User login
The Official Newspaper of the American Association for Thoracic Surgery
Drugmakers Dramatically Boosted Lobbying Spending In Trump’s First Quarter
Eight pharmaceutical companies more than doubled their lobbying spending in the first three months of 2017, when the Affordable Care Act was on the chopping block and high drug prices were clearly in the crosshairs of Congress and President Donald Trump.
Congressional records show that those eight, including Celgene and Mylan, kicked in an extra $4.42 million versus that quarter last year. Industry giant Teva Pharmaceutical Industries spent $2.67 million, up 115% from a year ago as several companies embroiled in controversies raised their outlays significantly.
“It’s certainly a rare event” when lobbying dollars double, noted Timothy LaPira, PhD, an associate professor of political science at James Madison University. “These spikes are usually timed when Congress in particular is going to be really hammering home on a particular issue. Right now, that’s health care and taxes.”
Trump has come down hard on drugmakers, stating in a press conference before his inauguration that the industry is “getting away with murder.” He has promised to lower drug prices and increase competition with faster approvals and fewer regulations. Sen. Bernie Sanders (I-Vt.), Sen. John McCain (R-Ariz.), and Rep. Elijah E. Cummings (D-Md.) have introduced bills to allow lower-cost drug imports from Canada or other countries.
Lobbyists weren’t expecting much by way of big policy changes during the comparatively sleepy end of the Obama administration this time last year, but, with a surprise Trump administration and a Republican-controlled House and Senate, trade groups and companies are probably “going all in,” Dr. LaPira said.
Thirty-eight major drugmakers and trade groups spent a total of $50.9 million, up $10.1 million from the first quarter of last year, according to a Kaiser Health News analysis. They deployed 600 lobbyists in all.
PhRMA, the drug industry’s largest trade group, spent $7.98 million during the quarter – more than in any single quarter in almost a decade, congressional records show, topping even its quarterly lobbying ahead of the Affordable Care Act’s passage in 2010.
In their congressional disclosures, companies listed Medicare price negotiation, the American Health Care Act, drug importation, and the orphan drug program as issues they were lobbying for or against. They do not have to disclose on which side of an issue they lobbied.
When Medicare prices are on the table, it should come as no surprise that pharmaceutical companies are interested in influencing congress.
“It’s quite literally hitting their bottom line,” LaPira said.
Drugmakers, under fire, more than doubled their lobbying dollars. Mylan spent $1.45 million during the quarter, up from $610,000 last year. The company’s CEO faced a congressional hearing in the fall when it raised the price of EpiPen to over $600.
Marathon Pharmaceuticals spent $230,000, which was $120,000 more than last year. Marathon was criticized in February after setting the price of Emflaza, a steroid to treat Duchenne muscular dystrophy, at $89,000 a year. That angered advocates, Congress, and patients who had been importing the same drug for as little as $1,000 a year. Marathon has since sold the drug to another company, and the price may come down.
Teva and Shire also more than doubled their spending. Teva was accused, as part of an alleged generic price-fixing scheme in December, and the Federal Trade Commission sued Shire because one of its recently acquired companies allegedly filed “sham” petitions with the Food and Drug Administration to stave off generics.
Companies that make drugs for rare diseases also more than doubled lobbying dollars as congressional leaders and the Government Accountability Office work to determine whether the Orphan Drug Act is being abused. Those firms include BioMarin, Celgene, and Vertex Pharmaceuticals. Celgene, which makes a rare cancer drug, more than tripled its first quarter lobbying to more than $1 million.
Despite efforts to make good on campaign promises to repeal the Affordable Care Act, House Republicans canceled a floor vote on the American Health Care Act in March after multiple studies estimated that millions of people would lose coverage if it passed, and neither Democrats nor ultraconservatives lined up in opposition to the bill’s provisions. Drug prices weren’t a key part of the package.
KHN’s coverage of prescription drug development, costs, and pricing is supported in part by the Laura and John Arnold Foundation. Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Eight pharmaceutical companies more than doubled their lobbying spending in the first three months of 2017, when the Affordable Care Act was on the chopping block and high drug prices were clearly in the crosshairs of Congress and President Donald Trump.
Congressional records show that those eight, including Celgene and Mylan, kicked in an extra $4.42 million versus that quarter last year. Industry giant Teva Pharmaceutical Industries spent $2.67 million, up 115% from a year ago as several companies embroiled in controversies raised their outlays significantly.
“It’s certainly a rare event” when lobbying dollars double, noted Timothy LaPira, PhD, an associate professor of political science at James Madison University. “These spikes are usually timed when Congress in particular is going to be really hammering home on a particular issue. Right now, that’s health care and taxes.”
Trump has come down hard on drugmakers, stating in a press conference before his inauguration that the industry is “getting away with murder.” He has promised to lower drug prices and increase competition with faster approvals and fewer regulations. Sen. Bernie Sanders (I-Vt.), Sen. John McCain (R-Ariz.), and Rep. Elijah E. Cummings (D-Md.) have introduced bills to allow lower-cost drug imports from Canada or other countries.
Lobbyists weren’t expecting much by way of big policy changes during the comparatively sleepy end of the Obama administration this time last year, but, with a surprise Trump administration and a Republican-controlled House and Senate, trade groups and companies are probably “going all in,” Dr. LaPira said.
Thirty-eight major drugmakers and trade groups spent a total of $50.9 million, up $10.1 million from the first quarter of last year, according to a Kaiser Health News analysis. They deployed 600 lobbyists in all.
PhRMA, the drug industry’s largest trade group, spent $7.98 million during the quarter – more than in any single quarter in almost a decade, congressional records show, topping even its quarterly lobbying ahead of the Affordable Care Act’s passage in 2010.
In their congressional disclosures, companies listed Medicare price negotiation, the American Health Care Act, drug importation, and the orphan drug program as issues they were lobbying for or against. They do not have to disclose on which side of an issue they lobbied.
When Medicare prices are on the table, it should come as no surprise that pharmaceutical companies are interested in influencing congress.
“It’s quite literally hitting their bottom line,” LaPira said.
Drugmakers, under fire, more than doubled their lobbying dollars. Mylan spent $1.45 million during the quarter, up from $610,000 last year. The company’s CEO faced a congressional hearing in the fall when it raised the price of EpiPen to over $600.
Marathon Pharmaceuticals spent $230,000, which was $120,000 more than last year. Marathon was criticized in February after setting the price of Emflaza, a steroid to treat Duchenne muscular dystrophy, at $89,000 a year. That angered advocates, Congress, and patients who had been importing the same drug for as little as $1,000 a year. Marathon has since sold the drug to another company, and the price may come down.
Teva and Shire also more than doubled their spending. Teva was accused, as part of an alleged generic price-fixing scheme in December, and the Federal Trade Commission sued Shire because one of its recently acquired companies allegedly filed “sham” petitions with the Food and Drug Administration to stave off generics.
Companies that make drugs for rare diseases also more than doubled lobbying dollars as congressional leaders and the Government Accountability Office work to determine whether the Orphan Drug Act is being abused. Those firms include BioMarin, Celgene, and Vertex Pharmaceuticals. Celgene, which makes a rare cancer drug, more than tripled its first quarter lobbying to more than $1 million.
Despite efforts to make good on campaign promises to repeal the Affordable Care Act, House Republicans canceled a floor vote on the American Health Care Act in March after multiple studies estimated that millions of people would lose coverage if it passed, and neither Democrats nor ultraconservatives lined up in opposition to the bill’s provisions. Drug prices weren’t a key part of the package.
KHN’s coverage of prescription drug development, costs, and pricing is supported in part by the Laura and John Arnold Foundation. Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Eight pharmaceutical companies more than doubled their lobbying spending in the first three months of 2017, when the Affordable Care Act was on the chopping block and high drug prices were clearly in the crosshairs of Congress and President Donald Trump.
Congressional records show that those eight, including Celgene and Mylan, kicked in an extra $4.42 million versus that quarter last year. Industry giant Teva Pharmaceutical Industries spent $2.67 million, up 115% from a year ago as several companies embroiled in controversies raised their outlays significantly.
“It’s certainly a rare event” when lobbying dollars double, noted Timothy LaPira, PhD, an associate professor of political science at James Madison University. “These spikes are usually timed when Congress in particular is going to be really hammering home on a particular issue. Right now, that’s health care and taxes.”
Trump has come down hard on drugmakers, stating in a press conference before his inauguration that the industry is “getting away with murder.” He has promised to lower drug prices and increase competition with faster approvals and fewer regulations. Sen. Bernie Sanders (I-Vt.), Sen. John McCain (R-Ariz.), and Rep. Elijah E. Cummings (D-Md.) have introduced bills to allow lower-cost drug imports from Canada or other countries.
Lobbyists weren’t expecting much by way of big policy changes during the comparatively sleepy end of the Obama administration this time last year, but, with a surprise Trump administration and a Republican-controlled House and Senate, trade groups and companies are probably “going all in,” Dr. LaPira said.
Thirty-eight major drugmakers and trade groups spent a total of $50.9 million, up $10.1 million from the first quarter of last year, according to a Kaiser Health News analysis. They deployed 600 lobbyists in all.
PhRMA, the drug industry’s largest trade group, spent $7.98 million during the quarter – more than in any single quarter in almost a decade, congressional records show, topping even its quarterly lobbying ahead of the Affordable Care Act’s passage in 2010.
In their congressional disclosures, companies listed Medicare price negotiation, the American Health Care Act, drug importation, and the orphan drug program as issues they were lobbying for or against. They do not have to disclose on which side of an issue they lobbied.
When Medicare prices are on the table, it should come as no surprise that pharmaceutical companies are interested in influencing congress.
“It’s quite literally hitting their bottom line,” LaPira said.
Drugmakers, under fire, more than doubled their lobbying dollars. Mylan spent $1.45 million during the quarter, up from $610,000 last year. The company’s CEO faced a congressional hearing in the fall when it raised the price of EpiPen to over $600.
Marathon Pharmaceuticals spent $230,000, which was $120,000 more than last year. Marathon was criticized in February after setting the price of Emflaza, a steroid to treat Duchenne muscular dystrophy, at $89,000 a year. That angered advocates, Congress, and patients who had been importing the same drug for as little as $1,000 a year. Marathon has since sold the drug to another company, and the price may come down.
Teva and Shire also more than doubled their spending. Teva was accused, as part of an alleged generic price-fixing scheme in December, and the Federal Trade Commission sued Shire because one of its recently acquired companies allegedly filed “sham” petitions with the Food and Drug Administration to stave off generics.
Companies that make drugs for rare diseases also more than doubled lobbying dollars as congressional leaders and the Government Accountability Office work to determine whether the Orphan Drug Act is being abused. Those firms include BioMarin, Celgene, and Vertex Pharmaceuticals. Celgene, which makes a rare cancer drug, more than tripled its first quarter lobbying to more than $1 million.
Despite efforts to make good on campaign promises to repeal the Affordable Care Act, House Republicans canceled a floor vote on the American Health Care Act in March after multiple studies estimated that millions of people would lose coverage if it passed, and neither Democrats nor ultraconservatives lined up in opposition to the bill’s provisions. Drug prices weren’t a key part of the package.
KHN’s coverage of prescription drug development, costs, and pricing is supported in part by the Laura and John Arnold Foundation. Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Blood donor age, sex do not affect recipient survival
The age and sex of blood donors do not affect the recipient’s survival and do not need to be considered in blood allocation, according to a report published online April 24 in JAMA Internal Medicine.
A recent observational Canadian study suggested that blood from young donors and female donors increased the recipients’ risk of death – a finding which, if confirmed, would have immediate implications for medical practice.
A separate group of Scandinavian researchers attempted to replicate these findings by performing a retrospective cohort study using similar but more nuanced statistical methods. Gustaf Edgren, MD, PhD, of the department of medical epidemiology and biostatistics, Karolinska Institutet, Stockholm, and his associates analyzed information collected on 968,264 patients over a 10-year period from a Swedish and Danish transfusion database.
In initial, unadjusted analyses, both extremes of age (young and old) and female sex in the donor were associated with reduced survival in the recipient. However, that association disappeared when the data were adjusted to account for the total number of transfusions a patient received, a marker of their severity of illness. The hazard ratio per transfusion from a donor younger than age 20 was 0.98, and the hazard ratio per transfusion from a female donor was 0.99. This pattern also occurred in sensitivity analyses, the investigators noted (JAMA Intern. Med. 2017 April 24. doi: 10.1001/jamainternmed.2017.0890).
“When studying associations between ... transfusions with a particular characteristic and the risk of death in the recipient, [the] underlying disease severity ... may still confound the association. However, with meticulous adjustment for total number of transfusions, it should be possible to block the confounding effect of patient disease severity entirely,” they noted.
“We believe that, rather than reflecting true biologic effects, the Canadian results can be explained by residual confounding (i.e., that the observations resulted from incomplete adjustment for the number of transfusions),” Dr. Edgren and his associates said.
“In addition, we believe these data reinforce the importance of extreme caution in assessing epidemiologic analyses in this field, given the tremendous clinical and logistical implications of false-positive findings,” they added.
The findings of Edgren et al. provide reassurance regarding the safety of current transfusion practice.
They present a convincing argument that differences in the statistical approach for controlling confounding likely explained the discrepant results of the Canadian study and their study.
This subtle confounding stems from the fact that increased transfusions expose the recipient to a greater total number of blood products, which in turn is associated with higher comorbidity, greater severity of illness, and higher mortality.
Nareg Roubinian, MD, is at the Blood Systems Research Institute, San Francisco, and in the division of research at Kaiser Permanente Northern California, Oakland. He and his associates reported having no relevant financial disclosures. They made these remarks in an invited commentary accompanying Dr. Edgren’s report (JAMA Intern. Med. 2017 April 24. doi: 10.1001/jamainternmed.2017.0914).
The findings of Edgren et al. provide reassurance regarding the safety of current transfusion practice.
They present a convincing argument that differences in the statistical approach for controlling confounding likely explained the discrepant results of the Canadian study and their study.
This subtle confounding stems from the fact that increased transfusions expose the recipient to a greater total number of blood products, which in turn is associated with higher comorbidity, greater severity of illness, and higher mortality.
Nareg Roubinian, MD, is at the Blood Systems Research Institute, San Francisco, and in the division of research at Kaiser Permanente Northern California, Oakland. He and his associates reported having no relevant financial disclosures. They made these remarks in an invited commentary accompanying Dr. Edgren’s report (JAMA Intern. Med. 2017 April 24. doi: 10.1001/jamainternmed.2017.0914).
The findings of Edgren et al. provide reassurance regarding the safety of current transfusion practice.
They present a convincing argument that differences in the statistical approach for controlling confounding likely explained the discrepant results of the Canadian study and their study.
This subtle confounding stems from the fact that increased transfusions expose the recipient to a greater total number of blood products, which in turn is associated with higher comorbidity, greater severity of illness, and higher mortality.
Nareg Roubinian, MD, is at the Blood Systems Research Institute, San Francisco, and in the division of research at Kaiser Permanente Northern California, Oakland. He and his associates reported having no relevant financial disclosures. They made these remarks in an invited commentary accompanying Dr. Edgren’s report (JAMA Intern. Med. 2017 April 24. doi: 10.1001/jamainternmed.2017.0914).
The age and sex of blood donors do not affect the recipient’s survival and do not need to be considered in blood allocation, according to a report published online April 24 in JAMA Internal Medicine.
A recent observational Canadian study suggested that blood from young donors and female donors increased the recipients’ risk of death – a finding which, if confirmed, would have immediate implications for medical practice.
A separate group of Scandinavian researchers attempted to replicate these findings by performing a retrospective cohort study using similar but more nuanced statistical methods. Gustaf Edgren, MD, PhD, of the department of medical epidemiology and biostatistics, Karolinska Institutet, Stockholm, and his associates analyzed information collected on 968,264 patients over a 10-year period from a Swedish and Danish transfusion database.
In initial, unadjusted analyses, both extremes of age (young and old) and female sex in the donor were associated with reduced survival in the recipient. However, that association disappeared when the data were adjusted to account for the total number of transfusions a patient received, a marker of their severity of illness. The hazard ratio per transfusion from a donor younger than age 20 was 0.98, and the hazard ratio per transfusion from a female donor was 0.99. This pattern also occurred in sensitivity analyses, the investigators noted (JAMA Intern. Med. 2017 April 24. doi: 10.1001/jamainternmed.2017.0890).
“When studying associations between ... transfusions with a particular characteristic and the risk of death in the recipient, [the] underlying disease severity ... may still confound the association. However, with meticulous adjustment for total number of transfusions, it should be possible to block the confounding effect of patient disease severity entirely,” they noted.
“We believe that, rather than reflecting true biologic effects, the Canadian results can be explained by residual confounding (i.e., that the observations resulted from incomplete adjustment for the number of transfusions),” Dr. Edgren and his associates said.
“In addition, we believe these data reinforce the importance of extreme caution in assessing epidemiologic analyses in this field, given the tremendous clinical and logistical implications of false-positive findings,” they added.
The age and sex of blood donors do not affect the recipient’s survival and do not need to be considered in blood allocation, according to a report published online April 24 in JAMA Internal Medicine.
A recent observational Canadian study suggested that blood from young donors and female donors increased the recipients’ risk of death – a finding which, if confirmed, would have immediate implications for medical practice.
A separate group of Scandinavian researchers attempted to replicate these findings by performing a retrospective cohort study using similar but more nuanced statistical methods. Gustaf Edgren, MD, PhD, of the department of medical epidemiology and biostatistics, Karolinska Institutet, Stockholm, and his associates analyzed information collected on 968,264 patients over a 10-year period from a Swedish and Danish transfusion database.
In initial, unadjusted analyses, both extremes of age (young and old) and female sex in the donor were associated with reduced survival in the recipient. However, that association disappeared when the data were adjusted to account for the total number of transfusions a patient received, a marker of their severity of illness. The hazard ratio per transfusion from a donor younger than age 20 was 0.98, and the hazard ratio per transfusion from a female donor was 0.99. This pattern also occurred in sensitivity analyses, the investigators noted (JAMA Intern. Med. 2017 April 24. doi: 10.1001/jamainternmed.2017.0890).
“When studying associations between ... transfusions with a particular characteristic and the risk of death in the recipient, [the] underlying disease severity ... may still confound the association. However, with meticulous adjustment for total number of transfusions, it should be possible to block the confounding effect of patient disease severity entirely,” they noted.
“We believe that, rather than reflecting true biologic effects, the Canadian results can be explained by residual confounding (i.e., that the observations resulted from incomplete adjustment for the number of transfusions),” Dr. Edgren and his associates said.
“In addition, we believe these data reinforce the importance of extreme caution in assessing epidemiologic analyses in this field, given the tremendous clinical and logistical implications of false-positive findings,” they added.
Key clinical point: The age and sex of blood donors do not affect the recipient’s survival and do not need to be considered in blood allocation.
Major finding: The hazard ratio per transfusion from a donor younger than age 20 was 0.98, and the hazard ratio per transfusion from a female donor was 0.99.
Data source: A retrospective cohort study involving 968,264 transfusion recipients in Sweden and Denmark during a 10-year period.
Disclosures: The Swedish Research Council, the Swedish Heart-Lung Foundation, the Swedish Society for Medical Research, Karolinska Institutet’s Strategic Research Program, and the Danish Council for Independent Research supported the study. Dr. Edgren and his associates reported having no relevant financial disclosures.
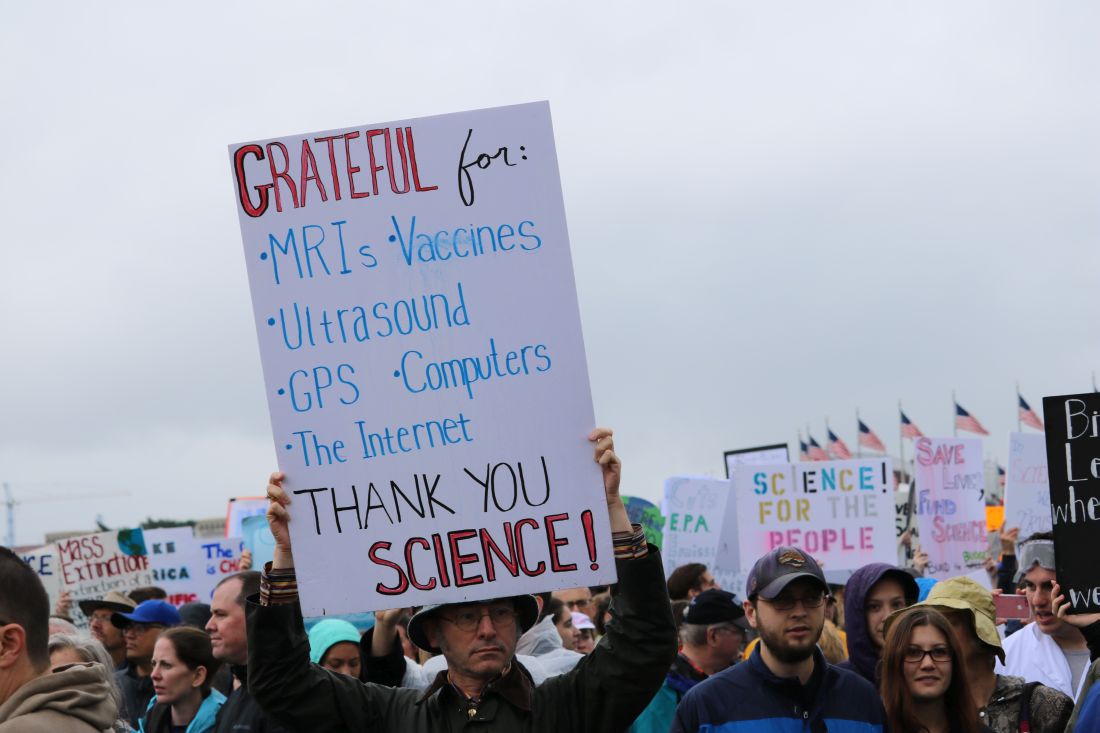
Science advocates take to D.C. streets in March for Science
WASHINGTON – Crowds of protesters packed the Washington’s National Mall for the March for Science, joining participants in 600 cities across the world on Saturday, April 22.
Advocates came in droves, braving the rain armed with homemade signs, chants, and a passion for peer review, to champion the scientific method and the importance of its role in society and policy making.
The event, organized by March for Science, Earth Day Network, and a robust list of advocacy groups and think tanks, started with learning sessions hosted in tents located beyond the Washington Monument, where experts in topics from physics to environmental science informed attendees about the importance of their subjects.
To the left of the tents, directly across from the White House, scores gathered around a large stage, where 56 science professionals from different fields came together to promote the importance of scientific research and science-based policy.
The main stage event was emceed by musician Questlove and Tyler DeWitt, PhD, host of the YouTube science education show “Science with Tyler DeWitt.”
“You cannot criticize a public that doesn’t understand science if we can’t explain it,” said Dr. DeWitt.
“A strong commitment to research is absolutely essential to crafting evidence-based policies to protect us from serious health threats,” said Georges C. Benjamin, MD, executive director of the America Public Health Association. “A nation that ignores science, that denies science, that underfunds science, does so at its own peril.”
Speakers like Kellan Baker, senior fellow with the LGBT Research and Communications Project at the Center for American Progress, promoted political action, echoing organizers’ intentions of being bipartisan but not shying away from promoting political action.
“Advocacy is not a dirty word” said Mr. Baker. “Science is objective, but it is not neutral.”
Other speakers included Mona Hanna-Attisha, MD, the pediatrician who helped expose the lead poisoning situation in Flint, Mich., and Bill Nye, CEO of the Planetary Society and host of the Netflix series “Bill Nye Saves the World.”
After speeches, protesters marched from the Washington Monument to the U.S. Capitol, chanting loudly and waving signs.
March for Science and its partners are continuing to promote advocacy through a “week of action” scheduled to run through April 29.
*This article was updated May 2, 2017.
[email protected]
On Twitter @eaztweets
WASHINGTON – Crowds of protesters packed the Washington’s National Mall for the March for Science, joining participants in 600 cities across the world on Saturday, April 22.
Advocates came in droves, braving the rain armed with homemade signs, chants, and a passion for peer review, to champion the scientific method and the importance of its role in society and policy making.
The event, organized by March for Science, Earth Day Network, and a robust list of advocacy groups and think tanks, started with learning sessions hosted in tents located beyond the Washington Monument, where experts in topics from physics to environmental science informed attendees about the importance of their subjects.
To the left of the tents, directly across from the White House, scores gathered around a large stage, where 56 science professionals from different fields came together to promote the importance of scientific research and science-based policy.
The main stage event was emceed by musician Questlove and Tyler DeWitt, PhD, host of the YouTube science education show “Science with Tyler DeWitt.”
“You cannot criticize a public that doesn’t understand science if we can’t explain it,” said Dr. DeWitt.
“A strong commitment to research is absolutely essential to crafting evidence-based policies to protect us from serious health threats,” said Georges C. Benjamin, MD, executive director of the America Public Health Association. “A nation that ignores science, that denies science, that underfunds science, does so at its own peril.”
Speakers like Kellan Baker, senior fellow with the LGBT Research and Communications Project at the Center for American Progress, promoted political action, echoing organizers’ intentions of being bipartisan but not shying away from promoting political action.
“Advocacy is not a dirty word” said Mr. Baker. “Science is objective, but it is not neutral.”
Other speakers included Mona Hanna-Attisha, MD, the pediatrician who helped expose the lead poisoning situation in Flint, Mich., and Bill Nye, CEO of the Planetary Society and host of the Netflix series “Bill Nye Saves the World.”
After speeches, protesters marched from the Washington Monument to the U.S. Capitol, chanting loudly and waving signs.
March for Science and its partners are continuing to promote advocacy through a “week of action” scheduled to run through April 29.
*This article was updated May 2, 2017.
[email protected]
On Twitter @eaztweets
WASHINGTON – Crowds of protesters packed the Washington’s National Mall for the March for Science, joining participants in 600 cities across the world on Saturday, April 22.
Advocates came in droves, braving the rain armed with homemade signs, chants, and a passion for peer review, to champion the scientific method and the importance of its role in society and policy making.
The event, organized by March for Science, Earth Day Network, and a robust list of advocacy groups and think tanks, started with learning sessions hosted in tents located beyond the Washington Monument, where experts in topics from physics to environmental science informed attendees about the importance of their subjects.
To the left of the tents, directly across from the White House, scores gathered around a large stage, where 56 science professionals from different fields came together to promote the importance of scientific research and science-based policy.
The main stage event was emceed by musician Questlove and Tyler DeWitt, PhD, host of the YouTube science education show “Science with Tyler DeWitt.”
“You cannot criticize a public that doesn’t understand science if we can’t explain it,” said Dr. DeWitt.
“A strong commitment to research is absolutely essential to crafting evidence-based policies to protect us from serious health threats,” said Georges C. Benjamin, MD, executive director of the America Public Health Association. “A nation that ignores science, that denies science, that underfunds science, does so at its own peril.”
Speakers like Kellan Baker, senior fellow with the LGBT Research and Communications Project at the Center for American Progress, promoted political action, echoing organizers’ intentions of being bipartisan but not shying away from promoting political action.
“Advocacy is not a dirty word” said Mr. Baker. “Science is objective, but it is not neutral.”
Other speakers included Mona Hanna-Attisha, MD, the pediatrician who helped expose the lead poisoning situation in Flint, Mich., and Bill Nye, CEO of the Planetary Society and host of the Netflix series “Bill Nye Saves the World.”
After speeches, protesters marched from the Washington Monument to the U.S. Capitol, chanting loudly and waving signs.
March for Science and its partners are continuing to promote advocacy through a “week of action” scheduled to run through April 29.
*This article was updated May 2, 2017.
[email protected]
On Twitter @eaztweets
VIDEO: Geeks brave rain to March for Science
WASHINGTON – Peaceful protesters in hundreds of cities around the globe gathered on Earth Day, April 22, to voice their support for evidence-based policies and funding for scientific research at the March for Science.
In Washington, thousands of participants gathered on the rainy National Mall for teach-ins and speeches, then marched from the Washington Monument to Capitol Hill. A key concern for marchers here was cuts in science agency funding in the Trump administration’s budget proposal for fiscal year 2018.
Organizers now are calling on supporters to participate in a week of action to continue to demonstrate widespread support for their positions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @denisefulton
WASHINGTON – Peaceful protesters in hundreds of cities around the globe gathered on Earth Day, April 22, to voice their support for evidence-based policies and funding for scientific research at the March for Science.
In Washington, thousands of participants gathered on the rainy National Mall for teach-ins and speeches, then marched from the Washington Monument to Capitol Hill. A key concern for marchers here was cuts in science agency funding in the Trump administration’s budget proposal for fiscal year 2018.
Organizers now are calling on supporters to participate in a week of action to continue to demonstrate widespread support for their positions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @denisefulton
WASHINGTON – Peaceful protesters in hundreds of cities around the globe gathered on Earth Day, April 22, to voice their support for evidence-based policies and funding for scientific research at the March for Science.
In Washington, thousands of participants gathered on the rainy National Mall for teach-ins and speeches, then marched from the Washington Monument to Capitol Hill. A key concern for marchers here was cuts in science agency funding in the Trump administration’s budget proposal for fiscal year 2018.
Organizers now are calling on supporters to participate in a week of action to continue to demonstrate widespread support for their positions.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @denisefulton
EHR price alert doesn’t reduce lab orders
Displaying Medicare allowable fees in the electronic health record at the time of order entry did not significantly reduce the number of inpatient lab tests at three Philadelphia hospitals.
In a study involving 98,529 patients and 142,921 admissions, Medicare payment information popped up randomly in the EHR when standard tests including complete blood cell counts, metabolic panels, and liver function tests were ordered. The costs of the labs varied depending on their extent. The message mentioned that “the dollar amount represents Medicare reimbursement for the test. Actual costs to the consumer may vary by patient insurance status.” Just over a third of the patients were actually on Medicare; most had private insurance.
The idea of the study was to see if cost information would curb unnecessary testing, and save money. “There is growing interest in using price transparency to influence medical decision-making toward higher value care,” Mina Sedrak, MD, and her colleagues said in a paper presented at the annual meeting of the Society of General Internal Medicine.
It didn’t work out that way. Four tests ordered per patient day when the messages appeared, and 2.34 when they did not. With messaging, the mean lab fee per patient day was $38.85, versus $27.59 without it. In an adjusted analyses comparing the intervention to the control group, there were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
In a subset analysis, the investigators did find a small decrease orders for the most expensive labs and a small but significant increase in orders for the least expensive ones when physicians aware of cost (top quartile of tests based on fee value: -0.01; P = .04; bottom quartile: 0.03, P = .04).
Despite the overall negative results, there’s still a likely role for cost information in value improvement programs; what the study shows is that there’s a better way to use it, according to Dr. Sedrak, currently of the City of Hope Comprehensive Cancer Center in Duarte, Calif., and colleagues.
The investigators made several suggestions when reviewing their work.
“First, the price transparency intervention in this study was always displayed regardless of the clinical scenario. The presence of this information for appropriate tests may have diminished its impact when tests were inappropriate. Future efforts may consider more selective targeting of price transparency.” It might also be a good idea to price out different testing options for providers, and use actual charges and other more on-point forms of cost estimates, they said, instead of Medicare fees that have little to do with what many patients are actually charged. Targeting only the most expensive tests might also help (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1144).
The investigators also noticed a problem when labs are ordered to repeat automatically; clinicians did not see the price information every day, and so missed cost information “when it would be most salient.”
The mean age in the study was 54.7 years; 52% of the patients were white, 39% black, and 57% women. The mean length of stay was about 6 days, and over 80% of the patients were discharged home.
The authors evaluated what happens when one randomizes which tests have price information; other studies examine what happens when one randomizes which physicians have price information. All contemporary studies conclude the same – no effect of price information on physician ordering behavior.
One possible conclusion is that making health care prices available at the point of care is not an effective strategy to decrease wasteful spending, yet we believe this is not the case.
The disconnect suggests that current price transparency initiatives are not enough to infuse clinical care with price information and encourage consumers and physicians to consider the value of health care decisions. This does not mean we should give up on increased price transparency in health care. Rather, a more thoughtful approach to the design, point of delivery, and context for health care price information is needed to achieve the promise of price transparency.
Little has been done to deliver [out-of-pocket cost] information to patients at the time when patients are making health care decisions. Also, if both patients and physicians could see prices for episodes or bundles of care, then it could allow them to assess value together. Future interventions need to deliver price and quality information together.
Anna Sinaiko, PhD, is a research scientist at the Harvard School of Public Health, Boston. Alyna Chien, MD, is an assistant professor of pediatrics at the Harvard Medical School and a healthcare quality researcher. They made their comments in an editorial, and had no relevant disclosures (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1676 ).
The authors evaluated what happens when one randomizes which tests have price information; other studies examine what happens when one randomizes which physicians have price information. All contemporary studies conclude the same – no effect of price information on physician ordering behavior.
One possible conclusion is that making health care prices available at the point of care is not an effective strategy to decrease wasteful spending, yet we believe this is not the case.
The disconnect suggests that current price transparency initiatives are not enough to infuse clinical care with price information and encourage consumers and physicians to consider the value of health care decisions. This does not mean we should give up on increased price transparency in health care. Rather, a more thoughtful approach to the design, point of delivery, and context for health care price information is needed to achieve the promise of price transparency.
Little has been done to deliver [out-of-pocket cost] information to patients at the time when patients are making health care decisions. Also, if both patients and physicians could see prices for episodes or bundles of care, then it could allow them to assess value together. Future interventions need to deliver price and quality information together.
Anna Sinaiko, PhD, is a research scientist at the Harvard School of Public Health, Boston. Alyna Chien, MD, is an assistant professor of pediatrics at the Harvard Medical School and a healthcare quality researcher. They made their comments in an editorial, and had no relevant disclosures (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1676 ).
The authors evaluated what happens when one randomizes which tests have price information; other studies examine what happens when one randomizes which physicians have price information. All contemporary studies conclude the same – no effect of price information on physician ordering behavior.
One possible conclusion is that making health care prices available at the point of care is not an effective strategy to decrease wasteful spending, yet we believe this is not the case.
The disconnect suggests that current price transparency initiatives are not enough to infuse clinical care with price information and encourage consumers and physicians to consider the value of health care decisions. This does not mean we should give up on increased price transparency in health care. Rather, a more thoughtful approach to the design, point of delivery, and context for health care price information is needed to achieve the promise of price transparency.
Little has been done to deliver [out-of-pocket cost] information to patients at the time when patients are making health care decisions. Also, if both patients and physicians could see prices for episodes or bundles of care, then it could allow them to assess value together. Future interventions need to deliver price and quality information together.
Anna Sinaiko, PhD, is a research scientist at the Harvard School of Public Health, Boston. Alyna Chien, MD, is an assistant professor of pediatrics at the Harvard Medical School and a healthcare quality researcher. They made their comments in an editorial, and had no relevant disclosures (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1676 ).
Displaying Medicare allowable fees in the electronic health record at the time of order entry did not significantly reduce the number of inpatient lab tests at three Philadelphia hospitals.
In a study involving 98,529 patients and 142,921 admissions, Medicare payment information popped up randomly in the EHR when standard tests including complete blood cell counts, metabolic panels, and liver function tests were ordered. The costs of the labs varied depending on their extent. The message mentioned that “the dollar amount represents Medicare reimbursement for the test. Actual costs to the consumer may vary by patient insurance status.” Just over a third of the patients were actually on Medicare; most had private insurance.
The idea of the study was to see if cost information would curb unnecessary testing, and save money. “There is growing interest in using price transparency to influence medical decision-making toward higher value care,” Mina Sedrak, MD, and her colleagues said in a paper presented at the annual meeting of the Society of General Internal Medicine.
It didn’t work out that way. Four tests ordered per patient day when the messages appeared, and 2.34 when they did not. With messaging, the mean lab fee per patient day was $38.85, versus $27.59 without it. In an adjusted analyses comparing the intervention to the control group, there were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
In a subset analysis, the investigators did find a small decrease orders for the most expensive labs and a small but significant increase in orders for the least expensive ones when physicians aware of cost (top quartile of tests based on fee value: -0.01; P = .04; bottom quartile: 0.03, P = .04).
Despite the overall negative results, there’s still a likely role for cost information in value improvement programs; what the study shows is that there’s a better way to use it, according to Dr. Sedrak, currently of the City of Hope Comprehensive Cancer Center in Duarte, Calif., and colleagues.
The investigators made several suggestions when reviewing their work.
“First, the price transparency intervention in this study was always displayed regardless of the clinical scenario. The presence of this information for appropriate tests may have diminished its impact when tests were inappropriate. Future efforts may consider more selective targeting of price transparency.” It might also be a good idea to price out different testing options for providers, and use actual charges and other more on-point forms of cost estimates, they said, instead of Medicare fees that have little to do with what many patients are actually charged. Targeting only the most expensive tests might also help (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1144).
The investigators also noticed a problem when labs are ordered to repeat automatically; clinicians did not see the price information every day, and so missed cost information “when it would be most salient.”
The mean age in the study was 54.7 years; 52% of the patients were white, 39% black, and 57% women. The mean length of stay was about 6 days, and over 80% of the patients were discharged home.
Displaying Medicare allowable fees in the electronic health record at the time of order entry did not significantly reduce the number of inpatient lab tests at three Philadelphia hospitals.
In a study involving 98,529 patients and 142,921 admissions, Medicare payment information popped up randomly in the EHR when standard tests including complete blood cell counts, metabolic panels, and liver function tests were ordered. The costs of the labs varied depending on their extent. The message mentioned that “the dollar amount represents Medicare reimbursement for the test. Actual costs to the consumer may vary by patient insurance status.” Just over a third of the patients were actually on Medicare; most had private insurance.
The idea of the study was to see if cost information would curb unnecessary testing, and save money. “There is growing interest in using price transparency to influence medical decision-making toward higher value care,” Mina Sedrak, MD, and her colleagues said in a paper presented at the annual meeting of the Society of General Internal Medicine.
It didn’t work out that way. Four tests ordered per patient day when the messages appeared, and 2.34 when they did not. With messaging, the mean lab fee per patient day was $38.85, versus $27.59 without it. In an adjusted analyses comparing the intervention to the control group, there were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
In a subset analysis, the investigators did find a small decrease orders for the most expensive labs and a small but significant increase in orders for the least expensive ones when physicians aware of cost (top quartile of tests based on fee value: -0.01; P = .04; bottom quartile: 0.03, P = .04).
Despite the overall negative results, there’s still a likely role for cost information in value improvement programs; what the study shows is that there’s a better way to use it, according to Dr. Sedrak, currently of the City of Hope Comprehensive Cancer Center in Duarte, Calif., and colleagues.
The investigators made several suggestions when reviewing their work.
“First, the price transparency intervention in this study was always displayed regardless of the clinical scenario. The presence of this information for appropriate tests may have diminished its impact when tests were inappropriate. Future efforts may consider more selective targeting of price transparency.” It might also be a good idea to price out different testing options for providers, and use actual charges and other more on-point forms of cost estimates, they said, instead of Medicare fees that have little to do with what many patients are actually charged. Targeting only the most expensive tests might also help (JAMA Intern Med. 2017 April 21. doi: 10.1001/jamainternmed.2017.1144).
The investigators also noticed a problem when labs are ordered to repeat automatically; clinicians did not see the price information every day, and so missed cost information “when it would be most salient.”
The mean age in the study was 54.7 years; 52% of the patients were white, 39% black, and 57% women. The mean length of stay was about 6 days, and over 80% of the patients were discharged home.
Key clinical point:
Major finding: There were no significant changes in overall test ordering (0.05 tests ordered per patient day, P = .06) or associated fees when pricing information was displayed ($0.24 per patient day; P = .47).
Data source: Analysis involving 98,529 patients and 142,921 admissions of the effect of Medicare reimbursement information on lab test ordering
Disclosures: This study was funded by the University of Pennsylvania Health System. The senior investigator Mitesh Patel, MD, an assistant professor of medicine at the University of Pennsylvania, Philadelphia, is a principal at Catalyst Health, a technology and behavioral change consulting firm. The authors had no other disclosures.
High early stroke risk for adult congenital heart disease
WASHINGTON – Adults with congenital heart disease are at fourfold greater risk of experiencing an ischemic stroke by age 60 than is the general population, Mette Glavind reported at the annual meeting of the American College of Cardiology.
She presented a population-based study that included all 14,710 Danish adults with congenital heart disease (ACHD) diagnosed in 1963-1994. Taking advantage of Denmark’s comprehensive system of linked national registries, she and her coinvestigators created a control group consisting of 144,735 age- and birth year–matched individuals from the general population.
During follow-up, a total of 2,868 Danes included in the study had an ischemic stroke. The cumulative incidence of ischemic stroke in the ACHD cohort was 0.8% by age 30 and 8.2% by age 60, compared with 0.09% and 2.9%, respectively, in controls, according to Ms. Glavind, a medical student at Aarhus (Denmark) University.
The median age at diagnosis of stroke was 52 years in the ACHD group and 69 years in controls. The risk of early ischemic stroke – defined as stroke at age 18-60 – was increased by 3.97-fold in the ACHD group, compared with controls. The risk of stroke after age 60 was increased by 1.68-fold.
Stroke was more likely to prove fatal in the ACHD group. Their 30-day stroke mortality rate was 10%, compared with 9.6% in controls. This corresponded to an adjusted 44% increased risk of stroke mortality, which was statistically significant.
The severity of congenital heart disease modified the stroke risk. Patients with mild or moderate ACHD had a 3.25-fold increased risk of early stroke, compared with controls, while those with severe or univentricular ACHD were at 5.97-fold greater risk.
For purposes of this study, mild ACHD was defined as a biventricular defect that was not repaired surgically or percutaneously. Moderate ACHD was considered to have biventricular pathophysiology with surgical or percutaneous intervention. The severe ACHD category was reserved for cases involving complex biventricular abnormalities.
By these definitions, 41% of patients had mild ACHD, 21% moderate, 22% severe, and 1% univentricular ACHD; the rest of the patients were unclassified.
This study was supported by Aarhus University and Cincinnati Children’s Hospital. Ms. Glavind reported having no financial conflicts.
WASHINGTON – Adults with congenital heart disease are at fourfold greater risk of experiencing an ischemic stroke by age 60 than is the general population, Mette Glavind reported at the annual meeting of the American College of Cardiology.
She presented a population-based study that included all 14,710 Danish adults with congenital heart disease (ACHD) diagnosed in 1963-1994. Taking advantage of Denmark’s comprehensive system of linked national registries, she and her coinvestigators created a control group consisting of 144,735 age- and birth year–matched individuals from the general population.
During follow-up, a total of 2,868 Danes included in the study had an ischemic stroke. The cumulative incidence of ischemic stroke in the ACHD cohort was 0.8% by age 30 and 8.2% by age 60, compared with 0.09% and 2.9%, respectively, in controls, according to Ms. Glavind, a medical student at Aarhus (Denmark) University.
The median age at diagnosis of stroke was 52 years in the ACHD group and 69 years in controls. The risk of early ischemic stroke – defined as stroke at age 18-60 – was increased by 3.97-fold in the ACHD group, compared with controls. The risk of stroke after age 60 was increased by 1.68-fold.
Stroke was more likely to prove fatal in the ACHD group. Their 30-day stroke mortality rate was 10%, compared with 9.6% in controls. This corresponded to an adjusted 44% increased risk of stroke mortality, which was statistically significant.
The severity of congenital heart disease modified the stroke risk. Patients with mild or moderate ACHD had a 3.25-fold increased risk of early stroke, compared with controls, while those with severe or univentricular ACHD were at 5.97-fold greater risk.
For purposes of this study, mild ACHD was defined as a biventricular defect that was not repaired surgically or percutaneously. Moderate ACHD was considered to have biventricular pathophysiology with surgical or percutaneous intervention. The severe ACHD category was reserved for cases involving complex biventricular abnormalities.
By these definitions, 41% of patients had mild ACHD, 21% moderate, 22% severe, and 1% univentricular ACHD; the rest of the patients were unclassified.
This study was supported by Aarhus University and Cincinnati Children’s Hospital. Ms. Glavind reported having no financial conflicts.
WASHINGTON – Adults with congenital heart disease are at fourfold greater risk of experiencing an ischemic stroke by age 60 than is the general population, Mette Glavind reported at the annual meeting of the American College of Cardiology.
She presented a population-based study that included all 14,710 Danish adults with congenital heart disease (ACHD) diagnosed in 1963-1994. Taking advantage of Denmark’s comprehensive system of linked national registries, she and her coinvestigators created a control group consisting of 144,735 age- and birth year–matched individuals from the general population.
During follow-up, a total of 2,868 Danes included in the study had an ischemic stroke. The cumulative incidence of ischemic stroke in the ACHD cohort was 0.8% by age 30 and 8.2% by age 60, compared with 0.09% and 2.9%, respectively, in controls, according to Ms. Glavind, a medical student at Aarhus (Denmark) University.
The median age at diagnosis of stroke was 52 years in the ACHD group and 69 years in controls. The risk of early ischemic stroke – defined as stroke at age 18-60 – was increased by 3.97-fold in the ACHD group, compared with controls. The risk of stroke after age 60 was increased by 1.68-fold.
Stroke was more likely to prove fatal in the ACHD group. Their 30-day stroke mortality rate was 10%, compared with 9.6% in controls. This corresponded to an adjusted 44% increased risk of stroke mortality, which was statistically significant.
The severity of congenital heart disease modified the stroke risk. Patients with mild or moderate ACHD had a 3.25-fold increased risk of early stroke, compared with controls, while those with severe or univentricular ACHD were at 5.97-fold greater risk.
For purposes of this study, mild ACHD was defined as a biventricular defect that was not repaired surgically or percutaneously. Moderate ACHD was considered to have biventricular pathophysiology with surgical or percutaneous intervention. The severe ACHD category was reserved for cases involving complex biventricular abnormalities.
By these definitions, 41% of patients had mild ACHD, 21% moderate, 22% severe, and 1% univentricular ACHD; the rest of the patients were unclassified.
This study was supported by Aarhus University and Cincinnati Children’s Hospital. Ms. Glavind reported having no financial conflicts.
AT ACC 2017
Key clinical point:
Major finding: Danish adults with complex biventricular congenital heart disease were sixfold more likely to have an ischemic stroke by age 60 years, compared with the general population.
Data source: A population-based registry study that included all Danish adults with congenital heart disease diagnosed in 1963-1994 and nearly 145,000 age- and birth year–matched controls drawn from the general Danish population.
Disclosures: This study was supported by Aarhus University and Cincinnati Children’s Hospital. The presenter reported having no financial conflicts.
Can public reporting improve pediatric heart surgery?
Public reporting of cardiac surgery outcomes has been a disruptive force in cardiology, and especially daunting in pediatric cardiac surgery because of low case volumes and rare mortality. To ensure that public reporting achieves its original goals – providing transparency to the patient care process, holding providers accountable, informing decision making for health care consumers, reducing costs, encouraging more efficient use of health system resources, and improving patient care and outcomes – further study that includes use of appropriate risk adjustment is needed, according to commentaries in the April issue of the Journal of Thoracic and Cardiovascular Surgery.
The journal asked two groups to provide perspective on a study Adam D. DeVore, MD, of Duke University in Durham, N.C., and his coauthors published last year (J Am Coll Cardiol. 2016 Mar 1;67:963-72). The study analyzed Medicare claims data from 2006 to 2012 for 37,829 hospitalizations for heart attack, 100,189 for heart failure (HF), and 79,076 for pneumonia. Dr. DeVore and his colleagues found readmission rates for the three conditions did not significantly improve after public reporting protocols were implemented in 2009. However, the study did show a significant decrease in ED visits and observation stays for those with HF: from 2.3% to –0.8% for the former (P = .007); and from 15% to 4% for the latter (P = .04).
• The metrics must be accurate, reliably discern hospital quality, and account for high-risk cases without penalizing hospitals. “In pediatric cardiac surgery, this can be particularly challenging, owing to the very wide heterogeneity of disease and variability in case mix and volumes across centers,” Dr. Gaynor and his coauthors wrote. While methodology for case mix and patient characteristics have improved in recent years, further improvement is needed.
• Metrics must be clearly reported and easy for stakeholders to interpret. “This is critical if the data are to be used to steer patients toward higher-performing centers and/or to provide incentives for hospitals with lower performance to make improvements,” the researchers said.
• Regional reporting or a methodology that indicates where a hospital ranks within larger categories deserve further investigation as tools to help families choose a high-performing center, “ideally based on geography and on the particular type and complexity of disease,” Dr. Gaynor and his coauthors stated (J Thorac Cardiovasc Surg. 2017 Apr;153:904-7).
• Indirect standardization, a statistical methodology used to calculate risk-adjusted performance, could help consumers to interpret hospital performance more easily. This methodology might help classify a hospital with a low-complexity population as a high performer. “Developing better methods to convey this information to consumers is vital,” according to the researchers.
The perspective acknowledged several reports of an unintended consequence of public reporting: surgeons and centers avoiding higher-risk cases to skew their performance scores higher, thus restricting access to care. However, in a separate perspective on Dr. DeVore’s study, James S. Tweddell, MD, of Cincinnati Children’s Hospital Medical Center, and his coauthors, questioned the quality of the evidence on which Dr. Gaynor and his colleagues based their conclusion of risk aversion and limited access to care: a newspaper report from the United Kingdom.
Dr. Tweddell and his coauthors noted, “The predominance of data suggest an overall beneficial impact of public reporting.” They cited a trial that showed a decrease in heart attack–related deaths after public reporting had been implemented (JAMA. 2009 Dec 2;302:2330-7); a 2012 Agency for Healthcare Research and Quality systemic review (Evidence Report No. 208) that showed that research on harm is limited, and most studies do not confirm potential harm; and a meta-analysis that found a 15% reduction in adverse events associated with public reporting (BMC Health Serv Res. 2016;16:296).
“Appropriate risk adjustment is critical to achieve effective and fair transparency, but there is little objective data of harm associated with public reporting,” Dr. Tweddell and his coauthors concluded. While examination of public reporting must continue, they said, “these efforts are likely to result in minor course changes and the effort to inform and educate our patients and their families must continue.”
Ds. Gaynor, Dr. Tweddell, and their coauthors reported having no financial disclosures.
Public reporting of cardiac surgery outcomes has been a disruptive force in cardiology, and especially daunting in pediatric cardiac surgery because of low case volumes and rare mortality. To ensure that public reporting achieves its original goals – providing transparency to the patient care process, holding providers accountable, informing decision making for health care consumers, reducing costs, encouraging more efficient use of health system resources, and improving patient care and outcomes – further study that includes use of appropriate risk adjustment is needed, according to commentaries in the April issue of the Journal of Thoracic and Cardiovascular Surgery.
The journal asked two groups to provide perspective on a study Adam D. DeVore, MD, of Duke University in Durham, N.C., and his coauthors published last year (J Am Coll Cardiol. 2016 Mar 1;67:963-72). The study analyzed Medicare claims data from 2006 to 2012 for 37,829 hospitalizations for heart attack, 100,189 for heart failure (HF), and 79,076 for pneumonia. Dr. DeVore and his colleagues found readmission rates for the three conditions did not significantly improve after public reporting protocols were implemented in 2009. However, the study did show a significant decrease in ED visits and observation stays for those with HF: from 2.3% to –0.8% for the former (P = .007); and from 15% to 4% for the latter (P = .04).
• The metrics must be accurate, reliably discern hospital quality, and account for high-risk cases without penalizing hospitals. “In pediatric cardiac surgery, this can be particularly challenging, owing to the very wide heterogeneity of disease and variability in case mix and volumes across centers,” Dr. Gaynor and his coauthors wrote. While methodology for case mix and patient characteristics have improved in recent years, further improvement is needed.
• Metrics must be clearly reported and easy for stakeholders to interpret. “This is critical if the data are to be used to steer patients toward higher-performing centers and/or to provide incentives for hospitals with lower performance to make improvements,” the researchers said.
• Regional reporting or a methodology that indicates where a hospital ranks within larger categories deserve further investigation as tools to help families choose a high-performing center, “ideally based on geography and on the particular type and complexity of disease,” Dr. Gaynor and his coauthors stated (J Thorac Cardiovasc Surg. 2017 Apr;153:904-7).
• Indirect standardization, a statistical methodology used to calculate risk-adjusted performance, could help consumers to interpret hospital performance more easily. This methodology might help classify a hospital with a low-complexity population as a high performer. “Developing better methods to convey this information to consumers is vital,” according to the researchers.
The perspective acknowledged several reports of an unintended consequence of public reporting: surgeons and centers avoiding higher-risk cases to skew their performance scores higher, thus restricting access to care. However, in a separate perspective on Dr. DeVore’s study, James S. Tweddell, MD, of Cincinnati Children’s Hospital Medical Center, and his coauthors, questioned the quality of the evidence on which Dr. Gaynor and his colleagues based their conclusion of risk aversion and limited access to care: a newspaper report from the United Kingdom.
Dr. Tweddell and his coauthors noted, “The predominance of data suggest an overall beneficial impact of public reporting.” They cited a trial that showed a decrease in heart attack–related deaths after public reporting had been implemented (JAMA. 2009 Dec 2;302:2330-7); a 2012 Agency for Healthcare Research and Quality systemic review (Evidence Report No. 208) that showed that research on harm is limited, and most studies do not confirm potential harm; and a meta-analysis that found a 15% reduction in adverse events associated with public reporting (BMC Health Serv Res. 2016;16:296).
“Appropriate risk adjustment is critical to achieve effective and fair transparency, but there is little objective data of harm associated with public reporting,” Dr. Tweddell and his coauthors concluded. While examination of public reporting must continue, they said, “these efforts are likely to result in minor course changes and the effort to inform and educate our patients and their families must continue.”
Ds. Gaynor, Dr. Tweddell, and their coauthors reported having no financial disclosures.
Public reporting of cardiac surgery outcomes has been a disruptive force in cardiology, and especially daunting in pediatric cardiac surgery because of low case volumes and rare mortality. To ensure that public reporting achieves its original goals – providing transparency to the patient care process, holding providers accountable, informing decision making for health care consumers, reducing costs, encouraging more efficient use of health system resources, and improving patient care and outcomes – further study that includes use of appropriate risk adjustment is needed, according to commentaries in the April issue of the Journal of Thoracic and Cardiovascular Surgery.
The journal asked two groups to provide perspective on a study Adam D. DeVore, MD, of Duke University in Durham, N.C., and his coauthors published last year (J Am Coll Cardiol. 2016 Mar 1;67:963-72). The study analyzed Medicare claims data from 2006 to 2012 for 37,829 hospitalizations for heart attack, 100,189 for heart failure (HF), and 79,076 for pneumonia. Dr. DeVore and his colleagues found readmission rates for the three conditions did not significantly improve after public reporting protocols were implemented in 2009. However, the study did show a significant decrease in ED visits and observation stays for those with HF: from 2.3% to –0.8% for the former (P = .007); and from 15% to 4% for the latter (P = .04).
• The metrics must be accurate, reliably discern hospital quality, and account for high-risk cases without penalizing hospitals. “In pediatric cardiac surgery, this can be particularly challenging, owing to the very wide heterogeneity of disease and variability in case mix and volumes across centers,” Dr. Gaynor and his coauthors wrote. While methodology for case mix and patient characteristics have improved in recent years, further improvement is needed.
• Metrics must be clearly reported and easy for stakeholders to interpret. “This is critical if the data are to be used to steer patients toward higher-performing centers and/or to provide incentives for hospitals with lower performance to make improvements,” the researchers said.
• Regional reporting or a methodology that indicates where a hospital ranks within larger categories deserve further investigation as tools to help families choose a high-performing center, “ideally based on geography and on the particular type and complexity of disease,” Dr. Gaynor and his coauthors stated (J Thorac Cardiovasc Surg. 2017 Apr;153:904-7).
• Indirect standardization, a statistical methodology used to calculate risk-adjusted performance, could help consumers to interpret hospital performance more easily. This methodology might help classify a hospital with a low-complexity population as a high performer. “Developing better methods to convey this information to consumers is vital,” according to the researchers.
The perspective acknowledged several reports of an unintended consequence of public reporting: surgeons and centers avoiding higher-risk cases to skew their performance scores higher, thus restricting access to care. However, in a separate perspective on Dr. DeVore’s study, James S. Tweddell, MD, of Cincinnati Children’s Hospital Medical Center, and his coauthors, questioned the quality of the evidence on which Dr. Gaynor and his colleagues based their conclusion of risk aversion and limited access to care: a newspaper report from the United Kingdom.
Dr. Tweddell and his coauthors noted, “The predominance of data suggest an overall beneficial impact of public reporting.” They cited a trial that showed a decrease in heart attack–related deaths after public reporting had been implemented (JAMA. 2009 Dec 2;302:2330-7); a 2012 Agency for Healthcare Research and Quality systemic review (Evidence Report No. 208) that showed that research on harm is limited, and most studies do not confirm potential harm; and a meta-analysis that found a 15% reduction in adverse events associated with public reporting (BMC Health Serv Res. 2016;16:296).
“Appropriate risk adjustment is critical to achieve effective and fair transparency, but there is little objective data of harm associated with public reporting,” Dr. Tweddell and his coauthors concluded. While examination of public reporting must continue, they said, “these efforts are likely to result in minor course changes and the effort to inform and educate our patients and their families must continue.”
Ds. Gaynor, Dr. Tweddell, and their coauthors reported having no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Public reporting of outcomes in cardiac surgery in children requires further investigation but has also been associated with improved outcomes.
Major finding: Emergency department visits for patients with heart failure declined from 2.3% before public reporting to –0.8% after implementation, and observation stays declined from 15.1% to 4.1%.
Data source: Analysis of Medicare claims data from 2006 to 2012 for 271,094 patients discharged after hospitalization for heart attack, heart failure or pneumonia.
Disclosures: Dr. Gaynor and Dr. Tweddell had no financial relationships to disclose.
AATS publishes guidelines for infective endocarditis
Infective endocarditis (IE) is a devastating complication of heart valve disease that, left untreated, can be fatal. Management requires a multidisciplinary approach, and many of the respective medical societies that represent the participating specialties have developed guidelines. Now, the American Association for Thoracic Surgery has published “Consensus Guidelines for the Surgical Treatment of Infective Endocarditis” to guide thoracic and cardiovascular surgeons in making decisions of when to operate in cases of IE (J Thorac Cardiovasc Surg. 2017 Jan 24. doi: 10.1016/j.jtcvs.2016.09.093).
The rationale for developing the guidelines is a growing prevalence of IE, including in patients with normal valves and no previous diagnosis of heart disease. “These new AATS consensus guidelines primarily address questions related to active and suspected active IE affective valves and intracardiac structures,” Dr. Pettersson and his coauthors said. The AATS guidelines for infective endocarditis address complications including risk of embolism and the timing of surgery in patients with neurological complications, while acknowledging the the need for additional research into these topics.* “It is understood that surgery is beneficial only if the patient’s complications and other comorbidities do not preclude survival and meaningful recovery,” the guideline authors said.
The guidelines confirm the team approach for managing patients with IE. The team should include cardiology, infectious disease, cardiac surgery, and other specialties needed to handle IE-related complications (class of recommendation [COR] I, level of evidence [LOE] B). Before surgery, the surgeon should know the patient is on effective antimicrobial therapy (COR I, LOE B). Transesophageal echocardiography (TEE) is indicated to yield the clearest understanding of the pathology (COR I, LOE B).
Dr. Pettersson and the guideline writing team also clarified indications for surgery in patients with IE. They include when valve dysfunction causes heart failure (COR I, LOE B); when, after a full course of antibiotics, the patient has signs of heart block, annular or aortic abscess or destructive penetrating lesions (COR I, LOE B); and in the setting of recurrent emboli and persistent vegetations despite appropriate antibiotic therapy (COR IIA, LOE B).
The guideline writers acknowledged potential disagreement between the AATS guidelines and those of the American College of Cardiology/American Heart Association with regard to early surgery in IE. Debate surrounds whether to operate early or wait for symptoms of heart failure to manifest in patients with native valve endocarditis (NVE). The AATS guideline authors cite work by Duk-Hyun Kang, MD, PhD, and coauthors in South Korea (N Engl J Med. 2012;366;2466-73) and others advocating for early surgery. “For this reason, once a surgical indication is evident, surgery should not be delayed,” Dr. Pettersson and his coauthors said.
Several conditions can influence the timing of surgery. Patients with cerebral mycotic aneurysm should be managed closely with neurology or neurosurgery (COR I, LOE C). Patients with a recent intracranial hemorrhage should wait at least 3 weeks for surgery (COR IIA, LOE B), but those with nonhemorrhagic strokes could go in for urgent surgery (COR IIA, LOE B). Brain imaging is indicated for IE patients with neurological symptoms (COR I, LOE B), but anticoagulation management requires a nuanced approach that takes all risks and benefits into consideration (COR I, LOE C).
Key steps during surgery involve mandatory intraoperative TEE (COR I, LOE B), median sternotomy with few exceptions (COR I, LOE B), and radical debridement and removal of all infected and necrotic tissue (COR I, LOE B). The writers also provided four guidelines for reconstruction and valve replacement:
- Repair when possible for patients with NVE (COR I, LOE B).
- When replacement is indicated, the surgeon should base valve choice on normal criteria – age, life expectancy, comorbidities, and expected compliance with anticoagulation (COR I, LOE B).
- Avoid use of mechanical valves in patients with intracranial bleeding or who have had a major stroke (COR IIA, LOE C).
- In patients with invasive disease and deconstruction, reconstruction should depend on the involved valve, severity of destruction, and available options for cardiac reconstruction (COR I, LOE B).
The AATS guidelines also challenge conventional thinking on the practice of soaking a gel-impregnated graft with antimicrobials targeting a specific organism. “We found no evidence to support this practice,” Dr. Pettersson and his coauthors said (COR IIB, LOE B). They came to the same conclusion with regard to the use of local antimicrobials or antiseptics during irrigation after debridement and local injection of antimicrobials around the infected area (COR I, LOE C).
The guidelines provide direction on a host of other surgical issues in IE: use of aortic valve grafts; when to remove or replace noninfected grafts; when to remove pacemakers; the role of drainage; postoperative management; follow-up; and additional screening. They also shed insight into what the guideline authors call “residual controversies,” including surgery for injection drug users (use “all available resources and options for drug rehabilitation”) and dialysis patients (“it is reasonable to offer surgery when the additional burden of comorbidities is not overwhelming”). They also acknowledge seven different scenarios that lack clear evidence for intervention but require the surgeon to determine the need for surgery, ranging from timing of surgery for IE in patients with neurologic complications to how to treat patients with functional valve issues after being cured of IE.
The guideline writers acknowledged that institutional funds supported the work. Dr. Pettersson had no financial relationships to disclose.
*Correction 5/172017: It was incorrectly stated that these complications were not addressed in the guidelines due to lack of evidence
Whether they’re intended to or not, guidelines like the AATS Consensus Guidelines for the Surgical Treatment of Infected Endocarditis “can evolve into hard and fast principles, sometimes leading to incorrect decision making and even creating medicolegal problems for treating physicians,” Gus J. Vlahakes, MD, of Harvard Medical School and Massachusetts General Hospital, Boston, said in his invited commentary (J Thorac Cardiovasc Surg. 2016 Nov 3. doi: 10.1016/j.jtcvs.2016.10.041).
Guidelines cannot “integrate all the necessary considerations,” Dr. Vlahakes said, so surgeons should view them as “a set of general principles to guide decision making.” In IE, that means having an experienced cardiac surgeon who can apply the guidelines on a case-by-case basis and a multidisciplinary team that includes an infectious disease specialist, he said. The surgeon must participate in preoperative management.
Dr. Vlahakes had no relevant financial disclosures.
Whether they’re intended to or not, guidelines like the AATS Consensus Guidelines for the Surgical Treatment of Infected Endocarditis “can evolve into hard and fast principles, sometimes leading to incorrect decision making and even creating medicolegal problems for treating physicians,” Gus J. Vlahakes, MD, of Harvard Medical School and Massachusetts General Hospital, Boston, said in his invited commentary (J Thorac Cardiovasc Surg. 2016 Nov 3. doi: 10.1016/j.jtcvs.2016.10.041).
Guidelines cannot “integrate all the necessary considerations,” Dr. Vlahakes said, so surgeons should view them as “a set of general principles to guide decision making.” In IE, that means having an experienced cardiac surgeon who can apply the guidelines on a case-by-case basis and a multidisciplinary team that includes an infectious disease specialist, he said. The surgeon must participate in preoperative management.
Dr. Vlahakes had no relevant financial disclosures.
Whether they’re intended to or not, guidelines like the AATS Consensus Guidelines for the Surgical Treatment of Infected Endocarditis “can evolve into hard and fast principles, sometimes leading to incorrect decision making and even creating medicolegal problems for treating physicians,” Gus J. Vlahakes, MD, of Harvard Medical School and Massachusetts General Hospital, Boston, said in his invited commentary (J Thorac Cardiovasc Surg. 2016 Nov 3. doi: 10.1016/j.jtcvs.2016.10.041).
Guidelines cannot “integrate all the necessary considerations,” Dr. Vlahakes said, so surgeons should view them as “a set of general principles to guide decision making.” In IE, that means having an experienced cardiac surgeon who can apply the guidelines on a case-by-case basis and a multidisciplinary team that includes an infectious disease specialist, he said. The surgeon must participate in preoperative management.
Dr. Vlahakes had no relevant financial disclosures.
Infective endocarditis (IE) is a devastating complication of heart valve disease that, left untreated, can be fatal. Management requires a multidisciplinary approach, and many of the respective medical societies that represent the participating specialties have developed guidelines. Now, the American Association for Thoracic Surgery has published “Consensus Guidelines for the Surgical Treatment of Infective Endocarditis” to guide thoracic and cardiovascular surgeons in making decisions of when to operate in cases of IE (J Thorac Cardiovasc Surg. 2017 Jan 24. doi: 10.1016/j.jtcvs.2016.09.093).
The rationale for developing the guidelines is a growing prevalence of IE, including in patients with normal valves and no previous diagnosis of heart disease. “These new AATS consensus guidelines primarily address questions related to active and suspected active IE affective valves and intracardiac structures,” Dr. Pettersson and his coauthors said. The AATS guidelines for infective endocarditis address complications including risk of embolism and the timing of surgery in patients with neurological complications, while acknowledging the the need for additional research into these topics.* “It is understood that surgery is beneficial only if the patient’s complications and other comorbidities do not preclude survival and meaningful recovery,” the guideline authors said.
The guidelines confirm the team approach for managing patients with IE. The team should include cardiology, infectious disease, cardiac surgery, and other specialties needed to handle IE-related complications (class of recommendation [COR] I, level of evidence [LOE] B). Before surgery, the surgeon should know the patient is on effective antimicrobial therapy (COR I, LOE B). Transesophageal echocardiography (TEE) is indicated to yield the clearest understanding of the pathology (COR I, LOE B).
Dr. Pettersson and the guideline writing team also clarified indications for surgery in patients with IE. They include when valve dysfunction causes heart failure (COR I, LOE B); when, after a full course of antibiotics, the patient has signs of heart block, annular or aortic abscess or destructive penetrating lesions (COR I, LOE B); and in the setting of recurrent emboli and persistent vegetations despite appropriate antibiotic therapy (COR IIA, LOE B).
The guideline writers acknowledged potential disagreement between the AATS guidelines and those of the American College of Cardiology/American Heart Association with regard to early surgery in IE. Debate surrounds whether to operate early or wait for symptoms of heart failure to manifest in patients with native valve endocarditis (NVE). The AATS guideline authors cite work by Duk-Hyun Kang, MD, PhD, and coauthors in South Korea (N Engl J Med. 2012;366;2466-73) and others advocating for early surgery. “For this reason, once a surgical indication is evident, surgery should not be delayed,” Dr. Pettersson and his coauthors said.
Several conditions can influence the timing of surgery. Patients with cerebral mycotic aneurysm should be managed closely with neurology or neurosurgery (COR I, LOE C). Patients with a recent intracranial hemorrhage should wait at least 3 weeks for surgery (COR IIA, LOE B), but those with nonhemorrhagic strokes could go in for urgent surgery (COR IIA, LOE B). Brain imaging is indicated for IE patients with neurological symptoms (COR I, LOE B), but anticoagulation management requires a nuanced approach that takes all risks and benefits into consideration (COR I, LOE C).
Key steps during surgery involve mandatory intraoperative TEE (COR I, LOE B), median sternotomy with few exceptions (COR I, LOE B), and radical debridement and removal of all infected and necrotic tissue (COR I, LOE B). The writers also provided four guidelines for reconstruction and valve replacement:
- Repair when possible for patients with NVE (COR I, LOE B).
- When replacement is indicated, the surgeon should base valve choice on normal criteria – age, life expectancy, comorbidities, and expected compliance with anticoagulation (COR I, LOE B).
- Avoid use of mechanical valves in patients with intracranial bleeding or who have had a major stroke (COR IIA, LOE C).
- In patients with invasive disease and deconstruction, reconstruction should depend on the involved valve, severity of destruction, and available options for cardiac reconstruction (COR I, LOE B).
The AATS guidelines also challenge conventional thinking on the practice of soaking a gel-impregnated graft with antimicrobials targeting a specific organism. “We found no evidence to support this practice,” Dr. Pettersson and his coauthors said (COR IIB, LOE B). They came to the same conclusion with regard to the use of local antimicrobials or antiseptics during irrigation after debridement and local injection of antimicrobials around the infected area (COR I, LOE C).
The guidelines provide direction on a host of other surgical issues in IE: use of aortic valve grafts; when to remove or replace noninfected grafts; when to remove pacemakers; the role of drainage; postoperative management; follow-up; and additional screening. They also shed insight into what the guideline authors call “residual controversies,” including surgery for injection drug users (use “all available resources and options for drug rehabilitation”) and dialysis patients (“it is reasonable to offer surgery when the additional burden of comorbidities is not overwhelming”). They also acknowledge seven different scenarios that lack clear evidence for intervention but require the surgeon to determine the need for surgery, ranging from timing of surgery for IE in patients with neurologic complications to how to treat patients with functional valve issues after being cured of IE.
The guideline writers acknowledged that institutional funds supported the work. Dr. Pettersson had no financial relationships to disclose.
*Correction 5/172017: It was incorrectly stated that these complications were not addressed in the guidelines due to lack of evidence
Infective endocarditis (IE) is a devastating complication of heart valve disease that, left untreated, can be fatal. Management requires a multidisciplinary approach, and many of the respective medical societies that represent the participating specialties have developed guidelines. Now, the American Association for Thoracic Surgery has published “Consensus Guidelines for the Surgical Treatment of Infective Endocarditis” to guide thoracic and cardiovascular surgeons in making decisions of when to operate in cases of IE (J Thorac Cardiovasc Surg. 2017 Jan 24. doi: 10.1016/j.jtcvs.2016.09.093).
The rationale for developing the guidelines is a growing prevalence of IE, including in patients with normal valves and no previous diagnosis of heart disease. “These new AATS consensus guidelines primarily address questions related to active and suspected active IE affective valves and intracardiac structures,” Dr. Pettersson and his coauthors said. The AATS guidelines for infective endocarditis address complications including risk of embolism and the timing of surgery in patients with neurological complications, while acknowledging the the need for additional research into these topics.* “It is understood that surgery is beneficial only if the patient’s complications and other comorbidities do not preclude survival and meaningful recovery,” the guideline authors said.
The guidelines confirm the team approach for managing patients with IE. The team should include cardiology, infectious disease, cardiac surgery, and other specialties needed to handle IE-related complications (class of recommendation [COR] I, level of evidence [LOE] B). Before surgery, the surgeon should know the patient is on effective antimicrobial therapy (COR I, LOE B). Transesophageal echocardiography (TEE) is indicated to yield the clearest understanding of the pathology (COR I, LOE B).
Dr. Pettersson and the guideline writing team also clarified indications for surgery in patients with IE. They include when valve dysfunction causes heart failure (COR I, LOE B); when, after a full course of antibiotics, the patient has signs of heart block, annular or aortic abscess or destructive penetrating lesions (COR I, LOE B); and in the setting of recurrent emboli and persistent vegetations despite appropriate antibiotic therapy (COR IIA, LOE B).
The guideline writers acknowledged potential disagreement between the AATS guidelines and those of the American College of Cardiology/American Heart Association with regard to early surgery in IE. Debate surrounds whether to operate early or wait for symptoms of heart failure to manifest in patients with native valve endocarditis (NVE). The AATS guideline authors cite work by Duk-Hyun Kang, MD, PhD, and coauthors in South Korea (N Engl J Med. 2012;366;2466-73) and others advocating for early surgery. “For this reason, once a surgical indication is evident, surgery should not be delayed,” Dr. Pettersson and his coauthors said.
Several conditions can influence the timing of surgery. Patients with cerebral mycotic aneurysm should be managed closely with neurology or neurosurgery (COR I, LOE C). Patients with a recent intracranial hemorrhage should wait at least 3 weeks for surgery (COR IIA, LOE B), but those with nonhemorrhagic strokes could go in for urgent surgery (COR IIA, LOE B). Brain imaging is indicated for IE patients with neurological symptoms (COR I, LOE B), but anticoagulation management requires a nuanced approach that takes all risks and benefits into consideration (COR I, LOE C).
Key steps during surgery involve mandatory intraoperative TEE (COR I, LOE B), median sternotomy with few exceptions (COR I, LOE B), and radical debridement and removal of all infected and necrotic tissue (COR I, LOE B). The writers also provided four guidelines for reconstruction and valve replacement:
- Repair when possible for patients with NVE (COR I, LOE B).
- When replacement is indicated, the surgeon should base valve choice on normal criteria – age, life expectancy, comorbidities, and expected compliance with anticoagulation (COR I, LOE B).
- Avoid use of mechanical valves in patients with intracranial bleeding or who have had a major stroke (COR IIA, LOE C).
- In patients with invasive disease and deconstruction, reconstruction should depend on the involved valve, severity of destruction, and available options for cardiac reconstruction (COR I, LOE B).
The AATS guidelines also challenge conventional thinking on the practice of soaking a gel-impregnated graft with antimicrobials targeting a specific organism. “We found no evidence to support this practice,” Dr. Pettersson and his coauthors said (COR IIB, LOE B). They came to the same conclusion with regard to the use of local antimicrobials or antiseptics during irrigation after debridement and local injection of antimicrobials around the infected area (COR I, LOE C).
The guidelines provide direction on a host of other surgical issues in IE: use of aortic valve grafts; when to remove or replace noninfected grafts; when to remove pacemakers; the role of drainage; postoperative management; follow-up; and additional screening. They also shed insight into what the guideline authors call “residual controversies,” including surgery for injection drug users (use “all available resources and options for drug rehabilitation”) and dialysis patients (“it is reasonable to offer surgery when the additional burden of comorbidities is not overwhelming”). They also acknowledge seven different scenarios that lack clear evidence for intervention but require the surgeon to determine the need for surgery, ranging from timing of surgery for IE in patients with neurologic complications to how to treat patients with functional valve issues after being cured of IE.
The guideline writers acknowledged that institutional funds supported the work. Dr. Pettersson had no financial relationships to disclose.
*Correction 5/172017: It was incorrectly stated that these complications were not addressed in the guidelines due to lack of evidence
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The American Association for Thoracic Surgery charged a committee of eight members to author “Consensus Guidelines: Surgical Treatment of Infective Endocarditis.”
Major finding: Patients with infective endocarditis need early input from the responsible cardiac surgeon, who must also lead the care team in evaluation, decision- making, and ultimately carrying out surgery as needed.
Data source: The writing committee followed Institute of Medicine standards for clinical practice guidelines, invited comment from a group of 12 multidisciplinary specialists and reviewed 288 articles in drafting the guidelines.
Disclosures: Institutional funds supported the work. Dr. Pettersson and his coauthors had no financial relationships to disclose.
As some holdout states revisit Medicaid expansion, new data show it pays off
Although the GOP-controlled Congress is pledging its continued interest – despite stalls and snags – in dismantling Obamacare, some “red state” legislatures are changing course and showing a newfound interest in embracing the health law’s Medicaid expansion.
And a study published April 12 in Health Affairs adds to these discussions, percolating in places such as Kansas, Georgia, Virginia, North Carolina, and Maine. Thirty-one states plus the District of Columbia already opted to pursue the expansion, which provided federal funding to broaden eligibility to include most low-income adults with incomes up to 138 percent of the federal poverty level (about $16,000 for an individual).
Researchers analyzed data from the National Association of State Budget Officers for fiscal years 2010-2015 to assess the fiscal effects of expansion’s first 2 years.
Their findings address arguments put forth by some GOP lawmakers, who say the expansion will add to the nation’s budget deficit and saddle states with additional coverage costs, forcing them to skimp on other budget priorities like education or transportation.
The researchers concluded that when states expanded eligibility for the low-income health insurance program they did see larger health care expenditures – but those costs were covered with federal funding. In addition, expansion states didn’t have to skimp on other policy priorities – such as environment, housing, and other public health initiatives – to make ends meet.
“This is a potential big benefit, not only to people who get coverage, but to state economies,” said Benjamin Sommers, MD, PhD, an associate professor of health policy and economics at Harvard University’s public health school, and the study’s first author.
This finding – that states expanding Medicaid didn’t encounter unforeseen budget problems – shouldn’t be surprising.
“Expansion is basically free” to the states, agreed Massachusetts Institute of Technology economist Jonathan Gruber, PhD, one of Obamacare’s architects who worked with Dr. Sommers to systematically compare the budgets of all 50 states to examine Medicaid expansion’s impact. “That’s the big insight,” he said. “There’s no sort of hidden downside.”
And that may be part of what’s fueling this renewed interest, said Edwin Park, vice president for health policy at the left-leaning Center for Budget and Policy Priorities. These states are seeing the federal windfall their neighbors received while trying to navigate public health concerns like opioid addiction, he said. They “are looking at how their neighbors or expansion states have done and see the benefits,” Mr. Park said. “The primary argument against the expansion on the state level has been it’s going to break the bank. The research demonstrates that’s not the case.”
But a caveat: The data used in this analysis reflected only years during which the federal government picked up 100% of the tab for expanding Medicaid eligibility and therefore could overestimate the benefit to state budgets. That’s because in 2017 that federal support begins to taper off, and by 2020 states have to pay 10 percent of the expansion costs themselves.
That means policymakers should exert caution in reading too much into this study, said Tom Miller, a resident fellow at the conservative American Enterprise Institute. Because states will eventually shoulder more of the cost, he said, studies that assess its budgetary impact are preliminary at best. Plus, Miller said, other factors such as relative economic growth could have padded state budgets in the years studied – masking any unintended costs with a bigger Medicaid program. It’s unclear whether in times of downturn Medicaid would take a bigger bite out of state budgets.
“It’s just the beginning of this – it’s an early snapshot,” he said.
Dr. Sommers argued the limited data set means researchers should continue to track how state budgets compare between expansion and nonexpansion states. But even when states do take on more of Medicaid’s cost, that may not pose such a burden, suggested Sara Rosenbaum, a professor of health law and policy at George Washington University. Expanding Medicaid brings in other potential economic benefits that this paper doesn’t account for – less uncompensated care in hospitals, for instance – that could offset the expenditures states ultimately take up.
A bigger concern, some experts say, is that – even without the Obamacare repeal – some GOP health proposals would change the federal government’s Medicaid funding mechanism from being an open-ended match to a block grant or per-capita cap in an effort to curb national spending. Those proposals would take away at least some of the federal dollars that have insulated state budgets.
“Ironically, all the arguments that have been made against expansion for years – like creating a hole in the state budget or breaking the bank – that’s exactly what a per-capita grant or block grant does,” Park said.
As more states take on the Medicaid debate, those consequences matter, both Dr. Sommers and Dr. Gruber said. And not just for state budgets – for consumers, too.
“The main lesson is there’s no sort of big hidden cost of expanding Medicaid. What you see is what you get,” Dr. Gruber said. “You get free health insurance for your citizens.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Although the GOP-controlled Congress is pledging its continued interest – despite stalls and snags – in dismantling Obamacare, some “red state” legislatures are changing course and showing a newfound interest in embracing the health law’s Medicaid expansion.
And a study published April 12 in Health Affairs adds to these discussions, percolating in places such as Kansas, Georgia, Virginia, North Carolina, and Maine. Thirty-one states plus the District of Columbia already opted to pursue the expansion, which provided federal funding to broaden eligibility to include most low-income adults with incomes up to 138 percent of the federal poverty level (about $16,000 for an individual).
Researchers analyzed data from the National Association of State Budget Officers for fiscal years 2010-2015 to assess the fiscal effects of expansion’s first 2 years.
Their findings address arguments put forth by some GOP lawmakers, who say the expansion will add to the nation’s budget deficit and saddle states with additional coverage costs, forcing them to skimp on other budget priorities like education or transportation.
The researchers concluded that when states expanded eligibility for the low-income health insurance program they did see larger health care expenditures – but those costs were covered with federal funding. In addition, expansion states didn’t have to skimp on other policy priorities – such as environment, housing, and other public health initiatives – to make ends meet.
“This is a potential big benefit, not only to people who get coverage, but to state economies,” said Benjamin Sommers, MD, PhD, an associate professor of health policy and economics at Harvard University’s public health school, and the study’s first author.
This finding – that states expanding Medicaid didn’t encounter unforeseen budget problems – shouldn’t be surprising.
“Expansion is basically free” to the states, agreed Massachusetts Institute of Technology economist Jonathan Gruber, PhD, one of Obamacare’s architects who worked with Dr. Sommers to systematically compare the budgets of all 50 states to examine Medicaid expansion’s impact. “That’s the big insight,” he said. “There’s no sort of hidden downside.”
And that may be part of what’s fueling this renewed interest, said Edwin Park, vice president for health policy at the left-leaning Center for Budget and Policy Priorities. These states are seeing the federal windfall their neighbors received while trying to navigate public health concerns like opioid addiction, he said. They “are looking at how their neighbors or expansion states have done and see the benefits,” Mr. Park said. “The primary argument against the expansion on the state level has been it’s going to break the bank. The research demonstrates that’s not the case.”
But a caveat: The data used in this analysis reflected only years during which the federal government picked up 100% of the tab for expanding Medicaid eligibility and therefore could overestimate the benefit to state budgets. That’s because in 2017 that federal support begins to taper off, and by 2020 states have to pay 10 percent of the expansion costs themselves.
That means policymakers should exert caution in reading too much into this study, said Tom Miller, a resident fellow at the conservative American Enterprise Institute. Because states will eventually shoulder more of the cost, he said, studies that assess its budgetary impact are preliminary at best. Plus, Miller said, other factors such as relative economic growth could have padded state budgets in the years studied – masking any unintended costs with a bigger Medicaid program. It’s unclear whether in times of downturn Medicaid would take a bigger bite out of state budgets.
“It’s just the beginning of this – it’s an early snapshot,” he said.
Dr. Sommers argued the limited data set means researchers should continue to track how state budgets compare between expansion and nonexpansion states. But even when states do take on more of Medicaid’s cost, that may not pose such a burden, suggested Sara Rosenbaum, a professor of health law and policy at George Washington University. Expanding Medicaid brings in other potential economic benefits that this paper doesn’t account for – less uncompensated care in hospitals, for instance – that could offset the expenditures states ultimately take up.
A bigger concern, some experts say, is that – even without the Obamacare repeal – some GOP health proposals would change the federal government’s Medicaid funding mechanism from being an open-ended match to a block grant or per-capita cap in an effort to curb national spending. Those proposals would take away at least some of the federal dollars that have insulated state budgets.
“Ironically, all the arguments that have been made against expansion for years – like creating a hole in the state budget or breaking the bank – that’s exactly what a per-capita grant or block grant does,” Park said.
As more states take on the Medicaid debate, those consequences matter, both Dr. Sommers and Dr. Gruber said. And not just for state budgets – for consumers, too.
“The main lesson is there’s no sort of big hidden cost of expanding Medicaid. What you see is what you get,” Dr. Gruber said. “You get free health insurance for your citizens.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Although the GOP-controlled Congress is pledging its continued interest – despite stalls and snags – in dismantling Obamacare, some “red state” legislatures are changing course and showing a newfound interest in embracing the health law’s Medicaid expansion.
And a study published April 12 in Health Affairs adds to these discussions, percolating in places such as Kansas, Georgia, Virginia, North Carolina, and Maine. Thirty-one states plus the District of Columbia already opted to pursue the expansion, which provided federal funding to broaden eligibility to include most low-income adults with incomes up to 138 percent of the federal poverty level (about $16,000 for an individual).
Researchers analyzed data from the National Association of State Budget Officers for fiscal years 2010-2015 to assess the fiscal effects of expansion’s first 2 years.
Their findings address arguments put forth by some GOP lawmakers, who say the expansion will add to the nation’s budget deficit and saddle states with additional coverage costs, forcing them to skimp on other budget priorities like education or transportation.
The researchers concluded that when states expanded eligibility for the low-income health insurance program they did see larger health care expenditures – but those costs were covered with federal funding. In addition, expansion states didn’t have to skimp on other policy priorities – such as environment, housing, and other public health initiatives – to make ends meet.
“This is a potential big benefit, not only to people who get coverage, but to state economies,” said Benjamin Sommers, MD, PhD, an associate professor of health policy and economics at Harvard University’s public health school, and the study’s first author.
This finding – that states expanding Medicaid didn’t encounter unforeseen budget problems – shouldn’t be surprising.
“Expansion is basically free” to the states, agreed Massachusetts Institute of Technology economist Jonathan Gruber, PhD, one of Obamacare’s architects who worked with Dr. Sommers to systematically compare the budgets of all 50 states to examine Medicaid expansion’s impact. “That’s the big insight,” he said. “There’s no sort of hidden downside.”
And that may be part of what’s fueling this renewed interest, said Edwin Park, vice president for health policy at the left-leaning Center for Budget and Policy Priorities. These states are seeing the federal windfall their neighbors received while trying to navigate public health concerns like opioid addiction, he said. They “are looking at how their neighbors or expansion states have done and see the benefits,” Mr. Park said. “The primary argument against the expansion on the state level has been it’s going to break the bank. The research demonstrates that’s not the case.”
But a caveat: The data used in this analysis reflected only years during which the federal government picked up 100% of the tab for expanding Medicaid eligibility and therefore could overestimate the benefit to state budgets. That’s because in 2017 that federal support begins to taper off, and by 2020 states have to pay 10 percent of the expansion costs themselves.
That means policymakers should exert caution in reading too much into this study, said Tom Miller, a resident fellow at the conservative American Enterprise Institute. Because states will eventually shoulder more of the cost, he said, studies that assess its budgetary impact are preliminary at best. Plus, Miller said, other factors such as relative economic growth could have padded state budgets in the years studied – masking any unintended costs with a bigger Medicaid program. It’s unclear whether in times of downturn Medicaid would take a bigger bite out of state budgets.
“It’s just the beginning of this – it’s an early snapshot,” he said.
Dr. Sommers argued the limited data set means researchers should continue to track how state budgets compare between expansion and nonexpansion states. But even when states do take on more of Medicaid’s cost, that may not pose such a burden, suggested Sara Rosenbaum, a professor of health law and policy at George Washington University. Expanding Medicaid brings in other potential economic benefits that this paper doesn’t account for – less uncompensated care in hospitals, for instance – that could offset the expenditures states ultimately take up.
A bigger concern, some experts say, is that – even without the Obamacare repeal – some GOP health proposals would change the federal government’s Medicaid funding mechanism from being an open-ended match to a block grant or per-capita cap in an effort to curb national spending. Those proposals would take away at least some of the federal dollars that have insulated state budgets.
“Ironically, all the arguments that have been made against expansion for years – like creating a hole in the state budget or breaking the bank – that’s exactly what a per-capita grant or block grant does,” Park said.
As more states take on the Medicaid debate, those consequences matter, both Dr. Sommers and Dr. Gruber said. And not just for state budgets – for consumers, too.
“The main lesson is there’s no sort of big hidden cost of expanding Medicaid. What you see is what you get,” Dr. Gruber said. “You get free health insurance for your citizens.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Time to reexamine surgery for nonlocalized bronchiectasis
Nonlocalized bronchiectasis is becoming more common in developing countries and has been difficult to treat. While surgery for localized bronchiectasis has been proven, its role in nonlocalized disease is less established; researchers from China are advocating for a reexamination of surgical resection in this disease based on results of a small cohort study at their academic center.
“Lobectomy for the predominant lesion is a safe procedure in the surgical treatment of nonlocalized bronchiectasis and leads to significant relief of symptoms with good rates of satisfaction,” Jie Dai, PhD, of Shanghai (China) Pulmonary Hospital Tongji University and his coauthors reported in the Journal of Thoracic and Cardiovascular Surgery (2017 Apr;153:979-85).
The researchers reviewed the medical records of 37 consecutive patients – 10 men and 27 women – with nonlocalized bronchiectasis who had lobectomies via thoracotomies during 2010-2013. Twenty-three patients (62.2%) were symptom free after surgery and 10 (27%) reported that their symptoms had improved. Four (10.8%) said their symptoms either did not improve or worsened, but three of them also had chronic occlusive pulmonary disease. There were no deaths, and the morbidity rate was 21.6%.
The researchers used three criteria to select candidates for surgery: persistent symptoms despite medical treatment; an identifiable predominant lesion; and cardiopulmonary function compatible with anesthetic risk. Average age was 54.5 years and more than half (19) had no smoking history.
The surgical technique involved a posterolateral thoracotomy and a double-lumen endotracheal tube to avoid contamination of the opposite side of the lung during surgery. Surgery avoided excessive bronchial dissection and preserved peribronchial tissues. Extrapleural dissection avoided spillage of lung contents into the pleural space.
Treatment of the hilum followed an order from the pulmonary artery to the pulmonary vein and then to the bronchus. An ultrasonic device helped isolate and then ligate or sever distorted bronchial arteries. A mechanical stapler was used to close the bronchial stump. Reinforcement involved an intercostal muscle flap in 16 cases and a pedicled parietal pleural flap in 21. If any sign of pleural infection appeared after hemostasis, pleural space irrigation with 0.5% neomycin (500 mg/L) was initiated. Two chest drains were placed at the bronchial stump, and the bronchial suture checked with bronchoscopy. Airway secretions were removed, and pathology confirmed bronchiectasis all specimens.
The frequency of acute infection and hemoptysis decreased significantly at 1 year postoperatively, from 5.3% to 1.8% and 4.9% to 1.1%, respectively, (P less than .01 for both). Daily sputum volume decreased an average of 26.3 mL (P less than .01) and sputum cultures became sterile in 13 (35%) of patients (P less than .01).
Previously, surgery for nonlocalized bronchiectasis had been reserved for life-threatening symptoms only, but Dr. Dai and his coauthors fashioned their study on previous studies of lobectomy that included patients with nonlocalized bronchiectasis (Br J Surg. 2005;92:836-9; Ann Thorac Surg. 2003;75:382-7).
Two major complications occurred in the Shanghai cohort: empyema and persistent air leak, both of which were managed without a reoperation and had been reported in previous series. Dr. Dai and his coauthors have adopted protocols to reduce complications, among them, requiring that patients have sputum output greater than 20 mL/day with little purulence and no engorgement or edema in the tunica mucosa bronchiorum on bronchoscopy.
But the researchers are not ready to extend surgery as a blanket indication for nonlocalized bronchiectasis. “It is worth mentioning that the surgical benefit is limited to patients who have only one predominant area of bronchiectatic disease that can be localized by CT instead of those with diffuse bronchiectasis,” they wrote. “The ideal surgical candidate has a heterogeneous distribution of diseased areas.”
The investigators pointed out that the study was limited by its small size and lack of information on etiologies of disease.
Dr. Dai and his coauthors had no financial relationships to disclose.
The study by Dr. Dai and his coauthors “is an important contribution to the literature” despite its limitations, Steven Milman, MD, and Thomas Ng, MD, of Brown University, Providence, R.I., said in their invited commentary (J Thorac Cardiovasc Surg. 2017 Apr;153:986). However, they added, “Several important points need to be stressed.”
Among those points: The researchers studied a “highly selected group” of young patients with good pulmonary functions; mean follow-up was short (15 months); the etiology of bronchiectasis was unknown; and lobectomy was not the optimal treatment for nonlocalized bronchiectasis. “It must be remembered that these patients first failed medical therapy and that the study population received lobectomy due to the extent of the dominant disease and not as routine treatment,” Dr. Milman and Dr. Ng wrote.
To validate the findings, Dr. Milman and Dr. Ng said, not only do more patients need to be studied with longer follow-up but future investigators also should study minimally invasive approaches to see if that would improve the outcomes.
Dr. Milman and Dr. Ng had no financial relationships to disclose.
The study by Dr. Dai and his coauthors “is an important contribution to the literature” despite its limitations, Steven Milman, MD, and Thomas Ng, MD, of Brown University, Providence, R.I., said in their invited commentary (J Thorac Cardiovasc Surg. 2017 Apr;153:986). However, they added, “Several important points need to be stressed.”
Among those points: The researchers studied a “highly selected group” of young patients with good pulmonary functions; mean follow-up was short (15 months); the etiology of bronchiectasis was unknown; and lobectomy was not the optimal treatment for nonlocalized bronchiectasis. “It must be remembered that these patients first failed medical therapy and that the study population received lobectomy due to the extent of the dominant disease and not as routine treatment,” Dr. Milman and Dr. Ng wrote.
To validate the findings, Dr. Milman and Dr. Ng said, not only do more patients need to be studied with longer follow-up but future investigators also should study minimally invasive approaches to see if that would improve the outcomes.
Dr. Milman and Dr. Ng had no financial relationships to disclose.
The study by Dr. Dai and his coauthors “is an important contribution to the literature” despite its limitations, Steven Milman, MD, and Thomas Ng, MD, of Brown University, Providence, R.I., said in their invited commentary (J Thorac Cardiovasc Surg. 2017 Apr;153:986). However, they added, “Several important points need to be stressed.”
Among those points: The researchers studied a “highly selected group” of young patients with good pulmonary functions; mean follow-up was short (15 months); the etiology of bronchiectasis was unknown; and lobectomy was not the optimal treatment for nonlocalized bronchiectasis. “It must be remembered that these patients first failed medical therapy and that the study population received lobectomy due to the extent of the dominant disease and not as routine treatment,” Dr. Milman and Dr. Ng wrote.
To validate the findings, Dr. Milman and Dr. Ng said, not only do more patients need to be studied with longer follow-up but future investigators also should study minimally invasive approaches to see if that would improve the outcomes.
Dr. Milman and Dr. Ng had no financial relationships to disclose.
Nonlocalized bronchiectasis is becoming more common in developing countries and has been difficult to treat. While surgery for localized bronchiectasis has been proven, its role in nonlocalized disease is less established; researchers from China are advocating for a reexamination of surgical resection in this disease based on results of a small cohort study at their academic center.
“Lobectomy for the predominant lesion is a safe procedure in the surgical treatment of nonlocalized bronchiectasis and leads to significant relief of symptoms with good rates of satisfaction,” Jie Dai, PhD, of Shanghai (China) Pulmonary Hospital Tongji University and his coauthors reported in the Journal of Thoracic and Cardiovascular Surgery (2017 Apr;153:979-85).
The researchers reviewed the medical records of 37 consecutive patients – 10 men and 27 women – with nonlocalized bronchiectasis who had lobectomies via thoracotomies during 2010-2013. Twenty-three patients (62.2%) were symptom free after surgery and 10 (27%) reported that their symptoms had improved. Four (10.8%) said their symptoms either did not improve or worsened, but three of them also had chronic occlusive pulmonary disease. There were no deaths, and the morbidity rate was 21.6%.
The researchers used three criteria to select candidates for surgery: persistent symptoms despite medical treatment; an identifiable predominant lesion; and cardiopulmonary function compatible with anesthetic risk. Average age was 54.5 years and more than half (19) had no smoking history.
The surgical technique involved a posterolateral thoracotomy and a double-lumen endotracheal tube to avoid contamination of the opposite side of the lung during surgery. Surgery avoided excessive bronchial dissection and preserved peribronchial tissues. Extrapleural dissection avoided spillage of lung contents into the pleural space.
Treatment of the hilum followed an order from the pulmonary artery to the pulmonary vein and then to the bronchus. An ultrasonic device helped isolate and then ligate or sever distorted bronchial arteries. A mechanical stapler was used to close the bronchial stump. Reinforcement involved an intercostal muscle flap in 16 cases and a pedicled parietal pleural flap in 21. If any sign of pleural infection appeared after hemostasis, pleural space irrigation with 0.5% neomycin (500 mg/L) was initiated. Two chest drains were placed at the bronchial stump, and the bronchial suture checked with bronchoscopy. Airway secretions were removed, and pathology confirmed bronchiectasis all specimens.
The frequency of acute infection and hemoptysis decreased significantly at 1 year postoperatively, from 5.3% to 1.8% and 4.9% to 1.1%, respectively, (P less than .01 for both). Daily sputum volume decreased an average of 26.3 mL (P less than .01) and sputum cultures became sterile in 13 (35%) of patients (P less than .01).
Previously, surgery for nonlocalized bronchiectasis had been reserved for life-threatening symptoms only, but Dr. Dai and his coauthors fashioned their study on previous studies of lobectomy that included patients with nonlocalized bronchiectasis (Br J Surg. 2005;92:836-9; Ann Thorac Surg. 2003;75:382-7).
Two major complications occurred in the Shanghai cohort: empyema and persistent air leak, both of which were managed without a reoperation and had been reported in previous series. Dr. Dai and his coauthors have adopted protocols to reduce complications, among them, requiring that patients have sputum output greater than 20 mL/day with little purulence and no engorgement or edema in the tunica mucosa bronchiorum on bronchoscopy.
But the researchers are not ready to extend surgery as a blanket indication for nonlocalized bronchiectasis. “It is worth mentioning that the surgical benefit is limited to patients who have only one predominant area of bronchiectatic disease that can be localized by CT instead of those with diffuse bronchiectasis,” they wrote. “The ideal surgical candidate has a heterogeneous distribution of diseased areas.”
The investigators pointed out that the study was limited by its small size and lack of information on etiologies of disease.
Dr. Dai and his coauthors had no financial relationships to disclose.
Nonlocalized bronchiectasis is becoming more common in developing countries and has been difficult to treat. While surgery for localized bronchiectasis has been proven, its role in nonlocalized disease is less established; researchers from China are advocating for a reexamination of surgical resection in this disease based on results of a small cohort study at their academic center.
“Lobectomy for the predominant lesion is a safe procedure in the surgical treatment of nonlocalized bronchiectasis and leads to significant relief of symptoms with good rates of satisfaction,” Jie Dai, PhD, of Shanghai (China) Pulmonary Hospital Tongji University and his coauthors reported in the Journal of Thoracic and Cardiovascular Surgery (2017 Apr;153:979-85).
The researchers reviewed the medical records of 37 consecutive patients – 10 men and 27 women – with nonlocalized bronchiectasis who had lobectomies via thoracotomies during 2010-2013. Twenty-three patients (62.2%) were symptom free after surgery and 10 (27%) reported that their symptoms had improved. Four (10.8%) said their symptoms either did not improve or worsened, but three of them also had chronic occlusive pulmonary disease. There were no deaths, and the morbidity rate was 21.6%.
The researchers used three criteria to select candidates for surgery: persistent symptoms despite medical treatment; an identifiable predominant lesion; and cardiopulmonary function compatible with anesthetic risk. Average age was 54.5 years and more than half (19) had no smoking history.
The surgical technique involved a posterolateral thoracotomy and a double-lumen endotracheal tube to avoid contamination of the opposite side of the lung during surgery. Surgery avoided excessive bronchial dissection and preserved peribronchial tissues. Extrapleural dissection avoided spillage of lung contents into the pleural space.
Treatment of the hilum followed an order from the pulmonary artery to the pulmonary vein and then to the bronchus. An ultrasonic device helped isolate and then ligate or sever distorted bronchial arteries. A mechanical stapler was used to close the bronchial stump. Reinforcement involved an intercostal muscle flap in 16 cases and a pedicled parietal pleural flap in 21. If any sign of pleural infection appeared after hemostasis, pleural space irrigation with 0.5% neomycin (500 mg/L) was initiated. Two chest drains were placed at the bronchial stump, and the bronchial suture checked with bronchoscopy. Airway secretions were removed, and pathology confirmed bronchiectasis all specimens.
The frequency of acute infection and hemoptysis decreased significantly at 1 year postoperatively, from 5.3% to 1.8% and 4.9% to 1.1%, respectively, (P less than .01 for both). Daily sputum volume decreased an average of 26.3 mL (P less than .01) and sputum cultures became sterile in 13 (35%) of patients (P less than .01).
Previously, surgery for nonlocalized bronchiectasis had been reserved for life-threatening symptoms only, but Dr. Dai and his coauthors fashioned their study on previous studies of lobectomy that included patients with nonlocalized bronchiectasis (Br J Surg. 2005;92:836-9; Ann Thorac Surg. 2003;75:382-7).
Two major complications occurred in the Shanghai cohort: empyema and persistent air leak, both of which were managed without a reoperation and had been reported in previous series. Dr. Dai and his coauthors have adopted protocols to reduce complications, among them, requiring that patients have sputum output greater than 20 mL/day with little purulence and no engorgement or edema in the tunica mucosa bronchiorum on bronchoscopy.
But the researchers are not ready to extend surgery as a blanket indication for nonlocalized bronchiectasis. “It is worth mentioning that the surgical benefit is limited to patients who have only one predominant area of bronchiectatic disease that can be localized by CT instead of those with diffuse bronchiectasis,” they wrote. “The ideal surgical candidate has a heterogeneous distribution of diseased areas.”
The investigators pointed out that the study was limited by its small size and lack of information on etiologies of disease.
Dr. Dai and his coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Lobectomy for nonlocalized bronchiectasis can improve symptoms significantly.
Major finding: Among 37 patients who had lobectomy, 62.2% were asymptomatic after surgery.
Data source: Single-center retrospective review of 37 patients who had lobectomy for nonlocalized bronchiectasis from January 2010 to December 2013.
Disclosure: Dr. Dai and his coauthors had no financial relationships to disclose.