User login
TALKING OUT CHILDHOOD OBESITY
Resnicow K, McMaster F, Bocian A, et al. Motivational interviewing and dietary counseling for obesity in primary care: an RCT. Pediatrics. 2015;135(4):649-657.
Counseling parents of overweight children using motivational interviewing from both health care providers and registered dietitians can significantly improve BMI, according to a study of 42 practices in the Pediatric Research in Office Settings Network of the American Academy of Pediatrics.
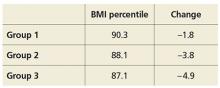
Researchers randomly assigned parents of overweight children, ages 2 through 8, to one of three groups: (1) usual care, (2) four provider-delivered motivational interviewing sessions over two years, or (3) four provider-delivered motivational interviewing sessions plus six sessions with a registered dietitian over two years. At study end, BMI percentile and change in BMI for the different groups were as follows:
COMMENTARY
The results of this study are exciting. Motivational interviewing is a technique in which the practitioner asks questions of a patient and allows the patient to discover his/her own conclusions about the topic. By so doing, the patient is more engaged in the discussion and is less resistant to input. This technique, with excellent evidence of effectiveness in the area of drug and alcohol abuse, has been shown to facilitate effective behavioral change in many areas and is recommended by the American Heart Association for behavioral change in adults.1,2 This is an exciting paper demonstrating evidence-based efficacy in addressing childhood obesity—a critical health issue—and is worth trying in the office.
1. Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305-312.
2. Spring B, Ockene JK, Gidding SS, et al; American Heart Association Behavior Change Committee of the Council on Epidemiology and Prevention, Council on Lifestyle and Cardiometabolic Health, Council for High Blood Pressure Research, and Council on Cardiovascular and Stroke Nursing. Better population health through behavior change in adults: a call to action. Circulation. 2013;128(19):2169-2176. doi: 10.1161/01.cir.0000435173.25936.e1.
Continue for long-acting reversible contraception among teens >>
LONG-ACTING REVERSIBLE CONTRACEPTION AMONG TEENS
Romero L, Pazol K, Warner L, et al. Vital signs: trends in use of long-acting reversible contraception among teens aged 15-19 years seeking contraceptive services – United States, 2005-2013. MMWR Morb Mortal Wkly Rep. 2015;64(13):363-369.
Efforts to improve teen access to long-acting reversible contraception (LARC) have increased use of these methods, according to a CDC review of services provided at Title X National Family Planning Program centers. The report found
• LARC rates among teen patients increased from 0.4% in 2005 to 7.2% in 2013.
• In 2013, 2.8% of those seeking contraception used IUDs and 4.3% used implants.
• Among Title X patients, 7.6% of 18- and 19-year-olds used LARC, compared with 6.5% of 15- to 17-year-olds.
• Rates of LARC were lowest in Mississippi (0.7%) and highest in Colorado (25.8%).
COMMENTARY
LARCs, which include IUD and implantable hormonal contraceptive devices, require no effort for adherence on the part of the user; once in place, they are effective without further action. Current CDC guidelines on contraceptive use clearly recommend LARC for teenagers based on the efficacy and safety.1 LARCs are favored for teenagers because poor compliance has yielded suboptimal effectiveness of oral contraceptives and condoms in teenagers, who often forget to take their birth control pills or don’t use condoms when they should. Many clinicians have been slow to recommend LARCs in teenagers based on safety concerns related to adverse experience with IUDs 20 to 30 years ago. According to CDC guidelines, IUDs and implantable contraceptive devices now have robust safety data, and this article shows that they are being increasingly made available to teenagers who need them.
1. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. US Selected Practice Recommendations for Contraceptive Use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd edition. MMWR Recomm Rep. 2013;62(RR-05):1-60.
Continue to testing for celiac in pediatric rheumatology patients >>
TESTING FOR CELIAC IN PEDIATRIC RHEUMATOLOGY PATIENTS
Sherman Y, Karanicolas R, DiMarco B, et al. Unrecognized celiac disease in children presenting for rheumatology evaluation. Pediatrics. 2015; [Epub ahead of print].
Children presenting for rheumatology evaluation should be screened for celiac disease, according to a review of 2,125 pediatric patients who were screened for celiac as part of the standard initial serologic evaluation.
Researchers identified 36 new cases of celiac disease (2.0% prevalence rate). The most common presenting complaints among these patients were myalgia, arthralgia, and rash. Less frequent complaints included gastrointestinal complaints of abdominal pain, nausea, and diarrhea.
After initiating a gluten-free diet, all of the patients with celiac disease reported improvement or complete resolution of musculoskeletal symptoms.
COMMENTARY
Celiac disease has a prevalence of 0.5% to 1% in the US and can present with a range of symptoms that include diarrhea, abdominal discomfort, and weight loss. In addition to these typical symptoms, celiac disease can cause a wide range of systemic symptoms, including osteopenia, abnormal liver function tests, anemia, neurologic symptoms, and general malaise and fatigue.1 This study suggests that celiac testing be considered in children presenting with rheumatologic symptoms, including myalgia, arthralgia, and rash.
1. Presutti RJ, Cangemi JR, Cassidy HD, et al. Celiac disease. Am Fam Physician. 2007;76(12):1795-1802, 1809-1810.
Continue for educating parents about antibiotic use >>
EDUCATING PARENTS ABOUT ANTIBIOTIC USE
Vaz LE, Kleinman KP, Lakoma MD, et al. Prevalence of parental misconceptions about antibiotic use. Pediatrics. 2015;136:221-231.
Misperceptions about antibiotic use persist and continue to be more prevalent among parents of Medicaid-insured children, according to a study of 1,500 Massachusetts parents.
Investigators examined antibiotic-related knowledge and attitudes among both Medicaid-insured and private-insured parents and found
• Fewer Medicaid parents answered questions correctly, except for one regarding bronchitis.
• Medicaid patients were more likely to request unnecessary antibiotics.
• More parents in 2013 understood that green nasal discharge did not require antibiotics than in 2000.
• Medicaid-insured parents were younger, less likely to be white, and had less education than those commercially insured.
COMMENTARY
Decreasing the unnecessary use of antibiotics for viral infections is an important component of decreasing the development of antibiotic-resistant organisms. An important driver of clinician use of antibiotics is patients’ expectations for antibiotics. This study shows that much work remains to be done in changing patient expectations, which is not surprising to any practicing clinician. This study also suggests that the expectation for antibiotics is greater among those individuals with Medicaid insurance, which suggests that an opportunity exists for Medicaid insurance plans to do targeted patient education on this issue—which should improve patient outcomes, decrease cost from use of unneeded antibiotics, and decrease the development of antibiotic-resistant organisms.
Continue for newborn pulmonary hypertension and maternal antidepressant use >>
NEWBORN PULMONARY HYPERTENSION AND MATERNAL ANTIDEPRESSANT USE
Huybrechts KF, Bateman BT, Palmsten K, et al. Antidepressant use late in pregnancy and risk of persistent pulmonary hypertension of the newborn. JAMA. 2015;313(21):2142-2151.
Taking antidepressants during late pregnancy may increase the risk for persistent pulmonary hypertension of the newborn (PPHN), according to a nested cohort study of more than 3.7 million pregnant women in the 2000-2010 Medicaid Analytic eXtract.
Investigators compared offspring of mothers who used selective serotonin reuptake inhibitors (SSRIs) or non-SSRI monotherapy in the last 90 days of pregnancy to those who did not and found 3.4% of women filled at least one prescription for antidepressants late in pregnancy, primarily SSRIs.
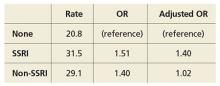
Rates and odds ratios (ORs) of PPHN stratified by use and type of antidepressant were as follows:
The study authors note the absolute risk is small, and the increased risk is more modest than previous studies found.
COMMENTARY
Depression affects more than 12% of pregnancies and has important consequences, including increased risk for suicide, preterm birth, poor fetal growth, and impaired fetal and infant development.1 PPHN is a serious condition that can require intubation and can be fatal in 10% to 20% of cases. This study adds to the conflicting data suggesting that SSRI use in pregnancy can lead to an increase in this rare condition. The decision to use an antidepressant during pregnancy is a difficult one, because depression has serious consequences but so, potentially, does treatment. The treatment of depression during pregnancy requires thoughtful, informed discussion between patient and provider.
1. Stewart DE. Clinical practice. Depression during pregnancy. N Engl J Med. 2011;365(17):1605-1611. doi:10.1056/NEJMcp1102730.
Continue for new infant vaccine treats 6 diseases >>
NEW INFANT VACCINE TREATS 6 DISEASES
Marshall GS, Adams GL, Leonardi ML, et al. Immunogenicity, safety, and tolerability of a hexavalent vaccine in infants. Pediatrics. 2015:136(2):323-332.
The safety and immunogenicity of DTaP5-IPV-Hib-HepB fully liquid investigational hexavalent vaccine are comparable with the analogous licensed component vaccines and provide a new combination vaccine option aligned with the recommended US infant immunization schedule, according to a phase III study of 1,465 participants. Overall, 981 healthy infants were vaccinated in group 1 with the hexavalent vaccine and 484 in group 2 with the analogous licensed component vaccines.
The study found
• Immune responses in group 1 to all antigens contained in the vaccine one month after dose 3 were essentially noninferior to those in group 2.
• Adverse event rates after any dose were similar in both groups.
COMMENTARY
Vaccine administration has led to many diseases, including Haemophilus influenzae type b, polio, and measles, becoming quite rare. As we have recently seen with the resurgence of measles, continued vigilance and high immunization rates are important in ensuring that these diseases remain rare. The development of a hexavalent vaccine is another step in making immunization easier for clinicians to administer and for patients to accept.
Continue for treating infants with bronchiolitis >>
TREATING INFANTS WITH BRONCHIOLITIS
Silver AH, Esteban-Cruciani N, Azzarone G, et al. 3% hypertonic saline versus normal saline in inpatient bronchiolitis: a randomized controlled trial. Pediatrics. 2015;136:1036-1043.
Infants hospitalized with bronchiolitis saw no difference in length of stay or seven-day readmission rates when treated with nebulized 3% hypertonic saline (HS) compared with nebulized normal saline (NS), according to a randomized, controlled study of 227 infants who were younger than 12 months when admitted. Patients received either 4 mL nebulized 3% HS (113 infants) or 4 mL 0.9% NS (114 infants) every four hours from enrollment until hospital discharge. Researchers found
• Median length of stay of HS and NS groups was 2.1 days vs 2.1 days, respectively.
• Seven-day readmission rates for HS and NS groups were 4.3% vs 3.1%, respectively.
• Clinical worsening events were similar between groups.
COMMENTARY
Bronchiolitis, the most common lower respiratory tract infection in infants, is usually due to a viral infection, most often respiratory syncytial virus, and can cause disease that ranges in severity from mild to life-threatening. Infants with bronchiolitis typically present with rhinitis, tachypnea, wheezing, and cough, and occasionally crackles and use of accessory muscles. While many medications are used, supportive care and monitoring are the mainstays of therapy. Maintaining pulse above 90% is important, using supplemental oxygen when needed to achieve this. Alpha-adrenergic and beta-adrenergic bronchodilators are often used; though the evidence suggests that they are not usually helpful, they can be tried and continued if they appear to help. Systemic steroids are often used, but they too lack evidence of efficacy.1 This study shows that hypertonic saline can now join the list of interventions used with evidence of a lack of efficacy.
1. Diagnosis and management of bronchiolitis. Subcommittee on diagnosis and management of bronchiolitis. Pediatrics. 2006;118(4):1774-1793. doi:10.1542/peds.2006-2223.
Continue for azithromycin and preschool children >>
AZITHROMYCIN AND PRESCHOOL CHILDREN: CAN ANTIBIOTICS LESSEN ONSET OF SEVERE LRTIs?
Bacharier LB, Guilbert TW, Mauger DT, et al. Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses: a randomized clinical trial. JAMA. 2015;314(19):2034-2044.
The use of azithromycin early during an apparent respiratory tract illness (RTI) reduced the likelihood of severe lower RTI (LRTI) among young children with a history of recurrent severe LRTI, compared with placebo, according to a study of 607 children ages 12 to 71 months. Participants were randomized in a 1:1 ratio to receive either azithromycin (12 mg/kg/d for 5 d) or matching placebo at the start of an RTI. Researchers found
• A total of 937 treated RTIs were experienced by 443 children, including 92 severe LRTIs (azithromycin group, 35; placebo group, 57).
• Azithromycin significantly reduced the risk for progression to severe LRTI relative to placebo (HR, 0.64).
• Induction of azithromycin-resistant organisms and adverse events were infrequent.
COMMENTARY
Recurrent episodes of severe wheezing with RTI are an important and common occurrence, affecting up to 15% to 20% of children prior to age 6.1 LRTI was defined in this study as RTI that required the use of additional rescue medication. The current approach to RTI is to try to minimize the use of antibiotics unless an infection is clearly bacterial in origin, and to treat severe LRTI when it occurs. The results of this trial suggest that in children at high risk for severe LRTI, identified by their episodes of recurrent wheezing, early treatment of RTI with azithromycin may decrease the development of severe LRTI by more than 35%—an important result. It is important to recognize that this study does not suggest treating all RTIs with antibiotics, but rather that the use of a macrolide antibiotic may be considered, perhaps, in the select group of children similar to those studied, with a history of recurrent wheezing with previous RTIs.
1. Ly NP, Gold DR, Weiss ST, Celedón JC. Recurrent wheeze in early childhood and asthma among children at risk for atopy. Pediatrics. 2006;117(6):e1132-e1138.
TALKING OUT CHILDHOOD OBESITY
Resnicow K, McMaster F, Bocian A, et al. Motivational interviewing and dietary counseling for obesity in primary care: an RCT. Pediatrics. 2015;135(4):649-657.
Counseling parents of overweight children using motivational interviewing from both health care providers and registered dietitians can significantly improve BMI, according to a study of 42 practices in the Pediatric Research in Office Settings Network of the American Academy of Pediatrics.
Researchers randomly assigned parents of overweight children, ages 2 through 8, to one of three groups: (1) usual care, (2) four provider-delivered motivational interviewing sessions over two years, or (3) four provider-delivered motivational interviewing sessions plus six sessions with a registered dietitian over two years. At study end, BMI percentile and change in BMI for the different groups were as follows:
COMMENTARY
The results of this study are exciting. Motivational interviewing is a technique in which the practitioner asks questions of a patient and allows the patient to discover his/her own conclusions about the topic. By so doing, the patient is more engaged in the discussion and is less resistant to input. This technique, with excellent evidence of effectiveness in the area of drug and alcohol abuse, has been shown to facilitate effective behavioral change in many areas and is recommended by the American Heart Association for behavioral change in adults.1,2 This is an exciting paper demonstrating evidence-based efficacy in addressing childhood obesity—a critical health issue—and is worth trying in the office.
1. Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305-312.
2. Spring B, Ockene JK, Gidding SS, et al; American Heart Association Behavior Change Committee of the Council on Epidemiology and Prevention, Council on Lifestyle and Cardiometabolic Health, Council for High Blood Pressure Research, and Council on Cardiovascular and Stroke Nursing. Better population health through behavior change in adults: a call to action. Circulation. 2013;128(19):2169-2176. doi: 10.1161/01.cir.0000435173.25936.e1.
Continue for long-acting reversible contraception among teens >>
LONG-ACTING REVERSIBLE CONTRACEPTION AMONG TEENS
Romero L, Pazol K, Warner L, et al. Vital signs: trends in use of long-acting reversible contraception among teens aged 15-19 years seeking contraceptive services – United States, 2005-2013. MMWR Morb Mortal Wkly Rep. 2015;64(13):363-369.
Efforts to improve teen access to long-acting reversible contraception (LARC) have increased use of these methods, according to a CDC review of services provided at Title X National Family Planning Program centers. The report found
• LARC rates among teen patients increased from 0.4% in 2005 to 7.2% in 2013.
• In 2013, 2.8% of those seeking contraception used IUDs and 4.3% used implants.
• Among Title X patients, 7.6% of 18- and 19-year-olds used LARC, compared with 6.5% of 15- to 17-year-olds.
• Rates of LARC were lowest in Mississippi (0.7%) and highest in Colorado (25.8%).
COMMENTARY
LARCs, which include IUD and implantable hormonal contraceptive devices, require no effort for adherence on the part of the user; once in place, they are effective without further action. Current CDC guidelines on contraceptive use clearly recommend LARC for teenagers based on the efficacy and safety.1 LARCs are favored for teenagers because poor compliance has yielded suboptimal effectiveness of oral contraceptives and condoms in teenagers, who often forget to take their birth control pills or don’t use condoms when they should. Many clinicians have been slow to recommend LARCs in teenagers based on safety concerns related to adverse experience with IUDs 20 to 30 years ago. According to CDC guidelines, IUDs and implantable contraceptive devices now have robust safety data, and this article shows that they are being increasingly made available to teenagers who need them.
1. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. US Selected Practice Recommendations for Contraceptive Use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd edition. MMWR Recomm Rep. 2013;62(RR-05):1-60.
Continue to testing for celiac in pediatric rheumatology patients >>
TESTING FOR CELIAC IN PEDIATRIC RHEUMATOLOGY PATIENTS
Sherman Y, Karanicolas R, DiMarco B, et al. Unrecognized celiac disease in children presenting for rheumatology evaluation. Pediatrics. 2015; [Epub ahead of print].
Children presenting for rheumatology evaluation should be screened for celiac disease, according to a review of 2,125 pediatric patients who were screened for celiac as part of the standard initial serologic evaluation.
Researchers identified 36 new cases of celiac disease (2.0% prevalence rate). The most common presenting complaints among these patients were myalgia, arthralgia, and rash. Less frequent complaints included gastrointestinal complaints of abdominal pain, nausea, and diarrhea.
After initiating a gluten-free diet, all of the patients with celiac disease reported improvement or complete resolution of musculoskeletal symptoms.
COMMENTARY
Celiac disease has a prevalence of 0.5% to 1% in the US and can present with a range of symptoms that include diarrhea, abdominal discomfort, and weight loss. In addition to these typical symptoms, celiac disease can cause a wide range of systemic symptoms, including osteopenia, abnormal liver function tests, anemia, neurologic symptoms, and general malaise and fatigue.1 This study suggests that celiac testing be considered in children presenting with rheumatologic symptoms, including myalgia, arthralgia, and rash.
1. Presutti RJ, Cangemi JR, Cassidy HD, et al. Celiac disease. Am Fam Physician. 2007;76(12):1795-1802, 1809-1810.
Continue for educating parents about antibiotic use >>
EDUCATING PARENTS ABOUT ANTIBIOTIC USE
Vaz LE, Kleinman KP, Lakoma MD, et al. Prevalence of parental misconceptions about antibiotic use. Pediatrics. 2015;136:221-231.
Misperceptions about antibiotic use persist and continue to be more prevalent among parents of Medicaid-insured children, according to a study of 1,500 Massachusetts parents.
Investigators examined antibiotic-related knowledge and attitudes among both Medicaid-insured and private-insured parents and found
• Fewer Medicaid parents answered questions correctly, except for one regarding bronchitis.
• Medicaid patients were more likely to request unnecessary antibiotics.
• More parents in 2013 understood that green nasal discharge did not require antibiotics than in 2000.
• Medicaid-insured parents were younger, less likely to be white, and had less education than those commercially insured.
COMMENTARY
Decreasing the unnecessary use of antibiotics for viral infections is an important component of decreasing the development of antibiotic-resistant organisms. An important driver of clinician use of antibiotics is patients’ expectations for antibiotics. This study shows that much work remains to be done in changing patient expectations, which is not surprising to any practicing clinician. This study also suggests that the expectation for antibiotics is greater among those individuals with Medicaid insurance, which suggests that an opportunity exists for Medicaid insurance plans to do targeted patient education on this issue—which should improve patient outcomes, decrease cost from use of unneeded antibiotics, and decrease the development of antibiotic-resistant organisms.
Continue for newborn pulmonary hypertension and maternal antidepressant use >>
NEWBORN PULMONARY HYPERTENSION AND MATERNAL ANTIDEPRESSANT USE
Huybrechts KF, Bateman BT, Palmsten K, et al. Antidepressant use late in pregnancy and risk of persistent pulmonary hypertension of the newborn. JAMA. 2015;313(21):2142-2151.
Taking antidepressants during late pregnancy may increase the risk for persistent pulmonary hypertension of the newborn (PPHN), according to a nested cohort study of more than 3.7 million pregnant women in the 2000-2010 Medicaid Analytic eXtract.
Investigators compared offspring of mothers who used selective serotonin reuptake inhibitors (SSRIs) or non-SSRI monotherapy in the last 90 days of pregnancy to those who did not and found 3.4% of women filled at least one prescription for antidepressants late in pregnancy, primarily SSRIs.
Rates and odds ratios (ORs) of PPHN stratified by use and type of antidepressant were as follows:
The study authors note the absolute risk is small, and the increased risk is more modest than previous studies found.
COMMENTARY
Depression affects more than 12% of pregnancies and has important consequences, including increased risk for suicide, preterm birth, poor fetal growth, and impaired fetal and infant development.1 PPHN is a serious condition that can require intubation and can be fatal in 10% to 20% of cases. This study adds to the conflicting data suggesting that SSRI use in pregnancy can lead to an increase in this rare condition. The decision to use an antidepressant during pregnancy is a difficult one, because depression has serious consequences but so, potentially, does treatment. The treatment of depression during pregnancy requires thoughtful, informed discussion between patient and provider.
1. Stewart DE. Clinical practice. Depression during pregnancy. N Engl J Med. 2011;365(17):1605-1611. doi:10.1056/NEJMcp1102730.
Continue for new infant vaccine treats 6 diseases >>
NEW INFANT VACCINE TREATS 6 DISEASES
Marshall GS, Adams GL, Leonardi ML, et al. Immunogenicity, safety, and tolerability of a hexavalent vaccine in infants. Pediatrics. 2015:136(2):323-332.
The safety and immunogenicity of DTaP5-IPV-Hib-HepB fully liquid investigational hexavalent vaccine are comparable with the analogous licensed component vaccines and provide a new combination vaccine option aligned with the recommended US infant immunization schedule, according to a phase III study of 1,465 participants. Overall, 981 healthy infants were vaccinated in group 1 with the hexavalent vaccine and 484 in group 2 with the analogous licensed component vaccines.
The study found
• Immune responses in group 1 to all antigens contained in the vaccine one month after dose 3 were essentially noninferior to those in group 2.
• Adverse event rates after any dose were similar in both groups.
COMMENTARY
Vaccine administration has led to many diseases, including Haemophilus influenzae type b, polio, and measles, becoming quite rare. As we have recently seen with the resurgence of measles, continued vigilance and high immunization rates are important in ensuring that these diseases remain rare. The development of a hexavalent vaccine is another step in making immunization easier for clinicians to administer and for patients to accept.
Continue for treating infants with bronchiolitis >>
TREATING INFANTS WITH BRONCHIOLITIS
Silver AH, Esteban-Cruciani N, Azzarone G, et al. 3% hypertonic saline versus normal saline in inpatient bronchiolitis: a randomized controlled trial. Pediatrics. 2015;136:1036-1043.
Infants hospitalized with bronchiolitis saw no difference in length of stay or seven-day readmission rates when treated with nebulized 3% hypertonic saline (HS) compared with nebulized normal saline (NS), according to a randomized, controlled study of 227 infants who were younger than 12 months when admitted. Patients received either 4 mL nebulized 3% HS (113 infants) or 4 mL 0.9% NS (114 infants) every four hours from enrollment until hospital discharge. Researchers found
• Median length of stay of HS and NS groups was 2.1 days vs 2.1 days, respectively.
• Seven-day readmission rates for HS and NS groups were 4.3% vs 3.1%, respectively.
• Clinical worsening events were similar between groups.
COMMENTARY
Bronchiolitis, the most common lower respiratory tract infection in infants, is usually due to a viral infection, most often respiratory syncytial virus, and can cause disease that ranges in severity from mild to life-threatening. Infants with bronchiolitis typically present with rhinitis, tachypnea, wheezing, and cough, and occasionally crackles and use of accessory muscles. While many medications are used, supportive care and monitoring are the mainstays of therapy. Maintaining pulse above 90% is important, using supplemental oxygen when needed to achieve this. Alpha-adrenergic and beta-adrenergic bronchodilators are often used; though the evidence suggests that they are not usually helpful, they can be tried and continued if they appear to help. Systemic steroids are often used, but they too lack evidence of efficacy.1 This study shows that hypertonic saline can now join the list of interventions used with evidence of a lack of efficacy.
1. Diagnosis and management of bronchiolitis. Subcommittee on diagnosis and management of bronchiolitis. Pediatrics. 2006;118(4):1774-1793. doi:10.1542/peds.2006-2223.
Continue for azithromycin and preschool children >>
AZITHROMYCIN AND PRESCHOOL CHILDREN: CAN ANTIBIOTICS LESSEN ONSET OF SEVERE LRTIs?
Bacharier LB, Guilbert TW, Mauger DT, et al. Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses: a randomized clinical trial. JAMA. 2015;314(19):2034-2044.
The use of azithromycin early during an apparent respiratory tract illness (RTI) reduced the likelihood of severe lower RTI (LRTI) among young children with a history of recurrent severe LRTI, compared with placebo, according to a study of 607 children ages 12 to 71 months. Participants were randomized in a 1:1 ratio to receive either azithromycin (12 mg/kg/d for 5 d) or matching placebo at the start of an RTI. Researchers found
• A total of 937 treated RTIs were experienced by 443 children, including 92 severe LRTIs (azithromycin group, 35; placebo group, 57).
• Azithromycin significantly reduced the risk for progression to severe LRTI relative to placebo (HR, 0.64).
• Induction of azithromycin-resistant organisms and adverse events were infrequent.
COMMENTARY
Recurrent episodes of severe wheezing with RTI are an important and common occurrence, affecting up to 15% to 20% of children prior to age 6.1 LRTI was defined in this study as RTI that required the use of additional rescue medication. The current approach to RTI is to try to minimize the use of antibiotics unless an infection is clearly bacterial in origin, and to treat severe LRTI when it occurs. The results of this trial suggest that in children at high risk for severe LRTI, identified by their episodes of recurrent wheezing, early treatment of RTI with azithromycin may decrease the development of severe LRTI by more than 35%—an important result. It is important to recognize that this study does not suggest treating all RTIs with antibiotics, but rather that the use of a macrolide antibiotic may be considered, perhaps, in the select group of children similar to those studied, with a history of recurrent wheezing with previous RTIs.
1. Ly NP, Gold DR, Weiss ST, Celedón JC. Recurrent wheeze in early childhood and asthma among children at risk for atopy. Pediatrics. 2006;117(6):e1132-e1138.
TALKING OUT CHILDHOOD OBESITY
Resnicow K, McMaster F, Bocian A, et al. Motivational interviewing and dietary counseling for obesity in primary care: an RCT. Pediatrics. 2015;135(4):649-657.
Counseling parents of overweight children using motivational interviewing from both health care providers and registered dietitians can significantly improve BMI, according to a study of 42 practices in the Pediatric Research in Office Settings Network of the American Academy of Pediatrics.
Researchers randomly assigned parents of overweight children, ages 2 through 8, to one of three groups: (1) usual care, (2) four provider-delivered motivational interviewing sessions over two years, or (3) four provider-delivered motivational interviewing sessions plus six sessions with a registered dietitian over two years. At study end, BMI percentile and change in BMI for the different groups were as follows:
COMMENTARY
The results of this study are exciting. Motivational interviewing is a technique in which the practitioner asks questions of a patient and allows the patient to discover his/her own conclusions about the topic. By so doing, the patient is more engaged in the discussion and is less resistant to input. This technique, with excellent evidence of effectiveness in the area of drug and alcohol abuse, has been shown to facilitate effective behavioral change in many areas and is recommended by the American Heart Association for behavioral change in adults.1,2 This is an exciting paper demonstrating evidence-based efficacy in addressing childhood obesity—a critical health issue—and is worth trying in the office.
1. Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55(513):305-312.
2. Spring B, Ockene JK, Gidding SS, et al; American Heart Association Behavior Change Committee of the Council on Epidemiology and Prevention, Council on Lifestyle and Cardiometabolic Health, Council for High Blood Pressure Research, and Council on Cardiovascular and Stroke Nursing. Better population health through behavior change in adults: a call to action. Circulation. 2013;128(19):2169-2176. doi: 10.1161/01.cir.0000435173.25936.e1.
Continue for long-acting reversible contraception among teens >>
LONG-ACTING REVERSIBLE CONTRACEPTION AMONG TEENS
Romero L, Pazol K, Warner L, et al. Vital signs: trends in use of long-acting reversible contraception among teens aged 15-19 years seeking contraceptive services – United States, 2005-2013. MMWR Morb Mortal Wkly Rep. 2015;64(13):363-369.
Efforts to improve teen access to long-acting reversible contraception (LARC) have increased use of these methods, according to a CDC review of services provided at Title X National Family Planning Program centers. The report found
• LARC rates among teen patients increased from 0.4% in 2005 to 7.2% in 2013.
• In 2013, 2.8% of those seeking contraception used IUDs and 4.3% used implants.
• Among Title X patients, 7.6% of 18- and 19-year-olds used LARC, compared with 6.5% of 15- to 17-year-olds.
• Rates of LARC were lowest in Mississippi (0.7%) and highest in Colorado (25.8%).
COMMENTARY
LARCs, which include IUD and implantable hormonal contraceptive devices, require no effort for adherence on the part of the user; once in place, they are effective without further action. Current CDC guidelines on contraceptive use clearly recommend LARC for teenagers based on the efficacy and safety.1 LARCs are favored for teenagers because poor compliance has yielded suboptimal effectiveness of oral contraceptives and condoms in teenagers, who often forget to take their birth control pills or don’t use condoms when they should. Many clinicians have been slow to recommend LARCs in teenagers based on safety concerns related to adverse experience with IUDs 20 to 30 years ago. According to CDC guidelines, IUDs and implantable contraceptive devices now have robust safety data, and this article shows that they are being increasingly made available to teenagers who need them.
1. Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. US Selected Practice Recommendations for Contraceptive Use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd edition. MMWR Recomm Rep. 2013;62(RR-05):1-60.
Continue to testing for celiac in pediatric rheumatology patients >>
TESTING FOR CELIAC IN PEDIATRIC RHEUMATOLOGY PATIENTS
Sherman Y, Karanicolas R, DiMarco B, et al. Unrecognized celiac disease in children presenting for rheumatology evaluation. Pediatrics. 2015; [Epub ahead of print].
Children presenting for rheumatology evaluation should be screened for celiac disease, according to a review of 2,125 pediatric patients who were screened for celiac as part of the standard initial serologic evaluation.
Researchers identified 36 new cases of celiac disease (2.0% prevalence rate). The most common presenting complaints among these patients were myalgia, arthralgia, and rash. Less frequent complaints included gastrointestinal complaints of abdominal pain, nausea, and diarrhea.
After initiating a gluten-free diet, all of the patients with celiac disease reported improvement or complete resolution of musculoskeletal symptoms.
COMMENTARY
Celiac disease has a prevalence of 0.5% to 1% in the US and can present with a range of symptoms that include diarrhea, abdominal discomfort, and weight loss. In addition to these typical symptoms, celiac disease can cause a wide range of systemic symptoms, including osteopenia, abnormal liver function tests, anemia, neurologic symptoms, and general malaise and fatigue.1 This study suggests that celiac testing be considered in children presenting with rheumatologic symptoms, including myalgia, arthralgia, and rash.
1. Presutti RJ, Cangemi JR, Cassidy HD, et al. Celiac disease. Am Fam Physician. 2007;76(12):1795-1802, 1809-1810.
Continue for educating parents about antibiotic use >>
EDUCATING PARENTS ABOUT ANTIBIOTIC USE
Vaz LE, Kleinman KP, Lakoma MD, et al. Prevalence of parental misconceptions about antibiotic use. Pediatrics. 2015;136:221-231.
Misperceptions about antibiotic use persist and continue to be more prevalent among parents of Medicaid-insured children, according to a study of 1,500 Massachusetts parents.
Investigators examined antibiotic-related knowledge and attitudes among both Medicaid-insured and private-insured parents and found
• Fewer Medicaid parents answered questions correctly, except for one regarding bronchitis.
• Medicaid patients were more likely to request unnecessary antibiotics.
• More parents in 2013 understood that green nasal discharge did not require antibiotics than in 2000.
• Medicaid-insured parents were younger, less likely to be white, and had less education than those commercially insured.
COMMENTARY
Decreasing the unnecessary use of antibiotics for viral infections is an important component of decreasing the development of antibiotic-resistant organisms. An important driver of clinician use of antibiotics is patients’ expectations for antibiotics. This study shows that much work remains to be done in changing patient expectations, which is not surprising to any practicing clinician. This study also suggests that the expectation for antibiotics is greater among those individuals with Medicaid insurance, which suggests that an opportunity exists for Medicaid insurance plans to do targeted patient education on this issue—which should improve patient outcomes, decrease cost from use of unneeded antibiotics, and decrease the development of antibiotic-resistant organisms.
Continue for newborn pulmonary hypertension and maternal antidepressant use >>
NEWBORN PULMONARY HYPERTENSION AND MATERNAL ANTIDEPRESSANT USE
Huybrechts KF, Bateman BT, Palmsten K, et al. Antidepressant use late in pregnancy and risk of persistent pulmonary hypertension of the newborn. JAMA. 2015;313(21):2142-2151.
Taking antidepressants during late pregnancy may increase the risk for persistent pulmonary hypertension of the newborn (PPHN), according to a nested cohort study of more than 3.7 million pregnant women in the 2000-2010 Medicaid Analytic eXtract.
Investigators compared offspring of mothers who used selective serotonin reuptake inhibitors (SSRIs) or non-SSRI monotherapy in the last 90 days of pregnancy to those who did not and found 3.4% of women filled at least one prescription for antidepressants late in pregnancy, primarily SSRIs.
Rates and odds ratios (ORs) of PPHN stratified by use and type of antidepressant were as follows:
The study authors note the absolute risk is small, and the increased risk is more modest than previous studies found.
COMMENTARY
Depression affects more than 12% of pregnancies and has important consequences, including increased risk for suicide, preterm birth, poor fetal growth, and impaired fetal and infant development.1 PPHN is a serious condition that can require intubation and can be fatal in 10% to 20% of cases. This study adds to the conflicting data suggesting that SSRI use in pregnancy can lead to an increase in this rare condition. The decision to use an antidepressant during pregnancy is a difficult one, because depression has serious consequences but so, potentially, does treatment. The treatment of depression during pregnancy requires thoughtful, informed discussion between patient and provider.
1. Stewart DE. Clinical practice. Depression during pregnancy. N Engl J Med. 2011;365(17):1605-1611. doi:10.1056/NEJMcp1102730.
Continue for new infant vaccine treats 6 diseases >>
NEW INFANT VACCINE TREATS 6 DISEASES
Marshall GS, Adams GL, Leonardi ML, et al. Immunogenicity, safety, and tolerability of a hexavalent vaccine in infants. Pediatrics. 2015:136(2):323-332.
The safety and immunogenicity of DTaP5-IPV-Hib-HepB fully liquid investigational hexavalent vaccine are comparable with the analogous licensed component vaccines and provide a new combination vaccine option aligned with the recommended US infant immunization schedule, according to a phase III study of 1,465 participants. Overall, 981 healthy infants were vaccinated in group 1 with the hexavalent vaccine and 484 in group 2 with the analogous licensed component vaccines.
The study found
• Immune responses in group 1 to all antigens contained in the vaccine one month after dose 3 were essentially noninferior to those in group 2.
• Adverse event rates after any dose were similar in both groups.
COMMENTARY
Vaccine administration has led to many diseases, including Haemophilus influenzae type b, polio, and measles, becoming quite rare. As we have recently seen with the resurgence of measles, continued vigilance and high immunization rates are important in ensuring that these diseases remain rare. The development of a hexavalent vaccine is another step in making immunization easier for clinicians to administer and for patients to accept.
Continue for treating infants with bronchiolitis >>
TREATING INFANTS WITH BRONCHIOLITIS
Silver AH, Esteban-Cruciani N, Azzarone G, et al. 3% hypertonic saline versus normal saline in inpatient bronchiolitis: a randomized controlled trial. Pediatrics. 2015;136:1036-1043.
Infants hospitalized with bronchiolitis saw no difference in length of stay or seven-day readmission rates when treated with nebulized 3% hypertonic saline (HS) compared with nebulized normal saline (NS), according to a randomized, controlled study of 227 infants who were younger than 12 months when admitted. Patients received either 4 mL nebulized 3% HS (113 infants) or 4 mL 0.9% NS (114 infants) every four hours from enrollment until hospital discharge. Researchers found
• Median length of stay of HS and NS groups was 2.1 days vs 2.1 days, respectively.
• Seven-day readmission rates for HS and NS groups were 4.3% vs 3.1%, respectively.
• Clinical worsening events were similar between groups.
COMMENTARY
Bronchiolitis, the most common lower respiratory tract infection in infants, is usually due to a viral infection, most often respiratory syncytial virus, and can cause disease that ranges in severity from mild to life-threatening. Infants with bronchiolitis typically present with rhinitis, tachypnea, wheezing, and cough, and occasionally crackles and use of accessory muscles. While many medications are used, supportive care and monitoring are the mainstays of therapy. Maintaining pulse above 90% is important, using supplemental oxygen when needed to achieve this. Alpha-adrenergic and beta-adrenergic bronchodilators are often used; though the evidence suggests that they are not usually helpful, they can be tried and continued if they appear to help. Systemic steroids are often used, but they too lack evidence of efficacy.1 This study shows that hypertonic saline can now join the list of interventions used with evidence of a lack of efficacy.
1. Diagnosis and management of bronchiolitis. Subcommittee on diagnosis and management of bronchiolitis. Pediatrics. 2006;118(4):1774-1793. doi:10.1542/peds.2006-2223.
Continue for azithromycin and preschool children >>
AZITHROMYCIN AND PRESCHOOL CHILDREN: CAN ANTIBIOTICS LESSEN ONSET OF SEVERE LRTIs?
Bacharier LB, Guilbert TW, Mauger DT, et al. Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses: a randomized clinical trial. JAMA. 2015;314(19):2034-2044.
The use of azithromycin early during an apparent respiratory tract illness (RTI) reduced the likelihood of severe lower RTI (LRTI) among young children with a history of recurrent severe LRTI, compared with placebo, according to a study of 607 children ages 12 to 71 months. Participants were randomized in a 1:1 ratio to receive either azithromycin (12 mg/kg/d for 5 d) or matching placebo at the start of an RTI. Researchers found
• A total of 937 treated RTIs were experienced by 443 children, including 92 severe LRTIs (azithromycin group, 35; placebo group, 57).
• Azithromycin significantly reduced the risk for progression to severe LRTI relative to placebo (HR, 0.64).
• Induction of azithromycin-resistant organisms and adverse events were infrequent.
COMMENTARY
Recurrent episodes of severe wheezing with RTI are an important and common occurrence, affecting up to 15% to 20% of children prior to age 6.1 LRTI was defined in this study as RTI that required the use of additional rescue medication. The current approach to RTI is to try to minimize the use of antibiotics unless an infection is clearly bacterial in origin, and to treat severe LRTI when it occurs. The results of this trial suggest that in children at high risk for severe LRTI, identified by their episodes of recurrent wheezing, early treatment of RTI with azithromycin may decrease the development of severe LRTI by more than 35%—an important result. It is important to recognize that this study does not suggest treating all RTIs with antibiotics, but rather that the use of a macrolide antibiotic may be considered, perhaps, in the select group of children similar to those studied, with a history of recurrent wheezing with previous RTIs.
1. Ly NP, Gold DR, Weiss ST, Celedón JC. Recurrent wheeze in early childhood and asthma among children at risk for atopy. Pediatrics. 2006;117(6):e1132-e1138.