subject Headings (MeSH) vocabulary, which consists of sets of descriptive terms organized in a hierarchical structure to allow searching with various levels of specificity. For instance, entering the term heart attack will map to the MeSH term myocardial infarction and will also include more specific terms such as myocardial stunning and cardiogenic shock.
Google, in comparison, explores resources beyond journals without any clear boundary to its scope, and its advanced search functions can be occasionally unreliable. For instance, search results are occasionally marred by outdated citation information and may include materials that are not truly scholarly. However, search engines can search through the actual text of manuscripts and access the gray literature, which includes open‐source material that is usually original but not widely distributed or often easily available, such as technical reports and dissertations. A direct study comparing the results of searches in PubMed (one of the MEDLINE search engines) and Google Scholar is difficult, but the critical characteristics of each can be compared and contrasted (Table 3).
| Google Scholar | PubMed |
|---|---|
| 1. Database selection is clumped under subject areas, and it cannot be searched with unique identifiers: Con | 1. It allows one to choose a database at the outset and can search with a unique identifier (PubMed identifier): Pro |
| 2. Results cannot be filtered (ie, it does not allow multiple article selection): Con | 2. The single citation matcher allows retrieval of articles with pieces of information: Pro |
| 3. A search for related articles or similar pages is not available: Con | 3. It allows article selection by checkbox to reduce the number of articles relevant to the search query and to append the filter to search box: Pro |
| 4. It allows one to search by without words to exclude unwanted and confusing retrieved data: Pro | 4. It provides unique identifier (PubMed identifier) for each retrieved article for easy communicability: Pro |
| 5. It allows one to search a single journal/publication of interest: Pro | 5. Search are limited to journals only; it does not include the grey area of literature: Con |
| 6. Initial search results are those articles that are most cited by journals that themselves are the most cited: Pro | 6. It lists search results in chronological order and not by relevance: Con |
Internet searches may also suggest diagnoses from a compilation of clinical features, such as in this case. To be successful, such a search must complement the cognitive process; a search engine cannot completely replace clinical judgment. Clinicians must be able to identify salient clinical features and generate high‐yield search terms and then exercise skill in sifting through the citations to arrive at the appropriate diagnosis. A recent study found that Google searches revealed the correct diagnosis in 58% of the case records of the New England Journal of Medicine,12 although each search query resulted in many results, which then had to be manually reviewed for appropriateness within the case's context.
Like a traditional diagnostic test, a search can be described by sensitivity, specificity, and the number of articles needed to read.13 For example, in a study comparing the performance of search strategies to identify clinical practice guidelines in Google Scholar and SUMSearch (another freely accessible search engine), using the term guideline yielded the highest sensitivity, and using the term practice guideline generated the highest specificity and the lowest number of articles needed to read (Table 4).14
| Search Strategy | Sensitivity (%) | Specificity (%) | NNR |
|---|---|---|---|
| |||
| SUMSearch | |||
| Guideline* | 81.51 (74.5388.49) | 74.29 (72.6475.94) | 8.18 (6.9010.05) |
| Recommendation* | 60.50 (51.7269.28) | 76.28 (74.6777.89) | 9.93 (8.1412.72) |
| Practice guideline* | 40.34 (31.5249.16) | 89.45 (88.2990.61) | 6.96 (5.529.43) |
| Google Scholar | |||
| Guideline/s | 31.93 (23.5640.30) | 78.05 (76.5079.60) | 16.67 (12.7624.04) |
| Recommendation/s | 8.40 (3.4213.38) | 92.11 (91.0993.13) | 22.42 (13.9756.82) |
| Practice guideline/s | 11.76 (5.9817.54) | 95.72 (94.9696.48) | 9.29 (6.2118.38) |
Although there are several other popular hosts of web‐based search engines, a more robust decision‐support program may help physicians more efficiently consider relevant diagnoses. One program, named Isabel, has been developed through the indexing of a database of more than 11,000 diseases according to word patterns in journal articles associated with each disease, and it is updated as new and relevant articles emerge. One recent study demonstrated that the correct diagnosis was made in 48 of 50 cases (96%) with specific, key findings as search terms but in only 37 of the same 50 cases (74%) if the entire case history was simply pasted in, again emphasizing the importance of specific search terms.15
POEMS syndrome is a rare entity occasionally seen in middle‐aged individuals and marked by a multitude of nonspecific findings, particularly polyneuropathy and plasma cell dyscrasia. In this case, the diagnostic test was an internet search based on the most prominent clinical symptoms. Such a strategy can provide a powerful addition to traditional literature and MEDLINE resources. However, the efficiency of this process is heavily dependent on the quality of the search strategy and, therefore, the cognitive faculties of the treating physician to avoid the predictable shortcoming of low specificity. Garbage in, garbage out still applies whether the computer in question is the human mind or the desktop PC.
Teaching Points
-
POEMS syndrome, also known as Crow‐Fukase syndrome, is a rare multisystem disorder characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes.
-
Internet‐based searches, including Google and MEDLINE, are being used more frequently because they are widely available, quick, and freely accessed.
-
Internet searches appear most useful as adjuncts to PubMed and clinical reasoning in identifying case reports when a well‐constructed collection of symptoms and signs is used for searches.
The approach to clinical conundrums by an expert clinician is revealed through the presentation of an actual patient's case in an approach typical of a morning report. Similarly to patient care, sequential pieces of information are provided to the clinician, who is unfamiliar with the case. The focus is on the thought processes of both the clinical team caring for the patient and the discussant.
A 52‐year‐old woman presented with a 3‐month history of progressive bilateral leg edema and dyspnea while climbing a flight of stairs or while walking up a steep slope. She also complained of a tingling sensation in both hands and fingers, which started about 2 months prior to the onset of edema. She did not describe sensory problems in the lower extremities and did not have any other neurological complaints. She denied fever, cough, chest pain, palpitations, orthopnea, paroxysmal nocturnal dyspnea, and dark stools. She had no history of hypertension, diabetes, dyslipidemia, or asthma and had never been hospitalized. She did not smoke or consume alcohol and used no medications, including over‐the‐counter drugs or dietary supplements. The patient was born in Japan and had not traveled outside the country since her birth. She was a homemaker and had worked occasionally as a manual laborer in sugar cane agriculture. A review of systems revealed no history of polydipsia, polyuria, or cold or heat intolerance but did identify new hair growth, especially on the extremities.
This middle‐aged woman shows progressive changes in her general health status that are characterized by edema and dyspnea on effort. The differential diagnosis of edema includes a broad spectrum of illnesses, such as cardiac, lung, renal, endocrine, and hepatic diseases. Because of the life‐threatening potential, my first concern is cardiac disease, although the patient is not experiencing typical symptoms of ischemic heart disease or congestive failure. Bilateral and distal distribution of neuropathic symptoms is likely due to diseases of peripheral nerves rather than those of the central nervous system. Her complaint of a bilateral tingling sensation in the hands may suggest carpal tunnel syndrome as a result of her long‐term agricultural work. Other possible causes include radiculopathy of the cervical spine or polyneuropathy. Clues in the physical examination may help narrow the differential diagnosis to a cardiac, hepatic, or endocrine disorder.
The patient appeared ill. Her weight had increased from 48 to 61 kg since she was last weighed 6 months previously. Her blood pressure was 140/78 mm Hg, her heart rate was 72 beats/minute with a regular rhythm, her respiratory rate was 18/minute, and her temperature was 37.5C. The jugular venous pressure was elevated at 10 cm above the sternal angle. A grade III/VI systolic ejection murmur was evident at the second interspace along the left sternal border. The second heart sound was fixed and split. There were decreased breath sounds and complete dullness to percussion over both lower lung fields. Shifting dullness was noted on abdominal examination. There was pitting edema from the feet to the thighs, with slow pit‐recovery time in both legs, and she exhibited generalized hirsutism on the face, body, and extremities. There was no lymphadenopathy. On neurological examination, her mental status was normal. The cranial nerves were normal, as was coordination. There was mild generalized distal‐dominant motor weakness with generalized hyporeflexia. Sensory testing demonstrated glove‐and‐stocking type loss of sensation to pinpricks as well as dysesthesia in all extremities. Phalen and Tinel tests were negative.
The elevated venous pressure and pitting edema with slow recovery suggest high venous pressure edema rather than hypoproteinemic edema. Complete bilateral dullness of the chest and shifting dullness of the abdomen indicate the presence of bilateral pleural effusion and ascites. Edema from high venous pressure is usually caused by right, left, or biventricular cardiac failure. A fixed splitting of the second heart sound suggests an atrial septal defect, which is a rare cause of progressive right heart failure in adults. I recommend checking the patient's thyroid function to investigate the possibility of hypothyroidism, which is a common illness among middle‐aged women and could contribute to her edema as well as hirsutism. The neurological findings suggest a generalized polyneuropathy. The unusual combination of high venous pressure edema and polyneuropathy may indicate a rare multisystem disorder such as amyloidosis. Alternatively, the patient might have developed multiple diseases during the same time period. For instance, diabetic polyneuropathy is the most common cause of polyneuropathy among the middle‐aged. Finally, the differential diagnosis of hirsutism includes ovarian, adrenal, or pituitary sources of hyperandrogenism in addition to hypothyroidism. I would first evaluate for diabetes, thyroid disease, and cardiac disease and would like to see the results of laboratory tests for thyrotropin and plasma glucose as well as chest radiography and electrocardiography.
The white‐cell count was 5400/mm3 with a normal differential. Hemoglobin was 10.7 g/dL with normal red‐cell indices, and the platelet count was 276,000/mm3. The erythrocyte sedimentation rate was 29 mm/hour. Other laboratory tests revealed the following values: total protein, 6.2 g/dL; albumin, 3.3 g/dL; blood urea nitrogen, 12 mg/dL; creatinine, 0.7 mg/dL; aspartate aminotransferase, 6 U/L; alanine aminotransferase, 2 U/L; lactate dehydrogenase, 96 U/L; alkaline phosphatase, 115 U/L; creatine phosphokinase, 60 U/L; total bilirubin, 0.9 mg/dL; glucose, 96 mg/dL; hemoglobin A1c, 4.6%; total cholesterol, 111 mg/dL; and thyrotropin, 6.32 mIU/mL (normal range, 0.50‐5.00 mIU/mL). Serum free thyroxine, triiodothyronine, and urine testosterone were normal. Serum dehydroepiandrosterone sulfate was mildly elevated for her age (864 ng/mL: normal range, 180‐750 ng/mL). Serological studies for human immunodeficiency virus, human T‐lymphotrophic virus type 1, and syphilis were negative. Urinalysis was weakly positive for protein but negative for casts and occult blood. The stool was negative for occult blood.
A chest radiograph showed bilateral pleural effusions. Computed tomography demonstrated bilateral pleural effusions, ascites, mild hepatomegaly, and small, multiple, mediastinal lymph nodes. Her electrocardiogram was normal. A transesophageal echocardiogram with agitated saline contrast demonstrated normal ventricular systolic and diastolic function and no atrial septal defect. The inferior vena cava did not collapse with inspiration, and there was no evidence of infiltrative cardiomyopathy.
These laboratory results rule out diabetes as the cause of the polyneuropathy. The subclinical hypothyroidism would not explain profound edema and hirsutism. A serum albumin level of 3.3 g/dL confirms high venous pressure edema rather than hypoproteinemic edema. Normochromic, normocytic anemia and a mildly elevated sedimentation rate point to a chronic illness or inflammatory state. The mediastinal lymphadenopathy may reflect congestion as a result of the high venous pressure or reflect a systemic disease involving lymph nodes. Normal ventricular function with high venous pressure is suggestive of heart failure from diastolic dysfunction, although the patient does not have risk factors for diastolic dysfunction, such as hypertension, and has no other echocardiographic features of diastolic impairment. The combination of hyperandrogenism and neuropathy points to a systemic process, such as a paraneoplastic syndrome. I would next investigate the source of the excess androgens.
Because serum dehydroepiandrosterone sulfate was mildly elevated, I‐131 aldosterol scintigraphy was performed, and it was negative. Electromyography showed a pattern of generalized sensorimotor polyneuropathy.
At this point, it appears that cardiac, endocrine, hepatic, and renal diseases have been largely ruled out as a cause of her symptoms. Reframing and unifying the important clinical problems for this patient may be useful in resolving this diagnostic puzzle. They include (1) systemic high venous pressure edema; (2) generalized sensorimotor polyneuropathy; (3) hirsutism; (4) normocytic, normochromic anemia; (5) an elevated erythrocyte sedimentation rate; (6) mediastinal lymphadenopathy; and (7) subclinical hypothyroidism. At this point, I cannot unify these pieces of information into a single diagnosis. I would search the medical literature, focusing on these terms.
A general internist consultant performed MEDLINE and Google Scholar searches using the key words edema, polyneuropathy, and hirsutism. This search suggested the diagnosis of Crow‐Fukase syndrome, also known as POEMS (polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes) syndrome. Subsequent evaluations were performed. First, serum protein electrophoresis revealed the presence of monoclonal proteins, although hypergammaglobulinemia was not present. Second, a bone marrow examination demonstrated increased abnormal plasma cell proliferation (7%), although a radiographic skeletal survey found no lesions suggestive of plasmacytoma. Third, cerebrospinal fluid analysis showed normal cell counts but increased protein concentration (202 mg/dL). Fourth, a blood sample referred to an outside laboratory demonstrated elevated levels of vascular endothelial growth factor (3902 pg/mL: normal range, 150‐500 pg/mL). On the basis of these findings, the diagnosis of POEMS syndrome was made. After oral prednisolone (40 mg/day) was initiated, the systemic edema improved gradually, and she did well during the 2‐year follow‐up period.
Commentary
POEMS syndrome, also known as Crow‐Fukase syndrome, is a rare multisystem disorder first described by Crow in 1956.1, 2 It is characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes, as indicated by the acronym. The diagnosis of POEMS syndrome is difficult as this syndrome is rare and requires high clinical suspicion. According to a nationwide cross‐sectional survey in Japan, the prevalence of POEMS syndrome is very low (about 3 patients per 1,000,000 persons),3 and its prevalence in Western countries is considered even lower than that in Japan. The average age at onset is around 45 to 50 years old, and men are twice as likely to have this syndrome as women.46 Table 1 shows the diagnostic criteria of POEMS syndrome, based on research by Dispenzieri and others at the Mayo Clinic, and Table 2 presents the relative frequency of these clinical features.6, 7 The initial symptomatology generally includes polyneuropathy, skin changes, and generalized edema, which are nonspecific symptoms, as are other well‐recognized associated conditions such as clubbing, weight loss, thrombocytosis, polycythemia, and hyperhidrosis. Thus, it is important to consider this syndrome when one is facing an undiagnosed illness involving multiple organ systems and to distinguish it from other conditions such as multiple myeloma, amyloidosis, and monoclonal gammopathy of undetermined significance. Vascular endothelial growth factor is thought to be involved in the edema of POEMS syndrome, as massive release from aggregated platelets increases vascular permeability and venous pressure.710
| |
| Major criteria | Polyneuropathy |
| Monoclonal plasma cell‐proliferative disorder | |
| Minor criteria | Sclerotic bone lesions |
| Castleman disease | |
| Organomegaly (splenomegaly, hepatomegaly, or lymphadenopathy) | |
| Edema (peripheral edema, pleural effusion, or ascites) | |
| Endocrinopathy (adrenal, thyroid, pituitary, gonadal, parathyroid, or pancreatic) | |
| Skin changes (hyperpigmentation, hirsutism, plethora, hemangiomata, and white nails) | |
| Papilledema | |
| Characteristic | % |
|---|---|
| |
| Peripheral neuropathy | 100 |
| Monoclonal plasma cell dyscrasia | 100 |
| Sclerotic bone lesions | 97 |
| Endocrinopathy | 71 |
| Skin changes | 68 |
| Organomegaly | 46 |
| Extravascular volume overload | 39 |
| Papilledema | 29 |
| Castleman disease | 11 |
Data regarding treatment and survival are largely observational. Overall mean survival from diagnosis in the 2003 Dispenzieri cohort was 13.7 years, with death often due to infection or cardiorespiratory failure.6 When a solitary plasmacytoma or osteosclerotic myeloma is present, radiation to the lesion can often lead to clinical remission. Other treatment options include alkylating agents and/or high‐dose chemotherapy with peripheral stem‐cell transplantation, corticosteroids, and supportive care.7
Clinicians frequently use the internet to aid in the clinical decision process. In a survey of the Royal New Zealand College of General Practitioners,11 half reported that they used the Internet to search for clinical information. Two well‐known resources are MEDLINE, which contains over 11 million references dating back to the 1960s, and internet search engines such as Google (and a more recent product, Google Scholar, which attempts to sort search results by including factors such as the author, the publication in which the article appears, and how often the article has been cited).
MEDLINE searches a well‐defined set of journals and uses the Medical Subject Headings (MeSH) vocabulary, which consists of sets of descriptive terms organized in a hierarchical structure to allow searching with various levels of specificity. For instance, entering the term heart attack will map to the MeSH term myocardial infarction and will also include more specific terms such as myocardial stunning and cardiogenic shock.
Google, in comparison, explores resources beyond journals without any clear boundary to its scope, and its advanced search functions can be occasionally unreliable. For instance, search results are occasionally marred by outdated citation information and may include materials that are not truly scholarly. However, search engines can search through the actual text of manuscripts and access the gray literature, which includes open‐source material that is usually original but not widely distributed or often easily available, such as technical reports and dissertations. A direct study comparing the results of searches in PubMed (one of the MEDLINE search engines) and Google Scholar is difficult, but the critical characteristics of each can be compared and contrasted (Table 3).
| Google Scholar | PubMed |
|---|---|
| 1. Database selection is clumped under subject areas, and it cannot be searched with unique identifiers: Con | 1. It allows one to choose a database at the outset and can search with a unique identifier (PubMed identifier): Pro |
| 2. Results cannot be filtered (ie, it does not allow multiple article selection): Con | 2. The single citation matcher allows retrieval of articles with pieces of information: Pro |
| 3. A search for related articles or similar pages is not available: Con | 3. It allows article selection by checkbox to reduce the number of articles relevant to the search query and to append the filter to search box: Pro |
| 4. It allows one to search by without words to exclude unwanted and confusing retrieved data: Pro | 4. It provides unique identifier (PubMed identifier) for each retrieved article for easy communicability: Pro |
| 5. It allows one to search a single journal/publication of interest: Pro | 5. Search are limited to journals only; it does not include the grey area of literature: Con |
| 6. Initial search results are those articles that are most cited by journals that themselves are the most cited: Pro | 6. It lists search results in chronological order and not by relevance: Con |
Internet searches may also suggest diagnoses from a compilation of clinical features, such as in this case. To be successful, such a search must complement the cognitive process; a search engine cannot completely replace clinical judgment. Clinicians must be able to identify salient clinical features and generate high‐yield search terms and then exercise skill in sifting through the citations to arrive at the appropriate diagnosis. A recent study found that Google searches revealed the correct diagnosis in 58% of the case records of the New England Journal of Medicine,12 although each search query resulted in many results, which then had to be manually reviewed for appropriateness within the case's context.
Like a traditional diagnostic test, a search can be described by sensitivity, specificity, and the number of articles needed to read.13 For example, in a study comparing the performance of search strategies to identify clinical practice guidelines in Google Scholar and SUMSearch (another freely accessible search engine), using the term guideline yielded the highest sensitivity, and using the term practice guideline generated the highest specificity and the lowest number of articles needed to read (Table 4).14
| Search Strategy | Sensitivity (%) | Specificity (%) | NNR |
|---|---|---|---|
| |||
| SUMSearch | |||
| Guideline* | 81.51 (74.5388.49) | 74.29 (72.6475.94) | 8.18 (6.9010.05) |
| Recommendation* | 60.50 (51.7269.28) | 76.28 (74.6777.89) | 9.93 (8.1412.72) |
| Practice guideline* | 40.34 (31.5249.16) | 89.45 (88.2990.61) | 6.96 (5.529.43) |
| Google Scholar | |||
| Guideline/s | 31.93 (23.5640.30) | 78.05 (76.5079.60) | 16.67 (12.7624.04) |
| Recommendation/s | 8.40 (3.4213.38) | 92.11 (91.0993.13) | 22.42 (13.9756.82) |
| Practice guideline/s | 11.76 (5.9817.54) | 95.72 (94.9696.48) | 9.29 (6.2118.38) |
Although there are several other popular hosts of web‐based search engines, a more robust decision‐support program may help physicians more efficiently consider relevant diagnoses. One program, named Isabel, has been developed through the indexing of a database of more than 11,000 diseases according to word patterns in journal articles associated with each disease, and it is updated as new and relevant articles emerge. One recent study demonstrated that the correct diagnosis was made in 48 of 50 cases (96%) with specific, key findings as search terms but in only 37 of the same 50 cases (74%) if the entire case history was simply pasted in, again emphasizing the importance of specific search terms.15
POEMS syndrome is a rare entity occasionally seen in middle‐aged individuals and marked by a multitude of nonspecific findings, particularly polyneuropathy and plasma cell dyscrasia. In this case, the diagnostic test was an internet search based on the most prominent clinical symptoms. Such a strategy can provide a powerful addition to traditional literature and MEDLINE resources. However, the efficiency of this process is heavily dependent on the quality of the search strategy and, therefore, the cognitive faculties of the treating physician to avoid the predictable shortcoming of low specificity. Garbage in, garbage out still applies whether the computer in question is the human mind or the desktop PC.
Teaching Points
-
POEMS syndrome, also known as Crow‐Fukase syndrome, is a rare multisystem disorder characterized by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes.
-
Internet‐based searches, including Google and MEDLINE, are being used more frequently because they are widely available, quick, and freely accessed.
-
Internet searches appear most useful as adjuncts to PubMed and clinical reasoning in identifying case reports when a well‐constructed collection of symptoms and signs is used for searches.
- .Peripheral neuritis in myelomatosis.Br Med J.1956;2(4996):802–804.
- ,,,,,.Plasma cell dyscrasia with polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes: the POEMS syndrome. Report on two cases and a review of the literature.Medicine (Baltimore).1980;59(4):311–322.
- .Nationwide Epidemiologic Survey of Crow‐Fukase Syndrome in 2004.Tokyo, Japan:Japanese Ministry of Health and Welfare Government Report, 2004.
- ,,, et al.The Crow‐Fukase syndrome: a study of 102 cases in Japan.Neurology.1984;34(6):712–720.
- ,,.POEMS syndrome: a study of 25 cases and a review of the literature. French Study Group on POEMS Syndrome.Am J Med.1994;97(6):543–553.
- ,,, et al.POEMS syndrome: definitions and long‐term outcome.Blood.2003;101(7):2496–2506.
- .POEMS syndrome.Hematology.2005;1(1):360–367.
- ,,,,.Greatly raised vascular endothelial growth factor (VEGF) in POEMS syndrome.Lancet.1996;347(9002):702.
- ,.Assessment of hypoproteinaemic oedema: a simple physical sign.Br Med J.1978;1(6117):890–891.
- ,,, et al.Ratio of serum vascular endothelial growth factor to platelet count correlates with disease activity in a patient with POEMS syndrome.Eur J Intern Med.2002;13(1):70–74.
- .In search of evidence: family practitioners' use of the Internet for clinical information.J Med Libr Assoc.2002;90(4):370–379.
- ,.Googling for a diagnosis—use of Google as a diagnostic aid: internet based study.BMJ.2006;333(7579):1143–5114.
- ,,.The number needed to read—a new measure of journal value.Health Info Libr J.2005;22(2):81–82.
- ,,,.Developing search strategies for clinical practice guidelines in SUMSearch and Google Scholar and assessing their retrieval performance.BMC Med Res Methodol.2007;7:28.
- ,.Performance of a web‐based clinical diagnosis support system for internists.J Gen Intern Med.2008;23(suppl 1):37–40.
- .Peripheral neuritis in myelomatosis.Br Med J.1956;2(4996):802–804.
- ,,,,,.Plasma cell dyscrasia with polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes: the POEMS syndrome. Report on two cases and a review of the literature.Medicine (Baltimore).1980;59(4):311–322.
- .Nationwide Epidemiologic Survey of Crow‐Fukase Syndrome in 2004.Tokyo, Japan:Japanese Ministry of Health and Welfare Government Report, 2004.
- ,,, et al.The Crow‐Fukase syndrome: a study of 102 cases in Japan.Neurology.1984;34(6):712–720.
- ,,.POEMS syndrome: a study of 25 cases and a review of the literature. French Study Group on POEMS Syndrome.Am J Med.1994;97(6):543–553.
- ,,, et al.POEMS syndrome: definitions and long‐term outcome.Blood.2003;101(7):2496–2506.
- .POEMS syndrome.Hematology.2005;1(1):360–367.
- ,,,,.Greatly raised vascular endothelial growth factor (VEGF) in POEMS syndrome.Lancet.1996;347(9002):702.
- ,.Assessment of hypoproteinaemic oedema: a simple physical sign.Br Med J.1978;1(6117):890–891.
- ,,, et al.Ratio of serum vascular endothelial growth factor to platelet count correlates with disease activity in a patient with POEMS syndrome.Eur J Intern Med.2002;13(1):70–74.
- .In search of evidence: family practitioners' use of the Internet for clinical information.J Med Libr Assoc.2002;90(4):370–379.
- ,.Googling for a diagnosis—use of Google as a diagnostic aid: internet based study.BMJ.2006;333(7579):1143–5114.
- ,,.The number needed to read—a new measure of journal value.Health Info Libr J.2005;22(2):81–82.
- ,,,.Developing search strategies for clinical practice guidelines in SUMSearch and Google Scholar and assessing their retrieval performance.BMC Med Res Methodol.2007;7:28.
- ,.Performance of a web‐based clinical diagnosis support system for internists.J Gen Intern Med.2008;23(suppl 1):37–40.