User login
HOUSTON – The specificity of fibromyalgia as a marker for psychogenic nonepileptic seizures is less reliable than previously described, results from a large analysis showed.
“Fibromyalgia has been referred to as a reliable clinical indicator for differentiating psychogenic nonepileptic seizures from epilepsy, but there hasn’t been a lot of research looking into this idea,” Emily K. Acton said in an interview at the annual meeting of the American Epilepsy Society. In fact, the most recent study to investigate the association focused on a small patient cohort in a tertiary care epilepsy referral center and found that a diagnosis of fibromyalgia had a predictive value of 75% and a specificity of 99% for the diagnosis of psychogenic nonepileptic seizures (Epilepsy Behav. 2005; 6[2]:264-5).
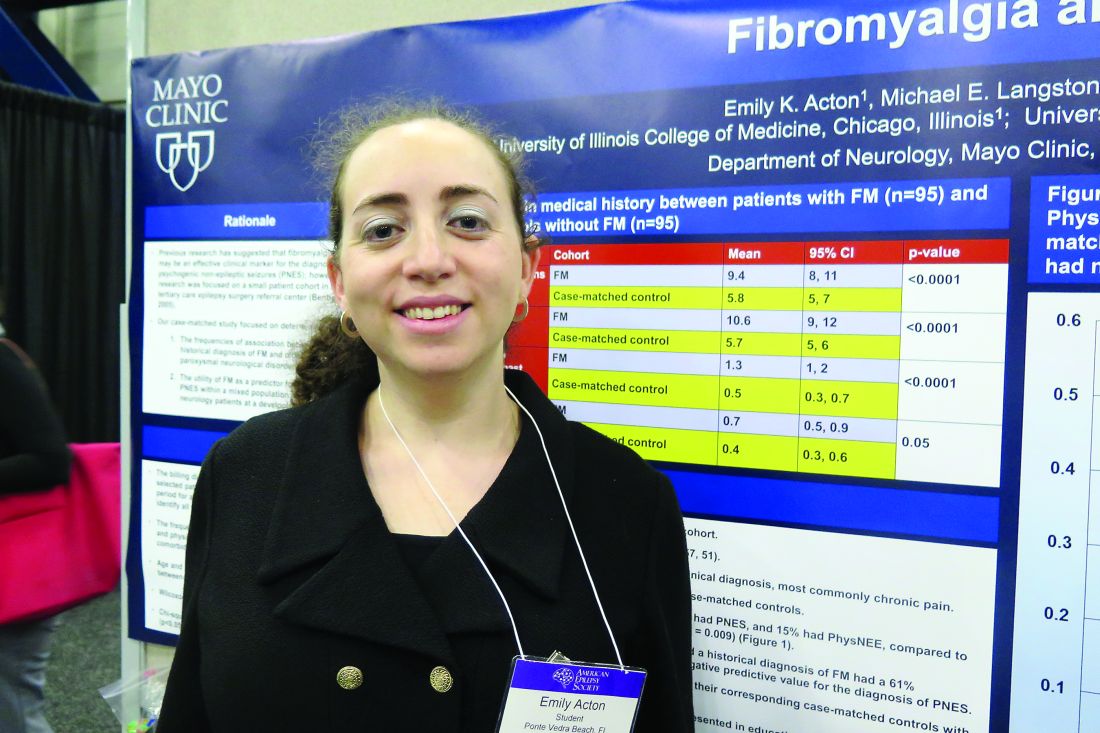
Ms. Acton reported that of the 1,730 patients studied, 95 (5.5%) had a medical history of fibromyalgia. A majority of the 95 patients (95%) were female, and the mean age was 53 years. In addition, 43% of fibromyalgia patients had a nonparoxysmal, neurologic primary clinical diagnosis, most commonly chronic pain. She said that no differences were seen between fibromyalgia patients and case-matched controls in terms of age, race, marital status, or reason for referral. However, compared with case-matched controls, fibromyalgia patients were underrepresented in education (P = .02) and employment (P = .009).
Paroxysmal events were present in 57% of fibromyalgia patients and in 54% of case-matched controls. Among fibromyalgia patients with paroxysmal disorders, 11% had epileptic seizures, 74% had PNES, and 15% had physiologic nonepileptic events. Among matched controls, 37% had epileptic seizures, 51% had PNES, and 12% had physiologic nonepileptic events (P = .009).
After comparing the two groups of patients, the researchers determined that a historical diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, 74% positive predictive value, and 49% negative predictive value for the diagnosis of PNES. “Another interesting finding was that quite a few of our fibromyalgia patients felt they didn’t have fibromyalgia,” Ms. Action said. “Unprompted, during the course of their first visit, about 10% of this cohort mentioned to a physician that they were diagnosed with fibromyalgia, but they didn’t believe it.”
In their abstract, the researchers wrote that the study design “and a larger sample size involving mixed general neurology patients may account for the lesser association seen between fibromyalgia and PNES in this study.” They reported having no financial disclosures.
HOUSTON – The specificity of fibromyalgia as a marker for psychogenic nonepileptic seizures is less reliable than previously described, results from a large analysis showed.
“Fibromyalgia has been referred to as a reliable clinical indicator for differentiating psychogenic nonepileptic seizures from epilepsy, but there hasn’t been a lot of research looking into this idea,” Emily K. Acton said in an interview at the annual meeting of the American Epilepsy Society. In fact, the most recent study to investigate the association focused on a small patient cohort in a tertiary care epilepsy referral center and found that a diagnosis of fibromyalgia had a predictive value of 75% and a specificity of 99% for the diagnosis of psychogenic nonepileptic seizures (Epilepsy Behav. 2005; 6[2]:264-5).
Ms. Acton reported that of the 1,730 patients studied, 95 (5.5%) had a medical history of fibromyalgia. A majority of the 95 patients (95%) were female, and the mean age was 53 years. In addition, 43% of fibromyalgia patients had a nonparoxysmal, neurologic primary clinical diagnosis, most commonly chronic pain. She said that no differences were seen between fibromyalgia patients and case-matched controls in terms of age, race, marital status, or reason for referral. However, compared with case-matched controls, fibromyalgia patients were underrepresented in education (P = .02) and employment (P = .009).
Paroxysmal events were present in 57% of fibromyalgia patients and in 54% of case-matched controls. Among fibromyalgia patients with paroxysmal disorders, 11% had epileptic seizures, 74% had PNES, and 15% had physiologic nonepileptic events. Among matched controls, 37% had epileptic seizures, 51% had PNES, and 12% had physiologic nonepileptic events (P = .009).
After comparing the two groups of patients, the researchers determined that a historical diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, 74% positive predictive value, and 49% negative predictive value for the diagnosis of PNES. “Another interesting finding was that quite a few of our fibromyalgia patients felt they didn’t have fibromyalgia,” Ms. Action said. “Unprompted, during the course of their first visit, about 10% of this cohort mentioned to a physician that they were diagnosed with fibromyalgia, but they didn’t believe it.”
In their abstract, the researchers wrote that the study design “and a larger sample size involving mixed general neurology patients may account for the lesser association seen between fibromyalgia and PNES in this study.” They reported having no financial disclosures.
HOUSTON – The specificity of fibromyalgia as a marker for psychogenic nonepileptic seizures is less reliable than previously described, results from a large analysis showed.
“Fibromyalgia has been referred to as a reliable clinical indicator for differentiating psychogenic nonepileptic seizures from epilepsy, but there hasn’t been a lot of research looking into this idea,” Emily K. Acton said in an interview at the annual meeting of the American Epilepsy Society. In fact, the most recent study to investigate the association focused on a small patient cohort in a tertiary care epilepsy referral center and found that a diagnosis of fibromyalgia had a predictive value of 75% and a specificity of 99% for the diagnosis of psychogenic nonepileptic seizures (Epilepsy Behav. 2005; 6[2]:264-5).
Ms. Acton reported that of the 1,730 patients studied, 95 (5.5%) had a medical history of fibromyalgia. A majority of the 95 patients (95%) were female, and the mean age was 53 years. In addition, 43% of fibromyalgia patients had a nonparoxysmal, neurologic primary clinical diagnosis, most commonly chronic pain. She said that no differences were seen between fibromyalgia patients and case-matched controls in terms of age, race, marital status, or reason for referral. However, compared with case-matched controls, fibromyalgia patients were underrepresented in education (P = .02) and employment (P = .009).
Paroxysmal events were present in 57% of fibromyalgia patients and in 54% of case-matched controls. Among fibromyalgia patients with paroxysmal disorders, 11% had epileptic seizures, 74% had PNES, and 15% had physiologic nonepileptic events. Among matched controls, 37% had epileptic seizures, 51% had PNES, and 12% had physiologic nonepileptic events (P = .009).
After comparing the two groups of patients, the researchers determined that a historical diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, 74% positive predictive value, and 49% negative predictive value for the diagnosis of PNES. “Another interesting finding was that quite a few of our fibromyalgia patients felt they didn’t have fibromyalgia,” Ms. Action said. “Unprompted, during the course of their first visit, about 10% of this cohort mentioned to a physician that they were diagnosed with fibromyalgia, but they didn’t believe it.”
In their abstract, the researchers wrote that the study design “and a larger sample size involving mixed general neurology patients may account for the lesser association seen between fibromyalgia and PNES in this study.” They reported having no financial disclosures.
AT AES 2016
Key clinical point:
Major finding: The diagnosis of fibromyalgia had a 61% sensitivity, 64% specificity, and a 74% positive predictive value for the diagnosis of PNES.
Data source: A retrospective review of 1,730 consecutive patients seen by a single epileptologist at a neurology clinic over a 3-year period.
Disclosures: The researchers reported having no financial disclosures.