User login
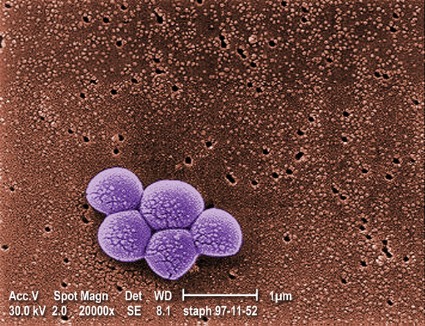
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
ORLANDO – The proportion of pediatric musculoskeletal infections involving methicillin-resistant Staphylococcus aureus vs. methicillin-sensitive S. aureus has increased dramatically over the past decade, according to a retrospective review of cases.
Between 2001 and 2010, 148 patients at the Children’s Hospital of Philadelphia presented with acute musculoskeletal S. aureus infection, and overall, 37 of those involved methicillin-resistant S. aureus (MRSA), Eric Sarkissian reported at the annual meeting of the American Academy of Pediatrics conference.
The proportion of musculoskeletal cases involving MRSA increased from 12% in 2001-2002 to about 35% in 2010, said Mr. Sarkissian, a 4th-year medical student at Drexel University, Philadelphia.
"Furthermore, we found that MRSA infections were associated with a significantly more complicated hospital stay," Mr. Sarkissian said.
MRSA and methicillin-sensitive S. aureus (MSSA) patients were undergoing magnetic resonance imaging at similar rates, but the average duration of hospitalization was longer for the MRSA patients (13 vs. 8 days), and more MRSA patients required multiple surgical procedures (38% vs. 15%), he said.
In addition, mean presenting C-reactive protein levels were higher in the MRSA vs. MSSA patients (14.7 mg/L vs. 9.8 mg/L), as were infection-related complications, including deep vein thrombosis, septic emboli, septic shock, recurrent infection, and/or avascular necrosis (22% vs. 6%).
MRSA patients also were more often admitted to the ICU for further treatment.
Patients included in this series – the largest known case series of children and adolescents presenting with culture-positive S. aureus osteomyelitis and/or septic arthritis – were consecutive patients with positive cultures of blood, bone, or joint aspirate. Those with postoperative and chronic infections were excluded in an effort to minimize bias caused by nosocomial infections, Mr. Sarkissian noted.
The findings support the ongoing concern that MRSA is evolving and becoming more virulent and invasive over time, compared with MSSA infections. In addition, the findings underscore the need for prompt recognition and aggressive treatment of MRSA musculoskeletal infections, as early recognition is paramount for avoiding sequelae and improving patient outcomes.
"A high index of suspicion is still necessary in the setting of musculoskeletal infections in pediatric patients. Multidisciplinary care provides the most successful opportunity for having improved patient outcomes, and this requires employing broad spectrum antibiotic coverage, using aggressive surgical management, and having an awareness of potential complications," Mr. Sarkissian said.
While clinical prediction models have been developed to help in detecting MRSA infections, outcomes using the models have varied geographically, suggesting that there are unknown regional differences among MRSA cases. It remains to be seen whether available models will be useful for identifying MRSA at presentation, he said.
Mr. Sarkissian reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: The proportion of musculoskeletal infection cases involving MRSA vs. MSSA increased from 12% to 35% between 2001 and 2010.
Data source: A retrospective study of 148 consecutive cases.
Disclosures: Mr. Sarkissian reported having no disclosures.