User login
American Heart Association (AHA): International Stroke Conference
Stroke: The brave new world of prevention and treatment
HONOLULU– What if you could scan your patients for stroke-susceptibility loci or implant a device in their brains to repair stroke-damaged pathways?
Those novel approaches may sound far-fetched, but such forward-thinking concepts are achievable, according to some of the best minds in the field of stroke medicine, who put forth these and other proposals at a special session at the International Stroke Conference. To spice things up even more, session organizers limited presentations to just 5 minutes and relied on the audience in some cases to keep on schedule and enthusiastically applaud the speakers off the stage. Here are just a few of the fascinating insights offered during the session, entitled "The Next Big Thing in Stroke."
Restorative therapies
Just 2 decades after scientists demonstrated the plasticity of the brain after stroke, the restorative processes that occur after the acute phase of stroke continue to be teased out, opening up potential targets for new drugs. At the same time, neurotechnology is maturing.
"We’re very quickly entering a brave new world of neuroengineering in the brain after stroke," said Randolph J. Nudo, Ph.D., director of the Landon Center on Aging at the University of Kansas Medical Center, Kansas City.
In the emerging field of robotics, a neural interface system implanted in two humans with long-standing tetraplegia recorded neural signals from the brain as input commands to control a robotic arm (Nature 2012;485:372-5).
A miniaturized closed-loop system implanted in the cerebral cortex of brain-injured rats has been shown to improve recovery. Dr. Nudo sees the potential of these advances for neurotransmitter sensing, open-and closed-loop drug delivery, and control of stem cell integration.
Dr. Joel Stein, chair of rehabilitative and regeneration medicine at Columbia University, New York, said robotics are being used to deliver rehabilitation therapy. Exoskeletal work stations (Hocoma) incorporate engaging games or virtual reality experiences to provide a large number of repetitions for the patient without therapist fatigue. Wearable "bionic legs" (Tibion) provide external force to supplement muscle strength and improve motor skills through practice.
Not all robotics have panned out, however. In a study of veterans, robot-assisted therapy provided only modest effects on poststroke upper-limb impairment (N. Engl. J. Med. 2010;362:1772-83). The robotic therapy also was somewhat more expensive than intensive human therapy ($9,977 vs. $8,269).
Robotics are not necessarily always going to be better; but when they are equally as good as traditional approaches, they provide us with new efficiencies in terms of delivery, said Dr. Stein. "The bottom line is that robots are coming, we should prepare for them and expect them to become a key piece of clinical practice in this field in the future."
Genetics
It’s still the early days in the search for genetic susceptibility loci for stroke, but we’re getting closer, said Dr. Ralph Sacco, professor and chair of neurology at Miller School of Medicine at the University of Miami.
The collaborative METASTROKE study offered some findings. The big push now, as the cost of these studies comes down, is moving from common variants to rare variants using next-generation sequencing and even whole-genome studies.
Large family studies that use next-generation sequencing such as the National Institute of Health–supported Life After Linkage study, should also help in smaller more homogenous groups.
"We really have to refine our phenotypes using extreme phenotypes, subgroups, and subclinical traits and make sure we get the phenotype right, so all this next-generation sequencing will make sense," Dr. Sacco said.
The ability to identify rare variants may open up unknown novel pathways that could serve as targets for drug therapy. Someday, clinicians could use genetic testing to identify "at-risk" patients for ultra-early stroke prevention therapies. Pharmacogenomic profiles will be used to personalize stroke prevention treatments.
A global preemptive strike
Several speakers looked to a prevention model to reverse the exploding global burden of stroke.
Dr. Valery Feigin, director of the National Institute for Stroke and Applied Neurosciences in Auckland, New Zealand, said that priority should be given to a population-based approach that includes legislative measures aimed at environmental risk factors such as reducing salt intake – something recently introduced in some European countries.
"A very small shift in the distribution of risk factors across the population will result in a major drop in stroke incidence," he said, noting, for example, that smoking cessation alone can reduce stroke risk by 12%-19%.
The suggestion elicited a flurry of comments during the discussion period including concerns about creating a "nanny state" and a reminder of the political price that New York City Mayor Michael Bloomberg paid for trying to reduce the size of soft drinks. Still others suggested that such measures need to be positively reinforced and that there is a civil obligation to act given the massive costs of poor public health.
Dr. Lewis Morgenstern, an epidemiologist and director of the stroke program at the University of Michigan, Ann Arbor, observed that even in the West where stroke incidence and mortality are declining, "Stoke is becoming more and more a disease of the poor and underserved."
He called on clinicians to address these disparities through global research agendas and advocacy, but also to reach out locally to poor and underserved populations with stroke prevention and preparedness messages. As for what they should emphasize, he highlighted a recent estimate that the cost of an endovascular procedure is at least $10,000, whereas a 1-month supply of the blood pressuring–lowering diuretic hydrochlorothiazide 25 mg costs $4.
Neuroprotection
After more than a decade developing a class of drugs called postsynaptic density-95 (PSD-95) protein inhibitors, the ENACT trial recently provided a positive signal that neuroprotection is achievable, said study coauthor Dr. Michael Tymianski, a neurosurgeon at the University of Toronto.
Like reperfusion therapies, however, neuroprotectants are emergency drugs that need to be administered in a prehospital setting. Only two trials, ENACT and the ongoing FAST-MAG, have recruited stroke patients in less than 4 hours. Thus, any new clinical trial design that waits 3-4 hours before administering neuroprotective agents is unlikely to detect the small effect size of delayed neuroprotection, he noted.
That said, we now have an effective drug and a feasible trial design. Planning is underway for a study that, if successful, may provide the necessary signal needed to determine whether neuroprotection is practical, Dr. Tymianski said.
‘Garbage in, garbage out’
Dr. Steven Warach, executive director of the Seton/University of Texas Southwestern Clinical Research Institute in Austin, made a plea for scientific rigor in future clinical trials to avoid the "garbage in, garbage out" type of research that just adds noise to the field.
Over the next 10 years, clinical trial enrollment and assessment will move away from the individual investigator. Instead, a "handful of on-call central adjudicators" will decide which patients get into trials based on both clinical and biologic case definitions and will assess outcomes.
"It’s all about three things. Whatever advances we talk about in clinical science, it’s about reducing bias, reducing variance, and increasing the power of the trials," he said.
The conference was sponsored by the American Heart Association.
Dr. Nudo reported research support from the National Institutes of Health and the Department of Defense and disclosed ties with Microtransponder. Dr. Stein disclosed research funding from Tibion, Tyromotion, and Myomo, and ties to Myomo. Dr. Sacco, Dr. Feigin, Dr. Morgenstern, Dr. Tymianski, and Dr. Warach reported having no disclosures.
HONOLULU– What if you could scan your patients for stroke-susceptibility loci or implant a device in their brains to repair stroke-damaged pathways?
Those novel approaches may sound far-fetched, but such forward-thinking concepts are achievable, according to some of the best minds in the field of stroke medicine, who put forth these and other proposals at a special session at the International Stroke Conference. To spice things up even more, session organizers limited presentations to just 5 minutes and relied on the audience in some cases to keep on schedule and enthusiastically applaud the speakers off the stage. Here are just a few of the fascinating insights offered during the session, entitled "The Next Big Thing in Stroke."
Restorative therapies
Just 2 decades after scientists demonstrated the plasticity of the brain after stroke, the restorative processes that occur after the acute phase of stroke continue to be teased out, opening up potential targets for new drugs. At the same time, neurotechnology is maturing.
"We’re very quickly entering a brave new world of neuroengineering in the brain after stroke," said Randolph J. Nudo, Ph.D., director of the Landon Center on Aging at the University of Kansas Medical Center, Kansas City.
In the emerging field of robotics, a neural interface system implanted in two humans with long-standing tetraplegia recorded neural signals from the brain as input commands to control a robotic arm (Nature 2012;485:372-5).
A miniaturized closed-loop system implanted in the cerebral cortex of brain-injured rats has been shown to improve recovery. Dr. Nudo sees the potential of these advances for neurotransmitter sensing, open-and closed-loop drug delivery, and control of stem cell integration.
Dr. Joel Stein, chair of rehabilitative and regeneration medicine at Columbia University, New York, said robotics are being used to deliver rehabilitation therapy. Exoskeletal work stations (Hocoma) incorporate engaging games or virtual reality experiences to provide a large number of repetitions for the patient without therapist fatigue. Wearable "bionic legs" (Tibion) provide external force to supplement muscle strength and improve motor skills through practice.
Not all robotics have panned out, however. In a study of veterans, robot-assisted therapy provided only modest effects on poststroke upper-limb impairment (N. Engl. J. Med. 2010;362:1772-83). The robotic therapy also was somewhat more expensive than intensive human therapy ($9,977 vs. $8,269).
Robotics are not necessarily always going to be better; but when they are equally as good as traditional approaches, they provide us with new efficiencies in terms of delivery, said Dr. Stein. "The bottom line is that robots are coming, we should prepare for them and expect them to become a key piece of clinical practice in this field in the future."
Genetics
It’s still the early days in the search for genetic susceptibility loci for stroke, but we’re getting closer, said Dr. Ralph Sacco, professor and chair of neurology at Miller School of Medicine at the University of Miami.
The collaborative METASTROKE study offered some findings. The big push now, as the cost of these studies comes down, is moving from common variants to rare variants using next-generation sequencing and even whole-genome studies.
Large family studies that use next-generation sequencing such as the National Institute of Health–supported Life After Linkage study, should also help in smaller more homogenous groups.
"We really have to refine our phenotypes using extreme phenotypes, subgroups, and subclinical traits and make sure we get the phenotype right, so all this next-generation sequencing will make sense," Dr. Sacco said.
The ability to identify rare variants may open up unknown novel pathways that could serve as targets for drug therapy. Someday, clinicians could use genetic testing to identify "at-risk" patients for ultra-early stroke prevention therapies. Pharmacogenomic profiles will be used to personalize stroke prevention treatments.
A global preemptive strike
Several speakers looked to a prevention model to reverse the exploding global burden of stroke.
Dr. Valery Feigin, director of the National Institute for Stroke and Applied Neurosciences in Auckland, New Zealand, said that priority should be given to a population-based approach that includes legislative measures aimed at environmental risk factors such as reducing salt intake – something recently introduced in some European countries.
"A very small shift in the distribution of risk factors across the population will result in a major drop in stroke incidence," he said, noting, for example, that smoking cessation alone can reduce stroke risk by 12%-19%.
The suggestion elicited a flurry of comments during the discussion period including concerns about creating a "nanny state" and a reminder of the political price that New York City Mayor Michael Bloomberg paid for trying to reduce the size of soft drinks. Still others suggested that such measures need to be positively reinforced and that there is a civil obligation to act given the massive costs of poor public health.
Dr. Lewis Morgenstern, an epidemiologist and director of the stroke program at the University of Michigan, Ann Arbor, observed that even in the West where stroke incidence and mortality are declining, "Stoke is becoming more and more a disease of the poor and underserved."
He called on clinicians to address these disparities through global research agendas and advocacy, but also to reach out locally to poor and underserved populations with stroke prevention and preparedness messages. As for what they should emphasize, he highlighted a recent estimate that the cost of an endovascular procedure is at least $10,000, whereas a 1-month supply of the blood pressuring–lowering diuretic hydrochlorothiazide 25 mg costs $4.
Neuroprotection
After more than a decade developing a class of drugs called postsynaptic density-95 (PSD-95) protein inhibitors, the ENACT trial recently provided a positive signal that neuroprotection is achievable, said study coauthor Dr. Michael Tymianski, a neurosurgeon at the University of Toronto.
Like reperfusion therapies, however, neuroprotectants are emergency drugs that need to be administered in a prehospital setting. Only two trials, ENACT and the ongoing FAST-MAG, have recruited stroke patients in less than 4 hours. Thus, any new clinical trial design that waits 3-4 hours before administering neuroprotective agents is unlikely to detect the small effect size of delayed neuroprotection, he noted.
That said, we now have an effective drug and a feasible trial design. Planning is underway for a study that, if successful, may provide the necessary signal needed to determine whether neuroprotection is practical, Dr. Tymianski said.
‘Garbage in, garbage out’
Dr. Steven Warach, executive director of the Seton/University of Texas Southwestern Clinical Research Institute in Austin, made a plea for scientific rigor in future clinical trials to avoid the "garbage in, garbage out" type of research that just adds noise to the field.
Over the next 10 years, clinical trial enrollment and assessment will move away from the individual investigator. Instead, a "handful of on-call central adjudicators" will decide which patients get into trials based on both clinical and biologic case definitions and will assess outcomes.
"It’s all about three things. Whatever advances we talk about in clinical science, it’s about reducing bias, reducing variance, and increasing the power of the trials," he said.
The conference was sponsored by the American Heart Association.
Dr. Nudo reported research support from the National Institutes of Health and the Department of Defense and disclosed ties with Microtransponder. Dr. Stein disclosed research funding from Tibion, Tyromotion, and Myomo, and ties to Myomo. Dr. Sacco, Dr. Feigin, Dr. Morgenstern, Dr. Tymianski, and Dr. Warach reported having no disclosures.
HONOLULU– What if you could scan your patients for stroke-susceptibility loci or implant a device in their brains to repair stroke-damaged pathways?
Those novel approaches may sound far-fetched, but such forward-thinking concepts are achievable, according to some of the best minds in the field of stroke medicine, who put forth these and other proposals at a special session at the International Stroke Conference. To spice things up even more, session organizers limited presentations to just 5 minutes and relied on the audience in some cases to keep on schedule and enthusiastically applaud the speakers off the stage. Here are just a few of the fascinating insights offered during the session, entitled "The Next Big Thing in Stroke."
Restorative therapies
Just 2 decades after scientists demonstrated the plasticity of the brain after stroke, the restorative processes that occur after the acute phase of stroke continue to be teased out, opening up potential targets for new drugs. At the same time, neurotechnology is maturing.
"We’re very quickly entering a brave new world of neuroengineering in the brain after stroke," said Randolph J. Nudo, Ph.D., director of the Landon Center on Aging at the University of Kansas Medical Center, Kansas City.
In the emerging field of robotics, a neural interface system implanted in two humans with long-standing tetraplegia recorded neural signals from the brain as input commands to control a robotic arm (Nature 2012;485:372-5).
A miniaturized closed-loop system implanted in the cerebral cortex of brain-injured rats has been shown to improve recovery. Dr. Nudo sees the potential of these advances for neurotransmitter sensing, open-and closed-loop drug delivery, and control of stem cell integration.
Dr. Joel Stein, chair of rehabilitative and regeneration medicine at Columbia University, New York, said robotics are being used to deliver rehabilitation therapy. Exoskeletal work stations (Hocoma) incorporate engaging games or virtual reality experiences to provide a large number of repetitions for the patient without therapist fatigue. Wearable "bionic legs" (Tibion) provide external force to supplement muscle strength and improve motor skills through practice.
Not all robotics have panned out, however. In a study of veterans, robot-assisted therapy provided only modest effects on poststroke upper-limb impairment (N. Engl. J. Med. 2010;362:1772-83). The robotic therapy also was somewhat more expensive than intensive human therapy ($9,977 vs. $8,269).
Robotics are not necessarily always going to be better; but when they are equally as good as traditional approaches, they provide us with new efficiencies in terms of delivery, said Dr. Stein. "The bottom line is that robots are coming, we should prepare for them and expect them to become a key piece of clinical practice in this field in the future."
Genetics
It’s still the early days in the search for genetic susceptibility loci for stroke, but we’re getting closer, said Dr. Ralph Sacco, professor and chair of neurology at Miller School of Medicine at the University of Miami.
The collaborative METASTROKE study offered some findings. The big push now, as the cost of these studies comes down, is moving from common variants to rare variants using next-generation sequencing and even whole-genome studies.
Large family studies that use next-generation sequencing such as the National Institute of Health–supported Life After Linkage study, should also help in smaller more homogenous groups.
"We really have to refine our phenotypes using extreme phenotypes, subgroups, and subclinical traits and make sure we get the phenotype right, so all this next-generation sequencing will make sense," Dr. Sacco said.
The ability to identify rare variants may open up unknown novel pathways that could serve as targets for drug therapy. Someday, clinicians could use genetic testing to identify "at-risk" patients for ultra-early stroke prevention therapies. Pharmacogenomic profiles will be used to personalize stroke prevention treatments.
A global preemptive strike
Several speakers looked to a prevention model to reverse the exploding global burden of stroke.
Dr. Valery Feigin, director of the National Institute for Stroke and Applied Neurosciences in Auckland, New Zealand, said that priority should be given to a population-based approach that includes legislative measures aimed at environmental risk factors such as reducing salt intake – something recently introduced in some European countries.
"A very small shift in the distribution of risk factors across the population will result in a major drop in stroke incidence," he said, noting, for example, that smoking cessation alone can reduce stroke risk by 12%-19%.
The suggestion elicited a flurry of comments during the discussion period including concerns about creating a "nanny state" and a reminder of the political price that New York City Mayor Michael Bloomberg paid for trying to reduce the size of soft drinks. Still others suggested that such measures need to be positively reinforced and that there is a civil obligation to act given the massive costs of poor public health.
Dr. Lewis Morgenstern, an epidemiologist and director of the stroke program at the University of Michigan, Ann Arbor, observed that even in the West where stroke incidence and mortality are declining, "Stoke is becoming more and more a disease of the poor and underserved."
He called on clinicians to address these disparities through global research agendas and advocacy, but also to reach out locally to poor and underserved populations with stroke prevention and preparedness messages. As for what they should emphasize, he highlighted a recent estimate that the cost of an endovascular procedure is at least $10,000, whereas a 1-month supply of the blood pressuring–lowering diuretic hydrochlorothiazide 25 mg costs $4.
Neuroprotection
After more than a decade developing a class of drugs called postsynaptic density-95 (PSD-95) protein inhibitors, the ENACT trial recently provided a positive signal that neuroprotection is achievable, said study coauthor Dr. Michael Tymianski, a neurosurgeon at the University of Toronto.
Like reperfusion therapies, however, neuroprotectants are emergency drugs that need to be administered in a prehospital setting. Only two trials, ENACT and the ongoing FAST-MAG, have recruited stroke patients in less than 4 hours. Thus, any new clinical trial design that waits 3-4 hours before administering neuroprotective agents is unlikely to detect the small effect size of delayed neuroprotection, he noted.
That said, we now have an effective drug and a feasible trial design. Planning is underway for a study that, if successful, may provide the necessary signal needed to determine whether neuroprotection is practical, Dr. Tymianski said.
‘Garbage in, garbage out’
Dr. Steven Warach, executive director of the Seton/University of Texas Southwestern Clinical Research Institute in Austin, made a plea for scientific rigor in future clinical trials to avoid the "garbage in, garbage out" type of research that just adds noise to the field.
Over the next 10 years, clinical trial enrollment and assessment will move away from the individual investigator. Instead, a "handful of on-call central adjudicators" will decide which patients get into trials based on both clinical and biologic case definitions and will assess outcomes.
"It’s all about three things. Whatever advances we talk about in clinical science, it’s about reducing bias, reducing variance, and increasing the power of the trials," he said.
The conference was sponsored by the American Heart Association.
Dr. Nudo reported research support from the National Institutes of Health and the Department of Defense and disclosed ties with Microtransponder. Dr. Stein disclosed research funding from Tibion, Tyromotion, and Myomo, and ties to Myomo. Dr. Sacco, Dr. Feigin, Dr. Morgenstern, Dr. Tymianski, and Dr. Warach reported having no disclosures.
EXPERT ANALYSIS FROM THE INTERNATIONAL STROKE CONFERENCE
Six questions flag risk for cardiovascular hospitalization
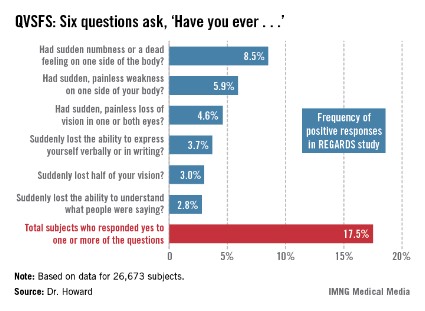
HONOLULU – The answers to six questions can identify 18% of the stroke-free general population as having a greater than 40% chance of hospitalization or an emergency department visit for cardiovascular disease within the next 5 years, according to a large national study.
New evidence from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study indicates that the predictive power of the six questions compares to that of traditional cardiovascular risk factors, Virginia J. Howard, Ph.D., said at the International Stroke Conference sponsored by the American Heart Association.

These six questions – called the Questionnaire for Verifying Stroke-Free Status, or QVSFS – can easily be asked by office staff during a routine patient evaluation. Although the questions relate to strokelike symptoms, they also were predictive of other cardiovascular events.
REGARDS is a prospective, population-based, longitudinal study of 30,239 African Americans and whites over age 45. The national study oversampled African Americans, who made up 40% of the study population.
Dr. Howard’s analysis was restricted to the 26,673 subjects, mean age 64 years, with no baseline history of stroke or transient ischemic attack (TIA). Of these participants, 49% characterized their general health as excellent or very good, and another 35% described it as good. Yet 57% of subjects had hypertension, 32% were dyslipidemic, and 21% had diabetes.
During a mean 5.6 years of follow-up, 30% of subjects were hospitalized or had an emergency department visit for heart disease, stroke (9%), or TIA.
Fully 17.5% of subjects answered one or more of the questions affirmatively at baseline (see chart). Their rate of hospitalization or an ED visit for cardiovascular disease during the follow-up period was nearly twice that of patients who answered ‘no’ to all six questions.
In a multivariate analysis fully adjusted for demographics, socioeconomic status, conventional cardiovascular risk factors, and self-reported general health, subjects with any positive answer on the QVSFS at baseline had a 62% greater incidence of hospitalization or an ED visit for cardiovascular disease and a 47% greater incidence of hospitalization or a trip to the ED for stroke than did those who answered ‘no’ to all six questions, reported Dr. Howard of the University of Alabama, Birmingham.
A positive response to a single QVSFS question was provided by 10.5% of subjects. Another 4.6% gave affirmative answers to two questions, 1.4% did so for three, and 0.9% gave four or more positive answers.
In the fully adjusted multivariate analysis, each additional positive response was associated with an additional 29% increase in the risk of a cardiovascular hospitalization or ED visit and a 22% increase in the risk of a hospitalization or ED visit for stroke.
Looking at traditional cardiovascular risk factors, subjects with hypertension had a 12% greater risk of cardiovascular hospitalization or an ED visit and a 17% greater risk of stroke hospitalization or an ED visit. Diabetes conveyed a 29% greater risk of cardiovascular hospitalization or an ED visit and a 43% increase in stroke risk.
The REGARDS study is funded by the National Institute of Neurological Disorders and Stroke. Dr. Howard reported having no financial conflicts.
HONOLULU – The answers to six questions can identify 18% of the stroke-free general population as having a greater than 40% chance of hospitalization or an emergency department visit for cardiovascular disease within the next 5 years, according to a large national study.
New evidence from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study indicates that the predictive power of the six questions compares to that of traditional cardiovascular risk factors, Virginia J. Howard, Ph.D., said at the International Stroke Conference sponsored by the American Heart Association.

These six questions – called the Questionnaire for Verifying Stroke-Free Status, or QVSFS – can easily be asked by office staff during a routine patient evaluation. Although the questions relate to strokelike symptoms, they also were predictive of other cardiovascular events.
REGARDS is a prospective, population-based, longitudinal study of 30,239 African Americans and whites over age 45. The national study oversampled African Americans, who made up 40% of the study population.
Dr. Howard’s analysis was restricted to the 26,673 subjects, mean age 64 years, with no baseline history of stroke or transient ischemic attack (TIA). Of these participants, 49% characterized their general health as excellent or very good, and another 35% described it as good. Yet 57% of subjects had hypertension, 32% were dyslipidemic, and 21% had diabetes.
During a mean 5.6 years of follow-up, 30% of subjects were hospitalized or had an emergency department visit for heart disease, stroke (9%), or TIA.
Fully 17.5% of subjects answered one or more of the questions affirmatively at baseline (see chart). Their rate of hospitalization or an ED visit for cardiovascular disease during the follow-up period was nearly twice that of patients who answered ‘no’ to all six questions.
In a multivariate analysis fully adjusted for demographics, socioeconomic status, conventional cardiovascular risk factors, and self-reported general health, subjects with any positive answer on the QVSFS at baseline had a 62% greater incidence of hospitalization or an ED visit for cardiovascular disease and a 47% greater incidence of hospitalization or a trip to the ED for stroke than did those who answered ‘no’ to all six questions, reported Dr. Howard of the University of Alabama, Birmingham.
A positive response to a single QVSFS question was provided by 10.5% of subjects. Another 4.6% gave affirmative answers to two questions, 1.4% did so for three, and 0.9% gave four or more positive answers.
In the fully adjusted multivariate analysis, each additional positive response was associated with an additional 29% increase in the risk of a cardiovascular hospitalization or ED visit and a 22% increase in the risk of a hospitalization or ED visit for stroke.
Looking at traditional cardiovascular risk factors, subjects with hypertension had a 12% greater risk of cardiovascular hospitalization or an ED visit and a 17% greater risk of stroke hospitalization or an ED visit. Diabetes conveyed a 29% greater risk of cardiovascular hospitalization or an ED visit and a 43% increase in stroke risk.
The REGARDS study is funded by the National Institute of Neurological Disorders and Stroke. Dr. Howard reported having no financial conflicts.
HONOLULU – The answers to six questions can identify 18% of the stroke-free general population as having a greater than 40% chance of hospitalization or an emergency department visit for cardiovascular disease within the next 5 years, according to a large national study.
New evidence from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study indicates that the predictive power of the six questions compares to that of traditional cardiovascular risk factors, Virginia J. Howard, Ph.D., said at the International Stroke Conference sponsored by the American Heart Association.

These six questions – called the Questionnaire for Verifying Stroke-Free Status, or QVSFS – can easily be asked by office staff during a routine patient evaluation. Although the questions relate to strokelike symptoms, they also were predictive of other cardiovascular events.
REGARDS is a prospective, population-based, longitudinal study of 30,239 African Americans and whites over age 45. The national study oversampled African Americans, who made up 40% of the study population.
Dr. Howard’s analysis was restricted to the 26,673 subjects, mean age 64 years, with no baseline history of stroke or transient ischemic attack (TIA). Of these participants, 49% characterized their general health as excellent or very good, and another 35% described it as good. Yet 57% of subjects had hypertension, 32% were dyslipidemic, and 21% had diabetes.
During a mean 5.6 years of follow-up, 30% of subjects were hospitalized or had an emergency department visit for heart disease, stroke (9%), or TIA.
Fully 17.5% of subjects answered one or more of the questions affirmatively at baseline (see chart). Their rate of hospitalization or an ED visit for cardiovascular disease during the follow-up period was nearly twice that of patients who answered ‘no’ to all six questions.
In a multivariate analysis fully adjusted for demographics, socioeconomic status, conventional cardiovascular risk factors, and self-reported general health, subjects with any positive answer on the QVSFS at baseline had a 62% greater incidence of hospitalization or an ED visit for cardiovascular disease and a 47% greater incidence of hospitalization or a trip to the ED for stroke than did those who answered ‘no’ to all six questions, reported Dr. Howard of the University of Alabama, Birmingham.
A positive response to a single QVSFS question was provided by 10.5% of subjects. Another 4.6% gave affirmative answers to two questions, 1.4% did so for three, and 0.9% gave four or more positive answers.
In the fully adjusted multivariate analysis, each additional positive response was associated with an additional 29% increase in the risk of a cardiovascular hospitalization or ED visit and a 22% increase in the risk of a hospitalization or ED visit for stroke.
Looking at traditional cardiovascular risk factors, subjects with hypertension had a 12% greater risk of cardiovascular hospitalization or an ED visit and a 17% greater risk of stroke hospitalization or an ED visit. Diabetes conveyed a 29% greater risk of cardiovascular hospitalization or an ED visit and a 43% increase in stroke risk.
The REGARDS study is funded by the National Institute of Neurological Disorders and Stroke. Dr. Howard reported having no financial conflicts.
AT THE INTERNATIONAL STROKE CONFERENCE
Major finding: Any positive answer on the QVSFS at baseline was associated with a 62% greater incidence of hospitalization or an ED visit for cardiovascular disease.
Data source: REGARDS, a national, prospective, population-based, longitudinal study of more than 32,000 African-American and white adults.
Disclosures: The REGARDS study is sponsored by the National Institute of Neurological Disorders and Stroke. The presenter reported having no conflicts of interest.
GI-friendly aspirin combo aces phase III trials
HONOLULU – A novel proprietary combination of aspirin and immediate-release omeprazole in a coordinated-delivery tablet resulted in markedly fewer gastroduodenal ulcers and treatment discontinuations than conventional enteric-coated aspirin in patients on antiplatelet therapy for secondary prevention of cerebrovascular events.
Two double-blind, 6-month, randomized phase III clinical trials totaling 1,049 patients with an indication for daily aspirin for secondary cardiovascular or cerebrovascular prevention included 215 subjects with prior ischemic stroke or transient ischemic attack (TIA). All participants in the phase III trials were at risk for upper GI ulcers by virtue of being at least 55 years of age or having a documented history of gastric or duodenal ulcer within 5 years prior to enrollment. Baseline endoscopy was negative in all subjects.
Study participants were randomized to conventional enteric-coated aspirin at 325 mg/day or to the investigational tablet, known for now as PA32540. This once-daily tablet contains 40 mg of immediate-release omeprazole layered around 325 mg of pH-sensitive aspirin, Dr. Mark J. Alberts explained at the International Stroke Conference sponsored by the American Heart Association.
He focused on the 215 study participants on aspirin for secondary cerebrovascular prevention. The primary study endpoint – the incidence of endoscopically confirmed gastroduodenal ulcers – occurred in 2.0% of patients on PA32540, compared with 12.4% of controls on enteric-coated aspirin.
Moreover, discontinuation of therapy due to dyspepsia, erosive gastritis, or other prespecified upper GI events occurred in 8% of controls and in none of the participants on the combo tablet, reported Dr. Alberts, professor of neurology at Northwestern University, Chicago, and director of the stroke program at Northwestern Memorial Hospital.
The major adverse cardiovascular event rate over the course of 6 months was 2.9% in the PA32540 group and 4.4% with enteric-coated aspirin, a nonsignificant difference.
These study findings support the hypothesis that a single tablet formulation of aspirin and GI-protective omeprazole may safely improve long-term compliance with aspirin therapy in patients at increased risk for upper GI toxicity, Dr. Alberts observed.
Pozen, which sponsored the phase III trials, has announced it will seek regulatory approval of the coordinated-delivery product with an indication for use in secondary cardiovascular and cerebrovascular prevention in the roughly 15% of patients at risk for aspirin-induced upper GI adverse events. The company is currently seeking strategic partners to help market the novel product on a wide scale at an affordable price after PA32540 receives regulatory approval.
Dr. Alberts reported serving as a consultant to Pozen.
HONOLULU – A novel proprietary combination of aspirin and immediate-release omeprazole in a coordinated-delivery tablet resulted in markedly fewer gastroduodenal ulcers and treatment discontinuations than conventional enteric-coated aspirin in patients on antiplatelet therapy for secondary prevention of cerebrovascular events.
Two double-blind, 6-month, randomized phase III clinical trials totaling 1,049 patients with an indication for daily aspirin for secondary cardiovascular or cerebrovascular prevention included 215 subjects with prior ischemic stroke or transient ischemic attack (TIA). All participants in the phase III trials were at risk for upper GI ulcers by virtue of being at least 55 years of age or having a documented history of gastric or duodenal ulcer within 5 years prior to enrollment. Baseline endoscopy was negative in all subjects.
Study participants were randomized to conventional enteric-coated aspirin at 325 mg/day or to the investigational tablet, known for now as PA32540. This once-daily tablet contains 40 mg of immediate-release omeprazole layered around 325 mg of pH-sensitive aspirin, Dr. Mark J. Alberts explained at the International Stroke Conference sponsored by the American Heart Association.
He focused on the 215 study participants on aspirin for secondary cerebrovascular prevention. The primary study endpoint – the incidence of endoscopically confirmed gastroduodenal ulcers – occurred in 2.0% of patients on PA32540, compared with 12.4% of controls on enteric-coated aspirin.
Moreover, discontinuation of therapy due to dyspepsia, erosive gastritis, or other prespecified upper GI events occurred in 8% of controls and in none of the participants on the combo tablet, reported Dr. Alberts, professor of neurology at Northwestern University, Chicago, and director of the stroke program at Northwestern Memorial Hospital.
The major adverse cardiovascular event rate over the course of 6 months was 2.9% in the PA32540 group and 4.4% with enteric-coated aspirin, a nonsignificant difference.
These study findings support the hypothesis that a single tablet formulation of aspirin and GI-protective omeprazole may safely improve long-term compliance with aspirin therapy in patients at increased risk for upper GI toxicity, Dr. Alberts observed.
Pozen, which sponsored the phase III trials, has announced it will seek regulatory approval of the coordinated-delivery product with an indication for use in secondary cardiovascular and cerebrovascular prevention in the roughly 15% of patients at risk for aspirin-induced upper GI adverse events. The company is currently seeking strategic partners to help market the novel product on a wide scale at an affordable price after PA32540 receives regulatory approval.
Dr. Alberts reported serving as a consultant to Pozen.
HONOLULU – A novel proprietary combination of aspirin and immediate-release omeprazole in a coordinated-delivery tablet resulted in markedly fewer gastroduodenal ulcers and treatment discontinuations than conventional enteric-coated aspirin in patients on antiplatelet therapy for secondary prevention of cerebrovascular events.
Two double-blind, 6-month, randomized phase III clinical trials totaling 1,049 patients with an indication for daily aspirin for secondary cardiovascular or cerebrovascular prevention included 215 subjects with prior ischemic stroke or transient ischemic attack (TIA). All participants in the phase III trials were at risk for upper GI ulcers by virtue of being at least 55 years of age or having a documented history of gastric or duodenal ulcer within 5 years prior to enrollment. Baseline endoscopy was negative in all subjects.
Study participants were randomized to conventional enteric-coated aspirin at 325 mg/day or to the investigational tablet, known for now as PA32540. This once-daily tablet contains 40 mg of immediate-release omeprazole layered around 325 mg of pH-sensitive aspirin, Dr. Mark J. Alberts explained at the International Stroke Conference sponsored by the American Heart Association.
He focused on the 215 study participants on aspirin for secondary cerebrovascular prevention. The primary study endpoint – the incidence of endoscopically confirmed gastroduodenal ulcers – occurred in 2.0% of patients on PA32540, compared with 12.4% of controls on enteric-coated aspirin.
Moreover, discontinuation of therapy due to dyspepsia, erosive gastritis, or other prespecified upper GI events occurred in 8% of controls and in none of the participants on the combo tablet, reported Dr. Alberts, professor of neurology at Northwestern University, Chicago, and director of the stroke program at Northwestern Memorial Hospital.
The major adverse cardiovascular event rate over the course of 6 months was 2.9% in the PA32540 group and 4.4% with enteric-coated aspirin, a nonsignificant difference.
These study findings support the hypothesis that a single tablet formulation of aspirin and GI-protective omeprazole may safely improve long-term compliance with aspirin therapy in patients at increased risk for upper GI toxicity, Dr. Alberts observed.
Pozen, which sponsored the phase III trials, has announced it will seek regulatory approval of the coordinated-delivery product with an indication for use in secondary cardiovascular and cerebrovascular prevention in the roughly 15% of patients at risk for aspirin-induced upper GI adverse events. The company is currently seeking strategic partners to help market the novel product on a wide scale at an affordable price after PA32540 receives regulatory approval.
Dr. Alberts reported serving as a consultant to Pozen.
AT THE INTERNATIONAL STROKE CONFERENCE
How to tell TIA/stroke from mimics
HONOLULU – The key to differentiating transient ischemic attacks and strokes from their main mimics – including partial seizures and complicated migraine – lies in the clinical history, Dr. Susan L. Hickenbottom said at the International Stroke Conference sponsored by the American Heart Association.
"The idea is that there are specific clinical presentations that go along with stroke and TIA. Almost always the vascular pathways are respected, as opposed to random patterns of symptoms that don’t really respect a vascular pathway," explained Dr. Hickenbottom, a neurologist who is director of the stroke program at St. Mercy Saline (Mich.) Hospital and a consortium of other community hospitals.
The timing of symptom onset provides important information. TIA/stroke symptoms typically start suddenly within seconds to minutes and don’t progress further. In contrast, the symptoms of complicated migraine or partial seizures often evolve in what neurologists call ‘the Jacksonian march,’ starting in one part of the body and then gradually spreading.
"The symptoms might start in, say, the hand, then over several minutes move up the arm and then to the face. Whereas typically with TIA or stroke, ‘boom,’ the patient has symptoms," she continued.
Complicated migraine is migraine with focal neurologic symptoms: weakness, tingling, or numbness on one side of the body or the other that can precede, accompany, or follow the actual headache. Complicated migraine is often accompanied by classic migraine symptoms, including nausea, photophobia, and visual aura phenomena such as scintillating scotoma or kaleidoscope vision.
It’s rare for a patient’s first-ever migraine episode to involve complicated migraine. Thus, a patient who presents with what looks like complicated migraine but no history of migraine is much more likely to have TIA/stroke.
Partial seizures can be divided into two types: complex partial seizures, which by definition are associated with an altered level or loss of consciousness; and simple partial seizures, which are not.
A patient experiencing a complex partial seizure will often stare off into space. Strange odors, ictal fear, the sensation of déjà vu or jamais vu, and automatic behaviors such as lip smacking or repetitive hand movements are common.
Notably, these symptoms are positive phenomena. In contrast, patients with TIA/stroke usually experience predominantly negative phenomena: loss of vision rather than seeing bursts of flashing lights, loss of speech, loss of motor function, and/or loss of sensation.
Dr. Hickenbottom said neurologists have changed their thinking about the distinction between TIA and stroke. It used to be that TIA was defined based upon duration: if symptoms in a vascular distribution pattern lasted less than 1 hour, it was a TIA. No longer. With the widespread availability of effective tissue plasminogen activator therapy for acute ischemic stroke, and the recognition that "time is brain" when it comes to reperfusion, stroke specialists are loath to stand around clocking symptom duration.
"The trend now is to move away from an arbitrary time cutoff and define TIA physiologically as an episode of neurologic dysfunction caused by focal brain, spinal cord, or retinal ischemia without evidence of acute infarction on imaging studies. And stroke is an episode with such evidence," she explained.
For primary care physicians, cardiologists, and emergency physicians to quickly distinguish TIA/stroke from its mimics, it’s important to learn to think like a neurologist, according to Dr. Hickenbottom. The first issue neurologists consider, she said, is whether the symptoms are focal or diffuse. The second is the temporal onset. And then neurologists want to see if the symptoms follow a characteristic vascular pathway informative of which brain artery is likely involved.
In the anterior circulation, vascular syndromes involving the internal carotid artery are characterized by the ipsilateral monocular temporary vision loss known as amaurosis fugax, which may or may not be accompanied by contralateral weakness or sensory changes.
Occlusion of the anterior cerebral artery brings contralateral weakness, possibly personality changes such as disinhibition or lack of motivation, and sensory changes, with the leg being more often affected than the face or arm.
Middle cerebral artery vascular syndromes entail contralateral weakness and sensory changes, with the face and arm more commonly involved than the leg. In some but not all cases, this is accompanied by a contralateral visual deficit. If the injury is in the dominant hemisphere it can result in aphasia: difficulty in speaking or understanding language. If the nondominant hemisphere is affected, people may experience visual/spatial difficulties on the opposite side of the body, even to the extent that they’re no longer aware of the existence of that side of the body.
In the posterior circulation, vascular syndromes involving the vertebrobasilar artery may manifest as ipsilateral cranial nerve deficits and ataxia involving the face along with contralateral or bilateral sensory changes or weakness on the body. The classic ‘5Ds’ of vertebrobasilar artery involvement, Dr. Hickenbottom observed, are diplopia, dysarthria, disequilibrium, drowsiness, and death. Vascular syndromes involving the posterior cerebral artery characteristically involve a contralateral visual field deficit.
While partial seizures and complicated migraine are the most common and important TIA/stroke mimics, on occasion panic attacks, conversion disorder, vertigo, and syncope can also be confused with TIA.
Panic attacks occasionally involve focal neurologic symptoms, but more typically the symptoms are vague and random. "It’s ‘I got numb and tingly all over,’ rather than ‘I got numb and tingly on one-half of my body,’ " the neurologist said.
Affected patients generally have a history of panic disorder or an anxiety disorder, and symptoms suggestive of a neurologic condition are accompanied by other panic symptoms, including shortness of breath, dizziness, palpitation, abdominal pain, or fear of dying.
Patients with conversion disorder–related symptoms that appear to be neurologic most often have a history of psychiatric disease of some other kind. On careful examination their seemingly neurologic symptoms don’t adhere to a physiologic pattern. Look for inconsistencies on examination: nonphysiologic sensory loss or weakness, or absence of tremor when the patient is distracted by a task. The distinctions can be subtle; a neurologic consultation can be very helpful when conversion disorder is suspected, according to Dr. Hickenbottom.
Isolated vertigo with no other accompanying neurologic symptoms is seldom vascular in nature.
"The brain stem is so small that to have a vascular episode that just affects the vestibular nuclei without getting double vision, or slurred speech, or a droopy face, or something else is pretty unlikely," she said.
Syncope is a diffuse/acute process rather than the focal/acute process which defines TIA/stroke. Neurologists get lots of consultations for patients with syncope, but the fact is syncope rarely has a neurologic cause. However, that possibility is heightened when a patient experiences more than a few minutes of confusion after waking up from a syncopal episode. Patients typically return to their normal mental status almost as soon as they wake up. Prolonged confusion raises the possibility of a seizure disorder with post-ictal confusion, according to Dr. Hickenbottom.
She reported having no financial conflicts.
HONOLULU – The key to differentiating transient ischemic attacks and strokes from their main mimics – including partial seizures and complicated migraine – lies in the clinical history, Dr. Susan L. Hickenbottom said at the International Stroke Conference sponsored by the American Heart Association.
"The idea is that there are specific clinical presentations that go along with stroke and TIA. Almost always the vascular pathways are respected, as opposed to random patterns of symptoms that don’t really respect a vascular pathway," explained Dr. Hickenbottom, a neurologist who is director of the stroke program at St. Mercy Saline (Mich.) Hospital and a consortium of other community hospitals.
The timing of symptom onset provides important information. TIA/stroke symptoms typically start suddenly within seconds to minutes and don’t progress further. In contrast, the symptoms of complicated migraine or partial seizures often evolve in what neurologists call ‘the Jacksonian march,’ starting in one part of the body and then gradually spreading.
"The symptoms might start in, say, the hand, then over several minutes move up the arm and then to the face. Whereas typically with TIA or stroke, ‘boom,’ the patient has symptoms," she continued.
Complicated migraine is migraine with focal neurologic symptoms: weakness, tingling, or numbness on one side of the body or the other that can precede, accompany, or follow the actual headache. Complicated migraine is often accompanied by classic migraine symptoms, including nausea, photophobia, and visual aura phenomena such as scintillating scotoma or kaleidoscope vision.
It’s rare for a patient’s first-ever migraine episode to involve complicated migraine. Thus, a patient who presents with what looks like complicated migraine but no history of migraine is much more likely to have TIA/stroke.
Partial seizures can be divided into two types: complex partial seizures, which by definition are associated with an altered level or loss of consciousness; and simple partial seizures, which are not.
A patient experiencing a complex partial seizure will often stare off into space. Strange odors, ictal fear, the sensation of déjà vu or jamais vu, and automatic behaviors such as lip smacking or repetitive hand movements are common.
Notably, these symptoms are positive phenomena. In contrast, patients with TIA/stroke usually experience predominantly negative phenomena: loss of vision rather than seeing bursts of flashing lights, loss of speech, loss of motor function, and/or loss of sensation.
Dr. Hickenbottom said neurologists have changed their thinking about the distinction between TIA and stroke. It used to be that TIA was defined based upon duration: if symptoms in a vascular distribution pattern lasted less than 1 hour, it was a TIA. No longer. With the widespread availability of effective tissue plasminogen activator therapy for acute ischemic stroke, and the recognition that "time is brain" when it comes to reperfusion, stroke specialists are loath to stand around clocking symptom duration.
"The trend now is to move away from an arbitrary time cutoff and define TIA physiologically as an episode of neurologic dysfunction caused by focal brain, spinal cord, or retinal ischemia without evidence of acute infarction on imaging studies. And stroke is an episode with such evidence," she explained.
For primary care physicians, cardiologists, and emergency physicians to quickly distinguish TIA/stroke from its mimics, it’s important to learn to think like a neurologist, according to Dr. Hickenbottom. The first issue neurologists consider, she said, is whether the symptoms are focal or diffuse. The second is the temporal onset. And then neurologists want to see if the symptoms follow a characteristic vascular pathway informative of which brain artery is likely involved.
In the anterior circulation, vascular syndromes involving the internal carotid artery are characterized by the ipsilateral monocular temporary vision loss known as amaurosis fugax, which may or may not be accompanied by contralateral weakness or sensory changes.
Occlusion of the anterior cerebral artery brings contralateral weakness, possibly personality changes such as disinhibition or lack of motivation, and sensory changes, with the leg being more often affected than the face or arm.
Middle cerebral artery vascular syndromes entail contralateral weakness and sensory changes, with the face and arm more commonly involved than the leg. In some but not all cases, this is accompanied by a contralateral visual deficit. If the injury is in the dominant hemisphere it can result in aphasia: difficulty in speaking or understanding language. If the nondominant hemisphere is affected, people may experience visual/spatial difficulties on the opposite side of the body, even to the extent that they’re no longer aware of the existence of that side of the body.
In the posterior circulation, vascular syndromes involving the vertebrobasilar artery may manifest as ipsilateral cranial nerve deficits and ataxia involving the face along with contralateral or bilateral sensory changes or weakness on the body. The classic ‘5Ds’ of vertebrobasilar artery involvement, Dr. Hickenbottom observed, are diplopia, dysarthria, disequilibrium, drowsiness, and death. Vascular syndromes involving the posterior cerebral artery characteristically involve a contralateral visual field deficit.
While partial seizures and complicated migraine are the most common and important TIA/stroke mimics, on occasion panic attacks, conversion disorder, vertigo, and syncope can also be confused with TIA.
Panic attacks occasionally involve focal neurologic symptoms, but more typically the symptoms are vague and random. "It’s ‘I got numb and tingly all over,’ rather than ‘I got numb and tingly on one-half of my body,’ " the neurologist said.
Affected patients generally have a history of panic disorder or an anxiety disorder, and symptoms suggestive of a neurologic condition are accompanied by other panic symptoms, including shortness of breath, dizziness, palpitation, abdominal pain, or fear of dying.
Patients with conversion disorder–related symptoms that appear to be neurologic most often have a history of psychiatric disease of some other kind. On careful examination their seemingly neurologic symptoms don’t adhere to a physiologic pattern. Look for inconsistencies on examination: nonphysiologic sensory loss or weakness, or absence of tremor when the patient is distracted by a task. The distinctions can be subtle; a neurologic consultation can be very helpful when conversion disorder is suspected, according to Dr. Hickenbottom.
Isolated vertigo with no other accompanying neurologic symptoms is seldom vascular in nature.
"The brain stem is so small that to have a vascular episode that just affects the vestibular nuclei without getting double vision, or slurred speech, or a droopy face, or something else is pretty unlikely," she said.
Syncope is a diffuse/acute process rather than the focal/acute process which defines TIA/stroke. Neurologists get lots of consultations for patients with syncope, but the fact is syncope rarely has a neurologic cause. However, that possibility is heightened when a patient experiences more than a few minutes of confusion after waking up from a syncopal episode. Patients typically return to their normal mental status almost as soon as they wake up. Prolonged confusion raises the possibility of a seizure disorder with post-ictal confusion, according to Dr. Hickenbottom.
She reported having no financial conflicts.
HONOLULU – The key to differentiating transient ischemic attacks and strokes from their main mimics – including partial seizures and complicated migraine – lies in the clinical history, Dr. Susan L. Hickenbottom said at the International Stroke Conference sponsored by the American Heart Association.
"The idea is that there are specific clinical presentations that go along with stroke and TIA. Almost always the vascular pathways are respected, as opposed to random patterns of symptoms that don’t really respect a vascular pathway," explained Dr. Hickenbottom, a neurologist who is director of the stroke program at St. Mercy Saline (Mich.) Hospital and a consortium of other community hospitals.
The timing of symptom onset provides important information. TIA/stroke symptoms typically start suddenly within seconds to minutes and don’t progress further. In contrast, the symptoms of complicated migraine or partial seizures often evolve in what neurologists call ‘the Jacksonian march,’ starting in one part of the body and then gradually spreading.
"The symptoms might start in, say, the hand, then over several minutes move up the arm and then to the face. Whereas typically with TIA or stroke, ‘boom,’ the patient has symptoms," she continued.
Complicated migraine is migraine with focal neurologic symptoms: weakness, tingling, or numbness on one side of the body or the other that can precede, accompany, or follow the actual headache. Complicated migraine is often accompanied by classic migraine symptoms, including nausea, photophobia, and visual aura phenomena such as scintillating scotoma or kaleidoscope vision.
It’s rare for a patient’s first-ever migraine episode to involve complicated migraine. Thus, a patient who presents with what looks like complicated migraine but no history of migraine is much more likely to have TIA/stroke.
Partial seizures can be divided into two types: complex partial seizures, which by definition are associated with an altered level or loss of consciousness; and simple partial seizures, which are not.
A patient experiencing a complex partial seizure will often stare off into space. Strange odors, ictal fear, the sensation of déjà vu or jamais vu, and automatic behaviors such as lip smacking or repetitive hand movements are common.
Notably, these symptoms are positive phenomena. In contrast, patients with TIA/stroke usually experience predominantly negative phenomena: loss of vision rather than seeing bursts of flashing lights, loss of speech, loss of motor function, and/or loss of sensation.
Dr. Hickenbottom said neurologists have changed their thinking about the distinction between TIA and stroke. It used to be that TIA was defined based upon duration: if symptoms in a vascular distribution pattern lasted less than 1 hour, it was a TIA. No longer. With the widespread availability of effective tissue plasminogen activator therapy for acute ischemic stroke, and the recognition that "time is brain" when it comes to reperfusion, stroke specialists are loath to stand around clocking symptom duration.
"The trend now is to move away from an arbitrary time cutoff and define TIA physiologically as an episode of neurologic dysfunction caused by focal brain, spinal cord, or retinal ischemia without evidence of acute infarction on imaging studies. And stroke is an episode with such evidence," she explained.
For primary care physicians, cardiologists, and emergency physicians to quickly distinguish TIA/stroke from its mimics, it’s important to learn to think like a neurologist, according to Dr. Hickenbottom. The first issue neurologists consider, she said, is whether the symptoms are focal or diffuse. The second is the temporal onset. And then neurologists want to see if the symptoms follow a characteristic vascular pathway informative of which brain artery is likely involved.
In the anterior circulation, vascular syndromes involving the internal carotid artery are characterized by the ipsilateral monocular temporary vision loss known as amaurosis fugax, which may or may not be accompanied by contralateral weakness or sensory changes.
Occlusion of the anterior cerebral artery brings contralateral weakness, possibly personality changes such as disinhibition or lack of motivation, and sensory changes, with the leg being more often affected than the face or arm.
Middle cerebral artery vascular syndromes entail contralateral weakness and sensory changes, with the face and arm more commonly involved than the leg. In some but not all cases, this is accompanied by a contralateral visual deficit. If the injury is in the dominant hemisphere it can result in aphasia: difficulty in speaking or understanding language. If the nondominant hemisphere is affected, people may experience visual/spatial difficulties on the opposite side of the body, even to the extent that they’re no longer aware of the existence of that side of the body.
In the posterior circulation, vascular syndromes involving the vertebrobasilar artery may manifest as ipsilateral cranial nerve deficits and ataxia involving the face along with contralateral or bilateral sensory changes or weakness on the body. The classic ‘5Ds’ of vertebrobasilar artery involvement, Dr. Hickenbottom observed, are diplopia, dysarthria, disequilibrium, drowsiness, and death. Vascular syndromes involving the posterior cerebral artery characteristically involve a contralateral visual field deficit.
While partial seizures and complicated migraine are the most common and important TIA/stroke mimics, on occasion panic attacks, conversion disorder, vertigo, and syncope can also be confused with TIA.
Panic attacks occasionally involve focal neurologic symptoms, but more typically the symptoms are vague and random. "It’s ‘I got numb and tingly all over,’ rather than ‘I got numb and tingly on one-half of my body,’ " the neurologist said.
Affected patients generally have a history of panic disorder or an anxiety disorder, and symptoms suggestive of a neurologic condition are accompanied by other panic symptoms, including shortness of breath, dizziness, palpitation, abdominal pain, or fear of dying.
Patients with conversion disorder–related symptoms that appear to be neurologic most often have a history of psychiatric disease of some other kind. On careful examination their seemingly neurologic symptoms don’t adhere to a physiologic pattern. Look for inconsistencies on examination: nonphysiologic sensory loss or weakness, or absence of tremor when the patient is distracted by a task. The distinctions can be subtle; a neurologic consultation can be very helpful when conversion disorder is suspected, according to Dr. Hickenbottom.
Isolated vertigo with no other accompanying neurologic symptoms is seldom vascular in nature.
"The brain stem is so small that to have a vascular episode that just affects the vestibular nuclei without getting double vision, or slurred speech, or a droopy face, or something else is pretty unlikely," she said.
Syncope is a diffuse/acute process rather than the focal/acute process which defines TIA/stroke. Neurologists get lots of consultations for patients with syncope, but the fact is syncope rarely has a neurologic cause. However, that possibility is heightened when a patient experiences more than a few minutes of confusion after waking up from a syncopal episode. Patients typically return to their normal mental status almost as soon as they wake up. Prolonged confusion raises the possibility of a seizure disorder with post-ictal confusion, according to Dr. Hickenbottom.
She reported having no financial conflicts.
EXPERT ANALYSIS FROM THE INTERNATIONAL STROKE CONFERENCE
Strokes pop up post aortic valve surgery
HONOLULU – Almost one-fifth of patients who underwent aortic valve surgery experienced a stroke in a prospective, cohort study of 196 patients.
"Stroke is a very prevalent complication of aortic valve replacement, and it’s much more common than prior series have suggested," Dr. Steven Messé said at the International Stroke Conference.
Based on the literature, the risk of periprocedural stroke varies widely from a low of less than 1% to 9% for cardiac valve replacement and 10% for heart transplant and left ventricular assist device placement, he said. If the number of times these procedures are performed each year is added to the equation, cardiac procedures account for about 5% of strokes annually in the United States.
"Unfortunately, the reality is probably worse than the literature," Dr. Messé said.
He observed that most risk estimates come from trials and case series rather than clinical practice, and that the vast majority of these studies did not include systematic evaluation by neurologists, who tend to be more sensitive to subtle yet meaningful deficits. Recent evidence also suggests that ischemic neurologic complications following surgery are increasing, "possibly related to the willingness of surgeons to undertake procedures with higher-risk patients," said Dr. Messé, a neurologist at the Hospital of the University of Pennsylvania, Philadelphia. To access their own stroke rates, neurologic, cognitive, and quality-of-life assessments were performed 1 week prior to surgery and at a 3- to 4-week and 9- to 12-month follow-up in 196 patients, aged at least 65 years, undergoing open surgical aortic valve replacement for moderate to severe aortic stenosis at two hospitals within the University of Pennsylvania Health System. Neurologic assessments were also performed on postoperative days 1, 3 and 7, and magnetic resonance imaging on day 5, plus or minus 2 days. Cerebrovascular end points in the study, led by colleague and radiologist Dr. Thomas Floyd, were independently adjudicated by two vascular neurologists.
Over the 4-year study period, 196 patients underwent aortic valve replacement, of which 36% were female and 6% nonwhite. Their average age was 76 years.
Ten (5%) died in hospital and 34 (17%) had a clinical stroke, defined as new focal neurologic symptoms lasting more than 24 hours determined to be of vascular origin or, if less than 24 hours, with evidence of infarction in the appropriate territory, Dr. Messé said. Most (32) were ischemic and 2 were hemorrhagic.
Most strokes were mild, with a median National Institutes of Health Stroke Score (NIHSS)of 3 (interquartile [IQR] range, 1-9).
Factors significantly associated with stroke in logistic regression were age (odds ratio, 1.07; P = .031), higher lowest mean arterial pressure (MAP) in the operating room (OR, 1.07; P = .019) and duration of cardiopulmonary bypass (OR, 1.12; P = .005).
"It’s not exactly clear why higher lowest MAP is associated with stroke, but I suspect it reflects that these patients have a higher burden of hypertension at baseline and that is a risk factor for stroke in general," Dr. Messé said.
Stroke was significantly associated with increased the length of stay (median 12 days vs. 10 days; P = .019). It was not statistically associated with mortality, although 9% of those with stroke died vs. 4% without (P = .28).
Moderate to severe stroke, present in eight patients and defined by a NIHSS of more than 10, however, was strongly associated with a ninefold increase in mortality (38% vs. 4%; P = .005), he said at the meeting, sponsored by the American Heart Association.
The investigators then queried the Society for Thoracic Surgery database, a national quality improvement initiative for cardiothoracic surgery, to look at the reported stroke outcomes in this cohort.
"It turns out that only 13 [patients], or 6.6%, were reported to have had a stroke," Dr. Messé said. "I should note that per protocol, when the neurologist evaluated the patient and suspected a stroke, the clinical team was informed of that."
Not surprising, strokes reported in the STS database were more severe (median NIHSS 5), although this was not statistically significant. Still, "they missed quite a few," with a quarter of unreported patients having a NIHSS score of 9 or more, he added.
Postoperative MRI was performed on 132 patients (67%). Use improved over time from 57% of the first 100 patients to 78% of the last 96 patients.
Of the 112 stroke-free subjects with postoperative imaging, silent infarct was identified in an additional 62 patients (55%). Silent infarct was not associated with in-hospital mortality or increased length of stay, he said.
Limitations of the study include the single academic health system experience, lack of MRI in a minority of patients, the homogeneous cohort, and the use of a bioprosthetic as opposed to a mechanical valve in the vast majority of patients, Dr. Messé said.
He noted that the longer-term cognitive and functional consequences of clinical stroke and silent infarct remain to be determined and that the team is planning on evaluating this data as it accumulates over the next year.
"Finally, I’d like to suggest that aortic valve replacement provides an excellent opportunity to test prophylactic neuroprotection medication," he concluded. "There’s a clinical need for this. The stroke burden in these patients is high."
The National Institutes of Health/National Heart, Lung, and Blood Institute funded the research. Dr. Messé and his coauthors report research funding from the National Institutes of Health.
HONOLULU – Almost one-fifth of patients who underwent aortic valve surgery experienced a stroke in a prospective, cohort study of 196 patients.
"Stroke is a very prevalent complication of aortic valve replacement, and it’s much more common than prior series have suggested," Dr. Steven Messé said at the International Stroke Conference.
Based on the literature, the risk of periprocedural stroke varies widely from a low of less than 1% to 9% for cardiac valve replacement and 10% for heart transplant and left ventricular assist device placement, he said. If the number of times these procedures are performed each year is added to the equation, cardiac procedures account for about 5% of strokes annually in the United States.
"Unfortunately, the reality is probably worse than the literature," Dr. Messé said.
He observed that most risk estimates come from trials and case series rather than clinical practice, and that the vast majority of these studies did not include systematic evaluation by neurologists, who tend to be more sensitive to subtle yet meaningful deficits. Recent evidence also suggests that ischemic neurologic complications following surgery are increasing, "possibly related to the willingness of surgeons to undertake procedures with higher-risk patients," said Dr. Messé, a neurologist at the Hospital of the University of Pennsylvania, Philadelphia. To access their own stroke rates, neurologic, cognitive, and quality-of-life assessments were performed 1 week prior to surgery and at a 3- to 4-week and 9- to 12-month follow-up in 196 patients, aged at least 65 years, undergoing open surgical aortic valve replacement for moderate to severe aortic stenosis at two hospitals within the University of Pennsylvania Health System. Neurologic assessments were also performed on postoperative days 1, 3 and 7, and magnetic resonance imaging on day 5, plus or minus 2 days. Cerebrovascular end points in the study, led by colleague and radiologist Dr. Thomas Floyd, were independently adjudicated by two vascular neurologists.
Over the 4-year study period, 196 patients underwent aortic valve replacement, of which 36% were female and 6% nonwhite. Their average age was 76 years.
Ten (5%) died in hospital and 34 (17%) had a clinical stroke, defined as new focal neurologic symptoms lasting more than 24 hours determined to be of vascular origin or, if less than 24 hours, with evidence of infarction in the appropriate territory, Dr. Messé said. Most (32) were ischemic and 2 were hemorrhagic.
Most strokes were mild, with a median National Institutes of Health Stroke Score (NIHSS)of 3 (interquartile [IQR] range, 1-9).
Factors significantly associated with stroke in logistic regression were age (odds ratio, 1.07; P = .031), higher lowest mean arterial pressure (MAP) in the operating room (OR, 1.07; P = .019) and duration of cardiopulmonary bypass (OR, 1.12; P = .005).
"It’s not exactly clear why higher lowest MAP is associated with stroke, but I suspect it reflects that these patients have a higher burden of hypertension at baseline and that is a risk factor for stroke in general," Dr. Messé said.
Stroke was significantly associated with increased the length of stay (median 12 days vs. 10 days; P = .019). It was not statistically associated with mortality, although 9% of those with stroke died vs. 4% without (P = .28).
Moderate to severe stroke, present in eight patients and defined by a NIHSS of more than 10, however, was strongly associated with a ninefold increase in mortality (38% vs. 4%; P = .005), he said at the meeting, sponsored by the American Heart Association.
The investigators then queried the Society for Thoracic Surgery database, a national quality improvement initiative for cardiothoracic surgery, to look at the reported stroke outcomes in this cohort.
"It turns out that only 13 [patients], or 6.6%, were reported to have had a stroke," Dr. Messé said. "I should note that per protocol, when the neurologist evaluated the patient and suspected a stroke, the clinical team was informed of that."
Not surprising, strokes reported in the STS database were more severe (median NIHSS 5), although this was not statistically significant. Still, "they missed quite a few," with a quarter of unreported patients having a NIHSS score of 9 or more, he added.
Postoperative MRI was performed on 132 patients (67%). Use improved over time from 57% of the first 100 patients to 78% of the last 96 patients.
Of the 112 stroke-free subjects with postoperative imaging, silent infarct was identified in an additional 62 patients (55%). Silent infarct was not associated with in-hospital mortality or increased length of stay, he said.
Limitations of the study include the single academic health system experience, lack of MRI in a minority of patients, the homogeneous cohort, and the use of a bioprosthetic as opposed to a mechanical valve in the vast majority of patients, Dr. Messé said.
He noted that the longer-term cognitive and functional consequences of clinical stroke and silent infarct remain to be determined and that the team is planning on evaluating this data as it accumulates over the next year.
"Finally, I’d like to suggest that aortic valve replacement provides an excellent opportunity to test prophylactic neuroprotection medication," he concluded. "There’s a clinical need for this. The stroke burden in these patients is high."
The National Institutes of Health/National Heart, Lung, and Blood Institute funded the research. Dr. Messé and his coauthors report research funding from the National Institutes of Health.
HONOLULU – Almost one-fifth of patients who underwent aortic valve surgery experienced a stroke in a prospective, cohort study of 196 patients.
"Stroke is a very prevalent complication of aortic valve replacement, and it’s much more common than prior series have suggested," Dr. Steven Messé said at the International Stroke Conference.
Based on the literature, the risk of periprocedural stroke varies widely from a low of less than 1% to 9% for cardiac valve replacement and 10% for heart transplant and left ventricular assist device placement, he said. If the number of times these procedures are performed each year is added to the equation, cardiac procedures account for about 5% of strokes annually in the United States.
"Unfortunately, the reality is probably worse than the literature," Dr. Messé said.
He observed that most risk estimates come from trials and case series rather than clinical practice, and that the vast majority of these studies did not include systematic evaluation by neurologists, who tend to be more sensitive to subtle yet meaningful deficits. Recent evidence also suggests that ischemic neurologic complications following surgery are increasing, "possibly related to the willingness of surgeons to undertake procedures with higher-risk patients," said Dr. Messé, a neurologist at the Hospital of the University of Pennsylvania, Philadelphia. To access their own stroke rates, neurologic, cognitive, and quality-of-life assessments were performed 1 week prior to surgery and at a 3- to 4-week and 9- to 12-month follow-up in 196 patients, aged at least 65 years, undergoing open surgical aortic valve replacement for moderate to severe aortic stenosis at two hospitals within the University of Pennsylvania Health System. Neurologic assessments were also performed on postoperative days 1, 3 and 7, and magnetic resonance imaging on day 5, plus or minus 2 days. Cerebrovascular end points in the study, led by colleague and radiologist Dr. Thomas Floyd, were independently adjudicated by two vascular neurologists.
Over the 4-year study period, 196 patients underwent aortic valve replacement, of which 36% were female and 6% nonwhite. Their average age was 76 years.
Ten (5%) died in hospital and 34 (17%) had a clinical stroke, defined as new focal neurologic symptoms lasting more than 24 hours determined to be of vascular origin or, if less than 24 hours, with evidence of infarction in the appropriate territory, Dr. Messé said. Most (32) were ischemic and 2 were hemorrhagic.
Most strokes were mild, with a median National Institutes of Health Stroke Score (NIHSS)of 3 (interquartile [IQR] range, 1-9).
Factors significantly associated with stroke in logistic regression were age (odds ratio, 1.07; P = .031), higher lowest mean arterial pressure (MAP) in the operating room (OR, 1.07; P = .019) and duration of cardiopulmonary bypass (OR, 1.12; P = .005).
"It’s not exactly clear why higher lowest MAP is associated with stroke, but I suspect it reflects that these patients have a higher burden of hypertension at baseline and that is a risk factor for stroke in general," Dr. Messé said.
Stroke was significantly associated with increased the length of stay (median 12 days vs. 10 days; P = .019). It was not statistically associated with mortality, although 9% of those with stroke died vs. 4% without (P = .28).
Moderate to severe stroke, present in eight patients and defined by a NIHSS of more than 10, however, was strongly associated with a ninefold increase in mortality (38% vs. 4%; P = .005), he said at the meeting, sponsored by the American Heart Association.
The investigators then queried the Society for Thoracic Surgery database, a national quality improvement initiative for cardiothoracic surgery, to look at the reported stroke outcomes in this cohort.
"It turns out that only 13 [patients], or 6.6%, were reported to have had a stroke," Dr. Messé said. "I should note that per protocol, when the neurologist evaluated the patient and suspected a stroke, the clinical team was informed of that."
Not surprising, strokes reported in the STS database were more severe (median NIHSS 5), although this was not statistically significant. Still, "they missed quite a few," with a quarter of unreported patients having a NIHSS score of 9 or more, he added.
Postoperative MRI was performed on 132 patients (67%). Use improved over time from 57% of the first 100 patients to 78% of the last 96 patients.
Of the 112 stroke-free subjects with postoperative imaging, silent infarct was identified in an additional 62 patients (55%). Silent infarct was not associated with in-hospital mortality or increased length of stay, he said.
Limitations of the study include the single academic health system experience, lack of MRI in a minority of patients, the homogeneous cohort, and the use of a bioprosthetic as opposed to a mechanical valve in the vast majority of patients, Dr. Messé said.
He noted that the longer-term cognitive and functional consequences of clinical stroke and silent infarct remain to be determined and that the team is planning on evaluating this data as it accumulates over the next year.
"Finally, I’d like to suggest that aortic valve replacement provides an excellent opportunity to test prophylactic neuroprotection medication," he concluded. "There’s a clinical need for this. The stroke burden in these patients is high."
The National Institutes of Health/National Heart, Lung, and Blood Institute funded the research. Dr. Messé and his coauthors report research funding from the National Institutes of Health.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: A clinical stroke was detected in 34 patients (17%) undergoing aortic valve repair.
Data Source: Prospective cohort study of 196 patients undergoing aortic valve surgery.
Disclosures: The National Institutes of Health/National Heart, Lung, and Blood Institute funded the research. Dr. Messé reported consulting for GlaxoSmithKline; his coauthors report grant funding from the National Institutes of Health.
Diet explains black Americans' high stroke risk
HONOLULU – Nearly two-thirds of the racial disparity in stroke risk is explainable by African Americans’ greater adherence to a dietary pattern high in fat, salt, and sugar, according to a major national study.
Investigators in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study named this dietary pattern the "Southern diet" because that’s where its following is greatest. It is one of five broad U.S. dietary patterns identified in the study, which involved detailed assessment of 30,239 black and white participants aged 45 years and older.
The Southern diet was the one that stood out in terms of increased stroke risk. It features heavy consumption of fried foods, including fried vegetables, as well as organ meats, processed meats, full-fat milk, and sugar-sweetened drinks, while downplaying fruits, salads, and whole grains.
The Southern diet is a dietary pattern that’s far more popular among blacks than whites, including blacks living in the so-called "stroke belt" in the Southeast. Enthusiasm for the dietary pattern, however, is by no means limited to the South: Among the top-10 states with the greatest adherence to the Southern diet are Delaware, Illinois, and Michigan, Suzanne Judd, Ph.D., noted at the International Stroke Conference, which was sponsored by the American Heart Association.
It is well established that African Americans are at sharply higher risk of stroke than are their same-age white counterparts. Mathematical modeling of the REGARDS data showed that the Southern diet explains 63% of the excess stroke risk among black Americans under age 65 years.
"That’s something we’re very excited to know because it’s something we could intervene in and make changes to reduce this racial disparity in stroke," observed Dr. Judd, a nutritional epidemiologist at the University of Alabama, Birmingham.
People who ate Southern diet–type foods six times per week had a 41% higher stroke risk than did those who ate such foods once a month. In a multivariate analysis that adjusted for age, race, gender, location, socioeconomic and educational status, total energy intake, smoking, and sedentary behavior, adherence to the Southern diet was independently associated with stroke risk in a dose-response fashion. The stroke rate climbed by 30% as adherence to the dietary pattern increased from the lowest to the highest quartile.
"I think that it’s a very positive message to show that even small changes in adding some of these plant-based foods into the diet seem to be protective against stroke in this population." -Dr. Suzanne Judd
Although it’s customary in dietary studies not to include factors that could lie in the causal pathway between diet and stroke, even when major known stroke risk factors such as hypertension, diabetes, atrial fibrillation, and prior MI were included in the modeling, there was still an association between adherence to the Southern dietary pattern and stroke risk, albeit an attenuated one, she noted.
The other four major dietary patterns identified by Dr. Judd and her associates were the Convenience pattern, typified by take-out pizza, Mexican and Chinese foods, and pastas – a diet favored by busy young working people; the Plant-based diet; the Sweets diet; and the Alcohol and Salads diet, which emphasizes beer, wine, liquor, salads, nuts and seeds, butter, and coffee. Dr. Judd conceded that the Alcohol and Salads pattern is poorly understood and is a construct that requires further study.
The Plant-based diet emphasizes cruciferous, green leafy, and other vegetables, fruits, beans, whole grains, yogurt, fish, and poultry. In the multivariate analysis, subjects in the second through fourth quartiles in terms of adherence to this dietary pattern enjoyed roughly a 20% reduction in stroke risk.
"I really want to highlight this Plant-based pattern. I think that it’s a very positive message to show that even small changes in adding some of these plant-based foods into the diet seem to be protective against stroke in this population," Dr. Judd said.
The REGARDS study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Judd reported having no financial conflicts.
HONOLULU – Nearly two-thirds of the racial disparity in stroke risk is explainable by African Americans’ greater adherence to a dietary pattern high in fat, salt, and sugar, according to a major national study.
Investigators in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study named this dietary pattern the "Southern diet" because that’s where its following is greatest. It is one of five broad U.S. dietary patterns identified in the study, which involved detailed assessment of 30,239 black and white participants aged 45 years and older.
The Southern diet was the one that stood out in terms of increased stroke risk. It features heavy consumption of fried foods, including fried vegetables, as well as organ meats, processed meats, full-fat milk, and sugar-sweetened drinks, while downplaying fruits, salads, and whole grains.
The Southern diet is a dietary pattern that’s far more popular among blacks than whites, including blacks living in the so-called "stroke belt" in the Southeast. Enthusiasm for the dietary pattern, however, is by no means limited to the South: Among the top-10 states with the greatest adherence to the Southern diet are Delaware, Illinois, and Michigan, Suzanne Judd, Ph.D., noted at the International Stroke Conference, which was sponsored by the American Heart Association.
It is well established that African Americans are at sharply higher risk of stroke than are their same-age white counterparts. Mathematical modeling of the REGARDS data showed that the Southern diet explains 63% of the excess stroke risk among black Americans under age 65 years.
"That’s something we’re very excited to know because it’s something we could intervene in and make changes to reduce this racial disparity in stroke," observed Dr. Judd, a nutritional epidemiologist at the University of Alabama, Birmingham.
People who ate Southern diet–type foods six times per week had a 41% higher stroke risk than did those who ate such foods once a month. In a multivariate analysis that adjusted for age, race, gender, location, socioeconomic and educational status, total energy intake, smoking, and sedentary behavior, adherence to the Southern diet was independently associated with stroke risk in a dose-response fashion. The stroke rate climbed by 30% as adherence to the dietary pattern increased from the lowest to the highest quartile.
"I think that it’s a very positive message to show that even small changes in adding some of these plant-based foods into the diet seem to be protective against stroke in this population." -Dr. Suzanne Judd
Although it’s customary in dietary studies not to include factors that could lie in the causal pathway between diet and stroke, even when major known stroke risk factors such as hypertension, diabetes, atrial fibrillation, and prior MI were included in the modeling, there was still an association between adherence to the Southern dietary pattern and stroke risk, albeit an attenuated one, she noted.
The other four major dietary patterns identified by Dr. Judd and her associates were the Convenience pattern, typified by take-out pizza, Mexican and Chinese foods, and pastas – a diet favored by busy young working people; the Plant-based diet; the Sweets diet; and the Alcohol and Salads diet, which emphasizes beer, wine, liquor, salads, nuts and seeds, butter, and coffee. Dr. Judd conceded that the Alcohol and Salads pattern is poorly understood and is a construct that requires further study.
The Plant-based diet emphasizes cruciferous, green leafy, and other vegetables, fruits, beans, whole grains, yogurt, fish, and poultry. In the multivariate analysis, subjects in the second through fourth quartiles in terms of adherence to this dietary pattern enjoyed roughly a 20% reduction in stroke risk.
"I really want to highlight this Plant-based pattern. I think that it’s a very positive message to show that even small changes in adding some of these plant-based foods into the diet seem to be protective against stroke in this population," Dr. Judd said.
The REGARDS study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Judd reported having no financial conflicts.
HONOLULU – Nearly two-thirds of the racial disparity in stroke risk is explainable by African Americans’ greater adherence to a dietary pattern high in fat, salt, and sugar, according to a major national study.
Investigators in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study named this dietary pattern the "Southern diet" because that’s where its following is greatest. It is one of five broad U.S. dietary patterns identified in the study, which involved detailed assessment of 30,239 black and white participants aged 45 years and older.
The Southern diet was the one that stood out in terms of increased stroke risk. It features heavy consumption of fried foods, including fried vegetables, as well as organ meats, processed meats, full-fat milk, and sugar-sweetened drinks, while downplaying fruits, salads, and whole grains.
The Southern diet is a dietary pattern that’s far more popular among blacks than whites, including blacks living in the so-called "stroke belt" in the Southeast. Enthusiasm for the dietary pattern, however, is by no means limited to the South: Among the top-10 states with the greatest adherence to the Southern diet are Delaware, Illinois, and Michigan, Suzanne Judd, Ph.D., noted at the International Stroke Conference, which was sponsored by the American Heart Association.
It is well established that African Americans are at sharply higher risk of stroke than are their same-age white counterparts. Mathematical modeling of the REGARDS data showed that the Southern diet explains 63% of the excess stroke risk among black Americans under age 65 years.
"That’s something we’re very excited to know because it’s something we could intervene in and make changes to reduce this racial disparity in stroke," observed Dr. Judd, a nutritional epidemiologist at the University of Alabama, Birmingham.
People who ate Southern diet–type foods six times per week had a 41% higher stroke risk than did those who ate such foods once a month. In a multivariate analysis that adjusted for age, race, gender, location, socioeconomic and educational status, total energy intake, smoking, and sedentary behavior, adherence to the Southern diet was independently associated with stroke risk in a dose-response fashion. The stroke rate climbed by 30% as adherence to the dietary pattern increased from the lowest to the highest quartile.
"I think that it’s a very positive message to show that even small changes in adding some of these plant-based foods into the diet seem to be protective against stroke in this population." -Dr. Suzanne Judd
Although it’s customary in dietary studies not to include factors that could lie in the causal pathway between diet and stroke, even when major known stroke risk factors such as hypertension, diabetes, atrial fibrillation, and prior MI were included in the modeling, there was still an association between adherence to the Southern dietary pattern and stroke risk, albeit an attenuated one, she noted.
The other four major dietary patterns identified by Dr. Judd and her associates were the Convenience pattern, typified by take-out pizza, Mexican and Chinese foods, and pastas – a diet favored by busy young working people; the Plant-based diet; the Sweets diet; and the Alcohol and Salads diet, which emphasizes beer, wine, liquor, salads, nuts and seeds, butter, and coffee. Dr. Judd conceded that the Alcohol and Salads pattern is poorly understood and is a construct that requires further study.
The Plant-based diet emphasizes cruciferous, green leafy, and other vegetables, fruits, beans, whole grains, yogurt, fish, and poultry. In the multivariate analysis, subjects in the second through fourth quartiles in terms of adherence to this dietary pattern enjoyed roughly a 20% reduction in stroke risk.
"I really want to highlight this Plant-based pattern. I think that it’s a very positive message to show that even small changes in adding some of these plant-based foods into the diet seem to be protective against stroke in this population," Dr. Judd said.
The REGARDS study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Judd reported having no financial conflicts.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Adherence to the so-called Southern diet explains 63% of the increased stroke risk in African Americans, compared with same-age whites.
Data Source: The REGARDS study examined the relationship between diet and stroke in 30,239 black and white Americans aged 45 years and older.
Disclosures: The study was sponsored by the National Institute of Neurological Disorders and Stroke. The presenter reported having no financial conflicts.
Poststroke depression often poorly managed
HONOLULU – Poststroke depression is a common condition that is underdiagnosed and inadequately treated, according to Dr. Linda S. Williams, a neurologist at Indiana University and the Roudebush VA Medical Center, both in Indianapolis.
But it doesn’t have to be this way. "There are many, many treatments, and they’re easy to give. It’s something that should be within the grasp of every provider to do," she said at the International Stroke Conference, sponsored by the American Heart Association.
Yet many of her fellow neurologists don’t see it this way. Dr. Williams said she faults her specialty for playing a major role in the generally poor management of poststroke depression (PSD).
"I’ve always wanted to write an editorial called, ‘What’s the ‘P’ in ABPN?’ because neurologists are boarded by the American Board of Psychiatry and Neurology, but many neurologists – even though we get some training in psychiatry – don’t want to initiate treatment for depression. We somehow think it’s not our job. That might be fine if you have great communication with the patient’s primary care doctor in an integrated health care system and you can be sure that doctor is going to see that the patient gets started on antidepressant therapy, but I think reality would suggest that’s not very often the case," she said.
"So I strongly feel that whoever detects the depression first should get the patient started on treatment and should make sure the patient is seen again in 6 weeks to see if there has been improvement in symptoms and to figure out who’ll get called if the patient has medication side effects and needs to switch," the neurologist continued.
An estimated 25%-30% of the 700,000 new stroke survivors each year will develop PSD, although it’s unclear how many cases are new onset after the neurovascular event, as opposed to undiagnosed depression present beforehand. Depression is, after all, an independent risk factor for both stroke and ischemic heart disease. In any case, PSD is associated with increased morbidity and mortality and greater health care utilization.
The keys to improved outcomes in PSD are to set up a systematic screening program for all patients beginning about 1 month after a stroke, start treatment promptly once the diagnosis is made, and then monitor symptomatic progress and adjust the antidepressant medication as needed, she said.
Lots of screening tools for depression are available. Dr. Williams said she favors the Patient Health Questionnaire-9 (PHQ-9) because it’s quick – just nine simple questions, it was developed specifically with primary care physicians in mind, and it’s one of the few screening tools that allows a busy nonpsychiatrist to reliably diagnose major depression based upon the results.
She conducted a study in which 316 stroke survivors were assessed for depression using both the PHQ-9 and the gold standard, time-consuming Structured Clinical Interview for DSM-IV Disorders (SCID). One hundred forty-five patients met SCID criteria for major depression. A PHQ-9 score of 10 or more out of a possible 27 had 91% sensitivity and 89% specificity for major depression. A PHQ-2 of 3 or more, in which only the first two of the nine questions are asked, had 83% sensitivity and 84% specificity for the diagnosis.
"Even in stroke patients, I feel pretty confident in using this scale and knowing it’s going to give me an accurate diagnosis," the neurologist said.
That being said, Dr. Williams acknowledged that the diagnosis of PSD is somewhat trickier than for other forms of depression because a stroke may have lingering physical or cognitive effects that can mimic the symptoms of the mood disorder. Conversely, stroke-induced severe right hemisphere damage or aphasia can mask depressive symptoms.
Epidemiologic studies suggest only about half of patients with PSD are diagnosed. It’s easy for busy physicians to forget to screen. That’s why a systematic screening plan is important, she said. An automated electronic reminder system to screen for PSD 1-6 months after a stroke is an effective way to boost detection and treatment rates. Dr. Williams and her coinvestigators developed such a system for primary care physicians and neurologists for inclusion in patients’ electronic medical record within the VA medical system. When the investigators put the automated reminder system to the test in a controlled trial, it boosted screening rates 1-6 months after a stroke by 6.2-fold and treatment rates in screen-positive patients by 2.45-fold, compared with usual care (J. Gen. Intern. Med. 2011;26:852-7).
PSD responds to the same therapies that are effective in nonstroke major depression. The recent literature suggests the proportion of patients with PSD who are on antidepressant therapy has been rising in the past few years; however, the majority of treated patients stop taking their medication after the first several weeks or stay on the initial dose without ever having it titrated upward. It’s crucial to check in with the patient after about 6 weeks of therapy to learn if symptoms are improving; if not, it’s time to switch to an antidepressant from another class, Dr. Williams said.
"I do think that ongoing monitoring of treatment and adjustment of medications is really fundamental to patients having good outcomes," she said.
A hot topic in the stroke literature in recent years has been whether it makes sense to simply initiate prophylactic antidepressant therapy in all poststroke patients as a means of preventing a full-blown depressive episode. "My answer is, ‘Not yet,’ " she said, noting that the randomized trials to date looking at this approach have been small and have yielded conflicting results.
Dr. Williams reported having no relevant financial conflicts.
HONOLULU – Poststroke depression is a common condition that is underdiagnosed and inadequately treated, according to Dr. Linda S. Williams, a neurologist at Indiana University and the Roudebush VA Medical Center, both in Indianapolis.
But it doesn’t have to be this way. "There are many, many treatments, and they’re easy to give. It’s something that should be within the grasp of every provider to do," she said at the International Stroke Conference, sponsored by the American Heart Association.
Yet many of her fellow neurologists don’t see it this way. Dr. Williams said she faults her specialty for playing a major role in the generally poor management of poststroke depression (PSD).
"I’ve always wanted to write an editorial called, ‘What’s the ‘P’ in ABPN?’ because neurologists are boarded by the American Board of Psychiatry and Neurology, but many neurologists – even though we get some training in psychiatry – don’t want to initiate treatment for depression. We somehow think it’s not our job. That might be fine if you have great communication with the patient’s primary care doctor in an integrated health care system and you can be sure that doctor is going to see that the patient gets started on antidepressant therapy, but I think reality would suggest that’s not very often the case," she said.
"So I strongly feel that whoever detects the depression first should get the patient started on treatment and should make sure the patient is seen again in 6 weeks to see if there has been improvement in symptoms and to figure out who’ll get called if the patient has medication side effects and needs to switch," the neurologist continued.
An estimated 25%-30% of the 700,000 new stroke survivors each year will develop PSD, although it’s unclear how many cases are new onset after the neurovascular event, as opposed to undiagnosed depression present beforehand. Depression is, after all, an independent risk factor for both stroke and ischemic heart disease. In any case, PSD is associated with increased morbidity and mortality and greater health care utilization.
The keys to improved outcomes in PSD are to set up a systematic screening program for all patients beginning about 1 month after a stroke, start treatment promptly once the diagnosis is made, and then monitor symptomatic progress and adjust the antidepressant medication as needed, she said.
Lots of screening tools for depression are available. Dr. Williams said she favors the Patient Health Questionnaire-9 (PHQ-9) because it’s quick – just nine simple questions, it was developed specifically with primary care physicians in mind, and it’s one of the few screening tools that allows a busy nonpsychiatrist to reliably diagnose major depression based upon the results.
She conducted a study in which 316 stroke survivors were assessed for depression using both the PHQ-9 and the gold standard, time-consuming Structured Clinical Interview for DSM-IV Disorders (SCID). One hundred forty-five patients met SCID criteria for major depression. A PHQ-9 score of 10 or more out of a possible 27 had 91% sensitivity and 89% specificity for major depression. A PHQ-2 of 3 or more, in which only the first two of the nine questions are asked, had 83% sensitivity and 84% specificity for the diagnosis.
"Even in stroke patients, I feel pretty confident in using this scale and knowing it’s going to give me an accurate diagnosis," the neurologist said.
That being said, Dr. Williams acknowledged that the diagnosis of PSD is somewhat trickier than for other forms of depression because a stroke may have lingering physical or cognitive effects that can mimic the symptoms of the mood disorder. Conversely, stroke-induced severe right hemisphere damage or aphasia can mask depressive symptoms.
Epidemiologic studies suggest only about half of patients with PSD are diagnosed. It’s easy for busy physicians to forget to screen. That’s why a systematic screening plan is important, she said. An automated electronic reminder system to screen for PSD 1-6 months after a stroke is an effective way to boost detection and treatment rates. Dr. Williams and her coinvestigators developed such a system for primary care physicians and neurologists for inclusion in patients’ electronic medical record within the VA medical system. When the investigators put the automated reminder system to the test in a controlled trial, it boosted screening rates 1-6 months after a stroke by 6.2-fold and treatment rates in screen-positive patients by 2.45-fold, compared with usual care (J. Gen. Intern. Med. 2011;26:852-7).
PSD responds to the same therapies that are effective in nonstroke major depression. The recent literature suggests the proportion of patients with PSD who are on antidepressant therapy has been rising in the past few years; however, the majority of treated patients stop taking their medication after the first several weeks or stay on the initial dose without ever having it titrated upward. It’s crucial to check in with the patient after about 6 weeks of therapy to learn if symptoms are improving; if not, it’s time to switch to an antidepressant from another class, Dr. Williams said.
"I do think that ongoing monitoring of treatment and adjustment of medications is really fundamental to patients having good outcomes," she said.
A hot topic in the stroke literature in recent years has been whether it makes sense to simply initiate prophylactic antidepressant therapy in all poststroke patients as a means of preventing a full-blown depressive episode. "My answer is, ‘Not yet,’ " she said, noting that the randomized trials to date looking at this approach have been small and have yielded conflicting results.
Dr. Williams reported having no relevant financial conflicts.
HONOLULU – Poststroke depression is a common condition that is underdiagnosed and inadequately treated, according to Dr. Linda S. Williams, a neurologist at Indiana University and the Roudebush VA Medical Center, both in Indianapolis.
But it doesn’t have to be this way. "There are many, many treatments, and they’re easy to give. It’s something that should be within the grasp of every provider to do," she said at the International Stroke Conference, sponsored by the American Heart Association.
Yet many of her fellow neurologists don’t see it this way. Dr. Williams said she faults her specialty for playing a major role in the generally poor management of poststroke depression (PSD).
"I’ve always wanted to write an editorial called, ‘What’s the ‘P’ in ABPN?’ because neurologists are boarded by the American Board of Psychiatry and Neurology, but many neurologists – even though we get some training in psychiatry – don’t want to initiate treatment for depression. We somehow think it’s not our job. That might be fine if you have great communication with the patient’s primary care doctor in an integrated health care system and you can be sure that doctor is going to see that the patient gets started on antidepressant therapy, but I think reality would suggest that’s not very often the case," she said.
"So I strongly feel that whoever detects the depression first should get the patient started on treatment and should make sure the patient is seen again in 6 weeks to see if there has been improvement in symptoms and to figure out who’ll get called if the patient has medication side effects and needs to switch," the neurologist continued.
An estimated 25%-30% of the 700,000 new stroke survivors each year will develop PSD, although it’s unclear how many cases are new onset after the neurovascular event, as opposed to undiagnosed depression present beforehand. Depression is, after all, an independent risk factor for both stroke and ischemic heart disease. In any case, PSD is associated with increased morbidity and mortality and greater health care utilization.
The keys to improved outcomes in PSD are to set up a systematic screening program for all patients beginning about 1 month after a stroke, start treatment promptly once the diagnosis is made, and then monitor symptomatic progress and adjust the antidepressant medication as needed, she said.
Lots of screening tools for depression are available. Dr. Williams said she favors the Patient Health Questionnaire-9 (PHQ-9) because it’s quick – just nine simple questions, it was developed specifically with primary care physicians in mind, and it’s one of the few screening tools that allows a busy nonpsychiatrist to reliably diagnose major depression based upon the results.
She conducted a study in which 316 stroke survivors were assessed for depression using both the PHQ-9 and the gold standard, time-consuming Structured Clinical Interview for DSM-IV Disorders (SCID). One hundred forty-five patients met SCID criteria for major depression. A PHQ-9 score of 10 or more out of a possible 27 had 91% sensitivity and 89% specificity for major depression. A PHQ-2 of 3 or more, in which only the first two of the nine questions are asked, had 83% sensitivity and 84% specificity for the diagnosis.
"Even in stroke patients, I feel pretty confident in using this scale and knowing it’s going to give me an accurate diagnosis," the neurologist said.
That being said, Dr. Williams acknowledged that the diagnosis of PSD is somewhat trickier than for other forms of depression because a stroke may have lingering physical or cognitive effects that can mimic the symptoms of the mood disorder. Conversely, stroke-induced severe right hemisphere damage or aphasia can mask depressive symptoms.
Epidemiologic studies suggest only about half of patients with PSD are diagnosed. It’s easy for busy physicians to forget to screen. That’s why a systematic screening plan is important, she said. An automated electronic reminder system to screen for PSD 1-6 months after a stroke is an effective way to boost detection and treatment rates. Dr. Williams and her coinvestigators developed such a system for primary care physicians and neurologists for inclusion in patients’ electronic medical record within the VA medical system. When the investigators put the automated reminder system to the test in a controlled trial, it boosted screening rates 1-6 months after a stroke by 6.2-fold and treatment rates in screen-positive patients by 2.45-fold, compared with usual care (J. Gen. Intern. Med. 2011;26:852-7).
PSD responds to the same therapies that are effective in nonstroke major depression. The recent literature suggests the proportion of patients with PSD who are on antidepressant therapy has been rising in the past few years; however, the majority of treated patients stop taking their medication after the first several weeks or stay on the initial dose without ever having it titrated upward. It’s crucial to check in with the patient after about 6 weeks of therapy to learn if symptoms are improving; if not, it’s time to switch to an antidepressant from another class, Dr. Williams said.
"I do think that ongoing monitoring of treatment and adjustment of medications is really fundamental to patients having good outcomes," she said.
A hot topic in the stroke literature in recent years has been whether it makes sense to simply initiate prophylactic antidepressant therapy in all poststroke patients as a means of preventing a full-blown depressive episode. "My answer is, ‘Not yet,’ " she said, noting that the randomized trials to date looking at this approach have been small and have yielded conflicting results.
Dr. Williams reported having no relevant financial conflicts.
EXPERT ANALYSIS FROM THE INTERNATIONAL STROKE CONFERENCE
Seizure risk substantial after pediatric intracerebral hemorrhage
HONOLULU – In the first 2 years following pediatric intracerebral hemorrhage, one-third of patients will experience a single remote symptomatic seizure and 13% will develop epilepsy, according to a large prospective study.
Twenty-eight percent of study participants who underwent continuous EEG monitoring were found to have subclinical EEG-only seizures. Additional follow-up will determine whether these subclinical seizures constitute a risk factor for later epilepsy, Dr. Lauren A. Beslow said at the International Stroke Conference sponsored by the American Heart Association.
She presented a three-center prospective cohort study involving 20 neonates and 53 other patients up to 18 years of age who experienced an intracerebral hemorrhage (ICH).
While 73 subjects may not sound like a lot, this is in fact an exceptionally large cohort, as pediatric ICH is an understudied topic. The incidence of stroke in U.S. children is 6.4 cases per 100,000 per year, a rate approaching that of pediatric brain tumors. And while intracerebral hemorrhage accounts for only about 15% of adult strokes, it is the cause of half of all strokes in children, according to Dr. Beslow, a pediatric neurologist at Yale University, New Haven, Conn.
Acute symptomatic seizures – that is, seizures occurring at presentation of ICH or up to 7 days afterward – were documented in 12 of 20 neonates (60%) and 23 of 53 older subjects (43%). The median age of non-neonates with acute symptomatic seizures was 2.2 years, compared with 10.8 years for subjects without such seizures.
Nine of 32 (28%) subjects placed on continuous EEG monitoring experienced EEG-only seizures. These subclinical seizures were treated medically in the same way that’s standard for symptomatic seizures.
Seizures occurring more than 7 days post ICH are deemed "remote." Eighteen percent of study participants experienced a remote symptomatic seizure during the first year of follow-up. At 2 years, 24 subjects (33%) had a remote symptomatic seizure.
Epilepsy, defined as two or more unprovoked remote symptomatic seizures, was diagnosed in 4% of patients during the first year. The cumulative rate through 2 years of follow-up was 13%.
This study contains several important new observations for clinical practice, Dr. Beslow said. One involves the high rate of EEG-only seizures. Previously, the decision to place a child on continuous EEG monitoring following ICH was often based upon physician intuition, and monitoring was more likely in those who presented with seizures at the time of their stroke.
"We hope our findings will encourage clinicians to consider more routine use of continuous EEG monitoring in children with ICH," she said.
The conventional wisdom has been that children who don’t have seizures at the time of their ICH are at reduced likelihood of developing seizures or epilepsy later on; these data suggest otherwise. Also, the parents of a young child with ICH are always deeply distraught and desperate to know what will happen to their child in the future. Now there are concrete risk figures for use in counseling, Dr. Beslow added.
Nearly a dozen prespecified potential risk factors for remote symptomatic seizures and epilepsy were scrutinized in the study. Only one proved statistically significant: elevated intracranial pressure requiring urgent intervention. The investigators anticipate that epilepsy rates will increase at planned 5- and 10-year follow-up. In addition, the researchers plan to recruit additional patients with pediatric ICH in order to strengthen the validity of their findings.
This ongoing study is funded by the National Institutes of Health. Dr. Beslow reported having no relevant financial interests.
HONOLULU – In the first 2 years following pediatric intracerebral hemorrhage, one-third of patients will experience a single remote symptomatic seizure and 13% will develop epilepsy, according to a large prospective study.
Twenty-eight percent of study participants who underwent continuous EEG monitoring were found to have subclinical EEG-only seizures. Additional follow-up will determine whether these subclinical seizures constitute a risk factor for later epilepsy, Dr. Lauren A. Beslow said at the International Stroke Conference sponsored by the American Heart Association.
She presented a three-center prospective cohort study involving 20 neonates and 53 other patients up to 18 years of age who experienced an intracerebral hemorrhage (ICH).
While 73 subjects may not sound like a lot, this is in fact an exceptionally large cohort, as pediatric ICH is an understudied topic. The incidence of stroke in U.S. children is 6.4 cases per 100,000 per year, a rate approaching that of pediatric brain tumors. And while intracerebral hemorrhage accounts for only about 15% of adult strokes, it is the cause of half of all strokes in children, according to Dr. Beslow, a pediatric neurologist at Yale University, New Haven, Conn.
Acute symptomatic seizures – that is, seizures occurring at presentation of ICH or up to 7 days afterward – were documented in 12 of 20 neonates (60%) and 23 of 53 older subjects (43%). The median age of non-neonates with acute symptomatic seizures was 2.2 years, compared with 10.8 years for subjects without such seizures.
Nine of 32 (28%) subjects placed on continuous EEG monitoring experienced EEG-only seizures. These subclinical seizures were treated medically in the same way that’s standard for symptomatic seizures.
Seizures occurring more than 7 days post ICH are deemed "remote." Eighteen percent of study participants experienced a remote symptomatic seizure during the first year of follow-up. At 2 years, 24 subjects (33%) had a remote symptomatic seizure.
Epilepsy, defined as two or more unprovoked remote symptomatic seizures, was diagnosed in 4% of patients during the first year. The cumulative rate through 2 years of follow-up was 13%.
This study contains several important new observations for clinical practice, Dr. Beslow said. One involves the high rate of EEG-only seizures. Previously, the decision to place a child on continuous EEG monitoring following ICH was often based upon physician intuition, and monitoring was more likely in those who presented with seizures at the time of their stroke.
"We hope our findings will encourage clinicians to consider more routine use of continuous EEG monitoring in children with ICH," she said.
The conventional wisdom has been that children who don’t have seizures at the time of their ICH are at reduced likelihood of developing seizures or epilepsy later on; these data suggest otherwise. Also, the parents of a young child with ICH are always deeply distraught and desperate to know what will happen to their child in the future. Now there are concrete risk figures for use in counseling, Dr. Beslow added.
Nearly a dozen prespecified potential risk factors for remote symptomatic seizures and epilepsy were scrutinized in the study. Only one proved statistically significant: elevated intracranial pressure requiring urgent intervention. The investigators anticipate that epilepsy rates will increase at planned 5- and 10-year follow-up. In addition, the researchers plan to recruit additional patients with pediatric ICH in order to strengthen the validity of their findings.
This ongoing study is funded by the National Institutes of Health. Dr. Beslow reported having no relevant financial interests.
HONOLULU – In the first 2 years following pediatric intracerebral hemorrhage, one-third of patients will experience a single remote symptomatic seizure and 13% will develop epilepsy, according to a large prospective study.
Twenty-eight percent of study participants who underwent continuous EEG monitoring were found to have subclinical EEG-only seizures. Additional follow-up will determine whether these subclinical seizures constitute a risk factor for later epilepsy, Dr. Lauren A. Beslow said at the International Stroke Conference sponsored by the American Heart Association.
She presented a three-center prospective cohort study involving 20 neonates and 53 other patients up to 18 years of age who experienced an intracerebral hemorrhage (ICH).
While 73 subjects may not sound like a lot, this is in fact an exceptionally large cohort, as pediatric ICH is an understudied topic. The incidence of stroke in U.S. children is 6.4 cases per 100,000 per year, a rate approaching that of pediatric brain tumors. And while intracerebral hemorrhage accounts for only about 15% of adult strokes, it is the cause of half of all strokes in children, according to Dr. Beslow, a pediatric neurologist at Yale University, New Haven, Conn.
Acute symptomatic seizures – that is, seizures occurring at presentation of ICH or up to 7 days afterward – were documented in 12 of 20 neonates (60%) and 23 of 53 older subjects (43%). The median age of non-neonates with acute symptomatic seizures was 2.2 years, compared with 10.8 years for subjects without such seizures.
Nine of 32 (28%) subjects placed on continuous EEG monitoring experienced EEG-only seizures. These subclinical seizures were treated medically in the same way that’s standard for symptomatic seizures.
Seizures occurring more than 7 days post ICH are deemed "remote." Eighteen percent of study participants experienced a remote symptomatic seizure during the first year of follow-up. At 2 years, 24 subjects (33%) had a remote symptomatic seizure.
Epilepsy, defined as two or more unprovoked remote symptomatic seizures, was diagnosed in 4% of patients during the first year. The cumulative rate through 2 years of follow-up was 13%.
This study contains several important new observations for clinical practice, Dr. Beslow said. One involves the high rate of EEG-only seizures. Previously, the decision to place a child on continuous EEG monitoring following ICH was often based upon physician intuition, and monitoring was more likely in those who presented with seizures at the time of their stroke.
"We hope our findings will encourage clinicians to consider more routine use of continuous EEG monitoring in children with ICH," she said.
The conventional wisdom has been that children who don’t have seizures at the time of their ICH are at reduced likelihood of developing seizures or epilepsy later on; these data suggest otherwise. Also, the parents of a young child with ICH are always deeply distraught and desperate to know what will happen to their child in the future. Now there are concrete risk figures for use in counseling, Dr. Beslow added.
Nearly a dozen prespecified potential risk factors for remote symptomatic seizures and epilepsy were scrutinized in the study. Only one proved statistically significant: elevated intracranial pressure requiring urgent intervention. The investigators anticipate that epilepsy rates will increase at planned 5- and 10-year follow-up. In addition, the researchers plan to recruit additional patients with pediatric ICH in order to strengthen the validity of their findings.
This ongoing study is funded by the National Institutes of Health. Dr. Beslow reported having no relevant financial interests.
AT THE INTERNATIONAL STROKE CONFERENCE
Major finding: Twenty-four of 73 (33%) children and adolescents who had a spontaneous intracerebral hemorrhage experienced a remote symptomatic seizure within the next 2 years.
Data source: This prospective cohort study includes 20 subjects who experienced an intracerebral hemorrhage as neonates and 53 who were older children or adolescents at the time of their stroke.
Disclosures: This ongoing study is funded by the National Institutes of Health. Dr. Beslow reported having no relevant financial interests.
Few preventable readmissions found after stroke
HONOLULU – Health care reformers looking to drive down preventable 30-day readmission rates will find slim pickings among the nation’s elderly hospitalized for ischemic stroke, according to Judith H. Lichtman, Ph.D.
An analysis of national fee-for-service Medicare data concluded that a mere 1.7% of patients hospitalized for ischemic stroke in 2006 had a potentially preventable readmission within 30 days of discharge, she reported at the International Stroke Conference sponsored by the American Heart Association.
"National programs aimed at reducing 30-day poststroke readmissions may have limited impact unless they focus on the small subset of potentially preventable readmissions. Identifying patients at greatest risk is an important first step for developing postdischarge interventions to minimize preventable readmissions and improve the care transitions for our stroke patients," said Dr. Lichtman of the department of epidemiology at Yale University, New Haven, Conn.
Toward that goal, she and her coinvestigators identified several strong predictors of preventable readmissions following ischemic stroke discharge. These included diabetes, heart failure, age greater than 85, black race, female gender, and prior MI, each of which was independently associated with a 1.4- to 2.3-fold increased risk.
Dr. Lichtman’s study included all 302,565 fee-for-service Medicare patients discharged alive after hospitalization for ischemic stroke in 2006. Of this group, 12.9% had at least one readmission within 30 days, of which 1.7% (5,322) were determined to be potentially preventable using evidence-based measures established by the Agency for Healthcare Research and Quality.
Potentially preventable readmission rates were slightly but statistically significantly higher in the Southeast and Mid-Atlantic states and lower than average in the Mountain and Pacific regions. But outlier hospitals with significantly higher-than-average rates were identified throughout the United States.
Patients deemed by AHRQ criteria to have had a potentially preventable readmission had significantly more comorbid conditions than those who weren’t rehospitalized within 30 days of discharge. For example, they had a 34% prevalence of heart failure and a 36% prevalence of diabetes, compared with 15% and 28% rates, respectively, in those without readmission.
Session cochair Dr. Cheryl Bushnell honed in on this finding, asking whether patients who are already sicker when they have their stroke are less able to withstand the rigors of the hospital experience, and therefore more likely to require early readmission.
"Stroke patients frequently don’t get much sleep in the hospital. They’re NPO until their swallowing status is established, so they’re not getting nutrition. They’re exposed to the risk of infections in the hospital environment. How many of these readmissions are due to the so-called posthospital syndrome – that is, once you’ve been in the hospital and subjected to all the things we need to do to people in the hospital, you’re basically at risk for anything?" commented Dr. Bushnell of Wake Forest University in Winston-Salem, N.C.
Point well taken, replied Dr. Lichtman. The fact is that it’s not at all clear as of yet how many so-called preventable readmissions truly are preventable and thus a quality-of-care problem. This is a hot issue for hospitals now with regard to acute MI because they’re starting to receive financial penalties for higher-than-expected early readmission rates after MI.
Dr. Lichtman’s study was funded by the National Institute of Neurological Disorders and Stroke. She reported having no relevant financial conflicts.
HONOLULU – Health care reformers looking to drive down preventable 30-day readmission rates will find slim pickings among the nation’s elderly hospitalized for ischemic stroke, according to Judith H. Lichtman, Ph.D.
An analysis of national fee-for-service Medicare data concluded that a mere 1.7% of patients hospitalized for ischemic stroke in 2006 had a potentially preventable readmission within 30 days of discharge, she reported at the International Stroke Conference sponsored by the American Heart Association.
"National programs aimed at reducing 30-day poststroke readmissions may have limited impact unless they focus on the small subset of potentially preventable readmissions. Identifying patients at greatest risk is an important first step for developing postdischarge interventions to minimize preventable readmissions and improve the care transitions for our stroke patients," said Dr. Lichtman of the department of epidemiology at Yale University, New Haven, Conn.
Toward that goal, she and her coinvestigators identified several strong predictors of preventable readmissions following ischemic stroke discharge. These included diabetes, heart failure, age greater than 85, black race, female gender, and prior MI, each of which was independently associated with a 1.4- to 2.3-fold increased risk.
Dr. Lichtman’s study included all 302,565 fee-for-service Medicare patients discharged alive after hospitalization for ischemic stroke in 2006. Of this group, 12.9% had at least one readmission within 30 days, of which 1.7% (5,322) were determined to be potentially preventable using evidence-based measures established by the Agency for Healthcare Research and Quality.
Potentially preventable readmission rates were slightly but statistically significantly higher in the Southeast and Mid-Atlantic states and lower than average in the Mountain and Pacific regions. But outlier hospitals with significantly higher-than-average rates were identified throughout the United States.
Patients deemed by AHRQ criteria to have had a potentially preventable readmission had significantly more comorbid conditions than those who weren’t rehospitalized within 30 days of discharge. For example, they had a 34% prevalence of heart failure and a 36% prevalence of diabetes, compared with 15% and 28% rates, respectively, in those without readmission.
Session cochair Dr. Cheryl Bushnell honed in on this finding, asking whether patients who are already sicker when they have their stroke are less able to withstand the rigors of the hospital experience, and therefore more likely to require early readmission.
"Stroke patients frequently don’t get much sleep in the hospital. They’re NPO until their swallowing status is established, so they’re not getting nutrition. They’re exposed to the risk of infections in the hospital environment. How many of these readmissions are due to the so-called posthospital syndrome – that is, once you’ve been in the hospital and subjected to all the things we need to do to people in the hospital, you’re basically at risk for anything?" commented Dr. Bushnell of Wake Forest University in Winston-Salem, N.C.
Point well taken, replied Dr. Lichtman. The fact is that it’s not at all clear as of yet how many so-called preventable readmissions truly are preventable and thus a quality-of-care problem. This is a hot issue for hospitals now with regard to acute MI because they’re starting to receive financial penalties for higher-than-expected early readmission rates after MI.
Dr. Lichtman’s study was funded by the National Institute of Neurological Disorders and Stroke. She reported having no relevant financial conflicts.
HONOLULU – Health care reformers looking to drive down preventable 30-day readmission rates will find slim pickings among the nation’s elderly hospitalized for ischemic stroke, according to Judith H. Lichtman, Ph.D.
An analysis of national fee-for-service Medicare data concluded that a mere 1.7% of patients hospitalized for ischemic stroke in 2006 had a potentially preventable readmission within 30 days of discharge, she reported at the International Stroke Conference sponsored by the American Heart Association.
"National programs aimed at reducing 30-day poststroke readmissions may have limited impact unless they focus on the small subset of potentially preventable readmissions. Identifying patients at greatest risk is an important first step for developing postdischarge interventions to minimize preventable readmissions and improve the care transitions for our stroke patients," said Dr. Lichtman of the department of epidemiology at Yale University, New Haven, Conn.
Toward that goal, she and her coinvestigators identified several strong predictors of preventable readmissions following ischemic stroke discharge. These included diabetes, heart failure, age greater than 85, black race, female gender, and prior MI, each of which was independently associated with a 1.4- to 2.3-fold increased risk.
Dr. Lichtman’s study included all 302,565 fee-for-service Medicare patients discharged alive after hospitalization for ischemic stroke in 2006. Of this group, 12.9% had at least one readmission within 30 days, of which 1.7% (5,322) were determined to be potentially preventable using evidence-based measures established by the Agency for Healthcare Research and Quality.
Potentially preventable readmission rates were slightly but statistically significantly higher in the Southeast and Mid-Atlantic states and lower than average in the Mountain and Pacific regions. But outlier hospitals with significantly higher-than-average rates were identified throughout the United States.
Patients deemed by AHRQ criteria to have had a potentially preventable readmission had significantly more comorbid conditions than those who weren’t rehospitalized within 30 days of discharge. For example, they had a 34% prevalence of heart failure and a 36% prevalence of diabetes, compared with 15% and 28% rates, respectively, in those without readmission.
Session cochair Dr. Cheryl Bushnell honed in on this finding, asking whether patients who are already sicker when they have their stroke are less able to withstand the rigors of the hospital experience, and therefore more likely to require early readmission.
"Stroke patients frequently don’t get much sleep in the hospital. They’re NPO until their swallowing status is established, so they’re not getting nutrition. They’re exposed to the risk of infections in the hospital environment. How many of these readmissions are due to the so-called posthospital syndrome – that is, once you’ve been in the hospital and subjected to all the things we need to do to people in the hospital, you’re basically at risk for anything?" commented Dr. Bushnell of Wake Forest University in Winston-Salem, N.C.
Point well taken, replied Dr. Lichtman. The fact is that it’s not at all clear as of yet how many so-called preventable readmissions truly are preventable and thus a quality-of-care problem. This is a hot issue for hospitals now with regard to acute MI because they’re starting to receive financial penalties for higher-than-expected early readmission rates after MI.
Dr. Lichtman’s study was funded by the National Institute of Neurological Disorders and Stroke. She reported having no relevant financial conflicts.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Only 1.7% of more than 300,000 consecutive Medicare patients discharged following hospitalization for ischemic stroke were judged to have had a potentially preventable readmission within 30 days.
Data Source: A retrospective study of all fee-for-service Medicare beneficiaries discharged alive with a primary diagnosis of ischemic stroke in 2006.
Disclosures: This study was funded by the National Institute of Neurological Disorders and Stroke. The presenter reported having no relevant financial conflicts.
Stroke thrombolysis can be done safely outside ICU
HONOLULU – Traditionally, acute ischemic stroke patients have been admitted to an ICU for administration of intravenous tissue plasminogen activator therapy. But it’s not necessary, according to Kisha C. Coleman.
Instead, these patients can safely undergo intravenous TPA therapy in a well-prepared stroke unit with excellent clinical outcomes – and big cost savings, said Ms. Coleman, a nurse at the University of Alabama at Birmingham comprehensive stroke center.
She presented what she and her coinvestigators said is the largest-ever series of non–ICU-managed stroke patients treated with intravenous TPA. The series consisted of 302 consecutive patients admitted from the emergency department to the university’s nine-bed intermediate-level stroke unit for intravenous TPA therapy during 2009-2011. During this 3-year period, another 31 acute ischemic stroke patients were sent from the ED to the ICU because of hemodynamic or pulmonary instability.
The stroke unit has flexible staffing, and the nurses have undergone extensive training. Their capabilities include management of intravenous TPA therapy, administration of nicardipine infusions when warranted for blood pressure control, management of bilevel positive airway pressure ventilation, and noninvasive or direct central arterial line and hardwired cardiac monitoring.
The median National Institutes of Health Stroke Scale score at admission to the stroke unit was 9, with a median modified Rankin score of 3 at discharge. Ten percent of patients received nicardipine infusions.
The overall symptomatic intracranial hemorrhage rate was 3.3%, with a systemic hemorrhage rate of 2.9%. The volume of patients admitted to the stroke unit for intravenous TPA increased over time from 86 patients in 2009 to 107 in 2010 and 109 in 2011. Meanwhile, the incidence of symptomatic intracranial hemorrhage dropped from 4.7% the first year to 2.8% in each of the next 2 years.
"We attribute that to increased nurse efficiency over time in caring for these types of patients," Ms. Coleman said at the International Stroke Conference, sponsored by the American Heart Association.
No patients required a transfer from the stroke unit to the ICU for continued management. No TPA-related deaths occurred.
Hospital length of stay decreased from a median 9.8 days in 2009 to 6.4 in 2010 and 5.2 days in 2011, she continued.
The 31 patients admitted to the ICU from the emergency department during the study period and the 302 managed in the stroke unit had similar admission NIH Stroke Scale severity scores, symptomatic intracranial hemorrhage and systemic hemorrhage rates, and average lengths of stay.
A day in the ICU costs about $1,200 more than does a day in the stroke unit, she noted. The estimated cost savings resulting from avoided ICU days during this 3-year period was $362,400, even after adjustment for the expense of the additional training for nurses. And that figure is a conservative one that probably significantly underestimates the true savings, according to Ms. Coleman.
"Use of the ICU solely for management of TPA monitoring may constitute a significant overuse of system resources at an expense that is not associated with additional safety benefit," she concluded.
Beyond the sizable cost savings, another advantage of managing intravenous TPA therapy in the stroke unit rather than the ICU is continuity of care. These patients are admitted to and discharged from the stroke unit, she noted.
Ms. Coleman reported having no relevant financial conflicts.
HONOLULU – Traditionally, acute ischemic stroke patients have been admitted to an ICU for administration of intravenous tissue plasminogen activator therapy. But it’s not necessary, according to Kisha C. Coleman.
Instead, these patients can safely undergo intravenous TPA therapy in a well-prepared stroke unit with excellent clinical outcomes – and big cost savings, said Ms. Coleman, a nurse at the University of Alabama at Birmingham comprehensive stroke center.
She presented what she and her coinvestigators said is the largest-ever series of non–ICU-managed stroke patients treated with intravenous TPA. The series consisted of 302 consecutive patients admitted from the emergency department to the university’s nine-bed intermediate-level stroke unit for intravenous TPA therapy during 2009-2011. During this 3-year period, another 31 acute ischemic stroke patients were sent from the ED to the ICU because of hemodynamic or pulmonary instability.
The stroke unit has flexible staffing, and the nurses have undergone extensive training. Their capabilities include management of intravenous TPA therapy, administration of nicardipine infusions when warranted for blood pressure control, management of bilevel positive airway pressure ventilation, and noninvasive or direct central arterial line and hardwired cardiac monitoring.
The median National Institutes of Health Stroke Scale score at admission to the stroke unit was 9, with a median modified Rankin score of 3 at discharge. Ten percent of patients received nicardipine infusions.
The overall symptomatic intracranial hemorrhage rate was 3.3%, with a systemic hemorrhage rate of 2.9%. The volume of patients admitted to the stroke unit for intravenous TPA increased over time from 86 patients in 2009 to 107 in 2010 and 109 in 2011. Meanwhile, the incidence of symptomatic intracranial hemorrhage dropped from 4.7% the first year to 2.8% in each of the next 2 years.
"We attribute that to increased nurse efficiency over time in caring for these types of patients," Ms. Coleman said at the International Stroke Conference, sponsored by the American Heart Association.
No patients required a transfer from the stroke unit to the ICU for continued management. No TPA-related deaths occurred.
Hospital length of stay decreased from a median 9.8 days in 2009 to 6.4 in 2010 and 5.2 days in 2011, she continued.
The 31 patients admitted to the ICU from the emergency department during the study period and the 302 managed in the stroke unit had similar admission NIH Stroke Scale severity scores, symptomatic intracranial hemorrhage and systemic hemorrhage rates, and average lengths of stay.
A day in the ICU costs about $1,200 more than does a day in the stroke unit, she noted. The estimated cost savings resulting from avoided ICU days during this 3-year period was $362,400, even after adjustment for the expense of the additional training for nurses. And that figure is a conservative one that probably significantly underestimates the true savings, according to Ms. Coleman.
"Use of the ICU solely for management of TPA monitoring may constitute a significant overuse of system resources at an expense that is not associated with additional safety benefit," she concluded.
Beyond the sizable cost savings, another advantage of managing intravenous TPA therapy in the stroke unit rather than the ICU is continuity of care. These patients are admitted to and discharged from the stroke unit, she noted.
Ms. Coleman reported having no relevant financial conflicts.
HONOLULU – Traditionally, acute ischemic stroke patients have been admitted to an ICU for administration of intravenous tissue plasminogen activator therapy. But it’s not necessary, according to Kisha C. Coleman.
Instead, these patients can safely undergo intravenous TPA therapy in a well-prepared stroke unit with excellent clinical outcomes – and big cost savings, said Ms. Coleman, a nurse at the University of Alabama at Birmingham comprehensive stroke center.
She presented what she and her coinvestigators said is the largest-ever series of non–ICU-managed stroke patients treated with intravenous TPA. The series consisted of 302 consecutive patients admitted from the emergency department to the university’s nine-bed intermediate-level stroke unit for intravenous TPA therapy during 2009-2011. During this 3-year period, another 31 acute ischemic stroke patients were sent from the ED to the ICU because of hemodynamic or pulmonary instability.
The stroke unit has flexible staffing, and the nurses have undergone extensive training. Their capabilities include management of intravenous TPA therapy, administration of nicardipine infusions when warranted for blood pressure control, management of bilevel positive airway pressure ventilation, and noninvasive or direct central arterial line and hardwired cardiac monitoring.
The median National Institutes of Health Stroke Scale score at admission to the stroke unit was 9, with a median modified Rankin score of 3 at discharge. Ten percent of patients received nicardipine infusions.
The overall symptomatic intracranial hemorrhage rate was 3.3%, with a systemic hemorrhage rate of 2.9%. The volume of patients admitted to the stroke unit for intravenous TPA increased over time from 86 patients in 2009 to 107 in 2010 and 109 in 2011. Meanwhile, the incidence of symptomatic intracranial hemorrhage dropped from 4.7% the first year to 2.8% in each of the next 2 years.
"We attribute that to increased nurse efficiency over time in caring for these types of patients," Ms. Coleman said at the International Stroke Conference, sponsored by the American Heart Association.
No patients required a transfer from the stroke unit to the ICU for continued management. No TPA-related deaths occurred.
Hospital length of stay decreased from a median 9.8 days in 2009 to 6.4 in 2010 and 5.2 days in 2011, she continued.
The 31 patients admitted to the ICU from the emergency department during the study period and the 302 managed in the stroke unit had similar admission NIH Stroke Scale severity scores, symptomatic intracranial hemorrhage and systemic hemorrhage rates, and average lengths of stay.
A day in the ICU costs about $1,200 more than does a day in the stroke unit, she noted. The estimated cost savings resulting from avoided ICU days during this 3-year period was $362,400, even after adjustment for the expense of the additional training for nurses. And that figure is a conservative one that probably significantly underestimates the true savings, according to Ms. Coleman.
"Use of the ICU solely for management of TPA monitoring may constitute a significant overuse of system resources at an expense that is not associated with additional safety benefit," she concluded.
Beyond the sizable cost savings, another advantage of managing intravenous TPA therapy in the stroke unit rather than the ICU is continuity of care. These patients are admitted to and discharged from the stroke unit, she noted.
Ms. Coleman reported having no relevant financial conflicts.
AT THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Three hundred and two consecutive acute ischemic stroke patients admitted to a stroke unit for intravenous tissue plasminogen activator therapy rather than to an ICU had impressively favorable outcomes, with an overall 3.3% symptomatic intracranial hemorrhage rate.
Data Source: A large case series consisting of 302 acute ischemic stroke patients admitted to an intermediate-level stroke unit for intravenous TPA and 31 others admitted to an ICU because they required intubation and mechanical ventilation.
Disclosures: The presenter reported having no relevant financial conflicts.