User login
American Academy of Pediatrics (AAP): 2013 National Conference and Exhibition
Pediatricians can play important role in crisis response
ORLANDO – Pediatricians can do a great deal to help their patients and communities in the wake of tragedies involving violence affecting children, according to Dr. David Schonfeld.
Unfortunately, it appears that such events are increasing in frequency, as evidenced by the headlines in recent months and years, Dr. Schonfeld, director of the National Center for School Crisis and Bereavement at St. Christopher’s Hospital in Philadelphia said at the annual meeting of the American Academy of Pediatrics.
It is important that when such events do occur, pediatricians work to address the impact of trauma on children; research suggests that supportive and nurturing adults can indeed mitigate the effects, said Dr. Schonfeld, a developmental and behavioral pediatrician and a member of the AAP Disaster Preparedness Advisory Council.
The available research, including both rat and human studies, highlights the role that nurturing by both mothers and other adults can play in protecting children.
In one set of experiments in rats, infants who experienced higher levels of maternal nurturing were less fearful and less reactive to stressful situations, and performed better on tasks thought to depend on optimal functioning of the hippocampus, Dr. Schonfeld explained.
Related studies showed that cross-fostering infant rats from mothers who provided less nurturing compensated for the lack of maternal nurturing.
This suggests that care and support provided by adults outside of the family can help promote the development and adjustment of children affected by a crisis, he said.
"These findings are directly applicable to humans. The National Collaborative Perinatal Project showed similar findings in humans at 8 months of age," he noted.
The project demonstrated that the degree of maternal nurturing in an experimental setting predicted the infants’ degree of emotional distress in adulthood.
An epigenetic phenomenon may explain how early parental nurturing results in less stress reactively in offspring in adulthood, he said, noting that this idea was supported by findings from recent postmortem analyses of the brains of suicide victims. Victims with a history of early-life adversity had lower levels of glucocorticoid receptor messenger RNA in their hippocampus and higher rates of DNA methylation in the same promoter region as in the rat model.
"A whole separate and growing body of research has also demonstrated that chronic severe stress, especially during critical periods of brain development, leads to long-term changes in brain function and structure," he said.
"If you take all of this together, it underscores the need to protect children from stressful situations as much as possible, to intervene quickly after stressful events occur, and to pay particular attention to minimizing subsequent stressors because of the particularly detrimental effects of chronic stress on children," he added.
He cautioned, however, that a child’s adjustment following a traumatic event is related not just to the trauma, but to what occurs as a result of the event.
For example, if a child loses a family member as a result of violence, difficulties experienced by the child may be a result of bereavement.
Dr. Schonfeld described one teen affected by the 2012 Aurora, Colo., shooting who was reluctant to return to school, and who declined offers of trauma counseling. Although many of his trauma-related symptoms – such as fidgeting and difficulty sleeping – had abated, he disclosed that he "just didn’t feel right, and felt sad and empty."
Further discussion revealed that his problem was one of bereavement; he had lost a close friend in the shooting.
"No one had suggested that might be an issue for him, and I have seen this in crisis event after crisis event when I’ve responded," Dr. Schonfeld said.
After a crisis, a "cascade of secondary losses" can occur, and any one of these can be the cause of difficulty for those affected, he added.
Also, keep in mind that even as such events seem to be occurring more often, children don’t "get used to it," he said.
"They simply learn that there is little benefit in asking for support or assistance from adults in these communities, because it is so infrequently offered to them," he said.
As a result, children may become fatalistic and engage in reactive risk-taking behaviors or counterphobic behaviors that place them at greater risk.
"But they don’t get used to it. And I would contend that neither should we," he said.
Pediatricians should, however, recognize and celebrate what they have done and can do every day to support children and families dealing with difficult situations.
"It makes a big difference. I don’t want you to get overwhelmed by all that could – and unfortunately does – happen, and the long-lasting and profound impact these violent events can have on children. Instead, I challenge you ... to commit to at least one strategy to advocate for violence prevention and/or readiness for your practice or your community to support those who have been impacted by these events," he said.
Such strategies can include:
• Working to decrease violence crisis and loss, and advocating for meaningful change.
• Giving voice to children impacted by these events, allowing them to tell their stories, and forcing a dialogue that can help move the agenda forward.
• Advocating for better systems and services for children affected by these events, and other adverse events in the lives of children, including poverty, exposure to urban violence, and food insecurity, for example.
• Becoming more skilled in supporting children who are grieving and traumatized.
• Ensuring that other professionals in positions to support children – such as teachers and other school staff – are better prepared, more skilled, and more effectively supported in helping children after these events (and introducing information that can help before such events occur).
• Inquiring about exposures and experiences routinely in the practice setting. (The Medical Home for Children Exposed to Violence project [MHCEV] is working to provide resources for identifying, treating, and referring affected children and youth.)
• Promptly identifying affected children at the time of an event, and facilitating discussion about the impact of the event, and offering "psychological first aid and psychoeducation." Attend to basic needs, provide triage and referral, and remember that services will be needed throughout the recovery period, which may be weeks, months, or years.
• Helping in one’s own community when events happen elsewhere, as communities struggle to understand and cope with the events, and deal with distress that can surface as a result of concerns and personal experience.
• Becoming aware of the resources and support efforts of the AAP with respect to disaster preparedness and response. The academy’s department of federal affairs has helped make the AAP one of the leading forces for positive change at the federal level, Dr. Schonfeld said.
"The [AAP] Friends of Children’s Fund in general, and specifically the disaster relief part of that fund, helps not only children, families, and communities recover, but also assists professionals with self-care after these events," he said, noting that it is important to recognize that "it is distressing to be with children in distress."
"Events that are troubling our patients and their families are troubling to us as pediatric health care providers, as well," he said.
Dr. Schonfeld recommended the following resources for additional information:
• The AAP Children and Disasters site.
• The AAP Children and Disasters site, Coping and Adjustment.
• The AAP Medical Home for Children Exposed to Violence.
• The National Center for School Crisis and Bereavement.
Dr. Schonfeld reported having no relevant financial disclosures.
ORLANDO – Pediatricians can do a great deal to help their patients and communities in the wake of tragedies involving violence affecting children, according to Dr. David Schonfeld.
Unfortunately, it appears that such events are increasing in frequency, as evidenced by the headlines in recent months and years, Dr. Schonfeld, director of the National Center for School Crisis and Bereavement at St. Christopher’s Hospital in Philadelphia said at the annual meeting of the American Academy of Pediatrics.
It is important that when such events do occur, pediatricians work to address the impact of trauma on children; research suggests that supportive and nurturing adults can indeed mitigate the effects, said Dr. Schonfeld, a developmental and behavioral pediatrician and a member of the AAP Disaster Preparedness Advisory Council.
The available research, including both rat and human studies, highlights the role that nurturing by both mothers and other adults can play in protecting children.
In one set of experiments in rats, infants who experienced higher levels of maternal nurturing were less fearful and less reactive to stressful situations, and performed better on tasks thought to depend on optimal functioning of the hippocampus, Dr. Schonfeld explained.
Related studies showed that cross-fostering infant rats from mothers who provided less nurturing compensated for the lack of maternal nurturing.
This suggests that care and support provided by adults outside of the family can help promote the development and adjustment of children affected by a crisis, he said.
"These findings are directly applicable to humans. The National Collaborative Perinatal Project showed similar findings in humans at 8 months of age," he noted.
The project demonstrated that the degree of maternal nurturing in an experimental setting predicted the infants’ degree of emotional distress in adulthood.
An epigenetic phenomenon may explain how early parental nurturing results in less stress reactively in offspring in adulthood, he said, noting that this idea was supported by findings from recent postmortem analyses of the brains of suicide victims. Victims with a history of early-life adversity had lower levels of glucocorticoid receptor messenger RNA in their hippocampus and higher rates of DNA methylation in the same promoter region as in the rat model.
"A whole separate and growing body of research has also demonstrated that chronic severe stress, especially during critical periods of brain development, leads to long-term changes in brain function and structure," he said.
"If you take all of this together, it underscores the need to protect children from stressful situations as much as possible, to intervene quickly after stressful events occur, and to pay particular attention to minimizing subsequent stressors because of the particularly detrimental effects of chronic stress on children," he added.
He cautioned, however, that a child’s adjustment following a traumatic event is related not just to the trauma, but to what occurs as a result of the event.
For example, if a child loses a family member as a result of violence, difficulties experienced by the child may be a result of bereavement.
Dr. Schonfeld described one teen affected by the 2012 Aurora, Colo., shooting who was reluctant to return to school, and who declined offers of trauma counseling. Although many of his trauma-related symptoms – such as fidgeting and difficulty sleeping – had abated, he disclosed that he "just didn’t feel right, and felt sad and empty."
Further discussion revealed that his problem was one of bereavement; he had lost a close friend in the shooting.
"No one had suggested that might be an issue for him, and I have seen this in crisis event after crisis event when I’ve responded," Dr. Schonfeld said.
After a crisis, a "cascade of secondary losses" can occur, and any one of these can be the cause of difficulty for those affected, he added.
Also, keep in mind that even as such events seem to be occurring more often, children don’t "get used to it," he said.
"They simply learn that there is little benefit in asking for support or assistance from adults in these communities, because it is so infrequently offered to them," he said.
As a result, children may become fatalistic and engage in reactive risk-taking behaviors or counterphobic behaviors that place them at greater risk.
"But they don’t get used to it. And I would contend that neither should we," he said.
Pediatricians should, however, recognize and celebrate what they have done and can do every day to support children and families dealing with difficult situations.
"It makes a big difference. I don’t want you to get overwhelmed by all that could – and unfortunately does – happen, and the long-lasting and profound impact these violent events can have on children. Instead, I challenge you ... to commit to at least one strategy to advocate for violence prevention and/or readiness for your practice or your community to support those who have been impacted by these events," he said.
Such strategies can include:
• Working to decrease violence crisis and loss, and advocating for meaningful change.
• Giving voice to children impacted by these events, allowing them to tell their stories, and forcing a dialogue that can help move the agenda forward.
• Advocating for better systems and services for children affected by these events, and other adverse events in the lives of children, including poverty, exposure to urban violence, and food insecurity, for example.
• Becoming more skilled in supporting children who are grieving and traumatized.
• Ensuring that other professionals in positions to support children – such as teachers and other school staff – are better prepared, more skilled, and more effectively supported in helping children after these events (and introducing information that can help before such events occur).
• Inquiring about exposures and experiences routinely in the practice setting. (The Medical Home for Children Exposed to Violence project [MHCEV] is working to provide resources for identifying, treating, and referring affected children and youth.)
• Promptly identifying affected children at the time of an event, and facilitating discussion about the impact of the event, and offering "psychological first aid and psychoeducation." Attend to basic needs, provide triage and referral, and remember that services will be needed throughout the recovery period, which may be weeks, months, or years.
• Helping in one’s own community when events happen elsewhere, as communities struggle to understand and cope with the events, and deal with distress that can surface as a result of concerns and personal experience.
• Becoming aware of the resources and support efforts of the AAP with respect to disaster preparedness and response. The academy’s department of federal affairs has helped make the AAP one of the leading forces for positive change at the federal level, Dr. Schonfeld said.
"The [AAP] Friends of Children’s Fund in general, and specifically the disaster relief part of that fund, helps not only children, families, and communities recover, but also assists professionals with self-care after these events," he said, noting that it is important to recognize that "it is distressing to be with children in distress."
"Events that are troubling our patients and their families are troubling to us as pediatric health care providers, as well," he said.
Dr. Schonfeld recommended the following resources for additional information:
• The AAP Children and Disasters site.
• The AAP Children and Disasters site, Coping and Adjustment.
• The AAP Medical Home for Children Exposed to Violence.
• The National Center for School Crisis and Bereavement.
Dr. Schonfeld reported having no relevant financial disclosures.
ORLANDO – Pediatricians can do a great deal to help their patients and communities in the wake of tragedies involving violence affecting children, according to Dr. David Schonfeld.
Unfortunately, it appears that such events are increasing in frequency, as evidenced by the headlines in recent months and years, Dr. Schonfeld, director of the National Center for School Crisis and Bereavement at St. Christopher’s Hospital in Philadelphia said at the annual meeting of the American Academy of Pediatrics.
It is important that when such events do occur, pediatricians work to address the impact of trauma on children; research suggests that supportive and nurturing adults can indeed mitigate the effects, said Dr. Schonfeld, a developmental and behavioral pediatrician and a member of the AAP Disaster Preparedness Advisory Council.
The available research, including both rat and human studies, highlights the role that nurturing by both mothers and other adults can play in protecting children.
In one set of experiments in rats, infants who experienced higher levels of maternal nurturing were less fearful and less reactive to stressful situations, and performed better on tasks thought to depend on optimal functioning of the hippocampus, Dr. Schonfeld explained.
Related studies showed that cross-fostering infant rats from mothers who provided less nurturing compensated for the lack of maternal nurturing.
This suggests that care and support provided by adults outside of the family can help promote the development and adjustment of children affected by a crisis, he said.
"These findings are directly applicable to humans. The National Collaborative Perinatal Project showed similar findings in humans at 8 months of age," he noted.
The project demonstrated that the degree of maternal nurturing in an experimental setting predicted the infants’ degree of emotional distress in adulthood.
An epigenetic phenomenon may explain how early parental nurturing results in less stress reactively in offspring in adulthood, he said, noting that this idea was supported by findings from recent postmortem analyses of the brains of suicide victims. Victims with a history of early-life adversity had lower levels of glucocorticoid receptor messenger RNA in their hippocampus and higher rates of DNA methylation in the same promoter region as in the rat model.
"A whole separate and growing body of research has also demonstrated that chronic severe stress, especially during critical periods of brain development, leads to long-term changes in brain function and structure," he said.
"If you take all of this together, it underscores the need to protect children from stressful situations as much as possible, to intervene quickly after stressful events occur, and to pay particular attention to minimizing subsequent stressors because of the particularly detrimental effects of chronic stress on children," he added.
He cautioned, however, that a child’s adjustment following a traumatic event is related not just to the trauma, but to what occurs as a result of the event.
For example, if a child loses a family member as a result of violence, difficulties experienced by the child may be a result of bereavement.
Dr. Schonfeld described one teen affected by the 2012 Aurora, Colo., shooting who was reluctant to return to school, and who declined offers of trauma counseling. Although many of his trauma-related symptoms – such as fidgeting and difficulty sleeping – had abated, he disclosed that he "just didn’t feel right, and felt sad and empty."
Further discussion revealed that his problem was one of bereavement; he had lost a close friend in the shooting.
"No one had suggested that might be an issue for him, and I have seen this in crisis event after crisis event when I’ve responded," Dr. Schonfeld said.
After a crisis, a "cascade of secondary losses" can occur, and any one of these can be the cause of difficulty for those affected, he added.
Also, keep in mind that even as such events seem to be occurring more often, children don’t "get used to it," he said.
"They simply learn that there is little benefit in asking for support or assistance from adults in these communities, because it is so infrequently offered to them," he said.
As a result, children may become fatalistic and engage in reactive risk-taking behaviors or counterphobic behaviors that place them at greater risk.
"But they don’t get used to it. And I would contend that neither should we," he said.
Pediatricians should, however, recognize and celebrate what they have done and can do every day to support children and families dealing with difficult situations.
"It makes a big difference. I don’t want you to get overwhelmed by all that could – and unfortunately does – happen, and the long-lasting and profound impact these violent events can have on children. Instead, I challenge you ... to commit to at least one strategy to advocate for violence prevention and/or readiness for your practice or your community to support those who have been impacted by these events," he said.
Such strategies can include:
• Working to decrease violence crisis and loss, and advocating for meaningful change.
• Giving voice to children impacted by these events, allowing them to tell their stories, and forcing a dialogue that can help move the agenda forward.
• Advocating for better systems and services for children affected by these events, and other adverse events in the lives of children, including poverty, exposure to urban violence, and food insecurity, for example.
• Becoming more skilled in supporting children who are grieving and traumatized.
• Ensuring that other professionals in positions to support children – such as teachers and other school staff – are better prepared, more skilled, and more effectively supported in helping children after these events (and introducing information that can help before such events occur).
• Inquiring about exposures and experiences routinely in the practice setting. (The Medical Home for Children Exposed to Violence project [MHCEV] is working to provide resources for identifying, treating, and referring affected children and youth.)
• Promptly identifying affected children at the time of an event, and facilitating discussion about the impact of the event, and offering "psychological first aid and psychoeducation." Attend to basic needs, provide triage and referral, and remember that services will be needed throughout the recovery period, which may be weeks, months, or years.
• Helping in one’s own community when events happen elsewhere, as communities struggle to understand and cope with the events, and deal with distress that can surface as a result of concerns and personal experience.
• Becoming aware of the resources and support efforts of the AAP with respect to disaster preparedness and response. The academy’s department of federal affairs has helped make the AAP one of the leading forces for positive change at the federal level, Dr. Schonfeld said.
"The [AAP] Friends of Children’s Fund in general, and specifically the disaster relief part of that fund, helps not only children, families, and communities recover, but also assists professionals with self-care after these events," he said, noting that it is important to recognize that "it is distressing to be with children in distress."
"Events that are troubling our patients and their families are troubling to us as pediatric health care providers, as well," he said.
Dr. Schonfeld recommended the following resources for additional information:
• The AAP Children and Disasters site.
• The AAP Children and Disasters site, Coping and Adjustment.
• The AAP Medical Home for Children Exposed to Violence.
• The National Center for School Crisis and Bereavement.
Dr. Schonfeld reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
Environmental stressors play major role in pediatric migraines
ORLANDO – Environmental stressors play a large role in triggering migraines in children, according to Dr. Eric Pearlman.
"Migraine is definitely a pediatric disorder. It peaks in young adulthood, but it definitely occurs in kids," Dr. Pearlman, chair of the department of pediatrics at Mercer University in Savannah, Ga., said at the annual meeting of the American Academy of Pediatrics.
Epidemiologic data suggest that migraine occurs in 10.5% of 10- to 15-year-old children and 3% of 7-year-olds, and that headaches – possibly including migraines – occur in 4% of 3-year-olds. By about 13 years of age, the prevalence of migraines starts reaching adult levels of about 6% in males, and 18% in females.
Environmental factors such as sleep deprivation, dehydration, dietary factors, school stressors, hidden stressors (like peers), and hormonal fluctuations represent triggers that can be particularly pronounced in children, he noted.
With International Classification of Headache Disorders, third edition (ICHD-III) criteria, migraines can be differentiated from acute, acute recurrent, and chronic progressive or chronic nonprogressive headaches if a child has experienced at least five attacks lasting up to 72 hours (whether untreated or unsuccessfully treated), if nausea and/or vomiting or photophobia and phonophobia are present, and if the child has at least two of four characteristics, including unilateral location, pulsating quality, moderate to severe intensity, and a tendency to be aggravated by – or avoid – routine physical activity.
In children, photophobia and phonophobia can be inferred (if they report having to lie down in a dark, quiet room, for example), as many have difficulty describing or understanding these symptoms
Unilateral headaches are rare in children, Dr. Pearlman noted.
If a diagnosis of migraine is established, it is important to make the diagnosis known to the child, and to educate the child about the condition and treatments.
Consider providing handouts and referring to websites (such as the American Headache Society or the National Headache Foundation sites), to help educate patients and to manage their expectations, as they need to understand you cannot cure their migraine, he advised.
Involving both the patient and their parents in decision making can improve compliance with treatment recommendations, he said.
Pharmacologic interventions can include nonspecific short-term therapies, migraine-specific therapies, and preventive treatment.
Nonspecific short-term therapies may include acetaminophen, nonsteroidal anti-inflammatory drugs, or combination drugs. Migraine-specific therapies include ergotamine and dihydroergotamine, and the "triptans."
Seven triptans are available, including two that are approved for use in children; rizitriptan (Maxalt) is approved for children older than age 6 years, and almitriptan (Axert) is approved for those aged 12-17 years.
Maxalt comes in both an oral and orally disintegrating form, and is available as a generic drug. Generic sumitriptan (Imitrex) also is available.
"There are good data for most of the triptans for adolescents aged 12 and older," Dr. Pearlman said.
Rescue medications for those who have an inadequate response to short-term therapy can include a combination of an analgesic like a nonsteroidal and an antiemetic, or an opiate and an antiemetic if the patient used a nonsteroidal initially. Rescue medications may be needed "because nothing is going to work 100% of the time," he said.
Preventive medications include beta-blockers, antidepressants, and antiseizure drugs.
The decision to use these medications should be based on attack frequency, disability associated with an attack, tolerance of short-term medication, and patient preference, and the choice of preventive medication depends on factors such as coexisting conditions, age, and prior medications use.
In a child with a sleep disorder, attention-deficit hyperactivity disorder, or depression, a tricyclic antidepressant such as amitriptyline might be considered; for a child with epilepsy, topirimate may be a good choice.
"If they have orthostatic intolerance, you think about a beta-blocker. If they are overweight, you want to stay away from medicine that causes weight gain – you might think about something like Topamax. For asthma and allergy you want to stay away from beta-blockers," he said, noting that these "are just some general principles."
Keep in mind that migraineurs are very sensitive to medicines, so it is important to start with a low dose and increase the dose slowly if needed, he said, also noting that the response to preventive medication takes time.
In studies of drugs that work for prevention, about 50% of patients had a 50% reduction in headaches, so managing expectations is important.
"You want to give a minimum of 2 months of a trial at a good dose," he said.
Treatment duration depends on response.
"Three months, 6 months, a year – sometimes longer if it takes a while to get them under control," he said, noting that he tends to take children off of preventives during the summer when they are less likely to experience the types of stress that can trigger migraines, and that he avoids taking them off of treatment at the beginning of the school year or during exams.
Nonpharmacologic preventive measures are important for all migraineurs.
"Headache hygiene" – regular sleep, regular meals, regular exercise – is particularly important, Dr. Pearlman said.
"The migraine brain doesn’t like changes. It doesn’t like disruption in routine or getting stressed," he said, noting that such disruptions can trigger an attack.
Stress management is easier said than done, but biofeedback, acupuncture, and massage (for those with a lot of tightness in the neck and shoulder muscles) may be helpful, he said.
Dr. Pearlman is a member of the speakers bureau for Allergan.
ORLANDO – Environmental stressors play a large role in triggering migraines in children, according to Dr. Eric Pearlman.
"Migraine is definitely a pediatric disorder. It peaks in young adulthood, but it definitely occurs in kids," Dr. Pearlman, chair of the department of pediatrics at Mercer University in Savannah, Ga., said at the annual meeting of the American Academy of Pediatrics.
Epidemiologic data suggest that migraine occurs in 10.5% of 10- to 15-year-old children and 3% of 7-year-olds, and that headaches – possibly including migraines – occur in 4% of 3-year-olds. By about 13 years of age, the prevalence of migraines starts reaching adult levels of about 6% in males, and 18% in females.
Environmental factors such as sleep deprivation, dehydration, dietary factors, school stressors, hidden stressors (like peers), and hormonal fluctuations represent triggers that can be particularly pronounced in children, he noted.
With International Classification of Headache Disorders, third edition (ICHD-III) criteria, migraines can be differentiated from acute, acute recurrent, and chronic progressive or chronic nonprogressive headaches if a child has experienced at least five attacks lasting up to 72 hours (whether untreated or unsuccessfully treated), if nausea and/or vomiting or photophobia and phonophobia are present, and if the child has at least two of four characteristics, including unilateral location, pulsating quality, moderate to severe intensity, and a tendency to be aggravated by – or avoid – routine physical activity.
In children, photophobia and phonophobia can be inferred (if they report having to lie down in a dark, quiet room, for example), as many have difficulty describing or understanding these symptoms
Unilateral headaches are rare in children, Dr. Pearlman noted.
If a diagnosis of migraine is established, it is important to make the diagnosis known to the child, and to educate the child about the condition and treatments.
Consider providing handouts and referring to websites (such as the American Headache Society or the National Headache Foundation sites), to help educate patients and to manage their expectations, as they need to understand you cannot cure their migraine, he advised.
Involving both the patient and their parents in decision making can improve compliance with treatment recommendations, he said.
Pharmacologic interventions can include nonspecific short-term therapies, migraine-specific therapies, and preventive treatment.
Nonspecific short-term therapies may include acetaminophen, nonsteroidal anti-inflammatory drugs, or combination drugs. Migraine-specific therapies include ergotamine and dihydroergotamine, and the "triptans."
Seven triptans are available, including two that are approved for use in children; rizitriptan (Maxalt) is approved for children older than age 6 years, and almitriptan (Axert) is approved for those aged 12-17 years.
Maxalt comes in both an oral and orally disintegrating form, and is available as a generic drug. Generic sumitriptan (Imitrex) also is available.
"There are good data for most of the triptans for adolescents aged 12 and older," Dr. Pearlman said.
Rescue medications for those who have an inadequate response to short-term therapy can include a combination of an analgesic like a nonsteroidal and an antiemetic, or an opiate and an antiemetic if the patient used a nonsteroidal initially. Rescue medications may be needed "because nothing is going to work 100% of the time," he said.
Preventive medications include beta-blockers, antidepressants, and antiseizure drugs.
The decision to use these medications should be based on attack frequency, disability associated with an attack, tolerance of short-term medication, and patient preference, and the choice of preventive medication depends on factors such as coexisting conditions, age, and prior medications use.
In a child with a sleep disorder, attention-deficit hyperactivity disorder, or depression, a tricyclic antidepressant such as amitriptyline might be considered; for a child with epilepsy, topirimate may be a good choice.
"If they have orthostatic intolerance, you think about a beta-blocker. If they are overweight, you want to stay away from medicine that causes weight gain – you might think about something like Topamax. For asthma and allergy you want to stay away from beta-blockers," he said, noting that these "are just some general principles."
Keep in mind that migraineurs are very sensitive to medicines, so it is important to start with a low dose and increase the dose slowly if needed, he said, also noting that the response to preventive medication takes time.
In studies of drugs that work for prevention, about 50% of patients had a 50% reduction in headaches, so managing expectations is important.
"You want to give a minimum of 2 months of a trial at a good dose," he said.
Treatment duration depends on response.
"Three months, 6 months, a year – sometimes longer if it takes a while to get them under control," he said, noting that he tends to take children off of preventives during the summer when they are less likely to experience the types of stress that can trigger migraines, and that he avoids taking them off of treatment at the beginning of the school year or during exams.
Nonpharmacologic preventive measures are important for all migraineurs.
"Headache hygiene" – regular sleep, regular meals, regular exercise – is particularly important, Dr. Pearlman said.
"The migraine brain doesn’t like changes. It doesn’t like disruption in routine or getting stressed," he said, noting that such disruptions can trigger an attack.
Stress management is easier said than done, but biofeedback, acupuncture, and massage (for those with a lot of tightness in the neck and shoulder muscles) may be helpful, he said.
Dr. Pearlman is a member of the speakers bureau for Allergan.
ORLANDO – Environmental stressors play a large role in triggering migraines in children, according to Dr. Eric Pearlman.
"Migraine is definitely a pediatric disorder. It peaks in young adulthood, but it definitely occurs in kids," Dr. Pearlman, chair of the department of pediatrics at Mercer University in Savannah, Ga., said at the annual meeting of the American Academy of Pediatrics.
Epidemiologic data suggest that migraine occurs in 10.5% of 10- to 15-year-old children and 3% of 7-year-olds, and that headaches – possibly including migraines – occur in 4% of 3-year-olds. By about 13 years of age, the prevalence of migraines starts reaching adult levels of about 6% in males, and 18% in females.
Environmental factors such as sleep deprivation, dehydration, dietary factors, school stressors, hidden stressors (like peers), and hormonal fluctuations represent triggers that can be particularly pronounced in children, he noted.
With International Classification of Headache Disorders, third edition (ICHD-III) criteria, migraines can be differentiated from acute, acute recurrent, and chronic progressive or chronic nonprogressive headaches if a child has experienced at least five attacks lasting up to 72 hours (whether untreated or unsuccessfully treated), if nausea and/or vomiting or photophobia and phonophobia are present, and if the child has at least two of four characteristics, including unilateral location, pulsating quality, moderate to severe intensity, and a tendency to be aggravated by – or avoid – routine physical activity.
In children, photophobia and phonophobia can be inferred (if they report having to lie down in a dark, quiet room, for example), as many have difficulty describing or understanding these symptoms
Unilateral headaches are rare in children, Dr. Pearlman noted.
If a diagnosis of migraine is established, it is important to make the diagnosis known to the child, and to educate the child about the condition and treatments.
Consider providing handouts and referring to websites (such as the American Headache Society or the National Headache Foundation sites), to help educate patients and to manage their expectations, as they need to understand you cannot cure their migraine, he advised.
Involving both the patient and their parents in decision making can improve compliance with treatment recommendations, he said.
Pharmacologic interventions can include nonspecific short-term therapies, migraine-specific therapies, and preventive treatment.
Nonspecific short-term therapies may include acetaminophen, nonsteroidal anti-inflammatory drugs, or combination drugs. Migraine-specific therapies include ergotamine and dihydroergotamine, and the "triptans."
Seven triptans are available, including two that are approved for use in children; rizitriptan (Maxalt) is approved for children older than age 6 years, and almitriptan (Axert) is approved for those aged 12-17 years.
Maxalt comes in both an oral and orally disintegrating form, and is available as a generic drug. Generic sumitriptan (Imitrex) also is available.
"There are good data for most of the triptans for adolescents aged 12 and older," Dr. Pearlman said.
Rescue medications for those who have an inadequate response to short-term therapy can include a combination of an analgesic like a nonsteroidal and an antiemetic, or an opiate and an antiemetic if the patient used a nonsteroidal initially. Rescue medications may be needed "because nothing is going to work 100% of the time," he said.
Preventive medications include beta-blockers, antidepressants, and antiseizure drugs.
The decision to use these medications should be based on attack frequency, disability associated with an attack, tolerance of short-term medication, and patient preference, and the choice of preventive medication depends on factors such as coexisting conditions, age, and prior medications use.
In a child with a sleep disorder, attention-deficit hyperactivity disorder, or depression, a tricyclic antidepressant such as amitriptyline might be considered; for a child with epilepsy, topirimate may be a good choice.
"If they have orthostatic intolerance, you think about a beta-blocker. If they are overweight, you want to stay away from medicine that causes weight gain – you might think about something like Topamax. For asthma and allergy you want to stay away from beta-blockers," he said, noting that these "are just some general principles."
Keep in mind that migraineurs are very sensitive to medicines, so it is important to start with a low dose and increase the dose slowly if needed, he said, also noting that the response to preventive medication takes time.
In studies of drugs that work for prevention, about 50% of patients had a 50% reduction in headaches, so managing expectations is important.
"You want to give a minimum of 2 months of a trial at a good dose," he said.
Treatment duration depends on response.
"Three months, 6 months, a year – sometimes longer if it takes a while to get them under control," he said, noting that he tends to take children off of preventives during the summer when they are less likely to experience the types of stress that can trigger migraines, and that he avoids taking them off of treatment at the beginning of the school year or during exams.
Nonpharmacologic preventive measures are important for all migraineurs.
"Headache hygiene" – regular sleep, regular meals, regular exercise – is particularly important, Dr. Pearlman said.
"The migraine brain doesn’t like changes. It doesn’t like disruption in routine or getting stressed," he said, noting that such disruptions can trigger an attack.
Stress management is easier said than done, but biofeedback, acupuncture, and massage (for those with a lot of tightness in the neck and shoulder muscles) may be helpful, he said.
Dr. Pearlman is a member of the speakers bureau for Allergan.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
Make the most of nonopioids: Managing acute pain in children
ORLANDO – Effective management of acute pain in children is important not only for improving comfort, but also for improving outcomes, according to Dr. Joseph D. Tobias.
"The important thing to realize is that there are many benefits (of pain management). Although we walk a fine line between adverse effects and benefits, many times with adequate analgesia we put patients in a better place, Dr. Tobias, chief of anesthesiology and pain medicine at Nationwide Children’s Hospital in Columbus, Ohio, said at the annual meeting of the American Academy of Pediatrics.
That’s because with inadequate analgesia there are a host of humoral factors, including increased endogenous catecholamines, that have adverse physiologic effects on oxygen consumption, CO2 production, and on the immune system, he explained.
Multiple studies have demonstrated that aggressive pain management has beneficial immune effects, he added, noting that patients with adequate pain management are less likely to experience infections and that neonates and infants without adequate pain management may experience chronic pain and pain syndromes later in life because of the neuroplasticity of the infant brain.
He recommends the classic "stepwise ladder" approach to pain management in pediatric patients with acute pain following surgery, trauma, or acute illness, for example. Step 1 involves administration of nonopioids and adjuvants.
"But even as we move to step 2 and add opioids, it’s very important to keep the nonopioids and adjuvants going. I don’t think anybody should ever be in the hospital on [patient-controlled analgesia] getting opioids and not getting nonsteroidal [drugs], acetaminophen, and other adjuvants, because what you’re going to do is decrease your opioid requirements, and as you do that, you then decrease opioid-related side effects," he said.
Keep in mind that the maximum dose of oral or rectal acetaminophen has been decreased from 4 to 3 grams, he said, noting that reports of significant toxicity with acetaminophen have been increasing, so it is important to limit the dose.
The same holds true for the new intravenous preparation of acetaminophen, given reports of 10-fold overdose (10 mg/mL concentration).
"We need to be cognizant of that," he said.
A number of salicylates and NSAIDs are also available for use in children. Ibuprofen is among the most commonly used, and also is now available in an intravenous formulation.
Ketorolac is another good treatment option, but intravenous acetaminophen is preferable in children under age 1 year, because of concerns regarding decreased renal perfusion, he said.
Other emerging options that are making their way from the adult to the pediatric pain-management arena are ketamine, gabapentin and pregabalin, dexamethasone, and dexmedetomidine, all of which appear to have some potential benefits for improving pain management and reducing the need for opioids.
Watch for interactions and adverse effects
Be sure to assess for potential drug interactions in children on several medications and to protect against the adverse gastrointestinal tract effects of nonsteroidal drugs, Dr. Tobias advised.
"If you’re using nonsteroidals, especially postoperatively in patients, it’s always a good idea to combine them with a proton pump inhibitor, or an H2 antagonist," he said, noting that that these can generally be discontinued once the patient is tolerating a regular diet.
Effects on renal function are also an important concern, particularly in those with preexisting renal dysfunction, concomitant use of other nephrotoxic agents, hypovolemia, hypoperfusion, and prolonged administration.
Bleeding is another concern, particularly in those receiving ketorolac, which shouldn’t be used in children undergoing tonsillectomy or in other cases involving increased bleeding risk, he said.
As for opioids, morphine and hydromorphone are the most commonly used in children, accounting for about 99% of usage.
Morphine is more often associated with pruritus in older children and adolescents, so hydromorphone may be a better option to start with in these patients.
"As far as dosing guidelines, I think it’s very important to adjust the dose based on the patient’s status and follow pain scores. I think everybody in the hospital needs to have their pain score checked. It doesn’t matter which (pain scale) you use," Dr. Tobias said.
Also, a steady-state serum concentration should be maintained with avoidance of peaks and troughs, and patients on opioids should be monitored for adverse effects, he said, noting that patient-controlled analgesia (PCA) devices are useful – after a loading dose – to maintain those concentrations. PCA devices can be used by children as young as 5 or 6 years of age; nurse-controlled analgesia is best for those who are younger or have cognitive impairment.
A lower basal infusion rate (4-5 mcg/kg per hour) allows for better sleep while reducing side effects, he said.
Among the concerning side effects of opioids are constipation and respiratory depression.
"Remember, you develop tolerance least quickly to their effects on the GI tract ... when you’re sending kids home from the hospital on opioids, make sure you focus on their bowel habits, or they’re going to be back, they’re going to be constipated, they’re not going to be ambulating, they may not be as well hydrated, so we really need to focus on the GI tract," he said.
Respiratory depression is recognized as an increasing concern.
"When these kids are getting PCA on the floor, make sure you have ready access to resuscitation equipment should you need it," he said.
"Especially as the population gets bigger, we may have more undiagnosed OSA [obstructive sleep apnea], so all of our patients get their respiratory rates checked, they’re on pulse oximetry. In really high-risk patients, we’re using end tidal transcutaneous CO2 monitoring," he said, adding: "Remember, hypoxemia is a late finding of opioid-related respiratory depression. You’re going to see a slight elevation in carbon dioxide first."
Adverse effects are most common in those at the extremes of age, in those with underlying systemic diseases, and in those receiving other agents that are central nervous system depressants.
Of course, the best way to limit side effects is to use adjunctive agents, Dr. Tobias said.
"Maximize the use of nonsteroidals and acetaminophen, and you’re going to use a lot less opioid," he said.
Another important approach to reducing opioid use is the perioperative use of regional anesthesia.
"If you’re working in the hospital taking care of kids after major surgical procedures, I think if you partner with the anesthesia team there’s a lot you can do perioperatively to almost eliminate the need for intravenous opioids," he said.
For a femur fracture patient, for example, a catheter can be placed near the femoral nerve to provide analgesia, or the lateral femoral cutaneous nerve can be blocked. Ultrasound has "really opened the door for regional anesthesia."
Home infusion devices are also available.
"So if you’re having your anterior cruciate ligament repaired, where I work, you’re going to go home with a femoral nerve catheter and a home infusion device that will work for 3 days and really limit your need for parenteral and oral opioids," he said.
Outside of the operating room, regional anesthesia can be used to treat pain that is unresponsive to opioids or if the opioids are causing side effects. Cases involving sickle cell vaso-occlusive crisis, multiple trauma, or burns are scenarios in which regional anesthesia can be particularly useful, he said.
Dr. Tobias reported having no disclosures.
ORLANDO – Effective management of acute pain in children is important not only for improving comfort, but also for improving outcomes, according to Dr. Joseph D. Tobias.
"The important thing to realize is that there are many benefits (of pain management). Although we walk a fine line between adverse effects and benefits, many times with adequate analgesia we put patients in a better place, Dr. Tobias, chief of anesthesiology and pain medicine at Nationwide Children’s Hospital in Columbus, Ohio, said at the annual meeting of the American Academy of Pediatrics.
That’s because with inadequate analgesia there are a host of humoral factors, including increased endogenous catecholamines, that have adverse physiologic effects on oxygen consumption, CO2 production, and on the immune system, he explained.
Multiple studies have demonstrated that aggressive pain management has beneficial immune effects, he added, noting that patients with adequate pain management are less likely to experience infections and that neonates and infants without adequate pain management may experience chronic pain and pain syndromes later in life because of the neuroplasticity of the infant brain.
He recommends the classic "stepwise ladder" approach to pain management in pediatric patients with acute pain following surgery, trauma, or acute illness, for example. Step 1 involves administration of nonopioids and adjuvants.
"But even as we move to step 2 and add opioids, it’s very important to keep the nonopioids and adjuvants going. I don’t think anybody should ever be in the hospital on [patient-controlled analgesia] getting opioids and not getting nonsteroidal [drugs], acetaminophen, and other adjuvants, because what you’re going to do is decrease your opioid requirements, and as you do that, you then decrease opioid-related side effects," he said.
Keep in mind that the maximum dose of oral or rectal acetaminophen has been decreased from 4 to 3 grams, he said, noting that reports of significant toxicity with acetaminophen have been increasing, so it is important to limit the dose.
The same holds true for the new intravenous preparation of acetaminophen, given reports of 10-fold overdose (10 mg/mL concentration).
"We need to be cognizant of that," he said.
A number of salicylates and NSAIDs are also available for use in children. Ibuprofen is among the most commonly used, and also is now available in an intravenous formulation.
Ketorolac is another good treatment option, but intravenous acetaminophen is preferable in children under age 1 year, because of concerns regarding decreased renal perfusion, he said.
Other emerging options that are making their way from the adult to the pediatric pain-management arena are ketamine, gabapentin and pregabalin, dexamethasone, and dexmedetomidine, all of which appear to have some potential benefits for improving pain management and reducing the need for opioids.
Watch for interactions and adverse effects
Be sure to assess for potential drug interactions in children on several medications and to protect against the adverse gastrointestinal tract effects of nonsteroidal drugs, Dr. Tobias advised.
"If you’re using nonsteroidals, especially postoperatively in patients, it’s always a good idea to combine them with a proton pump inhibitor, or an H2 antagonist," he said, noting that that these can generally be discontinued once the patient is tolerating a regular diet.
Effects on renal function are also an important concern, particularly in those with preexisting renal dysfunction, concomitant use of other nephrotoxic agents, hypovolemia, hypoperfusion, and prolonged administration.
Bleeding is another concern, particularly in those receiving ketorolac, which shouldn’t be used in children undergoing tonsillectomy or in other cases involving increased bleeding risk, he said.
As for opioids, morphine and hydromorphone are the most commonly used in children, accounting for about 99% of usage.
Morphine is more often associated with pruritus in older children and adolescents, so hydromorphone may be a better option to start with in these patients.
"As far as dosing guidelines, I think it’s very important to adjust the dose based on the patient’s status and follow pain scores. I think everybody in the hospital needs to have their pain score checked. It doesn’t matter which (pain scale) you use," Dr. Tobias said.
Also, a steady-state serum concentration should be maintained with avoidance of peaks and troughs, and patients on opioids should be monitored for adverse effects, he said, noting that patient-controlled analgesia (PCA) devices are useful – after a loading dose – to maintain those concentrations. PCA devices can be used by children as young as 5 or 6 years of age; nurse-controlled analgesia is best for those who are younger or have cognitive impairment.
A lower basal infusion rate (4-5 mcg/kg per hour) allows for better sleep while reducing side effects, he said.
Among the concerning side effects of opioids are constipation and respiratory depression.
"Remember, you develop tolerance least quickly to their effects on the GI tract ... when you’re sending kids home from the hospital on opioids, make sure you focus on their bowel habits, or they’re going to be back, they’re going to be constipated, they’re not going to be ambulating, they may not be as well hydrated, so we really need to focus on the GI tract," he said.
Respiratory depression is recognized as an increasing concern.
"When these kids are getting PCA on the floor, make sure you have ready access to resuscitation equipment should you need it," he said.
"Especially as the population gets bigger, we may have more undiagnosed OSA [obstructive sleep apnea], so all of our patients get their respiratory rates checked, they’re on pulse oximetry. In really high-risk patients, we’re using end tidal transcutaneous CO2 monitoring," he said, adding: "Remember, hypoxemia is a late finding of opioid-related respiratory depression. You’re going to see a slight elevation in carbon dioxide first."
Adverse effects are most common in those at the extremes of age, in those with underlying systemic diseases, and in those receiving other agents that are central nervous system depressants.
Of course, the best way to limit side effects is to use adjunctive agents, Dr. Tobias said.
"Maximize the use of nonsteroidals and acetaminophen, and you’re going to use a lot less opioid," he said.
Another important approach to reducing opioid use is the perioperative use of regional anesthesia.
"If you’re working in the hospital taking care of kids after major surgical procedures, I think if you partner with the anesthesia team there’s a lot you can do perioperatively to almost eliminate the need for intravenous opioids," he said.
For a femur fracture patient, for example, a catheter can be placed near the femoral nerve to provide analgesia, or the lateral femoral cutaneous nerve can be blocked. Ultrasound has "really opened the door for regional anesthesia."
Home infusion devices are also available.
"So if you’re having your anterior cruciate ligament repaired, where I work, you’re going to go home with a femoral nerve catheter and a home infusion device that will work for 3 days and really limit your need for parenteral and oral opioids," he said.
Outside of the operating room, regional anesthesia can be used to treat pain that is unresponsive to opioids or if the opioids are causing side effects. Cases involving sickle cell vaso-occlusive crisis, multiple trauma, or burns are scenarios in which regional anesthesia can be particularly useful, he said.
Dr. Tobias reported having no disclosures.
ORLANDO – Effective management of acute pain in children is important not only for improving comfort, but also for improving outcomes, according to Dr. Joseph D. Tobias.
"The important thing to realize is that there are many benefits (of pain management). Although we walk a fine line between adverse effects and benefits, many times with adequate analgesia we put patients in a better place, Dr. Tobias, chief of anesthesiology and pain medicine at Nationwide Children’s Hospital in Columbus, Ohio, said at the annual meeting of the American Academy of Pediatrics.
That’s because with inadequate analgesia there are a host of humoral factors, including increased endogenous catecholamines, that have adverse physiologic effects on oxygen consumption, CO2 production, and on the immune system, he explained.
Multiple studies have demonstrated that aggressive pain management has beneficial immune effects, he added, noting that patients with adequate pain management are less likely to experience infections and that neonates and infants without adequate pain management may experience chronic pain and pain syndromes later in life because of the neuroplasticity of the infant brain.
He recommends the classic "stepwise ladder" approach to pain management in pediatric patients with acute pain following surgery, trauma, or acute illness, for example. Step 1 involves administration of nonopioids and adjuvants.
"But even as we move to step 2 and add opioids, it’s very important to keep the nonopioids and adjuvants going. I don’t think anybody should ever be in the hospital on [patient-controlled analgesia] getting opioids and not getting nonsteroidal [drugs], acetaminophen, and other adjuvants, because what you’re going to do is decrease your opioid requirements, and as you do that, you then decrease opioid-related side effects," he said.
Keep in mind that the maximum dose of oral or rectal acetaminophen has been decreased from 4 to 3 grams, he said, noting that reports of significant toxicity with acetaminophen have been increasing, so it is important to limit the dose.
The same holds true for the new intravenous preparation of acetaminophen, given reports of 10-fold overdose (10 mg/mL concentration).
"We need to be cognizant of that," he said.
A number of salicylates and NSAIDs are also available for use in children. Ibuprofen is among the most commonly used, and also is now available in an intravenous formulation.
Ketorolac is another good treatment option, but intravenous acetaminophen is preferable in children under age 1 year, because of concerns regarding decreased renal perfusion, he said.
Other emerging options that are making their way from the adult to the pediatric pain-management arena are ketamine, gabapentin and pregabalin, dexamethasone, and dexmedetomidine, all of which appear to have some potential benefits for improving pain management and reducing the need for opioids.
Watch for interactions and adverse effects
Be sure to assess for potential drug interactions in children on several medications and to protect against the adverse gastrointestinal tract effects of nonsteroidal drugs, Dr. Tobias advised.
"If you’re using nonsteroidals, especially postoperatively in patients, it’s always a good idea to combine them with a proton pump inhibitor, or an H2 antagonist," he said, noting that that these can generally be discontinued once the patient is tolerating a regular diet.
Effects on renal function are also an important concern, particularly in those with preexisting renal dysfunction, concomitant use of other nephrotoxic agents, hypovolemia, hypoperfusion, and prolonged administration.
Bleeding is another concern, particularly in those receiving ketorolac, which shouldn’t be used in children undergoing tonsillectomy or in other cases involving increased bleeding risk, he said.
As for opioids, morphine and hydromorphone are the most commonly used in children, accounting for about 99% of usage.
Morphine is more often associated with pruritus in older children and adolescents, so hydromorphone may be a better option to start with in these patients.
"As far as dosing guidelines, I think it’s very important to adjust the dose based on the patient’s status and follow pain scores. I think everybody in the hospital needs to have their pain score checked. It doesn’t matter which (pain scale) you use," Dr. Tobias said.
Also, a steady-state serum concentration should be maintained with avoidance of peaks and troughs, and patients on opioids should be monitored for adverse effects, he said, noting that patient-controlled analgesia (PCA) devices are useful – after a loading dose – to maintain those concentrations. PCA devices can be used by children as young as 5 or 6 years of age; nurse-controlled analgesia is best for those who are younger or have cognitive impairment.
A lower basal infusion rate (4-5 mcg/kg per hour) allows for better sleep while reducing side effects, he said.
Among the concerning side effects of opioids are constipation and respiratory depression.
"Remember, you develop tolerance least quickly to their effects on the GI tract ... when you’re sending kids home from the hospital on opioids, make sure you focus on their bowel habits, or they’re going to be back, they’re going to be constipated, they’re not going to be ambulating, they may not be as well hydrated, so we really need to focus on the GI tract," he said.
Respiratory depression is recognized as an increasing concern.
"When these kids are getting PCA on the floor, make sure you have ready access to resuscitation equipment should you need it," he said.
"Especially as the population gets bigger, we may have more undiagnosed OSA [obstructive sleep apnea], so all of our patients get their respiratory rates checked, they’re on pulse oximetry. In really high-risk patients, we’re using end tidal transcutaneous CO2 monitoring," he said, adding: "Remember, hypoxemia is a late finding of opioid-related respiratory depression. You’re going to see a slight elevation in carbon dioxide first."
Adverse effects are most common in those at the extremes of age, in those with underlying systemic diseases, and in those receiving other agents that are central nervous system depressants.
Of course, the best way to limit side effects is to use adjunctive agents, Dr. Tobias said.
"Maximize the use of nonsteroidals and acetaminophen, and you’re going to use a lot less opioid," he said.
Another important approach to reducing opioid use is the perioperative use of regional anesthesia.
"If you’re working in the hospital taking care of kids after major surgical procedures, I think if you partner with the anesthesia team there’s a lot you can do perioperatively to almost eliminate the need for intravenous opioids," he said.
For a femur fracture patient, for example, a catheter can be placed near the femoral nerve to provide analgesia, or the lateral femoral cutaneous nerve can be blocked. Ultrasound has "really opened the door for regional anesthesia."
Home infusion devices are also available.
"So if you’re having your anterior cruciate ligament repaired, where I work, you’re going to go home with a femoral nerve catheter and a home infusion device that will work for 3 days and really limit your need for parenteral and oral opioids," he said.
Outside of the operating room, regional anesthesia can be used to treat pain that is unresponsive to opioids or if the opioids are causing side effects. Cases involving sickle cell vaso-occlusive crisis, multiple trauma, or burns are scenarios in which regional anesthesia can be particularly useful, he said.
Dr. Tobias reported having no disclosures.
EXPERT ANALYSIS AT THE AAP NATIONAL CONFERENCE
Equipping pediatricians to take on cancer survivor care
ORLANDO – Pediatricians need to be positioned to offer survivor care to the more than 80% of pediatric cancer patients who now survive their disease, according to Dr. Melissa Hudson.
"We have in excess of 479,000 individuals living in the United States diagnosed with cancer before the age of 21 ... and we know with those numbers increasing, you will be increasingly seeing them in your practices," Dr. Hudson, director of the cancer survivorship division, department of oncology at St. Jude Children’s Research Hospital, Memphis, Tenn., said at the annual meeting of the American Academy of Pediatrics.
Health-related issues that affect these cancer survivors include the risk for recurrence, potential late effects of treatment, and psychosocial effects related to the cancer experience, Importantly, health care needs in these patients change over time and across the spectrum of care. Ideally, pediatricians will provide these patients with risk-based survivor care that includes health education, anticipatory guidance based on cancer history and specific cancer-related health risks, and cancer and other health screening and surveillance as recommended based on the patient’s specific treatment exposures, she said.
In particular, patients need to be educated about the impact of their health behaviors on cancer-related health risk and about effective self-management of chronic health conditions.
The common chronic conditions that follow cancer often can impact growth and development – including linear growth, skeletal maturation, intellectual functioning, emotional and social maturation, and sexual development.
Recently published data from the St. Jude Lifetime Cohort Study showed that 95.5% of nearly 1,700 adult survivors of pediatric cancer had at least 1 chronic health condition by age 45 years, and nearly 81% had a serious disabling or life-threatening condition (J. Clin. Oncol. 2013;31:4242-51). Data from the retrospective Childhood Cancer Survivor Study similarly showed that, compared with population controls, survivors have a higher rate of premature mortality, largely from subsequent malignancies, which confer a 15-fold excess risk of death; cardiac conditions, which confer a sevenfold excess risk of death; and pulmonary conditions, which confer a nearly ninefold excess risk of death.
Survivor care also needs to consider that treatment-related issues, ongoing cancer risk, and the cancer experience in general can combine to have important psychosocial effects
Mental health factors can include body image issues, adverse effects of the cancer experience on educational and vocational goals, and late cognitive effects. Survivors also face insurance discrimination and access to care issues due to financial issues associated with medical bills and under- or unemployment.
Many survivors also struggle with ongoing symptoms such as fatigue, disrupted sleep, memory problems, concentration issues, and chronic pain; some have difficulty living independently because of the severity of these symptoms, and the effects can have a negative impact on social interactions with family and friends.
"We need to help them achieve access to resources to optimize their quality of life," Dr. Hudson said.
When cancer survivors return to primary care, they should present with a treatment summary. If they don’t, one should be requested from the cancer treatment center to help guide care, she said.
Become familiar with practice guidelines for caring for survivors of childhood cancers, and be prepared to work with either the oncology care center to help facilitate the transition to pediatric care, she said.
The Children’s Oncology Group (COG), a consortium of medical research institutions, provides numerous tools for care providers and patients. Dr. Hudson, who co-chaired the task force that established the care guidelines, said that they provide recommendations for screening and management of late effects that can arise in pediatric cancer survivors. These patient education handouts can be printed free of charge and many are available in Spanish and French as well as in English. An updated version (4.0) of the COG guidelines is pending release by early 2014, Dr. Hudson said.
Dr. Hudson reported having no disclosures.
ORLANDO – Pediatricians need to be positioned to offer survivor care to the more than 80% of pediatric cancer patients who now survive their disease, according to Dr. Melissa Hudson.
"We have in excess of 479,000 individuals living in the United States diagnosed with cancer before the age of 21 ... and we know with those numbers increasing, you will be increasingly seeing them in your practices," Dr. Hudson, director of the cancer survivorship division, department of oncology at St. Jude Children’s Research Hospital, Memphis, Tenn., said at the annual meeting of the American Academy of Pediatrics.
Health-related issues that affect these cancer survivors include the risk for recurrence, potential late effects of treatment, and psychosocial effects related to the cancer experience, Importantly, health care needs in these patients change over time and across the spectrum of care. Ideally, pediatricians will provide these patients with risk-based survivor care that includes health education, anticipatory guidance based on cancer history and specific cancer-related health risks, and cancer and other health screening and surveillance as recommended based on the patient’s specific treatment exposures, she said.
In particular, patients need to be educated about the impact of their health behaviors on cancer-related health risk and about effective self-management of chronic health conditions.
The common chronic conditions that follow cancer often can impact growth and development – including linear growth, skeletal maturation, intellectual functioning, emotional and social maturation, and sexual development.
Recently published data from the St. Jude Lifetime Cohort Study showed that 95.5% of nearly 1,700 adult survivors of pediatric cancer had at least 1 chronic health condition by age 45 years, and nearly 81% had a serious disabling or life-threatening condition (J. Clin. Oncol. 2013;31:4242-51). Data from the retrospective Childhood Cancer Survivor Study similarly showed that, compared with population controls, survivors have a higher rate of premature mortality, largely from subsequent malignancies, which confer a 15-fold excess risk of death; cardiac conditions, which confer a sevenfold excess risk of death; and pulmonary conditions, which confer a nearly ninefold excess risk of death.
Survivor care also needs to consider that treatment-related issues, ongoing cancer risk, and the cancer experience in general can combine to have important psychosocial effects
Mental health factors can include body image issues, adverse effects of the cancer experience on educational and vocational goals, and late cognitive effects. Survivors also face insurance discrimination and access to care issues due to financial issues associated with medical bills and under- or unemployment.
Many survivors also struggle with ongoing symptoms such as fatigue, disrupted sleep, memory problems, concentration issues, and chronic pain; some have difficulty living independently because of the severity of these symptoms, and the effects can have a negative impact on social interactions with family and friends.
"We need to help them achieve access to resources to optimize their quality of life," Dr. Hudson said.
When cancer survivors return to primary care, they should present with a treatment summary. If they don’t, one should be requested from the cancer treatment center to help guide care, she said.
Become familiar with practice guidelines for caring for survivors of childhood cancers, and be prepared to work with either the oncology care center to help facilitate the transition to pediatric care, she said.
The Children’s Oncology Group (COG), a consortium of medical research institutions, provides numerous tools for care providers and patients. Dr. Hudson, who co-chaired the task force that established the care guidelines, said that they provide recommendations for screening and management of late effects that can arise in pediatric cancer survivors. These patient education handouts can be printed free of charge and many are available in Spanish and French as well as in English. An updated version (4.0) of the COG guidelines is pending release by early 2014, Dr. Hudson said.
Dr. Hudson reported having no disclosures.
ORLANDO – Pediatricians need to be positioned to offer survivor care to the more than 80% of pediatric cancer patients who now survive their disease, according to Dr. Melissa Hudson.
"We have in excess of 479,000 individuals living in the United States diagnosed with cancer before the age of 21 ... and we know with those numbers increasing, you will be increasingly seeing them in your practices," Dr. Hudson, director of the cancer survivorship division, department of oncology at St. Jude Children’s Research Hospital, Memphis, Tenn., said at the annual meeting of the American Academy of Pediatrics.
Health-related issues that affect these cancer survivors include the risk for recurrence, potential late effects of treatment, and psychosocial effects related to the cancer experience, Importantly, health care needs in these patients change over time and across the spectrum of care. Ideally, pediatricians will provide these patients with risk-based survivor care that includes health education, anticipatory guidance based on cancer history and specific cancer-related health risks, and cancer and other health screening and surveillance as recommended based on the patient’s specific treatment exposures, she said.
In particular, patients need to be educated about the impact of their health behaviors on cancer-related health risk and about effective self-management of chronic health conditions.
The common chronic conditions that follow cancer often can impact growth and development – including linear growth, skeletal maturation, intellectual functioning, emotional and social maturation, and sexual development.
Recently published data from the St. Jude Lifetime Cohort Study showed that 95.5% of nearly 1,700 adult survivors of pediatric cancer had at least 1 chronic health condition by age 45 years, and nearly 81% had a serious disabling or life-threatening condition (J. Clin. Oncol. 2013;31:4242-51). Data from the retrospective Childhood Cancer Survivor Study similarly showed that, compared with population controls, survivors have a higher rate of premature mortality, largely from subsequent malignancies, which confer a 15-fold excess risk of death; cardiac conditions, which confer a sevenfold excess risk of death; and pulmonary conditions, which confer a nearly ninefold excess risk of death.
Survivor care also needs to consider that treatment-related issues, ongoing cancer risk, and the cancer experience in general can combine to have important psychosocial effects
Mental health factors can include body image issues, adverse effects of the cancer experience on educational and vocational goals, and late cognitive effects. Survivors also face insurance discrimination and access to care issues due to financial issues associated with medical bills and under- or unemployment.
Many survivors also struggle with ongoing symptoms such as fatigue, disrupted sleep, memory problems, concentration issues, and chronic pain; some have difficulty living independently because of the severity of these symptoms, and the effects can have a negative impact on social interactions with family and friends.
"We need to help them achieve access to resources to optimize their quality of life," Dr. Hudson said.
When cancer survivors return to primary care, they should present with a treatment summary. If they don’t, one should be requested from the cancer treatment center to help guide care, she said.
Become familiar with practice guidelines for caring for survivors of childhood cancers, and be prepared to work with either the oncology care center to help facilitate the transition to pediatric care, she said.
The Children’s Oncology Group (COG), a consortium of medical research institutions, provides numerous tools for care providers and patients. Dr. Hudson, who co-chaired the task force that established the care guidelines, said that they provide recommendations for screening and management of late effects that can arise in pediatric cancer survivors. These patient education handouts can be printed free of charge and many are available in Spanish and French as well as in English. An updated version (4.0) of the COG guidelines is pending release by early 2014, Dr. Hudson said.
Dr. Hudson reported having no disclosures.
AT THE AAP NATIONAL CONFERENCE
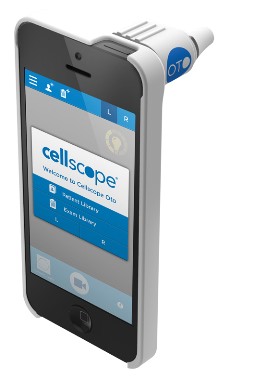
Online symptom checker, digital answering service add practice value
ORLANDO – Making the best use of the right technology can transform a primary care practice, according to Dr. Daniel Feiten.
Parents are living in a mobile world. They do their banking online, they order pizza online, and they want to manage some aspects of their family’s health care online when possible. Many pediatric practices, however, are still living in a typewriter world, said Dr. Feiten, a pediatrician in private practice in Centennial, Colo.
During a session on technology at the annual meeting of the American Academy of Pediatrics, he noted that it’s not always easy to incorporate new technology into an existing practice – and in some cases the transition can actually increase workload. Among those he recommended as potentially cost-effective and worth considering are a website with a symptom checker, and a digital answering service.
A survey of parents from his group practice showed that for 56%, the main reason for visiting the practice’s website was having a sick child. They wanted to know if their child needed to be seen by a doctor, and they wanted access to a symptom checker to help them determine that, Dr. Feiten said.
In another survey of 2,600 parents who have used such a symptom checker, 61% said the application saved them a call to the doctor’s office, 19% said it prompted them to call when they weren’t planning to do so, and 93% said they would prefer to find the symptom checker on the doctor’s website rather than having to use another source.
Furthermore, 93% of respondents said the symptom checker was the most important feature, and 72% listed patient portals (for appointment requests and other communications) as an important feature as well.
A third of them considered physician and staff photos to be important.
"What does that say? It says that we are moving away from the mentality of using a website or a web presence to get patients," Dr. Feiten said, explaining that the functionality parents want is a simple, quick way to determine whether their children need medical care.
"Websites should be functional tools rather than marketing tools," he said.
The symptom checker should be the prominent feature of the website – available on the home page, with easy access and drop-downs, he said.
An analysis in his practice showed that while the impact on answering service calls was minimal 5 years after launching a website with a symptom checker, the parents who said they used the website brought in $19,000 that year.
"That’s a nice return on investment for the little you would pay to have a symptom checker on your website," he said.
Dr. Feiten said that digital answering service applications allow patients to page an on-call physician via the website or a mobile phone. The applications direct parents to write concise descriptions of their children’s symptoms, and the programs can be adapted to direct pages "to the right person at the right time on the right device."
The relatively new technology offers a number of advantages over live answering services – not the least of which is improved accuracy for electronic health records. Consider the spelling of a patient’s name, for example. (How many ways are there to spell ‘Michaela?’ Dr. Feiten, mused). A parent will get it right, he said.
The applications are also easy to implement on a website or mobile device, and the cost is half (or less) that of live instant message answering services, according to Dr. Feiten, who predicted that "this will be the next revolution in after-hours."
Potential savings in the United States is $34 million each year, he said.
His practice has been using the service for 2 years, and an analysis showed that only 1 in 84 parents said they expected the availability of the service would increase the number of after-hours calls they make, and in fact, after implementation, visit volume increased 5%, but after-hours message volume increased by only 1.2%.
"The feedback that we get from parents is that they love this type of service," he said.
Many practices may find that it is best to make both types of answering services available, as not all parents will embrace this technology.
A related technology that has the potential to improve communications between physicians, and which a number of companies are currently developing, is message management software, he noted.
It will provide an efficient system to get messages quickly to the intended recipient, with criteria built in to ensure messages aren’t missed (such as live-agent validation for messages that aren’t picked up in a timely manner).
"I’m really excited about this," Dr. Feiten said, explaining that these "rules engine" applications are "the wave of the future."
Dr. Feiten is cofounder of MedSecure (an answering service), and cofounder and co-owner of Remedy Web Inc. (a web design and development company), but he receives no remuneration from these companies. He is on the board of directors of the Children’s Diabetes Foundation.
ORLANDO – Making the best use of the right technology can transform a primary care practice, according to Dr. Daniel Feiten.
Parents are living in a mobile world. They do their banking online, they order pizza online, and they want to manage some aspects of their family’s health care online when possible. Many pediatric practices, however, are still living in a typewriter world, said Dr. Feiten, a pediatrician in private practice in Centennial, Colo.
During a session on technology at the annual meeting of the American Academy of Pediatrics, he noted that it’s not always easy to incorporate new technology into an existing practice – and in some cases the transition can actually increase workload. Among those he recommended as potentially cost-effective and worth considering are a website with a symptom checker, and a digital answering service.
A survey of parents from his group practice showed that for 56%, the main reason for visiting the practice’s website was having a sick child. They wanted to know if their child needed to be seen by a doctor, and they wanted access to a symptom checker to help them determine that, Dr. Feiten said.
In another survey of 2,600 parents who have used such a symptom checker, 61% said the application saved them a call to the doctor’s office, 19% said it prompted them to call when they weren’t planning to do so, and 93% said they would prefer to find the symptom checker on the doctor’s website rather than having to use another source.
Furthermore, 93% of respondents said the symptom checker was the most important feature, and 72% listed patient portals (for appointment requests and other communications) as an important feature as well.
A third of them considered physician and staff photos to be important.
"What does that say? It says that we are moving away from the mentality of using a website or a web presence to get patients," Dr. Feiten said, explaining that the functionality parents want is a simple, quick way to determine whether their children need medical care.
"Websites should be functional tools rather than marketing tools," he said.
The symptom checker should be the prominent feature of the website – available on the home page, with easy access and drop-downs, he said.
An analysis in his practice showed that while the impact on answering service calls was minimal 5 years after launching a website with a symptom checker, the parents who said they used the website brought in $19,000 that year.
"That’s a nice return on investment for the little you would pay to have a symptom checker on your website," he said.
Dr. Feiten said that digital answering service applications allow patients to page an on-call physician via the website or a mobile phone. The applications direct parents to write concise descriptions of their children’s symptoms, and the programs can be adapted to direct pages "to the right person at the right time on the right device."
The relatively new technology offers a number of advantages over live answering services – not the least of which is improved accuracy for electronic health records. Consider the spelling of a patient’s name, for example. (How many ways are there to spell ‘Michaela?’ Dr. Feiten, mused). A parent will get it right, he said.
The applications are also easy to implement on a website or mobile device, and the cost is half (or less) that of live instant message answering services, according to Dr. Feiten, who predicted that "this will be the next revolution in after-hours."
Potential savings in the United States is $34 million each year, he said.
His practice has been using the service for 2 years, and an analysis showed that only 1 in 84 parents said they expected the availability of the service would increase the number of after-hours calls they make, and in fact, after implementation, visit volume increased 5%, but after-hours message volume increased by only 1.2%.
"The feedback that we get from parents is that they love this type of service," he said.
Many practices may find that it is best to make both types of answering services available, as not all parents will embrace this technology.
A related technology that has the potential to improve communications between physicians, and which a number of companies are currently developing, is message management software, he noted.
It will provide an efficient system to get messages quickly to the intended recipient, with criteria built in to ensure messages aren’t missed (such as live-agent validation for messages that aren’t picked up in a timely manner).
"I’m really excited about this," Dr. Feiten said, explaining that these "rules engine" applications are "the wave of the future."
Dr. Feiten is cofounder of MedSecure (an answering service), and cofounder and co-owner of Remedy Web Inc. (a web design and development company), but he receives no remuneration from these companies. He is on the board of directors of the Children’s Diabetes Foundation.
ORLANDO – Making the best use of the right technology can transform a primary care practice, according to Dr. Daniel Feiten.
Parents are living in a mobile world. They do their banking online, they order pizza online, and they want to manage some aspects of their family’s health care online when possible. Many pediatric practices, however, are still living in a typewriter world, said Dr. Feiten, a pediatrician in private practice in Centennial, Colo.
During a session on technology at the annual meeting of the American Academy of Pediatrics, he noted that it’s not always easy to incorporate new technology into an existing practice – and in some cases the transition can actually increase workload. Among those he recommended as potentially cost-effective and worth considering are a website with a symptom checker, and a digital answering service.
A survey of parents from his group practice showed that for 56%, the main reason for visiting the practice’s website was having a sick child. They wanted to know if their child needed to be seen by a doctor, and they wanted access to a symptom checker to help them determine that, Dr. Feiten said.
In another survey of 2,600 parents who have used such a symptom checker, 61% said the application saved them a call to the doctor’s office, 19% said it prompted them to call when they weren’t planning to do so, and 93% said they would prefer to find the symptom checker on the doctor’s website rather than having to use another source.
Furthermore, 93% of respondents said the symptom checker was the most important feature, and 72% listed patient portals (for appointment requests and other communications) as an important feature as well.
A third of them considered physician and staff photos to be important.
"What does that say? It says that we are moving away from the mentality of using a website or a web presence to get patients," Dr. Feiten said, explaining that the functionality parents want is a simple, quick way to determine whether their children need medical care.
"Websites should be functional tools rather than marketing tools," he said.
The symptom checker should be the prominent feature of the website – available on the home page, with easy access and drop-downs, he said.
An analysis in his practice showed that while the impact on answering service calls was minimal 5 years after launching a website with a symptom checker, the parents who said they used the website brought in $19,000 that year.
"That’s a nice return on investment for the little you would pay to have a symptom checker on your website," he said.
Dr. Feiten said that digital answering service applications allow patients to page an on-call physician via the website or a mobile phone. The applications direct parents to write concise descriptions of their children’s symptoms, and the programs can be adapted to direct pages "to the right person at the right time on the right device."
The relatively new technology offers a number of advantages over live answering services – not the least of which is improved accuracy for electronic health records. Consider the spelling of a patient’s name, for example. (How many ways are there to spell ‘Michaela?’ Dr. Feiten, mused). A parent will get it right, he said.
The applications are also easy to implement on a website or mobile device, and the cost is half (or less) that of live instant message answering services, according to Dr. Feiten, who predicted that "this will be the next revolution in after-hours."
Potential savings in the United States is $34 million each year, he said.
His practice has been using the service for 2 years, and an analysis showed that only 1 in 84 parents said they expected the availability of the service would increase the number of after-hours calls they make, and in fact, after implementation, visit volume increased 5%, but after-hours message volume increased by only 1.2%.
"The feedback that we get from parents is that they love this type of service," he said.
Many practices may find that it is best to make both types of answering services available, as not all parents will embrace this technology.
A related technology that has the potential to improve communications between physicians, and which a number of companies are currently developing, is message management software, he noted.
It will provide an efficient system to get messages quickly to the intended recipient, with criteria built in to ensure messages aren’t missed (such as live-agent validation for messages that aren’t picked up in a timely manner).
"I’m really excited about this," Dr. Feiten said, explaining that these "rules engine" applications are "the wave of the future."
Dr. Feiten is cofounder of MedSecure (an answering service), and cofounder and co-owner of Remedy Web Inc. (a web design and development company), but he receives no remuneration from these companies. He is on the board of directors of the Children’s Diabetes Foundation.
EXPERT ANALYSIS FROM THE AAP NATIONAL CONFERENCE
Early skin-to-skin contact promotes breastfeeding, benefits baby
ORLANDO – Early skin-to-skin contact between mothers and their newborns was associated with higher rates of exclusive breastfeeding in a retrospective study presented at the annual meeting of the American Academy of Pediatrics.
Of the 150 mothers included in the study, 72% intended to breastfeed exclusively, but only 28% did so. After adjustment for maternal age, mode of delivery, parity, and gestational age, the only factor significantly associated with exclusive breastfeeding other than intention to breastfeed exclusively was early skin-to-skin contact (odds ratio, 3.7), which occurred in 53% of cases, Dr. Darshna Bhatt of Cohen Children’s Medical Center of New York, New Hyde Park, reported.
For the study, Dr. Bhatt and her colleagues reviewed electronic medical records of consecutive admissions to the well baby nursery, including only singleton, late preterm, or term newborns whose records contained documentation regarding whether the newborn had early skin-to-skin contact with the mother. Early skin-to-skin contact is generally defined as mother-baby bare skin contact for a period of time right after delivery; exclusive breastfeeding was defined as receipt of no formula feedings during the hospital stay.
Early skin-to-skin contact between mother and infant in the delivery room has previously been shown to be associated with breastfeeding success, but not all newborns receive skin-to-skin contact in the critical postbirth period, Dr. Bhatt noted. The current findings suggest that promoting skin-to-skin contact in the delivery room may improve exclusive breastfeeding rates, she concluded.
Indeed, during a plenary session at the conference, Dr. Jae Kim, associate professor of pediatrics at the University of California, San Diego (UCSD), said that skin-to-skin contact promotes breastfeeding and provides a "rich experience in the first few minutes of life."
The benefits during this "early golden hour" are believed to be at least threefold, providing physical interaction that regulates the baby’s temperature and provides sensory stimuli; promoting an early breastfeeding response with access to colostrum, which improves both short- and long-term breastfeeding; and allowing for emotional bonding, which is difficult to measure but is "very, very critical to early infant development," he said.
Data suggest that this contact promotes body temperature regulation and physiological stability in the baby with respect to heart rate, breathing response, blood pressure, and blood sugar levels. It also is associated with less crying and a better breastfeeding response, Dr. Kim said, noting that a Cochrane review showed improved breastfeeding at 1 and 4 months, with trends toward longer duration of breastfeeding overall, in healthy term infants who experience early skin-to-skin contact. Improvement in terms of cardiorespiratory stability and blood glucose control also was seen in late pre-term infants.
Although better data – particularly on long-term effects – are needed, it is clear that skin-to-skin contact can "dramatically improve the breastfeeding success rate, halve the time to actually start breastfeeding, improve the satisfaction of both the mother and the family, and also [lead to] an increased amount of exclusive breastfeeding in those babies," he said.
Many hospitals, including his own institution, have moved toward a model that promotes early skin-to-skin contact, he said, adding that most babies at UCSD are coupled with their mother for early skin-to-skin contact.
The incidence of early skin-to-skin contact and establishment of breastfeeding at UCSD is very high for normal vaginal-birth babies and normal cesarean-section babies.
"We as pediatricians play an incredible role in really affecting this change. It’s not just the medical nurses that deliver this care, but it’s about the physicians sending a strong message about how important it is," he said, noting that the pediatricians at his hospital "make a very special point" to get babies back to their moms immediately after the physical examination and to emphasize the importance of skin-to-skin time.
Skin-to-skin contact can also be promoted in the neonatal intensive care unit (NICU), he said.
Data suggest that preterm and low-birth-weight infants do dramatically better with skin-to-skin contact, with improvements in mortality, sepsis, hypothermia, growth, mother-infant attachment, motor development, long-term cognitive development, stress and pain response, colic, sleep response, pain, breastfeeding, and length of stay.
This is an excellent model in limited-resource settings, and benefits have also been seen at UCSD.
"I think we can make a very strong case right now, especially in a family-centered model, the NICU, that we should be pushing for more and more skin-to-skin [contact time]," he said, noting that parents should be encouraged to request daily skin-to-skin therapy in the NICU.
A program at UCSD – the SPIN (Supporting Preterm Infant Nutrition) Program, which was designed to promote better preterm infant nutrition – has harnessed the benefits of early skin-to-skin contact and early human milk intake to move this approach from a regional program to a national platform, "where we can standardize how we deal with preterm infants and their nutrition," he said. Dialogue is encouraged to help improve standardization across the country, he said.
How can such a program be implemented?
It’s important to standardize the practice by gathering key stakeholders and empowering them to target certain objectives, take one step at a time, and develop a broad-based education program to teach everyone how to achieve the objectives. This is important for something like skin-to-skin contact, which involves the efforts of staff from many different areas (nurses from nursery, labor and delivery, NICU, etc.).
In addition, for quality improvement it is important to have some measure of the benchmarks you are targeting in order to measure success.
"A lot of the time, it’s just about getting everyone to the same table, having the same talk, and realizing the information is not that complicated, and that the practice is actually relatively easy to implement, even when it comes to very vulnerable babies in the NICU," he said.
Dr. Bhatt reported having no disclosures. Dr. Kim is on the speaker’s bureaus for Nestle Nutrition, Nutricia, Abbott Nutrition, and Medela, and has received honoraria or research grant support from Medela and GE Healthcare.
ORLANDO – Early skin-to-skin contact between mothers and their newborns was associated with higher rates of exclusive breastfeeding in a retrospective study presented at the annual meeting of the American Academy of Pediatrics.
Of the 150 mothers included in the study, 72% intended to breastfeed exclusively, but only 28% did so. After adjustment for maternal age, mode of delivery, parity, and gestational age, the only factor significantly associated with exclusive breastfeeding other than intention to breastfeed exclusively was early skin-to-skin contact (odds ratio, 3.7), which occurred in 53% of cases, Dr. Darshna Bhatt of Cohen Children’s Medical Center of New York, New Hyde Park, reported.
For the study, Dr. Bhatt and her colleagues reviewed electronic medical records of consecutive admissions to the well baby nursery, including only singleton, late preterm, or term newborns whose records contained documentation regarding whether the newborn had early skin-to-skin contact with the mother. Early skin-to-skin contact is generally defined as mother-baby bare skin contact for a period of time right after delivery; exclusive breastfeeding was defined as receipt of no formula feedings during the hospital stay.
Early skin-to-skin contact between mother and infant in the delivery room has previously been shown to be associated with breastfeeding success, but not all newborns receive skin-to-skin contact in the critical postbirth period, Dr. Bhatt noted. The current findings suggest that promoting skin-to-skin contact in the delivery room may improve exclusive breastfeeding rates, she concluded.
Indeed, during a plenary session at the conference, Dr. Jae Kim, associate professor of pediatrics at the University of California, San Diego (UCSD), said that skin-to-skin contact promotes breastfeeding and provides a "rich experience in the first few minutes of life."
The benefits during this "early golden hour" are believed to be at least threefold, providing physical interaction that regulates the baby’s temperature and provides sensory stimuli; promoting an early breastfeeding response with access to colostrum, which improves both short- and long-term breastfeeding; and allowing for emotional bonding, which is difficult to measure but is "very, very critical to early infant development," he said.
Data suggest that this contact promotes body temperature regulation and physiological stability in the baby with respect to heart rate, breathing response, blood pressure, and blood sugar levels. It also is associated with less crying and a better breastfeeding response, Dr. Kim said, noting that a Cochrane review showed improved breastfeeding at 1 and 4 months, with trends toward longer duration of breastfeeding overall, in healthy term infants who experience early skin-to-skin contact. Improvement in terms of cardiorespiratory stability and blood glucose control also was seen in late pre-term infants.
Although better data – particularly on long-term effects – are needed, it is clear that skin-to-skin contact can "dramatically improve the breastfeeding success rate, halve the time to actually start breastfeeding, improve the satisfaction of both the mother and the family, and also [lead to] an increased amount of exclusive breastfeeding in those babies," he said.
Many hospitals, including his own institution, have moved toward a model that promotes early skin-to-skin contact, he said, adding that most babies at UCSD are coupled with their mother for early skin-to-skin contact.
The incidence of early skin-to-skin contact and establishment of breastfeeding at UCSD is very high for normal vaginal-birth babies and normal cesarean-section babies.
"We as pediatricians play an incredible role in really affecting this change. It’s not just the medical nurses that deliver this care, but it’s about the physicians sending a strong message about how important it is," he said, noting that the pediatricians at his hospital "make a very special point" to get babies back to their moms immediately after the physical examination and to emphasize the importance of skin-to-skin time.
Skin-to-skin contact can also be promoted in the neonatal intensive care unit (NICU), he said.
Data suggest that preterm and low-birth-weight infants do dramatically better with skin-to-skin contact, with improvements in mortality, sepsis, hypothermia, growth, mother-infant attachment, motor development, long-term cognitive development, stress and pain response, colic, sleep response, pain, breastfeeding, and length of stay.
This is an excellent model in limited-resource settings, and benefits have also been seen at UCSD.
"I think we can make a very strong case right now, especially in a family-centered model, the NICU, that we should be pushing for more and more skin-to-skin [contact time]," he said, noting that parents should be encouraged to request daily skin-to-skin therapy in the NICU.
A program at UCSD – the SPIN (Supporting Preterm Infant Nutrition) Program, which was designed to promote better preterm infant nutrition – has harnessed the benefits of early skin-to-skin contact and early human milk intake to move this approach from a regional program to a national platform, "where we can standardize how we deal with preterm infants and their nutrition," he said. Dialogue is encouraged to help improve standardization across the country, he said.
How can such a program be implemented?
It’s important to standardize the practice by gathering key stakeholders and empowering them to target certain objectives, take one step at a time, and develop a broad-based education program to teach everyone how to achieve the objectives. This is important for something like skin-to-skin contact, which involves the efforts of staff from many different areas (nurses from nursery, labor and delivery, NICU, etc.).
In addition, for quality improvement it is important to have some measure of the benchmarks you are targeting in order to measure success.
"A lot of the time, it’s just about getting everyone to the same table, having the same talk, and realizing the information is not that complicated, and that the practice is actually relatively easy to implement, even when it comes to very vulnerable babies in the NICU," he said.
Dr. Bhatt reported having no disclosures. Dr. Kim is on the speaker’s bureaus for Nestle Nutrition, Nutricia, Abbott Nutrition, and Medela, and has received honoraria or research grant support from Medela and GE Healthcare.
ORLANDO – Early skin-to-skin contact between mothers and their newborns was associated with higher rates of exclusive breastfeeding in a retrospective study presented at the annual meeting of the American Academy of Pediatrics.
Of the 150 mothers included in the study, 72% intended to breastfeed exclusively, but only 28% did so. After adjustment for maternal age, mode of delivery, parity, and gestational age, the only factor significantly associated with exclusive breastfeeding other than intention to breastfeed exclusively was early skin-to-skin contact (odds ratio, 3.7), which occurred in 53% of cases, Dr. Darshna Bhatt of Cohen Children’s Medical Center of New York, New Hyde Park, reported.
For the study, Dr. Bhatt and her colleagues reviewed electronic medical records of consecutive admissions to the well baby nursery, including only singleton, late preterm, or term newborns whose records contained documentation regarding whether the newborn had early skin-to-skin contact with the mother. Early skin-to-skin contact is generally defined as mother-baby bare skin contact for a period of time right after delivery; exclusive breastfeeding was defined as receipt of no formula feedings during the hospital stay.
Early skin-to-skin contact between mother and infant in the delivery room has previously been shown to be associated with breastfeeding success, but not all newborns receive skin-to-skin contact in the critical postbirth period, Dr. Bhatt noted. The current findings suggest that promoting skin-to-skin contact in the delivery room may improve exclusive breastfeeding rates, she concluded.
Indeed, during a plenary session at the conference, Dr. Jae Kim, associate professor of pediatrics at the University of California, San Diego (UCSD), said that skin-to-skin contact promotes breastfeeding and provides a "rich experience in the first few minutes of life."
The benefits during this "early golden hour" are believed to be at least threefold, providing physical interaction that regulates the baby’s temperature and provides sensory stimuli; promoting an early breastfeeding response with access to colostrum, which improves both short- and long-term breastfeeding; and allowing for emotional bonding, which is difficult to measure but is "very, very critical to early infant development," he said.
Data suggest that this contact promotes body temperature regulation and physiological stability in the baby with respect to heart rate, breathing response, blood pressure, and blood sugar levels. It also is associated with less crying and a better breastfeeding response, Dr. Kim said, noting that a Cochrane review showed improved breastfeeding at 1 and 4 months, with trends toward longer duration of breastfeeding overall, in healthy term infants who experience early skin-to-skin contact. Improvement in terms of cardiorespiratory stability and blood glucose control also was seen in late pre-term infants.
Although better data – particularly on long-term effects – are needed, it is clear that skin-to-skin contact can "dramatically improve the breastfeeding success rate, halve the time to actually start breastfeeding, improve the satisfaction of both the mother and the family, and also [lead to] an increased amount of exclusive breastfeeding in those babies," he said.
Many hospitals, including his own institution, have moved toward a model that promotes early skin-to-skin contact, he said, adding that most babies at UCSD are coupled with their mother for early skin-to-skin contact.
The incidence of early skin-to-skin contact and establishment of breastfeeding at UCSD is very high for normal vaginal-birth babies and normal cesarean-section babies.
"We as pediatricians play an incredible role in really affecting this change. It’s not just the medical nurses that deliver this care, but it’s about the physicians sending a strong message about how important it is," he said, noting that the pediatricians at his hospital "make a very special point" to get babies back to their moms immediately after the physical examination and to emphasize the importance of skin-to-skin time.
Skin-to-skin contact can also be promoted in the neonatal intensive care unit (NICU), he said.
Data suggest that preterm and low-birth-weight infants do dramatically better with skin-to-skin contact, with improvements in mortality, sepsis, hypothermia, growth, mother-infant attachment, motor development, long-term cognitive development, stress and pain response, colic, sleep response, pain, breastfeeding, and length of stay.
This is an excellent model in limited-resource settings, and benefits have also been seen at UCSD.
"I think we can make a very strong case right now, especially in a family-centered model, the NICU, that we should be pushing for more and more skin-to-skin [contact time]," he said, noting that parents should be encouraged to request daily skin-to-skin therapy in the NICU.
A program at UCSD – the SPIN (Supporting Preterm Infant Nutrition) Program, which was designed to promote better preterm infant nutrition – has harnessed the benefits of early skin-to-skin contact and early human milk intake to move this approach from a regional program to a national platform, "where we can standardize how we deal with preterm infants and their nutrition," he said. Dialogue is encouraged to help improve standardization across the country, he said.
How can such a program be implemented?
It’s important to standardize the practice by gathering key stakeholders and empowering them to target certain objectives, take one step at a time, and develop a broad-based education program to teach everyone how to achieve the objectives. This is important for something like skin-to-skin contact, which involves the efforts of staff from many different areas (nurses from nursery, labor and delivery, NICU, etc.).
In addition, for quality improvement it is important to have some measure of the benchmarks you are targeting in order to measure success.
"A lot of the time, it’s just about getting everyone to the same table, having the same talk, and realizing the information is not that complicated, and that the practice is actually relatively easy to implement, even when it comes to very vulnerable babies in the NICU," he said.
Dr. Bhatt reported having no disclosures. Dr. Kim is on the speaker’s bureaus for Nestle Nutrition, Nutricia, Abbott Nutrition, and Medela, and has received honoraria or research grant support from Medela and GE Healthcare.
AT THE AAP NATIONAL CONFERENCE
Major finding: Early skin-to-skin contact was significantly associated with exclusive breastfeeding (odds ratio, 3.7).
Data source: A retrospective study of 150 mother-newborn pairs.
Disclosures: Dr. Bhatt reported having no disclosures. Dr. Kim is on the speaker’s bureaus for Nestle Nutrition, Nutricia, Abbott Nutrition, and Medela, and has received honoraria or research grant support from Medela and GE Healthcare.
No differences are seen in concussion risk, severity, by helmet brand
ORLANDO – A prospective comparison of three brands of football helmets and various types of mouth guards raises questions about manufacturers’ claims regarding protection against sport-related concussions, according to Dr. Alison Brooks.
During the 2012 football season, 115 of 1,332 (9%) football players from 36 high schools had 116 sport-related concussions (SRCs). More than half (52%) of the players wore Riddell helmets, 35% wore Schutt helmets, and 13% wore Xenith helmets. Thirty-nine percent of the helmets were purchased during 2011-2012, 33% during 2009-2010, and 28% during 2002-2008.
No difference was seen in the rate or severity (based on days lost) of sport-related concussion (SRC) by helmet type or helmet purchase year, Dr. Brooks of the University of Wisconsin, Madison, reported at the annual meeting of the American Academy of Pediatrics.
The incidence rates of SRC were 9.5, 8.1, and 6.7 for the Riddell, Schutt, and Xenith helmets, respectively, and the SRC rates by year purchased were 9.3, 7.9, and 8.8 for helmets purchased during 2011-2012, 2009-2010, and 2002-2008, respectively. Median days lost were 13.5, 13.0, and 13.5, respectively.
"Contrary to manufacturer claims, lower risk and severity of SRC were not associated with a specific helmet brand," Dr. Brooks said.
As for mouth guards, 61% of the players wore generic models provided by their school, and 39% wore specialized mouth guards custom fitted by a dental professional or specifically marketed to reduce SRC.
The SRC rate was actually higher for those who wore a specialized (12.7) or custom-fitted (11.3) mouth guard than for those who wore a generic mouth guard (6.4), Dr. Brooks said.
Students included in the study were 9th through 12th graders with a mean age of 15.9 years. The students – who completed a preseason demographic and injury questionnaire (with 171 reporting a concussion in the prior 12 months) – wore various models of the three football helmet brands. Athletic trainers recorded the incidence and severity of SRC throughout the football season.
Although limited by factors such as possible selection bias (as schools and players were aware of the study), and recall bias (with respect to previous concussion status), the findings are important, because about 40,000 SRCs occur in high school football players in the United States each year. Despite limited prospective data on how specific football helmets and mouth guards affect the incidence and severity of SRC, manufacturers often cite laboratory research – based on impact (drop) testing – showing that their brand and/or a specific model will lessen impact forces associated with SRC, and they often claim that players who use their equipment may have a reduced SRC risk, she said, noting that schools and parents may feel pressured to purchase newer, more expensive equipment.
The current findings suggest that caution should be used when considering these claims, Dr. Brooks said.
In an interview, she added, "These preliminary findings are important in helping parents and coaches understand that there is no compelling evidence that any particular helmet or mouth guard significantly reduces concussion risk."
Helmets and mouth guards are nonetheless effective for doing what they are designed to do – prevent skull fractures and intracranial bleeds and dental injuries – and are important pieces of equipment that need to be maintained in good condition, and be fit and worn properly. There is also always a role for trying to improve technology. However, it may not be possible to significantly reduce concussion risk using helmet technology, she said.
"I think focus could be better spent on rule enforcement and coaching education on tackling technique to limit/avoid contact to the head, perhaps limiting contact practices, and behavior change about the intent of tackling to injure or ‘punish’ the opponent," she added.
Dr. Brooks reported having no relevant financial disclosures.
ORLANDO – A prospective comparison of three brands of football helmets and various types of mouth guards raises questions about manufacturers’ claims regarding protection against sport-related concussions, according to Dr. Alison Brooks.
During the 2012 football season, 115 of 1,332 (9%) football players from 36 high schools had 116 sport-related concussions (SRCs). More than half (52%) of the players wore Riddell helmets, 35% wore Schutt helmets, and 13% wore Xenith helmets. Thirty-nine percent of the helmets were purchased during 2011-2012, 33% during 2009-2010, and 28% during 2002-2008.
No difference was seen in the rate or severity (based on days lost) of sport-related concussion (SRC) by helmet type or helmet purchase year, Dr. Brooks of the University of Wisconsin, Madison, reported at the annual meeting of the American Academy of Pediatrics.
The incidence rates of SRC were 9.5, 8.1, and 6.7 for the Riddell, Schutt, and Xenith helmets, respectively, and the SRC rates by year purchased were 9.3, 7.9, and 8.8 for helmets purchased during 2011-2012, 2009-2010, and 2002-2008, respectively. Median days lost were 13.5, 13.0, and 13.5, respectively.
"Contrary to manufacturer claims, lower risk and severity of SRC were not associated with a specific helmet brand," Dr. Brooks said.
As for mouth guards, 61% of the players wore generic models provided by their school, and 39% wore specialized mouth guards custom fitted by a dental professional or specifically marketed to reduce SRC.
The SRC rate was actually higher for those who wore a specialized (12.7) or custom-fitted (11.3) mouth guard than for those who wore a generic mouth guard (6.4), Dr. Brooks said.
Students included in the study were 9th through 12th graders with a mean age of 15.9 years. The students – who completed a preseason demographic and injury questionnaire (with 171 reporting a concussion in the prior 12 months) – wore various models of the three football helmet brands. Athletic trainers recorded the incidence and severity of SRC throughout the football season.
Although limited by factors such as possible selection bias (as schools and players were aware of the study), and recall bias (with respect to previous concussion status), the findings are important, because about 40,000 SRCs occur in high school football players in the United States each year. Despite limited prospective data on how specific football helmets and mouth guards affect the incidence and severity of SRC, manufacturers often cite laboratory research – based on impact (drop) testing – showing that their brand and/or a specific model will lessen impact forces associated with SRC, and they often claim that players who use their equipment may have a reduced SRC risk, she said, noting that schools and parents may feel pressured to purchase newer, more expensive equipment.
The current findings suggest that caution should be used when considering these claims, Dr. Brooks said.
In an interview, she added, "These preliminary findings are important in helping parents and coaches understand that there is no compelling evidence that any particular helmet or mouth guard significantly reduces concussion risk."
Helmets and mouth guards are nonetheless effective for doing what they are designed to do – prevent skull fractures and intracranial bleeds and dental injuries – and are important pieces of equipment that need to be maintained in good condition, and be fit and worn properly. There is also always a role for trying to improve technology. However, it may not be possible to significantly reduce concussion risk using helmet technology, she said.
"I think focus could be better spent on rule enforcement and coaching education on tackling technique to limit/avoid contact to the head, perhaps limiting contact practices, and behavior change about the intent of tackling to injure or ‘punish’ the opponent," she added.
Dr. Brooks reported having no relevant financial disclosures.
ORLANDO – A prospective comparison of three brands of football helmets and various types of mouth guards raises questions about manufacturers’ claims regarding protection against sport-related concussions, according to Dr. Alison Brooks.
During the 2012 football season, 115 of 1,332 (9%) football players from 36 high schools had 116 sport-related concussions (SRCs). More than half (52%) of the players wore Riddell helmets, 35% wore Schutt helmets, and 13% wore Xenith helmets. Thirty-nine percent of the helmets were purchased during 2011-2012, 33% during 2009-2010, and 28% during 2002-2008.
No difference was seen in the rate or severity (based on days lost) of sport-related concussion (SRC) by helmet type or helmet purchase year, Dr. Brooks of the University of Wisconsin, Madison, reported at the annual meeting of the American Academy of Pediatrics.
The incidence rates of SRC were 9.5, 8.1, and 6.7 for the Riddell, Schutt, and Xenith helmets, respectively, and the SRC rates by year purchased were 9.3, 7.9, and 8.8 for helmets purchased during 2011-2012, 2009-2010, and 2002-2008, respectively. Median days lost were 13.5, 13.0, and 13.5, respectively.
"Contrary to manufacturer claims, lower risk and severity of SRC were not associated with a specific helmet brand," Dr. Brooks said.
As for mouth guards, 61% of the players wore generic models provided by their school, and 39% wore specialized mouth guards custom fitted by a dental professional or specifically marketed to reduce SRC.
The SRC rate was actually higher for those who wore a specialized (12.7) or custom-fitted (11.3) mouth guard than for those who wore a generic mouth guard (6.4), Dr. Brooks said.
Students included in the study were 9th through 12th graders with a mean age of 15.9 years. The students – who completed a preseason demographic and injury questionnaire (with 171 reporting a concussion in the prior 12 months) – wore various models of the three football helmet brands. Athletic trainers recorded the incidence and severity of SRC throughout the football season.
Although limited by factors such as possible selection bias (as schools and players were aware of the study), and recall bias (with respect to previous concussion status), the findings are important, because about 40,000 SRCs occur in high school football players in the United States each year. Despite limited prospective data on how specific football helmets and mouth guards affect the incidence and severity of SRC, manufacturers often cite laboratory research – based on impact (drop) testing – showing that their brand and/or a specific model will lessen impact forces associated with SRC, and they often claim that players who use their equipment may have a reduced SRC risk, she said, noting that schools and parents may feel pressured to purchase newer, more expensive equipment.
The current findings suggest that caution should be used when considering these claims, Dr. Brooks said.
In an interview, she added, "These preliminary findings are important in helping parents and coaches understand that there is no compelling evidence that any particular helmet or mouth guard significantly reduces concussion risk."
Helmets and mouth guards are nonetheless effective for doing what they are designed to do – prevent skull fractures and intracranial bleeds and dental injuries – and are important pieces of equipment that need to be maintained in good condition, and be fit and worn properly. There is also always a role for trying to improve technology. However, it may not be possible to significantly reduce concussion risk using helmet technology, she said.
"I think focus could be better spent on rule enforcement and coaching education on tackling technique to limit/avoid contact to the head, perhaps limiting contact practices, and behavior change about the intent of tackling to injure or ‘punish’ the opponent," she added.
Dr. Brooks reported having no relevant financial disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: Sport-related concussion incidence rates were 9.5, 8.1, and 6.7 for the Riddell, Schutt, and Xenith helmets, respectively. SRC rates were 9.3, 7.9, and 8.8 for helmets by year purchased during 2011-2012, 2009-2010, and 2002-2008, respectively.
Data source: A prospective cohort study of 1,332 high school football players.
Disclosures: Dr. Brooks reported having no relevant financial disclosures.
Brief intervention promotes use of driving safety resource
ORLANDO – A brief intervention regarding driving safety is effective for encouraging the use of a new parent resource that promotes safe driving among teens, according to Jean Thatcher Shope, Ph.D.
In a prospective study, 133 trained pediatricians each delivered the 2-minute intervention to up to 35 individual parents, directing them to the Checkpoints web-based safe driving program. More than 50% of the parents visited the website. The parents clicked on an average of 4.2 pages and spent an average of 3.5 minutes at the site, Dr. Shope reported at the annual meeting of the American Academy of Pediatrics (AAP).
The Checkpoints Program is a free, evidence-based program that encourages parents to set limits on teen driving and to monitor novice drivers. It was developed by study coauthor Bruce Simons-Morton, Ed.D., at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The website includes teen driving statistics resources to help parents keep their teen drivers safe, and information about state-specific teen driving laws. It also includes an interactive component to help parents create a parent-teen driving agreement that addresses driving hours, number of passengers allowed, and other factors that can be modified over time as the driver becomes more experienced.
The website pages viewed most often were those on teen driving risks, site account registration, and state-specific teen driving laws, said Dr. Shope of the University of Michigan Transportation Research Institute, Ann Arbor.
Participating pediatricians were trained to deliver the brief intervention to parents of teens aged 14-17 years. The pediatricians used scripted materials, provided parents with a key chain imprinted with the website address, and referred parents to the website (youngdriverparenting.org), which will be sustained by the AAP. Parents were encouraged to register and use the interactive Checkpoints agreement and other materials.
The intervention was developed by Dr. Shope and her colleagues in collaboration with Pediatric Research in Office Settings (PROS) and the AAP’s practice-based research network.
Just a short message from a credible professional resource is effective for prompting the parents of teens to visit the Checkpoints website, Dr. Shope said, adding that with motor vehicle crashes topping the list of causes of death among teens, effective prevention measures above and beyond graduated driver licensing are needed.
Teen drivers whose parents are actively engaged in monitoring their driving are less risky drivers, and having a pediatrician deliver a brief intervention that guides parents to an evidence-based, web-based program has the potential to reach many families and to greatly enhance teen driver safety, she added.
This study was funded by the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
ORLANDO – A brief intervention regarding driving safety is effective for encouraging the use of a new parent resource that promotes safe driving among teens, according to Jean Thatcher Shope, Ph.D.
In a prospective study, 133 trained pediatricians each delivered the 2-minute intervention to up to 35 individual parents, directing them to the Checkpoints web-based safe driving program. More than 50% of the parents visited the website. The parents clicked on an average of 4.2 pages and spent an average of 3.5 minutes at the site, Dr. Shope reported at the annual meeting of the American Academy of Pediatrics (AAP).
The Checkpoints Program is a free, evidence-based program that encourages parents to set limits on teen driving and to monitor novice drivers. It was developed by study coauthor Bruce Simons-Morton, Ed.D., at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The website includes teen driving statistics resources to help parents keep their teen drivers safe, and information about state-specific teen driving laws. It also includes an interactive component to help parents create a parent-teen driving agreement that addresses driving hours, number of passengers allowed, and other factors that can be modified over time as the driver becomes more experienced.
The website pages viewed most often were those on teen driving risks, site account registration, and state-specific teen driving laws, said Dr. Shope of the University of Michigan Transportation Research Institute, Ann Arbor.
Participating pediatricians were trained to deliver the brief intervention to parents of teens aged 14-17 years. The pediatricians used scripted materials, provided parents with a key chain imprinted with the website address, and referred parents to the website (youngdriverparenting.org), which will be sustained by the AAP. Parents were encouraged to register and use the interactive Checkpoints agreement and other materials.
The intervention was developed by Dr. Shope and her colleagues in collaboration with Pediatric Research in Office Settings (PROS) and the AAP’s practice-based research network.
Just a short message from a credible professional resource is effective for prompting the parents of teens to visit the Checkpoints website, Dr. Shope said, adding that with motor vehicle crashes topping the list of causes of death among teens, effective prevention measures above and beyond graduated driver licensing are needed.
Teen drivers whose parents are actively engaged in monitoring their driving are less risky drivers, and having a pediatrician deliver a brief intervention that guides parents to an evidence-based, web-based program has the potential to reach many families and to greatly enhance teen driver safety, she added.
This study was funded by the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
ORLANDO – A brief intervention regarding driving safety is effective for encouraging the use of a new parent resource that promotes safe driving among teens, according to Jean Thatcher Shope, Ph.D.
In a prospective study, 133 trained pediatricians each delivered the 2-minute intervention to up to 35 individual parents, directing them to the Checkpoints web-based safe driving program. More than 50% of the parents visited the website. The parents clicked on an average of 4.2 pages and spent an average of 3.5 minutes at the site, Dr. Shope reported at the annual meeting of the American Academy of Pediatrics (AAP).
The Checkpoints Program is a free, evidence-based program that encourages parents to set limits on teen driving and to monitor novice drivers. It was developed by study coauthor Bruce Simons-Morton, Ed.D., at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The website includes teen driving statistics resources to help parents keep their teen drivers safe, and information about state-specific teen driving laws. It also includes an interactive component to help parents create a parent-teen driving agreement that addresses driving hours, number of passengers allowed, and other factors that can be modified over time as the driver becomes more experienced.
The website pages viewed most often were those on teen driving risks, site account registration, and state-specific teen driving laws, said Dr. Shope of the University of Michigan Transportation Research Institute, Ann Arbor.
Participating pediatricians were trained to deliver the brief intervention to parents of teens aged 14-17 years. The pediatricians used scripted materials, provided parents with a key chain imprinted with the website address, and referred parents to the website (youngdriverparenting.org), which will be sustained by the AAP. Parents were encouraged to register and use the interactive Checkpoints agreement and other materials.
The intervention was developed by Dr. Shope and her colleagues in collaboration with Pediatric Research in Office Settings (PROS) and the AAP’s practice-based research network.
Just a short message from a credible professional resource is effective for prompting the parents of teens to visit the Checkpoints website, Dr. Shope said, adding that with motor vehicle crashes topping the list of causes of death among teens, effective prevention measures above and beyond graduated driver licensing are needed.
Teen drivers whose parents are actively engaged in monitoring their driving are less risky drivers, and having a pediatrician deliver a brief intervention that guides parents to an evidence-based, web-based program has the potential to reach many families and to greatly enhance teen driver safety, she added.
This study was funded by the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
AT THE AAP ANNUAL CONFERENCE
Major finding: Fifty percent of parents, when prompted by a pediatrician, visited a website that promotes teen driving safety.
Data source: A prospective intervention involving 133 pediatricians and more than 4,000 parents.
Disclosures: This study was funded by the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control.
Age, atraumatic etiology, fever predict admission for limp
ORLANDO – Most children presenting to the emergency department with a limp have a traumatic etiology, and in most cases, a thorough history and physical examination coupled with radiographs are sufficient for diagnosis, a retrospective study of cases at a tertiary care pediatric emergency department showed.
Of 16,056 children aged 10 months to 18 years (mean, 2.2 years) who presented to the ED between Jan. 1, 2010, and April 1, 2010, 1,776 (11%) presented with a musculoskeletal complaint, and 779 had a lower-extremity injury, a limp, and/or an inability to bear weight. Among those 779 patients, the most common diagnoses were sprain or strain (26%), contusion (19%), fracture (14%), cellulitis/abscess (9%), and abrasion/laceration/puncture (8%), Dr. Johnathan J. Whitaker reported at the annual meeting of the American Academy of Pediatrics.
Of the 779 patients, 527 (68%) had a traumatic injury and 252 (32%) had an atraumatic etiology.
Transient synovitis was discovered in 15 patients (1.9%), and septic arthritis was discovered in 2 patients (0.3%). Other causes of a limp, from among more than 50 diagnoses, were animal bites, an ingrown or avulsed toenail, back spasm, sickle cell crisis, apophysitis, a burn injury, frostbite, slipped capital femoral epiphysis (SCFE), psoas abscess, deep venous thrombosis, rhabdomyolysis, and testicular torsion, said Dr. Whitaker of the Philadelphia College of Osteopathic Medicine.
Overall, 59 patients (7.6%) were admitted, with most of those having a fracture (36%) or an infection (27%). Others who were admitted had transient synovitis (8.5%), sickle cell crisis (6.8%), or SCFE (1.7%).
Several differences were seen between patients who were admitted and patients who were not admitted, including average age, mechanism of injury, presence of a fever, inability to bear weight, past medical history, serum white blood cell count level, and the use of advanced imaging or a laboratory work-up for diagnosis.
For example, among those with a traumatic etiology, the average age was 14 years; among those with an atraumatic etiology, the average age was 10 years. Only 1% of those with a traumatic etiology had a fever, compared with 5% of those with an atraumatic etiology, Dr. Whitaker said.
The inability to bear weight, the presence of a fever greater than 101.5 F, younger age, and an atraumatic mechanism of injury were significant predictors of admission; increased age and a traumatic mechanism of injury were significantly associated with a decreased likelihood of admission, Dr. Whitaker said.
"Limping primarily results from orthopedic diagnoses. However, limping is a chief complaint for a wide variety of other diagnoses," he said.
Though limited by a relatively small number of limp-related presenting complaints and the fact that the study was conducted during winter months – which may have an impact on the types of injuries seen, the findings suggest that laboratory studies and advanced imaging to assist in establishing a diagnosis that may require admission or urgent treatment are best utilized for younger children with an atraumatic mechanism of injury, the inability to bear weight, or a fever upon presentation, he said.
Dr. Whitaker reported having no relevant financial disclosures.
ORLANDO – Most children presenting to the emergency department with a limp have a traumatic etiology, and in most cases, a thorough history and physical examination coupled with radiographs are sufficient for diagnosis, a retrospective study of cases at a tertiary care pediatric emergency department showed.
Of 16,056 children aged 10 months to 18 years (mean, 2.2 years) who presented to the ED between Jan. 1, 2010, and April 1, 2010, 1,776 (11%) presented with a musculoskeletal complaint, and 779 had a lower-extremity injury, a limp, and/or an inability to bear weight. Among those 779 patients, the most common diagnoses were sprain or strain (26%), contusion (19%), fracture (14%), cellulitis/abscess (9%), and abrasion/laceration/puncture (8%), Dr. Johnathan J. Whitaker reported at the annual meeting of the American Academy of Pediatrics.
Of the 779 patients, 527 (68%) had a traumatic injury and 252 (32%) had an atraumatic etiology.
Transient synovitis was discovered in 15 patients (1.9%), and septic arthritis was discovered in 2 patients (0.3%). Other causes of a limp, from among more than 50 diagnoses, were animal bites, an ingrown or avulsed toenail, back spasm, sickle cell crisis, apophysitis, a burn injury, frostbite, slipped capital femoral epiphysis (SCFE), psoas abscess, deep venous thrombosis, rhabdomyolysis, and testicular torsion, said Dr. Whitaker of the Philadelphia College of Osteopathic Medicine.
Overall, 59 patients (7.6%) were admitted, with most of those having a fracture (36%) or an infection (27%). Others who were admitted had transient synovitis (8.5%), sickle cell crisis (6.8%), or SCFE (1.7%).
Several differences were seen between patients who were admitted and patients who were not admitted, including average age, mechanism of injury, presence of a fever, inability to bear weight, past medical history, serum white blood cell count level, and the use of advanced imaging or a laboratory work-up for diagnosis.
For example, among those with a traumatic etiology, the average age was 14 years; among those with an atraumatic etiology, the average age was 10 years. Only 1% of those with a traumatic etiology had a fever, compared with 5% of those with an atraumatic etiology, Dr. Whitaker said.
The inability to bear weight, the presence of a fever greater than 101.5 F, younger age, and an atraumatic mechanism of injury were significant predictors of admission; increased age and a traumatic mechanism of injury were significantly associated with a decreased likelihood of admission, Dr. Whitaker said.
"Limping primarily results from orthopedic diagnoses. However, limping is a chief complaint for a wide variety of other diagnoses," he said.
Though limited by a relatively small number of limp-related presenting complaints and the fact that the study was conducted during winter months – which may have an impact on the types of injuries seen, the findings suggest that laboratory studies and advanced imaging to assist in establishing a diagnosis that may require admission or urgent treatment are best utilized for younger children with an atraumatic mechanism of injury, the inability to bear weight, or a fever upon presentation, he said.
Dr. Whitaker reported having no relevant financial disclosures.
ORLANDO – Most children presenting to the emergency department with a limp have a traumatic etiology, and in most cases, a thorough history and physical examination coupled with radiographs are sufficient for diagnosis, a retrospective study of cases at a tertiary care pediatric emergency department showed.
Of 16,056 children aged 10 months to 18 years (mean, 2.2 years) who presented to the ED between Jan. 1, 2010, and April 1, 2010, 1,776 (11%) presented with a musculoskeletal complaint, and 779 had a lower-extremity injury, a limp, and/or an inability to bear weight. Among those 779 patients, the most common diagnoses were sprain or strain (26%), contusion (19%), fracture (14%), cellulitis/abscess (9%), and abrasion/laceration/puncture (8%), Dr. Johnathan J. Whitaker reported at the annual meeting of the American Academy of Pediatrics.
Of the 779 patients, 527 (68%) had a traumatic injury and 252 (32%) had an atraumatic etiology.
Transient synovitis was discovered in 15 patients (1.9%), and septic arthritis was discovered in 2 patients (0.3%). Other causes of a limp, from among more than 50 diagnoses, were animal bites, an ingrown or avulsed toenail, back spasm, sickle cell crisis, apophysitis, a burn injury, frostbite, slipped capital femoral epiphysis (SCFE), psoas abscess, deep venous thrombosis, rhabdomyolysis, and testicular torsion, said Dr. Whitaker of the Philadelphia College of Osteopathic Medicine.
Overall, 59 patients (7.6%) were admitted, with most of those having a fracture (36%) or an infection (27%). Others who were admitted had transient synovitis (8.5%), sickle cell crisis (6.8%), or SCFE (1.7%).
Several differences were seen between patients who were admitted and patients who were not admitted, including average age, mechanism of injury, presence of a fever, inability to bear weight, past medical history, serum white blood cell count level, and the use of advanced imaging or a laboratory work-up for diagnosis.
For example, among those with a traumatic etiology, the average age was 14 years; among those with an atraumatic etiology, the average age was 10 years. Only 1% of those with a traumatic etiology had a fever, compared with 5% of those with an atraumatic etiology, Dr. Whitaker said.
The inability to bear weight, the presence of a fever greater than 101.5 F, younger age, and an atraumatic mechanism of injury were significant predictors of admission; increased age and a traumatic mechanism of injury were significantly associated with a decreased likelihood of admission, Dr. Whitaker said.
"Limping primarily results from orthopedic diagnoses. However, limping is a chief complaint for a wide variety of other diagnoses," he said.
Though limited by a relatively small number of limp-related presenting complaints and the fact that the study was conducted during winter months – which may have an impact on the types of injuries seen, the findings suggest that laboratory studies and advanced imaging to assist in establishing a diagnosis that may require admission or urgent treatment are best utilized for younger children with an atraumatic mechanism of injury, the inability to bear weight, or a fever upon presentation, he said.
Dr. Whitaker reported having no relevant financial disclosures.
AT THE AAP NATIONAL CONFERENCE
Major finding: Fracture and infection were the most common reasons for admission (36% and 27%).
Data source: A retrospective investigation of ED cases presenting with a limp.
Disclosures: Dr. Whitaker reported having no relevant financial disclosures.
Remote Otitis Media Diagnosis
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
ORLANDO – A novel smartphone otoscope attachment provides clear, transmittable images of the ear drum or tympanic membrane, and could revolutionize the approach to diagnosing and managing ear infections, according to Dr. Kathryn Rappaport.
In a prospective study involving 63 children who presented to an emergency department between May and December 2012 with upper respiratory tract symptoms, the technology was as effective as a conventional otoscope, and was widely accepted by parents, Dr. Rappaport of Baylor College of Medicine, Houston, reported at the annual meeting of the American Academy of Pediatrics.
After receiving clinical care, each child in the study underwent bilateral otic videoscopy using both the smartphone otoscope (CellScope Oto) and a camera-fitted conventional otoscope. The procedures were performed in random order, said Dr. Rappaport, who was at Emory University in Atlanta when the study was conducted.
Of the children, who had a mean age of 2.9 years, 49 received a clinical diagnosis of acute otitis media by an ED practitioner. Based on independent scoring by four physicians who evaluated 31 CellScope Oto videos and 31 conventional otoscope videos from 26 subjects, there was no difference between the two technologies in either the diagnostic quality of the images or diagnosis confidence ratings.
Diagnosis and treatment decision making were similar with each device. Overall, the physician raters were in fair agreement regarding the clinical ED diagnosis of acute otitis media, while two of the raters had moderate to substantial agreement with the ED diagnosis and two had poor agreement with the ED diagnosis from images obtained via conventional otoscope, Dr. Rappaport said, noting that there was a significant correlation between antimicrobial use and image quality.
This indicated that higher-quality images were more likely to be associated with a definitive diagnosis, she said.
As for parent reactions to the use of the device, most (95%) responded favorably, stating that the CellScope Oto images improved their understanding of their child’s management. Also, 90% said they thought the technology would be easy to use, and they would feel comfortable using it remotely to transmit images to a provider.
The CellScope Oto has the potential to improve diagnosis and management, and to reduce costs associated with acute otitis media in children, Dr. Rappaport said.
The video images can provide a baseline, as well as ongoing documentation of a child’s condition. The video documentation could allow a child to be followed over a period of time – without the need for regular office visits – to help monitor for progression or resolution of middle ear effusion and to guide diagnosis and treatment decision making, she explained.
"Acute otitis media is the most common reason for antimicrobial prescriptions in children. In the future, we would like to study whether the ability to monitor for resolution of a patient’s middle ear effusion using digital imaging with the smartphone otoscope will lead to decreased antimicrobial prescriptions for acute otitis media in children," she said in an interview.
Dr. Rappaport reported having no relevant financial disclosures.
AT THE AAP NATIONAL CONFERENCE