User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Use of second-generation antidepressants in older adults is associated with increased hospitalization with hyponatremia
Clinical Question: Is there an increased risk of hyponatremia for older patients who are taking a second-generation antidepressant?
Background: Mood and anxiety disorders affect about one in eight older adults, and second-generation antidepressants are frequently recommended for treatment. A potential adverse effect of these agents is hyponatremia, which can lead to serious sequelae. The aim of this study was to investigate the 30-day risk for hospitalization with hyponatremia in older adults who were newly started on a second-generation antidepressant.
Setting: Ontario, Canada.
Synopsis: Multiple databases were utilized to obtain vital statistics and demographic information, diagnoses, prescriptions, and serum sodium measurements to establish a cohort population. One group of 172,552 was newly prescribed a second-generation antidepressant. A second control group of 297,501 was established in which patients were not prescribed antidepressants. Greedy matching was used to match each user to a nonuser based on similar characteristics of age, sex, evidence of mood disorder, chronic kidney disease, congestive heart failure, or diuretic use. After matching, 138,246 patients remained in each group and were nearly identical for all 10 0 measured characteristics. The primary outcome was that, compared with nonuse, second-generation antidepressant use was associated with higher 30-day risk of hospitalization with hyponatremia (relative risk, 5.46; 95% CI, 4.32-6.91). The secondary outcome showed that, compared with non-use, second-generation antidepressant use was associated with higher 30-day risk for hospitalization with concomitant hyponatremia and delirium (RR, 4.00; 95% CI, 1.74 - 9.16). Additionally, tests for specificity and temporality were employed.
Bottom Line: A robust association between second-generation antidepressant use and hospitalization with hyponatremia was determined in the large population-based cohort study.
Citation: Gandhi S, Shariff SZ, Al-Jaishi A, et al. “Second-generation antidepressants and hyponatremia risk: a population-based cohort study of older adults.” Am J Kidney Dis. 2017 Jan;69(1):87-96.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical Question: Is there an increased risk of hyponatremia for older patients who are taking a second-generation antidepressant?
Background: Mood and anxiety disorders affect about one in eight older adults, and second-generation antidepressants are frequently recommended for treatment. A potential adverse effect of these agents is hyponatremia, which can lead to serious sequelae. The aim of this study was to investigate the 30-day risk for hospitalization with hyponatremia in older adults who were newly started on a second-generation antidepressant.
Setting: Ontario, Canada.
Synopsis: Multiple databases were utilized to obtain vital statistics and demographic information, diagnoses, prescriptions, and serum sodium measurements to establish a cohort population. One group of 172,552 was newly prescribed a second-generation antidepressant. A second control group of 297,501 was established in which patients were not prescribed antidepressants. Greedy matching was used to match each user to a nonuser based on similar characteristics of age, sex, evidence of mood disorder, chronic kidney disease, congestive heart failure, or diuretic use. After matching, 138,246 patients remained in each group and were nearly identical for all 10 0 measured characteristics. The primary outcome was that, compared with nonuse, second-generation antidepressant use was associated with higher 30-day risk of hospitalization with hyponatremia (relative risk, 5.46; 95% CI, 4.32-6.91). The secondary outcome showed that, compared with non-use, second-generation antidepressant use was associated with higher 30-day risk for hospitalization with concomitant hyponatremia and delirium (RR, 4.00; 95% CI, 1.74 - 9.16). Additionally, tests for specificity and temporality were employed.
Bottom Line: A robust association between second-generation antidepressant use and hospitalization with hyponatremia was determined in the large population-based cohort study.
Citation: Gandhi S, Shariff SZ, Al-Jaishi A, et al. “Second-generation antidepressants and hyponatremia risk: a population-based cohort study of older adults.” Am J Kidney Dis. 2017 Jan;69(1):87-96.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical Question: Is there an increased risk of hyponatremia for older patients who are taking a second-generation antidepressant?
Background: Mood and anxiety disorders affect about one in eight older adults, and second-generation antidepressants are frequently recommended for treatment. A potential adverse effect of these agents is hyponatremia, which can lead to serious sequelae. The aim of this study was to investigate the 30-day risk for hospitalization with hyponatremia in older adults who were newly started on a second-generation antidepressant.
Setting: Ontario, Canada.
Synopsis: Multiple databases were utilized to obtain vital statistics and demographic information, diagnoses, prescriptions, and serum sodium measurements to establish a cohort population. One group of 172,552 was newly prescribed a second-generation antidepressant. A second control group of 297,501 was established in which patients were not prescribed antidepressants. Greedy matching was used to match each user to a nonuser based on similar characteristics of age, sex, evidence of mood disorder, chronic kidney disease, congestive heart failure, or diuretic use. After matching, 138,246 patients remained in each group and were nearly identical for all 10 0 measured characteristics. The primary outcome was that, compared with nonuse, second-generation antidepressant use was associated with higher 30-day risk of hospitalization with hyponatremia (relative risk, 5.46; 95% CI, 4.32-6.91). The secondary outcome showed that, compared with non-use, second-generation antidepressant use was associated with higher 30-day risk for hospitalization with concomitant hyponatremia and delirium (RR, 4.00; 95% CI, 1.74 - 9.16). Additionally, tests for specificity and temporality were employed.
Bottom Line: A robust association between second-generation antidepressant use and hospitalization with hyponatremia was determined in the large population-based cohort study.
Citation: Gandhi S, Shariff SZ, Al-Jaishi A, et al. “Second-generation antidepressants and hyponatremia risk: a population-based cohort study of older adults.” Am J Kidney Dis. 2017 Jan;69(1):87-96.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Hospital infections top WHO’s list of priority pathogens
The World Health Organization is urging governments to focus antibiotic research efforts on a list of urgent bacterial threats, topped by several increasingly powerful superbugs that cause hospital-based infections and other potentially deadly conditions.
The WHO listed the top 20 bacteria that it believes are most harmful to human health, other than mycobacteria such as Mycobacterium tuberculosis, which causes tuberculosis. The germ was not included in the list because it’s generally accepted to be the most urgent priority for new antibiotic research and development, Marie-Paule Kieny, PhD, a WHO assistant director, said at a press conference.
The priority list is needed because the antibiotic pipeline is “practically dry,” thanks to scientific research challenges and a lack of financial incentives, according to Dr. Kieny. “Antibiotics are generally used for the short term, unlike therapies for chronic diseases, which bring in much higher returns on investment,” she said. The list “is intended to signal to the scientific community and the pharmaceutical industry the areas they should focus on to address urgent public health threats.”
The WHO list begins with Priority 1/“Critical” pathogens that it believes most urgently need to be targeted through antibiotic research and development: Acinetobacter baumannii, carbapenem-resistant; Pseudomonas aeruginosa, carbapenem-resistant; and Enterobacteriaceae (including Klebsiella pneumonia, Escherichia coli, Enterobacter spp., Serratia spp., Proteus spp., Providencia spp., and Morganella spp.), carbapenem-resistant, extended-spectrum beta-lactamase–producing.
“These bacteria are responsible for severe infections and high mortality rates, mostly in hospitalized patients, transplant recipients, those receiving chemotherapy, or patients in intensive care units,” Dr. Kieny said. “While these bacteria are not widespread and do not generally affect healthy individuals, the burden for patients and society is now alarming – and new, effective therapies are imperative.”
Priority 2/”High” pathogens are Enterococcus faecium, vancomycin-resistant; Staphylococcus aureus, methicillin-resistant, vancomycin intermediate and resistant; Helicobacter pylori, clarithromycin-resistant; Campylobacter, fluoroquinolone-resistant; Salmonella spp., fluoroquinolone-resistant; Neisseria gonorrhoeae, third-generation cephalosporin-resistant and fluoroquinolone-resistant.
Pathogens in this category can infect healthy individuals, Dr. Kieny noted. “These infections, although not associated with significant mortality, have a dramatic health and economic impact on communities and, in particular, in low-income countries.”
Priority 3/”Medium” pathogens are Streptococcus pneumoniae, penicillin–non-susceptible; Haemophilus influenzae, ampicillin-resistant; and Shigella spp., fluoroquinolone-resistant.
These pathogens “represent a threat because of increasing resistance but still have some effective antibiotic options available,” Dr. Kieny said.
According to a statement provided by the WHO, the priority list doesn’t include streptococcus A and B or chlamydia, because resistance hasn’t reached the level of a public health threat.
One goal of the list is to focus attention on the development of small-market, gram-negative drugs that combat hospital-based infections, explained Nicola Magrini, MD, a WHO scientist who also spoke at the press conference.
Over the last decade, he said, the pipeline has instead focused more on gram-positive agents – mostly linked to beta-lactamase – that have wider market potential and generate less resistance.
“From a clinical point of view, these multidrug-resistant gram-negative clinical trials are very difficult and expensive to do, more than for gram-positive,” noted Evelina Tacconelli, MD, PhD, a contributor to the WHO report. “Because when we talk about gram-negative, we need to cover multiple pathogens and not just one or two, as in the case of gram-positive.”
Dr. Magrini said he couldn’t provide estimates about how many people worldwide are affected by the listed pathogens. However, he said a full report with numbers will be released by June.
It does appear that patients with severe infection from antibiotic-resistant germs face a mortality rate of up to 60%, while extended-spectrum beta-lactamase–positive E. coli accounts for up to 70% of urinary tract infections in many countries, explained Dr. Tacconelli, head of the division of infectious diseases at the University of Tübingen, Germany.
“Even if we don’t know exactly how many,” she said, “we are talking about millions of people affected.”
The World Health Organization is urging governments to focus antibiotic research efforts on a list of urgent bacterial threats, topped by several increasingly powerful superbugs that cause hospital-based infections and other potentially deadly conditions.
The WHO listed the top 20 bacteria that it believes are most harmful to human health, other than mycobacteria such as Mycobacterium tuberculosis, which causes tuberculosis. The germ was not included in the list because it’s generally accepted to be the most urgent priority for new antibiotic research and development, Marie-Paule Kieny, PhD, a WHO assistant director, said at a press conference.
The priority list is needed because the antibiotic pipeline is “practically dry,” thanks to scientific research challenges and a lack of financial incentives, according to Dr. Kieny. “Antibiotics are generally used for the short term, unlike therapies for chronic diseases, which bring in much higher returns on investment,” she said. The list “is intended to signal to the scientific community and the pharmaceutical industry the areas they should focus on to address urgent public health threats.”
The WHO list begins with Priority 1/“Critical” pathogens that it believes most urgently need to be targeted through antibiotic research and development: Acinetobacter baumannii, carbapenem-resistant; Pseudomonas aeruginosa, carbapenem-resistant; and Enterobacteriaceae (including Klebsiella pneumonia, Escherichia coli, Enterobacter spp., Serratia spp., Proteus spp., Providencia spp., and Morganella spp.), carbapenem-resistant, extended-spectrum beta-lactamase–producing.
“These bacteria are responsible for severe infections and high mortality rates, mostly in hospitalized patients, transplant recipients, those receiving chemotherapy, or patients in intensive care units,” Dr. Kieny said. “While these bacteria are not widespread and do not generally affect healthy individuals, the burden for patients and society is now alarming – and new, effective therapies are imperative.”
Priority 2/”High” pathogens are Enterococcus faecium, vancomycin-resistant; Staphylococcus aureus, methicillin-resistant, vancomycin intermediate and resistant; Helicobacter pylori, clarithromycin-resistant; Campylobacter, fluoroquinolone-resistant; Salmonella spp., fluoroquinolone-resistant; Neisseria gonorrhoeae, third-generation cephalosporin-resistant and fluoroquinolone-resistant.
Pathogens in this category can infect healthy individuals, Dr. Kieny noted. “These infections, although not associated with significant mortality, have a dramatic health and economic impact on communities and, in particular, in low-income countries.”
Priority 3/”Medium” pathogens are Streptococcus pneumoniae, penicillin–non-susceptible; Haemophilus influenzae, ampicillin-resistant; and Shigella spp., fluoroquinolone-resistant.
These pathogens “represent a threat because of increasing resistance but still have some effective antibiotic options available,” Dr. Kieny said.
According to a statement provided by the WHO, the priority list doesn’t include streptococcus A and B or chlamydia, because resistance hasn’t reached the level of a public health threat.
One goal of the list is to focus attention on the development of small-market, gram-negative drugs that combat hospital-based infections, explained Nicola Magrini, MD, a WHO scientist who also spoke at the press conference.
Over the last decade, he said, the pipeline has instead focused more on gram-positive agents – mostly linked to beta-lactamase – that have wider market potential and generate less resistance.
“From a clinical point of view, these multidrug-resistant gram-negative clinical trials are very difficult and expensive to do, more than for gram-positive,” noted Evelina Tacconelli, MD, PhD, a contributor to the WHO report. “Because when we talk about gram-negative, we need to cover multiple pathogens and not just one or two, as in the case of gram-positive.”
Dr. Magrini said he couldn’t provide estimates about how many people worldwide are affected by the listed pathogens. However, he said a full report with numbers will be released by June.
It does appear that patients with severe infection from antibiotic-resistant germs face a mortality rate of up to 60%, while extended-spectrum beta-lactamase–positive E. coli accounts for up to 70% of urinary tract infections in many countries, explained Dr. Tacconelli, head of the division of infectious diseases at the University of Tübingen, Germany.
“Even if we don’t know exactly how many,” she said, “we are talking about millions of people affected.”
The World Health Organization is urging governments to focus antibiotic research efforts on a list of urgent bacterial threats, topped by several increasingly powerful superbugs that cause hospital-based infections and other potentially deadly conditions.
The WHO listed the top 20 bacteria that it believes are most harmful to human health, other than mycobacteria such as Mycobacterium tuberculosis, which causes tuberculosis. The germ was not included in the list because it’s generally accepted to be the most urgent priority for new antibiotic research and development, Marie-Paule Kieny, PhD, a WHO assistant director, said at a press conference.
The priority list is needed because the antibiotic pipeline is “practically dry,” thanks to scientific research challenges and a lack of financial incentives, according to Dr. Kieny. “Antibiotics are generally used for the short term, unlike therapies for chronic diseases, which bring in much higher returns on investment,” she said. The list “is intended to signal to the scientific community and the pharmaceutical industry the areas they should focus on to address urgent public health threats.”
The WHO list begins with Priority 1/“Critical” pathogens that it believes most urgently need to be targeted through antibiotic research and development: Acinetobacter baumannii, carbapenem-resistant; Pseudomonas aeruginosa, carbapenem-resistant; and Enterobacteriaceae (including Klebsiella pneumonia, Escherichia coli, Enterobacter spp., Serratia spp., Proteus spp., Providencia spp., and Morganella spp.), carbapenem-resistant, extended-spectrum beta-lactamase–producing.
“These bacteria are responsible for severe infections and high mortality rates, mostly in hospitalized patients, transplant recipients, those receiving chemotherapy, or patients in intensive care units,” Dr. Kieny said. “While these bacteria are not widespread and do not generally affect healthy individuals, the burden for patients and society is now alarming – and new, effective therapies are imperative.”
Priority 2/”High” pathogens are Enterococcus faecium, vancomycin-resistant; Staphylococcus aureus, methicillin-resistant, vancomycin intermediate and resistant; Helicobacter pylori, clarithromycin-resistant; Campylobacter, fluoroquinolone-resistant; Salmonella spp., fluoroquinolone-resistant; Neisseria gonorrhoeae, third-generation cephalosporin-resistant and fluoroquinolone-resistant.
Pathogens in this category can infect healthy individuals, Dr. Kieny noted. “These infections, although not associated with significant mortality, have a dramatic health and economic impact on communities and, in particular, in low-income countries.”
Priority 3/”Medium” pathogens are Streptococcus pneumoniae, penicillin–non-susceptible; Haemophilus influenzae, ampicillin-resistant; and Shigella spp., fluoroquinolone-resistant.
These pathogens “represent a threat because of increasing resistance but still have some effective antibiotic options available,” Dr. Kieny said.
According to a statement provided by the WHO, the priority list doesn’t include streptococcus A and B or chlamydia, because resistance hasn’t reached the level of a public health threat.
One goal of the list is to focus attention on the development of small-market, gram-negative drugs that combat hospital-based infections, explained Nicola Magrini, MD, a WHO scientist who also spoke at the press conference.
Over the last decade, he said, the pipeline has instead focused more on gram-positive agents – mostly linked to beta-lactamase – that have wider market potential and generate less resistance.
“From a clinical point of view, these multidrug-resistant gram-negative clinical trials are very difficult and expensive to do, more than for gram-positive,” noted Evelina Tacconelli, MD, PhD, a contributor to the WHO report. “Because when we talk about gram-negative, we need to cover multiple pathogens and not just one or two, as in the case of gram-positive.”
Dr. Magrini said he couldn’t provide estimates about how many people worldwide are affected by the listed pathogens. However, he said a full report with numbers will be released by June.
It does appear that patients with severe infection from antibiotic-resistant germs face a mortality rate of up to 60%, while extended-spectrum beta-lactamase–positive E. coli accounts for up to 70% of urinary tract infections in many countries, explained Dr. Tacconelli, head of the division of infectious diseases at the University of Tübingen, Germany.
“Even if we don’t know exactly how many,” she said, “we are talking about millions of people affected.”
Battling biases with the 5 Rs of cultural humility
How do we, as hospitalists, win the hearts and minds of patients, families, and care team members whom we do not know? What are the obstacles that we face when encountering patients and gaining the trust needed to improve patient care and patient experience?
With these questions in mind, the Cultural Humility Work Group, part of SHM’s Practice Management Committee, set out to develop a simple, universal framework to provide a foundation for strengthening communication skills and raising awareness of the basic tenets of cultural humility. According to Tervalon and Murray-Garcia, cultural humility is defined as a “process that requires humility as individuals continually engage in self-reflection and self-critique as lifelong learners and reflective practitioners. It requires humility in how physicians bring into check the power imbalances that exist in the dynamics of physician-patient communication by using patient-focused interviewing and care, and it is a process that requires humility to develop and maintain mutually respectful and dynamic partnerships with communities” (Tervalon, M. & Murray-García, J. “Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education.” J Health Care Poor Underserved. 1998;9[2]:117-25).
How do we win this battle? The first step is to simply be aware that everyone is a victim of unconscious biases. Once we come to this (often uncomfortable) realization, we must make a conscious effort to change our mindset and make conscious decisions to not allow these biases to manifest.
Practicing cultural humility is extremely important in this process. It puts everyone on the same platform because there is no “minority,” “majority,” or “ethnicity” associated with it. It takes away the need to know everything about a certain culture and encourages us to approach every patient encounter acknowledging that we will humble ourselves, learn what is important to the patient, and leave having learned something from the interaction.
The work group developed “The 5 Rs of Cultural Humility” as a simple tool for hospitalists to incorporate into their practice. The first four Rs (Reflection, Respect, Regard and Relevance) are extrinsically focused, while the 5th R (Resiliency) is intrinsic. Our theory posits that, if you attain the first 4 Rs in every interaction, these will serve to build on and develop your own personal resiliency. Here are the 5 Rs:
- Reflection – Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Respect – Hospitalists will treat every person with the utmost respect and strive to preserve dignity at all times.
- Regard – Hospitalists will hold every person in their highest regard while being aware of and not allowing unconscious biases to interfere in any interactions.
- Relevance – Hospitalists will expect cultural humility to be relevant to the patient and apply this practice to every encounter.
- Resiliency – Hospitalists will embody the practice of cultural humility to enhance personal resilience and globally focused compassion.
The content will be available as a downloadable pocket card that can be easily referenced on rounds and shared with colleagues. Our hope is to achieve heightened awareness of effective interaction. In addition to the definitions of each of the Rs, the card will feature questions to ask yourself before, during, and after every interaction to aid in attaining cultural humility.
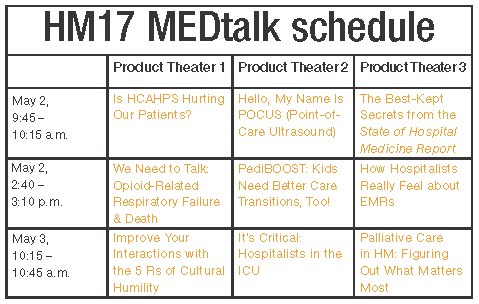
The card will be printed and disseminated at Hospital Medicine 2017, and the 5 Rs will be discussed in a few sessions: “Making ‘Everything We Say and Do’ a Positive Patient Experience” in the Practice Management track on Thursday, May 4, and during a 20-minute “MEDtalk” in Product Theater 1 on May 3, at 10:15 a.m.
Keep on the lookout for future blog posts, where you’ll read about the 5 R’s in action through vignettes and a deeper dive into each aspect.
For more information and the downloadable pocket card, visit www.hospitalmedicine.org/5Rs.
Dr. Ansari is associate professor and associate division director of hospital medicine at Loyola University Medical Center, Maywood, Ill., and serves on SHM’s Cultural Humility Work Group.
How do we, as hospitalists, win the hearts and minds of patients, families, and care team members whom we do not know? What are the obstacles that we face when encountering patients and gaining the trust needed to improve patient care and patient experience?
With these questions in mind, the Cultural Humility Work Group, part of SHM’s Practice Management Committee, set out to develop a simple, universal framework to provide a foundation for strengthening communication skills and raising awareness of the basic tenets of cultural humility. According to Tervalon and Murray-Garcia, cultural humility is defined as a “process that requires humility as individuals continually engage in self-reflection and self-critique as lifelong learners and reflective practitioners. It requires humility in how physicians bring into check the power imbalances that exist in the dynamics of physician-patient communication by using patient-focused interviewing and care, and it is a process that requires humility to develop and maintain mutually respectful and dynamic partnerships with communities” (Tervalon, M. & Murray-García, J. “Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education.” J Health Care Poor Underserved. 1998;9[2]:117-25).
How do we win this battle? The first step is to simply be aware that everyone is a victim of unconscious biases. Once we come to this (often uncomfortable) realization, we must make a conscious effort to change our mindset and make conscious decisions to not allow these biases to manifest.
Practicing cultural humility is extremely important in this process. It puts everyone on the same platform because there is no “minority,” “majority,” or “ethnicity” associated with it. It takes away the need to know everything about a certain culture and encourages us to approach every patient encounter acknowledging that we will humble ourselves, learn what is important to the patient, and leave having learned something from the interaction.
The work group developed “The 5 Rs of Cultural Humility” as a simple tool for hospitalists to incorporate into their practice. The first four Rs (Reflection, Respect, Regard and Relevance) are extrinsically focused, while the 5th R (Resiliency) is intrinsic. Our theory posits that, if you attain the first 4 Rs in every interaction, these will serve to build on and develop your own personal resiliency. Here are the 5 Rs:
- Reflection – Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Respect – Hospitalists will treat every person with the utmost respect and strive to preserve dignity at all times.
- Regard – Hospitalists will hold every person in their highest regard while being aware of and not allowing unconscious biases to interfere in any interactions.
- Relevance – Hospitalists will expect cultural humility to be relevant to the patient and apply this practice to every encounter.
- Resiliency – Hospitalists will embody the practice of cultural humility to enhance personal resilience and globally focused compassion.
The content will be available as a downloadable pocket card that can be easily referenced on rounds and shared with colleagues. Our hope is to achieve heightened awareness of effective interaction. In addition to the definitions of each of the Rs, the card will feature questions to ask yourself before, during, and after every interaction to aid in attaining cultural humility.
The card will be printed and disseminated at Hospital Medicine 2017, and the 5 Rs will be discussed in a few sessions: “Making ‘Everything We Say and Do’ a Positive Patient Experience” in the Practice Management track on Thursday, May 4, and during a 20-minute “MEDtalk” in Product Theater 1 on May 3, at 10:15 a.m.
Keep on the lookout for future blog posts, where you’ll read about the 5 R’s in action through vignettes and a deeper dive into each aspect.
For more information and the downloadable pocket card, visit www.hospitalmedicine.org/5Rs.
Dr. Ansari is associate professor and associate division director of hospital medicine at Loyola University Medical Center, Maywood, Ill., and serves on SHM’s Cultural Humility Work Group.
How do we, as hospitalists, win the hearts and minds of patients, families, and care team members whom we do not know? What are the obstacles that we face when encountering patients and gaining the trust needed to improve patient care and patient experience?
With these questions in mind, the Cultural Humility Work Group, part of SHM’s Practice Management Committee, set out to develop a simple, universal framework to provide a foundation for strengthening communication skills and raising awareness of the basic tenets of cultural humility. According to Tervalon and Murray-Garcia, cultural humility is defined as a “process that requires humility as individuals continually engage in self-reflection and self-critique as lifelong learners and reflective practitioners. It requires humility in how physicians bring into check the power imbalances that exist in the dynamics of physician-patient communication by using patient-focused interviewing and care, and it is a process that requires humility to develop and maintain mutually respectful and dynamic partnerships with communities” (Tervalon, M. & Murray-García, J. “Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education.” J Health Care Poor Underserved. 1998;9[2]:117-25).
How do we win this battle? The first step is to simply be aware that everyone is a victim of unconscious biases. Once we come to this (often uncomfortable) realization, we must make a conscious effort to change our mindset and make conscious decisions to not allow these biases to manifest.
Practicing cultural humility is extremely important in this process. It puts everyone on the same platform because there is no “minority,” “majority,” or “ethnicity” associated with it. It takes away the need to know everything about a certain culture and encourages us to approach every patient encounter acknowledging that we will humble ourselves, learn what is important to the patient, and leave having learned something from the interaction.
The work group developed “The 5 Rs of Cultural Humility” as a simple tool for hospitalists to incorporate into their practice. The first four Rs (Reflection, Respect, Regard and Relevance) are extrinsically focused, while the 5th R (Resiliency) is intrinsic. Our theory posits that, if you attain the first 4 Rs in every interaction, these will serve to build on and develop your own personal resiliency. Here are the 5 Rs:
- Reflection – Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Respect – Hospitalists will treat every person with the utmost respect and strive to preserve dignity at all times.
- Regard – Hospitalists will hold every person in their highest regard while being aware of and not allowing unconscious biases to interfere in any interactions.
- Relevance – Hospitalists will expect cultural humility to be relevant to the patient and apply this practice to every encounter.
- Resiliency – Hospitalists will embody the practice of cultural humility to enhance personal resilience and globally focused compassion.
The content will be available as a downloadable pocket card that can be easily referenced on rounds and shared with colleagues. Our hope is to achieve heightened awareness of effective interaction. In addition to the definitions of each of the Rs, the card will feature questions to ask yourself before, during, and after every interaction to aid in attaining cultural humility.
The card will be printed and disseminated at Hospital Medicine 2017, and the 5 Rs will be discussed in a few sessions: “Making ‘Everything We Say and Do’ a Positive Patient Experience” in the Practice Management track on Thursday, May 4, and during a 20-minute “MEDtalk” in Product Theater 1 on May 3, at 10:15 a.m.
Keep on the lookout for future blog posts, where you’ll read about the 5 R’s in action through vignettes and a deeper dive into each aspect.
For more information and the downloadable pocket card, visit www.hospitalmedicine.org/5Rs.
Dr. Ansari is associate professor and associate division director of hospital medicine at Loyola University Medical Center, Maywood, Ill., and serves on SHM’s Cultural Humility Work Group.
Guideline for reversal of antithrombotics in intracranial hemorrhage
Clinical Question: What is the current guideline for reversal of antithrombotics in intracranial hemorrhage (ICH)?
Background: Antithrombotics are used to treat or decrease the risk of thromboembolic events, and the use is expected to rise in the future because of an aging population and conditions such as atrial fibrillation. Patients on antithrombotics who experience spontaneous ICH have a higher risk of death or poor outcome, compared with those who are not. Rapid reversal of coagulopathy may help to improve outcomes.
Study design: A 13-person, multi-institutional, international committee with expertise in relevant medical fields reviewed a total of 488 articles to develop guidelines and treatment recommendations.
Synopsis: The committee developed guidelines for the reversal of antithrombotics after reviewing a total of 488 articles up through November 2015. The quality of evidence and treatment recommendations were drafted based on the GRADE system, as follows:
• Vitamin K antagonists: If international normalized ratio is greater than or equal to 1.4, administer vitamin K 10 mg IV, plus 3-4 factor prothrombin complex concentrate (PCC) or fresh frozen plasma.
• Direct factor Xa inhibitors: activated charcoal within 2 hr of ingestion, activated PCC or 4 factor PCC.
• Direct thrombin inhibitors – Dabigatran: activated charcoal within 2 hr of ingestion and Idarucizumab. Consider hemodialysis. Other DTIs: activated PCC or 4 factor PCC.
• Unfractionated heparin: protamine IV.
• Low-molecular-weight heparins – Enoxaparin: protamine IV, dose based on time of enoxaparin administration. Dalteparin/nadroparin/tinzaparin: protamine IV or recombinant factor (rF)VIIa.
• Danaparoid: rFVIIa.
• Pentasaccharides: activated PCC.
• Thrombolytic agents: cryoprecipitate 10 units or antifibrinolytics.
• Antiplatelet agents: desmopressin 0.4 mcg or platelet transfusion in neurosurgical procedure.
Bottom Line: This is a statement of the guideline for reversal of antithrombotics in intracranial hemorrhage from the Neurocritical Care Society and the Society of Critical Care Medicine.
Citation: Frontera J, Lewin JJ, Rabinstein AA, et al. “Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine.” Neurocrit Care. 2016 Feb;24(1):6-46.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical Question: What is the current guideline for reversal of antithrombotics in intracranial hemorrhage (ICH)?
Background: Antithrombotics are used to treat or decrease the risk of thromboembolic events, and the use is expected to rise in the future because of an aging population and conditions such as atrial fibrillation. Patients on antithrombotics who experience spontaneous ICH have a higher risk of death or poor outcome, compared with those who are not. Rapid reversal of coagulopathy may help to improve outcomes.
Study design: A 13-person, multi-institutional, international committee with expertise in relevant medical fields reviewed a total of 488 articles to develop guidelines and treatment recommendations.
Synopsis: The committee developed guidelines for the reversal of antithrombotics after reviewing a total of 488 articles up through November 2015. The quality of evidence and treatment recommendations were drafted based on the GRADE system, as follows:
• Vitamin K antagonists: If international normalized ratio is greater than or equal to 1.4, administer vitamin K 10 mg IV, plus 3-4 factor prothrombin complex concentrate (PCC) or fresh frozen plasma.
• Direct factor Xa inhibitors: activated charcoal within 2 hr of ingestion, activated PCC or 4 factor PCC.
• Direct thrombin inhibitors – Dabigatran: activated charcoal within 2 hr of ingestion and Idarucizumab. Consider hemodialysis. Other DTIs: activated PCC or 4 factor PCC.
• Unfractionated heparin: protamine IV.
• Low-molecular-weight heparins – Enoxaparin: protamine IV, dose based on time of enoxaparin administration. Dalteparin/nadroparin/tinzaparin: protamine IV or recombinant factor (rF)VIIa.
• Danaparoid: rFVIIa.
• Pentasaccharides: activated PCC.
• Thrombolytic agents: cryoprecipitate 10 units or antifibrinolytics.
• Antiplatelet agents: desmopressin 0.4 mcg or platelet transfusion in neurosurgical procedure.
Bottom Line: This is a statement of the guideline for reversal of antithrombotics in intracranial hemorrhage from the Neurocritical Care Society and the Society of Critical Care Medicine.
Citation: Frontera J, Lewin JJ, Rabinstein AA, et al. “Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine.” Neurocrit Care. 2016 Feb;24(1):6-46.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical Question: What is the current guideline for reversal of antithrombotics in intracranial hemorrhage (ICH)?
Background: Antithrombotics are used to treat or decrease the risk of thromboembolic events, and the use is expected to rise in the future because of an aging population and conditions such as atrial fibrillation. Patients on antithrombotics who experience spontaneous ICH have a higher risk of death or poor outcome, compared with those who are not. Rapid reversal of coagulopathy may help to improve outcomes.
Study design: A 13-person, multi-institutional, international committee with expertise in relevant medical fields reviewed a total of 488 articles to develop guidelines and treatment recommendations.
Synopsis: The committee developed guidelines for the reversal of antithrombotics after reviewing a total of 488 articles up through November 2015. The quality of evidence and treatment recommendations were drafted based on the GRADE system, as follows:
• Vitamin K antagonists: If international normalized ratio is greater than or equal to 1.4, administer vitamin K 10 mg IV, plus 3-4 factor prothrombin complex concentrate (PCC) or fresh frozen plasma.
• Direct factor Xa inhibitors: activated charcoal within 2 hr of ingestion, activated PCC or 4 factor PCC.
• Direct thrombin inhibitors – Dabigatran: activated charcoal within 2 hr of ingestion and Idarucizumab. Consider hemodialysis. Other DTIs: activated PCC or 4 factor PCC.
• Unfractionated heparin: protamine IV.
• Low-molecular-weight heparins – Enoxaparin: protamine IV, dose based on time of enoxaparin administration. Dalteparin/nadroparin/tinzaparin: protamine IV or recombinant factor (rF)VIIa.
• Danaparoid: rFVIIa.
• Pentasaccharides: activated PCC.
• Thrombolytic agents: cryoprecipitate 10 units or antifibrinolytics.
• Antiplatelet agents: desmopressin 0.4 mcg or platelet transfusion in neurosurgical procedure.
Bottom Line: This is a statement of the guideline for reversal of antithrombotics in intracranial hemorrhage from the Neurocritical Care Society and the Society of Critical Care Medicine.
Citation: Frontera J, Lewin JJ, Rabinstein AA, et al. “Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine.” Neurocrit Care. 2016 Feb;24(1):6-46.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Everything We Say and Do: Hospitalists are leaders in designing inpatient experience
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively affect patients’ experience of care. This column highlights key takeaways from the SHM track of the upcoming 2017 Cleveland Clinic Patient Experience Empathy and Innovation Summit, May 22-24. Three hospitalist leaders describe their approach to leading the design of the inpatient experience.
What we say and do, and why
Like many forms of care improvement, we have found that health care providers and patients alike engage most proactively when they are directly involved in codesigning an approach or intervention for improving the experience of care. Here are some examples of how hospitalists can be effective leaders in cocreating the inpatient experience with patients and interdisciplinary colleagues.
Dr. Sliwka is medical director of patient and provider experience at University of California, San Francisco, Health; Dr. Kneeland is medical director for patient and provider experience at University of Colorado, Aurora, Hospital; Dr. Hoffman is medical director for patient relations at University of Wisconsin-Madison, Health.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively affect patients’ experience of care. This column highlights key takeaways from the SHM track of the upcoming 2017 Cleveland Clinic Patient Experience Empathy and Innovation Summit, May 22-24. Three hospitalist leaders describe their approach to leading the design of the inpatient experience.
What we say and do, and why
Like many forms of care improvement, we have found that health care providers and patients alike engage most proactively when they are directly involved in codesigning an approach or intervention for improving the experience of care. Here are some examples of how hospitalists can be effective leaders in cocreating the inpatient experience with patients and interdisciplinary colleagues.
Dr. Sliwka is medical director of patient and provider experience at University of California, San Francisco, Health; Dr. Kneeland is medical director for patient and provider experience at University of Colorado, Aurora, Hospital; Dr. Hoffman is medical director for patient relations at University of Wisconsin-Madison, Health.
Editor’s note: “Everything We Say and Do” is an informational series developed by SHM’s Patient Experience Committee to provide readers with thoughtful and actionable communication tactics that have great potential to positively affect patients’ experience of care. This column highlights key takeaways from the SHM track of the upcoming 2017 Cleveland Clinic Patient Experience Empathy and Innovation Summit, May 22-24. Three hospitalist leaders describe their approach to leading the design of the inpatient experience.
What we say and do, and why
Like many forms of care improvement, we have found that health care providers and patients alike engage most proactively when they are directly involved in codesigning an approach or intervention for improving the experience of care. Here are some examples of how hospitalists can be effective leaders in cocreating the inpatient experience with patients and interdisciplinary colleagues.
Dr. Sliwka is medical director of patient and provider experience at University of California, San Francisco, Health; Dr. Kneeland is medical director for patient and provider experience at University of Colorado, Aurora, Hospital; Dr. Hoffman is medical director for patient relations at University of Wisconsin-Madison, Health.
Elimination of urine culture screening prior to elective joint arthroplasty
Clinical question: What is the clinical impact of implementing a policy to no longer process urine specimens for perioperative screening in patients undergoing elective joint arthroplasty (EJA)?
Background: Despite prior studies indicating the lack of clinical benefit, preoperative urine cultures are still frequently obtained in patients undergoing EJA in attempts to reduce the risk of periprosthetic joint infections (PJI).
Study Design: Time series analysis.
Setting: Holland Orthopedic and Arthritic Center (HOAC) of Sunnybrook Health Sciences Centre.
Synopsis: After a multidisciplinary meeting, obtaining routine urine culture screening was removed from the preoperative order set. A time series analysis was performed to review the frequency of screening urine cultures obtained and processed, the number of patients treated for asymptomatic bacteriuria (ASB), and the incidence of PJI before and after the new policy was implemented. After the policy change, only 129 screening urine cultures were obtained prior to 1,891 EJAs (7 per 100 EJA; 95% CI 6-8; P less than .0001) which is a drastic decrease from the 3,069 screening urine cultures obtained prior to 3,523 EJAs (87 per 100 EJA; 95% CI, 86-88) before the policy change. Prior to the policy change, of the 352 positive urine cultures, 43 received perioperative treatment for ASB, and PJI incidence was 1/3523 (0.03%; 95% CI, 0.001-02). After the policy change, no perioperative antibiotics were prescribed for ASB, and PJI rate did not significantly change at 3/1891 (0.2%; 95% CI, 0.05-0.5; P = .1).
The study was limited by its low power to detect for small differences in rates because of its small PJI rate occurrence.
Bottom Line: A multidisciplinary approach in eliminating routine urine screening prior to EJA resulted in a decrease of urine cultures obtained and a decrease in treatment for asymptomatic bacteriuria, with no significant change in PJI rate. This change in clinical practice is supported by current evidence and has a significant impact on cost savings.
References: Lamb MJ, Baillie L, Pajak D, et al. “Elimination of Screening Urine Cultures Prior to Elective Joint Arthroplasty.”
Dr. Libot is assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical question: What is the clinical impact of implementing a policy to no longer process urine specimens for perioperative screening in patients undergoing elective joint arthroplasty (EJA)?
Background: Despite prior studies indicating the lack of clinical benefit, preoperative urine cultures are still frequently obtained in patients undergoing EJA in attempts to reduce the risk of periprosthetic joint infections (PJI).
Study Design: Time series analysis.
Setting: Holland Orthopedic and Arthritic Center (HOAC) of Sunnybrook Health Sciences Centre.
Synopsis: After a multidisciplinary meeting, obtaining routine urine culture screening was removed from the preoperative order set. A time series analysis was performed to review the frequency of screening urine cultures obtained and processed, the number of patients treated for asymptomatic bacteriuria (ASB), and the incidence of PJI before and after the new policy was implemented. After the policy change, only 129 screening urine cultures were obtained prior to 1,891 EJAs (7 per 100 EJA; 95% CI 6-8; P less than .0001) which is a drastic decrease from the 3,069 screening urine cultures obtained prior to 3,523 EJAs (87 per 100 EJA; 95% CI, 86-88) before the policy change. Prior to the policy change, of the 352 positive urine cultures, 43 received perioperative treatment for ASB, and PJI incidence was 1/3523 (0.03%; 95% CI, 0.001-02). After the policy change, no perioperative antibiotics were prescribed for ASB, and PJI rate did not significantly change at 3/1891 (0.2%; 95% CI, 0.05-0.5; P = .1).
The study was limited by its low power to detect for small differences in rates because of its small PJI rate occurrence.
Bottom Line: A multidisciplinary approach in eliminating routine urine screening prior to EJA resulted in a decrease of urine cultures obtained and a decrease in treatment for asymptomatic bacteriuria, with no significant change in PJI rate. This change in clinical practice is supported by current evidence and has a significant impact on cost savings.
References: Lamb MJ, Baillie L, Pajak D, et al. “Elimination of Screening Urine Cultures Prior to Elective Joint Arthroplasty.”
Dr. Libot is assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical question: What is the clinical impact of implementing a policy to no longer process urine specimens for perioperative screening in patients undergoing elective joint arthroplasty (EJA)?
Background: Despite prior studies indicating the lack of clinical benefit, preoperative urine cultures are still frequently obtained in patients undergoing EJA in attempts to reduce the risk of periprosthetic joint infections (PJI).
Study Design: Time series analysis.
Setting: Holland Orthopedic and Arthritic Center (HOAC) of Sunnybrook Health Sciences Centre.
Synopsis: After a multidisciplinary meeting, obtaining routine urine culture screening was removed from the preoperative order set. A time series analysis was performed to review the frequency of screening urine cultures obtained and processed, the number of patients treated for asymptomatic bacteriuria (ASB), and the incidence of PJI before and after the new policy was implemented. After the policy change, only 129 screening urine cultures were obtained prior to 1,891 EJAs (7 per 100 EJA; 95% CI 6-8; P less than .0001) which is a drastic decrease from the 3,069 screening urine cultures obtained prior to 3,523 EJAs (87 per 100 EJA; 95% CI, 86-88) before the policy change. Prior to the policy change, of the 352 positive urine cultures, 43 received perioperative treatment for ASB, and PJI incidence was 1/3523 (0.03%; 95% CI, 0.001-02). After the policy change, no perioperative antibiotics were prescribed for ASB, and PJI rate did not significantly change at 3/1891 (0.2%; 95% CI, 0.05-0.5; P = .1).
The study was limited by its low power to detect for small differences in rates because of its small PJI rate occurrence.
Bottom Line: A multidisciplinary approach in eliminating routine urine screening prior to EJA resulted in a decrease of urine cultures obtained and a decrease in treatment for asymptomatic bacteriuria, with no significant change in PJI rate. This change in clinical practice is supported by current evidence and has a significant impact on cost savings.
References: Lamb MJ, Baillie L, Pajak D, et al. “Elimination of Screening Urine Cultures Prior to Elective Joint Arthroplasty.”
Dr. Libot is assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
In the lit: Short takes
Efficacy of ketorolac is similar at all the most commonly administered doses
A randomized, double-blind trial of IV ketorolac dosing found similar analgesic efficacy in patients aged 18-65 years with moderate to severe pain at the commonly ordered doses of 10 mg, 15 mg, and 30 mg with no increase in adverse effects.
Citation: Motov S, Yasavolian M, Likourezos A, et al. “Comparison of intravenous ketorolac at three single-dose regimens for treating acute pain in the emergency department: A randomized controlled trial.” Ann Emerg Med. 2016 Dec 16. doi: org/10.1016/j.annemergmed.2016.10.014.
-- Paula Marfia, MD, is assistant professor in the Division of Hospital Medicine, Loyola University Chicago, Maywood, Ill.
Viruses are common cause of nonventilated, hospital-acquired pneumonia
Retrospective analysis demonstrates that viruses are common etiology for nonventilated hospital-acquired pneumonia (NVHAP), as common as bacterial organisms. Clinicians should consider testing for viral etiologies in NVHAP in an effort to improve antibiotic stewardship.
Citation: Shorr AF, Zilberberg MD, Micek ST, Kollef MH. “Viruses are prevalent in non-ventilated hospital-acquired pneumonia.” Respir Med. 2017;122:76-80.
-- Anar Mashruwala, MD, FACP, is assistant professor in the Department of Medicine, Division of Hospital Medicine at Loyola University Medical Center, Maywood, Ill.
FDA issues important safety precautions for use of implantable infusions pumps in MRI
Serious adverse events, including patient injury and death, have been reported with the use of implantable infusion pumps in the MRI environment. The Food and Drug Administration has issued a safety communication for patients, caregivers, health care providers, and MRI technologists, outlining safety precautions and recommendations.
Citation: “Implantable Infusion Pumps in the Magnetic Resonance (MR) Environment: FDA Safety Communication – Important Safety Precautions.” FDA.gov. 2017 Jan 11.
-- Anar Mashruwala, MD, FACP, is assistant professor in the Department of Medicine, Division of Hospital Medicine at Loyola University Medical Center, Maywood, Ill.
Efficacy of ketorolac is similar at all the most commonly administered doses
A randomized, double-blind trial of IV ketorolac dosing found similar analgesic efficacy in patients aged 18-65 years with moderate to severe pain at the commonly ordered doses of 10 mg, 15 mg, and 30 mg with no increase in adverse effects.
Citation: Motov S, Yasavolian M, Likourezos A, et al. “Comparison of intravenous ketorolac at three single-dose regimens for treating acute pain in the emergency department: A randomized controlled trial.” Ann Emerg Med. 2016 Dec 16. doi: org/10.1016/j.annemergmed.2016.10.014.
-- Paula Marfia, MD, is assistant professor in the Division of Hospital Medicine, Loyola University Chicago, Maywood, Ill.
Viruses are common cause of nonventilated, hospital-acquired pneumonia
Retrospective analysis demonstrates that viruses are common etiology for nonventilated hospital-acquired pneumonia (NVHAP), as common as bacterial organisms. Clinicians should consider testing for viral etiologies in NVHAP in an effort to improve antibiotic stewardship.
Citation: Shorr AF, Zilberberg MD, Micek ST, Kollef MH. “Viruses are prevalent in non-ventilated hospital-acquired pneumonia.” Respir Med. 2017;122:76-80.
-- Anar Mashruwala, MD, FACP, is assistant professor in the Department of Medicine, Division of Hospital Medicine at Loyola University Medical Center, Maywood, Ill.
FDA issues important safety precautions for use of implantable infusions pumps in MRI
Serious adverse events, including patient injury and death, have been reported with the use of implantable infusion pumps in the MRI environment. The Food and Drug Administration has issued a safety communication for patients, caregivers, health care providers, and MRI technologists, outlining safety precautions and recommendations.
Citation: “Implantable Infusion Pumps in the Magnetic Resonance (MR) Environment: FDA Safety Communication – Important Safety Precautions.” FDA.gov. 2017 Jan 11.
-- Anar Mashruwala, MD, FACP, is assistant professor in the Department of Medicine, Division of Hospital Medicine at Loyola University Medical Center, Maywood, Ill.
Efficacy of ketorolac is similar at all the most commonly administered doses
A randomized, double-blind trial of IV ketorolac dosing found similar analgesic efficacy in patients aged 18-65 years with moderate to severe pain at the commonly ordered doses of 10 mg, 15 mg, and 30 mg with no increase in adverse effects.
Citation: Motov S, Yasavolian M, Likourezos A, et al. “Comparison of intravenous ketorolac at three single-dose regimens for treating acute pain in the emergency department: A randomized controlled trial.” Ann Emerg Med. 2016 Dec 16. doi: org/10.1016/j.annemergmed.2016.10.014.
-- Paula Marfia, MD, is assistant professor in the Division of Hospital Medicine, Loyola University Chicago, Maywood, Ill.
Viruses are common cause of nonventilated, hospital-acquired pneumonia
Retrospective analysis demonstrates that viruses are common etiology for nonventilated hospital-acquired pneumonia (NVHAP), as common as bacterial organisms. Clinicians should consider testing for viral etiologies in NVHAP in an effort to improve antibiotic stewardship.
Citation: Shorr AF, Zilberberg MD, Micek ST, Kollef MH. “Viruses are prevalent in non-ventilated hospital-acquired pneumonia.” Respir Med. 2017;122:76-80.
-- Anar Mashruwala, MD, FACP, is assistant professor in the Department of Medicine, Division of Hospital Medicine at Loyola University Medical Center, Maywood, Ill.
FDA issues important safety precautions for use of implantable infusions pumps in MRI
Serious adverse events, including patient injury and death, have been reported with the use of implantable infusion pumps in the MRI environment. The Food and Drug Administration has issued a safety communication for patients, caregivers, health care providers, and MRI technologists, outlining safety precautions and recommendations.
Citation: “Implantable Infusion Pumps in the Magnetic Resonance (MR) Environment: FDA Safety Communication – Important Safety Precautions.” FDA.gov. 2017 Jan 11.
-- Anar Mashruwala, MD, FACP, is assistant professor in the Department of Medicine, Division of Hospital Medicine at Loyola University Medical Center, Maywood, Ill.
Risks are reduced when angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers are held before noncardiac surgery
Clinical question: Is withholding angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers (ARBs) prior to noncardiac surgery associated with a lower risk of a 30-day composite outcome of all-cause death, myocardial injury after noncardiac surgery, and stroke when compared with continuing them on the day of surgery?
Background: The current American College of Cardiology/American Heart Association guidelines recommend continuing ACEI and ARBs for noncardiac surgery. However, many clinicians, including anesthesiologists, withhold these medications to prevent intraoperative hypotension. Because of the lack of strong evidence regarding clinical outcomes, the decision to withhold ACEI and ARBs prior to noncardiac surgery is currently dictated by physician preference and local policy.
Study Design: Prospective cohort study.
Setting: Analysis sample from the VISION study (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation), which included 12 centers in eight countries.
Synopsis: A sample analysis was performed on 14,687 patients from the VISION study, who were at least 45 years old and undergoing noncardiac surgery and who required an overnight hospital admission. A total of 4,802 patients were taking ACEI/ARBs at baseline, and, for 1,245 (25.9%) of those patients, ACEI/ARBs were withheld at least 24 hours before surgery. Using multivariable regression models, the authors found that patients for whom ACEI/ARBs were withheld were less likely to suffer from the primary composite outcome of 30-day all-cause death, myocardial injury after noncardiac surgery, and stroke (12% vs 12.9%; adjusted relative risk, 0.82; 95% confidence interval, 0.7-0.96; P = .01). Withholding ACEI/ARBs prior to surgery was also associated with less risk of clinically important intraoperative hypotension, while the risk of postoperative hypotension was similar between the two groups.
Given that this was an observational study, analysis is limited because of the inability to account for every potential confounding factor.
Bottom Line: The study suggests a lower risk of postoperative death, stroke, and myocardial injury in patients for whom ACEI/ARBs were withheld prior to noncardiac surgery. A large randomized trial is needed to confirm the findings suggested by this analysis.
Citation: Roshanov PS, Rochwerg B, Patel A, et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery.” Anesthesiology. 2017 Jan;126(1):16-27.
Dr. Libot is assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical question: Is withholding angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers (ARBs) prior to noncardiac surgery associated with a lower risk of a 30-day composite outcome of all-cause death, myocardial injury after noncardiac surgery, and stroke when compared with continuing them on the day of surgery?
Background: The current American College of Cardiology/American Heart Association guidelines recommend continuing ACEI and ARBs for noncardiac surgery. However, many clinicians, including anesthesiologists, withhold these medications to prevent intraoperative hypotension. Because of the lack of strong evidence regarding clinical outcomes, the decision to withhold ACEI and ARBs prior to noncardiac surgery is currently dictated by physician preference and local policy.
Study Design: Prospective cohort study.
Setting: Analysis sample from the VISION study (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation), which included 12 centers in eight countries.
Synopsis: A sample analysis was performed on 14,687 patients from the VISION study, who were at least 45 years old and undergoing noncardiac surgery and who required an overnight hospital admission. A total of 4,802 patients were taking ACEI/ARBs at baseline, and, for 1,245 (25.9%) of those patients, ACEI/ARBs were withheld at least 24 hours before surgery. Using multivariable regression models, the authors found that patients for whom ACEI/ARBs were withheld were less likely to suffer from the primary composite outcome of 30-day all-cause death, myocardial injury after noncardiac surgery, and stroke (12% vs 12.9%; adjusted relative risk, 0.82; 95% confidence interval, 0.7-0.96; P = .01). Withholding ACEI/ARBs prior to surgery was also associated with less risk of clinically important intraoperative hypotension, while the risk of postoperative hypotension was similar between the two groups.
Given that this was an observational study, analysis is limited because of the inability to account for every potential confounding factor.
Bottom Line: The study suggests a lower risk of postoperative death, stroke, and myocardial injury in patients for whom ACEI/ARBs were withheld prior to noncardiac surgery. A large randomized trial is needed to confirm the findings suggested by this analysis.
Citation: Roshanov PS, Rochwerg B, Patel A, et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery.” Anesthesiology. 2017 Jan;126(1):16-27.
Dr. Libot is assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical question: Is withholding angiotensin-converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers (ARBs) prior to noncardiac surgery associated with a lower risk of a 30-day composite outcome of all-cause death, myocardial injury after noncardiac surgery, and stroke when compared with continuing them on the day of surgery?
Background: The current American College of Cardiology/American Heart Association guidelines recommend continuing ACEI and ARBs for noncardiac surgery. However, many clinicians, including anesthesiologists, withhold these medications to prevent intraoperative hypotension. Because of the lack of strong evidence regarding clinical outcomes, the decision to withhold ACEI and ARBs prior to noncardiac surgery is currently dictated by physician preference and local policy.
Study Design: Prospective cohort study.
Setting: Analysis sample from the VISION study (Vascular Events in Noncardiac Surgery Patients Cohort Evaluation), which included 12 centers in eight countries.
Synopsis: A sample analysis was performed on 14,687 patients from the VISION study, who were at least 45 years old and undergoing noncardiac surgery and who required an overnight hospital admission. A total of 4,802 patients were taking ACEI/ARBs at baseline, and, for 1,245 (25.9%) of those patients, ACEI/ARBs were withheld at least 24 hours before surgery. Using multivariable regression models, the authors found that patients for whom ACEI/ARBs were withheld were less likely to suffer from the primary composite outcome of 30-day all-cause death, myocardial injury after noncardiac surgery, and stroke (12% vs 12.9%; adjusted relative risk, 0.82; 95% confidence interval, 0.7-0.96; P = .01). Withholding ACEI/ARBs prior to surgery was also associated with less risk of clinically important intraoperative hypotension, while the risk of postoperative hypotension was similar between the two groups.
Given that this was an observational study, analysis is limited because of the inability to account for every potential confounding factor.
Bottom Line: The study suggests a lower risk of postoperative death, stroke, and myocardial injury in patients for whom ACEI/ARBs were withheld prior to noncardiac surgery. A large randomized trial is needed to confirm the findings suggested by this analysis.
Citation: Roshanov PS, Rochwerg B, Patel A, et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery.” Anesthesiology. 2017 Jan;126(1):16-27.
Dr. Libot is assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Survey insights: Unwrapping the compensation package
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
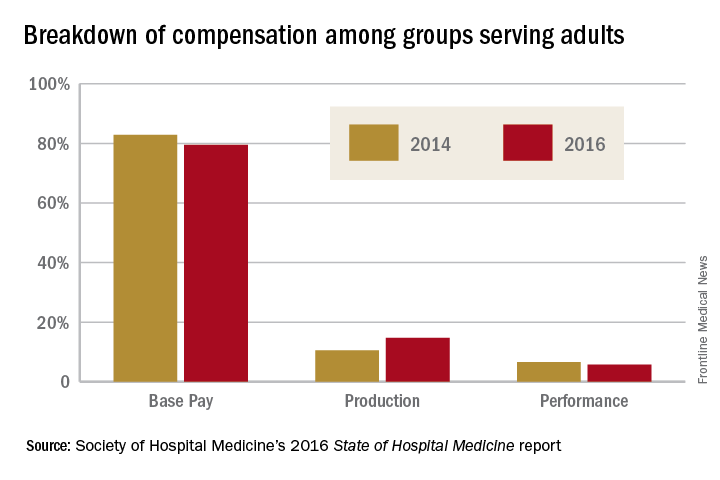
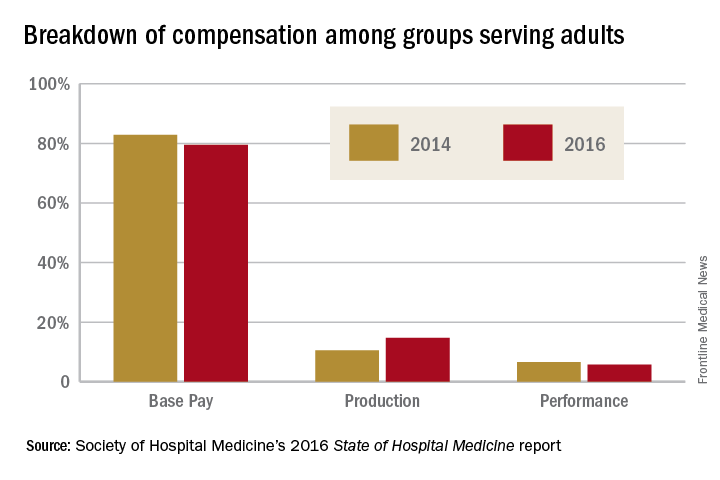
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
When approached for advice regarding the evaluation of job offers after completion of training, specific day-to-day duties (for example, shift length, teaching time, ICU coverage, and so on), and the overall gestalt of the interview experience, I find that location, lifestyle, and pay are the most consistent and common themes.
People often assume that pay is relatively straightforward, since it can be summarized in a number in the offer, whereas the other factors are harder to evaluate. However, it turns out pay is more complex. As a result, the last several State of Hospital Medicine reports have sought to evaluate compensation packages more thoroughly.
In 2016, the survey started including pay increases by years of experience, as well as CME dollars allotted per year per hospitalist. The goal was to gain deeper insight into the entire financial package, which is tied to a particular hospitalist job.
When looking at the 2014 and 2016 SHM survey results, there are several interesting findings. Base pay makes up the majority of earnings for all types of hospitalists (those seeing adults only, children only, and a mix of adults and children). In academic hospitalist groups, more of the total package of compensation comes from base pay, compared with nonacademic groups, where production and performance pay play a bigger role.
Of interest, despite the increased national attention on quality of care, productivity-based pay increased again (10.5%-14.7%), while performance-based pay (usually tied to quality and safety metrics) decreased (6.6%-5.7%) among groups serving adults. Consistent with prior trends for adults-only hospitalists, the Southern region of the country had the highest percentage of pay derived from productivity (18.8%), as well as of overall compensation in the 2016 report.
For hospitalists serving both adults and children, there was a smaller increase in pay derived from production (12.4%-13.2%), while pay derived from performance dropped more dramatically (8.9%-3.9%).
For hospitalists serving only children, the opposite occurred: Pay derived from production fell from 10.7% to 2.8%. While it is not yet clear why compensation, overall, is moving into closer alignment with productivity, rather than performance on quality and safety metrics, one hypothesis is that work relative value units used for calculating productivity are easier to tie to an individual hospitalist than are quality and safety outcomes.
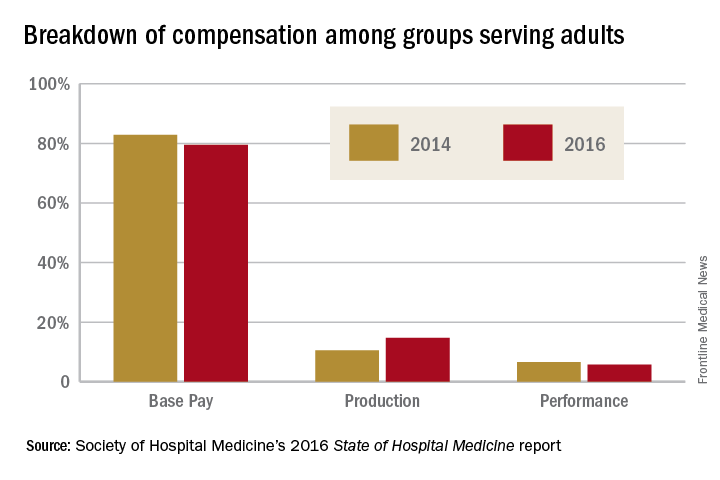
Employee benefits, as previously defined, increased among hospitalists caring for adults only and those caring for adults and children, with a mean increase in both groups of $5,000. The most generous benefits were typically seen at university-based academic medical centers. Amongst adult-only hospitalists, academic groups offer benefits worth $8,000-$9,000 more per year than in nonacademic groups. Lower benefits were common among practices in the Eastern region and in groups with four or fewer full-time hospitalists. The 2016 survey data on CME dollars revealed a median of $3,000-$4,000 per year, with higher amounts provided in nonacademic groups.
Paid time off (PTO) from work is an ongoing topic of interest on venues such as HMX forum, and, in the surveys, PTO remained fairly consistent among groups caring for adults only and those caring for adults and children, with only 30%-40% of groups offering PTO. The number of PTO hours offered vary substantially, however, ranging from a mean of 126 hours up to 216.4 hours annually. Future analysis of PTO will benefit from a deeper understanding of how many hours equate to a shift (the practical definition of a “day off” for most hospitalists).
Finally, the 2016 survey asked about automatic pay increases based strictly on overall experience or length of employment with the group. Roughly one-fifth to one-third of groups provided some sort of salary increase based on experience in 2015. This practice was more common in the Southern region and in nonteaching hospitals. These data raise the complex topic of seniority among hospitalists and how to define it: years since completing training, years with a particular hospital or group, academic rank, leadership roles, other? Further, if seniority is not recognized in pay, how commonly are groups recognizing it in other ways, such as in preferences related to time on certain services, shift type, or vacation requests?
The expanded survey on hospitalist pay, in addition to the biannual comparison of prior data, will likely continue to add value in assessing and exploring the entire package of compensation. Additional topics of interest moving forward might include better understanding of parental leave, sick time, and the comparison between compensation packages for physician hospitalists and those for inpatient Nurse Practitioners and Physician Assistants. Stay tuned for the next report.
Dr. Anoff is associate professor of clinical practice, division of hospital medicine, department of medicine, University of Colorado at Denver, Aurora.
References
1. (2014). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2014.
2. (2016). The State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine. Retrieved from www.hospitalmedicine.org/Survey2016.
MEDtalk presentations
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.
Is HCAHPS Hurting Our Patients?
Speakers: Suparna Dutta, MD, MS, MPH, and John Biebelhausen, MD, MBA
Explore the unintended consequences of assessing patient satisfaction and labeling pain as “the fifth vital sign” in the midst of a national opioid epidemic. The Hospital Consumer Assessment of Healthcare Providers and Systems, which was developed by the Centers for Medicare & Medicaid Services to assess the inpatient experience and impacts hospital reimbursement, includes directed questions about pain management.
Join us as we review the background of HCAHPS, its potential unintended impacts over the years, as well as current and future efforts of SHM toward improving health policy in this domain.
Hello, My Name Is POCUS (Point-of-Care Ultrasound)
Speaker: Nilam Soni, MD, MS, FHM
Point-of-care ultrasound is being used by more hospitalists to perform bedside diagnostics and to guide invasive procedures. However, most practicing hospitalists completed their training before point-of-care ultrasound education was common in medical school and residency curricula. This interactive session will:
- Explain what point-of-care ultrasonography is and how hospitalists are currently using it.
- Highlight some of the unique point-of-care ultrasound activities at HM17.
- Describe the launch of a new point-of-care ultrasound certification program offered by SHM & ACCP.
The Best-Kept Secrets from the State of Hospital Medicine Report
Speaker: Johnbuck Creamer, MD, SFHM
The State of Hospital Medicine Report is powered by SHM’s biannual survey that recently captured data from nearly 600 HM groups, augmented by additional hospitalist data licensed from MGMA. We’ll explore trends and difference among groups, including:
- Compensation per wRVU and use of nocturnists are increasing.
- Turnover rates are decreasing.
- Compensation for quality performance varies greatly among academic, nonacademic, and pediatric practice groups.
- NP/PA utilization rates are very different between East and West U.S. regions.
- Family Practice presence is increasing in adult-only practice groups.
- Academic groups are falling further behind in CPT coding levels.
We Need to Talk: Opioid-Related Respiratory Failure & Death
Speaker: Thomas Frederickson, MD, SFHM
Discussion topics:
- The opioid epidemic – not just an outpatient issue.
- How opioids can cause respiratory arrest and death, and why current screening and monitoring strategies can fail.
- What works – examples of successful strategies that have been implemented and have saved lives.
PediBOOST®: Kids Need Better Care Transitions, Too!
Speaker: James O’Callaghan, MD, SFHM
PediBOOST is a pediatric-specific adaption of the SHM Project BOOST® (Better Outcomes by Optimizing Safe Transitions) quality initiative. The goal is to improve poor discharge processes (demonstrated by low patient satisfaction and worse clinical outcomes, not just higher hospital readmission rates).
It considers unique problems for hospitalized children, including:
- Medication issues – palatability and adherence concerns, need for compounding.
- Equipment issues – portability use for home and school.
- Education issues – engagement of patient, as developmentally appropriate, along with training of all providers who might care for the patient (parents, teachers).
How Hospitalists Really Feel about EMRs
Speaker: Rupesh Prasad, MD, MPH, SFHM
Electronic medical record use has tremendously increased in the last few years.
- What are the potential benefits of use – have they been realized?
- What do the hospitalists think:
- How have EMRs impacted patient safety?
- How have EMRs impacted patient face to face time?
- What are hospitalists’ frustrations about EMRs?
Improve Your Interactions with the 5 Rs of Cultural Humility
Speaker: O’Neil Pyke, MD, SFHM
As the proverbial stranger at the bedside, HM providers are tasked with a very challenging proposition: meet a new patient in their most vulnerable state and quickly establish effective lines of communication and trust and provide patient-centric care, ultimately yielding a satisfied patient (and family) irrespective of the clinical outcome. With increased focus on patient experience and satisfaction, it is imperative that hospitals and health systems equip all hospitalists with the tools needed to deliver culturally competent care to all patients served.
The goal of the 5 Rs is to equip HM providers with tangible resources and easy to understand reminders that focus on encouraging awareness and, ultimately, deliver culturally “humble” care to all patients (and family members).
- Respect: Hospitalists will treat every person with the utmost respect and strive to preserve patient dignity.
- Regard: Hospitalists will hold every person in their highest regard and not allow unconscious biases to manifest, exercising utmost sensitivity to anticipated differences in beliefs, value systems, and preferences.
- Relevance: Hospitalists will expect cultural humility to be relevant and apply this practice to every encounter.
- Reflection: Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Resiliency: In order to provide better care for hospitalized patients, hospitalists will embody the practice of cultural humility to enhance personal resiliency and compassion for all.
It’s Critical: Hospitalists in the ICU
Speaker: Joseph Sweigart, MD
We hope to:
- Describe formation of purpose of the critical care task force within the Education Committee.
- Discuss the creation and execution of the SHM critical care survey.
- Present selected results including:
- Introduce strategies to address the practice gaps identified including:
Palliative Care in Hospital Medicine: Figuring Out What Matters Most
Speaker: Rab Razzak, MBBS, MD
We aim to:
- Discuss the overall definition of palliative care. It is for all seriously ill patients and focuses on human-centered care and quality of life, best provided early in an illness.
- Idea of primary palliative care and role of hospitalists. Most palliative care is provided by frontline clinicians, and hospitalists are optimally positioned to support seriously ill patients and their families. It is crucial for HM to involve palliative care specialists when needed.
- Effective communication about serious illness – words that work and how to operationalize human-centered care while honestly discussing serious illness.