User login
Advanced-Practice Providers Have More to Offer Hospital Medicine Groups
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
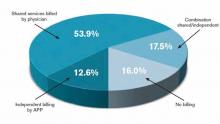
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
Advanced-practice providers (APPs) continue to make their presence felt in the world of hospital medicine. According to survey data from the 2012 State of Hospital Medicine report, more than half (53.9%) of respondent groups serving adults have nurse practitioners (NP) and/or physician assistants (PA) integrated into their practices. The median ratio of APPs to hospitalist physicians in these groups has remained about the same as in previous surveys, with respondents reporting 0.2 FTE NPs per FTE physician, and 0.1 FTE PAs per FTE physician. We’ve also learned that APPs tend to be stable members of most hospitalist practices, with more than 70% of groups reporting no turnover among their APPs during the survey period.
Unfortunately, we don’t yet have much information on the specific roles APPs are filling in HM practices; hopefully, this will be a subject for the next State of Hospital Medicine survey, scheduled to launch in January 2014.
The 2012 survey did provide new information about how APP work is billed by HM groups. More than half the time, APP work is billed as a shared service under a physician’s provider number (see Table 1). Only on rare occasions is APP work billed separately under the APP’s provider number.
Perhaps most surprising of all, 16% of adult HM groups with APPs reported that their APPs don’t generally provide billable services, or no charges were submitted to payors for their services. This figure rose to 23% for hospital-employed groups.
Almost everywhere I go in my consulting work, we are asked about the value APPs can provide to hospitalist practice, and what their optimal roles are. I am extremely supportive of integrating APPs into hospitalist practice and believe they can play valuable roles supporting both excellent patient care and overall group efficiency.
But in my experience, many HM groups fail to execute well on this promise. As the survey results suggest, sometimes APPs are relegated to nonbillable tasks that could be performed by individuals at a lower skill level. Sometimes the hospitalists tend to think of the APPs as “free” help, and no real attempt is made to account for their contribution or capture their billable work. And some groups are so focused on ensuring they capture the 100% reimbursement available by billing under the physician’s name (rather than the 85% reimbursement typically available to APPs) that they lose sight of the fact that the extra physician time and effort involved might cost more than the incremental additional reimbursement received.
As a specialty, we still have a lot to learn about the optimal ways to deploy APPs to support high-quality, effective hospitalist practice. In the meantime, it can be valuable for HM groups to ensure that APPs are functioning in roles that take advantage of their advanced skills and licensure scope, and that efforts are being made to ensure the capture of all billable services provided.
I hope you will plan to participate in the 2014 State of Hospital Medicine survey and share your own practice’s experience with APPs.
Leslie Flores is a partner in Nelson Flores Hospital Medicine Consultants and a member of SHM’s Practice Analysis Committee.
We Welcome the Newest SHM Members
- E. Canady, PA, Alabama
- D. Fico, MD, Alabama
- M. Hazin, DO, Arizona
- K. Ota, DO, Arizona
- T. Phan, Arizona
- M. Poquette, RN, Arizona
- T. Imran, MD, Arkansas
- S. Wooden, MD, Arkansas
- E. Agonafer, California
- S. Badger, MHA, California
- G. Buenaflor, DO, California
- H. Cao, California
- P. Cho, California
- N. Chua, MD, California
- W. Daines, California
- B. Gavi, MD, California
- R. Grant, MD, California
- R. Greysen, MD, California
- V. Hsiao, DO, California
- M. Karube, NP, California
- A. King, MD, California
- M. La, MD, California
- M. Lam, MD, California
- T. Moinizandi, MD, California
- C. Sather, MD, California
- K. Steinberg, MD, California
- S. Woo, MHA, California
- D. Abosh, Canada
- N. Cabilio, MD, Canada
- T. Gepraegs, MD, Canada
- G. Jeffries, CCFP, Canada
- W. Mayhew, MD, Canada
- W. Wilkins, Canada
- M. Braun, ACNP, Colorado
- E. Chu, MD, Colorado
- D. Katz, Colorado
- R. Kumar, Colorado
- A. Maclennan, MD, Colorado
- P. Ryan, Colorado
- O. Akande, MD, Connecticut
- L. Colabelli, Connecticut
- S. Green, ACNP, Connecticut
- S. Lin, Connecticut
- P. Patel, MD, Connecticut
- D. Sewell, MD, Connecticut
- R. Brogan, DO, Florida
- N. Dawson, MD, FACP, Florida
- P. Dhatt, MD, Florida
- N. Griffith, MBA, Florida
- S. Hanson, MD, Florida
- M. Hernandez, MD, Florida
- J. Mennie, MD, Florida
- M. Mohiuddin, MD, Florida
- A. Moynihan, ARNP, Florida
- Y. Patel, MD, Florida
- D. Reto, Florida
- C. Reyes, ARNP, Florida
- B. Fisher, PA-C, Georgia
- S. Fleming, ANP, Georgia
- J. Gilbert, MD, Georgia
- M. Holbrook, FNP, Georgia
- S. Hung, ANP, Georgia
- N. Maignan, MD, Georgia
- P. Nanda, MD, Georgia
- H. Pei, MD, Georgia
- K. Rangnow, NP, Georgia
- S. Shams, MD, Georgia
- L. Wilson, Georgia
- E. Allen, DO, Idaho
- E. Brennan, Illinois
- K. Gul, Illinois
- L. Hansen, MD, Illinois
- D. Nguyen, MD, Illinois
- F. Porter, MD,FACP, Illinois
- A. Ranadive, Illinois
- L. Shahani, MD, Illinois
- J. Tallcott, Illinois
- K. Tulla, Illinois
- N. Wiegley, Illinois
- R. Young, MD, MS, Illinois
- D. Yu, MD, Illinois
- Z. Alba, MD, Indiana
- G. Alcorn, MD, Indiana
- K. Dorairaj, MD, Indiana
- W. Harbin, DO, Indiana
- A. Patel, MD, Indiana
- J. Shamoun, MD, Indiana
- N. Wells, MD, Indiana
- J. Wynn, USA, Indiana
- N. Hartog, MD, Iowa
- K. Emoto, Japan
- M. Sakai, MD, Japan
- P. Poddutoori, MBBS, Kansas
- T. Stofferson, ACMPE, Kansas
- B. Huneycutt, MD, Kentucky
- S. Muldoon, MD, Kentucky
- W. Travis, MD, Kentucky
- B. Molbert, NP, Louisiana
- M. Jacquet, MD, Maine
- P. Pahel, FNP, Maine
- S. Albanez, Maryland
- A. Anigbo, MBBS, Maryland
- A. Antar, PhD, Maryland
- E. Bice, DO, Maryland
- J. Clark, Maryland
- T. Hall, Maryland
- B. Huntley, PA, Maryland
- J. Kaka, Maryland
- D. Kidd, Maryland
- R. Landis, BA, Maryland
- T. Lawgaw, PA-C, Maryland
- M. Singh, Maryland
- M. Baggett, MD, Massachusetts
- E. Barkoudah, MD, Massachusetts
- J. Bortinger, MD, Massachusetts
- J. Bukli, MD, Massachusetts
- S. Dhand, MD, Massachusetts
- L. DiPompo, Massachusetts
- J. Donze, MD, Massachusetts
- S. Ganatra, Massachusetts
- R. Goldberg, MD, Massachusetts
- R. Gumber, MD, Massachusetts
- J. Lawrason, MD, Massachusetts
- N. Lebaka, MD, Massachusetts
- M. Mahmoud, MD, Massachusetts
- G. Mills, Massachusetts
- M. Mohamed, MD, Massachusetts
- J. Parr, MPH, Massachusetts
- D. Ramirez, PA-C, Massachusetts
- L. Solis-Cohen, MD, Massachusetts
- C. Yu, MD, Massachusetts
- E. Bazan, Michigan
- J. Bedore, PA-C, Michigan
- P. Bradley, MD, Michigan
- L. Butz, MD, Michigan
- S. Chase, PharmD, Michigan
- A. Funk, MD, Michigan
- N. Khalid, MD, Michigan
- R. Patel, MD, Michigan
- I. Patsias, MD, Michigan
- P. Sanchez, Michigan
- D. Bowman, Minnesota
- M. Buchner, MD, Minnesota
- S. Mehmood, MD, Minnesota
- J. Ratelle, Minnesota
- M. Werpy, DO, Minnesota
- M. White, MD, Minnesota
- T. Willson, Minnesota
- H. Wood, MD, Minnesota
- S. Altmiller, Mississippi
- R. Andersson, Missouri
- K. Chuu, MD, Missouri
- M. Mullick, MD, Missouri
- C. Obi, MBBS, Missouri
- M. O’Dell, MD, Missouri
- D. Smith, MBA, Missouri
- J. Tyler, DO, Missouri
- S. Riggs, NP, Nebraska
- A. Bose, MD, New Hampshire
- F. Gaffney Comeau, New Hampshire
- C. Raymond, MSN, New Hampshire
- M. Balac, New Jersey
- A. Boa Hocbo, MD, New Jersey
- C. DeLuca, New Jersey
- P. Jadhav, MD, New Jersey
- S. Kishore, MBBS, New Jersey
- P. Krishnamoorthy, MD, New Jersey
- B. LaMotte, PharmD, New Jersey
- C. Maloy, PA-C, New Jersey
- A. Oakley, New Jersey
- K. Pratt, MD, New Jersey
- J. Yacco, New Jersey
- A. Zeff, New Jersey
- K. Caudell, PhD, New Mexico
- G. Ghuneim, MD, New Mexico
- J. Marley, DO, New Mexico
- B. Stricks, New Mexico
- L. Ahmed, New York
- G. Arora, MD, New York
- N. Bangiyeva, MD, New York
- A. Bansal, MD, New York
- L. Belletti, FACP, New York
- N. Bhatt, MPH, New York
- A. Blatt, MD, New York
- T. Chau, New York
- N. Chaudhry, MD, New York
- S. Collins, MD, New York
- L. Coryat, ANP, New York
- R. Dachs, MD, New York
- G. DeCastro, MD, New York
- J. Duffy, ANP, New York
- F. Farzan, MD, New York
- A. Gopal, MD, New York
- S. Hameed, New York
- A. Hanif, MD, New York
- A. Hassan, MD, New York
- A. Howe, New York
- M. Ip, New York
- M. Kelly, MD, New York
- S. Kovtunova, MD, New York
- J. Liu, MD, MPH, New York
- A. Maritato, MD, New York
- K. Mayer, MD, New York
- S. Mehra, New York
- K. Noshiro, MD, New York
- M. Panichas, New York
- V. Rakhvalchuk, DO, New York
- R. Ramkeesoon, New York
- M. Saluja, MD, New York
- P. Shanmugathasan, MD, New York
- S. Sherazi, MD, New York
- J. Shin, MD, New York
- S. Veeramachaneni, MD, New York
- S. Yang, MD, New York
- M. Ardison, MHS, North Carolina
- M. Banks, PA, North Carolina
- W. Brooks, MD, North Carolina
- M. Chadwick, MD, North Carolina
- J. Cowen, DO, North Carolina
- S. Hewitt, North Carolina
- S. Irvin, North Carolina
- J. Kornegay, MD, North Carolina
- K. Larbi-siaw, MD, North Carolina
- J. Pavon, MD, North Carolina
- D. Warner, PA-C, North Carolina
- S. Wells, PA, North Carolina
- S. Abdel-Ghani, MD, Ohio
- D. Abhyankar, Ohio
- A. Alahmar, MD, Ohio
- A. Andreadis, MD, Ohio
- M. Bajwa, Ohio
- A. Blankenship, RN, Ohio
- M. Constantiner, RPh, Ohio
- D. Djigbenou, MD, Ohio
- S. Evans, MD, Ohio
- J. Girard, Ohio
- J. Held, MD, Ohio
- K. Hilder, MD, Ohio
- R. Kanuru, MD, Ohio
- H. Mount, Ohio
- B. Pachmayer, MD, Ohio
- C. Rodehaver, RN, MS, Ohio
- C. Schelzig, MD, FAAP, Ohio
- M. Mathews, Oklahoma
- F. Escaro, Oregon
- S. Hale, MD, Oregon
- E. Meihoff, MD, Oregon
- B. Rainka, Oregon
- A. Behura, MD, Pennsylvania
- B. Bussler, Pennsylvania
- J. Chintanaboina, Pennsylvania
- I. Cirilo, MD, Pennsylvania
- S. Doomra, Pennsylvania
- G. Gabasan, MD, Pennsylvania
- J. Gengaro, DO, Pennsylvania
- D. Gondek, DO, Pennsylvania
- K. Gonzalez, NP, Pennsylvania
- A. Hellyer, Pennsylvania
- J. Julian, MD, MPH, Pennsylvania
- A. Kainz, Pennsylvania
- S. Kaur, MD, Pennsylvania
- P. Lange, MD, Pennsylvania
- S. Leslie, MD, Pennsylvania
- D. McBryan, MD, Pennsylvania
- A. Miller, CRNP, Pennsylvania
- S. Nichuls, PA-C, Pennsylvania
- T. Pellegrino, PharmD, Pennsylvania
- K. Reed, PharmD, Pennsylvania
- A. Seasock, PA-C, BS, Pennsylvania
- S. Soenen, Pennsylvania
- V. Subbiah, MD, Pennsylvania
- N. Thingalaya, MD, Pennsylvania
- E. Tuttle, PA, Pennsylvania
- G. Vadlamudi, MPH, MD, Pennsylvania
- B. Verma, MD, Pennsylvania
- E. Wannebo, MD, Pennsylvania
- A. Wesoly, PA, Pennsylvania
- L. Eddy, FNP, Rhode Island
- M. Antonatos, MD, South Carolina
- S. Connelly, South Carolina
- D. O’Briant, MD, South Carolina
- R. Agarwal, MD, MBA, Tennessee
- A. Aird, MD, Tennessee
- F. Dragila, MD, Tennessee
- S. Duncan, MD, Tennessee
- M. Flint, MPH, Tennessee
- A. Goldfeld, Tennessee
- R. Gusso, MD, Tennessee
- S. Lane, M.H.A., Tennessee
- C. Long, MD, Tennessee
- M. Naeem, MD, PhD, Tennessee
- C. Aiken, RN, Texas
- D. Berhane, Texas
- M. Cabello, MD, Texas
- A. Caruso, MD, Texas
- P. Desai, Texas
- J. Haygood, Texas
- R. Henderson, MD, Texas
- C. Inniss, Texas
- W. Mirza, DO, Texas
- C. Moreland, MD, Texas
- N. Mulukutla, MD, Texas
- G. Neil, MD, Texas
- I. Nwabude, MD, Texas
- T. Onishi, MD, Texas
- K. Patel, MD, Texas
- B. Pomeroy, MD, Texas
- S. Ray, Texas
- J. Tau, MD, Texas
- M. Blankenship, MD, Utah
- L. Porter, RN, Utah
- J. Strong, MD, Utah
- J. Van Blarcom, MD, Utah
- A. Wood, RN, Utah
- M. Wren, Utah
- M. Anawati, MD, Vermont
- S. Lee, Vermont
- C. Cook, MD, Virginia
- E. Deungwe Yonga, MD, Virginia
- F. Dieter, PA, Virginia
- P. Gill, MD, Virginia
- S. Goldwater, PharmD, Virginia
- R. Martin, MD, Virginia
- T. Masterson, Virginia
- P. Ouellette, MD, Virginia
- M. Plazarte, DO, Virginia
- C. Salamanca, NP, Virginia
- B. Seagroves, MD, Virginia
- G. Slitt, MD, Virginia
- F. Williams, MD, Virginia
- S. Won, NP, MSN, Virginia
- L. Alberts, MD, Washington
- E. Lopez, PA-C, Washington
- L. Lubinski, MD, Washington
- J. Oconer, MD, Washington
- K. Shulman, Washington
- S. Carpenter, MD, West Virginia
- Y. Jones, FAAP, West Virginia
- P. Cartier-Neely, PA, Wisconsin
- D. Johnson, MD, Wisconsin
- R. Johnson, MD, Wisconsin
- E. Canady, PA, Alabama
- D. Fico, MD, Alabama
- M. Hazin, DO, Arizona
- K. Ota, DO, Arizona
- T. Phan, Arizona
- M. Poquette, RN, Arizona
- T. Imran, MD, Arkansas
- S. Wooden, MD, Arkansas
- E. Agonafer, California
- S. Badger, MHA, California
- G. Buenaflor, DO, California
- H. Cao, California
- P. Cho, California
- N. Chua, MD, California
- W. Daines, California
- B. Gavi, MD, California
- R. Grant, MD, California
- R. Greysen, MD, California
- V. Hsiao, DO, California
- M. Karube, NP, California
- A. King, MD, California
- M. La, MD, California
- M. Lam, MD, California
- T. Moinizandi, MD, California
- C. Sather, MD, California
- K. Steinberg, MD, California
- S. Woo, MHA, California
- D. Abosh, Canada
- N. Cabilio, MD, Canada
- T. Gepraegs, MD, Canada
- G. Jeffries, CCFP, Canada
- W. Mayhew, MD, Canada
- W. Wilkins, Canada
- M. Braun, ACNP, Colorado
- E. Chu, MD, Colorado
- D. Katz, Colorado
- R. Kumar, Colorado
- A. Maclennan, MD, Colorado
- P. Ryan, Colorado
- O. Akande, MD, Connecticut
- L. Colabelli, Connecticut
- S. Green, ACNP, Connecticut
- S. Lin, Connecticut
- P. Patel, MD, Connecticut
- D. Sewell, MD, Connecticut
- R. Brogan, DO, Florida
- N. Dawson, MD, FACP, Florida
- P. Dhatt, MD, Florida
- N. Griffith, MBA, Florida
- S. Hanson, MD, Florida
- M. Hernandez, MD, Florida
- J. Mennie, MD, Florida
- M. Mohiuddin, MD, Florida
- A. Moynihan, ARNP, Florida
- Y. Patel, MD, Florida
- D. Reto, Florida
- C. Reyes, ARNP, Florida
- B. Fisher, PA-C, Georgia
- S. Fleming, ANP, Georgia
- J. Gilbert, MD, Georgia
- M. Holbrook, FNP, Georgia
- S. Hung, ANP, Georgia
- N. Maignan, MD, Georgia
- P. Nanda, MD, Georgia
- H. Pei, MD, Georgia
- K. Rangnow, NP, Georgia
- S. Shams, MD, Georgia
- L. Wilson, Georgia
- E. Allen, DO, Idaho
- E. Brennan, Illinois
- K. Gul, Illinois
- L. Hansen, MD, Illinois
- D. Nguyen, MD, Illinois
- F. Porter, MD,FACP, Illinois
- A. Ranadive, Illinois
- L. Shahani, MD, Illinois
- J. Tallcott, Illinois
- K. Tulla, Illinois
- N. Wiegley, Illinois
- R. Young, MD, MS, Illinois
- D. Yu, MD, Illinois
- Z. Alba, MD, Indiana
- G. Alcorn, MD, Indiana
- K. Dorairaj, MD, Indiana
- W. Harbin, DO, Indiana
- A. Patel, MD, Indiana
- J. Shamoun, MD, Indiana
- N. Wells, MD, Indiana
- J. Wynn, USA, Indiana
- N. Hartog, MD, Iowa
- K. Emoto, Japan
- M. Sakai, MD, Japan
- P. Poddutoori, MBBS, Kansas
- T. Stofferson, ACMPE, Kansas
- B. Huneycutt, MD, Kentucky
- S. Muldoon, MD, Kentucky
- W. Travis, MD, Kentucky
- B. Molbert, NP, Louisiana
- M. Jacquet, MD, Maine
- P. Pahel, FNP, Maine
- S. Albanez, Maryland
- A. Anigbo, MBBS, Maryland
- A. Antar, PhD, Maryland
- E. Bice, DO, Maryland
- J. Clark, Maryland
- T. Hall, Maryland
- B. Huntley, PA, Maryland
- J. Kaka, Maryland
- D. Kidd, Maryland
- R. Landis, BA, Maryland
- T. Lawgaw, PA-C, Maryland
- M. Singh, Maryland
- M. Baggett, MD, Massachusetts
- E. Barkoudah, MD, Massachusetts
- J. Bortinger, MD, Massachusetts
- J. Bukli, MD, Massachusetts
- S. Dhand, MD, Massachusetts
- L. DiPompo, Massachusetts
- J. Donze, MD, Massachusetts
- S. Ganatra, Massachusetts
- R. Goldberg, MD, Massachusetts
- R. Gumber, MD, Massachusetts
- J. Lawrason, MD, Massachusetts
- N. Lebaka, MD, Massachusetts
- M. Mahmoud, MD, Massachusetts
- G. Mills, Massachusetts
- M. Mohamed, MD, Massachusetts
- J. Parr, MPH, Massachusetts
- D. Ramirez, PA-C, Massachusetts
- L. Solis-Cohen, MD, Massachusetts
- C. Yu, MD, Massachusetts
- E. Bazan, Michigan
- J. Bedore, PA-C, Michigan
- P. Bradley, MD, Michigan
- L. Butz, MD, Michigan
- S. Chase, PharmD, Michigan
- A. Funk, MD, Michigan
- N. Khalid, MD, Michigan
- R. Patel, MD, Michigan
- I. Patsias, MD, Michigan
- P. Sanchez, Michigan
- D. Bowman, Minnesota
- M. Buchner, MD, Minnesota
- S. Mehmood, MD, Minnesota
- J. Ratelle, Minnesota
- M. Werpy, DO, Minnesota
- M. White, MD, Minnesota
- T. Willson, Minnesota
- H. Wood, MD, Minnesota
- S. Altmiller, Mississippi
- R. Andersson, Missouri
- K. Chuu, MD, Missouri
- M. Mullick, MD, Missouri
- C. Obi, MBBS, Missouri
- M. O’Dell, MD, Missouri
- D. Smith, MBA, Missouri
- J. Tyler, DO, Missouri
- S. Riggs, NP, Nebraska
- A. Bose, MD, New Hampshire
- F. Gaffney Comeau, New Hampshire
- C. Raymond, MSN, New Hampshire
- M. Balac, New Jersey
- A. Boa Hocbo, MD, New Jersey
- C. DeLuca, New Jersey
- P. Jadhav, MD, New Jersey
- S. Kishore, MBBS, New Jersey
- P. Krishnamoorthy, MD, New Jersey
- B. LaMotte, PharmD, New Jersey
- C. Maloy, PA-C, New Jersey
- A. Oakley, New Jersey
- K. Pratt, MD, New Jersey
- J. Yacco, New Jersey
- A. Zeff, New Jersey
- K. Caudell, PhD, New Mexico
- G. Ghuneim, MD, New Mexico
- J. Marley, DO, New Mexico
- B. Stricks, New Mexico
- L. Ahmed, New York
- G. Arora, MD, New York
- N. Bangiyeva, MD, New York
- A. Bansal, MD, New York
- L. Belletti, FACP, New York
- N. Bhatt, MPH, New York
- A. Blatt, MD, New York
- T. Chau, New York
- N. Chaudhry, MD, New York
- S. Collins, MD, New York
- L. Coryat, ANP, New York
- R. Dachs, MD, New York
- G. DeCastro, MD, New York
- J. Duffy, ANP, New York
- F. Farzan, MD, New York
- A. Gopal, MD, New York
- S. Hameed, New York
- A. Hanif, MD, New York
- A. Hassan, MD, New York
- A. Howe, New York
- M. Ip, New York
- M. Kelly, MD, New York
- S. Kovtunova, MD, New York
- J. Liu, MD, MPH, New York
- A. Maritato, MD, New York
- K. Mayer, MD, New York
- S. Mehra, New York
- K. Noshiro, MD, New York
- M. Panichas, New York
- V. Rakhvalchuk, DO, New York
- R. Ramkeesoon, New York
- M. Saluja, MD, New York
- P. Shanmugathasan, MD, New York
- S. Sherazi, MD, New York
- J. Shin, MD, New York
- S. Veeramachaneni, MD, New York
- S. Yang, MD, New York
- M. Ardison, MHS, North Carolina
- M. Banks, PA, North Carolina
- W. Brooks, MD, North Carolina
- M. Chadwick, MD, North Carolina
- J. Cowen, DO, North Carolina
- S. Hewitt, North Carolina
- S. Irvin, North Carolina
- J. Kornegay, MD, North Carolina
- K. Larbi-siaw, MD, North Carolina
- J. Pavon, MD, North Carolina
- D. Warner, PA-C, North Carolina
- S. Wells, PA, North Carolina
- S. Abdel-Ghani, MD, Ohio
- D. Abhyankar, Ohio
- A. Alahmar, MD, Ohio
- A. Andreadis, MD, Ohio
- M. Bajwa, Ohio
- A. Blankenship, RN, Ohio
- M. Constantiner, RPh, Ohio
- D. Djigbenou, MD, Ohio
- S. Evans, MD, Ohio
- J. Girard, Ohio
- J. Held, MD, Ohio
- K. Hilder, MD, Ohio
- R. Kanuru, MD, Ohio
- H. Mount, Ohio
- B. Pachmayer, MD, Ohio
- C. Rodehaver, RN, MS, Ohio
- C. Schelzig, MD, FAAP, Ohio
- M. Mathews, Oklahoma
- F. Escaro, Oregon
- S. Hale, MD, Oregon
- E. Meihoff, MD, Oregon
- B. Rainka, Oregon
- A. Behura, MD, Pennsylvania
- B. Bussler, Pennsylvania
- J. Chintanaboina, Pennsylvania
- I. Cirilo, MD, Pennsylvania
- S. Doomra, Pennsylvania
- G. Gabasan, MD, Pennsylvania
- J. Gengaro, DO, Pennsylvania
- D. Gondek, DO, Pennsylvania
- K. Gonzalez, NP, Pennsylvania
- A. Hellyer, Pennsylvania
- J. Julian, MD, MPH, Pennsylvania
- A. Kainz, Pennsylvania
- S. Kaur, MD, Pennsylvania
- P. Lange, MD, Pennsylvania
- S. Leslie, MD, Pennsylvania
- D. McBryan, MD, Pennsylvania
- A. Miller, CRNP, Pennsylvania
- S. Nichuls, PA-C, Pennsylvania
- T. Pellegrino, PharmD, Pennsylvania
- K. Reed, PharmD, Pennsylvania
- A. Seasock, PA-C, BS, Pennsylvania
- S. Soenen, Pennsylvania
- V. Subbiah, MD, Pennsylvania
- N. Thingalaya, MD, Pennsylvania
- E. Tuttle, PA, Pennsylvania
- G. Vadlamudi, MPH, MD, Pennsylvania
- B. Verma, MD, Pennsylvania
- E. Wannebo, MD, Pennsylvania
- A. Wesoly, PA, Pennsylvania
- L. Eddy, FNP, Rhode Island
- M. Antonatos, MD, South Carolina
- S. Connelly, South Carolina
- D. O’Briant, MD, South Carolina
- R. Agarwal, MD, MBA, Tennessee
- A. Aird, MD, Tennessee
- F. Dragila, MD, Tennessee
- S. Duncan, MD, Tennessee
- M. Flint, MPH, Tennessee
- A. Goldfeld, Tennessee
- R. Gusso, MD, Tennessee
- S. Lane, M.H.A., Tennessee
- C. Long, MD, Tennessee
- M. Naeem, MD, PhD, Tennessee
- C. Aiken, RN, Texas
- D. Berhane, Texas
- M. Cabello, MD, Texas
- A. Caruso, MD, Texas
- P. Desai, Texas
- J. Haygood, Texas
- R. Henderson, MD, Texas
- C. Inniss, Texas
- W. Mirza, DO, Texas
- C. Moreland, MD, Texas
- N. Mulukutla, MD, Texas
- G. Neil, MD, Texas
- I. Nwabude, MD, Texas
- T. Onishi, MD, Texas
- K. Patel, MD, Texas
- B. Pomeroy, MD, Texas
- S. Ray, Texas
- J. Tau, MD, Texas
- M. Blankenship, MD, Utah
- L. Porter, RN, Utah
- J. Strong, MD, Utah
- J. Van Blarcom, MD, Utah
- A. Wood, RN, Utah
- M. Wren, Utah
- M. Anawati, MD, Vermont
- S. Lee, Vermont
- C. Cook, MD, Virginia
- E. Deungwe Yonga, MD, Virginia
- F. Dieter, PA, Virginia
- P. Gill, MD, Virginia
- S. Goldwater, PharmD, Virginia
- R. Martin, MD, Virginia
- T. Masterson, Virginia
- P. Ouellette, MD, Virginia
- M. Plazarte, DO, Virginia
- C. Salamanca, NP, Virginia
- B. Seagroves, MD, Virginia
- G. Slitt, MD, Virginia
- F. Williams, MD, Virginia
- S. Won, NP, MSN, Virginia
- L. Alberts, MD, Washington
- E. Lopez, PA-C, Washington
- L. Lubinski, MD, Washington
- J. Oconer, MD, Washington
- K. Shulman, Washington
- S. Carpenter, MD, West Virginia
- Y. Jones, FAAP, West Virginia
- P. Cartier-Neely, PA, Wisconsin
- D. Johnson, MD, Wisconsin
- R. Johnson, MD, Wisconsin
- E. Canady, PA, Alabama
- D. Fico, MD, Alabama
- M. Hazin, DO, Arizona
- K. Ota, DO, Arizona
- T. Phan, Arizona
- M. Poquette, RN, Arizona
- T. Imran, MD, Arkansas
- S. Wooden, MD, Arkansas
- E. Agonafer, California
- S. Badger, MHA, California
- G. Buenaflor, DO, California
- H. Cao, California
- P. Cho, California
- N. Chua, MD, California
- W. Daines, California
- B. Gavi, MD, California
- R. Grant, MD, California
- R. Greysen, MD, California
- V. Hsiao, DO, California
- M. Karube, NP, California
- A. King, MD, California
- M. La, MD, California
- M. Lam, MD, California
- T. Moinizandi, MD, California
- C. Sather, MD, California
- K. Steinberg, MD, California
- S. Woo, MHA, California
- D. Abosh, Canada
- N. Cabilio, MD, Canada
- T. Gepraegs, MD, Canada
- G. Jeffries, CCFP, Canada
- W. Mayhew, MD, Canada
- W. Wilkins, Canada
- M. Braun, ACNP, Colorado
- E. Chu, MD, Colorado
- D. Katz, Colorado
- R. Kumar, Colorado
- A. Maclennan, MD, Colorado
- P. Ryan, Colorado
- O. Akande, MD, Connecticut
- L. Colabelli, Connecticut
- S. Green, ACNP, Connecticut
- S. Lin, Connecticut
- P. Patel, MD, Connecticut
- D. Sewell, MD, Connecticut
- R. Brogan, DO, Florida
- N. Dawson, MD, FACP, Florida
- P. Dhatt, MD, Florida
- N. Griffith, MBA, Florida
- S. Hanson, MD, Florida
- M. Hernandez, MD, Florida
- J. Mennie, MD, Florida
- M. Mohiuddin, MD, Florida
- A. Moynihan, ARNP, Florida
- Y. Patel, MD, Florida
- D. Reto, Florida
- C. Reyes, ARNP, Florida
- B. Fisher, PA-C, Georgia
- S. Fleming, ANP, Georgia
- J. Gilbert, MD, Georgia
- M. Holbrook, FNP, Georgia
- S. Hung, ANP, Georgia
- N. Maignan, MD, Georgia
- P. Nanda, MD, Georgia
- H. Pei, MD, Georgia
- K. Rangnow, NP, Georgia
- S. Shams, MD, Georgia
- L. Wilson, Georgia
- E. Allen, DO, Idaho
- E. Brennan, Illinois
- K. Gul, Illinois
- L. Hansen, MD, Illinois
- D. Nguyen, MD, Illinois
- F. Porter, MD,FACP, Illinois
- A. Ranadive, Illinois
- L. Shahani, MD, Illinois
- J. Tallcott, Illinois
- K. Tulla, Illinois
- N. Wiegley, Illinois
- R. Young, MD, MS, Illinois
- D. Yu, MD, Illinois
- Z. Alba, MD, Indiana
- G. Alcorn, MD, Indiana
- K. Dorairaj, MD, Indiana
- W. Harbin, DO, Indiana
- A. Patel, MD, Indiana
- J. Shamoun, MD, Indiana
- N. Wells, MD, Indiana
- J. Wynn, USA, Indiana
- N. Hartog, MD, Iowa
- K. Emoto, Japan
- M. Sakai, MD, Japan
- P. Poddutoori, MBBS, Kansas
- T. Stofferson, ACMPE, Kansas
- B. Huneycutt, MD, Kentucky
- S. Muldoon, MD, Kentucky
- W. Travis, MD, Kentucky
- B. Molbert, NP, Louisiana
- M. Jacquet, MD, Maine
- P. Pahel, FNP, Maine
- S. Albanez, Maryland
- A. Anigbo, MBBS, Maryland
- A. Antar, PhD, Maryland
- E. Bice, DO, Maryland
- J. Clark, Maryland
- T. Hall, Maryland
- B. Huntley, PA, Maryland
- J. Kaka, Maryland
- D. Kidd, Maryland
- R. Landis, BA, Maryland
- T. Lawgaw, PA-C, Maryland
- M. Singh, Maryland
- M. Baggett, MD, Massachusetts
- E. Barkoudah, MD, Massachusetts
- J. Bortinger, MD, Massachusetts
- J. Bukli, MD, Massachusetts
- S. Dhand, MD, Massachusetts
- L. DiPompo, Massachusetts
- J. Donze, MD, Massachusetts
- S. Ganatra, Massachusetts
- R. Goldberg, MD, Massachusetts
- R. Gumber, MD, Massachusetts
- J. Lawrason, MD, Massachusetts
- N. Lebaka, MD, Massachusetts
- M. Mahmoud, MD, Massachusetts
- G. Mills, Massachusetts
- M. Mohamed, MD, Massachusetts
- J. Parr, MPH, Massachusetts
- D. Ramirez, PA-C, Massachusetts
- L. Solis-Cohen, MD, Massachusetts
- C. Yu, MD, Massachusetts
- E. Bazan, Michigan
- J. Bedore, PA-C, Michigan
- P. Bradley, MD, Michigan
- L. Butz, MD, Michigan
- S. Chase, PharmD, Michigan
- A. Funk, MD, Michigan
- N. Khalid, MD, Michigan
- R. Patel, MD, Michigan
- I. Patsias, MD, Michigan
- P. Sanchez, Michigan
- D. Bowman, Minnesota
- M. Buchner, MD, Minnesota
- S. Mehmood, MD, Minnesota
- J. Ratelle, Minnesota
- M. Werpy, DO, Minnesota
- M. White, MD, Minnesota
- T. Willson, Minnesota
- H. Wood, MD, Minnesota
- S. Altmiller, Mississippi
- R. Andersson, Missouri
- K. Chuu, MD, Missouri
- M. Mullick, MD, Missouri
- C. Obi, MBBS, Missouri
- M. O’Dell, MD, Missouri
- D. Smith, MBA, Missouri
- J. Tyler, DO, Missouri
- S. Riggs, NP, Nebraska
- A. Bose, MD, New Hampshire
- F. Gaffney Comeau, New Hampshire
- C. Raymond, MSN, New Hampshire
- M. Balac, New Jersey
- A. Boa Hocbo, MD, New Jersey
- C. DeLuca, New Jersey
- P. Jadhav, MD, New Jersey
- S. Kishore, MBBS, New Jersey
- P. Krishnamoorthy, MD, New Jersey
- B. LaMotte, PharmD, New Jersey
- C. Maloy, PA-C, New Jersey
- A. Oakley, New Jersey
- K. Pratt, MD, New Jersey
- J. Yacco, New Jersey
- A. Zeff, New Jersey
- K. Caudell, PhD, New Mexico
- G. Ghuneim, MD, New Mexico
- J. Marley, DO, New Mexico
- B. Stricks, New Mexico
- L. Ahmed, New York
- G. Arora, MD, New York
- N. Bangiyeva, MD, New York
- A. Bansal, MD, New York
- L. Belletti, FACP, New York
- N. Bhatt, MPH, New York
- A. Blatt, MD, New York
- T. Chau, New York
- N. Chaudhry, MD, New York
- S. Collins, MD, New York
- L. Coryat, ANP, New York
- R. Dachs, MD, New York
- G. DeCastro, MD, New York
- J. Duffy, ANP, New York
- F. Farzan, MD, New York
- A. Gopal, MD, New York
- S. Hameed, New York
- A. Hanif, MD, New York
- A. Hassan, MD, New York
- A. Howe, New York
- M. Ip, New York
- M. Kelly, MD, New York
- S. Kovtunova, MD, New York
- J. Liu, MD, MPH, New York
- A. Maritato, MD, New York
- K. Mayer, MD, New York
- S. Mehra, New York
- K. Noshiro, MD, New York
- M. Panichas, New York
- V. Rakhvalchuk, DO, New York
- R. Ramkeesoon, New York
- M. Saluja, MD, New York
- P. Shanmugathasan, MD, New York
- S. Sherazi, MD, New York
- J. Shin, MD, New York
- S. Veeramachaneni, MD, New York
- S. Yang, MD, New York
- M. Ardison, MHS, North Carolina
- M. Banks, PA, North Carolina
- W. Brooks, MD, North Carolina
- M. Chadwick, MD, North Carolina
- J. Cowen, DO, North Carolina
- S. Hewitt, North Carolina
- S. Irvin, North Carolina
- J. Kornegay, MD, North Carolina
- K. Larbi-siaw, MD, North Carolina
- J. Pavon, MD, North Carolina
- D. Warner, PA-C, North Carolina
- S. Wells, PA, North Carolina
- S. Abdel-Ghani, MD, Ohio
- D. Abhyankar, Ohio
- A. Alahmar, MD, Ohio
- A. Andreadis, MD, Ohio
- M. Bajwa, Ohio
- A. Blankenship, RN, Ohio
- M. Constantiner, RPh, Ohio
- D. Djigbenou, MD, Ohio
- S. Evans, MD, Ohio
- J. Girard, Ohio
- J. Held, MD, Ohio
- K. Hilder, MD, Ohio
- R. Kanuru, MD, Ohio
- H. Mount, Ohio
- B. Pachmayer, MD, Ohio
- C. Rodehaver, RN, MS, Ohio
- C. Schelzig, MD, FAAP, Ohio
- M. Mathews, Oklahoma
- F. Escaro, Oregon
- S. Hale, MD, Oregon
- E. Meihoff, MD, Oregon
- B. Rainka, Oregon
- A. Behura, MD, Pennsylvania
- B. Bussler, Pennsylvania
- J. Chintanaboina, Pennsylvania
- I. Cirilo, MD, Pennsylvania
- S. Doomra, Pennsylvania
- G. Gabasan, MD, Pennsylvania
- J. Gengaro, DO, Pennsylvania
- D. Gondek, DO, Pennsylvania
- K. Gonzalez, NP, Pennsylvania
- A. Hellyer, Pennsylvania
- J. Julian, MD, MPH, Pennsylvania
- A. Kainz, Pennsylvania
- S. Kaur, MD, Pennsylvania
- P. Lange, MD, Pennsylvania
- S. Leslie, MD, Pennsylvania
- D. McBryan, MD, Pennsylvania
- A. Miller, CRNP, Pennsylvania
- S. Nichuls, PA-C, Pennsylvania
- T. Pellegrino, PharmD, Pennsylvania
- K. Reed, PharmD, Pennsylvania
- A. Seasock, PA-C, BS, Pennsylvania
- S. Soenen, Pennsylvania
- V. Subbiah, MD, Pennsylvania
- N. Thingalaya, MD, Pennsylvania
- E. Tuttle, PA, Pennsylvania
- G. Vadlamudi, MPH, MD, Pennsylvania
- B. Verma, MD, Pennsylvania
- E. Wannebo, MD, Pennsylvania
- A. Wesoly, PA, Pennsylvania
- L. Eddy, FNP, Rhode Island
- M. Antonatos, MD, South Carolina
- S. Connelly, South Carolina
- D. O’Briant, MD, South Carolina
- R. Agarwal, MD, MBA, Tennessee
- A. Aird, MD, Tennessee
- F. Dragila, MD, Tennessee
- S. Duncan, MD, Tennessee
- M. Flint, MPH, Tennessee
- A. Goldfeld, Tennessee
- R. Gusso, MD, Tennessee
- S. Lane, M.H.A., Tennessee
- C. Long, MD, Tennessee
- M. Naeem, MD, PhD, Tennessee
- C. Aiken, RN, Texas
- D. Berhane, Texas
- M. Cabello, MD, Texas
- A. Caruso, MD, Texas
- P. Desai, Texas
- J. Haygood, Texas
- R. Henderson, MD, Texas
- C. Inniss, Texas
- W. Mirza, DO, Texas
- C. Moreland, MD, Texas
- N. Mulukutla, MD, Texas
- G. Neil, MD, Texas
- I. Nwabude, MD, Texas
- T. Onishi, MD, Texas
- K. Patel, MD, Texas
- B. Pomeroy, MD, Texas
- S. Ray, Texas
- J. Tau, MD, Texas
- M. Blankenship, MD, Utah
- L. Porter, RN, Utah
- J. Strong, MD, Utah
- J. Van Blarcom, MD, Utah
- A. Wood, RN, Utah
- M. Wren, Utah
- M. Anawati, MD, Vermont
- S. Lee, Vermont
- C. Cook, MD, Virginia
- E. Deungwe Yonga, MD, Virginia
- F. Dieter, PA, Virginia
- P. Gill, MD, Virginia
- S. Goldwater, PharmD, Virginia
- R. Martin, MD, Virginia
- T. Masterson, Virginia
- P. Ouellette, MD, Virginia
- M. Plazarte, DO, Virginia
- C. Salamanca, NP, Virginia
- B. Seagroves, MD, Virginia
- G. Slitt, MD, Virginia
- F. Williams, MD, Virginia
- S. Won, NP, MSN, Virginia
- L. Alberts, MD, Washington
- E. Lopez, PA-C, Washington
- L. Lubinski, MD, Washington
- J. Oconer, MD, Washington
- K. Shulman, Washington
- S. Carpenter, MD, West Virginia
- Y. Jones, FAAP, West Virginia
- P. Cartier-Neely, PA, Wisconsin
- D. Johnson, MD, Wisconsin
- R. Johnson, MD, Wisconsin
Fellow in Hospital Medicine Spotlight: Rachel Thompson, MD, FHM

Dr. Thompson is an assistant professor in the Department of Medicine and the Department of Neurosurgery at the University of Washington in Seattle. She is director of the medicine consult service and the medicine operative consult clinic at Harborview Medical Center in Seattle. She also is president of SHM’s Pacific Northwest chapter and a member of the National Chapter Support Committee.
Undergraduate education: Amherst College, Amherst, Mass.
Medical school: University of Washington School of Medicine, Seattle.
Notable: Dr. Thompson says one of her greatest career achievements has been the development of collegial services with surgeons and researchers in order to look at surgical outcomes through the lens of a hospitalist. She also developed a glycemic-control center in her hospital to improve insulin ordering, a project for which she has been published and presented locally and nationally. She has served as a resident research project mentor since 2005, helping 13 students achieve their research goals. Dr. Thompson volunteers at the Mathematics Engineering Science Achievement (MESA) Saturday Academy, an inner-city high school program for advancement in math and science, for which she won the 2007 MESA Saturday Academy Outstanding Volunteer Award.
FYI: Dr. Thompson enjoys hiking and takes part in two soccer leagues. Her children are following in her footsteps: Both are on their own soccer teams.
Quotable: “Becoming an SHM fellow shows that you have what it takes to be engaged as a hospitalist. Hospital medicine is not just a job; it’s a career and a dedication.”

Dr. Thompson is an assistant professor in the Department of Medicine and the Department of Neurosurgery at the University of Washington in Seattle. She is director of the medicine consult service and the medicine operative consult clinic at Harborview Medical Center in Seattle. She also is president of SHM’s Pacific Northwest chapter and a member of the National Chapter Support Committee.
Undergraduate education: Amherst College, Amherst, Mass.
Medical school: University of Washington School of Medicine, Seattle.
Notable: Dr. Thompson says one of her greatest career achievements has been the development of collegial services with surgeons and researchers in order to look at surgical outcomes through the lens of a hospitalist. She also developed a glycemic-control center in her hospital to improve insulin ordering, a project for which she has been published and presented locally and nationally. She has served as a resident research project mentor since 2005, helping 13 students achieve their research goals. Dr. Thompson volunteers at the Mathematics Engineering Science Achievement (MESA) Saturday Academy, an inner-city high school program for advancement in math and science, for which she won the 2007 MESA Saturday Academy Outstanding Volunteer Award.
FYI: Dr. Thompson enjoys hiking and takes part in two soccer leagues. Her children are following in her footsteps: Both are on their own soccer teams.
Quotable: “Becoming an SHM fellow shows that you have what it takes to be engaged as a hospitalist. Hospital medicine is not just a job; it’s a career and a dedication.”

Dr. Thompson is an assistant professor in the Department of Medicine and the Department of Neurosurgery at the University of Washington in Seattle. She is director of the medicine consult service and the medicine operative consult clinic at Harborview Medical Center in Seattle. She also is president of SHM’s Pacific Northwest chapter and a member of the National Chapter Support Committee.
Undergraduate education: Amherst College, Amherst, Mass.
Medical school: University of Washington School of Medicine, Seattle.
Notable: Dr. Thompson says one of her greatest career achievements has been the development of collegial services with surgeons and researchers in order to look at surgical outcomes through the lens of a hospitalist. She also developed a glycemic-control center in her hospital to improve insulin ordering, a project for which she has been published and presented locally and nationally. She has served as a resident research project mentor since 2005, helping 13 students achieve their research goals. Dr. Thompson volunteers at the Mathematics Engineering Science Achievement (MESA) Saturday Academy, an inner-city high school program for advancement in math and science, for which she won the 2007 MESA Saturday Academy Outstanding Volunteer Award.
FYI: Dr. Thompson enjoys hiking and takes part in two soccer leagues. Her children are following in her footsteps: Both are on their own soccer teams.
Quotable: “Becoming an SHM fellow shows that you have what it takes to be engaged as a hospitalist. Hospital medicine is not just a job; it’s a career and a dedication.”
Start Planning Now for HM14
Whether you couldn’t make it to HM13 or you’re bringing back all the energy from the conference back to your hospital, now is the time to start planning for the next national conference exclusively designed for the nation’s 40,000 hospitalists.
For newcomers, HM14 will offer unprecedented access, networking, and CME-accredited educational sessions for hospitalists in all career stages. And for veterans of SHM’s annual meeting, 2014 will introduce two new pre-courses: “Cardiology and Evidence-Based Medicine” and “Bending the Cost Curve,” one of the hottest topics in public health, which will have its own dedicated track as well.
In addition to offering the best CME-accredited educational experience, HM14 will also give hospitalists the chance to enjoy an all-new official headquarters for the meeting: Mandalay Bay Hotel & Casino in Las Vegas.
Pre-Courses
Enhance the HM14 educational experience, broaden your skills, and earn additional CME credits. Choose from one of the following HM-focused topics:
- Medical Procedures for the Hospitalist;
- Portable Ultrasound for the Hospitalist;
- Perioperative Medicine;
- ABIM Maintenance of Certification;
- Practice Management;
- Neurology;
- Cardiology (new); and
- Evidence-Based Medicine (new).
Content Areas
The educational tracks offered at HM14 enable attendees to take courses in various designated tracks designed to better focus and enrich the annual meeting for attendees.
Tracks focus on the following cutting-edge content areas:
- Clinical;
- Rapid Fire;
- Practice Management;
- Academic/Research;
- Quality;
- Bending the Cost Curve (new);
- Pediatric;
- Potpourri;
- Comanagement; and
- Workshops.
Brendon Shank is SHM’s associate vice president of communications.
Whether you couldn’t make it to HM13 or you’re bringing back all the energy from the conference back to your hospital, now is the time to start planning for the next national conference exclusively designed for the nation’s 40,000 hospitalists.
For newcomers, HM14 will offer unprecedented access, networking, and CME-accredited educational sessions for hospitalists in all career stages. And for veterans of SHM’s annual meeting, 2014 will introduce two new pre-courses: “Cardiology and Evidence-Based Medicine” and “Bending the Cost Curve,” one of the hottest topics in public health, which will have its own dedicated track as well.
In addition to offering the best CME-accredited educational experience, HM14 will also give hospitalists the chance to enjoy an all-new official headquarters for the meeting: Mandalay Bay Hotel & Casino in Las Vegas.
Pre-Courses
Enhance the HM14 educational experience, broaden your skills, and earn additional CME credits. Choose from one of the following HM-focused topics:
- Medical Procedures for the Hospitalist;
- Portable Ultrasound for the Hospitalist;
- Perioperative Medicine;
- ABIM Maintenance of Certification;
- Practice Management;
- Neurology;
- Cardiology (new); and
- Evidence-Based Medicine (new).
Content Areas
The educational tracks offered at HM14 enable attendees to take courses in various designated tracks designed to better focus and enrich the annual meeting for attendees.
Tracks focus on the following cutting-edge content areas:
- Clinical;
- Rapid Fire;
- Practice Management;
- Academic/Research;
- Quality;
- Bending the Cost Curve (new);
- Pediatric;
- Potpourri;
- Comanagement; and
- Workshops.
Brendon Shank is SHM’s associate vice president of communications.
Whether you couldn’t make it to HM13 or you’re bringing back all the energy from the conference back to your hospital, now is the time to start planning for the next national conference exclusively designed for the nation’s 40,000 hospitalists.
For newcomers, HM14 will offer unprecedented access, networking, and CME-accredited educational sessions for hospitalists in all career stages. And for veterans of SHM’s annual meeting, 2014 will introduce two new pre-courses: “Cardiology and Evidence-Based Medicine” and “Bending the Cost Curve,” one of the hottest topics in public health, which will have its own dedicated track as well.
In addition to offering the best CME-accredited educational experience, HM14 will also give hospitalists the chance to enjoy an all-new official headquarters for the meeting: Mandalay Bay Hotel & Casino in Las Vegas.
Pre-Courses
Enhance the HM14 educational experience, broaden your skills, and earn additional CME credits. Choose from one of the following HM-focused topics:
- Medical Procedures for the Hospitalist;
- Portable Ultrasound for the Hospitalist;
- Perioperative Medicine;
- ABIM Maintenance of Certification;
- Practice Management;
- Neurology;
- Cardiology (new); and
- Evidence-Based Medicine (new).
Content Areas
The educational tracks offered at HM14 enable attendees to take courses in various designated tracks designed to better focus and enrich the annual meeting for attendees.
Tracks focus on the following cutting-edge content areas:
- Clinical;
- Rapid Fire;
- Practice Management;
- Academic/Research;
- Quality;
- Bending the Cost Curve (new);
- Pediatric;
- Potpourri;
- Comanagement; and
- Workshops.
Brendon Shank is SHM’s associate vice president of communications.
RIV Presenters at HM13 Explore Common Hospitalist Concerns
Two oral research poster presentations at HM13 explored malpractice concerns of hospitalists and the issue of defensive-medicine-related overutilization—popular topics considering how policymakers are attempting to bend the cost curve in the direction of greater efficiency and value.
Hospitalist Alan Kachalia, MD, JD, and colleagues at Brigham and Women’s Hospital in Boston conducted a randomized national survey of 1,020 hospitalists and analyzed their responses to common clinical scenarios. They found evidence of inappropriate overutilization and deviance from scientific evidence or recognized treatment guidelines, which the research team pegged to the practice of defensive medicine.
Dr. Kachalia’s presentation, “Overutilization and Defensive Medicine in U.S. Hospitals: A Randomized National Survey of Hospitalists,” was named best of the oral presentations in the research category.
“Our survey found substantial overutilization, frequently caused by defensive medicine,” in response to questions about practice patterns for two common clinical scenarios: preoperative evaluation and syncope, Dr. Kachalia said. Physicians who practiced at Veterans Affairs medical centers had less association with defensive medicine, while those who paid for their own liability insurance reported more. Overall, defensive medicine was reported for 37% of preoperative evaluations and 58% of the syncope scenarios.
More than 800 abstracts were submitted for HM13’s Research, Innovations, and Clinical Vignettes (RIV) competition. Nearly 600 were accepted, put on display at the annual meeting, and published online (www.shmabstracts.com). More than 100 abstracts were judged, with 15 of the Research and Innovations entries invited to make oral presentations of their projects. Three others gave “Best of RIV” plenary presentations at the conference.
The diversity and richness of HM13’s oral and poster presentations also will be highlighted in the Innovations department of The Hospitalist over the next year.
Asked to suggest policy responses to these findings, Dr. Kachalia said reform of the malpractice system is needed. “What a lot of us argue is that to get physicians to follow treatment guidelines, make them more clear and practical,” he said. “We’d also like to see safe harbors [from lawsuits] for following recognized guidelines.”
Adam Schaffer, MD, also a hospitalist at Brigham and Women’s Hospital in Boston, and colleagues reviewed a medical liability insurance carrier’s database of more than 30,000 closed claims for those in which a hospitalist was the attending of record. Dr. Schaffer’s retrospective, observational analysis, “Medical Malpractice: Causes and Outcomes of Claims Against Hospitalists,” of the claims database from 1997 to 2011 found 272 claims—almost 1%—for which the attending was a hospitalist.
“The claims rate was almost four times lower for hospitalists than for nonhospitalist internal-medicine physicians,” he said.
The average payment for claims against hospitalists also was smaller. He noted that the types of claims were similar and tended to fall in three general categories: errors in medical treatment, missed or delayed diagnoses, and medication-related errors (although claims also tended to have multiple contributing factors).
Research like Dr. Schaffer’s could help to inform patient-safety efforts and reduce legal malpractice risk, he said. If hospitalists have fewer malpractice claims, that information might also be used to argue for lower malpractice premium rates.
Larry Beresford is a freelance writer in Oakland, Calif.
Two oral research poster presentations at HM13 explored malpractice concerns of hospitalists and the issue of defensive-medicine-related overutilization—popular topics considering how policymakers are attempting to bend the cost curve in the direction of greater efficiency and value.
Hospitalist Alan Kachalia, MD, JD, and colleagues at Brigham and Women’s Hospital in Boston conducted a randomized national survey of 1,020 hospitalists and analyzed their responses to common clinical scenarios. They found evidence of inappropriate overutilization and deviance from scientific evidence or recognized treatment guidelines, which the research team pegged to the practice of defensive medicine.
Dr. Kachalia’s presentation, “Overutilization and Defensive Medicine in U.S. Hospitals: A Randomized National Survey of Hospitalists,” was named best of the oral presentations in the research category.
“Our survey found substantial overutilization, frequently caused by defensive medicine,” in response to questions about practice patterns for two common clinical scenarios: preoperative evaluation and syncope, Dr. Kachalia said. Physicians who practiced at Veterans Affairs medical centers had less association with defensive medicine, while those who paid for their own liability insurance reported more. Overall, defensive medicine was reported for 37% of preoperative evaluations and 58% of the syncope scenarios.
More than 800 abstracts were submitted for HM13’s Research, Innovations, and Clinical Vignettes (RIV) competition. Nearly 600 were accepted, put on display at the annual meeting, and published online (www.shmabstracts.com). More than 100 abstracts were judged, with 15 of the Research and Innovations entries invited to make oral presentations of their projects. Three others gave “Best of RIV” plenary presentations at the conference.
The diversity and richness of HM13’s oral and poster presentations also will be highlighted in the Innovations department of The Hospitalist over the next year.
Asked to suggest policy responses to these findings, Dr. Kachalia said reform of the malpractice system is needed. “What a lot of us argue is that to get physicians to follow treatment guidelines, make them more clear and practical,” he said. “We’d also like to see safe harbors [from lawsuits] for following recognized guidelines.”
Adam Schaffer, MD, also a hospitalist at Brigham and Women’s Hospital in Boston, and colleagues reviewed a medical liability insurance carrier’s database of more than 30,000 closed claims for those in which a hospitalist was the attending of record. Dr. Schaffer’s retrospective, observational analysis, “Medical Malpractice: Causes and Outcomes of Claims Against Hospitalists,” of the claims database from 1997 to 2011 found 272 claims—almost 1%—for which the attending was a hospitalist.
“The claims rate was almost four times lower for hospitalists than for nonhospitalist internal-medicine physicians,” he said.
The average payment for claims against hospitalists also was smaller. He noted that the types of claims were similar and tended to fall in three general categories: errors in medical treatment, missed or delayed diagnoses, and medication-related errors (although claims also tended to have multiple contributing factors).
Research like Dr. Schaffer’s could help to inform patient-safety efforts and reduce legal malpractice risk, he said. If hospitalists have fewer malpractice claims, that information might also be used to argue for lower malpractice premium rates.
Larry Beresford is a freelance writer in Oakland, Calif.
Two oral research poster presentations at HM13 explored malpractice concerns of hospitalists and the issue of defensive-medicine-related overutilization—popular topics considering how policymakers are attempting to bend the cost curve in the direction of greater efficiency and value.
Hospitalist Alan Kachalia, MD, JD, and colleagues at Brigham and Women’s Hospital in Boston conducted a randomized national survey of 1,020 hospitalists and analyzed their responses to common clinical scenarios. They found evidence of inappropriate overutilization and deviance from scientific evidence or recognized treatment guidelines, which the research team pegged to the practice of defensive medicine.
Dr. Kachalia’s presentation, “Overutilization and Defensive Medicine in U.S. Hospitals: A Randomized National Survey of Hospitalists,” was named best of the oral presentations in the research category.
“Our survey found substantial overutilization, frequently caused by defensive medicine,” in response to questions about practice patterns for two common clinical scenarios: preoperative evaluation and syncope, Dr. Kachalia said. Physicians who practiced at Veterans Affairs medical centers had less association with defensive medicine, while those who paid for their own liability insurance reported more. Overall, defensive medicine was reported for 37% of preoperative evaluations and 58% of the syncope scenarios.
More than 800 abstracts were submitted for HM13’s Research, Innovations, and Clinical Vignettes (RIV) competition. Nearly 600 were accepted, put on display at the annual meeting, and published online (www.shmabstracts.com). More than 100 abstracts were judged, with 15 of the Research and Innovations entries invited to make oral presentations of their projects. Three others gave “Best of RIV” plenary presentations at the conference.
The diversity and richness of HM13’s oral and poster presentations also will be highlighted in the Innovations department of The Hospitalist over the next year.
Asked to suggest policy responses to these findings, Dr. Kachalia said reform of the malpractice system is needed. “What a lot of us argue is that to get physicians to follow treatment guidelines, make them more clear and practical,” he said. “We’d also like to see safe harbors [from lawsuits] for following recognized guidelines.”
Adam Schaffer, MD, also a hospitalist at Brigham and Women’s Hospital in Boston, and colleagues reviewed a medical liability insurance carrier’s database of more than 30,000 closed claims for those in which a hospitalist was the attending of record. Dr. Schaffer’s retrospective, observational analysis, “Medical Malpractice: Causes and Outcomes of Claims Against Hospitalists,” of the claims database from 1997 to 2011 found 272 claims—almost 1%—for which the attending was a hospitalist.
“The claims rate was almost four times lower for hospitalists than for nonhospitalist internal-medicine physicians,” he said.
The average payment for claims against hospitalists also was smaller. He noted that the types of claims were similar and tended to fall in three general categories: errors in medical treatment, missed or delayed diagnoses, and medication-related errors (although claims also tended to have multiple contributing factors).
Research like Dr. Schaffer’s could help to inform patient-safety efforts and reduce legal malpractice risk, he said. If hospitalists have fewer malpractice claims, that information might also be used to argue for lower malpractice premium rates.
Larry Beresford is a freelance writer in Oakland, Calif.
Hospitalists Share Information, Insights Through RIV Posters at HM13
One of the busiest times of HM13—and, come to think of it, every recent annual meeting—is the poster session for the Research, Innovations, and Clinical Vignettes (RIV) competition. This year, more than 800 abstracts were submitted and reviewed, with nearly 600 being accepted for presentation at HM13. That meant thousands of hospitalists thumbtacking posters to rows and rows of portable bulletin boards in the Gaylord National Resort & Convention Center’s massive exhibit hall.
With all those posters and accompanying oral presentations, it’s impossible for RIV judges to chat with everybody, so they choose finalists based on the abstracts, then listen to quick-hit summaries before choosing a winner on site. And meeting attendees are just as strapped for time, so they do the best they can to see as many posters as they can, taking time to network with old connections and make new ones.
So with all the limitations on how many people will interact with your poster, the small chance of winning Best in Show, and the hundreds of work hours that go into a poster presentation, why do it?
“To share is what I think is really important,” says Todd Hecht, MD, FACP, SFHM, associate professor of clinical medicine at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. “If you don’t let other people know what you’re doing, they can’t bring it to their institutions, nor can you learn from others and bring their innovations to your own hospital.”
Dr. Hecht, director of the Anticoagulation Management Center and Anticoagulation Management Program at the Hospital of the University of Pennsylvania, takes the poster sessions very seriously. This year, he entered a poster in both the Innovations and Vignette categories. His Innovations poster, “Impact of a Multidisciplinary Safety Checklist on the Rate of Preventable Hospital Complications and Standardization of Care,” was a finalist.
That meant that, at the very least, he’d be able to explain to at least two judges what motivated his research team’s project. And what was the inspiration? A 90-year-old male patient with metastatic melanoma who, in the fall of 2011, refused to take medication for VTE prophylaxis, as lesions on his skin made the process rather painful. After refusing the doses for a bit, though, the high-risk patient unsurprisingly developed a pulmonary embolism (PE).
The man survived the PE, but Dr. Hecht and his colleagues began to wonder how many patients refuse VTE prophylaxis. So they investigated, and it turned out that from December 2010 to February 2011, 26.4% of the prescribed doses of prophylaxis on the medicine floors they studied were missed. Moreover, nearly 80% of all missed doses on the medicine floors were due to patient refusal.
“It was astonishing to me that it was that high,” Dr. Hecht says. “If there were 1,000 doses in a month, 260 of them were not being given—and 205 of them were not given because they were refused.”
Checklist Integration
So Dr. Hecht and colleagues set out to create a checklist that could be used daily on multidisciplinary rounds to help reduce the risk of VTE. First question on the list: Has prophylaxis been ordered, and if so, is the patient refusing it? Knowing that patients are “refusing” medication can lead to discussions about why that is happening, which in turn can lead to ways to convince the patient that the preventative measure is a good idea.
Dr. Hecht says the team also realized a checklist creates the opportunity to improve other quality metrics, such as hospital-associated infections (HAIs). Two questions on the checklist ask whether indwelling urinary catheters (IUCs) and central venous catheters (CVCs) can be removed. Two questions ask if telemetry can be stopped and whether there are any pain-management concerns. A final query asks whether there are any nursing, social work, or discharge-related questions—a step that, according to Dr. Hecht, loops the entire multidisciplinary team into the care-plan discussion.
“An ongoing challenge is making sure it’s not just questions being asked and being answered by rote,” Dr. Hecht says. “Just pause and think for just a second for each question. You can get through the checklist in 10 seconds, but you can’t go through the checklist in two seconds.”
The project’s results are what made it a finalist. After the checklist intervention, the number of missed doses of VTE prophylaxis plummeted 59% to just 10.9% (P<0.001) from September to November 2012; the number of “patient refused” doses dropped to 6.3% (P<0.001).
Not only was Dr. Hecht caught off guard by his findings, but so were the judges who visited his poster—Mangla Gulati, MD, FHM, of the University of Maryland School of Medicine and Rachel George, MD, MBA, FHM, of Cogent HMG.
“I wonder if it’s like that in every hospital,” Dr. George says. “I’d like to know.”
The positive reaction and feedback to Dr. Hecht’s poster, however, was not enough to win the Innovations category. That honor went to “SEPTRIS: Improving Sepsis Recognition and Management Through a Mobile Educational Game,” which was developed by a team of researchers at Stanford University in Palo Alto, Calif. The video game
(http://med.stanford.edu/septris/)—a mashup of sepsis and the once-popular Tetris puzzle game—already has been played 17,000 times and is on its way to being shared in other languages.
“Win or lose, it doesn’t matter,” Dr. Hecht says. “The goal is to share your information with other people and learn from them.”
Peter Watson, MD, FACP, FHM, sees it the same way. That’s why this year he was both judge and judged. The division head of hospital medicine for Henry Ford Medical Group in Detroit was part of a group presenting “Feasibility and Efficacy of a Specialized Pilot Training Program to Enhance Inpatient Communication Skills of Hospitalists.” He was a judge for the Research portion of the contest. He says he’s hard-pressed to say which process he enjoyed more, but one trick of the poster trade he passes along is that “judging actually makes you a better presenter on the back end,” especially when it comes to describing in less than five minutes a poster whose work may date back 12 to 18 months.
“In your brain,” he says, “you have a Tolstoy novel of information, but you have to break that down into a paragraph of CliffsNotes, and actually convince the people that are judging you that you have a really cool project that either is going to have a big impact in the field or may lead to other big studies or is going to impress somebody so much that they’re going to go back to their institution and say, ‘Hey, I’m going to do that.’”
Dr. Watson also urges people not to be discouraged by not winning the poster contest. First, all of the accepted abstracts get published online (www.shmabstracts.com) by the Journal of Hospital Medicine, a high point for medical students, residents, and early-career physicians looking to make a mark. Second, presenting information of value to one’s peers is the definition of a specialty that prides itself on collaboration.
“To see a second-year medical student presenting all the way up to a very senior division chief and everything in between is a really good example for our profession,” he says. “That’s really the magic of this meeting.”
Richard Quinn is a freelance writer in New Jersey.
One of the busiest times of HM13—and, come to think of it, every recent annual meeting—is the poster session for the Research, Innovations, and Clinical Vignettes (RIV) competition. This year, more than 800 abstracts were submitted and reviewed, with nearly 600 being accepted for presentation at HM13. That meant thousands of hospitalists thumbtacking posters to rows and rows of portable bulletin boards in the Gaylord National Resort & Convention Center’s massive exhibit hall.
With all those posters and accompanying oral presentations, it’s impossible for RIV judges to chat with everybody, so they choose finalists based on the abstracts, then listen to quick-hit summaries before choosing a winner on site. And meeting attendees are just as strapped for time, so they do the best they can to see as many posters as they can, taking time to network with old connections and make new ones.
So with all the limitations on how many people will interact with your poster, the small chance of winning Best in Show, and the hundreds of work hours that go into a poster presentation, why do it?
“To share is what I think is really important,” says Todd Hecht, MD, FACP, SFHM, associate professor of clinical medicine at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. “If you don’t let other people know what you’re doing, they can’t bring it to their institutions, nor can you learn from others and bring their innovations to your own hospital.”
Dr. Hecht, director of the Anticoagulation Management Center and Anticoagulation Management Program at the Hospital of the University of Pennsylvania, takes the poster sessions very seriously. This year, he entered a poster in both the Innovations and Vignette categories. His Innovations poster, “Impact of a Multidisciplinary Safety Checklist on the Rate of Preventable Hospital Complications and Standardization of Care,” was a finalist.
That meant that, at the very least, he’d be able to explain to at least two judges what motivated his research team’s project. And what was the inspiration? A 90-year-old male patient with metastatic melanoma who, in the fall of 2011, refused to take medication for VTE prophylaxis, as lesions on his skin made the process rather painful. After refusing the doses for a bit, though, the high-risk patient unsurprisingly developed a pulmonary embolism (PE).
The man survived the PE, but Dr. Hecht and his colleagues began to wonder how many patients refuse VTE prophylaxis. So they investigated, and it turned out that from December 2010 to February 2011, 26.4% of the prescribed doses of prophylaxis on the medicine floors they studied were missed. Moreover, nearly 80% of all missed doses on the medicine floors were due to patient refusal.
“It was astonishing to me that it was that high,” Dr. Hecht says. “If there were 1,000 doses in a month, 260 of them were not being given—and 205 of them were not given because they were refused.”
Checklist Integration
So Dr. Hecht and colleagues set out to create a checklist that could be used daily on multidisciplinary rounds to help reduce the risk of VTE. First question on the list: Has prophylaxis been ordered, and if so, is the patient refusing it? Knowing that patients are “refusing” medication can lead to discussions about why that is happening, which in turn can lead to ways to convince the patient that the preventative measure is a good idea.
Dr. Hecht says the team also realized a checklist creates the opportunity to improve other quality metrics, such as hospital-associated infections (HAIs). Two questions on the checklist ask whether indwelling urinary catheters (IUCs) and central venous catheters (CVCs) can be removed. Two questions ask if telemetry can be stopped and whether there are any pain-management concerns. A final query asks whether there are any nursing, social work, or discharge-related questions—a step that, according to Dr. Hecht, loops the entire multidisciplinary team into the care-plan discussion.
“An ongoing challenge is making sure it’s not just questions being asked and being answered by rote,” Dr. Hecht says. “Just pause and think for just a second for each question. You can get through the checklist in 10 seconds, but you can’t go through the checklist in two seconds.”
The project’s results are what made it a finalist. After the checklist intervention, the number of missed doses of VTE prophylaxis plummeted 59% to just 10.9% (P<0.001) from September to November 2012; the number of “patient refused” doses dropped to 6.3% (P<0.001).
Not only was Dr. Hecht caught off guard by his findings, but so were the judges who visited his poster—Mangla Gulati, MD, FHM, of the University of Maryland School of Medicine and Rachel George, MD, MBA, FHM, of Cogent HMG.
“I wonder if it’s like that in every hospital,” Dr. George says. “I’d like to know.”
The positive reaction and feedback to Dr. Hecht’s poster, however, was not enough to win the Innovations category. That honor went to “SEPTRIS: Improving Sepsis Recognition and Management Through a Mobile Educational Game,” which was developed by a team of researchers at Stanford University in Palo Alto, Calif. The video game
(http://med.stanford.edu/septris/)—a mashup of sepsis and the once-popular Tetris puzzle game—already has been played 17,000 times and is on its way to being shared in other languages.
“Win or lose, it doesn’t matter,” Dr. Hecht says. “The goal is to share your information with other people and learn from them.”
Peter Watson, MD, FACP, FHM, sees it the same way. That’s why this year he was both judge and judged. The division head of hospital medicine for Henry Ford Medical Group in Detroit was part of a group presenting “Feasibility and Efficacy of a Specialized Pilot Training Program to Enhance Inpatient Communication Skills of Hospitalists.” He was a judge for the Research portion of the contest. He says he’s hard-pressed to say which process he enjoyed more, but one trick of the poster trade he passes along is that “judging actually makes you a better presenter on the back end,” especially when it comes to describing in less than five minutes a poster whose work may date back 12 to 18 months.
“In your brain,” he says, “you have a Tolstoy novel of information, but you have to break that down into a paragraph of CliffsNotes, and actually convince the people that are judging you that you have a really cool project that either is going to have a big impact in the field or may lead to other big studies or is going to impress somebody so much that they’re going to go back to their institution and say, ‘Hey, I’m going to do that.’”
Dr. Watson also urges people not to be discouraged by not winning the poster contest. First, all of the accepted abstracts get published online (www.shmabstracts.com) by the Journal of Hospital Medicine, a high point for medical students, residents, and early-career physicians looking to make a mark. Second, presenting information of value to one’s peers is the definition of a specialty that prides itself on collaboration.
“To see a second-year medical student presenting all the way up to a very senior division chief and everything in between is a really good example for our profession,” he says. “That’s really the magic of this meeting.”
Richard Quinn is a freelance writer in New Jersey.
One of the busiest times of HM13—and, come to think of it, every recent annual meeting—is the poster session for the Research, Innovations, and Clinical Vignettes (RIV) competition. This year, more than 800 abstracts were submitted and reviewed, with nearly 600 being accepted for presentation at HM13. That meant thousands of hospitalists thumbtacking posters to rows and rows of portable bulletin boards in the Gaylord National Resort & Convention Center’s massive exhibit hall.
With all those posters and accompanying oral presentations, it’s impossible for RIV judges to chat with everybody, so they choose finalists based on the abstracts, then listen to quick-hit summaries before choosing a winner on site. And meeting attendees are just as strapped for time, so they do the best they can to see as many posters as they can, taking time to network with old connections and make new ones.
So with all the limitations on how many people will interact with your poster, the small chance of winning Best in Show, and the hundreds of work hours that go into a poster presentation, why do it?
“To share is what I think is really important,” says Todd Hecht, MD, FACP, SFHM, associate professor of clinical medicine at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. “If you don’t let other people know what you’re doing, they can’t bring it to their institutions, nor can you learn from others and bring their innovations to your own hospital.”
Dr. Hecht, director of the Anticoagulation Management Center and Anticoagulation Management Program at the Hospital of the University of Pennsylvania, takes the poster sessions very seriously. This year, he entered a poster in both the Innovations and Vignette categories. His Innovations poster, “Impact of a Multidisciplinary Safety Checklist on the Rate of Preventable Hospital Complications and Standardization of Care,” was a finalist.
That meant that, at the very least, he’d be able to explain to at least two judges what motivated his research team’s project. And what was the inspiration? A 90-year-old male patient with metastatic melanoma who, in the fall of 2011, refused to take medication for VTE prophylaxis, as lesions on his skin made the process rather painful. After refusing the doses for a bit, though, the high-risk patient unsurprisingly developed a pulmonary embolism (PE).
The man survived the PE, but Dr. Hecht and his colleagues began to wonder how many patients refuse VTE prophylaxis. So they investigated, and it turned out that from December 2010 to February 2011, 26.4% of the prescribed doses of prophylaxis on the medicine floors they studied were missed. Moreover, nearly 80% of all missed doses on the medicine floors were due to patient refusal.
“It was astonishing to me that it was that high,” Dr. Hecht says. “If there were 1,000 doses in a month, 260 of them were not being given—and 205 of them were not given because they were refused.”
Checklist Integration
So Dr. Hecht and colleagues set out to create a checklist that could be used daily on multidisciplinary rounds to help reduce the risk of VTE. First question on the list: Has prophylaxis been ordered, and if so, is the patient refusing it? Knowing that patients are “refusing” medication can lead to discussions about why that is happening, which in turn can lead to ways to convince the patient that the preventative measure is a good idea.
Dr. Hecht says the team also realized a checklist creates the opportunity to improve other quality metrics, such as hospital-associated infections (HAIs). Two questions on the checklist ask whether indwelling urinary catheters (IUCs) and central venous catheters (CVCs) can be removed. Two questions ask if telemetry can be stopped and whether there are any pain-management concerns. A final query asks whether there are any nursing, social work, or discharge-related questions—a step that, according to Dr. Hecht, loops the entire multidisciplinary team into the care-plan discussion.
“An ongoing challenge is making sure it’s not just questions being asked and being answered by rote,” Dr. Hecht says. “Just pause and think for just a second for each question. You can get through the checklist in 10 seconds, but you can’t go through the checklist in two seconds.”
The project’s results are what made it a finalist. After the checklist intervention, the number of missed doses of VTE prophylaxis plummeted 59% to just 10.9% (P<0.001) from September to November 2012; the number of “patient refused” doses dropped to 6.3% (P<0.001).
Not only was Dr. Hecht caught off guard by his findings, but so were the judges who visited his poster—Mangla Gulati, MD, FHM, of the University of Maryland School of Medicine and Rachel George, MD, MBA, FHM, of Cogent HMG.
“I wonder if it’s like that in every hospital,” Dr. George says. “I’d like to know.”
The positive reaction and feedback to Dr. Hecht’s poster, however, was not enough to win the Innovations category. That honor went to “SEPTRIS: Improving Sepsis Recognition and Management Through a Mobile Educational Game,” which was developed by a team of researchers at Stanford University in Palo Alto, Calif. The video game
(http://med.stanford.edu/septris/)—a mashup of sepsis and the once-popular Tetris puzzle game—already has been played 17,000 times and is on its way to being shared in other languages.
“Win or lose, it doesn’t matter,” Dr. Hecht says. “The goal is to share your information with other people and learn from them.”
Peter Watson, MD, FACP, FHM, sees it the same way. That’s why this year he was both judge and judged. The division head of hospital medicine for Henry Ford Medical Group in Detroit was part of a group presenting “Feasibility and Efficacy of a Specialized Pilot Training Program to Enhance Inpatient Communication Skills of Hospitalists.” He was a judge for the Research portion of the contest. He says he’s hard-pressed to say which process he enjoyed more, but one trick of the poster trade he passes along is that “judging actually makes you a better presenter on the back end,” especially when it comes to describing in less than five minutes a poster whose work may date back 12 to 18 months.
“In your brain,” he says, “you have a Tolstoy novel of information, but you have to break that down into a paragraph of CliffsNotes, and actually convince the people that are judging you that you have a really cool project that either is going to have a big impact in the field or may lead to other big studies or is going to impress somebody so much that they’re going to go back to their institution and say, ‘Hey, I’m going to do that.’”
Dr. Watson also urges people not to be discouraged by not winning the poster contest. First, all of the accepted abstracts get published online (www.shmabstracts.com) by the Journal of Hospital Medicine, a high point for medical students, residents, and early-career physicians looking to make a mark. Second, presenting information of value to one’s peers is the definition of a specialty that prides itself on collaboration.
“To see a second-year medical student presenting all the way up to a very senior division chief and everything in between is a really good example for our profession,” he says. “That’s really the magic of this meeting.”
Richard Quinn is a freelance writer in New Jersey.
Quality Improvement (QI) Remains a Central Theme at HM13
Like a grinning child at a carnival, Iqbal M. Binoj, MD, steps right up and gives it a try—except instead of tossing rings, he’s gripping an intraosseous infusion drill.
A tutor shows him how the device, which looks remarkably like a glue gun, inserts into the bones of the shoulder or knee and drills down until it hits the marrow. He is guided on using a steady speed to maintain the integrity of the cavity. He’s also taught about the maneuver’s low complication rates and ability to expedite workups.
“I’ve seen it used before, but I never did it,” says Dr. Binoj, a hospitalist with Cogent HMG at Genesis Medical Center in Davenport, Iowa.
Well, he never did it before a hands-on pre-course at HM13 that focused on improving hospitalists’ proficiency at such procedures as lumbar punctures and ultrasound-guided vascular access. Quality improvement (QI) is always a focus of SHM’s annual meeting, but sometimes the science of improving care is viewed from up on high.
Not everything needs to be a national imitative, an institution-wide project, or even a unit-based intervention. Sometimes, it’s as simple as teaching a room full of hospitalists how to use an intraosseous infusion drill, says Michelle Fox, RN, BSN, senior director of clinical affairs with Vidacare, which manufactures the drill used in the demonstration.
“Hospitalists have an increasing role in doing these procedures, not only in the environment they predominantly support but in other areas of the hospital,” Fox says, adding that “the primary goal of this course is to give them the opportunity to perfect those skills.”
Hospitalist Bradley Rosen, MD, MBA, FHM, medical of the inpatient specialty program at Cedars-Sinai in Los Angeles, says the point of hands-on demonstrations is to translate QI to the bedside. Take ultrasound devices, he says. In the past few years, the technology has become less expensive, better in resolution, more common, and more portable. Hospitalists must ensure hands-on training that keeps pace with that technology.
“We actually want people to get gloves on, hands on, learn where they may have challenges in terms of their own dexterity or workflow, which hand is dominant, and how to visualize on the ultrasound machine a three-dimensional structure in 2D,” he says. “We don’t want people watching from the sidelines. ... We try to get people in it and engaged.”
And once hospitalists master procedures or diagnostic maneuvers, they invariably are sought out by other physicians to pass that knowledge on to others, Dr. Rosen says.
“In so doing, we get involved in larger quality initiatives and systemwide changes that can go top-down,” he adds, “but from our perspective, it starts with the individual practitioner. And I think SHM has always advocated and preached the importance of the individual hospitalist doing the best possible job for your patient, and the group, and the institution.”
Shared Excellence
What’s best for individual institutions moving forward is what worries SHM immediate past president Shaun Frost, MD, SFHM. He fears CMS’ Value-Based Payment Modifier (VBPM) program could have the unintended consequence of spurring some hospitals to hang on to innovative ideas in order to keep a competitive business advantage.
In health care, where quality and affordability have long been viewed as valuable for nonmonetary reasons, “the medical profession willingly shares new information” to improve patient care, Dr. Frost said in his farewell speech. But he is concerned that commodification—imbuing monetary value into something that previously had none—could change that dynamic, a situation he says is “ethically not acceptable.”
“When somebody builds a better mousetrap, it should be freely shared so that all patients have the opportunity to benefit,” Dr. Frost said. “The pursuit of economic competitive advantage should not prevent us from collaborating and sharing new ideas that hopefully make the health system better.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque, N.M., says part of that improvement in quality and patient safety will come via hospitalists pushing for improvements to health information technology (HIT), particularly to maximize computerized physician order entry (CPOE) and order sets. He empathizes with those who complain about the operability of existing systems but urges physicians to stop complaining and take action.
“We need to stop accepting what our existing limitations are, and we need to be the innovators,” he says. “Many of us aren’t even thinking about, ‘What are the products we need?’ We’re just reacting to the products we currently have and stating how they don’t meet our needs.”
He suggests people communally report safety or troubleshooting issues, in part via Hospital Medicine Exchange (HMX), an online community SHM launched last year to discuss HM issues (www.hmxchange.org). He also wants hospitalists to push HIT vendors to provide improved functionality, and for institutions to provide necessary training.
“We just need to be vocal,” says Dr. Rogers, chair of SHM’s IT Executive Committee. “I do believe this is all leading us to a good place, but there’s a dip down before we have a swing up.”
Frustration Surge
In the long run, hospitalist Anuj Mehta, MD, medical director of the adult hospitalist program at Nyack Hospital in New York, agrees with Dr. Rogers. But as a provider seeing patients day after day, he says it’s often easier to not engage HIT than it is to slog through it.
“We try to work around the system, and sometimes it’s a much longer workaround,” he says. “So what happens is loss of productivity, greater length of stay, poor patient satisfaction, more screen time, and less bedside time.”
Dr. Mehta says frustration is building as society—outside of medicine—moves rapidly through such technology as smartphones, tablets, and other intuitive devices that make actions easier. He notes that his toddler daughter could learn how to navigate an iPad in a fraction of the time it takes him to complete an HIT training course.
“You cannot have physicians going through learning for four hours, learning a system to do step one before step two before step three,” he laments. “It should flow naturally. I don’t think the IT people have realized that as of yet.”
Richard Quinn is a freelance writer in New Jersey.
Like a grinning child at a carnival, Iqbal M. Binoj, MD, steps right up and gives it a try—except instead of tossing rings, he’s gripping an intraosseous infusion drill.
A tutor shows him how the device, which looks remarkably like a glue gun, inserts into the bones of the shoulder or knee and drills down until it hits the marrow. He is guided on using a steady speed to maintain the integrity of the cavity. He’s also taught about the maneuver’s low complication rates and ability to expedite workups.
“I’ve seen it used before, but I never did it,” says Dr. Binoj, a hospitalist with Cogent HMG at Genesis Medical Center in Davenport, Iowa.
Well, he never did it before a hands-on pre-course at HM13 that focused on improving hospitalists’ proficiency at such procedures as lumbar punctures and ultrasound-guided vascular access. Quality improvement (QI) is always a focus of SHM’s annual meeting, but sometimes the science of improving care is viewed from up on high.
Not everything needs to be a national imitative, an institution-wide project, or even a unit-based intervention. Sometimes, it’s as simple as teaching a room full of hospitalists how to use an intraosseous infusion drill, says Michelle Fox, RN, BSN, senior director of clinical affairs with Vidacare, which manufactures the drill used in the demonstration.
“Hospitalists have an increasing role in doing these procedures, not only in the environment they predominantly support but in other areas of the hospital,” Fox says, adding that “the primary goal of this course is to give them the opportunity to perfect those skills.”
Hospitalist Bradley Rosen, MD, MBA, FHM, medical of the inpatient specialty program at Cedars-Sinai in Los Angeles, says the point of hands-on demonstrations is to translate QI to the bedside. Take ultrasound devices, he says. In the past few years, the technology has become less expensive, better in resolution, more common, and more portable. Hospitalists must ensure hands-on training that keeps pace with that technology.
“We actually want people to get gloves on, hands on, learn where they may have challenges in terms of their own dexterity or workflow, which hand is dominant, and how to visualize on the ultrasound machine a three-dimensional structure in 2D,” he says. “We don’t want people watching from the sidelines. ... We try to get people in it and engaged.”
And once hospitalists master procedures or diagnostic maneuvers, they invariably are sought out by other physicians to pass that knowledge on to others, Dr. Rosen says.
“In so doing, we get involved in larger quality initiatives and systemwide changes that can go top-down,” he adds, “but from our perspective, it starts with the individual practitioner. And I think SHM has always advocated and preached the importance of the individual hospitalist doing the best possible job for your patient, and the group, and the institution.”
Shared Excellence
What’s best for individual institutions moving forward is what worries SHM immediate past president Shaun Frost, MD, SFHM. He fears CMS’ Value-Based Payment Modifier (VBPM) program could have the unintended consequence of spurring some hospitals to hang on to innovative ideas in order to keep a competitive business advantage.
In health care, where quality and affordability have long been viewed as valuable for nonmonetary reasons, “the medical profession willingly shares new information” to improve patient care, Dr. Frost said in his farewell speech. But he is concerned that commodification—imbuing monetary value into something that previously had none—could change that dynamic, a situation he says is “ethically not acceptable.”
“When somebody builds a better mousetrap, it should be freely shared so that all patients have the opportunity to benefit,” Dr. Frost said. “The pursuit of economic competitive advantage should not prevent us from collaborating and sharing new ideas that hopefully make the health system better.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque, N.M., says part of that improvement in quality and patient safety will come via hospitalists pushing for improvements to health information technology (HIT), particularly to maximize computerized physician order entry (CPOE) and order sets. He empathizes with those who complain about the operability of existing systems but urges physicians to stop complaining and take action.
“We need to stop accepting what our existing limitations are, and we need to be the innovators,” he says. “Many of us aren’t even thinking about, ‘What are the products we need?’ We’re just reacting to the products we currently have and stating how they don’t meet our needs.”
He suggests people communally report safety or troubleshooting issues, in part via Hospital Medicine Exchange (HMX), an online community SHM launched last year to discuss HM issues (www.hmxchange.org). He also wants hospitalists to push HIT vendors to provide improved functionality, and for institutions to provide necessary training.
“We just need to be vocal,” says Dr. Rogers, chair of SHM’s IT Executive Committee. “I do believe this is all leading us to a good place, but there’s a dip down before we have a swing up.”
Frustration Surge
In the long run, hospitalist Anuj Mehta, MD, medical director of the adult hospitalist program at Nyack Hospital in New York, agrees with Dr. Rogers. But as a provider seeing patients day after day, he says it’s often easier to not engage HIT than it is to slog through it.
“We try to work around the system, and sometimes it’s a much longer workaround,” he says. “So what happens is loss of productivity, greater length of stay, poor patient satisfaction, more screen time, and less bedside time.”
Dr. Mehta says frustration is building as society—outside of medicine—moves rapidly through such technology as smartphones, tablets, and other intuitive devices that make actions easier. He notes that his toddler daughter could learn how to navigate an iPad in a fraction of the time it takes him to complete an HIT training course.
“You cannot have physicians going through learning for four hours, learning a system to do step one before step two before step three,” he laments. “It should flow naturally. I don’t think the IT people have realized that as of yet.”
Richard Quinn is a freelance writer in New Jersey.
Like a grinning child at a carnival, Iqbal M. Binoj, MD, steps right up and gives it a try—except instead of tossing rings, he’s gripping an intraosseous infusion drill.
A tutor shows him how the device, which looks remarkably like a glue gun, inserts into the bones of the shoulder or knee and drills down until it hits the marrow. He is guided on using a steady speed to maintain the integrity of the cavity. He’s also taught about the maneuver’s low complication rates and ability to expedite workups.
“I’ve seen it used before, but I never did it,” says Dr. Binoj, a hospitalist with Cogent HMG at Genesis Medical Center in Davenport, Iowa.
Well, he never did it before a hands-on pre-course at HM13 that focused on improving hospitalists’ proficiency at such procedures as lumbar punctures and ultrasound-guided vascular access. Quality improvement (QI) is always a focus of SHM’s annual meeting, but sometimes the science of improving care is viewed from up on high.
Not everything needs to be a national imitative, an institution-wide project, or even a unit-based intervention. Sometimes, it’s as simple as teaching a room full of hospitalists how to use an intraosseous infusion drill, says Michelle Fox, RN, BSN, senior director of clinical affairs with Vidacare, which manufactures the drill used in the demonstration.
“Hospitalists have an increasing role in doing these procedures, not only in the environment they predominantly support but in other areas of the hospital,” Fox says, adding that “the primary goal of this course is to give them the opportunity to perfect those skills.”
Hospitalist Bradley Rosen, MD, MBA, FHM, medical of the inpatient specialty program at Cedars-Sinai in Los Angeles, says the point of hands-on demonstrations is to translate QI to the bedside. Take ultrasound devices, he says. In the past few years, the technology has become less expensive, better in resolution, more common, and more portable. Hospitalists must ensure hands-on training that keeps pace with that technology.
“We actually want people to get gloves on, hands on, learn where they may have challenges in terms of their own dexterity or workflow, which hand is dominant, and how to visualize on the ultrasound machine a three-dimensional structure in 2D,” he says. “We don’t want people watching from the sidelines. ... We try to get people in it and engaged.”
And once hospitalists master procedures or diagnostic maneuvers, they invariably are sought out by other physicians to pass that knowledge on to others, Dr. Rosen says.
“In so doing, we get involved in larger quality initiatives and systemwide changes that can go top-down,” he adds, “but from our perspective, it starts with the individual practitioner. And I think SHM has always advocated and preached the importance of the individual hospitalist doing the best possible job for your patient, and the group, and the institution.”
Shared Excellence
What’s best for individual institutions moving forward is what worries SHM immediate past president Shaun Frost, MD, SFHM. He fears CMS’ Value-Based Payment Modifier (VBPM) program could have the unintended consequence of spurring some hospitals to hang on to innovative ideas in order to keep a competitive business advantage.
In health care, where quality and affordability have long been viewed as valuable for nonmonetary reasons, “the medical profession willingly shares new information” to improve patient care, Dr. Frost said in his farewell speech. But he is concerned that commodification—imbuing monetary value into something that previously had none—could change that dynamic, a situation he says is “ethically not acceptable.”
“When somebody builds a better mousetrap, it should be freely shared so that all patients have the opportunity to benefit,” Dr. Frost said. “The pursuit of economic competitive advantage should not prevent us from collaborating and sharing new ideas that hopefully make the health system better.”
Kendall Rogers, MD, FACP, SFHM, chief of the division of hospital medicine at the University of New Mexico Health Sciences Center in Albuquerque, N.M., says part of that improvement in quality and patient safety will come via hospitalists pushing for improvements to health information technology (HIT), particularly to maximize computerized physician order entry (CPOE) and order sets. He empathizes with those who complain about the operability of existing systems but urges physicians to stop complaining and take action.
“We need to stop accepting what our existing limitations are, and we need to be the innovators,” he says. “Many of us aren’t even thinking about, ‘What are the products we need?’ We’re just reacting to the products we currently have and stating how they don’t meet our needs.”
He suggests people communally report safety or troubleshooting issues, in part via Hospital Medicine Exchange (HMX), an online community SHM launched last year to discuss HM issues (www.hmxchange.org). He also wants hospitalists to push HIT vendors to provide improved functionality, and for institutions to provide necessary training.
“We just need to be vocal,” says Dr. Rogers, chair of SHM’s IT Executive Committee. “I do believe this is all leading us to a good place, but there’s a dip down before we have a swing up.”
Frustration Surge
In the long run, hospitalist Anuj Mehta, MD, medical director of the adult hospitalist program at Nyack Hospital in New York, agrees with Dr. Rogers. But as a provider seeing patients day after day, he says it’s often easier to not engage HIT than it is to slog through it.
“We try to work around the system, and sometimes it’s a much longer workaround,” he says. “So what happens is loss of productivity, greater length of stay, poor patient satisfaction, more screen time, and less bedside time.”
Dr. Mehta says frustration is building as society—outside of medicine—moves rapidly through such technology as smartphones, tablets, and other intuitive devices that make actions easier. He notes that his toddler daughter could learn how to navigate an iPad in a fraction of the time it takes him to complete an HIT training course.
“You cannot have physicians going through learning for four hours, learning a system to do step one before step two before step three,” he laments. “It should flow naturally. I don’t think the IT people have realized that as of yet.”
Richard Quinn is a freelance writer in New Jersey.
Fix for Sustainable Growth Rate Formula a Top Priority
The Improving Access to Medicare Coverage Act isn’t the only legislative proposal on hospitalists’ radar right now. Republican members of the U.S. House of Representatives recently revised their plan to replace the sustainable growth rate (SGR) formula used to determine physician payments. A bill has not been introduced, but Beltway buzz hints one could be forthcoming this year.
“Fixing the flawed SGR physician payment is a top priority for the Committees on Energy and Commerce and Ways and Means,” GOP legislators said in an open letter to the “provider community.”2
The letter requested feedback from physicians and other stakeholders by April 15.
Any proposed fix would look to end the series of time-stamped delays that continue to delay a pending 27% cut to physician payments under Medicare. The latest delay was approved earlier this year, meaning that the new deadline for the SGR cut to be implemented is Dec. 31.
The SGR formula was created in 1997, but the pending cuts tied to the federal sequester were included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. But the cut also was considered a Draconian penalty that was never likely to actually happen.
Richard Quinn is a freelance writer in New Jersey.
References
- SHM. Letter to Congress members. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Letters_to_Congress_and_Regulatory_Agencies&Template=/CM/ContentDisplay.cfm&ContentID=33169. Accessed May 3, 2013.
- U.S. House of Representatives' Committee on Ways and Means, Energy and Commerce Committee, Health Subcommittee. Second draft of sustainable growth rate (SGR) repeal and reform proposal—request for feedback letter. U.S. House of Representatives' Committee on Ways and Means website. Available at: http://waysandmeans.house.gov/uploadedfiles/sgr_joint_release_document.pdf. Accessed May 3, 2013.
The Improving Access to Medicare Coverage Act isn’t the only legislative proposal on hospitalists’ radar right now. Republican members of the U.S. House of Representatives recently revised their plan to replace the sustainable growth rate (SGR) formula used to determine physician payments. A bill has not been introduced, but Beltway buzz hints one could be forthcoming this year.
“Fixing the flawed SGR physician payment is a top priority for the Committees on Energy and Commerce and Ways and Means,” GOP legislators said in an open letter to the “provider community.”2
The letter requested feedback from physicians and other stakeholders by April 15.
Any proposed fix would look to end the series of time-stamped delays that continue to delay a pending 27% cut to physician payments under Medicare. The latest delay was approved earlier this year, meaning that the new deadline for the SGR cut to be implemented is Dec. 31.
The SGR formula was created in 1997, but the pending cuts tied to the federal sequester were included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. But the cut also was considered a Draconian penalty that was never likely to actually happen.
Richard Quinn is a freelance writer in New Jersey.
References
- SHM. Letter to Congress members. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Letters_to_Congress_and_Regulatory_Agencies&Template=/CM/ContentDisplay.cfm&ContentID=33169. Accessed May 3, 2013.
- U.S. House of Representatives' Committee on Ways and Means, Energy and Commerce Committee, Health Subcommittee. Second draft of sustainable growth rate (SGR) repeal and reform proposal—request for feedback letter. U.S. House of Representatives' Committee on Ways and Means website. Available at: http://waysandmeans.house.gov/uploadedfiles/sgr_joint_release_document.pdf. Accessed May 3, 2013.
The Improving Access to Medicare Coverage Act isn’t the only legislative proposal on hospitalists’ radar right now. Republican members of the U.S. House of Representatives recently revised their plan to replace the sustainable growth rate (SGR) formula used to determine physician payments. A bill has not been introduced, but Beltway buzz hints one could be forthcoming this year.
“Fixing the flawed SGR physician payment is a top priority for the Committees on Energy and Commerce and Ways and Means,” GOP legislators said in an open letter to the “provider community.”2
The letter requested feedback from physicians and other stakeholders by April 15.
Any proposed fix would look to end the series of time-stamped delays that continue to delay a pending 27% cut to physician payments under Medicare. The latest delay was approved earlier this year, meaning that the new deadline for the SGR cut to be implemented is Dec. 31.
The SGR formula was created in 1997, but the pending cuts tied to the federal sequester were included in the Budget Control Act of 2011. At the time, the massive reduction to Medicare payments was tied to political brinksmanship over the country’s debt ceiling. But the cut also was considered a Draconian penalty that was never likely to actually happen.
Richard Quinn is a freelance writer in New Jersey.
References
- SHM. Letter to Congress members. SHM website. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Letters_to_Congress_and_Regulatory_Agencies&Template=/CM/ContentDisplay.cfm&ContentID=33169. Accessed May 3, 2013.
- U.S. House of Representatives' Committee on Ways and Means, Energy and Commerce Committee, Health Subcommittee. Second draft of sustainable growth rate (SGR) repeal and reform proposal—request for feedback letter. U.S. House of Representatives' Committee on Ways and Means website. Available at: http://waysandmeans.house.gov/uploadedfiles/sgr_joint_release_document.pdf. Accessed May 3, 2013.
Hospitalists Urge Congress to Reconsider Medicare’s “Observation Status” Rules

—Karim Godamunne, MD, MBA, SFHM
Hospitalists are pushing hard for a change to a Medicare rule requiring beneficiaries to accumulate at least three consecutive days of inpatient treatment at a hospital (not counting day of discharge) before it will cover care in a skilled nursing facility (SNF).
The issue was one of the talking points during last month’s Hospitalists on the Hill, SHM’s annual daylong advocacy campaign that this year coincided with the annual meeting in the nation’s capital. The issue gained attention from hospitalists and others in recent years, in part because of penalties hospitals face for readmissions—and also in part because hospitalists increasingly are providing care at SNFs and other post-acute-care facilities.
The spotlight is brighter now because a group of legislators is trying to identify Medicare beneficiaries previously given “observation status” as inpatients. The Improving Access to Medicare Coverage Act (H.R. 1179 and S. 569) also would establish a 90-day appeal period for those who have been denied the benefit.
SHM senior vice president Joe Miller says hospitalists used HM13 and the Hospitalists on the Hill advocacy day to discuss the issues and the proposed legislation with members of Congress, their staffs, and federal officials. He urges members to continue lobbying for changes. Although the topic might not have the resonance and impact of a fix to the sustainable growth rate (SGR), Miller says, “anybody that deals with admitting or discharging a patient will recognize the importance of this issue.”
The issue, according to Toby Edelman, a senior policy attorney for the Center for Medicare Advocacy in Washington, D.C, is that Medicare mandates that its program enrollees have at least three days of inpatient treatment before it will pay for SNF care. Medicare also covers the costs of post-acute care in other settings but does not require three days of inpatient treatment before doing so. The construct can be confusing to patients who spend time in a hospital but don’t realize that some or all of their stay is spent in “observation status,” meaning none of that time counts toward Medicare’s three-day threshold for reimbursement.
“Most people can’t believe you could be in a hospital bed for a week and then be told as you leave, ‘By the way, bring your checkbook to the nursing home because you weren’t an inpatient here and so now Medicare won’t pay for your stay in the nursing home,’” Edelman says. “This has been an issue for us for quite a while because the consequence for beneficiaries of being in observation is that people have to pay out of pocket for their nursing home care, and that cost is typically hundreds of dollars a day.”
The particular dilemma for hospitalists is managing transitions of care. Hospitalist Karim Godamunne, MD, MBA, SFHM, chief medical officer of North Fulton Hospital in Roswell, Ga., says hospitalists don’t want financial burdens to dictate care decisions, but they are caught in the middle of decisions that could saddle patients with uncovered costs.
He also worries that the issue will only grow in coming years as baby boomers put more pressure on the health-care system. “We have an aging population,” he adds. “This is not going to go away.”
That is one reason SHM is supporting the Improving Access to Medicare Coverage Act. SHM supported the bill when it was first introduced in March and it has been rapidly gaining cosponsors in recent weeks. This uptick in Congressional interest may be partly a response to the efforts of hospitalists during their time on the Hill. SHM staff and hospitalists are continuing their push now as society officials say hospitalists, who often handle both discharges from the hospital and care provided at SNFs, are in a position to lead discussions on how to sensibly fix the problem.
To that end, a recent SHM letter to the bill’s sponsors casts the issue as one of fiscal responsibility.1 Medicare not covering beneficiaries’ observation days cost patients out-of-pocket money and could cost hospitals in the long run.
“Patients who are admitted with observation status often choose to return home rather than paying out of pocket for a SNF stay,” SHM’s letter reads. “The resultant lack of appropriate post-acute SNF care can result in additional problems such as dehydration, falls, and many other avoidable complications. These complications can not only lead to otherwise preventable readmissions but also increase costs to Medicare for the treatment of conditions that were not present at the time of the original hospital stay.”
Given the debate on observation, Miller says, adopting the bill into law should be a no-brainer. The biggest sticking point likely is the perceived added cost to Medicare. Still, to streamline care and remove an added hurdle to coordinated care, Dr. Godamunne believes the bill should be embraced. He also says that many private insurers look to Medicare decisions to determine their own coverage approaches.
Basically, if Medicare changes its rules, that will carry a lot of weight in the private insurance world.
“This creates a lot of situations for the provider and the family,” Dr. Godamunne says. “You have to make a difficult decision, to try to help the family. You’re trying to provide good care, but on the other hand, there are rules and regulations and bylaws you work under. They don’t align that well, in this case.”
Richard Quinn is a freelance writer in New Jersey.
References

—Karim Godamunne, MD, MBA, SFHM
Hospitalists are pushing hard for a change to a Medicare rule requiring beneficiaries to accumulate at least three consecutive days of inpatient treatment at a hospital (not counting day of discharge) before it will cover care in a skilled nursing facility (SNF).
The issue was one of the talking points during last month’s Hospitalists on the Hill, SHM’s annual daylong advocacy campaign that this year coincided with the annual meeting in the nation’s capital. The issue gained attention from hospitalists and others in recent years, in part because of penalties hospitals face for readmissions—and also in part because hospitalists increasingly are providing care at SNFs and other post-acute-care facilities.
The spotlight is brighter now because a group of legislators is trying to identify Medicare beneficiaries previously given “observation status” as inpatients. The Improving Access to Medicare Coverage Act (H.R. 1179 and S. 569) also would establish a 90-day appeal period for those who have been denied the benefit.
SHM senior vice president Joe Miller says hospitalists used HM13 and the Hospitalists on the Hill advocacy day to discuss the issues and the proposed legislation with members of Congress, their staffs, and federal officials. He urges members to continue lobbying for changes. Although the topic might not have the resonance and impact of a fix to the sustainable growth rate (SGR), Miller says, “anybody that deals with admitting or discharging a patient will recognize the importance of this issue.”
The issue, according to Toby Edelman, a senior policy attorney for the Center for Medicare Advocacy in Washington, D.C, is that Medicare mandates that its program enrollees have at least three days of inpatient treatment before it will pay for SNF care. Medicare also covers the costs of post-acute care in other settings but does not require three days of inpatient treatment before doing so. The construct can be confusing to patients who spend time in a hospital but don’t realize that some or all of their stay is spent in “observation status,” meaning none of that time counts toward Medicare’s three-day threshold for reimbursement.
“Most people can’t believe you could be in a hospital bed for a week and then be told as you leave, ‘By the way, bring your checkbook to the nursing home because you weren’t an inpatient here and so now Medicare won’t pay for your stay in the nursing home,’” Edelman says. “This has been an issue for us for quite a while because the consequence for beneficiaries of being in observation is that people have to pay out of pocket for their nursing home care, and that cost is typically hundreds of dollars a day.”
The particular dilemma for hospitalists is managing transitions of care. Hospitalist Karim Godamunne, MD, MBA, SFHM, chief medical officer of North Fulton Hospital in Roswell, Ga., says hospitalists don’t want financial burdens to dictate care decisions, but they are caught in the middle of decisions that could saddle patients with uncovered costs.
He also worries that the issue will only grow in coming years as baby boomers put more pressure on the health-care system. “We have an aging population,” he adds. “This is not going to go away.”
That is one reason SHM is supporting the Improving Access to Medicare Coverage Act. SHM supported the bill when it was first introduced in March and it has been rapidly gaining cosponsors in recent weeks. This uptick in Congressional interest may be partly a response to the efforts of hospitalists during their time on the Hill. SHM staff and hospitalists are continuing their push now as society officials say hospitalists, who often handle both discharges from the hospital and care provided at SNFs, are in a position to lead discussions on how to sensibly fix the problem.
To that end, a recent SHM letter to the bill’s sponsors casts the issue as one of fiscal responsibility.1 Medicare not covering beneficiaries’ observation days cost patients out-of-pocket money and could cost hospitals in the long run.
“Patients who are admitted with observation status often choose to return home rather than paying out of pocket for a SNF stay,” SHM’s letter reads. “The resultant lack of appropriate post-acute SNF care can result in additional problems such as dehydration, falls, and many other avoidable complications. These complications can not only lead to otherwise preventable readmissions but also increase costs to Medicare for the treatment of conditions that were not present at the time of the original hospital stay.”
Given the debate on observation, Miller says, adopting the bill into law should be a no-brainer. The biggest sticking point likely is the perceived added cost to Medicare. Still, to streamline care and remove an added hurdle to coordinated care, Dr. Godamunne believes the bill should be embraced. He also says that many private insurers look to Medicare decisions to determine their own coverage approaches.
Basically, if Medicare changes its rules, that will carry a lot of weight in the private insurance world.
“This creates a lot of situations for the provider and the family,” Dr. Godamunne says. “You have to make a difficult decision, to try to help the family. You’re trying to provide good care, but on the other hand, there are rules and regulations and bylaws you work under. They don’t align that well, in this case.”
Richard Quinn is a freelance writer in New Jersey.
References

—Karim Godamunne, MD, MBA, SFHM
Hospitalists are pushing hard for a change to a Medicare rule requiring beneficiaries to accumulate at least three consecutive days of inpatient treatment at a hospital (not counting day of discharge) before it will cover care in a skilled nursing facility (SNF).
The issue was one of the talking points during last month’s Hospitalists on the Hill, SHM’s annual daylong advocacy campaign that this year coincided with the annual meeting in the nation’s capital. The issue gained attention from hospitalists and others in recent years, in part because of penalties hospitals face for readmissions—and also in part because hospitalists increasingly are providing care at SNFs and other post-acute-care facilities.
The spotlight is brighter now because a group of legislators is trying to identify Medicare beneficiaries previously given “observation status” as inpatients. The Improving Access to Medicare Coverage Act (H.R. 1179 and S. 569) also would establish a 90-day appeal period for those who have been denied the benefit.
SHM senior vice president Joe Miller says hospitalists used HM13 and the Hospitalists on the Hill advocacy day to discuss the issues and the proposed legislation with members of Congress, their staffs, and federal officials. He urges members to continue lobbying for changes. Although the topic might not have the resonance and impact of a fix to the sustainable growth rate (SGR), Miller says, “anybody that deals with admitting or discharging a patient will recognize the importance of this issue.”
The issue, according to Toby Edelman, a senior policy attorney for the Center for Medicare Advocacy in Washington, D.C, is that Medicare mandates that its program enrollees have at least three days of inpatient treatment before it will pay for SNF care. Medicare also covers the costs of post-acute care in other settings but does not require three days of inpatient treatment before doing so. The construct can be confusing to patients who spend time in a hospital but don’t realize that some or all of their stay is spent in “observation status,” meaning none of that time counts toward Medicare’s three-day threshold for reimbursement.
“Most people can’t believe you could be in a hospital bed for a week and then be told as you leave, ‘By the way, bring your checkbook to the nursing home because you weren’t an inpatient here and so now Medicare won’t pay for your stay in the nursing home,’” Edelman says. “This has been an issue for us for quite a while because the consequence for beneficiaries of being in observation is that people have to pay out of pocket for their nursing home care, and that cost is typically hundreds of dollars a day.”
The particular dilemma for hospitalists is managing transitions of care. Hospitalist Karim Godamunne, MD, MBA, SFHM, chief medical officer of North Fulton Hospital in Roswell, Ga., says hospitalists don’t want financial burdens to dictate care decisions, but they are caught in the middle of decisions that could saddle patients with uncovered costs.
He also worries that the issue will only grow in coming years as baby boomers put more pressure on the health-care system. “We have an aging population,” he adds. “This is not going to go away.”
That is one reason SHM is supporting the Improving Access to Medicare Coverage Act. SHM supported the bill when it was first introduced in March and it has been rapidly gaining cosponsors in recent weeks. This uptick in Congressional interest may be partly a response to the efforts of hospitalists during their time on the Hill. SHM staff and hospitalists are continuing their push now as society officials say hospitalists, who often handle both discharges from the hospital and care provided at SNFs, are in a position to lead discussions on how to sensibly fix the problem.
To that end, a recent SHM letter to the bill’s sponsors casts the issue as one of fiscal responsibility.1 Medicare not covering beneficiaries’ observation days cost patients out-of-pocket money and could cost hospitals in the long run.
“Patients who are admitted with observation status often choose to return home rather than paying out of pocket for a SNF stay,” SHM’s letter reads. “The resultant lack of appropriate post-acute SNF care can result in additional problems such as dehydration, falls, and many other avoidable complications. These complications can not only lead to otherwise preventable readmissions but also increase costs to Medicare for the treatment of conditions that were not present at the time of the original hospital stay.”
Given the debate on observation, Miller says, adopting the bill into law should be a no-brainer. The biggest sticking point likely is the perceived added cost to Medicare. Still, to streamline care and remove an added hurdle to coordinated care, Dr. Godamunne believes the bill should be embraced. He also says that many private insurers look to Medicare decisions to determine their own coverage approaches.
Basically, if Medicare changes its rules, that will carry a lot of weight in the private insurance world.
“This creates a lot of situations for the provider and the family,” Dr. Godamunne says. “You have to make a difficult decision, to try to help the family. You’re trying to provide good care, but on the other hand, there are rules and regulations and bylaws you work under. They don’t align that well, in this case.”
Richard Quinn is a freelance writer in New Jersey.
References
Pediatric Hospitalist Charts Decade-Long Journey in Health Care
Dear Mark,
I am pleased and excited that you are willing to abandon your plan for being a vagabond and will give serious consideration to joining the faculty of the Department of Pediatrics to become a core member of a new [general pediatric inpatient] program that I believe has exciting potential.
So reads the first line of my very first job offer letter. Obviously, my chairman had a sense of humor. But he also was not off target, as before May 21 of my third year of residency, I had no meaningful work lined up. Dreams of locum tenens work in Hawaii or a California coastal town quickly disappeared as I received only offers for work in small-town Mississippi and Oklahoma. Eleven years later, I don’t think I could have planned a more fulfilling early career, particularly when the alternative might have been surfing on the Mississippi River.
I would like this opportunity, in my final column as The Hospitalist’s pediatric editor, to reflect on this odyssey from vagabond to hospitalist.
The Early Years
As a new attending, I was appropriately terrified of how much I didn’t know. I also had ambitious goals at first, wanting to emulate my two favorite role models from residency, Charles Ginsburg and Heinz Eichenwald. We might call them hospitalists now, but back then they were old-fashioned, generalist inpatient clinician-educators, even while chairing the department of pediatrics over their separate tenures. They were the smartest and wisest teachers that I have ever met. These early years were a pseudo-fellowship of sorts; under their tutelage, I soaked up more than I ever had during residency.
Despite all of this learning, I remained sheltered in my clinician-educator bubble. The path to excellence for me was defined through frequent trips to the library (where journals used to be stored) and trying to teach as well as my mentors did. I largely was ignorant of the national hospitalist movement, until the 2007 SHM annual meeting was held in my backyard in Dallas. Listening to Bob Wachter that year, and then Don Berwick the following year, I suddenly realized the tremendous and intertwined importance of the quality movement and hospitalists. We were going to fix medicine. OK, maybe not all of medicine, but it happened to be the perfect time for me to learn about our health-care crisis, quality, and the role of hospital medicine.
If my first five years were about clinical medicine, the next five years were all about lessons in leadership. I had a new role, directing 8 15 20 25 hospitalists—and now was accountable for the group’s results. I’ve often said that an explicit leadership role is like stepping behind a curtain, where your own previous n=1 perspective is now the challenge of herding a group of n=25. And let’s be clear that it’s one thing to manage the group and keep the ship afloat, but it’s entirely another thing to lead the group toward success.
A Path for Me
Although the cacophony of managing that many voices was deafening early on, I found solace in the lessons of quality improvement (QI), where no project lives without a team that is all going the same direction. Between the national opportunities for collaborative improvement and the day-to-day experiences within my group, I found two simple principles worked well: 1) engage the team and 2) deliver objective results.
And just as I had craved a clinical learning environment early on, I now found myself learning from local and national peers putting their leadership skills in action to produce quality outcomes. The beauty of collaborative teamwork is that it creates self-sustaining capacity for more positive results.
Looking forward, the opportunities seem limitless for pediatric hospital medicine. From the inherent fulfillment of our day-to-day bedside work to the explicit leadership that we offer the complex hospital system, our family of pediatric hospitalists has blazed career paths in all directions. We are program directors. We are directors of quality and safety. We are division directors and section chiefs. We are professors. We are fellowship-trained. We are CEOs, of entire hospitals and the CMO of CMS. There has never been a better time to be a pediatric hospitalist.
This rapid ascent has to be the fastest in the history of medicine and might surprise the unsuspecting, but these career paths really should have been expected. Residents and students still identify the most with their ward months—we always will be leaders in education. Hospitals and health-care systems recognize the value of hospitalists as systems improvers and will forever need enlightened physicians to guide safer, better care. But we also remain generalists, perched over the exact intersection of acute illness and health. From this vantage point, we have the perfect perspective from which to lead the transformation of our health-care system. I’m not sure there is a leadership position in health care that a hospitalist will not fill in the near future.
A New Frontier
With all of this opportunity before us, there exists an imperative for true leadership. And unlike all of our past requirements for achievement, relying on our quantitative abilities will no longer be enough. Rather, we will need to focus on the qualitative “soft” skills, whether you call this emotional intelligence, interpersonal communication, or behavioral economics. The creation of value-based, care-delivery systems requires high-functioning units. We will need to design and lead teams from the bedside to the boardroom.
In the coming years, this leadership imperative will only intensify, as we all will be pressured to do more with less. We will be asked to improve quality and decrease costs. We will need to broaden our focus to health in addition to acute illness. Doing more with less will require courage and leadership. If you look at our growth curve to date, we have an abundance of both.
Dr. Shen is medical director of hospital medicine at Dell Children's Medical Center in Austin, Texas. He served as The Hospitalist's pediatric editor since 2010 and this marks his last column in his role as editor. In his newfound spare time, he looks forward to defining value in health care.
Dear Mark,
I am pleased and excited that you are willing to abandon your plan for being a vagabond and will give serious consideration to joining the faculty of the Department of Pediatrics to become a core member of a new [general pediatric inpatient] program that I believe has exciting potential.
So reads the first line of my very first job offer letter. Obviously, my chairman had a sense of humor. But he also was not off target, as before May 21 of my third year of residency, I had no meaningful work lined up. Dreams of locum tenens work in Hawaii or a California coastal town quickly disappeared as I received only offers for work in small-town Mississippi and Oklahoma. Eleven years later, I don’t think I could have planned a more fulfilling early career, particularly when the alternative might have been surfing on the Mississippi River.
I would like this opportunity, in my final column as The Hospitalist’s pediatric editor, to reflect on this odyssey from vagabond to hospitalist.
The Early Years
As a new attending, I was appropriately terrified of how much I didn’t know. I also had ambitious goals at first, wanting to emulate my two favorite role models from residency, Charles Ginsburg and Heinz Eichenwald. We might call them hospitalists now, but back then they were old-fashioned, generalist inpatient clinician-educators, even while chairing the department of pediatrics over their separate tenures. They were the smartest and wisest teachers that I have ever met. These early years were a pseudo-fellowship of sorts; under their tutelage, I soaked up more than I ever had during residency.
Despite all of this learning, I remained sheltered in my clinician-educator bubble. The path to excellence for me was defined through frequent trips to the library (where journals used to be stored) and trying to teach as well as my mentors did. I largely was ignorant of the national hospitalist movement, until the 2007 SHM annual meeting was held in my backyard in Dallas. Listening to Bob Wachter that year, and then Don Berwick the following year, I suddenly realized the tremendous and intertwined importance of the quality movement and hospitalists. We were going to fix medicine. OK, maybe not all of medicine, but it happened to be the perfect time for me to learn about our health-care crisis, quality, and the role of hospital medicine.
If my first five years were about clinical medicine, the next five years were all about lessons in leadership. I had a new role, directing 8 15 20 25 hospitalists—and now was accountable for the group’s results. I’ve often said that an explicit leadership role is like stepping behind a curtain, where your own previous n=1 perspective is now the challenge of herding a group of n=25. And let’s be clear that it’s one thing to manage the group and keep the ship afloat, but it’s entirely another thing to lead the group toward success.
A Path for Me
Although the cacophony of managing that many voices was deafening early on, I found solace in the lessons of quality improvement (QI), where no project lives without a team that is all going the same direction. Between the national opportunities for collaborative improvement and the day-to-day experiences within my group, I found two simple principles worked well: 1) engage the team and 2) deliver objective results.
And just as I had craved a clinical learning environment early on, I now found myself learning from local and national peers putting their leadership skills in action to produce quality outcomes. The beauty of collaborative teamwork is that it creates self-sustaining capacity for more positive results.
Looking forward, the opportunities seem limitless for pediatric hospital medicine. From the inherent fulfillment of our day-to-day bedside work to the explicit leadership that we offer the complex hospital system, our family of pediatric hospitalists has blazed career paths in all directions. We are program directors. We are directors of quality and safety. We are division directors and section chiefs. We are professors. We are fellowship-trained. We are CEOs, of entire hospitals and the CMO of CMS. There has never been a better time to be a pediatric hospitalist.
This rapid ascent has to be the fastest in the history of medicine and might surprise the unsuspecting, but these career paths really should have been expected. Residents and students still identify the most with their ward months—we always will be leaders in education. Hospitals and health-care systems recognize the value of hospitalists as systems improvers and will forever need enlightened physicians to guide safer, better care. But we also remain generalists, perched over the exact intersection of acute illness and health. From this vantage point, we have the perfect perspective from which to lead the transformation of our health-care system. I’m not sure there is a leadership position in health care that a hospitalist will not fill in the near future.
A New Frontier
With all of this opportunity before us, there exists an imperative for true leadership. And unlike all of our past requirements for achievement, relying on our quantitative abilities will no longer be enough. Rather, we will need to focus on the qualitative “soft” skills, whether you call this emotional intelligence, interpersonal communication, or behavioral economics. The creation of value-based, care-delivery systems requires high-functioning units. We will need to design and lead teams from the bedside to the boardroom.
In the coming years, this leadership imperative will only intensify, as we all will be pressured to do more with less. We will be asked to improve quality and decrease costs. We will need to broaden our focus to health in addition to acute illness. Doing more with less will require courage and leadership. If you look at our growth curve to date, we have an abundance of both.
Dr. Shen is medical director of hospital medicine at Dell Children's Medical Center in Austin, Texas. He served as The Hospitalist's pediatric editor since 2010 and this marks his last column in his role as editor. In his newfound spare time, he looks forward to defining value in health care.
Dear Mark,
I am pleased and excited that you are willing to abandon your plan for being a vagabond and will give serious consideration to joining the faculty of the Department of Pediatrics to become a core member of a new [general pediatric inpatient] program that I believe has exciting potential.
So reads the first line of my very first job offer letter. Obviously, my chairman had a sense of humor. But he also was not off target, as before May 21 of my third year of residency, I had no meaningful work lined up. Dreams of locum tenens work in Hawaii or a California coastal town quickly disappeared as I received only offers for work in small-town Mississippi and Oklahoma. Eleven years later, I don’t think I could have planned a more fulfilling early career, particularly when the alternative might have been surfing on the Mississippi River.
I would like this opportunity, in my final column as The Hospitalist’s pediatric editor, to reflect on this odyssey from vagabond to hospitalist.
The Early Years
As a new attending, I was appropriately terrified of how much I didn’t know. I also had ambitious goals at first, wanting to emulate my two favorite role models from residency, Charles Ginsburg and Heinz Eichenwald. We might call them hospitalists now, but back then they were old-fashioned, generalist inpatient clinician-educators, even while chairing the department of pediatrics over their separate tenures. They were the smartest and wisest teachers that I have ever met. These early years were a pseudo-fellowship of sorts; under their tutelage, I soaked up more than I ever had during residency.
Despite all of this learning, I remained sheltered in my clinician-educator bubble. The path to excellence for me was defined through frequent trips to the library (where journals used to be stored) and trying to teach as well as my mentors did. I largely was ignorant of the national hospitalist movement, until the 2007 SHM annual meeting was held in my backyard in Dallas. Listening to Bob Wachter that year, and then Don Berwick the following year, I suddenly realized the tremendous and intertwined importance of the quality movement and hospitalists. We were going to fix medicine. OK, maybe not all of medicine, but it happened to be the perfect time for me to learn about our health-care crisis, quality, and the role of hospital medicine.
If my first five years were about clinical medicine, the next five years were all about lessons in leadership. I had a new role, directing 8 15 20 25 hospitalists—and now was accountable for the group’s results. I’ve often said that an explicit leadership role is like stepping behind a curtain, where your own previous n=1 perspective is now the challenge of herding a group of n=25. And let’s be clear that it’s one thing to manage the group and keep the ship afloat, but it’s entirely another thing to lead the group toward success.
A Path for Me
Although the cacophony of managing that many voices was deafening early on, I found solace in the lessons of quality improvement (QI), where no project lives without a team that is all going the same direction. Between the national opportunities for collaborative improvement and the day-to-day experiences within my group, I found two simple principles worked well: 1) engage the team and 2) deliver objective results.
And just as I had craved a clinical learning environment early on, I now found myself learning from local and national peers putting their leadership skills in action to produce quality outcomes. The beauty of collaborative teamwork is that it creates self-sustaining capacity for more positive results.
Looking forward, the opportunities seem limitless for pediatric hospital medicine. From the inherent fulfillment of our day-to-day bedside work to the explicit leadership that we offer the complex hospital system, our family of pediatric hospitalists has blazed career paths in all directions. We are program directors. We are directors of quality and safety. We are division directors and section chiefs. We are professors. We are fellowship-trained. We are CEOs, of entire hospitals and the CMO of CMS. There has never been a better time to be a pediatric hospitalist.
This rapid ascent has to be the fastest in the history of medicine and might surprise the unsuspecting, but these career paths really should have been expected. Residents and students still identify the most with their ward months—we always will be leaders in education. Hospitals and health-care systems recognize the value of hospitalists as systems improvers and will forever need enlightened physicians to guide safer, better care. But we also remain generalists, perched over the exact intersection of acute illness and health. From this vantage point, we have the perfect perspective from which to lead the transformation of our health-care system. I’m not sure there is a leadership position in health care that a hospitalist will not fill in the near future.
A New Frontier
With all of this opportunity before us, there exists an imperative for true leadership. And unlike all of our past requirements for achievement, relying on our quantitative abilities will no longer be enough. Rather, we will need to focus on the qualitative “soft” skills, whether you call this emotional intelligence, interpersonal communication, or behavioral economics. The creation of value-based, care-delivery systems requires high-functioning units. We will need to design and lead teams from the bedside to the boardroom.
In the coming years, this leadership imperative will only intensify, as we all will be pressured to do more with less. We will be asked to improve quality and decrease costs. We will need to broaden our focus to health in addition to acute illness. Doing more with less will require courage and leadership. If you look at our growth curve to date, we have an abundance of both.
Dr. Shen is medical director of hospital medicine at Dell Children's Medical Center in Austin, Texas. He served as The Hospitalist's pediatric editor since 2010 and this marks his last column in his role as editor. In his newfound spare time, he looks forward to defining value in health care.