User login
Bone and Soft-Tissue Sarcomas
Supplement Co-Editors:
Steven A. Lietman, MD, and Risal Djohan, MD
Contents
Clinical presentation and imaging of bone and soft-tissue sarcomas
Hakan Ilaslan, MD; Jean Schils, MD; William Nageotte, PA-C; Steven A. Lietman, MD; and Murali Sundaram, MD
Bone sarcomas: Overview of management, with a focus on surgical treatment considerations
Steven A. Lietman, MD, and Michael J. Joyce, MD
Soft-tissue sarcomas: Overview of management, with a focus on surgical treatment considerations
Steven A. Lietman, MD
Considerations surrounding reconstruction after resection of musculoskeletal sarcomas
Andrea Moreira-Gonzalez, MD; Risal Djohan, MD; and Robert Lohman, MD
Use of chemotherapy for patients with bone and soft-tissue sarcomas
Robert Wesolowski, MD, and George Thomas Budd, MD
Use of radiation therapy for patients with soft-tissue and bone sarcomas
Lawrence J. Sheplan, MD, and Justin J. Juliano, MD
Supplement Co-Editors:
Steven A. Lietman, MD, and Risal Djohan, MD
Contents
Clinical presentation and imaging of bone and soft-tissue sarcomas
Hakan Ilaslan, MD; Jean Schils, MD; William Nageotte, PA-C; Steven A. Lietman, MD; and Murali Sundaram, MD
Bone sarcomas: Overview of management, with a focus on surgical treatment considerations
Steven A. Lietman, MD, and Michael J. Joyce, MD
Soft-tissue sarcomas: Overview of management, with a focus on surgical treatment considerations
Steven A. Lietman, MD
Considerations surrounding reconstruction after resection of musculoskeletal sarcomas
Andrea Moreira-Gonzalez, MD; Risal Djohan, MD; and Robert Lohman, MD
Use of chemotherapy for patients with bone and soft-tissue sarcomas
Robert Wesolowski, MD, and George Thomas Budd, MD
Use of radiation therapy for patients with soft-tissue and bone sarcomas
Lawrence J. Sheplan, MD, and Justin J. Juliano, MD
Supplement Co-Editors:
Steven A. Lietman, MD, and Risal Djohan, MD
Contents
Clinical presentation and imaging of bone and soft-tissue sarcomas
Hakan Ilaslan, MD; Jean Schils, MD; William Nageotte, PA-C; Steven A. Lietman, MD; and Murali Sundaram, MD
Bone sarcomas: Overview of management, with a focus on surgical treatment considerations
Steven A. Lietman, MD, and Michael J. Joyce, MD
Soft-tissue sarcomas: Overview of management, with a focus on surgical treatment considerations
Steven A. Lietman, MD
Considerations surrounding reconstruction after resection of musculoskeletal sarcomas
Andrea Moreira-Gonzalez, MD; Risal Djohan, MD; and Robert Lohman, MD
Use of chemotherapy for patients with bone and soft-tissue sarcomas
Robert Wesolowski, MD, and George Thomas Budd, MD
Use of radiation therapy for patients with soft-tissue and bone sarcomas
Lawrence J. Sheplan, MD, and Justin J. Juliano, MD
Clinical presentation and imaging of bone and soft-tissue sarcomas
Sarcomas are rare neoplasms arising from connective tissue elements of the body. Approximately 80% arise in soft tissue, while the remainder originate in bone.1 Soft-tissue sarcomas are tumors of the mesenchymal system, and about half develop in the extremities. Bone sarcomas are characterized by their location in bone and sometimes produce osteoid, or immature bone.
The most common types of soft-tissue sarcomas are malignant fibrous histiocytoma (although this term has lost favor with some pathologists) and liposarcoma.
The most common types of bone sarcomas are osteosarcoma (a sarcoma that makes osteoid or bone), Ewing sarcoma (composed of small round blue cells with a characteristic chromosomal translocation), and chondrosarcoma (a sarcoma that makes chondroid tissue, or cartilage).
EPIDEMIOLOGY AND PRIMARY BODY SITES
Approximately 10,600 new cases of soft-tissue sarcoma and 2,570 new cases of bone sarcoma were estimated to have been diagnosed in the United States in 2009.2,3 For perspective, the annual incidence of soft-tissue sarcoma is approximately 5.5% that of breast cancer and approximately 5% that of lung cancer.3
Most sarcomas develop in the lower extremities, although the age groups at greatest risk vary among sarcoma types.4
Soft-tissue sarcomas develop most commonly in the thigh and occur primarily in adults.2
Osteosarcomas are the most common bone sarcoma and develop most frequently in 10- to 20-year-olds; their most common location is the distal femur.5–8 Metastatic osteosarcoma is found in approximately 20% of patients at the time of osteosarcoma diagnosis. Osteosarcomas mainly spread hematogenously, and the lungs are the most common initial site of metastases, being affected in up to 90% of patients with metastatic disease.9
Ewing sarcomas develop most often in the long bones of the extremities or bones of the pelvis. The large majority of cases develop in patients aged 10 to 15 years. 5–8
Chondrosarcomas represent approximately 20% of all bone sarcomas and primarily affect older adults, with a peak incidence in the sixth decade of life.10
OVERVIEW OF PRESENTATION AND EVALUATION
Presentation is highly variable
The clinical presentation of patients with bone or soft-tissue sarcoma is highly variable. Patients often present with a mass, typically one that is increasing in size. In general, bone sarcomas are painful and soft-tissue sarcomas are not, but there are exceptions to this general rule. Constitutional symptoms are rare in patients with bone or soft-tissue sarcomas, but symptoms such as fever, malaise, and weight loss can be seen, especially in patients with Ewing sarcoma.11
Delayed presentation and diagnosis are common
Particularly when a sarcoma is painless, patients sometimes do not seek medical attention until a suspicious mass becomes quite large. Certain tumors, such as synovial sarcoma, a high-grade soft-tissue sarcoma often seen in young adults, may present as a slowly growing or stable-appearing mass over several years. In one study of 33 children with synovial sarcoma, the mean duration of symptoms was 98 weeks (range, 2–364), the mean patient delay before a doctor was seen was 43 weeks (0–156), the mean doctor delay before a correct diagnosis was made was 50 weeks (0–362), and the mean number of doctors seen before referral was 3 (1–6).12 For nearly half the patients in this study (15), the diagnosis was obtained only after unplanned excision, meaning that the surgeon did not expect a malignancy at the time of biopsy. Because delayed presentation is not uncommon in cases of bone or soft-tissue sarcoma, every patient with a mass with indeterminate imaging findings should be referred to or reviewed by an orthopedic or musculoskeletal oncologist.
Biopsy is gold standard for diagnosis
A comprehensive medical history and physical examination are essential at the initial presentation of patients with masses and/or pain suggestive of bone or soft-tissue sarcoma. Sarcoma simulators such as hematoma, metastatic disease, or infection can sometimes be ruled out by careful clinical examination, laboratory work-up, and appropriate imaging, but the gold standard for diagnosis is a biopsy. Moreover, an index of suspicion is required to rule out primary malignancy in any soft-tissue or bone lesion, and this index of suspicion will allow for referral or appropriate selection of the site for biopsy.
Biopsy considerations, as well as further detail on clinical presentation, are provided in the second and third articles in this supplement, which focus, respectively, on bone sarcoma and soft-tissue sarcoma. The remainder of this article reviews the use of imaging for the evaluation of suspected sarcomas, as imaging findings typically prompt or guide biopsy of a suspicious mass. Choosing the right imaging modality is critical to the diagnosis and management of patients with suspected sarcoma.
CONVENTIONAL IMAGING MODALITIES
Despite their utility for evaluating osseous lesions, radiographs have limited to no value in the evaluation of soft-tissue sarcomas but can demonstrate matrix mineralization and erosion or destruction of adjacent bone.
Angiography. In the past, angiography was frequently used to assess the vascularity of sarcomas preoperatively. Diagnostic angiography has been replaced by conventional MRI and magnetic resonance angiography, but some vascular sarcomas may require presurgical embolization to prevent excessive bleeding during surgery.
Radionuclide bone scans have long been a reliable tool for detecting multifocal or disseminated osseous lesions and remain the mainstay for evaluation of osseous metastases. They also are helpful in identifying skip lesions of osteosarcoma (ie, smaller discrete foci of osteosarcoma occurring in the same bone or on the opposing side of a joint).14 Advantages of this modality include whole-body scanning and low radiation at relatively low cost. Radionuclide bone scans demonstrate areas of bony repair and thus could be negative in purely lytic/destructive processes such as renal cell carcinoma metastases and multiple myeloma.
Chest radiographs are typically obtained in the initial stages of patient evaluation and are helpful in demonstrating large nodules or masses resulting from metastatic disease. In a patient with known sarcoma, a negative or equivocal chest radiograph should be followed by chest CT to definitively assess for metastasis.
CROSS-SECTIONAL IMAGING WITH MRI AND CT
MRI preferred for evaluation of most masses
MRI is the examination of choice in the evaluation of soft-tissue masses in light of its superior contrast resolution and ability to demonstrate subtle changes in soft tissues.
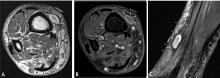
Predicting the histology of most soft-tissue masses is difficult, with the exception of some benign vascular lesions (eg, hemangioma), ganglia, neurogenic lesions, and well-differentiated lipomatous lesions. Aggressive features of a soft-tissue neoplasm include size greater than 5 cm,15 deep location, and absence of central enhancement, which is suggestive of necrosis (Figure 1). Yet one third of soft-tissue sarcomas are either superficial or smaller than 5 cm, which highlights the relative nonspecificity of these features.15
MRI is also the preferred modality in the evaluation of the majority of bone sarcomas, given its ability to accurately define the extent of marrow changes and soft-tissue involvement. MRI should be performed prior to a biopsy to prevent misinterpretation of biopsy-related signal changes in the surrounding tissues, which may negate the value of MRI in sarcoma staging.
Several distinct roles for CT
Chest CT should be obtained in all cases of known malignant neoplasms to evaluate for pulmonary nodules, masses, and lymphadenopathy. Despite the recent advances in MRI, CT remains the imaging modality of choice to evaluate the retroperitoneum, abdomen, and pelvis for masses, lymphadenopathy, or other signs of metastatic disease.
Post-treatment monitoring for recurrence
ULTRASONOGRAPHY
Ultrasonography has a limited role in the initial diagnosis and follow-up of musculoskeletal tumors. Its main advantages are a lack of ionizing radiation and dynamic imaging capabilities. Doppler ultrasonography allows direct visualization of tumor vascularity, which may be important for diagnosis and presurgical planning. Unfortunately, bone lesions cannot be evaluated with ultrasonography, owing to the inability of sound waves to penetrate the bony cortex. Poor sound wave penetration may prevent visualization of deep-seated lesions, such as retroperitoneal sarcomas.
Ultrasonography is best used for differentiating solid masses from cystic structures and can provide image guidance in solid tumor biopsy and cyst aspiration. It also may play a role in detecting suspected tumor recurrence in patients in whom artifact from implanted hardware precludes cross-sectional imaging, and it can be reliably used for following up unequivocal soft-tissue masses such as ganglia near joints.
POSITRON EMISSION TOMOGRAPHY
IMAGING-GUIDED INTERVENTIONS
Percutaneous imaging-guided procedures have increasingly replaced open surgical biopsies for bone and soft-tissue tumors. CT guidance is commonly used for percutaneous biopsy, whereas ultrasonographic guidance is sometimes used for superficial soft-tissue lesions. Although the shortest and most direct approach is desirable, this may not be possible in all cases due to the presence of nearby vital structures or the risk of contamination. Seeding of malignant cells along the biopsy tract is a well-known possible complication of image-guided biopsies, and en bloc resection of the needle tract is typically performed at the definitive surgery.
Knowledge of compartmental anatomy is paramount in planning the approach for these biopsies, and consultation with the referring orthopedic surgeon is recommended for optimal management. Expert histopathological interpretation of bone and soft-tissue specimens is essential for the efficacy and high success rates of percutaneous imaging-guided biopsies. Such expertise is integral to the broader interdisciplinary collaboration that is needed to arrive at the most plausible diagnosis, especially in the setting of uncommon or atypical neoplasms.
Currently, MRI-guided interventions are in the initial stage of evolution and could provide valuable guidance for subtle marrow or soft-tissue lesions visible on MRI but not well seen on CT.22 In the future, MRI could play an increasingly important role in imaging-guided procedures because of its lack of ionizing radiation and its ability to demonstrate subtle soft-tissue and bone marrow changes. Imaging-guided therapeutics are growing in their applications in musculoskeletal oncology. CT-guided radiofrequency ablation and cryoablation have been used in the treatment of a variety of tumors23 as well as in the palliation of metastatic bone pain.24
SUMMARY AND CONCLUSION
Bone and soft-tissue sarcomas are rare neoplasms with variable clinical presentations. A high index of suspicion is required for any unexplained mass with indeterminate imaging findings. Recent advances in imaging technology, including cross-sectional MRI and CT, have significantly refined the diagnosis and management of bone and soft-tissue sarcomas. When faced with a possible sarcoma, the clinician’s selection of imaging modalities has a direct impact on diagnosis, staging, and patient management.
- American Cancer Society. Cancer facts & figures 2009. Atlanta, GA: American Cancer Society; 2009.
- Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’ Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009; 59:225–249.
- Simon MA, Springfield DS, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Dahlin DC, Unni KK. Bone Tumors: General Aspects and Data on 8,542 Cases. 4th ed. Springfield, IL: Thomas; 1986.
- Unni KK. Bone Tumors. New York, NY: Churchill Livingstone; 1988.
- Unni KK. Atlas of Bone Pathology. New York, NY: Chapman & Hall; 1996:1 computer optical disc.
- Unni KK, Dahlin DC. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
- Kaste SC, Pratt CB, Cain AM, Jones-Wallace DJ, Rao BN. Metastases detected at the time of diagnosis of primary pediatric extremity osteosarcoma at diagnosis: imaging features. Cancer 1999; 86:1602–1608.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Kissane JM, Askin FB, Foulkes M, Stratton LB, Shirley SF. Ewing’s sarcoma of bone: clinicopathologic aspects of 303 cases from the Intergroup Ewing’s Sarcoma Study. Hum Pathol 1983; 14:773–779.
- Chotel F, Unnithan A, Chandrasekar CR, et al. Variability in the presentation of synovial sarcoma in children: a plea for greater awareness. J Bone Joint Surg Br 2008; 90:1090–1096.
- Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology 2008; 246:662–674.
- Richardson ML, Gillespy T. Magnetic resonance imaging. In: Kricun ME, ed. Imaging of Bone Tumors. Philadelphia, PA: WB Saunders; 1993:365.
- Fisher C. Soft tissue sarcomas: diagnosis, classification and prognostic factors. Br J Plast Surg 1996; 49:27–33.
- White LM, Wunder JS, Bell RS, et al. Histologic assessment of peritumoral edema in soft tissue sarcoma. Int J Radiat Oncol Biol Phys 2005; 61:1439–1445.
- White LM, Buckwalter KA. Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Semin Musculoskelet Radiol 2002; 6:5–17.
- Blodgett TM, Casagranda B, Townsend DW, Meltzer CC. Issues, controversies, and clinical utility of combined PET/CT imaging: what is the interpreting physician facing? AJR Am J Roentgenol 2005; 184(suppl 5):S138–S145.
- Shin DS, Shon OJ, Han DS, Choi JH, Chun KA, Cho IH. The clinical efficacy of 18F-FDG-PET/CT in benign and malignant musculoskeletal tumors. Ann Nucl Med 2008; 22:603–609.
- Benz MR, Czernin J, Allen-Auerbach MS, et al. FDG-PET/CT imaging predicts histopathologic treatment responses after the initial cycle of neoadjuvant chemotherapy in high-grade soft-tissue sarcomas. Clin Cancer Res 2009; 15:2856–2863.
- Aoki J, Watanabe H, Shinozaki T, et al. FDG-PET for preoperative differential diagnosis between benign and malignant soft tissue masses. Skeletal Radiol 2003; 32:133–138.
- Blanco Sequeiros R, Klemola R, Ojala R, et al. MRI-guided trephine biopsy and fine-needle aspiration in the diagnosis of bone lesions in low-field (0.23 T) MRI system using optical instrument tracking. Eur Radiol 2002; 12:830–835.
- Rosenthal DI. Radiofrequency treatment. Orthop Clin North Am 2006; 37:475–484.
- Callstrom MR, Charboneau JW. Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol 2007; 10:120–131.
Sarcomas are rare neoplasms arising from connective tissue elements of the body. Approximately 80% arise in soft tissue, while the remainder originate in bone.1 Soft-tissue sarcomas are tumors of the mesenchymal system, and about half develop in the extremities. Bone sarcomas are characterized by their location in bone and sometimes produce osteoid, or immature bone.
The most common types of soft-tissue sarcomas are malignant fibrous histiocytoma (although this term has lost favor with some pathologists) and liposarcoma.
The most common types of bone sarcomas are osteosarcoma (a sarcoma that makes osteoid or bone), Ewing sarcoma (composed of small round blue cells with a characteristic chromosomal translocation), and chondrosarcoma (a sarcoma that makes chondroid tissue, or cartilage).
EPIDEMIOLOGY AND PRIMARY BODY SITES
Approximately 10,600 new cases of soft-tissue sarcoma and 2,570 new cases of bone sarcoma were estimated to have been diagnosed in the United States in 2009.2,3 For perspective, the annual incidence of soft-tissue sarcoma is approximately 5.5% that of breast cancer and approximately 5% that of lung cancer.3
Most sarcomas develop in the lower extremities, although the age groups at greatest risk vary among sarcoma types.4
Soft-tissue sarcomas develop most commonly in the thigh and occur primarily in adults.2
Osteosarcomas are the most common bone sarcoma and develop most frequently in 10- to 20-year-olds; their most common location is the distal femur.5–8 Metastatic osteosarcoma is found in approximately 20% of patients at the time of osteosarcoma diagnosis. Osteosarcomas mainly spread hematogenously, and the lungs are the most common initial site of metastases, being affected in up to 90% of patients with metastatic disease.9
Ewing sarcomas develop most often in the long bones of the extremities or bones of the pelvis. The large majority of cases develop in patients aged 10 to 15 years. 5–8
Chondrosarcomas represent approximately 20% of all bone sarcomas and primarily affect older adults, with a peak incidence in the sixth decade of life.10
OVERVIEW OF PRESENTATION AND EVALUATION
Presentation is highly variable
The clinical presentation of patients with bone or soft-tissue sarcoma is highly variable. Patients often present with a mass, typically one that is increasing in size. In general, bone sarcomas are painful and soft-tissue sarcomas are not, but there are exceptions to this general rule. Constitutional symptoms are rare in patients with bone or soft-tissue sarcomas, but symptoms such as fever, malaise, and weight loss can be seen, especially in patients with Ewing sarcoma.11
Delayed presentation and diagnosis are common
Particularly when a sarcoma is painless, patients sometimes do not seek medical attention until a suspicious mass becomes quite large. Certain tumors, such as synovial sarcoma, a high-grade soft-tissue sarcoma often seen in young adults, may present as a slowly growing or stable-appearing mass over several years. In one study of 33 children with synovial sarcoma, the mean duration of symptoms was 98 weeks (range, 2–364), the mean patient delay before a doctor was seen was 43 weeks (0–156), the mean doctor delay before a correct diagnosis was made was 50 weeks (0–362), and the mean number of doctors seen before referral was 3 (1–6).12 For nearly half the patients in this study (15), the diagnosis was obtained only after unplanned excision, meaning that the surgeon did not expect a malignancy at the time of biopsy. Because delayed presentation is not uncommon in cases of bone or soft-tissue sarcoma, every patient with a mass with indeterminate imaging findings should be referred to or reviewed by an orthopedic or musculoskeletal oncologist.
Biopsy is gold standard for diagnosis
A comprehensive medical history and physical examination are essential at the initial presentation of patients with masses and/or pain suggestive of bone or soft-tissue sarcoma. Sarcoma simulators such as hematoma, metastatic disease, or infection can sometimes be ruled out by careful clinical examination, laboratory work-up, and appropriate imaging, but the gold standard for diagnosis is a biopsy. Moreover, an index of suspicion is required to rule out primary malignancy in any soft-tissue or bone lesion, and this index of suspicion will allow for referral or appropriate selection of the site for biopsy.
Biopsy considerations, as well as further detail on clinical presentation, are provided in the second and third articles in this supplement, which focus, respectively, on bone sarcoma and soft-tissue sarcoma. The remainder of this article reviews the use of imaging for the evaluation of suspected sarcomas, as imaging findings typically prompt or guide biopsy of a suspicious mass. Choosing the right imaging modality is critical to the diagnosis and management of patients with suspected sarcoma.
CONVENTIONAL IMAGING MODALITIES
Despite their utility for evaluating osseous lesions, radiographs have limited to no value in the evaluation of soft-tissue sarcomas but can demonstrate matrix mineralization and erosion or destruction of adjacent bone.
Angiography. In the past, angiography was frequently used to assess the vascularity of sarcomas preoperatively. Diagnostic angiography has been replaced by conventional MRI and magnetic resonance angiography, but some vascular sarcomas may require presurgical embolization to prevent excessive bleeding during surgery.
Radionuclide bone scans have long been a reliable tool for detecting multifocal or disseminated osseous lesions and remain the mainstay for evaluation of osseous metastases. They also are helpful in identifying skip lesions of osteosarcoma (ie, smaller discrete foci of osteosarcoma occurring in the same bone or on the opposing side of a joint).14 Advantages of this modality include whole-body scanning and low radiation at relatively low cost. Radionuclide bone scans demonstrate areas of bony repair and thus could be negative in purely lytic/destructive processes such as renal cell carcinoma metastases and multiple myeloma.
Chest radiographs are typically obtained in the initial stages of patient evaluation and are helpful in demonstrating large nodules or masses resulting from metastatic disease. In a patient with known sarcoma, a negative or equivocal chest radiograph should be followed by chest CT to definitively assess for metastasis.
CROSS-SECTIONAL IMAGING WITH MRI AND CT
MRI preferred for evaluation of most masses
MRI is the examination of choice in the evaluation of soft-tissue masses in light of its superior contrast resolution and ability to demonstrate subtle changes in soft tissues.
Predicting the histology of most soft-tissue masses is difficult, with the exception of some benign vascular lesions (eg, hemangioma), ganglia, neurogenic lesions, and well-differentiated lipomatous lesions. Aggressive features of a soft-tissue neoplasm include size greater than 5 cm,15 deep location, and absence of central enhancement, which is suggestive of necrosis (Figure 1). Yet one third of soft-tissue sarcomas are either superficial or smaller than 5 cm, which highlights the relative nonspecificity of these features.15
MRI is also the preferred modality in the evaluation of the majority of bone sarcomas, given its ability to accurately define the extent of marrow changes and soft-tissue involvement. MRI should be performed prior to a biopsy to prevent misinterpretation of biopsy-related signal changes in the surrounding tissues, which may negate the value of MRI in sarcoma staging.
Several distinct roles for CT
Chest CT should be obtained in all cases of known malignant neoplasms to evaluate for pulmonary nodules, masses, and lymphadenopathy. Despite the recent advances in MRI, CT remains the imaging modality of choice to evaluate the retroperitoneum, abdomen, and pelvis for masses, lymphadenopathy, or other signs of metastatic disease.
Post-treatment monitoring for recurrence
ULTRASONOGRAPHY
Ultrasonography has a limited role in the initial diagnosis and follow-up of musculoskeletal tumors. Its main advantages are a lack of ionizing radiation and dynamic imaging capabilities. Doppler ultrasonography allows direct visualization of tumor vascularity, which may be important for diagnosis and presurgical planning. Unfortunately, bone lesions cannot be evaluated with ultrasonography, owing to the inability of sound waves to penetrate the bony cortex. Poor sound wave penetration may prevent visualization of deep-seated lesions, such as retroperitoneal sarcomas.
Ultrasonography is best used for differentiating solid masses from cystic structures and can provide image guidance in solid tumor biopsy and cyst aspiration. It also may play a role in detecting suspected tumor recurrence in patients in whom artifact from implanted hardware precludes cross-sectional imaging, and it can be reliably used for following up unequivocal soft-tissue masses such as ganglia near joints.
POSITRON EMISSION TOMOGRAPHY
IMAGING-GUIDED INTERVENTIONS
Percutaneous imaging-guided procedures have increasingly replaced open surgical biopsies for bone and soft-tissue tumors. CT guidance is commonly used for percutaneous biopsy, whereas ultrasonographic guidance is sometimes used for superficial soft-tissue lesions. Although the shortest and most direct approach is desirable, this may not be possible in all cases due to the presence of nearby vital structures or the risk of contamination. Seeding of malignant cells along the biopsy tract is a well-known possible complication of image-guided biopsies, and en bloc resection of the needle tract is typically performed at the definitive surgery.
Knowledge of compartmental anatomy is paramount in planning the approach for these biopsies, and consultation with the referring orthopedic surgeon is recommended for optimal management. Expert histopathological interpretation of bone and soft-tissue specimens is essential for the efficacy and high success rates of percutaneous imaging-guided biopsies. Such expertise is integral to the broader interdisciplinary collaboration that is needed to arrive at the most plausible diagnosis, especially in the setting of uncommon or atypical neoplasms.
Currently, MRI-guided interventions are in the initial stage of evolution and could provide valuable guidance for subtle marrow or soft-tissue lesions visible on MRI but not well seen on CT.22 In the future, MRI could play an increasingly important role in imaging-guided procedures because of its lack of ionizing radiation and its ability to demonstrate subtle soft-tissue and bone marrow changes. Imaging-guided therapeutics are growing in their applications in musculoskeletal oncology. CT-guided radiofrequency ablation and cryoablation have been used in the treatment of a variety of tumors23 as well as in the palliation of metastatic bone pain.24
SUMMARY AND CONCLUSION
Bone and soft-tissue sarcomas are rare neoplasms with variable clinical presentations. A high index of suspicion is required for any unexplained mass with indeterminate imaging findings. Recent advances in imaging technology, including cross-sectional MRI and CT, have significantly refined the diagnosis and management of bone and soft-tissue sarcomas. When faced with a possible sarcoma, the clinician’s selection of imaging modalities has a direct impact on diagnosis, staging, and patient management.
Sarcomas are rare neoplasms arising from connective tissue elements of the body. Approximately 80% arise in soft tissue, while the remainder originate in bone.1 Soft-tissue sarcomas are tumors of the mesenchymal system, and about half develop in the extremities. Bone sarcomas are characterized by their location in bone and sometimes produce osteoid, or immature bone.
The most common types of soft-tissue sarcomas are malignant fibrous histiocytoma (although this term has lost favor with some pathologists) and liposarcoma.
The most common types of bone sarcomas are osteosarcoma (a sarcoma that makes osteoid or bone), Ewing sarcoma (composed of small round blue cells with a characteristic chromosomal translocation), and chondrosarcoma (a sarcoma that makes chondroid tissue, or cartilage).
EPIDEMIOLOGY AND PRIMARY BODY SITES
Approximately 10,600 new cases of soft-tissue sarcoma and 2,570 new cases of bone sarcoma were estimated to have been diagnosed in the United States in 2009.2,3 For perspective, the annual incidence of soft-tissue sarcoma is approximately 5.5% that of breast cancer and approximately 5% that of lung cancer.3
Most sarcomas develop in the lower extremities, although the age groups at greatest risk vary among sarcoma types.4
Soft-tissue sarcomas develop most commonly in the thigh and occur primarily in adults.2
Osteosarcomas are the most common bone sarcoma and develop most frequently in 10- to 20-year-olds; their most common location is the distal femur.5–8 Metastatic osteosarcoma is found in approximately 20% of patients at the time of osteosarcoma diagnosis. Osteosarcomas mainly spread hematogenously, and the lungs are the most common initial site of metastases, being affected in up to 90% of patients with metastatic disease.9
Ewing sarcomas develop most often in the long bones of the extremities or bones of the pelvis. The large majority of cases develop in patients aged 10 to 15 years. 5–8
Chondrosarcomas represent approximately 20% of all bone sarcomas and primarily affect older adults, with a peak incidence in the sixth decade of life.10
OVERVIEW OF PRESENTATION AND EVALUATION
Presentation is highly variable
The clinical presentation of patients with bone or soft-tissue sarcoma is highly variable. Patients often present with a mass, typically one that is increasing in size. In general, bone sarcomas are painful and soft-tissue sarcomas are not, but there are exceptions to this general rule. Constitutional symptoms are rare in patients with bone or soft-tissue sarcomas, but symptoms such as fever, malaise, and weight loss can be seen, especially in patients with Ewing sarcoma.11
Delayed presentation and diagnosis are common
Particularly when a sarcoma is painless, patients sometimes do not seek medical attention until a suspicious mass becomes quite large. Certain tumors, such as synovial sarcoma, a high-grade soft-tissue sarcoma often seen in young adults, may present as a slowly growing or stable-appearing mass over several years. In one study of 33 children with synovial sarcoma, the mean duration of symptoms was 98 weeks (range, 2–364), the mean patient delay before a doctor was seen was 43 weeks (0–156), the mean doctor delay before a correct diagnosis was made was 50 weeks (0–362), and the mean number of doctors seen before referral was 3 (1–6).12 For nearly half the patients in this study (15), the diagnosis was obtained only after unplanned excision, meaning that the surgeon did not expect a malignancy at the time of biopsy. Because delayed presentation is not uncommon in cases of bone or soft-tissue sarcoma, every patient with a mass with indeterminate imaging findings should be referred to or reviewed by an orthopedic or musculoskeletal oncologist.
Biopsy is gold standard for diagnosis
A comprehensive medical history and physical examination are essential at the initial presentation of patients with masses and/or pain suggestive of bone or soft-tissue sarcoma. Sarcoma simulators such as hematoma, metastatic disease, or infection can sometimes be ruled out by careful clinical examination, laboratory work-up, and appropriate imaging, but the gold standard for diagnosis is a biopsy. Moreover, an index of suspicion is required to rule out primary malignancy in any soft-tissue or bone lesion, and this index of suspicion will allow for referral or appropriate selection of the site for biopsy.
Biopsy considerations, as well as further detail on clinical presentation, are provided in the second and third articles in this supplement, which focus, respectively, on bone sarcoma and soft-tissue sarcoma. The remainder of this article reviews the use of imaging for the evaluation of suspected sarcomas, as imaging findings typically prompt or guide biopsy of a suspicious mass. Choosing the right imaging modality is critical to the diagnosis and management of patients with suspected sarcoma.
CONVENTIONAL IMAGING MODALITIES
Despite their utility for evaluating osseous lesions, radiographs have limited to no value in the evaluation of soft-tissue sarcomas but can demonstrate matrix mineralization and erosion or destruction of adjacent bone.
Angiography. In the past, angiography was frequently used to assess the vascularity of sarcomas preoperatively. Diagnostic angiography has been replaced by conventional MRI and magnetic resonance angiography, but some vascular sarcomas may require presurgical embolization to prevent excessive bleeding during surgery.
Radionuclide bone scans have long been a reliable tool for detecting multifocal or disseminated osseous lesions and remain the mainstay for evaluation of osseous metastases. They also are helpful in identifying skip lesions of osteosarcoma (ie, smaller discrete foci of osteosarcoma occurring in the same bone or on the opposing side of a joint).14 Advantages of this modality include whole-body scanning and low radiation at relatively low cost. Radionuclide bone scans demonstrate areas of bony repair and thus could be negative in purely lytic/destructive processes such as renal cell carcinoma metastases and multiple myeloma.
Chest radiographs are typically obtained in the initial stages of patient evaluation and are helpful in demonstrating large nodules or masses resulting from metastatic disease. In a patient with known sarcoma, a negative or equivocal chest radiograph should be followed by chest CT to definitively assess for metastasis.
CROSS-SECTIONAL IMAGING WITH MRI AND CT
MRI preferred for evaluation of most masses
MRI is the examination of choice in the evaluation of soft-tissue masses in light of its superior contrast resolution and ability to demonstrate subtle changes in soft tissues.
Predicting the histology of most soft-tissue masses is difficult, with the exception of some benign vascular lesions (eg, hemangioma), ganglia, neurogenic lesions, and well-differentiated lipomatous lesions. Aggressive features of a soft-tissue neoplasm include size greater than 5 cm,15 deep location, and absence of central enhancement, which is suggestive of necrosis (Figure 1). Yet one third of soft-tissue sarcomas are either superficial or smaller than 5 cm, which highlights the relative nonspecificity of these features.15
MRI is also the preferred modality in the evaluation of the majority of bone sarcomas, given its ability to accurately define the extent of marrow changes and soft-tissue involvement. MRI should be performed prior to a biopsy to prevent misinterpretation of biopsy-related signal changes in the surrounding tissues, which may negate the value of MRI in sarcoma staging.
Several distinct roles for CT
Chest CT should be obtained in all cases of known malignant neoplasms to evaluate for pulmonary nodules, masses, and lymphadenopathy. Despite the recent advances in MRI, CT remains the imaging modality of choice to evaluate the retroperitoneum, abdomen, and pelvis for masses, lymphadenopathy, or other signs of metastatic disease.
Post-treatment monitoring for recurrence
ULTRASONOGRAPHY
Ultrasonography has a limited role in the initial diagnosis and follow-up of musculoskeletal tumors. Its main advantages are a lack of ionizing radiation and dynamic imaging capabilities. Doppler ultrasonography allows direct visualization of tumor vascularity, which may be important for diagnosis and presurgical planning. Unfortunately, bone lesions cannot be evaluated with ultrasonography, owing to the inability of sound waves to penetrate the bony cortex. Poor sound wave penetration may prevent visualization of deep-seated lesions, such as retroperitoneal sarcomas.
Ultrasonography is best used for differentiating solid masses from cystic structures and can provide image guidance in solid tumor biopsy and cyst aspiration. It also may play a role in detecting suspected tumor recurrence in patients in whom artifact from implanted hardware precludes cross-sectional imaging, and it can be reliably used for following up unequivocal soft-tissue masses such as ganglia near joints.
POSITRON EMISSION TOMOGRAPHY
IMAGING-GUIDED INTERVENTIONS
Percutaneous imaging-guided procedures have increasingly replaced open surgical biopsies for bone and soft-tissue tumors. CT guidance is commonly used for percutaneous biopsy, whereas ultrasonographic guidance is sometimes used for superficial soft-tissue lesions. Although the shortest and most direct approach is desirable, this may not be possible in all cases due to the presence of nearby vital structures or the risk of contamination. Seeding of malignant cells along the biopsy tract is a well-known possible complication of image-guided biopsies, and en bloc resection of the needle tract is typically performed at the definitive surgery.
Knowledge of compartmental anatomy is paramount in planning the approach for these biopsies, and consultation with the referring orthopedic surgeon is recommended for optimal management. Expert histopathological interpretation of bone and soft-tissue specimens is essential for the efficacy and high success rates of percutaneous imaging-guided biopsies. Such expertise is integral to the broader interdisciplinary collaboration that is needed to arrive at the most plausible diagnosis, especially in the setting of uncommon or atypical neoplasms.
Currently, MRI-guided interventions are in the initial stage of evolution and could provide valuable guidance for subtle marrow or soft-tissue lesions visible on MRI but not well seen on CT.22 In the future, MRI could play an increasingly important role in imaging-guided procedures because of its lack of ionizing radiation and its ability to demonstrate subtle soft-tissue and bone marrow changes. Imaging-guided therapeutics are growing in their applications in musculoskeletal oncology. CT-guided radiofrequency ablation and cryoablation have been used in the treatment of a variety of tumors23 as well as in the palliation of metastatic bone pain.24
SUMMARY AND CONCLUSION
Bone and soft-tissue sarcomas are rare neoplasms with variable clinical presentations. A high index of suspicion is required for any unexplained mass with indeterminate imaging findings. Recent advances in imaging technology, including cross-sectional MRI and CT, have significantly refined the diagnosis and management of bone and soft-tissue sarcomas. When faced with a possible sarcoma, the clinician’s selection of imaging modalities has a direct impact on diagnosis, staging, and patient management.
- American Cancer Society. Cancer facts & figures 2009. Atlanta, GA: American Cancer Society; 2009.
- Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’ Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009; 59:225–249.
- Simon MA, Springfield DS, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Dahlin DC, Unni KK. Bone Tumors: General Aspects and Data on 8,542 Cases. 4th ed. Springfield, IL: Thomas; 1986.
- Unni KK. Bone Tumors. New York, NY: Churchill Livingstone; 1988.
- Unni KK. Atlas of Bone Pathology. New York, NY: Chapman & Hall; 1996:1 computer optical disc.
- Unni KK, Dahlin DC. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
- Kaste SC, Pratt CB, Cain AM, Jones-Wallace DJ, Rao BN. Metastases detected at the time of diagnosis of primary pediatric extremity osteosarcoma at diagnosis: imaging features. Cancer 1999; 86:1602–1608.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Kissane JM, Askin FB, Foulkes M, Stratton LB, Shirley SF. Ewing’s sarcoma of bone: clinicopathologic aspects of 303 cases from the Intergroup Ewing’s Sarcoma Study. Hum Pathol 1983; 14:773–779.
- Chotel F, Unnithan A, Chandrasekar CR, et al. Variability in the presentation of synovial sarcoma in children: a plea for greater awareness. J Bone Joint Surg Br 2008; 90:1090–1096.
- Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology 2008; 246:662–674.
- Richardson ML, Gillespy T. Magnetic resonance imaging. In: Kricun ME, ed. Imaging of Bone Tumors. Philadelphia, PA: WB Saunders; 1993:365.
- Fisher C. Soft tissue sarcomas: diagnosis, classification and prognostic factors. Br J Plast Surg 1996; 49:27–33.
- White LM, Wunder JS, Bell RS, et al. Histologic assessment of peritumoral edema in soft tissue sarcoma. Int J Radiat Oncol Biol Phys 2005; 61:1439–1445.
- White LM, Buckwalter KA. Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Semin Musculoskelet Radiol 2002; 6:5–17.
- Blodgett TM, Casagranda B, Townsend DW, Meltzer CC. Issues, controversies, and clinical utility of combined PET/CT imaging: what is the interpreting physician facing? AJR Am J Roentgenol 2005; 184(suppl 5):S138–S145.
- Shin DS, Shon OJ, Han DS, Choi JH, Chun KA, Cho IH. The clinical efficacy of 18F-FDG-PET/CT in benign and malignant musculoskeletal tumors. Ann Nucl Med 2008; 22:603–609.
- Benz MR, Czernin J, Allen-Auerbach MS, et al. FDG-PET/CT imaging predicts histopathologic treatment responses after the initial cycle of neoadjuvant chemotherapy in high-grade soft-tissue sarcomas. Clin Cancer Res 2009; 15:2856–2863.
- Aoki J, Watanabe H, Shinozaki T, et al. FDG-PET for preoperative differential diagnosis between benign and malignant soft tissue masses. Skeletal Radiol 2003; 32:133–138.
- Blanco Sequeiros R, Klemola R, Ojala R, et al. MRI-guided trephine biopsy and fine-needle aspiration in the diagnosis of bone lesions in low-field (0.23 T) MRI system using optical instrument tracking. Eur Radiol 2002; 12:830–835.
- Rosenthal DI. Radiofrequency treatment. Orthop Clin North Am 2006; 37:475–484.
- Callstrom MR, Charboneau JW. Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol 2007; 10:120–131.
- American Cancer Society. Cancer facts & figures 2009. Atlanta, GA: American Cancer Society; 2009.
- Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss’ Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin 2009; 59:225–249.
- Simon MA, Springfield DS, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Dahlin DC, Unni KK. Bone Tumors: General Aspects and Data on 8,542 Cases. 4th ed. Springfield, IL: Thomas; 1986.
- Unni KK. Bone Tumors. New York, NY: Churchill Livingstone; 1988.
- Unni KK. Atlas of Bone Pathology. New York, NY: Chapman & Hall; 1996:1 computer optical disc.
- Unni KK, Dahlin DC. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 5th ed. Philadelphia, PA: Lippincott-Raven; 1996.
- Kaste SC, Pratt CB, Cain AM, Jones-Wallace DJ, Rao BN. Metastases detected at the time of diagnosis of primary pediatric extremity osteosarcoma at diagnosis: imaging features. Cancer 1999; 86:1602–1608.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Kissane JM, Askin FB, Foulkes M, Stratton LB, Shirley SF. Ewing’s sarcoma of bone: clinicopathologic aspects of 303 cases from the Intergroup Ewing’s Sarcoma Study. Hum Pathol 1983; 14:773–779.
- Chotel F, Unnithan A, Chandrasekar CR, et al. Variability in the presentation of synovial sarcoma in children: a plea for greater awareness. J Bone Joint Surg Br 2008; 90:1090–1096.
- Miller TT. Bone tumors and tumorlike conditions: analysis with conventional radiography. Radiology 2008; 246:662–674.
- Richardson ML, Gillespy T. Magnetic resonance imaging. In: Kricun ME, ed. Imaging of Bone Tumors. Philadelphia, PA: WB Saunders; 1993:365.
- Fisher C. Soft tissue sarcomas: diagnosis, classification and prognostic factors. Br J Plast Surg 1996; 49:27–33.
- White LM, Wunder JS, Bell RS, et al. Histologic assessment of peritumoral edema in soft tissue sarcoma. Int J Radiat Oncol Biol Phys 2005; 61:1439–1445.
- White LM, Buckwalter KA. Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Semin Musculoskelet Radiol 2002; 6:5–17.
- Blodgett TM, Casagranda B, Townsend DW, Meltzer CC. Issues, controversies, and clinical utility of combined PET/CT imaging: what is the interpreting physician facing? AJR Am J Roentgenol 2005; 184(suppl 5):S138–S145.
- Shin DS, Shon OJ, Han DS, Choi JH, Chun KA, Cho IH. The clinical efficacy of 18F-FDG-PET/CT in benign and malignant musculoskeletal tumors. Ann Nucl Med 2008; 22:603–609.
- Benz MR, Czernin J, Allen-Auerbach MS, et al. FDG-PET/CT imaging predicts histopathologic treatment responses after the initial cycle of neoadjuvant chemotherapy in high-grade soft-tissue sarcomas. Clin Cancer Res 2009; 15:2856–2863.
- Aoki J, Watanabe H, Shinozaki T, et al. FDG-PET for preoperative differential diagnosis between benign and malignant soft tissue masses. Skeletal Radiol 2003; 32:133–138.
- Blanco Sequeiros R, Klemola R, Ojala R, et al. MRI-guided trephine biopsy and fine-needle aspiration in the diagnosis of bone lesions in low-field (0.23 T) MRI system using optical instrument tracking. Eur Radiol 2002; 12:830–835.
- Rosenthal DI. Radiofrequency treatment. Orthop Clin North Am 2006; 37:475–484.
- Callstrom MR, Charboneau JW. Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol 2007; 10:120–131.
Bone sarcomas: Overview of management, with a focus on surgical treatment considerations
Prior to the 1970s, bone sarcomas were routinely treated with amputation, yet most patients still died from metastatic disease.1 The advent of the use of chemotherapy for bone sarcomas in the 1970s was shown to increase long-term survival,2–5 contributing in part to tremendous subsequent advances in the treatment of the most common bone sarcomas—osteosarcoma and Ewing sarcoma. Today, long-term disease-free survival rates of about 60% to 80% are observed for patients with Ewing sarcoma or osteosarcoma with no metastasis at presentation.6,7 In addition to the chemotherapy advances, modular metallic prosthetic limb reconstruction systems are now readily available, eliminating the need to wait for custom reconstructive hardware. Moreover, these systems can be used in combination with large bone allografts or vascularized bone flaps.
The majority of patients with bone sarcomas require multimodal treatment, primarily with surgery and chemotherapy. Patients with chondrosarcomas are the primary exception, as chondrosarcomas are generally treated with resection alone. Thus, management of most patients with bone sarcomas requires a multidisciplinary team that includes orthopedic, medical, and radiation oncologists as well as plastic and reconstructive surgeons, physical therapy specialists, pathologists, and radiologists with expertise in bone tumors.
Despite this broad need for multimodal therapy, surgical resection is fundamental to the management of virtually all bone sarcomas and is the primary focus of this article. The roles of chemotherapy and radiation therapy for bone sarcomas are detailed in the final two articles in this supplement.
INITIAL EVALUATION OF SUSPICIOUS BONE MASSES
History and physical examination
As noted in the preceding article in this supplement, most bone sarcomas (particularly osteosarcomas and Ewing sarcomas) occur in pediatric patients and young adults and develop in the extremities (especially the distal femur) or pelvis.
In terms of history, most patients with a bone sarcoma will report pain, but pain is not a good indicator of malignancy, as some patients with no pain or an improvement in pain have sarcomas while many patients with pain do not have malignancies.1
The other most common finding in patients with a bone sarcoma is an enlarging mass. The presence of a mass, as well as its location, depth, size, and overlying skin quality, can be determined on physical examination. An accurate neurovascular exam should be performed as well, although damage to neurovascular structures is a late finding in sarcoma patients.
Imaging
Radiographs are important in any patient with prolonged unexplained bone pain and will almost always reveal an aggressive lesion in the patient with a bone sarcoma. Lengthy delays in the diagnosis of a bone sarcoma are nearly always explained by failure to obtain a radiograph.
Magnetic resonance imaging (MRI). Questions about whether a radiograph of a lesion is determinate or not are best resolved by MRI, which is the primary imaging method for evaluating bone lesions, their exact location, and their proximity to neurovascular structures. While “determinate” and “indeterminate” are most precisely used to refer to imaging studies of a lesion, these terms are often used in clinical parlance to refer to the lesions themselves. As such, “determinate lesions” by imaging are those that can be accurately judged malignant or benign with a high level of certainty. Determinate benign inactive lesions such as enchondromas and osteochondromas, if asymptomatic and without severe bony destruction, do not require a bone biopsy. “Indeterminate lesions” by imaging are those whose imaging findings are not clearly consistent with a single diagnosis, and nearly all of these lesions require a biopsy.
In general, any patient with a bone mass with indeterminate imaging results should be referred to an orthopedic oncologist.
Staging
When imaging findings are highly suggestive of bone sarcoma, efforts should be made to delineate how far the tumor extends and whether systemic disease is present. Bone sarcomas can metastasize to other bones, but their most common site for metastasis is the lung.
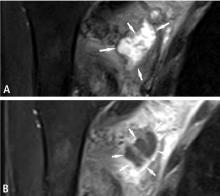
MRI of the lesion without gadolinium is indicated, and the entire bone is imaged to determine the extent of the external mass outside the bone and to look for medullary extension and skip lesions (eg, smaller foci of sarcoma occurring in the same bone or on the opposing side of a joint). The precision offered by MRI has dramatically increased surgeons’ ability to achieve negative margins during resection.
Radiography or computed tomography of the chest is required to accurately assess the lungs for metastasis. A nuclear medicine technetium scan can be obtained to look for other similar bone lesions (metachronous lesions) or metastatic bony disease.
Laboratory tests are not helpful in the staging of bone sarcomas.
BIOPSY
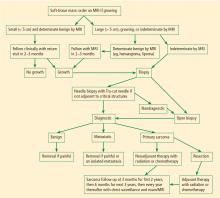
Biopsy is the gold standard for diagnosis of bone sarcoma (Figure 1). The primary biopsy methods used are needle or open biopsy techniques, and Tru-cut needles or core bone biopsy needles are increasingly used. If the core needle biopsy is diagnostically inconclusive, an open biopsy can promptly be performed. Biopsies yielding specimens that are too small can result in inconclusive pathology reports. Regardless of the biopsy technique, hemostasis is of paramount importance, and patients are generally advised to not use the affected limb for at least several days after the procedure to reduce the risk of a cancer cell–laden hematoma.
If a needle biopsy is performed, 2 to 10 minutes of gentle pressure is applied to the site. In an open biopsy, electrocauterization is used extensively. Aggressive hemostasis is achieved, and if a drain is placed it should be in proximity to the incision site itself so that the drain site will be resected with the specimen at the time of definitive resection. Open biopsies are performed in the operating room with regional or general anesthesia. Incisions are made longitudinally and never transversely.
Ideally, the biopsy should be performed or supervised by a physician experienced with limb salvage for bone sarcomas. Otherwise there is risk for an inappropriate biopsy tract or approach, misinterpretation of the radiographic studies, misinterpretation of the pathology, or biopsy complications. These errors may lead to undertreatment or even unnecessary amputation.8,9
RESECTION
For some bone sarcomas, such as osteosarcoma and Ewing sarcoma, there is a preference to treat the potential micrometastatic disease at the beginning of the course, prior to surgical treatment. This may result in reduction of the soft-tissue mass about the bone tumor and/or maturing of the mass, allowing for easier resection.
Importance of margins
The goal of resection is to achieve a margin or normal cuff of tissue around the pseudocapsule of the tumor. In general, the larger the margin, the less the chance of recurrence.10–12 Ideally, the tumor and pseudocapsule should not be violated or exposed and a margin of at least 1 cm should be obtained. It has been postulated that margins of less than 1 cm may be associated with a very low rate of recurrence, although no well-controlled study has proven this and such a study would be difficult to perform given the rarity and heterogeneity of bone sarcomas and the variability in their assessment and surgical treatment.
Intralesional surgery is generally to be avoided
Intralesional surgery should not be performed on high-grade bone sarcomas because it will lead to a high risk of local recurrence regardless of whether the patient receives perioperative radiation therapy or chemotherapy. If intralesional surgery has been performed for a high-grade sarcoma at an outside institution, re-excision of the tumor bed is recommended, as it has reduced the rate of recurrence following intralesional surgery.13 For low-grade chondrosarcomas, intralesional curettage (ie, violating the margin of the tumor by scraping it out thoroughly) with use of an adjuvant (freezing, phenol, methylmethacrylate, or argon beam) may be adequate and has been reported to have a low rate of recurrence.14
Preoperative planning
The resection procedure involves careful preoperative planning, typically guided by an MRI reviewed by a musculoskeletal tumor radiologist. General anesthesia is usually preferred because it can be used for a lengthy procedure, ensures complete muscle relaxation over the duration of the procedure, and allows for immediate postoperative nerve assessment. If neurovascular structures are not encased (ie, not more than 50% surrounded in the case of arteries or motor nerves), these structures are spared. If arteries are encased, arterial resection with reverse interpositional vein graft, synthetic graft, or vein allograft allows for bypass of the vessel and leaves the encased structure with the resection specimen for en bloc resection. In Ewing sarcoma, if the tumor is adjacent to but not encasing the neurovascular structures, the radiation oncologist is consulted about whether there is a preference for pre- or postoperative radiation therapy.
Limb salvage for Ewing sarcoma was originally with radiation only, but subsequently limb-salvaging surgery has been shown in several studies to have lower rates of local failure.6,15–18 Whether primary radiation or surgery is performed after the initiation of chemotherapy is generally determined by a discussion between the surgeon and radiation oncologist about the feasibility of a negative margin with surgery and the inherent functional loss with resection. There are particular concerns about radiation in younger patients, who have a relatively high rate of postradiation sarcoma.18
In osteosarcoma and chondrosarcoma, radiation has been found not to be effective, so resection with a negative margin is especially important for preventing local recurrence.
RECONSTRUCTION
Allograft or metallic prosthesis?
In the proximal and distal femur, modular metallic replacement prosthetic joint devices are used. Often a wafer of greater trochanter bone (if uninvolved in the tumor process) can be preserved and a “cable-claw” attachment to the metal component can be accomplished instead of using an allograft.
Since the proximal humerus is not weight-bearing and because of the importance of the rotator cuff, use of an APC in the proximal humerus can be most helpful. Function is not good with a metallic proximal humerus implant alone, and the dislocation rate is high over long-term follow-up, owing to lack of healing of the rotator cuff remnant to the metal prosthesis.
In patients with scapular sarcomas, allograft or prosthetic reconstruction has not been consistently better than simply repairing the remaining muscles to each other, so we generally do not use allografts or prostheses after sarcoma resection in these patients.
Growing bones of youth pose special challenges
In growing children, who represent a large share of bone sarcoma patients, reconstruction after resection in the lower extremity is challenging, particularly in terms of addressing leg length inequality. In general, a prosthesis is used and if the end growth discrepancy will be greater than 3 cm, use of an expandable prosthesis is considered. Use of these expandable prostheses has been fraught with complications, however, and by their nature they require revision because of breakage. An alternative is reoperation to disconnect the modular prosthesis and insert an additional 1- to 2-cm segment to increase length when necessary. Allograft bones are a common method of reconstruction when the resection does not involve the joint.
Rotationplasty
Rotationplasty—which involves saving the portion of the extremity distal to the resection site and reattaching it after being rotated 180 degrees—is rarely performed for leg reconstruction, in light of the disfiguring nature of the surgery as a result of the 180-degree rotation.
When rotationplasty is performed, the lower tibia and foot generally are brought up to the middle or proximal femoral area and attached to the short proximal femur. Rather than a short above-knee amputation, the reversed foot functions as a knee, allowing for better prosthetic function (ideally similar to a short below-knee prosthesis), and adds length to a short above-knee amputation.
Another alternative is a tibial turn-up to add length to a very short above-knee amputation if the vessels are not involved with the tumor and limb salvage is otherwise not practical. In this procedure the ankle can be turned up to the hip and the proximal tibia ends up distal to the ankle.
AMPUTATION
When curative surgery is possible and limb-salvaging resection is unlikely to obtain a negative margin or a functionally viable extremity, amputations are still performed. For example, amputation is recommended in a patient with a high-grade calcaneal (heel bone) sarcoma with a large soft-tissue mass. However, amputation is not the usual approach for most bone sarcomas today and it is not benign in outcome. Notably, phantom limb pain and stump pain have been reported after amputation in the typically sensate tumor patient.
Meticulous hemostasis is necessary in all amputations, and myodesis, or direct suturing of muscle to the distal end of the bone, is important for soft-tissue coverage over the distal stump. In general, a fish-mouth incision is used for the upper extremity and thigh, and a posterior flap is used, when possible, below the knee. However, the choice of technique depends on factors such as the presence or absence of a biopsy incision and the location of tumor soft-tissue mass, so local tissue rearrangement or flaps may need to be used for stable coverage or closure.
For all amputation patients, early involvement of an acute pain specialist reduces the incidence of phantom limb pain.
SURVEILLANCE AND FOLLOW-UP
Post-therapy follow-up of patients with bone sarcomas is critical. Even among patients who receive appropriate surgery with negative margins there is a recurrence rate of approximately 9% (personal communication from Dr. Dempsey Springfield), and previously undetectable metastatic disease may become detectable in the postoperative period. In general, patients are followed at 3-month intervals for the first 2 years, at 6-month intervals for the next 3 years, and at yearly intervals thereafter. Follow-up evaluations must include examination of the the involved extremity and imaging of the chest, with radiography or computed tomography, to assess for metastasis.
Rehabilitation is specific to the site of resection and the reconstruction. In general, range of motion is important around the knee, whereas in patients with resection and reconstruction involving the shoulder, hip, or pelvis, it is more important that the affected muscles be given time to heal (6–12 weeks) before aggressive rehabilitation is begun.
Many patients limp postoperatively, particularly in the initial period, and the degree of limp depends primarily on the amount of muscle and the bony insertion sites that are resected with the tumor. Improvements in function are common over time, even at several years after surgery.
FUTURE DIRECTIONS
Despite the advances in bone sarcoma outcomes in recent decades, sarcomas of the pelvis continue to carry a worse prognosis than those of the extremities and thus represent an opportunity for improvement. Among the improvements hoped for is an ability to accomplish partial pelvic resections—eg, of the wing, ischium, or ramus—without need for reconstruction for these smaller localized tumors. Options include amputation (hemipelvectomy) with loss of leg; internal hemipelvectomy (where the pelvis is resected but the leg is left attached without reconstruction of the defect); or resection of the pelvic/acetabular area but with reconstruction using pelvic allografts/total hip composites or large metallic prostheses.
- Simon MA, Springfield DS. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Cortes EP, Holland JF, Wang JJ, et al. Amputation and adriamycin in primary osteosarcoma. N Engl J Med 1974; 291:998–1000.
- Goorin AM, Abelson HT, Frei E III. Osteosarcoma: fifteen years later. N Engl J Med 1985; 313:1637–1643.
- Goorin AM, Frei E, Abelson HT. Adjuvant chemotherapy for osteosarcoma: a decade of experience. Surg Clin North Am 1981; 61:1379–1389.
- Jaffe N, Goorin A, Link M, et al. High-dose methotrexate in osteogenic sarcoma adjuvant chemotherapy and limb salvage results. Cancer Treat Rep 1981; 65(suppl 1):99–106.
- Rodriguez-Galindo C, Navid F, Liu T, et al. Prognostic factors for local and distant control in Ewing sarcoma family of tumors. Ann Oncol 2008; 19:814–820.
- Meyers PA, Schwartz CL, Krailo MD, et al. Osteosarcoma: the addition of muramyl tripeptide to chemotherapy improves overall survival: a report from the Children’s Oncology Group. J Clin Oncol 2008; 26:633–638.
- Mankin HJ, Mankin CJ, Simon MA. The hazards of the biopsy, revisited. Members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am 1996; 78:656–663.
- Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft-tissue tumors. J Bone Joint Surg Am 1982; 64:1121–1127.
- Blakely ML, Spurbeck WW, Pappo AS, et al. The impact of margin of resection on outcome in pediatric nonrhabdomyosarcoma soft tissue sarcoma. J Pediatr Surg 1999; 34:672–675.
- Davis AM, Kandel RA, Wunder JS, et al. The impact of residual disease on local recurrence in patients treated by initial unplanned resection for soft tissue sarcoma of the extremity. J Surg Oncol 1997; 66:81–87.
- Gupta GR, Yasko AW, Lewis VO, et al. Risk of local recurrence after deltoid-sparing resection for osteosarcoma of the proximal humerus. Cancer 2009; 115:3767–3773.
- Chandrasekar CR, Wafa H, Grimer RJ, Carter SR, Tillman RM, Abudu A. The effect of an unplanned excision of a soft-tissue sarcoma on prognosis. J Bone Joint Surg Br 2008; 90:203–208.
- Bauer HC, Brosjö O, Kreicbergs A, Lindholm J. Low risk of recurrence of enchondroma and low-grade chondrosarcoma in extremities: 80 patients followed for 2–25 years. Acta Orthop Scand 1995; 66:283–288.
- Graham-Pole J. Ewing sarcoma: treatment with high dose radiation and adjuvant chemotherapy. Med Pediatr Oncol 1979; 7:1–8.
- Merchant TE, Kushner BH, Sheldon JM, LaQuaglia M, Healey JH. Effect of low-dose radiation therapy when combined with surgical resection for Ewing sarcoma. Med Pediatr Oncol 1999; 33:65–70.
- Rosito P, Mancini AF, Rondelli R, et al. Italian Cooperative Study for the treatment of children and young adults with localized Ewing sarcoma of bone: a preliminary report of 6 years of experience. Cancer 1999; 86:421–428.
- Goldsby R, Burke C, Nagarajan R, et al. Second solid malignancies among children, adolescents, and young adults diagnosed with malignant bone tumors after 1976: follow-up of a Children’s Oncology Group cohort. Cancer 2008; 113:2597–2604.
Prior to the 1970s, bone sarcomas were routinely treated with amputation, yet most patients still died from metastatic disease.1 The advent of the use of chemotherapy for bone sarcomas in the 1970s was shown to increase long-term survival,2–5 contributing in part to tremendous subsequent advances in the treatment of the most common bone sarcomas—osteosarcoma and Ewing sarcoma. Today, long-term disease-free survival rates of about 60% to 80% are observed for patients with Ewing sarcoma or osteosarcoma with no metastasis at presentation.6,7 In addition to the chemotherapy advances, modular metallic prosthetic limb reconstruction systems are now readily available, eliminating the need to wait for custom reconstructive hardware. Moreover, these systems can be used in combination with large bone allografts or vascularized bone flaps.
The majority of patients with bone sarcomas require multimodal treatment, primarily with surgery and chemotherapy. Patients with chondrosarcomas are the primary exception, as chondrosarcomas are generally treated with resection alone. Thus, management of most patients with bone sarcomas requires a multidisciplinary team that includes orthopedic, medical, and radiation oncologists as well as plastic and reconstructive surgeons, physical therapy specialists, pathologists, and radiologists with expertise in bone tumors.
Despite this broad need for multimodal therapy, surgical resection is fundamental to the management of virtually all bone sarcomas and is the primary focus of this article. The roles of chemotherapy and radiation therapy for bone sarcomas are detailed in the final two articles in this supplement.
INITIAL EVALUATION OF SUSPICIOUS BONE MASSES
History and physical examination
As noted in the preceding article in this supplement, most bone sarcomas (particularly osteosarcomas and Ewing sarcomas) occur in pediatric patients and young adults and develop in the extremities (especially the distal femur) or pelvis.
In terms of history, most patients with a bone sarcoma will report pain, but pain is not a good indicator of malignancy, as some patients with no pain or an improvement in pain have sarcomas while many patients with pain do not have malignancies.1
The other most common finding in patients with a bone sarcoma is an enlarging mass. The presence of a mass, as well as its location, depth, size, and overlying skin quality, can be determined on physical examination. An accurate neurovascular exam should be performed as well, although damage to neurovascular structures is a late finding in sarcoma patients.
Imaging
Radiographs are important in any patient with prolonged unexplained bone pain and will almost always reveal an aggressive lesion in the patient with a bone sarcoma. Lengthy delays in the diagnosis of a bone sarcoma are nearly always explained by failure to obtain a radiograph.
Magnetic resonance imaging (MRI). Questions about whether a radiograph of a lesion is determinate or not are best resolved by MRI, which is the primary imaging method for evaluating bone lesions, their exact location, and their proximity to neurovascular structures. While “determinate” and “indeterminate” are most precisely used to refer to imaging studies of a lesion, these terms are often used in clinical parlance to refer to the lesions themselves. As such, “determinate lesions” by imaging are those that can be accurately judged malignant or benign with a high level of certainty. Determinate benign inactive lesions such as enchondromas and osteochondromas, if asymptomatic and without severe bony destruction, do not require a bone biopsy. “Indeterminate lesions” by imaging are those whose imaging findings are not clearly consistent with a single diagnosis, and nearly all of these lesions require a biopsy.
In general, any patient with a bone mass with indeterminate imaging results should be referred to an orthopedic oncologist.
Staging
When imaging findings are highly suggestive of bone sarcoma, efforts should be made to delineate how far the tumor extends and whether systemic disease is present. Bone sarcomas can metastasize to other bones, but their most common site for metastasis is the lung.
MRI of the lesion without gadolinium is indicated, and the entire bone is imaged to determine the extent of the external mass outside the bone and to look for medullary extension and skip lesions (eg, smaller foci of sarcoma occurring in the same bone or on the opposing side of a joint). The precision offered by MRI has dramatically increased surgeons’ ability to achieve negative margins during resection.
Radiography or computed tomography of the chest is required to accurately assess the lungs for metastasis. A nuclear medicine technetium scan can be obtained to look for other similar bone lesions (metachronous lesions) or metastatic bony disease.
Laboratory tests are not helpful in the staging of bone sarcomas.
BIOPSY
Biopsy is the gold standard for diagnosis of bone sarcoma (Figure 1). The primary biopsy methods used are needle or open biopsy techniques, and Tru-cut needles or core bone biopsy needles are increasingly used. If the core needle biopsy is diagnostically inconclusive, an open biopsy can promptly be performed. Biopsies yielding specimens that are too small can result in inconclusive pathology reports. Regardless of the biopsy technique, hemostasis is of paramount importance, and patients are generally advised to not use the affected limb for at least several days after the procedure to reduce the risk of a cancer cell–laden hematoma.
If a needle biopsy is performed, 2 to 10 minutes of gentle pressure is applied to the site. In an open biopsy, electrocauterization is used extensively. Aggressive hemostasis is achieved, and if a drain is placed it should be in proximity to the incision site itself so that the drain site will be resected with the specimen at the time of definitive resection. Open biopsies are performed in the operating room with regional or general anesthesia. Incisions are made longitudinally and never transversely.
Ideally, the biopsy should be performed or supervised by a physician experienced with limb salvage for bone sarcomas. Otherwise there is risk for an inappropriate biopsy tract or approach, misinterpretation of the radiographic studies, misinterpretation of the pathology, or biopsy complications. These errors may lead to undertreatment or even unnecessary amputation.8,9
RESECTION
For some bone sarcomas, such as osteosarcoma and Ewing sarcoma, there is a preference to treat the potential micrometastatic disease at the beginning of the course, prior to surgical treatment. This may result in reduction of the soft-tissue mass about the bone tumor and/or maturing of the mass, allowing for easier resection.
Importance of margins
The goal of resection is to achieve a margin or normal cuff of tissue around the pseudocapsule of the tumor. In general, the larger the margin, the less the chance of recurrence.10–12 Ideally, the tumor and pseudocapsule should not be violated or exposed and a margin of at least 1 cm should be obtained. It has been postulated that margins of less than 1 cm may be associated with a very low rate of recurrence, although no well-controlled study has proven this and such a study would be difficult to perform given the rarity and heterogeneity of bone sarcomas and the variability in their assessment and surgical treatment.
Intralesional surgery is generally to be avoided
Intralesional surgery should not be performed on high-grade bone sarcomas because it will lead to a high risk of local recurrence regardless of whether the patient receives perioperative radiation therapy or chemotherapy. If intralesional surgery has been performed for a high-grade sarcoma at an outside institution, re-excision of the tumor bed is recommended, as it has reduced the rate of recurrence following intralesional surgery.13 For low-grade chondrosarcomas, intralesional curettage (ie, violating the margin of the tumor by scraping it out thoroughly) with use of an adjuvant (freezing, phenol, methylmethacrylate, or argon beam) may be adequate and has been reported to have a low rate of recurrence.14
Preoperative planning
The resection procedure involves careful preoperative planning, typically guided by an MRI reviewed by a musculoskeletal tumor radiologist. General anesthesia is usually preferred because it can be used for a lengthy procedure, ensures complete muscle relaxation over the duration of the procedure, and allows for immediate postoperative nerve assessment. If neurovascular structures are not encased (ie, not more than 50% surrounded in the case of arteries or motor nerves), these structures are spared. If arteries are encased, arterial resection with reverse interpositional vein graft, synthetic graft, or vein allograft allows for bypass of the vessel and leaves the encased structure with the resection specimen for en bloc resection. In Ewing sarcoma, if the tumor is adjacent to but not encasing the neurovascular structures, the radiation oncologist is consulted about whether there is a preference for pre- or postoperative radiation therapy.
Limb salvage for Ewing sarcoma was originally with radiation only, but subsequently limb-salvaging surgery has been shown in several studies to have lower rates of local failure.6,15–18 Whether primary radiation or surgery is performed after the initiation of chemotherapy is generally determined by a discussion between the surgeon and radiation oncologist about the feasibility of a negative margin with surgery and the inherent functional loss with resection. There are particular concerns about radiation in younger patients, who have a relatively high rate of postradiation sarcoma.18
In osteosarcoma and chondrosarcoma, radiation has been found not to be effective, so resection with a negative margin is especially important for preventing local recurrence.
RECONSTRUCTION
Allograft or metallic prosthesis?
In the proximal and distal femur, modular metallic replacement prosthetic joint devices are used. Often a wafer of greater trochanter bone (if uninvolved in the tumor process) can be preserved and a “cable-claw” attachment to the metal component can be accomplished instead of using an allograft.
Since the proximal humerus is not weight-bearing and because of the importance of the rotator cuff, use of an APC in the proximal humerus can be most helpful. Function is not good with a metallic proximal humerus implant alone, and the dislocation rate is high over long-term follow-up, owing to lack of healing of the rotator cuff remnant to the metal prosthesis.
In patients with scapular sarcomas, allograft or prosthetic reconstruction has not been consistently better than simply repairing the remaining muscles to each other, so we generally do not use allografts or prostheses after sarcoma resection in these patients.
Growing bones of youth pose special challenges
In growing children, who represent a large share of bone sarcoma patients, reconstruction after resection in the lower extremity is challenging, particularly in terms of addressing leg length inequality. In general, a prosthesis is used and if the end growth discrepancy will be greater than 3 cm, use of an expandable prosthesis is considered. Use of these expandable prostheses has been fraught with complications, however, and by their nature they require revision because of breakage. An alternative is reoperation to disconnect the modular prosthesis and insert an additional 1- to 2-cm segment to increase length when necessary. Allograft bones are a common method of reconstruction when the resection does not involve the joint.
Rotationplasty
Rotationplasty—which involves saving the portion of the extremity distal to the resection site and reattaching it after being rotated 180 degrees—is rarely performed for leg reconstruction, in light of the disfiguring nature of the surgery as a result of the 180-degree rotation.
When rotationplasty is performed, the lower tibia and foot generally are brought up to the middle or proximal femoral area and attached to the short proximal femur. Rather than a short above-knee amputation, the reversed foot functions as a knee, allowing for better prosthetic function (ideally similar to a short below-knee prosthesis), and adds length to a short above-knee amputation.
Another alternative is a tibial turn-up to add length to a very short above-knee amputation if the vessels are not involved with the tumor and limb salvage is otherwise not practical. In this procedure the ankle can be turned up to the hip and the proximal tibia ends up distal to the ankle.
AMPUTATION
When curative surgery is possible and limb-salvaging resection is unlikely to obtain a negative margin or a functionally viable extremity, amputations are still performed. For example, amputation is recommended in a patient with a high-grade calcaneal (heel bone) sarcoma with a large soft-tissue mass. However, amputation is not the usual approach for most bone sarcomas today and it is not benign in outcome. Notably, phantom limb pain and stump pain have been reported after amputation in the typically sensate tumor patient.
Meticulous hemostasis is necessary in all amputations, and myodesis, or direct suturing of muscle to the distal end of the bone, is important for soft-tissue coverage over the distal stump. In general, a fish-mouth incision is used for the upper extremity and thigh, and a posterior flap is used, when possible, below the knee. However, the choice of technique depends on factors such as the presence or absence of a biopsy incision and the location of tumor soft-tissue mass, so local tissue rearrangement or flaps may need to be used for stable coverage or closure.
For all amputation patients, early involvement of an acute pain specialist reduces the incidence of phantom limb pain.
SURVEILLANCE AND FOLLOW-UP
Post-therapy follow-up of patients with bone sarcomas is critical. Even among patients who receive appropriate surgery with negative margins there is a recurrence rate of approximately 9% (personal communication from Dr. Dempsey Springfield), and previously undetectable metastatic disease may become detectable in the postoperative period. In general, patients are followed at 3-month intervals for the first 2 years, at 6-month intervals for the next 3 years, and at yearly intervals thereafter. Follow-up evaluations must include examination of the the involved extremity and imaging of the chest, with radiography or computed tomography, to assess for metastasis.
Rehabilitation is specific to the site of resection and the reconstruction. In general, range of motion is important around the knee, whereas in patients with resection and reconstruction involving the shoulder, hip, or pelvis, it is more important that the affected muscles be given time to heal (6–12 weeks) before aggressive rehabilitation is begun.
Many patients limp postoperatively, particularly in the initial period, and the degree of limp depends primarily on the amount of muscle and the bony insertion sites that are resected with the tumor. Improvements in function are common over time, even at several years after surgery.
FUTURE DIRECTIONS
Despite the advances in bone sarcoma outcomes in recent decades, sarcomas of the pelvis continue to carry a worse prognosis than those of the extremities and thus represent an opportunity for improvement. Among the improvements hoped for is an ability to accomplish partial pelvic resections—eg, of the wing, ischium, or ramus—without need for reconstruction for these smaller localized tumors. Options include amputation (hemipelvectomy) with loss of leg; internal hemipelvectomy (where the pelvis is resected but the leg is left attached without reconstruction of the defect); or resection of the pelvic/acetabular area but with reconstruction using pelvic allografts/total hip composites or large metallic prostheses.
Prior to the 1970s, bone sarcomas were routinely treated with amputation, yet most patients still died from metastatic disease.1 The advent of the use of chemotherapy for bone sarcomas in the 1970s was shown to increase long-term survival,2–5 contributing in part to tremendous subsequent advances in the treatment of the most common bone sarcomas—osteosarcoma and Ewing sarcoma. Today, long-term disease-free survival rates of about 60% to 80% are observed for patients with Ewing sarcoma or osteosarcoma with no metastasis at presentation.6,7 In addition to the chemotherapy advances, modular metallic prosthetic limb reconstruction systems are now readily available, eliminating the need to wait for custom reconstructive hardware. Moreover, these systems can be used in combination with large bone allografts or vascularized bone flaps.
The majority of patients with bone sarcomas require multimodal treatment, primarily with surgery and chemotherapy. Patients with chondrosarcomas are the primary exception, as chondrosarcomas are generally treated with resection alone. Thus, management of most patients with bone sarcomas requires a multidisciplinary team that includes orthopedic, medical, and radiation oncologists as well as plastic and reconstructive surgeons, physical therapy specialists, pathologists, and radiologists with expertise in bone tumors.
Despite this broad need for multimodal therapy, surgical resection is fundamental to the management of virtually all bone sarcomas and is the primary focus of this article. The roles of chemotherapy and radiation therapy for bone sarcomas are detailed in the final two articles in this supplement.
INITIAL EVALUATION OF SUSPICIOUS BONE MASSES
History and physical examination
As noted in the preceding article in this supplement, most bone sarcomas (particularly osteosarcomas and Ewing sarcomas) occur in pediatric patients and young adults and develop in the extremities (especially the distal femur) or pelvis.
In terms of history, most patients with a bone sarcoma will report pain, but pain is not a good indicator of malignancy, as some patients with no pain or an improvement in pain have sarcomas while many patients with pain do not have malignancies.1
The other most common finding in patients with a bone sarcoma is an enlarging mass. The presence of a mass, as well as its location, depth, size, and overlying skin quality, can be determined on physical examination. An accurate neurovascular exam should be performed as well, although damage to neurovascular structures is a late finding in sarcoma patients.
Imaging
Radiographs are important in any patient with prolonged unexplained bone pain and will almost always reveal an aggressive lesion in the patient with a bone sarcoma. Lengthy delays in the diagnosis of a bone sarcoma are nearly always explained by failure to obtain a radiograph.
Magnetic resonance imaging (MRI). Questions about whether a radiograph of a lesion is determinate or not are best resolved by MRI, which is the primary imaging method for evaluating bone lesions, their exact location, and their proximity to neurovascular structures. While “determinate” and “indeterminate” are most precisely used to refer to imaging studies of a lesion, these terms are often used in clinical parlance to refer to the lesions themselves. As such, “determinate lesions” by imaging are those that can be accurately judged malignant or benign with a high level of certainty. Determinate benign inactive lesions such as enchondromas and osteochondromas, if asymptomatic and without severe bony destruction, do not require a bone biopsy. “Indeterminate lesions” by imaging are those whose imaging findings are not clearly consistent with a single diagnosis, and nearly all of these lesions require a biopsy.
In general, any patient with a bone mass with indeterminate imaging results should be referred to an orthopedic oncologist.
Staging
When imaging findings are highly suggestive of bone sarcoma, efforts should be made to delineate how far the tumor extends and whether systemic disease is present. Bone sarcomas can metastasize to other bones, but their most common site for metastasis is the lung.
MRI of the lesion without gadolinium is indicated, and the entire bone is imaged to determine the extent of the external mass outside the bone and to look for medullary extension and skip lesions (eg, smaller foci of sarcoma occurring in the same bone or on the opposing side of a joint). The precision offered by MRI has dramatically increased surgeons’ ability to achieve negative margins during resection.
Radiography or computed tomography of the chest is required to accurately assess the lungs for metastasis. A nuclear medicine technetium scan can be obtained to look for other similar bone lesions (metachronous lesions) or metastatic bony disease.
Laboratory tests are not helpful in the staging of bone sarcomas.
BIOPSY
Biopsy is the gold standard for diagnosis of bone sarcoma (Figure 1). The primary biopsy methods used are needle or open biopsy techniques, and Tru-cut needles or core bone biopsy needles are increasingly used. If the core needle biopsy is diagnostically inconclusive, an open biopsy can promptly be performed. Biopsies yielding specimens that are too small can result in inconclusive pathology reports. Regardless of the biopsy technique, hemostasis is of paramount importance, and patients are generally advised to not use the affected limb for at least several days after the procedure to reduce the risk of a cancer cell–laden hematoma.
If a needle biopsy is performed, 2 to 10 minutes of gentle pressure is applied to the site. In an open biopsy, electrocauterization is used extensively. Aggressive hemostasis is achieved, and if a drain is placed it should be in proximity to the incision site itself so that the drain site will be resected with the specimen at the time of definitive resection. Open biopsies are performed in the operating room with regional or general anesthesia. Incisions are made longitudinally and never transversely.
Ideally, the biopsy should be performed or supervised by a physician experienced with limb salvage for bone sarcomas. Otherwise there is risk for an inappropriate biopsy tract or approach, misinterpretation of the radiographic studies, misinterpretation of the pathology, or biopsy complications. These errors may lead to undertreatment or even unnecessary amputation.8,9
RESECTION
For some bone sarcomas, such as osteosarcoma and Ewing sarcoma, there is a preference to treat the potential micrometastatic disease at the beginning of the course, prior to surgical treatment. This may result in reduction of the soft-tissue mass about the bone tumor and/or maturing of the mass, allowing for easier resection.
Importance of margins
The goal of resection is to achieve a margin or normal cuff of tissue around the pseudocapsule of the tumor. In general, the larger the margin, the less the chance of recurrence.10–12 Ideally, the tumor and pseudocapsule should not be violated or exposed and a margin of at least 1 cm should be obtained. It has been postulated that margins of less than 1 cm may be associated with a very low rate of recurrence, although no well-controlled study has proven this and such a study would be difficult to perform given the rarity and heterogeneity of bone sarcomas and the variability in their assessment and surgical treatment.
Intralesional surgery is generally to be avoided
Intralesional surgery should not be performed on high-grade bone sarcomas because it will lead to a high risk of local recurrence regardless of whether the patient receives perioperative radiation therapy or chemotherapy. If intralesional surgery has been performed for a high-grade sarcoma at an outside institution, re-excision of the tumor bed is recommended, as it has reduced the rate of recurrence following intralesional surgery.13 For low-grade chondrosarcomas, intralesional curettage (ie, violating the margin of the tumor by scraping it out thoroughly) with use of an adjuvant (freezing, phenol, methylmethacrylate, or argon beam) may be adequate and has been reported to have a low rate of recurrence.14
Preoperative planning
The resection procedure involves careful preoperative planning, typically guided by an MRI reviewed by a musculoskeletal tumor radiologist. General anesthesia is usually preferred because it can be used for a lengthy procedure, ensures complete muscle relaxation over the duration of the procedure, and allows for immediate postoperative nerve assessment. If neurovascular structures are not encased (ie, not more than 50% surrounded in the case of arteries or motor nerves), these structures are spared. If arteries are encased, arterial resection with reverse interpositional vein graft, synthetic graft, or vein allograft allows for bypass of the vessel and leaves the encased structure with the resection specimen for en bloc resection. In Ewing sarcoma, if the tumor is adjacent to but not encasing the neurovascular structures, the radiation oncologist is consulted about whether there is a preference for pre- or postoperative radiation therapy.
Limb salvage for Ewing sarcoma was originally with radiation only, but subsequently limb-salvaging surgery has been shown in several studies to have lower rates of local failure.6,15–18 Whether primary radiation or surgery is performed after the initiation of chemotherapy is generally determined by a discussion between the surgeon and radiation oncologist about the feasibility of a negative margin with surgery and the inherent functional loss with resection. There are particular concerns about radiation in younger patients, who have a relatively high rate of postradiation sarcoma.18
In osteosarcoma and chondrosarcoma, radiation has been found not to be effective, so resection with a negative margin is especially important for preventing local recurrence.
RECONSTRUCTION
Allograft or metallic prosthesis?
In the proximal and distal femur, modular metallic replacement prosthetic joint devices are used. Often a wafer of greater trochanter bone (if uninvolved in the tumor process) can be preserved and a “cable-claw” attachment to the metal component can be accomplished instead of using an allograft.
Since the proximal humerus is not weight-bearing and because of the importance of the rotator cuff, use of an APC in the proximal humerus can be most helpful. Function is not good with a metallic proximal humerus implant alone, and the dislocation rate is high over long-term follow-up, owing to lack of healing of the rotator cuff remnant to the metal prosthesis.
In patients with scapular sarcomas, allograft or prosthetic reconstruction has not been consistently better than simply repairing the remaining muscles to each other, so we generally do not use allografts or prostheses after sarcoma resection in these patients.
Growing bones of youth pose special challenges
In growing children, who represent a large share of bone sarcoma patients, reconstruction after resection in the lower extremity is challenging, particularly in terms of addressing leg length inequality. In general, a prosthesis is used and if the end growth discrepancy will be greater than 3 cm, use of an expandable prosthesis is considered. Use of these expandable prostheses has been fraught with complications, however, and by their nature they require revision because of breakage. An alternative is reoperation to disconnect the modular prosthesis and insert an additional 1- to 2-cm segment to increase length when necessary. Allograft bones are a common method of reconstruction when the resection does not involve the joint.
Rotationplasty
Rotationplasty—which involves saving the portion of the extremity distal to the resection site and reattaching it after being rotated 180 degrees—is rarely performed for leg reconstruction, in light of the disfiguring nature of the surgery as a result of the 180-degree rotation.
When rotationplasty is performed, the lower tibia and foot generally are brought up to the middle or proximal femoral area and attached to the short proximal femur. Rather than a short above-knee amputation, the reversed foot functions as a knee, allowing for better prosthetic function (ideally similar to a short below-knee prosthesis), and adds length to a short above-knee amputation.
Another alternative is a tibial turn-up to add length to a very short above-knee amputation if the vessels are not involved with the tumor and limb salvage is otherwise not practical. In this procedure the ankle can be turned up to the hip and the proximal tibia ends up distal to the ankle.
AMPUTATION
When curative surgery is possible and limb-salvaging resection is unlikely to obtain a negative margin or a functionally viable extremity, amputations are still performed. For example, amputation is recommended in a patient with a high-grade calcaneal (heel bone) sarcoma with a large soft-tissue mass. However, amputation is not the usual approach for most bone sarcomas today and it is not benign in outcome. Notably, phantom limb pain and stump pain have been reported after amputation in the typically sensate tumor patient.
Meticulous hemostasis is necessary in all amputations, and myodesis, or direct suturing of muscle to the distal end of the bone, is important for soft-tissue coverage over the distal stump. In general, a fish-mouth incision is used for the upper extremity and thigh, and a posterior flap is used, when possible, below the knee. However, the choice of technique depends on factors such as the presence or absence of a biopsy incision and the location of tumor soft-tissue mass, so local tissue rearrangement or flaps may need to be used for stable coverage or closure.
For all amputation patients, early involvement of an acute pain specialist reduces the incidence of phantom limb pain.
SURVEILLANCE AND FOLLOW-UP
Post-therapy follow-up of patients with bone sarcomas is critical. Even among patients who receive appropriate surgery with negative margins there is a recurrence rate of approximately 9% (personal communication from Dr. Dempsey Springfield), and previously undetectable metastatic disease may become detectable in the postoperative period. In general, patients are followed at 3-month intervals for the first 2 years, at 6-month intervals for the next 3 years, and at yearly intervals thereafter. Follow-up evaluations must include examination of the the involved extremity and imaging of the chest, with radiography or computed tomography, to assess for metastasis.
Rehabilitation is specific to the site of resection and the reconstruction. In general, range of motion is important around the knee, whereas in patients with resection and reconstruction involving the shoulder, hip, or pelvis, it is more important that the affected muscles be given time to heal (6–12 weeks) before aggressive rehabilitation is begun.
Many patients limp postoperatively, particularly in the initial period, and the degree of limp depends primarily on the amount of muscle and the bony insertion sites that are resected with the tumor. Improvements in function are common over time, even at several years after surgery.
FUTURE DIRECTIONS
Despite the advances in bone sarcoma outcomes in recent decades, sarcomas of the pelvis continue to carry a worse prognosis than those of the extremities and thus represent an opportunity for improvement. Among the improvements hoped for is an ability to accomplish partial pelvic resections—eg, of the wing, ischium, or ramus—without need for reconstruction for these smaller localized tumors. Options include amputation (hemipelvectomy) with loss of leg; internal hemipelvectomy (where the pelvis is resected but the leg is left attached without reconstruction of the defect); or resection of the pelvic/acetabular area but with reconstruction using pelvic allografts/total hip composites or large metallic prostheses.
- Simon MA, Springfield DS. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Cortes EP, Holland JF, Wang JJ, et al. Amputation and adriamycin in primary osteosarcoma. N Engl J Med 1974; 291:998–1000.
- Goorin AM, Abelson HT, Frei E III. Osteosarcoma: fifteen years later. N Engl J Med 1985; 313:1637–1643.
- Goorin AM, Frei E, Abelson HT. Adjuvant chemotherapy for osteosarcoma: a decade of experience. Surg Clin North Am 1981; 61:1379–1389.
- Jaffe N, Goorin A, Link M, et al. High-dose methotrexate in osteogenic sarcoma adjuvant chemotherapy and limb salvage results. Cancer Treat Rep 1981; 65(suppl 1):99–106.
- Rodriguez-Galindo C, Navid F, Liu T, et al. Prognostic factors for local and distant control in Ewing sarcoma family of tumors. Ann Oncol 2008; 19:814–820.
- Meyers PA, Schwartz CL, Krailo MD, et al. Osteosarcoma: the addition of muramyl tripeptide to chemotherapy improves overall survival: a report from the Children’s Oncology Group. J Clin Oncol 2008; 26:633–638.
- Mankin HJ, Mankin CJ, Simon MA. The hazards of the biopsy, revisited. Members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am 1996; 78:656–663.
- Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft-tissue tumors. J Bone Joint Surg Am 1982; 64:1121–1127.
- Blakely ML, Spurbeck WW, Pappo AS, et al. The impact of margin of resection on outcome in pediatric nonrhabdomyosarcoma soft tissue sarcoma. J Pediatr Surg 1999; 34:672–675.
- Davis AM, Kandel RA, Wunder JS, et al. The impact of residual disease on local recurrence in patients treated by initial unplanned resection for soft tissue sarcoma of the extremity. J Surg Oncol 1997; 66:81–87.
- Gupta GR, Yasko AW, Lewis VO, et al. Risk of local recurrence after deltoid-sparing resection for osteosarcoma of the proximal humerus. Cancer 2009; 115:3767–3773.
- Chandrasekar CR, Wafa H, Grimer RJ, Carter SR, Tillman RM, Abudu A. The effect of an unplanned excision of a soft-tissue sarcoma on prognosis. J Bone Joint Surg Br 2008; 90:203–208.
- Bauer HC, Brosjö O, Kreicbergs A, Lindholm J. Low risk of recurrence of enchondroma and low-grade chondrosarcoma in extremities: 80 patients followed for 2–25 years. Acta Orthop Scand 1995; 66:283–288.
- Graham-Pole J. Ewing sarcoma: treatment with high dose radiation and adjuvant chemotherapy. Med Pediatr Oncol 1979; 7:1–8.
- Merchant TE, Kushner BH, Sheldon JM, LaQuaglia M, Healey JH. Effect of low-dose radiation therapy when combined with surgical resection for Ewing sarcoma. Med Pediatr Oncol 1999; 33:65–70.
- Rosito P, Mancini AF, Rondelli R, et al. Italian Cooperative Study for the treatment of children and young adults with localized Ewing sarcoma of bone: a preliminary report of 6 years of experience. Cancer 1999; 86:421–428.
- Goldsby R, Burke C, Nagarajan R, et al. Second solid malignancies among children, adolescents, and young adults diagnosed with malignant bone tumors after 1976: follow-up of a Children’s Oncology Group cohort. Cancer 2008; 113:2597–2604.
- Simon MA, Springfield DS. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Cortes EP, Holland JF, Wang JJ, et al. Amputation and adriamycin in primary osteosarcoma. N Engl J Med 1974; 291:998–1000.
- Goorin AM, Abelson HT, Frei E III. Osteosarcoma: fifteen years later. N Engl J Med 1985; 313:1637–1643.
- Goorin AM, Frei E, Abelson HT. Adjuvant chemotherapy for osteosarcoma: a decade of experience. Surg Clin North Am 1981; 61:1379–1389.
- Jaffe N, Goorin A, Link M, et al. High-dose methotrexate in osteogenic sarcoma adjuvant chemotherapy and limb salvage results. Cancer Treat Rep 1981; 65(suppl 1):99–106.
- Rodriguez-Galindo C, Navid F, Liu T, et al. Prognostic factors for local and distant control in Ewing sarcoma family of tumors. Ann Oncol 2008; 19:814–820.
- Meyers PA, Schwartz CL, Krailo MD, et al. Osteosarcoma: the addition of muramyl tripeptide to chemotherapy improves overall survival: a report from the Children’s Oncology Group. J Clin Oncol 2008; 26:633–638.
- Mankin HJ, Mankin CJ, Simon MA. The hazards of the biopsy, revisited. Members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am 1996; 78:656–663.
- Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft-tissue tumors. J Bone Joint Surg Am 1982; 64:1121–1127.
- Blakely ML, Spurbeck WW, Pappo AS, et al. The impact of margin of resection on outcome in pediatric nonrhabdomyosarcoma soft tissue sarcoma. J Pediatr Surg 1999; 34:672–675.
- Davis AM, Kandel RA, Wunder JS, et al. The impact of residual disease on local recurrence in patients treated by initial unplanned resection for soft tissue sarcoma of the extremity. J Surg Oncol 1997; 66:81–87.
- Gupta GR, Yasko AW, Lewis VO, et al. Risk of local recurrence after deltoid-sparing resection for osteosarcoma of the proximal humerus. Cancer 2009; 115:3767–3773.
- Chandrasekar CR, Wafa H, Grimer RJ, Carter SR, Tillman RM, Abudu A. The effect of an unplanned excision of a soft-tissue sarcoma on prognosis. J Bone Joint Surg Br 2008; 90:203–208.
- Bauer HC, Brosjö O, Kreicbergs A, Lindholm J. Low risk of recurrence of enchondroma and low-grade chondrosarcoma in extremities: 80 patients followed for 2–25 years. Acta Orthop Scand 1995; 66:283–288.
- Graham-Pole J. Ewing sarcoma: treatment with high dose radiation and adjuvant chemotherapy. Med Pediatr Oncol 1979; 7:1–8.
- Merchant TE, Kushner BH, Sheldon JM, LaQuaglia M, Healey JH. Effect of low-dose radiation therapy when combined with surgical resection for Ewing sarcoma. Med Pediatr Oncol 1999; 33:65–70.
- Rosito P, Mancini AF, Rondelli R, et al. Italian Cooperative Study for the treatment of children and young adults with localized Ewing sarcoma of bone: a preliminary report of 6 years of experience. Cancer 1999; 86:421–428.
- Goldsby R, Burke C, Nagarajan R, et al. Second solid malignancies among children, adolescents, and young adults diagnosed with malignant bone tumors after 1976: follow-up of a Children’s Oncology Group cohort. Cancer 2008; 113:2597–2604.
Soft-tissue sarcomas: Overview of management, with a focus on surgical treatment considerations
Soft-tissue sarcomas are tumors of the mesenchymal system, and half develop in the extremities.1 Although patients with soft-tissue sarcomas have been treated with a combination of surgery, radiation therapy, and chemotherapy, it remains unclear whether either radiation or chemotherapy improves outcomes for these patients. Soft-tissue sarcomas are therefore currently treated with surgical resection when possible, with or without chemotherapy or radiation.
Even though multimodal therapy for patients with these tumors is controversial, a multidisciplinary conference among the many providers who may be involved in the management these patients—orthopedic, medical, and radiation oncologists, as well as the referring primary care physician, plastic and reconstructive surgeons, physical therapists, and radiologists and pathologists with expertise in these tumors—is helpful.2 This article presents an overview of the management of these patients, with a focus on the mainstay treatment, surgical resection. The roles of chemotherapy and radiation therapy for soft-tissue sarcomas, while touched upon here, are detailed in the final two articles in this supplement.
HISTOLOGIC GRADING AND THERAPY IMPLICATIONS
The prognosis of soft-tissue sarcomas correlates with histopathologic grade, and a three-grade system appears to be more accurate than a two-grade system.3 In general, low-grade lesions (grade 1) are unlikely to metastasize and are therefore less likely to need treatment with chemotherapy or radiation, as the risks of these therapies would most likely outweigh any benefit in terms of local control.
Specifically, the risk of radiation involves debilitation of local wound healing and the chance of dedifferentiation of low-grade lesions to higher-grade lesions with more metastatic potential. Grade 2 and 3 lesions are usually considered high-grade and are more likely to be treated with radiation and chemotherapy. Radiation is frequently used in patients with high-grade lesions when anticipated margins or actual margins are less than 1 cm.4–6
Chemotherapy’s lack of proven efficacy for soft-tissue sarcomas likely stems from poor understanding of the pathophysiology, molecular biology, and even some aspects of the natural history of these uncommon and heterogeneous tumors. There are more than 50 subtypes of soft-tissue sarcoma,7,8 and this heterogeneity has likely contributed to the difficulty of identifying chemotherapeutic agents that are highly active against these diseases.9
THE ROLE OF FAMILIAL GENETICS
Developing effective chemotherapeutic strategies may depend on grouping soft-tissue sarcomas more homogeneously. To compare like lesions with like lesions, molecular analysis and even molecular signatures may be of assistance. Along these lines, critical mutations and translocations have been described for several soft-tissue sarcoma subtypes.
Li-Fraumeni syndrome is an autosomal dominant cancer predisposition syndrome caused by germline mutations (ie, in every cell) in the p53 gene.10 Patients with Li-Fraumeni syndrome have an increased risk of developing soft-tissue sarcomas.1,11
Neurofibromatosis type 1 is caused by germline mutations in the NF1 gene, and malignant peripheral nerve sheath tumors occur within neurofibromas in neurofibromatosis patients and typically have additional mutations in CDKN2A or p53.9 INI1 loss is seen in all cases of extrarenal rhabdoid tumors and has been reported in a subset of epithelioid sarcomas (those occurring in proximal/axial regions).9,12 Delineation and greater understanding of these genetic abnormalities may lead to more effective medical therapy.
EVALUATION OF SUSPICIOUS SOFT-TISSUE MASSES
Figure 1 presents in flow chart form our general approach to the evaluation and management of patients with a soft-tissue mass suspicious for sarcoma—an approach detailed in the text below.
History and physical examination
Patients with soft-tissue sarcomas present with a mass that generally is increasing in size. The location and depth of the mass can be assessed on physical examination. In general, the deeper the mass, the more likely it is to be a sarcoma.13 Unlike bone sarcomas, soft-tissue sarcomas frequently are not associated with pain, so lack of pain does not make a mass more likely to be benign. In general, the only way to be sure that a mass is not malignant is to biopsy it. However, there are certain symptoms and signs that make a benign diagnosis much more likely. For example, very soft superficial masses that have not changed in size in years tend to be benign lipomas, and discolored lesions that go away with elevation of the affected body part tend to be hemangiomas.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is the primary imaging method for soft-tissue sarcomas. The benignity of a lesion such as a lipoma or hemangioma may be able to be determined with high certainty on MRI, in which case we call the imaging of the lesion “determinate.” Such lesions with determinate imaging (often referred to as “determinate lesions”) usually do not require a biopsy. However, the nature and identity of most lesions cannot be determined by MRI; although the MRI is still useful to help plan the biopsy in these cases, these lesions are termed “indeterminate” by MRI and should usually be biopsied.
Lesions that can be deemed determinate and usually be diagnosed as benign based on MRI findings include lipomas, hemangiomas, granuloma annulare, and ganglion cysts. However, most other soft-tissue lesions are indeterminate on MRI and, except in rare circumstances, require a biopsy to determine what they are and how they should be treated.
BIOPSY
The primary biopsy procedures for soft-tissue sarcomas are needle or open biopsy techniques and, in general, are similar to those for bone sarcomas, as reviewed in the previous article in this supplement. Regardless of the biopsy technique, hemostasis must be meticulous and patients are generally advised to not use the affected limb for at least several days after the biopsy to reduce the risk of a cancer cell–laden hematoma. It is preferable for the biopsy to be performed by or in consultation with the surgeon who will do the resection, if required.
Avoid transverse incisions
Lymph node biopsies
Lymph node biopsies are not generally indicated in patients with soft-tissue sarcoma. However, lymph node assessment and management should be considered in cases of clear cell sarcoma, epithelioid sarcoma, angiosarcoma, and embryonal/alveolar rhabdomyosarcoma, each of which has a greater than 10% incidence of lymph node metastasis.14 In this subset of soft-tissue sarcomas, a 5-year survival rate of 46% has been reported with therapeutic lymphadenectomy with curative intent versus nearly 0% with no lymphadenectomy or noncurative lymphadenectomy.14
Our approach in these sarcomas that go to the lymph nodes with increased relative frequency has been to first resect the sarcoma and then, after the margin is determined to be negative on the permanent pathology report, to schedule a nuclear medicine radiotracer study to analyze the drainage of the surgical bed. With this information we take the patient to the operating room and assess the location of the sentinel node (ie, node with the highest level of activity) through the skin using a radioactive counter with a sterile probe. We then make an incision in this area and find the lymph node. Upon removal of the “hot” lymph node, we reassess the radioactivity of the resected node and its node bed to be sure that we have the sentinel node. If this node or any node in the dissection has tumor in it, we do a therapeutic lymphadenectomy to remove all the lymph nodes in the area. For example, in the lower leg the lymphatic drainage is to the popliteal area, the inguinal area, or both. In the lower arm the lymphatic drainage is to the epitrochlear area and the axilla.
RESECTION
The resection surgery involves careful preoperative planning, almost always with an MRI and subsequent review by musculoskeletal tumor radiologists. In the operating room, general anesthesia is preferred to avoid ineffective blocks or overly effective blocks, which prevent neurologic examination immediately after the operation. If the functional loss is not too great, resection of the entire muscle or muscles involved is performed. If neurovascular structures are not encased (ie, not more than 50% surrounded in the case of arteries or motor nerves), then these structures are spared. If arteries are encased, the vessels are bypassed and the encased structure is left with the resection specimen. If the tumor is adjacent to but not encasing the neurovascular structures, the best course is to discuss with the radiation oncology team whether they prefer preoperative or postoperative radiation therapy. In general, for a high-grade lesion with adjacent neurovascular structues and no plane between the tumor and these structures, we ask our radiation oncologist colleagues to see the patient and discuss preoperative or perioperative (brachytherapy) radiation therapy. Postoperatively, where there is less than a 1-cm margin with no fascial boundary, we generally recommend radiation.
Margins
In our experience, margins of 1 cm or greater or resections with a fascial boundary are adequate and will leave patients with a much lower than 10% risk of recurrence. Others have postulated that margins that are smaller than this can have a very low rate of recurrence if perioperative (preoperative, intraoperative, or postoperative) radiation is given (personal communication from Drs. Jeffrey Eckardt and Dempsey Springfield). However, no well-controlled study has demonstrated how close the margin can be while still achieving an acceptable recurrence rate, and such a study would be very hard to perform given the rarity and heterogeneity of soft-tissue sarcomas and the variability in their assessment and surgical treatment.
Intralesional surgery leads to recurrence
Intralesional surgery will always lead to recurrence if the lesion is truly a soft-tissue sarcoma, even in spite of radiation therapy, chemotherapy, or both. Myomectomy and compartmental resections are frequently necessary to achieve a negative margin (normal tissue around the entire resection specimen). If intralesional surgery has been performed at an outside institution, we have generally recommended resection of the tumor bed, and in our experience this has reduced the recurrence rate after intralesional surgery to levels near those obtained when we perform the biopsy. In our experience, intralesional surgery without tumor bed resection will result in recurrence in nearly every case.
Reconstruction
Postoperative reconstruction of the defect involves closure of the fascia and skin with minimal tension, if possible. If there is tension, a vacuum-assisted closure dressing is placed on the wound and the patient returns for definitive closure, usually with a muscle flap. If the flap is a straightforward rotational flap, such as a medial gastrocnemius, or if only a split-thickness skin graft is required because there is healthy muscle in the floor of the open wound, this can be performed by experienced orthopedic surgeons. If these straightforward solutions are not possible, consultation with plastic surgeons is required, and they will cover the area with a complex rotational flap or, occasionally, with a free flap. For split-thickness skin grafts, it is prudent to make certain that the width of a #15 knife blade can pass between the blade and the housing of the Padgett dermatome and to take the skin from the extremity ipsilateral to the sarcoma (even with negative margins) to ensure that skin will not be contaminated with errant sarcoma cells.
Reconstruction following sarcoma resection is discussed in further detail in the next article in this supplement.
OUTCOMES AND FOLLOW-UP
The recurrence rate for soft-tissue sarcomas resected at Cleveland Clinic over the past 15 years has been less than 10%. This rate is comparable to the rates at other institutions that perform a high volume of sarcoma resections, but at institutions without a group dedicated to these procedures or without substantial experience in them, the recurrence rate is much higher, particularly with positive margins.15
Cure for soft-tissue sarcomas depends on being disease-free not only locally but also systemically. Most metastases from soft-tissue sarcomas are to the lung and, less commonly (as noted above), the lymph nodes. We assess local recurrence and metastatic disease at 3-month intervals for the first 2 years. Among patients who are disease-free at 2 years after the definitive surgery, the cure rate is 80% to 85%. After 2 years, we assess patients for presence of disease at 6-month intervals for the next 3 years and at yearly intervals thereafter.
Patients who have a recurrence are at increased risk for metastatic disease, and it is often very hard to achieve local control, as these patients frequently have had tumor contamination of the wound. At that point, unless the entire wound is excised or an amputation is performed, recurrences will continue. A nomogram has been validated for evaluating 10-year soft-tissue sarcoma–specific survival16 and is freely available at www.nomograms.org.
FUTURE DIRECTIONS
Future research challenges in this area include breaking down soft-tissue sarcoma subgroups more homogeneously, possibly with genetic markers, to better determine which lesions might benefit from chemotherapy. The goal of improved subtyping is to decrease the metastatic rate of soft-tissue sarcomas in much the same manner that directed chemotherapy has improved the metastasis and cure rates for patients with Ewing sarcoma and osteosarcoma.
- Simon MA, Springfield D, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Glencross J, Balasubramanian SP, Bacon J, Robinson MH, Reed MW. An audit of the management of soft tissue sarcoma within a health region in the UK. Eur J Surg Oncol 2003; 29:670–675.
- Kandel RA, Bell RS, Wunder JS, et al. Comparison between a 2- and 3-grade system in predicting metastatic-free survival in extremity soft-tissue sarcoma. J Surg Oncol 1999; 72:77–82.
- Suit HD, Spiro I. Role of radiation in the management of adult patients with sarcoma of soft tissue. Semin Surg Oncol 1994; 10:347–356.
- Suit H, Spiro I. Preoperative radiation therapy for patients with sarcoma of the soft tissues. Cancer Treat Res 1993; 67:99–105.
- Suit HD, Mankin HJ, Wood WC, et al. Treatment of the patient with stage M0 soft tissue sarcoma. J Clin Oncol 1988; 6:854–862.
- Fletcher CDM, Unni KK, Mertens F. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon, France: IARC Press; 2002.
- Brennan MF, Singer S, Maki RG, O’Sullivan B. Sarcomas of the soft tissue and bone. In: DeVita Jr VT, Lawrence TS, Rosenbert SA, eds. Cancer: Principles & Practice of Oncology. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
- Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Gonzalez KD, Buzin CH, Noltner KA, et al. High frequency of de novo mutations in Li-Fraumeni syndrome. J Med Genet 2009; 46:689–693.
- Gonzalez KD, Noltner KA, Buzin CH, et al. Beyond Li Fraumeni syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol 2009; 27:1250–1256.
- Modena P, Lualdi E, Facchinetti F, et al. SMARCB1/INI1 tumor suppressor gene is frequently inactivated in epithelioid sarcomas. Cancer Res 2005; 65:4012–4019.
- Peabody TD, Simon MA. Principles of staging of soft-tissue sarcomas. Clin Orthop Relat Res 1993; 289:19–31.
- Fong Y, Coit DG, Woodruff JM, Brennan MF. Lymph node metastasis from soft tissue sarcoma in adults: analysis of data from a prospective database of 1,772 sarcoma patients. Ann Surg 1993; 217:72–77.
- Potter BK, Adams SC, Pitcher JD Jr, Temple HT. Local recurrence of disease after unplanned excisions of high-grade soft tissue sarcomas. Clin Orthop Relat Res 2008; 466:3093–3100.
- Mariani L, Miceli R, Kattan MW, et al. Validation and adaptation of a nomogram for predicting the survival of patients with extremity soft tissue sarcoma using a three-grade system. Cancer 2005; 103:402–408.
Soft-tissue sarcomas are tumors of the mesenchymal system, and half develop in the extremities.1 Although patients with soft-tissue sarcomas have been treated with a combination of surgery, radiation therapy, and chemotherapy, it remains unclear whether either radiation or chemotherapy improves outcomes for these patients. Soft-tissue sarcomas are therefore currently treated with surgical resection when possible, with or without chemotherapy or radiation.
Even though multimodal therapy for patients with these tumors is controversial, a multidisciplinary conference among the many providers who may be involved in the management these patients—orthopedic, medical, and radiation oncologists, as well as the referring primary care physician, plastic and reconstructive surgeons, physical therapists, and radiologists and pathologists with expertise in these tumors—is helpful.2 This article presents an overview of the management of these patients, with a focus on the mainstay treatment, surgical resection. The roles of chemotherapy and radiation therapy for soft-tissue sarcomas, while touched upon here, are detailed in the final two articles in this supplement.
HISTOLOGIC GRADING AND THERAPY IMPLICATIONS
The prognosis of soft-tissue sarcomas correlates with histopathologic grade, and a three-grade system appears to be more accurate than a two-grade system.3 In general, low-grade lesions (grade 1) are unlikely to metastasize and are therefore less likely to need treatment with chemotherapy or radiation, as the risks of these therapies would most likely outweigh any benefit in terms of local control.
Specifically, the risk of radiation involves debilitation of local wound healing and the chance of dedifferentiation of low-grade lesions to higher-grade lesions with more metastatic potential. Grade 2 and 3 lesions are usually considered high-grade and are more likely to be treated with radiation and chemotherapy. Radiation is frequently used in patients with high-grade lesions when anticipated margins or actual margins are less than 1 cm.4–6
Chemotherapy’s lack of proven efficacy for soft-tissue sarcomas likely stems from poor understanding of the pathophysiology, molecular biology, and even some aspects of the natural history of these uncommon and heterogeneous tumors. There are more than 50 subtypes of soft-tissue sarcoma,7,8 and this heterogeneity has likely contributed to the difficulty of identifying chemotherapeutic agents that are highly active against these diseases.9
THE ROLE OF FAMILIAL GENETICS
Developing effective chemotherapeutic strategies may depend on grouping soft-tissue sarcomas more homogeneously. To compare like lesions with like lesions, molecular analysis and even molecular signatures may be of assistance. Along these lines, critical mutations and translocations have been described for several soft-tissue sarcoma subtypes.
Li-Fraumeni syndrome is an autosomal dominant cancer predisposition syndrome caused by germline mutations (ie, in every cell) in the p53 gene.10 Patients with Li-Fraumeni syndrome have an increased risk of developing soft-tissue sarcomas.1,11
Neurofibromatosis type 1 is caused by germline mutations in the NF1 gene, and malignant peripheral nerve sheath tumors occur within neurofibromas in neurofibromatosis patients and typically have additional mutations in CDKN2A or p53.9 INI1 loss is seen in all cases of extrarenal rhabdoid tumors and has been reported in a subset of epithelioid sarcomas (those occurring in proximal/axial regions).9,12 Delineation and greater understanding of these genetic abnormalities may lead to more effective medical therapy.
EVALUATION OF SUSPICIOUS SOFT-TISSUE MASSES
Figure 1 presents in flow chart form our general approach to the evaluation and management of patients with a soft-tissue mass suspicious for sarcoma—an approach detailed in the text below.
History and physical examination
Patients with soft-tissue sarcomas present with a mass that generally is increasing in size. The location and depth of the mass can be assessed on physical examination. In general, the deeper the mass, the more likely it is to be a sarcoma.13 Unlike bone sarcomas, soft-tissue sarcomas frequently are not associated with pain, so lack of pain does not make a mass more likely to be benign. In general, the only way to be sure that a mass is not malignant is to biopsy it. However, there are certain symptoms and signs that make a benign diagnosis much more likely. For example, very soft superficial masses that have not changed in size in years tend to be benign lipomas, and discolored lesions that go away with elevation of the affected body part tend to be hemangiomas.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is the primary imaging method for soft-tissue sarcomas. The benignity of a lesion such as a lipoma or hemangioma may be able to be determined with high certainty on MRI, in which case we call the imaging of the lesion “determinate.” Such lesions with determinate imaging (often referred to as “determinate lesions”) usually do not require a biopsy. However, the nature and identity of most lesions cannot be determined by MRI; although the MRI is still useful to help plan the biopsy in these cases, these lesions are termed “indeterminate” by MRI and should usually be biopsied.
Lesions that can be deemed determinate and usually be diagnosed as benign based on MRI findings include lipomas, hemangiomas, granuloma annulare, and ganglion cysts. However, most other soft-tissue lesions are indeterminate on MRI and, except in rare circumstances, require a biopsy to determine what they are and how they should be treated.
BIOPSY
The primary biopsy procedures for soft-tissue sarcomas are needle or open biopsy techniques and, in general, are similar to those for bone sarcomas, as reviewed in the previous article in this supplement. Regardless of the biopsy technique, hemostasis must be meticulous and patients are generally advised to not use the affected limb for at least several days after the biopsy to reduce the risk of a cancer cell–laden hematoma. It is preferable for the biopsy to be performed by or in consultation with the surgeon who will do the resection, if required.
Avoid transverse incisions
Lymph node biopsies
Lymph node biopsies are not generally indicated in patients with soft-tissue sarcoma. However, lymph node assessment and management should be considered in cases of clear cell sarcoma, epithelioid sarcoma, angiosarcoma, and embryonal/alveolar rhabdomyosarcoma, each of which has a greater than 10% incidence of lymph node metastasis.14 In this subset of soft-tissue sarcomas, a 5-year survival rate of 46% has been reported with therapeutic lymphadenectomy with curative intent versus nearly 0% with no lymphadenectomy or noncurative lymphadenectomy.14
Our approach in these sarcomas that go to the lymph nodes with increased relative frequency has been to first resect the sarcoma and then, after the margin is determined to be negative on the permanent pathology report, to schedule a nuclear medicine radiotracer study to analyze the drainage of the surgical bed. With this information we take the patient to the operating room and assess the location of the sentinel node (ie, node with the highest level of activity) through the skin using a radioactive counter with a sterile probe. We then make an incision in this area and find the lymph node. Upon removal of the “hot” lymph node, we reassess the radioactivity of the resected node and its node bed to be sure that we have the sentinel node. If this node or any node in the dissection has tumor in it, we do a therapeutic lymphadenectomy to remove all the lymph nodes in the area. For example, in the lower leg the lymphatic drainage is to the popliteal area, the inguinal area, or both. In the lower arm the lymphatic drainage is to the epitrochlear area and the axilla.
RESECTION
The resection surgery involves careful preoperative planning, almost always with an MRI and subsequent review by musculoskeletal tumor radiologists. In the operating room, general anesthesia is preferred to avoid ineffective blocks or overly effective blocks, which prevent neurologic examination immediately after the operation. If the functional loss is not too great, resection of the entire muscle or muscles involved is performed. If neurovascular structures are not encased (ie, not more than 50% surrounded in the case of arteries or motor nerves), then these structures are spared. If arteries are encased, the vessels are bypassed and the encased structure is left with the resection specimen. If the tumor is adjacent to but not encasing the neurovascular structures, the best course is to discuss with the radiation oncology team whether they prefer preoperative or postoperative radiation therapy. In general, for a high-grade lesion with adjacent neurovascular structues and no plane between the tumor and these structures, we ask our radiation oncologist colleagues to see the patient and discuss preoperative or perioperative (brachytherapy) radiation therapy. Postoperatively, where there is less than a 1-cm margin with no fascial boundary, we generally recommend radiation.
Margins
In our experience, margins of 1 cm or greater or resections with a fascial boundary are adequate and will leave patients with a much lower than 10% risk of recurrence. Others have postulated that margins that are smaller than this can have a very low rate of recurrence if perioperative (preoperative, intraoperative, or postoperative) radiation is given (personal communication from Drs. Jeffrey Eckardt and Dempsey Springfield). However, no well-controlled study has demonstrated how close the margin can be while still achieving an acceptable recurrence rate, and such a study would be very hard to perform given the rarity and heterogeneity of soft-tissue sarcomas and the variability in their assessment and surgical treatment.
Intralesional surgery leads to recurrence
Intralesional surgery will always lead to recurrence if the lesion is truly a soft-tissue sarcoma, even in spite of radiation therapy, chemotherapy, or both. Myomectomy and compartmental resections are frequently necessary to achieve a negative margin (normal tissue around the entire resection specimen). If intralesional surgery has been performed at an outside institution, we have generally recommended resection of the tumor bed, and in our experience this has reduced the recurrence rate after intralesional surgery to levels near those obtained when we perform the biopsy. In our experience, intralesional surgery without tumor bed resection will result in recurrence in nearly every case.
Reconstruction
Postoperative reconstruction of the defect involves closure of the fascia and skin with minimal tension, if possible. If there is tension, a vacuum-assisted closure dressing is placed on the wound and the patient returns for definitive closure, usually with a muscle flap. If the flap is a straightforward rotational flap, such as a medial gastrocnemius, or if only a split-thickness skin graft is required because there is healthy muscle in the floor of the open wound, this can be performed by experienced orthopedic surgeons. If these straightforward solutions are not possible, consultation with plastic surgeons is required, and they will cover the area with a complex rotational flap or, occasionally, with a free flap. For split-thickness skin grafts, it is prudent to make certain that the width of a #15 knife blade can pass between the blade and the housing of the Padgett dermatome and to take the skin from the extremity ipsilateral to the sarcoma (even with negative margins) to ensure that skin will not be contaminated with errant sarcoma cells.
Reconstruction following sarcoma resection is discussed in further detail in the next article in this supplement.
OUTCOMES AND FOLLOW-UP
The recurrence rate for soft-tissue sarcomas resected at Cleveland Clinic over the past 15 years has been less than 10%. This rate is comparable to the rates at other institutions that perform a high volume of sarcoma resections, but at institutions without a group dedicated to these procedures or without substantial experience in them, the recurrence rate is much higher, particularly with positive margins.15
Cure for soft-tissue sarcomas depends on being disease-free not only locally but also systemically. Most metastases from soft-tissue sarcomas are to the lung and, less commonly (as noted above), the lymph nodes. We assess local recurrence and metastatic disease at 3-month intervals for the first 2 years. Among patients who are disease-free at 2 years after the definitive surgery, the cure rate is 80% to 85%. After 2 years, we assess patients for presence of disease at 6-month intervals for the next 3 years and at yearly intervals thereafter.
Patients who have a recurrence are at increased risk for metastatic disease, and it is often very hard to achieve local control, as these patients frequently have had tumor contamination of the wound. At that point, unless the entire wound is excised or an amputation is performed, recurrences will continue. A nomogram has been validated for evaluating 10-year soft-tissue sarcoma–specific survival16 and is freely available at www.nomograms.org.
FUTURE DIRECTIONS
Future research challenges in this area include breaking down soft-tissue sarcoma subgroups more homogeneously, possibly with genetic markers, to better determine which lesions might benefit from chemotherapy. The goal of improved subtyping is to decrease the metastatic rate of soft-tissue sarcomas in much the same manner that directed chemotherapy has improved the metastasis and cure rates for patients with Ewing sarcoma and osteosarcoma.
Soft-tissue sarcomas are tumors of the mesenchymal system, and half develop in the extremities.1 Although patients with soft-tissue sarcomas have been treated with a combination of surgery, radiation therapy, and chemotherapy, it remains unclear whether either radiation or chemotherapy improves outcomes for these patients. Soft-tissue sarcomas are therefore currently treated with surgical resection when possible, with or without chemotherapy or radiation.
Even though multimodal therapy for patients with these tumors is controversial, a multidisciplinary conference among the many providers who may be involved in the management these patients—orthopedic, medical, and radiation oncologists, as well as the referring primary care physician, plastic and reconstructive surgeons, physical therapists, and radiologists and pathologists with expertise in these tumors—is helpful.2 This article presents an overview of the management of these patients, with a focus on the mainstay treatment, surgical resection. The roles of chemotherapy and radiation therapy for soft-tissue sarcomas, while touched upon here, are detailed in the final two articles in this supplement.
HISTOLOGIC GRADING AND THERAPY IMPLICATIONS
The prognosis of soft-tissue sarcomas correlates with histopathologic grade, and a three-grade system appears to be more accurate than a two-grade system.3 In general, low-grade lesions (grade 1) are unlikely to metastasize and are therefore less likely to need treatment with chemotherapy or radiation, as the risks of these therapies would most likely outweigh any benefit in terms of local control.
Specifically, the risk of radiation involves debilitation of local wound healing and the chance of dedifferentiation of low-grade lesions to higher-grade lesions with more metastatic potential. Grade 2 and 3 lesions are usually considered high-grade and are more likely to be treated with radiation and chemotherapy. Radiation is frequently used in patients with high-grade lesions when anticipated margins or actual margins are less than 1 cm.4–6
Chemotherapy’s lack of proven efficacy for soft-tissue sarcomas likely stems from poor understanding of the pathophysiology, molecular biology, and even some aspects of the natural history of these uncommon and heterogeneous tumors. There are more than 50 subtypes of soft-tissue sarcoma,7,8 and this heterogeneity has likely contributed to the difficulty of identifying chemotherapeutic agents that are highly active against these diseases.9
THE ROLE OF FAMILIAL GENETICS
Developing effective chemotherapeutic strategies may depend on grouping soft-tissue sarcomas more homogeneously. To compare like lesions with like lesions, molecular analysis and even molecular signatures may be of assistance. Along these lines, critical mutations and translocations have been described for several soft-tissue sarcoma subtypes.
Li-Fraumeni syndrome is an autosomal dominant cancer predisposition syndrome caused by germline mutations (ie, in every cell) in the p53 gene.10 Patients with Li-Fraumeni syndrome have an increased risk of developing soft-tissue sarcomas.1,11
Neurofibromatosis type 1 is caused by germline mutations in the NF1 gene, and malignant peripheral nerve sheath tumors occur within neurofibromas in neurofibromatosis patients and typically have additional mutations in CDKN2A or p53.9 INI1 loss is seen in all cases of extrarenal rhabdoid tumors and has been reported in a subset of epithelioid sarcomas (those occurring in proximal/axial regions).9,12 Delineation and greater understanding of these genetic abnormalities may lead to more effective medical therapy.
EVALUATION OF SUSPICIOUS SOFT-TISSUE MASSES
Figure 1 presents in flow chart form our general approach to the evaluation and management of patients with a soft-tissue mass suspicious for sarcoma—an approach detailed in the text below.
History and physical examination
Patients with soft-tissue sarcomas present with a mass that generally is increasing in size. The location and depth of the mass can be assessed on physical examination. In general, the deeper the mass, the more likely it is to be a sarcoma.13 Unlike bone sarcomas, soft-tissue sarcomas frequently are not associated with pain, so lack of pain does not make a mass more likely to be benign. In general, the only way to be sure that a mass is not malignant is to biopsy it. However, there are certain symptoms and signs that make a benign diagnosis much more likely. For example, very soft superficial masses that have not changed in size in years tend to be benign lipomas, and discolored lesions that go away with elevation of the affected body part tend to be hemangiomas.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is the primary imaging method for soft-tissue sarcomas. The benignity of a lesion such as a lipoma or hemangioma may be able to be determined with high certainty on MRI, in which case we call the imaging of the lesion “determinate.” Such lesions with determinate imaging (often referred to as “determinate lesions”) usually do not require a biopsy. However, the nature and identity of most lesions cannot be determined by MRI; although the MRI is still useful to help plan the biopsy in these cases, these lesions are termed “indeterminate” by MRI and should usually be biopsied.
Lesions that can be deemed determinate and usually be diagnosed as benign based on MRI findings include lipomas, hemangiomas, granuloma annulare, and ganglion cysts. However, most other soft-tissue lesions are indeterminate on MRI and, except in rare circumstances, require a biopsy to determine what they are and how they should be treated.
BIOPSY
The primary biopsy procedures for soft-tissue sarcomas are needle or open biopsy techniques and, in general, are similar to those for bone sarcomas, as reviewed in the previous article in this supplement. Regardless of the biopsy technique, hemostasis must be meticulous and patients are generally advised to not use the affected limb for at least several days after the biopsy to reduce the risk of a cancer cell–laden hematoma. It is preferable for the biopsy to be performed by or in consultation with the surgeon who will do the resection, if required.
Avoid transverse incisions
Lymph node biopsies
Lymph node biopsies are not generally indicated in patients with soft-tissue sarcoma. However, lymph node assessment and management should be considered in cases of clear cell sarcoma, epithelioid sarcoma, angiosarcoma, and embryonal/alveolar rhabdomyosarcoma, each of which has a greater than 10% incidence of lymph node metastasis.14 In this subset of soft-tissue sarcomas, a 5-year survival rate of 46% has been reported with therapeutic lymphadenectomy with curative intent versus nearly 0% with no lymphadenectomy or noncurative lymphadenectomy.14
Our approach in these sarcomas that go to the lymph nodes with increased relative frequency has been to first resect the sarcoma and then, after the margin is determined to be negative on the permanent pathology report, to schedule a nuclear medicine radiotracer study to analyze the drainage of the surgical bed. With this information we take the patient to the operating room and assess the location of the sentinel node (ie, node with the highest level of activity) through the skin using a radioactive counter with a sterile probe. We then make an incision in this area and find the lymph node. Upon removal of the “hot” lymph node, we reassess the radioactivity of the resected node and its node bed to be sure that we have the sentinel node. If this node or any node in the dissection has tumor in it, we do a therapeutic lymphadenectomy to remove all the lymph nodes in the area. For example, in the lower leg the lymphatic drainage is to the popliteal area, the inguinal area, or both. In the lower arm the lymphatic drainage is to the epitrochlear area and the axilla.
RESECTION
The resection surgery involves careful preoperative planning, almost always with an MRI and subsequent review by musculoskeletal tumor radiologists. In the operating room, general anesthesia is preferred to avoid ineffective blocks or overly effective blocks, which prevent neurologic examination immediately after the operation. If the functional loss is not too great, resection of the entire muscle or muscles involved is performed. If neurovascular structures are not encased (ie, not more than 50% surrounded in the case of arteries or motor nerves), then these structures are spared. If arteries are encased, the vessels are bypassed and the encased structure is left with the resection specimen. If the tumor is adjacent to but not encasing the neurovascular structures, the best course is to discuss with the radiation oncology team whether they prefer preoperative or postoperative radiation therapy. In general, for a high-grade lesion with adjacent neurovascular structues and no plane between the tumor and these structures, we ask our radiation oncologist colleagues to see the patient and discuss preoperative or perioperative (brachytherapy) radiation therapy. Postoperatively, where there is less than a 1-cm margin with no fascial boundary, we generally recommend radiation.
Margins
In our experience, margins of 1 cm or greater or resections with a fascial boundary are adequate and will leave patients with a much lower than 10% risk of recurrence. Others have postulated that margins that are smaller than this can have a very low rate of recurrence if perioperative (preoperative, intraoperative, or postoperative) radiation is given (personal communication from Drs. Jeffrey Eckardt and Dempsey Springfield). However, no well-controlled study has demonstrated how close the margin can be while still achieving an acceptable recurrence rate, and such a study would be very hard to perform given the rarity and heterogeneity of soft-tissue sarcomas and the variability in their assessment and surgical treatment.
Intralesional surgery leads to recurrence
Intralesional surgery will always lead to recurrence if the lesion is truly a soft-tissue sarcoma, even in spite of radiation therapy, chemotherapy, or both. Myomectomy and compartmental resections are frequently necessary to achieve a negative margin (normal tissue around the entire resection specimen). If intralesional surgery has been performed at an outside institution, we have generally recommended resection of the tumor bed, and in our experience this has reduced the recurrence rate after intralesional surgery to levels near those obtained when we perform the biopsy. In our experience, intralesional surgery without tumor bed resection will result in recurrence in nearly every case.
Reconstruction
Postoperative reconstruction of the defect involves closure of the fascia and skin with minimal tension, if possible. If there is tension, a vacuum-assisted closure dressing is placed on the wound and the patient returns for definitive closure, usually with a muscle flap. If the flap is a straightforward rotational flap, such as a medial gastrocnemius, or if only a split-thickness skin graft is required because there is healthy muscle in the floor of the open wound, this can be performed by experienced orthopedic surgeons. If these straightforward solutions are not possible, consultation with plastic surgeons is required, and they will cover the area with a complex rotational flap or, occasionally, with a free flap. For split-thickness skin grafts, it is prudent to make certain that the width of a #15 knife blade can pass between the blade and the housing of the Padgett dermatome and to take the skin from the extremity ipsilateral to the sarcoma (even with negative margins) to ensure that skin will not be contaminated with errant sarcoma cells.
Reconstruction following sarcoma resection is discussed in further detail in the next article in this supplement.
OUTCOMES AND FOLLOW-UP
The recurrence rate for soft-tissue sarcomas resected at Cleveland Clinic over the past 15 years has been less than 10%. This rate is comparable to the rates at other institutions that perform a high volume of sarcoma resections, but at institutions without a group dedicated to these procedures or without substantial experience in them, the recurrence rate is much higher, particularly with positive margins.15
Cure for soft-tissue sarcomas depends on being disease-free not only locally but also systemically. Most metastases from soft-tissue sarcomas are to the lung and, less commonly (as noted above), the lymph nodes. We assess local recurrence and metastatic disease at 3-month intervals for the first 2 years. Among patients who are disease-free at 2 years after the definitive surgery, the cure rate is 80% to 85%. After 2 years, we assess patients for presence of disease at 6-month intervals for the next 3 years and at yearly intervals thereafter.
Patients who have a recurrence are at increased risk for metastatic disease, and it is often very hard to achieve local control, as these patients frequently have had tumor contamination of the wound. At that point, unless the entire wound is excised or an amputation is performed, recurrences will continue. A nomogram has been validated for evaluating 10-year soft-tissue sarcoma–specific survival16 and is freely available at www.nomograms.org.
FUTURE DIRECTIONS
Future research challenges in this area include breaking down soft-tissue sarcoma subgroups more homogeneously, possibly with genetic markers, to better determine which lesions might benefit from chemotherapy. The goal of improved subtyping is to decrease the metastatic rate of soft-tissue sarcomas in much the same manner that directed chemotherapy has improved the metastasis and cure rates for patients with Ewing sarcoma and osteosarcoma.
- Simon MA, Springfield D, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Glencross J, Balasubramanian SP, Bacon J, Robinson MH, Reed MW. An audit of the management of soft tissue sarcoma within a health region in the UK. Eur J Surg Oncol 2003; 29:670–675.
- Kandel RA, Bell RS, Wunder JS, et al. Comparison between a 2- and 3-grade system in predicting metastatic-free survival in extremity soft-tissue sarcoma. J Surg Oncol 1999; 72:77–82.
- Suit HD, Spiro I. Role of radiation in the management of adult patients with sarcoma of soft tissue. Semin Surg Oncol 1994; 10:347–356.
- Suit H, Spiro I. Preoperative radiation therapy for patients with sarcoma of the soft tissues. Cancer Treat Res 1993; 67:99–105.
- Suit HD, Mankin HJ, Wood WC, et al. Treatment of the patient with stage M0 soft tissue sarcoma. J Clin Oncol 1988; 6:854–862.
- Fletcher CDM, Unni KK, Mertens F. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon, France: IARC Press; 2002.
- Brennan MF, Singer S, Maki RG, O’Sullivan B. Sarcomas of the soft tissue and bone. In: DeVita Jr VT, Lawrence TS, Rosenbert SA, eds. Cancer: Principles & Practice of Oncology. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
- Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Gonzalez KD, Buzin CH, Noltner KA, et al. High frequency of de novo mutations in Li-Fraumeni syndrome. J Med Genet 2009; 46:689–693.
- Gonzalez KD, Noltner KA, Buzin CH, et al. Beyond Li Fraumeni syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol 2009; 27:1250–1256.
- Modena P, Lualdi E, Facchinetti F, et al. SMARCB1/INI1 tumor suppressor gene is frequently inactivated in epithelioid sarcomas. Cancer Res 2005; 65:4012–4019.
- Peabody TD, Simon MA. Principles of staging of soft-tissue sarcomas. Clin Orthop Relat Res 1993; 289:19–31.
- Fong Y, Coit DG, Woodruff JM, Brennan MF. Lymph node metastasis from soft tissue sarcoma in adults: analysis of data from a prospective database of 1,772 sarcoma patients. Ann Surg 1993; 217:72–77.
- Potter BK, Adams SC, Pitcher JD Jr, Temple HT. Local recurrence of disease after unplanned excisions of high-grade soft tissue sarcomas. Clin Orthop Relat Res 2008; 466:3093–3100.
- Mariani L, Miceli R, Kattan MW, et al. Validation and adaptation of a nomogram for predicting the survival of patients with extremity soft tissue sarcoma using a three-grade system. Cancer 2005; 103:402–408.
- Simon MA, Springfield D, eds. Surgery for Bone and Soft-tissue Tumors. Philadelphia, PA: Lippincott-Raven; 1998.
- Glencross J, Balasubramanian SP, Bacon J, Robinson MH, Reed MW. An audit of the management of soft tissue sarcoma within a health region in the UK. Eur J Surg Oncol 2003; 29:670–675.
- Kandel RA, Bell RS, Wunder JS, et al. Comparison between a 2- and 3-grade system in predicting metastatic-free survival in extremity soft-tissue sarcoma. J Surg Oncol 1999; 72:77–82.
- Suit HD, Spiro I. Role of radiation in the management of adult patients with sarcoma of soft tissue. Semin Surg Oncol 1994; 10:347–356.
- Suit H, Spiro I. Preoperative radiation therapy for patients with sarcoma of the soft tissues. Cancer Treat Res 1993; 67:99–105.
- Suit HD, Mankin HJ, Wood WC, et al. Treatment of the patient with stage M0 soft tissue sarcoma. J Clin Oncol 1988; 6:854–862.
- Fletcher CDM, Unni KK, Mertens F. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. Lyon, France: IARC Press; 2002.
- Brennan MF, Singer S, Maki RG, O’Sullivan B. Sarcomas of the soft tissue and bone. In: DeVita Jr VT, Lawrence TS, Rosenbert SA, eds. Cancer: Principles & Practice of Oncology. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
- Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors. 5th ed. Philadelphia, PA: Mosby Elsevier; 2008.
- Gonzalez KD, Buzin CH, Noltner KA, et al. High frequency of de novo mutations in Li-Fraumeni syndrome. J Med Genet 2009; 46:689–693.
- Gonzalez KD, Noltner KA, Buzin CH, et al. Beyond Li Fraumeni syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol 2009; 27:1250–1256.
- Modena P, Lualdi E, Facchinetti F, et al. SMARCB1/INI1 tumor suppressor gene is frequently inactivated in epithelioid sarcomas. Cancer Res 2005; 65:4012–4019.
- Peabody TD, Simon MA. Principles of staging of soft-tissue sarcomas. Clin Orthop Relat Res 1993; 289:19–31.
- Fong Y, Coit DG, Woodruff JM, Brennan MF. Lymph node metastasis from soft tissue sarcoma in adults: analysis of data from a prospective database of 1,772 sarcoma patients. Ann Surg 1993; 217:72–77.
- Potter BK, Adams SC, Pitcher JD Jr, Temple HT. Local recurrence of disease after unplanned excisions of high-grade soft tissue sarcomas. Clin Orthop Relat Res 2008; 466:3093–3100.
- Mariani L, Miceli R, Kattan MW, et al. Validation and adaptation of a nomogram for predicting the survival of patients with extremity soft tissue sarcoma using a three-grade system. Cancer 2005; 103:402–408.
Considerations surrounding reconstruction after resection of musculoskeletal sarcomas
Advances in the management of soft-tissue and bone sarcomas—referred to collectively as “musculoskeletal sarcomas” hereafter—have resulted in significant improvements in survival and quality of life.1–3 Several factors have likely contributed to these advances, including improved surgical technique and the development of referral centers for sarcoma treatment that have embraced a multidisciplinary approach.1,2
The goal of treatment for musculoskeletal sarcomas is to optimize oncologic outcome and maximize functional restoration.2,3 Surgical resection has been the mainstay of therapy,1–7 as detailed earlier in this supplement. In patients with musculoskeletal sarcomas of the extremities, limb-sparing resection has been shown to be significantly superior to amputation.1,7–9 Wide local excision of the tumor along with its muscle compartment, followed by adjuvant chemotherapy and radiation therapy, has allowed limb salvage without an increased risk of recurrence in many patients.3 However, wide tumor resection can leave large defects that are not amenable to coverage by mobilization of the surrounding tissues, particularly if those tissues have been irradiated. As a result, resection can expose neurovascular structures, bone without periosteum, alloplastic materials, and internal fixation devices.
GOALS OF RECONSTRUCTION
Reconstructive surgery after musculoskeletal sarcoma resection aims to provide adequate wound coverage, preserve function, and optimize the cosmetic outcome.1–3 Tumors can be found on areas crucial to limb movement or may involve tissues vital to limb function. Reconstruction to repair these deficits can take many forms. In certain situations, amputation is still inevitable. In those cases, the reconstruction should provide stable stump coverage with durability and the ability to fit well with an external prosthesis.3
TIMING OF RECONSTRUCTION
Immediate reconstruction should be pursued if possible
Immediate reconstruction after a negative margin should always be considered and should be attempted when possible. Immediate reconstruction allows the reconstructive surgeon to benefit from better evaluation of the defect and exposed structures, as no scar tissue is present to distort the anatomy. Likewise, patients benefit from faster recovery and can receive adjuvant treatment (if necessary) sooner, as well as earlier rehabilitation. Patients may also benefit psychologically from immediate reconstruction.1,3
Indications for delayed reconstruction
Delayed reconstruction is primarily indicated when there are wound healing problems or there is uncertainty about the tumor margins. Secondary indications for delayed reconstruction are wound dehiscence and unstable soft-tissue coverage. If hardware is exposed, the recommendation is for early intervention and wound coverage with well-vascularized tissue to protect and cover the implant or prosthesis.
What about radiation therapy?
A very important consideration in reconstruction is the need for neoadjuvant or adjuvant radiation therapy.3,10,11 Irradiated wounds have a higher incidence of complications, including a tendency to dehisce. In patients who have been previously irradiated, the best practice is to perform immediate reconstruction with well-vascularized tissue, most likely a free tissue transfer.4,6,11,12 This practice reduces hospital stay, costs, and morbidity and increases limb salvage and patient satisfaction.13
SYSTEMATIC PREOPERATIVE PLANNING NEEDED
Reconstruction after musculoskeletal sarcoma resection should be planned systematically within a process that involves preoperative anticipation of the defect size and the resulting functional and cosmetic deficits that might need to be addressed. A preoperative visit to the reconstructive surgeon can be very helpful for presurgical planning.
During surgery it is usually preferable to allow the surgeon doing the tumor resection (eg, surgical oncologist or orthopedic oncologist) to complete the resection because the dimensions of the defect are not certain until negative margins are obtained.14 If tumor margins are unclear at the time of initial resection, the surgeon should consider delaying the definitive reconstruction until the permanent sections confirm negative margins. Temporary closure can be achieved with wound dressings, skin grafts (either allograft or autograft), or negative-pressure wound therapy. In the same context, if neurovascular structures are exposed it is reasonable to use a muscle flap without “tailoring” the flap to the defect. This approach allows the flap to be advanced or repositioned in case of positive margins, and the skin graft can be applied to the muscle surface in a second procedure.3
RECONSTRUCTIVE METHODS: A BRIEF OVERVIEW
Several methods can be used to close musculoskeletal sarcoma excision defects. Smaller defects can be closed primarily, although most defects are large and not amenable to primary closure. If fascia or muscle is preserved with only the skin coverage missing, the wound can be covered with either split-thickness or full-thickness skin grafts.1,4,6 Split-thickness skin grafts can be obtained in larger amounts and often heal faster than full-thickness skin grafts. However, most resections will require durable tissue coverage, particularly if adjuvant radiation therapy is planned.
In the case of long bone sarcoma resection, the resulting defect is usually large and complex and the traditional reconstruction is based on avascular allografts and local tissue flaps. However, allografts are associated with high rates of infection, nonunion, and fracture, leading to failure in about 50% of cases. Microvascular free flaps that contain bone, such as free fibula flaps, have been used instead of allografts with good success rates.2
Lately there has been growing interest in the use of the vacuum-assisted closure device (a form of negative-pressure wound therapy) to promote wound healing. It has been shown to improve the granulation and healing of open wounds by absorbing moisture, as well as to promote adherence after skin grafting, thereby reducing the risk of graft displacement.1,3 This device can be used immediately after musculoskeletal sarcoma resection while definitive tumor margin results are pending. It also can be used to prepare the wound bed for grafting in high-risk patients who would not tolerate more complex reconstructions.
Local or adjacent fascial, fasciocutaneous, and dermal flaps can also be used in lower-extremity reconstruction. However, muscle or musculocutaneous flaps are the mainstay of reconstruction after resection of musculoskeletal sarcomas. This group also includes perforator flaps, which have grown in popularity in the last few years.1,3
LOCATION-BASED WOUND RECONSTRUCTION
Musculoskeletal sarcomas can occur in virtually any region of the body, and myriad reconstructive options are available for various body sites. Since lower-extremity musculoskeletal sarcomas represent about 75% of cases,1 we will focus mainly on reconstruction of the lower extremity.
Factors driving choice of flap
Selection of an appropriate flap is essential to an optimal outcome. Flaps should be chosen with regard to donor site morbidity, functional requirements, length and diameter of the vascular pedicle, and aesthetic outcome.3 Usually physical examination, palpation of peripheral pulses, and Doppler ultrasonography are sufficient to evaluate the circulation. A preoperative angiogram should be considered in patients with severe peripheral vascular disease or previous trauma, which can potentially compromise the reconstructive outcome.15
Each region of the lower extremity possesses unique anatomic and functional characteristics that must be evaluated. It is useful to categorize the thigh, lower leg, and foot into separate anatomic units when planning reconstruction. We further divided these units into several subunits, as previously proposed by Sherman and Law15 and as outlined below.
Thigh
The thigh is usually well perfused and has several muscle groups, which facilitates reconstruction. Primary closure, skin grafts, or local flaps are acceptable options in most cases. The remaining musculature can be rotated or advanced to cover defects in the anterior or posterior thigh, providing bulk and adequate blood supply.
Hip and proximal/lateral thigh. Local muscle or myocutaneous flap options include tensor fascia lata, vastus lateralis, and rectus femoris flaps, all of which are based on the lateral circumflex femoral artery.
The tensor fascia lata flap is thin but has a long fascia extension that can be elevated from above the knee and can include a large skin paddle that is innervated by the lateral femoral cutaneous nerve. Some patients may experience knee instability after tensor fascia lata harvest.
The vastus lateralis muscle flap provides good bulk. Its arc of rotation reaches most of the inferior and posterior pelvis. It has little effect on ambulation.
The rectus femoris muscle flap is not so bulky, is easily mobilized, and has a wide arc of rotation. The donor site can be closed primarily. Harvest of this muscle can be associated with some strength loss during knee extension. For large defects of the upper third of the leg, a pedicled rectus abdominis muscle flap based on the deep inferior epigastric artery can be used. A vertically oriented skin island can be extended up to the costal margin, improving the reach. When the nature of the wound precludes use of pedicle flaps, free tissue transfer is indicated, with the latissimus dorsi muscle flap being used most commonly.15,16
Mid-thigh. Wounds in this location often can be closed with skin grafts or fasciocutaneous flaps. If the femur is exposed, however, a muscle flap will be required. As above, the tensor fascia lata, vastus lateralis, and rectus femoris can be used as flap options. If the lateral circumflex artery is unavailable, other flap options include the gracilis, vastus medialis, and rectus abdominis muscles. The gracilis muscle flap is based on the medial circumflex femoral artery and is useful for covering the medial aspect of the mid-thigh. Although this is a thin muscle, it can be used to cover long defects. The vastus medialis muscle flap is supplied by perforators from the profunda femoris and superficial femoral arteries. It can be rotated medially and advanced distally to cover patellar defects.
Supracondylar knee. The knee is a location where sarcoma resection is particularly likely to leave a defect with exposed bone, tendons, or ligaments that will need coverage. The gastrocnemius muscle flap combined with a split-thickness skin graft remains a consistent and reliable reconstructive option for this area. Other options are an extended medial gastrocnemius muscle flap or myocutaneous flap, which incorporates a random fasciocutaneous extension. For larger defects, free flaps should be considered, such as the anterior thigh flap, rectus abdominis muscle flap, or latissimus dorsi muscle flap. If tendons or ligaments need to be reconstructed, we favor autologous tissue, such as the fascia lata and plantaris tendons. These are easy to harvest and provide long-lasting joint stability.
Lower leg
Proximal third of the tibia. Defects here can usually be covered with a medial or lateral gastrocnemius muscle or myocutaneous flap, or a combination of the two. These muscles have a dominant vascular pedicle—the medial and lateral sural arteries. They can be harvested as an island for better reach, and they are reliable and have minimal donor site morbidity.15 The soleus muscle flap is another option that can be used alone or in combination with the medial or lateral gastrocnemius. Defects that are not amenable to closure by these flaps will most likely require free tissue transfer. The rectus abdominis or latissimus dorsi muscles are the first options. The latter can be combined with the serratus muscle if more bulk is needed.
Middle and lower thirds of the tibia. The soleus flap is frequently used for small or medium-sized mid-tibial defects. It is based on branches of the popliteal artery and posterior tibial artery. Larger defects require a combination of soleus and gastrocnemius muscle flaps or free tissue transfer.
Foot
Ideal reconstruction of the foot should provide thin and durable skin that will tolerate mechanical stress, and achieving this can be quite difficult. Skin grafts are seldom used for the foot, and are limited to non–weight-bearing portions with good underlying soft tissue.
Proximal non–weight-bearing areas (Achilles tendon and malleolar area). Local fasciocutaneous flaps are preferred. The lateral calcaneal artery flap, which is based on the peroneal artery branch, can cover exposed Achilles tendon, providing sensate coverage (sural nerve). The dorsalis pedis flap can be mobilized to cover the malleolar region and distal Achilles tendon, but donor site morbidity limits its use. Free tissue transfer is required for larger defects, and the the main options are flaps from the radial forearm, temporoparietal fascia, or lateral arm.
Heel and midplantar area. For heel reconstruction, the medial plantar artery flap, dorsalis pedis flap, abductor myocutaneous flap, peroneal artery flap, or anterior tibial artery flap can be used. The most versatile flap of the foot is the medial plantar artery flap, which is available only when the posterior tibial artery is intact. If local flaps are not suitable, microvascular tissue transfer is indicated. The radial forearm flap, scapular flap, lateral arm flap, or anterolateral thigh flap can be used. The radial forearm flap is usually the first choice because it is thin, has a long pedicle, and is easy to harvest.
If the foot defect is associated with a large cavity, muscle flaps are the first choices, specifically the gracilis or anterior serratus. A split latissimus muscle can also be applied. The full latissimus or the rectus abdominis are often too large for the type of defects observed.
Distal plantar area and forefoot. Most wounds in this region will require free tissue transfer. Free muscle flaps with split-thickness skin grafts provide the most stable and durable coverage.
Amputation vs limb salvage
It is important to evaluate the effects of lower-extremity salvage on ambulation. Salvage of a nonfunctional limb is of little value for the patient. Likewise, patients with severe medical problems may not be good candidates for limb salvage procedures. In those situations, amputation of the lower extremity is indicated. Adequate soft-tissue coverage and good distal perfusion are necessary to ensure healing of an amputation. If possible, local tissue rearrangement may be enough to provide a good amputation stump to fit an external prosthesis. In the case of radiation damage to the tissue, a free tissue transfer is necessary. The calcaneal-plantar unit from the amputated limb is frequently used as a free flap. Other flaps from the amputated limb, called fillet flaps, are harvested immediately and converted to flaps transferred to the defect site. Studies show that they are oncologically safe and reliable.17 Other flaps that provide good coverage for amputation defects are the latissimus dorsi muscle flap, the radial forearm flap, and the anterolateral thigh flap.
Upper extremities
POSTOPERATIVE CARE
Postoperative care following reconstruction after sarcoma resection requires a dedicated and trained team, particularly if a free flap is used for reconstruction.
Clinical evaluation of flaps includes color, temperature, and capillary refill. In cases of microsurgical reconstruction, postoperative care should include hourly examination of audible Doppler signals, at least for the first 36 hours. Free flap complications develop primarily in the first 24 hours, but they can occur during initial mobilization of the patient after a long period of bed rest. The surgical team should be aware of the potential problems and be able to act fast if necessary to reestablish blood flow to the flap.
In addition to flap monitoring, immobilization of the patient after surgery is extremely important. Postoperative swelling to the extremity should be avoided. Patients should be placed on bed rest until the postoperative swelling has subsided and the flap has adhered to the wound bed. Our protocol includes strict bed rest for about 7 days, followed by several days of dangling the extremity for short periods to ensure that dependent positioning will not alter the blood supply. A physical therapist should be involved to assist with crutches or a wheelchair. The patient should receive prophylactic anticoagulation during the resting period, in light of the high risk of deep vein thrombosis and pulmonary embolism. A compressive garment should be used to prevent lymphedema.
COMPLICATIONS ASSOCIATED WITH FLAPS
Once the flap is raised, it can still fail as a result of tension at insetting, inadequate blood flow, twisting of the pedicle, hematoma and/or infection, or the patient’s condition (eg, coagulopathy, poor nutritional status, anemia). Failure to correctly evaluate the direction of arterial flow, whether anterograde or retrograde, can cause flap loss. Instruments such as Doppler ultrasonographic equipment can be used to help to determine the flow. Partial or complete occlusion of the vascular pedicle can occur for several reasons (eg, twisting of the pedicle), and the consequences are disastrous if not recognized in time. If a pedicle problem is suspected in the case of a free flap, the patient should be taken to the operating room immediately and the flap should be explored. Rupture of the vascular anastomosis can occur as a result of technical problems, tension, and (in rare cases) infection.
Hematomas can cause mass effect, limit the venous return, and lead to flap necrosis. Hematoma formation also releases free radicals that can contribute to flap necrosis. Prevention is achieved through meticulous hemostasis. If a hematoma is suspected, the wound should be explored and the hematoma evacuated and washed out with normal saline.
The presence of an infected wound bed can also damage a flap by increasing its metabolic demand and causing the flap to be compromised by the infection itself. It is usually best to wait until the infection is controlled before planning the reconstruction.
Partial flap losses, skin graft losses, and wound dehiscence also are possible. Most of the time these require wound care, and patients’ nutrition and general health should be optimized to help the healing process. In the case of partial or complete flap loss, a new flap is often required and should be planned at a proper time.
CONCLUSIONS
Soft-tissue reconstruction following musculoskeletal sarcoma resection can be as simple as allowing the wound to heal by itself, which is less ideal, or as complex as coverage with a microsurgical osteocutaneous free flap. Limb salvage for sarcomas of the lower extremity has demonstrated good final functional outcomes without adversely affecting the oncologic results. Moreover, patients feel better psychologically and have higher quality of life.18,19
We believe that soft-tissue coverage after a wide resection is the most critical factor for avoiding postoperative complications of the tumor resection, such as infection or fractures. For this reason, we recommend the use of well-vascularized coverage at the time of the initial operation, if possible. Careful preoperative planning is especially important. We believe that reconstruction following musculoskeletal sarcoma resection can be done effectively only by using a team approach. Every such team should include, at minimum, an orthopedic surgeon and a reconstructive surgeon, with the mix of other providers dictated by the individual case.
- Misra A, Mistry N, Grimer R, Peart F. The management of soft tissue sarcoma. J Plast Reconstr Aesthet Surg 2009; 62:161–174.
- Morii T, Mochizuki K, Takushima A, Okazaki M, Satomi K. Soft tissue reconstruction using vascularized tissue transplantation following resection of musculoskeletal sarcoma: evaluation of oncologic and functional outcomes in 55 cases. Ann Plast Surg 2009; 62:252–257.
- Heller L, Kronowitz SJ. Lower extremity reconstruction. J Surg Oncol 2006; 94:479–489.
- Bannasch H, Haivas I, Momeni A, Stark GB. Oncosurgical and reconstructive concepts in the treatment of soft tissue sarcomas: a retrospective analysis. Arch Orthop Trauma Surg 2009; 129:43–49.
- Muramatsu K, Ihara K, Doi K, Hashimoto T, Taguchi T. Sarcoma in the forearm and hand: clinical outcomes and microsurgical reconstruction for limb salvage. Ann Plast Surg 2009; 62:28–33.
- Tukiainen E, Böhling T, Huuhtanen R. Soft tissue sarcoma of the trunk and extremities. Scand J Surg 2003; 92:257–263.
- Adelani MA, Holt GE, Dittus RS, Passman MA, Schwartz HS. Revascularization after segmental resection of lower extremity soft tissue sarcomas. J Surg Oncol 2007; 95:455–460.
- Lohman RF, Nabawi AS, Reece GP, Pollock RE, Evans GR. Soft tissue sarcoma of the upper extremity: a 5-year experience at two institutions emphasizing the role of soft tissue flap reconstruction. Cancer 2002; 94:2256–2264.
- Davis AM, Sennik S, Griffin AM, et al. Predictors of functional outcomes following limb salvage surgery for lower-extremity soft tissue sarcoma. J Surg Oncol 2000; 73:206–211.
- Heller L, Ballo MT, Cormier JN, Oates SD, Butler CE. Staged reconstruction for resection wounds in sarcoma patients treated with brachytherapy. Ann Plast Surg 2008; 60:58–63.
- Evans GR, Black JJ, Robb GL, et al. Adjuvant therapy: the effects on microvascular lower extremity reconstruction. Ann Plast Surg 1997; 39:141–144.
- Peat BG, Bell RS, Davis A, et al. Wound-healing complications after soft-tissue sarcoma surgery. Plast Reconstr Surg 1994; 93:980–987.
- Barwick WJ, Goldberg JA, Scully SP, Harrelson JM. Vascularized tissue transfer for closure of irradiated wounds after soft tissue sarcoma resection. Ann Surg 1992; 216:591–595.
- Masquelet AC, Romana MC. The medialis pedis flap: a new fasciocutaneous flap. Plast Reconstr Surg 1990; 85:765–772.
- Sherman R, Law M. Lower extremity reconstruction. In: Achauer BM, Eriksson E, Guyuron B, Coleman III JJ, Russell RC, Vander Kolk CA, eds. Plastic Surgery: Indications, Operations, and Outcomes. Vol 1. St. Louis, MO: Mosby; 2000:475–496.
- Innocenti M, Abed YY, Beltrami G, Delcroix L, Balatri A, Capanna R. Quadriceps muscle reconstruction with free functioning latissimus dorsi muscle flap after oncological resection. Microsurgery 2009; 29:189–198.
- Chiang YC, Wei FC, Wang JW, Chen WS. Reconstruction of below-knee stump using the salvaged foot fillet flap. Plast Reconstr Surg 1995; 96:731–738.
- Serletti JM, Carras AJ, O’Keefe RJ, Rosier RN. Functional outcome after soft-tissue reconstruction for limb salvage after sarcoma surgery. Plast Reconstr Surg 1998; 102:1576–1583.
- Niimi R, Matsumine A, Kusuzaki K, et al. Usefulness of limb salvage surgery for bone and soft tissue sarcomas of the distal lower leg. J Cancer Res Clin Oncol 2008; 134:1087–1095.
Advances in the management of soft-tissue and bone sarcomas—referred to collectively as “musculoskeletal sarcomas” hereafter—have resulted in significant improvements in survival and quality of life.1–3 Several factors have likely contributed to these advances, including improved surgical technique and the development of referral centers for sarcoma treatment that have embraced a multidisciplinary approach.1,2
The goal of treatment for musculoskeletal sarcomas is to optimize oncologic outcome and maximize functional restoration.2,3 Surgical resection has been the mainstay of therapy,1–7 as detailed earlier in this supplement. In patients with musculoskeletal sarcomas of the extremities, limb-sparing resection has been shown to be significantly superior to amputation.1,7–9 Wide local excision of the tumor along with its muscle compartment, followed by adjuvant chemotherapy and radiation therapy, has allowed limb salvage without an increased risk of recurrence in many patients.3 However, wide tumor resection can leave large defects that are not amenable to coverage by mobilization of the surrounding tissues, particularly if those tissues have been irradiated. As a result, resection can expose neurovascular structures, bone without periosteum, alloplastic materials, and internal fixation devices.
GOALS OF RECONSTRUCTION
Reconstructive surgery after musculoskeletal sarcoma resection aims to provide adequate wound coverage, preserve function, and optimize the cosmetic outcome.1–3 Tumors can be found on areas crucial to limb movement or may involve tissues vital to limb function. Reconstruction to repair these deficits can take many forms. In certain situations, amputation is still inevitable. In those cases, the reconstruction should provide stable stump coverage with durability and the ability to fit well with an external prosthesis.3
TIMING OF RECONSTRUCTION
Immediate reconstruction should be pursued if possible
Immediate reconstruction after a negative margin should always be considered and should be attempted when possible. Immediate reconstruction allows the reconstructive surgeon to benefit from better evaluation of the defect and exposed structures, as no scar tissue is present to distort the anatomy. Likewise, patients benefit from faster recovery and can receive adjuvant treatment (if necessary) sooner, as well as earlier rehabilitation. Patients may also benefit psychologically from immediate reconstruction.1,3
Indications for delayed reconstruction
Delayed reconstruction is primarily indicated when there are wound healing problems or there is uncertainty about the tumor margins. Secondary indications for delayed reconstruction are wound dehiscence and unstable soft-tissue coverage. If hardware is exposed, the recommendation is for early intervention and wound coverage with well-vascularized tissue to protect and cover the implant or prosthesis.
What about radiation therapy?
A very important consideration in reconstruction is the need for neoadjuvant or adjuvant radiation therapy.3,10,11 Irradiated wounds have a higher incidence of complications, including a tendency to dehisce. In patients who have been previously irradiated, the best practice is to perform immediate reconstruction with well-vascularized tissue, most likely a free tissue transfer.4,6,11,12 This practice reduces hospital stay, costs, and morbidity and increases limb salvage and patient satisfaction.13
SYSTEMATIC PREOPERATIVE PLANNING NEEDED
Reconstruction after musculoskeletal sarcoma resection should be planned systematically within a process that involves preoperative anticipation of the defect size and the resulting functional and cosmetic deficits that might need to be addressed. A preoperative visit to the reconstructive surgeon can be very helpful for presurgical planning.
During surgery it is usually preferable to allow the surgeon doing the tumor resection (eg, surgical oncologist or orthopedic oncologist) to complete the resection because the dimensions of the defect are not certain until negative margins are obtained.14 If tumor margins are unclear at the time of initial resection, the surgeon should consider delaying the definitive reconstruction until the permanent sections confirm negative margins. Temporary closure can be achieved with wound dressings, skin grafts (either allograft or autograft), or negative-pressure wound therapy. In the same context, if neurovascular structures are exposed it is reasonable to use a muscle flap without “tailoring” the flap to the defect. This approach allows the flap to be advanced or repositioned in case of positive margins, and the skin graft can be applied to the muscle surface in a second procedure.3
RECONSTRUCTIVE METHODS: A BRIEF OVERVIEW
Several methods can be used to close musculoskeletal sarcoma excision defects. Smaller defects can be closed primarily, although most defects are large and not amenable to primary closure. If fascia or muscle is preserved with only the skin coverage missing, the wound can be covered with either split-thickness or full-thickness skin grafts.1,4,6 Split-thickness skin grafts can be obtained in larger amounts and often heal faster than full-thickness skin grafts. However, most resections will require durable tissue coverage, particularly if adjuvant radiation therapy is planned.
In the case of long bone sarcoma resection, the resulting defect is usually large and complex and the traditional reconstruction is based on avascular allografts and local tissue flaps. However, allografts are associated with high rates of infection, nonunion, and fracture, leading to failure in about 50% of cases. Microvascular free flaps that contain bone, such as free fibula flaps, have been used instead of allografts with good success rates.2
Lately there has been growing interest in the use of the vacuum-assisted closure device (a form of negative-pressure wound therapy) to promote wound healing. It has been shown to improve the granulation and healing of open wounds by absorbing moisture, as well as to promote adherence after skin grafting, thereby reducing the risk of graft displacement.1,3 This device can be used immediately after musculoskeletal sarcoma resection while definitive tumor margin results are pending. It also can be used to prepare the wound bed for grafting in high-risk patients who would not tolerate more complex reconstructions.
Local or adjacent fascial, fasciocutaneous, and dermal flaps can also be used in lower-extremity reconstruction. However, muscle or musculocutaneous flaps are the mainstay of reconstruction after resection of musculoskeletal sarcomas. This group also includes perforator flaps, which have grown in popularity in the last few years.1,3
LOCATION-BASED WOUND RECONSTRUCTION
Musculoskeletal sarcomas can occur in virtually any region of the body, and myriad reconstructive options are available for various body sites. Since lower-extremity musculoskeletal sarcomas represent about 75% of cases,1 we will focus mainly on reconstruction of the lower extremity.
Factors driving choice of flap
Selection of an appropriate flap is essential to an optimal outcome. Flaps should be chosen with regard to donor site morbidity, functional requirements, length and diameter of the vascular pedicle, and aesthetic outcome.3 Usually physical examination, palpation of peripheral pulses, and Doppler ultrasonography are sufficient to evaluate the circulation. A preoperative angiogram should be considered in patients with severe peripheral vascular disease or previous trauma, which can potentially compromise the reconstructive outcome.15
Each region of the lower extremity possesses unique anatomic and functional characteristics that must be evaluated. It is useful to categorize the thigh, lower leg, and foot into separate anatomic units when planning reconstruction. We further divided these units into several subunits, as previously proposed by Sherman and Law15 and as outlined below.
Thigh
The thigh is usually well perfused and has several muscle groups, which facilitates reconstruction. Primary closure, skin grafts, or local flaps are acceptable options in most cases. The remaining musculature can be rotated or advanced to cover defects in the anterior or posterior thigh, providing bulk and adequate blood supply.
Hip and proximal/lateral thigh. Local muscle or myocutaneous flap options include tensor fascia lata, vastus lateralis, and rectus femoris flaps, all of which are based on the lateral circumflex femoral artery.
The tensor fascia lata flap is thin but has a long fascia extension that can be elevated from above the knee and can include a large skin paddle that is innervated by the lateral femoral cutaneous nerve. Some patients may experience knee instability after tensor fascia lata harvest.
The vastus lateralis muscle flap provides good bulk. Its arc of rotation reaches most of the inferior and posterior pelvis. It has little effect on ambulation.
The rectus femoris muscle flap is not so bulky, is easily mobilized, and has a wide arc of rotation. The donor site can be closed primarily. Harvest of this muscle can be associated with some strength loss during knee extension. For large defects of the upper third of the leg, a pedicled rectus abdominis muscle flap based on the deep inferior epigastric artery can be used. A vertically oriented skin island can be extended up to the costal margin, improving the reach. When the nature of the wound precludes use of pedicle flaps, free tissue transfer is indicated, with the latissimus dorsi muscle flap being used most commonly.15,16
Mid-thigh. Wounds in this location often can be closed with skin grafts or fasciocutaneous flaps. If the femur is exposed, however, a muscle flap will be required. As above, the tensor fascia lata, vastus lateralis, and rectus femoris can be used as flap options. If the lateral circumflex artery is unavailable, other flap options include the gracilis, vastus medialis, and rectus abdominis muscles. The gracilis muscle flap is based on the medial circumflex femoral artery and is useful for covering the medial aspect of the mid-thigh. Although this is a thin muscle, it can be used to cover long defects. The vastus medialis muscle flap is supplied by perforators from the profunda femoris and superficial femoral arteries. It can be rotated medially and advanced distally to cover patellar defects.
Supracondylar knee. The knee is a location where sarcoma resection is particularly likely to leave a defect with exposed bone, tendons, or ligaments that will need coverage. The gastrocnemius muscle flap combined with a split-thickness skin graft remains a consistent and reliable reconstructive option for this area. Other options are an extended medial gastrocnemius muscle flap or myocutaneous flap, which incorporates a random fasciocutaneous extension. For larger defects, free flaps should be considered, such as the anterior thigh flap, rectus abdominis muscle flap, or latissimus dorsi muscle flap. If tendons or ligaments need to be reconstructed, we favor autologous tissue, such as the fascia lata and plantaris tendons. These are easy to harvest and provide long-lasting joint stability.
Lower leg
Proximal third of the tibia. Defects here can usually be covered with a medial or lateral gastrocnemius muscle or myocutaneous flap, or a combination of the two. These muscles have a dominant vascular pedicle—the medial and lateral sural arteries. They can be harvested as an island for better reach, and they are reliable and have minimal donor site morbidity.15 The soleus muscle flap is another option that can be used alone or in combination with the medial or lateral gastrocnemius. Defects that are not amenable to closure by these flaps will most likely require free tissue transfer. The rectus abdominis or latissimus dorsi muscles are the first options. The latter can be combined with the serratus muscle if more bulk is needed.
Middle and lower thirds of the tibia. The soleus flap is frequently used for small or medium-sized mid-tibial defects. It is based on branches of the popliteal artery and posterior tibial artery. Larger defects require a combination of soleus and gastrocnemius muscle flaps or free tissue transfer.
Foot
Ideal reconstruction of the foot should provide thin and durable skin that will tolerate mechanical stress, and achieving this can be quite difficult. Skin grafts are seldom used for the foot, and are limited to non–weight-bearing portions with good underlying soft tissue.
Proximal non–weight-bearing areas (Achilles tendon and malleolar area). Local fasciocutaneous flaps are preferred. The lateral calcaneal artery flap, which is based on the peroneal artery branch, can cover exposed Achilles tendon, providing sensate coverage (sural nerve). The dorsalis pedis flap can be mobilized to cover the malleolar region and distal Achilles tendon, but donor site morbidity limits its use. Free tissue transfer is required for larger defects, and the the main options are flaps from the radial forearm, temporoparietal fascia, or lateral arm.
Heel and midplantar area. For heel reconstruction, the medial plantar artery flap, dorsalis pedis flap, abductor myocutaneous flap, peroneal artery flap, or anterior tibial artery flap can be used. The most versatile flap of the foot is the medial plantar artery flap, which is available only when the posterior tibial artery is intact. If local flaps are not suitable, microvascular tissue transfer is indicated. The radial forearm flap, scapular flap, lateral arm flap, or anterolateral thigh flap can be used. The radial forearm flap is usually the first choice because it is thin, has a long pedicle, and is easy to harvest.
If the foot defect is associated with a large cavity, muscle flaps are the first choices, specifically the gracilis or anterior serratus. A split latissimus muscle can also be applied. The full latissimus or the rectus abdominis are often too large for the type of defects observed.
Distal plantar area and forefoot. Most wounds in this region will require free tissue transfer. Free muscle flaps with split-thickness skin grafts provide the most stable and durable coverage.
Amputation vs limb salvage
It is important to evaluate the effects of lower-extremity salvage on ambulation. Salvage of a nonfunctional limb is of little value for the patient. Likewise, patients with severe medical problems may not be good candidates for limb salvage procedures. In those situations, amputation of the lower extremity is indicated. Adequate soft-tissue coverage and good distal perfusion are necessary to ensure healing of an amputation. If possible, local tissue rearrangement may be enough to provide a good amputation stump to fit an external prosthesis. In the case of radiation damage to the tissue, a free tissue transfer is necessary. The calcaneal-plantar unit from the amputated limb is frequently used as a free flap. Other flaps from the amputated limb, called fillet flaps, are harvested immediately and converted to flaps transferred to the defect site. Studies show that they are oncologically safe and reliable.17 Other flaps that provide good coverage for amputation defects are the latissimus dorsi muscle flap, the radial forearm flap, and the anterolateral thigh flap.
Upper extremities
POSTOPERATIVE CARE
Postoperative care following reconstruction after sarcoma resection requires a dedicated and trained team, particularly if a free flap is used for reconstruction.
Clinical evaluation of flaps includes color, temperature, and capillary refill. In cases of microsurgical reconstruction, postoperative care should include hourly examination of audible Doppler signals, at least for the first 36 hours. Free flap complications develop primarily in the first 24 hours, but they can occur during initial mobilization of the patient after a long period of bed rest. The surgical team should be aware of the potential problems and be able to act fast if necessary to reestablish blood flow to the flap.
In addition to flap monitoring, immobilization of the patient after surgery is extremely important. Postoperative swelling to the extremity should be avoided. Patients should be placed on bed rest until the postoperative swelling has subsided and the flap has adhered to the wound bed. Our protocol includes strict bed rest for about 7 days, followed by several days of dangling the extremity for short periods to ensure that dependent positioning will not alter the blood supply. A physical therapist should be involved to assist with crutches or a wheelchair. The patient should receive prophylactic anticoagulation during the resting period, in light of the high risk of deep vein thrombosis and pulmonary embolism. A compressive garment should be used to prevent lymphedema.
COMPLICATIONS ASSOCIATED WITH FLAPS
Once the flap is raised, it can still fail as a result of tension at insetting, inadequate blood flow, twisting of the pedicle, hematoma and/or infection, or the patient’s condition (eg, coagulopathy, poor nutritional status, anemia). Failure to correctly evaluate the direction of arterial flow, whether anterograde or retrograde, can cause flap loss. Instruments such as Doppler ultrasonographic equipment can be used to help to determine the flow. Partial or complete occlusion of the vascular pedicle can occur for several reasons (eg, twisting of the pedicle), and the consequences are disastrous if not recognized in time. If a pedicle problem is suspected in the case of a free flap, the patient should be taken to the operating room immediately and the flap should be explored. Rupture of the vascular anastomosis can occur as a result of technical problems, tension, and (in rare cases) infection.
Hematomas can cause mass effect, limit the venous return, and lead to flap necrosis. Hematoma formation also releases free radicals that can contribute to flap necrosis. Prevention is achieved through meticulous hemostasis. If a hematoma is suspected, the wound should be explored and the hematoma evacuated and washed out with normal saline.
The presence of an infected wound bed can also damage a flap by increasing its metabolic demand and causing the flap to be compromised by the infection itself. It is usually best to wait until the infection is controlled before planning the reconstruction.
Partial flap losses, skin graft losses, and wound dehiscence also are possible. Most of the time these require wound care, and patients’ nutrition and general health should be optimized to help the healing process. In the case of partial or complete flap loss, a new flap is often required and should be planned at a proper time.
CONCLUSIONS
Soft-tissue reconstruction following musculoskeletal sarcoma resection can be as simple as allowing the wound to heal by itself, which is less ideal, or as complex as coverage with a microsurgical osteocutaneous free flap. Limb salvage for sarcomas of the lower extremity has demonstrated good final functional outcomes without adversely affecting the oncologic results. Moreover, patients feel better psychologically and have higher quality of life.18,19
We believe that soft-tissue coverage after a wide resection is the most critical factor for avoiding postoperative complications of the tumor resection, such as infection or fractures. For this reason, we recommend the use of well-vascularized coverage at the time of the initial operation, if possible. Careful preoperative planning is especially important. We believe that reconstruction following musculoskeletal sarcoma resection can be done effectively only by using a team approach. Every such team should include, at minimum, an orthopedic surgeon and a reconstructive surgeon, with the mix of other providers dictated by the individual case.
Advances in the management of soft-tissue and bone sarcomas—referred to collectively as “musculoskeletal sarcomas” hereafter—have resulted in significant improvements in survival and quality of life.1–3 Several factors have likely contributed to these advances, including improved surgical technique and the development of referral centers for sarcoma treatment that have embraced a multidisciplinary approach.1,2
The goal of treatment for musculoskeletal sarcomas is to optimize oncologic outcome and maximize functional restoration.2,3 Surgical resection has been the mainstay of therapy,1–7 as detailed earlier in this supplement. In patients with musculoskeletal sarcomas of the extremities, limb-sparing resection has been shown to be significantly superior to amputation.1,7–9 Wide local excision of the tumor along with its muscle compartment, followed by adjuvant chemotherapy and radiation therapy, has allowed limb salvage without an increased risk of recurrence in many patients.3 However, wide tumor resection can leave large defects that are not amenable to coverage by mobilization of the surrounding tissues, particularly if those tissues have been irradiated. As a result, resection can expose neurovascular structures, bone without periosteum, alloplastic materials, and internal fixation devices.
GOALS OF RECONSTRUCTION
Reconstructive surgery after musculoskeletal sarcoma resection aims to provide adequate wound coverage, preserve function, and optimize the cosmetic outcome.1–3 Tumors can be found on areas crucial to limb movement or may involve tissues vital to limb function. Reconstruction to repair these deficits can take many forms. In certain situations, amputation is still inevitable. In those cases, the reconstruction should provide stable stump coverage with durability and the ability to fit well with an external prosthesis.3
TIMING OF RECONSTRUCTION
Immediate reconstruction should be pursued if possible
Immediate reconstruction after a negative margin should always be considered and should be attempted when possible. Immediate reconstruction allows the reconstructive surgeon to benefit from better evaluation of the defect and exposed structures, as no scar tissue is present to distort the anatomy. Likewise, patients benefit from faster recovery and can receive adjuvant treatment (if necessary) sooner, as well as earlier rehabilitation. Patients may also benefit psychologically from immediate reconstruction.1,3
Indications for delayed reconstruction
Delayed reconstruction is primarily indicated when there are wound healing problems or there is uncertainty about the tumor margins. Secondary indications for delayed reconstruction are wound dehiscence and unstable soft-tissue coverage. If hardware is exposed, the recommendation is for early intervention and wound coverage with well-vascularized tissue to protect and cover the implant or prosthesis.
What about radiation therapy?
A very important consideration in reconstruction is the need for neoadjuvant or adjuvant radiation therapy.3,10,11 Irradiated wounds have a higher incidence of complications, including a tendency to dehisce. In patients who have been previously irradiated, the best practice is to perform immediate reconstruction with well-vascularized tissue, most likely a free tissue transfer.4,6,11,12 This practice reduces hospital stay, costs, and morbidity and increases limb salvage and patient satisfaction.13
SYSTEMATIC PREOPERATIVE PLANNING NEEDED
Reconstruction after musculoskeletal sarcoma resection should be planned systematically within a process that involves preoperative anticipation of the defect size and the resulting functional and cosmetic deficits that might need to be addressed. A preoperative visit to the reconstructive surgeon can be very helpful for presurgical planning.
During surgery it is usually preferable to allow the surgeon doing the tumor resection (eg, surgical oncologist or orthopedic oncologist) to complete the resection because the dimensions of the defect are not certain until negative margins are obtained.14 If tumor margins are unclear at the time of initial resection, the surgeon should consider delaying the definitive reconstruction until the permanent sections confirm negative margins. Temporary closure can be achieved with wound dressings, skin grafts (either allograft or autograft), or negative-pressure wound therapy. In the same context, if neurovascular structures are exposed it is reasonable to use a muscle flap without “tailoring” the flap to the defect. This approach allows the flap to be advanced or repositioned in case of positive margins, and the skin graft can be applied to the muscle surface in a second procedure.3
RECONSTRUCTIVE METHODS: A BRIEF OVERVIEW
Several methods can be used to close musculoskeletal sarcoma excision defects. Smaller defects can be closed primarily, although most defects are large and not amenable to primary closure. If fascia or muscle is preserved with only the skin coverage missing, the wound can be covered with either split-thickness or full-thickness skin grafts.1,4,6 Split-thickness skin grafts can be obtained in larger amounts and often heal faster than full-thickness skin grafts. However, most resections will require durable tissue coverage, particularly if adjuvant radiation therapy is planned.
In the case of long bone sarcoma resection, the resulting defect is usually large and complex and the traditional reconstruction is based on avascular allografts and local tissue flaps. However, allografts are associated with high rates of infection, nonunion, and fracture, leading to failure in about 50% of cases. Microvascular free flaps that contain bone, such as free fibula flaps, have been used instead of allografts with good success rates.2
Lately there has been growing interest in the use of the vacuum-assisted closure device (a form of negative-pressure wound therapy) to promote wound healing. It has been shown to improve the granulation and healing of open wounds by absorbing moisture, as well as to promote adherence after skin grafting, thereby reducing the risk of graft displacement.1,3 This device can be used immediately after musculoskeletal sarcoma resection while definitive tumor margin results are pending. It also can be used to prepare the wound bed for grafting in high-risk patients who would not tolerate more complex reconstructions.
Local or adjacent fascial, fasciocutaneous, and dermal flaps can also be used in lower-extremity reconstruction. However, muscle or musculocutaneous flaps are the mainstay of reconstruction after resection of musculoskeletal sarcomas. This group also includes perforator flaps, which have grown in popularity in the last few years.1,3
LOCATION-BASED WOUND RECONSTRUCTION
Musculoskeletal sarcomas can occur in virtually any region of the body, and myriad reconstructive options are available for various body sites. Since lower-extremity musculoskeletal sarcomas represent about 75% of cases,1 we will focus mainly on reconstruction of the lower extremity.
Factors driving choice of flap
Selection of an appropriate flap is essential to an optimal outcome. Flaps should be chosen with regard to donor site morbidity, functional requirements, length and diameter of the vascular pedicle, and aesthetic outcome.3 Usually physical examination, palpation of peripheral pulses, and Doppler ultrasonography are sufficient to evaluate the circulation. A preoperative angiogram should be considered in patients with severe peripheral vascular disease or previous trauma, which can potentially compromise the reconstructive outcome.15
Each region of the lower extremity possesses unique anatomic and functional characteristics that must be evaluated. It is useful to categorize the thigh, lower leg, and foot into separate anatomic units when planning reconstruction. We further divided these units into several subunits, as previously proposed by Sherman and Law15 and as outlined below.
Thigh
The thigh is usually well perfused and has several muscle groups, which facilitates reconstruction. Primary closure, skin grafts, or local flaps are acceptable options in most cases. The remaining musculature can be rotated or advanced to cover defects in the anterior or posterior thigh, providing bulk and adequate blood supply.
Hip and proximal/lateral thigh. Local muscle or myocutaneous flap options include tensor fascia lata, vastus lateralis, and rectus femoris flaps, all of which are based on the lateral circumflex femoral artery.
The tensor fascia lata flap is thin but has a long fascia extension that can be elevated from above the knee and can include a large skin paddle that is innervated by the lateral femoral cutaneous nerve. Some patients may experience knee instability after tensor fascia lata harvest.
The vastus lateralis muscle flap provides good bulk. Its arc of rotation reaches most of the inferior and posterior pelvis. It has little effect on ambulation.
The rectus femoris muscle flap is not so bulky, is easily mobilized, and has a wide arc of rotation. The donor site can be closed primarily. Harvest of this muscle can be associated with some strength loss during knee extension. For large defects of the upper third of the leg, a pedicled rectus abdominis muscle flap based on the deep inferior epigastric artery can be used. A vertically oriented skin island can be extended up to the costal margin, improving the reach. When the nature of the wound precludes use of pedicle flaps, free tissue transfer is indicated, with the latissimus dorsi muscle flap being used most commonly.15,16
Mid-thigh. Wounds in this location often can be closed with skin grafts or fasciocutaneous flaps. If the femur is exposed, however, a muscle flap will be required. As above, the tensor fascia lata, vastus lateralis, and rectus femoris can be used as flap options. If the lateral circumflex artery is unavailable, other flap options include the gracilis, vastus medialis, and rectus abdominis muscles. The gracilis muscle flap is based on the medial circumflex femoral artery and is useful for covering the medial aspect of the mid-thigh. Although this is a thin muscle, it can be used to cover long defects. The vastus medialis muscle flap is supplied by perforators from the profunda femoris and superficial femoral arteries. It can be rotated medially and advanced distally to cover patellar defects.
Supracondylar knee. The knee is a location where sarcoma resection is particularly likely to leave a defect with exposed bone, tendons, or ligaments that will need coverage. The gastrocnemius muscle flap combined with a split-thickness skin graft remains a consistent and reliable reconstructive option for this area. Other options are an extended medial gastrocnemius muscle flap or myocutaneous flap, which incorporates a random fasciocutaneous extension. For larger defects, free flaps should be considered, such as the anterior thigh flap, rectus abdominis muscle flap, or latissimus dorsi muscle flap. If tendons or ligaments need to be reconstructed, we favor autologous tissue, such as the fascia lata and plantaris tendons. These are easy to harvest and provide long-lasting joint stability.
Lower leg
Proximal third of the tibia. Defects here can usually be covered with a medial or lateral gastrocnemius muscle or myocutaneous flap, or a combination of the two. These muscles have a dominant vascular pedicle—the medial and lateral sural arteries. They can be harvested as an island for better reach, and they are reliable and have minimal donor site morbidity.15 The soleus muscle flap is another option that can be used alone or in combination with the medial or lateral gastrocnemius. Defects that are not amenable to closure by these flaps will most likely require free tissue transfer. The rectus abdominis or latissimus dorsi muscles are the first options. The latter can be combined with the serratus muscle if more bulk is needed.
Middle and lower thirds of the tibia. The soleus flap is frequently used for small or medium-sized mid-tibial defects. It is based on branches of the popliteal artery and posterior tibial artery. Larger defects require a combination of soleus and gastrocnemius muscle flaps or free tissue transfer.
Foot
Ideal reconstruction of the foot should provide thin and durable skin that will tolerate mechanical stress, and achieving this can be quite difficult. Skin grafts are seldom used for the foot, and are limited to non–weight-bearing portions with good underlying soft tissue.
Proximal non–weight-bearing areas (Achilles tendon and malleolar area). Local fasciocutaneous flaps are preferred. The lateral calcaneal artery flap, which is based on the peroneal artery branch, can cover exposed Achilles tendon, providing sensate coverage (sural nerve). The dorsalis pedis flap can be mobilized to cover the malleolar region and distal Achilles tendon, but donor site morbidity limits its use. Free tissue transfer is required for larger defects, and the the main options are flaps from the radial forearm, temporoparietal fascia, or lateral arm.
Heel and midplantar area. For heel reconstruction, the medial plantar artery flap, dorsalis pedis flap, abductor myocutaneous flap, peroneal artery flap, or anterior tibial artery flap can be used. The most versatile flap of the foot is the medial plantar artery flap, which is available only when the posterior tibial artery is intact. If local flaps are not suitable, microvascular tissue transfer is indicated. The radial forearm flap, scapular flap, lateral arm flap, or anterolateral thigh flap can be used. The radial forearm flap is usually the first choice because it is thin, has a long pedicle, and is easy to harvest.
If the foot defect is associated with a large cavity, muscle flaps are the first choices, specifically the gracilis or anterior serratus. A split latissimus muscle can also be applied. The full latissimus or the rectus abdominis are often too large for the type of defects observed.
Distal plantar area and forefoot. Most wounds in this region will require free tissue transfer. Free muscle flaps with split-thickness skin grafts provide the most stable and durable coverage.
Amputation vs limb salvage
It is important to evaluate the effects of lower-extremity salvage on ambulation. Salvage of a nonfunctional limb is of little value for the patient. Likewise, patients with severe medical problems may not be good candidates for limb salvage procedures. In those situations, amputation of the lower extremity is indicated. Adequate soft-tissue coverage and good distal perfusion are necessary to ensure healing of an amputation. If possible, local tissue rearrangement may be enough to provide a good amputation stump to fit an external prosthesis. In the case of radiation damage to the tissue, a free tissue transfer is necessary. The calcaneal-plantar unit from the amputated limb is frequently used as a free flap. Other flaps from the amputated limb, called fillet flaps, are harvested immediately and converted to flaps transferred to the defect site. Studies show that they are oncologically safe and reliable.17 Other flaps that provide good coverage for amputation defects are the latissimus dorsi muscle flap, the radial forearm flap, and the anterolateral thigh flap.
Upper extremities
POSTOPERATIVE CARE
Postoperative care following reconstruction after sarcoma resection requires a dedicated and trained team, particularly if a free flap is used for reconstruction.
Clinical evaluation of flaps includes color, temperature, and capillary refill. In cases of microsurgical reconstruction, postoperative care should include hourly examination of audible Doppler signals, at least for the first 36 hours. Free flap complications develop primarily in the first 24 hours, but they can occur during initial mobilization of the patient after a long period of bed rest. The surgical team should be aware of the potential problems and be able to act fast if necessary to reestablish blood flow to the flap.
In addition to flap monitoring, immobilization of the patient after surgery is extremely important. Postoperative swelling to the extremity should be avoided. Patients should be placed on bed rest until the postoperative swelling has subsided and the flap has adhered to the wound bed. Our protocol includes strict bed rest for about 7 days, followed by several days of dangling the extremity for short periods to ensure that dependent positioning will not alter the blood supply. A physical therapist should be involved to assist with crutches or a wheelchair. The patient should receive prophylactic anticoagulation during the resting period, in light of the high risk of deep vein thrombosis and pulmonary embolism. A compressive garment should be used to prevent lymphedema.
COMPLICATIONS ASSOCIATED WITH FLAPS
Once the flap is raised, it can still fail as a result of tension at insetting, inadequate blood flow, twisting of the pedicle, hematoma and/or infection, or the patient’s condition (eg, coagulopathy, poor nutritional status, anemia). Failure to correctly evaluate the direction of arterial flow, whether anterograde or retrograde, can cause flap loss. Instruments such as Doppler ultrasonographic equipment can be used to help to determine the flow. Partial or complete occlusion of the vascular pedicle can occur for several reasons (eg, twisting of the pedicle), and the consequences are disastrous if not recognized in time. If a pedicle problem is suspected in the case of a free flap, the patient should be taken to the operating room immediately and the flap should be explored. Rupture of the vascular anastomosis can occur as a result of technical problems, tension, and (in rare cases) infection.
Hematomas can cause mass effect, limit the venous return, and lead to flap necrosis. Hematoma formation also releases free radicals that can contribute to flap necrosis. Prevention is achieved through meticulous hemostasis. If a hematoma is suspected, the wound should be explored and the hematoma evacuated and washed out with normal saline.
The presence of an infected wound bed can also damage a flap by increasing its metabolic demand and causing the flap to be compromised by the infection itself. It is usually best to wait until the infection is controlled before planning the reconstruction.
Partial flap losses, skin graft losses, and wound dehiscence also are possible. Most of the time these require wound care, and patients’ nutrition and general health should be optimized to help the healing process. In the case of partial or complete flap loss, a new flap is often required and should be planned at a proper time.
CONCLUSIONS
Soft-tissue reconstruction following musculoskeletal sarcoma resection can be as simple as allowing the wound to heal by itself, which is less ideal, or as complex as coverage with a microsurgical osteocutaneous free flap. Limb salvage for sarcomas of the lower extremity has demonstrated good final functional outcomes without adversely affecting the oncologic results. Moreover, patients feel better psychologically and have higher quality of life.18,19
We believe that soft-tissue coverage after a wide resection is the most critical factor for avoiding postoperative complications of the tumor resection, such as infection or fractures. For this reason, we recommend the use of well-vascularized coverage at the time of the initial operation, if possible. Careful preoperative planning is especially important. We believe that reconstruction following musculoskeletal sarcoma resection can be done effectively only by using a team approach. Every such team should include, at minimum, an orthopedic surgeon and a reconstructive surgeon, with the mix of other providers dictated by the individual case.
- Misra A, Mistry N, Grimer R, Peart F. The management of soft tissue sarcoma. J Plast Reconstr Aesthet Surg 2009; 62:161–174.
- Morii T, Mochizuki K, Takushima A, Okazaki M, Satomi K. Soft tissue reconstruction using vascularized tissue transplantation following resection of musculoskeletal sarcoma: evaluation of oncologic and functional outcomes in 55 cases. Ann Plast Surg 2009; 62:252–257.
- Heller L, Kronowitz SJ. Lower extremity reconstruction. J Surg Oncol 2006; 94:479–489.
- Bannasch H, Haivas I, Momeni A, Stark GB. Oncosurgical and reconstructive concepts in the treatment of soft tissue sarcomas: a retrospective analysis. Arch Orthop Trauma Surg 2009; 129:43–49.
- Muramatsu K, Ihara K, Doi K, Hashimoto T, Taguchi T. Sarcoma in the forearm and hand: clinical outcomes and microsurgical reconstruction for limb salvage. Ann Plast Surg 2009; 62:28–33.
- Tukiainen E, Böhling T, Huuhtanen R. Soft tissue sarcoma of the trunk and extremities. Scand J Surg 2003; 92:257–263.
- Adelani MA, Holt GE, Dittus RS, Passman MA, Schwartz HS. Revascularization after segmental resection of lower extremity soft tissue sarcomas. J Surg Oncol 2007; 95:455–460.
- Lohman RF, Nabawi AS, Reece GP, Pollock RE, Evans GR. Soft tissue sarcoma of the upper extremity: a 5-year experience at two institutions emphasizing the role of soft tissue flap reconstruction. Cancer 2002; 94:2256–2264.
- Davis AM, Sennik S, Griffin AM, et al. Predictors of functional outcomes following limb salvage surgery for lower-extremity soft tissue sarcoma. J Surg Oncol 2000; 73:206–211.
- Heller L, Ballo MT, Cormier JN, Oates SD, Butler CE. Staged reconstruction for resection wounds in sarcoma patients treated with brachytherapy. Ann Plast Surg 2008; 60:58–63.
- Evans GR, Black JJ, Robb GL, et al. Adjuvant therapy: the effects on microvascular lower extremity reconstruction. Ann Plast Surg 1997; 39:141–144.
- Peat BG, Bell RS, Davis A, et al. Wound-healing complications after soft-tissue sarcoma surgery. Plast Reconstr Surg 1994; 93:980–987.
- Barwick WJ, Goldberg JA, Scully SP, Harrelson JM. Vascularized tissue transfer for closure of irradiated wounds after soft tissue sarcoma resection. Ann Surg 1992; 216:591–595.
- Masquelet AC, Romana MC. The medialis pedis flap: a new fasciocutaneous flap. Plast Reconstr Surg 1990; 85:765–772.
- Sherman R, Law M. Lower extremity reconstruction. In: Achauer BM, Eriksson E, Guyuron B, Coleman III JJ, Russell RC, Vander Kolk CA, eds. Plastic Surgery: Indications, Operations, and Outcomes. Vol 1. St. Louis, MO: Mosby; 2000:475–496.
- Innocenti M, Abed YY, Beltrami G, Delcroix L, Balatri A, Capanna R. Quadriceps muscle reconstruction with free functioning latissimus dorsi muscle flap after oncological resection. Microsurgery 2009; 29:189–198.
- Chiang YC, Wei FC, Wang JW, Chen WS. Reconstruction of below-knee stump using the salvaged foot fillet flap. Plast Reconstr Surg 1995; 96:731–738.
- Serletti JM, Carras AJ, O’Keefe RJ, Rosier RN. Functional outcome after soft-tissue reconstruction for limb salvage after sarcoma surgery. Plast Reconstr Surg 1998; 102:1576–1583.
- Niimi R, Matsumine A, Kusuzaki K, et al. Usefulness of limb salvage surgery for bone and soft tissue sarcomas of the distal lower leg. J Cancer Res Clin Oncol 2008; 134:1087–1095.
- Misra A, Mistry N, Grimer R, Peart F. The management of soft tissue sarcoma. J Plast Reconstr Aesthet Surg 2009; 62:161–174.
- Morii T, Mochizuki K, Takushima A, Okazaki M, Satomi K. Soft tissue reconstruction using vascularized tissue transplantation following resection of musculoskeletal sarcoma: evaluation of oncologic and functional outcomes in 55 cases. Ann Plast Surg 2009; 62:252–257.
- Heller L, Kronowitz SJ. Lower extremity reconstruction. J Surg Oncol 2006; 94:479–489.
- Bannasch H, Haivas I, Momeni A, Stark GB. Oncosurgical and reconstructive concepts in the treatment of soft tissue sarcomas: a retrospective analysis. Arch Orthop Trauma Surg 2009; 129:43–49.
- Muramatsu K, Ihara K, Doi K, Hashimoto T, Taguchi T. Sarcoma in the forearm and hand: clinical outcomes and microsurgical reconstruction for limb salvage. Ann Plast Surg 2009; 62:28–33.
- Tukiainen E, Böhling T, Huuhtanen R. Soft tissue sarcoma of the trunk and extremities. Scand J Surg 2003; 92:257–263.
- Adelani MA, Holt GE, Dittus RS, Passman MA, Schwartz HS. Revascularization after segmental resection of lower extremity soft tissue sarcomas. J Surg Oncol 2007; 95:455–460.
- Lohman RF, Nabawi AS, Reece GP, Pollock RE, Evans GR. Soft tissue sarcoma of the upper extremity: a 5-year experience at two institutions emphasizing the role of soft tissue flap reconstruction. Cancer 2002; 94:2256–2264.
- Davis AM, Sennik S, Griffin AM, et al. Predictors of functional outcomes following limb salvage surgery for lower-extremity soft tissue sarcoma. J Surg Oncol 2000; 73:206–211.
- Heller L, Ballo MT, Cormier JN, Oates SD, Butler CE. Staged reconstruction for resection wounds in sarcoma patients treated with brachytherapy. Ann Plast Surg 2008; 60:58–63.
- Evans GR, Black JJ, Robb GL, et al. Adjuvant therapy: the effects on microvascular lower extremity reconstruction. Ann Plast Surg 1997; 39:141–144.
- Peat BG, Bell RS, Davis A, et al. Wound-healing complications after soft-tissue sarcoma surgery. Plast Reconstr Surg 1994; 93:980–987.
- Barwick WJ, Goldberg JA, Scully SP, Harrelson JM. Vascularized tissue transfer for closure of irradiated wounds after soft tissue sarcoma resection. Ann Surg 1992; 216:591–595.
- Masquelet AC, Romana MC. The medialis pedis flap: a new fasciocutaneous flap. Plast Reconstr Surg 1990; 85:765–772.
- Sherman R, Law M. Lower extremity reconstruction. In: Achauer BM, Eriksson E, Guyuron B, Coleman III JJ, Russell RC, Vander Kolk CA, eds. Plastic Surgery: Indications, Operations, and Outcomes. Vol 1. St. Louis, MO: Mosby; 2000:475–496.
- Innocenti M, Abed YY, Beltrami G, Delcroix L, Balatri A, Capanna R. Quadriceps muscle reconstruction with free functioning latissimus dorsi muscle flap after oncological resection. Microsurgery 2009; 29:189–198.
- Chiang YC, Wei FC, Wang JW, Chen WS. Reconstruction of below-knee stump using the salvaged foot fillet flap. Plast Reconstr Surg 1995; 96:731–738.
- Serletti JM, Carras AJ, O’Keefe RJ, Rosier RN. Functional outcome after soft-tissue reconstruction for limb salvage after sarcoma surgery. Plast Reconstr Surg 1998; 102:1576–1583.
- Niimi R, Matsumine A, Kusuzaki K, et al. Usefulness of limb salvage surgery for bone and soft tissue sarcomas of the distal lower leg. J Cancer Res Clin Oncol 2008; 134:1087–1095.
Use of chemotherapy for patients with bone and soft-tissue sarcomas
Surgical resection is the mainstay of treatment for musculoskeletal sarcomas, as detailed earlier in this supplement, but chemotherapy also has a proven role in the primary therapy of most bone sarcomas and a potential role for some patients with soft-tissue sarcomas. This article provides an overview of the roles of chemotherapy for patients with bone and soft-tissue sarcomas and addresses key considerations surrounding chemotherapy in the context of overall patient management.
BONE SARCOMAS
Because most bone sarcomas occur in pediatric patients and young adults, studies of chemotherapy in this disease have often enrolled predominantly young subjects. As a result, very limited data are available in older adults. Single-institution experiences indicate that adults with bone sarcomas have inferior outcomes compared with their pediatric and adolescent counterparts,1 but the literature on these tumors in adults is scant. Therefore, the following discussion on chemotherapy for bone sarcomas incorporates data from trials conducted predominantly in children and young adults (ie, generally younger than 30 years and with a very large majority younger than 20 years).
Chemotherapy for osteosarcoma
At present, neoadjuvant (preoperative) chemotherapy followed by definitive resection with subsequent adjuvant (postoperative) chemotherapy is the well-established approach to treatment of localized osteosarcomas. Chemotherapy can eradicate the micrometastatic disease that is believed to be present in the majority of patients with clinically resectable cancer.2
Efficacy. Historically, prior to the institution of effective chemotherapy, metastatic disease developed in 80% to 90% of patients who underwent curative resection with or without radiation therapy, which resulted in a long-term survival rate of less than 20%.3 In the 1980s, clinical trials that randomized patients with resectable osteosarcoma to surgery alone or to surgery plus chemotherapy found that the addition of perioperative chemotherapy led to significant improvements in recurrence rates and survival.4,5 More recent randomized trials have shown that treatment of such patients with modern multiagent chemotherapy regimens results in a 5-year survival rate of approximately 70%.6 Additionally, response to neoadjuvant (preoperative) treatment has become the most important predictor of outcome, as the median survival of osteosarcoma patients who have greater than 90% necrosis in the resected specimen following neoadjuvant chemotherapy is about 90% at 5 years.7,8
Toxicity. Current chemotherapy regimens are based on high doses of methotrexate and leucovorin in combination with doxorubicin, ifosfamide, and platinum. Long-term effects of such regimens include the following3:
- Azospermia (in 100% of patients who received a total ifosfamide dose > 75 g/m2)
- Subclinical renal impairment (in 48% of patients treated with high doses of ifosfamide)
- Hearing impairment (in 40% of patients treated with cisplatin)
- Second malignancies (in 2.1%)
- Cardiomyopathy (in 1.7%).3
In light of this, the development of equally effective but less intensive regimens for patients whose disease carries a better prognosis is highly desirable. Ongoing clinical trials are investigating this strategy.
Metastatic disease. Metastatic osteosarcoma is found in approximately 20% of patients at the time of diagnosis. Sarcoma mainly spreads hematogenously, and the lungs are the most common initial site of metastases, being affected in more than 60% of patients who develop metastatic disease.9 Patients with metachronous lung lesions are initially considered for aggressive treatment with neoadjuvant chemotherapy and subsequent resection of clinically apparent disease, which results in event-free survival rates of 20% to 30%.3
Patients with disease limited to the primary tumor and no more than one or two bone lesions fare best. The presence of multiple metastases is associated with the poorest prognosis, as few patients with this profile live past 2 years.10 In a review of 202 pediatric and adult patients with documented metastases at the time of osteosarcoma diagnosis, the presence of more than 5 metastatic lesions (which was reported in 91 patients) was associated with a 5-year overall survival rate of 19%.9
Chemotherapy for Ewing sarcoma
Perioperative chemotherapy in patients with localized Ewing sarcoma is believed to reduce the burden of micrometastasis that is thought to be present in most patients with early-stage disease. Five-year survival rates of 50% to 72% have been reported among patients with resectable Ewing sarcoma treated perioperatively with multiagent chemotherapy.11,12 Notably, randomized trials that studied intense multiagent chemotherapy regimens (consisting of doxorubicin, cyclophosphamide, vincristine, and dactinomycin alternating with etoposide and ifosfamide) reported the best outcomes despite significant but acceptable toxicity. In a large randomized trial involving 398 patients with resectable disease, a 5-year survival rate of 72% was achieved with the above regimen, compared with 61% in patients treated with a less intense regimen that did not contain ifosfamide and etoposide (p = .01).12
Compressing these standard regimens to an every-14-day instead of every-21-day schedule improved event-free survival at 3 years from 65% to 76% (p = .028) without any significant increase in toxicity in a randomized trial involving 568 patients.13 Data on overall survival from this trial are not yet published.
Metastatic disease. Metastatic Ewing sarcoma is found in 15% to 35% of patients with newly diagnosed disease and is treated with multiagent chemotherapy; resection of residual disease is considered in good responders.3 This approach produces objective responses to therapy, but long-term survival is rare.
Toxicity. Myelodysplastic syndrome and acute myeloid leukemia are the most dreaded long-term complications of intensive multiagent chemotherapy for Ewing sarcoma and develop in up to 8% of patients.14 Additionally, ifosfamide can lead to hematuria (~12% incidence), encephalopathy (mild somnolence and hallucinations to coma), chronic renal impairment (6% incidence), and hemorrhagic cystitis (though administration of mesna and generous intravenous hydration can minimize this latter complication).15 Recent efforts are therefore focused on testing less-intensive regimens in patients who have good prognostic features.
Chondrosarcoma: No role for chemotherapy
Chondrosarcoma, which represents approximately 20% of all bone sarcomas and has a peak incidence in older adults (ie, in the sixth decade of life), is insensitive to chemotherapy. Radiotherapy is also of limited value and is reserved for patients treated in the palliative setting.16 Definitive management of chondrosarcoma involves adequate surgical resection alone.
SOFT-TISSUE SARCOMAS
Aside from recent advances in the treatment of gastrointestinal stromal tumors with the small-molecule tyrosine kinase inhibitors imatinib and sunitinib (which are beyond the scope of this article), an overall survival advantage with chemotherapy has not been demonstrated in adults with soft-tissue sarcoma.17
Resectable disease
The decision to use chemotherapy needs to be weighed against the magnitude of potential clinical benefit and the acute and chronic toxicities that can develop.
Toxicity. Chemotherapy regimens with activity against soft-tissue sarcomas often contain anthracyclines, alkylating agents, and taxanes. These agents can produce serious long-term toxicities, which is especially important in patients treated with curative intent. Doxorubicin and other anthracyclines, for example, may result in cardiomyopathy, the risk of which rises with increasing cumulative dose.18 In addition, acute myeloid leukemia may develop in 2% to 12% of patients treated with anthracyclines or alkylating agents such as ifosfamide and dacarbazine.3,19 Renal failure and an elevated risk of bladder carcinoma are uncommonly reported in patients with a history of ifosfamide treatment.15 Sensory neuropathy associated with the use of taxanes (eg, paclitaxel and docetaxel) is dose dependent and reversible in more than half of patients. However, some patients treated with high doses of these agents can have persistent symptoms of paresthesias, burning, and decreased reflexes, which can be debilitating.20
Efficacy of adjuvant chemotherapy. Because chemotherapy puts patients at risk of such serious chronic toxicities, its use can be justified only if it results in significant benefit, such as prolongation of survival. A 1997 meta-analysis of 14 clinical trials evaluating adjuvant chemotherapy in patients with resectable soft-tissue sarcomas found chemotherapy to have an absolute benefit of 10% in recurrence-free survival at 10 years (ie, from 45% survival to 55% survival), with a hazard ratio of 0.75 (95% confidence interval [CI], 0.64–0.87; p = .0001) for recurrence or death.21 However, when the analysis was limited to overall survival at 10 years, the survival difference between patients who received adjuvant chemotherapy and those who did not (54% vs 50%, respectively) was not statistically significant (hazard ratio = 0.89; 95% CI, 0.76–1.03, p = .12).21
The concept of adjuvant therapy has been revisited since the antisarcoma activity of ifosfamide was established. A large European trial randomized 351 patients with resected soft-tissue sarcoma either to placebo or to doxorubicin and ifosfamide given every 21 days.22 The preliminary results, reported in abstract form at the 2007 annual meeting of the American Society of Clinical Oncology, showed a higher 5-year survival rate in the placebo arm (69%) compared with the chemotherapy arm (64%).22 This and other trials using ifosfamide in various drug combinations showed no difference in survival, suggesting that adjuvant chemotherapy should not be considered to be standard practice outside of a clinical trial.
Efficacy of neoadjuvant chemotherapy. Neoadjuvant chemotherapy also has been studied in patients with soft-tissue sarcomas. A retrospective analysis found that the greatest benefit is derived in patients with primary tumors larger than 10 cm, in whom neoadjuvant chemotherapy increased 3-year disease-specific survival from 62% to 83%.23 However, differing results came from a prospective multicenter trial that randomized patients with large primary and recurrent tumors to either surgery alone or surgery preceded by three cycles of neoadjuvant doxorubicin and ifosfamide (all patients could also receive adjuvant radiation therapy, depending on grade and adequacy of resection).24 The trial suffered from slow accrual, and only 150 patients were enrolled. At 5 years, survival was similar between the groups with and without neoadjuvant chemotherapy.24 Therefore, neoadjuvant chemotherapy is not yet recommended pending results of larger randomized trials.
No clear role for recurrent disease. Local recurrence of the primary tumor after resection occurs in 10% to 50% of cases of soft-tissue sarcoma, with the specific rate depending on the primary tumor location. The highest incidence of recurrence is found in patients with retroperitoneal and head and neck sarcoma (40% and 50%, respectively), mainly because of the difficulty of obtaining clear margins. Chemotherapy has not been well studied in this setting and is of uncertain value.3
Metastatic disease
Metastatic soft-tissue sarcomas may respond to chemotherapy, but there is a lack of evidence that chemotherapy improves overall survival. Pulmonary lesions are the most common site of distant recurrence, and resection of such metastases is sometimes undertaken in well-selected patients. However, there is no level 1 evidence supporting chemotherapy in this clinical setting despite its common preoperative use. There is a paucity of randomized phase 3 trials that compare established palliative chemotherapy regimens to best supportive care. It is believed that some groups of patients do benefit, however, including those who are young and have good performance status, low tumor grade, absence of liver metastasis or pulmonary metastasis only, and a long interval between treatment of the primary tumor and development of metastatic disease.3 Some histologies, such as uterine leiomyosarcomas and facial/scalp angiosarcomas, respond better to chemotherapy.17
Drugs found to have activity against metastatic sarcoma include doxorubicin, ifosfamide, platinum agents, gemcitabine, taxanes, and dacarbazine. Used either alone or in combinations, these drugs produce responses (ie, shrink metastatic tumors) in about 13% to 33% of patients.3 Use of chemotherapy is frequently curtailed by the acute toxicity of these agents, which includes pancytopenia, transfusion requirements, febrile neutropenia, nausea, alopecia, and significant fatigue, as well as renal failure with ifosfamide or cisplatin and peripheral neuropathy with platinum agents or taxanes. Appropriate patient selection for chemotherapy and exclusion of those who should be managed solely with best supportive care is an important challenge that oncologists often face when managing patients with metastatic soft-tissue sarcoma.
Future directions
Trabectedin (ET-743) is a novel compound with promising activity against soft-tissue sarcomas that acts by inhibiting cell-cycle transition from the G2 to M stages. The drug covalently binds to the minor grove of the DNA molecule, changing its three-dimensional structure and impairing transcription and possibly DNA repair.25 Phase 2 studies showed durable responses to trabectedin in 3% to 8% of heavily pretreated patients26–28 and in 17% of treatment-naïve patients with advanced soft-tissue sarcomas.25 Time to progression of up to 20 months has been reported in patients who respond or develop stable disease.3
Toxic effects of trabectedin include myelosuppression, fever, edema, arthralgias, hepatotoxicity, and (rarely) rhabdomyolysis. To date, these toxicities have been self-limiting. Larger clinical trials and longer follow-up is needed to assess whether this agent has any significant long-term toxicities.
Trabectedin has already been approved in Europe for treatment of chemotherapy-refractory soft-tissue sarcoma when given as a 24-hour infusion every 21 days.
More broadly, an active effort is under way to better understand the molecular derangements in a variety of soft-tissue sarcoma subtypes. The hope is that this understanding will lead to improved therapies that target aberrant proliferation, angiogenesis, and other biologic processes that drive the growth and metastasis of soft-tissue and bone sarcomas.
- Meyers PA, Heller G, Healey J, et al. Chemotherapy for nonmetastatic osteogenic sarcoma: the Memorial Sloan-Kettering experience. J Clin Oncol 1992; 10:5–15.
- Bruland OS, Høifødt H, Saeter G, Smeland S, Fodstad O. Hematogenous micrometastases in osteosarcoma patients. Clin Cancer Res 2005; 11:4666–4673.
- Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ, eds. Cancer Management: A Multidisciplinary Approach. 11th ed. Manhasset, NY: CMP Medica; 2009.
- Link MP, Goorin AM, Miser AW, et al. The effect of adjuvant chemotherapy on relapse-free survival in patients with osteosarcoma of the extremity. N Engl J Med 1986; 314:1600–1606.
- Eilber F, Giuliano A, Eckardt J, Patterson K, Moseley S, Goodnight J. Adjuvant chemotherapy for osteosarcoma: a randomized prospective trial. J Clin Oncol 1987; 5:21–26.
- Meyers PA, Schwartz CL, Krailo M, et al. Osteosarcoma: a randomized, prospective trial of the addition of ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate. J Clin Oncol 2005; 23:2004–2011.
- Winkler K, Beron G, Delling G, et al. Neoadjuvant chemotherapy of osteosarcomas: results of a randomized cooperative trial (COSS-82) with salvage chemotherapy based on histological tumor response. J Clin Oncol 1988; 6:329–337.
- Bramwell VH, Steward WP, Nooij M, et al. Neoadjuvant chemotherapy with doxorubicin and cisplatin in malignant fibrous histiocytoma of bone: a European Osteosarcoma Intergroup study. J Clin Oncol 1999; 17:3260–3269.
- Kager L, Zoubek A, Pötschger U, et al. Primary metastatic osteosarcoma: presentation and outcome of patients treated on Neoadjuvant Cooperative Osteosarcoma Study Group protocols. J Clin Oncol 2003; 21:2011–2018.
- Longhi A, Fabbri N, Donati D, et al. Neoadjuvant chemotherapy for patients with synchronous multifocal osteosarcoma: results in eleven cases. J Chemother 2001; 13:324–330.
- Nesbit ME Jr, Gehan EA, Burgert EO Jr, et al. Multimodal therapy for the management of primary, nonmetastatic Ewing’s sarcoma of bone: a long-term follow-up of the First Intergroup study. J Clin Oncol 1990; 8:1664–1674.
- Grier HE, Krailo MD, Tarbell NJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med 2003; 348:694–701.
- Womer RB, West DC, Krailo MD, et al; for the Children’s Oncology Group AEWS0031 Committee. Randomized comparison of every-two-week v. every-three-week chemotherapy in Ewing sarcoma family tumors. J Clin Oncol 2008; 26(May 20 suppl):10504. Abstract.
- Rodriguez-Galindo C, Poquette CA, Marina NM, et al. Hematologic abnormalities and acute myeloid leukemia in children and adolescents administered intensified chemotherapy for the Ewing sarcoma family of tumors. J Pediatr Hematol Oncol 2000; 22:321–329.
- Brade WP, Herdrich, K, Kachel-Fischer U, Araujo CE. Dosing and side-effects of ifosfamide plus mesna. J Cancer Res Clin Oncol 1991; 117(suppl 4):S164–S186.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Clark MA, Fisher C, Judson I, Thomas JM. Soft-tissue sarcomas in adults. N Engl J Med 2005; 353:701–711.
- Alexander J, Dainiak N, Berger HJ, et al. Serial assessment of doxorubicin cardiotoxicity with quantitative radionuclide angiocardiography. N Engl J Med 1979; 300:278–283.
- Felix CA. Secondary leukemias induced by topoisomerase-targeted drugs. Biochim Biophys Acta 1998; 1400:233–255.
- Postma TJ, Vermorken JB, Liefting AJ, Pinedo HM, Heimans JJ. Paclitaxel-induced neuropathy. Ann Oncol 1995; 6:489–494.
- Sarcoma Meta-analysis Collaboration. Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet 1997; 350:1647–1654.
- Woll PJ, van Glabbeke M, Hohenberger P, et al. Adjuvant chemotherapy (CT) with doxorubicin and ifosfamide in resected soft tissue sarcoma (STS): interim analysis of a randomised phase III trial. J Clin Oncol 2007; 25(June 20 suppl):10008. Abstract.
- Grobmyer SR, Maki RG, Demetri GD, et al. Neo-adjuvant chemotherapy for primary high-grade extremity soft tissue sarcoma. Ann Oncol 2004; 15:1667–1672.
- Gortzak E, Azzarelli A, Buesa J, et al. A randomised phase II study on neo-adjuvant chemotherapy for ‘high-risk’ adult soft-tissue sarcoma. Eur J Cancer 2001; 37:1096–1103.
- Garcia-Carbonero R, Supko JG, Maki RG, et al. Ecteinascidin-743 (ET-743) for chemotherapy-naive patients with advanced soft tissue sarcomas: multicenter phase II and pharmacokinetic study. J Clin Oncol 2005; 23:5484–5492.
- Yovine A, Riofrio M, Blay JY, et al. Phase II study of ecteinascidin-743 in advanced pretreated soft tissue sarcoma patients. J Clin Oncol 2004; 22:890–899.
- Garcia-Carbonero R, Supko JG, Manola J, et al. Phase II and pharmacokinetic study of ecteinascidin 743 in patients with progressive sarcomas of soft tissues refractory to chemotherapy. J Clin Oncol 2004; 22:1480–1490.
- Le Cesne A, Blay JY, Judson I, et al. Phase II study of ET-743 in advanced soft tissue sarcomas: a European Organisation for the Research and Treatment of Cancer (EORTC) soft tissue and bone sarcoma group trial. J Clin Oncol 2005; 23:576–584.
Surgical resection is the mainstay of treatment for musculoskeletal sarcomas, as detailed earlier in this supplement, but chemotherapy also has a proven role in the primary therapy of most bone sarcomas and a potential role for some patients with soft-tissue sarcomas. This article provides an overview of the roles of chemotherapy for patients with bone and soft-tissue sarcomas and addresses key considerations surrounding chemotherapy in the context of overall patient management.
BONE SARCOMAS
Because most bone sarcomas occur in pediatric patients and young adults, studies of chemotherapy in this disease have often enrolled predominantly young subjects. As a result, very limited data are available in older adults. Single-institution experiences indicate that adults with bone sarcomas have inferior outcomes compared with their pediatric and adolescent counterparts,1 but the literature on these tumors in adults is scant. Therefore, the following discussion on chemotherapy for bone sarcomas incorporates data from trials conducted predominantly in children and young adults (ie, generally younger than 30 years and with a very large majority younger than 20 years).
Chemotherapy for osteosarcoma
At present, neoadjuvant (preoperative) chemotherapy followed by definitive resection with subsequent adjuvant (postoperative) chemotherapy is the well-established approach to treatment of localized osteosarcomas. Chemotherapy can eradicate the micrometastatic disease that is believed to be present in the majority of patients with clinically resectable cancer.2
Efficacy. Historically, prior to the institution of effective chemotherapy, metastatic disease developed in 80% to 90% of patients who underwent curative resection with or without radiation therapy, which resulted in a long-term survival rate of less than 20%.3 In the 1980s, clinical trials that randomized patients with resectable osteosarcoma to surgery alone or to surgery plus chemotherapy found that the addition of perioperative chemotherapy led to significant improvements in recurrence rates and survival.4,5 More recent randomized trials have shown that treatment of such patients with modern multiagent chemotherapy regimens results in a 5-year survival rate of approximately 70%.6 Additionally, response to neoadjuvant (preoperative) treatment has become the most important predictor of outcome, as the median survival of osteosarcoma patients who have greater than 90% necrosis in the resected specimen following neoadjuvant chemotherapy is about 90% at 5 years.7,8
Toxicity. Current chemotherapy regimens are based on high doses of methotrexate and leucovorin in combination with doxorubicin, ifosfamide, and platinum. Long-term effects of such regimens include the following3:
- Azospermia (in 100% of patients who received a total ifosfamide dose > 75 g/m2)
- Subclinical renal impairment (in 48% of patients treated with high doses of ifosfamide)
- Hearing impairment (in 40% of patients treated with cisplatin)
- Second malignancies (in 2.1%)
- Cardiomyopathy (in 1.7%).3
In light of this, the development of equally effective but less intensive regimens for patients whose disease carries a better prognosis is highly desirable. Ongoing clinical trials are investigating this strategy.
Metastatic disease. Metastatic osteosarcoma is found in approximately 20% of patients at the time of diagnosis. Sarcoma mainly spreads hematogenously, and the lungs are the most common initial site of metastases, being affected in more than 60% of patients who develop metastatic disease.9 Patients with metachronous lung lesions are initially considered for aggressive treatment with neoadjuvant chemotherapy and subsequent resection of clinically apparent disease, which results in event-free survival rates of 20% to 30%.3
Patients with disease limited to the primary tumor and no more than one or two bone lesions fare best. The presence of multiple metastases is associated with the poorest prognosis, as few patients with this profile live past 2 years.10 In a review of 202 pediatric and adult patients with documented metastases at the time of osteosarcoma diagnosis, the presence of more than 5 metastatic lesions (which was reported in 91 patients) was associated with a 5-year overall survival rate of 19%.9
Chemotherapy for Ewing sarcoma
Perioperative chemotherapy in patients with localized Ewing sarcoma is believed to reduce the burden of micrometastasis that is thought to be present in most patients with early-stage disease. Five-year survival rates of 50% to 72% have been reported among patients with resectable Ewing sarcoma treated perioperatively with multiagent chemotherapy.11,12 Notably, randomized trials that studied intense multiagent chemotherapy regimens (consisting of doxorubicin, cyclophosphamide, vincristine, and dactinomycin alternating with etoposide and ifosfamide) reported the best outcomes despite significant but acceptable toxicity. In a large randomized trial involving 398 patients with resectable disease, a 5-year survival rate of 72% was achieved with the above regimen, compared with 61% in patients treated with a less intense regimen that did not contain ifosfamide and etoposide (p = .01).12
Compressing these standard regimens to an every-14-day instead of every-21-day schedule improved event-free survival at 3 years from 65% to 76% (p = .028) without any significant increase in toxicity in a randomized trial involving 568 patients.13 Data on overall survival from this trial are not yet published.
Metastatic disease. Metastatic Ewing sarcoma is found in 15% to 35% of patients with newly diagnosed disease and is treated with multiagent chemotherapy; resection of residual disease is considered in good responders.3 This approach produces objective responses to therapy, but long-term survival is rare.
Toxicity. Myelodysplastic syndrome and acute myeloid leukemia are the most dreaded long-term complications of intensive multiagent chemotherapy for Ewing sarcoma and develop in up to 8% of patients.14 Additionally, ifosfamide can lead to hematuria (~12% incidence), encephalopathy (mild somnolence and hallucinations to coma), chronic renal impairment (6% incidence), and hemorrhagic cystitis (though administration of mesna and generous intravenous hydration can minimize this latter complication).15 Recent efforts are therefore focused on testing less-intensive regimens in patients who have good prognostic features.
Chondrosarcoma: No role for chemotherapy
Chondrosarcoma, which represents approximately 20% of all bone sarcomas and has a peak incidence in older adults (ie, in the sixth decade of life), is insensitive to chemotherapy. Radiotherapy is also of limited value and is reserved for patients treated in the palliative setting.16 Definitive management of chondrosarcoma involves adequate surgical resection alone.
SOFT-TISSUE SARCOMAS
Aside from recent advances in the treatment of gastrointestinal stromal tumors with the small-molecule tyrosine kinase inhibitors imatinib and sunitinib (which are beyond the scope of this article), an overall survival advantage with chemotherapy has not been demonstrated in adults with soft-tissue sarcoma.17
Resectable disease
The decision to use chemotherapy needs to be weighed against the magnitude of potential clinical benefit and the acute and chronic toxicities that can develop.
Toxicity. Chemotherapy regimens with activity against soft-tissue sarcomas often contain anthracyclines, alkylating agents, and taxanes. These agents can produce serious long-term toxicities, which is especially important in patients treated with curative intent. Doxorubicin and other anthracyclines, for example, may result in cardiomyopathy, the risk of which rises with increasing cumulative dose.18 In addition, acute myeloid leukemia may develop in 2% to 12% of patients treated with anthracyclines or alkylating agents such as ifosfamide and dacarbazine.3,19 Renal failure and an elevated risk of bladder carcinoma are uncommonly reported in patients with a history of ifosfamide treatment.15 Sensory neuropathy associated with the use of taxanes (eg, paclitaxel and docetaxel) is dose dependent and reversible in more than half of patients. However, some patients treated with high doses of these agents can have persistent symptoms of paresthesias, burning, and decreased reflexes, which can be debilitating.20
Efficacy of adjuvant chemotherapy. Because chemotherapy puts patients at risk of such serious chronic toxicities, its use can be justified only if it results in significant benefit, such as prolongation of survival. A 1997 meta-analysis of 14 clinical trials evaluating adjuvant chemotherapy in patients with resectable soft-tissue sarcomas found chemotherapy to have an absolute benefit of 10% in recurrence-free survival at 10 years (ie, from 45% survival to 55% survival), with a hazard ratio of 0.75 (95% confidence interval [CI], 0.64–0.87; p = .0001) for recurrence or death.21 However, when the analysis was limited to overall survival at 10 years, the survival difference between patients who received adjuvant chemotherapy and those who did not (54% vs 50%, respectively) was not statistically significant (hazard ratio = 0.89; 95% CI, 0.76–1.03, p = .12).21
The concept of adjuvant therapy has been revisited since the antisarcoma activity of ifosfamide was established. A large European trial randomized 351 patients with resected soft-tissue sarcoma either to placebo or to doxorubicin and ifosfamide given every 21 days.22 The preliminary results, reported in abstract form at the 2007 annual meeting of the American Society of Clinical Oncology, showed a higher 5-year survival rate in the placebo arm (69%) compared with the chemotherapy arm (64%).22 This and other trials using ifosfamide in various drug combinations showed no difference in survival, suggesting that adjuvant chemotherapy should not be considered to be standard practice outside of a clinical trial.
Efficacy of neoadjuvant chemotherapy. Neoadjuvant chemotherapy also has been studied in patients with soft-tissue sarcomas. A retrospective analysis found that the greatest benefit is derived in patients with primary tumors larger than 10 cm, in whom neoadjuvant chemotherapy increased 3-year disease-specific survival from 62% to 83%.23 However, differing results came from a prospective multicenter trial that randomized patients with large primary and recurrent tumors to either surgery alone or surgery preceded by three cycles of neoadjuvant doxorubicin and ifosfamide (all patients could also receive adjuvant radiation therapy, depending on grade and adequacy of resection).24 The trial suffered from slow accrual, and only 150 patients were enrolled. At 5 years, survival was similar between the groups with and without neoadjuvant chemotherapy.24 Therefore, neoadjuvant chemotherapy is not yet recommended pending results of larger randomized trials.
No clear role for recurrent disease. Local recurrence of the primary tumor after resection occurs in 10% to 50% of cases of soft-tissue sarcoma, with the specific rate depending on the primary tumor location. The highest incidence of recurrence is found in patients with retroperitoneal and head and neck sarcoma (40% and 50%, respectively), mainly because of the difficulty of obtaining clear margins. Chemotherapy has not been well studied in this setting and is of uncertain value.3
Metastatic disease
Metastatic soft-tissue sarcomas may respond to chemotherapy, but there is a lack of evidence that chemotherapy improves overall survival. Pulmonary lesions are the most common site of distant recurrence, and resection of such metastases is sometimes undertaken in well-selected patients. However, there is no level 1 evidence supporting chemotherapy in this clinical setting despite its common preoperative use. There is a paucity of randomized phase 3 trials that compare established palliative chemotherapy regimens to best supportive care. It is believed that some groups of patients do benefit, however, including those who are young and have good performance status, low tumor grade, absence of liver metastasis or pulmonary metastasis only, and a long interval between treatment of the primary tumor and development of metastatic disease.3 Some histologies, such as uterine leiomyosarcomas and facial/scalp angiosarcomas, respond better to chemotherapy.17
Drugs found to have activity against metastatic sarcoma include doxorubicin, ifosfamide, platinum agents, gemcitabine, taxanes, and dacarbazine. Used either alone or in combinations, these drugs produce responses (ie, shrink metastatic tumors) in about 13% to 33% of patients.3 Use of chemotherapy is frequently curtailed by the acute toxicity of these agents, which includes pancytopenia, transfusion requirements, febrile neutropenia, nausea, alopecia, and significant fatigue, as well as renal failure with ifosfamide or cisplatin and peripheral neuropathy with platinum agents or taxanes. Appropriate patient selection for chemotherapy and exclusion of those who should be managed solely with best supportive care is an important challenge that oncologists often face when managing patients with metastatic soft-tissue sarcoma.
Future directions
Trabectedin (ET-743) is a novel compound with promising activity against soft-tissue sarcomas that acts by inhibiting cell-cycle transition from the G2 to M stages. The drug covalently binds to the minor grove of the DNA molecule, changing its three-dimensional structure and impairing transcription and possibly DNA repair.25 Phase 2 studies showed durable responses to trabectedin in 3% to 8% of heavily pretreated patients26–28 and in 17% of treatment-naïve patients with advanced soft-tissue sarcomas.25 Time to progression of up to 20 months has been reported in patients who respond or develop stable disease.3
Toxic effects of trabectedin include myelosuppression, fever, edema, arthralgias, hepatotoxicity, and (rarely) rhabdomyolysis. To date, these toxicities have been self-limiting. Larger clinical trials and longer follow-up is needed to assess whether this agent has any significant long-term toxicities.
Trabectedin has already been approved in Europe for treatment of chemotherapy-refractory soft-tissue sarcoma when given as a 24-hour infusion every 21 days.
More broadly, an active effort is under way to better understand the molecular derangements in a variety of soft-tissue sarcoma subtypes. The hope is that this understanding will lead to improved therapies that target aberrant proliferation, angiogenesis, and other biologic processes that drive the growth and metastasis of soft-tissue and bone sarcomas.
Surgical resection is the mainstay of treatment for musculoskeletal sarcomas, as detailed earlier in this supplement, but chemotherapy also has a proven role in the primary therapy of most bone sarcomas and a potential role for some patients with soft-tissue sarcomas. This article provides an overview of the roles of chemotherapy for patients with bone and soft-tissue sarcomas and addresses key considerations surrounding chemotherapy in the context of overall patient management.
BONE SARCOMAS
Because most bone sarcomas occur in pediatric patients and young adults, studies of chemotherapy in this disease have often enrolled predominantly young subjects. As a result, very limited data are available in older adults. Single-institution experiences indicate that adults with bone sarcomas have inferior outcomes compared with their pediatric and adolescent counterparts,1 but the literature on these tumors in adults is scant. Therefore, the following discussion on chemotherapy for bone sarcomas incorporates data from trials conducted predominantly in children and young adults (ie, generally younger than 30 years and with a very large majority younger than 20 years).
Chemotherapy for osteosarcoma
At present, neoadjuvant (preoperative) chemotherapy followed by definitive resection with subsequent adjuvant (postoperative) chemotherapy is the well-established approach to treatment of localized osteosarcomas. Chemotherapy can eradicate the micrometastatic disease that is believed to be present in the majority of patients with clinically resectable cancer.2
Efficacy. Historically, prior to the institution of effective chemotherapy, metastatic disease developed in 80% to 90% of patients who underwent curative resection with or without radiation therapy, which resulted in a long-term survival rate of less than 20%.3 In the 1980s, clinical trials that randomized patients with resectable osteosarcoma to surgery alone or to surgery plus chemotherapy found that the addition of perioperative chemotherapy led to significant improvements in recurrence rates and survival.4,5 More recent randomized trials have shown that treatment of such patients with modern multiagent chemotherapy regimens results in a 5-year survival rate of approximately 70%.6 Additionally, response to neoadjuvant (preoperative) treatment has become the most important predictor of outcome, as the median survival of osteosarcoma patients who have greater than 90% necrosis in the resected specimen following neoadjuvant chemotherapy is about 90% at 5 years.7,8
Toxicity. Current chemotherapy regimens are based on high doses of methotrexate and leucovorin in combination with doxorubicin, ifosfamide, and platinum. Long-term effects of such regimens include the following3:
- Azospermia (in 100% of patients who received a total ifosfamide dose > 75 g/m2)
- Subclinical renal impairment (in 48% of patients treated with high doses of ifosfamide)
- Hearing impairment (in 40% of patients treated with cisplatin)
- Second malignancies (in 2.1%)
- Cardiomyopathy (in 1.7%).3
In light of this, the development of equally effective but less intensive regimens for patients whose disease carries a better prognosis is highly desirable. Ongoing clinical trials are investigating this strategy.
Metastatic disease. Metastatic osteosarcoma is found in approximately 20% of patients at the time of diagnosis. Sarcoma mainly spreads hematogenously, and the lungs are the most common initial site of metastases, being affected in more than 60% of patients who develop metastatic disease.9 Patients with metachronous lung lesions are initially considered for aggressive treatment with neoadjuvant chemotherapy and subsequent resection of clinically apparent disease, which results in event-free survival rates of 20% to 30%.3
Patients with disease limited to the primary tumor and no more than one or two bone lesions fare best. The presence of multiple metastases is associated with the poorest prognosis, as few patients with this profile live past 2 years.10 In a review of 202 pediatric and adult patients with documented metastases at the time of osteosarcoma diagnosis, the presence of more than 5 metastatic lesions (which was reported in 91 patients) was associated with a 5-year overall survival rate of 19%.9
Chemotherapy for Ewing sarcoma
Perioperative chemotherapy in patients with localized Ewing sarcoma is believed to reduce the burden of micrometastasis that is thought to be present in most patients with early-stage disease. Five-year survival rates of 50% to 72% have been reported among patients with resectable Ewing sarcoma treated perioperatively with multiagent chemotherapy.11,12 Notably, randomized trials that studied intense multiagent chemotherapy regimens (consisting of doxorubicin, cyclophosphamide, vincristine, and dactinomycin alternating with etoposide and ifosfamide) reported the best outcomes despite significant but acceptable toxicity. In a large randomized trial involving 398 patients with resectable disease, a 5-year survival rate of 72% was achieved with the above regimen, compared with 61% in patients treated with a less intense regimen that did not contain ifosfamide and etoposide (p = .01).12
Compressing these standard regimens to an every-14-day instead of every-21-day schedule improved event-free survival at 3 years from 65% to 76% (p = .028) without any significant increase in toxicity in a randomized trial involving 568 patients.13 Data on overall survival from this trial are not yet published.
Metastatic disease. Metastatic Ewing sarcoma is found in 15% to 35% of patients with newly diagnosed disease and is treated with multiagent chemotherapy; resection of residual disease is considered in good responders.3 This approach produces objective responses to therapy, but long-term survival is rare.
Toxicity. Myelodysplastic syndrome and acute myeloid leukemia are the most dreaded long-term complications of intensive multiagent chemotherapy for Ewing sarcoma and develop in up to 8% of patients.14 Additionally, ifosfamide can lead to hematuria (~12% incidence), encephalopathy (mild somnolence and hallucinations to coma), chronic renal impairment (6% incidence), and hemorrhagic cystitis (though administration of mesna and generous intravenous hydration can minimize this latter complication).15 Recent efforts are therefore focused on testing less-intensive regimens in patients who have good prognostic features.
Chondrosarcoma: No role for chemotherapy
Chondrosarcoma, which represents approximately 20% of all bone sarcomas and has a peak incidence in older adults (ie, in the sixth decade of life), is insensitive to chemotherapy. Radiotherapy is also of limited value and is reserved for patients treated in the palliative setting.16 Definitive management of chondrosarcoma involves adequate surgical resection alone.
SOFT-TISSUE SARCOMAS
Aside from recent advances in the treatment of gastrointestinal stromal tumors with the small-molecule tyrosine kinase inhibitors imatinib and sunitinib (which are beyond the scope of this article), an overall survival advantage with chemotherapy has not been demonstrated in adults with soft-tissue sarcoma.17
Resectable disease
The decision to use chemotherapy needs to be weighed against the magnitude of potential clinical benefit and the acute and chronic toxicities that can develop.
Toxicity. Chemotherapy regimens with activity against soft-tissue sarcomas often contain anthracyclines, alkylating agents, and taxanes. These agents can produce serious long-term toxicities, which is especially important in patients treated with curative intent. Doxorubicin and other anthracyclines, for example, may result in cardiomyopathy, the risk of which rises with increasing cumulative dose.18 In addition, acute myeloid leukemia may develop in 2% to 12% of patients treated with anthracyclines or alkylating agents such as ifosfamide and dacarbazine.3,19 Renal failure and an elevated risk of bladder carcinoma are uncommonly reported in patients with a history of ifosfamide treatment.15 Sensory neuropathy associated with the use of taxanes (eg, paclitaxel and docetaxel) is dose dependent and reversible in more than half of patients. However, some patients treated with high doses of these agents can have persistent symptoms of paresthesias, burning, and decreased reflexes, which can be debilitating.20
Efficacy of adjuvant chemotherapy. Because chemotherapy puts patients at risk of such serious chronic toxicities, its use can be justified only if it results in significant benefit, such as prolongation of survival. A 1997 meta-analysis of 14 clinical trials evaluating adjuvant chemotherapy in patients with resectable soft-tissue sarcomas found chemotherapy to have an absolute benefit of 10% in recurrence-free survival at 10 years (ie, from 45% survival to 55% survival), with a hazard ratio of 0.75 (95% confidence interval [CI], 0.64–0.87; p = .0001) for recurrence or death.21 However, when the analysis was limited to overall survival at 10 years, the survival difference between patients who received adjuvant chemotherapy and those who did not (54% vs 50%, respectively) was not statistically significant (hazard ratio = 0.89; 95% CI, 0.76–1.03, p = .12).21
The concept of adjuvant therapy has been revisited since the antisarcoma activity of ifosfamide was established. A large European trial randomized 351 patients with resected soft-tissue sarcoma either to placebo or to doxorubicin and ifosfamide given every 21 days.22 The preliminary results, reported in abstract form at the 2007 annual meeting of the American Society of Clinical Oncology, showed a higher 5-year survival rate in the placebo arm (69%) compared with the chemotherapy arm (64%).22 This and other trials using ifosfamide in various drug combinations showed no difference in survival, suggesting that adjuvant chemotherapy should not be considered to be standard practice outside of a clinical trial.
Efficacy of neoadjuvant chemotherapy. Neoadjuvant chemotherapy also has been studied in patients with soft-tissue sarcomas. A retrospective analysis found that the greatest benefit is derived in patients with primary tumors larger than 10 cm, in whom neoadjuvant chemotherapy increased 3-year disease-specific survival from 62% to 83%.23 However, differing results came from a prospective multicenter trial that randomized patients with large primary and recurrent tumors to either surgery alone or surgery preceded by three cycles of neoadjuvant doxorubicin and ifosfamide (all patients could also receive adjuvant radiation therapy, depending on grade and adequacy of resection).24 The trial suffered from slow accrual, and only 150 patients were enrolled. At 5 years, survival was similar between the groups with and without neoadjuvant chemotherapy.24 Therefore, neoadjuvant chemotherapy is not yet recommended pending results of larger randomized trials.
No clear role for recurrent disease. Local recurrence of the primary tumor after resection occurs in 10% to 50% of cases of soft-tissue sarcoma, with the specific rate depending on the primary tumor location. The highest incidence of recurrence is found in patients with retroperitoneal and head and neck sarcoma (40% and 50%, respectively), mainly because of the difficulty of obtaining clear margins. Chemotherapy has not been well studied in this setting and is of uncertain value.3
Metastatic disease
Metastatic soft-tissue sarcomas may respond to chemotherapy, but there is a lack of evidence that chemotherapy improves overall survival. Pulmonary lesions are the most common site of distant recurrence, and resection of such metastases is sometimes undertaken in well-selected patients. However, there is no level 1 evidence supporting chemotherapy in this clinical setting despite its common preoperative use. There is a paucity of randomized phase 3 trials that compare established palliative chemotherapy regimens to best supportive care. It is believed that some groups of patients do benefit, however, including those who are young and have good performance status, low tumor grade, absence of liver metastasis or pulmonary metastasis only, and a long interval between treatment of the primary tumor and development of metastatic disease.3 Some histologies, such as uterine leiomyosarcomas and facial/scalp angiosarcomas, respond better to chemotherapy.17
Drugs found to have activity against metastatic sarcoma include doxorubicin, ifosfamide, platinum agents, gemcitabine, taxanes, and dacarbazine. Used either alone or in combinations, these drugs produce responses (ie, shrink metastatic tumors) in about 13% to 33% of patients.3 Use of chemotherapy is frequently curtailed by the acute toxicity of these agents, which includes pancytopenia, transfusion requirements, febrile neutropenia, nausea, alopecia, and significant fatigue, as well as renal failure with ifosfamide or cisplatin and peripheral neuropathy with platinum agents or taxanes. Appropriate patient selection for chemotherapy and exclusion of those who should be managed solely with best supportive care is an important challenge that oncologists often face when managing patients with metastatic soft-tissue sarcoma.
Future directions
Trabectedin (ET-743) is a novel compound with promising activity against soft-tissue sarcomas that acts by inhibiting cell-cycle transition from the G2 to M stages. The drug covalently binds to the minor grove of the DNA molecule, changing its three-dimensional structure and impairing transcription and possibly DNA repair.25 Phase 2 studies showed durable responses to trabectedin in 3% to 8% of heavily pretreated patients26–28 and in 17% of treatment-naïve patients with advanced soft-tissue sarcomas.25 Time to progression of up to 20 months has been reported in patients who respond or develop stable disease.3
Toxic effects of trabectedin include myelosuppression, fever, edema, arthralgias, hepatotoxicity, and (rarely) rhabdomyolysis. To date, these toxicities have been self-limiting. Larger clinical trials and longer follow-up is needed to assess whether this agent has any significant long-term toxicities.
Trabectedin has already been approved in Europe for treatment of chemotherapy-refractory soft-tissue sarcoma when given as a 24-hour infusion every 21 days.
More broadly, an active effort is under way to better understand the molecular derangements in a variety of soft-tissue sarcoma subtypes. The hope is that this understanding will lead to improved therapies that target aberrant proliferation, angiogenesis, and other biologic processes that drive the growth and metastasis of soft-tissue and bone sarcomas.
- Meyers PA, Heller G, Healey J, et al. Chemotherapy for nonmetastatic osteogenic sarcoma: the Memorial Sloan-Kettering experience. J Clin Oncol 1992; 10:5–15.
- Bruland OS, Høifødt H, Saeter G, Smeland S, Fodstad O. Hematogenous micrometastases in osteosarcoma patients. Clin Cancer Res 2005; 11:4666–4673.
- Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ, eds. Cancer Management: A Multidisciplinary Approach. 11th ed. Manhasset, NY: CMP Medica; 2009.
- Link MP, Goorin AM, Miser AW, et al. The effect of adjuvant chemotherapy on relapse-free survival in patients with osteosarcoma of the extremity. N Engl J Med 1986; 314:1600–1606.
- Eilber F, Giuliano A, Eckardt J, Patterson K, Moseley S, Goodnight J. Adjuvant chemotherapy for osteosarcoma: a randomized prospective trial. J Clin Oncol 1987; 5:21–26.
- Meyers PA, Schwartz CL, Krailo M, et al. Osteosarcoma: a randomized, prospective trial of the addition of ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate. J Clin Oncol 2005; 23:2004–2011.
- Winkler K, Beron G, Delling G, et al. Neoadjuvant chemotherapy of osteosarcomas: results of a randomized cooperative trial (COSS-82) with salvage chemotherapy based on histological tumor response. J Clin Oncol 1988; 6:329–337.
- Bramwell VH, Steward WP, Nooij M, et al. Neoadjuvant chemotherapy with doxorubicin and cisplatin in malignant fibrous histiocytoma of bone: a European Osteosarcoma Intergroup study. J Clin Oncol 1999; 17:3260–3269.
- Kager L, Zoubek A, Pötschger U, et al. Primary metastatic osteosarcoma: presentation and outcome of patients treated on Neoadjuvant Cooperative Osteosarcoma Study Group protocols. J Clin Oncol 2003; 21:2011–2018.
- Longhi A, Fabbri N, Donati D, et al. Neoadjuvant chemotherapy for patients with synchronous multifocal osteosarcoma: results in eleven cases. J Chemother 2001; 13:324–330.
- Nesbit ME Jr, Gehan EA, Burgert EO Jr, et al. Multimodal therapy for the management of primary, nonmetastatic Ewing’s sarcoma of bone: a long-term follow-up of the First Intergroup study. J Clin Oncol 1990; 8:1664–1674.
- Grier HE, Krailo MD, Tarbell NJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med 2003; 348:694–701.
- Womer RB, West DC, Krailo MD, et al; for the Children’s Oncology Group AEWS0031 Committee. Randomized comparison of every-two-week v. every-three-week chemotherapy in Ewing sarcoma family tumors. J Clin Oncol 2008; 26(May 20 suppl):10504. Abstract.
- Rodriguez-Galindo C, Poquette CA, Marina NM, et al. Hematologic abnormalities and acute myeloid leukemia in children and adolescents administered intensified chemotherapy for the Ewing sarcoma family of tumors. J Pediatr Hematol Oncol 2000; 22:321–329.
- Brade WP, Herdrich, K, Kachel-Fischer U, Araujo CE. Dosing and side-effects of ifosfamide plus mesna. J Cancer Res Clin Oncol 1991; 117(suppl 4):S164–S186.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Clark MA, Fisher C, Judson I, Thomas JM. Soft-tissue sarcomas in adults. N Engl J Med 2005; 353:701–711.
- Alexander J, Dainiak N, Berger HJ, et al. Serial assessment of doxorubicin cardiotoxicity with quantitative radionuclide angiocardiography. N Engl J Med 1979; 300:278–283.
- Felix CA. Secondary leukemias induced by topoisomerase-targeted drugs. Biochim Biophys Acta 1998; 1400:233–255.
- Postma TJ, Vermorken JB, Liefting AJ, Pinedo HM, Heimans JJ. Paclitaxel-induced neuropathy. Ann Oncol 1995; 6:489–494.
- Sarcoma Meta-analysis Collaboration. Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet 1997; 350:1647–1654.
- Woll PJ, van Glabbeke M, Hohenberger P, et al. Adjuvant chemotherapy (CT) with doxorubicin and ifosfamide in resected soft tissue sarcoma (STS): interim analysis of a randomised phase III trial. J Clin Oncol 2007; 25(June 20 suppl):10008. Abstract.
- Grobmyer SR, Maki RG, Demetri GD, et al. Neo-adjuvant chemotherapy for primary high-grade extremity soft tissue sarcoma. Ann Oncol 2004; 15:1667–1672.
- Gortzak E, Azzarelli A, Buesa J, et al. A randomised phase II study on neo-adjuvant chemotherapy for ‘high-risk’ adult soft-tissue sarcoma. Eur J Cancer 2001; 37:1096–1103.
- Garcia-Carbonero R, Supko JG, Maki RG, et al. Ecteinascidin-743 (ET-743) for chemotherapy-naive patients with advanced soft tissue sarcomas: multicenter phase II and pharmacokinetic study. J Clin Oncol 2005; 23:5484–5492.
- Yovine A, Riofrio M, Blay JY, et al. Phase II study of ecteinascidin-743 in advanced pretreated soft tissue sarcoma patients. J Clin Oncol 2004; 22:890–899.
- Garcia-Carbonero R, Supko JG, Manola J, et al. Phase II and pharmacokinetic study of ecteinascidin 743 in patients with progressive sarcomas of soft tissues refractory to chemotherapy. J Clin Oncol 2004; 22:1480–1490.
- Le Cesne A, Blay JY, Judson I, et al. Phase II study of ET-743 in advanced soft tissue sarcomas: a European Organisation for the Research and Treatment of Cancer (EORTC) soft tissue and bone sarcoma group trial. J Clin Oncol 2005; 23:576–584.
- Meyers PA, Heller G, Healey J, et al. Chemotherapy for nonmetastatic osteogenic sarcoma: the Memorial Sloan-Kettering experience. J Clin Oncol 1992; 10:5–15.
- Bruland OS, Høifødt H, Saeter G, Smeland S, Fodstad O. Hematogenous micrometastases in osteosarcoma patients. Clin Cancer Res 2005; 11:4666–4673.
- Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ, eds. Cancer Management: A Multidisciplinary Approach. 11th ed. Manhasset, NY: CMP Medica; 2009.
- Link MP, Goorin AM, Miser AW, et al. The effect of adjuvant chemotherapy on relapse-free survival in patients with osteosarcoma of the extremity. N Engl J Med 1986; 314:1600–1606.
- Eilber F, Giuliano A, Eckardt J, Patterson K, Moseley S, Goodnight J. Adjuvant chemotherapy for osteosarcoma: a randomized prospective trial. J Clin Oncol 1987; 5:21–26.
- Meyers PA, Schwartz CL, Krailo M, et al. Osteosarcoma: a randomized, prospective trial of the addition of ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate. J Clin Oncol 2005; 23:2004–2011.
- Winkler K, Beron G, Delling G, et al. Neoadjuvant chemotherapy of osteosarcomas: results of a randomized cooperative trial (COSS-82) with salvage chemotherapy based on histological tumor response. J Clin Oncol 1988; 6:329–337.
- Bramwell VH, Steward WP, Nooij M, et al. Neoadjuvant chemotherapy with doxorubicin and cisplatin in malignant fibrous histiocytoma of bone: a European Osteosarcoma Intergroup study. J Clin Oncol 1999; 17:3260–3269.
- Kager L, Zoubek A, Pötschger U, et al. Primary metastatic osteosarcoma: presentation and outcome of patients treated on Neoadjuvant Cooperative Osteosarcoma Study Group protocols. J Clin Oncol 2003; 21:2011–2018.
- Longhi A, Fabbri N, Donati D, et al. Neoadjuvant chemotherapy for patients with synchronous multifocal osteosarcoma: results in eleven cases. J Chemother 2001; 13:324–330.
- Nesbit ME Jr, Gehan EA, Burgert EO Jr, et al. Multimodal therapy for the management of primary, nonmetastatic Ewing’s sarcoma of bone: a long-term follow-up of the First Intergroup study. J Clin Oncol 1990; 8:1664–1674.
- Grier HE, Krailo MD, Tarbell NJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med 2003; 348:694–701.
- Womer RB, West DC, Krailo MD, et al; for the Children’s Oncology Group AEWS0031 Committee. Randomized comparison of every-two-week v. every-three-week chemotherapy in Ewing sarcoma family tumors. J Clin Oncol 2008; 26(May 20 suppl):10504. Abstract.
- Rodriguez-Galindo C, Poquette CA, Marina NM, et al. Hematologic abnormalities and acute myeloid leukemia in children and adolescents administered intensified chemotherapy for the Ewing sarcoma family of tumors. J Pediatr Hematol Oncol 2000; 22:321–329.
- Brade WP, Herdrich, K, Kachel-Fischer U, Araujo CE. Dosing and side-effects of ifosfamide plus mesna. J Cancer Res Clin Oncol 1991; 117(suppl 4):S164–S186.
- Healey JH, Lane JM. Chondrosarcoma. Clin Orthop Relat Res 1986; 204:119–129.
- Clark MA, Fisher C, Judson I, Thomas JM. Soft-tissue sarcomas in adults. N Engl J Med 2005; 353:701–711.
- Alexander J, Dainiak N, Berger HJ, et al. Serial assessment of doxorubicin cardiotoxicity with quantitative radionuclide angiocardiography. N Engl J Med 1979; 300:278–283.
- Felix CA. Secondary leukemias induced by topoisomerase-targeted drugs. Biochim Biophys Acta 1998; 1400:233–255.
- Postma TJ, Vermorken JB, Liefting AJ, Pinedo HM, Heimans JJ. Paclitaxel-induced neuropathy. Ann Oncol 1995; 6:489–494.
- Sarcoma Meta-analysis Collaboration. Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet 1997; 350:1647–1654.
- Woll PJ, van Glabbeke M, Hohenberger P, et al. Adjuvant chemotherapy (CT) with doxorubicin and ifosfamide in resected soft tissue sarcoma (STS): interim analysis of a randomised phase III trial. J Clin Oncol 2007; 25(June 20 suppl):10008. Abstract.
- Grobmyer SR, Maki RG, Demetri GD, et al. Neo-adjuvant chemotherapy for primary high-grade extremity soft tissue sarcoma. Ann Oncol 2004; 15:1667–1672.
- Gortzak E, Azzarelli A, Buesa J, et al. A randomised phase II study on neo-adjuvant chemotherapy for ‘high-risk’ adult soft-tissue sarcoma. Eur J Cancer 2001; 37:1096–1103.
- Garcia-Carbonero R, Supko JG, Maki RG, et al. Ecteinascidin-743 (ET-743) for chemotherapy-naive patients with advanced soft tissue sarcomas: multicenter phase II and pharmacokinetic study. J Clin Oncol 2005; 23:5484–5492.
- Yovine A, Riofrio M, Blay JY, et al. Phase II study of ecteinascidin-743 in advanced pretreated soft tissue sarcoma patients. J Clin Oncol 2004; 22:890–899.
- Garcia-Carbonero R, Supko JG, Manola J, et al. Phase II and pharmacokinetic study of ecteinascidin 743 in patients with progressive sarcomas of soft tissues refractory to chemotherapy. J Clin Oncol 2004; 22:1480–1490.
- Le Cesne A, Blay JY, Judson I, et al. Phase II study of ET-743 in advanced soft tissue sarcomas: a European Organisation for the Research and Treatment of Cancer (EORTC) soft tissue and bone sarcoma group trial. J Clin Oncol 2005; 23:576–584.
Use of radiation therapy for patients with soft-tissue and bone sarcomas
While radiation therapy (RT) has an integral role in the management of soft-tissue sarcoma, it has a limited role in that of bone sarcoma, with few exceptions (ie, Ewing sarcoma). In keeping with the rarity of these tumors, it has been demonstrated that patients treated at high-volume centers have significantly better survival and functional outcomes.1–3 Accordingly, treatment should be delivered by a multidisciplinary team including orthopedic, medical, and radiation oncologists, as well as plastic and reconstructive surgeons, physical therapy specialists, and pathologists and radiologists with expertise in musculoskeletal sarcomas.4 As the preceding articles in this supplement have addressed the major modalities in the treatment of sarcomas other than RT, this article will focus on how RT fits into the overall management mix, with a focus on soft-tissue sarcomas, where it figures most prominently.
BONE SARCOMAS: A LIMITED ROLE FOR RADIATION
The role of RT in the management of bone sarcomas is limited. Its primary application appears to be in Ewing sarcoma, for which curative treatment requires combined local and systemic therapy. For definitive therapy, limb-salvage surgery is preferable over amputation, but amputation may be an option for younger patients with lesions of the fibula, tibia, and foot. Based on the available data, postoperative RT is probably of benefit for all patients with Ewing sarcoma with close margins and/or those with a poor histologic response.5 Further discussion of Ewing sarcoma management is beyond the scope of this article (see the second and fifth articles in this supplement).
For osteosarcoma, the current standard of care is surgical resection combined with neoadjuvant and adjuvant chemotherapy. RT had been used years ago, prior to the advent of effective chemotherapy regimens, but its use for osteosarcoma has now been relegated to a few select situations. These include lesions not amenable to surgical resection and reconstruction, cases in which the patient refuses surgery, cases where there are positive margins after resection, and cases where palliation is needed for symptomatic lesions.
SOFT-TISSUE SARCOMAS: RADIATION HAS A CLEAR ADJUVANT ROLE
The primary management of localized soft-tissue sarcomas is surgical resection to achieve a negative margin when feasible. Historically, local excision of soft-tissue sarcomas resulted in local failure rates of 50% to 70%, even when a margin of normal tissue around the tumor was excised. As a result, amputation became standard treatment.6 In a landmark National Cancer Institute study 3 decades ago, patients were randomized to amputation or to limb-sparing surgery with the addition of RT.7 Notably, disease-free and overall survival were not compromised by limb-sparing surgery plus RT, demonstrating that although lesser surgery in the absence of RT may be insufficient, limb-sparing surgery with RT was equal to amputation. Consequently, limb-sparing approaches have become the favored surgery for the majority of cases of soft-tissue sarcoma, as advocated in a consensus statement from the National Institutes of Health.1
Indications vary by lesion grade
In general, adjuvant RT is recommended for all intermediate- and high-grade soft-tissue sarcoma lesions. A potential exception is a superficial tumor smaller than 5 cm with widely negative margins after resection. For low-grade lesions, re-excision is favored over adjuvant RT for positive or close margins, and RT is avoided in the setting of negative margins.
Optimal timing of radiation remains unclear
The optimal timing of adjuvant RT—preoperative versus postoperative—remains unknown. The relative advantages of preoperative RT include smaller and well-defined treatment volume, ability to use a lower dose, lack of tissue hypoxia, increased tumor resectability (smaller surgery), and improved limb function with less late fibrosis and edema. The disadvantages include inability to precisely stage patients and higher risk of acute wound-healing complications.
The National Cancer Institute of Canada compared outcomes with preoperative versus postoperative RT among 190 patients with soft-tissue sarcoma in a prospective randomized trial.8 Patients were stratified by tumor size (≤ 10 cm or > 10cm) and then randomized to preoperative RT (50 Gy in 25 fractions) or postoperative RT (66 Gy in 33 fractions).8 There was no difference between the groups in local control, distant control, or survival rates, but a higher rate of late complications, including fibrosis and edema, was observed with postoperative RT.8,9 On the other hand, the incidence of wound complications was higher in the preoperative group (35%) than in the postoperative group (17%).8
Likewise, the optimal sequencing and benefits of systemic therapy (chemotherapy) with relation to local therapy (surgery with pre- or postoperative RT) remain unclear. More than a dozen individual randomized trials of adjuvant chemotherapy, as well as a meta-analysis of 14 trials of doxorubicin-based adjuvant chemotherapy, have failed to demonstrate significant improvement in overall survival in patients with soft-tissue sarcomas.10 With regard to neoadjuvant chemotherapy for soft-tissue sarcomas, there are studies suggesting improvement in local control but no consistent survival benefit.11 Chemotherapy may yield a benefit in select cases, as detailed elsewhere in this supplement.
MECHANISMS OF ACTION: DIRECT AND INDIRECT
In simplified terms, radiation kills cancer cells through two basic mechanisms: indirect and direct.
The indirect effect (the most common mechanism) results from the generation of free radicals in the intracellular medium via ionization by photons. Free radicals, in turn, deposit large amounts of energy that damage DNA or some other vital component of the cell, resulting in cell death.
The direct effect is a consequence of photons themselves interacting directly with the cell in a lethal manner.
The goal of RT is to kill tumor cells selectively, without irreversibly injuring adjacent normal tissue. This is done by exploiting two abnormal aspects of tumor behavior: decreased ability for repair and increased susceptibility to ionizing radiation damage. Tumors are generally less able than normal tissue to repair DNA damage, owing to defective repair mechanisms. Tumor cells are also comparatively more radiosensitive than normal tissues, as they are more frequently in radiosensitive cell-cycle phases. Thus, dividing the radiation dose into a number of treatment fractions provides two advantages that further exploit the biologic differences between tumor and normal tissue: it allows DNA repair to take place within the normal tissues, and it allows proliferating tumor cells to redistribute through the cell cycle and move into the more radiosensitive phases.
TREATMENT PLANNING
Treatment simulation
Following initial consultation with a radiation oncologist, the eligible patient undergoes a simulation, or a treatment planning session in which he or she is positioned so as to allow treatment to be carefully designed and subsequently delivered with precision. This typically requires fabrication of a customized immobilization device to allow for consistent positioning over the treatment course. Sarcomas require that special care be taken to properly immobilize both the proximal and distal joints. Additionally, radiopaque wires are used to delineate the anatomic boundaries of the tumor or scar. Computed tomographic (CT) scans are then obtained to enable image-based three-dimensional treatment planning. The patient setup is photographed, and setup indicators are recorded and marked on the patient’s skin, some with freckle-size tattoos and some with indelible marker.
The treatment fields are then designed on the CT-simulation data set with the aid of virtual reality–type techniques. In addition to delineation of tumor volumes, three-dimensional treatment planning is used to contour all nearby normal structures on each slice. The resulting structures can then be used to specify dose constraints and help determine the optimal beam geometries to ensure proper tumor coverage and minimize the potential for side effects by reducing the dose to organs at risk. In the case of sarcomas, several strategies for reducing the risk of side effects are especially relevant: (1) carefully sparing a portion of the circumference of uninvolved bone to minimize the risk of fractures; (2) carefully sparing a strip of normal tissue to minimize edema by permitting undisrupted lymphatic drainage from the extremity; and (3) keeping dosing to joint spaces and other adjacent organs below tissue tolerances as defined by Emami et al.12
Determining target volume
The target volume for RT is determined on the basis of physical examination, radiologic studies, anatomical considerations, and the natural history of the sarcoma.
In the preoperative setting, longitudinal margins of 5 cm beyond the tumor and tumor-associated edema and radial margins of 2 cm are treated to 50 Gy in 25 fractions. Surgery is undertaken approximately 4 weeks after completion of RT to allow for repair in normal tissues and minimize operative and postoperative complications. Following surgery, an RT boost may be added for positive margins (16 Gy) or gross residual disease (25 Gy).
In the postoperative setting, details on the extent of dissection or observations from the surgeons themselves must be considered. Information regarding the surgical approach must be noted and can influence the effectiveness of postoperative RT as well as the incidence of late side effects. When experienced surgeons are involved, scars and drain sites, which are at risk for subclinical disease, can be planned so that their inclusion in the RT portal allows for sparing a strip of skin to minimize complications. Surgical clip placement at the boundaries of the tumor bed also facilitates RT planning.13 Finally, prophylactic bone stabilization may reduce the risk of subsequent fracture in cases where circumferential bone radiation in high-risk sites is anticipated.
Recommendations on the volume that must be treated vary among different authorities. Some advocate treating the entire compartment because of the risk for microscopic seeding.14 Others recommend margins around the tumor or tumor bed ranging from less than 5 cm up to 15 cm.15 Most often the postoperative approach is to include the resection bed with a 2-cm radial margin, the incision, and any drain sites in the initial treatment volume and to base the longitudinal margin on the grade and size of the primary tumor (5–15 cm). This volume is treated to 50 Gy in 25 fractions followed by two sequential reductions in field size, with the total dose determined by the extent of resection: 60 Gy for negative margins, 66 Gy for microscopically positive margins, and 75 Gy for gross residual disease.
TREATMENT DELIVERY
Once treatment planning is completed, treatments begin and are given daily Monday through Friday. Each day, the patient is positioned in the immobilization device, the field measurements are set, and positioning is checked with measurement tools and external marking of the field borders on the skin. Daily image guidance techniques may be used to increase setup reproducibility. Typical treatment times, including setup and actual delivery, are roughly 20 to 30 minutes daily.
While external beam RT is most commonly delivered as described above, brachytherapy, or intraoperative electron beam techniques, as well as proton or other charged-particle therapies, are also applied in selected cases.16–18
SIDE EFFECTS
Side effects of RT in the setting of sarcomas can be divided according to their onset—ie, acute versus delayed.
Acute effects. Skin changes ranging from erythema to moist desquamation in the skin overlying the high-dose volume are common. Major wound complications (delayed wound healing or need for surgical intervention) occur in approximately 17% of patients after surgical resection with postoperative RT, and perhaps more commonly (35%) with preoperative RT,8 though these rates vary widely in the literature. Another frequently reported acute side effect is fatigue.
Delayed sequelae after conservative resection and RT of extremity lesions include a reduction in range of motion secondary to joint contracture, edema, and fibrosis, as well as pain and bone fractures, all of which can significantly limit function of the preserved limb. In centers treating high volumes of patients with soft-tissue sarcoma, the incidence of moderate to severe late effects is less than 10%.19 In contrast to acute wound complications, a higher rate of late complications, including fibrosis and edema, have been observed with postoperative RT relative to preoperative RT.9 When necessary, high-dose RT does not appear to compromise the viability of skin grafts used to repair defects after sarcoma surgery if adequate time is allowed for healing.20
Regardless of the management approach, intensive rehabilitation led by physical therapy specialists is imperative in minimizing disabilities after treatment of soft-tissue sarcomas.
CONCLUSION
Outcomes of patients with musculoskeletal sarcomas are optimized at specialized sarcoma centers. For patients with soft-tissue sarcomas, effectively implementing an approach that combines conservative surgery and RT—and, in select cases, chemotherapy—achieves excellent local control rates while minimizing morbidity and maximizing long-term extremity function relative to aggressive surgery alone.
- Consensus conference. Limb-sparing treatment of adult soft-tissue sarcomas and osteosarcomas. JAMA 1985; 254:1791–1794.
- Gutierrez JC, Perez EA, Moffat FL, et al. Should soft tissue sarcomas be treated at high-volume centers? An analysis of 4,205 patients. Ann Surg 2007; 245:952–958.
- Halperin EC, Perez CA, Brady LW, eds. Perez and Brady’s Principles and Practice of Radiation Oncology. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
- Glencross J, Balasubramanian SP, Bacon J, Robinson MH, Reed MW. An audit of the management of soft tissue sarcoma within a health region in the UK. Eur J Surg Oncol 2003; 29:670–675.
- Dunst J, Schuck A. Role of radiotherapy in Ewing tumors. Pediatr Blood Cancer 2004; 42:465–470.
- Schwartz SI, Brunicardi FC, eds. Schwartz’s Principles of Surgery. 9th ed. New York: McGraw-Hill, Medical Pub. Division; 2010.
- Rosenberg SA, Tepper J, Glatstein E, et al. The treatment of soft-tissue sarcomas of the extremities: prospective randomized evaluations of (1) limb-sparing surgery plus radiation therapy compared with amputation and (2) the role of adjuvant chemotherapy. Ann Surg 1982; 196:305–315.
- O’Sullivan B, Davis AM, Turcotte R, et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 2002; 359:2235–2241.
- Davis AM, O’Sullivan B, Turcotte R, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol 2005; 75:48–53.
- Sarcoma Meta-analysis Collaboration. Adjuvant chemotherapy for localised respectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet 1997; 350:1647–1654.
- Eilber FC, Tap WD, Nelson SD, Eckardt JJ, Eilber FR. Advances in chemotherapy for patients with extremity soft tissue sarcoma. Orthop Clin North Am 2006; 37:15–22.
- Emami B, Lyman J, Brown A, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 1991; 21:109–122.
- Tepper J, Rosenberg SA, Glatstein E. Radiation therapy technique in soft tissue sarcomas of the extremity: policies of treatment at the National Cancer Institute. Int J Radiat Oncol Biol Phys 1982; 8:263–273.
- DeVita VT Jr, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles & Practice of Oncology. 8th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2008.
- Suit HD, Spiro I. Role of radiation in the management of adult patients with sarcoma of soft tissue. Semin Surg Oncol 1994; 10:347–356.
- DeLaney TF, Trofimov AV, Engelsman M, Suit HD. Advanced-technology radiation therapy in the management of bone and soft tissue sarcomas. Cancer Control 2005; 12:27–35.
- DeLaney TF, Liebsch NJ, Pedlow FX, et al. Phase II study of high-dose photon/proton radiotherapy in the management of spine sarcomas. Int J Radiat Oncol Biol Phys 2009; 74:732–739.
- Ishigami N, Suzuki K, Takahashi T, et al. Intimal sarcoma of aortic arch treated with proton therapy following surgery. Asian Cardiovasc Thorac Ann 2008; 16:e12–e14.
- Pollack A, Zagars GK, Goswitz MS, et al. Preoperative vs. postoperative radiotherapy in the treatment of soft tissue sarcomas: a matter of presentation. Int J Radiat Oncol Biol Phys 1998; 42:563–572.
- Lawrence WT, Zabell A, McDonald HD. The tolerance of skin grafts to postoperative radiation therapy in patients with soft-tissue sarcoma. Ann Plast Surg 1986; 16:204–210.
While radiation therapy (RT) has an integral role in the management of soft-tissue sarcoma, it has a limited role in that of bone sarcoma, with few exceptions (ie, Ewing sarcoma). In keeping with the rarity of these tumors, it has been demonstrated that patients treated at high-volume centers have significantly better survival and functional outcomes.1–3 Accordingly, treatment should be delivered by a multidisciplinary team including orthopedic, medical, and radiation oncologists, as well as plastic and reconstructive surgeons, physical therapy specialists, and pathologists and radiologists with expertise in musculoskeletal sarcomas.4 As the preceding articles in this supplement have addressed the major modalities in the treatment of sarcomas other than RT, this article will focus on how RT fits into the overall management mix, with a focus on soft-tissue sarcomas, where it figures most prominently.
BONE SARCOMAS: A LIMITED ROLE FOR RADIATION
The role of RT in the management of bone sarcomas is limited. Its primary application appears to be in Ewing sarcoma, for which curative treatment requires combined local and systemic therapy. For definitive therapy, limb-salvage surgery is preferable over amputation, but amputation may be an option for younger patients with lesions of the fibula, tibia, and foot. Based on the available data, postoperative RT is probably of benefit for all patients with Ewing sarcoma with close margins and/or those with a poor histologic response.5 Further discussion of Ewing sarcoma management is beyond the scope of this article (see the second and fifth articles in this supplement).
For osteosarcoma, the current standard of care is surgical resection combined with neoadjuvant and adjuvant chemotherapy. RT had been used years ago, prior to the advent of effective chemotherapy regimens, but its use for osteosarcoma has now been relegated to a few select situations. These include lesions not amenable to surgical resection and reconstruction, cases in which the patient refuses surgery, cases where there are positive margins after resection, and cases where palliation is needed for symptomatic lesions.
SOFT-TISSUE SARCOMAS: RADIATION HAS A CLEAR ADJUVANT ROLE
The primary management of localized soft-tissue sarcomas is surgical resection to achieve a negative margin when feasible. Historically, local excision of soft-tissue sarcomas resulted in local failure rates of 50% to 70%, even when a margin of normal tissue around the tumor was excised. As a result, amputation became standard treatment.6 In a landmark National Cancer Institute study 3 decades ago, patients were randomized to amputation or to limb-sparing surgery with the addition of RT.7 Notably, disease-free and overall survival were not compromised by limb-sparing surgery plus RT, demonstrating that although lesser surgery in the absence of RT may be insufficient, limb-sparing surgery with RT was equal to amputation. Consequently, limb-sparing approaches have become the favored surgery for the majority of cases of soft-tissue sarcoma, as advocated in a consensus statement from the National Institutes of Health.1
Indications vary by lesion grade
In general, adjuvant RT is recommended for all intermediate- and high-grade soft-tissue sarcoma lesions. A potential exception is a superficial tumor smaller than 5 cm with widely negative margins after resection. For low-grade lesions, re-excision is favored over adjuvant RT for positive or close margins, and RT is avoided in the setting of negative margins.
Optimal timing of radiation remains unclear
The optimal timing of adjuvant RT—preoperative versus postoperative—remains unknown. The relative advantages of preoperative RT include smaller and well-defined treatment volume, ability to use a lower dose, lack of tissue hypoxia, increased tumor resectability (smaller surgery), and improved limb function with less late fibrosis and edema. The disadvantages include inability to precisely stage patients and higher risk of acute wound-healing complications.
The National Cancer Institute of Canada compared outcomes with preoperative versus postoperative RT among 190 patients with soft-tissue sarcoma in a prospective randomized trial.8 Patients were stratified by tumor size (≤ 10 cm or > 10cm) and then randomized to preoperative RT (50 Gy in 25 fractions) or postoperative RT (66 Gy in 33 fractions).8 There was no difference between the groups in local control, distant control, or survival rates, but a higher rate of late complications, including fibrosis and edema, was observed with postoperative RT.8,9 On the other hand, the incidence of wound complications was higher in the preoperative group (35%) than in the postoperative group (17%).8
Likewise, the optimal sequencing and benefits of systemic therapy (chemotherapy) with relation to local therapy (surgery with pre- or postoperative RT) remain unclear. More than a dozen individual randomized trials of adjuvant chemotherapy, as well as a meta-analysis of 14 trials of doxorubicin-based adjuvant chemotherapy, have failed to demonstrate significant improvement in overall survival in patients with soft-tissue sarcomas.10 With regard to neoadjuvant chemotherapy for soft-tissue sarcomas, there are studies suggesting improvement in local control but no consistent survival benefit.11 Chemotherapy may yield a benefit in select cases, as detailed elsewhere in this supplement.
MECHANISMS OF ACTION: DIRECT AND INDIRECT
In simplified terms, radiation kills cancer cells through two basic mechanisms: indirect and direct.
The indirect effect (the most common mechanism) results from the generation of free radicals in the intracellular medium via ionization by photons. Free radicals, in turn, deposit large amounts of energy that damage DNA or some other vital component of the cell, resulting in cell death.
The direct effect is a consequence of photons themselves interacting directly with the cell in a lethal manner.
The goal of RT is to kill tumor cells selectively, without irreversibly injuring adjacent normal tissue. This is done by exploiting two abnormal aspects of tumor behavior: decreased ability for repair and increased susceptibility to ionizing radiation damage. Tumors are generally less able than normal tissue to repair DNA damage, owing to defective repair mechanisms. Tumor cells are also comparatively more radiosensitive than normal tissues, as they are more frequently in radiosensitive cell-cycle phases. Thus, dividing the radiation dose into a number of treatment fractions provides two advantages that further exploit the biologic differences between tumor and normal tissue: it allows DNA repair to take place within the normal tissues, and it allows proliferating tumor cells to redistribute through the cell cycle and move into the more radiosensitive phases.
TREATMENT PLANNING
Treatment simulation
Following initial consultation with a radiation oncologist, the eligible patient undergoes a simulation, or a treatment planning session in which he or she is positioned so as to allow treatment to be carefully designed and subsequently delivered with precision. This typically requires fabrication of a customized immobilization device to allow for consistent positioning over the treatment course. Sarcomas require that special care be taken to properly immobilize both the proximal and distal joints. Additionally, radiopaque wires are used to delineate the anatomic boundaries of the tumor or scar. Computed tomographic (CT) scans are then obtained to enable image-based three-dimensional treatment planning. The patient setup is photographed, and setup indicators are recorded and marked on the patient’s skin, some with freckle-size tattoos and some with indelible marker.
The treatment fields are then designed on the CT-simulation data set with the aid of virtual reality–type techniques. In addition to delineation of tumor volumes, three-dimensional treatment planning is used to contour all nearby normal structures on each slice. The resulting structures can then be used to specify dose constraints and help determine the optimal beam geometries to ensure proper tumor coverage and minimize the potential for side effects by reducing the dose to organs at risk. In the case of sarcomas, several strategies for reducing the risk of side effects are especially relevant: (1) carefully sparing a portion of the circumference of uninvolved bone to minimize the risk of fractures; (2) carefully sparing a strip of normal tissue to minimize edema by permitting undisrupted lymphatic drainage from the extremity; and (3) keeping dosing to joint spaces and other adjacent organs below tissue tolerances as defined by Emami et al.12
Determining target volume
The target volume for RT is determined on the basis of physical examination, radiologic studies, anatomical considerations, and the natural history of the sarcoma.
In the preoperative setting, longitudinal margins of 5 cm beyond the tumor and tumor-associated edema and radial margins of 2 cm are treated to 50 Gy in 25 fractions. Surgery is undertaken approximately 4 weeks after completion of RT to allow for repair in normal tissues and minimize operative and postoperative complications. Following surgery, an RT boost may be added for positive margins (16 Gy) or gross residual disease (25 Gy).
In the postoperative setting, details on the extent of dissection or observations from the surgeons themselves must be considered. Information regarding the surgical approach must be noted and can influence the effectiveness of postoperative RT as well as the incidence of late side effects. When experienced surgeons are involved, scars and drain sites, which are at risk for subclinical disease, can be planned so that their inclusion in the RT portal allows for sparing a strip of skin to minimize complications. Surgical clip placement at the boundaries of the tumor bed also facilitates RT planning.13 Finally, prophylactic bone stabilization may reduce the risk of subsequent fracture in cases where circumferential bone radiation in high-risk sites is anticipated.
Recommendations on the volume that must be treated vary among different authorities. Some advocate treating the entire compartment because of the risk for microscopic seeding.14 Others recommend margins around the tumor or tumor bed ranging from less than 5 cm up to 15 cm.15 Most often the postoperative approach is to include the resection bed with a 2-cm radial margin, the incision, and any drain sites in the initial treatment volume and to base the longitudinal margin on the grade and size of the primary tumor (5–15 cm). This volume is treated to 50 Gy in 25 fractions followed by two sequential reductions in field size, with the total dose determined by the extent of resection: 60 Gy for negative margins, 66 Gy for microscopically positive margins, and 75 Gy for gross residual disease.
TREATMENT DELIVERY
Once treatment planning is completed, treatments begin and are given daily Monday through Friday. Each day, the patient is positioned in the immobilization device, the field measurements are set, and positioning is checked with measurement tools and external marking of the field borders on the skin. Daily image guidance techniques may be used to increase setup reproducibility. Typical treatment times, including setup and actual delivery, are roughly 20 to 30 minutes daily.
While external beam RT is most commonly delivered as described above, brachytherapy, or intraoperative electron beam techniques, as well as proton or other charged-particle therapies, are also applied in selected cases.16–18
SIDE EFFECTS
Side effects of RT in the setting of sarcomas can be divided according to their onset—ie, acute versus delayed.
Acute effects. Skin changes ranging from erythema to moist desquamation in the skin overlying the high-dose volume are common. Major wound complications (delayed wound healing or need for surgical intervention) occur in approximately 17% of patients after surgical resection with postoperative RT, and perhaps more commonly (35%) with preoperative RT,8 though these rates vary widely in the literature. Another frequently reported acute side effect is fatigue.
Delayed sequelae after conservative resection and RT of extremity lesions include a reduction in range of motion secondary to joint contracture, edema, and fibrosis, as well as pain and bone fractures, all of which can significantly limit function of the preserved limb. In centers treating high volumes of patients with soft-tissue sarcoma, the incidence of moderate to severe late effects is less than 10%.19 In contrast to acute wound complications, a higher rate of late complications, including fibrosis and edema, have been observed with postoperative RT relative to preoperative RT.9 When necessary, high-dose RT does not appear to compromise the viability of skin grafts used to repair defects after sarcoma surgery if adequate time is allowed for healing.20
Regardless of the management approach, intensive rehabilitation led by physical therapy specialists is imperative in minimizing disabilities after treatment of soft-tissue sarcomas.
CONCLUSION
Outcomes of patients with musculoskeletal sarcomas are optimized at specialized sarcoma centers. For patients with soft-tissue sarcomas, effectively implementing an approach that combines conservative surgery and RT—and, in select cases, chemotherapy—achieves excellent local control rates while minimizing morbidity and maximizing long-term extremity function relative to aggressive surgery alone.
While radiation therapy (RT) has an integral role in the management of soft-tissue sarcoma, it has a limited role in that of bone sarcoma, with few exceptions (ie, Ewing sarcoma). In keeping with the rarity of these tumors, it has been demonstrated that patients treated at high-volume centers have significantly better survival and functional outcomes.1–3 Accordingly, treatment should be delivered by a multidisciplinary team including orthopedic, medical, and radiation oncologists, as well as plastic and reconstructive surgeons, physical therapy specialists, and pathologists and radiologists with expertise in musculoskeletal sarcomas.4 As the preceding articles in this supplement have addressed the major modalities in the treatment of sarcomas other than RT, this article will focus on how RT fits into the overall management mix, with a focus on soft-tissue sarcomas, where it figures most prominently.
BONE SARCOMAS: A LIMITED ROLE FOR RADIATION
The role of RT in the management of bone sarcomas is limited. Its primary application appears to be in Ewing sarcoma, for which curative treatment requires combined local and systemic therapy. For definitive therapy, limb-salvage surgery is preferable over amputation, but amputation may be an option for younger patients with lesions of the fibula, tibia, and foot. Based on the available data, postoperative RT is probably of benefit for all patients with Ewing sarcoma with close margins and/or those with a poor histologic response.5 Further discussion of Ewing sarcoma management is beyond the scope of this article (see the second and fifth articles in this supplement).
For osteosarcoma, the current standard of care is surgical resection combined with neoadjuvant and adjuvant chemotherapy. RT had been used years ago, prior to the advent of effective chemotherapy regimens, but its use for osteosarcoma has now been relegated to a few select situations. These include lesions not amenable to surgical resection and reconstruction, cases in which the patient refuses surgery, cases where there are positive margins after resection, and cases where palliation is needed for symptomatic lesions.
SOFT-TISSUE SARCOMAS: RADIATION HAS A CLEAR ADJUVANT ROLE
The primary management of localized soft-tissue sarcomas is surgical resection to achieve a negative margin when feasible. Historically, local excision of soft-tissue sarcomas resulted in local failure rates of 50% to 70%, even when a margin of normal tissue around the tumor was excised. As a result, amputation became standard treatment.6 In a landmark National Cancer Institute study 3 decades ago, patients were randomized to amputation or to limb-sparing surgery with the addition of RT.7 Notably, disease-free and overall survival were not compromised by limb-sparing surgery plus RT, demonstrating that although lesser surgery in the absence of RT may be insufficient, limb-sparing surgery with RT was equal to amputation. Consequently, limb-sparing approaches have become the favored surgery for the majority of cases of soft-tissue sarcoma, as advocated in a consensus statement from the National Institutes of Health.1
Indications vary by lesion grade
In general, adjuvant RT is recommended for all intermediate- and high-grade soft-tissue sarcoma lesions. A potential exception is a superficial tumor smaller than 5 cm with widely negative margins after resection. For low-grade lesions, re-excision is favored over adjuvant RT for positive or close margins, and RT is avoided in the setting of negative margins.
Optimal timing of radiation remains unclear
The optimal timing of adjuvant RT—preoperative versus postoperative—remains unknown. The relative advantages of preoperative RT include smaller and well-defined treatment volume, ability to use a lower dose, lack of tissue hypoxia, increased tumor resectability (smaller surgery), and improved limb function with less late fibrosis and edema. The disadvantages include inability to precisely stage patients and higher risk of acute wound-healing complications.
The National Cancer Institute of Canada compared outcomes with preoperative versus postoperative RT among 190 patients with soft-tissue sarcoma in a prospective randomized trial.8 Patients were stratified by tumor size (≤ 10 cm or > 10cm) and then randomized to preoperative RT (50 Gy in 25 fractions) or postoperative RT (66 Gy in 33 fractions).8 There was no difference between the groups in local control, distant control, or survival rates, but a higher rate of late complications, including fibrosis and edema, was observed with postoperative RT.8,9 On the other hand, the incidence of wound complications was higher in the preoperative group (35%) than in the postoperative group (17%).8
Likewise, the optimal sequencing and benefits of systemic therapy (chemotherapy) with relation to local therapy (surgery with pre- or postoperative RT) remain unclear. More than a dozen individual randomized trials of adjuvant chemotherapy, as well as a meta-analysis of 14 trials of doxorubicin-based adjuvant chemotherapy, have failed to demonstrate significant improvement in overall survival in patients with soft-tissue sarcomas.10 With regard to neoadjuvant chemotherapy for soft-tissue sarcomas, there are studies suggesting improvement in local control but no consistent survival benefit.11 Chemotherapy may yield a benefit in select cases, as detailed elsewhere in this supplement.
MECHANISMS OF ACTION: DIRECT AND INDIRECT
In simplified terms, radiation kills cancer cells through two basic mechanisms: indirect and direct.
The indirect effect (the most common mechanism) results from the generation of free radicals in the intracellular medium via ionization by photons. Free radicals, in turn, deposit large amounts of energy that damage DNA or some other vital component of the cell, resulting in cell death.
The direct effect is a consequence of photons themselves interacting directly with the cell in a lethal manner.
The goal of RT is to kill tumor cells selectively, without irreversibly injuring adjacent normal tissue. This is done by exploiting two abnormal aspects of tumor behavior: decreased ability for repair and increased susceptibility to ionizing radiation damage. Tumors are generally less able than normal tissue to repair DNA damage, owing to defective repair mechanisms. Tumor cells are also comparatively more radiosensitive than normal tissues, as they are more frequently in radiosensitive cell-cycle phases. Thus, dividing the radiation dose into a number of treatment fractions provides two advantages that further exploit the biologic differences between tumor and normal tissue: it allows DNA repair to take place within the normal tissues, and it allows proliferating tumor cells to redistribute through the cell cycle and move into the more radiosensitive phases.
TREATMENT PLANNING
Treatment simulation
Following initial consultation with a radiation oncologist, the eligible patient undergoes a simulation, or a treatment planning session in which he or she is positioned so as to allow treatment to be carefully designed and subsequently delivered with precision. This typically requires fabrication of a customized immobilization device to allow for consistent positioning over the treatment course. Sarcomas require that special care be taken to properly immobilize both the proximal and distal joints. Additionally, radiopaque wires are used to delineate the anatomic boundaries of the tumor or scar. Computed tomographic (CT) scans are then obtained to enable image-based three-dimensional treatment planning. The patient setup is photographed, and setup indicators are recorded and marked on the patient’s skin, some with freckle-size tattoos and some with indelible marker.
The treatment fields are then designed on the CT-simulation data set with the aid of virtual reality–type techniques. In addition to delineation of tumor volumes, three-dimensional treatment planning is used to contour all nearby normal structures on each slice. The resulting structures can then be used to specify dose constraints and help determine the optimal beam geometries to ensure proper tumor coverage and minimize the potential for side effects by reducing the dose to organs at risk. In the case of sarcomas, several strategies for reducing the risk of side effects are especially relevant: (1) carefully sparing a portion of the circumference of uninvolved bone to minimize the risk of fractures; (2) carefully sparing a strip of normal tissue to minimize edema by permitting undisrupted lymphatic drainage from the extremity; and (3) keeping dosing to joint spaces and other adjacent organs below tissue tolerances as defined by Emami et al.12
Determining target volume
The target volume for RT is determined on the basis of physical examination, radiologic studies, anatomical considerations, and the natural history of the sarcoma.
In the preoperative setting, longitudinal margins of 5 cm beyond the tumor and tumor-associated edema and radial margins of 2 cm are treated to 50 Gy in 25 fractions. Surgery is undertaken approximately 4 weeks after completion of RT to allow for repair in normal tissues and minimize operative and postoperative complications. Following surgery, an RT boost may be added for positive margins (16 Gy) or gross residual disease (25 Gy).
In the postoperative setting, details on the extent of dissection or observations from the surgeons themselves must be considered. Information regarding the surgical approach must be noted and can influence the effectiveness of postoperative RT as well as the incidence of late side effects. When experienced surgeons are involved, scars and drain sites, which are at risk for subclinical disease, can be planned so that their inclusion in the RT portal allows for sparing a strip of skin to minimize complications. Surgical clip placement at the boundaries of the tumor bed also facilitates RT planning.13 Finally, prophylactic bone stabilization may reduce the risk of subsequent fracture in cases where circumferential bone radiation in high-risk sites is anticipated.
Recommendations on the volume that must be treated vary among different authorities. Some advocate treating the entire compartment because of the risk for microscopic seeding.14 Others recommend margins around the tumor or tumor bed ranging from less than 5 cm up to 15 cm.15 Most often the postoperative approach is to include the resection bed with a 2-cm radial margin, the incision, and any drain sites in the initial treatment volume and to base the longitudinal margin on the grade and size of the primary tumor (5–15 cm). This volume is treated to 50 Gy in 25 fractions followed by two sequential reductions in field size, with the total dose determined by the extent of resection: 60 Gy for negative margins, 66 Gy for microscopically positive margins, and 75 Gy for gross residual disease.
TREATMENT DELIVERY
Once treatment planning is completed, treatments begin and are given daily Monday through Friday. Each day, the patient is positioned in the immobilization device, the field measurements are set, and positioning is checked with measurement tools and external marking of the field borders on the skin. Daily image guidance techniques may be used to increase setup reproducibility. Typical treatment times, including setup and actual delivery, are roughly 20 to 30 minutes daily.
While external beam RT is most commonly delivered as described above, brachytherapy, or intraoperative electron beam techniques, as well as proton or other charged-particle therapies, are also applied in selected cases.16–18
SIDE EFFECTS
Side effects of RT in the setting of sarcomas can be divided according to their onset—ie, acute versus delayed.
Acute effects. Skin changes ranging from erythema to moist desquamation in the skin overlying the high-dose volume are common. Major wound complications (delayed wound healing or need for surgical intervention) occur in approximately 17% of patients after surgical resection with postoperative RT, and perhaps more commonly (35%) with preoperative RT,8 though these rates vary widely in the literature. Another frequently reported acute side effect is fatigue.
Delayed sequelae after conservative resection and RT of extremity lesions include a reduction in range of motion secondary to joint contracture, edema, and fibrosis, as well as pain and bone fractures, all of which can significantly limit function of the preserved limb. In centers treating high volumes of patients with soft-tissue sarcoma, the incidence of moderate to severe late effects is less than 10%.19 In contrast to acute wound complications, a higher rate of late complications, including fibrosis and edema, have been observed with postoperative RT relative to preoperative RT.9 When necessary, high-dose RT does not appear to compromise the viability of skin grafts used to repair defects after sarcoma surgery if adequate time is allowed for healing.20
Regardless of the management approach, intensive rehabilitation led by physical therapy specialists is imperative in minimizing disabilities after treatment of soft-tissue sarcomas.
CONCLUSION
Outcomes of patients with musculoskeletal sarcomas are optimized at specialized sarcoma centers. For patients with soft-tissue sarcomas, effectively implementing an approach that combines conservative surgery and RT—and, in select cases, chemotherapy—achieves excellent local control rates while minimizing morbidity and maximizing long-term extremity function relative to aggressive surgery alone.
- Consensus conference. Limb-sparing treatment of adult soft-tissue sarcomas and osteosarcomas. JAMA 1985; 254:1791–1794.
- Gutierrez JC, Perez EA, Moffat FL, et al. Should soft tissue sarcomas be treated at high-volume centers? An analysis of 4,205 patients. Ann Surg 2007; 245:952–958.
- Halperin EC, Perez CA, Brady LW, eds. Perez and Brady’s Principles and Practice of Radiation Oncology. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
- Glencross J, Balasubramanian SP, Bacon J, Robinson MH, Reed MW. An audit of the management of soft tissue sarcoma within a health region in the UK. Eur J Surg Oncol 2003; 29:670–675.
- Dunst J, Schuck A. Role of radiotherapy in Ewing tumors. Pediatr Blood Cancer 2004; 42:465–470.
- Schwartz SI, Brunicardi FC, eds. Schwartz’s Principles of Surgery. 9th ed. New York: McGraw-Hill, Medical Pub. Division; 2010.
- Rosenberg SA, Tepper J, Glatstein E, et al. The treatment of soft-tissue sarcomas of the extremities: prospective randomized evaluations of (1) limb-sparing surgery plus radiation therapy compared with amputation and (2) the role of adjuvant chemotherapy. Ann Surg 1982; 196:305–315.
- O’Sullivan B, Davis AM, Turcotte R, et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 2002; 359:2235–2241.
- Davis AM, O’Sullivan B, Turcotte R, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol 2005; 75:48–53.
- Sarcoma Meta-analysis Collaboration. Adjuvant chemotherapy for localised respectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet 1997; 350:1647–1654.
- Eilber FC, Tap WD, Nelson SD, Eckardt JJ, Eilber FR. Advances in chemotherapy for patients with extremity soft tissue sarcoma. Orthop Clin North Am 2006; 37:15–22.
- Emami B, Lyman J, Brown A, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 1991; 21:109–122.
- Tepper J, Rosenberg SA, Glatstein E. Radiation therapy technique in soft tissue sarcomas of the extremity: policies of treatment at the National Cancer Institute. Int J Radiat Oncol Biol Phys 1982; 8:263–273.
- DeVita VT Jr, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles & Practice of Oncology. 8th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2008.
- Suit HD, Spiro I. Role of radiation in the management of adult patients with sarcoma of soft tissue. Semin Surg Oncol 1994; 10:347–356.
- DeLaney TF, Trofimov AV, Engelsman M, Suit HD. Advanced-technology radiation therapy in the management of bone and soft tissue sarcomas. Cancer Control 2005; 12:27–35.
- DeLaney TF, Liebsch NJ, Pedlow FX, et al. Phase II study of high-dose photon/proton radiotherapy in the management of spine sarcomas. Int J Radiat Oncol Biol Phys 2009; 74:732–739.
- Ishigami N, Suzuki K, Takahashi T, et al. Intimal sarcoma of aortic arch treated with proton therapy following surgery. Asian Cardiovasc Thorac Ann 2008; 16:e12–e14.
- Pollack A, Zagars GK, Goswitz MS, et al. Preoperative vs. postoperative radiotherapy in the treatment of soft tissue sarcomas: a matter of presentation. Int J Radiat Oncol Biol Phys 1998; 42:563–572.
- Lawrence WT, Zabell A, McDonald HD. The tolerance of skin grafts to postoperative radiation therapy in patients with soft-tissue sarcoma. Ann Plast Surg 1986; 16:204–210.
- Consensus conference. Limb-sparing treatment of adult soft-tissue sarcomas and osteosarcomas. JAMA 1985; 254:1791–1794.
- Gutierrez JC, Perez EA, Moffat FL, et al. Should soft tissue sarcomas be treated at high-volume centers? An analysis of 4,205 patients. Ann Surg 2007; 245:952–958.
- Halperin EC, Perez CA, Brady LW, eds. Perez and Brady’s Principles and Practice of Radiation Oncology. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
- Glencross J, Balasubramanian SP, Bacon J, Robinson MH, Reed MW. An audit of the management of soft tissue sarcoma within a health region in the UK. Eur J Surg Oncol 2003; 29:670–675.
- Dunst J, Schuck A. Role of radiotherapy in Ewing tumors. Pediatr Blood Cancer 2004; 42:465–470.
- Schwartz SI, Brunicardi FC, eds. Schwartz’s Principles of Surgery. 9th ed. New York: McGraw-Hill, Medical Pub. Division; 2010.
- Rosenberg SA, Tepper J, Glatstein E, et al. The treatment of soft-tissue sarcomas of the extremities: prospective randomized evaluations of (1) limb-sparing surgery plus radiation therapy compared with amputation and (2) the role of adjuvant chemotherapy. Ann Surg 1982; 196:305–315.
- O’Sullivan B, Davis AM, Turcotte R, et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 2002; 359:2235–2241.
- Davis AM, O’Sullivan B, Turcotte R, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol 2005; 75:48–53.
- Sarcoma Meta-analysis Collaboration. Adjuvant chemotherapy for localised respectable soft-tissue sarcoma of adults: meta-analysis of individual data. Lancet 1997; 350:1647–1654.
- Eilber FC, Tap WD, Nelson SD, Eckardt JJ, Eilber FR. Advances in chemotherapy for patients with extremity soft tissue sarcoma. Orthop Clin North Am 2006; 37:15–22.
- Emami B, Lyman J, Brown A, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 1991; 21:109–122.
- Tepper J, Rosenberg SA, Glatstein E. Radiation therapy technique in soft tissue sarcomas of the extremity: policies of treatment at the National Cancer Institute. Int J Radiat Oncol Biol Phys 1982; 8:263–273.
- DeVita VT Jr, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles & Practice of Oncology. 8th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2008.
- Suit HD, Spiro I. Role of radiation in the management of adult patients with sarcoma of soft tissue. Semin Surg Oncol 1994; 10:347–356.
- DeLaney TF, Trofimov AV, Engelsman M, Suit HD. Advanced-technology radiation therapy in the management of bone and soft tissue sarcomas. Cancer Control 2005; 12:27–35.
- DeLaney TF, Liebsch NJ, Pedlow FX, et al. Phase II study of high-dose photon/proton radiotherapy in the management of spine sarcomas. Int J Radiat Oncol Biol Phys 2009; 74:732–739.
- Ishigami N, Suzuki K, Takahashi T, et al. Intimal sarcoma of aortic arch treated with proton therapy following surgery. Asian Cardiovasc Thorac Ann 2008; 16:e12–e14.
- Pollack A, Zagars GK, Goswitz MS, et al. Preoperative vs. postoperative radiotherapy in the treatment of soft tissue sarcomas: a matter of presentation. Int J Radiat Oncol Biol Phys 1998; 42:563–572.
- Lawrence WT, Zabell A, McDonald HD. The tolerance of skin grafts to postoperative radiation therapy in patients with soft-tissue sarcoma. Ann Plast Surg 1986; 16:204–210.
Palpable purpura
Q: Which is the most likely diagnosis?
- Idiopathic thrombocytopenic purpura
- Vitamin C deficiency (scurvy)
- Kaposi sarcoma not related to human immunodeficiency virus (HIV) infection
- Henoch-Schönlein purpura
- Polyarteritis nodosa
A: The correct answer is Henoch-Schönlein purpura.
Idiopathic thrombocytopenic purpura is an autoimmune disease caused by specific antibodies against platelet-membrane glycoproteins. It is characterized by thrombocytopenia not explainable by contact with toxic substances or by other causes. Along with nonpalpable purpura, other common signs are epistaxis, gingival bleeding, menorrhagia, and retinal hemorrhage.
Scurvy is an uncommon deficiency of ascorbic acid (vitamin C). The elderly and alcoholics are at higher risk, as they do not take in enough vitamin C in the diet. Patients usually show perifollicular hemorrhages of the skin and mucous membranes, typically petechial hemorrhage or ecchymosis of the gums around the upper incisors. Other cutaneous signs are follicular hyperkeratosis on the forearms, small corkscrew hairs, and sicca syndrome, which is more common in adults.
Non-HIV Kaposi sarcoma usually affects elderly patients, with pink, red, or brown papules or nodules on the legs and, less commonly, on the head and neck. Histopathologic examination shows newly formed irregular blood vessels with an inflammatory infiltrate of plasma cells and lymphocytes; immunohistochemical human herpes virus staining is usually positive.
Polyarteritis nodosa is a systemic vasculitis that affects medium or small arteries with necrotizing inflammation; renal glomeruli and arterioles, capillaries, and venules are unaffected. Skin manifestations include palpable purpura, livedo reticularis, ulcers, and distal gangrene. The condition also usually affects the kidneys, the heart, and the musculoskeletal and nervous systems.
A SYSTEMIC VASCULITIS
Henoch-Schönlein purpura is a systemic vasculitis affecting the skin, gastrointestinal tract, kidneys, and joints. Palpable purpura and joint pain are the most common and consistent presenting symptoms. The kidneys are affected in about one-third of children and in 60% of adults, and this is the major factor determining the long-term outcome.1
In our patient, laboratory testing that included a complete blood cell count, biochemical testing (including IgA levels), urinary sediment, and coagulation studies showed no abnormalities except elevations of the erythrocyte sedimentation rate and the concentration of C-reactive protein (an acute-phase reactant). These can be normal in some patients. Renal involvement was also not present.
DIAGNOSIS
The diagnosis relies on clinical manifestations. Because Henoch-Schönlein purpura is less common in adults, biopsy plays a more important role in establishing the diagnosis in this age group, and it does this by demonstrating leukocytoclastic vasculitis with a predominance of IgA deposition under immunofluorescence. Recent studies in children showed that an elevated IgA concentration along with reduced IgM levels was associated with a higher rate of severe complications.2 However, depending on the age of the biopsied lesion, IgA may not be detected.
TREATMENT DIRECTED AT SYMPTOMS
Our patient received oral corticosteroids 0.5 mg/kg per day for 20 days, and the lesions resolved by 4 weeks.
Management of Henoch-Schönlein purpura is mainly directed at the symptoms, with oral hydration and nonsteroidal anti-inflammatory drugs. For severe cases, a short course of corticosteroids (0.5–1 mg/kg) may be used.
Although no controlled clinical trial has proven that Henoch-Schönlein purpura responds to corticosteroids, colchicine, or other drugs, corticosteroids are used most often, especially in patients with renal disease. Patients with severe renal insufficiency, abdominal pain, joint involvement, or bleeding should be hospitalized. Plasmapheresis3 has been used in severe cases.
HENOCH-SCHÖNLEIN PURPURA AND MALIGNANCY
During a follow-up evaluation 1 month later, our patient was diagnosed with adenocarcinoma of the breast. This highlights the value of a workup for cancer in adults with cutaneous vasculitis.
Cutaneous vasculitis can represent a paraneoplastic syndrome associated with a malignant tumor. The pathophysiology of this association is unclear, but one proposed mechanism is the exaggerated production of antibodies that react against tumor neoantigens, leading to the formation of immune complexes, or that occasionally recognize endothelial cells because of similarities with tumor antigens. Another theory is that abnormally high levels of inflammatory cytokines are produced by neoplastic cells or in response to decreased immune complex clearance.
Yet another theory is that hyperviscosity of the blood, seen in some cancers, increases the contact time for deposition of immune complexes and causes endothelial damage. Drugs used to treat cancer have also been reported to produce Henoch-Schönlein purpura.4
Although hematologic malignancy is three to five times more common than solid tumors in patients with small-vessel vasculitis, the disease has been associated with solid tumors of the liver, skin, colon, and breast in adults over age 40.5 An evaluation for neoplasm is therefore reasonable in adults with Henoch-Schönlein purpura, as is an evaluation for tumor recurrence or metastasis if the patient has been previously treated for a malignant tumor.
- Rieu P, Noël LH. Henoch-Schönlein nephritis in children and adults. Morphological features and clinicopathological correlations. Ann Med Interne (Paris) 1999; 150:151–159.
- Fretzayas A, Sionti I, Moustaki M, Nicolaidou P. Clinical impact of altered immunoglobulin levels in Henoch-Schönlein purpura. Pediatr Int 2009; 51:381–384.
- Donghi D, Schanz U, Sahrbacher U, et al. Life-threatening or organimpairing Henoch-Schönlein purpura: plasmapheresis may save lives and limit organ damage. Dermatology 2009; 219:167–170.
- Mitsui H, Shibagaki N, Kawamura T, Matsue H, Shimada S. A clinical study of Henoch-Schönlein purpura associated with malignancy. J Eur Acad Dermatol Venereol 2009; 23:394–401.
- Maestri A, Malacarne P, Santini A. Henoch-Schönlein syndrome associated with breast cancer. A case report. Angiology 1995; 46:625–627.
Q: Which is the most likely diagnosis?
- Idiopathic thrombocytopenic purpura
- Vitamin C deficiency (scurvy)
- Kaposi sarcoma not related to human immunodeficiency virus (HIV) infection
- Henoch-Schönlein purpura
- Polyarteritis nodosa
A: The correct answer is Henoch-Schönlein purpura.
Idiopathic thrombocytopenic purpura is an autoimmune disease caused by specific antibodies against platelet-membrane glycoproteins. It is characterized by thrombocytopenia not explainable by contact with toxic substances or by other causes. Along with nonpalpable purpura, other common signs are epistaxis, gingival bleeding, menorrhagia, and retinal hemorrhage.
Scurvy is an uncommon deficiency of ascorbic acid (vitamin C). The elderly and alcoholics are at higher risk, as they do not take in enough vitamin C in the diet. Patients usually show perifollicular hemorrhages of the skin and mucous membranes, typically petechial hemorrhage or ecchymosis of the gums around the upper incisors. Other cutaneous signs are follicular hyperkeratosis on the forearms, small corkscrew hairs, and sicca syndrome, which is more common in adults.
Non-HIV Kaposi sarcoma usually affects elderly patients, with pink, red, or brown papules or nodules on the legs and, less commonly, on the head and neck. Histopathologic examination shows newly formed irregular blood vessels with an inflammatory infiltrate of plasma cells and lymphocytes; immunohistochemical human herpes virus staining is usually positive.
Polyarteritis nodosa is a systemic vasculitis that affects medium or small arteries with necrotizing inflammation; renal glomeruli and arterioles, capillaries, and venules are unaffected. Skin manifestations include palpable purpura, livedo reticularis, ulcers, and distal gangrene. The condition also usually affects the kidneys, the heart, and the musculoskeletal and nervous systems.
A SYSTEMIC VASCULITIS
Henoch-Schönlein purpura is a systemic vasculitis affecting the skin, gastrointestinal tract, kidneys, and joints. Palpable purpura and joint pain are the most common and consistent presenting symptoms. The kidneys are affected in about one-third of children and in 60% of adults, and this is the major factor determining the long-term outcome.1
In our patient, laboratory testing that included a complete blood cell count, biochemical testing (including IgA levels), urinary sediment, and coagulation studies showed no abnormalities except elevations of the erythrocyte sedimentation rate and the concentration of C-reactive protein (an acute-phase reactant). These can be normal in some patients. Renal involvement was also not present.
DIAGNOSIS
The diagnosis relies on clinical manifestations. Because Henoch-Schönlein purpura is less common in adults, biopsy plays a more important role in establishing the diagnosis in this age group, and it does this by demonstrating leukocytoclastic vasculitis with a predominance of IgA deposition under immunofluorescence. Recent studies in children showed that an elevated IgA concentration along with reduced IgM levels was associated with a higher rate of severe complications.2 However, depending on the age of the biopsied lesion, IgA may not be detected.
TREATMENT DIRECTED AT SYMPTOMS
Our patient received oral corticosteroids 0.5 mg/kg per day for 20 days, and the lesions resolved by 4 weeks.
Management of Henoch-Schönlein purpura is mainly directed at the symptoms, with oral hydration and nonsteroidal anti-inflammatory drugs. For severe cases, a short course of corticosteroids (0.5–1 mg/kg) may be used.
Although no controlled clinical trial has proven that Henoch-Schönlein purpura responds to corticosteroids, colchicine, or other drugs, corticosteroids are used most often, especially in patients with renal disease. Patients with severe renal insufficiency, abdominal pain, joint involvement, or bleeding should be hospitalized. Plasmapheresis3 has been used in severe cases.
HENOCH-SCHÖNLEIN PURPURA AND MALIGNANCY
During a follow-up evaluation 1 month later, our patient was diagnosed with adenocarcinoma of the breast. This highlights the value of a workup for cancer in adults with cutaneous vasculitis.
Cutaneous vasculitis can represent a paraneoplastic syndrome associated with a malignant tumor. The pathophysiology of this association is unclear, but one proposed mechanism is the exaggerated production of antibodies that react against tumor neoantigens, leading to the formation of immune complexes, or that occasionally recognize endothelial cells because of similarities with tumor antigens. Another theory is that abnormally high levels of inflammatory cytokines are produced by neoplastic cells or in response to decreased immune complex clearance.
Yet another theory is that hyperviscosity of the blood, seen in some cancers, increases the contact time for deposition of immune complexes and causes endothelial damage. Drugs used to treat cancer have also been reported to produce Henoch-Schönlein purpura.4
Although hematologic malignancy is three to five times more common than solid tumors in patients with small-vessel vasculitis, the disease has been associated with solid tumors of the liver, skin, colon, and breast in adults over age 40.5 An evaluation for neoplasm is therefore reasonable in adults with Henoch-Schönlein purpura, as is an evaluation for tumor recurrence or metastasis if the patient has been previously treated for a malignant tumor.
Q: Which is the most likely diagnosis?
- Idiopathic thrombocytopenic purpura
- Vitamin C deficiency (scurvy)
- Kaposi sarcoma not related to human immunodeficiency virus (HIV) infection
- Henoch-Schönlein purpura
- Polyarteritis nodosa
A: The correct answer is Henoch-Schönlein purpura.
Idiopathic thrombocytopenic purpura is an autoimmune disease caused by specific antibodies against platelet-membrane glycoproteins. It is characterized by thrombocytopenia not explainable by contact with toxic substances or by other causes. Along with nonpalpable purpura, other common signs are epistaxis, gingival bleeding, menorrhagia, and retinal hemorrhage.
Scurvy is an uncommon deficiency of ascorbic acid (vitamin C). The elderly and alcoholics are at higher risk, as they do not take in enough vitamin C in the diet. Patients usually show perifollicular hemorrhages of the skin and mucous membranes, typically petechial hemorrhage or ecchymosis of the gums around the upper incisors. Other cutaneous signs are follicular hyperkeratosis on the forearms, small corkscrew hairs, and sicca syndrome, which is more common in adults.
Non-HIV Kaposi sarcoma usually affects elderly patients, with pink, red, or brown papules or nodules on the legs and, less commonly, on the head and neck. Histopathologic examination shows newly formed irregular blood vessels with an inflammatory infiltrate of plasma cells and lymphocytes; immunohistochemical human herpes virus staining is usually positive.
Polyarteritis nodosa is a systemic vasculitis that affects medium or small arteries with necrotizing inflammation; renal glomeruli and arterioles, capillaries, and venules are unaffected. Skin manifestations include palpable purpura, livedo reticularis, ulcers, and distal gangrene. The condition also usually affects the kidneys, the heart, and the musculoskeletal and nervous systems.
A SYSTEMIC VASCULITIS
Henoch-Schönlein purpura is a systemic vasculitis affecting the skin, gastrointestinal tract, kidneys, and joints. Palpable purpura and joint pain are the most common and consistent presenting symptoms. The kidneys are affected in about one-third of children and in 60% of adults, and this is the major factor determining the long-term outcome.1
In our patient, laboratory testing that included a complete blood cell count, biochemical testing (including IgA levels), urinary sediment, and coagulation studies showed no abnormalities except elevations of the erythrocyte sedimentation rate and the concentration of C-reactive protein (an acute-phase reactant). These can be normal in some patients. Renal involvement was also not present.
DIAGNOSIS
The diagnosis relies on clinical manifestations. Because Henoch-Schönlein purpura is less common in adults, biopsy plays a more important role in establishing the diagnosis in this age group, and it does this by demonstrating leukocytoclastic vasculitis with a predominance of IgA deposition under immunofluorescence. Recent studies in children showed that an elevated IgA concentration along with reduced IgM levels was associated with a higher rate of severe complications.2 However, depending on the age of the biopsied lesion, IgA may not be detected.
TREATMENT DIRECTED AT SYMPTOMS
Our patient received oral corticosteroids 0.5 mg/kg per day for 20 days, and the lesions resolved by 4 weeks.
Management of Henoch-Schönlein purpura is mainly directed at the symptoms, with oral hydration and nonsteroidal anti-inflammatory drugs. For severe cases, a short course of corticosteroids (0.5–1 mg/kg) may be used.
Although no controlled clinical trial has proven that Henoch-Schönlein purpura responds to corticosteroids, colchicine, or other drugs, corticosteroids are used most often, especially in patients with renal disease. Patients with severe renal insufficiency, abdominal pain, joint involvement, or bleeding should be hospitalized. Plasmapheresis3 has been used in severe cases.
HENOCH-SCHÖNLEIN PURPURA AND MALIGNANCY
During a follow-up evaluation 1 month later, our patient was diagnosed with adenocarcinoma of the breast. This highlights the value of a workup for cancer in adults with cutaneous vasculitis.
Cutaneous vasculitis can represent a paraneoplastic syndrome associated with a malignant tumor. The pathophysiology of this association is unclear, but one proposed mechanism is the exaggerated production of antibodies that react against tumor neoantigens, leading to the formation of immune complexes, or that occasionally recognize endothelial cells because of similarities with tumor antigens. Another theory is that abnormally high levels of inflammatory cytokines are produced by neoplastic cells or in response to decreased immune complex clearance.
Yet another theory is that hyperviscosity of the blood, seen in some cancers, increases the contact time for deposition of immune complexes and causes endothelial damage. Drugs used to treat cancer have also been reported to produce Henoch-Schönlein purpura.4
Although hematologic malignancy is three to five times more common than solid tumors in patients with small-vessel vasculitis, the disease has been associated with solid tumors of the liver, skin, colon, and breast in adults over age 40.5 An evaluation for neoplasm is therefore reasonable in adults with Henoch-Schönlein purpura, as is an evaluation for tumor recurrence or metastasis if the patient has been previously treated for a malignant tumor.
- Rieu P, Noël LH. Henoch-Schönlein nephritis in children and adults. Morphological features and clinicopathological correlations. Ann Med Interne (Paris) 1999; 150:151–159.
- Fretzayas A, Sionti I, Moustaki M, Nicolaidou P. Clinical impact of altered immunoglobulin levels in Henoch-Schönlein purpura. Pediatr Int 2009; 51:381–384.
- Donghi D, Schanz U, Sahrbacher U, et al. Life-threatening or organimpairing Henoch-Schönlein purpura: plasmapheresis may save lives and limit organ damage. Dermatology 2009; 219:167–170.
- Mitsui H, Shibagaki N, Kawamura T, Matsue H, Shimada S. A clinical study of Henoch-Schönlein purpura associated with malignancy. J Eur Acad Dermatol Venereol 2009; 23:394–401.
- Maestri A, Malacarne P, Santini A. Henoch-Schönlein syndrome associated with breast cancer. A case report. Angiology 1995; 46:625–627.
- Rieu P, Noël LH. Henoch-Schönlein nephritis in children and adults. Morphological features and clinicopathological correlations. Ann Med Interne (Paris) 1999; 150:151–159.
- Fretzayas A, Sionti I, Moustaki M, Nicolaidou P. Clinical impact of altered immunoglobulin levels in Henoch-Schönlein purpura. Pediatr Int 2009; 51:381–384.
- Donghi D, Schanz U, Sahrbacher U, et al. Life-threatening or organimpairing Henoch-Schönlein purpura: plasmapheresis may save lives and limit organ damage. Dermatology 2009; 219:167–170.
- Mitsui H, Shibagaki N, Kawamura T, Matsue H, Shimada S. A clinical study of Henoch-Schönlein purpura associated with malignancy. J Eur Acad Dermatol Venereol 2009; 23:394–401.
- Maestri A, Malacarne P, Santini A. Henoch-Schönlein syndrome associated with breast cancer. A case report. Angiology 1995; 46:625–627.
Interpreting The JUPITER Trial: Statins can prevent VTE, but more study is needed
A major placebo-controlled trial has found that a statin can reduce the risk of venous thromboembolism (VTE).1
We do not recommend prescribing this class of drugs for this purpose until much more research has been done, and we certainly do not recommend substituting a statin for anticoagulant therapy in a patient at risk of VTE.
Nevertheless, we are excited by the latest findings, and we find comfort in knowing that if a patient is taking a statin for an approved indication, ie, reducing the risk of cardiovascular disease in a patient with hyperlipidemia or a previous cardiovascular event, the drug will also reduce the risk of VTE.
In the pages that follow, we describe and comment on what is known about the effect of statins on the risk of VTE.
ARTERIAL AND VENOUS THROMBOSIS: HOW ARE THEY LINKED?
The causes of arterial thrombosis may not be entirely distinct from those of deep vein thrombosis and pulmonary embolism, collectively referred to as VTE. Some studies have found that risk factors for arterial thrombosis overlap with those for VTE.2–4 However, other studies have shown no association between venous and arterial events.5–10
Hyperlipidemia, in particular, has been evaluated to see if it is a risk factor for VTE. As with other risk factors for arterial thrombosis, the data have been mixed, with some reports favoring an association with VTE and others not.4,5,11 Even so, preventive strategies targeting arterial risk factors have shown promise in reducing VTE events.12
Although commonly used to treat hyperlipidemia, statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors) are believed to reduce the incidence of thrombosis by a number of mechanisms13:
- Decreasing platelet aggregation
- Inhibiting expression of tissue factor and plasminogen activator inhibitor 1
- Increasing expression of tissue plasminogen activator
- Increasing expression of thrombomodulin, which can activate protein C and prevent thrombin-induced platelet and factor V activation and fibrinogen clotting.
STATINS AND VTE IN OBSERVATIONAL AND CASE-CONTROL STUDIES
In view of the multiple effects of statins, several studies have looked at whether these drugs reduce the occurrence of both arterial thrombosis and VTE.14–19
Two prospective observational studies and four case-control studies found that statins reduced the risk of VTE by 20% to 60%.14–19 Interestingly, two of the case-control studies found that antiplatelet therapy did not reduce the risk of VTE.18,19
THE JUPITER STUDY
The Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) study primarily sought to determine if rosuvastatin (Crestor) 20 mg/day, compared with placebo, would reduce the rate of first major cardiovascular events.22 A prespecified secondary end point of the trial was VTE, making JUPITER the first randomized, placebo-controlled trial to specifically test whether statins prevent VTE.1
Inclusion criteria: Normal LDL, high CRP
The study included men age 50 and older and women age 60 and older with no history of cardiovascular disease. In addition, their lowdensity lipoprotein (LDL) cholesterol levels had to be lower than 130 mg/dL (3.4 mmol/L), their triglyceride levels had to be lower than 500 mg/dL (5.6 mmol/L), and their highsensitivity C-reactive protein (hs-CRP) levels had to be 2.0 mg/L or higher.
Since high levels of hs-CRP, a marker of inflammation, predict cardiovascular events and since statins lower hs-CRP levels, the investigators hypothesized that people with elevated hs-CRP but without hyperlipidemia might benefit from statin treatment.21
Patients were excluded if they had received lipid-lowering therapy within 6 weeks of the trial screening, had diabetes mellitus or uncontrolled hypertension, were currently using postmenopausal hormone-replacement therapy, or had had cancer within the previous 5 years, except for certain skin cancers.
Candidates who complied well during a 4-week placebo run-in phase were randomly assigned to receive either rosuvastatin 20 mg daily (an intermediate dose) or a matching placebo. In all, 17,802 people were randomized. The two assigned groups appeared to be well matched.
Patients were to come in for visits twice a year for 60 months after randomization to be assessed for symptomatic deep venous thrombosis and pulmonary embolism. New cases of VTE were confirmed by imaging studies, by the initiation of anticoagulation therapy, or by death ascribed to pulmonary embolism.
Idiopathic VTE was classified as unprovoked if it occurred in the absence of trauma, hospitalization, or surgery within 3 months before the event, and in the absence of any diagnosed cancer within 3 months before and after the event. Provoked VTE events were those that occurred in a participant with cancer or when a precipitating event was associated with trauma, hospitalization, or surgery.
Rosuvastatin prevents heart attack, stroke
On the recommendation of the trial’s independent data and safety monitoring board, JUPITER was stopped early because the trial drug showed evidence of efficacy in preventing the combined primary end point of a first major cardiovascular event—ie, nonfatal myocardial infarction, nonfatal stroke, hospitalization for unstable angina, an arterial revascularization procedure, or confirmed death from a cardiovascular cause.22 (The cardiovascular outcomes of the JUPITER study were reviewed by Shishehbor and Hazen23 in the January 2009 issue of the Cleveland Clinic Journal of Medicine; see doi:10.3949/ccjm.75a.08105).
Formal follow-up for the trial's primary and secondary efficacy end points ended then, but data on VTE continued to be collected until each patient’s closeout visit as part of a safety monitoring protocol. The last closeout visit occurred on August 20, 2008. The primary analysis focused on events occurring up to March 30, 2008, the date the study was stopped.
Secondary end point results: Rosuvastatin prevents VTE
At a median follow-up of 1.9 years, an episode of VTE had occurred in 94 (0.53%) of the 17,802 patients—34 in the rosuvastatin group and 60 in the placebo group.1 This translates to 0.18 and 0.32 events per 100 person-years of follow-up in the rosuvastatin and placebo groups, respectively (hazard ratio for the rosuvastatin group 0.57, 95% confidence interval [CI] 0.37–0.86, P = .007).
Forty-four cases of VTE were classified as provoked and 50 cases were categorized as unprovoked. The risk reduction was statistically significant for provoked cases (hazard ratio 0.52, 95% CI 0.28–0.96, P = .03), but not for unprovoked events (hazard ratio 0.61, 95% CI 0.35–1.09, P = .09).
Subgroup analysis revealed no significant association between patient characteristics and the impact of rosuvastatin on the risk of a VTE event, but, as expected, more benefit was associated with higher baseline lipid levels.
STILL TOO SOON TO ADVISE ROUTINE STATIN USE TO PREVENT VTE
While the JUPITER trial data show an apparent benefit of statin use on the rate of VTE events, advising routine use of statins to prevent VTE is premature, for three main reasons.
Many must be treated to prevent one case of VTE. The number needed to treat (NNT) with rosuvastatin for 5 years to prevent either a case of VTE or a cardiovascular event was 21, and the NNT to prevent one cardiovascular event was 25. In a review of the two most recent case-control studies investigating the effects of statins on VTE,18,19 Cushman24 calculated that the NNT to prevent one VTE event each year was 333 for those age 75 and older. Though the Jupiter data did not provide the specific incidence of VTE at 1 year, except graphically, we can estimate that the NNT to prevent one VTE event at 1 year in the study is also very high.
Practically speaking, the perceived benefits of VTE prevention require large numbers to be treated, and the net clinical gain is still largely in preventing arterial events such as heart attack and stroke rather than VTE.
Statins, though safe, can still have adverse effects. The JUPITER study found a trend (albeit nonsignificant) toward more muscle complaints and elevations on liver function testing in apparently healthy persons taking a statin.22 Although severe complications of statin therapy such as rhabdomyolysis and elevations of creatine phosphokinase are rare, patients taking a statin have a 39% higher risk of an adverse event, most commonly myalgias or abnormalities on liver function testing.25 Were statins to be given routinely to even more people than they are now, more adverse outcomes would be likely.
More study is needed. The JUPITER study did not address a high risk of VTE. In fact, the investigators provided no information as to the VTE history of those enrolled.
Clearly, statins should not be substituted for proven prophylaxis and anticoagulation without further investigation, especially for patients with recurrent deep venous thrombosis, hospitalized patients, postoperative patients, and other patients prone to VTE.
OUR VIEW
The JUPITER study is an important leap forward in adding to our knowledge of how to prevent VTE. For people with another indication for taking a statin (eg, a previous cardiovascular event, hyperlipidemia), it is helpful to know that their risk of VTE may be reduced without exposure to the risks of other kinds of conventional thromboprophylaxis.
We look forward to additional studies to elaborate on the benefits of statins in both the prevention and treatment of VTE for averagerisk and VTE-prone populations.
- Glynn RJ, Danielson E, Fonseca FA, et al. A randomized trial of rosuvastatin in the prevention of venous thromboembolism. N Engl J Med 2009; 360:1851–1861.
- Prandoni P, Bilora F, Marchiori A, et al. An association between atherosclerosis and venous thrombosis. N Engl J Med 2003; 348:1435–1441.
- Prandoni P, Ghirarduzzi A, Prins MH, et al. Venous thromboembolism and the risk of subsequent symptomatic atherosclerosis. J Thromb Haemost 2006; 4:1891–1896.
- Braekkan SK, Mathiesen EB, Njolstad I, Wilsgaard T, Stormer J, Hansen JB. Family history of myocardial infarction is an independent risk factor for venous thromboembolism: the Tromso study. J Thromb Haemost 2008; 6:1851–1857.
- Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med 2002; 162:1182–1189.
- van der Hagen PB, Folsom AR, Jenny NS, et al. Subclinical atherosclerosis and the risk of future venous thrombosis in the Cardiovascular Health Study. J Thromb Haemost 2006; 4:1903–1908.
- Reich LM, Folsom AR, Key NS, et al. Prospective study of subclinical atherosclerosis as a risk factor for venous thromboembolism. J Thromb Haemost 2006; 4:1909–1913.
- Huerta C, Johansson S, Wallander MA, Rodriguez LA. Risk of myocardial infarction and overall mortality in survivors of venous thromboembolism. Thromb J 2008; 6:10.
- Linnemann B, Schindewolf M, Zgouras D, Erbe M, Jarosch-Preusche M, Lindhoff-Last E. Are patients with thrombophilia and previous venous thromboembolism at higher risk to arterial thrombosis? Thromb Res 2008; 121:743–750.
- Schwaiger J, Kiechl S, Stockner H, et al. Burden of atherosclerosis and risk of venous thromboembolism in patients with migraine. Neurology 2008; 71:937–943.
- Linnemann B, Zgouras D, Schindewolf M, Schwonberg J, Jarosch-Preusche M, Lindhoff-Last E. Impact of sex and traditional cardiovascular risk factors on the risk of recurrent venous thromboembolism: results from the German MAISTHRO Registry. Blood Coagul Fibrinolysis 2008; 19:159–165.
- Steffen LM, Folsom AR, Cushman M, Jacobs DR, Rosamond WD. Greater fish, fruit, and vegetable intakes are related to lower incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology. Circulation 2007; 115:188–195.
- Arslan F, Pasterkamp G, de Kleijn DP. Unraveling pleiotropic effects of statins: bit by bit, a slow case with perspective. Circ Res 2008; 103:334–336.
- Grady D, Wenger NK, Herrington D, et al. Postmenopausal hormone therapy increases risk for venous thromboembolic disease. The Heart and Estrogen/progestin Replacement Study. Ann Intern Med 2000; 132:689–696.
- Ray JG, Mamdani M, Tsuyuki RT, Anderson DR, Yeo EL, Laupacis A. Use of statins and the subsequent development of deep vein thrombosis. Arch Intern Med 2001; 161:1405–1410.
- Doggen CJ, Lemaitre RN, Smith NL, Heckbert SR, Psaty BM. HMG CoA reductase inhibitors and the risk of venous thrombosis among postmenopausal women. J Thromb Haemost 2004; 2:700–701.
- Lacut K, Oger E, Le Gal G, et al. Statins but not fibrates are associated with a reduced risk of venous thromboembolism: a hospitalbased case-control study. Fundam Clin Pharmacol 2004; 18:477–482.
- Ramcharan AS, Van Stralen KJ, Snoep JD, Mantel-Teeuwisse AK, Rosendaal FR, Doggen CJ. HMG-CoA reductase inhibitors, other lipid-lowering medication, antiplatelet therapy, and the risk of venous thrombosis. J Thromb Haemost 2009; 7:514–520.
- Sørensen HT, Horvath-Puho E, Sogaard KK, et al. Arterial cardiovascular events, statins, low-dose aspirin and subsequent risk of venous thromboembolism: a population-based case-control study. J Thromb Haemost 2009; 7:521–528.
- Yang CC, Jick SS, Jick H. Statins and the risk of idiopathic venous thromboembolism. Br J Clin Pharmacol 2002; 53:101–105.
- Smeeth L, Douglas I, Hall AJ, Hubbard R, Evans S. Effect of statins on a wide range of health outcomes: a cohort study validated by comparison with randomized trials. Br J Clin Pharmacol 2009; 67:99–109.
- Ridker PM, Danielson E, Fonseca FA, et al; JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.
- Shishehbor MH, Hazen SL. JUPITER to Earth: A statin helps peole with normal LDL-C and high hs-CRP, but what does it mean? Cleve Clin J Med 2009; 76:37–44.
- Cushman M. A new indication for statins to prevent venous thromboembolism? Not yet. J Thromb Haemost 2009; 7:511–513.
- Silva MA, Swanson AC, Gandhi PJ, Tataronis GR. Statin-related adverse events: a meta-analysis. Clin Ther 2006; 28:26–35.
A major placebo-controlled trial has found that a statin can reduce the risk of venous thromboembolism (VTE).1
We do not recommend prescribing this class of drugs for this purpose until much more research has been done, and we certainly do not recommend substituting a statin for anticoagulant therapy in a patient at risk of VTE.
Nevertheless, we are excited by the latest findings, and we find comfort in knowing that if a patient is taking a statin for an approved indication, ie, reducing the risk of cardiovascular disease in a patient with hyperlipidemia or a previous cardiovascular event, the drug will also reduce the risk of VTE.
In the pages that follow, we describe and comment on what is known about the effect of statins on the risk of VTE.
ARTERIAL AND VENOUS THROMBOSIS: HOW ARE THEY LINKED?
The causes of arterial thrombosis may not be entirely distinct from those of deep vein thrombosis and pulmonary embolism, collectively referred to as VTE. Some studies have found that risk factors for arterial thrombosis overlap with those for VTE.2–4 However, other studies have shown no association between venous and arterial events.5–10
Hyperlipidemia, in particular, has been evaluated to see if it is a risk factor for VTE. As with other risk factors for arterial thrombosis, the data have been mixed, with some reports favoring an association with VTE and others not.4,5,11 Even so, preventive strategies targeting arterial risk factors have shown promise in reducing VTE events.12
Although commonly used to treat hyperlipidemia, statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors) are believed to reduce the incidence of thrombosis by a number of mechanisms13:
- Decreasing platelet aggregation
- Inhibiting expression of tissue factor and plasminogen activator inhibitor 1
- Increasing expression of tissue plasminogen activator
- Increasing expression of thrombomodulin, which can activate protein C and prevent thrombin-induced platelet and factor V activation and fibrinogen clotting.
STATINS AND VTE IN OBSERVATIONAL AND CASE-CONTROL STUDIES
In view of the multiple effects of statins, several studies have looked at whether these drugs reduce the occurrence of both arterial thrombosis and VTE.14–19
Two prospective observational studies and four case-control studies found that statins reduced the risk of VTE by 20% to 60%.14–19 Interestingly, two of the case-control studies found that antiplatelet therapy did not reduce the risk of VTE.18,19
THE JUPITER STUDY
The Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) study primarily sought to determine if rosuvastatin (Crestor) 20 mg/day, compared with placebo, would reduce the rate of first major cardiovascular events.22 A prespecified secondary end point of the trial was VTE, making JUPITER the first randomized, placebo-controlled trial to specifically test whether statins prevent VTE.1
Inclusion criteria: Normal LDL, high CRP
The study included men age 50 and older and women age 60 and older with no history of cardiovascular disease. In addition, their lowdensity lipoprotein (LDL) cholesterol levels had to be lower than 130 mg/dL (3.4 mmol/L), their triglyceride levels had to be lower than 500 mg/dL (5.6 mmol/L), and their highsensitivity C-reactive protein (hs-CRP) levels had to be 2.0 mg/L or higher.
Since high levels of hs-CRP, a marker of inflammation, predict cardiovascular events and since statins lower hs-CRP levels, the investigators hypothesized that people with elevated hs-CRP but without hyperlipidemia might benefit from statin treatment.21
Patients were excluded if they had received lipid-lowering therapy within 6 weeks of the trial screening, had diabetes mellitus or uncontrolled hypertension, were currently using postmenopausal hormone-replacement therapy, or had had cancer within the previous 5 years, except for certain skin cancers.
Candidates who complied well during a 4-week placebo run-in phase were randomly assigned to receive either rosuvastatin 20 mg daily (an intermediate dose) or a matching placebo. In all, 17,802 people were randomized. The two assigned groups appeared to be well matched.
Patients were to come in for visits twice a year for 60 months after randomization to be assessed for symptomatic deep venous thrombosis and pulmonary embolism. New cases of VTE were confirmed by imaging studies, by the initiation of anticoagulation therapy, or by death ascribed to pulmonary embolism.
Idiopathic VTE was classified as unprovoked if it occurred in the absence of trauma, hospitalization, or surgery within 3 months before the event, and in the absence of any diagnosed cancer within 3 months before and after the event. Provoked VTE events were those that occurred in a participant with cancer or when a precipitating event was associated with trauma, hospitalization, or surgery.
Rosuvastatin prevents heart attack, stroke
On the recommendation of the trial’s independent data and safety monitoring board, JUPITER was stopped early because the trial drug showed evidence of efficacy in preventing the combined primary end point of a first major cardiovascular event—ie, nonfatal myocardial infarction, nonfatal stroke, hospitalization for unstable angina, an arterial revascularization procedure, or confirmed death from a cardiovascular cause.22 (The cardiovascular outcomes of the JUPITER study were reviewed by Shishehbor and Hazen23 in the January 2009 issue of the Cleveland Clinic Journal of Medicine; see doi:10.3949/ccjm.75a.08105).
Formal follow-up for the trial's primary and secondary efficacy end points ended then, but data on VTE continued to be collected until each patient’s closeout visit as part of a safety monitoring protocol. The last closeout visit occurred on August 20, 2008. The primary analysis focused on events occurring up to March 30, 2008, the date the study was stopped.
Secondary end point results: Rosuvastatin prevents VTE
At a median follow-up of 1.9 years, an episode of VTE had occurred in 94 (0.53%) of the 17,802 patients—34 in the rosuvastatin group and 60 in the placebo group.1 This translates to 0.18 and 0.32 events per 100 person-years of follow-up in the rosuvastatin and placebo groups, respectively (hazard ratio for the rosuvastatin group 0.57, 95% confidence interval [CI] 0.37–0.86, P = .007).
Forty-four cases of VTE were classified as provoked and 50 cases were categorized as unprovoked. The risk reduction was statistically significant for provoked cases (hazard ratio 0.52, 95% CI 0.28–0.96, P = .03), but not for unprovoked events (hazard ratio 0.61, 95% CI 0.35–1.09, P = .09).
Subgroup analysis revealed no significant association between patient characteristics and the impact of rosuvastatin on the risk of a VTE event, but, as expected, more benefit was associated with higher baseline lipid levels.
STILL TOO SOON TO ADVISE ROUTINE STATIN USE TO PREVENT VTE
While the JUPITER trial data show an apparent benefit of statin use on the rate of VTE events, advising routine use of statins to prevent VTE is premature, for three main reasons.
Many must be treated to prevent one case of VTE. The number needed to treat (NNT) with rosuvastatin for 5 years to prevent either a case of VTE or a cardiovascular event was 21, and the NNT to prevent one cardiovascular event was 25. In a review of the two most recent case-control studies investigating the effects of statins on VTE,18,19 Cushman24 calculated that the NNT to prevent one VTE event each year was 333 for those age 75 and older. Though the Jupiter data did not provide the specific incidence of VTE at 1 year, except graphically, we can estimate that the NNT to prevent one VTE event at 1 year in the study is also very high.
Practically speaking, the perceived benefits of VTE prevention require large numbers to be treated, and the net clinical gain is still largely in preventing arterial events such as heart attack and stroke rather than VTE.
Statins, though safe, can still have adverse effects. The JUPITER study found a trend (albeit nonsignificant) toward more muscle complaints and elevations on liver function testing in apparently healthy persons taking a statin.22 Although severe complications of statin therapy such as rhabdomyolysis and elevations of creatine phosphokinase are rare, patients taking a statin have a 39% higher risk of an adverse event, most commonly myalgias or abnormalities on liver function testing.25 Were statins to be given routinely to even more people than they are now, more adverse outcomes would be likely.
More study is needed. The JUPITER study did not address a high risk of VTE. In fact, the investigators provided no information as to the VTE history of those enrolled.
Clearly, statins should not be substituted for proven prophylaxis and anticoagulation without further investigation, especially for patients with recurrent deep venous thrombosis, hospitalized patients, postoperative patients, and other patients prone to VTE.
OUR VIEW
The JUPITER study is an important leap forward in adding to our knowledge of how to prevent VTE. For people with another indication for taking a statin (eg, a previous cardiovascular event, hyperlipidemia), it is helpful to know that their risk of VTE may be reduced without exposure to the risks of other kinds of conventional thromboprophylaxis.
We look forward to additional studies to elaborate on the benefits of statins in both the prevention and treatment of VTE for averagerisk and VTE-prone populations.
A major placebo-controlled trial has found that a statin can reduce the risk of venous thromboembolism (VTE).1
We do not recommend prescribing this class of drugs for this purpose until much more research has been done, and we certainly do not recommend substituting a statin for anticoagulant therapy in a patient at risk of VTE.
Nevertheless, we are excited by the latest findings, and we find comfort in knowing that if a patient is taking a statin for an approved indication, ie, reducing the risk of cardiovascular disease in a patient with hyperlipidemia or a previous cardiovascular event, the drug will also reduce the risk of VTE.
In the pages that follow, we describe and comment on what is known about the effect of statins on the risk of VTE.
ARTERIAL AND VENOUS THROMBOSIS: HOW ARE THEY LINKED?
The causes of arterial thrombosis may not be entirely distinct from those of deep vein thrombosis and pulmonary embolism, collectively referred to as VTE. Some studies have found that risk factors for arterial thrombosis overlap with those for VTE.2–4 However, other studies have shown no association between venous and arterial events.5–10
Hyperlipidemia, in particular, has been evaluated to see if it is a risk factor for VTE. As with other risk factors for arterial thrombosis, the data have been mixed, with some reports favoring an association with VTE and others not.4,5,11 Even so, preventive strategies targeting arterial risk factors have shown promise in reducing VTE events.12
Although commonly used to treat hyperlipidemia, statins (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors) are believed to reduce the incidence of thrombosis by a number of mechanisms13:
- Decreasing platelet aggregation
- Inhibiting expression of tissue factor and plasminogen activator inhibitor 1
- Increasing expression of tissue plasminogen activator
- Increasing expression of thrombomodulin, which can activate protein C and prevent thrombin-induced platelet and factor V activation and fibrinogen clotting.
STATINS AND VTE IN OBSERVATIONAL AND CASE-CONTROL STUDIES
In view of the multiple effects of statins, several studies have looked at whether these drugs reduce the occurrence of both arterial thrombosis and VTE.14–19
Two prospective observational studies and four case-control studies found that statins reduced the risk of VTE by 20% to 60%.14–19 Interestingly, two of the case-control studies found that antiplatelet therapy did not reduce the risk of VTE.18,19
THE JUPITER STUDY
The Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) study primarily sought to determine if rosuvastatin (Crestor) 20 mg/day, compared with placebo, would reduce the rate of first major cardiovascular events.22 A prespecified secondary end point of the trial was VTE, making JUPITER the first randomized, placebo-controlled trial to specifically test whether statins prevent VTE.1
Inclusion criteria: Normal LDL, high CRP
The study included men age 50 and older and women age 60 and older with no history of cardiovascular disease. In addition, their lowdensity lipoprotein (LDL) cholesterol levels had to be lower than 130 mg/dL (3.4 mmol/L), their triglyceride levels had to be lower than 500 mg/dL (5.6 mmol/L), and their highsensitivity C-reactive protein (hs-CRP) levels had to be 2.0 mg/L or higher.
Since high levels of hs-CRP, a marker of inflammation, predict cardiovascular events and since statins lower hs-CRP levels, the investigators hypothesized that people with elevated hs-CRP but without hyperlipidemia might benefit from statin treatment.21
Patients were excluded if they had received lipid-lowering therapy within 6 weeks of the trial screening, had diabetes mellitus or uncontrolled hypertension, were currently using postmenopausal hormone-replacement therapy, or had had cancer within the previous 5 years, except for certain skin cancers.
Candidates who complied well during a 4-week placebo run-in phase were randomly assigned to receive either rosuvastatin 20 mg daily (an intermediate dose) or a matching placebo. In all, 17,802 people were randomized. The two assigned groups appeared to be well matched.
Patients were to come in for visits twice a year for 60 months after randomization to be assessed for symptomatic deep venous thrombosis and pulmonary embolism. New cases of VTE were confirmed by imaging studies, by the initiation of anticoagulation therapy, or by death ascribed to pulmonary embolism.
Idiopathic VTE was classified as unprovoked if it occurred in the absence of trauma, hospitalization, or surgery within 3 months before the event, and in the absence of any diagnosed cancer within 3 months before and after the event. Provoked VTE events were those that occurred in a participant with cancer or when a precipitating event was associated with trauma, hospitalization, or surgery.
Rosuvastatin prevents heart attack, stroke
On the recommendation of the trial’s independent data and safety monitoring board, JUPITER was stopped early because the trial drug showed evidence of efficacy in preventing the combined primary end point of a first major cardiovascular event—ie, nonfatal myocardial infarction, nonfatal stroke, hospitalization for unstable angina, an arterial revascularization procedure, or confirmed death from a cardiovascular cause.22 (The cardiovascular outcomes of the JUPITER study were reviewed by Shishehbor and Hazen23 in the January 2009 issue of the Cleveland Clinic Journal of Medicine; see doi:10.3949/ccjm.75a.08105).
Formal follow-up for the trial's primary and secondary efficacy end points ended then, but data on VTE continued to be collected until each patient’s closeout visit as part of a safety monitoring protocol. The last closeout visit occurred on August 20, 2008. The primary analysis focused on events occurring up to March 30, 2008, the date the study was stopped.
Secondary end point results: Rosuvastatin prevents VTE
At a median follow-up of 1.9 years, an episode of VTE had occurred in 94 (0.53%) of the 17,802 patients—34 in the rosuvastatin group and 60 in the placebo group.1 This translates to 0.18 and 0.32 events per 100 person-years of follow-up in the rosuvastatin and placebo groups, respectively (hazard ratio for the rosuvastatin group 0.57, 95% confidence interval [CI] 0.37–0.86, P = .007).
Forty-four cases of VTE were classified as provoked and 50 cases were categorized as unprovoked. The risk reduction was statistically significant for provoked cases (hazard ratio 0.52, 95% CI 0.28–0.96, P = .03), but not for unprovoked events (hazard ratio 0.61, 95% CI 0.35–1.09, P = .09).
Subgroup analysis revealed no significant association between patient characteristics and the impact of rosuvastatin on the risk of a VTE event, but, as expected, more benefit was associated with higher baseline lipid levels.
STILL TOO SOON TO ADVISE ROUTINE STATIN USE TO PREVENT VTE
While the JUPITER trial data show an apparent benefit of statin use on the rate of VTE events, advising routine use of statins to prevent VTE is premature, for three main reasons.
Many must be treated to prevent one case of VTE. The number needed to treat (NNT) with rosuvastatin for 5 years to prevent either a case of VTE or a cardiovascular event was 21, and the NNT to prevent one cardiovascular event was 25. In a review of the two most recent case-control studies investigating the effects of statins on VTE,18,19 Cushman24 calculated that the NNT to prevent one VTE event each year was 333 for those age 75 and older. Though the Jupiter data did not provide the specific incidence of VTE at 1 year, except graphically, we can estimate that the NNT to prevent one VTE event at 1 year in the study is also very high.
Practically speaking, the perceived benefits of VTE prevention require large numbers to be treated, and the net clinical gain is still largely in preventing arterial events such as heart attack and stroke rather than VTE.
Statins, though safe, can still have adverse effects. The JUPITER study found a trend (albeit nonsignificant) toward more muscle complaints and elevations on liver function testing in apparently healthy persons taking a statin.22 Although severe complications of statin therapy such as rhabdomyolysis and elevations of creatine phosphokinase are rare, patients taking a statin have a 39% higher risk of an adverse event, most commonly myalgias or abnormalities on liver function testing.25 Were statins to be given routinely to even more people than they are now, more adverse outcomes would be likely.
More study is needed. The JUPITER study did not address a high risk of VTE. In fact, the investigators provided no information as to the VTE history of those enrolled.
Clearly, statins should not be substituted for proven prophylaxis and anticoagulation without further investigation, especially for patients with recurrent deep venous thrombosis, hospitalized patients, postoperative patients, and other patients prone to VTE.
OUR VIEW
The JUPITER study is an important leap forward in adding to our knowledge of how to prevent VTE. For people with another indication for taking a statin (eg, a previous cardiovascular event, hyperlipidemia), it is helpful to know that their risk of VTE may be reduced without exposure to the risks of other kinds of conventional thromboprophylaxis.
We look forward to additional studies to elaborate on the benefits of statins in both the prevention and treatment of VTE for averagerisk and VTE-prone populations.
- Glynn RJ, Danielson E, Fonseca FA, et al. A randomized trial of rosuvastatin in the prevention of venous thromboembolism. N Engl J Med 2009; 360:1851–1861.
- Prandoni P, Bilora F, Marchiori A, et al. An association between atherosclerosis and venous thrombosis. N Engl J Med 2003; 348:1435–1441.
- Prandoni P, Ghirarduzzi A, Prins MH, et al. Venous thromboembolism and the risk of subsequent symptomatic atherosclerosis. J Thromb Haemost 2006; 4:1891–1896.
- Braekkan SK, Mathiesen EB, Njolstad I, Wilsgaard T, Stormer J, Hansen JB. Family history of myocardial infarction is an independent risk factor for venous thromboembolism: the Tromso study. J Thromb Haemost 2008; 6:1851–1857.
- Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med 2002; 162:1182–1189.
- van der Hagen PB, Folsom AR, Jenny NS, et al. Subclinical atherosclerosis and the risk of future venous thrombosis in the Cardiovascular Health Study. J Thromb Haemost 2006; 4:1903–1908.
- Reich LM, Folsom AR, Key NS, et al. Prospective study of subclinical atherosclerosis as a risk factor for venous thromboembolism. J Thromb Haemost 2006; 4:1909–1913.
- Huerta C, Johansson S, Wallander MA, Rodriguez LA. Risk of myocardial infarction and overall mortality in survivors of venous thromboembolism. Thromb J 2008; 6:10.
- Linnemann B, Schindewolf M, Zgouras D, Erbe M, Jarosch-Preusche M, Lindhoff-Last E. Are patients with thrombophilia and previous venous thromboembolism at higher risk to arterial thrombosis? Thromb Res 2008; 121:743–750.
- Schwaiger J, Kiechl S, Stockner H, et al. Burden of atherosclerosis and risk of venous thromboembolism in patients with migraine. Neurology 2008; 71:937–943.
- Linnemann B, Zgouras D, Schindewolf M, Schwonberg J, Jarosch-Preusche M, Lindhoff-Last E. Impact of sex and traditional cardiovascular risk factors on the risk of recurrent venous thromboembolism: results from the German MAISTHRO Registry. Blood Coagul Fibrinolysis 2008; 19:159–165.
- Steffen LM, Folsom AR, Cushman M, Jacobs DR, Rosamond WD. Greater fish, fruit, and vegetable intakes are related to lower incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology. Circulation 2007; 115:188–195.
- Arslan F, Pasterkamp G, de Kleijn DP. Unraveling pleiotropic effects of statins: bit by bit, a slow case with perspective. Circ Res 2008; 103:334–336.
- Grady D, Wenger NK, Herrington D, et al. Postmenopausal hormone therapy increases risk for venous thromboembolic disease. The Heart and Estrogen/progestin Replacement Study. Ann Intern Med 2000; 132:689–696.
- Ray JG, Mamdani M, Tsuyuki RT, Anderson DR, Yeo EL, Laupacis A. Use of statins and the subsequent development of deep vein thrombosis. Arch Intern Med 2001; 161:1405–1410.
- Doggen CJ, Lemaitre RN, Smith NL, Heckbert SR, Psaty BM. HMG CoA reductase inhibitors and the risk of venous thrombosis among postmenopausal women. J Thromb Haemost 2004; 2:700–701.
- Lacut K, Oger E, Le Gal G, et al. Statins but not fibrates are associated with a reduced risk of venous thromboembolism: a hospitalbased case-control study. Fundam Clin Pharmacol 2004; 18:477–482.
- Ramcharan AS, Van Stralen KJ, Snoep JD, Mantel-Teeuwisse AK, Rosendaal FR, Doggen CJ. HMG-CoA reductase inhibitors, other lipid-lowering medication, antiplatelet therapy, and the risk of venous thrombosis. J Thromb Haemost 2009; 7:514–520.
- Sørensen HT, Horvath-Puho E, Sogaard KK, et al. Arterial cardiovascular events, statins, low-dose aspirin and subsequent risk of venous thromboembolism: a population-based case-control study. J Thromb Haemost 2009; 7:521–528.
- Yang CC, Jick SS, Jick H. Statins and the risk of idiopathic venous thromboembolism. Br J Clin Pharmacol 2002; 53:101–105.
- Smeeth L, Douglas I, Hall AJ, Hubbard R, Evans S. Effect of statins on a wide range of health outcomes: a cohort study validated by comparison with randomized trials. Br J Clin Pharmacol 2009; 67:99–109.
- Ridker PM, Danielson E, Fonseca FA, et al; JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.
- Shishehbor MH, Hazen SL. JUPITER to Earth: A statin helps peole with normal LDL-C and high hs-CRP, but what does it mean? Cleve Clin J Med 2009; 76:37–44.
- Cushman M. A new indication for statins to prevent venous thromboembolism? Not yet. J Thromb Haemost 2009; 7:511–513.
- Silva MA, Swanson AC, Gandhi PJ, Tataronis GR. Statin-related adverse events: a meta-analysis. Clin Ther 2006; 28:26–35.
- Glynn RJ, Danielson E, Fonseca FA, et al. A randomized trial of rosuvastatin in the prevention of venous thromboembolism. N Engl J Med 2009; 360:1851–1861.
- Prandoni P, Bilora F, Marchiori A, et al. An association between atherosclerosis and venous thrombosis. N Engl J Med 2003; 348:1435–1441.
- Prandoni P, Ghirarduzzi A, Prins MH, et al. Venous thromboembolism and the risk of subsequent symptomatic atherosclerosis. J Thromb Haemost 2006; 4:1891–1896.
- Braekkan SK, Mathiesen EB, Njolstad I, Wilsgaard T, Stormer J, Hansen JB. Family history of myocardial infarction is an independent risk factor for venous thromboembolism: the Tromso study. J Thromb Haemost 2008; 6:1851–1857.
- Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med 2002; 162:1182–1189.
- van der Hagen PB, Folsom AR, Jenny NS, et al. Subclinical atherosclerosis and the risk of future venous thrombosis in the Cardiovascular Health Study. J Thromb Haemost 2006; 4:1903–1908.
- Reich LM, Folsom AR, Key NS, et al. Prospective study of subclinical atherosclerosis as a risk factor for venous thromboembolism. J Thromb Haemost 2006; 4:1909–1913.
- Huerta C, Johansson S, Wallander MA, Rodriguez LA. Risk of myocardial infarction and overall mortality in survivors of venous thromboembolism. Thromb J 2008; 6:10.
- Linnemann B, Schindewolf M, Zgouras D, Erbe M, Jarosch-Preusche M, Lindhoff-Last E. Are patients with thrombophilia and previous venous thromboembolism at higher risk to arterial thrombosis? Thromb Res 2008; 121:743–750.
- Schwaiger J, Kiechl S, Stockner H, et al. Burden of atherosclerosis and risk of venous thromboembolism in patients with migraine. Neurology 2008; 71:937–943.
- Linnemann B, Zgouras D, Schindewolf M, Schwonberg J, Jarosch-Preusche M, Lindhoff-Last E. Impact of sex and traditional cardiovascular risk factors on the risk of recurrent venous thromboembolism: results from the German MAISTHRO Registry. Blood Coagul Fibrinolysis 2008; 19:159–165.
- Steffen LM, Folsom AR, Cushman M, Jacobs DR, Rosamond WD. Greater fish, fruit, and vegetable intakes are related to lower incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology. Circulation 2007; 115:188–195.
- Arslan F, Pasterkamp G, de Kleijn DP. Unraveling pleiotropic effects of statins: bit by bit, a slow case with perspective. Circ Res 2008; 103:334–336.
- Grady D, Wenger NK, Herrington D, et al. Postmenopausal hormone therapy increases risk for venous thromboembolic disease. The Heart and Estrogen/progestin Replacement Study. Ann Intern Med 2000; 132:689–696.
- Ray JG, Mamdani M, Tsuyuki RT, Anderson DR, Yeo EL, Laupacis A. Use of statins and the subsequent development of deep vein thrombosis. Arch Intern Med 2001; 161:1405–1410.
- Doggen CJ, Lemaitre RN, Smith NL, Heckbert SR, Psaty BM. HMG CoA reductase inhibitors and the risk of venous thrombosis among postmenopausal women. J Thromb Haemost 2004; 2:700–701.
- Lacut K, Oger E, Le Gal G, et al. Statins but not fibrates are associated with a reduced risk of venous thromboembolism: a hospitalbased case-control study. Fundam Clin Pharmacol 2004; 18:477–482.
- Ramcharan AS, Van Stralen KJ, Snoep JD, Mantel-Teeuwisse AK, Rosendaal FR, Doggen CJ. HMG-CoA reductase inhibitors, other lipid-lowering medication, antiplatelet therapy, and the risk of venous thrombosis. J Thromb Haemost 2009; 7:514–520.
- Sørensen HT, Horvath-Puho E, Sogaard KK, et al. Arterial cardiovascular events, statins, low-dose aspirin and subsequent risk of venous thromboembolism: a population-based case-control study. J Thromb Haemost 2009; 7:521–528.
- Yang CC, Jick SS, Jick H. Statins and the risk of idiopathic venous thromboembolism. Br J Clin Pharmacol 2002; 53:101–105.
- Smeeth L, Douglas I, Hall AJ, Hubbard R, Evans S. Effect of statins on a wide range of health outcomes: a cohort study validated by comparison with randomized trials. Br J Clin Pharmacol 2009; 67:99–109.
- Ridker PM, Danielson E, Fonseca FA, et al; JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 2008; 359:2195–2207.
- Shishehbor MH, Hazen SL. JUPITER to Earth: A statin helps peole with normal LDL-C and high hs-CRP, but what does it mean? Cleve Clin J Med 2009; 76:37–44.
- Cushman M. A new indication for statins to prevent venous thromboembolism? Not yet. J Thromb Haemost 2009; 7:511–513.
- Silva MA, Swanson AC, Gandhi PJ, Tataronis GR. Statin-related adverse events: a meta-analysis. Clin Ther 2006; 28:26–35.
KEY POINTS
- Risk factors for VTE overlap with those for arterial thrombosis, although the data are mixed.
- The statin drugs have a number of effects on factors other than lipid levels, notably on markers of inflammation and on clotting factors.
- In the JUPITER trial, the incidence of VTE in people taking rosuvastatin (Crestor) 20 mg/day was about half that in people taking placebo. This was a relatively healthy population, and the incidence in both groups was low.
- Further study is needed in patients at risk of VTE.
Stenting for atherosclerotic renal artery stenosis: One poorly designed trial after another
The role of stenting for atherosclerotic renal artery stenosis is hotly debated among different specialties.1,2 If we may generalize a bit, interventionalists (cardiologists, interventional radiologists, vascular surgeons, and vascular medicine specialists) have been in favor of liberal use of stenting, and nephrologists often favor medical therapy alone. And as with all controversial issues, each group feels rather strongly about its position.
Because few prospective randomized trials have been completed, the management of atherosclerotic renal artery stenosis has been guided by retrospective studies and case series. 3
In this issue of the Cleveland Clinic Journal of Medicine, Dr. James Simon4 provides an excellent overview of the prevalence, natural history, and clinical presentation of atherosclerotic renal artery stenosis. In addition, he does an admirable job of reviewing the available prospective randomized trials and providing editorial commentary about the role of the various specialists in the management of renal artery disease. And while the title of his paper says that it is “time to be less aggressive,” Dr. Simon ultimately comes to the same conclusions that we do5 on the indications for renal artery stenting (see Table 3 of Dr. Simon’s article), which are those of the multidisciplinary 2006 American College of Cardiology/American Heart Association guidelines on the management of peripheral artery disease.3
So what then is all the controversy about? We all agree that prospective randomized trials that provide class I, level A evidence impart the only unbiased scientific information on the best treatment strategy for patients with renal artery disease. The basic controversial issue is the interpretation of these trials. We contend that the three randomized trials of stenting vs medical therapy published so far6–8 (see below) are so seriously flawed that it is impossible to make treatment decisions based on their results.
Since these trials were published in wellrespected journals, their results are often taken as gospel. However, careful review of each of these will reveal the flaws in study design and implementation.
THE DRASTIC TRIAL
In the Dutch Renal Artery Stenosis Intervention Cooperative (DRASTIC) trial,6 106 patients with renal artery stenosis and hypertension (diastolic blood pressure > 95 mm Hg) despite treatment with two antihypertensive medications were randomly assigned to either renal angioplasty (n = 56) or drug therapy (n = 50).
Authors’ conclusions
“In the treatment of patients with hypertension and renal-artery stenosis, angioplasty has little advantage over antihypertensive-drug therapy.”6
Four serious problems
As we discussed in a letter to the editor of the New England Journal of Medicine on August 10, 2000, this study had four serious problems that invalidate its authors’ conclusions.9
The sample size was insufficient to detect a significant difference between treatment groups. In other words, the chance of a type 2 statistical error is high.
Balloon angioplasty without stenting was used as the method of revascularization. Experts now recognize that stenting is required for renal artery intervention to have a durable result.3,5
Renal artery stenosis was defined as greater than 50% stenosis. This allowed a large number of patients to enter the trial who had hemodynamically and clinically insignificant lesions. Most clinicians believe that stenosis of less than 70% is not hemodynamically important.5,10,11
Twenty-two of the 50 patients randomized to medical therapy crossed over to the angioplasty group because their blood pressure became difficult to control. In other words, 44% of the patients in the medical group underwent angioplasty, an astounding percentage in an intention-to-treat analysis comparing one therapy with another.
Despite these serious flaws, the results of DRASTIC influenced therapy for years after its publication.
THE STAR TRIAL
In the Stent Placement in Patients With Atherosclerotic Renal Artery Stenosis and Impaired Renal Function (STAR) trial,7 140 patients with a creatinine clearance of less than 80 mL/min/1.73m2, renal artery stenosis greater than 50%, and well-controlled blood pressure were randomized to either renal artery stenting plus medical therapy (n = 64) or medical therapy alone (n = 76). The primary end point was a 20% or greater decrease in creatinine clearance. Secondary end points included measures of safety and cardiovascular morbidity and mortality.
Authors’ conclusions
“Stent placement with medical treatment had no clear effect on progression of impaired renal function but led to a small number of significant procedure-related complications. The study findings favor a conservative approach to patients with [atherosclerotic renal artery stenosis], focused on cardiovascular risk factor management and avoiding stenting.”7
Serious flaws
A number of serious flaws render this study uninterpretable.
Mild renal artery stenosis. At least 33% of the patients in the study had mild renal artery stenosis (50%–70%), and 12 (19%) of the 64 patients in the group randomized to stenting actually had stenosis of less than 50%. How can one expect there to be a benefit to stenting in patients with mild (and hemodynamically insignificant) renal artery stenosis? This is especially true when the primary end point is a change in renal function.
More than half of the patients had unilateral disease. It seems intuitive that if one were to plan a trial with a primary end point of a change in renal function, only patients with bilateral renal artery stenosis of greater than 70% or with stenosis of greater than 70% to a solitary functioning kidney would be included. One would not expect that patients with unilateral disease and a stenosis of less than 70% would derive any benefit from revascularization.
Not all “stent” patients received stents. All of the patients in the medical group received medication and there were no crossovers. However, only 46 (72%) of the 64 patients randomized to stenting actually received a stent, while 18 (28%) did not. There were two technical failures, and 12 patients should not have been randomized because they had less than 50% stenosis on angiography and thus were not stented. Yet all 64 patients were analyzed (by intention to treat) in the stent group. With these numbers, one could predict that the results would be negative.
Like DRASTIC, this trial was underpowered, meaning that the chance of a type 2 statistical error is high. In fact, the editors of the Annals of Internal Medicine, in a note accompanying the article, cautioned that the study “was underpowered to provide a definitive estimate of efficacy.”7 If the study was underpowered to answer the question at hand, why was it deemed worthy of publication?
High complication rates. The periprocedural complication and death rates were much higher than in many other reports on renal artery stenting (see details below).5
THE ASTRAL TRIAL
In the Angioplasty and Stenting for Renal Artery Lesions (ASTRAL) trial,8 the primary outcome measure was the change in renal function over time as assessed by the mean slope of the reciprocal of the serum creatinine. In this trial, 806 patients with atherosclerotic renal artery stenosis were randomized to either stent-based revascularization combined with medical therapy or medical therapy alone.
Authors’ conclusions
“We found substantial risks but no evidence of a worthwhile clinical benefit from revascularization in patients with atherosclerotic renovascular disease.”8
Despite size, flaws remain
Unlike the other trials, ASTRAL had a sample size large enough to provide an answer. However, numerous flaws in study design and implementation invalidate its results for the overall population of patients with renal artery stenosis. The major flaws in ASTRAL were:
Selection bias. For a patient to be enrolled, the treating physician had to be undecided on whether the patient should undergo revascularization or medical management alone. However, the treatment of atherosclerotic renal artery stenosis is so controversial that physicians of different specialties cannot agree on the most effective treatment strategy for most patients.1,2 Therefore, to exclude patients when their physicians were sure they needed or did not need renal artery revascularization is incomprehensible and introduces considerable selection bias into the trial design.
Normal renal function at baseline. The primary outcome was a change in renal function over time. Yet 25% of patients had normal renal function at the outset of the trial. In addition, a significant number had unilateral disease, and 41% had a stenosis less than 70%. What made the investigators think that stent implantation could possibly be shown to be beneficial if they entered patients into a renal function study who had near-normal renal function, unilateral disease, and mild renal artery stenosis? These are patients whose condition would not be expected to worsen with medical therapy nor to improve with stenting. Most clinicians would not consider stenting a patient to preserve renal function if the patient has unilateral mild renal artery stenosis.
There was no core laboratory to adjudicate the interpretation of the imaging studies. To determine the degree of stenosis of an artery in an accurate and unbiased fashion, a core laboratory must be used.
The reason this is so important is that visual assessment of the degree of stenosis on angiography is not accurate and almost always overestimates the degree of stenosis.12,13 In a study assessing the physiologic importance of renal artery lesions, the lesion severity by visual estimation was 74.9% ± 11.5% (range 50%–90%), which exceeded the quantitative vascular angiographic lesion severity of 56.6% ± 10.8% (range 45%–76%).13
Therefore, in ASTRAL, some patients in the 50%–70% stenosis group (about 40% of patients entered) actually had a stenosis of less than 50%. And some patients in the group with stenosis greater than 70% had stenosis of less than 70%. This further illustrates that, for the most part, the patients in ASTRAL had mild to moderate renal artery stenosis.
A high adverse event rate. The major adverse event rate in the first 24 hours was 9%, whereas the usual rate is 2% or less.14–18 Of the 280 patients in the revascularization group for whom data on adverse events were available at 1 month, 55 (20%) suffered a serious adverse event (including two patients who died) between 24 hours and 1 month after the procedure. This is in contrast to a major complication rate of 1.99% in five reports involving 727 patients.5
The trial centers were not high-volume centers. During the 7 years of recruitment, 24 centers (42% of all participating centers) randomized between one and five patients, and 32 centers (61% of all participating centers) randomized nine patients or fewer. This means that many participating centers randomized, on average, less than one patient per year! This was not a group of high-volume operators.
WILL CORAL GIVE US THE ANSWER?
The CORAL (Cardiovascular Outcomes in Renal Atherosclerotic Lesions) trial is under way.19 Enrollment was to have ended on January 31, 2010, and it will be several years before the data are available for analysis.
CORAL, a multicenter study funded in 2004 by the National Institutes of Health, will have randomized more than 900 patients with greater than 60% stenosis to optimal medical therapy alone or optimal medical therapy plus renal artery stenting. Inclusion criteria are a documented history of hypertension on two or more antihypertensive drugs or renal dysfunction, defined as stage 3 or greater chronic kidney disease based on the National Kidney Foundation classification (estimated glomerular filtration rate < 60 mL/min/1.73 m2 calculated by the modified Modification of Diet in Renal Disease [MDRD] formula) and stenosis of 60% or greater but less than 100%, as assessed by a core laboratory. The primary end point is survival free of cardiovascular and renal adverse events, defined as a composite of cardiovascular or renal death, stroke, myocardial infarction, hospitalization for congestive heart failure, progressive renal insufficiency, or need for permanent renal replacement therapy.
We hope this trial will give us a clear answer to the question of whether renal artery stenting is beneficial in the patient population studied. One note of caution: recruitment for this trial was difficult and slow. Thus, there were a number of protocol amendments throughout the trial in order to make recruitment easier. Hopefully, this will not be a problem when analyzing the results.
WE ALL AGREE ON THE INDICATIONS FOR STENTING
So, are we really so far apart in our thinking? And is it really “time to be less aggressive” if we follow the precepts below?
All renal arteries with stenosis do not need to be (and should not be) stented.
There must be a good clinical indicationandhemodynamically significant stenosis. This means the degree of stenosis should be more than 70% on angiography or intravascular ultrasonography.
Indications for stenting. Until more data from compelling randomized trials become available, adherence to the American College of Cardiology/American Heart Association guidelines on indications for renal artery stenting is advised3:
- Hypertension: class IIa, level of evidence B. Percutaneous revascularization is reasonable for patients with hemodynamically significant renal artery stenosis and accelerated hypertension, resistant hypertension, and malignant hypertension.
- Preservation of renal function: class IIa, level of evidence B. Percutaneous revascularization is reasonable for patients with renal artery stenosis and progressive chronic kidney disease with bilateral renal artery stenosis or a stenosis to a solitary functioning kidney.
- Congestive heart failure: class I, level of evidence B. Percutaneous revascularization is indicated for patients with hemodynamically significant renal artery stenosis (ie, > 70% stenosis on angiography or intravascular ultrasonography) and recurrent, unexplained congestive heart failure or sudden, unexplained pulmonary edema.
- Cooper CJ, Murphy TP. Is renal artery stenting the correct treatment of renal artery stenosis? The case for renal artery stenting for treatment of renal artery stenosis. Circulation 2007; 115:263–269.
- Dworkin LD, Jamerson KA. Is renal artery stenting the correct treatment of renal artery stenosis? Case against angioplasty and stenting of atherosclerotic renal artery stenosis. Circulation 2007; 115:271–276.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al ACC/AHA Guidelines for the Management of Patients with Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic): A Collaborative Report from the American Association of Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Interventional Radiology, Society for Vascular Medicine and Biology and the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2006; 113:e463–e654.
- Simon JF. Stenting atherosclerotic renal arteries: time to be less aggressive. Cleve Clin J Med 2010; 77:178–189.
- White CJ, Olin JW. Diagnosis and management of atherosclerotic renal artery stenosis: improving patient selection and outcomes. Nat Clin Pract Cardiovasc Med 2009; 6:176–190.
- van Jaarsveld BC, Krijnen P, Pieterman H, et al The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis. Dutch Renal Artery Stenosis Intervention Cooperative Study Group. N Engl J Med 2000; 342:1007–1014.
- Bax L, Woittiez AJ, Kouwenberg HJ, et al Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 2009; 150:840–841.
- Wheatley K, Ives N, Gray R, et al Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Tan WA, Wholey MH, Olin JW. The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis [letter]. N Engl J Med 2000; 343:438.
- Rocha-Singh KJ, Eisenhauer AC, Textor SC, et al Atherosclerotic Peripheral Vascular Disease Symposium II: intervention for renal artery disease. Circulation 2008; 118:2873–2878.
- Textor SC, Lerman L, McKusick M. The uncertain value of renal artery interventions: where are we now? JACC Cardiovasc Intervent 2009; 2:175–182.
- Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation 1995; 92:2333–2342.
- Subramanian R, White CJ, Rosenfield K, et al Renal fractional flow reserve: a hemodynamic evaluation of moderate renal artery stenoses. Catheter Cardiovasc Interv 2005; 64:480–486.
- Burket MW, Cooper CJ, Kennedy DJ, et al Renal artery angioplasty and stent placement: predictors of a favorable outcome. Am Heart J 2000; 139:64–71.
- Dorros G, Jaff M, Mathiak L, et al Four-year follow-up of Palmaz-Schatz stent revascularization as treatment for atherosclerotic renal artery stenosis. Circulation 1998; 98:642–647.
- Rocha-Singh K, Jaff MR, Rosenfield K. Evaluation of the safety and effectiveness of renal artery stenting after unsuccessful balloon angioplasty: the ASPIRE-2 study. J Am Coll Cardiol 2005; 46:776–783.
- Tuttle KR, Chouinard RF, Webber JT, et al Treatment of atherosclerotic ostial renal artery stenosis with the intravascular stent. Am J Kidney Dis 1998; 32:611–622.
- White CJ, Ramee SR, Collins TJ, Jenkins JS, Escobar A, Shaw D. Renal artery stent placement: utility in lesions difficult to treat with balloon angioplasty. J Am Coll Cardiol 1997; 30:1445–1450.
- Cooper CJ, Murphy TP, Matsumoto A, et al Stent revascularization for the prevention of cardiovascular and renal events among patients with renal artery stenosis and systolic hypertension: rationale and design of the CORAL trial. Am Heart J 2006; 152:59–66.
The role of stenting for atherosclerotic renal artery stenosis is hotly debated among different specialties.1,2 If we may generalize a bit, interventionalists (cardiologists, interventional radiologists, vascular surgeons, and vascular medicine specialists) have been in favor of liberal use of stenting, and nephrologists often favor medical therapy alone. And as with all controversial issues, each group feels rather strongly about its position.
Because few prospective randomized trials have been completed, the management of atherosclerotic renal artery stenosis has been guided by retrospective studies and case series. 3
In this issue of the Cleveland Clinic Journal of Medicine, Dr. James Simon4 provides an excellent overview of the prevalence, natural history, and clinical presentation of atherosclerotic renal artery stenosis. In addition, he does an admirable job of reviewing the available prospective randomized trials and providing editorial commentary about the role of the various specialists in the management of renal artery disease. And while the title of his paper says that it is “time to be less aggressive,” Dr. Simon ultimately comes to the same conclusions that we do5 on the indications for renal artery stenting (see Table 3 of Dr. Simon’s article), which are those of the multidisciplinary 2006 American College of Cardiology/American Heart Association guidelines on the management of peripheral artery disease.3
So what then is all the controversy about? We all agree that prospective randomized trials that provide class I, level A evidence impart the only unbiased scientific information on the best treatment strategy for patients with renal artery disease. The basic controversial issue is the interpretation of these trials. We contend that the three randomized trials of stenting vs medical therapy published so far6–8 (see below) are so seriously flawed that it is impossible to make treatment decisions based on their results.
Since these trials were published in wellrespected journals, their results are often taken as gospel. However, careful review of each of these will reveal the flaws in study design and implementation.
THE DRASTIC TRIAL
In the Dutch Renal Artery Stenosis Intervention Cooperative (DRASTIC) trial,6 106 patients with renal artery stenosis and hypertension (diastolic blood pressure > 95 mm Hg) despite treatment with two antihypertensive medications were randomly assigned to either renal angioplasty (n = 56) or drug therapy (n = 50).
Authors’ conclusions
“In the treatment of patients with hypertension and renal-artery stenosis, angioplasty has little advantage over antihypertensive-drug therapy.”6
Four serious problems
As we discussed in a letter to the editor of the New England Journal of Medicine on August 10, 2000, this study had four serious problems that invalidate its authors’ conclusions.9
The sample size was insufficient to detect a significant difference between treatment groups. In other words, the chance of a type 2 statistical error is high.
Balloon angioplasty without stenting was used as the method of revascularization. Experts now recognize that stenting is required for renal artery intervention to have a durable result.3,5
Renal artery stenosis was defined as greater than 50% stenosis. This allowed a large number of patients to enter the trial who had hemodynamically and clinically insignificant lesions. Most clinicians believe that stenosis of less than 70% is not hemodynamically important.5,10,11
Twenty-two of the 50 patients randomized to medical therapy crossed over to the angioplasty group because their blood pressure became difficult to control. In other words, 44% of the patients in the medical group underwent angioplasty, an astounding percentage in an intention-to-treat analysis comparing one therapy with another.
Despite these serious flaws, the results of DRASTIC influenced therapy for years after its publication.
THE STAR TRIAL
In the Stent Placement in Patients With Atherosclerotic Renal Artery Stenosis and Impaired Renal Function (STAR) trial,7 140 patients with a creatinine clearance of less than 80 mL/min/1.73m2, renal artery stenosis greater than 50%, and well-controlled blood pressure were randomized to either renal artery stenting plus medical therapy (n = 64) or medical therapy alone (n = 76). The primary end point was a 20% or greater decrease in creatinine clearance. Secondary end points included measures of safety and cardiovascular morbidity and mortality.
Authors’ conclusions
“Stent placement with medical treatment had no clear effect on progression of impaired renal function but led to a small number of significant procedure-related complications. The study findings favor a conservative approach to patients with [atherosclerotic renal artery stenosis], focused on cardiovascular risk factor management and avoiding stenting.”7
Serious flaws
A number of serious flaws render this study uninterpretable.
Mild renal artery stenosis. At least 33% of the patients in the study had mild renal artery stenosis (50%–70%), and 12 (19%) of the 64 patients in the group randomized to stenting actually had stenosis of less than 50%. How can one expect there to be a benefit to stenting in patients with mild (and hemodynamically insignificant) renal artery stenosis? This is especially true when the primary end point is a change in renal function.
More than half of the patients had unilateral disease. It seems intuitive that if one were to plan a trial with a primary end point of a change in renal function, only patients with bilateral renal artery stenosis of greater than 70% or with stenosis of greater than 70% to a solitary functioning kidney would be included. One would not expect that patients with unilateral disease and a stenosis of less than 70% would derive any benefit from revascularization.
Not all “stent” patients received stents. All of the patients in the medical group received medication and there were no crossovers. However, only 46 (72%) of the 64 patients randomized to stenting actually received a stent, while 18 (28%) did not. There were two technical failures, and 12 patients should not have been randomized because they had less than 50% stenosis on angiography and thus were not stented. Yet all 64 patients were analyzed (by intention to treat) in the stent group. With these numbers, one could predict that the results would be negative.
Like DRASTIC, this trial was underpowered, meaning that the chance of a type 2 statistical error is high. In fact, the editors of the Annals of Internal Medicine, in a note accompanying the article, cautioned that the study “was underpowered to provide a definitive estimate of efficacy.”7 If the study was underpowered to answer the question at hand, why was it deemed worthy of publication?
High complication rates. The periprocedural complication and death rates were much higher than in many other reports on renal artery stenting (see details below).5
THE ASTRAL TRIAL
In the Angioplasty and Stenting for Renal Artery Lesions (ASTRAL) trial,8 the primary outcome measure was the change in renal function over time as assessed by the mean slope of the reciprocal of the serum creatinine. In this trial, 806 patients with atherosclerotic renal artery stenosis were randomized to either stent-based revascularization combined with medical therapy or medical therapy alone.
Authors’ conclusions
“We found substantial risks but no evidence of a worthwhile clinical benefit from revascularization in patients with atherosclerotic renovascular disease.”8
Despite size, flaws remain
Unlike the other trials, ASTRAL had a sample size large enough to provide an answer. However, numerous flaws in study design and implementation invalidate its results for the overall population of patients with renal artery stenosis. The major flaws in ASTRAL were:
Selection bias. For a patient to be enrolled, the treating physician had to be undecided on whether the patient should undergo revascularization or medical management alone. However, the treatment of atherosclerotic renal artery stenosis is so controversial that physicians of different specialties cannot agree on the most effective treatment strategy for most patients.1,2 Therefore, to exclude patients when their physicians were sure they needed or did not need renal artery revascularization is incomprehensible and introduces considerable selection bias into the trial design.
Normal renal function at baseline. The primary outcome was a change in renal function over time. Yet 25% of patients had normal renal function at the outset of the trial. In addition, a significant number had unilateral disease, and 41% had a stenosis less than 70%. What made the investigators think that stent implantation could possibly be shown to be beneficial if they entered patients into a renal function study who had near-normal renal function, unilateral disease, and mild renal artery stenosis? These are patients whose condition would not be expected to worsen with medical therapy nor to improve with stenting. Most clinicians would not consider stenting a patient to preserve renal function if the patient has unilateral mild renal artery stenosis.
There was no core laboratory to adjudicate the interpretation of the imaging studies. To determine the degree of stenosis of an artery in an accurate and unbiased fashion, a core laboratory must be used.
The reason this is so important is that visual assessment of the degree of stenosis on angiography is not accurate and almost always overestimates the degree of stenosis.12,13 In a study assessing the physiologic importance of renal artery lesions, the lesion severity by visual estimation was 74.9% ± 11.5% (range 50%–90%), which exceeded the quantitative vascular angiographic lesion severity of 56.6% ± 10.8% (range 45%–76%).13
Therefore, in ASTRAL, some patients in the 50%–70% stenosis group (about 40% of patients entered) actually had a stenosis of less than 50%. And some patients in the group with stenosis greater than 70% had stenosis of less than 70%. This further illustrates that, for the most part, the patients in ASTRAL had mild to moderate renal artery stenosis.
A high adverse event rate. The major adverse event rate in the first 24 hours was 9%, whereas the usual rate is 2% or less.14–18 Of the 280 patients in the revascularization group for whom data on adverse events were available at 1 month, 55 (20%) suffered a serious adverse event (including two patients who died) between 24 hours and 1 month after the procedure. This is in contrast to a major complication rate of 1.99% in five reports involving 727 patients.5
The trial centers were not high-volume centers. During the 7 years of recruitment, 24 centers (42% of all participating centers) randomized between one and five patients, and 32 centers (61% of all participating centers) randomized nine patients or fewer. This means that many participating centers randomized, on average, less than one patient per year! This was not a group of high-volume operators.
WILL CORAL GIVE US THE ANSWER?
The CORAL (Cardiovascular Outcomes in Renal Atherosclerotic Lesions) trial is under way.19 Enrollment was to have ended on January 31, 2010, and it will be several years before the data are available for analysis.
CORAL, a multicenter study funded in 2004 by the National Institutes of Health, will have randomized more than 900 patients with greater than 60% stenosis to optimal medical therapy alone or optimal medical therapy plus renal artery stenting. Inclusion criteria are a documented history of hypertension on two or more antihypertensive drugs or renal dysfunction, defined as stage 3 or greater chronic kidney disease based on the National Kidney Foundation classification (estimated glomerular filtration rate < 60 mL/min/1.73 m2 calculated by the modified Modification of Diet in Renal Disease [MDRD] formula) and stenosis of 60% or greater but less than 100%, as assessed by a core laboratory. The primary end point is survival free of cardiovascular and renal adverse events, defined as a composite of cardiovascular or renal death, stroke, myocardial infarction, hospitalization for congestive heart failure, progressive renal insufficiency, or need for permanent renal replacement therapy.
We hope this trial will give us a clear answer to the question of whether renal artery stenting is beneficial in the patient population studied. One note of caution: recruitment for this trial was difficult and slow. Thus, there were a number of protocol amendments throughout the trial in order to make recruitment easier. Hopefully, this will not be a problem when analyzing the results.
WE ALL AGREE ON THE INDICATIONS FOR STENTING
So, are we really so far apart in our thinking? And is it really “time to be less aggressive” if we follow the precepts below?
All renal arteries with stenosis do not need to be (and should not be) stented.
There must be a good clinical indicationandhemodynamically significant stenosis. This means the degree of stenosis should be more than 70% on angiography or intravascular ultrasonography.
Indications for stenting. Until more data from compelling randomized trials become available, adherence to the American College of Cardiology/American Heart Association guidelines on indications for renal artery stenting is advised3:
- Hypertension: class IIa, level of evidence B. Percutaneous revascularization is reasonable for patients with hemodynamically significant renal artery stenosis and accelerated hypertension, resistant hypertension, and malignant hypertension.
- Preservation of renal function: class IIa, level of evidence B. Percutaneous revascularization is reasonable for patients with renal artery stenosis and progressive chronic kidney disease with bilateral renal artery stenosis or a stenosis to a solitary functioning kidney.
- Congestive heart failure: class I, level of evidence B. Percutaneous revascularization is indicated for patients with hemodynamically significant renal artery stenosis (ie, > 70% stenosis on angiography or intravascular ultrasonography) and recurrent, unexplained congestive heart failure or sudden, unexplained pulmonary edema.
The role of stenting for atherosclerotic renal artery stenosis is hotly debated among different specialties.1,2 If we may generalize a bit, interventionalists (cardiologists, interventional radiologists, vascular surgeons, and vascular medicine specialists) have been in favor of liberal use of stenting, and nephrologists often favor medical therapy alone. And as with all controversial issues, each group feels rather strongly about its position.
Because few prospective randomized trials have been completed, the management of atherosclerotic renal artery stenosis has been guided by retrospective studies and case series. 3
In this issue of the Cleveland Clinic Journal of Medicine, Dr. James Simon4 provides an excellent overview of the prevalence, natural history, and clinical presentation of atherosclerotic renal artery stenosis. In addition, he does an admirable job of reviewing the available prospective randomized trials and providing editorial commentary about the role of the various specialists in the management of renal artery disease. And while the title of his paper says that it is “time to be less aggressive,” Dr. Simon ultimately comes to the same conclusions that we do5 on the indications for renal artery stenting (see Table 3 of Dr. Simon’s article), which are those of the multidisciplinary 2006 American College of Cardiology/American Heart Association guidelines on the management of peripheral artery disease.3
So what then is all the controversy about? We all agree that prospective randomized trials that provide class I, level A evidence impart the only unbiased scientific information on the best treatment strategy for patients with renal artery disease. The basic controversial issue is the interpretation of these trials. We contend that the three randomized trials of stenting vs medical therapy published so far6–8 (see below) are so seriously flawed that it is impossible to make treatment decisions based on their results.
Since these trials were published in wellrespected journals, their results are often taken as gospel. However, careful review of each of these will reveal the flaws in study design and implementation.
THE DRASTIC TRIAL
In the Dutch Renal Artery Stenosis Intervention Cooperative (DRASTIC) trial,6 106 patients with renal artery stenosis and hypertension (diastolic blood pressure > 95 mm Hg) despite treatment with two antihypertensive medications were randomly assigned to either renal angioplasty (n = 56) or drug therapy (n = 50).
Authors’ conclusions
“In the treatment of patients with hypertension and renal-artery stenosis, angioplasty has little advantage over antihypertensive-drug therapy.”6
Four serious problems
As we discussed in a letter to the editor of the New England Journal of Medicine on August 10, 2000, this study had four serious problems that invalidate its authors’ conclusions.9
The sample size was insufficient to detect a significant difference between treatment groups. In other words, the chance of a type 2 statistical error is high.
Balloon angioplasty without stenting was used as the method of revascularization. Experts now recognize that stenting is required for renal artery intervention to have a durable result.3,5
Renal artery stenosis was defined as greater than 50% stenosis. This allowed a large number of patients to enter the trial who had hemodynamically and clinically insignificant lesions. Most clinicians believe that stenosis of less than 70% is not hemodynamically important.5,10,11
Twenty-two of the 50 patients randomized to medical therapy crossed over to the angioplasty group because their blood pressure became difficult to control. In other words, 44% of the patients in the medical group underwent angioplasty, an astounding percentage in an intention-to-treat analysis comparing one therapy with another.
Despite these serious flaws, the results of DRASTIC influenced therapy for years after its publication.
THE STAR TRIAL
In the Stent Placement in Patients With Atherosclerotic Renal Artery Stenosis and Impaired Renal Function (STAR) trial,7 140 patients with a creatinine clearance of less than 80 mL/min/1.73m2, renal artery stenosis greater than 50%, and well-controlled blood pressure were randomized to either renal artery stenting plus medical therapy (n = 64) or medical therapy alone (n = 76). The primary end point was a 20% or greater decrease in creatinine clearance. Secondary end points included measures of safety and cardiovascular morbidity and mortality.
Authors’ conclusions
“Stent placement with medical treatment had no clear effect on progression of impaired renal function but led to a small number of significant procedure-related complications. The study findings favor a conservative approach to patients with [atherosclerotic renal artery stenosis], focused on cardiovascular risk factor management and avoiding stenting.”7
Serious flaws
A number of serious flaws render this study uninterpretable.
Mild renal artery stenosis. At least 33% of the patients in the study had mild renal artery stenosis (50%–70%), and 12 (19%) of the 64 patients in the group randomized to stenting actually had stenosis of less than 50%. How can one expect there to be a benefit to stenting in patients with mild (and hemodynamically insignificant) renal artery stenosis? This is especially true when the primary end point is a change in renal function.
More than half of the patients had unilateral disease. It seems intuitive that if one were to plan a trial with a primary end point of a change in renal function, only patients with bilateral renal artery stenosis of greater than 70% or with stenosis of greater than 70% to a solitary functioning kidney would be included. One would not expect that patients with unilateral disease and a stenosis of less than 70% would derive any benefit from revascularization.
Not all “stent” patients received stents. All of the patients in the medical group received medication and there were no crossovers. However, only 46 (72%) of the 64 patients randomized to stenting actually received a stent, while 18 (28%) did not. There were two technical failures, and 12 patients should not have been randomized because they had less than 50% stenosis on angiography and thus were not stented. Yet all 64 patients were analyzed (by intention to treat) in the stent group. With these numbers, one could predict that the results would be negative.
Like DRASTIC, this trial was underpowered, meaning that the chance of a type 2 statistical error is high. In fact, the editors of the Annals of Internal Medicine, in a note accompanying the article, cautioned that the study “was underpowered to provide a definitive estimate of efficacy.”7 If the study was underpowered to answer the question at hand, why was it deemed worthy of publication?
High complication rates. The periprocedural complication and death rates were much higher than in many other reports on renal artery stenting (see details below).5
THE ASTRAL TRIAL
In the Angioplasty and Stenting for Renal Artery Lesions (ASTRAL) trial,8 the primary outcome measure was the change in renal function over time as assessed by the mean slope of the reciprocal of the serum creatinine. In this trial, 806 patients with atherosclerotic renal artery stenosis were randomized to either stent-based revascularization combined with medical therapy or medical therapy alone.
Authors’ conclusions
“We found substantial risks but no evidence of a worthwhile clinical benefit from revascularization in patients with atherosclerotic renovascular disease.”8
Despite size, flaws remain
Unlike the other trials, ASTRAL had a sample size large enough to provide an answer. However, numerous flaws in study design and implementation invalidate its results for the overall population of patients with renal artery stenosis. The major flaws in ASTRAL were:
Selection bias. For a patient to be enrolled, the treating physician had to be undecided on whether the patient should undergo revascularization or medical management alone. However, the treatment of atherosclerotic renal artery stenosis is so controversial that physicians of different specialties cannot agree on the most effective treatment strategy for most patients.1,2 Therefore, to exclude patients when their physicians were sure they needed or did not need renal artery revascularization is incomprehensible and introduces considerable selection bias into the trial design.
Normal renal function at baseline. The primary outcome was a change in renal function over time. Yet 25% of patients had normal renal function at the outset of the trial. In addition, a significant number had unilateral disease, and 41% had a stenosis less than 70%. What made the investigators think that stent implantation could possibly be shown to be beneficial if they entered patients into a renal function study who had near-normal renal function, unilateral disease, and mild renal artery stenosis? These are patients whose condition would not be expected to worsen with medical therapy nor to improve with stenting. Most clinicians would not consider stenting a patient to preserve renal function if the patient has unilateral mild renal artery stenosis.
There was no core laboratory to adjudicate the interpretation of the imaging studies. To determine the degree of stenosis of an artery in an accurate and unbiased fashion, a core laboratory must be used.
The reason this is so important is that visual assessment of the degree of stenosis on angiography is not accurate and almost always overestimates the degree of stenosis.12,13 In a study assessing the physiologic importance of renal artery lesions, the lesion severity by visual estimation was 74.9% ± 11.5% (range 50%–90%), which exceeded the quantitative vascular angiographic lesion severity of 56.6% ± 10.8% (range 45%–76%).13
Therefore, in ASTRAL, some patients in the 50%–70% stenosis group (about 40% of patients entered) actually had a stenosis of less than 50%. And some patients in the group with stenosis greater than 70% had stenosis of less than 70%. This further illustrates that, for the most part, the patients in ASTRAL had mild to moderate renal artery stenosis.
A high adverse event rate. The major adverse event rate in the first 24 hours was 9%, whereas the usual rate is 2% or less.14–18 Of the 280 patients in the revascularization group for whom data on adverse events were available at 1 month, 55 (20%) suffered a serious adverse event (including two patients who died) between 24 hours and 1 month after the procedure. This is in contrast to a major complication rate of 1.99% in five reports involving 727 patients.5
The trial centers were not high-volume centers. During the 7 years of recruitment, 24 centers (42% of all participating centers) randomized between one and five patients, and 32 centers (61% of all participating centers) randomized nine patients or fewer. This means that many participating centers randomized, on average, less than one patient per year! This was not a group of high-volume operators.
WILL CORAL GIVE US THE ANSWER?
The CORAL (Cardiovascular Outcomes in Renal Atherosclerotic Lesions) trial is under way.19 Enrollment was to have ended on January 31, 2010, and it will be several years before the data are available for analysis.
CORAL, a multicenter study funded in 2004 by the National Institutes of Health, will have randomized more than 900 patients with greater than 60% stenosis to optimal medical therapy alone or optimal medical therapy plus renal artery stenting. Inclusion criteria are a documented history of hypertension on two or more antihypertensive drugs or renal dysfunction, defined as stage 3 or greater chronic kidney disease based on the National Kidney Foundation classification (estimated glomerular filtration rate < 60 mL/min/1.73 m2 calculated by the modified Modification of Diet in Renal Disease [MDRD] formula) and stenosis of 60% or greater but less than 100%, as assessed by a core laboratory. The primary end point is survival free of cardiovascular and renal adverse events, defined as a composite of cardiovascular or renal death, stroke, myocardial infarction, hospitalization for congestive heart failure, progressive renal insufficiency, or need for permanent renal replacement therapy.
We hope this trial will give us a clear answer to the question of whether renal artery stenting is beneficial in the patient population studied. One note of caution: recruitment for this trial was difficult and slow. Thus, there were a number of protocol amendments throughout the trial in order to make recruitment easier. Hopefully, this will not be a problem when analyzing the results.
WE ALL AGREE ON THE INDICATIONS FOR STENTING
So, are we really so far apart in our thinking? And is it really “time to be less aggressive” if we follow the precepts below?
All renal arteries with stenosis do not need to be (and should not be) stented.
There must be a good clinical indicationandhemodynamically significant stenosis. This means the degree of stenosis should be more than 70% on angiography or intravascular ultrasonography.
Indications for stenting. Until more data from compelling randomized trials become available, adherence to the American College of Cardiology/American Heart Association guidelines on indications for renal artery stenting is advised3:
- Hypertension: class IIa, level of evidence B. Percutaneous revascularization is reasonable for patients with hemodynamically significant renal artery stenosis and accelerated hypertension, resistant hypertension, and malignant hypertension.
- Preservation of renal function: class IIa, level of evidence B. Percutaneous revascularization is reasonable for patients with renal artery stenosis and progressive chronic kidney disease with bilateral renal artery stenosis or a stenosis to a solitary functioning kidney.
- Congestive heart failure: class I, level of evidence B. Percutaneous revascularization is indicated for patients with hemodynamically significant renal artery stenosis (ie, > 70% stenosis on angiography or intravascular ultrasonography) and recurrent, unexplained congestive heart failure or sudden, unexplained pulmonary edema.
- Cooper CJ, Murphy TP. Is renal artery stenting the correct treatment of renal artery stenosis? The case for renal artery stenting for treatment of renal artery stenosis. Circulation 2007; 115:263–269.
- Dworkin LD, Jamerson KA. Is renal artery stenting the correct treatment of renal artery stenosis? Case against angioplasty and stenting of atherosclerotic renal artery stenosis. Circulation 2007; 115:271–276.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al ACC/AHA Guidelines for the Management of Patients with Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic): A Collaborative Report from the American Association of Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Interventional Radiology, Society for Vascular Medicine and Biology and the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2006; 113:e463–e654.
- Simon JF. Stenting atherosclerotic renal arteries: time to be less aggressive. Cleve Clin J Med 2010; 77:178–189.
- White CJ, Olin JW. Diagnosis and management of atherosclerotic renal artery stenosis: improving patient selection and outcomes. Nat Clin Pract Cardiovasc Med 2009; 6:176–190.
- van Jaarsveld BC, Krijnen P, Pieterman H, et al The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis. Dutch Renal Artery Stenosis Intervention Cooperative Study Group. N Engl J Med 2000; 342:1007–1014.
- Bax L, Woittiez AJ, Kouwenberg HJ, et al Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 2009; 150:840–841.
- Wheatley K, Ives N, Gray R, et al Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Tan WA, Wholey MH, Olin JW. The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis [letter]. N Engl J Med 2000; 343:438.
- Rocha-Singh KJ, Eisenhauer AC, Textor SC, et al Atherosclerotic Peripheral Vascular Disease Symposium II: intervention for renal artery disease. Circulation 2008; 118:2873–2878.
- Textor SC, Lerman L, McKusick M. The uncertain value of renal artery interventions: where are we now? JACC Cardiovasc Intervent 2009; 2:175–182.
- Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation 1995; 92:2333–2342.
- Subramanian R, White CJ, Rosenfield K, et al Renal fractional flow reserve: a hemodynamic evaluation of moderate renal artery stenoses. Catheter Cardiovasc Interv 2005; 64:480–486.
- Burket MW, Cooper CJ, Kennedy DJ, et al Renal artery angioplasty and stent placement: predictors of a favorable outcome. Am Heart J 2000; 139:64–71.
- Dorros G, Jaff M, Mathiak L, et al Four-year follow-up of Palmaz-Schatz stent revascularization as treatment for atherosclerotic renal artery stenosis. Circulation 1998; 98:642–647.
- Rocha-Singh K, Jaff MR, Rosenfield K. Evaluation of the safety and effectiveness of renal artery stenting after unsuccessful balloon angioplasty: the ASPIRE-2 study. J Am Coll Cardiol 2005; 46:776–783.
- Tuttle KR, Chouinard RF, Webber JT, et al Treatment of atherosclerotic ostial renal artery stenosis with the intravascular stent. Am J Kidney Dis 1998; 32:611–622.
- White CJ, Ramee SR, Collins TJ, Jenkins JS, Escobar A, Shaw D. Renal artery stent placement: utility in lesions difficult to treat with balloon angioplasty. J Am Coll Cardiol 1997; 30:1445–1450.
- Cooper CJ, Murphy TP, Matsumoto A, et al Stent revascularization for the prevention of cardiovascular and renal events among patients with renal artery stenosis and systolic hypertension: rationale and design of the CORAL trial. Am Heart J 2006; 152:59–66.
- Cooper CJ, Murphy TP. Is renal artery stenting the correct treatment of renal artery stenosis? The case for renal artery stenting for treatment of renal artery stenosis. Circulation 2007; 115:263–269.
- Dworkin LD, Jamerson KA. Is renal artery stenting the correct treatment of renal artery stenosis? Case against angioplasty and stenting of atherosclerotic renal artery stenosis. Circulation 2007; 115:271–276.
- Hirsch AT, Haskal ZJ, Hertzer NR, et al ACC/AHA Guidelines for the Management of Patients with Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic): A Collaborative Report from the American Association of Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Interventional Radiology, Society for Vascular Medicine and Biology and the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2006; 113:e463–e654.
- Simon JF. Stenting atherosclerotic renal arteries: time to be less aggressive. Cleve Clin J Med 2010; 77:178–189.
- White CJ, Olin JW. Diagnosis and management of atherosclerotic renal artery stenosis: improving patient selection and outcomes. Nat Clin Pract Cardiovasc Med 2009; 6:176–190.
- van Jaarsveld BC, Krijnen P, Pieterman H, et al The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis. Dutch Renal Artery Stenosis Intervention Cooperative Study Group. N Engl J Med 2000; 342:1007–1014.
- Bax L, Woittiez AJ, Kouwenberg HJ, et al Stent placement in patients with atherosclerotic renal artery stenosis and impaired renal function: a randomized trial. Ann Intern Med 2009; 150:840–841.
- Wheatley K, Ives N, Gray R, et al Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med 2009; 361:1953–1962.
- Tan WA, Wholey MH, Olin JW. The effect of balloon angioplasty on hypertension in atherosclerotic renal-artery stenosis [letter]. N Engl J Med 2000; 343:438.
- Rocha-Singh KJ, Eisenhauer AC, Textor SC, et al Atherosclerotic Peripheral Vascular Disease Symposium II: intervention for renal artery disease. Circulation 2008; 118:2873–2878.
- Textor SC, Lerman L, McKusick M. The uncertain value of renal artery interventions: where are we now? JACC Cardiovasc Intervent 2009; 2:175–182.
- Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation 1995; 92:2333–2342.
- Subramanian R, White CJ, Rosenfield K, et al Renal fractional flow reserve: a hemodynamic evaluation of moderate renal artery stenoses. Catheter Cardiovasc Interv 2005; 64:480–486.
- Burket MW, Cooper CJ, Kennedy DJ, et al Renal artery angioplasty and stent placement: predictors of a favorable outcome. Am Heart J 2000; 139:64–71.
- Dorros G, Jaff M, Mathiak L, et al Four-year follow-up of Palmaz-Schatz stent revascularization as treatment for atherosclerotic renal artery stenosis. Circulation 1998; 98:642–647.
- Rocha-Singh K, Jaff MR, Rosenfield K. Evaluation of the safety and effectiveness of renal artery stenting after unsuccessful balloon angioplasty: the ASPIRE-2 study. J Am Coll Cardiol 2005; 46:776–783.
- Tuttle KR, Chouinard RF, Webber JT, et al Treatment of atherosclerotic ostial renal artery stenosis with the intravascular stent. Am J Kidney Dis 1998; 32:611–622.
- White CJ, Ramee SR, Collins TJ, Jenkins JS, Escobar A, Shaw D. Renal artery stent placement: utility in lesions difficult to treat with balloon angioplasty. J Am Coll Cardiol 1997; 30:1445–1450.
- Cooper CJ, Murphy TP, Matsumoto A, et al Stent revascularization for the prevention of cardiovascular and renal events among patients with renal artery stenosis and systolic hypertension: rationale and design of the CORAL trial. Am Heart J 2006; 152:59–66.