User login
Growing the pool of academic vascular surgeons
NEW YORK – Strategies for growing the pool of academic vascular surgeons might help avert the expected scarcity of physicians in this specialty, according to Peter K. Henke, MD, a professor of vascular surgery at the University of Michigan, Ann Arbor.
Dr. Henke recounted in a video interview key messages he delivered at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. He argued for going back to basics to enlist residents and fellows completing their training to stay in the specialty and consider an academic position.
Many of these steps are known, such as verifying that mentors are available to encourage skill acquisition and providing adequate time to achieve an acceptable balance of research and clinical work.
However, a successful program would not solely focus on luring young and promising junior faculty, he said. A supportive atmosphere requires collaboration and support to flow both up and down the ranks of seniority where everyone benefits.As an example, he singled out midlevel faculty as vulnerable when programs are not developed to ensure support is equally distributed. He explained that midlevel faculty members denied the encouragement available to surgeons just initiating their career can feel abandoned when they are skilled but not yet leaders in their program.
The Society of Vascular Surgery is pursing several initiatives to address the projected shortage within this specialty, according to Dr. Henke, but he argues that leaders of academic programs have a role to play in helping make the specialty attractive, particularly for those considering an academic career.
NEW YORK – Strategies for growing the pool of academic vascular surgeons might help avert the expected scarcity of physicians in this specialty, according to Peter K. Henke, MD, a professor of vascular surgery at the University of Michigan, Ann Arbor.
Dr. Henke recounted in a video interview key messages he delivered at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. He argued for going back to basics to enlist residents and fellows completing their training to stay in the specialty and consider an academic position.
Many of these steps are known, such as verifying that mentors are available to encourage skill acquisition and providing adequate time to achieve an acceptable balance of research and clinical work.
However, a successful program would not solely focus on luring young and promising junior faculty, he said. A supportive atmosphere requires collaboration and support to flow both up and down the ranks of seniority where everyone benefits.As an example, he singled out midlevel faculty as vulnerable when programs are not developed to ensure support is equally distributed. He explained that midlevel faculty members denied the encouragement available to surgeons just initiating their career can feel abandoned when they are skilled but not yet leaders in their program.
The Society of Vascular Surgery is pursing several initiatives to address the projected shortage within this specialty, according to Dr. Henke, but he argues that leaders of academic programs have a role to play in helping make the specialty attractive, particularly for those considering an academic career.
NEW YORK – Strategies for growing the pool of academic vascular surgeons might help avert the expected scarcity of physicians in this specialty, according to Peter K. Henke, MD, a professor of vascular surgery at the University of Michigan, Ann Arbor.
Dr. Henke recounted in a video interview key messages he delivered at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. He argued for going back to basics to enlist residents and fellows completing their training to stay in the specialty and consider an academic position.
Many of these steps are known, such as verifying that mentors are available to encourage skill acquisition and providing adequate time to achieve an acceptable balance of research and clinical work.
However, a successful program would not solely focus on luring young and promising junior faculty, he said. A supportive atmosphere requires collaboration and support to flow both up and down the ranks of seniority where everyone benefits.As an example, he singled out midlevel faculty as vulnerable when programs are not developed to ensure support is equally distributed. He explained that midlevel faculty members denied the encouragement available to surgeons just initiating their career can feel abandoned when they are skilled but not yet leaders in their program.
The Society of Vascular Surgery is pursing several initiatives to address the projected shortage within this specialty, according to Dr. Henke, but he argues that leaders of academic programs have a role to play in helping make the specialty attractive, particularly for those considering an academic career.
REPORTING FROM VEITHSYMPOSIUM
Drug-coated balloon advantage persists in femoral artery disease
NEW YORK – John Laird, MD, of the Adventist Heart Institute, St. Helena, Calif., presented the data at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The data were drawn from the IN.PACT trial. In this trial, 331 patients were randomized to a paclitaxel-coated DCB device or standard percutaneous balloon angioplasty (PCBA), Dr. Laird explained.
The 5-year results are consistent with those previously reported at 1, 2, and 3 years. According to Dr. Laird, DCB continues to show an advantage for major outcomes over PCBA, and adverse events remain low.
Three DCB devices now available in the United States for dilatation of narrowed SFA. Although all have been associated with a reduced risk of target lesion revascularization relative to standard PCBA, the long-term follow-up presented from IN.PACT by Dr. Laird are the first to document 5-year outcomes.
In a video interview, Dr. Laird reported that there have been no thrombotic events since the 3-year results were presented.
Overall, he explains that the long-term outcomes provide additional confirmation that DCB is a safe procedure that reduces the need for stenting in SFA occlusions. Although he believes there might be clinically significant differences between available DCB devices, he concludes that DCB can be considered the first-line therapy for treating occluded femoral-popliteal arteries.
NEW YORK – John Laird, MD, of the Adventist Heart Institute, St. Helena, Calif., presented the data at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The data were drawn from the IN.PACT trial. In this trial, 331 patients were randomized to a paclitaxel-coated DCB device or standard percutaneous balloon angioplasty (PCBA), Dr. Laird explained.
The 5-year results are consistent with those previously reported at 1, 2, and 3 years. According to Dr. Laird, DCB continues to show an advantage for major outcomes over PCBA, and adverse events remain low.
Three DCB devices now available in the United States for dilatation of narrowed SFA. Although all have been associated with a reduced risk of target lesion revascularization relative to standard PCBA, the long-term follow-up presented from IN.PACT by Dr. Laird are the first to document 5-year outcomes.
In a video interview, Dr. Laird reported that there have been no thrombotic events since the 3-year results were presented.
Overall, he explains that the long-term outcomes provide additional confirmation that DCB is a safe procedure that reduces the need for stenting in SFA occlusions. Although he believes there might be clinically significant differences between available DCB devices, he concludes that DCB can be considered the first-line therapy for treating occluded femoral-popliteal arteries.
NEW YORK – John Laird, MD, of the Adventist Heart Institute, St. Helena, Calif., presented the data at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The data were drawn from the IN.PACT trial. In this trial, 331 patients were randomized to a paclitaxel-coated DCB device or standard percutaneous balloon angioplasty (PCBA), Dr. Laird explained.
The 5-year results are consistent with those previously reported at 1, 2, and 3 years. According to Dr. Laird, DCB continues to show an advantage for major outcomes over PCBA, and adverse events remain low.
Three DCB devices now available in the United States for dilatation of narrowed SFA. Although all have been associated with a reduced risk of target lesion revascularization relative to standard PCBA, the long-term follow-up presented from IN.PACT by Dr. Laird are the first to document 5-year outcomes.
In a video interview, Dr. Laird reported that there have been no thrombotic events since the 3-year results were presented.
Overall, he explains that the long-term outcomes provide additional confirmation that DCB is a safe procedure that reduces the need for stenting in SFA occlusions. Although he believes there might be clinically significant differences between available DCB devices, he concludes that DCB can be considered the first-line therapy for treating occluded femoral-popliteal arteries.
REPORTING FROM VEITHSYMPOSIUM
Don’t just work hard; work hard at living
NEW YORK – “A physician falls overboard on a large cruise ship and passengers gather at the guard rail. The first passenger at the guardrail shakes his finger down at the drowning physician and says, ‘You need to learn how to swim!’ Another passenger says, ‘No, man, throw him a life preserver.’ ... Finally, a passenger says, ‘We need better guard rails.’ ”
That’s the analogy Cynthia K. Shortell, MD used to kick off her presentation on physician burnout and the need for resilience at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
“Which of these is right? Well, of course, the answer is they all are,” said Dr. Shortell, who is a professor of surgery at Duke University Durham, N.C. But certainly, only the life preserver answer was appropriate at that time for the drowning physician, she added.
Continuing the analogy, Dr. Shortell pointed out that surely there is a man overboard, with 1 in 20 surgeons reporting suicidal ideation. That rate jumps threefold if the surgeon has had a recent medical error. In addition, vascular surgeons in particular are within the top tier of specialties at risk for burnout.
“We do need better guardrails,” she said, and described the need to actively engage with the health care system to help solve these issues, including those involving electronic medical records and operating room inefficiency and use. In addition, there is a great need for additional services that are provided to other high-end professionals, including food, concierge service, gym access, and other services that help with tasks of daily life when physicians need to spend most of their time at the hospital.
But, in the end, Dr. Shortell said, “We do need to learn to swim. Ultimately, we do need to take a role in having responsibility to solve this problem on our own. We need to change the way we think about our work, and the way we think about our health, and the way our culture values working hard instead of working hard at living.”
Dr. Shortell also highlighted the need to deal with musculoskeletal issues arising from the way that surgeons operate. This, along with good leadership, are key factors in preventing and remediating burnout.
Dr. Shortell had no disclosures relevant to her talk.
NEW YORK – “A physician falls overboard on a large cruise ship and passengers gather at the guard rail. The first passenger at the guardrail shakes his finger down at the drowning physician and says, ‘You need to learn how to swim!’ Another passenger says, ‘No, man, throw him a life preserver.’ ... Finally, a passenger says, ‘We need better guard rails.’ ”
That’s the analogy Cynthia K. Shortell, MD used to kick off her presentation on physician burnout and the need for resilience at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
“Which of these is right? Well, of course, the answer is they all are,” said Dr. Shortell, who is a professor of surgery at Duke University Durham, N.C. But certainly, only the life preserver answer was appropriate at that time for the drowning physician, she added.
Continuing the analogy, Dr. Shortell pointed out that surely there is a man overboard, with 1 in 20 surgeons reporting suicidal ideation. That rate jumps threefold if the surgeon has had a recent medical error. In addition, vascular surgeons in particular are within the top tier of specialties at risk for burnout.
“We do need better guardrails,” she said, and described the need to actively engage with the health care system to help solve these issues, including those involving electronic medical records and operating room inefficiency and use. In addition, there is a great need for additional services that are provided to other high-end professionals, including food, concierge service, gym access, and other services that help with tasks of daily life when physicians need to spend most of their time at the hospital.
But, in the end, Dr. Shortell said, “We do need to learn to swim. Ultimately, we do need to take a role in having responsibility to solve this problem on our own. We need to change the way we think about our work, and the way we think about our health, and the way our culture values working hard instead of working hard at living.”
Dr. Shortell also highlighted the need to deal with musculoskeletal issues arising from the way that surgeons operate. This, along with good leadership, are key factors in preventing and remediating burnout.
Dr. Shortell had no disclosures relevant to her talk.
NEW YORK – “A physician falls overboard on a large cruise ship and passengers gather at the guard rail. The first passenger at the guardrail shakes his finger down at the drowning physician and says, ‘You need to learn how to swim!’ Another passenger says, ‘No, man, throw him a life preserver.’ ... Finally, a passenger says, ‘We need better guard rails.’ ”
That’s the analogy Cynthia K. Shortell, MD used to kick off her presentation on physician burnout and the need for resilience at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
“Which of these is right? Well, of course, the answer is they all are,” said Dr. Shortell, who is a professor of surgery at Duke University Durham, N.C. But certainly, only the life preserver answer was appropriate at that time for the drowning physician, she added.
Continuing the analogy, Dr. Shortell pointed out that surely there is a man overboard, with 1 in 20 surgeons reporting suicidal ideation. That rate jumps threefold if the surgeon has had a recent medical error. In addition, vascular surgeons in particular are within the top tier of specialties at risk for burnout.
“We do need better guardrails,” she said, and described the need to actively engage with the health care system to help solve these issues, including those involving electronic medical records and operating room inefficiency and use. In addition, there is a great need for additional services that are provided to other high-end professionals, including food, concierge service, gym access, and other services that help with tasks of daily life when physicians need to spend most of their time at the hospital.
But, in the end, Dr. Shortell said, “We do need to learn to swim. Ultimately, we do need to take a role in having responsibility to solve this problem on our own. We need to change the way we think about our work, and the way we think about our health, and the way our culture values working hard instead of working hard at living.”
Dr. Shortell also highlighted the need to deal with musculoskeletal issues arising from the way that surgeons operate. This, along with good leadership, are key factors in preventing and remediating burnout.
Dr. Shortell had no disclosures relevant to her talk.
REPORTING FROM THE VEITHSYMPOSIUM
What’s new with the SVS VQI?
NEW YORK – The Vascular Quality Initiative (VQI) is designed to improve the quality, safety, and effectiveness of vascular health care, but also reduce costs through the collection and exchange of information, according to Larry W. Kraiss, MD, professor of surgery, University of Utah, Salt Lake City.
The VQI consists of three major components: a federally accredited patient safety organization (PSO), a registry, and a distributed network of quality groups, which can also serve as a platform for internal quality improvement efforts.
Even though registries are considered less reliable than the venerated randomized clinical trial models are, registries have some unique advantages, according to Dr. Kraiss, who spoke at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. Randomized clinical trials (RCTs) are very expensive to conduct and are criticized for potentially not being generalizable because of their rigidly defined inclusion/exclusion criteria. Despite inherent problems with registry data, especially bias, there are now statistical methods to help account for the biases. Registry-controlled trials are going to be important to answer many questions that cannot be answered by RCTs. Such trials can be too costly or actually unethical to randomize under certain circumstances. Registries, however, provide real-world patient populations in greater numbers than RCTs can manage, including access to rare events that would otherwise not be detected.
The VQI holds an important place in this second tier and is an important source of information for clinical care.
The VQI has grown steadily since its inception, and there are more than 500 centers now participating, including 6 international centers, and 18 regional groups, according to Dr. Kraiss. There are more than 530,000 procedures contained within the VQI’s 12 registries, with more than half of them involving peripheral vascular interventions and carotid endarterectomies. “But there [are] a healthy number of cases in all of the other registries, which provide a very rich resource and evidence base,” he added.
The VQI is becoming very important in the regulatory framework, with the Food and Drug Administration embracing “real-world evidence” as a way to justify some of its decisions, and the VQI has been involved in this process. The VQI has coordinated several post-market surveillance programs, the two most important being in the areas of thoracic endovascular aortic repair (TEVAR) and transcarotid artery revascularization (TCAR), said Dr. Kraiss.
One of the important values of the VQI is the ability to examine benchmarks and to compare performance across centers. For example, looking at aortic abdominal aneurysm (AAA) repair data, the results showed that a number of centers were not following established Society for Vascular Society guidelines and that there were a substantial number of AAAs reported in the VQI that were treated when they were below the threshold for intervention and should have received routine observation only.
So, ultimately two of the greatest values of the VQI are the ability to use it as a means of local quality improvement, and to provide an avenue for important clinical research, Dr. Kraiss concluded.
Dr. Kraiss reported that they had no disclosures.
NEW YORK – The Vascular Quality Initiative (VQI) is designed to improve the quality, safety, and effectiveness of vascular health care, but also reduce costs through the collection and exchange of information, according to Larry W. Kraiss, MD, professor of surgery, University of Utah, Salt Lake City.
The VQI consists of three major components: a federally accredited patient safety organization (PSO), a registry, and a distributed network of quality groups, which can also serve as a platform for internal quality improvement efforts.
Even though registries are considered less reliable than the venerated randomized clinical trial models are, registries have some unique advantages, according to Dr. Kraiss, who spoke at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. Randomized clinical trials (RCTs) are very expensive to conduct and are criticized for potentially not being generalizable because of their rigidly defined inclusion/exclusion criteria. Despite inherent problems with registry data, especially bias, there are now statistical methods to help account for the biases. Registry-controlled trials are going to be important to answer many questions that cannot be answered by RCTs. Such trials can be too costly or actually unethical to randomize under certain circumstances. Registries, however, provide real-world patient populations in greater numbers than RCTs can manage, including access to rare events that would otherwise not be detected.
The VQI holds an important place in this second tier and is an important source of information for clinical care.
The VQI has grown steadily since its inception, and there are more than 500 centers now participating, including 6 international centers, and 18 regional groups, according to Dr. Kraiss. There are more than 530,000 procedures contained within the VQI’s 12 registries, with more than half of them involving peripheral vascular interventions and carotid endarterectomies. “But there [are] a healthy number of cases in all of the other registries, which provide a very rich resource and evidence base,” he added.
The VQI is becoming very important in the regulatory framework, with the Food and Drug Administration embracing “real-world evidence” as a way to justify some of its decisions, and the VQI has been involved in this process. The VQI has coordinated several post-market surveillance programs, the two most important being in the areas of thoracic endovascular aortic repair (TEVAR) and transcarotid artery revascularization (TCAR), said Dr. Kraiss.
One of the important values of the VQI is the ability to examine benchmarks and to compare performance across centers. For example, looking at aortic abdominal aneurysm (AAA) repair data, the results showed that a number of centers were not following established Society for Vascular Society guidelines and that there were a substantial number of AAAs reported in the VQI that were treated when they were below the threshold for intervention and should have received routine observation only.
So, ultimately two of the greatest values of the VQI are the ability to use it as a means of local quality improvement, and to provide an avenue for important clinical research, Dr. Kraiss concluded.
Dr. Kraiss reported that they had no disclosures.
NEW YORK – The Vascular Quality Initiative (VQI) is designed to improve the quality, safety, and effectiveness of vascular health care, but also reduce costs through the collection and exchange of information, according to Larry W. Kraiss, MD, professor of surgery, University of Utah, Salt Lake City.
The VQI consists of three major components: a federally accredited patient safety organization (PSO), a registry, and a distributed network of quality groups, which can also serve as a platform for internal quality improvement efforts.
Even though registries are considered less reliable than the venerated randomized clinical trial models are, registries have some unique advantages, according to Dr. Kraiss, who spoke at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. Randomized clinical trials (RCTs) are very expensive to conduct and are criticized for potentially not being generalizable because of their rigidly defined inclusion/exclusion criteria. Despite inherent problems with registry data, especially bias, there are now statistical methods to help account for the biases. Registry-controlled trials are going to be important to answer many questions that cannot be answered by RCTs. Such trials can be too costly or actually unethical to randomize under certain circumstances. Registries, however, provide real-world patient populations in greater numbers than RCTs can manage, including access to rare events that would otherwise not be detected.
The VQI holds an important place in this second tier and is an important source of information for clinical care.
The VQI has grown steadily since its inception, and there are more than 500 centers now participating, including 6 international centers, and 18 regional groups, according to Dr. Kraiss. There are more than 530,000 procedures contained within the VQI’s 12 registries, with more than half of them involving peripheral vascular interventions and carotid endarterectomies. “But there [are] a healthy number of cases in all of the other registries, which provide a very rich resource and evidence base,” he added.
The VQI is becoming very important in the regulatory framework, with the Food and Drug Administration embracing “real-world evidence” as a way to justify some of its decisions, and the VQI has been involved in this process. The VQI has coordinated several post-market surveillance programs, the two most important being in the areas of thoracic endovascular aortic repair (TEVAR) and transcarotid artery revascularization (TCAR), said Dr. Kraiss.
One of the important values of the VQI is the ability to examine benchmarks and to compare performance across centers. For example, looking at aortic abdominal aneurysm (AAA) repair data, the results showed that a number of centers were not following established Society for Vascular Society guidelines and that there were a substantial number of AAAs reported in the VQI that were treated when they were below the threshold for intervention and should have received routine observation only.
So, ultimately two of the greatest values of the VQI are the ability to use it as a means of local quality improvement, and to provide an avenue for important clinical research, Dr. Kraiss concluded.
Dr. Kraiss reported that they had no disclosures.
REPORTING FROM THE VEITHSYMPOSIUM
Update on integrated vascular surgery residencies
NEW YORK – In March 2005, the Accreditation Council for Graduate Medical Education approved the primary certificate in vascular surgery, and the first integrated vascular surgery residencies (0+5) were approved shortly thereafter. By 2015, there was more than a 900% increase in both the number of programs and positions, which were offered for matriculation in July 2016, according to Murray L. Shames, MD, professor of surgery and radiology at the University of South Florida, Tampa, and chief of the division of vascular surgery at Tampa General Hospital.
In 2009, Dr. Shames and his colleagues first looked at the issue to try to better understand the applicant pool, and they found that there was a 900% increase in demand for the 0+5 residency positions, compared with the traditional 5+2 vascular fellowships, and that there was a 0+5 applicant-to-position ratio of 8:1 that year. “Despite initial concerns regarding the shortened training, studies have demonstrated equivalent case volumes and job opportunities for integrated vascular residents and vascular fellows,” Dr. Shames stated at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
His current presentation was an update of that assessment done for the 2015 data, as integrated vascular surgery residents have begun to enter the workforce. They looked at the current supply and demand for 0+5 training programs (as well as the traditional 5+2 programs), and the quality and attributes of the 0+5 residency applicants. They obtained data for applicants for both types of programs: 2008-2015 for 0+2 and 2007-2016 for 5+2) and comparable match data were queried for 2008-2016. They looked at the number of programs, the number of positions, the total number of applicants, sex of the applicants, applications/program and applications/position, and the U.S. versus international applicant ratios.
They found that the number of integrated programs increased from 4 to 48, with an increase from 4 to 56 positions, during the study period, said Dr. Shames. Demand for integrated vascular residencies has increased nearly 300%, from 112 applicants in 2008 to 434 in 2015. The total number of U.S. medical school graduate applicants to these programs has increased from 40 in 2008 to 2,030 in 2015, with the increase in program applicants driven primarily by these U.S. medical school graduates; the number of international applicants per program decrease over this time period from 57 to 37. The percentage of women applicants has steadily increased, from 16% to 27%, and currently women constitute 41% of all integrated vascular surgery residents.
“Overall, the supply for integrated vascular surgery residency positions continues to be outnumbered by the number of applicants, with increasing applicant to position ratios at 7.8:1 in 2015, while the total number for vascular surgery fellowships has remained stable at about 1:1,” Dr. Shames concluded.
Dr. Shames reported having no relevant disclosures for his presentation.
NEW YORK – In March 2005, the Accreditation Council for Graduate Medical Education approved the primary certificate in vascular surgery, and the first integrated vascular surgery residencies (0+5) were approved shortly thereafter. By 2015, there was more than a 900% increase in both the number of programs and positions, which were offered for matriculation in July 2016, according to Murray L. Shames, MD, professor of surgery and radiology at the University of South Florida, Tampa, and chief of the division of vascular surgery at Tampa General Hospital.
In 2009, Dr. Shames and his colleagues first looked at the issue to try to better understand the applicant pool, and they found that there was a 900% increase in demand for the 0+5 residency positions, compared with the traditional 5+2 vascular fellowships, and that there was a 0+5 applicant-to-position ratio of 8:1 that year. “Despite initial concerns regarding the shortened training, studies have demonstrated equivalent case volumes and job opportunities for integrated vascular residents and vascular fellows,” Dr. Shames stated at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
His current presentation was an update of that assessment done for the 2015 data, as integrated vascular surgery residents have begun to enter the workforce. They looked at the current supply and demand for 0+5 training programs (as well as the traditional 5+2 programs), and the quality and attributes of the 0+5 residency applicants. They obtained data for applicants for both types of programs: 2008-2015 for 0+2 and 2007-2016 for 5+2) and comparable match data were queried for 2008-2016. They looked at the number of programs, the number of positions, the total number of applicants, sex of the applicants, applications/program and applications/position, and the U.S. versus international applicant ratios.
They found that the number of integrated programs increased from 4 to 48, with an increase from 4 to 56 positions, during the study period, said Dr. Shames. Demand for integrated vascular residencies has increased nearly 300%, from 112 applicants in 2008 to 434 in 2015. The total number of U.S. medical school graduate applicants to these programs has increased from 40 in 2008 to 2,030 in 2015, with the increase in program applicants driven primarily by these U.S. medical school graduates; the number of international applicants per program decrease over this time period from 57 to 37. The percentage of women applicants has steadily increased, from 16% to 27%, and currently women constitute 41% of all integrated vascular surgery residents.
“Overall, the supply for integrated vascular surgery residency positions continues to be outnumbered by the number of applicants, with increasing applicant to position ratios at 7.8:1 in 2015, while the total number for vascular surgery fellowships has remained stable at about 1:1,” Dr. Shames concluded.
Dr. Shames reported having no relevant disclosures for his presentation.
NEW YORK – In March 2005, the Accreditation Council for Graduate Medical Education approved the primary certificate in vascular surgery, and the first integrated vascular surgery residencies (0+5) were approved shortly thereafter. By 2015, there was more than a 900% increase in both the number of programs and positions, which were offered for matriculation in July 2016, according to Murray L. Shames, MD, professor of surgery and radiology at the University of South Florida, Tampa, and chief of the division of vascular surgery at Tampa General Hospital.
In 2009, Dr. Shames and his colleagues first looked at the issue to try to better understand the applicant pool, and they found that there was a 900% increase in demand for the 0+5 residency positions, compared with the traditional 5+2 vascular fellowships, and that there was a 0+5 applicant-to-position ratio of 8:1 that year. “Despite initial concerns regarding the shortened training, studies have demonstrated equivalent case volumes and job opportunities for integrated vascular residents and vascular fellows,” Dr. Shames stated at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
His current presentation was an update of that assessment done for the 2015 data, as integrated vascular surgery residents have begun to enter the workforce. They looked at the current supply and demand for 0+5 training programs (as well as the traditional 5+2 programs), and the quality and attributes of the 0+5 residency applicants. They obtained data for applicants for both types of programs: 2008-2015 for 0+2 and 2007-2016 for 5+2) and comparable match data were queried for 2008-2016. They looked at the number of programs, the number of positions, the total number of applicants, sex of the applicants, applications/program and applications/position, and the U.S. versus international applicant ratios.
They found that the number of integrated programs increased from 4 to 48, with an increase from 4 to 56 positions, during the study period, said Dr. Shames. Demand for integrated vascular residencies has increased nearly 300%, from 112 applicants in 2008 to 434 in 2015. The total number of U.S. medical school graduate applicants to these programs has increased from 40 in 2008 to 2,030 in 2015, with the increase in program applicants driven primarily by these U.S. medical school graduates; the number of international applicants per program decrease over this time period from 57 to 37. The percentage of women applicants has steadily increased, from 16% to 27%, and currently women constitute 41% of all integrated vascular surgery residents.
“Overall, the supply for integrated vascular surgery residency positions continues to be outnumbered by the number of applicants, with increasing applicant to position ratios at 7.8:1 in 2015, while the total number for vascular surgery fellowships has remained stable at about 1:1,” Dr. Shames concluded.
Dr. Shames reported having no relevant disclosures for his presentation.
REPORTING FROM THE VEITHSYMPOSIUM
What are the barriers to solving the upcoming vascular surgeon shortage?
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
NEW YORK – Increasing the number of 0+5 integrated vascular surgery residency programs would help to alleviate a projected shortage of vascular surgeons, according to William D. Jordan, Jr., MD, professor of surgery, Emory University, Atlanta.*
“Ultimately the question is whether the workforce pipeline is large enough,” Dr. Jordan said at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation. “When you consider that there are little more than 600 vascular trainees right now, and almost 600 planned retirements over the next 5 years, the answer to the question is no. Our workforce pipeline is not big enough.”
Dr. Jordan pointed out that, in addition, if one considers the current geographic distribution of vascular surgeons across the country, and go with the new standard that 1.4 surgeons are needed per 100,000 population, there is not a single state in the country that matches up to that goal. “So we are clearly going to have a shortage,” he commented. The only way to fill that shortage is to produce more vascular surgeons. But how does the change to a 0+5 residency program model impact that need?
In a survey conducted by the Association of Program Directors in Vascular Surgery in 2016, regarding challenges as perceived by the trainees, the top two concerns expressed were regarding competing specialties and physician burnout. Statistics bear out the concern regarding competing specialties, for example, there is an increase of 85% in interventional cardiology trainees being produced and a nearly 50% increase in interventional radiology trainees. However, in vascular, it is only 18%. With regard to the goals of those vascular trainees, 90% indicated that they wanted to be attached to some academic or teaching environment. “They don’t want to be the lone wolf out there,” Dr. Jordan said, and this is from concerns regarding workload, mentorship, and camaraderie, as well as regulatory and administrative obligations that are steadily increasing and can be handled more easily in a large institution. This will not fill the need for vascular surgeons in community hospitals, creating a shortage of distribution as well as actual numbers.
One key problem with current training is the fact that the new form of student comes with almost no real surgical skills and there is a dearth of vascular surgery cases available to fully accommodate many of them throughout their training career. This is a problem exacerbated by some residency review committees, which are loathe to give vascular surgery cases to new trainees.
Integrated vascular surgery residency programs have grown and there is a substantially greater interest in them, receiving even more applicants than orthopedics or neurosurgery. U.S. interest exceeds the number of 0+5 positions available. One way to deal with the projected 31% deficit in vascular surgeons by 2025 would thus be to increase the number of these training positions. The financial accommodations to do this would be large, but perhaps the creation of an independent vascular surgery specialty board would facilitate dealing with that issue, he concluded.
Dr. Jordan reported no disclosures relevant to his talk.
Correction, 11/19/18: An earlier version of this article misidentified the speaker in the session. The speaker was William D. Jordan, Jr., MD.
REPORTING FROM THE VEITHSYMPOSIUM
A bovine arch predicts worse outcomes with type B aortic dissections
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
NEW YORK – The presence of a bovine arch predicts higher mortality in patients with a type B aortic dissection (TBAD), according to a study presented by Jan S. Brunkwall, MD, at a symposium on vascular and endovascular issues sponsored by the Cleveland Clinic Foundation.
The bovine arch is a congenital interruption in the evolution of the arch, and is a misnomer because it does not actually reflect the arch branching pattern found in cattle. It represents the most common variation of the aortic arch, with a prevalence of 1%-41%, depending on the literature, according to a study published by Dr. Brunkwall, chairman of the department of vascular and endovascular surgery at the University of Cologne (Germany), and his colleagues (Eur J Vasc Endovasc Surg. 2018; 55:385-391).
In order to assess the effect of the bovine arch on survival, Dr. Brunkwall and his colleagues performed a retrospective cohort analysis of patients with TBAD admitted at two centers. CT angiograms (CTAs) of patients referred because of aortic dissection were also reevaluated with regard to the presence of a bovine arch.
A total of 154 patients with TBAD and 168 with type A aortic dissection were assessed, and 110 oncologic patients who had undergone a chest CTA for disease staging during the study period acted as a control group.
There was an overall prevalence of 17.6% for bovine arch variants, with no statistical difference in prevalence between patients with a dissection and those in the control group, or between patients with a type A or type B dissection. However, mortality was 34.5% in patients with TBAD who had a bovine arch versus 16% in patients without a bovine arch. This was a significant difference (P =.04), according to Dr. Brunkwall.
Multivariate analysis showed that the presence of a bovine arch with TBAD was an independent predictor of mortality. “The reason for the high mortality cannot be explained by our data,” said Dr. Brunkwall, “but there has been a suggestion that the shear stress is different and higher in patients with a bovine arch leading to a stiffer aorta and more endothelial damage.”
Dr. Brunkwall reported that he had no disclosures.
REPORTING FROM VEITHSYMPOSIUM
Venous Venous Venous @VEITHsymposium
The Venous Venous Venous @VEITHsymposium program has become a popular staple of the meeting. With a mixture of didactic sessions and workshops, the Venous Venous Venous program, which will be held on Thursday, Friday, and Saturday, will cover the full gamut of venous disorders and their treatments, surgical, endovascular, and medical.
The didactic Program J (Sessions 63-67) on Superficial Venous Disease will be held on Thursday morning and early afternoon and will detail the latest developments in venous clinical examinations and imaging, superficial vein strategies and techniques, thermal and non-thermal ablation, and there will be a special session on venous societal issues and governance. Moderated by Elna M. Masuda, MD, and Marc A. Passman, MD, this special session will feature discussions of the Centers for Medicare & Medicaid policy update on venous ablation, dealing with MACRA, the RUC, and the reevaluation of phlebectomy, and more.
The didactic Program N (Sessions 88-92) on Deep Venous Disease will be all day Friday and will cover pelvic venous disorders, femoro-iliocaval interventions, deep vein reflux, wounds, and endovascular and open solutions for inferior vena cava disorders, and more.
The didactic Program R (Sessions 109-114) on Superficial Venous Disease will be held on Thursday morning and early afternoon and will cover all aspects of venous disease, from venous imaging, thrombophilia, schelrotherapy, phlebectomy, and more.
This year’s workshops will be held on Thursday afternoon and early evening, Nov. 15, and will feature video case presentations, and lectures and demonstrations on managing venous disease by leading experts in the field. In addition, there will be hands-on work station opportunities for participants to work with trained professionals to hone their skills.Two workshop modules are being offered this year:
1) Thrombus Management, which will focus on thromolysis, thrombectomry, the latest in stents and filters, difficult recanalizations, and issues in anticoagulation.
2) Superficial Venous Disease and Compression Management, which will deal with venous ablation, phelebctomy, schlerotherapy, and the critical areas of lymphedema, lipedema, and venous edema treatment, as well as wound care and compression.
The Venous Venous Venous @VEITHsymposium program has become a popular staple of the meeting. With a mixture of didactic sessions and workshops, the Venous Venous Venous program, which will be held on Thursday, Friday, and Saturday, will cover the full gamut of venous disorders and their treatments, surgical, endovascular, and medical.
The didactic Program J (Sessions 63-67) on Superficial Venous Disease will be held on Thursday morning and early afternoon and will detail the latest developments in venous clinical examinations and imaging, superficial vein strategies and techniques, thermal and non-thermal ablation, and there will be a special session on venous societal issues and governance. Moderated by Elna M. Masuda, MD, and Marc A. Passman, MD, this special session will feature discussions of the Centers for Medicare & Medicaid policy update on venous ablation, dealing with MACRA, the RUC, and the reevaluation of phlebectomy, and more.
The didactic Program N (Sessions 88-92) on Deep Venous Disease will be all day Friday and will cover pelvic venous disorders, femoro-iliocaval interventions, deep vein reflux, wounds, and endovascular and open solutions for inferior vena cava disorders, and more.
The didactic Program R (Sessions 109-114) on Superficial Venous Disease will be held on Thursday morning and early afternoon and will cover all aspects of venous disease, from venous imaging, thrombophilia, schelrotherapy, phlebectomy, and more.
This year’s workshops will be held on Thursday afternoon and early evening, Nov. 15, and will feature video case presentations, and lectures and demonstrations on managing venous disease by leading experts in the field. In addition, there will be hands-on work station opportunities for participants to work with trained professionals to hone their skills.Two workshop modules are being offered this year:
1) Thrombus Management, which will focus on thromolysis, thrombectomry, the latest in stents and filters, difficult recanalizations, and issues in anticoagulation.
2) Superficial Venous Disease and Compression Management, which will deal with venous ablation, phelebctomy, schlerotherapy, and the critical areas of lymphedema, lipedema, and venous edema treatment, as well as wound care and compression.
The Venous Venous Venous @VEITHsymposium program has become a popular staple of the meeting. With a mixture of didactic sessions and workshops, the Venous Venous Venous program, which will be held on Thursday, Friday, and Saturday, will cover the full gamut of venous disorders and their treatments, surgical, endovascular, and medical.
The didactic Program J (Sessions 63-67) on Superficial Venous Disease will be held on Thursday morning and early afternoon and will detail the latest developments in venous clinical examinations and imaging, superficial vein strategies and techniques, thermal and non-thermal ablation, and there will be a special session on venous societal issues and governance. Moderated by Elna M. Masuda, MD, and Marc A. Passman, MD, this special session will feature discussions of the Centers for Medicare & Medicaid policy update on venous ablation, dealing with MACRA, the RUC, and the reevaluation of phlebectomy, and more.
The didactic Program N (Sessions 88-92) on Deep Venous Disease will be all day Friday and will cover pelvic venous disorders, femoro-iliocaval interventions, deep vein reflux, wounds, and endovascular and open solutions for inferior vena cava disorders, and more.
The didactic Program R (Sessions 109-114) on Superficial Venous Disease will be held on Thursday morning and early afternoon and will cover all aspects of venous disease, from venous imaging, thrombophilia, schelrotherapy, phlebectomy, and more.
This year’s workshops will be held on Thursday afternoon and early evening, Nov. 15, and will feature video case presentations, and lectures and demonstrations on managing venous disease by leading experts in the field. In addition, there will be hands-on work station opportunities for participants to work with trained professionals to hone their skills.Two workshop modules are being offered this year:
1) Thrombus Management, which will focus on thromolysis, thrombectomry, the latest in stents and filters, difficult recanalizations, and issues in anticoagulation.
2) Superficial Venous Disease and Compression Management, which will deal with venous ablation, phelebctomy, schlerotherapy, and the critical areas of lymphedema, lipedema, and venous edema treatment, as well as wound care and compression.
VEITHsymposium: Focusing on (clinical) trials and tribulations
A hallmark of the VEITHsymposium has always been its focus on the results of recent and ongoing clinical trials, and this year is no exception. These trials will be presented by experts in their various fields who will discuss how the results will affect your daily practice.
A plethora of such clinical trials take center stage throughout the week and Tuesday alone has its fair share of highlighted studies.
For example, Tuesday morning, Jan D. Blankensteijn, MD, will discuss how and why the late results of the Dutch Randomised Endovascular Aneurysm Management (DREAM) and the Standard Open Surgery Versus Endovascular Repair of Abdominal Aortic Aneurysm (OVER) randomized controlled trials did not show the same late survival benefit for open repair as for EVAR and will address the issue of whether EVAR should be the treatment of choice for all anatomically suitable AAA patients.
Intracranial treatments for stroke will be a key interest of three trial presentations: Colin P. Derdeyn, MD, will present new findings from the Stenting vs. Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) randomized controlled trial comparing intracranial stenting to best medical treatments, highlighting the high incidence of in-stent restenosis causing strokes that were observed. Alejandro M. Spiotta, MD, will discuss how the COMPASS Trial: a Direct Aspiration First Pass Technique (COMPASS) shows that new aspiration systems are equivalent to stentrievers for removing intracranial clots to treat acute strokes, and address when they appear to be actually better. In addition, L. Nelson Hopkins, MD, will present an update on the value of intracranial clot removal for acute strokes, highlighting the question of when a longer window after symptom onset (up to 24 hours) is acceptable, as seen in recent trials such as the Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo (DAWN) and Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke (EXTEND-IA TNK) studies.
Switching gears later in the day, the 1-year results of the Bare Metal Stent Versus Paclitaxel Eluting Stent in the Setting of Primary Stenting of Intermediate Length Femoropopliteal Lesions (BATTLE) multicenter randomized controlled trial, will be presented by Yann Gouëffic, MD, PhD.
Be sure to catch up with these trial results and others on Tuesday and the host of trials to be presented and discussed throughout the week at the 2018 VEITHsymposium.
A hallmark of the VEITHsymposium has always been its focus on the results of recent and ongoing clinical trials, and this year is no exception. These trials will be presented by experts in their various fields who will discuss how the results will affect your daily practice.
A plethora of such clinical trials take center stage throughout the week and Tuesday alone has its fair share of highlighted studies.
For example, Tuesday morning, Jan D. Blankensteijn, MD, will discuss how and why the late results of the Dutch Randomised Endovascular Aneurysm Management (DREAM) and the Standard Open Surgery Versus Endovascular Repair of Abdominal Aortic Aneurysm (OVER) randomized controlled trials did not show the same late survival benefit for open repair as for EVAR and will address the issue of whether EVAR should be the treatment of choice for all anatomically suitable AAA patients.
Intracranial treatments for stroke will be a key interest of three trial presentations: Colin P. Derdeyn, MD, will present new findings from the Stenting vs. Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) randomized controlled trial comparing intracranial stenting to best medical treatments, highlighting the high incidence of in-stent restenosis causing strokes that were observed. Alejandro M. Spiotta, MD, will discuss how the COMPASS Trial: a Direct Aspiration First Pass Technique (COMPASS) shows that new aspiration systems are equivalent to stentrievers for removing intracranial clots to treat acute strokes, and address when they appear to be actually better. In addition, L. Nelson Hopkins, MD, will present an update on the value of intracranial clot removal for acute strokes, highlighting the question of when a longer window after symptom onset (up to 24 hours) is acceptable, as seen in recent trials such as the Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo (DAWN) and Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke (EXTEND-IA TNK) studies.
Switching gears later in the day, the 1-year results of the Bare Metal Stent Versus Paclitaxel Eluting Stent in the Setting of Primary Stenting of Intermediate Length Femoropopliteal Lesions (BATTLE) multicenter randomized controlled trial, will be presented by Yann Gouëffic, MD, PhD.
Be sure to catch up with these trial results and others on Tuesday and the host of trials to be presented and discussed throughout the week at the 2018 VEITHsymposium.
A hallmark of the VEITHsymposium has always been its focus on the results of recent and ongoing clinical trials, and this year is no exception. These trials will be presented by experts in their various fields who will discuss how the results will affect your daily practice.
A plethora of such clinical trials take center stage throughout the week and Tuesday alone has its fair share of highlighted studies.
For example, Tuesday morning, Jan D. Blankensteijn, MD, will discuss how and why the late results of the Dutch Randomised Endovascular Aneurysm Management (DREAM) and the Standard Open Surgery Versus Endovascular Repair of Abdominal Aortic Aneurysm (OVER) randomized controlled trials did not show the same late survival benefit for open repair as for EVAR and will address the issue of whether EVAR should be the treatment of choice for all anatomically suitable AAA patients.
Intracranial treatments for stroke will be a key interest of three trial presentations: Colin P. Derdeyn, MD, will present new findings from the Stenting vs. Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) randomized controlled trial comparing intracranial stenting to best medical treatments, highlighting the high incidence of in-stent restenosis causing strokes that were observed. Alejandro M. Spiotta, MD, will discuss how the COMPASS Trial: a Direct Aspiration First Pass Technique (COMPASS) shows that new aspiration systems are equivalent to stentrievers for removing intracranial clots to treat acute strokes, and address when they appear to be actually better. In addition, L. Nelson Hopkins, MD, will present an update on the value of intracranial clot removal for acute strokes, highlighting the question of when a longer window after symptom onset (up to 24 hours) is acceptable, as seen in recent trials such as the Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo (DAWN) and Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke (EXTEND-IA TNK) studies.
Switching gears later in the day, the 1-year results of the Bare Metal Stent Versus Paclitaxel Eluting Stent in the Setting of Primary Stenting of Intermediate Length Femoropopliteal Lesions (BATTLE) multicenter randomized controlled trial, will be presented by Yann Gouëffic, MD, PhD.
Be sure to catch up with these trial results and others on Tuesday and the host of trials to be presented and discussed throughout the week at the 2018 VEITHsymposium.
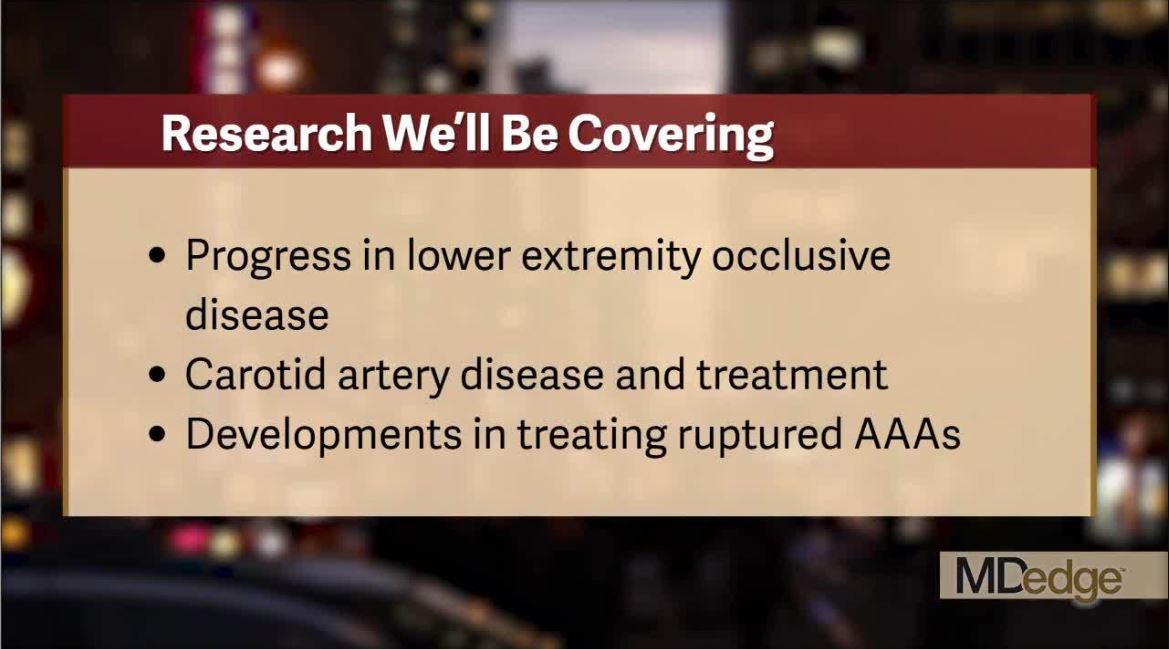
Catch all the action at the VEITHsymposium
The VEITHsymposium, held yearly in New York City, is a world-class meeting that covers the full range of vascular surgery and treatment. Frontline Medical Communications on behalf of our publication, Vascular Specialist, will be there to cover the newest and the best in devices, drugs, and surgical treatments for arterial and venous disease and the biological systems they impact.
Check out this video and get a flavor of what we will be covering live once the meeting starts. And be sure follow our continuing coverage next week at on our website and @VascularTweets. Also, check out our in depth reporting from the meeting afterward in the upcoming pages of Vascular Specialist.
The VEITHsymposium, held yearly in New York City, is a world-class meeting that covers the full range of vascular surgery and treatment. Frontline Medical Communications on behalf of our publication, Vascular Specialist, will be there to cover the newest and the best in devices, drugs, and surgical treatments for arterial and venous disease and the biological systems they impact.
Check out this video and get a flavor of what we will be covering live once the meeting starts. And be sure follow our continuing coverage next week at on our website and @VascularTweets. Also, check out our in depth reporting from the meeting afterward in the upcoming pages of Vascular Specialist.
The VEITHsymposium, held yearly in New York City, is a world-class meeting that covers the full range of vascular surgery and treatment. Frontline Medical Communications on behalf of our publication, Vascular Specialist, will be there to cover the newest and the best in devices, drugs, and surgical treatments for arterial and venous disease and the biological systems they impact.
Check out this video and get a flavor of what we will be covering live once the meeting starts. And be sure follow our continuing coverage next week at on our website and @VascularTweets. Also, check out our in depth reporting from the meeting afterward in the upcoming pages of Vascular Specialist.