User login
It’s all in the P wave
A 49-year-old man with rheumatic mitral valve stenosis, which had been diagnosed 3 years previously, presented to the outpatient department with worsening exertional dyspnea, fatigue, and cough.
At rest, he appeared comfortable; his pulse rate was 94 bpm and his blood pressure was 117/82 mm Hg. Cardiac auscultation revealed a loud first heart sound, a mid-diastolic murmur with presystolic accentuation at the cardiac apex, and a pansystolic murmur at the left lower sternal border that increased in intensity with inspiration. A prominent left parasternal heave was present.
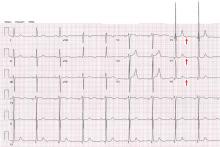
His 12-lead electrocardiogram is shown in Figure 1.
Transthoracic echocardiography confirmed severe mitral stenosis with an estimated mitral valve area of 0.7 cm2 without significant mitral regurgitation. In addition, right ventricular dilatation with moderately severe systolic dysfunction and 4+ (severe) tricuspid regurgitation were present. On the basis of the peak tricuspid regurgitant velocity, the right ventricular systolic pressure was calculated to be 80 mm Hg, consistent with severe pulmonary hypertension. The left ventricular end-diastolic volume was reduced and the ejection fraction was normal.
On right heart catheterization, the pulmonary artery pressure was 92/51 mm Hg.
Q: Electrocardiographic findings that support a diagnosis of pulmonary hypertension include which of the following?
- QRS complex axis of +110°
- R/S (QRS complex) ratio greater than 1 in lead V1
- Sum of the amplitudes of the R wave in lead V1 and the S wave in lead V6 greater than 1.0 mV
- All of the above
A: The correct answer is all of the above. Regardless of the cause, patients with long-standing pulmonary hypertension possess varying degrees of right ventricular hypertrophy that may be accompanied by right ventricular enlargement and systolic dysfunction. A QRS complex axis of 110° or more, an R/S (QRS complex) ratio greater than 1 in lead V1, and the sum of the amplitudes of the R wave in lead V1 and the S wave in lead V6 greater than 1.0 mV all support right ventricular hypertrophy.1
As noted in this electrocardiogram, T-wave inversion in leads V1 and V2 supports a right ventricular repolarization abnormality secondary to the hypertrophy.2
Q: Important electrocardiographic findings in this patient that support secondary pulmonary hypertension due to mitral stenosis include which of the following?
- Tall peaked P waves in lead II of at least 0.25 mV and positive P waves in V1 greater than 0.15 mV
- Prolonged P waves of at least 120 ms in lead II and terminal negative P waves in V1 greater than 40 ms
- Right ventricular hypertrophy
- All of the above
A: The correct answer is prolonged P waves of at least 120 ms in lead II and terminal negative P waves in V1 greater than 40 ms.
Abnormal surface electrocardiographic findings reflecting atrial enlargement or slowed atrial conduction are difficult to differentiate and are best characterized as “atrial abnormalities.” On surface electrocardiography, an atrial abnormality is represented by a P wave morphology that is best studied in leads II and V1. In lead II, a tall peaked P wave of at least 0.25 mV supports right atrial abnormality, and a prolonged P wave (≥ 120 ms) supports left atrial abnormality. In lead V1, right atrial abnormality is suggested by a positive P wave in V1 greater than 0.15 mV, and a terminally negative P wave greater than 40 ms in duration and greater than 0.1 mV deep supports left atrial abnormality.3
It is well recognized that the pathophysiology of pulmonary hypertension involves both the right ventricle and the right atrium.4,5 Therefore, irrespective of the cause of pulmonary hypertension, electrocardiography may additionally reveal right atrial abnormality.6
When the findings suggest pulmonary hypertension (ie, right ventricular hypertrophy with or without right atrial abnormality), it is also important to evaluate for concurrent left atrial abnormality. If present, concomitant left atrial abnormality is a valuable, more specific clue that may help characterize secondary pulmonary hypertension from left-sided heart disease, as illustrated in this example with long-standing severe mitral stenosis.2
- Hancock EW, Deal BJ, Mirvis DM, et al; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009; 53:992–1002.
- Goldberger AL. Atrial and ventricular enlargement. In: Clinical Electrocardiography: A Simplified Approach. 7th ed. Philadelphia, PA: Mosby Elsevier; 2006:59–71.
- Bayés-de-Luna A, Goldwasser D, Fiol M, Bayés-Genis A. Surface electrocardiography. In: Hurst’s The Heart. 13th ed. New York, NY: McGraw-Hill Medical; 2011.
- Cioffi G, de Simone G, Mureddu G, Tarantini L, Stefenelli C. Right atrial size and function in patients with pulmonary hypertension associated with disorders of respiratory system or hypoxemia. Eur J Echocardiogr 2007; 8:322–331.
- Raymond RJ, Hinderliter AL, Willis PW, et al. Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol 2002; 39:1214–1219.
- Al-Naamani K, Hijal T, Nguyen V, Andrew S, Nguyen T, Huynh T. Predictive values of the electrocardiogram in diagnosing pulmonary hypertension. Int J Cardiol 2008; 127:214–218.
A 49-year-old man with rheumatic mitral valve stenosis, which had been diagnosed 3 years previously, presented to the outpatient department with worsening exertional dyspnea, fatigue, and cough.
At rest, he appeared comfortable; his pulse rate was 94 bpm and his blood pressure was 117/82 mm Hg. Cardiac auscultation revealed a loud first heart sound, a mid-diastolic murmur with presystolic accentuation at the cardiac apex, and a pansystolic murmur at the left lower sternal border that increased in intensity with inspiration. A prominent left parasternal heave was present.
His 12-lead electrocardiogram is shown in Figure 1.
Transthoracic echocardiography confirmed severe mitral stenosis with an estimated mitral valve area of 0.7 cm2 without significant mitral regurgitation. In addition, right ventricular dilatation with moderately severe systolic dysfunction and 4+ (severe) tricuspid regurgitation were present. On the basis of the peak tricuspid regurgitant velocity, the right ventricular systolic pressure was calculated to be 80 mm Hg, consistent with severe pulmonary hypertension. The left ventricular end-diastolic volume was reduced and the ejection fraction was normal.
On right heart catheterization, the pulmonary artery pressure was 92/51 mm Hg.
Q: Electrocardiographic findings that support a diagnosis of pulmonary hypertension include which of the following?
- QRS complex axis of +110°
- R/S (QRS complex) ratio greater than 1 in lead V1
- Sum of the amplitudes of the R wave in lead V1 and the S wave in lead V6 greater than 1.0 mV
- All of the above
A: The correct answer is all of the above. Regardless of the cause, patients with long-standing pulmonary hypertension possess varying degrees of right ventricular hypertrophy that may be accompanied by right ventricular enlargement and systolic dysfunction. A QRS complex axis of 110° or more, an R/S (QRS complex) ratio greater than 1 in lead V1, and the sum of the amplitudes of the R wave in lead V1 and the S wave in lead V6 greater than 1.0 mV all support right ventricular hypertrophy.1
As noted in this electrocardiogram, T-wave inversion in leads V1 and V2 supports a right ventricular repolarization abnormality secondary to the hypertrophy.2
Q: Important electrocardiographic findings in this patient that support secondary pulmonary hypertension due to mitral stenosis include which of the following?
- Tall peaked P waves in lead II of at least 0.25 mV and positive P waves in V1 greater than 0.15 mV
- Prolonged P waves of at least 120 ms in lead II and terminal negative P waves in V1 greater than 40 ms
- Right ventricular hypertrophy
- All of the above
A: The correct answer is prolonged P waves of at least 120 ms in lead II and terminal negative P waves in V1 greater than 40 ms.
Abnormal surface electrocardiographic findings reflecting atrial enlargement or slowed atrial conduction are difficult to differentiate and are best characterized as “atrial abnormalities.” On surface electrocardiography, an atrial abnormality is represented by a P wave morphology that is best studied in leads II and V1. In lead II, a tall peaked P wave of at least 0.25 mV supports right atrial abnormality, and a prolonged P wave (≥ 120 ms) supports left atrial abnormality. In lead V1, right atrial abnormality is suggested by a positive P wave in V1 greater than 0.15 mV, and a terminally negative P wave greater than 40 ms in duration and greater than 0.1 mV deep supports left atrial abnormality.3
It is well recognized that the pathophysiology of pulmonary hypertension involves both the right ventricle and the right atrium.4,5 Therefore, irrespective of the cause of pulmonary hypertension, electrocardiography may additionally reveal right atrial abnormality.6
When the findings suggest pulmonary hypertension (ie, right ventricular hypertrophy with or without right atrial abnormality), it is also important to evaluate for concurrent left atrial abnormality. If present, concomitant left atrial abnormality is a valuable, more specific clue that may help characterize secondary pulmonary hypertension from left-sided heart disease, as illustrated in this example with long-standing severe mitral stenosis.2
A 49-year-old man with rheumatic mitral valve stenosis, which had been diagnosed 3 years previously, presented to the outpatient department with worsening exertional dyspnea, fatigue, and cough.
At rest, he appeared comfortable; his pulse rate was 94 bpm and his blood pressure was 117/82 mm Hg. Cardiac auscultation revealed a loud first heart sound, a mid-diastolic murmur with presystolic accentuation at the cardiac apex, and a pansystolic murmur at the left lower sternal border that increased in intensity with inspiration. A prominent left parasternal heave was present.
His 12-lead electrocardiogram is shown in Figure 1.
Transthoracic echocardiography confirmed severe mitral stenosis with an estimated mitral valve area of 0.7 cm2 without significant mitral regurgitation. In addition, right ventricular dilatation with moderately severe systolic dysfunction and 4+ (severe) tricuspid regurgitation were present. On the basis of the peak tricuspid regurgitant velocity, the right ventricular systolic pressure was calculated to be 80 mm Hg, consistent with severe pulmonary hypertension. The left ventricular end-diastolic volume was reduced and the ejection fraction was normal.
On right heart catheterization, the pulmonary artery pressure was 92/51 mm Hg.
Q: Electrocardiographic findings that support a diagnosis of pulmonary hypertension include which of the following?
- QRS complex axis of +110°
- R/S (QRS complex) ratio greater than 1 in lead V1
- Sum of the amplitudes of the R wave in lead V1 and the S wave in lead V6 greater than 1.0 mV
- All of the above
A: The correct answer is all of the above. Regardless of the cause, patients with long-standing pulmonary hypertension possess varying degrees of right ventricular hypertrophy that may be accompanied by right ventricular enlargement and systolic dysfunction. A QRS complex axis of 110° or more, an R/S (QRS complex) ratio greater than 1 in lead V1, and the sum of the amplitudes of the R wave in lead V1 and the S wave in lead V6 greater than 1.0 mV all support right ventricular hypertrophy.1
As noted in this electrocardiogram, T-wave inversion in leads V1 and V2 supports a right ventricular repolarization abnormality secondary to the hypertrophy.2
Q: Important electrocardiographic findings in this patient that support secondary pulmonary hypertension due to mitral stenosis include which of the following?
- Tall peaked P waves in lead II of at least 0.25 mV and positive P waves in V1 greater than 0.15 mV
- Prolonged P waves of at least 120 ms in lead II and terminal negative P waves in V1 greater than 40 ms
- Right ventricular hypertrophy
- All of the above
A: The correct answer is prolonged P waves of at least 120 ms in lead II and terminal negative P waves in V1 greater than 40 ms.
Abnormal surface electrocardiographic findings reflecting atrial enlargement or slowed atrial conduction are difficult to differentiate and are best characterized as “atrial abnormalities.” On surface electrocardiography, an atrial abnormality is represented by a P wave morphology that is best studied in leads II and V1. In lead II, a tall peaked P wave of at least 0.25 mV supports right atrial abnormality, and a prolonged P wave (≥ 120 ms) supports left atrial abnormality. In lead V1, right atrial abnormality is suggested by a positive P wave in V1 greater than 0.15 mV, and a terminally negative P wave greater than 40 ms in duration and greater than 0.1 mV deep supports left atrial abnormality.3
It is well recognized that the pathophysiology of pulmonary hypertension involves both the right ventricle and the right atrium.4,5 Therefore, irrespective of the cause of pulmonary hypertension, electrocardiography may additionally reveal right atrial abnormality.6
When the findings suggest pulmonary hypertension (ie, right ventricular hypertrophy with or without right atrial abnormality), it is also important to evaluate for concurrent left atrial abnormality. If present, concomitant left atrial abnormality is a valuable, more specific clue that may help characterize secondary pulmonary hypertension from left-sided heart disease, as illustrated in this example with long-standing severe mitral stenosis.2
- Hancock EW, Deal BJ, Mirvis DM, et al; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009; 53:992–1002.
- Goldberger AL. Atrial and ventricular enlargement. In: Clinical Electrocardiography: A Simplified Approach. 7th ed. Philadelphia, PA: Mosby Elsevier; 2006:59–71.
- Bayés-de-Luna A, Goldwasser D, Fiol M, Bayés-Genis A. Surface electrocardiography. In: Hurst’s The Heart. 13th ed. New York, NY: McGraw-Hill Medical; 2011.
- Cioffi G, de Simone G, Mureddu G, Tarantini L, Stefenelli C. Right atrial size and function in patients with pulmonary hypertension associated with disorders of respiratory system or hypoxemia. Eur J Echocardiogr 2007; 8:322–331.
- Raymond RJ, Hinderliter AL, Willis PW, et al. Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol 2002; 39:1214–1219.
- Al-Naamani K, Hijal T, Nguyen V, Andrew S, Nguyen T, Huynh T. Predictive values of the electrocardiogram in diagnosing pulmonary hypertension. Int J Cardiol 2008; 127:214–218.
- Hancock EW, Deal BJ, Mirvis DM, et al; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009; 53:992–1002.
- Goldberger AL. Atrial and ventricular enlargement. In: Clinical Electrocardiography: A Simplified Approach. 7th ed. Philadelphia, PA: Mosby Elsevier; 2006:59–71.
- Bayés-de-Luna A, Goldwasser D, Fiol M, Bayés-Genis A. Surface electrocardiography. In: Hurst’s The Heart. 13th ed. New York, NY: McGraw-Hill Medical; 2011.
- Cioffi G, de Simone G, Mureddu G, Tarantini L, Stefenelli C. Right atrial size and function in patients with pulmonary hypertension associated with disorders of respiratory system or hypoxemia. Eur J Echocardiogr 2007; 8:322–331.
- Raymond RJ, Hinderliter AL, Willis PW, et al. Echocardiographic predictors of adverse outcomes in primary pulmonary hypertension. J Am Coll Cardiol 2002; 39:1214–1219.
- Al-Naamani K, Hijal T, Nguyen V, Andrew S, Nguyen T, Huynh T. Predictive values of the electrocardiogram in diagnosing pulmonary hypertension. Int J Cardiol 2008; 127:214–218.
Electrocardiography in aortic regurgitation: It’s in the details
A 72-year-old man with a 15-year history of a heart murmur presents to his cardiologist with shortness of breath on exertion over the past 12 months. He otherwise feels well and reports no chest discomfort, palpitations, or swelling of his legs or feet. He is not taking any cardiac drugs, and his health has previously been excellent.
Q: Which of the following findings on 12-lead ECG is not commonly reported in chronic severe aortic regurgitation?
- Left ventricular hypertrophy
- QRS complex left-axis deviation
- A negative U wave
- Atrial fibrillation
A: The correct answer is a negative U wave.
In long-standing left ventricular volume overload, such as in chronic aortic regurgitation, characteristic findings on ECG include lateral precordial narrow Q waves and left ventricular hypertrophy. The ST segment and T wave are often normal or nearly normal. The QRS complex vector may demonstrate left-axis deviation, but this is not absolute. In contrast, pressure overload conditions such as aortic stenosis and systemic hypertension commonly manifest as left ventricular hypertrophy with strain pattern of ST depression in lateral precordial leads and asymmetric T-wave inversion.
A negative U wave, best identified in leads V4 to V6, is a common finding in left ventricular volume overload. A negative U wave represents a negative deflection of small amplitude (normally < 0.1 to 3 mV) immediately following the T wave. Although not routinely reported, the negative U wave is an indicator of underlying structural heart disease.1
Q: A negative U wave has been associated with which of the following conditions?
- Aortic or mitral regurgitation
- Myocardial ischemia
- Hypertension
- All of the above
A: The correct answer is all of the above.
Negative U waves have been identified in regurgitant valvular heart disease with left ventricular volume overload, in myocardial ischemia, 2,3 and in hypertension.4 During exercise stress testing, the transient appearance of negative U waves strongly suggests flow-limiting coronary artery disease. Moreover, changes in the U wave during exercise stress testing may be a sign of well-developed coronary collaterals.5 Therefore, it is prudent to note their presence on resting ECG and to investigate further with cardiac stress testing and imaging.
The pathogenesis of the negative U wave remains unclear. Of the various hypotheses put forth, a mechano-electric phenomenon may best explain its diverse pathology.
- Correale E, Battista R, Ricciardiello V, Martone A. The negative U wave: a pathogenetic enigma but a useful, often overlooked bedside diagnostic and prognostic clue in ischemic heart disease. Clin Cardiol 2004; 27:674–677.
- Rimmerman CM. A 62-year-old man with an abnormal electrocardiogram. Cleve Clin J Med 2001; 68:975–976.
- Gerson MC, Phillips JF, Morris SN, McHenry PL. Exercise-induced U-wave inversion as a marker of stenosis of the left anterior descending coronary artery. Circulation 1979; 60:1014–1020.
- Lambert J. Clinical study of the abnormalities of the terminal complex TU-U of the electrocardiogram. Circulation 1957; 15:102–104.
- Miwa K, Nakagawa K, Hirai T, Inoue H. Exercise-induced U-wave alterations as a marker of well-developed and well-functioning collateral vessels in patients with effort angina. J Am Coll Cardiol 2000; 35:757–763.
A 72-year-old man with a 15-year history of a heart murmur presents to his cardiologist with shortness of breath on exertion over the past 12 months. He otherwise feels well and reports no chest discomfort, palpitations, or swelling of his legs or feet. He is not taking any cardiac drugs, and his health has previously been excellent.
Q: Which of the following findings on 12-lead ECG is not commonly reported in chronic severe aortic regurgitation?
- Left ventricular hypertrophy
- QRS complex left-axis deviation
- A negative U wave
- Atrial fibrillation
A: The correct answer is a negative U wave.
In long-standing left ventricular volume overload, such as in chronic aortic regurgitation, characteristic findings on ECG include lateral precordial narrow Q waves and left ventricular hypertrophy. The ST segment and T wave are often normal or nearly normal. The QRS complex vector may demonstrate left-axis deviation, but this is not absolute. In contrast, pressure overload conditions such as aortic stenosis and systemic hypertension commonly manifest as left ventricular hypertrophy with strain pattern of ST depression in lateral precordial leads and asymmetric T-wave inversion.
A negative U wave, best identified in leads V4 to V6, is a common finding in left ventricular volume overload. A negative U wave represents a negative deflection of small amplitude (normally < 0.1 to 3 mV) immediately following the T wave. Although not routinely reported, the negative U wave is an indicator of underlying structural heart disease.1
Q: A negative U wave has been associated with which of the following conditions?
- Aortic or mitral regurgitation
- Myocardial ischemia
- Hypertension
- All of the above
A: The correct answer is all of the above.
Negative U waves have been identified in regurgitant valvular heart disease with left ventricular volume overload, in myocardial ischemia, 2,3 and in hypertension.4 During exercise stress testing, the transient appearance of negative U waves strongly suggests flow-limiting coronary artery disease. Moreover, changes in the U wave during exercise stress testing may be a sign of well-developed coronary collaterals.5 Therefore, it is prudent to note their presence on resting ECG and to investigate further with cardiac stress testing and imaging.
The pathogenesis of the negative U wave remains unclear. Of the various hypotheses put forth, a mechano-electric phenomenon may best explain its diverse pathology.
A 72-year-old man with a 15-year history of a heart murmur presents to his cardiologist with shortness of breath on exertion over the past 12 months. He otherwise feels well and reports no chest discomfort, palpitations, or swelling of his legs or feet. He is not taking any cardiac drugs, and his health has previously been excellent.
Q: Which of the following findings on 12-lead ECG is not commonly reported in chronic severe aortic regurgitation?
- Left ventricular hypertrophy
- QRS complex left-axis deviation
- A negative U wave
- Atrial fibrillation
A: The correct answer is a negative U wave.
In long-standing left ventricular volume overload, such as in chronic aortic regurgitation, characteristic findings on ECG include lateral precordial narrow Q waves and left ventricular hypertrophy. The ST segment and T wave are often normal or nearly normal. The QRS complex vector may demonstrate left-axis deviation, but this is not absolute. In contrast, pressure overload conditions such as aortic stenosis and systemic hypertension commonly manifest as left ventricular hypertrophy with strain pattern of ST depression in lateral precordial leads and asymmetric T-wave inversion.
A negative U wave, best identified in leads V4 to V6, is a common finding in left ventricular volume overload. A negative U wave represents a negative deflection of small amplitude (normally < 0.1 to 3 mV) immediately following the T wave. Although not routinely reported, the negative U wave is an indicator of underlying structural heart disease.1
Q: A negative U wave has been associated with which of the following conditions?
- Aortic or mitral regurgitation
- Myocardial ischemia
- Hypertension
- All of the above
A: The correct answer is all of the above.
Negative U waves have been identified in regurgitant valvular heart disease with left ventricular volume overload, in myocardial ischemia, 2,3 and in hypertension.4 During exercise stress testing, the transient appearance of negative U waves strongly suggests flow-limiting coronary artery disease. Moreover, changes in the U wave during exercise stress testing may be a sign of well-developed coronary collaterals.5 Therefore, it is prudent to note their presence on resting ECG and to investigate further with cardiac stress testing and imaging.
The pathogenesis of the negative U wave remains unclear. Of the various hypotheses put forth, a mechano-electric phenomenon may best explain its diverse pathology.
- Correale E, Battista R, Ricciardiello V, Martone A. The negative U wave: a pathogenetic enigma but a useful, often overlooked bedside diagnostic and prognostic clue in ischemic heart disease. Clin Cardiol 2004; 27:674–677.
- Rimmerman CM. A 62-year-old man with an abnormal electrocardiogram. Cleve Clin J Med 2001; 68:975–976.
- Gerson MC, Phillips JF, Morris SN, McHenry PL. Exercise-induced U-wave inversion as a marker of stenosis of the left anterior descending coronary artery. Circulation 1979; 60:1014–1020.
- Lambert J. Clinical study of the abnormalities of the terminal complex TU-U of the electrocardiogram. Circulation 1957; 15:102–104.
- Miwa K, Nakagawa K, Hirai T, Inoue H. Exercise-induced U-wave alterations as a marker of well-developed and well-functioning collateral vessels in patients with effort angina. J Am Coll Cardiol 2000; 35:757–763.
- Correale E, Battista R, Ricciardiello V, Martone A. The negative U wave: a pathogenetic enigma but a useful, often overlooked bedside diagnostic and prognostic clue in ischemic heart disease. Clin Cardiol 2004; 27:674–677.
- Rimmerman CM. A 62-year-old man with an abnormal electrocardiogram. Cleve Clin J Med 2001; 68:975–976.
- Gerson MC, Phillips JF, Morris SN, McHenry PL. Exercise-induced U-wave inversion as a marker of stenosis of the left anterior descending coronary artery. Circulation 1979; 60:1014–1020.
- Lambert J. Clinical study of the abnormalities of the terminal complex TU-U of the electrocardiogram. Circulation 1957; 15:102–104.
- Miwa K, Nakagawa K, Hirai T, Inoue H. Exercise-induced U-wave alterations as a marker of well-developed and well-functioning collateral vessels in patients with effort angina. J Am Coll Cardiol 2000; 35:757–763.