User login
The Obesity Society: Annual Scientific Meeting (Obesity 2013)
The politics of food addiction: Who wins, who 'loses'
ATLANTA – It’s too soon to disrupt current obesity treatment by declaring food addiction to be a clinical condition, according to Dr. Paul Fletcher.
"If we are to employ [the term] food addiction ... it needs a firm scientific basis," said Dr. Fletcher, who is the Bernard Wolfe Professor of Health Neuroscience in the department of psychiatry at University of Cambridge (England).
Organized medicine took the first step toward recognizing food addiction as a clinical diagnosis with the 2013 inclusion of binge eating disorder (BED) in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). That recognition has the potential to set the stage for an overhaul in delivery and funding of obesity treatment as well as how people with pathologic eating behaviors are viewed.
Obesogenic environment
For some, the answer to obesity and food addiction is to remove unhealthful foods from the environment. And to address "powerful environmental drives to consume them," Dr. Hisham Ziauddeen, a Wellcome Trust Fellow in Translational Medicine and Therapeutics at Cambridge, said in an interview.
In a separate presentation at a meeting, sponsored by the Obesity Society and the Society for the Study of Ingestive Behavior, Ashley Gearhardt, Ph.D., noted that researchers do not know whether food addiction exists. "The science is emerging." Foods high in fat and sugar, especially when aggressively marketed to children, are the chief culprits of the obesity epidemic, according to Dr. Gearhardt, a clinical psychologist at the University of Michigan, Ann Arbor.
"If scientific evidence identifies that certain foods are also capable of hijacking the brain in an addictive manner, it would likely be a landmark change that would support bold policy approaches that focus on improving the food environment," she has said (Biol. Psychiatry 2013;73:802-3).
Current research in the field is focused on the individual risk factors for compulsive eating, such as impulsivity or reward sensitivity, Dr. Gearhardt said. However, the lack of addictive behaviors associated with "minimally processed foods that are relatively low in sugar and fat, such as apples or chicken breasts," means research now needs to determine if there is something about the food or behavior "that leads to compulsive problematic use," she said in an interview.
"Individual approaches may be helpful in developing clinical interventions but will touch the lives of far fewer people than will policy changes that affect entire populations," she said.
Dr. Gearhardt and her associates sought to link obesity to addictive patterning in the brain through the combined use of functional neuroimaging (fMRI) and scores on the Yale Food Addiction Scale (YFAS), which applies substance-dependence criteria in the DSM-IV-TR as a type of metric for addictive eating behaviors.
The investigators used fMRI maps of participants’ brain activation when they were given food cues of either a tasteless substance or a chocolate milkshake high in fat and sugar. These images were then compared with the participants’ scores from the YFAS. The group was a mixture of both lean and obese women (Arch. Gen. Psychiatry. 2011;68:808-16).
The researchers found that when presented with a chocolate milkshake, those with higher YFAS scores, regardless of body mass index, experienced "significantly greater activation" in brain regions associated with dopaminergic release, including the anterior cingulate cortex. Those with the highest YFAS scores experienced a significant increase in activity of the dorsolateral prefrontal cortex.
‘Elegant experiments’
While fMRI research into the neurobiologic response to food has "generated some very elegant experiments," according to Dr. Fletcher, he is concerned that food addiction proponents have neglected to see these data in a larger context. "The literature is hugely inconsistent, and ignoring this fact may be inconvenient ... but if we continue to do so, it will come back to slap us in the face."
Because neuroimages "are often ambiguous, unless they are constrained by a specific hypothesis, it becomes more like reading tarot cards than interpreting scientific data," he said. "There is a dangerous tendency for people to have a particular perspective and then, no matter what the fMRI data show, to interpret them according to the perspective with which they started out."
And while this free hand with data interpretation happens generally, Dr. Fletcher said he has been "particularly struck" by its occurrence in the food addiction field. "There seem to be very few constraints on interpretation of the regional activation," he said, noting that whether researchers are looking at obesity, binge-eating, or anyone assumed to have a food addition. "Inevitably, [the researchers] find differences in neural activation in such groups but the interpretations of those activations are often post hoc and heavily biased by what the researchers believed in the first place."
As an example, he cited how activity in the anterior cingulate cortex in overweight people given food cues may be interpreted as a sign of craving. "But this is an unjustified inference because we do not know what the anterior cingulate cortex does and it far more frequently related to other processes than to craving."
Dr. Fletcher and his colleagues’ alarm over this "oversimplification of data" prompted a polite, but impassioned, back and forth with Dr. Gearhardt and her associates, published in Nature Reviews Neuroscience (2012;13:279-86 [doi:10.1038/nrn3212]); (2012;13:514 [doi:10.1038/nrn3212-c1]); (2012;13:514 [doi:10.1038/nrn3212-c2]).
In the first of these editorials, Dr. Fletcher and his coauthors wrote that "the messages now emerging from the neuroscientific research community may therefore have an unprecedented impact on policy development," and in another, urged the adoption of "a more detailed consideration" of how to explore food addiction, particularly since cognitive neuroscience is already moving the field beyond ideas based "purely on clinical overlap" and the model of addiction as delineated in the DSM-IV-TR.
Obesity subsets
"Dr. Fletcher and I agree that the concept of ‘food addiction’ is still an open question," Dr. Gearhardt said in an interview. "My group believes that there is evidence building that suggests it is plausible that an addictive process contributes to problematic eating in some circumstances, especially for eaters who exhibit behavioral phenotypes."
Binge eating, emotional eating, and other pathologies surrounding attitudes toward food also were noted in participants with high YFAS scores in Dr. Gearhardt’s study. "We see evidence of addictive-like processes contributing to problematic eating even for individuals who do not meet the criteria for BED," she said.
Dr. Fletcher noted that "there is a clear degree of clinical overlap between obesity and binge eating, particularly binge eating disorder and drug addiction." Specifically, tolerance, withdrawal, persistent desire for food, eating more than intended, and the diminishment of social engagement in exchange for more time spent acquiring and ingesting food all parallel drug addiction. "However, we don’t know what the overlap is," said Dr. Fletcher. "Is it sugar? Is it fat? Is it a combination? We really don’t know yet."
Populations vs. individuals
"If certain foods are addictive, this may partially explain the difficulty people experience in achieving sustainable weight loss," according to Dr. Gearhardt in commenting on the fMRI study results. "Ubiquitous food advertising and the availability of inexpensive palatable foods may make it extremely difficult to adhere to healthier food choices because the omnipresent food cues trigger the reward system."
Dr. Gearhardt speculated that a focus on specific food ingredients being at the root of addiction-linked obesity may spur activism by manufacturers. "The food industry will likely use any inconsistency in the food addiction literature to plant doubt, attack scientists’ credibility, or fund negative studies," they wrote.
By focusing on how detrimental the food environment has become as a result of "heavily marketed foods that interact with the brain in harmful ways," the public may be more likely to support restrictive policies such as "taxing addictive foods, limiting marketing of these foods to children, and enacting zoning laws that limit the number of vendors selling such foods" among other measures, she wrote.
Dr. Fletcher acknowledged that there is likely a legitimate "battle to be joined" against marketers of junk food and other agents contributing to a deleterious food environment, but attacking the problem at the societal level without consideration of the potential impact on the individual will ultimately backfire. "We must be very careful about how we line up our troops," he said.
"Changing behavior at a population level, which indubitably is required, is not going to be easy," said Dr. Ziauddeen. "As well as the resistance of those with vested interests, such changes will be considered widely unacceptable if they are perceived to entail a loss of liberty."
Although Dr. Fletcher and Dr. Ziauddeen agree a lack of willpower and moral frailty are antiquated notions of why people become obese, assuming that diagnosing people as food addicts will protect them, either from stigmatization or any unforeseen effects of policy changes, is short-sighted.
"Based on our experience with drug addictions over the centuries, it is hard to think that food addiction will not come with some stigma and the consequences thereof," he said.
And Dr. Ziauddeen agreed that, "If the science is shaky and hard to defend, it will be ripped apart." Beyond it possibly being "indefensible" in the face of the opposition from processed food manufacturers, thus setting the field back on its heels, there is the danger of a loss of personal liberty that results, not for the sake of the greater good, but solely from policies based on shoddy science.
"The removal of choice is less threatening if it is done to protect against a situation in which the individual has no real choice anyway, as is the case with addictive substances," said Dr. Ziauddeen. "In short, if there is an addictive agent in some foods, then policy change and legislation can be seen as protective rather than restrictive." This is only possible however, he said, if there is "clear, consistent evidence that there is indeed an addictive substance in food."
And yet, regarding a connection between obesity and food addiction, "the most striking finding is complete inconsistency," said Dr. Fletcher. "I would like to see the same sorts of changes that those supporting food addiction would like, but I do not think that we are going to succeed by using a poorly specified concept with little real evidence to back it up."
Dopamine response not reliable measure
"Food addiction may well exist, [but] even then, it may only explain a tiny fraction of obesity and overeating," according to Dr. Fletcher. "Perhaps the major problem is our general limitations in our often dopaminergically centered views of what constitutes addiction."
A full understanding of the brain’s pathophysiology is still under development, he said. But in addition to classic behavioral manifestations, such as persistent use of a substance, accepted components of addiction include reduced dopamine-receptor density in the ventral striatum and a flip in the neurocircuitry for decision making from the ventral to the dorsal striatum.
Otherwise, he said, conclusive statements about the neurobiology of addiction are suspect. "When we run a functional neuroimaging experiment, we are looking at many different brain regions and, for pretty much all of these, there is a fairly dense ambiguity about what processes they carry out."
In addition, said Dr. Fletcher, although several researchers have tried to replicate one particular study showing that that showed those with severe obesity had reduced raclopride, an indication their dopamine reception was suppressed, the various findings have been inconsistent, thus, said Dr. Fletcher, "there is no proof that there is reduced dopamine in obesity" (Lancet 2001;357:354-7).
As the field of addiction research advances, there will be a shift in the viewpoint that dopamine is the "end all and be all," in part because there will be a deeper understanding of individual variability to different substances that lead to different forms of eating pathologies, he said. "We need to entertain the notion that no single characteristic will define the nature of reward-processing in obesity and that there may be many routes to positive calorie balance."
Longitudinal studies of individual variability to certain foods also could help better determine the impact of certain foods on the brain, he said.
Winners and ‘losers’
"In terms of those who stand to gain from the acceptance of food addiction," said Dr. Fletcher, "At first glance, this would seem to be the people who offer treatments for food addiction and the people who might make some money by suing [processed food] companies."
Yet, for Dr. Gearhardt, if food addiction is proved, and a direct line can be drawn between the food industry’s intentional manipulation of ingredients to profit from this "brain hijacking," Dr. Gearhardt said, "This brings up the question of industry culpability and the ethics of aggressively marketing it to children."
Dr. Gearhardt also believes the possibility of a clinical food addiction diagnosis for those who struggle with pathological eating might "encourage more people ... to receive professional help rather than beat themselves up for not being able to stick to diet after diet on their own."
Conversely, Dr. Ziauddeen noted what while a food addiction diagnosis may offer someone consolation and motivation to seek help, "What if the person is subject to restrictions or treatments based on the diagnosis?" Specifically, he cited ineligibility for bariatric surgery or less clout in the eyes of the court for child custody. "This does not require a stretch of the imagination," he said. "If you have a diagnosis of alcohol dependence, it influences your chances of receiving a liver transplant. If you have a diagnosis of drug or alcohol addiction, it impacts social care decisions made about your children."
Accepting food addiction as real will affect not only those given the diagnosis, but also the so-called "unaffected" public, said Dr. Fletcher. "If food ‘X’ is addictive, to what extent should it be controlled?" He also suggested that health care provision would experience overhaul: "What will be the effect of diverting funding to food addiction treatment from other obesity-related treatments?"
Food addiction "may help us think of novel and hopefully more effective strategies for treating eating-related concerns," said Dr. Gearhardt.
Regardless, Dr. Fletcher warned that because obesity is multifactorial, and includes molecular, metabolic, behavioral, societal and environmental elements, we should not rush to accept "simplistic" answers, or force things to fit where they actually might not. "The thing I think we need to stop right now is this selective citing because we like the narrative."
Dr. Fletcher, Dr. Ziauddeen, and Dr. Gearhardt had no relevant disclosures.
ATLANTA – It’s too soon to disrupt current obesity treatment by declaring food addiction to be a clinical condition, according to Dr. Paul Fletcher.
"If we are to employ [the term] food addiction ... it needs a firm scientific basis," said Dr. Fletcher, who is the Bernard Wolfe Professor of Health Neuroscience in the department of psychiatry at University of Cambridge (England).
Organized medicine took the first step toward recognizing food addiction as a clinical diagnosis with the 2013 inclusion of binge eating disorder (BED) in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). That recognition has the potential to set the stage for an overhaul in delivery and funding of obesity treatment as well as how people with pathologic eating behaviors are viewed.
Obesogenic environment
For some, the answer to obesity and food addiction is to remove unhealthful foods from the environment. And to address "powerful environmental drives to consume them," Dr. Hisham Ziauddeen, a Wellcome Trust Fellow in Translational Medicine and Therapeutics at Cambridge, said in an interview.
In a separate presentation at a meeting, sponsored by the Obesity Society and the Society for the Study of Ingestive Behavior, Ashley Gearhardt, Ph.D., noted that researchers do not know whether food addiction exists. "The science is emerging." Foods high in fat and sugar, especially when aggressively marketed to children, are the chief culprits of the obesity epidemic, according to Dr. Gearhardt, a clinical psychologist at the University of Michigan, Ann Arbor.
"If scientific evidence identifies that certain foods are also capable of hijacking the brain in an addictive manner, it would likely be a landmark change that would support bold policy approaches that focus on improving the food environment," she has said (Biol. Psychiatry 2013;73:802-3).
Current research in the field is focused on the individual risk factors for compulsive eating, such as impulsivity or reward sensitivity, Dr. Gearhardt said. However, the lack of addictive behaviors associated with "minimally processed foods that are relatively low in sugar and fat, such as apples or chicken breasts," means research now needs to determine if there is something about the food or behavior "that leads to compulsive problematic use," she said in an interview.
"Individual approaches may be helpful in developing clinical interventions but will touch the lives of far fewer people than will policy changes that affect entire populations," she said.
Dr. Gearhardt and her associates sought to link obesity to addictive patterning in the brain through the combined use of functional neuroimaging (fMRI) and scores on the Yale Food Addiction Scale (YFAS), which applies substance-dependence criteria in the DSM-IV-TR as a type of metric for addictive eating behaviors.
The investigators used fMRI maps of participants’ brain activation when they were given food cues of either a tasteless substance or a chocolate milkshake high in fat and sugar. These images were then compared with the participants’ scores from the YFAS. The group was a mixture of both lean and obese women (Arch. Gen. Psychiatry. 2011;68:808-16).
The researchers found that when presented with a chocolate milkshake, those with higher YFAS scores, regardless of body mass index, experienced "significantly greater activation" in brain regions associated with dopaminergic release, including the anterior cingulate cortex. Those with the highest YFAS scores experienced a significant increase in activity of the dorsolateral prefrontal cortex.
‘Elegant experiments’
While fMRI research into the neurobiologic response to food has "generated some very elegant experiments," according to Dr. Fletcher, he is concerned that food addiction proponents have neglected to see these data in a larger context. "The literature is hugely inconsistent, and ignoring this fact may be inconvenient ... but if we continue to do so, it will come back to slap us in the face."
Because neuroimages "are often ambiguous, unless they are constrained by a specific hypothesis, it becomes more like reading tarot cards than interpreting scientific data," he said. "There is a dangerous tendency for people to have a particular perspective and then, no matter what the fMRI data show, to interpret them according to the perspective with which they started out."
And while this free hand with data interpretation happens generally, Dr. Fletcher said he has been "particularly struck" by its occurrence in the food addiction field. "There seem to be very few constraints on interpretation of the regional activation," he said, noting that whether researchers are looking at obesity, binge-eating, or anyone assumed to have a food addition. "Inevitably, [the researchers] find differences in neural activation in such groups but the interpretations of those activations are often post hoc and heavily biased by what the researchers believed in the first place."
As an example, he cited how activity in the anterior cingulate cortex in overweight people given food cues may be interpreted as a sign of craving. "But this is an unjustified inference because we do not know what the anterior cingulate cortex does and it far more frequently related to other processes than to craving."
Dr. Fletcher and his colleagues’ alarm over this "oversimplification of data" prompted a polite, but impassioned, back and forth with Dr. Gearhardt and her associates, published in Nature Reviews Neuroscience (2012;13:279-86 [doi:10.1038/nrn3212]); (2012;13:514 [doi:10.1038/nrn3212-c1]); (2012;13:514 [doi:10.1038/nrn3212-c2]).
In the first of these editorials, Dr. Fletcher and his coauthors wrote that "the messages now emerging from the neuroscientific research community may therefore have an unprecedented impact on policy development," and in another, urged the adoption of "a more detailed consideration" of how to explore food addiction, particularly since cognitive neuroscience is already moving the field beyond ideas based "purely on clinical overlap" and the model of addiction as delineated in the DSM-IV-TR.
Obesity subsets
"Dr. Fletcher and I agree that the concept of ‘food addiction’ is still an open question," Dr. Gearhardt said in an interview. "My group believes that there is evidence building that suggests it is plausible that an addictive process contributes to problematic eating in some circumstances, especially for eaters who exhibit behavioral phenotypes."
Binge eating, emotional eating, and other pathologies surrounding attitudes toward food also were noted in participants with high YFAS scores in Dr. Gearhardt’s study. "We see evidence of addictive-like processes contributing to problematic eating even for individuals who do not meet the criteria for BED," she said.
Dr. Fletcher noted that "there is a clear degree of clinical overlap between obesity and binge eating, particularly binge eating disorder and drug addiction." Specifically, tolerance, withdrawal, persistent desire for food, eating more than intended, and the diminishment of social engagement in exchange for more time spent acquiring and ingesting food all parallel drug addiction. "However, we don’t know what the overlap is," said Dr. Fletcher. "Is it sugar? Is it fat? Is it a combination? We really don’t know yet."
Populations vs. individuals
"If certain foods are addictive, this may partially explain the difficulty people experience in achieving sustainable weight loss," according to Dr. Gearhardt in commenting on the fMRI study results. "Ubiquitous food advertising and the availability of inexpensive palatable foods may make it extremely difficult to adhere to healthier food choices because the omnipresent food cues trigger the reward system."
Dr. Gearhardt speculated that a focus on specific food ingredients being at the root of addiction-linked obesity may spur activism by manufacturers. "The food industry will likely use any inconsistency in the food addiction literature to plant doubt, attack scientists’ credibility, or fund negative studies," they wrote.
By focusing on how detrimental the food environment has become as a result of "heavily marketed foods that interact with the brain in harmful ways," the public may be more likely to support restrictive policies such as "taxing addictive foods, limiting marketing of these foods to children, and enacting zoning laws that limit the number of vendors selling such foods" among other measures, she wrote.
Dr. Fletcher acknowledged that there is likely a legitimate "battle to be joined" against marketers of junk food and other agents contributing to a deleterious food environment, but attacking the problem at the societal level without consideration of the potential impact on the individual will ultimately backfire. "We must be very careful about how we line up our troops," he said.
"Changing behavior at a population level, which indubitably is required, is not going to be easy," said Dr. Ziauddeen. "As well as the resistance of those with vested interests, such changes will be considered widely unacceptable if they are perceived to entail a loss of liberty."
Although Dr. Fletcher and Dr. Ziauddeen agree a lack of willpower and moral frailty are antiquated notions of why people become obese, assuming that diagnosing people as food addicts will protect them, either from stigmatization or any unforeseen effects of policy changes, is short-sighted.
"Based on our experience with drug addictions over the centuries, it is hard to think that food addiction will not come with some stigma and the consequences thereof," he said.
And Dr. Ziauddeen agreed that, "If the science is shaky and hard to defend, it will be ripped apart." Beyond it possibly being "indefensible" in the face of the opposition from processed food manufacturers, thus setting the field back on its heels, there is the danger of a loss of personal liberty that results, not for the sake of the greater good, but solely from policies based on shoddy science.
"The removal of choice is less threatening if it is done to protect against a situation in which the individual has no real choice anyway, as is the case with addictive substances," said Dr. Ziauddeen. "In short, if there is an addictive agent in some foods, then policy change and legislation can be seen as protective rather than restrictive." This is only possible however, he said, if there is "clear, consistent evidence that there is indeed an addictive substance in food."
And yet, regarding a connection between obesity and food addiction, "the most striking finding is complete inconsistency," said Dr. Fletcher. "I would like to see the same sorts of changes that those supporting food addiction would like, but I do not think that we are going to succeed by using a poorly specified concept with little real evidence to back it up."
Dopamine response not reliable measure
"Food addiction may well exist, [but] even then, it may only explain a tiny fraction of obesity and overeating," according to Dr. Fletcher. "Perhaps the major problem is our general limitations in our often dopaminergically centered views of what constitutes addiction."
A full understanding of the brain’s pathophysiology is still under development, he said. But in addition to classic behavioral manifestations, such as persistent use of a substance, accepted components of addiction include reduced dopamine-receptor density in the ventral striatum and a flip in the neurocircuitry for decision making from the ventral to the dorsal striatum.
Otherwise, he said, conclusive statements about the neurobiology of addiction are suspect. "When we run a functional neuroimaging experiment, we are looking at many different brain regions and, for pretty much all of these, there is a fairly dense ambiguity about what processes they carry out."
In addition, said Dr. Fletcher, although several researchers have tried to replicate one particular study showing that that showed those with severe obesity had reduced raclopride, an indication their dopamine reception was suppressed, the various findings have been inconsistent, thus, said Dr. Fletcher, "there is no proof that there is reduced dopamine in obesity" (Lancet 2001;357:354-7).
As the field of addiction research advances, there will be a shift in the viewpoint that dopamine is the "end all and be all," in part because there will be a deeper understanding of individual variability to different substances that lead to different forms of eating pathologies, he said. "We need to entertain the notion that no single characteristic will define the nature of reward-processing in obesity and that there may be many routes to positive calorie balance."
Longitudinal studies of individual variability to certain foods also could help better determine the impact of certain foods on the brain, he said.
Winners and ‘losers’
"In terms of those who stand to gain from the acceptance of food addiction," said Dr. Fletcher, "At first glance, this would seem to be the people who offer treatments for food addiction and the people who might make some money by suing [processed food] companies."
Yet, for Dr. Gearhardt, if food addiction is proved, and a direct line can be drawn between the food industry’s intentional manipulation of ingredients to profit from this "brain hijacking," Dr. Gearhardt said, "This brings up the question of industry culpability and the ethics of aggressively marketing it to children."
Dr. Gearhardt also believes the possibility of a clinical food addiction diagnosis for those who struggle with pathological eating might "encourage more people ... to receive professional help rather than beat themselves up for not being able to stick to diet after diet on their own."
Conversely, Dr. Ziauddeen noted what while a food addiction diagnosis may offer someone consolation and motivation to seek help, "What if the person is subject to restrictions or treatments based on the diagnosis?" Specifically, he cited ineligibility for bariatric surgery or less clout in the eyes of the court for child custody. "This does not require a stretch of the imagination," he said. "If you have a diagnosis of alcohol dependence, it influences your chances of receiving a liver transplant. If you have a diagnosis of drug or alcohol addiction, it impacts social care decisions made about your children."
Accepting food addiction as real will affect not only those given the diagnosis, but also the so-called "unaffected" public, said Dr. Fletcher. "If food ‘X’ is addictive, to what extent should it be controlled?" He also suggested that health care provision would experience overhaul: "What will be the effect of diverting funding to food addiction treatment from other obesity-related treatments?"
Food addiction "may help us think of novel and hopefully more effective strategies for treating eating-related concerns," said Dr. Gearhardt.
Regardless, Dr. Fletcher warned that because obesity is multifactorial, and includes molecular, metabolic, behavioral, societal and environmental elements, we should not rush to accept "simplistic" answers, or force things to fit where they actually might not. "The thing I think we need to stop right now is this selective citing because we like the narrative."
Dr. Fletcher, Dr. Ziauddeen, and Dr. Gearhardt had no relevant disclosures.
ATLANTA – It’s too soon to disrupt current obesity treatment by declaring food addiction to be a clinical condition, according to Dr. Paul Fletcher.
"If we are to employ [the term] food addiction ... it needs a firm scientific basis," said Dr. Fletcher, who is the Bernard Wolfe Professor of Health Neuroscience in the department of psychiatry at University of Cambridge (England).
Organized medicine took the first step toward recognizing food addiction as a clinical diagnosis with the 2013 inclusion of binge eating disorder (BED) in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). That recognition has the potential to set the stage for an overhaul in delivery and funding of obesity treatment as well as how people with pathologic eating behaviors are viewed.
Obesogenic environment
For some, the answer to obesity and food addiction is to remove unhealthful foods from the environment. And to address "powerful environmental drives to consume them," Dr. Hisham Ziauddeen, a Wellcome Trust Fellow in Translational Medicine and Therapeutics at Cambridge, said in an interview.
In a separate presentation at a meeting, sponsored by the Obesity Society and the Society for the Study of Ingestive Behavior, Ashley Gearhardt, Ph.D., noted that researchers do not know whether food addiction exists. "The science is emerging." Foods high in fat and sugar, especially when aggressively marketed to children, are the chief culprits of the obesity epidemic, according to Dr. Gearhardt, a clinical psychologist at the University of Michigan, Ann Arbor.
"If scientific evidence identifies that certain foods are also capable of hijacking the brain in an addictive manner, it would likely be a landmark change that would support bold policy approaches that focus on improving the food environment," she has said (Biol. Psychiatry 2013;73:802-3).
Current research in the field is focused on the individual risk factors for compulsive eating, such as impulsivity or reward sensitivity, Dr. Gearhardt said. However, the lack of addictive behaviors associated with "minimally processed foods that are relatively low in sugar and fat, such as apples or chicken breasts," means research now needs to determine if there is something about the food or behavior "that leads to compulsive problematic use," she said in an interview.
"Individual approaches may be helpful in developing clinical interventions but will touch the lives of far fewer people than will policy changes that affect entire populations," she said.
Dr. Gearhardt and her associates sought to link obesity to addictive patterning in the brain through the combined use of functional neuroimaging (fMRI) and scores on the Yale Food Addiction Scale (YFAS), which applies substance-dependence criteria in the DSM-IV-TR as a type of metric for addictive eating behaviors.
The investigators used fMRI maps of participants’ brain activation when they were given food cues of either a tasteless substance or a chocolate milkshake high in fat and sugar. These images were then compared with the participants’ scores from the YFAS. The group was a mixture of both lean and obese women (Arch. Gen. Psychiatry. 2011;68:808-16).
The researchers found that when presented with a chocolate milkshake, those with higher YFAS scores, regardless of body mass index, experienced "significantly greater activation" in brain regions associated with dopaminergic release, including the anterior cingulate cortex. Those with the highest YFAS scores experienced a significant increase in activity of the dorsolateral prefrontal cortex.
‘Elegant experiments’
While fMRI research into the neurobiologic response to food has "generated some very elegant experiments," according to Dr. Fletcher, he is concerned that food addiction proponents have neglected to see these data in a larger context. "The literature is hugely inconsistent, and ignoring this fact may be inconvenient ... but if we continue to do so, it will come back to slap us in the face."
Because neuroimages "are often ambiguous, unless they are constrained by a specific hypothesis, it becomes more like reading tarot cards than interpreting scientific data," he said. "There is a dangerous tendency for people to have a particular perspective and then, no matter what the fMRI data show, to interpret them according to the perspective with which they started out."
And while this free hand with data interpretation happens generally, Dr. Fletcher said he has been "particularly struck" by its occurrence in the food addiction field. "There seem to be very few constraints on interpretation of the regional activation," he said, noting that whether researchers are looking at obesity, binge-eating, or anyone assumed to have a food addition. "Inevitably, [the researchers] find differences in neural activation in such groups but the interpretations of those activations are often post hoc and heavily biased by what the researchers believed in the first place."
As an example, he cited how activity in the anterior cingulate cortex in overweight people given food cues may be interpreted as a sign of craving. "But this is an unjustified inference because we do not know what the anterior cingulate cortex does and it far more frequently related to other processes than to craving."
Dr. Fletcher and his colleagues’ alarm over this "oversimplification of data" prompted a polite, but impassioned, back and forth with Dr. Gearhardt and her associates, published in Nature Reviews Neuroscience (2012;13:279-86 [doi:10.1038/nrn3212]); (2012;13:514 [doi:10.1038/nrn3212-c1]); (2012;13:514 [doi:10.1038/nrn3212-c2]).
In the first of these editorials, Dr. Fletcher and his coauthors wrote that "the messages now emerging from the neuroscientific research community may therefore have an unprecedented impact on policy development," and in another, urged the adoption of "a more detailed consideration" of how to explore food addiction, particularly since cognitive neuroscience is already moving the field beyond ideas based "purely on clinical overlap" and the model of addiction as delineated in the DSM-IV-TR.
Obesity subsets
"Dr. Fletcher and I agree that the concept of ‘food addiction’ is still an open question," Dr. Gearhardt said in an interview. "My group believes that there is evidence building that suggests it is plausible that an addictive process contributes to problematic eating in some circumstances, especially for eaters who exhibit behavioral phenotypes."
Binge eating, emotional eating, and other pathologies surrounding attitudes toward food also were noted in participants with high YFAS scores in Dr. Gearhardt’s study. "We see evidence of addictive-like processes contributing to problematic eating even for individuals who do not meet the criteria for BED," she said.
Dr. Fletcher noted that "there is a clear degree of clinical overlap between obesity and binge eating, particularly binge eating disorder and drug addiction." Specifically, tolerance, withdrawal, persistent desire for food, eating more than intended, and the diminishment of social engagement in exchange for more time spent acquiring and ingesting food all parallel drug addiction. "However, we don’t know what the overlap is," said Dr. Fletcher. "Is it sugar? Is it fat? Is it a combination? We really don’t know yet."
Populations vs. individuals
"If certain foods are addictive, this may partially explain the difficulty people experience in achieving sustainable weight loss," according to Dr. Gearhardt in commenting on the fMRI study results. "Ubiquitous food advertising and the availability of inexpensive palatable foods may make it extremely difficult to adhere to healthier food choices because the omnipresent food cues trigger the reward system."
Dr. Gearhardt speculated that a focus on specific food ingredients being at the root of addiction-linked obesity may spur activism by manufacturers. "The food industry will likely use any inconsistency in the food addiction literature to plant doubt, attack scientists’ credibility, or fund negative studies," they wrote.
By focusing on how detrimental the food environment has become as a result of "heavily marketed foods that interact with the brain in harmful ways," the public may be more likely to support restrictive policies such as "taxing addictive foods, limiting marketing of these foods to children, and enacting zoning laws that limit the number of vendors selling such foods" among other measures, she wrote.
Dr. Fletcher acknowledged that there is likely a legitimate "battle to be joined" against marketers of junk food and other agents contributing to a deleterious food environment, but attacking the problem at the societal level without consideration of the potential impact on the individual will ultimately backfire. "We must be very careful about how we line up our troops," he said.
"Changing behavior at a population level, which indubitably is required, is not going to be easy," said Dr. Ziauddeen. "As well as the resistance of those with vested interests, such changes will be considered widely unacceptable if they are perceived to entail a loss of liberty."
Although Dr. Fletcher and Dr. Ziauddeen agree a lack of willpower and moral frailty are antiquated notions of why people become obese, assuming that diagnosing people as food addicts will protect them, either from stigmatization or any unforeseen effects of policy changes, is short-sighted.
"Based on our experience with drug addictions over the centuries, it is hard to think that food addiction will not come with some stigma and the consequences thereof," he said.
And Dr. Ziauddeen agreed that, "If the science is shaky and hard to defend, it will be ripped apart." Beyond it possibly being "indefensible" in the face of the opposition from processed food manufacturers, thus setting the field back on its heels, there is the danger of a loss of personal liberty that results, not for the sake of the greater good, but solely from policies based on shoddy science.
"The removal of choice is less threatening if it is done to protect against a situation in which the individual has no real choice anyway, as is the case with addictive substances," said Dr. Ziauddeen. "In short, if there is an addictive agent in some foods, then policy change and legislation can be seen as protective rather than restrictive." This is only possible however, he said, if there is "clear, consistent evidence that there is indeed an addictive substance in food."
And yet, regarding a connection between obesity and food addiction, "the most striking finding is complete inconsistency," said Dr. Fletcher. "I would like to see the same sorts of changes that those supporting food addiction would like, but I do not think that we are going to succeed by using a poorly specified concept with little real evidence to back it up."
Dopamine response not reliable measure
"Food addiction may well exist, [but] even then, it may only explain a tiny fraction of obesity and overeating," according to Dr. Fletcher. "Perhaps the major problem is our general limitations in our often dopaminergically centered views of what constitutes addiction."
A full understanding of the brain’s pathophysiology is still under development, he said. But in addition to classic behavioral manifestations, such as persistent use of a substance, accepted components of addiction include reduced dopamine-receptor density in the ventral striatum and a flip in the neurocircuitry for decision making from the ventral to the dorsal striatum.
Otherwise, he said, conclusive statements about the neurobiology of addiction are suspect. "When we run a functional neuroimaging experiment, we are looking at many different brain regions and, for pretty much all of these, there is a fairly dense ambiguity about what processes they carry out."
In addition, said Dr. Fletcher, although several researchers have tried to replicate one particular study showing that that showed those with severe obesity had reduced raclopride, an indication their dopamine reception was suppressed, the various findings have been inconsistent, thus, said Dr. Fletcher, "there is no proof that there is reduced dopamine in obesity" (Lancet 2001;357:354-7).
As the field of addiction research advances, there will be a shift in the viewpoint that dopamine is the "end all and be all," in part because there will be a deeper understanding of individual variability to different substances that lead to different forms of eating pathologies, he said. "We need to entertain the notion that no single characteristic will define the nature of reward-processing in obesity and that there may be many routes to positive calorie balance."
Longitudinal studies of individual variability to certain foods also could help better determine the impact of certain foods on the brain, he said.
Winners and ‘losers’
"In terms of those who stand to gain from the acceptance of food addiction," said Dr. Fletcher, "At first glance, this would seem to be the people who offer treatments for food addiction and the people who might make some money by suing [processed food] companies."
Yet, for Dr. Gearhardt, if food addiction is proved, and a direct line can be drawn between the food industry’s intentional manipulation of ingredients to profit from this "brain hijacking," Dr. Gearhardt said, "This brings up the question of industry culpability and the ethics of aggressively marketing it to children."
Dr. Gearhardt also believes the possibility of a clinical food addiction diagnosis for those who struggle with pathological eating might "encourage more people ... to receive professional help rather than beat themselves up for not being able to stick to diet after diet on their own."
Conversely, Dr. Ziauddeen noted what while a food addiction diagnosis may offer someone consolation and motivation to seek help, "What if the person is subject to restrictions or treatments based on the diagnosis?" Specifically, he cited ineligibility for bariatric surgery or less clout in the eyes of the court for child custody. "This does not require a stretch of the imagination," he said. "If you have a diagnosis of alcohol dependence, it influences your chances of receiving a liver transplant. If you have a diagnosis of drug or alcohol addiction, it impacts social care decisions made about your children."
Accepting food addiction as real will affect not only those given the diagnosis, but also the so-called "unaffected" public, said Dr. Fletcher. "If food ‘X’ is addictive, to what extent should it be controlled?" He also suggested that health care provision would experience overhaul: "What will be the effect of diverting funding to food addiction treatment from other obesity-related treatments?"
Food addiction "may help us think of novel and hopefully more effective strategies for treating eating-related concerns," said Dr. Gearhardt.
Regardless, Dr. Fletcher warned that because obesity is multifactorial, and includes molecular, metabolic, behavioral, societal and environmental elements, we should not rush to accept "simplistic" answers, or force things to fit where they actually might not. "The thing I think we need to stop right now is this selective citing because we like the narrative."
Dr. Fletcher, Dr. Ziauddeen, and Dr. Gearhardt had no relevant disclosures.
EXPERT ANALYSIS FROM OBESITY WEEK
Bariatric surgery may have favorable outcomes in patients with HIV
ATLANTA – Bariatric surgery was associated with lowered viral loads and resolution of some antiretroviral-related comorbidities, such as type 2 diabetes, in patients with the human immunodeficiency virus, according to Dr. Raul J. Rosenthal.
Patients with HIV who have extended their life expectancy through highly antiretroviral treatment are now living long enough to develop lipohypertrophy, similar to metabolic syndrome, said Dr. Rosenthal, a bariatric surgeon at the Cleveland Clinic Florida in Weston.
"[Some obese patients with HIV] are developing hypertriglyceridemia, type 2 diabetes, hypercholesterolemia, and coronary artery disease," said Dr. Rosenthal. "We are not surprised that infectious disease and primary care doctors send these patients to us for surgery."
To determine whether bariatric surgery was improving the course of the HIV infection in this patient population, Dr. Rosenthal and his associates reviewed the records of 11 asymptomatic patients with HIV who underwent a bariatric procedure at a single surgery center in the past 10 years.
The researchers found that none of the patients had perioperative complications, and all reduced their preoperative mean body mass index (BMI) from 52 kg/m2 to 36 kg/m2. The patients’ preoperative mean weight dropped, on average, by 50%, Dr. Rosenthal said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The patients’ total preoperative mean CD4 count went from 825 cells/mm3 to 504 cells/mm3; the viral load went from a preoperative mean of 813 copies/mL plasma to 684 copies/mL plasma. "I think this is the most important part of the whole study," said Dr. Rosenthal, who said that in patients with the HIV infection, it is important to always keep the CD4 (T-cell) level above 200 cells/mm3 and the viral load under 10,000 copies/mL plasma.
Five patients were followed for 2 years postoperatively. None had complications, although one patient did experience a long-term marginal ulcer with malnutrition.
Although the literature about bariatric surgery in this patient population is "scant" said Dr. Rosenthal, the data from his study were comparable to the findings from at least two other small studies that indicated bariatric surgery may be an effective treatment for obesity and its attendant comorbidities in HIV, without negatively impacting virologic suppression (Surg. Obes. Relat. Dis. 2005;1:73-6).
The best bariatric treatment in this patient population may be the sleeve because it was the least likely to preclude future treatments.
"The sleeve has a morbidity rate of 1.6%, and I am not going to fight that," given the unpredictable prognosis in this patient population, Dr. Rosenthal said.
Although larger studies are necessary, "so far, HIV does not appear to increase the rate of perioperative complications, and it does alter the course of HIV infection," he noted.
ATLANTA – Bariatric surgery was associated with lowered viral loads and resolution of some antiretroviral-related comorbidities, such as type 2 diabetes, in patients with the human immunodeficiency virus, according to Dr. Raul J. Rosenthal.
Patients with HIV who have extended their life expectancy through highly antiretroviral treatment are now living long enough to develop lipohypertrophy, similar to metabolic syndrome, said Dr. Rosenthal, a bariatric surgeon at the Cleveland Clinic Florida in Weston.
"[Some obese patients with HIV] are developing hypertriglyceridemia, type 2 diabetes, hypercholesterolemia, and coronary artery disease," said Dr. Rosenthal. "We are not surprised that infectious disease and primary care doctors send these patients to us for surgery."
To determine whether bariatric surgery was improving the course of the HIV infection in this patient population, Dr. Rosenthal and his associates reviewed the records of 11 asymptomatic patients with HIV who underwent a bariatric procedure at a single surgery center in the past 10 years.
The researchers found that none of the patients had perioperative complications, and all reduced their preoperative mean body mass index (BMI) from 52 kg/m2 to 36 kg/m2. The patients’ preoperative mean weight dropped, on average, by 50%, Dr. Rosenthal said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The patients’ total preoperative mean CD4 count went from 825 cells/mm3 to 504 cells/mm3; the viral load went from a preoperative mean of 813 copies/mL plasma to 684 copies/mL plasma. "I think this is the most important part of the whole study," said Dr. Rosenthal, who said that in patients with the HIV infection, it is important to always keep the CD4 (T-cell) level above 200 cells/mm3 and the viral load under 10,000 copies/mL plasma.
Five patients were followed for 2 years postoperatively. None had complications, although one patient did experience a long-term marginal ulcer with malnutrition.
Although the literature about bariatric surgery in this patient population is "scant" said Dr. Rosenthal, the data from his study were comparable to the findings from at least two other small studies that indicated bariatric surgery may be an effective treatment for obesity and its attendant comorbidities in HIV, without negatively impacting virologic suppression (Surg. Obes. Relat. Dis. 2005;1:73-6).
The best bariatric treatment in this patient population may be the sleeve because it was the least likely to preclude future treatments.
"The sleeve has a morbidity rate of 1.6%, and I am not going to fight that," given the unpredictable prognosis in this patient population, Dr. Rosenthal said.
Although larger studies are necessary, "so far, HIV does not appear to increase the rate of perioperative complications, and it does alter the course of HIV infection," he noted.
ATLANTA – Bariatric surgery was associated with lowered viral loads and resolution of some antiretroviral-related comorbidities, such as type 2 diabetes, in patients with the human immunodeficiency virus, according to Dr. Raul J. Rosenthal.
Patients with HIV who have extended their life expectancy through highly antiretroviral treatment are now living long enough to develop lipohypertrophy, similar to metabolic syndrome, said Dr. Rosenthal, a bariatric surgeon at the Cleveland Clinic Florida in Weston.
"[Some obese patients with HIV] are developing hypertriglyceridemia, type 2 diabetes, hypercholesterolemia, and coronary artery disease," said Dr. Rosenthal. "We are not surprised that infectious disease and primary care doctors send these patients to us for surgery."
To determine whether bariatric surgery was improving the course of the HIV infection in this patient population, Dr. Rosenthal and his associates reviewed the records of 11 asymptomatic patients with HIV who underwent a bariatric procedure at a single surgery center in the past 10 years.
The researchers found that none of the patients had perioperative complications, and all reduced their preoperative mean body mass index (BMI) from 52 kg/m2 to 36 kg/m2. The patients’ preoperative mean weight dropped, on average, by 50%, Dr. Rosenthal said at the meeting, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The patients’ total preoperative mean CD4 count went from 825 cells/mm3 to 504 cells/mm3; the viral load went from a preoperative mean of 813 copies/mL plasma to 684 copies/mL plasma. "I think this is the most important part of the whole study," said Dr. Rosenthal, who said that in patients with the HIV infection, it is important to always keep the CD4 (T-cell) level above 200 cells/mm3 and the viral load under 10,000 copies/mL plasma.
Five patients were followed for 2 years postoperatively. None had complications, although one patient did experience a long-term marginal ulcer with malnutrition.
Although the literature about bariatric surgery in this patient population is "scant" said Dr. Rosenthal, the data from his study were comparable to the findings from at least two other small studies that indicated bariatric surgery may be an effective treatment for obesity and its attendant comorbidities in HIV, without negatively impacting virologic suppression (Surg. Obes. Relat. Dis. 2005;1:73-6).
The best bariatric treatment in this patient population may be the sleeve because it was the least likely to preclude future treatments.
"The sleeve has a morbidity rate of 1.6%, and I am not going to fight that," given the unpredictable prognosis in this patient population, Dr. Rosenthal said.
Although larger studies are necessary, "so far, HIV does not appear to increase the rate of perioperative complications, and it does alter the course of HIV infection," he noted.
AT OBESITY WEEK
Major finding: Bariatric surgery in HIV was not found to negatively impact the course of infection in HIV patients, and had no significant adverse outcomes.
Data source: A retrospective study of 11 patients at a single site, in addition to an analysis of the literature.
Disclosures: Dr. Rosenthal did not report any financial disclosures.
Obesity Treatment Costs
ATLANTA – Obesity and its comorbidities loom, threatening to become an expensive national crisis, given that its treatment costs are nearly double that of other chronic diseases, and third party payers so far have failed to invest in its prevention.
"Obese individuals are about 42% more expensive than their normal weight counterparts," accounting for 9% of all medical expenditures, Eric Finkelstein, Ph.D., said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
With close to half the population expected to have a BMI greater or equal to 40 kg/m2 by 2030, even the slightest reversal of trends can save billions, according to Dr. Finkelstein, a health policy research analyst and professor at the Duke-National University of Singapore Global Health Institute (Am. J. Prev. Med. 2012;42:563-70).
‘Bend the curve’
"By 2020, if you could bend even just the cost percentage point by 1 per year, you could have 2.6 million fewer obese adults, and $3.9 billion less in medical expenditures," said Dr. Finkelstein. "By 2030, the numbers go up to 2.9 million fewer obese adults, and $9.5 billion in savings."
The way to bend the curve is through prevention, said Dr. Finkelstein. But, just what constitutes prevention and who should pay for it are not so straightforward.
Although the Affordable Care Act expanded the Centers for Medicare and Medicaid’s coverage of obesity screening and prevention, "there is some debate as to whether the ACA will help this problem," said Dr. Finkelstein.
A trifecta of politics, prejudice, and inconsistent health insurance policies may undermine the legislation’s ability to meet the challenges posed by obesity, according to the symposium presenters.
‘Ounce of prevention, pound of cure’
"Grandma was right. An ounce of prevention equals a pound of cure," noted Dr. Richard Wild, chief medical officer of the CMS in Atlanta.
To that end, he said that under the ACA, there is "more flexibility to [cover prevention] with no cost sharing to patients." CMS obesity screening, prevention, and treatment are largely tied to the U. S. Preventive Services Task Force advisory committee, said Dr. Wild.
A significant percentage of individuals in their mid-20s with class 1 obesity (BMI between 30 and 35 kg/m2) will have BMIs of 40 kg/m2 or greater before they reach their 40s, according to Dr. Finkelstein. By the time they enter their 40s, 63% of males and 78% of women will have an obesity-related comorbidity. Many of those in the 30 to 35 BMI group are likely to continue to a significant weight gain that will make them eligible for bariatric surgery fairly soon," he said.
Early intervention is key to preventing the cost of comorbidities, Dr. Finkelstein said (Surg. Obes. Relat. Dis. 2013;9:547-53).
However, CMS limits Medicare coverage of bariatric surgery to those with a BMI greater than 35 kg/m2, who have at least one related comorbidity and have proven unsuccessful at past attempts to control their weight.
Beyond that, following the USPTF Recommendation Statement (grade B) for screening and treatment of obesity in adults, behavioral intervention is covered when a person has a BMI of 30 kg/m2. If, after 6 months, the person has demonstrated a 3-kg weight loss, continued "face-to-face" weekly visits with a primary care provider of behavioral intervention can continue up to another 6 months.
Politics over patients
Regardless of the point at which intervention is deemed appropriate, access to all available treatments is still not equal, said Dr. John Morton of Stanford (Calif.) University and president elect of ASBMS.
"Let’s make the playing field level," said Dr. Morton. "Everybody should have the same benefits. One Constitution for all of us, one health care benefit for all of us."
Access to bariatric surgery is limited by a number of factors, including the type of health exchange available in the state where a person lives, or whether their employer-backed health plan offers bariatric surgery and if so, at what cost.
"We believe that a big part of any sort of package should definitely be bariatric surgery," said Dr. Morton, citing data on the "tertiary prevention" provided by bariatric surgery. "We hear about statins and all the good they do. If you look at how much mortality they decrease in 5 years, it’s in the single digits. We’re talking about a 40% decrease in mortality in bariatric surgery." said Dr. Morton (N. Engl. J. Med. 2007; 357:753-61).
Noting that as BMI goes up, costs go up, Dr. Morton said that with bariatric surgery, there is a return on investment in a short amount of time. But politics gets in the way of allowing the cost-saving measures of weight reduction surgery to be applied, he said.
Since the presidential election of 2012, "a lot of states have held their fire about implementing these programs," said Dr. Morton. "But at the end of the day, you need to do what’s right for the patient."
Because bariatric surgery coverage is not mandated at the federal level, millions of American do not have access to obesity care, said Dr. Morton.
Role of prejudice
"The biggest problem we have had with this for 50 years is prejudice," Dr. Henry Buchwald, professor emeritus of the Owen H. and Sarah Davidson Wangensteen Chair in Experimental Surgery at the University of Minnesota, Minneapolis. "People are prejudiced against the obese."
Dr. Morton said that even though obesity is a disease recognized by the AMA, it is often described in exclusionary terms by third-party payers.
"When you look at the ACA, there’s language that says it cannot discriminate on the basis of a health condition, but if you look at some of these [insurance] plans, there is actually language that says ‘we will not cover obesity treatment.’ That’s exclusionary language, and we need to figure out why this is occurring."
However, Dr. Finkelstein suggested that part of the problem with getting coverage for weight loss surgery might be how the field frames their argument in favor of it.
"I think the obesity community has done themselves a disservice by pushing [return on investment] for bariatric procedures," said Dr. Finkelstein. "I don’t think bariatric surgery should be talked about in terms of value for money. The [health] value is there just like any other procedure, and so it should be covered."
Little incentive
Despite the fact that the costs of obesity over a lifetime are high in the aggregate, Dr. Finkelstein said that the costs are highest later in life. That, plus the current trend of employees changing jobs an average of every 3 years, means obesity is often overlooked.
"Even though the net costs from a lifetime perspective are significant, there is not a lot of incentive for any particular payer to do any obesity prevention because the costs are eventually shifted down the line," said Dr. Finkelstein. When the federal government picks up paying for the health care costs of everyone 65 years of age or older, you are unlikely to "see significant investments in prevention," he said.
In cases in which the individual has had no insurance prior to qualifying for Medicare, the costs are even higher, and the cases more complex. "About 25% of patients who have chronic disease with multiple comorbidities make up 85% of our costs," Dr. Wild said, adding that of those 25%, 5% are "superusers" who make up 50% of all CMS costs.
The CMS spends $1.5 billion a day, or $900 billion annually, on health care, according to Dr. Wild.
"When we talk about bending the cost curve and saving money, we need to focus on those patients with multiple comorbidities and chronic diseases," said Dr. Wild.
The agreement on this point brought the panel back to the question of what is the sweet spot for prevention and intervention, and who should pay for it.
Surgery not the only answer
"We’re not going to solve the obesity problem by surgery alone," Dr. Buchwald said, adding that a combination of approaches, including prevention, medical, and other approaches. "We have to look for things that will work together."
Dr. Morton agreed that more research into complimentary medical interventions for obesity was needed. "We have been hamstrung by not having a lot of options," he said.
"Diet and exercise do work, but we don’t diet or exercise as much as we used to and that’s part of the reason we’re in this situation," Dr. Finkelstein said.
The data support bariatric surgery as a viable way to cut costs, said Dr. Morton. "The data are on our side," he said. "We have a lot of patients in need, and I would call for some rational coverage decisions when it comes to health exchanges. I think the government can be our partners in this."
Dr. Finkelstein noted several disclosures including, Jenny Craig, Johnson & Johnson, and Sanofi-Aventis, among several others. Dr. Morton has worked with Covidien. Dr. Buchwald and Dr. Wild did not have any relevant disclosures
ATLANTA – Obesity and its comorbidities loom, threatening to become an expensive national crisis, given that its treatment costs are nearly double that of other chronic diseases, and third party payers so far have failed to invest in its prevention.
"Obese individuals are about 42% more expensive than their normal weight counterparts," accounting for 9% of all medical expenditures, Eric Finkelstein, Ph.D., said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
With close to half the population expected to have a BMI greater or equal to 40 kg/m2 by 2030, even the slightest reversal of trends can save billions, according to Dr. Finkelstein, a health policy research analyst and professor at the Duke-National University of Singapore Global Health Institute (Am. J. Prev. Med. 2012;42:563-70).
‘Bend the curve’
"By 2020, if you could bend even just the cost percentage point by 1 per year, you could have 2.6 million fewer obese adults, and $3.9 billion less in medical expenditures," said Dr. Finkelstein. "By 2030, the numbers go up to 2.9 million fewer obese adults, and $9.5 billion in savings."
The way to bend the curve is through prevention, said Dr. Finkelstein. But, just what constitutes prevention and who should pay for it are not so straightforward.
Although the Affordable Care Act expanded the Centers for Medicare and Medicaid’s coverage of obesity screening and prevention, "there is some debate as to whether the ACA will help this problem," said Dr. Finkelstein.
A trifecta of politics, prejudice, and inconsistent health insurance policies may undermine the legislation’s ability to meet the challenges posed by obesity, according to the symposium presenters.
‘Ounce of prevention, pound of cure’
"Grandma was right. An ounce of prevention equals a pound of cure," noted Dr. Richard Wild, chief medical officer of the CMS in Atlanta.
To that end, he said that under the ACA, there is "more flexibility to [cover prevention] with no cost sharing to patients." CMS obesity screening, prevention, and treatment are largely tied to the U. S. Preventive Services Task Force advisory committee, said Dr. Wild.
A significant percentage of individuals in their mid-20s with class 1 obesity (BMI between 30 and 35 kg/m2) will have BMIs of 40 kg/m2 or greater before they reach their 40s, according to Dr. Finkelstein. By the time they enter their 40s, 63% of males and 78% of women will have an obesity-related comorbidity. Many of those in the 30 to 35 BMI group are likely to continue to a significant weight gain that will make them eligible for bariatric surgery fairly soon," he said.
Early intervention is key to preventing the cost of comorbidities, Dr. Finkelstein said (Surg. Obes. Relat. Dis. 2013;9:547-53).
However, CMS limits Medicare coverage of bariatric surgery to those with a BMI greater than 35 kg/m2, who have at least one related comorbidity and have proven unsuccessful at past attempts to control their weight.
Beyond that, following the USPTF Recommendation Statement (grade B) for screening and treatment of obesity in adults, behavioral intervention is covered when a person has a BMI of 30 kg/m2. If, after 6 months, the person has demonstrated a 3-kg weight loss, continued "face-to-face" weekly visits with a primary care provider of behavioral intervention can continue up to another 6 months.
Politics over patients
Regardless of the point at which intervention is deemed appropriate, access to all available treatments is still not equal, said Dr. John Morton of Stanford (Calif.) University and president elect of ASBMS.
"Let’s make the playing field level," said Dr. Morton. "Everybody should have the same benefits. One Constitution for all of us, one health care benefit for all of us."
Access to bariatric surgery is limited by a number of factors, including the type of health exchange available in the state where a person lives, or whether their employer-backed health plan offers bariatric surgery and if so, at what cost.
"We believe that a big part of any sort of package should definitely be bariatric surgery," said Dr. Morton, citing data on the "tertiary prevention" provided by bariatric surgery. "We hear about statins and all the good they do. If you look at how much mortality they decrease in 5 years, it’s in the single digits. We’re talking about a 40% decrease in mortality in bariatric surgery." said Dr. Morton (N. Engl. J. Med. 2007; 357:753-61).
Noting that as BMI goes up, costs go up, Dr. Morton said that with bariatric surgery, there is a return on investment in a short amount of time. But politics gets in the way of allowing the cost-saving measures of weight reduction surgery to be applied, he said.
Since the presidential election of 2012, "a lot of states have held their fire about implementing these programs," said Dr. Morton. "But at the end of the day, you need to do what’s right for the patient."
Because bariatric surgery coverage is not mandated at the federal level, millions of American do not have access to obesity care, said Dr. Morton.
Role of prejudice
"The biggest problem we have had with this for 50 years is prejudice," Dr. Henry Buchwald, professor emeritus of the Owen H. and Sarah Davidson Wangensteen Chair in Experimental Surgery at the University of Minnesota, Minneapolis. "People are prejudiced against the obese."
Dr. Morton said that even though obesity is a disease recognized by the AMA, it is often described in exclusionary terms by third-party payers.
"When you look at the ACA, there’s language that says it cannot discriminate on the basis of a health condition, but if you look at some of these [insurance] plans, there is actually language that says ‘we will not cover obesity treatment.’ That’s exclusionary language, and we need to figure out why this is occurring."
However, Dr. Finkelstein suggested that part of the problem with getting coverage for weight loss surgery might be how the field frames their argument in favor of it.
"I think the obesity community has done themselves a disservice by pushing [return on investment] for bariatric procedures," said Dr. Finkelstein. "I don’t think bariatric surgery should be talked about in terms of value for money. The [health] value is there just like any other procedure, and so it should be covered."
Little incentive
Despite the fact that the costs of obesity over a lifetime are high in the aggregate, Dr. Finkelstein said that the costs are highest later in life. That, plus the current trend of employees changing jobs an average of every 3 years, means obesity is often overlooked.
"Even though the net costs from a lifetime perspective are significant, there is not a lot of incentive for any particular payer to do any obesity prevention because the costs are eventually shifted down the line," said Dr. Finkelstein. When the federal government picks up paying for the health care costs of everyone 65 years of age or older, you are unlikely to "see significant investments in prevention," he said.
In cases in which the individual has had no insurance prior to qualifying for Medicare, the costs are even higher, and the cases more complex. "About 25% of patients who have chronic disease with multiple comorbidities make up 85% of our costs," Dr. Wild said, adding that of those 25%, 5% are "superusers" who make up 50% of all CMS costs.
The CMS spends $1.5 billion a day, or $900 billion annually, on health care, according to Dr. Wild.
"When we talk about bending the cost curve and saving money, we need to focus on those patients with multiple comorbidities and chronic diseases," said Dr. Wild.
The agreement on this point brought the panel back to the question of what is the sweet spot for prevention and intervention, and who should pay for it.
Surgery not the only answer
"We’re not going to solve the obesity problem by surgery alone," Dr. Buchwald said, adding that a combination of approaches, including prevention, medical, and other approaches. "We have to look for things that will work together."
Dr. Morton agreed that more research into complimentary medical interventions for obesity was needed. "We have been hamstrung by not having a lot of options," he said.
"Diet and exercise do work, but we don’t diet or exercise as much as we used to and that’s part of the reason we’re in this situation," Dr. Finkelstein said.
The data support bariatric surgery as a viable way to cut costs, said Dr. Morton. "The data are on our side," he said. "We have a lot of patients in need, and I would call for some rational coverage decisions when it comes to health exchanges. I think the government can be our partners in this."
Dr. Finkelstein noted several disclosures including, Jenny Craig, Johnson & Johnson, and Sanofi-Aventis, among several others. Dr. Morton has worked with Covidien. Dr. Buchwald and Dr. Wild did not have any relevant disclosures
ATLANTA – Obesity and its comorbidities loom, threatening to become an expensive national crisis, given that its treatment costs are nearly double that of other chronic diseases, and third party payers so far have failed to invest in its prevention.
"Obese individuals are about 42% more expensive than their normal weight counterparts," accounting for 9% of all medical expenditures, Eric Finkelstein, Ph.D., said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
With close to half the population expected to have a BMI greater or equal to 40 kg/m2 by 2030, even the slightest reversal of trends can save billions, according to Dr. Finkelstein, a health policy research analyst and professor at the Duke-National University of Singapore Global Health Institute (Am. J. Prev. Med. 2012;42:563-70).
‘Bend the curve’
"By 2020, if you could bend even just the cost percentage point by 1 per year, you could have 2.6 million fewer obese adults, and $3.9 billion less in medical expenditures," said Dr. Finkelstein. "By 2030, the numbers go up to 2.9 million fewer obese adults, and $9.5 billion in savings."
The way to bend the curve is through prevention, said Dr. Finkelstein. But, just what constitutes prevention and who should pay for it are not so straightforward.
Although the Affordable Care Act expanded the Centers for Medicare and Medicaid’s coverage of obesity screening and prevention, "there is some debate as to whether the ACA will help this problem," said Dr. Finkelstein.
A trifecta of politics, prejudice, and inconsistent health insurance policies may undermine the legislation’s ability to meet the challenges posed by obesity, according to the symposium presenters.
‘Ounce of prevention, pound of cure’
"Grandma was right. An ounce of prevention equals a pound of cure," noted Dr. Richard Wild, chief medical officer of the CMS in Atlanta.
To that end, he said that under the ACA, there is "more flexibility to [cover prevention] with no cost sharing to patients." CMS obesity screening, prevention, and treatment are largely tied to the U. S. Preventive Services Task Force advisory committee, said Dr. Wild.
A significant percentage of individuals in their mid-20s with class 1 obesity (BMI between 30 and 35 kg/m2) will have BMIs of 40 kg/m2 or greater before they reach their 40s, according to Dr. Finkelstein. By the time they enter their 40s, 63% of males and 78% of women will have an obesity-related comorbidity. Many of those in the 30 to 35 BMI group are likely to continue to a significant weight gain that will make them eligible for bariatric surgery fairly soon," he said.
Early intervention is key to preventing the cost of comorbidities, Dr. Finkelstein said (Surg. Obes. Relat. Dis. 2013;9:547-53).
However, CMS limits Medicare coverage of bariatric surgery to those with a BMI greater than 35 kg/m2, who have at least one related comorbidity and have proven unsuccessful at past attempts to control their weight.
Beyond that, following the USPTF Recommendation Statement (grade B) for screening and treatment of obesity in adults, behavioral intervention is covered when a person has a BMI of 30 kg/m2. If, after 6 months, the person has demonstrated a 3-kg weight loss, continued "face-to-face" weekly visits with a primary care provider of behavioral intervention can continue up to another 6 months.
Politics over patients
Regardless of the point at which intervention is deemed appropriate, access to all available treatments is still not equal, said Dr. John Morton of Stanford (Calif.) University and president elect of ASBMS.
"Let’s make the playing field level," said Dr. Morton. "Everybody should have the same benefits. One Constitution for all of us, one health care benefit for all of us."
Access to bariatric surgery is limited by a number of factors, including the type of health exchange available in the state where a person lives, or whether their employer-backed health plan offers bariatric surgery and if so, at what cost.
"We believe that a big part of any sort of package should definitely be bariatric surgery," said Dr. Morton, citing data on the "tertiary prevention" provided by bariatric surgery. "We hear about statins and all the good they do. If you look at how much mortality they decrease in 5 years, it’s in the single digits. We’re talking about a 40% decrease in mortality in bariatric surgery." said Dr. Morton (N. Engl. J. Med. 2007; 357:753-61).
Noting that as BMI goes up, costs go up, Dr. Morton said that with bariatric surgery, there is a return on investment in a short amount of time. But politics gets in the way of allowing the cost-saving measures of weight reduction surgery to be applied, he said.
Since the presidential election of 2012, "a lot of states have held their fire about implementing these programs," said Dr. Morton. "But at the end of the day, you need to do what’s right for the patient."
Because bariatric surgery coverage is not mandated at the federal level, millions of American do not have access to obesity care, said Dr. Morton.
Role of prejudice
"The biggest problem we have had with this for 50 years is prejudice," Dr. Henry Buchwald, professor emeritus of the Owen H. and Sarah Davidson Wangensteen Chair in Experimental Surgery at the University of Minnesota, Minneapolis. "People are prejudiced against the obese."
Dr. Morton said that even though obesity is a disease recognized by the AMA, it is often described in exclusionary terms by third-party payers.
"When you look at the ACA, there’s language that says it cannot discriminate on the basis of a health condition, but if you look at some of these [insurance] plans, there is actually language that says ‘we will not cover obesity treatment.’ That’s exclusionary language, and we need to figure out why this is occurring."
However, Dr. Finkelstein suggested that part of the problem with getting coverage for weight loss surgery might be how the field frames their argument in favor of it.
"I think the obesity community has done themselves a disservice by pushing [return on investment] for bariatric procedures," said Dr. Finkelstein. "I don’t think bariatric surgery should be talked about in terms of value for money. The [health] value is there just like any other procedure, and so it should be covered."
Little incentive
Despite the fact that the costs of obesity over a lifetime are high in the aggregate, Dr. Finkelstein said that the costs are highest later in life. That, plus the current trend of employees changing jobs an average of every 3 years, means obesity is often overlooked.
"Even though the net costs from a lifetime perspective are significant, there is not a lot of incentive for any particular payer to do any obesity prevention because the costs are eventually shifted down the line," said Dr. Finkelstein. When the federal government picks up paying for the health care costs of everyone 65 years of age or older, you are unlikely to "see significant investments in prevention," he said.
In cases in which the individual has had no insurance prior to qualifying for Medicare, the costs are even higher, and the cases more complex. "About 25% of patients who have chronic disease with multiple comorbidities make up 85% of our costs," Dr. Wild said, adding that of those 25%, 5% are "superusers" who make up 50% of all CMS costs.
The CMS spends $1.5 billion a day, or $900 billion annually, on health care, according to Dr. Wild.
"When we talk about bending the cost curve and saving money, we need to focus on those patients with multiple comorbidities and chronic diseases," said Dr. Wild.
The agreement on this point brought the panel back to the question of what is the sweet spot for prevention and intervention, and who should pay for it.
Surgery not the only answer
"We’re not going to solve the obesity problem by surgery alone," Dr. Buchwald said, adding that a combination of approaches, including prevention, medical, and other approaches. "We have to look for things that will work together."
Dr. Morton agreed that more research into complimentary medical interventions for obesity was needed. "We have been hamstrung by not having a lot of options," he said.
"Diet and exercise do work, but we don’t diet or exercise as much as we used to and that’s part of the reason we’re in this situation," Dr. Finkelstein said.
The data support bariatric surgery as a viable way to cut costs, said Dr. Morton. "The data are on our side," he said. "We have a lot of patients in need, and I would call for some rational coverage decisions when it comes to health exchanges. I think the government can be our partners in this."
Dr. Finkelstein noted several disclosures including, Jenny Craig, Johnson & Johnson, and Sanofi-Aventis, among several others. Dr. Morton has worked with Covidien. Dr. Buchwald and Dr. Wild did not have any relevant disclosures
EXPERT ANALYSIS FROM OBESITY WEEK
Politics, prejudice, inconsistent policies wreak havoc with obesity treatment costs
ATLANTA – Obesity and its comorbidities loom, threatening to become an expensive national crisis, given that its treatment costs are nearly double that of other chronic diseases, and third party payers so far have failed to invest in its prevention.
"Obese individuals are about 42% more expensive than their normal weight counterparts," accounting for 9% of all medical expenditures, Eric Finkelstein, Ph.D., said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
With close to half the population expected to have a BMI greater or equal to 40 kg/m2 by 2030, even the slightest reversal of trends can save billions, according to Dr. Finkelstein, a health policy research analyst and professor at the Duke-National University of Singapore Global Health Institute (Am. J. Prev. Med. 2012;42:563-70).
‘Bend the curve’
"By 2020, if you could bend even just the cost percentage point by 1 per year, you could have 2.6 million fewer obese adults, and $3.9 billion less in medical expenditures," said Dr. Finkelstein. "By 2030, the numbers go up to 2.9 million fewer obese adults, and $9.5 billion in savings."
The way to bend the curve is through prevention, said Dr. Finkelstein. But, just what constitutes prevention and who should pay for it are not so straightforward.
Although the Affordable Care Act expanded the Centers for Medicare and Medicaid’s coverage of obesity screening and prevention, "there is some debate as to whether the ACA will help this problem," said Dr. Finkelstein.
A trifecta of politics, prejudice, and inconsistent health insurance policies may undermine the legislation’s ability to meet the challenges posed by obesity, according to the symposium presenters.
‘Ounce of prevention, pound of cure’
"Grandma was right. An ounce of prevention equals a pound of cure," noted Dr. Richard Wild, chief medical officer of the CMS in Atlanta.
To that end, he said that under the ACA, there is "more flexibility to [cover prevention] with no cost sharing to patients." CMS obesity screening, prevention, and treatment are largely tied to the U. S. Preventive Services Task Force advisory committee, said Dr. Wild.
A significant percentage of individuals in their mid-20s with class 1 obesity (BMI between 30 and 35 kg/m2) will have BMIs of 40 kg/m2 or greater before they reach their 40s, according to Dr. Finkelstein. By the time they enter their 40s, 63% of males and 78% of women will have an obesity-related comorbidity. Many of those in the 30 to 35 BMI group are likely to continue to a significant weight gain that will make them eligible for bariatric surgery fairly soon," he said.
Early intervention is key to preventing the cost of comorbidities, Dr. Finkelstein said (Surg. Obes. Relat. Dis. 2013;9:547-53).
However, CMS limits Medicare coverage of bariatric surgery to those with a BMI greater than 35 kg/m2, who have at least one related comorbidity and have proven unsuccessful at past attempts to control their weight.
Beyond that, following the USPTF Recommendation Statement (grade B) for screening and treatment of obesity in adults, behavioral intervention is covered when a person has a BMI of 30 kg/m2. If, after 6 months, the person has demonstrated a 3-kg weight loss, continued "face-to-face" weekly visits with a primary care provider of behavioral intervention can continue up to another 6 months.
Politics over patients
Regardless of the point at which intervention is deemed appropriate, access to all available treatments is still not equal, said Dr. John Morton of Stanford (Calif.) University and president elect of ASBMS.
"Let’s make the playing field level," said Dr. Morton. "Everybody should have the same benefits. One Constitution for all of us, one health care benefit for all of us."
Access to bariatric surgery is limited by a number of factors, including the type of health exchange available in the state where a person lives, or whether their employer-backed health plan offers bariatric surgery and if so, at what cost.
"We believe that a big part of any sort of package should definitely be bariatric surgery," said Dr. Morton, citing data on the "tertiary prevention" provided by bariatric surgery. "We hear about statins and all the good they do. If you look at how much mortality they decrease in 5 years, it’s in the single digits. We’re talking about a 40% decrease in mortality in bariatric surgery." said Dr. Morton (N. Engl. J. Med. 2007; 357:753-61).
Noting that as BMI goes up, costs go up, Dr. Morton said that with bariatric surgery, there is a return on investment in a short amount of time. But politics gets in the way of allowing the cost-saving measures of weight reduction surgery to be applied, he said.
Since the presidential election of 2012, "a lot of states have held their fire about implementing these programs," said Dr. Morton. "But at the end of the day, you need to do what’s right for the patient."
Because bariatric surgery coverage is not mandated at the federal level, millions of American do not have access to obesity care, said Dr. Morton.
Role of prejudice
"The biggest problem we have had with this for 50 years is prejudice," Dr. Henry Buchwald, professor emeritus of the Owen H. and Sarah Davidson Wangensteen Chair in Experimental Surgery at the University of Minnesota, Minneapolis. "People are prejudiced against the obese."
Dr. Morton said that even though obesity is a disease recognized by the AMA, it is often described in exclusionary terms by third-party payers.
"When you look at the ACA, there’s language that says it cannot discriminate on the basis of a health condition, but if you look at some of these [insurance] plans, there is actually language that says ‘we will not cover obesity treatment.’ That’s exclusionary language, and we need to figure out why this is occurring."
However, Dr. Finkelstein suggested that part of the problem with getting coverage for weight loss surgery might be how the field frames their argument in favor of it.
"I think the obesity community has done themselves a disservice by pushing [return on investment] for bariatric procedures," said Dr. Finkelstein. "I don’t think bariatric surgery should be talked about in terms of value for money. The [health] value is there just like any other procedure, and so it should be covered."
Little incentive
Despite the fact that the costs of obesity over a lifetime are high in the aggregate, Dr. Finkelstein said that the costs are highest later in life. That, plus the current trend of employees changing jobs an average of every 3 years, means obesity is often overlooked.
"Even though the net costs from a lifetime perspective are significant, there is not a lot of incentive for any particular payer to do any obesity prevention because the costs are eventually shifted down the line," said Dr. Finkelstein. When the federal government picks up paying for the health care costs of everyone 65 years of age or older, you are unlikely to "see significant investments in prevention," he said.
In cases in which the individual has had no insurance prior to qualifying for Medicare, the costs are even higher, and the cases more complex. "About 25% of patients who have chronic disease with multiple comorbidities make up 85% of our costs," Dr. Wild said, adding that of those 25%, 5% are "superusers" who make up 50% of all CMS costs.
The CMS spends $1.5 billion a day, or $900 billion annually, on health care, according to Dr. Wild.
"When we talk about bending the cost curve and saving money, we need to focus on those patients with multiple comorbidities and chronic diseases," said Dr. Wild.
The agreement on this point brought the panel back to the question of what is the sweet spot for prevention and intervention, and who should pay for it.
Surgery not the only answer
"We’re not going to solve the obesity problem by surgery alone," Dr. Buchwald said, adding that a combination of approaches, including prevention, medical, and other approaches. "We have to look for things that will work together."
Dr. Morton agreed that more research into complimentary medical interventions for obesity was needed. "We have been hamstrung by not having a lot of options," he said.
"Diet and exercise do work, but we don’t diet or exercise as much as we used to and that’s part of the reason we’re in this situation," Dr. Finkelstein said.
The data support bariatric surgery as a viable way to cut costs, said Dr. Morton. "The data are on our side," he said. "We have a lot of patients in need, and I would call for some rational coverage decisions when it comes to health exchanges. I think the government can be our partners in this."
Dr. Finkelstein noted several disclosures including, Jenny Craig, Johnson & Johnson, and Sanofi-Aventis, among several others. Dr. Morton has worked with Covidien. Dr. Buchwald and Dr. Wild did not have any relevant disclosures
ATLANTA – Obesity and its comorbidities loom, threatening to become an expensive national crisis, given that its treatment costs are nearly double that of other chronic diseases, and third party payers so far have failed to invest in its prevention.
"Obese individuals are about 42% more expensive than their normal weight counterparts," accounting for 9% of all medical expenditures, Eric Finkelstein, Ph.D., said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
With close to half the population expected to have a BMI greater or equal to 40 kg/m2 by 2030, even the slightest reversal of trends can save billions, according to Dr. Finkelstein, a health policy research analyst and professor at the Duke-National University of Singapore Global Health Institute (Am. J. Prev. Med. 2012;42:563-70).
‘Bend the curve’
"By 2020, if you could bend even just the cost percentage point by 1 per year, you could have 2.6 million fewer obese adults, and $3.9 billion less in medical expenditures," said Dr. Finkelstein. "By 2030, the numbers go up to 2.9 million fewer obese adults, and $9.5 billion in savings."
The way to bend the curve is through prevention, said Dr. Finkelstein. But, just what constitutes prevention and who should pay for it are not so straightforward.
Although the Affordable Care Act expanded the Centers for Medicare and Medicaid’s coverage of obesity screening and prevention, "there is some debate as to whether the ACA will help this problem," said Dr. Finkelstein.
A trifecta of politics, prejudice, and inconsistent health insurance policies may undermine the legislation’s ability to meet the challenges posed by obesity, according to the symposium presenters.
‘Ounce of prevention, pound of cure’
"Grandma was right. An ounce of prevention equals a pound of cure," noted Dr. Richard Wild, chief medical officer of the CMS in Atlanta.
To that end, he said that under the ACA, there is "more flexibility to [cover prevention] with no cost sharing to patients." CMS obesity screening, prevention, and treatment are largely tied to the U. S. Preventive Services Task Force advisory committee, said Dr. Wild.
A significant percentage of individuals in their mid-20s with class 1 obesity (BMI between 30 and 35 kg/m2) will have BMIs of 40 kg/m2 or greater before they reach their 40s, according to Dr. Finkelstein. By the time they enter their 40s, 63% of males and 78% of women will have an obesity-related comorbidity. Many of those in the 30 to 35 BMI group are likely to continue to a significant weight gain that will make them eligible for bariatric surgery fairly soon," he said.
Early intervention is key to preventing the cost of comorbidities, Dr. Finkelstein said (Surg. Obes. Relat. Dis. 2013;9:547-53).
However, CMS limits Medicare coverage of bariatric surgery to those with a BMI greater than 35 kg/m2, who have at least one related comorbidity and have proven unsuccessful at past attempts to control their weight.
Beyond that, following the USPTF Recommendation Statement (grade B) for screening and treatment of obesity in adults, behavioral intervention is covered when a person has a BMI of 30 kg/m2. If, after 6 months, the person has demonstrated a 3-kg weight loss, continued "face-to-face" weekly visits with a primary care provider of behavioral intervention can continue up to another 6 months.
Politics over patients
Regardless of the point at which intervention is deemed appropriate, access to all available treatments is still not equal, said Dr. John Morton of Stanford (Calif.) University and president elect of ASBMS.
"Let’s make the playing field level," said Dr. Morton. "Everybody should have the same benefits. One Constitution for all of us, one health care benefit for all of us."
Access to bariatric surgery is limited by a number of factors, including the type of health exchange available in the state where a person lives, or whether their employer-backed health plan offers bariatric surgery and if so, at what cost.
"We believe that a big part of any sort of package should definitely be bariatric surgery," said Dr. Morton, citing data on the "tertiary prevention" provided by bariatric surgery. "We hear about statins and all the good they do. If you look at how much mortality they decrease in 5 years, it’s in the single digits. We’re talking about a 40% decrease in mortality in bariatric surgery." said Dr. Morton (N. Engl. J. Med. 2007; 357:753-61).
Noting that as BMI goes up, costs go up, Dr. Morton said that with bariatric surgery, there is a return on investment in a short amount of time. But politics gets in the way of allowing the cost-saving measures of weight reduction surgery to be applied, he said.
Since the presidential election of 2012, "a lot of states have held their fire about implementing these programs," said Dr. Morton. "But at the end of the day, you need to do what’s right for the patient."
Because bariatric surgery coverage is not mandated at the federal level, millions of American do not have access to obesity care, said Dr. Morton.
Role of prejudice
"The biggest problem we have had with this for 50 years is prejudice," Dr. Henry Buchwald, professor emeritus of the Owen H. and Sarah Davidson Wangensteen Chair in Experimental Surgery at the University of Minnesota, Minneapolis. "People are prejudiced against the obese."
Dr. Morton said that even though obesity is a disease recognized by the AMA, it is often described in exclusionary terms by third-party payers.
"When you look at the ACA, there’s language that says it cannot discriminate on the basis of a health condition, but if you look at some of these [insurance] plans, there is actually language that says ‘we will not cover obesity treatment.’ That’s exclusionary language, and we need to figure out why this is occurring."
However, Dr. Finkelstein suggested that part of the problem with getting coverage for weight loss surgery might be how the field frames their argument in favor of it.
"I think the obesity community has done themselves a disservice by pushing [return on investment] for bariatric procedures," said Dr. Finkelstein. "I don’t think bariatric surgery should be talked about in terms of value for money. The [health] value is there just like any other procedure, and so it should be covered."
Little incentive
Despite the fact that the costs of obesity over a lifetime are high in the aggregate, Dr. Finkelstein said that the costs are highest later in life. That, plus the current trend of employees changing jobs an average of every 3 years, means obesity is often overlooked.
"Even though the net costs from a lifetime perspective are significant, there is not a lot of incentive for any particular payer to do any obesity prevention because the costs are eventually shifted down the line," said Dr. Finkelstein. When the federal government picks up paying for the health care costs of everyone 65 years of age or older, you are unlikely to "see significant investments in prevention," he said.
In cases in which the individual has had no insurance prior to qualifying for Medicare, the costs are even higher, and the cases more complex. "About 25% of patients who have chronic disease with multiple comorbidities make up 85% of our costs," Dr. Wild said, adding that of those 25%, 5% are "superusers" who make up 50% of all CMS costs.
The CMS spends $1.5 billion a day, or $900 billion annually, on health care, according to Dr. Wild.
"When we talk about bending the cost curve and saving money, we need to focus on those patients with multiple comorbidities and chronic diseases," said Dr. Wild.
The agreement on this point brought the panel back to the question of what is the sweet spot for prevention and intervention, and who should pay for it.
Surgery not the only answer
"We’re not going to solve the obesity problem by surgery alone," Dr. Buchwald said, adding that a combination of approaches, including prevention, medical, and other approaches. "We have to look for things that will work together."
Dr. Morton agreed that more research into complimentary medical interventions for obesity was needed. "We have been hamstrung by not having a lot of options," he said.
"Diet and exercise do work, but we don’t diet or exercise as much as we used to and that’s part of the reason we’re in this situation," Dr. Finkelstein said.
The data support bariatric surgery as a viable way to cut costs, said Dr. Morton. "The data are on our side," he said. "We have a lot of patients in need, and I would call for some rational coverage decisions when it comes to health exchanges. I think the government can be our partners in this."
Dr. Finkelstein noted several disclosures including, Jenny Craig, Johnson & Johnson, and Sanofi-Aventis, among several others. Dr. Morton has worked with Covidien. Dr. Buchwald and Dr. Wild did not have any relevant disclosures
ATLANTA – Obesity and its comorbidities loom, threatening to become an expensive national crisis, given that its treatment costs are nearly double that of other chronic diseases, and third party payers so far have failed to invest in its prevention.
"Obese individuals are about 42% more expensive than their normal weight counterparts," accounting for 9% of all medical expenditures, Eric Finkelstein, Ph.D., said at the meeting presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
With close to half the population expected to have a BMI greater or equal to 40 kg/m2 by 2030, even the slightest reversal of trends can save billions, according to Dr. Finkelstein, a health policy research analyst and professor at the Duke-National University of Singapore Global Health Institute (Am. J. Prev. Med. 2012;42:563-70).
‘Bend the curve’
"By 2020, if you could bend even just the cost percentage point by 1 per year, you could have 2.6 million fewer obese adults, and $3.9 billion less in medical expenditures," said Dr. Finkelstein. "By 2030, the numbers go up to 2.9 million fewer obese adults, and $9.5 billion in savings."
The way to bend the curve is through prevention, said Dr. Finkelstein. But, just what constitutes prevention and who should pay for it are not so straightforward.
Although the Affordable Care Act expanded the Centers for Medicare and Medicaid’s coverage of obesity screening and prevention, "there is some debate as to whether the ACA will help this problem," said Dr. Finkelstein.
A trifecta of politics, prejudice, and inconsistent health insurance policies may undermine the legislation’s ability to meet the challenges posed by obesity, according to the symposium presenters.
‘Ounce of prevention, pound of cure’
"Grandma was right. An ounce of prevention equals a pound of cure," noted Dr. Richard Wild, chief medical officer of the CMS in Atlanta.
To that end, he said that under the ACA, there is "more flexibility to [cover prevention] with no cost sharing to patients." CMS obesity screening, prevention, and treatment are largely tied to the U. S. Preventive Services Task Force advisory committee, said Dr. Wild.
A significant percentage of individuals in their mid-20s with class 1 obesity (BMI between 30 and 35 kg/m2) will have BMIs of 40 kg/m2 or greater before they reach their 40s, according to Dr. Finkelstein. By the time they enter their 40s, 63% of males and 78% of women will have an obesity-related comorbidity. Many of those in the 30 to 35 BMI group are likely to continue to a significant weight gain that will make them eligible for bariatric surgery fairly soon," he said.
Early intervention is key to preventing the cost of comorbidities, Dr. Finkelstein said (Surg. Obes. Relat. Dis. 2013;9:547-53).
However, CMS limits Medicare coverage of bariatric surgery to those with a BMI greater than 35 kg/m2, who have at least one related comorbidity and have proven unsuccessful at past attempts to control their weight.
Beyond that, following the USPTF Recommendation Statement (grade B) for screening and treatment of obesity in adults, behavioral intervention is covered when a person has a BMI of 30 kg/m2. If, after 6 months, the person has demonstrated a 3-kg weight loss, continued "face-to-face" weekly visits with a primary care provider of behavioral intervention can continue up to another 6 months.
Politics over patients
Regardless of the point at which intervention is deemed appropriate, access to all available treatments is still not equal, said Dr. John Morton of Stanford (Calif.) University and president elect of ASBMS.
"Let’s make the playing field level," said Dr. Morton. "Everybody should have the same benefits. One Constitution for all of us, one health care benefit for all of us."
Access to bariatric surgery is limited by a number of factors, including the type of health exchange available in the state where a person lives, or whether their employer-backed health plan offers bariatric surgery and if so, at what cost.
"We believe that a big part of any sort of package should definitely be bariatric surgery," said Dr. Morton, citing data on the "tertiary prevention" provided by bariatric surgery. "We hear about statins and all the good they do. If you look at how much mortality they decrease in 5 years, it’s in the single digits. We’re talking about a 40% decrease in mortality in bariatric surgery." said Dr. Morton (N. Engl. J. Med. 2007; 357:753-61).
Noting that as BMI goes up, costs go up, Dr. Morton said that with bariatric surgery, there is a return on investment in a short amount of time. But politics gets in the way of allowing the cost-saving measures of weight reduction surgery to be applied, he said.
Since the presidential election of 2012, "a lot of states have held their fire about implementing these programs," said Dr. Morton. "But at the end of the day, you need to do what’s right for the patient."
Because bariatric surgery coverage is not mandated at the federal level, millions of American do not have access to obesity care, said Dr. Morton.
Role of prejudice
"The biggest problem we have had with this for 50 years is prejudice," Dr. Henry Buchwald, professor emeritus of the Owen H. and Sarah Davidson Wangensteen Chair in Experimental Surgery at the University of Minnesota, Minneapolis. "People are prejudiced against the obese."
Dr. Morton said that even though obesity is a disease recognized by the AMA, it is often described in exclusionary terms by third-party payers.
"When you look at the ACA, there’s language that says it cannot discriminate on the basis of a health condition, but if you look at some of these [insurance] plans, there is actually language that says ‘we will not cover obesity treatment.’ That’s exclusionary language, and we need to figure out why this is occurring."
However, Dr. Finkelstein suggested that part of the problem with getting coverage for weight loss surgery might be how the field frames their argument in favor of it.
"I think the obesity community has done themselves a disservice by pushing [return on investment] for bariatric procedures," said Dr. Finkelstein. "I don’t think bariatric surgery should be talked about in terms of value for money. The [health] value is there just like any other procedure, and so it should be covered."
Little incentive
Despite the fact that the costs of obesity over a lifetime are high in the aggregate, Dr. Finkelstein said that the costs are highest later in life. That, plus the current trend of employees changing jobs an average of every 3 years, means obesity is often overlooked.
"Even though the net costs from a lifetime perspective are significant, there is not a lot of incentive for any particular payer to do any obesity prevention because the costs are eventually shifted down the line," said Dr. Finkelstein. When the federal government picks up paying for the health care costs of everyone 65 years of age or older, you are unlikely to "see significant investments in prevention," he said.
In cases in which the individual has had no insurance prior to qualifying for Medicare, the costs are even higher, and the cases more complex. "About 25% of patients who have chronic disease with multiple comorbidities make up 85% of our costs," Dr. Wild said, adding that of those 25%, 5% are "superusers" who make up 50% of all CMS costs.
The CMS spends $1.5 billion a day, or $900 billion annually, on health care, according to Dr. Wild.
"When we talk about bending the cost curve and saving money, we need to focus on those patients with multiple comorbidities and chronic diseases," said Dr. Wild.
The agreement on this point brought the panel back to the question of what is the sweet spot for prevention and intervention, and who should pay for it.
Surgery not the only answer
"We’re not going to solve the obesity problem by surgery alone," Dr. Buchwald said, adding that a combination of approaches, including prevention, medical, and other approaches. "We have to look for things that will work together."
Dr. Morton agreed that more research into complimentary medical interventions for obesity was needed. "We have been hamstrung by not having a lot of options," he said.
"Diet and exercise do work, but we don’t diet or exercise as much as we used to and that’s part of the reason we’re in this situation," Dr. Finkelstein said.
The data support bariatric surgery as a viable way to cut costs, said Dr. Morton. "The data are on our side," he said. "We have a lot of patients in need, and I would call for some rational coverage decisions when it comes to health exchanges. I think the government can be our partners in this."
Dr. Finkelstein noted several disclosures including, Jenny Craig, Johnson & Johnson, and Sanofi-Aventis, among several others. Dr. Morton has worked with Covidien. Dr. Buchwald and Dr. Wild did not have any relevant disclosures
EXPERT ANALYSIS FROM OBESITY WEEK
Psychoeducation, compliance contracts curb postsurgery alcohol abuse
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
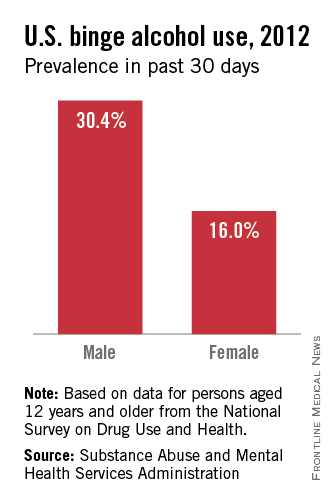
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
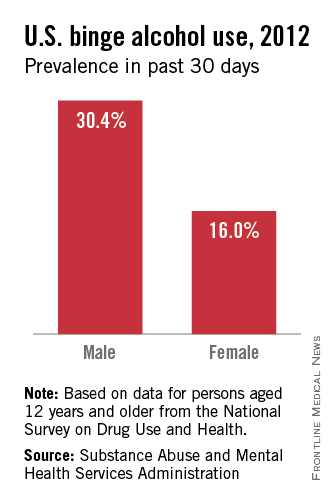
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
ATLANTA – Pre–bariatric surgery psychoeducation and compliance contracts are two ways to help lower the risk of patient alcohol abuse after surgery.
"Surgery itself changes a patient’s susceptibility to alcohol," said Leslie Heinberg, Ph.D., director of behavioral services for the Bariatric and Metabolic Institute at Cleveland Clinic. "There’s going to be increased sensitivity to alcohol and decreased tolerance," Dr. Heinberg said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
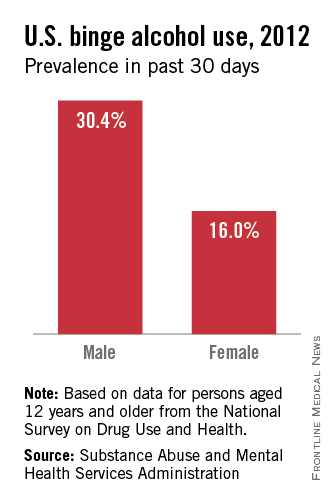
Programs that screen and triage bariatric surgery candidates, as well as inform them of how alcohol will affect them post surgery, can help manage their risk, according to Dr. Heinberg.
"I tell patients: ‘You’re going to get drunk very easily, very quickly, and it’s going to last a very long time.’ "
Dr. Heinberg cited a case cross-over trial that showed how at 6 months post gastric bypass surgery, patients had higher postoperative peak blood alcohol content levels after drinking one 5-ounce glass of red wine, and took longer to recover than they did before surgery.
"Patients that have one glass of red wine before surgery, they’re about at .02 [blood alcohol content], and they’re legally fine," she said. "Six months after surgery, they’re legally drunk." (J. Am. Coll. Surg. 2011;212:209-14).
The physical experience of drinking alcohol changes post surgery, too. "Postop, people are more likely to report that they feel dizzy and lightheaded and have double vision," said Dr. Heinberg, also professor of medicine in the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University.
‘Addiction transfer’
Reasons for the increased susceptibility in this patient population include the change in ratio between body weight and alcohol concentration, as well as the physiologic change inherent to gastric bypass where a pouch is placed in the jejunum. "There is a bolus of alcohol that hits and hits very quickly," said Dr. Heinberg.
Another reason is that in weight-loss surgery, one of the body’s primary sources of antialcohol dehydrogenase, the stomach, has been reduced in volume, she said.
Dr. Heinberg also said new data suggest "addiction transfer," thought to be the result of the body’s shared neural pathways for compulsive eating and substance abuse, might lead to either relapse in patients with histories of alcohol abuse or new-onset alcoholism in those who may not have abused alcohol, but who were compulsive eaters (Arch. Gen. Psychiatry. 2011;68:808-16).
Risk predictors
Dr. Heinberg cited a longitudinal study showing that predictors of risk included being male; presurgery use of tobacco, alcohol, and recreational drugs; having weak social support networks; and having gastric bypass surgery rather than other surgical weight loss procedures (JAMA 2012;307:2516-25).
The "good news," said Dr. Heinberg, is that contrary to her own hypothesis, a study of 400 patients with a history of substance abuse, controlled for presurgical body mass index, surgery type, gender, and race showed that people with a history of substance abuse had lost more weight 2 years after surgery (Surg. Obes. Relat. Dis. 2012 8:357-63).
"I think people who achieve abstinence have figured out how to completely change their lifestyle," said Dr. Heinberg. "Maybe those skills that helped them quit drinking are helping them post surgery."
Improved compliance
In an online questionnaire, 84% of 318 bariatric surgery patients surveyed admitted they continued to drink after their surgery, said Dr. Heinberg. "I think it’s important to screen each and every patient for all kinds of alcohol problems."
To help ensure compliance, she suggested clinics use free screening tools and guidelines available from the National Institute on Alcohol Abuse and Alcoholism. She described various levels of psychoeducation in use at her clinic, depending upon how severe the risk per the screening.
Participants deemed by her clinic to be at greater risk are given substance risk reduction education, which includes pre- and posttests. This helps avoid patients’ claims that they were unaware of the risks of alcohol after the surgery, said Dr. Heinberg. "We just pull out the test and say, ‘You got a 100%."
In some cases, she suggested that asking a patient who is a compliance risk concern to sign a contract agreeing not to drink after the surgery might help "get around risk management."
Dr. Heinberg concluded that this is a "vulnerable" patient population that may not be aware of the risks posed by alcohol post surgery. "Most programs need to think about putting this in their informed consent and providing more psychoeducation prior to surgery, sometimes even behavioral contracts," she said.
EXPERT ANALYSIS FROM OBESITY WEEK
Diet drinks’ link to cardiometabolic disease elusive
ATLANTA – Diet drinks might be protective rather than causative in cardiometabolic diseases such as obesity and type 2 diabetes, but definitive data are lacking.
"I would say that based on the scientific evidence to date, it might be a good idea to switch to artificially sweetened beverages, but I don’t see the evidence to either promote or avoid them," said Mark Pereira, Ph.D., of the School of Public Health at the University of Minnesota, Minneapolis.
There are data linking sugar-sweetened beverages to metabolic disorders. Findings from a recent, small, but "pretty provocative" randomized pilot study point to a relationship between sugar-sweetened beverages’ strong effect on visceral fat, particularly in the intra-abdominal cavity, he said. Diet drinks were not found in the study to have a positive association with this kind of adiposity (Am. J. Clin. Nutr. 2012;95:283-9).
The significance of this is that visceral adipose tissue in the gut "is consistent with a higher cardiometabolic risk profile," he said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The study supports findings from the National Heart, Blood, and Lung Institute’s prospective Coronary Artery Risk Development in Young Adults (CARDIA) study of 3,000 individuals. Imaging done across the cohort at year 25 of the study showed a weak association between artificially sweetened beverages and the volume of fat in the visceral cavity, but a "really, really strong" association with sugar-sweetened beverages and visceral cavity adipose tissue, said Dr. Pereira.
"If you look at the true drivers of metabolic risk, the visceral fat, it’s not there with the artificially sweetened drinks, it’s only there with the sugar-sweetened ones," he said.
Although both diet and sugar-sweetened drinks have positive associations with incident diabetes and other metabolic disturbances, the relationship between "diet drinks and cardiometabolic risk may be an anomaly of reverse causality," Dr. Pereira said.
While findings from the CARDIA study show an association between waist circumference and consumption of diet drinks, there was not an association with blood sugar, lipids, or blood pressure. "So, the question is, ‘Why isn’t [diet drink consumption] driving the risk factors?" asked Dr. Pereira.
The reason may be that consumers of high amounts of diet drinks "are more likely to be overweight and obese, and are more likely to be at high risk for chronic disease so they choose beverages with low calories to try to lower their risk," he suggested.
However, the extent of reverse causality in this patient population, said Dr. Pereira, is still unknown: "There could be an increased risk [of cardiometabolic disease] with a higher intake of artificially sweetened drinks, but you could also say it is protective."
The lack of certainty, according to Dr. Pereira, is due to a drought of data from well designed studies.
"I argue with some of my colleagues who believe that we can learn just as much or more on this from observational prospective epidemiological studies," he said, adding, "I am kind of steadfast that this is a topic that should be clearly addressed in terms of mechanisms and causality through better randomized controlled trials."
Dr. Pereira reported he has received support from the Robert Wood Johnson Foundation.
ATLANTA – Diet drinks might be protective rather than causative in cardiometabolic diseases such as obesity and type 2 diabetes, but definitive data are lacking.
"I would say that based on the scientific evidence to date, it might be a good idea to switch to artificially sweetened beverages, but I don’t see the evidence to either promote or avoid them," said Mark Pereira, Ph.D., of the School of Public Health at the University of Minnesota, Minneapolis.
There are data linking sugar-sweetened beverages to metabolic disorders. Findings from a recent, small, but "pretty provocative" randomized pilot study point to a relationship between sugar-sweetened beverages’ strong effect on visceral fat, particularly in the intra-abdominal cavity, he said. Diet drinks were not found in the study to have a positive association with this kind of adiposity (Am. J. Clin. Nutr. 2012;95:283-9).
The significance of this is that visceral adipose tissue in the gut "is consistent with a higher cardiometabolic risk profile," he said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The study supports findings from the National Heart, Blood, and Lung Institute’s prospective Coronary Artery Risk Development in Young Adults (CARDIA) study of 3,000 individuals. Imaging done across the cohort at year 25 of the study showed a weak association between artificially sweetened beverages and the volume of fat in the visceral cavity, but a "really, really strong" association with sugar-sweetened beverages and visceral cavity adipose tissue, said Dr. Pereira.
"If you look at the true drivers of metabolic risk, the visceral fat, it’s not there with the artificially sweetened drinks, it’s only there with the sugar-sweetened ones," he said.
Although both diet and sugar-sweetened drinks have positive associations with incident diabetes and other metabolic disturbances, the relationship between "diet drinks and cardiometabolic risk may be an anomaly of reverse causality," Dr. Pereira said.
While findings from the CARDIA study show an association between waist circumference and consumption of diet drinks, there was not an association with blood sugar, lipids, or blood pressure. "So, the question is, ‘Why isn’t [diet drink consumption] driving the risk factors?" asked Dr. Pereira.
The reason may be that consumers of high amounts of diet drinks "are more likely to be overweight and obese, and are more likely to be at high risk for chronic disease so they choose beverages with low calories to try to lower their risk," he suggested.
However, the extent of reverse causality in this patient population, said Dr. Pereira, is still unknown: "There could be an increased risk [of cardiometabolic disease] with a higher intake of artificially sweetened drinks, but you could also say it is protective."
The lack of certainty, according to Dr. Pereira, is due to a drought of data from well designed studies.
"I argue with some of my colleagues who believe that we can learn just as much or more on this from observational prospective epidemiological studies," he said, adding, "I am kind of steadfast that this is a topic that should be clearly addressed in terms of mechanisms and causality through better randomized controlled trials."
Dr. Pereira reported he has received support from the Robert Wood Johnson Foundation.
ATLANTA – Diet drinks might be protective rather than causative in cardiometabolic diseases such as obesity and type 2 diabetes, but definitive data are lacking.
"I would say that based on the scientific evidence to date, it might be a good idea to switch to artificially sweetened beverages, but I don’t see the evidence to either promote or avoid them," said Mark Pereira, Ph.D., of the School of Public Health at the University of Minnesota, Minneapolis.
There are data linking sugar-sweetened beverages to metabolic disorders. Findings from a recent, small, but "pretty provocative" randomized pilot study point to a relationship between sugar-sweetened beverages’ strong effect on visceral fat, particularly in the intra-abdominal cavity, he said. Diet drinks were not found in the study to have a positive association with this kind of adiposity (Am. J. Clin. Nutr. 2012;95:283-9).
The significance of this is that visceral adipose tissue in the gut "is consistent with a higher cardiometabolic risk profile," he said at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
The study supports findings from the National Heart, Blood, and Lung Institute’s prospective Coronary Artery Risk Development in Young Adults (CARDIA) study of 3,000 individuals. Imaging done across the cohort at year 25 of the study showed a weak association between artificially sweetened beverages and the volume of fat in the visceral cavity, but a "really, really strong" association with sugar-sweetened beverages and visceral cavity adipose tissue, said Dr. Pereira.
"If you look at the true drivers of metabolic risk, the visceral fat, it’s not there with the artificially sweetened drinks, it’s only there with the sugar-sweetened ones," he said.
Although both diet and sugar-sweetened drinks have positive associations with incident diabetes and other metabolic disturbances, the relationship between "diet drinks and cardiometabolic risk may be an anomaly of reverse causality," Dr. Pereira said.
While findings from the CARDIA study show an association between waist circumference and consumption of diet drinks, there was not an association with blood sugar, lipids, or blood pressure. "So, the question is, ‘Why isn’t [diet drink consumption] driving the risk factors?" asked Dr. Pereira.
The reason may be that consumers of high amounts of diet drinks "are more likely to be overweight and obese, and are more likely to be at high risk for chronic disease so they choose beverages with low calories to try to lower their risk," he suggested.
However, the extent of reverse causality in this patient population, said Dr. Pereira, is still unknown: "There could be an increased risk [of cardiometabolic disease] with a higher intake of artificially sweetened drinks, but you could also say it is protective."
The lack of certainty, according to Dr. Pereira, is due to a drought of data from well designed studies.
"I argue with some of my colleagues who believe that we can learn just as much or more on this from observational prospective epidemiological studies," he said, adding, "I am kind of steadfast that this is a topic that should be clearly addressed in terms of mechanisms and causality through better randomized controlled trials."
Dr. Pereira reported he has received support from the Robert Wood Johnson Foundation.
EXPERT ANALYSIS FROM OBESITY WEEK
Cognitive impairment at baseline linked to poorer bariatric surgery outcomes
ATLANTA – Higher baseline levels of cognitive impairment are associated with poorer weight loss outcomes after bariatric surgery.
"People with problems of memory, problem solving, or attention prior to surgery show reduced ability to lose weight," said John Gunstad, Ph.D., at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
In a prospective study of 109 bariatric surgery patients enrolled in the LABS (Longitudinal Assessment of Bariatric Surgery) study and 41 obese matched controls who’d not had surgery, Dr. Gunstad, who is professor and chairman of neuroscience at Kent (Ohio) State University, and his colleagues assessed all participants’ cognitive function at baseline, at 12 weeks, and at 12, 24, and 36 months.
They found that 25% of all surgical patients had baseline cognitive impairment. "These were individuals who were at least 1.5 standard deviations below normal-weight persons in at least one cognitive domain," said Dr. Gunstad. "If these individuals came to my clinic, I would have to diagnose them with some kind of cognitive disorder."
Expanding the criteria to 1 standard deviation meant that 40% of participants had subtle impairment. "Patients who are coming in for bariatric surgery are between 5 and 8 times more likely to have cognitive impairment than their normal-weight counterparts. That’s a remarkable number," said Dr. Gunstad.
At 12 weeks, surgery patients who’d lost an average of 48 pounds showed gains in cognitive functioning. Overall, the study showed initial, rapid cognitive improvement, and then either continued or sustained improvement 3 years out.
"We went from a quarter of patients being clinically impaired prior to surgery," said Dr. Gunstad. "At 3 years after surgery, that number was down to 4%."
However, in a related study, Dr. Gunstad and his colleagues found that greater levels of cognitive impairment correlated to less weight loss at all follow-up points (Surg. Obes. Relat. Dis. 2013;9:765-70).
Dr. Gunstad said this was likely due to patient adherence issues after the tumult of bariatric surgery. "You have to eat in a different way. You have to think in a different way. You have to restructure every moment of your life," said Dr. Gunstad. "If you have problems with memory, problem solving, or organizing, it will be much more difficult to make and persist with those changes."
The clinical implication, said Dr. Gunstad, is that better screening of bariatric surgery candidates might be helpful. "If we know the cognitive status of our patients, it’s likely we will know what the outcomes will be," he said.
The drawback, he said, is that even though most third-party payers will cover the costs of evaluations, if a physician has a large practice of hundreds of patients, then the number of referrals might be overwhelming to the system, which might not have enough neuropsychologists to perform the tests.
Self-reporting might also be an issue because of the phenomenon of the "worried well" – the patients who overreport their problems – or because the patients with cognitive impairment won’t necessarily recognize the symptoms they need to report, said Dr. Gunstad.
By next year, said Dr. Gunstad, he hoped he and his colleagues will have finalized a better screening tool for clinicians who treat bariatric surgery patients.
Dr. Gunstad did not report any financial disclosures.
ATLANTA – Higher baseline levels of cognitive impairment are associated with poorer weight loss outcomes after bariatric surgery.
"People with problems of memory, problem solving, or attention prior to surgery show reduced ability to lose weight," said John Gunstad, Ph.D., at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
In a prospective study of 109 bariatric surgery patients enrolled in the LABS (Longitudinal Assessment of Bariatric Surgery) study and 41 obese matched controls who’d not had surgery, Dr. Gunstad, who is professor and chairman of neuroscience at Kent (Ohio) State University, and his colleagues assessed all participants’ cognitive function at baseline, at 12 weeks, and at 12, 24, and 36 months.
They found that 25% of all surgical patients had baseline cognitive impairment. "These were individuals who were at least 1.5 standard deviations below normal-weight persons in at least one cognitive domain," said Dr. Gunstad. "If these individuals came to my clinic, I would have to diagnose them with some kind of cognitive disorder."
Expanding the criteria to 1 standard deviation meant that 40% of participants had subtle impairment. "Patients who are coming in for bariatric surgery are between 5 and 8 times more likely to have cognitive impairment than their normal-weight counterparts. That’s a remarkable number," said Dr. Gunstad.
At 12 weeks, surgery patients who’d lost an average of 48 pounds showed gains in cognitive functioning. Overall, the study showed initial, rapid cognitive improvement, and then either continued or sustained improvement 3 years out.
"We went from a quarter of patients being clinically impaired prior to surgery," said Dr. Gunstad. "At 3 years after surgery, that number was down to 4%."
However, in a related study, Dr. Gunstad and his colleagues found that greater levels of cognitive impairment correlated to less weight loss at all follow-up points (Surg. Obes. Relat. Dis. 2013;9:765-70).
Dr. Gunstad said this was likely due to patient adherence issues after the tumult of bariatric surgery. "You have to eat in a different way. You have to think in a different way. You have to restructure every moment of your life," said Dr. Gunstad. "If you have problems with memory, problem solving, or organizing, it will be much more difficult to make and persist with those changes."
The clinical implication, said Dr. Gunstad, is that better screening of bariatric surgery candidates might be helpful. "If we know the cognitive status of our patients, it’s likely we will know what the outcomes will be," he said.
The drawback, he said, is that even though most third-party payers will cover the costs of evaluations, if a physician has a large practice of hundreds of patients, then the number of referrals might be overwhelming to the system, which might not have enough neuropsychologists to perform the tests.
Self-reporting might also be an issue because of the phenomenon of the "worried well" – the patients who overreport their problems – or because the patients with cognitive impairment won’t necessarily recognize the symptoms they need to report, said Dr. Gunstad.
By next year, said Dr. Gunstad, he hoped he and his colleagues will have finalized a better screening tool for clinicians who treat bariatric surgery patients.
Dr. Gunstad did not report any financial disclosures.
ATLANTA – Higher baseline levels of cognitive impairment are associated with poorer weight loss outcomes after bariatric surgery.
"People with problems of memory, problem solving, or attention prior to surgery show reduced ability to lose weight," said John Gunstad, Ph.D., at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
In a prospective study of 109 bariatric surgery patients enrolled in the LABS (Longitudinal Assessment of Bariatric Surgery) study and 41 obese matched controls who’d not had surgery, Dr. Gunstad, who is professor and chairman of neuroscience at Kent (Ohio) State University, and his colleagues assessed all participants’ cognitive function at baseline, at 12 weeks, and at 12, 24, and 36 months.
They found that 25% of all surgical patients had baseline cognitive impairment. "These were individuals who were at least 1.5 standard deviations below normal-weight persons in at least one cognitive domain," said Dr. Gunstad. "If these individuals came to my clinic, I would have to diagnose them with some kind of cognitive disorder."
Expanding the criteria to 1 standard deviation meant that 40% of participants had subtle impairment. "Patients who are coming in for bariatric surgery are between 5 and 8 times more likely to have cognitive impairment than their normal-weight counterparts. That’s a remarkable number," said Dr. Gunstad.
At 12 weeks, surgery patients who’d lost an average of 48 pounds showed gains in cognitive functioning. Overall, the study showed initial, rapid cognitive improvement, and then either continued or sustained improvement 3 years out.
"We went from a quarter of patients being clinically impaired prior to surgery," said Dr. Gunstad. "At 3 years after surgery, that number was down to 4%."
However, in a related study, Dr. Gunstad and his colleagues found that greater levels of cognitive impairment correlated to less weight loss at all follow-up points (Surg. Obes. Relat. Dis. 2013;9:765-70).
Dr. Gunstad said this was likely due to patient adherence issues after the tumult of bariatric surgery. "You have to eat in a different way. You have to think in a different way. You have to restructure every moment of your life," said Dr. Gunstad. "If you have problems with memory, problem solving, or organizing, it will be much more difficult to make and persist with those changes."
The clinical implication, said Dr. Gunstad, is that better screening of bariatric surgery candidates might be helpful. "If we know the cognitive status of our patients, it’s likely we will know what the outcomes will be," he said.
The drawback, he said, is that even though most third-party payers will cover the costs of evaluations, if a physician has a large practice of hundreds of patients, then the number of referrals might be overwhelming to the system, which might not have enough neuropsychologists to perform the tests.
Self-reporting might also be an issue because of the phenomenon of the "worried well" – the patients who overreport their problems – or because the patients with cognitive impairment won’t necessarily recognize the symptoms they need to report, said Dr. Gunstad.
By next year, said Dr. Gunstad, he hoped he and his colleagues will have finalized a better screening tool for clinicians who treat bariatric surgery patients.
Dr. Gunstad did not report any financial disclosures.
AT OBESITY WEEK
Vegetarian, Vegan Diets for Weight Loss?
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
AT OBESITY WEEK
Obese and overweight adults lost significant weight on vegetarian, vegan diets
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
ATLANTA – Vegetarian and vegan diets that did not emphasize counting calories led to more weight loss over 8 weeks and at 6 months than did diets that included meat, according to data presented at Obesity Week.
"We’re not trying to get people to lose weight just so they can look attractive," said Gabrielle Turner-McGrievy, Ph.D., in an interview. "We’re hoping they will choose a healthy body weight to prevent diabetes and cancer."
The results are from the first randomized study to directly compare the effect of vegan, vegetarian, and omnivorous diets, without caloric restrictions, on body weight, said Dr. Turner-McGrievy, of the department of health promotion, education, and behavior at the Arnold School of Public Health at the University of South Carolina in Columbia.
In the New DIETs (New Dietary Interventions to Enhance the Treatments for Weight Loss) study, 63 adults (73% female, 79% white) with a mean age of 49 years and a mean body mass index of 35 kg/m2 were randomly assigned to one of five diets: vegan, vegetarian, pesco-vegetarian, semi-vegetarian, and omnivorous*. All five dietary approaches emphasized low-fat, low-glycemic-index foods but did not require caloric restriction. All participants attended weekly meetings to learn more about the type of diet they had been assigned. All diets stressed consumption of foods that were as unprocessed as possible. Participants who screened positive for eating disorder–like behavior were not included in the study.
An intent-to-treat analysis showed that at 8 weeks, the groups that followed a plant-based diet had lost an average of 8-10 pounds, while those consuming some meat lost an average of 5 pounds.
At 6 months, the vegans had lost about 7% of their body weight, the semi-vegetarian group had lost about 4% of their body weight, the pesco-vegetarian group had lost about 3%, and the omnivorous group had lost about 3%, Dr. Turner-McGrievy reported.
"All groups lost a significant amount of weight without having to count calories, but it was greatest in the vegan group," she said. Compliance in the vegan group at 8 weeks averaged about half; at 6 months, it had dropped to 30%.
"Our message here is that adherence may not be completely necessary," she said. "We shifted people so far down the dietary spectrum that even if they added a little cheese or meat here or there, they still weren’t going back to where they were before."
The exact reason for the greater weight loss in the plant-based diet groups was not clear, said Dr. Turner-McGrievy, but she and her colleagues theorized that changes in macronutrient content, which were found to be significantly different across groups (P < .05), may be a factor. "When we looked at the nutritive changes of these five different diets, we saw a much greater decrease of saturated fat among the vegan diet group," she said. "Vegetarians and vegans also decreased their cholesterol more than the other groups."
When Dr. Turner-McGrievy was asked whether any groups consumed more food, on average, than other groups, she said her team had not determined if there were different levels of hunger between the groups. Study participants were enthusiastic about the "freedom" they had from calorie counting: "On calorie-restricted diets, if at the end of the day you’ve reached your calorie allotment, but you’re still hungry, then you go to bed hungry," she said.
Despite the limited sample size and duration of the NEW DIETs study, Dr. Turner-McGrievy said one of the study’s implications is that when it comes to treating obesity and its attendant comorbidities, there can be a focus on nutrition. "It moves this area of science forward and shows there is another approach that can be used instead of calorie restriction," she said. People with obesity could also be placed on a "stepwise" system, where they start out eating slightly less meat, and eventually move to a more plant-based diet, she noted.
Obesity Week was presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery.
Dr. Turner-McGrievy did not have any relevant disclosures.
*Correction, 12/11/2013: An earlier version of this article misstated one of the diets included in the New DIETs study.
AT OBESITY WEEK
Major finding: Plant-based diets, without calorie restriction, led to nearly twice as much weight loss as diets that included meat in 63 obese and overweight adults.
Data source: Randomized controlled pilot study conducted over 8 weeks and followed up at 6 months.
Disclosures: Dr. Turner-McGrievy did not have any relevant disclosures.
Gastric bypass associated with reversal of aging process
ATLANTA – Gastric bypass was associated with the lengthening of telomeres, an indication that surgical weight loss may reverse aging in obese patients.
The most significant changes in telomere length occurred in patients with biomarkers indicative of higher levels of preoperative inflammation and cholesterol, according to findings presented by bariatric surgeon John Morton at this year’s Obesity Week.
"Telomeres are unique markers for aging and are linked to chronic diseases and things like smoking and depression," Dr. Morton said in an interview. "There are a lot of things that can potentially affect telomeres, but there aren’t a lot of things that can affect them in a positive sense."
Dr. Morton and his colleagues at Stanford (Calif.) University measured the baseline telomere length, weight, C-reactive protein (CRP) levels, cholesterol levels, and fasting insulin levels in 51 gastric bypass surgery patients (77% female, average age 49 years). The group’s mean body mass index was 44 kg/m2. The measurements were taken again at 3, 6, and 12 months. Telomere length was determined using quantitative polymerase chain reaction testing.
In all patients, excess body weight loss at 12 months averaged 71%; CRP levels, indicative of inflammation, dropped an average of more than 60%. Fasting insulin levels decreased from 24 uIU/mL at baseline to 6 uIU/mL when measured 1 year after surgery. These results were consistent with those of previous studies, but this study was the first to correlate such changes with the body’s biomarkers for aging, telomeres, Dr. Morton said.
Unexpected results
Telomere length did not change significantly across the cohort, but when analyzed according to CRP and LDL levels, significant changes in telomere length were found in patients whose levels of both were higher at baseline (P = .0387 and P = .005). In those whose baseline CRP was high, there also was a significant positive correlation between telomere lengthening and weight loss (P = .0498) and increases in HDL cholesterol level (P = .0176).
The results were somewhat unexpected. "The thing that surprised me the most was that if there were going to be changes, then they should be across the board," said Dr. Morton. "But where it really made a difference was in those who had [high levels of markers of] inflammation. It was a pretty specific result in a pretty specific population."
At least one other longitudinal study has shown the impact of nonsurgical intervention, namely a change in diet, on the length of telomeres (PLoS One 2013;8:e62781[doi:10.1371/journal.pone.0062781]), but Dr. Morton said the study, which emphasized eating less red meat and more fish, fresh vegetables, and olive oil did not demonstrate results that were notably different from his findings.
"One thing that study’s diet, the Mediterranean Diet, is known to do is to raise HDL," said Dr. Morton. "In our study we also saw a correlation between telomere lengthening and increases in HDL. That’s really hard to do. There aren’t a lot of medicines that can really affect the ‘good’ cholesterol."
‘Unique ability’ of gastric bypass
The study did not examine the relationship between telomeres and other kinds of surgical interventions for weight loss, but Dr. Morton said future studies on bariatric procedures such as the sleeve gastrectomy need to be conducted before they can be equated with bypass.
"Gastric bypass has a unique affect on inflammation that is independent of the other operations," said Dr. Morton, referring to data he presented earlier this year at the American College of Surgeons annual meeting, discussing the relationship between bypass and diabetes. "We have shown that C-reactive protein decreases more with gastric bypass than with other operations."
That of all the surgical interventions, gastric bypass has the greatest impact on diabetes, independent of weight loss, points to future research on inflammation, said Dr. Morton. "People are starting to think that type 2 diabetes is not just a burned-out pancreas, but that a lot of inflammation is involved."
Calling bariatric surgery a "platform for investigation" that can help [us] understand the connection between inflammation and the processes of disease in the general population, not just those with obesity, Dr. Morton said, "I think the future will elucidate some of those processes, and will come up with different interventions such as drugs."
Dr. Morton said he did not have any relevant financial disclosures.
ATLANTA – Gastric bypass was associated with the lengthening of telomeres, an indication that surgical weight loss may reverse aging in obese patients.
The most significant changes in telomere length occurred in patients with biomarkers indicative of higher levels of preoperative inflammation and cholesterol, according to findings presented by bariatric surgeon John Morton at this year’s Obesity Week.
"Telomeres are unique markers for aging and are linked to chronic diseases and things like smoking and depression," Dr. Morton said in an interview. "There are a lot of things that can potentially affect telomeres, but there aren’t a lot of things that can affect them in a positive sense."
Dr. Morton and his colleagues at Stanford (Calif.) University measured the baseline telomere length, weight, C-reactive protein (CRP) levels, cholesterol levels, and fasting insulin levels in 51 gastric bypass surgery patients (77% female, average age 49 years). The group’s mean body mass index was 44 kg/m2. The measurements were taken again at 3, 6, and 12 months. Telomere length was determined using quantitative polymerase chain reaction testing.
In all patients, excess body weight loss at 12 months averaged 71%; CRP levels, indicative of inflammation, dropped an average of more than 60%. Fasting insulin levels decreased from 24 uIU/mL at baseline to 6 uIU/mL when measured 1 year after surgery. These results were consistent with those of previous studies, but this study was the first to correlate such changes with the body’s biomarkers for aging, telomeres, Dr. Morton said.
Unexpected results
Telomere length did not change significantly across the cohort, but when analyzed according to CRP and LDL levels, significant changes in telomere length were found in patients whose levels of both were higher at baseline (P = .0387 and P = .005). In those whose baseline CRP was high, there also was a significant positive correlation between telomere lengthening and weight loss (P = .0498) and increases in HDL cholesterol level (P = .0176).
The results were somewhat unexpected. "The thing that surprised me the most was that if there were going to be changes, then they should be across the board," said Dr. Morton. "But where it really made a difference was in those who had [high levels of markers of] inflammation. It was a pretty specific result in a pretty specific population."
At least one other longitudinal study has shown the impact of nonsurgical intervention, namely a change in diet, on the length of telomeres (PLoS One 2013;8:e62781[doi:10.1371/journal.pone.0062781]), but Dr. Morton said the study, which emphasized eating less red meat and more fish, fresh vegetables, and olive oil did not demonstrate results that were notably different from his findings.
"One thing that study’s diet, the Mediterranean Diet, is known to do is to raise HDL," said Dr. Morton. "In our study we also saw a correlation between telomere lengthening and increases in HDL. That’s really hard to do. There aren’t a lot of medicines that can really affect the ‘good’ cholesterol."
‘Unique ability’ of gastric bypass
The study did not examine the relationship between telomeres and other kinds of surgical interventions for weight loss, but Dr. Morton said future studies on bariatric procedures such as the sleeve gastrectomy need to be conducted before they can be equated with bypass.
"Gastric bypass has a unique affect on inflammation that is independent of the other operations," said Dr. Morton, referring to data he presented earlier this year at the American College of Surgeons annual meeting, discussing the relationship between bypass and diabetes. "We have shown that C-reactive protein decreases more with gastric bypass than with other operations."
That of all the surgical interventions, gastric bypass has the greatest impact on diabetes, independent of weight loss, points to future research on inflammation, said Dr. Morton. "People are starting to think that type 2 diabetes is not just a burned-out pancreas, but that a lot of inflammation is involved."
Calling bariatric surgery a "platform for investigation" that can help [us] understand the connection between inflammation and the processes of disease in the general population, not just those with obesity, Dr. Morton said, "I think the future will elucidate some of those processes, and will come up with different interventions such as drugs."
Dr. Morton said he did not have any relevant financial disclosures.
ATLANTA – Gastric bypass was associated with the lengthening of telomeres, an indication that surgical weight loss may reverse aging in obese patients.
The most significant changes in telomere length occurred in patients with biomarkers indicative of higher levels of preoperative inflammation and cholesterol, according to findings presented by bariatric surgeon John Morton at this year’s Obesity Week.
"Telomeres are unique markers for aging and are linked to chronic diseases and things like smoking and depression," Dr. Morton said in an interview. "There are a lot of things that can potentially affect telomeres, but there aren’t a lot of things that can affect them in a positive sense."
Dr. Morton and his colleagues at Stanford (Calif.) University measured the baseline telomere length, weight, C-reactive protein (CRP) levels, cholesterol levels, and fasting insulin levels in 51 gastric bypass surgery patients (77% female, average age 49 years). The group’s mean body mass index was 44 kg/m2. The measurements were taken again at 3, 6, and 12 months. Telomere length was determined using quantitative polymerase chain reaction testing.
In all patients, excess body weight loss at 12 months averaged 71%; CRP levels, indicative of inflammation, dropped an average of more than 60%. Fasting insulin levels decreased from 24 uIU/mL at baseline to 6 uIU/mL when measured 1 year after surgery. These results were consistent with those of previous studies, but this study was the first to correlate such changes with the body’s biomarkers for aging, telomeres, Dr. Morton said.
Unexpected results
Telomere length did not change significantly across the cohort, but when analyzed according to CRP and LDL levels, significant changes in telomere length were found in patients whose levels of both were higher at baseline (P = .0387 and P = .005). In those whose baseline CRP was high, there also was a significant positive correlation between telomere lengthening and weight loss (P = .0498) and increases in HDL cholesterol level (P = .0176).
The results were somewhat unexpected. "The thing that surprised me the most was that if there were going to be changes, then they should be across the board," said Dr. Morton. "But where it really made a difference was in those who had [high levels of markers of] inflammation. It was a pretty specific result in a pretty specific population."
At least one other longitudinal study has shown the impact of nonsurgical intervention, namely a change in diet, on the length of telomeres (PLoS One 2013;8:e62781[doi:10.1371/journal.pone.0062781]), but Dr. Morton said the study, which emphasized eating less red meat and more fish, fresh vegetables, and olive oil did not demonstrate results that were notably different from his findings.
"One thing that study’s diet, the Mediterranean Diet, is known to do is to raise HDL," said Dr. Morton. "In our study we also saw a correlation between telomere lengthening and increases in HDL. That’s really hard to do. There aren’t a lot of medicines that can really affect the ‘good’ cholesterol."
‘Unique ability’ of gastric bypass
The study did not examine the relationship between telomeres and other kinds of surgical interventions for weight loss, but Dr. Morton said future studies on bariatric procedures such as the sleeve gastrectomy need to be conducted before they can be equated with bypass.
"Gastric bypass has a unique affect on inflammation that is independent of the other operations," said Dr. Morton, referring to data he presented earlier this year at the American College of Surgeons annual meeting, discussing the relationship between bypass and diabetes. "We have shown that C-reactive protein decreases more with gastric bypass than with other operations."
That of all the surgical interventions, gastric bypass has the greatest impact on diabetes, independent of weight loss, points to future research on inflammation, said Dr. Morton. "People are starting to think that type 2 diabetes is not just a burned-out pancreas, but that a lot of inflammation is involved."
Calling bariatric surgery a "platform for investigation" that can help [us] understand the connection between inflammation and the processes of disease in the general population, not just those with obesity, Dr. Morton said, "I think the future will elucidate some of those processes, and will come up with different interventions such as drugs."
Dr. Morton said he did not have any relevant financial disclosures.
AT OBESITY WEEK
Major finding: Significant increases in telomere length were observed after gastric bypass in individuals with high baseline CRP or LDL cholesterol levels (P = .0387 and P = .005, respectively); weight loss and increased levels of HDL cholesterol were positively correlated with telomere length in patients with high baseline CRP (P = .0498 and P = .0176).
Data source: A prospective study of 51 gastric bypass patients (77% female) whose telomere lengths, LDL, and CRP levels were measured at baseline and at 3,6, and 12 months.
Disclosures: Dr. Morton said he did not have any relevant financial disclosures.
















