User login
American Heart Association (AHA): International Stroke Conference
DP-b99 dead in the water as stroke therapy
HONOLULU – The investigational agent DP-b99 provides no more neuroprotection than placebo for patients with acute ischemic stroke, according to the results of the phase III Membrane-Activated Chelator Stroke Intervention trial.
"There is no evidence that this drug offers any clinical benefit when administered within 9 hours of symptom onset," lead investigator Dr. Kennedy Lees said in a late-breaking abstract session at the International Stroke Conference.
DP-b99 is a first-in-class, membrane-activated ion chelator of zinc, which has been associated with cell signaling and, if overloaded, can be a precursor for cell death and subsequent brain degeneration following a stroke.
"The theory is that if you chelate the signaling within the membrane, you could improve the outcome and reduce the damage," said Dr. Lees, who is with the University of Glasgow, Scotland.
DP-b99 produced promising results in animal models and two phase II studies at a daily dose of 1 mg/kg for 4 days. In one of those trials, a 4-day course of DP-b99 failed to significantly alter the primary endpoint of change in National Institutes of Health Stroke Scale (NIHSS) score at 90 days, but significantly improved recovery at 90 days, as measured by modified Rankin Scale scores. In addition, patients with moderate stroke severity (NIHSS score of 10-16) appeared to gain a particular advantage from DP-b99 therapy, experiencing a significant change in NIHSS scores by day 90 (Stroke 2008;39:1774-8).
Based on these intriguing findings, the double-blind, multicenter phase III MACSI (Membrane-Activated Chelator Stroke Intervention) trial was restricted to patients within 9 hours of acute ischemic stroke onset who had a baseline NIHSS score of 10-16, were not treated with the recombinant TPA drug alteplase (Activase), and had cortical stroke findings. At the time of a preplanned futility analysis, 446 patients had been randomly assigned to intravenous DP-b99 for 4 consecutive days or placebo.
The 218 Dp-b99 patients and 219 controls with at least one outcome in the intent-to-treat analysis were reasonably balanced, with the exception of controls being slightly younger (69.7 years vs. 73 years) and less likely to have had a previous stroke (17% vs. 22%), noted Dr. Lees, professor of cerebrovascular medicine at the University of Glasgow, Scotland. Median NIHSS scores were 13 and 12.5, respectively.
The study’s primary endpoint, ordinal modified Rankin score distributions at 90 days, were not significantly different between the placebo and DP-b99 groups (P = .105), even when adjusted for baseline age and NIHSS score (P = .21).
Moreover, fewer patients treated with DP-b99 than placebo achieved a modified Rankin score of 0 or 1 (odds ratio, 0.64) or a NIHSS score of 0 or 1 (OR, 0.69), and both groups had similar time at home within the first 90 days (OR, 1.28) and mortality (OR, 0.90).
The trial was stopped due to futility, although the authors reluctantly went on to perform subgroup analyses at the behest of Stroke, which simultaneously published the results online (Stroke 2013 Feb. 7 [doi: 10.1161/strokeaha.111.000013]).
"The bottom line: no effect there," regardless of whether the data were cut by gender, history of prior stroke, premorbid modified Rankin Score 0 or deficit, onset to treatment time, or age, Dr. Lees said at the conference, sponsored by the American Heart Association.
D-Pharm sponsored the trial. The authors received fees and expenses for their role on the MACSI trial steering committee. Dr. Lees and his coauthors reported relationships with drug and device companies, but none directly related to MACSI.
HONOLULU – The investigational agent DP-b99 provides no more neuroprotection than placebo for patients with acute ischemic stroke, according to the results of the phase III Membrane-Activated Chelator Stroke Intervention trial.
"There is no evidence that this drug offers any clinical benefit when administered within 9 hours of symptom onset," lead investigator Dr. Kennedy Lees said in a late-breaking abstract session at the International Stroke Conference.
DP-b99 is a first-in-class, membrane-activated ion chelator of zinc, which has been associated with cell signaling and, if overloaded, can be a precursor for cell death and subsequent brain degeneration following a stroke.
"The theory is that if you chelate the signaling within the membrane, you could improve the outcome and reduce the damage," said Dr. Lees, who is with the University of Glasgow, Scotland.
DP-b99 produced promising results in animal models and two phase II studies at a daily dose of 1 mg/kg for 4 days. In one of those trials, a 4-day course of DP-b99 failed to significantly alter the primary endpoint of change in National Institutes of Health Stroke Scale (NIHSS) score at 90 days, but significantly improved recovery at 90 days, as measured by modified Rankin Scale scores. In addition, patients with moderate stroke severity (NIHSS score of 10-16) appeared to gain a particular advantage from DP-b99 therapy, experiencing a significant change in NIHSS scores by day 90 (Stroke 2008;39:1774-8).
Based on these intriguing findings, the double-blind, multicenter phase III MACSI (Membrane-Activated Chelator Stroke Intervention) trial was restricted to patients within 9 hours of acute ischemic stroke onset who had a baseline NIHSS score of 10-16, were not treated with the recombinant TPA drug alteplase (Activase), and had cortical stroke findings. At the time of a preplanned futility analysis, 446 patients had been randomly assigned to intravenous DP-b99 for 4 consecutive days or placebo.
The 218 Dp-b99 patients and 219 controls with at least one outcome in the intent-to-treat analysis were reasonably balanced, with the exception of controls being slightly younger (69.7 years vs. 73 years) and less likely to have had a previous stroke (17% vs. 22%), noted Dr. Lees, professor of cerebrovascular medicine at the University of Glasgow, Scotland. Median NIHSS scores were 13 and 12.5, respectively.
The study’s primary endpoint, ordinal modified Rankin score distributions at 90 days, were not significantly different between the placebo and DP-b99 groups (P = .105), even when adjusted for baseline age and NIHSS score (P = .21).
Moreover, fewer patients treated with DP-b99 than placebo achieved a modified Rankin score of 0 or 1 (odds ratio, 0.64) or a NIHSS score of 0 or 1 (OR, 0.69), and both groups had similar time at home within the first 90 days (OR, 1.28) and mortality (OR, 0.90).
The trial was stopped due to futility, although the authors reluctantly went on to perform subgroup analyses at the behest of Stroke, which simultaneously published the results online (Stroke 2013 Feb. 7 [doi: 10.1161/strokeaha.111.000013]).
"The bottom line: no effect there," regardless of whether the data were cut by gender, history of prior stroke, premorbid modified Rankin Score 0 or deficit, onset to treatment time, or age, Dr. Lees said at the conference, sponsored by the American Heart Association.
D-Pharm sponsored the trial. The authors received fees and expenses for their role on the MACSI trial steering committee. Dr. Lees and his coauthors reported relationships with drug and device companies, but none directly related to MACSI.
HONOLULU – The investigational agent DP-b99 provides no more neuroprotection than placebo for patients with acute ischemic stroke, according to the results of the phase III Membrane-Activated Chelator Stroke Intervention trial.
"There is no evidence that this drug offers any clinical benefit when administered within 9 hours of symptom onset," lead investigator Dr. Kennedy Lees said in a late-breaking abstract session at the International Stroke Conference.
DP-b99 is a first-in-class, membrane-activated ion chelator of zinc, which has been associated with cell signaling and, if overloaded, can be a precursor for cell death and subsequent brain degeneration following a stroke.
"The theory is that if you chelate the signaling within the membrane, you could improve the outcome and reduce the damage," said Dr. Lees, who is with the University of Glasgow, Scotland.
DP-b99 produced promising results in animal models and two phase II studies at a daily dose of 1 mg/kg for 4 days. In one of those trials, a 4-day course of DP-b99 failed to significantly alter the primary endpoint of change in National Institutes of Health Stroke Scale (NIHSS) score at 90 days, but significantly improved recovery at 90 days, as measured by modified Rankin Scale scores. In addition, patients with moderate stroke severity (NIHSS score of 10-16) appeared to gain a particular advantage from DP-b99 therapy, experiencing a significant change in NIHSS scores by day 90 (Stroke 2008;39:1774-8).
Based on these intriguing findings, the double-blind, multicenter phase III MACSI (Membrane-Activated Chelator Stroke Intervention) trial was restricted to patients within 9 hours of acute ischemic stroke onset who had a baseline NIHSS score of 10-16, were not treated with the recombinant TPA drug alteplase (Activase), and had cortical stroke findings. At the time of a preplanned futility analysis, 446 patients had been randomly assigned to intravenous DP-b99 for 4 consecutive days or placebo.
The 218 Dp-b99 patients and 219 controls with at least one outcome in the intent-to-treat analysis were reasonably balanced, with the exception of controls being slightly younger (69.7 years vs. 73 years) and less likely to have had a previous stroke (17% vs. 22%), noted Dr. Lees, professor of cerebrovascular medicine at the University of Glasgow, Scotland. Median NIHSS scores were 13 and 12.5, respectively.
The study’s primary endpoint, ordinal modified Rankin score distributions at 90 days, were not significantly different between the placebo and DP-b99 groups (P = .105), even when adjusted for baseline age and NIHSS score (P = .21).
Moreover, fewer patients treated with DP-b99 than placebo achieved a modified Rankin score of 0 or 1 (odds ratio, 0.64) or a NIHSS score of 0 or 1 (OR, 0.69), and both groups had similar time at home within the first 90 days (OR, 1.28) and mortality (OR, 0.90).
The trial was stopped due to futility, although the authors reluctantly went on to perform subgroup analyses at the behest of Stroke, which simultaneously published the results online (Stroke 2013 Feb. 7 [doi: 10.1161/strokeaha.111.000013]).
"The bottom line: no effect there," regardless of whether the data were cut by gender, history of prior stroke, premorbid modified Rankin Score 0 or deficit, onset to treatment time, or age, Dr. Lees said at the conference, sponsored by the American Heart Association.
D-Pharm sponsored the trial. The authors received fees and expenses for their role on the MACSI trial steering committee. Dr. Lees and his coauthors reported relationships with drug and device companies, but none directly related to MACSI.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Ordinal modified Rankin score distributions at 90 days were not significantly different between the placebo and DP-b99 groups (P = .105), even when adjusted for baseline age and NIHSS score (P = .21).
Data Source: Double-blind, multicenter phase III trial in 437 patients with acute ischemic stroke.
Disclosures: D-Pharm sponsored the trial. The authors received fees and expenses for their role on the MACSI trial steering committee. Dr. Lees and his coauthors reported relationships with drug and device companies, but none directly related to MACSI.
Aggressive BP lowering after lacunar stroke may reduce recurrence
HONOLULU – In patients with recent lacunar strokes, aggressive lowering of systolic blood pressure safely reduced the risk of recurrent stroke by about 20% in the BP intervention arm of the Secondary Prevention of Small Subcortical Strokes trial.
The primary endpoint of recurrent ischemic and hemorrhagic stroke was 2.3% per year in patients with a target systolic blood pressure of less than 130 mm Hg and 2.8% among those randomized to a target of 130-149 mm Hg (hazard ratio, 0.81; P = .08). Annual ischemic stroke rates also trended lower (2.0 vs. 2.4%; HR, 0.84; P = .19).
The lower blood pressure target, however, significantly reduced intracerebral hemorrhage by nearly two-thirds (0.11% vs. 0.29%; HR, 0.37; P = .03), Dr. Oscar R. Benavente reported on behalf of the Secondary Prevention of Small Subcortical Strokes (SPS3) investigators during a late-breaking plenary session at the International Stroke Conference.
The results are consistent with previous randomized controlled trials of BP lowering in stroke, but do not answer how low blood pressure should go or what the optimal target is, he said at a press briefing.
At 1-year follow-up, the average systolic BPs were 138 mm Hg and 127 mm Hg in the higher- and lower-target groups, having fallen from an average of 145 mm Hg and 144 mm Hg, respectively, at baseline.
Despite the lack of statistical significance for the primary endpoint, plenary session comoderator Dr. Steven Greenberg, professor of neurology at Harvard Medical School and director of hemorrhagic stroke research at Massachusetts General Hospital, both in Boston, told reporters, "as a clinician in practice, I would take these results very seriously."
He observed that clinicians often make decisions without a P value at the .05 level of certainty, and said the reduction in hemorrhagic stroke was a "very powerful finding" since studies have shown that the outcome from hemorrhagic stroke is even worse than that from ischemic stroke.
"This very much reinforces the impression that many of us already have – but now that the data are stronger – that we should aim for a lower blood pressure target in our patients," he said at the press briefing.
While the hemorrhagic stroke finding is important, the problem is that ischemic strokes make up the vast majority of recurrent strokes, commented Dr. Philip Gorelick, professor of translation science and molecular medicine, Michigan State University, and medical director of the Hauenstein Neuroscience Center, both in Grand Rapids, Mich.
"There wasn’t a clear-cut significance there, and so we’re still wrestling with this issue of where to drop that blood pressure point [to]," he said in an interview.
The intervention was well tolerated, however, "so you are not trading strokes for major safety events," pointed out Dr. Benavente of the brain research center, University of British Columbia, Vancouver.
As previously reported, the dual-therapy arm of SPS3 was stopped early because treatment with clopidogrel plus aspirin not only failed to significantly reduce the risk of recurrent stroke, but significantly increased the risk of all-cause mortality and major hemorrhage, compared with aspirin alone.
In the BP intervention arm, the higher- and lower-target groups had similar rates of serious complications of hypotension (15 events vs. 23 events; HR, 1.53; P = .20), including orthostatic syncope (5 events vs. 11 events; HR, 2.18; P = .14), stroke (1 event vs. 2 events; HR, 2.00; P = .57), myocardial infarction (0 events in both groups), and fall with injury (0 events vs. 3 events; HR and P not available).
Serious complications related to BP medications were limited to one case of bradycardia requiring hospitalization in the lower-target group, Dr. Benavente said at the conference, sponsored by the American Heart Association.
He also noted that there was no interaction between the BP intervention and diabetes, which was present in a little more than one-third of patients in both groups.
This finding is important since the American Diabetes Association recently raised its BP treatment goal from less than 130 mm Hg to less than 140 mm Hg to reflect clinical trial data showing limited benefit to more-intensive BP treatment in patients with diabetes, Dr. Gorelick observed. In the PROGRESS trial in which Dr. Gorelick served on the steering committee, he noted that it took at least 6 months for the curves to begin to separate for stroke recurrence.
"I think that blood pressures in the 130-139 [mm Hg] range is where you want to be, because you’re not going to know who’s going to have a hemorrhage; you’re not going to know who’s going to have a heart attack necessarily or a stroke; so I think we need to be reasonable here," he said.
Dr. Benavente told reporters that while BP lowering is recommended for stroke patients in other guidelines, there are no set BP targets.
Patients in SPS3 had an imaging-verified lacunar stroke within 180 days of study entry and were followed for a mean of 3.7 years. There were 1,519 patients in the higher-target group and 1,501 in the lower-target group. Their baseline diastolic BPs were 80 mm Hg and 78 mm Hg. They were on an average of 1.4 and 1.2 BP medications at study entry, and 1.4 and 1.3 at 1 year. Blood pressure medications were not specified by protocol.
Antihypertensives were not discontinued at study entry. At last visit, 60% of the higher-target group and 78% of the lower-target group were on an angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, 39% vs. 43% on a calcium channel blocker, and 38% vs. 54% on thiazides.
At the last observed visit, the average systolic BP difference between groups was 11 mm Hg. Major vascular events, defined as stroke, MI, and vascular deaths, occurred in 3.4% of the higher-target group (188 events) vs. 3.0% of the lower-target group (160 events) (HR,0.84; P = .10), Dr. Benavente said.
SPS3 is sponsored by the National Institute of Neurological Disorders and Stroke (NINDS). Sanofi-Aventis and Bristol-Myers Squibb donated the study drugs. Dr. Benavente has received research support from NINDS. Dr. Greenberg reported receiving research grants from the National Institutes of Health and serving as a consultant/advisory board member for Hoffman-La Roche. Dr. Gorelick reported having no relevant financial disclosures.
HONOLULU – In patients with recent lacunar strokes, aggressive lowering of systolic blood pressure safely reduced the risk of recurrent stroke by about 20% in the BP intervention arm of the Secondary Prevention of Small Subcortical Strokes trial.
The primary endpoint of recurrent ischemic and hemorrhagic stroke was 2.3% per year in patients with a target systolic blood pressure of less than 130 mm Hg and 2.8% among those randomized to a target of 130-149 mm Hg (hazard ratio, 0.81; P = .08). Annual ischemic stroke rates also trended lower (2.0 vs. 2.4%; HR, 0.84; P = .19).
The lower blood pressure target, however, significantly reduced intracerebral hemorrhage by nearly two-thirds (0.11% vs. 0.29%; HR, 0.37; P = .03), Dr. Oscar R. Benavente reported on behalf of the Secondary Prevention of Small Subcortical Strokes (SPS3) investigators during a late-breaking plenary session at the International Stroke Conference.
The results are consistent with previous randomized controlled trials of BP lowering in stroke, but do not answer how low blood pressure should go or what the optimal target is, he said at a press briefing.
At 1-year follow-up, the average systolic BPs were 138 mm Hg and 127 mm Hg in the higher- and lower-target groups, having fallen from an average of 145 mm Hg and 144 mm Hg, respectively, at baseline.
Despite the lack of statistical significance for the primary endpoint, plenary session comoderator Dr. Steven Greenberg, professor of neurology at Harvard Medical School and director of hemorrhagic stroke research at Massachusetts General Hospital, both in Boston, told reporters, "as a clinician in practice, I would take these results very seriously."
He observed that clinicians often make decisions without a P value at the .05 level of certainty, and said the reduction in hemorrhagic stroke was a "very powerful finding" since studies have shown that the outcome from hemorrhagic stroke is even worse than that from ischemic stroke.
"This very much reinforces the impression that many of us already have – but now that the data are stronger – that we should aim for a lower blood pressure target in our patients," he said at the press briefing.
While the hemorrhagic stroke finding is important, the problem is that ischemic strokes make up the vast majority of recurrent strokes, commented Dr. Philip Gorelick, professor of translation science and molecular medicine, Michigan State University, and medical director of the Hauenstein Neuroscience Center, both in Grand Rapids, Mich.
"There wasn’t a clear-cut significance there, and so we’re still wrestling with this issue of where to drop that blood pressure point [to]," he said in an interview.
The intervention was well tolerated, however, "so you are not trading strokes for major safety events," pointed out Dr. Benavente of the brain research center, University of British Columbia, Vancouver.
As previously reported, the dual-therapy arm of SPS3 was stopped early because treatment with clopidogrel plus aspirin not only failed to significantly reduce the risk of recurrent stroke, but significantly increased the risk of all-cause mortality and major hemorrhage, compared with aspirin alone.
In the BP intervention arm, the higher- and lower-target groups had similar rates of serious complications of hypotension (15 events vs. 23 events; HR, 1.53; P = .20), including orthostatic syncope (5 events vs. 11 events; HR, 2.18; P = .14), stroke (1 event vs. 2 events; HR, 2.00; P = .57), myocardial infarction (0 events in both groups), and fall with injury (0 events vs. 3 events; HR and P not available).
Serious complications related to BP medications were limited to one case of bradycardia requiring hospitalization in the lower-target group, Dr. Benavente said at the conference, sponsored by the American Heart Association.
He also noted that there was no interaction between the BP intervention and diabetes, which was present in a little more than one-third of patients in both groups.
This finding is important since the American Diabetes Association recently raised its BP treatment goal from less than 130 mm Hg to less than 140 mm Hg to reflect clinical trial data showing limited benefit to more-intensive BP treatment in patients with diabetes, Dr. Gorelick observed. In the PROGRESS trial in which Dr. Gorelick served on the steering committee, he noted that it took at least 6 months for the curves to begin to separate for stroke recurrence.
"I think that blood pressures in the 130-139 [mm Hg] range is where you want to be, because you’re not going to know who’s going to have a hemorrhage; you’re not going to know who’s going to have a heart attack necessarily or a stroke; so I think we need to be reasonable here," he said.
Dr. Benavente told reporters that while BP lowering is recommended for stroke patients in other guidelines, there are no set BP targets.
Patients in SPS3 had an imaging-verified lacunar stroke within 180 days of study entry and were followed for a mean of 3.7 years. There were 1,519 patients in the higher-target group and 1,501 in the lower-target group. Their baseline diastolic BPs were 80 mm Hg and 78 mm Hg. They were on an average of 1.4 and 1.2 BP medications at study entry, and 1.4 and 1.3 at 1 year. Blood pressure medications were not specified by protocol.
Antihypertensives were not discontinued at study entry. At last visit, 60% of the higher-target group and 78% of the lower-target group were on an angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, 39% vs. 43% on a calcium channel blocker, and 38% vs. 54% on thiazides.
At the last observed visit, the average systolic BP difference between groups was 11 mm Hg. Major vascular events, defined as stroke, MI, and vascular deaths, occurred in 3.4% of the higher-target group (188 events) vs. 3.0% of the lower-target group (160 events) (HR,0.84; P = .10), Dr. Benavente said.
SPS3 is sponsored by the National Institute of Neurological Disorders and Stroke (NINDS). Sanofi-Aventis and Bristol-Myers Squibb donated the study drugs. Dr. Benavente has received research support from NINDS. Dr. Greenberg reported receiving research grants from the National Institutes of Health and serving as a consultant/advisory board member for Hoffman-La Roche. Dr. Gorelick reported having no relevant financial disclosures.
HONOLULU – In patients with recent lacunar strokes, aggressive lowering of systolic blood pressure safely reduced the risk of recurrent stroke by about 20% in the BP intervention arm of the Secondary Prevention of Small Subcortical Strokes trial.
The primary endpoint of recurrent ischemic and hemorrhagic stroke was 2.3% per year in patients with a target systolic blood pressure of less than 130 mm Hg and 2.8% among those randomized to a target of 130-149 mm Hg (hazard ratio, 0.81; P = .08). Annual ischemic stroke rates also trended lower (2.0 vs. 2.4%; HR, 0.84; P = .19).
The lower blood pressure target, however, significantly reduced intracerebral hemorrhage by nearly two-thirds (0.11% vs. 0.29%; HR, 0.37; P = .03), Dr. Oscar R. Benavente reported on behalf of the Secondary Prevention of Small Subcortical Strokes (SPS3) investigators during a late-breaking plenary session at the International Stroke Conference.
The results are consistent with previous randomized controlled trials of BP lowering in stroke, but do not answer how low blood pressure should go or what the optimal target is, he said at a press briefing.
At 1-year follow-up, the average systolic BPs were 138 mm Hg and 127 mm Hg in the higher- and lower-target groups, having fallen from an average of 145 mm Hg and 144 mm Hg, respectively, at baseline.
Despite the lack of statistical significance for the primary endpoint, plenary session comoderator Dr. Steven Greenberg, professor of neurology at Harvard Medical School and director of hemorrhagic stroke research at Massachusetts General Hospital, both in Boston, told reporters, "as a clinician in practice, I would take these results very seriously."
He observed that clinicians often make decisions without a P value at the .05 level of certainty, and said the reduction in hemorrhagic stroke was a "very powerful finding" since studies have shown that the outcome from hemorrhagic stroke is even worse than that from ischemic stroke.
"This very much reinforces the impression that many of us already have – but now that the data are stronger – that we should aim for a lower blood pressure target in our patients," he said at the press briefing.
While the hemorrhagic stroke finding is important, the problem is that ischemic strokes make up the vast majority of recurrent strokes, commented Dr. Philip Gorelick, professor of translation science and molecular medicine, Michigan State University, and medical director of the Hauenstein Neuroscience Center, both in Grand Rapids, Mich.
"There wasn’t a clear-cut significance there, and so we’re still wrestling with this issue of where to drop that blood pressure point [to]," he said in an interview.
The intervention was well tolerated, however, "so you are not trading strokes for major safety events," pointed out Dr. Benavente of the brain research center, University of British Columbia, Vancouver.
As previously reported, the dual-therapy arm of SPS3 was stopped early because treatment with clopidogrel plus aspirin not only failed to significantly reduce the risk of recurrent stroke, but significantly increased the risk of all-cause mortality and major hemorrhage, compared with aspirin alone.
In the BP intervention arm, the higher- and lower-target groups had similar rates of serious complications of hypotension (15 events vs. 23 events; HR, 1.53; P = .20), including orthostatic syncope (5 events vs. 11 events; HR, 2.18; P = .14), stroke (1 event vs. 2 events; HR, 2.00; P = .57), myocardial infarction (0 events in both groups), and fall with injury (0 events vs. 3 events; HR and P not available).
Serious complications related to BP medications were limited to one case of bradycardia requiring hospitalization in the lower-target group, Dr. Benavente said at the conference, sponsored by the American Heart Association.
He also noted that there was no interaction between the BP intervention and diabetes, which was present in a little more than one-third of patients in both groups.
This finding is important since the American Diabetes Association recently raised its BP treatment goal from less than 130 mm Hg to less than 140 mm Hg to reflect clinical trial data showing limited benefit to more-intensive BP treatment in patients with diabetes, Dr. Gorelick observed. In the PROGRESS trial in which Dr. Gorelick served on the steering committee, he noted that it took at least 6 months for the curves to begin to separate for stroke recurrence.
"I think that blood pressures in the 130-139 [mm Hg] range is where you want to be, because you’re not going to know who’s going to have a hemorrhage; you’re not going to know who’s going to have a heart attack necessarily or a stroke; so I think we need to be reasonable here," he said.
Dr. Benavente told reporters that while BP lowering is recommended for stroke patients in other guidelines, there are no set BP targets.
Patients in SPS3 had an imaging-verified lacunar stroke within 180 days of study entry and were followed for a mean of 3.7 years. There were 1,519 patients in the higher-target group and 1,501 in the lower-target group. Their baseline diastolic BPs were 80 mm Hg and 78 mm Hg. They were on an average of 1.4 and 1.2 BP medications at study entry, and 1.4 and 1.3 at 1 year. Blood pressure medications were not specified by protocol.
Antihypertensives were not discontinued at study entry. At last visit, 60% of the higher-target group and 78% of the lower-target group were on an angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, 39% vs. 43% on a calcium channel blocker, and 38% vs. 54% on thiazides.
At the last observed visit, the average systolic BP difference between groups was 11 mm Hg. Major vascular events, defined as stroke, MI, and vascular deaths, occurred in 3.4% of the higher-target group (188 events) vs. 3.0% of the lower-target group (160 events) (HR,0.84; P = .10), Dr. Benavente said.
SPS3 is sponsored by the National Institute of Neurological Disorders and Stroke (NINDS). Sanofi-Aventis and Bristol-Myers Squibb donated the study drugs. Dr. Benavente has received research support from NINDS. Dr. Greenberg reported receiving research grants from the National Institutes of Health and serving as a consultant/advisory board member for Hoffman-La Roche. Dr. Gorelick reported having no relevant financial disclosures.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Annual rates of recurrent ischemic and hemorrhagic stroke were 2.3% in patients with a target systolic BP of less than 130 mm Hg and 2.8% in those with a target of 130-149 mm Hg (HR, 0.81; P = .08).
Data Source: Randomized, multicenter, international trial in 3,020 patients with lacunar strokes.
Disclosures: The SPS3 trial is sponsored by the National Institute of Neurological Disorders and Stroke. Sanofi-Aventis and Bristol-Myers Squibb donated the study drugs. Dr. Benavente has received research support from NINDS. Dr. Greenberg reported receiving research grants from the National Institutes of Health and serving as a consultant/advisory board member for Hoffman-La Roche. Dr. Gorelick reported having no relevant financial disclosures.
Eptifibatide combo passes phase II hurdle
HONOLULU – Eptifibatide plus medium-dose tissue plasminogen activator was safe in a phase IIb study, and a larger, phase III trial is now needed to determine whether the combination can improve ischemic stroke outcomes.
Symptomatic intracerebral hemorrhage (ICH) within 36 hours, the primary safety end point of the trial, occurred in 2% of patients randomized to the combination and in 12% given standard intravenous recombinant tissue plasminogen activator (rt-PA) alone.
A modified Rankin Scale score of 0 or 1 or return to baseline mRS at 90 days, the primary efficacy outcome, was achieved by 36% on rt-PA alone and by 49.5% on the combination. The outcome values far exceeded the 33% prespecified "no-go" criterion set for phase III evaluation, Dr. Opeolu Adeoye said on behalf of the CLEAR-ER (Combined Approach to Lysis Utilizing Eptifibatide and rt-PA in Acute Ischemic Stroke- Enhanced Regimen) trial investigators at the International Stroke Conference.
Dr. Adeoye acknowledged that "unexpected imbalances," however, existed between groups. The combination therapy group tended to be younger than the rt-PA only group (mean, 68.9 years vs. 70.9 years), had less severe strokes based on NIHSS scores (median 12 vs. 17), and had a slightly higher proportion of patients with a baseline mRS of 0 or 1 (84.2% vs. 72%).
The unadjusted odds ratio for the primary efficacy end point was 1.74, and the odds ratio was 1.38 after adjustment for age, baseline NIHSS (National Institutes of Health Stroke Scale) score, time to rt-PA, and baseline mRS. After adjustment for all but baseline mRS, the relative risk was 1.16.
"Obviously, this is a phase II study and was not designed to assess efficacy, but after adjusting for these imbalances, what we think is a clinically meaningful treatment effect persisted between groups," said Dr. Adeoye, of the University of Cincinnati Neuroscience Institute.
He noted that no obvious efficacy signal was observed in the dose-escalation, safety CLEAR Stroke trial, which was stopped early due to safety concerns about dosing rt-PA at 0.45 mg/kg over 60 minutes with a 75-mcg/kg bolus of eptifibatide followed by a 2-hour infusion at 0.75 mcg/kg/min (Stroke 2008;39:3268-76).
Among patients with myocardial infarction, combining the glycoprotein IIb/IIIa receptor inhibitor plus unfractionated heparin offered no added benefit and significantly increased the rate of bleeding in the ASSIST trial.
In CLEAR-ER, 126 ischemic stroke patients, aged 18-85 years, with an NIHSS score of more than 5 were randomized 5:1 to rt-PA 0.6 mg/kg over 40 minutes plus eptifibatide 135 mcg/kg bolus followed by a 2-hour infusion at 0.75 mcg/kg/min or standard-dose rt-PA 0.9 mg/kg. Treatment was initiated within 3 hours of symptom onset.
At day 7, symptomatic ICH rates held constant in the combination and rt-PA only groups at 2% and 12%, respectively (OR, 0.15), while asymptomatic ICH was seen in 15.8% and 12% (OR, 1.38).
At 90 days, at least one serious adverse event was reported in 26% of the combination group and 28% of the rt-PA only group. All-cause mortality rates were 20% vs. 16%, respectively, and were 15% vs. 16% for stroke-related death.
Dr. Andrei Alexandrov, director of the division of cerebrovascular disease at the University of Alabama, Birmingham, who moderated the late-breaking abstract session, questioned whether a phase III trial may be premature given that vascular imaging was not used in the current trial to determine whether vessel occlusions were present.
Dr. Adeoye responded that at the time the trial was designed, the standard of care was variable at the nine participating sites. Moreover, the data were stratified using an NIHSS score of more than or less than 12, and showed that "the bulk of the treatment effect actually appeared to be in the patients with a higher stroke scale. Not having imaging, I can’t speak to whether or not that definitely means those strokes were open; but clinically, I would venture to suggest that is what’s going on."
The conference was sponsored by the American Heart Association.
The National Heart, Lung and Blood Institute funded the study. Genentech and Merck supplied the study drugs. Dr. Adeoye reported serving as a speaker for Genentech; his coauthors reported no disclosures.
HONOLULU – Eptifibatide plus medium-dose tissue plasminogen activator was safe in a phase IIb study, and a larger, phase III trial is now needed to determine whether the combination can improve ischemic stroke outcomes.
Symptomatic intracerebral hemorrhage (ICH) within 36 hours, the primary safety end point of the trial, occurred in 2% of patients randomized to the combination and in 12% given standard intravenous recombinant tissue plasminogen activator (rt-PA) alone.
A modified Rankin Scale score of 0 or 1 or return to baseline mRS at 90 days, the primary efficacy outcome, was achieved by 36% on rt-PA alone and by 49.5% on the combination. The outcome values far exceeded the 33% prespecified "no-go" criterion set for phase III evaluation, Dr. Opeolu Adeoye said on behalf of the CLEAR-ER (Combined Approach to Lysis Utilizing Eptifibatide and rt-PA in Acute Ischemic Stroke- Enhanced Regimen) trial investigators at the International Stroke Conference.
Dr. Adeoye acknowledged that "unexpected imbalances," however, existed between groups. The combination therapy group tended to be younger than the rt-PA only group (mean, 68.9 years vs. 70.9 years), had less severe strokes based on NIHSS scores (median 12 vs. 17), and had a slightly higher proportion of patients with a baseline mRS of 0 or 1 (84.2% vs. 72%).
The unadjusted odds ratio for the primary efficacy end point was 1.74, and the odds ratio was 1.38 after adjustment for age, baseline NIHSS (National Institutes of Health Stroke Scale) score, time to rt-PA, and baseline mRS. After adjustment for all but baseline mRS, the relative risk was 1.16.
"Obviously, this is a phase II study and was not designed to assess efficacy, but after adjusting for these imbalances, what we think is a clinically meaningful treatment effect persisted between groups," said Dr. Adeoye, of the University of Cincinnati Neuroscience Institute.
He noted that no obvious efficacy signal was observed in the dose-escalation, safety CLEAR Stroke trial, which was stopped early due to safety concerns about dosing rt-PA at 0.45 mg/kg over 60 minutes with a 75-mcg/kg bolus of eptifibatide followed by a 2-hour infusion at 0.75 mcg/kg/min (Stroke 2008;39:3268-76).
Among patients with myocardial infarction, combining the glycoprotein IIb/IIIa receptor inhibitor plus unfractionated heparin offered no added benefit and significantly increased the rate of bleeding in the ASSIST trial.
In CLEAR-ER, 126 ischemic stroke patients, aged 18-85 years, with an NIHSS score of more than 5 were randomized 5:1 to rt-PA 0.6 mg/kg over 40 minutes plus eptifibatide 135 mcg/kg bolus followed by a 2-hour infusion at 0.75 mcg/kg/min or standard-dose rt-PA 0.9 mg/kg. Treatment was initiated within 3 hours of symptom onset.
At day 7, symptomatic ICH rates held constant in the combination and rt-PA only groups at 2% and 12%, respectively (OR, 0.15), while asymptomatic ICH was seen in 15.8% and 12% (OR, 1.38).
At 90 days, at least one serious adverse event was reported in 26% of the combination group and 28% of the rt-PA only group. All-cause mortality rates were 20% vs. 16%, respectively, and were 15% vs. 16% for stroke-related death.
Dr. Andrei Alexandrov, director of the division of cerebrovascular disease at the University of Alabama, Birmingham, who moderated the late-breaking abstract session, questioned whether a phase III trial may be premature given that vascular imaging was not used in the current trial to determine whether vessel occlusions were present.
Dr. Adeoye responded that at the time the trial was designed, the standard of care was variable at the nine participating sites. Moreover, the data were stratified using an NIHSS score of more than or less than 12, and showed that "the bulk of the treatment effect actually appeared to be in the patients with a higher stroke scale. Not having imaging, I can’t speak to whether or not that definitely means those strokes were open; but clinically, I would venture to suggest that is what’s going on."
The conference was sponsored by the American Heart Association.
The National Heart, Lung and Blood Institute funded the study. Genentech and Merck supplied the study drugs. Dr. Adeoye reported serving as a speaker for Genentech; his coauthors reported no disclosures.
HONOLULU – Eptifibatide plus medium-dose tissue plasminogen activator was safe in a phase IIb study, and a larger, phase III trial is now needed to determine whether the combination can improve ischemic stroke outcomes.
Symptomatic intracerebral hemorrhage (ICH) within 36 hours, the primary safety end point of the trial, occurred in 2% of patients randomized to the combination and in 12% given standard intravenous recombinant tissue plasminogen activator (rt-PA) alone.
A modified Rankin Scale score of 0 or 1 or return to baseline mRS at 90 days, the primary efficacy outcome, was achieved by 36% on rt-PA alone and by 49.5% on the combination. The outcome values far exceeded the 33% prespecified "no-go" criterion set for phase III evaluation, Dr. Opeolu Adeoye said on behalf of the CLEAR-ER (Combined Approach to Lysis Utilizing Eptifibatide and rt-PA in Acute Ischemic Stroke- Enhanced Regimen) trial investigators at the International Stroke Conference.
Dr. Adeoye acknowledged that "unexpected imbalances," however, existed between groups. The combination therapy group tended to be younger than the rt-PA only group (mean, 68.9 years vs. 70.9 years), had less severe strokes based on NIHSS scores (median 12 vs. 17), and had a slightly higher proportion of patients with a baseline mRS of 0 or 1 (84.2% vs. 72%).
The unadjusted odds ratio for the primary efficacy end point was 1.74, and the odds ratio was 1.38 after adjustment for age, baseline NIHSS (National Institutes of Health Stroke Scale) score, time to rt-PA, and baseline mRS. After adjustment for all but baseline mRS, the relative risk was 1.16.
"Obviously, this is a phase II study and was not designed to assess efficacy, but after adjusting for these imbalances, what we think is a clinically meaningful treatment effect persisted between groups," said Dr. Adeoye, of the University of Cincinnati Neuroscience Institute.
He noted that no obvious efficacy signal was observed in the dose-escalation, safety CLEAR Stroke trial, which was stopped early due to safety concerns about dosing rt-PA at 0.45 mg/kg over 60 minutes with a 75-mcg/kg bolus of eptifibatide followed by a 2-hour infusion at 0.75 mcg/kg/min (Stroke 2008;39:3268-76).
Among patients with myocardial infarction, combining the glycoprotein IIb/IIIa receptor inhibitor plus unfractionated heparin offered no added benefit and significantly increased the rate of bleeding in the ASSIST trial.
In CLEAR-ER, 126 ischemic stroke patients, aged 18-85 years, with an NIHSS score of more than 5 were randomized 5:1 to rt-PA 0.6 mg/kg over 40 minutes plus eptifibatide 135 mcg/kg bolus followed by a 2-hour infusion at 0.75 mcg/kg/min or standard-dose rt-PA 0.9 mg/kg. Treatment was initiated within 3 hours of symptom onset.
At day 7, symptomatic ICH rates held constant in the combination and rt-PA only groups at 2% and 12%, respectively (OR, 0.15), while asymptomatic ICH was seen in 15.8% and 12% (OR, 1.38).
At 90 days, at least one serious adverse event was reported in 26% of the combination group and 28% of the rt-PA only group. All-cause mortality rates were 20% vs. 16%, respectively, and were 15% vs. 16% for stroke-related death.
Dr. Andrei Alexandrov, director of the division of cerebrovascular disease at the University of Alabama, Birmingham, who moderated the late-breaking abstract session, questioned whether a phase III trial may be premature given that vascular imaging was not used in the current trial to determine whether vessel occlusions were present.
Dr. Adeoye responded that at the time the trial was designed, the standard of care was variable at the nine participating sites. Moreover, the data were stratified using an NIHSS score of more than or less than 12, and showed that "the bulk of the treatment effect actually appeared to be in the patients with a higher stroke scale. Not having imaging, I can’t speak to whether or not that definitely means those strokes were open; but clinically, I would venture to suggest that is what’s going on."
The conference was sponsored by the American Heart Association.
The National Heart, Lung and Blood Institute funded the study. Genentech and Merck supplied the study drugs. Dr. Adeoye reported serving as a speaker for Genentech; his coauthors reported no disclosures.
AT THE INTERNATIONAL STROKE CONFERENCE
Major finding: Symptomatic intracerebral hemorrhage within 36 hours occurred in 2% of patients on medium-dose rt-PA plus eptifibatide and in 12% of those on standard rt-PA alone (OR, 0.15).
Data source: Prospective, multicenter, double-blind phase IIb study of 126 patients with acute ischemic stroke.
Disclosures: The National Heart, Lung and Blood Institute funded the study. Genentech and Merck supplied the study drugs. Dr. Adeoye reported serving as a speaker for Genentech; his coauthors reported no disclosures.
The TIAs you need to worry about
HONOLULU – A patient comes to your office because of what sounds very much like a recent TIA. As a busy primary care physician on the health care front lines, you need to be able to quickly assess this individual’s near-term risk of a full-blown stroke. The ABCD2 score is the right tool for this task, according to Dr. S. Claiborne Johnston.
The ABCD2 score is a simple tool for predicting the risk of stroke within 2 days after a TIA. It requires no special training and takes just seconds to calculate based upon patient history. With a score of 3 or more on the 0-7 scale, tell the patient to go straight to the emergency department. No referral to the neurologist for a consultation is necessary, he said at the International Stroke Conference sponsored by the American Stroke Association.
"If you’re talking to the patient on the phone, she doesn’t need to come into the office at all. Have her go straight to the ED. With a score of 3 or more, her stroke risk in the next 2 days is pretty high – and, really, what are you going to do in the clinic to reduce that risk?" said Dr. Johnston, professor of neurology and epidemiology and director of the stroke center at the University of California, San Francisco.
In the emergency department, physicians can obtain a brain scan to further define the short-term risk. And it’s likely they will admit the patient for observation during that very high-risk 2-day period.
"If you look at the cost effectiveness of observing these people in the hospital, the cost of hospitalization is justified by the opportunity to treat promptly with IV TPA [tissue plasminogen activator] should a stroke occur," Dr. Johnston added.
He and his coworkers developed the ABCD2 score through analysis of large patient data sets (Lancet 2007;369:283-92). The score has since been validated in numerous studies in varied populations. And it is endorsed in various stroke guidelines. For example, the American Heart Association/American Stroke Association guidelines state: "It is reasonable to hospitalize patients with an ABCD2 score of 3 or more presenting within 72 hours of symptoms, or with lower scores if work-up cannot be done as an outpatient within 2 days or if there is other evidence for focused ischemia."
The ABCD2 score assesses five parameters: age, blood pressure, clinical features, duration, and diabetes. Each has been shown to be an independent risk factor for stroke within 2 days after a TIA, with an associated roughly twofold increased risk. A patient gets 1 point for being age 60 or more, 1 point for having a blood pressure above 140/90 mm Hg in the office at the time of the TIA evaluation, 2 points if focal weakness was a clinical feature of the TIA, 1 point for speech impairment without weakness, 1 point for a TIA duration of 10-59 minutes, and 2 points for a duration of 60 minutes or more.
Multiple studies by Dr. Johnston and others have established that roughly 34% of TIA patients have an ABCD2 score of 0-3, putting them in a low short-term risk category, with an associated 1% risk of stroke within the first 2 days after their TIA. Another 45% of patients will have a score of 4-5, with an associated 4% 2-day stroke risk. And 21% of TIA patients are very high risk, with a score of 6-7 and an 8% incidence of stroke within 2 days.
How does the ABCD2 score predict stroke risk? Most likely in part by identifying people who’ve had a true TIA rather than migraine or another TIA mimic. Neurologist-confirmed TIAs have been shown to have higher ABCD2 scores.
"We think ABCD2 scores are just a simple way of doing the complex work that neurologists try to do when they’re diagnosing a specific event," Dr. Johnston explained.
He presented the case of a 72-year-old diabetic woman who phones the office because she has just had a 90-minute episode of difficulty in speaking and arm weakness. She stresses that she feels completely normal now. But even without knowing her current blood pressure, her ABCD2 score is still 6, giving her an 8% risk of stroke within the next 2 days. She needs to go to the ED immediately.
"Some day there’s going to be a blood test for this risk assessment, and I hope it’s soon. It will be sort of a troponin for the brain, but even more sensitive so we can look at transient ischemia as opposed to infarction. There are groups working on this, and there are a couple of leads. It would be wonderful if we got that. Until then we have this – and it works. It’s not perfect. It’s not great. But it’s better than the other things we have now," the neurologist said.
He was quick to add, however, that the ABCD2 score is no substitute for clinical judgment. Certain patients with a TIA should be sent straightaway to the ED regardless of their ABCD2 score. They include individuals with a hypercoagulable state, endocarditis, a crescendo event, known ipsilateral large-vessel stenosis or occlusion, or CT or MRI evidence of recent infarction.
"The ABCD2 score is not magic. A young person who is an IV drug user and has a 1-minute spell of diplopia is someone you’d worry about, and yet that person probably has an ABCD2 score of 0," Dr. Johnston noted.
He reported having no relevant financial conflicts.
predicting the risk of stroke, International Stroke Conference, American Stroke Association, neurology,
HONOLULU – A patient comes to your office because of what sounds very much like a recent TIA. As a busy primary care physician on the health care front lines, you need to be able to quickly assess this individual’s near-term risk of a full-blown stroke. The ABCD2 score is the right tool for this task, according to Dr. S. Claiborne Johnston.
The ABCD2 score is a simple tool for predicting the risk of stroke within 2 days after a TIA. It requires no special training and takes just seconds to calculate based upon patient history. With a score of 3 or more on the 0-7 scale, tell the patient to go straight to the emergency department. No referral to the neurologist for a consultation is necessary, he said at the International Stroke Conference sponsored by the American Stroke Association.
"If you’re talking to the patient on the phone, she doesn’t need to come into the office at all. Have her go straight to the ED. With a score of 3 or more, her stroke risk in the next 2 days is pretty high – and, really, what are you going to do in the clinic to reduce that risk?" said Dr. Johnston, professor of neurology and epidemiology and director of the stroke center at the University of California, San Francisco.
In the emergency department, physicians can obtain a brain scan to further define the short-term risk. And it’s likely they will admit the patient for observation during that very high-risk 2-day period.
"If you look at the cost effectiveness of observing these people in the hospital, the cost of hospitalization is justified by the opportunity to treat promptly with IV TPA [tissue plasminogen activator] should a stroke occur," Dr. Johnston added.
He and his coworkers developed the ABCD2 score through analysis of large patient data sets (Lancet 2007;369:283-92). The score has since been validated in numerous studies in varied populations. And it is endorsed in various stroke guidelines. For example, the American Heart Association/American Stroke Association guidelines state: "It is reasonable to hospitalize patients with an ABCD2 score of 3 or more presenting within 72 hours of symptoms, or with lower scores if work-up cannot be done as an outpatient within 2 days or if there is other evidence for focused ischemia."
The ABCD2 score assesses five parameters: age, blood pressure, clinical features, duration, and diabetes. Each has been shown to be an independent risk factor for stroke within 2 days after a TIA, with an associated roughly twofold increased risk. A patient gets 1 point for being age 60 or more, 1 point for having a blood pressure above 140/90 mm Hg in the office at the time of the TIA evaluation, 2 points if focal weakness was a clinical feature of the TIA, 1 point for speech impairment without weakness, 1 point for a TIA duration of 10-59 minutes, and 2 points for a duration of 60 minutes or more.
Multiple studies by Dr. Johnston and others have established that roughly 34% of TIA patients have an ABCD2 score of 0-3, putting them in a low short-term risk category, with an associated 1% risk of stroke within the first 2 days after their TIA. Another 45% of patients will have a score of 4-5, with an associated 4% 2-day stroke risk. And 21% of TIA patients are very high risk, with a score of 6-7 and an 8% incidence of stroke within 2 days.
How does the ABCD2 score predict stroke risk? Most likely in part by identifying people who’ve had a true TIA rather than migraine or another TIA mimic. Neurologist-confirmed TIAs have been shown to have higher ABCD2 scores.
"We think ABCD2 scores are just a simple way of doing the complex work that neurologists try to do when they’re diagnosing a specific event," Dr. Johnston explained.
He presented the case of a 72-year-old diabetic woman who phones the office because she has just had a 90-minute episode of difficulty in speaking and arm weakness. She stresses that she feels completely normal now. But even without knowing her current blood pressure, her ABCD2 score is still 6, giving her an 8% risk of stroke within the next 2 days. She needs to go to the ED immediately.
"Some day there’s going to be a blood test for this risk assessment, and I hope it’s soon. It will be sort of a troponin for the brain, but even more sensitive so we can look at transient ischemia as opposed to infarction. There are groups working on this, and there are a couple of leads. It would be wonderful if we got that. Until then we have this – and it works. It’s not perfect. It’s not great. But it’s better than the other things we have now," the neurologist said.
He was quick to add, however, that the ABCD2 score is no substitute for clinical judgment. Certain patients with a TIA should be sent straightaway to the ED regardless of their ABCD2 score. They include individuals with a hypercoagulable state, endocarditis, a crescendo event, known ipsilateral large-vessel stenosis or occlusion, or CT or MRI evidence of recent infarction.
"The ABCD2 score is not magic. A young person who is an IV drug user and has a 1-minute spell of diplopia is someone you’d worry about, and yet that person probably has an ABCD2 score of 0," Dr. Johnston noted.
He reported having no relevant financial conflicts.
HONOLULU – A patient comes to your office because of what sounds very much like a recent TIA. As a busy primary care physician on the health care front lines, you need to be able to quickly assess this individual’s near-term risk of a full-blown stroke. The ABCD2 score is the right tool for this task, according to Dr. S. Claiborne Johnston.
The ABCD2 score is a simple tool for predicting the risk of stroke within 2 days after a TIA. It requires no special training and takes just seconds to calculate based upon patient history. With a score of 3 or more on the 0-7 scale, tell the patient to go straight to the emergency department. No referral to the neurologist for a consultation is necessary, he said at the International Stroke Conference sponsored by the American Stroke Association.
"If you’re talking to the patient on the phone, she doesn’t need to come into the office at all. Have her go straight to the ED. With a score of 3 or more, her stroke risk in the next 2 days is pretty high – and, really, what are you going to do in the clinic to reduce that risk?" said Dr. Johnston, professor of neurology and epidemiology and director of the stroke center at the University of California, San Francisco.
In the emergency department, physicians can obtain a brain scan to further define the short-term risk. And it’s likely they will admit the patient for observation during that very high-risk 2-day period.
"If you look at the cost effectiveness of observing these people in the hospital, the cost of hospitalization is justified by the opportunity to treat promptly with IV TPA [tissue plasminogen activator] should a stroke occur," Dr. Johnston added.
He and his coworkers developed the ABCD2 score through analysis of large patient data sets (Lancet 2007;369:283-92). The score has since been validated in numerous studies in varied populations. And it is endorsed in various stroke guidelines. For example, the American Heart Association/American Stroke Association guidelines state: "It is reasonable to hospitalize patients with an ABCD2 score of 3 or more presenting within 72 hours of symptoms, or with lower scores if work-up cannot be done as an outpatient within 2 days or if there is other evidence for focused ischemia."
The ABCD2 score assesses five parameters: age, blood pressure, clinical features, duration, and diabetes. Each has been shown to be an independent risk factor for stroke within 2 days after a TIA, with an associated roughly twofold increased risk. A patient gets 1 point for being age 60 or more, 1 point for having a blood pressure above 140/90 mm Hg in the office at the time of the TIA evaluation, 2 points if focal weakness was a clinical feature of the TIA, 1 point for speech impairment without weakness, 1 point for a TIA duration of 10-59 minutes, and 2 points for a duration of 60 minutes or more.
Multiple studies by Dr. Johnston and others have established that roughly 34% of TIA patients have an ABCD2 score of 0-3, putting them in a low short-term risk category, with an associated 1% risk of stroke within the first 2 days after their TIA. Another 45% of patients will have a score of 4-5, with an associated 4% 2-day stroke risk. And 21% of TIA patients are very high risk, with a score of 6-7 and an 8% incidence of stroke within 2 days.
How does the ABCD2 score predict stroke risk? Most likely in part by identifying people who’ve had a true TIA rather than migraine or another TIA mimic. Neurologist-confirmed TIAs have been shown to have higher ABCD2 scores.
"We think ABCD2 scores are just a simple way of doing the complex work that neurologists try to do when they’re diagnosing a specific event," Dr. Johnston explained.
He presented the case of a 72-year-old diabetic woman who phones the office because she has just had a 90-minute episode of difficulty in speaking and arm weakness. She stresses that she feels completely normal now. But even without knowing her current blood pressure, her ABCD2 score is still 6, giving her an 8% risk of stroke within the next 2 days. She needs to go to the ED immediately.
"Some day there’s going to be a blood test for this risk assessment, and I hope it’s soon. It will be sort of a troponin for the brain, but even more sensitive so we can look at transient ischemia as opposed to infarction. There are groups working on this, and there are a couple of leads. It would be wonderful if we got that. Until then we have this – and it works. It’s not perfect. It’s not great. But it’s better than the other things we have now," the neurologist said.
He was quick to add, however, that the ABCD2 score is no substitute for clinical judgment. Certain patients with a TIA should be sent straightaway to the ED regardless of their ABCD2 score. They include individuals with a hypercoagulable state, endocarditis, a crescendo event, known ipsilateral large-vessel stenosis or occlusion, or CT or MRI evidence of recent infarction.
"The ABCD2 score is not magic. A young person who is an IV drug user and has a 1-minute spell of diplopia is someone you’d worry about, and yet that person probably has an ABCD2 score of 0," Dr. Johnston noted.
He reported having no relevant financial conflicts.
predicting the risk of stroke, International Stroke Conference, American Stroke Association, neurology,
predicting the risk of stroke, International Stroke Conference, American Stroke Association, neurology,
EXPERT OPINION FROM THE INTERNATIONAL STROKE CONFERENCE
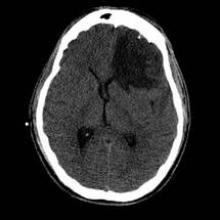
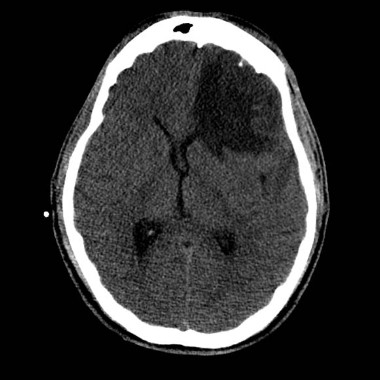
Novel hemorrhagic stroke therapy bests medical management
A minimally invasive surgical procedure that enables direct local delivery of tissue plasminogen activator to the blood clot in patients with intracerebral hemorrhage safely resulted in markedly improved functional ability, greater independence, and dramatically lower costs than conventional medical management at 1 year of follow-up, in the randomized multicenter MISTIE trial.
"The procedure is simple, rapid, and easy to generalize. There is now real hope we have a treatment for the last form of stroke that doesn’t have a treatment: brain hemorrhage," Dr. Daniel F. Hanley said at the International Stroke Conference sponsored by the American Stroke Association.
That being said, MISTIE (Minimally Invasive Surgery plus rTPA for Intracerebral Hemorrhage Evacuation) was a modestly sized, phase II proof-of-concept study, the concept being that reducing clot size should improve outcomes in patients with intracerebral hemorrhage (ICH). Based on the encouraging 1-year MISTIE results, the plan is to ramp up to a 500-patient definitive phase III trial, said Dr. Hanley, professor of neurology and director of the brain injury outcomes division at Johns Hopkins University, Baltimore.
The trial involved 96 patients with ICH at 26 hospitals who were randomized to the minimally invasive surgical procedure or medical management. The "most startling" finding to emerge from the trial, in Dr. Hanley’s view, was that the benefits of the surgical intervention documented at 6 months’ follow-up and reported at last year’s International Stroke Conference are even greater at 1 year.
"The benefits of surgery are expanding over time," the neurologist observed. "It takes a long time to resolve brain injury, even though we’re getting the majority of the clot out in the first 3 days."
The procedure entails cutting a dime-sized hole in the patient’s skull, snaking a catheter through it and into the bulk of the clot, then delivering a dose of tissue plasminogen activator (TPA) every 8 hours for 2-3 days. As TPA dissolves the clot, the material is evacuated through the catheter. The surgical procedure took an average of 42 minutes compared with 3 hours, typically, for a craniotomy.
Among the key findings from the MISTIE 1-year update:
• Non-ICU hospital length of stay averaged 38 days less in the surgically managed group.
• The cost of acute care averaged $44,000 less per patient, a 35% reduction, compared with medical management.
• At 1 year, 21% of patients in the medically managed group were in a nursing home, compared with just 8% of the surgically managed group.
• The average Stroke Impact Scale mobility score in the surgical group doubled from 40 at 6 months to 80 at 1 year while plateauing at about 20 between days 80 and 90 in the medically managed patients. A score of 80 on this scale means a patient can do what he wants most of the time; a score of 20 means he seldom can
• The average Stroke Impact Scale activities of daily living score similarly showed progressive, roughly linear improvement in the surgical group between 6 months and 1 year while plateauing at a low performance level at 90-180 days in the medically managed group.
• The proportion of patients with functional independence as defined by a modified Rankin score of 0-2 was an absolute 14% greater in surgically managed compared with medically managed patients at 1 year.
The average baseline clot volume was 46 mL. The surgical goal was to remove 60% of the clot volume; this was achieved in 72% of treated patients. On average 28 mL of clot were removed over a period of 3 days.
"The surgeons are consistently able to achieve 20- to 40-mL reductions in clot volume. Twenty-nine surgeons have done the procedure, and we don’t see a learning curve. That’s good. It means this is a pretty simple procedure to do. In point of fact, the training consisted of a single 1-hour conference with the lead neurosurgeon and a short self-learning computer program," according to Dr. Hanley.
Roughly 60% of patients whose clot volume was reduced to less than 10 mL had functional independence as reflected in a modified Rankin score of 0-2 at 180 days, compared with a 10% rate in those with a residual clot volume in excess of 35 mL.
Outcomes were similar regardless of whether the surgery was done within 36 hours after stroke onset or later.
"To me it looks like the time consideration for this surgery is going to be permissive. That’s very important for the 1 million people in the world each year who have an ICH," the neurologist noted.
The MISTIE trial was funded by the National Institute of Neurological Disorders and Stroke. Dr. Hanley reported having no relevant financial conflicts.
A minimally invasive surgical procedure that enables direct local delivery of tissue plasminogen activator to the blood clot in patients with intracerebral hemorrhage safely resulted in markedly improved functional ability, greater independence, and dramatically lower costs than conventional medical management at 1 year of follow-up, in the randomized multicenter MISTIE trial.
"The procedure is simple, rapid, and easy to generalize. There is now real hope we have a treatment for the last form of stroke that doesn’t have a treatment: brain hemorrhage," Dr. Daniel F. Hanley said at the International Stroke Conference sponsored by the American Stroke Association.
That being said, MISTIE (Minimally Invasive Surgery plus rTPA for Intracerebral Hemorrhage Evacuation) was a modestly sized, phase II proof-of-concept study, the concept being that reducing clot size should improve outcomes in patients with intracerebral hemorrhage (ICH). Based on the encouraging 1-year MISTIE results, the plan is to ramp up to a 500-patient definitive phase III trial, said Dr. Hanley, professor of neurology and director of the brain injury outcomes division at Johns Hopkins University, Baltimore.
The trial involved 96 patients with ICH at 26 hospitals who were randomized to the minimally invasive surgical procedure or medical management. The "most startling" finding to emerge from the trial, in Dr. Hanley’s view, was that the benefits of the surgical intervention documented at 6 months’ follow-up and reported at last year’s International Stroke Conference are even greater at 1 year.
"The benefits of surgery are expanding over time," the neurologist observed. "It takes a long time to resolve brain injury, even though we’re getting the majority of the clot out in the first 3 days."
The procedure entails cutting a dime-sized hole in the patient’s skull, snaking a catheter through it and into the bulk of the clot, then delivering a dose of tissue plasminogen activator (TPA) every 8 hours for 2-3 days. As TPA dissolves the clot, the material is evacuated through the catheter. The surgical procedure took an average of 42 minutes compared with 3 hours, typically, for a craniotomy.
Among the key findings from the MISTIE 1-year update:
• Non-ICU hospital length of stay averaged 38 days less in the surgically managed group.
• The cost of acute care averaged $44,000 less per patient, a 35% reduction, compared with medical management.
• At 1 year, 21% of patients in the medically managed group were in a nursing home, compared with just 8% of the surgically managed group.
• The average Stroke Impact Scale mobility score in the surgical group doubled from 40 at 6 months to 80 at 1 year while plateauing at about 20 between days 80 and 90 in the medically managed patients. A score of 80 on this scale means a patient can do what he wants most of the time; a score of 20 means he seldom can
• The average Stroke Impact Scale activities of daily living score similarly showed progressive, roughly linear improvement in the surgical group between 6 months and 1 year while plateauing at a low performance level at 90-180 days in the medically managed group.
• The proportion of patients with functional independence as defined by a modified Rankin score of 0-2 was an absolute 14% greater in surgically managed compared with medically managed patients at 1 year.
The average baseline clot volume was 46 mL. The surgical goal was to remove 60% of the clot volume; this was achieved in 72% of treated patients. On average 28 mL of clot were removed over a period of 3 days.
"The surgeons are consistently able to achieve 20- to 40-mL reductions in clot volume. Twenty-nine surgeons have done the procedure, and we don’t see a learning curve. That’s good. It means this is a pretty simple procedure to do. In point of fact, the training consisted of a single 1-hour conference with the lead neurosurgeon and a short self-learning computer program," according to Dr. Hanley.
Roughly 60% of patients whose clot volume was reduced to less than 10 mL had functional independence as reflected in a modified Rankin score of 0-2 at 180 days, compared with a 10% rate in those with a residual clot volume in excess of 35 mL.
Outcomes were similar regardless of whether the surgery was done within 36 hours after stroke onset or later.
"To me it looks like the time consideration for this surgery is going to be permissive. That’s very important for the 1 million people in the world each year who have an ICH," the neurologist noted.
The MISTIE trial was funded by the National Institute of Neurological Disorders and Stroke. Dr. Hanley reported having no relevant financial conflicts.
A minimally invasive surgical procedure that enables direct local delivery of tissue plasminogen activator to the blood clot in patients with intracerebral hemorrhage safely resulted in markedly improved functional ability, greater independence, and dramatically lower costs than conventional medical management at 1 year of follow-up, in the randomized multicenter MISTIE trial.
"The procedure is simple, rapid, and easy to generalize. There is now real hope we have a treatment for the last form of stroke that doesn’t have a treatment: brain hemorrhage," Dr. Daniel F. Hanley said at the International Stroke Conference sponsored by the American Stroke Association.
That being said, MISTIE (Minimally Invasive Surgery plus rTPA for Intracerebral Hemorrhage Evacuation) was a modestly sized, phase II proof-of-concept study, the concept being that reducing clot size should improve outcomes in patients with intracerebral hemorrhage (ICH). Based on the encouraging 1-year MISTIE results, the plan is to ramp up to a 500-patient definitive phase III trial, said Dr. Hanley, professor of neurology and director of the brain injury outcomes division at Johns Hopkins University, Baltimore.
The trial involved 96 patients with ICH at 26 hospitals who were randomized to the minimally invasive surgical procedure or medical management. The "most startling" finding to emerge from the trial, in Dr. Hanley’s view, was that the benefits of the surgical intervention documented at 6 months’ follow-up and reported at last year’s International Stroke Conference are even greater at 1 year.
"The benefits of surgery are expanding over time," the neurologist observed. "It takes a long time to resolve brain injury, even though we’re getting the majority of the clot out in the first 3 days."
The procedure entails cutting a dime-sized hole in the patient’s skull, snaking a catheter through it and into the bulk of the clot, then delivering a dose of tissue plasminogen activator (TPA) every 8 hours for 2-3 days. As TPA dissolves the clot, the material is evacuated through the catheter. The surgical procedure took an average of 42 minutes compared with 3 hours, typically, for a craniotomy.
Among the key findings from the MISTIE 1-year update:
• Non-ICU hospital length of stay averaged 38 days less in the surgically managed group.
• The cost of acute care averaged $44,000 less per patient, a 35% reduction, compared with medical management.
• At 1 year, 21% of patients in the medically managed group were in a nursing home, compared with just 8% of the surgically managed group.
• The average Stroke Impact Scale mobility score in the surgical group doubled from 40 at 6 months to 80 at 1 year while plateauing at about 20 between days 80 and 90 in the medically managed patients. A score of 80 on this scale means a patient can do what he wants most of the time; a score of 20 means he seldom can
• The average Stroke Impact Scale activities of daily living score similarly showed progressive, roughly linear improvement in the surgical group between 6 months and 1 year while plateauing at a low performance level at 90-180 days in the medically managed group.
• The proportion of patients with functional independence as defined by a modified Rankin score of 0-2 was an absolute 14% greater in surgically managed compared with medically managed patients at 1 year.
The average baseline clot volume was 46 mL. The surgical goal was to remove 60% of the clot volume; this was achieved in 72% of treated patients. On average 28 mL of clot were removed over a period of 3 days.
"The surgeons are consistently able to achieve 20- to 40-mL reductions in clot volume. Twenty-nine surgeons have done the procedure, and we don’t see a learning curve. That’s good. It means this is a pretty simple procedure to do. In point of fact, the training consisted of a single 1-hour conference with the lead neurosurgeon and a short self-learning computer program," according to Dr. Hanley.
Roughly 60% of patients whose clot volume was reduced to less than 10 mL had functional independence as reflected in a modified Rankin score of 0-2 at 180 days, compared with a 10% rate in those with a residual clot volume in excess of 35 mL.
Outcomes were similar regardless of whether the surgery was done within 36 hours after stroke onset or later.
"To me it looks like the time consideration for this surgery is going to be permissive. That’s very important for the 1 million people in the world each year who have an ICH," the neurologist noted.
The MISTIE trial was funded by the National Institute of Neurological Disorders and Stroke. Dr. Hanley reported having no relevant financial conflicts.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: One year after undergoing a novel minimally invasive surgical procedure for treatment of intracerebral hemorrhage, patients had significantly better outcomes than those randomized to medical management – and the disparity in outcomes was significantly greater than at 6 months’ follow-up.
Data Source: MISTIE, a randomized multicenter trial in which 96 patients with intracerebral hemorrhage were randomized to standard medical management or to a novel surgical procedure.
Disclosures: MISTIE was sponsored by the National Institute of Neurological Disorders and Stroke. The study presenter said he had no relevant financial conflicts.
Hemodynamic complications commonly found in veterans after TBI
HONOLULU – Cerebral vasospasm and intracranial hypertension may be frequent secondary insults following wartime traumatic brain injury, according to a retrospective study of 122 consecutive veterans.
Transcranial Doppler (TCD) ultrasonography signs of mild, moderate, and severe vasospasm involving anterior circulation vessels were observed in 71%, 42%, and 16% of the veterans with traumatic brain injury (TBI), respectively.
TCD signs involving posterior circulation vessels were observed in 57%, 32%, and 14%, respectively.
Intracranial hypertension was recorded in 43% of patients, lead author Alexander Razumovsky, Ph.D., reported at the International Stroke Conference.
"Cerebral blood flow velocity measurements permit detection of early signs of cerebral vasospasm and allow physicians to better define management strategies," he said.
TCD monitoring is routinely used by the U.S. Army, but it has not been fully embraced elsewhere because many physicians are unaware of how it can be used within the continuum of TBI care to help reverse outcomes, said study coauthor Col. Rocco Armonda, MC, USA.
"There’s this lack of drive to change outcomes because people haven’t seen how you can take someone who is in a comatose state and eventually gain functional independence," said Dr. Armonda, who is the director of cerebrovascular surgery and interventional neuroradiology at the National Naval Medical Center in Bethesda, Md.
A recent study from Walter Reed National Military Medical Center (J. Trauma Acute Care Surg. 2012;73:1525-30), however, reported that 63% of veterans with a penetrating TBI and a mean discharge Glasgow Coma Scale (GCS) score of 6-8 progressed to functional independence – a number twice as high as would be expected, Dr. Armonda remarked.
Dr. Razumovsky said that simple, noninvasive TCD monitoring should be performed in the daily management of hospitalized TBI patients to complement other monitoring strategies, and it can be used alone in emergency situations when intracranial pressure monitoring is contraindicated or not readily available.
TCD monitoring is not necessary during outpatient follow-up of patients with TBI, with the exception of the subset who’ve undergone hemicraniectomy, Dr. Armonda said.
"In those patients who’ve had hemicraniectomy, some of them suffer prolonged duration from atmospheric pressure of the cranial defect, and TCD has actually been helpful to look at the cerebral blood flow dynamics," he said at a press briefing on the study.
The results confirm earlier data that TBI is associated with a high incidence of cerebral vasospasm, particularly in patients with severe TBI, and are applicable to civilian TBI patients because a significant number will experience post-traumatic bleeding that will lead to vasospasm and intracranial hypertension, said Dr. Razumovsky, director of Sentient NeuroCare Services in Hunt Valley, Md., which provides services to the National Naval Medical Hospital.
In the current study, patients were admitted to Walter Reed a mean of 6.7 days after injury from Oct. 1, 2008, to Nov. 30, 2012. Mean cerebral blood flow velocity (CBFV) of 100-139 cm/s was used to define mild vasospasm, 140-199 cm/s moderate vasospasm, and more than 200 cm/s severe vasospasm.
In all, 88 patients had penetrating head injury, of whom 45 (51%) had a secondary diagnosis of blast injury; and 34 patients had a closed head injury, of whom 15 (44%) had a secondary diagnosis of blast injury. Their mean age was 26 years.
In the mild vasospasm group, the mean anterior circulation CBFV was 122.5 cm/s and mean posterior CBFV was 61 cm/s. Their average GCS score changed from 8 at baseline to 6.1 at discharge, Dr. Razumovsky said.
In the moderate vasospasm group, the mean anterior circulation CBFV was 156.6 cm/s and mean posterior CBFV was 77.5 cm/s. Their average GCS score changed from 5.9 at baseline to 5.3 at discharge.
Patients with severe vasospasm had an average anterior circulation CBFV of 241.9 cm/s and a mean posterior CBFV of 101.8 cm/s. Their average GCS score was 4.8 at both time periods.
Eight patients (7%) underwent transluminal angioplasty for post-traumatic symptomatic vasospasm, he said at the meeting, sponsored by the American Heart Association.
Dr. Larry Goldstein, director of the Duke Stroke Center in Durham, N.C., said in an interview that the detection of vasospasm by TCD was potentially important because there is an increased risk of vasospasm after subarachnoid hemorrhage that can lead to delayed ischemic neurological deficits. Although it was unclear from the data how many patients had traumatic subarachnoid hemorrhage associated with their brain injury, he noted that the risk of vasospasm seems to be similar for traumatic and nontraumatic subarachnoid hemorrhage.
"In many centers, both groups of patients are routinely monitored with transcranial Dopplers over the first couple of weeks or so, which is when the peak period of vasospasm develops," Dr. Goldstein said. "Showing that monitoring leads to interventions that then change outcome, that’s not so straightforward."
The study was supported in part by the U.S. Army Medical Research and Materiel Command’s Telemedicine and Advanced Technology Research Center. Dr. Razumovsky and two of his coauthors reported financial remuneration from private practice.
posterior circulation vessels, Alexander Razumovsky, Ph.D., the International Stroke Conference, Cerebral blood flow velocity, U.S. Army, Col. Rocco Armonda, MC, USA,
HONOLULU – Cerebral vasospasm and intracranial hypertension may be frequent secondary insults following wartime traumatic brain injury, according to a retrospective study of 122 consecutive veterans.
Transcranial Doppler (TCD) ultrasonography signs of mild, moderate, and severe vasospasm involving anterior circulation vessels were observed in 71%, 42%, and 16% of the veterans with traumatic brain injury (TBI), respectively.
TCD signs involving posterior circulation vessels were observed in 57%, 32%, and 14%, respectively.
Intracranial hypertension was recorded in 43% of patients, lead author Alexander Razumovsky, Ph.D., reported at the International Stroke Conference.
"Cerebral blood flow velocity measurements permit detection of early signs of cerebral vasospasm and allow physicians to better define management strategies," he said.
TCD monitoring is routinely used by the U.S. Army, but it has not been fully embraced elsewhere because many physicians are unaware of how it can be used within the continuum of TBI care to help reverse outcomes, said study coauthor Col. Rocco Armonda, MC, USA.
"There’s this lack of drive to change outcomes because people haven’t seen how you can take someone who is in a comatose state and eventually gain functional independence," said Dr. Armonda, who is the director of cerebrovascular surgery and interventional neuroradiology at the National Naval Medical Center in Bethesda, Md.
A recent study from Walter Reed National Military Medical Center (J. Trauma Acute Care Surg. 2012;73:1525-30), however, reported that 63% of veterans with a penetrating TBI and a mean discharge Glasgow Coma Scale (GCS) score of 6-8 progressed to functional independence – a number twice as high as would be expected, Dr. Armonda remarked.
Dr. Razumovsky said that simple, noninvasive TCD monitoring should be performed in the daily management of hospitalized TBI patients to complement other monitoring strategies, and it can be used alone in emergency situations when intracranial pressure monitoring is contraindicated or not readily available.
TCD monitoring is not necessary during outpatient follow-up of patients with TBI, with the exception of the subset who’ve undergone hemicraniectomy, Dr. Armonda said.
"In those patients who’ve had hemicraniectomy, some of them suffer prolonged duration from atmospheric pressure of the cranial defect, and TCD has actually been helpful to look at the cerebral blood flow dynamics," he said at a press briefing on the study.
The results confirm earlier data that TBI is associated with a high incidence of cerebral vasospasm, particularly in patients with severe TBI, and are applicable to civilian TBI patients because a significant number will experience post-traumatic bleeding that will lead to vasospasm and intracranial hypertension, said Dr. Razumovsky, director of Sentient NeuroCare Services in Hunt Valley, Md., which provides services to the National Naval Medical Hospital.
In the current study, patients were admitted to Walter Reed a mean of 6.7 days after injury from Oct. 1, 2008, to Nov. 30, 2012. Mean cerebral blood flow velocity (CBFV) of 100-139 cm/s was used to define mild vasospasm, 140-199 cm/s moderate vasospasm, and more than 200 cm/s severe vasospasm.
In all, 88 patients had penetrating head injury, of whom 45 (51%) had a secondary diagnosis of blast injury; and 34 patients had a closed head injury, of whom 15 (44%) had a secondary diagnosis of blast injury. Their mean age was 26 years.
In the mild vasospasm group, the mean anterior circulation CBFV was 122.5 cm/s and mean posterior CBFV was 61 cm/s. Their average GCS score changed from 8 at baseline to 6.1 at discharge, Dr. Razumovsky said.
In the moderate vasospasm group, the mean anterior circulation CBFV was 156.6 cm/s and mean posterior CBFV was 77.5 cm/s. Their average GCS score changed from 5.9 at baseline to 5.3 at discharge.
Patients with severe vasospasm had an average anterior circulation CBFV of 241.9 cm/s and a mean posterior CBFV of 101.8 cm/s. Their average GCS score was 4.8 at both time periods.
Eight patients (7%) underwent transluminal angioplasty for post-traumatic symptomatic vasospasm, he said at the meeting, sponsored by the American Heart Association.
Dr. Larry Goldstein, director of the Duke Stroke Center in Durham, N.C., said in an interview that the detection of vasospasm by TCD was potentially important because there is an increased risk of vasospasm after subarachnoid hemorrhage that can lead to delayed ischemic neurological deficits. Although it was unclear from the data how many patients had traumatic subarachnoid hemorrhage associated with their brain injury, he noted that the risk of vasospasm seems to be similar for traumatic and nontraumatic subarachnoid hemorrhage.
"In many centers, both groups of patients are routinely monitored with transcranial Dopplers over the first couple of weeks or so, which is when the peak period of vasospasm develops," Dr. Goldstein said. "Showing that monitoring leads to interventions that then change outcome, that’s not so straightforward."
The study was supported in part by the U.S. Army Medical Research and Materiel Command’s Telemedicine and Advanced Technology Research Center. Dr. Razumovsky and two of his coauthors reported financial remuneration from private practice.
HONOLULU – Cerebral vasospasm and intracranial hypertension may be frequent secondary insults following wartime traumatic brain injury, according to a retrospective study of 122 consecutive veterans.
Transcranial Doppler (TCD) ultrasonography signs of mild, moderate, and severe vasospasm involving anterior circulation vessels were observed in 71%, 42%, and 16% of the veterans with traumatic brain injury (TBI), respectively.
TCD signs involving posterior circulation vessels were observed in 57%, 32%, and 14%, respectively.
Intracranial hypertension was recorded in 43% of patients, lead author Alexander Razumovsky, Ph.D., reported at the International Stroke Conference.
"Cerebral blood flow velocity measurements permit detection of early signs of cerebral vasospasm and allow physicians to better define management strategies," he said.
TCD monitoring is routinely used by the U.S. Army, but it has not been fully embraced elsewhere because many physicians are unaware of how it can be used within the continuum of TBI care to help reverse outcomes, said study coauthor Col. Rocco Armonda, MC, USA.
"There’s this lack of drive to change outcomes because people haven’t seen how you can take someone who is in a comatose state and eventually gain functional independence," said Dr. Armonda, who is the director of cerebrovascular surgery and interventional neuroradiology at the National Naval Medical Center in Bethesda, Md.
A recent study from Walter Reed National Military Medical Center (J. Trauma Acute Care Surg. 2012;73:1525-30), however, reported that 63% of veterans with a penetrating TBI and a mean discharge Glasgow Coma Scale (GCS) score of 6-8 progressed to functional independence – a number twice as high as would be expected, Dr. Armonda remarked.
Dr. Razumovsky said that simple, noninvasive TCD monitoring should be performed in the daily management of hospitalized TBI patients to complement other monitoring strategies, and it can be used alone in emergency situations when intracranial pressure monitoring is contraindicated or not readily available.
TCD monitoring is not necessary during outpatient follow-up of patients with TBI, with the exception of the subset who’ve undergone hemicraniectomy, Dr. Armonda said.
"In those patients who’ve had hemicraniectomy, some of them suffer prolonged duration from atmospheric pressure of the cranial defect, and TCD has actually been helpful to look at the cerebral blood flow dynamics," he said at a press briefing on the study.
The results confirm earlier data that TBI is associated with a high incidence of cerebral vasospasm, particularly in patients with severe TBI, and are applicable to civilian TBI patients because a significant number will experience post-traumatic bleeding that will lead to vasospasm and intracranial hypertension, said Dr. Razumovsky, director of Sentient NeuroCare Services in Hunt Valley, Md., which provides services to the National Naval Medical Hospital.
In the current study, patients were admitted to Walter Reed a mean of 6.7 days after injury from Oct. 1, 2008, to Nov. 30, 2012. Mean cerebral blood flow velocity (CBFV) of 100-139 cm/s was used to define mild vasospasm, 140-199 cm/s moderate vasospasm, and more than 200 cm/s severe vasospasm.
In all, 88 patients had penetrating head injury, of whom 45 (51%) had a secondary diagnosis of blast injury; and 34 patients had a closed head injury, of whom 15 (44%) had a secondary diagnosis of blast injury. Their mean age was 26 years.
In the mild vasospasm group, the mean anterior circulation CBFV was 122.5 cm/s and mean posterior CBFV was 61 cm/s. Their average GCS score changed from 8 at baseline to 6.1 at discharge, Dr. Razumovsky said.
In the moderate vasospasm group, the mean anterior circulation CBFV was 156.6 cm/s and mean posterior CBFV was 77.5 cm/s. Their average GCS score changed from 5.9 at baseline to 5.3 at discharge.
Patients with severe vasospasm had an average anterior circulation CBFV of 241.9 cm/s and a mean posterior CBFV of 101.8 cm/s. Their average GCS score was 4.8 at both time periods.
Eight patients (7%) underwent transluminal angioplasty for post-traumatic symptomatic vasospasm, he said at the meeting, sponsored by the American Heart Association.
Dr. Larry Goldstein, director of the Duke Stroke Center in Durham, N.C., said in an interview that the detection of vasospasm by TCD was potentially important because there is an increased risk of vasospasm after subarachnoid hemorrhage that can lead to delayed ischemic neurological deficits. Although it was unclear from the data how many patients had traumatic subarachnoid hemorrhage associated with their brain injury, he noted that the risk of vasospasm seems to be similar for traumatic and nontraumatic subarachnoid hemorrhage.
"In many centers, both groups of patients are routinely monitored with transcranial Dopplers over the first couple of weeks or so, which is when the peak period of vasospasm develops," Dr. Goldstein said. "Showing that monitoring leads to interventions that then change outcome, that’s not so straightforward."
The study was supported in part by the U.S. Army Medical Research and Materiel Command’s Telemedicine and Advanced Technology Research Center. Dr. Razumovsky and two of his coauthors reported financial remuneration from private practice.
posterior circulation vessels, Alexander Razumovsky, Ph.D., the International Stroke Conference, Cerebral blood flow velocity, U.S. Army, Col. Rocco Armonda, MC, USA,
posterior circulation vessels, Alexander Razumovsky, Ph.D., the International Stroke Conference, Cerebral blood flow velocity, U.S. Army, Col. Rocco Armonda, MC, USA,
AT THE INTERNATIONAL STROKE CONFERENCE
Major finding: Transcranial Doppler ultrasonography revealed signs of mild, moderate, and severe vasospasm involving anterior circulation vessels in 71%, 42%, and 16% of patients, respectively, but slightly less often in posterior circulation vessels (57%, 32%, and 14%).
Data source: A retrospective study of 122 consecutive patients with combat-related traumatic brain injury.
Disclosures: The study was supported in part by the U.S. Army Medical Research and Materiel Command’s Telemedicine and Advanced Technology Research Center. Dr. Razumovsky and two of his coauthors reported financial remuneration from private practice.
'Target: Stroke' improves door-to-needle TPA times
HONOLULU – Applying the American Heart Association’s "Target: Stroke" best practices more than doubled the percentages of patients receiving CT imaging and lifesaving, clot-busting therapy in a study of 2,338 patients.
The percentage of patients who underwent CT imaging within 25 minutes of hospital arrival increased from 12.6% to 27.7% post intervention, while receipt of intravenous tissue plasminogen activator (TPA) within 60 minutes of arrival jumped from 32% to 70.3% (both P less than .001), Dr. Ilana Ruff reported at the International Stroke Conference.
"Target: Stroke best practices are feasible to implement but require a dedicated team effort, including the ED [emergency department], to be most successful," said Dr. Ruff, a vascular neurology fellow at Massachusetts General Hospital in Boston.
The preintervention data are somewhat surprising given that hospitals with high annual volumes of TPA-treated patients have been shown to be associated with lower door-to-needle times, but Dr. Ruff points out that they are not alone. The pivotal University of California, Los Angeles, study that prompted the creation of Target: Stroke in 2010 reported that hospitals had door-to-needle times within 60 minutes in only 29.1% of patients treated with intravenous TPA in 2009, with a range of 0% to 79.2% (Circulation 2011;123:750-8).
The newly updated American Heart Association/American Stroke Association acute ischemic stroke guidelines put a strong emphasis on the 60-minute treatment window for TPA and the need to streamline initial testing to avoid delays in its administration.
The guidelines also feature a new recommendation calling on health care institutions to create a multidisciplinary quality improvement committee to review and monitor stroke care quality benchmarks, evidence-based practices, and outcomes.
Massachusetts General Hospital implemented a new institutional acute stroke care model in 2007 that included 10 best practices, all of which were later included in the Target: Stroke program. Some of those changes included sending stroke patients to the acute area of the ED; using a group paging system to notify the entire stroke team, including radiology technicians, nurses, pharmacy, and the laboratory; sending all labs as "super stat"; storing TPA in an ED drug-dispensing machine or a TPA box; having neuroradiologists in the ED bay; having a pharmacist at the bedside during the entire stroke code to mix TPA for eligible patients; and holding monthly case reviews, Dr. Ruff said.
Structurally, the hospital also shifted sole ownership of stroke patients from the stroke fellow by naming the ED attending the team captain to handle door-to-CT flow and the stroke fellow to facilitate CT-to-TPA administration.
"We realized that the emergency department is best equipped to handle emergency protocols," she said.
The investigators analyzed the median ED door-to-CT and door-to-needle within 60 minutes (DTN60) times in 2,338 patients who arrived within 4.5 hours of an acute ischemic stroke and were enrolled in the hospital’s Get with the Guidelines Stroke registry from 2003 to 2011.
In all, 281 patients received TPA, of which 155 were treated within 60 minutes and 126 beyond 60 minutes.
Patients’ characteristics for those treated with TPA were similar, including average National Institutes of Health Stroke Scale (NIHSS) score (mean 13; range 8-19) and prevalence of hypertension (about 75%) and diabetes mellitus (about 25%). The median age was 72.
Among all patients, the median time from the ED to CT decreased from 71 minutes in the 2003-2006 preintervention period to 59 minutes in the 2008-2011 postintervention period (P less than .001), Dr. Ruff said. Among TPA-treated patients, the median time to CT dropped from 26 minutes to 18 minutes over the same time period (P less than .001).
Median DTN60 times decreased from 70 minutes before intervention to 47 minutes post intervention (P less than .001). Specifically, the median time to TPA was 51.5 minutes in 2007 and reached a low of 40 minutes in 2010 before an uptick to 51 minutes in 2011 (both P less than .001).
It’s unclear why the DTN60 time increased in 2011, although it’s possible, but unlikely, that a new neurology unit further from the ED may have played a role, she said in an interview.
In univariate analysis, patients with a DTN60 did not differ significantly in age, gender, race, comorbidities or NIHSS scores. Only calendar year was associated with achieving DTN60, suggesting that changes at the hospital level, rather than patient-related factors, are driving the improvement, she said at the meeting sponsored by the American Heart Association.
Dr. Ruff and her coauthors reported no disclosures.
HONOLULU – Applying the American Heart Association’s "Target: Stroke" best practices more than doubled the percentages of patients receiving CT imaging and lifesaving, clot-busting therapy in a study of 2,338 patients.
The percentage of patients who underwent CT imaging within 25 minutes of hospital arrival increased from 12.6% to 27.7% post intervention, while receipt of intravenous tissue plasminogen activator (TPA) within 60 minutes of arrival jumped from 32% to 70.3% (both P less than .001), Dr. Ilana Ruff reported at the International Stroke Conference.
"Target: Stroke best practices are feasible to implement but require a dedicated team effort, including the ED [emergency department], to be most successful," said Dr. Ruff, a vascular neurology fellow at Massachusetts General Hospital in Boston.
The preintervention data are somewhat surprising given that hospitals with high annual volumes of TPA-treated patients have been shown to be associated with lower door-to-needle times, but Dr. Ruff points out that they are not alone. The pivotal University of California, Los Angeles, study that prompted the creation of Target: Stroke in 2010 reported that hospitals had door-to-needle times within 60 minutes in only 29.1% of patients treated with intravenous TPA in 2009, with a range of 0% to 79.2% (Circulation 2011;123:750-8).
The newly updated American Heart Association/American Stroke Association acute ischemic stroke guidelines put a strong emphasis on the 60-minute treatment window for TPA and the need to streamline initial testing to avoid delays in its administration.
The guidelines also feature a new recommendation calling on health care institutions to create a multidisciplinary quality improvement committee to review and monitor stroke care quality benchmarks, evidence-based practices, and outcomes.
Massachusetts General Hospital implemented a new institutional acute stroke care model in 2007 that included 10 best practices, all of which were later included in the Target: Stroke program. Some of those changes included sending stroke patients to the acute area of the ED; using a group paging system to notify the entire stroke team, including radiology technicians, nurses, pharmacy, and the laboratory; sending all labs as "super stat"; storing TPA in an ED drug-dispensing machine or a TPA box; having neuroradiologists in the ED bay; having a pharmacist at the bedside during the entire stroke code to mix TPA for eligible patients; and holding monthly case reviews, Dr. Ruff said.
Structurally, the hospital also shifted sole ownership of stroke patients from the stroke fellow by naming the ED attending the team captain to handle door-to-CT flow and the stroke fellow to facilitate CT-to-TPA administration.
"We realized that the emergency department is best equipped to handle emergency protocols," she said.
The investigators analyzed the median ED door-to-CT and door-to-needle within 60 minutes (DTN60) times in 2,338 patients who arrived within 4.5 hours of an acute ischemic stroke and were enrolled in the hospital’s Get with the Guidelines Stroke registry from 2003 to 2011.
In all, 281 patients received TPA, of which 155 were treated within 60 minutes and 126 beyond 60 minutes.
Patients’ characteristics for those treated with TPA were similar, including average National Institutes of Health Stroke Scale (NIHSS) score (mean 13; range 8-19) and prevalence of hypertension (about 75%) and diabetes mellitus (about 25%). The median age was 72.
Among all patients, the median time from the ED to CT decreased from 71 minutes in the 2003-2006 preintervention period to 59 minutes in the 2008-2011 postintervention period (P less than .001), Dr. Ruff said. Among TPA-treated patients, the median time to CT dropped from 26 minutes to 18 minutes over the same time period (P less than .001).
Median DTN60 times decreased from 70 minutes before intervention to 47 minutes post intervention (P less than .001). Specifically, the median time to TPA was 51.5 minutes in 2007 and reached a low of 40 minutes in 2010 before an uptick to 51 minutes in 2011 (both P less than .001).
It’s unclear why the DTN60 time increased in 2011, although it’s possible, but unlikely, that a new neurology unit further from the ED may have played a role, she said in an interview.
In univariate analysis, patients with a DTN60 did not differ significantly in age, gender, race, comorbidities or NIHSS scores. Only calendar year was associated with achieving DTN60, suggesting that changes at the hospital level, rather than patient-related factors, are driving the improvement, she said at the meeting sponsored by the American Heart Association.
Dr. Ruff and her coauthors reported no disclosures.
HONOLULU – Applying the American Heart Association’s "Target: Stroke" best practices more than doubled the percentages of patients receiving CT imaging and lifesaving, clot-busting therapy in a study of 2,338 patients.
The percentage of patients who underwent CT imaging within 25 minutes of hospital arrival increased from 12.6% to 27.7% post intervention, while receipt of intravenous tissue plasminogen activator (TPA) within 60 minutes of arrival jumped from 32% to 70.3% (both P less than .001), Dr. Ilana Ruff reported at the International Stroke Conference.
"Target: Stroke best practices are feasible to implement but require a dedicated team effort, including the ED [emergency department], to be most successful," said Dr. Ruff, a vascular neurology fellow at Massachusetts General Hospital in Boston.
The preintervention data are somewhat surprising given that hospitals with high annual volumes of TPA-treated patients have been shown to be associated with lower door-to-needle times, but Dr. Ruff points out that they are not alone. The pivotal University of California, Los Angeles, study that prompted the creation of Target: Stroke in 2010 reported that hospitals had door-to-needle times within 60 minutes in only 29.1% of patients treated with intravenous TPA in 2009, with a range of 0% to 79.2% (Circulation 2011;123:750-8).
The newly updated American Heart Association/American Stroke Association acute ischemic stroke guidelines put a strong emphasis on the 60-minute treatment window for TPA and the need to streamline initial testing to avoid delays in its administration.
The guidelines also feature a new recommendation calling on health care institutions to create a multidisciplinary quality improvement committee to review and monitor stroke care quality benchmarks, evidence-based practices, and outcomes.
Massachusetts General Hospital implemented a new institutional acute stroke care model in 2007 that included 10 best practices, all of which were later included in the Target: Stroke program. Some of those changes included sending stroke patients to the acute area of the ED; using a group paging system to notify the entire stroke team, including radiology technicians, nurses, pharmacy, and the laboratory; sending all labs as "super stat"; storing TPA in an ED drug-dispensing machine or a TPA box; having neuroradiologists in the ED bay; having a pharmacist at the bedside during the entire stroke code to mix TPA for eligible patients; and holding monthly case reviews, Dr. Ruff said.
Structurally, the hospital also shifted sole ownership of stroke patients from the stroke fellow by naming the ED attending the team captain to handle door-to-CT flow and the stroke fellow to facilitate CT-to-TPA administration.
"We realized that the emergency department is best equipped to handle emergency protocols," she said.
The investigators analyzed the median ED door-to-CT and door-to-needle within 60 minutes (DTN60) times in 2,338 patients who arrived within 4.5 hours of an acute ischemic stroke and were enrolled in the hospital’s Get with the Guidelines Stroke registry from 2003 to 2011.
In all, 281 patients received TPA, of which 155 were treated within 60 minutes and 126 beyond 60 minutes.
Patients’ characteristics for those treated with TPA were similar, including average National Institutes of Health Stroke Scale (NIHSS) score (mean 13; range 8-19) and prevalence of hypertension (about 75%) and diabetes mellitus (about 25%). The median age was 72.
Among all patients, the median time from the ED to CT decreased from 71 minutes in the 2003-2006 preintervention period to 59 minutes in the 2008-2011 postintervention period (P less than .001), Dr. Ruff said. Among TPA-treated patients, the median time to CT dropped from 26 minutes to 18 minutes over the same time period (P less than .001).
Median DTN60 times decreased from 70 minutes before intervention to 47 minutes post intervention (P less than .001). Specifically, the median time to TPA was 51.5 minutes in 2007 and reached a low of 40 minutes in 2010 before an uptick to 51 minutes in 2011 (both P less than .001).
It’s unclear why the DTN60 time increased in 2011, although it’s possible, but unlikely, that a new neurology unit further from the ED may have played a role, she said in an interview.
In univariate analysis, patients with a DTN60 did not differ significantly in age, gender, race, comorbidities or NIHSS scores. Only calendar year was associated with achieving DTN60, suggesting that changes at the hospital level, rather than patient-related factors, are driving the improvement, she said at the meeting sponsored by the American Heart Association.
Dr. Ruff and her coauthors reported no disclosures.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: The percentage of stroke patients receiving a CT scan within 25 minutes of hospital arrival increased from 12.6% to 27.7% postintervention, and receipt of TPA within 60 minutes of arrival increased from 32% to 70.3% (both P less than .001).
Data Source: Single-center, retrospective study of 2,338 patients presenting with acute ischemic stroke from 2003 to 2011.
Disclosures: Dr. Ruff and her coauthors reported no disclosures.
No benefit of endovascular therapy added to TPA for stroke
Functional outcomes in patients treated with intravenous tissue plasminogen activator with or without endovascular therapy after a moderate to severe acute ischemic stroke were not significantly different, and safety outcomes were similar, in a study that was stopped early because of these results.
In the IMS (Interventional Management of Stroke) III study, 40.8% of patients randomized to receive endovascular therapy plus intravenous TPA met the primary endpoint, a measure of functional independence – a modified Rankin score of 2 or less at 90 days – compared with 38.7% among those who had intravenous TPA alone, a difference that was not statistically significant, reported Dr. Joseph Broderick of the University of Cincinnati Neuroscience Institute, and the other IMS III investigators.
Mortality and other safety outcomes were also not significantly different between the two groups of patients in the study, which was stopped early because of futility after 656 of the planned 900 patients had been randomized. The study is being published online on Feb. 7 to coincide with the presentation of the results at the International Stroke Conference (N. Engl. J. Med. 2013 [doi:10.1056/NEJMoa1214300]).
Referring to the lack of randomized clinical trial data, the authors pointed out that it is uncertain whether endovascular therapy (which includes endovascular pharmacologic thrombolysis and, more recently, the use of stent retrievers) alone or combined with intravenous TPA is a more effective treatment of acute stroke than intravenous TPA alone, "the only proven reperfusion therapy for acute ischemic stroke."
In the study, conducted at 58 centers in the United States, Canada, Australia, and Europe, 434 patients were randomized to endovascular therapy plus intravenous TPA and 222 were randomized to standard treatment with intravenous TPA alone (started within 3 hours of stroke onset). The median age of those enrolled was 68-69 years (range, 23-89 years), a little over half were men, about 14% were black or Hispanic, and the median the National Institute of Health Stroke Scale (NIHSS) score was 16-17 (8-19 is a moderately severe stroke and 20 or greater is a severe stroke At the beginning of the study, only one thrombectomy device had been cleared by the Food and Drug Administration and, as the trial continued, other devices were used as they became cleared for use in the different countries.
In addition to the main finding, there were no differences in the primary outcome among those patients with an NIHSS score of 20 or more, and those with a score of 19 or lower, said the authors, who had hypothesized that endovascular therapy would have greater efficacy in patients with more-severe strokes since they "have the highest likelihood of occlusion in a major intracranial artery and the greatest volume of ischemic brain at risk."
They had also hypothesized that receiving endovascular therapy earlier would be associated with a greater benefit, but this was also not a significant factor in outcomes.
Mortality at 90 days was 19.1% in the endovascular therapy group and 21.6% in the intravenous TPA–alone group. Within 30 hours of TPA initiation, 6.2% of those on endovascular therapy and 5.9% of those on TPA alone had a symptomatic intracerebral hemorrhage. The differences in mortality at 7 days and in parenchymal hematoma rates were also not significantly different between the two groups. The rate of asymptomatic intracerebral hemorrhage, however, was significantly higher in the endovascular group.
Outcomes consistently trended better with combined therapy in patients with strokes involving larger artery occlusions and those with the shortest times from stroke onset to initiation of treatment, although because of small patient numbers the differences didn’t achieve statistical significance. These will be the subgroups that ought to be the focus of future clinical trials, Dr. Broderick said in a press briefing at the conference.
The underlying rationale for combined therapy is that intravenous TPA can quickly be started in the emergency department while the endovascular device therapy team is assembling, often at another hospital, which entails time-consuming patient transfer.
Intravenous TPA is the only proven therapy for acute ischemic stroke, but endovascular therapy is more effective at achieving recanalization. The study results bore this out: for example, the rate of partial or complete recanalization at 24 hours for an occlusion in the internal carotid artery was 81% with combined therapy compared to 35% with intravenous TPA alone. Yet this higher recanalization rate bore no clinical benefit, possibly because recanalization occurred too late, after ischemia had turned into infarction, Dr. Broderick explained.
"ISM III is going to be disappointing for a lot of people who are proponents of endovascular therapy. However, there is a light at the end of the tunnel in that there are these subgroups who may benefit," Dr. Brian Silver, who was not involved in the trial, said in an interview.
"The most critical feature is to treat the patients as soon as possible when they arrive in the emergency department, perhaps within 90 minutes. I think that’s the best chance for recovery. We are nowhere near what’s being done in cardiology, where there are door-to-balloon times of an hour. We need to do that in stroke. Since we’re dealing with an organ that’s more sensitive than the heart to ischemia, we probably need to be even faster than what’s being done in cardiology. There is definitely room for improvement in our systems, perhaps by having the endovascular team stay in the hospital. Expense will be the limitation," according to Dr. Silver, director of the stroke center at Brown University, Providence, R.I.
ISM III investigator and interventional neuroradiologist Dr. Thomas A. Tomsick said in an interview that the study results won’t change his own clinical practice.
"ISM III is by no means the final word on combined therapy. In Cincinnati tomorrow, if a patient with a large NIH Stroke Severity score shows up and we’re treating him with IV TPA at 2 hours from stroke onset, we’re not going to do a CT angiogram to evaluate that patient. He’s going to the cath lab for angiography to see if there’s a clot suitable for endovascular therapy," said Dr. Tomsick, professor of radiology at the University of Cincinnati.
Five different endovascular device therapies were utilized in IMS III. As new devices reached clinical practice, their use was allowed by investigators in order to keep the randomized trial clinically relevant. But recruitment for the study was slow because so many clinicians were already convinced by anecdotal experience that combined therapy is better. So the endovascular therapies used most frequently in IMS III aren’t the ones widely used in clinical practice today. Major new randomized trials are now getting underway comparing combined therapy using state-of-the-art, more effective stent clot retriever devices to intravenous TPA alone, he added.
In the New England Journal of Medicine report, the authors noted that "the use of randomization in ongoing and future stroke trials, rather than the treatment of eligible patients with endovascular therapy outside any trial, and minimization of the time to treatment will be essential for assessing the potential benefit of endovascular therapy for acute ischemic stroke."
No matter how future trials of combined therapy turn out, endovascular therapy is not going away, Dr. Broderick observed.
"It’s a very good tool. The reason why is there are patients who can’t get TPA. For example, roughly 5% of patients who undergo coronary artery bypass surgery have a stroke. If you have somebody with a big stroke 2 days after having their chest cracked, you can’t use TPA. In that case, those endovascular devices are the way we can get up in there and get rid of the clot," he explained.
In an editorial accompanying the report in the New England Journal of Medicine (doi:10.1056/NEJMe1215730), Dr. Marc I. Chimowitz declared that the clinical implication of IMS III is that endovascular therapy remains unproven and IV-tPA should continue to be the first-line treatment for patients with acute ischemic stroke within 4.5 hours after stroke onset.
While new clinical trials featuring more effective IV clot busters, such as tenecteplase, and next-generation endovascular devices are urgently needed in an effort to improve stroke outcomes, patient recruitment is likely to continue to be a challenge in the current environment. This could be overcome if Medicare were to place a moratorium on reimbursement for endovascular therapy of acute ischemic stroke except as part of a randomized trial, according to Dr. Chimowitz, professor of neurology at the Medical University of South Carolina, Charleston.
The study was supported with grants from NIH and the National Institute of Neurological Disorders and Stroke; and by Genentech (which supplied the TPA); and EKOS, Concentric Medical, and Cordis Neurovascular (which supplied catheters); and Actilyse (alteplase) manufacturer Boehringer Ingelheim (which, along with Genentech and EKOS, provided support for investigator meetings). Dr. Broderick disclosed consulting fees from PhotoThera. Of the 28 other authors, disclosures for 14 were listed and included having received consulting fees, grant support, and/or lecture fees from a variety of device and pharmaceutical companies that include Genentech. Dr. Chimowitz, Dr. Silver, and Dr. Tomsick reported having no financial conflicts.
* This story was updated February 8, 2013.
Functional outcomes in patients treated with intravenous tissue plasminogen activator with or without endovascular therapy after a moderate to severe acute ischemic stroke were not significantly different, and safety outcomes were similar, in a study that was stopped early because of these results.
In the IMS (Interventional Management of Stroke) III study, 40.8% of patients randomized to receive endovascular therapy plus intravenous TPA met the primary endpoint, a measure of functional independence – a modified Rankin score of 2 or less at 90 days – compared with 38.7% among those who had intravenous TPA alone, a difference that was not statistically significant, reported Dr. Joseph Broderick of the University of Cincinnati Neuroscience Institute, and the other IMS III investigators.
Mortality and other safety outcomes were also not significantly different between the two groups of patients in the study, which was stopped early because of futility after 656 of the planned 900 patients had been randomized. The study is being published online on Feb. 7 to coincide with the presentation of the results at the International Stroke Conference (N. Engl. J. Med. 2013 [doi:10.1056/NEJMoa1214300]).
Referring to the lack of randomized clinical trial data, the authors pointed out that it is uncertain whether endovascular therapy (which includes endovascular pharmacologic thrombolysis and, more recently, the use of stent retrievers) alone or combined with intravenous TPA is a more effective treatment of acute stroke than intravenous TPA alone, "the only proven reperfusion therapy for acute ischemic stroke."
In the study, conducted at 58 centers in the United States, Canada, Australia, and Europe, 434 patients were randomized to endovascular therapy plus intravenous TPA and 222 were randomized to standard treatment with intravenous TPA alone (started within 3 hours of stroke onset). The median age of those enrolled was 68-69 years (range, 23-89 years), a little over half were men, about 14% were black or Hispanic, and the median the National Institute of Health Stroke Scale (NIHSS) score was 16-17 (8-19 is a moderately severe stroke and 20 or greater is a severe stroke At the beginning of the study, only one thrombectomy device had been cleared by the Food and Drug Administration and, as the trial continued, other devices were used as they became cleared for use in the different countries.
In addition to the main finding, there were no differences in the primary outcome among those patients with an NIHSS score of 20 or more, and those with a score of 19 or lower, said the authors, who had hypothesized that endovascular therapy would have greater efficacy in patients with more-severe strokes since they "have the highest likelihood of occlusion in a major intracranial artery and the greatest volume of ischemic brain at risk."
They had also hypothesized that receiving endovascular therapy earlier would be associated with a greater benefit, but this was also not a significant factor in outcomes.
Mortality at 90 days was 19.1% in the endovascular therapy group and 21.6% in the intravenous TPA–alone group. Within 30 hours of TPA initiation, 6.2% of those on endovascular therapy and 5.9% of those on TPA alone had a symptomatic intracerebral hemorrhage. The differences in mortality at 7 days and in parenchymal hematoma rates were also not significantly different between the two groups. The rate of asymptomatic intracerebral hemorrhage, however, was significantly higher in the endovascular group.
Outcomes consistently trended better with combined therapy in patients with strokes involving larger artery occlusions and those with the shortest times from stroke onset to initiation of treatment, although because of small patient numbers the differences didn’t achieve statistical significance. These will be the subgroups that ought to be the focus of future clinical trials, Dr. Broderick said in a press briefing at the conference.
The underlying rationale for combined therapy is that intravenous TPA can quickly be started in the emergency department while the endovascular device therapy team is assembling, often at another hospital, which entails time-consuming patient transfer.
Intravenous TPA is the only proven therapy for acute ischemic stroke, but endovascular therapy is more effective at achieving recanalization. The study results bore this out: for example, the rate of partial or complete recanalization at 24 hours for an occlusion in the internal carotid artery was 81% with combined therapy compared to 35% with intravenous TPA alone. Yet this higher recanalization rate bore no clinical benefit, possibly because recanalization occurred too late, after ischemia had turned into infarction, Dr. Broderick explained.
"ISM III is going to be disappointing for a lot of people who are proponents of endovascular therapy. However, there is a light at the end of the tunnel in that there are these subgroups who may benefit," Dr. Brian Silver, who was not involved in the trial, said in an interview.
"The most critical feature is to treat the patients as soon as possible when they arrive in the emergency department, perhaps within 90 minutes. I think that’s the best chance for recovery. We are nowhere near what’s being done in cardiology, where there are door-to-balloon times of an hour. We need to do that in stroke. Since we’re dealing with an organ that’s more sensitive than the heart to ischemia, we probably need to be even faster than what’s being done in cardiology. There is definitely room for improvement in our systems, perhaps by having the endovascular team stay in the hospital. Expense will be the limitation," according to Dr. Silver, director of the stroke center at Brown University, Providence, R.I.
ISM III investigator and interventional neuroradiologist Dr. Thomas A. Tomsick said in an interview that the study results won’t change his own clinical practice.
"ISM III is by no means the final word on combined therapy. In Cincinnati tomorrow, if a patient with a large NIH Stroke Severity score shows up and we’re treating him with IV TPA at 2 hours from stroke onset, we’re not going to do a CT angiogram to evaluate that patient. He’s going to the cath lab for angiography to see if there’s a clot suitable for endovascular therapy," said Dr. Tomsick, professor of radiology at the University of Cincinnati.
Five different endovascular device therapies were utilized in IMS III. As new devices reached clinical practice, their use was allowed by investigators in order to keep the randomized trial clinically relevant. But recruitment for the study was slow because so many clinicians were already convinced by anecdotal experience that combined therapy is better. So the endovascular therapies used most frequently in IMS III aren’t the ones widely used in clinical practice today. Major new randomized trials are now getting underway comparing combined therapy using state-of-the-art, more effective stent clot retriever devices to intravenous TPA alone, he added.
In the New England Journal of Medicine report, the authors noted that "the use of randomization in ongoing and future stroke trials, rather than the treatment of eligible patients with endovascular therapy outside any trial, and minimization of the time to treatment will be essential for assessing the potential benefit of endovascular therapy for acute ischemic stroke."
No matter how future trials of combined therapy turn out, endovascular therapy is not going away, Dr. Broderick observed.
"It’s a very good tool. The reason why is there are patients who can’t get TPA. For example, roughly 5% of patients who undergo coronary artery bypass surgery have a stroke. If you have somebody with a big stroke 2 days after having their chest cracked, you can’t use TPA. In that case, those endovascular devices are the way we can get up in there and get rid of the clot," he explained.
In an editorial accompanying the report in the New England Journal of Medicine (doi:10.1056/NEJMe1215730), Dr. Marc I. Chimowitz declared that the clinical implication of IMS III is that endovascular therapy remains unproven and IV-tPA should continue to be the first-line treatment for patients with acute ischemic stroke within 4.5 hours after stroke onset.
While new clinical trials featuring more effective IV clot busters, such as tenecteplase, and next-generation endovascular devices are urgently needed in an effort to improve stroke outcomes, patient recruitment is likely to continue to be a challenge in the current environment. This could be overcome if Medicare were to place a moratorium on reimbursement for endovascular therapy of acute ischemic stroke except as part of a randomized trial, according to Dr. Chimowitz, professor of neurology at the Medical University of South Carolina, Charleston.
The study was supported with grants from NIH and the National Institute of Neurological Disorders and Stroke; and by Genentech (which supplied the TPA); and EKOS, Concentric Medical, and Cordis Neurovascular (which supplied catheters); and Actilyse (alteplase) manufacturer Boehringer Ingelheim (which, along with Genentech and EKOS, provided support for investigator meetings). Dr. Broderick disclosed consulting fees from PhotoThera. Of the 28 other authors, disclosures for 14 were listed and included having received consulting fees, grant support, and/or lecture fees from a variety of device and pharmaceutical companies that include Genentech. Dr. Chimowitz, Dr. Silver, and Dr. Tomsick reported having no financial conflicts.
* This story was updated February 8, 2013.
Functional outcomes in patients treated with intravenous tissue plasminogen activator with or without endovascular therapy after a moderate to severe acute ischemic stroke were not significantly different, and safety outcomes were similar, in a study that was stopped early because of these results.
In the IMS (Interventional Management of Stroke) III study, 40.8% of patients randomized to receive endovascular therapy plus intravenous TPA met the primary endpoint, a measure of functional independence – a modified Rankin score of 2 or less at 90 days – compared with 38.7% among those who had intravenous TPA alone, a difference that was not statistically significant, reported Dr. Joseph Broderick of the University of Cincinnati Neuroscience Institute, and the other IMS III investigators.
Mortality and other safety outcomes were also not significantly different between the two groups of patients in the study, which was stopped early because of futility after 656 of the planned 900 patients had been randomized. The study is being published online on Feb. 7 to coincide with the presentation of the results at the International Stroke Conference (N. Engl. J. Med. 2013 [doi:10.1056/NEJMoa1214300]).
Referring to the lack of randomized clinical trial data, the authors pointed out that it is uncertain whether endovascular therapy (which includes endovascular pharmacologic thrombolysis and, more recently, the use of stent retrievers) alone or combined with intravenous TPA is a more effective treatment of acute stroke than intravenous TPA alone, "the only proven reperfusion therapy for acute ischemic stroke."
In the study, conducted at 58 centers in the United States, Canada, Australia, and Europe, 434 patients were randomized to endovascular therapy plus intravenous TPA and 222 were randomized to standard treatment with intravenous TPA alone (started within 3 hours of stroke onset). The median age of those enrolled was 68-69 years (range, 23-89 years), a little over half were men, about 14% were black or Hispanic, and the median the National Institute of Health Stroke Scale (NIHSS) score was 16-17 (8-19 is a moderately severe stroke and 20 or greater is a severe stroke At the beginning of the study, only one thrombectomy device had been cleared by the Food and Drug Administration and, as the trial continued, other devices were used as they became cleared for use in the different countries.
In addition to the main finding, there were no differences in the primary outcome among those patients with an NIHSS score of 20 or more, and those with a score of 19 or lower, said the authors, who had hypothesized that endovascular therapy would have greater efficacy in patients with more-severe strokes since they "have the highest likelihood of occlusion in a major intracranial artery and the greatest volume of ischemic brain at risk."
They had also hypothesized that receiving endovascular therapy earlier would be associated with a greater benefit, but this was also not a significant factor in outcomes.
Mortality at 90 days was 19.1% in the endovascular therapy group and 21.6% in the intravenous TPA–alone group. Within 30 hours of TPA initiation, 6.2% of those on endovascular therapy and 5.9% of those on TPA alone had a symptomatic intracerebral hemorrhage. The differences in mortality at 7 days and in parenchymal hematoma rates were also not significantly different between the two groups. The rate of asymptomatic intracerebral hemorrhage, however, was significantly higher in the endovascular group.
Outcomes consistently trended better with combined therapy in patients with strokes involving larger artery occlusions and those with the shortest times from stroke onset to initiation of treatment, although because of small patient numbers the differences didn’t achieve statistical significance. These will be the subgroups that ought to be the focus of future clinical trials, Dr. Broderick said in a press briefing at the conference.
The underlying rationale for combined therapy is that intravenous TPA can quickly be started in the emergency department while the endovascular device therapy team is assembling, often at another hospital, which entails time-consuming patient transfer.
Intravenous TPA is the only proven therapy for acute ischemic stroke, but endovascular therapy is more effective at achieving recanalization. The study results bore this out: for example, the rate of partial or complete recanalization at 24 hours for an occlusion in the internal carotid artery was 81% with combined therapy compared to 35% with intravenous TPA alone. Yet this higher recanalization rate bore no clinical benefit, possibly because recanalization occurred too late, after ischemia had turned into infarction, Dr. Broderick explained.
"ISM III is going to be disappointing for a lot of people who are proponents of endovascular therapy. However, there is a light at the end of the tunnel in that there are these subgroups who may benefit," Dr. Brian Silver, who was not involved in the trial, said in an interview.
"The most critical feature is to treat the patients as soon as possible when they arrive in the emergency department, perhaps within 90 minutes. I think that’s the best chance for recovery. We are nowhere near what’s being done in cardiology, where there are door-to-balloon times of an hour. We need to do that in stroke. Since we’re dealing with an organ that’s more sensitive than the heart to ischemia, we probably need to be even faster than what’s being done in cardiology. There is definitely room for improvement in our systems, perhaps by having the endovascular team stay in the hospital. Expense will be the limitation," according to Dr. Silver, director of the stroke center at Brown University, Providence, R.I.
ISM III investigator and interventional neuroradiologist Dr. Thomas A. Tomsick said in an interview that the study results won’t change his own clinical practice.
"ISM III is by no means the final word on combined therapy. In Cincinnati tomorrow, if a patient with a large NIH Stroke Severity score shows up and we’re treating him with IV TPA at 2 hours from stroke onset, we’re not going to do a CT angiogram to evaluate that patient. He’s going to the cath lab for angiography to see if there’s a clot suitable for endovascular therapy," said Dr. Tomsick, professor of radiology at the University of Cincinnati.
Five different endovascular device therapies were utilized in IMS III. As new devices reached clinical practice, their use was allowed by investigators in order to keep the randomized trial clinically relevant. But recruitment for the study was slow because so many clinicians were already convinced by anecdotal experience that combined therapy is better. So the endovascular therapies used most frequently in IMS III aren’t the ones widely used in clinical practice today. Major new randomized trials are now getting underway comparing combined therapy using state-of-the-art, more effective stent clot retriever devices to intravenous TPA alone, he added.
In the New England Journal of Medicine report, the authors noted that "the use of randomization in ongoing and future stroke trials, rather than the treatment of eligible patients with endovascular therapy outside any trial, and minimization of the time to treatment will be essential for assessing the potential benefit of endovascular therapy for acute ischemic stroke."
No matter how future trials of combined therapy turn out, endovascular therapy is not going away, Dr. Broderick observed.
"It’s a very good tool. The reason why is there are patients who can’t get TPA. For example, roughly 5% of patients who undergo coronary artery bypass surgery have a stroke. If you have somebody with a big stroke 2 days after having their chest cracked, you can’t use TPA. In that case, those endovascular devices are the way we can get up in there and get rid of the clot," he explained.
In an editorial accompanying the report in the New England Journal of Medicine (doi:10.1056/NEJMe1215730), Dr. Marc I. Chimowitz declared that the clinical implication of IMS III is that endovascular therapy remains unproven and IV-tPA should continue to be the first-line treatment for patients with acute ischemic stroke within 4.5 hours after stroke onset.
While new clinical trials featuring more effective IV clot busters, such as tenecteplase, and next-generation endovascular devices are urgently needed in an effort to improve stroke outcomes, patient recruitment is likely to continue to be a challenge in the current environment. This could be overcome if Medicare were to place a moratorium on reimbursement for endovascular therapy of acute ischemic stroke except as part of a randomized trial, according to Dr. Chimowitz, professor of neurology at the Medical University of South Carolina, Charleston.
The study was supported with grants from NIH and the National Institute of Neurological Disorders and Stroke; and by Genentech (which supplied the TPA); and EKOS, Concentric Medical, and Cordis Neurovascular (which supplied catheters); and Actilyse (alteplase) manufacturer Boehringer Ingelheim (which, along with Genentech and EKOS, provided support for investigator meetings). Dr. Broderick disclosed consulting fees from PhotoThera. Of the 28 other authors, disclosures for 14 were listed and included having received consulting fees, grant support, and/or lecture fees from a variety of device and pharmaceutical companies that include Genentech. Dr. Chimowitz, Dr. Silver, and Dr. Tomsick reported having no financial conflicts.
* This story was updated February 8, 2013.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Endovascular therapy plus intravenous TPA showed no added outcome benefits, compared with TPA alone, with 40.8% and 38.7% of patients, respectively, reaching functional independence at 90 days.
Data Source: An international, phase III study of 656 patients with an acute moderate to severe ischemic stroke randomized 2:1 to IV TPA with endovascular therapy or IV TPA alone.
Disclosures: The study was supported with grants from NIH and the National Institute of Neurological Disorders and Stroke, and by Genentech (supplier of TPA), and EKOS, Concentric Medical, and Cordis Neurovascular (which supplied catheters). Dr. Broderick's disclosed consulting fees from PhotoThera. Of the 28 other authors, disclosures for 14 were listed and included having received consulting fees, grant support, and/or lecture fees from a variety of device and pharmaceutical companies that included Genentech.