User login
Helping adolescents get enough quality sleep
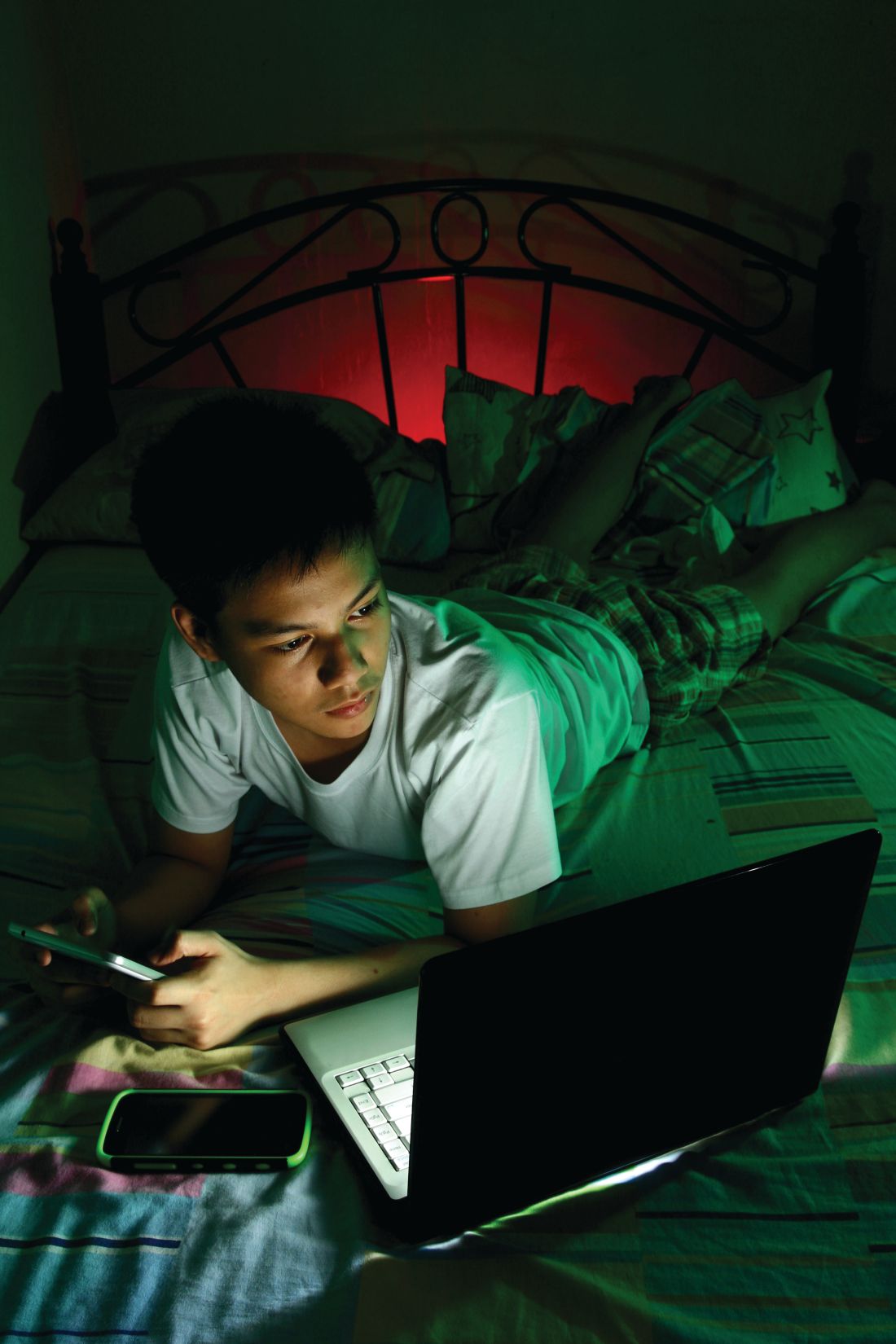
NEW ORLEANS – Social media and electronics aren’t the only barriers to a good night’s sleep for teens, according to Adiaha I. A. Spinks-Franklin, MD, MPH, a pediatrician at Texas Children’s Hospital in Houston.
Another half-dozen “sleep enemies” interfere with adolescents’ sleep and can contribute to insomnia or other sleep disorders, she told attendees at the annual meeting of the American Academy of Pediatrics.
Knowing what normal sleep physiology looks like in youth and understanding the most common sleep enemies and sleep-behavior problems can help you use effective interventions to help your patients get the sleep they need, she said.
Infants need the most sleep, about 12-16 hours each 24-hour period, including naps, for those aged 4-12 months. As they grow into toddlerhood and preschool age, children gradually need less: Children aged 1-2 years need 11-14 hours and children aged 3-5 years need 10-13 hours, including naps. By the time children are in school, ages 6-12, they should have dropped their naps and need 9-12 hours a night.
In fact, 75% of high school seniors get less than 8 hours of sleep a day and live with a chronic sleep debt, Dr. Spinks-Franklin said.
Although social media use and electronics in the bedroom – TVs, computers, cell phones, and video games – can certainly contribute to inadequate sleep, a heavy academic load and extracurricular activities can be just as problematic, Dr. Spinks-Franklin said. Teens who work after school also may have difficulty getting enough sleep, especially if they also have to balance a heavier academic load or even one or two extracurricular activities.
Socializing with friends also can interfere with sleep, especially when get-togethers run late; drinking caffeinated drinks in the afternoon onward can make it difficult for adolescents to get the sleep they need as well. Less-modifiable contributors to too little sleep are stress and early school start times, Dr. Spinks-Franklin said.
The two most common sleep problems seen in teens are insomnia and delayed sleep phase syndrome. Addressing these is important because the effects of chronic insufficient sleep can have far-reaching consequences. Obesity and related chronic health conditions are associated with inadequate sleep, as are poor academic performance, poor judgment, poor executive functioning, and mental health disorders like depression.
Short-term effects of insufficient sleep also can be problematic and can exacerbate existing sleep problems, such as sleeping in on the weekends to “catch up” on sleep or drinking more caffeine to try to stay awake during the day. Increased caffeine intake can interfere with non-REM deep sleep, Dr. Spinks-Franklin said, and therefore reduce the quality of sleep even if the person gets the total hours they need.
Insomnia in adolescents
Insomnia can refer to difficulty falling asleep, staying asleep, sleeping for long enough, or getting enough sleep in one period of time even when the opportunity is there. Some people may have no trouble falling asleep, but they wake up too early – before they have had gotten the sleep they need – and cannot return to sleep.
To be insomnia, the problem must occur “despite having enough time available for sleep,” Dr. Spinks-Franklin said. “Patient who restrict the amount of time for sleep due to work or social commitments may have trouble sleeping and daytime sleepiness but do not have insomnia.”
Daytime impairment also is part of the American Academy of Sleep Medicine’s definition of insomnia. The rare teen who doesn’t need as much sleep as average and functions without difficulty during the day does not necessarily have insomnia.
But the impairment may not necessarily just be fatigue or sleepiness. In fact, many of the symptoms are the same as those seen with ADHD.
Daytime consequences of insomnia can include the following:
- Depression, feeling sad or “blue,” or emotional hypersensitivity.
- Mood swings, crankiness, or irritability.
- Difficulty concentrating or paying attention, poor memory, mind wandering, or even inability to sit still.
- Job or school problems, such as not being able to finish homework, not finishing tasks they start, or forgetfulness.
- Difficulty in social situations, such as discomfort with others or problems with friends.
- Daytime sleepiness, even when unable to actually take a nap.
- Behavioral problems, such as hyperactivity, impulsivity, or aggression.
- Frequent mistakes, especially at work, at school, or while driving (often “errors of omission,” such as not seeing a street sign or not hearing an instruction).
- Lower levels of motivation or initiative, feeling less energetic.
- Excessive worry about sleep.
Evaluation of insomnia can be framed with “the three-factor model,” which includes predisposing factors, precipitating factors, and perpetuating factors.
Predisposing factors – those that indicate a person already may be at risk for insomnia – include potential genetic influences as well as their typical response to stress. “Do they sleep more or less?” Dr. Spinks-Franklin said. Even teens predisposed to insomnia may not develop it, however, without a precipitating trigger.
These triggers could include stress, anxiety, poor initial sleep hygiene that becomes a pattern, dietary intake or behaviors (such as drinking caffeine or eating too much or too late in the evening), changes to their schedule, or side effects of medications.
Once insomnia begins, various factors can then perpetuate the cycle, including some of those that triggered it, such as anxiety or a school or work schedule. Sometimes it can be difficult to pinpoint the factor prolonging insomnia, such as the unconscious reward of going to work or school late with few or no consequences.
Delayed sleep phase syndrome
Delayed sleep phase syndrome occurs when someone has a delayed onset of melatonin secretion that pushes back the time when they can fall asleep. Melatonin is the neurotransmitter produced by the pineal gland that signals the start of nighttime. Although it has a hereditary component, delayed sleep phase syndrome also can result from a pattern of poor sleep onset and sleeping in on the weekends.
Dr. Spinks-Franklin described the typical cycle: A teen doesn’t go to sleep until after midnight and then wants to sleep in later in the morning. Because they have to wake up early for school, they sleep in on the weekends to try to regain the sleep they lost. Sleeping in pushes their circadian rhythm even later, perpetuating the problem.
Interventions for sleep disorders
The recommended treatment for insomnia is cognitive-behavior therapy for insomnia, for which strong evidence exists. Before seeking cognitive-behavior therapy, however, families can work to improve sleep hygiene and reduce stimuli that contribute to insomnia.
Teens should avoid screens for at least 1 hour before bedtime and avoid caffeine and exercise for at least 4 hours before going to bed. They also need to develop a schedule with a consistent bedtime and wake-up time, including on the weekends. They should avoid sleeping in on the weekends or taking naps during the day, Dr. Spinks-Franklin said.
Delayed sleep phase syndrome is more resistant to treatment and has a high recurrence rate, she said, and it requires commitment from the parent and their child to address it successfully. Teens with this condition also can start with sleep hygiene practices: a consistent wake-up time that they maintain on the weekends and no daytime naps. Phototherapy in the morning can be added to hopefully induce an earlier onset of melatonin release in the evening.
The next step is making changes to the youth’s schedule, particularly evening and/or weekend activities. They can try to gradually advance their biological clock by changing their sleep schedule.
Dr. Spinks-Franklin also briefly addressed the use of over-the-counter melatonin supplements for treating sleep problems. Melatonin can be effective for treating insomnia by improving sleep onset and sleep quality, particularly in children and teens with autism spectrum disorder or ADHD.
Dr. Spinks-Franklin had no disclosures, and her presentation used no outside funding.
NEW ORLEANS – Social media and electronics aren’t the only barriers to a good night’s sleep for teens, according to Adiaha I. A. Spinks-Franklin, MD, MPH, a pediatrician at Texas Children’s Hospital in Houston.
Another half-dozen “sleep enemies” interfere with adolescents’ sleep and can contribute to insomnia or other sleep disorders, she told attendees at the annual meeting of the American Academy of Pediatrics.
Knowing what normal sleep physiology looks like in youth and understanding the most common sleep enemies and sleep-behavior problems can help you use effective interventions to help your patients get the sleep they need, she said.
Infants need the most sleep, about 12-16 hours each 24-hour period, including naps, for those aged 4-12 months. As they grow into toddlerhood and preschool age, children gradually need less: Children aged 1-2 years need 11-14 hours and children aged 3-5 years need 10-13 hours, including naps. By the time children are in school, ages 6-12, they should have dropped their naps and need 9-12 hours a night.
In fact, 75% of high school seniors get less than 8 hours of sleep a day and live with a chronic sleep debt, Dr. Spinks-Franklin said.
Although social media use and electronics in the bedroom – TVs, computers, cell phones, and video games – can certainly contribute to inadequate sleep, a heavy academic load and extracurricular activities can be just as problematic, Dr. Spinks-Franklin said. Teens who work after school also may have difficulty getting enough sleep, especially if they also have to balance a heavier academic load or even one or two extracurricular activities.
Socializing with friends also can interfere with sleep, especially when get-togethers run late; drinking caffeinated drinks in the afternoon onward can make it difficult for adolescents to get the sleep they need as well. Less-modifiable contributors to too little sleep are stress and early school start times, Dr. Spinks-Franklin said.
The two most common sleep problems seen in teens are insomnia and delayed sleep phase syndrome. Addressing these is important because the effects of chronic insufficient sleep can have far-reaching consequences. Obesity and related chronic health conditions are associated with inadequate sleep, as are poor academic performance, poor judgment, poor executive functioning, and mental health disorders like depression.
Short-term effects of insufficient sleep also can be problematic and can exacerbate existing sleep problems, such as sleeping in on the weekends to “catch up” on sleep or drinking more caffeine to try to stay awake during the day. Increased caffeine intake can interfere with non-REM deep sleep, Dr. Spinks-Franklin said, and therefore reduce the quality of sleep even if the person gets the total hours they need.
Insomnia in adolescents
Insomnia can refer to difficulty falling asleep, staying asleep, sleeping for long enough, or getting enough sleep in one period of time even when the opportunity is there. Some people may have no trouble falling asleep, but they wake up too early – before they have had gotten the sleep they need – and cannot return to sleep.
To be insomnia, the problem must occur “despite having enough time available for sleep,” Dr. Spinks-Franklin said. “Patient who restrict the amount of time for sleep due to work or social commitments may have trouble sleeping and daytime sleepiness but do not have insomnia.”
Daytime impairment also is part of the American Academy of Sleep Medicine’s definition of insomnia. The rare teen who doesn’t need as much sleep as average and functions without difficulty during the day does not necessarily have insomnia.
But the impairment may not necessarily just be fatigue or sleepiness. In fact, many of the symptoms are the same as those seen with ADHD.
Daytime consequences of insomnia can include the following:
- Depression, feeling sad or “blue,” or emotional hypersensitivity.
- Mood swings, crankiness, or irritability.
- Difficulty concentrating or paying attention, poor memory, mind wandering, or even inability to sit still.
- Job or school problems, such as not being able to finish homework, not finishing tasks they start, or forgetfulness.
- Difficulty in social situations, such as discomfort with others or problems with friends.
- Daytime sleepiness, even when unable to actually take a nap.
- Behavioral problems, such as hyperactivity, impulsivity, or aggression.
- Frequent mistakes, especially at work, at school, or while driving (often “errors of omission,” such as not seeing a street sign or not hearing an instruction).
- Lower levels of motivation or initiative, feeling less energetic.
- Excessive worry about sleep.
Evaluation of insomnia can be framed with “the three-factor model,” which includes predisposing factors, precipitating factors, and perpetuating factors.
Predisposing factors – those that indicate a person already may be at risk for insomnia – include potential genetic influences as well as their typical response to stress. “Do they sleep more or less?” Dr. Spinks-Franklin said. Even teens predisposed to insomnia may not develop it, however, without a precipitating trigger.
These triggers could include stress, anxiety, poor initial sleep hygiene that becomes a pattern, dietary intake or behaviors (such as drinking caffeine or eating too much or too late in the evening), changes to their schedule, or side effects of medications.
Once insomnia begins, various factors can then perpetuate the cycle, including some of those that triggered it, such as anxiety or a school or work schedule. Sometimes it can be difficult to pinpoint the factor prolonging insomnia, such as the unconscious reward of going to work or school late with few or no consequences.
Delayed sleep phase syndrome
Delayed sleep phase syndrome occurs when someone has a delayed onset of melatonin secretion that pushes back the time when they can fall asleep. Melatonin is the neurotransmitter produced by the pineal gland that signals the start of nighttime. Although it has a hereditary component, delayed sleep phase syndrome also can result from a pattern of poor sleep onset and sleeping in on the weekends.
Dr. Spinks-Franklin described the typical cycle: A teen doesn’t go to sleep until after midnight and then wants to sleep in later in the morning. Because they have to wake up early for school, they sleep in on the weekends to try to regain the sleep they lost. Sleeping in pushes their circadian rhythm even later, perpetuating the problem.
Interventions for sleep disorders
The recommended treatment for insomnia is cognitive-behavior therapy for insomnia, for which strong evidence exists. Before seeking cognitive-behavior therapy, however, families can work to improve sleep hygiene and reduce stimuli that contribute to insomnia.
Teens should avoid screens for at least 1 hour before bedtime and avoid caffeine and exercise for at least 4 hours before going to bed. They also need to develop a schedule with a consistent bedtime and wake-up time, including on the weekends. They should avoid sleeping in on the weekends or taking naps during the day, Dr. Spinks-Franklin said.
Delayed sleep phase syndrome is more resistant to treatment and has a high recurrence rate, she said, and it requires commitment from the parent and their child to address it successfully. Teens with this condition also can start with sleep hygiene practices: a consistent wake-up time that they maintain on the weekends and no daytime naps. Phototherapy in the morning can be added to hopefully induce an earlier onset of melatonin release in the evening.
The next step is making changes to the youth’s schedule, particularly evening and/or weekend activities. They can try to gradually advance their biological clock by changing their sleep schedule.
Dr. Spinks-Franklin also briefly addressed the use of over-the-counter melatonin supplements for treating sleep problems. Melatonin can be effective for treating insomnia by improving sleep onset and sleep quality, particularly in children and teens with autism spectrum disorder or ADHD.
Dr. Spinks-Franklin had no disclosures, and her presentation used no outside funding.
NEW ORLEANS – Social media and electronics aren’t the only barriers to a good night’s sleep for teens, according to Adiaha I. A. Spinks-Franklin, MD, MPH, a pediatrician at Texas Children’s Hospital in Houston.
Another half-dozen “sleep enemies” interfere with adolescents’ sleep and can contribute to insomnia or other sleep disorders, she told attendees at the annual meeting of the American Academy of Pediatrics.
Knowing what normal sleep physiology looks like in youth and understanding the most common sleep enemies and sleep-behavior problems can help you use effective interventions to help your patients get the sleep they need, she said.
Infants need the most sleep, about 12-16 hours each 24-hour period, including naps, for those aged 4-12 months. As they grow into toddlerhood and preschool age, children gradually need less: Children aged 1-2 years need 11-14 hours and children aged 3-5 years need 10-13 hours, including naps. By the time children are in school, ages 6-12, they should have dropped their naps and need 9-12 hours a night.
In fact, 75% of high school seniors get less than 8 hours of sleep a day and live with a chronic sleep debt, Dr. Spinks-Franklin said.
Although social media use and electronics in the bedroom – TVs, computers, cell phones, and video games – can certainly contribute to inadequate sleep, a heavy academic load and extracurricular activities can be just as problematic, Dr. Spinks-Franklin said. Teens who work after school also may have difficulty getting enough sleep, especially if they also have to balance a heavier academic load or even one or two extracurricular activities.
Socializing with friends also can interfere with sleep, especially when get-togethers run late; drinking caffeinated drinks in the afternoon onward can make it difficult for adolescents to get the sleep they need as well. Less-modifiable contributors to too little sleep are stress and early school start times, Dr. Spinks-Franklin said.
The two most common sleep problems seen in teens are insomnia and delayed sleep phase syndrome. Addressing these is important because the effects of chronic insufficient sleep can have far-reaching consequences. Obesity and related chronic health conditions are associated with inadequate sleep, as are poor academic performance, poor judgment, poor executive functioning, and mental health disorders like depression.
Short-term effects of insufficient sleep also can be problematic and can exacerbate existing sleep problems, such as sleeping in on the weekends to “catch up” on sleep or drinking more caffeine to try to stay awake during the day. Increased caffeine intake can interfere with non-REM deep sleep, Dr. Spinks-Franklin said, and therefore reduce the quality of sleep even if the person gets the total hours they need.
Insomnia in adolescents
Insomnia can refer to difficulty falling asleep, staying asleep, sleeping for long enough, or getting enough sleep in one period of time even when the opportunity is there. Some people may have no trouble falling asleep, but they wake up too early – before they have had gotten the sleep they need – and cannot return to sleep.
To be insomnia, the problem must occur “despite having enough time available for sleep,” Dr. Spinks-Franklin said. “Patient who restrict the amount of time for sleep due to work or social commitments may have trouble sleeping and daytime sleepiness but do not have insomnia.”
Daytime impairment also is part of the American Academy of Sleep Medicine’s definition of insomnia. The rare teen who doesn’t need as much sleep as average and functions without difficulty during the day does not necessarily have insomnia.
But the impairment may not necessarily just be fatigue or sleepiness. In fact, many of the symptoms are the same as those seen with ADHD.
Daytime consequences of insomnia can include the following:
- Depression, feeling sad or “blue,” or emotional hypersensitivity.
- Mood swings, crankiness, or irritability.
- Difficulty concentrating or paying attention, poor memory, mind wandering, or even inability to sit still.
- Job or school problems, such as not being able to finish homework, not finishing tasks they start, or forgetfulness.
- Difficulty in social situations, such as discomfort with others or problems with friends.
- Daytime sleepiness, even when unable to actually take a nap.
- Behavioral problems, such as hyperactivity, impulsivity, or aggression.
- Frequent mistakes, especially at work, at school, or while driving (often “errors of omission,” such as not seeing a street sign or not hearing an instruction).
- Lower levels of motivation or initiative, feeling less energetic.
- Excessive worry about sleep.
Evaluation of insomnia can be framed with “the three-factor model,” which includes predisposing factors, precipitating factors, and perpetuating factors.
Predisposing factors – those that indicate a person already may be at risk for insomnia – include potential genetic influences as well as their typical response to stress. “Do they sleep more or less?” Dr. Spinks-Franklin said. Even teens predisposed to insomnia may not develop it, however, without a precipitating trigger.
These triggers could include stress, anxiety, poor initial sleep hygiene that becomes a pattern, dietary intake or behaviors (such as drinking caffeine or eating too much or too late in the evening), changes to their schedule, or side effects of medications.
Once insomnia begins, various factors can then perpetuate the cycle, including some of those that triggered it, such as anxiety or a school or work schedule. Sometimes it can be difficult to pinpoint the factor prolonging insomnia, such as the unconscious reward of going to work or school late with few or no consequences.
Delayed sleep phase syndrome
Delayed sleep phase syndrome occurs when someone has a delayed onset of melatonin secretion that pushes back the time when they can fall asleep. Melatonin is the neurotransmitter produced by the pineal gland that signals the start of nighttime. Although it has a hereditary component, delayed sleep phase syndrome also can result from a pattern of poor sleep onset and sleeping in on the weekends.
Dr. Spinks-Franklin described the typical cycle: A teen doesn’t go to sleep until after midnight and then wants to sleep in later in the morning. Because they have to wake up early for school, they sleep in on the weekends to try to regain the sleep they lost. Sleeping in pushes their circadian rhythm even later, perpetuating the problem.
Interventions for sleep disorders
The recommended treatment for insomnia is cognitive-behavior therapy for insomnia, for which strong evidence exists. Before seeking cognitive-behavior therapy, however, families can work to improve sleep hygiene and reduce stimuli that contribute to insomnia.
Teens should avoid screens for at least 1 hour before bedtime and avoid caffeine and exercise for at least 4 hours before going to bed. They also need to develop a schedule with a consistent bedtime and wake-up time, including on the weekends. They should avoid sleeping in on the weekends or taking naps during the day, Dr. Spinks-Franklin said.
Delayed sleep phase syndrome is more resistant to treatment and has a high recurrence rate, she said, and it requires commitment from the parent and their child to address it successfully. Teens with this condition also can start with sleep hygiene practices: a consistent wake-up time that they maintain on the weekends and no daytime naps. Phototherapy in the morning can be added to hopefully induce an earlier onset of melatonin release in the evening.
The next step is making changes to the youth’s schedule, particularly evening and/or weekend activities. They can try to gradually advance their biological clock by changing their sleep schedule.
Dr. Spinks-Franklin also briefly addressed the use of over-the-counter melatonin supplements for treating sleep problems. Melatonin can be effective for treating insomnia by improving sleep onset and sleep quality, particularly in children and teens with autism spectrum disorder or ADHD.
Dr. Spinks-Franklin had no disclosures, and her presentation used no outside funding.
EXPERT ANALYSIS FROM AAP 19
Pediatricians uniquely qualified to treat adolescents with opioid use disorder
NEW ORLEANS –
“One of the real benefits of treatment in primary care is that it removes the stigma so that these patients aren’t isolated into addiction clinics; they’re being treated by providers that they know well and that their family knows well,” Dr. Reynolds, a pediatrician who practices in Wareham, Mass., said at the annual meeting of the American Academy of Pediatrics. “That feels a lot better to them, and I think it makes a statement in the community that these people don’t need to be isolated. Anything we can do to reduce the stigma of opioid use disorder is important. We in primary care are well suited to manage chronic disease over the continuum.”
In 2016, the AAP released a policy statement advocating for pediatricians to consider providing medication-assisted treatment to patients with OUD (Pediatrics. 2016;138[3]e20161893). The statement cited results from a nationally representative sample of 345 addiction treatment programs serving adolescents and adults. It found that fewer than 50% of those programs used medication-assisted treatment (J Addict Med. 2011;5[1]:21-7). “When they looked at patients who actually had opioid dependence, the numbers were even lower,” said Dr. Reynolds, who was not involved with the study. “In fact, 34% of opioid-dependent patients received medication-assisted treatment. When they stratified it by age, the younger you were, the less likely you were to be treated. Only 11.5% of youth under 18 are actually being treated. We know that youth with opioid use disorders have very bad health outcomes over their lifetime. The fact that such few patients receive what is considered to be a gold-standard treatment is really alarming.”
Dr. Reynolds acknowledged that many perceived barriers exist to providing treatment of OUD in pediatric primary care, including the fact that patients with addiction are not easy to treat. “They can be manipulative and can make you feel both sad for them and angry at them within the same visit,” he said. “They also have complex needs. For many of these patients, it’s not just that they use opiates; they have medical problems and psychological diagnoses, and oftentimes they have social issues such as being in foster care. They also may have issues with their parents, employer, or their school, so there are many needs that need to be juggled. That can be overwhelming.”
However, he said that such patients “are actually in our wheelhouse, because as primary care physicians we’re used to coordinating care. These are the perfect patients to have a medical home. We manage chronic disease over the continuum of care. This is a chronic disease, and we have to help patients.”
Another perceived barrier for treating adolescents with OUD relates to reimbursement. While most patients with OUD have insurance, Dr. Reynolds finds that the requirement for prior authorizations can result in delay of treatment and poses an unnecessary burden on care providers. “It’s an administrative task that either the physician or the office staff has to take care of,” he said. “Interestingly, reimbursement ranks as a low concern in studies of buprenorphine providers. That tells me that this is not a major hurdle.”
Pediatricians also cite a lack of knowledge as a reason they’re leery of providing OUD treatment in their office. “They wonder: ‘How do I do this? What’s the right way to do it? Are there best practices?’ ” Dr. Reynolds said. “There’s a feeling that it must be dangerous, the idea that if I don’t do it right I’m going to hurt somebody. The reality is, buprenorphine is no more dangerous than any of the other opiates. Technically, because it’s a partial agonist, it’s probably less dangerous than some of the opiates that we prescribe. It’s no more dangerous than prescribing amitriptyline for chronic pain.”
One key resource, the Providers Clinical Support System (www.pcssnow.org), provides resources for clinicians and family members, education and training, and access to mentoring. Another resource, the American Society of Addiction Medicine (www.asam.org), includes clinical practice guidelines, online courses and training on the treatment of OUD, and sample consent and opioid-withdrawal forms. Dr. Reynolds characterized learning how to treat patients with OUD as no different than learning step therapy for asthma. “Once you look into it, you realize that there’s no sort of magic behind this,” he said. “It’s something that any of us can do. Staff can be trained. There are modules to train your staff into the protocols. Learn the knowledge and put it into action. Have the confidence and the knowledge.”
The Drug Addiction and Treatment Act of 2000 set up the waiver process by which physicians can obtain a waiver from the Drug Enforcement Agency after completing an 8-hour CME course on substance abuse disorder and buprenorphine prescribing. To receive a waiver to practice opioid dependency treatment with approved buprenorphine medications, a clinician must notify the SAMHSA Center for Substance Abuse Treatment of their intent to practice this form of medication-assisted treatment.
Dr. Reynolds acknowledged that not every practice is equipped to provide psychosocial support for complex patients with OUD. “When I first started this in 2017, I wanted to make sure that my patients were in some form of counseling,” he said. “However, the medical literature shows that you can treat OUD without counseling, and some of those patients will be fine, too. There have been reports that just going to Narcotics Anonymous meetings weekly has been shown to improve the effectiveness of medication-assisted treatment.”
For clinicians concerned about having backup when they face challenging cases, data shows that having more than one waivered provider in a practice is associated with completing waiver training. “This makes sense,” Dr. Reynolds said. “We like to be able to discuss our cases with colleagues, but a lot of us don’t want to be on call 365 days a year for our patients. Shared responsibility makes it easier. Access to specialty telemedicine consult has also been identified as a facilitator to physicians prescribing medical-assisted therapy.”
He concluded his presentation by noting that increasing numbers of OUD patients are initiating buprenorphine treatment in the ED. “That takes advantage of the fact that most of these patients present to the emergency room after receiving Narcan for an overdose,” Dr. Reynolds said. “In the emergency room, they’re counseled and instructed on how to start buprenorphine, they’re given the first dose, and they’re told to go home and avoid using any other opiates for 24 hours, start the buprenorphine, and follow up with their primary care doctor or an addiction medicine specialist in 3 days. In my community, this is what our local emergency department is doing for adult patients, except they’re not referring back to primary care. They’re referring to a hospital-based addiction medicine specialist. This is a way to increase access and get people started on buprenorphine treatment.”
Dr. Reynolds reported having no financial disclosures.
NEW ORLEANS –
“One of the real benefits of treatment in primary care is that it removes the stigma so that these patients aren’t isolated into addiction clinics; they’re being treated by providers that they know well and that their family knows well,” Dr. Reynolds, a pediatrician who practices in Wareham, Mass., said at the annual meeting of the American Academy of Pediatrics. “That feels a lot better to them, and I think it makes a statement in the community that these people don’t need to be isolated. Anything we can do to reduce the stigma of opioid use disorder is important. We in primary care are well suited to manage chronic disease over the continuum.”
In 2016, the AAP released a policy statement advocating for pediatricians to consider providing medication-assisted treatment to patients with OUD (Pediatrics. 2016;138[3]e20161893). The statement cited results from a nationally representative sample of 345 addiction treatment programs serving adolescents and adults. It found that fewer than 50% of those programs used medication-assisted treatment (J Addict Med. 2011;5[1]:21-7). “When they looked at patients who actually had opioid dependence, the numbers were even lower,” said Dr. Reynolds, who was not involved with the study. “In fact, 34% of opioid-dependent patients received medication-assisted treatment. When they stratified it by age, the younger you were, the less likely you were to be treated. Only 11.5% of youth under 18 are actually being treated. We know that youth with opioid use disorders have very bad health outcomes over their lifetime. The fact that such few patients receive what is considered to be a gold-standard treatment is really alarming.”
Dr. Reynolds acknowledged that many perceived barriers exist to providing treatment of OUD in pediatric primary care, including the fact that patients with addiction are not easy to treat. “They can be manipulative and can make you feel both sad for them and angry at them within the same visit,” he said. “They also have complex needs. For many of these patients, it’s not just that they use opiates; they have medical problems and psychological diagnoses, and oftentimes they have social issues such as being in foster care. They also may have issues with their parents, employer, or their school, so there are many needs that need to be juggled. That can be overwhelming.”
However, he said that such patients “are actually in our wheelhouse, because as primary care physicians we’re used to coordinating care. These are the perfect patients to have a medical home. We manage chronic disease over the continuum of care. This is a chronic disease, and we have to help patients.”
Another perceived barrier for treating adolescents with OUD relates to reimbursement. While most patients with OUD have insurance, Dr. Reynolds finds that the requirement for prior authorizations can result in delay of treatment and poses an unnecessary burden on care providers. “It’s an administrative task that either the physician or the office staff has to take care of,” he said. “Interestingly, reimbursement ranks as a low concern in studies of buprenorphine providers. That tells me that this is not a major hurdle.”
Pediatricians also cite a lack of knowledge as a reason they’re leery of providing OUD treatment in their office. “They wonder: ‘How do I do this? What’s the right way to do it? Are there best practices?’ ” Dr. Reynolds said. “There’s a feeling that it must be dangerous, the idea that if I don’t do it right I’m going to hurt somebody. The reality is, buprenorphine is no more dangerous than any of the other opiates. Technically, because it’s a partial agonist, it’s probably less dangerous than some of the opiates that we prescribe. It’s no more dangerous than prescribing amitriptyline for chronic pain.”
One key resource, the Providers Clinical Support System (www.pcssnow.org), provides resources for clinicians and family members, education and training, and access to mentoring. Another resource, the American Society of Addiction Medicine (www.asam.org), includes clinical practice guidelines, online courses and training on the treatment of OUD, and sample consent and opioid-withdrawal forms. Dr. Reynolds characterized learning how to treat patients with OUD as no different than learning step therapy for asthma. “Once you look into it, you realize that there’s no sort of magic behind this,” he said. “It’s something that any of us can do. Staff can be trained. There are modules to train your staff into the protocols. Learn the knowledge and put it into action. Have the confidence and the knowledge.”
The Drug Addiction and Treatment Act of 2000 set up the waiver process by which physicians can obtain a waiver from the Drug Enforcement Agency after completing an 8-hour CME course on substance abuse disorder and buprenorphine prescribing. To receive a waiver to practice opioid dependency treatment with approved buprenorphine medications, a clinician must notify the SAMHSA Center for Substance Abuse Treatment of their intent to practice this form of medication-assisted treatment.
Dr. Reynolds acknowledged that not every practice is equipped to provide psychosocial support for complex patients with OUD. “When I first started this in 2017, I wanted to make sure that my patients were in some form of counseling,” he said. “However, the medical literature shows that you can treat OUD without counseling, and some of those patients will be fine, too. There have been reports that just going to Narcotics Anonymous meetings weekly has been shown to improve the effectiveness of medication-assisted treatment.”
For clinicians concerned about having backup when they face challenging cases, data shows that having more than one waivered provider in a practice is associated with completing waiver training. “This makes sense,” Dr. Reynolds said. “We like to be able to discuss our cases with colleagues, but a lot of us don’t want to be on call 365 days a year for our patients. Shared responsibility makes it easier. Access to specialty telemedicine consult has also been identified as a facilitator to physicians prescribing medical-assisted therapy.”
He concluded his presentation by noting that increasing numbers of OUD patients are initiating buprenorphine treatment in the ED. “That takes advantage of the fact that most of these patients present to the emergency room after receiving Narcan for an overdose,” Dr. Reynolds said. “In the emergency room, they’re counseled and instructed on how to start buprenorphine, they’re given the first dose, and they’re told to go home and avoid using any other opiates for 24 hours, start the buprenorphine, and follow up with their primary care doctor or an addiction medicine specialist in 3 days. In my community, this is what our local emergency department is doing for adult patients, except they’re not referring back to primary care. They’re referring to a hospital-based addiction medicine specialist. This is a way to increase access and get people started on buprenorphine treatment.”
Dr. Reynolds reported having no financial disclosures.
NEW ORLEANS –
“One of the real benefits of treatment in primary care is that it removes the stigma so that these patients aren’t isolated into addiction clinics; they’re being treated by providers that they know well and that their family knows well,” Dr. Reynolds, a pediatrician who practices in Wareham, Mass., said at the annual meeting of the American Academy of Pediatrics. “That feels a lot better to them, and I think it makes a statement in the community that these people don’t need to be isolated. Anything we can do to reduce the stigma of opioid use disorder is important. We in primary care are well suited to manage chronic disease over the continuum.”
In 2016, the AAP released a policy statement advocating for pediatricians to consider providing medication-assisted treatment to patients with OUD (Pediatrics. 2016;138[3]e20161893). The statement cited results from a nationally representative sample of 345 addiction treatment programs serving adolescents and adults. It found that fewer than 50% of those programs used medication-assisted treatment (J Addict Med. 2011;5[1]:21-7). “When they looked at patients who actually had opioid dependence, the numbers were even lower,” said Dr. Reynolds, who was not involved with the study. “In fact, 34% of opioid-dependent patients received medication-assisted treatment. When they stratified it by age, the younger you were, the less likely you were to be treated. Only 11.5% of youth under 18 are actually being treated. We know that youth with opioid use disorders have very bad health outcomes over their lifetime. The fact that such few patients receive what is considered to be a gold-standard treatment is really alarming.”
Dr. Reynolds acknowledged that many perceived barriers exist to providing treatment of OUD in pediatric primary care, including the fact that patients with addiction are not easy to treat. “They can be manipulative and can make you feel both sad for them and angry at them within the same visit,” he said. “They also have complex needs. For many of these patients, it’s not just that they use opiates; they have medical problems and psychological diagnoses, and oftentimes they have social issues such as being in foster care. They also may have issues with their parents, employer, or their school, so there are many needs that need to be juggled. That can be overwhelming.”
However, he said that such patients “are actually in our wheelhouse, because as primary care physicians we’re used to coordinating care. These are the perfect patients to have a medical home. We manage chronic disease over the continuum of care. This is a chronic disease, and we have to help patients.”
Another perceived barrier for treating adolescents with OUD relates to reimbursement. While most patients with OUD have insurance, Dr. Reynolds finds that the requirement for prior authorizations can result in delay of treatment and poses an unnecessary burden on care providers. “It’s an administrative task that either the physician or the office staff has to take care of,” he said. “Interestingly, reimbursement ranks as a low concern in studies of buprenorphine providers. That tells me that this is not a major hurdle.”
Pediatricians also cite a lack of knowledge as a reason they’re leery of providing OUD treatment in their office. “They wonder: ‘How do I do this? What’s the right way to do it? Are there best practices?’ ” Dr. Reynolds said. “There’s a feeling that it must be dangerous, the idea that if I don’t do it right I’m going to hurt somebody. The reality is, buprenorphine is no more dangerous than any of the other opiates. Technically, because it’s a partial agonist, it’s probably less dangerous than some of the opiates that we prescribe. It’s no more dangerous than prescribing amitriptyline for chronic pain.”
One key resource, the Providers Clinical Support System (www.pcssnow.org), provides resources for clinicians and family members, education and training, and access to mentoring. Another resource, the American Society of Addiction Medicine (www.asam.org), includes clinical practice guidelines, online courses and training on the treatment of OUD, and sample consent and opioid-withdrawal forms. Dr. Reynolds characterized learning how to treat patients with OUD as no different than learning step therapy for asthma. “Once you look into it, you realize that there’s no sort of magic behind this,” he said. “It’s something that any of us can do. Staff can be trained. There are modules to train your staff into the protocols. Learn the knowledge and put it into action. Have the confidence and the knowledge.”
The Drug Addiction and Treatment Act of 2000 set up the waiver process by which physicians can obtain a waiver from the Drug Enforcement Agency after completing an 8-hour CME course on substance abuse disorder and buprenorphine prescribing. To receive a waiver to practice opioid dependency treatment with approved buprenorphine medications, a clinician must notify the SAMHSA Center for Substance Abuse Treatment of their intent to practice this form of medication-assisted treatment.
Dr. Reynolds acknowledged that not every practice is equipped to provide psychosocial support for complex patients with OUD. “When I first started this in 2017, I wanted to make sure that my patients were in some form of counseling,” he said. “However, the medical literature shows that you can treat OUD without counseling, and some of those patients will be fine, too. There have been reports that just going to Narcotics Anonymous meetings weekly has been shown to improve the effectiveness of medication-assisted treatment.”
For clinicians concerned about having backup when they face challenging cases, data shows that having more than one waivered provider in a practice is associated with completing waiver training. “This makes sense,” Dr. Reynolds said. “We like to be able to discuss our cases with colleagues, but a lot of us don’t want to be on call 365 days a year for our patients. Shared responsibility makes it easier. Access to specialty telemedicine consult has also been identified as a facilitator to physicians prescribing medical-assisted therapy.”
He concluded his presentation by noting that increasing numbers of OUD patients are initiating buprenorphine treatment in the ED. “That takes advantage of the fact that most of these patients present to the emergency room after receiving Narcan for an overdose,” Dr. Reynolds said. “In the emergency room, they’re counseled and instructed on how to start buprenorphine, they’re given the first dose, and they’re told to go home and avoid using any other opiates for 24 hours, start the buprenorphine, and follow up with their primary care doctor or an addiction medicine specialist in 3 days. In my community, this is what our local emergency department is doing for adult patients, except they’re not referring back to primary care. They’re referring to a hospital-based addiction medicine specialist. This is a way to increase access and get people started on buprenorphine treatment.”
Dr. Reynolds reported having no financial disclosures.
EXPERT ANALYSIS FROM AAP 19
Adding mental health clinicians to your practice is full of benefits
NEW ORLEANS – The way Jay Rabinowitz, MD, MPH, sees it, providing mental and behavioral health care services in your primary care pediatrics practice is a win-win for patients, parents, and clinicians.
For one thing, children with mental and behavioral issues – especially depression and anxiety – make up a good chunk of any pediatrician’s workday. Dr. Rabinowitz, clinical professor of pediatrics at the University of Colorado, Aurora, said at the annual meeting of the American Academy of Pediatrics. “It is the most costly issue in children’s health care today.”
According to “Behavioral Health Integration in Pediatric Primary Care,” a report supported by the Milbank Memorial Fund, one in five children aged 9-17 years have a diagnosable psychiatric disorder, and up to 70% of children in the juvenile justice system have a mental health disorder. The report also found that the treatment of mental health disorders accounts for the most costly childhood medical expenditure, and that between 15% and 20% of children with psychiatric disorders receive specialty care; the rest see their primary care provider. A long-term cost analysis showed significant cost savings: $1 spent on collaborative care saves $6.50 on health care costs.
More recently, the Guidelines for Adolescent Depression in Primary Care (GLAD-PC) found that only 50% of adolescents with depression are diagnosed before reaching adulthood (Pediatrics. March 2018;141[3]:e20174081). As many as two out of three youth with depression are not identified by their pediatrician and do not receive any kind of care.
“Even when diagnosed, only half of these patients are treated appropriately,” said Dr. Rabinowitz, who also practices at Parker (Colo.) Pediatrics and Adolescents.
The guidelines also found that reliance on self-report depression checklists alone lead to substantial numbers of false-positive and false-negative cases. “Primary care providers will benefit from having access to ongoing consultation with mental health providers,” according to the guidelines.
“Integrative care was associated with significant decreases in depression scores, and improved response and remission rates at 12 months, compared with treatment as usual,” Dr. Rabinowitz said.
Providing mental health services in a primary care pediatrics setting also makes sense because there’s a shortage of psychiatrists and psychologists to see them, and it enables patients to get evaluated quicker. “It’s convenient, and it reduces stigma,” he added. “It’s a familiar setting, a familiar provider, and they’re more likely to initiate counseling. Nationwide, 50% of patients who are referred for mental health do not make their initial appointment. Think about that. If you had diabetics in your practice and only 50% would go to the endocrinologist, what would you think?”
How Dr. Rabinowitz and his partners got started
Dr. Rabinowitz and his colleagues created an integrated care model in 2008 by adding a psychologist to their practice, but before doing that, they asked parents of children with mental and behavioral health issues what type of insurance they had. Then they obtained a referral list from the family’s insurer and hoped for the best. “Sometimes I referred to someone I may not have heard of,” Dr. Rabinowitz said. “Usually I did not get follow-up reports, or even know for sure if the patient ever went.”
Today, Parker Pediatrics and Adolescents employs three doctoral-level psychologists: one full-time, one three-quarter time, and one half-time, as well as one master’s-level therapist who works half-time.
“On any given day, we have at least two counselors in our office,” said Lindsey Einhorn, PhD, a licensed clinical psychologist who joined the practice in 2011. She and her colleagues care for children and teens with ADHD, depression, anxiety, behavioral and adjustment disorders, drug counseling, behavioral addictions, social struggles such as bullying, obsessive compulsive disorder (OCD), loss, hair or eyelash pulling, mood dysregulation, and sibling conflict. They refer for educational testing, comprehensive psychological evaluations, difficult divorce cases, play therapy, complex cases requiring more than 20 sessions, and children of staff employed by the practice.
The practice features a separate waiting room for psychology patients and front office staff dedicated to managing their schedules. “For anyone who’s trying to make a psychology appointment but can’t be seen in an efficient manner or wants a different day or time, we keep an ongoing move-up list,” Dr. Einhorn said. “If a family calls to cancel an appointment, the front desk person who makes that cancellation will fill out a slip and give it to one of our psychology schedulers. That person will create a move-up list and start filling that appointment. If there’s a cancellation, it’s rare that it goes unfilled.”
Key forms for parents to complete include informed consent, a notice of privacy practices, a late cancel/no show policy, an initial intake agreement, and a summary of parent concerns.
Patient and clinician reaction
According to results from a recent survey of parents whose children were seen by a psychologist at Parker Pediatrics and Adolescents, 89% said it was important for their children to receive mental health services in the same location as their medical care, and 96% were satisfied with the services provided. In addition, 93% said that the experience benefited their child, 72% were satisfied with appointment times, and 55% expressed interest in virtual visits via telemedicine. Meanwhile, a survey of parents whose children have not been seen by a psychologist at the practice found that 65% knew a psychologist was on staff, and only 9% said that there were barriers to their child seeing a psychologist there.
Clinicians themselves benefit from having mental health specialists on site for referrals. “It enables you to be more efficient, and it saves time,” Dr. Rabinowitz said. “There’s knowledge and confidence gained, and it improves satisfaction because physicians don’t have to stay at the office later filling out referral forms. It meets the needs of your patients and their families, it attracts new patients, and you may be able to make some income on this.”
How to get started
Dr. Rabinowitz recommended that, once clinicians at a pediatric practice commit to expanding their services to include mental and behavioral health care, they should hold a corporate/partner meeting, assign responsibilities, and establish a timeline for implementation. “This is all very important,” he said. “Then you have to talk about what kind of arrangement you want to have. You could employ someone to join your practice, hire an independent contractor, establish a space share agreement, or have an out-of-office arrangement.”
For many years, clinicians at Parker Pediatrics and Adolescents had a psychologist perform ADHD evaluations on a consultative basis. “Then, as we saw a need for mental health services about a decade ago, we hired a part-time psychologist who did testing as well as counseling,” Dr. Rabinowitz said. “But that psychologist got very busy, so we hired a full-time psychologist. We continued to hire additional psychologists as need increased.”
Reimbursement issues
Numerous reimbursement barriers to providing mental health services in pediatric primary care exist, he noted, including a lack of payment if mental health codes are used, a lack of “incident to” payments in some areas of the country, existing reimbursement levels, and the fact that same-day billing of physical and mental health often is not allowed. “However, we have found that if we give flu shots during their mental health visit, [insurers] will cover the flu shot,” he said. “Reimbursement for screening is sometimes not covered very well.”
One reimbursement option is the fee-for-service/concierge model, “but that’s not an economic option for many,” he said. “You can’t see Medicaid patients in that model.” Joining a mental health networks is feasible, “but there is poor reimbursement,” he said. “It also creates another layer of administration.”
He recommends financial integration, “but you need to research your options because a lot of it is state dependent.” Other options include grants, insurance contracts, and seeking permission from Medicaid.
Mental health CPT codes that mental health clinicians at the practice commonly use include bill by time (CPT code 99214/15); psychotherapy session that lasts 16-37 minutes (CPT code 90832); psychotherapy session that lasts 38-52 minutes (CPT code 90834); and psychotherapy session that lasts more than 53 minutes (CPT code 90837). Clinicians also can bill by interactive complexity (CPT code 90785) and psychotherapy for crisis (CPT code 90839).
Dr. Rabinowitz and Dr. Einhorn reported having no financial disclosures.
NEW ORLEANS – The way Jay Rabinowitz, MD, MPH, sees it, providing mental and behavioral health care services in your primary care pediatrics practice is a win-win for patients, parents, and clinicians.
For one thing, children with mental and behavioral issues – especially depression and anxiety – make up a good chunk of any pediatrician’s workday. Dr. Rabinowitz, clinical professor of pediatrics at the University of Colorado, Aurora, said at the annual meeting of the American Academy of Pediatrics. “It is the most costly issue in children’s health care today.”
According to “Behavioral Health Integration in Pediatric Primary Care,” a report supported by the Milbank Memorial Fund, one in five children aged 9-17 years have a diagnosable psychiatric disorder, and up to 70% of children in the juvenile justice system have a mental health disorder. The report also found that the treatment of mental health disorders accounts for the most costly childhood medical expenditure, and that between 15% and 20% of children with psychiatric disorders receive specialty care; the rest see their primary care provider. A long-term cost analysis showed significant cost savings: $1 spent on collaborative care saves $6.50 on health care costs.
More recently, the Guidelines for Adolescent Depression in Primary Care (GLAD-PC) found that only 50% of adolescents with depression are diagnosed before reaching adulthood (Pediatrics. March 2018;141[3]:e20174081). As many as two out of three youth with depression are not identified by their pediatrician and do not receive any kind of care.
“Even when diagnosed, only half of these patients are treated appropriately,” said Dr. Rabinowitz, who also practices at Parker (Colo.) Pediatrics and Adolescents.
The guidelines also found that reliance on self-report depression checklists alone lead to substantial numbers of false-positive and false-negative cases. “Primary care providers will benefit from having access to ongoing consultation with mental health providers,” according to the guidelines.
“Integrative care was associated with significant decreases in depression scores, and improved response and remission rates at 12 months, compared with treatment as usual,” Dr. Rabinowitz said.
Providing mental health services in a primary care pediatrics setting also makes sense because there’s a shortage of psychiatrists and psychologists to see them, and it enables patients to get evaluated quicker. “It’s convenient, and it reduces stigma,” he added. “It’s a familiar setting, a familiar provider, and they’re more likely to initiate counseling. Nationwide, 50% of patients who are referred for mental health do not make their initial appointment. Think about that. If you had diabetics in your practice and only 50% would go to the endocrinologist, what would you think?”
How Dr. Rabinowitz and his partners got started
Dr. Rabinowitz and his colleagues created an integrated care model in 2008 by adding a psychologist to their practice, but before doing that, they asked parents of children with mental and behavioral health issues what type of insurance they had. Then they obtained a referral list from the family’s insurer and hoped for the best. “Sometimes I referred to someone I may not have heard of,” Dr. Rabinowitz said. “Usually I did not get follow-up reports, or even know for sure if the patient ever went.”
Today, Parker Pediatrics and Adolescents employs three doctoral-level psychologists: one full-time, one three-quarter time, and one half-time, as well as one master’s-level therapist who works half-time.
“On any given day, we have at least two counselors in our office,” said Lindsey Einhorn, PhD, a licensed clinical psychologist who joined the practice in 2011. She and her colleagues care for children and teens with ADHD, depression, anxiety, behavioral and adjustment disorders, drug counseling, behavioral addictions, social struggles such as bullying, obsessive compulsive disorder (OCD), loss, hair or eyelash pulling, mood dysregulation, and sibling conflict. They refer for educational testing, comprehensive psychological evaluations, difficult divorce cases, play therapy, complex cases requiring more than 20 sessions, and children of staff employed by the practice.
The practice features a separate waiting room for psychology patients and front office staff dedicated to managing their schedules. “For anyone who’s trying to make a psychology appointment but can’t be seen in an efficient manner or wants a different day or time, we keep an ongoing move-up list,” Dr. Einhorn said. “If a family calls to cancel an appointment, the front desk person who makes that cancellation will fill out a slip and give it to one of our psychology schedulers. That person will create a move-up list and start filling that appointment. If there’s a cancellation, it’s rare that it goes unfilled.”
Key forms for parents to complete include informed consent, a notice of privacy practices, a late cancel/no show policy, an initial intake agreement, and a summary of parent concerns.
Patient and clinician reaction
According to results from a recent survey of parents whose children were seen by a psychologist at Parker Pediatrics and Adolescents, 89% said it was important for their children to receive mental health services in the same location as their medical care, and 96% were satisfied with the services provided. In addition, 93% said that the experience benefited their child, 72% were satisfied with appointment times, and 55% expressed interest in virtual visits via telemedicine. Meanwhile, a survey of parents whose children have not been seen by a psychologist at the practice found that 65% knew a psychologist was on staff, and only 9% said that there were barriers to their child seeing a psychologist there.
Clinicians themselves benefit from having mental health specialists on site for referrals. “It enables you to be more efficient, and it saves time,” Dr. Rabinowitz said. “There’s knowledge and confidence gained, and it improves satisfaction because physicians don’t have to stay at the office later filling out referral forms. It meets the needs of your patients and their families, it attracts new patients, and you may be able to make some income on this.”
How to get started
Dr. Rabinowitz recommended that, once clinicians at a pediatric practice commit to expanding their services to include mental and behavioral health care, they should hold a corporate/partner meeting, assign responsibilities, and establish a timeline for implementation. “This is all very important,” he said. “Then you have to talk about what kind of arrangement you want to have. You could employ someone to join your practice, hire an independent contractor, establish a space share agreement, or have an out-of-office arrangement.”
For many years, clinicians at Parker Pediatrics and Adolescents had a psychologist perform ADHD evaluations on a consultative basis. “Then, as we saw a need for mental health services about a decade ago, we hired a part-time psychologist who did testing as well as counseling,” Dr. Rabinowitz said. “But that psychologist got very busy, so we hired a full-time psychologist. We continued to hire additional psychologists as need increased.”
Reimbursement issues
Numerous reimbursement barriers to providing mental health services in pediatric primary care exist, he noted, including a lack of payment if mental health codes are used, a lack of “incident to” payments in some areas of the country, existing reimbursement levels, and the fact that same-day billing of physical and mental health often is not allowed. “However, we have found that if we give flu shots during their mental health visit, [insurers] will cover the flu shot,” he said. “Reimbursement for screening is sometimes not covered very well.”
One reimbursement option is the fee-for-service/concierge model, “but that’s not an economic option for many,” he said. “You can’t see Medicaid patients in that model.” Joining a mental health networks is feasible, “but there is poor reimbursement,” he said. “It also creates another layer of administration.”
He recommends financial integration, “but you need to research your options because a lot of it is state dependent.” Other options include grants, insurance contracts, and seeking permission from Medicaid.
Mental health CPT codes that mental health clinicians at the practice commonly use include bill by time (CPT code 99214/15); psychotherapy session that lasts 16-37 minutes (CPT code 90832); psychotherapy session that lasts 38-52 minutes (CPT code 90834); and psychotherapy session that lasts more than 53 minutes (CPT code 90837). Clinicians also can bill by interactive complexity (CPT code 90785) and psychotherapy for crisis (CPT code 90839).
Dr. Rabinowitz and Dr. Einhorn reported having no financial disclosures.
NEW ORLEANS – The way Jay Rabinowitz, MD, MPH, sees it, providing mental and behavioral health care services in your primary care pediatrics practice is a win-win for patients, parents, and clinicians.
For one thing, children with mental and behavioral issues – especially depression and anxiety – make up a good chunk of any pediatrician’s workday. Dr. Rabinowitz, clinical professor of pediatrics at the University of Colorado, Aurora, said at the annual meeting of the American Academy of Pediatrics. “It is the most costly issue in children’s health care today.”
According to “Behavioral Health Integration in Pediatric Primary Care,” a report supported by the Milbank Memorial Fund, one in five children aged 9-17 years have a diagnosable psychiatric disorder, and up to 70% of children in the juvenile justice system have a mental health disorder. The report also found that the treatment of mental health disorders accounts for the most costly childhood medical expenditure, and that between 15% and 20% of children with psychiatric disorders receive specialty care; the rest see their primary care provider. A long-term cost analysis showed significant cost savings: $1 spent on collaborative care saves $6.50 on health care costs.
More recently, the Guidelines for Adolescent Depression in Primary Care (GLAD-PC) found that only 50% of adolescents with depression are diagnosed before reaching adulthood (Pediatrics. March 2018;141[3]:e20174081). As many as two out of three youth with depression are not identified by their pediatrician and do not receive any kind of care.
“Even when diagnosed, only half of these patients are treated appropriately,” said Dr. Rabinowitz, who also practices at Parker (Colo.) Pediatrics and Adolescents.
The guidelines also found that reliance on self-report depression checklists alone lead to substantial numbers of false-positive and false-negative cases. “Primary care providers will benefit from having access to ongoing consultation with mental health providers,” according to the guidelines.
“Integrative care was associated with significant decreases in depression scores, and improved response and remission rates at 12 months, compared with treatment as usual,” Dr. Rabinowitz said.
Providing mental health services in a primary care pediatrics setting also makes sense because there’s a shortage of psychiatrists and psychologists to see them, and it enables patients to get evaluated quicker. “It’s convenient, and it reduces stigma,” he added. “It’s a familiar setting, a familiar provider, and they’re more likely to initiate counseling. Nationwide, 50% of patients who are referred for mental health do not make their initial appointment. Think about that. If you had diabetics in your practice and only 50% would go to the endocrinologist, what would you think?”
How Dr. Rabinowitz and his partners got started
Dr. Rabinowitz and his colleagues created an integrated care model in 2008 by adding a psychologist to their practice, but before doing that, they asked parents of children with mental and behavioral health issues what type of insurance they had. Then they obtained a referral list from the family’s insurer and hoped for the best. “Sometimes I referred to someone I may not have heard of,” Dr. Rabinowitz said. “Usually I did not get follow-up reports, or even know for sure if the patient ever went.”
Today, Parker Pediatrics and Adolescents employs three doctoral-level psychologists: one full-time, one three-quarter time, and one half-time, as well as one master’s-level therapist who works half-time.
“On any given day, we have at least two counselors in our office,” said Lindsey Einhorn, PhD, a licensed clinical psychologist who joined the practice in 2011. She and her colleagues care for children and teens with ADHD, depression, anxiety, behavioral and adjustment disorders, drug counseling, behavioral addictions, social struggles such as bullying, obsessive compulsive disorder (OCD), loss, hair or eyelash pulling, mood dysregulation, and sibling conflict. They refer for educational testing, comprehensive psychological evaluations, difficult divorce cases, play therapy, complex cases requiring more than 20 sessions, and children of staff employed by the practice.
The practice features a separate waiting room for psychology patients and front office staff dedicated to managing their schedules. “For anyone who’s trying to make a psychology appointment but can’t be seen in an efficient manner or wants a different day or time, we keep an ongoing move-up list,” Dr. Einhorn said. “If a family calls to cancel an appointment, the front desk person who makes that cancellation will fill out a slip and give it to one of our psychology schedulers. That person will create a move-up list and start filling that appointment. If there’s a cancellation, it’s rare that it goes unfilled.”
Key forms for parents to complete include informed consent, a notice of privacy practices, a late cancel/no show policy, an initial intake agreement, and a summary of parent concerns.
Patient and clinician reaction
According to results from a recent survey of parents whose children were seen by a psychologist at Parker Pediatrics and Adolescents, 89% said it was important for their children to receive mental health services in the same location as their medical care, and 96% were satisfied with the services provided. In addition, 93% said that the experience benefited their child, 72% were satisfied with appointment times, and 55% expressed interest in virtual visits via telemedicine. Meanwhile, a survey of parents whose children have not been seen by a psychologist at the practice found that 65% knew a psychologist was on staff, and only 9% said that there were barriers to their child seeing a psychologist there.
Clinicians themselves benefit from having mental health specialists on site for referrals. “It enables you to be more efficient, and it saves time,” Dr. Rabinowitz said. “There’s knowledge and confidence gained, and it improves satisfaction because physicians don’t have to stay at the office later filling out referral forms. It meets the needs of your patients and their families, it attracts new patients, and you may be able to make some income on this.”
How to get started
Dr. Rabinowitz recommended that, once clinicians at a pediatric practice commit to expanding their services to include mental and behavioral health care, they should hold a corporate/partner meeting, assign responsibilities, and establish a timeline for implementation. “This is all very important,” he said. “Then you have to talk about what kind of arrangement you want to have. You could employ someone to join your practice, hire an independent contractor, establish a space share agreement, or have an out-of-office arrangement.”
For many years, clinicians at Parker Pediatrics and Adolescents had a psychologist perform ADHD evaluations on a consultative basis. “Then, as we saw a need for mental health services about a decade ago, we hired a part-time psychologist who did testing as well as counseling,” Dr. Rabinowitz said. “But that psychologist got very busy, so we hired a full-time psychologist. We continued to hire additional psychologists as need increased.”
Reimbursement issues
Numerous reimbursement barriers to providing mental health services in pediatric primary care exist, he noted, including a lack of payment if mental health codes are used, a lack of “incident to” payments in some areas of the country, existing reimbursement levels, and the fact that same-day billing of physical and mental health often is not allowed. “However, we have found that if we give flu shots during their mental health visit, [insurers] will cover the flu shot,” he said. “Reimbursement for screening is sometimes not covered very well.”
One reimbursement option is the fee-for-service/concierge model, “but that’s not an economic option for many,” he said. “You can’t see Medicaid patients in that model.” Joining a mental health networks is feasible, “but there is poor reimbursement,” he said. “It also creates another layer of administration.”
He recommends financial integration, “but you need to research your options because a lot of it is state dependent.” Other options include grants, insurance contracts, and seeking permission from Medicaid.
Mental health CPT codes that mental health clinicians at the practice commonly use include bill by time (CPT code 99214/15); psychotherapy session that lasts 16-37 minutes (CPT code 90832); psychotherapy session that lasts 38-52 minutes (CPT code 90834); and psychotherapy session that lasts more than 53 minutes (CPT code 90837). Clinicians also can bill by interactive complexity (CPT code 90785) and psychotherapy for crisis (CPT code 90839).
Dr. Rabinowitz and Dr. Einhorn reported having no financial disclosures.
EXPERT ANALYSIS FROM AAP 2019
Tide beginning to turn on vaccine hesitancy
NEW ORLEANS –
The shift began with the measles outbreak in Southern California in late 2014, he said. According to the Centers for Disease Control and Prevention, 125 measles cases with rash that occurred between Dec. 28, 2014, and Feb. 8, 2015, were confirmed in U.S. residents. Of these, 100 were California residents (MMWR. 2015 Feb 20;64[06];153-4).
“This outbreak spread ultimately to 25 states and involved 189 people,” Dr. Offit said at the annual meeting of the American Academy of Pediatrics. “It was in the news almost every day. As a consequence, there were measles outbreaks in New York, New Jersey, Florida, Oregon, and Texas, and Washington, which began to turn the public sentiment against the antivaccine movement.”
Even longstanding skeptics are changing their tune. Dr. Offit, professor of pediatrics in the division of infectious diseases at the Children’s Hospital of Philadelphia, cited a recent study from the Autism Science Foundation which found that 85% of parents of children with autism spectrum disorder don’t believe that vaccines cause the condition. “Although there will be parents who continue to believe that vaccines cause autism, most parents of children with autism don’t believe that,” he said. “Also, it’s a little hard to make your case that vaccines are dangerous and that you shouldn’t get them in the midst of outbreaks.”
Perhaps the greatest pushback against antivaccination efforts has been made in the legal arena. In 2019 alone, legislators in California banned parents from not vaccinating their kids because of personal beliefs, while lawmakers in New York repealed the religious exemption to vaccinate, those in Maine repealed the religious and philosophical exemption, those in New Jersey required detailed written explanation for religious exemption, and those in Washington State repealed the philosophical exemption for the MMR vaccine.
Pushback also is apparent on various social media platforms. For example, Dr. Offit said, Pinterest restricts vaccine search results to curb the spread of misinformation, YouTube removes ads from antivaccine channels, Amazon Prime has pulled antivaccination documentaries from its video service, and Facebook has taken steps to curb misinformation about vaccines. “With outbreaks and with children suffering, the media and public sentiment has largely turned against those who are vehemently against vaccines,” he said. “I’m talking about an angry, politically connected, lawyer-backed group of people who are conspiracy theorists, [those] who no matter what you say, they’re going to believe there’s a conspiracy theory to hurt their children and not believe you. When that group becomes big enough and you start to see outbreaks like we’ve seen, then it becomes an issue. That’s where it comes down to legislation. Is it your inalienable right as a U.S. citizen to allow your child to catch and transmit a potentially fatal infection? That’s what we’re struggling with now.”
When meeting with parents who are skeptical about vaccines or refuse their children to have them, Dr. Offit advises clinicians to “go down swinging” in favor of vaccination. He shared how his wife, Bonnie, a pediatrician who practices in suburban Philadelphia, counsels parents who raise such concerns. “The way she handled it initially was to do the best she could to eventually get people vaccinated,” he said. “She was successful about one-quarter of the time. Then she drew a line. She started saying to parents, ‘Look; don’t put me in a position where you are asking me to practice substandard care. I can’t send them out of this room knowing that there’s more measles out there, knowing that there’s mumps out there, knowing that there’s whooping cough out there, knowing that there’s pneumococcus and varicella out there. If this child leaves this office and is hurt by any of those viruses or bacteria and I knew I could have done something to prevent it, I couldn’t live with myself. If you’re going to let this child out without being vaccinated I can’t see you anymore because I’m responsible for the health of this child.’ With that [approach], she has been far more successful. Because at some level, if you continue to see that patient, you’re tacitly agreeing that it’s okay to [not vaccinate].”
In 2000, Dr. Offit and colleagues created the Vaccine Education Center at Children’s Hospital of Philadelphia, which provides complete, up-to-date, and reliable information about vaccines to parents and clinicians. It summarizes the purpose of each vaccine, and the relative risks and benefits in easy-to-read language. The CDC also maintains updated information about vaccines and immunizations on its web site. For his part, Dr. Offit tells parents that passing on an opportunity to vaccinate their child is not a risk-free choice. “If you choose not to get a vaccine you probably will get away with it, but you might not,” he said. “You are playing a game of Russian roulette. It may not be five empty chambers and one bullet, but maybe it’s 100,000 empty chambers and one bullet. There’s a bullet there.”
Dr. Offit reported having no relevant financial disclosures.
NEW ORLEANS –
The shift began with the measles outbreak in Southern California in late 2014, he said. According to the Centers for Disease Control and Prevention, 125 measles cases with rash that occurred between Dec. 28, 2014, and Feb. 8, 2015, were confirmed in U.S. residents. Of these, 100 were California residents (MMWR. 2015 Feb 20;64[06];153-4).
“This outbreak spread ultimately to 25 states and involved 189 people,” Dr. Offit said at the annual meeting of the American Academy of Pediatrics. “It was in the news almost every day. As a consequence, there were measles outbreaks in New York, New Jersey, Florida, Oregon, and Texas, and Washington, which began to turn the public sentiment against the antivaccine movement.”
Even longstanding skeptics are changing their tune. Dr. Offit, professor of pediatrics in the division of infectious diseases at the Children’s Hospital of Philadelphia, cited a recent study from the Autism Science Foundation which found that 85% of parents of children with autism spectrum disorder don’t believe that vaccines cause the condition. “Although there will be parents who continue to believe that vaccines cause autism, most parents of children with autism don’t believe that,” he said. “Also, it’s a little hard to make your case that vaccines are dangerous and that you shouldn’t get them in the midst of outbreaks.”
Perhaps the greatest pushback against antivaccination efforts has been made in the legal arena. In 2019 alone, legislators in California banned parents from not vaccinating their kids because of personal beliefs, while lawmakers in New York repealed the religious exemption to vaccinate, those in Maine repealed the religious and philosophical exemption, those in New Jersey required detailed written explanation for religious exemption, and those in Washington State repealed the philosophical exemption for the MMR vaccine.
Pushback also is apparent on various social media platforms. For example, Dr. Offit said, Pinterest restricts vaccine search results to curb the spread of misinformation, YouTube removes ads from antivaccine channels, Amazon Prime has pulled antivaccination documentaries from its video service, and Facebook has taken steps to curb misinformation about vaccines. “With outbreaks and with children suffering, the media and public sentiment has largely turned against those who are vehemently against vaccines,” he said. “I’m talking about an angry, politically connected, lawyer-backed group of people who are conspiracy theorists, [those] who no matter what you say, they’re going to believe there’s a conspiracy theory to hurt their children and not believe you. When that group becomes big enough and you start to see outbreaks like we’ve seen, then it becomes an issue. That’s where it comes down to legislation. Is it your inalienable right as a U.S. citizen to allow your child to catch and transmit a potentially fatal infection? That’s what we’re struggling with now.”
When meeting with parents who are skeptical about vaccines or refuse their children to have them, Dr. Offit advises clinicians to “go down swinging” in favor of vaccination. He shared how his wife, Bonnie, a pediatrician who practices in suburban Philadelphia, counsels parents who raise such concerns. “The way she handled it initially was to do the best she could to eventually get people vaccinated,” he said. “She was successful about one-quarter of the time. Then she drew a line. She started saying to parents, ‘Look; don’t put me in a position where you are asking me to practice substandard care. I can’t send them out of this room knowing that there’s more measles out there, knowing that there’s mumps out there, knowing that there’s whooping cough out there, knowing that there’s pneumococcus and varicella out there. If this child leaves this office and is hurt by any of those viruses or bacteria and I knew I could have done something to prevent it, I couldn’t live with myself. If you’re going to let this child out without being vaccinated I can’t see you anymore because I’m responsible for the health of this child.’ With that [approach], she has been far more successful. Because at some level, if you continue to see that patient, you’re tacitly agreeing that it’s okay to [not vaccinate].”
In 2000, Dr. Offit and colleagues created the Vaccine Education Center at Children’s Hospital of Philadelphia, which provides complete, up-to-date, and reliable information about vaccines to parents and clinicians. It summarizes the purpose of each vaccine, and the relative risks and benefits in easy-to-read language. The CDC also maintains updated information about vaccines and immunizations on its web site. For his part, Dr. Offit tells parents that passing on an opportunity to vaccinate their child is not a risk-free choice. “If you choose not to get a vaccine you probably will get away with it, but you might not,” he said. “You are playing a game of Russian roulette. It may not be five empty chambers and one bullet, but maybe it’s 100,000 empty chambers and one bullet. There’s a bullet there.”
Dr. Offit reported having no relevant financial disclosures.
NEW ORLEANS –
The shift began with the measles outbreak in Southern California in late 2014, he said. According to the Centers for Disease Control and Prevention, 125 measles cases with rash that occurred between Dec. 28, 2014, and Feb. 8, 2015, were confirmed in U.S. residents. Of these, 100 were California residents (MMWR. 2015 Feb 20;64[06];153-4).
“This outbreak spread ultimately to 25 states and involved 189 people,” Dr. Offit said at the annual meeting of the American Academy of Pediatrics. “It was in the news almost every day. As a consequence, there were measles outbreaks in New York, New Jersey, Florida, Oregon, and Texas, and Washington, which began to turn the public sentiment against the antivaccine movement.”
Even longstanding skeptics are changing their tune. Dr. Offit, professor of pediatrics in the division of infectious diseases at the Children’s Hospital of Philadelphia, cited a recent study from the Autism Science Foundation which found that 85% of parents of children with autism spectrum disorder don’t believe that vaccines cause the condition. “Although there will be parents who continue to believe that vaccines cause autism, most parents of children with autism don’t believe that,” he said. “Also, it’s a little hard to make your case that vaccines are dangerous and that you shouldn’t get them in the midst of outbreaks.”
Perhaps the greatest pushback against antivaccination efforts has been made in the legal arena. In 2019 alone, legislators in California banned parents from not vaccinating their kids because of personal beliefs, while lawmakers in New York repealed the religious exemption to vaccinate, those in Maine repealed the religious and philosophical exemption, those in New Jersey required detailed written explanation for religious exemption, and those in Washington State repealed the philosophical exemption for the MMR vaccine.
Pushback also is apparent on various social media platforms. For example, Dr. Offit said, Pinterest restricts vaccine search results to curb the spread of misinformation, YouTube removes ads from antivaccine channels, Amazon Prime has pulled antivaccination documentaries from its video service, and Facebook has taken steps to curb misinformation about vaccines. “With outbreaks and with children suffering, the media and public sentiment has largely turned against those who are vehemently against vaccines,” he said. “I’m talking about an angry, politically connected, lawyer-backed group of people who are conspiracy theorists, [those] who no matter what you say, they’re going to believe there’s a conspiracy theory to hurt their children and not believe you. When that group becomes big enough and you start to see outbreaks like we’ve seen, then it becomes an issue. That’s where it comes down to legislation. Is it your inalienable right as a U.S. citizen to allow your child to catch and transmit a potentially fatal infection? That’s what we’re struggling with now.”
When meeting with parents who are skeptical about vaccines or refuse their children to have them, Dr. Offit advises clinicians to “go down swinging” in favor of vaccination. He shared how his wife, Bonnie, a pediatrician who practices in suburban Philadelphia, counsels parents who raise such concerns. “The way she handled it initially was to do the best she could to eventually get people vaccinated,” he said. “She was successful about one-quarter of the time. Then she drew a line. She started saying to parents, ‘Look; don’t put me in a position where you are asking me to practice substandard care. I can’t send them out of this room knowing that there’s more measles out there, knowing that there’s mumps out there, knowing that there’s whooping cough out there, knowing that there’s pneumococcus and varicella out there. If this child leaves this office and is hurt by any of those viruses or bacteria and I knew I could have done something to prevent it, I couldn’t live with myself. If you’re going to let this child out without being vaccinated I can’t see you anymore because I’m responsible for the health of this child.’ With that [approach], she has been far more successful. Because at some level, if you continue to see that patient, you’re tacitly agreeing that it’s okay to [not vaccinate].”
In 2000, Dr. Offit and colleagues created the Vaccine Education Center at Children’s Hospital of Philadelphia, which provides complete, up-to-date, and reliable information about vaccines to parents and clinicians. It summarizes the purpose of each vaccine, and the relative risks and benefits in easy-to-read language. The CDC also maintains updated information about vaccines and immunizations on its web site. For his part, Dr. Offit tells parents that passing on an opportunity to vaccinate their child is not a risk-free choice. “If you choose not to get a vaccine you probably will get away with it, but you might not,” he said. “You are playing a game of Russian roulette. It may not be five empty chambers and one bullet, but maybe it’s 100,000 empty chambers and one bullet. There’s a bullet there.”
Dr. Offit reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM AAP 2019
Tips for helping children improve adherence to asthma treatment
NEW ORLEANS – Up to 50% of children with asthma struggle to control their condition, yet fewer than 5% of pediatric asthma is severe and truly resistant to therapy, according to Susan Laubach, MD.
Other factors may make asthma difficult to control and may be modifiable, especially nonadherence to recommended treatment. In fact, up to 70% of patients report poor adherence to recommended treatment, Dr. Laubach said at the annual meeting of the American Academy of Pediatrics.
“Barriers to adherence may be related to the treatments themselves,” she said. “These include complex treatment schedules, lack of an immediately discernible beneficial effect, adverse effects of the medication, and prohibitive costs.”
Dr. Laubach, who directs the allergy clinic at Rady Children’s Hospital in San Diego, said that clinician-related barriers also influence patient adherence to recommended treatment, including difficulty scheduling appointments or seeing the same physician, a perceived lack of empathy, or failure to discuss the family’s concerns or answer questions. Common patient-related barriers include poor understanding of how the medication may help or how to use the inhalers.
“Some families have a lack of trust in the health care system, or certain beliefs about illness or medication that may hamper motivation to adhere,” she added. “Social issues such as poverty, lack of insurance, or a chaotic home environment may make it difficult for a patient to adhere to recommended treatment.”
In 2013, researchers led by Ted Klok, MD, PhD, of Princess Amalia Children’s Clinic in the Netherlands, explored practical ways to improve treatment adherence in children with pediatric respiratory disease (Breathe. 2013;9:268-77). One of their recommendations involves “five E’s” of ensuring optimal adherence. They include:
Ensure close and repeated follow-up to help build trust and partnership. “I’ll often follow up every month until I know a patient has gained good control of his or her asthma,” said Dr. Laubach, who was not involved in developing the recommendations. “Then I’ll follow up every 3 months.”
Explore the patient’s views, beliefs, and preferences. “You can do this by inviting questions or following up on comments or remarks made about the treatment plan,” she said. “This doesn’t have to take long. You can simply ask, ‘What are you concerned might happen if your child uses an inhaled corticosteroid?’ Or, ‘What have you heard about inhaled steroids?’ ”
Express empathy using active listening techniques tailored to the patient’s needs. Consider phrasing like, “I understand what you’re saying. In a perfect world, your child would not have to use any medications. But when he can’t sleep because he’s coughing so much, the benefit of this medication probably outweighs any potential risks.”
Exercise shared decision making. For example, if the parent of one of your patients has to leave for work very early in the morning, “maybe find a way to adjust to once-daily dosing so that appropriate doses can be given at bedtime when the parent is consistently available,” Dr. Laubach said.
Evaluate adherence in a nonjudgmental fashion. Evidence suggests that most patients with asthma miss a couple of medication doses now and then. She makes it a point to ask patients, “If you’re supposed to take 14 doses a week, how many do you think you actually take?” Their response “gives me an idea about their level of adherence and it opens a discussion into why they may miss doses, so that we can find a solution to help improve adherence.”
The Childhood Asthma Management Program (CAMP) study found a significant reduction in height velocity in patients treated with budesonide, compared with placebo (N Engl J Med. 2012;367[10]:904-12). “However, most of this reduction occurred in the first year of treatment, was not additive over time, and led in average to a 1-cm difference in height as an adult,” said Dr. Laubach, who is also of the department of pediatrics at the University of California, San Diego. “So while it must be acknowledged that high-dose inhaled corticosteroids may affect growth, who do we put on inhaled corticosteroids? People who can’t breathe.”
Studies have demonstrated that the regular use of inhaled corticosteroids is associated with a decreased risk of death from asthma (N Engl J Med. 2000;343:332-6). “I suspect that most parents would trade 1 cm of height to reduce the risk of death in their child,” Dr. Laubach said.
She reported having no financial disclosures.
NEW ORLEANS – Up to 50% of children with asthma struggle to control their condition, yet fewer than 5% of pediatric asthma is severe and truly resistant to therapy, according to Susan Laubach, MD.
Other factors may make asthma difficult to control and may be modifiable, especially nonadherence to recommended treatment. In fact, up to 70% of patients report poor adherence to recommended treatment, Dr. Laubach said at the annual meeting of the American Academy of Pediatrics.
“Barriers to adherence may be related to the treatments themselves,” she said. “These include complex treatment schedules, lack of an immediately discernible beneficial effect, adverse effects of the medication, and prohibitive costs.”
Dr. Laubach, who directs the allergy clinic at Rady Children’s Hospital in San Diego, said that clinician-related barriers also influence patient adherence to recommended treatment, including difficulty scheduling appointments or seeing the same physician, a perceived lack of empathy, or failure to discuss the family’s concerns or answer questions. Common patient-related barriers include poor understanding of how the medication may help or how to use the inhalers.
“Some families have a lack of trust in the health care system, or certain beliefs about illness or medication that may hamper motivation to adhere,” she added. “Social issues such as poverty, lack of insurance, or a chaotic home environment may make it difficult for a patient to adhere to recommended treatment.”
In 2013, researchers led by Ted Klok, MD, PhD, of Princess Amalia Children’s Clinic in the Netherlands, explored practical ways to improve treatment adherence in children with pediatric respiratory disease (Breathe. 2013;9:268-77). One of their recommendations involves “five E’s” of ensuring optimal adherence. They include:
Ensure close and repeated follow-up to help build trust and partnership. “I’ll often follow up every month until I know a patient has gained good control of his or her asthma,” said Dr. Laubach, who was not involved in developing the recommendations. “Then I’ll follow up every 3 months.”
Explore the patient’s views, beliefs, and preferences. “You can do this by inviting questions or following up on comments or remarks made about the treatment plan,” she said. “This doesn’t have to take long. You can simply ask, ‘What are you concerned might happen if your child uses an inhaled corticosteroid?’ Or, ‘What have you heard about inhaled steroids?’ ”
Express empathy using active listening techniques tailored to the patient’s needs. Consider phrasing like, “I understand what you’re saying. In a perfect world, your child would not have to use any medications. But when he can’t sleep because he’s coughing so much, the benefit of this medication probably outweighs any potential risks.”
Exercise shared decision making. For example, if the parent of one of your patients has to leave for work very early in the morning, “maybe find a way to adjust to once-daily dosing so that appropriate doses can be given at bedtime when the parent is consistently available,” Dr. Laubach said.
Evaluate adherence in a nonjudgmental fashion. Evidence suggests that most patients with asthma miss a couple of medication doses now and then. She makes it a point to ask patients, “If you’re supposed to take 14 doses a week, how many do you think you actually take?” Their response “gives me an idea about their level of adherence and it opens a discussion into why they may miss doses, so that we can find a solution to help improve adherence.”
The Childhood Asthma Management Program (CAMP) study found a significant reduction in height velocity in patients treated with budesonide, compared with placebo (N Engl J Med. 2012;367[10]:904-12). “However, most of this reduction occurred in the first year of treatment, was not additive over time, and led in average to a 1-cm difference in height as an adult,” said Dr. Laubach, who is also of the department of pediatrics at the University of California, San Diego. “So while it must be acknowledged that high-dose inhaled corticosteroids may affect growth, who do we put on inhaled corticosteroids? People who can’t breathe.”
Studies have demonstrated that the regular use of inhaled corticosteroids is associated with a decreased risk of death from asthma (N Engl J Med. 2000;343:332-6). “I suspect that most parents would trade 1 cm of height to reduce the risk of death in their child,” Dr. Laubach said.
She reported having no financial disclosures.
NEW ORLEANS – Up to 50% of children with asthma struggle to control their condition, yet fewer than 5% of pediatric asthma is severe and truly resistant to therapy, according to Susan Laubach, MD.
Other factors may make asthma difficult to control and may be modifiable, especially nonadherence to recommended treatment. In fact, up to 70% of patients report poor adherence to recommended treatment, Dr. Laubach said at the annual meeting of the American Academy of Pediatrics.
“Barriers to adherence may be related to the treatments themselves,” she said. “These include complex treatment schedules, lack of an immediately discernible beneficial effect, adverse effects of the medication, and prohibitive costs.”
Dr. Laubach, who directs the allergy clinic at Rady Children’s Hospital in San Diego, said that clinician-related barriers also influence patient adherence to recommended treatment, including difficulty scheduling appointments or seeing the same physician, a perceived lack of empathy, or failure to discuss the family’s concerns or answer questions. Common patient-related barriers include poor understanding of how the medication may help or how to use the inhalers.
“Some families have a lack of trust in the health care system, or certain beliefs about illness or medication that may hamper motivation to adhere,” she added. “Social issues such as poverty, lack of insurance, or a chaotic home environment may make it difficult for a patient to adhere to recommended treatment.”
In 2013, researchers led by Ted Klok, MD, PhD, of Princess Amalia Children’s Clinic in the Netherlands, explored practical ways to improve treatment adherence in children with pediatric respiratory disease (Breathe. 2013;9:268-77). One of their recommendations involves “five E’s” of ensuring optimal adherence. They include:
Ensure close and repeated follow-up to help build trust and partnership. “I’ll often follow up every month until I know a patient has gained good control of his or her asthma,” said Dr. Laubach, who was not involved in developing the recommendations. “Then I’ll follow up every 3 months.”
Explore the patient’s views, beliefs, and preferences. “You can do this by inviting questions or following up on comments or remarks made about the treatment plan,” she said. “This doesn’t have to take long. You can simply ask, ‘What are you concerned might happen if your child uses an inhaled corticosteroid?’ Or, ‘What have you heard about inhaled steroids?’ ”
Express empathy using active listening techniques tailored to the patient’s needs. Consider phrasing like, “I understand what you’re saying. In a perfect world, your child would not have to use any medications. But when he can’t sleep because he’s coughing so much, the benefit of this medication probably outweighs any potential risks.”
Exercise shared decision making. For example, if the parent of one of your patients has to leave for work very early in the morning, “maybe find a way to adjust to once-daily dosing so that appropriate doses can be given at bedtime when the parent is consistently available,” Dr. Laubach said.
Evaluate adherence in a nonjudgmental fashion. Evidence suggests that most patients with asthma miss a couple of medication doses now and then. She makes it a point to ask patients, “If you’re supposed to take 14 doses a week, how many do you think you actually take?” Their response “gives me an idea about their level of adherence and it opens a discussion into why they may miss doses, so that we can find a solution to help improve adherence.”
The Childhood Asthma Management Program (CAMP) study found a significant reduction in height velocity in patients treated with budesonide, compared with placebo (N Engl J Med. 2012;367[10]:904-12). “However, most of this reduction occurred in the first year of treatment, was not additive over time, and led in average to a 1-cm difference in height as an adult,” said Dr. Laubach, who is also of the department of pediatrics at the University of California, San Diego. “So while it must be acknowledged that high-dose inhaled corticosteroids may affect growth, who do we put on inhaled corticosteroids? People who can’t breathe.”
Studies have demonstrated that the regular use of inhaled corticosteroids is associated with a decreased risk of death from asthma (N Engl J Med. 2000;343:332-6). “I suspect that most parents would trade 1 cm of height to reduce the risk of death in their child,” Dr. Laubach said.
She reported having no financial disclosures.
EXPERT ANALYSIS FROM AAP 2019
Children with single ventricle CHD at risk for behavioral, emotional problems
NEW ORLEANS – Single ventricle congenital heart disease (CHD) and worse social determinants of health are associated with more behavior problems and less total competency in children, and this relationship is mediated by disease-related chronic stress, self-perception, and family environment.
Those are key findings from a large analysis of existing cross-sectional data presented at the annual meeting of the American Academy of Pediatrics. The study set out to assess what factors mediate the relationship between CHD severity, social determinants of health, and behavioral and emotional outcomes.
“We know that worse CHD severity is associated with worse parent-reported and self-reported behavioral and emotional functioning in children and adolescents survivors,” lead author Asad Qadir, MD, said in an interview. “ by taking measures that would decrease their and their caregivers’ disease-related chronic stress, improve family functioning, and improve the self-perception of the child. While social determinants of health are not modifiable, they are important for predicting which children may be at risk for behavior problems.”
Dr. Qadir, a cardiology fellow in the department of pediatrics at Northwestern University, Chicago, and colleagues performed a corollary analysis of the Pediatric Cardiac Quality of Life Inventory Testing study, an international, multicenter, cross-sectional study in which parents and patients with CHD completed questionnaires measuring behavioral and emotional functioning, self-perception, family environment, family coping, posttraumatic stress, and illness-related parenting stress (see Qual Life Res. 2008;17:613-26, Pediatrics. 2010;126[3]:498-508, and Cardiol Young. 2014;[2]:220-8). They assessed the relationships between CHD severity and social determinants of health (predictors), disease-related stress and psychosocial adaptation (mediators), and behavioral and emotional outcomes. They used structural equation modeling to determine the effects of predictors and mediators on outcomes, and created multivariable models for each patient- and parent-reported outcome.
The analysis included 981 patient-parent dyads. Of these, 210 patients had mild biventricular CHD, 620 had moderate biventricular CHD, and 151 had single ventricle CHD. The mean age of patients was 13 years and 55% were male. The researchers found that single ventricle CHD and worse social determinants of health were significant predictors of greater disease-related chronic stress for patients and caregivers and worse psychosocial adaptation in CHD survivors, including self-perception and family functioning constructs of cohesion and expressiveness (P less than .001 for all associations). In addition, single ventricle CHD and worse social determinants of health were associated with worse behavioral and emotional outcomes as reported by patients and parents, including internalizing behaviors, externalizing behaviors, and total competency (P less than .001 for all associations).
In multivariable models for all parent-reported outcomes, significant associations were observed between single ventricle CHD, social determinants of health, disease-related stress, child receiving mental health services, and cohesion/conflict in the family environment (P less than .001). In multivariable models for all patient-reported outcomes, significant associations were seen between single ventricle CHD, self-perception, and cohesion/conflict in the family environment (P less than 0.001).
Patient disease-related stress had the strongest association with externalizing problems, and worse social determinants of health significantly lowered patient-reported total competency.
“Many of the relationships found in the study make intuitive sense,” Dr. Qadir said. “For example, less favorable social determinants of health were associated with more parent disease-related chronic stress, which in turn was associated with parent-reported behavior problems in children. What was surprising was that worse behavioral outcomes were specifically associated with single ventricle disease only. Complex biventricular congenital heart disease patients (CHD that required a surgical- or catheter-based intervention) often have worse behavioral and emotional outcomes, similar to single ventricle patients. However, our model would argue that biventricular congenital heart disease complexity patients have more behavioral and emotional issues not because of their disease complexity, but due to their social determinants of health and the amount of disease-related chronic stress in the child and the parent and the amount of psychosocial adaptation found in the child and parent.”
Parent and patient disease-related chronic stress was not only an important mediator of the effect of CHD severity and social determinants of health on behavioral and emotional outcomes, he added, but it also had indirect effects that were mediated by family cohesion/conflict and patient self-perception.
“These data suggest that for those children with worse social determinants of health and single ventricle congenital heart disease, interventions that mitigate disease-related chronic stress, promote family functioning, and promote self-perception in the child may improve or optimize behavioral and emotional functioning during childhood and adolescence in CHD surgical survivors,” Dr. Qadir concluded.
He acknowledged certain limitations of the analysis, including the fact that it was a corollary cross-sectional analysis of an existing data set. “The results do not reflect possible changes over time,” he added. “There was also selection bias as non-English speakers were excluded, and the study population had a greater percentage of Caucasian and highly educated parents with higher income than the general population, which may affect the generalizability of our results.”
The researchers reported having no relevant financial disclosures.
NEW ORLEANS – Single ventricle congenital heart disease (CHD) and worse social determinants of health are associated with more behavior problems and less total competency in children, and this relationship is mediated by disease-related chronic stress, self-perception, and family environment.
Those are key findings from a large analysis of existing cross-sectional data presented at the annual meeting of the American Academy of Pediatrics. The study set out to assess what factors mediate the relationship between CHD severity, social determinants of health, and behavioral and emotional outcomes.
“We know that worse CHD severity is associated with worse parent-reported and self-reported behavioral and emotional functioning in children and adolescents survivors,” lead author Asad Qadir, MD, said in an interview. “ by taking measures that would decrease their and their caregivers’ disease-related chronic stress, improve family functioning, and improve the self-perception of the child. While social determinants of health are not modifiable, they are important for predicting which children may be at risk for behavior problems.”
Dr. Qadir, a cardiology fellow in the department of pediatrics at Northwestern University, Chicago, and colleagues performed a corollary analysis of the Pediatric Cardiac Quality of Life Inventory Testing study, an international, multicenter, cross-sectional study in which parents and patients with CHD completed questionnaires measuring behavioral and emotional functioning, self-perception, family environment, family coping, posttraumatic stress, and illness-related parenting stress (see Qual Life Res. 2008;17:613-26, Pediatrics. 2010;126[3]:498-508, and Cardiol Young. 2014;[2]:220-8). They assessed the relationships between CHD severity and social determinants of health (predictors), disease-related stress and psychosocial adaptation (mediators), and behavioral and emotional outcomes. They used structural equation modeling to determine the effects of predictors and mediators on outcomes, and created multivariable models for each patient- and parent-reported outcome.
The analysis included 981 patient-parent dyads. Of these, 210 patients had mild biventricular CHD, 620 had moderate biventricular CHD, and 151 had single ventricle CHD. The mean age of patients was 13 years and 55% were male. The researchers found that single ventricle CHD and worse social determinants of health were significant predictors of greater disease-related chronic stress for patients and caregivers and worse psychosocial adaptation in CHD survivors, including self-perception and family functioning constructs of cohesion and expressiveness (P less than .001 for all associations). In addition, single ventricle CHD and worse social determinants of health were associated with worse behavioral and emotional outcomes as reported by patients and parents, including internalizing behaviors, externalizing behaviors, and total competency (P less than .001 for all associations).
In multivariable models for all parent-reported outcomes, significant associations were observed between single ventricle CHD, social determinants of health, disease-related stress, child receiving mental health services, and cohesion/conflict in the family environment (P less than .001). In multivariable models for all patient-reported outcomes, significant associations were seen between single ventricle CHD, self-perception, and cohesion/conflict in the family environment (P less than 0.001).
Patient disease-related stress had the strongest association with externalizing problems, and worse social determinants of health significantly lowered patient-reported total competency.
“Many of the relationships found in the study make intuitive sense,” Dr. Qadir said. “For example, less favorable social determinants of health were associated with more parent disease-related chronic stress, which in turn was associated with parent-reported behavior problems in children. What was surprising was that worse behavioral outcomes were specifically associated with single ventricle disease only. Complex biventricular congenital heart disease patients (CHD that required a surgical- or catheter-based intervention) often have worse behavioral and emotional outcomes, similar to single ventricle patients. However, our model would argue that biventricular congenital heart disease complexity patients have more behavioral and emotional issues not because of their disease complexity, but due to their social determinants of health and the amount of disease-related chronic stress in the child and the parent and the amount of psychosocial adaptation found in the child and parent.”
Parent and patient disease-related chronic stress was not only an important mediator of the effect of CHD severity and social determinants of health on behavioral and emotional outcomes, he added, but it also had indirect effects that were mediated by family cohesion/conflict and patient self-perception.
“These data suggest that for those children with worse social determinants of health and single ventricle congenital heart disease, interventions that mitigate disease-related chronic stress, promote family functioning, and promote self-perception in the child may improve or optimize behavioral and emotional functioning during childhood and adolescence in CHD surgical survivors,” Dr. Qadir concluded.
He acknowledged certain limitations of the analysis, including the fact that it was a corollary cross-sectional analysis of an existing data set. “The results do not reflect possible changes over time,” he added. “There was also selection bias as non-English speakers were excluded, and the study population had a greater percentage of Caucasian and highly educated parents with higher income than the general population, which may affect the generalizability of our results.”
The researchers reported having no relevant financial disclosures.
NEW ORLEANS – Single ventricle congenital heart disease (CHD) and worse social determinants of health are associated with more behavior problems and less total competency in children, and this relationship is mediated by disease-related chronic stress, self-perception, and family environment.
Those are key findings from a large analysis of existing cross-sectional data presented at the annual meeting of the American Academy of Pediatrics. The study set out to assess what factors mediate the relationship between CHD severity, social determinants of health, and behavioral and emotional outcomes.
“We know that worse CHD severity is associated with worse parent-reported and self-reported behavioral and emotional functioning in children and adolescents survivors,” lead author Asad Qadir, MD, said in an interview. “ by taking measures that would decrease their and their caregivers’ disease-related chronic stress, improve family functioning, and improve the self-perception of the child. While social determinants of health are not modifiable, they are important for predicting which children may be at risk for behavior problems.”
Dr. Qadir, a cardiology fellow in the department of pediatrics at Northwestern University, Chicago, and colleagues performed a corollary analysis of the Pediatric Cardiac Quality of Life Inventory Testing study, an international, multicenter, cross-sectional study in which parents and patients with CHD completed questionnaires measuring behavioral and emotional functioning, self-perception, family environment, family coping, posttraumatic stress, and illness-related parenting stress (see Qual Life Res. 2008;17:613-26, Pediatrics. 2010;126[3]:498-508, and Cardiol Young. 2014;[2]:220-8). They assessed the relationships between CHD severity and social determinants of health (predictors), disease-related stress and psychosocial adaptation (mediators), and behavioral and emotional outcomes. They used structural equation modeling to determine the effects of predictors and mediators on outcomes, and created multivariable models for each patient- and parent-reported outcome.
The analysis included 981 patient-parent dyads. Of these, 210 patients had mild biventricular CHD, 620 had moderate biventricular CHD, and 151 had single ventricle CHD. The mean age of patients was 13 years and 55% were male. The researchers found that single ventricle CHD and worse social determinants of health were significant predictors of greater disease-related chronic stress for patients and caregivers and worse psychosocial adaptation in CHD survivors, including self-perception and family functioning constructs of cohesion and expressiveness (P less than .001 for all associations). In addition, single ventricle CHD and worse social determinants of health were associated with worse behavioral and emotional outcomes as reported by patients and parents, including internalizing behaviors, externalizing behaviors, and total competency (P less than .001 for all associations).
In multivariable models for all parent-reported outcomes, significant associations were observed between single ventricle CHD, social determinants of health, disease-related stress, child receiving mental health services, and cohesion/conflict in the family environment (P less than .001). In multivariable models for all patient-reported outcomes, significant associations were seen between single ventricle CHD, self-perception, and cohesion/conflict in the family environment (P less than 0.001).
Patient disease-related stress had the strongest association with externalizing problems, and worse social determinants of health significantly lowered patient-reported total competency.
“Many of the relationships found in the study make intuitive sense,” Dr. Qadir said. “For example, less favorable social determinants of health were associated with more parent disease-related chronic stress, which in turn was associated with parent-reported behavior problems in children. What was surprising was that worse behavioral outcomes were specifically associated with single ventricle disease only. Complex biventricular congenital heart disease patients (CHD that required a surgical- or catheter-based intervention) often have worse behavioral and emotional outcomes, similar to single ventricle patients. However, our model would argue that biventricular congenital heart disease complexity patients have more behavioral and emotional issues not because of their disease complexity, but due to their social determinants of health and the amount of disease-related chronic stress in the child and the parent and the amount of psychosocial adaptation found in the child and parent.”
Parent and patient disease-related chronic stress was not only an important mediator of the effect of CHD severity and social determinants of health on behavioral and emotional outcomes, he added, but it also had indirect effects that were mediated by family cohesion/conflict and patient self-perception.
“These data suggest that for those children with worse social determinants of health and single ventricle congenital heart disease, interventions that mitigate disease-related chronic stress, promote family functioning, and promote self-perception in the child may improve or optimize behavioral and emotional functioning during childhood and adolescence in CHD surgical survivors,” Dr. Qadir concluded.
He acknowledged certain limitations of the analysis, including the fact that it was a corollary cross-sectional analysis of an existing data set. “The results do not reflect possible changes over time,” he added. “There was also selection bias as non-English speakers were excluded, and the study population had a greater percentage of Caucasian and highly educated parents with higher income than the general population, which may affect the generalizability of our results.”
The researchers reported having no relevant financial disclosures.
AT AAP 2019
Understanding your LGBTQ patients’ needs
NEW ORLEANS – One of the most important things pediatricians can do to support their lesbian, gay, bisexual, transgender (LGBT) and other gender-nonconforming patients is to ask all their patients about their feelings, preferences and experiences when it comes to gender and sexuality, according to Julie Finger, MD, MPH.
It’s equally important not to make assumptions, she told attendees at the annual meeting of the American Academy of Pediatrics. Biology and sexual and gender identity and expression can be very diverse, she said. Specifically, doctors should not assume patients are heterosexual, that bisexuality is a phase, that orientation or attraction translates directly to behavior or vice versa, or that LGBTQ patients have unsupportive families or are engaging in risky behavior. Research suggests LGB youth have slightly higher rates of early sexual debut, sexual activity or multiple partners than straight or uncertain youth, but only marginally so.
Pediatricians also cannot assume a patient’s sexual orientation based on their partner’s gender or determine a patient’s sexual orientation or gender identity based on appearance – or even that either is the same as it was on the previous visit.
What doctors can be sure of is that they do have LGBTQ patients, said Dr. Finger, and assistant professor of clinical pediatrics at Tulane University in New Orleans. According to a 2016 Morbidity and Mortality Weekly Report (2016 Aug 12; 65[9]), about 1 in 10 students in grades 9-12 are a sexual minority. About 2% of respondents identify as gay or lesbian, 6% identify as bisexual and 3% say they aren’t sure.
Knowing the terminology
Dr. Finger defined key terminology regarding gender and sexuality. She first clarified that LGBT is not the full spectrum for sexual orientation. Pansexual (fluid attraction to any sex or gender) and asexual (lack of feeling sexual attraction) can also describe sexuality, and the Q on the end of LGBTQ is often an umbrella term for “queer” or “questioning” that encompasses anyone who fits outside conventional social norms of sexual identity and gender expression.
Sexual behaviors – which include “young men who have sex with men” and “young women who have sex with women” – do not necessarily correspond as one might expect with sexual orientation or identity, which is one’s concept of their romantic or sexual feelings, attractions and desires, again reinforcing the importance of asking patients their identity and preferences.
In terms of gender, a person’s natal or biologic gender is the one assigned people at birth based on their body parts and hormones. Gender identity is a person’s understanding of their own gender, and gender expression refers to how someone acts or presents themselves and communicates their gender within their culture.
Those who identify as “gender nonconforming, genderqueer, gender fluid, or nonbinary” see their gender on a spectrum, not within the binary “male” or “female.” A cisgender person’s gender identity matches both their biological sex assigned at birth and conventional cultural norms, while a transgender person’s gender differs from the sex they were assigned at birth. Transgender women (male to female, MTF) and men (female to men, FTM) go through the process of transition, a time that can occur in weeks or years when they shift from living as one gender to another.
While it’s unclear what leads to a person’s sexual orientation – likely a combination of genetic, hormonal and environmental factors—there is no question that sexual orientation is not a “choice,” Dr Finger said. Research has also clarified that one’s sexual orientation does not result from parenting behaviors or a history of sexual abuse.
“But I would urge all of you, instead of focusing on why someone is LGBTQ, to focus on what that means for them in their life,” Dr Finger said. “How is this bearing out in terms of their relationships and their behaviors, and how do they feel about it? How are they being supported by their family or their community, and how is it impacting their lives?”
She cited findings from a Human Rights Campaign survey in 2012 of 10,000 youth aged 13-17, which found that most LGBTQ respondents became aware of their same-sex attraction at 9 years of age, though the average age of disclosures is 16, an improvement from age 21 in the 1980s.
How and what to ask
Although children start becoming conscious of gender at ages 1-2, their sense of gender usually stabilizes by age 4.
“Who should we be screening for gender nonconformity? Quite frankly, all children, because all of them have some gender identity, so we should be asking them about that,” Dr Finger said.
When children are younger, doctors can ask parents about their child’s social interactions, forms of play, dress preferences, and mood. Questions for patients themselves, adapted for their age, might include, “Do you feel more like a girl, boy, neither or both?”, “How would you like to play, cut your hair and dress?” And “What name or pronoun (he or she) fits you?”
While such conversations do not necessarily need to happen annually, doctors should especially ask youth who dress or behave in non–gender-conforming ways or who appear to have mood, behavior or social difficulties.
To understand a patient’s sexuality, ask whether they are attracted to people of their own gender or sex, a different gender or sex, both or all genders or no one, or if they’re not sure yet. Doctors can then ask how comfortable they are with their attraction and whether they have told family members or friends about them.
Sexual behavior questions should be developmentally appropriate and lead to counsel but not judgment, Dr Finger said. Her method, with adjustments for age and development, starts, “There are many way of being sexual or intimate with someone: kissing, hugging and touching, and oral sex, anal sex and vaginal sex. Have you ever had any of these experiences? Which ones? With males or females or both, or other genders?”
Then she gets more specific while remaining sensitive. Doctors can ask younger children if they have held hands or cuddled with someone, if they have kissed someone, or if they have touched another person’s private parts. They can ask teens about oral sex, vaginal sex and anal sex and then gather more details about what parts went where, which helps determine what screenings or treatment options a patient may need or desire.
Doctors can use their judgment about whether to ask questions with parents in the room or not, but as kids grow older, it’s good practice to speak to patients without their caregivers present. Doctors should also explain the rules of confidentiality to their patients and be aware of the risks of “coming out,” including family discord or rejection, problems at school or work, social stigma, bullying and harassment, physical violence and risk-taking behaviors, such as substance use, self-injury and risky sexual behaviors. A HEADSSS screen can help doctors learn if any of these are present.
Making your practice inclusive and welcoming
Fewer than one in five teens who are “out” as LGBTQ have come out to their doctor, Dr Finger cited. Most are out to their friends and classmates, and more than half are out to their family, but teens are less likely to tell their doctors.
Research suggests one reason for this is the fact that pediatricians often don’t ask. One study found that only 20% of pediatricians discussed sexual orientation with their patients (Pediatrics 2010 Apr;125:e741-7). Similarly, only 30% of family physicians brought up sexual orientation, found another study (Fam. Med. 2001 May;33[5]:376-81). The studies found physicians more often discussed condoms, HIV, sexually transmitted infections, abstinence, violence, contraception or, in the case of family physicians, sexual behaviors, and relationships.
But another reason for not being out to doctors is a history of poor experiences. A Lambda Legal Survey in 2009 of 4,916 LGBT respondents found that 8% of LGB and 27% of transgender and gender nonconforming patients had been denied care because of their identity of orientation. Eleven percent said “providers refused to touch them or used excessive precautions,” Dr Finger reported. LGBTQ patients may fear the doctor’s reaction or not keeping their identity confidential. Patients may also have internalized shame or guilt due to societal norms or homophobia, and all these barriers can reduce LGBTQ people’s willingness to seek and access to competent care.
The first step to making LGBTQ patients comfortable in your practice is to confront your own personal biases, Dr Finger said. Understand what they are and that a provider’s discomfort, even unconscious, can be damaging to the patient-provider relationship.
“If you find that this is just not something that you’re going to be comfortable doing, at the very least, I would suggest that you find providers in your area who are comfortable working with this patient population and you refer your patients to them so that they can have a good, trusting patient-provider relationship with somebody who can provide the care that they need,” Dr Finger said.
The next step is creating a safe place with zero tolerance for insensitivity by training staff to be welcoming and inclusive, assuring patients confidentiality, providing support and resources and displaying LGBTQ-affirming materials. These youth need active, visible evidence that the office will be a safe place for them.
Ways pediatricians can communicate an inclusive environment include having gender-neutral restrooms, using “parent” instead of “mother/father” and using forms and EMR prompts with gender-neutral language or multiple options for gender selection.
Screening and LGBTQ patients’ health needs
LGB youth and those who aren’t sure of their sexual orientation tend to have higher rates of substance use, including tobacco, alcohol and illicit drugs, and are more often victims of rape and other sexual violence. Their rates of depressive symptoms, bullying victimization, and suicidality are also significantly higher than in their heterosexual cisgender peers. Homelessness rates are also considerably higher in LGBTQ youth than in heterosexual cisgender youth.
One thing pediatricians can do is work with parents to ensure a patient’s school is meeting their needs. The greater risks LGBTQ youth typically face are mediated by social support, resiliency, supportive friends and family and a supportive school environment, including inclusive curricula and supportive staff.
Lesbian and bisexual women are considerably more at risk for poor sexual or reproductive outcomes, Dr Finger said. Their rates of unplanned pregnancy are double that of straight women, contributing to their higher rates of emergency contraception and abortion. They are also more likely to have more partners (male and females), to have a younger sexual debut and to be forced into sex by a male partner—yet they are far less likely to perceive themselves as at risk for a sexually transmitted infection than their peers.
This patient population therefore may need contraception counseling, including discussing their current methods and reviewing their options, including emergency contraception and possibly an advance prescription. Dr Finger also suggests having male and female condoms available in the office.
Doctors should screen all their female patients, regardless of sexuality, for chlamydia and gonorrhea, and offer routine cervical cancer screening and the HPV vaccine, as recommended by the CDC. They might consider screening for trichomoniasis, bacterial vaginosis, herpes simplex, human papillomavirus and HIV.
For men who have sex with men, the CDC recommends HIV and syphilis serology, urine/pharyngeal/rectal gonorrhea nucleic acid amplification test (NAAT), urine/rectal chlamydia NAAT, and hepatitis C screening for those who are HIV-positive—all at least once a year.
For transgender patients, doctors need to assess their STI- and HIV-related risks based on their current anatomy and sexual behaviors.
Doctors should also consider discussing pre-exposure prophylaxis (PrEP) for any youth at high risk for HIV infection if they are at least 77 pounds (35 kg). Emtricitabine/tenofovir (Truvada, Descovy) reduces the chance of sexually acquired infection by 99%, and infection acquired via drug injection by 74% when taken as prescribed.
Resources
Dr Finger noted a range of resources for LGBTQ youth and their families and providers, including the Family Acceptance Project, Gay and Lesbian Medical Association, Gay, Lesbian and Straight Education Network, GLBTQ Legal Advocates and Defenders (GLAD), Human Rights Campaign, It Gets Better Project, LGBTQ Student Resources and Support, National Center for Lesbian Rights, Parents and Friends of Lesbians and Gays (PFLAG), Safe Schools Coalition and The Trevor Project (concerning suicide risk).
NEW ORLEANS – One of the most important things pediatricians can do to support their lesbian, gay, bisexual, transgender (LGBT) and other gender-nonconforming patients is to ask all their patients about their feelings, preferences and experiences when it comes to gender and sexuality, according to Julie Finger, MD, MPH.
It’s equally important not to make assumptions, she told attendees at the annual meeting of the American Academy of Pediatrics. Biology and sexual and gender identity and expression can be very diverse, she said. Specifically, doctors should not assume patients are heterosexual, that bisexuality is a phase, that orientation or attraction translates directly to behavior or vice versa, or that LGBTQ patients have unsupportive families or are engaging in risky behavior. Research suggests LGB youth have slightly higher rates of early sexual debut, sexual activity or multiple partners than straight or uncertain youth, but only marginally so.
Pediatricians also cannot assume a patient’s sexual orientation based on their partner’s gender or determine a patient’s sexual orientation or gender identity based on appearance – or even that either is the same as it was on the previous visit.
What doctors can be sure of is that they do have LGBTQ patients, said Dr. Finger, and assistant professor of clinical pediatrics at Tulane University in New Orleans. According to a 2016 Morbidity and Mortality Weekly Report (2016 Aug 12; 65[9]), about 1 in 10 students in grades 9-12 are a sexual minority. About 2% of respondents identify as gay or lesbian, 6% identify as bisexual and 3% say they aren’t sure.
Knowing the terminology
Dr. Finger defined key terminology regarding gender and sexuality. She first clarified that LGBT is not the full spectrum for sexual orientation. Pansexual (fluid attraction to any sex or gender) and asexual (lack of feeling sexual attraction) can also describe sexuality, and the Q on the end of LGBTQ is often an umbrella term for “queer” or “questioning” that encompasses anyone who fits outside conventional social norms of sexual identity and gender expression.
Sexual behaviors – which include “young men who have sex with men” and “young women who have sex with women” – do not necessarily correspond as one might expect with sexual orientation or identity, which is one’s concept of their romantic or sexual feelings, attractions and desires, again reinforcing the importance of asking patients their identity and preferences.
In terms of gender, a person’s natal or biologic gender is the one assigned people at birth based on their body parts and hormones. Gender identity is a person’s understanding of their own gender, and gender expression refers to how someone acts or presents themselves and communicates their gender within their culture.
Those who identify as “gender nonconforming, genderqueer, gender fluid, or nonbinary” see their gender on a spectrum, not within the binary “male” or “female.” A cisgender person’s gender identity matches both their biological sex assigned at birth and conventional cultural norms, while a transgender person’s gender differs from the sex they were assigned at birth. Transgender women (male to female, MTF) and men (female to men, FTM) go through the process of transition, a time that can occur in weeks or years when they shift from living as one gender to another.
While it’s unclear what leads to a person’s sexual orientation – likely a combination of genetic, hormonal and environmental factors—there is no question that sexual orientation is not a “choice,” Dr Finger said. Research has also clarified that one’s sexual orientation does not result from parenting behaviors or a history of sexual abuse.
“But I would urge all of you, instead of focusing on why someone is LGBTQ, to focus on what that means for them in their life,” Dr Finger said. “How is this bearing out in terms of their relationships and their behaviors, and how do they feel about it? How are they being supported by their family or their community, and how is it impacting their lives?”
She cited findings from a Human Rights Campaign survey in 2012 of 10,000 youth aged 13-17, which found that most LGBTQ respondents became aware of their same-sex attraction at 9 years of age, though the average age of disclosures is 16, an improvement from age 21 in the 1980s.
How and what to ask
Although children start becoming conscious of gender at ages 1-2, their sense of gender usually stabilizes by age 4.
“Who should we be screening for gender nonconformity? Quite frankly, all children, because all of them have some gender identity, so we should be asking them about that,” Dr Finger said.
When children are younger, doctors can ask parents about their child’s social interactions, forms of play, dress preferences, and mood. Questions for patients themselves, adapted for their age, might include, “Do you feel more like a girl, boy, neither or both?”, “How would you like to play, cut your hair and dress?” And “What name or pronoun (he or she) fits you?”
While such conversations do not necessarily need to happen annually, doctors should especially ask youth who dress or behave in non–gender-conforming ways or who appear to have mood, behavior or social difficulties.
To understand a patient’s sexuality, ask whether they are attracted to people of their own gender or sex, a different gender or sex, both or all genders or no one, or if they’re not sure yet. Doctors can then ask how comfortable they are with their attraction and whether they have told family members or friends about them.
Sexual behavior questions should be developmentally appropriate and lead to counsel but not judgment, Dr Finger said. Her method, with adjustments for age and development, starts, “There are many way of being sexual or intimate with someone: kissing, hugging and touching, and oral sex, anal sex and vaginal sex. Have you ever had any of these experiences? Which ones? With males or females or both, or other genders?”
Then she gets more specific while remaining sensitive. Doctors can ask younger children if they have held hands or cuddled with someone, if they have kissed someone, or if they have touched another person’s private parts. They can ask teens about oral sex, vaginal sex and anal sex and then gather more details about what parts went where, which helps determine what screenings or treatment options a patient may need or desire.
Doctors can use their judgment about whether to ask questions with parents in the room or not, but as kids grow older, it’s good practice to speak to patients without their caregivers present. Doctors should also explain the rules of confidentiality to their patients and be aware of the risks of “coming out,” including family discord or rejection, problems at school or work, social stigma, bullying and harassment, physical violence and risk-taking behaviors, such as substance use, self-injury and risky sexual behaviors. A HEADSSS screen can help doctors learn if any of these are present.
Making your practice inclusive and welcoming
Fewer than one in five teens who are “out” as LGBTQ have come out to their doctor, Dr Finger cited. Most are out to their friends and classmates, and more than half are out to their family, but teens are less likely to tell their doctors.
Research suggests one reason for this is the fact that pediatricians often don’t ask. One study found that only 20% of pediatricians discussed sexual orientation with their patients (Pediatrics 2010 Apr;125:e741-7). Similarly, only 30% of family physicians brought up sexual orientation, found another study (Fam. Med. 2001 May;33[5]:376-81). The studies found physicians more often discussed condoms, HIV, sexually transmitted infections, abstinence, violence, contraception or, in the case of family physicians, sexual behaviors, and relationships.
But another reason for not being out to doctors is a history of poor experiences. A Lambda Legal Survey in 2009 of 4,916 LGBT respondents found that 8% of LGB and 27% of transgender and gender nonconforming patients had been denied care because of their identity of orientation. Eleven percent said “providers refused to touch them or used excessive precautions,” Dr Finger reported. LGBTQ patients may fear the doctor’s reaction or not keeping their identity confidential. Patients may also have internalized shame or guilt due to societal norms or homophobia, and all these barriers can reduce LGBTQ people’s willingness to seek and access to competent care.
The first step to making LGBTQ patients comfortable in your practice is to confront your own personal biases, Dr Finger said. Understand what they are and that a provider’s discomfort, even unconscious, can be damaging to the patient-provider relationship.
“If you find that this is just not something that you’re going to be comfortable doing, at the very least, I would suggest that you find providers in your area who are comfortable working with this patient population and you refer your patients to them so that they can have a good, trusting patient-provider relationship with somebody who can provide the care that they need,” Dr Finger said.
The next step is creating a safe place with zero tolerance for insensitivity by training staff to be welcoming and inclusive, assuring patients confidentiality, providing support and resources and displaying LGBTQ-affirming materials. These youth need active, visible evidence that the office will be a safe place for them.
Ways pediatricians can communicate an inclusive environment include having gender-neutral restrooms, using “parent” instead of “mother/father” and using forms and EMR prompts with gender-neutral language or multiple options for gender selection.
Screening and LGBTQ patients’ health needs
LGB youth and those who aren’t sure of their sexual orientation tend to have higher rates of substance use, including tobacco, alcohol and illicit drugs, and are more often victims of rape and other sexual violence. Their rates of depressive symptoms, bullying victimization, and suicidality are also significantly higher than in their heterosexual cisgender peers. Homelessness rates are also considerably higher in LGBTQ youth than in heterosexual cisgender youth.
One thing pediatricians can do is work with parents to ensure a patient’s school is meeting their needs. The greater risks LGBTQ youth typically face are mediated by social support, resiliency, supportive friends and family and a supportive school environment, including inclusive curricula and supportive staff.
Lesbian and bisexual women are considerably more at risk for poor sexual or reproductive outcomes, Dr Finger said. Their rates of unplanned pregnancy are double that of straight women, contributing to their higher rates of emergency contraception and abortion. They are also more likely to have more partners (male and females), to have a younger sexual debut and to be forced into sex by a male partner—yet they are far less likely to perceive themselves as at risk for a sexually transmitted infection than their peers.
This patient population therefore may need contraception counseling, including discussing their current methods and reviewing their options, including emergency contraception and possibly an advance prescription. Dr Finger also suggests having male and female condoms available in the office.
Doctors should screen all their female patients, regardless of sexuality, for chlamydia and gonorrhea, and offer routine cervical cancer screening and the HPV vaccine, as recommended by the CDC. They might consider screening for trichomoniasis, bacterial vaginosis, herpes simplex, human papillomavirus and HIV.
For men who have sex with men, the CDC recommends HIV and syphilis serology, urine/pharyngeal/rectal gonorrhea nucleic acid amplification test (NAAT), urine/rectal chlamydia NAAT, and hepatitis C screening for those who are HIV-positive—all at least once a year.
For transgender patients, doctors need to assess their STI- and HIV-related risks based on their current anatomy and sexual behaviors.
Doctors should also consider discussing pre-exposure prophylaxis (PrEP) for any youth at high risk for HIV infection if they are at least 77 pounds (35 kg). Emtricitabine/tenofovir (Truvada, Descovy) reduces the chance of sexually acquired infection by 99%, and infection acquired via drug injection by 74% when taken as prescribed.
Resources
Dr Finger noted a range of resources for LGBTQ youth and their families and providers, including the Family Acceptance Project, Gay and Lesbian Medical Association, Gay, Lesbian and Straight Education Network, GLBTQ Legal Advocates and Defenders (GLAD), Human Rights Campaign, It Gets Better Project, LGBTQ Student Resources and Support, National Center for Lesbian Rights, Parents and Friends of Lesbians and Gays (PFLAG), Safe Schools Coalition and The Trevor Project (concerning suicide risk).
NEW ORLEANS – One of the most important things pediatricians can do to support their lesbian, gay, bisexual, transgender (LGBT) and other gender-nonconforming patients is to ask all their patients about their feelings, preferences and experiences when it comes to gender and sexuality, according to Julie Finger, MD, MPH.
It’s equally important not to make assumptions, she told attendees at the annual meeting of the American Academy of Pediatrics. Biology and sexual and gender identity and expression can be very diverse, she said. Specifically, doctors should not assume patients are heterosexual, that bisexuality is a phase, that orientation or attraction translates directly to behavior or vice versa, or that LGBTQ patients have unsupportive families or are engaging in risky behavior. Research suggests LGB youth have slightly higher rates of early sexual debut, sexual activity or multiple partners than straight or uncertain youth, but only marginally so.
Pediatricians also cannot assume a patient’s sexual orientation based on their partner’s gender or determine a patient’s sexual orientation or gender identity based on appearance – or even that either is the same as it was on the previous visit.
What doctors can be sure of is that they do have LGBTQ patients, said Dr. Finger, and assistant professor of clinical pediatrics at Tulane University in New Orleans. According to a 2016 Morbidity and Mortality Weekly Report (2016 Aug 12; 65[9]), about 1 in 10 students in grades 9-12 are a sexual minority. About 2% of respondents identify as gay or lesbian, 6% identify as bisexual and 3% say they aren’t sure.
Knowing the terminology
Dr. Finger defined key terminology regarding gender and sexuality. She first clarified that LGBT is not the full spectrum for sexual orientation. Pansexual (fluid attraction to any sex or gender) and asexual (lack of feeling sexual attraction) can also describe sexuality, and the Q on the end of LGBTQ is often an umbrella term for “queer” or “questioning” that encompasses anyone who fits outside conventional social norms of sexual identity and gender expression.
Sexual behaviors – which include “young men who have sex with men” and “young women who have sex with women” – do not necessarily correspond as one might expect with sexual orientation or identity, which is one’s concept of their romantic or sexual feelings, attractions and desires, again reinforcing the importance of asking patients their identity and preferences.
In terms of gender, a person’s natal or biologic gender is the one assigned people at birth based on their body parts and hormones. Gender identity is a person’s understanding of their own gender, and gender expression refers to how someone acts or presents themselves and communicates their gender within their culture.
Those who identify as “gender nonconforming, genderqueer, gender fluid, or nonbinary” see their gender on a spectrum, not within the binary “male” or “female.” A cisgender person’s gender identity matches both their biological sex assigned at birth and conventional cultural norms, while a transgender person’s gender differs from the sex they were assigned at birth. Transgender women (male to female, MTF) and men (female to men, FTM) go through the process of transition, a time that can occur in weeks or years when they shift from living as one gender to another.
While it’s unclear what leads to a person’s sexual orientation – likely a combination of genetic, hormonal and environmental factors—there is no question that sexual orientation is not a “choice,” Dr Finger said. Research has also clarified that one’s sexual orientation does not result from parenting behaviors or a history of sexual abuse.
“But I would urge all of you, instead of focusing on why someone is LGBTQ, to focus on what that means for them in their life,” Dr Finger said. “How is this bearing out in terms of their relationships and their behaviors, and how do they feel about it? How are they being supported by their family or their community, and how is it impacting their lives?”
She cited findings from a Human Rights Campaign survey in 2012 of 10,000 youth aged 13-17, which found that most LGBTQ respondents became aware of their same-sex attraction at 9 years of age, though the average age of disclosures is 16, an improvement from age 21 in the 1980s.
How and what to ask
Although children start becoming conscious of gender at ages 1-2, their sense of gender usually stabilizes by age 4.
“Who should we be screening for gender nonconformity? Quite frankly, all children, because all of them have some gender identity, so we should be asking them about that,” Dr Finger said.
When children are younger, doctors can ask parents about their child’s social interactions, forms of play, dress preferences, and mood. Questions for patients themselves, adapted for their age, might include, “Do you feel more like a girl, boy, neither or both?”, “How would you like to play, cut your hair and dress?” And “What name or pronoun (he or she) fits you?”
While such conversations do not necessarily need to happen annually, doctors should especially ask youth who dress or behave in non–gender-conforming ways or who appear to have mood, behavior or social difficulties.
To understand a patient’s sexuality, ask whether they are attracted to people of their own gender or sex, a different gender or sex, both or all genders or no one, or if they’re not sure yet. Doctors can then ask how comfortable they are with their attraction and whether they have told family members or friends about them.
Sexual behavior questions should be developmentally appropriate and lead to counsel but not judgment, Dr Finger said. Her method, with adjustments for age and development, starts, “There are many way of being sexual or intimate with someone: kissing, hugging and touching, and oral sex, anal sex and vaginal sex. Have you ever had any of these experiences? Which ones? With males or females or both, or other genders?”
Then she gets more specific while remaining sensitive. Doctors can ask younger children if they have held hands or cuddled with someone, if they have kissed someone, or if they have touched another person’s private parts. They can ask teens about oral sex, vaginal sex and anal sex and then gather more details about what parts went where, which helps determine what screenings or treatment options a patient may need or desire.
Doctors can use their judgment about whether to ask questions with parents in the room or not, but as kids grow older, it’s good practice to speak to patients without their caregivers present. Doctors should also explain the rules of confidentiality to their patients and be aware of the risks of “coming out,” including family discord or rejection, problems at school or work, social stigma, bullying and harassment, physical violence and risk-taking behaviors, such as substance use, self-injury and risky sexual behaviors. A HEADSSS screen can help doctors learn if any of these are present.
Making your practice inclusive and welcoming
Fewer than one in five teens who are “out” as LGBTQ have come out to their doctor, Dr Finger cited. Most are out to their friends and classmates, and more than half are out to their family, but teens are less likely to tell their doctors.
Research suggests one reason for this is the fact that pediatricians often don’t ask. One study found that only 20% of pediatricians discussed sexual orientation with their patients (Pediatrics 2010 Apr;125:e741-7). Similarly, only 30% of family physicians brought up sexual orientation, found another study (Fam. Med. 2001 May;33[5]:376-81). The studies found physicians more often discussed condoms, HIV, sexually transmitted infections, abstinence, violence, contraception or, in the case of family physicians, sexual behaviors, and relationships.
But another reason for not being out to doctors is a history of poor experiences. A Lambda Legal Survey in 2009 of 4,916 LGBT respondents found that 8% of LGB and 27% of transgender and gender nonconforming patients had been denied care because of their identity of orientation. Eleven percent said “providers refused to touch them or used excessive precautions,” Dr Finger reported. LGBTQ patients may fear the doctor’s reaction or not keeping their identity confidential. Patients may also have internalized shame or guilt due to societal norms or homophobia, and all these barriers can reduce LGBTQ people’s willingness to seek and access to competent care.
The first step to making LGBTQ patients comfortable in your practice is to confront your own personal biases, Dr Finger said. Understand what they are and that a provider’s discomfort, even unconscious, can be damaging to the patient-provider relationship.
“If you find that this is just not something that you’re going to be comfortable doing, at the very least, I would suggest that you find providers in your area who are comfortable working with this patient population and you refer your patients to them so that they can have a good, trusting patient-provider relationship with somebody who can provide the care that they need,” Dr Finger said.
The next step is creating a safe place with zero tolerance for insensitivity by training staff to be welcoming and inclusive, assuring patients confidentiality, providing support and resources and displaying LGBTQ-affirming materials. These youth need active, visible evidence that the office will be a safe place for them.
Ways pediatricians can communicate an inclusive environment include having gender-neutral restrooms, using “parent” instead of “mother/father” and using forms and EMR prompts with gender-neutral language or multiple options for gender selection.
Screening and LGBTQ patients’ health needs
LGB youth and those who aren’t sure of their sexual orientation tend to have higher rates of substance use, including tobacco, alcohol and illicit drugs, and are more often victims of rape and other sexual violence. Their rates of depressive symptoms, bullying victimization, and suicidality are also significantly higher than in their heterosexual cisgender peers. Homelessness rates are also considerably higher in LGBTQ youth than in heterosexual cisgender youth.
One thing pediatricians can do is work with parents to ensure a patient’s school is meeting their needs. The greater risks LGBTQ youth typically face are mediated by social support, resiliency, supportive friends and family and a supportive school environment, including inclusive curricula and supportive staff.
Lesbian and bisexual women are considerably more at risk for poor sexual or reproductive outcomes, Dr Finger said. Their rates of unplanned pregnancy are double that of straight women, contributing to their higher rates of emergency contraception and abortion. They are also more likely to have more partners (male and females), to have a younger sexual debut and to be forced into sex by a male partner—yet they are far less likely to perceive themselves as at risk for a sexually transmitted infection than their peers.
This patient population therefore may need contraception counseling, including discussing their current methods and reviewing their options, including emergency contraception and possibly an advance prescription. Dr Finger also suggests having male and female condoms available in the office.
Doctors should screen all their female patients, regardless of sexuality, for chlamydia and gonorrhea, and offer routine cervical cancer screening and the HPV vaccine, as recommended by the CDC. They might consider screening for trichomoniasis, bacterial vaginosis, herpes simplex, human papillomavirus and HIV.
For men who have sex with men, the CDC recommends HIV and syphilis serology, urine/pharyngeal/rectal gonorrhea nucleic acid amplification test (NAAT), urine/rectal chlamydia NAAT, and hepatitis C screening for those who are HIV-positive—all at least once a year.
For transgender patients, doctors need to assess their STI- and HIV-related risks based on their current anatomy and sexual behaviors.
Doctors should also consider discussing pre-exposure prophylaxis (PrEP) for any youth at high risk for HIV infection if they are at least 77 pounds (35 kg). Emtricitabine/tenofovir (Truvada, Descovy) reduces the chance of sexually acquired infection by 99%, and infection acquired via drug injection by 74% when taken as prescribed.
Resources
Dr Finger noted a range of resources for LGBTQ youth and their families and providers, including the Family Acceptance Project, Gay and Lesbian Medical Association, Gay, Lesbian and Straight Education Network, GLBTQ Legal Advocates and Defenders (GLAD), Human Rights Campaign, It Gets Better Project, LGBTQ Student Resources and Support, National Center for Lesbian Rights, Parents and Friends of Lesbians and Gays (PFLAG), Safe Schools Coalition and The Trevor Project (concerning suicide risk).
EXPERT ANALYSIS FROM AAP 2019
Recurrent intussusception rare in young children
NEW ORLEANS – Recurrent intussusception after discharge may be far less common in young children than previously reported, and significant morbidity associated with the condition is rare, results from an analysis of national data show.
“Recurrent intussusception following successful nonoperative reduction has previously been reported with a frequency of 8-12% based on data from individual institutions,” researchers led by Anthony R. Ferrantella, MD, wrote in an abstract presented at the annual meeting of the American Academy of Pediatrics. “Timing of discharge following successful non-operative reduction continues to be debated, but recent studies suggest it is safe to discharge home from the emergency department. However, the practice of hospital admission for an observation period of 24-48 hours following successful nonoperative reduction persists today among many pediatric surgeons.”
In an effort to evaluate readmissions for recurrent intussusception in young children on a large scale, Dr. Ferrantella, a surgery resident at the University of Miami, and his colleagues queried the Nationwide Readmissions Database during 2010-2014 to identify children younger than 5 years of age diagnosed with ileocolic intussusception. They compared the management during index admission and frequency of readmissions for recurrent intussusception up to one year after discharge. They excluded patients lacking procedure data, weighted the results for national estimates, and used chi-square analysis to compare cohorts.
The search yielded 8,289 young children who were diagnosed with ileocolic intussusception during an index admission. Of these, 43% received definitive treatment with nonoperative reduction alone, 42% underwent surgical reduction without bowel resection, and 15% underwent surgery with bowel resection. Among the hospitals where patients were treated, 75% were large, 80% were not-for-profit, and 94% were metropolitan teaching hospitals.
The researchers found that readmission for recurrent intussusception was required for only 4% of patients managed with nonoperative reduction alone, 2% of patients who underwent surgical reduction, and 0% of those who underwent bowel resection. The median time to readmission was 4 days for those managed with nonoperative reduction only and 64 days for those managed with surgery.
Among patients managed with nonoperative reduction alone during index admission, 71% were again managed successfully with nonoperative reduction alone, 24 underwent surgical reduction, and only 5% required bowel resection. No deaths occurred during any readmissions.
The findings “suggest and support the idea that if you can successfully perform a nonoperative reduction on a child that comes in with an intussusception, you can safely discharge them,” Dr. Ferrantella said in an interview. “If you were to keep them in the hospital, the [rate] of recurrences are very low. Even when they do recur, only 30%-40% will happen within the first 24-48 hours, so the majority will not benefit from a hospital admission.”
He acknowledged certain limitations of the analysis, including that the data came from a retrospectively collected database and that he and his colleagues were unable to track readmissions across state lines.
Dr. Ferrantella reported having no financial disclosures.
SOURCE: Ferrantella A. AAP 2019, Section on Surgery session.
NEW ORLEANS – Recurrent intussusception after discharge may be far less common in young children than previously reported, and significant morbidity associated with the condition is rare, results from an analysis of national data show.
“Recurrent intussusception following successful nonoperative reduction has previously been reported with a frequency of 8-12% based on data from individual institutions,” researchers led by Anthony R. Ferrantella, MD, wrote in an abstract presented at the annual meeting of the American Academy of Pediatrics. “Timing of discharge following successful non-operative reduction continues to be debated, but recent studies suggest it is safe to discharge home from the emergency department. However, the practice of hospital admission for an observation period of 24-48 hours following successful nonoperative reduction persists today among many pediatric surgeons.”
In an effort to evaluate readmissions for recurrent intussusception in young children on a large scale, Dr. Ferrantella, a surgery resident at the University of Miami, and his colleagues queried the Nationwide Readmissions Database during 2010-2014 to identify children younger than 5 years of age diagnosed with ileocolic intussusception. They compared the management during index admission and frequency of readmissions for recurrent intussusception up to one year after discharge. They excluded patients lacking procedure data, weighted the results for national estimates, and used chi-square analysis to compare cohorts.
The search yielded 8,289 young children who were diagnosed with ileocolic intussusception during an index admission. Of these, 43% received definitive treatment with nonoperative reduction alone, 42% underwent surgical reduction without bowel resection, and 15% underwent surgery with bowel resection. Among the hospitals where patients were treated, 75% were large, 80% were not-for-profit, and 94% were metropolitan teaching hospitals.
The researchers found that readmission for recurrent intussusception was required for only 4% of patients managed with nonoperative reduction alone, 2% of patients who underwent surgical reduction, and 0% of those who underwent bowel resection. The median time to readmission was 4 days for those managed with nonoperative reduction only and 64 days for those managed with surgery.
Among patients managed with nonoperative reduction alone during index admission, 71% were again managed successfully with nonoperative reduction alone, 24 underwent surgical reduction, and only 5% required bowel resection. No deaths occurred during any readmissions.
The findings “suggest and support the idea that if you can successfully perform a nonoperative reduction on a child that comes in with an intussusception, you can safely discharge them,” Dr. Ferrantella said in an interview. “If you were to keep them in the hospital, the [rate] of recurrences are very low. Even when they do recur, only 30%-40% will happen within the first 24-48 hours, so the majority will not benefit from a hospital admission.”
He acknowledged certain limitations of the analysis, including that the data came from a retrospectively collected database and that he and his colleagues were unable to track readmissions across state lines.
Dr. Ferrantella reported having no financial disclosures.
SOURCE: Ferrantella A. AAP 2019, Section on Surgery session.
NEW ORLEANS – Recurrent intussusception after discharge may be far less common in young children than previously reported, and significant morbidity associated with the condition is rare, results from an analysis of national data show.
“Recurrent intussusception following successful nonoperative reduction has previously been reported with a frequency of 8-12% based on data from individual institutions,” researchers led by Anthony R. Ferrantella, MD, wrote in an abstract presented at the annual meeting of the American Academy of Pediatrics. “Timing of discharge following successful non-operative reduction continues to be debated, but recent studies suggest it is safe to discharge home from the emergency department. However, the practice of hospital admission for an observation period of 24-48 hours following successful nonoperative reduction persists today among many pediatric surgeons.”
In an effort to evaluate readmissions for recurrent intussusception in young children on a large scale, Dr. Ferrantella, a surgery resident at the University of Miami, and his colleagues queried the Nationwide Readmissions Database during 2010-2014 to identify children younger than 5 years of age diagnosed with ileocolic intussusception. They compared the management during index admission and frequency of readmissions for recurrent intussusception up to one year after discharge. They excluded patients lacking procedure data, weighted the results for national estimates, and used chi-square analysis to compare cohorts.
The search yielded 8,289 young children who were diagnosed with ileocolic intussusception during an index admission. Of these, 43% received definitive treatment with nonoperative reduction alone, 42% underwent surgical reduction without bowel resection, and 15% underwent surgery with bowel resection. Among the hospitals where patients were treated, 75% were large, 80% were not-for-profit, and 94% were metropolitan teaching hospitals.
The researchers found that readmission for recurrent intussusception was required for only 4% of patients managed with nonoperative reduction alone, 2% of patients who underwent surgical reduction, and 0% of those who underwent bowel resection. The median time to readmission was 4 days for those managed with nonoperative reduction only and 64 days for those managed with surgery.
Among patients managed with nonoperative reduction alone during index admission, 71% were again managed successfully with nonoperative reduction alone, 24 underwent surgical reduction, and only 5% required bowel resection. No deaths occurred during any readmissions.
The findings “suggest and support the idea that if you can successfully perform a nonoperative reduction on a child that comes in with an intussusception, you can safely discharge them,” Dr. Ferrantella said in an interview. “If you were to keep them in the hospital, the [rate] of recurrences are very low. Even when they do recur, only 30%-40% will happen within the first 24-48 hours, so the majority will not benefit from a hospital admission.”
He acknowledged certain limitations of the analysis, including that the data came from a retrospectively collected database and that he and his colleagues were unable to track readmissions across state lines.
Dr. Ferrantella reported having no financial disclosures.
SOURCE: Ferrantella A. AAP 2019, Section on Surgery session.
AT AAP 2016
Wandering is underrecognized, serious problem for autistic children
NEW ORLEANS – Nearly half of all children with autism spectrum disorder wander off from safe supervision at some point in their childhood or adolescence, reported Paul Lipkin, MD, at the annual meeting of the American Academy of Pediatrics.
Though such behavior is developmentally normal in toddlers, it’s rarer for older children to leave a supervised, safe space for a longer period than just running away for a bit, he said.
Far more than an inconvenience, wandering, also called elopement, puts these children at high risk for injury or victimization. In fact, statistics from a survey by the National Autism Foundation suggest that nearly a third of autism-related wandering cases resulted in death or serious enough injury to require medical attention, said Dr. Lipkin, an associate professor of pediatrics at the Kennedy Krieger Institute and Johns Hopkins Medicine in Baltimore.
“Drowning is overwhelmingly the main cause of death in children with autism,” he said, sharing the data from National Autism Association, which relied on parent report and media reports. In that data, 71% of deaths from autistic children who wandered from 2011-2016 were drowning, and of those deaths, 76% of the drownings occurred in a natural body of water or drainage water. At a distant second, 18% of deaths were traffic accidents. The remaining causes were being hit by a train (4%), hypothermia or hyperthermia (3%), falling (1%) or other trauma (3%) (J Autism Dev Disord. 2019 Mar 5. doi: 10.1007/s10803-019-03961-x).
Academic research has found similar statistics to those from the National Autism Association. In one study, 53% of autistic youth who attempted to run off succeeded and were missing long enough to cause safety concerns (Pediatrics. 2012 Nov;130[5]:870-7). Among these youth – representing about a quarter of all families surveyed in the study – the police were called in 31% of cases. In addition, 65% had a “close call” with a traffic injury and 24% had a close call with drowning.
The children wandered off in various settings, including home; another’s home; a store or other public place; or school, daycare or camp. A 2019 study found that 70% of parents reported their children wandering off from home at least once in the past 2 years (J Autism Dev Disorders. 2019 Mar 5; doi: 10.1107/s10803-019-03961-x).
Although most cases occur in children and teens, with the highest rate of death among children aged 5-9, the National Autism Association has received reports of wandering occur throughout autistic people’s lifetime.
Yet this issue doesn’t appear to be on the radar of many pediatricians, and those who are aware of it may not know the best strategies to share with parents to prevent wandering and subsequent injury, Dr Lipkin explained. In one study, only one-third of parents reported receiving guidance from a health provider related to wandering (J Dev Behav Pediatr. 2018 Sep;39[7]:538-46).
That research found that only 10% received advice from a pediatrician or other primary care provider, 12% received advice from a developmental pediatrician or neurologist and 10% received advance from a psychologist or psychiatrist. The largest source of guidance in that study was autism advocacy organizations, whom 22% of parents cited. Others included a teacher or other school staff member (15%), a personal contact (13%), law enforcement (8%) or another source (1%).
Role of the pediatrician
Pediatricians have an important role to play in prevention of elopement, Dr Lipkin said. They can screen autistic patients for wandering and elopement during visits, work with community stakeholders such as schools and law enforcement, advocate for awareness, and provider education and resources for families.
Perhaps the most valuable resource, he said, is the Big Red Safety Box, available from the National Autism Association. This resource, sponsored by more than a half dozen autism advocacy organizations, includes three digital safety toolkits: one for caregivers, one for first responders, and one for teachers. Parents can therefore share the toolkits for first responders and teachers with those respective community members.
Pediatricians can also help families develop a Family Wandering Emergency Plan (FWEP), a template for which is in the Big Red Safety Box. Parents and community members should know the steps to take if someone wanders: Stay calm, call 911, search nearby water first and then implement the FWEP.
It’s first helpful to understand why these youth wander off. In the National Autism Association survey, the most common reasons were to escape an anxious situation, particularly for those with Asperger’s, or simply to run, explore, or go to a favorite place, particularly among those with autism or pervasive developmental disorder-not otherwise specified (PDD-NOS).
Researchers have found similar reasons: 43% of elopement situations occurred when children were trying to escape an anxious situation, 39% left while in a stressful environment, and 24% were in an environment with conflict, found one study (J Autism Dev Disord. 2019 Mar 5. doi: 10.1007/s10803-019-03961-x).
Sensory overload was also a trigger, with 38% of elopements occurring when it was too noisy, and 34% when it was a generally uncomfortable sensory experience. Just over a quarter (27%) of children left when they were understimulated or in a “boring” environment, Dr Lipkin reported. The remaining reason was goal-directed: 27% left to pursue a special interest, 18% sought a place where they enjoyed playing, and 11% were after their favorite food.
Prevention Strategies
Most data about effective strategies to prevent wandering comes from research that relies on parents, Dr Lipkin said. In general, environmental interventions tend to be the most effective, and medication tends to be the least effective.
One study on elopement prevention found that 96% of caregivers use at least some type of intervention, and the vast majority (83%) were using environmental interventions such as dead bolts (51%), latches (49%) and gates (36%). An equal proportion used behavioral services (83%), such as a behavioral psychologist (41%), social stories (40%) or an aide (39%). Just under a third used an ID bracelet or shoe tag (31%), and 19% used GPS trackers, according to Dr. Lipkin.
Although parents reported environmental interventions to be very effective, 68% said they were highly burdensome, though the median cost over 2 years was less than $1,000. The least expensive intervention was home behavioral specialists (when covered by insurance) and school aides, and the most expensive and burdensome – albeit highly effective – was a service animal.
Interventions with the least cost effectiveness included security cameras and GPS trackers, which only 15% of parents reported as being effective.
Although nearly half of parents reported their child had taken any psychiatric medication (48%), only 16% had taken medication explicitly to prevent wandering. Few reported the medication was very effective, however. Among the small number who did (less than 10), lorazepam, diazepam and atomoxetine appeared best.
Teaching children survival skills, as developmentally appropriate and possible, can also help. These include swimming lessons as well as learning how to interact in traffic, knowing their home address, and learning how to navigate around their neighborhood.
Dr. Lipkin no disclosures and used no external funding for this presentation.
NEW ORLEANS – Nearly half of all children with autism spectrum disorder wander off from safe supervision at some point in their childhood or adolescence, reported Paul Lipkin, MD, at the annual meeting of the American Academy of Pediatrics.
Though such behavior is developmentally normal in toddlers, it’s rarer for older children to leave a supervised, safe space for a longer period than just running away for a bit, he said.
Far more than an inconvenience, wandering, also called elopement, puts these children at high risk for injury or victimization. In fact, statistics from a survey by the National Autism Foundation suggest that nearly a third of autism-related wandering cases resulted in death or serious enough injury to require medical attention, said Dr. Lipkin, an associate professor of pediatrics at the Kennedy Krieger Institute and Johns Hopkins Medicine in Baltimore.
“Drowning is overwhelmingly the main cause of death in children with autism,” he said, sharing the data from National Autism Association, which relied on parent report and media reports. In that data, 71% of deaths from autistic children who wandered from 2011-2016 were drowning, and of those deaths, 76% of the drownings occurred in a natural body of water or drainage water. At a distant second, 18% of deaths were traffic accidents. The remaining causes were being hit by a train (4%), hypothermia or hyperthermia (3%), falling (1%) or other trauma (3%) (J Autism Dev Disord. 2019 Mar 5. doi: 10.1007/s10803-019-03961-x).
Academic research has found similar statistics to those from the National Autism Association. In one study, 53% of autistic youth who attempted to run off succeeded and were missing long enough to cause safety concerns (Pediatrics. 2012 Nov;130[5]:870-7). Among these youth – representing about a quarter of all families surveyed in the study – the police were called in 31% of cases. In addition, 65% had a “close call” with a traffic injury and 24% had a close call with drowning.
The children wandered off in various settings, including home; another’s home; a store or other public place; or school, daycare or camp. A 2019 study found that 70% of parents reported their children wandering off from home at least once in the past 2 years (J Autism Dev Disorders. 2019 Mar 5; doi: 10.1107/s10803-019-03961-x).
Although most cases occur in children and teens, with the highest rate of death among children aged 5-9, the National Autism Association has received reports of wandering occur throughout autistic people’s lifetime.
Yet this issue doesn’t appear to be on the radar of many pediatricians, and those who are aware of it may not know the best strategies to share with parents to prevent wandering and subsequent injury, Dr Lipkin explained. In one study, only one-third of parents reported receiving guidance from a health provider related to wandering (J Dev Behav Pediatr. 2018 Sep;39[7]:538-46).
That research found that only 10% received advice from a pediatrician or other primary care provider, 12% received advice from a developmental pediatrician or neurologist and 10% received advance from a psychologist or psychiatrist. The largest source of guidance in that study was autism advocacy organizations, whom 22% of parents cited. Others included a teacher or other school staff member (15%), a personal contact (13%), law enforcement (8%) or another source (1%).
Role of the pediatrician
Pediatricians have an important role to play in prevention of elopement, Dr Lipkin said. They can screen autistic patients for wandering and elopement during visits, work with community stakeholders such as schools and law enforcement, advocate for awareness, and provider education and resources for families.
Perhaps the most valuable resource, he said, is the Big Red Safety Box, available from the National Autism Association. This resource, sponsored by more than a half dozen autism advocacy organizations, includes three digital safety toolkits: one for caregivers, one for first responders, and one for teachers. Parents can therefore share the toolkits for first responders and teachers with those respective community members.
Pediatricians can also help families develop a Family Wandering Emergency Plan (FWEP), a template for which is in the Big Red Safety Box. Parents and community members should know the steps to take if someone wanders: Stay calm, call 911, search nearby water first and then implement the FWEP.
It’s first helpful to understand why these youth wander off. In the National Autism Association survey, the most common reasons were to escape an anxious situation, particularly for those with Asperger’s, or simply to run, explore, or go to a favorite place, particularly among those with autism or pervasive developmental disorder-not otherwise specified (PDD-NOS).
Researchers have found similar reasons: 43% of elopement situations occurred when children were trying to escape an anxious situation, 39% left while in a stressful environment, and 24% were in an environment with conflict, found one study (J Autism Dev Disord. 2019 Mar 5. doi: 10.1007/s10803-019-03961-x).
Sensory overload was also a trigger, with 38% of elopements occurring when it was too noisy, and 34% when it was a generally uncomfortable sensory experience. Just over a quarter (27%) of children left when they were understimulated or in a “boring” environment, Dr Lipkin reported. The remaining reason was goal-directed: 27% left to pursue a special interest, 18% sought a place where they enjoyed playing, and 11% were after their favorite food.
Prevention Strategies
Most data about effective strategies to prevent wandering comes from research that relies on parents, Dr Lipkin said. In general, environmental interventions tend to be the most effective, and medication tends to be the least effective.
One study on elopement prevention found that 96% of caregivers use at least some type of intervention, and the vast majority (83%) were using environmental interventions such as dead bolts (51%), latches (49%) and gates (36%). An equal proportion used behavioral services (83%), such as a behavioral psychologist (41%), social stories (40%) or an aide (39%). Just under a third used an ID bracelet or shoe tag (31%), and 19% used GPS trackers, according to Dr. Lipkin.
Although parents reported environmental interventions to be very effective, 68% said they were highly burdensome, though the median cost over 2 years was less than $1,000. The least expensive intervention was home behavioral specialists (when covered by insurance) and school aides, and the most expensive and burdensome – albeit highly effective – was a service animal.
Interventions with the least cost effectiveness included security cameras and GPS trackers, which only 15% of parents reported as being effective.
Although nearly half of parents reported their child had taken any psychiatric medication (48%), only 16% had taken medication explicitly to prevent wandering. Few reported the medication was very effective, however. Among the small number who did (less than 10), lorazepam, diazepam and atomoxetine appeared best.
Teaching children survival skills, as developmentally appropriate and possible, can also help. These include swimming lessons as well as learning how to interact in traffic, knowing their home address, and learning how to navigate around their neighborhood.
Dr. Lipkin no disclosures and used no external funding for this presentation.
NEW ORLEANS – Nearly half of all children with autism spectrum disorder wander off from safe supervision at some point in their childhood or adolescence, reported Paul Lipkin, MD, at the annual meeting of the American Academy of Pediatrics.
Though such behavior is developmentally normal in toddlers, it’s rarer for older children to leave a supervised, safe space for a longer period than just running away for a bit, he said.
Far more than an inconvenience, wandering, also called elopement, puts these children at high risk for injury or victimization. In fact, statistics from a survey by the National Autism Foundation suggest that nearly a third of autism-related wandering cases resulted in death or serious enough injury to require medical attention, said Dr. Lipkin, an associate professor of pediatrics at the Kennedy Krieger Institute and Johns Hopkins Medicine in Baltimore.
“Drowning is overwhelmingly the main cause of death in children with autism,” he said, sharing the data from National Autism Association, which relied on parent report and media reports. In that data, 71% of deaths from autistic children who wandered from 2011-2016 were drowning, and of those deaths, 76% of the drownings occurred in a natural body of water or drainage water. At a distant second, 18% of deaths were traffic accidents. The remaining causes were being hit by a train (4%), hypothermia or hyperthermia (3%), falling (1%) or other trauma (3%) (J Autism Dev Disord. 2019 Mar 5. doi: 10.1007/s10803-019-03961-x).
Academic research has found similar statistics to those from the National Autism Association. In one study, 53% of autistic youth who attempted to run off succeeded and were missing long enough to cause safety concerns (Pediatrics. 2012 Nov;130[5]:870-7). Among these youth – representing about a quarter of all families surveyed in the study – the police were called in 31% of cases. In addition, 65% had a “close call” with a traffic injury and 24% had a close call with drowning.
The children wandered off in various settings, including home; another’s home; a store or other public place; or school, daycare or camp. A 2019 study found that 70% of parents reported their children wandering off from home at least once in the past 2 years (J Autism Dev Disorders. 2019 Mar 5; doi: 10.1107/s10803-019-03961-x).
Although most cases occur in children and teens, with the highest rate of death among children aged 5-9, the National Autism Association has received reports of wandering occur throughout autistic people’s lifetime.
Yet this issue doesn’t appear to be on the radar of many pediatricians, and those who are aware of it may not know the best strategies to share with parents to prevent wandering and subsequent injury, Dr Lipkin explained. In one study, only one-third of parents reported receiving guidance from a health provider related to wandering (J Dev Behav Pediatr. 2018 Sep;39[7]:538-46).
That research found that only 10% received advice from a pediatrician or other primary care provider, 12% received advice from a developmental pediatrician or neurologist and 10% received advance from a psychologist or psychiatrist. The largest source of guidance in that study was autism advocacy organizations, whom 22% of parents cited. Others included a teacher or other school staff member (15%), a personal contact (13%), law enforcement (8%) or another source (1%).
Role of the pediatrician
Pediatricians have an important role to play in prevention of elopement, Dr Lipkin said. They can screen autistic patients for wandering and elopement during visits, work with community stakeholders such as schools and law enforcement, advocate for awareness, and provider education and resources for families.
Perhaps the most valuable resource, he said, is the Big Red Safety Box, available from the National Autism Association. This resource, sponsored by more than a half dozen autism advocacy organizations, includes three digital safety toolkits: one for caregivers, one for first responders, and one for teachers. Parents can therefore share the toolkits for first responders and teachers with those respective community members.
Pediatricians can also help families develop a Family Wandering Emergency Plan (FWEP), a template for which is in the Big Red Safety Box. Parents and community members should know the steps to take if someone wanders: Stay calm, call 911, search nearby water first and then implement the FWEP.
It’s first helpful to understand why these youth wander off. In the National Autism Association survey, the most common reasons were to escape an anxious situation, particularly for those with Asperger’s, or simply to run, explore, or go to a favorite place, particularly among those with autism or pervasive developmental disorder-not otherwise specified (PDD-NOS).
Researchers have found similar reasons: 43% of elopement situations occurred when children were trying to escape an anxious situation, 39% left while in a stressful environment, and 24% were in an environment with conflict, found one study (J Autism Dev Disord. 2019 Mar 5. doi: 10.1007/s10803-019-03961-x).
Sensory overload was also a trigger, with 38% of elopements occurring when it was too noisy, and 34% when it was a generally uncomfortable sensory experience. Just over a quarter (27%) of children left when they were understimulated or in a “boring” environment, Dr Lipkin reported. The remaining reason was goal-directed: 27% left to pursue a special interest, 18% sought a place where they enjoyed playing, and 11% were after their favorite food.
Prevention Strategies
Most data about effective strategies to prevent wandering comes from research that relies on parents, Dr Lipkin said. In general, environmental interventions tend to be the most effective, and medication tends to be the least effective.
One study on elopement prevention found that 96% of caregivers use at least some type of intervention, and the vast majority (83%) were using environmental interventions such as dead bolts (51%), latches (49%) and gates (36%). An equal proportion used behavioral services (83%), such as a behavioral psychologist (41%), social stories (40%) or an aide (39%). Just under a third used an ID bracelet or shoe tag (31%), and 19% used GPS trackers, according to Dr. Lipkin.
Although parents reported environmental interventions to be very effective, 68% said they were highly burdensome, though the median cost over 2 years was less than $1,000. The least expensive intervention was home behavioral specialists (when covered by insurance) and school aides, and the most expensive and burdensome – albeit highly effective – was a service animal.
Interventions with the least cost effectiveness included security cameras and GPS trackers, which only 15% of parents reported as being effective.
Although nearly half of parents reported their child had taken any psychiatric medication (48%), only 16% had taken medication explicitly to prevent wandering. Few reported the medication was very effective, however. Among the small number who did (less than 10), lorazepam, diazepam and atomoxetine appeared best.
Teaching children survival skills, as developmentally appropriate and possible, can also help. These include swimming lessons as well as learning how to interact in traffic, knowing their home address, and learning how to navigate around their neighborhood.
Dr. Lipkin no disclosures and used no external funding for this presentation.
FROM AAP
Urban or rural, children’s gun-related injuries equally deadly
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
NEW ORLEANS – Accidental firearm-related injuries among children occur more frequently in rural than in urban locations, and nearly 60% of such cases are potentially preventable, results from a single-center study suggest.
Furthermore, these gun injuries carry the same mortality and disability risk.
“Firearm-related injury is an understudied topic,” lead study author Amelia Lucisano, MD, said in an interview in advance of the annual meeting of the American Academy of Pediatrics. “In particular there is a lack of granular level research on firearm-related injury in the population.”
At the meeting, she presented findings from an analysis which set out to investigate the location, preventability, and temporal trends of pediatric firearm-related injury in 184 patients age 18 and younger who were treated in the pediatric trauma program at University of Pittsburgh Medical Center during 2008-2017. Dr. Lucisano, a surgical resident at the university, and her colleagues focused their work on efforts to illustrate the differences and similarities in the demographics, injury-related characteristics, and outcomes between the rural and urban populations of children who are injured by firearms in Southwestern Pennsylvania. They classified the location as rural if the injury occurred outside the region’s central metropolitan county, and classified the injury as potentially preventable if the firearm was not stored securely and was used without permission. Statistical analyses included Wilcoxon rank-sum and chi-square analyses.
Of the 184 children who sustained a firearm-related injury during the study period, 43% occurred in a rural location. Compared with children who were injured in an urban setting, those who were injured in a rural setting were younger (a mean of 13 vs. 14 years; P = 0.0003), were more frequently white (81% vs. 14%; P less than 0.0001), and were more frequently injured by accident (70% vs. 15%; P less than 0.0001). They were also more likely to be injured by rifle or shotgun (24.1% vs. 6.67%; P = 0.001).
The rates of death or disability and lengths of stay did not differ significantly based on location of injury, occurring in 16.5% of rural and 13.3% of urban patients.
Nearly three-quarters of accidental injuries (72%) occurred on the gun-owner’s property and 58% were considered by the researchers to be potentially preventable.
“As expected, rural injuries are more frequently unintentional while urban injuries are more frequently assaults,” Dr. Lucisano said. “However, markers of injury severity and outcomes are equivalent between the groups, meaning that morbidity and mortality of injuries in the rural setting are similar to those in the urban setting.”
She emphasized that while clinician bias may be to consider rural firearm-based injuries as less severe, “our study shows that they carry the same burden of morbidity and mortality as urban injuries and thus should be cared for with the same intensity and anticipation of a possible poor outcome. Furthermore, the large number of potentially preventable injuries among those that were unintentional represents a significant burden of morbidity and mortality that could have been avoided through safer firearm storage. Programs to promote safe firearm storage should be targeted to populations that have high rates of potentially preventable injuries.”
Dr. Lucisano and her colleagues observed that the rates of all forms of firearm-related injury appear to be on the rise in both rural and urban areas: accidental, self-inflicted, and assault, in particular. She acknowledged certain limitations of the study, including its retrospective, single-center design. “We did not capture children who died in the field or who were treated at other hospitals, though as our center is the only pediatric Level 1 trauma center, we capture a large majority of pediatric trauma patients in the region,” she said.
The researchers reported having no disclosures.
SOURCE: Lucisano A. AAP 2019, Section on Surgery program.
AT AAP 2019