User login
In the Literature: The Latest Research You Need to Know
Clinical question: Do certain patient characteristics predict increased risk for mechanical ventilation or death among patients with acute exacerbations of chronic obstructive pulmonary disease (COPD)?
Background: Hospitalizations for acute COPD exacerbations are costly and impair quality of life. A validated tool has not been developed to help physicians risk-stratify and predict outcomes for patients presenting with acute exacerbations of COPD.
Study design: Retrospective cohort.
Setting: 191 U.S. hospitals, of which 41% were academic hospitals and 76% were urban hospitals.
Synopsis: Researchers used the Cardinal Health Clinical Outcomes Research Database to analyze the hospital admissions of 88,074 patients aged 40 years and older with acute exacerbations of COPD. The research team identified risk factors that predicted in-hospital mortality (primary endpoint) and the need for mechanical ventilation (secondary endpoint).
The main risk factors were a BUN level higher than 25 mg/dL, altered mental status, and pulse >109/minute. Patients <65 were found to be at lowest risk. Patients age <65 without any of the three main risk factors had a mortality rate of 0.3%, while patients with all three main risk factors had a mortality rate of 13.8%.
Similarly, patients with two or three primary risk characteristics were more likely to undergo mechanical ventilation. Researchers proposed a risk score known as BAP-65 (BUN, altered mental status, pulse, and age), and patients were placed into risk classes 1 through 5 based on their risk factors.
Bottom line: The BAP-65 score might be useful to predict the risk of death or need for mechanical ventilation in COPD patients with acute exacerbation.
Citation: Tabak YP, Sun X, Johannes RS, Gupta V, Shorr AF. Mortality and need for mechanical ventilation in acute exacerbations of chronic obstructive pulmonary disease: development and validation of a simple risk score. Arch Intern Med. 2009;169(17):1595-1602.
Reviewed for TH eWire by Anneliese M. Schleyer, MD, MHA, Mark C. Zaros, MD, Angelena Labella, MD, Heather L. Davidson, MD, Reena K. Julka, MD, Anna S. Loge, MD, and Paul R. Sutton, MD, PhD, University of Washington Medicine Hospital and Consultative Medicine Program, Seattle
For more HM-related literature reviews, visit our Web site.
Clinical question: Do certain patient characteristics predict increased risk for mechanical ventilation or death among patients with acute exacerbations of chronic obstructive pulmonary disease (COPD)?
Background: Hospitalizations for acute COPD exacerbations are costly and impair quality of life. A validated tool has not been developed to help physicians risk-stratify and predict outcomes for patients presenting with acute exacerbations of COPD.
Study design: Retrospective cohort.
Setting: 191 U.S. hospitals, of which 41% were academic hospitals and 76% were urban hospitals.
Synopsis: Researchers used the Cardinal Health Clinical Outcomes Research Database to analyze the hospital admissions of 88,074 patients aged 40 years and older with acute exacerbations of COPD. The research team identified risk factors that predicted in-hospital mortality (primary endpoint) and the need for mechanical ventilation (secondary endpoint).
The main risk factors were a BUN level higher than 25 mg/dL, altered mental status, and pulse >109/minute. Patients <65 were found to be at lowest risk. Patients age <65 without any of the three main risk factors had a mortality rate of 0.3%, while patients with all three main risk factors had a mortality rate of 13.8%.
Similarly, patients with two or three primary risk characteristics were more likely to undergo mechanical ventilation. Researchers proposed a risk score known as BAP-65 (BUN, altered mental status, pulse, and age), and patients were placed into risk classes 1 through 5 based on their risk factors.
Bottom line: The BAP-65 score might be useful to predict the risk of death or need for mechanical ventilation in COPD patients with acute exacerbation.
Citation: Tabak YP, Sun X, Johannes RS, Gupta V, Shorr AF. Mortality and need for mechanical ventilation in acute exacerbations of chronic obstructive pulmonary disease: development and validation of a simple risk score. Arch Intern Med. 2009;169(17):1595-1602.
Reviewed for TH eWire by Anneliese M. Schleyer, MD, MHA, Mark C. Zaros, MD, Angelena Labella, MD, Heather L. Davidson, MD, Reena K. Julka, MD, Anna S. Loge, MD, and Paul R. Sutton, MD, PhD, University of Washington Medicine Hospital and Consultative Medicine Program, Seattle
For more HM-related literature reviews, visit our Web site.
Clinical question: Do certain patient characteristics predict increased risk for mechanical ventilation or death among patients with acute exacerbations of chronic obstructive pulmonary disease (COPD)?
Background: Hospitalizations for acute COPD exacerbations are costly and impair quality of life. A validated tool has not been developed to help physicians risk-stratify and predict outcomes for patients presenting with acute exacerbations of COPD.
Study design: Retrospective cohort.
Setting: 191 U.S. hospitals, of which 41% were academic hospitals and 76% were urban hospitals.
Synopsis: Researchers used the Cardinal Health Clinical Outcomes Research Database to analyze the hospital admissions of 88,074 patients aged 40 years and older with acute exacerbations of COPD. The research team identified risk factors that predicted in-hospital mortality (primary endpoint) and the need for mechanical ventilation (secondary endpoint).
The main risk factors were a BUN level higher than 25 mg/dL, altered mental status, and pulse >109/minute. Patients <65 were found to be at lowest risk. Patients age <65 without any of the three main risk factors had a mortality rate of 0.3%, while patients with all three main risk factors had a mortality rate of 13.8%.
Similarly, patients with two or three primary risk characteristics were more likely to undergo mechanical ventilation. Researchers proposed a risk score known as BAP-65 (BUN, altered mental status, pulse, and age), and patients were placed into risk classes 1 through 5 based on their risk factors.
Bottom line: The BAP-65 score might be useful to predict the risk of death or need for mechanical ventilation in COPD patients with acute exacerbation.
Citation: Tabak YP, Sun X, Johannes RS, Gupta V, Shorr AF. Mortality and need for mechanical ventilation in acute exacerbations of chronic obstructive pulmonary disease: development and validation of a simple risk score. Arch Intern Med. 2009;169(17):1595-1602.
Reviewed for TH eWire by Anneliese M. Schleyer, MD, MHA, Mark C. Zaros, MD, Angelena Labella, MD, Heather L. Davidson, MD, Reena K. Julka, MD, Anna S. Loge, MD, and Paul R. Sutton, MD, PhD, University of Washington Medicine Hospital and Consultative Medicine Program, Seattle
For more HM-related literature reviews, visit our Web site.
BEST PRACTICES IN: Approaches to Pruritus
A supplement to Skin & Allergy News. This supplement was supported by Ferndale Laboratories Inc.
• Impact of Pruritus on Quality of Life
• Screening for Psychogenic Causes
• Palpation
• Medication History
• Xerosis (dry skin)
• Cutaneous Infestations
• Systemic Diseases
• Malignancy
• Neuropathic Pruritus
• Atypical Causes
• Diagnostic Workup
• Managing Pruritus
• Summary
Faculty/Faculty Disclosure
Joseph B. Bikowski, MD
Clinical Assistant Professor
Dermatology
Ohio State University
Columbus, OH
Director
Bikowski Skin Care Center
Sewickley, PA
Dr. Bikowski has received honoraria from Allergan, Inc., Coria Laboratories, Ltd., Galderma Laboratories, L.P., Intendis GmbH, Medicis Pharmaceutical Corporation, OrthoDermatologics, Quinnova Pharmaceuticals, Inc., Stiefel Laboratories, Inc., and Warner Chilcott; served on advisory boards for Coria, Galderma, Intendis, Ranbaxy Pharmaceuticals Inc., Stiefel, and Warner Chilcott; has been a speaker for Allergan, Coria, Galderma, Intendis, Promius Pharma, LLC, Ranbaxy, and Stiefel; has a consulting agreement with Allergan, Coria, Galderma, Intendis, Medicis, Promius, OrthoDermatologics, and Stiefel; and is a stockholder for Quinnova.
A supplement to Skin & Allergy News. This supplement was supported by Ferndale Laboratories Inc.
• Impact of Pruritus on Quality of Life
• Screening for Psychogenic Causes
• Palpation
• Medication History
• Xerosis (dry skin)
• Cutaneous Infestations
• Systemic Diseases
• Malignancy
• Neuropathic Pruritus
• Atypical Causes
• Diagnostic Workup
• Managing Pruritus
• Summary
Faculty/Faculty Disclosure
Joseph B. Bikowski, MD
Clinical Assistant Professor
Dermatology
Ohio State University
Columbus, OH
Director
Bikowski Skin Care Center
Sewickley, PA
Dr. Bikowski has received honoraria from Allergan, Inc., Coria Laboratories, Ltd., Galderma Laboratories, L.P., Intendis GmbH, Medicis Pharmaceutical Corporation, OrthoDermatologics, Quinnova Pharmaceuticals, Inc., Stiefel Laboratories, Inc., and Warner Chilcott; served on advisory boards for Coria, Galderma, Intendis, Ranbaxy Pharmaceuticals Inc., Stiefel, and Warner Chilcott; has been a speaker for Allergan, Coria, Galderma, Intendis, Promius Pharma, LLC, Ranbaxy, and Stiefel; has a consulting agreement with Allergan, Coria, Galderma, Intendis, Medicis, Promius, OrthoDermatologics, and Stiefel; and is a stockholder for Quinnova.
A supplement to Skin & Allergy News. This supplement was supported by Ferndale Laboratories Inc.
• Impact of Pruritus on Quality of Life
• Screening for Psychogenic Causes
• Palpation
• Medication History
• Xerosis (dry skin)
• Cutaneous Infestations
• Systemic Diseases
• Malignancy
• Neuropathic Pruritus
• Atypical Causes
• Diagnostic Workup
• Managing Pruritus
• Summary
Faculty/Faculty Disclosure
Joseph B. Bikowski, MD
Clinical Assistant Professor
Dermatology
Ohio State University
Columbus, OH
Director
Bikowski Skin Care Center
Sewickley, PA
Dr. Bikowski has received honoraria from Allergan, Inc., Coria Laboratories, Ltd., Galderma Laboratories, L.P., Intendis GmbH, Medicis Pharmaceutical Corporation, OrthoDermatologics, Quinnova Pharmaceuticals, Inc., Stiefel Laboratories, Inc., and Warner Chilcott; served on advisory boards for Coria, Galderma, Intendis, Ranbaxy Pharmaceuticals Inc., Stiefel, and Warner Chilcott; has been a speaker for Allergan, Coria, Galderma, Intendis, Promius Pharma, LLC, Ranbaxy, and Stiefel; has a consulting agreement with Allergan, Coria, Galderma, Intendis, Medicis, Promius, OrthoDermatologics, and Stiefel; and is a stockholder for Quinnova.
Congenital Anomalies in Infant HSV
Herpes simplex virus (HSV) is a significant cause of pediatric hospitalization, morbidity and mortality, particularly in infants under 60 days of age, where HSV can present as meningoencephalitis, skin disease, or sepsis.14 Most prior studies use data from registries taken from single centers or a restricted group of hospitals. Thus, there is a paucity of recent, nationally‐representative information about the outcome of infants infected with HSV, especially those treated at nonteaching hospitals or with rarer comorbid conditions. The goal of this project was to determine the patient and hospital characteristics associated with worse clinical outcomes in infants under the age of 60 days admitted with HSV disease. We hypothesized that younger infants, infants with a concurrent congenital anomaly, and infants treated at non‐children's hospitals would have worse clinical outcomes. To answer these questions, we used 2003 panel data from the Healthcare Cost and Utilization Project (HCUP) Kids' Inpatient Database (KID), a nationally representative sample of inpatient hospitalizations in the United States.
Methods
Study Population and Data Collection
We conducted a retrospective population cohort study of all infants admitted at 60 days of age who were discharged with a diagnosis of HSV disease between January 1, 2003 and December 31, 2003, using the 2003 KID. The KID is a collaborative project between the Agency for Healthcare Research and Quality AHRQ and 36 states, which includes approximately 2.9 million pediatric discharge records from 3438 hospitals.5 The KID is the only national, all‐payer database of pediatric hospitalizations in the United States.
Patient Eligibility
As in prior studies,611 children were eligible for this project if they were discharged with an International Classification of Disease, ninth edition, Clinical Modification (ICD‐9CM) discharge code of 054.xx (herpes simplex virus), where xx represented any combination of one or two‐digit codes, or 771.2 (neonatal viral infection including HSV). However, the 771.2 code may also contain other perinatal infections of relatively rare frequency, such as toxoplasmosis. Thus, we also performed the same set of analyses on the cohort of children who had an 054.xx code alone. No results presented in this study changed in statistical significance when this smaller cohort of infants was examined.
Data Variables and Outcomes
Outcome Variables
We examined 2 primary clinical outcomes in this study: in‐hospital death and the occurrence of a serious complication. Complications were identified using ICD‐9CM codes from both prior work12 and examination of all diagnosis and procedure codes for eligible infants by the 2 principal investigators (Appendix). These 2 reviewers had to independently agree on the inclusion of an ICD‐9CM code as a complication. In‐hospital deaths were captured through a disposition code of 20 in the KID dataset. Length of stay (LOS) and in‐hospital costs were examined as secondary outcome measures for specific risk factors of interest.
Demographic and Comorbidity Variables
Demographic and comorbidity variables were included in the analyses to control for the increased cost, LOS, or risk of a complication that result from these factors.1315 Demographic information available in the KID included gender, age at admission, race, low birth weight infants, and insurance status. Age at admission was grouped into 4 categories: 07 days, 814 days, 1528 days, and 2960 days. Infants were classified as low birth weight if they had an ICD‐9CM code for a birth weight <2000 g (ICD‐9CM codes 765.01‐07, 765.11‐17, or 765.21‐27). We used the ICD‐9CM codes shown in the Appendix to classify various comorbid conditions. Because of the young age of the cohort, all comorbid conditions consisted of congenital anomalies that were grouped according to the involved organ system. To help classify patients by their illness severity, we used the All‐Patient Refined Diagnosis‐Related Group (APR‐DRG) severity of illness classification for each hospital admission (3M Corporation, St. Paul, MN). The APR‐DRG classification system used discharge diagnoses, procedures, and demographic information to assign patients to 4 severity of illness categories.
Hospital Characteristics
We identified the following hospital characteristics from the KID: total bed size, divided as small, medium, and large; hospital status (children's hospital vs. non‐children's hospital, teaching hospital vs. nonteaching hospital); source of admission (emergency department, clinic, other hospitals); and location (rural vs. urban). Children's hospitals were identified by the AHRQ using information from the National Association of Children's Hospitals and Related Institutions, while teaching hospital status was determined by the presence of an approved residency program and a ratio of full‐time residents to beds of 0.25 or greater.5
Statistical Analysis
All analyses accounted for the complex sampling design with the survey commands included in STATA 9.2 (Statacorp, College Station, TX) and report national estimates from the data available in the 36 surveyed states. Because of the complex sampling design, the Wald test was used to determine significant differences for each outcome in univariable analysis. Variance estimates were reported as standard errors of the mean. We constructed multivariable logistic regression models to assess the adjusted impact of patient and hospital‐level characteristics on each primary outcome measure; ie, in‐hospital death and development of a serious complication. Negative binomial models were used for our secondary outcomes, LOS and costs, because of their rightward skew. Variance estimates for each model accounted for the clustering of data at the hospital level, and data were analyzed as per the latest AHRQ statistical update.16
Results
The 2003 KID identified 1587 hospitalizations for HSV in infants admitted at an age of 60 days or less in the entire United States. These infants had a total hospital cost of $27,147,000. Of the cohort, 10% had a concurrent congenital anomaly. Most infants (73.5%) were admitted within 14 days of birth, and 15.5% were transferred from another hospital. Based on APR‐DRG criteria, 33% of the infants were classified as having a moderate risk of death, 24% as major risk, and 12.2% as extreme risk. The majority of infants were treated at non‐children's hospitals (85.3%) in urban locations (91.5%). The average LOS was 12.0 0.6 days and the average total hospital cost was $17,382 1269. After admission, 267 of the infants, or 16.8%, had at least 1 serious complication. Fifty infants died during the hospitalization included in the KID.
Risk Factor Analysis
Serious Complications
Univariable (Table 1) analysis identified several factors associated with higher rates of serious complications. Younger age at admission was associated with a higher risk of serious complications. This trend was greatest for infants admitted under 14 days of age, of which 20.2% had a serious complication, compared with 10.2% of the infants admitted between 29 and 60 days of age. Infants with any identified congenital anomaly had significantly higher rates of serious complication (41.1% vs. 14.8% for infants without a congenital anomaly). Similar findings were seen with low birth weight infants. Infants who were transferred prior to the hospitalization captured in the KID had a higher complication rate (38.7%) than infants admitted as a routine admission (15.9%) or via the emergency room (8.8%). Among hospital‐level factors, infants admitted to children's or teaching hospitals had higher rates of serious complications, although only the difference between teaching and nonteaching hospitals reached statistical significance (Table 1).
| Patient‐Level Factors | % of Cohort | % with Serious Complication | % Death |
|---|---|---|---|
| |||
| Age at presentation | |||
| 7 days | 58.4 | 21.6* | 4.2* |
| 814 days | 15.1 | 15.8 | 3.6 |
| 1528 days | 16.4 | 9.7 | 2.1 |
| 2960 days | 10.1 | 10.2 | 0 |
| Low birth weight | |||
| Yes | 10.6 | 44.2* | 9.0* |
| No | 89.4 | 14.3 | 2.7 |
| Type of insurance | |||
| Private | 47.4 | 15.6 | 2.1* |
| Medicaid | 49.0 | 19.2 | 4.8 |
| Self pay | 3.6 | 17.0 | 0 |
| Race | |||
| White | 52.8 | 17.7 | 3.5 |
| Black | 18.9 | 17.6 | 4.2 |
| Other | 28.3 | 19.2 | 4.5 |
| Gender | |||
| Female | 45.4 | 15.7 | 2.2 |
| Male | 54.6 | 18.9 | 4.3 |
| Any congenital anomaly | |||
| Yes | 10.0 | 41.1* | 10.4* |
| No | 90.0 | 14.8 | 2.6 |
| Admission type | |||
| Routine | 62.3 | 15.9* | 2.8* |
| Emergency room | 22.2 | 8.8 | 1.1 |
| Transfer from another hospital | 15.5 | 38.7 | 9.6 |
| APR‐DRG risk | |||
| Mild | 3.0 | 0.3* | 0* |
| Moderate | 33.0 | 2.0 | 0.5 |
| Major | 24.0 | 24.7 | 2.3 |
| Extreme | 12.2 | 85.0 | 20.8 |
| Hospital‐level factors | |||
| Children's hospital | |||
| Yes | 14.7 | 27.0 | 6.4 |
| No | 85.3 | 16.3 | 3.1 |
| Teaching hospital | |||
| Yes | 68.4 | 21.3* | 4.3* |
| No | 31.7 | 8.5 | 1.5 |
| Location | |||
| Urban | 91.5 | 18.0* | 3.6 |
| Rural | 8.5 | 9.0 | 1.6 |
| Hospital size | |||
| Small | 14.1 | 19.3 | 4.2 |
| Medium | 25.9 | 14.3 | 3.2 |
| Large | 60.0 | 18.1 | 3.3 |
Many of these factors were independently associated with increased complication rates in multivariable analysis (Table 2). Infants under 7 days of age on admission (odds ratio [OR], 2.68; 95% confidence interval [CI], 1.112.47), low birth weight (OR, 5.17; 95% CI, 2.988.98), and the concurrent presence of a congenital anomaly (OR, 3.09; 95% CI, 1.805.33) were associated with higher odds of a serious complication. Site of care lost its statistical significance once our models adjusted for differences in illness severity. Insurance status, gender, and race were not associated with a change in complication rates for these infants.
| Risk Factor | Serious Complication | Mortality | ||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| ||||
| Age at admission | ||||
| 7 days | 2.68 | 1.112.47 | 1.63 | 0.347.73 |
| 814 days | 1.22 | 0.403.73 | 2.15 | 0.3612.9 |
| 1428 days | 0.87 | 0.322.37 | Reference* | |
| 2960 days | Reference | |||
| Racial/ethnic status | ||||
| White | Reference | Reference | ||
| Black | 0.90 | 0.451.82 | 1.30 | 0.433.89 |
| Other | 0.99 | 0.571.70 | 1.19 | 0.482.99 |
| Treatment at children's hospital | 2.33 | 0.836.18 | 2.59 | 0.6510.2 |
| Treatment at teaching hospital | 1.71 | 0.943.12 | 1.86 | 0.566.25 |
| Female gender | 0.96 | 0.631.48 | 0.28 | 0.100.82 |
| Medicaid insurance | 1.51 | 0.912.50 | 1.69 | 0.634.53 |
| Transferred from another hospital | 3.76 | 2.036.98 | 3.47 | 1.428.46 |
| Transferred to another hospital | 1.35 | 0.672.73 | ||
| Presence of a congenital anomaly | 3.09 | 1.805.33 | 4.26 | 1.7610.3 |
| Low birth weight infant | 5.17 | 2.988.98 | 5.33 | 1.9015.0 |
Death
Risk factors for higher mortality rates followed similar trends as those for the risk of a serious complication. Younger age at admission, low birth weight status, the presence of a serious complication, admission from another hospital, and treatment at a children's hospital or teaching hospital were all associated with higher mortality rates. In multivariable analysis, the concurrent presence of a congenital anomaly was associated with higher odds of death (OR, 4.26; 95% CI, 1.7610.3). The cause of increased death in infants with congenital anomalies appeared to be a higher rate of serious complications, as including serious complications in the multivariable regression model resulted in the association between congenital anomalies and death losing statistical significance (OR in revised model 1.95; 95% CI, 0.636.05). Site of care again was not associated with differences in mortality after controlling for patient case‐mix.
Concurrent Congenital Anomalies
Based on the higher complication and mortality rates seen in infants with HSV who had a concurrent congenital anomaly, we then investigated how the presence of specific congenital anomalies influenced clinical outcomes, LOS, and total hospital costs with HSV disease. Using the congenital anomaly groups listed in the Appendix, we found that congenital heart disease, central nervous system anomalies, pulmonary anomalies, and gastrointestinal anomalies were each associated with either higher rates of serious complications, longer LOS, or higher total hospital costs compared to infants without congenital anomalies (Table 3). Serious complications occurred most commonly in patients with central nervous system anomalies (55.6%) and congenital heart disease (50.8%), while infants with pulmonary anomalies had the longest LOS (37.1 10.0 days) and highest total hospital costs of all anomaly categories. The types of complications differed by the anomaly group: infants with cardiac and pulmonary anomalies had the highest rates of respiratory complications (45% and 40%, respectively), whereas those with central nervous system anomalies had the highest rates of cardiac complications (51%). Each anomaly class had a similar rate of neurological complications, between 30% and 40%.
| Number* | % With Serious Complication | LOS (days) | Total Hospital Costs (2003 dollars) | |
|---|---|---|---|---|
| ||||
| No congenital anomaly | 1391 | 14.8 | 11.3 0.6 | 15,118 1158 |
| Type of congenital anomaly | ||||
| Congenital heart disease | 73 | 50.8 | 23.5 4.6 | 46,760 9340 |
| Central nervous system anomaly | 31 | 55.6 | 15.4 3.0 | 23,962 5037 |
| Head/neck anomaly | 13 | 40.6 | 11.1 4.6 | 14,132 7860 |
| Pulmonary anomaly | 13 | 34.1 | 37.1 10.0 | 67,234 21,002 |
| Gastrointestinal anomaly | 20 | 33.5 | 21.6 4.9 | 41,207 13,878 |
| Genitourinary anomaly | 19 | 24.1 | 11.0 2.5 | 10,906 1890 |
| Musculoskeletal anomaly | ||||
| Genetic anomaly | 18 | 10.2 | 12.2 2.4 | 15,990 3808 |
Site of Care
Finally, we examined the LOS and costs of receiving care at a children's hospital. The data shown in Tables 1 and 2 suggest that receiving treatment at a children's hospital does not result in improved clinical outcomes for infants admitted with HSV. One potential advantage, though, is improved efficiency of care, which would result in a shorter LOS or lower costs. Using negative binomial multivariable regression models to account for differences in patient characteristics, regional variation, and insurance status, treatment at a children's hospital was associated with an 18% shorter LOS (95% CI, 1%34%) compared to non‐children's hospitals after accounting for the generally sicker infants treated at children's hospitals. Children's hospitals, though, were more expensive than non‐children's hospitals (increase of $642 per day; 95% CI, $2321052). These results remained consistent when we omitted transferred patients from the model, instead of controlling for them in the analysis.
Conclusions
There has been little prior information to guide practitioners and parents about factors that potentially influence clinical outcome of infants hospitalized with HSV in non‐children's hospitals, although over 80% of infants are managed at non‐children's hospitals. These studies also did not have the power to characterize the risk of poor clinical outcome associated with rarer clinical factors.1, 2, 6 This study, using nationally representative data, found that these rarer clinical factors and site of care may influence the outcomes of infants hospitalized with HSV, albeit in different methods. Younger age at admission and a coexisting congenital anomaly remained statistically significant predictors of worse clinical outcomes after controlling for various patient and hospital factors. Not all congenital anomalies increased the risk of death or serious complications; rather, anomalies that affected either the cardiopulmonary system or the central nervous system appeared to result in the highest increases in risk. This study also found that treatment of infants with HSV at a children's hospital was associated with a 28% shorter LOS after accounting for the sicker patients cared for by children's hospitals. This finding is in contrast to prior studies of common pediatric conditions, where there were no differences in the LOS between children's and non‐children's hospitals,17, 18 and severe sepsis, where children's hospitals had longer LOSs.19 These results confirm the importance of specific risk factors in predicting the likelihood that an infant admitted with HSV may have a poor clinical outcome. Also, these results emphasize the differences in outcomes that may occur at different types of hospitals.
This study is the first to find that certain congenital anomalies or conditions may be associated with worse clinical outcomes from HSV. There is little information in the literature to explain these findings. Those anomalies that affect the cardiopulmonary or central nervous system may either worsen the symptoms of HSV or predispose infants to have a serious complication, such as shock or respiratory failure. This finding would be similar to the increased risk of serious complications seen in infants with congenital heart disease who contract respiratory syncytial virus20 or infants with genetic syndromes who undergo heart surgery.21 Alternatively, because we do not have information on do‐not‐resuscitate status, the presence of one of these congenital anomalies may result in more withdrawal of care when an infant is infected with HSV and has a serious complication; the LOS of these children may not reflect these decisions because the decision to withdrawal care may only occur after the child's condition worsens significantly, which may happen any time during the disease course. However, this theory is less likely because we failed to find similar results with other congenital anomalies such as genetic or chromosomal syndromes. Further examination of these infants and their overall response to insults such as HSV is needed to understand how these anomalies influence the outcomes of a serious, unrelated illness.
Age upon admission was another important predictor of poor outcomes when analyzed in univariable or multivariable analysis. This result is consistent with prior work,14 which suggests that younger children are more likely to be hospitalized with either congenitally acquired HSV or systemic disease. The information contained in the KID does not allow us to determine whether young age is a risk factor for poor outcome irrespective of the clinical presentation of HSV, or whether age serves as a proxy for the appearance of more severe clinical disease. This effect of age remained present even after controlling for the higher risk of a serious complication and death in low birth weight infants. There are limited data that suggest that premature birth is an independent risk factor for worse outcomes associated with perinatal or congenital infection; 1 previous case study of Enterobacter sakazakii infections found a higher fatality rate for premature infants compared to term infants.22 This study supports these findings.
This study found that treatment at a children's hospital resulted in a 28% shorter LOS without a statistically significant difference in clinical outcomes after controlling for case‐mix differences. This finding is in contrast to prior studies of common pediatric conditions17, 18 and severe sepsis.19 There are several potential explanations for the difference in findings. For common pediatric conditions, there may be fewer variations in treatment style and less need for new diagnostic modalities that are more available at academic centers. For HSV disease, though, children's hospitals may also be more likely than non‐children's hospitals to perform polymerase‐chain reaction (PCR) testing for the diagnosis of perinatally acquired HSV, correctly identify the disorder, or receive the test results in a timely fashion. Pediatric subspecialists, such as infectious disease physicians or neurologists, are also likely to be more available at children's hospitals than at other centers. While the role of subspecialty consultation in improving outcomes for neonates with HSV is not known, improved outcomes at children's hospitals has been described for other serious conditions such as splenic injuries.23 Children's hospitals had higher daily costs than non‐children's hospitals, as has been found in other work.17, 19 Children's hospitals may be treating sicker patients, for whom we are unable to adequately adjust for their illness severity with hospital administrative data.17, 19 Also, there may be a greater use of medical tests and treatments that increase the costs of care. These costs do not include indirect costs to the families such as loss of work and travel costs. In light of the shorter LOS in children's hospitals, policy makers will need to balance the potentially higher daily costs of care with more efficient management of the disease process.
Because this study used hospital administrative records, there are a few limitations. We used ICD‐9CM diagnosis codes to identify patients, congenital anomalies, and complications. The diagnosis of some infants with HSV or less significant congenital anomalies could have been missed because clinicians either overlooked the disease or did not make the diagnosis before discharge. This form of spectrum bias would likely miss the infants with the least severe disease and make it more difficult to find the results that we found in this study.24 Prior work successfully used and validated similar ICD‐9CM codes to identify HSV cases among the different types of hospitals included in the KID.611 Our study design estimated 1587 cases of neonatal HSV in 2003. A prospective study of maternal serologic and virologic status during pregnancy estimated 480 to 2160 new cases of neonatal HSV per year.25 Thus, while miscoding is a potential limitation to our study, the overall numbers of patients in this study were similar to past annual estimates. One potential area of miscounting, though, was the inability of the KID to link the records of 16% of the identified infants with HSV whose care was transferred between hospitals. These infants may result in misleading LOS or cost information: lower for the transferring hospital, because they only kept the child a short period of time, or lower for the accepting hospital, as some of the total hospital stay is not accounted for in the KID. We accounted for this issue in 2 ways. First, we included a variable for being transferred in the multivariable models, and found no difference in any results when we omitted these patients from the analysis. Second, we performed a univariable analysis stratified by transfer status, which did not differ substantially from our main model for most variables. Accurate linkage of all the hospital records for an infant's hospital course, likely only through a mandatory reporting system for infant HSV, would help confirm the associations we identified in this study.
In conclusion, infants with congenital anomalies should be closely monitored for the development of serious complications associated with HSV, particularly those infants with congenital heart disease, pulmonary anomalies, or central nervous system anomalies. Closer investigation of the care practices that children's hospitals use in the management of infants with HSV is needed to improve the efficiency of care delivered to these infants, as HSV disease remains a significant public health problem.
- ,,, et al.Natural history of neonatal herpes simplex virus infections in the acyclovir era.Pediatrics.2001;108:223–229.
- ,,.Herpes simplex viruses.Clin Infect Dis.1998;26:541–553.
- ,,.Herpes simplex virus infections. In: Remington JS, Wilson CB, Baker CJ, editors.Infectious Diseases of the Fetus and Newborn Infant.5th ed.Philadelphia, PA:W.B. Saunders;2001. p425–446.
- ,,, et al.Changing presentation of herpes simplex virus infection in neonates.J Infect Dis.1988;158:109–116.
- Design of the HCUP Kids' Inpatient Database (KID), 2003. Healthcare Cost and Utilization Project (HCUP).Rockville, MD:Agency for Healthcare Research and Quality;2003. Revised January 30, 2006. Available at: http://www.hcup‐us.ahrq.gov/db/nation/kid/reports/KID_2003_Design_Edited_013006.pdf. Accessed October 2009.
- ,,.Incidence of neonatal herpes simplex virus infections in a managed‐care population.Sex Transm Dis.2007;34:704–708.
- ,,, et al.Targeted prenatal herpes simplex virus testing: can we identify women at risk of transmission to the neonate.Am J Obstet Gynecol.2006;194:408–414.
- ,,, et al.The estimated economic burden of genital herpes in the united states.BMC Infect Dis.2001;1:5.
- ,,, et al.Accuracy of obstetric diagnoses and procedures in hospital discharge data.Am J Obstet Gynecol.2006;194:992–1001.
- ,,, et al.The epidemiology of neonatal herpes simplex virus infections in California from 1985 to 1995.J Infect Dis.1999;180:199–202.
- ,,.Medical care expenditures for genital herpes in the United States.Sex Transm Dis.2000;27:32–38.
- ,,, et al.The epidemiology of sepsis in the United States from 1979 through 2000.N Engl J Med.2003;348:1546–1554.
- ,,, et al.The importance of comorbidities in explaining differences in patient costs.Med Care.1996;34:767–782.
- ,,, et al.Contribution of birth defects and genetic diseases to pediatric hospitalizations. A population‐based study.Arch Pediatr Adolesc Med.1997;151:1096–1103.
- ,,.The influence of chronic disease on resource utilization in common acute pediatric conditions. Financial concerns for children's hospitals.Arch Pediatr Adolesc Med.1999;153:169–179.
- Health Care Cost and Utility Project.Calculating Kids' Inpatient Database (KID) Variances. December 16, 2005. Methods Series Report # 2005‐5.Rockville, MD:Agency for Healthcare Research and Quality. Available at: http://www.hcup‐us.ahrq.gov/db/nation/kid/reports/CalculatingKIDVariances.pdf. Accessed October2009.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
- ,.Length of stay for common pediatric conditions: teaching versus nonteaching hospitals.Pediatrics.2003;112:278–281.
- ,,.Patient and hospital correlates of clinical outcomes and resource utilization in severe pediatric sepsis.Pediatrics.2007;119:487–494.
- .Review of epidemiology and clinical risk factors for severe respiratory syncytial virus (RSV) infection.J Pediatr.2003;143:S112–S117.
- ,,, et al.Patient characteristics are important determinants of neurodevelopmental outcome at one year of age after neonatal and infant cardiac surgery.J Thorac Cardiovasc Surg.2007;133:1344–1353,1353,e1341–e1343.
- .Enterobacter sakazakii infections among neonates, infants, children, and adults. Case reports and a review of the literature.Medicine.2001;80:113–122.
- ,,, et al.Hospital characteristics associated with the management of pediatric splenic injuries.JAMA.2005;294:2611–2617.
- ,.Spectrum bias or spectrum effect? Subgroup variation in diagnostic test evaluation.Ann Intern Med.2002;137:598–602.
- ,,, et al.Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant.JAMA.2003;289:203–209.
Herpes simplex virus (HSV) is a significant cause of pediatric hospitalization, morbidity and mortality, particularly in infants under 60 days of age, where HSV can present as meningoencephalitis, skin disease, or sepsis.14 Most prior studies use data from registries taken from single centers or a restricted group of hospitals. Thus, there is a paucity of recent, nationally‐representative information about the outcome of infants infected with HSV, especially those treated at nonteaching hospitals or with rarer comorbid conditions. The goal of this project was to determine the patient and hospital characteristics associated with worse clinical outcomes in infants under the age of 60 days admitted with HSV disease. We hypothesized that younger infants, infants with a concurrent congenital anomaly, and infants treated at non‐children's hospitals would have worse clinical outcomes. To answer these questions, we used 2003 panel data from the Healthcare Cost and Utilization Project (HCUP) Kids' Inpatient Database (KID), a nationally representative sample of inpatient hospitalizations in the United States.
Methods
Study Population and Data Collection
We conducted a retrospective population cohort study of all infants admitted at 60 days of age who were discharged with a diagnosis of HSV disease between January 1, 2003 and December 31, 2003, using the 2003 KID. The KID is a collaborative project between the Agency for Healthcare Research and Quality AHRQ and 36 states, which includes approximately 2.9 million pediatric discharge records from 3438 hospitals.5 The KID is the only national, all‐payer database of pediatric hospitalizations in the United States.
Patient Eligibility
As in prior studies,611 children were eligible for this project if they were discharged with an International Classification of Disease, ninth edition, Clinical Modification (ICD‐9CM) discharge code of 054.xx (herpes simplex virus), where xx represented any combination of one or two‐digit codes, or 771.2 (neonatal viral infection including HSV). However, the 771.2 code may also contain other perinatal infections of relatively rare frequency, such as toxoplasmosis. Thus, we also performed the same set of analyses on the cohort of children who had an 054.xx code alone. No results presented in this study changed in statistical significance when this smaller cohort of infants was examined.
Data Variables and Outcomes
Outcome Variables
We examined 2 primary clinical outcomes in this study: in‐hospital death and the occurrence of a serious complication. Complications were identified using ICD‐9CM codes from both prior work12 and examination of all diagnosis and procedure codes for eligible infants by the 2 principal investigators (Appendix). These 2 reviewers had to independently agree on the inclusion of an ICD‐9CM code as a complication. In‐hospital deaths were captured through a disposition code of 20 in the KID dataset. Length of stay (LOS) and in‐hospital costs were examined as secondary outcome measures for specific risk factors of interest.
Demographic and Comorbidity Variables
Demographic and comorbidity variables were included in the analyses to control for the increased cost, LOS, or risk of a complication that result from these factors.1315 Demographic information available in the KID included gender, age at admission, race, low birth weight infants, and insurance status. Age at admission was grouped into 4 categories: 07 days, 814 days, 1528 days, and 2960 days. Infants were classified as low birth weight if they had an ICD‐9CM code for a birth weight <2000 g (ICD‐9CM codes 765.01‐07, 765.11‐17, or 765.21‐27). We used the ICD‐9CM codes shown in the Appendix to classify various comorbid conditions. Because of the young age of the cohort, all comorbid conditions consisted of congenital anomalies that were grouped according to the involved organ system. To help classify patients by their illness severity, we used the All‐Patient Refined Diagnosis‐Related Group (APR‐DRG) severity of illness classification for each hospital admission (3M Corporation, St. Paul, MN). The APR‐DRG classification system used discharge diagnoses, procedures, and demographic information to assign patients to 4 severity of illness categories.
Hospital Characteristics
We identified the following hospital characteristics from the KID: total bed size, divided as small, medium, and large; hospital status (children's hospital vs. non‐children's hospital, teaching hospital vs. nonteaching hospital); source of admission (emergency department, clinic, other hospitals); and location (rural vs. urban). Children's hospitals were identified by the AHRQ using information from the National Association of Children's Hospitals and Related Institutions, while teaching hospital status was determined by the presence of an approved residency program and a ratio of full‐time residents to beds of 0.25 or greater.5
Statistical Analysis
All analyses accounted for the complex sampling design with the survey commands included in STATA 9.2 (Statacorp, College Station, TX) and report national estimates from the data available in the 36 surveyed states. Because of the complex sampling design, the Wald test was used to determine significant differences for each outcome in univariable analysis. Variance estimates were reported as standard errors of the mean. We constructed multivariable logistic regression models to assess the adjusted impact of patient and hospital‐level characteristics on each primary outcome measure; ie, in‐hospital death and development of a serious complication. Negative binomial models were used for our secondary outcomes, LOS and costs, because of their rightward skew. Variance estimates for each model accounted for the clustering of data at the hospital level, and data were analyzed as per the latest AHRQ statistical update.16
Results
The 2003 KID identified 1587 hospitalizations for HSV in infants admitted at an age of 60 days or less in the entire United States. These infants had a total hospital cost of $27,147,000. Of the cohort, 10% had a concurrent congenital anomaly. Most infants (73.5%) were admitted within 14 days of birth, and 15.5% were transferred from another hospital. Based on APR‐DRG criteria, 33% of the infants were classified as having a moderate risk of death, 24% as major risk, and 12.2% as extreme risk. The majority of infants were treated at non‐children's hospitals (85.3%) in urban locations (91.5%). The average LOS was 12.0 0.6 days and the average total hospital cost was $17,382 1269. After admission, 267 of the infants, or 16.8%, had at least 1 serious complication. Fifty infants died during the hospitalization included in the KID.
Risk Factor Analysis
Serious Complications
Univariable (Table 1) analysis identified several factors associated with higher rates of serious complications. Younger age at admission was associated with a higher risk of serious complications. This trend was greatest for infants admitted under 14 days of age, of which 20.2% had a serious complication, compared with 10.2% of the infants admitted between 29 and 60 days of age. Infants with any identified congenital anomaly had significantly higher rates of serious complication (41.1% vs. 14.8% for infants without a congenital anomaly). Similar findings were seen with low birth weight infants. Infants who were transferred prior to the hospitalization captured in the KID had a higher complication rate (38.7%) than infants admitted as a routine admission (15.9%) or via the emergency room (8.8%). Among hospital‐level factors, infants admitted to children's or teaching hospitals had higher rates of serious complications, although only the difference between teaching and nonteaching hospitals reached statistical significance (Table 1).
| Patient‐Level Factors | % of Cohort | % with Serious Complication | % Death |
|---|---|---|---|
| |||
| Age at presentation | |||
| 7 days | 58.4 | 21.6* | 4.2* |
| 814 days | 15.1 | 15.8 | 3.6 |
| 1528 days | 16.4 | 9.7 | 2.1 |
| 2960 days | 10.1 | 10.2 | 0 |
| Low birth weight | |||
| Yes | 10.6 | 44.2* | 9.0* |
| No | 89.4 | 14.3 | 2.7 |
| Type of insurance | |||
| Private | 47.4 | 15.6 | 2.1* |
| Medicaid | 49.0 | 19.2 | 4.8 |
| Self pay | 3.6 | 17.0 | 0 |
| Race | |||
| White | 52.8 | 17.7 | 3.5 |
| Black | 18.9 | 17.6 | 4.2 |
| Other | 28.3 | 19.2 | 4.5 |
| Gender | |||
| Female | 45.4 | 15.7 | 2.2 |
| Male | 54.6 | 18.9 | 4.3 |
| Any congenital anomaly | |||
| Yes | 10.0 | 41.1* | 10.4* |
| No | 90.0 | 14.8 | 2.6 |
| Admission type | |||
| Routine | 62.3 | 15.9* | 2.8* |
| Emergency room | 22.2 | 8.8 | 1.1 |
| Transfer from another hospital | 15.5 | 38.7 | 9.6 |
| APR‐DRG risk | |||
| Mild | 3.0 | 0.3* | 0* |
| Moderate | 33.0 | 2.0 | 0.5 |
| Major | 24.0 | 24.7 | 2.3 |
| Extreme | 12.2 | 85.0 | 20.8 |
| Hospital‐level factors | |||
| Children's hospital | |||
| Yes | 14.7 | 27.0 | 6.4 |
| No | 85.3 | 16.3 | 3.1 |
| Teaching hospital | |||
| Yes | 68.4 | 21.3* | 4.3* |
| No | 31.7 | 8.5 | 1.5 |
| Location | |||
| Urban | 91.5 | 18.0* | 3.6 |
| Rural | 8.5 | 9.0 | 1.6 |
| Hospital size | |||
| Small | 14.1 | 19.3 | 4.2 |
| Medium | 25.9 | 14.3 | 3.2 |
| Large | 60.0 | 18.1 | 3.3 |
Many of these factors were independently associated with increased complication rates in multivariable analysis (Table 2). Infants under 7 days of age on admission (odds ratio [OR], 2.68; 95% confidence interval [CI], 1.112.47), low birth weight (OR, 5.17; 95% CI, 2.988.98), and the concurrent presence of a congenital anomaly (OR, 3.09; 95% CI, 1.805.33) were associated with higher odds of a serious complication. Site of care lost its statistical significance once our models adjusted for differences in illness severity. Insurance status, gender, and race were not associated with a change in complication rates for these infants.
| Risk Factor | Serious Complication | Mortality | ||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| ||||
| Age at admission | ||||
| 7 days | 2.68 | 1.112.47 | 1.63 | 0.347.73 |
| 814 days | 1.22 | 0.403.73 | 2.15 | 0.3612.9 |
| 1428 days | 0.87 | 0.322.37 | Reference* | |
| 2960 days | Reference | |||
| Racial/ethnic status | ||||
| White | Reference | Reference | ||
| Black | 0.90 | 0.451.82 | 1.30 | 0.433.89 |
| Other | 0.99 | 0.571.70 | 1.19 | 0.482.99 |
| Treatment at children's hospital | 2.33 | 0.836.18 | 2.59 | 0.6510.2 |
| Treatment at teaching hospital | 1.71 | 0.943.12 | 1.86 | 0.566.25 |
| Female gender | 0.96 | 0.631.48 | 0.28 | 0.100.82 |
| Medicaid insurance | 1.51 | 0.912.50 | 1.69 | 0.634.53 |
| Transferred from another hospital | 3.76 | 2.036.98 | 3.47 | 1.428.46 |
| Transferred to another hospital | 1.35 | 0.672.73 | ||
| Presence of a congenital anomaly | 3.09 | 1.805.33 | 4.26 | 1.7610.3 |
| Low birth weight infant | 5.17 | 2.988.98 | 5.33 | 1.9015.0 |
Death
Risk factors for higher mortality rates followed similar trends as those for the risk of a serious complication. Younger age at admission, low birth weight status, the presence of a serious complication, admission from another hospital, and treatment at a children's hospital or teaching hospital were all associated with higher mortality rates. In multivariable analysis, the concurrent presence of a congenital anomaly was associated with higher odds of death (OR, 4.26; 95% CI, 1.7610.3). The cause of increased death in infants with congenital anomalies appeared to be a higher rate of serious complications, as including serious complications in the multivariable regression model resulted in the association between congenital anomalies and death losing statistical significance (OR in revised model 1.95; 95% CI, 0.636.05). Site of care again was not associated with differences in mortality after controlling for patient case‐mix.
Concurrent Congenital Anomalies
Based on the higher complication and mortality rates seen in infants with HSV who had a concurrent congenital anomaly, we then investigated how the presence of specific congenital anomalies influenced clinical outcomes, LOS, and total hospital costs with HSV disease. Using the congenital anomaly groups listed in the Appendix, we found that congenital heart disease, central nervous system anomalies, pulmonary anomalies, and gastrointestinal anomalies were each associated with either higher rates of serious complications, longer LOS, or higher total hospital costs compared to infants without congenital anomalies (Table 3). Serious complications occurred most commonly in patients with central nervous system anomalies (55.6%) and congenital heart disease (50.8%), while infants with pulmonary anomalies had the longest LOS (37.1 10.0 days) and highest total hospital costs of all anomaly categories. The types of complications differed by the anomaly group: infants with cardiac and pulmonary anomalies had the highest rates of respiratory complications (45% and 40%, respectively), whereas those with central nervous system anomalies had the highest rates of cardiac complications (51%). Each anomaly class had a similar rate of neurological complications, between 30% and 40%.
| Number* | % With Serious Complication | LOS (days) | Total Hospital Costs (2003 dollars) | |
|---|---|---|---|---|
| ||||
| No congenital anomaly | 1391 | 14.8 | 11.3 0.6 | 15,118 1158 |
| Type of congenital anomaly | ||||
| Congenital heart disease | 73 | 50.8 | 23.5 4.6 | 46,760 9340 |
| Central nervous system anomaly | 31 | 55.6 | 15.4 3.0 | 23,962 5037 |
| Head/neck anomaly | 13 | 40.6 | 11.1 4.6 | 14,132 7860 |
| Pulmonary anomaly | 13 | 34.1 | 37.1 10.0 | 67,234 21,002 |
| Gastrointestinal anomaly | 20 | 33.5 | 21.6 4.9 | 41,207 13,878 |
| Genitourinary anomaly | 19 | 24.1 | 11.0 2.5 | 10,906 1890 |
| Musculoskeletal anomaly | ||||
| Genetic anomaly | 18 | 10.2 | 12.2 2.4 | 15,990 3808 |
Site of Care
Finally, we examined the LOS and costs of receiving care at a children's hospital. The data shown in Tables 1 and 2 suggest that receiving treatment at a children's hospital does not result in improved clinical outcomes for infants admitted with HSV. One potential advantage, though, is improved efficiency of care, which would result in a shorter LOS or lower costs. Using negative binomial multivariable regression models to account for differences in patient characteristics, regional variation, and insurance status, treatment at a children's hospital was associated with an 18% shorter LOS (95% CI, 1%34%) compared to non‐children's hospitals after accounting for the generally sicker infants treated at children's hospitals. Children's hospitals, though, were more expensive than non‐children's hospitals (increase of $642 per day; 95% CI, $2321052). These results remained consistent when we omitted transferred patients from the model, instead of controlling for them in the analysis.
Conclusions
There has been little prior information to guide practitioners and parents about factors that potentially influence clinical outcome of infants hospitalized with HSV in non‐children's hospitals, although over 80% of infants are managed at non‐children's hospitals. These studies also did not have the power to characterize the risk of poor clinical outcome associated with rarer clinical factors.1, 2, 6 This study, using nationally representative data, found that these rarer clinical factors and site of care may influence the outcomes of infants hospitalized with HSV, albeit in different methods. Younger age at admission and a coexisting congenital anomaly remained statistically significant predictors of worse clinical outcomes after controlling for various patient and hospital factors. Not all congenital anomalies increased the risk of death or serious complications; rather, anomalies that affected either the cardiopulmonary system or the central nervous system appeared to result in the highest increases in risk. This study also found that treatment of infants with HSV at a children's hospital was associated with a 28% shorter LOS after accounting for the sicker patients cared for by children's hospitals. This finding is in contrast to prior studies of common pediatric conditions, where there were no differences in the LOS between children's and non‐children's hospitals,17, 18 and severe sepsis, where children's hospitals had longer LOSs.19 These results confirm the importance of specific risk factors in predicting the likelihood that an infant admitted with HSV may have a poor clinical outcome. Also, these results emphasize the differences in outcomes that may occur at different types of hospitals.
This study is the first to find that certain congenital anomalies or conditions may be associated with worse clinical outcomes from HSV. There is little information in the literature to explain these findings. Those anomalies that affect the cardiopulmonary or central nervous system may either worsen the symptoms of HSV or predispose infants to have a serious complication, such as shock or respiratory failure. This finding would be similar to the increased risk of serious complications seen in infants with congenital heart disease who contract respiratory syncytial virus20 or infants with genetic syndromes who undergo heart surgery.21 Alternatively, because we do not have information on do‐not‐resuscitate status, the presence of one of these congenital anomalies may result in more withdrawal of care when an infant is infected with HSV and has a serious complication; the LOS of these children may not reflect these decisions because the decision to withdrawal care may only occur after the child's condition worsens significantly, which may happen any time during the disease course. However, this theory is less likely because we failed to find similar results with other congenital anomalies such as genetic or chromosomal syndromes. Further examination of these infants and their overall response to insults such as HSV is needed to understand how these anomalies influence the outcomes of a serious, unrelated illness.
Age upon admission was another important predictor of poor outcomes when analyzed in univariable or multivariable analysis. This result is consistent with prior work,14 which suggests that younger children are more likely to be hospitalized with either congenitally acquired HSV or systemic disease. The information contained in the KID does not allow us to determine whether young age is a risk factor for poor outcome irrespective of the clinical presentation of HSV, or whether age serves as a proxy for the appearance of more severe clinical disease. This effect of age remained present even after controlling for the higher risk of a serious complication and death in low birth weight infants. There are limited data that suggest that premature birth is an independent risk factor for worse outcomes associated with perinatal or congenital infection; 1 previous case study of Enterobacter sakazakii infections found a higher fatality rate for premature infants compared to term infants.22 This study supports these findings.
This study found that treatment at a children's hospital resulted in a 28% shorter LOS without a statistically significant difference in clinical outcomes after controlling for case‐mix differences. This finding is in contrast to prior studies of common pediatric conditions17, 18 and severe sepsis.19 There are several potential explanations for the difference in findings. For common pediatric conditions, there may be fewer variations in treatment style and less need for new diagnostic modalities that are more available at academic centers. For HSV disease, though, children's hospitals may also be more likely than non‐children's hospitals to perform polymerase‐chain reaction (PCR) testing for the diagnosis of perinatally acquired HSV, correctly identify the disorder, or receive the test results in a timely fashion. Pediatric subspecialists, such as infectious disease physicians or neurologists, are also likely to be more available at children's hospitals than at other centers. While the role of subspecialty consultation in improving outcomes for neonates with HSV is not known, improved outcomes at children's hospitals has been described for other serious conditions such as splenic injuries.23 Children's hospitals had higher daily costs than non‐children's hospitals, as has been found in other work.17, 19 Children's hospitals may be treating sicker patients, for whom we are unable to adequately adjust for their illness severity with hospital administrative data.17, 19 Also, there may be a greater use of medical tests and treatments that increase the costs of care. These costs do not include indirect costs to the families such as loss of work and travel costs. In light of the shorter LOS in children's hospitals, policy makers will need to balance the potentially higher daily costs of care with more efficient management of the disease process.
Because this study used hospital administrative records, there are a few limitations. We used ICD‐9CM diagnosis codes to identify patients, congenital anomalies, and complications. The diagnosis of some infants with HSV or less significant congenital anomalies could have been missed because clinicians either overlooked the disease or did not make the diagnosis before discharge. This form of spectrum bias would likely miss the infants with the least severe disease and make it more difficult to find the results that we found in this study.24 Prior work successfully used and validated similar ICD‐9CM codes to identify HSV cases among the different types of hospitals included in the KID.611 Our study design estimated 1587 cases of neonatal HSV in 2003. A prospective study of maternal serologic and virologic status during pregnancy estimated 480 to 2160 new cases of neonatal HSV per year.25 Thus, while miscoding is a potential limitation to our study, the overall numbers of patients in this study were similar to past annual estimates. One potential area of miscounting, though, was the inability of the KID to link the records of 16% of the identified infants with HSV whose care was transferred between hospitals. These infants may result in misleading LOS or cost information: lower for the transferring hospital, because they only kept the child a short period of time, or lower for the accepting hospital, as some of the total hospital stay is not accounted for in the KID. We accounted for this issue in 2 ways. First, we included a variable for being transferred in the multivariable models, and found no difference in any results when we omitted these patients from the analysis. Second, we performed a univariable analysis stratified by transfer status, which did not differ substantially from our main model for most variables. Accurate linkage of all the hospital records for an infant's hospital course, likely only through a mandatory reporting system for infant HSV, would help confirm the associations we identified in this study.
In conclusion, infants with congenital anomalies should be closely monitored for the development of serious complications associated with HSV, particularly those infants with congenital heart disease, pulmonary anomalies, or central nervous system anomalies. Closer investigation of the care practices that children's hospitals use in the management of infants with HSV is needed to improve the efficiency of care delivered to these infants, as HSV disease remains a significant public health problem.
Herpes simplex virus (HSV) is a significant cause of pediatric hospitalization, morbidity and mortality, particularly in infants under 60 days of age, where HSV can present as meningoencephalitis, skin disease, or sepsis.14 Most prior studies use data from registries taken from single centers or a restricted group of hospitals. Thus, there is a paucity of recent, nationally‐representative information about the outcome of infants infected with HSV, especially those treated at nonteaching hospitals or with rarer comorbid conditions. The goal of this project was to determine the patient and hospital characteristics associated with worse clinical outcomes in infants under the age of 60 days admitted with HSV disease. We hypothesized that younger infants, infants with a concurrent congenital anomaly, and infants treated at non‐children's hospitals would have worse clinical outcomes. To answer these questions, we used 2003 panel data from the Healthcare Cost and Utilization Project (HCUP) Kids' Inpatient Database (KID), a nationally representative sample of inpatient hospitalizations in the United States.
Methods
Study Population and Data Collection
We conducted a retrospective population cohort study of all infants admitted at 60 days of age who were discharged with a diagnosis of HSV disease between January 1, 2003 and December 31, 2003, using the 2003 KID. The KID is a collaborative project between the Agency for Healthcare Research and Quality AHRQ and 36 states, which includes approximately 2.9 million pediatric discharge records from 3438 hospitals.5 The KID is the only national, all‐payer database of pediatric hospitalizations in the United States.
Patient Eligibility
As in prior studies,611 children were eligible for this project if they were discharged with an International Classification of Disease, ninth edition, Clinical Modification (ICD‐9CM) discharge code of 054.xx (herpes simplex virus), where xx represented any combination of one or two‐digit codes, or 771.2 (neonatal viral infection including HSV). However, the 771.2 code may also contain other perinatal infections of relatively rare frequency, such as toxoplasmosis. Thus, we also performed the same set of analyses on the cohort of children who had an 054.xx code alone. No results presented in this study changed in statistical significance when this smaller cohort of infants was examined.
Data Variables and Outcomes
Outcome Variables
We examined 2 primary clinical outcomes in this study: in‐hospital death and the occurrence of a serious complication. Complications were identified using ICD‐9CM codes from both prior work12 and examination of all diagnosis and procedure codes for eligible infants by the 2 principal investigators (Appendix). These 2 reviewers had to independently agree on the inclusion of an ICD‐9CM code as a complication. In‐hospital deaths were captured through a disposition code of 20 in the KID dataset. Length of stay (LOS) and in‐hospital costs were examined as secondary outcome measures for specific risk factors of interest.
Demographic and Comorbidity Variables
Demographic and comorbidity variables were included in the analyses to control for the increased cost, LOS, or risk of a complication that result from these factors.1315 Demographic information available in the KID included gender, age at admission, race, low birth weight infants, and insurance status. Age at admission was grouped into 4 categories: 07 days, 814 days, 1528 days, and 2960 days. Infants were classified as low birth weight if they had an ICD‐9CM code for a birth weight <2000 g (ICD‐9CM codes 765.01‐07, 765.11‐17, or 765.21‐27). We used the ICD‐9CM codes shown in the Appendix to classify various comorbid conditions. Because of the young age of the cohort, all comorbid conditions consisted of congenital anomalies that were grouped according to the involved organ system. To help classify patients by their illness severity, we used the All‐Patient Refined Diagnosis‐Related Group (APR‐DRG) severity of illness classification for each hospital admission (3M Corporation, St. Paul, MN). The APR‐DRG classification system used discharge diagnoses, procedures, and demographic information to assign patients to 4 severity of illness categories.
Hospital Characteristics
We identified the following hospital characteristics from the KID: total bed size, divided as small, medium, and large; hospital status (children's hospital vs. non‐children's hospital, teaching hospital vs. nonteaching hospital); source of admission (emergency department, clinic, other hospitals); and location (rural vs. urban). Children's hospitals were identified by the AHRQ using information from the National Association of Children's Hospitals and Related Institutions, while teaching hospital status was determined by the presence of an approved residency program and a ratio of full‐time residents to beds of 0.25 or greater.5
Statistical Analysis
All analyses accounted for the complex sampling design with the survey commands included in STATA 9.2 (Statacorp, College Station, TX) and report national estimates from the data available in the 36 surveyed states. Because of the complex sampling design, the Wald test was used to determine significant differences for each outcome in univariable analysis. Variance estimates were reported as standard errors of the mean. We constructed multivariable logistic regression models to assess the adjusted impact of patient and hospital‐level characteristics on each primary outcome measure; ie, in‐hospital death and development of a serious complication. Negative binomial models were used for our secondary outcomes, LOS and costs, because of their rightward skew. Variance estimates for each model accounted for the clustering of data at the hospital level, and data were analyzed as per the latest AHRQ statistical update.16
Results
The 2003 KID identified 1587 hospitalizations for HSV in infants admitted at an age of 60 days or less in the entire United States. These infants had a total hospital cost of $27,147,000. Of the cohort, 10% had a concurrent congenital anomaly. Most infants (73.5%) were admitted within 14 days of birth, and 15.5% were transferred from another hospital. Based on APR‐DRG criteria, 33% of the infants were classified as having a moderate risk of death, 24% as major risk, and 12.2% as extreme risk. The majority of infants were treated at non‐children's hospitals (85.3%) in urban locations (91.5%). The average LOS was 12.0 0.6 days and the average total hospital cost was $17,382 1269. After admission, 267 of the infants, or 16.8%, had at least 1 serious complication. Fifty infants died during the hospitalization included in the KID.
Risk Factor Analysis
Serious Complications
Univariable (Table 1) analysis identified several factors associated with higher rates of serious complications. Younger age at admission was associated with a higher risk of serious complications. This trend was greatest for infants admitted under 14 days of age, of which 20.2% had a serious complication, compared with 10.2% of the infants admitted between 29 and 60 days of age. Infants with any identified congenital anomaly had significantly higher rates of serious complication (41.1% vs. 14.8% for infants without a congenital anomaly). Similar findings were seen with low birth weight infants. Infants who were transferred prior to the hospitalization captured in the KID had a higher complication rate (38.7%) than infants admitted as a routine admission (15.9%) or via the emergency room (8.8%). Among hospital‐level factors, infants admitted to children's or teaching hospitals had higher rates of serious complications, although only the difference between teaching and nonteaching hospitals reached statistical significance (Table 1).
| Patient‐Level Factors | % of Cohort | % with Serious Complication | % Death |
|---|---|---|---|
| |||
| Age at presentation | |||
| 7 days | 58.4 | 21.6* | 4.2* |
| 814 days | 15.1 | 15.8 | 3.6 |
| 1528 days | 16.4 | 9.7 | 2.1 |
| 2960 days | 10.1 | 10.2 | 0 |
| Low birth weight | |||
| Yes | 10.6 | 44.2* | 9.0* |
| No | 89.4 | 14.3 | 2.7 |
| Type of insurance | |||
| Private | 47.4 | 15.6 | 2.1* |
| Medicaid | 49.0 | 19.2 | 4.8 |
| Self pay | 3.6 | 17.0 | 0 |
| Race | |||
| White | 52.8 | 17.7 | 3.5 |
| Black | 18.9 | 17.6 | 4.2 |
| Other | 28.3 | 19.2 | 4.5 |
| Gender | |||
| Female | 45.4 | 15.7 | 2.2 |
| Male | 54.6 | 18.9 | 4.3 |
| Any congenital anomaly | |||
| Yes | 10.0 | 41.1* | 10.4* |
| No | 90.0 | 14.8 | 2.6 |
| Admission type | |||
| Routine | 62.3 | 15.9* | 2.8* |
| Emergency room | 22.2 | 8.8 | 1.1 |
| Transfer from another hospital | 15.5 | 38.7 | 9.6 |
| APR‐DRG risk | |||
| Mild | 3.0 | 0.3* | 0* |
| Moderate | 33.0 | 2.0 | 0.5 |
| Major | 24.0 | 24.7 | 2.3 |
| Extreme | 12.2 | 85.0 | 20.8 |
| Hospital‐level factors | |||
| Children's hospital | |||
| Yes | 14.7 | 27.0 | 6.4 |
| No | 85.3 | 16.3 | 3.1 |
| Teaching hospital | |||
| Yes | 68.4 | 21.3* | 4.3* |
| No | 31.7 | 8.5 | 1.5 |
| Location | |||
| Urban | 91.5 | 18.0* | 3.6 |
| Rural | 8.5 | 9.0 | 1.6 |
| Hospital size | |||
| Small | 14.1 | 19.3 | 4.2 |
| Medium | 25.9 | 14.3 | 3.2 |
| Large | 60.0 | 18.1 | 3.3 |
Many of these factors were independently associated with increased complication rates in multivariable analysis (Table 2). Infants under 7 days of age on admission (odds ratio [OR], 2.68; 95% confidence interval [CI], 1.112.47), low birth weight (OR, 5.17; 95% CI, 2.988.98), and the concurrent presence of a congenital anomaly (OR, 3.09; 95% CI, 1.805.33) were associated with higher odds of a serious complication. Site of care lost its statistical significance once our models adjusted for differences in illness severity. Insurance status, gender, and race were not associated with a change in complication rates for these infants.
| Risk Factor | Serious Complication | Mortality | ||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| ||||
| Age at admission | ||||
| 7 days | 2.68 | 1.112.47 | 1.63 | 0.347.73 |
| 814 days | 1.22 | 0.403.73 | 2.15 | 0.3612.9 |
| 1428 days | 0.87 | 0.322.37 | Reference* | |
| 2960 days | Reference | |||
| Racial/ethnic status | ||||
| White | Reference | Reference | ||
| Black | 0.90 | 0.451.82 | 1.30 | 0.433.89 |
| Other | 0.99 | 0.571.70 | 1.19 | 0.482.99 |
| Treatment at children's hospital | 2.33 | 0.836.18 | 2.59 | 0.6510.2 |
| Treatment at teaching hospital | 1.71 | 0.943.12 | 1.86 | 0.566.25 |
| Female gender | 0.96 | 0.631.48 | 0.28 | 0.100.82 |
| Medicaid insurance | 1.51 | 0.912.50 | 1.69 | 0.634.53 |
| Transferred from another hospital | 3.76 | 2.036.98 | 3.47 | 1.428.46 |
| Transferred to another hospital | 1.35 | 0.672.73 | ||
| Presence of a congenital anomaly | 3.09 | 1.805.33 | 4.26 | 1.7610.3 |
| Low birth weight infant | 5.17 | 2.988.98 | 5.33 | 1.9015.0 |
Death
Risk factors for higher mortality rates followed similar trends as those for the risk of a serious complication. Younger age at admission, low birth weight status, the presence of a serious complication, admission from another hospital, and treatment at a children's hospital or teaching hospital were all associated with higher mortality rates. In multivariable analysis, the concurrent presence of a congenital anomaly was associated with higher odds of death (OR, 4.26; 95% CI, 1.7610.3). The cause of increased death in infants with congenital anomalies appeared to be a higher rate of serious complications, as including serious complications in the multivariable regression model resulted in the association between congenital anomalies and death losing statistical significance (OR in revised model 1.95; 95% CI, 0.636.05). Site of care again was not associated with differences in mortality after controlling for patient case‐mix.
Concurrent Congenital Anomalies
Based on the higher complication and mortality rates seen in infants with HSV who had a concurrent congenital anomaly, we then investigated how the presence of specific congenital anomalies influenced clinical outcomes, LOS, and total hospital costs with HSV disease. Using the congenital anomaly groups listed in the Appendix, we found that congenital heart disease, central nervous system anomalies, pulmonary anomalies, and gastrointestinal anomalies were each associated with either higher rates of serious complications, longer LOS, or higher total hospital costs compared to infants without congenital anomalies (Table 3). Serious complications occurred most commonly in patients with central nervous system anomalies (55.6%) and congenital heart disease (50.8%), while infants with pulmonary anomalies had the longest LOS (37.1 10.0 days) and highest total hospital costs of all anomaly categories. The types of complications differed by the anomaly group: infants with cardiac and pulmonary anomalies had the highest rates of respiratory complications (45% and 40%, respectively), whereas those with central nervous system anomalies had the highest rates of cardiac complications (51%). Each anomaly class had a similar rate of neurological complications, between 30% and 40%.
| Number* | % With Serious Complication | LOS (days) | Total Hospital Costs (2003 dollars) | |
|---|---|---|---|---|
| ||||
| No congenital anomaly | 1391 | 14.8 | 11.3 0.6 | 15,118 1158 |
| Type of congenital anomaly | ||||
| Congenital heart disease | 73 | 50.8 | 23.5 4.6 | 46,760 9340 |
| Central nervous system anomaly | 31 | 55.6 | 15.4 3.0 | 23,962 5037 |
| Head/neck anomaly | 13 | 40.6 | 11.1 4.6 | 14,132 7860 |
| Pulmonary anomaly | 13 | 34.1 | 37.1 10.0 | 67,234 21,002 |
| Gastrointestinal anomaly | 20 | 33.5 | 21.6 4.9 | 41,207 13,878 |
| Genitourinary anomaly | 19 | 24.1 | 11.0 2.5 | 10,906 1890 |
| Musculoskeletal anomaly | ||||
| Genetic anomaly | 18 | 10.2 | 12.2 2.4 | 15,990 3808 |
Site of Care
Finally, we examined the LOS and costs of receiving care at a children's hospital. The data shown in Tables 1 and 2 suggest that receiving treatment at a children's hospital does not result in improved clinical outcomes for infants admitted with HSV. One potential advantage, though, is improved efficiency of care, which would result in a shorter LOS or lower costs. Using negative binomial multivariable regression models to account for differences in patient characteristics, regional variation, and insurance status, treatment at a children's hospital was associated with an 18% shorter LOS (95% CI, 1%34%) compared to non‐children's hospitals after accounting for the generally sicker infants treated at children's hospitals. Children's hospitals, though, were more expensive than non‐children's hospitals (increase of $642 per day; 95% CI, $2321052). These results remained consistent when we omitted transferred patients from the model, instead of controlling for them in the analysis.
Conclusions
There has been little prior information to guide practitioners and parents about factors that potentially influence clinical outcome of infants hospitalized with HSV in non‐children's hospitals, although over 80% of infants are managed at non‐children's hospitals. These studies also did not have the power to characterize the risk of poor clinical outcome associated with rarer clinical factors.1, 2, 6 This study, using nationally representative data, found that these rarer clinical factors and site of care may influence the outcomes of infants hospitalized with HSV, albeit in different methods. Younger age at admission and a coexisting congenital anomaly remained statistically significant predictors of worse clinical outcomes after controlling for various patient and hospital factors. Not all congenital anomalies increased the risk of death or serious complications; rather, anomalies that affected either the cardiopulmonary system or the central nervous system appeared to result in the highest increases in risk. This study also found that treatment of infants with HSV at a children's hospital was associated with a 28% shorter LOS after accounting for the sicker patients cared for by children's hospitals. This finding is in contrast to prior studies of common pediatric conditions, where there were no differences in the LOS between children's and non‐children's hospitals,17, 18 and severe sepsis, where children's hospitals had longer LOSs.19 These results confirm the importance of specific risk factors in predicting the likelihood that an infant admitted with HSV may have a poor clinical outcome. Also, these results emphasize the differences in outcomes that may occur at different types of hospitals.
This study is the first to find that certain congenital anomalies or conditions may be associated with worse clinical outcomes from HSV. There is little information in the literature to explain these findings. Those anomalies that affect the cardiopulmonary or central nervous system may either worsen the symptoms of HSV or predispose infants to have a serious complication, such as shock or respiratory failure. This finding would be similar to the increased risk of serious complications seen in infants with congenital heart disease who contract respiratory syncytial virus20 or infants with genetic syndromes who undergo heart surgery.21 Alternatively, because we do not have information on do‐not‐resuscitate status, the presence of one of these congenital anomalies may result in more withdrawal of care when an infant is infected with HSV and has a serious complication; the LOS of these children may not reflect these decisions because the decision to withdrawal care may only occur after the child's condition worsens significantly, which may happen any time during the disease course. However, this theory is less likely because we failed to find similar results with other congenital anomalies such as genetic or chromosomal syndromes. Further examination of these infants and their overall response to insults such as HSV is needed to understand how these anomalies influence the outcomes of a serious, unrelated illness.
Age upon admission was another important predictor of poor outcomes when analyzed in univariable or multivariable analysis. This result is consistent with prior work,14 which suggests that younger children are more likely to be hospitalized with either congenitally acquired HSV or systemic disease. The information contained in the KID does not allow us to determine whether young age is a risk factor for poor outcome irrespective of the clinical presentation of HSV, or whether age serves as a proxy for the appearance of more severe clinical disease. This effect of age remained present even after controlling for the higher risk of a serious complication and death in low birth weight infants. There are limited data that suggest that premature birth is an independent risk factor for worse outcomes associated with perinatal or congenital infection; 1 previous case study of Enterobacter sakazakii infections found a higher fatality rate for premature infants compared to term infants.22 This study supports these findings.
This study found that treatment at a children's hospital resulted in a 28% shorter LOS without a statistically significant difference in clinical outcomes after controlling for case‐mix differences. This finding is in contrast to prior studies of common pediatric conditions17, 18 and severe sepsis.19 There are several potential explanations for the difference in findings. For common pediatric conditions, there may be fewer variations in treatment style and less need for new diagnostic modalities that are more available at academic centers. For HSV disease, though, children's hospitals may also be more likely than non‐children's hospitals to perform polymerase‐chain reaction (PCR) testing for the diagnosis of perinatally acquired HSV, correctly identify the disorder, or receive the test results in a timely fashion. Pediatric subspecialists, such as infectious disease physicians or neurologists, are also likely to be more available at children's hospitals than at other centers. While the role of subspecialty consultation in improving outcomes for neonates with HSV is not known, improved outcomes at children's hospitals has been described for other serious conditions such as splenic injuries.23 Children's hospitals had higher daily costs than non‐children's hospitals, as has been found in other work.17, 19 Children's hospitals may be treating sicker patients, for whom we are unable to adequately adjust for their illness severity with hospital administrative data.17, 19 Also, there may be a greater use of medical tests and treatments that increase the costs of care. These costs do not include indirect costs to the families such as loss of work and travel costs. In light of the shorter LOS in children's hospitals, policy makers will need to balance the potentially higher daily costs of care with more efficient management of the disease process.
Because this study used hospital administrative records, there are a few limitations. We used ICD‐9CM diagnosis codes to identify patients, congenital anomalies, and complications. The diagnosis of some infants with HSV or less significant congenital anomalies could have been missed because clinicians either overlooked the disease or did not make the diagnosis before discharge. This form of spectrum bias would likely miss the infants with the least severe disease and make it more difficult to find the results that we found in this study.24 Prior work successfully used and validated similar ICD‐9CM codes to identify HSV cases among the different types of hospitals included in the KID.611 Our study design estimated 1587 cases of neonatal HSV in 2003. A prospective study of maternal serologic and virologic status during pregnancy estimated 480 to 2160 new cases of neonatal HSV per year.25 Thus, while miscoding is a potential limitation to our study, the overall numbers of patients in this study were similar to past annual estimates. One potential area of miscounting, though, was the inability of the KID to link the records of 16% of the identified infants with HSV whose care was transferred between hospitals. These infants may result in misleading LOS or cost information: lower for the transferring hospital, because they only kept the child a short period of time, or lower for the accepting hospital, as some of the total hospital stay is not accounted for in the KID. We accounted for this issue in 2 ways. First, we included a variable for being transferred in the multivariable models, and found no difference in any results when we omitted these patients from the analysis. Second, we performed a univariable analysis stratified by transfer status, which did not differ substantially from our main model for most variables. Accurate linkage of all the hospital records for an infant's hospital course, likely only through a mandatory reporting system for infant HSV, would help confirm the associations we identified in this study.
In conclusion, infants with congenital anomalies should be closely monitored for the development of serious complications associated with HSV, particularly those infants with congenital heart disease, pulmonary anomalies, or central nervous system anomalies. Closer investigation of the care practices that children's hospitals use in the management of infants with HSV is needed to improve the efficiency of care delivered to these infants, as HSV disease remains a significant public health problem.
- ,,, et al.Natural history of neonatal herpes simplex virus infections in the acyclovir era.Pediatrics.2001;108:223–229.
- ,,.Herpes simplex viruses.Clin Infect Dis.1998;26:541–553.
- ,,.Herpes simplex virus infections. In: Remington JS, Wilson CB, Baker CJ, editors.Infectious Diseases of the Fetus and Newborn Infant.5th ed.Philadelphia, PA:W.B. Saunders;2001. p425–446.
- ,,, et al.Changing presentation of herpes simplex virus infection in neonates.J Infect Dis.1988;158:109–116.
- Design of the HCUP Kids' Inpatient Database (KID), 2003. Healthcare Cost and Utilization Project (HCUP).Rockville, MD:Agency for Healthcare Research and Quality;2003. Revised January 30, 2006. Available at: http://www.hcup‐us.ahrq.gov/db/nation/kid/reports/KID_2003_Design_Edited_013006.pdf. Accessed October 2009.
- ,,.Incidence of neonatal herpes simplex virus infections in a managed‐care population.Sex Transm Dis.2007;34:704–708.
- ,,, et al.Targeted prenatal herpes simplex virus testing: can we identify women at risk of transmission to the neonate.Am J Obstet Gynecol.2006;194:408–414.
- ,,, et al.The estimated economic burden of genital herpes in the united states.BMC Infect Dis.2001;1:5.
- ,,, et al.Accuracy of obstetric diagnoses and procedures in hospital discharge data.Am J Obstet Gynecol.2006;194:992–1001.
- ,,, et al.The epidemiology of neonatal herpes simplex virus infections in California from 1985 to 1995.J Infect Dis.1999;180:199–202.
- ,,.Medical care expenditures for genital herpes in the United States.Sex Transm Dis.2000;27:32–38.
- ,,, et al.The epidemiology of sepsis in the United States from 1979 through 2000.N Engl J Med.2003;348:1546–1554.
- ,,, et al.The importance of comorbidities in explaining differences in patient costs.Med Care.1996;34:767–782.
- ,,, et al.Contribution of birth defects and genetic diseases to pediatric hospitalizations. A population‐based study.Arch Pediatr Adolesc Med.1997;151:1096–1103.
- ,,.The influence of chronic disease on resource utilization in common acute pediatric conditions. Financial concerns for children's hospitals.Arch Pediatr Adolesc Med.1999;153:169–179.
- Health Care Cost and Utility Project.Calculating Kids' Inpatient Database (KID) Variances. December 16, 2005. Methods Series Report # 2005‐5.Rockville, MD:Agency for Healthcare Research and Quality. Available at: http://www.hcup‐us.ahrq.gov/db/nation/kid/reports/CalculatingKIDVariances.pdf. Accessed October2009.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
- ,.Length of stay for common pediatric conditions: teaching versus nonteaching hospitals.Pediatrics.2003;112:278–281.
- ,,.Patient and hospital correlates of clinical outcomes and resource utilization in severe pediatric sepsis.Pediatrics.2007;119:487–494.
- .Review of epidemiology and clinical risk factors for severe respiratory syncytial virus (RSV) infection.J Pediatr.2003;143:S112–S117.
- ,,, et al.Patient characteristics are important determinants of neurodevelopmental outcome at one year of age after neonatal and infant cardiac surgery.J Thorac Cardiovasc Surg.2007;133:1344–1353,1353,e1341–e1343.
- .Enterobacter sakazakii infections among neonates, infants, children, and adults. Case reports and a review of the literature.Medicine.2001;80:113–122.
- ,,, et al.Hospital characteristics associated with the management of pediatric splenic injuries.JAMA.2005;294:2611–2617.
- ,.Spectrum bias or spectrum effect? Subgroup variation in diagnostic test evaluation.Ann Intern Med.2002;137:598–602.
- ,,, et al.Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant.JAMA.2003;289:203–209.
- ,,, et al.Natural history of neonatal herpes simplex virus infections in the acyclovir era.Pediatrics.2001;108:223–229.
- ,,.Herpes simplex viruses.Clin Infect Dis.1998;26:541–553.
- ,,.Herpes simplex virus infections. In: Remington JS, Wilson CB, Baker CJ, editors.Infectious Diseases of the Fetus and Newborn Infant.5th ed.Philadelphia, PA:W.B. Saunders;2001. p425–446.
- ,,, et al.Changing presentation of herpes simplex virus infection in neonates.J Infect Dis.1988;158:109–116.
- Design of the HCUP Kids' Inpatient Database (KID), 2003. Healthcare Cost and Utilization Project (HCUP).Rockville, MD:Agency for Healthcare Research and Quality;2003. Revised January 30, 2006. Available at: http://www.hcup‐us.ahrq.gov/db/nation/kid/reports/KID_2003_Design_Edited_013006.pdf. Accessed October 2009.
- ,,.Incidence of neonatal herpes simplex virus infections in a managed‐care population.Sex Transm Dis.2007;34:704–708.
- ,,, et al.Targeted prenatal herpes simplex virus testing: can we identify women at risk of transmission to the neonate.Am J Obstet Gynecol.2006;194:408–414.
- ,,, et al.The estimated economic burden of genital herpes in the united states.BMC Infect Dis.2001;1:5.
- ,,, et al.Accuracy of obstetric diagnoses and procedures in hospital discharge data.Am J Obstet Gynecol.2006;194:992–1001.
- ,,, et al.The epidemiology of neonatal herpes simplex virus infections in California from 1985 to 1995.J Infect Dis.1999;180:199–202.
- ,,.Medical care expenditures for genital herpes in the United States.Sex Transm Dis.2000;27:32–38.
- ,,, et al.The epidemiology of sepsis in the United States from 1979 through 2000.N Engl J Med.2003;348:1546–1554.
- ,,, et al.The importance of comorbidities in explaining differences in patient costs.Med Care.1996;34:767–782.
- ,,, et al.Contribution of birth defects and genetic diseases to pediatric hospitalizations. A population‐based study.Arch Pediatr Adolesc Med.1997;151:1096–1103.
- ,,.The influence of chronic disease on resource utilization in common acute pediatric conditions. Financial concerns for children's hospitals.Arch Pediatr Adolesc Med.1999;153:169–179.
- Health Care Cost and Utility Project.Calculating Kids' Inpatient Database (KID) Variances. December 16, 2005. Methods Series Report # 2005‐5.Rockville, MD:Agency for Healthcare Research and Quality. Available at: http://www.hcup‐us.ahrq.gov/db/nation/kid/reports/CalculatingKIDVariances.pdf. Accessed October2009.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
- ,.Length of stay for common pediatric conditions: teaching versus nonteaching hospitals.Pediatrics.2003;112:278–281.
- ,,.Patient and hospital correlates of clinical outcomes and resource utilization in severe pediatric sepsis.Pediatrics.2007;119:487–494.
- .Review of epidemiology and clinical risk factors for severe respiratory syncytial virus (RSV) infection.J Pediatr.2003;143:S112–S117.
- ,,, et al.Patient characteristics are important determinants of neurodevelopmental outcome at one year of age after neonatal and infant cardiac surgery.J Thorac Cardiovasc Surg.2007;133:1344–1353,1353,e1341–e1343.
- .Enterobacter sakazakii infections among neonates, infants, children, and adults. Case reports and a review of the literature.Medicine.2001;80:113–122.
- ,,, et al.Hospital characteristics associated with the management of pediatric splenic injuries.JAMA.2005;294:2611–2617.
- ,.Spectrum bias or spectrum effect? Subgroup variation in diagnostic test evaluation.Ann Intern Med.2002;137:598–602.
- ,,, et al.Effect of serologic status and cesarean delivery on transmission rates of herpes simplex virus from mother to infant.JAMA.2003;289:203–209.
Copyright © 2010 Society of Hospital Medicine
Erythema with Leukemia and Bacteremia
A previously healthy 66‐year‐old man was admitted with a 4‐day history of high fever and an extensive, nonpruritic, nonmigratory, erythematous rash with areas of induration over his torso (Figure 1A). Biopsy of the rash, which spontaneously subsided within 8 days, revealed only nonspecific superficial and deep perivascular lymphocytic infiltration, without vasculitis, granulomas, or immunohistochemical evidence of malignant cells (Figure 1B). Blood cultures grew spiral‐shaped Gram‐negative rods (Figure 1C), which were identified as Helicobacter cinaedi by polymerase chain reaction (PCR). H. cinaedi is a rare pathogen that is reported to cause bacteremia in immunocompromised hosts. Peripheral blood showed more than 2000/L of lymphocytes with prominent hyperlobulated flower‐like nuclei (Figure 1D), which were CD4+/CD8 and CD25+ by flow cytometry. Human T‐lymphotropic virus 1 (HTLV‐1) antibody was positive, highlighting the fact that the patient's mother was from southern Kyushu, Japan, where HTLV‐1 is endemic. Diagnosis of adult T‐cell leukemia was confirmed by southern blot hybridization analysis. We believe that this case makes an important addition to the library of annular or gyrate erythemas, which can be secondary to bacteremia, leukemia, or both.

A previously healthy 66‐year‐old man was admitted with a 4‐day history of high fever and an extensive, nonpruritic, nonmigratory, erythematous rash with areas of induration over his torso (Figure 1A). Biopsy of the rash, which spontaneously subsided within 8 days, revealed only nonspecific superficial and deep perivascular lymphocytic infiltration, without vasculitis, granulomas, or immunohistochemical evidence of malignant cells (Figure 1B). Blood cultures grew spiral‐shaped Gram‐negative rods (Figure 1C), which were identified as Helicobacter cinaedi by polymerase chain reaction (PCR). H. cinaedi is a rare pathogen that is reported to cause bacteremia in immunocompromised hosts. Peripheral blood showed more than 2000/L of lymphocytes with prominent hyperlobulated flower‐like nuclei (Figure 1D), which were CD4+/CD8 and CD25+ by flow cytometry. Human T‐lymphotropic virus 1 (HTLV‐1) antibody was positive, highlighting the fact that the patient's mother was from southern Kyushu, Japan, where HTLV‐1 is endemic. Diagnosis of adult T‐cell leukemia was confirmed by southern blot hybridization analysis. We believe that this case makes an important addition to the library of annular or gyrate erythemas, which can be secondary to bacteremia, leukemia, or both.

A previously healthy 66‐year‐old man was admitted with a 4‐day history of high fever and an extensive, nonpruritic, nonmigratory, erythematous rash with areas of induration over his torso (Figure 1A). Biopsy of the rash, which spontaneously subsided within 8 days, revealed only nonspecific superficial and deep perivascular lymphocytic infiltration, without vasculitis, granulomas, or immunohistochemical evidence of malignant cells (Figure 1B). Blood cultures grew spiral‐shaped Gram‐negative rods (Figure 1C), which were identified as Helicobacter cinaedi by polymerase chain reaction (PCR). H. cinaedi is a rare pathogen that is reported to cause bacteremia in immunocompromised hosts. Peripheral blood showed more than 2000/L of lymphocytes with prominent hyperlobulated flower‐like nuclei (Figure 1D), which were CD4+/CD8 and CD25+ by flow cytometry. Human T‐lymphotropic virus 1 (HTLV‐1) antibody was positive, highlighting the fact that the patient's mother was from southern Kyushu, Japan, where HTLV‐1 is endemic. Diagnosis of adult T‐cell leukemia was confirmed by southern blot hybridization analysis. We believe that this case makes an important addition to the library of annular or gyrate erythemas, which can be secondary to bacteremia, leukemia, or both.

Antimicrobial Prescription in Pneumonia
Pneumonia is the second most common infection in nursing home residents after urinary tract infection, and is the most common reason for transfer to the hospital.1 Although it remains difficult to determine the incidence of pneumonia in institutionalized elderly patients, an estimated 4 million cases of nursing homeacquired pneumonia (NHAP) occur annually in the United States and result in more than 600,000 emergency department visits.2 In the past 2 decades, multiple studies have documented the rapid rise in drug resistance among common pathogens responsible for pneumonia in the elderly and the acquisition of multidrug‐resistant organisms in residents of long‐term care facilities.3, 4 Health care practitioners are faced with the dilemma of attempting to limit broad‐spectrum antimicrobial drug use while striving to maximize therapeutic efficacy in individual patients.5 The current practice guidelines for the management of NHAP from various professional societies provide mixed messages on the class of antibiotics for patients requiring hospitalization.2, 68 While the 2000 Canadian and the 2003 Infectious Disease Society of America (IDSA) guidelines advocate a community‐acquired pneumonia‐like approach to therapy, the 2005 American Thoracic Society (ATS)/IDSA guidelines and the 2007 IDSA/ATS guidelines consider drug‐resistant pathogens (DRPs) (ie, methicillin‐resistant Staphylococcus aureus [MRSA] and Pseudomonas aeruginosa) to be major etiologic agents in NHAP and thus the empiric treatment recommendations focus specifically on these pathogens (Table 1).
|
| 2003 IDSA |
| 1. Parenteral third‐generation cephalosporin or ampicillin sulbactam + macrolide; or |
| 2. Parenteral fluoroquinolone alone |
| 2000 Canadian |
| 1. Parenteral fluoroquinolone alone; or |
| 2. Parenteral third‐generation, or fourth‐generation cephalosporin + macrolide |
| 2005 ATS/IDSA |
| 1. Antipseudomonal cephalosporin or antipseudomonal carbapenem or antipseudomonal penicillin + antipseudomonal fluoroquinolone or aminoglycoside + anti‐methicillin‐resistant Staphylococcus agents |
Given these differences in antibiotic recommendations among the various guidelines, we sought to examine the antimicrobial prescription patterns in hospitalized non‐critically‐ill patients with NHAP in multiple tertiary care facilities vis‐‐vis the population demographics and clinical characteristics.
Methods
Study Population
This retrospective study was conducted in 3 tertiary‐care hospitals (Erie County Medical Center, Millard Fillmore Hospital, and Buffalo General Hospital) in the city of Buffalo, New York. These hospitals account for 96% of admissions from nursing homes in Erie County. The Institutional Review Board approved the study and certified that it met the criteria for a waiver of the requirement to obtain informed consent. All medical charts of adult patients with pneumonia listed under admission diagnosis or discharge diagnosis (International Classification of Diseases, ninth revision, Clinical Modification Codes [ICD‐9‐CM] [35] codes 480.0480.9, 481, 482.0482.9, 483.0483.8, 485, 486, 487.0, and 507.0) between April 2005 and December 2007 were abstracted. The records were searched for place of residence prior to admission and all patients residing in nursing homes for 30 days or more were selected for review. Inclusion criteria included the presence of new or increased radiographic abnormalities plus 2 or more of the following symptoms and signs: new or increased cough, new or increased sputum production, and temperature greater than 38C. Patients who met at least one of the following criteria were excluded: (1) admission to a critical care unit from the emergency department; (2) discharge within 24 hours; (3) human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS) or immunocompromised; (4) transfer from another hospital; or (5) receiving active chemotherapy. Patients with multiple admissions were included only once to ensure independence of observations.
Data Collection
Data collected included information on sociodemographic characteristics, admitting service (University‐affiliated or private service), comorbidities, preadmission functional status, do not resuscitate (DNR) order, and prior antibiotic therapy. Antibiotic information was comprised of the name of the antibiotic, start and stop dates (including postdischarge), monotherapy or combination therapy, and route of administration. Antimicrobials were assigned to 1 of the following categories: macrolides (azithromycin, clarithromycin), lincosamide (clindamycin), fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin), carbapenems (ertapenem, imipenem), cephalosporins (ceftriaxone, cefpodoxime, cefepime), and ureidopenicillins (piperacillin‐tazobactam). Patients who died during the hospital stay before completion of therapy were assigned 14 days of antibiotic therapy.
The burden of comorbidities was assessed by the Charlson Index.9 The Activity of Daily Living (ADL) score was abstracted from a standardized patient‐review instrument included in all patients' charts.10 Patients were assigned an ADL score in each of the 6 major areas of activity: eating, toileting, feeding, bathing, mobility, and continence; ranging from 1 if they were fully independent, 2 if they were partially independent, and 3 if they were completely dependent. The ADL score was calculated by adding the points assigned for each activity, and it ranged from 6 to 18. Three categories were arbitrarily created: ADL I, corresponding to ADL scores from 6 to 8; ADL II, scores from 9 to 13; and ADL III, scores from 14 to 18.4
The Pneumonia Severity Index Score (PSI)11 was also calculated. The PSI is a validated disease‐severity classification system based on age, sex, nursing home residence, 5 comorbid illnesses, vital signs on admission, mental status, 7 laboratory values, and the findings on chest roentgenograms. Based on the scoring system, patients were stratified into 5 categories or classes of risk for in‐hospital mortality. Class I patients have the lowest disease severity while class V have the highest disease severity.
Statistics
Data were analyzed using the NCSS 2000 Statistical Analysis System (NCSS, Kaysville, UT). Continuous variables were tested for normal distribution using the Kolmogorov‐Smirnov test. Results are expressed as means standard deviation (SD). Univariate analysis was carried out using the chi‐square test and Fisher's exact test for categorical data and the t test for independent samples for continuous variables. Missing values for ADL and Charlson scores were encountered at <3% of the total population sample. Multiple regression models of available variables were utilized to predict missing values as described by Little and Rubin.12 All tests were 2‐tailed and statistical significance was determined at the 5% level.
Results
A total of 397 subjects with NHAP were included in the study. The mean age of the cohort group was 76.8 13.5 years. Eighty percent had 2 or more chronic diseases. Degenerative nervous system, cardiac, and pulmonary diseases accounted for the majority of underlying comorbidities. Demographic and clinical characteristics of the study population are presented in Table 2. At the time of admission, 17% of patients had received antimicrobial therapy for a respiratory ailment within the last week prior to transfer to an acute care facility. The most commonly prescribed agents at the nursing home were an oral fluoroquinolone (81%), a cephalosporin (14%), or a macrolide (3%).
| |
| Characteristic (n = 397) | |
| Age (years), mean (SD) | 76.8 (13.5) |
| Male, n (%) | 162 (41) |
| Underlying comorbidities, n (%) | |
| Cardiac diseases | 135 (34) |
| Pulmonary diseases | 129 (32) |
| Cerebrovascular accident | 98 (25) |
| Diabetes mellitus | 138 (35) |
| Dementia | 179 (45) |
| DNR, n (%) | 42 (11) |
| Activity of daily living, n (%) | |
| ADL I | 57 (14) |
| ADL II | 150 (38) |
| ADL III | 190 (48) |
| Pneumonia Severity Index, n (%) | |
| Class II | 13 (3) |
| Class III | 34 (8) |
| Class IV | 177 (45) |
| Class V | 173 (44) |
| Bacteremia, n (%) | 48 (12) |
Of the 397 patients who met the criteria for NHAP, all but 5 patients received antimicrobial therapy. The 3 most commonly used antimicrobial compounds for inpatient treatment were fluoroquinolones (51.4%), ceftriaxone (45.0%), and azithromycin (42.1%). None of the participating hospitals had an antibiotic restriction policy for the use of fluoroquinolones or vancomycin.
Monotherapy was prescribed in 57.4%. Fluoroquinolones represented 79.5% of these cases. The other monotherapy choices included a third‐generation cephalosporin (10.7%), piperacillin/tazobactam (8%), and vancomycin (0.2%). Combination therapy consisted mainly of a macrolide plus a third‐generation cephalosporin (74/168; 44%). Other combination regimens included vancomycin plus piperacillin/tazobactam plus ciprofloxacin (35%), vancomycin plus imipenem plus ciprofloxacin (9%), vancomycin plus piperacillin/tazobactam plus azithromycin (4%), vancomycin plus piperacillin/tazobactam (7%), and piperacillin/tazobactam plus azithromycin (1%). Figure 1 shows the distribution of vancomycin and fluoroquinolones use across the different age groups. While the use of fluoroquinolones (P = 0.76) was comparable between groups, there was a significant trend in prescribing less vancomycin with increasing age (P < 0.001). As for the rest of the antibiotics, there was no difference in the overall use of macrolides (P = 0.53), cephalosporins (P = 0.84), or carbapenems (P = 0.67) among age groups. Clindamycin was only used in 9 (2%) out of 392 patients. None of the patients had an aminoglycoside or a sulfa drug prescribed. We also found no difference in terms of antibiotic choice or use of combination therapy among the 3 hospitals (P = 0.78, and P = 0.52; respectively).
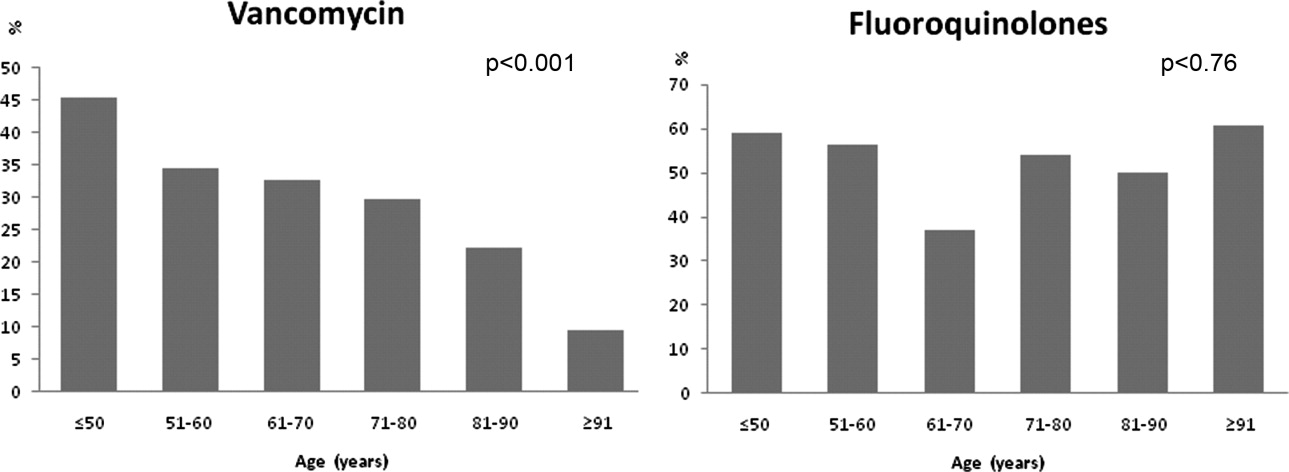
Antibiotic choices were influenced by severity of illness. There was an inverse relationship between PSI classes and the use of either fluoroquinolones or ceftriaxone plus azithromycin (P = 0.02) (Figure 2). Patients with higher acuity of illness were more likely to receive combination regimens that include vancomycin plus piperacillin/tazobactam than those with lower acuity of illness (P < 0.001). Neither the comorbidity index nor the ADL scores had a significant impact on the use of combination therapy (P = 0.49 and P = 0.2; respectively). There was a trend toward association between increasing ADL score and the use of vancomycin plus piperacillin/tazobactam but it did not reach statistical significance (P = 0.06). Of interest, patients who were admitted on the University‐affiliated service were more likely to receive combination therapy than those who were under the care of private service (P < 0.001) (Figure 3). Ceftriaxone plus azithromycin accounted for the majority of combination regimens irrespective of physicians' affiliation.
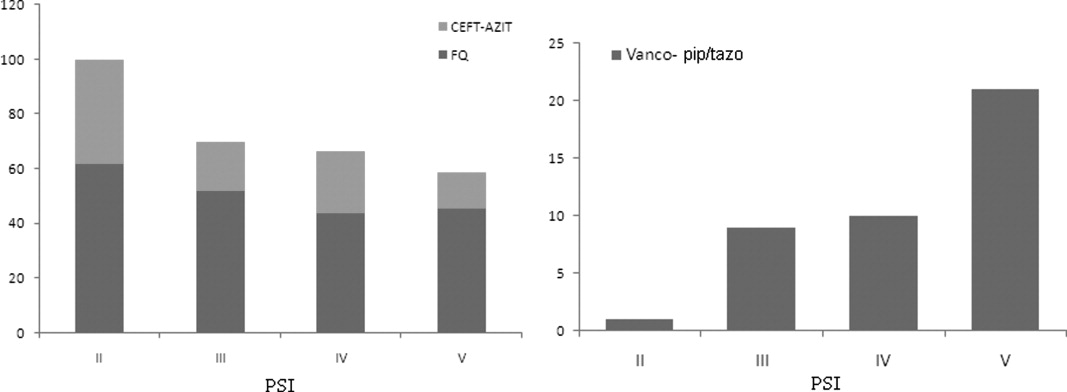
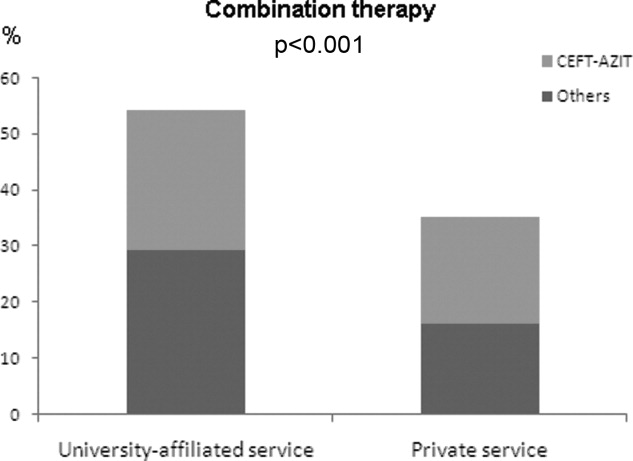
Overall, there were more patients who received antibiotic therapy in compliance with the 2003 IDSA guidelines6 compared with the 2005 ATS/IDSA guidelines7 (65% vs. 19%, respectively; P < 0.001). A positive correlation was noted between severity of illness and adherence to the 2005 ATS/IDSA antimicrobial recommendations (P = 0.02). However, neither the burden of comorbidities nor the functional status was associated with the use of guidelines (P = 0.76 and P = 0.43; respectively).
Duration of therapy ranged from 3 to 21 days with a median of 8 days. The choice of antibiotics, burden of comorbidities, DNR status, or PSI scores had no correlation with antibiotic duration. Only the presence of bacteremia was associated with more than 8 days of antibiotic duration (P < 0.001) (Figure 4). On average, bacteremic patients received 10.1 3.3 (range, 6‐21) days of antimicrobial therapy compared to 7.8 4.1 (range, 319) days for nonbacteremic cases (P < 0.001). During the course of hospitalization, change in antibiotics occurred in 35 (9%) out of the 392 patients, with the majority of substitutions affecting those who were initially prescribed a regimen that included vancomycin plus piperacillin/tazobactam. In these cases, patients were most commonly switched to fluoroquinolones (n = 20), followed by cephalosporins (n = 11).
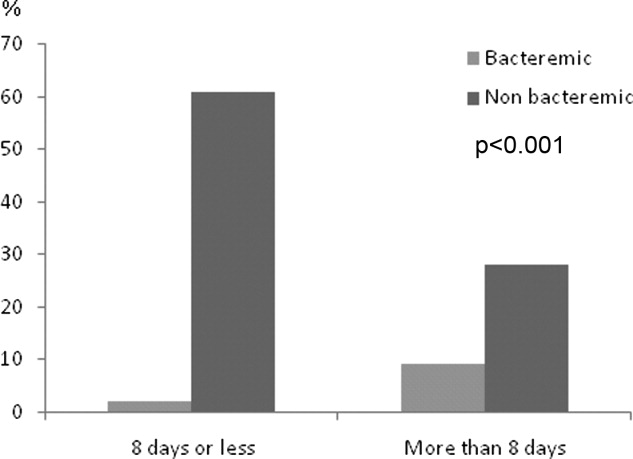
Discussion
Our study suggests that antimicrobial selection among hospitalized nursing homes patients with pneumonia is influenced by patients' age, severity of illness, and provider's academic affiliation.
This is the first comprehensive study, to our knowledge, to report on the type, distribution, and pattern of antimicrobials prescribed among institutionalized patients requiring hospital admission. Various treatment regimens have been investigated in the last 2 decades using both retrospective and prospective randomized clinical trials to examine the efficacy and safety of parenteral and oral antibiotics in nursing homes.1316 However, there are no randomized controlled clinical trials for the treatment of hospitalized NHAP on which to base treatment recommendations. For some healthcare providers, the treatment parallels the coverage of patients with community‐acquired pneumonia; for others, broad‐spectrum coverage is the norm. In the absence of validated guidelines, the present investigation shows that prescription patterns varied across demographic and clinical characteristics. Fluoroquinolones were the preferred agents for the initial therapy of NHAP across all age groups, probably because of their single daily dosing, broad spectrum coverage against typical and atypical pathogens, and favorable side effect profile. Conversely, the use of vancomycin tended to decline in older age groups. This decline could be attributed to the need for frequent monitoring of trough levels when venous access can be difficult, lack of oral formulation, or potential toxicity. Further studies are needed to examine the validity of this pattern.
To our knowledge, compliance with guidelines regarding treatment of NHAP has not been previously reported. Despite recent studies suggesting that adherence to community‐acquired pneumonia guidelines resulted in reduced need for hospitalization, shorter stays, and lower mortality,1721 our findings indicated a rather low compliance with the most recently published guidelines. Potential reasons for the low levels of compliance include lack of awareness, time lag for the information to be disseminated in the medical community, lack of endorsement by local opinion leaders, or local barriers to implementation of these guidelines. Unfortunately, little is known about physicians' familiarity and attitude toward NHAP guidelines use. Efforts to improve the effectiveness of pneumonia care will depend on future studies aiming at identifying factors that influence nonadherence.
Severity of illness had a significant influence on the prescription pattern of antimicrobial therapy. As the PSI increased, treatment with a fluoroquinolone or with combination therapy of nonpseudomonal third‐generation cephalosporin plus macrolide was replaced by a broader spectrum of antimicrobial coverage. We believe that healthcare providers' prescriptions may be influenced by the recommendations of the ATS guidelines for the treatment of health care associated pneumonia,7 in which antimicrobial therapy for severely ill patients admitted from long‐term care facilities is directed toward multidrug resistant pathogens. The validity of this practice, however, remains the subject of intense debate,2225 driven by the absence of randomized trials showing improved morbidity and mortality.
Few formal clinical trials exist to guide the length of therapy of hospitalized patients with NHAP. The usual recommendation ranges from 7 to 14 days.16, 26 The median duration of 8 days observed in the current study is consistent with length of therapy advocated in the literature.16 Yet, prolonging antibiotic duration has been suggested when clinical severity of illness is high, comorbid illnesses are multiple, and expected resolution is delayed.27 Arguing against such a practice is evidence from meta‐analysis,28 expert reviews,29 and clinical investigation.30 Prescribing principles are nevertheless unlikely to induce substantial change unless their dissemination and promotion is sustained through intensive continuing educational programs for physicians and pharmacists.3133
Our study has a number of limitations. First, the cohort group described in this investigation consists of institutionalized patients in Western New York and hence the antibiotic prescribing patterns may vary in other locations. Second, we did not have adequate microbial information to fully assess the appropriateness of antimicrobial therapy. Third, the absence of microbial etiology may have resulted in incorrect identification of patients with pneumonia. Further, retrospective data extraction is notoriously imperfect, and pneumonia cases may have been missed because of either coding errors or atypical manifestations. However, we have used strict inclusion criteria in to minimize any potential bias. Fourth, the results of this study describe patterns of antibiotic utilization in the treatment of NHAP but do not provide reasoning for such a practice. The rationale behind these practices can only be discerned by a survey of healthcare providers.
In conclusion, we have observed in this study a poor compliance with the current guidelines for the treatment of NHAP. It is generally accepted that physicians' prescribing habits are influenced by their understanding of the pathophysiology and epidemiology of the infection being treated, as well as the pharmacology and spectrum of available antimicrobials. In the absence of outcome data, translation of this knowledge into practice may be influenced by a number of factors, such as the physician's preference, the academic milieu in which the practice occurs, and more importantly, by the patients' clinical condition.
- .Pneumonia in the long‐term‐care facility.Infect Control Hosp Epidemiol.2002;23:159–164.
- ,,,,.Canadian guidelines for the initial management of an evidence based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Pneumonia Working Group.Clin Infect Dis.2000;31:383–421.
- ,,, et al.Antimicrobial resistance in long‐term care facilities.Infect Control Hosp Epidemiol.1996;17:129–140.
- ,,,.Etiology of severe pneumonia in the very elderly.Am J Respir Crit Care Med.2001;163:645–651.
- ,,,.Tensions in antibiotic prescribing: pitting social concerns against the interests of individual patients.J Gen Intern Med.2002;17:87–94.
- ,,,,,.Update of practice guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433.
- American Thoracic Society and Infectious Diseases Society of America. Guidelines for the management of adults with hospital acquired, ventilator‐associated, and health care associated pneumonia.Am J Respir Crit Care Med.2005;171:388–416.
- ,,, et al.Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the management of community‐acquired pneumonia in adults.Clin Infect Dis.2007;44:S27–S72.
- ,,,.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.J Chron Dis.1987;40:373–383.
- New York State Department of Health. Hospital and Community Patient Review Instrument. DOH‐694.Albany, NY:Department of Health;1989.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,.Statistical Analysis with Missing Data.New York:John Wiley 1987.
- ,,,,.A randomized study of ciprofloxacin versus ceftriaxone in the treatment of nursing home‐acquired lower respiratory tract infections.J Am Geriatr Soc.1991;39:979–985.
- ,,, et al.Prospective study of lower respiratory tract infections in an extended‐care nursing home program: potential role of oral ciprofloxacin.Am J Med.1988;85:164–171.
- ,,.Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial.JAMA2006;295:2503–2510.
- ,.Treatment guideline for nursing‐home acquired pneumonia based on community practice.J Am Geriatr Soc.2000;48:82–88.
- ,,,,,.Decreased mortality after implementation of a treatment guideline for community‐acquired pneumonia.Am J Med.2001;110:451–457.
- ,,,,,.A controlled trial of a critical pathway for treatment of community‐acquired pneumonia. CAPITAL Study Investigators. Community‐Acquired Pneumonia Intervention Trial Assessing Levofloxacin.JAMA.2000;283:749–755.
- ,,, et al.Improvement of process‐of‐care and outcomes after implementing a guideline for the management of community‐acquired pneumonia: a controlled before‐and‐after design study.Clin Infect Dis.2004;39:955–963.
- ,,, et al.Guidelines for the treatment of community‐acquired pneumonia: predictors of adherence and outcome.Am J Respir Crit Care Med.2005;172:757–762.
- ,,, et al.Antibiotic prescription for community‐acquired pneumonia in the intensive care unit: impact of adherence to Infectious Diseases Society of America guidelines on survival.Clin Infect Dis.2005;41:1709–1716.
- ,,.Nosocomial or healthcare facility‐related pneumonia in adults.Curr Infect Dis Rep.2000;2:215–223.
- ,.Pneumonia in the older patient.Clin Chest Med.2007;28:751–771.
- .Guidelines for the management of adults with health care‐associated pneumonia: implications for nursing facility residents.Consult Pharm.2006;21:719–725.
- ,,, et al.Health‐care associated pneumonia: a critical appraisal to improve identification, management, and outcomes‐proceedings of the HCAP summit.Clin Infect Dis.2008;46:S296–S334.
- ,,,.Pneumonia in a long term care facility: a prospective study of outcome.Arch Intern Med.1996;156:2365–2370.
- .Understanding the natural history of community‐acquired pneumonia resolution: vital information for optimizing duration of therapy.Clin Infect Dis.2004;39:1791–1793.
- ,,,.Efficacy of short course antibiotic regimens for community‐acquired pneumonia: a meta‐analysis.Am J Med.2007;120:783–790.
- ,.How long should we treat community‐acquired pneumonia?Curr Opin Infect Dis.2007;20:177–181.
- ,,.High‐dose, short course levofloxacin for community‐acquired pneumonia: a new treatment paradigm.Clin Infect Dis.2003;37:752–760.
- ,,,,.Improving the quality of antibiotic prescription patterns in general practice: the role of educational intervention.Med J Aust.1994;160:502–505.
- ,,,,,.Drug prescription attitudes and behaviour of general practitioners: effects of a problem oriented educational programme.Eur J Clin Pharmacol.1995;47:381–387.
- ,,, et al.Interventions to improve antibiotic prescribing practices for hospital inpatients.Cochrane Database Syst Rev.2005;CD003543.
Pneumonia is the second most common infection in nursing home residents after urinary tract infection, and is the most common reason for transfer to the hospital.1 Although it remains difficult to determine the incidence of pneumonia in institutionalized elderly patients, an estimated 4 million cases of nursing homeacquired pneumonia (NHAP) occur annually in the United States and result in more than 600,000 emergency department visits.2 In the past 2 decades, multiple studies have documented the rapid rise in drug resistance among common pathogens responsible for pneumonia in the elderly and the acquisition of multidrug‐resistant organisms in residents of long‐term care facilities.3, 4 Health care practitioners are faced with the dilemma of attempting to limit broad‐spectrum antimicrobial drug use while striving to maximize therapeutic efficacy in individual patients.5 The current practice guidelines for the management of NHAP from various professional societies provide mixed messages on the class of antibiotics for patients requiring hospitalization.2, 68 While the 2000 Canadian and the 2003 Infectious Disease Society of America (IDSA) guidelines advocate a community‐acquired pneumonia‐like approach to therapy, the 2005 American Thoracic Society (ATS)/IDSA guidelines and the 2007 IDSA/ATS guidelines consider drug‐resistant pathogens (DRPs) (ie, methicillin‐resistant Staphylococcus aureus [MRSA] and Pseudomonas aeruginosa) to be major etiologic agents in NHAP and thus the empiric treatment recommendations focus specifically on these pathogens (Table 1).
|
| 2003 IDSA |
| 1. Parenteral third‐generation cephalosporin or ampicillin sulbactam + macrolide; or |
| 2. Parenteral fluoroquinolone alone |
| 2000 Canadian |
| 1. Parenteral fluoroquinolone alone; or |
| 2. Parenteral third‐generation, or fourth‐generation cephalosporin + macrolide |
| 2005 ATS/IDSA |
| 1. Antipseudomonal cephalosporin or antipseudomonal carbapenem or antipseudomonal penicillin + antipseudomonal fluoroquinolone or aminoglycoside + anti‐methicillin‐resistant Staphylococcus agents |
Given these differences in antibiotic recommendations among the various guidelines, we sought to examine the antimicrobial prescription patterns in hospitalized non‐critically‐ill patients with NHAP in multiple tertiary care facilities vis‐‐vis the population demographics and clinical characteristics.
Methods
Study Population
This retrospective study was conducted in 3 tertiary‐care hospitals (Erie County Medical Center, Millard Fillmore Hospital, and Buffalo General Hospital) in the city of Buffalo, New York. These hospitals account for 96% of admissions from nursing homes in Erie County. The Institutional Review Board approved the study and certified that it met the criteria for a waiver of the requirement to obtain informed consent. All medical charts of adult patients with pneumonia listed under admission diagnosis or discharge diagnosis (International Classification of Diseases, ninth revision, Clinical Modification Codes [ICD‐9‐CM] [35] codes 480.0480.9, 481, 482.0482.9, 483.0483.8, 485, 486, 487.0, and 507.0) between April 2005 and December 2007 were abstracted. The records were searched for place of residence prior to admission and all patients residing in nursing homes for 30 days or more were selected for review. Inclusion criteria included the presence of new or increased radiographic abnormalities plus 2 or more of the following symptoms and signs: new or increased cough, new or increased sputum production, and temperature greater than 38C. Patients who met at least one of the following criteria were excluded: (1) admission to a critical care unit from the emergency department; (2) discharge within 24 hours; (3) human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS) or immunocompromised; (4) transfer from another hospital; or (5) receiving active chemotherapy. Patients with multiple admissions were included only once to ensure independence of observations.
Data Collection
Data collected included information on sociodemographic characteristics, admitting service (University‐affiliated or private service), comorbidities, preadmission functional status, do not resuscitate (DNR) order, and prior antibiotic therapy. Antibiotic information was comprised of the name of the antibiotic, start and stop dates (including postdischarge), monotherapy or combination therapy, and route of administration. Antimicrobials were assigned to 1 of the following categories: macrolides (azithromycin, clarithromycin), lincosamide (clindamycin), fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin), carbapenems (ertapenem, imipenem), cephalosporins (ceftriaxone, cefpodoxime, cefepime), and ureidopenicillins (piperacillin‐tazobactam). Patients who died during the hospital stay before completion of therapy were assigned 14 days of antibiotic therapy.
The burden of comorbidities was assessed by the Charlson Index.9 The Activity of Daily Living (ADL) score was abstracted from a standardized patient‐review instrument included in all patients' charts.10 Patients were assigned an ADL score in each of the 6 major areas of activity: eating, toileting, feeding, bathing, mobility, and continence; ranging from 1 if they were fully independent, 2 if they were partially independent, and 3 if they were completely dependent. The ADL score was calculated by adding the points assigned for each activity, and it ranged from 6 to 18. Three categories were arbitrarily created: ADL I, corresponding to ADL scores from 6 to 8; ADL II, scores from 9 to 13; and ADL III, scores from 14 to 18.4
The Pneumonia Severity Index Score (PSI)11 was also calculated. The PSI is a validated disease‐severity classification system based on age, sex, nursing home residence, 5 comorbid illnesses, vital signs on admission, mental status, 7 laboratory values, and the findings on chest roentgenograms. Based on the scoring system, patients were stratified into 5 categories or classes of risk for in‐hospital mortality. Class I patients have the lowest disease severity while class V have the highest disease severity.
Statistics
Data were analyzed using the NCSS 2000 Statistical Analysis System (NCSS, Kaysville, UT). Continuous variables were tested for normal distribution using the Kolmogorov‐Smirnov test. Results are expressed as means standard deviation (SD). Univariate analysis was carried out using the chi‐square test and Fisher's exact test for categorical data and the t test for independent samples for continuous variables. Missing values for ADL and Charlson scores were encountered at <3% of the total population sample. Multiple regression models of available variables were utilized to predict missing values as described by Little and Rubin.12 All tests were 2‐tailed and statistical significance was determined at the 5% level.
Results
A total of 397 subjects with NHAP were included in the study. The mean age of the cohort group was 76.8 13.5 years. Eighty percent had 2 or more chronic diseases. Degenerative nervous system, cardiac, and pulmonary diseases accounted for the majority of underlying comorbidities. Demographic and clinical characteristics of the study population are presented in Table 2. At the time of admission, 17% of patients had received antimicrobial therapy for a respiratory ailment within the last week prior to transfer to an acute care facility. The most commonly prescribed agents at the nursing home were an oral fluoroquinolone (81%), a cephalosporin (14%), or a macrolide (3%).
| |
| Characteristic (n = 397) | |
| Age (years), mean (SD) | 76.8 (13.5) |
| Male, n (%) | 162 (41) |
| Underlying comorbidities, n (%) | |
| Cardiac diseases | 135 (34) |
| Pulmonary diseases | 129 (32) |
| Cerebrovascular accident | 98 (25) |
| Diabetes mellitus | 138 (35) |
| Dementia | 179 (45) |
| DNR, n (%) | 42 (11) |
| Activity of daily living, n (%) | |
| ADL I | 57 (14) |
| ADL II | 150 (38) |
| ADL III | 190 (48) |
| Pneumonia Severity Index, n (%) | |
| Class II | 13 (3) |
| Class III | 34 (8) |
| Class IV | 177 (45) |
| Class V | 173 (44) |
| Bacteremia, n (%) | 48 (12) |
Of the 397 patients who met the criteria for NHAP, all but 5 patients received antimicrobial therapy. The 3 most commonly used antimicrobial compounds for inpatient treatment were fluoroquinolones (51.4%), ceftriaxone (45.0%), and azithromycin (42.1%). None of the participating hospitals had an antibiotic restriction policy for the use of fluoroquinolones or vancomycin.
Monotherapy was prescribed in 57.4%. Fluoroquinolones represented 79.5% of these cases. The other monotherapy choices included a third‐generation cephalosporin (10.7%), piperacillin/tazobactam (8%), and vancomycin (0.2%). Combination therapy consisted mainly of a macrolide plus a third‐generation cephalosporin (74/168; 44%). Other combination regimens included vancomycin plus piperacillin/tazobactam plus ciprofloxacin (35%), vancomycin plus imipenem plus ciprofloxacin (9%), vancomycin plus piperacillin/tazobactam plus azithromycin (4%), vancomycin plus piperacillin/tazobactam (7%), and piperacillin/tazobactam plus azithromycin (1%). Figure 1 shows the distribution of vancomycin and fluoroquinolones use across the different age groups. While the use of fluoroquinolones (P = 0.76) was comparable between groups, there was a significant trend in prescribing less vancomycin with increasing age (P < 0.001). As for the rest of the antibiotics, there was no difference in the overall use of macrolides (P = 0.53), cephalosporins (P = 0.84), or carbapenems (P = 0.67) among age groups. Clindamycin was only used in 9 (2%) out of 392 patients. None of the patients had an aminoglycoside or a sulfa drug prescribed. We also found no difference in terms of antibiotic choice or use of combination therapy among the 3 hospitals (P = 0.78, and P = 0.52; respectively).
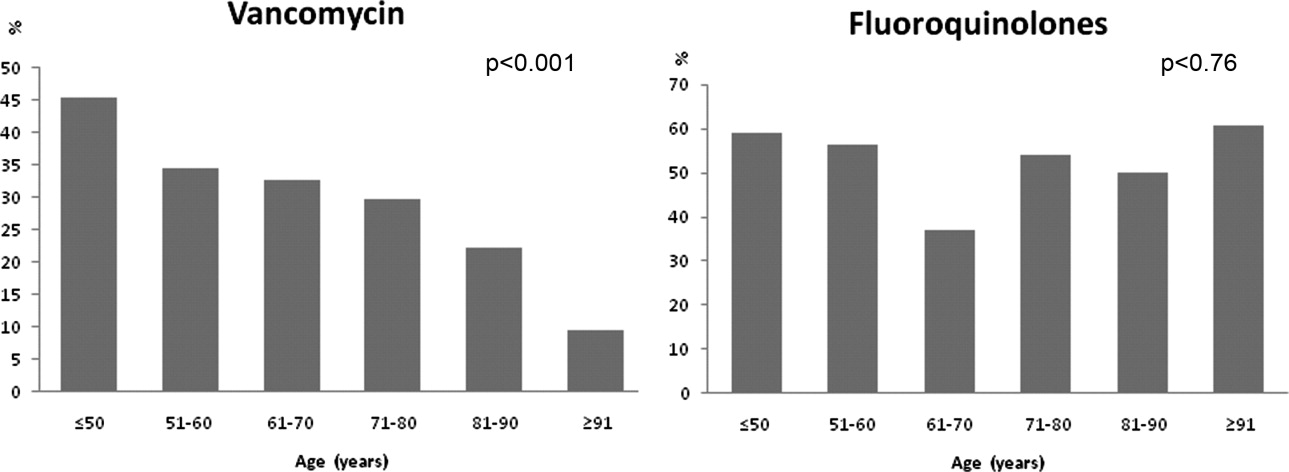
Antibiotic choices were influenced by severity of illness. There was an inverse relationship between PSI classes and the use of either fluoroquinolones or ceftriaxone plus azithromycin (P = 0.02) (Figure 2). Patients with higher acuity of illness were more likely to receive combination regimens that include vancomycin plus piperacillin/tazobactam than those with lower acuity of illness (P < 0.001). Neither the comorbidity index nor the ADL scores had a significant impact on the use of combination therapy (P = 0.49 and P = 0.2; respectively). There was a trend toward association between increasing ADL score and the use of vancomycin plus piperacillin/tazobactam but it did not reach statistical significance (P = 0.06). Of interest, patients who were admitted on the University‐affiliated service were more likely to receive combination therapy than those who were under the care of private service (P < 0.001) (Figure 3). Ceftriaxone plus azithromycin accounted for the majority of combination regimens irrespective of physicians' affiliation.
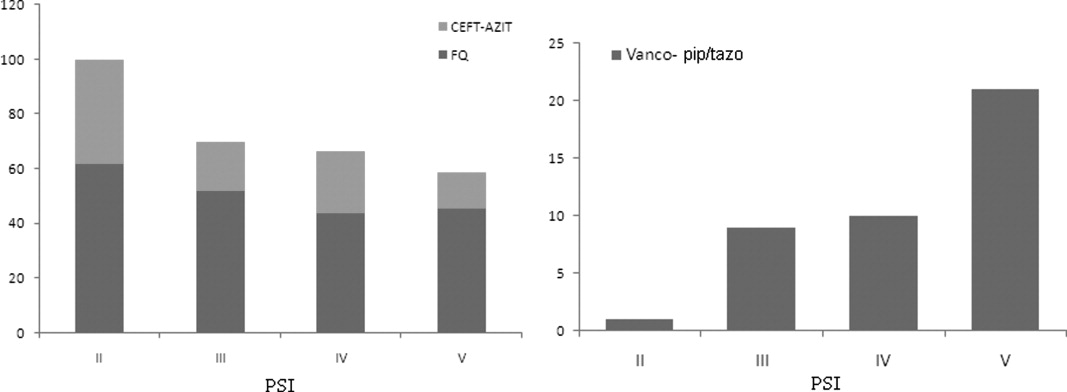
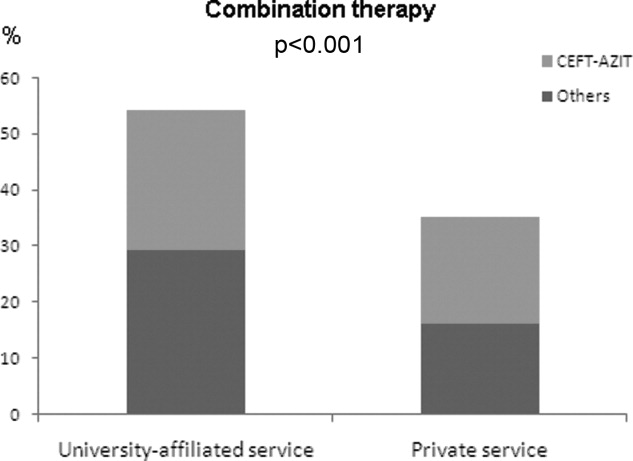
Overall, there were more patients who received antibiotic therapy in compliance with the 2003 IDSA guidelines6 compared with the 2005 ATS/IDSA guidelines7 (65% vs. 19%, respectively; P < 0.001). A positive correlation was noted between severity of illness and adherence to the 2005 ATS/IDSA antimicrobial recommendations (P = 0.02). However, neither the burden of comorbidities nor the functional status was associated with the use of guidelines (P = 0.76 and P = 0.43; respectively).
Duration of therapy ranged from 3 to 21 days with a median of 8 days. The choice of antibiotics, burden of comorbidities, DNR status, or PSI scores had no correlation with antibiotic duration. Only the presence of bacteremia was associated with more than 8 days of antibiotic duration (P < 0.001) (Figure 4). On average, bacteremic patients received 10.1 3.3 (range, 6‐21) days of antimicrobial therapy compared to 7.8 4.1 (range, 319) days for nonbacteremic cases (P < 0.001). During the course of hospitalization, change in antibiotics occurred in 35 (9%) out of the 392 patients, with the majority of substitutions affecting those who were initially prescribed a regimen that included vancomycin plus piperacillin/tazobactam. In these cases, patients were most commonly switched to fluoroquinolones (n = 20), followed by cephalosporins (n = 11).
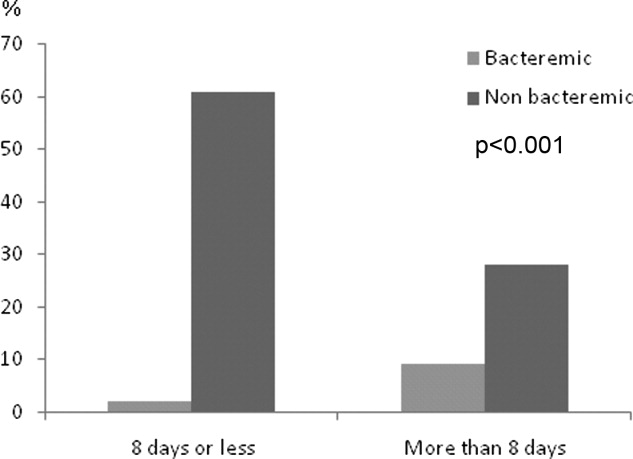
Discussion
Our study suggests that antimicrobial selection among hospitalized nursing homes patients with pneumonia is influenced by patients' age, severity of illness, and provider's academic affiliation.
This is the first comprehensive study, to our knowledge, to report on the type, distribution, and pattern of antimicrobials prescribed among institutionalized patients requiring hospital admission. Various treatment regimens have been investigated in the last 2 decades using both retrospective and prospective randomized clinical trials to examine the efficacy and safety of parenteral and oral antibiotics in nursing homes.1316 However, there are no randomized controlled clinical trials for the treatment of hospitalized NHAP on which to base treatment recommendations. For some healthcare providers, the treatment parallels the coverage of patients with community‐acquired pneumonia; for others, broad‐spectrum coverage is the norm. In the absence of validated guidelines, the present investigation shows that prescription patterns varied across demographic and clinical characteristics. Fluoroquinolones were the preferred agents for the initial therapy of NHAP across all age groups, probably because of their single daily dosing, broad spectrum coverage against typical and atypical pathogens, and favorable side effect profile. Conversely, the use of vancomycin tended to decline in older age groups. This decline could be attributed to the need for frequent monitoring of trough levels when venous access can be difficult, lack of oral formulation, or potential toxicity. Further studies are needed to examine the validity of this pattern.
To our knowledge, compliance with guidelines regarding treatment of NHAP has not been previously reported. Despite recent studies suggesting that adherence to community‐acquired pneumonia guidelines resulted in reduced need for hospitalization, shorter stays, and lower mortality,1721 our findings indicated a rather low compliance with the most recently published guidelines. Potential reasons for the low levels of compliance include lack of awareness, time lag for the information to be disseminated in the medical community, lack of endorsement by local opinion leaders, or local barriers to implementation of these guidelines. Unfortunately, little is known about physicians' familiarity and attitude toward NHAP guidelines use. Efforts to improve the effectiveness of pneumonia care will depend on future studies aiming at identifying factors that influence nonadherence.
Severity of illness had a significant influence on the prescription pattern of antimicrobial therapy. As the PSI increased, treatment with a fluoroquinolone or with combination therapy of nonpseudomonal third‐generation cephalosporin plus macrolide was replaced by a broader spectrum of antimicrobial coverage. We believe that healthcare providers' prescriptions may be influenced by the recommendations of the ATS guidelines for the treatment of health care associated pneumonia,7 in which antimicrobial therapy for severely ill patients admitted from long‐term care facilities is directed toward multidrug resistant pathogens. The validity of this practice, however, remains the subject of intense debate,2225 driven by the absence of randomized trials showing improved morbidity and mortality.
Few formal clinical trials exist to guide the length of therapy of hospitalized patients with NHAP. The usual recommendation ranges from 7 to 14 days.16, 26 The median duration of 8 days observed in the current study is consistent with length of therapy advocated in the literature.16 Yet, prolonging antibiotic duration has been suggested when clinical severity of illness is high, comorbid illnesses are multiple, and expected resolution is delayed.27 Arguing against such a practice is evidence from meta‐analysis,28 expert reviews,29 and clinical investigation.30 Prescribing principles are nevertheless unlikely to induce substantial change unless their dissemination and promotion is sustained through intensive continuing educational programs for physicians and pharmacists.3133
Our study has a number of limitations. First, the cohort group described in this investigation consists of institutionalized patients in Western New York and hence the antibiotic prescribing patterns may vary in other locations. Second, we did not have adequate microbial information to fully assess the appropriateness of antimicrobial therapy. Third, the absence of microbial etiology may have resulted in incorrect identification of patients with pneumonia. Further, retrospective data extraction is notoriously imperfect, and pneumonia cases may have been missed because of either coding errors or atypical manifestations. However, we have used strict inclusion criteria in to minimize any potential bias. Fourth, the results of this study describe patterns of antibiotic utilization in the treatment of NHAP but do not provide reasoning for such a practice. The rationale behind these practices can only be discerned by a survey of healthcare providers.
In conclusion, we have observed in this study a poor compliance with the current guidelines for the treatment of NHAP. It is generally accepted that physicians' prescribing habits are influenced by their understanding of the pathophysiology and epidemiology of the infection being treated, as well as the pharmacology and spectrum of available antimicrobials. In the absence of outcome data, translation of this knowledge into practice may be influenced by a number of factors, such as the physician's preference, the academic milieu in which the practice occurs, and more importantly, by the patients' clinical condition.
Pneumonia is the second most common infection in nursing home residents after urinary tract infection, and is the most common reason for transfer to the hospital.1 Although it remains difficult to determine the incidence of pneumonia in institutionalized elderly patients, an estimated 4 million cases of nursing homeacquired pneumonia (NHAP) occur annually in the United States and result in more than 600,000 emergency department visits.2 In the past 2 decades, multiple studies have documented the rapid rise in drug resistance among common pathogens responsible for pneumonia in the elderly and the acquisition of multidrug‐resistant organisms in residents of long‐term care facilities.3, 4 Health care practitioners are faced with the dilemma of attempting to limit broad‐spectrum antimicrobial drug use while striving to maximize therapeutic efficacy in individual patients.5 The current practice guidelines for the management of NHAP from various professional societies provide mixed messages on the class of antibiotics for patients requiring hospitalization.2, 68 While the 2000 Canadian and the 2003 Infectious Disease Society of America (IDSA) guidelines advocate a community‐acquired pneumonia‐like approach to therapy, the 2005 American Thoracic Society (ATS)/IDSA guidelines and the 2007 IDSA/ATS guidelines consider drug‐resistant pathogens (DRPs) (ie, methicillin‐resistant Staphylococcus aureus [MRSA] and Pseudomonas aeruginosa) to be major etiologic agents in NHAP and thus the empiric treatment recommendations focus specifically on these pathogens (Table 1).
|
| 2003 IDSA |
| 1. Parenteral third‐generation cephalosporin or ampicillin sulbactam + macrolide; or |
| 2. Parenteral fluoroquinolone alone |
| 2000 Canadian |
| 1. Parenteral fluoroquinolone alone; or |
| 2. Parenteral third‐generation, or fourth‐generation cephalosporin + macrolide |
| 2005 ATS/IDSA |
| 1. Antipseudomonal cephalosporin or antipseudomonal carbapenem or antipseudomonal penicillin + antipseudomonal fluoroquinolone or aminoglycoside + anti‐methicillin‐resistant Staphylococcus agents |
Given these differences in antibiotic recommendations among the various guidelines, we sought to examine the antimicrobial prescription patterns in hospitalized non‐critically‐ill patients with NHAP in multiple tertiary care facilities vis‐‐vis the population demographics and clinical characteristics.
Methods
Study Population
This retrospective study was conducted in 3 tertiary‐care hospitals (Erie County Medical Center, Millard Fillmore Hospital, and Buffalo General Hospital) in the city of Buffalo, New York. These hospitals account for 96% of admissions from nursing homes in Erie County. The Institutional Review Board approved the study and certified that it met the criteria for a waiver of the requirement to obtain informed consent. All medical charts of adult patients with pneumonia listed under admission diagnosis or discharge diagnosis (International Classification of Diseases, ninth revision, Clinical Modification Codes [ICD‐9‐CM] [35] codes 480.0480.9, 481, 482.0482.9, 483.0483.8, 485, 486, 487.0, and 507.0) between April 2005 and December 2007 were abstracted. The records were searched for place of residence prior to admission and all patients residing in nursing homes for 30 days or more were selected for review. Inclusion criteria included the presence of new or increased radiographic abnormalities plus 2 or more of the following symptoms and signs: new or increased cough, new or increased sputum production, and temperature greater than 38C. Patients who met at least one of the following criteria were excluded: (1) admission to a critical care unit from the emergency department; (2) discharge within 24 hours; (3) human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS) or immunocompromised; (4) transfer from another hospital; or (5) receiving active chemotherapy. Patients with multiple admissions were included only once to ensure independence of observations.
Data Collection
Data collected included information on sociodemographic characteristics, admitting service (University‐affiliated or private service), comorbidities, preadmission functional status, do not resuscitate (DNR) order, and prior antibiotic therapy. Antibiotic information was comprised of the name of the antibiotic, start and stop dates (including postdischarge), monotherapy or combination therapy, and route of administration. Antimicrobials were assigned to 1 of the following categories: macrolides (azithromycin, clarithromycin), lincosamide (clindamycin), fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin), carbapenems (ertapenem, imipenem), cephalosporins (ceftriaxone, cefpodoxime, cefepime), and ureidopenicillins (piperacillin‐tazobactam). Patients who died during the hospital stay before completion of therapy were assigned 14 days of antibiotic therapy.
The burden of comorbidities was assessed by the Charlson Index.9 The Activity of Daily Living (ADL) score was abstracted from a standardized patient‐review instrument included in all patients' charts.10 Patients were assigned an ADL score in each of the 6 major areas of activity: eating, toileting, feeding, bathing, mobility, and continence; ranging from 1 if they were fully independent, 2 if they were partially independent, and 3 if they were completely dependent. The ADL score was calculated by adding the points assigned for each activity, and it ranged from 6 to 18. Three categories were arbitrarily created: ADL I, corresponding to ADL scores from 6 to 8; ADL II, scores from 9 to 13; and ADL III, scores from 14 to 18.4
The Pneumonia Severity Index Score (PSI)11 was also calculated. The PSI is a validated disease‐severity classification system based on age, sex, nursing home residence, 5 comorbid illnesses, vital signs on admission, mental status, 7 laboratory values, and the findings on chest roentgenograms. Based on the scoring system, patients were stratified into 5 categories or classes of risk for in‐hospital mortality. Class I patients have the lowest disease severity while class V have the highest disease severity.
Statistics
Data were analyzed using the NCSS 2000 Statistical Analysis System (NCSS, Kaysville, UT). Continuous variables were tested for normal distribution using the Kolmogorov‐Smirnov test. Results are expressed as means standard deviation (SD). Univariate analysis was carried out using the chi‐square test and Fisher's exact test for categorical data and the t test for independent samples for continuous variables. Missing values for ADL and Charlson scores were encountered at <3% of the total population sample. Multiple regression models of available variables were utilized to predict missing values as described by Little and Rubin.12 All tests were 2‐tailed and statistical significance was determined at the 5% level.
Results
A total of 397 subjects with NHAP were included in the study. The mean age of the cohort group was 76.8 13.5 years. Eighty percent had 2 or more chronic diseases. Degenerative nervous system, cardiac, and pulmonary diseases accounted for the majority of underlying comorbidities. Demographic and clinical characteristics of the study population are presented in Table 2. At the time of admission, 17% of patients had received antimicrobial therapy for a respiratory ailment within the last week prior to transfer to an acute care facility. The most commonly prescribed agents at the nursing home were an oral fluoroquinolone (81%), a cephalosporin (14%), or a macrolide (3%).
| |
| Characteristic (n = 397) | |
| Age (years), mean (SD) | 76.8 (13.5) |
| Male, n (%) | 162 (41) |
| Underlying comorbidities, n (%) | |
| Cardiac diseases | 135 (34) |
| Pulmonary diseases | 129 (32) |
| Cerebrovascular accident | 98 (25) |
| Diabetes mellitus | 138 (35) |
| Dementia | 179 (45) |
| DNR, n (%) | 42 (11) |
| Activity of daily living, n (%) | |
| ADL I | 57 (14) |
| ADL II | 150 (38) |
| ADL III | 190 (48) |
| Pneumonia Severity Index, n (%) | |
| Class II | 13 (3) |
| Class III | 34 (8) |
| Class IV | 177 (45) |
| Class V | 173 (44) |
| Bacteremia, n (%) | 48 (12) |
Of the 397 patients who met the criteria for NHAP, all but 5 patients received antimicrobial therapy. The 3 most commonly used antimicrobial compounds for inpatient treatment were fluoroquinolones (51.4%), ceftriaxone (45.0%), and azithromycin (42.1%). None of the participating hospitals had an antibiotic restriction policy for the use of fluoroquinolones or vancomycin.
Monotherapy was prescribed in 57.4%. Fluoroquinolones represented 79.5% of these cases. The other monotherapy choices included a third‐generation cephalosporin (10.7%), piperacillin/tazobactam (8%), and vancomycin (0.2%). Combination therapy consisted mainly of a macrolide plus a third‐generation cephalosporin (74/168; 44%). Other combination regimens included vancomycin plus piperacillin/tazobactam plus ciprofloxacin (35%), vancomycin plus imipenem plus ciprofloxacin (9%), vancomycin plus piperacillin/tazobactam plus azithromycin (4%), vancomycin plus piperacillin/tazobactam (7%), and piperacillin/tazobactam plus azithromycin (1%). Figure 1 shows the distribution of vancomycin and fluoroquinolones use across the different age groups. While the use of fluoroquinolones (P = 0.76) was comparable between groups, there was a significant trend in prescribing less vancomycin with increasing age (P < 0.001). As for the rest of the antibiotics, there was no difference in the overall use of macrolides (P = 0.53), cephalosporins (P = 0.84), or carbapenems (P = 0.67) among age groups. Clindamycin was only used in 9 (2%) out of 392 patients. None of the patients had an aminoglycoside or a sulfa drug prescribed. We also found no difference in terms of antibiotic choice or use of combination therapy among the 3 hospitals (P = 0.78, and P = 0.52; respectively).
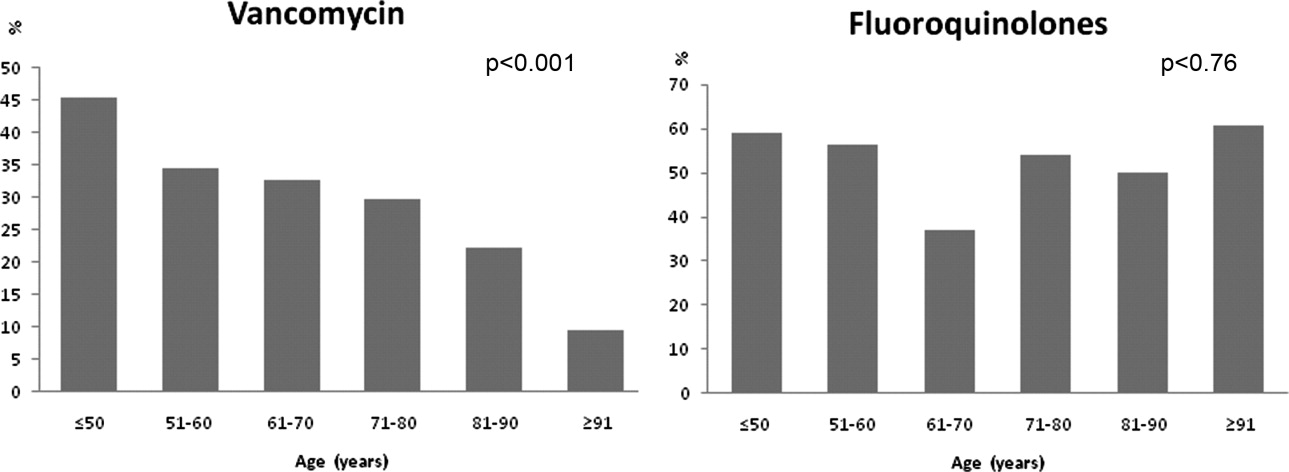
Antibiotic choices were influenced by severity of illness. There was an inverse relationship between PSI classes and the use of either fluoroquinolones or ceftriaxone plus azithromycin (P = 0.02) (Figure 2). Patients with higher acuity of illness were more likely to receive combination regimens that include vancomycin plus piperacillin/tazobactam than those with lower acuity of illness (P < 0.001). Neither the comorbidity index nor the ADL scores had a significant impact on the use of combination therapy (P = 0.49 and P = 0.2; respectively). There was a trend toward association between increasing ADL score and the use of vancomycin plus piperacillin/tazobactam but it did not reach statistical significance (P = 0.06). Of interest, patients who were admitted on the University‐affiliated service were more likely to receive combination therapy than those who were under the care of private service (P < 0.001) (Figure 3). Ceftriaxone plus azithromycin accounted for the majority of combination regimens irrespective of physicians' affiliation.
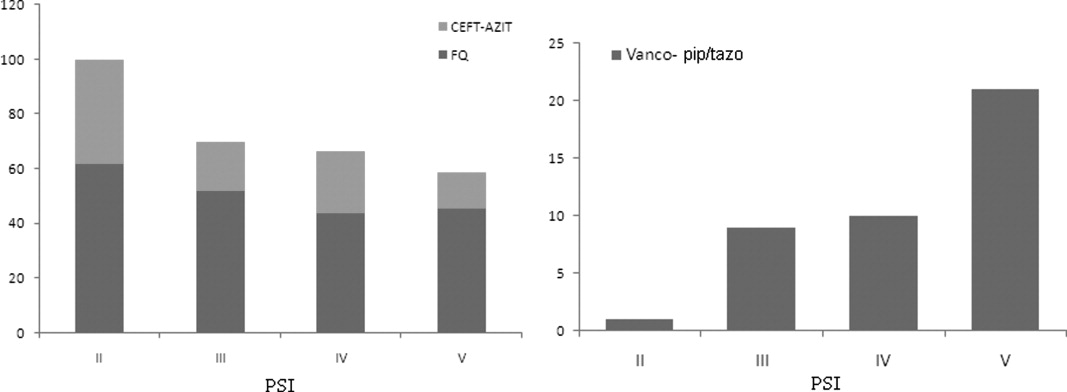
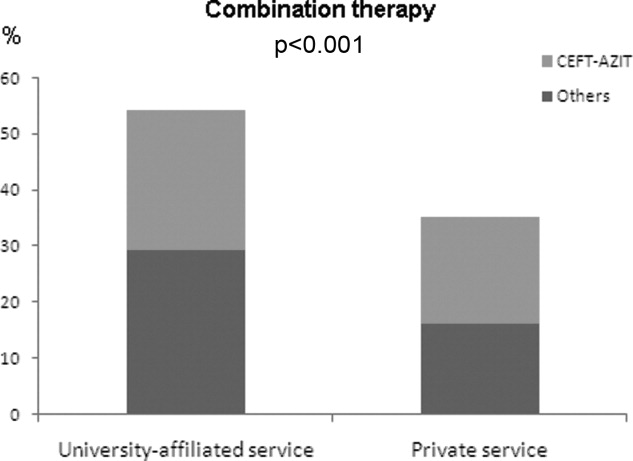
Overall, there were more patients who received antibiotic therapy in compliance with the 2003 IDSA guidelines6 compared with the 2005 ATS/IDSA guidelines7 (65% vs. 19%, respectively; P < 0.001). A positive correlation was noted between severity of illness and adherence to the 2005 ATS/IDSA antimicrobial recommendations (P = 0.02). However, neither the burden of comorbidities nor the functional status was associated with the use of guidelines (P = 0.76 and P = 0.43; respectively).
Duration of therapy ranged from 3 to 21 days with a median of 8 days. The choice of antibiotics, burden of comorbidities, DNR status, or PSI scores had no correlation with antibiotic duration. Only the presence of bacteremia was associated with more than 8 days of antibiotic duration (P < 0.001) (Figure 4). On average, bacteremic patients received 10.1 3.3 (range, 6‐21) days of antimicrobial therapy compared to 7.8 4.1 (range, 319) days for nonbacteremic cases (P < 0.001). During the course of hospitalization, change in antibiotics occurred in 35 (9%) out of the 392 patients, with the majority of substitutions affecting those who were initially prescribed a regimen that included vancomycin plus piperacillin/tazobactam. In these cases, patients were most commonly switched to fluoroquinolones (n = 20), followed by cephalosporins (n = 11).
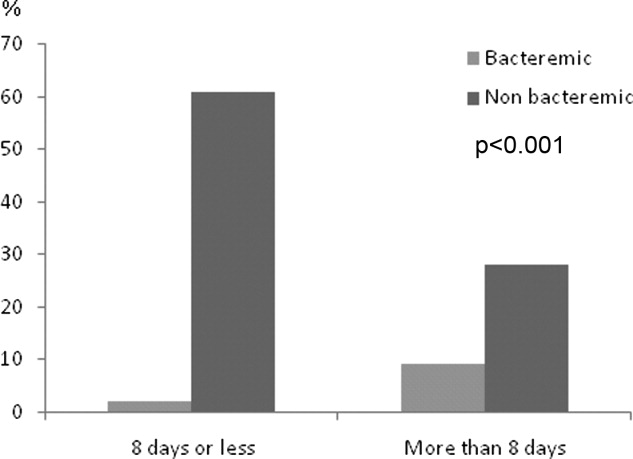
Discussion
Our study suggests that antimicrobial selection among hospitalized nursing homes patients with pneumonia is influenced by patients' age, severity of illness, and provider's academic affiliation.
This is the first comprehensive study, to our knowledge, to report on the type, distribution, and pattern of antimicrobials prescribed among institutionalized patients requiring hospital admission. Various treatment regimens have been investigated in the last 2 decades using both retrospective and prospective randomized clinical trials to examine the efficacy and safety of parenteral and oral antibiotics in nursing homes.1316 However, there are no randomized controlled clinical trials for the treatment of hospitalized NHAP on which to base treatment recommendations. For some healthcare providers, the treatment parallels the coverage of patients with community‐acquired pneumonia; for others, broad‐spectrum coverage is the norm. In the absence of validated guidelines, the present investigation shows that prescription patterns varied across demographic and clinical characteristics. Fluoroquinolones were the preferred agents for the initial therapy of NHAP across all age groups, probably because of their single daily dosing, broad spectrum coverage against typical and atypical pathogens, and favorable side effect profile. Conversely, the use of vancomycin tended to decline in older age groups. This decline could be attributed to the need for frequent monitoring of trough levels when venous access can be difficult, lack of oral formulation, or potential toxicity. Further studies are needed to examine the validity of this pattern.
To our knowledge, compliance with guidelines regarding treatment of NHAP has not been previously reported. Despite recent studies suggesting that adherence to community‐acquired pneumonia guidelines resulted in reduced need for hospitalization, shorter stays, and lower mortality,1721 our findings indicated a rather low compliance with the most recently published guidelines. Potential reasons for the low levels of compliance include lack of awareness, time lag for the information to be disseminated in the medical community, lack of endorsement by local opinion leaders, or local barriers to implementation of these guidelines. Unfortunately, little is known about physicians' familiarity and attitude toward NHAP guidelines use. Efforts to improve the effectiveness of pneumonia care will depend on future studies aiming at identifying factors that influence nonadherence.
Severity of illness had a significant influence on the prescription pattern of antimicrobial therapy. As the PSI increased, treatment with a fluoroquinolone or with combination therapy of nonpseudomonal third‐generation cephalosporin plus macrolide was replaced by a broader spectrum of antimicrobial coverage. We believe that healthcare providers' prescriptions may be influenced by the recommendations of the ATS guidelines for the treatment of health care associated pneumonia,7 in which antimicrobial therapy for severely ill patients admitted from long‐term care facilities is directed toward multidrug resistant pathogens. The validity of this practice, however, remains the subject of intense debate,2225 driven by the absence of randomized trials showing improved morbidity and mortality.
Few formal clinical trials exist to guide the length of therapy of hospitalized patients with NHAP. The usual recommendation ranges from 7 to 14 days.16, 26 The median duration of 8 days observed in the current study is consistent with length of therapy advocated in the literature.16 Yet, prolonging antibiotic duration has been suggested when clinical severity of illness is high, comorbid illnesses are multiple, and expected resolution is delayed.27 Arguing against such a practice is evidence from meta‐analysis,28 expert reviews,29 and clinical investigation.30 Prescribing principles are nevertheless unlikely to induce substantial change unless their dissemination and promotion is sustained through intensive continuing educational programs for physicians and pharmacists.3133
Our study has a number of limitations. First, the cohort group described in this investigation consists of institutionalized patients in Western New York and hence the antibiotic prescribing patterns may vary in other locations. Second, we did not have adequate microbial information to fully assess the appropriateness of antimicrobial therapy. Third, the absence of microbial etiology may have resulted in incorrect identification of patients with pneumonia. Further, retrospective data extraction is notoriously imperfect, and pneumonia cases may have been missed because of either coding errors or atypical manifestations. However, we have used strict inclusion criteria in to minimize any potential bias. Fourth, the results of this study describe patterns of antibiotic utilization in the treatment of NHAP but do not provide reasoning for such a practice. The rationale behind these practices can only be discerned by a survey of healthcare providers.
In conclusion, we have observed in this study a poor compliance with the current guidelines for the treatment of NHAP. It is generally accepted that physicians' prescribing habits are influenced by their understanding of the pathophysiology and epidemiology of the infection being treated, as well as the pharmacology and spectrum of available antimicrobials. In the absence of outcome data, translation of this knowledge into practice may be influenced by a number of factors, such as the physician's preference, the academic milieu in which the practice occurs, and more importantly, by the patients' clinical condition.
- .Pneumonia in the long‐term‐care facility.Infect Control Hosp Epidemiol.2002;23:159–164.
- ,,,,.Canadian guidelines for the initial management of an evidence based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Pneumonia Working Group.Clin Infect Dis.2000;31:383–421.
- ,,, et al.Antimicrobial resistance in long‐term care facilities.Infect Control Hosp Epidemiol.1996;17:129–140.
- ,,,.Etiology of severe pneumonia in the very elderly.Am J Respir Crit Care Med.2001;163:645–651.
- ,,,.Tensions in antibiotic prescribing: pitting social concerns against the interests of individual patients.J Gen Intern Med.2002;17:87–94.
- ,,,,,.Update of practice guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433.
- American Thoracic Society and Infectious Diseases Society of America. Guidelines for the management of adults with hospital acquired, ventilator‐associated, and health care associated pneumonia.Am J Respir Crit Care Med.2005;171:388–416.
- ,,, et al.Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the management of community‐acquired pneumonia in adults.Clin Infect Dis.2007;44:S27–S72.
- ,,,.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.J Chron Dis.1987;40:373–383.
- New York State Department of Health. Hospital and Community Patient Review Instrument. DOH‐694.Albany, NY:Department of Health;1989.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,.Statistical Analysis with Missing Data.New York:John Wiley 1987.
- ,,,,.A randomized study of ciprofloxacin versus ceftriaxone in the treatment of nursing home‐acquired lower respiratory tract infections.J Am Geriatr Soc.1991;39:979–985.
- ,,, et al.Prospective study of lower respiratory tract infections in an extended‐care nursing home program: potential role of oral ciprofloxacin.Am J Med.1988;85:164–171.
- ,,.Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial.JAMA2006;295:2503–2510.
- ,.Treatment guideline for nursing‐home acquired pneumonia based on community practice.J Am Geriatr Soc.2000;48:82–88.
- ,,,,,.Decreased mortality after implementation of a treatment guideline for community‐acquired pneumonia.Am J Med.2001;110:451–457.
- ,,,,,.A controlled trial of a critical pathway for treatment of community‐acquired pneumonia. CAPITAL Study Investigators. Community‐Acquired Pneumonia Intervention Trial Assessing Levofloxacin.JAMA.2000;283:749–755.
- ,,, et al.Improvement of process‐of‐care and outcomes after implementing a guideline for the management of community‐acquired pneumonia: a controlled before‐and‐after design study.Clin Infect Dis.2004;39:955–963.
- ,,, et al.Guidelines for the treatment of community‐acquired pneumonia: predictors of adherence and outcome.Am J Respir Crit Care Med.2005;172:757–762.
- ,,, et al.Antibiotic prescription for community‐acquired pneumonia in the intensive care unit: impact of adherence to Infectious Diseases Society of America guidelines on survival.Clin Infect Dis.2005;41:1709–1716.
- ,,.Nosocomial or healthcare facility‐related pneumonia in adults.Curr Infect Dis Rep.2000;2:215–223.
- ,.Pneumonia in the older patient.Clin Chest Med.2007;28:751–771.
- .Guidelines for the management of adults with health care‐associated pneumonia: implications for nursing facility residents.Consult Pharm.2006;21:719–725.
- ,,, et al.Health‐care associated pneumonia: a critical appraisal to improve identification, management, and outcomes‐proceedings of the HCAP summit.Clin Infect Dis.2008;46:S296–S334.
- ,,,.Pneumonia in a long term care facility: a prospective study of outcome.Arch Intern Med.1996;156:2365–2370.
- .Understanding the natural history of community‐acquired pneumonia resolution: vital information for optimizing duration of therapy.Clin Infect Dis.2004;39:1791–1793.
- ,,,.Efficacy of short course antibiotic regimens for community‐acquired pneumonia: a meta‐analysis.Am J Med.2007;120:783–790.
- ,.How long should we treat community‐acquired pneumonia?Curr Opin Infect Dis.2007;20:177–181.
- ,,.High‐dose, short course levofloxacin for community‐acquired pneumonia: a new treatment paradigm.Clin Infect Dis.2003;37:752–760.
- ,,,,.Improving the quality of antibiotic prescription patterns in general practice: the role of educational intervention.Med J Aust.1994;160:502–505.
- ,,,,,.Drug prescription attitudes and behaviour of general practitioners: effects of a problem oriented educational programme.Eur J Clin Pharmacol.1995;47:381–387.
- ,,, et al.Interventions to improve antibiotic prescribing practices for hospital inpatients.Cochrane Database Syst Rev.2005;CD003543.
- .Pneumonia in the long‐term‐care facility.Infect Control Hosp Epidemiol.2002;23:159–164.
- ,,,,.Canadian guidelines for the initial management of an evidence based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Pneumonia Working Group.Clin Infect Dis.2000;31:383–421.
- ,,, et al.Antimicrobial resistance in long‐term care facilities.Infect Control Hosp Epidemiol.1996;17:129–140.
- ,,,.Etiology of severe pneumonia in the very elderly.Am J Respir Crit Care Med.2001;163:645–651.
- ,,,.Tensions in antibiotic prescribing: pitting social concerns against the interests of individual patients.J Gen Intern Med.2002;17:87–94.
- ,,,,,.Update of practice guidelines for the management of community‐acquired pneumonia in immunocompetent adults.Clin Infect Dis.2003;37:1405–1433.
- American Thoracic Society and Infectious Diseases Society of America. Guidelines for the management of adults with hospital acquired, ventilator‐associated, and health care associated pneumonia.Am J Respir Crit Care Med.2005;171:388–416.
- ,,, et al.Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the management of community‐acquired pneumonia in adults.Clin Infect Dis.2007;44:S27–S72.
- ,,,.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.J Chron Dis.1987;40:373–383.
- New York State Department of Health. Hospital and Community Patient Review Instrument. DOH‐694.Albany, NY:Department of Health;1989.
- ,,, et al.A prediction rule to identify low‐risk patients with community‐acquired pneumonia.N Engl J Med.1997;336:243–250.
- ,.Statistical Analysis with Missing Data.New York:John Wiley 1987.
- ,,,,.A randomized study of ciprofloxacin versus ceftriaxone in the treatment of nursing home‐acquired lower respiratory tract infections.J Am Geriatr Soc.1991;39:979–985.
- ,,, et al.Prospective study of lower respiratory tract infections in an extended‐care nursing home program: potential role of oral ciprofloxacin.Am J Med.1988;85:164–171.
- ,,.Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial.JAMA2006;295:2503–2510.
- ,.Treatment guideline for nursing‐home acquired pneumonia based on community practice.J Am Geriatr Soc.2000;48:82–88.
- ,,,,,.Decreased mortality after implementation of a treatment guideline for community‐acquired pneumonia.Am J Med.2001;110:451–457.
- ,,,,,.A controlled trial of a critical pathway for treatment of community‐acquired pneumonia. CAPITAL Study Investigators. Community‐Acquired Pneumonia Intervention Trial Assessing Levofloxacin.JAMA.2000;283:749–755.
- ,,, et al.Improvement of process‐of‐care and outcomes after implementing a guideline for the management of community‐acquired pneumonia: a controlled before‐and‐after design study.Clin Infect Dis.2004;39:955–963.
- ,,, et al.Guidelines for the treatment of community‐acquired pneumonia: predictors of adherence and outcome.Am J Respir Crit Care Med.2005;172:757–762.
- ,,, et al.Antibiotic prescription for community‐acquired pneumonia in the intensive care unit: impact of adherence to Infectious Diseases Society of America guidelines on survival.Clin Infect Dis.2005;41:1709–1716.
- ,,.Nosocomial or healthcare facility‐related pneumonia in adults.Curr Infect Dis Rep.2000;2:215–223.
- ,.Pneumonia in the older patient.Clin Chest Med.2007;28:751–771.
- .Guidelines for the management of adults with health care‐associated pneumonia: implications for nursing facility residents.Consult Pharm.2006;21:719–725.
- ,,, et al.Health‐care associated pneumonia: a critical appraisal to improve identification, management, and outcomes‐proceedings of the HCAP summit.Clin Infect Dis.2008;46:S296–S334.
- ,,,.Pneumonia in a long term care facility: a prospective study of outcome.Arch Intern Med.1996;156:2365–2370.
- .Understanding the natural history of community‐acquired pneumonia resolution: vital information for optimizing duration of therapy.Clin Infect Dis.2004;39:1791–1793.
- ,,,.Efficacy of short course antibiotic regimens for community‐acquired pneumonia: a meta‐analysis.Am J Med.2007;120:783–790.
- ,.How long should we treat community‐acquired pneumonia?Curr Opin Infect Dis.2007;20:177–181.
- ,,.High‐dose, short course levofloxacin for community‐acquired pneumonia: a new treatment paradigm.Clin Infect Dis.2003;37:752–760.
- ,,,,.Improving the quality of antibiotic prescription patterns in general practice: the role of educational intervention.Med J Aust.1994;160:502–505.
- ,,,,,.Drug prescription attitudes and behaviour of general practitioners: effects of a problem oriented educational programme.Eur J Clin Pharmacol.1995;47:381–387.
- ,,, et al.Interventions to improve antibiotic prescribing practices for hospital inpatients.Cochrane Database Syst Rev.2005;CD003543.
Copyright © 2010 Society of Hospital Medicine
Lower Extremity Ulcers
A 62‐year‐old man with hypertension, diabetes mellitus, and coronary artery disease (CAD), on peritoneal dialysis, presented with a nonhealing left lower extremity ulcer (Figure 1). Treatment with empiric antibiotics showed no improvement and cultures remained persistently negative. A surgical specimen revealed pathological changes consistent with calciphylaxis (Figures 2 and 3).

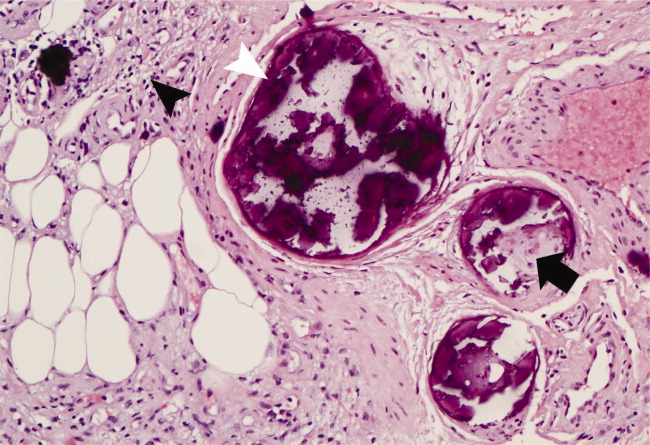
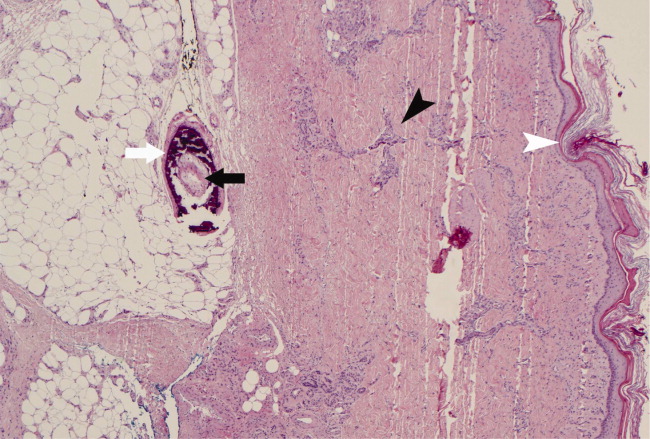
With a mortality between 30% and 80% and a 5‐year survival of 40%,1‐3 calciphylaxis, or calcific uremic arteriolopathy, is devastating. Dialysis and a calcium‐phosphate product above 60 mg2/dL2 increased the index of suspicion (our patient = 70).4 As visual findings may resemble vasculitis or atherosclerotic vascular lesions, biopsy remains the mainstay of diagnosis. Findings include intimal fibrosis, medial calcification, panniculitis, and fat necrosis.5
Management involves aggressive phosphate binding, preventing superinfection, and surgical debridement.6 The evidence for newer therapies (sodium thiosulfate, cinacalcet) appears promising,7‐10 while the benefit of parathyroidectomy is equivocal.11 Despite therapy, our patient developed new lesions (right lower extremity, penis) and opted for hospice services.
- ,,,.Cecil Essentials of Medicine.6th ed.New York:W.B. Saunders;2003.
- .Calciphylaxis: pathogenesis and therapy.J Cutan Med Surg.1998;2(4):245‐248.
- ,.Calciphylaxis: diagnosis and treatment.Adv Skin Wound Care.2001;14(6):309‐312.
- ,,.Calciphylaxis.Postgrad Med J.2001;77(911):557‐561.
- Silverberg SG, DeLellis RA, Frable WJ, LiVolsi VA, Wick MR, eds.Silverberg's Principles and Practice of Surgical Pathology and Cytopathology. Vol.1‐2.4th ed.Philadelphia:Elsevier Churchill Livingstone;2006.
- ,,,.Calciphylaxis: medical and surgical management of chronic extensive wounds in a renal dialysis population.Plast Reconstr Surg.2004;113(1):304‐312.
- ,,, et al.Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis.N Engl J Med.2004;350(15):1516‐1525.
- ,,.Rapid resolution of calciphylaxis with intravenous sodium thiosulfate and continuous venovenous haemofiltration using low calcium replacement fluid: case report.Nephrol Dial Transplant.2005;20(6):1260‐1262.
- ,,,.Successful treatment of calciphylaxis with intravenous sodium thiosulfate.Am J Kidney Dis.2004;43(6):1104‐1108.
- ,.Intraperitoneal sodium thiosulfate for the treatment of calciphylaxis.Ren Fail.2006;28(4):361‐363.
- ,,,,.Therapy for calciphylaxis: an outcome analysis.Surgery.2003;134(6):941‐944; discussion 944‐945.
A 62‐year‐old man with hypertension, diabetes mellitus, and coronary artery disease (CAD), on peritoneal dialysis, presented with a nonhealing left lower extremity ulcer (Figure 1). Treatment with empiric antibiotics showed no improvement and cultures remained persistently negative. A surgical specimen revealed pathological changes consistent with calciphylaxis (Figures 2 and 3).

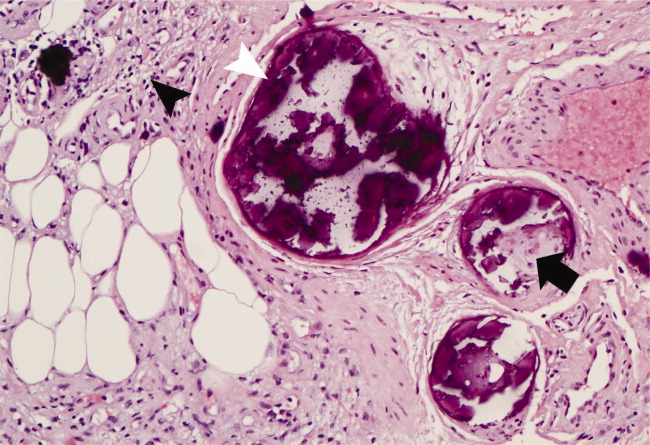
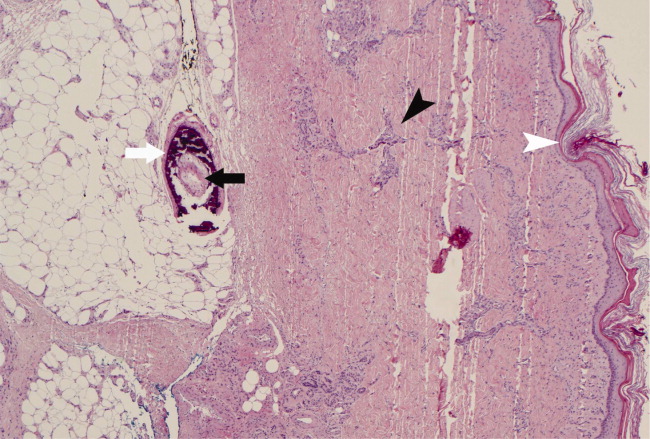
With a mortality between 30% and 80% and a 5‐year survival of 40%,1‐3 calciphylaxis, or calcific uremic arteriolopathy, is devastating. Dialysis and a calcium‐phosphate product above 60 mg2/dL2 increased the index of suspicion (our patient = 70).4 As visual findings may resemble vasculitis or atherosclerotic vascular lesions, biopsy remains the mainstay of diagnosis. Findings include intimal fibrosis, medial calcification, panniculitis, and fat necrosis.5
Management involves aggressive phosphate binding, preventing superinfection, and surgical debridement.6 The evidence for newer therapies (sodium thiosulfate, cinacalcet) appears promising,7‐10 while the benefit of parathyroidectomy is equivocal.11 Despite therapy, our patient developed new lesions (right lower extremity, penis) and opted for hospice services.
A 62‐year‐old man with hypertension, diabetes mellitus, and coronary artery disease (CAD), on peritoneal dialysis, presented with a nonhealing left lower extremity ulcer (Figure 1). Treatment with empiric antibiotics showed no improvement and cultures remained persistently negative. A surgical specimen revealed pathological changes consistent with calciphylaxis (Figures 2 and 3).

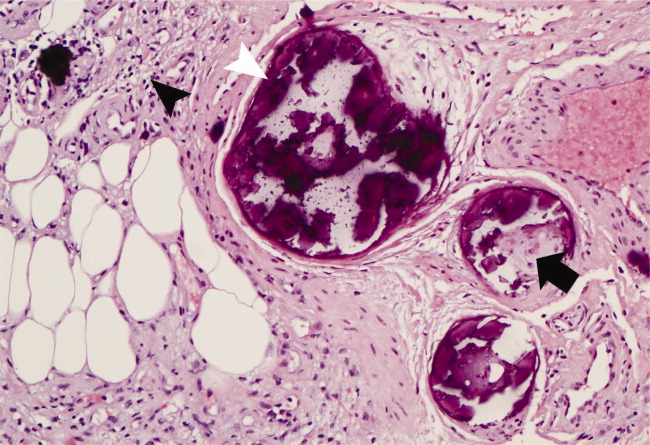
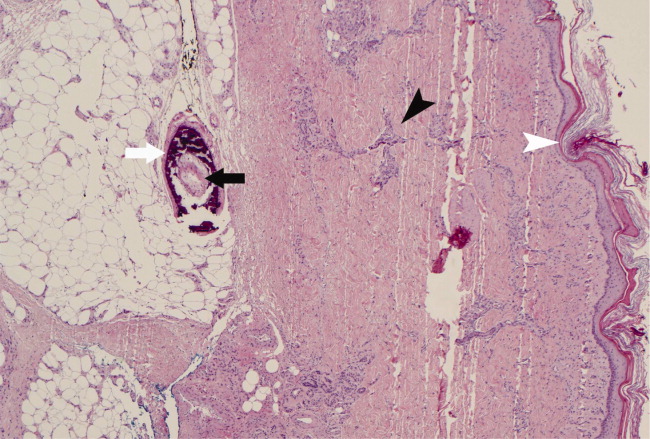
With a mortality between 30% and 80% and a 5‐year survival of 40%,1‐3 calciphylaxis, or calcific uremic arteriolopathy, is devastating. Dialysis and a calcium‐phosphate product above 60 mg2/dL2 increased the index of suspicion (our patient = 70).4 As visual findings may resemble vasculitis or atherosclerotic vascular lesions, biopsy remains the mainstay of diagnosis. Findings include intimal fibrosis, medial calcification, panniculitis, and fat necrosis.5
Management involves aggressive phosphate binding, preventing superinfection, and surgical debridement.6 The evidence for newer therapies (sodium thiosulfate, cinacalcet) appears promising,7‐10 while the benefit of parathyroidectomy is equivocal.11 Despite therapy, our patient developed new lesions (right lower extremity, penis) and opted for hospice services.
- ,,,.Cecil Essentials of Medicine.6th ed.New York:W.B. Saunders;2003.
- .Calciphylaxis: pathogenesis and therapy.J Cutan Med Surg.1998;2(4):245‐248.
- ,.Calciphylaxis: diagnosis and treatment.Adv Skin Wound Care.2001;14(6):309‐312.
- ,,.Calciphylaxis.Postgrad Med J.2001;77(911):557‐561.
- Silverberg SG, DeLellis RA, Frable WJ, LiVolsi VA, Wick MR, eds.Silverberg's Principles and Practice of Surgical Pathology and Cytopathology. Vol.1‐2.4th ed.Philadelphia:Elsevier Churchill Livingstone;2006.
- ,,,.Calciphylaxis: medical and surgical management of chronic extensive wounds in a renal dialysis population.Plast Reconstr Surg.2004;113(1):304‐312.
- ,,, et al.Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis.N Engl J Med.2004;350(15):1516‐1525.
- ,,.Rapid resolution of calciphylaxis with intravenous sodium thiosulfate and continuous venovenous haemofiltration using low calcium replacement fluid: case report.Nephrol Dial Transplant.2005;20(6):1260‐1262.
- ,,,.Successful treatment of calciphylaxis with intravenous sodium thiosulfate.Am J Kidney Dis.2004;43(6):1104‐1108.
- ,.Intraperitoneal sodium thiosulfate for the treatment of calciphylaxis.Ren Fail.2006;28(4):361‐363.
- ,,,,.Therapy for calciphylaxis: an outcome analysis.Surgery.2003;134(6):941‐944; discussion 944‐945.
- ,,,.Cecil Essentials of Medicine.6th ed.New York:W.B. Saunders;2003.
- .Calciphylaxis: pathogenesis and therapy.J Cutan Med Surg.1998;2(4):245‐248.
- ,.Calciphylaxis: diagnosis and treatment.Adv Skin Wound Care.2001;14(6):309‐312.
- ,,.Calciphylaxis.Postgrad Med J.2001;77(911):557‐561.
- Silverberg SG, DeLellis RA, Frable WJ, LiVolsi VA, Wick MR, eds.Silverberg's Principles and Practice of Surgical Pathology and Cytopathology. Vol.1‐2.4th ed.Philadelphia:Elsevier Churchill Livingstone;2006.
- ,,,.Calciphylaxis: medical and surgical management of chronic extensive wounds in a renal dialysis population.Plast Reconstr Surg.2004;113(1):304‐312.
- ,,, et al.Cinacalcet for secondary hyperparathyroidism in patients receiving hemodialysis.N Engl J Med.2004;350(15):1516‐1525.
- ,,.Rapid resolution of calciphylaxis with intravenous sodium thiosulfate and continuous venovenous haemofiltration using low calcium replacement fluid: case report.Nephrol Dial Transplant.2005;20(6):1260‐1262.
- ,,,.Successful treatment of calciphylaxis with intravenous sodium thiosulfate.Am J Kidney Dis.2004;43(6):1104‐1108.
- ,.Intraperitoneal sodium thiosulfate for the treatment of calciphylaxis.Ren Fail.2006;28(4):361‐363.
- ,,,,.Therapy for calciphylaxis: an outcome analysis.Surgery.2003;134(6):941‐944; discussion 944‐945.
Healthcare Costs
Let's think about what we need to do ourselves. We have to acknowledge that orders we write drive up health care costs.1 AMA President, Nancy H. Nielsen, MD, PhD
As the most prominent providers of inpatient care, hospitalists should be aware that, of the total annual expenditures on US healthcare ($2.3 trillion in 2007),2 approximately one‐third goes to hospital‐based medical care, over one‐half of which (57%) is covered by public funds through Medicare and Medicaid3; this high cost of healthcare is increasingly being blamed for unnecessarily burdening our economy and preventing our industries from being globally competitive. I believe that the high proportion of spending on inpatient care places hospitalists firmly in the center of the debate on how to reduce healthcare costs. It is well known that the United States spends about twice as much per capita as other industrialized countries on healthcare,4 without evidence of superior health outcomes.5 However, it is also known that remarkable local and regional variations in healthcare spending also exist within the US, again, without evidence of superior health outcomes in the higher‐spending regions.6 Both of these observations suggest that we are spending many healthcare dollars on things that evidently do not improve the health of our patients. How much of this waste is administrative, operational, or clinical is debatable and remains the focus of growing national healthcare reform efforts.711 However, from the hospitalist perspective, we should be especially wary of providing so‐called flat‐of‐the‐curve medicine, that is, a level of intensity of care that provides no incremental health benefit.12 The purpose of this editorial is to challenge hospitalists to collectively examine how much of our inpatient spending is potentially unnecessary, and how we, as specialists in inpatient medicine, can assume a critical role in controlling healthcare costs.
To illustrate the issue, consider the following clinical scenario, managed in different ways by different hospitalists, with approximate costs itemized in Table 1. The patient is an elderly woman who presents to the emergency room with syncope occurring at church. The first hospitalist takes time to gather history from the patient, family, eyewitnesses, and the primary care physician, and requests a medication list and outside medical records, which reveal several recent and relevant cardiac and imaging studies. He performs a careful examination, discovers orthostatic hypotension, and his final diagnosis is syncope related to volume depletion from a recently added diuretic as well as a mild gastroenteritis. The patient is rehydrated and discharged home from the emergency room in the care of her family, and asked to hold her diuretic until seen by her family physician in 1 or 2 days. The second hospitalist receives the call from the emergency room and tells the staff to get the patient a telemetry bed. He sees the patient 2 hours later when she gets to the floor. The family has gone home and the mildly demented patient does not recall much of the event or her past medical history. The busy hospitalist constructs a broad differential diagnosis and writes some quick orders to evaluate the patient for possible stroke, seizure, pulmonary embolism, and cardiac ischemia or arrhythmia. He also asks cardiology and neurology to give an opinion. The testing is normal, and the patient is discharged with a cardiac event monitor and an outpatient tilt‐table test scheduled.
| Mrs. Syncope #1 | Cost | Mrs. Syncope #2 | Cost |
|---|---|---|---|
| |||
| Level 4 emergency room visit | $745 | Level 4 emergency room visit | $745 |
| Level 4 internal medicine consultation | $190 | Level 3 history and physical | $190 |
| Laboratory evaluation: CBC, CMP, cardiac panel, urinalysis, D‐dimer | $843 | ||
| EKG | $150 | ||
| Head CT | $1426 | ||
| Chest CT angiogram | $2120 | ||
| Brain MRI | $3388 | ||
| Echocardiogram | $687 | ||
| Carotid ultrasound | $911 | ||
| Level 4 neurology consult | $190 | ||
| Subsequent visits day 2, day 3 | $150 | ||
| EEG | $520 | ||
| Level 4 cardiology consult | $190 | ||
| Nuclear stress test | $1359 | ||
| Specialist subsequent visits | $150 | ||
| Telemetry bed, 3 days | $3453 | ||
| Discharge, low‐level | $90 | ||
| Cardiac event monitor | $421 | ||
| Tilt‐table test | $1766 | ||
| $935 | $18,749 | ||
Although the above scenarios purposely demonstrate 2 extremes of care, I suspect most readers would agree that each hospitalist has his or her own style of practice, and that these differences in style inevitably result in significant differences in the total cost of healthcare delivered. This variation in spending among individual physicians is perhaps more easily understood than the striking variations in healthcare spending seen when different states, regions, and hospitals are compared. For example, annual Medicare spending per beneficiary has varied widely from state to state, from $5436 in Iowa to $7995 in New York (in 2004), a 47% difference.13 Specific analysis of inpatient spending variations is presented in the Dartmouth Atlas of Health Care 2008, which reports healthcare spending in the last 2 years of life for patients with at least 1 chronic illness.14 While the average Medicare inpatient spending per capita for these patients was about $25,000, the state‐specific spending varied widely from $37,040 in New Jersey to $17,135 in Idaho. There was also significant variation in spending within individual states (ie, New York: Binghamton, $18,339; Manhattan, $57,000) and between similar types of hospitals (UCLA Medical Center, $63,900; Massachusetts General Hospital, $43,058). Yet there is no evidence that higher‐spending regions produce better health outcomes.6 Interestingly, the observed differences in spending within the US were primarily due to the volume and intensity of care, not the price of care, as has been seen in some comparisons of the US with other industrialized countries.8, 15 In overall Medicare expenditures, higher‐spending locations tended to have a more inpatient‐based and specialist‐oriented pattern of practice, with higher utilization of inpatient consultations, diagnostic testing, and minor procedures.6
Although the wide variation in spending observed is a bit baffling, the encouraging aspect of this data is that some places are apparently doing it right; that is, providing their patients with a much higher value per healthcare dollar. Ultimately, if the higher‐spending locations modeled the lower‐spending locations, we would have the potential to reduce overall healthcare costs by as much as 30% without harming health.9
What are the possible reasons that we are providing unnecessary care? There are both environment‐dependent and physician‐dependent reasons, which I will outline here. The first 3 reasons represent areas that would seem to require system‐wide change, whereas the remaining 7 reasons are perhaps more amenable to local and/or national hospitalist‐directed efforts.
-
Working in a litigious environment promotes unnecessary testing and consultations with the intent of reducing our exposure to malpractice liability, so‐called defensive medicine.16
-
A reimbursement system that is primarily fee‐for‐service encourages physicians to provide more care and involve more physicians in the care of each patient, with little or no incentive to spend less, a core problem that was recently highlighted in a public Society of Hospital Management (SHM) statement.17
-
The lack of integrated medical record systems promotes waste by leading to duplicate testing, simply because we cannot easily obtain old records to confirm whether tests were previously done. Interestingly, data from the Commonwealth Fund conclude that US physicians order duplicate diagnostic tests (a test repeated within 2 years) at more than twice the rate of Canada and the United Kingdom, while the nation with the lowest rate of duplicate testing, The Netherlands, has the highest rate of electronic medical record use (98%).18
-
Working with patients (or families) with high expectations who insist upon aggressive testing, treatment, and referral to specialists inflates spending, especially if associated with futile and expensive end‐of‐life care.
-
The involvement of one or more specialists may subsequently lead to even more aggressive care ordered by each specialist.
-
The availability and promotion of new technology (diagnostic testing, medical devices, etc.) may prompt us to make use of it simply because it is there, with or without evidence of a health benefit. Our natural curiosity or fascination with information, or our desire to do an overly complete evaluation, works against cost containment.
-
Local trends or traditions within our specific work environment, as suggested by the variability data, may have a strong influence on our individual practice. In such a setting, inadequate knowledge of the cost‐effectiveness of various tests and treatment options likely leads to unnecessary health care spending.
-
A hospitalist work environment in which a high patient load is carried will inevitably result in less time to gather a detailed history and obtain old records or other information that could help narrow a differential diagnosis and minimize unnecessary or duplicate testing.
-
Preventable readmissions resulting from inadequate coordination of care add cost,19 a phenomenon highly dependent on efficient information systems and proper physician‐physician communication.20
-
An overestimation of the need for inpatient evaluation and treatment (vs. outpatient) leads to unnecessary admissions and a longer average length‐of‐stay, each of which add dramatically to total healthcare costs. This is not only dependent on our individual threshold for admitting and discharging patients, but also on our efficiency in diagnosing and treating acute conditions. The fact that the average length‐of‐stay for congestive heart failure admissions, for example, ranges in different regions from 4.9 to 6.1 days (with costs of $9143 and $12,528, respectively)21 is enough to show that there is room for progress.
What joint efforts could be made to minimize unnecessary inpatient spending? The following are my personal opinions and suggestions (Table 2). Most importantly, I believe every physician deserves prompt and accurate feedback regarding their spending patterns, accompanied by valid comparisons to national and local standards, to demonstrate where they stand on the spectrum of healthcare spending. We are currently far behind other industries in our ability, as physicians, to evaluate what we are spending money on, how much, and why. If I knew, for example, that my spending was in the 95th percentile of all hospitalists in community hospitals similar to mine, I would be prompted to investigate where the differences were and why. In an informal survey of hospitalist colleagues, I found that the majority do not receive any data on the costs associated with their care, and are largely unaware of the actual cost of the inpatient tests they commonly order. Developing a secure, user‐friendly database of individual physician spending patterns relative to national and local standards could be a preliminary step, and would likely require a unified effort between government agencies, professional societies, hospitals, and the insurance industry. However, once available, the increased transparency and clarity of spending variations would hopefully prompt introspection and change. In the absence of hard data, however, individual self‐assessment on spending patterns could also be offered through the development of an online simulated case‐based examination in which a physician could gain a general idea of how his evaluation and treatment of a case scenario compares to his hospitalist colleagues, and to what degree each of his clinical decisions affects the overall cost of care. There are many excellent quality improvement tools offered through SHM but none that specifically address the cost of care.
| Spending Data | Guidelines | Patient Education | Advocacy | Professional Development | |
|---|---|---|---|---|---|
| |||||
| Defensive medicine | ✓ | ✓ | ✓✓ | ||
| Patient expectations | ✓ | ✓✓ | |||
| Specialist consultations | ✓ | ✓ | ✓ | ✓✓ | |
| Fee‐for‐service environment | ✓✓ | ||||
| Availability of technology | ✓✓ | ✓✓ | ✓ | ✓ | |
| Poor access to medical records | ✓✓ | ||||
| Local medical culture | ✓✓ | ✓✓ | ✓ | ||
| Insufficient knowledge of evidence‐based guidelines | ✓✓ | ✓ | ✓✓ | ||
| Lack of available value‐based data | ✓ | ✓✓ | |||
| High patient load | ✓ | ✓✓ | ✓ | ||
| Preventable readmissions from poor coordination | ✓ | ✓✓ | |||
| Overestimation of the need for inpatient care | ✓ | ✓✓ | ✓ | ✓✓ | |
Second, hospitalists need quick access to current evidence‐based guidelines regarding the true clinical value, or cost‐effectiveness, of testing and treatment for common inpatient conditions, including specific admission criteria. A single source or clearinghouse of guidelines, sponsored by SHM, may be particularly helpful, especially if it focuses on clarifying areas of highest variability in inpatient spending. In addition, I believe that, given the critically important interface between emergency medicine and hospital medicine, joint guidelines between the 2 groups would potentially be very helpful in controlling costs by limiting unnecessary admissions. Advocacy for comparative effectiveness research to establish validity in these guidelines will be fundamental22, 23; however, I suspect the common sense question: Will this added cost improve my patient's outcome? also needs to be applied more generously, since many individual clinical scenarios will not likely lend themselves to formal study. For discussion, some sample case scenarios are presented (Table 3).
| |
| An 82‐year‐old nursing home patient limited to a wheelchair due to severe osteoarthritis presents with new‐onset expressive aphasia and mild right‐sided hemiparesis. Head CT is negative for bleed, but shows an acute left middle cerebral artery infarct. | Would your stroke workup include an MRI/MRA of the brain, carotid ultrasound, echocardiogram, and neurology consultation? |
| A 68‐year‐old with known ischemic cardiomyopathy is admitted with a CHF exacerbation clearly due to medication noncompliance. The last echocardiogram was done 18 months ago and showed an ejection fraction of 20% with moderate to severe mitral regurgitation. | Would you order a repeat echocardiogram? Would you consult cardiology? |
| A 35‐year‐old construction worker presents with sharp chest pain that is partially reproducible on examination, and no other physical findings. Vital signs, EKG, and cardiac markers are normal. The patient had a negative stress test last year. However, his D‐dimer is slightly elevated. | Would you order a CT angiogram of the chest? If he had a normal one last month for the same symptoms, would you repeat it? In either case, would you admit him to the hospital? |
| A 42‐year‐old man presents with chest pain associated with recent cocaine use. His chest pain resolves in the emergency room and his repeat troponin is normal at 6 hours. | Would you order a nuclear stress test for the patient? Would your management change if a stress test was normal a year ago? Would you admit him? |
| A 58‐year‐old man admitted with community‐acquired pneumonia of the right lower lobe has improved clinically with empiric treatment. Before discharge, he asks for a repeat radiograph to make sure it is getting better. | Would you comply with the patient's request? |
| A 68‐year‐old woman who underwent left total knee arthroplasty 2 weeks ago presents with a left proximal DVT. She has no other symptoms and vitals are normal. She has no personal or family history of clotting. | Would you admit the patient to the hospital? Would you order a CT angiogram of the chest? Would you order a hypercoagulable workup? |
| A 43‐year‐old is admitted for atypical chest pain. Serial cardiac enzymes and nuclear stress test are negative. However, his transaminases are elevated at twice the normal upper limits. He takes a statin for dyslipidemia. | Would you order further laboratory tests or imaging to evaluate for hepatic disorders or discharge the patient? |
| A 63‐year‐old receiving chemotherapy for colon cancer with multiple liver metastases presents with new‐onset dyspnea and is found to have a large left‐sided pleural effusion on chest radiograph. You perform a thoracentesis and malignant cells are present. | Would you order a chest CT? Would you consult pulmonology and/or thoracic surgery (for chest tube and/or pleurodesis)? |
| A 78‐year‐old with severe oxygen‐dependent obstructive lung disease (FEV1 of 1.0 L) has a new 1‐cm nodule on his chest radiograph when admitted for a COPD exacerbation. | Would you order a chest CT? Would you arrange for a biopsy? Would you consult oncology or pulmonology? |
| A 45‐year‐old woke up with severe low‐back pain with right‐sided radiculitis after shoveling heavy snow yesterday. He is unable to walk due to pain, but no focal neurologic symptoms are identified on exam. | Would you order an MRI of the spine? Would you consult orthopedics? |
| A 68‐year‐old man on coumadin for chronic atrial fibrillation is incidentally found to have an INR of 6.5 in clinic. He is currently asymptomatic without evidence of bleeding and with normal vital signs. His hemoglobin is 10.1 compared to 10.8 last month. Digital rectal exam results in a hemoccult‐positive smear. | Would you admit him to the hospital? Would you give fresh frozen plasma? Would you consult gastroenterology? |
| A 58‐year old truck driver presents with acute PE, identified on CT angiogram. There is no previous history of DVT. The patient's arterial blood gas shows a pH of 7.45, pCO2 of 35 mmHg, and pO2 of 55 mmHg on room air. The heart rate is 75. | Would you order a lower extremity duplex to assess for DVT? Would you ask interventional radiology to place an IVC filter if a DVT was present? |
| A 26‐year‐old presents with fever, headache, and meningismus. Head CT is normal. | Would you perform a bedside spinal tap or send the patient for a fluoroscopically‐guided procedure in radiology? |
| A 68‐year‐old smoker presents with right‐sided pneumonia with a small parapneumonic effusion. He is afebrile after 24 hours of IV antibiotics and clinically feels much better. | Would you order a thoracentesis? If so, would you perform it bedside or send the patient to radiology for an ultrasound‐guided procedure? Would you consult a pulmonologist? |
| An 82‐year‐old severely demented nursing home resident who has required total care for the past few months presents with dehydration and a sodium of 158 after increasingly poor oral intake. No other illness is identified. | Would you begin IV fluids immediately and consider gastrostomy tube placement to maintain adequate hydration at the nursing home or would you contact family to discuss end‐of‐life care goals first? Would your management change if a UTI or pneumonia was diagnosed? |
Third, hospitalists could potentially benefit from the development of patient education materials, available through SHM, that address the cost‐effectiveness of common inpatient tests and treatments with the goal of decreasing patient demand for unnecessary testing. Education regarding advanced directives and end‐of‐life care decision‐making could be particularly valuable in minimizing futile care, as it is well‐documented that transitioning to palliative care as soon as it is appropriate reduces healthcare spending greatly during the end‐of‐life period.2427 At the same time, we need to be careful to reassure our patients that we are not trying to ration care, but are instead minimizing the risks and costs for them associated with unnecessary care. In my experience, most patients, if given appropriate time, attention, and education, are willing to accept the final recommendation of their physician.
Fourth, intensified federal and state advocacy in several areas could help reduce spending. For example, advocacy for medical liability reform may reduce the atmosphere of defensive medicine, although I suspect that because old habits die hard, it may take a full generation of decreased liability risk to actually change practice patterns. Advocacy for the development of a national, or at least more uniform, electronic medical record, may decrease duplicate testing and improve efficiency. Advocacy for value‐based reimbursement models may help dampen costs resulting from a predominantly fee‐for‐service environment.28
Fifth, and perhaps most fundamental to the future of our specialty, encouraging the broad professional development of hospitalists as a true specialists in inpatient medicine (based on the SHM Core Competencies,)29 could help minimize the unnecessary costs associated with specialist‐oriented care.6 With the desire to create, in the near future, a formal board‐certification in hospital medicine comes an obligation to develop broad knowledge and broad skill sets that are truly unique to our profession, whereas deferring to a specialist‐oriented pattern of care actually shrinks us down to something less than a traditional internist, rather than a unique entity.30 With our 24/7 focus on inpatient care, we should easily be able to demonstrate our superiority in safety, quality, and efficiency, all of which are closely linked to increased value per healthcare dollar. If, however, our focus is blurred by an overly productivity‐based practice, in which patient volume and procedures take precedence, we will not be able to claim any special value to the system.
Last, supporting efforts to improve coordination of care and transitions of care could reduce costs associated with unnecessary readmissions or posthospital complications. A recent policy statement from several professional societies, including SHM, highlights the importance of these transitions,20, 31 and within the past year, SHM has launched the successful Project BOOST (Better Outcomes for Older adults through Safe Transitions) to help in this effort.32
Unfortunately, there is an inherent problem with all of the above proposals: the assumption that physicians actually want to reduce healthcare spending. Since everyone who works in the medical industry benefits financially in some way from the current high levels of spending on healthcare, reducing spending is counterintuitive for many, and the incentives to spend more will likely persist until some form of spending targets or limits are set.33 Moreover, since physicians traditionally do not like to be told how to practice medicine, history would predict that, without attractive incentives, nothing will change. This is the fundamental and unfortunate dilemma that has apparently pushed us to the eleventh hour of a healthcare crisis.
Another concern with an extreme atmosphere of cost cutting is the risk of swinging too far in the opposite direction, focusing so intently on cost that we begin to compromise quality or access to care in order to achieve spending targets. Reassuringly, however, the data suggest that there is plenty of room for us to cut costs without harming health outcomes.
Despite these obstacles, during this historic time in US healthcare, I believe hospitalists have a unique and perhaps transient opportunity to demonstrate their singular commitment to rational healthcare spending and by doing so to gain significant influence in shaping the impending healthcare reforms. If we speak and act with one voice, with transparency, and with the proper data, we could be the first and only professional society to not only demonstrate our current pattern of spending, but also our potential for reducing spending and our plan on how to get there.
Acknowledgements
Judy Knight, MLS, provided valuable research and technical support.
- Medicare pay overhaul can no longer wait. American Medical News.2009. Available at: http://www.ama‐assn.org/amednews/2009/01/12/edsa0112.htm. Accessed July 2009.
- ,,, et al.Health spending projections through 2017: the baby‐boom generation is coming to Medicare.Health Aff (Millwood).2008;27(2):w145–w155.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:380.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:374.
- National Scorecard on U.S. Health System Performance, 2008 Chartpack.New York, NY:The Commonwealth Fund;2008:6.
- ,,,,,.The implications of regional variations in medicare spending. Part 1: The content, quality, and accessibility of care.Ann Intern Med.2003;138(4):273–287.
- ,,,.Waste in the U.S. health care system: a conceptual framework.Milbank Q.2008;86(4):629–659.
- ,,,.It's the prices, stupid: why the United States is so different from other countries.Health Aff (Millwood).2003;22(3):89–105.
- . Health Care and the budget: issues and challenges for reform.2007. Available at: http://www.cbo.gov/ftpdocs/82xx/doc8255/06–21‐HealthCareReform.pdf. Accessed July 2009.
- .Overtreated: Why Too Much Medicine Is Making Us Sicker and Poorer.1st ed.New York, NY:Bloomsbury;2007.
- ,,,. Slowing the growth of U.S. health care expensitures: what are the options?2007. Available at: http://www.commonwealthfund.org/publications/publications_show.htm?doc_id=449510. Accessed July 2009.
- .More variation in use of care, more flat‐of‐the‐curve medicine.Health Aff (Millwood).2004;(Suppl Web Exclusives):VAR104–VAR107.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:419.
- ,.Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care 2008.Lebanon, NH:Dartmouth Institute for Health Policy and Clinical Practice, Center for Health Policy Research;2008:25–32.
- ,.Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care 2008.Lebanon, NH:Dartmouth Institute for Health Policy and Clinical Practice, Center for Health Policy Research;2008:2–4.
- ,,.Effects of the medical liability system in Australia, the UK, and the USA.Lancet.2006;368(9531):240–246.
- Comments on the centers for Medicare and Medicaid services plan to transition to a Medicare value‐based purchasing program for physicians and other professional services.2008. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Issues_in_the_Spotlight12008:62,73.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Transitions of Care Consensus Policy Statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine.J Gen Intern Med.2009;24(8):971–976.
- Hospitals like mine: 2006 national statistics.2006. Available at: http://www.hcupnet.ahrq.gov. Accessed July 2009.
- ,,.Evidence‐Based to Value‐Based Medicine.Chicago, IL:AMA Press;2005.
- Improved Availability of Comparative Effectiveness Information: An Essential Feature for a High‐Quality and Efficient United States Health Care System.Philadelphia, PA:American College of Physicians;2008.
- ,.Clinical practice. Palliative care.N Engl J Med.2004;350(25):2582–2590.
- ,,.The health economics of palliative care.Oncology (Williston Park).2002;16(6):801–808; discussion 808, 811–802.
- .Cost savings at the end of life. What do the data show?JAMA.1996;275(24):1907–1914.
- ,,, et al.Cost savings associated with US hospital palliative care consultation programs.Arch Intern Med.2008;168(16):1783–1790.
- ,,, et al.Toward a 21st‐century health care system: recommendations for health care reform.Ann Intern Med.2009;150(7):493–495.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- .The expanding or shrinking universe of the hospitalist.J Hosp Med.2008;3(4):288–291.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- Project BOOST.2009. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. Accessed Julyyear="2009"2009.
- ,,.The Obama administration's options for health care cost control: hope versus reality.Ann Intern Med.2009;150(7):485–489.
Let's think about what we need to do ourselves. We have to acknowledge that orders we write drive up health care costs.1 AMA President, Nancy H. Nielsen, MD, PhD
As the most prominent providers of inpatient care, hospitalists should be aware that, of the total annual expenditures on US healthcare ($2.3 trillion in 2007),2 approximately one‐third goes to hospital‐based medical care, over one‐half of which (57%) is covered by public funds through Medicare and Medicaid3; this high cost of healthcare is increasingly being blamed for unnecessarily burdening our economy and preventing our industries from being globally competitive. I believe that the high proportion of spending on inpatient care places hospitalists firmly in the center of the debate on how to reduce healthcare costs. It is well known that the United States spends about twice as much per capita as other industrialized countries on healthcare,4 without evidence of superior health outcomes.5 However, it is also known that remarkable local and regional variations in healthcare spending also exist within the US, again, without evidence of superior health outcomes in the higher‐spending regions.6 Both of these observations suggest that we are spending many healthcare dollars on things that evidently do not improve the health of our patients. How much of this waste is administrative, operational, or clinical is debatable and remains the focus of growing national healthcare reform efforts.711 However, from the hospitalist perspective, we should be especially wary of providing so‐called flat‐of‐the‐curve medicine, that is, a level of intensity of care that provides no incremental health benefit.12 The purpose of this editorial is to challenge hospitalists to collectively examine how much of our inpatient spending is potentially unnecessary, and how we, as specialists in inpatient medicine, can assume a critical role in controlling healthcare costs.
To illustrate the issue, consider the following clinical scenario, managed in different ways by different hospitalists, with approximate costs itemized in Table 1. The patient is an elderly woman who presents to the emergency room with syncope occurring at church. The first hospitalist takes time to gather history from the patient, family, eyewitnesses, and the primary care physician, and requests a medication list and outside medical records, which reveal several recent and relevant cardiac and imaging studies. He performs a careful examination, discovers orthostatic hypotension, and his final diagnosis is syncope related to volume depletion from a recently added diuretic as well as a mild gastroenteritis. The patient is rehydrated and discharged home from the emergency room in the care of her family, and asked to hold her diuretic until seen by her family physician in 1 or 2 days. The second hospitalist receives the call from the emergency room and tells the staff to get the patient a telemetry bed. He sees the patient 2 hours later when she gets to the floor. The family has gone home and the mildly demented patient does not recall much of the event or her past medical history. The busy hospitalist constructs a broad differential diagnosis and writes some quick orders to evaluate the patient for possible stroke, seizure, pulmonary embolism, and cardiac ischemia or arrhythmia. He also asks cardiology and neurology to give an opinion. The testing is normal, and the patient is discharged with a cardiac event monitor and an outpatient tilt‐table test scheduled.
| Mrs. Syncope #1 | Cost | Mrs. Syncope #2 | Cost |
|---|---|---|---|
| |||
| Level 4 emergency room visit | $745 | Level 4 emergency room visit | $745 |
| Level 4 internal medicine consultation | $190 | Level 3 history and physical | $190 |
| Laboratory evaluation: CBC, CMP, cardiac panel, urinalysis, D‐dimer | $843 | ||
| EKG | $150 | ||
| Head CT | $1426 | ||
| Chest CT angiogram | $2120 | ||
| Brain MRI | $3388 | ||
| Echocardiogram | $687 | ||
| Carotid ultrasound | $911 | ||
| Level 4 neurology consult | $190 | ||
| Subsequent visits day 2, day 3 | $150 | ||
| EEG | $520 | ||
| Level 4 cardiology consult | $190 | ||
| Nuclear stress test | $1359 | ||
| Specialist subsequent visits | $150 | ||
| Telemetry bed, 3 days | $3453 | ||
| Discharge, low‐level | $90 | ||
| Cardiac event monitor | $421 | ||
| Tilt‐table test | $1766 | ||
| $935 | $18,749 | ||
Although the above scenarios purposely demonstrate 2 extremes of care, I suspect most readers would agree that each hospitalist has his or her own style of practice, and that these differences in style inevitably result in significant differences in the total cost of healthcare delivered. This variation in spending among individual physicians is perhaps more easily understood than the striking variations in healthcare spending seen when different states, regions, and hospitals are compared. For example, annual Medicare spending per beneficiary has varied widely from state to state, from $5436 in Iowa to $7995 in New York (in 2004), a 47% difference.13 Specific analysis of inpatient spending variations is presented in the Dartmouth Atlas of Health Care 2008, which reports healthcare spending in the last 2 years of life for patients with at least 1 chronic illness.14 While the average Medicare inpatient spending per capita for these patients was about $25,000, the state‐specific spending varied widely from $37,040 in New Jersey to $17,135 in Idaho. There was also significant variation in spending within individual states (ie, New York: Binghamton, $18,339; Manhattan, $57,000) and between similar types of hospitals (UCLA Medical Center, $63,900; Massachusetts General Hospital, $43,058). Yet there is no evidence that higher‐spending regions produce better health outcomes.6 Interestingly, the observed differences in spending within the US were primarily due to the volume and intensity of care, not the price of care, as has been seen in some comparisons of the US with other industrialized countries.8, 15 In overall Medicare expenditures, higher‐spending locations tended to have a more inpatient‐based and specialist‐oriented pattern of practice, with higher utilization of inpatient consultations, diagnostic testing, and minor procedures.6
Although the wide variation in spending observed is a bit baffling, the encouraging aspect of this data is that some places are apparently doing it right; that is, providing their patients with a much higher value per healthcare dollar. Ultimately, if the higher‐spending locations modeled the lower‐spending locations, we would have the potential to reduce overall healthcare costs by as much as 30% without harming health.9
What are the possible reasons that we are providing unnecessary care? There are both environment‐dependent and physician‐dependent reasons, which I will outline here. The first 3 reasons represent areas that would seem to require system‐wide change, whereas the remaining 7 reasons are perhaps more amenable to local and/or national hospitalist‐directed efforts.
-
Working in a litigious environment promotes unnecessary testing and consultations with the intent of reducing our exposure to malpractice liability, so‐called defensive medicine.16
-
A reimbursement system that is primarily fee‐for‐service encourages physicians to provide more care and involve more physicians in the care of each patient, with little or no incentive to spend less, a core problem that was recently highlighted in a public Society of Hospital Management (SHM) statement.17
-
The lack of integrated medical record systems promotes waste by leading to duplicate testing, simply because we cannot easily obtain old records to confirm whether tests were previously done. Interestingly, data from the Commonwealth Fund conclude that US physicians order duplicate diagnostic tests (a test repeated within 2 years) at more than twice the rate of Canada and the United Kingdom, while the nation with the lowest rate of duplicate testing, The Netherlands, has the highest rate of electronic medical record use (98%).18
-
Working with patients (or families) with high expectations who insist upon aggressive testing, treatment, and referral to specialists inflates spending, especially if associated with futile and expensive end‐of‐life care.
-
The involvement of one or more specialists may subsequently lead to even more aggressive care ordered by each specialist.
-
The availability and promotion of new technology (diagnostic testing, medical devices, etc.) may prompt us to make use of it simply because it is there, with or without evidence of a health benefit. Our natural curiosity or fascination with information, or our desire to do an overly complete evaluation, works against cost containment.
-
Local trends or traditions within our specific work environment, as suggested by the variability data, may have a strong influence on our individual practice. In such a setting, inadequate knowledge of the cost‐effectiveness of various tests and treatment options likely leads to unnecessary health care spending.
-
A hospitalist work environment in which a high patient load is carried will inevitably result in less time to gather a detailed history and obtain old records or other information that could help narrow a differential diagnosis and minimize unnecessary or duplicate testing.
-
Preventable readmissions resulting from inadequate coordination of care add cost,19 a phenomenon highly dependent on efficient information systems and proper physician‐physician communication.20
-
An overestimation of the need for inpatient evaluation and treatment (vs. outpatient) leads to unnecessary admissions and a longer average length‐of‐stay, each of which add dramatically to total healthcare costs. This is not only dependent on our individual threshold for admitting and discharging patients, but also on our efficiency in diagnosing and treating acute conditions. The fact that the average length‐of‐stay for congestive heart failure admissions, for example, ranges in different regions from 4.9 to 6.1 days (with costs of $9143 and $12,528, respectively)21 is enough to show that there is room for progress.
What joint efforts could be made to minimize unnecessary inpatient spending? The following are my personal opinions and suggestions (Table 2). Most importantly, I believe every physician deserves prompt and accurate feedback regarding their spending patterns, accompanied by valid comparisons to national and local standards, to demonstrate where they stand on the spectrum of healthcare spending. We are currently far behind other industries in our ability, as physicians, to evaluate what we are spending money on, how much, and why. If I knew, for example, that my spending was in the 95th percentile of all hospitalists in community hospitals similar to mine, I would be prompted to investigate where the differences were and why. In an informal survey of hospitalist colleagues, I found that the majority do not receive any data on the costs associated with their care, and are largely unaware of the actual cost of the inpatient tests they commonly order. Developing a secure, user‐friendly database of individual physician spending patterns relative to national and local standards could be a preliminary step, and would likely require a unified effort between government agencies, professional societies, hospitals, and the insurance industry. However, once available, the increased transparency and clarity of spending variations would hopefully prompt introspection and change. In the absence of hard data, however, individual self‐assessment on spending patterns could also be offered through the development of an online simulated case‐based examination in which a physician could gain a general idea of how his evaluation and treatment of a case scenario compares to his hospitalist colleagues, and to what degree each of his clinical decisions affects the overall cost of care. There are many excellent quality improvement tools offered through SHM but none that specifically address the cost of care.
| Spending Data | Guidelines | Patient Education | Advocacy | Professional Development | |
|---|---|---|---|---|---|
| |||||
| Defensive medicine | ✓ | ✓ | ✓✓ | ||
| Patient expectations | ✓ | ✓✓ | |||
| Specialist consultations | ✓ | ✓ | ✓ | ✓✓ | |
| Fee‐for‐service environment | ✓✓ | ||||
| Availability of technology | ✓✓ | ✓✓ | ✓ | ✓ | |
| Poor access to medical records | ✓✓ | ||||
| Local medical culture | ✓✓ | ✓✓ | ✓ | ||
| Insufficient knowledge of evidence‐based guidelines | ✓✓ | ✓ | ✓✓ | ||
| Lack of available value‐based data | ✓ | ✓✓ | |||
| High patient load | ✓ | ✓✓ | ✓ | ||
| Preventable readmissions from poor coordination | ✓ | ✓✓ | |||
| Overestimation of the need for inpatient care | ✓ | ✓✓ | ✓ | ✓✓ | |
Second, hospitalists need quick access to current evidence‐based guidelines regarding the true clinical value, or cost‐effectiveness, of testing and treatment for common inpatient conditions, including specific admission criteria. A single source or clearinghouse of guidelines, sponsored by SHM, may be particularly helpful, especially if it focuses on clarifying areas of highest variability in inpatient spending. In addition, I believe that, given the critically important interface between emergency medicine and hospital medicine, joint guidelines between the 2 groups would potentially be very helpful in controlling costs by limiting unnecessary admissions. Advocacy for comparative effectiveness research to establish validity in these guidelines will be fundamental22, 23; however, I suspect the common sense question: Will this added cost improve my patient's outcome? also needs to be applied more generously, since many individual clinical scenarios will not likely lend themselves to formal study. For discussion, some sample case scenarios are presented (Table 3).
| |
| An 82‐year‐old nursing home patient limited to a wheelchair due to severe osteoarthritis presents with new‐onset expressive aphasia and mild right‐sided hemiparesis. Head CT is negative for bleed, but shows an acute left middle cerebral artery infarct. | Would your stroke workup include an MRI/MRA of the brain, carotid ultrasound, echocardiogram, and neurology consultation? |
| A 68‐year‐old with known ischemic cardiomyopathy is admitted with a CHF exacerbation clearly due to medication noncompliance. The last echocardiogram was done 18 months ago and showed an ejection fraction of 20% with moderate to severe mitral regurgitation. | Would you order a repeat echocardiogram? Would you consult cardiology? |
| A 35‐year‐old construction worker presents with sharp chest pain that is partially reproducible on examination, and no other physical findings. Vital signs, EKG, and cardiac markers are normal. The patient had a negative stress test last year. However, his D‐dimer is slightly elevated. | Would you order a CT angiogram of the chest? If he had a normal one last month for the same symptoms, would you repeat it? In either case, would you admit him to the hospital? |
| A 42‐year‐old man presents with chest pain associated with recent cocaine use. His chest pain resolves in the emergency room and his repeat troponin is normal at 6 hours. | Would you order a nuclear stress test for the patient? Would your management change if a stress test was normal a year ago? Would you admit him? |
| A 58‐year‐old man admitted with community‐acquired pneumonia of the right lower lobe has improved clinically with empiric treatment. Before discharge, he asks for a repeat radiograph to make sure it is getting better. | Would you comply with the patient's request? |
| A 68‐year‐old woman who underwent left total knee arthroplasty 2 weeks ago presents with a left proximal DVT. She has no other symptoms and vitals are normal. She has no personal or family history of clotting. | Would you admit the patient to the hospital? Would you order a CT angiogram of the chest? Would you order a hypercoagulable workup? |
| A 43‐year‐old is admitted for atypical chest pain. Serial cardiac enzymes and nuclear stress test are negative. However, his transaminases are elevated at twice the normal upper limits. He takes a statin for dyslipidemia. | Would you order further laboratory tests or imaging to evaluate for hepatic disorders or discharge the patient? |
| A 63‐year‐old receiving chemotherapy for colon cancer with multiple liver metastases presents with new‐onset dyspnea and is found to have a large left‐sided pleural effusion on chest radiograph. You perform a thoracentesis and malignant cells are present. | Would you order a chest CT? Would you consult pulmonology and/or thoracic surgery (for chest tube and/or pleurodesis)? |
| A 78‐year‐old with severe oxygen‐dependent obstructive lung disease (FEV1 of 1.0 L) has a new 1‐cm nodule on his chest radiograph when admitted for a COPD exacerbation. | Would you order a chest CT? Would you arrange for a biopsy? Would you consult oncology or pulmonology? |
| A 45‐year‐old woke up with severe low‐back pain with right‐sided radiculitis after shoveling heavy snow yesterday. He is unable to walk due to pain, but no focal neurologic symptoms are identified on exam. | Would you order an MRI of the spine? Would you consult orthopedics? |
| A 68‐year‐old man on coumadin for chronic atrial fibrillation is incidentally found to have an INR of 6.5 in clinic. He is currently asymptomatic without evidence of bleeding and with normal vital signs. His hemoglobin is 10.1 compared to 10.8 last month. Digital rectal exam results in a hemoccult‐positive smear. | Would you admit him to the hospital? Would you give fresh frozen plasma? Would you consult gastroenterology? |
| A 58‐year old truck driver presents with acute PE, identified on CT angiogram. There is no previous history of DVT. The patient's arterial blood gas shows a pH of 7.45, pCO2 of 35 mmHg, and pO2 of 55 mmHg on room air. The heart rate is 75. | Would you order a lower extremity duplex to assess for DVT? Would you ask interventional radiology to place an IVC filter if a DVT was present? |
| A 26‐year‐old presents with fever, headache, and meningismus. Head CT is normal. | Would you perform a bedside spinal tap or send the patient for a fluoroscopically‐guided procedure in radiology? |
| A 68‐year‐old smoker presents with right‐sided pneumonia with a small parapneumonic effusion. He is afebrile after 24 hours of IV antibiotics and clinically feels much better. | Would you order a thoracentesis? If so, would you perform it bedside or send the patient to radiology for an ultrasound‐guided procedure? Would you consult a pulmonologist? |
| An 82‐year‐old severely demented nursing home resident who has required total care for the past few months presents with dehydration and a sodium of 158 after increasingly poor oral intake. No other illness is identified. | Would you begin IV fluids immediately and consider gastrostomy tube placement to maintain adequate hydration at the nursing home or would you contact family to discuss end‐of‐life care goals first? Would your management change if a UTI or pneumonia was diagnosed? |
Third, hospitalists could potentially benefit from the development of patient education materials, available through SHM, that address the cost‐effectiveness of common inpatient tests and treatments with the goal of decreasing patient demand for unnecessary testing. Education regarding advanced directives and end‐of‐life care decision‐making could be particularly valuable in minimizing futile care, as it is well‐documented that transitioning to palliative care as soon as it is appropriate reduces healthcare spending greatly during the end‐of‐life period.2427 At the same time, we need to be careful to reassure our patients that we are not trying to ration care, but are instead minimizing the risks and costs for them associated with unnecessary care. In my experience, most patients, if given appropriate time, attention, and education, are willing to accept the final recommendation of their physician.
Fourth, intensified federal and state advocacy in several areas could help reduce spending. For example, advocacy for medical liability reform may reduce the atmosphere of defensive medicine, although I suspect that because old habits die hard, it may take a full generation of decreased liability risk to actually change practice patterns. Advocacy for the development of a national, or at least more uniform, electronic medical record, may decrease duplicate testing and improve efficiency. Advocacy for value‐based reimbursement models may help dampen costs resulting from a predominantly fee‐for‐service environment.28
Fifth, and perhaps most fundamental to the future of our specialty, encouraging the broad professional development of hospitalists as a true specialists in inpatient medicine (based on the SHM Core Competencies,)29 could help minimize the unnecessary costs associated with specialist‐oriented care.6 With the desire to create, in the near future, a formal board‐certification in hospital medicine comes an obligation to develop broad knowledge and broad skill sets that are truly unique to our profession, whereas deferring to a specialist‐oriented pattern of care actually shrinks us down to something less than a traditional internist, rather than a unique entity.30 With our 24/7 focus on inpatient care, we should easily be able to demonstrate our superiority in safety, quality, and efficiency, all of which are closely linked to increased value per healthcare dollar. If, however, our focus is blurred by an overly productivity‐based practice, in which patient volume and procedures take precedence, we will not be able to claim any special value to the system.
Last, supporting efforts to improve coordination of care and transitions of care could reduce costs associated with unnecessary readmissions or posthospital complications. A recent policy statement from several professional societies, including SHM, highlights the importance of these transitions,20, 31 and within the past year, SHM has launched the successful Project BOOST (Better Outcomes for Older adults through Safe Transitions) to help in this effort.32
Unfortunately, there is an inherent problem with all of the above proposals: the assumption that physicians actually want to reduce healthcare spending. Since everyone who works in the medical industry benefits financially in some way from the current high levels of spending on healthcare, reducing spending is counterintuitive for many, and the incentives to spend more will likely persist until some form of spending targets or limits are set.33 Moreover, since physicians traditionally do not like to be told how to practice medicine, history would predict that, without attractive incentives, nothing will change. This is the fundamental and unfortunate dilemma that has apparently pushed us to the eleventh hour of a healthcare crisis.
Another concern with an extreme atmosphere of cost cutting is the risk of swinging too far in the opposite direction, focusing so intently on cost that we begin to compromise quality or access to care in order to achieve spending targets. Reassuringly, however, the data suggest that there is plenty of room for us to cut costs without harming health outcomes.
Despite these obstacles, during this historic time in US healthcare, I believe hospitalists have a unique and perhaps transient opportunity to demonstrate their singular commitment to rational healthcare spending and by doing so to gain significant influence in shaping the impending healthcare reforms. If we speak and act with one voice, with transparency, and with the proper data, we could be the first and only professional society to not only demonstrate our current pattern of spending, but also our potential for reducing spending and our plan on how to get there.
Acknowledgements
Judy Knight, MLS, provided valuable research and technical support.
Let's think about what we need to do ourselves. We have to acknowledge that orders we write drive up health care costs.1 AMA President, Nancy H. Nielsen, MD, PhD
As the most prominent providers of inpatient care, hospitalists should be aware that, of the total annual expenditures on US healthcare ($2.3 trillion in 2007),2 approximately one‐third goes to hospital‐based medical care, over one‐half of which (57%) is covered by public funds through Medicare and Medicaid3; this high cost of healthcare is increasingly being blamed for unnecessarily burdening our economy and preventing our industries from being globally competitive. I believe that the high proportion of spending on inpatient care places hospitalists firmly in the center of the debate on how to reduce healthcare costs. It is well known that the United States spends about twice as much per capita as other industrialized countries on healthcare,4 without evidence of superior health outcomes.5 However, it is also known that remarkable local and regional variations in healthcare spending also exist within the US, again, without evidence of superior health outcomes in the higher‐spending regions.6 Both of these observations suggest that we are spending many healthcare dollars on things that evidently do not improve the health of our patients. How much of this waste is administrative, operational, or clinical is debatable and remains the focus of growing national healthcare reform efforts.711 However, from the hospitalist perspective, we should be especially wary of providing so‐called flat‐of‐the‐curve medicine, that is, a level of intensity of care that provides no incremental health benefit.12 The purpose of this editorial is to challenge hospitalists to collectively examine how much of our inpatient spending is potentially unnecessary, and how we, as specialists in inpatient medicine, can assume a critical role in controlling healthcare costs.
To illustrate the issue, consider the following clinical scenario, managed in different ways by different hospitalists, with approximate costs itemized in Table 1. The patient is an elderly woman who presents to the emergency room with syncope occurring at church. The first hospitalist takes time to gather history from the patient, family, eyewitnesses, and the primary care physician, and requests a medication list and outside medical records, which reveal several recent and relevant cardiac and imaging studies. He performs a careful examination, discovers orthostatic hypotension, and his final diagnosis is syncope related to volume depletion from a recently added diuretic as well as a mild gastroenteritis. The patient is rehydrated and discharged home from the emergency room in the care of her family, and asked to hold her diuretic until seen by her family physician in 1 or 2 days. The second hospitalist receives the call from the emergency room and tells the staff to get the patient a telemetry bed. He sees the patient 2 hours later when she gets to the floor. The family has gone home and the mildly demented patient does not recall much of the event or her past medical history. The busy hospitalist constructs a broad differential diagnosis and writes some quick orders to evaluate the patient for possible stroke, seizure, pulmonary embolism, and cardiac ischemia or arrhythmia. He also asks cardiology and neurology to give an opinion. The testing is normal, and the patient is discharged with a cardiac event monitor and an outpatient tilt‐table test scheduled.
| Mrs. Syncope #1 | Cost | Mrs. Syncope #2 | Cost |
|---|---|---|---|
| |||
| Level 4 emergency room visit | $745 | Level 4 emergency room visit | $745 |
| Level 4 internal medicine consultation | $190 | Level 3 history and physical | $190 |
| Laboratory evaluation: CBC, CMP, cardiac panel, urinalysis, D‐dimer | $843 | ||
| EKG | $150 | ||
| Head CT | $1426 | ||
| Chest CT angiogram | $2120 | ||
| Brain MRI | $3388 | ||
| Echocardiogram | $687 | ||
| Carotid ultrasound | $911 | ||
| Level 4 neurology consult | $190 | ||
| Subsequent visits day 2, day 3 | $150 | ||
| EEG | $520 | ||
| Level 4 cardiology consult | $190 | ||
| Nuclear stress test | $1359 | ||
| Specialist subsequent visits | $150 | ||
| Telemetry bed, 3 days | $3453 | ||
| Discharge, low‐level | $90 | ||
| Cardiac event monitor | $421 | ||
| Tilt‐table test | $1766 | ||
| $935 | $18,749 | ||
Although the above scenarios purposely demonstrate 2 extremes of care, I suspect most readers would agree that each hospitalist has his or her own style of practice, and that these differences in style inevitably result in significant differences in the total cost of healthcare delivered. This variation in spending among individual physicians is perhaps more easily understood than the striking variations in healthcare spending seen when different states, regions, and hospitals are compared. For example, annual Medicare spending per beneficiary has varied widely from state to state, from $5436 in Iowa to $7995 in New York (in 2004), a 47% difference.13 Specific analysis of inpatient spending variations is presented in the Dartmouth Atlas of Health Care 2008, which reports healthcare spending in the last 2 years of life for patients with at least 1 chronic illness.14 While the average Medicare inpatient spending per capita for these patients was about $25,000, the state‐specific spending varied widely from $37,040 in New Jersey to $17,135 in Idaho. There was also significant variation in spending within individual states (ie, New York: Binghamton, $18,339; Manhattan, $57,000) and between similar types of hospitals (UCLA Medical Center, $63,900; Massachusetts General Hospital, $43,058). Yet there is no evidence that higher‐spending regions produce better health outcomes.6 Interestingly, the observed differences in spending within the US were primarily due to the volume and intensity of care, not the price of care, as has been seen in some comparisons of the US with other industrialized countries.8, 15 In overall Medicare expenditures, higher‐spending locations tended to have a more inpatient‐based and specialist‐oriented pattern of practice, with higher utilization of inpatient consultations, diagnostic testing, and minor procedures.6
Although the wide variation in spending observed is a bit baffling, the encouraging aspect of this data is that some places are apparently doing it right; that is, providing their patients with a much higher value per healthcare dollar. Ultimately, if the higher‐spending locations modeled the lower‐spending locations, we would have the potential to reduce overall healthcare costs by as much as 30% without harming health.9
What are the possible reasons that we are providing unnecessary care? There are both environment‐dependent and physician‐dependent reasons, which I will outline here. The first 3 reasons represent areas that would seem to require system‐wide change, whereas the remaining 7 reasons are perhaps more amenable to local and/or national hospitalist‐directed efforts.
-
Working in a litigious environment promotes unnecessary testing and consultations with the intent of reducing our exposure to malpractice liability, so‐called defensive medicine.16
-
A reimbursement system that is primarily fee‐for‐service encourages physicians to provide more care and involve more physicians in the care of each patient, with little or no incentive to spend less, a core problem that was recently highlighted in a public Society of Hospital Management (SHM) statement.17
-
The lack of integrated medical record systems promotes waste by leading to duplicate testing, simply because we cannot easily obtain old records to confirm whether tests were previously done. Interestingly, data from the Commonwealth Fund conclude that US physicians order duplicate diagnostic tests (a test repeated within 2 years) at more than twice the rate of Canada and the United Kingdom, while the nation with the lowest rate of duplicate testing, The Netherlands, has the highest rate of electronic medical record use (98%).18
-
Working with patients (or families) with high expectations who insist upon aggressive testing, treatment, and referral to specialists inflates spending, especially if associated with futile and expensive end‐of‐life care.
-
The involvement of one or more specialists may subsequently lead to even more aggressive care ordered by each specialist.
-
The availability and promotion of new technology (diagnostic testing, medical devices, etc.) may prompt us to make use of it simply because it is there, with or without evidence of a health benefit. Our natural curiosity or fascination with information, or our desire to do an overly complete evaluation, works against cost containment.
-
Local trends or traditions within our specific work environment, as suggested by the variability data, may have a strong influence on our individual practice. In such a setting, inadequate knowledge of the cost‐effectiveness of various tests and treatment options likely leads to unnecessary health care spending.
-
A hospitalist work environment in which a high patient load is carried will inevitably result in less time to gather a detailed history and obtain old records or other information that could help narrow a differential diagnosis and minimize unnecessary or duplicate testing.
-
Preventable readmissions resulting from inadequate coordination of care add cost,19 a phenomenon highly dependent on efficient information systems and proper physician‐physician communication.20
-
An overestimation of the need for inpatient evaluation and treatment (vs. outpatient) leads to unnecessary admissions and a longer average length‐of‐stay, each of which add dramatically to total healthcare costs. This is not only dependent on our individual threshold for admitting and discharging patients, but also on our efficiency in diagnosing and treating acute conditions. The fact that the average length‐of‐stay for congestive heart failure admissions, for example, ranges in different regions from 4.9 to 6.1 days (with costs of $9143 and $12,528, respectively)21 is enough to show that there is room for progress.
What joint efforts could be made to minimize unnecessary inpatient spending? The following are my personal opinions and suggestions (Table 2). Most importantly, I believe every physician deserves prompt and accurate feedback regarding their spending patterns, accompanied by valid comparisons to national and local standards, to demonstrate where they stand on the spectrum of healthcare spending. We are currently far behind other industries in our ability, as physicians, to evaluate what we are spending money on, how much, and why. If I knew, for example, that my spending was in the 95th percentile of all hospitalists in community hospitals similar to mine, I would be prompted to investigate where the differences were and why. In an informal survey of hospitalist colleagues, I found that the majority do not receive any data on the costs associated with their care, and are largely unaware of the actual cost of the inpatient tests they commonly order. Developing a secure, user‐friendly database of individual physician spending patterns relative to national and local standards could be a preliminary step, and would likely require a unified effort between government agencies, professional societies, hospitals, and the insurance industry. However, once available, the increased transparency and clarity of spending variations would hopefully prompt introspection and change. In the absence of hard data, however, individual self‐assessment on spending patterns could also be offered through the development of an online simulated case‐based examination in which a physician could gain a general idea of how his evaluation and treatment of a case scenario compares to his hospitalist colleagues, and to what degree each of his clinical decisions affects the overall cost of care. There are many excellent quality improvement tools offered through SHM but none that specifically address the cost of care.
| Spending Data | Guidelines | Patient Education | Advocacy | Professional Development | |
|---|---|---|---|---|---|
| |||||
| Defensive medicine | ✓ | ✓ | ✓✓ | ||
| Patient expectations | ✓ | ✓✓ | |||
| Specialist consultations | ✓ | ✓ | ✓ | ✓✓ | |
| Fee‐for‐service environment | ✓✓ | ||||
| Availability of technology | ✓✓ | ✓✓ | ✓ | ✓ | |
| Poor access to medical records | ✓✓ | ||||
| Local medical culture | ✓✓ | ✓✓ | ✓ | ||
| Insufficient knowledge of evidence‐based guidelines | ✓✓ | ✓ | ✓✓ | ||
| Lack of available value‐based data | ✓ | ✓✓ | |||
| High patient load | ✓ | ✓✓ | ✓ | ||
| Preventable readmissions from poor coordination | ✓ | ✓✓ | |||
| Overestimation of the need for inpatient care | ✓ | ✓✓ | ✓ | ✓✓ | |
Second, hospitalists need quick access to current evidence‐based guidelines regarding the true clinical value, or cost‐effectiveness, of testing and treatment for common inpatient conditions, including specific admission criteria. A single source or clearinghouse of guidelines, sponsored by SHM, may be particularly helpful, especially if it focuses on clarifying areas of highest variability in inpatient spending. In addition, I believe that, given the critically important interface between emergency medicine and hospital medicine, joint guidelines between the 2 groups would potentially be very helpful in controlling costs by limiting unnecessary admissions. Advocacy for comparative effectiveness research to establish validity in these guidelines will be fundamental22, 23; however, I suspect the common sense question: Will this added cost improve my patient's outcome? also needs to be applied more generously, since many individual clinical scenarios will not likely lend themselves to formal study. For discussion, some sample case scenarios are presented (Table 3).
| |
| An 82‐year‐old nursing home patient limited to a wheelchair due to severe osteoarthritis presents with new‐onset expressive aphasia and mild right‐sided hemiparesis. Head CT is negative for bleed, but shows an acute left middle cerebral artery infarct. | Would your stroke workup include an MRI/MRA of the brain, carotid ultrasound, echocardiogram, and neurology consultation? |
| A 68‐year‐old with known ischemic cardiomyopathy is admitted with a CHF exacerbation clearly due to medication noncompliance. The last echocardiogram was done 18 months ago and showed an ejection fraction of 20% with moderate to severe mitral regurgitation. | Would you order a repeat echocardiogram? Would you consult cardiology? |
| A 35‐year‐old construction worker presents with sharp chest pain that is partially reproducible on examination, and no other physical findings. Vital signs, EKG, and cardiac markers are normal. The patient had a negative stress test last year. However, his D‐dimer is slightly elevated. | Would you order a CT angiogram of the chest? If he had a normal one last month for the same symptoms, would you repeat it? In either case, would you admit him to the hospital? |
| A 42‐year‐old man presents with chest pain associated with recent cocaine use. His chest pain resolves in the emergency room and his repeat troponin is normal at 6 hours. | Would you order a nuclear stress test for the patient? Would your management change if a stress test was normal a year ago? Would you admit him? |
| A 58‐year‐old man admitted with community‐acquired pneumonia of the right lower lobe has improved clinically with empiric treatment. Before discharge, he asks for a repeat radiograph to make sure it is getting better. | Would you comply with the patient's request? |
| A 68‐year‐old woman who underwent left total knee arthroplasty 2 weeks ago presents with a left proximal DVT. She has no other symptoms and vitals are normal. She has no personal or family history of clotting. | Would you admit the patient to the hospital? Would you order a CT angiogram of the chest? Would you order a hypercoagulable workup? |
| A 43‐year‐old is admitted for atypical chest pain. Serial cardiac enzymes and nuclear stress test are negative. However, his transaminases are elevated at twice the normal upper limits. He takes a statin for dyslipidemia. | Would you order further laboratory tests or imaging to evaluate for hepatic disorders or discharge the patient? |
| A 63‐year‐old receiving chemotherapy for colon cancer with multiple liver metastases presents with new‐onset dyspnea and is found to have a large left‐sided pleural effusion on chest radiograph. You perform a thoracentesis and malignant cells are present. | Would you order a chest CT? Would you consult pulmonology and/or thoracic surgery (for chest tube and/or pleurodesis)? |
| A 78‐year‐old with severe oxygen‐dependent obstructive lung disease (FEV1 of 1.0 L) has a new 1‐cm nodule on his chest radiograph when admitted for a COPD exacerbation. | Would you order a chest CT? Would you arrange for a biopsy? Would you consult oncology or pulmonology? |
| A 45‐year‐old woke up with severe low‐back pain with right‐sided radiculitis after shoveling heavy snow yesterday. He is unable to walk due to pain, but no focal neurologic symptoms are identified on exam. | Would you order an MRI of the spine? Would you consult orthopedics? |
| A 68‐year‐old man on coumadin for chronic atrial fibrillation is incidentally found to have an INR of 6.5 in clinic. He is currently asymptomatic without evidence of bleeding and with normal vital signs. His hemoglobin is 10.1 compared to 10.8 last month. Digital rectal exam results in a hemoccult‐positive smear. | Would you admit him to the hospital? Would you give fresh frozen plasma? Would you consult gastroenterology? |
| A 58‐year old truck driver presents with acute PE, identified on CT angiogram. There is no previous history of DVT. The patient's arterial blood gas shows a pH of 7.45, pCO2 of 35 mmHg, and pO2 of 55 mmHg on room air. The heart rate is 75. | Would you order a lower extremity duplex to assess for DVT? Would you ask interventional radiology to place an IVC filter if a DVT was present? |
| A 26‐year‐old presents with fever, headache, and meningismus. Head CT is normal. | Would you perform a bedside spinal tap or send the patient for a fluoroscopically‐guided procedure in radiology? |
| A 68‐year‐old smoker presents with right‐sided pneumonia with a small parapneumonic effusion. He is afebrile after 24 hours of IV antibiotics and clinically feels much better. | Would you order a thoracentesis? If so, would you perform it bedside or send the patient to radiology for an ultrasound‐guided procedure? Would you consult a pulmonologist? |
| An 82‐year‐old severely demented nursing home resident who has required total care for the past few months presents with dehydration and a sodium of 158 after increasingly poor oral intake. No other illness is identified. | Would you begin IV fluids immediately and consider gastrostomy tube placement to maintain adequate hydration at the nursing home or would you contact family to discuss end‐of‐life care goals first? Would your management change if a UTI or pneumonia was diagnosed? |
Third, hospitalists could potentially benefit from the development of patient education materials, available through SHM, that address the cost‐effectiveness of common inpatient tests and treatments with the goal of decreasing patient demand for unnecessary testing. Education regarding advanced directives and end‐of‐life care decision‐making could be particularly valuable in minimizing futile care, as it is well‐documented that transitioning to palliative care as soon as it is appropriate reduces healthcare spending greatly during the end‐of‐life period.2427 At the same time, we need to be careful to reassure our patients that we are not trying to ration care, but are instead minimizing the risks and costs for them associated with unnecessary care. In my experience, most patients, if given appropriate time, attention, and education, are willing to accept the final recommendation of their physician.
Fourth, intensified federal and state advocacy in several areas could help reduce spending. For example, advocacy for medical liability reform may reduce the atmosphere of defensive medicine, although I suspect that because old habits die hard, it may take a full generation of decreased liability risk to actually change practice patterns. Advocacy for the development of a national, or at least more uniform, electronic medical record, may decrease duplicate testing and improve efficiency. Advocacy for value‐based reimbursement models may help dampen costs resulting from a predominantly fee‐for‐service environment.28
Fifth, and perhaps most fundamental to the future of our specialty, encouraging the broad professional development of hospitalists as a true specialists in inpatient medicine (based on the SHM Core Competencies,)29 could help minimize the unnecessary costs associated with specialist‐oriented care.6 With the desire to create, in the near future, a formal board‐certification in hospital medicine comes an obligation to develop broad knowledge and broad skill sets that are truly unique to our profession, whereas deferring to a specialist‐oriented pattern of care actually shrinks us down to something less than a traditional internist, rather than a unique entity.30 With our 24/7 focus on inpatient care, we should easily be able to demonstrate our superiority in safety, quality, and efficiency, all of which are closely linked to increased value per healthcare dollar. If, however, our focus is blurred by an overly productivity‐based practice, in which patient volume and procedures take precedence, we will not be able to claim any special value to the system.
Last, supporting efforts to improve coordination of care and transitions of care could reduce costs associated with unnecessary readmissions or posthospital complications. A recent policy statement from several professional societies, including SHM, highlights the importance of these transitions,20, 31 and within the past year, SHM has launched the successful Project BOOST (Better Outcomes for Older adults through Safe Transitions) to help in this effort.32
Unfortunately, there is an inherent problem with all of the above proposals: the assumption that physicians actually want to reduce healthcare spending. Since everyone who works in the medical industry benefits financially in some way from the current high levels of spending on healthcare, reducing spending is counterintuitive for many, and the incentives to spend more will likely persist until some form of spending targets or limits are set.33 Moreover, since physicians traditionally do not like to be told how to practice medicine, history would predict that, without attractive incentives, nothing will change. This is the fundamental and unfortunate dilemma that has apparently pushed us to the eleventh hour of a healthcare crisis.
Another concern with an extreme atmosphere of cost cutting is the risk of swinging too far in the opposite direction, focusing so intently on cost that we begin to compromise quality or access to care in order to achieve spending targets. Reassuringly, however, the data suggest that there is plenty of room for us to cut costs without harming health outcomes.
Despite these obstacles, during this historic time in US healthcare, I believe hospitalists have a unique and perhaps transient opportunity to demonstrate their singular commitment to rational healthcare spending and by doing so to gain significant influence in shaping the impending healthcare reforms. If we speak and act with one voice, with transparency, and with the proper data, we could be the first and only professional society to not only demonstrate our current pattern of spending, but also our potential for reducing spending and our plan on how to get there.
Acknowledgements
Judy Knight, MLS, provided valuable research and technical support.
- Medicare pay overhaul can no longer wait. American Medical News.2009. Available at: http://www.ama‐assn.org/amednews/2009/01/12/edsa0112.htm. Accessed July 2009.
- ,,, et al.Health spending projections through 2017: the baby‐boom generation is coming to Medicare.Health Aff (Millwood).2008;27(2):w145–w155.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:380.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:374.
- National Scorecard on U.S. Health System Performance, 2008 Chartpack.New York, NY:The Commonwealth Fund;2008:6.
- ,,,,,.The implications of regional variations in medicare spending. Part 1: The content, quality, and accessibility of care.Ann Intern Med.2003;138(4):273–287.
- ,,,.Waste in the U.S. health care system: a conceptual framework.Milbank Q.2008;86(4):629–659.
- ,,,.It's the prices, stupid: why the United States is so different from other countries.Health Aff (Millwood).2003;22(3):89–105.
- . Health Care and the budget: issues and challenges for reform.2007. Available at: http://www.cbo.gov/ftpdocs/82xx/doc8255/06–21‐HealthCareReform.pdf. Accessed July 2009.
- .Overtreated: Why Too Much Medicine Is Making Us Sicker and Poorer.1st ed.New York, NY:Bloomsbury;2007.
- ,,,. Slowing the growth of U.S. health care expensitures: what are the options?2007. Available at: http://www.commonwealthfund.org/publications/publications_show.htm?doc_id=449510. Accessed July 2009.
- .More variation in use of care, more flat‐of‐the‐curve medicine.Health Aff (Millwood).2004;(Suppl Web Exclusives):VAR104–VAR107.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:419.
- ,.Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care 2008.Lebanon, NH:Dartmouth Institute for Health Policy and Clinical Practice, Center for Health Policy Research;2008:25–32.
- ,.Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care 2008.Lebanon, NH:Dartmouth Institute for Health Policy and Clinical Practice, Center for Health Policy Research;2008:2–4.
- ,,.Effects of the medical liability system in Australia, the UK, and the USA.Lancet.2006;368(9531):240–246.
- Comments on the centers for Medicare and Medicaid services plan to transition to a Medicare value‐based purchasing program for physicians and other professional services.2008. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Issues_in_the_Spotlight12008:62,73.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Transitions of Care Consensus Policy Statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine.J Gen Intern Med.2009;24(8):971–976.
- Hospitals like mine: 2006 national statistics.2006. Available at: http://www.hcupnet.ahrq.gov. Accessed July 2009.
- ,,.Evidence‐Based to Value‐Based Medicine.Chicago, IL:AMA Press;2005.
- Improved Availability of Comparative Effectiveness Information: An Essential Feature for a High‐Quality and Efficient United States Health Care System.Philadelphia, PA:American College of Physicians;2008.
- ,.Clinical practice. Palliative care.N Engl J Med.2004;350(25):2582–2590.
- ,,.The health economics of palliative care.Oncology (Williston Park).2002;16(6):801–808; discussion 808, 811–802.
- .Cost savings at the end of life. What do the data show?JAMA.1996;275(24):1907–1914.
- ,,, et al.Cost savings associated with US hospital palliative care consultation programs.Arch Intern Med.2008;168(16):1783–1790.
- ,,, et al.Toward a 21st‐century health care system: recommendations for health care reform.Ann Intern Med.2009;150(7):493–495.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- .The expanding or shrinking universe of the hospitalist.J Hosp Med.2008;3(4):288–291.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- Project BOOST.2009. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. Accessed Julyyear="2009"2009.
- ,,.The Obama administration's options for health care cost control: hope versus reality.Ann Intern Med.2009;150(7):485–489.
- Medicare pay overhaul can no longer wait. American Medical News.2009. Available at: http://www.ama‐assn.org/amednews/2009/01/12/edsa0112.htm. Accessed July 2009.
- ,,, et al.Health spending projections through 2017: the baby‐boom generation is coming to Medicare.Health Aff (Millwood).2008;27(2):w145–w155.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:380.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:374.
- National Scorecard on U.S. Health System Performance, 2008 Chartpack.New York, NY:The Commonwealth Fund;2008:6.
- ,,,,,.The implications of regional variations in medicare spending. Part 1: The content, quality, and accessibility of care.Ann Intern Med.2003;138(4):273–287.
- ,,,.Waste in the U.S. health care system: a conceptual framework.Milbank Q.2008;86(4):629–659.
- ,,,.It's the prices, stupid: why the United States is so different from other countries.Health Aff (Millwood).2003;22(3):89–105.
- . Health Care and the budget: issues and challenges for reform.2007. Available at: http://www.cbo.gov/ftpdocs/82xx/doc8255/06–21‐HealthCareReform.pdf. Accessed July 2009.
- .Overtreated: Why Too Much Medicine Is Making Us Sicker and Poorer.1st ed.New York, NY:Bloomsbury;2007.
- ,,,. Slowing the growth of U.S. health care expensitures: what are the options?2007. Available at: http://www.commonwealthfund.org/publications/publications_show.htm?doc_id=449510. Accessed July 2009.
- .More variation in use of care, more flat‐of‐the‐curve medicine.Health Aff (Millwood).2004;(Suppl Web Exclusives):VAR104–VAR107.
- Health, United States, 2007: Chartbook on Trends in the Health of Americans.Hyattsville, MD:National Center for Health Statistics;2007:419.
- ,.Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care 2008.Lebanon, NH:Dartmouth Institute for Health Policy and Clinical Practice, Center for Health Policy Research;2008:25–32.
- ,.Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care 2008.Lebanon, NH:Dartmouth Institute for Health Policy and Clinical Practice, Center for Health Policy Research;2008:2–4.
- ,,.Effects of the medical liability system in Australia, the UK, and the USA.Lancet.2006;368(9531):240–246.
- Comments on the centers for Medicare and Medicaid services plan to transition to a Medicare value‐based purchasing program for physicians and other professional services.2008. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Issues_in_the_Spotlight12008:62,73.
- ,,, et al.A reengineered hospital discharge program to decrease rehospitalization: a randomized trial.Ann Intern Med.2009;150(3):178–187.
- ,,, et al.Transitions of Care Consensus Policy Statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine.J Gen Intern Med.2009;24(8):971–976.
- Hospitals like mine: 2006 national statistics.2006. Available at: http://www.hcupnet.ahrq.gov. Accessed July 2009.
- ,,.Evidence‐Based to Value‐Based Medicine.Chicago, IL:AMA Press;2005.
- Improved Availability of Comparative Effectiveness Information: An Essential Feature for a High‐Quality and Efficient United States Health Care System.Philadelphia, PA:American College of Physicians;2008.
- ,.Clinical practice. Palliative care.N Engl J Med.2004;350(25):2582–2590.
- ,,.The health economics of palliative care.Oncology (Williston Park).2002;16(6):801–808; discussion 808, 811–802.
- .Cost savings at the end of life. What do the data show?JAMA.1996;275(24):1907–1914.
- ,,, et al.Cost savings associated with US hospital palliative care consultation programs.Arch Intern Med.2008;168(16):1783–1790.
- ,,, et al.Toward a 21st‐century health care system: recommendations for health care reform.Ann Intern Med.2009;150(7):493–495.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- .The expanding or shrinking universe of the hospitalist.J Hosp Med.2008;3(4):288–291.
- ,,,.Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists.J Hosp Med.2007;2(5):314–323.
- Project BOOST.2009. Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/CT_Home.cfm. Accessed Julyyear="2009"2009.
- ,,.The Obama administration's options for health care cost control: hope versus reality.Ann Intern Med.2009;150(7):485–489.
Heart Failure Program Readmissions
Congestive heart failure (CHF) is a common disease with high mortality and morbidity.1, 2 Better physiological understanding has led to significant advances in therapy in recent years, with synthesis of this evidence into widely available treatment guidelines.3, 4 However, patients who have had an acute hospitalization with heart failure continue to have a high rate of symptomatic relapse, with up to 25% readmitted within 3 months.2 One of the major challenges in heart failure therapy is to avert these relapses to prevent hospital readmission.
Angiotensin‐converting enzyme (ACE) inhibitors, beta‐blockers, and spironolactone have promised a reduction in hospitalization rates as well as mortality; however, suboptimal prescribing5 and adherence to therapy6, 7 may limit their anticipated benefits. This has led to interest in improved systems of care to reduce hospital utilization. Such approaches have included improved systems for optimizing medications,68 comprehensive discharge planning and postdischarge support,914 and self‐management and case management strategies1517 to enhance patient participation in care.
Combinations of these strategies are known as disease management programs (DMPs), and trials of such combination strategies to improve patient outcomes have been promising.1823 Recognized features4 include skilled multidisciplinary team care; individualized guideline‐based treatment plans that may include dietary and exercise programs as well as optimal pharmacological therapy; patient education and self‐management strategies; improved integration between hospital and community care providers; vigilant follow‐up including prompt review after hospitalization; ready access to expert assessment in the event of deterioration; and regular monitoring with expert titration of therapy, through clinics, home visits, or telemonitoring. Several randomized controlled trials have suggested that DMPs may reduce heart failure‐related9, 1517 and all‐cause9, 10 readmissions. Meta‐analyses12, 1823 have demonstrated reduction in risk of all‐cause readmission of 12% to 25% as well as a reduction in mortality of 14% to 25%.
Trials of DMPs have generally involved careful participant selection, and differences in methods and outcome reporting have led some reviewers to be circumspect in their interpretation of the impact of these programs on readmission rates.23 A large, real‐world quality improvement program conducted as part of the Royal Australasian College of Physicians Clinical Support Systems Project provided an opportunity to measure whether a multifaceted program targeting a representative group of patients with CHF and their healthcare providers could reduce readmission rates. As previously published, this program delivered measurable improvements in processes of care including evidence‐based prescribing, adherence, multidisciplinary involvement, and discharge communication, associated with a reduction in 12‐month mortality.24
Objective
The Brisbane Cardiac Consortium sought to improve processes of care for patients with CHF by using evidence‐based strategies targeting patients and their healthcare providers to optimize uptake of management guidelines, improve discharge processes between hospital and primary care, and increase patient participation in care. We hypothesized that the program would reduce hospital readmissions in the intervention patients in the first 12 months following discharge.
Methods
Setting
The program was conducted in 3 metropolitan public teaching hospitals in Brisbane, Australia (Royal Brisbane, Princess Alexandra, and Queen Elizabeth II Hospitals) and their associated Divisions of General Practice, targeting the hospital and posthospital care of patients with CHF.
Design
The study was a prospective time series study. Consecutive participants were enrolled continuously between October 1, 2000 and August 31, 2002. Interventions were introduced progressively as systems matured. For evaluation purposes, we predefined a baseline cohort (October 1, 2000 to April 17, 2001) who were admitted prior to implementation of any interventions, and an intervention cohort (February 15, 2002 to August 31, 2002) who were admitted after all interventions were mature. The study was approved by the Ethics Committees of all participating institutions.
Participants
All patients with a recorded clinical diagnosis of CHF within 48 hours of hospital presentation, and evidence of at least 2 supporting clinical signs (raised jugular venous pressure, third or fourth heart sounds, bilateral chest crackles, dependent edema, or cardiomegaly and/or pulmonary edema on chest x‐ray) were identified prospectively by trained research nurses. Patients were ineligible for reevaluation if they had already been enrolled in the study. Detailed data were abstracted from the medical record including demographics, illness characteristics, and comorbid conditions.
Interventions
Provider‐directed Interventions
Provider‐directed interventions aimed to improve clinician compliance with agreed management guidelines using decision support tools, reminders, education and academic detailing, and regular performance feedback. These interventions were delivered by project staff and local clinical leaders and were directed toward both hospital clinicians (internists and cardiologists) and general practitioners providing community care.
Patient‐directed Interventions
Patient‐directed interventions included written evidence‐based patient education, pharmacist discharge medication review and inpatient education, and patient diaries. Comprehensive discharge summaries including target‐directed management plans were provided to the general practitioner and community pharmacist.
Participants were considered suitable for more intensive posthospital intervention and follow‐up if they: (1) did not have cognitive impairment or psychiatric illness which would preclude participation in self‐care; (2) did not have a life expectancy due to comorbidities estimated to be less than 6 months; (3) had a stable residence in the community where they could be contacted by telephone; (4) attended a general practitioner within the greater Brisbane area; and (5) consented to more detailed follow‐up. In the baseline phase, this intensive group was contacted by nursing staff at 1, 3, 6, and 12 months for data collection purposes; in the intervention phase, these participants received enhanced predischarge pharmacist education; postdischarge pharmacist telephone follow‐up of medication understanding and adherence; telephone reminders from project nursing staff at 1, 3, 6, and 12 months to attend their general practitioner; and individualized, written, guideline‐based reminders sent to participating general practitioners.
Measures and Analysis
The primary outcome measure was all‐cause hospital readmission over 12 months. Secondary outcomes included 12‐month all‐cause mortality, 12‐month readmissions due to CHF, total hospital days, and the combined endpoint of death or readmission (ie, readmission‐free survival) at 12 months.
Readmission data were obtained from the Queensland Health Information Centre by matching patient data with the Queensland Hospital Admitted Patient Data Collection. Admission to any Queensland hospital is captured in this database. Readmission was defined as due to CHF (same‐cause) if a principal diagnosis code from ICD‐10‐AM code chapter I50 was assigned. Mortality data were obtained from the Australian Institute of Health and Welfare (AIHW) National Death Index.
Processes of inpatient care were collected by trained research nurses using a standardized structured chart abstraction tool. Data items were based on guideline recommendations for patient assessment, investigation, and management.
All analyses were conducted using SAS version for Windows 9.1 (SAS Institute, Cary, NC). Baseline and intervention patient characteristics were compared using independent samples t test for continuous variables and contingency tables with chi‐square tests for proportions.
Logistic regression models adjusted for hospital and posthospital intensity (considered to be significant potential confounders) were used to test the strength of association between the intervention and readmission (or death and readmission); Cox proportional hazards model was used to assess the time to first readmission or death. A Wilcoxon 2‐sample test was used to compare total number of days in hospital over the 12‐month follow‐up period, as these data were highly positively skewed; means rather than medians are reported, as the median was 0 in each group and hence uninformative. Frequency of readmission was compared using Poisson regression adjusted for hospital. A P value of 0.05 was considered significant in all analyses.
Preliminary analysis revealed a number of differences in baseline clinical characteristics between the 2 groups. To account for measured differences other than hospital and intervention intensity, propensity scores (the conditional probability of assignment to a particular treatment group given a vector of observed covariates) were developed using a logistic model with the control or intervention group as the dependent variable and baseline patient characteristic variables with P < 0.2 (as shown in Table 1) as the independent variables. The equation obtained from this model was used to estimate a propensity score for each patient. These scores along with hospital and intervention intensity were then used to provide estimates adjusted for baseline differences between the control and intervention groups.25
| Characteristic | Baseline (n = 197) | Intervention (n = 219) | P Value |
|---|---|---|---|
| |||
| Hospital, n (%) | 0.001 | ||
| 1 | 75 (38) | 100 (46) | |
| 2 | 40 (20) | 17 (8) | |
| 3 | 82 (42) | 102 (46) | |
| Age (years), mean (range) | 75 (24‐100) | 78 (32‐102) | 0.059 |
| Female, n (%) | 103 (52) | 118 (54) | 0.74 |
| Hostel resident, n (%) | 15 (8) | 38 (17) | <0.01 |
| Previous CHF admission, n (%) | 52 (26) | 26 (12) | <0.01 |
| Contributing factors, n (%) | |||
| Hypertension | 104 (53) | 139 (63) | 0.027 |
| Coronary disease | 107 (54) | 118 (54) | 0.93 |
| Valvular disease | 20 (10) | 45 (21) | <0.01 |
| Cardiomyopathy | 29 (15) | 33 (15) | 0.92 |
| NYHA class III/IV, n (%) | 143 (73) | 155 (71) | 0.68 |
| Atrial fibrillation, n (%) | 65 (33) | 78 (36) | 0.57 |
| LVEF % (mean) | 24 | 28 | 0.10 |
| Cardiologist care, n (%) | 42 (21) | 61 (28) | 0.12 |
| Comorbidity score | 2.6 (1,8) | 2.7 (1,10) | 0.52 |
Results
There were 220 patients identified with a clinical diagnosis of CHF during the baseline period, and 235 during the intervention period. Figure 1 shows ascertainment, in‐hospital mortality, and eligibility rates for the 2 cohorts. Eighty‐nine (45%) of baseline patients and 76 (35%) of intervention patients received intensive posthospital follow‐up as described above. Information on readmission was available for 197 baseline patients and 219 intervention patients discharged alive; this is the sample used for all analyses in this report. Table 1 shows the demographic and clinical characteristics of these patients. Table 2 summarizes the previously reported improvements in processes of care.
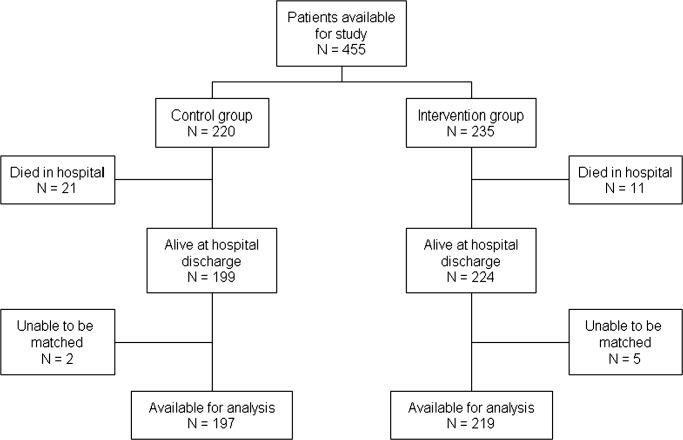
| Process indicator | Baseline (n = 220) [n (%)>] | Intervention (n = 235) [n (%)] | P Value |
|---|---|---|---|
| |||
| Assessment of reversible triggers | 166 (75) | 211 (90) | <0.001 |
| DVT prophylaxis | 57 (26) | 148 (63) | <0.001 |
| Imaging of left ventricular function | 135 (61) | 164 (70) | 0.002 |
| Scheduled outpatient visit within 30 days | 87 (46)* | 130 (59) | 0.005 |
| ACE inhibitor prescription at discharge | 136 (71)* | 163 (74) | 0.46 |
| Beta‐blocker prescription at discharge | 61 (32)* | 113 (52) | <0.001 |
| Avoid deleterious agents at discharge | 180 (94)* | 214 (98) | 0.79 |
Duing the 12‐month follow‐up, 107 (49%) of intervention patients were readmitted to the hospital compared to 71 (36%) of control patients, representing a 1.7‐fold increase in the adjusted probability of readmission in the intervention group (odds ratio [OR] = 1.71, 95% confidence interval [CI] = 1.14‐2.56; P = 0.009). As shown in Table 3, this was partly balanced by a trend toward reduced post‐hospital mortality, such that no significant difference was seen in readmission‐free survival.
| Baseline (%) | Intervention (%) | OR (95% CI) | P Value | |
|---|---|---|---|---|
| ||||
| Readmitted within 12 months | 71/197 (36) | 107/219 (49) | 1.71* (1.14, 2.56); 1.90 (1.24, 2.91) | 0.009; 0.004 |
| Death within 12 months | 59/197 (30) | 53/219 (24) | 0.68* (0.44, 1.07) | 0.099 |
| Death or readmission within 12 months | 104/197 (53) | 133/219 (61) | 1.30* (0.87, 1.93); 1.36 (0.89, 2.08) | 0.20; 0.15 |
Time‐to‐event analysis (Figures 2 and 3) demonstrated similar findings, with a significant reduction in time to first readmission in the intervention group (adjusted hazard ratio [HR] = 1.43; 95% CI = 1.04‐1.97; P = 0.046) but no difference in time to death or first readmission (adjusted HR = 1.14; 95% CI = 0.86‐1.46; P = 0.36).
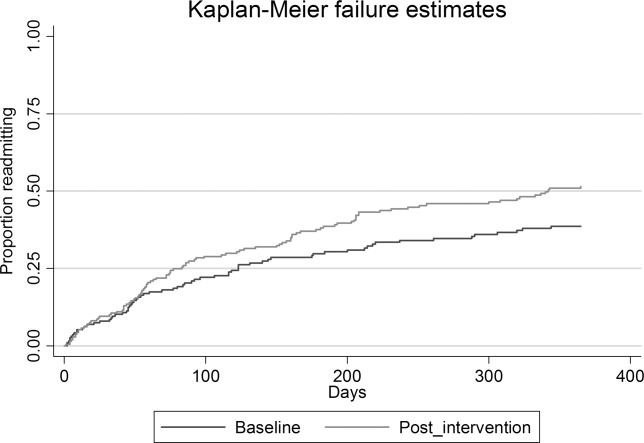
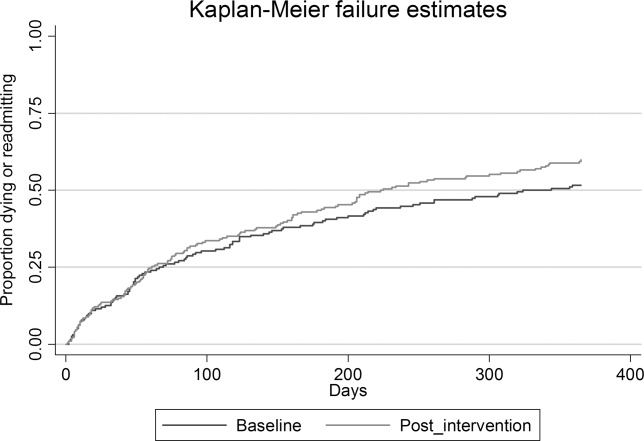
There was a trend to increased readmissions attributed to heart failure: 47 (21.5%) of intervention patients compared to 33 (16.7%) in the baseline group (OR = 1.30; 95% CI = 0.87‐1.93; P = 0.20). No significant difference was demonstrated in the frequency of readmissions (average 0.75 admission per participant per year in baseline, compared to 0.93 intervention; P = 0.32) nor the mean number of days in hospital in 12 months subsequent to the index admission (5.9 in the baseline group compared to 6.5 in the intervention group; P = 0.1).
Subgroup analysis by intervention intensity showed similar results, with 42 of 76 (55.3%) intensive group participants in the intervention group and 36 of 89 (40.4%) in the baseline group requiring hospital readmission within 12 months. The HR for death or readmission was estimated to be 1.27 (95% CI = 0.85‐1.9).
Discussion
In this study, heart failure patients who received a multidisciplinary intervention (including inpatient education, self‐management support, improved timely medical follow‐up, and better integration between hospital and primary care) showed a trend to improved 1‐year post‐hospital survival, but this appeared to be at the cost of increased readmissions among survivors. This occurred despite our previously reported improved optimization of pharmacological therapy both in‐hospital and posthospital with this program.18
There are a number of potential explanations for this finding, which have important implications for adoption of disease management programs. First, the intervention may not have been of sufficient intensity. Programs primarily aimed at educating providers and patients in evidence‐based guidelines, without structured postdischarge support, have not always improved clinical outcomes.26 In our study, general practitioners were supported to provide improved postdischarge care to their CHF patients, but direct postdischarge patient support was only provided to consenting patients and was limited in scope. There is still some debate about which elements of successful DMPs are most important for efficacy. Most authorities support the central importance of medication optimization, intensive education, and self‐care support. Taylor et al.23 found stronger evidence for programs using individual case management or outreach rather than clinic‐based interventions. Yu et al.27 concluded that outpatient drug titration and ready access to specialist review were factors contributing to success. In our program, even the more intensive intervention did not include regular clinical review by specialist nurses, a system for rapid review in the event of deterioration or supervised drug titration protocols. Furthermore, strategies which prompted more frequent primary care review and improved patient, carer, and general practitioner recognition of disease deterioration may have provided more opportunities to initiate readmission, especially in the absence of an alternative care pathway such as rapid‐access clinics or outreach services.28
Second, this study may reflect the reality of generalizing randomized controlled trial data to an unselected population. Many trials enrolled patients with high anticipated event rates but excluded patients with complex comorbidities, poor life expectancy, and cognitive impairment. Such studies enrolled a high‐risk population (10%‐48% of screened patients randomized) who had a relatively high readmission rate (50%‐60% at 6‐12 months) compared to our unselected population. These studies may overstate the benefits of applying heart failure DMPs in an unselected population. Galbreath et al.29 enrolled a self‐selected community sample of heart failure patients into a disease management program incorporating education, self‐management, telephone support, and advice to primary care providers and home health providers. Like our model, they demonstrated a survival benefit in the intervention group but no reduction in hospital or other healthcare utilization.
Third, only about one‐half of the readmissions were due to heart failure, again reflecting the complexity of this real‐world patient group. Interventions that focus on a single disease in patients with complex comorbidities might be expected to have only limited impact on their subsequent healthcare needs.
Fourth, findings may reflect differences in patient characteristics between the 2 cohorts. While statistical adjustment for measured differences did not have any significant impact on results, unmeasured patient characteristics may have introduced bias. The beforeafter nature of the study also raises the possibility that temporal trends in care practices influenced patient outcomes, such as changing patterns of drug and device therapies. There is conflicting evidence in the literature regarding trends in CHF readmission rates,3032 but it is possible that health system factors external to the study contributed to a higher readmission rate in the later cohort.
Finally, there was a trend toward reduction in mortality within the intervention cohort. These additional survivors might be expected to have more advanced heart failure or other comorbid disease, and therefore may have been more susceptible to deterioration and the need for inpatient care.
Conclusions
We acknowledge the weaknesses inherent in this nonrandomized study design, including convenience sampling, measured and unmeasured confounders and temporal trends in processes and systems of care. Nonetheless, this real world study suggests a note of caution in the widespread enthusiasm for chronic disease management programs. A complex bundle of interventions that resulted in measurable improvements in adherence to evidence‐based guidelines, discharge processes, integration between care providers, and patient education appeared to prolong life expectancy but increase hospital utilization. Mortality reduction in an incurable chronic disease such as heart failure will increase the burden of disease (and therefore treatment costs) unless treatments concurrently reduce disability and the frequency of symptomatic relapse.33 Whether this balance is achieved will depend on patient selection and the intensity and/or components of the intervention. These factors have not been fully defined in the literature to date.
Our study suggests that a widely applied, discharge‐focused intervention which primarily augmented the CHF management knowledge of care providers and patients, and enhanced attendance within the existing care model of primary care and internal medicine/cardiology outpatient services, improved the quality of care and may have reduced mortality at the cost of higher hospital utilization. It raises questions about whether a disease management service can achieve the uncertain promise of reduced readmissions in a cost‐effective manner outside of a high‐risk experimental population.
Acknowledgements
The authors acknowledge the contribution of the advisory and working groups of the Brisbane Cardiac Consortium. The authors appreciate the support of clinicians from the Internal Medicine, Cardiology, and Pharmacy Departments of the participating hospitals as well as staff from the Brisbane North and Brisbane Inner South Divisions of General Practice. The authors are grateful for the efforts of the staff of the PAH Clinical Services Evaluation Unit and the RBWH Internal Medicine Research Unit for data collection and data management; and the Queensland Health Information Centre and Australian Institute of Health and Welfare (AIHW) National Death Index for data matching.
- ,,,,.More ‘malignant’ than cancer? Five‐year survival following a first admission with heart failure.Eur J Heart Fail.2001;3:315–322.
- ,,, et al.;Study Group on Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology The EuroHeart Failure survey programme—a survey on the quality of care among patients with heart failure in Europe.Part 1: patient characteristics and diagnosis.Eur Heart J.2003;24(5):442–463.
- National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand Chronic Heart Failure Clinical Practice Guidelines Writing Panel.Guidelines for management of patients with chronic heart failure in Australia.Med J Aust.2001;174:459–466.
- ,,.Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology.Eur Heart J.2005;26(11):1115–1140.
- ,,, et al.Quality of care of patients hospitalized with congestive heart failure.Intern Med J.2003;33(4):140–151.
- ,,, et al.Improvements in 1‐year cardiovascular clinical outcomes associated with a hospital‐based discharge medication program.Ann Intern Med.2004;141(6):446–453.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team.Arch Intern Med.1999;159(16):1939–1945.
- .Impact of pharmacist interventions on hospital readmissions for heart failure.Am J Health Syst Pharm.1999;56:1339–1342.
- ,,.Effects of a multidisciplinary, home‐based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study.Lancet.1999;354:1077–1083.
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,.Home‐based intervention in congestive heart failure. Long‐term implications on readmission and survival.Circulation.2002;105(24):2861–2866.
- ,,,,,.Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure. A meta‐analysis.JAMA.2004;291(11):1358–1367.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders. A randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,,,,.Quality of life of individuals with heart failure. A randomized trial of the effectiveness of two models of hospital‐to‐home transition.Med Care.2002;40(4):271–282.
- ,,, et al.Randomised controlled trial of specialist nurse intervention in heart failure.BMJ.2001;323(7315):715–718.
- ,,,,,.Effect of a standardised nurse case‐management telephone intervention on resource use in patients with chronic heart failure.Arch Intern Med.2002;162:705–712.
- ,,,,,.Randomized trial of an education and support intervention to prevent readmission of patients with heart failure.J Am Coll Cardiol.2002;39:83–89.
- ,,,.A systematic review of randomized trials of disease management programs in heart failure.Am J Med.2001;2001(110):378–384.
- ,,,.Multidisciplinary strategies for the management of heart failure patients at high risk for admission.J Am Coll Cardiol.2004;44(4):810–819.
- ,,,,.Effectiveness of comprehensive disease management programmes in improving clinical outcomes in heart failure patients. A meta‐analysis.Eur J Heart Fail.2005;7:1133–1144.
- ,,,.The effectiveness of disease management programmes in reducing hospital re‐admission in older patients with heart failure: a systematic review and meta‐analysis of published reports.Eur Heart J.2004;25:1570–1595.
- ,,,,,.Systematic review of multidisciplinary interventions in heart failure.Heart.2005;91:899–906.
- ,,, et al.Clinical service organisation for heart failure.Cochrane Database Syst Rev.2005(2):CD002752.pub2.
- ,,, et al.Achieving better in‐hospital and after‐hospital care of patients with acute cardiac disease.Med J Aust.2004;180:S83–S88.
- .Propensity score methods for bias reduction in the comparison of a treatment to a non‐randomized control group.Stat Med.1998;17:2265–2281.
- ,,,,,.The results of a randomized trial of a quality improvement intervention in the care of patients with heart failure.Am J Med.2000;109(6):443–449.
- ,,.Disease management programmes for older people with heart failure: crucial characteristics which improve post‐discharge outcomes.Eur Heart J.2006;27:596–612.
- ,,.Does increased access to primary care reduce hospital readmissions?N Engl J Med.1996;334:1441–1447.
- ,,, et al.Long‐term healthcare and cost outcomes of disease management in a large, randomized, community‐based population with heart failure.Circulation.2004;110(23):3518–3526.
- ,,,.Trends in postdischarge mortality and readmissions. Has length of stay declined too far?Arch Intern Med.2004;164:538–544.
- ,,,.Is the prognosis of heart failure improving?Eur J Heart Fail.1999;1(3):229–241.
- ,,, et al.Trends in heart failure outcomes and pharmacotherapy: 1992 to 2000.Am J Med.2004;116(9):581–589.
- ,,.Repeated hospitalization for the same disease: a multiplier of national health costs.Milbank Mem Fund Q.1908;58(3):454–471.
Congestive heart failure (CHF) is a common disease with high mortality and morbidity.1, 2 Better physiological understanding has led to significant advances in therapy in recent years, with synthesis of this evidence into widely available treatment guidelines.3, 4 However, patients who have had an acute hospitalization with heart failure continue to have a high rate of symptomatic relapse, with up to 25% readmitted within 3 months.2 One of the major challenges in heart failure therapy is to avert these relapses to prevent hospital readmission.
Angiotensin‐converting enzyme (ACE) inhibitors, beta‐blockers, and spironolactone have promised a reduction in hospitalization rates as well as mortality; however, suboptimal prescribing5 and adherence to therapy6, 7 may limit their anticipated benefits. This has led to interest in improved systems of care to reduce hospital utilization. Such approaches have included improved systems for optimizing medications,68 comprehensive discharge planning and postdischarge support,914 and self‐management and case management strategies1517 to enhance patient participation in care.
Combinations of these strategies are known as disease management programs (DMPs), and trials of such combination strategies to improve patient outcomes have been promising.1823 Recognized features4 include skilled multidisciplinary team care; individualized guideline‐based treatment plans that may include dietary and exercise programs as well as optimal pharmacological therapy; patient education and self‐management strategies; improved integration between hospital and community care providers; vigilant follow‐up including prompt review after hospitalization; ready access to expert assessment in the event of deterioration; and regular monitoring with expert titration of therapy, through clinics, home visits, or telemonitoring. Several randomized controlled trials have suggested that DMPs may reduce heart failure‐related9, 1517 and all‐cause9, 10 readmissions. Meta‐analyses12, 1823 have demonstrated reduction in risk of all‐cause readmission of 12% to 25% as well as a reduction in mortality of 14% to 25%.
Trials of DMPs have generally involved careful participant selection, and differences in methods and outcome reporting have led some reviewers to be circumspect in their interpretation of the impact of these programs on readmission rates.23 A large, real‐world quality improvement program conducted as part of the Royal Australasian College of Physicians Clinical Support Systems Project provided an opportunity to measure whether a multifaceted program targeting a representative group of patients with CHF and their healthcare providers could reduce readmission rates. As previously published, this program delivered measurable improvements in processes of care including evidence‐based prescribing, adherence, multidisciplinary involvement, and discharge communication, associated with a reduction in 12‐month mortality.24
Objective
The Brisbane Cardiac Consortium sought to improve processes of care for patients with CHF by using evidence‐based strategies targeting patients and their healthcare providers to optimize uptake of management guidelines, improve discharge processes between hospital and primary care, and increase patient participation in care. We hypothesized that the program would reduce hospital readmissions in the intervention patients in the first 12 months following discharge.
Methods
Setting
The program was conducted in 3 metropolitan public teaching hospitals in Brisbane, Australia (Royal Brisbane, Princess Alexandra, and Queen Elizabeth II Hospitals) and their associated Divisions of General Practice, targeting the hospital and posthospital care of patients with CHF.
Design
The study was a prospective time series study. Consecutive participants were enrolled continuously between October 1, 2000 and August 31, 2002. Interventions were introduced progressively as systems matured. For evaluation purposes, we predefined a baseline cohort (October 1, 2000 to April 17, 2001) who were admitted prior to implementation of any interventions, and an intervention cohort (February 15, 2002 to August 31, 2002) who were admitted after all interventions were mature. The study was approved by the Ethics Committees of all participating institutions.
Participants
All patients with a recorded clinical diagnosis of CHF within 48 hours of hospital presentation, and evidence of at least 2 supporting clinical signs (raised jugular venous pressure, third or fourth heart sounds, bilateral chest crackles, dependent edema, or cardiomegaly and/or pulmonary edema on chest x‐ray) were identified prospectively by trained research nurses. Patients were ineligible for reevaluation if they had already been enrolled in the study. Detailed data were abstracted from the medical record including demographics, illness characteristics, and comorbid conditions.
Interventions
Provider‐directed Interventions
Provider‐directed interventions aimed to improve clinician compliance with agreed management guidelines using decision support tools, reminders, education and academic detailing, and regular performance feedback. These interventions were delivered by project staff and local clinical leaders and were directed toward both hospital clinicians (internists and cardiologists) and general practitioners providing community care.
Patient‐directed Interventions
Patient‐directed interventions included written evidence‐based patient education, pharmacist discharge medication review and inpatient education, and patient diaries. Comprehensive discharge summaries including target‐directed management plans were provided to the general practitioner and community pharmacist.
Participants were considered suitable for more intensive posthospital intervention and follow‐up if they: (1) did not have cognitive impairment or psychiatric illness which would preclude participation in self‐care; (2) did not have a life expectancy due to comorbidities estimated to be less than 6 months; (3) had a stable residence in the community where they could be contacted by telephone; (4) attended a general practitioner within the greater Brisbane area; and (5) consented to more detailed follow‐up. In the baseline phase, this intensive group was contacted by nursing staff at 1, 3, 6, and 12 months for data collection purposes; in the intervention phase, these participants received enhanced predischarge pharmacist education; postdischarge pharmacist telephone follow‐up of medication understanding and adherence; telephone reminders from project nursing staff at 1, 3, 6, and 12 months to attend their general practitioner; and individualized, written, guideline‐based reminders sent to participating general practitioners.
Measures and Analysis
The primary outcome measure was all‐cause hospital readmission over 12 months. Secondary outcomes included 12‐month all‐cause mortality, 12‐month readmissions due to CHF, total hospital days, and the combined endpoint of death or readmission (ie, readmission‐free survival) at 12 months.
Readmission data were obtained from the Queensland Health Information Centre by matching patient data with the Queensland Hospital Admitted Patient Data Collection. Admission to any Queensland hospital is captured in this database. Readmission was defined as due to CHF (same‐cause) if a principal diagnosis code from ICD‐10‐AM code chapter I50 was assigned. Mortality data were obtained from the Australian Institute of Health and Welfare (AIHW) National Death Index.
Processes of inpatient care were collected by trained research nurses using a standardized structured chart abstraction tool. Data items were based on guideline recommendations for patient assessment, investigation, and management.
All analyses were conducted using SAS version for Windows 9.1 (SAS Institute, Cary, NC). Baseline and intervention patient characteristics were compared using independent samples t test for continuous variables and contingency tables with chi‐square tests for proportions.
Logistic regression models adjusted for hospital and posthospital intensity (considered to be significant potential confounders) were used to test the strength of association between the intervention and readmission (or death and readmission); Cox proportional hazards model was used to assess the time to first readmission or death. A Wilcoxon 2‐sample test was used to compare total number of days in hospital over the 12‐month follow‐up period, as these data were highly positively skewed; means rather than medians are reported, as the median was 0 in each group and hence uninformative. Frequency of readmission was compared using Poisson regression adjusted for hospital. A P value of 0.05 was considered significant in all analyses.
Preliminary analysis revealed a number of differences in baseline clinical characteristics between the 2 groups. To account for measured differences other than hospital and intervention intensity, propensity scores (the conditional probability of assignment to a particular treatment group given a vector of observed covariates) were developed using a logistic model with the control or intervention group as the dependent variable and baseline patient characteristic variables with P < 0.2 (as shown in Table 1) as the independent variables. The equation obtained from this model was used to estimate a propensity score for each patient. These scores along with hospital and intervention intensity were then used to provide estimates adjusted for baseline differences between the control and intervention groups.25
| Characteristic | Baseline (n = 197) | Intervention (n = 219) | P Value |
|---|---|---|---|
| |||
| Hospital, n (%) | 0.001 | ||
| 1 | 75 (38) | 100 (46) | |
| 2 | 40 (20) | 17 (8) | |
| 3 | 82 (42) | 102 (46) | |
| Age (years), mean (range) | 75 (24‐100) | 78 (32‐102) | 0.059 |
| Female, n (%) | 103 (52) | 118 (54) | 0.74 |
| Hostel resident, n (%) | 15 (8) | 38 (17) | <0.01 |
| Previous CHF admission, n (%) | 52 (26) | 26 (12) | <0.01 |
| Contributing factors, n (%) | |||
| Hypertension | 104 (53) | 139 (63) | 0.027 |
| Coronary disease | 107 (54) | 118 (54) | 0.93 |
| Valvular disease | 20 (10) | 45 (21) | <0.01 |
| Cardiomyopathy | 29 (15) | 33 (15) | 0.92 |
| NYHA class III/IV, n (%) | 143 (73) | 155 (71) | 0.68 |
| Atrial fibrillation, n (%) | 65 (33) | 78 (36) | 0.57 |
| LVEF % (mean) | 24 | 28 | 0.10 |
| Cardiologist care, n (%) | 42 (21) | 61 (28) | 0.12 |
| Comorbidity score | 2.6 (1,8) | 2.7 (1,10) | 0.52 |
Results
There were 220 patients identified with a clinical diagnosis of CHF during the baseline period, and 235 during the intervention period. Figure 1 shows ascertainment, in‐hospital mortality, and eligibility rates for the 2 cohorts. Eighty‐nine (45%) of baseline patients and 76 (35%) of intervention patients received intensive posthospital follow‐up as described above. Information on readmission was available for 197 baseline patients and 219 intervention patients discharged alive; this is the sample used for all analyses in this report. Table 1 shows the demographic and clinical characteristics of these patients. Table 2 summarizes the previously reported improvements in processes of care.
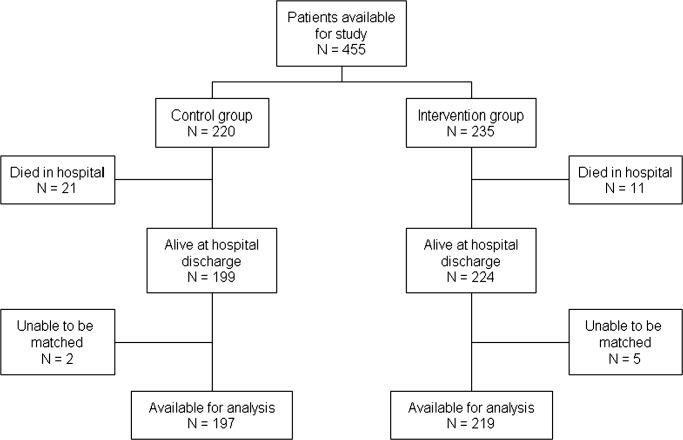
| Process indicator | Baseline (n = 220) [n (%)>] | Intervention (n = 235) [n (%)] | P Value |
|---|---|---|---|
| |||
| Assessment of reversible triggers | 166 (75) | 211 (90) | <0.001 |
| DVT prophylaxis | 57 (26) | 148 (63) | <0.001 |
| Imaging of left ventricular function | 135 (61) | 164 (70) | 0.002 |
| Scheduled outpatient visit within 30 days | 87 (46)* | 130 (59) | 0.005 |
| ACE inhibitor prescription at discharge | 136 (71)* | 163 (74) | 0.46 |
| Beta‐blocker prescription at discharge | 61 (32)* | 113 (52) | <0.001 |
| Avoid deleterious agents at discharge | 180 (94)* | 214 (98) | 0.79 |
Duing the 12‐month follow‐up, 107 (49%) of intervention patients were readmitted to the hospital compared to 71 (36%) of control patients, representing a 1.7‐fold increase in the adjusted probability of readmission in the intervention group (odds ratio [OR] = 1.71, 95% confidence interval [CI] = 1.14‐2.56; P = 0.009). As shown in Table 3, this was partly balanced by a trend toward reduced post‐hospital mortality, such that no significant difference was seen in readmission‐free survival.
| Baseline (%) | Intervention (%) | OR (95% CI) | P Value | |
|---|---|---|---|---|
| ||||
| Readmitted within 12 months | 71/197 (36) | 107/219 (49) | 1.71* (1.14, 2.56); 1.90 (1.24, 2.91) | 0.009; 0.004 |
| Death within 12 months | 59/197 (30) | 53/219 (24) | 0.68* (0.44, 1.07) | 0.099 |
| Death or readmission within 12 months | 104/197 (53) | 133/219 (61) | 1.30* (0.87, 1.93); 1.36 (0.89, 2.08) | 0.20; 0.15 |
Time‐to‐event analysis (Figures 2 and 3) demonstrated similar findings, with a significant reduction in time to first readmission in the intervention group (adjusted hazard ratio [HR] = 1.43; 95% CI = 1.04‐1.97; P = 0.046) but no difference in time to death or first readmission (adjusted HR = 1.14; 95% CI = 0.86‐1.46; P = 0.36).
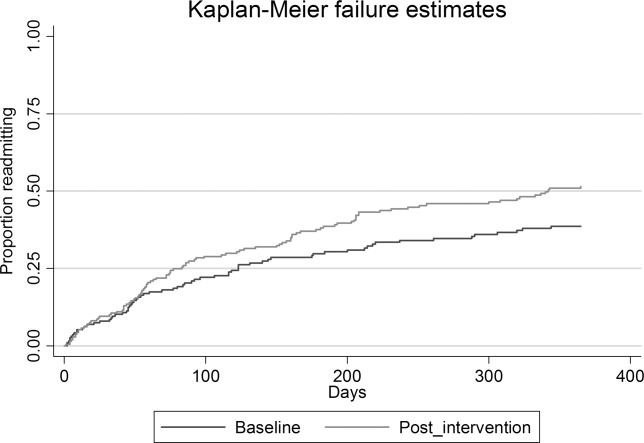
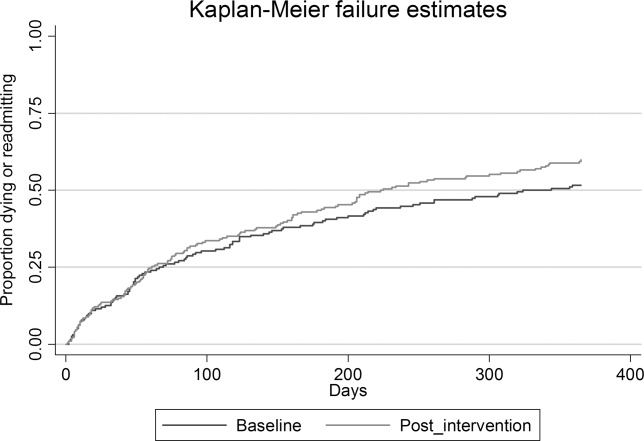
There was a trend to increased readmissions attributed to heart failure: 47 (21.5%) of intervention patients compared to 33 (16.7%) in the baseline group (OR = 1.30; 95% CI = 0.87‐1.93; P = 0.20). No significant difference was demonstrated in the frequency of readmissions (average 0.75 admission per participant per year in baseline, compared to 0.93 intervention; P = 0.32) nor the mean number of days in hospital in 12 months subsequent to the index admission (5.9 in the baseline group compared to 6.5 in the intervention group; P = 0.1).
Subgroup analysis by intervention intensity showed similar results, with 42 of 76 (55.3%) intensive group participants in the intervention group and 36 of 89 (40.4%) in the baseline group requiring hospital readmission within 12 months. The HR for death or readmission was estimated to be 1.27 (95% CI = 0.85‐1.9).
Discussion
In this study, heart failure patients who received a multidisciplinary intervention (including inpatient education, self‐management support, improved timely medical follow‐up, and better integration between hospital and primary care) showed a trend to improved 1‐year post‐hospital survival, but this appeared to be at the cost of increased readmissions among survivors. This occurred despite our previously reported improved optimization of pharmacological therapy both in‐hospital and posthospital with this program.18
There are a number of potential explanations for this finding, which have important implications for adoption of disease management programs. First, the intervention may not have been of sufficient intensity. Programs primarily aimed at educating providers and patients in evidence‐based guidelines, without structured postdischarge support, have not always improved clinical outcomes.26 In our study, general practitioners were supported to provide improved postdischarge care to their CHF patients, but direct postdischarge patient support was only provided to consenting patients and was limited in scope. There is still some debate about which elements of successful DMPs are most important for efficacy. Most authorities support the central importance of medication optimization, intensive education, and self‐care support. Taylor et al.23 found stronger evidence for programs using individual case management or outreach rather than clinic‐based interventions. Yu et al.27 concluded that outpatient drug titration and ready access to specialist review were factors contributing to success. In our program, even the more intensive intervention did not include regular clinical review by specialist nurses, a system for rapid review in the event of deterioration or supervised drug titration protocols. Furthermore, strategies which prompted more frequent primary care review and improved patient, carer, and general practitioner recognition of disease deterioration may have provided more opportunities to initiate readmission, especially in the absence of an alternative care pathway such as rapid‐access clinics or outreach services.28
Second, this study may reflect the reality of generalizing randomized controlled trial data to an unselected population. Many trials enrolled patients with high anticipated event rates but excluded patients with complex comorbidities, poor life expectancy, and cognitive impairment. Such studies enrolled a high‐risk population (10%‐48% of screened patients randomized) who had a relatively high readmission rate (50%‐60% at 6‐12 months) compared to our unselected population. These studies may overstate the benefits of applying heart failure DMPs in an unselected population. Galbreath et al.29 enrolled a self‐selected community sample of heart failure patients into a disease management program incorporating education, self‐management, telephone support, and advice to primary care providers and home health providers. Like our model, they demonstrated a survival benefit in the intervention group but no reduction in hospital or other healthcare utilization.
Third, only about one‐half of the readmissions were due to heart failure, again reflecting the complexity of this real‐world patient group. Interventions that focus on a single disease in patients with complex comorbidities might be expected to have only limited impact on their subsequent healthcare needs.
Fourth, findings may reflect differences in patient characteristics between the 2 cohorts. While statistical adjustment for measured differences did not have any significant impact on results, unmeasured patient characteristics may have introduced bias. The beforeafter nature of the study also raises the possibility that temporal trends in care practices influenced patient outcomes, such as changing patterns of drug and device therapies. There is conflicting evidence in the literature regarding trends in CHF readmission rates,3032 but it is possible that health system factors external to the study contributed to a higher readmission rate in the later cohort.
Finally, there was a trend toward reduction in mortality within the intervention cohort. These additional survivors might be expected to have more advanced heart failure or other comorbid disease, and therefore may have been more susceptible to deterioration and the need for inpatient care.
Conclusions
We acknowledge the weaknesses inherent in this nonrandomized study design, including convenience sampling, measured and unmeasured confounders and temporal trends in processes and systems of care. Nonetheless, this real world study suggests a note of caution in the widespread enthusiasm for chronic disease management programs. A complex bundle of interventions that resulted in measurable improvements in adherence to evidence‐based guidelines, discharge processes, integration between care providers, and patient education appeared to prolong life expectancy but increase hospital utilization. Mortality reduction in an incurable chronic disease such as heart failure will increase the burden of disease (and therefore treatment costs) unless treatments concurrently reduce disability and the frequency of symptomatic relapse.33 Whether this balance is achieved will depend on patient selection and the intensity and/or components of the intervention. These factors have not been fully defined in the literature to date.
Our study suggests that a widely applied, discharge‐focused intervention which primarily augmented the CHF management knowledge of care providers and patients, and enhanced attendance within the existing care model of primary care and internal medicine/cardiology outpatient services, improved the quality of care and may have reduced mortality at the cost of higher hospital utilization. It raises questions about whether a disease management service can achieve the uncertain promise of reduced readmissions in a cost‐effective manner outside of a high‐risk experimental population.
Acknowledgements
The authors acknowledge the contribution of the advisory and working groups of the Brisbane Cardiac Consortium. The authors appreciate the support of clinicians from the Internal Medicine, Cardiology, and Pharmacy Departments of the participating hospitals as well as staff from the Brisbane North and Brisbane Inner South Divisions of General Practice. The authors are grateful for the efforts of the staff of the PAH Clinical Services Evaluation Unit and the RBWH Internal Medicine Research Unit for data collection and data management; and the Queensland Health Information Centre and Australian Institute of Health and Welfare (AIHW) National Death Index for data matching.
Congestive heart failure (CHF) is a common disease with high mortality and morbidity.1, 2 Better physiological understanding has led to significant advances in therapy in recent years, with synthesis of this evidence into widely available treatment guidelines.3, 4 However, patients who have had an acute hospitalization with heart failure continue to have a high rate of symptomatic relapse, with up to 25% readmitted within 3 months.2 One of the major challenges in heart failure therapy is to avert these relapses to prevent hospital readmission.
Angiotensin‐converting enzyme (ACE) inhibitors, beta‐blockers, and spironolactone have promised a reduction in hospitalization rates as well as mortality; however, suboptimal prescribing5 and adherence to therapy6, 7 may limit their anticipated benefits. This has led to interest in improved systems of care to reduce hospital utilization. Such approaches have included improved systems for optimizing medications,68 comprehensive discharge planning and postdischarge support,914 and self‐management and case management strategies1517 to enhance patient participation in care.
Combinations of these strategies are known as disease management programs (DMPs), and trials of such combination strategies to improve patient outcomes have been promising.1823 Recognized features4 include skilled multidisciplinary team care; individualized guideline‐based treatment plans that may include dietary and exercise programs as well as optimal pharmacological therapy; patient education and self‐management strategies; improved integration between hospital and community care providers; vigilant follow‐up including prompt review after hospitalization; ready access to expert assessment in the event of deterioration; and regular monitoring with expert titration of therapy, through clinics, home visits, or telemonitoring. Several randomized controlled trials have suggested that DMPs may reduce heart failure‐related9, 1517 and all‐cause9, 10 readmissions. Meta‐analyses12, 1823 have demonstrated reduction in risk of all‐cause readmission of 12% to 25% as well as a reduction in mortality of 14% to 25%.
Trials of DMPs have generally involved careful participant selection, and differences in methods and outcome reporting have led some reviewers to be circumspect in their interpretation of the impact of these programs on readmission rates.23 A large, real‐world quality improvement program conducted as part of the Royal Australasian College of Physicians Clinical Support Systems Project provided an opportunity to measure whether a multifaceted program targeting a representative group of patients with CHF and their healthcare providers could reduce readmission rates. As previously published, this program delivered measurable improvements in processes of care including evidence‐based prescribing, adherence, multidisciplinary involvement, and discharge communication, associated with a reduction in 12‐month mortality.24
Objective
The Brisbane Cardiac Consortium sought to improve processes of care for patients with CHF by using evidence‐based strategies targeting patients and their healthcare providers to optimize uptake of management guidelines, improve discharge processes between hospital and primary care, and increase patient participation in care. We hypothesized that the program would reduce hospital readmissions in the intervention patients in the first 12 months following discharge.
Methods
Setting
The program was conducted in 3 metropolitan public teaching hospitals in Brisbane, Australia (Royal Brisbane, Princess Alexandra, and Queen Elizabeth II Hospitals) and their associated Divisions of General Practice, targeting the hospital and posthospital care of patients with CHF.
Design
The study was a prospective time series study. Consecutive participants were enrolled continuously between October 1, 2000 and August 31, 2002. Interventions were introduced progressively as systems matured. For evaluation purposes, we predefined a baseline cohort (October 1, 2000 to April 17, 2001) who were admitted prior to implementation of any interventions, and an intervention cohort (February 15, 2002 to August 31, 2002) who were admitted after all interventions were mature. The study was approved by the Ethics Committees of all participating institutions.
Participants
All patients with a recorded clinical diagnosis of CHF within 48 hours of hospital presentation, and evidence of at least 2 supporting clinical signs (raised jugular venous pressure, third or fourth heart sounds, bilateral chest crackles, dependent edema, or cardiomegaly and/or pulmonary edema on chest x‐ray) were identified prospectively by trained research nurses. Patients were ineligible for reevaluation if they had already been enrolled in the study. Detailed data were abstracted from the medical record including demographics, illness characteristics, and comorbid conditions.
Interventions
Provider‐directed Interventions
Provider‐directed interventions aimed to improve clinician compliance with agreed management guidelines using decision support tools, reminders, education and academic detailing, and regular performance feedback. These interventions were delivered by project staff and local clinical leaders and were directed toward both hospital clinicians (internists and cardiologists) and general practitioners providing community care.
Patient‐directed Interventions
Patient‐directed interventions included written evidence‐based patient education, pharmacist discharge medication review and inpatient education, and patient diaries. Comprehensive discharge summaries including target‐directed management plans were provided to the general practitioner and community pharmacist.
Participants were considered suitable for more intensive posthospital intervention and follow‐up if they: (1) did not have cognitive impairment or psychiatric illness which would preclude participation in self‐care; (2) did not have a life expectancy due to comorbidities estimated to be less than 6 months; (3) had a stable residence in the community where they could be contacted by telephone; (4) attended a general practitioner within the greater Brisbane area; and (5) consented to more detailed follow‐up. In the baseline phase, this intensive group was contacted by nursing staff at 1, 3, 6, and 12 months for data collection purposes; in the intervention phase, these participants received enhanced predischarge pharmacist education; postdischarge pharmacist telephone follow‐up of medication understanding and adherence; telephone reminders from project nursing staff at 1, 3, 6, and 12 months to attend their general practitioner; and individualized, written, guideline‐based reminders sent to participating general practitioners.
Measures and Analysis
The primary outcome measure was all‐cause hospital readmission over 12 months. Secondary outcomes included 12‐month all‐cause mortality, 12‐month readmissions due to CHF, total hospital days, and the combined endpoint of death or readmission (ie, readmission‐free survival) at 12 months.
Readmission data were obtained from the Queensland Health Information Centre by matching patient data with the Queensland Hospital Admitted Patient Data Collection. Admission to any Queensland hospital is captured in this database. Readmission was defined as due to CHF (same‐cause) if a principal diagnosis code from ICD‐10‐AM code chapter I50 was assigned. Mortality data were obtained from the Australian Institute of Health and Welfare (AIHW) National Death Index.
Processes of inpatient care were collected by trained research nurses using a standardized structured chart abstraction tool. Data items were based on guideline recommendations for patient assessment, investigation, and management.
All analyses were conducted using SAS version for Windows 9.1 (SAS Institute, Cary, NC). Baseline and intervention patient characteristics were compared using independent samples t test for continuous variables and contingency tables with chi‐square tests for proportions.
Logistic regression models adjusted for hospital and posthospital intensity (considered to be significant potential confounders) were used to test the strength of association between the intervention and readmission (or death and readmission); Cox proportional hazards model was used to assess the time to first readmission or death. A Wilcoxon 2‐sample test was used to compare total number of days in hospital over the 12‐month follow‐up period, as these data were highly positively skewed; means rather than medians are reported, as the median was 0 in each group and hence uninformative. Frequency of readmission was compared using Poisson regression adjusted for hospital. A P value of 0.05 was considered significant in all analyses.
Preliminary analysis revealed a number of differences in baseline clinical characteristics between the 2 groups. To account for measured differences other than hospital and intervention intensity, propensity scores (the conditional probability of assignment to a particular treatment group given a vector of observed covariates) were developed using a logistic model with the control or intervention group as the dependent variable and baseline patient characteristic variables with P < 0.2 (as shown in Table 1) as the independent variables. The equation obtained from this model was used to estimate a propensity score for each patient. These scores along with hospital and intervention intensity were then used to provide estimates adjusted for baseline differences between the control and intervention groups.25
| Characteristic | Baseline (n = 197) | Intervention (n = 219) | P Value |
|---|---|---|---|
| |||
| Hospital, n (%) | 0.001 | ||
| 1 | 75 (38) | 100 (46) | |
| 2 | 40 (20) | 17 (8) | |
| 3 | 82 (42) | 102 (46) | |
| Age (years), mean (range) | 75 (24‐100) | 78 (32‐102) | 0.059 |
| Female, n (%) | 103 (52) | 118 (54) | 0.74 |
| Hostel resident, n (%) | 15 (8) | 38 (17) | <0.01 |
| Previous CHF admission, n (%) | 52 (26) | 26 (12) | <0.01 |
| Contributing factors, n (%) | |||
| Hypertension | 104 (53) | 139 (63) | 0.027 |
| Coronary disease | 107 (54) | 118 (54) | 0.93 |
| Valvular disease | 20 (10) | 45 (21) | <0.01 |
| Cardiomyopathy | 29 (15) | 33 (15) | 0.92 |
| NYHA class III/IV, n (%) | 143 (73) | 155 (71) | 0.68 |
| Atrial fibrillation, n (%) | 65 (33) | 78 (36) | 0.57 |
| LVEF % (mean) | 24 | 28 | 0.10 |
| Cardiologist care, n (%) | 42 (21) | 61 (28) | 0.12 |
| Comorbidity score | 2.6 (1,8) | 2.7 (1,10) | 0.52 |
Results
There were 220 patients identified with a clinical diagnosis of CHF during the baseline period, and 235 during the intervention period. Figure 1 shows ascertainment, in‐hospital mortality, and eligibility rates for the 2 cohorts. Eighty‐nine (45%) of baseline patients and 76 (35%) of intervention patients received intensive posthospital follow‐up as described above. Information on readmission was available for 197 baseline patients and 219 intervention patients discharged alive; this is the sample used for all analyses in this report. Table 1 shows the demographic and clinical characteristics of these patients. Table 2 summarizes the previously reported improvements in processes of care.
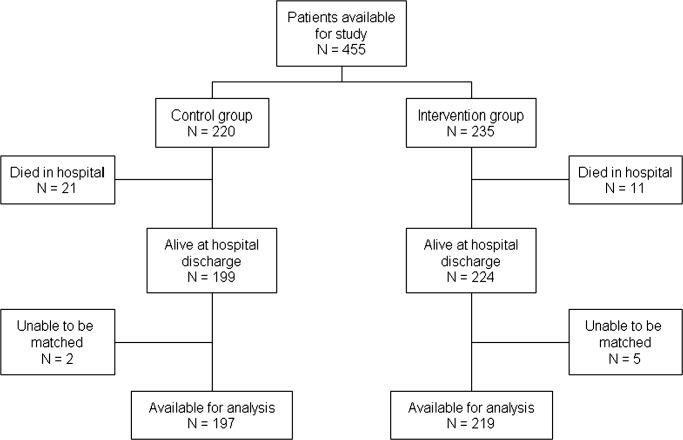
| Process indicator | Baseline (n = 220) [n (%)>] | Intervention (n = 235) [n (%)] | P Value |
|---|---|---|---|
| |||
| Assessment of reversible triggers | 166 (75) | 211 (90) | <0.001 |
| DVT prophylaxis | 57 (26) | 148 (63) | <0.001 |
| Imaging of left ventricular function | 135 (61) | 164 (70) | 0.002 |
| Scheduled outpatient visit within 30 days | 87 (46)* | 130 (59) | 0.005 |
| ACE inhibitor prescription at discharge | 136 (71)* | 163 (74) | 0.46 |
| Beta‐blocker prescription at discharge | 61 (32)* | 113 (52) | <0.001 |
| Avoid deleterious agents at discharge | 180 (94)* | 214 (98) | 0.79 |
Duing the 12‐month follow‐up, 107 (49%) of intervention patients were readmitted to the hospital compared to 71 (36%) of control patients, representing a 1.7‐fold increase in the adjusted probability of readmission in the intervention group (odds ratio [OR] = 1.71, 95% confidence interval [CI] = 1.14‐2.56; P = 0.009). As shown in Table 3, this was partly balanced by a trend toward reduced post‐hospital mortality, such that no significant difference was seen in readmission‐free survival.
| Baseline (%) | Intervention (%) | OR (95% CI) | P Value | |
|---|---|---|---|---|
| ||||
| Readmitted within 12 months | 71/197 (36) | 107/219 (49) | 1.71* (1.14, 2.56); 1.90 (1.24, 2.91) | 0.009; 0.004 |
| Death within 12 months | 59/197 (30) | 53/219 (24) | 0.68* (0.44, 1.07) | 0.099 |
| Death or readmission within 12 months | 104/197 (53) | 133/219 (61) | 1.30* (0.87, 1.93); 1.36 (0.89, 2.08) | 0.20; 0.15 |
Time‐to‐event analysis (Figures 2 and 3) demonstrated similar findings, with a significant reduction in time to first readmission in the intervention group (adjusted hazard ratio [HR] = 1.43; 95% CI = 1.04‐1.97; P = 0.046) but no difference in time to death or first readmission (adjusted HR = 1.14; 95% CI = 0.86‐1.46; P = 0.36).
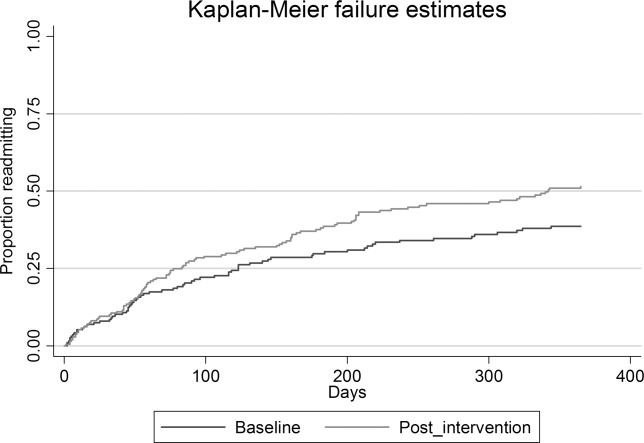
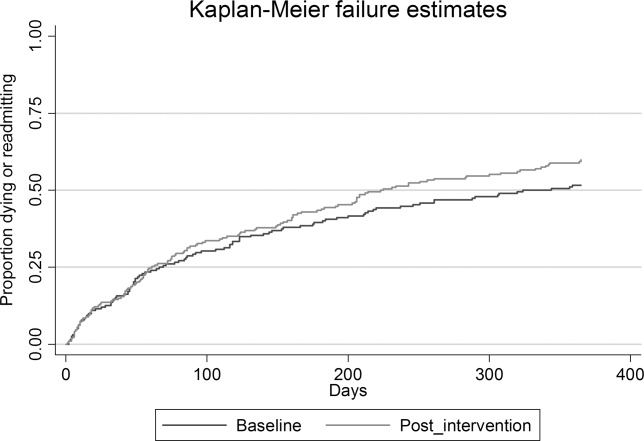
There was a trend to increased readmissions attributed to heart failure: 47 (21.5%) of intervention patients compared to 33 (16.7%) in the baseline group (OR = 1.30; 95% CI = 0.87‐1.93; P = 0.20). No significant difference was demonstrated in the frequency of readmissions (average 0.75 admission per participant per year in baseline, compared to 0.93 intervention; P = 0.32) nor the mean number of days in hospital in 12 months subsequent to the index admission (5.9 in the baseline group compared to 6.5 in the intervention group; P = 0.1).
Subgroup analysis by intervention intensity showed similar results, with 42 of 76 (55.3%) intensive group participants in the intervention group and 36 of 89 (40.4%) in the baseline group requiring hospital readmission within 12 months. The HR for death or readmission was estimated to be 1.27 (95% CI = 0.85‐1.9).
Discussion
In this study, heart failure patients who received a multidisciplinary intervention (including inpatient education, self‐management support, improved timely medical follow‐up, and better integration between hospital and primary care) showed a trend to improved 1‐year post‐hospital survival, but this appeared to be at the cost of increased readmissions among survivors. This occurred despite our previously reported improved optimization of pharmacological therapy both in‐hospital and posthospital with this program.18
There are a number of potential explanations for this finding, which have important implications for adoption of disease management programs. First, the intervention may not have been of sufficient intensity. Programs primarily aimed at educating providers and patients in evidence‐based guidelines, without structured postdischarge support, have not always improved clinical outcomes.26 In our study, general practitioners were supported to provide improved postdischarge care to their CHF patients, but direct postdischarge patient support was only provided to consenting patients and was limited in scope. There is still some debate about which elements of successful DMPs are most important for efficacy. Most authorities support the central importance of medication optimization, intensive education, and self‐care support. Taylor et al.23 found stronger evidence for programs using individual case management or outreach rather than clinic‐based interventions. Yu et al.27 concluded that outpatient drug titration and ready access to specialist review were factors contributing to success. In our program, even the more intensive intervention did not include regular clinical review by specialist nurses, a system for rapid review in the event of deterioration or supervised drug titration protocols. Furthermore, strategies which prompted more frequent primary care review and improved patient, carer, and general practitioner recognition of disease deterioration may have provided more opportunities to initiate readmission, especially in the absence of an alternative care pathway such as rapid‐access clinics or outreach services.28
Second, this study may reflect the reality of generalizing randomized controlled trial data to an unselected population. Many trials enrolled patients with high anticipated event rates but excluded patients with complex comorbidities, poor life expectancy, and cognitive impairment. Such studies enrolled a high‐risk population (10%‐48% of screened patients randomized) who had a relatively high readmission rate (50%‐60% at 6‐12 months) compared to our unselected population. These studies may overstate the benefits of applying heart failure DMPs in an unselected population. Galbreath et al.29 enrolled a self‐selected community sample of heart failure patients into a disease management program incorporating education, self‐management, telephone support, and advice to primary care providers and home health providers. Like our model, they demonstrated a survival benefit in the intervention group but no reduction in hospital or other healthcare utilization.
Third, only about one‐half of the readmissions were due to heart failure, again reflecting the complexity of this real‐world patient group. Interventions that focus on a single disease in patients with complex comorbidities might be expected to have only limited impact on their subsequent healthcare needs.
Fourth, findings may reflect differences in patient characteristics between the 2 cohorts. While statistical adjustment for measured differences did not have any significant impact on results, unmeasured patient characteristics may have introduced bias. The beforeafter nature of the study also raises the possibility that temporal trends in care practices influenced patient outcomes, such as changing patterns of drug and device therapies. There is conflicting evidence in the literature regarding trends in CHF readmission rates,3032 but it is possible that health system factors external to the study contributed to a higher readmission rate in the later cohort.
Finally, there was a trend toward reduction in mortality within the intervention cohort. These additional survivors might be expected to have more advanced heart failure or other comorbid disease, and therefore may have been more susceptible to deterioration and the need for inpatient care.
Conclusions
We acknowledge the weaknesses inherent in this nonrandomized study design, including convenience sampling, measured and unmeasured confounders and temporal trends in processes and systems of care. Nonetheless, this real world study suggests a note of caution in the widespread enthusiasm for chronic disease management programs. A complex bundle of interventions that resulted in measurable improvements in adherence to evidence‐based guidelines, discharge processes, integration between care providers, and patient education appeared to prolong life expectancy but increase hospital utilization. Mortality reduction in an incurable chronic disease such as heart failure will increase the burden of disease (and therefore treatment costs) unless treatments concurrently reduce disability and the frequency of symptomatic relapse.33 Whether this balance is achieved will depend on patient selection and the intensity and/or components of the intervention. These factors have not been fully defined in the literature to date.
Our study suggests that a widely applied, discharge‐focused intervention which primarily augmented the CHF management knowledge of care providers and patients, and enhanced attendance within the existing care model of primary care and internal medicine/cardiology outpatient services, improved the quality of care and may have reduced mortality at the cost of higher hospital utilization. It raises questions about whether a disease management service can achieve the uncertain promise of reduced readmissions in a cost‐effective manner outside of a high‐risk experimental population.
Acknowledgements
The authors acknowledge the contribution of the advisory and working groups of the Brisbane Cardiac Consortium. The authors appreciate the support of clinicians from the Internal Medicine, Cardiology, and Pharmacy Departments of the participating hospitals as well as staff from the Brisbane North and Brisbane Inner South Divisions of General Practice. The authors are grateful for the efforts of the staff of the PAH Clinical Services Evaluation Unit and the RBWH Internal Medicine Research Unit for data collection and data management; and the Queensland Health Information Centre and Australian Institute of Health and Welfare (AIHW) National Death Index for data matching.
- ,,,,.More ‘malignant’ than cancer? Five‐year survival following a first admission with heart failure.Eur J Heart Fail.2001;3:315–322.
- ,,, et al.;Study Group on Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology The EuroHeart Failure survey programme—a survey on the quality of care among patients with heart failure in Europe.Part 1: patient characteristics and diagnosis.Eur Heart J.2003;24(5):442–463.
- National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand Chronic Heart Failure Clinical Practice Guidelines Writing Panel.Guidelines for management of patients with chronic heart failure in Australia.Med J Aust.2001;174:459–466.
- ,,.Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology.Eur Heart J.2005;26(11):1115–1140.
- ,,, et al.Quality of care of patients hospitalized with congestive heart failure.Intern Med J.2003;33(4):140–151.
- ,,, et al.Improvements in 1‐year cardiovascular clinical outcomes associated with a hospital‐based discharge medication program.Ann Intern Med.2004;141(6):446–453.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team.Arch Intern Med.1999;159(16):1939–1945.
- .Impact of pharmacist interventions on hospital readmissions for heart failure.Am J Health Syst Pharm.1999;56:1339–1342.
- ,,.Effects of a multidisciplinary, home‐based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study.Lancet.1999;354:1077–1083.
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,.Home‐based intervention in congestive heart failure. Long‐term implications on readmission and survival.Circulation.2002;105(24):2861–2866.
- ,,,,,.Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure. A meta‐analysis.JAMA.2004;291(11):1358–1367.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders. A randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,,,,.Quality of life of individuals with heart failure. A randomized trial of the effectiveness of two models of hospital‐to‐home transition.Med Care.2002;40(4):271–282.
- ,,, et al.Randomised controlled trial of specialist nurse intervention in heart failure.BMJ.2001;323(7315):715–718.
- ,,,,,.Effect of a standardised nurse case‐management telephone intervention on resource use in patients with chronic heart failure.Arch Intern Med.2002;162:705–712.
- ,,,,,.Randomized trial of an education and support intervention to prevent readmission of patients with heart failure.J Am Coll Cardiol.2002;39:83–89.
- ,,,.A systematic review of randomized trials of disease management programs in heart failure.Am J Med.2001;2001(110):378–384.
- ,,,.Multidisciplinary strategies for the management of heart failure patients at high risk for admission.J Am Coll Cardiol.2004;44(4):810–819.
- ,,,,.Effectiveness of comprehensive disease management programmes in improving clinical outcomes in heart failure patients. A meta‐analysis.Eur J Heart Fail.2005;7:1133–1144.
- ,,,.The effectiveness of disease management programmes in reducing hospital re‐admission in older patients with heart failure: a systematic review and meta‐analysis of published reports.Eur Heart J.2004;25:1570–1595.
- ,,,,,.Systematic review of multidisciplinary interventions in heart failure.Heart.2005;91:899–906.
- ,,, et al.Clinical service organisation for heart failure.Cochrane Database Syst Rev.2005(2):CD002752.pub2.
- ,,, et al.Achieving better in‐hospital and after‐hospital care of patients with acute cardiac disease.Med J Aust.2004;180:S83–S88.
- .Propensity score methods for bias reduction in the comparison of a treatment to a non‐randomized control group.Stat Med.1998;17:2265–2281.
- ,,,,,.The results of a randomized trial of a quality improvement intervention in the care of patients with heart failure.Am J Med.2000;109(6):443–449.
- ,,.Disease management programmes for older people with heart failure: crucial characteristics which improve post‐discharge outcomes.Eur Heart J.2006;27:596–612.
- ,,.Does increased access to primary care reduce hospital readmissions?N Engl J Med.1996;334:1441–1447.
- ,,, et al.Long‐term healthcare and cost outcomes of disease management in a large, randomized, community‐based population with heart failure.Circulation.2004;110(23):3518–3526.
- ,,,.Trends in postdischarge mortality and readmissions. Has length of stay declined too far?Arch Intern Med.2004;164:538–544.
- ,,,.Is the prognosis of heart failure improving?Eur J Heart Fail.1999;1(3):229–241.
- ,,, et al.Trends in heart failure outcomes and pharmacotherapy: 1992 to 2000.Am J Med.2004;116(9):581–589.
- ,,.Repeated hospitalization for the same disease: a multiplier of national health costs.Milbank Mem Fund Q.1908;58(3):454–471.
- ,,,,.More ‘malignant’ than cancer? Five‐year survival following a first admission with heart failure.Eur J Heart Fail.2001;3:315–322.
- ,,, et al.;Study Group on Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology The EuroHeart Failure survey programme—a survey on the quality of care among patients with heart failure in Europe.Part 1: patient characteristics and diagnosis.Eur Heart J.2003;24(5):442–463.
- National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand Chronic Heart Failure Clinical Practice Guidelines Writing Panel.Guidelines for management of patients with chronic heart failure in Australia.Med J Aust.2001;174:459–466.
- ,,.Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology.Eur Heart J.2005;26(11):1115–1140.
- ,,, et al.Quality of care of patients hospitalized with congestive heart failure.Intern Med J.2003;33(4):140–151.
- ,,, et al.Improvements in 1‐year cardiovascular clinical outcomes associated with a hospital‐based discharge medication program.Ann Intern Med.2004;141(6):446–453.
- ,,,.Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team.Arch Intern Med.1999;159(16):1939–1945.
- .Impact of pharmacist interventions on hospital readmissions for heart failure.Am J Health Syst Pharm.1999;56:1339–1342.
- ,,.Effects of a multidisciplinary, home‐based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study.Lancet.1999;354:1077–1083.
- ,,,,,.A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure.N Engl J Med.1995;333(18):1190–1195.
- ,.Home‐based intervention in congestive heart failure. Long‐term implications on readmission and survival.Circulation.2002;105(24):2861–2866.
- ,,,,,.Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure. A meta‐analysis.JAMA.2004;291(11):1358–1367.
- ,,, et al.Comprehensive discharge planning and home follow‐up of hospitalized elders. A randomized clinical trial.JAMA.1999;281(7):613–620.
- ,,,,,.Quality of life of individuals with heart failure. A randomized trial of the effectiveness of two models of hospital‐to‐home transition.Med Care.2002;40(4):271–282.
- ,,, et al.Randomised controlled trial of specialist nurse intervention in heart failure.BMJ.2001;323(7315):715–718.
- ,,,,,.Effect of a standardised nurse case‐management telephone intervention on resource use in patients with chronic heart failure.Arch Intern Med.2002;162:705–712.
- ,,,,,.Randomized trial of an education and support intervention to prevent readmission of patients with heart failure.J Am Coll Cardiol.2002;39:83–89.
- ,,,.A systematic review of randomized trials of disease management programs in heart failure.Am J Med.2001;2001(110):378–384.
- ,,,.Multidisciplinary strategies for the management of heart failure patients at high risk for admission.J Am Coll Cardiol.2004;44(4):810–819.
- ,,,,.Effectiveness of comprehensive disease management programmes in improving clinical outcomes in heart failure patients. A meta‐analysis.Eur J Heart Fail.2005;7:1133–1144.
- ,,,.The effectiveness of disease management programmes in reducing hospital re‐admission in older patients with heart failure: a systematic review and meta‐analysis of published reports.Eur Heart J.2004;25:1570–1595.
- ,,,,,.Systematic review of multidisciplinary interventions in heart failure.Heart.2005;91:899–906.
- ,,, et al.Clinical service organisation for heart failure.Cochrane Database Syst Rev.2005(2):CD002752.pub2.
- ,,, et al.Achieving better in‐hospital and after‐hospital care of patients with acute cardiac disease.Med J Aust.2004;180:S83–S88.
- .Propensity score methods for bias reduction in the comparison of a treatment to a non‐randomized control group.Stat Med.1998;17:2265–2281.
- ,,,,,.The results of a randomized trial of a quality improvement intervention in the care of patients with heart failure.Am J Med.2000;109(6):443–449.
- ,,.Disease management programmes for older people with heart failure: crucial characteristics which improve post‐discharge outcomes.Eur Heart J.2006;27:596–612.
- ,,.Does increased access to primary care reduce hospital readmissions?N Engl J Med.1996;334:1441–1447.
- ,,, et al.Long‐term healthcare and cost outcomes of disease management in a large, randomized, community‐based population with heart failure.Circulation.2004;110(23):3518–3526.
- ,,,.Trends in postdischarge mortality and readmissions. Has length of stay declined too far?Arch Intern Med.2004;164:538–544.
- ,,,.Is the prognosis of heart failure improving?Eur J Heart Fail.1999;1(3):229–241.
- ,,, et al.Trends in heart failure outcomes and pharmacotherapy: 1992 to 2000.Am J Med.2004;116(9):581–589.
- ,,.Repeated hospitalization for the same disease: a multiplier of national health costs.Milbank Mem Fund Q.1908;58(3):454–471.
Copyright © 2010 Society of Hospital Medicine
UGIB vs. LGIB
Gastrointestinal bleeding (GIB) is a frequent reason for acute hospitalization, with estimated rates of hospitalization at 375 per 100,000 per year in the United States.1 GIB is not a specific disease but rather a diverse set of conditions that lead to the clinical manifestations associated with bleeding into the gastrointestinal tract. One of the most commonly used organizing frameworks in gastrointestinal bleeding is the differentiation between upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB). There are important differences in the etiologies between the 2 sources. For example, acid‐related disease is a common etiology in UGIB but does not occur in LGIB. While some aspects of the acute management are shared between UGIB and LGIB, important differences exist in the management, including initial endoscopy and medication choice. There have been few direct comparisons of rates, resource use, and clinical outcomes between UGIB and LGIB.
Historically, rates of UGIB have been reported to exceed those of LGIB by 2‐fold to 8‐fold.25 Protocols, clinical practice guidelines, and policy decisions reflect this emphasis on UGIB.68 Among 9 guidelines hosted by National Guideline Clearinghouse addressing GIB, 6 were focused on UGIB, 2 on both UGIB and LGIB, and only 1 on LGIB.9 There are several reasons to believe that these relative incidence rates may not be accurate. First, recent advances in therapy and prevention of UGIB, such as the treatment of Helicobacter pylori infection; proton pump inhibitors (PPIs); and selective cyclooxygenase‐2 (COX‐2) inhibitors, may have affected the epidemiology of gastrointestinal bleeding.1016 Among these therapies, only COX‐2 inhibitors may also reduce the incidence of LGIB.14, 1618 Therefore, these advances may result in a disproportionate drop in UGIB relative to LGIB. In addition, known risk factors for both LGIB and UGIB, including advancing age and renal failure, are increasing in the general population.5, 19, 20 Finally, given the recent increased recommendations for aspirin therapy and systemic anticoagulation, exposure to aspirin and warfarin have increased, both risk factors for LGIB and UGIB.2124 Indeed, recent studies in the epidemiology of UGIB do suggest a changing pattern of etiologies of UGIB reflecting these advances.25 One study examining rates of both UGIB and LGIB demonstrate a decrease in hospitalizations overall for GIB driven by a reduction in UGIB while at the same time reporting an increase in the incidence of hospitalization for LGIB.1
In addition to a changing epidemiology, a second reason for a potential underestimation of LGIB incidence is one of methodology. There are well‐recognized limitations with using purely administrative data due to difficulties in accurately identifying patients with LGIB.26
Studies using large administrative databases may not accurately identify LGIB because of the poor sensitivity and specificity of International Classification of Diseases, Ninth revision, Clinical Modification (ICD‐9) codes for LGIB.5 While there are standard methods of identifying patients with UGIB using ICD‐9 codes,19 there is not an accepted standard for LGIB. Thus, estimates using only ICD‐9 codes may overidentify or underidentify patients with LGIB. Prior studies that have most accurately identified patients with LGIB used a 2‐step method to address this issue. The initial ICD‐9 identification included a high sensitivity/low specificity approach. These identified patient charts undergo chart review to confirm the presence of an LGIB.5 This method is labor intensive and cannot be done using administrative databases. No direct comparison of UGIB to LGIB among hospitalized patients using this 2‐step method has been done recently.
The current emphasis on UGIB as seen in the published guidelines could also be supported if patients with UGIB had greater resource utilization or worse clinical outcomes. Limited direct comparisons for these outcomes are available. However, 1 administrative database study reported similar mortality rates for UGIB (2.7%) and LGIB (2.9%) in 2006.1 No direct comparisons of other clinical outcomes or resource use outcomes are available. Therefore, the emphasis on UGIB in publications and guidelines is best supported by the incidence rates that are, as has already been discussed, problematic.
We conducted a retrospective cohort study to examine the incidences of UGIB and LGIB among patients admitted to an academic medical center over 2 years using methods designed to optimally identify patients with either UGIB or LGIB. Our study also examined differences in clinical outcomes and resource utilization between subjects with UGIB and LGIB to examine the relative severity of these 2 clinical entities. These results may be useful in determining the need to reconsider clinical approaches as well as protocols and guidelines among patients with gastrointestinal bleeding.
Patients and Methods
Patients
This retrospective cohort study evaluated all patients who were admitted with GIB to a large urban academic medical center from July 1, 2001 to June 30, 2003 and who consented to a larger study examining the effects of hospitalists on patient care. Subjects unable to provide consent due to death or lack of decisional capacity were consented via proxy. To identify patients with GIB, all patients were screened for a primary or secondary diagnosis of GIB using ICD 9 codes. These codes were selected for a very high sensitivity threshold to assure that all potential subjects with GIB were identified. All subjects identified using these codes underwent chart abstraction to determine if they met criteria for GIB. These inclusion criteria required documentation in any portion of the chart (including emergency department [ED] clinician documentation, admission note, nursing intake note, etc.) of signs or symptoms of GI hemorrhage upon admission, including: hematemesis, coffee ground emesis, gastrooccult‐positive emesis, melena, hematochezia, maroon stools, and hemoccult‐positive stools interpreted by the treating physician team as an acute GIB. Subjects identified using the ICD‐9 codes and confirmed to have an acute GIB by chart review were included in the study and underwent additional chart abstraction and administrative data analysis.
ICD‐9 codes for GIB included: esophageal varices with hemorrhage (456.0, 456.20), Mallory‐Weiss syndrome (530.7), gastric ulcer with hemorrhage (531.00531.61), duodenal ulcer with hemorrhage (532.00532.61), peptic ulcer, site unspecified, with hemorrhage (533.00533.61), gastrojejunal ulcer with hemorrhage (534.00534.61), gastritis with hemorrhage (535.61), angiodysplasia of stomach/duodenum with hemorrhage (537.83), hematemesis (578.0578.9), diverticular disease (562.00562.9), other disorders of the intestine (569.00569.9), congenital anomalies of the digestive system (751.00), proctocolitis (556.00), hemorrhoids (455.00455.6), nondysenteric colitis (006.2), noninfectious gastroenteritis and colitis (558.0558.9), salmonella gastroenteritis (003.3), malignant neoplasm of colon (153), familial adenomatous polyposis (211.3), and gastric varices (456.8).
Data
Trained research assistants performed chart abstraction with validation by the principal investigators (PIs) of the first 15 charts to ensure accuracy. Subsequently, research assistants consulted with PIs with any questions during abstracting with final decisions being made by PIs. Detailed chart abstraction collected admission medication lists as obtained by the admitting physician team, including the use of PPIs, histamine‐2 (H‐2) blockers, COX‐2 inhibitors, and medications known to increase the risk of GIB, such as nonselective NSAIDs (nsNSAIDs), aspirin, and other anticoagulants. Other clinical data including risk factors, comorbid illnesses, laboratory tests, and vital signs were also abstracted from subjects' charts.
The source (UGIB vs. LGIB) and etiology (peptic ulcer disease [PUD], varices, diverticula, etc.) of bleeding were assessed using endoscopic reports as the primary source. When no clear source was identified on endoscopy or no endoscopy was done, the abstracter would review all progress notes, discharge summaries, and other diagnostic test results such as angiography in order to identify the source of bleeding (UGIB vs. LGIB). Endoscopic reports that identified a patient as having a UGIB or LGIB but no confirmed etiology were classified as undetermined etiology unless review of the other clinical documentation provided a specific etiology.
Tachycardia was defined as pulse greater than 100 beats per minute. Orthostasis was defined by either a drop in systolic blood pressure of 20 mmHg or an increase in pulse of 10 beats per minute. Hospital administrative databases were utilized to obtain resource utilization (ie, length of stay [LOS], total cost of care, intensive care transfers), Charlson comorbidity index,27 30‐day readmission rate, and in‐hospital mortality. Hospital costs were determined using TSI cost accounting software (Transition Systems Incorporated [now Eclypsis Corporation], Boston, MA), a validated system to assess actual direct and indirect costs of care.
Statistical Analysis
Descriptive statistics (means and proportions) were calculated by location of GIB for all variables describing patient characteristics, clinical presentation, clinical outcomes, and resource utilization. Differences in age and Charlson comorbidity index by GIB location were evaluated using t tests. Differences in gender, race, and medication use were evaluated using chi‐squared tests of independence.
We fit generalized linear models to investigate differences by location of bleed for those variables measuring clinical outcomes (inpatient mortality, intensive care unit [ICU] transfer, emergency surgery, 30‐day readmission, change in hemoglobin) and those variables measuring resource outcomes (total cost, LOS, number of procedures, number of correct scopes, repeat scope indicator, incorrect scope indicator, number of red blood cell [RBC] transfusions). The repeat scope indicator was used to denote a repeat scope (either esophagogastroduodenoscopy [EGD] or colonoscopy) and the incorrect scope indicator was used to denote when the initial scope was negative and a follow‐up scope from the other direction was positive (negative EGD followed by positive colonoscopy or negative colonoscopy followed by positive EGD). For each variable we fit 2 regression models, the first model (unadjusted effect) only included location of bleed as a covariate. The second model (adjusted effect) included location of bleed, age, gender, race (black/not black) and Charlson comorbidity index as covariates. Binary outcomes were modeled using logistic regressions. For continuous variables, we determined the distribution and link of the outcome variable using residual diagnostics and by comparing the log likelihood and information criteria of competing models. All analyses were performed using STATA SE Version 9.0 (StataCorp, College Station, TX)
This study was approved by the University of Chicago Institutional Review Board.
Results
During the 2 years of observation, a total of 7741 subjects were admitted to the internal medicine service and enrolled in the hospitalist study. Of these, 1014 had a primary or secondary ICD‐9 code that may be consistent with UGIB or LGIB and underwent chart review to determine if they had an acute GIB. Out of 1014 subjects, 647 were determined not to have an acute GI hemorrhage and were excluded from the remaining analyses; 367 of the 1104 subjects identified by ICD‐9 codes were found to have a clinical presentation consistent with GIB and were included in this study. A total of 180 of these 367 had UGIB and 187 had LGIB. The mean age was 62.4 years, 56.7% were female, 82.6% were African American, 12.7% were Caucasian, and the mean Charlson index was 1.5. (Table 1) Among baseline characteristics, both gender and age were statistically associated with a difference in rates of upper vs. lower source bleeding, with LGIB patients more likely to be female (P = 0.01) and older (P < 0.001). Etiologies of UGIB include erosive disease, peptic ulcer disease, variceal bleeding, arteriovenous malformation, and malignancy. Etiologies of LGIB include: diverticulosis, colitis, arteriovenous malformation, cancer, ischemic colitis, polyp, hemorrhoidal bleed, ulcer, inflammatory bowel disease, other, and not determined (Table 2).
| Upper and Lower GI Bleeding (n = 367) | Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | P Value | |
|---|---|---|---|---|
| ||||
| Age (years), mean (SD) | 62.4 (18.0) | 58.6 (18.2) | 66.0 (17.1) | <0.001 |
| Female gender (%) | 56.7 | 50.0 | 63.1 | 0.01 |
| Race (%) | ||||
| African American | 82.6 | 85.3 | 80.1 | 0.43 |
| White | 12.7 | 10.7 | 14.5 | |
| Other | 4.7 | 4.0 | 5.4 | |
| Charlson comorbidity index, mean (SD) | 1.5 (1.5) | 1.6 (1.6) | 1.4 (1.5) | 0.44 |
| Lower GI Bleed (n = 187) | Upper GI Bleed (n = 180) | ||||
|---|---|---|---|---|---|
| Etiology | Frequency | Percent of Total (%) | Etiology | Frequency | Percent of Total (%) |
| |||||
| Diverticulosis | 76 | 41 | Erosive disease | 86 | 48 |
| Not identified | 38 | 20 | Peptic ulcer | 51 | 28 |
| Colitis, NOS | 14 | 7 | Not identified | 26 | 14 |
| AVM | 13 | 7 | Mallory Weiss | 17 | 9 |
| Cancer | 11 | 6 | Varices | 8 | 4 |
| Ischemic colitis | 9 | 5 | AVMs | 5 | 3 |
| Polyp | 9 | 5 | Mass/cancer | 5 | 3 |
| Hemorrhoid | 8 | 4 | |||
| Ulcer | 5 | 3 | |||
| Other | 3 | 1 | |||
| IBD | 1 | <1 | |||
Baseline use of medications known to be associated with either increased or decreased risk of GIB was common. Approximately one‐third of subjects with both LGIB and UGIB used aspirin and 10% used warfarin. LGIB subjects were less likely to use an nsNSAID (P < 0.001), but more likely to use a proton pump inhibitor (PPI) (P = 0.06) (Table 3).
| Upper and Lower GI Bleeding (%) (n = 367) | Upper GI Bleeding (%) (n = 180) | Lower GI Bleeding (%) (n = 187) | P Value* | |
|---|---|---|---|---|
| ||||
| Aspirin | 34.9 | 31.8 | 37.4 | 0.28 |
| nsNSAID | 12.9 | 20.8 | 6.4 | < 0.001 |
| COX‐2 selective inhibitor | 8.2 | 6.5 | 9.6 | 0.29 |
| Warfarin | 10.9 | 8.4 | 12.8 | 0.19 |
| PPI | 24.3 | 19.5 | 28.3 | 0.06 |
| nsNSAID + PPI | 1.8 | 1.3 | 2.1 | 0.56 |
| COX‐2 + PPI | 2.9 | 1.3 | 4.3 | 0.11 |
Key initial clinical presentation findings included vital sign abnormalities and admission hemoglobin levels. While hypotension was not common (4.7%), resting tachycardia (37%) and orthostasis (16%) were seen frequently. Subjects with LGIB were significantly less likely than those with UGIB to present with orthostasis (8.8% vs. 21.0%, respectively; P = 0.006) and resting tachycardia (32.3% vs. 42.5%, respectively; P = 0.04). Subjects with LGIB had a higher admission hemoglobin than those with UGIB (10.7 vs. 9.7, respectively; P < 0.001) (Table 4).
| Clinical Finding | Upper and Lower GI Bleeding (n = 367) | Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | P Value* |
|---|---|---|---|---|
| ||||
| Hypotension (%) | 4.7 | 5.7 | 3.8 | 0.39 |
| Resting tachycardia (%) | 37.3 | 42.5 | 32.3 | 0.04 |
| Orthostatic hypotension (%) | 16.2 | 21.0 | 8.8 | 0.006 |
| Admission hemoglobin (g/dL), mean (SD) | 10.2 (2.6) | 9.7 (2.7) | 10.7 (2.5) | <0.001 |
We also examined several clinical outcomes. When comparing LGIB to UGIB patients for these clinical outcomes using bivariate and multivariate statistics, there was no difference for in‐hospital mortality (1.1% vs. 1.1%), transfer to ICU (16.0% vs. 13.9%), 30‐day readmission (5.9% vs.7.8%), number of red blood cell (RBC) transfusions (2.7 vs. 2.4), or need for GI surgery (1.1% vs. 0.0%). The mean drop in hemoglobin was greater among subjects with LGIB compared to UGIB (1.9 g/dL vs. 1.5 g/dL, respectively) by both bivariate (P = 0.01) and multivariate (P = 0.003) analyses (Table 5).
| Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | Bivariate P Value | Multivariate P Value | |
|---|---|---|---|---|
| ||||
| In‐hospital mortality (%)* | 1.1 | 1.1 | 0.97 | 0.74 |
| Transfer to ICU (%)* | 13.9 | 16.0 | 0.56 | 0.44 |
| Drop in hemoglobin (g/dL), mean (SD) | 1.5 (1.5) | 1.9 (1.6) | 0.01 | 0.003 |
| Packed RBC transfusions required (units), mean (SD)* | 2.4 (2.9) | 2.7 (3.7) | 0.36 | 0.33 |
| Surgery for GI bleeding (%) | 0.0% | 1.1 | ||
| 30‐day readmission rate (%)* | 7.8 | 5.9 | 0.49 | 0.45 |
Mean costs were $11,892 for LGIB and $14,301 for UGIB and median costs were $7,890 for LGIB and $9,548 for UGIB, but were not statistically different. LOS was also similar between subjects with LGIB (5.1 days) and UGIB (5.7 days). In bivariate and multivariate analyses, UGIB subjects had a similar mean number of endoscopic procedures (1.3) compared to LGIB subjects (1.2). Thirteen percent of subjects with UGIB required a second EGD while only 8% of subjects with LGIB required 2 colonoscopies. In addition, 29% of subjects with LGIB received an EGD while only 16% of subjects with an UGIB received a colonoscopy (P = 0.001) (Table 6).
| Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | Bivariate P Value | Multivariate P Value | |
|---|---|---|---|---|
| ||||
| Cost ($), mean (SD)* | 14,301 (17,196) | 11,892 (13,100) | 0.13 | 0.21 |
| Cost ($), median | $9,548 | $7,890 | ||
| Length of stay (days), mean (SD)* | 5.7 (7.0) | 5.1 (5.3) | 0.37 | 0.72 |
| Number of endoscopies/ patient, mean (SD) | 1.3 (0.5) | 1.2 (0.9) | 0.18 | 0.20 |
Conclusions
This study represents one of the largest direct comparisons of LGIB to UGIB not based on administrative databases. The most striking finding was the nearly equal rates of LGIB and UGIB. There are 2 likely explanations for this surprising result. First, there may be methodological reasons that we identified a greater proportion of true LGIBs; our study used a highly sensitive search strategy of ICD‐9 coding with confirmatory chart abstraction to ensure that as many LGIB and UGIB cases would be identified as possible while also excluding cases not meeting accepted criteria for GIB. The second possibility is that there is an actual change in epidemiology of GIB. Known risk factors for LGIB are increasing such as advancing age, increased use of chronic aspirin therapy, and renal disease. At the same time, significant advances in the treatment and prevention of UGIB have been made. Recent studies have demonstrated similar trends in admissions for upper and lower GI complications, suggesting that there may be a changing epidemiology due primarily to reductions in upper GI complications.1, 16
Either explanation would have implications for the care of patients with GIB. Clinical decision‐making based on prior literature would support that in ambiguous clinical situations and initial evaluation for an UGIB is appropriate. Most risk stratification literature and clinical guidelines focus on UGIB. If rates of LGIB and UGIB are similar, then existing clinical decision protocols may need to be reevaluated to incorporate the higher likelihood of LGIB. This reevaluation would be less important if the clinical outcomes or resource utilization of UGIB was significantly greater than that for LGIB, but we did not find this was the case. Similarly, if the ability to distinguish between LGIB and UGIB were robust on clinical signs and symptoms, then a reevaluation would be less important. However, we found fairly similar numbers of patients initially receiving evaluation for UGIB then being evaluated for LGIB as we found patients initially receiving evaluation for LGIB then being evaluated for UGIB. This suggests the potential benefit of clinical decision protocols that could better distinguish between UGIB and LGIB and account for the potentially higher incidence of LGIB than previously thought.
In addition to affecting the attention paid to LGIB for acute management, a changed understanding of incidence could also affect the attention paid to prevention of LGIB. Of the recent nonendoscopic advances in the treatment and prevention of GIB, only the use of COX‐2s (when used in place of traditional nsNSAIDs) reduces the risk of both LGIB and UGIB;14, 1618 H .pylori treatment and PPIs only prevent UGIB. Therefore, if the clinical and financial burdens of LGIB are similar to those seen in UGIB, more attention may need to be focused on preventing LGIB.
Baseline medication use was notable primarily for the similarities between UGIB and LGIB. Agents known to affect the rates of GIB were common in both groups. Over one‐third of the population was using aspirin and 10% were taking warfarin. Over 20% of subjects were taking an nsNSAID or a COX‐2 inhibitor. Almost one‐quarter of subjects were taking a PPI, agents known to decrease rates of UGIB and potentially increase LGIB through the risk of C. difficile colitis. Notably, the only statistically significant difference in baseline medication use between subjects with UGIB and LGIB was the more than 3‐fold higher use of nsNSAIDs in patients with UGIB as compared to LGIB. While current guidelines are not clear and consistent about which populations of at‐risk patients should receive GI prophylaxis,2830 these results suggest that patients admitted with GIB are very likely to be taking medications which impact the risk of GIB.
In terms of disease severity, the clinical presentation at admission suggests a greater degree of hemodynamic instability among subjects with UGIB. Rates of orthostatic hypotension and resting tachycardia are higher in UGIB subjects, as well as having a lower mean hemoglobin levels at presentation. However, despite the more severe clinical presentation, clinical outcomes did not differ significantly between the 2 bleeding sources. Thus, the most relevant clinical outcomes suggest that the severity of both LGIB and UGIB are similar. This similarity again suggest that the clinical burden of LGIB is not significantly different than UGIB.
Our results concerning resource utilization demonstrate a similar pattern. While the point estimates for costs and LOS suggest that UGIB may be associated with higher resource utilization, these differences were not significant in either bivariate or multivariate analyses. Those subjects with UGIB did receive more total endoscopic procedures than subjects with LGIB. More interesting though was that 24% of all subjects received an endoscopy of the opposite site (LGIB with EGD and UGIB with colonoscopy). These results suggest that the site of bleeding is not clear in a significant proportion of patients who present with GIB. These additional endoscopies are associated with increased risk, costs, LOS, and discomfort to patients. Improving our ability to accurately predict the source (upper vs. lower) of bleeding would allow us to reduce the number of these excess endoscopies. Additionally, it is interesting that despite the almost universal use of endoscopies, 20% of LGIB and 14% of UGIB subjects could not have a specific etiology identified during endoscopy or subsequent workup.
There are some important limitations to this study. While the sample size is among the largest of its type involving chart abstraction, it may be underpowered to detect some differences. Additionally, our results are from a single urban academic medical center with a patient population that is predominantly African American, which may limit generalizability. This study required consent and therefore only examines a subset of patients admitted to the medical center with GIB, which could potentially introduce bias into the sample. However, it is not clear why there would be systematic differences in subjects who choose to consent vs. those who decide not to consent that would affect the results of this study in substantive ways.
Despite significant efforts at identifying all subjects with GIB admitted during this time period, there were potential methodological reasons that may have resulted in some cases being missed. Only subjects admitted to a medicine service were approached for consent. All subjects in this medical center with GIB are admitted to a medicine service. We captured all subjects who were initially admitted to a medicine service as well as those admitted initially to an ICU and then transferred to the floor at any point prior to discharge. It is possible, though, that a subject would be admitted to an ICU for GIB and die prior to being transferred to the floor. While it is the impression of the director of the ICU that this would be a very unusual event, as most of the patients would be discharged to the floor prior to death (personal communication), given the very low mortality rate seen in this study, small numbers of missed events could have a significant impact on the interpretation of in‐hospital mortality results. It is also important to note that this medical center did not have the ability to perform endoscopy prior to admission for patients with GIB at the time of the study; all patients who presented with GIB would have been admitted and identified for this study. Finally, we were unable to routinely identify the rationale for obtaining an endoscopic exam. We assumed that all endoscopic exams were done for the purpose of evaluating and/or treating the GIB for which the subject was admitted. It is possible that some subjects had additional endoscopies for other reasons, which would have led to our overestimating the rates of additional endoscopies for GIB.
This study highlights the similarities between LGIB and UGIB rather than the differences. There were few significant differences between the 2 bleeding sources in terms of incidence, clinical outcomes, and resource utilization. In fact, the study also suggests that determining the source of bleeding may not be clear, given the high rates of opposite site endoscopies. While this study did reveal several similarities between UGIB and LGIB, it also highlights the need to identify improved strategies to improve the sensitivity and specificity of identification of LGIB compared to UGIB, both for clinical purposes and for research. The value of such improved clinical algorithms have the potential to improve both the cost and outcomes of care, while better algorithms for separating UGIB and LGIB using administrative data might help produce more precise estimates of costs and clinical outcomes, and aid in the development of risk stratification models.
- ,.Hospitalizations for Gastrointestinal Bleeding in 1998 and 2006. HCUP Statistical Brief #65, December 2008.Rockville, MD:Agency for Healthcare Research and Quality.
- ,.Causes and outcome of upper and lower gastrointestinal bleeding: The Grady Hospital Experience.South Med J.1999;92(1):44–50.
- ,,, et al.Acute upper gastrointestinal haemorrhage in west of Scotland: case ascertainment study.BMJ.1997;315:510–540.
- ,.A cost‐effective approach to the patient with peptic ulcer bleeding.Surg Clin North Am.1996;76:83–103.
- .Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population based study.Am J Gastroenterol.1997;92:419–424.
- ,,.Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding.Ann Int Med.2003;139:843–857.
- ,.Incremental value of upper endoscopy for triage of patients with acute non‐variceal upper‐GI hemorrhage.Gastrointest Endosc2004;60:9–14.
- ,,, et al.Upper gastrointestinal hemorrhage clinical guideline‐determining the optimal hospital length of stay.Am J Med.1996;100:313–322.
- National Guideline Clearinghouse. Available at: http://www.guideline.gov. Accessed August2009.
- ,,, et al.Prevention of ulcer recurrence after eradication of Helicobacter pylori: a prospective long‐term follow‐up study.Gastroenterology.1997;113:1082–1086.
- ,,, et al.Treatment of Helicobacter pylori in patients with duodenal ulcer hemorrhage‐a long‐term randomized, controlled study.Am J Gastroenterol.2000;95:2225–2232.
- ,,, et al.Preventing recurrent upper gastrointestinal bleeding in patients with Helicobacter pylori infection who are taking low‐dose aspirin or naproxen.N Engl J Med.2001;344:967–973.
- ,,, et al.Lansoprazole for the prevention of recurrences of ulcer complications from long‐term low‐dose aspirin use.N Engl J Med.2002;346:2033–2038.
- ,,, et al.Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group.N Engl J Med.2000;343:1520–1528.
- ,,, et al.Gastrointestinal toxicity with celecoxib vs nonsteroidal anti‐inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long‐Term Arthritis Safety Study.JAMA.2000;284:1247–1255.
- ,,, et al.Time trends and clinical impact of upper and lower gastrointestinal complications. Digestive Disease Week National Meeting,2008. San Diego, CA, May 17–22.
- ,,, et al.Video capsule endoscopy to prospectively assess small bowel injury with celecoxib, naproxen plus omeprazole, and placebo.Clin Gastroenterol Hepatol.2005;3:133–141.
- ,,, et al.Serious lower gastrointestinal clinical events with nonselective NSAID or Coxib use.Gastroenterology.2003;124:288–292.
- ,,, et al.Risk factors for upper gastrointestinal bleeding among end‐stage renal disease patients.Kidney Int.2003;64:1455–1461.
- ,,, et al.Risk factors for hospitalized bleeding among older patients.J Am Geriatr Soc.2001;49:126–133.
- Institute for Clinical Systems Improvement (ICSI). Preventive services in adults. Bloomington, MN: Institute for Clinical Systems Improvement (ICSI).2005. Available at http://www.isci.org/guidelines_and_more/guidelines_order_sets_protocol/for_patients_families/preventive_services_for_adults_for_patients_families_.html. Accessed Month year.
- .NSAID‐associated deaths: the rise and fall of NSAID‐associated GI mortality.Am J Gastroenterol.2005;100:1694–1695.
- ,.Effects of very low doses of daily long‐term aspirin therapy on gastric, duodenal, and rectal prostaglandins on mucosal injury in healthy humans.Gastroenterology. 199;117:17–25.
- ,,, et al.A nationwide study of mortality associated with hospital admission due to severe gastrointestinal events and those associated with nonsteroidal antiinflammatory drug use.Am J Gastroenterol.2005;100:1685–1693.
- ,,, et al.Acute upper GI bleeding: did anything change?Am J Gastroenterol.2003;98:1494–1499.
- ,.Lower intestinal bleeding.Best Pract Res Clin Gastroenterol.2001;15:135–153.
- ,,,.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.J Chronic Dis.1987;40:373–383.
- AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons.J Am Geriatr Soc.2002;50(6 suppl):S205–S224.
- ,,, et al.Pain in Osteoarthritis, Rheumatoid Arthritis and Juvenile Chronic Arthritis.2nd ed.Clinical practice guideline no. 2.Glenview, IL:American Pain Society (APS);2002:179.
- American College of Rheumatology Subcommittee on Osteoarthritis Guidelines.Recommendations for the Medical Management of Osteoarthritis of the Hip and Knee.Arthritis Rheum.2000;43:1905–1915.
Gastrointestinal bleeding (GIB) is a frequent reason for acute hospitalization, with estimated rates of hospitalization at 375 per 100,000 per year in the United States.1 GIB is not a specific disease but rather a diverse set of conditions that lead to the clinical manifestations associated with bleeding into the gastrointestinal tract. One of the most commonly used organizing frameworks in gastrointestinal bleeding is the differentiation between upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB). There are important differences in the etiologies between the 2 sources. For example, acid‐related disease is a common etiology in UGIB but does not occur in LGIB. While some aspects of the acute management are shared between UGIB and LGIB, important differences exist in the management, including initial endoscopy and medication choice. There have been few direct comparisons of rates, resource use, and clinical outcomes between UGIB and LGIB.
Historically, rates of UGIB have been reported to exceed those of LGIB by 2‐fold to 8‐fold.25 Protocols, clinical practice guidelines, and policy decisions reflect this emphasis on UGIB.68 Among 9 guidelines hosted by National Guideline Clearinghouse addressing GIB, 6 were focused on UGIB, 2 on both UGIB and LGIB, and only 1 on LGIB.9 There are several reasons to believe that these relative incidence rates may not be accurate. First, recent advances in therapy and prevention of UGIB, such as the treatment of Helicobacter pylori infection; proton pump inhibitors (PPIs); and selective cyclooxygenase‐2 (COX‐2) inhibitors, may have affected the epidemiology of gastrointestinal bleeding.1016 Among these therapies, only COX‐2 inhibitors may also reduce the incidence of LGIB.14, 1618 Therefore, these advances may result in a disproportionate drop in UGIB relative to LGIB. In addition, known risk factors for both LGIB and UGIB, including advancing age and renal failure, are increasing in the general population.5, 19, 20 Finally, given the recent increased recommendations for aspirin therapy and systemic anticoagulation, exposure to aspirin and warfarin have increased, both risk factors for LGIB and UGIB.2124 Indeed, recent studies in the epidemiology of UGIB do suggest a changing pattern of etiologies of UGIB reflecting these advances.25 One study examining rates of both UGIB and LGIB demonstrate a decrease in hospitalizations overall for GIB driven by a reduction in UGIB while at the same time reporting an increase in the incidence of hospitalization for LGIB.1
In addition to a changing epidemiology, a second reason for a potential underestimation of LGIB incidence is one of methodology. There are well‐recognized limitations with using purely administrative data due to difficulties in accurately identifying patients with LGIB.26
Studies using large administrative databases may not accurately identify LGIB because of the poor sensitivity and specificity of International Classification of Diseases, Ninth revision, Clinical Modification (ICD‐9) codes for LGIB.5 While there are standard methods of identifying patients with UGIB using ICD‐9 codes,19 there is not an accepted standard for LGIB. Thus, estimates using only ICD‐9 codes may overidentify or underidentify patients with LGIB. Prior studies that have most accurately identified patients with LGIB used a 2‐step method to address this issue. The initial ICD‐9 identification included a high sensitivity/low specificity approach. These identified patient charts undergo chart review to confirm the presence of an LGIB.5 This method is labor intensive and cannot be done using administrative databases. No direct comparison of UGIB to LGIB among hospitalized patients using this 2‐step method has been done recently.
The current emphasis on UGIB as seen in the published guidelines could also be supported if patients with UGIB had greater resource utilization or worse clinical outcomes. Limited direct comparisons for these outcomes are available. However, 1 administrative database study reported similar mortality rates for UGIB (2.7%) and LGIB (2.9%) in 2006.1 No direct comparisons of other clinical outcomes or resource use outcomes are available. Therefore, the emphasis on UGIB in publications and guidelines is best supported by the incidence rates that are, as has already been discussed, problematic.
We conducted a retrospective cohort study to examine the incidences of UGIB and LGIB among patients admitted to an academic medical center over 2 years using methods designed to optimally identify patients with either UGIB or LGIB. Our study also examined differences in clinical outcomes and resource utilization between subjects with UGIB and LGIB to examine the relative severity of these 2 clinical entities. These results may be useful in determining the need to reconsider clinical approaches as well as protocols and guidelines among patients with gastrointestinal bleeding.
Patients and Methods
Patients
This retrospective cohort study evaluated all patients who were admitted with GIB to a large urban academic medical center from July 1, 2001 to June 30, 2003 and who consented to a larger study examining the effects of hospitalists on patient care. Subjects unable to provide consent due to death or lack of decisional capacity were consented via proxy. To identify patients with GIB, all patients were screened for a primary or secondary diagnosis of GIB using ICD 9 codes. These codes were selected for a very high sensitivity threshold to assure that all potential subjects with GIB were identified. All subjects identified using these codes underwent chart abstraction to determine if they met criteria for GIB. These inclusion criteria required documentation in any portion of the chart (including emergency department [ED] clinician documentation, admission note, nursing intake note, etc.) of signs or symptoms of GI hemorrhage upon admission, including: hematemesis, coffee ground emesis, gastrooccult‐positive emesis, melena, hematochezia, maroon stools, and hemoccult‐positive stools interpreted by the treating physician team as an acute GIB. Subjects identified using the ICD‐9 codes and confirmed to have an acute GIB by chart review were included in the study and underwent additional chart abstraction and administrative data analysis.
ICD‐9 codes for GIB included: esophageal varices with hemorrhage (456.0, 456.20), Mallory‐Weiss syndrome (530.7), gastric ulcer with hemorrhage (531.00531.61), duodenal ulcer with hemorrhage (532.00532.61), peptic ulcer, site unspecified, with hemorrhage (533.00533.61), gastrojejunal ulcer with hemorrhage (534.00534.61), gastritis with hemorrhage (535.61), angiodysplasia of stomach/duodenum with hemorrhage (537.83), hematemesis (578.0578.9), diverticular disease (562.00562.9), other disorders of the intestine (569.00569.9), congenital anomalies of the digestive system (751.00), proctocolitis (556.00), hemorrhoids (455.00455.6), nondysenteric colitis (006.2), noninfectious gastroenteritis and colitis (558.0558.9), salmonella gastroenteritis (003.3), malignant neoplasm of colon (153), familial adenomatous polyposis (211.3), and gastric varices (456.8).
Data
Trained research assistants performed chart abstraction with validation by the principal investigators (PIs) of the first 15 charts to ensure accuracy. Subsequently, research assistants consulted with PIs with any questions during abstracting with final decisions being made by PIs. Detailed chart abstraction collected admission medication lists as obtained by the admitting physician team, including the use of PPIs, histamine‐2 (H‐2) blockers, COX‐2 inhibitors, and medications known to increase the risk of GIB, such as nonselective NSAIDs (nsNSAIDs), aspirin, and other anticoagulants. Other clinical data including risk factors, comorbid illnesses, laboratory tests, and vital signs were also abstracted from subjects' charts.
The source (UGIB vs. LGIB) and etiology (peptic ulcer disease [PUD], varices, diverticula, etc.) of bleeding were assessed using endoscopic reports as the primary source. When no clear source was identified on endoscopy or no endoscopy was done, the abstracter would review all progress notes, discharge summaries, and other diagnostic test results such as angiography in order to identify the source of bleeding (UGIB vs. LGIB). Endoscopic reports that identified a patient as having a UGIB or LGIB but no confirmed etiology were classified as undetermined etiology unless review of the other clinical documentation provided a specific etiology.
Tachycardia was defined as pulse greater than 100 beats per minute. Orthostasis was defined by either a drop in systolic blood pressure of 20 mmHg or an increase in pulse of 10 beats per minute. Hospital administrative databases were utilized to obtain resource utilization (ie, length of stay [LOS], total cost of care, intensive care transfers), Charlson comorbidity index,27 30‐day readmission rate, and in‐hospital mortality. Hospital costs were determined using TSI cost accounting software (Transition Systems Incorporated [now Eclypsis Corporation], Boston, MA), a validated system to assess actual direct and indirect costs of care.
Statistical Analysis
Descriptive statistics (means and proportions) were calculated by location of GIB for all variables describing patient characteristics, clinical presentation, clinical outcomes, and resource utilization. Differences in age and Charlson comorbidity index by GIB location were evaluated using t tests. Differences in gender, race, and medication use were evaluated using chi‐squared tests of independence.
We fit generalized linear models to investigate differences by location of bleed for those variables measuring clinical outcomes (inpatient mortality, intensive care unit [ICU] transfer, emergency surgery, 30‐day readmission, change in hemoglobin) and those variables measuring resource outcomes (total cost, LOS, number of procedures, number of correct scopes, repeat scope indicator, incorrect scope indicator, number of red blood cell [RBC] transfusions). The repeat scope indicator was used to denote a repeat scope (either esophagogastroduodenoscopy [EGD] or colonoscopy) and the incorrect scope indicator was used to denote when the initial scope was negative and a follow‐up scope from the other direction was positive (negative EGD followed by positive colonoscopy or negative colonoscopy followed by positive EGD). For each variable we fit 2 regression models, the first model (unadjusted effect) only included location of bleed as a covariate. The second model (adjusted effect) included location of bleed, age, gender, race (black/not black) and Charlson comorbidity index as covariates. Binary outcomes were modeled using logistic regressions. For continuous variables, we determined the distribution and link of the outcome variable using residual diagnostics and by comparing the log likelihood and information criteria of competing models. All analyses were performed using STATA SE Version 9.0 (StataCorp, College Station, TX)
This study was approved by the University of Chicago Institutional Review Board.
Results
During the 2 years of observation, a total of 7741 subjects were admitted to the internal medicine service and enrolled in the hospitalist study. Of these, 1014 had a primary or secondary ICD‐9 code that may be consistent with UGIB or LGIB and underwent chart review to determine if they had an acute GIB. Out of 1014 subjects, 647 were determined not to have an acute GI hemorrhage and were excluded from the remaining analyses; 367 of the 1104 subjects identified by ICD‐9 codes were found to have a clinical presentation consistent with GIB and were included in this study. A total of 180 of these 367 had UGIB and 187 had LGIB. The mean age was 62.4 years, 56.7% were female, 82.6% were African American, 12.7% were Caucasian, and the mean Charlson index was 1.5. (Table 1) Among baseline characteristics, both gender and age were statistically associated with a difference in rates of upper vs. lower source bleeding, with LGIB patients more likely to be female (P = 0.01) and older (P < 0.001). Etiologies of UGIB include erosive disease, peptic ulcer disease, variceal bleeding, arteriovenous malformation, and malignancy. Etiologies of LGIB include: diverticulosis, colitis, arteriovenous malformation, cancer, ischemic colitis, polyp, hemorrhoidal bleed, ulcer, inflammatory bowel disease, other, and not determined (Table 2).
| Upper and Lower GI Bleeding (n = 367) | Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | P Value | |
|---|---|---|---|---|
| ||||
| Age (years), mean (SD) | 62.4 (18.0) | 58.6 (18.2) | 66.0 (17.1) | <0.001 |
| Female gender (%) | 56.7 | 50.0 | 63.1 | 0.01 |
| Race (%) | ||||
| African American | 82.6 | 85.3 | 80.1 | 0.43 |
| White | 12.7 | 10.7 | 14.5 | |
| Other | 4.7 | 4.0 | 5.4 | |
| Charlson comorbidity index, mean (SD) | 1.5 (1.5) | 1.6 (1.6) | 1.4 (1.5) | 0.44 |
| Lower GI Bleed (n = 187) | Upper GI Bleed (n = 180) | ||||
|---|---|---|---|---|---|
| Etiology | Frequency | Percent of Total (%) | Etiology | Frequency | Percent of Total (%) |
| |||||
| Diverticulosis | 76 | 41 | Erosive disease | 86 | 48 |
| Not identified | 38 | 20 | Peptic ulcer | 51 | 28 |
| Colitis, NOS | 14 | 7 | Not identified | 26 | 14 |
| AVM | 13 | 7 | Mallory Weiss | 17 | 9 |
| Cancer | 11 | 6 | Varices | 8 | 4 |
| Ischemic colitis | 9 | 5 | AVMs | 5 | 3 |
| Polyp | 9 | 5 | Mass/cancer | 5 | 3 |
| Hemorrhoid | 8 | 4 | |||
| Ulcer | 5 | 3 | |||
| Other | 3 | 1 | |||
| IBD | 1 | <1 | |||
Baseline use of medications known to be associated with either increased or decreased risk of GIB was common. Approximately one‐third of subjects with both LGIB and UGIB used aspirin and 10% used warfarin. LGIB subjects were less likely to use an nsNSAID (P < 0.001), but more likely to use a proton pump inhibitor (PPI) (P = 0.06) (Table 3).
| Upper and Lower GI Bleeding (%) (n = 367) | Upper GI Bleeding (%) (n = 180) | Lower GI Bleeding (%) (n = 187) | P Value* | |
|---|---|---|---|---|
| ||||
| Aspirin | 34.9 | 31.8 | 37.4 | 0.28 |
| nsNSAID | 12.9 | 20.8 | 6.4 | < 0.001 |
| COX‐2 selective inhibitor | 8.2 | 6.5 | 9.6 | 0.29 |
| Warfarin | 10.9 | 8.4 | 12.8 | 0.19 |
| PPI | 24.3 | 19.5 | 28.3 | 0.06 |
| nsNSAID + PPI | 1.8 | 1.3 | 2.1 | 0.56 |
| COX‐2 + PPI | 2.9 | 1.3 | 4.3 | 0.11 |
Key initial clinical presentation findings included vital sign abnormalities and admission hemoglobin levels. While hypotension was not common (4.7%), resting tachycardia (37%) and orthostasis (16%) were seen frequently. Subjects with LGIB were significantly less likely than those with UGIB to present with orthostasis (8.8% vs. 21.0%, respectively; P = 0.006) and resting tachycardia (32.3% vs. 42.5%, respectively; P = 0.04). Subjects with LGIB had a higher admission hemoglobin than those with UGIB (10.7 vs. 9.7, respectively; P < 0.001) (Table 4).
| Clinical Finding | Upper and Lower GI Bleeding (n = 367) | Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | P Value* |
|---|---|---|---|---|
| ||||
| Hypotension (%) | 4.7 | 5.7 | 3.8 | 0.39 |
| Resting tachycardia (%) | 37.3 | 42.5 | 32.3 | 0.04 |
| Orthostatic hypotension (%) | 16.2 | 21.0 | 8.8 | 0.006 |
| Admission hemoglobin (g/dL), mean (SD) | 10.2 (2.6) | 9.7 (2.7) | 10.7 (2.5) | <0.001 |
We also examined several clinical outcomes. When comparing LGIB to UGIB patients for these clinical outcomes using bivariate and multivariate statistics, there was no difference for in‐hospital mortality (1.1% vs. 1.1%), transfer to ICU (16.0% vs. 13.9%), 30‐day readmission (5.9% vs.7.8%), number of red blood cell (RBC) transfusions (2.7 vs. 2.4), or need for GI surgery (1.1% vs. 0.0%). The mean drop in hemoglobin was greater among subjects with LGIB compared to UGIB (1.9 g/dL vs. 1.5 g/dL, respectively) by both bivariate (P = 0.01) and multivariate (P = 0.003) analyses (Table 5).
| Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | Bivariate P Value | Multivariate P Value | |
|---|---|---|---|---|
| ||||
| In‐hospital mortality (%)* | 1.1 | 1.1 | 0.97 | 0.74 |
| Transfer to ICU (%)* | 13.9 | 16.0 | 0.56 | 0.44 |
| Drop in hemoglobin (g/dL), mean (SD) | 1.5 (1.5) | 1.9 (1.6) | 0.01 | 0.003 |
| Packed RBC transfusions required (units), mean (SD)* | 2.4 (2.9) | 2.7 (3.7) | 0.36 | 0.33 |
| Surgery for GI bleeding (%) | 0.0% | 1.1 | ||
| 30‐day readmission rate (%)* | 7.8 | 5.9 | 0.49 | 0.45 |
Mean costs were $11,892 for LGIB and $14,301 for UGIB and median costs were $7,890 for LGIB and $9,548 for UGIB, but were not statistically different. LOS was also similar between subjects with LGIB (5.1 days) and UGIB (5.7 days). In bivariate and multivariate analyses, UGIB subjects had a similar mean number of endoscopic procedures (1.3) compared to LGIB subjects (1.2). Thirteen percent of subjects with UGIB required a second EGD while only 8% of subjects with LGIB required 2 colonoscopies. In addition, 29% of subjects with LGIB received an EGD while only 16% of subjects with an UGIB received a colonoscopy (P = 0.001) (Table 6).
| Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | Bivariate P Value | Multivariate P Value | |
|---|---|---|---|---|
| ||||
| Cost ($), mean (SD)* | 14,301 (17,196) | 11,892 (13,100) | 0.13 | 0.21 |
| Cost ($), median | $9,548 | $7,890 | ||
| Length of stay (days), mean (SD)* | 5.7 (7.0) | 5.1 (5.3) | 0.37 | 0.72 |
| Number of endoscopies/ patient, mean (SD) | 1.3 (0.5) | 1.2 (0.9) | 0.18 | 0.20 |
Conclusions
This study represents one of the largest direct comparisons of LGIB to UGIB not based on administrative databases. The most striking finding was the nearly equal rates of LGIB and UGIB. There are 2 likely explanations for this surprising result. First, there may be methodological reasons that we identified a greater proportion of true LGIBs; our study used a highly sensitive search strategy of ICD‐9 coding with confirmatory chart abstraction to ensure that as many LGIB and UGIB cases would be identified as possible while also excluding cases not meeting accepted criteria for GIB. The second possibility is that there is an actual change in epidemiology of GIB. Known risk factors for LGIB are increasing such as advancing age, increased use of chronic aspirin therapy, and renal disease. At the same time, significant advances in the treatment and prevention of UGIB have been made. Recent studies have demonstrated similar trends in admissions for upper and lower GI complications, suggesting that there may be a changing epidemiology due primarily to reductions in upper GI complications.1, 16
Either explanation would have implications for the care of patients with GIB. Clinical decision‐making based on prior literature would support that in ambiguous clinical situations and initial evaluation for an UGIB is appropriate. Most risk stratification literature and clinical guidelines focus on UGIB. If rates of LGIB and UGIB are similar, then existing clinical decision protocols may need to be reevaluated to incorporate the higher likelihood of LGIB. This reevaluation would be less important if the clinical outcomes or resource utilization of UGIB was significantly greater than that for LGIB, but we did not find this was the case. Similarly, if the ability to distinguish between LGIB and UGIB were robust on clinical signs and symptoms, then a reevaluation would be less important. However, we found fairly similar numbers of patients initially receiving evaluation for UGIB then being evaluated for LGIB as we found patients initially receiving evaluation for LGIB then being evaluated for UGIB. This suggests the potential benefit of clinical decision protocols that could better distinguish between UGIB and LGIB and account for the potentially higher incidence of LGIB than previously thought.
In addition to affecting the attention paid to LGIB for acute management, a changed understanding of incidence could also affect the attention paid to prevention of LGIB. Of the recent nonendoscopic advances in the treatment and prevention of GIB, only the use of COX‐2s (when used in place of traditional nsNSAIDs) reduces the risk of both LGIB and UGIB;14, 1618 H .pylori treatment and PPIs only prevent UGIB. Therefore, if the clinical and financial burdens of LGIB are similar to those seen in UGIB, more attention may need to be focused on preventing LGIB.
Baseline medication use was notable primarily for the similarities between UGIB and LGIB. Agents known to affect the rates of GIB were common in both groups. Over one‐third of the population was using aspirin and 10% were taking warfarin. Over 20% of subjects were taking an nsNSAID or a COX‐2 inhibitor. Almost one‐quarter of subjects were taking a PPI, agents known to decrease rates of UGIB and potentially increase LGIB through the risk of C. difficile colitis. Notably, the only statistically significant difference in baseline medication use between subjects with UGIB and LGIB was the more than 3‐fold higher use of nsNSAIDs in patients with UGIB as compared to LGIB. While current guidelines are not clear and consistent about which populations of at‐risk patients should receive GI prophylaxis,2830 these results suggest that patients admitted with GIB are very likely to be taking medications which impact the risk of GIB.
In terms of disease severity, the clinical presentation at admission suggests a greater degree of hemodynamic instability among subjects with UGIB. Rates of orthostatic hypotension and resting tachycardia are higher in UGIB subjects, as well as having a lower mean hemoglobin levels at presentation. However, despite the more severe clinical presentation, clinical outcomes did not differ significantly between the 2 bleeding sources. Thus, the most relevant clinical outcomes suggest that the severity of both LGIB and UGIB are similar. This similarity again suggest that the clinical burden of LGIB is not significantly different than UGIB.
Our results concerning resource utilization demonstrate a similar pattern. While the point estimates for costs and LOS suggest that UGIB may be associated with higher resource utilization, these differences were not significant in either bivariate or multivariate analyses. Those subjects with UGIB did receive more total endoscopic procedures than subjects with LGIB. More interesting though was that 24% of all subjects received an endoscopy of the opposite site (LGIB with EGD and UGIB with colonoscopy). These results suggest that the site of bleeding is not clear in a significant proportion of patients who present with GIB. These additional endoscopies are associated with increased risk, costs, LOS, and discomfort to patients. Improving our ability to accurately predict the source (upper vs. lower) of bleeding would allow us to reduce the number of these excess endoscopies. Additionally, it is interesting that despite the almost universal use of endoscopies, 20% of LGIB and 14% of UGIB subjects could not have a specific etiology identified during endoscopy or subsequent workup.
There are some important limitations to this study. While the sample size is among the largest of its type involving chart abstraction, it may be underpowered to detect some differences. Additionally, our results are from a single urban academic medical center with a patient population that is predominantly African American, which may limit generalizability. This study required consent and therefore only examines a subset of patients admitted to the medical center with GIB, which could potentially introduce bias into the sample. However, it is not clear why there would be systematic differences in subjects who choose to consent vs. those who decide not to consent that would affect the results of this study in substantive ways.
Despite significant efforts at identifying all subjects with GIB admitted during this time period, there were potential methodological reasons that may have resulted in some cases being missed. Only subjects admitted to a medicine service were approached for consent. All subjects in this medical center with GIB are admitted to a medicine service. We captured all subjects who were initially admitted to a medicine service as well as those admitted initially to an ICU and then transferred to the floor at any point prior to discharge. It is possible, though, that a subject would be admitted to an ICU for GIB and die prior to being transferred to the floor. While it is the impression of the director of the ICU that this would be a very unusual event, as most of the patients would be discharged to the floor prior to death (personal communication), given the very low mortality rate seen in this study, small numbers of missed events could have a significant impact on the interpretation of in‐hospital mortality results. It is also important to note that this medical center did not have the ability to perform endoscopy prior to admission for patients with GIB at the time of the study; all patients who presented with GIB would have been admitted and identified for this study. Finally, we were unable to routinely identify the rationale for obtaining an endoscopic exam. We assumed that all endoscopic exams were done for the purpose of evaluating and/or treating the GIB for which the subject was admitted. It is possible that some subjects had additional endoscopies for other reasons, which would have led to our overestimating the rates of additional endoscopies for GIB.
This study highlights the similarities between LGIB and UGIB rather than the differences. There were few significant differences between the 2 bleeding sources in terms of incidence, clinical outcomes, and resource utilization. In fact, the study also suggests that determining the source of bleeding may not be clear, given the high rates of opposite site endoscopies. While this study did reveal several similarities between UGIB and LGIB, it also highlights the need to identify improved strategies to improve the sensitivity and specificity of identification of LGIB compared to UGIB, both for clinical purposes and for research. The value of such improved clinical algorithms have the potential to improve both the cost and outcomes of care, while better algorithms for separating UGIB and LGIB using administrative data might help produce more precise estimates of costs and clinical outcomes, and aid in the development of risk stratification models.
Gastrointestinal bleeding (GIB) is a frequent reason for acute hospitalization, with estimated rates of hospitalization at 375 per 100,000 per year in the United States.1 GIB is not a specific disease but rather a diverse set of conditions that lead to the clinical manifestations associated with bleeding into the gastrointestinal tract. One of the most commonly used organizing frameworks in gastrointestinal bleeding is the differentiation between upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB). There are important differences in the etiologies between the 2 sources. For example, acid‐related disease is a common etiology in UGIB but does not occur in LGIB. While some aspects of the acute management are shared between UGIB and LGIB, important differences exist in the management, including initial endoscopy and medication choice. There have been few direct comparisons of rates, resource use, and clinical outcomes between UGIB and LGIB.
Historically, rates of UGIB have been reported to exceed those of LGIB by 2‐fold to 8‐fold.25 Protocols, clinical practice guidelines, and policy decisions reflect this emphasis on UGIB.68 Among 9 guidelines hosted by National Guideline Clearinghouse addressing GIB, 6 were focused on UGIB, 2 on both UGIB and LGIB, and only 1 on LGIB.9 There are several reasons to believe that these relative incidence rates may not be accurate. First, recent advances in therapy and prevention of UGIB, such as the treatment of Helicobacter pylori infection; proton pump inhibitors (PPIs); and selective cyclooxygenase‐2 (COX‐2) inhibitors, may have affected the epidemiology of gastrointestinal bleeding.1016 Among these therapies, only COX‐2 inhibitors may also reduce the incidence of LGIB.14, 1618 Therefore, these advances may result in a disproportionate drop in UGIB relative to LGIB. In addition, known risk factors for both LGIB and UGIB, including advancing age and renal failure, are increasing in the general population.5, 19, 20 Finally, given the recent increased recommendations for aspirin therapy and systemic anticoagulation, exposure to aspirin and warfarin have increased, both risk factors for LGIB and UGIB.2124 Indeed, recent studies in the epidemiology of UGIB do suggest a changing pattern of etiologies of UGIB reflecting these advances.25 One study examining rates of both UGIB and LGIB demonstrate a decrease in hospitalizations overall for GIB driven by a reduction in UGIB while at the same time reporting an increase in the incidence of hospitalization for LGIB.1
In addition to a changing epidemiology, a second reason for a potential underestimation of LGIB incidence is one of methodology. There are well‐recognized limitations with using purely administrative data due to difficulties in accurately identifying patients with LGIB.26
Studies using large administrative databases may not accurately identify LGIB because of the poor sensitivity and specificity of International Classification of Diseases, Ninth revision, Clinical Modification (ICD‐9) codes for LGIB.5 While there are standard methods of identifying patients with UGIB using ICD‐9 codes,19 there is not an accepted standard for LGIB. Thus, estimates using only ICD‐9 codes may overidentify or underidentify patients with LGIB. Prior studies that have most accurately identified patients with LGIB used a 2‐step method to address this issue. The initial ICD‐9 identification included a high sensitivity/low specificity approach. These identified patient charts undergo chart review to confirm the presence of an LGIB.5 This method is labor intensive and cannot be done using administrative databases. No direct comparison of UGIB to LGIB among hospitalized patients using this 2‐step method has been done recently.
The current emphasis on UGIB as seen in the published guidelines could also be supported if patients with UGIB had greater resource utilization or worse clinical outcomes. Limited direct comparisons for these outcomes are available. However, 1 administrative database study reported similar mortality rates for UGIB (2.7%) and LGIB (2.9%) in 2006.1 No direct comparisons of other clinical outcomes or resource use outcomes are available. Therefore, the emphasis on UGIB in publications and guidelines is best supported by the incidence rates that are, as has already been discussed, problematic.
We conducted a retrospective cohort study to examine the incidences of UGIB and LGIB among patients admitted to an academic medical center over 2 years using methods designed to optimally identify patients with either UGIB or LGIB. Our study also examined differences in clinical outcomes and resource utilization between subjects with UGIB and LGIB to examine the relative severity of these 2 clinical entities. These results may be useful in determining the need to reconsider clinical approaches as well as protocols and guidelines among patients with gastrointestinal bleeding.
Patients and Methods
Patients
This retrospective cohort study evaluated all patients who were admitted with GIB to a large urban academic medical center from July 1, 2001 to June 30, 2003 and who consented to a larger study examining the effects of hospitalists on patient care. Subjects unable to provide consent due to death or lack of decisional capacity were consented via proxy. To identify patients with GIB, all patients were screened for a primary or secondary diagnosis of GIB using ICD 9 codes. These codes were selected for a very high sensitivity threshold to assure that all potential subjects with GIB were identified. All subjects identified using these codes underwent chart abstraction to determine if they met criteria for GIB. These inclusion criteria required documentation in any portion of the chart (including emergency department [ED] clinician documentation, admission note, nursing intake note, etc.) of signs or symptoms of GI hemorrhage upon admission, including: hematemesis, coffee ground emesis, gastrooccult‐positive emesis, melena, hematochezia, maroon stools, and hemoccult‐positive stools interpreted by the treating physician team as an acute GIB. Subjects identified using the ICD‐9 codes and confirmed to have an acute GIB by chart review were included in the study and underwent additional chart abstraction and administrative data analysis.
ICD‐9 codes for GIB included: esophageal varices with hemorrhage (456.0, 456.20), Mallory‐Weiss syndrome (530.7), gastric ulcer with hemorrhage (531.00531.61), duodenal ulcer with hemorrhage (532.00532.61), peptic ulcer, site unspecified, with hemorrhage (533.00533.61), gastrojejunal ulcer with hemorrhage (534.00534.61), gastritis with hemorrhage (535.61), angiodysplasia of stomach/duodenum with hemorrhage (537.83), hematemesis (578.0578.9), diverticular disease (562.00562.9), other disorders of the intestine (569.00569.9), congenital anomalies of the digestive system (751.00), proctocolitis (556.00), hemorrhoids (455.00455.6), nondysenteric colitis (006.2), noninfectious gastroenteritis and colitis (558.0558.9), salmonella gastroenteritis (003.3), malignant neoplasm of colon (153), familial adenomatous polyposis (211.3), and gastric varices (456.8).
Data
Trained research assistants performed chart abstraction with validation by the principal investigators (PIs) of the first 15 charts to ensure accuracy. Subsequently, research assistants consulted with PIs with any questions during abstracting with final decisions being made by PIs. Detailed chart abstraction collected admission medication lists as obtained by the admitting physician team, including the use of PPIs, histamine‐2 (H‐2) blockers, COX‐2 inhibitors, and medications known to increase the risk of GIB, such as nonselective NSAIDs (nsNSAIDs), aspirin, and other anticoagulants. Other clinical data including risk factors, comorbid illnesses, laboratory tests, and vital signs were also abstracted from subjects' charts.
The source (UGIB vs. LGIB) and etiology (peptic ulcer disease [PUD], varices, diverticula, etc.) of bleeding were assessed using endoscopic reports as the primary source. When no clear source was identified on endoscopy or no endoscopy was done, the abstracter would review all progress notes, discharge summaries, and other diagnostic test results such as angiography in order to identify the source of bleeding (UGIB vs. LGIB). Endoscopic reports that identified a patient as having a UGIB or LGIB but no confirmed etiology were classified as undetermined etiology unless review of the other clinical documentation provided a specific etiology.
Tachycardia was defined as pulse greater than 100 beats per minute. Orthostasis was defined by either a drop in systolic blood pressure of 20 mmHg or an increase in pulse of 10 beats per minute. Hospital administrative databases were utilized to obtain resource utilization (ie, length of stay [LOS], total cost of care, intensive care transfers), Charlson comorbidity index,27 30‐day readmission rate, and in‐hospital mortality. Hospital costs were determined using TSI cost accounting software (Transition Systems Incorporated [now Eclypsis Corporation], Boston, MA), a validated system to assess actual direct and indirect costs of care.
Statistical Analysis
Descriptive statistics (means and proportions) were calculated by location of GIB for all variables describing patient characteristics, clinical presentation, clinical outcomes, and resource utilization. Differences in age and Charlson comorbidity index by GIB location were evaluated using t tests. Differences in gender, race, and medication use were evaluated using chi‐squared tests of independence.
We fit generalized linear models to investigate differences by location of bleed for those variables measuring clinical outcomes (inpatient mortality, intensive care unit [ICU] transfer, emergency surgery, 30‐day readmission, change in hemoglobin) and those variables measuring resource outcomes (total cost, LOS, number of procedures, number of correct scopes, repeat scope indicator, incorrect scope indicator, number of red blood cell [RBC] transfusions). The repeat scope indicator was used to denote a repeat scope (either esophagogastroduodenoscopy [EGD] or colonoscopy) and the incorrect scope indicator was used to denote when the initial scope was negative and a follow‐up scope from the other direction was positive (negative EGD followed by positive colonoscopy or negative colonoscopy followed by positive EGD). For each variable we fit 2 regression models, the first model (unadjusted effect) only included location of bleed as a covariate. The second model (adjusted effect) included location of bleed, age, gender, race (black/not black) and Charlson comorbidity index as covariates. Binary outcomes were modeled using logistic regressions. For continuous variables, we determined the distribution and link of the outcome variable using residual diagnostics and by comparing the log likelihood and information criteria of competing models. All analyses were performed using STATA SE Version 9.0 (StataCorp, College Station, TX)
This study was approved by the University of Chicago Institutional Review Board.
Results
During the 2 years of observation, a total of 7741 subjects were admitted to the internal medicine service and enrolled in the hospitalist study. Of these, 1014 had a primary or secondary ICD‐9 code that may be consistent with UGIB or LGIB and underwent chart review to determine if they had an acute GIB. Out of 1014 subjects, 647 were determined not to have an acute GI hemorrhage and were excluded from the remaining analyses; 367 of the 1104 subjects identified by ICD‐9 codes were found to have a clinical presentation consistent with GIB and were included in this study. A total of 180 of these 367 had UGIB and 187 had LGIB. The mean age was 62.4 years, 56.7% were female, 82.6% were African American, 12.7% were Caucasian, and the mean Charlson index was 1.5. (Table 1) Among baseline characteristics, both gender and age were statistically associated with a difference in rates of upper vs. lower source bleeding, with LGIB patients more likely to be female (P = 0.01) and older (P < 0.001). Etiologies of UGIB include erosive disease, peptic ulcer disease, variceal bleeding, arteriovenous malformation, and malignancy. Etiologies of LGIB include: diverticulosis, colitis, arteriovenous malformation, cancer, ischemic colitis, polyp, hemorrhoidal bleed, ulcer, inflammatory bowel disease, other, and not determined (Table 2).
| Upper and Lower GI Bleeding (n = 367) | Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | P Value | |
|---|---|---|---|---|
| ||||
| Age (years), mean (SD) | 62.4 (18.0) | 58.6 (18.2) | 66.0 (17.1) | <0.001 |
| Female gender (%) | 56.7 | 50.0 | 63.1 | 0.01 |
| Race (%) | ||||
| African American | 82.6 | 85.3 | 80.1 | 0.43 |
| White | 12.7 | 10.7 | 14.5 | |
| Other | 4.7 | 4.0 | 5.4 | |
| Charlson comorbidity index, mean (SD) | 1.5 (1.5) | 1.6 (1.6) | 1.4 (1.5) | 0.44 |
| Lower GI Bleed (n = 187) | Upper GI Bleed (n = 180) | ||||
|---|---|---|---|---|---|
| Etiology | Frequency | Percent of Total (%) | Etiology | Frequency | Percent of Total (%) |
| |||||
| Diverticulosis | 76 | 41 | Erosive disease | 86 | 48 |
| Not identified | 38 | 20 | Peptic ulcer | 51 | 28 |
| Colitis, NOS | 14 | 7 | Not identified | 26 | 14 |
| AVM | 13 | 7 | Mallory Weiss | 17 | 9 |
| Cancer | 11 | 6 | Varices | 8 | 4 |
| Ischemic colitis | 9 | 5 | AVMs | 5 | 3 |
| Polyp | 9 | 5 | Mass/cancer | 5 | 3 |
| Hemorrhoid | 8 | 4 | |||
| Ulcer | 5 | 3 | |||
| Other | 3 | 1 | |||
| IBD | 1 | <1 | |||
Baseline use of medications known to be associated with either increased or decreased risk of GIB was common. Approximately one‐third of subjects with both LGIB and UGIB used aspirin and 10% used warfarin. LGIB subjects were less likely to use an nsNSAID (P < 0.001), but more likely to use a proton pump inhibitor (PPI) (P = 0.06) (Table 3).
| Upper and Lower GI Bleeding (%) (n = 367) | Upper GI Bleeding (%) (n = 180) | Lower GI Bleeding (%) (n = 187) | P Value* | |
|---|---|---|---|---|
| ||||
| Aspirin | 34.9 | 31.8 | 37.4 | 0.28 |
| nsNSAID | 12.9 | 20.8 | 6.4 | < 0.001 |
| COX‐2 selective inhibitor | 8.2 | 6.5 | 9.6 | 0.29 |
| Warfarin | 10.9 | 8.4 | 12.8 | 0.19 |
| PPI | 24.3 | 19.5 | 28.3 | 0.06 |
| nsNSAID + PPI | 1.8 | 1.3 | 2.1 | 0.56 |
| COX‐2 + PPI | 2.9 | 1.3 | 4.3 | 0.11 |
Key initial clinical presentation findings included vital sign abnormalities and admission hemoglobin levels. While hypotension was not common (4.7%), resting tachycardia (37%) and orthostasis (16%) were seen frequently. Subjects with LGIB were significantly less likely than those with UGIB to present with orthostasis (8.8% vs. 21.0%, respectively; P = 0.006) and resting tachycardia (32.3% vs. 42.5%, respectively; P = 0.04). Subjects with LGIB had a higher admission hemoglobin than those with UGIB (10.7 vs. 9.7, respectively; P < 0.001) (Table 4).
| Clinical Finding | Upper and Lower GI Bleeding (n = 367) | Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | P Value* |
|---|---|---|---|---|
| ||||
| Hypotension (%) | 4.7 | 5.7 | 3.8 | 0.39 |
| Resting tachycardia (%) | 37.3 | 42.5 | 32.3 | 0.04 |
| Orthostatic hypotension (%) | 16.2 | 21.0 | 8.8 | 0.006 |
| Admission hemoglobin (g/dL), mean (SD) | 10.2 (2.6) | 9.7 (2.7) | 10.7 (2.5) | <0.001 |
We also examined several clinical outcomes. When comparing LGIB to UGIB patients for these clinical outcomes using bivariate and multivariate statistics, there was no difference for in‐hospital mortality (1.1% vs. 1.1%), transfer to ICU (16.0% vs. 13.9%), 30‐day readmission (5.9% vs.7.8%), number of red blood cell (RBC) transfusions (2.7 vs. 2.4), or need for GI surgery (1.1% vs. 0.0%). The mean drop in hemoglobin was greater among subjects with LGIB compared to UGIB (1.9 g/dL vs. 1.5 g/dL, respectively) by both bivariate (P = 0.01) and multivariate (P = 0.003) analyses (Table 5).
| Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | Bivariate P Value | Multivariate P Value | |
|---|---|---|---|---|
| ||||
| In‐hospital mortality (%)* | 1.1 | 1.1 | 0.97 | 0.74 |
| Transfer to ICU (%)* | 13.9 | 16.0 | 0.56 | 0.44 |
| Drop in hemoglobin (g/dL), mean (SD) | 1.5 (1.5) | 1.9 (1.6) | 0.01 | 0.003 |
| Packed RBC transfusions required (units), mean (SD)* | 2.4 (2.9) | 2.7 (3.7) | 0.36 | 0.33 |
| Surgery for GI bleeding (%) | 0.0% | 1.1 | ||
| 30‐day readmission rate (%)* | 7.8 | 5.9 | 0.49 | 0.45 |
Mean costs were $11,892 for LGIB and $14,301 for UGIB and median costs were $7,890 for LGIB and $9,548 for UGIB, but were not statistically different. LOS was also similar between subjects with LGIB (5.1 days) and UGIB (5.7 days). In bivariate and multivariate analyses, UGIB subjects had a similar mean number of endoscopic procedures (1.3) compared to LGIB subjects (1.2). Thirteen percent of subjects with UGIB required a second EGD while only 8% of subjects with LGIB required 2 colonoscopies. In addition, 29% of subjects with LGIB received an EGD while only 16% of subjects with an UGIB received a colonoscopy (P = 0.001) (Table 6).
| Upper GI Bleeding (n = 180) | Lower GI Bleeding (n = 187) | Bivariate P Value | Multivariate P Value | |
|---|---|---|---|---|
| ||||
| Cost ($), mean (SD)* | 14,301 (17,196) | 11,892 (13,100) | 0.13 | 0.21 |
| Cost ($), median | $9,548 | $7,890 | ||
| Length of stay (days), mean (SD)* | 5.7 (7.0) | 5.1 (5.3) | 0.37 | 0.72 |
| Number of endoscopies/ patient, mean (SD) | 1.3 (0.5) | 1.2 (0.9) | 0.18 | 0.20 |
Conclusions
This study represents one of the largest direct comparisons of LGIB to UGIB not based on administrative databases. The most striking finding was the nearly equal rates of LGIB and UGIB. There are 2 likely explanations for this surprising result. First, there may be methodological reasons that we identified a greater proportion of true LGIBs; our study used a highly sensitive search strategy of ICD‐9 coding with confirmatory chart abstraction to ensure that as many LGIB and UGIB cases would be identified as possible while also excluding cases not meeting accepted criteria for GIB. The second possibility is that there is an actual change in epidemiology of GIB. Known risk factors for LGIB are increasing such as advancing age, increased use of chronic aspirin therapy, and renal disease. At the same time, significant advances in the treatment and prevention of UGIB have been made. Recent studies have demonstrated similar trends in admissions for upper and lower GI complications, suggesting that there may be a changing epidemiology due primarily to reductions in upper GI complications.1, 16
Either explanation would have implications for the care of patients with GIB. Clinical decision‐making based on prior literature would support that in ambiguous clinical situations and initial evaluation for an UGIB is appropriate. Most risk stratification literature and clinical guidelines focus on UGIB. If rates of LGIB and UGIB are similar, then existing clinical decision protocols may need to be reevaluated to incorporate the higher likelihood of LGIB. This reevaluation would be less important if the clinical outcomes or resource utilization of UGIB was significantly greater than that for LGIB, but we did not find this was the case. Similarly, if the ability to distinguish between LGIB and UGIB were robust on clinical signs and symptoms, then a reevaluation would be less important. However, we found fairly similar numbers of patients initially receiving evaluation for UGIB then being evaluated for LGIB as we found patients initially receiving evaluation for LGIB then being evaluated for UGIB. This suggests the potential benefit of clinical decision protocols that could better distinguish between UGIB and LGIB and account for the potentially higher incidence of LGIB than previously thought.
In addition to affecting the attention paid to LGIB for acute management, a changed understanding of incidence could also affect the attention paid to prevention of LGIB. Of the recent nonendoscopic advances in the treatment and prevention of GIB, only the use of COX‐2s (when used in place of traditional nsNSAIDs) reduces the risk of both LGIB and UGIB;14, 1618 H .pylori treatment and PPIs only prevent UGIB. Therefore, if the clinical and financial burdens of LGIB are similar to those seen in UGIB, more attention may need to be focused on preventing LGIB.
Baseline medication use was notable primarily for the similarities between UGIB and LGIB. Agents known to affect the rates of GIB were common in both groups. Over one‐third of the population was using aspirin and 10% were taking warfarin. Over 20% of subjects were taking an nsNSAID or a COX‐2 inhibitor. Almost one‐quarter of subjects were taking a PPI, agents known to decrease rates of UGIB and potentially increase LGIB through the risk of C. difficile colitis. Notably, the only statistically significant difference in baseline medication use between subjects with UGIB and LGIB was the more than 3‐fold higher use of nsNSAIDs in patients with UGIB as compared to LGIB. While current guidelines are not clear and consistent about which populations of at‐risk patients should receive GI prophylaxis,2830 these results suggest that patients admitted with GIB are very likely to be taking medications which impact the risk of GIB.
In terms of disease severity, the clinical presentation at admission suggests a greater degree of hemodynamic instability among subjects with UGIB. Rates of orthostatic hypotension and resting tachycardia are higher in UGIB subjects, as well as having a lower mean hemoglobin levels at presentation. However, despite the more severe clinical presentation, clinical outcomes did not differ significantly between the 2 bleeding sources. Thus, the most relevant clinical outcomes suggest that the severity of both LGIB and UGIB are similar. This similarity again suggest that the clinical burden of LGIB is not significantly different than UGIB.
Our results concerning resource utilization demonstrate a similar pattern. While the point estimates for costs and LOS suggest that UGIB may be associated with higher resource utilization, these differences were not significant in either bivariate or multivariate analyses. Those subjects with UGIB did receive more total endoscopic procedures than subjects with LGIB. More interesting though was that 24% of all subjects received an endoscopy of the opposite site (LGIB with EGD and UGIB with colonoscopy). These results suggest that the site of bleeding is not clear in a significant proportion of patients who present with GIB. These additional endoscopies are associated with increased risk, costs, LOS, and discomfort to patients. Improving our ability to accurately predict the source (upper vs. lower) of bleeding would allow us to reduce the number of these excess endoscopies. Additionally, it is interesting that despite the almost universal use of endoscopies, 20% of LGIB and 14% of UGIB subjects could not have a specific etiology identified during endoscopy or subsequent workup.
There are some important limitations to this study. While the sample size is among the largest of its type involving chart abstraction, it may be underpowered to detect some differences. Additionally, our results are from a single urban academic medical center with a patient population that is predominantly African American, which may limit generalizability. This study required consent and therefore only examines a subset of patients admitted to the medical center with GIB, which could potentially introduce bias into the sample. However, it is not clear why there would be systematic differences in subjects who choose to consent vs. those who decide not to consent that would affect the results of this study in substantive ways.
Despite significant efforts at identifying all subjects with GIB admitted during this time period, there were potential methodological reasons that may have resulted in some cases being missed. Only subjects admitted to a medicine service were approached for consent. All subjects in this medical center with GIB are admitted to a medicine service. We captured all subjects who were initially admitted to a medicine service as well as those admitted initially to an ICU and then transferred to the floor at any point prior to discharge. It is possible, though, that a subject would be admitted to an ICU for GIB and die prior to being transferred to the floor. While it is the impression of the director of the ICU that this would be a very unusual event, as most of the patients would be discharged to the floor prior to death (personal communication), given the very low mortality rate seen in this study, small numbers of missed events could have a significant impact on the interpretation of in‐hospital mortality results. It is also important to note that this medical center did not have the ability to perform endoscopy prior to admission for patients with GIB at the time of the study; all patients who presented with GIB would have been admitted and identified for this study. Finally, we were unable to routinely identify the rationale for obtaining an endoscopic exam. We assumed that all endoscopic exams were done for the purpose of evaluating and/or treating the GIB for which the subject was admitted. It is possible that some subjects had additional endoscopies for other reasons, which would have led to our overestimating the rates of additional endoscopies for GIB.
This study highlights the similarities between LGIB and UGIB rather than the differences. There were few significant differences between the 2 bleeding sources in terms of incidence, clinical outcomes, and resource utilization. In fact, the study also suggests that determining the source of bleeding may not be clear, given the high rates of opposite site endoscopies. While this study did reveal several similarities between UGIB and LGIB, it also highlights the need to identify improved strategies to improve the sensitivity and specificity of identification of LGIB compared to UGIB, both for clinical purposes and for research. The value of such improved clinical algorithms have the potential to improve both the cost and outcomes of care, while better algorithms for separating UGIB and LGIB using administrative data might help produce more precise estimates of costs and clinical outcomes, and aid in the development of risk stratification models.
- ,.Hospitalizations for Gastrointestinal Bleeding in 1998 and 2006. HCUP Statistical Brief #65, December 2008.Rockville, MD:Agency for Healthcare Research and Quality.
- ,.Causes and outcome of upper and lower gastrointestinal bleeding: The Grady Hospital Experience.South Med J.1999;92(1):44–50.
- ,,, et al.Acute upper gastrointestinal haemorrhage in west of Scotland: case ascertainment study.BMJ.1997;315:510–540.
- ,.A cost‐effective approach to the patient with peptic ulcer bleeding.Surg Clin North Am.1996;76:83–103.
- .Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population based study.Am J Gastroenterol.1997;92:419–424.
- ,,.Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding.Ann Int Med.2003;139:843–857.
- ,.Incremental value of upper endoscopy for triage of patients with acute non‐variceal upper‐GI hemorrhage.Gastrointest Endosc2004;60:9–14.
- ,,, et al.Upper gastrointestinal hemorrhage clinical guideline‐determining the optimal hospital length of stay.Am J Med.1996;100:313–322.
- National Guideline Clearinghouse. Available at: http://www.guideline.gov. Accessed August2009.
- ,,, et al.Prevention of ulcer recurrence after eradication of Helicobacter pylori: a prospective long‐term follow‐up study.Gastroenterology.1997;113:1082–1086.
- ,,, et al.Treatment of Helicobacter pylori in patients with duodenal ulcer hemorrhage‐a long‐term randomized, controlled study.Am J Gastroenterol.2000;95:2225–2232.
- ,,, et al.Preventing recurrent upper gastrointestinal bleeding in patients with Helicobacter pylori infection who are taking low‐dose aspirin or naproxen.N Engl J Med.2001;344:967–973.
- ,,, et al.Lansoprazole for the prevention of recurrences of ulcer complications from long‐term low‐dose aspirin use.N Engl J Med.2002;346:2033–2038.
- ,,, et al.Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group.N Engl J Med.2000;343:1520–1528.
- ,,, et al.Gastrointestinal toxicity with celecoxib vs nonsteroidal anti‐inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long‐Term Arthritis Safety Study.JAMA.2000;284:1247–1255.
- ,,, et al.Time trends and clinical impact of upper and lower gastrointestinal complications. Digestive Disease Week National Meeting,2008. San Diego, CA, May 17–22.
- ,,, et al.Video capsule endoscopy to prospectively assess small bowel injury with celecoxib, naproxen plus omeprazole, and placebo.Clin Gastroenterol Hepatol.2005;3:133–141.
- ,,, et al.Serious lower gastrointestinal clinical events with nonselective NSAID or Coxib use.Gastroenterology.2003;124:288–292.
- ,,, et al.Risk factors for upper gastrointestinal bleeding among end‐stage renal disease patients.Kidney Int.2003;64:1455–1461.
- ,,, et al.Risk factors for hospitalized bleeding among older patients.J Am Geriatr Soc.2001;49:126–133.
- Institute for Clinical Systems Improvement (ICSI). Preventive services in adults. Bloomington, MN: Institute for Clinical Systems Improvement (ICSI).2005. Available at http://www.isci.org/guidelines_and_more/guidelines_order_sets_protocol/for_patients_families/preventive_services_for_adults_for_patients_families_.html. Accessed Month year.
- .NSAID‐associated deaths: the rise and fall of NSAID‐associated GI mortality.Am J Gastroenterol.2005;100:1694–1695.
- ,.Effects of very low doses of daily long‐term aspirin therapy on gastric, duodenal, and rectal prostaglandins on mucosal injury in healthy humans.Gastroenterology. 199;117:17–25.
- ,,, et al.A nationwide study of mortality associated with hospital admission due to severe gastrointestinal events and those associated with nonsteroidal antiinflammatory drug use.Am J Gastroenterol.2005;100:1685–1693.
- ,,, et al.Acute upper GI bleeding: did anything change?Am J Gastroenterol.2003;98:1494–1499.
- ,.Lower intestinal bleeding.Best Pract Res Clin Gastroenterol.2001;15:135–153.
- ,,,.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.J Chronic Dis.1987;40:373–383.
- AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons.J Am Geriatr Soc.2002;50(6 suppl):S205–S224.
- ,,, et al.Pain in Osteoarthritis, Rheumatoid Arthritis and Juvenile Chronic Arthritis.2nd ed.Clinical practice guideline no. 2.Glenview, IL:American Pain Society (APS);2002:179.
- American College of Rheumatology Subcommittee on Osteoarthritis Guidelines.Recommendations for the Medical Management of Osteoarthritis of the Hip and Knee.Arthritis Rheum.2000;43:1905–1915.
- ,.Hospitalizations for Gastrointestinal Bleeding in 1998 and 2006. HCUP Statistical Brief #65, December 2008.Rockville, MD:Agency for Healthcare Research and Quality.
- ,.Causes and outcome of upper and lower gastrointestinal bleeding: The Grady Hospital Experience.South Med J.1999;92(1):44–50.
- ,,, et al.Acute upper gastrointestinal haemorrhage in west of Scotland: case ascertainment study.BMJ.1997;315:510–540.
- ,.A cost‐effective approach to the patient with peptic ulcer bleeding.Surg Clin North Am.1996;76:83–103.
- .Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population based study.Am J Gastroenterol.1997;92:419–424.
- ,,.Consensus recommendations for managing patients with nonvariceal upper gastrointestinal bleeding.Ann Int Med.2003;139:843–857.
- ,.Incremental value of upper endoscopy for triage of patients with acute non‐variceal upper‐GI hemorrhage.Gastrointest Endosc2004;60:9–14.
- ,,, et al.Upper gastrointestinal hemorrhage clinical guideline‐determining the optimal hospital length of stay.Am J Med.1996;100:313–322.
- National Guideline Clearinghouse. Available at: http://www.guideline.gov. Accessed August2009.
- ,,, et al.Prevention of ulcer recurrence after eradication of Helicobacter pylori: a prospective long‐term follow‐up study.Gastroenterology.1997;113:1082–1086.
- ,,, et al.Treatment of Helicobacter pylori in patients with duodenal ulcer hemorrhage‐a long‐term randomized, controlled study.Am J Gastroenterol.2000;95:2225–2232.
- ,,, et al.Preventing recurrent upper gastrointestinal bleeding in patients with Helicobacter pylori infection who are taking low‐dose aspirin or naproxen.N Engl J Med.2001;344:967–973.
- ,,, et al.Lansoprazole for the prevention of recurrences of ulcer complications from long‐term low‐dose aspirin use.N Engl J Med.2002;346:2033–2038.
- ,,, et al.Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group.N Engl J Med.2000;343:1520–1528.
- ,,, et al.Gastrointestinal toxicity with celecoxib vs nonsteroidal anti‐inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long‐Term Arthritis Safety Study.JAMA.2000;284:1247–1255.
- ,,, et al.Time trends and clinical impact of upper and lower gastrointestinal complications. Digestive Disease Week National Meeting,2008. San Diego, CA, May 17–22.
- ,,, et al.Video capsule endoscopy to prospectively assess small bowel injury with celecoxib, naproxen plus omeprazole, and placebo.Clin Gastroenterol Hepatol.2005;3:133–141.
- ,,, et al.Serious lower gastrointestinal clinical events with nonselective NSAID or Coxib use.Gastroenterology.2003;124:288–292.
- ,,, et al.Risk factors for upper gastrointestinal bleeding among end‐stage renal disease patients.Kidney Int.2003;64:1455–1461.
- ,,, et al.Risk factors for hospitalized bleeding among older patients.J Am Geriatr Soc.2001;49:126–133.
- Institute for Clinical Systems Improvement (ICSI). Preventive services in adults. Bloomington, MN: Institute for Clinical Systems Improvement (ICSI).2005. Available at http://www.isci.org/guidelines_and_more/guidelines_order_sets_protocol/for_patients_families/preventive_services_for_adults_for_patients_families_.html. Accessed Month year.
- .NSAID‐associated deaths: the rise and fall of NSAID‐associated GI mortality.Am J Gastroenterol.2005;100:1694–1695.
- ,.Effects of very low doses of daily long‐term aspirin therapy on gastric, duodenal, and rectal prostaglandins on mucosal injury in healthy humans.Gastroenterology. 199;117:17–25.
- ,,, et al.A nationwide study of mortality associated with hospital admission due to severe gastrointestinal events and those associated with nonsteroidal antiinflammatory drug use.Am J Gastroenterol.2005;100:1685–1693.
- ,,, et al.Acute upper GI bleeding: did anything change?Am J Gastroenterol.2003;98:1494–1499.
- ,.Lower intestinal bleeding.Best Pract Res Clin Gastroenterol.2001;15:135–153.
- ,,,.A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.J Chronic Dis.1987;40:373–383.
- AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons.J Am Geriatr Soc.2002;50(6 suppl):S205–S224.
- ,,, et al.Pain in Osteoarthritis, Rheumatoid Arthritis and Juvenile Chronic Arthritis.2nd ed.Clinical practice guideline no. 2.Glenview, IL:American Pain Society (APS);2002:179.
- American College of Rheumatology Subcommittee on Osteoarthritis Guidelines.Recommendations for the Medical Management of Osteoarthritis of the Hip and Knee.Arthritis Rheum.2000;43:1905–1915.
Copyright © 2010 Society of Hospital Medicine
Hospitalist Effects on Acute IGIH Patients
Acute upper gastrointestinal hemorrhage (UGIH) is one of the most common hospital admissions for acute care. Estimates indicate that 300,000 patients (100‐150 cases per 100,000 adults) are admitted annually with an associated economic impact of $2.5 billion.15 The current standard management of UGIH requires hospital admission and esophagogastroduodenoscopy (EGD) by a gastroenterologist for diagnosis and/or treatment. This management strategy results in a high consumption of hospital resources and costs.
Simultaneously, hospitalists have dramatically changed the delivery of inpatient care in the United States and are recognized as a location‐driven subspecialty for the care of acute hospitalized patients, similar to emergency medicine. Currently there are 20,000 hospitalists, and more than one‐third of general medicine inpatients are cared for by hospitalists.6, 7
Previous studies have shown that hospitalist care offers better or comparable outcomes, with lower overall length of stay (LOS) and costs compared to traditional providers.810 However, most of these studies were performed in single institutions, had weak designs or little‐to‐no adjustment for severity of illness, or were limited to 7 specific diseases (pneumonia, congestive heart failure [CHF], chest pain, ischemic stroke, urinary tract infection, chronic obstructive lung disease [COPD], and acute myocardial infarction [AMI]).8
Furthermore, less is known about the effect of hospitalists on conditions that may be dependent upon specialist consultation for procedures and/or treatment plans. In this study, gastroenterologists performed diagnostic and/or therapeutic endoscopy work as consultants to the attending physicians in the management of acute inpatient UGIH.
To explore the effects of hospitalists on care of patients with acute UGIH, we examined data from the Multicenter Hospitalist (MCH) trial. The objectives of our study were to compare clinical outcomesin‐hospital mortality and complications (ie, recurrent bleeding, intensive care unit [ICU] transfer, decompensation, transfusion, reendoscopy, 30‐day readmission)and efficiency (LOS and costs) in hospitalized acute UGIH patients cared for by hospitalists and nonhospitalists in 6 academic centers in the United States during a 2‐year period.
Patients and Methods
Study Sites
From July 1, 2001 to June 30, 2003, the MCH trial1113 was a prospective, multicenter, observational trial of the care provided by hospitalists to patients admitted to general medical services at 6 academic medical institutions. There were 31,000 consecutive admissions to the general medical services of these participating sites: University of Chicago (Chicago, IL), University of Wisconsin Hospital (Madison, WI), University of Iowa (Iowa City, IA), University of California at San Francisco (San Francisco, CA), University of New Mexico (Albuquerque, NM), and Brigham and Women's Hospital (Boston, MA). The study was approved by the institutional review boards (IRBs) at each of the 6 participating institutions.
MCH Study Patients
Patients were eligible if they were admitted to the general medical services under the care of a hospitalist or nonhospitalist physician. Regardless of the admitting provider, each medical service was composed of rotating senior and junior resident physicians in all 6 sites. Furthermore, patients were 18 years of age or older, and were able to give consent themselves or had an appropriate proxy. Patients with mini‐mental status score of 17 (out of 22), admitted under their primary care physician or to an inpatient gastroenterology service, or transferred from another hospital, were excluded. The MCH study was designed to study the outcomes and efficiency in patients admitted for CHF, pneumonia, UGIH, and end‐of‐life care.
Acute UGIH Patients
Within the MCH‐eligible patients, we identified those with acute UGIH using the following International Classification of Diseases, 9th edition (ICD‐9) codes assigned at discharge: esophageal varices with hemorrhage (456.0, 456.20); Mallory‐Weiss syndrome (530.7); gastric ulcer with hemorrhage (531.00531.61); duodenal ulcer with hemorrhage (532.00532.61); peptic ulcer, site unspecified, with hemorrhage (533.00533.61); gastrojejunal ulcer with hemorrhage (534.00534.61); gastritis with hemorrhage (535.61); angiodysplasia of stomach/duodenum with hemorrhage (537.83); and hematemesis (578.0, 578.9). We also confirmed the diagnosis of UGIH by reviewing patient medical records for observed hematemesis, nasogastric tube aspirate with gross or hemoccult blood, or clinical history of hematemesis, melena, or hematochezia.14, 15
Data
All data were obtained from the 6 hospitals' administrative records, patient interviews, and medical chart abstractions. Dates of admission and discharge, ICD‐9 diagnosis codes, insurance type, age, race, and gender were obtained from administrative data. One‐month follow‐up telephone interviews assessed whether or not patient had any follow‐up appointment or hospital readmissions. Trained abstractors from each site performed manual chart reviews using a standard data collection sheet. The ICD‐9 code designation and chart abstraction methodology were developed prior to the initiation of the study to ensure consistent data collection and reduce bias.
The following data elements were collected: comorbidities, endoscopic findings, inpatient mortality, clinical evidence of rebleeding, endoscopic treatment or gastrointestinal (GI) surgery to control bleeding, repeat EGD, ICU transfer, decompensated comorbid illness requiring continued hospitalization, and blood transfusion (packed red cells, plasma, platelets). Clinical evidence of rebleeding was defined as either hematemesis or melena with decrease in hemoglobin of 2 g in 24 hours with or without hemodynamic compromise.14, 15 For the purpose of this study, recurrent bleeding was defined as clinical evidence of rebleeding, emergency GI surgery for control of UGIH, or repeat EGD before discharge. Furthermore, a composite endpoint termed total complications encompassed all adverse outcomes related to the UGIH hospitalization. The 30‐day readmission variable was defined using readmission identified in administrative records and a 30‐day follow‐up phone call. To guard against recall bias, self‐report data was only included for nonsite admissions.
We defined efficiency in terms of costs and LOS. Total hospital costs were measured using the TSI cost accounting system (Transition Systems, Inc., Boston, MA; now Eclipsys Corporation)16, 17 at 5 out of the 6 participating sites. TSI is a hospital cost accounting software system that integrates resource utilization and financial data already recorded in other hospital databases (such as the billing system, payroll system, and general ledger system).17 Hospital LOS was defined as the number of days from patient admission to the general medicine service until patient discharge.
Provider Specialization: Hospitalists vs. Nonhospitalists
The study was designed as a natural experiment based on a call cycle. The hospitalist‐led teams at each institution alternated in a 4‐day or 5‐day general medicine call cycle with teams led by traditional academic internal medicine attending physicians. All patients were assigned to teams according to their position in the call cycle without regard to whether the attending physician was a hospitalist or a nonhospitalist. Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients.18, 19 As previously reported in a related MCH work,11 a hospitalist was also defined as a provider who spends at least 25% of his or her time on an academic inpatient general medicine service. Nonhospitalist physicians were most often outpatient general internal medicine faculty or subspecialists, who attended 1 month per year. Physicians were classified as hospitalists or nonhospitalists according to the designations provided by each site.
UGIH‐specific Confounders
From chart abstraction, we captured severity of illness, comorbidity, and performance of early EGD, variables that can confound analysis in UGIH. To capture severity of illness, a complete Rockall risk score was calculated for each patient. The complete Rockall uses 3 clinical variables (age, shock, and comorbidity) and 2 endoscopic variables (endoscopic diagnosis and stigmata of recent hemorrhage).5, 20 A complete Rockall score of 2 is considered low‐risk for rebleeding or death following admission.21, 22 The accepted definition of low‐risk is <5% recurrent bleeding and <1% mortality risk. A complete Rockall score of 3 to 5 is considered moderate‐risk while 6 is considered high‐risk. Comorbidity was measured using the Charlson comorbidity index.23 Performance of early endoscopy, usually defined as endoscopy performed within 24 hours from presentation, was previously shown to decrease LOS and need for surgical intervention in patients with acute UGIH.24, 25 Documented times of presentation to the emergency department and time of endoscopy performance were collected to calculate for the rate of early endoscopy in our study population.
Statistical Analysis
All statistical analyses were performed using SAS Version 9.1 for Windows (SAS Institute, Cary, NC).
Differences in baseline demographic characteristics of patients and their endoscopic findings were compared between the 2 types of providers. Univariate analyses were also performed to compare the differences in adverse outcomes, LOS, and costs between patients cared for by hospitalists and nonhospitalists. Chi‐square tests were used for categorical variables; while both Wilcoxon rank sum test and Student's t test were used in the analysis of continuous variables.
Next, we performed multivariable analyses to determine the independent association between hospitalist care and the odds of the patients having certain outcomes. However, to prevent overfitting, we only developed regression models for adverse outcomes that have at least 20% event rate.
Multivariable regression models were developed separately for LOS and costs. In contrast with the models on outcomes, analyses of LOS and costs were restricted to: (1) patients who were discharged alive; and (2) to cases with LOS and costs values within 3 standard deviations (SDs) of the mean because of the skewed nature of these data.
All models were adjusted for age, gender, race, insurance type, complete Rockall risk score, performance of early EGD, Charlson comorbidity index, and study site. Final candidate variables in the models were chosen based on stepwise selection, a method very similar to forward selection except that variables selected for the model do not necessarily remain in the model. Effects were entered into and then removed from the model in such a way that each forward selection step can be followed by 1 or more backward elimination steps. The stepwise selection was terminated if no further effect can be added to the model or if the current model was identical to the previous model. The stepwise selection model was generated using statistical criterion of alpha = 0.05 for entry and elimination from the model. Variables that can be a profound source of variation, such as study site and treating physician, were included in the model irrespective of their statistical significance.
To account for clustering of patients treated by the same physician, we used multilevel modeling with SAS PROC GLIMMIX (with random effects). For outcomes (categorical variables), we utilized models with logit‐link and binomial‐distributed errors. As for efficiency (continuous variables with skewed distribution), the multivariable analyses used a generalized linear model with log‐link and assuming gamma‐distributed errors.
Results
Patient Characteristics and Endoscopic Diagnoses
Out of 31,000 patients, the study identified a total of 566 patients (1.8%) with acute UGIH (Table 1). However, 116 patients transferred from another hospital were excluded as their initial management was provided elsewhere, giving a final study sample of 450 patients. Overall, there are 163 admitting physicians from 6 sites, with 39 (24%) classified as hospitalists and 124 (76%) as nonhospitalists. Forty‐two percent (177/450) of patients were cared for by hospitalists. Compared to nonhospitalists, patients admitted to the hospitalist service were older (62.8 vs. 57.7 years, P < 0.01) and with third‐party payor mix differences (P < 0.01). However, there were no statistical differences between patients attended by hospitalists and nonhospitalists with regard to Complete Rockall risk score, Charlson comorbidity index, performance of early endoscopy, and mean hemoglobin values on admission. Upper endoscopy was performed in all patients with distribution of the 3 most common diagnoses being similar (P > 0.05) between hospitalists and nonhospitalists: erosive disease (49.7% vs. 54.6%), peptic ulcer disease (PUD) (48% vs. 46.9%), and varices (18.6% vs. 14.7%).
| Variable | Admitting Service | P | |
|---|---|---|---|
| Hospitalist (n = 177) | Nonhospitalist (n = 273) | ||
| |||
| Age, years (meanSD) | 62.817.4 | 57.718.5 | <0.01 |
| Male sex, n (%) | 104 (58.8) | 169 (61.9) | 0.50 |
| Ethnicity, n (%) | 0.13 | ||
| White | 83 (46.9) | 102 (37.4) | |
| African‐American | 34 (19.2) | 75 (27.5) | |
| Hispanic | 21 (11.9) | 40 (14.7) | |
| Asian/Pacific Islander | 24 (13.6) | 29 (10.6) | |
| Others/unknown | 15 (8.5) | 27 (9.9) | |
| Insurance, n (%) | <0.01 | ||
| Medicare | 86 (48.6) | 104 (38.1) | |
| Medicaid | 15 (8.5) | 33 (12.1) | |
| No payer | 18 (10.2) | 36 (13.2) | |
| Private | 46 (26) | 52 (19.1) | |
| Unknown | 12 (6.8) | 48 (17.5) | |
| Charlson Comorbidity Index (meanSD) | 1.91.6 | 1.81.7 | 0.51 |
| Complete Rockall, n (%) | 0.11 | ||
| Low‐risk (0‐2) | 82 (46.3) | 103 (37.7) | |
| Moderate‐risk (3‐5) | 71 (40.1) | 137 (50.2) | |
| High‐risk (6) | 24 (14.6) | 33 (12.1) | |
| Early endoscopy (<24 hours) | 82 (46.3) | 133 (48.7) | 0.62 |
| Endoscopic diagnosis, n (%)* | |||
| Erosive disease | 88 (49.7) | 149 (54.6) | 0.31 |
| Peptic ulcer disease | 85 (48.0) | 128 (46.9) | 0.81 |
| Varices | 33 (18.6) | 40 (14.7) | 0.26 |
| Mallory‐Weiss tear | 9 (5.1) | 21 (7.7) | 0.28 |
| Angiodysplasia | 9 (5.1) | 13 (4.8) | 0.88 |
| GI mass | 1 (0.6) | 4 (1.5) | 0.65 |
| Normal | 7 (4.0) | 8 (2.9) | 0.55 |
| Admission hemoglobin values (meanSD) | 10.22.9 | 10.22.9 | 0.78 |
Clinical Outcomes
Between hospitalists and nonhospitalists, unadjusted outcomes were similar (P > 0.05) for mortality (2.3% vs. 0.4%), recurrent bleeding (11% vs. 11%), need for endoscopic therapy (24% vs. 22%), ICU‐transfer and decompensation (15% vs. 15%), as well as an overall composite measure of any complication (79% vs. 72%) (Table 2). However, the hospitalist‐led teams performed more blood transfusions (74% vs. 63%, P = 0.02) and readmission rates were higher (7.3% vs. 3.3%, P = 0.05).
| Outcomes, n (%) | Admitting Service | P | |
|---|---|---|---|
| Hospitalist (n = 177) | Nonhospitalist (n = 273) | ||
| |||
| Inpatient mortality | 4 (2.3) | 1 (0.4) | 0.08 |
| Recurrent bleeding* | 20 (11.3) | 29 (10.6) | 0.88 |
| Endoscopic therapy | 43 (24.3) | 60 (22.0) | 0.57 |
| ICU transfers | 23 (13) | 24 (8.8) | 0.20 |
| Decompensated comorbidities that required continued hospitalization | 26 (14.7) | 41 (15.0) | 0.92 |
| Any transfusion | 131 (74.0) | 172 (63.0) | 0.02 |
| Total complications | 139 (78.5) | 196 (71.8) | 0.11 |
| 30‐day all‐cause readmissions | 13 (7.3) | 9 (3.3) | 0.05 |
| Efficiency | Hospitalist (n = 164) | Nonhospitalist (n = 259) | P |
| LOS, days | |||
| MeanSD | 4.83.5 | 4.53.0 | 0.30 |
| Median (interquartile range) | 4 (36) | 4 (26) | 0.69 |
| Total costs, U.S. $ | |||
| MeanSD | 10,466.669191.00 | 7926.716065.00 | <0.01 |
| Median (interquartile range) | 7359.00 (4,698.0012,550.00) | 6181.00 (3744.0010,344.00) | <0.01 |
Because of the low event rate of certain adverse outcomes (<20%), we were only able to perform adjusted analyses on 4 outcomes: need for endoscopic therapy (odds ratio [OR], 0.82; 95% confidence interval [CI], 0.491.37), ICU transfer and decompensation (OR, 0.82; 95% CI, 0.451.52), blood transfusion (OR, 1.30; 95% CI, 0.822.04), and any complication (OR, 1.18; 95% CI, 0.711.96). Since outcome differences disappeared after controlling for confounders, the data suggest that overall care provided by hospitalists and nonhospitalists might be equivalenteven in certain outcomes that we were unable to substantiate using multivariable methods.
Efficiency
Efficiency, as measured by LOS and costs, are presented both as means and medians in univariate analyses in Table 2. Median LOS was similar for hospitalist‐led and nonhospitalist‐led teams (4 days). Despite having similar LOS, the median costs of acute UGIH in patients cared for by hospitalists were higher ($7,359.00 vs. $6,181.00; P < 0.01).
After adjusting for demographic factors, Rockall risk score, comorbidity, early EGD, and hospital site, LOS remained similar between the 2 groups. On the other hand, the adjusted cost for UGIH patients cared for by hospitalists and nonhospitalists persisted, with hospitalist care costs $1,502.40 more than their nonhospitalist counterparts (Table 3).
| Efficiency | Treatment Provider | P | |
|---|---|---|---|
| Hospitalist (n = 164) | Nonhospitalist (n = 259) | ||
| |||
| Adjusted length of stay, days (mean SD) | 5.2 (4.95.6) | 4.7 (4.55.0) | 0.15 |
| Adjusted total cost, U.S. $ (mean SD) | 9006.50 (8366.609693.60) | 7504.10 (7069.907964.20) | 0.03 |
Discussion
This is the first study that has looked at the effect of hospitalists on clinical outcomes and efficiency in patients admitted for acute UGIH, a condition highly dependent upon another specialty for procedures and management. This is also one of only a few studies on UGIH that adjusted for severity of illness (Rockall score), comorbidity, performance of early endoscopypatient‐level confounders usually unaccounted for in prior research.
We show that hospitalists and nonhospitalists caring for acute UGIH patients had overall similar unadjusted outcomes; except for blood transfusion and 30‐day readmission rates. Unfortunately, due to the small number of events for readmissions, we were unable to perform adjusted analysis for readmission. Differences between hospitalists and nonhospitalists on blood transfusion rates were not substantiated on multivariable adjustments.
As for efficiency, univariable and multivariable analyses revealed that LOS was similar between provider types while costs were greater in UGIH patients attended by hospitalists.
Reductions in resource use, particularly costs, may be achieved by increasing throughput (eg, reducing LOS) or by decreasing service intensity (eg, using fewer ancillary services and specialty consultations).26 Specifically in acute UGIH, LOS is significantly affected by performance of early EGD.27, 28 In these studies, gastroenterologist‐led teams, compared to internists and surgeons, have easier access to endoscopy, thus reducing LOS and overall costs.27, 28
Similarly, prior studies have shown that the mechanism by which hospitalists lower costs is by decreasing LOS.810, 29 There are several hypotheses on how hospitalists affect LOS. Hospitalists, by being available all day, are thought to respond quickly to acute symptoms or new test results, are more efficient in navigating the complex hospital environment, or develop greater expertise as a result of added inpatient experience.8 On the downside, although the hospitalist model reduces overall LOS and costs, they also provide higher intensity of care as reflected by greater costs when broken down per hospital day.29 Thus, the cost differential we found may represent higher intensity of care by hospitalists in their management of acute UGIH, as higher intensity care without decreasing LOS can translate to higher costs.
In addition, patients with acute UGIH are unique in several respects. In contrast to diseases like heart failure, COPD, and pneumonia, in which the admitting provider has the option to request a subspecialist consultation, all patients with acute UGIH need a gastroenterologist to perform endoscopy as part of the management. These patients are usually admitted to general medicine wards, aggressively resuscitated with intravenous fluids, with a nonurgent gastroenterology consult or EGD performed on the next available schedule.
Aside from LOS being greatly affected by performance of early EGD and/or delay in consulting gastroenterology, sicker patients require longer hospitalization and drive LOS and healthcare costs up. It was therefore crucial that we accounted for severity of illness, comorbidity, and performance of early EGD in our regression models for LOS and costs. This approach allows us to acquire a more accurate estimate on the effects of hospitalist on LOS and costs in patients admitted with acute UGIH.
Our findings suggest that the academic hospitalist model of care may not have as great of an impact on hospital efficiency in certain patient groups that require nonurgent subspecialty consultations. Future studies should focus on elucidating these relationships.
Limitations
This study has several limitations. First, clinical data were abstracted at 6 sites by different abstractors so it is possible there were variations in how data were collected. To reduce variation, a standardized abstraction form with instructions was developed and the primary investigator (PI) was available for specific questions during the abstraction process. Second, only 5 out of the 6 sites used TSI accounting systems. Although similar, interhospital costs captured by TSI may vary among sites in terms of classifying direct and indirect costs, potentially resulting in misclassification bias in our cost estimates.17 We addressed these issues by including the hospital site variable in our regression models, regardless of its significance. Third, consent rates across sites vary from 70% to 85%. It is possible that patients who refused enrollment in the MCH trial are systematically different and may introduce bias in our analysis.
Furthermore, the study was designed as a natural experiment based on a rotational call cycle between hospitalist‐led and nonhospitalist‐led teams. It is possible that the order of patient assignment might not be completely naturally random as we intended. However, the study period was for 2 years and we expect the effect of order would have averaged out in time.
There are many hospitalist models of care. In terms of generalizability, the study pertains only to academic hospitalists and may not be applicable to hospitalists practicing in community hospitals. For example, the nonhospitalist comparison group is likely different in the community and academic settings. Community nonhospitalists (traditional practitioners) are usually internists covering both inpatient and outpatient responsibilities at the same time. In contrast, academic nonhospitalists are internists or subspecialists serving as ward attendings for a limited period (usually 1 month) with considerable variation in their nonattending responsibilities (eg, research, clinic, administration). Furthermore, academic nonhospitalist providers might be a self‐selected group by their willingness to serve as a ward attending, making them more hospitalist‐like. Changes and variability of inpatient attendings may also affect our findings when compared to prior work. Finally, it is also possible that having residents at academic medical centers may attenuate the effect of hospitalists more than in community‐based models.
Conclusions/Implications
Compared to nonhospitalists, academic hospitalist care of acute UGIH patients had similar overall clinical outcomes. However, our finding of similar LOS yet higher costs for patients cared for by hospitalists support 1 proposed mechanism in which hospitalists decrease healthcare costs: providing higher intensity of care per day of hospitalization. However, in academic hospitalist models, this higher intensity hypothesis should be revisited, especially in certain patient groups in which timing and involvement of subspecialists may influence discharge decisions, affecting LOS and overall costs.
Due to inherent limitations in this observational study, future studies should focus on verifying and elucidating these relationships further. Lastly, understanding which patient groups receive the greatest potential benefit from this model will help guide both organizational efforts and quality improvement strategies.
- ,.Bleeding peptic ulcer.N Engl J Med.1994;331(11):717–727.
- .Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population‐based study.Am J Gastroenterol.1995;90(2):206–210.
- ,,, et al.Variation in outcome after acute upper gastrointestinal haemorrhage. the national audit of acute upper gastrointestinal haemorrhage.Lancet.1995;346(8971):346–350.
- ,,, et al.Influencing the practice and outcome in acute upper gastrointestinal haemorrhage. Steering committee of the National Audit of Acute Upper Gastrointestinal Haemorrhage.Gut.1997;41(5):606–611.
- ,,, et al.Risk assessment after acute upper gastrointestinal haemorrhage.Gut.1996;38(3):316–321.
- ,,, et al.The potential size of the hospitalist workforce in the united states.Am J Med.1999;106(4):441–445.
- Society of Hospital Medicine. About SHM. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information357(25):2589–2600.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137(11):866–874.
- .A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists.Mayo Clin Proc.2009;84(3):248–254.
- ,,, et al.Do hospitalists or physicians with greater inpatient HIV experience improve HIV care in the era of highly active antiretroviral therapy? Results from a multicenter trial of academic hospitalists.Clin Infect Dis.2008;46(7):1085–1092.
- ,,, et al.Quality of care for decompensated heart failure: comparable performance between academic hospitalists and non‐hospitalists. J Gen Intern Med.2008;23(9):1399–1406.
- ,,, et al.Factors associated with discussion of care plans and code status at the time of hospital admission: results from the Multicenter Hospitalist Study.J Hosp Med.2008;3(6):437–445.
- ,,, et al.Upper gastrointestinal hemorrhage clinical guideline determining the optimal hospital length of stay.Am J Med.1996;100(3):313–322.
- ,,, et al.Prospective evaluation of a clinical guideline recommending hospital length of stay in upper gastrointestinal tract hemorrhage.JAMA.1997;278(24):2151–2156.
- ,,, et al.In‐hospital cost of abdominal aortic aneurysm repair in Canada and the United States.Arch Intern Med.2003;163(20):2500–2504.
- ,,, et al.The use of transition cost accounting system in health services research.Cost Eff Resour Alloc.2007;5:11.
- Society of Hospital Medicine. Definition of a Hospitalist. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information335(7):514–517.
- ,,, et al.Selection of patients for early discharge or outpatient care after acute upper gastrointestinal haemorrhage. National Audit of Acute Upper Gastrointestinal Haemorrhage.Lancet.1996;347(9009):1138–1140.
- ,,, et al.Utilization of health care resources for low‐risk patients with acute, nonvariceal upper GI hemorrhage: an historical cohort study.Gastrointest Endosc.2002;55(3):321–327.
- ,.Incremental value of upper endoscopy for triage of patients with acute non‐variceal upper‐GI hemorrhage.Gastrointest Endosc.2004;60(1):9–14.
- ,,, et al.The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients.J Clin Epidemiol.2008;61(12):1234–1240.
- ,,, et al.The effectiveness of early endoscopy for upper gastrointestinal hemorrhage: a community‐based analysis.Med Care.1998;36(4):462–474.
- ,,, et al.Early endoscopy in upper gastrointestinal hemorrhage: associations with recurrent bleeding, surgery, and length of hospital stay.Gastrointest Endosc.1999;49(2):145–152.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the united states: a research synthesis.Med Care Res Rev.2005;62(4):379–406.
- ,,, et al.Physician specialty and variations in the cost of treating patients with acute upper gastrointestinal bleeding.Gastroenterology.1997;113(5):1443–1448.
- ,,, et al.Impact of physician specialty on the cost of nonvariceal upper GI bleeding care.Am J Gastroenterol.2002;97(6):1535–1542.
- ,,.Associations with reduced length of stay and costs on an academic hospitalist service.Am J Manag Care.2004;10(8):561–568.
Acute upper gastrointestinal hemorrhage (UGIH) is one of the most common hospital admissions for acute care. Estimates indicate that 300,000 patients (100‐150 cases per 100,000 adults) are admitted annually with an associated economic impact of $2.5 billion.15 The current standard management of UGIH requires hospital admission and esophagogastroduodenoscopy (EGD) by a gastroenterologist for diagnosis and/or treatment. This management strategy results in a high consumption of hospital resources and costs.
Simultaneously, hospitalists have dramatically changed the delivery of inpatient care in the United States and are recognized as a location‐driven subspecialty for the care of acute hospitalized patients, similar to emergency medicine. Currently there are 20,000 hospitalists, and more than one‐third of general medicine inpatients are cared for by hospitalists.6, 7
Previous studies have shown that hospitalist care offers better or comparable outcomes, with lower overall length of stay (LOS) and costs compared to traditional providers.810 However, most of these studies were performed in single institutions, had weak designs or little‐to‐no adjustment for severity of illness, or were limited to 7 specific diseases (pneumonia, congestive heart failure [CHF], chest pain, ischemic stroke, urinary tract infection, chronic obstructive lung disease [COPD], and acute myocardial infarction [AMI]).8
Furthermore, less is known about the effect of hospitalists on conditions that may be dependent upon specialist consultation for procedures and/or treatment plans. In this study, gastroenterologists performed diagnostic and/or therapeutic endoscopy work as consultants to the attending physicians in the management of acute inpatient UGIH.
To explore the effects of hospitalists on care of patients with acute UGIH, we examined data from the Multicenter Hospitalist (MCH) trial. The objectives of our study were to compare clinical outcomesin‐hospital mortality and complications (ie, recurrent bleeding, intensive care unit [ICU] transfer, decompensation, transfusion, reendoscopy, 30‐day readmission)and efficiency (LOS and costs) in hospitalized acute UGIH patients cared for by hospitalists and nonhospitalists in 6 academic centers in the United States during a 2‐year period.
Patients and Methods
Study Sites
From July 1, 2001 to June 30, 2003, the MCH trial1113 was a prospective, multicenter, observational trial of the care provided by hospitalists to patients admitted to general medical services at 6 academic medical institutions. There were 31,000 consecutive admissions to the general medical services of these participating sites: University of Chicago (Chicago, IL), University of Wisconsin Hospital (Madison, WI), University of Iowa (Iowa City, IA), University of California at San Francisco (San Francisco, CA), University of New Mexico (Albuquerque, NM), and Brigham and Women's Hospital (Boston, MA). The study was approved by the institutional review boards (IRBs) at each of the 6 participating institutions.
MCH Study Patients
Patients were eligible if they were admitted to the general medical services under the care of a hospitalist or nonhospitalist physician. Regardless of the admitting provider, each medical service was composed of rotating senior and junior resident physicians in all 6 sites. Furthermore, patients were 18 years of age or older, and were able to give consent themselves or had an appropriate proxy. Patients with mini‐mental status score of 17 (out of 22), admitted under their primary care physician or to an inpatient gastroenterology service, or transferred from another hospital, were excluded. The MCH study was designed to study the outcomes and efficiency in patients admitted for CHF, pneumonia, UGIH, and end‐of‐life care.
Acute UGIH Patients
Within the MCH‐eligible patients, we identified those with acute UGIH using the following International Classification of Diseases, 9th edition (ICD‐9) codes assigned at discharge: esophageal varices with hemorrhage (456.0, 456.20); Mallory‐Weiss syndrome (530.7); gastric ulcer with hemorrhage (531.00531.61); duodenal ulcer with hemorrhage (532.00532.61); peptic ulcer, site unspecified, with hemorrhage (533.00533.61); gastrojejunal ulcer with hemorrhage (534.00534.61); gastritis with hemorrhage (535.61); angiodysplasia of stomach/duodenum with hemorrhage (537.83); and hematemesis (578.0, 578.9). We also confirmed the diagnosis of UGIH by reviewing patient medical records for observed hematemesis, nasogastric tube aspirate with gross or hemoccult blood, or clinical history of hematemesis, melena, or hematochezia.14, 15
Data
All data were obtained from the 6 hospitals' administrative records, patient interviews, and medical chart abstractions. Dates of admission and discharge, ICD‐9 diagnosis codes, insurance type, age, race, and gender were obtained from administrative data. One‐month follow‐up telephone interviews assessed whether or not patient had any follow‐up appointment or hospital readmissions. Trained abstractors from each site performed manual chart reviews using a standard data collection sheet. The ICD‐9 code designation and chart abstraction methodology were developed prior to the initiation of the study to ensure consistent data collection and reduce bias.
The following data elements were collected: comorbidities, endoscopic findings, inpatient mortality, clinical evidence of rebleeding, endoscopic treatment or gastrointestinal (GI) surgery to control bleeding, repeat EGD, ICU transfer, decompensated comorbid illness requiring continued hospitalization, and blood transfusion (packed red cells, plasma, platelets). Clinical evidence of rebleeding was defined as either hematemesis or melena with decrease in hemoglobin of 2 g in 24 hours with or without hemodynamic compromise.14, 15 For the purpose of this study, recurrent bleeding was defined as clinical evidence of rebleeding, emergency GI surgery for control of UGIH, or repeat EGD before discharge. Furthermore, a composite endpoint termed total complications encompassed all adverse outcomes related to the UGIH hospitalization. The 30‐day readmission variable was defined using readmission identified in administrative records and a 30‐day follow‐up phone call. To guard against recall bias, self‐report data was only included for nonsite admissions.
We defined efficiency in terms of costs and LOS. Total hospital costs were measured using the TSI cost accounting system (Transition Systems, Inc., Boston, MA; now Eclipsys Corporation)16, 17 at 5 out of the 6 participating sites. TSI is a hospital cost accounting software system that integrates resource utilization and financial data already recorded in other hospital databases (such as the billing system, payroll system, and general ledger system).17 Hospital LOS was defined as the number of days from patient admission to the general medicine service until patient discharge.
Provider Specialization: Hospitalists vs. Nonhospitalists
The study was designed as a natural experiment based on a call cycle. The hospitalist‐led teams at each institution alternated in a 4‐day or 5‐day general medicine call cycle with teams led by traditional academic internal medicine attending physicians. All patients were assigned to teams according to their position in the call cycle without regard to whether the attending physician was a hospitalist or a nonhospitalist. Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients.18, 19 As previously reported in a related MCH work,11 a hospitalist was also defined as a provider who spends at least 25% of his or her time on an academic inpatient general medicine service. Nonhospitalist physicians were most often outpatient general internal medicine faculty or subspecialists, who attended 1 month per year. Physicians were classified as hospitalists or nonhospitalists according to the designations provided by each site.
UGIH‐specific Confounders
From chart abstraction, we captured severity of illness, comorbidity, and performance of early EGD, variables that can confound analysis in UGIH. To capture severity of illness, a complete Rockall risk score was calculated for each patient. The complete Rockall uses 3 clinical variables (age, shock, and comorbidity) and 2 endoscopic variables (endoscopic diagnosis and stigmata of recent hemorrhage).5, 20 A complete Rockall score of 2 is considered low‐risk for rebleeding or death following admission.21, 22 The accepted definition of low‐risk is <5% recurrent bleeding and <1% mortality risk. A complete Rockall score of 3 to 5 is considered moderate‐risk while 6 is considered high‐risk. Comorbidity was measured using the Charlson comorbidity index.23 Performance of early endoscopy, usually defined as endoscopy performed within 24 hours from presentation, was previously shown to decrease LOS and need for surgical intervention in patients with acute UGIH.24, 25 Documented times of presentation to the emergency department and time of endoscopy performance were collected to calculate for the rate of early endoscopy in our study population.
Statistical Analysis
All statistical analyses were performed using SAS Version 9.1 for Windows (SAS Institute, Cary, NC).
Differences in baseline demographic characteristics of patients and their endoscopic findings were compared between the 2 types of providers. Univariate analyses were also performed to compare the differences in adverse outcomes, LOS, and costs between patients cared for by hospitalists and nonhospitalists. Chi‐square tests were used for categorical variables; while both Wilcoxon rank sum test and Student's t test were used in the analysis of continuous variables.
Next, we performed multivariable analyses to determine the independent association between hospitalist care and the odds of the patients having certain outcomes. However, to prevent overfitting, we only developed regression models for adverse outcomes that have at least 20% event rate.
Multivariable regression models were developed separately for LOS and costs. In contrast with the models on outcomes, analyses of LOS and costs were restricted to: (1) patients who were discharged alive; and (2) to cases with LOS and costs values within 3 standard deviations (SDs) of the mean because of the skewed nature of these data.
All models were adjusted for age, gender, race, insurance type, complete Rockall risk score, performance of early EGD, Charlson comorbidity index, and study site. Final candidate variables in the models were chosen based on stepwise selection, a method very similar to forward selection except that variables selected for the model do not necessarily remain in the model. Effects were entered into and then removed from the model in such a way that each forward selection step can be followed by 1 or more backward elimination steps. The stepwise selection was terminated if no further effect can be added to the model or if the current model was identical to the previous model. The stepwise selection model was generated using statistical criterion of alpha = 0.05 for entry and elimination from the model. Variables that can be a profound source of variation, such as study site and treating physician, were included in the model irrespective of their statistical significance.
To account for clustering of patients treated by the same physician, we used multilevel modeling with SAS PROC GLIMMIX (with random effects). For outcomes (categorical variables), we utilized models with logit‐link and binomial‐distributed errors. As for efficiency (continuous variables with skewed distribution), the multivariable analyses used a generalized linear model with log‐link and assuming gamma‐distributed errors.
Results
Patient Characteristics and Endoscopic Diagnoses
Out of 31,000 patients, the study identified a total of 566 patients (1.8%) with acute UGIH (Table 1). However, 116 patients transferred from another hospital were excluded as their initial management was provided elsewhere, giving a final study sample of 450 patients. Overall, there are 163 admitting physicians from 6 sites, with 39 (24%) classified as hospitalists and 124 (76%) as nonhospitalists. Forty‐two percent (177/450) of patients were cared for by hospitalists. Compared to nonhospitalists, patients admitted to the hospitalist service were older (62.8 vs. 57.7 years, P < 0.01) and with third‐party payor mix differences (P < 0.01). However, there were no statistical differences between patients attended by hospitalists and nonhospitalists with regard to Complete Rockall risk score, Charlson comorbidity index, performance of early endoscopy, and mean hemoglobin values on admission. Upper endoscopy was performed in all patients with distribution of the 3 most common diagnoses being similar (P > 0.05) between hospitalists and nonhospitalists: erosive disease (49.7% vs. 54.6%), peptic ulcer disease (PUD) (48% vs. 46.9%), and varices (18.6% vs. 14.7%).
| Variable | Admitting Service | P | |
|---|---|---|---|
| Hospitalist (n = 177) | Nonhospitalist (n = 273) | ||
| |||
| Age, years (meanSD) | 62.817.4 | 57.718.5 | <0.01 |
| Male sex, n (%) | 104 (58.8) | 169 (61.9) | 0.50 |
| Ethnicity, n (%) | 0.13 | ||
| White | 83 (46.9) | 102 (37.4) | |
| African‐American | 34 (19.2) | 75 (27.5) | |
| Hispanic | 21 (11.9) | 40 (14.7) | |
| Asian/Pacific Islander | 24 (13.6) | 29 (10.6) | |
| Others/unknown | 15 (8.5) | 27 (9.9) | |
| Insurance, n (%) | <0.01 | ||
| Medicare | 86 (48.6) | 104 (38.1) | |
| Medicaid | 15 (8.5) | 33 (12.1) | |
| No payer | 18 (10.2) | 36 (13.2) | |
| Private | 46 (26) | 52 (19.1) | |
| Unknown | 12 (6.8) | 48 (17.5) | |
| Charlson Comorbidity Index (meanSD) | 1.91.6 | 1.81.7 | 0.51 |
| Complete Rockall, n (%) | 0.11 | ||
| Low‐risk (0‐2) | 82 (46.3) | 103 (37.7) | |
| Moderate‐risk (3‐5) | 71 (40.1) | 137 (50.2) | |
| High‐risk (6) | 24 (14.6) | 33 (12.1) | |
| Early endoscopy (<24 hours) | 82 (46.3) | 133 (48.7) | 0.62 |
| Endoscopic diagnosis, n (%)* | |||
| Erosive disease | 88 (49.7) | 149 (54.6) | 0.31 |
| Peptic ulcer disease | 85 (48.0) | 128 (46.9) | 0.81 |
| Varices | 33 (18.6) | 40 (14.7) | 0.26 |
| Mallory‐Weiss tear | 9 (5.1) | 21 (7.7) | 0.28 |
| Angiodysplasia | 9 (5.1) | 13 (4.8) | 0.88 |
| GI mass | 1 (0.6) | 4 (1.5) | 0.65 |
| Normal | 7 (4.0) | 8 (2.9) | 0.55 |
| Admission hemoglobin values (meanSD) | 10.22.9 | 10.22.9 | 0.78 |
Clinical Outcomes
Between hospitalists and nonhospitalists, unadjusted outcomes were similar (P > 0.05) for mortality (2.3% vs. 0.4%), recurrent bleeding (11% vs. 11%), need for endoscopic therapy (24% vs. 22%), ICU‐transfer and decompensation (15% vs. 15%), as well as an overall composite measure of any complication (79% vs. 72%) (Table 2). However, the hospitalist‐led teams performed more blood transfusions (74% vs. 63%, P = 0.02) and readmission rates were higher (7.3% vs. 3.3%, P = 0.05).
| Outcomes, n (%) | Admitting Service | P | |
|---|---|---|---|
| Hospitalist (n = 177) | Nonhospitalist (n = 273) | ||
| |||
| Inpatient mortality | 4 (2.3) | 1 (0.4) | 0.08 |
| Recurrent bleeding* | 20 (11.3) | 29 (10.6) | 0.88 |
| Endoscopic therapy | 43 (24.3) | 60 (22.0) | 0.57 |
| ICU transfers | 23 (13) | 24 (8.8) | 0.20 |
| Decompensated comorbidities that required continued hospitalization | 26 (14.7) | 41 (15.0) | 0.92 |
| Any transfusion | 131 (74.0) | 172 (63.0) | 0.02 |
| Total complications | 139 (78.5) | 196 (71.8) | 0.11 |
| 30‐day all‐cause readmissions | 13 (7.3) | 9 (3.3) | 0.05 |
| Efficiency | Hospitalist (n = 164) | Nonhospitalist (n = 259) | P |
| LOS, days | |||
| MeanSD | 4.83.5 | 4.53.0 | 0.30 |
| Median (interquartile range) | 4 (36) | 4 (26) | 0.69 |
| Total costs, U.S. $ | |||
| MeanSD | 10,466.669191.00 | 7926.716065.00 | <0.01 |
| Median (interquartile range) | 7359.00 (4,698.0012,550.00) | 6181.00 (3744.0010,344.00) | <0.01 |
Because of the low event rate of certain adverse outcomes (<20%), we were only able to perform adjusted analyses on 4 outcomes: need for endoscopic therapy (odds ratio [OR], 0.82; 95% confidence interval [CI], 0.491.37), ICU transfer and decompensation (OR, 0.82; 95% CI, 0.451.52), blood transfusion (OR, 1.30; 95% CI, 0.822.04), and any complication (OR, 1.18; 95% CI, 0.711.96). Since outcome differences disappeared after controlling for confounders, the data suggest that overall care provided by hospitalists and nonhospitalists might be equivalenteven in certain outcomes that we were unable to substantiate using multivariable methods.
Efficiency
Efficiency, as measured by LOS and costs, are presented both as means and medians in univariate analyses in Table 2. Median LOS was similar for hospitalist‐led and nonhospitalist‐led teams (4 days). Despite having similar LOS, the median costs of acute UGIH in patients cared for by hospitalists were higher ($7,359.00 vs. $6,181.00; P < 0.01).
After adjusting for demographic factors, Rockall risk score, comorbidity, early EGD, and hospital site, LOS remained similar between the 2 groups. On the other hand, the adjusted cost for UGIH patients cared for by hospitalists and nonhospitalists persisted, with hospitalist care costs $1,502.40 more than their nonhospitalist counterparts (Table 3).
| Efficiency | Treatment Provider | P | |
|---|---|---|---|
| Hospitalist (n = 164) | Nonhospitalist (n = 259) | ||
| |||
| Adjusted length of stay, days (mean SD) | 5.2 (4.95.6) | 4.7 (4.55.0) | 0.15 |
| Adjusted total cost, U.S. $ (mean SD) | 9006.50 (8366.609693.60) | 7504.10 (7069.907964.20) | 0.03 |
Discussion
This is the first study that has looked at the effect of hospitalists on clinical outcomes and efficiency in patients admitted for acute UGIH, a condition highly dependent upon another specialty for procedures and management. This is also one of only a few studies on UGIH that adjusted for severity of illness (Rockall score), comorbidity, performance of early endoscopypatient‐level confounders usually unaccounted for in prior research.
We show that hospitalists and nonhospitalists caring for acute UGIH patients had overall similar unadjusted outcomes; except for blood transfusion and 30‐day readmission rates. Unfortunately, due to the small number of events for readmissions, we were unable to perform adjusted analysis for readmission. Differences between hospitalists and nonhospitalists on blood transfusion rates were not substantiated on multivariable adjustments.
As for efficiency, univariable and multivariable analyses revealed that LOS was similar between provider types while costs were greater in UGIH patients attended by hospitalists.
Reductions in resource use, particularly costs, may be achieved by increasing throughput (eg, reducing LOS) or by decreasing service intensity (eg, using fewer ancillary services and specialty consultations).26 Specifically in acute UGIH, LOS is significantly affected by performance of early EGD.27, 28 In these studies, gastroenterologist‐led teams, compared to internists and surgeons, have easier access to endoscopy, thus reducing LOS and overall costs.27, 28
Similarly, prior studies have shown that the mechanism by which hospitalists lower costs is by decreasing LOS.810, 29 There are several hypotheses on how hospitalists affect LOS. Hospitalists, by being available all day, are thought to respond quickly to acute symptoms or new test results, are more efficient in navigating the complex hospital environment, or develop greater expertise as a result of added inpatient experience.8 On the downside, although the hospitalist model reduces overall LOS and costs, they also provide higher intensity of care as reflected by greater costs when broken down per hospital day.29 Thus, the cost differential we found may represent higher intensity of care by hospitalists in their management of acute UGIH, as higher intensity care without decreasing LOS can translate to higher costs.
In addition, patients with acute UGIH are unique in several respects. In contrast to diseases like heart failure, COPD, and pneumonia, in which the admitting provider has the option to request a subspecialist consultation, all patients with acute UGIH need a gastroenterologist to perform endoscopy as part of the management. These patients are usually admitted to general medicine wards, aggressively resuscitated with intravenous fluids, with a nonurgent gastroenterology consult or EGD performed on the next available schedule.
Aside from LOS being greatly affected by performance of early EGD and/or delay in consulting gastroenterology, sicker patients require longer hospitalization and drive LOS and healthcare costs up. It was therefore crucial that we accounted for severity of illness, comorbidity, and performance of early EGD in our regression models for LOS and costs. This approach allows us to acquire a more accurate estimate on the effects of hospitalist on LOS and costs in patients admitted with acute UGIH.
Our findings suggest that the academic hospitalist model of care may not have as great of an impact on hospital efficiency in certain patient groups that require nonurgent subspecialty consultations. Future studies should focus on elucidating these relationships.
Limitations
This study has several limitations. First, clinical data were abstracted at 6 sites by different abstractors so it is possible there were variations in how data were collected. To reduce variation, a standardized abstraction form with instructions was developed and the primary investigator (PI) was available for specific questions during the abstraction process. Second, only 5 out of the 6 sites used TSI accounting systems. Although similar, interhospital costs captured by TSI may vary among sites in terms of classifying direct and indirect costs, potentially resulting in misclassification bias in our cost estimates.17 We addressed these issues by including the hospital site variable in our regression models, regardless of its significance. Third, consent rates across sites vary from 70% to 85%. It is possible that patients who refused enrollment in the MCH trial are systematically different and may introduce bias in our analysis.
Furthermore, the study was designed as a natural experiment based on a rotational call cycle between hospitalist‐led and nonhospitalist‐led teams. It is possible that the order of patient assignment might not be completely naturally random as we intended. However, the study period was for 2 years and we expect the effect of order would have averaged out in time.
There are many hospitalist models of care. In terms of generalizability, the study pertains only to academic hospitalists and may not be applicable to hospitalists practicing in community hospitals. For example, the nonhospitalist comparison group is likely different in the community and academic settings. Community nonhospitalists (traditional practitioners) are usually internists covering both inpatient and outpatient responsibilities at the same time. In contrast, academic nonhospitalists are internists or subspecialists serving as ward attendings for a limited period (usually 1 month) with considerable variation in their nonattending responsibilities (eg, research, clinic, administration). Furthermore, academic nonhospitalist providers might be a self‐selected group by their willingness to serve as a ward attending, making them more hospitalist‐like. Changes and variability of inpatient attendings may also affect our findings when compared to prior work. Finally, it is also possible that having residents at academic medical centers may attenuate the effect of hospitalists more than in community‐based models.
Conclusions/Implications
Compared to nonhospitalists, academic hospitalist care of acute UGIH patients had similar overall clinical outcomes. However, our finding of similar LOS yet higher costs for patients cared for by hospitalists support 1 proposed mechanism in which hospitalists decrease healthcare costs: providing higher intensity of care per day of hospitalization. However, in academic hospitalist models, this higher intensity hypothesis should be revisited, especially in certain patient groups in which timing and involvement of subspecialists may influence discharge decisions, affecting LOS and overall costs.
Due to inherent limitations in this observational study, future studies should focus on verifying and elucidating these relationships further. Lastly, understanding which patient groups receive the greatest potential benefit from this model will help guide both organizational efforts and quality improvement strategies.
Acute upper gastrointestinal hemorrhage (UGIH) is one of the most common hospital admissions for acute care. Estimates indicate that 300,000 patients (100‐150 cases per 100,000 adults) are admitted annually with an associated economic impact of $2.5 billion.15 The current standard management of UGIH requires hospital admission and esophagogastroduodenoscopy (EGD) by a gastroenterologist for diagnosis and/or treatment. This management strategy results in a high consumption of hospital resources and costs.
Simultaneously, hospitalists have dramatically changed the delivery of inpatient care in the United States and are recognized as a location‐driven subspecialty for the care of acute hospitalized patients, similar to emergency medicine. Currently there are 20,000 hospitalists, and more than one‐third of general medicine inpatients are cared for by hospitalists.6, 7
Previous studies have shown that hospitalist care offers better or comparable outcomes, with lower overall length of stay (LOS) and costs compared to traditional providers.810 However, most of these studies were performed in single institutions, had weak designs or little‐to‐no adjustment for severity of illness, or were limited to 7 specific diseases (pneumonia, congestive heart failure [CHF], chest pain, ischemic stroke, urinary tract infection, chronic obstructive lung disease [COPD], and acute myocardial infarction [AMI]).8
Furthermore, less is known about the effect of hospitalists on conditions that may be dependent upon specialist consultation for procedures and/or treatment plans. In this study, gastroenterologists performed diagnostic and/or therapeutic endoscopy work as consultants to the attending physicians in the management of acute inpatient UGIH.
To explore the effects of hospitalists on care of patients with acute UGIH, we examined data from the Multicenter Hospitalist (MCH) trial. The objectives of our study were to compare clinical outcomesin‐hospital mortality and complications (ie, recurrent bleeding, intensive care unit [ICU] transfer, decompensation, transfusion, reendoscopy, 30‐day readmission)and efficiency (LOS and costs) in hospitalized acute UGIH patients cared for by hospitalists and nonhospitalists in 6 academic centers in the United States during a 2‐year period.
Patients and Methods
Study Sites
From July 1, 2001 to June 30, 2003, the MCH trial1113 was a prospective, multicenter, observational trial of the care provided by hospitalists to patients admitted to general medical services at 6 academic medical institutions. There were 31,000 consecutive admissions to the general medical services of these participating sites: University of Chicago (Chicago, IL), University of Wisconsin Hospital (Madison, WI), University of Iowa (Iowa City, IA), University of California at San Francisco (San Francisco, CA), University of New Mexico (Albuquerque, NM), and Brigham and Women's Hospital (Boston, MA). The study was approved by the institutional review boards (IRBs) at each of the 6 participating institutions.
MCH Study Patients
Patients were eligible if they were admitted to the general medical services under the care of a hospitalist or nonhospitalist physician. Regardless of the admitting provider, each medical service was composed of rotating senior and junior resident physicians in all 6 sites. Furthermore, patients were 18 years of age or older, and were able to give consent themselves or had an appropriate proxy. Patients with mini‐mental status score of 17 (out of 22), admitted under their primary care physician or to an inpatient gastroenterology service, or transferred from another hospital, were excluded. The MCH study was designed to study the outcomes and efficiency in patients admitted for CHF, pneumonia, UGIH, and end‐of‐life care.
Acute UGIH Patients
Within the MCH‐eligible patients, we identified those with acute UGIH using the following International Classification of Diseases, 9th edition (ICD‐9) codes assigned at discharge: esophageal varices with hemorrhage (456.0, 456.20); Mallory‐Weiss syndrome (530.7); gastric ulcer with hemorrhage (531.00531.61); duodenal ulcer with hemorrhage (532.00532.61); peptic ulcer, site unspecified, with hemorrhage (533.00533.61); gastrojejunal ulcer with hemorrhage (534.00534.61); gastritis with hemorrhage (535.61); angiodysplasia of stomach/duodenum with hemorrhage (537.83); and hematemesis (578.0, 578.9). We also confirmed the diagnosis of UGIH by reviewing patient medical records for observed hematemesis, nasogastric tube aspirate with gross or hemoccult blood, or clinical history of hematemesis, melena, or hematochezia.14, 15
Data
All data were obtained from the 6 hospitals' administrative records, patient interviews, and medical chart abstractions. Dates of admission and discharge, ICD‐9 diagnosis codes, insurance type, age, race, and gender were obtained from administrative data. One‐month follow‐up telephone interviews assessed whether or not patient had any follow‐up appointment or hospital readmissions. Trained abstractors from each site performed manual chart reviews using a standard data collection sheet. The ICD‐9 code designation and chart abstraction methodology were developed prior to the initiation of the study to ensure consistent data collection and reduce bias.
The following data elements were collected: comorbidities, endoscopic findings, inpatient mortality, clinical evidence of rebleeding, endoscopic treatment or gastrointestinal (GI) surgery to control bleeding, repeat EGD, ICU transfer, decompensated comorbid illness requiring continued hospitalization, and blood transfusion (packed red cells, plasma, platelets). Clinical evidence of rebleeding was defined as either hematemesis or melena with decrease in hemoglobin of 2 g in 24 hours with or without hemodynamic compromise.14, 15 For the purpose of this study, recurrent bleeding was defined as clinical evidence of rebleeding, emergency GI surgery for control of UGIH, or repeat EGD before discharge. Furthermore, a composite endpoint termed total complications encompassed all adverse outcomes related to the UGIH hospitalization. The 30‐day readmission variable was defined using readmission identified in administrative records and a 30‐day follow‐up phone call. To guard against recall bias, self‐report data was only included for nonsite admissions.
We defined efficiency in terms of costs and LOS. Total hospital costs were measured using the TSI cost accounting system (Transition Systems, Inc., Boston, MA; now Eclipsys Corporation)16, 17 at 5 out of the 6 participating sites. TSI is a hospital cost accounting software system that integrates resource utilization and financial data already recorded in other hospital databases (such as the billing system, payroll system, and general ledger system).17 Hospital LOS was defined as the number of days from patient admission to the general medicine service until patient discharge.
Provider Specialization: Hospitalists vs. Nonhospitalists
The study was designed as a natural experiment based on a call cycle. The hospitalist‐led teams at each institution alternated in a 4‐day or 5‐day general medicine call cycle with teams led by traditional academic internal medicine attending physicians. All patients were assigned to teams according to their position in the call cycle without regard to whether the attending physician was a hospitalist or a nonhospitalist. Hospitalists are physicians whose primary professional focus is the general medical care of hospitalized patients.18, 19 As previously reported in a related MCH work,11 a hospitalist was also defined as a provider who spends at least 25% of his or her time on an academic inpatient general medicine service. Nonhospitalist physicians were most often outpatient general internal medicine faculty or subspecialists, who attended 1 month per year. Physicians were classified as hospitalists or nonhospitalists according to the designations provided by each site.
UGIH‐specific Confounders
From chart abstraction, we captured severity of illness, comorbidity, and performance of early EGD, variables that can confound analysis in UGIH. To capture severity of illness, a complete Rockall risk score was calculated for each patient. The complete Rockall uses 3 clinical variables (age, shock, and comorbidity) and 2 endoscopic variables (endoscopic diagnosis and stigmata of recent hemorrhage).5, 20 A complete Rockall score of 2 is considered low‐risk for rebleeding or death following admission.21, 22 The accepted definition of low‐risk is <5% recurrent bleeding and <1% mortality risk. A complete Rockall score of 3 to 5 is considered moderate‐risk while 6 is considered high‐risk. Comorbidity was measured using the Charlson comorbidity index.23 Performance of early endoscopy, usually defined as endoscopy performed within 24 hours from presentation, was previously shown to decrease LOS and need for surgical intervention in patients with acute UGIH.24, 25 Documented times of presentation to the emergency department and time of endoscopy performance were collected to calculate for the rate of early endoscopy in our study population.
Statistical Analysis
All statistical analyses were performed using SAS Version 9.1 for Windows (SAS Institute, Cary, NC).
Differences in baseline demographic characteristics of patients and their endoscopic findings were compared between the 2 types of providers. Univariate analyses were also performed to compare the differences in adverse outcomes, LOS, and costs between patients cared for by hospitalists and nonhospitalists. Chi‐square tests were used for categorical variables; while both Wilcoxon rank sum test and Student's t test were used in the analysis of continuous variables.
Next, we performed multivariable analyses to determine the independent association between hospitalist care and the odds of the patients having certain outcomes. However, to prevent overfitting, we only developed regression models for adverse outcomes that have at least 20% event rate.
Multivariable regression models were developed separately for LOS and costs. In contrast with the models on outcomes, analyses of LOS and costs were restricted to: (1) patients who were discharged alive; and (2) to cases with LOS and costs values within 3 standard deviations (SDs) of the mean because of the skewed nature of these data.
All models were adjusted for age, gender, race, insurance type, complete Rockall risk score, performance of early EGD, Charlson comorbidity index, and study site. Final candidate variables in the models were chosen based on stepwise selection, a method very similar to forward selection except that variables selected for the model do not necessarily remain in the model. Effects were entered into and then removed from the model in such a way that each forward selection step can be followed by 1 or more backward elimination steps. The stepwise selection was terminated if no further effect can be added to the model or if the current model was identical to the previous model. The stepwise selection model was generated using statistical criterion of alpha = 0.05 for entry and elimination from the model. Variables that can be a profound source of variation, such as study site and treating physician, were included in the model irrespective of their statistical significance.
To account for clustering of patients treated by the same physician, we used multilevel modeling with SAS PROC GLIMMIX (with random effects). For outcomes (categorical variables), we utilized models with logit‐link and binomial‐distributed errors. As for efficiency (continuous variables with skewed distribution), the multivariable analyses used a generalized linear model with log‐link and assuming gamma‐distributed errors.
Results
Patient Characteristics and Endoscopic Diagnoses
Out of 31,000 patients, the study identified a total of 566 patients (1.8%) with acute UGIH (Table 1). However, 116 patients transferred from another hospital were excluded as their initial management was provided elsewhere, giving a final study sample of 450 patients. Overall, there are 163 admitting physicians from 6 sites, with 39 (24%) classified as hospitalists and 124 (76%) as nonhospitalists. Forty‐two percent (177/450) of patients were cared for by hospitalists. Compared to nonhospitalists, patients admitted to the hospitalist service were older (62.8 vs. 57.7 years, P < 0.01) and with third‐party payor mix differences (P < 0.01). However, there were no statistical differences between patients attended by hospitalists and nonhospitalists with regard to Complete Rockall risk score, Charlson comorbidity index, performance of early endoscopy, and mean hemoglobin values on admission. Upper endoscopy was performed in all patients with distribution of the 3 most common diagnoses being similar (P > 0.05) between hospitalists and nonhospitalists: erosive disease (49.7% vs. 54.6%), peptic ulcer disease (PUD) (48% vs. 46.9%), and varices (18.6% vs. 14.7%).
| Variable | Admitting Service | P | |
|---|---|---|---|
| Hospitalist (n = 177) | Nonhospitalist (n = 273) | ||
| |||
| Age, years (meanSD) | 62.817.4 | 57.718.5 | <0.01 |
| Male sex, n (%) | 104 (58.8) | 169 (61.9) | 0.50 |
| Ethnicity, n (%) | 0.13 | ||
| White | 83 (46.9) | 102 (37.4) | |
| African‐American | 34 (19.2) | 75 (27.5) | |
| Hispanic | 21 (11.9) | 40 (14.7) | |
| Asian/Pacific Islander | 24 (13.6) | 29 (10.6) | |
| Others/unknown | 15 (8.5) | 27 (9.9) | |
| Insurance, n (%) | <0.01 | ||
| Medicare | 86 (48.6) | 104 (38.1) | |
| Medicaid | 15 (8.5) | 33 (12.1) | |
| No payer | 18 (10.2) | 36 (13.2) | |
| Private | 46 (26) | 52 (19.1) | |
| Unknown | 12 (6.8) | 48 (17.5) | |
| Charlson Comorbidity Index (meanSD) | 1.91.6 | 1.81.7 | 0.51 |
| Complete Rockall, n (%) | 0.11 | ||
| Low‐risk (0‐2) | 82 (46.3) | 103 (37.7) | |
| Moderate‐risk (3‐5) | 71 (40.1) | 137 (50.2) | |
| High‐risk (6) | 24 (14.6) | 33 (12.1) | |
| Early endoscopy (<24 hours) | 82 (46.3) | 133 (48.7) | 0.62 |
| Endoscopic diagnosis, n (%)* | |||
| Erosive disease | 88 (49.7) | 149 (54.6) | 0.31 |
| Peptic ulcer disease | 85 (48.0) | 128 (46.9) | 0.81 |
| Varices | 33 (18.6) | 40 (14.7) | 0.26 |
| Mallory‐Weiss tear | 9 (5.1) | 21 (7.7) | 0.28 |
| Angiodysplasia | 9 (5.1) | 13 (4.8) | 0.88 |
| GI mass | 1 (0.6) | 4 (1.5) | 0.65 |
| Normal | 7 (4.0) | 8 (2.9) | 0.55 |
| Admission hemoglobin values (meanSD) | 10.22.9 | 10.22.9 | 0.78 |
Clinical Outcomes
Between hospitalists and nonhospitalists, unadjusted outcomes were similar (P > 0.05) for mortality (2.3% vs. 0.4%), recurrent bleeding (11% vs. 11%), need for endoscopic therapy (24% vs. 22%), ICU‐transfer and decompensation (15% vs. 15%), as well as an overall composite measure of any complication (79% vs. 72%) (Table 2). However, the hospitalist‐led teams performed more blood transfusions (74% vs. 63%, P = 0.02) and readmission rates were higher (7.3% vs. 3.3%, P = 0.05).
| Outcomes, n (%) | Admitting Service | P | |
|---|---|---|---|
| Hospitalist (n = 177) | Nonhospitalist (n = 273) | ||
| |||
| Inpatient mortality | 4 (2.3) | 1 (0.4) | 0.08 |
| Recurrent bleeding* | 20 (11.3) | 29 (10.6) | 0.88 |
| Endoscopic therapy | 43 (24.3) | 60 (22.0) | 0.57 |
| ICU transfers | 23 (13) | 24 (8.8) | 0.20 |
| Decompensated comorbidities that required continued hospitalization | 26 (14.7) | 41 (15.0) | 0.92 |
| Any transfusion | 131 (74.0) | 172 (63.0) | 0.02 |
| Total complications | 139 (78.5) | 196 (71.8) | 0.11 |
| 30‐day all‐cause readmissions | 13 (7.3) | 9 (3.3) | 0.05 |
| Efficiency | Hospitalist (n = 164) | Nonhospitalist (n = 259) | P |
| LOS, days | |||
| MeanSD | 4.83.5 | 4.53.0 | 0.30 |
| Median (interquartile range) | 4 (36) | 4 (26) | 0.69 |
| Total costs, U.S. $ | |||
| MeanSD | 10,466.669191.00 | 7926.716065.00 | <0.01 |
| Median (interquartile range) | 7359.00 (4,698.0012,550.00) | 6181.00 (3744.0010,344.00) | <0.01 |
Because of the low event rate of certain adverse outcomes (<20%), we were only able to perform adjusted analyses on 4 outcomes: need for endoscopic therapy (odds ratio [OR], 0.82; 95% confidence interval [CI], 0.491.37), ICU transfer and decompensation (OR, 0.82; 95% CI, 0.451.52), blood transfusion (OR, 1.30; 95% CI, 0.822.04), and any complication (OR, 1.18; 95% CI, 0.711.96). Since outcome differences disappeared after controlling for confounders, the data suggest that overall care provided by hospitalists and nonhospitalists might be equivalenteven in certain outcomes that we were unable to substantiate using multivariable methods.
Efficiency
Efficiency, as measured by LOS and costs, are presented both as means and medians in univariate analyses in Table 2. Median LOS was similar for hospitalist‐led and nonhospitalist‐led teams (4 days). Despite having similar LOS, the median costs of acute UGIH in patients cared for by hospitalists were higher ($7,359.00 vs. $6,181.00; P < 0.01).
After adjusting for demographic factors, Rockall risk score, comorbidity, early EGD, and hospital site, LOS remained similar between the 2 groups. On the other hand, the adjusted cost for UGIH patients cared for by hospitalists and nonhospitalists persisted, with hospitalist care costs $1,502.40 more than their nonhospitalist counterparts (Table 3).
| Efficiency | Treatment Provider | P | |
|---|---|---|---|
| Hospitalist (n = 164) | Nonhospitalist (n = 259) | ||
| |||
| Adjusted length of stay, days (mean SD) | 5.2 (4.95.6) | 4.7 (4.55.0) | 0.15 |
| Adjusted total cost, U.S. $ (mean SD) | 9006.50 (8366.609693.60) | 7504.10 (7069.907964.20) | 0.03 |
Discussion
This is the first study that has looked at the effect of hospitalists on clinical outcomes and efficiency in patients admitted for acute UGIH, a condition highly dependent upon another specialty for procedures and management. This is also one of only a few studies on UGIH that adjusted for severity of illness (Rockall score), comorbidity, performance of early endoscopypatient‐level confounders usually unaccounted for in prior research.
We show that hospitalists and nonhospitalists caring for acute UGIH patients had overall similar unadjusted outcomes; except for blood transfusion and 30‐day readmission rates. Unfortunately, due to the small number of events for readmissions, we were unable to perform adjusted analysis for readmission. Differences between hospitalists and nonhospitalists on blood transfusion rates were not substantiated on multivariable adjustments.
As for efficiency, univariable and multivariable analyses revealed that LOS was similar between provider types while costs were greater in UGIH patients attended by hospitalists.
Reductions in resource use, particularly costs, may be achieved by increasing throughput (eg, reducing LOS) or by decreasing service intensity (eg, using fewer ancillary services and specialty consultations).26 Specifically in acute UGIH, LOS is significantly affected by performance of early EGD.27, 28 In these studies, gastroenterologist‐led teams, compared to internists and surgeons, have easier access to endoscopy, thus reducing LOS and overall costs.27, 28
Similarly, prior studies have shown that the mechanism by which hospitalists lower costs is by decreasing LOS.810, 29 There are several hypotheses on how hospitalists affect LOS. Hospitalists, by being available all day, are thought to respond quickly to acute symptoms or new test results, are more efficient in navigating the complex hospital environment, or develop greater expertise as a result of added inpatient experience.8 On the downside, although the hospitalist model reduces overall LOS and costs, they also provide higher intensity of care as reflected by greater costs when broken down per hospital day.29 Thus, the cost differential we found may represent higher intensity of care by hospitalists in their management of acute UGIH, as higher intensity care without decreasing LOS can translate to higher costs.
In addition, patients with acute UGIH are unique in several respects. In contrast to diseases like heart failure, COPD, and pneumonia, in which the admitting provider has the option to request a subspecialist consultation, all patients with acute UGIH need a gastroenterologist to perform endoscopy as part of the management. These patients are usually admitted to general medicine wards, aggressively resuscitated with intravenous fluids, with a nonurgent gastroenterology consult or EGD performed on the next available schedule.
Aside from LOS being greatly affected by performance of early EGD and/or delay in consulting gastroenterology, sicker patients require longer hospitalization and drive LOS and healthcare costs up. It was therefore crucial that we accounted for severity of illness, comorbidity, and performance of early EGD in our regression models for LOS and costs. This approach allows us to acquire a more accurate estimate on the effects of hospitalist on LOS and costs in patients admitted with acute UGIH.
Our findings suggest that the academic hospitalist model of care may not have as great of an impact on hospital efficiency in certain patient groups that require nonurgent subspecialty consultations. Future studies should focus on elucidating these relationships.
Limitations
This study has several limitations. First, clinical data were abstracted at 6 sites by different abstractors so it is possible there were variations in how data were collected. To reduce variation, a standardized abstraction form with instructions was developed and the primary investigator (PI) was available for specific questions during the abstraction process. Second, only 5 out of the 6 sites used TSI accounting systems. Although similar, interhospital costs captured by TSI may vary among sites in terms of classifying direct and indirect costs, potentially resulting in misclassification bias in our cost estimates.17 We addressed these issues by including the hospital site variable in our regression models, regardless of its significance. Third, consent rates across sites vary from 70% to 85%. It is possible that patients who refused enrollment in the MCH trial are systematically different and may introduce bias in our analysis.
Furthermore, the study was designed as a natural experiment based on a rotational call cycle between hospitalist‐led and nonhospitalist‐led teams. It is possible that the order of patient assignment might not be completely naturally random as we intended. However, the study period was for 2 years and we expect the effect of order would have averaged out in time.
There are many hospitalist models of care. In terms of generalizability, the study pertains only to academic hospitalists and may not be applicable to hospitalists practicing in community hospitals. For example, the nonhospitalist comparison group is likely different in the community and academic settings. Community nonhospitalists (traditional practitioners) are usually internists covering both inpatient and outpatient responsibilities at the same time. In contrast, academic nonhospitalists are internists or subspecialists serving as ward attendings for a limited period (usually 1 month) with considerable variation in their nonattending responsibilities (eg, research, clinic, administration). Furthermore, academic nonhospitalist providers might be a self‐selected group by their willingness to serve as a ward attending, making them more hospitalist‐like. Changes and variability of inpatient attendings may also affect our findings when compared to prior work. Finally, it is also possible that having residents at academic medical centers may attenuate the effect of hospitalists more than in community‐based models.
Conclusions/Implications
Compared to nonhospitalists, academic hospitalist care of acute UGIH patients had similar overall clinical outcomes. However, our finding of similar LOS yet higher costs for patients cared for by hospitalists support 1 proposed mechanism in which hospitalists decrease healthcare costs: providing higher intensity of care per day of hospitalization. However, in academic hospitalist models, this higher intensity hypothesis should be revisited, especially in certain patient groups in which timing and involvement of subspecialists may influence discharge decisions, affecting LOS and overall costs.
Due to inherent limitations in this observational study, future studies should focus on verifying and elucidating these relationships further. Lastly, understanding which patient groups receive the greatest potential benefit from this model will help guide both organizational efforts and quality improvement strategies.
- ,.Bleeding peptic ulcer.N Engl J Med.1994;331(11):717–727.
- .Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population‐based study.Am J Gastroenterol.1995;90(2):206–210.
- ,,, et al.Variation in outcome after acute upper gastrointestinal haemorrhage. the national audit of acute upper gastrointestinal haemorrhage.Lancet.1995;346(8971):346–350.
- ,,, et al.Influencing the practice and outcome in acute upper gastrointestinal haemorrhage. Steering committee of the National Audit of Acute Upper Gastrointestinal Haemorrhage.Gut.1997;41(5):606–611.
- ,,, et al.Risk assessment after acute upper gastrointestinal haemorrhage.Gut.1996;38(3):316–321.
- ,,, et al.The potential size of the hospitalist workforce in the united states.Am J Med.1999;106(4):441–445.
- Society of Hospital Medicine. About SHM. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information357(25):2589–2600.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137(11):866–874.
- .A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists.Mayo Clin Proc.2009;84(3):248–254.
- ,,, et al.Do hospitalists or physicians with greater inpatient HIV experience improve HIV care in the era of highly active antiretroviral therapy? Results from a multicenter trial of academic hospitalists.Clin Infect Dis.2008;46(7):1085–1092.
- ,,, et al.Quality of care for decompensated heart failure: comparable performance between academic hospitalists and non‐hospitalists. J Gen Intern Med.2008;23(9):1399–1406.
- ,,, et al.Factors associated with discussion of care plans and code status at the time of hospital admission: results from the Multicenter Hospitalist Study.J Hosp Med.2008;3(6):437–445.
- ,,, et al.Upper gastrointestinal hemorrhage clinical guideline determining the optimal hospital length of stay.Am J Med.1996;100(3):313–322.
- ,,, et al.Prospective evaluation of a clinical guideline recommending hospital length of stay in upper gastrointestinal tract hemorrhage.JAMA.1997;278(24):2151–2156.
- ,,, et al.In‐hospital cost of abdominal aortic aneurysm repair in Canada and the United States.Arch Intern Med.2003;163(20):2500–2504.
- ,,, et al.The use of transition cost accounting system in health services research.Cost Eff Resour Alloc.2007;5:11.
- Society of Hospital Medicine. Definition of a Hospitalist. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information335(7):514–517.
- ,,, et al.Selection of patients for early discharge or outpatient care after acute upper gastrointestinal haemorrhage. National Audit of Acute Upper Gastrointestinal Haemorrhage.Lancet.1996;347(9009):1138–1140.
- ,,, et al.Utilization of health care resources for low‐risk patients with acute, nonvariceal upper GI hemorrhage: an historical cohort study.Gastrointest Endosc.2002;55(3):321–327.
- ,.Incremental value of upper endoscopy for triage of patients with acute non‐variceal upper‐GI hemorrhage.Gastrointest Endosc.2004;60(1):9–14.
- ,,, et al.The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients.J Clin Epidemiol.2008;61(12):1234–1240.
- ,,, et al.The effectiveness of early endoscopy for upper gastrointestinal hemorrhage: a community‐based analysis.Med Care.1998;36(4):462–474.
- ,,, et al.Early endoscopy in upper gastrointestinal hemorrhage: associations with recurrent bleeding, surgery, and length of hospital stay.Gastrointest Endosc.1999;49(2):145–152.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the united states: a research synthesis.Med Care Res Rev.2005;62(4):379–406.
- ,,, et al.Physician specialty and variations in the cost of treating patients with acute upper gastrointestinal bleeding.Gastroenterology.1997;113(5):1443–1448.
- ,,, et al.Impact of physician specialty on the cost of nonvariceal upper GI bleeding care.Am J Gastroenterol.2002;97(6):1535–1542.
- ,,.Associations with reduced length of stay and costs on an academic hospitalist service.Am J Manag Care.2004;10(8):561–568.
- ,.Bleeding peptic ulcer.N Engl J Med.1994;331(11):717–727.
- .Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population‐based study.Am J Gastroenterol.1995;90(2):206–210.
- ,,, et al.Variation in outcome after acute upper gastrointestinal haemorrhage. the national audit of acute upper gastrointestinal haemorrhage.Lancet.1995;346(8971):346–350.
- ,,, et al.Influencing the practice and outcome in acute upper gastrointestinal haemorrhage. Steering committee of the National Audit of Acute Upper Gastrointestinal Haemorrhage.Gut.1997;41(5):606–611.
- ,,, et al.Risk assessment after acute upper gastrointestinal haemorrhage.Gut.1996;38(3):316–321.
- ,,, et al.The potential size of the hospitalist workforce in the united states.Am J Med.1999;106(4):441–445.
- Society of Hospital Medicine. About SHM. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information357(25):2589–2600.
- ,,, et al.Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists.Ann Intern Med.2002;137(11):866–874.
- .A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists.Mayo Clin Proc.2009;84(3):248–254.
- ,,, et al.Do hospitalists or physicians with greater inpatient HIV experience improve HIV care in the era of highly active antiretroviral therapy? Results from a multicenter trial of academic hospitalists.Clin Infect Dis.2008;46(7):1085–1092.
- ,,, et al.Quality of care for decompensated heart failure: comparable performance between academic hospitalists and non‐hospitalists. J Gen Intern Med.2008;23(9):1399–1406.
- ,,, et al.Factors associated with discussion of care plans and code status at the time of hospital admission: results from the Multicenter Hospitalist Study.J Hosp Med.2008;3(6):437–445.
- ,,, et al.Upper gastrointestinal hemorrhage clinical guideline determining the optimal hospital length of stay.Am J Med.1996;100(3):313–322.
- ,,, et al.Prospective evaluation of a clinical guideline recommending hospital length of stay in upper gastrointestinal tract hemorrhage.JAMA.1997;278(24):2151–2156.
- ,,, et al.In‐hospital cost of abdominal aortic aneurysm repair in Canada and the United States.Arch Intern Med.2003;163(20):2500–2504.
- ,,, et al.The use of transition cost accounting system in health services research.Cost Eff Resour Alloc.2007;5:11.
- Society of Hospital Medicine. Definition of a Hospitalist. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_Information335(7):514–517.
- ,,, et al.Selection of patients for early discharge or outpatient care after acute upper gastrointestinal haemorrhage. National Audit of Acute Upper Gastrointestinal Haemorrhage.Lancet.1996;347(9009):1138–1140.
- ,,, et al.Utilization of health care resources for low‐risk patients with acute, nonvariceal upper GI hemorrhage: an historical cohort study.Gastrointest Endosc.2002;55(3):321–327.
- ,.Incremental value of upper endoscopy for triage of patients with acute non‐variceal upper‐GI hemorrhage.Gastrointest Endosc.2004;60(1):9–14.
- ,,, et al.The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients.J Clin Epidemiol.2008;61(12):1234–1240.
- ,,, et al.The effectiveness of early endoscopy for upper gastrointestinal hemorrhage: a community‐based analysis.Med Care.1998;36(4):462–474.
- ,,, et al.Early endoscopy in upper gastrointestinal hemorrhage: associations with recurrent bleeding, surgery, and length of hospital stay.Gastrointest Endosc.1999;49(2):145–152.
- ,.The impact of hospitalists on the cost and quality of inpatient care in the united states: a research synthesis.Med Care Res Rev.2005;62(4):379–406.
- ,,, et al.Physician specialty and variations in the cost of treating patients with acute upper gastrointestinal bleeding.Gastroenterology.1997;113(5):1443–1448.
- ,,, et al.Impact of physician specialty on the cost of nonvariceal upper GI bleeding care.Am J Gastroenterol.2002;97(6):1535–1542.
- ,,.Associations with reduced length of stay and costs on an academic hospitalist service.Am J Manag Care.2004;10(8):561–568.
Copyright © 2010 Society of Hospital Medicine