User login
A 72-year-old man with a 15-year history of a heart murmur presents to his cardiologist with shortness of breath on exertion over the past 12 months. He otherwise feels well and reports no chest discomfort, palpitations, or swelling of his legs or feet. He is not taking any cardiac drugs, and his health has previously been excellent.
Q: Which of the following findings on 12-lead ECG is not commonly reported in chronic severe aortic regurgitation?
- Left ventricular hypertrophy
- QRS complex left-axis deviation
- A negative U wave
- Atrial fibrillation
A: The correct answer is a negative U wave.
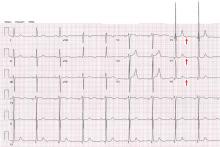
In long-standing left ventricular volume overload, such as in chronic aortic regurgitation, characteristic findings on ECG include lateral precordial narrow Q waves and left ventricular hypertrophy. The ST segment and T wave are often normal or nearly normal. The QRS complex vector may demonstrate left-axis deviation, but this is not absolute. In contrast, pressure overload conditions such as aortic stenosis and systemic hypertension commonly manifest as left ventricular hypertrophy with strain pattern of ST depression in lateral precordial leads and asymmetric T-wave inversion.
A negative U wave, best identified in leads V4 to V6, is a common finding in left ventricular volume overload. A negative U wave represents a negative deflection of small amplitude (normally < 0.1 to 3 mV) immediately following the T wave. Although not routinely reported, the negative U wave is an indicator of underlying structural heart disease.1
Q: A negative U wave has been associated with which of the following conditions?
- Aortic or mitral regurgitation
- Myocardial ischemia
- Hypertension
- All of the above
A: The correct answer is all of the above.
Negative U waves have been identified in regurgitant valvular heart disease with left ventricular volume overload, in myocardial ischemia, 2,3 and in hypertension.4 During exercise stress testing, the transient appearance of negative U waves strongly suggests flow-limiting coronary artery disease. Moreover, changes in the U wave during exercise stress testing may be a sign of well-developed coronary collaterals.5 Therefore, it is prudent to note their presence on resting ECG and to investigate further with cardiac stress testing and imaging.
The pathogenesis of the negative U wave remains unclear. Of the various hypotheses put forth, a mechano-electric phenomenon may best explain its diverse pathology.
- Correale E, Battista R, Ricciardiello V, Martone A. The negative U wave: a pathogenetic enigma but a useful, often overlooked bedside diagnostic and prognostic clue in ischemic heart disease. Clin Cardiol 2004; 27:674–677.
- Rimmerman CM. A 62-year-old man with an abnormal electrocardiogram. Cleve Clin J Med 2001; 68:975–976.
- Gerson MC, Phillips JF, Morris SN, McHenry PL. Exercise-induced U-wave inversion as a marker of stenosis of the left anterior descending coronary artery. Circulation 1979; 60:1014–1020.
- Lambert J. Clinical study of the abnormalities of the terminal complex TU-U of the electrocardiogram. Circulation 1957; 15:102–104.
- Miwa K, Nakagawa K, Hirai T, Inoue H. Exercise-induced U-wave alterations as a marker of well-developed and well-functioning collateral vessels in patients with effort angina. J Am Coll Cardiol 2000; 35:757–763.
A 72-year-old man with a 15-year history of a heart murmur presents to his cardiologist with shortness of breath on exertion over the past 12 months. He otherwise feels well and reports no chest discomfort, palpitations, or swelling of his legs or feet. He is not taking any cardiac drugs, and his health has previously been excellent.
Q: Which of the following findings on 12-lead ECG is not commonly reported in chronic severe aortic regurgitation?
- Left ventricular hypertrophy
- QRS complex left-axis deviation
- A negative U wave
- Atrial fibrillation
A: The correct answer is a negative U wave.
In long-standing left ventricular volume overload, such as in chronic aortic regurgitation, characteristic findings on ECG include lateral precordial narrow Q waves and left ventricular hypertrophy. The ST segment and T wave are often normal or nearly normal. The QRS complex vector may demonstrate left-axis deviation, but this is not absolute. In contrast, pressure overload conditions such as aortic stenosis and systemic hypertension commonly manifest as left ventricular hypertrophy with strain pattern of ST depression in lateral precordial leads and asymmetric T-wave inversion.
A negative U wave, best identified in leads V4 to V6, is a common finding in left ventricular volume overload. A negative U wave represents a negative deflection of small amplitude (normally < 0.1 to 3 mV) immediately following the T wave. Although not routinely reported, the negative U wave is an indicator of underlying structural heart disease.1
Q: A negative U wave has been associated with which of the following conditions?
- Aortic or mitral regurgitation
- Myocardial ischemia
- Hypertension
- All of the above
A: The correct answer is all of the above.
Negative U waves have been identified in regurgitant valvular heart disease with left ventricular volume overload, in myocardial ischemia, 2,3 and in hypertension.4 During exercise stress testing, the transient appearance of negative U waves strongly suggests flow-limiting coronary artery disease. Moreover, changes in the U wave during exercise stress testing may be a sign of well-developed coronary collaterals.5 Therefore, it is prudent to note their presence on resting ECG and to investigate further with cardiac stress testing and imaging.
The pathogenesis of the negative U wave remains unclear. Of the various hypotheses put forth, a mechano-electric phenomenon may best explain its diverse pathology.
A 72-year-old man with a 15-year history of a heart murmur presents to his cardiologist with shortness of breath on exertion over the past 12 months. He otherwise feels well and reports no chest discomfort, palpitations, or swelling of his legs or feet. He is not taking any cardiac drugs, and his health has previously been excellent.
Q: Which of the following findings on 12-lead ECG is not commonly reported in chronic severe aortic regurgitation?
- Left ventricular hypertrophy
- QRS complex left-axis deviation
- A negative U wave
- Atrial fibrillation
A: The correct answer is a negative U wave.
In long-standing left ventricular volume overload, such as in chronic aortic regurgitation, characteristic findings on ECG include lateral precordial narrow Q waves and left ventricular hypertrophy. The ST segment and T wave are often normal or nearly normal. The QRS complex vector may demonstrate left-axis deviation, but this is not absolute. In contrast, pressure overload conditions such as aortic stenosis and systemic hypertension commonly manifest as left ventricular hypertrophy with strain pattern of ST depression in lateral precordial leads and asymmetric T-wave inversion.
A negative U wave, best identified in leads V4 to V6, is a common finding in left ventricular volume overload. A negative U wave represents a negative deflection of small amplitude (normally < 0.1 to 3 mV) immediately following the T wave. Although not routinely reported, the negative U wave is an indicator of underlying structural heart disease.1
Q: A negative U wave has been associated with which of the following conditions?
- Aortic or mitral regurgitation
- Myocardial ischemia
- Hypertension
- All of the above
A: The correct answer is all of the above.
Negative U waves have been identified in regurgitant valvular heart disease with left ventricular volume overload, in myocardial ischemia, 2,3 and in hypertension.4 During exercise stress testing, the transient appearance of negative U waves strongly suggests flow-limiting coronary artery disease. Moreover, changes in the U wave during exercise stress testing may be a sign of well-developed coronary collaterals.5 Therefore, it is prudent to note their presence on resting ECG and to investigate further with cardiac stress testing and imaging.
The pathogenesis of the negative U wave remains unclear. Of the various hypotheses put forth, a mechano-electric phenomenon may best explain its diverse pathology.
- Correale E, Battista R, Ricciardiello V, Martone A. The negative U wave: a pathogenetic enigma but a useful, often overlooked bedside diagnostic and prognostic clue in ischemic heart disease. Clin Cardiol 2004; 27:674–677.
- Rimmerman CM. A 62-year-old man with an abnormal electrocardiogram. Cleve Clin J Med 2001; 68:975–976.
- Gerson MC, Phillips JF, Morris SN, McHenry PL. Exercise-induced U-wave inversion as a marker of stenosis of the left anterior descending coronary artery. Circulation 1979; 60:1014–1020.
- Lambert J. Clinical study of the abnormalities of the terminal complex TU-U of the electrocardiogram. Circulation 1957; 15:102–104.
- Miwa K, Nakagawa K, Hirai T, Inoue H. Exercise-induced U-wave alterations as a marker of well-developed and well-functioning collateral vessels in patients with effort angina. J Am Coll Cardiol 2000; 35:757–763.
- Correale E, Battista R, Ricciardiello V, Martone A. The negative U wave: a pathogenetic enigma but a useful, often overlooked bedside diagnostic and prognostic clue in ischemic heart disease. Clin Cardiol 2004; 27:674–677.
- Rimmerman CM. A 62-year-old man with an abnormal electrocardiogram. Cleve Clin J Med 2001; 68:975–976.
- Gerson MC, Phillips JF, Morris SN, McHenry PL. Exercise-induced U-wave inversion as a marker of stenosis of the left anterior descending coronary artery. Circulation 1979; 60:1014–1020.
- Lambert J. Clinical study of the abnormalities of the terminal complex TU-U of the electrocardiogram. Circulation 1957; 15:102–104.
- Miwa K, Nakagawa K, Hirai T, Inoue H. Exercise-induced U-wave alterations as a marker of well-developed and well-functioning collateral vessels in patients with effort angina. J Am Coll Cardiol 2000; 35:757–763.