User login
VTE Studies Win Grants
Two pharmacist-hospitalist teams each won $50,000 grants June 12 from the American Society of Health-System Pharmacists (ASHP) Research and Education Foundation (Bethesda, Md.) to support development of screening tools and order sets to prevent and treat hospital-acquired venous thromboembolism (VTE).
The grant winners and lead co-investigators from each team:
- Robert Weibert, PharmD, health sciences clinical professor and director of the Anticoagulation Clinic, School of Pharmacy, and Gregory Maynard, MD, MS, head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego (UCSD); and
- Rachel Hroncich, PharmD, pharmacy clinical coordinator of Presbyterian Healthcare Service, and Randle Adair, DO, PhD, a PMG hospitalist in adult medicine from Albuquerque, N.M.
The ASHP, a nonprofit organization, fosters safe medication use.
“We are thrilled that our grant application was selected by the ASHP and excited about the opportunity for our research to improve patient care,” says Dr. Hroncich.
The ASHP Research and Education Foundation grant program, sponsored by Sanofi-Aventis, supports research by hospitalists and hospital pharmacists to treat VTE, with a focus on hospitalized patients and post-discharge follow-up. The grants are geared to help hospitalists and pharmacists reduce hospital-acquired VTE, a significant cause of morbidity and mortality in hospitals.
VTE-related treatment costs $1.5 billion a year, according to researchers at the University of Washington School of Pharmacy in Seattle. ASHP statistics indicate VTE affects more than 450,000 hospitalized patients annually. The condition—an amalgam of deep vein thrombosis (DVT) and pulmonary embolism (PE)—affects a range of hospitalized patients. Gynecologic, orthopedic, urologic, vascular, trauma, and cancer patients all are at risk—as are those with other medical conditions such as congestive heart failure, severe respiratory disease, and obesity, or those who are bedridden.
The ASHP grants help pharmacist-hospitalist teams find tools to screen for VTE. Such tools let clinicians intervene early with at-risk patients. Better screening and intervention requires sound clinical, administrative, and IT processes.
The trick is to encourage busy hospitalists to use a consensus-based VTE screening tool for all hospitalized patients.
While most VTE research involves retrospective chart review of diagnostic codes, Drs. Weibert and Maynard’s grant research goes beyond such studies by identifying patients at risk concurrent with their hospitalizations. Dr. Maynard says the need is urgent: “Hospitals grossly underestimate the risk of VTE. In a 300-bed hospital, at least 150 patients are at risk of hospital-acquired VTE at any time.”
The UCSD team hopes to improve VTE screening by integrating an order set into the hospital’s computer physician order entry (CPOE) system. “The literature points to a bundle of best practices for VTE,” says Dr. Maynard, “including baseline lab work, use of compression stockings, using heparin for an optimal time period, patient education for those on anticoagulants, timely follow-up post discharge, the Society of Hospital Medicine collaborative, etc.”
Based on that body of knowledge and the input of its 15 full-time equivalent hospitalists, UCSD stakeholders in VTE screening debate what is practical and workable, conduct small, paper-based pilot projects, and fine-tune the protocol to integrate it with patient flow through admissions. “As we transition fully to a CPOE in our health system, we will incorporate a VTE order set that is doable and user-friendly,” adds Dr. Maynard.
UCSD’s pharmacist-hospitalist collaboration also encourages residents from both disciplines to work together on integrating protocols into clinical care processes. The team hopes that the VTE protocol will go beyond the inpatient stay by wrapping the protocol into the discharge plan. Dr. Weibert’s anticoagulation and pulmonary embolism clinics also help “build on our strengths,” he says.
The second team is led by newcomers to the grant winner’s circle, Drs. Hroncich (pharmacist) and Adair (hospitalist) from Presbyterian Healthcare Services, Albuquerque, N.M. They base their research on this question: Is it more efficient for the system’s 34 hospitalists to screen out those at low risk of VTE than to screen everyone for high risk?
The investigators have been collecting baseline data on compliance with VTE screening since 2003. Hospitalist use of a VTE screening tool on admissions was 60%, improving to 88% with reminders. “The implication is that 12% of the hospitalists didn’t use the screening tool,” says Dr. Adair. “We found that they were resistant to another piece of paper.” PHS data also showed that seven out of 10 patients had some VTE risk, that co-morbidities and hospitalization increase VTE risk, and that the age at which patients fall prey to VTE is dropping to between 50 and 60.
For the ASHP grant, Drs. Hroncich and Adair will monitor VTE screening on admission to all PHS general medical units. All patients 18 or older admitted to those units during a three-month period will be routinely screened on admission for VTE risk. Drs. Hroncich and Adair will make two VTE-related admission order sets available to hospitalists to complete. The current screening tool is designed to identify patients at risk of developing a VTE based on the presence of risk factors. The second, shorter admission order set will contain a screening tool that assumes that all patients need VTE prophylaxis, except low-risk patients and those with VTE prophylaxis contraindications. “The shorter tool should take only one or two minutes to complete,” says Dr. Hroncich.
The PHS team hopes that the shorter screening tool will overcome resistance to VTE screening. Dr. Hroncich says there are many barriers to VTE screening. They include lack of consensus on the best screening tool on admission, the misperception that VTE isn’t a big problem, lack of reliable processes so at-risk patients don’t fall through the cracks, and a misperception that anti-coagulant therapy is dangerous.
“It’s one thing to treat COPD and heart failure,” adds Dr. Adair, “but if I can prevent VTE with less than a 60-second screening, I can prevent a disease state from happening.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Two pharmacist-hospitalist teams each won $50,000 grants June 12 from the American Society of Health-System Pharmacists (ASHP) Research and Education Foundation (Bethesda, Md.) to support development of screening tools and order sets to prevent and treat hospital-acquired venous thromboembolism (VTE).
The grant winners and lead co-investigators from each team:
- Robert Weibert, PharmD, health sciences clinical professor and director of the Anticoagulation Clinic, School of Pharmacy, and Gregory Maynard, MD, MS, head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego (UCSD); and
- Rachel Hroncich, PharmD, pharmacy clinical coordinator of Presbyterian Healthcare Service, and Randle Adair, DO, PhD, a PMG hospitalist in adult medicine from Albuquerque, N.M.
The ASHP, a nonprofit organization, fosters safe medication use.
“We are thrilled that our grant application was selected by the ASHP and excited about the opportunity for our research to improve patient care,” says Dr. Hroncich.
The ASHP Research and Education Foundation grant program, sponsored by Sanofi-Aventis, supports research by hospitalists and hospital pharmacists to treat VTE, with a focus on hospitalized patients and post-discharge follow-up. The grants are geared to help hospitalists and pharmacists reduce hospital-acquired VTE, a significant cause of morbidity and mortality in hospitals.
VTE-related treatment costs $1.5 billion a year, according to researchers at the University of Washington School of Pharmacy in Seattle. ASHP statistics indicate VTE affects more than 450,000 hospitalized patients annually. The condition—an amalgam of deep vein thrombosis (DVT) and pulmonary embolism (PE)—affects a range of hospitalized patients. Gynecologic, orthopedic, urologic, vascular, trauma, and cancer patients all are at risk—as are those with other medical conditions such as congestive heart failure, severe respiratory disease, and obesity, or those who are bedridden.
The ASHP grants help pharmacist-hospitalist teams find tools to screen for VTE. Such tools let clinicians intervene early with at-risk patients. Better screening and intervention requires sound clinical, administrative, and IT processes.
The trick is to encourage busy hospitalists to use a consensus-based VTE screening tool for all hospitalized patients.
While most VTE research involves retrospective chart review of diagnostic codes, Drs. Weibert and Maynard’s grant research goes beyond such studies by identifying patients at risk concurrent with their hospitalizations. Dr. Maynard says the need is urgent: “Hospitals grossly underestimate the risk of VTE. In a 300-bed hospital, at least 150 patients are at risk of hospital-acquired VTE at any time.”
The UCSD team hopes to improve VTE screening by integrating an order set into the hospital’s computer physician order entry (CPOE) system. “The literature points to a bundle of best practices for VTE,” says Dr. Maynard, “including baseline lab work, use of compression stockings, using heparin for an optimal time period, patient education for those on anticoagulants, timely follow-up post discharge, the Society of Hospital Medicine collaborative, etc.”
Based on that body of knowledge and the input of its 15 full-time equivalent hospitalists, UCSD stakeholders in VTE screening debate what is practical and workable, conduct small, paper-based pilot projects, and fine-tune the protocol to integrate it with patient flow through admissions. “As we transition fully to a CPOE in our health system, we will incorporate a VTE order set that is doable and user-friendly,” adds Dr. Maynard.
UCSD’s pharmacist-hospitalist collaboration also encourages residents from both disciplines to work together on integrating protocols into clinical care processes. The team hopes that the VTE protocol will go beyond the inpatient stay by wrapping the protocol into the discharge plan. Dr. Weibert’s anticoagulation and pulmonary embolism clinics also help “build on our strengths,” he says.
The second team is led by newcomers to the grant winner’s circle, Drs. Hroncich (pharmacist) and Adair (hospitalist) from Presbyterian Healthcare Services, Albuquerque, N.M. They base their research on this question: Is it more efficient for the system’s 34 hospitalists to screen out those at low risk of VTE than to screen everyone for high risk?
The investigators have been collecting baseline data on compliance with VTE screening since 2003. Hospitalist use of a VTE screening tool on admissions was 60%, improving to 88% with reminders. “The implication is that 12% of the hospitalists didn’t use the screening tool,” says Dr. Adair. “We found that they were resistant to another piece of paper.” PHS data also showed that seven out of 10 patients had some VTE risk, that co-morbidities and hospitalization increase VTE risk, and that the age at which patients fall prey to VTE is dropping to between 50 and 60.
For the ASHP grant, Drs. Hroncich and Adair will monitor VTE screening on admission to all PHS general medical units. All patients 18 or older admitted to those units during a three-month period will be routinely screened on admission for VTE risk. Drs. Hroncich and Adair will make two VTE-related admission order sets available to hospitalists to complete. The current screening tool is designed to identify patients at risk of developing a VTE based on the presence of risk factors. The second, shorter admission order set will contain a screening tool that assumes that all patients need VTE prophylaxis, except low-risk patients and those with VTE prophylaxis contraindications. “The shorter tool should take only one or two minutes to complete,” says Dr. Hroncich.
The PHS team hopes that the shorter screening tool will overcome resistance to VTE screening. Dr. Hroncich says there are many barriers to VTE screening. They include lack of consensus on the best screening tool on admission, the misperception that VTE isn’t a big problem, lack of reliable processes so at-risk patients don’t fall through the cracks, and a misperception that anti-coagulant therapy is dangerous.
“It’s one thing to treat COPD and heart failure,” adds Dr. Adair, “but if I can prevent VTE with less than a 60-second screening, I can prevent a disease state from happening.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Two pharmacist-hospitalist teams each won $50,000 grants June 12 from the American Society of Health-System Pharmacists (ASHP) Research and Education Foundation (Bethesda, Md.) to support development of screening tools and order sets to prevent and treat hospital-acquired venous thromboembolism (VTE).
The grant winners and lead co-investigators from each team:
- Robert Weibert, PharmD, health sciences clinical professor and director of the Anticoagulation Clinic, School of Pharmacy, and Gregory Maynard, MD, MS, head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego (UCSD); and
- Rachel Hroncich, PharmD, pharmacy clinical coordinator of Presbyterian Healthcare Service, and Randle Adair, DO, PhD, a PMG hospitalist in adult medicine from Albuquerque, N.M.
The ASHP, a nonprofit organization, fosters safe medication use.
“We are thrilled that our grant application was selected by the ASHP and excited about the opportunity for our research to improve patient care,” says Dr. Hroncich.
The ASHP Research and Education Foundation grant program, sponsored by Sanofi-Aventis, supports research by hospitalists and hospital pharmacists to treat VTE, with a focus on hospitalized patients and post-discharge follow-up. The grants are geared to help hospitalists and pharmacists reduce hospital-acquired VTE, a significant cause of morbidity and mortality in hospitals.
VTE-related treatment costs $1.5 billion a year, according to researchers at the University of Washington School of Pharmacy in Seattle. ASHP statistics indicate VTE affects more than 450,000 hospitalized patients annually. The condition—an amalgam of deep vein thrombosis (DVT) and pulmonary embolism (PE)—affects a range of hospitalized patients. Gynecologic, orthopedic, urologic, vascular, trauma, and cancer patients all are at risk—as are those with other medical conditions such as congestive heart failure, severe respiratory disease, and obesity, or those who are bedridden.
The ASHP grants help pharmacist-hospitalist teams find tools to screen for VTE. Such tools let clinicians intervene early with at-risk patients. Better screening and intervention requires sound clinical, administrative, and IT processes.
The trick is to encourage busy hospitalists to use a consensus-based VTE screening tool for all hospitalized patients.
While most VTE research involves retrospective chart review of diagnostic codes, Drs. Weibert and Maynard’s grant research goes beyond such studies by identifying patients at risk concurrent with their hospitalizations. Dr. Maynard says the need is urgent: “Hospitals grossly underestimate the risk of VTE. In a 300-bed hospital, at least 150 patients are at risk of hospital-acquired VTE at any time.”
The UCSD team hopes to improve VTE screening by integrating an order set into the hospital’s computer physician order entry (CPOE) system. “The literature points to a bundle of best practices for VTE,” says Dr. Maynard, “including baseline lab work, use of compression stockings, using heparin for an optimal time period, patient education for those on anticoagulants, timely follow-up post discharge, the Society of Hospital Medicine collaborative, etc.”
Based on that body of knowledge and the input of its 15 full-time equivalent hospitalists, UCSD stakeholders in VTE screening debate what is practical and workable, conduct small, paper-based pilot projects, and fine-tune the protocol to integrate it with patient flow through admissions. “As we transition fully to a CPOE in our health system, we will incorporate a VTE order set that is doable and user-friendly,” adds Dr. Maynard.
UCSD’s pharmacist-hospitalist collaboration also encourages residents from both disciplines to work together on integrating protocols into clinical care processes. The team hopes that the VTE protocol will go beyond the inpatient stay by wrapping the protocol into the discharge plan. Dr. Weibert’s anticoagulation and pulmonary embolism clinics also help “build on our strengths,” he says.
The second team is led by newcomers to the grant winner’s circle, Drs. Hroncich (pharmacist) and Adair (hospitalist) from Presbyterian Healthcare Services, Albuquerque, N.M. They base their research on this question: Is it more efficient for the system’s 34 hospitalists to screen out those at low risk of VTE than to screen everyone for high risk?
The investigators have been collecting baseline data on compliance with VTE screening since 2003. Hospitalist use of a VTE screening tool on admissions was 60%, improving to 88% with reminders. “The implication is that 12% of the hospitalists didn’t use the screening tool,” says Dr. Adair. “We found that they were resistant to another piece of paper.” PHS data also showed that seven out of 10 patients had some VTE risk, that co-morbidities and hospitalization increase VTE risk, and that the age at which patients fall prey to VTE is dropping to between 50 and 60.
For the ASHP grant, Drs. Hroncich and Adair will monitor VTE screening on admission to all PHS general medical units. All patients 18 or older admitted to those units during a three-month period will be routinely screened on admission for VTE risk. Drs. Hroncich and Adair will make two VTE-related admission order sets available to hospitalists to complete. The current screening tool is designed to identify patients at risk of developing a VTE based on the presence of risk factors. The second, shorter admission order set will contain a screening tool that assumes that all patients need VTE prophylaxis, except low-risk patients and those with VTE prophylaxis contraindications. “The shorter tool should take only one or two minutes to complete,” says Dr. Hroncich.
The PHS team hopes that the shorter screening tool will overcome resistance to VTE screening. Dr. Hroncich says there are many barriers to VTE screening. They include lack of consensus on the best screening tool on admission, the misperception that VTE isn’t a big problem, lack of reliable processes so at-risk patients don’t fall through the cracks, and a misperception that anti-coagulant therapy is dangerous.
“It’s one thing to treat COPD and heart failure,” adds Dr. Adair, “but if I can prevent VTE with less than a 60-second screening, I can prevent a disease state from happening.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Get Clear on Delirium
Delirium—also known as acute confusional state—is a common and potentially serious condition for hospitalized geriatric patients. It is believed to complicate hospital stays for more than 2.3 million older people, account for more than 17.5 million in patient days, and cost more than $4 billion in Medicare expenditures.1
Many experts believe the numbers may be higher because clinical staff too often automatically attribute patients’ symptoms to age-related dementia.
Delirium is many times more likely to occur in older people.2 Because patients older than 65 account for nearly half of all inpatient days, hospitalists must be readily able to identify the signs and symptoms of delirium—as well as what factors put certain patients at an increased risk for developing delirium. Hospitalists with this knowledge and ability will be better equipped to reduce the risk for delirium in their patients and more effectively treat delirium when it occurs.
“Assuming that the patient’s confusion is a normal state for him or her, without speaking to the patient’s family or caregivers to establish the baseline mental status for the patient, is probably the biggest reason delirium is so often misdiagnosed and, consequently, left untreated,” says Sharon Inouye, MD, of the Institute for Aging Research, Hebrew SeniorLife and Harvard Medical School.
Define and Diagnose Delirium
Delirium is a temporary state of mental confusion and fluctuating consciousness. Patients are unable to focus their thoughts or pay attention, are confused about their environment and individuals, and unsure about their daily routines. They may exhibit subtle or startling personality changes. Some people may become withdrawn and lethargic, while others become agitated or hyperactive. Some patients experience visual and/or auditory hallucinations and become paranoid.
Changes in sleep patterns are a typical manifestation of delirium. The patient may experience anything from mild insomnia to complete reversal of the sleep-wake cycle. All symptoms may fluctuate in severity as the day progresses, and it is common for delirious patients to become more agitated and confused at night.
Dementia is a chronic problem that develops over time. Delirium is acute—usually developing over hours or days. While patients with pre-existing dementia, brain trauma, cerebrovascular accident, or brain tumor are at higher risk for developing delirium, don’t automatically attribute unusual behavior in a geriatric patient to one of these diagnoses—especially if the behavioral change is sudden.
It is vital to obtain a solid history to determine the patient’s baseline mental status. The patient may not be the most reliable source of information regarding his or her normal level of cognition—particularly if he or she is beginning to show signs that may indicate delirium. Make every effort to question the patient’s family members and caregivers thoroughly to determine the patient’s normal level of functioning.
“The trick is that you have to have a nursing staff you can trust and who is attentive enough to changes in behavior—keeping in mind that they’ve only known the patient for a short time,” says Jonathan Flacker, MD, assistant professor of medicine at Emory University in Atlanta. “You have to rely a lot on the families and caregivers. You have to know whether the patient’s behavior is new or not, and sometimes that’s hard to establish.”
A simple tool nursing staff can use to monitor the patient’s mental status is the Confusion Assessment Method (CAM). The CAM is easy to use and interpret and only takes moments to complete. When staff on each shift use this tool and accurately document the results, it can help identify early changes that may indicate the onset of delirium.3
In addition to the CAM, other tools that can assist in cognitive assessment of the patient can include The Mini-Cog Assessment Instrument for Dementia, The Clock Draw Test, The Short Portable Mental Status Questionnaire (SPMSQ), The Geriatric Depression Scale, The Folstein Mini-Mental Status Exam, and The Digit Span Test.
Identify Etiology
Once the physician has determined that a patient is suffering from delirium, the challenge is to identify and treat the cause.
“It is important to remember that older folks often have atypical presentation of symptoms for medical problems,” says Dr. Inouye. “Physicians and clinical staff need to carefully consider all of the patient’s signs and symptoms, regardless of how insignificant they may seem.”
The physician can then order additional diagnostic tests based on the findings of the physical examination, which may include CBC, serum chemistry group, urinalysis, serum and urine drug screens, and possibly diagnostic radiographic studies as indicated.
Assessment must also include a careful review of the patient’s medications—possibly with input from a pharmacist. To do this, obtain a complete list of medications the patient was taking prior to admission to compare with the medications the patient is taking currently. Consider the possible effects of:
- Medications that have been discontinued;
- New medications;
- Changes in dosage;
- Possible drug interactions; and
- Possible drug toxicities that may require additional lab testing.
Pay attention to psychoactive medications the patient is taking, such as sedative-hypnotic agents, narcotics, and antidepressants. It is important to note whether the patient has recently received anesthesia or pain medications.4 It is also important to determine whether the patient has a history of alcohol or drug dependency.
“The first thing I would think if a patient is not acting right is drugs—some new drug that we’re administering or some drug that he or she is withdrawing from,” says O’Neil Pyke, MD, medical director of the Hamot Hospitalist Group in Erie, Pa. “You have to consider the possibility of side effects, drug interactions, and withdrawals. You also have to recognize polypharmacology as a major risk factor and try to curtail unnecessary medications.”
Dr. Flacker cautions that even once a problem has been identified, the physician must follow through on the complete examination and evaluation of the patient, keeping in mind that the cause for delirium may be multifactorial. “The problem is that like a lot of things in older folks, if you look for ‘the’ cause, you’re likely to be frustrated,” he says. “It’s often a combination of stressors causing the patient’s delirium.”
Treatment
Once the underlying problem or problems have been identified, treat those medical conditions accordingly—by administering antibiotics, fluids, and electrolytes as needed and adjusting or discontinuing medications.
However, resolution of the etiologic cause does not necessarily mean the symptoms of delirium will spontaneously resolve. These symptoms likely will require specific interventions to reorient the patient.
Encourage family members to participate in these efforts and spend as much time as possible with the patient. It may also be helpful to have family members bring in a few familiar items from the patient’s home—such as family photographs—to help calm and reassure the patient.
David Meyers, MD, hospitalist and chief of inpatient medicine at the Veterans Administration Medical Center in Madison, Wis., says: “You can use very simple modifications that really don’t take much time or effort. It’s really trying to recreate the patient’s environment and getting him or her to identify with certain things.”
To help the patient remain oriented to time and assist with disturbances in sleep patterns, staff should turn lights on and off and open and close curtains and blinds at the appropriate times. Make wall calendars and clocks visible to the patient. Try to keep the patient as active as possible during the day and minimize sleep interruptions.
Maintain as calm an environment for the patient as possible, minimizing ambient noise and activity. Place the patient in a room without a roommate if possible, close enough to the nurses’ station to facilitate close observation—but not so close that they’re disturbed by beepers, telephones, monitors, and other noises. Keep televisions at a reasonable volume and turned off when no one is watching. However, don’t isolate or abandon the patient, or let him/her spend too much time in bed. Assist the patient with mobilization several times daily.
If the patient has a vision or hearing impairment, staff and family should make every effort to ensure that the patient has access to and uses the appropriate corrective devices.4 Staff will also need to pay special attention to ensure that the patient eats appropriately, maintains an adequate fluid intake, and is assisted to the restroom regularly.
If safety concerns make it absolutely necessary to use physical restraints on a delirious patient, remember to explain all actions and instructions in clear, simple terms, using a low, calm tone of voice. Apply restraints carefully, release at frequent intervals, and discontinue as soon as possible. The patient likely will not understand why he or she is being restrained—and this lack of comprehension can worsen the patient’s fear and agitation.4,5
If nonpharmacologic interventions are not effective in controlling the patient’s agitation, physicians may prescribe antipsychotic agents and intermediate-acting benzodiazepines to immediately control an extremely agitated patient. However, some antipsychotic drugs can have anticholinergic side effects, which may aggravate delirium. Benzodiazepines can also exacerbate the patient’s delirious symptoms in the long term. Use these medications only for initial control of the patient’s behavior, and reduce and discontinue as soon as possible.
Dr. Meyers encourages consultation by a geriatrician. “The biggest consult service I utilize for suggestion of treatment options is geriatrics,” he says. “They’re very good at working with the patient and family and thinking of other behavioral and medical modifications.
“We can’t give a pill to reverse delirium. This is a shift in paradigm from what physicians are taught. In this setting, you actually want to get rid of medications and limit interventions.”
Remember to reassure patients and their families that most people recover fully if delirium is rapidly identified and treated. However, also caution them that some of the patient’s symptoms may persist for weeks or months, and improvement may occur slowly. Discharge from the hospital may be in the patient’s best interest—but the persistence of symptoms may necessitate home healthcare or temporary nursing home placement.
“In the absence of an acute medical problem, it may be preferable to get the patient to a less acute setting that can be more orienting and more therapeutic,” says Dr. Flacker.
While experts agree that it is not possible to prevent every case of delirium, knowing what puts patients at higher risk gives us the ability to reduce that risk for many patients.
In 1999, Dr. Inouye and her colleagues at the Yale University School of Medicine developed The Hospital Elder Life Program (HELP). The HELP program utilizes a trained interdisciplinary team consisting of a geriatric nurse-specialist, specially trained Elder Life specialists, trained volunteers, geriatrician, and other consultants (such as a certified therapeutic recreation specialist, a physical therapist, a pharmacist, and a nutritionist) to address six facets of delirium risk:
- Orientation. Provide daily communication and a daily schedule on a dry-erase board or chalkboard;
- Therapeutic activities. A variety of cognitively stimulating, fun activities like word games, reminiscence, trivia, or current events;
- Early mobilization. Get all patients up and walking three times a day;
- Vision and hearing adaptations;
- Feeding assistance and hydration assistance with encouragement/companionship during meals; and
- Sleep enhancement. Provide a nonpharmacologic sleep protocol, such as warm milk or herbal tea, backrub, and relaxation music.
A study of the HELP program published in The New England Journal of Medicine showed a 40% reduction in risk for delirium when these measures were applied to at-risk patients included in the study. Implementing the program cost $6,341 per case of delirium prevented. That is significantly less than the estimated cost associated with preventing other hospital complications, such as falls and myocardial infarction.
Prevention is preferable to treatment. But when delirium cannot be prevented, Dr. Inouye concludes with this advice for hospitalists: “Recognition is huge. The single most important thing that hospitalists can do for patients suffering from delirium is to know the signs and symptoms and recognize them when they occur. Earlier recognition means earlier intervention—and that is what’s in the best interest of the patient.” TH
Sheri Polley is a frequent contributor to The Hospitalist.
References
- Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med.1999 Mar 4;340:669-676.
- Rummans TA, Evans JM, Krahn LE, Fleming KC. Delirium in elderly patients: Evaluation and management. Mayo Clinic Web site. Available at www.mayoclinicproceedings.com/inside.asp?AID=4031&UID. Last accessed May 14, 2007.
- Clinical Toolbox for Geriatric Care. Society of Hospital Medicine Web site. Available at www.hospitalmedicine.org/geriresource/toolbox/howto.htm. Last accessed May 2, 2007.
- McGowan NC, Locala JA. Delirium. The Cleveland Clinic Web site. Available at www.clevelandclinicmeded.com/diseasemanagement/psychiatry/delirium/delirum1.htm. Last accessed May 15, 2007.
- Restraint Alternative Menu. Clinical Toolbox for Geriatric Care 2004 Society of Hospital Medicine. Available at www.hospitalmedicine.org/geriresource/toolbox/howto.htm. Last accessed May 2, 2007.
Delirium—also known as acute confusional state—is a common and potentially serious condition for hospitalized geriatric patients. It is believed to complicate hospital stays for more than 2.3 million older people, account for more than 17.5 million in patient days, and cost more than $4 billion in Medicare expenditures.1
Many experts believe the numbers may be higher because clinical staff too often automatically attribute patients’ symptoms to age-related dementia.
Delirium is many times more likely to occur in older people.2 Because patients older than 65 account for nearly half of all inpatient days, hospitalists must be readily able to identify the signs and symptoms of delirium—as well as what factors put certain patients at an increased risk for developing delirium. Hospitalists with this knowledge and ability will be better equipped to reduce the risk for delirium in their patients and more effectively treat delirium when it occurs.
“Assuming that the patient’s confusion is a normal state for him or her, without speaking to the patient’s family or caregivers to establish the baseline mental status for the patient, is probably the biggest reason delirium is so often misdiagnosed and, consequently, left untreated,” says Sharon Inouye, MD, of the Institute for Aging Research, Hebrew SeniorLife and Harvard Medical School.
Define and Diagnose Delirium
Delirium is a temporary state of mental confusion and fluctuating consciousness. Patients are unable to focus their thoughts or pay attention, are confused about their environment and individuals, and unsure about their daily routines. They may exhibit subtle or startling personality changes. Some people may become withdrawn and lethargic, while others become agitated or hyperactive. Some patients experience visual and/or auditory hallucinations and become paranoid.
Changes in sleep patterns are a typical manifestation of delirium. The patient may experience anything from mild insomnia to complete reversal of the sleep-wake cycle. All symptoms may fluctuate in severity as the day progresses, and it is common for delirious patients to become more agitated and confused at night.
Dementia is a chronic problem that develops over time. Delirium is acute—usually developing over hours or days. While patients with pre-existing dementia, brain trauma, cerebrovascular accident, or brain tumor are at higher risk for developing delirium, don’t automatically attribute unusual behavior in a geriatric patient to one of these diagnoses—especially if the behavioral change is sudden.
It is vital to obtain a solid history to determine the patient’s baseline mental status. The patient may not be the most reliable source of information regarding his or her normal level of cognition—particularly if he or she is beginning to show signs that may indicate delirium. Make every effort to question the patient’s family members and caregivers thoroughly to determine the patient’s normal level of functioning.
“The trick is that you have to have a nursing staff you can trust and who is attentive enough to changes in behavior—keeping in mind that they’ve only known the patient for a short time,” says Jonathan Flacker, MD, assistant professor of medicine at Emory University in Atlanta. “You have to rely a lot on the families and caregivers. You have to know whether the patient’s behavior is new or not, and sometimes that’s hard to establish.”
A simple tool nursing staff can use to monitor the patient’s mental status is the Confusion Assessment Method (CAM). The CAM is easy to use and interpret and only takes moments to complete. When staff on each shift use this tool and accurately document the results, it can help identify early changes that may indicate the onset of delirium.3
In addition to the CAM, other tools that can assist in cognitive assessment of the patient can include The Mini-Cog Assessment Instrument for Dementia, The Clock Draw Test, The Short Portable Mental Status Questionnaire (SPMSQ), The Geriatric Depression Scale, The Folstein Mini-Mental Status Exam, and The Digit Span Test.
Identify Etiology
Once the physician has determined that a patient is suffering from delirium, the challenge is to identify and treat the cause.
“It is important to remember that older folks often have atypical presentation of symptoms for medical problems,” says Dr. Inouye. “Physicians and clinical staff need to carefully consider all of the patient’s signs and symptoms, regardless of how insignificant they may seem.”
The physician can then order additional diagnostic tests based on the findings of the physical examination, which may include CBC, serum chemistry group, urinalysis, serum and urine drug screens, and possibly diagnostic radiographic studies as indicated.
Assessment must also include a careful review of the patient’s medications—possibly with input from a pharmacist. To do this, obtain a complete list of medications the patient was taking prior to admission to compare with the medications the patient is taking currently. Consider the possible effects of:
- Medications that have been discontinued;
- New medications;
- Changes in dosage;
- Possible drug interactions; and
- Possible drug toxicities that may require additional lab testing.
Pay attention to psychoactive medications the patient is taking, such as sedative-hypnotic agents, narcotics, and antidepressants. It is important to note whether the patient has recently received anesthesia or pain medications.4 It is also important to determine whether the patient has a history of alcohol or drug dependency.
“The first thing I would think if a patient is not acting right is drugs—some new drug that we’re administering or some drug that he or she is withdrawing from,” says O’Neil Pyke, MD, medical director of the Hamot Hospitalist Group in Erie, Pa. “You have to consider the possibility of side effects, drug interactions, and withdrawals. You also have to recognize polypharmacology as a major risk factor and try to curtail unnecessary medications.”
Dr. Flacker cautions that even once a problem has been identified, the physician must follow through on the complete examination and evaluation of the patient, keeping in mind that the cause for delirium may be multifactorial. “The problem is that like a lot of things in older folks, if you look for ‘the’ cause, you’re likely to be frustrated,” he says. “It’s often a combination of stressors causing the patient’s delirium.”
Treatment
Once the underlying problem or problems have been identified, treat those medical conditions accordingly—by administering antibiotics, fluids, and electrolytes as needed and adjusting or discontinuing medications.
However, resolution of the etiologic cause does not necessarily mean the symptoms of delirium will spontaneously resolve. These symptoms likely will require specific interventions to reorient the patient.
Encourage family members to participate in these efforts and spend as much time as possible with the patient. It may also be helpful to have family members bring in a few familiar items from the patient’s home—such as family photographs—to help calm and reassure the patient.
David Meyers, MD, hospitalist and chief of inpatient medicine at the Veterans Administration Medical Center in Madison, Wis., says: “You can use very simple modifications that really don’t take much time or effort. It’s really trying to recreate the patient’s environment and getting him or her to identify with certain things.”
To help the patient remain oriented to time and assist with disturbances in sleep patterns, staff should turn lights on and off and open and close curtains and blinds at the appropriate times. Make wall calendars and clocks visible to the patient. Try to keep the patient as active as possible during the day and minimize sleep interruptions.
Maintain as calm an environment for the patient as possible, minimizing ambient noise and activity. Place the patient in a room without a roommate if possible, close enough to the nurses’ station to facilitate close observation—but not so close that they’re disturbed by beepers, telephones, monitors, and other noises. Keep televisions at a reasonable volume and turned off when no one is watching. However, don’t isolate or abandon the patient, or let him/her spend too much time in bed. Assist the patient with mobilization several times daily.
If the patient has a vision or hearing impairment, staff and family should make every effort to ensure that the patient has access to and uses the appropriate corrective devices.4 Staff will also need to pay special attention to ensure that the patient eats appropriately, maintains an adequate fluid intake, and is assisted to the restroom regularly.
If safety concerns make it absolutely necessary to use physical restraints on a delirious patient, remember to explain all actions and instructions in clear, simple terms, using a low, calm tone of voice. Apply restraints carefully, release at frequent intervals, and discontinue as soon as possible. The patient likely will not understand why he or she is being restrained—and this lack of comprehension can worsen the patient’s fear and agitation.4,5
If nonpharmacologic interventions are not effective in controlling the patient’s agitation, physicians may prescribe antipsychotic agents and intermediate-acting benzodiazepines to immediately control an extremely agitated patient. However, some antipsychotic drugs can have anticholinergic side effects, which may aggravate delirium. Benzodiazepines can also exacerbate the patient’s delirious symptoms in the long term. Use these medications only for initial control of the patient’s behavior, and reduce and discontinue as soon as possible.
Dr. Meyers encourages consultation by a geriatrician. “The biggest consult service I utilize for suggestion of treatment options is geriatrics,” he says. “They’re very good at working with the patient and family and thinking of other behavioral and medical modifications.
“We can’t give a pill to reverse delirium. This is a shift in paradigm from what physicians are taught. In this setting, you actually want to get rid of medications and limit interventions.”
Remember to reassure patients and their families that most people recover fully if delirium is rapidly identified and treated. However, also caution them that some of the patient’s symptoms may persist for weeks or months, and improvement may occur slowly. Discharge from the hospital may be in the patient’s best interest—but the persistence of symptoms may necessitate home healthcare or temporary nursing home placement.
“In the absence of an acute medical problem, it may be preferable to get the patient to a less acute setting that can be more orienting and more therapeutic,” says Dr. Flacker.
While experts agree that it is not possible to prevent every case of delirium, knowing what puts patients at higher risk gives us the ability to reduce that risk for many patients.
In 1999, Dr. Inouye and her colleagues at the Yale University School of Medicine developed The Hospital Elder Life Program (HELP). The HELP program utilizes a trained interdisciplinary team consisting of a geriatric nurse-specialist, specially trained Elder Life specialists, trained volunteers, geriatrician, and other consultants (such as a certified therapeutic recreation specialist, a physical therapist, a pharmacist, and a nutritionist) to address six facets of delirium risk:
- Orientation. Provide daily communication and a daily schedule on a dry-erase board or chalkboard;
- Therapeutic activities. A variety of cognitively stimulating, fun activities like word games, reminiscence, trivia, or current events;
- Early mobilization. Get all patients up and walking three times a day;
- Vision and hearing adaptations;
- Feeding assistance and hydration assistance with encouragement/companionship during meals; and
- Sleep enhancement. Provide a nonpharmacologic sleep protocol, such as warm milk or herbal tea, backrub, and relaxation music.
A study of the HELP program published in The New England Journal of Medicine showed a 40% reduction in risk for delirium when these measures were applied to at-risk patients included in the study. Implementing the program cost $6,341 per case of delirium prevented. That is significantly less than the estimated cost associated with preventing other hospital complications, such as falls and myocardial infarction.
Prevention is preferable to treatment. But when delirium cannot be prevented, Dr. Inouye concludes with this advice for hospitalists: “Recognition is huge. The single most important thing that hospitalists can do for patients suffering from delirium is to know the signs and symptoms and recognize them when they occur. Earlier recognition means earlier intervention—and that is what’s in the best interest of the patient.” TH
Sheri Polley is a frequent contributor to The Hospitalist.
References
- Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med.1999 Mar 4;340:669-676.
- Rummans TA, Evans JM, Krahn LE, Fleming KC. Delirium in elderly patients: Evaluation and management. Mayo Clinic Web site. Available at www.mayoclinicproceedings.com/inside.asp?AID=4031&UID. Last accessed May 14, 2007.
- Clinical Toolbox for Geriatric Care. Society of Hospital Medicine Web site. Available at www.hospitalmedicine.org/geriresource/toolbox/howto.htm. Last accessed May 2, 2007.
- McGowan NC, Locala JA. Delirium. The Cleveland Clinic Web site. Available at www.clevelandclinicmeded.com/diseasemanagement/psychiatry/delirium/delirum1.htm. Last accessed May 15, 2007.
- Restraint Alternative Menu. Clinical Toolbox for Geriatric Care 2004 Society of Hospital Medicine. Available at www.hospitalmedicine.org/geriresource/toolbox/howto.htm. Last accessed May 2, 2007.
Delirium—also known as acute confusional state—is a common and potentially serious condition for hospitalized geriatric patients. It is believed to complicate hospital stays for more than 2.3 million older people, account for more than 17.5 million in patient days, and cost more than $4 billion in Medicare expenditures.1
Many experts believe the numbers may be higher because clinical staff too often automatically attribute patients’ symptoms to age-related dementia.
Delirium is many times more likely to occur in older people.2 Because patients older than 65 account for nearly half of all inpatient days, hospitalists must be readily able to identify the signs and symptoms of delirium—as well as what factors put certain patients at an increased risk for developing delirium. Hospitalists with this knowledge and ability will be better equipped to reduce the risk for delirium in their patients and more effectively treat delirium when it occurs.
“Assuming that the patient’s confusion is a normal state for him or her, without speaking to the patient’s family or caregivers to establish the baseline mental status for the patient, is probably the biggest reason delirium is so often misdiagnosed and, consequently, left untreated,” says Sharon Inouye, MD, of the Institute for Aging Research, Hebrew SeniorLife and Harvard Medical School.
Define and Diagnose Delirium
Delirium is a temporary state of mental confusion and fluctuating consciousness. Patients are unable to focus their thoughts or pay attention, are confused about their environment and individuals, and unsure about their daily routines. They may exhibit subtle or startling personality changes. Some people may become withdrawn and lethargic, while others become agitated or hyperactive. Some patients experience visual and/or auditory hallucinations and become paranoid.
Changes in sleep patterns are a typical manifestation of delirium. The patient may experience anything from mild insomnia to complete reversal of the sleep-wake cycle. All symptoms may fluctuate in severity as the day progresses, and it is common for delirious patients to become more agitated and confused at night.
Dementia is a chronic problem that develops over time. Delirium is acute—usually developing over hours or days. While patients with pre-existing dementia, brain trauma, cerebrovascular accident, or brain tumor are at higher risk for developing delirium, don’t automatically attribute unusual behavior in a geriatric patient to one of these diagnoses—especially if the behavioral change is sudden.
It is vital to obtain a solid history to determine the patient’s baseline mental status. The patient may not be the most reliable source of information regarding his or her normal level of cognition—particularly if he or she is beginning to show signs that may indicate delirium. Make every effort to question the patient’s family members and caregivers thoroughly to determine the patient’s normal level of functioning.
“The trick is that you have to have a nursing staff you can trust and who is attentive enough to changes in behavior—keeping in mind that they’ve only known the patient for a short time,” says Jonathan Flacker, MD, assistant professor of medicine at Emory University in Atlanta. “You have to rely a lot on the families and caregivers. You have to know whether the patient’s behavior is new or not, and sometimes that’s hard to establish.”
A simple tool nursing staff can use to monitor the patient’s mental status is the Confusion Assessment Method (CAM). The CAM is easy to use and interpret and only takes moments to complete. When staff on each shift use this tool and accurately document the results, it can help identify early changes that may indicate the onset of delirium.3
In addition to the CAM, other tools that can assist in cognitive assessment of the patient can include The Mini-Cog Assessment Instrument for Dementia, The Clock Draw Test, The Short Portable Mental Status Questionnaire (SPMSQ), The Geriatric Depression Scale, The Folstein Mini-Mental Status Exam, and The Digit Span Test.
Identify Etiology
Once the physician has determined that a patient is suffering from delirium, the challenge is to identify and treat the cause.
“It is important to remember that older folks often have atypical presentation of symptoms for medical problems,” says Dr. Inouye. “Physicians and clinical staff need to carefully consider all of the patient’s signs and symptoms, regardless of how insignificant they may seem.”
The physician can then order additional diagnostic tests based on the findings of the physical examination, which may include CBC, serum chemistry group, urinalysis, serum and urine drug screens, and possibly diagnostic radiographic studies as indicated.
Assessment must also include a careful review of the patient’s medications—possibly with input from a pharmacist. To do this, obtain a complete list of medications the patient was taking prior to admission to compare with the medications the patient is taking currently. Consider the possible effects of:
- Medications that have been discontinued;
- New medications;
- Changes in dosage;
- Possible drug interactions; and
- Possible drug toxicities that may require additional lab testing.
Pay attention to psychoactive medications the patient is taking, such as sedative-hypnotic agents, narcotics, and antidepressants. It is important to note whether the patient has recently received anesthesia or pain medications.4 It is also important to determine whether the patient has a history of alcohol or drug dependency.
“The first thing I would think if a patient is not acting right is drugs—some new drug that we’re administering or some drug that he or she is withdrawing from,” says O’Neil Pyke, MD, medical director of the Hamot Hospitalist Group in Erie, Pa. “You have to consider the possibility of side effects, drug interactions, and withdrawals. You also have to recognize polypharmacology as a major risk factor and try to curtail unnecessary medications.”
Dr. Flacker cautions that even once a problem has been identified, the physician must follow through on the complete examination and evaluation of the patient, keeping in mind that the cause for delirium may be multifactorial. “The problem is that like a lot of things in older folks, if you look for ‘the’ cause, you’re likely to be frustrated,” he says. “It’s often a combination of stressors causing the patient’s delirium.”
Treatment
Once the underlying problem or problems have been identified, treat those medical conditions accordingly—by administering antibiotics, fluids, and electrolytes as needed and adjusting or discontinuing medications.
However, resolution of the etiologic cause does not necessarily mean the symptoms of delirium will spontaneously resolve. These symptoms likely will require specific interventions to reorient the patient.
Encourage family members to participate in these efforts and spend as much time as possible with the patient. It may also be helpful to have family members bring in a few familiar items from the patient’s home—such as family photographs—to help calm and reassure the patient.
David Meyers, MD, hospitalist and chief of inpatient medicine at the Veterans Administration Medical Center in Madison, Wis., says: “You can use very simple modifications that really don’t take much time or effort. It’s really trying to recreate the patient’s environment and getting him or her to identify with certain things.”
To help the patient remain oriented to time and assist with disturbances in sleep patterns, staff should turn lights on and off and open and close curtains and blinds at the appropriate times. Make wall calendars and clocks visible to the patient. Try to keep the patient as active as possible during the day and minimize sleep interruptions.
Maintain as calm an environment for the patient as possible, minimizing ambient noise and activity. Place the patient in a room without a roommate if possible, close enough to the nurses’ station to facilitate close observation—but not so close that they’re disturbed by beepers, telephones, monitors, and other noises. Keep televisions at a reasonable volume and turned off when no one is watching. However, don’t isolate or abandon the patient, or let him/her spend too much time in bed. Assist the patient with mobilization several times daily.
If the patient has a vision or hearing impairment, staff and family should make every effort to ensure that the patient has access to and uses the appropriate corrective devices.4 Staff will also need to pay special attention to ensure that the patient eats appropriately, maintains an adequate fluid intake, and is assisted to the restroom regularly.
If safety concerns make it absolutely necessary to use physical restraints on a delirious patient, remember to explain all actions and instructions in clear, simple terms, using a low, calm tone of voice. Apply restraints carefully, release at frequent intervals, and discontinue as soon as possible. The patient likely will not understand why he or she is being restrained—and this lack of comprehension can worsen the patient’s fear and agitation.4,5
If nonpharmacologic interventions are not effective in controlling the patient’s agitation, physicians may prescribe antipsychotic agents and intermediate-acting benzodiazepines to immediately control an extremely agitated patient. However, some antipsychotic drugs can have anticholinergic side effects, which may aggravate delirium. Benzodiazepines can also exacerbate the patient’s delirious symptoms in the long term. Use these medications only for initial control of the patient’s behavior, and reduce and discontinue as soon as possible.
Dr. Meyers encourages consultation by a geriatrician. “The biggest consult service I utilize for suggestion of treatment options is geriatrics,” he says. “They’re very good at working with the patient and family and thinking of other behavioral and medical modifications.
“We can’t give a pill to reverse delirium. This is a shift in paradigm from what physicians are taught. In this setting, you actually want to get rid of medications and limit interventions.”
Remember to reassure patients and their families that most people recover fully if delirium is rapidly identified and treated. However, also caution them that some of the patient’s symptoms may persist for weeks or months, and improvement may occur slowly. Discharge from the hospital may be in the patient’s best interest—but the persistence of symptoms may necessitate home healthcare or temporary nursing home placement.
“In the absence of an acute medical problem, it may be preferable to get the patient to a less acute setting that can be more orienting and more therapeutic,” says Dr. Flacker.
While experts agree that it is not possible to prevent every case of delirium, knowing what puts patients at higher risk gives us the ability to reduce that risk for many patients.
In 1999, Dr. Inouye and her colleagues at the Yale University School of Medicine developed The Hospital Elder Life Program (HELP). The HELP program utilizes a trained interdisciplinary team consisting of a geriatric nurse-specialist, specially trained Elder Life specialists, trained volunteers, geriatrician, and other consultants (such as a certified therapeutic recreation specialist, a physical therapist, a pharmacist, and a nutritionist) to address six facets of delirium risk:
- Orientation. Provide daily communication and a daily schedule on a dry-erase board or chalkboard;
- Therapeutic activities. A variety of cognitively stimulating, fun activities like word games, reminiscence, trivia, or current events;
- Early mobilization. Get all patients up and walking three times a day;
- Vision and hearing adaptations;
- Feeding assistance and hydration assistance with encouragement/companionship during meals; and
- Sleep enhancement. Provide a nonpharmacologic sleep protocol, such as warm milk or herbal tea, backrub, and relaxation music.
A study of the HELP program published in The New England Journal of Medicine showed a 40% reduction in risk for delirium when these measures were applied to at-risk patients included in the study. Implementing the program cost $6,341 per case of delirium prevented. That is significantly less than the estimated cost associated with preventing other hospital complications, such as falls and myocardial infarction.
Prevention is preferable to treatment. But when delirium cannot be prevented, Dr. Inouye concludes with this advice for hospitalists: “Recognition is huge. The single most important thing that hospitalists can do for patients suffering from delirium is to know the signs and symptoms and recognize them when they occur. Earlier recognition means earlier intervention—and that is what’s in the best interest of the patient.” TH
Sheri Polley is a frequent contributor to The Hospitalist.
References
- Inouye SK, Bogardus ST, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med.1999 Mar 4;340:669-676.
- Rummans TA, Evans JM, Krahn LE, Fleming KC. Delirium in elderly patients: Evaluation and management. Mayo Clinic Web site. Available at www.mayoclinicproceedings.com/inside.asp?AID=4031&UID. Last accessed May 14, 2007.
- Clinical Toolbox for Geriatric Care. Society of Hospital Medicine Web site. Available at www.hospitalmedicine.org/geriresource/toolbox/howto.htm. Last accessed May 2, 2007.
- McGowan NC, Locala JA. Delirium. The Cleveland Clinic Web site. Available at www.clevelandclinicmeded.com/diseasemanagement/psychiatry/delirium/delirum1.htm. Last accessed May 15, 2007.
- Restraint Alternative Menu. Clinical Toolbox for Geriatric Care 2004 Society of Hospital Medicine. Available at www.hospitalmedicine.org/geriresource/toolbox/howto.htm. Last accessed May 2, 2007.
Bullied into Botched Care
Bullying, intimidation, verbal abuse—these behaviors negatively affect self-esteem, feelings of competence, and workplace morale. And they can devastate hospital professionals and their patients.
When 2,095 healthcare providers (1,565 nurses, 354 pharmacists, and 176 others) responded to an Institute for Safe Medication Practices (ISMP) survey on intimidation in their healthcare setting, remarkable data were collected.1
Perhaps the most alarming statistic in the 2003-2004 study was that 7% of respondents (n=147) reported they had been involved in a medication error allowed to occur partly because the respondents were afraid to question the prescriber’s decision. At a large urban trauma center in the northeastern United States, nurses listed intimidation as one of the barriers to implementing a sharps safety program.2
Nurses’ Perceptions
Research over the past decade has spotlighted intimidation in healthcare.3
“Bullying and harassment still happen in many areas of medicine,” says David M. Pressel, MD, PhD, hospitalist and director, Inpatient Service, Division of General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. “The question is, how do you monitor yourself to make sure you aren’t falling into that hierarchical frame of mind that could intervene in great teaching and learning and great patient care?”
Dr. Pressel and his partner, David I. Rappaport, MD, also a pediatric hospitalist at duPont, have focused on the literature pertaining to nurse-physician relationships. Research shows that intimidation impedes nurse recruitment, retention, and satisfaction. In one study, 90% of nurses reported experiencing at least one episode of verbal abuse.4 A 1997 study examining the effects of intimidation on 35 pediatric nurses over a three-month period found that 25 (71.4%) of them reported being yelled at or loudly admonished. Sixteen (45.7%) had been victims of insults. Thirty (85.7%) were spoken to in a condescending manner. One-third of nurses believed that such behavior was “part of the job.”
Although studies have differed as to the most common source of this abuse—patients and families or physicians—a study of pediatric nurses reported a similar incidence from both sources.5 And, nurses are often guilty of verbally abusing each other.6
When the duPont pediatric hospitalist team began performing more family-centered rounds, they began to appreciate the nurse-physician relationship. “We have worked hard to have a charge nurse and oftentimes the bedside nurse with us when we round,” Dr. Rappaport says. Speculating that rounding with hospitalists allowed nurses to feel more part of the team, Dr. Rappaport says know the medical plan, consolidate efforts such that pages to residents were reduced, and generally improve communication. They heard from participating nurses that it made a tremendous difference. This prompted them to conduct their research.
“Our study looked at the nurse-physician relationship globally, not intimidation or abuse specifically,” says Dr. Rappaport. Along with their nurse colleague Norine Watson, RN, Drs. Pressel and Rappaport are examining the relationship between nurses and different categories of physicians: how nurses perceive interactions between nurses and surgical residents, surgical attendings, community physicians, pediatric residents, and pediatric hospitalists.
“Early data suggest that hospitalists may work more effectively with nurses because they share many of the same goals,” says Dr. Rappaport. “As hospital leaders, hospitalists can also improve working conditions for nurses by providing more accessible, efficient, and effective care. Presumably, improved collaboration will also include decreased intimidation or abuse from physicians and also probably from dissatisfied patients and families.”
Avoiding the trap of communicating in a manner that is too direct and might be construed as abusive requires self-awareness and the realization that people receive information in different ways, says Dr. Pressel. Standard professional behavior is the key. Beyond that, the challenge is giving feedback constructively and in a positive manner.
“Hospitalists [may be] more in tune with the needs of nurses than nonhospitalists,” says Dr. Rappaport. “I think that is one of our strengths. We need to continue to facilitate very strong relationships between nurses and physicians because without good nursing care, hospitalists simply cannot provide good medical care.”
There is another way hospitalists can help address verbal abuse. “Studies consistently show that nurses are hesitant to report episodes of verbal abuse,” Dr. Rappaport says, “whether it is from a family, a patient, a physician, or a fellow nurse. Fewer than one in five nurses reports these episodes. One thing that hospitalists can do is work with hospital administration to create an environment that is more proactive in addressing these concerns and allowing nurses to feel more support in this area.”
Only 60% of respondents to the ISMP survey felt their organization had clearly defined an effective process for handling disagreements with a medication order’s safety. Only about a third felt the process facilitated their bypassing an intimidating prescriber or their own supervisor if necessary. Although 70% of respondents reported that they thought their organization or manager would support them if they reported intimidating behavior, only 39% of respondents believed their organization was dealing effectively with intimidating behavior.
Untapped Source
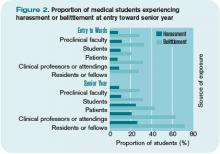
Perceptions of intimidation also occur among trainees. When 2,884 students from the class of 2003 at 16 U.S. medical schools completed questionnaires at various times during training, 27% reported having been “harassed” by house staff, 21% by faculty, and 25% by patients.7 Further, 71% reported having been “belittled” by house staff, 63% by faculty, and 43% by patients.
Mistreated students were significantly more likely to have suffered stress, be depressed or suicidal, and less likely to report being glad they trained as a physician.

—David I. Rappaport, MD, pediatric hospitalist, Alfred I. Dupont Hospital for Children, Wilmington, Del.
This may have an underlying effect on the potential to monitor for patient safety.8,9 Because errors and near misses often result from miscommunication, medical students may be adept at preventing certain types of errors. Students’ observation skills may be just as keen, if not more so, than their more clinically proficient healthcare teammates.8 In four cases from two U.S. academic health centers reported by medical students Samuel Seiden, Cynthia Galvan, and Ruth Lamm in 2006, medical students demonstrated keen attention to detail and appropriately characterized problematic situations with patients—adding another layer of defense within systems safeguarding against patient harm.8 Yet of the 76% of medical students who had observed a medical error, only about half of the students reported the errors to a resident or an attending, despite having received patient-safety training; only 7% reported having used an electronic medical error reporting system.10
By Example
Some intimidation in medical education may be the result of anger toward students and residents over a lack of medical knowledge, says Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University in New Orleans and member of the SHM Board of Directors. “It is natural to feel [that anger]; people abhor in others what they most detest in themselves,’’ he says. “As physicians, a lack of medical knowledge is what we detest in ourselves. But a student’s ignorance is usually a product of where she is in her training; that’s why she is with you.”
—Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University, New Orleans
Anger alienates students, absolving them of the guilt of not knowing the information, and demotivating them from learning it. “The lesson to be communicated is that it is OK not to know, but it is not OK to continue to not know,” Dr. Wiese says. “Reprimands should be reserved for the student who does not know, and then after being taught or asked to look it up, continues to not know.”
“The average physician who practices for 30 years will take care of roughly 80,000 people,” estimates Dr. Wiese. “That’s an arithmetic contribution and there is nothing wrong with that. But if you really want to change the world, teaching is the rule. The same 30 years invested in teaching will indirectly affect 400 million people,” he says. “Even better, if you can train your students and residents in the value of coaching their students and residents, well, now you’re talking about 10 billion people that you can affect over the course of a career.”
The question to ask yourself, says Dr. Wiese, is: Do you want to change the world? “If you do, this is the way to do it,” he says.
“For the 30 years in your career, focus on clinical coaching and getting others to clinically coach. That way, especially if you have the right motives in your heart, the right vision for the way you want to see the profession practiced, and the way you want patient care performed, that’s your shot at changing the world.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I). Available at w.ismp.org/Newsletters/acutecare/articles/20040311_2.asp. Last accessed June 27, 2007.
- Hagstrom AM. Perceived barriers to implementation of a successful sharps safety program. AORN J. 2006;83(2):391-7.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthc. 2006 Jul-Aug;3:16-24.
- Manderino MA, Berkey N. Verbal abuse of staff nurses by physicians. J Prof Nurs. 1997;13(1):48-55.
- Pejic AR. Verbal abuse: A problem for pediatric nurses. Pediatr Nurs. 2005;31(4):271-279.
- Rowe MM, Sherlock H. Stress and verbal abuse in nursing: do burned out nurses eat their young? J Nurs Manag. 2005May;13(3):242-248.
- Frank E, Carrera JS, Stratton T, et al. Experiences of belittlement and harassment and their correlates among medical students in the United States: longitudinal survey. BMJ. 2006 Sep 30;333(7570):682.
- Seiden SC, Galvan C, Lamm R. Role of medical students in preventing patient harm and enhancing patient safety. Qual Saf Health Care. 2006 Aug;15(4):272-276.
- Wood DF. Bullying and harassment in medical schools. BMJ. 2006 Sep 30;333(7570):664-665.
- Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006 Jan;81(1):94-101.
- Institute for Safe Medication Practice. Intimidation: Mapping a plan for cultural change in healthcare (Part II). Available at www.ismp.org/Newsletters/acutecare/articles/20040325.asp Last accessed July 2, 2007.
Bullying, intimidation, verbal abuse—these behaviors negatively affect self-esteem, feelings of competence, and workplace morale. And they can devastate hospital professionals and their patients.
When 2,095 healthcare providers (1,565 nurses, 354 pharmacists, and 176 others) responded to an Institute for Safe Medication Practices (ISMP) survey on intimidation in their healthcare setting, remarkable data were collected.1
Perhaps the most alarming statistic in the 2003-2004 study was that 7% of respondents (n=147) reported they had been involved in a medication error allowed to occur partly because the respondents were afraid to question the prescriber’s decision. At a large urban trauma center in the northeastern United States, nurses listed intimidation as one of the barriers to implementing a sharps safety program.2
Nurses’ Perceptions
Research over the past decade has spotlighted intimidation in healthcare.3
“Bullying and harassment still happen in many areas of medicine,” says David M. Pressel, MD, PhD, hospitalist and director, Inpatient Service, Division of General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. “The question is, how do you monitor yourself to make sure you aren’t falling into that hierarchical frame of mind that could intervene in great teaching and learning and great patient care?”
Dr. Pressel and his partner, David I. Rappaport, MD, also a pediatric hospitalist at duPont, have focused on the literature pertaining to nurse-physician relationships. Research shows that intimidation impedes nurse recruitment, retention, and satisfaction. In one study, 90% of nurses reported experiencing at least one episode of verbal abuse.4 A 1997 study examining the effects of intimidation on 35 pediatric nurses over a three-month period found that 25 (71.4%) of them reported being yelled at or loudly admonished. Sixteen (45.7%) had been victims of insults. Thirty (85.7%) were spoken to in a condescending manner. One-third of nurses believed that such behavior was “part of the job.”
Although studies have differed as to the most common source of this abuse—patients and families or physicians—a study of pediatric nurses reported a similar incidence from both sources.5 And, nurses are often guilty of verbally abusing each other.6
When the duPont pediatric hospitalist team began performing more family-centered rounds, they began to appreciate the nurse-physician relationship. “We have worked hard to have a charge nurse and oftentimes the bedside nurse with us when we round,” Dr. Rappaport says. Speculating that rounding with hospitalists allowed nurses to feel more part of the team, Dr. Rappaport says know the medical plan, consolidate efforts such that pages to residents were reduced, and generally improve communication. They heard from participating nurses that it made a tremendous difference. This prompted them to conduct their research.
“Our study looked at the nurse-physician relationship globally, not intimidation or abuse specifically,” says Dr. Rappaport. Along with their nurse colleague Norine Watson, RN, Drs. Pressel and Rappaport are examining the relationship between nurses and different categories of physicians: how nurses perceive interactions between nurses and surgical residents, surgical attendings, community physicians, pediatric residents, and pediatric hospitalists.
“Early data suggest that hospitalists may work more effectively with nurses because they share many of the same goals,” says Dr. Rappaport. “As hospital leaders, hospitalists can also improve working conditions for nurses by providing more accessible, efficient, and effective care. Presumably, improved collaboration will also include decreased intimidation or abuse from physicians and also probably from dissatisfied patients and families.”
Avoiding the trap of communicating in a manner that is too direct and might be construed as abusive requires self-awareness and the realization that people receive information in different ways, says Dr. Pressel. Standard professional behavior is the key. Beyond that, the challenge is giving feedback constructively and in a positive manner.
“Hospitalists [may be] more in tune with the needs of nurses than nonhospitalists,” says Dr. Rappaport. “I think that is one of our strengths. We need to continue to facilitate very strong relationships between nurses and physicians because without good nursing care, hospitalists simply cannot provide good medical care.”
There is another way hospitalists can help address verbal abuse. “Studies consistently show that nurses are hesitant to report episodes of verbal abuse,” Dr. Rappaport says, “whether it is from a family, a patient, a physician, or a fellow nurse. Fewer than one in five nurses reports these episodes. One thing that hospitalists can do is work with hospital administration to create an environment that is more proactive in addressing these concerns and allowing nurses to feel more support in this area.”
Only 60% of respondents to the ISMP survey felt their organization had clearly defined an effective process for handling disagreements with a medication order’s safety. Only about a third felt the process facilitated their bypassing an intimidating prescriber or their own supervisor if necessary. Although 70% of respondents reported that they thought their organization or manager would support them if they reported intimidating behavior, only 39% of respondents believed their organization was dealing effectively with intimidating behavior.
Untapped Source
Perceptions of intimidation also occur among trainees. When 2,884 students from the class of 2003 at 16 U.S. medical schools completed questionnaires at various times during training, 27% reported having been “harassed” by house staff, 21% by faculty, and 25% by patients.7 Further, 71% reported having been “belittled” by house staff, 63% by faculty, and 43% by patients.
Mistreated students were significantly more likely to have suffered stress, be depressed or suicidal, and less likely to report being glad they trained as a physician.

—David I. Rappaport, MD, pediatric hospitalist, Alfred I. Dupont Hospital for Children, Wilmington, Del.
This may have an underlying effect on the potential to monitor for patient safety.8,9 Because errors and near misses often result from miscommunication, medical students may be adept at preventing certain types of errors. Students’ observation skills may be just as keen, if not more so, than their more clinically proficient healthcare teammates.8 In four cases from two U.S. academic health centers reported by medical students Samuel Seiden, Cynthia Galvan, and Ruth Lamm in 2006, medical students demonstrated keen attention to detail and appropriately characterized problematic situations with patients—adding another layer of defense within systems safeguarding against patient harm.8 Yet of the 76% of medical students who had observed a medical error, only about half of the students reported the errors to a resident or an attending, despite having received patient-safety training; only 7% reported having used an electronic medical error reporting system.10
By Example
Some intimidation in medical education may be the result of anger toward students and residents over a lack of medical knowledge, says Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University in New Orleans and member of the SHM Board of Directors. “It is natural to feel [that anger]; people abhor in others what they most detest in themselves,’’ he says. “As physicians, a lack of medical knowledge is what we detest in ourselves. But a student’s ignorance is usually a product of where she is in her training; that’s why she is with you.”
—Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University, New Orleans
Anger alienates students, absolving them of the guilt of not knowing the information, and demotivating them from learning it. “The lesson to be communicated is that it is OK not to know, but it is not OK to continue to not know,” Dr. Wiese says. “Reprimands should be reserved for the student who does not know, and then after being taught or asked to look it up, continues to not know.”
“The average physician who practices for 30 years will take care of roughly 80,000 people,” estimates Dr. Wiese. “That’s an arithmetic contribution and there is nothing wrong with that. But if you really want to change the world, teaching is the rule. The same 30 years invested in teaching will indirectly affect 400 million people,” he says. “Even better, if you can train your students and residents in the value of coaching their students and residents, well, now you’re talking about 10 billion people that you can affect over the course of a career.”
The question to ask yourself, says Dr. Wiese, is: Do you want to change the world? “If you do, this is the way to do it,” he says.
“For the 30 years in your career, focus on clinical coaching and getting others to clinically coach. That way, especially if you have the right motives in your heart, the right vision for the way you want to see the profession practiced, and the way you want patient care performed, that’s your shot at changing the world.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I). Available at w.ismp.org/Newsletters/acutecare/articles/20040311_2.asp. Last accessed June 27, 2007.
- Hagstrom AM. Perceived barriers to implementation of a successful sharps safety program. AORN J. 2006;83(2):391-7.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthc. 2006 Jul-Aug;3:16-24.
- Manderino MA, Berkey N. Verbal abuse of staff nurses by physicians. J Prof Nurs. 1997;13(1):48-55.
- Pejic AR. Verbal abuse: A problem for pediatric nurses. Pediatr Nurs. 2005;31(4):271-279.
- Rowe MM, Sherlock H. Stress and verbal abuse in nursing: do burned out nurses eat their young? J Nurs Manag. 2005May;13(3):242-248.
- Frank E, Carrera JS, Stratton T, et al. Experiences of belittlement and harassment and their correlates among medical students in the United States: longitudinal survey. BMJ. 2006 Sep 30;333(7570):682.
- Seiden SC, Galvan C, Lamm R. Role of medical students in preventing patient harm and enhancing patient safety. Qual Saf Health Care. 2006 Aug;15(4):272-276.
- Wood DF. Bullying and harassment in medical schools. BMJ. 2006 Sep 30;333(7570):664-665.
- Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006 Jan;81(1):94-101.
- Institute for Safe Medication Practice. Intimidation: Mapping a plan for cultural change in healthcare (Part II). Available at www.ismp.org/Newsletters/acutecare/articles/20040325.asp Last accessed July 2, 2007.
Bullying, intimidation, verbal abuse—these behaviors negatively affect self-esteem, feelings of competence, and workplace morale. And they can devastate hospital professionals and their patients.
When 2,095 healthcare providers (1,565 nurses, 354 pharmacists, and 176 others) responded to an Institute for Safe Medication Practices (ISMP) survey on intimidation in their healthcare setting, remarkable data were collected.1
Perhaps the most alarming statistic in the 2003-2004 study was that 7% of respondents (n=147) reported they had been involved in a medication error allowed to occur partly because the respondents were afraid to question the prescriber’s decision. At a large urban trauma center in the northeastern United States, nurses listed intimidation as one of the barriers to implementing a sharps safety program.2
Nurses’ Perceptions
Research over the past decade has spotlighted intimidation in healthcare.3
“Bullying and harassment still happen in many areas of medicine,” says David M. Pressel, MD, PhD, hospitalist and director, Inpatient Service, Division of General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del. “The question is, how do you monitor yourself to make sure you aren’t falling into that hierarchical frame of mind that could intervene in great teaching and learning and great patient care?”
Dr. Pressel and his partner, David I. Rappaport, MD, also a pediatric hospitalist at duPont, have focused on the literature pertaining to nurse-physician relationships. Research shows that intimidation impedes nurse recruitment, retention, and satisfaction. In one study, 90% of nurses reported experiencing at least one episode of verbal abuse.4 A 1997 study examining the effects of intimidation on 35 pediatric nurses over a three-month period found that 25 (71.4%) of them reported being yelled at or loudly admonished. Sixteen (45.7%) had been victims of insults. Thirty (85.7%) were spoken to in a condescending manner. One-third of nurses believed that such behavior was “part of the job.”
Although studies have differed as to the most common source of this abuse—patients and families or physicians—a study of pediatric nurses reported a similar incidence from both sources.5 And, nurses are often guilty of verbally abusing each other.6
When the duPont pediatric hospitalist team began performing more family-centered rounds, they began to appreciate the nurse-physician relationship. “We have worked hard to have a charge nurse and oftentimes the bedside nurse with us when we round,” Dr. Rappaport says. Speculating that rounding with hospitalists allowed nurses to feel more part of the team, Dr. Rappaport says know the medical plan, consolidate efforts such that pages to residents were reduced, and generally improve communication. They heard from participating nurses that it made a tremendous difference. This prompted them to conduct their research.
“Our study looked at the nurse-physician relationship globally, not intimidation or abuse specifically,” says Dr. Rappaport. Along with their nurse colleague Norine Watson, RN, Drs. Pressel and Rappaport are examining the relationship between nurses and different categories of physicians: how nurses perceive interactions between nurses and surgical residents, surgical attendings, community physicians, pediatric residents, and pediatric hospitalists.
“Early data suggest that hospitalists may work more effectively with nurses because they share many of the same goals,” says Dr. Rappaport. “As hospital leaders, hospitalists can also improve working conditions for nurses by providing more accessible, efficient, and effective care. Presumably, improved collaboration will also include decreased intimidation or abuse from physicians and also probably from dissatisfied patients and families.”
Avoiding the trap of communicating in a manner that is too direct and might be construed as abusive requires self-awareness and the realization that people receive information in different ways, says Dr. Pressel. Standard professional behavior is the key. Beyond that, the challenge is giving feedback constructively and in a positive manner.
“Hospitalists [may be] more in tune with the needs of nurses than nonhospitalists,” says Dr. Rappaport. “I think that is one of our strengths. We need to continue to facilitate very strong relationships between nurses and physicians because without good nursing care, hospitalists simply cannot provide good medical care.”
There is another way hospitalists can help address verbal abuse. “Studies consistently show that nurses are hesitant to report episodes of verbal abuse,” Dr. Rappaport says, “whether it is from a family, a patient, a physician, or a fellow nurse. Fewer than one in five nurses reports these episodes. One thing that hospitalists can do is work with hospital administration to create an environment that is more proactive in addressing these concerns and allowing nurses to feel more support in this area.”
Only 60% of respondents to the ISMP survey felt their organization had clearly defined an effective process for handling disagreements with a medication order’s safety. Only about a third felt the process facilitated their bypassing an intimidating prescriber or their own supervisor if necessary. Although 70% of respondents reported that they thought their organization or manager would support them if they reported intimidating behavior, only 39% of respondents believed their organization was dealing effectively with intimidating behavior.
Untapped Source
Perceptions of intimidation also occur among trainees. When 2,884 students from the class of 2003 at 16 U.S. medical schools completed questionnaires at various times during training, 27% reported having been “harassed” by house staff, 21% by faculty, and 25% by patients.7 Further, 71% reported having been “belittled” by house staff, 63% by faculty, and 43% by patients.
Mistreated students were significantly more likely to have suffered stress, be depressed or suicidal, and less likely to report being glad they trained as a physician.

—David I. Rappaport, MD, pediatric hospitalist, Alfred I. Dupont Hospital for Children, Wilmington, Del.
This may have an underlying effect on the potential to monitor for patient safety.8,9 Because errors and near misses often result from miscommunication, medical students may be adept at preventing certain types of errors. Students’ observation skills may be just as keen, if not more so, than their more clinically proficient healthcare teammates.8 In four cases from two U.S. academic health centers reported by medical students Samuel Seiden, Cynthia Galvan, and Ruth Lamm in 2006, medical students demonstrated keen attention to detail and appropriately characterized problematic situations with patients—adding another layer of defense within systems safeguarding against patient harm.8 Yet of the 76% of medical students who had observed a medical error, only about half of the students reported the errors to a resident or an attending, despite having received patient-safety training; only 7% reported having used an electronic medical error reporting system.10
By Example
Some intimidation in medical education may be the result of anger toward students and residents over a lack of medical knowledge, says Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University in New Orleans and member of the SHM Board of Directors. “It is natural to feel [that anger]; people abhor in others what they most detest in themselves,’’ he says. “As physicians, a lack of medical knowledge is what we detest in ourselves. But a student’s ignorance is usually a product of where she is in her training; that’s why she is with you.”
—Jeffery G. Wiese, MD, associate professor of Medicine at Tulane University, New Orleans
Anger alienates students, absolving them of the guilt of not knowing the information, and demotivating them from learning it. “The lesson to be communicated is that it is OK not to know, but it is not OK to continue to not know,” Dr. Wiese says. “Reprimands should be reserved for the student who does not know, and then after being taught or asked to look it up, continues to not know.”
“The average physician who practices for 30 years will take care of roughly 80,000 people,” estimates Dr. Wiese. “That’s an arithmetic contribution and there is nothing wrong with that. But if you really want to change the world, teaching is the rule. The same 30 years invested in teaching will indirectly affect 400 million people,” he says. “Even better, if you can train your students and residents in the value of coaching their students and residents, well, now you’re talking about 10 billion people that you can affect over the course of a career.”
The question to ask yourself, says Dr. Wiese, is: Do you want to change the world? “If you do, this is the way to do it,” he says.
“For the 30 years in your career, focus on clinical coaching and getting others to clinically coach. That way, especially if you have the right motives in your heart, the right vision for the way you want to see the profession practiced, and the way you want patient care performed, that’s your shot at changing the world.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I). Available at w.ismp.org/Newsletters/acutecare/articles/20040311_2.asp. Last accessed June 27, 2007.
- Hagstrom AM. Perceived barriers to implementation of a successful sharps safety program. AORN J. 2006;83(2):391-7.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthc. 2006 Jul-Aug;3:16-24.
- Manderino MA, Berkey N. Verbal abuse of staff nurses by physicians. J Prof Nurs. 1997;13(1):48-55.
- Pejic AR. Verbal abuse: A problem for pediatric nurses. Pediatr Nurs. 2005;31(4):271-279.
- Rowe MM, Sherlock H. Stress and verbal abuse in nursing: do burned out nurses eat their young? J Nurs Manag. 2005May;13(3):242-248.
- Frank E, Carrera JS, Stratton T, et al. Experiences of belittlement and harassment and their correlates among medical students in the United States: longitudinal survey. BMJ. 2006 Sep 30;333(7570):682.
- Seiden SC, Galvan C, Lamm R. Role of medical students in preventing patient harm and enhancing patient safety. Qual Saf Health Care. 2006 Aug;15(4):272-276.
- Wood DF. Bullying and harassment in medical schools. BMJ. 2006 Sep 30;333(7570):664-665.
- Madigosky WS, Headrick LA, Nelson K, et al. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006 Jan;81(1):94-101.
- Institute for Safe Medication Practice. Intimidation: Mapping a plan for cultural change in healthcare (Part II). Available at www.ismp.org/Newsletters/acutecare/articles/20040325.asp Last accessed July 2, 2007.
Pediatric Predictions
In reflecting on the history of pediatric hospital medicine (HM), I have identified a widening schism between inpatient and outpatient pediatrics as the major threat to HM. Here, I follow Bob Wachter’s lead from SHM’s May annual meeting and detail key steps for pediatric HM in the upcoming 10 years.
Define the field: The SHM Pediatric Committee and the Ambulatory Pediatric Association’s (APA) hospital medicine special interest group are collaborating to publish a list of core clinical procedural and systems domains for pediatric hospital medicine.
This will provide a blueprint of how we have defined our field and supply a framework for pediatric acute care residency tracks, hospitalist electives, hospitalist fellowships, and maintenance of certification (MOC). Related characterizations of the field are available through pediatric hospital medicine textbooks. The Pediatric Research in Inpatient Settings (PRIS) network is studying the epidemiology of pediatric HM practice to provide an evidence basis for these expert decrees.
Individual programs should use these resources to help develop program-specific hospitalist privilege materials based on documented patient acuity, volume, and hospital medicine CME activities. The specific criteria and privileges will differ based on differences in job description between and within tertiary care centers and community hospitals—but all will include the general pediatric ward.
Develop MOC Appropriate for Pediatric Hospitalists: The American Board of Internal Medicine has officially approved the creation of a Focused Recognition of Hospital Medicine through its MOC system. A final decision rests with the American Board of Medical Specialties.
Pediatric hospitalists will do well to wait several years to examine the results of these efforts before deciding whether to pursue a similar designation from the American Board of Pediatrics. In the meantime, we should be on a fast track to create specific pediatric HM materials that will meet the 2010 MOC requirements.
There are at least 1,500 practicing pediatric hospitalists. This is equal to the number of board-certified pediatric ED physicians (1,446) and considerably more than the number of pulmonologists (821). Certainly these numbers merit development of MOC materials specifical to pediatric HM. The American Academy of Pediatrics (AAP) is developing an inpatient Education in Quality Improvement for Pediatric Practice (eQIPP) asthma model. SHM may be able to develop a transitions-of-care personal information manager and/or self-evaluation program (SEP) module appropriate for adult and pediatric hospitalists.
The only things missing are a comprehensive inpatient SEP and a closed-book exam. Pediatric hospitalists are here to stay. The American Board of Pediatrics (ABP) will best fulfill its responsibility to the public by creating an MOC program germane to pediatric HM. The actual designation on the MOC doesn’t need to be changed in 2010, but hospitalists recertifying in 2010 should be participating in relevant activities.
Expand pediatric HM (post-) graduate medical education: The increasing number of hospitalists will undoubtedly influence pediatric graduate medical education.
The ABP’s Residency Review and Redesign in Pediatrics project, which looks at global reform of pediatric residency training, should allow for acute care pediatric residency tracks. These would be amenable to pediatricians planning careers in HM, emergency medicine, and critical care.
Overall, most pediatric hospitalists will continue to begin their careers directly out of residency. Although pediatric hospitalist fellowship programs are likely to increase in number, formal fellowship training will not be required for one to practice as a pediatric hospitalist. These programs will benefit individuals choosing either an academic or administrative career. Frontline hospitalists should be able to gain suitable experience through appropriately mentored and supported clinical practice and focused CME activities—much as a new office-based pediatrician matures during his or her initial years in practice.
Publish, publish, publish: Success within the academic and research environment is crucial to being viewed as equal among subspecialties.
Perceptions of our field improve with each paper published in Pediatrics and the Journal of Hospital Medicine and each plenary presentation at a national meeting. Within our professional community, writing articles for The Hospitalist and the AAP Section on Hospital Medicine newsletter and presenting our work in poster form or hospitalist platform presentation advances knowledge and creates group identity.
Additionally, these activities promote the pediatric HM group and the authors. Some of us have made a career out of LISTSERV postings.
Continue to grow PRIS: We must all contribute to the growth of PRIS over the next decade.
Ultimately, PRIS promises to answer clinical questions faced by hospitalists the same way the Vermont Oxford Network helps neonatology and the Pediatric Emergency Care Applied Research Network helps pediatric emergency medicine. Academic hospitalists can use PRIS to pursue their research interests. Community hospitalists can pick and choose from available projects to identify a study relevant and suitable for them. We all must participate.
My hope is that in 10 to 20 years PRIS will coordinate randomized, controlled clinical trials and universal, integrated, HIPPA-compliant, electronic medical record systems that facilitate real-time analysis of outcomes and practice variation.
Own our diseases: Defining The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, creating a research base, and publishing must lead to the recognition of pediatric hospitalists as the experts for a core set of illnesses.
Potential starting points include bronchiolitis, the ruling out of sepsis in less than 30 days, apparent life-threatening events (ALTE), and the medically complex/technologically dependent child. We’ll know we’ve hit it big when the nationally recognized speakers and authors on these topics identify themselves as hospitalists rather than infectious disease physicians or pulmonologists. For this to occur, hospitalists must participate in research efforts, speak at regional and national meetings, and participate on national consensus panels.
On a purely local program level, individual physicians within a hospital medicine group should cultivate areas of clinical, administrative, and educational expertise. This is particularly valuable in community hospital settings where pediatric infectious disease or pulmonary specialists may not be available—but is equally important to career development in larger academic centers where hospitalists are ideal for quality improvement, safety, and educational roles.
Identify and publicly report national benchmarks: Our adult colleagues suffer and benefit from the public reporting mandated by the Centers for Medicare and Medicaid Services. One hopes the adult tribulations with data collection, attribution, and risk adjustment will make pediatric public reporting easier.
The wide variation in management of ALTE, osteomyelitis, and complicated pneumonias documented by Pediatric Health Information System researchers at the Toronto Pediatric Academic Societies meetings is a clarion call for evidence-based medicine. Parents have a right to make an informed choice about where and how their child is treated based on reliable data. Rational expenditure of limited State Children’s Health Insurance Program (SCHIP) funds requires practicing evidence-based medicine
Pediatric quality measures and standards are being developed through the National Quality Forum as well as the Alliance for Pediatric Quality. This movement will significantly affect pediatric HM. On the positive side, reporting will require that more resources be devoted to pediatric quality improvement (QI) efforts. Pediatric hospitalists are ideally suited to lead inpatient QI efforts. Creation of a hospitalist physician specialty identification code will facilitate comparison of hospitalist with non-hospitalist care in large multicenter data sets. These studies will be key descriptors of the cost and quality outcomes of pediatric HM programs.
Public reporting will highlight variation among hospitals, programs, and, possibly, physicians. Parents and payers will vote with their feet. Overall, this will create less variation in care as best practices are identified and adopted. Shortcomings will be revealed in programs that fail to practice state-of-the-art pediatrics or that are inadequately staffed from either the physician or nursing perspective. This likely will result in a consolidation of pediatric care. Smaller units closer to larger pediatric centers probably will close or become affiliates of the referral center. Geographic proximity will be a secondary concern to outcomes for parents and office-based pediatricians.
The methodological and political considerations of pay for performance are beyond most of us. Nonetheless, we in pediatric HM can begin to prepare for these changes by identifying the benchmarks that highlight our successes and failures as hospitalists, groups, hospitals, and the field as a whole. Potential clinical, quality, economic, and logistic metrics include severity-adjusted lengths of stay (LOS) for asthma and bronchiolitis, readmission rates, time to antibiotics for ruling out sepsis less than 30 days, patient and referring physician satisfaction, and coordination of transitions of care.
Expand children’s health insurance: SCHIP and universal insurance for children enjoys significant support.
The AAP’s efforts in this area deserve praise and demand continued support. As noted previously, large public expenditures on SCHIP likely will be linked to public reporting of outcomes. It is crucial to the economic viability of pediatrics that SCHIP reimbursement is equivalent to Medicare reimbursement on a code-for-code basis. It is indefensible to suggest that we as a nation value the care of children less than the care of the elderly.
Ultimately, SCHIP and state Medicaid programs would do well to move beyond a per diem-based system of reimbursement for pediatric inpatient care to a system based either on diagnosis-related groups (DRGs) or disease episodes. This would benefit HM programs by rewarding hospitals that can shorten LOS while providing the same high-quality outcomes. Current per diem reimbursement paradigms at best fail to maximally encourage efficiency and at worst create perverse incentives to prolong LOS.
Relentlessly pursue career satisfaction: Many programs are asking pediatric hospitalists to work at a clinical pace not sustainable over a 20- to 30-year career. Particularly efficient programs can produce burnout in one to three years of excessive workloads and call obligations.
SHM’s “A White Paper on Hospitalist Career Satisfaction” identifies four pillars: reward/recognition, workload/schedule, autonomy/control, and community/environment. (Each pillar has been featured in the “Career Development” section, starting with the June issue.) In pediatrics we can turn to neonatology, pediatric critical care, and (pediatric) emergency medicine for help in establishing realistic guidelines for clinical hours in house.
The harder question to answer is: What is a reasonable number of patients for a hospitalist to cover at a time? This depends on patient acuity, patient and family expectations, teaching responsibilities, hospitalist responsibilities outside the ward, and physician style. It is unlikely that prospective randomized controlled trials will be conducted to answer this question. The answer is likely to come from individual programs, hospitalists, and—regrettably—patients suffering the consequences of pushing the limits too far. We will learn from our mistakes. Failed models will not be repeated. To the extent that quality rather than economics becomes the overriding driver for HM programs, I favor 15 encounters per hospitalist per day over 20.
Hospitalists also must diversify beyond pure clinical practice for long-term career satisfaction. Focusing on a specific clinical interest, subspecialty, or practice environment can provide some variety.
Teaching and research is another source of career satisfaction. Each hospitalist within a group should be involved in at least one QI project and/or committee—if only to appreciate the importance and complexity of a systems approach to improving overall outcomes. Job descriptions must include protected time for these nonclinical activities. Career growth and satisfaction will be stifled without these additional outlets.
Expand beyond traditional roles: The push for improved quality will lead to expanded roles for pediatric hospitalists—some of which may be unwelcome.
In particular, larger programs will move to 24/7 in-house hospitalist presence. Given the acuity and complexity of the patients we care for, particularly in tertiary care centers, the quality argument for 24/7 in-house coverage will quickly trump the economic argument against it. The choice is obvious in terms of quality and safety and from the perspective of the most important “decider” when it comes to healthcare—the patient.
As educators exploit the opportunities of 24/7 coverage, resident teaching will increase and academic hospitalists will master the art of promoting autonomy 24/7 while providing appropriate supervision. If we learned to teach with family-centered rounds, we can learn to teach at 3 a.m.
In addition to expanded hours, we will follow the lead of adult hospitalists and increase our co-management role beyond the traditional general medical patient on the hospitalist service. This will include surgical and subspecialty patients. From the patient’s and family’s perspective the improved care that can result is valuable. It may not be necessary for every patient or for every surgeon or subspecialist, but on the whole hospitalists provide added value.
Within individual programs and among various physicians, the rules of engagement will need to be defined to promote collegial, respectful relationships with clear lines of communication and defined clinical responsibilities. “Inappropriate behavior” from “difficult” physicians (surgeons, subspecialists, and hospitalists) will need to be addressed. Specific arrangements will need to be defined (co-management versus specialist/surgeon attending with hospitalist consultation or hospitalist attending with specialist/surgeon consultant). But once the rules of engagement are established and appropriate resources allotted, it becomes impossible for hospitalists to argue that it’s not within our job description to contribute to improved quality of care for hospitalized patients. Improving patient care is not scutwork.
In particular, given the limited availability of pediatric sub-specialists and surgeons, to the extent that we as hospitalists can increase the efficiency of our subspecialty and surgical colleagues, we can improve access to pediatric subspecialty care within both the inpatient and outpatient settings These manpower issues will also drive involvement of pediatric hospitalists into other parts of the hospital such as sedation services, the ED, the NICU, and PICU. As these other services become vocal advocates for pediatric hospitalists, the economic viability of pediatric hospital medicine programs will increase.
Make the economic argument for value-added services: Pediatric hospitalists must do better at the economic arguments of value-added services.
Until pediatric inpatient stays are reimbursed on a DRG basis or physician charges are based on a global fee, we most move beyond the simple formulation of decreased costs for inpatient stays. We must highlight the value of our critical roles in coordination of care; quality and safety; 24/7 coverage; improved throughput in the emergency department (ED), ward, and PICU; and increased efficiency for surgeons and subspecialists.
Success for pediatric HM in these arenas will come only at the cost of failed individual programs. As implied above, it is only natural for non-hospitalist administrators and department leaders to push the limits of hospitalist programs to the maximum. Programs that place excessive demands on hospitalists will implode. Good hospitalists will leave for positions that offer them respect, autonomy, and a reasonable workload and lifestyle. Small community programs with low-volume services may not be economically viable. As we develop a history of successful programs and failed programs, hospitalists and administrators will have more realistic expectations of the ingredients of success.
Conclusion
Programs that meet the above challenges will succeed. Pediatric HM is a tremendously rewarding and challenging field. National recognition of pediatric HM as a unique field combined with the respect of local pediatricians, subspecialists, and surgeons will create the pride and ownership among hospitalists necessary for us to raise the bar for standards of inpatient care.
Public reporting will provide the external pull for the same high-quality outcomes. Divisions of HM led by hospitalists in which each hospitalist has an additional clinical, administrative, or academic focus will create the workload, autonomy, and diversity necessary for long-term career satisfaction and support the research and QI activities necessary for the evidence-based practice of high-quality pediatric inpatient care by hospitalists and non-hospitalists alike. Universal access, economic parity with Medicare, and a full understanding of the value-added nature of pediatric hospital medicine practice will provide the margin necessary for this mission. It will be a challenging but rewarding 10 years. TH
Dr. Percelay is SHM’s treasurer and a pediatric hospitalist.
In reflecting on the history of pediatric hospital medicine (HM), I have identified a widening schism between inpatient and outpatient pediatrics as the major threat to HM. Here, I follow Bob Wachter’s lead from SHM’s May annual meeting and detail key steps for pediatric HM in the upcoming 10 years.
Define the field: The SHM Pediatric Committee and the Ambulatory Pediatric Association’s (APA) hospital medicine special interest group are collaborating to publish a list of core clinical procedural and systems domains for pediatric hospital medicine.
This will provide a blueprint of how we have defined our field and supply a framework for pediatric acute care residency tracks, hospitalist electives, hospitalist fellowships, and maintenance of certification (MOC). Related characterizations of the field are available through pediatric hospital medicine textbooks. The Pediatric Research in Inpatient Settings (PRIS) network is studying the epidemiology of pediatric HM practice to provide an evidence basis for these expert decrees.
Individual programs should use these resources to help develop program-specific hospitalist privilege materials based on documented patient acuity, volume, and hospital medicine CME activities. The specific criteria and privileges will differ based on differences in job description between and within tertiary care centers and community hospitals—but all will include the general pediatric ward.
Develop MOC Appropriate for Pediatric Hospitalists: The American Board of Internal Medicine has officially approved the creation of a Focused Recognition of Hospital Medicine through its MOC system. A final decision rests with the American Board of Medical Specialties.
Pediatric hospitalists will do well to wait several years to examine the results of these efforts before deciding whether to pursue a similar designation from the American Board of Pediatrics. In the meantime, we should be on a fast track to create specific pediatric HM materials that will meet the 2010 MOC requirements.
There are at least 1,500 practicing pediatric hospitalists. This is equal to the number of board-certified pediatric ED physicians (1,446) and considerably more than the number of pulmonologists (821). Certainly these numbers merit development of MOC materials specifical to pediatric HM. The American Academy of Pediatrics (AAP) is developing an inpatient Education in Quality Improvement for Pediatric Practice (eQIPP) asthma model. SHM may be able to develop a transitions-of-care personal information manager and/or self-evaluation program (SEP) module appropriate for adult and pediatric hospitalists.
The only things missing are a comprehensive inpatient SEP and a closed-book exam. Pediatric hospitalists are here to stay. The American Board of Pediatrics (ABP) will best fulfill its responsibility to the public by creating an MOC program germane to pediatric HM. The actual designation on the MOC doesn’t need to be changed in 2010, but hospitalists recertifying in 2010 should be participating in relevant activities.
Expand pediatric HM (post-) graduate medical education: The increasing number of hospitalists will undoubtedly influence pediatric graduate medical education.
The ABP’s Residency Review and Redesign in Pediatrics project, which looks at global reform of pediatric residency training, should allow for acute care pediatric residency tracks. These would be amenable to pediatricians planning careers in HM, emergency medicine, and critical care.
Overall, most pediatric hospitalists will continue to begin their careers directly out of residency. Although pediatric hospitalist fellowship programs are likely to increase in number, formal fellowship training will not be required for one to practice as a pediatric hospitalist. These programs will benefit individuals choosing either an academic or administrative career. Frontline hospitalists should be able to gain suitable experience through appropriately mentored and supported clinical practice and focused CME activities—much as a new office-based pediatrician matures during his or her initial years in practice.
Publish, publish, publish: Success within the academic and research environment is crucial to being viewed as equal among subspecialties.
Perceptions of our field improve with each paper published in Pediatrics and the Journal of Hospital Medicine and each plenary presentation at a national meeting. Within our professional community, writing articles for The Hospitalist and the AAP Section on Hospital Medicine newsletter and presenting our work in poster form or hospitalist platform presentation advances knowledge and creates group identity.
Additionally, these activities promote the pediatric HM group and the authors. Some of us have made a career out of LISTSERV postings.
Continue to grow PRIS: We must all contribute to the growth of PRIS over the next decade.
Ultimately, PRIS promises to answer clinical questions faced by hospitalists the same way the Vermont Oxford Network helps neonatology and the Pediatric Emergency Care Applied Research Network helps pediatric emergency medicine. Academic hospitalists can use PRIS to pursue their research interests. Community hospitalists can pick and choose from available projects to identify a study relevant and suitable for them. We all must participate.
My hope is that in 10 to 20 years PRIS will coordinate randomized, controlled clinical trials and universal, integrated, HIPPA-compliant, electronic medical record systems that facilitate real-time analysis of outcomes and practice variation.
Own our diseases: Defining The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, creating a research base, and publishing must lead to the recognition of pediatric hospitalists as the experts for a core set of illnesses.
Potential starting points include bronchiolitis, the ruling out of sepsis in less than 30 days, apparent life-threatening events (ALTE), and the medically complex/technologically dependent child. We’ll know we’ve hit it big when the nationally recognized speakers and authors on these topics identify themselves as hospitalists rather than infectious disease physicians or pulmonologists. For this to occur, hospitalists must participate in research efforts, speak at regional and national meetings, and participate on national consensus panels.
On a purely local program level, individual physicians within a hospital medicine group should cultivate areas of clinical, administrative, and educational expertise. This is particularly valuable in community hospital settings where pediatric infectious disease or pulmonary specialists may not be available—but is equally important to career development in larger academic centers where hospitalists are ideal for quality improvement, safety, and educational roles.
Identify and publicly report national benchmarks: Our adult colleagues suffer and benefit from the public reporting mandated by the Centers for Medicare and Medicaid Services. One hopes the adult tribulations with data collection, attribution, and risk adjustment will make pediatric public reporting easier.
The wide variation in management of ALTE, osteomyelitis, and complicated pneumonias documented by Pediatric Health Information System researchers at the Toronto Pediatric Academic Societies meetings is a clarion call for evidence-based medicine. Parents have a right to make an informed choice about where and how their child is treated based on reliable data. Rational expenditure of limited State Children’s Health Insurance Program (SCHIP) funds requires practicing evidence-based medicine
Pediatric quality measures and standards are being developed through the National Quality Forum as well as the Alliance for Pediatric Quality. This movement will significantly affect pediatric HM. On the positive side, reporting will require that more resources be devoted to pediatric quality improvement (QI) efforts. Pediatric hospitalists are ideally suited to lead inpatient QI efforts. Creation of a hospitalist physician specialty identification code will facilitate comparison of hospitalist with non-hospitalist care in large multicenter data sets. These studies will be key descriptors of the cost and quality outcomes of pediatric HM programs.
Public reporting will highlight variation among hospitals, programs, and, possibly, physicians. Parents and payers will vote with their feet. Overall, this will create less variation in care as best practices are identified and adopted. Shortcomings will be revealed in programs that fail to practice state-of-the-art pediatrics or that are inadequately staffed from either the physician or nursing perspective. This likely will result in a consolidation of pediatric care. Smaller units closer to larger pediatric centers probably will close or become affiliates of the referral center. Geographic proximity will be a secondary concern to outcomes for parents and office-based pediatricians.
The methodological and political considerations of pay for performance are beyond most of us. Nonetheless, we in pediatric HM can begin to prepare for these changes by identifying the benchmarks that highlight our successes and failures as hospitalists, groups, hospitals, and the field as a whole. Potential clinical, quality, economic, and logistic metrics include severity-adjusted lengths of stay (LOS) for asthma and bronchiolitis, readmission rates, time to antibiotics for ruling out sepsis less than 30 days, patient and referring physician satisfaction, and coordination of transitions of care.
Expand children’s health insurance: SCHIP and universal insurance for children enjoys significant support.
The AAP’s efforts in this area deserve praise and demand continued support. As noted previously, large public expenditures on SCHIP likely will be linked to public reporting of outcomes. It is crucial to the economic viability of pediatrics that SCHIP reimbursement is equivalent to Medicare reimbursement on a code-for-code basis. It is indefensible to suggest that we as a nation value the care of children less than the care of the elderly.
Ultimately, SCHIP and state Medicaid programs would do well to move beyond a per diem-based system of reimbursement for pediatric inpatient care to a system based either on diagnosis-related groups (DRGs) or disease episodes. This would benefit HM programs by rewarding hospitals that can shorten LOS while providing the same high-quality outcomes. Current per diem reimbursement paradigms at best fail to maximally encourage efficiency and at worst create perverse incentives to prolong LOS.
Relentlessly pursue career satisfaction: Many programs are asking pediatric hospitalists to work at a clinical pace not sustainable over a 20- to 30-year career. Particularly efficient programs can produce burnout in one to three years of excessive workloads and call obligations.
SHM’s “A White Paper on Hospitalist Career Satisfaction” identifies four pillars: reward/recognition, workload/schedule, autonomy/control, and community/environment. (Each pillar has been featured in the “Career Development” section, starting with the June issue.) In pediatrics we can turn to neonatology, pediatric critical care, and (pediatric) emergency medicine for help in establishing realistic guidelines for clinical hours in house.
The harder question to answer is: What is a reasonable number of patients for a hospitalist to cover at a time? This depends on patient acuity, patient and family expectations, teaching responsibilities, hospitalist responsibilities outside the ward, and physician style. It is unlikely that prospective randomized controlled trials will be conducted to answer this question. The answer is likely to come from individual programs, hospitalists, and—regrettably—patients suffering the consequences of pushing the limits too far. We will learn from our mistakes. Failed models will not be repeated. To the extent that quality rather than economics becomes the overriding driver for HM programs, I favor 15 encounters per hospitalist per day over 20.
Hospitalists also must diversify beyond pure clinical practice for long-term career satisfaction. Focusing on a specific clinical interest, subspecialty, or practice environment can provide some variety.
Teaching and research is another source of career satisfaction. Each hospitalist within a group should be involved in at least one QI project and/or committee—if only to appreciate the importance and complexity of a systems approach to improving overall outcomes. Job descriptions must include protected time for these nonclinical activities. Career growth and satisfaction will be stifled without these additional outlets.
Expand beyond traditional roles: The push for improved quality will lead to expanded roles for pediatric hospitalists—some of which may be unwelcome.
In particular, larger programs will move to 24/7 in-house hospitalist presence. Given the acuity and complexity of the patients we care for, particularly in tertiary care centers, the quality argument for 24/7 in-house coverage will quickly trump the economic argument against it. The choice is obvious in terms of quality and safety and from the perspective of the most important “decider” when it comes to healthcare—the patient.
As educators exploit the opportunities of 24/7 coverage, resident teaching will increase and academic hospitalists will master the art of promoting autonomy 24/7 while providing appropriate supervision. If we learned to teach with family-centered rounds, we can learn to teach at 3 a.m.
In addition to expanded hours, we will follow the lead of adult hospitalists and increase our co-management role beyond the traditional general medical patient on the hospitalist service. This will include surgical and subspecialty patients. From the patient’s and family’s perspective the improved care that can result is valuable. It may not be necessary for every patient or for every surgeon or subspecialist, but on the whole hospitalists provide added value.
Within individual programs and among various physicians, the rules of engagement will need to be defined to promote collegial, respectful relationships with clear lines of communication and defined clinical responsibilities. “Inappropriate behavior” from “difficult” physicians (surgeons, subspecialists, and hospitalists) will need to be addressed. Specific arrangements will need to be defined (co-management versus specialist/surgeon attending with hospitalist consultation or hospitalist attending with specialist/surgeon consultant). But once the rules of engagement are established and appropriate resources allotted, it becomes impossible for hospitalists to argue that it’s not within our job description to contribute to improved quality of care for hospitalized patients. Improving patient care is not scutwork.
In particular, given the limited availability of pediatric sub-specialists and surgeons, to the extent that we as hospitalists can increase the efficiency of our subspecialty and surgical colleagues, we can improve access to pediatric subspecialty care within both the inpatient and outpatient settings These manpower issues will also drive involvement of pediatric hospitalists into other parts of the hospital such as sedation services, the ED, the NICU, and PICU. As these other services become vocal advocates for pediatric hospitalists, the economic viability of pediatric hospital medicine programs will increase.
Make the economic argument for value-added services: Pediatric hospitalists must do better at the economic arguments of value-added services.
Until pediatric inpatient stays are reimbursed on a DRG basis or physician charges are based on a global fee, we most move beyond the simple formulation of decreased costs for inpatient stays. We must highlight the value of our critical roles in coordination of care; quality and safety; 24/7 coverage; improved throughput in the emergency department (ED), ward, and PICU; and increased efficiency for surgeons and subspecialists.
Success for pediatric HM in these arenas will come only at the cost of failed individual programs. As implied above, it is only natural for non-hospitalist administrators and department leaders to push the limits of hospitalist programs to the maximum. Programs that place excessive demands on hospitalists will implode. Good hospitalists will leave for positions that offer them respect, autonomy, and a reasonable workload and lifestyle. Small community programs with low-volume services may not be economically viable. As we develop a history of successful programs and failed programs, hospitalists and administrators will have more realistic expectations of the ingredients of success.
Conclusion
Programs that meet the above challenges will succeed. Pediatric HM is a tremendously rewarding and challenging field. National recognition of pediatric HM as a unique field combined with the respect of local pediatricians, subspecialists, and surgeons will create the pride and ownership among hospitalists necessary for us to raise the bar for standards of inpatient care.
Public reporting will provide the external pull for the same high-quality outcomes. Divisions of HM led by hospitalists in which each hospitalist has an additional clinical, administrative, or academic focus will create the workload, autonomy, and diversity necessary for long-term career satisfaction and support the research and QI activities necessary for the evidence-based practice of high-quality pediatric inpatient care by hospitalists and non-hospitalists alike. Universal access, economic parity with Medicare, and a full understanding of the value-added nature of pediatric hospital medicine practice will provide the margin necessary for this mission. It will be a challenging but rewarding 10 years. TH
Dr. Percelay is SHM’s treasurer and a pediatric hospitalist.
In reflecting on the history of pediatric hospital medicine (HM), I have identified a widening schism between inpatient and outpatient pediatrics as the major threat to HM. Here, I follow Bob Wachter’s lead from SHM’s May annual meeting and detail key steps for pediatric HM in the upcoming 10 years.
Define the field: The SHM Pediatric Committee and the Ambulatory Pediatric Association’s (APA) hospital medicine special interest group are collaborating to publish a list of core clinical procedural and systems domains for pediatric hospital medicine.
This will provide a blueprint of how we have defined our field and supply a framework for pediatric acute care residency tracks, hospitalist electives, hospitalist fellowships, and maintenance of certification (MOC). Related characterizations of the field are available through pediatric hospital medicine textbooks. The Pediatric Research in Inpatient Settings (PRIS) network is studying the epidemiology of pediatric HM practice to provide an evidence basis for these expert decrees.
Individual programs should use these resources to help develop program-specific hospitalist privilege materials based on documented patient acuity, volume, and hospital medicine CME activities. The specific criteria and privileges will differ based on differences in job description between and within tertiary care centers and community hospitals—but all will include the general pediatric ward.
Develop MOC Appropriate for Pediatric Hospitalists: The American Board of Internal Medicine has officially approved the creation of a Focused Recognition of Hospital Medicine through its MOC system. A final decision rests with the American Board of Medical Specialties.
Pediatric hospitalists will do well to wait several years to examine the results of these efforts before deciding whether to pursue a similar designation from the American Board of Pediatrics. In the meantime, we should be on a fast track to create specific pediatric HM materials that will meet the 2010 MOC requirements.
There are at least 1,500 practicing pediatric hospitalists. This is equal to the number of board-certified pediatric ED physicians (1,446) and considerably more than the number of pulmonologists (821). Certainly these numbers merit development of MOC materials specifical to pediatric HM. The American Academy of Pediatrics (AAP) is developing an inpatient Education in Quality Improvement for Pediatric Practice (eQIPP) asthma model. SHM may be able to develop a transitions-of-care personal information manager and/or self-evaluation program (SEP) module appropriate for adult and pediatric hospitalists.
The only things missing are a comprehensive inpatient SEP and a closed-book exam. Pediatric hospitalists are here to stay. The American Board of Pediatrics (ABP) will best fulfill its responsibility to the public by creating an MOC program germane to pediatric HM. The actual designation on the MOC doesn’t need to be changed in 2010, but hospitalists recertifying in 2010 should be participating in relevant activities.
Expand pediatric HM (post-) graduate medical education: The increasing number of hospitalists will undoubtedly influence pediatric graduate medical education.
The ABP’s Residency Review and Redesign in Pediatrics project, which looks at global reform of pediatric residency training, should allow for acute care pediatric residency tracks. These would be amenable to pediatricians planning careers in HM, emergency medicine, and critical care.
Overall, most pediatric hospitalists will continue to begin their careers directly out of residency. Although pediatric hospitalist fellowship programs are likely to increase in number, formal fellowship training will not be required for one to practice as a pediatric hospitalist. These programs will benefit individuals choosing either an academic or administrative career. Frontline hospitalists should be able to gain suitable experience through appropriately mentored and supported clinical practice and focused CME activities—much as a new office-based pediatrician matures during his or her initial years in practice.
Publish, publish, publish: Success within the academic and research environment is crucial to being viewed as equal among subspecialties.
Perceptions of our field improve with each paper published in Pediatrics and the Journal of Hospital Medicine and each plenary presentation at a national meeting. Within our professional community, writing articles for The Hospitalist and the AAP Section on Hospital Medicine newsletter and presenting our work in poster form or hospitalist platform presentation advances knowledge and creates group identity.
Additionally, these activities promote the pediatric HM group and the authors. Some of us have made a career out of LISTSERV postings.
Continue to grow PRIS: We must all contribute to the growth of PRIS over the next decade.
Ultimately, PRIS promises to answer clinical questions faced by hospitalists the same way the Vermont Oxford Network helps neonatology and the Pediatric Emergency Care Applied Research Network helps pediatric emergency medicine. Academic hospitalists can use PRIS to pursue their research interests. Community hospitalists can pick and choose from available projects to identify a study relevant and suitable for them. We all must participate.
My hope is that in 10 to 20 years PRIS will coordinate randomized, controlled clinical trials and universal, integrated, HIPPA-compliant, electronic medical record systems that facilitate real-time analysis of outcomes and practice variation.
Own our diseases: Defining The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, creating a research base, and publishing must lead to the recognition of pediatric hospitalists as the experts for a core set of illnesses.
Potential starting points include bronchiolitis, the ruling out of sepsis in less than 30 days, apparent life-threatening events (ALTE), and the medically complex/technologically dependent child. We’ll know we’ve hit it big when the nationally recognized speakers and authors on these topics identify themselves as hospitalists rather than infectious disease physicians or pulmonologists. For this to occur, hospitalists must participate in research efforts, speak at regional and national meetings, and participate on national consensus panels.
On a purely local program level, individual physicians within a hospital medicine group should cultivate areas of clinical, administrative, and educational expertise. This is particularly valuable in community hospital settings where pediatric infectious disease or pulmonary specialists may not be available—but is equally important to career development in larger academic centers where hospitalists are ideal for quality improvement, safety, and educational roles.
Identify and publicly report national benchmarks: Our adult colleagues suffer and benefit from the public reporting mandated by the Centers for Medicare and Medicaid Services. One hopes the adult tribulations with data collection, attribution, and risk adjustment will make pediatric public reporting easier.
The wide variation in management of ALTE, osteomyelitis, and complicated pneumonias documented by Pediatric Health Information System researchers at the Toronto Pediatric Academic Societies meetings is a clarion call for evidence-based medicine. Parents have a right to make an informed choice about where and how their child is treated based on reliable data. Rational expenditure of limited State Children’s Health Insurance Program (SCHIP) funds requires practicing evidence-based medicine
Pediatric quality measures and standards are being developed through the National Quality Forum as well as the Alliance for Pediatric Quality. This movement will significantly affect pediatric HM. On the positive side, reporting will require that more resources be devoted to pediatric quality improvement (QI) efforts. Pediatric hospitalists are ideally suited to lead inpatient QI efforts. Creation of a hospitalist physician specialty identification code will facilitate comparison of hospitalist with non-hospitalist care in large multicenter data sets. These studies will be key descriptors of the cost and quality outcomes of pediatric HM programs.
Public reporting will highlight variation among hospitals, programs, and, possibly, physicians. Parents and payers will vote with their feet. Overall, this will create less variation in care as best practices are identified and adopted. Shortcomings will be revealed in programs that fail to practice state-of-the-art pediatrics or that are inadequately staffed from either the physician or nursing perspective. This likely will result in a consolidation of pediatric care. Smaller units closer to larger pediatric centers probably will close or become affiliates of the referral center. Geographic proximity will be a secondary concern to outcomes for parents and office-based pediatricians.
The methodological and political considerations of pay for performance are beyond most of us. Nonetheless, we in pediatric HM can begin to prepare for these changes by identifying the benchmarks that highlight our successes and failures as hospitalists, groups, hospitals, and the field as a whole. Potential clinical, quality, economic, and logistic metrics include severity-adjusted lengths of stay (LOS) for asthma and bronchiolitis, readmission rates, time to antibiotics for ruling out sepsis less than 30 days, patient and referring physician satisfaction, and coordination of transitions of care.
Expand children’s health insurance: SCHIP and universal insurance for children enjoys significant support.
The AAP’s efforts in this area deserve praise and demand continued support. As noted previously, large public expenditures on SCHIP likely will be linked to public reporting of outcomes. It is crucial to the economic viability of pediatrics that SCHIP reimbursement is equivalent to Medicare reimbursement on a code-for-code basis. It is indefensible to suggest that we as a nation value the care of children less than the care of the elderly.
Ultimately, SCHIP and state Medicaid programs would do well to move beyond a per diem-based system of reimbursement for pediatric inpatient care to a system based either on diagnosis-related groups (DRGs) or disease episodes. This would benefit HM programs by rewarding hospitals that can shorten LOS while providing the same high-quality outcomes. Current per diem reimbursement paradigms at best fail to maximally encourage efficiency and at worst create perverse incentives to prolong LOS.
Relentlessly pursue career satisfaction: Many programs are asking pediatric hospitalists to work at a clinical pace not sustainable over a 20- to 30-year career. Particularly efficient programs can produce burnout in one to three years of excessive workloads and call obligations.
SHM’s “A White Paper on Hospitalist Career Satisfaction” identifies four pillars: reward/recognition, workload/schedule, autonomy/control, and community/environment. (Each pillar has been featured in the “Career Development” section, starting with the June issue.) In pediatrics we can turn to neonatology, pediatric critical care, and (pediatric) emergency medicine for help in establishing realistic guidelines for clinical hours in house.
The harder question to answer is: What is a reasonable number of patients for a hospitalist to cover at a time? This depends on patient acuity, patient and family expectations, teaching responsibilities, hospitalist responsibilities outside the ward, and physician style. It is unlikely that prospective randomized controlled trials will be conducted to answer this question. The answer is likely to come from individual programs, hospitalists, and—regrettably—patients suffering the consequences of pushing the limits too far. We will learn from our mistakes. Failed models will not be repeated. To the extent that quality rather than economics becomes the overriding driver for HM programs, I favor 15 encounters per hospitalist per day over 20.
Hospitalists also must diversify beyond pure clinical practice for long-term career satisfaction. Focusing on a specific clinical interest, subspecialty, or practice environment can provide some variety.
Teaching and research is another source of career satisfaction. Each hospitalist within a group should be involved in at least one QI project and/or committee—if only to appreciate the importance and complexity of a systems approach to improving overall outcomes. Job descriptions must include protected time for these nonclinical activities. Career growth and satisfaction will be stifled without these additional outlets.
Expand beyond traditional roles: The push for improved quality will lead to expanded roles for pediatric hospitalists—some of which may be unwelcome.
In particular, larger programs will move to 24/7 in-house hospitalist presence. Given the acuity and complexity of the patients we care for, particularly in tertiary care centers, the quality argument for 24/7 in-house coverage will quickly trump the economic argument against it. The choice is obvious in terms of quality and safety and from the perspective of the most important “decider” when it comes to healthcare—the patient.
As educators exploit the opportunities of 24/7 coverage, resident teaching will increase and academic hospitalists will master the art of promoting autonomy 24/7 while providing appropriate supervision. If we learned to teach with family-centered rounds, we can learn to teach at 3 a.m.
In addition to expanded hours, we will follow the lead of adult hospitalists and increase our co-management role beyond the traditional general medical patient on the hospitalist service. This will include surgical and subspecialty patients. From the patient’s and family’s perspective the improved care that can result is valuable. It may not be necessary for every patient or for every surgeon or subspecialist, but on the whole hospitalists provide added value.
Within individual programs and among various physicians, the rules of engagement will need to be defined to promote collegial, respectful relationships with clear lines of communication and defined clinical responsibilities. “Inappropriate behavior” from “difficult” physicians (surgeons, subspecialists, and hospitalists) will need to be addressed. Specific arrangements will need to be defined (co-management versus specialist/surgeon attending with hospitalist consultation or hospitalist attending with specialist/surgeon consultant). But once the rules of engagement are established and appropriate resources allotted, it becomes impossible for hospitalists to argue that it’s not within our job description to contribute to improved quality of care for hospitalized patients. Improving patient care is not scutwork.
In particular, given the limited availability of pediatric sub-specialists and surgeons, to the extent that we as hospitalists can increase the efficiency of our subspecialty and surgical colleagues, we can improve access to pediatric subspecialty care within both the inpatient and outpatient settings These manpower issues will also drive involvement of pediatric hospitalists into other parts of the hospital such as sedation services, the ED, the NICU, and PICU. As these other services become vocal advocates for pediatric hospitalists, the economic viability of pediatric hospital medicine programs will increase.
Make the economic argument for value-added services: Pediatric hospitalists must do better at the economic arguments of value-added services.
Until pediatric inpatient stays are reimbursed on a DRG basis or physician charges are based on a global fee, we most move beyond the simple formulation of decreased costs for inpatient stays. We must highlight the value of our critical roles in coordination of care; quality and safety; 24/7 coverage; improved throughput in the emergency department (ED), ward, and PICU; and increased efficiency for surgeons and subspecialists.
Success for pediatric HM in these arenas will come only at the cost of failed individual programs. As implied above, it is only natural for non-hospitalist administrators and department leaders to push the limits of hospitalist programs to the maximum. Programs that place excessive demands on hospitalists will implode. Good hospitalists will leave for positions that offer them respect, autonomy, and a reasonable workload and lifestyle. Small community programs with low-volume services may not be economically viable. As we develop a history of successful programs and failed programs, hospitalists and administrators will have more realistic expectations of the ingredients of success.
Conclusion
Programs that meet the above challenges will succeed. Pediatric HM is a tremendously rewarding and challenging field. National recognition of pediatric HM as a unique field combined with the respect of local pediatricians, subspecialists, and surgeons will create the pride and ownership among hospitalists necessary for us to raise the bar for standards of inpatient care.
Public reporting will provide the external pull for the same high-quality outcomes. Divisions of HM led by hospitalists in which each hospitalist has an additional clinical, administrative, or academic focus will create the workload, autonomy, and diversity necessary for long-term career satisfaction and support the research and QI activities necessary for the evidence-based practice of high-quality pediatric inpatient care by hospitalists and non-hospitalists alike. Universal access, economic parity with Medicare, and a full understanding of the value-added nature of pediatric hospital medicine practice will provide the margin necessary for this mission. It will be a challenging but rewarding 10 years. TH
Dr. Percelay is SHM’s treasurer and a pediatric hospitalist.
Efficiency Rules
While nationwide demand for hospitalists outstrips supply, hospitals across the country are looking at how their hospitalists and their hospital medicine groups weigh in on efficiency.
The notion of efficiency at a time of rapid growth may seem counterintuitive, but healthcare dollars are always hotly contested, and an efficient hospitalist program has a better chance of capturing them than a less-efficient one.
Even the definition of efficiency is being refined. Stakeholders scrutinizing compensation packages, key clinical indicators, productivity and quality metrics, scheduling, average daily census, and patient handoffs to gauge whether or not their group has a competitive edge over others. And hospital medicine group (HMG) leaders are scrutinizing themselves because they know hospitals increasingly are inviting more than one HMG to work under their roofs—the better to serve different populations and compare one with another.
How to Measure Efficiency
An evolving medical discipline that aspires to specialize in internal medicine, hospital medicine is in the process of developing a consensus definition of efficiency for itself. Major variables included in the calculation are obvious: average daily census, length of stay (LOS), case mix-adjusted costs, severity, and readmission rates. Other, harder-to-quantify dimensions include how a hospitalist group practice affects mortality, and how scheduling, variable costs, hospitalist group type, subsidies, and level of expertise play out.
The foundation on which hospitalist groups build their efficiencies is the group type. In itself, how a hospitalist group chooses to organize itself reflects a maturing marketplace. SHM’s 2005-2006 productivity survey shows an increase in multistate hospitalist groups, up from 9% in ’03-’04 to 19% in the latest survey. Local private hospitalist groups fell from 20% in ’03-’04 to 12% in ’05-’06. The percentage of academic hospitalist groups rose from 16% to 20% in the same period.
It’s unclear how to interpret the shift from local to multistate hospitalist groups and the increase in academic medical center programs, but these trends bear watching. Comparison of the two most recent SHM surveys shows compensation models are also growing up, reflecting the need to balance base salary with productivity.
A major indicator of hospital group efficiency is the performance of groups with hospitalists on duty 24 hours a day, seven days a week. Although hospital administrators and hospitalist leaders struggle with the economics of providing night coverage when admissions are slow, such coverage pays off in quality and efficiency.
Stacy Goldsholl, MD, president of TeamHealth Hospital Medicine, a healthcare outsourcing firm based in Knoxville, Tenn., has long advocated 24/7 coverage as a crucial element in HMG efficiency. Even though she estimates that night coverage adds approximately $10,000 in subsidies to an average compensation package for a full-time hospitalist, such coverage improves efficiency in length of stay adjusted for severity and in readmissions. Full coverage allows hospitalists to be better integrated into the hospital in a way that fewer hours don’t.
“How hospitalists who cover 24/7 are used varies,” says Dr. Goldsholl. “Doing night admissions for community doctors, [working] as intensivist extenders, helping with ED [emergency department] throughput, being on rapid response teams—all are important contributors to improved efficiency,” says Dr. Goldsholl.
For Dr. Goldsholl, who has at least one academic medical center—Good Samaritan in Los Angeles at the University of Southern California Keck School of Medicine—on her roster, hospitalist group efficiency and productivity are major concerns for academic and community hospital administrators footing the bill for such services.
“Usually, TeamHealth is the exclusive hospitalist medicine provider contracting with a community hospital,” she explains. “Once we have been in a hospital for a while, we tend to see a progression in our responsibilities. Mostly we start with unassigned patients, then we expand to cover private primary care physicians’ patients. Then we co-manage complex cases with sub-specialists.”
Despite operating mostly in community hospitals, Dr. Goldsholl has fielded more queries from academic medical centers (AMCs) in the past several years.
“We’re definitely getting more interest from AMCs,” Dr. Goldsholl notes. “The work-hours restriction on residents—faculty who are uninterested in being hospitalists—whatever is driving their interest, they’re looking for solutions for handling their unassigned patients and beyond. To outsource to a private hospitalist company, an academic medical center would have to be in some pain, but interest is definitely picking up.”
Cogent Healthcare’s June 2006 contract with Temple University Hospital (TUH), Philadelphia, to provide a 24/7 hospitalist program of teaching and non-teaching services is another example of hospitals striving for efficiency. To better reach its clinical, economic, and regulatory goals, TUH switched from its own academic hospitalist group to partner with Cogent to manage its adult medical/surgical population. It’s too soon to gauge the results.
Despite stakeholders’ need to know more about which hospitalist group structure is most efficient, there’s little published data on AMC versus private group efficiency. One important study, published in the American Journal of Medicine (AJM) in May 2005, compared an academic hospitalist group with a private hospitalist group and community internists on several efficiency measures. The academic hospitalists’ patients had a 13% shorter LOS than those patients cared for by other groups and academic hospitalists had lowered costs by $173 per case, versus $109 for the private hospitalist group. The academic hospitalists also had a 20% relative risk reduction for severity of illness over the community physicians.
Lakshmi Halasyamani, MD, the AJM study’s lead author and chair of the Hospital Quality and Patient Safety Committee for SHM, speculated that the academic hospitalist groups’ efficiency resulted from fewer handoffs and that academic hospitalists’ relationships with their hospitals were more aligned than those of outsiders, both from financial and quality perspectives. Additionally, the academic hospitalist group used the hospital’s computerized physician order entry system and followed its protocols for clinical pathways and core measures. Scheduling also made a difference. The academic group worked in half-month blocks for an average of 14 weeks, while the private hospitalists worked from 8 a.m. to 6 p.m. on weekdays and some nights and weekends, leaving moonlighters to cover 75% of nights, weekends, and holidays and providing for rockier handoffs.
Another study comparing a traditional pediatric faculty group with two private hospitalist groups at St. Joseph’s Hospital and Medical Center of Phoenix showed that the faculty group outperformed the private hospitalists on all measures.
The authors concluded that faculty models can be as efficient as or more efficient than private groups in terms of direct costs and LOS.
Fine Tuning
Although academic hospitalist groups have been thought of as less efficient than private hospitalist groups because the former tend to use salaried employees while the latter tend to compensate employees based more on performance, the data cited above indicate academic hospitalist groups may have a competitive edge with regard to efficiency. What may account for the difference is that academic hospitalists are familiar with and often products of their hospital’s culture and mores. Unlike physicians working for private hospitalist groups with their own structure and culture, academic hospitalists are of a piece with their hospital. It’s common to find academic hospitalists who return to their medical school alma mater after a stint in an office-based practice. Some never left, joining the academic hospitalist group directly from residency.
For the chief of a hospitalist program, being so attuned to the hospital’s rhythms can be a mixed blessing.
Pat Cawley, MD, is the hospitalist program director and founder of the academic hospitalist group at the Charleston-based Medical University of South Carolina’s Hospital. He has a hard time focusing on hospitalist group efficiency, though, when he’s still flat-out recruiting.
“Demand for hospitalists is still way outstripping supply,” says Dr. Cawley. “We currently have nine hospitalists and plan to add five more this year, but we could actually use 10 more.”
The South Carolina market is competitive, with other hospitals planning to establish hospitalist medicine programs and vying with Dr. Cawley’s program for fresh physicians. Medical University Hospital’s hospitalist group started in July 2003 with four physicians and has kept growing. The hospitalists spend most of their time functioning as a teaching service and also cover a long-term acute-care facility at another hospital.
Defining efficiency in South Carolina’s booming market is secondary to recruiting and incorporating new physicians as team members. Dr. Cawley uses average daily census (ADC) as an efficiency benchmark: 15-20 patients per hospitalist is productive, although many doctors are comfortable at 12.
“We looked at our learning curve, about 10-12,” points out Dr. Cawley. “We think 15-20 is better, although some places are reporting an ADC of 22. But after a certain point, performance doesn’t appear to improve.”
A big problem with improving hospitalist group efficiency, according to Dr. Cawley, is hospital inefficiency: “Lack of IT to get lab results quickly, not enough nursing and secretarial support for admissions and discharges, policies on contacting the primary doc versus having a standing order for a procedure—all decrease efficiency.”
He’d also like his hospital administrators to allow nurses to pronounce death (common in community hospitals but less so in AMCs). “The power of hospitalists is to challenge the hospital’s inefficiencies, to break down the barriers to more efficient practices,” adds Dr. Cawley. “Many institutions need huge culture change, and hospitalists must lead the way.”
A close watcher of hospitalist performance, Scott Oxenhandler, MD, medical director of the Memorial Hospitalist Group in Hollywood, Fla., heads a hospitalist group he started in June 2004 that now has 23 physicians and two nurse practitioners. Memorial Hospital also has two other private hospitalist groups. While Dr. Oxenhandler’s group handles unassigned patients (55%) and Medicaid/Medicare patients (45%), the other hospitalist groups have captured the more lucrative business of managed care and other commercially insured patients.
—Per Danielsson, MD, medical director, Swedish Medical Center Adult Hospitalist Program, Seattle
Dr. Oxenhandler says efficiency is a complicated issue involving several key components. “Following evidence-based medicine protocols and CMS core measures are fairly straightforward [ideas] for all of us,” he says, “but financial measures are more complex.”
He has taken aim at adjusted variable costs per discharge on lab tests, pharmacy, and radiology, “three areas where I know that our group can improve,” he adds.
As for how hard and how efficiently a hospitalist works, Dr. Oxenhandler is taking a closer look at that as his group and the field mature. “We know that average daily census can be deceiving and RVUs [relative value units] are more relevant to efficiency but not perfect,” he says. “Another factor is tenure with the hospitalist group. For the physician to excel and to mature clinically, he or she needs to stay with a hospitalist group long enough to improve readmission rates and to get a sense of how to better manage clinical resources.’’
Dr. Oxenhandler describes a patient presenting with heart failure and anemia to show how a hospitalist’s clinical skills might mature. After several days of repeated hemoglobin studies indicating anemia, the hospitalist might refer the patient—once stabilized and discharged—to his primary physician for an outpatient work-up for possible colon cancer—rather than do so during the hospitalization.
Dr. Oxenhandler has contemplated pursuing managed care contracts but hesitates because his hospitalist group’s clinical and cost performance is equal to that of the hospitalist group that currently holds such contracts. “Why should they switch to us unless we can outperform the other group?” he muses. “Plus, there would be added cost for us in more paperwork and administration, and we’d have to improve our efficiency to make it worthwhile.”
Per Danielsson, MD, Swedish Medical Center’s Adult Hospitalist Program’s medical director, has hospitalists rotating among the First Hill, Cherry Hill, and Ballard campuses in Seattle, Wash. Demand for hospitalist services at the sites keeps growing, and Dr. Danielsson sees no end in sight. “Today’s hospital stays are getting shorter, and the patients are sicker, and there is increasing pressure for greater efficiency here,” he says.
Overall, clinicians, administrators, and researchers need to zero in on the organizational factors of hospitalist groups—from scheduling to 24/7 coverage, handoffs, and use of in-hospital resources—to improve efficiency. At present, academic hospitalist groups appear to have a slight edge because they’re tied more closely to hospital personnel, technology, and care pathways than private groups that come from outside the hospital. But there isn’t enough data either way to say which group type is the most efficient. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
While nationwide demand for hospitalists outstrips supply, hospitals across the country are looking at how their hospitalists and their hospital medicine groups weigh in on efficiency.
The notion of efficiency at a time of rapid growth may seem counterintuitive, but healthcare dollars are always hotly contested, and an efficient hospitalist program has a better chance of capturing them than a less-efficient one.
Even the definition of efficiency is being refined. Stakeholders scrutinizing compensation packages, key clinical indicators, productivity and quality metrics, scheduling, average daily census, and patient handoffs to gauge whether or not their group has a competitive edge over others. And hospital medicine group (HMG) leaders are scrutinizing themselves because they know hospitals increasingly are inviting more than one HMG to work under their roofs—the better to serve different populations and compare one with another.
How to Measure Efficiency
An evolving medical discipline that aspires to specialize in internal medicine, hospital medicine is in the process of developing a consensus definition of efficiency for itself. Major variables included in the calculation are obvious: average daily census, length of stay (LOS), case mix-adjusted costs, severity, and readmission rates. Other, harder-to-quantify dimensions include how a hospitalist group practice affects mortality, and how scheduling, variable costs, hospitalist group type, subsidies, and level of expertise play out.
The foundation on which hospitalist groups build their efficiencies is the group type. In itself, how a hospitalist group chooses to organize itself reflects a maturing marketplace. SHM’s 2005-2006 productivity survey shows an increase in multistate hospitalist groups, up from 9% in ’03-’04 to 19% in the latest survey. Local private hospitalist groups fell from 20% in ’03-’04 to 12% in ’05-’06. The percentage of academic hospitalist groups rose from 16% to 20% in the same period.
It’s unclear how to interpret the shift from local to multistate hospitalist groups and the increase in academic medical center programs, but these trends bear watching. Comparison of the two most recent SHM surveys shows compensation models are also growing up, reflecting the need to balance base salary with productivity.
A major indicator of hospital group efficiency is the performance of groups with hospitalists on duty 24 hours a day, seven days a week. Although hospital administrators and hospitalist leaders struggle with the economics of providing night coverage when admissions are slow, such coverage pays off in quality and efficiency.
Stacy Goldsholl, MD, president of TeamHealth Hospital Medicine, a healthcare outsourcing firm based in Knoxville, Tenn., has long advocated 24/7 coverage as a crucial element in HMG efficiency. Even though she estimates that night coverage adds approximately $10,000 in subsidies to an average compensation package for a full-time hospitalist, such coverage improves efficiency in length of stay adjusted for severity and in readmissions. Full coverage allows hospitalists to be better integrated into the hospital in a way that fewer hours don’t.
“How hospitalists who cover 24/7 are used varies,” says Dr. Goldsholl. “Doing night admissions for community doctors, [working] as intensivist extenders, helping with ED [emergency department] throughput, being on rapid response teams—all are important contributors to improved efficiency,” says Dr. Goldsholl.
For Dr. Goldsholl, who has at least one academic medical center—Good Samaritan in Los Angeles at the University of Southern California Keck School of Medicine—on her roster, hospitalist group efficiency and productivity are major concerns for academic and community hospital administrators footing the bill for such services.
“Usually, TeamHealth is the exclusive hospitalist medicine provider contracting with a community hospital,” she explains. “Once we have been in a hospital for a while, we tend to see a progression in our responsibilities. Mostly we start with unassigned patients, then we expand to cover private primary care physicians’ patients. Then we co-manage complex cases with sub-specialists.”
Despite operating mostly in community hospitals, Dr. Goldsholl has fielded more queries from academic medical centers (AMCs) in the past several years.
“We’re definitely getting more interest from AMCs,” Dr. Goldsholl notes. “The work-hours restriction on residents—faculty who are uninterested in being hospitalists—whatever is driving their interest, they’re looking for solutions for handling their unassigned patients and beyond. To outsource to a private hospitalist company, an academic medical center would have to be in some pain, but interest is definitely picking up.”
Cogent Healthcare’s June 2006 contract with Temple University Hospital (TUH), Philadelphia, to provide a 24/7 hospitalist program of teaching and non-teaching services is another example of hospitals striving for efficiency. To better reach its clinical, economic, and regulatory goals, TUH switched from its own academic hospitalist group to partner with Cogent to manage its adult medical/surgical population. It’s too soon to gauge the results.
Despite stakeholders’ need to know more about which hospitalist group structure is most efficient, there’s little published data on AMC versus private group efficiency. One important study, published in the American Journal of Medicine (AJM) in May 2005, compared an academic hospitalist group with a private hospitalist group and community internists on several efficiency measures. The academic hospitalists’ patients had a 13% shorter LOS than those patients cared for by other groups and academic hospitalists had lowered costs by $173 per case, versus $109 for the private hospitalist group. The academic hospitalists also had a 20% relative risk reduction for severity of illness over the community physicians.
Lakshmi Halasyamani, MD, the AJM study’s lead author and chair of the Hospital Quality and Patient Safety Committee for SHM, speculated that the academic hospitalist groups’ efficiency resulted from fewer handoffs and that academic hospitalists’ relationships with their hospitals were more aligned than those of outsiders, both from financial and quality perspectives. Additionally, the academic hospitalist group used the hospital’s computerized physician order entry system and followed its protocols for clinical pathways and core measures. Scheduling also made a difference. The academic group worked in half-month blocks for an average of 14 weeks, while the private hospitalists worked from 8 a.m. to 6 p.m. on weekdays and some nights and weekends, leaving moonlighters to cover 75% of nights, weekends, and holidays and providing for rockier handoffs.
Another study comparing a traditional pediatric faculty group with two private hospitalist groups at St. Joseph’s Hospital and Medical Center of Phoenix showed that the faculty group outperformed the private hospitalists on all measures.
The authors concluded that faculty models can be as efficient as or more efficient than private groups in terms of direct costs and LOS.
Fine Tuning
Although academic hospitalist groups have been thought of as less efficient than private hospitalist groups because the former tend to use salaried employees while the latter tend to compensate employees based more on performance, the data cited above indicate academic hospitalist groups may have a competitive edge with regard to efficiency. What may account for the difference is that academic hospitalists are familiar with and often products of their hospital’s culture and mores. Unlike physicians working for private hospitalist groups with their own structure and culture, academic hospitalists are of a piece with their hospital. It’s common to find academic hospitalists who return to their medical school alma mater after a stint in an office-based practice. Some never left, joining the academic hospitalist group directly from residency.
For the chief of a hospitalist program, being so attuned to the hospital’s rhythms can be a mixed blessing.
Pat Cawley, MD, is the hospitalist program director and founder of the academic hospitalist group at the Charleston-based Medical University of South Carolina’s Hospital. He has a hard time focusing on hospitalist group efficiency, though, when he’s still flat-out recruiting.
“Demand for hospitalists is still way outstripping supply,” says Dr. Cawley. “We currently have nine hospitalists and plan to add five more this year, but we could actually use 10 more.”
The South Carolina market is competitive, with other hospitals planning to establish hospitalist medicine programs and vying with Dr. Cawley’s program for fresh physicians. Medical University Hospital’s hospitalist group started in July 2003 with four physicians and has kept growing. The hospitalists spend most of their time functioning as a teaching service and also cover a long-term acute-care facility at another hospital.
Defining efficiency in South Carolina’s booming market is secondary to recruiting and incorporating new physicians as team members. Dr. Cawley uses average daily census (ADC) as an efficiency benchmark: 15-20 patients per hospitalist is productive, although many doctors are comfortable at 12.
“We looked at our learning curve, about 10-12,” points out Dr. Cawley. “We think 15-20 is better, although some places are reporting an ADC of 22. But after a certain point, performance doesn’t appear to improve.”
A big problem with improving hospitalist group efficiency, according to Dr. Cawley, is hospital inefficiency: “Lack of IT to get lab results quickly, not enough nursing and secretarial support for admissions and discharges, policies on contacting the primary doc versus having a standing order for a procedure—all decrease efficiency.”
He’d also like his hospital administrators to allow nurses to pronounce death (common in community hospitals but less so in AMCs). “The power of hospitalists is to challenge the hospital’s inefficiencies, to break down the barriers to more efficient practices,” adds Dr. Cawley. “Many institutions need huge culture change, and hospitalists must lead the way.”
A close watcher of hospitalist performance, Scott Oxenhandler, MD, medical director of the Memorial Hospitalist Group in Hollywood, Fla., heads a hospitalist group he started in June 2004 that now has 23 physicians and two nurse practitioners. Memorial Hospital also has two other private hospitalist groups. While Dr. Oxenhandler’s group handles unassigned patients (55%) and Medicaid/Medicare patients (45%), the other hospitalist groups have captured the more lucrative business of managed care and other commercially insured patients.
—Per Danielsson, MD, medical director, Swedish Medical Center Adult Hospitalist Program, Seattle
Dr. Oxenhandler says efficiency is a complicated issue involving several key components. “Following evidence-based medicine protocols and CMS core measures are fairly straightforward [ideas] for all of us,” he says, “but financial measures are more complex.”
He has taken aim at adjusted variable costs per discharge on lab tests, pharmacy, and radiology, “three areas where I know that our group can improve,” he adds.
As for how hard and how efficiently a hospitalist works, Dr. Oxenhandler is taking a closer look at that as his group and the field mature. “We know that average daily census can be deceiving and RVUs [relative value units] are more relevant to efficiency but not perfect,” he says. “Another factor is tenure with the hospitalist group. For the physician to excel and to mature clinically, he or she needs to stay with a hospitalist group long enough to improve readmission rates and to get a sense of how to better manage clinical resources.’’
Dr. Oxenhandler describes a patient presenting with heart failure and anemia to show how a hospitalist’s clinical skills might mature. After several days of repeated hemoglobin studies indicating anemia, the hospitalist might refer the patient—once stabilized and discharged—to his primary physician for an outpatient work-up for possible colon cancer—rather than do so during the hospitalization.
Dr. Oxenhandler has contemplated pursuing managed care contracts but hesitates because his hospitalist group’s clinical and cost performance is equal to that of the hospitalist group that currently holds such contracts. “Why should they switch to us unless we can outperform the other group?” he muses. “Plus, there would be added cost for us in more paperwork and administration, and we’d have to improve our efficiency to make it worthwhile.”
Per Danielsson, MD, Swedish Medical Center’s Adult Hospitalist Program’s medical director, has hospitalists rotating among the First Hill, Cherry Hill, and Ballard campuses in Seattle, Wash. Demand for hospitalist services at the sites keeps growing, and Dr. Danielsson sees no end in sight. “Today’s hospital stays are getting shorter, and the patients are sicker, and there is increasing pressure for greater efficiency here,” he says.
Overall, clinicians, administrators, and researchers need to zero in on the organizational factors of hospitalist groups—from scheduling to 24/7 coverage, handoffs, and use of in-hospital resources—to improve efficiency. At present, academic hospitalist groups appear to have a slight edge because they’re tied more closely to hospital personnel, technology, and care pathways than private groups that come from outside the hospital. But there isn’t enough data either way to say which group type is the most efficient. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
While nationwide demand for hospitalists outstrips supply, hospitals across the country are looking at how their hospitalists and their hospital medicine groups weigh in on efficiency.
The notion of efficiency at a time of rapid growth may seem counterintuitive, but healthcare dollars are always hotly contested, and an efficient hospitalist program has a better chance of capturing them than a less-efficient one.
Even the definition of efficiency is being refined. Stakeholders scrutinizing compensation packages, key clinical indicators, productivity and quality metrics, scheduling, average daily census, and patient handoffs to gauge whether or not their group has a competitive edge over others. And hospital medicine group (HMG) leaders are scrutinizing themselves because they know hospitals increasingly are inviting more than one HMG to work under their roofs—the better to serve different populations and compare one with another.
How to Measure Efficiency
An evolving medical discipline that aspires to specialize in internal medicine, hospital medicine is in the process of developing a consensus definition of efficiency for itself. Major variables included in the calculation are obvious: average daily census, length of stay (LOS), case mix-adjusted costs, severity, and readmission rates. Other, harder-to-quantify dimensions include how a hospitalist group practice affects mortality, and how scheduling, variable costs, hospitalist group type, subsidies, and level of expertise play out.
The foundation on which hospitalist groups build their efficiencies is the group type. In itself, how a hospitalist group chooses to organize itself reflects a maturing marketplace. SHM’s 2005-2006 productivity survey shows an increase in multistate hospitalist groups, up from 9% in ’03-’04 to 19% in the latest survey. Local private hospitalist groups fell from 20% in ’03-’04 to 12% in ’05-’06. The percentage of academic hospitalist groups rose from 16% to 20% in the same period.
It’s unclear how to interpret the shift from local to multistate hospitalist groups and the increase in academic medical center programs, but these trends bear watching. Comparison of the two most recent SHM surveys shows compensation models are also growing up, reflecting the need to balance base salary with productivity.
A major indicator of hospital group efficiency is the performance of groups with hospitalists on duty 24 hours a day, seven days a week. Although hospital administrators and hospitalist leaders struggle with the economics of providing night coverage when admissions are slow, such coverage pays off in quality and efficiency.
Stacy Goldsholl, MD, president of TeamHealth Hospital Medicine, a healthcare outsourcing firm based in Knoxville, Tenn., has long advocated 24/7 coverage as a crucial element in HMG efficiency. Even though she estimates that night coverage adds approximately $10,000 in subsidies to an average compensation package for a full-time hospitalist, such coverage improves efficiency in length of stay adjusted for severity and in readmissions. Full coverage allows hospitalists to be better integrated into the hospital in a way that fewer hours don’t.
“How hospitalists who cover 24/7 are used varies,” says Dr. Goldsholl. “Doing night admissions for community doctors, [working] as intensivist extenders, helping with ED [emergency department] throughput, being on rapid response teams—all are important contributors to improved efficiency,” says Dr. Goldsholl.
For Dr. Goldsholl, who has at least one academic medical center—Good Samaritan in Los Angeles at the University of Southern California Keck School of Medicine—on her roster, hospitalist group efficiency and productivity are major concerns for academic and community hospital administrators footing the bill for such services.
“Usually, TeamHealth is the exclusive hospitalist medicine provider contracting with a community hospital,” she explains. “Once we have been in a hospital for a while, we tend to see a progression in our responsibilities. Mostly we start with unassigned patients, then we expand to cover private primary care physicians’ patients. Then we co-manage complex cases with sub-specialists.”
Despite operating mostly in community hospitals, Dr. Goldsholl has fielded more queries from academic medical centers (AMCs) in the past several years.
“We’re definitely getting more interest from AMCs,” Dr. Goldsholl notes. “The work-hours restriction on residents—faculty who are uninterested in being hospitalists—whatever is driving their interest, they’re looking for solutions for handling their unassigned patients and beyond. To outsource to a private hospitalist company, an academic medical center would have to be in some pain, but interest is definitely picking up.”
Cogent Healthcare’s June 2006 contract with Temple University Hospital (TUH), Philadelphia, to provide a 24/7 hospitalist program of teaching and non-teaching services is another example of hospitals striving for efficiency. To better reach its clinical, economic, and regulatory goals, TUH switched from its own academic hospitalist group to partner with Cogent to manage its adult medical/surgical population. It’s too soon to gauge the results.
Despite stakeholders’ need to know more about which hospitalist group structure is most efficient, there’s little published data on AMC versus private group efficiency. One important study, published in the American Journal of Medicine (AJM) in May 2005, compared an academic hospitalist group with a private hospitalist group and community internists on several efficiency measures. The academic hospitalists’ patients had a 13% shorter LOS than those patients cared for by other groups and academic hospitalists had lowered costs by $173 per case, versus $109 for the private hospitalist group. The academic hospitalists also had a 20% relative risk reduction for severity of illness over the community physicians.
Lakshmi Halasyamani, MD, the AJM study’s lead author and chair of the Hospital Quality and Patient Safety Committee for SHM, speculated that the academic hospitalist groups’ efficiency resulted from fewer handoffs and that academic hospitalists’ relationships with their hospitals were more aligned than those of outsiders, both from financial and quality perspectives. Additionally, the academic hospitalist group used the hospital’s computerized physician order entry system and followed its protocols for clinical pathways and core measures. Scheduling also made a difference. The academic group worked in half-month blocks for an average of 14 weeks, while the private hospitalists worked from 8 a.m. to 6 p.m. on weekdays and some nights and weekends, leaving moonlighters to cover 75% of nights, weekends, and holidays and providing for rockier handoffs.
Another study comparing a traditional pediatric faculty group with two private hospitalist groups at St. Joseph’s Hospital and Medical Center of Phoenix showed that the faculty group outperformed the private hospitalists on all measures.
The authors concluded that faculty models can be as efficient as or more efficient than private groups in terms of direct costs and LOS.
Fine Tuning
Although academic hospitalist groups have been thought of as less efficient than private hospitalist groups because the former tend to use salaried employees while the latter tend to compensate employees based more on performance, the data cited above indicate academic hospitalist groups may have a competitive edge with regard to efficiency. What may account for the difference is that academic hospitalists are familiar with and often products of their hospital’s culture and mores. Unlike physicians working for private hospitalist groups with their own structure and culture, academic hospitalists are of a piece with their hospital. It’s common to find academic hospitalists who return to their medical school alma mater after a stint in an office-based practice. Some never left, joining the academic hospitalist group directly from residency.
For the chief of a hospitalist program, being so attuned to the hospital’s rhythms can be a mixed blessing.
Pat Cawley, MD, is the hospitalist program director and founder of the academic hospitalist group at the Charleston-based Medical University of South Carolina’s Hospital. He has a hard time focusing on hospitalist group efficiency, though, when he’s still flat-out recruiting.
“Demand for hospitalists is still way outstripping supply,” says Dr. Cawley. “We currently have nine hospitalists and plan to add five more this year, but we could actually use 10 more.”
The South Carolina market is competitive, with other hospitals planning to establish hospitalist medicine programs and vying with Dr. Cawley’s program for fresh physicians. Medical University Hospital’s hospitalist group started in July 2003 with four physicians and has kept growing. The hospitalists spend most of their time functioning as a teaching service and also cover a long-term acute-care facility at another hospital.
Defining efficiency in South Carolina’s booming market is secondary to recruiting and incorporating new physicians as team members. Dr. Cawley uses average daily census (ADC) as an efficiency benchmark: 15-20 patients per hospitalist is productive, although many doctors are comfortable at 12.
“We looked at our learning curve, about 10-12,” points out Dr. Cawley. “We think 15-20 is better, although some places are reporting an ADC of 22. But after a certain point, performance doesn’t appear to improve.”
A big problem with improving hospitalist group efficiency, according to Dr. Cawley, is hospital inefficiency: “Lack of IT to get lab results quickly, not enough nursing and secretarial support for admissions and discharges, policies on contacting the primary doc versus having a standing order for a procedure—all decrease efficiency.”
He’d also like his hospital administrators to allow nurses to pronounce death (common in community hospitals but less so in AMCs). “The power of hospitalists is to challenge the hospital’s inefficiencies, to break down the barriers to more efficient practices,” adds Dr. Cawley. “Many institutions need huge culture change, and hospitalists must lead the way.”
A close watcher of hospitalist performance, Scott Oxenhandler, MD, medical director of the Memorial Hospitalist Group in Hollywood, Fla., heads a hospitalist group he started in June 2004 that now has 23 physicians and two nurse practitioners. Memorial Hospital also has two other private hospitalist groups. While Dr. Oxenhandler’s group handles unassigned patients (55%) and Medicaid/Medicare patients (45%), the other hospitalist groups have captured the more lucrative business of managed care and other commercially insured patients.
—Per Danielsson, MD, medical director, Swedish Medical Center Adult Hospitalist Program, Seattle
Dr. Oxenhandler says efficiency is a complicated issue involving several key components. “Following evidence-based medicine protocols and CMS core measures are fairly straightforward [ideas] for all of us,” he says, “but financial measures are more complex.”
He has taken aim at adjusted variable costs per discharge on lab tests, pharmacy, and radiology, “three areas where I know that our group can improve,” he adds.
As for how hard and how efficiently a hospitalist works, Dr. Oxenhandler is taking a closer look at that as his group and the field mature. “We know that average daily census can be deceiving and RVUs [relative value units] are more relevant to efficiency but not perfect,” he says. “Another factor is tenure with the hospitalist group. For the physician to excel and to mature clinically, he or she needs to stay with a hospitalist group long enough to improve readmission rates and to get a sense of how to better manage clinical resources.’’
Dr. Oxenhandler describes a patient presenting with heart failure and anemia to show how a hospitalist’s clinical skills might mature. After several days of repeated hemoglobin studies indicating anemia, the hospitalist might refer the patient—once stabilized and discharged—to his primary physician for an outpatient work-up for possible colon cancer—rather than do so during the hospitalization.
Dr. Oxenhandler has contemplated pursuing managed care contracts but hesitates because his hospitalist group’s clinical and cost performance is equal to that of the hospitalist group that currently holds such contracts. “Why should they switch to us unless we can outperform the other group?” he muses. “Plus, there would be added cost for us in more paperwork and administration, and we’d have to improve our efficiency to make it worthwhile.”
Per Danielsson, MD, Swedish Medical Center’s Adult Hospitalist Program’s medical director, has hospitalists rotating among the First Hill, Cherry Hill, and Ballard campuses in Seattle, Wash. Demand for hospitalist services at the sites keeps growing, and Dr. Danielsson sees no end in sight. “Today’s hospital stays are getting shorter, and the patients are sicker, and there is increasing pressure for greater efficiency here,” he says.
Overall, clinicians, administrators, and researchers need to zero in on the organizational factors of hospitalist groups—from scheduling to 24/7 coverage, handoffs, and use of in-hospital resources—to improve efficiency. At present, academic hospitalist groups appear to have a slight edge because they’re tied more closely to hospital personnel, technology, and care pathways than private groups that come from outside the hospital. But there isn’t enough data either way to say which group type is the most efficient. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
A Cure for Rabies
In September 2004, animal-loving Wisconsin teenager Jeanna Giese picked up a bat trapped inside her church and took it outside. As she tried to set it free, the bat sank its teeth into her left index finger for an instant before she shook it loose.
Back at home, her mother rinsed the tiny wound with hydrogen peroxide and thought no more about it. A month later, the girl, a star student and athlete, developed fatigue, double vision from bilateral sixth nerve palsies, and paresthesias in her left arm. She deteriorated rapidly over the next few days, with high fever, ataxia, confusion, tremor, drooling, and spasm with swallowing, and was intubated for airway protection. Rabies antibody was found in her spinal fluid and serum.
The Fond du Lac girl’s doctors at Children’s Hospital of Wisconsin (Milwaukee) offered the family a dismal choice. She could receive hospice care for the gruesome and invariably fatal consequences of rabies in unvaccinated patients. Or, the doctors could embark on experimental treatment, with no guarantee she would have any meaningful neurological function or quality of life should she survive.
Parents Chose Treatment
On the basis of data indicating rabies patients are capable of clearing the virus, but die largely of secondary complications (e.g., autonomic dysfunction and excitatory neurotoxicity), the team administered massive doses of ketamine, midazolam, and phenobarbital, the antivirals ribavirin and amantadine, and supplementation with coenzyme Q to counter the possible mitochondrial toxicity of ribavirin. Ketamine blocks the neuroexcitatory NMDA receptor, possibly a receptor for rabies virus.
After a stormy, four-week intensive-care course characterized by autonomic instability and other complications, Giese was extubated and went home on New Year’s Day 2005. She made a remarkable recovery, eventually returning to school full time— although she was unable to participate in athletics. At 17, she has been accepted to college to study biology starting this fall.1-3
While the Wisconsin protocol has achieved the previously impossible, it is not yet a surefire cure for rabies. Two U.S. children treated last year with the Wisconsin protocol and meticulous supportive care died—one with cerebral edema, the other with cerebral and cerebellar herniation.4 Additional clinical experience and further tinkering with the protocol are likely required to optimize outcomes.
What To Know
While rabies is rare is the U.S., it retains a disproportionate importance because of its historic 100% fatality rate. Hospitalists should know this about rabies:
Suspect rabies in all patients with undiagnosed neurological disease. Making the diagnosis of rabies as early as possible is more critical than ever, now that a potential treatment exists. Unfortunately, in the United States rabies is rarely considered when patients first present for medical attention.
During the prodromal phase of rabies, which lasts about four days, patients have non-specific symptoms of fever, malaise, and nausea. This is quickly followed by paresthesias at the bite or wound site, personality change and hallucinations, and the classic manifestations of “furious rabies”: agitation, delirium, hydrophobia, aerophobia, aggression, and spasms affecting swallowing and respiration.
In up to 20% of patients, the disease may present in atypical form as “dumb rabies,” an ascending paralysis that may mimic Guillain-Barré syndrome. Tests for rabies include polymerase chain reaction of cerebrospinal fluid or saliva, antibody testing of serum and CSF, and direct fluorescent antibody of biopsy from the nape of the neck, where the virus congregates in hair follicles.
Ask all patients about bat and animal exposure when rabies is in the differential. Worldwide, there are 55,000 cases of human rabies a year. The vast majority of these occur in developing countries as a result of dog bites. In the United States, there is only a handful of human cases of rabies each year, almost always associated with bat exposure. It is not necessary to get a bat bite or scratch to be at risk for rabies. Some U.S. patients seem to have contracted rabies after exposure to bat saliva or vapors, sometimes having been bitten while asleep. Any patient who wakes up in a room or cabin and finds a bat should be considered at risk for rabies.
Other animals commonly infected with rabies in the U.S. include raccoons, skunks, and foxes. Unvaccinated dogs and cats also are at risk of rabies.
Consider prevention the best treatment. Wash bite wounds with 20% soap and irrigate with povidone-iodine to reduce the risk of rabies by up to 90%. If the biting animal is available for observation, the rabies vaccine may be deferred or not administered at all if the animal is well after 10 days. Many state laboratories will also perform rabies testing on euthanized animals. If the biting animal is unavailable for observation, promptly give the rabies vaccine and immune globulin. Current rabies vaccines are safe and highly effective in preventing infection after exposure, provided they are given in a timely fashion. Vaccine and immune globulin have no role in treatment once rabies symptoms have developed. TH
Dr. Ross is an associate physician and hospitalist at Brigham and Women’s Hospital, Boston, and a fellow of the Infectious Diseases Society of America. Contact him at [email protected].
References
- Willoughby RE Jr, Tieves KS, Hoffman GM, et al. Survival after treatment of rabies with induction of coma. N Engl J Med. 2005;352(24):2508-2514.
- Johnson M, Nelson K. Down to a prayer. Milwaukee Journal Sentinel. June 18, 2005.
- Nelson K. Potential cure for rabies fails in others. Milwaukee Journal Sentinel. April 22, 2007.
- Centers for Disease Control and Prevention. Human rabies Indiana and California, 2006. MMWR. 2007;56(15):361-365.
In September 2004, animal-loving Wisconsin teenager Jeanna Giese picked up a bat trapped inside her church and took it outside. As she tried to set it free, the bat sank its teeth into her left index finger for an instant before she shook it loose.
Back at home, her mother rinsed the tiny wound with hydrogen peroxide and thought no more about it. A month later, the girl, a star student and athlete, developed fatigue, double vision from bilateral sixth nerve palsies, and paresthesias in her left arm. She deteriorated rapidly over the next few days, with high fever, ataxia, confusion, tremor, drooling, and spasm with swallowing, and was intubated for airway protection. Rabies antibody was found in her spinal fluid and serum.
The Fond du Lac girl’s doctors at Children’s Hospital of Wisconsin (Milwaukee) offered the family a dismal choice. She could receive hospice care for the gruesome and invariably fatal consequences of rabies in unvaccinated patients. Or, the doctors could embark on experimental treatment, with no guarantee she would have any meaningful neurological function or quality of life should she survive.
Parents Chose Treatment
On the basis of data indicating rabies patients are capable of clearing the virus, but die largely of secondary complications (e.g., autonomic dysfunction and excitatory neurotoxicity), the team administered massive doses of ketamine, midazolam, and phenobarbital, the antivirals ribavirin and amantadine, and supplementation with coenzyme Q to counter the possible mitochondrial toxicity of ribavirin. Ketamine blocks the neuroexcitatory NMDA receptor, possibly a receptor for rabies virus.
After a stormy, four-week intensive-care course characterized by autonomic instability and other complications, Giese was extubated and went home on New Year’s Day 2005. She made a remarkable recovery, eventually returning to school full time— although she was unable to participate in athletics. At 17, she has been accepted to college to study biology starting this fall.1-3
While the Wisconsin protocol has achieved the previously impossible, it is not yet a surefire cure for rabies. Two U.S. children treated last year with the Wisconsin protocol and meticulous supportive care died—one with cerebral edema, the other with cerebral and cerebellar herniation.4 Additional clinical experience and further tinkering with the protocol are likely required to optimize outcomes.
What To Know
While rabies is rare is the U.S., it retains a disproportionate importance because of its historic 100% fatality rate. Hospitalists should know this about rabies:
Suspect rabies in all patients with undiagnosed neurological disease. Making the diagnosis of rabies as early as possible is more critical than ever, now that a potential treatment exists. Unfortunately, in the United States rabies is rarely considered when patients first present for medical attention.
During the prodromal phase of rabies, which lasts about four days, patients have non-specific symptoms of fever, malaise, and nausea. This is quickly followed by paresthesias at the bite or wound site, personality change and hallucinations, and the classic manifestations of “furious rabies”: agitation, delirium, hydrophobia, aerophobia, aggression, and spasms affecting swallowing and respiration.
In up to 20% of patients, the disease may present in atypical form as “dumb rabies,” an ascending paralysis that may mimic Guillain-Barré syndrome. Tests for rabies include polymerase chain reaction of cerebrospinal fluid or saliva, antibody testing of serum and CSF, and direct fluorescent antibody of biopsy from the nape of the neck, where the virus congregates in hair follicles.
Ask all patients about bat and animal exposure when rabies is in the differential. Worldwide, there are 55,000 cases of human rabies a year. The vast majority of these occur in developing countries as a result of dog bites. In the United States, there is only a handful of human cases of rabies each year, almost always associated with bat exposure. It is not necessary to get a bat bite or scratch to be at risk for rabies. Some U.S. patients seem to have contracted rabies after exposure to bat saliva or vapors, sometimes having been bitten while asleep. Any patient who wakes up in a room or cabin and finds a bat should be considered at risk for rabies.
Other animals commonly infected with rabies in the U.S. include raccoons, skunks, and foxes. Unvaccinated dogs and cats also are at risk of rabies.
Consider prevention the best treatment. Wash bite wounds with 20% soap and irrigate with povidone-iodine to reduce the risk of rabies by up to 90%. If the biting animal is available for observation, the rabies vaccine may be deferred or not administered at all if the animal is well after 10 days. Many state laboratories will also perform rabies testing on euthanized animals. If the biting animal is unavailable for observation, promptly give the rabies vaccine and immune globulin. Current rabies vaccines are safe and highly effective in preventing infection after exposure, provided they are given in a timely fashion. Vaccine and immune globulin have no role in treatment once rabies symptoms have developed. TH
Dr. Ross is an associate physician and hospitalist at Brigham and Women’s Hospital, Boston, and a fellow of the Infectious Diseases Society of America. Contact him at [email protected].
References
- Willoughby RE Jr, Tieves KS, Hoffman GM, et al. Survival after treatment of rabies with induction of coma. N Engl J Med. 2005;352(24):2508-2514.
- Johnson M, Nelson K. Down to a prayer. Milwaukee Journal Sentinel. June 18, 2005.
- Nelson K. Potential cure for rabies fails in others. Milwaukee Journal Sentinel. April 22, 2007.
- Centers for Disease Control and Prevention. Human rabies Indiana and California, 2006. MMWR. 2007;56(15):361-365.
In September 2004, animal-loving Wisconsin teenager Jeanna Giese picked up a bat trapped inside her church and took it outside. As she tried to set it free, the bat sank its teeth into her left index finger for an instant before she shook it loose.
Back at home, her mother rinsed the tiny wound with hydrogen peroxide and thought no more about it. A month later, the girl, a star student and athlete, developed fatigue, double vision from bilateral sixth nerve palsies, and paresthesias in her left arm. She deteriorated rapidly over the next few days, with high fever, ataxia, confusion, tremor, drooling, and spasm with swallowing, and was intubated for airway protection. Rabies antibody was found in her spinal fluid and serum.
The Fond du Lac girl’s doctors at Children’s Hospital of Wisconsin (Milwaukee) offered the family a dismal choice. She could receive hospice care for the gruesome and invariably fatal consequences of rabies in unvaccinated patients. Or, the doctors could embark on experimental treatment, with no guarantee she would have any meaningful neurological function or quality of life should she survive.
Parents Chose Treatment
On the basis of data indicating rabies patients are capable of clearing the virus, but die largely of secondary complications (e.g., autonomic dysfunction and excitatory neurotoxicity), the team administered massive doses of ketamine, midazolam, and phenobarbital, the antivirals ribavirin and amantadine, and supplementation with coenzyme Q to counter the possible mitochondrial toxicity of ribavirin. Ketamine blocks the neuroexcitatory NMDA receptor, possibly a receptor for rabies virus.
After a stormy, four-week intensive-care course characterized by autonomic instability and other complications, Giese was extubated and went home on New Year’s Day 2005. She made a remarkable recovery, eventually returning to school full time— although she was unable to participate in athletics. At 17, she has been accepted to college to study biology starting this fall.1-3
While the Wisconsin protocol has achieved the previously impossible, it is not yet a surefire cure for rabies. Two U.S. children treated last year with the Wisconsin protocol and meticulous supportive care died—one with cerebral edema, the other with cerebral and cerebellar herniation.4 Additional clinical experience and further tinkering with the protocol are likely required to optimize outcomes.
What To Know
While rabies is rare is the U.S., it retains a disproportionate importance because of its historic 100% fatality rate. Hospitalists should know this about rabies:
Suspect rabies in all patients with undiagnosed neurological disease. Making the diagnosis of rabies as early as possible is more critical than ever, now that a potential treatment exists. Unfortunately, in the United States rabies is rarely considered when patients first present for medical attention.
During the prodromal phase of rabies, which lasts about four days, patients have non-specific symptoms of fever, malaise, and nausea. This is quickly followed by paresthesias at the bite or wound site, personality change and hallucinations, and the classic manifestations of “furious rabies”: agitation, delirium, hydrophobia, aerophobia, aggression, and spasms affecting swallowing and respiration.
In up to 20% of patients, the disease may present in atypical form as “dumb rabies,” an ascending paralysis that may mimic Guillain-Barré syndrome. Tests for rabies include polymerase chain reaction of cerebrospinal fluid or saliva, antibody testing of serum and CSF, and direct fluorescent antibody of biopsy from the nape of the neck, where the virus congregates in hair follicles.
Ask all patients about bat and animal exposure when rabies is in the differential. Worldwide, there are 55,000 cases of human rabies a year. The vast majority of these occur in developing countries as a result of dog bites. In the United States, there is only a handful of human cases of rabies each year, almost always associated with bat exposure. It is not necessary to get a bat bite or scratch to be at risk for rabies. Some U.S. patients seem to have contracted rabies after exposure to bat saliva or vapors, sometimes having been bitten while asleep. Any patient who wakes up in a room or cabin and finds a bat should be considered at risk for rabies.
Other animals commonly infected with rabies in the U.S. include raccoons, skunks, and foxes. Unvaccinated dogs and cats also are at risk of rabies.
Consider prevention the best treatment. Wash bite wounds with 20% soap and irrigate with povidone-iodine to reduce the risk of rabies by up to 90%. If the biting animal is available for observation, the rabies vaccine may be deferred or not administered at all if the animal is well after 10 days. Many state laboratories will also perform rabies testing on euthanized animals. If the biting animal is unavailable for observation, promptly give the rabies vaccine and immune globulin. Current rabies vaccines are safe and highly effective in preventing infection after exposure, provided they are given in a timely fashion. Vaccine and immune globulin have no role in treatment once rabies symptoms have developed. TH
Dr. Ross is an associate physician and hospitalist at Brigham and Women’s Hospital, Boston, and a fellow of the Infectious Diseases Society of America. Contact him at [email protected].
References
- Willoughby RE Jr, Tieves KS, Hoffman GM, et al. Survival after treatment of rabies with induction of coma. N Engl J Med. 2005;352(24):2508-2514.
- Johnson M, Nelson K. Down to a prayer. Milwaukee Journal Sentinel. June 18, 2005.
- Nelson K. Potential cure for rabies fails in others. Milwaukee Journal Sentinel. April 22, 2007.
- Centers for Disease Control and Prevention. Human rabies Indiana and California, 2006. MMWR. 2007;56(15):361-365.
Dare to Compare
A new concept on Capitol Hill could reshape physicians’ treatment choices: comparative effectiveness research, or CER.
CER is a set of standards for examining the effectiveness of different therapies for a specific medical condition or set of patients to determine the best option. It may involve comparing competing medications or analyzing treatment approaches, such as surgery, devices, and drug therapies.
The healthcare community—and Capitol Hill—should keep an eye on CER.
“We need to look at evidence-based medicine and see what is the most effective treatment,” says Andrew Fishmann, MD, FCCP, FACP, co-founder of Cogent Healthcare and director of intensive care at Good Samaritan Hospital in Los Angeles. “The answer may also be the most expensive, but other factors such as decreased length of stay and fewer complications can help bring that cost down.”
One example that CER might address is back surgery—an issue many physicians cannot agree on. “There are billions of dollars spent on back surgery that may not be necessary,” Dr. Fishmann points out.
CER could ultimately provide guidelines that would standardize treatments for all types of conditions: “A big organization like Cogent would like to think that a patient with pneumonia receives the same treatment whether he’s in California or in Mississippi—but there are many reasons this is probably not true,” says Dr. Fishmann.
CER So Far
The Medicare Modernization Act of 2003 gave CER a jumpstart with $65 million in appropriations and authorized the Agency for Healthcare Research and Quality (AHRQ) to conduct research.
“Since 2004, [the AHRQ has] received $15 million a year for CER,” says Emily Rowe, director of government relations for the Coalition for Health Services Research in Washington, D.C., and a member of the Friends of AHRQ coalition. “They’re pretty limited in what they can produce on that budget, but to date they’ve done some interesting work.”
That work includes eight published reports on treatment options for breast cancer, gastroesophageal reflux disease (GERD), cancer-related anemia, low-bone density, depression, and more, with 20 additional reports “in the pipeline,” says Rowe.
All available reports can be downloaded from http://effectivehealthcare. ahrq.gov, where results have been published in separate versions for physicians and consumers.
“The most interesting example of [CER from AHRQ] is synthesized research that shows that drugs can be as effective as surgery for severe heart burn,” or GERD, says Rowe. “This shows the promise of CER.”
So AHRQ is at work on CER projects but, says Rowe, “It needs a more serious investment.” Some in Congress agree.
New Laws, More Money
The Enhanced Health Care Value for All Act of 2007 (HR 2184) was introduced by Reps. Tom Allen, D-Maine, and Jo Ann Emerson, R-Mo, in May. This bill would provide $3 billion over five years to fund CER.
Under the legislation, the AHRQ would remain the federal agency charged with supporting CER, but a new comparative effectiveness advisory board would be established, comprising employers, consumers, healthcare providers, researchers, and others. The board would offer advice on research priorities and methodologies.
Some, including the Blue Cross Blue Shield Association (BCBSA), have called for a new executive-branch agency or a new coalition to oversee CER. Dr. Fishmann, who is serving a second term on the National Advisory Council for AHRQ, strongly disagrees. “This is evidence-based medicine,” he stresses. “AHRQ is the perfect entity for this. What an organization like AHRQ will do is look at everything and address the issue impartially.”
Quality, Costs, Results
Congress views CER as a means of saving costs in healthcare, but CER would not provide immediate savings; rather, it’s a first step toward lowering healthcare costs. In fact, House Ways and Means Subcommittee Chairman Pete Stark, R-Calif., expressed concern about “moving” CER legislation this year, because it would require immediate investment without immediate savings.
“I don’t know where you come up with that money when everyone else in healthcare is fighting for more funds,” Dr. Fishmann says of the current legislation. “But Congress can come up with the funds if they want to.”
Rowe won’t speculate on whether the House bill will pass but does say: “The appropriators and budgeters are getting ready to fund this, so that if the legislation passes the money will be there. And interest in CER is gaining in both parties of Congress.”
While legislators focus on costs and savings, healthcare professionals are interested in improving quality.
“It is a quality issue, but a better term is value,” says Rowe. “The idea is, ‘Let’s get what we pay for.’ The U.S. needs better medical outcomes, and the idea of CER is not what treatments costs less but that it’s worth it if you have to spend more if the outcomes are improved.”
And Dr. Fishmann thinks CER will change how we provide care. “It’s going to standardize the delivery of healthcare,” he predicts. “If you don’t follow these standards, someone is going to ask why not—it might be the payer, your colleagues, your hospital.” Once CER reports are available and shared with the public, he points out, “as patients get educated, and payers too, they’ll stop paying for treatments that go against the standard.”
—Emily Rowe, director of government relations for the Coalition for Health Services Research, Washington, D.C.
Hospitalists and CER
How will comparative effectiveness affect hospital medicine?
“They’re looking at ischemic heart disease, pneumonia, diabetes, stroke—all hospitalized diseases,” says Dr. Fishmann of current CER projects. “Right now, everyone is practicing their trade, and everyone is doing things differently. I think in terms of hospitalists, it clearly will affect how you treat patients, and for how long.”
Regardless of the current House bill, it seems CER is on the horizon, for hospitalists and for all of healthcare.
“The good news is, I don’t think this is going away any time soon,” says Rowe of CER. “The train has left the station and it’s steaming away.” TH
A new concept on Capitol Hill could reshape physicians’ treatment choices: comparative effectiveness research, or CER.
CER is a set of standards for examining the effectiveness of different therapies for a specific medical condition or set of patients to determine the best option. It may involve comparing competing medications or analyzing treatment approaches, such as surgery, devices, and drug therapies.
The healthcare community—and Capitol Hill—should keep an eye on CER.
“We need to look at evidence-based medicine and see what is the most effective treatment,” says Andrew Fishmann, MD, FCCP, FACP, co-founder of Cogent Healthcare and director of intensive care at Good Samaritan Hospital in Los Angeles. “The answer may also be the most expensive, but other factors such as decreased length of stay and fewer complications can help bring that cost down.”
One example that CER might address is back surgery—an issue many physicians cannot agree on. “There are billions of dollars spent on back surgery that may not be necessary,” Dr. Fishmann points out.
CER could ultimately provide guidelines that would standardize treatments for all types of conditions: “A big organization like Cogent would like to think that a patient with pneumonia receives the same treatment whether he’s in California or in Mississippi—but there are many reasons this is probably not true,” says Dr. Fishmann.
CER So Far
The Medicare Modernization Act of 2003 gave CER a jumpstart with $65 million in appropriations and authorized the Agency for Healthcare Research and Quality (AHRQ) to conduct research.
“Since 2004, [the AHRQ has] received $15 million a year for CER,” says Emily Rowe, director of government relations for the Coalition for Health Services Research in Washington, D.C., and a member of the Friends of AHRQ coalition. “They’re pretty limited in what they can produce on that budget, but to date they’ve done some interesting work.”
That work includes eight published reports on treatment options for breast cancer, gastroesophageal reflux disease (GERD), cancer-related anemia, low-bone density, depression, and more, with 20 additional reports “in the pipeline,” says Rowe.
All available reports can be downloaded from http://effectivehealthcare. ahrq.gov, where results have been published in separate versions for physicians and consumers.
“The most interesting example of [CER from AHRQ] is synthesized research that shows that drugs can be as effective as surgery for severe heart burn,” or GERD, says Rowe. “This shows the promise of CER.”
So AHRQ is at work on CER projects but, says Rowe, “It needs a more serious investment.” Some in Congress agree.
New Laws, More Money
The Enhanced Health Care Value for All Act of 2007 (HR 2184) was introduced by Reps. Tom Allen, D-Maine, and Jo Ann Emerson, R-Mo, in May. This bill would provide $3 billion over five years to fund CER.
Under the legislation, the AHRQ would remain the federal agency charged with supporting CER, but a new comparative effectiveness advisory board would be established, comprising employers, consumers, healthcare providers, researchers, and others. The board would offer advice on research priorities and methodologies.
Some, including the Blue Cross Blue Shield Association (BCBSA), have called for a new executive-branch agency or a new coalition to oversee CER. Dr. Fishmann, who is serving a second term on the National Advisory Council for AHRQ, strongly disagrees. “This is evidence-based medicine,” he stresses. “AHRQ is the perfect entity for this. What an organization like AHRQ will do is look at everything and address the issue impartially.”
Quality, Costs, Results
Congress views CER as a means of saving costs in healthcare, but CER would not provide immediate savings; rather, it’s a first step toward lowering healthcare costs. In fact, House Ways and Means Subcommittee Chairman Pete Stark, R-Calif., expressed concern about “moving” CER legislation this year, because it would require immediate investment without immediate savings.
“I don’t know where you come up with that money when everyone else in healthcare is fighting for more funds,” Dr. Fishmann says of the current legislation. “But Congress can come up with the funds if they want to.”
Rowe won’t speculate on whether the House bill will pass but does say: “The appropriators and budgeters are getting ready to fund this, so that if the legislation passes the money will be there. And interest in CER is gaining in both parties of Congress.”
While legislators focus on costs and savings, healthcare professionals are interested in improving quality.
“It is a quality issue, but a better term is value,” says Rowe. “The idea is, ‘Let’s get what we pay for.’ The U.S. needs better medical outcomes, and the idea of CER is not what treatments costs less but that it’s worth it if you have to spend more if the outcomes are improved.”
And Dr. Fishmann thinks CER will change how we provide care. “It’s going to standardize the delivery of healthcare,” he predicts. “If you don’t follow these standards, someone is going to ask why not—it might be the payer, your colleagues, your hospital.” Once CER reports are available and shared with the public, he points out, “as patients get educated, and payers too, they’ll stop paying for treatments that go against the standard.”
—Emily Rowe, director of government relations for the Coalition for Health Services Research, Washington, D.C.
Hospitalists and CER
How will comparative effectiveness affect hospital medicine?
“They’re looking at ischemic heart disease, pneumonia, diabetes, stroke—all hospitalized diseases,” says Dr. Fishmann of current CER projects. “Right now, everyone is practicing their trade, and everyone is doing things differently. I think in terms of hospitalists, it clearly will affect how you treat patients, and for how long.”
Regardless of the current House bill, it seems CER is on the horizon, for hospitalists and for all of healthcare.
“The good news is, I don’t think this is going away any time soon,” says Rowe of CER. “The train has left the station and it’s steaming away.” TH
A new concept on Capitol Hill could reshape physicians’ treatment choices: comparative effectiveness research, or CER.
CER is a set of standards for examining the effectiveness of different therapies for a specific medical condition or set of patients to determine the best option. It may involve comparing competing medications or analyzing treatment approaches, such as surgery, devices, and drug therapies.
The healthcare community—and Capitol Hill—should keep an eye on CER.
“We need to look at evidence-based medicine and see what is the most effective treatment,” says Andrew Fishmann, MD, FCCP, FACP, co-founder of Cogent Healthcare and director of intensive care at Good Samaritan Hospital in Los Angeles. “The answer may also be the most expensive, but other factors such as decreased length of stay and fewer complications can help bring that cost down.”
One example that CER might address is back surgery—an issue many physicians cannot agree on. “There are billions of dollars spent on back surgery that may not be necessary,” Dr. Fishmann points out.
CER could ultimately provide guidelines that would standardize treatments for all types of conditions: “A big organization like Cogent would like to think that a patient with pneumonia receives the same treatment whether he’s in California or in Mississippi—but there are many reasons this is probably not true,” says Dr. Fishmann.
CER So Far
The Medicare Modernization Act of 2003 gave CER a jumpstart with $65 million in appropriations and authorized the Agency for Healthcare Research and Quality (AHRQ) to conduct research.
“Since 2004, [the AHRQ has] received $15 million a year for CER,” says Emily Rowe, director of government relations for the Coalition for Health Services Research in Washington, D.C., and a member of the Friends of AHRQ coalition. “They’re pretty limited in what they can produce on that budget, but to date they’ve done some interesting work.”
That work includes eight published reports on treatment options for breast cancer, gastroesophageal reflux disease (GERD), cancer-related anemia, low-bone density, depression, and more, with 20 additional reports “in the pipeline,” says Rowe.
All available reports can be downloaded from http://effectivehealthcare. ahrq.gov, where results have been published in separate versions for physicians and consumers.
“The most interesting example of [CER from AHRQ] is synthesized research that shows that drugs can be as effective as surgery for severe heart burn,” or GERD, says Rowe. “This shows the promise of CER.”
So AHRQ is at work on CER projects but, says Rowe, “It needs a more serious investment.” Some in Congress agree.
New Laws, More Money
The Enhanced Health Care Value for All Act of 2007 (HR 2184) was introduced by Reps. Tom Allen, D-Maine, and Jo Ann Emerson, R-Mo, in May. This bill would provide $3 billion over five years to fund CER.
Under the legislation, the AHRQ would remain the federal agency charged with supporting CER, but a new comparative effectiveness advisory board would be established, comprising employers, consumers, healthcare providers, researchers, and others. The board would offer advice on research priorities and methodologies.
Some, including the Blue Cross Blue Shield Association (BCBSA), have called for a new executive-branch agency or a new coalition to oversee CER. Dr. Fishmann, who is serving a second term on the National Advisory Council for AHRQ, strongly disagrees. “This is evidence-based medicine,” he stresses. “AHRQ is the perfect entity for this. What an organization like AHRQ will do is look at everything and address the issue impartially.”
Quality, Costs, Results
Congress views CER as a means of saving costs in healthcare, but CER would not provide immediate savings; rather, it’s a first step toward lowering healthcare costs. In fact, House Ways and Means Subcommittee Chairman Pete Stark, R-Calif., expressed concern about “moving” CER legislation this year, because it would require immediate investment without immediate savings.
“I don’t know where you come up with that money when everyone else in healthcare is fighting for more funds,” Dr. Fishmann says of the current legislation. “But Congress can come up with the funds if they want to.”
Rowe won’t speculate on whether the House bill will pass but does say: “The appropriators and budgeters are getting ready to fund this, so that if the legislation passes the money will be there. And interest in CER is gaining in both parties of Congress.”
While legislators focus on costs and savings, healthcare professionals are interested in improving quality.
“It is a quality issue, but a better term is value,” says Rowe. “The idea is, ‘Let’s get what we pay for.’ The U.S. needs better medical outcomes, and the idea of CER is not what treatments costs less but that it’s worth it if you have to spend more if the outcomes are improved.”
And Dr. Fishmann thinks CER will change how we provide care. “It’s going to standardize the delivery of healthcare,” he predicts. “If you don’t follow these standards, someone is going to ask why not—it might be the payer, your colleagues, your hospital.” Once CER reports are available and shared with the public, he points out, “as patients get educated, and payers too, they’ll stop paying for treatments that go against the standard.”
—Emily Rowe, director of government relations for the Coalition for Health Services Research, Washington, D.C.
Hospitalists and CER
How will comparative effectiveness affect hospital medicine?
“They’re looking at ischemic heart disease, pneumonia, diabetes, stroke—all hospitalized diseases,” says Dr. Fishmann of current CER projects. “Right now, everyone is practicing their trade, and everyone is doing things differently. I think in terms of hospitalists, it clearly will affect how you treat patients, and for how long.”
Regardless of the current House bill, it seems CER is on the horizon, for hospitalists and for all of healthcare.
“The good news is, I don’t think this is going away any time soon,” says Rowe of CER. “The train has left the station and it’s steaming away.” TH
Group Growth
This is the last article in a series on the four pillars of career satisfaction in hospital medicine.
What kind of support do you get from your hospital medicine group? From your hospital? How cohesive is your group? Do these things really matter?
The answers can be found in the SHM white paper “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available online at www.hospitalmedicine.org). SHM’s Career Satisfaction Task Force (CSTF) drafted the document to be used by hospitalists and hospital medicine practices as a toolkit for ensuring or improving job satisfaction. It outlines the four pillars of career satisfaction: autonomy/control (see the June edition of The Hospitalist, p. 14), workload/ schedule (July edition, p. 10), reward/ recognition (August edition, p. 10), and community/environment. This article looks at the last of these.
The Fourth Pillar
Hospitalists belong, in some sense, to four communities and must address the expectations of each group: administration, referring and nonreferring physicians, house staff and other healthcare staff, and medical students.
The hospitalist’s community includes his/her practice as well as hospitalists from other groups. The patient community is not just patients and their family members, but the broader public community served by the hospital medicine group and the hospital. The home community, consisting of the hospitalist’s family and friends, is also a vital part of the individual’s environment.
Each of these communities contributes to job satisfaction. A sense of shared values and connection with others, as well as social and work support, can ensure satisfaction; a sense of isolation, lack of support, and unresolved conflict can lead to unhappiness with a job.
Working within a strong community “makes everything else easier,” says CSTF member Noah Harris, MD, a hospitalist at Presbyterian Hospital, Albuquerque, N.M.
“Twenty years ago, there was a medical community in hospitals where physicians came together,” recalls Dr. Harris. “With managed care, physicians have become much less invested in the hospital and you see fewer [primary care] physicians there. Hospitalists have filled that gap. The question is how to restructure the hospital medical community.”
A hospitalist might struggle with the issue this way:
“I’m one of only three hospitalists at a hospital in a rural community. I feel it’s important to work as a team with primary care physicians, the emergency department, and other medical subspecialists.”
“How do hospitalists come in as the new kid on the block and reach out to other physicians?” asks Dr. Harris. “This is important, and if hospitalists feel like they’re more a part of the community, then that makes [their work] easier.”
According to Dr. Harris, the key to building a community in your workplace is communication. Strengthen it or establish it where there is none. When you communicate, focus on common goals with the other parties.
“Community has to do with shared expectations,” Dr. Harris points out. “Everyone—particularly the various types of physicians in the hospital—has to know what they expect from hospitalists.” It may be up to individual hospitalists to educate others as to what those expectations should be.
Of course, communication should start at the top. “On one level, there has to be formal communication with administrators and [physician leaders],” says Dr. Harris. “There has to be some sort of ongoing communication with the hospital administrators because they work with all the other groups as well.”
However, less formal communication is up to the hospitalist. The more you communicate with others, the more you’ll build your community.
Here are tips for how the hospitalist in the aforementioned example might work with each group of physicians:
ED doctors: “This hospitalist needs to get to know the other physicians and healthcare professionals,” Dr. Harris advises. “Make yourself available. When you have a minute, go down to the emergency department to update the ED physicians on admissions they’ve seen. Make a point to chat.”
Primary care physicians (PCPs): It may be more difficult to initiate informal communications with these docs if they’re not often in the hospital.
“One thing that helps is for the hospitalist to focus on communicating by phone, fax, or e-mail to PCPs when their patients are in the hospital,” says Dr. Harris. “In our office, we assigned a secretary to make sure PCPs get discharge summaries. That really helped with the community.”
If you want to strengthen ties to your community PCPs, issue an invitation to an event. “Our group would have an annual holiday party and invite all our referring physicians,” says Dr. Harris. “We’d have a speaker and get to know each other a little better.”
Surgeons: Dr. Harris suggests hospitalists can guide surgeons’ expectations for their working relationship with you and strengthen a sense of community.
“If there’s a particular issue, you can use that,” says Dr. Harris. “We were seeing a lot of elderly patients admitted with hip fractures. One thing we did to get a working relationship [with orthopedic surgeons] is we came up with a set of orders for these patients. The surgeons welcomed this because they wanted help with elderly patients who had multiple conditions. This was a way to work with them in a kind of formal way that helps patients. “It’s good to come up with order sets, but the big part of this is the negotiation with the other physicians that leads up to the order sets,” Dr. Harris says.
If you’re doing something like this to help in obstetrics, neurosurgery, or orthopedics, make it a two-way conversation.
“Above all else, it’s important to work with nonphysician healthcare workers,” says Dr. Harris, “especially nurses and physical therapists.”
The Rural Factor
The example above involves a small hospital medicine program in a rural area. Are there built-in problems with building community in this environment?
“I don’t think [it’s] necessarily more difficult” to build community in this setting, says Dr. Harris, “particularly if the hospital and physicians are on board with bringing in hospitalists. They might even be easier because you have fewer folks to deal with.”
But there may be an underlying problem with working at a smaller hospital. “If you’re the only hospitalist, or even the only hospitalist on a given shift, you’re practicing in a vacuum,” says Dr. Harris. If this is the case, you can broaden your hospitalist community by establishing a network with nearby hospitals and/or hospital medicine groups, and by becoming active in a regional or national group. TH
This is the last article in a series on the four pillars of career satisfaction in hospital medicine.
What kind of support do you get from your hospital medicine group? From your hospital? How cohesive is your group? Do these things really matter?
The answers can be found in the SHM white paper “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available online at www.hospitalmedicine.org). SHM’s Career Satisfaction Task Force (CSTF) drafted the document to be used by hospitalists and hospital medicine practices as a toolkit for ensuring or improving job satisfaction. It outlines the four pillars of career satisfaction: autonomy/control (see the June edition of The Hospitalist, p. 14), workload/ schedule (July edition, p. 10), reward/ recognition (August edition, p. 10), and community/environment. This article looks at the last of these.
The Fourth Pillar
Hospitalists belong, in some sense, to four communities and must address the expectations of each group: administration, referring and nonreferring physicians, house staff and other healthcare staff, and medical students.
The hospitalist’s community includes his/her practice as well as hospitalists from other groups. The patient community is not just patients and their family members, but the broader public community served by the hospital medicine group and the hospital. The home community, consisting of the hospitalist’s family and friends, is also a vital part of the individual’s environment.
Each of these communities contributes to job satisfaction. A sense of shared values and connection with others, as well as social and work support, can ensure satisfaction; a sense of isolation, lack of support, and unresolved conflict can lead to unhappiness with a job.
Working within a strong community “makes everything else easier,” says CSTF member Noah Harris, MD, a hospitalist at Presbyterian Hospital, Albuquerque, N.M.
“Twenty years ago, there was a medical community in hospitals where physicians came together,” recalls Dr. Harris. “With managed care, physicians have become much less invested in the hospital and you see fewer [primary care] physicians there. Hospitalists have filled that gap. The question is how to restructure the hospital medical community.”
A hospitalist might struggle with the issue this way:
“I’m one of only three hospitalists at a hospital in a rural community. I feel it’s important to work as a team with primary care physicians, the emergency department, and other medical subspecialists.”
“How do hospitalists come in as the new kid on the block and reach out to other physicians?” asks Dr. Harris. “This is important, and if hospitalists feel like they’re more a part of the community, then that makes [their work] easier.”
According to Dr. Harris, the key to building a community in your workplace is communication. Strengthen it or establish it where there is none. When you communicate, focus on common goals with the other parties.
“Community has to do with shared expectations,” Dr. Harris points out. “Everyone—particularly the various types of physicians in the hospital—has to know what they expect from hospitalists.” It may be up to individual hospitalists to educate others as to what those expectations should be.
Of course, communication should start at the top. “On one level, there has to be formal communication with administrators and [physician leaders],” says Dr. Harris. “There has to be some sort of ongoing communication with the hospital administrators because they work with all the other groups as well.”
However, less formal communication is up to the hospitalist. The more you communicate with others, the more you’ll build your community.
Here are tips for how the hospitalist in the aforementioned example might work with each group of physicians:
ED doctors: “This hospitalist needs to get to know the other physicians and healthcare professionals,” Dr. Harris advises. “Make yourself available. When you have a minute, go down to the emergency department to update the ED physicians on admissions they’ve seen. Make a point to chat.”
Primary care physicians (PCPs): It may be more difficult to initiate informal communications with these docs if they’re not often in the hospital.
“One thing that helps is for the hospitalist to focus on communicating by phone, fax, or e-mail to PCPs when their patients are in the hospital,” says Dr. Harris. “In our office, we assigned a secretary to make sure PCPs get discharge summaries. That really helped with the community.”
If you want to strengthen ties to your community PCPs, issue an invitation to an event. “Our group would have an annual holiday party and invite all our referring physicians,” says Dr. Harris. “We’d have a speaker and get to know each other a little better.”
Surgeons: Dr. Harris suggests hospitalists can guide surgeons’ expectations for their working relationship with you and strengthen a sense of community.
“If there’s a particular issue, you can use that,” says Dr. Harris. “We were seeing a lot of elderly patients admitted with hip fractures. One thing we did to get a working relationship [with orthopedic surgeons] is we came up with a set of orders for these patients. The surgeons welcomed this because they wanted help with elderly patients who had multiple conditions. This was a way to work with them in a kind of formal way that helps patients. “It’s good to come up with order sets, but the big part of this is the negotiation with the other physicians that leads up to the order sets,” Dr. Harris says.
If you’re doing something like this to help in obstetrics, neurosurgery, or orthopedics, make it a two-way conversation.
“Above all else, it’s important to work with nonphysician healthcare workers,” says Dr. Harris, “especially nurses and physical therapists.”
The Rural Factor
The example above involves a small hospital medicine program in a rural area. Are there built-in problems with building community in this environment?
“I don’t think [it’s] necessarily more difficult” to build community in this setting, says Dr. Harris, “particularly if the hospital and physicians are on board with bringing in hospitalists. They might even be easier because you have fewer folks to deal with.”
But there may be an underlying problem with working at a smaller hospital. “If you’re the only hospitalist, or even the only hospitalist on a given shift, you’re practicing in a vacuum,” says Dr. Harris. If this is the case, you can broaden your hospitalist community by establishing a network with nearby hospitals and/or hospital medicine groups, and by becoming active in a regional or national group. TH
This is the last article in a series on the four pillars of career satisfaction in hospital medicine.
What kind of support do you get from your hospital medicine group? From your hospital? How cohesive is your group? Do these things really matter?
The answers can be found in the SHM white paper “A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction” (available online at www.hospitalmedicine.org). SHM’s Career Satisfaction Task Force (CSTF) drafted the document to be used by hospitalists and hospital medicine practices as a toolkit for ensuring or improving job satisfaction. It outlines the four pillars of career satisfaction: autonomy/control (see the June edition of The Hospitalist, p. 14), workload/ schedule (July edition, p. 10), reward/ recognition (August edition, p. 10), and community/environment. This article looks at the last of these.
The Fourth Pillar
Hospitalists belong, in some sense, to four communities and must address the expectations of each group: administration, referring and nonreferring physicians, house staff and other healthcare staff, and medical students.
The hospitalist’s community includes his/her practice as well as hospitalists from other groups. The patient community is not just patients and their family members, but the broader public community served by the hospital medicine group and the hospital. The home community, consisting of the hospitalist’s family and friends, is also a vital part of the individual’s environment.
Each of these communities contributes to job satisfaction. A sense of shared values and connection with others, as well as social and work support, can ensure satisfaction; a sense of isolation, lack of support, and unresolved conflict can lead to unhappiness with a job.
Working within a strong community “makes everything else easier,” says CSTF member Noah Harris, MD, a hospitalist at Presbyterian Hospital, Albuquerque, N.M.
“Twenty years ago, there was a medical community in hospitals where physicians came together,” recalls Dr. Harris. “With managed care, physicians have become much less invested in the hospital and you see fewer [primary care] physicians there. Hospitalists have filled that gap. The question is how to restructure the hospital medical community.”
A hospitalist might struggle with the issue this way:
“I’m one of only three hospitalists at a hospital in a rural community. I feel it’s important to work as a team with primary care physicians, the emergency department, and other medical subspecialists.”
“How do hospitalists come in as the new kid on the block and reach out to other physicians?” asks Dr. Harris. “This is important, and if hospitalists feel like they’re more a part of the community, then that makes [their work] easier.”
According to Dr. Harris, the key to building a community in your workplace is communication. Strengthen it or establish it where there is none. When you communicate, focus on common goals with the other parties.
“Community has to do with shared expectations,” Dr. Harris points out. “Everyone—particularly the various types of physicians in the hospital—has to know what they expect from hospitalists.” It may be up to individual hospitalists to educate others as to what those expectations should be.
Of course, communication should start at the top. “On one level, there has to be formal communication with administrators and [physician leaders],” says Dr. Harris. “There has to be some sort of ongoing communication with the hospital administrators because they work with all the other groups as well.”
However, less formal communication is up to the hospitalist. The more you communicate with others, the more you’ll build your community.
Here are tips for how the hospitalist in the aforementioned example might work with each group of physicians:
ED doctors: “This hospitalist needs to get to know the other physicians and healthcare professionals,” Dr. Harris advises. “Make yourself available. When you have a minute, go down to the emergency department to update the ED physicians on admissions they’ve seen. Make a point to chat.”
Primary care physicians (PCPs): It may be more difficult to initiate informal communications with these docs if they’re not often in the hospital.
“One thing that helps is for the hospitalist to focus on communicating by phone, fax, or e-mail to PCPs when their patients are in the hospital,” says Dr. Harris. “In our office, we assigned a secretary to make sure PCPs get discharge summaries. That really helped with the community.”
If you want to strengthen ties to your community PCPs, issue an invitation to an event. “Our group would have an annual holiday party and invite all our referring physicians,” says Dr. Harris. “We’d have a speaker and get to know each other a little better.”
Surgeons: Dr. Harris suggests hospitalists can guide surgeons’ expectations for their working relationship with you and strengthen a sense of community.
“If there’s a particular issue, you can use that,” says Dr. Harris. “We were seeing a lot of elderly patients admitted with hip fractures. One thing we did to get a working relationship [with orthopedic surgeons] is we came up with a set of orders for these patients. The surgeons welcomed this because they wanted help with elderly patients who had multiple conditions. This was a way to work with them in a kind of formal way that helps patients. “It’s good to come up with order sets, but the big part of this is the negotiation with the other physicians that leads up to the order sets,” Dr. Harris says.
If you’re doing something like this to help in obstetrics, neurosurgery, or orthopedics, make it a two-way conversation.
“Above all else, it’s important to work with nonphysician healthcare workers,” says Dr. Harris, “especially nurses and physical therapists.”
The Rural Factor
The example above involves a small hospital medicine program in a rural area. Are there built-in problems with building community in this environment?
“I don’t think [it’s] necessarily more difficult” to build community in this setting, says Dr. Harris, “particularly if the hospital and physicians are on board with bringing in hospitalists. They might even be easier because you have fewer folks to deal with.”
But there may be an underlying problem with working at a smaller hospital. “If you’re the only hospitalist, or even the only hospitalist on a given shift, you’re practicing in a vacuum,” says Dr. Harris. If this is the case, you can broaden your hospitalist community by establishing a network with nearby hospitals and/or hospital medicine groups, and by becoming active in a regional or national group. TH
After the Discharge
Hospital discharge and transition, whether back into the community or to other levels of care, are burdened by a lack of standardization and can be executed poorly—making them treacherous periods for patients.
Indeed, 20% of discharges are complicated by adverse events within 30 days, often resulting in avoidable trips to the emergency department and rehospitalization. Nationwide, 25% of patients are readmitted within 90 days, often because the fragmented discharge process leaves them vulnerable to iatrogenic complications.
Yet few studies have examined the discharge process in depth. Until now, none have looked at it from the patient’s point of view, lead author Lee Strunin, PhD, and colleagues Meg Stone, MPH, and Brian Jack, MD, write in the September-October edition of the Journal of Hospital Medicine. They interviewed 21 low-income patients in an inner-city hospital in Boston to identify the factors most closely associated with the risk of readmission.
The patients had a mean age of 46, and all had been hospitalized at least once within the previous six months. Twenty of the 21 patients were in the hospital for the same primary problem they were admitted for on their previous stay. The interviews lasted 20 to 45 minutes with each patient and addressed the patient’s ability to obtain follow-up care, care after discharge, and social support.
In most cases, inability to understand discharge instructions was not a problem. All participants could describe those instructions as well as their medical condition, why they were admitted to the hospital, and the medications they were taking.
—Brian Jack, MD, associate professor of family medicine, Boston University Medical Center
“For the participants in this study, difficult life circumstances posed a greater barrier to recuperation than lack of medical knowledge,” the investigators write. Patients complained of little or no support in such areas as child care, transportation to medical appointments, or attempts to overcome alcoholism or drug abuse. Many patients could not follow instructions to rest because they had to work or care for young children.
Half the patients reported psychological conditions such as depression and stress, which interfered with their ability to follow their treatment plan. For example, an 18-year-old black woman with diabetes told of how she would do well for a while, following diet and medication recommendations and monitoring her blood sugar regularly, only to become depressed and lose motivation. She was not receiving treatment for her depression. Another woman with polycystic kidney disease described pain that was sometimes so intense she had to delegate the housekeeping chores to her 5-year-old son.
Even though the patients in this study appeared to understand their illnesses and what to do (under ideal circumstances) after they went home, poor health literacy could be one explanation for these findings, senior author Dr. Jack tells The Hospitalist.
“We have data now that patients with low health literacy are less ready for discharge,” says Dr. Jack, associate professor of family medicine, Boston University Medical Center, and the department’s founding vice chair for academic affairs. He and his colleagues are developing patient-centered interventions to mitigate the discrepancies between people who are more or less health-literate. “To the degree that the middle-class population has higher health literacy, [outcomes after discharge] might vary,” he says.
These findings demonstrate the critical effect life circumstances outside the hospital have on a patient’s recovery, the authors say in the paper, adding that the patients’ experiences “clearly demonstrate the ways in which stresses make it difficult or impossible to attain sufficient rest to heal, maintain behavior change necessary to improve health, and follow instructions given by clinicians at the time of discharge.”
They further point out that interventions aimed at low-income patients should include social support and assistance with daily responsibilities.
“A focus on each patient’s life circumstance is critical,” Dr. Jack explains. For example, it isn’t sufficient simply to tell the patient when to come back for a stress test. Hospitals or caseworkers should also determine if “it is a day the patient can go, do they have a ride, daycare, do they know where the test is, which doctor will follow up the results, will they be seeing that doctor, and so on. There are now recent data suggesting that most tests ordered after discharge are never done.”
From this and other studies on the subject, it seems intuitive that providing these supports for at-risk patients should reduce rehospitalization rates. Is there any evidence this is the case?
“Not yet,” Dr. Jack says. “But stay tuned.” TH
Norra MacReady is a medical writer based in California.
Hospital discharge and transition, whether back into the community or to other levels of care, are burdened by a lack of standardization and can be executed poorly—making them treacherous periods for patients.
Indeed, 20% of discharges are complicated by adverse events within 30 days, often resulting in avoidable trips to the emergency department and rehospitalization. Nationwide, 25% of patients are readmitted within 90 days, often because the fragmented discharge process leaves them vulnerable to iatrogenic complications.
Yet few studies have examined the discharge process in depth. Until now, none have looked at it from the patient’s point of view, lead author Lee Strunin, PhD, and colleagues Meg Stone, MPH, and Brian Jack, MD, write in the September-October edition of the Journal of Hospital Medicine. They interviewed 21 low-income patients in an inner-city hospital in Boston to identify the factors most closely associated with the risk of readmission.
The patients had a mean age of 46, and all had been hospitalized at least once within the previous six months. Twenty of the 21 patients were in the hospital for the same primary problem they were admitted for on their previous stay. The interviews lasted 20 to 45 minutes with each patient and addressed the patient’s ability to obtain follow-up care, care after discharge, and social support.
In most cases, inability to understand discharge instructions was not a problem. All participants could describe those instructions as well as their medical condition, why they were admitted to the hospital, and the medications they were taking.
—Brian Jack, MD, associate professor of family medicine, Boston University Medical Center
“For the participants in this study, difficult life circumstances posed a greater barrier to recuperation than lack of medical knowledge,” the investigators write. Patients complained of little or no support in such areas as child care, transportation to medical appointments, or attempts to overcome alcoholism or drug abuse. Many patients could not follow instructions to rest because they had to work or care for young children.
Half the patients reported psychological conditions such as depression and stress, which interfered with their ability to follow their treatment plan. For example, an 18-year-old black woman with diabetes told of how she would do well for a while, following diet and medication recommendations and monitoring her blood sugar regularly, only to become depressed and lose motivation. She was not receiving treatment for her depression. Another woman with polycystic kidney disease described pain that was sometimes so intense she had to delegate the housekeeping chores to her 5-year-old son.
Even though the patients in this study appeared to understand their illnesses and what to do (under ideal circumstances) after they went home, poor health literacy could be one explanation for these findings, senior author Dr. Jack tells The Hospitalist.
“We have data now that patients with low health literacy are less ready for discharge,” says Dr. Jack, associate professor of family medicine, Boston University Medical Center, and the department’s founding vice chair for academic affairs. He and his colleagues are developing patient-centered interventions to mitigate the discrepancies between people who are more or less health-literate. “To the degree that the middle-class population has higher health literacy, [outcomes after discharge] might vary,” he says.
These findings demonstrate the critical effect life circumstances outside the hospital have on a patient’s recovery, the authors say in the paper, adding that the patients’ experiences “clearly demonstrate the ways in which stresses make it difficult or impossible to attain sufficient rest to heal, maintain behavior change necessary to improve health, and follow instructions given by clinicians at the time of discharge.”
They further point out that interventions aimed at low-income patients should include social support and assistance with daily responsibilities.
“A focus on each patient’s life circumstance is critical,” Dr. Jack explains. For example, it isn’t sufficient simply to tell the patient when to come back for a stress test. Hospitals or caseworkers should also determine if “it is a day the patient can go, do they have a ride, daycare, do they know where the test is, which doctor will follow up the results, will they be seeing that doctor, and so on. There are now recent data suggesting that most tests ordered after discharge are never done.”
From this and other studies on the subject, it seems intuitive that providing these supports for at-risk patients should reduce rehospitalization rates. Is there any evidence this is the case?
“Not yet,” Dr. Jack says. “But stay tuned.” TH
Norra MacReady is a medical writer based in California.
Hospital discharge and transition, whether back into the community or to other levels of care, are burdened by a lack of standardization and can be executed poorly—making them treacherous periods for patients.
Indeed, 20% of discharges are complicated by adverse events within 30 days, often resulting in avoidable trips to the emergency department and rehospitalization. Nationwide, 25% of patients are readmitted within 90 days, often because the fragmented discharge process leaves them vulnerable to iatrogenic complications.
Yet few studies have examined the discharge process in depth. Until now, none have looked at it from the patient’s point of view, lead author Lee Strunin, PhD, and colleagues Meg Stone, MPH, and Brian Jack, MD, write in the September-October edition of the Journal of Hospital Medicine. They interviewed 21 low-income patients in an inner-city hospital in Boston to identify the factors most closely associated with the risk of readmission.
The patients had a mean age of 46, and all had been hospitalized at least once within the previous six months. Twenty of the 21 patients were in the hospital for the same primary problem they were admitted for on their previous stay. The interviews lasted 20 to 45 minutes with each patient and addressed the patient’s ability to obtain follow-up care, care after discharge, and social support.
In most cases, inability to understand discharge instructions was not a problem. All participants could describe those instructions as well as their medical condition, why they were admitted to the hospital, and the medications they were taking.
—Brian Jack, MD, associate professor of family medicine, Boston University Medical Center
“For the participants in this study, difficult life circumstances posed a greater barrier to recuperation than lack of medical knowledge,” the investigators write. Patients complained of little or no support in such areas as child care, transportation to medical appointments, or attempts to overcome alcoholism or drug abuse. Many patients could not follow instructions to rest because they had to work or care for young children.
Half the patients reported psychological conditions such as depression and stress, which interfered with their ability to follow their treatment plan. For example, an 18-year-old black woman with diabetes told of how she would do well for a while, following diet and medication recommendations and monitoring her blood sugar regularly, only to become depressed and lose motivation. She was not receiving treatment for her depression. Another woman with polycystic kidney disease described pain that was sometimes so intense she had to delegate the housekeeping chores to her 5-year-old son.
Even though the patients in this study appeared to understand their illnesses and what to do (under ideal circumstances) after they went home, poor health literacy could be one explanation for these findings, senior author Dr. Jack tells The Hospitalist.
“We have data now that patients with low health literacy are less ready for discharge,” says Dr. Jack, associate professor of family medicine, Boston University Medical Center, and the department’s founding vice chair for academic affairs. He and his colleagues are developing patient-centered interventions to mitigate the discrepancies between people who are more or less health-literate. “To the degree that the middle-class population has higher health literacy, [outcomes after discharge] might vary,” he says.
These findings demonstrate the critical effect life circumstances outside the hospital have on a patient’s recovery, the authors say in the paper, adding that the patients’ experiences “clearly demonstrate the ways in which stresses make it difficult or impossible to attain sufficient rest to heal, maintain behavior change necessary to improve health, and follow instructions given by clinicians at the time of discharge.”
They further point out that interventions aimed at low-income patients should include social support and assistance with daily responsibilities.
“A focus on each patient’s life circumstance is critical,” Dr. Jack explains. For example, it isn’t sufficient simply to tell the patient when to come back for a stress test. Hospitals or caseworkers should also determine if “it is a day the patient can go, do they have a ride, daycare, do they know where the test is, which doctor will follow up the results, will they be seeing that doctor, and so on. There are now recent data suggesting that most tests ordered after discharge are never done.”
From this and other studies on the subject, it seems intuitive that providing these supports for at-risk patients should reduce rehospitalization rates. Is there any evidence this is the case?
“Not yet,” Dr. Jack says. “But stay tuned.” TH
Norra MacReady is a medical writer based in California.
Steroid Stress Dosing
Adrenal response to stress can vary broadly from patient to patient. For hospitalists, the challenge is predicting patients’ cortisol needs.
The variability exists whether one is dealing with a healthy patient or a patient with adrenal insufficiency (AI).1 Glucocorticoid use is even more complicated in patients with chronic autoimmune or inflammatory disorders who have been treated with high doses of glucocorticoids, or with those who are hypothalamic-pituitary-adrenal (HPA) axis suppressed.
Additionally, glucocorticoid administration is the most common cause of AI. Guidelines for adrenal supplementation therapy published in JAMA in 2002 note the difficulty in determining exact patient needs. JAMA’s review of guidelines for adrenal supplementation therapy is based on expert opinion, extrapolation from research literature, and clinical experience rather than clinical trials and should be consulted for more specific patient recommendations.2
Around the same time, similar guidelines on the management of rheumatoid arthritis (RA) patients on chronic glucocorticoids were published in the Bulletin on the Rheumatic Diseases.3 The guidelines suggest lower doses and shorter therapy than many textbooks advocate to counter problems associated with excessive steroid dosing. Problems such as immunosuppression, hyperglycemia, hypertension, acute psychosis, and accelerated protein catabolism lead to poor wound healing.
Additionally, the guidelines recommend that all patients receiving chronic glucocorticoids with an illness or while undergoing any procedure continue their normal daily glucocorticoid therapy. The authors caution that in patients with rheumatic disease, discontinuation of even low glucocorticoid doses may lead to a significant disease flare. Patients who receive 5 mg or less of prednisone daily do not require additional supplementation—regardless of whether they are undergoing a procedure or have an intercurrent illness. Patients undergoing superficial surgical procedures while less than an hour under local anesthesia (e.g., routine dental work, skin biopsy, minor orthopedic surgery) require their normal daily glucocorticoid dose without additional supplementation.
Patients with primary AI should receive individualized supplemental homeostatic glucocorticoid replacement therapy—usually with 20 to 30 mg of hydrocortisone two to three times daily in divided doses. Adjust based on patient factors and use of concomitant medications. Also consider that mineralocorticoid replacement may be necessary in these patients.
When considering patients for potential use of corticosteroids in the hospital, identify those who may be HPA-axis suppressed versus those who are not. The time to achieve HPA-axis suppression varies among patients. Patients can be considered not suppressed if:
- They have received any glucocorticoid doses for less than weeks; and
- They have received alternate-day glucocorticoid therapy. 4-6
- On the contrary, patients should be assumed to have HPA-axis suppression if they:
- Have received less than 20 mg of prednisone or its equivalent daily for more than three weeks (e.g., 16 mg/day methylprednisolone, 2 mg/ day dexamethasone, 80 mg/ day hydrocortisone); and/or
- Have clinical Cushing’s syndrome (e.g., centripetal obesity, glucose intolerance, proximal myopathy, hypertension, psychological chan-ges, and easy bruisability).
Intermediate patient categories may require HPA axis function testing with cosyntropin to determine if AI is present. TH
Michele Kaufman is a clinical/managed care consultant and medical writer based in New York City.
References
- Lamberts SWJ, Bruining HA, de Jong FK. Corticosteroid therapy in severe illness. N Engl J Med. 1997 Oct 30;337(18):1285-1292.
- Coursin DB, Wood KE. Corticosteroid supplementation for adrenal insufficiency. JAMA. 2002 Jan 9;287(2):236-240.
- Kelley JT, Conn DL. Perioperative management of the rheumatic disease patient. Bull Rheum Dis. 2002;51(6).
- Nieman LK, Kovacs WJ. Pharmacologic use of glucocorticoids. UpToDate. Waltham, Mass. 2007. Available at: www.pharmacologic use of glucocorticoids
- Nieman LK. Clinical manifestations of Cushing’s syndrome. UpToDate. Waltham, Mass. 2007.
- Welsh GA, Manzullo EF, Nieman LK. The surgical patient taking glucocorticoids. UpToDate. Waltham, Mass. 2007. Available at: www.patients.uptodate.com/topic.asp?file=adrenal
Adrenal response to stress can vary broadly from patient to patient. For hospitalists, the challenge is predicting patients’ cortisol needs.
The variability exists whether one is dealing with a healthy patient or a patient with adrenal insufficiency (AI).1 Glucocorticoid use is even more complicated in patients with chronic autoimmune or inflammatory disorders who have been treated with high doses of glucocorticoids, or with those who are hypothalamic-pituitary-adrenal (HPA) axis suppressed.
Additionally, glucocorticoid administration is the most common cause of AI. Guidelines for adrenal supplementation therapy published in JAMA in 2002 note the difficulty in determining exact patient needs. JAMA’s review of guidelines for adrenal supplementation therapy is based on expert opinion, extrapolation from research literature, and clinical experience rather than clinical trials and should be consulted for more specific patient recommendations.2
Around the same time, similar guidelines on the management of rheumatoid arthritis (RA) patients on chronic glucocorticoids were published in the Bulletin on the Rheumatic Diseases.3 The guidelines suggest lower doses and shorter therapy than many textbooks advocate to counter problems associated with excessive steroid dosing. Problems such as immunosuppression, hyperglycemia, hypertension, acute psychosis, and accelerated protein catabolism lead to poor wound healing.
Additionally, the guidelines recommend that all patients receiving chronic glucocorticoids with an illness or while undergoing any procedure continue their normal daily glucocorticoid therapy. The authors caution that in patients with rheumatic disease, discontinuation of even low glucocorticoid doses may lead to a significant disease flare. Patients who receive 5 mg or less of prednisone daily do not require additional supplementation—regardless of whether they are undergoing a procedure or have an intercurrent illness. Patients undergoing superficial surgical procedures while less than an hour under local anesthesia (e.g., routine dental work, skin biopsy, minor orthopedic surgery) require their normal daily glucocorticoid dose without additional supplementation.
Patients with primary AI should receive individualized supplemental homeostatic glucocorticoid replacement therapy—usually with 20 to 30 mg of hydrocortisone two to three times daily in divided doses. Adjust based on patient factors and use of concomitant medications. Also consider that mineralocorticoid replacement may be necessary in these patients.
When considering patients for potential use of corticosteroids in the hospital, identify those who may be HPA-axis suppressed versus those who are not. The time to achieve HPA-axis suppression varies among patients. Patients can be considered not suppressed if:
- They have received any glucocorticoid doses for less than weeks; and
- They have received alternate-day glucocorticoid therapy. 4-6
- On the contrary, patients should be assumed to have HPA-axis suppression if they:
- Have received less than 20 mg of prednisone or its equivalent daily for more than three weeks (e.g., 16 mg/day methylprednisolone, 2 mg/ day dexamethasone, 80 mg/ day hydrocortisone); and/or
- Have clinical Cushing’s syndrome (e.g., centripetal obesity, glucose intolerance, proximal myopathy, hypertension, psychological chan-ges, and easy bruisability).
Intermediate patient categories may require HPA axis function testing with cosyntropin to determine if AI is present. TH
Michele Kaufman is a clinical/managed care consultant and medical writer based in New York City.
References
- Lamberts SWJ, Bruining HA, de Jong FK. Corticosteroid therapy in severe illness. N Engl J Med. 1997 Oct 30;337(18):1285-1292.
- Coursin DB, Wood KE. Corticosteroid supplementation for adrenal insufficiency. JAMA. 2002 Jan 9;287(2):236-240.
- Kelley JT, Conn DL. Perioperative management of the rheumatic disease patient. Bull Rheum Dis. 2002;51(6).
- Nieman LK, Kovacs WJ. Pharmacologic use of glucocorticoids. UpToDate. Waltham, Mass. 2007. Available at: www.pharmacologic use of glucocorticoids
- Nieman LK. Clinical manifestations of Cushing’s syndrome. UpToDate. Waltham, Mass. 2007.
- Welsh GA, Manzullo EF, Nieman LK. The surgical patient taking glucocorticoids. UpToDate. Waltham, Mass. 2007. Available at: www.patients.uptodate.com/topic.asp?file=adrenal
Adrenal response to stress can vary broadly from patient to patient. For hospitalists, the challenge is predicting patients’ cortisol needs.
The variability exists whether one is dealing with a healthy patient or a patient with adrenal insufficiency (AI).1 Glucocorticoid use is even more complicated in patients with chronic autoimmune or inflammatory disorders who have been treated with high doses of glucocorticoids, or with those who are hypothalamic-pituitary-adrenal (HPA) axis suppressed.
Additionally, glucocorticoid administration is the most common cause of AI. Guidelines for adrenal supplementation therapy published in JAMA in 2002 note the difficulty in determining exact patient needs. JAMA’s review of guidelines for adrenal supplementation therapy is based on expert opinion, extrapolation from research literature, and clinical experience rather than clinical trials and should be consulted for more specific patient recommendations.2
Around the same time, similar guidelines on the management of rheumatoid arthritis (RA) patients on chronic glucocorticoids were published in the Bulletin on the Rheumatic Diseases.3 The guidelines suggest lower doses and shorter therapy than many textbooks advocate to counter problems associated with excessive steroid dosing. Problems such as immunosuppression, hyperglycemia, hypertension, acute psychosis, and accelerated protein catabolism lead to poor wound healing.
Additionally, the guidelines recommend that all patients receiving chronic glucocorticoids with an illness or while undergoing any procedure continue their normal daily glucocorticoid therapy. The authors caution that in patients with rheumatic disease, discontinuation of even low glucocorticoid doses may lead to a significant disease flare. Patients who receive 5 mg or less of prednisone daily do not require additional supplementation—regardless of whether they are undergoing a procedure or have an intercurrent illness. Patients undergoing superficial surgical procedures while less than an hour under local anesthesia (e.g., routine dental work, skin biopsy, minor orthopedic surgery) require their normal daily glucocorticoid dose without additional supplementation.
Patients with primary AI should receive individualized supplemental homeostatic glucocorticoid replacement therapy—usually with 20 to 30 mg of hydrocortisone two to three times daily in divided doses. Adjust based on patient factors and use of concomitant medications. Also consider that mineralocorticoid replacement may be necessary in these patients.
When considering patients for potential use of corticosteroids in the hospital, identify those who may be HPA-axis suppressed versus those who are not. The time to achieve HPA-axis suppression varies among patients. Patients can be considered not suppressed if:
- They have received any glucocorticoid doses for less than weeks; and
- They have received alternate-day glucocorticoid therapy. 4-6
- On the contrary, patients should be assumed to have HPA-axis suppression if they:
- Have received less than 20 mg of prednisone or its equivalent daily for more than three weeks (e.g., 16 mg/day methylprednisolone, 2 mg/ day dexamethasone, 80 mg/ day hydrocortisone); and/or
- Have clinical Cushing’s syndrome (e.g., centripetal obesity, glucose intolerance, proximal myopathy, hypertension, psychological chan-ges, and easy bruisability).
Intermediate patient categories may require HPA axis function testing with cosyntropin to determine if AI is present. TH
Michele Kaufman is a clinical/managed care consultant and medical writer based in New York City.
References
- Lamberts SWJ, Bruining HA, de Jong FK. Corticosteroid therapy in severe illness. N Engl J Med. 1997 Oct 30;337(18):1285-1292.
- Coursin DB, Wood KE. Corticosteroid supplementation for adrenal insufficiency. JAMA. 2002 Jan 9;287(2):236-240.
- Kelley JT, Conn DL. Perioperative management of the rheumatic disease patient. Bull Rheum Dis. 2002;51(6).
- Nieman LK, Kovacs WJ. Pharmacologic use of glucocorticoids. UpToDate. Waltham, Mass. 2007. Available at: www.pharmacologic use of glucocorticoids
- Nieman LK. Clinical manifestations of Cushing’s syndrome. UpToDate. Waltham, Mass. 2007.
- Welsh GA, Manzullo EF, Nieman LK. The surgical patient taking glucocorticoids. UpToDate. Waltham, Mass. 2007. Available at: www.patients.uptodate.com/topic.asp?file=adrenal