User login
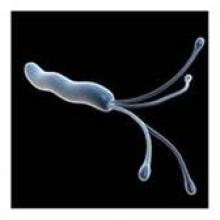
H. Pylori Infection, Colonic Neoplasms Linked
SAN DIEGO – Patients with Helicobacter pylori infection face a significantly increased risk for developing colonic neoplasms, according to what is believed to be the largest investigation of the association.
Several studies have suggested that H. pylori infection is a risk factor for colonic neoplasms, but all of them involved relatively small case populations, Dr. Amnon Sonnenberg explained at the annual Digestive Disease Week.
Dr. Sonnenberg, a gastroenterologist with the Portland (Ore.) VA Medical Center, investigated the relationship between H. pylori infection and the presence of colonic neoplasms in 156,269 patients who had undergone both a colonoscopy and an esophagogastroduodenoscopy. Surgical pathology samples from all the patients were stored in an electronic database at the Miraca Research Institute, a specialized gastrointestinal lab that serves private outpatient endoscopy centers throughout the United States. More than 1,500 gastroenterologists contributed to the database between January 2008 and December 2011.
Patients were an average age of 58 years, and 59% were female. Among the total, 16,759 (11%) had H. pylori gastritis on immunochemistry. The prevalence of H. pylori gastritis was 9% in patients without polyps, 11% in patients with hyperplastic polyps, 12% in patients with adenoma, 14% in patients with advanced adenoma, 15% in patients with villous adenoma or polyps with high-grade dysplasia, and 18% in patients with colonic adenocarcinoma.
There was a slight trend for the prevalence of H. pylori to rise with the increasing number, as well as the size, of adenomatous polyps. The prevalence of H. pylori was similar for all colon sites.
Significant associations also were noted between the development of colonic adenoma and the following other types of gastric histopathology: intestinal metaplasia, gastric adenoma, gastric cancer, and gastric lymphoma. Similar but even more significant associations were seen between advanced adenoma and these types of gastric histopathology.
Multivariate logistic regression confirmed that the development of H. pylori gastritis was associated with advanced age, male gender, hyperplastic polyps, adenoma, villous adenoma or high-grade dysplasia, and adenocarcinoma.
"H. pylori gastritis confers an increased risk for colonic neoplasm," concluded Dr. Sonnenberg, who is also professor of medicine in the division of gastroenterology and hepatology at Oregon Health and Science University.
"The risk applies to all types of colonic neoplasms and appears to increase with advancing stage of the neoplasm from hyperplastic and adenomatous polyps to tubulovillous adenoma, adenoma with high-grade dysplasia, and adenocarcinoma. Such risk is not limited to chronic active gastritis but is found in other types of gastric histopathology related to H. pylori, such as gastric intestinal metaplasia, gastric adenoma, gastric lymphoma, and gastric cancer," he said.
Long-term infection with H. pylori "may be related to elevated gastrin levels that may act as a growth factor," he speculated.
Dr. Sonnenberg disclosed having received a research grant from Takeda Pharmaceutical Company. No support was received for this study.
SAN DIEGO – Patients with Helicobacter pylori infection face a significantly increased risk for developing colonic neoplasms, according to what is believed to be the largest investigation of the association.
Several studies have suggested that H. pylori infection is a risk factor for colonic neoplasms, but all of them involved relatively small case populations, Dr. Amnon Sonnenberg explained at the annual Digestive Disease Week.
Dr. Sonnenberg, a gastroenterologist with the Portland (Ore.) VA Medical Center, investigated the relationship between H. pylori infection and the presence of colonic neoplasms in 156,269 patients who had undergone both a colonoscopy and an esophagogastroduodenoscopy. Surgical pathology samples from all the patients were stored in an electronic database at the Miraca Research Institute, a specialized gastrointestinal lab that serves private outpatient endoscopy centers throughout the United States. More than 1,500 gastroenterologists contributed to the database between January 2008 and December 2011.
Patients were an average age of 58 years, and 59% were female. Among the total, 16,759 (11%) had H. pylori gastritis on immunochemistry. The prevalence of H. pylori gastritis was 9% in patients without polyps, 11% in patients with hyperplastic polyps, 12% in patients with adenoma, 14% in patients with advanced adenoma, 15% in patients with villous adenoma or polyps with high-grade dysplasia, and 18% in patients with colonic adenocarcinoma.
There was a slight trend for the prevalence of H. pylori to rise with the increasing number, as well as the size, of adenomatous polyps. The prevalence of H. pylori was similar for all colon sites.
Significant associations also were noted between the development of colonic adenoma and the following other types of gastric histopathology: intestinal metaplasia, gastric adenoma, gastric cancer, and gastric lymphoma. Similar but even more significant associations were seen between advanced adenoma and these types of gastric histopathology.
Multivariate logistic regression confirmed that the development of H. pylori gastritis was associated with advanced age, male gender, hyperplastic polyps, adenoma, villous adenoma or high-grade dysplasia, and adenocarcinoma.
"H. pylori gastritis confers an increased risk for colonic neoplasm," concluded Dr. Sonnenberg, who is also professor of medicine in the division of gastroenterology and hepatology at Oregon Health and Science University.
"The risk applies to all types of colonic neoplasms and appears to increase with advancing stage of the neoplasm from hyperplastic and adenomatous polyps to tubulovillous adenoma, adenoma with high-grade dysplasia, and adenocarcinoma. Such risk is not limited to chronic active gastritis but is found in other types of gastric histopathology related to H. pylori, such as gastric intestinal metaplasia, gastric adenoma, gastric lymphoma, and gastric cancer," he said.
Long-term infection with H. pylori "may be related to elevated gastrin levels that may act as a growth factor," he speculated.
Dr. Sonnenberg disclosed having received a research grant from Takeda Pharmaceutical Company. No support was received for this study.
SAN DIEGO – Patients with Helicobacter pylori infection face a significantly increased risk for developing colonic neoplasms, according to what is believed to be the largest investigation of the association.
Several studies have suggested that H. pylori infection is a risk factor for colonic neoplasms, but all of them involved relatively small case populations, Dr. Amnon Sonnenberg explained at the annual Digestive Disease Week.
Dr. Sonnenberg, a gastroenterologist with the Portland (Ore.) VA Medical Center, investigated the relationship between H. pylori infection and the presence of colonic neoplasms in 156,269 patients who had undergone both a colonoscopy and an esophagogastroduodenoscopy. Surgical pathology samples from all the patients were stored in an electronic database at the Miraca Research Institute, a specialized gastrointestinal lab that serves private outpatient endoscopy centers throughout the United States. More than 1,500 gastroenterologists contributed to the database between January 2008 and December 2011.
Patients were an average age of 58 years, and 59% were female. Among the total, 16,759 (11%) had H. pylori gastritis on immunochemistry. The prevalence of H. pylori gastritis was 9% in patients without polyps, 11% in patients with hyperplastic polyps, 12% in patients with adenoma, 14% in patients with advanced adenoma, 15% in patients with villous adenoma or polyps with high-grade dysplasia, and 18% in patients with colonic adenocarcinoma.
There was a slight trend for the prevalence of H. pylori to rise with the increasing number, as well as the size, of adenomatous polyps. The prevalence of H. pylori was similar for all colon sites.
Significant associations also were noted between the development of colonic adenoma and the following other types of gastric histopathology: intestinal metaplasia, gastric adenoma, gastric cancer, and gastric lymphoma. Similar but even more significant associations were seen between advanced adenoma and these types of gastric histopathology.
Multivariate logistic regression confirmed that the development of H. pylori gastritis was associated with advanced age, male gender, hyperplastic polyps, adenoma, villous adenoma or high-grade dysplasia, and adenocarcinoma.
"H. pylori gastritis confers an increased risk for colonic neoplasm," concluded Dr. Sonnenberg, who is also professor of medicine in the division of gastroenterology and hepatology at Oregon Health and Science University.
"The risk applies to all types of colonic neoplasms and appears to increase with advancing stage of the neoplasm from hyperplastic and adenomatous polyps to tubulovillous adenoma, adenoma with high-grade dysplasia, and adenocarcinoma. Such risk is not limited to chronic active gastritis but is found in other types of gastric histopathology related to H. pylori, such as gastric intestinal metaplasia, gastric adenoma, gastric lymphoma, and gastric cancer," he said.
Long-term infection with H. pylori "may be related to elevated gastrin levels that may act as a growth factor," he speculated.
Dr. Sonnenberg disclosed having received a research grant from Takeda Pharmaceutical Company. No support was received for this study.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: The prevalence of H. pylori gastritis was 9% in patients without polyps, 11% in patients with hyperplastic polyps, 12% in patients with adenoma, 14% in patients with advanced adenoma, 15% in patients with villous adenoma or polyps with high-grade dysplasia, and 18% in patients with colonic adenocarcinoma.
Data Source: Findings are based on an analysis of pathology data from 156,269 patients who had undergone both a colonoscopy and an esophagogastroduodenoscopy.
Disclosures: Dr. Sonnenberg disclosed having received a research grant from Takeda Pharmaceutical Company. No support was received for this study.
Fundoplication Doesn't Diminish Efficacy of Ablation in Barrett's Patients
SAN DIEGO – Radiofrequency ablation was found to be safe and effective in treating Barrett’s esophagus patients, whether or not they had undergone a prior fundoplication, based on results from a multicenter registry study.
"Gastroesophageal reflux causes esophageal mucosal injury and inflammation that may impair healing and squamous re-epithelialization after treatment of Barrett’s esophagus [BE] with radiofrequency ablation [RFA]," Dr. Nicholas J. Shaheen said at the annual Digestive Disease Week.
"It is unclear if fundoplication surgery, as a mechanical barrier to all reflux, improves treatment outcomes of RFA for BE. Similarly, some have postulated that change in the conformation of the hiatus with surgery might make ablation problematic."
Dr. Shaheen, director of the Center for Esophageal Diseases and Swallowing at the University of North Carolina, Chapel Hill, and his associates conducted the largest study of its kind, he said. They evaluated records from the RFA Patient Registry to assess the relationship between prior fundoplication and both efficacy and safety outcomes in patients with BE who were treated with RFA.
The registry comprises 113 community-based and 35 academic-affiliated medical institutions in the United States. "About 75% of these institutions are private practices, so this is an interesting snapshot of RFA as it’s practiced outside of tertiary care centers," Dr. Shaheen said.
All study patients had BE confirmed by endoscopy and histology, and had undergone treatment with RFA. Enrollment commenced in July 2007 and ended in July 2011. Data were gleaned from standard case report forms and included demographics; relevant medical history; histologic grade prior to treatment; endoscopic findings; dates and total number of RFA treatment sessions; and ablation outcomes and complications.
"The vast amount of data is prospective, but less than 15% is retrospective," Dr. Shaheen said. "This is a registry study, so we could not mandate treatment, but a treatment protocol was suggested." Twice-daily use of proton pump inhibitors (PPIs) was recommended to everyone in the study, including those post fundoplication.
The mean age of patients was 61 years, and the majority were white. The mean pretreatment length of BE was about 4 cm, and patients received an average of 2.5 treatments with RFA. "Importantly, in this registry, about half of the patients had nondysplastic disease," Dr. Shaheen said. "Also, roughly 20% in each group had low- and high-grade dysplasia."
Dr. Shaheen reported results from the safety cohort, which included 5,537 patients who received RFA, and results from the efficacy cohort, which included 2,466 patients with biopsies performed 12 months after enrollment. Safety outcomes included perforation, stricture that required dilation, bleeding that required hospitalization or transfusion, and hospitalization. Efficacy outcomes included complete eradication of intestinal metaplasia and dysplasia.
Among patients in the safety cohort, 301 had a prior fundoplication, whereas 5,236 had received medical therapy only. Patients in the fundoplication group had a somewhat lower mean age than those in the medical therapy group (59 vs. 62 years, P = .0002), and were slightly less likely to be African American (0.3% vs. 1.6%, P = .03) or Hispanic (0.7% vs. 2.6%, P = .03). In the fundoplication group, the length of BE was greater (5.0 cm vs. 4.1 cm, P less than .0001), and the prevalence of nondysplastic BE was higher (53% vs. 49%, P = .05).
In addition, fewer patients in the fundoplication group were taking twice-daily PPIs compared with those in the medical therapy group (82% vs. 95%, P less than .001). There were no significant between-group differences in the rates of bleeding, hospitalization, or stricture.
Among patients in the efficacy cohort, 136 had a prior fundoplication and 2,330 had received medical therapy only. The fundoplication patients were slightly younger than the medical therapy patients (59 vs. 62 years, P = .004), had a somewhat greater length of BE (5.0 cm vs. 4.3 cm, P = .009), and were less likely to be taking twice-daily PPIs (75% vs. 93%, P less than .001).
Rates of complete eradication of intestinal metaplasia were 71% in the fundoplication group vs. 73% in the medical therapy group, a nonsignificant difference, while the rate of complete eradication of dysplasia was identical in both groups at 87%.
Among patients who had nondysplastic BE, 75% in the fundoplication group achieved complete eradication of intestinal metaplasia, compared with 81% in the medical therapy group, a nonsignificant difference.
Regarding combined efficacy for dysplastic BE and intramucosal carcinoma, 67% of patients in the fundoplication group achieved complete eradication of intestinal metaplasia, compared with 66% in the medical therapy group, and both groups had a rate of 87% for complete eradication of dysplasia; none of these differences were significant.
Dr. Shaheen acknowledged certain limitations of the study, including the fact that the functional status of the fundoplications was not known. "All we know is that some patients had them," he said. "These are observational data and subject to selection bias. Also note that this is hardly a pure comparison, because the people who got fundoplication were also getting PPIs. However, one might expect that to bias the study in favor of fundoplication, to the degree that the addition of PPIs helps."
The study was funded by Covidien, which provided the RFA equipment used in the study, and by grants from the National Institutes of Health. Dr. Shaheen disclosed that he has consulting relationships with numerous pharmaceutical and medical device companies, but none with Covidien.
SAN DIEGO – Radiofrequency ablation was found to be safe and effective in treating Barrett’s esophagus patients, whether or not they had undergone a prior fundoplication, based on results from a multicenter registry study.
"Gastroesophageal reflux causes esophageal mucosal injury and inflammation that may impair healing and squamous re-epithelialization after treatment of Barrett’s esophagus [BE] with radiofrequency ablation [RFA]," Dr. Nicholas J. Shaheen said at the annual Digestive Disease Week.
"It is unclear if fundoplication surgery, as a mechanical barrier to all reflux, improves treatment outcomes of RFA for BE. Similarly, some have postulated that change in the conformation of the hiatus with surgery might make ablation problematic."
Dr. Shaheen, director of the Center for Esophageal Diseases and Swallowing at the University of North Carolina, Chapel Hill, and his associates conducted the largest study of its kind, he said. They evaluated records from the RFA Patient Registry to assess the relationship between prior fundoplication and both efficacy and safety outcomes in patients with BE who were treated with RFA.
The registry comprises 113 community-based and 35 academic-affiliated medical institutions in the United States. "About 75% of these institutions are private practices, so this is an interesting snapshot of RFA as it’s practiced outside of tertiary care centers," Dr. Shaheen said.
All study patients had BE confirmed by endoscopy and histology, and had undergone treatment with RFA. Enrollment commenced in July 2007 and ended in July 2011. Data were gleaned from standard case report forms and included demographics; relevant medical history; histologic grade prior to treatment; endoscopic findings; dates and total number of RFA treatment sessions; and ablation outcomes and complications.
"The vast amount of data is prospective, but less than 15% is retrospective," Dr. Shaheen said. "This is a registry study, so we could not mandate treatment, but a treatment protocol was suggested." Twice-daily use of proton pump inhibitors (PPIs) was recommended to everyone in the study, including those post fundoplication.
The mean age of patients was 61 years, and the majority were white. The mean pretreatment length of BE was about 4 cm, and patients received an average of 2.5 treatments with RFA. "Importantly, in this registry, about half of the patients had nondysplastic disease," Dr. Shaheen said. "Also, roughly 20% in each group had low- and high-grade dysplasia."
Dr. Shaheen reported results from the safety cohort, which included 5,537 patients who received RFA, and results from the efficacy cohort, which included 2,466 patients with biopsies performed 12 months after enrollment. Safety outcomes included perforation, stricture that required dilation, bleeding that required hospitalization or transfusion, and hospitalization. Efficacy outcomes included complete eradication of intestinal metaplasia and dysplasia.
Among patients in the safety cohort, 301 had a prior fundoplication, whereas 5,236 had received medical therapy only. Patients in the fundoplication group had a somewhat lower mean age than those in the medical therapy group (59 vs. 62 years, P = .0002), and were slightly less likely to be African American (0.3% vs. 1.6%, P = .03) or Hispanic (0.7% vs. 2.6%, P = .03). In the fundoplication group, the length of BE was greater (5.0 cm vs. 4.1 cm, P less than .0001), and the prevalence of nondysplastic BE was higher (53% vs. 49%, P = .05).
In addition, fewer patients in the fundoplication group were taking twice-daily PPIs compared with those in the medical therapy group (82% vs. 95%, P less than .001). There were no significant between-group differences in the rates of bleeding, hospitalization, or stricture.
Among patients in the efficacy cohort, 136 had a prior fundoplication and 2,330 had received medical therapy only. The fundoplication patients were slightly younger than the medical therapy patients (59 vs. 62 years, P = .004), had a somewhat greater length of BE (5.0 cm vs. 4.3 cm, P = .009), and were less likely to be taking twice-daily PPIs (75% vs. 93%, P less than .001).
Rates of complete eradication of intestinal metaplasia were 71% in the fundoplication group vs. 73% in the medical therapy group, a nonsignificant difference, while the rate of complete eradication of dysplasia was identical in both groups at 87%.
Among patients who had nondysplastic BE, 75% in the fundoplication group achieved complete eradication of intestinal metaplasia, compared with 81% in the medical therapy group, a nonsignificant difference.
Regarding combined efficacy for dysplastic BE and intramucosal carcinoma, 67% of patients in the fundoplication group achieved complete eradication of intestinal metaplasia, compared with 66% in the medical therapy group, and both groups had a rate of 87% for complete eradication of dysplasia; none of these differences were significant.
Dr. Shaheen acknowledged certain limitations of the study, including the fact that the functional status of the fundoplications was not known. "All we know is that some patients had them," he said. "These are observational data and subject to selection bias. Also note that this is hardly a pure comparison, because the people who got fundoplication were also getting PPIs. However, one might expect that to bias the study in favor of fundoplication, to the degree that the addition of PPIs helps."
The study was funded by Covidien, which provided the RFA equipment used in the study, and by grants from the National Institutes of Health. Dr. Shaheen disclosed that he has consulting relationships with numerous pharmaceutical and medical device companies, but none with Covidien.
SAN DIEGO – Radiofrequency ablation was found to be safe and effective in treating Barrett’s esophagus patients, whether or not they had undergone a prior fundoplication, based on results from a multicenter registry study.
"Gastroesophageal reflux causes esophageal mucosal injury and inflammation that may impair healing and squamous re-epithelialization after treatment of Barrett’s esophagus [BE] with radiofrequency ablation [RFA]," Dr. Nicholas J. Shaheen said at the annual Digestive Disease Week.
"It is unclear if fundoplication surgery, as a mechanical barrier to all reflux, improves treatment outcomes of RFA for BE. Similarly, some have postulated that change in the conformation of the hiatus with surgery might make ablation problematic."
Dr. Shaheen, director of the Center for Esophageal Diseases and Swallowing at the University of North Carolina, Chapel Hill, and his associates conducted the largest study of its kind, he said. They evaluated records from the RFA Patient Registry to assess the relationship between prior fundoplication and both efficacy and safety outcomes in patients with BE who were treated with RFA.
The registry comprises 113 community-based and 35 academic-affiliated medical institutions in the United States. "About 75% of these institutions are private practices, so this is an interesting snapshot of RFA as it’s practiced outside of tertiary care centers," Dr. Shaheen said.
All study patients had BE confirmed by endoscopy and histology, and had undergone treatment with RFA. Enrollment commenced in July 2007 and ended in July 2011. Data were gleaned from standard case report forms and included demographics; relevant medical history; histologic grade prior to treatment; endoscopic findings; dates and total number of RFA treatment sessions; and ablation outcomes and complications.
"The vast amount of data is prospective, but less than 15% is retrospective," Dr. Shaheen said. "This is a registry study, so we could not mandate treatment, but a treatment protocol was suggested." Twice-daily use of proton pump inhibitors (PPIs) was recommended to everyone in the study, including those post fundoplication.
The mean age of patients was 61 years, and the majority were white. The mean pretreatment length of BE was about 4 cm, and patients received an average of 2.5 treatments with RFA. "Importantly, in this registry, about half of the patients had nondysplastic disease," Dr. Shaheen said. "Also, roughly 20% in each group had low- and high-grade dysplasia."
Dr. Shaheen reported results from the safety cohort, which included 5,537 patients who received RFA, and results from the efficacy cohort, which included 2,466 patients with biopsies performed 12 months after enrollment. Safety outcomes included perforation, stricture that required dilation, bleeding that required hospitalization or transfusion, and hospitalization. Efficacy outcomes included complete eradication of intestinal metaplasia and dysplasia.
Among patients in the safety cohort, 301 had a prior fundoplication, whereas 5,236 had received medical therapy only. Patients in the fundoplication group had a somewhat lower mean age than those in the medical therapy group (59 vs. 62 years, P = .0002), and were slightly less likely to be African American (0.3% vs. 1.6%, P = .03) or Hispanic (0.7% vs. 2.6%, P = .03). In the fundoplication group, the length of BE was greater (5.0 cm vs. 4.1 cm, P less than .0001), and the prevalence of nondysplastic BE was higher (53% vs. 49%, P = .05).
In addition, fewer patients in the fundoplication group were taking twice-daily PPIs compared with those in the medical therapy group (82% vs. 95%, P less than .001). There were no significant between-group differences in the rates of bleeding, hospitalization, or stricture.
Among patients in the efficacy cohort, 136 had a prior fundoplication and 2,330 had received medical therapy only. The fundoplication patients were slightly younger than the medical therapy patients (59 vs. 62 years, P = .004), had a somewhat greater length of BE (5.0 cm vs. 4.3 cm, P = .009), and were less likely to be taking twice-daily PPIs (75% vs. 93%, P less than .001).
Rates of complete eradication of intestinal metaplasia were 71% in the fundoplication group vs. 73% in the medical therapy group, a nonsignificant difference, while the rate of complete eradication of dysplasia was identical in both groups at 87%.
Among patients who had nondysplastic BE, 75% in the fundoplication group achieved complete eradication of intestinal metaplasia, compared with 81% in the medical therapy group, a nonsignificant difference.
Regarding combined efficacy for dysplastic BE and intramucosal carcinoma, 67% of patients in the fundoplication group achieved complete eradication of intestinal metaplasia, compared with 66% in the medical therapy group, and both groups had a rate of 87% for complete eradication of dysplasia; none of these differences were significant.
Dr. Shaheen acknowledged certain limitations of the study, including the fact that the functional status of the fundoplications was not known. "All we know is that some patients had them," he said. "These are observational data and subject to selection bias. Also note that this is hardly a pure comparison, because the people who got fundoplication were also getting PPIs. However, one might expect that to bias the study in favor of fundoplication, to the degree that the addition of PPIs helps."
The study was funded by Covidien, which provided the RFA equipment used in the study, and by grants from the National Institutes of Health. Dr. Shaheen disclosed that he has consulting relationships with numerous pharmaceutical and medical device companies, but none with Covidien.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Blocking GI Acid Linked to Lower Pouchitis Risk
SAN DIEGO – Changing the acid content of the gastrointestinal tract may reduce the risk of developing pouchitis following ileal pouch anal anastomosis, based on a review of 85 patients at one U.S. center.
After patients underwent ileal pouch anal anastomosis (IPAA) for ulcerative colitis, those who did not develop pouchitis used a proton pump inhibitor (PPI) or histamine2 (H2) blocker on a daily basis significantly more often than did patients who developed pouchitis during follow-up, Dr. Lisa S. Poritz said at the annual Digestive Disease Week.
Patients who did not develop pouchitis also regularly used an antacid significantly more often than did those with pouchitis during follow-up, but "occasional" use of a PPI or H2 blocker showed no statistically significant association with reduced pouchitis incidence, said Dr. Poritz, a colon and rectal surgeon at Pennsylvania State University, Hershey.
Pouchitis is the most common complication of IPAA, occurring in about half of these patients, and chronic pouchitis develops in 5%-19% of them, Dr. Poritz said. Pouchitis produces urgency, bloody bowel movements, and abdominal pain.
IPAA patients who require chronic antibiotic treatment for pouchitis are the subgroup with the best chance to benefit from daily treatment to stop or neutralize acid secretion, a strategy that would "hopefully get them off chronic antibiotics," she said.
The study reviewed ulcerative colitis patients from the Penn State Familial IBD Registry who had undergone IPAA and had at least 2 subsequent years of follow-up. In all, 45 patients developed no pouchitis, and 40 had pouchitis. The registry data showed no demographic or clinical differences between the two subgroups.
The researchers limited their analysis of acid treatment associations to the subgroup of patients for whom data were available. In all, 15 of 30 patients who had no pouchitis following IPAA and 5 of 35 who developed pouchitis received daily treatment with a PPI or H2 blocker, a statistically significant difference. And 12 of 21 patients with no pouchitis took an antacid more than once a week, compared with 3 of 25 patients who developed pouchitis, also a statistically significant difference.
The analysis showed very similar usage rates among the pouchitis and no-pouchitis subgroups for a variety of other agents that could potentially influence this complication, including probiotics, NSAIDs, fiber supplements, antidiarrheal drugs, and immunosuppressive drugs.
The treatment effects of a PPI or H2 blocker on the incidence of pouchitis may be mediated by changes in fecal flora, but clear evidence for the mechanism of action will require further study, she said.
Dr. Poritz said that she had no disclosures.
SAN DIEGO – Changing the acid content of the gastrointestinal tract may reduce the risk of developing pouchitis following ileal pouch anal anastomosis, based on a review of 85 patients at one U.S. center.
After patients underwent ileal pouch anal anastomosis (IPAA) for ulcerative colitis, those who did not develop pouchitis used a proton pump inhibitor (PPI) or histamine2 (H2) blocker on a daily basis significantly more often than did patients who developed pouchitis during follow-up, Dr. Lisa S. Poritz said at the annual Digestive Disease Week.
Patients who did not develop pouchitis also regularly used an antacid significantly more often than did those with pouchitis during follow-up, but "occasional" use of a PPI or H2 blocker showed no statistically significant association with reduced pouchitis incidence, said Dr. Poritz, a colon and rectal surgeon at Pennsylvania State University, Hershey.
Pouchitis is the most common complication of IPAA, occurring in about half of these patients, and chronic pouchitis develops in 5%-19% of them, Dr. Poritz said. Pouchitis produces urgency, bloody bowel movements, and abdominal pain.
IPAA patients who require chronic antibiotic treatment for pouchitis are the subgroup with the best chance to benefit from daily treatment to stop or neutralize acid secretion, a strategy that would "hopefully get them off chronic antibiotics," she said.
The study reviewed ulcerative colitis patients from the Penn State Familial IBD Registry who had undergone IPAA and had at least 2 subsequent years of follow-up. In all, 45 patients developed no pouchitis, and 40 had pouchitis. The registry data showed no demographic or clinical differences between the two subgroups.
The researchers limited their analysis of acid treatment associations to the subgroup of patients for whom data were available. In all, 15 of 30 patients who had no pouchitis following IPAA and 5 of 35 who developed pouchitis received daily treatment with a PPI or H2 blocker, a statistically significant difference. And 12 of 21 patients with no pouchitis took an antacid more than once a week, compared with 3 of 25 patients who developed pouchitis, also a statistically significant difference.
The analysis showed very similar usage rates among the pouchitis and no-pouchitis subgroups for a variety of other agents that could potentially influence this complication, including probiotics, NSAIDs, fiber supplements, antidiarrheal drugs, and immunosuppressive drugs.
The treatment effects of a PPI or H2 blocker on the incidence of pouchitis may be mediated by changes in fecal flora, but clear evidence for the mechanism of action will require further study, she said.
Dr. Poritz said that she had no disclosures.
SAN DIEGO – Changing the acid content of the gastrointestinal tract may reduce the risk of developing pouchitis following ileal pouch anal anastomosis, based on a review of 85 patients at one U.S. center.
After patients underwent ileal pouch anal anastomosis (IPAA) for ulcerative colitis, those who did not develop pouchitis used a proton pump inhibitor (PPI) or histamine2 (H2) blocker on a daily basis significantly more often than did patients who developed pouchitis during follow-up, Dr. Lisa S. Poritz said at the annual Digestive Disease Week.
Patients who did not develop pouchitis also regularly used an antacid significantly more often than did those with pouchitis during follow-up, but "occasional" use of a PPI or H2 blocker showed no statistically significant association with reduced pouchitis incidence, said Dr. Poritz, a colon and rectal surgeon at Pennsylvania State University, Hershey.
Pouchitis is the most common complication of IPAA, occurring in about half of these patients, and chronic pouchitis develops in 5%-19% of them, Dr. Poritz said. Pouchitis produces urgency, bloody bowel movements, and abdominal pain.
IPAA patients who require chronic antibiotic treatment for pouchitis are the subgroup with the best chance to benefit from daily treatment to stop or neutralize acid secretion, a strategy that would "hopefully get them off chronic antibiotics," she said.
The study reviewed ulcerative colitis patients from the Penn State Familial IBD Registry who had undergone IPAA and had at least 2 subsequent years of follow-up. In all, 45 patients developed no pouchitis, and 40 had pouchitis. The registry data showed no demographic or clinical differences between the two subgroups.
The researchers limited their analysis of acid treatment associations to the subgroup of patients for whom data were available. In all, 15 of 30 patients who had no pouchitis following IPAA and 5 of 35 who developed pouchitis received daily treatment with a PPI or H2 blocker, a statistically significant difference. And 12 of 21 patients with no pouchitis took an antacid more than once a week, compared with 3 of 25 patients who developed pouchitis, also a statistically significant difference.
The analysis showed very similar usage rates among the pouchitis and no-pouchitis subgroups for a variety of other agents that could potentially influence this complication, including probiotics, NSAIDs, fiber supplements, antidiarrheal drugs, and immunosuppressive drugs.
The treatment effects of a PPI or H2 blocker on the incidence of pouchitis may be mediated by changes in fecal flora, but clear evidence for the mechanism of action will require further study, she said.
Dr. Poritz said that she had no disclosures.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: Following ileal pouch anal anastomosis, significantly more patients with no pouchitis regularly used acid suppression compared with patients who developed pouchitis.
Data Source: The data came from a review of 85 patients who underwent ileal pouch anal anastomosis at one U.S. center.
Disclosures: Dr. Poritz said that she had no disclosures.
Antireflux Procedures Increasingly Performed at Low-Volume Centers
SAN DIEGO – Since the late 1990s, when the annual number of antireflux procedures performed in the United States peaked, the overall rate of complications has increased, operations have shifted to more complex procedures in sicker patients, and the largest gains in caseload have occurred at urban nonteaching hospitals.
Those are three key findings from a large analysis of National Inpatient Sample (NIS) data reported by Dr. Paul D. Colavita at the annual Digestive Disease Week.
"Around the same time that antireflux surgery surged in the late 1990s, the Leapfrog Group – a large consortium of public and private health care purchasers – emerged as leaders in the national call for regionalization of complex surgical procedures in 2000," said Dr. Colavita, of the general surgery department at Carolinas Medical Center, Charlotte, N.C. "The objective of our study was to measure the extent of regionalization from its peak in 1998-1999 with data from 2008-2009."
He and his associates examined NIS data from 1998-1999 and 2008-2009 for antireflux procedures performed on patients with a diagnosis of gastroesophageal reflux, esophagitis, esophageal ulcer, and hiatal hernia. They excluded cases of achalasia, gangrenous/incarcerated diaphragmatic hernia, and patients younger than 18 years.
To measure the effect of regionalization, the researchers used 1998-1999 annual hospital volume of antireflux operations stratified into one of three baseline terciles: low-volume centers, defined as 1-14 annual procedures; medium-volume centers (15-37 annual procedures); and high-volume centers (38 or more annual procedures). The researchers also compared complications and outcomes that occurred in 1998-99 (time period 1) with those that occurred in 2008-09 (time period 2).
Dr. Colavita reported that 11,803 procedures were performed in time period 1, compared with 8,855 in time period 2. The proportion of procedures performed at low-volume centers increased between time periods 1 and 2 (from 33.3% to 40.4%) and declined at high-volume centers (from 33.4% to 25.3%).
As has been found with other surgical procedures, outcomes improved in high-volume centers, he said. The researchers attribute the lack of regionalization, in part, to the increased number of surgeons trained to perform these procedures. "In the past decade, surgical residents have been trained to perform antireflux procedures," Dr. Colavita said. "These former residents are now general surgeons who are performing these procedures in a variety of hospitals in different locations, both urban and rural."
Certain baseline characteristics differed significantly between time periods 1 and 2, including age (a mean of 50 vs. 57 years, respectively), percentage of women (57% vs. 69%), percentage of white patients (91% vs. 85%), and those with a Charlson comorbidity index score of more than 1 (5% vs. 10%). All differences had a P value of less than .0001.
There was no difference in inpatient mortality between time periods 1 and 2 (0.41% vs. 0.34%, respectively; P = .433), but there were significant increases in the rate of complications (4% vs. 6%) and total charges ($16,000 vs. $40,000), while the frequency of routine discharge decreased (95% vs. 92%). All differences had a P value of less than .0001. The average length of stay increased by 0.15 days (P = .001).
Multivariate regression analysis revealed that between time periods 1 and 2, low-volume centers remained independently associated with increased complications (odds ratio 1.8 vs. 1.9, respectively), nonroutine discharge (OR 2.0 vs. 1.8), length of stay (0.82 vs. 0.94 days), and higher total charges ($2,700 vs. $3,200).
"Taking these findings into consideration, we as health care providers must decide whether or not to call for increased referrals to high-volume centers," Dr. Colavita said.
Multivariate regression revealed two significant predictors of antireflux procedures performed at low-volume centers during time periods 1 and 2: emergent admission (OR 3.7 vs. 3.0, respectively) and lack of private insurance (OR 1.3 in both). Nonwhite race was a significant predictor in time period 1 only (OR 1.8), while significant predictors in time period 2 only included residing in the poorest vs. wealthiest zip code (OR 1.2), decreasing age (OR 1.1), and female gender (OR 1.2).
Dr. Colavita also reported that rural hospitals had decreased surgical volume between time periods 1 and 2 (19% to 10%), while the volume increased at urban nonteaching hospitals (from 33% to 39%) and at urban teaching hospitals (from 48% to 51%).
"Urban teaching hospitals had the highest proportion of high-volume cases in both eras, while urban nonteaching hospitals had the highest proportion of low-volume cases in both eras," he said.
Dr. Colavita acknowledged certain limitations of the study, including the lack of opportunity for follow-up in the NIS database and the fact that there are no codes for redo fundoplications. Also, "higher volumes have a shorter length of stay," he said. "This is a smaller window to detect death, complications, and overall cost. We also lack operative details such as operative time."
Dr. Colavita said he had no relevant financial conflicts to disclose.
SAN DIEGO – Since the late 1990s, when the annual number of antireflux procedures performed in the United States peaked, the overall rate of complications has increased, operations have shifted to more complex procedures in sicker patients, and the largest gains in caseload have occurred at urban nonteaching hospitals.
Those are three key findings from a large analysis of National Inpatient Sample (NIS) data reported by Dr. Paul D. Colavita at the annual Digestive Disease Week.
"Around the same time that antireflux surgery surged in the late 1990s, the Leapfrog Group – a large consortium of public and private health care purchasers – emerged as leaders in the national call for regionalization of complex surgical procedures in 2000," said Dr. Colavita, of the general surgery department at Carolinas Medical Center, Charlotte, N.C. "The objective of our study was to measure the extent of regionalization from its peak in 1998-1999 with data from 2008-2009."
He and his associates examined NIS data from 1998-1999 and 2008-2009 for antireflux procedures performed on patients with a diagnosis of gastroesophageal reflux, esophagitis, esophageal ulcer, and hiatal hernia. They excluded cases of achalasia, gangrenous/incarcerated diaphragmatic hernia, and patients younger than 18 years.
To measure the effect of regionalization, the researchers used 1998-1999 annual hospital volume of antireflux operations stratified into one of three baseline terciles: low-volume centers, defined as 1-14 annual procedures; medium-volume centers (15-37 annual procedures); and high-volume centers (38 or more annual procedures). The researchers also compared complications and outcomes that occurred in 1998-99 (time period 1) with those that occurred in 2008-09 (time period 2).
Dr. Colavita reported that 11,803 procedures were performed in time period 1, compared with 8,855 in time period 2. The proportion of procedures performed at low-volume centers increased between time periods 1 and 2 (from 33.3% to 40.4%) and declined at high-volume centers (from 33.4% to 25.3%).
As has been found with other surgical procedures, outcomes improved in high-volume centers, he said. The researchers attribute the lack of regionalization, in part, to the increased number of surgeons trained to perform these procedures. "In the past decade, surgical residents have been trained to perform antireflux procedures," Dr. Colavita said. "These former residents are now general surgeons who are performing these procedures in a variety of hospitals in different locations, both urban and rural."
Certain baseline characteristics differed significantly between time periods 1 and 2, including age (a mean of 50 vs. 57 years, respectively), percentage of women (57% vs. 69%), percentage of white patients (91% vs. 85%), and those with a Charlson comorbidity index score of more than 1 (5% vs. 10%). All differences had a P value of less than .0001.
There was no difference in inpatient mortality between time periods 1 and 2 (0.41% vs. 0.34%, respectively; P = .433), but there were significant increases in the rate of complications (4% vs. 6%) and total charges ($16,000 vs. $40,000), while the frequency of routine discharge decreased (95% vs. 92%). All differences had a P value of less than .0001. The average length of stay increased by 0.15 days (P = .001).
Multivariate regression analysis revealed that between time periods 1 and 2, low-volume centers remained independently associated with increased complications (odds ratio 1.8 vs. 1.9, respectively), nonroutine discharge (OR 2.0 vs. 1.8), length of stay (0.82 vs. 0.94 days), and higher total charges ($2,700 vs. $3,200).
"Taking these findings into consideration, we as health care providers must decide whether or not to call for increased referrals to high-volume centers," Dr. Colavita said.
Multivariate regression revealed two significant predictors of antireflux procedures performed at low-volume centers during time periods 1 and 2: emergent admission (OR 3.7 vs. 3.0, respectively) and lack of private insurance (OR 1.3 in both). Nonwhite race was a significant predictor in time period 1 only (OR 1.8), while significant predictors in time period 2 only included residing in the poorest vs. wealthiest zip code (OR 1.2), decreasing age (OR 1.1), and female gender (OR 1.2).
Dr. Colavita also reported that rural hospitals had decreased surgical volume between time periods 1 and 2 (19% to 10%), while the volume increased at urban nonteaching hospitals (from 33% to 39%) and at urban teaching hospitals (from 48% to 51%).
"Urban teaching hospitals had the highest proportion of high-volume cases in both eras, while urban nonteaching hospitals had the highest proportion of low-volume cases in both eras," he said.
Dr. Colavita acknowledged certain limitations of the study, including the lack of opportunity for follow-up in the NIS database and the fact that there are no codes for redo fundoplications. Also, "higher volumes have a shorter length of stay," he said. "This is a smaller window to detect death, complications, and overall cost. We also lack operative details such as operative time."
Dr. Colavita said he had no relevant financial conflicts to disclose.
SAN DIEGO – Since the late 1990s, when the annual number of antireflux procedures performed in the United States peaked, the overall rate of complications has increased, operations have shifted to more complex procedures in sicker patients, and the largest gains in caseload have occurred at urban nonteaching hospitals.
Those are three key findings from a large analysis of National Inpatient Sample (NIS) data reported by Dr. Paul D. Colavita at the annual Digestive Disease Week.
"Around the same time that antireflux surgery surged in the late 1990s, the Leapfrog Group – a large consortium of public and private health care purchasers – emerged as leaders in the national call for regionalization of complex surgical procedures in 2000," said Dr. Colavita, of the general surgery department at Carolinas Medical Center, Charlotte, N.C. "The objective of our study was to measure the extent of regionalization from its peak in 1998-1999 with data from 2008-2009."
He and his associates examined NIS data from 1998-1999 and 2008-2009 for antireflux procedures performed on patients with a diagnosis of gastroesophageal reflux, esophagitis, esophageal ulcer, and hiatal hernia. They excluded cases of achalasia, gangrenous/incarcerated diaphragmatic hernia, and patients younger than 18 years.
To measure the effect of regionalization, the researchers used 1998-1999 annual hospital volume of antireflux operations stratified into one of three baseline terciles: low-volume centers, defined as 1-14 annual procedures; medium-volume centers (15-37 annual procedures); and high-volume centers (38 or more annual procedures). The researchers also compared complications and outcomes that occurred in 1998-99 (time period 1) with those that occurred in 2008-09 (time period 2).
Dr. Colavita reported that 11,803 procedures were performed in time period 1, compared with 8,855 in time period 2. The proportion of procedures performed at low-volume centers increased between time periods 1 and 2 (from 33.3% to 40.4%) and declined at high-volume centers (from 33.4% to 25.3%).
As has been found with other surgical procedures, outcomes improved in high-volume centers, he said. The researchers attribute the lack of regionalization, in part, to the increased number of surgeons trained to perform these procedures. "In the past decade, surgical residents have been trained to perform antireflux procedures," Dr. Colavita said. "These former residents are now general surgeons who are performing these procedures in a variety of hospitals in different locations, both urban and rural."
Certain baseline characteristics differed significantly between time periods 1 and 2, including age (a mean of 50 vs. 57 years, respectively), percentage of women (57% vs. 69%), percentage of white patients (91% vs. 85%), and those with a Charlson comorbidity index score of more than 1 (5% vs. 10%). All differences had a P value of less than .0001.
There was no difference in inpatient mortality between time periods 1 and 2 (0.41% vs. 0.34%, respectively; P = .433), but there were significant increases in the rate of complications (4% vs. 6%) and total charges ($16,000 vs. $40,000), while the frequency of routine discharge decreased (95% vs. 92%). All differences had a P value of less than .0001. The average length of stay increased by 0.15 days (P = .001).
Multivariate regression analysis revealed that between time periods 1 and 2, low-volume centers remained independently associated with increased complications (odds ratio 1.8 vs. 1.9, respectively), nonroutine discharge (OR 2.0 vs. 1.8), length of stay (0.82 vs. 0.94 days), and higher total charges ($2,700 vs. $3,200).
"Taking these findings into consideration, we as health care providers must decide whether or not to call for increased referrals to high-volume centers," Dr. Colavita said.
Multivariate regression revealed two significant predictors of antireflux procedures performed at low-volume centers during time periods 1 and 2: emergent admission (OR 3.7 vs. 3.0, respectively) and lack of private insurance (OR 1.3 in both). Nonwhite race was a significant predictor in time period 1 only (OR 1.8), while significant predictors in time period 2 only included residing in the poorest vs. wealthiest zip code (OR 1.2), decreasing age (OR 1.1), and female gender (OR 1.2).
Dr. Colavita also reported that rural hospitals had decreased surgical volume between time periods 1 and 2 (19% to 10%), while the volume increased at urban nonteaching hospitals (from 33% to 39%) and at urban teaching hospitals (from 48% to 51%).
"Urban teaching hospitals had the highest proportion of high-volume cases in both eras, while urban nonteaching hospitals had the highest proportion of low-volume cases in both eras," he said.
Dr. Colavita acknowledged certain limitations of the study, including the lack of opportunity for follow-up in the NIS database and the fact that there are no codes for redo fundoplications. Also, "higher volumes have a shorter length of stay," he said. "This is a smaller window to detect death, complications, and overall cost. We also lack operative details such as operative time."
Dr. Colavita said he had no relevant financial conflicts to disclose.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Screening Colonoscopy Can Benefit Selected Elderly People
SAN DIEGO – Elderly patients who never previously underwent screening colonoscopy have a high prevalence of colorectal cancer and could benefit from screening if they are healthy and functional and have a life expectancy of at least about 7 years, based on a review of colonoscopies done on people aged 76-85 at one U.S. center.
The results also showed a reasonable detection rate for colorectal cancers in the same age group when their prior colonoscopy had last been done 10 or more years before, Dr. Therese G. Kerwel said at the annual Digestive Disease Week meeting.
"The U.S. Preventive Services Task Force says that you don’t see benefit [from screening colonoscopy] until about 7 years so that’s the benchmark. If you think the person will live for another 7 or more years, then screen. If not, then it’s not worth the resources," said Dr. Kerwel, a surgeon at Spectrum Health in Grand Rapids, Mich.
"The headline from the U.S. Preventive Services Task Force is to stop screening at age 75; that’s what everyone knows. A lot of people don’t read the fine print, the loophole that you can screen elderly people if they are healthy and functional," Dr. Kerwel said in an interview.
Another reason to strongly consider screening elderly patients who are healthy enough to potentially benefit is that if they develop colorectal cancer, they have an increased risk for an emergency presentation compared with younger adults, with the potential to develop bleeding, obstruction, or perforation, she said.
"It’s always a balance of risk and benefit, but there is definitely a subset of the elderly who need to be focused on a little more."
The review also showed a sizeable percent of elderly people underwent colonoscopy at Spectrum Health roughly 5 years following a prior procedure, with no cases of colorectal cancer detected, indicating that a significant number of elderly people had been subjected to overly aggressive colonoscopy, Dr. Kerwel said.
She and her associates reviewed 903 people, aged 76-85 years, who underwent colonoscopy at Spectrum Health during January 2009 to December 2010. The colonoscopy occurred purely for screening in 19%, for surveillance in 42%, for symptoms in 35%, and for other reasons in 4%.
Fifty-three of the people had never previously undergone colonoscopy (in this subgroup roughly half the procedures were for screening and half were for symptoms). Colonoscopy identified colorectal carcinoma in 9%. An additional 56 people from the study group had not had a prior colonoscopy for at least 10 years; in this group the new procedure detected carcinoma in 5%.
The remaining 88% of the procedures reviewed occurred within 9 years or less of prior colonoscopy. The largest subgroup was 247 people (27% of the study group) examined 4-5 years after a prior colonoscopy. In this subgroup the procedure identified no carcinomas, and in everyone else examined 9 or fewer years after their prior examination, about 3% had cancers identified.
These results suggest that repeat colonoscopies at intervals shorter than 10 years may have questionable utility in the elderly, Dr. Kerwel said.
She said that she had no relevant financial disclosures.
SAN DIEGO – Elderly patients who never previously underwent screening colonoscopy have a high prevalence of colorectal cancer and could benefit from screening if they are healthy and functional and have a life expectancy of at least about 7 years, based on a review of colonoscopies done on people aged 76-85 at one U.S. center.
The results also showed a reasonable detection rate for colorectal cancers in the same age group when their prior colonoscopy had last been done 10 or more years before, Dr. Therese G. Kerwel said at the annual Digestive Disease Week meeting.
"The U.S. Preventive Services Task Force says that you don’t see benefit [from screening colonoscopy] until about 7 years so that’s the benchmark. If you think the person will live for another 7 or more years, then screen. If not, then it’s not worth the resources," said Dr. Kerwel, a surgeon at Spectrum Health in Grand Rapids, Mich.
"The headline from the U.S. Preventive Services Task Force is to stop screening at age 75; that’s what everyone knows. A lot of people don’t read the fine print, the loophole that you can screen elderly people if they are healthy and functional," Dr. Kerwel said in an interview.
Another reason to strongly consider screening elderly patients who are healthy enough to potentially benefit is that if they develop colorectal cancer, they have an increased risk for an emergency presentation compared with younger adults, with the potential to develop bleeding, obstruction, or perforation, she said.
"It’s always a balance of risk and benefit, but there is definitely a subset of the elderly who need to be focused on a little more."
The review also showed a sizeable percent of elderly people underwent colonoscopy at Spectrum Health roughly 5 years following a prior procedure, with no cases of colorectal cancer detected, indicating that a significant number of elderly people had been subjected to overly aggressive colonoscopy, Dr. Kerwel said.
She and her associates reviewed 903 people, aged 76-85 years, who underwent colonoscopy at Spectrum Health during January 2009 to December 2010. The colonoscopy occurred purely for screening in 19%, for surveillance in 42%, for symptoms in 35%, and for other reasons in 4%.
Fifty-three of the people had never previously undergone colonoscopy (in this subgroup roughly half the procedures were for screening and half were for symptoms). Colonoscopy identified colorectal carcinoma in 9%. An additional 56 people from the study group had not had a prior colonoscopy for at least 10 years; in this group the new procedure detected carcinoma in 5%.
The remaining 88% of the procedures reviewed occurred within 9 years or less of prior colonoscopy. The largest subgroup was 247 people (27% of the study group) examined 4-5 years after a prior colonoscopy. In this subgroup the procedure identified no carcinomas, and in everyone else examined 9 or fewer years after their prior examination, about 3% had cancers identified.
These results suggest that repeat colonoscopies at intervals shorter than 10 years may have questionable utility in the elderly, Dr. Kerwel said.
She said that she had no relevant financial disclosures.
SAN DIEGO – Elderly patients who never previously underwent screening colonoscopy have a high prevalence of colorectal cancer and could benefit from screening if they are healthy and functional and have a life expectancy of at least about 7 years, based on a review of colonoscopies done on people aged 76-85 at one U.S. center.
The results also showed a reasonable detection rate for colorectal cancers in the same age group when their prior colonoscopy had last been done 10 or more years before, Dr. Therese G. Kerwel said at the annual Digestive Disease Week meeting.
"The U.S. Preventive Services Task Force says that you don’t see benefit [from screening colonoscopy] until about 7 years so that’s the benchmark. If you think the person will live for another 7 or more years, then screen. If not, then it’s not worth the resources," said Dr. Kerwel, a surgeon at Spectrum Health in Grand Rapids, Mich.
"The headline from the U.S. Preventive Services Task Force is to stop screening at age 75; that’s what everyone knows. A lot of people don’t read the fine print, the loophole that you can screen elderly people if they are healthy and functional," Dr. Kerwel said in an interview.
Another reason to strongly consider screening elderly patients who are healthy enough to potentially benefit is that if they develop colorectal cancer, they have an increased risk for an emergency presentation compared with younger adults, with the potential to develop bleeding, obstruction, or perforation, she said.
"It’s always a balance of risk and benefit, but there is definitely a subset of the elderly who need to be focused on a little more."
The review also showed a sizeable percent of elderly people underwent colonoscopy at Spectrum Health roughly 5 years following a prior procedure, with no cases of colorectal cancer detected, indicating that a significant number of elderly people had been subjected to overly aggressive colonoscopy, Dr. Kerwel said.
She and her associates reviewed 903 people, aged 76-85 years, who underwent colonoscopy at Spectrum Health during January 2009 to December 2010. The colonoscopy occurred purely for screening in 19%, for surveillance in 42%, for symptoms in 35%, and for other reasons in 4%.
Fifty-three of the people had never previously undergone colonoscopy (in this subgroup roughly half the procedures were for screening and half were for symptoms). Colonoscopy identified colorectal carcinoma in 9%. An additional 56 people from the study group had not had a prior colonoscopy for at least 10 years; in this group the new procedure detected carcinoma in 5%.
The remaining 88% of the procedures reviewed occurred within 9 years or less of prior colonoscopy. The largest subgroup was 247 people (27% of the study group) examined 4-5 years after a prior colonoscopy. In this subgroup the procedure identified no carcinomas, and in everyone else examined 9 or fewer years after their prior examination, about 3% had cancers identified.
These results suggest that repeat colonoscopies at intervals shorter than 10 years may have questionable utility in the elderly, Dr. Kerwel said.
She said that she had no relevant financial disclosures.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: Colonoscopy detected carcinoma in 9% of people 76-85 years old who never previously underwent colonoscopy.
Data Source: Data came from a review of 903 people, aged 76-85 years, who underwent colonoscopy at a single U.S. center during 2009 or 2010.
Disclosures: Dr. Kerwel said that she had no relevant financial disclosures.
Laparoscopy Tops Open Resection for Most Gastric Tumors
SAN DIEGO – Patients who underwent laparoscopic resection of gastric submucosal neoplasms had shorter operative times, less blood loss, lower postoperative morbidity, and shorter hospital lengths of stay compared with those who underwent open resection, according to results from a single-center study.
"Numerous reports not only have assessed the feasibility, but confirmed the long-term oncologic efficacy of laparoscopic resection for gastrointestinal stromal tumors [GISTs]," Dr. Sabha Ganai said at the annual Digestive Disease Week.
"However, in 2004, the European Society of Medical Oncology published a consensus report suggesting that laparoscopic surgery may result in a higher risk of tumor rupture and peritoneal seeding, and suggested that laparoscopic resection may be acceptable in cases of small intramural tumors – those 2 cm or smaller," she added (Ann. Oncol. 2005;16:566-78).
Dr. Ganai, a fellow in surgical oncology and clinical medical ethics at the University of Chicago, noted that concerns exist "regarding the ability to generalize laparoscopic techniques to the spectra of gastric submucosal neoplasms, specifically related to tumor size and location, particularly the GE junction/cardia, the antrum/pylorus, and posteriorly based lesions."
To evaluate patient selection for a minimally invasive approach to resection, Dr. Ganai and her associates compared laparoscopic and open techniques used in the resection of gastric submucosal neoplasms. "We hypothesized that there are predictors of unsuccessful laparoscopic resection, with failures defined by conversions, complications, and recurrences," she said.
The retrospective study involved 106 patients with gastric submucosal neoplasms who underwent operative management at the university from October 2002 to March 2012. There were 79 patients in the laparoscopic group and 27 in the open group. The mean age was 63 years, the mean body mass index was 29 kg/m2, and 57% were male.
There was less preoperative use of ultrasound in the open group vs. the laparoscopic group (67% vs. 87%, respectively), and greater pretreatment lesion size (9.5 cm vs. 3.9 cm). In addition, the open group had a 6-month greater interval from diagnosis to surgery (10.1 months vs. 4.4 months), and more neoadjuvant imatinib was used in the open group (26% vs. 5%).
Most tumors (76%) were GISTs; the rest were leiomyomas (9%), schwannomas (6%), carcinoids (3%), and other types (6%).
There were no significant differences between the groups in terms of tumor location; most were found in the greater curvature (41% open vs. 32% laparoscopic). "There were slightly more posterior lesions in the open group, but this was not statistically significant," she said. "On presentation, patients in the open group had a significantly greater presentation with abdominal pain, while those in the laparoscopic group were more likely to present with GI bleed."
Most patients underwent sleeve or wedge resection, with 11% of patients undergoing transgastric wedge resections. A higher proportion of the open group required a gastroenteric anastomosis (37% vs. 6%) and a multivisceral resection (41% vs. 1%). Overall, operative time was significantly greater in the open group (a mean of 230 minutes vs. 132 minutes), as was the amount of estimated blood loss (a mean of 364 mL vs. 35 mL).
Most GISTs in the laparoscopic group (64%) ranged in size from 2 cm to 5 cm, while the majority in the open group (58%) were greater than 5 cm. In addition, the open group had a higher mitotic index (44% vs. 20%).
Postoperatively, hospital length of stay was significantly shorter in the laparoscopic group (a mean of 3.3 days) than in the open group (a mean of 8.4 days). The laparoscopic group also had significantly fewer surgical site infections (1% vs. 22%), anastomotic leaks (0% vs. 7%), and postoperative arrhythmias (0% vs. 15%).
Overall complications, evaluated on the basis of the Accordion Severity Grading System of surgical complications, were less severe in the laparoscopic group. "However, there was one perioperative death in the laparoscopic group related to a massive myocardial infarction, as well as two reoperations, one related to a port site hernia and one related to a gastric outlet obstruction in an antral lesion," Dr. Ganai said.
On multivariate analysis, conversion was predicted by tumor size greater than 8 cm (odds ratio, 18.48), while recurrence was predicted by having a mitotic rate of greater than 5 mitoses per 50 high-power fields (OR, 4.68). Laparoscopic resection resulted in better perioperative outcomes, with less morbidity, shorter operative times, less blood loss, and shorter lengths of stay (P less than .05). No significant difference was seen in survival; 90% and 81% of patients were alive 3 years after laparoscopic and open resection, respectively (hazard ratio, 0.4; P = .13). "Tumor biology and imatinib may play a greater role in oncologic outcome than technical considerations," Dr. Ganai suggested.
She acknowledged certain limitations of the study, including its retrospective design, the potential for selection bias, and limited follow-up, "especially in the lower-risk tumors."
Dr. Ganai said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who underwent laparoscopic resection of gastric submucosal neoplasms had shorter operative times, less blood loss, lower postoperative morbidity, and shorter hospital lengths of stay compared with those who underwent open resection, according to results from a single-center study.
"Numerous reports not only have assessed the feasibility, but confirmed the long-term oncologic efficacy of laparoscopic resection for gastrointestinal stromal tumors [GISTs]," Dr. Sabha Ganai said at the annual Digestive Disease Week.
"However, in 2004, the European Society of Medical Oncology published a consensus report suggesting that laparoscopic surgery may result in a higher risk of tumor rupture and peritoneal seeding, and suggested that laparoscopic resection may be acceptable in cases of small intramural tumors – those 2 cm or smaller," she added (Ann. Oncol. 2005;16:566-78).
Dr. Ganai, a fellow in surgical oncology and clinical medical ethics at the University of Chicago, noted that concerns exist "regarding the ability to generalize laparoscopic techniques to the spectra of gastric submucosal neoplasms, specifically related to tumor size and location, particularly the GE junction/cardia, the antrum/pylorus, and posteriorly based lesions."
To evaluate patient selection for a minimally invasive approach to resection, Dr. Ganai and her associates compared laparoscopic and open techniques used in the resection of gastric submucosal neoplasms. "We hypothesized that there are predictors of unsuccessful laparoscopic resection, with failures defined by conversions, complications, and recurrences," she said.
The retrospective study involved 106 patients with gastric submucosal neoplasms who underwent operative management at the university from October 2002 to March 2012. There were 79 patients in the laparoscopic group and 27 in the open group. The mean age was 63 years, the mean body mass index was 29 kg/m2, and 57% were male.
There was less preoperative use of ultrasound in the open group vs. the laparoscopic group (67% vs. 87%, respectively), and greater pretreatment lesion size (9.5 cm vs. 3.9 cm). In addition, the open group had a 6-month greater interval from diagnosis to surgery (10.1 months vs. 4.4 months), and more neoadjuvant imatinib was used in the open group (26% vs. 5%).
Most tumors (76%) were GISTs; the rest were leiomyomas (9%), schwannomas (6%), carcinoids (3%), and other types (6%).
There were no significant differences between the groups in terms of tumor location; most were found in the greater curvature (41% open vs. 32% laparoscopic). "There were slightly more posterior lesions in the open group, but this was not statistically significant," she said. "On presentation, patients in the open group had a significantly greater presentation with abdominal pain, while those in the laparoscopic group were more likely to present with GI bleed."
Most patients underwent sleeve or wedge resection, with 11% of patients undergoing transgastric wedge resections. A higher proportion of the open group required a gastroenteric anastomosis (37% vs. 6%) and a multivisceral resection (41% vs. 1%). Overall, operative time was significantly greater in the open group (a mean of 230 minutes vs. 132 minutes), as was the amount of estimated blood loss (a mean of 364 mL vs. 35 mL).
Most GISTs in the laparoscopic group (64%) ranged in size from 2 cm to 5 cm, while the majority in the open group (58%) were greater than 5 cm. In addition, the open group had a higher mitotic index (44% vs. 20%).
Postoperatively, hospital length of stay was significantly shorter in the laparoscopic group (a mean of 3.3 days) than in the open group (a mean of 8.4 days). The laparoscopic group also had significantly fewer surgical site infections (1% vs. 22%), anastomotic leaks (0% vs. 7%), and postoperative arrhythmias (0% vs. 15%).
Overall complications, evaluated on the basis of the Accordion Severity Grading System of surgical complications, were less severe in the laparoscopic group. "However, there was one perioperative death in the laparoscopic group related to a massive myocardial infarction, as well as two reoperations, one related to a port site hernia and one related to a gastric outlet obstruction in an antral lesion," Dr. Ganai said.
On multivariate analysis, conversion was predicted by tumor size greater than 8 cm (odds ratio, 18.48), while recurrence was predicted by having a mitotic rate of greater than 5 mitoses per 50 high-power fields (OR, 4.68). Laparoscopic resection resulted in better perioperative outcomes, with less morbidity, shorter operative times, less blood loss, and shorter lengths of stay (P less than .05). No significant difference was seen in survival; 90% and 81% of patients were alive 3 years after laparoscopic and open resection, respectively (hazard ratio, 0.4; P = .13). "Tumor biology and imatinib may play a greater role in oncologic outcome than technical considerations," Dr. Ganai suggested.
She acknowledged certain limitations of the study, including its retrospective design, the potential for selection bias, and limited follow-up, "especially in the lower-risk tumors."
Dr. Ganai said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who underwent laparoscopic resection of gastric submucosal neoplasms had shorter operative times, less blood loss, lower postoperative morbidity, and shorter hospital lengths of stay compared with those who underwent open resection, according to results from a single-center study.
"Numerous reports not only have assessed the feasibility, but confirmed the long-term oncologic efficacy of laparoscopic resection for gastrointestinal stromal tumors [GISTs]," Dr. Sabha Ganai said at the annual Digestive Disease Week.
"However, in 2004, the European Society of Medical Oncology published a consensus report suggesting that laparoscopic surgery may result in a higher risk of tumor rupture and peritoneal seeding, and suggested that laparoscopic resection may be acceptable in cases of small intramural tumors – those 2 cm or smaller," she added (Ann. Oncol. 2005;16:566-78).
Dr. Ganai, a fellow in surgical oncology and clinical medical ethics at the University of Chicago, noted that concerns exist "regarding the ability to generalize laparoscopic techniques to the spectra of gastric submucosal neoplasms, specifically related to tumor size and location, particularly the GE junction/cardia, the antrum/pylorus, and posteriorly based lesions."
To evaluate patient selection for a minimally invasive approach to resection, Dr. Ganai and her associates compared laparoscopic and open techniques used in the resection of gastric submucosal neoplasms. "We hypothesized that there are predictors of unsuccessful laparoscopic resection, with failures defined by conversions, complications, and recurrences," she said.
The retrospective study involved 106 patients with gastric submucosal neoplasms who underwent operative management at the university from October 2002 to March 2012. There were 79 patients in the laparoscopic group and 27 in the open group. The mean age was 63 years, the mean body mass index was 29 kg/m2, and 57% were male.
There was less preoperative use of ultrasound in the open group vs. the laparoscopic group (67% vs. 87%, respectively), and greater pretreatment lesion size (9.5 cm vs. 3.9 cm). In addition, the open group had a 6-month greater interval from diagnosis to surgery (10.1 months vs. 4.4 months), and more neoadjuvant imatinib was used in the open group (26% vs. 5%).
Most tumors (76%) were GISTs; the rest were leiomyomas (9%), schwannomas (6%), carcinoids (3%), and other types (6%).
There were no significant differences between the groups in terms of tumor location; most were found in the greater curvature (41% open vs. 32% laparoscopic). "There were slightly more posterior lesions in the open group, but this was not statistically significant," she said. "On presentation, patients in the open group had a significantly greater presentation with abdominal pain, while those in the laparoscopic group were more likely to present with GI bleed."
Most patients underwent sleeve or wedge resection, with 11% of patients undergoing transgastric wedge resections. A higher proportion of the open group required a gastroenteric anastomosis (37% vs. 6%) and a multivisceral resection (41% vs. 1%). Overall, operative time was significantly greater in the open group (a mean of 230 minutes vs. 132 minutes), as was the amount of estimated blood loss (a mean of 364 mL vs. 35 mL).
Most GISTs in the laparoscopic group (64%) ranged in size from 2 cm to 5 cm, while the majority in the open group (58%) were greater than 5 cm. In addition, the open group had a higher mitotic index (44% vs. 20%).
Postoperatively, hospital length of stay was significantly shorter in the laparoscopic group (a mean of 3.3 days) than in the open group (a mean of 8.4 days). The laparoscopic group also had significantly fewer surgical site infections (1% vs. 22%), anastomotic leaks (0% vs. 7%), and postoperative arrhythmias (0% vs. 15%).
Overall complications, evaluated on the basis of the Accordion Severity Grading System of surgical complications, were less severe in the laparoscopic group. "However, there was one perioperative death in the laparoscopic group related to a massive myocardial infarction, as well as two reoperations, one related to a port site hernia and one related to a gastric outlet obstruction in an antral lesion," Dr. Ganai said.
On multivariate analysis, conversion was predicted by tumor size greater than 8 cm (odds ratio, 18.48), while recurrence was predicted by having a mitotic rate of greater than 5 mitoses per 50 high-power fields (OR, 4.68). Laparoscopic resection resulted in better perioperative outcomes, with less morbidity, shorter operative times, less blood loss, and shorter lengths of stay (P less than .05). No significant difference was seen in survival; 90% and 81% of patients were alive 3 years after laparoscopic and open resection, respectively (hazard ratio, 0.4; P = .13). "Tumor biology and imatinib may play a greater role in oncologic outcome than technical considerations," Dr. Ganai suggested.
She acknowledged certain limitations of the study, including its retrospective design, the potential for selection bias, and limited follow-up, "especially in the lower-risk tumors."
Dr. Ganai said that she had no relevant financial conflicts to disclose.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Quality of Life Undiminished by Telaprevir in Chronic Hepatitis C
SAN DIEGO – Although the addition of telaprevir to peginterferon/ribavirin therapy for treatment of chronic hepatitis C exacerbates treatment-related side effects, the triple combination does not diminish patient quality of life relative to treatment with the peginterferon/ribavirin regimen alone, a study has shown.
In other words, adding the protease inhibitor "does not further diminish patient quality of life," lead investigator Dr. Zobair Younossi explained at the annual Digestive Disease Week. "The most important contributor to the quality of life measurement in interferon therapy is interferon itself, which is so overwhelming in terms of side effects, especially grade 4 and 5 effects, that it probably overshadows everything else," he said.
Studies have shown that the addition of telaprevir to standard peginterferon alfa-2a/ribavirin (PR) significantly improves treatment efficacy in treatment-naive patients with genotype 1 hepatitis C virus (HCV), but there is a perception that the additional side effect burden from adding telaprevir is prohibitive in some patients, said Dr. Younossi, chairman of the department of medicine at Inova Health System in Falls Church, Va.
Dr. Younossi and colleagues conducted post hoc analyses of data from the ADVANCE trial, in which adding telaprevir to the treatment mix significantly improved patients’ sustained virologic response compared with standard PR therapy.
In the ADVANCE study, 1,088 treatment naive HCV genotype 1 patients were assigned to one of three treatment arms: 48 weeks of standard PR therapy; 12 weeks of telaprevir plus 24 weeks PR; or 12 weeks of telaprevir plus 48 weeks of PR. Nearly 80% of patients in both telaprevir groups achieved sustained virologic response, compared with 46% of patients in the standard PR treatment group (N. Engl. J. Med. 2011;364:2405-16).
In terms of side effects, "across all phase III studies, the incidence of rash and anemia (which are the effects we’re talking about with the protease inhibitors) was 56% and 34%, respectively, among telaprevir-treated patients, and 36% and 17% in patients receiving standard treatment," Dr. Younossi said.
To assess whether and to what degree these increases played a role in patient quality of life, Dr. Younossi and colleagues analyzed the results of EQ-5D quality of life questionnaires completed at baseline and at weeks 4, 12, 24, 36, 48, and 72 by 722 patients. They derived a summary index by calculating the percentages of patients reporting problems for each of the five health-related quality of life dimensions measured (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression).
After adjustment for age and sex, the baseline mean index values for the EQ-5D were 0.92 for the telaprevir plus 24-week PR group, 0.90 for the telaprevir plus 48-week PR group, and 0.91 for the 48-week PR-only group. The percentages of patients reporting any problems in each of the five qualitative dimensions at baseline were 8.2% for mobility, 2.0% for self-care, 12.9% for usual activities, 25.7% for pain/discomfort, and 25.6% for anxiety/depression, he said.
Across all the treatment groups, the EQ-5D index scores worsened during the first 12 weeks of treatment initiation. Specifically, mean values were 0.80 for the pooled-telaprevir groups and 0.83 for the PR-only group, according to Dr. Younossi.
Also, the respective percentages of patients in the pooled-telaprevir and PR-only groups reporting any problems at week 12 were 56% and 50% for usual activities, 51% and 42% for anxiety/depression, and 60% and 63% for pain/discomfort, he said. Change from baseline in terms of reported impact on mobility and self-care were small and not reported.
At week 48, the corresponding mean EQ-5D values were 0.93 for the telaprevir plus 24-week PR group, 0.83 for the telaprevir plus 48-week PR group, and 0.84 for the PR-only group.
By week 72 the EQ-5D index values returned to baseline levels, Dr. Younossi said.
Adjusted for age and sex, the mean EQ-5D index at week 72 was higher among the patients achieving sustained virologic response (SVR) compared with those who did not, with respective values of 0.90 and 0.86. "The 4% difference is within the range of published values for the minimal clinically important difference for the EQ-5D," he said.
Furthermore, at week 72, there were fewer patients among those who experienced SVR and reported problems in each dimension, compared with those who did not experience SVR.
At week 72, after adjustment for the index at baseline, patient age, sex, race, advanced liver disease, self-reported comorbidities, and the number of adverse events during treatment, only SVR was a positive predictor of the EQ-5D index. "We saw that [SVR] was a statistically significant and meaningful predictor of health-related quality of life," he said.
The study findings are consistent with the published research on the impacts of interferon-based regimens on health-related quality of life in this patient population, "and support the value of shorter treatment duration and [SVR] from a patient-reported outcomes perspective," said Dr. Younossi.
"We certainly cannot say that adding telaprevir causes fewer side effects. It’s clear there are more side effects, but it appears that the most troublesome side effects are related to the interferon therapy," he explained. When considered in the context of the improved SVR, "the burden of the increased incidence of anemia and rash associated with telaprevir, of which few cases are severe, appears to be outweighed by the overall treatment response."
This study was sponsored by Vertex. Dr. Younossi disclosed relationships with Biolex, Vertex, Salix, GlaxoSmithKline, and Tibotec.
SAN DIEGO – Although the addition of telaprevir to peginterferon/ribavirin therapy for treatment of chronic hepatitis C exacerbates treatment-related side effects, the triple combination does not diminish patient quality of life relative to treatment with the peginterferon/ribavirin regimen alone, a study has shown.
In other words, adding the protease inhibitor "does not further diminish patient quality of life," lead investigator Dr. Zobair Younossi explained at the annual Digestive Disease Week. "The most important contributor to the quality of life measurement in interferon therapy is interferon itself, which is so overwhelming in terms of side effects, especially grade 4 and 5 effects, that it probably overshadows everything else," he said.
Studies have shown that the addition of telaprevir to standard peginterferon alfa-2a/ribavirin (PR) significantly improves treatment efficacy in treatment-naive patients with genotype 1 hepatitis C virus (HCV), but there is a perception that the additional side effect burden from adding telaprevir is prohibitive in some patients, said Dr. Younossi, chairman of the department of medicine at Inova Health System in Falls Church, Va.
Dr. Younossi and colleagues conducted post hoc analyses of data from the ADVANCE trial, in which adding telaprevir to the treatment mix significantly improved patients’ sustained virologic response compared with standard PR therapy.
In the ADVANCE study, 1,088 treatment naive HCV genotype 1 patients were assigned to one of three treatment arms: 48 weeks of standard PR therapy; 12 weeks of telaprevir plus 24 weeks PR; or 12 weeks of telaprevir plus 48 weeks of PR. Nearly 80% of patients in both telaprevir groups achieved sustained virologic response, compared with 46% of patients in the standard PR treatment group (N. Engl. J. Med. 2011;364:2405-16).
In terms of side effects, "across all phase III studies, the incidence of rash and anemia (which are the effects we’re talking about with the protease inhibitors) was 56% and 34%, respectively, among telaprevir-treated patients, and 36% and 17% in patients receiving standard treatment," Dr. Younossi said.
To assess whether and to what degree these increases played a role in patient quality of life, Dr. Younossi and colleagues analyzed the results of EQ-5D quality of life questionnaires completed at baseline and at weeks 4, 12, 24, 36, 48, and 72 by 722 patients. They derived a summary index by calculating the percentages of patients reporting problems for each of the five health-related quality of life dimensions measured (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression).
After adjustment for age and sex, the baseline mean index values for the EQ-5D were 0.92 for the telaprevir plus 24-week PR group, 0.90 for the telaprevir plus 48-week PR group, and 0.91 for the 48-week PR-only group. The percentages of patients reporting any problems in each of the five qualitative dimensions at baseline were 8.2% for mobility, 2.0% for self-care, 12.9% for usual activities, 25.7% for pain/discomfort, and 25.6% for anxiety/depression, he said.
Across all the treatment groups, the EQ-5D index scores worsened during the first 12 weeks of treatment initiation. Specifically, mean values were 0.80 for the pooled-telaprevir groups and 0.83 for the PR-only group, according to Dr. Younossi.
Also, the respective percentages of patients in the pooled-telaprevir and PR-only groups reporting any problems at week 12 were 56% and 50% for usual activities, 51% and 42% for anxiety/depression, and 60% and 63% for pain/discomfort, he said. Change from baseline in terms of reported impact on mobility and self-care were small and not reported.
At week 48, the corresponding mean EQ-5D values were 0.93 for the telaprevir plus 24-week PR group, 0.83 for the telaprevir plus 48-week PR group, and 0.84 for the PR-only group.
By week 72 the EQ-5D index values returned to baseline levels, Dr. Younossi said.
Adjusted for age and sex, the mean EQ-5D index at week 72 was higher among the patients achieving sustained virologic response (SVR) compared with those who did not, with respective values of 0.90 and 0.86. "The 4% difference is within the range of published values for the minimal clinically important difference for the EQ-5D," he said.
Furthermore, at week 72, there were fewer patients among those who experienced SVR and reported problems in each dimension, compared with those who did not experience SVR.
At week 72, after adjustment for the index at baseline, patient age, sex, race, advanced liver disease, self-reported comorbidities, and the number of adverse events during treatment, only SVR was a positive predictor of the EQ-5D index. "We saw that [SVR] was a statistically significant and meaningful predictor of health-related quality of life," he said.
The study findings are consistent with the published research on the impacts of interferon-based regimens on health-related quality of life in this patient population, "and support the value of shorter treatment duration and [SVR] from a patient-reported outcomes perspective," said Dr. Younossi.
"We certainly cannot say that adding telaprevir causes fewer side effects. It’s clear there are more side effects, but it appears that the most troublesome side effects are related to the interferon therapy," he explained. When considered in the context of the improved SVR, "the burden of the increased incidence of anemia and rash associated with telaprevir, of which few cases are severe, appears to be outweighed by the overall treatment response."
This study was sponsored by Vertex. Dr. Younossi disclosed relationships with Biolex, Vertex, Salix, GlaxoSmithKline, and Tibotec.
SAN DIEGO – Although the addition of telaprevir to peginterferon/ribavirin therapy for treatment of chronic hepatitis C exacerbates treatment-related side effects, the triple combination does not diminish patient quality of life relative to treatment with the peginterferon/ribavirin regimen alone, a study has shown.
In other words, adding the protease inhibitor "does not further diminish patient quality of life," lead investigator Dr. Zobair Younossi explained at the annual Digestive Disease Week. "The most important contributor to the quality of life measurement in interferon therapy is interferon itself, which is so overwhelming in terms of side effects, especially grade 4 and 5 effects, that it probably overshadows everything else," he said.
Studies have shown that the addition of telaprevir to standard peginterferon alfa-2a/ribavirin (PR) significantly improves treatment efficacy in treatment-naive patients with genotype 1 hepatitis C virus (HCV), but there is a perception that the additional side effect burden from adding telaprevir is prohibitive in some patients, said Dr. Younossi, chairman of the department of medicine at Inova Health System in Falls Church, Va.
Dr. Younossi and colleagues conducted post hoc analyses of data from the ADVANCE trial, in which adding telaprevir to the treatment mix significantly improved patients’ sustained virologic response compared with standard PR therapy.
In the ADVANCE study, 1,088 treatment naive HCV genotype 1 patients were assigned to one of three treatment arms: 48 weeks of standard PR therapy; 12 weeks of telaprevir plus 24 weeks PR; or 12 weeks of telaprevir plus 48 weeks of PR. Nearly 80% of patients in both telaprevir groups achieved sustained virologic response, compared with 46% of patients in the standard PR treatment group (N. Engl. J. Med. 2011;364:2405-16).
In terms of side effects, "across all phase III studies, the incidence of rash and anemia (which are the effects we’re talking about with the protease inhibitors) was 56% and 34%, respectively, among telaprevir-treated patients, and 36% and 17% in patients receiving standard treatment," Dr. Younossi said.
To assess whether and to what degree these increases played a role in patient quality of life, Dr. Younossi and colleagues analyzed the results of EQ-5D quality of life questionnaires completed at baseline and at weeks 4, 12, 24, 36, 48, and 72 by 722 patients. They derived a summary index by calculating the percentages of patients reporting problems for each of the five health-related quality of life dimensions measured (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression).
After adjustment for age and sex, the baseline mean index values for the EQ-5D were 0.92 for the telaprevir plus 24-week PR group, 0.90 for the telaprevir plus 48-week PR group, and 0.91 for the 48-week PR-only group. The percentages of patients reporting any problems in each of the five qualitative dimensions at baseline were 8.2% for mobility, 2.0% for self-care, 12.9% for usual activities, 25.7% for pain/discomfort, and 25.6% for anxiety/depression, he said.
Across all the treatment groups, the EQ-5D index scores worsened during the first 12 weeks of treatment initiation. Specifically, mean values were 0.80 for the pooled-telaprevir groups and 0.83 for the PR-only group, according to Dr. Younossi.
Also, the respective percentages of patients in the pooled-telaprevir and PR-only groups reporting any problems at week 12 were 56% and 50% for usual activities, 51% and 42% for anxiety/depression, and 60% and 63% for pain/discomfort, he said. Change from baseline in terms of reported impact on mobility and self-care were small and not reported.
At week 48, the corresponding mean EQ-5D values were 0.93 for the telaprevir plus 24-week PR group, 0.83 for the telaprevir plus 48-week PR group, and 0.84 for the PR-only group.
By week 72 the EQ-5D index values returned to baseline levels, Dr. Younossi said.
Adjusted for age and sex, the mean EQ-5D index at week 72 was higher among the patients achieving sustained virologic response (SVR) compared with those who did not, with respective values of 0.90 and 0.86. "The 4% difference is within the range of published values for the minimal clinically important difference for the EQ-5D," he said.
Furthermore, at week 72, there were fewer patients among those who experienced SVR and reported problems in each dimension, compared with those who did not experience SVR.
At week 72, after adjustment for the index at baseline, patient age, sex, race, advanced liver disease, self-reported comorbidities, and the number of adverse events during treatment, only SVR was a positive predictor of the EQ-5D index. "We saw that [SVR] was a statistically significant and meaningful predictor of health-related quality of life," he said.
The study findings are consistent with the published research on the impacts of interferon-based regimens on health-related quality of life in this patient population, "and support the value of shorter treatment duration and [SVR] from a patient-reported outcomes perspective," said Dr. Younossi.
"We certainly cannot say that adding telaprevir causes fewer side effects. It’s clear there are more side effects, but it appears that the most troublesome side effects are related to the interferon therapy," he explained. When considered in the context of the improved SVR, "the burden of the increased incidence of anemia and rash associated with telaprevir, of which few cases are severe, appears to be outweighed by the overall treatment response."
This study was sponsored by Vertex. Dr. Younossi disclosed relationships with Biolex, Vertex, Salix, GlaxoSmithKline, and Tibotec.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: After adjustment for age and sex in treatment-naive chronic HCV patients, the baseline mean index values for health-related quality of life on the EQ-5D were 0.92 for the telaprevir plus 24-week PR group, 0.90 for the telaprevir plus 48-week PR group, and 0.91 for the 48-week PR-only group. At treatment week 12, mean values dropped to 0.80 for the pooled telaprevir groups and to 0.83 for the PR-only group, and then rebounded to baseline levels at 72 weeks, indicating that the addition of telaprevir to PR did not further impair quality of life.
Data Source: Findings are based on post hoc analyses of the ADVANCE randomized controlled trial comparing telaprevir plus PR vs. PR alone in chronic HCV.
Disclosures: This study was sponsored by Vertex. Dr. Younossi disclosed relationships with Biolex, Vertex, Salix, GlaxoSmithKline, and Tibotec.
Liver Cancer Rates Continue to Rise, Vigilance Warranted
SAN DIEGO – The U.S. incidence of hepatocellular carcinoma continues to soar, and will likely remain on that trajectory for at least a couple of decades, fed in large part by the obesity and type 2 diabetes epidemics, as well as by infections with hepatitis virus types C and B.
"I think rates will increase for another 10-20 years," predicted Dr. Alita Mishra, one of two researchers who reported results at the meeting from independent studies that documented increased rates of U.S. hepatocellular carcinoma (HCC) cases during the 2000s.
Greater vigilance is therefore needed to spot incident cases early, she said in an interview. While patients infected with hepatitis C virus who develop cirrhosis usually undergo routine, serial ultrasound screening for liver lesions, regular surveillance occurs less often in patients with cirrhosis who are infected with hepatitis B virus, or those with cirrhosis due to non-alcoholic fatty liver disease (NAFLD) secondary to obesity or type two diabetes. "Patients with cirrhosis should undergo regular HCC screening regardless of the underlying cause," Dr. Mishra said at the annual Digestive Disease Week.
One analysis, based on data collected by the Surveillance Epidemiology and End Results (SEER) registry of the National Cancer Institute, showed that U.S. HCC rates rose three-fold from 1975-2007, including a 33% rise during 1998-2007, Jessica A. Davila, Ph.D. reported at the meeting.
The second analysis, using data collected by the Nationwide Inpatient Sample (NIS), showed that the number of patients hospitalized with HCC per 100,000 hospital discharges jumped from 148 in 2005 to 213, said Dr. Mishra, a hospitalist at Inova Farifax (Va.) Hospital.
"HCC is rising because of hepatitis C viral infection, especially in people born during 1945-1965," Dr. Mishra said in an interview. Many of these people don’t know they are infected, and it usually takes decades for them to develop HCC.
The second big factor is the rising prevalence of obesity and type 2 diabetes. "Hepatitis C infections are now falling, so perhaps the rise in new HCC cases will eventually peak, but not if other factors like obesity and type 2 diabetes continue to push it up," she said.
"What is driving a lot of the increase is hepatitis C virus, and the high prevalence of hepatitis B virus in foreign-born Asians," said Dr. Davila, a clinical epidemiologist at the Houston VA Medical Center and Baylor College of Medicine in Houston.
"A lot also has to do with obesity and type 2 diabetes and their association with non-alcoholic fatty liver disease, especially in middle-aged, Hispanic women. I think we’ll see the greatest increase in HCC in women during the next 2 decades," Dr. Davila said. She also predicted increasing numbers of hepatitis C virus-driven HCC cases in the short term "as the [infected] cohort ages, increasing numbers will develop advanced fibrosis and eventually HCC," she said.
Dr. Davila’s study used data from SEER, which the National Cancer Institute began in 1973 to collect data on cancer cases from about 14% of the U.S. population in selected states and metropolitan areas. During 1975-2007, SEER tallied a total of 21,472 HCC cases, about 80% of which occurred in people aged 50-79 years, and about three-quarters of cases in men.
HCC incidence rose from 1.6 cases per 100,000 people during 1975-1977 to 4.8 per 100,000 in 2005-2007. Roughly a tripling of cases during the three decades occurred in both men and in women. The greatest increase occurred among people aged 50-59 years, which jumped nearly fivefold, from 2.6 per 100,000 in 1975-1977 to 12.6 per 100,000 in 2005-2007. The smallest rise was 2.4-fold among people aged 70-79 years.
By 2005-2007, the highest rate was among Asians, 10.3 per 100,000, followed by 8.2 per 100,000 in Hispanics, 7.5 per 100,000 in blacks, and 3.7/100,000 in whites (see table).
Dr. Mishra’s study used data collected in NIS by the federal Agency for Healthcare Research and Quality from about 1,000 hospitals in 44 states. The number of patients hospitalized with HCC (not confined to incident cases) rose from 9,537 in 2005 to 13,689 in 2009. During the 5-year period, in-hospital mortality of HCC cases dropped from 120 per 1,000 cases in 2005 to 95 per 1,000 cases in 2009, and the median length of stay fell by about 0.5 days.
Despite reduced hospitalized time, median hospital charges for each HCC hospitalized case rose from about $21,000 in 2005 to nearly $29,000 in 2009. Paralleling this increase was an uptick in the percent of cases having "major" or "extreme" illness, from 52% in 2005 to 63% in 2009, and the average number of comorbidities also rose steadily during the 5 years studied.
Hospitalized patients with HCC "are getting sicker, more complicated, and have more comorbidities," Dr. Mishra said. She also noted that the rate of liver transplants remained "very low" during the period studied.
Dr. Davila and Dr. Mishra reported having no conflicts of interest.
SAN DIEGO – The U.S. incidence of hepatocellular carcinoma continues to soar, and will likely remain on that trajectory for at least a couple of decades, fed in large part by the obesity and type 2 diabetes epidemics, as well as by infections with hepatitis virus types C and B.
"I think rates will increase for another 10-20 years," predicted Dr. Alita Mishra, one of two researchers who reported results at the meeting from independent studies that documented increased rates of U.S. hepatocellular carcinoma (HCC) cases during the 2000s.
Greater vigilance is therefore needed to spot incident cases early, she said in an interview. While patients infected with hepatitis C virus who develop cirrhosis usually undergo routine, serial ultrasound screening for liver lesions, regular surveillance occurs less often in patients with cirrhosis who are infected with hepatitis B virus, or those with cirrhosis due to non-alcoholic fatty liver disease (NAFLD) secondary to obesity or type two diabetes. "Patients with cirrhosis should undergo regular HCC screening regardless of the underlying cause," Dr. Mishra said at the annual Digestive Disease Week.
One analysis, based on data collected by the Surveillance Epidemiology and End Results (SEER) registry of the National Cancer Institute, showed that U.S. HCC rates rose three-fold from 1975-2007, including a 33% rise during 1998-2007, Jessica A. Davila, Ph.D. reported at the meeting.
The second analysis, using data collected by the Nationwide Inpatient Sample (NIS), showed that the number of patients hospitalized with HCC per 100,000 hospital discharges jumped from 148 in 2005 to 213, said Dr. Mishra, a hospitalist at Inova Farifax (Va.) Hospital.
"HCC is rising because of hepatitis C viral infection, especially in people born during 1945-1965," Dr. Mishra said in an interview. Many of these people don’t know they are infected, and it usually takes decades for them to develop HCC.
The second big factor is the rising prevalence of obesity and type 2 diabetes. "Hepatitis C infections are now falling, so perhaps the rise in new HCC cases will eventually peak, but not if other factors like obesity and type 2 diabetes continue to push it up," she said.
"What is driving a lot of the increase is hepatitis C virus, and the high prevalence of hepatitis B virus in foreign-born Asians," said Dr. Davila, a clinical epidemiologist at the Houston VA Medical Center and Baylor College of Medicine in Houston.
"A lot also has to do with obesity and type 2 diabetes and their association with non-alcoholic fatty liver disease, especially in middle-aged, Hispanic women. I think we’ll see the greatest increase in HCC in women during the next 2 decades," Dr. Davila said. She also predicted increasing numbers of hepatitis C virus-driven HCC cases in the short term "as the [infected] cohort ages, increasing numbers will develop advanced fibrosis and eventually HCC," she said.
Dr. Davila’s study used data from SEER, which the National Cancer Institute began in 1973 to collect data on cancer cases from about 14% of the U.S. population in selected states and metropolitan areas. During 1975-2007, SEER tallied a total of 21,472 HCC cases, about 80% of which occurred in people aged 50-79 years, and about three-quarters of cases in men.
HCC incidence rose from 1.6 cases per 100,000 people during 1975-1977 to 4.8 per 100,000 in 2005-2007. Roughly a tripling of cases during the three decades occurred in both men and in women. The greatest increase occurred among people aged 50-59 years, which jumped nearly fivefold, from 2.6 per 100,000 in 1975-1977 to 12.6 per 100,000 in 2005-2007. The smallest rise was 2.4-fold among people aged 70-79 years.
By 2005-2007, the highest rate was among Asians, 10.3 per 100,000, followed by 8.2 per 100,000 in Hispanics, 7.5 per 100,000 in blacks, and 3.7/100,000 in whites (see table).
Dr. Mishra’s study used data collected in NIS by the federal Agency for Healthcare Research and Quality from about 1,000 hospitals in 44 states. The number of patients hospitalized with HCC (not confined to incident cases) rose from 9,537 in 2005 to 13,689 in 2009. During the 5-year period, in-hospital mortality of HCC cases dropped from 120 per 1,000 cases in 2005 to 95 per 1,000 cases in 2009, and the median length of stay fell by about 0.5 days.
Despite reduced hospitalized time, median hospital charges for each HCC hospitalized case rose from about $21,000 in 2005 to nearly $29,000 in 2009. Paralleling this increase was an uptick in the percent of cases having "major" or "extreme" illness, from 52% in 2005 to 63% in 2009, and the average number of comorbidities also rose steadily during the 5 years studied.
Hospitalized patients with HCC "are getting sicker, more complicated, and have more comorbidities," Dr. Mishra said. She also noted that the rate of liver transplants remained "very low" during the period studied.
Dr. Davila and Dr. Mishra reported having no conflicts of interest.
SAN DIEGO – The U.S. incidence of hepatocellular carcinoma continues to soar, and will likely remain on that trajectory for at least a couple of decades, fed in large part by the obesity and type 2 diabetes epidemics, as well as by infections with hepatitis virus types C and B.
"I think rates will increase for another 10-20 years," predicted Dr. Alita Mishra, one of two researchers who reported results at the meeting from independent studies that documented increased rates of U.S. hepatocellular carcinoma (HCC) cases during the 2000s.
Greater vigilance is therefore needed to spot incident cases early, she said in an interview. While patients infected with hepatitis C virus who develop cirrhosis usually undergo routine, serial ultrasound screening for liver lesions, regular surveillance occurs less often in patients with cirrhosis who are infected with hepatitis B virus, or those with cirrhosis due to non-alcoholic fatty liver disease (NAFLD) secondary to obesity or type two diabetes. "Patients with cirrhosis should undergo regular HCC screening regardless of the underlying cause," Dr. Mishra said at the annual Digestive Disease Week.
One analysis, based on data collected by the Surveillance Epidemiology and End Results (SEER) registry of the National Cancer Institute, showed that U.S. HCC rates rose three-fold from 1975-2007, including a 33% rise during 1998-2007, Jessica A. Davila, Ph.D. reported at the meeting.
The second analysis, using data collected by the Nationwide Inpatient Sample (NIS), showed that the number of patients hospitalized with HCC per 100,000 hospital discharges jumped from 148 in 2005 to 213, said Dr. Mishra, a hospitalist at Inova Farifax (Va.) Hospital.
"HCC is rising because of hepatitis C viral infection, especially in people born during 1945-1965," Dr. Mishra said in an interview. Many of these people don’t know they are infected, and it usually takes decades for them to develop HCC.
The second big factor is the rising prevalence of obesity and type 2 diabetes. "Hepatitis C infections are now falling, so perhaps the rise in new HCC cases will eventually peak, but not if other factors like obesity and type 2 diabetes continue to push it up," she said.
"What is driving a lot of the increase is hepatitis C virus, and the high prevalence of hepatitis B virus in foreign-born Asians," said Dr. Davila, a clinical epidemiologist at the Houston VA Medical Center and Baylor College of Medicine in Houston.
"A lot also has to do with obesity and type 2 diabetes and their association with non-alcoholic fatty liver disease, especially in middle-aged, Hispanic women. I think we’ll see the greatest increase in HCC in women during the next 2 decades," Dr. Davila said. She also predicted increasing numbers of hepatitis C virus-driven HCC cases in the short term "as the [infected] cohort ages, increasing numbers will develop advanced fibrosis and eventually HCC," she said.
Dr. Davila’s study used data from SEER, which the National Cancer Institute began in 1973 to collect data on cancer cases from about 14% of the U.S. population in selected states and metropolitan areas. During 1975-2007, SEER tallied a total of 21,472 HCC cases, about 80% of which occurred in people aged 50-79 years, and about three-quarters of cases in men.
HCC incidence rose from 1.6 cases per 100,000 people during 1975-1977 to 4.8 per 100,000 in 2005-2007. Roughly a tripling of cases during the three decades occurred in both men and in women. The greatest increase occurred among people aged 50-59 years, which jumped nearly fivefold, from 2.6 per 100,000 in 1975-1977 to 12.6 per 100,000 in 2005-2007. The smallest rise was 2.4-fold among people aged 70-79 years.
By 2005-2007, the highest rate was among Asians, 10.3 per 100,000, followed by 8.2 per 100,000 in Hispanics, 7.5 per 100,000 in blacks, and 3.7/100,000 in whites (see table).
Dr. Mishra’s study used data collected in NIS by the federal Agency for Healthcare Research and Quality from about 1,000 hospitals in 44 states. The number of patients hospitalized with HCC (not confined to incident cases) rose from 9,537 in 2005 to 13,689 in 2009. During the 5-year period, in-hospital mortality of HCC cases dropped from 120 per 1,000 cases in 2005 to 95 per 1,000 cases in 2009, and the median length of stay fell by about 0.5 days.
Despite reduced hospitalized time, median hospital charges for each HCC hospitalized case rose from about $21,000 in 2005 to nearly $29,000 in 2009. Paralleling this increase was an uptick in the percent of cases having "major" or "extreme" illness, from 52% in 2005 to 63% in 2009, and the average number of comorbidities also rose steadily during the 5 years studied.
Hospitalized patients with HCC "are getting sicker, more complicated, and have more comorbidities," Dr. Mishra said. She also noted that the rate of liver transplants remained "very low" during the period studied.
Dr. Davila and Dr. Mishra reported having no conflicts of interest.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: U.S. hepatocellular carcinoma cases rose threefold during 1975-2007, while hospitalized cases rose by more than a third during 2005-2009.
Data Source: Data came from a review of U.S. HCC cases collected by the SEER registry during 1975-2007, and from a review of hospitalized U.S. HCC cases collected in the NIS registry during 2005-2009.
Disclosures: Dr. Davila and Dr. Mishra reported having no conflicts of interest.
Scope Matches Pathology in Diminutive Colorectal Polyps
SAN DIEGO – Researchers have taken a major step toward eliminating the need for routine pathology on every polyp removed during colonoscopy.
Use of a high-definition, dual-focus colonoscope allowed endoscopists to perform "significantly more accurate, high-confidence endoscopic diagnosis of diminutive polyps," Dr. Tonya Kaltenbach said at the annual Digestive Disease Week.
"In many hospitals, about 20%-25% of all pathology samples are small colon polyps, almost all of which are benign. This is a lot of money that can be saved," said Dr. Kaltenbach in a written statement. About 80% of all polyps found during screening colonoscopy are diminutive, 5 mm in diameter or less, and the current standard of care is to do a pathology analysis on each of these polyps.
As used by five gastroenterologists who participated in the study at three U.S. centers to assess 530 polyps in 277 people, the high-definition scope produced a 95.9% agreement in polyp assignment for follow-up surveillance, compared with pathology-laboratory analysis of the same polyps, and a 96.4% negative predictive value for adenomas, said Dr. Kaltenbach, a gastroenterologist at the VA Medical Center in Palo Alto, Calif.
These performance levels surpassed the greater than 90% targets for colonoscopic assessment of diminutive polyps set last year by a committee organized by the American Society of Gastrointestinal Endoscopy (Gastrointest. Endosc. 2011;73:419-22). Notably, the 90% threshold for assignment of postpolypectomy surveillance accuracy and negative predictive value was set by the ASGE committee before dual-focus colonoscopies like the one used in the current study were in widespread use, said Dr. Roy Soetikno, chief of endoscopy at the Palo Alto VA and senior investigator on the study.
Today, some of the scopes used in routine U.S. practice have the high-definition, dual focus features of the one used in the study, and within the next 5 years essentially all U.S. colonoscopies will have these performance characteristics, he said in an interview.
Although the new study results showed that endoscopists can surpass the thresholds set by the ASGE for visual assessment, widespread use of the method will require further validation, Dr. Soetikno said. "We need to develop programs to teach gastroenterologists and incorporate them into fellowship programs. We also need a way to store the images so that people can document their diagnoses. But [our study] is the beginning," he said.
Dr. Soetikno also noted that the idea of visual assessment of potentially cancerous or precancerous lesions is not new, as the same approach is routinely used in dermatology. With new technologies, gastroenterologists "may be able to do the same thing. We can save our resources, and not spend money on evaluating polyps of no consequence."
Dr. Soetikno, Dr. Kaltenbach, and their associates designed the Veterans Affairs Colorectal Lesion Interpretation and Diagnosis (VALID) study to test the hypothesis that colonoscopy using a high-definition, narrow-band imaging, dual focus colonoscope could increase the rate of accurate, high-confidence histology predictions of diminutive polyps. Five endoscopists working at three VA Medical Centers randomized 558 patients scheduled to undergo routine colonoscopy. The patients averaged 63 years old, 95% were men, and about 80% were white. Roughly 38% underwent colonoscopy for screening, 44% for surveillance following a history of polyps, and for 19% the examination was symptom driven (total is 101% due to rounding).
The protocol randomized 277 people to high-definition colonoscopy with an Olympus model CF-HQ190, and 281 people to examination with an older model without dual-focus capability, the Olympus CF-H180. Examination of the people in the dual-focus group found 710 polyps, including 530 diminutive lesions; the control group had 599 polyps, including 445 that were 5 mm or less.
The endoscopists made accurate, high-confidence endoscopic predictions on 75% of the diminutive polyps that they saw using the dual-focus device, compared with a 63% when they used the less advanced endoscope, a statistically significant difference. When compared with the pathologic assessments, 95.9% of the high-confidence, dual-focus diagnoses produced correct surveillance-interval recommendations, compared with a 95.2% rate using the standard-focus device. Negative predictive value was 96.4% using the dual-focus scope and 92.0% for the more conventional scope. In addition, the dual-focus scope produced no misdiagnoses of advanced histology as non-neoplasia, and use of this scope did not result in any meaningful increase in examination time, nor did it produce any bleeding or perforation.
The VALID study received partial funding from Olympus America, the company that markets the dual-focus, high-definition colonoscope tested. Dr. Soetikno said that he has been a consultant to Olympus. Dr. Kaltenbach and Dr. Kochman said they had no disclosures.
The Preservation and Incorporation of Valuable Endoscopic Innovations (PIVI) statement issued last year by the American Society of Gastrointestinal Endoscopy threw down a challenge to companies to come up with a colonoscope technology that could meet the threshold for clinical application of the "cut and discard" approach to managing diminutive colorectal polyp. The new report by Drs. Kaltenbach, Dr. Soetikno, and their associates is a major step in that direction. Their findings show that endoscopists really can see and accurately predict the histologic profile of colorectal polyps without producing any major adverse outcomes.

|
Mitchel L. Zoler/IMNG Medical Media
|
However, despite the success reported in this study, it is premature to extrapolate the efficacy of the colonoscopic methods they used to routine practice. Results are always better when physicians participate in a study and know they are being watched. We worry that there will be a fall in efficacy as the method diffuses out more widely. A better approach is what Dr. Soetikno suggested: waiting until a generation of endoscopists come into practice who have undergone thorough training with the new, high-definition scopes.
Dr. Michael L. Kochman is a gastroenterologist and professor of medicine at the University of Pennsylvania in Philadelphia. He said that he had no relevant disclosures. He made these remarks in a press conference during the DDW meeting.
The Preservation and Incorporation of Valuable Endoscopic Innovations (PIVI) statement issued last year by the American Society of Gastrointestinal Endoscopy threw down a challenge to companies to come up with a colonoscope technology that could meet the threshold for clinical application of the "cut and discard" approach to managing diminutive colorectal polyp. The new report by Drs. Kaltenbach, Dr. Soetikno, and their associates is a major step in that direction. Their findings show that endoscopists really can see and accurately predict the histologic profile of colorectal polyps without producing any major adverse outcomes.

|
Mitchel L. Zoler/IMNG Medical Media
|
However, despite the success reported in this study, it is premature to extrapolate the efficacy of the colonoscopic methods they used to routine practice. Results are always better when physicians participate in a study and know they are being watched. We worry that there will be a fall in efficacy as the method diffuses out more widely. A better approach is what Dr. Soetikno suggested: waiting until a generation of endoscopists come into practice who have undergone thorough training with the new, high-definition scopes.
Dr. Michael L. Kochman is a gastroenterologist and professor of medicine at the University of Pennsylvania in Philadelphia. He said that he had no relevant disclosures. He made these remarks in a press conference during the DDW meeting.
The Preservation and Incorporation of Valuable Endoscopic Innovations (PIVI) statement issued last year by the American Society of Gastrointestinal Endoscopy threw down a challenge to companies to come up with a colonoscope technology that could meet the threshold for clinical application of the "cut and discard" approach to managing diminutive colorectal polyp. The new report by Drs. Kaltenbach, Dr. Soetikno, and their associates is a major step in that direction. Their findings show that endoscopists really can see and accurately predict the histologic profile of colorectal polyps without producing any major adverse outcomes.

|
Mitchel L. Zoler/IMNG Medical Media
|
However, despite the success reported in this study, it is premature to extrapolate the efficacy of the colonoscopic methods they used to routine practice. Results are always better when physicians participate in a study and know they are being watched. We worry that there will be a fall in efficacy as the method diffuses out more widely. A better approach is what Dr. Soetikno suggested: waiting until a generation of endoscopists come into practice who have undergone thorough training with the new, high-definition scopes.
Dr. Michael L. Kochman is a gastroenterologist and professor of medicine at the University of Pennsylvania in Philadelphia. He said that he had no relevant disclosures. He made these remarks in a press conference during the DDW meeting.
SAN DIEGO – Researchers have taken a major step toward eliminating the need for routine pathology on every polyp removed during colonoscopy.
Use of a high-definition, dual-focus colonoscope allowed endoscopists to perform "significantly more accurate, high-confidence endoscopic diagnosis of diminutive polyps," Dr. Tonya Kaltenbach said at the annual Digestive Disease Week.
"In many hospitals, about 20%-25% of all pathology samples are small colon polyps, almost all of which are benign. This is a lot of money that can be saved," said Dr. Kaltenbach in a written statement. About 80% of all polyps found during screening colonoscopy are diminutive, 5 mm in diameter or less, and the current standard of care is to do a pathology analysis on each of these polyps.
As used by five gastroenterologists who participated in the study at three U.S. centers to assess 530 polyps in 277 people, the high-definition scope produced a 95.9% agreement in polyp assignment for follow-up surveillance, compared with pathology-laboratory analysis of the same polyps, and a 96.4% negative predictive value for adenomas, said Dr. Kaltenbach, a gastroenterologist at the VA Medical Center in Palo Alto, Calif.
These performance levels surpassed the greater than 90% targets for colonoscopic assessment of diminutive polyps set last year by a committee organized by the American Society of Gastrointestinal Endoscopy (Gastrointest. Endosc. 2011;73:419-22). Notably, the 90% threshold for assignment of postpolypectomy surveillance accuracy and negative predictive value was set by the ASGE committee before dual-focus colonoscopies like the one used in the current study were in widespread use, said Dr. Roy Soetikno, chief of endoscopy at the Palo Alto VA and senior investigator on the study.
Today, some of the scopes used in routine U.S. practice have the high-definition, dual focus features of the one used in the study, and within the next 5 years essentially all U.S. colonoscopies will have these performance characteristics, he said in an interview.
Although the new study results showed that endoscopists can surpass the thresholds set by the ASGE for visual assessment, widespread use of the method will require further validation, Dr. Soetikno said. "We need to develop programs to teach gastroenterologists and incorporate them into fellowship programs. We also need a way to store the images so that people can document their diagnoses. But [our study] is the beginning," he said.
Dr. Soetikno also noted that the idea of visual assessment of potentially cancerous or precancerous lesions is not new, as the same approach is routinely used in dermatology. With new technologies, gastroenterologists "may be able to do the same thing. We can save our resources, and not spend money on evaluating polyps of no consequence."
Dr. Soetikno, Dr. Kaltenbach, and their associates designed the Veterans Affairs Colorectal Lesion Interpretation and Diagnosis (VALID) study to test the hypothesis that colonoscopy using a high-definition, narrow-band imaging, dual focus colonoscope could increase the rate of accurate, high-confidence histology predictions of diminutive polyps. Five endoscopists working at three VA Medical Centers randomized 558 patients scheduled to undergo routine colonoscopy. The patients averaged 63 years old, 95% were men, and about 80% were white. Roughly 38% underwent colonoscopy for screening, 44% for surveillance following a history of polyps, and for 19% the examination was symptom driven (total is 101% due to rounding).
The protocol randomized 277 people to high-definition colonoscopy with an Olympus model CF-HQ190, and 281 people to examination with an older model without dual-focus capability, the Olympus CF-H180. Examination of the people in the dual-focus group found 710 polyps, including 530 diminutive lesions; the control group had 599 polyps, including 445 that were 5 mm or less.
The endoscopists made accurate, high-confidence endoscopic predictions on 75% of the diminutive polyps that they saw using the dual-focus device, compared with a 63% when they used the less advanced endoscope, a statistically significant difference. When compared with the pathologic assessments, 95.9% of the high-confidence, dual-focus diagnoses produced correct surveillance-interval recommendations, compared with a 95.2% rate using the standard-focus device. Negative predictive value was 96.4% using the dual-focus scope and 92.0% for the more conventional scope. In addition, the dual-focus scope produced no misdiagnoses of advanced histology as non-neoplasia, and use of this scope did not result in any meaningful increase in examination time, nor did it produce any bleeding or perforation.
The VALID study received partial funding from Olympus America, the company that markets the dual-focus, high-definition colonoscope tested. Dr. Soetikno said that he has been a consultant to Olympus. Dr. Kaltenbach and Dr. Kochman said they had no disclosures.
SAN DIEGO – Researchers have taken a major step toward eliminating the need for routine pathology on every polyp removed during colonoscopy.
Use of a high-definition, dual-focus colonoscope allowed endoscopists to perform "significantly more accurate, high-confidence endoscopic diagnosis of diminutive polyps," Dr. Tonya Kaltenbach said at the annual Digestive Disease Week.
"In many hospitals, about 20%-25% of all pathology samples are small colon polyps, almost all of which are benign. This is a lot of money that can be saved," said Dr. Kaltenbach in a written statement. About 80% of all polyps found during screening colonoscopy are diminutive, 5 mm in diameter or less, and the current standard of care is to do a pathology analysis on each of these polyps.
As used by five gastroenterologists who participated in the study at three U.S. centers to assess 530 polyps in 277 people, the high-definition scope produced a 95.9% agreement in polyp assignment for follow-up surveillance, compared with pathology-laboratory analysis of the same polyps, and a 96.4% negative predictive value for adenomas, said Dr. Kaltenbach, a gastroenterologist at the VA Medical Center in Palo Alto, Calif.
These performance levels surpassed the greater than 90% targets for colonoscopic assessment of diminutive polyps set last year by a committee organized by the American Society of Gastrointestinal Endoscopy (Gastrointest. Endosc. 2011;73:419-22). Notably, the 90% threshold for assignment of postpolypectomy surveillance accuracy and negative predictive value was set by the ASGE committee before dual-focus colonoscopies like the one used in the current study were in widespread use, said Dr. Roy Soetikno, chief of endoscopy at the Palo Alto VA and senior investigator on the study.
Today, some of the scopes used in routine U.S. practice have the high-definition, dual focus features of the one used in the study, and within the next 5 years essentially all U.S. colonoscopies will have these performance characteristics, he said in an interview.
Although the new study results showed that endoscopists can surpass the thresholds set by the ASGE for visual assessment, widespread use of the method will require further validation, Dr. Soetikno said. "We need to develop programs to teach gastroenterologists and incorporate them into fellowship programs. We also need a way to store the images so that people can document their diagnoses. But [our study] is the beginning," he said.
Dr. Soetikno also noted that the idea of visual assessment of potentially cancerous or precancerous lesions is not new, as the same approach is routinely used in dermatology. With new technologies, gastroenterologists "may be able to do the same thing. We can save our resources, and not spend money on evaluating polyps of no consequence."
Dr. Soetikno, Dr. Kaltenbach, and their associates designed the Veterans Affairs Colorectal Lesion Interpretation and Diagnosis (VALID) study to test the hypothesis that colonoscopy using a high-definition, narrow-band imaging, dual focus colonoscope could increase the rate of accurate, high-confidence histology predictions of diminutive polyps. Five endoscopists working at three VA Medical Centers randomized 558 patients scheduled to undergo routine colonoscopy. The patients averaged 63 years old, 95% were men, and about 80% were white. Roughly 38% underwent colonoscopy for screening, 44% for surveillance following a history of polyps, and for 19% the examination was symptom driven (total is 101% due to rounding).
The protocol randomized 277 people to high-definition colonoscopy with an Olympus model CF-HQ190, and 281 people to examination with an older model without dual-focus capability, the Olympus CF-H180. Examination of the people in the dual-focus group found 710 polyps, including 530 diminutive lesions; the control group had 599 polyps, including 445 that were 5 mm or less.
The endoscopists made accurate, high-confidence endoscopic predictions on 75% of the diminutive polyps that they saw using the dual-focus device, compared with a 63% when they used the less advanced endoscope, a statistically significant difference. When compared with the pathologic assessments, 95.9% of the high-confidence, dual-focus diagnoses produced correct surveillance-interval recommendations, compared with a 95.2% rate using the standard-focus device. Negative predictive value was 96.4% using the dual-focus scope and 92.0% for the more conventional scope. In addition, the dual-focus scope produced no misdiagnoses of advanced histology as non-neoplasia, and use of this scope did not result in any meaningful increase in examination time, nor did it produce any bleeding or perforation.
The VALID study received partial funding from Olympus America, the company that markets the dual-focus, high-definition colonoscope tested. Dr. Soetikno said that he has been a consultant to Olympus. Dr. Kaltenbach and Dr. Kochman said they had no disclosures.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: High-definition, dual-focus colonoscopy produced 75% accurate, high-confidence diagnoses of diminutive polyps, vs. 63% using an older-model scope.
Data Source: Data came from a randomized, controlled trial with 558 people who underwent colonoscopy at three U.S. centers.
Disclosures: The VALID study received partial funding from Olympus America, the company that markets the dual-focus, high-definition colonoscope tested. Dr. Soetikno said that he has been a consultant to Olympus. Dr. Kaltenbach said that she had no disclosures.
Statins Appear Safe, Even Beneficial, in Cirrhosis
SAN DIEGO – Statin therapy is not only safe for patients with cirrhosis, it may slow the progression of their liver disease to hepatic decompensation and help them live longer, a study has shown.
The findings, reported at the annual Digestive Disease Week, should help allay fears that decreased hepatic clearance of statins could lead to complications in patients with advanced liver disease, as was previously hypothesized, said lead investigator Dr. Sonal Kumar.
"In fact, it seems the opposite may be true," said Dr. Kumar of Brigham and Women’s Hospital, Boston, referring to the results of her retrospective study in which statin therapy in cirrhosis patients was associated with a decreased risk of hepatic decompensation, a delay in the time to decompensation, and reduced all-cause mortality, compared with cirrhosis patients not taking statins.
The investigators were aware that some clinicians either do not initiate statin therapy or discontinue statins in patients with advanced liver disease because of perceived safety concerns. Dr. Kumar and her colleagues sought to determine the actual effect of statin therapy on the risk of hepatic decomposition in cirrhosis.
They identified all patients with biopsy-proven cirrhosis who had taken statins for a minimum of 3 months for treatment of dyslipidemia. A control population of cirrhosis patients not on statins was matched 2:1 for age, gender, and Child-Pugh class from the Partners HealthCare System Research Patient Data Registry, which includes demographic and diagnostic information on patients treated at Massachusetts General Hospital and Brigham and Women’s Hospital.
The primary outcomes of the study were hepatic decompensation, defined as the development of ascites, jaundice (bilirubin greater than 2.5 mg/dL), hepatic encephalopathy, or variceal hemorrhage, and time to decompensation. Mortality was a secondary outcome, Dr. Kumar explained.
The investigators created a Cox proportional hazards model for decompensation to control for age, Child-Pugh class, diabetes, coronary artery disease, and hepatocellular carcinoma, and they used conditional logistic regression to assess mortality, she said.
Of 243 cirrhosis patients included in the analysis, 81 were statin users and 162 were matched controls. "In each group, approximately 70% of patients were Child-Pugh A and 30% were Child-Pugh B/C, and the MELD [Model for End-Stage Liver Disease] score, albumin, presence of varices, and beta-blocker use were similar between groups," Dr. Kumar noted. In the statin group, which was followed for a mean of 1,756 days, decompensation was reported in 31 patients (38.2%), compared with 80 patients (50.62%) in the control group.
The control patients were followed for a mean of 1,503 days, and on Cox analysis, "statin therapy was the only factor significantly associated with lower decompensation risk, with a hazard ratio of 0.46." Additionally, Kaplan-Meier curves showed a significantly longer time to decompensation in patients receiving statin therapy, she said. In subgroup analyses, significantly longer time to decompensation was observed in Child-Pugh A and Child-Pugh B/C patients.
Overall mortality was significantly lower in the statin group, at 37.0%, than in the control group, at 50.6%, said Dr. Kumar. Statin use remained significantly associated with decreased mortality in multivariate analysis, with an odds ratio of 0.36, while coronary artery disease and hepatocellular carcinoma were associated with increased mortality, with respective odds ratios of 3.6 and 4.9.
There were no statistically significant differences in cause of death between the two groups, "however it is important to note that cause of death was not documented for approximately one-third of the study patients, so we cannot make definitive statements about whether patients on statins were less likely to die of liver-related or cardiovascular causes than patients in the control group," said Dr. Kumar.
The apparent hepatoprotective effect of statin therapy in cirrhosis patients may be a function of previously observed hemodynamic and molecular effects of statins, Dr. Kumar hypothesized. Sinusoidal endothelial dysfunction with decreased nitric oxide production contributes to increased hepatic resistance in cirrhosis, she explained. Just as statins improve endothelial dysfunction in the peripheral vasculature, they may also improve the vascular disturbances that contribute to portal hypertension in cirrhosis by selectively increasing nitric oxide availability in the liver, thus reducing pressures, she said.
The retrospective design of the study limits the conclusions that can be taken from it. Specifically, "we can’t say that all patients with liver disease should be prescribed statins," Dr. Kumar said. "What we can say is that statin therapy is safe in this population, it may be beneficial for its effects on the liver as well as the cardiovascular system, and clinicians should not hesitate to prescribe it for appropriate cardiovascular indications in cirrhosis patients." The findings also indicate that prospective studies are warranted to clarify the role of statins in advanced liver disease, she stressed.
Dr. Kumar disclosed no relevant financial conflicts of interest.
SAN DIEGO – Statin therapy is not only safe for patients with cirrhosis, it may slow the progression of their liver disease to hepatic decompensation and help them live longer, a study has shown.
The findings, reported at the annual Digestive Disease Week, should help allay fears that decreased hepatic clearance of statins could lead to complications in patients with advanced liver disease, as was previously hypothesized, said lead investigator Dr. Sonal Kumar.
"In fact, it seems the opposite may be true," said Dr. Kumar of Brigham and Women’s Hospital, Boston, referring to the results of her retrospective study in which statin therapy in cirrhosis patients was associated with a decreased risk of hepatic decompensation, a delay in the time to decompensation, and reduced all-cause mortality, compared with cirrhosis patients not taking statins.
The investigators were aware that some clinicians either do not initiate statin therapy or discontinue statins in patients with advanced liver disease because of perceived safety concerns. Dr. Kumar and her colleagues sought to determine the actual effect of statin therapy on the risk of hepatic decomposition in cirrhosis.
They identified all patients with biopsy-proven cirrhosis who had taken statins for a minimum of 3 months for treatment of dyslipidemia. A control population of cirrhosis patients not on statins was matched 2:1 for age, gender, and Child-Pugh class from the Partners HealthCare System Research Patient Data Registry, which includes demographic and diagnostic information on patients treated at Massachusetts General Hospital and Brigham and Women’s Hospital.
The primary outcomes of the study were hepatic decompensation, defined as the development of ascites, jaundice (bilirubin greater than 2.5 mg/dL), hepatic encephalopathy, or variceal hemorrhage, and time to decompensation. Mortality was a secondary outcome, Dr. Kumar explained.
The investigators created a Cox proportional hazards model for decompensation to control for age, Child-Pugh class, diabetes, coronary artery disease, and hepatocellular carcinoma, and they used conditional logistic regression to assess mortality, she said.
Of 243 cirrhosis patients included in the analysis, 81 were statin users and 162 were matched controls. "In each group, approximately 70% of patients were Child-Pugh A and 30% were Child-Pugh B/C, and the MELD [Model for End-Stage Liver Disease] score, albumin, presence of varices, and beta-blocker use were similar between groups," Dr. Kumar noted. In the statin group, which was followed for a mean of 1,756 days, decompensation was reported in 31 patients (38.2%), compared with 80 patients (50.62%) in the control group.
The control patients were followed for a mean of 1,503 days, and on Cox analysis, "statin therapy was the only factor significantly associated with lower decompensation risk, with a hazard ratio of 0.46." Additionally, Kaplan-Meier curves showed a significantly longer time to decompensation in patients receiving statin therapy, she said. In subgroup analyses, significantly longer time to decompensation was observed in Child-Pugh A and Child-Pugh B/C patients.
Overall mortality was significantly lower in the statin group, at 37.0%, than in the control group, at 50.6%, said Dr. Kumar. Statin use remained significantly associated with decreased mortality in multivariate analysis, with an odds ratio of 0.36, while coronary artery disease and hepatocellular carcinoma were associated with increased mortality, with respective odds ratios of 3.6 and 4.9.
There were no statistically significant differences in cause of death between the two groups, "however it is important to note that cause of death was not documented for approximately one-third of the study patients, so we cannot make definitive statements about whether patients on statins were less likely to die of liver-related or cardiovascular causes than patients in the control group," said Dr. Kumar.
The apparent hepatoprotective effect of statin therapy in cirrhosis patients may be a function of previously observed hemodynamic and molecular effects of statins, Dr. Kumar hypothesized. Sinusoidal endothelial dysfunction with decreased nitric oxide production contributes to increased hepatic resistance in cirrhosis, she explained. Just as statins improve endothelial dysfunction in the peripheral vasculature, they may also improve the vascular disturbances that contribute to portal hypertension in cirrhosis by selectively increasing nitric oxide availability in the liver, thus reducing pressures, she said.
The retrospective design of the study limits the conclusions that can be taken from it. Specifically, "we can’t say that all patients with liver disease should be prescribed statins," Dr. Kumar said. "What we can say is that statin therapy is safe in this population, it may be beneficial for its effects on the liver as well as the cardiovascular system, and clinicians should not hesitate to prescribe it for appropriate cardiovascular indications in cirrhosis patients." The findings also indicate that prospective studies are warranted to clarify the role of statins in advanced liver disease, she stressed.
Dr. Kumar disclosed no relevant financial conflicts of interest.
SAN DIEGO – Statin therapy is not only safe for patients with cirrhosis, it may slow the progression of their liver disease to hepatic decompensation and help them live longer, a study has shown.
The findings, reported at the annual Digestive Disease Week, should help allay fears that decreased hepatic clearance of statins could lead to complications in patients with advanced liver disease, as was previously hypothesized, said lead investigator Dr. Sonal Kumar.
"In fact, it seems the opposite may be true," said Dr. Kumar of Brigham and Women’s Hospital, Boston, referring to the results of her retrospective study in which statin therapy in cirrhosis patients was associated with a decreased risk of hepatic decompensation, a delay in the time to decompensation, and reduced all-cause mortality, compared with cirrhosis patients not taking statins.
The investigators were aware that some clinicians either do not initiate statin therapy or discontinue statins in patients with advanced liver disease because of perceived safety concerns. Dr. Kumar and her colleagues sought to determine the actual effect of statin therapy on the risk of hepatic decomposition in cirrhosis.
They identified all patients with biopsy-proven cirrhosis who had taken statins for a minimum of 3 months for treatment of dyslipidemia. A control population of cirrhosis patients not on statins was matched 2:1 for age, gender, and Child-Pugh class from the Partners HealthCare System Research Patient Data Registry, which includes demographic and diagnostic information on patients treated at Massachusetts General Hospital and Brigham and Women’s Hospital.
The primary outcomes of the study were hepatic decompensation, defined as the development of ascites, jaundice (bilirubin greater than 2.5 mg/dL), hepatic encephalopathy, or variceal hemorrhage, and time to decompensation. Mortality was a secondary outcome, Dr. Kumar explained.
The investigators created a Cox proportional hazards model for decompensation to control for age, Child-Pugh class, diabetes, coronary artery disease, and hepatocellular carcinoma, and they used conditional logistic regression to assess mortality, she said.
Of 243 cirrhosis patients included in the analysis, 81 were statin users and 162 were matched controls. "In each group, approximately 70% of patients were Child-Pugh A and 30% were Child-Pugh B/C, and the MELD [Model for End-Stage Liver Disease] score, albumin, presence of varices, and beta-blocker use were similar between groups," Dr. Kumar noted. In the statin group, which was followed for a mean of 1,756 days, decompensation was reported in 31 patients (38.2%), compared with 80 patients (50.62%) in the control group.
The control patients were followed for a mean of 1,503 days, and on Cox analysis, "statin therapy was the only factor significantly associated with lower decompensation risk, with a hazard ratio of 0.46." Additionally, Kaplan-Meier curves showed a significantly longer time to decompensation in patients receiving statin therapy, she said. In subgroup analyses, significantly longer time to decompensation was observed in Child-Pugh A and Child-Pugh B/C patients.
Overall mortality was significantly lower in the statin group, at 37.0%, than in the control group, at 50.6%, said Dr. Kumar. Statin use remained significantly associated with decreased mortality in multivariate analysis, with an odds ratio of 0.36, while coronary artery disease and hepatocellular carcinoma were associated with increased mortality, with respective odds ratios of 3.6 and 4.9.
There were no statistically significant differences in cause of death between the two groups, "however it is important to note that cause of death was not documented for approximately one-third of the study patients, so we cannot make definitive statements about whether patients on statins were less likely to die of liver-related or cardiovascular causes than patients in the control group," said Dr. Kumar.
The apparent hepatoprotective effect of statin therapy in cirrhosis patients may be a function of previously observed hemodynamic and molecular effects of statins, Dr. Kumar hypothesized. Sinusoidal endothelial dysfunction with decreased nitric oxide production contributes to increased hepatic resistance in cirrhosis, she explained. Just as statins improve endothelial dysfunction in the peripheral vasculature, they may also improve the vascular disturbances that contribute to portal hypertension in cirrhosis by selectively increasing nitric oxide availability in the liver, thus reducing pressures, she said.
The retrospective design of the study limits the conclusions that can be taken from it. Specifically, "we can’t say that all patients with liver disease should be prescribed statins," Dr. Kumar said. "What we can say is that statin therapy is safe in this population, it may be beneficial for its effects on the liver as well as the cardiovascular system, and clinicians should not hesitate to prescribe it for appropriate cardiovascular indications in cirrhosis patients." The findings also indicate that prospective studies are warranted to clarify the role of statins in advanced liver disease, she stressed.
Dr. Kumar disclosed no relevant financial conflicts of interest.
FROM THE ANNUAL DIGESTIVE DISEASE WEEK
Major Finding: Among patients with advanced liver disease, the hepatic decompensation rate was 38.2% in patients on statin therapy and 50.6% in those not using statins.
Data Source: This was a retrospective analysis of medical record data for 243 patients with biopsy-proven cirrhosis: 81 taking statins for dyslipidemia and 162 controls.
Disclosures: Dr. Kumar disclosed no relevant financial conflicts of interest.