User login
Vasovagal syncope is usually benign, and although it often recurs, increasing fluid and salt intake and performing counter-pressure maneuvers are usually sufficient.1 However, if patients continue to have syncopal episodes despite these first-line measures, other options include drug therapy with midodrine, fludrocortisone, beta-blockers, or selective serotonin reuptake inhibitors; orthostatic training; and, in some cases, pacemaker implantation. The 2017 guidelines from the American College of Cardiology, American Heart Association, and Heart Rhythm Society (ACC/AHA/HRS) are helpful in the management of these patients.1
RATIONALE
Although vasovagal syncope is considered benign, it can result in injury and can significantly affect quality of life.
The diagnosis can often be established in the initial evaluation with a structured history, physical examination, and electrocardiography. If the diagnosis is still unclear, tilt-table testing can be useful and has an ACC/AHA/HRS class IIa (moderate) recommendation.1 Once the diagnosis of vasovagal syncope is made, first-line measures can be instituted.
FIRST-LINE MEASURES
An explanation of the diagnosis, education on avoiding triggers such as prolonged standing and warm environments, coping with potentially stressful visits to the doctor or dentist, and reassurance that the condition is benign are all strongly recommended (class I).1
Initial measures include performing physical counter-pressure maneuvers (class IIa), increasing salt and fluid intake (class IIb) in the absence of contraindications, and, in selected patients, reducing or withdrawing hypotensive medications when appropriate (class IIb).
Physical counter-pressure maneuvers are recommended for patients whose syncopal episodes have a sufficiently long prodromal period. Maneuvers include the following:
- Leg crossing: crossing the legs while tensing leg, abdominal, and buttock muscles
- Handgrip: maximally contracting a rubber ball or other object in the dominant hand
- Squatting
- Limb or abdominal contractions
- Arm tensing: contracting both arms by gripping one hand with the other and abducting both arms.2
The effectiveness of counter-pressure maneuvers was studied by van Dijk et al2 in a multicenter prospective randomized clinical trial that included 223 patients with recurrent vasovagal syncope associated with prodromal symptoms. They concluded that these maneuvers decreased the recurrence of syncopal episodes, with a relative risk reduction of 0.36 (95% confidence interval 0.11–0.53, P < .005) and were low-cost and risk-free.
Confirming the diagnosis of vasovagal syncope with tilt-table testing may reassure the patient. It can also help the patient learn to identify the symptoms associated with a vasovagal episode, which in turn may encourage timely use of physical counter-pressure maneuvers at the onset.
The evidence for increasing salt and fluid intake for patients with vasovagal syncope is limited. But in the absence of a contraindication such as hypertension, renal disease, or heart failure, it may be reasonable to encourage the ingestion of 2 L to 3 L of fluid per day and a total of 6 g to 9 g of salt per day (around 1 to 2 heaping teaspoons of salt).1
MEDICAL THERAPY
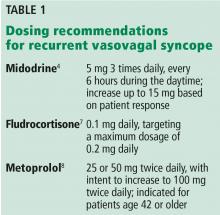
In patients who continue to have syncopal episodes despite adequate use of first-line measures, medical therapy can be considered. Unfortunately, evidence supporting drug therapy for recurrent syncope is limited.3 Options include midodrine (class IIa), fludrocortisone (class IIb), beta-blockers (class IIb), and selective serotonin reuptake inhibitors (class IIb).1
Midodrine has the strongest recommendation and is a reasonable option if there is no history of hypertension, heart failure, or urinary retention. It is a peripheral alpha-agonist that ameliorates the reduction in peripheral sympathetic neural outflow responsible for venous pooling and vasodepression in vasovagal syncope.4–6
Fludrocortisone results in increased blood volume due to mineralocorticoid activity. In the Prevention of Syncope Trial 2 of fludrocortisone vs placebo, patients on fludrocortisone had a “marginally nonsignificant” reduction in recurrence of syncope over 1 year (hazard ratio 0.69, P = .069).7
Overall, beta-blockers have failed to prevent syncope in randomized controlled trials. But in a meta-analysis that included patients from the Prevention of Syncope Trial,8 an age-dependent benefit of beta-blockers was noted in patients age 42 and older.9 Therefore, a beta-blocker may be a reasonable option in patients in this age group with recurrent vasovagal syncope.1
Serotonin has central effects on blood pressure and heart rate that can induce syncope. However, evidence for the effectiveness of selective serotonin reuptake inhibitors in the prevention of recurrent vasovagal syncope has been contradictory in small trials.10,11
When choosing a drug, contraindications should be considered, including possible effects during pregnancy in women of childbearing age.
OTHER MEASURES
Orthostatic training, with repetitive tilt-table testing until a test is negative, or with daily standing quietly against a wall for prolonged periods of time, has not been shown to have sustained benefit in reducing the recurrence of syncopal episodes (class IIb recommendation).1
Dual-chamber pacing can be considered in carefully selected patients age 40 or older with syncope and documented asystole of at least 3 seconds or spontaneous pauses of at least 6 seconds without syncope on implantable loop recorder monitoring (class IIb recommendation).1,12,13 Strict patient selection increases the likelihood that pacing will be effective.1 For example, patients with documented asystole during syncope and a tilt-table test that induces minimal or no vasodepressor response are more likely to respond than patients with a positive tilt-table test with a vasodepressor (hypotensive) response.13
Tilt-table testing may also be considered to identify patients with a hypotensive response who would be less likely to respond to permanent cardiac pacing.14
Compression garments carry a class IIa recommendation for orthostatic hypotension,1 but they have not been adequately studied in vasovagal syncope.
- Shen WK, Sheldon RS, Benditt DG, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2017; 136(5):e60–e122. doi:10.1161/CIR.0000000000000499
- van Dijk N, Quartieri F, Blanc JJ, Garcia-Civera R, Brignole M, Moya A, Wieling W; PC-Trial Investigators. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: the Physical Counterpressure Manoeuvres Trial (PC-Trial). J Am Coll Cardiol 2006; 48(8):1652–1657. doi:10.1016/j.jacc.2006.06.059
- Romme JJ, Reitsma JB, Black CN, et al. Drugs and pacemakers for vasovagal, carotid sinus and situational syncope. Cochrane Database Syst Rev 2011; (10):CD004194. doi:10.1002/14651858.CD004194.pub3
- Perez-Lugones A, Schweikert R, Pavia S, et al. Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: a randomized control study. J Cardiovasc Electrophysiol 2001; 12(8):935–938. pmid:11513446
- Romme JJ, van Dijk N, Go-Schön IK, Reitsma JB, Wieling W. Effectiveness of midodrine treatment in patients with recurrent vasovagal syncope not responding to non-pharmacological treatment (STAND-trial). Europace 2011; 13(11):1639–1647. doi:10.1093/europace/eur200
- Samniah N, Sakaguchi S, Lurie KG, Iskos D, Benditt DG. Efficacy and safety of midodrine hydrochloride in patients with refractory vasovagal syncope. Am J Cardiol 2001; 88(1):A7, 80–83. pmid:11423066
- Sheldon R, Raj SR, Rose MS, et al; POST 2 Investigators. Fludrocortisone for the prevention of vasovagal syncope: a randomized, placebo-controlled trial. J Am Coll Cardiol 2016; 68(1):1–9. doi:10.1016/j.jacc.2016.04.030
- Sheldon R, Connolly S, Rose S, et al; POST Investigators. Prevention of Syncope Trial (POST): a randomized, placebo-controlled study of metoprolol in the prevention of vasovagal syncope. Circulation 2006; 113(9):1164–1170. doi:10.1161/CIRCULATIONAHA.105.535161
- Sheldon RS, Morillo CA, Klingenheben T, Krahn AD, Sheldon A, Rose MS. Age-dependent effect of beta-blockers in preventing vasovagal syncope. Circ Arrhythm Electrophysiol 2012; 5(5):920–926. doi:10.1161/CIRCEP.112.974386
- Takata TS, Wasmund SL, Smith ML, et al. Serotonin reuptake inhibitor (Paxil) does not prevent the vasovagal reaction associated with carotid sinus massage and/or lower body negative pressure in healthy volunteers. Circulation 2002; 106(12):1500–1504. pmid:12234955
- Di Girolamo E, Di Iorio C, Sabatini P, Leonzio L, Barbone C, Barsotti A. Effects of paroxetine hydrochloride, a selective serotonin reuptake inhibitor, on refractory vasovagal syncope: a randomized, double-blind, placebo-controlled study. J Am Coll Cardiol 1999; 33(5):1227–1230. pmid:10193720
- Brignole M, Menozzi C, Moya A, et al; International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators. Pacemaker therapy in patients with neurally mediated syncope and documented asystole: third International Study on Syncope of Uncertain Etiology (ISSUE-3): a randomized trial. Circulation 2012; 125(21):2566–2571. doi:10.1161/CIRCULATIONAHA.111.082313
- Brignole M, Donateo P, Tomaino M, et al; International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators. Benefit of pacemaker therapy in patients with presumed neurally mediated syncope and documented asystole is greater when tilt test is negative: an analysis from the third International Study on Syncope of Uncertain Etiology (ISSUE-3). Circ Arrhythm Electrophysiol 2014; 7(1):10–16. doi:10.1161/CIRCEP.113.001103
- Sheldon RS, Grubb BP, Olshansky B, et al. 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 2015; 12(6):e41–e63. doi:10.1016/j.hrthm.2015.03.029
Vasovagal syncope is usually benign, and although it often recurs, increasing fluid and salt intake and performing counter-pressure maneuvers are usually sufficient.1 However, if patients continue to have syncopal episodes despite these first-line measures, other options include drug therapy with midodrine, fludrocortisone, beta-blockers, or selective serotonin reuptake inhibitors; orthostatic training; and, in some cases, pacemaker implantation. The 2017 guidelines from the American College of Cardiology, American Heart Association, and Heart Rhythm Society (ACC/AHA/HRS) are helpful in the management of these patients.1
RATIONALE
Although vasovagal syncope is considered benign, it can result in injury and can significantly affect quality of life.
The diagnosis can often be established in the initial evaluation with a structured history, physical examination, and electrocardiography. If the diagnosis is still unclear, tilt-table testing can be useful and has an ACC/AHA/HRS class IIa (moderate) recommendation.1 Once the diagnosis of vasovagal syncope is made, first-line measures can be instituted.
FIRST-LINE MEASURES
An explanation of the diagnosis, education on avoiding triggers such as prolonged standing and warm environments, coping with potentially stressful visits to the doctor or dentist, and reassurance that the condition is benign are all strongly recommended (class I).1
Initial measures include performing physical counter-pressure maneuvers (class IIa), increasing salt and fluid intake (class IIb) in the absence of contraindications, and, in selected patients, reducing or withdrawing hypotensive medications when appropriate (class IIb).
Physical counter-pressure maneuvers are recommended for patients whose syncopal episodes have a sufficiently long prodromal period. Maneuvers include the following:
- Leg crossing: crossing the legs while tensing leg, abdominal, and buttock muscles
- Handgrip: maximally contracting a rubber ball or other object in the dominant hand
- Squatting
- Limb or abdominal contractions
- Arm tensing: contracting both arms by gripping one hand with the other and abducting both arms.2
The effectiveness of counter-pressure maneuvers was studied by van Dijk et al2 in a multicenter prospective randomized clinical trial that included 223 patients with recurrent vasovagal syncope associated with prodromal symptoms. They concluded that these maneuvers decreased the recurrence of syncopal episodes, with a relative risk reduction of 0.36 (95% confidence interval 0.11–0.53, P < .005) and were low-cost and risk-free.
Confirming the diagnosis of vasovagal syncope with tilt-table testing may reassure the patient. It can also help the patient learn to identify the symptoms associated with a vasovagal episode, which in turn may encourage timely use of physical counter-pressure maneuvers at the onset.
The evidence for increasing salt and fluid intake for patients with vasovagal syncope is limited. But in the absence of a contraindication such as hypertension, renal disease, or heart failure, it may be reasonable to encourage the ingestion of 2 L to 3 L of fluid per day and a total of 6 g to 9 g of salt per day (around 1 to 2 heaping teaspoons of salt).1
MEDICAL THERAPY
In patients who continue to have syncopal episodes despite adequate use of first-line measures, medical therapy can be considered. Unfortunately, evidence supporting drug therapy for recurrent syncope is limited.3 Options include midodrine (class IIa), fludrocortisone (class IIb), beta-blockers (class IIb), and selective serotonin reuptake inhibitors (class IIb).1
Midodrine has the strongest recommendation and is a reasonable option if there is no history of hypertension, heart failure, or urinary retention. It is a peripheral alpha-agonist that ameliorates the reduction in peripheral sympathetic neural outflow responsible for venous pooling and vasodepression in vasovagal syncope.4–6
Fludrocortisone results in increased blood volume due to mineralocorticoid activity. In the Prevention of Syncope Trial 2 of fludrocortisone vs placebo, patients on fludrocortisone had a “marginally nonsignificant” reduction in recurrence of syncope over 1 year (hazard ratio 0.69, P = .069).7
Overall, beta-blockers have failed to prevent syncope in randomized controlled trials. But in a meta-analysis that included patients from the Prevention of Syncope Trial,8 an age-dependent benefit of beta-blockers was noted in patients age 42 and older.9 Therefore, a beta-blocker may be a reasonable option in patients in this age group with recurrent vasovagal syncope.1
Serotonin has central effects on blood pressure and heart rate that can induce syncope. However, evidence for the effectiveness of selective serotonin reuptake inhibitors in the prevention of recurrent vasovagal syncope has been contradictory in small trials.10,11
When choosing a drug, contraindications should be considered, including possible effects during pregnancy in women of childbearing age.
OTHER MEASURES
Orthostatic training, with repetitive tilt-table testing until a test is negative, or with daily standing quietly against a wall for prolonged periods of time, has not been shown to have sustained benefit in reducing the recurrence of syncopal episodes (class IIb recommendation).1
Dual-chamber pacing can be considered in carefully selected patients age 40 or older with syncope and documented asystole of at least 3 seconds or spontaneous pauses of at least 6 seconds without syncope on implantable loop recorder monitoring (class IIb recommendation).1,12,13 Strict patient selection increases the likelihood that pacing will be effective.1 For example, patients with documented asystole during syncope and a tilt-table test that induces minimal or no vasodepressor response are more likely to respond than patients with a positive tilt-table test with a vasodepressor (hypotensive) response.13
Tilt-table testing may also be considered to identify patients with a hypotensive response who would be less likely to respond to permanent cardiac pacing.14
Compression garments carry a class IIa recommendation for orthostatic hypotension,1 but they have not been adequately studied in vasovagal syncope.
Vasovagal syncope is usually benign, and although it often recurs, increasing fluid and salt intake and performing counter-pressure maneuvers are usually sufficient.1 However, if patients continue to have syncopal episodes despite these first-line measures, other options include drug therapy with midodrine, fludrocortisone, beta-blockers, or selective serotonin reuptake inhibitors; orthostatic training; and, in some cases, pacemaker implantation. The 2017 guidelines from the American College of Cardiology, American Heart Association, and Heart Rhythm Society (ACC/AHA/HRS) are helpful in the management of these patients.1
RATIONALE
Although vasovagal syncope is considered benign, it can result in injury and can significantly affect quality of life.
The diagnosis can often be established in the initial evaluation with a structured history, physical examination, and electrocardiography. If the diagnosis is still unclear, tilt-table testing can be useful and has an ACC/AHA/HRS class IIa (moderate) recommendation.1 Once the diagnosis of vasovagal syncope is made, first-line measures can be instituted.
FIRST-LINE MEASURES
An explanation of the diagnosis, education on avoiding triggers such as prolonged standing and warm environments, coping with potentially stressful visits to the doctor or dentist, and reassurance that the condition is benign are all strongly recommended (class I).1
Initial measures include performing physical counter-pressure maneuvers (class IIa), increasing salt and fluid intake (class IIb) in the absence of contraindications, and, in selected patients, reducing or withdrawing hypotensive medications when appropriate (class IIb).
Physical counter-pressure maneuvers are recommended for patients whose syncopal episodes have a sufficiently long prodromal period. Maneuvers include the following:
- Leg crossing: crossing the legs while tensing leg, abdominal, and buttock muscles
- Handgrip: maximally contracting a rubber ball or other object in the dominant hand
- Squatting
- Limb or abdominal contractions
- Arm tensing: contracting both arms by gripping one hand with the other and abducting both arms.2
The effectiveness of counter-pressure maneuvers was studied by van Dijk et al2 in a multicenter prospective randomized clinical trial that included 223 patients with recurrent vasovagal syncope associated with prodromal symptoms. They concluded that these maneuvers decreased the recurrence of syncopal episodes, with a relative risk reduction of 0.36 (95% confidence interval 0.11–0.53, P < .005) and were low-cost and risk-free.
Confirming the diagnosis of vasovagal syncope with tilt-table testing may reassure the patient. It can also help the patient learn to identify the symptoms associated with a vasovagal episode, which in turn may encourage timely use of physical counter-pressure maneuvers at the onset.
The evidence for increasing salt and fluid intake for patients with vasovagal syncope is limited. But in the absence of a contraindication such as hypertension, renal disease, or heart failure, it may be reasonable to encourage the ingestion of 2 L to 3 L of fluid per day and a total of 6 g to 9 g of salt per day (around 1 to 2 heaping teaspoons of salt).1
MEDICAL THERAPY
In patients who continue to have syncopal episodes despite adequate use of first-line measures, medical therapy can be considered. Unfortunately, evidence supporting drug therapy for recurrent syncope is limited.3 Options include midodrine (class IIa), fludrocortisone (class IIb), beta-blockers (class IIb), and selective serotonin reuptake inhibitors (class IIb).1
Midodrine has the strongest recommendation and is a reasonable option if there is no history of hypertension, heart failure, or urinary retention. It is a peripheral alpha-agonist that ameliorates the reduction in peripheral sympathetic neural outflow responsible for venous pooling and vasodepression in vasovagal syncope.4–6
Fludrocortisone results in increased blood volume due to mineralocorticoid activity. In the Prevention of Syncope Trial 2 of fludrocortisone vs placebo, patients on fludrocortisone had a “marginally nonsignificant” reduction in recurrence of syncope over 1 year (hazard ratio 0.69, P = .069).7
Overall, beta-blockers have failed to prevent syncope in randomized controlled trials. But in a meta-analysis that included patients from the Prevention of Syncope Trial,8 an age-dependent benefit of beta-blockers was noted in patients age 42 and older.9 Therefore, a beta-blocker may be a reasonable option in patients in this age group with recurrent vasovagal syncope.1
Serotonin has central effects on blood pressure and heart rate that can induce syncope. However, evidence for the effectiveness of selective serotonin reuptake inhibitors in the prevention of recurrent vasovagal syncope has been contradictory in small trials.10,11
When choosing a drug, contraindications should be considered, including possible effects during pregnancy in women of childbearing age.
OTHER MEASURES
Orthostatic training, with repetitive tilt-table testing until a test is negative, or with daily standing quietly against a wall for prolonged periods of time, has not been shown to have sustained benefit in reducing the recurrence of syncopal episodes (class IIb recommendation).1
Dual-chamber pacing can be considered in carefully selected patients age 40 or older with syncope and documented asystole of at least 3 seconds or spontaneous pauses of at least 6 seconds without syncope on implantable loop recorder monitoring (class IIb recommendation).1,12,13 Strict patient selection increases the likelihood that pacing will be effective.1 For example, patients with documented asystole during syncope and a tilt-table test that induces minimal or no vasodepressor response are more likely to respond than patients with a positive tilt-table test with a vasodepressor (hypotensive) response.13
Tilt-table testing may also be considered to identify patients with a hypotensive response who would be less likely to respond to permanent cardiac pacing.14
Compression garments carry a class IIa recommendation for orthostatic hypotension,1 but they have not been adequately studied in vasovagal syncope.
- Shen WK, Sheldon RS, Benditt DG, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2017; 136(5):e60–e122. doi:10.1161/CIR.0000000000000499
- van Dijk N, Quartieri F, Blanc JJ, Garcia-Civera R, Brignole M, Moya A, Wieling W; PC-Trial Investigators. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: the Physical Counterpressure Manoeuvres Trial (PC-Trial). J Am Coll Cardiol 2006; 48(8):1652–1657. doi:10.1016/j.jacc.2006.06.059
- Romme JJ, Reitsma JB, Black CN, et al. Drugs and pacemakers for vasovagal, carotid sinus and situational syncope. Cochrane Database Syst Rev 2011; (10):CD004194. doi:10.1002/14651858.CD004194.pub3
- Perez-Lugones A, Schweikert R, Pavia S, et al. Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: a randomized control study. J Cardiovasc Electrophysiol 2001; 12(8):935–938. pmid:11513446
- Romme JJ, van Dijk N, Go-Schön IK, Reitsma JB, Wieling W. Effectiveness of midodrine treatment in patients with recurrent vasovagal syncope not responding to non-pharmacological treatment (STAND-trial). Europace 2011; 13(11):1639–1647. doi:10.1093/europace/eur200
- Samniah N, Sakaguchi S, Lurie KG, Iskos D, Benditt DG. Efficacy and safety of midodrine hydrochloride in patients with refractory vasovagal syncope. Am J Cardiol 2001; 88(1):A7, 80–83. pmid:11423066
- Sheldon R, Raj SR, Rose MS, et al; POST 2 Investigators. Fludrocortisone for the prevention of vasovagal syncope: a randomized, placebo-controlled trial. J Am Coll Cardiol 2016; 68(1):1–9. doi:10.1016/j.jacc.2016.04.030
- Sheldon R, Connolly S, Rose S, et al; POST Investigators. Prevention of Syncope Trial (POST): a randomized, placebo-controlled study of metoprolol in the prevention of vasovagal syncope. Circulation 2006; 113(9):1164–1170. doi:10.1161/CIRCULATIONAHA.105.535161
- Sheldon RS, Morillo CA, Klingenheben T, Krahn AD, Sheldon A, Rose MS. Age-dependent effect of beta-blockers in preventing vasovagal syncope. Circ Arrhythm Electrophysiol 2012; 5(5):920–926. doi:10.1161/CIRCEP.112.974386
- Takata TS, Wasmund SL, Smith ML, et al. Serotonin reuptake inhibitor (Paxil) does not prevent the vasovagal reaction associated with carotid sinus massage and/or lower body negative pressure in healthy volunteers. Circulation 2002; 106(12):1500–1504. pmid:12234955
- Di Girolamo E, Di Iorio C, Sabatini P, Leonzio L, Barbone C, Barsotti A. Effects of paroxetine hydrochloride, a selective serotonin reuptake inhibitor, on refractory vasovagal syncope: a randomized, double-blind, placebo-controlled study. J Am Coll Cardiol 1999; 33(5):1227–1230. pmid:10193720
- Brignole M, Menozzi C, Moya A, et al; International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators. Pacemaker therapy in patients with neurally mediated syncope and documented asystole: third International Study on Syncope of Uncertain Etiology (ISSUE-3): a randomized trial. Circulation 2012; 125(21):2566–2571. doi:10.1161/CIRCULATIONAHA.111.082313
- Brignole M, Donateo P, Tomaino M, et al; International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators. Benefit of pacemaker therapy in patients with presumed neurally mediated syncope and documented asystole is greater when tilt test is negative: an analysis from the third International Study on Syncope of Uncertain Etiology (ISSUE-3). Circ Arrhythm Electrophysiol 2014; 7(1):10–16. doi:10.1161/CIRCEP.113.001103
- Sheldon RS, Grubb BP, Olshansky B, et al. 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 2015; 12(6):e41–e63. doi:10.1016/j.hrthm.2015.03.029
- Shen WK, Sheldon RS, Benditt DG, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2017; 136(5):e60–e122. doi:10.1161/CIR.0000000000000499
- van Dijk N, Quartieri F, Blanc JJ, Garcia-Civera R, Brignole M, Moya A, Wieling W; PC-Trial Investigators. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: the Physical Counterpressure Manoeuvres Trial (PC-Trial). J Am Coll Cardiol 2006; 48(8):1652–1657. doi:10.1016/j.jacc.2006.06.059
- Romme JJ, Reitsma JB, Black CN, et al. Drugs and pacemakers for vasovagal, carotid sinus and situational syncope. Cochrane Database Syst Rev 2011; (10):CD004194. doi:10.1002/14651858.CD004194.pub3
- Perez-Lugones A, Schweikert R, Pavia S, et al. Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: a randomized control study. J Cardiovasc Electrophysiol 2001; 12(8):935–938. pmid:11513446
- Romme JJ, van Dijk N, Go-Schön IK, Reitsma JB, Wieling W. Effectiveness of midodrine treatment in patients with recurrent vasovagal syncope not responding to non-pharmacological treatment (STAND-trial). Europace 2011; 13(11):1639–1647. doi:10.1093/europace/eur200
- Samniah N, Sakaguchi S, Lurie KG, Iskos D, Benditt DG. Efficacy and safety of midodrine hydrochloride in patients with refractory vasovagal syncope. Am J Cardiol 2001; 88(1):A7, 80–83. pmid:11423066
- Sheldon R, Raj SR, Rose MS, et al; POST 2 Investigators. Fludrocortisone for the prevention of vasovagal syncope: a randomized, placebo-controlled trial. J Am Coll Cardiol 2016; 68(1):1–9. doi:10.1016/j.jacc.2016.04.030
- Sheldon R, Connolly S, Rose S, et al; POST Investigators. Prevention of Syncope Trial (POST): a randomized, placebo-controlled study of metoprolol in the prevention of vasovagal syncope. Circulation 2006; 113(9):1164–1170. doi:10.1161/CIRCULATIONAHA.105.535161
- Sheldon RS, Morillo CA, Klingenheben T, Krahn AD, Sheldon A, Rose MS. Age-dependent effect of beta-blockers in preventing vasovagal syncope. Circ Arrhythm Electrophysiol 2012; 5(5):920–926. doi:10.1161/CIRCEP.112.974386
- Takata TS, Wasmund SL, Smith ML, et al. Serotonin reuptake inhibitor (Paxil) does not prevent the vasovagal reaction associated with carotid sinus massage and/or lower body negative pressure in healthy volunteers. Circulation 2002; 106(12):1500–1504. pmid:12234955
- Di Girolamo E, Di Iorio C, Sabatini P, Leonzio L, Barbone C, Barsotti A. Effects of paroxetine hydrochloride, a selective serotonin reuptake inhibitor, on refractory vasovagal syncope: a randomized, double-blind, placebo-controlled study. J Am Coll Cardiol 1999; 33(5):1227–1230. pmid:10193720
- Brignole M, Menozzi C, Moya A, et al; International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators. Pacemaker therapy in patients with neurally mediated syncope and documented asystole: third International Study on Syncope of Uncertain Etiology (ISSUE-3): a randomized trial. Circulation 2012; 125(21):2566–2571. doi:10.1161/CIRCULATIONAHA.111.082313
- Brignole M, Donateo P, Tomaino M, et al; International Study on Syncope of Uncertain Etiology 3 (ISSUE-3) Investigators. Benefit of pacemaker therapy in patients with presumed neurally mediated syncope and documented asystole is greater when tilt test is negative: an analysis from the third International Study on Syncope of Uncertain Etiology (ISSUE-3). Circ Arrhythm Electrophysiol 2014; 7(1):10–16. doi:10.1161/CIRCEP.113.001103
- Sheldon RS, Grubb BP, Olshansky B, et al. 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 2015; 12(6):e41–e63. doi:10.1016/j.hrthm.2015.03.029