User login
Gastric Bypass Tops Banding in Weight Loss
SAN DIEGO – Laparoscopic Roux-en-Y gastric bypass produced long-term weight loss results that were statistically superior to those of laparoscopic adjustable gastric banding, based on 10-years’ follow-up in a prospective randomized study.
Dr. Luigi Angrisani and his colleagues compared 10-year outcomes in 27 patients who underwent the Lap-Band via pars flaccida (group A) vs. those in 24 patients who underwent laparoscopic Roux-en-Y gastric bypass (group B) at San Giovanni Bosco Hospital, Naples, Italy, from January to November 2000.
Patients were included in the study if they had a body mass index (BMI) greater than 35 but less than 50 kg/m2, if they were older than age 19 years but younger than age 50, and if they lacked a hiatal hernia and had no previous abdominal surgery, Dr. Angrisani said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
At baseline, the mean age of patients was 34 years, their mean BMI was 44, their mean percentage of excess weight was 83%, and their mean weight was 118 kg.
Dr. Angrisani, who directs the general and laparoscopic surgery unit at San Giovanni Bosco Hospital, reported that the mean operative times were 60 minutes for group A and 220 minutes for group B (P greater than.001). There was no mortality, but five patients in group A and three in group B were lost to follow-up. The rate of reoperation was 41% in group A and 29% in group B.
After 10 years, the mean weight of patients in group A and B was 101 kg and 83 kg, respectively, their mean BMI was 37 vs. 30, and their mean loss of excess body weight was 46% vs. 69% (all P less than .05).
Reported compliance with the intake of multivitamins among patients in group B decreased over time. Compliance was 80% at 3 years, 66% at 5 years, 50% at 7 years, and just 33% at 10 years.
"Surgical complications in gastric bypass patients were life threatening, and long-term nutritional consequences remain to be defined, such as low compliance to vitamin supplementation," Dr. Angrisani said.
In his practice, potential candidates for gastric banding include "young and motivated" patients with a BMI of 40 or less; adolescents regardless of BMI; patients with BMI of 35 or less; high-risk patients, and those fearful of more-invasive procedures such as sleeve gastrectomy and Roux-en-Y gastric bypass.
Dr. Angrisani said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Laparoscopic Roux-en-Y gastric bypass produced long-term weight loss results that were statistically superior to those of laparoscopic adjustable gastric banding, based on 10-years’ follow-up in a prospective randomized study.
Dr. Luigi Angrisani and his colleagues compared 10-year outcomes in 27 patients who underwent the Lap-Band via pars flaccida (group A) vs. those in 24 patients who underwent laparoscopic Roux-en-Y gastric bypass (group B) at San Giovanni Bosco Hospital, Naples, Italy, from January to November 2000.
Patients were included in the study if they had a body mass index (BMI) greater than 35 but less than 50 kg/m2, if they were older than age 19 years but younger than age 50, and if they lacked a hiatal hernia and had no previous abdominal surgery, Dr. Angrisani said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
At baseline, the mean age of patients was 34 years, their mean BMI was 44, their mean percentage of excess weight was 83%, and their mean weight was 118 kg.
Dr. Angrisani, who directs the general and laparoscopic surgery unit at San Giovanni Bosco Hospital, reported that the mean operative times were 60 minutes for group A and 220 minutes for group B (P greater than.001). There was no mortality, but five patients in group A and three in group B were lost to follow-up. The rate of reoperation was 41% in group A and 29% in group B.
After 10 years, the mean weight of patients in group A and B was 101 kg and 83 kg, respectively, their mean BMI was 37 vs. 30, and their mean loss of excess body weight was 46% vs. 69% (all P less than .05).
Reported compliance with the intake of multivitamins among patients in group B decreased over time. Compliance was 80% at 3 years, 66% at 5 years, 50% at 7 years, and just 33% at 10 years.
"Surgical complications in gastric bypass patients were life threatening, and long-term nutritional consequences remain to be defined, such as low compliance to vitamin supplementation," Dr. Angrisani said.
In his practice, potential candidates for gastric banding include "young and motivated" patients with a BMI of 40 or less; adolescents regardless of BMI; patients with BMI of 35 or less; high-risk patients, and those fearful of more-invasive procedures such as sleeve gastrectomy and Roux-en-Y gastric bypass.
Dr. Angrisani said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Laparoscopic Roux-en-Y gastric bypass produced long-term weight loss results that were statistically superior to those of laparoscopic adjustable gastric banding, based on 10-years’ follow-up in a prospective randomized study.
Dr. Luigi Angrisani and his colleagues compared 10-year outcomes in 27 patients who underwent the Lap-Band via pars flaccida (group A) vs. those in 24 patients who underwent laparoscopic Roux-en-Y gastric bypass (group B) at San Giovanni Bosco Hospital, Naples, Italy, from January to November 2000.
Patients were included in the study if they had a body mass index (BMI) greater than 35 but less than 50 kg/m2, if they were older than age 19 years but younger than age 50, and if they lacked a hiatal hernia and had no previous abdominal surgery, Dr. Angrisani said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
At baseline, the mean age of patients was 34 years, their mean BMI was 44, their mean percentage of excess weight was 83%, and their mean weight was 118 kg.
Dr. Angrisani, who directs the general and laparoscopic surgery unit at San Giovanni Bosco Hospital, reported that the mean operative times were 60 minutes for group A and 220 minutes for group B (P greater than.001). There was no mortality, but five patients in group A and three in group B were lost to follow-up. The rate of reoperation was 41% in group A and 29% in group B.
After 10 years, the mean weight of patients in group A and B was 101 kg and 83 kg, respectively, their mean BMI was 37 vs. 30, and their mean loss of excess body weight was 46% vs. 69% (all P less than .05).
Reported compliance with the intake of multivitamins among patients in group B decreased over time. Compliance was 80% at 3 years, 66% at 5 years, 50% at 7 years, and just 33% at 10 years.
"Surgical complications in gastric bypass patients were life threatening, and long-term nutritional consequences remain to be defined, such as low compliance to vitamin supplementation," Dr. Angrisani said.
In his practice, potential candidates for gastric banding include "young and motivated" patients with a BMI of 40 or less; adolescents regardless of BMI; patients with BMI of 35 or less; high-risk patients, and those fearful of more-invasive procedures such as sleeve gastrectomy and Roux-en-Y gastric bypass.
Dr. Angrisani said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: At 10 years of follow-up, the mean weight among patients who underwent gastric banding was 101 kg, compared with 83 kg among those who underwent laparoscopic Roux-en-Y gastric bypass. In addition, their mean BMI was 37 vs. 30, respectively, and their mean loss of excess body weight was 46% vs. 69% (all P less than .05).
Data Source: This was a randomized, single-center study of 51 patients who underwent either procedure from January to November 2000.
Disclosures: Dr. Angrisani said that he had no relevant financial conflicts to disclose.
Reversal of Lap-Band to Sleeve Gastrectomy Feasible
SAN DIEGO – Laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy is a safe and feasible operation, results from a two-center study showed.
"Since the Lap-Band was introduced in the United States in 2001, it has been a popular minimally invasive procedure for weight loss," Dr. Abdelkader A. Hawasli said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "However, recent reports have shown that there’s an increased rate of explantation (up to 49%)" because of complications or failure to lose weight. Options are removal, reversion, or reversal to a nonphysiological procedure, "such as Roux-en-Y gastric bypass or biliopancreatic diversion. However, recent reports have been showing that sleeve gastrectomy could be a possible physiologic alternative."
For the current study, Dr. Hawasli, a surgeon at St. John Hospital and Medical Center in Detroit and Beaumont Hospital in Grosse Pointe, Mich., and his associates set out to evaluate the safety of the laparoscopic reversal of the Lap-Band to sleeve gastrectomy, the feasibility of performing simultaneous laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy, and the results of the sleeve gastrectomy after reversal as the final bariatric procedure in continuing or maintaining weight loss.
Dr. Hawasli reported on 485 patients who had undergone Lap-Band placement at St. John Hospital and Medical Center and 4 who had undergone the procedure at another institution from January 2004 to October 2011.
Of the 489 patients, 34 (7%) had reversal of the Lap-Band to sleeve gastrectomy. Of these, 20 patients (group 1) underwent reversal because of slippage in 15 cases, erosion in 3 cases, and infection in 2 cases, whereas 14 patients (group 2) underwent reversal because they were dissatisfied with their weight loss. The mean time of the reversal to sleeve gastrectomy was more than 3 years from Lap-Band insertion among the slippage subset patients in group 1 and among all patients in group 2 (36.5 vs. 43.3 months, respectively).
The majority of patients (32) underwent simultaneous removal of the band with reversal to sleeve gastrectomy, whereas 2 underwent a staged sleeve gastrectomy.
Dr. Hawasli reported that there were just two complications in group 1: one leak, which occurred because of erosion, and one narrowing. Both cases were treated conservatively. There were no complications in group 2. There were no readmissions in group 1, whereas in group 2 one patient was readmitted for nausea and one for dehydration.
Patients in both groups lost weight after the reversal, but the loss was more pronounced in group 1, compared with group 2 (mean total body mass index loss, –15.8 kg/m2 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
To explain this difference in weight loss, Dr. Hawasli said that patients in group 1 lost most of their weight before the reversal (mean BMI loss, –11.7) and lost additional weight after the reversal (mean BMI loss, –3.8). However, group 2 patients struggled with weight loss before the reversal (mean BMI loss, –3.6) and they may have continued to struggle after the reversal, even though they lost more weight after the reversal than did group 1 patients (mean BMI loss, –7.2 vs. –3.8, respectively), which is expected.
"Another reason could be the short postreversal follow-up period (a mean of 9 months)," during which they did not get enough time to lose more weight, he explained.
In group 1, the mean operative time was 159 minutes for patients with Lap-Band slippage and 174 minutes for those with erosion or infection. The mean operative time in group 2 was 106 minutes.
Length of stay was about 2 days in both groups, but reached a mean of 3.6 days for the subset of group 1 patients who had reversal because of infection or erosion.
"The short-term results of weight loss after the reversal are better in patients who had the reversal secondary to complications," Dr. Hawasli concluded. "Concomitant removal of the band and reversal to sleeve gastrectomy did not increase the risk of complications except in patients with erosion. Thus, patients with erosion may benefit better from staged reversal."
Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.
SAN DIEGO – Laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy is a safe and feasible operation, results from a two-center study showed.
"Since the Lap-Band was introduced in the United States in 2001, it has been a popular minimally invasive procedure for weight loss," Dr. Abdelkader A. Hawasli said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "However, recent reports have shown that there’s an increased rate of explantation (up to 49%)" because of complications or failure to lose weight. Options are removal, reversion, or reversal to a nonphysiological procedure, "such as Roux-en-Y gastric bypass or biliopancreatic diversion. However, recent reports have been showing that sleeve gastrectomy could be a possible physiologic alternative."
For the current study, Dr. Hawasli, a surgeon at St. John Hospital and Medical Center in Detroit and Beaumont Hospital in Grosse Pointe, Mich., and his associates set out to evaluate the safety of the laparoscopic reversal of the Lap-Band to sleeve gastrectomy, the feasibility of performing simultaneous laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy, and the results of the sleeve gastrectomy after reversal as the final bariatric procedure in continuing or maintaining weight loss.
Dr. Hawasli reported on 485 patients who had undergone Lap-Band placement at St. John Hospital and Medical Center and 4 who had undergone the procedure at another institution from January 2004 to October 2011.
Of the 489 patients, 34 (7%) had reversal of the Lap-Band to sleeve gastrectomy. Of these, 20 patients (group 1) underwent reversal because of slippage in 15 cases, erosion in 3 cases, and infection in 2 cases, whereas 14 patients (group 2) underwent reversal because they were dissatisfied with their weight loss. The mean time of the reversal to sleeve gastrectomy was more than 3 years from Lap-Band insertion among the slippage subset patients in group 1 and among all patients in group 2 (36.5 vs. 43.3 months, respectively).
The majority of patients (32) underwent simultaneous removal of the band with reversal to sleeve gastrectomy, whereas 2 underwent a staged sleeve gastrectomy.
Dr. Hawasli reported that there were just two complications in group 1: one leak, which occurred because of erosion, and one narrowing. Both cases were treated conservatively. There were no complications in group 2. There were no readmissions in group 1, whereas in group 2 one patient was readmitted for nausea and one for dehydration.
Patients in both groups lost weight after the reversal, but the loss was more pronounced in group 1, compared with group 2 (mean total body mass index loss, –15.8 kg/m2 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
To explain this difference in weight loss, Dr. Hawasli said that patients in group 1 lost most of their weight before the reversal (mean BMI loss, –11.7) and lost additional weight after the reversal (mean BMI loss, –3.8). However, group 2 patients struggled with weight loss before the reversal (mean BMI loss, –3.6) and they may have continued to struggle after the reversal, even though they lost more weight after the reversal than did group 1 patients (mean BMI loss, –7.2 vs. –3.8, respectively), which is expected.
"Another reason could be the short postreversal follow-up period (a mean of 9 months)," during which they did not get enough time to lose more weight, he explained.
In group 1, the mean operative time was 159 minutes for patients with Lap-Band slippage and 174 minutes for those with erosion or infection. The mean operative time in group 2 was 106 minutes.
Length of stay was about 2 days in both groups, but reached a mean of 3.6 days for the subset of group 1 patients who had reversal because of infection or erosion.
"The short-term results of weight loss after the reversal are better in patients who had the reversal secondary to complications," Dr. Hawasli concluded. "Concomitant removal of the band and reversal to sleeve gastrectomy did not increase the risk of complications except in patients with erosion. Thus, patients with erosion may benefit better from staged reversal."
Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.
SAN DIEGO – Laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy is a safe and feasible operation, results from a two-center study showed.
"Since the Lap-Band was introduced in the United States in 2001, it has been a popular minimally invasive procedure for weight loss," Dr. Abdelkader A. Hawasli said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "However, recent reports have shown that there’s an increased rate of explantation (up to 49%)" because of complications or failure to lose weight. Options are removal, reversion, or reversal to a nonphysiological procedure, "such as Roux-en-Y gastric bypass or biliopancreatic diversion. However, recent reports have been showing that sleeve gastrectomy could be a possible physiologic alternative."
For the current study, Dr. Hawasli, a surgeon at St. John Hospital and Medical Center in Detroit and Beaumont Hospital in Grosse Pointe, Mich., and his associates set out to evaluate the safety of the laparoscopic reversal of the Lap-Band to sleeve gastrectomy, the feasibility of performing simultaneous laparoscopic removal of the Lap-Band and reversal to sleeve gastrectomy, and the results of the sleeve gastrectomy after reversal as the final bariatric procedure in continuing or maintaining weight loss.
Dr. Hawasli reported on 485 patients who had undergone Lap-Band placement at St. John Hospital and Medical Center and 4 who had undergone the procedure at another institution from January 2004 to October 2011.
Of the 489 patients, 34 (7%) had reversal of the Lap-Band to sleeve gastrectomy. Of these, 20 patients (group 1) underwent reversal because of slippage in 15 cases, erosion in 3 cases, and infection in 2 cases, whereas 14 patients (group 2) underwent reversal because they were dissatisfied with their weight loss. The mean time of the reversal to sleeve gastrectomy was more than 3 years from Lap-Band insertion among the slippage subset patients in group 1 and among all patients in group 2 (36.5 vs. 43.3 months, respectively).
The majority of patients (32) underwent simultaneous removal of the band with reversal to sleeve gastrectomy, whereas 2 underwent a staged sleeve gastrectomy.
Dr. Hawasli reported that there were just two complications in group 1: one leak, which occurred because of erosion, and one narrowing. Both cases were treated conservatively. There were no complications in group 2. There were no readmissions in group 1, whereas in group 2 one patient was readmitted for nausea and one for dehydration.
Patients in both groups lost weight after the reversal, but the loss was more pronounced in group 1, compared with group 2 (mean total body mass index loss, –15.8 kg/m2 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
To explain this difference in weight loss, Dr. Hawasli said that patients in group 1 lost most of their weight before the reversal (mean BMI loss, –11.7) and lost additional weight after the reversal (mean BMI loss, –3.8). However, group 2 patients struggled with weight loss before the reversal (mean BMI loss, –3.6) and they may have continued to struggle after the reversal, even though they lost more weight after the reversal than did group 1 patients (mean BMI loss, –7.2 vs. –3.8, respectively), which is expected.
"Another reason could be the short postreversal follow-up period (a mean of 9 months)," during which they did not get enough time to lose more weight, he explained.
In group 1, the mean operative time was 159 minutes for patients with Lap-Band slippage and 174 minutes for those with erosion or infection. The mean operative time in group 2 was 106 minutes.
Length of stay was about 2 days in both groups, but reached a mean of 3.6 days for the subset of group 1 patients who had reversal because of infection or erosion.
"The short-term results of weight loss after the reversal are better in patients who had the reversal secondary to complications," Dr. Hawasli concluded. "Concomitant removal of the band and reversal to sleeve gastrectomy did not increase the risk of complications except in patients with erosion. Thus, patients with erosion may benefit better from staged reversal."
Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: Weight loss was more pronounced among patients who underwent reversal of Lap-Band to sleeve gastrectomy because of band slippage, erosion, or infection than because of dissatisfaction with weight loss (mean total BMI loss, –15.8 vs. –10.8, respectively; mean percentage of excess BMI loss, –66.5% vs. –44.6%; all P less than .05).
Data Source: The study consisted of 34 patients who underwent reversal of Lap-Band to sleeve gastrectomy at two centers from January 2004 to October 2011.
Disclosures: Dr. Hawasli disclosed that he receives compensation from Covidien as a proctor.
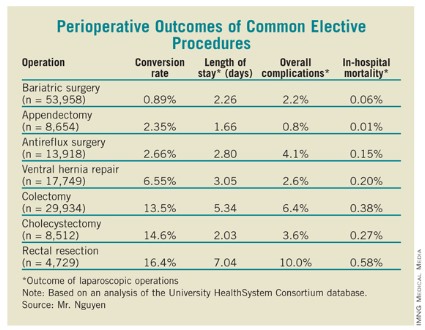
Bariatric Surgery Most Common Elective Surgical Procedure
SAN DIEGO – Within the setting of academic medical centers, bariatric surgery is the most common elective general surgical operation and it has the highest use of laparoscopy.
In addition, the in-hospital mortality rate of laparoscopic bariatric surgery is now comparable to those of laparoscopic appendectomy and antireflux surgery, and is currently lower than that of laparoscopic cholecystectomy.
Those are main findings from an analysis of data from the University HealthSystem Consortium database, which contains data from 114 academic centers and 250 major teaching affiliates in the United States.
"Laparoscopy has revolutionized the performance of most intra-abdominal operations [and] is now widely utilized in many different types of general surgical operations," Brian Nguyen, a research student at the University of California, Irvine, said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
He and his associates searched the University HealthSystem database to determine the rate of laparoscopy use in seven common elective general surgical operations performed between Oct. 1, 2008, and March 31, 2012: antireflux surgery for gastroesophageal reflux disease (GERD) or hiatal hernia, cholecystectomy for chronic cholecystitis, bariatric surgery for morbid obesity, ventral hernia repair for incisional hernia, appendectomy for acute appendicitis, rectal resection for rectal cancer, and colectomy for colon cancer or diverticulitis. Secondary objectives were to determine the rate of conversion to open surgery, length of stay, overall complications, and in-hospital mortality.
The most common elective surgical procedure performed during the study period was bariatric surgery (53,958 cases), followed by colectomy (29,934 cases), ventral hernia repair (17,749 cases), antireflux surgery (13,918 cases), appendectomy (8,654 cases), cholecystectomy (8,512 cases), and rectal resection (4,729). Bariatric surgery also led the way with the highest rate of laparoscopy use (94%), followed by antireflux surgery (83%), appendectomy (79%), cholecystectomy (77%), colectomy (52%), ventral hernia repair (28%), and rectal resection (18%).
As for perioperative outcomes (see table), Mr. Nguyen reported that patients who underwent bariatric surgery had the lowest conversion rate to open procedures (0.89%). The overall complication rate of 2.2% and the in-hospital mortality rate of 0.06% associated with bariatric surgery were lower only in appendectomy, which had rates of 0.8% and 0.01%, respectively. The mean length of stay for bariatric surgery patients was 2.26 days, which was higher than that for appendectomy and cholecystectomy patients (a mean of 1.66 and 2.03 days, respectively), but lower than that for antireflux surgery (a mean of 2.80 days).
Mr. Nguyen acknowledged that the study was limited by the fact that it represented only inpatients at academic medical centers and affiliated hospitals.
He said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Within the setting of academic medical centers, bariatric surgery is the most common elective general surgical operation and it has the highest use of laparoscopy.
In addition, the in-hospital mortality rate of laparoscopic bariatric surgery is now comparable to those of laparoscopic appendectomy and antireflux surgery, and is currently lower than that of laparoscopic cholecystectomy.
Those are main findings from an analysis of data from the University HealthSystem Consortium database, which contains data from 114 academic centers and 250 major teaching affiliates in the United States.
"Laparoscopy has revolutionized the performance of most intra-abdominal operations [and] is now widely utilized in many different types of general surgical operations," Brian Nguyen, a research student at the University of California, Irvine, said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
He and his associates searched the University HealthSystem database to determine the rate of laparoscopy use in seven common elective general surgical operations performed between Oct. 1, 2008, and March 31, 2012: antireflux surgery for gastroesophageal reflux disease (GERD) or hiatal hernia, cholecystectomy for chronic cholecystitis, bariatric surgery for morbid obesity, ventral hernia repair for incisional hernia, appendectomy for acute appendicitis, rectal resection for rectal cancer, and colectomy for colon cancer or diverticulitis. Secondary objectives were to determine the rate of conversion to open surgery, length of stay, overall complications, and in-hospital mortality.
The most common elective surgical procedure performed during the study period was bariatric surgery (53,958 cases), followed by colectomy (29,934 cases), ventral hernia repair (17,749 cases), antireflux surgery (13,918 cases), appendectomy (8,654 cases), cholecystectomy (8,512 cases), and rectal resection (4,729). Bariatric surgery also led the way with the highest rate of laparoscopy use (94%), followed by antireflux surgery (83%), appendectomy (79%), cholecystectomy (77%), colectomy (52%), ventral hernia repair (28%), and rectal resection (18%).
As for perioperative outcomes (see table), Mr. Nguyen reported that patients who underwent bariatric surgery had the lowest conversion rate to open procedures (0.89%). The overall complication rate of 2.2% and the in-hospital mortality rate of 0.06% associated with bariatric surgery were lower only in appendectomy, which had rates of 0.8% and 0.01%, respectively. The mean length of stay for bariatric surgery patients was 2.26 days, which was higher than that for appendectomy and cholecystectomy patients (a mean of 1.66 and 2.03 days, respectively), but lower than that for antireflux surgery (a mean of 2.80 days).
Mr. Nguyen acknowledged that the study was limited by the fact that it represented only inpatients at academic medical centers and affiliated hospitals.
He said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Within the setting of academic medical centers, bariatric surgery is the most common elective general surgical operation and it has the highest use of laparoscopy.
In addition, the in-hospital mortality rate of laparoscopic bariatric surgery is now comparable to those of laparoscopic appendectomy and antireflux surgery, and is currently lower than that of laparoscopic cholecystectomy.
Those are main findings from an analysis of data from the University HealthSystem Consortium database, which contains data from 114 academic centers and 250 major teaching affiliates in the United States.
"Laparoscopy has revolutionized the performance of most intra-abdominal operations [and] is now widely utilized in many different types of general surgical operations," Brian Nguyen, a research student at the University of California, Irvine, said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
He and his associates searched the University HealthSystem database to determine the rate of laparoscopy use in seven common elective general surgical operations performed between Oct. 1, 2008, and March 31, 2012: antireflux surgery for gastroesophageal reflux disease (GERD) or hiatal hernia, cholecystectomy for chronic cholecystitis, bariatric surgery for morbid obesity, ventral hernia repair for incisional hernia, appendectomy for acute appendicitis, rectal resection for rectal cancer, and colectomy for colon cancer or diverticulitis. Secondary objectives were to determine the rate of conversion to open surgery, length of stay, overall complications, and in-hospital mortality.
The most common elective surgical procedure performed during the study period was bariatric surgery (53,958 cases), followed by colectomy (29,934 cases), ventral hernia repair (17,749 cases), antireflux surgery (13,918 cases), appendectomy (8,654 cases), cholecystectomy (8,512 cases), and rectal resection (4,729). Bariatric surgery also led the way with the highest rate of laparoscopy use (94%), followed by antireflux surgery (83%), appendectomy (79%), cholecystectomy (77%), colectomy (52%), ventral hernia repair (28%), and rectal resection (18%).
As for perioperative outcomes (see table), Mr. Nguyen reported that patients who underwent bariatric surgery had the lowest conversion rate to open procedures (0.89%). The overall complication rate of 2.2% and the in-hospital mortality rate of 0.06% associated with bariatric surgery were lower only in appendectomy, which had rates of 0.8% and 0.01%, respectively. The mean length of stay for bariatric surgery patients was 2.26 days, which was higher than that for appendectomy and cholecystectomy patients (a mean of 1.66 and 2.03 days, respectively), but lower than that for antireflux surgery (a mean of 2.80 days).
Mr. Nguyen acknowledged that the study was limited by the fact that it represented only inpatients at academic medical centers and affiliated hospitals.
He said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: Between Oct. 1, 2008, and March 31, 2012, bariatric surgery ranked as the most common elective surgical procedure performed (53,958 cases), and led the way with use of laparoscopy (94% of cases).
Data Source: This study of seven common surgical elective procedures was based on a search of the University HealthSystem Consortium database, which is limited to 114 academic centers and 250 major teaching affiliates in the United States.
Disclosures: Mr. Nguyen said that he had no relevant financial conflicts to disclose.
Sleeve Gastrectomy Feasible in Obese Transplant Candidates
SAN DIEGO – Laparoscopic sleeve gastrectomy is safe and effective in obese candidates for organ transplantation, results from a novel pilot study demonstrated.
Nationwide, 15%-20% of patients on the transplant waiting list are morbidly obese, with a body mass index of greater than 35 kg/m2, "but many cannot be transplanted unless they lose weight," said Dr. Matthew Y. Lin of the surgery department at the University of California, San Francisco (UCSF). "Morbid obesity can contribute to end-stage kidney or liver failure. For example, obesity-related nonalcoholic steatohepatitis is now the third most common indication for liver transplant in the United States and will likely become first in the future."
In what Dr. Lin said is the only reported case series of bariatric surgery in obese transplant candidates, he and his associates conducted a pilot study of 26 morbidly obese patients with liver or kidney failure who underwent laparoscopic sleeve gastrectomy at UCSF from 2006 to 2012. They chose sleeve gastrectomy over gastric banding "to avoid foreign body implantation, in anticipation of post-transplant immunosuppression," Dr. Lin explained at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
"We chose sleeve gastrectomy over gastric bypass to maintain endoscopic access to the biliary system, to reduce surgical complexity, and to avoid unpredictable immunosuppression absorption," he said.
Morbid obesity is a relative contraindication for solid organ transplantation at most centers because of poor post-transplant outcomes, according to Dr. Lin. "At UCSF, the selection criteria are a BMI of less than 40 for liver transplant, less than 38 for kidney transplant, and less than 34 for kidney transplant in patients with diabetes." The researchers hypothesized that laparoscopic sleeve gastrectomy could be safely performed in high-risk patients with liver or kidney failure and achieve enough weight loss to allow for transplantation.
The 26 patients had a mean age of 57 years, 17 were women, 20 were white, and their average preoperative BMI was 48. Twenty patients had liver insufficiency with a mean Model for End-Stage Liver Disease (MELD) score of 11, and 6 had kidney insufficiency with a mean glomerular filtration rate of 10 mL/min. Five of these patients were on hemodialysis.
All 26 patients had laparoscopic sleeve gastrectomy performed by the same surgeon. The mean operative time was 151 minutes, and the mean length of stay was 4.2 days. Complications that occurred within 30 days were two cases of superficial wound infection and one case each of worsened hepatic encephalopathy, acute renal insufficiency, need for blood transfusion, and staple line leak. There was no mortality within 30 days, but after that period two patients died awaiting transplant and one patient died from complications of the staple line leak and progressive liver failure 4 years after surgery.
After 2 years, the average BMI of study participants dropped from a mean of 48 to a mean of 29. "Between the 6- and 12-month marks, most patients were able to achieve a BMI that would make them acceptable for transplant," Dr. Lin said.
At 1, 3, 12, and 24 months, the percent of excess body weight lost was 17%, 26%, 50%, and 66%, respectively. "The weight-loss profile is similar to [those of] the general bariatric sleeve gastrectomy population," he noted.
Of the 13 patients who had diabetes preoperatively, 7 had complete resolution after the procedure and 1 had partial resolution. Mean postoperative albumin levels for all 26 patients after sleeve gastrectomy were 3.1 g/dL at 6 months and 3.3 g/dL at 12 months.
Eight patients went on to receive their organ transplant, Dr. Lin said. Their mean age was 56 years, and six were women. They waited a mean of 17 months for their procedures, which included six liver transplants, one liver and kidney transplant, and one kidney transplant. Their mean BMI before sleeve gastrectomy was 46, and their mean BMI prior to transplantation was 31. Immediately before transplant, their mean albumin level was 3.2 g/dL, and the most current measurement remained the same. "No increased acute rejection or difficulty maintaining immunosuppression was observed," he said.
Dr. Lin acknowledged certain limitations of the study, including its single-center design, lack of a control population, and the fact that "there is very little statistical power to estimate the true complication rate in this high-risk surgical group. Furthermore, we only have short-term follow-up."
Dr. Lin said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Laparoscopic sleeve gastrectomy is safe and effective in obese candidates for organ transplantation, results from a novel pilot study demonstrated.
Nationwide, 15%-20% of patients on the transplant waiting list are morbidly obese, with a body mass index of greater than 35 kg/m2, "but many cannot be transplanted unless they lose weight," said Dr. Matthew Y. Lin of the surgery department at the University of California, San Francisco (UCSF). "Morbid obesity can contribute to end-stage kidney or liver failure. For example, obesity-related nonalcoholic steatohepatitis is now the third most common indication for liver transplant in the United States and will likely become first in the future."
In what Dr. Lin said is the only reported case series of bariatric surgery in obese transplant candidates, he and his associates conducted a pilot study of 26 morbidly obese patients with liver or kidney failure who underwent laparoscopic sleeve gastrectomy at UCSF from 2006 to 2012. They chose sleeve gastrectomy over gastric banding "to avoid foreign body implantation, in anticipation of post-transplant immunosuppression," Dr. Lin explained at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
"We chose sleeve gastrectomy over gastric bypass to maintain endoscopic access to the biliary system, to reduce surgical complexity, and to avoid unpredictable immunosuppression absorption," he said.
Morbid obesity is a relative contraindication for solid organ transplantation at most centers because of poor post-transplant outcomes, according to Dr. Lin. "At UCSF, the selection criteria are a BMI of less than 40 for liver transplant, less than 38 for kidney transplant, and less than 34 for kidney transplant in patients with diabetes." The researchers hypothesized that laparoscopic sleeve gastrectomy could be safely performed in high-risk patients with liver or kidney failure and achieve enough weight loss to allow for transplantation.
The 26 patients had a mean age of 57 years, 17 were women, 20 were white, and their average preoperative BMI was 48. Twenty patients had liver insufficiency with a mean Model for End-Stage Liver Disease (MELD) score of 11, and 6 had kidney insufficiency with a mean glomerular filtration rate of 10 mL/min. Five of these patients were on hemodialysis.
All 26 patients had laparoscopic sleeve gastrectomy performed by the same surgeon. The mean operative time was 151 minutes, and the mean length of stay was 4.2 days. Complications that occurred within 30 days were two cases of superficial wound infection and one case each of worsened hepatic encephalopathy, acute renal insufficiency, need for blood transfusion, and staple line leak. There was no mortality within 30 days, but after that period two patients died awaiting transplant and one patient died from complications of the staple line leak and progressive liver failure 4 years after surgery.
After 2 years, the average BMI of study participants dropped from a mean of 48 to a mean of 29. "Between the 6- and 12-month marks, most patients were able to achieve a BMI that would make them acceptable for transplant," Dr. Lin said.
At 1, 3, 12, and 24 months, the percent of excess body weight lost was 17%, 26%, 50%, and 66%, respectively. "The weight-loss profile is similar to [those of] the general bariatric sleeve gastrectomy population," he noted.
Of the 13 patients who had diabetes preoperatively, 7 had complete resolution after the procedure and 1 had partial resolution. Mean postoperative albumin levels for all 26 patients after sleeve gastrectomy were 3.1 g/dL at 6 months and 3.3 g/dL at 12 months.
Eight patients went on to receive their organ transplant, Dr. Lin said. Their mean age was 56 years, and six were women. They waited a mean of 17 months for their procedures, which included six liver transplants, one liver and kidney transplant, and one kidney transplant. Their mean BMI before sleeve gastrectomy was 46, and their mean BMI prior to transplantation was 31. Immediately before transplant, their mean albumin level was 3.2 g/dL, and the most current measurement remained the same. "No increased acute rejection or difficulty maintaining immunosuppression was observed," he said.
Dr. Lin acknowledged certain limitations of the study, including its single-center design, lack of a control population, and the fact that "there is very little statistical power to estimate the true complication rate in this high-risk surgical group. Furthermore, we only have short-term follow-up."
Dr. Lin said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Laparoscopic sleeve gastrectomy is safe and effective in obese candidates for organ transplantation, results from a novel pilot study demonstrated.
Nationwide, 15%-20% of patients on the transplant waiting list are morbidly obese, with a body mass index of greater than 35 kg/m2, "but many cannot be transplanted unless they lose weight," said Dr. Matthew Y. Lin of the surgery department at the University of California, San Francisco (UCSF). "Morbid obesity can contribute to end-stage kidney or liver failure. For example, obesity-related nonalcoholic steatohepatitis is now the third most common indication for liver transplant in the United States and will likely become first in the future."
In what Dr. Lin said is the only reported case series of bariatric surgery in obese transplant candidates, he and his associates conducted a pilot study of 26 morbidly obese patients with liver or kidney failure who underwent laparoscopic sleeve gastrectomy at UCSF from 2006 to 2012. They chose sleeve gastrectomy over gastric banding "to avoid foreign body implantation, in anticipation of post-transplant immunosuppression," Dr. Lin explained at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
"We chose sleeve gastrectomy over gastric bypass to maintain endoscopic access to the biliary system, to reduce surgical complexity, and to avoid unpredictable immunosuppression absorption," he said.
Morbid obesity is a relative contraindication for solid organ transplantation at most centers because of poor post-transplant outcomes, according to Dr. Lin. "At UCSF, the selection criteria are a BMI of less than 40 for liver transplant, less than 38 for kidney transplant, and less than 34 for kidney transplant in patients with diabetes." The researchers hypothesized that laparoscopic sleeve gastrectomy could be safely performed in high-risk patients with liver or kidney failure and achieve enough weight loss to allow for transplantation.
The 26 patients had a mean age of 57 years, 17 were women, 20 were white, and their average preoperative BMI was 48. Twenty patients had liver insufficiency with a mean Model for End-Stage Liver Disease (MELD) score of 11, and 6 had kidney insufficiency with a mean glomerular filtration rate of 10 mL/min. Five of these patients were on hemodialysis.
All 26 patients had laparoscopic sleeve gastrectomy performed by the same surgeon. The mean operative time was 151 minutes, and the mean length of stay was 4.2 days. Complications that occurred within 30 days were two cases of superficial wound infection and one case each of worsened hepatic encephalopathy, acute renal insufficiency, need for blood transfusion, and staple line leak. There was no mortality within 30 days, but after that period two patients died awaiting transplant and one patient died from complications of the staple line leak and progressive liver failure 4 years after surgery.
After 2 years, the average BMI of study participants dropped from a mean of 48 to a mean of 29. "Between the 6- and 12-month marks, most patients were able to achieve a BMI that would make them acceptable for transplant," Dr. Lin said.
At 1, 3, 12, and 24 months, the percent of excess body weight lost was 17%, 26%, 50%, and 66%, respectively. "The weight-loss profile is similar to [those of] the general bariatric sleeve gastrectomy population," he noted.
Of the 13 patients who had diabetes preoperatively, 7 had complete resolution after the procedure and 1 had partial resolution. Mean postoperative albumin levels for all 26 patients after sleeve gastrectomy were 3.1 g/dL at 6 months and 3.3 g/dL at 12 months.
Eight patients went on to receive their organ transplant, Dr. Lin said. Their mean age was 56 years, and six were women. They waited a mean of 17 months for their procedures, which included six liver transplants, one liver and kidney transplant, and one kidney transplant. Their mean BMI before sleeve gastrectomy was 46, and their mean BMI prior to transplantation was 31. Immediately before transplant, their mean albumin level was 3.2 g/dL, and the most current measurement remained the same. "No increased acute rejection or difficulty maintaining immunosuppression was observed," he said.
Dr. Lin acknowledged certain limitations of the study, including its single-center design, lack of a control population, and the fact that "there is very little statistical power to estimate the true complication rate in this high-risk surgical group. Furthermore, we only have short-term follow-up."
Dr. Lin said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Survey: Long Surgical Career Raises Likelihood of Lawsuit
SAN DIEGO – The most experienced bariatric surgeons are those who are most likely to be sued, judging by responses to a survey from more than 300 members of the American Society for Metabolic and Bariatric Surgery.
"There are no resources, national registries, or easily accessible databases to analyze bariatric-specific medical malpractice claims in the United States," Dr. Ramsey M. Dallal said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "Without the ability to analyze aggregate data, surgeons cannot easily study common causes of medical malpractice litigation and develop patient safety improvements. Nor do there exist easily accessible measures of trends in bariatric surgery litigation."
In an effort to obtain a snapshot of the liability landscape in bariatric surgery, Dr. Dallal and other members of the ASMBS Patient Safety Committee e-mailed a survey to 1,672 surgeon members of the ASMBS in July 2011. A total of 330 surgeons in 46 states responded, for a response rate of 20%. Their mean number of years in practice was 15, which represented 5,042 years of bariatric surgery–specific liability exposure. Most respondents (38%) practiced in a hospital or academic group, 26% in a single specialty group, 20% in solo practice, 13% in a multispecialty group, and 3% in other settings.
Nine respondents chose not to have malpractice insurance. Those who were insured reported a mean yearly cost of malpractice insurance of $59,200.
Nearly half of respondents (48%) reported having no malpractice insurance cases since their careers began, but the average number of lifetime cases reported by their counterparts was 1.5.
Of the 464 lawsuits reported by 156 surgeons, 54% were dropped or dismissed, 27% were settled out of court, and 19% went to trial or arbitration.
Of those cases that went to trial, 72% were found in favor of the surgeon-defendant. The mean lifetime amount paid in lawsuits was $250,000, including one settlement for $7,000,000. The total amount paid by the respondents was $70,871,998.
Using multivariate logistic regression analysis, the researchers determined that the probability of reporting at least one lawsuit independently increased with the number of years in practice (odds ratio, 1.03; P = .03) and among those who have performed more than 1,000 cases (OR, 8.5%; P = .01). "In essence, our most experienced surgeons are the ones being sued the most," said Dr. Dallal, chief of bariatric/minimally invasive surgery at Einstein Healthcare Network, Philadelphia.
The odds of having lost a malpractice case that resulted in monetary compensation independently increased with the number of years in practice (OR, 1.09; P less than .0005), and the number of lawsuits experienced (OR, 1.42; P = .02). "The type of practice and the lack of a bariatric surgeon expert witness did not independently predict a payout," Dr. Dallal said.
Nearly 7% of survey respondents reported that the primary expert witness in determining the standard of bariatric surgery care was not a bariatric surgeon. In such cases, the surgeon-defendant had an 11-fold increased risk of having a lawsuit (P = .018). However, the use of an expert witness who was not a bariatric surgeon was not associated with the chance of settlement or the case’s going to trial.
Dr. Dallal noted that many lawsuits are filed about 2 years after the alleged injury, and another 1-2 years may pass before resolution of that lawsuit occurs. "So, there is a built-in bias against surgeons who have been in practice longer," he said.
He noted that successful lawsuits that are based on patient harm "do occur and are devastating to all involved. Improving the patient safety culture is the mainstay of reducing liability risk."
Dr. Dallal said that he had no relevant financial conflicts to disclose.
SAN DIEGO – The most experienced bariatric surgeons are those who are most likely to be sued, judging by responses to a survey from more than 300 members of the American Society for Metabolic and Bariatric Surgery.
"There are no resources, national registries, or easily accessible databases to analyze bariatric-specific medical malpractice claims in the United States," Dr. Ramsey M. Dallal said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "Without the ability to analyze aggregate data, surgeons cannot easily study common causes of medical malpractice litigation and develop patient safety improvements. Nor do there exist easily accessible measures of trends in bariatric surgery litigation."
In an effort to obtain a snapshot of the liability landscape in bariatric surgery, Dr. Dallal and other members of the ASMBS Patient Safety Committee e-mailed a survey to 1,672 surgeon members of the ASMBS in July 2011. A total of 330 surgeons in 46 states responded, for a response rate of 20%. Their mean number of years in practice was 15, which represented 5,042 years of bariatric surgery–specific liability exposure. Most respondents (38%) practiced in a hospital or academic group, 26% in a single specialty group, 20% in solo practice, 13% in a multispecialty group, and 3% in other settings.
Nine respondents chose not to have malpractice insurance. Those who were insured reported a mean yearly cost of malpractice insurance of $59,200.
Nearly half of respondents (48%) reported having no malpractice insurance cases since their careers began, but the average number of lifetime cases reported by their counterparts was 1.5.
Of the 464 lawsuits reported by 156 surgeons, 54% were dropped or dismissed, 27% were settled out of court, and 19% went to trial or arbitration.
Of those cases that went to trial, 72% were found in favor of the surgeon-defendant. The mean lifetime amount paid in lawsuits was $250,000, including one settlement for $7,000,000. The total amount paid by the respondents was $70,871,998.
Using multivariate logistic regression analysis, the researchers determined that the probability of reporting at least one lawsuit independently increased with the number of years in practice (odds ratio, 1.03; P = .03) and among those who have performed more than 1,000 cases (OR, 8.5%; P = .01). "In essence, our most experienced surgeons are the ones being sued the most," said Dr. Dallal, chief of bariatric/minimally invasive surgery at Einstein Healthcare Network, Philadelphia.
The odds of having lost a malpractice case that resulted in monetary compensation independently increased with the number of years in practice (OR, 1.09; P less than .0005), and the number of lawsuits experienced (OR, 1.42; P = .02). "The type of practice and the lack of a bariatric surgeon expert witness did not independently predict a payout," Dr. Dallal said.
Nearly 7% of survey respondents reported that the primary expert witness in determining the standard of bariatric surgery care was not a bariatric surgeon. In such cases, the surgeon-defendant had an 11-fold increased risk of having a lawsuit (P = .018). However, the use of an expert witness who was not a bariatric surgeon was not associated with the chance of settlement or the case’s going to trial.
Dr. Dallal noted that many lawsuits are filed about 2 years after the alleged injury, and another 1-2 years may pass before resolution of that lawsuit occurs. "So, there is a built-in bias against surgeons who have been in practice longer," he said.
He noted that successful lawsuits that are based on patient harm "do occur and are devastating to all involved. Improving the patient safety culture is the mainstay of reducing liability risk."
Dr. Dallal said that he had no relevant financial conflicts to disclose.
SAN DIEGO – The most experienced bariatric surgeons are those who are most likely to be sued, judging by responses to a survey from more than 300 members of the American Society for Metabolic and Bariatric Surgery.
"There are no resources, national registries, or easily accessible databases to analyze bariatric-specific medical malpractice claims in the United States," Dr. Ramsey M. Dallal said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "Without the ability to analyze aggregate data, surgeons cannot easily study common causes of medical malpractice litigation and develop patient safety improvements. Nor do there exist easily accessible measures of trends in bariatric surgery litigation."
In an effort to obtain a snapshot of the liability landscape in bariatric surgery, Dr. Dallal and other members of the ASMBS Patient Safety Committee e-mailed a survey to 1,672 surgeon members of the ASMBS in July 2011. A total of 330 surgeons in 46 states responded, for a response rate of 20%. Their mean number of years in practice was 15, which represented 5,042 years of bariatric surgery–specific liability exposure. Most respondents (38%) practiced in a hospital or academic group, 26% in a single specialty group, 20% in solo practice, 13% in a multispecialty group, and 3% in other settings.
Nine respondents chose not to have malpractice insurance. Those who were insured reported a mean yearly cost of malpractice insurance of $59,200.
Nearly half of respondents (48%) reported having no malpractice insurance cases since their careers began, but the average number of lifetime cases reported by their counterparts was 1.5.
Of the 464 lawsuits reported by 156 surgeons, 54% were dropped or dismissed, 27% were settled out of court, and 19% went to trial or arbitration.
Of those cases that went to trial, 72% were found in favor of the surgeon-defendant. The mean lifetime amount paid in lawsuits was $250,000, including one settlement for $7,000,000. The total amount paid by the respondents was $70,871,998.
Using multivariate logistic regression analysis, the researchers determined that the probability of reporting at least one lawsuit independently increased with the number of years in practice (odds ratio, 1.03; P = .03) and among those who have performed more than 1,000 cases (OR, 8.5%; P = .01). "In essence, our most experienced surgeons are the ones being sued the most," said Dr. Dallal, chief of bariatric/minimally invasive surgery at Einstein Healthcare Network, Philadelphia.
The odds of having lost a malpractice case that resulted in monetary compensation independently increased with the number of years in practice (OR, 1.09; P less than .0005), and the number of lawsuits experienced (OR, 1.42; P = .02). "The type of practice and the lack of a bariatric surgeon expert witness did not independently predict a payout," Dr. Dallal said.
Nearly 7% of survey respondents reported that the primary expert witness in determining the standard of bariatric surgery care was not a bariatric surgeon. In such cases, the surgeon-defendant had an 11-fold increased risk of having a lawsuit (P = .018). However, the use of an expert witness who was not a bariatric surgeon was not associated with the chance of settlement or the case’s going to trial.
Dr. Dallal noted that many lawsuits are filed about 2 years after the alleged injury, and another 1-2 years may pass before resolution of that lawsuit occurs. "So, there is a built-in bias against surgeons who have been in practice longer," he said.
He noted that successful lawsuits that are based on patient harm "do occur and are devastating to all involved. Improving the patient safety culture is the mainstay of reducing liability risk."
Dr. Dallal said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: The probability of reporting at least one lawsuit independently increased with the number of years in practice (OR, 1.03; P = .03) and among those who have performed more than 1,000 cases (OR, 8.5%; P = .01).
Data Source: The findings are based on responses to a survey from 330 members of the American Society of Metabolic and Bariatric Surgery.
Disclosures: Dr. Dallal said that he had no relevant financial conflicts to disclose.
Endoscopy Exposure Generally Low Among Surgical Trainees
SAN DIEGO – Exposure to endoscopy is generally low among surgical trainees, yet most bariatric surgeons continue to perform endoscopy and manage complications, responses to a survey indicate.
"There is a varying amount of endoscopic training during surgical residency and fellowship, and endoscopic practices are not standardized," Dr. Bipan Chand said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "Surgeons today perform varying degrees of endoscopy, pre- and postoperatively, as well as diagnostic and therapeutic procedures."
Dr. Chand and his associates sent a 19-question online survey to 1,670 active surgeon members of the ASMBS during a 1-month time frame in an effort to "obtain a better understanding on the current amount of exposure to endoscopy, to obtain information on the amount of diagnostic and therapeutic procedures being performed, by whom and [what the] the comfort level [is]."
Of the 1,670 members, 291 (17%) completed the survey, said Dr. Chand, director of metabolic surgery and bariatric care at Loyola University, Chicago. The largest proportion of respondents (30.9%) were more than 15 years removed from surgical training, whereas 18.9% were 11-15 years removed, 23.4% were 6-10 years removed, 23.4% were 1-5 years removed, and 3.4% were less than 1 year removed.
Nearly 60% of respondents completed a postresidency fellowship. Of these, 38% completed a fellowship in bariatric surgery with an emphasis in minimally invasive surgery (MIS), and 31% completed a fellowship in general MIS.
Dr. Chand, who chairs the ASMBS Emerging Technology and Procedures Committee, reported that during their combined residency and fellowship training, 25% of respondents performed fewer than 25 diagnostic procedures and 55% performed fewer than 5 therapeutic procedures such as dilation and treatment of bleeding.
After completing their training, 41% of respondents reported performing routine preoperative endoscopy for primary bariatric procedures, and 90% reported performing routine preoperative upper endoscopy for revisional bariatric procedures. More than 70% of these procedures were being done by the respondents or by their surgical partners.
Overall, 49% of respondents said they felt "very comfortable" with endoscopic management of bariatric complications, including bleeding, dilation of strictures, removal of foreign bodies, and stent placement.
More than three-quarters of respondents (78%) expressed interest in additional endoscopy training via postgraduate courses, particularly those related to advanced training techniques, whereas 53% and 56%, respectively, predicted that endoscopic procedures will play a role as primary and revisional endoluminal bariatric therapies.
More than two-thirds of surgeons (69%) said that they plan to increase the amount of endoscopy in their practice. "The ASMBS will continue to offer training labs to surgeons to help [them] acquire and refine these important skills," Dr. Chand said. "One such lab was offered at this year’s annual meeting."
Dr. Chand said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Exposure to endoscopy is generally low among surgical trainees, yet most bariatric surgeons continue to perform endoscopy and manage complications, responses to a survey indicate.
"There is a varying amount of endoscopic training during surgical residency and fellowship, and endoscopic practices are not standardized," Dr. Bipan Chand said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "Surgeons today perform varying degrees of endoscopy, pre- and postoperatively, as well as diagnostic and therapeutic procedures."
Dr. Chand and his associates sent a 19-question online survey to 1,670 active surgeon members of the ASMBS during a 1-month time frame in an effort to "obtain a better understanding on the current amount of exposure to endoscopy, to obtain information on the amount of diagnostic and therapeutic procedures being performed, by whom and [what the] the comfort level [is]."
Of the 1,670 members, 291 (17%) completed the survey, said Dr. Chand, director of metabolic surgery and bariatric care at Loyola University, Chicago. The largest proportion of respondents (30.9%) were more than 15 years removed from surgical training, whereas 18.9% were 11-15 years removed, 23.4% were 6-10 years removed, 23.4% were 1-5 years removed, and 3.4% were less than 1 year removed.
Nearly 60% of respondents completed a postresidency fellowship. Of these, 38% completed a fellowship in bariatric surgery with an emphasis in minimally invasive surgery (MIS), and 31% completed a fellowship in general MIS.
Dr. Chand, who chairs the ASMBS Emerging Technology and Procedures Committee, reported that during their combined residency and fellowship training, 25% of respondents performed fewer than 25 diagnostic procedures and 55% performed fewer than 5 therapeutic procedures such as dilation and treatment of bleeding.
After completing their training, 41% of respondents reported performing routine preoperative endoscopy for primary bariatric procedures, and 90% reported performing routine preoperative upper endoscopy for revisional bariatric procedures. More than 70% of these procedures were being done by the respondents or by their surgical partners.
Overall, 49% of respondents said they felt "very comfortable" with endoscopic management of bariatric complications, including bleeding, dilation of strictures, removal of foreign bodies, and stent placement.
More than three-quarters of respondents (78%) expressed interest in additional endoscopy training via postgraduate courses, particularly those related to advanced training techniques, whereas 53% and 56%, respectively, predicted that endoscopic procedures will play a role as primary and revisional endoluminal bariatric therapies.
More than two-thirds of surgeons (69%) said that they plan to increase the amount of endoscopy in their practice. "The ASMBS will continue to offer training labs to surgeons to help [them] acquire and refine these important skills," Dr. Chand said. "One such lab was offered at this year’s annual meeting."
Dr. Chand said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Exposure to endoscopy is generally low among surgical trainees, yet most bariatric surgeons continue to perform endoscopy and manage complications, responses to a survey indicate.
"There is a varying amount of endoscopic training during surgical residency and fellowship, and endoscopic practices are not standardized," Dr. Bipan Chand said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "Surgeons today perform varying degrees of endoscopy, pre- and postoperatively, as well as diagnostic and therapeutic procedures."
Dr. Chand and his associates sent a 19-question online survey to 1,670 active surgeon members of the ASMBS during a 1-month time frame in an effort to "obtain a better understanding on the current amount of exposure to endoscopy, to obtain information on the amount of diagnostic and therapeutic procedures being performed, by whom and [what the] the comfort level [is]."
Of the 1,670 members, 291 (17%) completed the survey, said Dr. Chand, director of metabolic surgery and bariatric care at Loyola University, Chicago. The largest proportion of respondents (30.9%) were more than 15 years removed from surgical training, whereas 18.9% were 11-15 years removed, 23.4% were 6-10 years removed, 23.4% were 1-5 years removed, and 3.4% were less than 1 year removed.
Nearly 60% of respondents completed a postresidency fellowship. Of these, 38% completed a fellowship in bariatric surgery with an emphasis in minimally invasive surgery (MIS), and 31% completed a fellowship in general MIS.
Dr. Chand, who chairs the ASMBS Emerging Technology and Procedures Committee, reported that during their combined residency and fellowship training, 25% of respondents performed fewer than 25 diagnostic procedures and 55% performed fewer than 5 therapeutic procedures such as dilation and treatment of bleeding.
After completing their training, 41% of respondents reported performing routine preoperative endoscopy for primary bariatric procedures, and 90% reported performing routine preoperative upper endoscopy for revisional bariatric procedures. More than 70% of these procedures were being done by the respondents or by their surgical partners.
Overall, 49% of respondents said they felt "very comfortable" with endoscopic management of bariatric complications, including bleeding, dilation of strictures, removal of foreign bodies, and stent placement.
More than three-quarters of respondents (78%) expressed interest in additional endoscopy training via postgraduate courses, particularly those related to advanced training techniques, whereas 53% and 56%, respectively, predicted that endoscopic procedures will play a role as primary and revisional endoluminal bariatric therapies.
More than two-thirds of surgeons (69%) said that they plan to increase the amount of endoscopy in their practice. "The ASMBS will continue to offer training labs to surgeons to help [them] acquire and refine these important skills," Dr. Chand said. "One such lab was offered at this year’s annual meeting."
Dr. Chand said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: During their combined residency and fellowship training, 25% of surgeons performed fewer than 25 diagnostic endoscopic procedures and 55% performed fewer than 5 endoscopic therapeutic procedures such as dilation and treatment of bleeding.
Data Source: The study was based on responses from 291 surgeons to an online survey sent to members of the American Society for Metabolic and Bariatric Surgery.
Disclosures: Dr. Chand said he had no relevant financial conflicts to disclose.
Men Benefit Most From Combined Weight-Loss Procedure
SAN DIEGO – Significantly greater reductions in weight, body mass index, and adipose tissue were seen in men vs. women who underwent biliopancreatic diversion with duodenal switch surgery, a single-center study indicated.
The study, which was conducted at the Institute of Pneumology and Cardiology at Laval University in Quebec City, was designed to assess the impact of sex on weight loss along with changes in adiposity and skeletal muscle in 42 severely obese men and women who underwent biliopancreatic diversion with duodenal switch (BPD-DS) surgery. Audrey Auclair, a Ph.D. student in pharmacy at the university, presented the study results on behalf of her colleagues at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
At baseline and 6 months, the 12 men and 30 women (mean age, 46 years) underwent anthropometric measurements and a midthigh CT scan. At baseline, the men and women were similar in terms of thickness of total, deep, and subcutaneous adipose tissue. However, the men weighed significantly more(mean, 156 vs. 118 kg, respectively), and had a higher body mass index (51.2 vs. 46.2 kg/m2) as well as greater midthigh composition in terms of total muscle (193 vs. 130 cm2), normal-density muscle (115 vs. 79 cm2), and low-density muscle (54 vs. 37 cm2), compared with the women (all P less than.001).
At 6 months, after adjustment for baseline weight, the researchers found that the men had a significantly greater reduction in weight (–30% vs. –26%, respectively), BMI (–30% vs. –26%), subcutaneous adipose tissue (–45% vs. –31%), and deep adipose tissue (–50% vs. –31%) than did the women (all P less than or equal to .05). There were no significant differences between the sexes in the percent decline at 6 months in total muscle, normal-density muscle, and low-density muscle.
"The BPD-DS has a major impact on weight and on both thigh muscle and fat mass in both sexes," Ms. Auclair concluded.
In a later interview, she speculated that the outcome differences between sexes may be attributable to greater physical activity among men compared with women, which would explain a similar loss in midthigh muscle between the sexes, despite a greater reduction in body weight and midthigh adipose tissue among men.
"In order to confirm this hypothesis, we plan to begin a new study to determine the effectiveness of a supervised exercise program on the maintenance of muscle mass in months after the BPD-DS," she said.
Ms. Auclair said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Significantly greater reductions in weight, body mass index, and adipose tissue were seen in men vs. women who underwent biliopancreatic diversion with duodenal switch surgery, a single-center study indicated.
The study, which was conducted at the Institute of Pneumology and Cardiology at Laval University in Quebec City, was designed to assess the impact of sex on weight loss along with changes in adiposity and skeletal muscle in 42 severely obese men and women who underwent biliopancreatic diversion with duodenal switch (BPD-DS) surgery. Audrey Auclair, a Ph.D. student in pharmacy at the university, presented the study results on behalf of her colleagues at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
At baseline and 6 months, the 12 men and 30 women (mean age, 46 years) underwent anthropometric measurements and a midthigh CT scan. At baseline, the men and women were similar in terms of thickness of total, deep, and subcutaneous adipose tissue. However, the men weighed significantly more(mean, 156 vs. 118 kg, respectively), and had a higher body mass index (51.2 vs. 46.2 kg/m2) as well as greater midthigh composition in terms of total muscle (193 vs. 130 cm2), normal-density muscle (115 vs. 79 cm2), and low-density muscle (54 vs. 37 cm2), compared with the women (all P less than.001).
At 6 months, after adjustment for baseline weight, the researchers found that the men had a significantly greater reduction in weight (–30% vs. –26%, respectively), BMI (–30% vs. –26%), subcutaneous adipose tissue (–45% vs. –31%), and deep adipose tissue (–50% vs. –31%) than did the women (all P less than or equal to .05). There were no significant differences between the sexes in the percent decline at 6 months in total muscle, normal-density muscle, and low-density muscle.
"The BPD-DS has a major impact on weight and on both thigh muscle and fat mass in both sexes," Ms. Auclair concluded.
In a later interview, she speculated that the outcome differences between sexes may be attributable to greater physical activity among men compared with women, which would explain a similar loss in midthigh muscle between the sexes, despite a greater reduction in body weight and midthigh adipose tissue among men.
"In order to confirm this hypothesis, we plan to begin a new study to determine the effectiveness of a supervised exercise program on the maintenance of muscle mass in months after the BPD-DS," she said.
Ms. Auclair said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Significantly greater reductions in weight, body mass index, and adipose tissue were seen in men vs. women who underwent biliopancreatic diversion with duodenal switch surgery, a single-center study indicated.
The study, which was conducted at the Institute of Pneumology and Cardiology at Laval University in Quebec City, was designed to assess the impact of sex on weight loss along with changes in adiposity and skeletal muscle in 42 severely obese men and women who underwent biliopancreatic diversion with duodenal switch (BPD-DS) surgery. Audrey Auclair, a Ph.D. student in pharmacy at the university, presented the study results on behalf of her colleagues at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
At baseline and 6 months, the 12 men and 30 women (mean age, 46 years) underwent anthropometric measurements and a midthigh CT scan. At baseline, the men and women were similar in terms of thickness of total, deep, and subcutaneous adipose tissue. However, the men weighed significantly more(mean, 156 vs. 118 kg, respectively), and had a higher body mass index (51.2 vs. 46.2 kg/m2) as well as greater midthigh composition in terms of total muscle (193 vs. 130 cm2), normal-density muscle (115 vs. 79 cm2), and low-density muscle (54 vs. 37 cm2), compared with the women (all P less than.001).
At 6 months, after adjustment for baseline weight, the researchers found that the men had a significantly greater reduction in weight (–30% vs. –26%, respectively), BMI (–30% vs. –26%), subcutaneous adipose tissue (–45% vs. –31%), and deep adipose tissue (–50% vs. –31%) than did the women (all P less than or equal to .05). There were no significant differences between the sexes in the percent decline at 6 months in total muscle, normal-density muscle, and low-density muscle.
"The BPD-DS has a major impact on weight and on both thigh muscle and fat mass in both sexes," Ms. Auclair concluded.
In a later interview, she speculated that the outcome differences between sexes may be attributable to greater physical activity among men compared with women, which would explain a similar loss in midthigh muscle between the sexes, despite a greater reduction in body weight and midthigh adipose tissue among men.
"In order to confirm this hypothesis, we plan to begin a new study to determine the effectiveness of a supervised exercise program on the maintenance of muscle mass in months after the BPD-DS," she said.
Ms. Auclair said that she had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: At 6 months after undergoing BPD-DS surgery, men had a significantly greater reduction in weight (–-30% vs. –26%, respectively), body mass index (–30% vs. –26%), subcutaneous adipose tissue (–45% vs. –31%), and deep adipose tissue (–50% vs. –31%) than did women.
Data Source: The results are based on a single-center study of 42 severely obese patients who underwent BPD-DS.
Disclosures: Ms. Auclair said that she had no relevant financial conflicts to disclose.
Largest Series of Robotic-Assisted Gastric Bypass Reported
SAN DIEGO – At 30 days, the mortality rate from robotic-assisted gastric bypass surgery was zero and the rate of leak or abscess was just 0.3%, a multicenter study showed.
"Complications are few and may be less than with conventional laparoscopic techniques, even in different centers," Dr. Erik B. Wilson said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
In what he said is the largest reported series of its kind, Dr. Wilson and his associates reviewed 1,695 robotic-assisted Roux-en-Y gastric bypass procedures performed with the da Vinci Surgical System (Intuitive Surgical) between February 2003 and September 2011. The operations were performed at three centers: the University of Texas Health Science Center at Houston (578 procedures), Eastern Maine Medical Center, Bangor (708 procedures), and Florida Hospital Celebration Health (409). The mean body mass index of patients was 48.9 kg/m2, and the researchers evaluated complications and outcomes that occurred within the first 30 days of surgery.
Dr. Wilson, associate professor of surgery at the University of Texas Health Science Center at Houston, reported that the average length of stay was 2.2 days. Within the first 30 days of surgery there were 81 readmissions (4.8%), "which is not too different from what you’d expect in most populations," he said. Of these, 49 (2.9%) were for dehydration, 27 (1.6%) were for nausea/vomiting, and 5 (0.3%) were for stricture requiring dilation.
There were 46 reoperations (2.7%) within the first 30 days of surgery. Of these, 18 (1.06%) were for bowel obstruction/hernia, 17 (1%) were for bleeding/hematoma, 6 (0.35%) were for negative exploration of patients the surgeons were concerned about, and 5 (0.29%) were for abscess/leak.
There were 26 early major complications (1.5%). Of these, 14 (0.83%) were bleeding requiring transfusion, 5 (0.29%) were stricture requiring dilation, 3 (0.18%) were abscesses, 2 (0.12%) were anastomotic leaks, and 2 (0.12%) were cases of pulmonary embolism/infarct. There was no mortality, "which we think is very favorable," Dr. Wilson said.
Average operating times varied by center: 156 minutes in Houston, 128 minutes in Florida, and 104 minutes in Maine. "As time has gone on, and as we engage each other on how we do things, these operative times have continued to decrease, with current times approaching 90 minutes," Dr. Wilson said. "So long operative times are not necessary when you do robotic surgery."
He concluded by describing robotic-assisted bypass surgery as "an enabling technology that allows for excellent reproducible outcomes, because we have multiple centers doing it well. Future studies should focus on revisional and more complex procedures such as biliopancreatic conversion."
Dr. Wilson disclosed that he is a consultant for Intuitive Surgical, Ethicon Endo-Surgery, Apollo Endosurgery, and EndoGastric Solutions. He is also a proctor for Intuitive Surgical, and has received an educational grant from Gore.
SAN DIEGO – At 30 days, the mortality rate from robotic-assisted gastric bypass surgery was zero and the rate of leak or abscess was just 0.3%, a multicenter study showed.
"Complications are few and may be less than with conventional laparoscopic techniques, even in different centers," Dr. Erik B. Wilson said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
In what he said is the largest reported series of its kind, Dr. Wilson and his associates reviewed 1,695 robotic-assisted Roux-en-Y gastric bypass procedures performed with the da Vinci Surgical System (Intuitive Surgical) between February 2003 and September 2011. The operations were performed at three centers: the University of Texas Health Science Center at Houston (578 procedures), Eastern Maine Medical Center, Bangor (708 procedures), and Florida Hospital Celebration Health (409). The mean body mass index of patients was 48.9 kg/m2, and the researchers evaluated complications and outcomes that occurred within the first 30 days of surgery.
Dr. Wilson, associate professor of surgery at the University of Texas Health Science Center at Houston, reported that the average length of stay was 2.2 days. Within the first 30 days of surgery there were 81 readmissions (4.8%), "which is not too different from what you’d expect in most populations," he said. Of these, 49 (2.9%) were for dehydration, 27 (1.6%) were for nausea/vomiting, and 5 (0.3%) were for stricture requiring dilation.
There were 46 reoperations (2.7%) within the first 30 days of surgery. Of these, 18 (1.06%) were for bowel obstruction/hernia, 17 (1%) were for bleeding/hematoma, 6 (0.35%) were for negative exploration of patients the surgeons were concerned about, and 5 (0.29%) were for abscess/leak.
There were 26 early major complications (1.5%). Of these, 14 (0.83%) were bleeding requiring transfusion, 5 (0.29%) were stricture requiring dilation, 3 (0.18%) were abscesses, 2 (0.12%) were anastomotic leaks, and 2 (0.12%) were cases of pulmonary embolism/infarct. There was no mortality, "which we think is very favorable," Dr. Wilson said.
Average operating times varied by center: 156 minutes in Houston, 128 minutes in Florida, and 104 minutes in Maine. "As time has gone on, and as we engage each other on how we do things, these operative times have continued to decrease, with current times approaching 90 minutes," Dr. Wilson said. "So long operative times are not necessary when you do robotic surgery."
He concluded by describing robotic-assisted bypass surgery as "an enabling technology that allows for excellent reproducible outcomes, because we have multiple centers doing it well. Future studies should focus on revisional and more complex procedures such as biliopancreatic conversion."
Dr. Wilson disclosed that he is a consultant for Intuitive Surgical, Ethicon Endo-Surgery, Apollo Endosurgery, and EndoGastric Solutions. He is also a proctor for Intuitive Surgical, and has received an educational grant from Gore.
SAN DIEGO – At 30 days, the mortality rate from robotic-assisted gastric bypass surgery was zero and the rate of leak or abscess was just 0.3%, a multicenter study showed.
"Complications are few and may be less than with conventional laparoscopic techniques, even in different centers," Dr. Erik B. Wilson said at the annual meeting of the American Society for Metabolic and Bariatric Surgery.
In what he said is the largest reported series of its kind, Dr. Wilson and his associates reviewed 1,695 robotic-assisted Roux-en-Y gastric bypass procedures performed with the da Vinci Surgical System (Intuitive Surgical) between February 2003 and September 2011. The operations were performed at three centers: the University of Texas Health Science Center at Houston (578 procedures), Eastern Maine Medical Center, Bangor (708 procedures), and Florida Hospital Celebration Health (409). The mean body mass index of patients was 48.9 kg/m2, and the researchers evaluated complications and outcomes that occurred within the first 30 days of surgery.
Dr. Wilson, associate professor of surgery at the University of Texas Health Science Center at Houston, reported that the average length of stay was 2.2 days. Within the first 30 days of surgery there were 81 readmissions (4.8%), "which is not too different from what you’d expect in most populations," he said. Of these, 49 (2.9%) were for dehydration, 27 (1.6%) were for nausea/vomiting, and 5 (0.3%) were for stricture requiring dilation.
There were 46 reoperations (2.7%) within the first 30 days of surgery. Of these, 18 (1.06%) were for bowel obstruction/hernia, 17 (1%) were for bleeding/hematoma, 6 (0.35%) were for negative exploration of patients the surgeons were concerned about, and 5 (0.29%) were for abscess/leak.
There were 26 early major complications (1.5%). Of these, 14 (0.83%) were bleeding requiring transfusion, 5 (0.29%) were stricture requiring dilation, 3 (0.18%) were abscesses, 2 (0.12%) were anastomotic leaks, and 2 (0.12%) were cases of pulmonary embolism/infarct. There was no mortality, "which we think is very favorable," Dr. Wilson said.
Average operating times varied by center: 156 minutes in Houston, 128 minutes in Florida, and 104 minutes in Maine. "As time has gone on, and as we engage each other on how we do things, these operative times have continued to decrease, with current times approaching 90 minutes," Dr. Wilson said. "So long operative times are not necessary when you do robotic surgery."
He concluded by describing robotic-assisted bypass surgery as "an enabling technology that allows for excellent reproducible outcomes, because we have multiple centers doing it well. Future studies should focus on revisional and more complex procedures such as biliopancreatic conversion."
Dr. Wilson disclosed that he is a consultant for Intuitive Surgical, Ethicon Endo-Surgery, Apollo Endosurgery, and EndoGastric Solutions. He is also a proctor for Intuitive Surgical, and has received an educational grant from Gore.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Bariatric Surgery Yields Durable Results for Diabetic Nephropathy
SAN DIEGO – Bariatric surgery induced a significant and durable improvement in diabetic nephropathy after 5 years of follow-up, results from a single-center study showed.
"In addition to significant weight loss, [bariatric surgery] achieves profound metabolic effects, including improvements in glycemic control and insulin sensitivity, as well as a decrease in cardiovascular disease risk and mortality," lead author Dr. Helen M. Heneghan said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "We hypothesized that improving diabetic control with bariatric surgery may have positive effects on the end-organ complications of this disease, such as diabetic nephropathy. We also wanted to address one of the prevailing questions in this field: whether or not the effects of bariatric surgery on diabetes and its complications are durable."
Dr. Heneghan, a bariatric surgery fellow at the Cleveland Clinic Bariatric and Metabolic Institute, and her associates identified 52 patients who underwent bariatric surgery at the institute and had completed the 5-year follow-up. At baseline, the mean age of patients was 51 years, and 75% were women. Their preoperative mean body mass index was 49 kg/m2, 84% had hypertension, and 71% had hyperlipidemia. Preoperatively, the mean duration of diabetes was 8.6 years, and 29% were already taking insulin. Their mean hemoglobin A1c level was 7.7%, and 38% had diabetic nephropathy as indicated by microalbuminuria (30-299 mg of albumin per g of creatinine) or macroalbuminura (greater than 300 mg/g), and 22% of patients were prescribed an ACE inhibitor or angiotensin receptor blocker.
The majority of patients (69%) underwent gastric bypass; 25% had laparoscopic gastric banding and 6% had sleeve gastrectomy. Dr. Heneghan reported that 5 years after their surgery, 44% of patients had sustained remission of their type 2 diabetes, 33% had a significant improvement, and 23% had no change or worsening of their disease. This latter cohort "had the least amount of weight loss and were those who had the longest standing duration of diabetes preoperatively."
The rates of patients with remission, improvement, or change in hypertension were 16%, 50%, and 34%, respectively, whereas the rates for patients with dyslipidemia were 39%, 20%, and 41%.
Only 25% of patients who did not have diabetic nephropathy at the time of surgery went on to develop the condition. Among patients with preoperative microalbuminuria, 42% remained stable whereas 58% regressed and had no albuminuria 5 years after surgery. Similarly, among patients with preoperative macroalbuminuria, 50% remained stable and 50% regressed and had no albuminuria at 5 years.*
There were no preoperative differences in the mean urinary albumin to creatinine ratio (ACR) between patients who were and patients who were not prescribed a renoprotective agent. However, postoperatively, patients who were not on a renoprotective agent had a significantly lower urinary ACR, compared with those who remained on a renoprotective agent (P = .039). "This probably reflects the fact that patients who had improvement of their diabetes and regression or nonprogression of their nephropathy status also had a significant improvement in – or remission of – hypertension, and were no longer prescribed an antihypertensive medication," Dr. Heneghan explained.
She characterized the study’s overall findings as "remarkable, considering that diabetes is a chronic, progressive disease, and certainly warrant further investigation in the form of a prospective and larger study."
Dr. Heneghan said that she had no relevant financial conflicts to disclose.
*CORRECTION 8/28/12: The original sentence contained an error in describing the patients. The sentence should read" "Similarly, among patients with preoperative macroalbuminuria, 50% remained stable and 50% regressed and had no albuminuria at 5 years."
SAN DIEGO – Bariatric surgery induced a significant and durable improvement in diabetic nephropathy after 5 years of follow-up, results from a single-center study showed.
"In addition to significant weight loss, [bariatric surgery] achieves profound metabolic effects, including improvements in glycemic control and insulin sensitivity, as well as a decrease in cardiovascular disease risk and mortality," lead author Dr. Helen M. Heneghan said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "We hypothesized that improving diabetic control with bariatric surgery may have positive effects on the end-organ complications of this disease, such as diabetic nephropathy. We also wanted to address one of the prevailing questions in this field: whether or not the effects of bariatric surgery on diabetes and its complications are durable."
Dr. Heneghan, a bariatric surgery fellow at the Cleveland Clinic Bariatric and Metabolic Institute, and her associates identified 52 patients who underwent bariatric surgery at the institute and had completed the 5-year follow-up. At baseline, the mean age of patients was 51 years, and 75% were women. Their preoperative mean body mass index was 49 kg/m2, 84% had hypertension, and 71% had hyperlipidemia. Preoperatively, the mean duration of diabetes was 8.6 years, and 29% were already taking insulin. Their mean hemoglobin A1c level was 7.7%, and 38% had diabetic nephropathy as indicated by microalbuminuria (30-299 mg of albumin per g of creatinine) or macroalbuminura (greater than 300 mg/g), and 22% of patients were prescribed an ACE inhibitor or angiotensin receptor blocker.
The majority of patients (69%) underwent gastric bypass; 25% had laparoscopic gastric banding and 6% had sleeve gastrectomy. Dr. Heneghan reported that 5 years after their surgery, 44% of patients had sustained remission of their type 2 diabetes, 33% had a significant improvement, and 23% had no change or worsening of their disease. This latter cohort "had the least amount of weight loss and were those who had the longest standing duration of diabetes preoperatively."
The rates of patients with remission, improvement, or change in hypertension were 16%, 50%, and 34%, respectively, whereas the rates for patients with dyslipidemia were 39%, 20%, and 41%.
Only 25% of patients who did not have diabetic nephropathy at the time of surgery went on to develop the condition. Among patients with preoperative microalbuminuria, 42% remained stable whereas 58% regressed and had no albuminuria 5 years after surgery. Similarly, among patients with preoperative macroalbuminuria, 50% remained stable and 50% regressed and had no albuminuria at 5 years.*
There were no preoperative differences in the mean urinary albumin to creatinine ratio (ACR) between patients who were and patients who were not prescribed a renoprotective agent. However, postoperatively, patients who were not on a renoprotective agent had a significantly lower urinary ACR, compared with those who remained on a renoprotective agent (P = .039). "This probably reflects the fact that patients who had improvement of their diabetes and regression or nonprogression of their nephropathy status also had a significant improvement in – or remission of – hypertension, and were no longer prescribed an antihypertensive medication," Dr. Heneghan explained.
She characterized the study’s overall findings as "remarkable, considering that diabetes is a chronic, progressive disease, and certainly warrant further investigation in the form of a prospective and larger study."
Dr. Heneghan said that she had no relevant financial conflicts to disclose.
*CORRECTION 8/28/12: The original sentence contained an error in describing the patients. The sentence should read" "Similarly, among patients with preoperative macroalbuminuria, 50% remained stable and 50% regressed and had no albuminuria at 5 years."
SAN DIEGO – Bariatric surgery induced a significant and durable improvement in diabetic nephropathy after 5 years of follow-up, results from a single-center study showed.
"In addition to significant weight loss, [bariatric surgery] achieves profound metabolic effects, including improvements in glycemic control and insulin sensitivity, as well as a decrease in cardiovascular disease risk and mortality," lead author Dr. Helen M. Heneghan said at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "We hypothesized that improving diabetic control with bariatric surgery may have positive effects on the end-organ complications of this disease, such as diabetic nephropathy. We also wanted to address one of the prevailing questions in this field: whether or not the effects of bariatric surgery on diabetes and its complications are durable."
Dr. Heneghan, a bariatric surgery fellow at the Cleveland Clinic Bariatric and Metabolic Institute, and her associates identified 52 patients who underwent bariatric surgery at the institute and had completed the 5-year follow-up. At baseline, the mean age of patients was 51 years, and 75% were women. Their preoperative mean body mass index was 49 kg/m2, 84% had hypertension, and 71% had hyperlipidemia. Preoperatively, the mean duration of diabetes was 8.6 years, and 29% were already taking insulin. Their mean hemoglobin A1c level was 7.7%, and 38% had diabetic nephropathy as indicated by microalbuminuria (30-299 mg of albumin per g of creatinine) or macroalbuminura (greater than 300 mg/g), and 22% of patients were prescribed an ACE inhibitor or angiotensin receptor blocker.
The majority of patients (69%) underwent gastric bypass; 25% had laparoscopic gastric banding and 6% had sleeve gastrectomy. Dr. Heneghan reported that 5 years after their surgery, 44% of patients had sustained remission of their type 2 diabetes, 33% had a significant improvement, and 23% had no change or worsening of their disease. This latter cohort "had the least amount of weight loss and were those who had the longest standing duration of diabetes preoperatively."
The rates of patients with remission, improvement, or change in hypertension were 16%, 50%, and 34%, respectively, whereas the rates for patients with dyslipidemia were 39%, 20%, and 41%.
Only 25% of patients who did not have diabetic nephropathy at the time of surgery went on to develop the condition. Among patients with preoperative microalbuminuria, 42% remained stable whereas 58% regressed and had no albuminuria 5 years after surgery. Similarly, among patients with preoperative macroalbuminuria, 50% remained stable and 50% regressed and had no albuminuria at 5 years.*
There were no preoperative differences in the mean urinary albumin to creatinine ratio (ACR) between patients who were and patients who were not prescribed a renoprotective agent. However, postoperatively, patients who were not on a renoprotective agent had a significantly lower urinary ACR, compared with those who remained on a renoprotective agent (P = .039). "This probably reflects the fact that patients who had improvement of their diabetes and regression or nonprogression of their nephropathy status also had a significant improvement in – or remission of – hypertension, and were no longer prescribed an antihypertensive medication," Dr. Heneghan explained.
She characterized the study’s overall findings as "remarkable, considering that diabetes is a chronic, progressive disease, and certainly warrant further investigation in the form of a prospective and larger study."
Dr. Heneghan said that she had no relevant financial conflicts to disclose.
*CORRECTION 8/28/12: The original sentence contained an error in describing the patients. The sentence should read" "Similarly, among patients with preoperative macroalbuminuria, 50% remained stable and 50% regressed and had no albuminuria at 5 years."
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: Among patients with preoperative microalbuminuria, 42% remained stable 5 years after their bariatric surgery, whereas 58% regressed and had no albuminuria. Similarly, among patients with preoperative macroalbuminuria, 50% remained stable, and 50% regressed and had no albuminuria at 5 years.
Data Source: The study included 52 patients who underwent bariatric surgery at the Cleveland Clinic and had completed the 5-year follow-up.
Disclosures: Dr. Heneghan said that she had no relevant financial conflicts to disclose.
BOLD Analysis Backs Safety of Sleeve Gastrectomy
SAN DIEGO – Laparoscopic sleeve gastrectomy is positioned between gastric banding and the laparoscopic gastric bypass for both safety and efficacy, results from the largest comparative study of its kind demonstrated.
The finding comes at a time when the Centers for Medicare and Medicaid Services is reviewing evidence to consider including sleeve gastrectomy as a covered benefit. Currently, gastric bypass, vertical banded gastroplasty, duodenal switch, and gastric banding are the only CMS-sanctioned bariatric procedures.
The study, which involved nearly 300,000 patients, "shows that across the board, regardless of the procedure, bariatric surgery is safe and effective," Dr. John M. Morton said in an interview at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "The emerging new procedure, the sleeve gastrectomy, is shown to be right between the bypass and the band. As a result, we have seen more interest from payers to cover it. In fact there are about 100 million lives that are covered. Our only outlier is CMS in deciding to cover. We hope that these data will help influence CMS in granting coverage for the sleeve gastrectomy."
Dr. Morton, associate professor of surgery and director of bariatric surgery at Stanford Hospitals and Clinics at Stanford (Calif.) University, and his associates examined BOLD (Bariatric Outcomes Longitudinal Database) to identify patients who had undergone laparoscopic Roux-en-Y gastric bypass (LRNYGB), gastric banding (LAGB), and sleeve gastrectomy (LSG) from June 2007 to December 2010. BOLD, the largest bariatric-specific database, is maintained by the ASMBS Bariatric Surgery Center of Excellence program, and includes more than 1,200 surgeons at 540 hospitals. Dr. Morton described the data as a "clinically rich" variable set that includes age, gender, race, insurance status, body mass index, excess body weight, and comorbidities.
"There is a definite need for more data around comparison of different procedures," Dr. Morton said at the meeting. "Our study hypothesis is very straightforward: Do demographics and outcomes for bariatric surgery vary by procedure?"
The primary outcomes were 30-day mortality, serious complications, and readmissions. The definitions of serious complications included death, anastomotic leakage, cardiac arrest, deep venous thrombosis, evisceration, heart failure and/or pulmonary edema, liver failure, and bleeding requiring transfusion.
Dr. Morton reported outcomes from 117,365 patients in the LAGB group, 138,222 in the LRNYGB group, and 16,139 in the LSG group. Patients in each group were generally the same age (a mean of 45, 46, and 45 years, respectively), mostly female (78%, 79%, and 74%), and mostly white (72%, 73%, and 72%). "The one area where there was a sizable difference was around self-pay," Dr. Morton said. About 21% of patients in the LSG group paid out-of-pocket, compared with 6% of those in the LAGB group and 2% of those in the LRNYGB group.
The proportion of preoperative comorbidities was similar among the three groups, with two exceptions. The prevalence of diabetes was highest in the LRNYGB group (37%, compared with 30% in the LSG group and 28% in the LAGB group; P less than .0001). A similar association was seen in the proportion of patients with five or more preoperative comorbidities (62%, 55%, and 52%, respectively; P less than .0001).
The mean length of stay was 0.7 days for the LAGB group, 1.9 days for the LSG group, and 2.3 days for the LRNYGB group. The percent change in BMI at 12 months was 7.6%, 13.4%, and 16.4%, respectively; the rate of 30-day serious complications was 0.25%, 0.96%, and 1.25%; and the rate of 30-day mortality was 0.03%, 0.08%, and 0.14%. All differences between the groups were significant (P less than .0001).
"If you look at the remainder of the safety outcomes – everything from 30-day readmission to 30-day reoperation – it’s pretty much the same order, with the band group having the lowest [percentage], and the bypass having the highest, and the sleeve being right in between," Dr. Morton said. "When we looked at age greater than 65 in isolation, we found that the order of safety remains, with the banding having the least amount of mortality and the sleeve being right between the band procedure and the bypass."
Logistic regression analysis revealed several significant factors that predicted serious adverse events at 30 days: male gender (odds ratio, 1.67), having nonprivate insurance (OR, 1.15), stepwise progression with increasing age (for example, an OR of 1.27 for those aged 26-35 years and an OR of 4.42 for those above age 65), and stepwise progression with increasing BMI (for example, an OR of 1.37 for those with a BMI of 46-55 kg/m2 and an OR of 3.03 for those with a BMI greater than 65).
The invited discussant, Dr. Matthew M. Hutter, of Massachusetts General Hospital, Boston, described the size of the overall study cohort as remarkable. "What I find most interesting about this study is that it shows that sleeve gastrectomy – a brand-new, very complex procedure – can be introduced safely and effectively when performed under the standards of a bariatric accreditation program," Dr. Hutter said. "Other surgical procedures such as laparoscopic cholecystectomy or laparoscopic colectomy had very high morbidity and conversion rates when they were first implemented. However, this new complex procedure has been safe and effective from the get-go, and that is really quite impressive. The other remarkable finding is how consistent this is with all of the other major [bariatric surgery] data collection programs."
Dr. Morton acknowledged certain limitations of the study, including the fact that 1-year follow-up was available in only 60% of patients, while 30-day follow-up was available in 98% of the cohort. "Potentially, patients could have been admitted to other hospitals," he added. "These are research-consented patients, so about 70% consented. Some of this is surgeon-directed reporting."
Dr. Morton said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Laparoscopic sleeve gastrectomy is positioned between gastric banding and the laparoscopic gastric bypass for both safety and efficacy, results from the largest comparative study of its kind demonstrated.
The finding comes at a time when the Centers for Medicare and Medicaid Services is reviewing evidence to consider including sleeve gastrectomy as a covered benefit. Currently, gastric bypass, vertical banded gastroplasty, duodenal switch, and gastric banding are the only CMS-sanctioned bariatric procedures.
The study, which involved nearly 300,000 patients, "shows that across the board, regardless of the procedure, bariatric surgery is safe and effective," Dr. John M. Morton said in an interview at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "The emerging new procedure, the sleeve gastrectomy, is shown to be right between the bypass and the band. As a result, we have seen more interest from payers to cover it. In fact there are about 100 million lives that are covered. Our only outlier is CMS in deciding to cover. We hope that these data will help influence CMS in granting coverage for the sleeve gastrectomy."
Dr. Morton, associate professor of surgery and director of bariatric surgery at Stanford Hospitals and Clinics at Stanford (Calif.) University, and his associates examined BOLD (Bariatric Outcomes Longitudinal Database) to identify patients who had undergone laparoscopic Roux-en-Y gastric bypass (LRNYGB), gastric banding (LAGB), and sleeve gastrectomy (LSG) from June 2007 to December 2010. BOLD, the largest bariatric-specific database, is maintained by the ASMBS Bariatric Surgery Center of Excellence program, and includes more than 1,200 surgeons at 540 hospitals. Dr. Morton described the data as a "clinically rich" variable set that includes age, gender, race, insurance status, body mass index, excess body weight, and comorbidities.
"There is a definite need for more data around comparison of different procedures," Dr. Morton said at the meeting. "Our study hypothesis is very straightforward: Do demographics and outcomes for bariatric surgery vary by procedure?"
The primary outcomes were 30-day mortality, serious complications, and readmissions. The definitions of serious complications included death, anastomotic leakage, cardiac arrest, deep venous thrombosis, evisceration, heart failure and/or pulmonary edema, liver failure, and bleeding requiring transfusion.
Dr. Morton reported outcomes from 117,365 patients in the LAGB group, 138,222 in the LRNYGB group, and 16,139 in the LSG group. Patients in each group were generally the same age (a mean of 45, 46, and 45 years, respectively), mostly female (78%, 79%, and 74%), and mostly white (72%, 73%, and 72%). "The one area where there was a sizable difference was around self-pay," Dr. Morton said. About 21% of patients in the LSG group paid out-of-pocket, compared with 6% of those in the LAGB group and 2% of those in the LRNYGB group.
The proportion of preoperative comorbidities was similar among the three groups, with two exceptions. The prevalence of diabetes was highest in the LRNYGB group (37%, compared with 30% in the LSG group and 28% in the LAGB group; P less than .0001). A similar association was seen in the proportion of patients with five or more preoperative comorbidities (62%, 55%, and 52%, respectively; P less than .0001).
The mean length of stay was 0.7 days for the LAGB group, 1.9 days for the LSG group, and 2.3 days for the LRNYGB group. The percent change in BMI at 12 months was 7.6%, 13.4%, and 16.4%, respectively; the rate of 30-day serious complications was 0.25%, 0.96%, and 1.25%; and the rate of 30-day mortality was 0.03%, 0.08%, and 0.14%. All differences between the groups were significant (P less than .0001).
"If you look at the remainder of the safety outcomes – everything from 30-day readmission to 30-day reoperation – it’s pretty much the same order, with the band group having the lowest [percentage], and the bypass having the highest, and the sleeve being right in between," Dr. Morton said. "When we looked at age greater than 65 in isolation, we found that the order of safety remains, with the banding having the least amount of mortality and the sleeve being right between the band procedure and the bypass."
Logistic regression analysis revealed several significant factors that predicted serious adverse events at 30 days: male gender (odds ratio, 1.67), having nonprivate insurance (OR, 1.15), stepwise progression with increasing age (for example, an OR of 1.27 for those aged 26-35 years and an OR of 4.42 for those above age 65), and stepwise progression with increasing BMI (for example, an OR of 1.37 for those with a BMI of 46-55 kg/m2 and an OR of 3.03 for those with a BMI greater than 65).
The invited discussant, Dr. Matthew M. Hutter, of Massachusetts General Hospital, Boston, described the size of the overall study cohort as remarkable. "What I find most interesting about this study is that it shows that sleeve gastrectomy – a brand-new, very complex procedure – can be introduced safely and effectively when performed under the standards of a bariatric accreditation program," Dr. Hutter said. "Other surgical procedures such as laparoscopic cholecystectomy or laparoscopic colectomy had very high morbidity and conversion rates when they were first implemented. However, this new complex procedure has been safe and effective from the get-go, and that is really quite impressive. The other remarkable finding is how consistent this is with all of the other major [bariatric surgery] data collection programs."
Dr. Morton acknowledged certain limitations of the study, including the fact that 1-year follow-up was available in only 60% of patients, while 30-day follow-up was available in 98% of the cohort. "Potentially, patients could have been admitted to other hospitals," he added. "These are research-consented patients, so about 70% consented. Some of this is surgeon-directed reporting."
Dr. Morton said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Laparoscopic sleeve gastrectomy is positioned between gastric banding and the laparoscopic gastric bypass for both safety and efficacy, results from the largest comparative study of its kind demonstrated.
The finding comes at a time when the Centers for Medicare and Medicaid Services is reviewing evidence to consider including sleeve gastrectomy as a covered benefit. Currently, gastric bypass, vertical banded gastroplasty, duodenal switch, and gastric banding are the only CMS-sanctioned bariatric procedures.
The study, which involved nearly 300,000 patients, "shows that across the board, regardless of the procedure, bariatric surgery is safe and effective," Dr. John M. Morton said in an interview at the annual meeting of the American Society for Metabolic and Bariatric Surgery. "The emerging new procedure, the sleeve gastrectomy, is shown to be right between the bypass and the band. As a result, we have seen more interest from payers to cover it. In fact there are about 100 million lives that are covered. Our only outlier is CMS in deciding to cover. We hope that these data will help influence CMS in granting coverage for the sleeve gastrectomy."
Dr. Morton, associate professor of surgery and director of bariatric surgery at Stanford Hospitals and Clinics at Stanford (Calif.) University, and his associates examined BOLD (Bariatric Outcomes Longitudinal Database) to identify patients who had undergone laparoscopic Roux-en-Y gastric bypass (LRNYGB), gastric banding (LAGB), and sleeve gastrectomy (LSG) from June 2007 to December 2010. BOLD, the largest bariatric-specific database, is maintained by the ASMBS Bariatric Surgery Center of Excellence program, and includes more than 1,200 surgeons at 540 hospitals. Dr. Morton described the data as a "clinically rich" variable set that includes age, gender, race, insurance status, body mass index, excess body weight, and comorbidities.
"There is a definite need for more data around comparison of different procedures," Dr. Morton said at the meeting. "Our study hypothesis is very straightforward: Do demographics and outcomes for bariatric surgery vary by procedure?"
The primary outcomes were 30-day mortality, serious complications, and readmissions. The definitions of serious complications included death, anastomotic leakage, cardiac arrest, deep venous thrombosis, evisceration, heart failure and/or pulmonary edema, liver failure, and bleeding requiring transfusion.
Dr. Morton reported outcomes from 117,365 patients in the LAGB group, 138,222 in the LRNYGB group, and 16,139 in the LSG group. Patients in each group were generally the same age (a mean of 45, 46, and 45 years, respectively), mostly female (78%, 79%, and 74%), and mostly white (72%, 73%, and 72%). "The one area where there was a sizable difference was around self-pay," Dr. Morton said. About 21% of patients in the LSG group paid out-of-pocket, compared with 6% of those in the LAGB group and 2% of those in the LRNYGB group.
The proportion of preoperative comorbidities was similar among the three groups, with two exceptions. The prevalence of diabetes was highest in the LRNYGB group (37%, compared with 30% in the LSG group and 28% in the LAGB group; P less than .0001). A similar association was seen in the proportion of patients with five or more preoperative comorbidities (62%, 55%, and 52%, respectively; P less than .0001).
The mean length of stay was 0.7 days for the LAGB group, 1.9 days for the LSG group, and 2.3 days for the LRNYGB group. The percent change in BMI at 12 months was 7.6%, 13.4%, and 16.4%, respectively; the rate of 30-day serious complications was 0.25%, 0.96%, and 1.25%; and the rate of 30-day mortality was 0.03%, 0.08%, and 0.14%. All differences between the groups were significant (P less than .0001).
"If you look at the remainder of the safety outcomes – everything from 30-day readmission to 30-day reoperation – it’s pretty much the same order, with the band group having the lowest [percentage], and the bypass having the highest, and the sleeve being right in between," Dr. Morton said. "When we looked at age greater than 65 in isolation, we found that the order of safety remains, with the banding having the least amount of mortality and the sleeve being right between the band procedure and the bypass."
Logistic regression analysis revealed several significant factors that predicted serious adverse events at 30 days: male gender (odds ratio, 1.67), having nonprivate insurance (OR, 1.15), stepwise progression with increasing age (for example, an OR of 1.27 for those aged 26-35 years and an OR of 4.42 for those above age 65), and stepwise progression with increasing BMI (for example, an OR of 1.37 for those with a BMI of 46-55 kg/m2 and an OR of 3.03 for those with a BMI greater than 65).
The invited discussant, Dr. Matthew M. Hutter, of Massachusetts General Hospital, Boston, described the size of the overall study cohort as remarkable. "What I find most interesting about this study is that it shows that sleeve gastrectomy – a brand-new, very complex procedure – can be introduced safely and effectively when performed under the standards of a bariatric accreditation program," Dr. Hutter said. "Other surgical procedures such as laparoscopic cholecystectomy or laparoscopic colectomy had very high morbidity and conversion rates when they were first implemented. However, this new complex procedure has been safe and effective from the get-go, and that is really quite impressive. The other remarkable finding is how consistent this is with all of the other major [bariatric surgery] data collection programs."
Dr. Morton acknowledged certain limitations of the study, including the fact that 1-year follow-up was available in only 60% of patients, while 30-day follow-up was available in 98% of the cohort. "Potentially, patients could have been admitted to other hospitals," he added. "These are research-consented patients, so about 70% consented. Some of this is surgeon-directed reporting."
Dr. Morton said that he had no relevant financial conflicts to disclose.
AT THE ANNUAL MEETING OF THE AMERICAN SOCIETY FOR METABOLIC AND BARIATRIC SURGERY
Major Finding: The rate of 30-day serious complications was 0.25% among those who underwent laparoscopic gastric banding, 0.96% among those who underwent laparoscopic sleeve gastrectomy, and 1.25% among those who underwent laparoscopic Roux-en-Y gastric bypass, while the rate of 30-day mortality was 0.03%, 0.08%, and 0.14%, respectively.
Data Source: The data analysis was based on 271,726 patients from the Bariatric Outcomes Longitudinal Database who underwent bariatric surgery from June 2007 to December 2010.
Disclosures: Dr. Morton said that he had no relevant financial conflicts to disclose.