User login
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
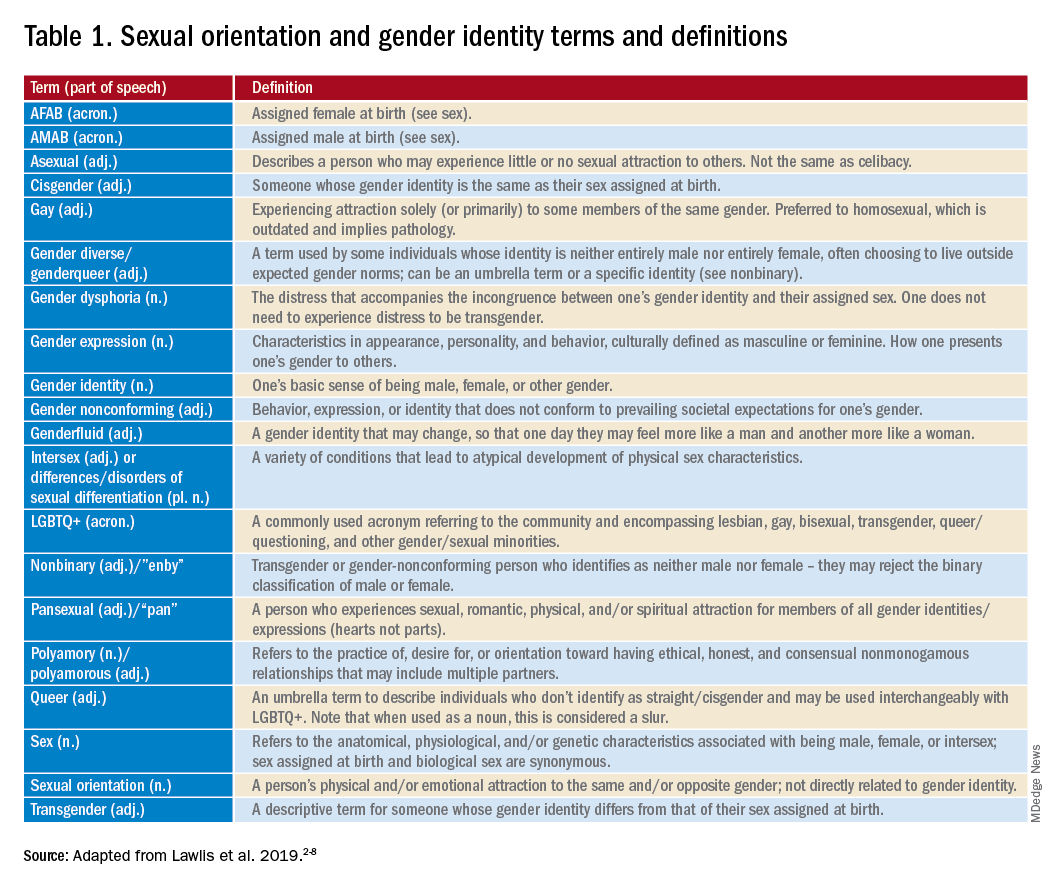
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
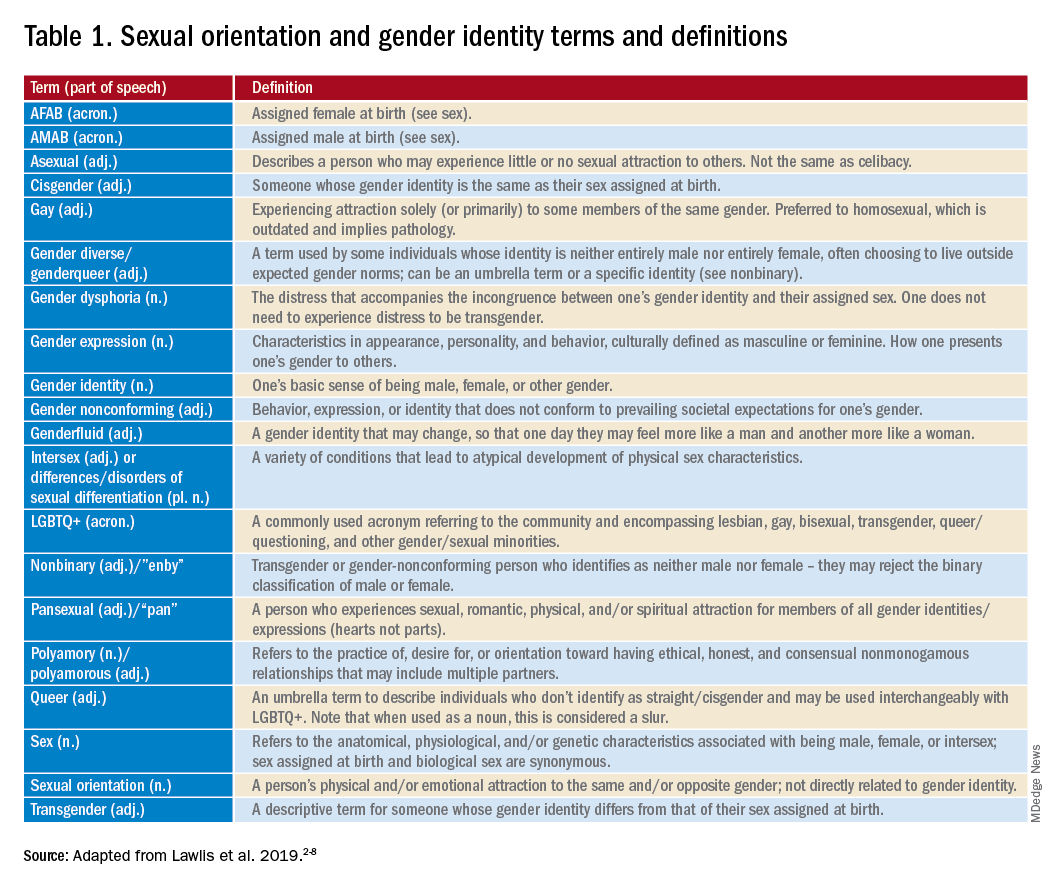
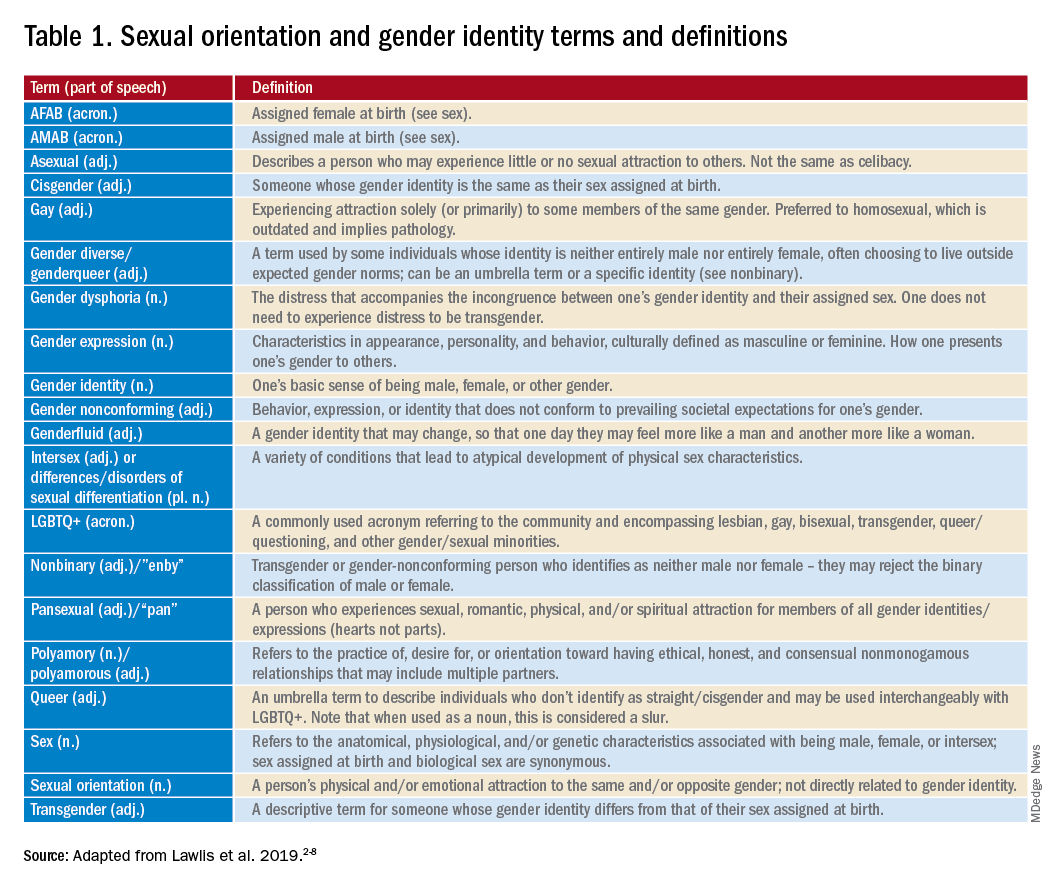
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.

