User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
COVID-19 mortality in hospitalized HF patients: Nearly 1 in 4
Patients with heart failure who are infected with SARS-CoV-2 are at high risk for complications, with nearly 1 in 4 dying during hospitalization, according to a large database analysis that included more than 8,000 patients who had heart failure and COVID-19.
In-hospital mortality was 24.2% for patients who had a history of heart failure and were hospitalized with COVID-19, as compared with 14.2% for individuals without heart failure who were hospitalized with COVID-19.
For perspective, the researchers compared the patients with heart failure and COVID-19 with patients who had a history of heart failure and were hospitalized for an acute worsening episode: the risk for death was about 10-fold higher with COVID-19.
“These patients really face remarkably high risk, and when we compare that to the risk of in-hospital death with something we are a lot more familiar with – acute heart failure – we see that the risk was about 10-fold greater,” said first author Ankeet S. Bhatt, MD, MBA, from Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
In an article published online in JACC Heart Failure on Dec. 28, a group led by Dr. Bhatt and senior author Scott D. Solomon, MD, reported an analysis of administrative data on a total of 2,041,855 incident hospitalizations logged in the Premier Healthcare Database between April 1, 2020, and Sept. 30, 2020.
The Premier Healthcare Database comprises data from more than 1 billion patient encounters, which equates to approximately 1 in every 5 of all inpatient discharges in the United States.
Of 132,312 hospitalizations of patients with a history of heart failure, 23,843 (18.0%) were hospitalized with acute heart failure, 8,383 patients (6.4%) were hospitalized with COVID-19, and 100,068 (75.6%) were hospitalized for other reasons.
Outcomes and resource utilization were compared with 141,895 COVID-19 hospitalizations of patients who did not have heart failure.
Patients were deemed to have a history of heart failure if they were hospitalized at least once for heart failure from Jan. 1, 2019, to March 21, 2020, or had at least two heart failure outpatient visits during that period.
In a comment, Dr. Solomon noted some of the pros and cons of the data used in this study.
“Premier is a huge database, encompassing about one-quarter of all the health care facilities in the United States and one-fifth of all inpatient visits, so for that reason we’re able to look at things that are very difficult to look at in smaller hospital systems, but the data are also limited in that you don’t have as much granular detail as you might in smaller datasets,” said Dr. Solomon.
“One thing to recognize is that our data start at the point of hospital admission, so were looking only at individuals who have crossed the threshold in terms of their illness and been admitted,” he added.
Use of in-hospital resources was significantly greater for patients with heart failure hospitalized for COVID-19, compared with patients hospitalized for acute heart failure or for other reasons. This included “multifold” higher rates of ICU care (29% vs. 15%), mechanical ventilation (17% vs. 6%), and central venous catheter insertion (19% vs. 7%; P < .001 for all).
The proportion of patients who required mechanical ventilation and care in the ICU in the group with COVID-19 but who did not have no heart failure was similar to those who had both conditions.
The greater odds of in-hospital mortality among patients with both heart failure and COVID-19, compared with individuals with heart failure hospitalized for other reasons, was strongest in April, with an adjusted odds ratio of 14.48, compared with subsequent months (adjusted OR for May-September, 10.11; P for interaction < .001).
“We’re obviously not able to say with certainty what was happening in April, but I think that maybe the patients who were most vulnerable to COVID-19 may be more represented in that population, so the patients with comorbidities or who are immunosuppressed or otherwise,” said Dr. Bhatt in an interview.
“The other thing we think is that there may be a learning curve in terms of how to care for patients with acute severe respiratory illness. That includes increased institutional knowledge – like the use of prone ventilation – but also therapies that were subsequently shown to have benefit in randomized clinical trials, such as dexamethasone,” he added.
“These results should remind us to be innovative and thoughtful in our management of patients with heart failure while trying to maintain equity and good health for all,” wrote Nasrien E. Ibrahim, MD, from Massachusetts General Hospital, Boston; Ersilia DeFillipis, MD, Columbia University, New York; and Mitchel Psotka, MD, PhD, Innova Heart and Vascular Institute, Falls Church, Va., in an editorial accompanying the study.
The data emphasize the importance of ensuring equal access to services such as telemedicine, virtual visits, home nursing visits, and remote monitoring, they noted.
“As the COVID-19 pandemic rages on and disproportionately ravages socioeconomically disadvantaged communities, we should focus our efforts on strategies that minimize these inequities,” the editorialists wrote.
Dr. Solomon noted that, although Black and Hispanic patients were overrepresented in the population of heart failure patients hospitalized with COVID-19, once in the hospital, race was not a predictor of in-hospital mortality or the need for mechanical ventilation.
Dr. Bhatt has received speaker fees from Sanofi Pasteur and is supported by a National Institutes of Health/National Heart, Lung, and Blood Institute postdoctoral training grant. Dr. Solomon has received grant support and/or speaking fees from a number of companies and from the NIH/NHLBI. The editorialists disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with heart failure who are infected with SARS-CoV-2 are at high risk for complications, with nearly 1 in 4 dying during hospitalization, according to a large database analysis that included more than 8,000 patients who had heart failure and COVID-19.
In-hospital mortality was 24.2% for patients who had a history of heart failure and were hospitalized with COVID-19, as compared with 14.2% for individuals without heart failure who were hospitalized with COVID-19.
For perspective, the researchers compared the patients with heart failure and COVID-19 with patients who had a history of heart failure and were hospitalized for an acute worsening episode: the risk for death was about 10-fold higher with COVID-19.
“These patients really face remarkably high risk, and when we compare that to the risk of in-hospital death with something we are a lot more familiar with – acute heart failure – we see that the risk was about 10-fold greater,” said first author Ankeet S. Bhatt, MD, MBA, from Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
In an article published online in JACC Heart Failure on Dec. 28, a group led by Dr. Bhatt and senior author Scott D. Solomon, MD, reported an analysis of administrative data on a total of 2,041,855 incident hospitalizations logged in the Premier Healthcare Database between April 1, 2020, and Sept. 30, 2020.
The Premier Healthcare Database comprises data from more than 1 billion patient encounters, which equates to approximately 1 in every 5 of all inpatient discharges in the United States.
Of 132,312 hospitalizations of patients with a history of heart failure, 23,843 (18.0%) were hospitalized with acute heart failure, 8,383 patients (6.4%) were hospitalized with COVID-19, and 100,068 (75.6%) were hospitalized for other reasons.
Outcomes and resource utilization were compared with 141,895 COVID-19 hospitalizations of patients who did not have heart failure.
Patients were deemed to have a history of heart failure if they were hospitalized at least once for heart failure from Jan. 1, 2019, to March 21, 2020, or had at least two heart failure outpatient visits during that period.
In a comment, Dr. Solomon noted some of the pros and cons of the data used in this study.
“Premier is a huge database, encompassing about one-quarter of all the health care facilities in the United States and one-fifth of all inpatient visits, so for that reason we’re able to look at things that are very difficult to look at in smaller hospital systems, but the data are also limited in that you don’t have as much granular detail as you might in smaller datasets,” said Dr. Solomon.
“One thing to recognize is that our data start at the point of hospital admission, so were looking only at individuals who have crossed the threshold in terms of their illness and been admitted,” he added.
Use of in-hospital resources was significantly greater for patients with heart failure hospitalized for COVID-19, compared with patients hospitalized for acute heart failure or for other reasons. This included “multifold” higher rates of ICU care (29% vs. 15%), mechanical ventilation (17% vs. 6%), and central venous catheter insertion (19% vs. 7%; P < .001 for all).
The proportion of patients who required mechanical ventilation and care in the ICU in the group with COVID-19 but who did not have no heart failure was similar to those who had both conditions.
The greater odds of in-hospital mortality among patients with both heart failure and COVID-19, compared with individuals with heart failure hospitalized for other reasons, was strongest in April, with an adjusted odds ratio of 14.48, compared with subsequent months (adjusted OR for May-September, 10.11; P for interaction < .001).
“We’re obviously not able to say with certainty what was happening in April, but I think that maybe the patients who were most vulnerable to COVID-19 may be more represented in that population, so the patients with comorbidities or who are immunosuppressed or otherwise,” said Dr. Bhatt in an interview.
“The other thing we think is that there may be a learning curve in terms of how to care for patients with acute severe respiratory illness. That includes increased institutional knowledge – like the use of prone ventilation – but also therapies that were subsequently shown to have benefit in randomized clinical trials, such as dexamethasone,” he added.
“These results should remind us to be innovative and thoughtful in our management of patients with heart failure while trying to maintain equity and good health for all,” wrote Nasrien E. Ibrahim, MD, from Massachusetts General Hospital, Boston; Ersilia DeFillipis, MD, Columbia University, New York; and Mitchel Psotka, MD, PhD, Innova Heart and Vascular Institute, Falls Church, Va., in an editorial accompanying the study.
The data emphasize the importance of ensuring equal access to services such as telemedicine, virtual visits, home nursing visits, and remote monitoring, they noted.
“As the COVID-19 pandemic rages on and disproportionately ravages socioeconomically disadvantaged communities, we should focus our efforts on strategies that minimize these inequities,” the editorialists wrote.
Dr. Solomon noted that, although Black and Hispanic patients were overrepresented in the population of heart failure patients hospitalized with COVID-19, once in the hospital, race was not a predictor of in-hospital mortality or the need for mechanical ventilation.
Dr. Bhatt has received speaker fees from Sanofi Pasteur and is supported by a National Institutes of Health/National Heart, Lung, and Blood Institute postdoctoral training grant. Dr. Solomon has received grant support and/or speaking fees from a number of companies and from the NIH/NHLBI. The editorialists disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Patients with heart failure who are infected with SARS-CoV-2 are at high risk for complications, with nearly 1 in 4 dying during hospitalization, according to a large database analysis that included more than 8,000 patients who had heart failure and COVID-19.
In-hospital mortality was 24.2% for patients who had a history of heart failure and were hospitalized with COVID-19, as compared with 14.2% for individuals without heart failure who were hospitalized with COVID-19.
For perspective, the researchers compared the patients with heart failure and COVID-19 with patients who had a history of heart failure and were hospitalized for an acute worsening episode: the risk for death was about 10-fold higher with COVID-19.
“These patients really face remarkably high risk, and when we compare that to the risk of in-hospital death with something we are a lot more familiar with – acute heart failure – we see that the risk was about 10-fold greater,” said first author Ankeet S. Bhatt, MD, MBA, from Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
In an article published online in JACC Heart Failure on Dec. 28, a group led by Dr. Bhatt and senior author Scott D. Solomon, MD, reported an analysis of administrative data on a total of 2,041,855 incident hospitalizations logged in the Premier Healthcare Database between April 1, 2020, and Sept. 30, 2020.
The Premier Healthcare Database comprises data from more than 1 billion patient encounters, which equates to approximately 1 in every 5 of all inpatient discharges in the United States.
Of 132,312 hospitalizations of patients with a history of heart failure, 23,843 (18.0%) were hospitalized with acute heart failure, 8,383 patients (6.4%) were hospitalized with COVID-19, and 100,068 (75.6%) were hospitalized for other reasons.
Outcomes and resource utilization were compared with 141,895 COVID-19 hospitalizations of patients who did not have heart failure.
Patients were deemed to have a history of heart failure if they were hospitalized at least once for heart failure from Jan. 1, 2019, to March 21, 2020, or had at least two heart failure outpatient visits during that period.
In a comment, Dr. Solomon noted some of the pros and cons of the data used in this study.
“Premier is a huge database, encompassing about one-quarter of all the health care facilities in the United States and one-fifth of all inpatient visits, so for that reason we’re able to look at things that are very difficult to look at in smaller hospital systems, but the data are also limited in that you don’t have as much granular detail as you might in smaller datasets,” said Dr. Solomon.
“One thing to recognize is that our data start at the point of hospital admission, so were looking only at individuals who have crossed the threshold in terms of their illness and been admitted,” he added.
Use of in-hospital resources was significantly greater for patients with heart failure hospitalized for COVID-19, compared with patients hospitalized for acute heart failure or for other reasons. This included “multifold” higher rates of ICU care (29% vs. 15%), mechanical ventilation (17% vs. 6%), and central venous catheter insertion (19% vs. 7%; P < .001 for all).
The proportion of patients who required mechanical ventilation and care in the ICU in the group with COVID-19 but who did not have no heart failure was similar to those who had both conditions.
The greater odds of in-hospital mortality among patients with both heart failure and COVID-19, compared with individuals with heart failure hospitalized for other reasons, was strongest in April, with an adjusted odds ratio of 14.48, compared with subsequent months (adjusted OR for May-September, 10.11; P for interaction < .001).
“We’re obviously not able to say with certainty what was happening in April, but I think that maybe the patients who were most vulnerable to COVID-19 may be more represented in that population, so the patients with comorbidities or who are immunosuppressed or otherwise,” said Dr. Bhatt in an interview.
“The other thing we think is that there may be a learning curve in terms of how to care for patients with acute severe respiratory illness. That includes increased institutional knowledge – like the use of prone ventilation – but also therapies that were subsequently shown to have benefit in randomized clinical trials, such as dexamethasone,” he added.
“These results should remind us to be innovative and thoughtful in our management of patients with heart failure while trying to maintain equity and good health for all,” wrote Nasrien E. Ibrahim, MD, from Massachusetts General Hospital, Boston; Ersilia DeFillipis, MD, Columbia University, New York; and Mitchel Psotka, MD, PhD, Innova Heart and Vascular Institute, Falls Church, Va., in an editorial accompanying the study.
The data emphasize the importance of ensuring equal access to services such as telemedicine, virtual visits, home nursing visits, and remote monitoring, they noted.
“As the COVID-19 pandemic rages on and disproportionately ravages socioeconomically disadvantaged communities, we should focus our efforts on strategies that minimize these inequities,” the editorialists wrote.
Dr. Solomon noted that, although Black and Hispanic patients were overrepresented in the population of heart failure patients hospitalized with COVID-19, once in the hospital, race was not a predictor of in-hospital mortality or the need for mechanical ventilation.
Dr. Bhatt has received speaker fees from Sanofi Pasteur and is supported by a National Institutes of Health/National Heart, Lung, and Blood Institute postdoctoral training grant. Dr. Solomon has received grant support and/or speaking fees from a number of companies and from the NIH/NHLBI. The editorialists disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NETs a possible therapeutic target for COVID-19 thrombosis?
Researchers in Madrid may have found a clue to the pathogenesis of ST-segment elevation myocardial infarction (STEMI) in patients with COVID-19; it might also offer a therapeutic target to counter the hypercoagulability seen with COVID-19.
In a case series of five patients with COVID-19 who had an STEMI, neutrophil extracellular traps (NETs) were detected in coronary thrombi of all five patients. The median density was 66%, which is significantly higher than that seen in a historical series of patients with STEMI. In that series, NETs were found in only two-thirds of patients; in that series, the median density was 19%.
In the patients with COVID-19 and STEMI and in the patients reported in the prepandemic historical series from 2015, intracoronary aspirates were obtained during percutaneous coronary intervention using a thrombus aspiration device.
Histologically, findings in the patients from 2015 differed from those of patients with COVID-19. In the patients with COVID, thrombi were composed mostly of fibrin and polymorphonuclear cells. None showed fragments of atherosclerotic plaque or iron deposits indicative of previous episodes of plaque rupture. In contrast, 65% of thrombi from the 2015 series contained plaque fragments.
Ana Blasco, MD, PhD, Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, and colleagues report their findings in an article published online Dec. 29 in JAMA Cardiology.
Commenting on the findings in an interview, Irene Lang, MD, from the Medical University of Vienna said, “This is really a very small series, purely observational, and suffering from the problem that acute STEMI is uncommon in COVID-19, but it does serve to demonstrate once more the abundance of NETs in acute myocardial infarction.”
“NETs are very much at the cutting edge of thrombosis research, and NET formation provides yet another link between inflammation and clot formation,” added Peter Libby, MD, from Harvard Medical School and Brigham and Women’s Hospital, Boston.
“Multiple observations have shown thrombosis of arteries large and small, microvessels, and veins in COVID-19. The observations of Blasco et al. add to the growing literature about NETs as contributors to the havoc wrought in multiple organs in advanced COVID-19,” he added in an email exchange with this news organization.
Neither Dr. Lang nor Dr. Libby were involved in this research; both have been actively studying NETs and their contribution to cardiothrombotic disease in recent years.
NETs are newly recognized contributors to venous and arterial thrombosis. These weblike DNA strands are extruded by activated or dying neutrophils and have protein mediators that ensnare pathogens while minimizing damage to the host cell.
First described in 2004, exaggerated NET formation has also been linked to the initiation and accretion of inflammation and thrombosis.
“NETs thus furnish a previously unsuspected link between inflammation, innate immunity, thrombosis, oxidative stress, and cardiovascular diseases,” Dr. Libby and his coauthors wrote in an article on the topic published in Circulation Research earlier this year.
Limiting NET formation or “dissolving” existing NETs could provide a therapeutic avenue not just for patients with COVID-19 but for all patients with thrombotic disease.
“The concept of NETs as a therapeutic target is appealing, in and out of COVID times,” said Dr. Lang.
“I personally believe that the work helps to raise awareness for the potential use of deoxyribonuclease (DNase), an enzyme that acts to clear NETs by dissolving the DNA strands, in the acute treatment of STEMI. Rapid injection of engineered recombinant DNases could potentially wipe away coronary obstructions, ideally before they may cause damage to the myocardium,” she added.
Dr. Blasco and colleagues and Dr. Lang have disclosed no relevant financial relationships. Dr. Libby is an unpaid consultant or member of the advisory board for a number of companies.
A version of this article first appeared on Medscape.com.
Researchers in Madrid may have found a clue to the pathogenesis of ST-segment elevation myocardial infarction (STEMI) in patients with COVID-19; it might also offer a therapeutic target to counter the hypercoagulability seen with COVID-19.
In a case series of five patients with COVID-19 who had an STEMI, neutrophil extracellular traps (NETs) were detected in coronary thrombi of all five patients. The median density was 66%, which is significantly higher than that seen in a historical series of patients with STEMI. In that series, NETs were found in only two-thirds of patients; in that series, the median density was 19%.
In the patients with COVID-19 and STEMI and in the patients reported in the prepandemic historical series from 2015, intracoronary aspirates were obtained during percutaneous coronary intervention using a thrombus aspiration device.
Histologically, findings in the patients from 2015 differed from those of patients with COVID-19. In the patients with COVID, thrombi were composed mostly of fibrin and polymorphonuclear cells. None showed fragments of atherosclerotic plaque or iron deposits indicative of previous episodes of plaque rupture. In contrast, 65% of thrombi from the 2015 series contained plaque fragments.
Ana Blasco, MD, PhD, Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, and colleagues report their findings in an article published online Dec. 29 in JAMA Cardiology.
Commenting on the findings in an interview, Irene Lang, MD, from the Medical University of Vienna said, “This is really a very small series, purely observational, and suffering from the problem that acute STEMI is uncommon in COVID-19, but it does serve to demonstrate once more the abundance of NETs in acute myocardial infarction.”
“NETs are very much at the cutting edge of thrombosis research, and NET formation provides yet another link between inflammation and clot formation,” added Peter Libby, MD, from Harvard Medical School and Brigham and Women’s Hospital, Boston.
“Multiple observations have shown thrombosis of arteries large and small, microvessels, and veins in COVID-19. The observations of Blasco et al. add to the growing literature about NETs as contributors to the havoc wrought in multiple organs in advanced COVID-19,” he added in an email exchange with this news organization.
Neither Dr. Lang nor Dr. Libby were involved in this research; both have been actively studying NETs and their contribution to cardiothrombotic disease in recent years.
NETs are newly recognized contributors to venous and arterial thrombosis. These weblike DNA strands are extruded by activated or dying neutrophils and have protein mediators that ensnare pathogens while minimizing damage to the host cell.
First described in 2004, exaggerated NET formation has also been linked to the initiation and accretion of inflammation and thrombosis.
“NETs thus furnish a previously unsuspected link between inflammation, innate immunity, thrombosis, oxidative stress, and cardiovascular diseases,” Dr. Libby and his coauthors wrote in an article on the topic published in Circulation Research earlier this year.
Limiting NET formation or “dissolving” existing NETs could provide a therapeutic avenue not just for patients with COVID-19 but for all patients with thrombotic disease.
“The concept of NETs as a therapeutic target is appealing, in and out of COVID times,” said Dr. Lang.
“I personally believe that the work helps to raise awareness for the potential use of deoxyribonuclease (DNase), an enzyme that acts to clear NETs by dissolving the DNA strands, in the acute treatment of STEMI. Rapid injection of engineered recombinant DNases could potentially wipe away coronary obstructions, ideally before they may cause damage to the myocardium,” she added.
Dr. Blasco and colleagues and Dr. Lang have disclosed no relevant financial relationships. Dr. Libby is an unpaid consultant or member of the advisory board for a number of companies.
A version of this article first appeared on Medscape.com.
Researchers in Madrid may have found a clue to the pathogenesis of ST-segment elevation myocardial infarction (STEMI) in patients with COVID-19; it might also offer a therapeutic target to counter the hypercoagulability seen with COVID-19.
In a case series of five patients with COVID-19 who had an STEMI, neutrophil extracellular traps (NETs) were detected in coronary thrombi of all five patients. The median density was 66%, which is significantly higher than that seen in a historical series of patients with STEMI. In that series, NETs were found in only two-thirds of patients; in that series, the median density was 19%.
In the patients with COVID-19 and STEMI and in the patients reported in the prepandemic historical series from 2015, intracoronary aspirates were obtained during percutaneous coronary intervention using a thrombus aspiration device.
Histologically, findings in the patients from 2015 differed from those of patients with COVID-19. In the patients with COVID, thrombi were composed mostly of fibrin and polymorphonuclear cells. None showed fragments of atherosclerotic plaque or iron deposits indicative of previous episodes of plaque rupture. In contrast, 65% of thrombi from the 2015 series contained plaque fragments.
Ana Blasco, MD, PhD, Hospital Universitario Puerta de Hierro-Majadahonda, Madrid, and colleagues report their findings in an article published online Dec. 29 in JAMA Cardiology.
Commenting on the findings in an interview, Irene Lang, MD, from the Medical University of Vienna said, “This is really a very small series, purely observational, and suffering from the problem that acute STEMI is uncommon in COVID-19, but it does serve to demonstrate once more the abundance of NETs in acute myocardial infarction.”
“NETs are very much at the cutting edge of thrombosis research, and NET formation provides yet another link between inflammation and clot formation,” added Peter Libby, MD, from Harvard Medical School and Brigham and Women’s Hospital, Boston.
“Multiple observations have shown thrombosis of arteries large and small, microvessels, and veins in COVID-19. The observations of Blasco et al. add to the growing literature about NETs as contributors to the havoc wrought in multiple organs in advanced COVID-19,” he added in an email exchange with this news organization.
Neither Dr. Lang nor Dr. Libby were involved in this research; both have been actively studying NETs and their contribution to cardiothrombotic disease in recent years.
NETs are newly recognized contributors to venous and arterial thrombosis. These weblike DNA strands are extruded by activated or dying neutrophils and have protein mediators that ensnare pathogens while minimizing damage to the host cell.
First described in 2004, exaggerated NET formation has also been linked to the initiation and accretion of inflammation and thrombosis.
“NETs thus furnish a previously unsuspected link between inflammation, innate immunity, thrombosis, oxidative stress, and cardiovascular diseases,” Dr. Libby and his coauthors wrote in an article on the topic published in Circulation Research earlier this year.
Limiting NET formation or “dissolving” existing NETs could provide a therapeutic avenue not just for patients with COVID-19 but for all patients with thrombotic disease.
“The concept of NETs as a therapeutic target is appealing, in and out of COVID times,” said Dr. Lang.
“I personally believe that the work helps to raise awareness for the potential use of deoxyribonuclease (DNase), an enzyme that acts to clear NETs by dissolving the DNA strands, in the acute treatment of STEMI. Rapid injection of engineered recombinant DNases could potentially wipe away coronary obstructions, ideally before they may cause damage to the myocardium,” she added.
Dr. Blasco and colleagues and Dr. Lang have disclosed no relevant financial relationships. Dr. Libby is an unpaid consultant or member of the advisory board for a number of companies.
A version of this article first appeared on Medscape.com.
COVID-19 vaccine rollout faces delays
If the current pace of vaccination continues, “it’s going to take years, not months, to vaccinate the American people,” President-elect Joe Biden said during a briefing Dec. 29.
In fact, at the current rate, it would take nearly 10 years to vaccinate enough Americans to bring the pandemic under control, according to NBC News. To reach 80% of the country by late June, 3 million people would need to receive a COVID-19 vaccine each day.
“As I long feared and warned, the effort to distribute and administer the vaccine is not progressing as it should,” Mr. Biden said, reemphasizing his pledge to get 100 million doses to Americans during his first 100 days as president.
So far, 11.4 million doses have been distributed and 2.1 million people have received a vaccine, according to the Centers for Disease Control and Prevention. Most states have administered a fraction of the doses they’ve received, according to data compiled by The New York Times.
Federal officials have said there’s an “expected lag” between delivery of doses, shots going into arms, and the data being reported to the CDC, according to CNN. The Food and Drug Administration must assess each shipment for quality control, which has slowed down distribution, and the CDC data are just now beginning to include the Moderna vaccine, which the FDA authorized for emergency use on Dec. 18.
The 2.1 million number is “an underestimate,” Brett Giroir, MD, the assistant secretary of the U.S. Department of Health & Human Services, told NBC News Dec. 29. At the same time, the U.S. won’t meet the goal of vaccinating 20 million people in the next few days, he said.
Another 30 million doses will go out in January, Dr. Giroir said, followed by 50 million in February.
Some vaccine experts have said they’re not surprised by the speed of vaccine distribution.
“It had to go this way,” Paul Offit, MD, a professor of pediatrics at Children’s Hospital of Philadelphia, told STAT. “We had to trip and fall and stumble and figure this out.”
To speed up distribution in 2021, the federal government will need to help states, Mr. Biden said Dec. 29. He plans to use the Defense Authorization Act to ramp up production of vaccine supplies. Even still, the process will take months, he said.
A version of this article first appeared on WebMD.com .
If the current pace of vaccination continues, “it’s going to take years, not months, to vaccinate the American people,” President-elect Joe Biden said during a briefing Dec. 29.
In fact, at the current rate, it would take nearly 10 years to vaccinate enough Americans to bring the pandemic under control, according to NBC News. To reach 80% of the country by late June, 3 million people would need to receive a COVID-19 vaccine each day.
“As I long feared and warned, the effort to distribute and administer the vaccine is not progressing as it should,” Mr. Biden said, reemphasizing his pledge to get 100 million doses to Americans during his first 100 days as president.
So far, 11.4 million doses have been distributed and 2.1 million people have received a vaccine, according to the Centers for Disease Control and Prevention. Most states have administered a fraction of the doses they’ve received, according to data compiled by The New York Times.
Federal officials have said there’s an “expected lag” between delivery of doses, shots going into arms, and the data being reported to the CDC, according to CNN. The Food and Drug Administration must assess each shipment for quality control, which has slowed down distribution, and the CDC data are just now beginning to include the Moderna vaccine, which the FDA authorized for emergency use on Dec. 18.
The 2.1 million number is “an underestimate,” Brett Giroir, MD, the assistant secretary of the U.S. Department of Health & Human Services, told NBC News Dec. 29. At the same time, the U.S. won’t meet the goal of vaccinating 20 million people in the next few days, he said.
Another 30 million doses will go out in January, Dr. Giroir said, followed by 50 million in February.
Some vaccine experts have said they’re not surprised by the speed of vaccine distribution.
“It had to go this way,” Paul Offit, MD, a professor of pediatrics at Children’s Hospital of Philadelphia, told STAT. “We had to trip and fall and stumble and figure this out.”
To speed up distribution in 2021, the federal government will need to help states, Mr. Biden said Dec. 29. He plans to use the Defense Authorization Act to ramp up production of vaccine supplies. Even still, the process will take months, he said.
A version of this article first appeared on WebMD.com .
If the current pace of vaccination continues, “it’s going to take years, not months, to vaccinate the American people,” President-elect Joe Biden said during a briefing Dec. 29.
In fact, at the current rate, it would take nearly 10 years to vaccinate enough Americans to bring the pandemic under control, according to NBC News. To reach 80% of the country by late June, 3 million people would need to receive a COVID-19 vaccine each day.
“As I long feared and warned, the effort to distribute and administer the vaccine is not progressing as it should,” Mr. Biden said, reemphasizing his pledge to get 100 million doses to Americans during his first 100 days as president.
So far, 11.4 million doses have been distributed and 2.1 million people have received a vaccine, according to the Centers for Disease Control and Prevention. Most states have administered a fraction of the doses they’ve received, according to data compiled by The New York Times.
Federal officials have said there’s an “expected lag” between delivery of doses, shots going into arms, and the data being reported to the CDC, according to CNN. The Food and Drug Administration must assess each shipment for quality control, which has slowed down distribution, and the CDC data are just now beginning to include the Moderna vaccine, which the FDA authorized for emergency use on Dec. 18.
The 2.1 million number is “an underestimate,” Brett Giroir, MD, the assistant secretary of the U.S. Department of Health & Human Services, told NBC News Dec. 29. At the same time, the U.S. won’t meet the goal of vaccinating 20 million people in the next few days, he said.
Another 30 million doses will go out in January, Dr. Giroir said, followed by 50 million in February.
Some vaccine experts have said they’re not surprised by the speed of vaccine distribution.
“It had to go this way,” Paul Offit, MD, a professor of pediatrics at Children’s Hospital of Philadelphia, told STAT. “We had to trip and fall and stumble and figure this out.”
To speed up distribution in 2021, the federal government will need to help states, Mr. Biden said Dec. 29. He plans to use the Defense Authorization Act to ramp up production of vaccine supplies. Even still, the process will take months, he said.
A version of this article first appeared on WebMD.com .
Complete blood count scoring can predict COVID-19 severity
A scoring system based on 10 parameters in a complete blood count with differential within 3 days of hospital presentation predict those with COVID-19 who are most likely to progress to critical illness, new evidence shows.
Advantages include prognosis based on a common and inexpensive clinical measure, as well as automatic generation of the score along with CBC results, noted investigators in the observational study conducted throughout 11 European hospitals.
“COVID-19 comes along with specific alterations in circulating blood cells that can be detected by a routine hematology analyzer, especially when that hematology analyzer is also capable to recognize activated immune cells and early circulating blood cells, such as erythroblast and immature granulocytes,” senior author Andre van der Ven, MD, PhD, infectious diseases specialist and professor of international health at Radboud University Medical Center’s Center for Infectious Diseases in Nijmegen, the Netherlands, said in an interview.
Furthermore, Dr. van der Ven said, “these specific changes are also seen in the early course of COVID-19 disease, and more in those that will develop serious disease compared to those with mild disease.”
The study was published online Dec. 21 in the journal eLife.
The study is “almost instinctively correct. It’s basically what clinicians do informally with complete blood count … looking at a combination of results to get the gestalt of what patients are going through,” Samuel Reichberg, MD, PhD, associate medical director of the Northwell Health Core Laboratory in Lake Success, N.Y., said in an interview.
“This is something that begs to be done for COVID-19. I’m surprised no one has done this before,” he added.
Dr. Van der Ven and colleagues created an algorithm based on 1,587 CBC assays from 923 adults. They also validated the scoring system in a second cohort of 217 CBC measurements in 202 people. The findings were concordant – the score accurately predicted the need for critical care within 14 days in 70.5% of the development cohort and 72% of the validation group.
The scoring system was superior to any of the 10 parameters alone. Over 14 days, the majority of those classified as noncritical within the first 3 days remained clinically stable, whereas the “clinical illness” group progressed. Clinical severity peaked on day 6.
Most previous COVID-19 prognosis research was geographically limited, carried a high risk for bias and/or did not validate the findings, Dr. Van der Ven and colleagues noted.
Early identification, early intervention
The aim of the score is “to assist with objective risk stratification to support patient management decision-making early on, and thus facilitate timely interventions, such as need for ICU or not, before symptoms of severe illness become clinically overt, with the intention to improve patient outcomes, and not to predict mortality,” the investigators noted.
Dr. Van der Ven and colleagues developed the score based on adults presenting from Feb. 21 to April 6, with outcomes followed until June 9. Median age of the 982 patients was 71 years and approximately two-thirds were men. They used a Sysmex Europe XN-1000 (Hamburg, Germany) hemocytometric analyzer in the study.
Only 7% of this cohort was not admitted to a hospital. Another 74% were admitted to a general ward and the remaining 19% were transferred directly to the ICU.
The scoring system includes parameters for neutrophils, monocytes, red blood cells and immature granulocytes, and when available, reticulocyte and iron bioavailability measures.
The researchers report significant differences over time in the neutrophil-to-lymphocyte ratio between the critical illness and noncritical groups (P < .001), for example. They also found significant differences in hemoglobin levels between cohorts after day 5.
The system generates a score from 0 to 28. Sensitivity for correctly predicting the need for critical care increased from 62% on day 1 to 93% on day 6.
A more objective assessment of risk
The study demonstrated that SARS-CoV-2 infection is characterized by hemocytometric changes over time. These changes, reflected together in the prognostic score, could aid in the early identification of patients whose clinical course is more likely to deteriorate over time.
The findings also support other work that shows men are more likely to present to the hospital with COVID-19, and that older age and presence of comorbidities add to overall risk. “However,” the researchers noted, “not all young patients had a mild course, and not all old patients with comorbidities were critical.”
Therefore, the prognostic score can help identify patients at risk for severe progression outside other risk factors and “support individualized treatment decisions with objective data,” they added.
Dr. Reichberg called the concept of combining CBC parameters into one score “very valuable.” However, he added that incorporating an index into clinical practice “has historically been tricky.”
The results “probably have to be replicated,” Dr. Reichberg said.
He added that it is likely a CBC-based score will be combined with other measures. “I would like to see an index that combines all the tests we do [for COVID-19], including complete blood count.”
Dr. Van der Ven shared the next step in his research. “The algorithm should be installed on the hematology analyzers so the prognostic score will be automatically generated if a full blood count is asked for in a COVID-19 patient,” he said. “So implementation of score is the main focus now.”
Dr. van der Ven disclosed an ad hoc consultancy agreement with Sysmex Europe. Sysmex Europe provided the reagents in the study free of charge; no other funders were involved. Dr. Reichberg has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A scoring system based on 10 parameters in a complete blood count with differential within 3 days of hospital presentation predict those with COVID-19 who are most likely to progress to critical illness, new evidence shows.
Advantages include prognosis based on a common and inexpensive clinical measure, as well as automatic generation of the score along with CBC results, noted investigators in the observational study conducted throughout 11 European hospitals.
“COVID-19 comes along with specific alterations in circulating blood cells that can be detected by a routine hematology analyzer, especially when that hematology analyzer is also capable to recognize activated immune cells and early circulating blood cells, such as erythroblast and immature granulocytes,” senior author Andre van der Ven, MD, PhD, infectious diseases specialist and professor of international health at Radboud University Medical Center’s Center for Infectious Diseases in Nijmegen, the Netherlands, said in an interview.
Furthermore, Dr. van der Ven said, “these specific changes are also seen in the early course of COVID-19 disease, and more in those that will develop serious disease compared to those with mild disease.”
The study was published online Dec. 21 in the journal eLife.
The study is “almost instinctively correct. It’s basically what clinicians do informally with complete blood count … looking at a combination of results to get the gestalt of what patients are going through,” Samuel Reichberg, MD, PhD, associate medical director of the Northwell Health Core Laboratory in Lake Success, N.Y., said in an interview.
“This is something that begs to be done for COVID-19. I’m surprised no one has done this before,” he added.
Dr. Van der Ven and colleagues created an algorithm based on 1,587 CBC assays from 923 adults. They also validated the scoring system in a second cohort of 217 CBC measurements in 202 people. The findings were concordant – the score accurately predicted the need for critical care within 14 days in 70.5% of the development cohort and 72% of the validation group.
The scoring system was superior to any of the 10 parameters alone. Over 14 days, the majority of those classified as noncritical within the first 3 days remained clinically stable, whereas the “clinical illness” group progressed. Clinical severity peaked on day 6.
Most previous COVID-19 prognosis research was geographically limited, carried a high risk for bias and/or did not validate the findings, Dr. Van der Ven and colleagues noted.
Early identification, early intervention
The aim of the score is “to assist with objective risk stratification to support patient management decision-making early on, and thus facilitate timely interventions, such as need for ICU or not, before symptoms of severe illness become clinically overt, with the intention to improve patient outcomes, and not to predict mortality,” the investigators noted.
Dr. Van der Ven and colleagues developed the score based on adults presenting from Feb. 21 to April 6, with outcomes followed until June 9. Median age of the 982 patients was 71 years and approximately two-thirds were men. They used a Sysmex Europe XN-1000 (Hamburg, Germany) hemocytometric analyzer in the study.
Only 7% of this cohort was not admitted to a hospital. Another 74% were admitted to a general ward and the remaining 19% were transferred directly to the ICU.
The scoring system includes parameters for neutrophils, monocytes, red blood cells and immature granulocytes, and when available, reticulocyte and iron bioavailability measures.
The researchers report significant differences over time in the neutrophil-to-lymphocyte ratio between the critical illness and noncritical groups (P < .001), for example. They also found significant differences in hemoglobin levels between cohorts after day 5.
The system generates a score from 0 to 28. Sensitivity for correctly predicting the need for critical care increased from 62% on day 1 to 93% on day 6.
A more objective assessment of risk
The study demonstrated that SARS-CoV-2 infection is characterized by hemocytometric changes over time. These changes, reflected together in the prognostic score, could aid in the early identification of patients whose clinical course is more likely to deteriorate over time.
The findings also support other work that shows men are more likely to present to the hospital with COVID-19, and that older age and presence of comorbidities add to overall risk. “However,” the researchers noted, “not all young patients had a mild course, and not all old patients with comorbidities were critical.”
Therefore, the prognostic score can help identify patients at risk for severe progression outside other risk factors and “support individualized treatment decisions with objective data,” they added.
Dr. Reichberg called the concept of combining CBC parameters into one score “very valuable.” However, he added that incorporating an index into clinical practice “has historically been tricky.”
The results “probably have to be replicated,” Dr. Reichberg said.
He added that it is likely a CBC-based score will be combined with other measures. “I would like to see an index that combines all the tests we do [for COVID-19], including complete blood count.”
Dr. Van der Ven shared the next step in his research. “The algorithm should be installed on the hematology analyzers so the prognostic score will be automatically generated if a full blood count is asked for in a COVID-19 patient,” he said. “So implementation of score is the main focus now.”
Dr. van der Ven disclosed an ad hoc consultancy agreement with Sysmex Europe. Sysmex Europe provided the reagents in the study free of charge; no other funders were involved. Dr. Reichberg has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A scoring system based on 10 parameters in a complete blood count with differential within 3 days of hospital presentation predict those with COVID-19 who are most likely to progress to critical illness, new evidence shows.
Advantages include prognosis based on a common and inexpensive clinical measure, as well as automatic generation of the score along with CBC results, noted investigators in the observational study conducted throughout 11 European hospitals.
“COVID-19 comes along with specific alterations in circulating blood cells that can be detected by a routine hematology analyzer, especially when that hematology analyzer is also capable to recognize activated immune cells and early circulating blood cells, such as erythroblast and immature granulocytes,” senior author Andre van der Ven, MD, PhD, infectious diseases specialist and professor of international health at Radboud University Medical Center’s Center for Infectious Diseases in Nijmegen, the Netherlands, said in an interview.
Furthermore, Dr. van der Ven said, “these specific changes are also seen in the early course of COVID-19 disease, and more in those that will develop serious disease compared to those with mild disease.”
The study was published online Dec. 21 in the journal eLife.
The study is “almost instinctively correct. It’s basically what clinicians do informally with complete blood count … looking at a combination of results to get the gestalt of what patients are going through,” Samuel Reichberg, MD, PhD, associate medical director of the Northwell Health Core Laboratory in Lake Success, N.Y., said in an interview.
“This is something that begs to be done for COVID-19. I’m surprised no one has done this before,” he added.
Dr. Van der Ven and colleagues created an algorithm based on 1,587 CBC assays from 923 adults. They also validated the scoring system in a second cohort of 217 CBC measurements in 202 people. The findings were concordant – the score accurately predicted the need for critical care within 14 days in 70.5% of the development cohort and 72% of the validation group.
The scoring system was superior to any of the 10 parameters alone. Over 14 days, the majority of those classified as noncritical within the first 3 days remained clinically stable, whereas the “clinical illness” group progressed. Clinical severity peaked on day 6.
Most previous COVID-19 prognosis research was geographically limited, carried a high risk for bias and/or did not validate the findings, Dr. Van der Ven and colleagues noted.
Early identification, early intervention
The aim of the score is “to assist with objective risk stratification to support patient management decision-making early on, and thus facilitate timely interventions, such as need for ICU or not, before symptoms of severe illness become clinically overt, with the intention to improve patient outcomes, and not to predict mortality,” the investigators noted.
Dr. Van der Ven and colleagues developed the score based on adults presenting from Feb. 21 to April 6, with outcomes followed until June 9. Median age of the 982 patients was 71 years and approximately two-thirds were men. They used a Sysmex Europe XN-1000 (Hamburg, Germany) hemocytometric analyzer in the study.
Only 7% of this cohort was not admitted to a hospital. Another 74% were admitted to a general ward and the remaining 19% were transferred directly to the ICU.
The scoring system includes parameters for neutrophils, monocytes, red blood cells and immature granulocytes, and when available, reticulocyte and iron bioavailability measures.
The researchers report significant differences over time in the neutrophil-to-lymphocyte ratio between the critical illness and noncritical groups (P < .001), for example. They also found significant differences in hemoglobin levels between cohorts after day 5.
The system generates a score from 0 to 28. Sensitivity for correctly predicting the need for critical care increased from 62% on day 1 to 93% on day 6.
A more objective assessment of risk
The study demonstrated that SARS-CoV-2 infection is characterized by hemocytometric changes over time. These changes, reflected together in the prognostic score, could aid in the early identification of patients whose clinical course is more likely to deteriorate over time.
The findings also support other work that shows men are more likely to present to the hospital with COVID-19, and that older age and presence of comorbidities add to overall risk. “However,” the researchers noted, “not all young patients had a mild course, and not all old patients with comorbidities were critical.”
Therefore, the prognostic score can help identify patients at risk for severe progression outside other risk factors and “support individualized treatment decisions with objective data,” they added.
Dr. Reichberg called the concept of combining CBC parameters into one score “very valuable.” However, he added that incorporating an index into clinical practice “has historically been tricky.”
The results “probably have to be replicated,” Dr. Reichberg said.
He added that it is likely a CBC-based score will be combined with other measures. “I would like to see an index that combines all the tests we do [for COVID-19], including complete blood count.”
Dr. Van der Ven shared the next step in his research. “The algorithm should be installed on the hematology analyzers so the prognostic score will be automatically generated if a full blood count is asked for in a COVID-19 patient,” he said. “So implementation of score is the main focus now.”
Dr. van der Ven disclosed an ad hoc consultancy agreement with Sysmex Europe. Sysmex Europe provided the reagents in the study free of charge; no other funders were involved. Dr. Reichberg has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
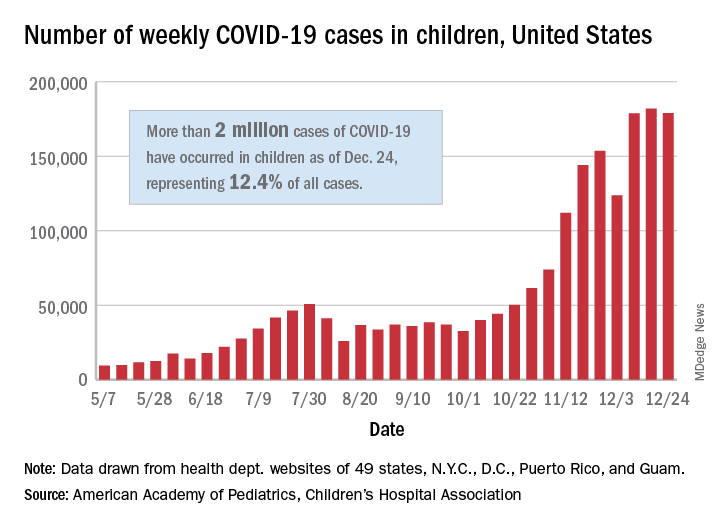
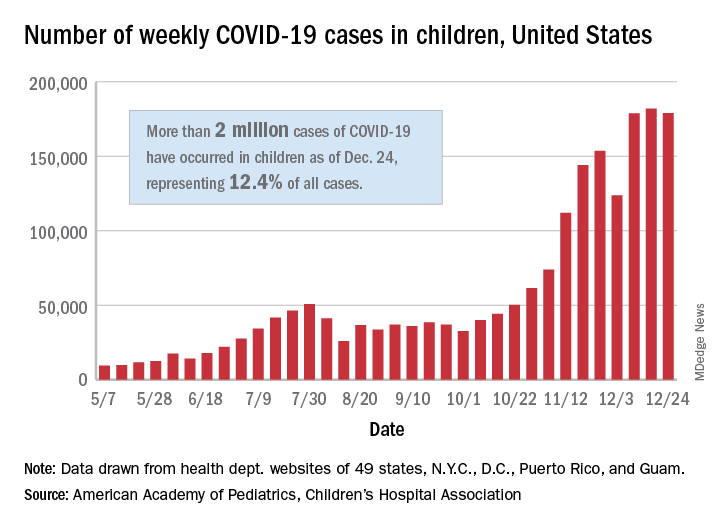
New pediatric cases down as U.S. tops 2 million children with COVID-19
The United States exceeded 2 million reported cases of COVID-19 in children just 6 weeks after recording its 1 millionth case, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
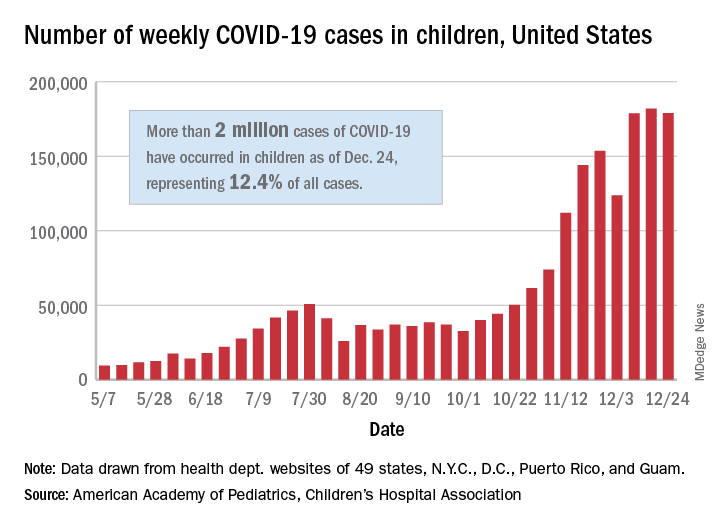
The total number of cases in children was 2,000,681 as of Dec. 24, which represents 12.4% of all cases reported by the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA stated Dec. 29.
The case count for just the latest week, 178,935, was actually down 1.7% from the 182,018 reported the week before, marking the second drop since the beginning of December. The first came during the week ending Dec. 3, when the number of cases dropped more than 19% from the previous week, based on data from the AAP/CHA report.
The cumulative national rate of coronavirus infection is now 2,658 cases per 100,000 children, and “13 states have reported more than 4,000 cases per 100,000,” the two groups said.
The highest rate for any state can be found in North Dakota, which has had 7,722 cases of COVID-19 per 100,000 children. Wyoming has the highest proportion of cases in children at 20.5%, and California has reported the most cases overall, 234,174, the report shows.
Data on testing, hospitalization, and mortality were not included in the Dec. 29 report because of the holiday but will be available in the next edition, scheduled for release on Jan. 5, 2021.
The United States exceeded 2 million reported cases of COVID-19 in children just 6 weeks after recording its 1 millionth case, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The total number of cases in children was 2,000,681 as of Dec. 24, which represents 12.4% of all cases reported by the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA stated Dec. 29.
The case count for just the latest week, 178,935, was actually down 1.7% from the 182,018 reported the week before, marking the second drop since the beginning of December. The first came during the week ending Dec. 3, when the number of cases dropped more than 19% from the previous week, based on data from the AAP/CHA report.
The cumulative national rate of coronavirus infection is now 2,658 cases per 100,000 children, and “13 states have reported more than 4,000 cases per 100,000,” the two groups said.
The highest rate for any state can be found in North Dakota, which has had 7,722 cases of COVID-19 per 100,000 children. Wyoming has the highest proportion of cases in children at 20.5%, and California has reported the most cases overall, 234,174, the report shows.
Data on testing, hospitalization, and mortality were not included in the Dec. 29 report because of the holiday but will be available in the next edition, scheduled for release on Jan. 5, 2021.
The United States exceeded 2 million reported cases of COVID-19 in children just 6 weeks after recording its 1 millionth case, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
The total number of cases in children was 2,000,681 as of Dec. 24, which represents 12.4% of all cases reported by the health departments of 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam, the AAP and CHA stated Dec. 29.
The case count for just the latest week, 178,935, was actually down 1.7% from the 182,018 reported the week before, marking the second drop since the beginning of December. The first came during the week ending Dec. 3, when the number of cases dropped more than 19% from the previous week, based on data from the AAP/CHA report.
The cumulative national rate of coronavirus infection is now 2,658 cases per 100,000 children, and “13 states have reported more than 4,000 cases per 100,000,” the two groups said.
The highest rate for any state can be found in North Dakota, which has had 7,722 cases of COVID-19 per 100,000 children. Wyoming has the highest proportion of cases in children at 20.5%, and California has reported the most cases overall, 234,174, the report shows.
Data on testing, hospitalization, and mortality were not included in the Dec. 29 report because of the holiday but will be available in the next edition, scheduled for release on Jan. 5, 2021.
2.1 Million COVID Vaccine Doses Given in U.S.
The U.S. has distributed more than 11.4 million doses of the Pfizer and Moderna COVID-19 vaccines, and more than 2.1 million of those had been given to people as of December 28, according to the CDC.
The CDC’s COVID Data Tracker showed the updated numbers as of 9 a.m. on that day. The distribution total is based on the CDC’s Vaccine Tracking System, and the administered total is based on reports from state and local public health departments, as well as updates from five federal agencies: the Bureau of Prisons, Veterans Administration, Department of Defense, Department of State, and Indian Health Services.
Health care providers report to public health agencies up to 72 hours after the vaccine is given, and public health agencies report to the CDC after that, so there may be a lag in the data. The CDC’s numbers will be updated on Mondays, Wednesdays, and Fridays.
“A large difference between the number of doses distributed and the number of doses administered is expected at this point in the COVID vaccination program due to several factors,” the CDC says.
Delays could occur due to the reporting of doses given, how states and local vaccine sites are managing vaccines, and the pending launch of vaccination through the federal Pharmacy Partnership for Long-Term Care Program.
“Numbers reported on other websites may differ from what is posted on CDC’s website because CDC’s overall numbers are validated through a data submission process with each jurisdiction,” the CDC says.
On Dec. 26, the agency’s tally showed that 9.5 million doses had been distributed and 1.9 million had been given, according to Reuters.
Public health officials and health care workers have begun to voice their concerns about the delay in giving the vaccines.
“We certainly are not at the numbers that we wanted to be at the end of December,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNNDec. 29.
Operation Warp Speed had planned for 20 million people to be vaccinated by the end of the year. Fauci said he hopes that number will be achieved next month.
“I believe that as we get into January, we are going to see an increase in the momentum,” he said.
Shipment delays have affected other priority groups as well. The New York Police Department anticipated a rollout Dec. 29, but it’s now been delayed since the department hasn’t received enough Moderna doses to start giving the shots, according to the New York Daily News.
“We’ve made numerous attempts to get updated information, and when we get further word on its availability, we will immediately keep our members appraised of the new date and the method of distribution,” Paul DiGiacomo, president of the Detectives’ Endowment Association, wrote in a memo to members on Dec. 28.
“Every detective squad has been crushed with [COVID-19],” he told the newspaper. “Within the last couple of weeks, we’ve had at least two detectives hospitalized.”
President-elect Joe Biden will receive a briefing from his COVID-19 advisory team, provide a general update on the pandemic, and describe his own plan for vaccinating people quickly during an address Dec. 29, a transition official told Axios. Biden has pledged to administer 100 million vaccine doses in his first 100 days in office.
A version of this article originally appeared on WebMd.
The U.S. has distributed more than 11.4 million doses of the Pfizer and Moderna COVID-19 vaccines, and more than 2.1 million of those had been given to people as of December 28, according to the CDC.
The CDC’s COVID Data Tracker showed the updated numbers as of 9 a.m. on that day. The distribution total is based on the CDC’s Vaccine Tracking System, and the administered total is based on reports from state and local public health departments, as well as updates from five federal agencies: the Bureau of Prisons, Veterans Administration, Department of Defense, Department of State, and Indian Health Services.
Health care providers report to public health agencies up to 72 hours after the vaccine is given, and public health agencies report to the CDC after that, so there may be a lag in the data. The CDC’s numbers will be updated on Mondays, Wednesdays, and Fridays.
“A large difference between the number of doses distributed and the number of doses administered is expected at this point in the COVID vaccination program due to several factors,” the CDC says.
Delays could occur due to the reporting of doses given, how states and local vaccine sites are managing vaccines, and the pending launch of vaccination through the federal Pharmacy Partnership for Long-Term Care Program.
“Numbers reported on other websites may differ from what is posted on CDC’s website because CDC’s overall numbers are validated through a data submission process with each jurisdiction,” the CDC says.
On Dec. 26, the agency’s tally showed that 9.5 million doses had been distributed and 1.9 million had been given, according to Reuters.
Public health officials and health care workers have begun to voice their concerns about the delay in giving the vaccines.
“We certainly are not at the numbers that we wanted to be at the end of December,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNNDec. 29.
Operation Warp Speed had planned for 20 million people to be vaccinated by the end of the year. Fauci said he hopes that number will be achieved next month.
“I believe that as we get into January, we are going to see an increase in the momentum,” he said.
Shipment delays have affected other priority groups as well. The New York Police Department anticipated a rollout Dec. 29, but it’s now been delayed since the department hasn’t received enough Moderna doses to start giving the shots, according to the New York Daily News.
“We’ve made numerous attempts to get updated information, and when we get further word on its availability, we will immediately keep our members appraised of the new date and the method of distribution,” Paul DiGiacomo, president of the Detectives’ Endowment Association, wrote in a memo to members on Dec. 28.
“Every detective squad has been crushed with [COVID-19],” he told the newspaper. “Within the last couple of weeks, we’ve had at least two detectives hospitalized.”
President-elect Joe Biden will receive a briefing from his COVID-19 advisory team, provide a general update on the pandemic, and describe his own plan for vaccinating people quickly during an address Dec. 29, a transition official told Axios. Biden has pledged to administer 100 million vaccine doses in his first 100 days in office.
A version of this article originally appeared on WebMd.
The U.S. has distributed more than 11.4 million doses of the Pfizer and Moderna COVID-19 vaccines, and more than 2.1 million of those had been given to people as of December 28, according to the CDC.
The CDC’s COVID Data Tracker showed the updated numbers as of 9 a.m. on that day. The distribution total is based on the CDC’s Vaccine Tracking System, and the administered total is based on reports from state and local public health departments, as well as updates from five federal agencies: the Bureau of Prisons, Veterans Administration, Department of Defense, Department of State, and Indian Health Services.
Health care providers report to public health agencies up to 72 hours after the vaccine is given, and public health agencies report to the CDC after that, so there may be a lag in the data. The CDC’s numbers will be updated on Mondays, Wednesdays, and Fridays.
“A large difference between the number of doses distributed and the number of doses administered is expected at this point in the COVID vaccination program due to several factors,” the CDC says.
Delays could occur due to the reporting of doses given, how states and local vaccine sites are managing vaccines, and the pending launch of vaccination through the federal Pharmacy Partnership for Long-Term Care Program.
“Numbers reported on other websites may differ from what is posted on CDC’s website because CDC’s overall numbers are validated through a data submission process with each jurisdiction,” the CDC says.
On Dec. 26, the agency’s tally showed that 9.5 million doses had been distributed and 1.9 million had been given, according to Reuters.
Public health officials and health care workers have begun to voice their concerns about the delay in giving the vaccines.
“We certainly are not at the numbers that we wanted to be at the end of December,” Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told CNNDec. 29.
Operation Warp Speed had planned for 20 million people to be vaccinated by the end of the year. Fauci said he hopes that number will be achieved next month.
“I believe that as we get into January, we are going to see an increase in the momentum,” he said.
Shipment delays have affected other priority groups as well. The New York Police Department anticipated a rollout Dec. 29, but it’s now been delayed since the department hasn’t received enough Moderna doses to start giving the shots, according to the New York Daily News.
“We’ve made numerous attempts to get updated information, and when we get further word on its availability, we will immediately keep our members appraised of the new date and the method of distribution,” Paul DiGiacomo, president of the Detectives’ Endowment Association, wrote in a memo to members on Dec. 28.
“Every detective squad has been crushed with [COVID-19],” he told the newspaper. “Within the last couple of weeks, we’ve had at least two detectives hospitalized.”
President-elect Joe Biden will receive a briefing from his COVID-19 advisory team, provide a general update on the pandemic, and describe his own plan for vaccinating people quickly during an address Dec. 29, a transition official told Axios. Biden has pledged to administer 100 million vaccine doses in his first 100 days in office.
A version of this article originally appeared on WebMd.
CDC issues COVID-19 vaccine guidance for underlying conditions
The Centers for Disease Control and Prevention has issued updated guidance for people with underlying medical conditions who are considering getting the coronavirus vaccine.
“Adults of any age with certain underlying medical conditions are at increased risk for severe illness from the virus that causes COVID-19,” the CDC said in the guidance, posted on Dec. 26. “mRNA COVID-19 vaccines may be administered to people with underlying medical conditions provided they have not had a severe allergic reaction to any of the ingredients in the vaccine.”
Both the Pfizer and Moderna vaccines use mRNA, or messenger RNA.
The CDC guidance had specific information for people with HIV, weakened immune systems, and autoimmune conditions such as Guillain-Barré syndrome (GBS) and Bell’s palsy who are thinking of getting the vaccine.
People with HIV and weakened immune systems “may receive a COVID-19 vaccine. However, they should be aware of the limited safety data,” the CDC said.
There’s no information available yet about the safety of the vaccines for people with weakened immune systems. People with HIV were included in clinical trials, but “safety data specific to this group are not yet available at this time,” the CDC said.
Cases of Bell’s palsy, a temporary facial paralysis, were reported in people receiving the Pfizer and Moderna vaccines in clinical trials, the Food and Drug Administration said Dec. 17.
But the new CDC guidance said that the FDA “does not consider these to be above the rate expected in the general population. They have not concluded these cases were caused by vaccination. Therefore, persons who have previously had Bell’s palsy may receive an mRNA COVID-19 vaccine.”
Researchers have determined the vaccines are safe for people with GBS, a rare autoimmune disorder in which the body’s immune system attacks nerves just as they leave the spinal cord, the CDC said.
“To date, no cases of GBS have been reported following vaccination among participants in the mRNA COVID-19 vaccine clinical trials,” the CDC guidance said. “With few exceptions, the independent Advisory Committee on Immunization Practices general best practice guidelines for immunization do not include a history of GBS as a precaution to vaccination with other vaccines.”
For months, the CDC and other health authorities have said that people with certain medical conditions are at an increased risk of developing severe cases of COVID-19.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention has issued updated guidance for people with underlying medical conditions who are considering getting the coronavirus vaccine.
“Adults of any age with certain underlying medical conditions are at increased risk for severe illness from the virus that causes COVID-19,” the CDC said in the guidance, posted on Dec. 26. “mRNA COVID-19 vaccines may be administered to people with underlying medical conditions provided they have not had a severe allergic reaction to any of the ingredients in the vaccine.”
Both the Pfizer and Moderna vaccines use mRNA, or messenger RNA.
The CDC guidance had specific information for people with HIV, weakened immune systems, and autoimmune conditions such as Guillain-Barré syndrome (GBS) and Bell’s palsy who are thinking of getting the vaccine.
People with HIV and weakened immune systems “may receive a COVID-19 vaccine. However, they should be aware of the limited safety data,” the CDC said.
There’s no information available yet about the safety of the vaccines for people with weakened immune systems. People with HIV were included in clinical trials, but “safety data specific to this group are not yet available at this time,” the CDC said.
Cases of Bell’s palsy, a temporary facial paralysis, were reported in people receiving the Pfizer and Moderna vaccines in clinical trials, the Food and Drug Administration said Dec. 17.
But the new CDC guidance said that the FDA “does not consider these to be above the rate expected in the general population. They have not concluded these cases were caused by vaccination. Therefore, persons who have previously had Bell’s palsy may receive an mRNA COVID-19 vaccine.”
Researchers have determined the vaccines are safe for people with GBS, a rare autoimmune disorder in which the body’s immune system attacks nerves just as they leave the spinal cord, the CDC said.
“To date, no cases of GBS have been reported following vaccination among participants in the mRNA COVID-19 vaccine clinical trials,” the CDC guidance said. “With few exceptions, the independent Advisory Committee on Immunization Practices general best practice guidelines for immunization do not include a history of GBS as a precaution to vaccination with other vaccines.”
For months, the CDC and other health authorities have said that people with certain medical conditions are at an increased risk of developing severe cases of COVID-19.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention has issued updated guidance for people with underlying medical conditions who are considering getting the coronavirus vaccine.
“Adults of any age with certain underlying medical conditions are at increased risk for severe illness from the virus that causes COVID-19,” the CDC said in the guidance, posted on Dec. 26. “mRNA COVID-19 vaccines may be administered to people with underlying medical conditions provided they have not had a severe allergic reaction to any of the ingredients in the vaccine.”
Both the Pfizer and Moderna vaccines use mRNA, or messenger RNA.
The CDC guidance had specific information for people with HIV, weakened immune systems, and autoimmune conditions such as Guillain-Barré syndrome (GBS) and Bell’s palsy who are thinking of getting the vaccine.
People with HIV and weakened immune systems “may receive a COVID-19 vaccine. However, they should be aware of the limited safety data,” the CDC said.
There’s no information available yet about the safety of the vaccines for people with weakened immune systems. People with HIV were included in clinical trials, but “safety data specific to this group are not yet available at this time,” the CDC said.
Cases of Bell’s palsy, a temporary facial paralysis, were reported in people receiving the Pfizer and Moderna vaccines in clinical trials, the Food and Drug Administration said Dec. 17.
But the new CDC guidance said that the FDA “does not consider these to be above the rate expected in the general population. They have not concluded these cases were caused by vaccination. Therefore, persons who have previously had Bell’s palsy may receive an mRNA COVID-19 vaccine.”
Researchers have determined the vaccines are safe for people with GBS, a rare autoimmune disorder in which the body’s immune system attacks nerves just as they leave the spinal cord, the CDC said.
“To date, no cases of GBS have been reported following vaccination among participants in the mRNA COVID-19 vaccine clinical trials,” the CDC guidance said. “With few exceptions, the independent Advisory Committee on Immunization Practices general best practice guidelines for immunization do not include a history of GBS as a precaution to vaccination with other vaccines.”
For months, the CDC and other health authorities have said that people with certain medical conditions are at an increased risk of developing severe cases of COVID-19.
A version of this article first appeared on Medscape.com.
Cancer treatment delays are deadly: 5- and 10-year data
The COVID-19 pandemic has meant delays in cancer screening, diagnosis, and treatment — and a new study shows just how deadly delaying cancer treatment can be.
The study found evidence that longer time to starting treatment after diagnosis was generally associated with higher mortality across several common cancers, most notably for colon and early-stage lung cancer.
“There is a limit to how long we can safely defer treatment for cancer therapies, pandemic or not, which may be shorter than we think,” lead author Eugene Cone, MD, Combined Harvard Program in Urologic Oncology, Massachusetts General Hospital and Brigham & Women’s Hospital, Boston, told Medscape Medical News.
“When you consider that cancer screening may have been delayed during the pandemic, which would further increase the period between developing a disease and getting therapy, timely treatment for cancer has never been more important,” Cone added.
The study was published online December 14 in JAMA Network Open.
The sooner the better
Using the National Cancer Database, Cone and colleagues identified roughly 2.24 million patients diagnosed with nonmetastatic breast (52%), prostate (38%), colon (4%) and non-small cell lung cancer (NSCLC, 6%) between 2004 and 2015. Treatment and outcome data were analyzed from January to March 2020.
The time-to-treatment initiation (TTI) – the interval between cancer diagnosis and receipt of curative-intent therapy – was categorized as 8 to 60 days (reference), 61 to 120 days, 121 to 180 days, and 181 to 365 days. Median TTI was 32 days for breast, 79 days for prostate, 41 days for NSCLC, and 26 days for colon cancer.
All four cancers benefitted to some degree from a short interval between diagnosis and therapy, the researchers found.
Across all four cancers, increasing TTI was generally associated with higher predicted mortality at 5 and 10 years, although the degree varied by cancer type and stage. The most pronounced association between increasing TTI and mortality was observed for colon and lung cancer.
For example, for stage III colon cancer, 5- and 10-year predicted mortality was 38.9% and 54%, respectively, with TTI of 61 to 120 days, and increased to 47.8% and 63.8%, respectively, with TTI of 181 to 365 days.
Each additional 60-day delay was associated with a 3.2% to 6% increase in 5-year mortality for stage III colon cancer and a 0.9% to 4.6% increase for stage I colon cancer, with a longer 10-year time horizon showing larger effect sizes with increasing TTI.
For stage I NSCLC, 5- and 10-year predicted mortality was 47.4% and 72.6%, respectively, with TTI of 61 to 120 days compared with 47.6% and 72.8%, respectively, with TTI of 181 to 365 days.
For stage I NSCLC, there was a 4% to 6.2% absolute increase in 5-year mortality for increased TTI groups compared with the 8- to 60-day reference group, with larger effect sizes on 10-year mortality. The data precluded conclusions about stage II NSCLC.
“For prostate cancer, deferral of treatment by even a few months was associated with a significant impact on mortality,” Cone told Medscape Medical News.
For high-risk prostate cancer, 5- and 10-year predicted mortality was 12.8% and 31.2%, respectively, with TTI of 61-120 days increasing to 14.1% and 33.8%, respectively with TTI at 181-365 days.
For intermediate-risk prostate cancer, 5- and 10-year predicted mortality was 7.4% and 20.4% with TTI of 61-120 days vs 8.3% and 22.6% with TTI at 181-365 days.
The data show all-cause mortality differences of 2.2% at 5 years and 4.6% at 10 years between high-risk prostate cancer patients who were treated expeditiously vs those waiting 4 to 6 months and differences of 0.9% at 5 years and 2.4% at 10 years for similar intermediate-risk patients.
No surprises
Turning to breast cancer, increased TTI was associated with the most negative survival effects for stage II and III breast cancer.
For stage II breast cancer, for example, 5- and 10-year predicted mortality was 17.7% and 30.5%, respectively, with TTI of 61-120 days vs 21.7% and 36.5% with TTI at 181-365 days.
Even for stage I breast cancer patients, there were significant differences in all-cause mortality with delayed definitive therapy, although the effect size is clinically small, the researchers report.
Patients with stage IA or IB breast cancer who were not treated until 61 to 120 days after diagnosis had 1.3% and 2.3% increased mortality at 5 years and 10 years, respectively, and those waiting longer suffered even greater increases in mortality. “As such, our analysis underscores the importance of timely definitive treatment, even for stage I breast cancer,” the authors write.
Charles Shapiro, MD, director of translational breast cancer research for the Mount Sinai Health System, New York City, was not surprised by the data.
The observation that delays in initiating cancer treatment are associated with worse survival is “not new, as delays in primary surgical treatments and chemotherapy for early-stage disease is an adverse prognostic factor for clinical outcomes,” Shapiro told Medscape Medical News.
“The bottom line is primary surgery and the start of chemotherapy should probably occur as soon as clinically feasible,” said Shapiro, who was not involved in the study.
The authors of an accompanying editorial agree.
This study supports avoiding unnecessary treatment delays and prioritizing timely cancer care, even during the COVID-19 pandemic, write Laura Van Metre Baum, MD, Division of Hematology and Oncology, Vanderbilt University, Nashville, Tennessee, and colleagues.
They note, however, that primary care, “the most important conduit for cancer screening and initial evaluation of new symptoms, has been the hardest hit economically and the most subject to profound disruption and restructuring during the current COVID-19 pandemic.
“In many centers, cancer care delivery has been disrupted and nonstandard therapies offered in an effort to minimize exposure of this high-risk group to the virus. The implications in appropriately balancing the urgency of cancer care and the threat of COVID-19 exposure in the pandemic are more complex,” the editorialists conclude.
Cone, Shapiro, and Van Metre Baum have disclosed no relevant financial relationships. This work won first prize in the Commission on Cancer 2020 Cancer Research Paper Competition and was virtually presented at the Commission on Cancer Plenary Session on October 30, 2020.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has meant delays in cancer screening, diagnosis, and treatment — and a new study shows just how deadly delaying cancer treatment can be.
The study found evidence that longer time to starting treatment after diagnosis was generally associated with higher mortality across several common cancers, most notably for colon and early-stage lung cancer.
“There is a limit to how long we can safely defer treatment for cancer therapies, pandemic or not, which may be shorter than we think,” lead author Eugene Cone, MD, Combined Harvard Program in Urologic Oncology, Massachusetts General Hospital and Brigham & Women’s Hospital, Boston, told Medscape Medical News.
“When you consider that cancer screening may have been delayed during the pandemic, which would further increase the period between developing a disease and getting therapy, timely treatment for cancer has never been more important,” Cone added.
The study was published online December 14 in JAMA Network Open.
The sooner the better
Using the National Cancer Database, Cone and colleagues identified roughly 2.24 million patients diagnosed with nonmetastatic breast (52%), prostate (38%), colon (4%) and non-small cell lung cancer (NSCLC, 6%) between 2004 and 2015. Treatment and outcome data were analyzed from January to March 2020.
The time-to-treatment initiation (TTI) – the interval between cancer diagnosis and receipt of curative-intent therapy – was categorized as 8 to 60 days (reference), 61 to 120 days, 121 to 180 days, and 181 to 365 days. Median TTI was 32 days for breast, 79 days for prostate, 41 days for NSCLC, and 26 days for colon cancer.
All four cancers benefitted to some degree from a short interval between diagnosis and therapy, the researchers found.
Across all four cancers, increasing TTI was generally associated with higher predicted mortality at 5 and 10 years, although the degree varied by cancer type and stage. The most pronounced association between increasing TTI and mortality was observed for colon and lung cancer.
For example, for stage III colon cancer, 5- and 10-year predicted mortality was 38.9% and 54%, respectively, with TTI of 61 to 120 days, and increased to 47.8% and 63.8%, respectively, with TTI of 181 to 365 days.
Each additional 60-day delay was associated with a 3.2% to 6% increase in 5-year mortality for stage III colon cancer and a 0.9% to 4.6% increase for stage I colon cancer, with a longer 10-year time horizon showing larger effect sizes with increasing TTI.
For stage I NSCLC, 5- and 10-year predicted mortality was 47.4% and 72.6%, respectively, with TTI of 61 to 120 days compared with 47.6% and 72.8%, respectively, with TTI of 181 to 365 days.
For stage I NSCLC, there was a 4% to 6.2% absolute increase in 5-year mortality for increased TTI groups compared with the 8- to 60-day reference group, with larger effect sizes on 10-year mortality. The data precluded conclusions about stage II NSCLC.
“For prostate cancer, deferral of treatment by even a few months was associated with a significant impact on mortality,” Cone told Medscape Medical News.
For high-risk prostate cancer, 5- and 10-year predicted mortality was 12.8% and 31.2%, respectively, with TTI of 61-120 days increasing to 14.1% and 33.8%, respectively with TTI at 181-365 days.
For intermediate-risk prostate cancer, 5- and 10-year predicted mortality was 7.4% and 20.4% with TTI of 61-120 days vs 8.3% and 22.6% with TTI at 181-365 days.
The data show all-cause mortality differences of 2.2% at 5 years and 4.6% at 10 years between high-risk prostate cancer patients who were treated expeditiously vs those waiting 4 to 6 months and differences of 0.9% at 5 years and 2.4% at 10 years for similar intermediate-risk patients.
No surprises
Turning to breast cancer, increased TTI was associated with the most negative survival effects for stage II and III breast cancer.
For stage II breast cancer, for example, 5- and 10-year predicted mortality was 17.7% and 30.5%, respectively, with TTI of 61-120 days vs 21.7% and 36.5% with TTI at 181-365 days.
Even for stage I breast cancer patients, there were significant differences in all-cause mortality with delayed definitive therapy, although the effect size is clinically small, the researchers report.
Patients with stage IA or IB breast cancer who were not treated until 61 to 120 days after diagnosis had 1.3% and 2.3% increased mortality at 5 years and 10 years, respectively, and those waiting longer suffered even greater increases in mortality. “As such, our analysis underscores the importance of timely definitive treatment, even for stage I breast cancer,” the authors write.
Charles Shapiro, MD, director of translational breast cancer research for the Mount Sinai Health System, New York City, was not surprised by the data.
The observation that delays in initiating cancer treatment are associated with worse survival is “not new, as delays in primary surgical treatments and chemotherapy for early-stage disease is an adverse prognostic factor for clinical outcomes,” Shapiro told Medscape Medical News.
“The bottom line is primary surgery and the start of chemotherapy should probably occur as soon as clinically feasible,” said Shapiro, who was not involved in the study.
The authors of an accompanying editorial agree.
This study supports avoiding unnecessary treatment delays and prioritizing timely cancer care, even during the COVID-19 pandemic, write Laura Van Metre Baum, MD, Division of Hematology and Oncology, Vanderbilt University, Nashville, Tennessee, and colleagues.
They note, however, that primary care, “the most important conduit for cancer screening and initial evaluation of new symptoms, has been the hardest hit economically and the most subject to profound disruption and restructuring during the current COVID-19 pandemic.
“In many centers, cancer care delivery has been disrupted and nonstandard therapies offered in an effort to minimize exposure of this high-risk group to the virus. The implications in appropriately balancing the urgency of cancer care and the threat of COVID-19 exposure in the pandemic are more complex,” the editorialists conclude.
Cone, Shapiro, and Van Metre Baum have disclosed no relevant financial relationships. This work won first prize in the Commission on Cancer 2020 Cancer Research Paper Competition and was virtually presented at the Commission on Cancer Plenary Session on October 30, 2020.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has meant delays in cancer screening, diagnosis, and treatment — and a new study shows just how deadly delaying cancer treatment can be.
The study found evidence that longer time to starting treatment after diagnosis was generally associated with higher mortality across several common cancers, most notably for colon and early-stage lung cancer.
“There is a limit to how long we can safely defer treatment for cancer therapies, pandemic or not, which may be shorter than we think,” lead author Eugene Cone, MD, Combined Harvard Program in Urologic Oncology, Massachusetts General Hospital and Brigham & Women’s Hospital, Boston, told Medscape Medical News.
“When you consider that cancer screening may have been delayed during the pandemic, which would further increase the period between developing a disease and getting therapy, timely treatment for cancer has never been more important,” Cone added.
The study was published online December 14 in JAMA Network Open.
The sooner the better
Using the National Cancer Database, Cone and colleagues identified roughly 2.24 million patients diagnosed with nonmetastatic breast (52%), prostate (38%), colon (4%) and non-small cell lung cancer (NSCLC, 6%) between 2004 and 2015. Treatment and outcome data were analyzed from January to March 2020.
The time-to-treatment initiation (TTI) – the interval between cancer diagnosis and receipt of curative-intent therapy – was categorized as 8 to 60 days (reference), 61 to 120 days, 121 to 180 days, and 181 to 365 days. Median TTI was 32 days for breast, 79 days for prostate, 41 days for NSCLC, and 26 days for colon cancer.
All four cancers benefitted to some degree from a short interval between diagnosis and therapy, the researchers found.
Across all four cancers, increasing TTI was generally associated with higher predicted mortality at 5 and 10 years, although the degree varied by cancer type and stage. The most pronounced association between increasing TTI and mortality was observed for colon and lung cancer.
For example, for stage III colon cancer, 5- and 10-year predicted mortality was 38.9% and 54%, respectively, with TTI of 61 to 120 days, and increased to 47.8% and 63.8%, respectively, with TTI of 181 to 365 days.
Each additional 60-day delay was associated with a 3.2% to 6% increase in 5-year mortality for stage III colon cancer and a 0.9% to 4.6% increase for stage I colon cancer, with a longer 10-year time horizon showing larger effect sizes with increasing TTI.
For stage I NSCLC, 5- and 10-year predicted mortality was 47.4% and 72.6%, respectively, with TTI of 61 to 120 days compared with 47.6% and 72.8%, respectively, with TTI of 181 to 365 days.
For stage I NSCLC, there was a 4% to 6.2% absolute increase in 5-year mortality for increased TTI groups compared with the 8- to 60-day reference group, with larger effect sizes on 10-year mortality. The data precluded conclusions about stage II NSCLC.
“For prostate cancer, deferral of treatment by even a few months was associated with a significant impact on mortality,” Cone told Medscape Medical News.
For high-risk prostate cancer, 5- and 10-year predicted mortality was 12.8% and 31.2%, respectively, with TTI of 61-120 days increasing to 14.1% and 33.8%, respectively with TTI at 181-365 days.
For intermediate-risk prostate cancer, 5- and 10-year predicted mortality was 7.4% and 20.4% with TTI of 61-120 days vs 8.3% and 22.6% with TTI at 181-365 days.
The data show all-cause mortality differences of 2.2% at 5 years and 4.6% at 10 years between high-risk prostate cancer patients who were treated expeditiously vs those waiting 4 to 6 months and differences of 0.9% at 5 years and 2.4% at 10 years for similar intermediate-risk patients.
No surprises
Turning to breast cancer, increased TTI was associated with the most negative survival effects for stage II and III breast cancer.
For stage II breast cancer, for example, 5- and 10-year predicted mortality was 17.7% and 30.5%, respectively, with TTI of 61-120 days vs 21.7% and 36.5% with TTI at 181-365 days.
Even for stage I breast cancer patients, there were significant differences in all-cause mortality with delayed definitive therapy, although the effect size is clinically small, the researchers report.
Patients with stage IA or IB breast cancer who were not treated until 61 to 120 days after diagnosis had 1.3% and 2.3% increased mortality at 5 years and 10 years, respectively, and those waiting longer suffered even greater increases in mortality. “As such, our analysis underscores the importance of timely definitive treatment, even for stage I breast cancer,” the authors write.
Charles Shapiro, MD, director of translational breast cancer research for the Mount Sinai Health System, New York City, was not surprised by the data.
The observation that delays in initiating cancer treatment are associated with worse survival is “not new, as delays in primary surgical treatments and chemotherapy for early-stage disease is an adverse prognostic factor for clinical outcomes,” Shapiro told Medscape Medical News.
“The bottom line is primary surgery and the start of chemotherapy should probably occur as soon as clinically feasible,” said Shapiro, who was not involved in the study.
The authors of an accompanying editorial agree.
This study supports avoiding unnecessary treatment delays and prioritizing timely cancer care, even during the COVID-19 pandemic, write Laura Van Metre Baum, MD, Division of Hematology and Oncology, Vanderbilt University, Nashville, Tennessee, and colleagues.
They note, however, that primary care, “the most important conduit for cancer screening and initial evaluation of new symptoms, has been the hardest hit economically and the most subject to profound disruption and restructuring during the current COVID-19 pandemic.
“In many centers, cancer care delivery has been disrupted and nonstandard therapies offered in an effort to minimize exposure of this high-risk group to the virus. The implications in appropriately balancing the urgency of cancer care and the threat of COVID-19 exposure in the pandemic are more complex,” the editorialists conclude.
Cone, Shapiro, and Van Metre Baum have disclosed no relevant financial relationships. This work won first prize in the Commission on Cancer 2020 Cancer Research Paper Competition and was virtually presented at the Commission on Cancer Plenary Session on October 30, 2020.
A version of this article first appeared on Medscape.com.
Scant risk for SARS-CoV-2 from hospital air
Everywhere they look within hospitals, researchers find RNA from SARS-CoV-2 in the air. But viable viruses typically are found only close to patients, according to a review of published studies.
The finding supports recommendations to use surgical masks in most parts of the hospital, reserving respirators (such as N95 or FFP2) for aerosol-generating procedures on patients’ respiratory tracts, said Gabriel Birgand, PhD, an infectious disease researcher at Imperial College London.
“When the virus is spreading a lot in the community, it’s probably more likely for you to be contaminated in your friends’ areas or in your building than in your work area, where you are well equipped and compliant with all the measures,” he said in an interview. “So it’s pretty good news.”
The systematic review by Dr. Birgand and colleagues was published in JAMA Network Open.
Recommended precautions to protect health care workers from SARS-CoV-2 infections remain controversial. Most authorities believe droplets are the primary route of transmission, which would mean surgical masks may be sufficient protection. But some research has suggested transmission by aerosols as well, making N95 respirators seem necessary. There is even disagreement about the definitions of the words “aerosol” and “droplet.”
To better understand where traces of the virus can be found in the air in hospitals, Dr. Birgand and colleagues analyzed all the studies they could find on the subject in English.
They identified 24 articles with original data. All of the studies used reverse transcription–polymerase chain reaction (PCR) tests to identify SARS-CoV-2 RNA. In five studies, attempts were also made to culture viable viruses. Three studies assessed the particle size relative to RNA concentration or viral titer.
Of 893 air samples across the 24 studies, 52.7% were taken from areas close to patients, 26.5% were taken in clinical areas, 13.7% in staff areas, 4.7% in public areas, and 2.4% in toilets or bathrooms.
Among those studies that quantified RNA, the median interquartile range of concentrations varied from 1.0 x 103 copies/m3 in clinical areas to 9.7 x 103 copies/m3 in toilets or bathrooms.
One study found an RNA concentration of 2.0 x 103 copies for particle sizes >4 mcm and 1.3 x 103 copies/m3 for particle sizes ≤4 mcm, both in patients’ rooms.
Three studies included viral cultures; of those, two resulted in positive cultures, both in a non-ICU setting. In one study, 3 of 39 samples were positive, and in the other, 4 of 4 were positive. Viral cultures in toilets, clinical areas, staff areas, and public areas were negative.
One of these studies assessed viral concentration and found that the median interquartile range was 4.8 tissue culture infectious dose (TCID50)/m3 for particles <1 mcm, 4.27 TCID50/m3 for particles 1-4 mcm, and 1.82 TCID50/m3 for particles >4 mcm.
Although viable viruses weren’t found in staff areas, the presence of viral RNA in places such as dining rooms and meeting rooms raises a concern, Dr. Birgand said.
“All of these staff areas are probably playing an important role in contamination,” he said. “It’s pretty easy to see when you are dining, you are not wearing a face mask, and it’s associated with a strong risk when there is a strong dissemination of the virus in the community.”
Studies on contact tracing among health care workers have also identified meeting rooms and dining rooms as the second most common source of infection after community contact, he said.
In general, the findings of the review correspond to epidemiologic studies, said Angela Rasmussen, PhD, a virologist with the Georgetown University Center for Global Health Science and Security, Washington, who was not involved in the review. “Absent aerosol-generating procedures, health care workers are largely not getting infected when they take droplet precautions.”
One reason may be that patients shed the most infectious viruses a couple of days before and after symptoms begin. By the time they’re hospitalized, they’re less likely to be contagious but may continue to shed viral RNA.
“We don’t really know the basis for the persistence of RNA being produced long after people have been infected and have recovered from the acute infection,” she said, “but it has been observed quite frequently.”
Although the virus cannot remain viable for very long in the air, remnants may still be detected in the form of RNA, Dr. Rasmussen said. In addition, hospitals often do a good job of ventilation.
She pointed out that it can be difficult to cultivate viruses in air samples because of contaminants such as bacteria and fungi. “That’s one of the limitations of a study like this. You’re not really sure if it’s because there’s no viable virus there or because you just aren’t able to collect samples that would allow you to determine that.”
Dr. Birgand and colleagues acknowledged other limitations. The studies they reviewed used different approaches to sampling. Different procedures may have been underway in the rooms being sampled, and factors such as temperature and humidity could have affected the results. In addition, the studies used different cycle thresholds for PCR positivity.
A version of this article first appeared on Medscape.com.
Everywhere they look within hospitals, researchers find RNA from SARS-CoV-2 in the air. But viable viruses typically are found only close to patients, according to a review of published studies.
The finding supports recommendations to use surgical masks in most parts of the hospital, reserving respirators (such as N95 or FFP2) for aerosol-generating procedures on patients’ respiratory tracts, said Gabriel Birgand, PhD, an infectious disease researcher at Imperial College London.
“When the virus is spreading a lot in the community, it’s probably more likely for you to be contaminated in your friends’ areas or in your building than in your work area, where you are well equipped and compliant with all the measures,” he said in an interview. “So it’s pretty good news.”
The systematic review by Dr. Birgand and colleagues was published in JAMA Network Open.
Recommended precautions to protect health care workers from SARS-CoV-2 infections remain controversial. Most authorities believe droplets are the primary route of transmission, which would mean surgical masks may be sufficient protection. But some research has suggested transmission by aerosols as well, making N95 respirators seem necessary. There is even disagreement about the definitions of the words “aerosol” and “droplet.”
To better understand where traces of the virus can be found in the air in hospitals, Dr. Birgand and colleagues analyzed all the studies they could find on the subject in English.
They identified 24 articles with original data. All of the studies used reverse transcription–polymerase chain reaction (PCR) tests to identify SARS-CoV-2 RNA. In five studies, attempts were also made to culture viable viruses. Three studies assessed the particle size relative to RNA concentration or viral titer.
Of 893 air samples across the 24 studies, 52.7% were taken from areas close to patients, 26.5% were taken in clinical areas, 13.7% in staff areas, 4.7% in public areas, and 2.4% in toilets or bathrooms.
Among those studies that quantified RNA, the median interquartile range of concentrations varied from 1.0 x 103 copies/m3 in clinical areas to 9.7 x 103 copies/m3 in toilets or bathrooms.
One study found an RNA concentration of 2.0 x 103 copies for particle sizes >4 mcm and 1.3 x 103 copies/m3 for particle sizes ≤4 mcm, both in patients’ rooms.
Three studies included viral cultures; of those, two resulted in positive cultures, both in a non-ICU setting. In one study, 3 of 39 samples were positive, and in the other, 4 of 4 were positive. Viral cultures in toilets, clinical areas, staff areas, and public areas were negative.
One of these studies assessed viral concentration and found that the median interquartile range was 4.8 tissue culture infectious dose (TCID50)/m3 for particles <1 mcm, 4.27 TCID50/m3 for particles 1-4 mcm, and 1.82 TCID50/m3 for particles >4 mcm.
Although viable viruses weren’t found in staff areas, the presence of viral RNA in places such as dining rooms and meeting rooms raises a concern, Dr. Birgand said.
“All of these staff areas are probably playing an important role in contamination,” he said. “It’s pretty easy to see when you are dining, you are not wearing a face mask, and it’s associated with a strong risk when there is a strong dissemination of the virus in the community.”
Studies on contact tracing among health care workers have also identified meeting rooms and dining rooms as the second most common source of infection after community contact, he said.
In general, the findings of the review correspond to epidemiologic studies, said Angela Rasmussen, PhD, a virologist with the Georgetown University Center for Global Health Science and Security, Washington, who was not involved in the review. “Absent aerosol-generating procedures, health care workers are largely not getting infected when they take droplet precautions.”
One reason may be that patients shed the most infectious viruses a couple of days before and after symptoms begin. By the time they’re hospitalized, they’re less likely to be contagious but may continue to shed viral RNA.
“We don’t really know the basis for the persistence of RNA being produced long after people have been infected and have recovered from the acute infection,” she said, “but it has been observed quite frequently.”
Although the virus cannot remain viable for very long in the air, remnants may still be detected in the form of RNA, Dr. Rasmussen said. In addition, hospitals often do a good job of ventilation.
She pointed out that it can be difficult to cultivate viruses in air samples because of contaminants such as bacteria and fungi. “That’s one of the limitations of a study like this. You’re not really sure if it’s because there’s no viable virus there or because you just aren’t able to collect samples that would allow you to determine that.”
Dr. Birgand and colleagues acknowledged other limitations. The studies they reviewed used different approaches to sampling. Different procedures may have been underway in the rooms being sampled, and factors such as temperature and humidity could have affected the results. In addition, the studies used different cycle thresholds for PCR positivity.
A version of this article first appeared on Medscape.com.
Everywhere they look within hospitals, researchers find RNA from SARS-CoV-2 in the air. But viable viruses typically are found only close to patients, according to a review of published studies.
The finding supports recommendations to use surgical masks in most parts of the hospital, reserving respirators (such as N95 or FFP2) for aerosol-generating procedures on patients’ respiratory tracts, said Gabriel Birgand, PhD, an infectious disease researcher at Imperial College London.
“When the virus is spreading a lot in the community, it’s probably more likely for you to be contaminated in your friends’ areas or in your building than in your work area, where you are well equipped and compliant with all the measures,” he said in an interview. “So it’s pretty good news.”
The systematic review by Dr. Birgand and colleagues was published in JAMA Network Open.
Recommended precautions to protect health care workers from SARS-CoV-2 infections remain controversial. Most authorities believe droplets are the primary route of transmission, which would mean surgical masks may be sufficient protection. But some research has suggested transmission by aerosols as well, making N95 respirators seem necessary. There is even disagreement about the definitions of the words “aerosol” and “droplet.”
To better understand where traces of the virus can be found in the air in hospitals, Dr. Birgand and colleagues analyzed all the studies they could find on the subject in English.
They identified 24 articles with original data. All of the studies used reverse transcription–polymerase chain reaction (PCR) tests to identify SARS-CoV-2 RNA. In five studies, attempts were also made to culture viable viruses. Three studies assessed the particle size relative to RNA concentration or viral titer.
Of 893 air samples across the 24 studies, 52.7% were taken from areas close to patients, 26.5% were taken in clinical areas, 13.7% in staff areas, 4.7% in public areas, and 2.4% in toilets or bathrooms.
Among those studies that quantified RNA, the median interquartile range of concentrations varied from 1.0 x 103 copies/m3 in clinical areas to 9.7 x 103 copies/m3 in toilets or bathrooms.
One study found an RNA concentration of 2.0 x 103 copies for particle sizes >4 mcm and 1.3 x 103 copies/m3 for particle sizes ≤4 mcm, both in patients’ rooms.
Three studies included viral cultures; of those, two resulted in positive cultures, both in a non-ICU setting. In one study, 3 of 39 samples were positive, and in the other, 4 of 4 were positive. Viral cultures in toilets, clinical areas, staff areas, and public areas were negative.
One of these studies assessed viral concentration and found that the median interquartile range was 4.8 tissue culture infectious dose (TCID50)/m3 for particles <1 mcm, 4.27 TCID50/m3 for particles 1-4 mcm, and 1.82 TCID50/m3 for particles >4 mcm.
Although viable viruses weren’t found in staff areas, the presence of viral RNA in places such as dining rooms and meeting rooms raises a concern, Dr. Birgand said.
“All of these staff areas are probably playing an important role in contamination,” he said. “It’s pretty easy to see when you are dining, you are not wearing a face mask, and it’s associated with a strong risk when there is a strong dissemination of the virus in the community.”
Studies on contact tracing among health care workers have also identified meeting rooms and dining rooms as the second most common source of infection after community contact, he said.
In general, the findings of the review correspond to epidemiologic studies, said Angela Rasmussen, PhD, a virologist with the Georgetown University Center for Global Health Science and Security, Washington, who was not involved in the review. “Absent aerosol-generating procedures, health care workers are largely not getting infected when they take droplet precautions.”
One reason may be that patients shed the most infectious viruses a couple of days before and after symptoms begin. By the time they’re hospitalized, they’re less likely to be contagious but may continue to shed viral RNA.
“We don’t really know the basis for the persistence of RNA being produced long after people have been infected and have recovered from the acute infection,” she said, “but it has been observed quite frequently.”
Although the virus cannot remain viable for very long in the air, remnants may still be detected in the form of RNA, Dr. Rasmussen said. In addition, hospitals often do a good job of ventilation.
She pointed out that it can be difficult to cultivate viruses in air samples because of contaminants such as bacteria and fungi. “That’s one of the limitations of a study like this. You’re not really sure if it’s because there’s no viable virus there or because you just aren’t able to collect samples that would allow you to determine that.”
Dr. Birgand and colleagues acknowledged other limitations. The studies they reviewed used different approaches to sampling. Different procedures may have been underway in the rooms being sampled, and factors such as temperature and humidity could have affected the results. In addition, the studies used different cycle thresholds for PCR positivity.
A version of this article first appeared on Medscape.com.
Does daily inhaler monitoring improve asthma outcomes in children?
Among children with moderate or severe persistent asthma, a randomized trial suggests.
But the intervention also may lead to more ED visits and increased hospitalization rates.
“We improved asthma symptom control but did not reduce health care use,” Ruchi S. Gupta, MD, MPH, and colleagues, wrote in a study published in Pediatrics.
The monitoring system alerted clinicians when a patient used a short-acting beta-agonist more than four times in a day. It could be that the “alerts enabled providers to detect asthma exacerbation virtually and refer for clinically appropriate care that included directing children to the ED,” the authors suggested. It also is possible that the intervention led caregivers to be more vigilant about symptoms and more empowered to seek care.
Adherence to preventive regimens
Many patients with asthma need to use preventive medications such as daily inhaled corticosteroids to control symptoms. Researchers have developed sensor-based inhaler monitoring interventions to improve treatment adherence, but the effectiveness of these interventions in improving asthma outcomes in urban and minority populations is unclear.
To assess the effectiveness of a clinically integrated, sensor-based inhaler monitoring intervention on improving asthma symptom control and related outcomes in children, Dr. Gupta, of Northwestern University and Ann & Robert H. Lurie Children’s Hospital of Chicago, and colleagues conducted a randomized, unblinded study, known as the Improving Technology-Assisted Recording of Asthma Control in Children (iTRACC) trial. They included 252 children: 127 in the control group and 125 in the intervention group.
Patients in the intervention group received Propeller Health’s Food and Drug Administration–cleared inhaler sensors for inhaled corticosteroids and short-acting beta-agonists. Caregivers could use a mobile application and clinicians could use a Web portal to track patients’ medication use. The app featured personalized insights, educational content, encouragement, surveys, and care team services.
Researchers recruited caregivers and children from five Chicago clinics for the study, which was conducted between 2016 and 2018. They included children aged 4-17 years who had a prescription for daily inhaled corticosteroids for at least 1 year before enrollment. In addition, participants had at least 1 exacerbation requiring oral corticosteroids in the previous year. They excluded children with other respiratory conditions. They also excluded participants who did not speak English because the app was available only in English.
“Sensors monitored inhaled medication use, capturing the date, time, and number of uses, and transmitted this information via Bluetooth to a paired smartphone and the provider portal in real-time,” the authors said.
Clinicians were alerted to call participants if a patient missed inhaled corticosteroid doses for 4 continuous days or used more than 4 short-acting beta-agonist doses per day. Clinicians could help guide asthma management, schedule an appointment, refill medications, and address technical difficulties with the sensors.
The intervention and control groups had similar baseline characteristics. About one-third of the patients were female, and the mean age was 9.3 years. In the control group, 28% identified as Hispanic, and 33% identified as non-Hispanic Black. In the intervention group, 40% identified as Hispanic, and 23% identified as non-Hispanic Black. About 59% reported Medicaid insurance. The intervention and control arms completed electronic surveys at 1, 3, 6, 9, and 12 months.
Average Asthma Control Test score increased from 19 to 22 in the intervention group, compared with an increase from 19 to 20 in the control group. Adjusted rates of emergency department visits and hospitalizations were greater in the intervention group (incidence rate ratios, 2.2 and 3.4, respectively). A measure of caregiver quality of life was greater in the intervention group, although the difference was not significant.
During the trial, more caregivers in the intervention group reported asthma attacks for which steroids were prescribed by a medical office (73% vs. 35%).
Some participants had to manually enter the number of daily puffs into the app because their inhalers were incompatible with the sensors. In addition, some data were missing because of incomplete or missing survey responses and sensor failure over time. “The number of intervention participants with actively transmitting sensors decreased from 102 at baseline to 56 at 12 months,” Dr. Gupta and associates noted.
Important area of research
“One interesting finding of this study is the increase in health care use in the intervention group to nearly twice as many emergency department (ED) visits and three times as many hospitalizations as the control group over 12 months,” Rachelle R. Ramsey, PhD, and Theresa W. Guilbert, MD, MS, of the University of Cincinnati, wrote in a related commentary. “Although it is plausible that, as the authors suggest, greater asthma knowledge and monitoring may have led to increased vigilance of asthma symptoms, it seems that this would have only led to an increase in ED visits but not hospitalizations.”
The mixture of objective electronic monitoring and subjective self-reported adherence may complicate interpretation of the results, they added.
“Overall, this article underscores the feasibility and importance of sensor-based electronic monitoring of adherence in pediatric asthma and encourages future research in this area,” Dr. Ramsey and Dr. Guilbert said.
The trial was supported by the UnitedHealth Group. Dr. Gupta has received grants from the National Institutes of Health, Rho, and other organizations, and has served as a medical consultant and adviser for a variety of companies. Dr. Ramsey is supported by the NIH. Dr. Guilbert reported fees from the American Board of Pediatrics, the Pediatric Pulmonary Subboard, and some pharmaceutical companies, plus grants from the NIH, grants and personal fees from Sanofi, Regeneron, and AstraZeneca, and royalties from UpToDate.
SOURCE: Gupta RS et al. Pediatrics. 2020 Dec 22. doi: 10.1542/peds.2020-1330.
Among children with moderate or severe persistent asthma, a randomized trial suggests.
But the intervention also may lead to more ED visits and increased hospitalization rates.
“We improved asthma symptom control but did not reduce health care use,” Ruchi S. Gupta, MD, MPH, and colleagues, wrote in a study published in Pediatrics.
The monitoring system alerted clinicians when a patient used a short-acting beta-agonist more than four times in a day. It could be that the “alerts enabled providers to detect asthma exacerbation virtually and refer for clinically appropriate care that included directing children to the ED,” the authors suggested. It also is possible that the intervention led caregivers to be more vigilant about symptoms and more empowered to seek care.
Adherence to preventive regimens
Many patients with asthma need to use preventive medications such as daily inhaled corticosteroids to control symptoms. Researchers have developed sensor-based inhaler monitoring interventions to improve treatment adherence, but the effectiveness of these interventions in improving asthma outcomes in urban and minority populations is unclear.
To assess the effectiveness of a clinically integrated, sensor-based inhaler monitoring intervention on improving asthma symptom control and related outcomes in children, Dr. Gupta, of Northwestern University and Ann & Robert H. Lurie Children’s Hospital of Chicago, and colleagues conducted a randomized, unblinded study, known as the Improving Technology-Assisted Recording of Asthma Control in Children (iTRACC) trial. They included 252 children: 127 in the control group and 125 in the intervention group.
Patients in the intervention group received Propeller Health’s Food and Drug Administration–cleared inhaler sensors for inhaled corticosteroids and short-acting beta-agonists. Caregivers could use a mobile application and clinicians could use a Web portal to track patients’ medication use. The app featured personalized insights, educational content, encouragement, surveys, and care team services.
Researchers recruited caregivers and children from five Chicago clinics for the study, which was conducted between 2016 and 2018. They included children aged 4-17 years who had a prescription for daily inhaled corticosteroids for at least 1 year before enrollment. In addition, participants had at least 1 exacerbation requiring oral corticosteroids in the previous year. They excluded children with other respiratory conditions. They also excluded participants who did not speak English because the app was available only in English.
“Sensors monitored inhaled medication use, capturing the date, time, and number of uses, and transmitted this information via Bluetooth to a paired smartphone and the provider portal in real-time,” the authors said.
Clinicians were alerted to call participants if a patient missed inhaled corticosteroid doses for 4 continuous days or used more than 4 short-acting beta-agonist doses per day. Clinicians could help guide asthma management, schedule an appointment, refill medications, and address technical difficulties with the sensors.
The intervention and control groups had similar baseline characteristics. About one-third of the patients were female, and the mean age was 9.3 years. In the control group, 28% identified as Hispanic, and 33% identified as non-Hispanic Black. In the intervention group, 40% identified as Hispanic, and 23% identified as non-Hispanic Black. About 59% reported Medicaid insurance. The intervention and control arms completed electronic surveys at 1, 3, 6, 9, and 12 months.
Average Asthma Control Test score increased from 19 to 22 in the intervention group, compared with an increase from 19 to 20 in the control group. Adjusted rates of emergency department visits and hospitalizations were greater in the intervention group (incidence rate ratios, 2.2 and 3.4, respectively). A measure of caregiver quality of life was greater in the intervention group, although the difference was not significant.
During the trial, more caregivers in the intervention group reported asthma attacks for which steroids were prescribed by a medical office (73% vs. 35%).
Some participants had to manually enter the number of daily puffs into the app because their inhalers were incompatible with the sensors. In addition, some data were missing because of incomplete or missing survey responses and sensor failure over time. “The number of intervention participants with actively transmitting sensors decreased from 102 at baseline to 56 at 12 months,” Dr. Gupta and associates noted.
Important area of research
“One interesting finding of this study is the increase in health care use in the intervention group to nearly twice as many emergency department (ED) visits and three times as many hospitalizations as the control group over 12 months,” Rachelle R. Ramsey, PhD, and Theresa W. Guilbert, MD, MS, of the University of Cincinnati, wrote in a related commentary. “Although it is plausible that, as the authors suggest, greater asthma knowledge and monitoring may have led to increased vigilance of asthma symptoms, it seems that this would have only led to an increase in ED visits but not hospitalizations.”
The mixture of objective electronic monitoring and subjective self-reported adherence may complicate interpretation of the results, they added.
“Overall, this article underscores the feasibility and importance of sensor-based electronic monitoring of adherence in pediatric asthma and encourages future research in this area,” Dr. Ramsey and Dr. Guilbert said.
The trial was supported by the UnitedHealth Group. Dr. Gupta has received grants from the National Institutes of Health, Rho, and other organizations, and has served as a medical consultant and adviser for a variety of companies. Dr. Ramsey is supported by the NIH. Dr. Guilbert reported fees from the American Board of Pediatrics, the Pediatric Pulmonary Subboard, and some pharmaceutical companies, plus grants from the NIH, grants and personal fees from Sanofi, Regeneron, and AstraZeneca, and royalties from UpToDate.
SOURCE: Gupta RS et al. Pediatrics. 2020 Dec 22. doi: 10.1542/peds.2020-1330.
Among children with moderate or severe persistent asthma, a randomized trial suggests.
But the intervention also may lead to more ED visits and increased hospitalization rates.
“We improved asthma symptom control but did not reduce health care use,” Ruchi S. Gupta, MD, MPH, and colleagues, wrote in a study published in Pediatrics.
The monitoring system alerted clinicians when a patient used a short-acting beta-agonist more than four times in a day. It could be that the “alerts enabled providers to detect asthma exacerbation virtually and refer for clinically appropriate care that included directing children to the ED,” the authors suggested. It also is possible that the intervention led caregivers to be more vigilant about symptoms and more empowered to seek care.
Adherence to preventive regimens
Many patients with asthma need to use preventive medications such as daily inhaled corticosteroids to control symptoms. Researchers have developed sensor-based inhaler monitoring interventions to improve treatment adherence, but the effectiveness of these interventions in improving asthma outcomes in urban and minority populations is unclear.
To assess the effectiveness of a clinically integrated, sensor-based inhaler monitoring intervention on improving asthma symptom control and related outcomes in children, Dr. Gupta, of Northwestern University and Ann & Robert H. Lurie Children’s Hospital of Chicago, and colleagues conducted a randomized, unblinded study, known as the Improving Technology-Assisted Recording of Asthma Control in Children (iTRACC) trial. They included 252 children: 127 in the control group and 125 in the intervention group.
Patients in the intervention group received Propeller Health’s Food and Drug Administration–cleared inhaler sensors for inhaled corticosteroids and short-acting beta-agonists. Caregivers could use a mobile application and clinicians could use a Web portal to track patients’ medication use. The app featured personalized insights, educational content, encouragement, surveys, and care team services.
Researchers recruited caregivers and children from five Chicago clinics for the study, which was conducted between 2016 and 2018. They included children aged 4-17 years who had a prescription for daily inhaled corticosteroids for at least 1 year before enrollment. In addition, participants had at least 1 exacerbation requiring oral corticosteroids in the previous year. They excluded children with other respiratory conditions. They also excluded participants who did not speak English because the app was available only in English.
“Sensors monitored inhaled medication use, capturing the date, time, and number of uses, and transmitted this information via Bluetooth to a paired smartphone and the provider portal in real-time,” the authors said.
Clinicians were alerted to call participants if a patient missed inhaled corticosteroid doses for 4 continuous days or used more than 4 short-acting beta-agonist doses per day. Clinicians could help guide asthma management, schedule an appointment, refill medications, and address technical difficulties with the sensors.
The intervention and control groups had similar baseline characteristics. About one-third of the patients were female, and the mean age was 9.3 years. In the control group, 28% identified as Hispanic, and 33% identified as non-Hispanic Black. In the intervention group, 40% identified as Hispanic, and 23% identified as non-Hispanic Black. About 59% reported Medicaid insurance. The intervention and control arms completed electronic surveys at 1, 3, 6, 9, and 12 months.
Average Asthma Control Test score increased from 19 to 22 in the intervention group, compared with an increase from 19 to 20 in the control group. Adjusted rates of emergency department visits and hospitalizations were greater in the intervention group (incidence rate ratios, 2.2 and 3.4, respectively). A measure of caregiver quality of life was greater in the intervention group, although the difference was not significant.
During the trial, more caregivers in the intervention group reported asthma attacks for which steroids were prescribed by a medical office (73% vs. 35%).
Some participants had to manually enter the number of daily puffs into the app because their inhalers were incompatible with the sensors. In addition, some data were missing because of incomplete or missing survey responses and sensor failure over time. “The number of intervention participants with actively transmitting sensors decreased from 102 at baseline to 56 at 12 months,” Dr. Gupta and associates noted.
Important area of research
“One interesting finding of this study is the increase in health care use in the intervention group to nearly twice as many emergency department (ED) visits and three times as many hospitalizations as the control group over 12 months,” Rachelle R. Ramsey, PhD, and Theresa W. Guilbert, MD, MS, of the University of Cincinnati, wrote in a related commentary. “Although it is plausible that, as the authors suggest, greater asthma knowledge and monitoring may have led to increased vigilance of asthma symptoms, it seems that this would have only led to an increase in ED visits but not hospitalizations.”
The mixture of objective electronic monitoring and subjective self-reported adherence may complicate interpretation of the results, they added.
“Overall, this article underscores the feasibility and importance of sensor-based electronic monitoring of adherence in pediatric asthma and encourages future research in this area,” Dr. Ramsey and Dr. Guilbert said.
The trial was supported by the UnitedHealth Group. Dr. Gupta has received grants from the National Institutes of Health, Rho, and other organizations, and has served as a medical consultant and adviser for a variety of companies. Dr. Ramsey is supported by the NIH. Dr. Guilbert reported fees from the American Board of Pediatrics, the Pediatric Pulmonary Subboard, and some pharmaceutical companies, plus grants from the NIH, grants and personal fees from Sanofi, Regeneron, and AstraZeneca, and royalties from UpToDate.
SOURCE: Gupta RS et al. Pediatrics. 2020 Dec 22. doi: 10.1542/peds.2020-1330.
FROM PEDIATRICS



