User login
Collateral Damage: How COVID-19 Is Adversely Impacting Women Physicians
The coronavirus disease of 2019 (COVID-19) pandemic has affected every facet of our work and personal lives. While many hope we will return to “normal” with the pandemic’s passing, there is reason to believe medicine, and society, will experience irrevocable changes. Although the number of women pursuing and practicing medicine has increased, inequities remain in compensation, academic rank, and leadership positions.1,2 Within the workplace, women are more likely to be in frontline clinical positions, are more likely to be integral in promoting positive interpersonal relationships and collaborative work environments, and often are less represented in the high-level, decision-making roles in leadership or administration.3,4 These well-described issues may be exacerbated during this pandemic crisis. We describe how the current COVID-19 pandemic may intensify workplace inequities for women, and propose solutions for hospitalist groups, leaders, and administrators to ensure female hospitalists continue to prosper and thrive in these tenuous times.
HOW THE PANDEMIC MAY EXACERBATE EXISTING INEQUITIES
Increasing Demands at Home
Female physicians are more likely to have partners who are employed full-time and report spending more time on household activities including cleaning, cooking, and the care of children, compared with their male counterparts.5 With school and daycare closings, as well as stay-at-home orders in many US states, there has been an increase in household responsibilities and care needs for children remaining at home with a marked decrease in options for stable or emergency childcare.6 As compared with primary care and subspecialty colleagues who can provide a large percentage of their care through telemedicine, this is not the case for hospitalists who must be physically present to care for their patients. Therefore, hospitalists are unable to clinically “work from home” in the same way as many of their colleagues in other specialties. Increased childcare and schooling obligations, coupled with disproportionate household responsibilities and an inability to work from home, will likely result in female hospitalists struggling to meet family needs while pandemic-related work responsibilities are ramping up.7 In addition, women who are involved with administrative, leadership, or research activities may struggle to execute their responsibilities as a result of increased domestic duties.
Many hospitalists are also concerned about contracting COVID-19 and exposing their families to the illness given the high infection rate among healthcare workers and the shortage of personal protective equipment (PPE).8,9 Institutions and national organizations, including the Society of Hospital Medicine, have partnered with industry to provide discounted or complimentary hotel rooms for members to aid self-isolation while providing clinical care.10 One famous photo in popular and social media showed a pulmonary and critical care physician in a tent in his garage in order to self-isolate from his family.11 However, since women are often the primary caregivers for their children or other family members and may also be responsible for other important household activities, they may be unable or unwilling to remove themselves from their children and families. As a result, female hospitalists may encounter feelings of guilt or inadequacy if they’re unable to isolate in the same manner as male colleagues.8
Exaggerating Leadership Gap
One of the keys to a robust response to this pandemic is strong, thoughtful, and strategic leadership.12 Institutional, regional, and national leaders are at the forefront of designing the solutions to the many problems the COVID-19 pandemic has created. The paucity of women at high-level leadership positions in institutions across the United States, including university-based, community, public, and private institutions, means that there is a lack of female representation when institutional policy is being discussed and decided.4 This lack of representation may lead to policies and procedures that negatively affect female hospitalists or, at best, fail to consider the needs of or support female physicians. For example, leaders of a hospital medicine group may create mandatory “backup” coverage for night and weekend shifts for their group during surge periods of the pandemic without considering implications for childcare. Finding weekday, daytime coverage is challenging for many during this time when daycares and school are closed, and finding coverage during weekend or overnight hours will be even more challenging. With increased risks for older adults with high-risk medical conditions, grandparents or other friends or family members that previously would have assisted with childcare may no longer be an option. If a female hospitalist is not a member of the leadership group that helped design this coverage structure, there could be a lack of recognition of the undue strain this coverage model could create for women in the group. Even if not intentional, such policies may hinder women’s career stability and opportunities for further advancement, as well as their ability to adequately provide care for their families. Having women as a part of the leadership group that creates policies and schedules and makes pivotal decisions is imperative, especially regarding topics of providing access and compensation for “emergency childcare,” hazard pay, shift length, work conditions, job security, sick leave, workers compensation, advancement opportunities, and hiring practices.
Compensation
The gender pay gap in medicine has been consistently demonstrated among many specialties.13,14 The reasons for this inequity are multifactorial, and the COVID-19 pandemic has the potential to further widen this gap. With the unequal burden of unpaid care provided by women and their higher prevalence as frontline workers, they are at greater risk of needing to take unpaid leave to care for a sick family member or themselves.6,7 Similarly, without hazard pay, those with direct clinical responsibilities bear the risk of illness for themselves and their families without adequate compensation.
Impact on Physical and Mental Health
The overall well-being of the hospitalist workforce is critical to continue to provide the highest level of care for our patients. With higher workloads at home and at work, female hospitalists are at risk for increased burnout. Burnout has been linked to many negative outcomes including poor performance, depression, suicide, and leaving the profession.15 Burnout is documented to be higher in female physicians with several contributing factors that are aggravated by gender inequities, including having children at home, gender bias, and real or perceived lack of fairness in promotion and compensation.16 The COVID-19 pandemic has amplified the stress of having children in the home, as well as concerns around fair compensation as described above. The consequences of this have yet to be fully realized but may be dire.
PROPOSED RECOMMENDATIONS
We propose the following recommendations to help mitigate the effects of this epidemic and to continue to move our field forward on our path to equity.
1. Closely monitor the direct and indirect effects of COVID-19 on female hospitalists. While there has been a recent increase in scholarship on the pre–COVID-19 state of gender disparities, there is still much that is unknown. As we experience this upheaval in the way our institutions function, it is even more imperative to track gender deaggregated key indicators of wellness, burnout, and productivity. This includes the use of burnout inventories, salary equity reviews, procedures that track progress toward promotion, and even focus groups of female hospitalists.
2. Inquire about the needs of women in your organization and secure the support they need. This may take the form of including women on key task forces that address personal protective equipment allocation, design new processes, and prepare for surge capacity, as well as providing wellness initiatives, fostering collaborative social networks, or connecting them with emergency childcare resources.
3. Provide a mechanism to account for lack of academic productivity during this time. This period of decreased academic productivity may disproportionately derail progress toward promotion for women. Academic institutions should consider extending deadlines for promotion or tenure, as well as increasing flexibility in metrics used to determine appropriate progress in annual performance reviews.
4. Recognize and reward increased efforts in the areas of clinical or administrative contribution. In this time of crisis, women may be stepping up and leading efforts without titles or positions in ways that are significant and meaningful for their group or organization. Recognizing the ways women are contributing in a tangible and explicit way can provide an avenue for fair compensation, recognition, and career advancement. Female hospitalists should also “manage up” by speaking up and ensuring that leaders are aware of contributions. Amplification is another powerful technique whereby unrecognized contributions can be called out by other women or men.17
5. Support diversity, inclusion, and equity efforts. Keeping equity targets at the top of priority lists for goals moving forward will be imperative. Many institutions struggled to support strong diversity, inclusion, and equity efforts prior to COVID-19; however, the pandemic has highlighted the stark racial and socioeconomic disparities that exist in healthcare.18,19 As healthcare institutions and providers work to mitigate these disparities for patients, there would be no better time to look internally at how they pay, support, and promote their own employees. This would include actively identifying and mitigating any disparities that exist for employees by gender, race, religion, sexual orientation, ethnicity, age, or disability status.
6. Advocate for fair compensation for providers caring for COVID-19 patients. Frontline clinicians are bearing significant risks and increased workload during this crisis and should be compensated accordingly. Hazard pay, paid sick leave, medical and supplemental life insurance, and strong workers’ compensation protections for hospitalists who become ill at work are important for all clinicians, including women. Other long-term plans should include institutional interventions such as salary corrections and ongoing monitoring.20
SUMMARY
The COVID-19 pandemic will have long-term effects that are yet to be realized, including potentially widening gender disparities in medicine. With the current health and economic crises facing our institutions and nations, it can be tempting for diversity, equity, and inclusion initiatives to fall by the wayside. However, it is imperative that hospitalists, leaders, and institutions monitor the effects of the COVID-19 pandemic on women and proactively work to mitigate worsening disparities. Without this focus there is a risk that the recent gains in equity and advancement for women may be lost.
1. Association of American Medical Colleges. Table 13: US medical school faculty by sex, rank, and department, 2017-2018. December 31, 2019. Accessed January 16, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144(5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Rouse LP, Nagy-Agren S, Gebhard RE, Bernstein WK. Women physicians: gender and the medical workplace. J Womens Health (Larchmt). 2020;29(3):297‐309. https://doi.org/10.1089/jwh.2018.7290
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Starmer AJ, Frintner MP, Matos K, Somberg C, Freed G, Byrne BJ. Gender discrepancies related to pediatrician work-life balance and household responsibilities. Pediatrics. 2019;144(4):e20182926. https://doi.org/10.1542/peds.2018-2926
6. Alon TM, Doepke M, Olmstead-Rumsey J, Tertilt Ml. The impact of COVID-19 on gender equality. NBER Working Paper Series. 2020. https://doi.org/10.3386/w26947
7. Addati L, Cattaneo U, Esquivel V, Valarino I. Care work and care jobs for the future of decent work. Geneva: International Labour Office; 2018.
8. Maguire P. Should you steer clear of your own family? Hospitalists weigh living in isolation. Today’s Hospitalist. May 2020. Accessed May 4, 2020. https://www.todayshospitalist.com/treating-covid-patients/
9. Burrer SL, de Perio MA, Hughes MM, et al. Characteristics of health care personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-481. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e6
10. SHM Teams Up with Hilton and American Express to Provide Hotel Rooms for Members. SHM. April 13, 2020. Accessed May 7, 2020. https://www.hospitalmedicine.org/about/press-releases/SHM-One-Million-Beds-Hilton-AMEX/
11. Fichtel C, Kaufman S. Fearing COVID-19 spread to families, health care workers self-isolate at home. NBC News. March 31, 2020. Accessed May 7, 2020. https://www.nbcnews.com/health/health-news/fearing-covid-19-spread-families-health-care-workers-self-isolate-n1171726
12. Meier KA, Jerardi KE, Statile AM, Shah SS. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020;15(5):308‐310. https://doi.org/10.12788/jhm.3435
13. Frintner MP, Sisk B, Byrne BJ, Freed GL, Starmer AJ, Olson LM. Gender differences in earnings of early- and midcareer pediatricians. Pediatrics. 2019;144(4):e20183955. https://doi.org/10.1542/peds.2018-3955
14. Read S, Butkus R, Weissman A, Moyer DV. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169(9):658-661. https://doi.org/10.7326/m18-0693
15. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. https://doi.org/10.1111/joim.12752
16. Templeton K, Halpern L, Jumper C, Carroll RG. Leading and sustaining curricular change: workshop proceedings from the 2018 Sex and Gender Health Education Summit. J Womens Health (Larchmt). 2019;28(12):1743-1747. https://doi.org/10.1089/jwh.2018.7387
17. Eilperin J. White House women want to be in the room where it happens. The Washington Post. September 13, 2016. Accessed April 24, 2020. https://www.washingtonpost.com/news/powerpost/wp/2016/09/13/white-house-women-are-now-in-the-room-where-it-happens/
18. Choo EK. COVID-19 fault lines. Lancet. 2020;395(10233):1333. https://doi.org/10.1016/s0140-6736(20)30812-6
19. Núñez A, Madison M, Schiavo R, Elk R, Prigerson HG. Responding to healthcare disparities and challenges with access to care during COVID-19. Health Equity. 2020;4(1):117-128. https://doi.org/10.1089/heq.2020.29000.rtl
20. Paturel A. Closing the gender pay gap in medicine. AAMC News. April 16, 2019. Accessed April 21, 2020. https://www.aamc.org/news-insights/closing-gender-pay-gap-medicine
The coronavirus disease of 2019 (COVID-19) pandemic has affected every facet of our work and personal lives. While many hope we will return to “normal” with the pandemic’s passing, there is reason to believe medicine, and society, will experience irrevocable changes. Although the number of women pursuing and practicing medicine has increased, inequities remain in compensation, academic rank, and leadership positions.1,2 Within the workplace, women are more likely to be in frontline clinical positions, are more likely to be integral in promoting positive interpersonal relationships and collaborative work environments, and often are less represented in the high-level, decision-making roles in leadership or administration.3,4 These well-described issues may be exacerbated during this pandemic crisis. We describe how the current COVID-19 pandemic may intensify workplace inequities for women, and propose solutions for hospitalist groups, leaders, and administrators to ensure female hospitalists continue to prosper and thrive in these tenuous times.
HOW THE PANDEMIC MAY EXACERBATE EXISTING INEQUITIES
Increasing Demands at Home
Female physicians are more likely to have partners who are employed full-time and report spending more time on household activities including cleaning, cooking, and the care of children, compared with their male counterparts.5 With school and daycare closings, as well as stay-at-home orders in many US states, there has been an increase in household responsibilities and care needs for children remaining at home with a marked decrease in options for stable or emergency childcare.6 As compared with primary care and subspecialty colleagues who can provide a large percentage of their care through telemedicine, this is not the case for hospitalists who must be physically present to care for their patients. Therefore, hospitalists are unable to clinically “work from home” in the same way as many of their colleagues in other specialties. Increased childcare and schooling obligations, coupled with disproportionate household responsibilities and an inability to work from home, will likely result in female hospitalists struggling to meet family needs while pandemic-related work responsibilities are ramping up.7 In addition, women who are involved with administrative, leadership, or research activities may struggle to execute their responsibilities as a result of increased domestic duties.
Many hospitalists are also concerned about contracting COVID-19 and exposing their families to the illness given the high infection rate among healthcare workers and the shortage of personal protective equipment (PPE).8,9 Institutions and national organizations, including the Society of Hospital Medicine, have partnered with industry to provide discounted or complimentary hotel rooms for members to aid self-isolation while providing clinical care.10 One famous photo in popular and social media showed a pulmonary and critical care physician in a tent in his garage in order to self-isolate from his family.11 However, since women are often the primary caregivers for their children or other family members and may also be responsible for other important household activities, they may be unable or unwilling to remove themselves from their children and families. As a result, female hospitalists may encounter feelings of guilt or inadequacy if they’re unable to isolate in the same manner as male colleagues.8
Exaggerating Leadership Gap
One of the keys to a robust response to this pandemic is strong, thoughtful, and strategic leadership.12 Institutional, regional, and national leaders are at the forefront of designing the solutions to the many problems the COVID-19 pandemic has created. The paucity of women at high-level leadership positions in institutions across the United States, including university-based, community, public, and private institutions, means that there is a lack of female representation when institutional policy is being discussed and decided.4 This lack of representation may lead to policies and procedures that negatively affect female hospitalists or, at best, fail to consider the needs of or support female physicians. For example, leaders of a hospital medicine group may create mandatory “backup” coverage for night and weekend shifts for their group during surge periods of the pandemic without considering implications for childcare. Finding weekday, daytime coverage is challenging for many during this time when daycares and school are closed, and finding coverage during weekend or overnight hours will be even more challenging. With increased risks for older adults with high-risk medical conditions, grandparents or other friends or family members that previously would have assisted with childcare may no longer be an option. If a female hospitalist is not a member of the leadership group that helped design this coverage structure, there could be a lack of recognition of the undue strain this coverage model could create for women in the group. Even if not intentional, such policies may hinder women’s career stability and opportunities for further advancement, as well as their ability to adequately provide care for their families. Having women as a part of the leadership group that creates policies and schedules and makes pivotal decisions is imperative, especially regarding topics of providing access and compensation for “emergency childcare,” hazard pay, shift length, work conditions, job security, sick leave, workers compensation, advancement opportunities, and hiring practices.
Compensation
The gender pay gap in medicine has been consistently demonstrated among many specialties.13,14 The reasons for this inequity are multifactorial, and the COVID-19 pandemic has the potential to further widen this gap. With the unequal burden of unpaid care provided by women and their higher prevalence as frontline workers, they are at greater risk of needing to take unpaid leave to care for a sick family member or themselves.6,7 Similarly, without hazard pay, those with direct clinical responsibilities bear the risk of illness for themselves and their families without adequate compensation.
Impact on Physical and Mental Health
The overall well-being of the hospitalist workforce is critical to continue to provide the highest level of care for our patients. With higher workloads at home and at work, female hospitalists are at risk for increased burnout. Burnout has been linked to many negative outcomes including poor performance, depression, suicide, and leaving the profession.15 Burnout is documented to be higher in female physicians with several contributing factors that are aggravated by gender inequities, including having children at home, gender bias, and real or perceived lack of fairness in promotion and compensation.16 The COVID-19 pandemic has amplified the stress of having children in the home, as well as concerns around fair compensation as described above. The consequences of this have yet to be fully realized but may be dire.
PROPOSED RECOMMENDATIONS
We propose the following recommendations to help mitigate the effects of this epidemic and to continue to move our field forward on our path to equity.
1. Closely monitor the direct and indirect effects of COVID-19 on female hospitalists. While there has been a recent increase in scholarship on the pre–COVID-19 state of gender disparities, there is still much that is unknown. As we experience this upheaval in the way our institutions function, it is even more imperative to track gender deaggregated key indicators of wellness, burnout, and productivity. This includes the use of burnout inventories, salary equity reviews, procedures that track progress toward promotion, and even focus groups of female hospitalists.
2. Inquire about the needs of women in your organization and secure the support they need. This may take the form of including women on key task forces that address personal protective equipment allocation, design new processes, and prepare for surge capacity, as well as providing wellness initiatives, fostering collaborative social networks, or connecting them with emergency childcare resources.
3. Provide a mechanism to account for lack of academic productivity during this time. This period of decreased academic productivity may disproportionately derail progress toward promotion for women. Academic institutions should consider extending deadlines for promotion or tenure, as well as increasing flexibility in metrics used to determine appropriate progress in annual performance reviews.
4. Recognize and reward increased efforts in the areas of clinical or administrative contribution. In this time of crisis, women may be stepping up and leading efforts without titles or positions in ways that are significant and meaningful for their group or organization. Recognizing the ways women are contributing in a tangible and explicit way can provide an avenue for fair compensation, recognition, and career advancement. Female hospitalists should also “manage up” by speaking up and ensuring that leaders are aware of contributions. Amplification is another powerful technique whereby unrecognized contributions can be called out by other women or men.17
5. Support diversity, inclusion, and equity efforts. Keeping equity targets at the top of priority lists for goals moving forward will be imperative. Many institutions struggled to support strong diversity, inclusion, and equity efforts prior to COVID-19; however, the pandemic has highlighted the stark racial and socioeconomic disparities that exist in healthcare.18,19 As healthcare institutions and providers work to mitigate these disparities for patients, there would be no better time to look internally at how they pay, support, and promote their own employees. This would include actively identifying and mitigating any disparities that exist for employees by gender, race, religion, sexual orientation, ethnicity, age, or disability status.
6. Advocate for fair compensation for providers caring for COVID-19 patients. Frontline clinicians are bearing significant risks and increased workload during this crisis and should be compensated accordingly. Hazard pay, paid sick leave, medical and supplemental life insurance, and strong workers’ compensation protections for hospitalists who become ill at work are important for all clinicians, including women. Other long-term plans should include institutional interventions such as salary corrections and ongoing monitoring.20
SUMMARY
The COVID-19 pandemic will have long-term effects that are yet to be realized, including potentially widening gender disparities in medicine. With the current health and economic crises facing our institutions and nations, it can be tempting for diversity, equity, and inclusion initiatives to fall by the wayside. However, it is imperative that hospitalists, leaders, and institutions monitor the effects of the COVID-19 pandemic on women and proactively work to mitigate worsening disparities. Without this focus there is a risk that the recent gains in equity and advancement for women may be lost.
The coronavirus disease of 2019 (COVID-19) pandemic has affected every facet of our work and personal lives. While many hope we will return to “normal” with the pandemic’s passing, there is reason to believe medicine, and society, will experience irrevocable changes. Although the number of women pursuing and practicing medicine has increased, inequities remain in compensation, academic rank, and leadership positions.1,2 Within the workplace, women are more likely to be in frontline clinical positions, are more likely to be integral in promoting positive interpersonal relationships and collaborative work environments, and often are less represented in the high-level, decision-making roles in leadership or administration.3,4 These well-described issues may be exacerbated during this pandemic crisis. We describe how the current COVID-19 pandemic may intensify workplace inequities for women, and propose solutions for hospitalist groups, leaders, and administrators to ensure female hospitalists continue to prosper and thrive in these tenuous times.
HOW THE PANDEMIC MAY EXACERBATE EXISTING INEQUITIES
Increasing Demands at Home
Female physicians are more likely to have partners who are employed full-time and report spending more time on household activities including cleaning, cooking, and the care of children, compared with their male counterparts.5 With school and daycare closings, as well as stay-at-home orders in many US states, there has been an increase in household responsibilities and care needs for children remaining at home with a marked decrease in options for stable or emergency childcare.6 As compared with primary care and subspecialty colleagues who can provide a large percentage of their care through telemedicine, this is not the case for hospitalists who must be physically present to care for their patients. Therefore, hospitalists are unable to clinically “work from home” in the same way as many of their colleagues in other specialties. Increased childcare and schooling obligations, coupled with disproportionate household responsibilities and an inability to work from home, will likely result in female hospitalists struggling to meet family needs while pandemic-related work responsibilities are ramping up.7 In addition, women who are involved with administrative, leadership, or research activities may struggle to execute their responsibilities as a result of increased domestic duties.
Many hospitalists are also concerned about contracting COVID-19 and exposing their families to the illness given the high infection rate among healthcare workers and the shortage of personal protective equipment (PPE).8,9 Institutions and national organizations, including the Society of Hospital Medicine, have partnered with industry to provide discounted or complimentary hotel rooms for members to aid self-isolation while providing clinical care.10 One famous photo in popular and social media showed a pulmonary and critical care physician in a tent in his garage in order to self-isolate from his family.11 However, since women are often the primary caregivers for their children or other family members and may also be responsible for other important household activities, they may be unable or unwilling to remove themselves from their children and families. As a result, female hospitalists may encounter feelings of guilt or inadequacy if they’re unable to isolate in the same manner as male colleagues.8
Exaggerating Leadership Gap
One of the keys to a robust response to this pandemic is strong, thoughtful, and strategic leadership.12 Institutional, regional, and national leaders are at the forefront of designing the solutions to the many problems the COVID-19 pandemic has created. The paucity of women at high-level leadership positions in institutions across the United States, including university-based, community, public, and private institutions, means that there is a lack of female representation when institutional policy is being discussed and decided.4 This lack of representation may lead to policies and procedures that negatively affect female hospitalists or, at best, fail to consider the needs of or support female physicians. For example, leaders of a hospital medicine group may create mandatory “backup” coverage for night and weekend shifts for their group during surge periods of the pandemic without considering implications for childcare. Finding weekday, daytime coverage is challenging for many during this time when daycares and school are closed, and finding coverage during weekend or overnight hours will be even more challenging. With increased risks for older adults with high-risk medical conditions, grandparents or other friends or family members that previously would have assisted with childcare may no longer be an option. If a female hospitalist is not a member of the leadership group that helped design this coverage structure, there could be a lack of recognition of the undue strain this coverage model could create for women in the group. Even if not intentional, such policies may hinder women’s career stability and opportunities for further advancement, as well as their ability to adequately provide care for their families. Having women as a part of the leadership group that creates policies and schedules and makes pivotal decisions is imperative, especially regarding topics of providing access and compensation for “emergency childcare,” hazard pay, shift length, work conditions, job security, sick leave, workers compensation, advancement opportunities, and hiring practices.
Compensation
The gender pay gap in medicine has been consistently demonstrated among many specialties.13,14 The reasons for this inequity are multifactorial, and the COVID-19 pandemic has the potential to further widen this gap. With the unequal burden of unpaid care provided by women and their higher prevalence as frontline workers, they are at greater risk of needing to take unpaid leave to care for a sick family member or themselves.6,7 Similarly, without hazard pay, those with direct clinical responsibilities bear the risk of illness for themselves and their families without adequate compensation.
Impact on Physical and Mental Health
The overall well-being of the hospitalist workforce is critical to continue to provide the highest level of care for our patients. With higher workloads at home and at work, female hospitalists are at risk for increased burnout. Burnout has been linked to many negative outcomes including poor performance, depression, suicide, and leaving the profession.15 Burnout is documented to be higher in female physicians with several contributing factors that are aggravated by gender inequities, including having children at home, gender bias, and real or perceived lack of fairness in promotion and compensation.16 The COVID-19 pandemic has amplified the stress of having children in the home, as well as concerns around fair compensation as described above. The consequences of this have yet to be fully realized but may be dire.
PROPOSED RECOMMENDATIONS
We propose the following recommendations to help mitigate the effects of this epidemic and to continue to move our field forward on our path to equity.
1. Closely monitor the direct and indirect effects of COVID-19 on female hospitalists. While there has been a recent increase in scholarship on the pre–COVID-19 state of gender disparities, there is still much that is unknown. As we experience this upheaval in the way our institutions function, it is even more imperative to track gender deaggregated key indicators of wellness, burnout, and productivity. This includes the use of burnout inventories, salary equity reviews, procedures that track progress toward promotion, and even focus groups of female hospitalists.
2. Inquire about the needs of women in your organization and secure the support they need. This may take the form of including women on key task forces that address personal protective equipment allocation, design new processes, and prepare for surge capacity, as well as providing wellness initiatives, fostering collaborative social networks, or connecting them with emergency childcare resources.
3. Provide a mechanism to account for lack of academic productivity during this time. This period of decreased academic productivity may disproportionately derail progress toward promotion for women. Academic institutions should consider extending deadlines for promotion or tenure, as well as increasing flexibility in metrics used to determine appropriate progress in annual performance reviews.
4. Recognize and reward increased efforts in the areas of clinical or administrative contribution. In this time of crisis, women may be stepping up and leading efforts without titles or positions in ways that are significant and meaningful for their group or organization. Recognizing the ways women are contributing in a tangible and explicit way can provide an avenue for fair compensation, recognition, and career advancement. Female hospitalists should also “manage up” by speaking up and ensuring that leaders are aware of contributions. Amplification is another powerful technique whereby unrecognized contributions can be called out by other women or men.17
5. Support diversity, inclusion, and equity efforts. Keeping equity targets at the top of priority lists for goals moving forward will be imperative. Many institutions struggled to support strong diversity, inclusion, and equity efforts prior to COVID-19; however, the pandemic has highlighted the stark racial and socioeconomic disparities that exist in healthcare.18,19 As healthcare institutions and providers work to mitigate these disparities for patients, there would be no better time to look internally at how they pay, support, and promote their own employees. This would include actively identifying and mitigating any disparities that exist for employees by gender, race, religion, sexual orientation, ethnicity, age, or disability status.
6. Advocate for fair compensation for providers caring for COVID-19 patients. Frontline clinicians are bearing significant risks and increased workload during this crisis and should be compensated accordingly. Hazard pay, paid sick leave, medical and supplemental life insurance, and strong workers’ compensation protections for hospitalists who become ill at work are important for all clinicians, including women. Other long-term plans should include institutional interventions such as salary corrections and ongoing monitoring.20
SUMMARY
The COVID-19 pandemic will have long-term effects that are yet to be realized, including potentially widening gender disparities in medicine. With the current health and economic crises facing our institutions and nations, it can be tempting for diversity, equity, and inclusion initiatives to fall by the wayside. However, it is imperative that hospitalists, leaders, and institutions monitor the effects of the COVID-19 pandemic on women and proactively work to mitigate worsening disparities. Without this focus there is a risk that the recent gains in equity and advancement for women may be lost.
1. Association of American Medical Colleges. Table 13: US medical school faculty by sex, rank, and department, 2017-2018. December 31, 2019. Accessed January 16, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144(5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Rouse LP, Nagy-Agren S, Gebhard RE, Bernstein WK. Women physicians: gender and the medical workplace. J Womens Health (Larchmt). 2020;29(3):297‐309. https://doi.org/10.1089/jwh.2018.7290
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Starmer AJ, Frintner MP, Matos K, Somberg C, Freed G, Byrne BJ. Gender discrepancies related to pediatrician work-life balance and household responsibilities. Pediatrics. 2019;144(4):e20182926. https://doi.org/10.1542/peds.2018-2926
6. Alon TM, Doepke M, Olmstead-Rumsey J, Tertilt Ml. The impact of COVID-19 on gender equality. NBER Working Paper Series. 2020. https://doi.org/10.3386/w26947
7. Addati L, Cattaneo U, Esquivel V, Valarino I. Care work and care jobs for the future of decent work. Geneva: International Labour Office; 2018.
8. Maguire P. Should you steer clear of your own family? Hospitalists weigh living in isolation. Today’s Hospitalist. May 2020. Accessed May 4, 2020. https://www.todayshospitalist.com/treating-covid-patients/
9. Burrer SL, de Perio MA, Hughes MM, et al. Characteristics of health care personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-481. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e6
10. SHM Teams Up with Hilton and American Express to Provide Hotel Rooms for Members. SHM. April 13, 2020. Accessed May 7, 2020. https://www.hospitalmedicine.org/about/press-releases/SHM-One-Million-Beds-Hilton-AMEX/
11. Fichtel C, Kaufman S. Fearing COVID-19 spread to families, health care workers self-isolate at home. NBC News. March 31, 2020. Accessed May 7, 2020. https://www.nbcnews.com/health/health-news/fearing-covid-19-spread-families-health-care-workers-self-isolate-n1171726
12. Meier KA, Jerardi KE, Statile AM, Shah SS. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020;15(5):308‐310. https://doi.org/10.12788/jhm.3435
13. Frintner MP, Sisk B, Byrne BJ, Freed GL, Starmer AJ, Olson LM. Gender differences in earnings of early- and midcareer pediatricians. Pediatrics. 2019;144(4):e20183955. https://doi.org/10.1542/peds.2018-3955
14. Read S, Butkus R, Weissman A, Moyer DV. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169(9):658-661. https://doi.org/10.7326/m18-0693
15. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. https://doi.org/10.1111/joim.12752
16. Templeton K, Halpern L, Jumper C, Carroll RG. Leading and sustaining curricular change: workshop proceedings from the 2018 Sex and Gender Health Education Summit. J Womens Health (Larchmt). 2019;28(12):1743-1747. https://doi.org/10.1089/jwh.2018.7387
17. Eilperin J. White House women want to be in the room where it happens. The Washington Post. September 13, 2016. Accessed April 24, 2020. https://www.washingtonpost.com/news/powerpost/wp/2016/09/13/white-house-women-are-now-in-the-room-where-it-happens/
18. Choo EK. COVID-19 fault lines. Lancet. 2020;395(10233):1333. https://doi.org/10.1016/s0140-6736(20)30812-6
19. Núñez A, Madison M, Schiavo R, Elk R, Prigerson HG. Responding to healthcare disparities and challenges with access to care during COVID-19. Health Equity. 2020;4(1):117-128. https://doi.org/10.1089/heq.2020.29000.rtl
20. Paturel A. Closing the gender pay gap in medicine. AAMC News. April 16, 2019. Accessed April 21, 2020. https://www.aamc.org/news-insights/closing-gender-pay-gap-medicine
1. Association of American Medical Colleges. Table 13: US medical school faculty by sex, rank, and department, 2017-2018. December 31, 2019. Accessed January 16, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144(5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Rouse LP, Nagy-Agren S, Gebhard RE, Bernstein WK. Women physicians: gender and the medical workplace. J Womens Health (Larchmt). 2020;29(3):297‐309. https://doi.org/10.1089/jwh.2018.7290
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Starmer AJ, Frintner MP, Matos K, Somberg C, Freed G, Byrne BJ. Gender discrepancies related to pediatrician work-life balance and household responsibilities. Pediatrics. 2019;144(4):e20182926. https://doi.org/10.1542/peds.2018-2926
6. Alon TM, Doepke M, Olmstead-Rumsey J, Tertilt Ml. The impact of COVID-19 on gender equality. NBER Working Paper Series. 2020. https://doi.org/10.3386/w26947
7. Addati L, Cattaneo U, Esquivel V, Valarino I. Care work and care jobs for the future of decent work. Geneva: International Labour Office; 2018.
8. Maguire P. Should you steer clear of your own family? Hospitalists weigh living in isolation. Today’s Hospitalist. May 2020. Accessed May 4, 2020. https://www.todayshospitalist.com/treating-covid-patients/
9. Burrer SL, de Perio MA, Hughes MM, et al. Characteristics of health care personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-481. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e6
10. SHM Teams Up with Hilton and American Express to Provide Hotel Rooms for Members. SHM. April 13, 2020. Accessed May 7, 2020. https://www.hospitalmedicine.org/about/press-releases/SHM-One-Million-Beds-Hilton-AMEX/
11. Fichtel C, Kaufman S. Fearing COVID-19 spread to families, health care workers self-isolate at home. NBC News. March 31, 2020. Accessed May 7, 2020. https://www.nbcnews.com/health/health-news/fearing-covid-19-spread-families-health-care-workers-self-isolate-n1171726
12. Meier KA, Jerardi KE, Statile AM, Shah SS. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020;15(5):308‐310. https://doi.org/10.12788/jhm.3435
13. Frintner MP, Sisk B, Byrne BJ, Freed GL, Starmer AJ, Olson LM. Gender differences in earnings of early- and midcareer pediatricians. Pediatrics. 2019;144(4):e20183955. https://doi.org/10.1542/peds.2018-3955
14. Read S, Butkus R, Weissman A, Moyer DV. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169(9):658-661. https://doi.org/10.7326/m18-0693
15. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. https://doi.org/10.1111/joim.12752
16. Templeton K, Halpern L, Jumper C, Carroll RG. Leading and sustaining curricular change: workshop proceedings from the 2018 Sex and Gender Health Education Summit. J Womens Health (Larchmt). 2019;28(12):1743-1747. https://doi.org/10.1089/jwh.2018.7387
17. Eilperin J. White House women want to be in the room where it happens. The Washington Post. September 13, 2016. Accessed April 24, 2020. https://www.washingtonpost.com/news/powerpost/wp/2016/09/13/white-house-women-are-now-in-the-room-where-it-happens/
18. Choo EK. COVID-19 fault lines. Lancet. 2020;395(10233):1333. https://doi.org/10.1016/s0140-6736(20)30812-6
19. Núñez A, Madison M, Schiavo R, Elk R, Prigerson HG. Responding to healthcare disparities and challenges with access to care during COVID-19. Health Equity. 2020;4(1):117-128. https://doi.org/10.1089/heq.2020.29000.rtl
20. Paturel A. Closing the gender pay gap in medicine. AAMC News. April 16, 2019. Accessed April 21, 2020. https://www.aamc.org/news-insights/closing-gender-pay-gap-medicine
© 2020 Society of Hospital Medicine
Leveraging the Outpatient Pharmacy to Reduce Medication Waste in Pediatric Asthma Hospitalizations
Asthma results in approximately 125,000 hospitalizations for children annually in the United States.1,2 The National Heart, Lung, and Blood Institute guidelines recommend that children with persistent asthma be treated with a daily controller medication, ie, an inhaled corticosteroid (ICS).3 Hospitalization for an asthma exacerbation provides an opportunity to optimize daily controller medications and improve disease self-management by providing access to medications and teaching appropriate use of complicated inhalation devices.
To reduce readmission4 by mitigating low rates of postdischarge filling of ICS prescriptions,5,6 a strategy of “meds-in-hand” was implemented at discharge. “Meds-in-hand” mitigates medication access as a barrier to adherence by ensuring that patients are discharged from the hospital with all required medications in hand, removing any barriers to filling their initial prescriptions.7 The Asthma Improvement Collaborative at Cincinnati Children’s Hospital Medical Center (CCHMC) previously applied quality improvement methodology to implement “meds-in-hand” as a key intervention in a broad strategy that successfully reduced asthma-specific utilization for the 30-day period following an asthma-related hospitalization of publicly insured children from 12% to 7%.8,9
At the onset of the work described in this manuscript, children hospitalized with an acute exacerbation of persistent asthma were most often treated with an ICS while inpatients in addition to a standard short course of oral systemic corticosteroids. Conceptually, inpatient administration of ICS provided the opportunity to teach effective device usage with each inpatient administration and to reinforce daily use of the ICS as part of the patient’s daily home medication regimen. However, a proportion of patients admitted for an asthma exacerbation were noted to receive more than one ICS inhaler during their admission, most commonly due to a change in dose or type of ICS. When this occurred, the initially dispensed inhaler was discarded despite weeks of potential doses remaining. While some hospitals preferentially dispense ICS devices marketed to institutions with fewer doses per device, our pharmacy primarily dispensed ICS devices identical to retail locations containing at least a one-month supply of medication. In addition to the wasted medication, this practice resulted in additional work by healthcare staff, unnecessary patient charges, and potentially contributed to confusion about the discharge medication regimen.
Our specific aim for this quality improvement study was to reduce the monthly percentage of admissions for an acute asthma exacerbation treated with >1 ICS from 7% to 4% over a six-month period.
METHODS
Context
CCHMC is a quaternary care pediatric health system with more than 600 inpatient beds and 800-900 inpatient admissions per year for acute asthma exacerbation. The Hospital Medicine service cares for patients with asthma on five clinical teams across two different campuses. Care teams are supervised by an attending physician and may include residents, fellows, or nurse practitioners. Patients hospitalized for an acute asthma exacerbation may receive a consult from the Asthma Center consult team, staffed by faculty from either the Pediatric Pulmonology or Allergy/Immunology divisions. Respiratory therapists (RTs) administer inhaled medications and provide asthma education.
Planning the Intervention
Our improvement team included physicians from Hospital Medicine and Pulmonary Medicine, an Asthma Education Coordinator, a Clinical Pharmacist, a Pediatric Chief Resident, and a clinical research coordinator. Initial interventions targeted a single resident team at the main campus before spreading improvement activities to all resident teams at the main campus and then the satellite campus by February 2017.
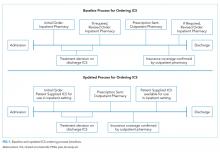
Development of our process map (Figure 1) revealed that the decision for ordering inpatient ICS treatment frequently occurred at admission. Subsequently, the care team or consulting team might make a change in the ICS to fine-tune the outpatient medication regimen given that admission for asthma often results from suboptimal chronic symptom control. Baseline analysis of changes in ICS orders revealed that 81% of ICS changes were associated with a step-up in therapy, defined as an increase in the daily dose of the ICS or the addition of a long-acting beta-agonist. The other common ICS adjustment, accounting for 17%, was a change in corticosteroid without a step-up in therapy, (ie, beclomethasone to fluticasone) that typically occurred near the end of the hospitalization to accommodate outpatient insurance formularies, independent of patient factors related to illness severity.
We utilized the model for improvement and sought to decrease the number of patients administered more than one ICS during an admission through a step-wise quality improvement approach, utilizing plan-do-study-act (PDSA) cycles.10 This study was reviewed and designated as not human subjects research by the CCHMC institutional review board.
Improvement Activities
We conceived key drivers or domains that would be necessary to address to effect change. Key drivers included a standardized process for delayed initiation of ICS and confirmation of outpatient insurance prescription drug coverage, prescriber education, and real-time failure notification.
PDSA Interventions
PDSA 1 & 2: Standardized Process for Initiation of ICS
Our initial tests of change targeted the timing of when an ICS was ordered during hospitalization for an asthma exacerbation. Providers were instructed to delay ordering an ICS until the patient’s albuterol treatments were spaced to every three hours and to include a standardized communication prompt within the albuterol order. The prompt instructed the RT to contact the provider once the patient’s albuterol treatments were spaced to every three hours and ask for an ICS order, if appropriate. This intervention was abandoned because it did not reliably occur.
The subsequent intervention delayed the start of ICS treatment by using a PRN indication advising that the ICS was to be administered once the patient’s albuterol treatments were spaced to every three hours. However, after an error resulted in the PRN indication being included on a discharge prescription for an ICS, the PRN indication was abandoned. Subsequent work to develop a standardized process for delayed initiation of ICS occurred as part of the workflow to address the confirmation of outpatient formulary coverage as described next.
PDSA 3: Prioritize the Use of the Institution’s Outpatient Pharmacy
Medication changes that occurred because of outpatient insurance formulary denials were a unique challenge; they required a medication change after the discharge treatment plan had been finalized, and a prescription was already submitted to the outpatient pharmacy. In addition, neither our inpatient electronic medical record nor our inpatient hospital pharmacy has access to decision support tools that incorporate outpatient prescription formulary coverage. Alternatively, outpatient pharmacies have a standard workflow that routinely confirms insurance coverage before dispensing medication. The institutional policy was modified to allow for the inpatient administration of patient-supplied medications, pursuant to an inpatient order. Patient-supplied medications include those brought from home or those supplied by the outpatient pharmacy.
Subsequently, we developed a standardized process to confirm outpatient prescription drug coverage by using our hospital-based outpatient pharmacy to dispense ICS for inpatient treatment and asthma education. This new workflow included placing an order for an ICS at admission as a patient-supplied medication with an administration comment to “please administer once available from the outpatient pharmacy” (Figure 1). Then, once the discharge medication plan is finalized, the prescription is submitted to the outpatient pharmacy. Following verification of insurance coverage, the outpatient pharmacy dispenses the ICS, allowing it to be used for patient education and inpatient administration. If the patient is ineligible to have their prescription filled by the outpatient pharmacy for reasons other than formulary coverage, the ICS is dispensed from the hospital inpatient pharmacy as per the previous standard workflow. Inpatient ICS inhalers are then relabeled for home use per the existing practice to support medications-in-hand.
Further workflow improvements occurred following the development of an algorithm to help the outpatient pharmacy contact the correct inpatient team, and augmentation of the medication delivery process included notification of the RT when the ICS was delivered to the inpatient unit.
PDSA 4: Prescriber Education
Prescribers received education regarding PDSA interventions before testing and throughout the improvement cycle. Education sessions included informal coaching by the Asthma Education Coordinator, e-mail reminders containing screenshots of the ordering process, and formal didactic sessions for ordering providers. The Asthma Education Coordinator also provided education to the nursing and respiratory therapy staff regarding the implemented process and workflow changes.
PDSA 5: Real-Time Failure Notification
To supplement education for the complicated process change, the improvement team utilized a decision support tool (Vigilanz Corp., Chicago, IL) linked to EMR data to provide notification of real-time process failures. When a patient with an admission diagnosis of asthma had a prescription for an ICS verified and dispensed by the inpatient pharmacy, an automated message with relevant patient information would be sent to a member of the improvement team. Following a brief chart review, directed feedback could be offered to the ordering provider, allowing the prescription to be redirected to the outpatient pharmacy.
Study of the Improvement
Patients of all ages, with the International Classification of Diseases, Ninth Revision, and Tenth Revision codes for asthma (493.xx or J45.xx) were included in data collection and analysis if they were treated by the Hospital Medicine service, as the first inpatient service or after transfer from the ICU, and prescribed an ICS with or without a long-acting beta-agonist. Data were collected retrospectively and aggregated monthly. The baseline period was from January 2015 through October 2016. The intervention period was from November 2016 through March 2018. The prolonged baseline and study periods were utilized to understand the seasonal nature of asthma exacerbations.
Measures
Our primary outcome measure was defined as the monthly number of patients admitted to Hospital Medicine for an acute asthma exacerbation administered more than one ICS divided by the total number of asthma patients administered at least one dose of an ICS (patient-supplied or dispensed from the inpatient pharmacy). A full list of ICS is included in the appendix Table.
A secondary process measure approximated our adherence to obtaining ICS from the outpatient pharmacy for inpatient use. All medications administered during hospitalization are documented in the medication administration report. However, only medications dispensed from the inpatient pharmacy are associated with a patient charge. Patient-supplied medications, including those dispensed from the hospital outpatient pharmacy, are not associated with an inpatient charge. Therefore, the secondary process measure was defined as the monthly number of asthma patients administered an ICS not associated with an inpatient charge divided by the total number of asthma patients administered an ICS.
A cost outcome measure was developed to track changes in the average cost of an ICS included on inpatient bills during hospitalization for an asthma exacerbation. This outcome measure was defined as the total monthly cost, using the average wholesale price, of the ICS included on the inpatient bill for an asthma exacerbation, divided by the total number of asthma patients administered at least one dose of an ICS (patient supplied or dispensed from the inpatient pharmacy).
Our a priori intent was to reduce ICS medication waste while maintaining a highly reliable system that included inpatient administration and education with ICS devices and maintain our medications-in-hand practice. A balancing measure was developed to monitor the reliability of inpatient administration of ICS. It was defined as the monthly number of patients who received a discharge prescription for an ICS and were administered an ICS while an inpatient divided by the total number of asthma patients with a discharge prescription for an ICS.
Analysis
Measures were evaluated using statistical process control charts and special cause variation was determined by previously established rules. Our primary, secondary, and balancing measures were all evaluated using a p-chart with variable subgroup size. The cost outcome measure was evaluated using an X-bar S control chart.11-13
RESULTS
Primary Outcome Measure
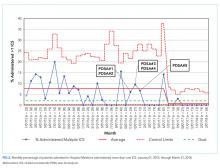
During the baseline period, 7.4% of patients admitted to Hospital Medicine for an acute asthma exacerbation were administered more than one ICS, ranging from 0%-20% of patients per month (Figure 2). Following the start of our interventions, we met criteria for special cause allowing adjustment of the centerline.13 The mean percentage of patients receiving more than one ICS decreased from 7.4% to 0.7%. Figure 2 includes the n-value displayed each month and represents all patients admitted to the Hospital Medicine service with an asthma exacerbation who were administered at least one ICS.
Secondary Process Measure
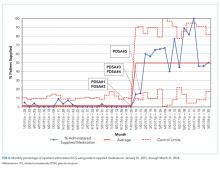
During the baseline period, there were only rare occurrences (less than 1%) of a patient-supplied ICS being administered during an asthma admission. Following the start of our intervention period, the frequency of inpatient administration of patient-supplied ICS showed a rapid increase and met rules for special cause with an increase in the mean percent from 0.7% to 50% (Figure 3). The n-value displayed each month represents all patients admitted to the Hospital Medicine service for an asthma exacerbation administered at least one ICS.
Cost Outcome Measure
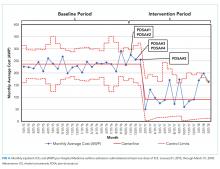
The average cost of an ICS billed during hospitalization for an acute asthma exacerbation was $236.57 per ICS during the baseline period. After the intervention period, the average inpatient cost for ICS decreased by 62% to $90.25 per ICS (Figure 4).
Balancing Measure
DISCUSSION
Our team reduced the monthly percent of children hospitalized with an acute asthma exacerbation administered more than one ICS from 7.4% to 0.7% after implementation of a new workflow process for ordering ICS utilizing the hospital-based outpatient pharmacy. The new workflow delayed ordering and administration of the initial inpatient ICS treatment, allowing time to consider a step-up in therapy. The brief delay in initiating ICS is not expected to have clinical consequence given the concomitant treatment with systemic corticosteroids. In addition, the outpatient pharmacy was utilized to verify insurance coverage reliably prior to dispensing ICS, reducing medication waste, and discharge delays due to outpatient medication formulary conflicts.
Our hospital’s previous approach to inpatient asthma care resulted in a highly reliable process to ensure patients were discharged with medications-in-hand as part of a broader system that effectively decreased reutilization. However, the previous process inadvertently resulted in medication waste. This waste included nearly full inhalers being discarded, additional work by the healthcare team (ordering providers, pharmacists, and RTs), and unnecessary patient charges.
While the primary driver of our decision to use the outpatient pharmacy was to adjudicate insurance prescription coverage reliably to prevent waste, this change likely resulted in a financial benefit to patients. The average cost per asthma admission of an inpatient billed for ICS using the average wholesale price, decreased by 62% following our interventions. The decrease in cost was primarily driven by using patient-supplied medications, including prescriptions newly filled by the on-site outpatient pharmacy, whose costs were not captured in this measure. While our secondary measure may underestimate the total expense incurred by families for an ICS, families likely receive their medications at a lower cost from the outpatient pharmacy than if the ICS was provided by an inpatient pharmacy. The average wholesale price is not what families are charged or pay for medications, partly due to differences in overhead costs that result in inpatient pharmacies having significantly higher charges than outpatient pharmacies. In addition, the 6.7% absolute reduction of our primary measure resulted in direct savings by reducing inpatient medication waste. Our process results in 67 fewer wasted ICS devices ($15,960) per 1,000 admissions for asthma exacerbation, extrapolated using the average cost ($238.20, average wholesale price) of each ICS during the baseline period.
Our quality improvement study had several limitations. (1) The interventions occurred at a single center with an established culture that embraces quality improvement, which may limit the generalizability of the work. (2) Our process verified insurance coverage with a hospital-based outpatient pharmacy. Some ICS prescriptions continued to be dispensed from the inpatient pharmacy, limiting our ability to verify insurance coverage. Local factors, including regulatory restrictions and delivery requirements, may limit the generalizability of using an outpatient pharmacy in this manner. (3) We achieved our goal of decreasing medication waste, but our a priori goal was to maintain our commitment to our established practice of interactive patient education with an ICS device as well as medications-in-hand at time of discharge. Our balancing measure showed a decrease in the percent of patients with a discharge prescription for an ICS who also received an inpatient dose of that ICS. This implies a decreased fidelity in our previously established education protocols. We had postulated that this occurred when the patient-supplied medication arrived on the day of discharge, but not close to when the medication was scheduled on the medication administration report, preventing administration. However, this is not a direct measure of patients receiving medications-in-hand or interactive medication education. Both may have occurred without administration of the ICS. (4) Despite a hospital culture that embraces quality improvement, this project required a significant change in the workflow that required considerable education at the time of implementation to integrate the new process reliably. However, once the process was in place, we have been able to sustain our improvement with limited educational investment.
CONCLUSIONS
Implementation of a new process for ordering ICS that emphasized delaying treatment until all necessary information was available and using an outpatient pharmacy to confirm insurance formulary coverage reduced the waste associated with more than one ICS being prescribed during a single admission.
Acknowledgments
The authors thank Sally Pope, MPH and Dr. Michael Carlisle, MD for their contribution to the quality improvement project. Thank you to Drs. Karen McDowell, MD and Carolyn Kercsmar, MD for advisement of our quality improvement project.
The authors appreciate the following individuals for their invaluable contributions. Dr. Hoefgen conceptualized and designed the study, was a member of the primary improvement team, carried out initial analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Drs. Jones and Torres Garcia, and Mr. Hare were members of the primary improvement team who contributed to the design of the quality improvement study and interventions, ongoing data interpretation, and critically reviewed the manuscript. Dr. Courter contributed to the conceptualization and designed the study, was a member of the primary improvement team, designed data collection instruments, and critically reviewed and revised the manuscript. Dr. Simmons conceptualized and designed the study, critically reviewed the manuscript for important intellectual content, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Disclaimer
The information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by the BHPR, HRSA, DHHS, or the U.S. Government.
1. Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):e20152354. https://doi.org/10.1542/peds.2015-2354.
2. HCUP Databases. Healthcare Cost and Utilization Project (HCUP). www.hcup.us.ahrq.gov/kidoverview.jsp. Published 2016. Accessed September 14, 2016.
3. NHLBI. Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma–summary report 2007. J Allergy Clin Immunol. 2007;120(5):S94-S138. https://doi.org/10.1016/j.jaci.2007.09.029.
4. Kenyon CC, Rubin DM, Zorc JJ, Mohamad Z, Faerber JA, Feudtner C. Childhood asthma hospital discharge medication fills and risk of subsequent readmission. J Pediatr. 2015;166(5):1121-1127. https://doi.org/10.1016/j.jpeds.2014.12.019.
5. Bollinger ME, Mudd KE, Boldt A, Hsu VD, Tsoukleris MG, Butz AM. Prescription fill patterns in underserved children with asthma receiving subspecialty care. Ann Allergy Asthma Immunol. 2013;111(3):185-189. https://doi.org/10.1016/j.anai.2013.06.009.
6. Cooper WO, Hickson GB. Corticosteroid prescription filling for children covered by Medicaid following an emergency department visit or a hospitalization for asthma. Arch Pediatr Adolesc Med. 2001;155(10):1111-1115. https://doi.org/10.1001/archpedi.155.10.1111.
7. Hatoun J, Bair-Merritt M, Cabral H, Moses J. Increasing medication possession at discharge for patients with asthma: the Meds-in-Hand Project. Pediatrics. 2016;137(3):e20150461-e20150461. https://doi.org/10.1542/peds.2015-0461.
8. Kercsmar CM, Beck AF, Sauers-Ford H, et al. Association of an asthma improvement collaborative with health care utilization in medicaid-insured pediatric patients in an urban community. JAMA Pediatr. 2017;171(11):1072-1080. https://doi.org/10.1001/jamapediatrics.2017.2600.
9. Sauers HS, Beck AF, Kahn RS, Simmons JM. Increasing recruitment rates in an inpatient clinical research study using quality improvement methods. Hosp Pediatr. 2014;4(6):335-341. https://doi.org/10.1542/hpeds.2014-0072.
10. Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Hoboken: John Wiley & Sons, Inc.; 2009.
11. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458-464. https://doi.org/10.1136/qhc.12.6.458.
12. Mohammed MA, Panesar JS, Laney DB, Wilson R. Statistical process control charts for attribute data involving very large sample sizes: a review of problems and solutions. BMJ Qual Saf. 2013;22(4):362-368. https://doi.org/10.1136/bmjqs-2012-001373.
13. Moen R, Nolan T, Provost L. Quality Improvement through Planned Experimentation. 2nd ed. New York City: McGraw-Hill Professional; 1998.
Asthma results in approximately 125,000 hospitalizations for children annually in the United States.1,2 The National Heart, Lung, and Blood Institute guidelines recommend that children with persistent asthma be treated with a daily controller medication, ie, an inhaled corticosteroid (ICS).3 Hospitalization for an asthma exacerbation provides an opportunity to optimize daily controller medications and improve disease self-management by providing access to medications and teaching appropriate use of complicated inhalation devices.
To reduce readmission4 by mitigating low rates of postdischarge filling of ICS prescriptions,5,6 a strategy of “meds-in-hand” was implemented at discharge. “Meds-in-hand” mitigates medication access as a barrier to adherence by ensuring that patients are discharged from the hospital with all required medications in hand, removing any barriers to filling their initial prescriptions.7 The Asthma Improvement Collaborative at Cincinnati Children’s Hospital Medical Center (CCHMC) previously applied quality improvement methodology to implement “meds-in-hand” as a key intervention in a broad strategy that successfully reduced asthma-specific utilization for the 30-day period following an asthma-related hospitalization of publicly insured children from 12% to 7%.8,9
At the onset of the work described in this manuscript, children hospitalized with an acute exacerbation of persistent asthma were most often treated with an ICS while inpatients in addition to a standard short course of oral systemic corticosteroids. Conceptually, inpatient administration of ICS provided the opportunity to teach effective device usage with each inpatient administration and to reinforce daily use of the ICS as part of the patient’s daily home medication regimen. However, a proportion of patients admitted for an asthma exacerbation were noted to receive more than one ICS inhaler during their admission, most commonly due to a change in dose or type of ICS. When this occurred, the initially dispensed inhaler was discarded despite weeks of potential doses remaining. While some hospitals preferentially dispense ICS devices marketed to institutions with fewer doses per device, our pharmacy primarily dispensed ICS devices identical to retail locations containing at least a one-month supply of medication. In addition to the wasted medication, this practice resulted in additional work by healthcare staff, unnecessary patient charges, and potentially contributed to confusion about the discharge medication regimen.
Our specific aim for this quality improvement study was to reduce the monthly percentage of admissions for an acute asthma exacerbation treated with >1 ICS from 7% to 4% over a six-month period.
METHODS
Context
CCHMC is a quaternary care pediatric health system with more than 600 inpatient beds and 800-900 inpatient admissions per year for acute asthma exacerbation. The Hospital Medicine service cares for patients with asthma on five clinical teams across two different campuses. Care teams are supervised by an attending physician and may include residents, fellows, or nurse practitioners. Patients hospitalized for an acute asthma exacerbation may receive a consult from the Asthma Center consult team, staffed by faculty from either the Pediatric Pulmonology or Allergy/Immunology divisions. Respiratory therapists (RTs) administer inhaled medications and provide asthma education.
Planning the Intervention
Our improvement team included physicians from Hospital Medicine and Pulmonary Medicine, an Asthma Education Coordinator, a Clinical Pharmacist, a Pediatric Chief Resident, and a clinical research coordinator. Initial interventions targeted a single resident team at the main campus before spreading improvement activities to all resident teams at the main campus and then the satellite campus by February 2017.
Development of our process map (Figure 1) revealed that the decision for ordering inpatient ICS treatment frequently occurred at admission. Subsequently, the care team or consulting team might make a change in the ICS to fine-tune the outpatient medication regimen given that admission for asthma often results from suboptimal chronic symptom control. Baseline analysis of changes in ICS orders revealed that 81% of ICS changes were associated with a step-up in therapy, defined as an increase in the daily dose of the ICS or the addition of a long-acting beta-agonist. The other common ICS adjustment, accounting for 17%, was a change in corticosteroid without a step-up in therapy, (ie, beclomethasone to fluticasone) that typically occurred near the end of the hospitalization to accommodate outpatient insurance formularies, independent of patient factors related to illness severity.
We utilized the model for improvement and sought to decrease the number of patients administered more than one ICS during an admission through a step-wise quality improvement approach, utilizing plan-do-study-act (PDSA) cycles.10 This study was reviewed and designated as not human subjects research by the CCHMC institutional review board.
Improvement Activities
We conceived key drivers or domains that would be necessary to address to effect change. Key drivers included a standardized process for delayed initiation of ICS and confirmation of outpatient insurance prescription drug coverage, prescriber education, and real-time failure notification.
PDSA Interventions
PDSA 1 & 2: Standardized Process for Initiation of ICS
Our initial tests of change targeted the timing of when an ICS was ordered during hospitalization for an asthma exacerbation. Providers were instructed to delay ordering an ICS until the patient’s albuterol treatments were spaced to every three hours and to include a standardized communication prompt within the albuterol order. The prompt instructed the RT to contact the provider once the patient’s albuterol treatments were spaced to every three hours and ask for an ICS order, if appropriate. This intervention was abandoned because it did not reliably occur.
The subsequent intervention delayed the start of ICS treatment by using a PRN indication advising that the ICS was to be administered once the patient’s albuterol treatments were spaced to every three hours. However, after an error resulted in the PRN indication being included on a discharge prescription for an ICS, the PRN indication was abandoned. Subsequent work to develop a standardized process for delayed initiation of ICS occurred as part of the workflow to address the confirmation of outpatient formulary coverage as described next.
PDSA 3: Prioritize the Use of the Institution’s Outpatient Pharmacy
Medication changes that occurred because of outpatient insurance formulary denials were a unique challenge; they required a medication change after the discharge treatment plan had been finalized, and a prescription was already submitted to the outpatient pharmacy. In addition, neither our inpatient electronic medical record nor our inpatient hospital pharmacy has access to decision support tools that incorporate outpatient prescription formulary coverage. Alternatively, outpatient pharmacies have a standard workflow that routinely confirms insurance coverage before dispensing medication. The institutional policy was modified to allow for the inpatient administration of patient-supplied medications, pursuant to an inpatient order. Patient-supplied medications include those brought from home or those supplied by the outpatient pharmacy.
Subsequently, we developed a standardized process to confirm outpatient prescription drug coverage by using our hospital-based outpatient pharmacy to dispense ICS for inpatient treatment and asthma education. This new workflow included placing an order for an ICS at admission as a patient-supplied medication with an administration comment to “please administer once available from the outpatient pharmacy” (Figure 1). Then, once the discharge medication plan is finalized, the prescription is submitted to the outpatient pharmacy. Following verification of insurance coverage, the outpatient pharmacy dispenses the ICS, allowing it to be used for patient education and inpatient administration. If the patient is ineligible to have their prescription filled by the outpatient pharmacy for reasons other than formulary coverage, the ICS is dispensed from the hospital inpatient pharmacy as per the previous standard workflow. Inpatient ICS inhalers are then relabeled for home use per the existing practice to support medications-in-hand.
Further workflow improvements occurred following the development of an algorithm to help the outpatient pharmacy contact the correct inpatient team, and augmentation of the medication delivery process included notification of the RT when the ICS was delivered to the inpatient unit.
PDSA 4: Prescriber Education
Prescribers received education regarding PDSA interventions before testing and throughout the improvement cycle. Education sessions included informal coaching by the Asthma Education Coordinator, e-mail reminders containing screenshots of the ordering process, and formal didactic sessions for ordering providers. The Asthma Education Coordinator also provided education to the nursing and respiratory therapy staff regarding the implemented process and workflow changes.
PDSA 5: Real-Time Failure Notification
To supplement education for the complicated process change, the improvement team utilized a decision support tool (Vigilanz Corp., Chicago, IL) linked to EMR data to provide notification of real-time process failures. When a patient with an admission diagnosis of asthma had a prescription for an ICS verified and dispensed by the inpatient pharmacy, an automated message with relevant patient information would be sent to a member of the improvement team. Following a brief chart review, directed feedback could be offered to the ordering provider, allowing the prescription to be redirected to the outpatient pharmacy.
Study of the Improvement
Patients of all ages, with the International Classification of Diseases, Ninth Revision, and Tenth Revision codes for asthma (493.xx or J45.xx) were included in data collection and analysis if they were treated by the Hospital Medicine service, as the first inpatient service or after transfer from the ICU, and prescribed an ICS with or without a long-acting beta-agonist. Data were collected retrospectively and aggregated monthly. The baseline period was from January 2015 through October 2016. The intervention period was from November 2016 through March 2018. The prolonged baseline and study periods were utilized to understand the seasonal nature of asthma exacerbations.
Measures
Our primary outcome measure was defined as the monthly number of patients admitted to Hospital Medicine for an acute asthma exacerbation administered more than one ICS divided by the total number of asthma patients administered at least one dose of an ICS (patient-supplied or dispensed from the inpatient pharmacy). A full list of ICS is included in the appendix Table.
A secondary process measure approximated our adherence to obtaining ICS from the outpatient pharmacy for inpatient use. All medications administered during hospitalization are documented in the medication administration report. However, only medications dispensed from the inpatient pharmacy are associated with a patient charge. Patient-supplied medications, including those dispensed from the hospital outpatient pharmacy, are not associated with an inpatient charge. Therefore, the secondary process measure was defined as the monthly number of asthma patients administered an ICS not associated with an inpatient charge divided by the total number of asthma patients administered an ICS.
A cost outcome measure was developed to track changes in the average cost of an ICS included on inpatient bills during hospitalization for an asthma exacerbation. This outcome measure was defined as the total monthly cost, using the average wholesale price, of the ICS included on the inpatient bill for an asthma exacerbation, divided by the total number of asthma patients administered at least one dose of an ICS (patient supplied or dispensed from the inpatient pharmacy).
Our a priori intent was to reduce ICS medication waste while maintaining a highly reliable system that included inpatient administration and education with ICS devices and maintain our medications-in-hand practice. A balancing measure was developed to monitor the reliability of inpatient administration of ICS. It was defined as the monthly number of patients who received a discharge prescription for an ICS and were administered an ICS while an inpatient divided by the total number of asthma patients with a discharge prescription for an ICS.
Analysis
Measures were evaluated using statistical process control charts and special cause variation was determined by previously established rules. Our primary, secondary, and balancing measures were all evaluated using a p-chart with variable subgroup size. The cost outcome measure was evaluated using an X-bar S control chart.11-13
RESULTS
Primary Outcome Measure
During the baseline period, 7.4% of patients admitted to Hospital Medicine for an acute asthma exacerbation were administered more than one ICS, ranging from 0%-20% of patients per month (Figure 2). Following the start of our interventions, we met criteria for special cause allowing adjustment of the centerline.13 The mean percentage of patients receiving more than one ICS decreased from 7.4% to 0.7%. Figure 2 includes the n-value displayed each month and represents all patients admitted to the Hospital Medicine service with an asthma exacerbation who were administered at least one ICS.
Secondary Process Measure
During the baseline period, there were only rare occurrences (less than 1%) of a patient-supplied ICS being administered during an asthma admission. Following the start of our intervention period, the frequency of inpatient administration of patient-supplied ICS showed a rapid increase and met rules for special cause with an increase in the mean percent from 0.7% to 50% (Figure 3). The n-value displayed each month represents all patients admitted to the Hospital Medicine service for an asthma exacerbation administered at least one ICS.
Cost Outcome Measure
The average cost of an ICS billed during hospitalization for an acute asthma exacerbation was $236.57 per ICS during the baseline period. After the intervention period, the average inpatient cost for ICS decreased by 62% to $90.25 per ICS (Figure 4).
Balancing Measure
DISCUSSION
Our team reduced the monthly percent of children hospitalized with an acute asthma exacerbation administered more than one ICS from 7.4% to 0.7% after implementation of a new workflow process for ordering ICS utilizing the hospital-based outpatient pharmacy. The new workflow delayed ordering and administration of the initial inpatient ICS treatment, allowing time to consider a step-up in therapy. The brief delay in initiating ICS is not expected to have clinical consequence given the concomitant treatment with systemic corticosteroids. In addition, the outpatient pharmacy was utilized to verify insurance coverage reliably prior to dispensing ICS, reducing medication waste, and discharge delays due to outpatient medication formulary conflicts.
Our hospital’s previous approach to inpatient asthma care resulted in a highly reliable process to ensure patients were discharged with medications-in-hand as part of a broader system that effectively decreased reutilization. However, the previous process inadvertently resulted in medication waste. This waste included nearly full inhalers being discarded, additional work by the healthcare team (ordering providers, pharmacists, and RTs), and unnecessary patient charges.
While the primary driver of our decision to use the outpatient pharmacy was to adjudicate insurance prescription coverage reliably to prevent waste, this change likely resulted in a financial benefit to patients. The average cost per asthma admission of an inpatient billed for ICS using the average wholesale price, decreased by 62% following our interventions. The decrease in cost was primarily driven by using patient-supplied medications, including prescriptions newly filled by the on-site outpatient pharmacy, whose costs were not captured in this measure. While our secondary measure may underestimate the total expense incurred by families for an ICS, families likely receive their medications at a lower cost from the outpatient pharmacy than if the ICS was provided by an inpatient pharmacy. The average wholesale price is not what families are charged or pay for medications, partly due to differences in overhead costs that result in inpatient pharmacies having significantly higher charges than outpatient pharmacies. In addition, the 6.7% absolute reduction of our primary measure resulted in direct savings by reducing inpatient medication waste. Our process results in 67 fewer wasted ICS devices ($15,960) per 1,000 admissions for asthma exacerbation, extrapolated using the average cost ($238.20, average wholesale price) of each ICS during the baseline period.
Our quality improvement study had several limitations. (1) The interventions occurred at a single center with an established culture that embraces quality improvement, which may limit the generalizability of the work. (2) Our process verified insurance coverage with a hospital-based outpatient pharmacy. Some ICS prescriptions continued to be dispensed from the inpatient pharmacy, limiting our ability to verify insurance coverage. Local factors, including regulatory restrictions and delivery requirements, may limit the generalizability of using an outpatient pharmacy in this manner. (3) We achieved our goal of decreasing medication waste, but our a priori goal was to maintain our commitment to our established practice of interactive patient education with an ICS device as well as medications-in-hand at time of discharge. Our balancing measure showed a decrease in the percent of patients with a discharge prescription for an ICS who also received an inpatient dose of that ICS. This implies a decreased fidelity in our previously established education protocols. We had postulated that this occurred when the patient-supplied medication arrived on the day of discharge, but not close to when the medication was scheduled on the medication administration report, preventing administration. However, this is not a direct measure of patients receiving medications-in-hand or interactive medication education. Both may have occurred without administration of the ICS. (4) Despite a hospital culture that embraces quality improvement, this project required a significant change in the workflow that required considerable education at the time of implementation to integrate the new process reliably. However, once the process was in place, we have been able to sustain our improvement with limited educational investment.
CONCLUSIONS
Implementation of a new process for ordering ICS that emphasized delaying treatment until all necessary information was available and using an outpatient pharmacy to confirm insurance formulary coverage reduced the waste associated with more than one ICS being prescribed during a single admission.
Acknowledgments
The authors thank Sally Pope, MPH and Dr. Michael Carlisle, MD for their contribution to the quality improvement project. Thank you to Drs. Karen McDowell, MD and Carolyn Kercsmar, MD for advisement of our quality improvement project.
The authors appreciate the following individuals for their invaluable contributions. Dr. Hoefgen conceptualized and designed the study, was a member of the primary improvement team, carried out initial analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Drs. Jones and Torres Garcia, and Mr. Hare were members of the primary improvement team who contributed to the design of the quality improvement study and interventions, ongoing data interpretation, and critically reviewed the manuscript. Dr. Courter contributed to the conceptualization and designed the study, was a member of the primary improvement team, designed data collection instruments, and critically reviewed and revised the manuscript. Dr. Simmons conceptualized and designed the study, critically reviewed the manuscript for important intellectual content, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Disclaimer
The information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by the BHPR, HRSA, DHHS, or the U.S. Government.
Asthma results in approximately 125,000 hospitalizations for children annually in the United States.1,2 The National Heart, Lung, and Blood Institute guidelines recommend that children with persistent asthma be treated with a daily controller medication, ie, an inhaled corticosteroid (ICS).3 Hospitalization for an asthma exacerbation provides an opportunity to optimize daily controller medications and improve disease self-management by providing access to medications and teaching appropriate use of complicated inhalation devices.
To reduce readmission4 by mitigating low rates of postdischarge filling of ICS prescriptions,5,6 a strategy of “meds-in-hand” was implemented at discharge. “Meds-in-hand” mitigates medication access as a barrier to adherence by ensuring that patients are discharged from the hospital with all required medications in hand, removing any barriers to filling their initial prescriptions.7 The Asthma Improvement Collaborative at Cincinnati Children’s Hospital Medical Center (CCHMC) previously applied quality improvement methodology to implement “meds-in-hand” as a key intervention in a broad strategy that successfully reduced asthma-specific utilization for the 30-day period following an asthma-related hospitalization of publicly insured children from 12% to 7%.8,9
At the onset of the work described in this manuscript, children hospitalized with an acute exacerbation of persistent asthma were most often treated with an ICS while inpatients in addition to a standard short course of oral systemic corticosteroids. Conceptually, inpatient administration of ICS provided the opportunity to teach effective device usage with each inpatient administration and to reinforce daily use of the ICS as part of the patient’s daily home medication regimen. However, a proportion of patients admitted for an asthma exacerbation were noted to receive more than one ICS inhaler during their admission, most commonly due to a change in dose or type of ICS. When this occurred, the initially dispensed inhaler was discarded despite weeks of potential doses remaining. While some hospitals preferentially dispense ICS devices marketed to institutions with fewer doses per device, our pharmacy primarily dispensed ICS devices identical to retail locations containing at least a one-month supply of medication. In addition to the wasted medication, this practice resulted in additional work by healthcare staff, unnecessary patient charges, and potentially contributed to confusion about the discharge medication regimen.
Our specific aim for this quality improvement study was to reduce the monthly percentage of admissions for an acute asthma exacerbation treated with >1 ICS from 7% to 4% over a six-month period.
METHODS
Context
CCHMC is a quaternary care pediatric health system with more than 600 inpatient beds and 800-900 inpatient admissions per year for acute asthma exacerbation. The Hospital Medicine service cares for patients with asthma on five clinical teams across two different campuses. Care teams are supervised by an attending physician and may include residents, fellows, or nurse practitioners. Patients hospitalized for an acute asthma exacerbation may receive a consult from the Asthma Center consult team, staffed by faculty from either the Pediatric Pulmonology or Allergy/Immunology divisions. Respiratory therapists (RTs) administer inhaled medications and provide asthma education.
Planning the Intervention
Our improvement team included physicians from Hospital Medicine and Pulmonary Medicine, an Asthma Education Coordinator, a Clinical Pharmacist, a Pediatric Chief Resident, and a clinical research coordinator. Initial interventions targeted a single resident team at the main campus before spreading improvement activities to all resident teams at the main campus and then the satellite campus by February 2017.
Development of our process map (Figure 1) revealed that the decision for ordering inpatient ICS treatment frequently occurred at admission. Subsequently, the care team or consulting team might make a change in the ICS to fine-tune the outpatient medication regimen given that admission for asthma often results from suboptimal chronic symptom control. Baseline analysis of changes in ICS orders revealed that 81% of ICS changes were associated with a step-up in therapy, defined as an increase in the daily dose of the ICS or the addition of a long-acting beta-agonist. The other common ICS adjustment, accounting for 17%, was a change in corticosteroid without a step-up in therapy, (ie, beclomethasone to fluticasone) that typically occurred near the end of the hospitalization to accommodate outpatient insurance formularies, independent of patient factors related to illness severity.
We utilized the model for improvement and sought to decrease the number of patients administered more than one ICS during an admission through a step-wise quality improvement approach, utilizing plan-do-study-act (PDSA) cycles.10 This study was reviewed and designated as not human subjects research by the CCHMC institutional review board.
Improvement Activities
We conceived key drivers or domains that would be necessary to address to effect change. Key drivers included a standardized process for delayed initiation of ICS and confirmation of outpatient insurance prescription drug coverage, prescriber education, and real-time failure notification.
PDSA Interventions
PDSA 1 & 2: Standardized Process for Initiation of ICS
Our initial tests of change targeted the timing of when an ICS was ordered during hospitalization for an asthma exacerbation. Providers were instructed to delay ordering an ICS until the patient’s albuterol treatments were spaced to every three hours and to include a standardized communication prompt within the albuterol order. The prompt instructed the RT to contact the provider once the patient’s albuterol treatments were spaced to every three hours and ask for an ICS order, if appropriate. This intervention was abandoned because it did not reliably occur.
The subsequent intervention delayed the start of ICS treatment by using a PRN indication advising that the ICS was to be administered once the patient’s albuterol treatments were spaced to every three hours. However, after an error resulted in the PRN indication being included on a discharge prescription for an ICS, the PRN indication was abandoned. Subsequent work to develop a standardized process for delayed initiation of ICS occurred as part of the workflow to address the confirmation of outpatient formulary coverage as described next.
PDSA 3: Prioritize the Use of the Institution’s Outpatient Pharmacy
Medication changes that occurred because of outpatient insurance formulary denials were a unique challenge; they required a medication change after the discharge treatment plan had been finalized, and a prescription was already submitted to the outpatient pharmacy. In addition, neither our inpatient electronic medical record nor our inpatient hospital pharmacy has access to decision support tools that incorporate outpatient prescription formulary coverage. Alternatively, outpatient pharmacies have a standard workflow that routinely confirms insurance coverage before dispensing medication. The institutional policy was modified to allow for the inpatient administration of patient-supplied medications, pursuant to an inpatient order. Patient-supplied medications include those brought from home or those supplied by the outpatient pharmacy.
Subsequently, we developed a standardized process to confirm outpatient prescription drug coverage by using our hospital-based outpatient pharmacy to dispense ICS for inpatient treatment and asthma education. This new workflow included placing an order for an ICS at admission as a patient-supplied medication with an administration comment to “please administer once available from the outpatient pharmacy” (Figure 1). Then, once the discharge medication plan is finalized, the prescription is submitted to the outpatient pharmacy. Following verification of insurance coverage, the outpatient pharmacy dispenses the ICS, allowing it to be used for patient education and inpatient administration. If the patient is ineligible to have their prescription filled by the outpatient pharmacy for reasons other than formulary coverage, the ICS is dispensed from the hospital inpatient pharmacy as per the previous standard workflow. Inpatient ICS inhalers are then relabeled for home use per the existing practice to support medications-in-hand.
Further workflow improvements occurred following the development of an algorithm to help the outpatient pharmacy contact the correct inpatient team, and augmentation of the medication delivery process included notification of the RT when the ICS was delivered to the inpatient unit.
PDSA 4: Prescriber Education
Prescribers received education regarding PDSA interventions before testing and throughout the improvement cycle. Education sessions included informal coaching by the Asthma Education Coordinator, e-mail reminders containing screenshots of the ordering process, and formal didactic sessions for ordering providers. The Asthma Education Coordinator also provided education to the nursing and respiratory therapy staff regarding the implemented process and workflow changes.
PDSA 5: Real-Time Failure Notification
To supplement education for the complicated process change, the improvement team utilized a decision support tool (Vigilanz Corp., Chicago, IL) linked to EMR data to provide notification of real-time process failures. When a patient with an admission diagnosis of asthma had a prescription for an ICS verified and dispensed by the inpatient pharmacy, an automated message with relevant patient information would be sent to a member of the improvement team. Following a brief chart review, directed feedback could be offered to the ordering provider, allowing the prescription to be redirected to the outpatient pharmacy.
Study of the Improvement
Patients of all ages, with the International Classification of Diseases, Ninth Revision, and Tenth Revision codes for asthma (493.xx or J45.xx) were included in data collection and analysis if they were treated by the Hospital Medicine service, as the first inpatient service or after transfer from the ICU, and prescribed an ICS with or without a long-acting beta-agonist. Data were collected retrospectively and aggregated monthly. The baseline period was from January 2015 through October 2016. The intervention period was from November 2016 through March 2018. The prolonged baseline and study periods were utilized to understand the seasonal nature of asthma exacerbations.
Measures
Our primary outcome measure was defined as the monthly number of patients admitted to Hospital Medicine for an acute asthma exacerbation administered more than one ICS divided by the total number of asthma patients administered at least one dose of an ICS (patient-supplied or dispensed from the inpatient pharmacy). A full list of ICS is included in the appendix Table.
A secondary process measure approximated our adherence to obtaining ICS from the outpatient pharmacy for inpatient use. All medications administered during hospitalization are documented in the medication administration report. However, only medications dispensed from the inpatient pharmacy are associated with a patient charge. Patient-supplied medications, including those dispensed from the hospital outpatient pharmacy, are not associated with an inpatient charge. Therefore, the secondary process measure was defined as the monthly number of asthma patients administered an ICS not associated with an inpatient charge divided by the total number of asthma patients administered an ICS.
A cost outcome measure was developed to track changes in the average cost of an ICS included on inpatient bills during hospitalization for an asthma exacerbation. This outcome measure was defined as the total monthly cost, using the average wholesale price, of the ICS included on the inpatient bill for an asthma exacerbation, divided by the total number of asthma patients administered at least one dose of an ICS (patient supplied or dispensed from the inpatient pharmacy).
Our a priori intent was to reduce ICS medication waste while maintaining a highly reliable system that included inpatient administration and education with ICS devices and maintain our medications-in-hand practice. A balancing measure was developed to monitor the reliability of inpatient administration of ICS. It was defined as the monthly number of patients who received a discharge prescription for an ICS and were administered an ICS while an inpatient divided by the total number of asthma patients with a discharge prescription for an ICS.
Analysis
Measures were evaluated using statistical process control charts and special cause variation was determined by previously established rules. Our primary, secondary, and balancing measures were all evaluated using a p-chart with variable subgroup size. The cost outcome measure was evaluated using an X-bar S control chart.11-13
RESULTS
Primary Outcome Measure
During the baseline period, 7.4% of patients admitted to Hospital Medicine for an acute asthma exacerbation were administered more than one ICS, ranging from 0%-20% of patients per month (Figure 2). Following the start of our interventions, we met criteria for special cause allowing adjustment of the centerline.13 The mean percentage of patients receiving more than one ICS decreased from 7.4% to 0.7%. Figure 2 includes the n-value displayed each month and represents all patients admitted to the Hospital Medicine service with an asthma exacerbation who were administered at least one ICS.
Secondary Process Measure
During the baseline period, there were only rare occurrences (less than 1%) of a patient-supplied ICS being administered during an asthma admission. Following the start of our intervention period, the frequency of inpatient administration of patient-supplied ICS showed a rapid increase and met rules for special cause with an increase in the mean percent from 0.7% to 50% (Figure 3). The n-value displayed each month represents all patients admitted to the Hospital Medicine service for an asthma exacerbation administered at least one ICS.
Cost Outcome Measure
The average cost of an ICS billed during hospitalization for an acute asthma exacerbation was $236.57 per ICS during the baseline period. After the intervention period, the average inpatient cost for ICS decreased by 62% to $90.25 per ICS (Figure 4).
Balancing Measure
DISCUSSION
Our team reduced the monthly percent of children hospitalized with an acute asthma exacerbation administered more than one ICS from 7.4% to 0.7% after implementation of a new workflow process for ordering ICS utilizing the hospital-based outpatient pharmacy. The new workflow delayed ordering and administration of the initial inpatient ICS treatment, allowing time to consider a step-up in therapy. The brief delay in initiating ICS is not expected to have clinical consequence given the concomitant treatment with systemic corticosteroids. In addition, the outpatient pharmacy was utilized to verify insurance coverage reliably prior to dispensing ICS, reducing medication waste, and discharge delays due to outpatient medication formulary conflicts.
Our hospital’s previous approach to inpatient asthma care resulted in a highly reliable process to ensure patients were discharged with medications-in-hand as part of a broader system that effectively decreased reutilization. However, the previous process inadvertently resulted in medication waste. This waste included nearly full inhalers being discarded, additional work by the healthcare team (ordering providers, pharmacists, and RTs), and unnecessary patient charges.
While the primary driver of our decision to use the outpatient pharmacy was to adjudicate insurance prescription coverage reliably to prevent waste, this change likely resulted in a financial benefit to patients. The average cost per asthma admission of an inpatient billed for ICS using the average wholesale price, decreased by 62% following our interventions. The decrease in cost was primarily driven by using patient-supplied medications, including prescriptions newly filled by the on-site outpatient pharmacy, whose costs were not captured in this measure. While our secondary measure may underestimate the total expense incurred by families for an ICS, families likely receive their medications at a lower cost from the outpatient pharmacy than if the ICS was provided by an inpatient pharmacy. The average wholesale price is not what families are charged or pay for medications, partly due to differences in overhead costs that result in inpatient pharmacies having significantly higher charges than outpatient pharmacies. In addition, the 6.7% absolute reduction of our primary measure resulted in direct savings by reducing inpatient medication waste. Our process results in 67 fewer wasted ICS devices ($15,960) per 1,000 admissions for asthma exacerbation, extrapolated using the average cost ($238.20, average wholesale price) of each ICS during the baseline period.
Our quality improvement study had several limitations. (1) The interventions occurred at a single center with an established culture that embraces quality improvement, which may limit the generalizability of the work. (2) Our process verified insurance coverage with a hospital-based outpatient pharmacy. Some ICS prescriptions continued to be dispensed from the inpatient pharmacy, limiting our ability to verify insurance coverage. Local factors, including regulatory restrictions and delivery requirements, may limit the generalizability of using an outpatient pharmacy in this manner. (3) We achieved our goal of decreasing medication waste, but our a priori goal was to maintain our commitment to our established practice of interactive patient education with an ICS device as well as medications-in-hand at time of discharge. Our balancing measure showed a decrease in the percent of patients with a discharge prescription for an ICS who also received an inpatient dose of that ICS. This implies a decreased fidelity in our previously established education protocols. We had postulated that this occurred when the patient-supplied medication arrived on the day of discharge, but not close to when the medication was scheduled on the medication administration report, preventing administration. However, this is not a direct measure of patients receiving medications-in-hand or interactive medication education. Both may have occurred without administration of the ICS. (4) Despite a hospital culture that embraces quality improvement, this project required a significant change in the workflow that required considerable education at the time of implementation to integrate the new process reliably. However, once the process was in place, we have been able to sustain our improvement with limited educational investment.
CONCLUSIONS
Implementation of a new process for ordering ICS that emphasized delaying treatment until all necessary information was available and using an outpatient pharmacy to confirm insurance formulary coverage reduced the waste associated with more than one ICS being prescribed during a single admission.
Acknowledgments
The authors thank Sally Pope, MPH and Dr. Michael Carlisle, MD for their contribution to the quality improvement project. Thank you to Drs. Karen McDowell, MD and Carolyn Kercsmar, MD for advisement of our quality improvement project.
The authors appreciate the following individuals for their invaluable contributions. Dr. Hoefgen conceptualized and designed the study, was a member of the primary improvement team, carried out initial analysis, drafted the initial manuscript, and reviewed and revised the manuscript. Drs. Jones and Torres Garcia, and Mr. Hare were members of the primary improvement team who contributed to the design of the quality improvement study and interventions, ongoing data interpretation, and critically reviewed the manuscript. Dr. Courter contributed to the conceptualization and designed the study, was a member of the primary improvement team, designed data collection instruments, and critically reviewed and revised the manuscript. Dr. Simmons conceptualized and designed the study, critically reviewed the manuscript for important intellectual content, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Disclaimer
The information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by the BHPR, HRSA, DHHS, or the U.S. Government.
1. Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):e20152354. https://doi.org/10.1542/peds.2015-2354.
2. HCUP Databases. Healthcare Cost and Utilization Project (HCUP). www.hcup.us.ahrq.gov/kidoverview.jsp. Published 2016. Accessed September 14, 2016.
3. NHLBI. Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma–summary report 2007. J Allergy Clin Immunol. 2007;120(5):S94-S138. https://doi.org/10.1016/j.jaci.2007.09.029.
4. Kenyon CC, Rubin DM, Zorc JJ, Mohamad Z, Faerber JA, Feudtner C. Childhood asthma hospital discharge medication fills and risk of subsequent readmission. J Pediatr. 2015;166(5):1121-1127. https://doi.org/10.1016/j.jpeds.2014.12.019.
5. Bollinger ME, Mudd KE, Boldt A, Hsu VD, Tsoukleris MG, Butz AM. Prescription fill patterns in underserved children with asthma receiving subspecialty care. Ann Allergy Asthma Immunol. 2013;111(3):185-189. https://doi.org/10.1016/j.anai.2013.06.009.
6. Cooper WO, Hickson GB. Corticosteroid prescription filling for children covered by Medicaid following an emergency department visit or a hospitalization for asthma. Arch Pediatr Adolesc Med. 2001;155(10):1111-1115. https://doi.org/10.1001/archpedi.155.10.1111.
7. Hatoun J, Bair-Merritt M, Cabral H, Moses J. Increasing medication possession at discharge for patients with asthma: the Meds-in-Hand Project. Pediatrics. 2016;137(3):e20150461-e20150461. https://doi.org/10.1542/peds.2015-0461.
8. Kercsmar CM, Beck AF, Sauers-Ford H, et al. Association of an asthma improvement collaborative with health care utilization in medicaid-insured pediatric patients in an urban community. JAMA Pediatr. 2017;171(11):1072-1080. https://doi.org/10.1001/jamapediatrics.2017.2600.
9. Sauers HS, Beck AF, Kahn RS, Simmons JM. Increasing recruitment rates in an inpatient clinical research study using quality improvement methods. Hosp Pediatr. 2014;4(6):335-341. https://doi.org/10.1542/hpeds.2014-0072.
10. Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Hoboken: John Wiley & Sons, Inc.; 2009.
11. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458-464. https://doi.org/10.1136/qhc.12.6.458.
12. Mohammed MA, Panesar JS, Laney DB, Wilson R. Statistical process control charts for attribute data involving very large sample sizes: a review of problems and solutions. BMJ Qual Saf. 2013;22(4):362-368. https://doi.org/10.1136/bmjqs-2012-001373.
13. Moen R, Nolan T, Provost L. Quality Improvement through Planned Experimentation. 2nd ed. New York City: McGraw-Hill Professional; 1998.
1. Akinbami LJ, Simon AE, Rossen LM. Changing trends in asthma prevalence among children. Pediatrics. 2016;137(1):e20152354. https://doi.org/10.1542/peds.2015-2354.
2. HCUP Databases. Healthcare Cost and Utilization Project (HCUP). www.hcup.us.ahrq.gov/kidoverview.jsp. Published 2016. Accessed September 14, 2016.
3. NHLBI. Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma–summary report 2007. J Allergy Clin Immunol. 2007;120(5):S94-S138. https://doi.org/10.1016/j.jaci.2007.09.029.
4. Kenyon CC, Rubin DM, Zorc JJ, Mohamad Z, Faerber JA, Feudtner C. Childhood asthma hospital discharge medication fills and risk of subsequent readmission. J Pediatr. 2015;166(5):1121-1127. https://doi.org/10.1016/j.jpeds.2014.12.019.
5. Bollinger ME, Mudd KE, Boldt A, Hsu VD, Tsoukleris MG, Butz AM. Prescription fill patterns in underserved children with asthma receiving subspecialty care. Ann Allergy Asthma Immunol. 2013;111(3):185-189. https://doi.org/10.1016/j.anai.2013.06.009.
6. Cooper WO, Hickson GB. Corticosteroid prescription filling for children covered by Medicaid following an emergency department visit or a hospitalization for asthma. Arch Pediatr Adolesc Med. 2001;155(10):1111-1115. https://doi.org/10.1001/archpedi.155.10.1111.
7. Hatoun J, Bair-Merritt M, Cabral H, Moses J. Increasing medication possession at discharge for patients with asthma: the Meds-in-Hand Project. Pediatrics. 2016;137(3):e20150461-e20150461. https://doi.org/10.1542/peds.2015-0461.
8. Kercsmar CM, Beck AF, Sauers-Ford H, et al. Association of an asthma improvement collaborative with health care utilization in medicaid-insured pediatric patients in an urban community. JAMA Pediatr. 2017;171(11):1072-1080. https://doi.org/10.1001/jamapediatrics.2017.2600.
9. Sauers HS, Beck AF, Kahn RS, Simmons JM. Increasing recruitment rates in an inpatient clinical research study using quality improvement methods. Hosp Pediatr. 2014;4(6):335-341. https://doi.org/10.1542/hpeds.2014-0072.
10. Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Hoboken: John Wiley & Sons, Inc.; 2009.
11. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458-464. https://doi.org/10.1136/qhc.12.6.458.
12. Mohammed MA, Panesar JS, Laney DB, Wilson R. Statistical process control charts for attribute data involving very large sample sizes: a review of problems and solutions. BMJ Qual Saf. 2013;22(4):362-368. https://doi.org/10.1136/bmjqs-2012-001373.
13. Moen R, Nolan T, Provost L. Quality Improvement through Planned Experimentation. 2nd ed. New York City: McGraw-Hill Professional; 1998.
© 2020 Society of Hospital Medicine