User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
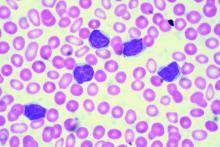
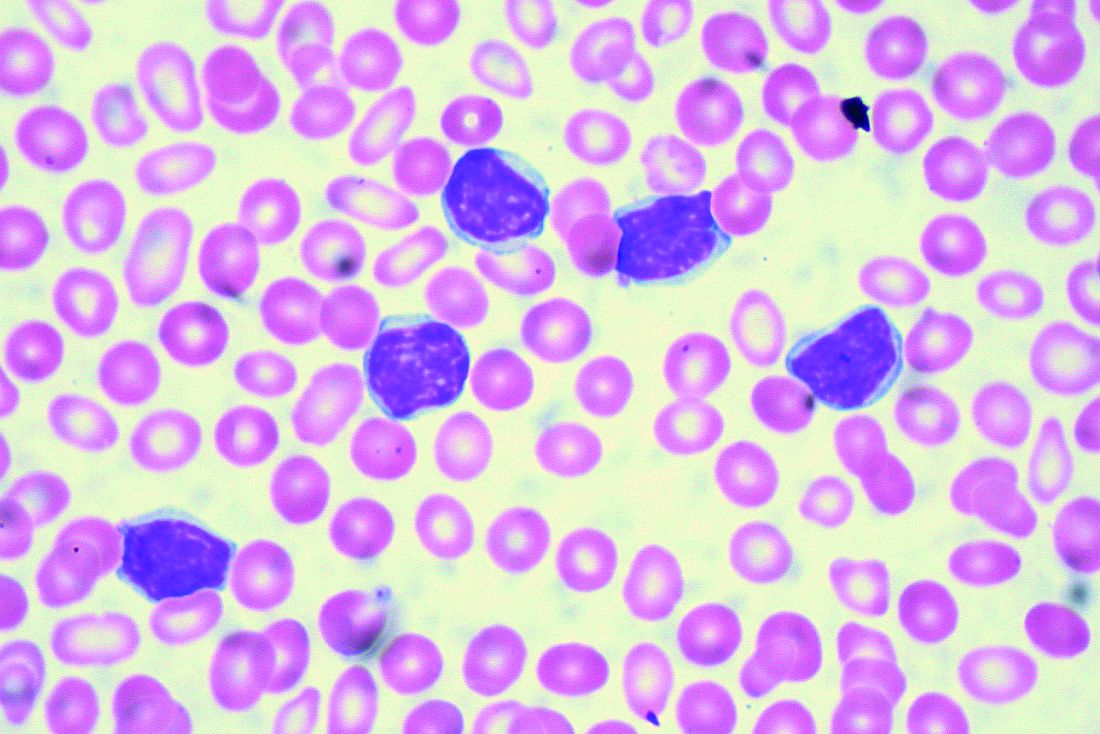
MCL treatment choices depend partly on age
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – Treatment for mantle cell lymphoma (MCL) depends at least in part on patient age, with some important differences in those aged 65 years or younger versus those over age 65, according to Kristie A. Blum, MD.
“For the [younger] early-stage patients I’ll think about radiation and maybe observation, although I think [observation] is pretty uncommon,” Dr. Blum, acting hematology and medical oncology professor at Emory University in Atlanta, said at the American Society of Hematology Meeting on Hematologic Malignancies.
For advanced-stage patients, a number of options, including observation, can be considered, she said.
Observation
Observation is acceptable in highly selected advanced stage cases. In a 2009 study of 97 mantle cell patients, 31 were observed for more than 3 months before treatment was initiated (median time to treatment, 12 months), and at median follow-up of 55 months, overall survival (OS) was significantly better in the observation group (not reached vs. 64 months in treated patients), she said (J Clin Oncol. 2009 Mar 10;27[8]:1209-13).
Observed patients had better performance status and lower-risk standard International Prognostic Index scores, compared with treated patients, and the authors concluded that a “watch-and-wait” approach is acceptable in select patients.
“In addition, if you looked at their overall survival from the time of first treatment, there was no difference in the groups, suggesting you really weren’t hurting people by delaying their therapy,” Dr. Blum said.
In a more recent series of 440 favorable-risk MCL patients, 17% were observed for at least 3 months (median time to treatment, 35 months), 80% were observed for at least 12 months, and 13% were observed for 5 years.
Again, median OS was better for observed patients than for those treated initially, at 72 months vs. 52.5 months (Ann Oncol. 2017;28[10]:2489-95).
“So I do think there is a subset of patients that can safely be observed with mantle cell [lymphoma],” she said.
Transplant-based approaches
Transplant-based approaches in younger patients with advanced disease include the Nordic regimen plus autologous stem cell transplant (ASCT), R-CHOP/R-DHAP plus ASCT, and R-bendamustine/R-cytarabine – all with post-ASCT maintenance rituximab, Dr. Blum said.
Cytarabine-containing induction was established as the pretransplant standard of care by the 474-patient MCL Younger trial, which demonstrated significantly prolonged time to treatment failure (9.1 vs. 3.9 years), with alternating pretransplant R-CHOP/R-DHAP versus R-CHOP for six cycles, though this was associated with increased toxicity. (Lancet. 2016 Aug 6;388[10044]:565-75).
For example, grade 3-4 thrombocytopenia occurred in 73% vs. 9% of patients, she noted.
The Nordic MCL2 trial showed that an intensive regimen involving alternating Maxi-CHOP and AraC followed by transplant results in median OS of about 12 years and PFS of about 8 years.
“I do want to highlight, though, that again, the high-risk patients don’t do very well,” she said, noting that median PFS even with this intensive approach was only 2.5 years in those at high risk based on MCL International Prognostic Index (MIPI) score, compared with 12.7 years for patients with a low-risk MIPI score.
Newer induction regimens also show some promise and appear feasible in younger patients based on early data, she said, noting that the SWOG S1106 trial comparing R-bendamustine and R-HyperCVAD showed a minimal residual disease (MRD) negativity rate of 78% in the R-bendamustine group. Another study evaluating R-bendamustine followed by AraC showed a 96% complete remission and PFS at 13 months of 96%, with MRD-negativity of 93% (Br J Haematol. 2016 Apr;173[1]:89-95).
Transplant also is an option in advanced stage patients aged 66-70 years who are fit and willing, Dr. Blum said.
“I spend a long time talking to these patients about whether they want a transplant or not,” she said.
For induction in those patients who choose transplant, Dr. Blum said she prefers bendamustine-based regimens, “because these have been published in patients up to the age of 70.”
Transplant timing is usually at the first complete remission.
Data show that 5-year OS after such early ASCT in patients with no more than two prior lines of chemotherapy is about 60%, compared with about 44% with late ASCT. For reduced intensity conditioning allogeneic stem cell transplant in that study, the 5-year OS was 62% for early transplant and 31% for late transplant (J Clin Oncol. 2014 Feb 1;32[4]:273-81).
R-HyperCVAD
R-HyperCVAD is another option in younger patients, and is usually given for eight cycles, followed by transplant only in those who aren’t in complete remission, Dr. Blum said.
Median failure-free survival among patients aged 65 years and younger in one study of this regimen was 6.5 years and OS was 13.4 years. In those over age 65, median failure-free survival was about 3 years (Br J Haematol. 2016 Jan;172[1]:80-88).
The SWOG 0213 study looked at this in a multicenter fashion, she said, noting that 39% of patients – 48% of whom were aged 65 and older – could not complete all eight cycles.
“Again, there was a high rate of this sort of infectious toxicity,” she said.
Median PFS was about 5 years in this study as well, and OS was nearly 7 years. For those over age 65, median PFS was just 1.6 years.
“So I don’t typically recommend this for the 65- to 70-year-olds,” she said.
Older nontransplant candidates
When treating patients who are unfit for transplant, Dr. Blum pointed to the results of the StiL and BRIGHT studies, which both showed that R-bendamustine was noninferior to R-CHOP as first-line treatment.
In addition, recent data on combined bendamustine and cytarabine (R-BAC500) showed that in 57 patients with a median age of 71 years, 95% received at least four cycles, and 67% completed six cycles. CR was 91% , and 2-year OS and PFS were 86% and 81%, respectively.
However, grade 3-4 neutropenia and thrombocytopenia occurred in 49% and 52% of patients, respectively (Lancet Haematol. 2017 Jan 1;4[1]:e15-e23).
The bortezomib-containing regimen VR-CAP has also been shown to be of benefit for older MCL patients not eligible for transplant, she said.
Median PFS with VR-CAP in a study of 487 newly diagnosed MCL patients was about 25 months vs. 14 months with R-CHOP (N Engl J Med. 2015 Mar 5;372:944-53).
“R-lenalidomide has activity in the front-line setting as well,” Dr. Blum said, citing a multicenter phase 2 study of 38 patients with a mean age of 65 years. The intention-to-treat analysis showed an overall response rate of 87%, CR rate of 61%, and 2-year PFS of 85% (N Engl J Med. 2015;373:1835-44).
Maintenance therapy
As for maintenance therapy in younger patients, a phase 3 study of 299 patients showed that rituximab maintenance was associated with significantly better 4-year PFS (83% vs. 64% with observation), and 4-year OS (89% vs. 80% with observation), she said (N Engl J Med. 2017 Sep 28;377:1250-60).
“I do think that rituximab maintenance is the standard of care now, based on this study,” Dr. Blum said, adding that there is also a role for rituximab maintenance in older patients.
A European Mantle Cell Network study of patients aged 60 and older (median age of 70) showed an OS of 62% with R-CHOP vs. 47% with R-FC (rituximab, fludarabine, and cyclophosphamide), and – among those then randomized to maintenance rituximab or interferon alpha – 4-year PFS of 58% vs. 29%, respectively (N Engl J Med. 2012;367:520-31).
“Now I will tell you that most of these patients are getting bendamustine. We don’t really know the role for rituximab maintenance after bendamustine-based induction, but at this point I think it’s reasonable to consider adding it,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
EXPERT ANALYSIS FROM MHM 2018
Some mutation testing can be useful at CLL diagnosis
CHICAGO – A number of mutation tests – including immunoglobulin heavy chain gene (IgVH), fluorescence in situ hybridization (FISH), and TP53 – provide useful prognostic information at the time of chronic lymphocytic leukemia (CLL) diagnosis, according to Paul M. Barr, MD.
“It’s understood that IgVH mutation status is certainly prognostic,” Dr. Barr, associate professor of hematology/oncology at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
The B-cell receptor of the CLL cells uses IgVH genes that may or may not have undergone somatic mutations, with unmutated being defined as 98% or more sequence homology to germline.
“This is indicative of stronger signaling through the B-cell receptor and, as we all know, predicts for an inferior prognosis,” he explained, citing a study that demonstrated superior survival rates with mutated IgVH genes (Blood. 1999;94[6]:1840-7).
“It’s also well understood and accepted that we should perform a FISH panel; we should look for interphase cytogenetics based on FISH in our patients,” Dr. Barr said. “Having said that, we, as medical oncologists, do not do a very good job of using this testing appropriately. Patterns of care studies have suggested that a significant number of patients don’t get FISH testing at diagnosis or before first-line therapy.”
In fact, a typical interphase FISH panel identifies cytogenetic lesions, including del(17p), del(11q), del(13q), and trisomy 12 in more than 80% of CLL cases, with del(13q) being the most common.
Another marker that can be assessed in CLL patients and has maintained prognostic value across multiple analyses is serum beta-2 microglobulin, Dr. Barr noted.
TP53 sequencing is valuable as well and has been associated with outcomes similar to those seen in patients with del(17p), he said, citing data from a study that found similarly poor outcomes with TP53 mutations or deletions and del(17p), even when minor subclones are identified using next-generation sequencing (Blood. 2014;123:2139-47).
“One of the primary reasons for this is that the two aberrations go together. Most often, if you have del(17p) you’re also going to find a TP53 mutation, but in about 30% of patients or so, only one allele is affected, so this is why it’s still important to test for TP53 mutations when you’re looking for a 17p deletion,” he said.
Numerous other recurrent mutations in CLL have been associated with poor overall survival and/or progression-free survival, including SF3B1, ATM, NOTCH1, POT1, BIRC3, and NFKBIE.
“The gut instinct is that maybe we should start testing for all of these mutations now, but I would caution everybody that we still need further validation before we can apply these to the majority of patients,” Dr. Barr said. “We still don’t know exactly what to do with all of these mutations – when and how often we should test for them, if the novel agents are truly better – so while, again, they can predict for inferior outcomes, I would say these are not yet standard of care to be tested in all patients.”
It is likely, though, that new prognostic systems will evolve as more is learned about how to use these molecular aberrations. Attempts are already being made to incorporate novel mutations into a prognostic system. Dr. Barr pointed to a report that looked at the integration of mutations and cytogenetic lesions to improve the accuracy of survival prediction in CLL (Blood. 2013;121:1403-12).
“But this still requires prospective testing, especially in patients getting the novel agents,” he said.
Conventional karyotyping also has potential, though a limited role in this setting, he said, noting that it can be reliably performed with stimulation of CLL cells.
“We also know additional aberrations are prognostic and that a complex karyotype predicts for a very poor outcome,” he said. The International Workshop on CLL (iwCLL) guidelines, which were recently updated for the first time in a decade, state that further validation is needed.
“I think it’s potentially useful in a very young patient you are considering taking to transplant, but again, I agree with the stance that this is not something that should be performed in every patient across the board,” he said.
The tests currently recommended by iwCLL before CLL treatment include IgVH mutation status; FISH for del(13q), del(11q), del(17p), and trisomy 12 in peripheral blood lymphocytes; and TP53.
“Some folks... don’t check a lot of these markers at diagnosis, but wait for patients to require therapy, and that’s a reasonable way to practice,” Dr. Barr said, noting, however, that he prefers knowing patients’ risk up front – especially for those patients he will see just once before they are “managed closer to home for the majority of their course.
“But if you [wait], then knowing what to repeat later is important,” he added. Namely, the FISH and TP53 tests are worth repeating as patients can acquire additional molecular aberrations over time.
Dr. Barr reported serving as a consultant for Pharmacyclics, AbbVie, Celgene, Gilead Sciences, Infinity Pharmaceuticals, Novartis, and Seattle Genetics. He also reported receiving research funding from Pharmacyclics and AbbVie.
CHICAGO – A number of mutation tests – including immunoglobulin heavy chain gene (IgVH), fluorescence in situ hybridization (FISH), and TP53 – provide useful prognostic information at the time of chronic lymphocytic leukemia (CLL) diagnosis, according to Paul M. Barr, MD.
“It’s understood that IgVH mutation status is certainly prognostic,” Dr. Barr, associate professor of hematology/oncology at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
The B-cell receptor of the CLL cells uses IgVH genes that may or may not have undergone somatic mutations, with unmutated being defined as 98% or more sequence homology to germline.
“This is indicative of stronger signaling through the B-cell receptor and, as we all know, predicts for an inferior prognosis,” he explained, citing a study that demonstrated superior survival rates with mutated IgVH genes (Blood. 1999;94[6]:1840-7).
“It’s also well understood and accepted that we should perform a FISH panel; we should look for interphase cytogenetics based on FISH in our patients,” Dr. Barr said. “Having said that, we, as medical oncologists, do not do a very good job of using this testing appropriately. Patterns of care studies have suggested that a significant number of patients don’t get FISH testing at diagnosis or before first-line therapy.”
In fact, a typical interphase FISH panel identifies cytogenetic lesions, including del(17p), del(11q), del(13q), and trisomy 12 in more than 80% of CLL cases, with del(13q) being the most common.
Another marker that can be assessed in CLL patients and has maintained prognostic value across multiple analyses is serum beta-2 microglobulin, Dr. Barr noted.
TP53 sequencing is valuable as well and has been associated with outcomes similar to those seen in patients with del(17p), he said, citing data from a study that found similarly poor outcomes with TP53 mutations or deletions and del(17p), even when minor subclones are identified using next-generation sequencing (Blood. 2014;123:2139-47).
“One of the primary reasons for this is that the two aberrations go together. Most often, if you have del(17p) you’re also going to find a TP53 mutation, but in about 30% of patients or so, only one allele is affected, so this is why it’s still important to test for TP53 mutations when you’re looking for a 17p deletion,” he said.
Numerous other recurrent mutations in CLL have been associated with poor overall survival and/or progression-free survival, including SF3B1, ATM, NOTCH1, POT1, BIRC3, and NFKBIE.
“The gut instinct is that maybe we should start testing for all of these mutations now, but I would caution everybody that we still need further validation before we can apply these to the majority of patients,” Dr. Barr said. “We still don’t know exactly what to do with all of these mutations – when and how often we should test for them, if the novel agents are truly better – so while, again, they can predict for inferior outcomes, I would say these are not yet standard of care to be tested in all patients.”
It is likely, though, that new prognostic systems will evolve as more is learned about how to use these molecular aberrations. Attempts are already being made to incorporate novel mutations into a prognostic system. Dr. Barr pointed to a report that looked at the integration of mutations and cytogenetic lesions to improve the accuracy of survival prediction in CLL (Blood. 2013;121:1403-12).
“But this still requires prospective testing, especially in patients getting the novel agents,” he said.
Conventional karyotyping also has potential, though a limited role in this setting, he said, noting that it can be reliably performed with stimulation of CLL cells.
“We also know additional aberrations are prognostic and that a complex karyotype predicts for a very poor outcome,” he said. The International Workshop on CLL (iwCLL) guidelines, which were recently updated for the first time in a decade, state that further validation is needed.
“I think it’s potentially useful in a very young patient you are considering taking to transplant, but again, I agree with the stance that this is not something that should be performed in every patient across the board,” he said.
The tests currently recommended by iwCLL before CLL treatment include IgVH mutation status; FISH for del(13q), del(11q), del(17p), and trisomy 12 in peripheral blood lymphocytes; and TP53.
“Some folks... don’t check a lot of these markers at diagnosis, but wait for patients to require therapy, and that’s a reasonable way to practice,” Dr. Barr said, noting, however, that he prefers knowing patients’ risk up front – especially for those patients he will see just once before they are “managed closer to home for the majority of their course.
“But if you [wait], then knowing what to repeat later is important,” he added. Namely, the FISH and TP53 tests are worth repeating as patients can acquire additional molecular aberrations over time.
Dr. Barr reported serving as a consultant for Pharmacyclics, AbbVie, Celgene, Gilead Sciences, Infinity Pharmaceuticals, Novartis, and Seattle Genetics. He also reported receiving research funding from Pharmacyclics and AbbVie.
CHICAGO – A number of mutation tests – including immunoglobulin heavy chain gene (IgVH), fluorescence in situ hybridization (FISH), and TP53 – provide useful prognostic information at the time of chronic lymphocytic leukemia (CLL) diagnosis, according to Paul M. Barr, MD.
“It’s understood that IgVH mutation status is certainly prognostic,” Dr. Barr, associate professor of hematology/oncology at the University of Rochester (N.Y.), said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
The B-cell receptor of the CLL cells uses IgVH genes that may or may not have undergone somatic mutations, with unmutated being defined as 98% or more sequence homology to germline.
“This is indicative of stronger signaling through the B-cell receptor and, as we all know, predicts for an inferior prognosis,” he explained, citing a study that demonstrated superior survival rates with mutated IgVH genes (Blood. 1999;94[6]:1840-7).
“It’s also well understood and accepted that we should perform a FISH panel; we should look for interphase cytogenetics based on FISH in our patients,” Dr. Barr said. “Having said that, we, as medical oncologists, do not do a very good job of using this testing appropriately. Patterns of care studies have suggested that a significant number of patients don’t get FISH testing at diagnosis or before first-line therapy.”
In fact, a typical interphase FISH panel identifies cytogenetic lesions, including del(17p), del(11q), del(13q), and trisomy 12 in more than 80% of CLL cases, with del(13q) being the most common.
Another marker that can be assessed in CLL patients and has maintained prognostic value across multiple analyses is serum beta-2 microglobulin, Dr. Barr noted.
TP53 sequencing is valuable as well and has been associated with outcomes similar to those seen in patients with del(17p), he said, citing data from a study that found similarly poor outcomes with TP53 mutations or deletions and del(17p), even when minor subclones are identified using next-generation sequencing (Blood. 2014;123:2139-47).
“One of the primary reasons for this is that the two aberrations go together. Most often, if you have del(17p) you’re also going to find a TP53 mutation, but in about 30% of patients or so, only one allele is affected, so this is why it’s still important to test for TP53 mutations when you’re looking for a 17p deletion,” he said.
Numerous other recurrent mutations in CLL have been associated with poor overall survival and/or progression-free survival, including SF3B1, ATM, NOTCH1, POT1, BIRC3, and NFKBIE.
“The gut instinct is that maybe we should start testing for all of these mutations now, but I would caution everybody that we still need further validation before we can apply these to the majority of patients,” Dr. Barr said. “We still don’t know exactly what to do with all of these mutations – when and how often we should test for them, if the novel agents are truly better – so while, again, they can predict for inferior outcomes, I would say these are not yet standard of care to be tested in all patients.”
It is likely, though, that new prognostic systems will evolve as more is learned about how to use these molecular aberrations. Attempts are already being made to incorporate novel mutations into a prognostic system. Dr. Barr pointed to a report that looked at the integration of mutations and cytogenetic lesions to improve the accuracy of survival prediction in CLL (Blood. 2013;121:1403-12).
“But this still requires prospective testing, especially in patients getting the novel agents,” he said.
Conventional karyotyping also has potential, though a limited role in this setting, he said, noting that it can be reliably performed with stimulation of CLL cells.
“We also know additional aberrations are prognostic and that a complex karyotype predicts for a very poor outcome,” he said. The International Workshop on CLL (iwCLL) guidelines, which were recently updated for the first time in a decade, state that further validation is needed.
“I think it’s potentially useful in a very young patient you are considering taking to transplant, but again, I agree with the stance that this is not something that should be performed in every patient across the board,” he said.
The tests currently recommended by iwCLL before CLL treatment include IgVH mutation status; FISH for del(13q), del(11q), del(17p), and trisomy 12 in peripheral blood lymphocytes; and TP53.
“Some folks... don’t check a lot of these markers at diagnosis, but wait for patients to require therapy, and that’s a reasonable way to practice,” Dr. Barr said, noting, however, that he prefers knowing patients’ risk up front – especially for those patients he will see just once before they are “managed closer to home for the majority of their course.
“But if you [wait], then knowing what to repeat later is important,” he added. Namely, the FISH and TP53 tests are worth repeating as patients can acquire additional molecular aberrations over time.
Dr. Barr reported serving as a consultant for Pharmacyclics, AbbVie, Celgene, Gilead Sciences, Infinity Pharmaceuticals, Novartis, and Seattle Genetics. He also reported receiving research funding from Pharmacyclics and AbbVie.
EXPERT ANALYSIS FROM MHM 2018
Frontline rituximab shows long-term success in indolent lymphoma
Advanced indolent lymphoma patients can be treated with a rituximab-containing regimen as first-line therapy and, in some cases, skip chemotherapy altogether, a study with 10 years of follow-up data suggests.
After a median of 10.6 years’ follow-up, almost three-quarters of patients (73%) in the study were alive, and 36% never required chemotherapy.
“This [overall survival] is at least as good as that observed in modern immunochemotherapy trials,” Sandra Lockmer, MD, of Karolinska University Hospital in Stockholm and her colleagues reported in the Journal of Clinical Oncology.
The study included 321 patients who were previously untreated and had been enrolled in two randomized clinical trials performed by the Nordic Lymphoma Group. The trials randomized patients to receive either rituximab monotherapy or rituximab combined with interferon alfa-2a. Neither trial used up-front chemotherapy.
Patients included in the follow-up analysis had follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, or indolent lymphoma not otherwise specified.
The overall survival rate at 10 years after trial assignment was 75% and 66% after 15 years. Similarly, the lymphoma-specific survival rate was 81% at 10 years after trial assignment and 77% at 15 years, the researchers reported.
Overall, 117 patients did not require treatment with chemotherapy, but 24 patients were further treated with antibodies and/or radiation. Of the 93 patients who received no additional therapies after frontline treatment, 9 patients died from causes unrelated to their lymphoma.
Among the 237 patients who failed initial treatment, the median time to treatment failure was 1.5 years.
In terms of transformation to aggressive lymphoma, the rate was 2.4%/person-year overall. The cumulative risk of transformation was 20% at 10 years after trial assignment and 24% at 15 years.
The study was funded in part by the Stockholm County Council and by the Nordic Lymphoma Group. The trials analyzed in the study were supported by Roche. Dr. Lockmer reported having no financial disclosures. Her coauthors reported relationships with Novartis, Gilead, Roche, and Takeda, among others.
[email protected]
SOURCE: Lockmer S et al. J Clin Oncol. 2018 Oct 4:JCO1800262. doi: 10.1200/JCO.18.00262.
Advanced indolent lymphoma patients can be treated with a rituximab-containing regimen as first-line therapy and, in some cases, skip chemotherapy altogether, a study with 10 years of follow-up data suggests.
After a median of 10.6 years’ follow-up, almost three-quarters of patients (73%) in the study were alive, and 36% never required chemotherapy.
“This [overall survival] is at least as good as that observed in modern immunochemotherapy trials,” Sandra Lockmer, MD, of Karolinska University Hospital in Stockholm and her colleagues reported in the Journal of Clinical Oncology.
The study included 321 patients who were previously untreated and had been enrolled in two randomized clinical trials performed by the Nordic Lymphoma Group. The trials randomized patients to receive either rituximab monotherapy or rituximab combined with interferon alfa-2a. Neither trial used up-front chemotherapy.
Patients included in the follow-up analysis had follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, or indolent lymphoma not otherwise specified.
The overall survival rate at 10 years after trial assignment was 75% and 66% after 15 years. Similarly, the lymphoma-specific survival rate was 81% at 10 years after trial assignment and 77% at 15 years, the researchers reported.
Overall, 117 patients did not require treatment with chemotherapy, but 24 patients were further treated with antibodies and/or radiation. Of the 93 patients who received no additional therapies after frontline treatment, 9 patients died from causes unrelated to their lymphoma.
Among the 237 patients who failed initial treatment, the median time to treatment failure was 1.5 years.
In terms of transformation to aggressive lymphoma, the rate was 2.4%/person-year overall. The cumulative risk of transformation was 20% at 10 years after trial assignment and 24% at 15 years.
The study was funded in part by the Stockholm County Council and by the Nordic Lymphoma Group. The trials analyzed in the study were supported by Roche. Dr. Lockmer reported having no financial disclosures. Her coauthors reported relationships with Novartis, Gilead, Roche, and Takeda, among others.
[email protected]
SOURCE: Lockmer S et al. J Clin Oncol. 2018 Oct 4:JCO1800262. doi: 10.1200/JCO.18.00262.
Advanced indolent lymphoma patients can be treated with a rituximab-containing regimen as first-line therapy and, in some cases, skip chemotherapy altogether, a study with 10 years of follow-up data suggests.
After a median of 10.6 years’ follow-up, almost three-quarters of patients (73%) in the study were alive, and 36% never required chemotherapy.
“This [overall survival] is at least as good as that observed in modern immunochemotherapy trials,” Sandra Lockmer, MD, of Karolinska University Hospital in Stockholm and her colleagues reported in the Journal of Clinical Oncology.
The study included 321 patients who were previously untreated and had been enrolled in two randomized clinical trials performed by the Nordic Lymphoma Group. The trials randomized patients to receive either rituximab monotherapy or rituximab combined with interferon alfa-2a. Neither trial used up-front chemotherapy.
Patients included in the follow-up analysis had follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, or indolent lymphoma not otherwise specified.
The overall survival rate at 10 years after trial assignment was 75% and 66% after 15 years. Similarly, the lymphoma-specific survival rate was 81% at 10 years after trial assignment and 77% at 15 years, the researchers reported.
Overall, 117 patients did not require treatment with chemotherapy, but 24 patients were further treated with antibodies and/or radiation. Of the 93 patients who received no additional therapies after frontline treatment, 9 patients died from causes unrelated to their lymphoma.
Among the 237 patients who failed initial treatment, the median time to treatment failure was 1.5 years.
In terms of transformation to aggressive lymphoma, the rate was 2.4%/person-year overall. The cumulative risk of transformation was 20% at 10 years after trial assignment and 24% at 15 years.
The study was funded in part by the Stockholm County Council and by the Nordic Lymphoma Group. The trials analyzed in the study were supported by Roche. Dr. Lockmer reported having no financial disclosures. Her coauthors reported relationships with Novartis, Gilead, Roche, and Takeda, among others.
[email protected]
SOURCE: Lockmer S et al. J Clin Oncol. 2018 Oct 4:JCO1800262. doi: 10.1200/JCO.18.00262.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: After a median of 10.6 years’ follow up, 73% of patients were alive, and 36% did not require chemotherapy.
Study details: Ten-year follow-up data from two trials on 321 previously untreated patients who had follicular lymphoma, marginal zone lymphoma, small lymphocytic lymphoma, or indolent lymphoma not otherwise specified.
Disclosures: The study was funded in part by the Stockholm County Council and by the Nordic Lymphoma Group. The trials analyzed in the study were supported by Roche. Dr. Lockmer reported having no financial disclosures. Her coauthors reported relationships with Novartis, Gilead, Roche, and Takeda, among others.
Source: Lockmer S et al. J Clin Oncol. 2018 Oct 4:JCO1800262. doi: 10.1200/JCO.18.00262.
AITL responds to 5-azacytidine in small series
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
FROM BLOOD
Key clinical point:
Major finding: The overall response rate was 75% among the 12 patients, with 6 patients achieving complete response.
Study details: A retrospective case series of 12 patients with angioimmunoblastic T cell lymphoma.
Disclosures: The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
Source: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Brentuximab vendotin plus CHP meets PFS endpoint in ECHELON-2
Takeda Pharmaceuticals and Seattle Genetics announced top-line results in the ECHELON-2 phase 3 trial of brentuximab vedotin plus CHP (cyclophosphamide, doxorubicin, prednisone) in the frontline treatment of CD-30 expressing peripheral T-cell lymphoma (PTCL).
The combination achieved statistically significant improvement in progression-free survival (PFS), compared with the control arm of standard chemotherapy alone using cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The PFS was assessed by an Independent Review Facility (hazard ratio, 0.71; P = .0110).
The combination of brentuximab vedotin plus CHP also outperformed CHOP in overall survival, a secondary endpoint of the trial (hazard ratio, 0.66, P = .0244), according to the drug sponsors.
Full results of ECHELON-2 will be presented in December 2018 at the annual meeting of the American Society of Hematology, according to the announcement from Seattle Genetics and Takeda.
Takeda Pharmaceuticals and Seattle Genetics announced top-line results in the ECHELON-2 phase 3 trial of brentuximab vedotin plus CHP (cyclophosphamide, doxorubicin, prednisone) in the frontline treatment of CD-30 expressing peripheral T-cell lymphoma (PTCL).
The combination achieved statistically significant improvement in progression-free survival (PFS), compared with the control arm of standard chemotherapy alone using cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The PFS was assessed by an Independent Review Facility (hazard ratio, 0.71; P = .0110).
The combination of brentuximab vedotin plus CHP also outperformed CHOP in overall survival, a secondary endpoint of the trial (hazard ratio, 0.66, P = .0244), according to the drug sponsors.
Full results of ECHELON-2 will be presented in December 2018 at the annual meeting of the American Society of Hematology, according to the announcement from Seattle Genetics and Takeda.
Takeda Pharmaceuticals and Seattle Genetics announced top-line results in the ECHELON-2 phase 3 trial of brentuximab vedotin plus CHP (cyclophosphamide, doxorubicin, prednisone) in the frontline treatment of CD-30 expressing peripheral T-cell lymphoma (PTCL).
The combination achieved statistically significant improvement in progression-free survival (PFS), compared with the control arm of standard chemotherapy alone using cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). The PFS was assessed by an Independent Review Facility (hazard ratio, 0.71; P = .0110).
The combination of brentuximab vedotin plus CHP also outperformed CHOP in overall survival, a secondary endpoint of the trial (hazard ratio, 0.66, P = .0244), according to the drug sponsors.
Full results of ECHELON-2 will be presented in December 2018 at the annual meeting of the American Society of Hematology, according to the announcement from Seattle Genetics and Takeda.
Novel options for treating hairy cell leukemia
NEW YORK – Ibrutinib, and now moxetumomab pasudotox, are two novel therapies that can be tried in patients with previously treated hairy cell leukemia, although data and experience with them are so far limited in this rare disease, experts said during a panel discussion at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
Since there are so few patients, data on the BTK inhibitor ibrutinib in hairy cell leukemia is largely “anecdotal,” said Andrew D. Zelenetz, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
The anti-CD22 monoclonal antibody moxetumomab pasudotox – approved for hairy cell leukemia in September – isn’t yet on the formulary at Memorial Sloan Kettering, Dr. Zelenetz added in a panel discussion of treatment options for a patient previously treated with purine analogueues and vemurafenib.
Between the two agents, moxetumomab pasudotox has more robust data in this disease, said John N. Allan, MD, of Weill Cornell Medicine, New York.
“I think if you can get access to the drug, that’s probably the best answer,” Dr. Allan said in the case discussion.
Hairy cell leukemia is an indolent B-cell lymphoma that makes up just 2% of all lymphoid leukemias, according to NCCN guidelines.
It is a chronic disease that requires long-term management, according to Dr. Allan.
First-line treatment is usually a purine analogue, either cladribine or pentostatin, and multiple treatments are possible as long as responses of greater than 2 years are achieved, he told attendees at the NCCN conference.
For relapses more than 2 years after first-line treatment, patients can be retreated with the same purine analogue, with or without rituximab, or can be switched to the alternative purine analogue, he said.
Vemurafenib, the BRAF inhibitor, is “surprisingly” effective in 90% of classic hairy cell leukemia patients with the BRAF V600E mutation, Dr. Allan added, though only about 40% of patients achieve complete response.
In discussing therapy options for a hairy cell leukemia patient previously treated with purine analogues and vemurafenib, Dr. Allan noted that the data behind ibrutinib includes case reports and early clinical investigations.
Several phase 1 studies with small numbers of patients show response rates “in the 50% range,” he said.
“This is an option,” he said. “It’s in the guidelines, and it’s something to consider.”
Moxetumomab pasudotox was recently approved for intravenous use in adults with relapsed or refractory hairy cell leukemia who have had at least two previous systemic treatments, including a purine nucleoside analogue. The CD22-directed cytotoxin is the first of its kind for treating patients with hairy cell leukemia, according to the Food and Drug Administration.
In a single-arm, open-label clinical trial including 80 patients with hairy cell leukemia who had previous treatment in line with that indication, 75% had a partial or complete response, of whom 30% had a durable complete response (CR), defined as maintaining hematologic remission for at least 180 days following CR.
Following the FDA’s approval of moxetumomab pasudotox, the NCCN updated its hairy cell leukemia clinical practice guidelines to include the drug as a category 2A recommendation for relapsed/refractory treatment. Other category 2A options in that setting include ibrutinib, vemurafenib with or without rituximab, or a clinical trial.
Along with that, NCCN guideline authors added a full page on special considerations for use of moxetumomab pasudotox. That includes advice on monitoring for capillary leak syndrome and hemolytic uremic syndrome, along with guidance on capillary leak syndrome grading and management by grade.
Dr. Zelenetz reported financial disclosures related to Adaptive Biotechnology, Amgen, AstraZeneca, Celgene, Genentech, Gilead, Hoffman La Roche, MEI Pharma, MorphoSys AG, Novartis, Pfizer, Pharmacyclics, Roche, and Verastem Oncology. Dr. Allan reported disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis, and Verastem Oncology.
NEW YORK – Ibrutinib, and now moxetumomab pasudotox, are two novel therapies that can be tried in patients with previously treated hairy cell leukemia, although data and experience with them are so far limited in this rare disease, experts said during a panel discussion at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
Since there are so few patients, data on the BTK inhibitor ibrutinib in hairy cell leukemia is largely “anecdotal,” said Andrew D. Zelenetz, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
The anti-CD22 monoclonal antibody moxetumomab pasudotox – approved for hairy cell leukemia in September – isn’t yet on the formulary at Memorial Sloan Kettering, Dr. Zelenetz added in a panel discussion of treatment options for a patient previously treated with purine analogueues and vemurafenib.
Between the two agents, moxetumomab pasudotox has more robust data in this disease, said John N. Allan, MD, of Weill Cornell Medicine, New York.
“I think if you can get access to the drug, that’s probably the best answer,” Dr. Allan said in the case discussion.
Hairy cell leukemia is an indolent B-cell lymphoma that makes up just 2% of all lymphoid leukemias, according to NCCN guidelines.
It is a chronic disease that requires long-term management, according to Dr. Allan.
First-line treatment is usually a purine analogue, either cladribine or pentostatin, and multiple treatments are possible as long as responses of greater than 2 years are achieved, he told attendees at the NCCN conference.
For relapses more than 2 years after first-line treatment, patients can be retreated with the same purine analogue, with or without rituximab, or can be switched to the alternative purine analogue, he said.
Vemurafenib, the BRAF inhibitor, is “surprisingly” effective in 90% of classic hairy cell leukemia patients with the BRAF V600E mutation, Dr. Allan added, though only about 40% of patients achieve complete response.
In discussing therapy options for a hairy cell leukemia patient previously treated with purine analogues and vemurafenib, Dr. Allan noted that the data behind ibrutinib includes case reports and early clinical investigations.
Several phase 1 studies with small numbers of patients show response rates “in the 50% range,” he said.
“This is an option,” he said. “It’s in the guidelines, and it’s something to consider.”
Moxetumomab pasudotox was recently approved for intravenous use in adults with relapsed or refractory hairy cell leukemia who have had at least two previous systemic treatments, including a purine nucleoside analogue. The CD22-directed cytotoxin is the first of its kind for treating patients with hairy cell leukemia, according to the Food and Drug Administration.
In a single-arm, open-label clinical trial including 80 patients with hairy cell leukemia who had previous treatment in line with that indication, 75% had a partial or complete response, of whom 30% had a durable complete response (CR), defined as maintaining hematologic remission for at least 180 days following CR.
Following the FDA’s approval of moxetumomab pasudotox, the NCCN updated its hairy cell leukemia clinical practice guidelines to include the drug as a category 2A recommendation for relapsed/refractory treatment. Other category 2A options in that setting include ibrutinib, vemurafenib with or without rituximab, or a clinical trial.
Along with that, NCCN guideline authors added a full page on special considerations for use of moxetumomab pasudotox. That includes advice on monitoring for capillary leak syndrome and hemolytic uremic syndrome, along with guidance on capillary leak syndrome grading and management by grade.
Dr. Zelenetz reported financial disclosures related to Adaptive Biotechnology, Amgen, AstraZeneca, Celgene, Genentech, Gilead, Hoffman La Roche, MEI Pharma, MorphoSys AG, Novartis, Pfizer, Pharmacyclics, Roche, and Verastem Oncology. Dr. Allan reported disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis, and Verastem Oncology.
NEW YORK – Ibrutinib, and now moxetumomab pasudotox, are two novel therapies that can be tried in patients with previously treated hairy cell leukemia, although data and experience with them are so far limited in this rare disease, experts said during a panel discussion at the National Comprehensive Cancer Network Hematologic Malignancies Annual Congress.
Since there are so few patients, data on the BTK inhibitor ibrutinib in hairy cell leukemia is largely “anecdotal,” said Andrew D. Zelenetz, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
The anti-CD22 monoclonal antibody moxetumomab pasudotox – approved for hairy cell leukemia in September – isn’t yet on the formulary at Memorial Sloan Kettering, Dr. Zelenetz added in a panel discussion of treatment options for a patient previously treated with purine analogueues and vemurafenib.
Between the two agents, moxetumomab pasudotox has more robust data in this disease, said John N. Allan, MD, of Weill Cornell Medicine, New York.
“I think if you can get access to the drug, that’s probably the best answer,” Dr. Allan said in the case discussion.
Hairy cell leukemia is an indolent B-cell lymphoma that makes up just 2% of all lymphoid leukemias, according to NCCN guidelines.
It is a chronic disease that requires long-term management, according to Dr. Allan.
First-line treatment is usually a purine analogue, either cladribine or pentostatin, and multiple treatments are possible as long as responses of greater than 2 years are achieved, he told attendees at the NCCN conference.
For relapses more than 2 years after first-line treatment, patients can be retreated with the same purine analogue, with or without rituximab, or can be switched to the alternative purine analogue, he said.
Vemurafenib, the BRAF inhibitor, is “surprisingly” effective in 90% of classic hairy cell leukemia patients with the BRAF V600E mutation, Dr. Allan added, though only about 40% of patients achieve complete response.
In discussing therapy options for a hairy cell leukemia patient previously treated with purine analogues and vemurafenib, Dr. Allan noted that the data behind ibrutinib includes case reports and early clinical investigations.
Several phase 1 studies with small numbers of patients show response rates “in the 50% range,” he said.
“This is an option,” he said. “It’s in the guidelines, and it’s something to consider.”
Moxetumomab pasudotox was recently approved for intravenous use in adults with relapsed or refractory hairy cell leukemia who have had at least two previous systemic treatments, including a purine nucleoside analogue. The CD22-directed cytotoxin is the first of its kind for treating patients with hairy cell leukemia, according to the Food and Drug Administration.
In a single-arm, open-label clinical trial including 80 patients with hairy cell leukemia who had previous treatment in line with that indication, 75% had a partial or complete response, of whom 30% had a durable complete response (CR), defined as maintaining hematologic remission for at least 180 days following CR.
Following the FDA’s approval of moxetumomab pasudotox, the NCCN updated its hairy cell leukemia clinical practice guidelines to include the drug as a category 2A recommendation for relapsed/refractory treatment. Other category 2A options in that setting include ibrutinib, vemurafenib with or without rituximab, or a clinical trial.
Along with that, NCCN guideline authors added a full page on special considerations for use of moxetumomab pasudotox. That includes advice on monitoring for capillary leak syndrome and hemolytic uremic syndrome, along with guidance on capillary leak syndrome grading and management by grade.
Dr. Zelenetz reported financial disclosures related to Adaptive Biotechnology, Amgen, AstraZeneca, Celgene, Genentech, Gilead, Hoffman La Roche, MEI Pharma, MorphoSys AG, Novartis, Pfizer, Pharmacyclics, Roche, and Verastem Oncology. Dr. Allan reported disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis, and Verastem Oncology.
EXPERT ANALYSIS FROM NCCN HEMATOLOGIC MALIGNANCIES
FDA lifts partial hold on tazemetostat trials
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
The U.S. Food and Drug Administration has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas, according to a press release from the drug’s developer Epizyme.
The patient had been on study for approximately 15 months and had achieved a confirmed partial response. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” Robert Bazemore, president and chief executive officer of Epizyme, said in a webcast on Sept. 24.
Epizyme assessed the risk of secondary malignancies, including T-LBL, as well as the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials. A panel of external scientific and medical experts who reviewed the findings concluded that T-LBL risks appear to be confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
“The team at Epizyme has worked diligently in collaboration with external experts and the FDA over the past several months,” Mr. Bazemore said.
The company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials. However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies. Mr. Bazemore said Epizyme hopes to submit a New Drug Application for tazemetostat in the treatment of epithelioid sarcoma.
Tazemetostat is under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid-tumor malignancies. The drug is also being studied as part of combination therapy for non–small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Epizyme is now working to resolve partial clinical holds placed on tazemetostat in France and Germany in order to resume trial enrollment in those countries.
Prognostic factors guide mantle cell treatment decisions
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
CHICAGO – The treatment options for patients with mantle cell lymphoma (MCL) vary based on age, but several prognostic factors can help guide treatment decision making in all patients, according to Kristie A. Blum, MD.
These include age, disease stage, disease sites, Mantle Cell Lymphoma International Prognostic Index (MIPI), biologic factors, and histology, Dr. Blum said during a presentation at the American Society of Hematology Meeting on Hematologic Malignancies.
Age
“I think the most important thing to recognize is there really isn’t any randomized transplant data for patients that are over 65. … There are very few transplant studies for patients [aged] 66-70,” said Dr. Blum, acting professor of hematology and medical oncology at Emory University in Atlanta.
The SWOG 0213 study did examine rituximab-hyperCVAD (R-HCVAD) in this age group, and showed that it has higher toxicity and lower efficacy in older versus younger patients, she said.
“Of course this is not typically a transplant approach, but an intensive-therapy approach,” she said, noting that progression-free and overall survival in patients aged 66-70 years were just 29% and 57%, respectively (Ann Oncol. 2013 Jun; 24[6]:1587-93).
The CALGB 59909 and 50403 studies of chemoimmunotherapy and autologous stem cell transplant (ASCT), with or without bortezomib, included only adults up to age 70.
“So while most of us think that transplant is probably okay and safe in patients up to 70, the question is what induction regimen to use,” she said.
Dr. Blum noted that a retrospective study from the Mayo Clinic looked at all 63 patients aged 65 years and older with MCL who underwent ASCT there (including 22 patients over age 70), and most (60%) were treated with R-CHOP. Just 19% received cytarabine-based regimens (Blood. 2017:130:4536).
Median overall survival after ASCT was 5 years, and median relapse-free survival was 3.2 years.
Stage
Like age, disease stage in MCL patients has not been well studied, Dr. Blum said.
“Most of the randomized transplant studies have been conducted in patients stage II-IV, so we don’t have a lot of data about the early-stage patients,” she said, adding, however, that there are some retrospective data on radiation therapy for stage I-II MCL in older adults.
An International Lymphoma Radiation Oncology Group study of 179 patients, for example, showed that overall survival was “really the same whether they got chemo, chemo plus radiation, or radiation alone,” she said.
The 10-year freedom from progression was 46%, 43%, and 31%, respectively (P = .64).
Location
“What about where the disease presents? We’ve all heard about indolent mantle cell – so there’s this leukemic ‘non-nodal’ variant that’s been described,” she said, noting that this variant has a chronic lymphocytic leukemia–like presentation (no nodal disease, blood and marrow involvement, and splenic involvement). “And they tend to be SOX11-negative with mutated [immunoglobulin variable region heavy chain gene].”
Another variant involves primarily nodal disease that typically presents without elevated white blood cell count, with low Ki-67 (10% or lower), with SOX11 positivity, and without TP53 mutations.
“But I would caution you that this is really not very well defined; there’s no clear marker that predicts for indolent disease,” Dr. Blum said. “If you have one of these patients and you’re thinking about observing them, my experience has been that the most important thing to do is make sure you look at their [gastrointestinal] tract. I’ve had a lot of these patients progress with colon masses over time.”
MIPI
MIPI is basically a risk score calculated based on age, performance status, lactate dehydrogenase levels, and white cell count, she said.
MIPI less than 5.70 indicates low risk, MIPI of 5.70-6.2 is considered intermediate risk, and MIPI greater than 6.2 is considered high risk. High-risk patients who were transplanted in one study had a median overall survival of about 2.8 years and a median time to treatment failure of 1.4 years (J Clin Oncol. 2014 May 1;32[13]:1338-46). Even among patients under age 65 with high risk, the median time to treatment failure was 2 years, she said.
“So I do wonder, are we really helping these patients by transplanting them?” she added. “Similarly, the low-risk patients had a median time to treatment failure of 6 years; I wonder if they didn’t need a transplant.”
Biology
Ki-67 protein, a cellular marker for proliferation, is another important prognostic factor. A European Mantle Cell network study showed that median overall survival for patients with a Ki-67 proliferation index of less than 30% was not reached, and 5-year survival was 75%. At the same time, the median overall survival (OS) for those with Ki-67 proliferation index of 30% or greater was just 3.4 years, and 5-year OS was only 41% (J Clin Oncol. 2016 Apr 20;34[12]:1386-94).
The prognostic effect was independent of induction treatment, Dr. Blum said.
Combining MIPI and the Ki-67 index (MIPI-C) provides further value in defining a very high-risk group; those with both high MIPI and high Ki-67 had a median overall survival of only 1.5 years, and those with both, but who were under age 65, had median OS of only 1.7 years.
Histology
Patients with blastoid MCL variants were shown in that same study to have median OS of about 2.8 years, compared with 8 years in those with nonblastoid variants. The 5-year OS and progression-free survival (PFS) for blastoid variants were 35% and 29%, respectively, and for nonblastoid variants were 68% and 44%, respectively.
“But when you look at this with respect to the Ki-67 – so those patients that were called nonblastoid, that had a high Ki-67 index – their median overall survival is still lower at 5 years,” she said, noting that median OS was not reached in blastic variant (low-Ki-67) patients. “So it seems like the prognostic effect of cytology is largely explained by the Ki-67 index.”
In terms of karyotype, several studies have shown that complex karyotype is associated with poorer outcomes. One recent multicenter study of 274 patients showed that median OS in 53 patients with at least three cytogenetic abnormalities versus the remaining patients was 4.5 years vs. 11.6 years, and median PFS was 1.9 vs. 4.4 years (Cancer. 2018 Jun 1;124[11]:2306-15).
TP53 deletions (which affect about 20% of MCL patients) and mutations (which affect about 10%), are also useful prognostic factors, she said, noting that each is associated with inferior outcomes, and in one study patients with both appeared to have the worst outcomes (Blood. 2017;130:1903-10).
Another study showed that high TP53 staining (greater than 50% positive) is also associated with inferior outcomes, including reduced time to treatment failure and lower overall survival (Blood. 2018;131:417-20).
Finally, the most important factor is the patient’s wishes, Dr. Blum said, noting that she has “a lot of long discussions with these patients.”
“I consider all of these factors with each patient that I see with mantle cell,” she said.
Dr. Blum is a consultant for Acerta, AstraZeneca, and Molecular Templates and has received research funding from Acerta, AstraZeneca, Celgene, Cephalon, Immunomedics, Janssen, Merck, Millennium, Molecular Templates, Novartis, Pharmacyclics, and Seattle Genetics.
REPORTING FROM MHM 2018
Real-world clues for optimal sequencing of CLL novel agents
NEW YORK – Although optimal sequencing strategies in chronic lymphocytic leukemia are still unclear, real-world data suggest an alternate kinase inhibitor or venetoclax is the best approach for a patient who has received ibrutinib or idelalisib, according to John N. Allan, MD, of Cornell University, New York.
“I think for the most part, there’s enough evidence,” Dr. Allan said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“If you had one to two lines of therapy, it still favors the novel agents rather than the chemotherapy arms in all these studies,” said Dr. Allan, referring to some of the pivotal trials supporting approval of novel agents in chronic lymphocytic leukemia (CLL). “The earlier we get to these drugs, I believe, the better.”
While venetoclax after ibrutinib is supported by multiple studies, “vice versa is unknown, but there’s seemingly no reason to think it wouldn’t work – different mechanisms of actions, different pathways,” Dr. Allan said.
What is clear, he added, is that retreating those patients with chemoimmunotherapy is not optimal.
In support of that, he cited a multicenter retrospective analysis, which is believed to be the largest real-world experience to date of novel agents in CLL looking at post–kinase inhibitor salvage strategies (Ann Oncol. 2017 May 1;28[5]:1050-6).
Using an alternate kinase inhibitor or venetoclax resulted in superior progression-free survival versus chemoimmunotherapy at the time of initial kinase inhibitor failure in that study, which looked at treatment strategies and outcomes for 683 patients.
Ibrutinib appeared to be superior to idelalisib as a first kinase inhibitor, with significantly better progression-free survival in both frontline and relapsed/refractory settings, and in both complex karyotype and del17p patients, according to the report. Additionally, the response rate to venetoclax seemed superior to that of idelalisib in patients who discontinued ibrutinib because of progression or toxicity.
All of that supports the need for trials to test various sequencing strategies and establish clear treatment algorithms, according to Dr. Allan. “Optimal sequencing is unknown, but real-world data gives us some idea.”
For relapsed/refractory patients, ibrutinib, idelalisib, and venetoclax all have lengthened responses, improved survival, and are approved by the Food and Drug Administration, he added, noting that the toxicity profiles vary and must be understood when dosing and prescribing these agents.
More novel treatments are on the way. On Sept. 24, just days after Dr. Allan’s NCCN presentation, the FDA granted approval to duvelisib for adults with relapsed or refractory CLL or small lymphocytic lymphoma following two or more previous lines of therapy.
Dr. Allan reported financial disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis Pharmaceuticals, and Verastem Oncology.
NEW YORK – Although optimal sequencing strategies in chronic lymphocytic leukemia are still unclear, real-world data suggest an alternate kinase inhibitor or venetoclax is the best approach for a patient who has received ibrutinib or idelalisib, according to John N. Allan, MD, of Cornell University, New York.
“I think for the most part, there’s enough evidence,” Dr. Allan said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“If you had one to two lines of therapy, it still favors the novel agents rather than the chemotherapy arms in all these studies,” said Dr. Allan, referring to some of the pivotal trials supporting approval of novel agents in chronic lymphocytic leukemia (CLL). “The earlier we get to these drugs, I believe, the better.”
While venetoclax after ibrutinib is supported by multiple studies, “vice versa is unknown, but there’s seemingly no reason to think it wouldn’t work – different mechanisms of actions, different pathways,” Dr. Allan said.
What is clear, he added, is that retreating those patients with chemoimmunotherapy is not optimal.
In support of that, he cited a multicenter retrospective analysis, which is believed to be the largest real-world experience to date of novel agents in CLL looking at post–kinase inhibitor salvage strategies (Ann Oncol. 2017 May 1;28[5]:1050-6).
Using an alternate kinase inhibitor or venetoclax resulted in superior progression-free survival versus chemoimmunotherapy at the time of initial kinase inhibitor failure in that study, which looked at treatment strategies and outcomes for 683 patients.
Ibrutinib appeared to be superior to idelalisib as a first kinase inhibitor, with significantly better progression-free survival in both frontline and relapsed/refractory settings, and in both complex karyotype and del17p patients, according to the report. Additionally, the response rate to venetoclax seemed superior to that of idelalisib in patients who discontinued ibrutinib because of progression or toxicity.
All of that supports the need for trials to test various sequencing strategies and establish clear treatment algorithms, according to Dr. Allan. “Optimal sequencing is unknown, but real-world data gives us some idea.”
For relapsed/refractory patients, ibrutinib, idelalisib, and venetoclax all have lengthened responses, improved survival, and are approved by the Food and Drug Administration, he added, noting that the toxicity profiles vary and must be understood when dosing and prescribing these agents.
More novel treatments are on the way. On Sept. 24, just days after Dr. Allan’s NCCN presentation, the FDA granted approval to duvelisib for adults with relapsed or refractory CLL or small lymphocytic lymphoma following two or more previous lines of therapy.
Dr. Allan reported financial disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis Pharmaceuticals, and Verastem Oncology.
NEW YORK – Although optimal sequencing strategies in chronic lymphocytic leukemia are still unclear, real-world data suggest an alternate kinase inhibitor or venetoclax is the best approach for a patient who has received ibrutinib or idelalisib, according to John N. Allan, MD, of Cornell University, New York.
“I think for the most part, there’s enough evidence,” Dr. Allan said at the annual congress on Hematologic Malignancies held by the National Comprehensive Cancer Network.
“If you had one to two lines of therapy, it still favors the novel agents rather than the chemotherapy arms in all these studies,” said Dr. Allan, referring to some of the pivotal trials supporting approval of novel agents in chronic lymphocytic leukemia (CLL). “The earlier we get to these drugs, I believe, the better.”
While venetoclax after ibrutinib is supported by multiple studies, “vice versa is unknown, but there’s seemingly no reason to think it wouldn’t work – different mechanisms of actions, different pathways,” Dr. Allan said.
What is clear, he added, is that retreating those patients with chemoimmunotherapy is not optimal.
In support of that, he cited a multicenter retrospective analysis, which is believed to be the largest real-world experience to date of novel agents in CLL looking at post–kinase inhibitor salvage strategies (Ann Oncol. 2017 May 1;28[5]:1050-6).
Using an alternate kinase inhibitor or venetoclax resulted in superior progression-free survival versus chemoimmunotherapy at the time of initial kinase inhibitor failure in that study, which looked at treatment strategies and outcomes for 683 patients.
Ibrutinib appeared to be superior to idelalisib as a first kinase inhibitor, with significantly better progression-free survival in both frontline and relapsed/refractory settings, and in both complex karyotype and del17p patients, according to the report. Additionally, the response rate to venetoclax seemed superior to that of idelalisib in patients who discontinued ibrutinib because of progression or toxicity.
All of that supports the need for trials to test various sequencing strategies and establish clear treatment algorithms, according to Dr. Allan. “Optimal sequencing is unknown, but real-world data gives us some idea.”
For relapsed/refractory patients, ibrutinib, idelalisib, and venetoclax all have lengthened responses, improved survival, and are approved by the Food and Drug Administration, he added, noting that the toxicity profiles vary and must be understood when dosing and prescribing these agents.
More novel treatments are on the way. On Sept. 24, just days after Dr. Allan’s NCCN presentation, the FDA granted approval to duvelisib for adults with relapsed or refractory CLL or small lymphocytic lymphoma following two or more previous lines of therapy.
Dr. Allan reported financial disclosures related to AbbVie, Acerta Pharma, Genentech, Pharmacyclics, Sunesis Pharmaceuticals, and Verastem Oncology.
EXPERT ANALYSIS FROM NCCN HEMATOLOGIC MALIGNANCIES CONGRESS
Outpatient lenalidomide/rituximab yields long-term MCL remission
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
After 5 years, the combination of lenalidomide and rituximab as first-line therapy for mantle cell lymphoma (MCL) continues to show durable responses with manageable toxicities, long-term results from a phase 2 clinical trial show.
After a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University, New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote. Their report was published in Blood.
In the multicenter, phase 2 single-arm study, 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase. Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P = .04).
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption. Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting, lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach,” the investigators wrote.
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
SOURCE: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.
FROM BLOOD
Key clinical point:
Major finding: After 64-months of median follow-up, 21 of 33 patients with initial responses remained in remission.
Study details: Five-year follow-up of a phase 2 single arm trial of lenalidomide/rituximab induction and maintenance in 38 patients with mantle cell lymphoma.
Disclosures: The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation. Dr. Ruan has received research support and been a consultant for Celgene, and other coauthors reported research support and consultant relationships with the company.
Source: Ruan J et al. Blood. 2018 Sep 4. doi: 10.1182/blood-2018-07-859769.