User login
Other Literature of Interest
1. Dexter PR, Perkins SM, Mahany KS, Jones K, McDonald CJ. Inpatient computer-based standing orders vs. physician reminders to increase influenza and pneumococcal vaccination rates: a randomized trial. JAMA. 2004; 292: 2366-71.
Past studies have suggested that most patients admitted with severe pneumococcal infections have been hospitalized in the preceding 5 years, and simply being hospitalized is a potential risk factor for later pneumococcal infection. Likewise, hospitalization provides an opportunity to vaccinate high-risk patients against influenza, and raising pneumococcal and influenza immunization rates is a CMS quality improvement priority. Prior investigations have supported the use of labor-intensive manual standing orders as well as computerized reminders, but this prospective trial was conducted in 1998 and 1999 to assess the effectiveness of a computer-based system to screen for eligible patients and then generate orders to perform pneumonia and influenza vaccinations on inpatients at the time of discharge.
Over 13 months, a total of 3777 inpatients were entered into the study. The hospital computer identified patients eligible for vaccination based on common criteria and randomized them to one of two groups of physician teams. For one group of teams, the computer order-entry system would automatically generate vaccination orders at the time of discharge for vaccine-eligible patients; for the other group of teams, only computer reminders were provided to physicians. The outcome measure was administration of vaccine; long-term outcomes such as incidence of subsequent disease or mortality were not measured.
During the study period, 50% of all hospitalized patients were identified as eligible for influenza vaccination; 22% were eligible for pneumococcal vaccination. In each case, the “standing order” group received vaccine more often (influenza: 42% vs. 30%, p<.001; pneumococcal vaccine: 51% vs. 31%). The numbers were subsequently adjusted to allow for patients who had previously received vaccine, but the impressive differences persisted. Nurses reported reasons for non-administration in 98% of the eligible patients who were not vaccinated; the most common reason was patient refusal. It is not clear if the physicians knew that a study was being conducted. No adverse reactions were reported.
CMS has pushed for the development of institutional standing order sets as a tool to improve compliance with vaccination rate targets. Where the technology is available, computer systems that can screen eligible patients and generate automatic orders are an effective tool in implementing many quality-improvement initiatives, and hospitalists are in a crucial position to take an active role in their development and implementation.
2. Fang MC, Chang Y, Hylek EM, et al. Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for a trial fibrillation. Ann Intern Med. 2004; 141: 745-52.
Warfarin has been shown to reduce risk of stroke in patients with chronic and paroxysmal atrial fibrillation. Intracranial hemorrhage remains one of the most feared complications of warfarin, especially among older patients, prompting suggestions to consider lower intensity anticoagulation among patients older than 75 years who have atrial fibrillation.
This study evaluated the relationship between the intensity of anticoagulation, risk of intracranial hemorrhage, and age of patients with atrial fibrillation.
This was a retrospective case control study conducted at a tertiary care medical center. One-hundred and seventy patients on warfarin and admitted with intracranial hemorrhage from 1993 to 2002 were matched with 1020 patients who were on warfarin but without intracranial bleed. After controlling for comorbid conditions and aspirin use, authors conducted multivariable logistic regression analysis to determine the odds of intracranial hemorrhage with regard to age and INR. The risk of intracranial hemorrhage increased at 85 years of age and at INR values of 3.5 or greater. The risk of intracranial hemorrhage at INR less than 2.0 did not differ statistically from the risk at INR of 2.0–3.0.
This study shows the risk of intracranial hemorrhage is not decreased by choosing lower intensity anticoagulation, and target INR should still be kept at 2.5 among elderly patients. However, patients older than 85 years should be counseled about their higher risk of intracranial hemorrhage.
3. Heeschen C, Hamm CW, Mitrovic V, et al. N-terminal pro-B-type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation. 2004;110: 3206-12.
Recent data demonstrate the prognostic value of assessment of neurohormonal activation in patients with acute coronary syndromes (ACS). B-type natriuretic peptide levels (BNP) and levels of the N-terminal fragment of the BNP prohormone (NT-proBNP) predict adverse long-term outcomes in patients with ACS. Investigators reviewed plasma samples of Troponin T (TnT) and NT-proBNP obtained from patients with ACS enrolled in the Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) trial, which randomized patients to tirofiban or heparin for 48 hours and assessed mortality and myocardial infarction at 30 day follow-up. TnT and NT-proBNP determinations were available at baseline for 1791 patients, and at 48 and 72 hours from 1401 patients. Baseline NT-proBNP levels >250 ng/L were associated with significantly higher rates of death and myocardial infarction at 7 and 30 day follow-up. After adjustment for TnT and C-reactive protein levels, elevated NTproBNP levels maintained its predictive value (OR 2.7; p<.001). In patients with normal TnT levels, NT-proBNP levels identified a subgroup of patients at increased risk (OR 3.0; p=.004). However, in patients with high TnT levels (>0.1 mcg/L), NT-proBNP lost its predictive value (p=.58). More importantly, patients with normal levels of both TnT and NT-proBNP were at very low risk (0.6% event rate at 30 day follow-up).
Serial determinations of NT-proBNP levels at 48 and 72 hours were reviewed in patients without major adverse cardiac events (death or myocardial infarction); these patients were subdivided into groups with and without refractory ischemia. Patients without refractory ischemia showed a significant decline in NT-proBNP levels, whereas patients with refractory ischemia had no significant change. Persistently elevated NT-proBNP levels at 72 hours were associated with a 17.2% risk of death or MI at 30 days, compared with 0.6% risk if NT-proBNP returned to normal at 72 hours (p<.001). Neither TnT nor C-reactive protein demonstrated similar predictive value.
The study is limited by its retrospective nature, by potential selection bias by including only patients with direct evidence of coronary artery disease, and by limitations of the generalizability of its findings (e.g., to emergency department patients with chest pain).
As BNP and NT-proBNP are counter-regulatory hormones that play an active role in the response to ischemic injury, the authors suggest that NT-proBNP is a promising tool for dynamic risk assessment in patients with ACS. The authors also do not differentiate between BNP and NT-proBNP with regard to use in risk stratification, which might lead one to believe that these tests share similar predictive value. (Of note, the study was entirely funded by a company that produces an assay for NT-proBNP). Prospective trials to validate this tool are warranted
4. Heuschmann PU, Kolominsky-Rabas PL, Roether J, et al. Predictors of in-hospital mortality in patients with acute ischemic stroke treated with thrombolytic therapy. JAMA. 2004;292:1831-38.
The objective of this study was to identify factors associated with in-hospital mortality in ischemic stroke patients treated with recombinant tissue plasminogen activator (tPA). It was a prospective observational cohort study of 1658 patients conducted at 225 community and academic hospitals throughout Germany with main outcome of in-hospital mortality.
In this study 10% of patients who were treated with tPA died during their hospital stay, with 2/3 of deaths occurring in the first 7 days. Relative probability of in-hospital mortality increased with increasing patient age, with an odds ratio (OR) of 1.6 for each 10-year increment in age. Age was an independent predictor of in hospital mortality irrespective of tPA administration, with patients older than 75 years age having 4 fold higher mortality than the youngest cohort of less than 55 years age.
Other factors predicting in hospital mortality were altered level of consciousness and relative lack of experience with tPA treatment in the center. Altered level of consciousness was a predictor of stroke severity and an independent predictor of in-hospital mortality (OR 3.4). The increase in mortality in centers with limited experience with tPA administration (OR 0.97) reflected learning curve issues with these patients. The study was not designed to separate out the confounders of operator experience curve from institutional experience curves, or to derive the exact relationship between experience and outcomes.
5. McAlister FA, Bertsch K, Man J, et al. Incidence of and risk factors for pulmonary complications after non-thoracic surgery. Am J Respir Crit Care Med. 2004; published ahead of print on November 24, 2004 as doi:10.1164/rccm.200408-1069OC. Accessed January 27, 2005.
Postoperative pulmonary complications after nonthoracic surgery are a cause of significant morbidity and increased length of hospital stay. Previous studies of preoperative pulmonary assessment were limited by non-representative patient samples, conflicting results, and lack of explicit definitions of these complications. The authors conducted a prospective cohort study of 1055 patients seen in a Pre-Admission Clinic of a tertiary care university hospital. Mean age was 55 years, 50% male, and the cohort consisted of patients scheduled for intermediate risk elective surgery (upper abdominal, lower abdominal, orthopedic). They evaluated physical exam maneuvers (cough test, wheeze test, maximal laryngeal height, and forced expiratory time, all of which are described in an online data supplement) and preoperative spirometry values, and collected information on clinically significant postoperative pulmonary complications, including pneumonia, respiratory failure requiring mechanical ventilation, atelectasis requiring bronchoscopy, or pneumothorax or pleural effusion requiring percutaneous intervention. Twenty-eight patients (2.7%) suffered a pulmonary complication within 7 days of surgery, one of whom died. Length of stay was significantly prolonged in this group (mean 27.9 days vs 4.5 days, p=.006). Multivariate regression analysis revealed four variables that were independently associated with increased risk for postoperative pulmonary complications: age > 65 years, positive cough test (repeated coughing after asking the patient to inhale deeply and cough once), perioperative nasogastric tube, and anesthesia duration 2.5 hours or greater. Number of pack years smoked, FEV1, FEV1/FVC ratio, and upper abdominal surgery were associated with postoperative pulmonary complications but were not found to be independently associated by multivariate analysis.
While it is not surprising that the above risk factors are predictive of postoperative complications, this is the first study to incorporate specific exam maneuvers and spirometry into a risk prediction analysis. Limitations of this model are lack of independent validation and lack of generalizability to other populations, e.g., inpatients awaiting urgent surgery. Of note, the study further provides further support for not routinely obtaining pulmonary function testing for risk stratification prior to noncardiac surgery.
6. Mortenson, EM, Restrepo M, Anzeuto A, Pugh J. Effects of guideline-concordant antimicrobial therapy on mortality among patients with community-acquired pneumonia. Am J Med. 2004;117:726-31.
The American Thoracic Society (ATS) and the Infectious Diseases Society of America (IDSA) have published guidelines for the management of community acquired pneumonia that include recommendations for antibiotic selection. This retrospective cohort study attempted to measure the association between adherence to such guidelines and 30-day mortality in patients admitted with pneumonia to two Texas hospitals.
The characteristics of the patients studied reflect a reasonable cross-section of typical pneumonia patients, with the exception that the patients were mostly (85%) men. Of the study population, 78% were admitted through the ER, 20% admitted to the ICU, and 9% were nursing home residents. Antibiotics were considered “concordant” if they were consistent with either the most recent IDSA or ATS recommendations. The “nonconcordant” group was slightly older (66 vs. 61), generally sicker (higher rate of comorbid COPD and CVD), had more cerebrovascular disease, was more likely to present with altered mental status, and less frequently received antibiotics within 8 hours of presentation. The study did not comment on patients’ vaccination status. Thirty-day mortality was 6.2% in the guideline-concordant group, versus 21.7% in the other group (p < .001). The most common “non-concordant” regimen described was use of a beta-lactam alone, although specific antibiotic regimens were not evaluated.
While the results of this study are not surprising, they provide us with both the validation to continue practice according to existing recommendations, particularly the avoidance of monotherapy with beta-lactam antibiotics. The study also provides us with the imperative to take the lead in developing evidence-based pneumonia pathways at our own hospitals.
7. Pham MX, Whooley MA, Evans GT Jr, et al. Prognostic value of low-level cardiac troponin-I elevations in patients without definite acute coronary syndromes. Am Heart J. 2004;148: 776-82.
With the availability of rapid and highly sensitive and specific troponin testing, many patients admitted to the hospital with non-cardiac diagnoses have been recognized as having abnormal serum troponin-I or troponin-T levels, often just slightly above the reference cutoff for “normal.” While the clinical assumption is often that the elevated enzyme level does not reflect an acute coronary syndrome per se, its significance regarding the patient’s underlying cardiac health is often unclear.
Pham et al. retrospectively reviewed the 1-year mortality of 366 patients who were admitted to the San Francisco VA without evidence of acute MI or ACS either clinically or by EKG, but who had low-level troponin-I elevations (up to 3.0 ng/mL—a level that the authors state was reached by institutional consensus, and which was measured by a “first-generation” assay). These patients were admitted for a broad spectrum of diagnoses ranging from CHF to COPD to sepsis. Ninety-six percent of the patients were men; their average age was 69.
Follow-up was accomplished after a mean of 288 days and included 97% of patients. The primary endpoint was MI or death due to cardiac disease at one year; secondary endpoints were revascularization or admission for unstable angina. The primary endpoint was reached by 11% of patients with cTn-I between 1.0 and 3.0 ng/mL, and 4% of the patients with cTn-I up to 1.0 ng/mL (adjusted HR 3.4, 95% CI, 1.3 to 9.4), and the higher the cTn-I, the higher the risk. However, the authors did not test for the level of risk by specific diagnosis, so they caution against overgeneralizing their findings.
The findings of this study add to the evidence that any evidence of myocardial injury implies an increased risk of underlying heart disease and accompanying long—term cardiac complications– even if such injury occurs in the absence of ACS or known heart disease. Hospitalists often see such injury in the setting of acute infection and pulmonary disease and may be the first to recognize the possibility of CHD in a given patient. To date, guidelines addressing optimal prospective risk stratification have not been developed. Until they are, hospitalists should be aware of the ramifications of “troponin leak” and be prepared to initiate necessary inpatient monitoring and treatments, and to coordinate appropriate follow-up for these patients.
8. Saposnik G, Young B, Silver B, et al. Lack of improvement in patients with acute stroke after treatment with thrombolytic therapy: predictors and association with outcome. JAMA. 2004; 292: 1839-44.
Recombinant tissue plasminogen activator (tPA) has been shown to be one of the most efficacious therapies for acute stroke treatment. This was a systematic evaluation of predictors for outcomes at 24 hours after tPA therapy and of the prognostic significance of lack of improvement at 24 hours for long-term outcomes at 3 months.
The trial was a prospective cohort study of 216 consecutive patients admitted with acute ischemic stroke to a university hospital. The decision to treat with tPA was based on the NINDS protocol with one difference: patients with involvement of more than one third of the middle cerebral artery on the baseline CT scan were excluded. A control CT scan was performed at 24 hours to determine the presence of new infarction, cortical involvement, and extension of the ischemic lesion.
Lack of improvement was defined as a difference between the NIHSS score at baseline and at 24 hours of 3 points or less. Poor outcome at 3 months was defined by a modified Rankin Scale score of 3 to 5 or death.
After adjusting for age, gender, and stroke severity, hyperglycemia at admission (glucose > 144 mg/dL), cortical involvement, and time to treatment were independent predictors of lack of improvement at 24 hours. After adjusting for age, gender, and stroke severity, lack of improvement at 24 hours was an independent predictor of poor outcome and death at 3 months. Patients with lack of improvement at 24 hours also had longer lengths of hospitalization.
9. Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049-57.
Neurohormonal changes, endothelial dysfunction, impaired nitric oxide availability, and oxidant stress all contribute to the structural remodeling of the left ventricle in congestive heart failure. The combination of isosorbide dinitrate, an organic nitrate that stimulates nitric oxide signaling, and the antioxidant and vasodilator hydralazine improves survival in heart failure. Based on more recent data that black patients have a clinically significant response to this combination therapy, the authors of the African-American Heart Failure Trial (A-HeFT) evaluated 1050 black patients with congestive heart failure in a randomized, double-blind, placebo controlled trial. Patients were randomized to fixed doses of isosorbide dinitrate and hydralazine plus background therapy (i.e., digoxin, ACE inhibitors, beta-blockers, diuretics, angiotensin receptor blockers) or to placebo plus background therapy. After 18 months, the trial was stopped due to a significantly higher mortality rate in the placebo group (10.2% in the placebo group vs. 6.2% with combination
therapy, p=.02); survival differences emerged at 180 days and increased progressively thereafter. The combination therapy group reported more headache and dizziness but suffered fewer exacerbations of congestive heart failure and reported improvement in subjective assessments of quality of life as measured by questionnaires. Accompanying editorials discuss the role of nitric oxide and prevention of oxidative stress in the treatment of heart failure, as well as the controversial issues surrounding race-based therapeutics.
1. Dexter PR, Perkins SM, Mahany KS, Jones K, McDonald CJ. Inpatient computer-based standing orders vs. physician reminders to increase influenza and pneumococcal vaccination rates: a randomized trial. JAMA. 2004; 292: 2366-71.
Past studies have suggested that most patients admitted with severe pneumococcal infections have been hospitalized in the preceding 5 years, and simply being hospitalized is a potential risk factor for later pneumococcal infection. Likewise, hospitalization provides an opportunity to vaccinate high-risk patients against influenza, and raising pneumococcal and influenza immunization rates is a CMS quality improvement priority. Prior investigations have supported the use of labor-intensive manual standing orders as well as computerized reminders, but this prospective trial was conducted in 1998 and 1999 to assess the effectiveness of a computer-based system to screen for eligible patients and then generate orders to perform pneumonia and influenza vaccinations on inpatients at the time of discharge.
Over 13 months, a total of 3777 inpatients were entered into the study. The hospital computer identified patients eligible for vaccination based on common criteria and randomized them to one of two groups of physician teams. For one group of teams, the computer order-entry system would automatically generate vaccination orders at the time of discharge for vaccine-eligible patients; for the other group of teams, only computer reminders were provided to physicians. The outcome measure was administration of vaccine; long-term outcomes such as incidence of subsequent disease or mortality were not measured.
During the study period, 50% of all hospitalized patients were identified as eligible for influenza vaccination; 22% were eligible for pneumococcal vaccination. In each case, the “standing order” group received vaccine more often (influenza: 42% vs. 30%, p<.001; pneumococcal vaccine: 51% vs. 31%). The numbers were subsequently adjusted to allow for patients who had previously received vaccine, but the impressive differences persisted. Nurses reported reasons for non-administration in 98% of the eligible patients who were not vaccinated; the most common reason was patient refusal. It is not clear if the physicians knew that a study was being conducted. No adverse reactions were reported.
CMS has pushed for the development of institutional standing order sets as a tool to improve compliance with vaccination rate targets. Where the technology is available, computer systems that can screen eligible patients and generate automatic orders are an effective tool in implementing many quality-improvement initiatives, and hospitalists are in a crucial position to take an active role in their development and implementation.
2. Fang MC, Chang Y, Hylek EM, et al. Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for a trial fibrillation. Ann Intern Med. 2004; 141: 745-52.
Warfarin has been shown to reduce risk of stroke in patients with chronic and paroxysmal atrial fibrillation. Intracranial hemorrhage remains one of the most feared complications of warfarin, especially among older patients, prompting suggestions to consider lower intensity anticoagulation among patients older than 75 years who have atrial fibrillation.
This study evaluated the relationship between the intensity of anticoagulation, risk of intracranial hemorrhage, and age of patients with atrial fibrillation.
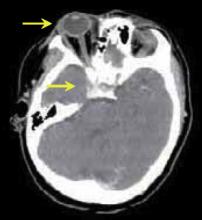
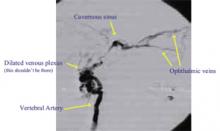
This was a retrospective case control study conducted at a tertiary care medical center. One-hundred and seventy patients on warfarin and admitted with intracranial hemorrhage from 1993 to 2002 were matched with 1020 patients who were on warfarin but without intracranial bleed. After controlling for comorbid conditions and aspirin use, authors conducted multivariable logistic regression analysis to determine the odds of intracranial hemorrhage with regard to age and INR. The risk of intracranial hemorrhage increased at 85 years of age and at INR values of 3.5 or greater. The risk of intracranial hemorrhage at INR less than 2.0 did not differ statistically from the risk at INR of 2.0–3.0.
This study shows the risk of intracranial hemorrhage is not decreased by choosing lower intensity anticoagulation, and target INR should still be kept at 2.5 among elderly patients. However, patients older than 85 years should be counseled about their higher risk of intracranial hemorrhage.
3. Heeschen C, Hamm CW, Mitrovic V, et al. N-terminal pro-B-type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation. 2004;110: 3206-12.
Recent data demonstrate the prognostic value of assessment of neurohormonal activation in patients with acute coronary syndromes (ACS). B-type natriuretic peptide levels (BNP) and levels of the N-terminal fragment of the BNP prohormone (NT-proBNP) predict adverse long-term outcomes in patients with ACS. Investigators reviewed plasma samples of Troponin T (TnT) and NT-proBNP obtained from patients with ACS enrolled in the Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) trial, which randomized patients to tirofiban or heparin for 48 hours and assessed mortality and myocardial infarction at 30 day follow-up. TnT and NT-proBNP determinations were available at baseline for 1791 patients, and at 48 and 72 hours from 1401 patients. Baseline NT-proBNP levels >250 ng/L were associated with significantly higher rates of death and myocardial infarction at 7 and 30 day follow-up. After adjustment for TnT and C-reactive protein levels, elevated NTproBNP levels maintained its predictive value (OR 2.7; p<.001). In patients with normal TnT levels, NT-proBNP levels identified a subgroup of patients at increased risk (OR 3.0; p=.004). However, in patients with high TnT levels (>0.1 mcg/L), NT-proBNP lost its predictive value (p=.58). More importantly, patients with normal levels of both TnT and NT-proBNP were at very low risk (0.6% event rate at 30 day follow-up).
Serial determinations of NT-proBNP levels at 48 and 72 hours were reviewed in patients without major adverse cardiac events (death or myocardial infarction); these patients were subdivided into groups with and without refractory ischemia. Patients without refractory ischemia showed a significant decline in NT-proBNP levels, whereas patients with refractory ischemia had no significant change. Persistently elevated NT-proBNP levels at 72 hours were associated with a 17.2% risk of death or MI at 30 days, compared with 0.6% risk if NT-proBNP returned to normal at 72 hours (p<.001). Neither TnT nor C-reactive protein demonstrated similar predictive value.
The study is limited by its retrospective nature, by potential selection bias by including only patients with direct evidence of coronary artery disease, and by limitations of the generalizability of its findings (e.g., to emergency department patients with chest pain).
As BNP and NT-proBNP are counter-regulatory hormones that play an active role in the response to ischemic injury, the authors suggest that NT-proBNP is a promising tool for dynamic risk assessment in patients with ACS. The authors also do not differentiate between BNP and NT-proBNP with regard to use in risk stratification, which might lead one to believe that these tests share similar predictive value. (Of note, the study was entirely funded by a company that produces an assay for NT-proBNP). Prospective trials to validate this tool are warranted
4. Heuschmann PU, Kolominsky-Rabas PL, Roether J, et al. Predictors of in-hospital mortality in patients with acute ischemic stroke treated with thrombolytic therapy. JAMA. 2004;292:1831-38.
The objective of this study was to identify factors associated with in-hospital mortality in ischemic stroke patients treated with recombinant tissue plasminogen activator (tPA). It was a prospective observational cohort study of 1658 patients conducted at 225 community and academic hospitals throughout Germany with main outcome of in-hospital mortality.
In this study 10% of patients who were treated with tPA died during their hospital stay, with 2/3 of deaths occurring in the first 7 days. Relative probability of in-hospital mortality increased with increasing patient age, with an odds ratio (OR) of 1.6 for each 10-year increment in age. Age was an independent predictor of in hospital mortality irrespective of tPA administration, with patients older than 75 years age having 4 fold higher mortality than the youngest cohort of less than 55 years age.
Other factors predicting in hospital mortality were altered level of consciousness and relative lack of experience with tPA treatment in the center. Altered level of consciousness was a predictor of stroke severity and an independent predictor of in-hospital mortality (OR 3.4). The increase in mortality in centers with limited experience with tPA administration (OR 0.97) reflected learning curve issues with these patients. The study was not designed to separate out the confounders of operator experience curve from institutional experience curves, or to derive the exact relationship between experience and outcomes.
5. McAlister FA, Bertsch K, Man J, et al. Incidence of and risk factors for pulmonary complications after non-thoracic surgery. Am J Respir Crit Care Med. 2004; published ahead of print on November 24, 2004 as doi:10.1164/rccm.200408-1069OC. Accessed January 27, 2005.
Postoperative pulmonary complications after nonthoracic surgery are a cause of significant morbidity and increased length of hospital stay. Previous studies of preoperative pulmonary assessment were limited by non-representative patient samples, conflicting results, and lack of explicit definitions of these complications. The authors conducted a prospective cohort study of 1055 patients seen in a Pre-Admission Clinic of a tertiary care university hospital. Mean age was 55 years, 50% male, and the cohort consisted of patients scheduled for intermediate risk elective surgery (upper abdominal, lower abdominal, orthopedic). They evaluated physical exam maneuvers (cough test, wheeze test, maximal laryngeal height, and forced expiratory time, all of which are described in an online data supplement) and preoperative spirometry values, and collected information on clinically significant postoperative pulmonary complications, including pneumonia, respiratory failure requiring mechanical ventilation, atelectasis requiring bronchoscopy, or pneumothorax or pleural effusion requiring percutaneous intervention. Twenty-eight patients (2.7%) suffered a pulmonary complication within 7 days of surgery, one of whom died. Length of stay was significantly prolonged in this group (mean 27.9 days vs 4.5 days, p=.006). Multivariate regression analysis revealed four variables that were independently associated with increased risk for postoperative pulmonary complications: age > 65 years, positive cough test (repeated coughing after asking the patient to inhale deeply and cough once), perioperative nasogastric tube, and anesthesia duration 2.5 hours or greater. Number of pack years smoked, FEV1, FEV1/FVC ratio, and upper abdominal surgery were associated with postoperative pulmonary complications but were not found to be independently associated by multivariate analysis.
While it is not surprising that the above risk factors are predictive of postoperative complications, this is the first study to incorporate specific exam maneuvers and spirometry into a risk prediction analysis. Limitations of this model are lack of independent validation and lack of generalizability to other populations, e.g., inpatients awaiting urgent surgery. Of note, the study further provides further support for not routinely obtaining pulmonary function testing for risk stratification prior to noncardiac surgery.
6. Mortenson, EM, Restrepo M, Anzeuto A, Pugh J. Effects of guideline-concordant antimicrobial therapy on mortality among patients with community-acquired pneumonia. Am J Med. 2004;117:726-31.
The American Thoracic Society (ATS) and the Infectious Diseases Society of America (IDSA) have published guidelines for the management of community acquired pneumonia that include recommendations for antibiotic selection. This retrospective cohort study attempted to measure the association between adherence to such guidelines and 30-day mortality in patients admitted with pneumonia to two Texas hospitals.
The characteristics of the patients studied reflect a reasonable cross-section of typical pneumonia patients, with the exception that the patients were mostly (85%) men. Of the study population, 78% were admitted through the ER, 20% admitted to the ICU, and 9% were nursing home residents. Antibiotics were considered “concordant” if they were consistent with either the most recent IDSA or ATS recommendations. The “nonconcordant” group was slightly older (66 vs. 61), generally sicker (higher rate of comorbid COPD and CVD), had more cerebrovascular disease, was more likely to present with altered mental status, and less frequently received antibiotics within 8 hours of presentation. The study did not comment on patients’ vaccination status. Thirty-day mortality was 6.2% in the guideline-concordant group, versus 21.7% in the other group (p < .001). The most common “non-concordant” regimen described was use of a beta-lactam alone, although specific antibiotic regimens were not evaluated.
While the results of this study are not surprising, they provide us with both the validation to continue practice according to existing recommendations, particularly the avoidance of monotherapy with beta-lactam antibiotics. The study also provides us with the imperative to take the lead in developing evidence-based pneumonia pathways at our own hospitals.
7. Pham MX, Whooley MA, Evans GT Jr, et al. Prognostic value of low-level cardiac troponin-I elevations in patients without definite acute coronary syndromes. Am Heart J. 2004;148: 776-82.
With the availability of rapid and highly sensitive and specific troponin testing, many patients admitted to the hospital with non-cardiac diagnoses have been recognized as having abnormal serum troponin-I or troponin-T levels, often just slightly above the reference cutoff for “normal.” While the clinical assumption is often that the elevated enzyme level does not reflect an acute coronary syndrome per se, its significance regarding the patient’s underlying cardiac health is often unclear.
Pham et al. retrospectively reviewed the 1-year mortality of 366 patients who were admitted to the San Francisco VA without evidence of acute MI or ACS either clinically or by EKG, but who had low-level troponin-I elevations (up to 3.0 ng/mL—a level that the authors state was reached by institutional consensus, and which was measured by a “first-generation” assay). These patients were admitted for a broad spectrum of diagnoses ranging from CHF to COPD to sepsis. Ninety-six percent of the patients were men; their average age was 69.
Follow-up was accomplished after a mean of 288 days and included 97% of patients. The primary endpoint was MI or death due to cardiac disease at one year; secondary endpoints were revascularization or admission for unstable angina. The primary endpoint was reached by 11% of patients with cTn-I between 1.0 and 3.0 ng/mL, and 4% of the patients with cTn-I up to 1.0 ng/mL (adjusted HR 3.4, 95% CI, 1.3 to 9.4), and the higher the cTn-I, the higher the risk. However, the authors did not test for the level of risk by specific diagnosis, so they caution against overgeneralizing their findings.
The findings of this study add to the evidence that any evidence of myocardial injury implies an increased risk of underlying heart disease and accompanying long—term cardiac complications– even if such injury occurs in the absence of ACS or known heart disease. Hospitalists often see such injury in the setting of acute infection and pulmonary disease and may be the first to recognize the possibility of CHD in a given patient. To date, guidelines addressing optimal prospective risk stratification have not been developed. Until they are, hospitalists should be aware of the ramifications of “troponin leak” and be prepared to initiate necessary inpatient monitoring and treatments, and to coordinate appropriate follow-up for these patients.
8. Saposnik G, Young B, Silver B, et al. Lack of improvement in patients with acute stroke after treatment with thrombolytic therapy: predictors and association with outcome. JAMA. 2004; 292: 1839-44.
Recombinant tissue plasminogen activator (tPA) has been shown to be one of the most efficacious therapies for acute stroke treatment. This was a systematic evaluation of predictors for outcomes at 24 hours after tPA therapy and of the prognostic significance of lack of improvement at 24 hours for long-term outcomes at 3 months.
The trial was a prospective cohort study of 216 consecutive patients admitted with acute ischemic stroke to a university hospital. The decision to treat with tPA was based on the NINDS protocol with one difference: patients with involvement of more than one third of the middle cerebral artery on the baseline CT scan were excluded. A control CT scan was performed at 24 hours to determine the presence of new infarction, cortical involvement, and extension of the ischemic lesion.
Lack of improvement was defined as a difference between the NIHSS score at baseline and at 24 hours of 3 points or less. Poor outcome at 3 months was defined by a modified Rankin Scale score of 3 to 5 or death.
After adjusting for age, gender, and stroke severity, hyperglycemia at admission (glucose > 144 mg/dL), cortical involvement, and time to treatment were independent predictors of lack of improvement at 24 hours. After adjusting for age, gender, and stroke severity, lack of improvement at 24 hours was an independent predictor of poor outcome and death at 3 months. Patients with lack of improvement at 24 hours also had longer lengths of hospitalization.
9. Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049-57.
Neurohormonal changes, endothelial dysfunction, impaired nitric oxide availability, and oxidant stress all contribute to the structural remodeling of the left ventricle in congestive heart failure. The combination of isosorbide dinitrate, an organic nitrate that stimulates nitric oxide signaling, and the antioxidant and vasodilator hydralazine improves survival in heart failure. Based on more recent data that black patients have a clinically significant response to this combination therapy, the authors of the African-American Heart Failure Trial (A-HeFT) evaluated 1050 black patients with congestive heart failure in a randomized, double-blind, placebo controlled trial. Patients were randomized to fixed doses of isosorbide dinitrate and hydralazine plus background therapy (i.e., digoxin, ACE inhibitors, beta-blockers, diuretics, angiotensin receptor blockers) or to placebo plus background therapy. After 18 months, the trial was stopped due to a significantly higher mortality rate in the placebo group (10.2% in the placebo group vs. 6.2% with combination
therapy, p=.02); survival differences emerged at 180 days and increased progressively thereafter. The combination therapy group reported more headache and dizziness but suffered fewer exacerbations of congestive heart failure and reported improvement in subjective assessments of quality of life as measured by questionnaires. Accompanying editorials discuss the role of nitric oxide and prevention of oxidative stress in the treatment of heart failure, as well as the controversial issues surrounding race-based therapeutics.
1. Dexter PR, Perkins SM, Mahany KS, Jones K, McDonald CJ. Inpatient computer-based standing orders vs. physician reminders to increase influenza and pneumococcal vaccination rates: a randomized trial. JAMA. 2004; 292: 2366-71.
Past studies have suggested that most patients admitted with severe pneumococcal infections have been hospitalized in the preceding 5 years, and simply being hospitalized is a potential risk factor for later pneumococcal infection. Likewise, hospitalization provides an opportunity to vaccinate high-risk patients against influenza, and raising pneumococcal and influenza immunization rates is a CMS quality improvement priority. Prior investigations have supported the use of labor-intensive manual standing orders as well as computerized reminders, but this prospective trial was conducted in 1998 and 1999 to assess the effectiveness of a computer-based system to screen for eligible patients and then generate orders to perform pneumonia and influenza vaccinations on inpatients at the time of discharge.
Over 13 months, a total of 3777 inpatients were entered into the study. The hospital computer identified patients eligible for vaccination based on common criteria and randomized them to one of two groups of physician teams. For one group of teams, the computer order-entry system would automatically generate vaccination orders at the time of discharge for vaccine-eligible patients; for the other group of teams, only computer reminders were provided to physicians. The outcome measure was administration of vaccine; long-term outcomes such as incidence of subsequent disease or mortality were not measured.
During the study period, 50% of all hospitalized patients were identified as eligible for influenza vaccination; 22% were eligible for pneumococcal vaccination. In each case, the “standing order” group received vaccine more often (influenza: 42% vs. 30%, p<.001; pneumococcal vaccine: 51% vs. 31%). The numbers were subsequently adjusted to allow for patients who had previously received vaccine, but the impressive differences persisted. Nurses reported reasons for non-administration in 98% of the eligible patients who were not vaccinated; the most common reason was patient refusal. It is not clear if the physicians knew that a study was being conducted. No adverse reactions were reported.
CMS has pushed for the development of institutional standing order sets as a tool to improve compliance with vaccination rate targets. Where the technology is available, computer systems that can screen eligible patients and generate automatic orders are an effective tool in implementing many quality-improvement initiatives, and hospitalists are in a crucial position to take an active role in their development and implementation.
2. Fang MC, Chang Y, Hylek EM, et al. Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for a trial fibrillation. Ann Intern Med. 2004; 141: 745-52.
Warfarin has been shown to reduce risk of stroke in patients with chronic and paroxysmal atrial fibrillation. Intracranial hemorrhage remains one of the most feared complications of warfarin, especially among older patients, prompting suggestions to consider lower intensity anticoagulation among patients older than 75 years who have atrial fibrillation.
This study evaluated the relationship between the intensity of anticoagulation, risk of intracranial hemorrhage, and age of patients with atrial fibrillation.
This was a retrospective case control study conducted at a tertiary care medical center. One-hundred and seventy patients on warfarin and admitted with intracranial hemorrhage from 1993 to 2002 were matched with 1020 patients who were on warfarin but without intracranial bleed. After controlling for comorbid conditions and aspirin use, authors conducted multivariable logistic regression analysis to determine the odds of intracranial hemorrhage with regard to age and INR. The risk of intracranial hemorrhage increased at 85 years of age and at INR values of 3.5 or greater. The risk of intracranial hemorrhage at INR less than 2.0 did not differ statistically from the risk at INR of 2.0–3.0.
This study shows the risk of intracranial hemorrhage is not decreased by choosing lower intensity anticoagulation, and target INR should still be kept at 2.5 among elderly patients. However, patients older than 85 years should be counseled about their higher risk of intracranial hemorrhage.
3. Heeschen C, Hamm CW, Mitrovic V, et al. N-terminal pro-B-type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation. 2004;110: 3206-12.
Recent data demonstrate the prognostic value of assessment of neurohormonal activation in patients with acute coronary syndromes (ACS). B-type natriuretic peptide levels (BNP) and levels of the N-terminal fragment of the BNP prohormone (NT-proBNP) predict adverse long-term outcomes in patients with ACS. Investigators reviewed plasma samples of Troponin T (TnT) and NT-proBNP obtained from patients with ACS enrolled in the Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) trial, which randomized patients to tirofiban or heparin for 48 hours and assessed mortality and myocardial infarction at 30 day follow-up. TnT and NT-proBNP determinations were available at baseline for 1791 patients, and at 48 and 72 hours from 1401 patients. Baseline NT-proBNP levels >250 ng/L were associated with significantly higher rates of death and myocardial infarction at 7 and 30 day follow-up. After adjustment for TnT and C-reactive protein levels, elevated NTproBNP levels maintained its predictive value (OR 2.7; p<.001). In patients with normal TnT levels, NT-proBNP levels identified a subgroup of patients at increased risk (OR 3.0; p=.004). However, in patients with high TnT levels (>0.1 mcg/L), NT-proBNP lost its predictive value (p=.58). More importantly, patients with normal levels of both TnT and NT-proBNP were at very low risk (0.6% event rate at 30 day follow-up).
Serial determinations of NT-proBNP levels at 48 and 72 hours were reviewed in patients without major adverse cardiac events (death or myocardial infarction); these patients were subdivided into groups with and without refractory ischemia. Patients without refractory ischemia showed a significant decline in NT-proBNP levels, whereas patients with refractory ischemia had no significant change. Persistently elevated NT-proBNP levels at 72 hours were associated with a 17.2% risk of death or MI at 30 days, compared with 0.6% risk if NT-proBNP returned to normal at 72 hours (p<.001). Neither TnT nor C-reactive protein demonstrated similar predictive value.
The study is limited by its retrospective nature, by potential selection bias by including only patients with direct evidence of coronary artery disease, and by limitations of the generalizability of its findings (e.g., to emergency department patients with chest pain).
As BNP and NT-proBNP are counter-regulatory hormones that play an active role in the response to ischemic injury, the authors suggest that NT-proBNP is a promising tool for dynamic risk assessment in patients with ACS. The authors also do not differentiate between BNP and NT-proBNP with regard to use in risk stratification, which might lead one to believe that these tests share similar predictive value. (Of note, the study was entirely funded by a company that produces an assay for NT-proBNP). Prospective trials to validate this tool are warranted
4. Heuschmann PU, Kolominsky-Rabas PL, Roether J, et al. Predictors of in-hospital mortality in patients with acute ischemic stroke treated with thrombolytic therapy. JAMA. 2004;292:1831-38.
The objective of this study was to identify factors associated with in-hospital mortality in ischemic stroke patients treated with recombinant tissue plasminogen activator (tPA). It was a prospective observational cohort study of 1658 patients conducted at 225 community and academic hospitals throughout Germany with main outcome of in-hospital mortality.
In this study 10% of patients who were treated with tPA died during their hospital stay, with 2/3 of deaths occurring in the first 7 days. Relative probability of in-hospital mortality increased with increasing patient age, with an odds ratio (OR) of 1.6 for each 10-year increment in age. Age was an independent predictor of in hospital mortality irrespective of tPA administration, with patients older than 75 years age having 4 fold higher mortality than the youngest cohort of less than 55 years age.
Other factors predicting in hospital mortality were altered level of consciousness and relative lack of experience with tPA treatment in the center. Altered level of consciousness was a predictor of stroke severity and an independent predictor of in-hospital mortality (OR 3.4). The increase in mortality in centers with limited experience with tPA administration (OR 0.97) reflected learning curve issues with these patients. The study was not designed to separate out the confounders of operator experience curve from institutional experience curves, or to derive the exact relationship between experience and outcomes.
5. McAlister FA, Bertsch K, Man J, et al. Incidence of and risk factors for pulmonary complications after non-thoracic surgery. Am J Respir Crit Care Med. 2004; published ahead of print on November 24, 2004 as doi:10.1164/rccm.200408-1069OC. Accessed January 27, 2005.
Postoperative pulmonary complications after nonthoracic surgery are a cause of significant morbidity and increased length of hospital stay. Previous studies of preoperative pulmonary assessment were limited by non-representative patient samples, conflicting results, and lack of explicit definitions of these complications. The authors conducted a prospective cohort study of 1055 patients seen in a Pre-Admission Clinic of a tertiary care university hospital. Mean age was 55 years, 50% male, and the cohort consisted of patients scheduled for intermediate risk elective surgery (upper abdominal, lower abdominal, orthopedic). They evaluated physical exam maneuvers (cough test, wheeze test, maximal laryngeal height, and forced expiratory time, all of which are described in an online data supplement) and preoperative spirometry values, and collected information on clinically significant postoperative pulmonary complications, including pneumonia, respiratory failure requiring mechanical ventilation, atelectasis requiring bronchoscopy, or pneumothorax or pleural effusion requiring percutaneous intervention. Twenty-eight patients (2.7%) suffered a pulmonary complication within 7 days of surgery, one of whom died. Length of stay was significantly prolonged in this group (mean 27.9 days vs 4.5 days, p=.006). Multivariate regression analysis revealed four variables that were independently associated with increased risk for postoperative pulmonary complications: age > 65 years, positive cough test (repeated coughing after asking the patient to inhale deeply and cough once), perioperative nasogastric tube, and anesthesia duration 2.5 hours or greater. Number of pack years smoked, FEV1, FEV1/FVC ratio, and upper abdominal surgery were associated with postoperative pulmonary complications but were not found to be independently associated by multivariate analysis.
While it is not surprising that the above risk factors are predictive of postoperative complications, this is the first study to incorporate specific exam maneuvers and spirometry into a risk prediction analysis. Limitations of this model are lack of independent validation and lack of generalizability to other populations, e.g., inpatients awaiting urgent surgery. Of note, the study further provides further support for not routinely obtaining pulmonary function testing for risk stratification prior to noncardiac surgery.
6. Mortenson, EM, Restrepo M, Anzeuto A, Pugh J. Effects of guideline-concordant antimicrobial therapy on mortality among patients with community-acquired pneumonia. Am J Med. 2004;117:726-31.
The American Thoracic Society (ATS) and the Infectious Diseases Society of America (IDSA) have published guidelines for the management of community acquired pneumonia that include recommendations for antibiotic selection. This retrospective cohort study attempted to measure the association between adherence to such guidelines and 30-day mortality in patients admitted with pneumonia to two Texas hospitals.
The characteristics of the patients studied reflect a reasonable cross-section of typical pneumonia patients, with the exception that the patients were mostly (85%) men. Of the study population, 78% were admitted through the ER, 20% admitted to the ICU, and 9% were nursing home residents. Antibiotics were considered “concordant” if they were consistent with either the most recent IDSA or ATS recommendations. The “nonconcordant” group was slightly older (66 vs. 61), generally sicker (higher rate of comorbid COPD and CVD), had more cerebrovascular disease, was more likely to present with altered mental status, and less frequently received antibiotics within 8 hours of presentation. The study did not comment on patients’ vaccination status. Thirty-day mortality was 6.2% in the guideline-concordant group, versus 21.7% in the other group (p < .001). The most common “non-concordant” regimen described was use of a beta-lactam alone, although specific antibiotic regimens were not evaluated.
While the results of this study are not surprising, they provide us with both the validation to continue practice according to existing recommendations, particularly the avoidance of monotherapy with beta-lactam antibiotics. The study also provides us with the imperative to take the lead in developing evidence-based pneumonia pathways at our own hospitals.
7. Pham MX, Whooley MA, Evans GT Jr, et al. Prognostic value of low-level cardiac troponin-I elevations in patients without definite acute coronary syndromes. Am Heart J. 2004;148: 776-82.
With the availability of rapid and highly sensitive and specific troponin testing, many patients admitted to the hospital with non-cardiac diagnoses have been recognized as having abnormal serum troponin-I or troponin-T levels, often just slightly above the reference cutoff for “normal.” While the clinical assumption is often that the elevated enzyme level does not reflect an acute coronary syndrome per se, its significance regarding the patient’s underlying cardiac health is often unclear.
Pham et al. retrospectively reviewed the 1-year mortality of 366 patients who were admitted to the San Francisco VA without evidence of acute MI or ACS either clinically or by EKG, but who had low-level troponin-I elevations (up to 3.0 ng/mL—a level that the authors state was reached by institutional consensus, and which was measured by a “first-generation” assay). These patients were admitted for a broad spectrum of diagnoses ranging from CHF to COPD to sepsis. Ninety-six percent of the patients were men; their average age was 69.
Follow-up was accomplished after a mean of 288 days and included 97% of patients. The primary endpoint was MI or death due to cardiac disease at one year; secondary endpoints were revascularization or admission for unstable angina. The primary endpoint was reached by 11% of patients with cTn-I between 1.0 and 3.0 ng/mL, and 4% of the patients with cTn-I up to 1.0 ng/mL (adjusted HR 3.4, 95% CI, 1.3 to 9.4), and the higher the cTn-I, the higher the risk. However, the authors did not test for the level of risk by specific diagnosis, so they caution against overgeneralizing their findings.
The findings of this study add to the evidence that any evidence of myocardial injury implies an increased risk of underlying heart disease and accompanying long—term cardiac complications– even if such injury occurs in the absence of ACS or known heart disease. Hospitalists often see such injury in the setting of acute infection and pulmonary disease and may be the first to recognize the possibility of CHD in a given patient. To date, guidelines addressing optimal prospective risk stratification have not been developed. Until they are, hospitalists should be aware of the ramifications of “troponin leak” and be prepared to initiate necessary inpatient monitoring and treatments, and to coordinate appropriate follow-up for these patients.
8. Saposnik G, Young B, Silver B, et al. Lack of improvement in patients with acute stroke after treatment with thrombolytic therapy: predictors and association with outcome. JAMA. 2004; 292: 1839-44.
Recombinant tissue plasminogen activator (tPA) has been shown to be one of the most efficacious therapies for acute stroke treatment. This was a systematic evaluation of predictors for outcomes at 24 hours after tPA therapy and of the prognostic significance of lack of improvement at 24 hours for long-term outcomes at 3 months.
The trial was a prospective cohort study of 216 consecutive patients admitted with acute ischemic stroke to a university hospital. The decision to treat with tPA was based on the NINDS protocol with one difference: patients with involvement of more than one third of the middle cerebral artery on the baseline CT scan were excluded. A control CT scan was performed at 24 hours to determine the presence of new infarction, cortical involvement, and extension of the ischemic lesion.
Lack of improvement was defined as a difference between the NIHSS score at baseline and at 24 hours of 3 points or less. Poor outcome at 3 months was defined by a modified Rankin Scale score of 3 to 5 or death.
After adjusting for age, gender, and stroke severity, hyperglycemia at admission (glucose > 144 mg/dL), cortical involvement, and time to treatment were independent predictors of lack of improvement at 24 hours. After adjusting for age, gender, and stroke severity, lack of improvement at 24 hours was an independent predictor of poor outcome and death at 3 months. Patients with lack of improvement at 24 hours also had longer lengths of hospitalization.
9. Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351:2049-57.
Neurohormonal changes, endothelial dysfunction, impaired nitric oxide availability, and oxidant stress all contribute to the structural remodeling of the left ventricle in congestive heart failure. The combination of isosorbide dinitrate, an organic nitrate that stimulates nitric oxide signaling, and the antioxidant and vasodilator hydralazine improves survival in heart failure. Based on more recent data that black patients have a clinically significant response to this combination therapy, the authors of the African-American Heart Failure Trial (A-HeFT) evaluated 1050 black patients with congestive heart failure in a randomized, double-blind, placebo controlled trial. Patients were randomized to fixed doses of isosorbide dinitrate and hydralazine plus background therapy (i.e., digoxin, ACE inhibitors, beta-blockers, diuretics, angiotensin receptor blockers) or to placebo plus background therapy. After 18 months, the trial was stopped due to a significantly higher mortality rate in the placebo group (10.2% in the placebo group vs. 6.2% with combination
therapy, p=.02); survival differences emerged at 180 days and increased progressively thereafter. The combination therapy group reported more headache and dizziness but suffered fewer exacerbations of congestive heart failure and reported improvement in subjective assessments of quality of life as measured by questionnaires. Accompanying editorials discuss the role of nitric oxide and prevention of oxidative stress in the treatment of heart failure, as well as the controversial issues surrounding race-based therapeutics.
In the Literature
CARP Trial Suggests No Benefit to Revascularization Before Vascular Surgery
McFalls, EO, Ward HB, Mortiz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2795-2804.
Recent studies have presented evidence that treatment with beta-blockers for patients with CAD could reduce the risk of perioperative cardiac complications. Beta-blockers have since become a critical part of the management plan for the perioperative patient. Evidence-based practice guidelines for cardiac risk assessment have been published by both the American College of Physicians and the American College of Cardiology/American Heart Association. However, practice patterns continue to vary between physicians and cardiologists, particularly for patients clinically stratified into the intermediate-risk category. Some physicians feel comfortable with a conservative approach of medical optimization even in the setting of established CAD, while others favor more aggressive treatment, even though the prospective data supporting cardiac revascularization before major surgery has been lacking. The study investigators sought to clarify this uncertainty.
The prospective trial enrolled 510 patients at 18 VA centers. Patients scheduled for major vascular operations were eligible, and were preoperatively assessed via clinical criteria, stress imaging, and angiography when appropriate. Eligible patients had significant (at least 70%) stenosis of at least one coronary artery. High-risk patients (i.e., those with left main disease, severe aortic stenosis, and LVEF <20%) were excluded. Patients were then randomized to one
of two groups. The first group underwent revascularization with PTCA or CABG plus medical optimization; the second group received only medical optimization. Most patients in both groups received beta-blockers, and more than half in each received statins. The patient populations were appropriately randomized, although overwhelmingly male (98%). Most patients had one- or two-vessel CAD. The primary endpoint was long-term mortality. Secondary endpoints included MI, stroke, renal failure requiring dialysis, and limb loss. Follow-up rates were similar in both groups (86% and 85%).
The major finding of the study was the lack of difference in mortality between the two groups at an average follow-up of 2.7 years (22% vs. 23%, RR= 0.98, 95% CI 0.70 to 1.37, p = 0.92). Analyzing by “treatment-received” instead of “intention-to-treat” did not significantly change this result. Of note, ten patients in the revascularization arm died between the revascularization procedure and the vascular surgery. Not surprisingly, revascularization also delayed the time to surgery for patients in that arm of the study. In the authors’ analysis, the patients were also divided into subgroups based on high-risk variables (prior CABG, category of Revised Cardiac Risk Index, etc.), but the study was not powered to detect mortality differences between the two arms within these subgroups. The authors concluded that there was no benefit to revascularization in patients with stable coronary syndromes prior to elective vascular surgeries.
The results of this study validate the conservative practice recommended by the existing guidelines— that is, to perform revascularization procedures in the preoperative setting only when indicated by clinical criteria such as unstable ischemic symptoms, and if likely to improve long-term survival. Beta-blockers, and based on recent studies probably “statins,” should continue to be the mainstay of perioperative risk optimization for patients with stable coronary disease.
There were, however, several important considerations: first, the study group was exclusively male, although there is little reason to believe that women would have better outcomes from revascularization. And second, the highest-risk patients were excluded, and therefore the results should not be extrapolated to that population. Prospective identification of the group of patients who may benefit from aggressive intervention should remain a target of risk assessment and further research. (BH)
Blood Transfusion May Increase Mortality in Acute Coronary Syndrome
Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292:1555-62.
The increased use of invasive procedures and anticoagulant and fibrinolytic drugs in patients with ischemic heart disease in recent years predictably increases the potential for bleeding and perceived need for transfusion. Studies evaluating the association between transfusion and mortality have produced mixed results. A more pertinent clinical question is whether transfusion is beneficial or harmful in patients with acute coronary syndromes who acutely develop anemia during their hospitalization.
The authors used clinical data from three large international trials of patients with acute coronary syndromes (GUSTO IIb, PURSUIT, and PARAGON B) to determine the association between blood transfusion and outcomes among patients who developed moderate to severe bleeding, anemia, or both during their hospitalization.
Assessment of clinically significant bleeding complications was based on the GUSTO definition of severe (intracranial hemorrhage or hemodynamic compromise and requiring intervention) or moderate (hemodynamically stable but requiring blood transfusion) bleeding. The GUSTO IIb and PURSUIT trials used the above definition; PARAGON B categorized bleeding as “major or life threatening” (intracranial hemorrhage or bleeding leading to hemodynamic compromise requiring intervention) or “intermediate” (requiring transfusion or a decrease in hemoglobin of 5 g/dL or more, or a decrease in hematocrit ( 15%). Major or life-threatening bleeding episodes and intermediate bleeding episodes in PARAGON B were deemed equivalent to severe and moderate bleeding episodes in GUSTO.
Data were collected on the date, time, severity, and location of each bleeding event, and on the date and number of units of packed red blood cells and whole blood transfused. The primary end-point was 30-day all-cause mortality. Secondary end-points were occurrence of the composite of 30-day death or MI.
The unadjusted rates of 30-day death, MI, and composite death/MI were significantly higher among patients who received a transfusion (30-day death, 8.00% vs. 3.08%; p<.001; 30-day MI, 25.16% vs. 8.16%; p<.001; 30-day composite death/MI, 29.24% vs. 10.02%; p<.001).
After adjustment for baseline characteristics, bleeding and transfusion propensity, and nadir hematocrit, blood transfusion was associated with a hazard ratio for death of 3.94 (95% confidence interval, 3.26–4.75).
No significant association was found between transfusion and 30-day mortality at a nadir hematocrit of 25% or less (adjusted OR 1.13; 95% CI 0.70-1.82). However, at a nadir hematocrit higher than 25%, transfusion was associated with significantly higher odds of 30-day death, even after excluding patients who underwent CABG or those who died within the first 5 days of follow-up.
These findings differ from the findings of Wu et al. (1) who noted that blood transfusion was associated with lower 30-day mortality among elderly patients with MI if the admission hematocrit was 30% or lower. The current authors propose that their data is more robust due to meticulous collection through clinical trial records, and that their analysis accounts for timing of transfusion and indications for transfusion.
Many clinicians logically believe that augmentation of oxygen carrying capacity via transfusion would be beneficial to patients with active ischemia. However, the authors note that red blood cells in stored blood may be depleted of both 2,3-diphosphoglyceric acid and nitric oxide, both of which are critical components to oxygen delivery and exchange. These cells then function as nitric oxide “sinks,” promoting vasoconstriction, platelet aggregation, and impaired oxygen delivery to tissues. In addition, inflammatory mediators associated with exacerbation of myocardial ischemia may remain in transfused blood, potentially contributing to adverse outcomes.
As this is a nonrandomized, post hoc observational study, further prescriptive conclusions regarding transfusion cannot be made. However, the authors, along with an accompanying editorial, call for prospective randomized trials of transfusion in anemic patients with acute coronary syndromes to better define the role of this commonly used therapy. (CW)
- Wu WC, Rathore SS, Wang Y, Radford MJ, Krumholz HM. Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med. 2001;345:1230-6.
Cost-effectiveness of Rhythm Versus Rate Control in Atrial Fibrillation
Marshall DA, Levy AR, Vidaillet H, et al. Cost-effectiveness of rhythm versus rate control in atrial fibrillation. Ann Intern Med. 2004;141:653-61.
Atrial fibrillation is the most common arrhythmia treated by physicians. It afflicts nearly 10% of patients age 80 years or older. There are two primary modalities of managing patients with atrial fibrillation; rate control versus cardioversion into sinus rhythm.
AFFIRM was a multicenter randomized controlled trial involving 213 centers in USA and Canada that compared rate versus rhythm control in 4060 patients. These patients had a mean age of 70 years. Sixty-one percent of the enrolled patients were men, and 66% had recurrent atrial fibrillation. Seventy-one percent of patients had hypertension, 39% had coronary artery disease, and 9% had congestive heart failure. Patients were block randomized by center to either rate control or rhythm control and followed for an average of 3.5 years. AFFIRM results showed no significant mortality difference between the two groups (hazard ratio for rate versus rhythm control, 0.87 with 95% CI, 0.75 to 1.01).
Primary data on survival and resource utilization were used to conduct the economic analysis from a third party payer perspective. Authors used intention to treat data for the economic analysis.
For resource utilization estimates, US healthcare cost figures for the year 2002 were used. All earlier costs were appropriately adjusted using Consumer Price Index, Medical Care component to estimate their nominal values in year 2002. Hospital costs were taken as the mean charges per day from Healthcare Cost and Utilization Project statistics for Diseases of the Circulatory System for patients older than 18 years age. Low and high end of these costs were assumed to be equivalent to 25th and 75th percentiles of the mean costs, respectively. Physician costs were assumed to be equivalent to be the average of all carriers’ payments for the relative value units of the services rendered based on a generic current procedural terminology code. Sensitivity analysis was conducted on these physician costs using minimum payment among these carriers as the low cost estimate and the standard charges for Marshfield Clinic for the high end. Costs of pacemaker and implantable cardioverter defibrillators were based on manufacturers’ list prices. For sensitivity analysis, hardware costs were excluded for low cost estimates and the maximum manufacturers’ list price for the high estimate was used.
At each follow-up visit during the AFFIRM trial, the number of cardioversion attempts since the prior visit was recorded. Costs of cardioversion were based on average payment to Marshfield Clinic for outpatient electrical cardioversion for the year 2002. Authors assigned no costs for low cost estimate and used billed charges for high costs for sensitivity analysis.
At each follow-up visit, the number of short stay and emergency department visits since the prior visit was recorded. Weighted average Medicare costs for level I and II facilities were used as the baseline estimate for these visits. Estimates for sensitivity analysis were the minimum and maximum Medicare payments for these visits. Physician fees were based on level III emergency department visit with low and high cost estimates assigned as described above.
Medication costs were based on the least average wholesale price (AWP) for a generic medication. Low and high cost estimates were taken from lowest quoted US Internet pharmacy price and highest AWP for the most expensive drug in the class respectively. Only medications used for atrial fibrillation and anticoagulation were considered for analysis.
The authors calculated the mean cost per patient In the Literature (continued) and the mean survival time between the two interventions. Future costs were discounted by 3%. For the base estimate, rhythm control was more expensive and less effective than rate control, i.e., dominated by the rate control. Rate control dominated rhythm control even for high and low estimates of the sensitivity analysis demonstrating stability of the results. Authors used 10,000 simulations to perform non-parametric bootstrapping analysis to find the 95% credible intervals around the base estimate. The bootstrap results showed that for 95% of the results rate control had higher survival time and was less costly than rhythm control. These simulation results clearly showed rate control is more cost-effective for patient population resembling that of AFFIRM trial.
The study has some limitations. These results are robust for patients similar to those in AFFIRM trial, i.e., older patients with cardiovascular defects that are at risk of cerebrovascular embolism. However these results may not be applicable to younger patients and those with “lone atrial fibrillation.” The study had a follow-up period of 3.5 years, and the cost-effectiveness analysis is confined to this period. It is difficult to determine mortality advantage of one treatment over another within the limited duration of the AFFIRM study. Most of the patients were on multiple pharmacologic agents for rhythm control and had a high incidence of cross-over from rhythm control to rate control reflecting modest benefits of the current agents. These results may not be applicable to patients whose atrial fibrillation is well controlled by a single agent or by non-pharmacological treatment. Patients on rhythm control agents had, as expected, more hospitalization days from the side effects and treatment protocols of the agents (especially pharmacologic) used to control the rhythm. With advances in both pharmacologic as well as nonpharmacologic methods for rhythm control generating safer and more efficacious technologies, the results of this analysis may become less valid in the future. The analysis was conducted from a third-party payer perspective, without accounting for the quality of life. Thus patients who have symptomatic atrial fibrillation and those with diastolic dysfunction may have improved quality of life from rhythm control over just rate control. The results may not be applicable to these patients. (SS)
CARP Trial Suggests No Benefit to Revascularization Before Vascular Surgery
McFalls, EO, Ward HB, Mortiz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2795-2804.
Recent studies have presented evidence that treatment with beta-blockers for patients with CAD could reduce the risk of perioperative cardiac complications. Beta-blockers have since become a critical part of the management plan for the perioperative patient. Evidence-based practice guidelines for cardiac risk assessment have been published by both the American College of Physicians and the American College of Cardiology/American Heart Association. However, practice patterns continue to vary between physicians and cardiologists, particularly for patients clinically stratified into the intermediate-risk category. Some physicians feel comfortable with a conservative approach of medical optimization even in the setting of established CAD, while others favor more aggressive treatment, even though the prospective data supporting cardiac revascularization before major surgery has been lacking. The study investigators sought to clarify this uncertainty.
The prospective trial enrolled 510 patients at 18 VA centers. Patients scheduled for major vascular operations were eligible, and were preoperatively assessed via clinical criteria, stress imaging, and angiography when appropriate. Eligible patients had significant (at least 70%) stenosis of at least one coronary artery. High-risk patients (i.e., those with left main disease, severe aortic stenosis, and LVEF <20%) were excluded. Patients were then randomized to one
of two groups. The first group underwent revascularization with PTCA or CABG plus medical optimization; the second group received only medical optimization. Most patients in both groups received beta-blockers, and more than half in each received statins. The patient populations were appropriately randomized, although overwhelmingly male (98%). Most patients had one- or two-vessel CAD. The primary endpoint was long-term mortality. Secondary endpoints included MI, stroke, renal failure requiring dialysis, and limb loss. Follow-up rates were similar in both groups (86% and 85%).
The major finding of the study was the lack of difference in mortality between the two groups at an average follow-up of 2.7 years (22% vs. 23%, RR= 0.98, 95% CI 0.70 to 1.37, p = 0.92). Analyzing by “treatment-received” instead of “intention-to-treat” did not significantly change this result. Of note, ten patients in the revascularization arm died between the revascularization procedure and the vascular surgery. Not surprisingly, revascularization also delayed the time to surgery for patients in that arm of the study. In the authors’ analysis, the patients were also divided into subgroups based on high-risk variables (prior CABG, category of Revised Cardiac Risk Index, etc.), but the study was not powered to detect mortality differences between the two arms within these subgroups. The authors concluded that there was no benefit to revascularization in patients with stable coronary syndromes prior to elective vascular surgeries.
The results of this study validate the conservative practice recommended by the existing guidelines— that is, to perform revascularization procedures in the preoperative setting only when indicated by clinical criteria such as unstable ischemic symptoms, and if likely to improve long-term survival. Beta-blockers, and based on recent studies probably “statins,” should continue to be the mainstay of perioperative risk optimization for patients with stable coronary disease.
There were, however, several important considerations: first, the study group was exclusively male, although there is little reason to believe that women would have better outcomes from revascularization. And second, the highest-risk patients were excluded, and therefore the results should not be extrapolated to that population. Prospective identification of the group of patients who may benefit from aggressive intervention should remain a target of risk assessment and further research. (BH)
Blood Transfusion May Increase Mortality in Acute Coronary Syndrome
Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292:1555-62.
The increased use of invasive procedures and anticoagulant and fibrinolytic drugs in patients with ischemic heart disease in recent years predictably increases the potential for bleeding and perceived need for transfusion. Studies evaluating the association between transfusion and mortality have produced mixed results. A more pertinent clinical question is whether transfusion is beneficial or harmful in patients with acute coronary syndromes who acutely develop anemia during their hospitalization.
The authors used clinical data from three large international trials of patients with acute coronary syndromes (GUSTO IIb, PURSUIT, and PARAGON B) to determine the association between blood transfusion and outcomes among patients who developed moderate to severe bleeding, anemia, or both during their hospitalization.
Assessment of clinically significant bleeding complications was based on the GUSTO definition of severe (intracranial hemorrhage or hemodynamic compromise and requiring intervention) or moderate (hemodynamically stable but requiring blood transfusion) bleeding. The GUSTO IIb and PURSUIT trials used the above definition; PARAGON B categorized bleeding as “major or life threatening” (intracranial hemorrhage or bleeding leading to hemodynamic compromise requiring intervention) or “intermediate” (requiring transfusion or a decrease in hemoglobin of 5 g/dL or more, or a decrease in hematocrit ( 15%). Major or life-threatening bleeding episodes and intermediate bleeding episodes in PARAGON B were deemed equivalent to severe and moderate bleeding episodes in GUSTO.
Data were collected on the date, time, severity, and location of each bleeding event, and on the date and number of units of packed red blood cells and whole blood transfused. The primary end-point was 30-day all-cause mortality. Secondary end-points were occurrence of the composite of 30-day death or MI.
The unadjusted rates of 30-day death, MI, and composite death/MI were significantly higher among patients who received a transfusion (30-day death, 8.00% vs. 3.08%; p<.001; 30-day MI, 25.16% vs. 8.16%; p<.001; 30-day composite death/MI, 29.24% vs. 10.02%; p<.001).
After adjustment for baseline characteristics, bleeding and transfusion propensity, and nadir hematocrit, blood transfusion was associated with a hazard ratio for death of 3.94 (95% confidence interval, 3.26–4.75).
No significant association was found between transfusion and 30-day mortality at a nadir hematocrit of 25% or less (adjusted OR 1.13; 95% CI 0.70-1.82). However, at a nadir hematocrit higher than 25%, transfusion was associated with significantly higher odds of 30-day death, even after excluding patients who underwent CABG or those who died within the first 5 days of follow-up.
These findings differ from the findings of Wu et al. (1) who noted that blood transfusion was associated with lower 30-day mortality among elderly patients with MI if the admission hematocrit was 30% or lower. The current authors propose that their data is more robust due to meticulous collection through clinical trial records, and that their analysis accounts for timing of transfusion and indications for transfusion.
Many clinicians logically believe that augmentation of oxygen carrying capacity via transfusion would be beneficial to patients with active ischemia. However, the authors note that red blood cells in stored blood may be depleted of both 2,3-diphosphoglyceric acid and nitric oxide, both of which are critical components to oxygen delivery and exchange. These cells then function as nitric oxide “sinks,” promoting vasoconstriction, platelet aggregation, and impaired oxygen delivery to tissues. In addition, inflammatory mediators associated with exacerbation of myocardial ischemia may remain in transfused blood, potentially contributing to adverse outcomes.
As this is a nonrandomized, post hoc observational study, further prescriptive conclusions regarding transfusion cannot be made. However, the authors, along with an accompanying editorial, call for prospective randomized trials of transfusion in anemic patients with acute coronary syndromes to better define the role of this commonly used therapy. (CW)
- Wu WC, Rathore SS, Wang Y, Radford MJ, Krumholz HM. Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med. 2001;345:1230-6.
Cost-effectiveness of Rhythm Versus Rate Control in Atrial Fibrillation
Marshall DA, Levy AR, Vidaillet H, et al. Cost-effectiveness of rhythm versus rate control in atrial fibrillation. Ann Intern Med. 2004;141:653-61.
Atrial fibrillation is the most common arrhythmia treated by physicians. It afflicts nearly 10% of patients age 80 years or older. There are two primary modalities of managing patients with atrial fibrillation; rate control versus cardioversion into sinus rhythm.
AFFIRM was a multicenter randomized controlled trial involving 213 centers in USA and Canada that compared rate versus rhythm control in 4060 patients. These patients had a mean age of 70 years. Sixty-one percent of the enrolled patients were men, and 66% had recurrent atrial fibrillation. Seventy-one percent of patients had hypertension, 39% had coronary artery disease, and 9% had congestive heart failure. Patients were block randomized by center to either rate control or rhythm control and followed for an average of 3.5 years. AFFIRM results showed no significant mortality difference between the two groups (hazard ratio for rate versus rhythm control, 0.87 with 95% CI, 0.75 to 1.01).
Primary data on survival and resource utilization were used to conduct the economic analysis from a third party payer perspective. Authors used intention to treat data for the economic analysis.
For resource utilization estimates, US healthcare cost figures for the year 2002 were used. All earlier costs were appropriately adjusted using Consumer Price Index, Medical Care component to estimate their nominal values in year 2002. Hospital costs were taken as the mean charges per day from Healthcare Cost and Utilization Project statistics for Diseases of the Circulatory System for patients older than 18 years age. Low and high end of these costs were assumed to be equivalent to 25th and 75th percentiles of the mean costs, respectively. Physician costs were assumed to be equivalent to be the average of all carriers’ payments for the relative value units of the services rendered based on a generic current procedural terminology code. Sensitivity analysis was conducted on these physician costs using minimum payment among these carriers as the low cost estimate and the standard charges for Marshfield Clinic for the high end. Costs of pacemaker and implantable cardioverter defibrillators were based on manufacturers’ list prices. For sensitivity analysis, hardware costs were excluded for low cost estimates and the maximum manufacturers’ list price for the high estimate was used.
At each follow-up visit during the AFFIRM trial, the number of cardioversion attempts since the prior visit was recorded. Costs of cardioversion were based on average payment to Marshfield Clinic for outpatient electrical cardioversion for the year 2002. Authors assigned no costs for low cost estimate and used billed charges for high costs for sensitivity analysis.
At each follow-up visit, the number of short stay and emergency department visits since the prior visit was recorded. Weighted average Medicare costs for level I and II facilities were used as the baseline estimate for these visits. Estimates for sensitivity analysis were the minimum and maximum Medicare payments for these visits. Physician fees were based on level III emergency department visit with low and high cost estimates assigned as described above.
Medication costs were based on the least average wholesale price (AWP) for a generic medication. Low and high cost estimates were taken from lowest quoted US Internet pharmacy price and highest AWP for the most expensive drug in the class respectively. Only medications used for atrial fibrillation and anticoagulation were considered for analysis.
The authors calculated the mean cost per patient In the Literature (continued) and the mean survival time between the two interventions. Future costs were discounted by 3%. For the base estimate, rhythm control was more expensive and less effective than rate control, i.e., dominated by the rate control. Rate control dominated rhythm control even for high and low estimates of the sensitivity analysis demonstrating stability of the results. Authors used 10,000 simulations to perform non-parametric bootstrapping analysis to find the 95% credible intervals around the base estimate. The bootstrap results showed that for 95% of the results rate control had higher survival time and was less costly than rhythm control. These simulation results clearly showed rate control is more cost-effective for patient population resembling that of AFFIRM trial.
The study has some limitations. These results are robust for patients similar to those in AFFIRM trial, i.e., older patients with cardiovascular defects that are at risk of cerebrovascular embolism. However these results may not be applicable to younger patients and those with “lone atrial fibrillation.” The study had a follow-up period of 3.5 years, and the cost-effectiveness analysis is confined to this period. It is difficult to determine mortality advantage of one treatment over another within the limited duration of the AFFIRM study. Most of the patients were on multiple pharmacologic agents for rhythm control and had a high incidence of cross-over from rhythm control to rate control reflecting modest benefits of the current agents. These results may not be applicable to patients whose atrial fibrillation is well controlled by a single agent or by non-pharmacological treatment. Patients on rhythm control agents had, as expected, more hospitalization days from the side effects and treatment protocols of the agents (especially pharmacologic) used to control the rhythm. With advances in both pharmacologic as well as nonpharmacologic methods for rhythm control generating safer and more efficacious technologies, the results of this analysis may become less valid in the future. The analysis was conducted from a third-party payer perspective, without accounting for the quality of life. Thus patients who have symptomatic atrial fibrillation and those with diastolic dysfunction may have improved quality of life from rhythm control over just rate control. The results may not be applicable to these patients. (SS)
CARP Trial Suggests No Benefit to Revascularization Before Vascular Surgery
McFalls, EO, Ward HB, Mortiz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351:2795-2804.
Recent studies have presented evidence that treatment with beta-blockers for patients with CAD could reduce the risk of perioperative cardiac complications. Beta-blockers have since become a critical part of the management plan for the perioperative patient. Evidence-based practice guidelines for cardiac risk assessment have been published by both the American College of Physicians and the American College of Cardiology/American Heart Association. However, practice patterns continue to vary between physicians and cardiologists, particularly for patients clinically stratified into the intermediate-risk category. Some physicians feel comfortable with a conservative approach of medical optimization even in the setting of established CAD, while others favor more aggressive treatment, even though the prospective data supporting cardiac revascularization before major surgery has been lacking. The study investigators sought to clarify this uncertainty.
The prospective trial enrolled 510 patients at 18 VA centers. Patients scheduled for major vascular operations were eligible, and were preoperatively assessed via clinical criteria, stress imaging, and angiography when appropriate. Eligible patients had significant (at least 70%) stenosis of at least one coronary artery. High-risk patients (i.e., those with left main disease, severe aortic stenosis, and LVEF <20%) were excluded. Patients were then randomized to one
of two groups. The first group underwent revascularization with PTCA or CABG plus medical optimization; the second group received only medical optimization. Most patients in both groups received beta-blockers, and more than half in each received statins. The patient populations were appropriately randomized, although overwhelmingly male (98%). Most patients had one- or two-vessel CAD. The primary endpoint was long-term mortality. Secondary endpoints included MI, stroke, renal failure requiring dialysis, and limb loss. Follow-up rates were similar in both groups (86% and 85%).
The major finding of the study was the lack of difference in mortality between the two groups at an average follow-up of 2.7 years (22% vs. 23%, RR= 0.98, 95% CI 0.70 to 1.37, p = 0.92). Analyzing by “treatment-received” instead of “intention-to-treat” did not significantly change this result. Of note, ten patients in the revascularization arm died between the revascularization procedure and the vascular surgery. Not surprisingly, revascularization also delayed the time to surgery for patients in that arm of the study. In the authors’ analysis, the patients were also divided into subgroups based on high-risk variables (prior CABG, category of Revised Cardiac Risk Index, etc.), but the study was not powered to detect mortality differences between the two arms within these subgroups. The authors concluded that there was no benefit to revascularization in patients with stable coronary syndromes prior to elective vascular surgeries.
The results of this study validate the conservative practice recommended by the existing guidelines— that is, to perform revascularization procedures in the preoperative setting only when indicated by clinical criteria such as unstable ischemic symptoms, and if likely to improve long-term survival. Beta-blockers, and based on recent studies probably “statins,” should continue to be the mainstay of perioperative risk optimization for patients with stable coronary disease.
There were, however, several important considerations: first, the study group was exclusively male, although there is little reason to believe that women would have better outcomes from revascularization. And second, the highest-risk patients were excluded, and therefore the results should not be extrapolated to that population. Prospective identification of the group of patients who may benefit from aggressive intervention should remain a target of risk assessment and further research. (BH)
Blood Transfusion May Increase Mortality in Acute Coronary Syndrome
Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292:1555-62.
The increased use of invasive procedures and anticoagulant and fibrinolytic drugs in patients with ischemic heart disease in recent years predictably increases the potential for bleeding and perceived need for transfusion. Studies evaluating the association between transfusion and mortality have produced mixed results. A more pertinent clinical question is whether transfusion is beneficial or harmful in patients with acute coronary syndromes who acutely develop anemia during their hospitalization.
The authors used clinical data from three large international trials of patients with acute coronary syndromes (GUSTO IIb, PURSUIT, and PARAGON B) to determine the association between blood transfusion and outcomes among patients who developed moderate to severe bleeding, anemia, or both during their hospitalization.
Assessment of clinically significant bleeding complications was based on the GUSTO definition of severe (intracranial hemorrhage or hemodynamic compromise and requiring intervention) or moderate (hemodynamically stable but requiring blood transfusion) bleeding. The GUSTO IIb and PURSUIT trials used the above definition; PARAGON B categorized bleeding as “major or life threatening” (intracranial hemorrhage or bleeding leading to hemodynamic compromise requiring intervention) or “intermediate” (requiring transfusion or a decrease in hemoglobin of 5 g/dL or more, or a decrease in hematocrit ( 15%). Major or life-threatening bleeding episodes and intermediate bleeding episodes in PARAGON B were deemed equivalent to severe and moderate bleeding episodes in GUSTO.
Data were collected on the date, time, severity, and location of each bleeding event, and on the date and number of units of packed red blood cells and whole blood transfused. The primary end-point was 30-day all-cause mortality. Secondary end-points were occurrence of the composite of 30-day death or MI.
The unadjusted rates of 30-day death, MI, and composite death/MI were significantly higher among patients who received a transfusion (30-day death, 8.00% vs. 3.08%; p<.001; 30-day MI, 25.16% vs. 8.16%; p<.001; 30-day composite death/MI, 29.24% vs. 10.02%; p<.001).
After adjustment for baseline characteristics, bleeding and transfusion propensity, and nadir hematocrit, blood transfusion was associated with a hazard ratio for death of 3.94 (95% confidence interval, 3.26–4.75).
No significant association was found between transfusion and 30-day mortality at a nadir hematocrit of 25% or less (adjusted OR 1.13; 95% CI 0.70-1.82). However, at a nadir hematocrit higher than 25%, transfusion was associated with significantly higher odds of 30-day death, even after excluding patients who underwent CABG or those who died within the first 5 days of follow-up.
These findings differ from the findings of Wu et al. (1) who noted that blood transfusion was associated with lower 30-day mortality among elderly patients with MI if the admission hematocrit was 30% or lower. The current authors propose that their data is more robust due to meticulous collection through clinical trial records, and that their analysis accounts for timing of transfusion and indications for transfusion.
Many clinicians logically believe that augmentation of oxygen carrying capacity via transfusion would be beneficial to patients with active ischemia. However, the authors note that red blood cells in stored blood may be depleted of both 2,3-diphosphoglyceric acid and nitric oxide, both of which are critical components to oxygen delivery and exchange. These cells then function as nitric oxide “sinks,” promoting vasoconstriction, platelet aggregation, and impaired oxygen delivery to tissues. In addition, inflammatory mediators associated with exacerbation of myocardial ischemia may remain in transfused blood, potentially contributing to adverse outcomes.
As this is a nonrandomized, post hoc observational study, further prescriptive conclusions regarding transfusion cannot be made. However, the authors, along with an accompanying editorial, call for prospective randomized trials of transfusion in anemic patients with acute coronary syndromes to better define the role of this commonly used therapy. (CW)
- Wu WC, Rathore SS, Wang Y, Radford MJ, Krumholz HM. Blood transfusion in elderly patients with acute myocardial infarction. N Engl J Med. 2001;345:1230-6.
Cost-effectiveness of Rhythm Versus Rate Control in Atrial Fibrillation
Marshall DA, Levy AR, Vidaillet H, et al. Cost-effectiveness of rhythm versus rate control in atrial fibrillation. Ann Intern Med. 2004;141:653-61.
Atrial fibrillation is the most common arrhythmia treated by physicians. It afflicts nearly 10% of patients age 80 years or older. There are two primary modalities of managing patients with atrial fibrillation; rate control versus cardioversion into sinus rhythm.
AFFIRM was a multicenter randomized controlled trial involving 213 centers in USA and Canada that compared rate versus rhythm control in 4060 patients. These patients had a mean age of 70 years. Sixty-one percent of the enrolled patients were men, and 66% had recurrent atrial fibrillation. Seventy-one percent of patients had hypertension, 39% had coronary artery disease, and 9% had congestive heart failure. Patients were block randomized by center to either rate control or rhythm control and followed for an average of 3.5 years. AFFIRM results showed no significant mortality difference between the two groups (hazard ratio for rate versus rhythm control, 0.87 with 95% CI, 0.75 to 1.01).
Primary data on survival and resource utilization were used to conduct the economic analysis from a third party payer perspective. Authors used intention to treat data for the economic analysis.
For resource utilization estimates, US healthcare cost figures for the year 2002 were used. All earlier costs were appropriately adjusted using Consumer Price Index, Medical Care component to estimate their nominal values in year 2002. Hospital costs were taken as the mean charges per day from Healthcare Cost and Utilization Project statistics for Diseases of the Circulatory System for patients older than 18 years age. Low and high end of these costs were assumed to be equivalent to 25th and 75th percentiles of the mean costs, respectively. Physician costs were assumed to be equivalent to be the average of all carriers’ payments for the relative value units of the services rendered based on a generic current procedural terminology code. Sensitivity analysis was conducted on these physician costs using minimum payment among these carriers as the low cost estimate and the standard charges for Marshfield Clinic for the high end. Costs of pacemaker and implantable cardioverter defibrillators were based on manufacturers’ list prices. For sensitivity analysis, hardware costs were excluded for low cost estimates and the maximum manufacturers’ list price for the high estimate was used.
At each follow-up visit during the AFFIRM trial, the number of cardioversion attempts since the prior visit was recorded. Costs of cardioversion were based on average payment to Marshfield Clinic for outpatient electrical cardioversion for the year 2002. Authors assigned no costs for low cost estimate and used billed charges for high costs for sensitivity analysis.
At each follow-up visit, the number of short stay and emergency department visits since the prior visit was recorded. Weighted average Medicare costs for level I and II facilities were used as the baseline estimate for these visits. Estimates for sensitivity analysis were the minimum and maximum Medicare payments for these visits. Physician fees were based on level III emergency department visit with low and high cost estimates assigned as described above.
Medication costs were based on the least average wholesale price (AWP) for a generic medication. Low and high cost estimates were taken from lowest quoted US Internet pharmacy price and highest AWP for the most expensive drug in the class respectively. Only medications used for atrial fibrillation and anticoagulation were considered for analysis.
The authors calculated the mean cost per patient In the Literature (continued) and the mean survival time between the two interventions. Future costs were discounted by 3%. For the base estimate, rhythm control was more expensive and less effective than rate control, i.e., dominated by the rate control. Rate control dominated rhythm control even for high and low estimates of the sensitivity analysis demonstrating stability of the results. Authors used 10,000 simulations to perform non-parametric bootstrapping analysis to find the 95% credible intervals around the base estimate. The bootstrap results showed that for 95% of the results rate control had higher survival time and was less costly than rhythm control. These simulation results clearly showed rate control is more cost-effective for patient population resembling that of AFFIRM trial.
The study has some limitations. These results are robust for patients similar to those in AFFIRM trial, i.e., older patients with cardiovascular defects that are at risk of cerebrovascular embolism. However these results may not be applicable to younger patients and those with “lone atrial fibrillation.” The study had a follow-up period of 3.5 years, and the cost-effectiveness analysis is confined to this period. It is difficult to determine mortality advantage of one treatment over another within the limited duration of the AFFIRM study. Most of the patients were on multiple pharmacologic agents for rhythm control and had a high incidence of cross-over from rhythm control to rate control reflecting modest benefits of the current agents. These results may not be applicable to patients whose atrial fibrillation is well controlled by a single agent or by non-pharmacological treatment. Patients on rhythm control agents had, as expected, more hospitalization days from the side effects and treatment protocols of the agents (especially pharmacologic) used to control the rhythm. With advances in both pharmacologic as well as nonpharmacologic methods for rhythm control generating safer and more efficacious technologies, the results of this analysis may become less valid in the future. The analysis was conducted from a third-party payer perspective, without accounting for the quality of life. Thus patients who have symptomatic atrial fibrillation and those with diastolic dysfunction may have improved quality of life from rhythm control over just rate control. The results may not be applicable to these patients. (SS)
Practice Profile
Contact
Michael J. Pistoria, DO
Medical Director, Lehigh Valley Hospitalist Services
Associate Program Director, Internal Medicine Residency
Assistant Professor of Medicine, Penn State College of Medicine
Kevin Flynn, MS, Administrative Director
Lehigh Valley Hospital
Cedar Crest Boulevard and I-78
Allentown, PA 18105
Phone: 610-402-8045
Fax: 610-402-1675
Website: www.lvhhn.org
E-mail: [email protected]
Start Up
July 2003
Practitioners
Lehigh Valley Hospital - Cedar Crest
Ardeth Copeland, MD
Shoban Dave, MD
John Davidyock, MD
William Ford, MD
Arvind Gupta, MD (site leader)
Kweku Hayford, MD
Lehigh Valley Hospital - Muhlenberg
Donna Dowlatshahi, Coordinator
Jeff rey Faidley, MD
Melissa Geitz, DO
Wayne Howard, DO (site leader)
Melissa Liu, MD
Dan Mulcahy, DO
Gonzalo Pimentel, MD
Deborah Sterner, Coordinator
Training
All ABIM certified
Employed By
Lehigh Valley Physician Group and Specialty Physicians of LVHHN, PC
Lehigh Valley Hospital and Health Network (LVHHN) is one of the largest teaching facilities in Pennsylvania. LVHHN consists of three clinical campuses, two of which focus on inpatient care: Lehigh Valley Hospital-Cedar Crest (LVHCC) and Lehigh Valley Hospital-Muhlenberg (LVH-M). The Network has more than 1,100 physicians and is a major clinical campus for Penn State’s College of Medicine. LVH-M opens a new patient care, tower in March 2005 and has approximately 200 inpatient beds on campus. The campus offers cardiac catheterization and open heart surgery capabilities, and its intensive care unit is augmented by a tele-intensivist system. A 24/7 hospitalist program was launched at LVH-M in July 2003 and is presently staffed by six full-time physicians.
The LVH-CC campus is preparing to undergo a major expansion that will bring its total beds to approximately 800 by 2007. This campus is a tertiary care center, featuring medical and surgical intensive care, a Level I trauma unit, a burn center, open heart surgery, perinatal care and renal transplantation services. LVHHN also boasts active teaching programs, with residencies in internal medicine, surgery, OB/GYN, family medicine, and emergency medicine. There are also fellowships in cardiology, pulmonary/critical care, and hematology/oncology. The LVHCC hospitalist program provides 24/7 service staffed by six physicians and was launched in July 2004.
Finances
All LVHS physicians are salaried employees. A bonus was paid to the physicians at LVH-M at the end of the first year of services. A bonus structure is being defined for both campuses, focusing on clinical, quality, and service measures. Each hospitalist receives 4 weeks vacation and 5 days of CME. A stipend is also provided for CME. Hospitalists receive malpractice coverage and reimbursement for licensure expenses. Physicians are also entitled to a benefits package that includes disability insurance, a supplemental retirement plan, and a 401(k)/403(b).
Chart abstraction and billing is done by the employer. At the end of each shift, the hospitalist submits a list of the patients seen and/or admitted. Each campus has a program coordinator certified in coding who reviews the charts for documentation and submits for the appropriate level of care. This system has worked well in ensuring proper billing and in allowing prompt feedback to the hospitalists regarding their documentation.
Referrals
LVH-M: The LVH-M hospitalist program was developed to provide a resource for primary care physicians in the community who wished to focus on outpatient care. Primary care physicians were identified and ranked in terms of their willingness to refer patients to the hospitalist program. Care was taken not to target groups who already had referral patterns to existing LVH-M groups to minimize the adverse impact of the hospitalist program on these groups. Hospitalists then made visits to these offices to explain the hospitalist program and answer questions from the PCPs. The program quickly became successful and now has a well-established referral base.
LVH-CC: The major driver of the hospitalist program at the Cedar Crest campus was assisting with the residency program. The existing faculty group staffed two of the five inpatient teaching services and was becoming increasingly busy as a result of new referrals. The hospitalist program helped decompress some of the volume from the existing faculty services by taking over one of the other inpatient teaching slots and establishing an overflow service. The program also seeks referrals from physicians outside the hospital’s traditional referral radius. The hospitalists have also worked with the medical and surgical subspecialists, developing standards for admission of subspecialty patients to the hospitalist service.
Teaching
LVH-CC: The LVH-CC hospitalists are intimately involved in the internal medicine residency program. They staff one of five inpatient teaching services during the morning. In the afternoon and overnight hours, the hospitalists cover their own service and the two pre-existing academic inpatient services. The hospitalists round either formally or informally with the residents of these three teams in the afternoon. They also review each new admission between noon and 8 a.m. to the three inpatient teams and provide bedside teaching on these patients.
A second daytime hospitalist also staff s an overflow service to ensure compliance with Residency Review Committee guidelines regarding service and admission caps. If the three teaching services hit their respective caps, any new patients are admitted by the hospitalists to this overflow service. In addition to rounding on the overflow patients, the second hospitalist staff s a consultative medicine service with a PGY-2 or PGY-3 resident.
The hospitalists participate in morning report and the resident lectures. The hospitalists are also involved in faculty development with the academic general internists as well as other residency initiatives.
LVH-M: Hospitalists at the LVH-M campus have no formal involvement in the teaching programs (osteopathic rotating internship and emergency medicine residency) at that campus. They are an available resource for housestaff, however, and have received many positive compliments from the housestaff for their assistance with difficult patients.
Schedule
LVH-M: The primary rounding hospitalist works Monday through Friday from 7 a.m. to 3 p.m. A second hospitalist works Monday through Friday from 10 a.m. to 7 p.m. and is available on Saturday if the census is high. This hospitalist also works the Sunday night shift beginning at 7 p.m. and ending 7 a.m. Monday. The overnight hospitalist works from 7 p.m. to 7 a.m. Monday through Saturday. There is always a back-up hospitalist available in case of emergency or significant influx of patients that overwhelms the system. The hospitalists work an average of 16 shifts per month.
LVH-CC: There are two hospitalists scheduled during the daytime hours. The hospitalist rounding with the resident team works 7 a.m. to 7 p.m. Monday through Sunday. The overflow/consult hospitalist works 8 a.m. to 8 p.m. Monday through Friday and 7 p.m. to 7 a.m. Saturday and Sunday. The overnight hospitalist works 7 p.m. to 7 a.m. Monday through Friday. The hospitalists work an average of 16 shifts per month.
Future Directions
LVH-M: As the campus continues to grow, the hospitalists aim to become more intricately involved in process improvement and quality-improvement measures. The program is exploring ways of becoming active in the teaching program, either with residents and medical students or with physician assistant students. Additionally, as the Network’s tele-intensivist initiative develops, the hospitalists are working closely with their critical care colleagues to provide top-quality ICU care for patients.
LVH-CC: The LVH-CC hospitalists are becoming increasingly involved in efforts to maximize institutional efficiency and throughput. This program is also seeking to establish itself as a premier research program, in both the educational and clinical realms.
Hospitalists at both campuses are becoming involved in various hospital committees such as Therapeutics and Quality Assurance. Their expertise has also been utilized in various throughput initiatives such as an automated discharge instruction process and electronic signout development.
Given the rapid growth of both programs, staffing needs are expected to increase considerably. One long-term goal is to make it possible for hospitalists to rotate between the two campuses to allow them a variety of experiences. A hospital medicine elective is being developed for PGY-3 residents interested in a career in hospital medicine. There has also been some preliminary discussion of a hospital medicine fellowship that would emphasize teaching, research, and palliative care.
Contact
Michael J. Pistoria, DO
Medical Director, Lehigh Valley Hospitalist Services
Associate Program Director, Internal Medicine Residency
Assistant Professor of Medicine, Penn State College of Medicine
Kevin Flynn, MS, Administrative Director
Lehigh Valley Hospital
Cedar Crest Boulevard and I-78
Allentown, PA 18105
Phone: 610-402-8045
Fax: 610-402-1675
Website: www.lvhhn.org
E-mail: [email protected]
Start Up
July 2003
Practitioners
Lehigh Valley Hospital - Cedar Crest
Ardeth Copeland, MD
Shoban Dave, MD
John Davidyock, MD
William Ford, MD
Arvind Gupta, MD (site leader)
Kweku Hayford, MD
Lehigh Valley Hospital - Muhlenberg
Donna Dowlatshahi, Coordinator
Jeff rey Faidley, MD
Melissa Geitz, DO
Wayne Howard, DO (site leader)
Melissa Liu, MD
Dan Mulcahy, DO
Gonzalo Pimentel, MD
Deborah Sterner, Coordinator
Training
All ABIM certified
Employed By
Lehigh Valley Physician Group and Specialty Physicians of LVHHN, PC
Lehigh Valley Hospital and Health Network (LVHHN) is one of the largest teaching facilities in Pennsylvania. LVHHN consists of three clinical campuses, two of which focus on inpatient care: Lehigh Valley Hospital-Cedar Crest (LVHCC) and Lehigh Valley Hospital-Muhlenberg (LVH-M). The Network has more than 1,100 physicians and is a major clinical campus for Penn State’s College of Medicine. LVH-M opens a new patient care, tower in March 2005 and has approximately 200 inpatient beds on campus. The campus offers cardiac catheterization and open heart surgery capabilities, and its intensive care unit is augmented by a tele-intensivist system. A 24/7 hospitalist program was launched at LVH-M in July 2003 and is presently staffed by six full-time physicians.
The LVH-CC campus is preparing to undergo a major expansion that will bring its total beds to approximately 800 by 2007. This campus is a tertiary care center, featuring medical and surgical intensive care, a Level I trauma unit, a burn center, open heart surgery, perinatal care and renal transplantation services. LVHHN also boasts active teaching programs, with residencies in internal medicine, surgery, OB/GYN, family medicine, and emergency medicine. There are also fellowships in cardiology, pulmonary/critical care, and hematology/oncology. The LVHCC hospitalist program provides 24/7 service staffed by six physicians and was launched in July 2004.
Finances
All LVHS physicians are salaried employees. A bonus was paid to the physicians at LVH-M at the end of the first year of services. A bonus structure is being defined for both campuses, focusing on clinical, quality, and service measures. Each hospitalist receives 4 weeks vacation and 5 days of CME. A stipend is also provided for CME. Hospitalists receive malpractice coverage and reimbursement for licensure expenses. Physicians are also entitled to a benefits package that includes disability insurance, a supplemental retirement plan, and a 401(k)/403(b).
Chart abstraction and billing is done by the employer. At the end of each shift, the hospitalist submits a list of the patients seen and/or admitted. Each campus has a program coordinator certified in coding who reviews the charts for documentation and submits for the appropriate level of care. This system has worked well in ensuring proper billing and in allowing prompt feedback to the hospitalists regarding their documentation.
Referrals
LVH-M: The LVH-M hospitalist program was developed to provide a resource for primary care physicians in the community who wished to focus on outpatient care. Primary care physicians were identified and ranked in terms of their willingness to refer patients to the hospitalist program. Care was taken not to target groups who already had referral patterns to existing LVH-M groups to minimize the adverse impact of the hospitalist program on these groups. Hospitalists then made visits to these offices to explain the hospitalist program and answer questions from the PCPs. The program quickly became successful and now has a well-established referral base.
LVH-CC: The major driver of the hospitalist program at the Cedar Crest campus was assisting with the residency program. The existing faculty group staffed two of the five inpatient teaching services and was becoming increasingly busy as a result of new referrals. The hospitalist program helped decompress some of the volume from the existing faculty services by taking over one of the other inpatient teaching slots and establishing an overflow service. The program also seeks referrals from physicians outside the hospital’s traditional referral radius. The hospitalists have also worked with the medical and surgical subspecialists, developing standards for admission of subspecialty patients to the hospitalist service.
Teaching
LVH-CC: The LVH-CC hospitalists are intimately involved in the internal medicine residency program. They staff one of five inpatient teaching services during the morning. In the afternoon and overnight hours, the hospitalists cover their own service and the two pre-existing academic inpatient services. The hospitalists round either formally or informally with the residents of these three teams in the afternoon. They also review each new admission between noon and 8 a.m. to the three inpatient teams and provide bedside teaching on these patients.
A second daytime hospitalist also staff s an overflow service to ensure compliance with Residency Review Committee guidelines regarding service and admission caps. If the three teaching services hit their respective caps, any new patients are admitted by the hospitalists to this overflow service. In addition to rounding on the overflow patients, the second hospitalist staff s a consultative medicine service with a PGY-2 or PGY-3 resident.
The hospitalists participate in morning report and the resident lectures. The hospitalists are also involved in faculty development with the academic general internists as well as other residency initiatives.
LVH-M: Hospitalists at the LVH-M campus have no formal involvement in the teaching programs (osteopathic rotating internship and emergency medicine residency) at that campus. They are an available resource for housestaff, however, and have received many positive compliments from the housestaff for their assistance with difficult patients.
Schedule
LVH-M: The primary rounding hospitalist works Monday through Friday from 7 a.m. to 3 p.m. A second hospitalist works Monday through Friday from 10 a.m. to 7 p.m. and is available on Saturday if the census is high. This hospitalist also works the Sunday night shift beginning at 7 p.m. and ending 7 a.m. Monday. The overnight hospitalist works from 7 p.m. to 7 a.m. Monday through Saturday. There is always a back-up hospitalist available in case of emergency or significant influx of patients that overwhelms the system. The hospitalists work an average of 16 shifts per month.
LVH-CC: There are two hospitalists scheduled during the daytime hours. The hospitalist rounding with the resident team works 7 a.m. to 7 p.m. Monday through Sunday. The overflow/consult hospitalist works 8 a.m. to 8 p.m. Monday through Friday and 7 p.m. to 7 a.m. Saturday and Sunday. The overnight hospitalist works 7 p.m. to 7 a.m. Monday through Friday. The hospitalists work an average of 16 shifts per month.
Future Directions
LVH-M: As the campus continues to grow, the hospitalists aim to become more intricately involved in process improvement and quality-improvement measures. The program is exploring ways of becoming active in the teaching program, either with residents and medical students or with physician assistant students. Additionally, as the Network’s tele-intensivist initiative develops, the hospitalists are working closely with their critical care colleagues to provide top-quality ICU care for patients.
LVH-CC: The LVH-CC hospitalists are becoming increasingly involved in efforts to maximize institutional efficiency and throughput. This program is also seeking to establish itself as a premier research program, in both the educational and clinical realms.
Hospitalists at both campuses are becoming involved in various hospital committees such as Therapeutics and Quality Assurance. Their expertise has also been utilized in various throughput initiatives such as an automated discharge instruction process and electronic signout development.
Given the rapid growth of both programs, staffing needs are expected to increase considerably. One long-term goal is to make it possible for hospitalists to rotate between the two campuses to allow them a variety of experiences. A hospital medicine elective is being developed for PGY-3 residents interested in a career in hospital medicine. There has also been some preliminary discussion of a hospital medicine fellowship that would emphasize teaching, research, and palliative care.
Contact
Michael J. Pistoria, DO
Medical Director, Lehigh Valley Hospitalist Services
Associate Program Director, Internal Medicine Residency
Assistant Professor of Medicine, Penn State College of Medicine
Kevin Flynn, MS, Administrative Director
Lehigh Valley Hospital
Cedar Crest Boulevard and I-78
Allentown, PA 18105
Phone: 610-402-8045
Fax: 610-402-1675
Website: www.lvhhn.org
E-mail: [email protected]
Start Up
July 2003
Practitioners
Lehigh Valley Hospital - Cedar Crest
Ardeth Copeland, MD
Shoban Dave, MD
John Davidyock, MD
William Ford, MD
Arvind Gupta, MD (site leader)
Kweku Hayford, MD
Lehigh Valley Hospital - Muhlenberg
Donna Dowlatshahi, Coordinator
Jeff rey Faidley, MD
Melissa Geitz, DO
Wayne Howard, DO (site leader)
Melissa Liu, MD
Dan Mulcahy, DO
Gonzalo Pimentel, MD
Deborah Sterner, Coordinator
Training
All ABIM certified
Employed By
Lehigh Valley Physician Group and Specialty Physicians of LVHHN, PC
Lehigh Valley Hospital and Health Network (LVHHN) is one of the largest teaching facilities in Pennsylvania. LVHHN consists of three clinical campuses, two of which focus on inpatient care: Lehigh Valley Hospital-Cedar Crest (LVHCC) and Lehigh Valley Hospital-Muhlenberg (LVH-M). The Network has more than 1,100 physicians and is a major clinical campus for Penn State’s College of Medicine. LVH-M opens a new patient care, tower in March 2005 and has approximately 200 inpatient beds on campus. The campus offers cardiac catheterization and open heart surgery capabilities, and its intensive care unit is augmented by a tele-intensivist system. A 24/7 hospitalist program was launched at LVH-M in July 2003 and is presently staffed by six full-time physicians.
The LVH-CC campus is preparing to undergo a major expansion that will bring its total beds to approximately 800 by 2007. This campus is a tertiary care center, featuring medical and surgical intensive care, a Level I trauma unit, a burn center, open heart surgery, perinatal care and renal transplantation services. LVHHN also boasts active teaching programs, with residencies in internal medicine, surgery, OB/GYN, family medicine, and emergency medicine. There are also fellowships in cardiology, pulmonary/critical care, and hematology/oncology. The LVHCC hospitalist program provides 24/7 service staffed by six physicians and was launched in July 2004.
Finances
All LVHS physicians are salaried employees. A bonus was paid to the physicians at LVH-M at the end of the first year of services. A bonus structure is being defined for both campuses, focusing on clinical, quality, and service measures. Each hospitalist receives 4 weeks vacation and 5 days of CME. A stipend is also provided for CME. Hospitalists receive malpractice coverage and reimbursement for licensure expenses. Physicians are also entitled to a benefits package that includes disability insurance, a supplemental retirement plan, and a 401(k)/403(b).
Chart abstraction and billing is done by the employer. At the end of each shift, the hospitalist submits a list of the patients seen and/or admitted. Each campus has a program coordinator certified in coding who reviews the charts for documentation and submits for the appropriate level of care. This system has worked well in ensuring proper billing and in allowing prompt feedback to the hospitalists regarding their documentation.
Referrals
LVH-M: The LVH-M hospitalist program was developed to provide a resource for primary care physicians in the community who wished to focus on outpatient care. Primary care physicians were identified and ranked in terms of their willingness to refer patients to the hospitalist program. Care was taken not to target groups who already had referral patterns to existing LVH-M groups to minimize the adverse impact of the hospitalist program on these groups. Hospitalists then made visits to these offices to explain the hospitalist program and answer questions from the PCPs. The program quickly became successful and now has a well-established referral base.
LVH-CC: The major driver of the hospitalist program at the Cedar Crest campus was assisting with the residency program. The existing faculty group staffed two of the five inpatient teaching services and was becoming increasingly busy as a result of new referrals. The hospitalist program helped decompress some of the volume from the existing faculty services by taking over one of the other inpatient teaching slots and establishing an overflow service. The program also seeks referrals from physicians outside the hospital’s traditional referral radius. The hospitalists have also worked with the medical and surgical subspecialists, developing standards for admission of subspecialty patients to the hospitalist service.
Teaching
LVH-CC: The LVH-CC hospitalists are intimately involved in the internal medicine residency program. They staff one of five inpatient teaching services during the morning. In the afternoon and overnight hours, the hospitalists cover their own service and the two pre-existing academic inpatient services. The hospitalists round either formally or informally with the residents of these three teams in the afternoon. They also review each new admission between noon and 8 a.m. to the three inpatient teams and provide bedside teaching on these patients.
A second daytime hospitalist also staff s an overflow service to ensure compliance with Residency Review Committee guidelines regarding service and admission caps. If the three teaching services hit their respective caps, any new patients are admitted by the hospitalists to this overflow service. In addition to rounding on the overflow patients, the second hospitalist staff s a consultative medicine service with a PGY-2 or PGY-3 resident.
The hospitalists participate in morning report and the resident lectures. The hospitalists are also involved in faculty development with the academic general internists as well as other residency initiatives.
LVH-M: Hospitalists at the LVH-M campus have no formal involvement in the teaching programs (osteopathic rotating internship and emergency medicine residency) at that campus. They are an available resource for housestaff, however, and have received many positive compliments from the housestaff for their assistance with difficult patients.
Schedule
LVH-M: The primary rounding hospitalist works Monday through Friday from 7 a.m. to 3 p.m. A second hospitalist works Monday through Friday from 10 a.m. to 7 p.m. and is available on Saturday if the census is high. This hospitalist also works the Sunday night shift beginning at 7 p.m. and ending 7 a.m. Monday. The overnight hospitalist works from 7 p.m. to 7 a.m. Monday through Saturday. There is always a back-up hospitalist available in case of emergency or significant influx of patients that overwhelms the system. The hospitalists work an average of 16 shifts per month.
LVH-CC: There are two hospitalists scheduled during the daytime hours. The hospitalist rounding with the resident team works 7 a.m. to 7 p.m. Monday through Sunday. The overflow/consult hospitalist works 8 a.m. to 8 p.m. Monday through Friday and 7 p.m. to 7 a.m. Saturday and Sunday. The overnight hospitalist works 7 p.m. to 7 a.m. Monday through Friday. The hospitalists work an average of 16 shifts per month.
Future Directions
LVH-M: As the campus continues to grow, the hospitalists aim to become more intricately involved in process improvement and quality-improvement measures. The program is exploring ways of becoming active in the teaching program, either with residents and medical students or with physician assistant students. Additionally, as the Network’s tele-intensivist initiative develops, the hospitalists are working closely with their critical care colleagues to provide top-quality ICU care for patients.
LVH-CC: The LVH-CC hospitalists are becoming increasingly involved in efforts to maximize institutional efficiency and throughput. This program is also seeking to establish itself as a premier research program, in both the educational and clinical realms.
Hospitalists at both campuses are becoming involved in various hospital committees such as Therapeutics and Quality Assurance. Their expertise has also been utilized in various throughput initiatives such as an automated discharge instruction process and electronic signout development.
Given the rapid growth of both programs, staffing needs are expected to increase considerably. One long-term goal is to make it possible for hospitalists to rotate between the two campuses to allow them a variety of experiences. A hospital medicine elective is being developed for PGY-3 residents interested in a career in hospital medicine. There has also been some preliminary discussion of a hospital medicine fellowship that would emphasize teaching, research, and palliative care.
The Quality and Patient Safety Track at the 2005 SHM Annual Meeting
Quality and Patient Safety have become the cornerstone of the ways that hospitalists can improve inpatient care delivery. At this year’s annual meeting, the focus on quality and safety is represented through a series of dynamic workshops that will allow practicing hospitalists to learn practical skills in quality improvement, to contribute to the development of standards on the discharge process, and to understand emerging models of care delivery that may impact inpatient mortality. Below is a brief summary of the workshops and their objectives:
- Hospital Mortality Reduction— the Role of Rapid Response Teams: Faculty from the Institute for Healthcare Improvement and leading patient safety programs will present an overview of the concept of rapid response teams, data their effectiveness, and examples of their implementation. Hospitalists are often advocates for patient safety and quality in their institution and will be critical in the development of initiatives to reduce inpatient mortality.
- The Role of Information Technology in Quality Improvement and Safety: A dynamic team of physician leaders in quality and safety will review the literature in the use of information technology to improve quality and safety. Examples of IT approaches to improve inpatient care will be described and discussed. In addition, potential barriers in the use of IT-based approaches to quality and safety will be outlined. Hospitalists will learn about how to integrate existing IT support into quality initiatives and when IT may not be essential to process change.
- A Primer on Root Cause Analysis: Hospitalists may be asked to be part of interdisciplinary teams that review sentinel events through root cause analysis using tools such as Failure Mode Effects Analysis (FMEA). This process can often uncover system-issues that contribute to quality and safety issues. However, it is critical for hospitalists to understand the root cause analysis process, its limitations, and how to maximize the potential of FMEA to identify underlying issues critical to improving patient care and safety.
- Consensus Group/Workshop to Develop the Ideal Discharge Process: Discharging patients from the hospital is a necessary task in every hospital admission, but one that has had very little study or standardization. Hospitalists are critical agents of change in reframing the discharge process and in developing and implementing tools to make that process as safe and efficient as possible. A panel of hospitalists and experts on patient safety especially at care transition points will moderate an open forum to establish guidelines for the ideal hospital discharge. Input from participants will be used to shape guidelines and tools for discharge.
- Quality Improvement for the Clinical Hospitalist: This workshop is targeted at bringing quality improvement from the ivory tower to the practicing hospitalist. Participants will be exposed to basic quality improvement tools and strategies that can be applied in myriad settings to improve care. Examples of successful projects will be presented for discussion.
We will be evaluating participation in the quality and patients safety track at the meeting to help determine the need for more in-depth sessions such as a pre-course on quality assessment and improvement methodology. We are excited to offer such a diverse series of workshops and look forward to your active participation!
Quality and Patient Safety have become the cornerstone of the ways that hospitalists can improve inpatient care delivery. At this year’s annual meeting, the focus on quality and safety is represented through a series of dynamic workshops that will allow practicing hospitalists to learn practical skills in quality improvement, to contribute to the development of standards on the discharge process, and to understand emerging models of care delivery that may impact inpatient mortality. Below is a brief summary of the workshops and their objectives:
- Hospital Mortality Reduction— the Role of Rapid Response Teams: Faculty from the Institute for Healthcare Improvement and leading patient safety programs will present an overview of the concept of rapid response teams, data their effectiveness, and examples of their implementation. Hospitalists are often advocates for patient safety and quality in their institution and will be critical in the development of initiatives to reduce inpatient mortality.
- The Role of Information Technology in Quality Improvement and Safety: A dynamic team of physician leaders in quality and safety will review the literature in the use of information technology to improve quality and safety. Examples of IT approaches to improve inpatient care will be described and discussed. In addition, potential barriers in the use of IT-based approaches to quality and safety will be outlined. Hospitalists will learn about how to integrate existing IT support into quality initiatives and when IT may not be essential to process change.
- A Primer on Root Cause Analysis: Hospitalists may be asked to be part of interdisciplinary teams that review sentinel events through root cause analysis using tools such as Failure Mode Effects Analysis (FMEA). This process can often uncover system-issues that contribute to quality and safety issues. However, it is critical for hospitalists to understand the root cause analysis process, its limitations, and how to maximize the potential of FMEA to identify underlying issues critical to improving patient care and safety.
- Consensus Group/Workshop to Develop the Ideal Discharge Process: Discharging patients from the hospital is a necessary task in every hospital admission, but one that has had very little study or standardization. Hospitalists are critical agents of change in reframing the discharge process and in developing and implementing tools to make that process as safe and efficient as possible. A panel of hospitalists and experts on patient safety especially at care transition points will moderate an open forum to establish guidelines for the ideal hospital discharge. Input from participants will be used to shape guidelines and tools for discharge.
- Quality Improvement for the Clinical Hospitalist: This workshop is targeted at bringing quality improvement from the ivory tower to the practicing hospitalist. Participants will be exposed to basic quality improvement tools and strategies that can be applied in myriad settings to improve care. Examples of successful projects will be presented for discussion.
We will be evaluating participation in the quality and patients safety track at the meeting to help determine the need for more in-depth sessions such as a pre-course on quality assessment and improvement methodology. We are excited to offer such a diverse series of workshops and look forward to your active participation!
Quality and Patient Safety have become the cornerstone of the ways that hospitalists can improve inpatient care delivery. At this year’s annual meeting, the focus on quality and safety is represented through a series of dynamic workshops that will allow practicing hospitalists to learn practical skills in quality improvement, to contribute to the development of standards on the discharge process, and to understand emerging models of care delivery that may impact inpatient mortality. Below is a brief summary of the workshops and their objectives:
- Hospital Mortality Reduction— the Role of Rapid Response Teams: Faculty from the Institute for Healthcare Improvement and leading patient safety programs will present an overview of the concept of rapid response teams, data their effectiveness, and examples of their implementation. Hospitalists are often advocates for patient safety and quality in their institution and will be critical in the development of initiatives to reduce inpatient mortality.
- The Role of Information Technology in Quality Improvement and Safety: A dynamic team of physician leaders in quality and safety will review the literature in the use of information technology to improve quality and safety. Examples of IT approaches to improve inpatient care will be described and discussed. In addition, potential barriers in the use of IT-based approaches to quality and safety will be outlined. Hospitalists will learn about how to integrate existing IT support into quality initiatives and when IT may not be essential to process change.
- A Primer on Root Cause Analysis: Hospitalists may be asked to be part of interdisciplinary teams that review sentinel events through root cause analysis using tools such as Failure Mode Effects Analysis (FMEA). This process can often uncover system-issues that contribute to quality and safety issues. However, it is critical for hospitalists to understand the root cause analysis process, its limitations, and how to maximize the potential of FMEA to identify underlying issues critical to improving patient care and safety.
- Consensus Group/Workshop to Develop the Ideal Discharge Process: Discharging patients from the hospital is a necessary task in every hospital admission, but one that has had very little study or standardization. Hospitalists are critical agents of change in reframing the discharge process and in developing and implementing tools to make that process as safe and efficient as possible. A panel of hospitalists and experts on patient safety especially at care transition points will moderate an open forum to establish guidelines for the ideal hospital discharge. Input from participants will be used to shape guidelines and tools for discharge.
- Quality Improvement for the Clinical Hospitalist: This workshop is targeted at bringing quality improvement from the ivory tower to the practicing hospitalist. Participants will be exposed to basic quality improvement tools and strategies that can be applied in myriad settings to improve care. Examples of successful projects will be presented for discussion.
We will be evaluating participation in the quality and patients safety track at the meeting to help determine the need for more in-depth sessions such as a pre-course on quality assessment and improvement methodology. We are excited to offer such a diverse series of workshops and look forward to your active participation!
The Informed Hospitalist and the Pharmaceutical Industry
The ideal patient-physician relationship is one of choice, competence, communication, compassion, and continuity, and is free of any conflict of interest. There is heated controversy about whether the relationship between the pharmaceutical industry and medical professionals betrays this ideal. The heart of this debate lies in the fundamental difference in priorities and goals of the pharmaceutical industry and hospitalists. Hospitalists are trusted with the lives and well-being of patients. A physician is expected to make an unbiased analysis of the treatment options for a given patient and to apply that treatment to the best of his or her abilities. In contrast, the ultimate interest of the pharmaceutical industry lies with the shareholders, and the primary goal is to maximize profit. Many feel that these two goals are mutually exclusive (1,2). Medical educators believe that it is the responsibility of the medical profession, not pharmaceutical companies, to educate physicians. The entanglement of the pharmaceutical industry with physicians calls into question the credibility of information obtained from any pharmaceutical-sponsored event and casts doubt over the medical profession as a whole. Governmental regulation and legislative initiatives such as the Bayh-Dole Act (3) have furthered the commercialization of academic research and realigned academic centers’ approach to clinical research.
The pharmaceutical industry argues that its goals and the goals of the medical profession are complementary (4) and that their involvement optimizes the benefit to the patient. The pharmaceutical industry is quick to point out that pharmaceutical companies are an important source of funding for clinical trials and are the leading sponsors of continuing medical education, and that it is the most research-intensive industry in the United States supported by private funds (5). Corporate contributions to research and development in academia have increased by 900% between 1980 and 2000. The pharmaceutical industry devoted 18% of profits in 2002 to research, development, and testing activities (6). The pharmaceutical industry claims that these are designed to serve the mutual interests of the pharmaceutical industry and the medical community by providing accurate and up-to-date information to maximize patient care. The advances made as a result of commercial development have dramatically altered the landscape of research. Pharmaceutical courtship of hospitalists, who find themselves on the front line in clinical settings as prescribers or researchers, is part of an aggressive marketing campaign that some believe contributes little to the common good.
Hospitalists have increased their financial incentives with stock options, fees for consultation, speaking arrangements, and memberships on advisory boards for pharmaceutical companies. Disclosure of financial conflicts is becoming an empty ritual providing a false sense of security. Pharmaceutical research is increasingly organized by Contract Research Organizations, written up with the help of ghostwriters, and published under the name of established investigators (7,8). Not all industry-funded studies are necessarily fl awed and without scientific merit, but the fact that negative consequences can be devastating to the financial health of a corporation has to be considered.
A leading catalyst for continued pharmaceutical industry/hospitalist interaction is continuing medical education (CME). In 2003, the pharmaceutical industry provided 900 million of the one billion dollars spent on CME in the United States. Currently, the pharmaceutical industry funds approximately 60% of all CME activities in the United States (9). Information provided to physicians by a pharmaceutical representative has an inaccuracy rating of 13% (10). Not surprisingly, many of these inaccuracies favor the product being presented and casts an unfavorable light on competing drugs (10,11). This has led some to believe that this pharmaceutical representative/physician interaction is having a negative impact on patients (12) through the dissemination of inaccurate information. In addition, misleading advertisements have been found to overstate the effectiveness and minimize the risks of a given drug (11). Another form of bias is the selective publication of research studies by the pharmaceutical industry (13).
Bedside and Conference Detailing
Interactions with pharmaceutical representatives (drug detailers) often begin in medical school and proceed throughout a physician’s career (12,14). In 2003, the pharmaceutical industry spent more than 13 billion dollars on promotional activities for doctors, an average of about $10,500 per physician. There is one drug detailer for every 4.7 office-based physicians. Interactions include conferences with free lunch, personal visits by drug detailers, sponsored CME workshops/seminars, sponsored dinners, sponsored scientific conferences, sponsored research, direct gifts (e.g., cash payments for prescribing a given medication), and indirect gifts (e.g., subsidizing a trip to a medical conference). These interactions evolve from merely lunches and pens early in a physician’s career to positions as a consultant and advisory board honoree as the relationship matures. Some physicians view such exchanges as helpful and informative while others view it as unethical (2) and harmful.
Hospitalists, residents, and medical students alike believe their interactions with drug detailers, and the small gifts that they receive, do not influence their behavior (14,15). Wazana found that as physicians continue to receive gifts from drug detailers, they become even less likely to believe that the gifts can influence their behavior (16). Many physicians believe that their interactions with drug companies are beneficial not only to them but also to their patients. However, studies have found that this is in fact not the case. Physicians who interact with pharmaceutical representatives prescribe newer and more expensive drugs, rather than cheaper and equally effective generic drugs (16,17). There are a significantly higher number of prescriptions written for the drugs manufactured by pharmaceutical companies who sponsor a given CME activity than pharmaceutical companies who do not. A rise in prescription expenditures (17), as well as an increase in irrational prescribing, often follows in-house exposure to drug detailers (16).
The enormous amount spent on marketing can also be used as further proof of the pharmaceutical industry’s avarice. However, we often fail to acknowledge the role that medical educators and professionals play in this problem. Pharmaceutical companies are profitable because of our prescribing habits. For example, many medical professionals prescribe expensive “me too” drugs that often offer little if any benefit over cheaper established or prototypical drugs. Our actions encourage what we claim to be bad behavior by the pharmaceutical industry.
It is often argued by the pharmaceutical industry that these “me too” drugs have a different side effect profile, may improve compliance in long-term treatment, or will reduce cost when compared to the prototype drug. This is true in some instances, as exemplified by the wide array of anti-hypertensives and the even wider array of side effect profiles. However, there are many instances when this is far from the case. If a financial incentive did not exist for pharmaceutical companies to introduce “me too” drugs, the pharmaceutical industry would not do so unless the drug being introduced provided a substantial clinical advantage over the prototype drug. As a result, the pharmaceutical industry would be spending their time, effort, and finances on research aimed at finding new and innovative cures.
Proposed Solution to the Problem
In an effort to remedy this situation, many professional societies (as well as the pharmaceutical industry itself) have established guidelines on the interactions between the pharmaceutical industry and physicians. The AMA has established guidelines responsible for the regulation of gifts bestowed on physicians by industry (18). The Pharmaceutical Research Manufacturers of America has established similar guidelines known as the PhRMA Code (19). Increasingly, many professional organizations have taken it upon themselves to establish their own code of conduct. However, there remains a low level of awareness of the guidelines (15) that are currently in place, and some of the pharmaceutical companies have chosen not to abide by the PhRMA Code. In response to the increasing influence pharmaceutical companies are having on the medical decision-making process, many training programs are adopting policies to limit the contact between pharmaceutical representatives and physicians in training. This is being carried out at both the undergraduate and graduate medical education levels (20). The effects of such restrictions are currently unknown. McCormick found that physicians who trained in institutions with such policies were less likely to find information from pharmaceutical company representatives useful (20). However, Ferguson found that being trained in a program with a policy that limited access to pharmaceutical sales representatives did not affect the subsequent likelihood of future physician-pharmaceutical representative interactions (21).
The Informed Hospitalist in the 21st Century
The literature clearly documents that the pharmaceutical industry influences physician prescribing habits. Hospitalists can take a four-prong approach to help counteract these effects:
1. Academic Detailing
Medical educators can shield residents and medical students from the influence of pharmaceutical representatives by limiting or prohibiting contact, or they can teach trainees how to effectively manage such interactions through academic detailing. As stated above, Ferguson found that policies limiting access to drug detailers did not affect the subsequent likelihood of future physician and pharmaceutical representative interactions (21). It might be wiser to teach trainees how to manage their interactions with the drug representatives and thereby take control of the situation. In order for doctors to effectively manage such interactions, we must learn how to evaluate the literature and interpret the information given to us by representatives. Watkins found that both attendings and residents feel that they should learn how to critically evaluate promotional materials, recognize potential conflicts of interest, and consider how patients perceive physician-pharmaceutical relationships (22). Previous studies have found that educational interventions can have a significant effect on the attitudes of medical students and residents towards pharmaceutical marketing and drug detailers (23,24).
One way to evaluate pharmaceutical literature is to have academic detailing of the clinical studies and statements made by pharmaceutical detailers at sponsored events. During these academic detailing conferences the drug in question can be compared to other drugs in the class, and indications and differences should be mentioned if they exist. This should be done in the presence of both an attending who is very familiar with the drug and drug class in question and a hospital pharmacist. If this is done in a small setting, the medical students and residents can take turns critically evaluating the presentations. This approach is comparable to teaching medicine at the bedside; learners develop a deeper appreciation and understanding by experiencing various situations first-hand.
An additional benefit of critically evaluating pharmaceutical representative presentations is that when they know that the information they provide will be closely scrutinized, pharmaceutical representatives will have an incentive to provide more accurate information.
2. Cost Sensitivity
One of the many topics that can be discussed by the hospital pharmacist or attending is the price of the given drug. In discussing price, two critical points must be evaluated. The first is the price-benefit ratio of the given drug and the second is the financial situation of the patient. Physicians should always have the patient’s best interest in mind. However, this does not mean that cost should not be considered when making therapeutic decisions. Rather, a more practical therapeutic decision can be made with cost in mind. Cost is the major factor to some patients when determining whether they will fill their prescriptions. In such an instance, if cost is taken into consideration when writing the prescription, a physician is more apt to write a prescription for a less expensive medication (if one exists).
3. Three-Way Transparency
In order for hospitalists to effectively interact with the pharmaceutical industry, it must be realized that medical professionals are not victims of the marketing strategies of the pharmaceutical industry; rather, we are accomplices. We often fail to acknowledge the role medical educators and professionals play in this problem. Many years ago, Troyan Brennan called for transparency, stating “Conflict will remain with us. Physicians’ relationship with the pharmaceutical industry must be better managed” (25). However, Brennan did not offer any proposals on a better management system. Our current management system of disclosure of conflict has become obsolete. It has become a ritual practice in academia to acknowledge that one may have a conflict of interest, but this does nothing to address the real issue: the conflict of interest itself. Hospitalists can adopt a three-way transparency between the patient, colleagues, and the pharmaceutical industry where all conflicts are fully disclosed, rather than simply stating that a conflict might exist.
4. High Threshold for Rationalization
Most medical professionals, to some degree, rationalize interactions with the pharmaceutical industry. Almost all physicians insist that these interactions do not influence their judgment. The simple fact that the industry spends thousands of dollars per doctor per year indicates that we are wrong. If physicians were not being influenced, the pharmaceutical companies would not be spending such a considerable amount of money marketing to us. Patients trust physicians to make the best decision for them, they depend on researchers to publish impartial studies, and they count on educators to present unbiased truths. The cost of betrayal is paid in human lives. We should learn from the past, as well as the recent coxib debacle.
Conclusion
The interaction between hospitalists and the pharmaceutical industry continues to evolve. With increasing scrutiny from the medical profession and the government, many of the marketing practices that were considered acceptable in the past are now viewed as unacceptable and even criminal. As the relationship evolves, new conflicts are sure to arise as long as the fundamental difference between the medical profession and pharmaceutical industry continues to exist. As medical professionals, we must keep in mind that the pharmaceutical industry is a for-profit industry whose interest lies with its shareholders. It is to be expected that the pharmaceutical industry will try to maximize profits through marketing efforts directed at physicians and patients.
Medical educators must take on the responsibility of preparing medical students, residents, and fellow attendings on how to manage their interactions with the pharmaceutical industry and not just shield them from the issue. In applying the four-point approach of academic detailing, cost sensitivity, three-way transparency, and a high threshold for justification, we can better manage such interactions.
We would like to thank Dr. Anna Headly and Emily Hartsough for their constructive comments in the preparation of the manuscript.
Disclaimer: The content of the article is solely the responsibility of the authors and does not necessarily represent the official view of the Society of Hospital Medicine.
Dr. Rajput can be contacted at [email protected].
References
- Abbasi K, Smith R. No more free lunch: patients will benefit from doctors and drug companies disentangling. BMJ. 2003;326:1155-6.
- Relman AS. Separating continuing medical education from pharmaceutical marketing. JAMA. 2001;285:2009-12.
- Thursby JG, Thursby MC. Intellectual property. University licensing and the Bayh-Dole Act. Science. 2003;301:1052.
- Holmer AF. Industry strongly supports continuing medical education. JAMA. 2001;285:2012-4.
- Scherer FM. The pharmaceutical industry: price and progress. N Engl J Med. 2004;351:927-32.
- Pharmaceutical industry profiles 2003. Washinton, DC; 2003.
- Moynihan R. Who pays for the pizza? Redefining the relationships between doctors and drug companies. 2: Disentanglement. BMJ. 2003;326:1193-6.
- Smith R. Medical journals and pharmaceutical companies: uneasy bedfellows. BMJ. 2003;326:1202-5.
- Relman AS. Defending professional independence: ACCME’s proposed new guidelines for commercial support of CME. JAMA. 2003;289:2418-20.
- Ziegler MG, Lew P, Singer BC. The accuracy of drug information from pharmaceutical sales representatives. JAMA. 1995;273:1296-8.
- Gottlieb S. Congress criticises drug industry for misleading advertising. BMJ. 2002;325:1379.
- Rogers WA, Mansfield PR, Braunack-Mayer AJ, Jureidini JN. The ethics of pharmaceutical industry relationships with medical students. Med J Aust. 2004;180:411-4.
- Melander H, Ahlqvist-Rastad J, Me&er G, Beermann B. Evidence b(i)ased medicine—selective reporting from studies sponsored by pharmaceutical industry: review of studies in new drug applications. BMJ. 2003;326:1171-3.
- Lexchin J. Interactions between physician and the pharmaceutical industry: what does the literatue say? Can Med Assoc J. 1993;149:1401-7.
- Steinman MA, Shlipak MG, McPhee SJ. Of principles and pens: attitudes and practices of medicine housestaff toward pharmaceutical industry promotions. Am J Med. 2001;110:551-7.
- Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283:373-80.
- Watkins C, Moore L, Harvey I, Carthy P, Robinson E, Brawn R. Characteristics of general practitioners who frequently see drug industry representatives: national cross sectional study. BMJ. 2003;326:1178-9.
- Guidelines on gifts to physicians from industry: an update. Food Drug Law J. 2001;56:27-40.
- PhRMA CODE On Interactions with Health Care Professionals. Infectious Diseases in Clinical Practice. 2002;(11):153-4.
- McCormick BB, Tomlinson G, Brill-Edwards P, Detsky AS. Effect of restricting contact between pharmaceutical company representatives and internal medicine residents on posttraining attitudes and behavior. JAMA. 2001;286:1994-9.
- Ferguson RP, Rhim E, Belizaire W, Egede L, Carter K, Lansdale T. Encounters with pharmaceutical sales representatives among practicing internists. Am J Med. 1999;107:149-52.
- Watkins RS, Kimberly JJ. What residents don’t know about physician-pharmaceutical industry interactions. Acad Med. 2004;79:432-7.
- Wilkes MS, Hoffman JR. An innovative approach to educating medical students about pharmaceutical promotion. Acad Med. 2001;76:1271-7.
- Vinson DC, McCandless B, Hosokawa MC. Medical students’ attitudes toward pharmaceutical marketing: possibilities for change. Fam Med. 1993;25:31-3.
- Brennan TA. Buying editorials. N Engl J Med. 1994;331: 673-5; discussion 76.
The ideal patient-physician relationship is one of choice, competence, communication, compassion, and continuity, and is free of any conflict of interest. There is heated controversy about whether the relationship between the pharmaceutical industry and medical professionals betrays this ideal. The heart of this debate lies in the fundamental difference in priorities and goals of the pharmaceutical industry and hospitalists. Hospitalists are trusted with the lives and well-being of patients. A physician is expected to make an unbiased analysis of the treatment options for a given patient and to apply that treatment to the best of his or her abilities. In contrast, the ultimate interest of the pharmaceutical industry lies with the shareholders, and the primary goal is to maximize profit. Many feel that these two goals are mutually exclusive (1,2). Medical educators believe that it is the responsibility of the medical profession, not pharmaceutical companies, to educate physicians. The entanglement of the pharmaceutical industry with physicians calls into question the credibility of information obtained from any pharmaceutical-sponsored event and casts doubt over the medical profession as a whole. Governmental regulation and legislative initiatives such as the Bayh-Dole Act (3) have furthered the commercialization of academic research and realigned academic centers’ approach to clinical research.
The pharmaceutical industry argues that its goals and the goals of the medical profession are complementary (4) and that their involvement optimizes the benefit to the patient. The pharmaceutical industry is quick to point out that pharmaceutical companies are an important source of funding for clinical trials and are the leading sponsors of continuing medical education, and that it is the most research-intensive industry in the United States supported by private funds (5). Corporate contributions to research and development in academia have increased by 900% between 1980 and 2000. The pharmaceutical industry devoted 18% of profits in 2002 to research, development, and testing activities (6). The pharmaceutical industry claims that these are designed to serve the mutual interests of the pharmaceutical industry and the medical community by providing accurate and up-to-date information to maximize patient care. The advances made as a result of commercial development have dramatically altered the landscape of research. Pharmaceutical courtship of hospitalists, who find themselves on the front line in clinical settings as prescribers or researchers, is part of an aggressive marketing campaign that some believe contributes little to the common good.
Hospitalists have increased their financial incentives with stock options, fees for consultation, speaking arrangements, and memberships on advisory boards for pharmaceutical companies. Disclosure of financial conflicts is becoming an empty ritual providing a false sense of security. Pharmaceutical research is increasingly organized by Contract Research Organizations, written up with the help of ghostwriters, and published under the name of established investigators (7,8). Not all industry-funded studies are necessarily fl awed and without scientific merit, but the fact that negative consequences can be devastating to the financial health of a corporation has to be considered.
A leading catalyst for continued pharmaceutical industry/hospitalist interaction is continuing medical education (CME). In 2003, the pharmaceutical industry provided 900 million of the one billion dollars spent on CME in the United States. Currently, the pharmaceutical industry funds approximately 60% of all CME activities in the United States (9). Information provided to physicians by a pharmaceutical representative has an inaccuracy rating of 13% (10). Not surprisingly, many of these inaccuracies favor the product being presented and casts an unfavorable light on competing drugs (10,11). This has led some to believe that this pharmaceutical representative/physician interaction is having a negative impact on patients (12) through the dissemination of inaccurate information. In addition, misleading advertisements have been found to overstate the effectiveness and minimize the risks of a given drug (11). Another form of bias is the selective publication of research studies by the pharmaceutical industry (13).
Bedside and Conference Detailing
Interactions with pharmaceutical representatives (drug detailers) often begin in medical school and proceed throughout a physician’s career (12,14). In 2003, the pharmaceutical industry spent more than 13 billion dollars on promotional activities for doctors, an average of about $10,500 per physician. There is one drug detailer for every 4.7 office-based physicians. Interactions include conferences with free lunch, personal visits by drug detailers, sponsored CME workshops/seminars, sponsored dinners, sponsored scientific conferences, sponsored research, direct gifts (e.g., cash payments for prescribing a given medication), and indirect gifts (e.g., subsidizing a trip to a medical conference). These interactions evolve from merely lunches and pens early in a physician’s career to positions as a consultant and advisory board honoree as the relationship matures. Some physicians view such exchanges as helpful and informative while others view it as unethical (2) and harmful.
Hospitalists, residents, and medical students alike believe their interactions with drug detailers, and the small gifts that they receive, do not influence their behavior (14,15). Wazana found that as physicians continue to receive gifts from drug detailers, they become even less likely to believe that the gifts can influence their behavior (16). Many physicians believe that their interactions with drug companies are beneficial not only to them but also to their patients. However, studies have found that this is in fact not the case. Physicians who interact with pharmaceutical representatives prescribe newer and more expensive drugs, rather than cheaper and equally effective generic drugs (16,17). There are a significantly higher number of prescriptions written for the drugs manufactured by pharmaceutical companies who sponsor a given CME activity than pharmaceutical companies who do not. A rise in prescription expenditures (17), as well as an increase in irrational prescribing, often follows in-house exposure to drug detailers (16).
The enormous amount spent on marketing can also be used as further proof of the pharmaceutical industry’s avarice. However, we often fail to acknowledge the role that medical educators and professionals play in this problem. Pharmaceutical companies are profitable because of our prescribing habits. For example, many medical professionals prescribe expensive “me too” drugs that often offer little if any benefit over cheaper established or prototypical drugs. Our actions encourage what we claim to be bad behavior by the pharmaceutical industry.
It is often argued by the pharmaceutical industry that these “me too” drugs have a different side effect profile, may improve compliance in long-term treatment, or will reduce cost when compared to the prototype drug. This is true in some instances, as exemplified by the wide array of anti-hypertensives and the even wider array of side effect profiles. However, there are many instances when this is far from the case. If a financial incentive did not exist for pharmaceutical companies to introduce “me too” drugs, the pharmaceutical industry would not do so unless the drug being introduced provided a substantial clinical advantage over the prototype drug. As a result, the pharmaceutical industry would be spending their time, effort, and finances on research aimed at finding new and innovative cures.
Proposed Solution to the Problem
In an effort to remedy this situation, many professional societies (as well as the pharmaceutical industry itself) have established guidelines on the interactions between the pharmaceutical industry and physicians. The AMA has established guidelines responsible for the regulation of gifts bestowed on physicians by industry (18). The Pharmaceutical Research Manufacturers of America has established similar guidelines known as the PhRMA Code (19). Increasingly, many professional organizations have taken it upon themselves to establish their own code of conduct. However, there remains a low level of awareness of the guidelines (15) that are currently in place, and some of the pharmaceutical companies have chosen not to abide by the PhRMA Code. In response to the increasing influence pharmaceutical companies are having on the medical decision-making process, many training programs are adopting policies to limit the contact between pharmaceutical representatives and physicians in training. This is being carried out at both the undergraduate and graduate medical education levels (20). The effects of such restrictions are currently unknown. McCormick found that physicians who trained in institutions with such policies were less likely to find information from pharmaceutical company representatives useful (20). However, Ferguson found that being trained in a program with a policy that limited access to pharmaceutical sales representatives did not affect the subsequent likelihood of future physician-pharmaceutical representative interactions (21).
The Informed Hospitalist in the 21st Century
The literature clearly documents that the pharmaceutical industry influences physician prescribing habits. Hospitalists can take a four-prong approach to help counteract these effects:
1. Academic Detailing
Medical educators can shield residents and medical students from the influence of pharmaceutical representatives by limiting or prohibiting contact, or they can teach trainees how to effectively manage such interactions through academic detailing. As stated above, Ferguson found that policies limiting access to drug detailers did not affect the subsequent likelihood of future physician and pharmaceutical representative interactions (21). It might be wiser to teach trainees how to manage their interactions with the drug representatives and thereby take control of the situation. In order for doctors to effectively manage such interactions, we must learn how to evaluate the literature and interpret the information given to us by representatives. Watkins found that both attendings and residents feel that they should learn how to critically evaluate promotional materials, recognize potential conflicts of interest, and consider how patients perceive physician-pharmaceutical relationships (22). Previous studies have found that educational interventions can have a significant effect on the attitudes of medical students and residents towards pharmaceutical marketing and drug detailers (23,24).
One way to evaluate pharmaceutical literature is to have academic detailing of the clinical studies and statements made by pharmaceutical detailers at sponsored events. During these academic detailing conferences the drug in question can be compared to other drugs in the class, and indications and differences should be mentioned if they exist. This should be done in the presence of both an attending who is very familiar with the drug and drug class in question and a hospital pharmacist. If this is done in a small setting, the medical students and residents can take turns critically evaluating the presentations. This approach is comparable to teaching medicine at the bedside; learners develop a deeper appreciation and understanding by experiencing various situations first-hand.
An additional benefit of critically evaluating pharmaceutical representative presentations is that when they know that the information they provide will be closely scrutinized, pharmaceutical representatives will have an incentive to provide more accurate information.
2. Cost Sensitivity
One of the many topics that can be discussed by the hospital pharmacist or attending is the price of the given drug. In discussing price, two critical points must be evaluated. The first is the price-benefit ratio of the given drug and the second is the financial situation of the patient. Physicians should always have the patient’s best interest in mind. However, this does not mean that cost should not be considered when making therapeutic decisions. Rather, a more practical therapeutic decision can be made with cost in mind. Cost is the major factor to some patients when determining whether they will fill their prescriptions. In such an instance, if cost is taken into consideration when writing the prescription, a physician is more apt to write a prescription for a less expensive medication (if one exists).
3. Three-Way Transparency
In order for hospitalists to effectively interact with the pharmaceutical industry, it must be realized that medical professionals are not victims of the marketing strategies of the pharmaceutical industry; rather, we are accomplices. We often fail to acknowledge the role medical educators and professionals play in this problem. Many years ago, Troyan Brennan called for transparency, stating “Conflict will remain with us. Physicians’ relationship with the pharmaceutical industry must be better managed” (25). However, Brennan did not offer any proposals on a better management system. Our current management system of disclosure of conflict has become obsolete. It has become a ritual practice in academia to acknowledge that one may have a conflict of interest, but this does nothing to address the real issue: the conflict of interest itself. Hospitalists can adopt a three-way transparency between the patient, colleagues, and the pharmaceutical industry where all conflicts are fully disclosed, rather than simply stating that a conflict might exist.
4. High Threshold for Rationalization
Most medical professionals, to some degree, rationalize interactions with the pharmaceutical industry. Almost all physicians insist that these interactions do not influence their judgment. The simple fact that the industry spends thousands of dollars per doctor per year indicates that we are wrong. If physicians were not being influenced, the pharmaceutical companies would not be spending such a considerable amount of money marketing to us. Patients trust physicians to make the best decision for them, they depend on researchers to publish impartial studies, and they count on educators to present unbiased truths. The cost of betrayal is paid in human lives. We should learn from the past, as well as the recent coxib debacle.
Conclusion
The interaction between hospitalists and the pharmaceutical industry continues to evolve. With increasing scrutiny from the medical profession and the government, many of the marketing practices that were considered acceptable in the past are now viewed as unacceptable and even criminal. As the relationship evolves, new conflicts are sure to arise as long as the fundamental difference between the medical profession and pharmaceutical industry continues to exist. As medical professionals, we must keep in mind that the pharmaceutical industry is a for-profit industry whose interest lies with its shareholders. It is to be expected that the pharmaceutical industry will try to maximize profits through marketing efforts directed at physicians and patients.
Medical educators must take on the responsibility of preparing medical students, residents, and fellow attendings on how to manage their interactions with the pharmaceutical industry and not just shield them from the issue. In applying the four-point approach of academic detailing, cost sensitivity, three-way transparency, and a high threshold for justification, we can better manage such interactions.
We would like to thank Dr. Anna Headly and Emily Hartsough for their constructive comments in the preparation of the manuscript.
Disclaimer: The content of the article is solely the responsibility of the authors and does not necessarily represent the official view of the Society of Hospital Medicine.
Dr. Rajput can be contacted at [email protected].
References
- Abbasi K, Smith R. No more free lunch: patients will benefit from doctors and drug companies disentangling. BMJ. 2003;326:1155-6.
- Relman AS. Separating continuing medical education from pharmaceutical marketing. JAMA. 2001;285:2009-12.
- Thursby JG, Thursby MC. Intellectual property. University licensing and the Bayh-Dole Act. Science. 2003;301:1052.
- Holmer AF. Industry strongly supports continuing medical education. JAMA. 2001;285:2012-4.
- Scherer FM. The pharmaceutical industry: price and progress. N Engl J Med. 2004;351:927-32.
- Pharmaceutical industry profiles 2003. Washinton, DC; 2003.
- Moynihan R. Who pays for the pizza? Redefining the relationships between doctors and drug companies. 2: Disentanglement. BMJ. 2003;326:1193-6.
- Smith R. Medical journals and pharmaceutical companies: uneasy bedfellows. BMJ. 2003;326:1202-5.
- Relman AS. Defending professional independence: ACCME’s proposed new guidelines for commercial support of CME. JAMA. 2003;289:2418-20.
- Ziegler MG, Lew P, Singer BC. The accuracy of drug information from pharmaceutical sales representatives. JAMA. 1995;273:1296-8.
- Gottlieb S. Congress criticises drug industry for misleading advertising. BMJ. 2002;325:1379.
- Rogers WA, Mansfield PR, Braunack-Mayer AJ, Jureidini JN. The ethics of pharmaceutical industry relationships with medical students. Med J Aust. 2004;180:411-4.
- Melander H, Ahlqvist-Rastad J, Me&er G, Beermann B. Evidence b(i)ased medicine—selective reporting from studies sponsored by pharmaceutical industry: review of studies in new drug applications. BMJ. 2003;326:1171-3.
- Lexchin J. Interactions between physician and the pharmaceutical industry: what does the literatue say? Can Med Assoc J. 1993;149:1401-7.
- Steinman MA, Shlipak MG, McPhee SJ. Of principles and pens: attitudes and practices of medicine housestaff toward pharmaceutical industry promotions. Am J Med. 2001;110:551-7.
- Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283:373-80.
- Watkins C, Moore L, Harvey I, Carthy P, Robinson E, Brawn R. Characteristics of general practitioners who frequently see drug industry representatives: national cross sectional study. BMJ. 2003;326:1178-9.
- Guidelines on gifts to physicians from industry: an update. Food Drug Law J. 2001;56:27-40.
- PhRMA CODE On Interactions with Health Care Professionals. Infectious Diseases in Clinical Practice. 2002;(11):153-4.
- McCormick BB, Tomlinson G, Brill-Edwards P, Detsky AS. Effect of restricting contact between pharmaceutical company representatives and internal medicine residents on posttraining attitudes and behavior. JAMA. 2001;286:1994-9.
- Ferguson RP, Rhim E, Belizaire W, Egede L, Carter K, Lansdale T. Encounters with pharmaceutical sales representatives among practicing internists. Am J Med. 1999;107:149-52.
- Watkins RS, Kimberly JJ. What residents don’t know about physician-pharmaceutical industry interactions. Acad Med. 2004;79:432-7.
- Wilkes MS, Hoffman JR. An innovative approach to educating medical students about pharmaceutical promotion. Acad Med. 2001;76:1271-7.
- Vinson DC, McCandless B, Hosokawa MC. Medical students’ attitudes toward pharmaceutical marketing: possibilities for change. Fam Med. 1993;25:31-3.
- Brennan TA. Buying editorials. N Engl J Med. 1994;331: 673-5; discussion 76.
The ideal patient-physician relationship is one of choice, competence, communication, compassion, and continuity, and is free of any conflict of interest. There is heated controversy about whether the relationship between the pharmaceutical industry and medical professionals betrays this ideal. The heart of this debate lies in the fundamental difference in priorities and goals of the pharmaceutical industry and hospitalists. Hospitalists are trusted with the lives and well-being of patients. A physician is expected to make an unbiased analysis of the treatment options for a given patient and to apply that treatment to the best of his or her abilities. In contrast, the ultimate interest of the pharmaceutical industry lies with the shareholders, and the primary goal is to maximize profit. Many feel that these two goals are mutually exclusive (1,2). Medical educators believe that it is the responsibility of the medical profession, not pharmaceutical companies, to educate physicians. The entanglement of the pharmaceutical industry with physicians calls into question the credibility of information obtained from any pharmaceutical-sponsored event and casts doubt over the medical profession as a whole. Governmental regulation and legislative initiatives such as the Bayh-Dole Act (3) have furthered the commercialization of academic research and realigned academic centers’ approach to clinical research.
The pharmaceutical industry argues that its goals and the goals of the medical profession are complementary (4) and that their involvement optimizes the benefit to the patient. The pharmaceutical industry is quick to point out that pharmaceutical companies are an important source of funding for clinical trials and are the leading sponsors of continuing medical education, and that it is the most research-intensive industry in the United States supported by private funds (5). Corporate contributions to research and development in academia have increased by 900% between 1980 and 2000. The pharmaceutical industry devoted 18% of profits in 2002 to research, development, and testing activities (6). The pharmaceutical industry claims that these are designed to serve the mutual interests of the pharmaceutical industry and the medical community by providing accurate and up-to-date information to maximize patient care. The advances made as a result of commercial development have dramatically altered the landscape of research. Pharmaceutical courtship of hospitalists, who find themselves on the front line in clinical settings as prescribers or researchers, is part of an aggressive marketing campaign that some believe contributes little to the common good.
Hospitalists have increased their financial incentives with stock options, fees for consultation, speaking arrangements, and memberships on advisory boards for pharmaceutical companies. Disclosure of financial conflicts is becoming an empty ritual providing a false sense of security. Pharmaceutical research is increasingly organized by Contract Research Organizations, written up with the help of ghostwriters, and published under the name of established investigators (7,8). Not all industry-funded studies are necessarily fl awed and without scientific merit, but the fact that negative consequences can be devastating to the financial health of a corporation has to be considered.
A leading catalyst for continued pharmaceutical industry/hospitalist interaction is continuing medical education (CME). In 2003, the pharmaceutical industry provided 900 million of the one billion dollars spent on CME in the United States. Currently, the pharmaceutical industry funds approximately 60% of all CME activities in the United States (9). Information provided to physicians by a pharmaceutical representative has an inaccuracy rating of 13% (10). Not surprisingly, many of these inaccuracies favor the product being presented and casts an unfavorable light on competing drugs (10,11). This has led some to believe that this pharmaceutical representative/physician interaction is having a negative impact on patients (12) through the dissemination of inaccurate information. In addition, misleading advertisements have been found to overstate the effectiveness and minimize the risks of a given drug (11). Another form of bias is the selective publication of research studies by the pharmaceutical industry (13).
Bedside and Conference Detailing
Interactions with pharmaceutical representatives (drug detailers) often begin in medical school and proceed throughout a physician’s career (12,14). In 2003, the pharmaceutical industry spent more than 13 billion dollars on promotional activities for doctors, an average of about $10,500 per physician. There is one drug detailer for every 4.7 office-based physicians. Interactions include conferences with free lunch, personal visits by drug detailers, sponsored CME workshops/seminars, sponsored dinners, sponsored scientific conferences, sponsored research, direct gifts (e.g., cash payments for prescribing a given medication), and indirect gifts (e.g., subsidizing a trip to a medical conference). These interactions evolve from merely lunches and pens early in a physician’s career to positions as a consultant and advisory board honoree as the relationship matures. Some physicians view such exchanges as helpful and informative while others view it as unethical (2) and harmful.
Hospitalists, residents, and medical students alike believe their interactions with drug detailers, and the small gifts that they receive, do not influence their behavior (14,15). Wazana found that as physicians continue to receive gifts from drug detailers, they become even less likely to believe that the gifts can influence their behavior (16). Many physicians believe that their interactions with drug companies are beneficial not only to them but also to their patients. However, studies have found that this is in fact not the case. Physicians who interact with pharmaceutical representatives prescribe newer and more expensive drugs, rather than cheaper and equally effective generic drugs (16,17). There are a significantly higher number of prescriptions written for the drugs manufactured by pharmaceutical companies who sponsor a given CME activity than pharmaceutical companies who do not. A rise in prescription expenditures (17), as well as an increase in irrational prescribing, often follows in-house exposure to drug detailers (16).
The enormous amount spent on marketing can also be used as further proof of the pharmaceutical industry’s avarice. However, we often fail to acknowledge the role that medical educators and professionals play in this problem. Pharmaceutical companies are profitable because of our prescribing habits. For example, many medical professionals prescribe expensive “me too” drugs that often offer little if any benefit over cheaper established or prototypical drugs. Our actions encourage what we claim to be bad behavior by the pharmaceutical industry.
It is often argued by the pharmaceutical industry that these “me too” drugs have a different side effect profile, may improve compliance in long-term treatment, or will reduce cost when compared to the prototype drug. This is true in some instances, as exemplified by the wide array of anti-hypertensives and the even wider array of side effect profiles. However, there are many instances when this is far from the case. If a financial incentive did not exist for pharmaceutical companies to introduce “me too” drugs, the pharmaceutical industry would not do so unless the drug being introduced provided a substantial clinical advantage over the prototype drug. As a result, the pharmaceutical industry would be spending their time, effort, and finances on research aimed at finding new and innovative cures.
Proposed Solution to the Problem
In an effort to remedy this situation, many professional societies (as well as the pharmaceutical industry itself) have established guidelines on the interactions between the pharmaceutical industry and physicians. The AMA has established guidelines responsible for the regulation of gifts bestowed on physicians by industry (18). The Pharmaceutical Research Manufacturers of America has established similar guidelines known as the PhRMA Code (19). Increasingly, many professional organizations have taken it upon themselves to establish their own code of conduct. However, there remains a low level of awareness of the guidelines (15) that are currently in place, and some of the pharmaceutical companies have chosen not to abide by the PhRMA Code. In response to the increasing influence pharmaceutical companies are having on the medical decision-making process, many training programs are adopting policies to limit the contact between pharmaceutical representatives and physicians in training. This is being carried out at both the undergraduate and graduate medical education levels (20). The effects of such restrictions are currently unknown. McCormick found that physicians who trained in institutions with such policies were less likely to find information from pharmaceutical company representatives useful (20). However, Ferguson found that being trained in a program with a policy that limited access to pharmaceutical sales representatives did not affect the subsequent likelihood of future physician-pharmaceutical representative interactions (21).
The Informed Hospitalist in the 21st Century
The literature clearly documents that the pharmaceutical industry influences physician prescribing habits. Hospitalists can take a four-prong approach to help counteract these effects:
1. Academic Detailing
Medical educators can shield residents and medical students from the influence of pharmaceutical representatives by limiting or prohibiting contact, or they can teach trainees how to effectively manage such interactions through academic detailing. As stated above, Ferguson found that policies limiting access to drug detailers did not affect the subsequent likelihood of future physician and pharmaceutical representative interactions (21). It might be wiser to teach trainees how to manage their interactions with the drug representatives and thereby take control of the situation. In order for doctors to effectively manage such interactions, we must learn how to evaluate the literature and interpret the information given to us by representatives. Watkins found that both attendings and residents feel that they should learn how to critically evaluate promotional materials, recognize potential conflicts of interest, and consider how patients perceive physician-pharmaceutical relationships (22). Previous studies have found that educational interventions can have a significant effect on the attitudes of medical students and residents towards pharmaceutical marketing and drug detailers (23,24).
One way to evaluate pharmaceutical literature is to have academic detailing of the clinical studies and statements made by pharmaceutical detailers at sponsored events. During these academic detailing conferences the drug in question can be compared to other drugs in the class, and indications and differences should be mentioned if they exist. This should be done in the presence of both an attending who is very familiar with the drug and drug class in question and a hospital pharmacist. If this is done in a small setting, the medical students and residents can take turns critically evaluating the presentations. This approach is comparable to teaching medicine at the bedside; learners develop a deeper appreciation and understanding by experiencing various situations first-hand.
An additional benefit of critically evaluating pharmaceutical representative presentations is that when they know that the information they provide will be closely scrutinized, pharmaceutical representatives will have an incentive to provide more accurate information.
2. Cost Sensitivity
One of the many topics that can be discussed by the hospital pharmacist or attending is the price of the given drug. In discussing price, two critical points must be evaluated. The first is the price-benefit ratio of the given drug and the second is the financial situation of the patient. Physicians should always have the patient’s best interest in mind. However, this does not mean that cost should not be considered when making therapeutic decisions. Rather, a more practical therapeutic decision can be made with cost in mind. Cost is the major factor to some patients when determining whether they will fill their prescriptions. In such an instance, if cost is taken into consideration when writing the prescription, a physician is more apt to write a prescription for a less expensive medication (if one exists).
3. Three-Way Transparency
In order for hospitalists to effectively interact with the pharmaceutical industry, it must be realized that medical professionals are not victims of the marketing strategies of the pharmaceutical industry; rather, we are accomplices. We often fail to acknowledge the role medical educators and professionals play in this problem. Many years ago, Troyan Brennan called for transparency, stating “Conflict will remain with us. Physicians’ relationship with the pharmaceutical industry must be better managed” (25). However, Brennan did not offer any proposals on a better management system. Our current management system of disclosure of conflict has become obsolete. It has become a ritual practice in academia to acknowledge that one may have a conflict of interest, but this does nothing to address the real issue: the conflict of interest itself. Hospitalists can adopt a three-way transparency between the patient, colleagues, and the pharmaceutical industry where all conflicts are fully disclosed, rather than simply stating that a conflict might exist.
4. High Threshold for Rationalization
Most medical professionals, to some degree, rationalize interactions with the pharmaceutical industry. Almost all physicians insist that these interactions do not influence their judgment. The simple fact that the industry spends thousands of dollars per doctor per year indicates that we are wrong. If physicians were not being influenced, the pharmaceutical companies would not be spending such a considerable amount of money marketing to us. Patients trust physicians to make the best decision for them, they depend on researchers to publish impartial studies, and they count on educators to present unbiased truths. The cost of betrayal is paid in human lives. We should learn from the past, as well as the recent coxib debacle.
Conclusion
The interaction between hospitalists and the pharmaceutical industry continues to evolve. With increasing scrutiny from the medical profession and the government, many of the marketing practices that were considered acceptable in the past are now viewed as unacceptable and even criminal. As the relationship evolves, new conflicts are sure to arise as long as the fundamental difference between the medical profession and pharmaceutical industry continues to exist. As medical professionals, we must keep in mind that the pharmaceutical industry is a for-profit industry whose interest lies with its shareholders. It is to be expected that the pharmaceutical industry will try to maximize profits through marketing efforts directed at physicians and patients.
Medical educators must take on the responsibility of preparing medical students, residents, and fellow attendings on how to manage their interactions with the pharmaceutical industry and not just shield them from the issue. In applying the four-point approach of academic detailing, cost sensitivity, three-way transparency, and a high threshold for justification, we can better manage such interactions.
We would like to thank Dr. Anna Headly and Emily Hartsough for their constructive comments in the preparation of the manuscript.
Disclaimer: The content of the article is solely the responsibility of the authors and does not necessarily represent the official view of the Society of Hospital Medicine.
Dr. Rajput can be contacted at [email protected].
References
- Abbasi K, Smith R. No more free lunch: patients will benefit from doctors and drug companies disentangling. BMJ. 2003;326:1155-6.
- Relman AS. Separating continuing medical education from pharmaceutical marketing. JAMA. 2001;285:2009-12.
- Thursby JG, Thursby MC. Intellectual property. University licensing and the Bayh-Dole Act. Science. 2003;301:1052.
- Holmer AF. Industry strongly supports continuing medical education. JAMA. 2001;285:2012-4.
- Scherer FM. The pharmaceutical industry: price and progress. N Engl J Med. 2004;351:927-32.
- Pharmaceutical industry profiles 2003. Washinton, DC; 2003.
- Moynihan R. Who pays for the pizza? Redefining the relationships between doctors and drug companies. 2: Disentanglement. BMJ. 2003;326:1193-6.
- Smith R. Medical journals and pharmaceutical companies: uneasy bedfellows. BMJ. 2003;326:1202-5.
- Relman AS. Defending professional independence: ACCME’s proposed new guidelines for commercial support of CME. JAMA. 2003;289:2418-20.
- Ziegler MG, Lew P, Singer BC. The accuracy of drug information from pharmaceutical sales representatives. JAMA. 1995;273:1296-8.
- Gottlieb S. Congress criticises drug industry for misleading advertising. BMJ. 2002;325:1379.
- Rogers WA, Mansfield PR, Braunack-Mayer AJ, Jureidini JN. The ethics of pharmaceutical industry relationships with medical students. Med J Aust. 2004;180:411-4.
- Melander H, Ahlqvist-Rastad J, Me&er G, Beermann B. Evidence b(i)ased medicine—selective reporting from studies sponsored by pharmaceutical industry: review of studies in new drug applications. BMJ. 2003;326:1171-3.
- Lexchin J. Interactions between physician and the pharmaceutical industry: what does the literatue say? Can Med Assoc J. 1993;149:1401-7.
- Steinman MA, Shlipak MG, McPhee SJ. Of principles and pens: attitudes and practices of medicine housestaff toward pharmaceutical industry promotions. Am J Med. 2001;110:551-7.
- Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283:373-80.
- Watkins C, Moore L, Harvey I, Carthy P, Robinson E, Brawn R. Characteristics of general practitioners who frequently see drug industry representatives: national cross sectional study. BMJ. 2003;326:1178-9.
- Guidelines on gifts to physicians from industry: an update. Food Drug Law J. 2001;56:27-40.
- PhRMA CODE On Interactions with Health Care Professionals. Infectious Diseases in Clinical Practice. 2002;(11):153-4.
- McCormick BB, Tomlinson G, Brill-Edwards P, Detsky AS. Effect of restricting contact between pharmaceutical company representatives and internal medicine residents on posttraining attitudes and behavior. JAMA. 2001;286:1994-9.
- Ferguson RP, Rhim E, Belizaire W, Egede L, Carter K, Lansdale T. Encounters with pharmaceutical sales representatives among practicing internists. Am J Med. 1999;107:149-52.
- Watkins RS, Kimberly JJ. What residents don’t know about physician-pharmaceutical industry interactions. Acad Med. 2004;79:432-7.
- Wilkes MS, Hoffman JR. An innovative approach to educating medical students about pharmaceutical promotion. Acad Med. 2001;76:1271-7.
- Vinson DC, McCandless B, Hosokawa MC. Medical students’ attitudes toward pharmaceutical marketing: possibilities for change. Fam Med. 1993;25:31-3.
- Brennan TA. Buying editorials. N Engl J Med. 1994;331: 673-5; discussion 76.
Tackling the Underlying Problems of Failure to Rescue
A recent HealthGrades Quality Study titled Patient Safety in American Hospitals (July 2004) highlighted the frequency of patients dying from complications that develop while in hospitals. Failure to rescue, according to the 3-year study, accounts for 60,000 deaths each year in Medicare patients under the age of 75.
Based on my experience as a pulmonary and critical care physician, this statistic quantifies an important problem. Deaths from complications of illness, or care, during a hospital stay happen more than we’d like to admit. However, the good news is that by identifying the underlying problem and deploying some targeted, systemic changes, hospitalists can begin to handle decompensation quickly, proactively, and before it’s too late.
Moving forward, hospitals need to build an effective patient safety net, which requires three important elements: point-of care tools for caregivers, proactive clinical surveillance, and real-time process monitoring.
Reasons for Failure to Rescue
A huge effort, and amount of money, has been focused on finding errors that lead to harm. Unfortunately, we’re tackling the wrong errors. New tools like barcode medication administration or CPOE tackle errors of commission. These errors might occur when a doctor or nurse administers a wrong dose or wrong medication. Errors of commission are much easier to identify and solve, but clinically significant errors of commission that cause harm are relatively rare events and don’t affect overall hospital mortality.
Errors of omission, however, are much more insidious. An error of omission is an error that occurs when an action is not taken or an important step in the process is left out. Examples of an error of omission include sub-optimal patient care resulting from the inadequate availability of patient information for decision-making, or a more blatant example, when a patient’s vital signs indicate decompensation but the clinical response is inadequate or delayed.
Errors of omission continue in today’s hospitals for two very important reasons: First, we lack a systematic way to handle clinical decompensation. While we have “code” teams, their efforts often come into play too late. Second, lacking a way to recognize and respond to the issue, we have accepted that failure to rescue is in some ways inevitable and excusable.
The basic, first step is to replace the inherently unreliable paper patient chart. Paper patient charts get misplaced, information is sometimes missing and/or illegible, and they make it impossible for a team effort to optimize care.
Hospitals need to get patient data such as vital signs and medication usage in electronic form. That way, it is effortless and time-efficient to determine a patient’s status and check up on patients even when not physically near them. Making this change alone, even in only one hospital unit, hospitalists can begin to effect significant positive changes in patient safety outcomes.
Catastrophes Aren’t Inevitable
Often, the first time physicians become aware of a problem is when they receive a frantic call to come to the bedside. The patient is decompensating and needs immediate, dramatic intervention to save their life. However, when we take the time to look back at the patient chart and “connect the dots,” we see that instability had been developing for hours before an urgent summons for assistance.
Even with the best care, patients’ clinical needs often change after admission. Patient status can change rapidly, so a perfect assessment earlier in the day can quickly become dated. Further, bedside staff have many other patients, and staffing assignments don’t build in “slack time” to permit paying extra attention when problems develop. Consequently, signs of clinical deterioration are often missed or not acted upon until there’s a code on the unit and dramatic measures are needed to save a life.
Proactive clinical surveillance tools are the second big step in creating a safety net for patients. With patient data in electronic form, hands-on caregivers, nurses, and supervisors can use specially designed “dashboard views” to quickly identify which patients are exhibiting warning signs of clinical decline and exactly where they are located.
To be most effective, staff should view clinical surveillance information in a variety of useful ways:
- Hospital–wide for a big picture of where the trouble spots are
- By unit, to scan through patients and see the values that are triggering an alert
- By provider, so doctors and nurses can scan their list of patients and see which have triggered alerts
- By patient, drilling into all the details of that patient’s current status and previous care
- By patient, drilling into all the details of that patient’s current status and previous care
tion, which are out of range or trending in the wrong direction, should automatically highlight patients. With the complete clinical record on-line, staff can prioritize which patients to visit next and what type of supplemental resources might be needed to enhance care.
For hospitalists, clinical surveillance tools save an immense amount of time and help prioritize patient care. Typically hospitalists manage a large number of patients who are scattered around the hospital. Determining where to start rounds and which patients should be seen first is often difficult. Even worse, patients’ conditions suddenly change for the worse soon after you’ve checked on them. There are just too many patients to continually be looking at patient charts and relying on verbal information: that’s why there are computers!
Supervisory staff can provide an additional safety net, if they have the tools to do so effectively. Typically, they rely on “report” and walking around, visiting staff, looking for an opportunity where their intervention could be helpful. By referring to “hot spots” indicated on a clinical surveillance dashboard view, they would know where they’re needed and spend their time helping, rather than prospecting.
Some hospitals have formalized their response to the failure to rescue problem by creating “rapid response teams.” Such teams can also rely on clinical surveillance tools to identify patients in need, rather than waiting for a phone call from an overwhelmed primary caregiver.
Making Best Practices Work
Organizational performance can be dramatically improved when patient outcomes and staff activity can be measured and analyzed. Traditionally, this has been done retrospectively.
By evaluating outcomes of patients and compliance with processes, many sites have been able to improve processes for future patients. However, because reporting has been periodic, results become available only months later, and implementation of care enhancements are delayed.
With comprehensive patient data in electronic form, real-time monitoring of compliance with intended processes and best practices becomes possible. For example, if there is a consensus that the head of the bed of ventilated patients should be elevated to reduce the incidence of ventilator-associated pneumonia, then the monitoring system can show, by ICU, the percentage compliance with that protocol at any given moment.
Since the report is available real-time, non-compliance can be addressed immediately, benefiting the patient and directing education about the protocol precisely when and where it is needed for maximum impact.
Creating a Reliable Patient Safety System
An electronic medical record forms the very foundation of a patient safety system. This electronic data provides the capability for proactive clinical monitoring and much more sophisticated process analysis that happens in days or weeks, not over a course of months or years.
Capture patient data electronically, set up a set of effective alerts based on hospital-defined triggers, and enact process monitoring to improve outcomes and fix problems as they occur. With these three elements, hospitals have the best antidote for failure to rescue and are able to create a safety net for patients.
Dr. Kremsdorf can be contacted at [email protected].
A recent HealthGrades Quality Study titled Patient Safety in American Hospitals (July 2004) highlighted the frequency of patients dying from complications that develop while in hospitals. Failure to rescue, according to the 3-year study, accounts for 60,000 deaths each year in Medicare patients under the age of 75.
Based on my experience as a pulmonary and critical care physician, this statistic quantifies an important problem. Deaths from complications of illness, or care, during a hospital stay happen more than we’d like to admit. However, the good news is that by identifying the underlying problem and deploying some targeted, systemic changes, hospitalists can begin to handle decompensation quickly, proactively, and before it’s too late.
Moving forward, hospitals need to build an effective patient safety net, which requires three important elements: point-of care tools for caregivers, proactive clinical surveillance, and real-time process monitoring.
Reasons for Failure to Rescue
A huge effort, and amount of money, has been focused on finding errors that lead to harm. Unfortunately, we’re tackling the wrong errors. New tools like barcode medication administration or CPOE tackle errors of commission. These errors might occur when a doctor or nurse administers a wrong dose or wrong medication. Errors of commission are much easier to identify and solve, but clinically significant errors of commission that cause harm are relatively rare events and don’t affect overall hospital mortality.
Errors of omission, however, are much more insidious. An error of omission is an error that occurs when an action is not taken or an important step in the process is left out. Examples of an error of omission include sub-optimal patient care resulting from the inadequate availability of patient information for decision-making, or a more blatant example, when a patient’s vital signs indicate decompensation but the clinical response is inadequate or delayed.
Errors of omission continue in today’s hospitals for two very important reasons: First, we lack a systematic way to handle clinical decompensation. While we have “code” teams, their efforts often come into play too late. Second, lacking a way to recognize and respond to the issue, we have accepted that failure to rescue is in some ways inevitable and excusable.
The basic, first step is to replace the inherently unreliable paper patient chart. Paper patient charts get misplaced, information is sometimes missing and/or illegible, and they make it impossible for a team effort to optimize care.
Hospitals need to get patient data such as vital signs and medication usage in electronic form. That way, it is effortless and time-efficient to determine a patient’s status and check up on patients even when not physically near them. Making this change alone, even in only one hospital unit, hospitalists can begin to effect significant positive changes in patient safety outcomes.
Catastrophes Aren’t Inevitable
Often, the first time physicians become aware of a problem is when they receive a frantic call to come to the bedside. The patient is decompensating and needs immediate, dramatic intervention to save their life. However, when we take the time to look back at the patient chart and “connect the dots,” we see that instability had been developing for hours before an urgent summons for assistance.
Even with the best care, patients’ clinical needs often change after admission. Patient status can change rapidly, so a perfect assessment earlier in the day can quickly become dated. Further, bedside staff have many other patients, and staffing assignments don’t build in “slack time” to permit paying extra attention when problems develop. Consequently, signs of clinical deterioration are often missed or not acted upon until there’s a code on the unit and dramatic measures are needed to save a life.
Proactive clinical surveillance tools are the second big step in creating a safety net for patients. With patient data in electronic form, hands-on caregivers, nurses, and supervisors can use specially designed “dashboard views” to quickly identify which patients are exhibiting warning signs of clinical decline and exactly where they are located.
To be most effective, staff should view clinical surveillance information in a variety of useful ways:
- Hospital–wide for a big picture of where the trouble spots are
- By unit, to scan through patients and see the values that are triggering an alert
- By provider, so doctors and nurses can scan their list of patients and see which have triggered alerts
- By patient, drilling into all the details of that patient’s current status and previous care
- By patient, drilling into all the details of that patient’s current status and previous care
tion, which are out of range or trending in the wrong direction, should automatically highlight patients. With the complete clinical record on-line, staff can prioritize which patients to visit next and what type of supplemental resources might be needed to enhance care.
For hospitalists, clinical surveillance tools save an immense amount of time and help prioritize patient care. Typically hospitalists manage a large number of patients who are scattered around the hospital. Determining where to start rounds and which patients should be seen first is often difficult. Even worse, patients’ conditions suddenly change for the worse soon after you’ve checked on them. There are just too many patients to continually be looking at patient charts and relying on verbal information: that’s why there are computers!
Supervisory staff can provide an additional safety net, if they have the tools to do so effectively. Typically, they rely on “report” and walking around, visiting staff, looking for an opportunity where their intervention could be helpful. By referring to “hot spots” indicated on a clinical surveillance dashboard view, they would know where they’re needed and spend their time helping, rather than prospecting.
Some hospitals have formalized their response to the failure to rescue problem by creating “rapid response teams.” Such teams can also rely on clinical surveillance tools to identify patients in need, rather than waiting for a phone call from an overwhelmed primary caregiver.
Making Best Practices Work
Organizational performance can be dramatically improved when patient outcomes and staff activity can be measured and analyzed. Traditionally, this has been done retrospectively.
By evaluating outcomes of patients and compliance with processes, many sites have been able to improve processes for future patients. However, because reporting has been periodic, results become available only months later, and implementation of care enhancements are delayed.
With comprehensive patient data in electronic form, real-time monitoring of compliance with intended processes and best practices becomes possible. For example, if there is a consensus that the head of the bed of ventilated patients should be elevated to reduce the incidence of ventilator-associated pneumonia, then the monitoring system can show, by ICU, the percentage compliance with that protocol at any given moment.
Since the report is available real-time, non-compliance can be addressed immediately, benefiting the patient and directing education about the protocol precisely when and where it is needed for maximum impact.
Creating a Reliable Patient Safety System
An electronic medical record forms the very foundation of a patient safety system. This electronic data provides the capability for proactive clinical monitoring and much more sophisticated process analysis that happens in days or weeks, not over a course of months or years.
Capture patient data electronically, set up a set of effective alerts based on hospital-defined triggers, and enact process monitoring to improve outcomes and fix problems as they occur. With these three elements, hospitals have the best antidote for failure to rescue and are able to create a safety net for patients.
Dr. Kremsdorf can be contacted at [email protected].
A recent HealthGrades Quality Study titled Patient Safety in American Hospitals (July 2004) highlighted the frequency of patients dying from complications that develop while in hospitals. Failure to rescue, according to the 3-year study, accounts for 60,000 deaths each year in Medicare patients under the age of 75.
Based on my experience as a pulmonary and critical care physician, this statistic quantifies an important problem. Deaths from complications of illness, or care, during a hospital stay happen more than we’d like to admit. However, the good news is that by identifying the underlying problem and deploying some targeted, systemic changes, hospitalists can begin to handle decompensation quickly, proactively, and before it’s too late.
Moving forward, hospitals need to build an effective patient safety net, which requires three important elements: point-of care tools for caregivers, proactive clinical surveillance, and real-time process monitoring.
Reasons for Failure to Rescue
A huge effort, and amount of money, has been focused on finding errors that lead to harm. Unfortunately, we’re tackling the wrong errors. New tools like barcode medication administration or CPOE tackle errors of commission. These errors might occur when a doctor or nurse administers a wrong dose or wrong medication. Errors of commission are much easier to identify and solve, but clinically significant errors of commission that cause harm are relatively rare events and don’t affect overall hospital mortality.
Errors of omission, however, are much more insidious. An error of omission is an error that occurs when an action is not taken or an important step in the process is left out. Examples of an error of omission include sub-optimal patient care resulting from the inadequate availability of patient information for decision-making, or a more blatant example, when a patient’s vital signs indicate decompensation but the clinical response is inadequate or delayed.
Errors of omission continue in today’s hospitals for two very important reasons: First, we lack a systematic way to handle clinical decompensation. While we have “code” teams, their efforts often come into play too late. Second, lacking a way to recognize and respond to the issue, we have accepted that failure to rescue is in some ways inevitable and excusable.
The basic, first step is to replace the inherently unreliable paper patient chart. Paper patient charts get misplaced, information is sometimes missing and/or illegible, and they make it impossible for a team effort to optimize care.
Hospitals need to get patient data such as vital signs and medication usage in electronic form. That way, it is effortless and time-efficient to determine a patient’s status and check up on patients even when not physically near them. Making this change alone, even in only one hospital unit, hospitalists can begin to effect significant positive changes in patient safety outcomes.
Catastrophes Aren’t Inevitable
Often, the first time physicians become aware of a problem is when they receive a frantic call to come to the bedside. The patient is decompensating and needs immediate, dramatic intervention to save their life. However, when we take the time to look back at the patient chart and “connect the dots,” we see that instability had been developing for hours before an urgent summons for assistance.
Even with the best care, patients’ clinical needs often change after admission. Patient status can change rapidly, so a perfect assessment earlier in the day can quickly become dated. Further, bedside staff have many other patients, and staffing assignments don’t build in “slack time” to permit paying extra attention when problems develop. Consequently, signs of clinical deterioration are often missed or not acted upon until there’s a code on the unit and dramatic measures are needed to save a life.
Proactive clinical surveillance tools are the second big step in creating a safety net for patients. With patient data in electronic form, hands-on caregivers, nurses, and supervisors can use specially designed “dashboard views” to quickly identify which patients are exhibiting warning signs of clinical decline and exactly where they are located.
To be most effective, staff should view clinical surveillance information in a variety of useful ways:
- Hospital–wide for a big picture of where the trouble spots are
- By unit, to scan through patients and see the values that are triggering an alert
- By provider, so doctors and nurses can scan their list of patients and see which have triggered alerts
- By patient, drilling into all the details of that patient’s current status and previous care
- By patient, drilling into all the details of that patient’s current status and previous care
tion, which are out of range or trending in the wrong direction, should automatically highlight patients. With the complete clinical record on-line, staff can prioritize which patients to visit next and what type of supplemental resources might be needed to enhance care.
For hospitalists, clinical surveillance tools save an immense amount of time and help prioritize patient care. Typically hospitalists manage a large number of patients who are scattered around the hospital. Determining where to start rounds and which patients should be seen first is often difficult. Even worse, patients’ conditions suddenly change for the worse soon after you’ve checked on them. There are just too many patients to continually be looking at patient charts and relying on verbal information: that’s why there are computers!
Supervisory staff can provide an additional safety net, if they have the tools to do so effectively. Typically, they rely on “report” and walking around, visiting staff, looking for an opportunity where their intervention could be helpful. By referring to “hot spots” indicated on a clinical surveillance dashboard view, they would know where they’re needed and spend their time helping, rather than prospecting.
Some hospitals have formalized their response to the failure to rescue problem by creating “rapid response teams.” Such teams can also rely on clinical surveillance tools to identify patients in need, rather than waiting for a phone call from an overwhelmed primary caregiver.
Making Best Practices Work
Organizational performance can be dramatically improved when patient outcomes and staff activity can be measured and analyzed. Traditionally, this has been done retrospectively.
By evaluating outcomes of patients and compliance with processes, many sites have been able to improve processes for future patients. However, because reporting has been periodic, results become available only months later, and implementation of care enhancements are delayed.
With comprehensive patient data in electronic form, real-time monitoring of compliance with intended processes and best practices becomes possible. For example, if there is a consensus that the head of the bed of ventilated patients should be elevated to reduce the incidence of ventilator-associated pneumonia, then the monitoring system can show, by ICU, the percentage compliance with that protocol at any given moment.
Since the report is available real-time, non-compliance can be addressed immediately, benefiting the patient and directing education about the protocol precisely when and where it is needed for maximum impact.
Creating a Reliable Patient Safety System
An electronic medical record forms the very foundation of a patient safety system. This electronic data provides the capability for proactive clinical monitoring and much more sophisticated process analysis that happens in days or weeks, not over a course of months or years.
Capture patient data electronically, set up a set of effective alerts based on hospital-defined triggers, and enact process monitoring to improve outcomes and fix problems as they occur. With these three elements, hospitals have the best antidote for failure to rescue and are able to create a safety net for patients.
Dr. Kremsdorf can be contacted at [email protected].
Clinicians’ Perspectives on Work-Hour Restrictions and House Officer Errors
Background: Concerned about the impact of house officer (HO) fatigue on education and the quality of patient care, the ACGME instituted work restrictions for HOs effective July 1, 2003. Proponents believe HO fatigue contributes to in-hospital errors. Opponents argue that decreasing HO work hours will increase errors due to patient handoffs and HO cross-coverage. We surveyed internal medicine faculty and HOs to understand clinician perceptions of the impact of the ACGME regulations.
Methods: We created a written survey instrument based on a literature review, expert opinion, and focus groups of HOs, staff internists, and nurses. The survey asked respondents to recall types of errors and contributing factors that occurred in the 3 months prior to work-hour restrictions,and to predict how the restrictions would affect patient care and HO education. We administered the survey in July and August 2003 via email and in person to PGY2/3 medical HOs and medical ward and ICU attending physicians at Beth Israel Deaconess Medical Center. Responses were scored on the Likert scale. We calculated the percentage of respondents who agreed/strongly agreed or disagreed/strongly disagreed with statements and used the rank sum test to compare HO and attending physician responses.
Results: We received completed surveys from 81 of 95 HOs and 40 of 104 attending physicians, including all 11 staff hospitalists who, together, accounted for approximately 65% of inpatient medical admissions. HOs were more likely than attendings to attribute errors to high census (70% vs. 22%, p=0.001) and fatigue (52% vs. 38%, p=0.02); HOs were less likely than attendings to attribute errors to cross-coverage (53% vs. 79%, p<0.001) and lack of experience or knowledge (54% vs. 68%, p=0.03).
Fifty-two percent of HOs and 22% of attending physicians agreed that fatigue contributed to HO errors in the previous 3 months, but only 20% of HOs and 10% of attendings predicted that fatigue would contribute to errors after implementing work-hour restrictions. Despite this expected reduction in HO fatigue, a majority of HOs and attendings disagreed that quality of care (55% and 69%) and continuity of care (89% and 89%) would improve. Ninetyfive percent of HOs and 98% of attendings predicted that in the new system errors would occur as a result of cross-coverage, compared with 53% and 79%, respectively, at baseline. Half the HOs (55%) and attendings (50%) believed that HO errors would increase overall after the change.
Conclusion: Clinicians were skeptical that ACGME work-hour restrictions would improve care or decrease errors. Instead, many HOs and attendings predicted that the new regulations would change the underlying cause of error from fatigue to cross-coverage, and that the total number of errors would increase. If academic medical centers and their patients are to reap the intended benefits of work-hour restrictions, residency directors will need to develop and implement skill-building initiatives focused on cross-coverage.
Dr. Kripalani can be contacted at [email protected].
Background: Concerned about the impact of house officer (HO) fatigue on education and the quality of patient care, the ACGME instituted work restrictions for HOs effective July 1, 2003. Proponents believe HO fatigue contributes to in-hospital errors. Opponents argue that decreasing HO work hours will increase errors due to patient handoffs and HO cross-coverage. We surveyed internal medicine faculty and HOs to understand clinician perceptions of the impact of the ACGME regulations.
Methods: We created a written survey instrument based on a literature review, expert opinion, and focus groups of HOs, staff internists, and nurses. The survey asked respondents to recall types of errors and contributing factors that occurred in the 3 months prior to work-hour restrictions,and to predict how the restrictions would affect patient care and HO education. We administered the survey in July and August 2003 via email and in person to PGY2/3 medical HOs and medical ward and ICU attending physicians at Beth Israel Deaconess Medical Center. Responses were scored on the Likert scale. We calculated the percentage of respondents who agreed/strongly agreed or disagreed/strongly disagreed with statements and used the rank sum test to compare HO and attending physician responses.
Results: We received completed surveys from 81 of 95 HOs and 40 of 104 attending physicians, including all 11 staff hospitalists who, together, accounted for approximately 65% of inpatient medical admissions. HOs were more likely than attendings to attribute errors to high census (70% vs. 22%, p=0.001) and fatigue (52% vs. 38%, p=0.02); HOs were less likely than attendings to attribute errors to cross-coverage (53% vs. 79%, p<0.001) and lack of experience or knowledge (54% vs. 68%, p=0.03).
Fifty-two percent of HOs and 22% of attending physicians agreed that fatigue contributed to HO errors in the previous 3 months, but only 20% of HOs and 10% of attendings predicted that fatigue would contribute to errors after implementing work-hour restrictions. Despite this expected reduction in HO fatigue, a majority of HOs and attendings disagreed that quality of care (55% and 69%) and continuity of care (89% and 89%) would improve. Ninetyfive percent of HOs and 98% of attendings predicted that in the new system errors would occur as a result of cross-coverage, compared with 53% and 79%, respectively, at baseline. Half the HOs (55%) and attendings (50%) believed that HO errors would increase overall after the change.
Conclusion: Clinicians were skeptical that ACGME work-hour restrictions would improve care or decrease errors. Instead, many HOs and attendings predicted that the new regulations would change the underlying cause of error from fatigue to cross-coverage, and that the total number of errors would increase. If academic medical centers and their patients are to reap the intended benefits of work-hour restrictions, residency directors will need to develop and implement skill-building initiatives focused on cross-coverage.
Dr. Kripalani can be contacted at [email protected].
Background: Concerned about the impact of house officer (HO) fatigue on education and the quality of patient care, the ACGME instituted work restrictions for HOs effective July 1, 2003. Proponents believe HO fatigue contributes to in-hospital errors. Opponents argue that decreasing HO work hours will increase errors due to patient handoffs and HO cross-coverage. We surveyed internal medicine faculty and HOs to understand clinician perceptions of the impact of the ACGME regulations.
Methods: We created a written survey instrument based on a literature review, expert opinion, and focus groups of HOs, staff internists, and nurses. The survey asked respondents to recall types of errors and contributing factors that occurred in the 3 months prior to work-hour restrictions,and to predict how the restrictions would affect patient care and HO education. We administered the survey in July and August 2003 via email and in person to PGY2/3 medical HOs and medical ward and ICU attending physicians at Beth Israel Deaconess Medical Center. Responses were scored on the Likert scale. We calculated the percentage of respondents who agreed/strongly agreed or disagreed/strongly disagreed with statements and used the rank sum test to compare HO and attending physician responses.
Results: We received completed surveys from 81 of 95 HOs and 40 of 104 attending physicians, including all 11 staff hospitalists who, together, accounted for approximately 65% of inpatient medical admissions. HOs were more likely than attendings to attribute errors to high census (70% vs. 22%, p=0.001) and fatigue (52% vs. 38%, p=0.02); HOs were less likely than attendings to attribute errors to cross-coverage (53% vs. 79%, p<0.001) and lack of experience or knowledge (54% vs. 68%, p=0.03).
Fifty-two percent of HOs and 22% of attending physicians agreed that fatigue contributed to HO errors in the previous 3 months, but only 20% of HOs and 10% of attendings predicted that fatigue would contribute to errors after implementing work-hour restrictions. Despite this expected reduction in HO fatigue, a majority of HOs and attendings disagreed that quality of care (55% and 69%) and continuity of care (89% and 89%) would improve. Ninetyfive percent of HOs and 98% of attendings predicted that in the new system errors would occur as a result of cross-coverage, compared with 53% and 79%, respectively, at baseline. Half the HOs (55%) and attendings (50%) believed that HO errors would increase overall after the change.
Conclusion: Clinicians were skeptical that ACGME work-hour restrictions would improve care or decrease errors. Instead, many HOs and attendings predicted that the new regulations would change the underlying cause of error from fatigue to cross-coverage, and that the total number of errors would increase. If academic medical centers and their patients are to reap the intended benefits of work-hour restrictions, residency directors will need to develop and implement skill-building initiatives focused on cross-coverage.
Dr. Kripalani can be contacted at [email protected].
Listen to the Eye
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at [email protected].
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at [email protected].
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.
A 57-year-old woman with no previous medical history was admitted with weakness. The patient complained of 2 months of ascending bilateral lower extremity weakness followed by subjective “numbness” of both legs. She had a normal lumbosacral MRI as an outpatient and presented to the ED with progressive symptoms. She denied back pain, bowel or bladder problems, diplopia, ataxia, or confusion. As well, there were no fevers, chills, muscle pain, or weight loss. She had no risk factors for HIV and no toxic exposures.
On admission, her vital signs were normal and her general physical exam was unremarkable. Her neurologic exam was notable for diffuse symmetric 3/5 bilateral lower extremity weakness and symmetric bilateral sensory loss in a “stocking” distribution. She had bilateral lower extremity hyperreflexia and plantar reflexes were extensor bilaterally. She had normal upper extremities, cranial nerves, and mental status. Screening laboratories including fasting glucose, B12, RPR, TSH, HIV, SPEP, and UPEP were negative. A repeat lumbosacral MRI and a lumbar puncture were nondiagnostic.
While hospitalized, the patient suffered progressive ascending weakness involving the upper extremities and the diaphragm, necessitating intubation. She was treated with high-dose steroids, IVIG, and plasmapheresis for the possibility of Guillain-Barre or transverse myelitis; there was no change in her symptoms. With no clear diagnosis, on hospital day 10, she complained of diplopia and was found to have right eye chemosis, proptosis, right abducens nerve palsy, and a loud bruit over the right eye. A CT scan revealed dilated right ophthalmic veins and an engorged cavernous sinus (Figure 1). A cerebral angiogram was performed and showed a distal right vertebral arteriovenous fistula (Figure 2), and an MRI showed increased signal in the entire cord secondary to venous hypertension.
What is the diagnosis?
Vertebral Arterio-Venous Fistula (AVF) with arterialized venous drainage to the cavernous sinus, ophthalmic veins, and the cervical epidural veins leading to her ocular symptoms and a cervical myelopathy.
She had no history of trauma and the AVF was thought to be spontaneous. She underwent successful transarterial embolization of the right vertebral artery (see Figure 3). Her ocular symptoms rapidly improved and she was transferred to a rehabilitation facility with improving motor and sensory function.
Discussion: Vertebral arteriovenous fistulas (AVFs) are rare vascular malformations characterized by abnormal shunting between the extracranial vertebral artery and a neighboring vein. Vertebral AVFs are most often secondary to trauma including penetrating gunshot or stab wounds to the neck. Fibromuscular dysplasia and neurofibromatosis are predisposing conditions but vertebral AVFs can be spontaneous as in this case. Patients with vertebral AVFs may present with tinnitus, but frequently they have no symptoms and their fistulas are discovered as cervical bruits on routine auscultation. Neurologic syndromes in the setting of a vertebral AVF are rare and typically secondary to arterialization of venous drainage leading to local ischemia and nerve damage. There are case reports of vertigo and vertebrobasilar insufficiency, cervical radiculopathy related to nerve-root compression from engorged vertebral veins, and cervical myelopathy from venous hypertension similar to this patient. As well, there is only one case report of a vertebral AVF leading to exophthalmos, chemosis, and a bruit, mimicking a carotid-cavernous fistula. This is the first reported case of a vertebral AVF leading to both cervical cord and ocular pathology.
Vertebral AVFs can be suspected based on CT and MRI findings, but angiography is the gold standard for diagnosis. Transarterial embolization is the safest and most effective treatment, allowing for occlusion of the fistula while maintaining patency of the vertebral artery. If treated expediently, most patients experience total recovery.
Dr. Baudendistel can be contacted at [email protected].
References
- Ammirati M, Mirzai S, Samii M. Vertebral arteriovenous fistulae: report of two cases and review of the literature. Acta Neurochir. 1989;99:122-6.
- Gobin YP, Duckwiler GR, Vinuela F. Direct arteriovenous fistulas: diagnosis and intervention. Neuroimaging Clin North Am. 1998;8:425-43.
- Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR. 1988;150:405-12.
Navigating the Nuances of Consult Coding
Introduction
Hospitalists often have questions related to coding for consultative services and subsequent hospital visits, especially when other specialists are managing the patient “concurrently.” If the hospitalist is practicing in a teaching hospital the guidelines can be yet more confusing, due to the need to apply Medicare’s teaching physician guidelines. Even after reading informative articles or attending educational sessions, hospitalists may encounter unique scenarios that can frustrate the most experienced physician and/or coder. The goal of this article is to present some basic principles regarding coding for consultations and concurrent care, and to provide several case scenarios that can be applied in clinical practice as a guide.
Objectives of the article include answering the following questions:
- Is it appropriate as a hospitalist to bill a consultation code when requested by a surgeon who really wants you to manage the patient’s chronic medical conditions?
- Can a hospitalist charge for services provided to a postoperative patient at the request of the surgeon, even though there are no real medical conditions or complications?
- Can two internists (different subspecialties) treat and bill the same patient on the same day and get paid?
- Can two internists (same specialty) treat and bill the same patient on the same day?
- What if my group performs preoperative evaluations and will also be managing the patient postoperatively for his/her medical conditions? When the surgeon requests a “consult” may I use the consultation codes?
Consultations
An inpatient consultation is a service provided by a physician whose opinion or advice regarding evaluation and/or management of a specific problem(s) is requested by another physician. There has been a tremendous amount of confusion in interpreting the rules regarding consultations in general, and this is particularly true for hospitalists given frequent blurring of the distinction between classic consultation and co-management. In August of 1999, Medicare clarified for its carriers when an encounter qualified as a consultation. Here’s what the manual states:
Consultation followed by treatment: “…Payment for a consultation may be made regardless of treatment initiation UNLESS A TRANSFER OF CARE OCCURS. A transfer of care occurs when the referring physician transfers the responsibility for the patient’s complete care to the receiving physician at the time of referral and the receiving physician documents approval of the transfer of care in advance. “ (reference MCM 15506 B.)
Inpatient consultant services are coded using initial consult codes (99251-99255).
Scenario # 1
A psychiatrist asks you to see a 36-year-old man for “uncontrolled hypertension” who was admitted with a manic episode. The patient stopped taking his anti-hypertensive medications 6 weeks before, and his systolic blood pressure has been consistently running 160–170 since admission. You perform an in-depth review of his medical records, along with a thorough history and physical examination (made challenging by his poorly controlled mania) and review of his laboratory studies. After your evaluation, you agree to manage the patient’s hypertension problem.
Question # 1: Should this be coded as a consultation or a subsequent visit?
Answer: Since a request was made to evaluate a patient for a problem and you did not in advance of the consultation (in writing) accept transfer of the patient’s medical care, a consultation may be coded as long as all of the criteria have been met. The fact that you decide to manage the patient’s hypertension subsequent to the initial consult does not impact your ability to use the initial consult code for this patient. Remember the requirements for a consultation—
- Request for consult. (A written order by the psychiatrist should be documented in the record and the consulting physician should document “Consult requested by Dr. Smith for evaluation of patient’s uncontrolled hypertension.”)
- Written report of his or her findings in the inpatient medical record. (The note may serve as a “report” and should clearly define the recommendations made by you, the consultant.)
Question # 2: Can the degree of complexity be considered higher than a typical patient with “uncontrolled hypertension” due to the difficulties in obtaining the information for this patient?
Answer: The complexity of data reviewed can have an impact on the level of service billed. The uncontrolled nature of the underlying problem, and the summarizing of the patient’s history from the record when the patient is unable to provide the information would be indicative of moderate complexity decision-making. Note that in situations where the level of service is much lower than the time spent with the patient due to extenuating circumstances such as these, it may be appropriate to consider “prolonged care” codes as long as the time thresholds are met and time is documented in the record.
Scenario # 2
A patient with stable hypertension and diabetes has been seen by one of the other members of your group and specialty for a preoperative consultation. The consultation was performed and the patient was deemed to be medically optimized. After the surgery, you are asked to co-manage the patient’s SAME medical conditions.
Question: Can I code an initial consult?
Answer: This is a situation where Medicare has a special rule for those physicians (same specialty and in the same group practice) who perform pre-operative consultations. A consult code (either initial or follow up) should not be used but rather a subsequent visit code should be used. An assumption is made that the physician who performed the preoperative consult will have developed a treatment plan for that problem and will have assumed responsibility for any postoperative care requested by the surgeon. HOWEVER, if a new problem has arisen and a consult is requested by the physician postoperatively, then an initial consult code may be used.
Postoperative Management of Medical Problems
According to Medicare’s carrier manual, “If a surgeon asks a physician to take responsibility for the management of an aspect of the patient’s condition during the postoperative period, the physician may not bill a consultation because the surgeon is not asking the physician’s opinion or advice for the surgeon’s use in treating the patient. The physician’s services would constitute concurrent care and should be billed using the appropriate level subsequent visit codes.” (MCM 15506 G) This often is reflected by an order from the surgeon that says “notify Dr. X of patient’s transfer to RNF” or perhaps a telephone call to place a patient on the hospitalist’s schedule. So what is “concurrent care”?
Concurrent Care
Concurrent care exists where services “more extensive than consultative services are rendered by more than one physician during a period of time” (MCM 2020E). Basically this means that more than one physician has primary responsibility for managing a portion of the patient’s care (concurrently) during the patient’s inpatient stay. For Medicare and other payers, this is considered appropriate when these “concurrent” services are “reasonable and necessary.”
- The condition(s) or diagnoses warrant the service and the specialty or expertise of the other physician(s) and at a reasonable frequency or duration.
- Duplicate services (i.e., services provided by two different providers of the same specialty for the same or similar conditions) will typically not be considered necessary unless a special circumstance is noted. For many payers, the internist and subspecialist who co-manage the same problem may have services performed on the same day denied, and documentation would need to show there were “special circumstances.” However, if the hospitalist is treating additional issues, then there should be no problem with separate payment. Medicare does recognize the endocrinology and internal medicine specialties separately and would probably pay both even if for the same condition. But if both are really “co-managing” the same problem without any additional issues daily, most payers are going to question this, either at the time of billing or retrospectively through audits.
Inpatient Concurrent care then is coded with subsequent hospital codes in the hospital setting (Codes 99231 through 99233).
Scenario # 3
A 73-year-old man with a past medical history notable for chronic renal insufficiency, hypertension, and Alzheimer’s type dementia undergoes a right open nephrectomy for renal cell carcinoma. His early postoperative course is marked by hypotension in the post-anesthesia care unit, and he is admitted to the SICU. His course there is significant for worsening of his baseline creatinine of 1.9 to 3.8, the development of delirium, and labile blood pressure. He is transferred from the SICU to a regular nursing floor on postoperative day 2, and the attending urologist requests that you assume management of the patient’s hypertension, delirium, and acute renal failure.
Question: Does this meet the definition of appropriate concurrent care or a consultation?
Answer: Although this constitutes something of a gray area, the request as worded indicates that the hospitalist will be providing concurrent care, and the initial visit should thus be billed as a Level 3 subsequent visit (99233). If the hospitalist’s role is, rather, to provide recommendations regarding management of these problems, the initial visit should be billed as an initial inpatient consult at the appropriate level.
Scenario # 4
A 66-year-old woman with a history of coronary artery disease 3 years after stenting of the left anterior descending coronary artery, moderate aortic stenosis, well-controlled diabetes mellitus, and hyperlipidemia undergoes a left modified radical mastectomy. On the morning of her first postoperative day, she experiences substernal chest pain, with T wave inversions in the inferior leads of her ECG. Her breast surgeon consults cardiology for her chest pain, endocrinology for “diabetic control,” and the hospitalist to “oversee the medical issues.”
Question: Can the hospitalist successfully bill in this setting? If so, what needs to be done to allow this?
Answer: Because of the various specialists who are treating this patient’s medical conditions, it will be difficult to demonstrate to a payer that an additional physician should be managing the patient’s care on a daily basis for the same medical problems. Such billing would probably be considered “duplicate care” and one of the physicians’ charges will be appropriately denied. However, if the specialists have been consulted only and have not assumed management for these medical conditions, then the hospitalist who has assumed management may bill for these services. As with scenario #3, the surgeon’s request as worded in this scenario indicates the hospitalist is providing concurrent care and a consultation is not being requested.
Scenario #5:
The hospital medicine consult team is asked to see a 31-year-old woman who is postoperative day 3 after a total proctocolectomy for refractory ulcerative colitis. Her past medical history is remarkable for iron-deficiency anemia, steroid-induced diabetes, and depression. You are asked to evaluate the patient for shortness of breath that began that day. The PGY-3 resident working with you evaluates the patient initially, reviews all available records from this admission as well as the past, performs an exhaustive history and physical, personally reviews the ECG and chest X-ray that have just been completed, and documents all of the above. You then discuss the case with the resident, and personally confirm critical portions of the history and examination. You agree with the resident’s assessment that the patient has most likely sustained a pulmonary embolism, as well as her recommendation for empiric anticoagulation and an urgent V/Q scan.
Question #1: What must be done documentation-wise by the attending physician to ensure that the optimum billing level is captured for this patient? What is not acceptable in this setting?
Answer: Redocumentation by the teaching physician is relatively minimal since CMS revised its guidelines [Transmittal 1780 dated 11/22/02], which allows substantial reference to the resident’s note in addition to a personal note, however, documentation must clearly demonstrate that the teaching physician was physically present during the key portions of the service billed. Examples of documentation provided by CMS are:
“I performed a history and examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
Or
“I saw and evaluated the patient. I agree with the findings and plan of care documented in the resident’s note.”
Or
“I saw and evaluated the patient. I agree w/ the resident’s note except…” while noting the difference in plan, etc.
Question #2: If the hospitalist/medical resident write the orders for the heparin and V/Q scan, does this constitute comanagement and prevent billing this as a consult?
Answer: A consultant may initiate treatment at the conclusion of his evaluation and still bill a consultation code as long as the other requirements have been met (i.e., a request for opinion regarding evaluation and treatment and no advance transfer of care). There are no specific rules related to medical residents in this scenario, so if the teaching physician is performing the consult in a timely manner with the resident, a consultation could still be coded appropriately.
Summary
Although efforts have been made by Medicare to clarify the vagaries of coding for consultative work, existing guidelines remain complex and not necessarily intuitive. This article has attempted to shed light on some of the more commonly encountered situations with which hospitalists grapple, but is unable to address all of the questions that may arise. Hospitalists and hospital medicine groups are encouraged to familiarize themselves with current coding guidelines and to establish and maintain strong relationships with local coding professionals. Future issues of The Hospitalist will tackle additional coding questions.
Dr. Pfeiffer can be contacted at [email protected].
Introduction
Hospitalists often have questions related to coding for consultative services and subsequent hospital visits, especially when other specialists are managing the patient “concurrently.” If the hospitalist is practicing in a teaching hospital the guidelines can be yet more confusing, due to the need to apply Medicare’s teaching physician guidelines. Even after reading informative articles or attending educational sessions, hospitalists may encounter unique scenarios that can frustrate the most experienced physician and/or coder. The goal of this article is to present some basic principles regarding coding for consultations and concurrent care, and to provide several case scenarios that can be applied in clinical practice as a guide.
Objectives of the article include answering the following questions:
- Is it appropriate as a hospitalist to bill a consultation code when requested by a surgeon who really wants you to manage the patient’s chronic medical conditions?
- Can a hospitalist charge for services provided to a postoperative patient at the request of the surgeon, even though there are no real medical conditions or complications?
- Can two internists (different subspecialties) treat and bill the same patient on the same day and get paid?
- Can two internists (same specialty) treat and bill the same patient on the same day?
- What if my group performs preoperative evaluations and will also be managing the patient postoperatively for his/her medical conditions? When the surgeon requests a “consult” may I use the consultation codes?
Consultations
An inpatient consultation is a service provided by a physician whose opinion or advice regarding evaluation and/or management of a specific problem(s) is requested by another physician. There has been a tremendous amount of confusion in interpreting the rules regarding consultations in general, and this is particularly true for hospitalists given frequent blurring of the distinction between classic consultation and co-management. In August of 1999, Medicare clarified for its carriers when an encounter qualified as a consultation. Here’s what the manual states:
Consultation followed by treatment: “…Payment for a consultation may be made regardless of treatment initiation UNLESS A TRANSFER OF CARE OCCURS. A transfer of care occurs when the referring physician transfers the responsibility for the patient’s complete care to the receiving physician at the time of referral and the receiving physician documents approval of the transfer of care in advance. “ (reference MCM 15506 B.)
Inpatient consultant services are coded using initial consult codes (99251-99255).
Scenario # 1
A psychiatrist asks you to see a 36-year-old man for “uncontrolled hypertension” who was admitted with a manic episode. The patient stopped taking his anti-hypertensive medications 6 weeks before, and his systolic blood pressure has been consistently running 160–170 since admission. You perform an in-depth review of his medical records, along with a thorough history and physical examination (made challenging by his poorly controlled mania) and review of his laboratory studies. After your evaluation, you agree to manage the patient’s hypertension problem.
Question # 1: Should this be coded as a consultation or a subsequent visit?
Answer: Since a request was made to evaluate a patient for a problem and you did not in advance of the consultation (in writing) accept transfer of the patient’s medical care, a consultation may be coded as long as all of the criteria have been met. The fact that you decide to manage the patient’s hypertension subsequent to the initial consult does not impact your ability to use the initial consult code for this patient. Remember the requirements for a consultation—
- Request for consult. (A written order by the psychiatrist should be documented in the record and the consulting physician should document “Consult requested by Dr. Smith for evaluation of patient’s uncontrolled hypertension.”)
- Written report of his or her findings in the inpatient medical record. (The note may serve as a “report” and should clearly define the recommendations made by you, the consultant.)
Question # 2: Can the degree of complexity be considered higher than a typical patient with “uncontrolled hypertension” due to the difficulties in obtaining the information for this patient?
Answer: The complexity of data reviewed can have an impact on the level of service billed. The uncontrolled nature of the underlying problem, and the summarizing of the patient’s history from the record when the patient is unable to provide the information would be indicative of moderate complexity decision-making. Note that in situations where the level of service is much lower than the time spent with the patient due to extenuating circumstances such as these, it may be appropriate to consider “prolonged care” codes as long as the time thresholds are met and time is documented in the record.
Scenario # 2
A patient with stable hypertension and diabetes has been seen by one of the other members of your group and specialty for a preoperative consultation. The consultation was performed and the patient was deemed to be medically optimized. After the surgery, you are asked to co-manage the patient’s SAME medical conditions.
Question: Can I code an initial consult?
Answer: This is a situation where Medicare has a special rule for those physicians (same specialty and in the same group practice) who perform pre-operative consultations. A consult code (either initial or follow up) should not be used but rather a subsequent visit code should be used. An assumption is made that the physician who performed the preoperative consult will have developed a treatment plan for that problem and will have assumed responsibility for any postoperative care requested by the surgeon. HOWEVER, if a new problem has arisen and a consult is requested by the physician postoperatively, then an initial consult code may be used.
Postoperative Management of Medical Problems
According to Medicare’s carrier manual, “If a surgeon asks a physician to take responsibility for the management of an aspect of the patient’s condition during the postoperative period, the physician may not bill a consultation because the surgeon is not asking the physician’s opinion or advice for the surgeon’s use in treating the patient. The physician’s services would constitute concurrent care and should be billed using the appropriate level subsequent visit codes.” (MCM 15506 G) This often is reflected by an order from the surgeon that says “notify Dr. X of patient’s transfer to RNF” or perhaps a telephone call to place a patient on the hospitalist’s schedule. So what is “concurrent care”?
Concurrent Care
Concurrent care exists where services “more extensive than consultative services are rendered by more than one physician during a period of time” (MCM 2020E). Basically this means that more than one physician has primary responsibility for managing a portion of the patient’s care (concurrently) during the patient’s inpatient stay. For Medicare and other payers, this is considered appropriate when these “concurrent” services are “reasonable and necessary.”
- The condition(s) or diagnoses warrant the service and the specialty or expertise of the other physician(s) and at a reasonable frequency or duration.
- Duplicate services (i.e., services provided by two different providers of the same specialty for the same or similar conditions) will typically not be considered necessary unless a special circumstance is noted. For many payers, the internist and subspecialist who co-manage the same problem may have services performed on the same day denied, and documentation would need to show there were “special circumstances.” However, if the hospitalist is treating additional issues, then there should be no problem with separate payment. Medicare does recognize the endocrinology and internal medicine specialties separately and would probably pay both even if for the same condition. But if both are really “co-managing” the same problem without any additional issues daily, most payers are going to question this, either at the time of billing or retrospectively through audits.
Inpatient Concurrent care then is coded with subsequent hospital codes in the hospital setting (Codes 99231 through 99233).
Scenario # 3
A 73-year-old man with a past medical history notable for chronic renal insufficiency, hypertension, and Alzheimer’s type dementia undergoes a right open nephrectomy for renal cell carcinoma. His early postoperative course is marked by hypotension in the post-anesthesia care unit, and he is admitted to the SICU. His course there is significant for worsening of his baseline creatinine of 1.9 to 3.8, the development of delirium, and labile blood pressure. He is transferred from the SICU to a regular nursing floor on postoperative day 2, and the attending urologist requests that you assume management of the patient’s hypertension, delirium, and acute renal failure.
Question: Does this meet the definition of appropriate concurrent care or a consultation?
Answer: Although this constitutes something of a gray area, the request as worded indicates that the hospitalist will be providing concurrent care, and the initial visit should thus be billed as a Level 3 subsequent visit (99233). If the hospitalist’s role is, rather, to provide recommendations regarding management of these problems, the initial visit should be billed as an initial inpatient consult at the appropriate level.
Scenario # 4
A 66-year-old woman with a history of coronary artery disease 3 years after stenting of the left anterior descending coronary artery, moderate aortic stenosis, well-controlled diabetes mellitus, and hyperlipidemia undergoes a left modified radical mastectomy. On the morning of her first postoperative day, she experiences substernal chest pain, with T wave inversions in the inferior leads of her ECG. Her breast surgeon consults cardiology for her chest pain, endocrinology for “diabetic control,” and the hospitalist to “oversee the medical issues.”
Question: Can the hospitalist successfully bill in this setting? If so, what needs to be done to allow this?
Answer: Because of the various specialists who are treating this patient’s medical conditions, it will be difficult to demonstrate to a payer that an additional physician should be managing the patient’s care on a daily basis for the same medical problems. Such billing would probably be considered “duplicate care” and one of the physicians’ charges will be appropriately denied. However, if the specialists have been consulted only and have not assumed management for these medical conditions, then the hospitalist who has assumed management may bill for these services. As with scenario #3, the surgeon’s request as worded in this scenario indicates the hospitalist is providing concurrent care and a consultation is not being requested.
Scenario #5:
The hospital medicine consult team is asked to see a 31-year-old woman who is postoperative day 3 after a total proctocolectomy for refractory ulcerative colitis. Her past medical history is remarkable for iron-deficiency anemia, steroid-induced diabetes, and depression. You are asked to evaluate the patient for shortness of breath that began that day. The PGY-3 resident working with you evaluates the patient initially, reviews all available records from this admission as well as the past, performs an exhaustive history and physical, personally reviews the ECG and chest X-ray that have just been completed, and documents all of the above. You then discuss the case with the resident, and personally confirm critical portions of the history and examination. You agree with the resident’s assessment that the patient has most likely sustained a pulmonary embolism, as well as her recommendation for empiric anticoagulation and an urgent V/Q scan.
Question #1: What must be done documentation-wise by the attending physician to ensure that the optimum billing level is captured for this patient? What is not acceptable in this setting?
Answer: Redocumentation by the teaching physician is relatively minimal since CMS revised its guidelines [Transmittal 1780 dated 11/22/02], which allows substantial reference to the resident’s note in addition to a personal note, however, documentation must clearly demonstrate that the teaching physician was physically present during the key portions of the service billed. Examples of documentation provided by CMS are:
“I performed a history and examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
Or
“I saw and evaluated the patient. I agree with the findings and plan of care documented in the resident’s note.”
Or
“I saw and evaluated the patient. I agree w/ the resident’s note except…” while noting the difference in plan, etc.
Question #2: If the hospitalist/medical resident write the orders for the heparin and V/Q scan, does this constitute comanagement and prevent billing this as a consult?
Answer: A consultant may initiate treatment at the conclusion of his evaluation and still bill a consultation code as long as the other requirements have been met (i.e., a request for opinion regarding evaluation and treatment and no advance transfer of care). There are no specific rules related to medical residents in this scenario, so if the teaching physician is performing the consult in a timely manner with the resident, a consultation could still be coded appropriately.
Summary
Although efforts have been made by Medicare to clarify the vagaries of coding for consultative work, existing guidelines remain complex and not necessarily intuitive. This article has attempted to shed light on some of the more commonly encountered situations with which hospitalists grapple, but is unable to address all of the questions that may arise. Hospitalists and hospital medicine groups are encouraged to familiarize themselves with current coding guidelines and to establish and maintain strong relationships with local coding professionals. Future issues of The Hospitalist will tackle additional coding questions.
Dr. Pfeiffer can be contacted at [email protected].
Introduction
Hospitalists often have questions related to coding for consultative services and subsequent hospital visits, especially when other specialists are managing the patient “concurrently.” If the hospitalist is practicing in a teaching hospital the guidelines can be yet more confusing, due to the need to apply Medicare’s teaching physician guidelines. Even after reading informative articles or attending educational sessions, hospitalists may encounter unique scenarios that can frustrate the most experienced physician and/or coder. The goal of this article is to present some basic principles regarding coding for consultations and concurrent care, and to provide several case scenarios that can be applied in clinical practice as a guide.
Objectives of the article include answering the following questions:
- Is it appropriate as a hospitalist to bill a consultation code when requested by a surgeon who really wants you to manage the patient’s chronic medical conditions?
- Can a hospitalist charge for services provided to a postoperative patient at the request of the surgeon, even though there are no real medical conditions or complications?
- Can two internists (different subspecialties) treat and bill the same patient on the same day and get paid?
- Can two internists (same specialty) treat and bill the same patient on the same day?
- What if my group performs preoperative evaluations and will also be managing the patient postoperatively for his/her medical conditions? When the surgeon requests a “consult” may I use the consultation codes?
Consultations
An inpatient consultation is a service provided by a physician whose opinion or advice regarding evaluation and/or management of a specific problem(s) is requested by another physician. There has been a tremendous amount of confusion in interpreting the rules regarding consultations in general, and this is particularly true for hospitalists given frequent blurring of the distinction between classic consultation and co-management. In August of 1999, Medicare clarified for its carriers when an encounter qualified as a consultation. Here’s what the manual states:
Consultation followed by treatment: “…Payment for a consultation may be made regardless of treatment initiation UNLESS A TRANSFER OF CARE OCCURS. A transfer of care occurs when the referring physician transfers the responsibility for the patient’s complete care to the receiving physician at the time of referral and the receiving physician documents approval of the transfer of care in advance. “ (reference MCM 15506 B.)
Inpatient consultant services are coded using initial consult codes (99251-99255).
Scenario # 1
A psychiatrist asks you to see a 36-year-old man for “uncontrolled hypertension” who was admitted with a manic episode. The patient stopped taking his anti-hypertensive medications 6 weeks before, and his systolic blood pressure has been consistently running 160–170 since admission. You perform an in-depth review of his medical records, along with a thorough history and physical examination (made challenging by his poorly controlled mania) and review of his laboratory studies. After your evaluation, you agree to manage the patient’s hypertension problem.
Question # 1: Should this be coded as a consultation or a subsequent visit?
Answer: Since a request was made to evaluate a patient for a problem and you did not in advance of the consultation (in writing) accept transfer of the patient’s medical care, a consultation may be coded as long as all of the criteria have been met. The fact that you decide to manage the patient’s hypertension subsequent to the initial consult does not impact your ability to use the initial consult code for this patient. Remember the requirements for a consultation—
- Request for consult. (A written order by the psychiatrist should be documented in the record and the consulting physician should document “Consult requested by Dr. Smith for evaluation of patient’s uncontrolled hypertension.”)
- Written report of his or her findings in the inpatient medical record. (The note may serve as a “report” and should clearly define the recommendations made by you, the consultant.)
Question # 2: Can the degree of complexity be considered higher than a typical patient with “uncontrolled hypertension” due to the difficulties in obtaining the information for this patient?
Answer: The complexity of data reviewed can have an impact on the level of service billed. The uncontrolled nature of the underlying problem, and the summarizing of the patient’s history from the record when the patient is unable to provide the information would be indicative of moderate complexity decision-making. Note that in situations where the level of service is much lower than the time spent with the patient due to extenuating circumstances such as these, it may be appropriate to consider “prolonged care” codes as long as the time thresholds are met and time is documented in the record.
Scenario # 2
A patient with stable hypertension and diabetes has been seen by one of the other members of your group and specialty for a preoperative consultation. The consultation was performed and the patient was deemed to be medically optimized. After the surgery, you are asked to co-manage the patient’s SAME medical conditions.
Question: Can I code an initial consult?
Answer: This is a situation where Medicare has a special rule for those physicians (same specialty and in the same group practice) who perform pre-operative consultations. A consult code (either initial or follow up) should not be used but rather a subsequent visit code should be used. An assumption is made that the physician who performed the preoperative consult will have developed a treatment plan for that problem and will have assumed responsibility for any postoperative care requested by the surgeon. HOWEVER, if a new problem has arisen and a consult is requested by the physician postoperatively, then an initial consult code may be used.
Postoperative Management of Medical Problems
According to Medicare’s carrier manual, “If a surgeon asks a physician to take responsibility for the management of an aspect of the patient’s condition during the postoperative period, the physician may not bill a consultation because the surgeon is not asking the physician’s opinion or advice for the surgeon’s use in treating the patient. The physician’s services would constitute concurrent care and should be billed using the appropriate level subsequent visit codes.” (MCM 15506 G) This often is reflected by an order from the surgeon that says “notify Dr. X of patient’s transfer to RNF” or perhaps a telephone call to place a patient on the hospitalist’s schedule. So what is “concurrent care”?
Concurrent Care
Concurrent care exists where services “more extensive than consultative services are rendered by more than one physician during a period of time” (MCM 2020E). Basically this means that more than one physician has primary responsibility for managing a portion of the patient’s care (concurrently) during the patient’s inpatient stay. For Medicare and other payers, this is considered appropriate when these “concurrent” services are “reasonable and necessary.”
- The condition(s) or diagnoses warrant the service and the specialty or expertise of the other physician(s) and at a reasonable frequency or duration.
- Duplicate services (i.e., services provided by two different providers of the same specialty for the same or similar conditions) will typically not be considered necessary unless a special circumstance is noted. For many payers, the internist and subspecialist who co-manage the same problem may have services performed on the same day denied, and documentation would need to show there were “special circumstances.” However, if the hospitalist is treating additional issues, then there should be no problem with separate payment. Medicare does recognize the endocrinology and internal medicine specialties separately and would probably pay both even if for the same condition. But if both are really “co-managing” the same problem without any additional issues daily, most payers are going to question this, either at the time of billing or retrospectively through audits.
Inpatient Concurrent care then is coded with subsequent hospital codes in the hospital setting (Codes 99231 through 99233).
Scenario # 3
A 73-year-old man with a past medical history notable for chronic renal insufficiency, hypertension, and Alzheimer’s type dementia undergoes a right open nephrectomy for renal cell carcinoma. His early postoperative course is marked by hypotension in the post-anesthesia care unit, and he is admitted to the SICU. His course there is significant for worsening of his baseline creatinine of 1.9 to 3.8, the development of delirium, and labile blood pressure. He is transferred from the SICU to a regular nursing floor on postoperative day 2, and the attending urologist requests that you assume management of the patient’s hypertension, delirium, and acute renal failure.
Question: Does this meet the definition of appropriate concurrent care or a consultation?
Answer: Although this constitutes something of a gray area, the request as worded indicates that the hospitalist will be providing concurrent care, and the initial visit should thus be billed as a Level 3 subsequent visit (99233). If the hospitalist’s role is, rather, to provide recommendations regarding management of these problems, the initial visit should be billed as an initial inpatient consult at the appropriate level.
Scenario # 4
A 66-year-old woman with a history of coronary artery disease 3 years after stenting of the left anterior descending coronary artery, moderate aortic stenosis, well-controlled diabetes mellitus, and hyperlipidemia undergoes a left modified radical mastectomy. On the morning of her first postoperative day, she experiences substernal chest pain, with T wave inversions in the inferior leads of her ECG. Her breast surgeon consults cardiology for her chest pain, endocrinology for “diabetic control,” and the hospitalist to “oversee the medical issues.”
Question: Can the hospitalist successfully bill in this setting? If so, what needs to be done to allow this?
Answer: Because of the various specialists who are treating this patient’s medical conditions, it will be difficult to demonstrate to a payer that an additional physician should be managing the patient’s care on a daily basis for the same medical problems. Such billing would probably be considered “duplicate care” and one of the physicians’ charges will be appropriately denied. However, if the specialists have been consulted only and have not assumed management for these medical conditions, then the hospitalist who has assumed management may bill for these services. As with scenario #3, the surgeon’s request as worded in this scenario indicates the hospitalist is providing concurrent care and a consultation is not being requested.
Scenario #5:
The hospital medicine consult team is asked to see a 31-year-old woman who is postoperative day 3 after a total proctocolectomy for refractory ulcerative colitis. Her past medical history is remarkable for iron-deficiency anemia, steroid-induced diabetes, and depression. You are asked to evaluate the patient for shortness of breath that began that day. The PGY-3 resident working with you evaluates the patient initially, reviews all available records from this admission as well as the past, performs an exhaustive history and physical, personally reviews the ECG and chest X-ray that have just been completed, and documents all of the above. You then discuss the case with the resident, and personally confirm critical portions of the history and examination. You agree with the resident’s assessment that the patient has most likely sustained a pulmonary embolism, as well as her recommendation for empiric anticoagulation and an urgent V/Q scan.
Question #1: What must be done documentation-wise by the attending physician to ensure that the optimum billing level is captured for this patient? What is not acceptable in this setting?
Answer: Redocumentation by the teaching physician is relatively minimal since CMS revised its guidelines [Transmittal 1780 dated 11/22/02], which allows substantial reference to the resident’s note in addition to a personal note, however, documentation must clearly demonstrate that the teaching physician was physically present during the key portions of the service billed. Examples of documentation provided by CMS are:
“I performed a history and examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
Or
“I saw and evaluated the patient. I agree with the findings and plan of care documented in the resident’s note.”
Or
“I saw and evaluated the patient. I agree w/ the resident’s note except…” while noting the difference in plan, etc.
Question #2: If the hospitalist/medical resident write the orders for the heparin and V/Q scan, does this constitute comanagement and prevent billing this as a consult?
Answer: A consultant may initiate treatment at the conclusion of his evaluation and still bill a consultation code as long as the other requirements have been met (i.e., a request for opinion regarding evaluation and treatment and no advance transfer of care). There are no specific rules related to medical residents in this scenario, so if the teaching physician is performing the consult in a timely manner with the resident, a consultation could still be coded appropriately.
Summary
Although efforts have been made by Medicare to clarify the vagaries of coding for consultative work, existing guidelines remain complex and not necessarily intuitive. This article has attempted to shed light on some of the more commonly encountered situations with which hospitalists grapple, but is unable to address all of the questions that may arise. Hospitalists and hospital medicine groups are encouraged to familiarize themselves with current coding guidelines and to establish and maintain strong relationships with local coding professionals. Future issues of The Hospitalist will tackle additional coding questions.
Dr. Pfeiffer can be contacted at [email protected].
Resource Utilization: How Hospitalists Add Value to the Bottom Line
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibilityfor the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term hospitalist in an article in the New England Journal of Medicine in 1996 (15). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8: 1 when a hospitalist program is utilized (See Table 1 for details) (14).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (11).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (12).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (7). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings. “Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (9).
In the role of inpatient leader, the hospitalist also facilitates emergency department (ED) throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes ,and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available and services more patients, eventually helping the hospital’s bottom line,” says Coppola (2).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (13).
A recently published study (6) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (17), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low-intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes, and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company, has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines (also) support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (5).
Stacy Goldsholl, Director of the Covenant Health-Care Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and nonhospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides the following benefits to each of the listed stakeholder (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective and prospective data analysis have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians, and hospital medicine. The following studies represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization (Table 3).
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent—if not superior—quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at [email protected].
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org
- Coppola P. Email interview, December 15, 2004.
- Everett GD, Anton MP, Jackson BK, Swigert C, Uddin N. “Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital.” Am J Manag Care. 2004;10:626-30.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3): 905-18; discussion 919-22.
- Greeno, Ron, MD, FCCP, chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview, December 16, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10: 561-8.
- Miller LC. Telephone interview, November 16, 2004.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111: 627-632.
- Rifkin WD. Telephone interview. December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichorn A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- Shallash A. Email interview, December 17, 2004.
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002.
- Wachter RM and Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM and Goldman L. “The hospitalist movement five years later.” J Am Med Assoc. 2002;287:0487-94.
- “Why less really can be more when it comes to teaching hospitals.” Today’s Hospitalist. 2004 December
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibilityfor the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term hospitalist in an article in the New England Journal of Medicine in 1996 (15). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8: 1 when a hospitalist program is utilized (See Table 1 for details) (14).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (11).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (12).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (7). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings. “Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (9).
In the role of inpatient leader, the hospitalist also facilitates emergency department (ED) throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes ,and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available and services more patients, eventually helping the hospital’s bottom line,” says Coppola (2).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (13).
A recently published study (6) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (17), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low-intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes, and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company, has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines (also) support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (5).
Stacy Goldsholl, Director of the Covenant Health-Care Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and nonhospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides the following benefits to each of the listed stakeholder (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective and prospective data analysis have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians, and hospital medicine. The following studies represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization (Table 3).
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent—if not superior—quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at [email protected].
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org
- Coppola P. Email interview, December 15, 2004.
- Everett GD, Anton MP, Jackson BK, Swigert C, Uddin N. “Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital.” Am J Manag Care. 2004;10:626-30.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3): 905-18; discussion 919-22.
- Greeno, Ron, MD, FCCP, chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview, December 16, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10: 561-8.
- Miller LC. Telephone interview, November 16, 2004.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111: 627-632.
- Rifkin WD. Telephone interview. December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichorn A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- Shallash A. Email interview, December 17, 2004.
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002.
- Wachter RM and Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM and Goldman L. “The hospitalist movement five years later.” J Am Med Assoc. 2002;287:0487-94.
- “Why less really can be more when it comes to teaching hospitals.” Today’s Hospitalist. 2004 December
Today’s hospitals must address a variety of challenges stemming from the expectation to provide more services and better quality with fewer financial, material, and human resources. According to the annual survey conducted by the American Hospital Association (AHA) in 2003, total expenses for all U.S. community hospitals were more than $450 billion. In managing these expenditures, hospitals face the following pressures:
- Cost increases in medical supplies and pharmaceuticals.
- Record shortages of nurses, pharmacists, and technicians.
- A growing uncompensated patient pool.
- Annual potential reductions in Medicare and Medicaid reimbursements.
- Rising bad debt resulting from greater patient responsibilityfor the cost of care.
- The diversion of more profitable cases to specialty and freestanding ambulatory care facilities and surgery centers.
- Soaring costs associated with adequately serving high-risk conditions, such as cancer, heart disease, and HIV/AIDS.
- Discounted reimbursement rates with insurers.
- Increasing pressure to commit financial resources to clinical information technology.
- The need to fund infrastructure improvements and physical plant renovations as well as expansions to address increasing demand (1).
To overcome these challenges, hospitals must find innovative ways to balance revenues and expenses, fund necessary capital investments, and satisfy the public’s demand for quality, safety, and accessibility.
Hospitalist Programs: A Good Investment
One solution to the above-mentioned situations is a hospitalist program, which, in its short history, has already had a profound impact on inpatient care. Robert M. Wachter, MD, associate chair in the department of medicine at the University of California, San Francisco (UCSF) and medical service chief at Moffitt-Long Hospitals, coined the term hospitalist in an article in the New England Journal of Medicine in 1996 (15). At the 2002 annual meeting of the Society of Hospital Medicine (SHM), Wachter presented findings from a study conducted at his institution. The results demonstrate a significant return on investment (ROI) of 5.8: 1 when a hospitalist program is utilized (See Table 1 for details) (14).
How do hospitalists reduce length of stay (LOS) and cost per stay? William David Rifkin, MD, associate director of the Yale Primary Care Residency Program, offers three basic reasons why hospitalist programs contribute to effective and efficient use of resources. Since hospitalists are physically onsite, they are better able to react to condition changes and requests for consultations in a timely manner, he asserts. Also, being familiar with the hospital’s systems of care, the hospitalist knows who to call and how to utilize the services of social workers and other contingency staff when arranging for post-discharge care. Third, Rifkin indicates that inpatients today are sicker than they were in past years, a fact well known and understood by hospitalists. “There is an increased level of acuity,” he says. “Hospitalists are used to seeing these kinds of patients. They are more comfortable taking care of these patients and will see more of them with any given diagnosis” (11).
In one of his studies, Rifkin noted a reduction in LOS for inpatients with a pneumonia diagnosis. “The hospitalist had switched the patient from IV (intravenous) to oral antibiotics,” he says. Reacting quickly to indications that the patient was ready for a change in treatment modality facilitated an earlier discharge (12).
L. Craig Miller, MD, senior vice president of medical affairs at Baptist Health Care, reports that his hospital saved $2.56 million in 2 years as a direct result of its inpatient management program (7). Although attention to technical and clinical details is important, Miller emphasizes the critical role the human factor plays, specifically the impact of teamwork, on achieving resource utilization savings. “Hospitalists work as a team, collaborating with physicians and ED doctors,” he says. This cooperative spirit enables the efficient use of manpower in patient care. Miller adds that at Baptist, as is the case at most hospitals, the medical complexity of patients dictates a need for cooperation in order to successfully treat illness. The presence of hospitalists facilitates the team effort, causing a positive trickle down effect regarding LOS, readmission and mortality rates, he affirms. “The hospitalist provides focused leadership to utilization resource management,” says Miller (9).
In the role of inpatient leader, the hospitalist also facilitates emergency department (ED) throughput, which results in another area of cost savings for the hospital. Paola Coppola, MD, ED director at Brookhaven Memorial Hospital Medical Center, says, “From an ER perspective, a call to the hospitalist replaces multiple calls to specialists. In general, hospitalists feel much more comfortable treating a wide array of conditions including infectious disease, pneumonias, strokes ,and chest pain without the intervention of specialists in that field. Hence, hospital consumption of resources decreases, which in turn lowers length of stay.” He echoes Rifkin’s thoughts on quick response time. “Hospitalists provide an immediately available service, thus saving ER physicians valuable time. This ensures faster turnover, better throughput, makes more ER beds available and services more patients, eventually helping the hospital’s bottom line,” says Coppola (2).
In addition to teamwork, 24/7 availability is vital to the wise utilization of resources, according to Anthony Shallash, MD, vice president of medical affairs at Brookhaven. “The fact of 24/7 presence allows rapid responses to patient condition and problems. Continuous and close monitoring of patients allows them to be upgraded or downgraded as needed,” he says. “As such, LOS is decreased and quite favorable as compared to peer practitioners for similar disease severity. Resources consumed and tests ordered also show a favorable trend” (13).
A recently published study (6) by researchers at Dartmouth Medical School documents the variation in the volume and cost of services that academic medical centers use in treating patients. Hospitals were categorized as low- and high-intensity, with significant differences in cost per case. For example, the high-intensity hospitals spent up to 47% more on care for acute myocardial infarction. In an interview in Today’s Hospitalist (17), the lead author, Elliott S. Fisher, MD, professor of medicine and community and family medicine at Dartmouth Medical School, described the importance of coordination in achieving efficient care. Fisher says, “I think there’s a real opportunity for hospitalists to improve the care of patients in both high- and low-intensity hospitals. Having ten doctors involved in a given patient’s care may not be a good thing, unless someone [i.e., the hospitalist] is doing a really good job of coordinating that care.”
Hospitalists focus only on inpatient medicine. They are familiar with managing the most common medical diagnoses, such as community acquired pneumonia, diabetes, and congestive heart failure. Hospitalist programs often develop uniform and consistent ways of treating these patients. Cogent Healthcare, a national hospitalist management company, has implemented the “Cogent Care Guides,” best practice guidelines for high-volume hospital diagnoses. Ron Greeno, MD, FCCP and Cogent’s chief medical officer, says “The Cogent Care Guides ensure best practices are implemented at critical points in the patient’s care… decreasing the variability of care that results in inefficiencies.” Greeno added, “The care guidelines (also) support the timely notification of the primary care physician of nine critical landmark events related to patient status that can affect outcomes” (5).
Stacy Goldsholl, Director of the Covenant Health-Care Hospital Medicine Program in Saginaw, MI, suggests other ways that hospitalists can generate utilization savings for their hospitals. “Hospitalists often eliminate unnecessary admissions and shift work-ups to the ambulatory setting. For example, I recently arranged an outpatient colonoscopy for a pneumonia patient with a stable hemoglobin and heme positive stool. Because of my experience treating patients with pneumonia, I was able to determine that the circumstances did not require an inpatient stay.” In addition, Dr. Goldsholl has found that the hospitalists in her program are quite effective in classifying “observation” patients, eliminating reimbursement conflicts with Medicare, Medicaid, and other insurers.
Finally, because they are always in the hospital rather than sharing time between the office and hospital, hospitalists can improve inpatient continuity of care, resulting in lower costs and better outcomes. Adrienne Bennett, MD, chief of the hospital medicine service at Newton-Wellesley Hospital near Boston, examined cases managed by hospitalists and nonhospitalist community physicians, comparing the number of “handoffs” of responsibility that occur among attending physicians. Community physicians share inpatient responsibility in their practices and sometimes their partners round on their patients. Every time another physician assumes responsibility for a patient, there is the potential for a loss of information and a discontinuity of care. At Newton-Wellesley Hospital, the hospitalists work a schedule of 14 days on, followed by 7 days off. “We found that hospitalists averaged less than half the number of handoffs as the community physicians,” says Bennett. “This may be one of the reasons that hospitalists have better case mix adjusted utilization performance.”
Stakeholder Analysis
Anecdotal evidence, as well as documented studies, has demonstrated that hospitalists provide value to a wide range of stakeholders involved in the inpatient care process. With regard to resource utilization savings, the hospitalist provides the following benefits to each of the listed stakeholder (Table 2).
Published Research Results
Dozens of studies demonstrate the positive effects hospitalist programs have on resource utilization. Observational, retrospective and prospective data analysis have been conducted at community-based hospitals as well as at academic medical institutions. Findings consistently indicate that hospitalist programs result in resource savings for patients, physicians, and hospital medicine. The following studies represent the most recent efforts at tracking hospitalist programs and their effects on resource utilization (Table 3).
Conclusion
According to the AHA’s 2003 survey of healthcare trends, the fiscal health of the nation’s hospitals will most likely remain fragile and variable in the coming years. The survey cites declining operating margins, a continued decrease in reimbursement, labor shortages, and rising insurance and pharmaceutical costs, as well as the need to invest in technology and facility maintenance and upkeep as key factors. However, hospitalists have proven time and again in clinical studies that they can bring value to the operation of a healthcare facility. With reduced lengths of stay, decreased overall hospital costs, and equivalent—if not superior—quality, hospitalists can contribute significantly to a hospital’s healthy bottom line.
Dr. Syed can be contacted at [email protected].
References
- ACP Research Center, Environmental Assessment: Trends in hospital financing. 2003. www.aha.org
- Coppola P. Email interview, December 15, 2004.
- Everett GD, Anton MP, Jackson BK, Swigert C, Uddin N. “Comparison of hospital costs and length of stay associated with general internists and hospitalist physicians at a community hospital.” Am J Manag Care. 2004;10:626-30.
- Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Services Research. 2003:38(3): 905-18; discussion 919-22.
- Greeno, Ron, MD, FCCP, chief medical officer, Cogent Healthcare, Irvine, California. Telephone interview, December 16, 2004.
- Healthaffairs.org, “Use of Medicare claims data to monitor provider-specific performance among patients with severe chronic illness.” 10.1377/hlthaff.var.5. Posting date: October 7, 2004.
- “Hospitalists save $2.5 million and decrease LOS.” Healthcare Benchmarks and Quality Improvement, May 2004.
- Kaboli PJ, Barnett MJ, Rosenthal GE. Associations with reduced length of stay and costs on an academic hospitalist service. Am J Manag Care. 2004;10: 561-8.
- Miller LC. Telephone interview, November 16, 2004.
- Palmer HC, Armistead NS, Elnicki DM, et al. The effect of a hospitalist service with nurse discharge planner on patient care in an academic teaching hospital. Am J Med. 2001;111: 627-632.
- Rifkin WD. Telephone interview. December 15, 2004.
- Rifkin WD, Conner D, Silver A, Eichorn A. Comparison of processes and outcomes of pneumonia care between hospitalists and community-based primary care physicians. Mayo Clin Proc. 2002;77:1053-8.
- Shallash A. Email interview, December 17, 2004.
- Wachter RM. Presentation, Society of Hospital Medicine (SHM) annual meeting 2002.
- Wachter RM and Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335:514-7
- Wachter RM and Goldman L. “The hospitalist movement five years later.” J Am Med Assoc. 2002;287:0487-94.
- “Why less really can be more when it comes to teaching hospitals.” Today’s Hospitalist. 2004 December